User login
Adverse Events and Rural Discharges
The Center on Patient Safety at Florida State University College of Medicine in Tallahassee has been awarded a two-year, $908,000 grant from the federal Agency for Healthcare Research and Quality to study adverse events during the three weeks following hospital discharge, both for urban patients and, for the first time, those returning to rural settings.
Center director Dennis Tsilimingras, MD, MPH, says the project will enroll 600 patients, half urban and half rural, discharged by the Tallahassee Memorial Hospitalist Group, and track injuries resulting from medical errors, including medication errors, procedure-related injuries, nosocomial infections, and pressure ulcers.
Errors or injuries to patients may occur in the hospital but not be identified until after the patient goes home, he says, and such errors could contribute to rehospitalizations. “Our hypothesis is that the rate of adverse events post-discharge may be greater among rural patients because they have less access to follow-up care,” he adds.
Dr. Tsilimingras will be working closely with hospitalists, and Phase 2 of the research will use the hospital’s post-discharge transitional care clinic (see “Is a Post-Discharge Clinic in Your Hospital’s Future?,” December 2011) as an intervention strategy.
The eventual goal is to develop a screening tool to flag risk for post-discharge adverse events and develop strategies to reduce post-discharge problems, including readmissions, a quarter of which may be related to post-discharge adverse events, Dr. Tsilimingras says. He encourages hospitalists to reevaluate their patients and review their charts at the time of discharge, to see if post-discharge problems loom, and to reach out to primary care physicians by telephone, rather than just sending discharge summaries.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Armellino D, Hussain E, Schilling ME, et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare [published online ahead of print Nov. 21, 2011. Clin Infect Dis. doi;10.1093/cid/cir773.
- Fuller C, Savage J, Besser S, et al. “The dirty handin the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32(12):1194-1199.
The Center on Patient Safety at Florida State University College of Medicine in Tallahassee has been awarded a two-year, $908,000 grant from the federal Agency for Healthcare Research and Quality to study adverse events during the three weeks following hospital discharge, both for urban patients and, for the first time, those returning to rural settings.
Center director Dennis Tsilimingras, MD, MPH, says the project will enroll 600 patients, half urban and half rural, discharged by the Tallahassee Memorial Hospitalist Group, and track injuries resulting from medical errors, including medication errors, procedure-related injuries, nosocomial infections, and pressure ulcers.
Errors or injuries to patients may occur in the hospital but not be identified until after the patient goes home, he says, and such errors could contribute to rehospitalizations. “Our hypothesis is that the rate of adverse events post-discharge may be greater among rural patients because they have less access to follow-up care,” he adds.
Dr. Tsilimingras will be working closely with hospitalists, and Phase 2 of the research will use the hospital’s post-discharge transitional care clinic (see “Is a Post-Discharge Clinic in Your Hospital’s Future?,” December 2011) as an intervention strategy.
The eventual goal is to develop a screening tool to flag risk for post-discharge adverse events and develop strategies to reduce post-discharge problems, including readmissions, a quarter of which may be related to post-discharge adverse events, Dr. Tsilimingras says. He encourages hospitalists to reevaluate their patients and review their charts at the time of discharge, to see if post-discharge problems loom, and to reach out to primary care physicians by telephone, rather than just sending discharge summaries.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Armellino D, Hussain E, Schilling ME, et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare [published online ahead of print Nov. 21, 2011. Clin Infect Dis. doi;10.1093/cid/cir773.
- Fuller C, Savage J, Besser S, et al. “The dirty handin the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32(12):1194-1199.
The Center on Patient Safety at Florida State University College of Medicine in Tallahassee has been awarded a two-year, $908,000 grant from the federal Agency for Healthcare Research and Quality to study adverse events during the three weeks following hospital discharge, both for urban patients and, for the first time, those returning to rural settings.
Center director Dennis Tsilimingras, MD, MPH, says the project will enroll 600 patients, half urban and half rural, discharged by the Tallahassee Memorial Hospitalist Group, and track injuries resulting from medical errors, including medication errors, procedure-related injuries, nosocomial infections, and pressure ulcers.
Errors or injuries to patients may occur in the hospital but not be identified until after the patient goes home, he says, and such errors could contribute to rehospitalizations. “Our hypothesis is that the rate of adverse events post-discharge may be greater among rural patients because they have less access to follow-up care,” he adds.
Dr. Tsilimingras will be working closely with hospitalists, and Phase 2 of the research will use the hospital’s post-discharge transitional care clinic (see “Is a Post-Discharge Clinic in Your Hospital’s Future?,” December 2011) as an intervention strategy.
The eventual goal is to develop a screening tool to flag risk for post-discharge adverse events and develop strategies to reduce post-discharge problems, including readmissions, a quarter of which may be related to post-discharge adverse events, Dr. Tsilimingras says. He encourages hospitalists to reevaluate their patients and review their charts at the time of discharge, to see if post-discharge problems loom, and to reach out to primary care physicians by telephone, rather than just sending discharge summaries.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Armellino D, Hussain E, Schilling ME, et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare [published online ahead of print Nov. 21, 2011. Clin Infect Dis. doi;10.1093/cid/cir773.
- Fuller C, Savage J, Besser S, et al. “The dirty handin the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32(12):1194-1199.
Hand Hygiene Makes Headlines
Recent efforts to raise awareness about proper hand hygiene in health facilities in order to prevent disease transmission, range from the ScrubUp! campaign in Ohio to the World Health Organization’s global Clean Care is Safer Care campaign (www.who.int/gpsc/en/), which advocates for improving hand hygiene practices of health care workers around the world.
Twenty hospitals in Central Ohio staged ScrubUp! rallies on Dec. 5, 2011, during National Handwashing Awareness Week, not only to raise awareness of the hospitals’ commitment to hand hygiene, but also to encourage hospital visitors to wash their hands. The Ohio Hospital Association estimates that 50,000 people were exposed to these messages via a full-page ad in the Columbus Dispatch, overhead announcements and distribution tables in each hospital, handing out hand sanitizers to visitors, and engaging staff with humor, food, and prizes.
A recent study conducted at North Shore University Hospital in Manhasset, N.Y., found that hand hygiene compliance rates improve when remote video auditing platforms provide professionals with continuous feedback.1 During 16 weeks of real-time feedback on compliance with strict hand hygiene (i.e. within 10 seconds of entering/leaving patients’ rooms) via LED screens mounted on the walls of a MICU, compliance jumped to more than 80%.
A British study of 7,000 contacts in ICUs and geriatric units found that wearing latex gloves may discourage guideline-recommended hand washing, even though such failures to wash may contribute to spreading disease.2 Compliance was 47.7% without gloves, and 41% with gloves.
One of the study’s authors calls for further study of the behavioral reasons why healthcare workers are less likely to wash their hands when gloved, but urges that hand hygiene associated with gloving be part of educational campaigns.
Recent efforts to raise awareness about proper hand hygiene in health facilities in order to prevent disease transmission, range from the ScrubUp! campaign in Ohio to the World Health Organization’s global Clean Care is Safer Care campaign (www.who.int/gpsc/en/), which advocates for improving hand hygiene practices of health care workers around the world.
Twenty hospitals in Central Ohio staged ScrubUp! rallies on Dec. 5, 2011, during National Handwashing Awareness Week, not only to raise awareness of the hospitals’ commitment to hand hygiene, but also to encourage hospital visitors to wash their hands. The Ohio Hospital Association estimates that 50,000 people were exposed to these messages via a full-page ad in the Columbus Dispatch, overhead announcements and distribution tables in each hospital, handing out hand sanitizers to visitors, and engaging staff with humor, food, and prizes.
A recent study conducted at North Shore University Hospital in Manhasset, N.Y., found that hand hygiene compliance rates improve when remote video auditing platforms provide professionals with continuous feedback.1 During 16 weeks of real-time feedback on compliance with strict hand hygiene (i.e. within 10 seconds of entering/leaving patients’ rooms) via LED screens mounted on the walls of a MICU, compliance jumped to more than 80%.
A British study of 7,000 contacts in ICUs and geriatric units found that wearing latex gloves may discourage guideline-recommended hand washing, even though such failures to wash may contribute to spreading disease.2 Compliance was 47.7% without gloves, and 41% with gloves.
One of the study’s authors calls for further study of the behavioral reasons why healthcare workers are less likely to wash their hands when gloved, but urges that hand hygiene associated with gloving be part of educational campaigns.
Recent efforts to raise awareness about proper hand hygiene in health facilities in order to prevent disease transmission, range from the ScrubUp! campaign in Ohio to the World Health Organization’s global Clean Care is Safer Care campaign (www.who.int/gpsc/en/), which advocates for improving hand hygiene practices of health care workers around the world.
Twenty hospitals in Central Ohio staged ScrubUp! rallies on Dec. 5, 2011, during National Handwashing Awareness Week, not only to raise awareness of the hospitals’ commitment to hand hygiene, but also to encourage hospital visitors to wash their hands. The Ohio Hospital Association estimates that 50,000 people were exposed to these messages via a full-page ad in the Columbus Dispatch, overhead announcements and distribution tables in each hospital, handing out hand sanitizers to visitors, and engaging staff with humor, food, and prizes.
A recent study conducted at North Shore University Hospital in Manhasset, N.Y., found that hand hygiene compliance rates improve when remote video auditing platforms provide professionals with continuous feedback.1 During 16 weeks of real-time feedback on compliance with strict hand hygiene (i.e. within 10 seconds of entering/leaving patients’ rooms) via LED screens mounted on the walls of a MICU, compliance jumped to more than 80%.
A British study of 7,000 contacts in ICUs and geriatric units found that wearing latex gloves may discourage guideline-recommended hand washing, even though such failures to wash may contribute to spreading disease.2 Compliance was 47.7% without gloves, and 41% with gloves.
One of the study’s authors calls for further study of the behavioral reasons why healthcare workers are less likely to wash their hands when gloved, but urges that hand hygiene associated with gloving be part of educational campaigns.
By the Numbers: 57
Percentage of responding physicians who say they are using electronic health records (EHR), according to a survey of 10,000 office-based physicians by the National Center for Health Statistics, up from 51% usage in 2010. More than half say they intend to apply for meaningful use incentives offered by the government for implementing EHR, and 43% of those respondents report having computerized systems meeting Stage 1 Core Set criteria to qualify.
Percentage of responding physicians who say they are using electronic health records (EHR), according to a survey of 10,000 office-based physicians by the National Center for Health Statistics, up from 51% usage in 2010. More than half say they intend to apply for meaningful use incentives offered by the government for implementing EHR, and 43% of those respondents report having computerized systems meeting Stage 1 Core Set criteria to qualify.
Percentage of responding physicians who say they are using electronic health records (EHR), according to a survey of 10,000 office-based physicians by the National Center for Health Statistics, up from 51% usage in 2010. More than half say they intend to apply for meaningful use incentives offered by the government for implementing EHR, and 43% of those respondents report having computerized systems meeting Stage 1 Core Set criteria to qualify.
Resume Red Flags
Fifteen seconds: That’s approximately how long an employer looks at a CV. Recruiters and employers know what they want; they skim even the best resumes. They are on the lookout for applicants who meet their requirements; sometimes they’ll take a chance on a long shot whose pitch catches their eye.
So what happens when a resume stands out for the wrong reasons? Work histories aren’t always perfect, and recruiters and prospective employers will notice any blemishes.
“The thing about red flags is they’re just an indicator that the applicant is an outlier,” says Kim Bell, MD, FACP, SFHM, regional medical director of the Pacific West Region for EmCare, a Dallas-based company that provides outsourced physician services to more than 500 hospitals in 40 states. “It doesn’t necessarily rule them out.”
Preempt Suspicion
For hospitalists, resume imperfections that attract attention include:
- Gaps in employment;
- Frequent changes in employment;
- Changes in residency;
- Medical board sanctions or probation;
- Failures on the board exam; and
- Forced resignations or firings.
—Cheryl O’Malley, MD, FACP, program director, Department of Internal Medicine and Pediatrics, Banner Good Samaritan Medical Center, Phoenix
When recruiters or employers notice a red flag, they look for other problems to see if patterns emerge and to discern if the applicant exhibited bad judgment, has character flaws, or shows an inability to learn from a mistake, says Jeff Kaplan, PhD, MBA, MCC, a licensed psychologist and Philadelphia-based executive coach whose clients include healthcare industry executives. If such signs exist, the applicant is generally eliminated from consideration. Therefore, it’s critical that applicants explain clearly and succinctly the reason for any resume shortcoming.
“A good way is to actually write a cover letter to explain some uniqueness in their CV that they want [recruiters] to understand,” says Alpesh Amin, MD, MBA, FACP, SFHM, professor and chairman of the Department of Medicine and executive director of the hospitalist program at the University of California at Irvine.
By explaining the situation, Dr. Bell says, the hospitalist doesn’t give the employer a chance to guess a reason for the red flag—and potentially guess wrong.
“There’s a big difference between there’s been some sort of serious censure and they’ve been driven out, versus they thought another setting might be more interesting or they just wanted to make a geographic move,” says Thomas E. Thorsheim, PhD, a licensed psychologist and physician leadership coach based in Greenville, S.C. “It’s important to preempt any concerns about how reliable or stable they’re going to be.”
Applicants with resume red flags should show that they’ve taken responsibility for what happened and grown from the experience, say Dr. Thorsheim and Cheryl O’Malley, MD, FACP, program director in the department of internal medicine and pediatrics at Banner Good Samaritan Medical Center in Phoenix.
“Everyone wants to know that you have learned from your mistakes. Try to have a demonstrated remediation of the concern and go above and beyond the minimum requirements,” Dr. O’Malley says. “For example, if the red flag is academic concerns or not passing your board exams, then bring in documentation of your schedule for reading daily and all of the CME and MKSAP you complete. If it is interpersonal issues, then give examples of recent successes that show how you have improved.”
Brand Recognition
Physicians with a resume blemish should concentrate on highlighting their strengths and “branding” themselves as a workplace contributor, says Bernadette Norz, MBA, ACC, a certified physician development coach. While this advice applies to all applicants, it is particularly critical for those with resume problems, as it will demonstrate they have skills that set them apart from others.
“What people are really looking for is what did you do and what was the result,” Norz says. “Things that one accomplished as a volunteer or on a committee count, too, because that’s where people gain a lot of leadership skills.”
Resumes should not be recitations of job descriptions, she advises. They should be lists of achievements described with action verbs that give the applicant a clear identity and brand. “When you read a resume, you should walk away from it knowing who this person is,” says Dr. Kaplan. “If you don’t see that on their resume, then you’ve got to question it.”
The best applicants network. The more you can develop a relationship and rapport with peers and potential employers, the more likely you will be given a greater chance to sell your strengths and explain weaknesses, says career strategist Ellen Dunagan, president of Traverse Management Solutions in Arlington, Va. “You really want to step it up and be much more active with your own pitch,” she says.
Attitude Matters
But before a hospitalist or any applicant with a resume shortcoming begins to look for a job, they must resolve the issue internally, Dr. Kaplan notes. Taking responsibility will allow you to speak clearly and comfortably about what happened, without negativity or blame.
“If you don’t, you will fumble,” he says. “The prospective employer will start seeing those red flags and they will ask you about it, and you thought you had your pitch ready. Then they ask you two more questions, and before you know it, they’re not going to feel a sense of transparency with you.”
More and more, what employers are looking for is positivity, Dunagan says. It’s a trait applicants won’t have if they still harbor negative feelings toward a previous employer. “It’s just very important to be not only a team player, but to have a really good attitude,” she says. “So present yourself in the best possible light.”
Lisa Ryan is a freelance writer based in New Jersey.
Fifteen seconds: That’s approximately how long an employer looks at a CV. Recruiters and employers know what they want; they skim even the best resumes. They are on the lookout for applicants who meet their requirements; sometimes they’ll take a chance on a long shot whose pitch catches their eye.
So what happens when a resume stands out for the wrong reasons? Work histories aren’t always perfect, and recruiters and prospective employers will notice any blemishes.
“The thing about red flags is they’re just an indicator that the applicant is an outlier,” says Kim Bell, MD, FACP, SFHM, regional medical director of the Pacific West Region for EmCare, a Dallas-based company that provides outsourced physician services to more than 500 hospitals in 40 states. “It doesn’t necessarily rule them out.”
Preempt Suspicion
For hospitalists, resume imperfections that attract attention include:
- Gaps in employment;
- Frequent changes in employment;
- Changes in residency;
- Medical board sanctions or probation;
- Failures on the board exam; and
- Forced resignations or firings.
—Cheryl O’Malley, MD, FACP, program director, Department of Internal Medicine and Pediatrics, Banner Good Samaritan Medical Center, Phoenix
When recruiters or employers notice a red flag, they look for other problems to see if patterns emerge and to discern if the applicant exhibited bad judgment, has character flaws, or shows an inability to learn from a mistake, says Jeff Kaplan, PhD, MBA, MCC, a licensed psychologist and Philadelphia-based executive coach whose clients include healthcare industry executives. If such signs exist, the applicant is generally eliminated from consideration. Therefore, it’s critical that applicants explain clearly and succinctly the reason for any resume shortcoming.
“A good way is to actually write a cover letter to explain some uniqueness in their CV that they want [recruiters] to understand,” says Alpesh Amin, MD, MBA, FACP, SFHM, professor and chairman of the Department of Medicine and executive director of the hospitalist program at the University of California at Irvine.
By explaining the situation, Dr. Bell says, the hospitalist doesn’t give the employer a chance to guess a reason for the red flag—and potentially guess wrong.
“There’s a big difference between there’s been some sort of serious censure and they’ve been driven out, versus they thought another setting might be more interesting or they just wanted to make a geographic move,” says Thomas E. Thorsheim, PhD, a licensed psychologist and physician leadership coach based in Greenville, S.C. “It’s important to preempt any concerns about how reliable or stable they’re going to be.”
Applicants with resume red flags should show that they’ve taken responsibility for what happened and grown from the experience, say Dr. Thorsheim and Cheryl O’Malley, MD, FACP, program director in the department of internal medicine and pediatrics at Banner Good Samaritan Medical Center in Phoenix.
“Everyone wants to know that you have learned from your mistakes. Try to have a demonstrated remediation of the concern and go above and beyond the minimum requirements,” Dr. O’Malley says. “For example, if the red flag is academic concerns or not passing your board exams, then bring in documentation of your schedule for reading daily and all of the CME and MKSAP you complete. If it is interpersonal issues, then give examples of recent successes that show how you have improved.”
Brand Recognition
Physicians with a resume blemish should concentrate on highlighting their strengths and “branding” themselves as a workplace contributor, says Bernadette Norz, MBA, ACC, a certified physician development coach. While this advice applies to all applicants, it is particularly critical for those with resume problems, as it will demonstrate they have skills that set them apart from others.
“What people are really looking for is what did you do and what was the result,” Norz says. “Things that one accomplished as a volunteer or on a committee count, too, because that’s where people gain a lot of leadership skills.”
Resumes should not be recitations of job descriptions, she advises. They should be lists of achievements described with action verbs that give the applicant a clear identity and brand. “When you read a resume, you should walk away from it knowing who this person is,” says Dr. Kaplan. “If you don’t see that on their resume, then you’ve got to question it.”
The best applicants network. The more you can develop a relationship and rapport with peers and potential employers, the more likely you will be given a greater chance to sell your strengths and explain weaknesses, says career strategist Ellen Dunagan, president of Traverse Management Solutions in Arlington, Va. “You really want to step it up and be much more active with your own pitch,” she says.
Attitude Matters
But before a hospitalist or any applicant with a resume shortcoming begins to look for a job, they must resolve the issue internally, Dr. Kaplan notes. Taking responsibility will allow you to speak clearly and comfortably about what happened, without negativity or blame.
“If you don’t, you will fumble,” he says. “The prospective employer will start seeing those red flags and they will ask you about it, and you thought you had your pitch ready. Then they ask you two more questions, and before you know it, they’re not going to feel a sense of transparency with you.”
More and more, what employers are looking for is positivity, Dunagan says. It’s a trait applicants won’t have if they still harbor negative feelings toward a previous employer. “It’s just very important to be not only a team player, but to have a really good attitude,” she says. “So present yourself in the best possible light.”
Lisa Ryan is a freelance writer based in New Jersey.
Fifteen seconds: That’s approximately how long an employer looks at a CV. Recruiters and employers know what they want; they skim even the best resumes. They are on the lookout for applicants who meet their requirements; sometimes they’ll take a chance on a long shot whose pitch catches their eye.
So what happens when a resume stands out for the wrong reasons? Work histories aren’t always perfect, and recruiters and prospective employers will notice any blemishes.
“The thing about red flags is they’re just an indicator that the applicant is an outlier,” says Kim Bell, MD, FACP, SFHM, regional medical director of the Pacific West Region for EmCare, a Dallas-based company that provides outsourced physician services to more than 500 hospitals in 40 states. “It doesn’t necessarily rule them out.”
Preempt Suspicion
For hospitalists, resume imperfections that attract attention include:
- Gaps in employment;
- Frequent changes in employment;
- Changes in residency;
- Medical board sanctions or probation;
- Failures on the board exam; and
- Forced resignations or firings.
—Cheryl O’Malley, MD, FACP, program director, Department of Internal Medicine and Pediatrics, Banner Good Samaritan Medical Center, Phoenix
When recruiters or employers notice a red flag, they look for other problems to see if patterns emerge and to discern if the applicant exhibited bad judgment, has character flaws, or shows an inability to learn from a mistake, says Jeff Kaplan, PhD, MBA, MCC, a licensed psychologist and Philadelphia-based executive coach whose clients include healthcare industry executives. If such signs exist, the applicant is generally eliminated from consideration. Therefore, it’s critical that applicants explain clearly and succinctly the reason for any resume shortcoming.
“A good way is to actually write a cover letter to explain some uniqueness in their CV that they want [recruiters] to understand,” says Alpesh Amin, MD, MBA, FACP, SFHM, professor and chairman of the Department of Medicine and executive director of the hospitalist program at the University of California at Irvine.
By explaining the situation, Dr. Bell says, the hospitalist doesn’t give the employer a chance to guess a reason for the red flag—and potentially guess wrong.
“There’s a big difference between there’s been some sort of serious censure and they’ve been driven out, versus they thought another setting might be more interesting or they just wanted to make a geographic move,” says Thomas E. Thorsheim, PhD, a licensed psychologist and physician leadership coach based in Greenville, S.C. “It’s important to preempt any concerns about how reliable or stable they’re going to be.”
Applicants with resume red flags should show that they’ve taken responsibility for what happened and grown from the experience, say Dr. Thorsheim and Cheryl O’Malley, MD, FACP, program director in the department of internal medicine and pediatrics at Banner Good Samaritan Medical Center in Phoenix.
“Everyone wants to know that you have learned from your mistakes. Try to have a demonstrated remediation of the concern and go above and beyond the minimum requirements,” Dr. O’Malley says. “For example, if the red flag is academic concerns or not passing your board exams, then bring in documentation of your schedule for reading daily and all of the CME and MKSAP you complete. If it is interpersonal issues, then give examples of recent successes that show how you have improved.”
Brand Recognition
Physicians with a resume blemish should concentrate on highlighting their strengths and “branding” themselves as a workplace contributor, says Bernadette Norz, MBA, ACC, a certified physician development coach. While this advice applies to all applicants, it is particularly critical for those with resume problems, as it will demonstrate they have skills that set them apart from others.
“What people are really looking for is what did you do and what was the result,” Norz says. “Things that one accomplished as a volunteer or on a committee count, too, because that’s where people gain a lot of leadership skills.”
Resumes should not be recitations of job descriptions, she advises. They should be lists of achievements described with action verbs that give the applicant a clear identity and brand. “When you read a resume, you should walk away from it knowing who this person is,” says Dr. Kaplan. “If you don’t see that on their resume, then you’ve got to question it.”
The best applicants network. The more you can develop a relationship and rapport with peers and potential employers, the more likely you will be given a greater chance to sell your strengths and explain weaknesses, says career strategist Ellen Dunagan, president of Traverse Management Solutions in Arlington, Va. “You really want to step it up and be much more active with your own pitch,” she says.
Attitude Matters
But before a hospitalist or any applicant with a resume shortcoming begins to look for a job, they must resolve the issue internally, Dr. Kaplan notes. Taking responsibility will allow you to speak clearly and comfortably about what happened, without negativity or blame.
“If you don’t, you will fumble,” he says. “The prospective employer will start seeing those red flags and they will ask you about it, and you thought you had your pitch ready. Then they ask you two more questions, and before you know it, they’re not going to feel a sense of transparency with you.”
More and more, what employers are looking for is positivity, Dunagan says. It’s a trait applicants won’t have if they still harbor negative feelings toward a previous employer. “It’s just very important to be not only a team player, but to have a really good attitude,” she says. “So present yourself in the best possible light.”
Lisa Ryan is a freelance writer based in New Jersey.
Medical Decision-Making Factors Include Quantity of Information, Complexity
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
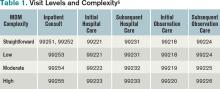
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
IPAB is Medicare's New Hammer for Spending Accountability
Now that the latest annual “doc fix” is in, physicians have been granted another reprieve from potentially crippling cuts to their Medicare reimbursement under the flawed sustainable growth rate (SGR) payment formula.
Beginning this year, there’s a new player in town that will have the authority to achieve what Congress has consistently failed to do—cut Medicare provider spending to keep it below a cap—and it can do so with unprecedented autonomy.
Say hello to the Independent Payment Advisory Board (IPAB), a creature of the Affordable Care Act (ACA) that will propose ways to reduce “overpayment” to Medicare providers if target-spending levels are exceeded.
What distinguishes the IPAB from the Medicare Payment Advisory Commission (MedPAC) is that its proposals will automatically become law, unless Congress enacts its own proposals that reduce Medicare provider spending by at least as much as IPAB’s, or the Senate musters a three-fifths majority vote to override IPAB’s proposals entirely. Further, the IPAB’s changes to Medicare cannot be overruled by the executive branch or a court of law.
MedPAC never wielded such authority; in fact, many of its cost-control recommendations were ignored.

—Judith Feder, PhD, professor of public policy, Georgetown University, Washington, D.C., former dean, Georgetown Public Policy Institute, fellow, the Urban Institute
The IPAB comes to life this year, with a $15 million appropriation from the ACA, and begins ramping up its operations (see “The IPAB Timetable,” p. 26). The board will be comprised of a 15-member, multi-stakeholder group—expected to include physicians, nurses, medical experts, economists, consumer advocates, and others—appointed by the President and subject to Senate confirmation.
Incendiary Reactions
Dubbed by its most vociferous and largely Republican critics as “dangerously powerful,” “the real death panel,” and “bureaucrats deciding whether you get care,” the IPAB even has some Democrats decrying its power grab. Rep. Pete Stark (D-Calif.) called the IPAB “an unprecedented abrogation of Congressional authority to an unelected, unaccountable body of so-called experts.”1
Even Allyson Schwartz (D-Pa.), who helped draft the ACA, has come out against the IPAB, joining a handful of Democrats and more than 200 Republicans in signing on to a bill (H.R. 452) to repeal the ACA’s IPAB provision. The Senate has a similar bill (S. 668).
Although the IPAB legally is barred from formally making recommendations to ration care, increase beneficiary premiums or cost sharing, and from restricting benefits or eligibility criteria, critics worry that its authority to control prices could hurt patients by driving Medicare payments so low that physicians cease to offer certain services to them.
Enforcement Power
IPAB will have unprecedented power to enforce Medicare’s provider spending benchmarks. Beginning in 2014, if Medicare’s projected spending growth rate per beneficiary rises above an inflation threshold of Gross Domestic Product per capita plus 1%, the IPAB would be triggered and would propose ways to trim provider payments. President Obama has since proposed a lower threshold of GDP per capita plus 0.5%, meaning that the IPAB would be triggered earlier and likely would have deeper cuts to make.
It is unclear how the spending growth benchmark will be affected by the $123 billion in Medicare payment cuts to hospitals and other providers over nine years, which were triggered when the so-called “super committee” failed to reach a budget-cutting consensus last fall.
U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius describes the IPAB as a “backstop to ensure that rising costs don’t accelerate out of control, threatening Medicare’s stability,” and she maintains that the board is a necessary fallback mechanism to enforce Medicare spending within budget while healthcare providers continue to prove the effectiveness of various value-based delivery and reimbursement reform projects the ACA is funding.2
Impact on Physicians
“The IPAB is a structural intervention to put pressure on Congress, the Executive, and CMS [Centers for Medicare & Medicaid Services] to guarantee the ACA’s investment in cost-containment, and it gives physicians the incentive to act on its principles,” says Judith Feder, PhD, professor of public policy at Georgetown University, former dean of the Georgetown Public Policy Institute, and a fellow at the Urban Institute.
Dr. Feder was a co-signer of a letter sent by 100 health policy experts and economists—including Congressional Budget Office founding director Alice Rivlin, now with the Brookings Institute—to congressional leaders last May urging them to abandon attempts to repeal the IPAB provision. Dr. Feder maintains that the IPAB will marshal “the expertise of professionals who can weigh evidence on how payment incentives affect care delivery and suggest sensible improvements, while forcing debate on difficult choices that Congress has thus far failed to address.”
Because of the changes the ACA has already made to provider reimbursement and Medicare Advantage plan funding, Feder says that Medicare’s average annual growth rate for the next decade is projected to be a full percentage point below per capita growth in GDP. On top of that, she says, “the ACA’s other payment reform experiments have the potential to improve quality and cut spending growth even further by reducing payment for overpriced or undesirable care–like unnecessary hospital readmissions–and rewarding efficiently provided, coordinated care.” By Feder’s analysis, the IPAB would not likely be triggered for a decade, but stands ready as a backup, if needed. Indeed, she favors extending IPAB’s authority beyond Medicare, to allow a system-wide spending target that creates an all-payer incentive to assure that providers really change their behavior to boost quality and efficiency.
Impact on Hospitalists
If the IPAB does come into play, Feder believes that hospitalists have less to worry about than other physician specialists, because the Board’s cost-reduction proposals would likely focus on services where overpayment is the most acute – like imaging and high-cost specialty procedures. “If hospitalists are promoting efficient, coordinated care, their position can only be enhanced by IPAB’s recommendations, to the extent that they can demonstrate value for the healthcare dollar spent,” she says.
Necessary quality and cost reforms that patients deserve, and physicians want to deliver, have been stymied for too long by a crippled Congress, and by powerful special interest agendas, says SHM Public Policy Committee member Bradley Flansbaum DO, MPH, FACP, SFHM, director of the HM program at Lenox Hill Hospital in New York City, and clinical assistant professor of medicine at NYU School of Medicine. Reform requires some real enforcement authority to put value-based quality above the fray, he adds.
“CMS just does not have the teeth to do that right now; they are in the cross-hairs, and an IPAB-like body is needed to insulate Congress from the politically-risky choices, bring evidence and expertise to the decisions, bust through the politics, and get the job done,” Dr. Flansbaum says.
Dr. Flansbaum illustrates the problem by pointing to recent clinical studies that show percutaneous vertebroplasty, which injects bone cement into the spine to treat fractures, to be no better than a placebo in relieving pain. Medicare and private health insurers have been covering vertebroplasty for many years, despite the absence of rigorous study of its effectiveness. The same likely holds true for scores of other expensive treatments and surgical procedures. “Who, exactly, is going to put the kibosh on this?” Dr. Flansbaum asks. “The free market, which includes surgeons, hospitals, and device companies, each with their agendas, or regulators?”
Dr. Flansbaum believes that, in order to effectively bring down costs, the IPAB should not be restricted to supply-side proposals (i.e. provider reimbursement), but also should be allowed to propose demand-side changes to Medicare’s benefit plans, such as tiered network pricing with higher premiums to cover the latest and most expensive technologies.
SHM supports the need for an independent entity to check the growth in Medicare spending, but it does not support the IPAB as it is currently established under the ACA because certain groups (including hospitals) are protected from its scrutiny during its first several years—a limitation that SHM says puts the board’s legitimacy into question and seriously weakens its potential cost-saving effectiveness. SHM supports replacing the IPAB with an independent board that (1) subjects all Medicare providers and suppliers to the same scrutiny without special interest carve-outs, (2) balances cost-saving with QI considerations, (3) protects delivery of quality services, and (4) ensures board membership that represents all potentially affected groups, including physicians. (Read the entire statement in the “Where We Stand” section of SHM’s Advocacy microsite at www.hospitalmedicine.org/advocacy.)
By removing the IPAB’s present handcuffs—opening its scope to all providers, as well as to demand-side changes in Medicare’s benefit structure—an IPAB-like entity with the proper staff and expertise can rationally think-out the choices that Congress will never make, according to Dr. Flansbaum.
“For the sake of our economy and our future generations, healthcare costs have to come down, even if that means some short-term pain,” he says. “Hospitals may take a hit. Some physician income might take a hit. Otherwise, there won’t be any hospitals or salaries to be hit.”
Christopher Guadagnino is a freelance writer in Philadelphia.
Reference
- Statement of Congressman Pete Stark Supporting Health Care Reform, March 21, 2010. Available at: http://www.stark.house.gov/index.php?option=com_content&view=article&id=1534:statement-of-congressman-pete-stark-supporting-health-care-reform&catid=67:floor-statements-2010-. Accessed Jan. 5, 2012.
- Kathleen Sebelius, “IPAB Will Protect Medicare.” Politico, June 23, 2011. Available at: http://dyn.politico.com/printstory.cfm?uuid=FDE594BA-87EE-4DA5-9841-33804926EF36. Accessed Jan. 5, 2012.
Now that the latest annual “doc fix” is in, physicians have been granted another reprieve from potentially crippling cuts to their Medicare reimbursement under the flawed sustainable growth rate (SGR) payment formula.
Beginning this year, there’s a new player in town that will have the authority to achieve what Congress has consistently failed to do—cut Medicare provider spending to keep it below a cap—and it can do so with unprecedented autonomy.
Say hello to the Independent Payment Advisory Board (IPAB), a creature of the Affordable Care Act (ACA) that will propose ways to reduce “overpayment” to Medicare providers if target-spending levels are exceeded.
What distinguishes the IPAB from the Medicare Payment Advisory Commission (MedPAC) is that its proposals will automatically become law, unless Congress enacts its own proposals that reduce Medicare provider spending by at least as much as IPAB’s, or the Senate musters a three-fifths majority vote to override IPAB’s proposals entirely. Further, the IPAB’s changes to Medicare cannot be overruled by the executive branch or a court of law.
MedPAC never wielded such authority; in fact, many of its cost-control recommendations were ignored.

—Judith Feder, PhD, professor of public policy, Georgetown University, Washington, D.C., former dean, Georgetown Public Policy Institute, fellow, the Urban Institute
The IPAB comes to life this year, with a $15 million appropriation from the ACA, and begins ramping up its operations (see “The IPAB Timetable,” p. 26). The board will be comprised of a 15-member, multi-stakeholder group—expected to include physicians, nurses, medical experts, economists, consumer advocates, and others—appointed by the President and subject to Senate confirmation.
Incendiary Reactions
Dubbed by its most vociferous and largely Republican critics as “dangerously powerful,” “the real death panel,” and “bureaucrats deciding whether you get care,” the IPAB even has some Democrats decrying its power grab. Rep. Pete Stark (D-Calif.) called the IPAB “an unprecedented abrogation of Congressional authority to an unelected, unaccountable body of so-called experts.”1
Even Allyson Schwartz (D-Pa.), who helped draft the ACA, has come out against the IPAB, joining a handful of Democrats and more than 200 Republicans in signing on to a bill (H.R. 452) to repeal the ACA’s IPAB provision. The Senate has a similar bill (S. 668).
Although the IPAB legally is barred from formally making recommendations to ration care, increase beneficiary premiums or cost sharing, and from restricting benefits or eligibility criteria, critics worry that its authority to control prices could hurt patients by driving Medicare payments so low that physicians cease to offer certain services to them.
Enforcement Power
IPAB will have unprecedented power to enforce Medicare’s provider spending benchmarks. Beginning in 2014, if Medicare’s projected spending growth rate per beneficiary rises above an inflation threshold of Gross Domestic Product per capita plus 1%, the IPAB would be triggered and would propose ways to trim provider payments. President Obama has since proposed a lower threshold of GDP per capita plus 0.5%, meaning that the IPAB would be triggered earlier and likely would have deeper cuts to make.
It is unclear how the spending growth benchmark will be affected by the $123 billion in Medicare payment cuts to hospitals and other providers over nine years, which were triggered when the so-called “super committee” failed to reach a budget-cutting consensus last fall.
U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius describes the IPAB as a “backstop to ensure that rising costs don’t accelerate out of control, threatening Medicare’s stability,” and she maintains that the board is a necessary fallback mechanism to enforce Medicare spending within budget while healthcare providers continue to prove the effectiveness of various value-based delivery and reimbursement reform projects the ACA is funding.2
Impact on Physicians
“The IPAB is a structural intervention to put pressure on Congress, the Executive, and CMS [Centers for Medicare & Medicaid Services] to guarantee the ACA’s investment in cost-containment, and it gives physicians the incentive to act on its principles,” says Judith Feder, PhD, professor of public policy at Georgetown University, former dean of the Georgetown Public Policy Institute, and a fellow at the Urban Institute.
Dr. Feder was a co-signer of a letter sent by 100 health policy experts and economists—including Congressional Budget Office founding director Alice Rivlin, now with the Brookings Institute—to congressional leaders last May urging them to abandon attempts to repeal the IPAB provision. Dr. Feder maintains that the IPAB will marshal “the expertise of professionals who can weigh evidence on how payment incentives affect care delivery and suggest sensible improvements, while forcing debate on difficult choices that Congress has thus far failed to address.”
Because of the changes the ACA has already made to provider reimbursement and Medicare Advantage plan funding, Feder says that Medicare’s average annual growth rate for the next decade is projected to be a full percentage point below per capita growth in GDP. On top of that, she says, “the ACA’s other payment reform experiments have the potential to improve quality and cut spending growth even further by reducing payment for overpriced or undesirable care–like unnecessary hospital readmissions–and rewarding efficiently provided, coordinated care.” By Feder’s analysis, the IPAB would not likely be triggered for a decade, but stands ready as a backup, if needed. Indeed, she favors extending IPAB’s authority beyond Medicare, to allow a system-wide spending target that creates an all-payer incentive to assure that providers really change their behavior to boost quality and efficiency.
Impact on Hospitalists
If the IPAB does come into play, Feder believes that hospitalists have less to worry about than other physician specialists, because the Board’s cost-reduction proposals would likely focus on services where overpayment is the most acute – like imaging and high-cost specialty procedures. “If hospitalists are promoting efficient, coordinated care, their position can only be enhanced by IPAB’s recommendations, to the extent that they can demonstrate value for the healthcare dollar spent,” she says.
Necessary quality and cost reforms that patients deserve, and physicians want to deliver, have been stymied for too long by a crippled Congress, and by powerful special interest agendas, says SHM Public Policy Committee member Bradley Flansbaum DO, MPH, FACP, SFHM, director of the HM program at Lenox Hill Hospital in New York City, and clinical assistant professor of medicine at NYU School of Medicine. Reform requires some real enforcement authority to put value-based quality above the fray, he adds.
“CMS just does not have the teeth to do that right now; they are in the cross-hairs, and an IPAB-like body is needed to insulate Congress from the politically-risky choices, bring evidence and expertise to the decisions, bust through the politics, and get the job done,” Dr. Flansbaum says.
Dr. Flansbaum illustrates the problem by pointing to recent clinical studies that show percutaneous vertebroplasty, which injects bone cement into the spine to treat fractures, to be no better than a placebo in relieving pain. Medicare and private health insurers have been covering vertebroplasty for many years, despite the absence of rigorous study of its effectiveness. The same likely holds true for scores of other expensive treatments and surgical procedures. “Who, exactly, is going to put the kibosh on this?” Dr. Flansbaum asks. “The free market, which includes surgeons, hospitals, and device companies, each with their agendas, or regulators?”
Dr. Flansbaum believes that, in order to effectively bring down costs, the IPAB should not be restricted to supply-side proposals (i.e. provider reimbursement), but also should be allowed to propose demand-side changes to Medicare’s benefit plans, such as tiered network pricing with higher premiums to cover the latest and most expensive technologies.
SHM supports the need for an independent entity to check the growth in Medicare spending, but it does not support the IPAB as it is currently established under the ACA because certain groups (including hospitals) are protected from its scrutiny during its first several years—a limitation that SHM says puts the board’s legitimacy into question and seriously weakens its potential cost-saving effectiveness. SHM supports replacing the IPAB with an independent board that (1) subjects all Medicare providers and suppliers to the same scrutiny without special interest carve-outs, (2) balances cost-saving with QI considerations, (3) protects delivery of quality services, and (4) ensures board membership that represents all potentially affected groups, including physicians. (Read the entire statement in the “Where We Stand” section of SHM’s Advocacy microsite at www.hospitalmedicine.org/advocacy.)
By removing the IPAB’s present handcuffs—opening its scope to all providers, as well as to demand-side changes in Medicare’s benefit structure—an IPAB-like entity with the proper staff and expertise can rationally think-out the choices that Congress will never make, according to Dr. Flansbaum.
“For the sake of our economy and our future generations, healthcare costs have to come down, even if that means some short-term pain,” he says. “Hospitals may take a hit. Some physician income might take a hit. Otherwise, there won’t be any hospitals or salaries to be hit.”
Christopher Guadagnino is a freelance writer in Philadelphia.
Reference
- Statement of Congressman Pete Stark Supporting Health Care Reform, March 21, 2010. Available at: http://www.stark.house.gov/index.php?option=com_content&view=article&id=1534:statement-of-congressman-pete-stark-supporting-health-care-reform&catid=67:floor-statements-2010-. Accessed Jan. 5, 2012.
- Kathleen Sebelius, “IPAB Will Protect Medicare.” Politico, June 23, 2011. Available at: http://dyn.politico.com/printstory.cfm?uuid=FDE594BA-87EE-4DA5-9841-33804926EF36. Accessed Jan. 5, 2012.
Now that the latest annual “doc fix” is in, physicians have been granted another reprieve from potentially crippling cuts to their Medicare reimbursement under the flawed sustainable growth rate (SGR) payment formula.
Beginning this year, there’s a new player in town that will have the authority to achieve what Congress has consistently failed to do—cut Medicare provider spending to keep it below a cap—and it can do so with unprecedented autonomy.
Say hello to the Independent Payment Advisory Board (IPAB), a creature of the Affordable Care Act (ACA) that will propose ways to reduce “overpayment” to Medicare providers if target-spending levels are exceeded.
What distinguishes the IPAB from the Medicare Payment Advisory Commission (MedPAC) is that its proposals will automatically become law, unless Congress enacts its own proposals that reduce Medicare provider spending by at least as much as IPAB’s, or the Senate musters a three-fifths majority vote to override IPAB’s proposals entirely. Further, the IPAB’s changes to Medicare cannot be overruled by the executive branch or a court of law.
MedPAC never wielded such authority; in fact, many of its cost-control recommendations were ignored.

—Judith Feder, PhD, professor of public policy, Georgetown University, Washington, D.C., former dean, Georgetown Public Policy Institute, fellow, the Urban Institute
The IPAB comes to life this year, with a $15 million appropriation from the ACA, and begins ramping up its operations (see “The IPAB Timetable,” p. 26). The board will be comprised of a 15-member, multi-stakeholder group—expected to include physicians, nurses, medical experts, economists, consumer advocates, and others—appointed by the President and subject to Senate confirmation.
Incendiary Reactions
Dubbed by its most vociferous and largely Republican critics as “dangerously powerful,” “the real death panel,” and “bureaucrats deciding whether you get care,” the IPAB even has some Democrats decrying its power grab. Rep. Pete Stark (D-Calif.) called the IPAB “an unprecedented abrogation of Congressional authority to an unelected, unaccountable body of so-called experts.”1
Even Allyson Schwartz (D-Pa.), who helped draft the ACA, has come out against the IPAB, joining a handful of Democrats and more than 200 Republicans in signing on to a bill (H.R. 452) to repeal the ACA’s IPAB provision. The Senate has a similar bill (S. 668).
Although the IPAB legally is barred from formally making recommendations to ration care, increase beneficiary premiums or cost sharing, and from restricting benefits or eligibility criteria, critics worry that its authority to control prices could hurt patients by driving Medicare payments so low that physicians cease to offer certain services to them.
Enforcement Power
IPAB will have unprecedented power to enforce Medicare’s provider spending benchmarks. Beginning in 2014, if Medicare’s projected spending growth rate per beneficiary rises above an inflation threshold of Gross Domestic Product per capita plus 1%, the IPAB would be triggered and would propose ways to trim provider payments. President Obama has since proposed a lower threshold of GDP per capita plus 0.5%, meaning that the IPAB would be triggered earlier and likely would have deeper cuts to make.
It is unclear how the spending growth benchmark will be affected by the $123 billion in Medicare payment cuts to hospitals and other providers over nine years, which were triggered when the so-called “super committee” failed to reach a budget-cutting consensus last fall.
U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius describes the IPAB as a “backstop to ensure that rising costs don’t accelerate out of control, threatening Medicare’s stability,” and she maintains that the board is a necessary fallback mechanism to enforce Medicare spending within budget while healthcare providers continue to prove the effectiveness of various value-based delivery and reimbursement reform projects the ACA is funding.2
Impact on Physicians
“The IPAB is a structural intervention to put pressure on Congress, the Executive, and CMS [Centers for Medicare & Medicaid Services] to guarantee the ACA’s investment in cost-containment, and it gives physicians the incentive to act on its principles,” says Judith Feder, PhD, professor of public policy at Georgetown University, former dean of the Georgetown Public Policy Institute, and a fellow at the Urban Institute.
Dr. Feder was a co-signer of a letter sent by 100 health policy experts and economists—including Congressional Budget Office founding director Alice Rivlin, now with the Brookings Institute—to congressional leaders last May urging them to abandon attempts to repeal the IPAB provision. Dr. Feder maintains that the IPAB will marshal “the expertise of professionals who can weigh evidence on how payment incentives affect care delivery and suggest sensible improvements, while forcing debate on difficult choices that Congress has thus far failed to address.”
Because of the changes the ACA has already made to provider reimbursement and Medicare Advantage plan funding, Feder says that Medicare’s average annual growth rate for the next decade is projected to be a full percentage point below per capita growth in GDP. On top of that, she says, “the ACA’s other payment reform experiments have the potential to improve quality and cut spending growth even further by reducing payment for overpriced or undesirable care–like unnecessary hospital readmissions–and rewarding efficiently provided, coordinated care.” By Feder’s analysis, the IPAB would not likely be triggered for a decade, but stands ready as a backup, if needed. Indeed, she favors extending IPAB’s authority beyond Medicare, to allow a system-wide spending target that creates an all-payer incentive to assure that providers really change their behavior to boost quality and efficiency.
Impact on Hospitalists
If the IPAB does come into play, Feder believes that hospitalists have less to worry about than other physician specialists, because the Board’s cost-reduction proposals would likely focus on services where overpayment is the most acute – like imaging and high-cost specialty procedures. “If hospitalists are promoting efficient, coordinated care, their position can only be enhanced by IPAB’s recommendations, to the extent that they can demonstrate value for the healthcare dollar spent,” she says.
Necessary quality and cost reforms that patients deserve, and physicians want to deliver, have been stymied for too long by a crippled Congress, and by powerful special interest agendas, says SHM Public Policy Committee member Bradley Flansbaum DO, MPH, FACP, SFHM, director of the HM program at Lenox Hill Hospital in New York City, and clinical assistant professor of medicine at NYU School of Medicine. Reform requires some real enforcement authority to put value-based quality above the fray, he adds.
“CMS just does not have the teeth to do that right now; they are in the cross-hairs, and an IPAB-like body is needed to insulate Congress from the politically-risky choices, bring evidence and expertise to the decisions, bust through the politics, and get the job done,” Dr. Flansbaum says.
Dr. Flansbaum illustrates the problem by pointing to recent clinical studies that show percutaneous vertebroplasty, which injects bone cement into the spine to treat fractures, to be no better than a placebo in relieving pain. Medicare and private health insurers have been covering vertebroplasty for many years, despite the absence of rigorous study of its effectiveness. The same likely holds true for scores of other expensive treatments and surgical procedures. “Who, exactly, is going to put the kibosh on this?” Dr. Flansbaum asks. “The free market, which includes surgeons, hospitals, and device companies, each with their agendas, or regulators?”
Dr. Flansbaum believes that, in order to effectively bring down costs, the IPAB should not be restricted to supply-side proposals (i.e. provider reimbursement), but also should be allowed to propose demand-side changes to Medicare’s benefit plans, such as tiered network pricing with higher premiums to cover the latest and most expensive technologies.
SHM supports the need for an independent entity to check the growth in Medicare spending, but it does not support the IPAB as it is currently established under the ACA because certain groups (including hospitals) are protected from its scrutiny during its first several years—a limitation that SHM says puts the board’s legitimacy into question and seriously weakens its potential cost-saving effectiveness. SHM supports replacing the IPAB with an independent board that (1) subjects all Medicare providers and suppliers to the same scrutiny without special interest carve-outs, (2) balances cost-saving with QI considerations, (3) protects delivery of quality services, and (4) ensures board membership that represents all potentially affected groups, including physicians. (Read the entire statement in the “Where We Stand” section of SHM’s Advocacy microsite at www.hospitalmedicine.org/advocacy.)
By removing the IPAB’s present handcuffs—opening its scope to all providers, as well as to demand-side changes in Medicare’s benefit structure—an IPAB-like entity with the proper staff and expertise can rationally think-out the choices that Congress will never make, according to Dr. Flansbaum.
“For the sake of our economy and our future generations, healthcare costs have to come down, even if that means some short-term pain,” he says. “Hospitals may take a hit. Some physician income might take a hit. Otherwise, there won’t be any hospitals or salaries to be hit.”
Christopher Guadagnino is a freelance writer in Philadelphia.
Reference
- Statement of Congressman Pete Stark Supporting Health Care Reform, March 21, 2010. Available at: http://www.stark.house.gov/index.php?option=com_content&view=article&id=1534:statement-of-congressman-pete-stark-supporting-health-care-reform&catid=67:floor-statements-2010-. Accessed Jan. 5, 2012.
- Kathleen Sebelius, “IPAB Will Protect Medicare.” Politico, June 23, 2011. Available at: http://dyn.politico.com/printstory.cfm?uuid=FDE594BA-87EE-4DA5-9841-33804926EF36. Accessed Jan. 5, 2012.
Seven-Day Schedule Could Improve Hospital Quality, Capacity
A new study evaluating outcomes for hospitals participating in the American Heart Association’s Get with the Guidelines program found no correlation between high performance on adhering to measures and care standards for acute myocardial infarction and for heart failure despite overlap between the sets of care processes (J Am Coll Cardio. 2011;58:637-644).
A total of 400,000 heart patients were studied, and 283 participating hospitals were stratified into thirds based on their adherence to core quality measures for each disease, with the upper third labeled superior in performance. Lead author Tracy Wang, MD, MHS, MSc, of the Duke Clinical Research Institute in Durham, N.C., and colleagues found that superior performance for only one of the two diseases led to such end-result outcomes as in-hospital mortality that were no better than for hospitals that were not high performers for either condition. But hospitals with superior performance for both conditions had lower in-hospital mortality rates.
“Perhaps quality is more than just following checklists,” Dr. Wang says. “There’s something special about these high-performing hospitals across the board, with better QI, perhaps a little more investment in infrastructure for quality.”
This result, Dr. Wang says, should give ammunition for hospitalists and other physicians to go to their hospital administrators to request more investment in quality improvement overall, not just for specific conditions.
A new study evaluating outcomes for hospitals participating in the American Heart Association’s Get with the Guidelines program found no correlation between high performance on adhering to measures and care standards for acute myocardial infarction and for heart failure despite overlap between the sets of care processes (J Am Coll Cardio. 2011;58:637-644).
A total of 400,000 heart patients were studied, and 283 participating hospitals were stratified into thirds based on their adherence to core quality measures for each disease, with the upper third labeled superior in performance. Lead author Tracy Wang, MD, MHS, MSc, of the Duke Clinical Research Institute in Durham, N.C., and colleagues found that superior performance for only one of the two diseases led to such end-result outcomes as in-hospital mortality that were no better than for hospitals that were not high performers for either condition. But hospitals with superior performance for both conditions had lower in-hospital mortality rates.
“Perhaps quality is more than just following checklists,” Dr. Wang says. “There’s something special about these high-performing hospitals across the board, with better QI, perhaps a little more investment in infrastructure for quality.”
This result, Dr. Wang says, should give ammunition for hospitalists and other physicians to go to their hospital administrators to request more investment in quality improvement overall, not just for specific conditions.
A new study evaluating outcomes for hospitals participating in the American Heart Association’s Get with the Guidelines program found no correlation between high performance on adhering to measures and care standards for acute myocardial infarction and for heart failure despite overlap between the sets of care processes (J Am Coll Cardio. 2011;58:637-644).
A total of 400,000 heart patients were studied, and 283 participating hospitals were stratified into thirds based on their adherence to core quality measures for each disease, with the upper third labeled superior in performance. Lead author Tracy Wang, MD, MHS, MSc, of the Duke Clinical Research Institute in Durham, N.C., and colleagues found that superior performance for only one of the two diseases led to such end-result outcomes as in-hospital mortality that were no better than for hospitals that were not high performers for either condition. But hospitals with superior performance for both conditions had lower in-hospital mortality rates.
“Perhaps quality is more than just following checklists,” Dr. Wang says. “There’s something special about these high-performing hospitals across the board, with better QI, perhaps a little more investment in infrastructure for quality.”
This result, Dr. Wang says, should give ammunition for hospitalists and other physicians to go to their hospital administrators to request more investment in quality improvement overall, not just for specific conditions.
Massive Acetylcysteine Overdose to Treat Acetaminophen Overdose
Cases reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
A 21-year-old North Carolina woman presented to the emergency department (ED) with nausea after taking too much acetaminophen during her menstrual cycle. She was given IV acetylcysteine by the emergency physician, who had never before administered this agent intravenously; the ED pharmacy had never previously dispensed the drug.
According to the pharmacist’s prescription, the drug was to be given in three stages and should run “times” four hours during the second stage and “times” 16 hours during the final stage. The prescription should have said that a single dose of acetylcysteine was to be given “over” a certain time period.
The emergency physician signed and entered the order written by the pharmacist without checking it. The nurse who initiated the IV had never administered acetylcysteine before. The result was a four-times overdosage during the second stage and a 16-times overdosage during the final stage of transfusion.
The patient was moved to the hospital medical floor. After 20 hours of treatment, lab results showed that her acetaminophen level had fallen to a safe concentration. When the original order expired, however, a nurse called another physician, who ordered that the drug be continued at the 16-times overdosage rate. This physician was unfamiliar with the patient or with acetylcysteine. The woman became sluggish and then agitated, pulling at her clothing and finally yanking out her IV. A nurse contacted the doctor on duty and received an order for an injection of haloperidol. Although hospital protocol required the doctor to actually evaluate the patient before ordering haloperidol, the order was placed by phone.
Within five minutes of receiving the haloperidol injection, the woman began to experience seizure. The doctor on duty did not come to her bedside. Her condition worsened, and she was transferred to the ICU. Four hours passed before another physician came to see her although her seizures continued. The doctor on duty was also unfamiliar with acetylcysteine but wrote another order for the 16-times overdosage rate.
After eight hours, the treatment was discontinued for two hours, although no change had been made in the doctor orders. When the treatment resumed, the dosage was significantly lower than it had been, although no explanation for this was recorded in the patient’s chart.
She was transferred from the ICU to another hospital. Her brain herniated after the transfer, leaving her in a persistent vegetative state.
Plaintiff for the patient claimed that the discharge information included no information for the receiving hospital regarding an overdose of acetylcysteine. The plaintiff claimed that the maximum dose for acetylcysteine is 14,600 mg, but the patient received 180,000 mg. In addition to the drug overdose, the plaintiff claimed that the patient had received a fluid overdose (6,000 mL of fluid had been infused, whereas no more than 160 mL should have been infused). The pharmacy charged more than $15,000 for the acetylcysteine and dispensed so much of the drug that the pharmacy’s supply was emptied; the drug had to be reordered on an emergency basis.
OUTCOME
According to a published account, a $15.5 million settlement was reached.
COMMENT
Patients and jurors expect clinicians to calculate and monitor medication dosages with care. This is a tragic case, resulting in a substantial settlement.
It is helpful to have multiple layers to check and confirm dosing, but in this case, unfortunately, every one of those layers (at least one pharmacist, two nurses, and two physicians) missed an opportunity to detect and correct a fatal error. The initial problem appears to have been a miscommunication between the pharmacy, the prescribing physician, and the nurse, in which “times” was misinterpreted as an independent dose rather than duration. The use of “times” here is confusing and “over” should have been used instead. Still, despite the initial confusion, several prescribing practices could have prevented the overdose.
First, if you have any question regarding a substance, look it up. If the prescriber in this case had checked the recommended dosing instructions, he or she would have noted the dosing for acetylcysteine for patients weighing more than 40 kg as follows: loading dose 150 mg/kg over 60 minutes, 50 mg/kg over 4 hours, and 100 mg/kg over 16 hours (that is, 300 mg/kg total over 21 hours). It would have been clear that “times” referred to duration, not a discrete administration for each hour. A subsequent short confirmatory call to the pharmacy would have revealed that “times” referred to duration.
Second, it is always prudent to get a second opinion before prescribing an unfamiliar medication. It would have been reasonable for the physician and nurse to double-check with a colleague to make sure the dosing and administration sounded right. As acetaminophen overdose is common, it should have been relatively easy to find an experienced clinician in the department who would know that hourly administration of acetylcysteine is not required. There is no shame or weakness in checking with colleagues or looking up information. Your practice environment should permit reasonable research or allow a “second set of eyes” to consult on any issue. If your practice environment does not foster such cooperative practice, it is broken and must be fixed.
Third, when execution of any order appears to call for an unusual medication amount or frequency, revisit the order or prescription and secure a second opinion. The hospital’s stores were depleted, underscoring the fact that the amount being dispensed to a single patient was excessive. Acetylcysteine is prepared as 200 mg/mL in 30-mL glass vials. Correct treatment for this patient would have required about 2.5 vials, but she was administered 30 vials. Quite practically, this should have raised red flags. If you bring 30 vials of one substance into a room, find yourself reconstituting 11 vials of a drug, or preparing a dozen syringes for one patient, recheck your dosing and get a second opinion before administering.
Fourth, whenever possible, verify that the dose to be administered is “in the ballpark” and generally reasonable to avoid excessive overdose—such as the dreaded 10-fold dosing error. Here, we know the patient weighed 48 kg (106 lb), and that her 21-hour dosing was 14,600 mg; a 70-kg patient (154 lb) would get a 21,000-mg total over 21 hours—in the same general ballpark. It should be clear that 180,000 mg is approximately 10 times out of the ballpark. Of course, use appropriate substance-specific judgment: When medications have a narrow therapeutic range or are titrated to effect, a general ballpark concept is inappropriate. Though useful, a fast check to estimate that your calculations aren’t wildly off may not suffice to detect smaller-scale yet important errors.
Fifth, always use caution when continuing orders from another clinician. You are prescribing under your authority, and it is important to independently check the order and not blindly ratify the actions of another. You owe the patient an individual analysis, and jurors will hold you individually responsible for medication errors. When you are called upon to continue an order, make your own assessment and, though sometimes difficult, be prepared to question an order if you are concerned. Consider seeking a colleague’s opinion on the propriety of the initial order as well.
Lastly, to minimize the risk for medication errors, follow good general prescriptive and ordering practices. Write legibly, spell out directions or terms commonly misinterpreted (and a source of litigation): Use “daily” instead of “qd,” “international units” or “units” instead of “IU.” Spell out “magnesium sulfate” or “morphine sulfate,” not “MgSO4” or “MSO4.” Include indications (to avoid prescribing the wrong drug and to remind the patient of the medication’s function) and with decimal points, “always lead, never trail” (eg, write “10 mg,” not “10.0 mg”; write “0.5 mg,” not “.5 mg”). Dispense the correct substance-specific amount, with refills only when appropriate, and confirm the patient’s identity.
Regarding allergies, I have always used a burst of three questions: Do you have any allergies? Are there any medications you cannot take? Have you ever been told that you should not take any medication? I have been surprised when a patient answers affirmatively to one question but negatively to the other two.
Recommend that patients use one pharmacy to allow the pharmacist and pharmacy professionals to monitor for duplications, interactions, and allergies to prescriptions issued by different prescribers. Technology continually brings us more medications, and patients commonly have prescription lists in the double digits; respond with technology of your own. Use multidrug interaction checkers, such as Medscape.com or Epocrates.com, which offer free browser-based and app options. Employ these assets in conjunction with and not in lieu of your own training, skill, and experience to minimize adverse drug interactions. —DML
Cases reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
A 21-year-old North Carolina woman presented to the emergency department (ED) with nausea after taking too much acetaminophen during her menstrual cycle. She was given IV acetylcysteine by the emergency physician, who had never before administered this agent intravenously; the ED pharmacy had never previously dispensed the drug.
According to the pharmacist’s prescription, the drug was to be given in three stages and should run “times” four hours during the second stage and “times” 16 hours during the final stage. The prescription should have said that a single dose of acetylcysteine was to be given “over” a certain time period.
The emergency physician signed and entered the order written by the pharmacist without checking it. The nurse who initiated the IV had never administered acetylcysteine before. The result was a four-times overdosage during the second stage and a 16-times overdosage during the final stage of transfusion.
The patient was moved to the hospital medical floor. After 20 hours of treatment, lab results showed that her acetaminophen level had fallen to a safe concentration. When the original order expired, however, a nurse called another physician, who ordered that the drug be continued at the 16-times overdosage rate. This physician was unfamiliar with the patient or with acetylcysteine. The woman became sluggish and then agitated, pulling at her clothing and finally yanking out her IV. A nurse contacted the doctor on duty and received an order for an injection of haloperidol. Although hospital protocol required the doctor to actually evaluate the patient before ordering haloperidol, the order was placed by phone.
Within five minutes of receiving the haloperidol injection, the woman began to experience seizure. The doctor on duty did not come to her bedside. Her condition worsened, and she was transferred to the ICU. Four hours passed before another physician came to see her although her seizures continued. The doctor on duty was also unfamiliar with acetylcysteine but wrote another order for the 16-times overdosage rate.
After eight hours, the treatment was discontinued for two hours, although no change had been made in the doctor orders. When the treatment resumed, the dosage was significantly lower than it had been, although no explanation for this was recorded in the patient’s chart.
She was transferred from the ICU to another hospital. Her brain herniated after the transfer, leaving her in a persistent vegetative state.
Plaintiff for the patient claimed that the discharge information included no information for the receiving hospital regarding an overdose of acetylcysteine. The plaintiff claimed that the maximum dose for acetylcysteine is 14,600 mg, but the patient received 180,000 mg. In addition to the drug overdose, the plaintiff claimed that the patient had received a fluid overdose (6,000 mL of fluid had been infused, whereas no more than 160 mL should have been infused). The pharmacy charged more than $15,000 for the acetylcysteine and dispensed so much of the drug that the pharmacy’s supply was emptied; the drug had to be reordered on an emergency basis.
OUTCOME
According to a published account, a $15.5 million settlement was reached.
COMMENT
Patients and jurors expect clinicians to calculate and monitor medication dosages with care. This is a tragic case, resulting in a substantial settlement.
It is helpful to have multiple layers to check and confirm dosing, but in this case, unfortunately, every one of those layers (at least one pharmacist, two nurses, and two physicians) missed an opportunity to detect and correct a fatal error. The initial problem appears to have been a miscommunication between the pharmacy, the prescribing physician, and the nurse, in which “times” was misinterpreted as an independent dose rather than duration. The use of “times” here is confusing and “over” should have been used instead. Still, despite the initial confusion, several prescribing practices could have prevented the overdose.
First, if you have any question regarding a substance, look it up. If the prescriber in this case had checked the recommended dosing instructions, he or she would have noted the dosing for acetylcysteine for patients weighing more than 40 kg as follows: loading dose 150 mg/kg over 60 minutes, 50 mg/kg over 4 hours, and 100 mg/kg over 16 hours (that is, 300 mg/kg total over 21 hours). It would have been clear that “times” referred to duration, not a discrete administration for each hour. A subsequent short confirmatory call to the pharmacy would have revealed that “times” referred to duration.
Second, it is always prudent to get a second opinion before prescribing an unfamiliar medication. It would have been reasonable for the physician and nurse to double-check with a colleague to make sure the dosing and administration sounded right. As acetaminophen overdose is common, it should have been relatively easy to find an experienced clinician in the department who would know that hourly administration of acetylcysteine is not required. There is no shame or weakness in checking with colleagues or looking up information. Your practice environment should permit reasonable research or allow a “second set of eyes” to consult on any issue. If your practice environment does not foster such cooperative practice, it is broken and must be fixed.
Third, when execution of any order appears to call for an unusual medication amount or frequency, revisit the order or prescription and secure a second opinion. The hospital’s stores were depleted, underscoring the fact that the amount being dispensed to a single patient was excessive. Acetylcysteine is prepared as 200 mg/mL in 30-mL glass vials. Correct treatment for this patient would have required about 2.5 vials, but she was administered 30 vials. Quite practically, this should have raised red flags. If you bring 30 vials of one substance into a room, find yourself reconstituting 11 vials of a drug, or preparing a dozen syringes for one patient, recheck your dosing and get a second opinion before administering.
Fourth, whenever possible, verify that the dose to be administered is “in the ballpark” and generally reasonable to avoid excessive overdose—such as the dreaded 10-fold dosing error. Here, we know the patient weighed 48 kg (106 lb), and that her 21-hour dosing was 14,600 mg; a 70-kg patient (154 lb) would get a 21,000-mg total over 21 hours—in the same general ballpark. It should be clear that 180,000 mg is approximately 10 times out of the ballpark. Of course, use appropriate substance-specific judgment: When medications have a narrow therapeutic range or are titrated to effect, a general ballpark concept is inappropriate. Though useful, a fast check to estimate that your calculations aren’t wildly off may not suffice to detect smaller-scale yet important errors.
Fifth, always use caution when continuing orders from another clinician. You are prescribing under your authority, and it is important to independently check the order and not blindly ratify the actions of another. You owe the patient an individual analysis, and jurors will hold you individually responsible for medication errors. When you are called upon to continue an order, make your own assessment and, though sometimes difficult, be prepared to question an order if you are concerned. Consider seeking a colleague’s opinion on the propriety of the initial order as well.
Lastly, to minimize the risk for medication errors, follow good general prescriptive and ordering practices. Write legibly, spell out directions or terms commonly misinterpreted (and a source of litigation): Use “daily” instead of “qd,” “international units” or “units” instead of “IU.” Spell out “magnesium sulfate” or “morphine sulfate,” not “MgSO4” or “MSO4.” Include indications (to avoid prescribing the wrong drug and to remind the patient of the medication’s function) and with decimal points, “always lead, never trail” (eg, write “10 mg,” not “10.0 mg”; write “0.5 mg,” not “.5 mg”). Dispense the correct substance-specific amount, with refills only when appropriate, and confirm the patient’s identity.
Regarding allergies, I have always used a burst of three questions: Do you have any allergies? Are there any medications you cannot take? Have you ever been told that you should not take any medication? I have been surprised when a patient answers affirmatively to one question but negatively to the other two.
Recommend that patients use one pharmacy to allow the pharmacist and pharmacy professionals to monitor for duplications, interactions, and allergies to prescriptions issued by different prescribers. Technology continually brings us more medications, and patients commonly have prescription lists in the double digits; respond with technology of your own. Use multidrug interaction checkers, such as Medscape.com or Epocrates.com, which offer free browser-based and app options. Employ these assets in conjunction with and not in lieu of your own training, skill, and experience to minimize adverse drug interactions. —DML
Cases reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
A 21-year-old North Carolina woman presented to the emergency department (ED) with nausea after taking too much acetaminophen during her menstrual cycle. She was given IV acetylcysteine by the emergency physician, who had never before administered this agent intravenously; the ED pharmacy had never previously dispensed the drug.
According to the pharmacist’s prescription, the drug was to be given in three stages and should run “times” four hours during the second stage and “times” 16 hours during the final stage. The prescription should have said that a single dose of acetylcysteine was to be given “over” a certain time period.
The emergency physician signed and entered the order written by the pharmacist without checking it. The nurse who initiated the IV had never administered acetylcysteine before. The result was a four-times overdosage during the second stage and a 16-times overdosage during the final stage of transfusion.
The patient was moved to the hospital medical floor. After 20 hours of treatment, lab results showed that her acetaminophen level had fallen to a safe concentration. When the original order expired, however, a nurse called another physician, who ordered that the drug be continued at the 16-times overdosage rate. This physician was unfamiliar with the patient or with acetylcysteine. The woman became sluggish and then agitated, pulling at her clothing and finally yanking out her IV. A nurse contacted the doctor on duty and received an order for an injection of haloperidol. Although hospital protocol required the doctor to actually evaluate the patient before ordering haloperidol, the order was placed by phone.
Within five minutes of receiving the haloperidol injection, the woman began to experience seizure. The doctor on duty did not come to her bedside. Her condition worsened, and she was transferred to the ICU. Four hours passed before another physician came to see her although her seizures continued. The doctor on duty was also unfamiliar with acetylcysteine but wrote another order for the 16-times overdosage rate.
After eight hours, the treatment was discontinued for two hours, although no change had been made in the doctor orders. When the treatment resumed, the dosage was significantly lower than it had been, although no explanation for this was recorded in the patient’s chart.
She was transferred from the ICU to another hospital. Her brain herniated after the transfer, leaving her in a persistent vegetative state.
Plaintiff for the patient claimed that the discharge information included no information for the receiving hospital regarding an overdose of acetylcysteine. The plaintiff claimed that the maximum dose for acetylcysteine is 14,600 mg, but the patient received 180,000 mg. In addition to the drug overdose, the plaintiff claimed that the patient had received a fluid overdose (6,000 mL of fluid had been infused, whereas no more than 160 mL should have been infused). The pharmacy charged more than $15,000 for the acetylcysteine and dispensed so much of the drug that the pharmacy’s supply was emptied; the drug had to be reordered on an emergency basis.
OUTCOME
According to a published account, a $15.5 million settlement was reached.
COMMENT
Patients and jurors expect clinicians to calculate and monitor medication dosages with care. This is a tragic case, resulting in a substantial settlement.
It is helpful to have multiple layers to check and confirm dosing, but in this case, unfortunately, every one of those layers (at least one pharmacist, two nurses, and two physicians) missed an opportunity to detect and correct a fatal error. The initial problem appears to have been a miscommunication between the pharmacy, the prescribing physician, and the nurse, in which “times” was misinterpreted as an independent dose rather than duration. The use of “times” here is confusing and “over” should have been used instead. Still, despite the initial confusion, several prescribing practices could have prevented the overdose.
First, if you have any question regarding a substance, look it up. If the prescriber in this case had checked the recommended dosing instructions, he or she would have noted the dosing for acetylcysteine for patients weighing more than 40 kg as follows: loading dose 150 mg/kg over 60 minutes, 50 mg/kg over 4 hours, and 100 mg/kg over 16 hours (that is, 300 mg/kg total over 21 hours). It would have been clear that “times” referred to duration, not a discrete administration for each hour. A subsequent short confirmatory call to the pharmacy would have revealed that “times” referred to duration.
Second, it is always prudent to get a second opinion before prescribing an unfamiliar medication. It would have been reasonable for the physician and nurse to double-check with a colleague to make sure the dosing and administration sounded right. As acetaminophen overdose is common, it should have been relatively easy to find an experienced clinician in the department who would know that hourly administration of acetylcysteine is not required. There is no shame or weakness in checking with colleagues or looking up information. Your practice environment should permit reasonable research or allow a “second set of eyes” to consult on any issue. If your practice environment does not foster such cooperative practice, it is broken and must be fixed.
Third, when execution of any order appears to call for an unusual medication amount or frequency, revisit the order or prescription and secure a second opinion. The hospital’s stores were depleted, underscoring the fact that the amount being dispensed to a single patient was excessive. Acetylcysteine is prepared as 200 mg/mL in 30-mL glass vials. Correct treatment for this patient would have required about 2.5 vials, but she was administered 30 vials. Quite practically, this should have raised red flags. If you bring 30 vials of one substance into a room, find yourself reconstituting 11 vials of a drug, or preparing a dozen syringes for one patient, recheck your dosing and get a second opinion before administering.
Fourth, whenever possible, verify that the dose to be administered is “in the ballpark” and generally reasonable to avoid excessive overdose—such as the dreaded 10-fold dosing error. Here, we know the patient weighed 48 kg (106 lb), and that her 21-hour dosing was 14,600 mg; a 70-kg patient (154 lb) would get a 21,000-mg total over 21 hours—in the same general ballpark. It should be clear that 180,000 mg is approximately 10 times out of the ballpark. Of course, use appropriate substance-specific judgment: When medications have a narrow therapeutic range or are titrated to effect, a general ballpark concept is inappropriate. Though useful, a fast check to estimate that your calculations aren’t wildly off may not suffice to detect smaller-scale yet important errors.
Fifth, always use caution when continuing orders from another clinician. You are prescribing under your authority, and it is important to independently check the order and not blindly ratify the actions of another. You owe the patient an individual analysis, and jurors will hold you individually responsible for medication errors. When you are called upon to continue an order, make your own assessment and, though sometimes difficult, be prepared to question an order if you are concerned. Consider seeking a colleague’s opinion on the propriety of the initial order as well.
Lastly, to minimize the risk for medication errors, follow good general prescriptive and ordering practices. Write legibly, spell out directions or terms commonly misinterpreted (and a source of litigation): Use “daily” instead of “qd,” “international units” or “units” instead of “IU.” Spell out “magnesium sulfate” or “morphine sulfate,” not “MgSO4” or “MSO4.” Include indications (to avoid prescribing the wrong drug and to remind the patient of the medication’s function) and with decimal points, “always lead, never trail” (eg, write “10 mg,” not “10.0 mg”; write “0.5 mg,” not “.5 mg”). Dispense the correct substance-specific amount, with refills only when appropriate, and confirm the patient’s identity.
Regarding allergies, I have always used a burst of three questions: Do you have any allergies? Are there any medications you cannot take? Have you ever been told that you should not take any medication? I have been surprised when a patient answers affirmatively to one question but negatively to the other two.
Recommend that patients use one pharmacy to allow the pharmacist and pharmacy professionals to monitor for duplications, interactions, and allergies to prescriptions issued by different prescribers. Technology continually brings us more medications, and patients commonly have prescription lists in the double digits; respond with technology of your own. Use multidrug interaction checkers, such as Medscape.com or Epocrates.com, which offer free browser-based and app options. Employ these assets in conjunction with and not in lieu of your own training, skill, and experience to minimize adverse drug interactions. —DML
Data on liability claims offer bright spots for ObGyns— and sobering statistics
Good news on the medical liability front, Doctor!
Yes, that’s right, good news.
According to data from the Physician Insurers Association of America (PIAA), the number of claims that were paid in the ObGyn category between 2006 and 2011 was 44% lower than the number of claims paid between 1986 and 1991.
The percentage of claims that were paid also decreased over the same quarter century. During 1986–1990, 37.25% of all claims were paid in the ObGyn category, compared with 31.73% during 2006–2010.1
And when claims for both periods are calculated in 2010 dollars, the amount paid also declined—by more than $138 million!
These are three of the findings that reflect “significant improvement” in obstetrics and gynecology in medical liability, says John B. Stanchfield, MD, an endocrinologist who, for 25 years, was medical director of the Utah Medical Insurance Association (UMIA)—a member company of PIAA. PIAA is the insurance industry trade association.
PIAA member companies in the United States “include large national insurance companies, mid-size regional writers, single-state insurers, and specialty companies that serve specific health care–provider niche markets. Collectively, these companies provide insurance protection to more than 60% of America’s private practice physicians and write approximately 46%, or $5.2 billion, of the total industry premium.”2
The improvement in ObGyn comes as no surprise to Dr. Stanchfield because the specialty was “the first group that got ‘risk-managed’ almost universally across the country,” he says. “In our little company out here in Utah, in 1985, we were told that if we didn’t do something [about lawsuits in obstetrics and gynecology], we weren’t going to be able to insure that class anymore because we wouldn’t be able to collect enough money. That’s what the actuaries told us, but it wasn’t unique to us—it was a nationwide problem.”
Why was the ObGyn specialty, in particular, in need of aggressive risk management? What made ObGyn claims unique?
“It’s infant injury,” says Dr. Stanchfield. “It’s injury to the baby. Those claims, you start talking at a million dollars.”
Another reason may be that some claims in this specialty category involve doctors other than ObGyns who provide obstetric care—for example, family practice physicians.

A risk manager’s perspective
After receiving the warning about ObGyn claims, UMIA got busy. First, it formed a committee comprising perinatologists, ObGyns, family practice physicians, claims specialists, and attorneys. “We analyzed all claims that were paid, looking for common denominators,” says Dr. Stanchfield. Improvement was clearly needed in about 10 areas, so “we basically created a risk-management program and then mandated it.” In the process, the organization published a booklet entitled Insurance Recommendations for Obstetrical Practice, of which Dr. Stanchfield was the editor.3
The booklet offers guidance on 10 potential “problem” areas:
- antepartum testing
- hypertension and pregnancy
- operative vaginal delivery
- breech delivery
- oxytocin administration
- vaginal birth after cesarean
- use of misoprostol
- shoulder dystocia
- preterm labor
- hospital standards.
Fewer claims and more physicians
The declining number and percentage of paid claims in obstetrics and gynecology over 25 years may be even more impressive than the figures suggest, says Dr. Stanchfield.
“Gestalt tells me that through the years there are more practicing physicians rather than fewer,” so the denominator is increasing even as these claims are declining—making the decrease “even more powerful.”
The numbers haven’t improved to the same degree in other specialties, Dr. Stanchfield says. “If you look at global data, the decrease in paid claims might have been 10% to 15%. In ObGyn, if you compare the last 5-year block of data with the first 5-year block, the number of paid claims is almost cut in half.”
What brought about this improvement?
“There weren’t any groundbreaking medical or surgical technological advances during this period. It was just doing it better. And the main push to doing it better in this country, in my opinion, is risk management.”
Slicing the data
Now for the not-so-great news: In 2010 alone, more than $55 million was paid out in the ObGyn category for 10 patient conditions. Topping the list were “pregnancy” and “brain-damaged infant.” The $55 million figure represents the money paid for the top 10 most commonly cited conditions in cases closed during 2010 (TABLE 1).
TABLE 1
Claims categorized under the rather broad category of pregnancy usually were placed there because a more appropriate category was lacking, says Dr. Stanchfield. These claims typically involve “things that happen—usually to the baby—that result in a lawsuit other than brain damage per se.” For example, a claim that involved skull fracture without brain damage might fall into this zone, he says.
Problematic procedures
Slicing the data a different way, problems related to the 10 most commonly cited ObGyn procedures cost PIAA companies more than $120 million dollars in 2010—and that figure is only for the top 10.1 The top three procedures, in terms of number of claims closed in 2010, were operative procedures on the uterus, manually assisted delivery, and cesarean delivery (TABLE 2).
TABLE 2
Manually assisted delivery does not include vacuum extraction or forceps delivery, notes Dr. Stanchfield. “Manually assisted delivery is basically standing there like a quarterback and catching the baby.”
Top 10 “medical misadventures”
And another slice of data reveals the 10 most prevalent medical misadventures in the ObGyn specialty in 2010 (TABLE 3):
- improper performance of a procedure
- no medical misadventure (i.e., no misadventure was identifiable)
- errors in diagnosis
- failure to supervise or monitor a case
- delay in performance of a procedure
- failure to recognize a complication
- surgical foreign body left in a patient after a procedure
- necessary treatment or management was “not performed”
- failure to instruct or communicate with a patient
- medication errors.
The total indemnity paid for these so-called misadventures was more than $136 million.1
TABLE 3
Putting the dollars in perspective
PIAA also collects data on the number of claims reported, and indemnity dollars paid, for other specialties.
“Of the 28 specialty groups included in the database, ObGyn ranks second”—behind internal medicine—“in the number of claims closed between 1985 and 2010,” a PIAA report notes. The ObGyn specialty also ranks second—behind dentists—in the percentage (35%) of those claims that were paid (for dentists, the figure was 46%). Obstetrics and gynecology was also responsible for the single largest indemnity payment—$13,000,000.1
Medical liability: A national disaster?
According to figures from the PIAA Data Sharing Project, an ongoing claim study that includes 22 PIAA member companies, $19.7 billion in losses (total indemnity plus expenses) were reported during the period from 1985 through 2008. Those losses represented approximately 25% of the physicians who were practicing during that time.
“So if you multiply that $19.7 billion figure by four”—to extrapolate it to the full spectrum of physicians practicing between 1985 and 2008—“you’ve got almost $80 billion coming out of the pockets of the doctors in this country,” says Dr. Stanchfield. If you compare that $80 billion figure to the World Trade Center disaster, which involved approximately $42 billion in losses, the need for federal tort reform is highlighted, he says. In 24 years, the physicians “in this country have paid for almost two World Trade Center disasters. That’s an incredible dollar cost.”
From Dr. Stanchfield’s perspective as a risk manager, the best thing physicians can do to protect themselves is to practice medicine wisely.
“One of our speakers used to say, ‘Look, just practice good, middle-of-the-road medicine. Don’t get yourself out on the fringes where you’re doing something questionable. Just practice rock-solid, conservative, safe medicine.’”
We want to hear from you! Tell us what you think.
1. Physician Insurers Association of America. 2011 Risk Management Review. Rockville, Md: PIAA; 2011.
2. Physician Insurers Association of America. PIAA Backgrounder. Rockville, Md: PIAA; 2011.
3. Stanchfied JB, ed. Insurance Recommendations for Obstetrical Practice. Revised ed. Salt Lake City, Utah: Utah Medical Insurance Association; 2009.
Good news on the medical liability front, Doctor!
Yes, that’s right, good news.
According to data from the Physician Insurers Association of America (PIAA), the number of claims that were paid in the ObGyn category between 2006 and 2011 was 44% lower than the number of claims paid between 1986 and 1991.
The percentage of claims that were paid also decreased over the same quarter century. During 1986–1990, 37.25% of all claims were paid in the ObGyn category, compared with 31.73% during 2006–2010.1
And when claims for both periods are calculated in 2010 dollars, the amount paid also declined—by more than $138 million!
These are three of the findings that reflect “significant improvement” in obstetrics and gynecology in medical liability, says John B. Stanchfield, MD, an endocrinologist who, for 25 years, was medical director of the Utah Medical Insurance Association (UMIA)—a member company of PIAA. PIAA is the insurance industry trade association.
PIAA member companies in the United States “include large national insurance companies, mid-size regional writers, single-state insurers, and specialty companies that serve specific health care–provider niche markets. Collectively, these companies provide insurance protection to more than 60% of America’s private practice physicians and write approximately 46%, or $5.2 billion, of the total industry premium.”2
The improvement in ObGyn comes as no surprise to Dr. Stanchfield because the specialty was “the first group that got ‘risk-managed’ almost universally across the country,” he says. “In our little company out here in Utah, in 1985, we were told that if we didn’t do something [about lawsuits in obstetrics and gynecology], we weren’t going to be able to insure that class anymore because we wouldn’t be able to collect enough money. That’s what the actuaries told us, but it wasn’t unique to us—it was a nationwide problem.”
Why was the ObGyn specialty, in particular, in need of aggressive risk management? What made ObGyn claims unique?
“It’s infant injury,” says Dr. Stanchfield. “It’s injury to the baby. Those claims, you start talking at a million dollars.”
Another reason may be that some claims in this specialty category involve doctors other than ObGyns who provide obstetric care—for example, family practice physicians.

A risk manager’s perspective
After receiving the warning about ObGyn claims, UMIA got busy. First, it formed a committee comprising perinatologists, ObGyns, family practice physicians, claims specialists, and attorneys. “We analyzed all claims that were paid, looking for common denominators,” says Dr. Stanchfield. Improvement was clearly needed in about 10 areas, so “we basically created a risk-management program and then mandated it.” In the process, the organization published a booklet entitled Insurance Recommendations for Obstetrical Practice, of which Dr. Stanchfield was the editor.3
The booklet offers guidance on 10 potential “problem” areas:
- antepartum testing
- hypertension and pregnancy
- operative vaginal delivery
- breech delivery
- oxytocin administration
- vaginal birth after cesarean
- use of misoprostol
- shoulder dystocia
- preterm labor
- hospital standards.
Fewer claims and more physicians
The declining number and percentage of paid claims in obstetrics and gynecology over 25 years may be even more impressive than the figures suggest, says Dr. Stanchfield.
“Gestalt tells me that through the years there are more practicing physicians rather than fewer,” so the denominator is increasing even as these claims are declining—making the decrease “even more powerful.”
The numbers haven’t improved to the same degree in other specialties, Dr. Stanchfield says. “If you look at global data, the decrease in paid claims might have been 10% to 15%. In ObGyn, if you compare the last 5-year block of data with the first 5-year block, the number of paid claims is almost cut in half.”
What brought about this improvement?
“There weren’t any groundbreaking medical or surgical technological advances during this period. It was just doing it better. And the main push to doing it better in this country, in my opinion, is risk management.”
Slicing the data
Now for the not-so-great news: In 2010 alone, more than $55 million was paid out in the ObGyn category for 10 patient conditions. Topping the list were “pregnancy” and “brain-damaged infant.” The $55 million figure represents the money paid for the top 10 most commonly cited conditions in cases closed during 2010 (TABLE 1).
TABLE 1
Claims categorized under the rather broad category of pregnancy usually were placed there because a more appropriate category was lacking, says Dr. Stanchfield. These claims typically involve “things that happen—usually to the baby—that result in a lawsuit other than brain damage per se.” For example, a claim that involved skull fracture without brain damage might fall into this zone, he says.
Problematic procedures
Slicing the data a different way, problems related to the 10 most commonly cited ObGyn procedures cost PIAA companies more than $120 million dollars in 2010—and that figure is only for the top 10.1 The top three procedures, in terms of number of claims closed in 2010, were operative procedures on the uterus, manually assisted delivery, and cesarean delivery (TABLE 2).
TABLE 2
Manually assisted delivery does not include vacuum extraction or forceps delivery, notes Dr. Stanchfield. “Manually assisted delivery is basically standing there like a quarterback and catching the baby.”
Top 10 “medical misadventures”
And another slice of data reveals the 10 most prevalent medical misadventures in the ObGyn specialty in 2010 (TABLE 3):
- improper performance of a procedure
- no medical misadventure (i.e., no misadventure was identifiable)
- errors in diagnosis
- failure to supervise or monitor a case
- delay in performance of a procedure
- failure to recognize a complication
- surgical foreign body left in a patient after a procedure
- necessary treatment or management was “not performed”
- failure to instruct or communicate with a patient
- medication errors.
The total indemnity paid for these so-called misadventures was more than $136 million.1
TABLE 3
Putting the dollars in perspective
PIAA also collects data on the number of claims reported, and indemnity dollars paid, for other specialties.
“Of the 28 specialty groups included in the database, ObGyn ranks second”—behind internal medicine—“in the number of claims closed between 1985 and 2010,” a PIAA report notes. The ObGyn specialty also ranks second—behind dentists—in the percentage (35%) of those claims that were paid (for dentists, the figure was 46%). Obstetrics and gynecology was also responsible for the single largest indemnity payment—$13,000,000.1
Medical liability: A national disaster?
According to figures from the PIAA Data Sharing Project, an ongoing claim study that includes 22 PIAA member companies, $19.7 billion in losses (total indemnity plus expenses) were reported during the period from 1985 through 2008. Those losses represented approximately 25% of the physicians who were practicing during that time.
“So if you multiply that $19.7 billion figure by four”—to extrapolate it to the full spectrum of physicians practicing between 1985 and 2008—“you’ve got almost $80 billion coming out of the pockets of the doctors in this country,” says Dr. Stanchfield. If you compare that $80 billion figure to the World Trade Center disaster, which involved approximately $42 billion in losses, the need for federal tort reform is highlighted, he says. In 24 years, the physicians “in this country have paid for almost two World Trade Center disasters. That’s an incredible dollar cost.”
From Dr. Stanchfield’s perspective as a risk manager, the best thing physicians can do to protect themselves is to practice medicine wisely.
“One of our speakers used to say, ‘Look, just practice good, middle-of-the-road medicine. Don’t get yourself out on the fringes where you’re doing something questionable. Just practice rock-solid, conservative, safe medicine.’”
We want to hear from you! Tell us what you think.
Good news on the medical liability front, Doctor!
Yes, that’s right, good news.
According to data from the Physician Insurers Association of America (PIAA), the number of claims that were paid in the ObGyn category between 2006 and 2011 was 44% lower than the number of claims paid between 1986 and 1991.
The percentage of claims that were paid also decreased over the same quarter century. During 1986–1990, 37.25% of all claims were paid in the ObGyn category, compared with 31.73% during 2006–2010.1
And when claims for both periods are calculated in 2010 dollars, the amount paid also declined—by more than $138 million!
These are three of the findings that reflect “significant improvement” in obstetrics and gynecology in medical liability, says John B. Stanchfield, MD, an endocrinologist who, for 25 years, was medical director of the Utah Medical Insurance Association (UMIA)—a member company of PIAA. PIAA is the insurance industry trade association.
PIAA member companies in the United States “include large national insurance companies, mid-size regional writers, single-state insurers, and specialty companies that serve specific health care–provider niche markets. Collectively, these companies provide insurance protection to more than 60% of America’s private practice physicians and write approximately 46%, or $5.2 billion, of the total industry premium.”2
The improvement in ObGyn comes as no surprise to Dr. Stanchfield because the specialty was “the first group that got ‘risk-managed’ almost universally across the country,” he says. “In our little company out here in Utah, in 1985, we were told that if we didn’t do something [about lawsuits in obstetrics and gynecology], we weren’t going to be able to insure that class anymore because we wouldn’t be able to collect enough money. That’s what the actuaries told us, but it wasn’t unique to us—it was a nationwide problem.”
Why was the ObGyn specialty, in particular, in need of aggressive risk management? What made ObGyn claims unique?
“It’s infant injury,” says Dr. Stanchfield. “It’s injury to the baby. Those claims, you start talking at a million dollars.”
Another reason may be that some claims in this specialty category involve doctors other than ObGyns who provide obstetric care—for example, family practice physicians.

A risk manager’s perspective
After receiving the warning about ObGyn claims, UMIA got busy. First, it formed a committee comprising perinatologists, ObGyns, family practice physicians, claims specialists, and attorneys. “We analyzed all claims that were paid, looking for common denominators,” says Dr. Stanchfield. Improvement was clearly needed in about 10 areas, so “we basically created a risk-management program and then mandated it.” In the process, the organization published a booklet entitled Insurance Recommendations for Obstetrical Practice, of which Dr. Stanchfield was the editor.3
The booklet offers guidance on 10 potential “problem” areas:
- antepartum testing
- hypertension and pregnancy
- operative vaginal delivery
- breech delivery
- oxytocin administration
- vaginal birth after cesarean
- use of misoprostol
- shoulder dystocia
- preterm labor
- hospital standards.
Fewer claims and more physicians
The declining number and percentage of paid claims in obstetrics and gynecology over 25 years may be even more impressive than the figures suggest, says Dr. Stanchfield.
“Gestalt tells me that through the years there are more practicing physicians rather than fewer,” so the denominator is increasing even as these claims are declining—making the decrease “even more powerful.”
The numbers haven’t improved to the same degree in other specialties, Dr. Stanchfield says. “If you look at global data, the decrease in paid claims might have been 10% to 15%. In ObGyn, if you compare the last 5-year block of data with the first 5-year block, the number of paid claims is almost cut in half.”
What brought about this improvement?
“There weren’t any groundbreaking medical or surgical technological advances during this period. It was just doing it better. And the main push to doing it better in this country, in my opinion, is risk management.”
Slicing the data
Now for the not-so-great news: In 2010 alone, more than $55 million was paid out in the ObGyn category for 10 patient conditions. Topping the list were “pregnancy” and “brain-damaged infant.” The $55 million figure represents the money paid for the top 10 most commonly cited conditions in cases closed during 2010 (TABLE 1).
TABLE 1
Claims categorized under the rather broad category of pregnancy usually were placed there because a more appropriate category was lacking, says Dr. Stanchfield. These claims typically involve “things that happen—usually to the baby—that result in a lawsuit other than brain damage per se.” For example, a claim that involved skull fracture without brain damage might fall into this zone, he says.
Problematic procedures
Slicing the data a different way, problems related to the 10 most commonly cited ObGyn procedures cost PIAA companies more than $120 million dollars in 2010—and that figure is only for the top 10.1 The top three procedures, in terms of number of claims closed in 2010, were operative procedures on the uterus, manually assisted delivery, and cesarean delivery (TABLE 2).
TABLE 2
Manually assisted delivery does not include vacuum extraction or forceps delivery, notes Dr. Stanchfield. “Manually assisted delivery is basically standing there like a quarterback and catching the baby.”
Top 10 “medical misadventures”
And another slice of data reveals the 10 most prevalent medical misadventures in the ObGyn specialty in 2010 (TABLE 3):
- improper performance of a procedure
- no medical misadventure (i.e., no misadventure was identifiable)
- errors in diagnosis
- failure to supervise or monitor a case
- delay in performance of a procedure
- failure to recognize a complication
- surgical foreign body left in a patient after a procedure
- necessary treatment or management was “not performed”
- failure to instruct or communicate with a patient
- medication errors.
The total indemnity paid for these so-called misadventures was more than $136 million.1
TABLE 3
Putting the dollars in perspective
PIAA also collects data on the number of claims reported, and indemnity dollars paid, for other specialties.
“Of the 28 specialty groups included in the database, ObGyn ranks second”—behind internal medicine—“in the number of claims closed between 1985 and 2010,” a PIAA report notes. The ObGyn specialty also ranks second—behind dentists—in the percentage (35%) of those claims that were paid (for dentists, the figure was 46%). Obstetrics and gynecology was also responsible for the single largest indemnity payment—$13,000,000.1
Medical liability: A national disaster?
According to figures from the PIAA Data Sharing Project, an ongoing claim study that includes 22 PIAA member companies, $19.7 billion in losses (total indemnity plus expenses) were reported during the period from 1985 through 2008. Those losses represented approximately 25% of the physicians who were practicing during that time.
“So if you multiply that $19.7 billion figure by four”—to extrapolate it to the full spectrum of physicians practicing between 1985 and 2008—“you’ve got almost $80 billion coming out of the pockets of the doctors in this country,” says Dr. Stanchfield. If you compare that $80 billion figure to the World Trade Center disaster, which involved approximately $42 billion in losses, the need for federal tort reform is highlighted, he says. In 24 years, the physicians “in this country have paid for almost two World Trade Center disasters. That’s an incredible dollar cost.”
From Dr. Stanchfield’s perspective as a risk manager, the best thing physicians can do to protect themselves is to practice medicine wisely.
“One of our speakers used to say, ‘Look, just practice good, middle-of-the-road medicine. Don’t get yourself out on the fringes where you’re doing something questionable. Just practice rock-solid, conservative, safe medicine.’”
We want to hear from you! Tell us what you think.
1. Physician Insurers Association of America. 2011 Risk Management Review. Rockville, Md: PIAA; 2011.
2. Physician Insurers Association of America. PIAA Backgrounder. Rockville, Md: PIAA; 2011.
3. Stanchfied JB, ed. Insurance Recommendations for Obstetrical Practice. Revised ed. Salt Lake City, Utah: Utah Medical Insurance Association; 2009.
1. Physician Insurers Association of America. 2011 Risk Management Review. Rockville, Md: PIAA; 2011.
2. Physician Insurers Association of America. PIAA Backgrounder. Rockville, Md: PIAA; 2011.
3. Stanchfied JB, ed. Insurance Recommendations for Obstetrical Practice. Revised ed. Salt Lake City, Utah: Utah Medical Insurance Association; 2009.
Head entrapment in premature baby ... more

DURING BREECH VAGINAL DELIVERY of a premature infant, the child’s head became entrapped. A maternal-fetal medicine specialist was called in. Delivery took 22 minutes. The child has cerebral palsy, with severe developmental delays, and requires a gastrostomy tube and tracheotomy.
PATIENT’S CLAIM Lack of oxygen for 22 minutes before delivery caused brain damage. Inappropriate maneuvers used by the physicians and nurses to relieve head entrapment also contributed to the injury. An emergency cesarean delivery should have been performed when vaginal delivery was delayed.
DEFENDANTS’ DEFENSE The appropriate maneuvers were performed to release the entrapped head. The child’s problems were due to her prematurity and fetal inflammatory response syndrome.
VERDICT In Illinois, a summary judgment was granted for the maternal-fetal medicine physician. A directed verdict was given for one nurse. A jury returned a defense verdict for the hospital, a labor and delivery nurse, and one of the ObGyns. The jury deadlocked on the claims against a second ObGyn.
Stenotic os thwarts two biopsies
AT HER ANNUAL VISIT in June 2006, a 48-year-old woman reported heavy bleeding. Her ObGyn asked the woman to return for re-examination. Twelve days later, ultrasonography revealed an enlarged uterus. The ObGyn attempted to perform a biopsy, but failed because of a stenotic os.
In September 2006, after a course of hormones, the ObGyn again tried to obtain a biopsy, but once more encountered the stenotic os. A hysterectomy was discussed, but the patient declined. In October 2007, the woman agreed to a hysterectomy. During surgery, the ObGyn identified cancer, and a gynecologic oncologist was called in. The woman was found to have stage-IV endometrial cancer. She underwent chemotherapy; at trial, the cancer was in remission.
PATIENT’S CLAIM Cancer should have been diagnosed earlier.
PHYSICIAN’S DEFENSE There was no negligence; the patient had rejected hysterectomy in September 2006. In addition, the cancer initially was not endometrial, but had started in an area of adenomyosis deep in the uterine wall.
VERDICT A Kentucky defense verdict was returned.
Brachial plexus injury after shoulder dystocia
AN OBESE WOMAN had gestational diabetes; the fetus was estimated to be macrosomic. When shoulder dystocia was encountered at delivery, the ObGyn delivered the child using several maneuvers. The child was born with a brachial plexus injury.
PATIENT’S CLAIM The physician was negligent in not scheduling a cesarean delivery because the fetus was large. When dystocia occurred, the ObGyn continued to apply traction to the infant’s head and neck, causing injury.
PHYSICIAN’S DEFENSE The proper maneuvers were undertaken to deliver the child as quickly and safely as possible.
VERDICT A $72,500 Texas settlement was reached.
Was informed consent neglected?
A 35-YEAR-OLD WOMAN underwent diagnostic laparoscopy in March 2005 because of severe pelvic pain. During surgery, the ObGyn observed adhesions and scarring that obstructed visualization of the pelvic area. He converted to an open procedure and discovered advanced-stage endometriosis. Because of his concern that endometriosis might perforate the patient’s colon, he performed supracervical hysterectomy.
PATIENT’S CLAIM The ObGyn was negligent in converting to an open procedure and performing the hysterectomy without obtaining informed consent. She suffered post-traumatic stress disorder because of the surgery.
PHYSICIAN’S DEFENSE The only option for treating the conditions he found was a hysterectomy. The patient had a history of anxiety prior to surgery.
VERDICT A Tennessee defense verdict was returned.
Nipples “too high” after breast reduction surgery
A 25-YEAR-OLD WOMAN underwent breast reduction surgery.
PATIENT’S CLAIM The plastic surgeon placed her nipples too high on her chest, making it impossible to find a bra that covered them, and making it difficult to find clothing to wear.
PHYSICIAN’S DEFENSE Unforeseeable postoperative changes caused the woman’s breasts to drop, giving the appearance of the nipples being too high. The nipples were properly located during surgery.
VERDICT A $170,000 Georgia verdict was returned.
Placental abruption; stillbirth follows
A 24-YEAR-OLD WOMAN AWOKE one day during the 39th week of pregnancy with abrupt onset of vaginal bleeding. She arrived at the emergency department (ED) at 12:30 am, and was transferred to labor and delivery at 1:12 am. A sonogram at 1:24 am revealed a fetal heart rate of 2 beats in 40 seconds, and a fetal scalp electrode did not register a heartbeat.
The mother was immediately prepped for emergency cesarean delivery, but a second sonogram performed in the OR showed no fetal heartbeat. Cesarean delivery was cancelled and labor was induced. The stillborn fetus was delivered vaginally several hours later, when a >60% placental abruption was found.
PATIENT’S CLAIM She was not treated in a timely manner in the ED or on labor and delivery. An emergency cesarean delivery should have been performed earlier.
DEFENDANTS’ DEFENSE All treatment had been timely. Placental abruption was the cause of fetal demise; the child was not viable shortly after the mother’s arrival. The time allowed for transfer from the ED to labor and delivery, evaluation, and emergency cesarean preparation was appropriate. The child could not possibly have been born alive.
VERDICT An Illinois defense verdict was returned.
Child’s enlarged heart unnoticed; lethal result
A WOMAN UNDERWENT four prenatal sonograms because she was found to have a single umbilical artery. Delivery was uneventful.
At 26 days, the infant became ill and was vomiting. The pediatrician sent the parents and baby to the emergency department, where Dr. A undertook his care. A radiologist read a three-view plain radiograph remotely and reported nothing abnormal. The infant was discharged.
When the parents returned the child to the ED the next morning, he was in cardiac failure related to an enlarged heart. He died before he could be transported to another hospital.
PATIENT’S CLAIM The ObGyn failed to diagnose the child’s defective heart in utero. Dr. A relied on the radiologist’s report; he should have personally viewed the radiograph, as it clearly showed the defective and enlarged heart. The defect could have been surgically repaired. The hospital nurses and radiologist were also negligent.
DEFENDANTS’ DEFENSE The hospital and radiologist settled for undisclosed amounts, and the trial proceeded against the ObGyn and Dr. A.
The ObGyn maintained that none of the prenatal sonograms was troubling; she had complied with the standard of care. Dr. A claimed that it was reasonable to rely on the radiologist’s report. Both physicians claimed they could not have done anything to avoid the child’s death; the hospital, radiologist, and pediatrician were at fault.
VERDICT A Kentucky defense verdict was returned.
Death from occult uterine Ca
A WOMAN SAW HER GYNECOLOGIST in January 1999 with postmenopausal bleeding and severe pelvic pain, but the physician could not determine a source of the problems.
Several months later, another gynecologist found that she had uterine sarcoma. She died of metastatic leiomyosarcoma at age 52 in July 2000.
ESTATE’S CLAIM The first gynecologist was negligent in failing to diagnose and treat the cancer, failing to consult or refer her to a specialist, and in prescribing hormones, which are contraindicated and caused the cancer to grow more rapidly.
PHYSICIAN’S DEFENSE The cancer had metastasized before the woman’s first visit, but was too small to be detected at that time. The decedent was already taking hormones when he saw her in January 1999; he only changed the type and brand. Hormones would not cause this type of cancer to grow more rapidly.
VERDICT A Texas defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.

DURING BREECH VAGINAL DELIVERY of a premature infant, the child’s head became entrapped. A maternal-fetal medicine specialist was called in. Delivery took 22 minutes. The child has cerebral palsy, with severe developmental delays, and requires a gastrostomy tube and tracheotomy.
PATIENT’S CLAIM Lack of oxygen for 22 minutes before delivery caused brain damage. Inappropriate maneuvers used by the physicians and nurses to relieve head entrapment also contributed to the injury. An emergency cesarean delivery should have been performed when vaginal delivery was delayed.
DEFENDANTS’ DEFENSE The appropriate maneuvers were performed to release the entrapped head. The child’s problems were due to her prematurity and fetal inflammatory response syndrome.
VERDICT In Illinois, a summary judgment was granted for the maternal-fetal medicine physician. A directed verdict was given for one nurse. A jury returned a defense verdict for the hospital, a labor and delivery nurse, and one of the ObGyns. The jury deadlocked on the claims against a second ObGyn.
Stenotic os thwarts two biopsies
AT HER ANNUAL VISIT in June 2006, a 48-year-old woman reported heavy bleeding. Her ObGyn asked the woman to return for re-examination. Twelve days later, ultrasonography revealed an enlarged uterus. The ObGyn attempted to perform a biopsy, but failed because of a stenotic os.
In September 2006, after a course of hormones, the ObGyn again tried to obtain a biopsy, but once more encountered the stenotic os. A hysterectomy was discussed, but the patient declined. In October 2007, the woman agreed to a hysterectomy. During surgery, the ObGyn identified cancer, and a gynecologic oncologist was called in. The woman was found to have stage-IV endometrial cancer. She underwent chemotherapy; at trial, the cancer was in remission.
PATIENT’S CLAIM Cancer should have been diagnosed earlier.
PHYSICIAN’S DEFENSE There was no negligence; the patient had rejected hysterectomy in September 2006. In addition, the cancer initially was not endometrial, but had started in an area of adenomyosis deep in the uterine wall.
VERDICT A Kentucky defense verdict was returned.
Brachial plexus injury after shoulder dystocia
AN OBESE WOMAN had gestational diabetes; the fetus was estimated to be macrosomic. When shoulder dystocia was encountered at delivery, the ObGyn delivered the child using several maneuvers. The child was born with a brachial plexus injury.
PATIENT’S CLAIM The physician was negligent in not scheduling a cesarean delivery because the fetus was large. When dystocia occurred, the ObGyn continued to apply traction to the infant’s head and neck, causing injury.
PHYSICIAN’S DEFENSE The proper maneuvers were undertaken to deliver the child as quickly and safely as possible.
VERDICT A $72,500 Texas settlement was reached.
Was informed consent neglected?
A 35-YEAR-OLD WOMAN underwent diagnostic laparoscopy in March 2005 because of severe pelvic pain. During surgery, the ObGyn observed adhesions and scarring that obstructed visualization of the pelvic area. He converted to an open procedure and discovered advanced-stage endometriosis. Because of his concern that endometriosis might perforate the patient’s colon, he performed supracervical hysterectomy.
PATIENT’S CLAIM The ObGyn was negligent in converting to an open procedure and performing the hysterectomy without obtaining informed consent. She suffered post-traumatic stress disorder because of the surgery.
PHYSICIAN’S DEFENSE The only option for treating the conditions he found was a hysterectomy. The patient had a history of anxiety prior to surgery.
VERDICT A Tennessee defense verdict was returned.
Nipples “too high” after breast reduction surgery
A 25-YEAR-OLD WOMAN underwent breast reduction surgery.
PATIENT’S CLAIM The plastic surgeon placed her nipples too high on her chest, making it impossible to find a bra that covered them, and making it difficult to find clothing to wear.
PHYSICIAN’S DEFENSE Unforeseeable postoperative changes caused the woman’s breasts to drop, giving the appearance of the nipples being too high. The nipples were properly located during surgery.
VERDICT A $170,000 Georgia verdict was returned.
Placental abruption; stillbirth follows
A 24-YEAR-OLD WOMAN AWOKE one day during the 39th week of pregnancy with abrupt onset of vaginal bleeding. She arrived at the emergency department (ED) at 12:30 am, and was transferred to labor and delivery at 1:12 am. A sonogram at 1:24 am revealed a fetal heart rate of 2 beats in 40 seconds, and a fetal scalp electrode did not register a heartbeat.
The mother was immediately prepped for emergency cesarean delivery, but a second sonogram performed in the OR showed no fetal heartbeat. Cesarean delivery was cancelled and labor was induced. The stillborn fetus was delivered vaginally several hours later, when a >60% placental abruption was found.
PATIENT’S CLAIM She was not treated in a timely manner in the ED or on labor and delivery. An emergency cesarean delivery should have been performed earlier.
DEFENDANTS’ DEFENSE All treatment had been timely. Placental abruption was the cause of fetal demise; the child was not viable shortly after the mother’s arrival. The time allowed for transfer from the ED to labor and delivery, evaluation, and emergency cesarean preparation was appropriate. The child could not possibly have been born alive.
VERDICT An Illinois defense verdict was returned.
Child’s enlarged heart unnoticed; lethal result
A WOMAN UNDERWENT four prenatal sonograms because she was found to have a single umbilical artery. Delivery was uneventful.
At 26 days, the infant became ill and was vomiting. The pediatrician sent the parents and baby to the emergency department, where Dr. A undertook his care. A radiologist read a three-view plain radiograph remotely and reported nothing abnormal. The infant was discharged.
When the parents returned the child to the ED the next morning, he was in cardiac failure related to an enlarged heart. He died before he could be transported to another hospital.
PATIENT’S CLAIM The ObGyn failed to diagnose the child’s defective heart in utero. Dr. A relied on the radiologist’s report; he should have personally viewed the radiograph, as it clearly showed the defective and enlarged heart. The defect could have been surgically repaired. The hospital nurses and radiologist were also negligent.
DEFENDANTS’ DEFENSE The hospital and radiologist settled for undisclosed amounts, and the trial proceeded against the ObGyn and Dr. A.
The ObGyn maintained that none of the prenatal sonograms was troubling; she had complied with the standard of care. Dr. A claimed that it was reasonable to rely on the radiologist’s report. Both physicians claimed they could not have done anything to avoid the child’s death; the hospital, radiologist, and pediatrician were at fault.
VERDICT A Kentucky defense verdict was returned.
Death from occult uterine Ca
A WOMAN SAW HER GYNECOLOGIST in January 1999 with postmenopausal bleeding and severe pelvic pain, but the physician could not determine a source of the problems.
Several months later, another gynecologist found that she had uterine sarcoma. She died of metastatic leiomyosarcoma at age 52 in July 2000.
ESTATE’S CLAIM The first gynecologist was negligent in failing to diagnose and treat the cancer, failing to consult or refer her to a specialist, and in prescribing hormones, which are contraindicated and caused the cancer to grow more rapidly.
PHYSICIAN’S DEFENSE The cancer had metastasized before the woman’s first visit, but was too small to be detected at that time. The decedent was already taking hormones when he saw her in January 1999; he only changed the type and brand. Hormones would not cause this type of cancer to grow more rapidly.
VERDICT A Texas defense verdict was returned.

DURING BREECH VAGINAL DELIVERY of a premature infant, the child’s head became entrapped. A maternal-fetal medicine specialist was called in. Delivery took 22 minutes. The child has cerebral palsy, with severe developmental delays, and requires a gastrostomy tube and tracheotomy.
PATIENT’S CLAIM Lack of oxygen for 22 minutes before delivery caused brain damage. Inappropriate maneuvers used by the physicians and nurses to relieve head entrapment also contributed to the injury. An emergency cesarean delivery should have been performed when vaginal delivery was delayed.
DEFENDANTS’ DEFENSE The appropriate maneuvers were performed to release the entrapped head. The child’s problems were due to her prematurity and fetal inflammatory response syndrome.
VERDICT In Illinois, a summary judgment was granted for the maternal-fetal medicine physician. A directed verdict was given for one nurse. A jury returned a defense verdict for the hospital, a labor and delivery nurse, and one of the ObGyns. The jury deadlocked on the claims against a second ObGyn.
Stenotic os thwarts two biopsies
AT HER ANNUAL VISIT in June 2006, a 48-year-old woman reported heavy bleeding. Her ObGyn asked the woman to return for re-examination. Twelve days later, ultrasonography revealed an enlarged uterus. The ObGyn attempted to perform a biopsy, but failed because of a stenotic os.
In September 2006, after a course of hormones, the ObGyn again tried to obtain a biopsy, but once more encountered the stenotic os. A hysterectomy was discussed, but the patient declined. In October 2007, the woman agreed to a hysterectomy. During surgery, the ObGyn identified cancer, and a gynecologic oncologist was called in. The woman was found to have stage-IV endometrial cancer. She underwent chemotherapy; at trial, the cancer was in remission.
PATIENT’S CLAIM Cancer should have been diagnosed earlier.
PHYSICIAN’S DEFENSE There was no negligence; the patient had rejected hysterectomy in September 2006. In addition, the cancer initially was not endometrial, but had started in an area of adenomyosis deep in the uterine wall.
VERDICT A Kentucky defense verdict was returned.
Brachial plexus injury after shoulder dystocia
AN OBESE WOMAN had gestational diabetes; the fetus was estimated to be macrosomic. When shoulder dystocia was encountered at delivery, the ObGyn delivered the child using several maneuvers. The child was born with a brachial plexus injury.
PATIENT’S CLAIM The physician was negligent in not scheduling a cesarean delivery because the fetus was large. When dystocia occurred, the ObGyn continued to apply traction to the infant’s head and neck, causing injury.
PHYSICIAN’S DEFENSE The proper maneuvers were undertaken to deliver the child as quickly and safely as possible.
VERDICT A $72,500 Texas settlement was reached.
Was informed consent neglected?
A 35-YEAR-OLD WOMAN underwent diagnostic laparoscopy in March 2005 because of severe pelvic pain. During surgery, the ObGyn observed adhesions and scarring that obstructed visualization of the pelvic area. He converted to an open procedure and discovered advanced-stage endometriosis. Because of his concern that endometriosis might perforate the patient’s colon, he performed supracervical hysterectomy.
PATIENT’S CLAIM The ObGyn was negligent in converting to an open procedure and performing the hysterectomy without obtaining informed consent. She suffered post-traumatic stress disorder because of the surgery.
PHYSICIAN’S DEFENSE The only option for treating the conditions he found was a hysterectomy. The patient had a history of anxiety prior to surgery.
VERDICT A Tennessee defense verdict was returned.
Nipples “too high” after breast reduction surgery
A 25-YEAR-OLD WOMAN underwent breast reduction surgery.
PATIENT’S CLAIM The plastic surgeon placed her nipples too high on her chest, making it impossible to find a bra that covered them, and making it difficult to find clothing to wear.
PHYSICIAN’S DEFENSE Unforeseeable postoperative changes caused the woman’s breasts to drop, giving the appearance of the nipples being too high. The nipples were properly located during surgery.
VERDICT A $170,000 Georgia verdict was returned.
Placental abruption; stillbirth follows
A 24-YEAR-OLD WOMAN AWOKE one day during the 39th week of pregnancy with abrupt onset of vaginal bleeding. She arrived at the emergency department (ED) at 12:30 am, and was transferred to labor and delivery at 1:12 am. A sonogram at 1:24 am revealed a fetal heart rate of 2 beats in 40 seconds, and a fetal scalp electrode did not register a heartbeat.
The mother was immediately prepped for emergency cesarean delivery, but a second sonogram performed in the OR showed no fetal heartbeat. Cesarean delivery was cancelled and labor was induced. The stillborn fetus was delivered vaginally several hours later, when a >60% placental abruption was found.
PATIENT’S CLAIM She was not treated in a timely manner in the ED or on labor and delivery. An emergency cesarean delivery should have been performed earlier.
DEFENDANTS’ DEFENSE All treatment had been timely. Placental abruption was the cause of fetal demise; the child was not viable shortly after the mother’s arrival. The time allowed for transfer from the ED to labor and delivery, evaluation, and emergency cesarean preparation was appropriate. The child could not possibly have been born alive.
VERDICT An Illinois defense verdict was returned.
Child’s enlarged heart unnoticed; lethal result
A WOMAN UNDERWENT four prenatal sonograms because she was found to have a single umbilical artery. Delivery was uneventful.
At 26 days, the infant became ill and was vomiting. The pediatrician sent the parents and baby to the emergency department, where Dr. A undertook his care. A radiologist read a three-view plain radiograph remotely and reported nothing abnormal. The infant was discharged.
When the parents returned the child to the ED the next morning, he was in cardiac failure related to an enlarged heart. He died before he could be transported to another hospital.
PATIENT’S CLAIM The ObGyn failed to diagnose the child’s defective heart in utero. Dr. A relied on the radiologist’s report; he should have personally viewed the radiograph, as it clearly showed the defective and enlarged heart. The defect could have been surgically repaired. The hospital nurses and radiologist were also negligent.
DEFENDANTS’ DEFENSE The hospital and radiologist settled for undisclosed amounts, and the trial proceeded against the ObGyn and Dr. A.
The ObGyn maintained that none of the prenatal sonograms was troubling; she had complied with the standard of care. Dr. A claimed that it was reasonable to rely on the radiologist’s report. Both physicians claimed they could not have done anything to avoid the child’s death; the hospital, radiologist, and pediatrician were at fault.
VERDICT A Kentucky defense verdict was returned.
Death from occult uterine Ca
A WOMAN SAW HER GYNECOLOGIST in January 1999 with postmenopausal bleeding and severe pelvic pain, but the physician could not determine a source of the problems.
Several months later, another gynecologist found that she had uterine sarcoma. She died of metastatic leiomyosarcoma at age 52 in July 2000.
ESTATE’S CLAIM The first gynecologist was negligent in failing to diagnose and treat the cancer, failing to consult or refer her to a specialist, and in prescribing hormones, which are contraindicated and caused the cancer to grow more rapidly.
PHYSICIAN’S DEFENSE The cancer had metastasized before the woman’s first visit, but was too small to be detected at that time. The decedent was already taking hormones when he saw her in January 1999; he only changed the type and brand. Hormones would not cause this type of cancer to grow more rapidly.
VERDICT A Texas defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.