User login
Outcomes of audit-enhanced monitoring of patients with type 2 diabetes
OBJECTIVE: To assess the outcome of diabetes care in a practice-based research network after the introduction of an audit-enhanced monitoring system (AEMS).
STUDY DESIGN: An AEMS was introduced into family practices participating in the academic research network of Nijmegen University, Nijmegen, the Netherlands. One and 7 years later, a cross-sectional analysis was performed on the outcome of care in all type 2 diabetes patients under treatment by their family physicians.
POPULATION: Approximately 42,500 patients in 1993 and approximately 46,000 patients in 1999 at 10 family practices participating in the university’s academic research network.
OUTCOMES MEASURED: Targets of care were Hb A1c< 8.5% and blood pressure < 150/85 mm Hg. Targets for lipids depended on age, cardiovascular morbidity, and smoking status.
RESULTS: In 1993, 540 type 2 diabetes patients were included; in 1999, 851 such patients were included, representing a prevalence of 1.3% and 1.9%, respectively. Glycemic control improved statistically significantly by the percentage of patients with Hb A1c< 8.5% (87% vs 59%, P = .0001) and the mean Hb A1c (7.1% vs 8.2%, P = .0001) from the first to the second cohort. Mean blood pressure and the percentage of patients above the target blood pressure did not change. The mean cholesterol level (207 mg/dL vs 238 mg/dL [5.4 mmol/L vs 6.2 mmol/L], P = .0001) and the percentage of patients who met their target lipid levels (72% vs 52%, P = .001) also improved between 1993 and 1999. In addition, an increased percentage of patients attended an annual review in the past year (73% vs 84%).
CONCLUSIONS: Outcomes of diabetes care in a family practice research setting using an AEMS were comparable with those reported under randomized controlled trial conditions.
- Guidelines recommend tight metabolic control in combination with state-of-the-art management of other risk factors in order to prevent macrovascular and microvascular complications in patients with type 2 diabetes.
- The formulation of clinical guidelines alone, however, is insufficient to improve actual care.
- Monitoring and feedback with systematic follow-up of treatment targets of diabetes care in a family practice setting can produce outcomes comparable with those reported under randomized controlled trial conditions.
Recent studies have emphasized the importance of tight metabolic control in combination with state-of-the-art management of other risk factors to prevent macrovascular and microvascular complications in patients with type 2 diabetes mellitus.1-5 Guidelines for diabetes care recommend systematic monitoring of patients’ health status, including metabolic control, cardiovascular risk factors, and desired outcome of care.6-8
The formulation of clinical guidelines alone, however, is insufficient to improve actual care.9,10 Strategies to reinforce the guidelines in daily practice include monitoring the patient’s clinical condition over a given period of time, feedback to the clinician about the outcome, audit of clinical performance, academic detailing by peers, and evidence-based guidelines.10-12 Monitoring and feedback with systematic follow-up of relevant treatment targets enhanced a proactive approach to patients,13 which is a key factor for successful diabetes care.14 As large numbers of patients with type 2 diabetes are treated in family practice, it is important that target-specific monitoring fit into the overall primary care function of family practice and that it answer the needs, demands, and expectations of patients.
Since 1985, the Nijmegen University Department of Family Practice has been developing a computer-assisted practice network, the Nijmegen Academic Research Network CMR/NMP, to study chronic diseases.15,16 The objectives of this network are to support care for patients with chronic diseases and to create an optimal setting for clinical research under family practice conditions. This paper analyzes the outcome of diabetes care in the CMR/NMP 7 years after the introduction of an audit-enhanced monitoring system (AEMS).17
The aims were to assess (1) the outcome of care compared with external guideline criteria and the results of clinical trials, and (2) the relationship of outcome to process of care measures and to patient-related and practice-related factors.
Methods
Study population
Data were collected at the 10 family practices in the CMR/NMP, with 25 family physicians and a patient list of approximately 46,000 in 1999.16 All patients meeting World Health Organization criteria for the diagnosis of type 2 diabetes mellitus and under treatment by a family physician in 1993 and 1999 were included in the AEMS.15,18 Patients who were treated with insulin within 1 year of diagnosis and who continued to take it were considered to have type 1 diabetes mellitus. All other patients were regarded as type 2, regardless of current treatment. For this study we included all type 2 diabetes patients under treatment by their family physician in 1993 and 1999. Patients who had died or who had moved to another area or been admitted to a residential nursing home before the end of the year were excluded, as were those who had been newly diagnosed during the year.
Audit-enhanced monitoring system
Since 1989, data have been collected on all type 2 diabetes patients at the time of diagnosis and during all regular (quarterly) diabetes-related outpatient visits. In 1992, a structured annual review, based on guidelines from the Dutch College of Family Physicians,19 was added. Starting in 1992, monitoring has consisted of the assessment of (1) compliance with 3 monthly control visits and an annual review visit; (2) glycemic control (ie, fasting blood glucose and Hb A1c); (3) diabetes-related complications (ie, retinopathy, creatinine clearance, and foot problems); (4) cardiovascular risk factors (ie, smoking behavior, blood pressure, and lipid profile); (5) cardiovascular morbidity (ie, myocardial infarction, angina pectoris, heart failure, peripheral vascular disease, transient ischemic attack, or cerebrovascular accident). In addition, all reasons for dropping out, including cause of death, were recorded. Morbidity and causes of death were defined as in the International Classification of Health Problems in Primary Care.
To facilitate data collection, a computerized Research Registration System (RRS) was developed. The system was integrated into a standard Dutch electronic record system for family practice (Promedico, Euroned). The RRS generates templates for recording data at the quarterly or annual diabetes control visits into the patient’s electronic record. Templates guide the delivery of care and a reminder system is integrated into the RRS. Office assistants contact patients who do not come in for visits at regular intervals, both those (< 1%) who usually do not come in and those who are supposed to but fail to do so.
Family physicians sent the RRS data files to the University Department of Family Practice, where they were processed into a feedback report on process of care and outcome of care measures on 3 levels: (1) total study population; (2) practice population; (3) individual patient. Process and outcome measures were compared with external criteria based on guidelines from the Dutch College of Family Medicine and with average performance at the other practices. Feedback items were selected in consultation with the participating physicians. In this way, feedback corresponded with daily practice needs. During the project, the feedback was gradually extended from process to outcome measures. The feedback was standard to all practices.
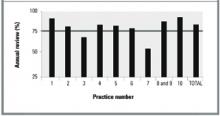
Feedback was discussed at University Department of Family Medicine meetings, which maintained uniform registration and safeguarded the progress of the project. The feedback was also sent to every practice and participating GP. This report contained practice-level as well as physician-level data. The Figure demonstrates one way in which data are presented at the meetings and shows the percentage of patients who attended their annual diabetes control visit in the year studied.
Targets for care
Targets for care consisted of 2 elements: process and outcome measures. The key marker for process of care was compliance to the annual diabetes control visit. Key markers for desired outcome of care were (1) Hb A1c < 8.5%,19 (2) blood pressure less than 160/90 mm Hg (revised to 150/85 mm Hg in 1999),8,19 and (3) lipids in accordance with Dutch guidelines for general practice8: (a) cholesterol < 5 mmol (192 mg/dL) for patients with cardiovascular morbidity; (b) cholesterol/HDL ratio < 5.0 in smokers without cardiovascular morbidity; and (c) cholesterol/HDL < 6.0 in nonsmokers without cardiovascular morbidity. These guidelines for lipid-lowering therapy are based on sex, a life expectancy of at least 5 years, smoking status, presence of cardiovascular morbidity, total cholesterol levels, high-density lipoprotein (HDL) cholesterol levels, and triglyceride levels. If even 1 of these variables is absent, the potential value of lipid lowering cannot be determined.8
Analysis
Cross-sectional analysis was performed on the outcome of diabetes care in patients with type 2 diabetes who were treated by their family physicians in 1993 and 1999. The comparison was based on all patients who had been treated for the full calendar year in 1993 and 1999; therefore, it was based on a dynamic population. Process and outcome measures are compared using the chi-squared, unpaired t, or Mann–Whitney test, as appropriate. Results are expressed as means plus or minus standard deviations or as proportions. Multilevel analysis was performed to assess factors that contributed to the variance in compliance with the annual review and the desired glycemic level (Hb A1c < 8.5%).
Results
In 1993, 540 type 2 diabetes patients (prevalence 1.3%) were included in the AEMS. Of these, 51 had been newly diagnosed (incidence 1.2/1000); 37 had been treated by a specialist (7%); and 20 did not participate (4%). Excluding the 108 patients in the latter 3 categories left a total of 432 patients for analysis. In 1999, 851 patients were included (prevalence 1.9%). Of these, 138 had been newly diagnosed (incidence 3.0/1000); 88 had been treated by a specialist (10%); and 31 did not participate (4%). Excluding the 257 patients in those 3 categories left 594 for analysis. Table 1 shows the baseline characteristics of patients included in the analysis.
Annual review was attended by 73% of patients in 1993 and 84% of patients in 1999 (Table 2). Increased compliance was achieved at all the practices, although differences between practices remained in 1999 (Figure). Univariate analysis showed that compliance with the annual review in 1999 was related to the practice (P = .001) but not to patient factors such as sex, age, duration of diabetes, therapy regimen, or cardiovascular morbidity, even after adjusting for blood glucose levels. Patients who did not attend their annual diabetes control visit had statistically significantly higher fasting blood glucose levels than patients who did comply (8.9 mmol/L [160 mg/dL] vs 8.2 mmol [147 mg/dL], P = .03). In 1993, 59% of patients had visited an ophthalmologist in the previous 2 years versus 80% in 1999.
In 1993, Hb A1c was measured in 51% of patients with a mean of 8.2%. In 1999, compliance in measurement of Hb A1c improved to 82%, with a mean Hb A1c level of 7.1% (P = .0001, Table 3). The percentages of patients with an Hb A1c level of more than 8.5% decreased from 41% to 13% (P = .001). These outcomes were associated with changes in treatment (P = .001): a decrease in patients treated with diet only (22% in 1993 vs 13% in 1999) and with oral hypoglycemic monotherapy (45% in 1993 vs 37% in 1999); an increase in patients treated with combination therapy using 2 or more oral hypoglycemic agents (22% in 1993 vs 31% in 1999); and an increase in insulin therapy (11% in 1993 vs 19% in 1999). Univariate analysis showed that poor glycemic control (Hb A1c > 8.5%) in 1999 was related to the therapy regimen (P = .001) but not to sex, age, duration of diabetes, cardiovascular morbidity, or practice. The glycemic control in patients treated with combination therapy or insulin was poorer than in patients treated with diet only or oral hypoglycemic monotherapy, probably reflecting the fact that patients with less severe disease are managed with single agents and diet.
Compliance with measurement of blood pressure improved from 72% to 83% during the study period (Table 3). However, the percentage of patients with a systolic blood pressure below 150 mm Hg or a diastolic blood pressure below 85 mm Hg did not change between 1993 and 1999 whether patients were hypertensive or not. In hypertensive patients with type 2 diabetes, the mean diastolic blood pressure decreased from 88 mm Hg to 85 mm Hg (P = .004), but mean systolic blood pressure did not change.
The mean cholesterol level was lower in 1999 than in 1993 (6.2 vs 5.4 mmol/L; 238 mg/dL vs 207 mg/dL, P = .0001), as was the mean triglyceride level (2.54 mmol/L vs 2.07 mmol/L; 221 mg/dL vs 180 mg/dL, P = .0003). In both years, data regarding which patients could be considered for lipid-lowering therapy were available for 63% and 82%, respectively. In 1993, a far higher proportion of patients had failed to reach lipid target levels than was the case in 1999 (48% vs 28%, respectively, P = .001).
Multilevel analysis showed that paying an annual diabetes control visit (a process outcome) was related to the practice (intraclass correlation coefficient [ICC] = 0.29) but not to patient factors. Reaching the glycemic target level of Hb A1c < 8.5%, however, was not related to practice factors (ICC = 0.003).
TABLE 1
Chacteristics of type 2 diabetes patients under family physician care in 1993 and 1999
| Characteristic | 1993 (n = 432) | 1999 (n = 594) | P |
|---|---|---|---|
| Mean age (years) | 68 | 67 | .34 |
| Male, % | 38 | 44 | .06 |
| Mean duration of diabetes (years) | 6.2 | 6.7 | .08 |
| Cardiovascular morbidity,% | 31 | 27 | .08 |
| Hypertension,% | 36 | 39 | .51 |
| Mean body mass index (kg/m2) | 28.3 | 29.2 | .02 |
| NOTE: Table excludes those patients newly diagnosed during the previous year. | |||
TABLE 2
Process of care for type 2 diabetes patients under family physician care, 1993 vs 1999
| Process of care | Compliance to criterion, % (range between practices) | |
|---|---|---|
| 1993* | 1999† | |
| Any visit addressing diabetic control in past year | 97 (89–100) | 96 (91–100) |
| Annual review in past year | 73 (34–90) | 84 (64–100) |
| Visit to ophthalmologist in previous 2 years | 59 (40–79) | 80 (60–94) |
| *n = 432. | ||
| † n = 594. | ||
TABLE 3
Outcomes of care for type 2 diabetes patients under family physician care, 1993 vs 1999
| Outcome | 1993 (n = 432) | Missing* (%) | 1999 (n = 594) | Missing* (%) | P |
|---|---|---|---|---|---|
| Mean fasting glucose (mmol/L) | 8.6 (2.9) | 3 | 8.3 (2.6) | 4 | .07 |
| Mean Hb A1c (percentage) | 8.3 (2.2) | 50 | 7.1 (1.5) | 18 | .0001 |
| Hb A1c | |||||
| < 7% | 30% | 52% | ┐ | ||
| 7% to 8.5% | 29% | 35% | .001 | ||
| > 8.5% | 41% | 13% | ┘ | ||
| Blood pressure in patients with hypertension | n = 112 (36%) | 28 | n = 195(39%) | 17 | |
| •Mean systolic blood pressure (mm Hg) | 161 (19) | 158 (20) | .2 | ||
| •Mean diastolic blood pressure (mm Hg) | 88 (9) | 85 (9) | .004 | ||
| •Systolic blood pressure > 150 mm Hg | 68% | 62% | .3 | ||
| •Diastolic blood pressure > 85 mm Hg | 51% | 48% | .7 | ||
| Blood pressure in patients without hypertension | n = 197 (64%) | 28 | n = 299 (61%) | 17 | |
| •Mean systolic blood pressure (mm Hg) | 145 (18) | 145 (19) | .7 | ||
| •Mean diastolic blood pressure (mm Hg) | 80 (9) | 79 (9) | .5 | ||
| •Systolic blood pressure > 150 mm Hg | 34% | 35% | .6 | ||
| •Diastolic blood pressure > 85 mm Hg | 23% | 23% | .9 | ||
| Mean cholesterol (mmol/L /mg/dL) | 6.2 (1.3) / 238 (49) | 31 | 5.4 (1.1) / 207 (42) | 17 | .0001 |
| Mean HDL (mmol/L /mg/dL) | 1.2 (0.6) / 46.5 (23.2) | 62 | 1.2 (0.4) / 46.5 (15.5) | 23 | .59 |
| Mean triglycerides (mmol /mg/dL) | 2.6 (1.5) / 226 (130) | 58 | 2.1 (1.3) / 182 (113) | 23 | .0001 |
| Patients with cardiovascular morbidity > 5 mmol/L and cholesterol >192 mg/L | 31% | ┐ | 17% | ┐ | ┐ |
| Patients without cardiovascular morbidity, smokers, and those with cholesterol/HDL ratio > 5.0 | 4% | 37 | 5% | 18 | .001 |
| Patients without cardiovascular morbidity, nonsmokers, and those with cholesterol/HDL ratio > 6.0 | 13% | ┘ | 6% | ┘ | ┘ |
| *Refers to the percentage of patients with missing data for this variable. | |||||
FIGURE
Percentage of patients with annual review (target = 75%) in 1999 (n=594)
Discussion
During 7 years of structured audit-enhanced monitoring of patients with type 2 diabetes in an academic family practice research network, the intermediate measures of diabetes care improved. In particular, the mean Hb A1c of 7.1% can be seen as a measure of good quality of care. The number of patients treated according to Dutch family practice guidelines (a process of care outcome) also increased.8
While our data were collected during normal daily care (effectiveness), the findings come close to the outcome of care under ideal trial conditions (efficacy).21 In the UK Prospective Diabetes Study (UKPDS), the median Hb A1c level for all newly diagnosed patients in the group with intensive blood glucose control over 10 years reached a comparable level of 7.0%.1 Thus, the outcome of our study approaches that achieved under trial conditions. When we analyzed patients without outcome data as poorly controlled (worst-case scenario), Hb A1c was less than 8.5% in 28%.
The trend of improvement in glycemic control could have been a result of improved overall diabetes care in the Netherlands during the study period. Data about the outcome of diabetes care in the family medicine setting in the Netherlands during the study period are scarce and, when available, are derived from other research networks. In these networks a mean Hb A1c of 7.0% to 7.6% was reached.22 Yet indicators from other studies suggest that our results were far better than outcome from usual care. Recently published data on such outcomes in family medicine in the Netherlands showed that Hb A1c, blood pressure, and lipids were measured in less than 30% of patients.23,24 Outcomes from usual care as reported in research studies appear to be strongly biased by selection and probably cannot serve as a valid reference value.
The disappointing effect on the percentage of patients who reached the target blood pressure could have resulted from evaluating the data prematurely. When the study began, the primary objective was to improve glycemic control. Shortly after the publication of the Scandinavian Simvastatin Survival Study (4S)3 and the UKPDS,12 the guidelines of the Dutch College of Family Physicians were changed8 and more attention was paid to blood pressure and lipid control. This new approach was discussed with the participating family physicians. Consequently, the target for blood pressure was revised from 160/90 mm Hg to 150/85 mm Hg and lipid-lowering therapy was tailored to each patient’s cardiovascular risk profile. The 1999 outcome with respect to blood pressure and lipid control was measured only 1 year after these changes had been announced. Nevertheless, mean diastolic blood pressure in hypertensive patients and total cholesterol and triglyceride levels decreased significantly, and more patients reached target levels for lipids in 1999 than in 1993.
Our outcome was reached through enhanced compliance to guidelines. Therefore, the outcome in 1999 was based on a larger percentage of available patients. Because the AEMS studied a dynamic group of patients, the study groups in 1993 and 1999 were not identical. Theoretically, improvement in outcome could have been reached by including more easily manageable patients. However, no patient factors such as sex, age, duration of diabetes, treatment modality, or cardiovascular morbidity were related to compliance with annual review. The higher fasting blood glucose levels in patients who were noncompliant with annual review probably reflected under-treatment rather than more severe illness status. Therefore, we are confident that the findings reflect improved overall diabetes care.
The data on process measures in this study compare favorably with those of multipractice audits of diabetes care in the United Kingdom.25-29 The high prevalence rate of 2.0% (exclusively patients with type 2 diabetes) supports the validity of our data.25-27 Among our patients, 96% had been seen at least once during the previous year. In the large studies by Khunti and Bennett, only 85% had been seen during the previous year.25,26 The mean annual compliance rate of nearly 85% with Hb A1c and blood pressure measurements in our study was high. In particular, compliance with lipid control25,26,28 and funduscopy26,28 was better in our study. In 2 longitudinal studies that used an organized care system in which feedback was provided to the participating family physicians, compliance rates in process measures of up to 75% were reported.30,31
The outcomes of this study were achieved in an academic family practice research network, with specific facilities for the proactive supervision of patients with chronic diseases. These results cannot and should not be generalized to “routine” family practice. Monitoring and feedback in routine family practice are in themselves insufficient to improve the quality of care.10 Care assessment should preferably take a more comprehensive approach in which evidence-based goals for care are formulated, care is improved to reach those goals, and care is measured to see whether those goals have been achieved.11 Our academic network provides this comprehensive approach.
The electronic Research Registration System played an important role in the audit-enhanced monitoring. In the pilot phase of the project, paper records were used. Although using paper records had clear disadvantages, one could expect to achieve similar results using such records in combination with a central electronic data bank.
Conclusions
Outcomes of diabetes care in our family research setting were comparable with those reported in randomized controlled trials. Therefore, it is possible for the management of diabetes in family practice to be efficacious. This finding should encourage more efforts by physicians in family practice to bridge the gap between efficacy and effectiveness.
Important differences remained in achieved process measures between the academic family practices. While the outcome of diabetes care in the network was favorable, the outcome of treatment was unsatisfactory in a substantial number of patients. Further implementation strategies must be developed. The differences in achieved process measures were probably unrelated to socioeconomic differences between the practice populations, since the practice pairs 1/3 and 7/10 served comparable communities and had different levels of compliance.
Our study demonstrated that a high quality of diabetes care in family practice can be achieved. Audit-enhanced monitoring, which will provide the greatest benefit to the most patients with type 2 diabetes mellitus, should be implemented as part of a quality improvement system.
ACKNOWLEDGMENTS
The authors wish to thank the family physicians and practice nurses for their continuing support and data collection.
1. UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-53.
2. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;327:703-13.
3. Pyörälä K, Pedersen T, Klekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetes patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care 1997;20:614-20.
4. Adler AI, Stratton IM, Niel HAW, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405-12.
5. Adler AI, Stratton IM, Niel HAW, et al. Association of systolic blood pressure glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412-9.
6. American Diabetes Association. Standards of Medical Care for patients with diabetes mellitus (position statement). Diabetes Care 1999;22(suppl 1):S32-9.
7. European Diabetes Policy Group 1999. A desktop guide to type 2 diabetes mellitus. Diabet Med 1999;16:716-30.
8. Rutten GEHM, Verhoeven S, Heine RJ, et al. NHG-standaard diabetes mellitus type 2 (eerste herziening). Huisarts Wet 1999;42:67-84.Available in English at: http://www.diabetesinprimarycare.com.
9. Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of guidelines. BMJ 1999;318:527-30.
10. Grol R, Jones R. Twenty years of implementation research. Fam Pract 2000;17:S32-5.
11. Grol R. Between evidence-based practice and total quality management: the implementation of cost-effective care. Int J Qual Health Care 2000;12:297-304.
12. Thomson O’Brien MA, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. Audit and feedback: effects on professional practice and health care outcomes (Cochrane Review). In: The Cochrane Library, Issue 3, 2000. Oxford, England: Update Software.
13. Hart JT. Reactive and proactive care: a crisis. Br J Gen Pract 1990;40:4-9.
14. Greenhalgh PM. Shared care for diabetes: a systematic review. Occasional Paper 67. Royal College of General Practitioners; 1994.
15. Weel van C. Validating long-term morbidity recording. J Epidemiol Community Health 1995;49(suppl 1):29-32.
16. Weel van C, Smith H, Beasly JW. Family practice research networks: experience from three countries. J Fam Pract 2000;49:938-43.
17. Grauw de WJC, Lisdonk van de EH, Hoogen van den HJM, Weel van C. Monitoring of non-insulin dependent diabetes mellitus in general practice. Diabetes Nutr Metab 1991;4(suppl):67-71.
18. World Health Organization, Expert Committee on Diabetes Mellitus. WHO Technical Report No.727. Geneva, Switzerland: WHO; 1985.
19. Nederlands Huisartsen Genootschap. Standaard diabetes mellitus type II. Huisarts Wet 1989;32:15-8.
20. ICHPPC-2 Defined WONCA, 3rd ed. Oxford, England: Oxford University Press; 1983.
21. Weel van C, Knottnerus JA. Evidence-based interventions and comprehensive treatment. Lancet 1999;353:916-8.
22. Rutten G.H.E.M. Diabetiker-versorgung in den Nierderlanden. In: Lauterbach K, Ziegenhagen DJ. Diabetes mellitus—evidenz basierte diagnostik und therapie. Stuttgart, Germany: Schattauer; 2000;110-21.
23. Renders CM, Valk GD, Franse LV, Schellevis FG, Eijk van JThM, Wal van der G. Long-term effectiveness of a quality improvement program for patients with type 2 diabetes in general practice. Diabetes Care 2001;24:1365-70.
24. Dam van HA, Crebolder HFJM, Eijkelberg I, Nunen van M, Horst van der FG. Wegblijven van patienten met diabetes mellitus type 2—een echt probleem? Huisarts Wet 2000;43:380-4.
25. Khunti K, Baker R, Rumsey M, Lakhani M. Quality of care of patients with diabetes: collation of data from multi-practice audits of diabetes in primary care. Fam Pract 1999;16:54-9.
26. Benett IJ, Lambert C, Hinds G, Kirton C. Emerging standards for diabetes care from a city-wide primary care audit. Diabet Med 1994;11:489-92.
27. Howitt AJ, Cheales NA. Diabetes registers: a grassroots approach. BMJ 1993;307:1047-8.
28. Dunn NR, Bough P. Standards of care of diabetes patients in a typical English community. Br J Gen Pract 1996;46:401-5.
29. Turnbridge FKE, Millar JP, Schofield PJ, Spencer JA, Young G, Home PD. Diabetes care in general practice: an approach to audit of process and outcome. Br J Gen Pract 1993;34:291-5.
30. Butler CB, Smithers M, Stott N, Peters J. Audit-enhanced, districtwide primary care for people with diabetes mellitus. Eur J Gen Pract 1997;3:23-7.
31. Foulkes A, Kinmonth A, Frost S, Macdonald D. Organized personal care—an effective choice for managing diabetes in general practice. J R Coll Gen Pract 1989;39:444-7.
OBJECTIVE: To assess the outcome of diabetes care in a practice-based research network after the introduction of an audit-enhanced monitoring system (AEMS).
STUDY DESIGN: An AEMS was introduced into family practices participating in the academic research network of Nijmegen University, Nijmegen, the Netherlands. One and 7 years later, a cross-sectional analysis was performed on the outcome of care in all type 2 diabetes patients under treatment by their family physicians.
POPULATION: Approximately 42,500 patients in 1993 and approximately 46,000 patients in 1999 at 10 family practices participating in the university’s academic research network.
OUTCOMES MEASURED: Targets of care were Hb A1c< 8.5% and blood pressure < 150/85 mm Hg. Targets for lipids depended on age, cardiovascular morbidity, and smoking status.
RESULTS: In 1993, 540 type 2 diabetes patients were included; in 1999, 851 such patients were included, representing a prevalence of 1.3% and 1.9%, respectively. Glycemic control improved statistically significantly by the percentage of patients with Hb A1c< 8.5% (87% vs 59%, P = .0001) and the mean Hb A1c (7.1% vs 8.2%, P = .0001) from the first to the second cohort. Mean blood pressure and the percentage of patients above the target blood pressure did not change. The mean cholesterol level (207 mg/dL vs 238 mg/dL [5.4 mmol/L vs 6.2 mmol/L], P = .0001) and the percentage of patients who met their target lipid levels (72% vs 52%, P = .001) also improved between 1993 and 1999. In addition, an increased percentage of patients attended an annual review in the past year (73% vs 84%).
CONCLUSIONS: Outcomes of diabetes care in a family practice research setting using an AEMS were comparable with those reported under randomized controlled trial conditions.
- Guidelines recommend tight metabolic control in combination with state-of-the-art management of other risk factors in order to prevent macrovascular and microvascular complications in patients with type 2 diabetes.
- The formulation of clinical guidelines alone, however, is insufficient to improve actual care.
- Monitoring and feedback with systematic follow-up of treatment targets of diabetes care in a family practice setting can produce outcomes comparable with those reported under randomized controlled trial conditions.
Recent studies have emphasized the importance of tight metabolic control in combination with state-of-the-art management of other risk factors to prevent macrovascular and microvascular complications in patients with type 2 diabetes mellitus.1-5 Guidelines for diabetes care recommend systematic monitoring of patients’ health status, including metabolic control, cardiovascular risk factors, and desired outcome of care.6-8
The formulation of clinical guidelines alone, however, is insufficient to improve actual care.9,10 Strategies to reinforce the guidelines in daily practice include monitoring the patient’s clinical condition over a given period of time, feedback to the clinician about the outcome, audit of clinical performance, academic detailing by peers, and evidence-based guidelines.10-12 Monitoring and feedback with systematic follow-up of relevant treatment targets enhanced a proactive approach to patients,13 which is a key factor for successful diabetes care.14 As large numbers of patients with type 2 diabetes are treated in family practice, it is important that target-specific monitoring fit into the overall primary care function of family practice and that it answer the needs, demands, and expectations of patients.
Since 1985, the Nijmegen University Department of Family Practice has been developing a computer-assisted practice network, the Nijmegen Academic Research Network CMR/NMP, to study chronic diseases.15,16 The objectives of this network are to support care for patients with chronic diseases and to create an optimal setting for clinical research under family practice conditions. This paper analyzes the outcome of diabetes care in the CMR/NMP 7 years after the introduction of an audit-enhanced monitoring system (AEMS).17
The aims were to assess (1) the outcome of care compared with external guideline criteria and the results of clinical trials, and (2) the relationship of outcome to process of care measures and to patient-related and practice-related factors.
Methods
Study population
Data were collected at the 10 family practices in the CMR/NMP, with 25 family physicians and a patient list of approximately 46,000 in 1999.16 All patients meeting World Health Organization criteria for the diagnosis of type 2 diabetes mellitus and under treatment by a family physician in 1993 and 1999 were included in the AEMS.15,18 Patients who were treated with insulin within 1 year of diagnosis and who continued to take it were considered to have type 1 diabetes mellitus. All other patients were regarded as type 2, regardless of current treatment. For this study we included all type 2 diabetes patients under treatment by their family physician in 1993 and 1999. Patients who had died or who had moved to another area or been admitted to a residential nursing home before the end of the year were excluded, as were those who had been newly diagnosed during the year.
Audit-enhanced monitoring system
Since 1989, data have been collected on all type 2 diabetes patients at the time of diagnosis and during all regular (quarterly) diabetes-related outpatient visits. In 1992, a structured annual review, based on guidelines from the Dutch College of Family Physicians,19 was added. Starting in 1992, monitoring has consisted of the assessment of (1) compliance with 3 monthly control visits and an annual review visit; (2) glycemic control (ie, fasting blood glucose and Hb A1c); (3) diabetes-related complications (ie, retinopathy, creatinine clearance, and foot problems); (4) cardiovascular risk factors (ie, smoking behavior, blood pressure, and lipid profile); (5) cardiovascular morbidity (ie, myocardial infarction, angina pectoris, heart failure, peripheral vascular disease, transient ischemic attack, or cerebrovascular accident). In addition, all reasons for dropping out, including cause of death, were recorded. Morbidity and causes of death were defined as in the International Classification of Health Problems in Primary Care.
To facilitate data collection, a computerized Research Registration System (RRS) was developed. The system was integrated into a standard Dutch electronic record system for family practice (Promedico, Euroned). The RRS generates templates for recording data at the quarterly or annual diabetes control visits into the patient’s electronic record. Templates guide the delivery of care and a reminder system is integrated into the RRS. Office assistants contact patients who do not come in for visits at regular intervals, both those (< 1%) who usually do not come in and those who are supposed to but fail to do so.
Family physicians sent the RRS data files to the University Department of Family Practice, where they were processed into a feedback report on process of care and outcome of care measures on 3 levels: (1) total study population; (2) practice population; (3) individual patient. Process and outcome measures were compared with external criteria based on guidelines from the Dutch College of Family Medicine and with average performance at the other practices. Feedback items were selected in consultation with the participating physicians. In this way, feedback corresponded with daily practice needs. During the project, the feedback was gradually extended from process to outcome measures. The feedback was standard to all practices.
Feedback was discussed at University Department of Family Medicine meetings, which maintained uniform registration and safeguarded the progress of the project. The feedback was also sent to every practice and participating GP. This report contained practice-level as well as physician-level data. The Figure demonstrates one way in which data are presented at the meetings and shows the percentage of patients who attended their annual diabetes control visit in the year studied.
Targets for care
Targets for care consisted of 2 elements: process and outcome measures. The key marker for process of care was compliance to the annual diabetes control visit. Key markers for desired outcome of care were (1) Hb A1c < 8.5%,19 (2) blood pressure less than 160/90 mm Hg (revised to 150/85 mm Hg in 1999),8,19 and (3) lipids in accordance with Dutch guidelines for general practice8: (a) cholesterol < 5 mmol (192 mg/dL) for patients with cardiovascular morbidity; (b) cholesterol/HDL ratio < 5.0 in smokers without cardiovascular morbidity; and (c) cholesterol/HDL < 6.0 in nonsmokers without cardiovascular morbidity. These guidelines for lipid-lowering therapy are based on sex, a life expectancy of at least 5 years, smoking status, presence of cardiovascular morbidity, total cholesterol levels, high-density lipoprotein (HDL) cholesterol levels, and triglyceride levels. If even 1 of these variables is absent, the potential value of lipid lowering cannot be determined.8
Analysis
Cross-sectional analysis was performed on the outcome of diabetes care in patients with type 2 diabetes who were treated by their family physicians in 1993 and 1999. The comparison was based on all patients who had been treated for the full calendar year in 1993 and 1999; therefore, it was based on a dynamic population. Process and outcome measures are compared using the chi-squared, unpaired t, or Mann–Whitney test, as appropriate. Results are expressed as means plus or minus standard deviations or as proportions. Multilevel analysis was performed to assess factors that contributed to the variance in compliance with the annual review and the desired glycemic level (Hb A1c < 8.5%).
Results
In 1993, 540 type 2 diabetes patients (prevalence 1.3%) were included in the AEMS. Of these, 51 had been newly diagnosed (incidence 1.2/1000); 37 had been treated by a specialist (7%); and 20 did not participate (4%). Excluding the 108 patients in the latter 3 categories left a total of 432 patients for analysis. In 1999, 851 patients were included (prevalence 1.9%). Of these, 138 had been newly diagnosed (incidence 3.0/1000); 88 had been treated by a specialist (10%); and 31 did not participate (4%). Excluding the 257 patients in those 3 categories left 594 for analysis. Table 1 shows the baseline characteristics of patients included in the analysis.
Annual review was attended by 73% of patients in 1993 and 84% of patients in 1999 (Table 2). Increased compliance was achieved at all the practices, although differences between practices remained in 1999 (Figure). Univariate analysis showed that compliance with the annual review in 1999 was related to the practice (P = .001) but not to patient factors such as sex, age, duration of diabetes, therapy regimen, or cardiovascular morbidity, even after adjusting for blood glucose levels. Patients who did not attend their annual diabetes control visit had statistically significantly higher fasting blood glucose levels than patients who did comply (8.9 mmol/L [160 mg/dL] vs 8.2 mmol [147 mg/dL], P = .03). In 1993, 59% of patients had visited an ophthalmologist in the previous 2 years versus 80% in 1999.
In 1993, Hb A1c was measured in 51% of patients with a mean of 8.2%. In 1999, compliance in measurement of Hb A1c improved to 82%, with a mean Hb A1c level of 7.1% (P = .0001, Table 3). The percentages of patients with an Hb A1c level of more than 8.5% decreased from 41% to 13% (P = .001). These outcomes were associated with changes in treatment (P = .001): a decrease in patients treated with diet only (22% in 1993 vs 13% in 1999) and with oral hypoglycemic monotherapy (45% in 1993 vs 37% in 1999); an increase in patients treated with combination therapy using 2 or more oral hypoglycemic agents (22% in 1993 vs 31% in 1999); and an increase in insulin therapy (11% in 1993 vs 19% in 1999). Univariate analysis showed that poor glycemic control (Hb A1c > 8.5%) in 1999 was related to the therapy regimen (P = .001) but not to sex, age, duration of diabetes, cardiovascular morbidity, or practice. The glycemic control in patients treated with combination therapy or insulin was poorer than in patients treated with diet only or oral hypoglycemic monotherapy, probably reflecting the fact that patients with less severe disease are managed with single agents and diet.
Compliance with measurement of blood pressure improved from 72% to 83% during the study period (Table 3). However, the percentage of patients with a systolic blood pressure below 150 mm Hg or a diastolic blood pressure below 85 mm Hg did not change between 1993 and 1999 whether patients were hypertensive or not. In hypertensive patients with type 2 diabetes, the mean diastolic blood pressure decreased from 88 mm Hg to 85 mm Hg (P = .004), but mean systolic blood pressure did not change.
The mean cholesterol level was lower in 1999 than in 1993 (6.2 vs 5.4 mmol/L; 238 mg/dL vs 207 mg/dL, P = .0001), as was the mean triglyceride level (2.54 mmol/L vs 2.07 mmol/L; 221 mg/dL vs 180 mg/dL, P = .0003). In both years, data regarding which patients could be considered for lipid-lowering therapy were available for 63% and 82%, respectively. In 1993, a far higher proportion of patients had failed to reach lipid target levels than was the case in 1999 (48% vs 28%, respectively, P = .001).
Multilevel analysis showed that paying an annual diabetes control visit (a process outcome) was related to the practice (intraclass correlation coefficient [ICC] = 0.29) but not to patient factors. Reaching the glycemic target level of Hb A1c < 8.5%, however, was not related to practice factors (ICC = 0.003).
TABLE 1
Chacteristics of type 2 diabetes patients under family physician care in 1993 and 1999
| Characteristic | 1993 (n = 432) | 1999 (n = 594) | P |
|---|---|---|---|
| Mean age (years) | 68 | 67 | .34 |
| Male, % | 38 | 44 | .06 |
| Mean duration of diabetes (years) | 6.2 | 6.7 | .08 |
| Cardiovascular morbidity,% | 31 | 27 | .08 |
| Hypertension,% | 36 | 39 | .51 |
| Mean body mass index (kg/m2) | 28.3 | 29.2 | .02 |
| NOTE: Table excludes those patients newly diagnosed during the previous year. | |||
TABLE 2
Process of care for type 2 diabetes patients under family physician care, 1993 vs 1999
| Process of care | Compliance to criterion, % (range between practices) | |
|---|---|---|
| 1993* | 1999† | |
| Any visit addressing diabetic control in past year | 97 (89–100) | 96 (91–100) |
| Annual review in past year | 73 (34–90) | 84 (64–100) |
| Visit to ophthalmologist in previous 2 years | 59 (40–79) | 80 (60–94) |
| *n = 432. | ||
| † n = 594. | ||
TABLE 3
Outcomes of care for type 2 diabetes patients under family physician care, 1993 vs 1999
| Outcome | 1993 (n = 432) | Missing* (%) | 1999 (n = 594) | Missing* (%) | P |
|---|---|---|---|---|---|
| Mean fasting glucose (mmol/L) | 8.6 (2.9) | 3 | 8.3 (2.6) | 4 | .07 |
| Mean Hb A1c (percentage) | 8.3 (2.2) | 50 | 7.1 (1.5) | 18 | .0001 |
| Hb A1c | |||||
| < 7% | 30% | 52% | ┐ | ||
| 7% to 8.5% | 29% | 35% | .001 | ||
| > 8.5% | 41% | 13% | ┘ | ||
| Blood pressure in patients with hypertension | n = 112 (36%) | 28 | n = 195(39%) | 17 | |
| •Mean systolic blood pressure (mm Hg) | 161 (19) | 158 (20) | .2 | ||
| •Mean diastolic blood pressure (mm Hg) | 88 (9) | 85 (9) | .004 | ||
| •Systolic blood pressure > 150 mm Hg | 68% | 62% | .3 | ||
| •Diastolic blood pressure > 85 mm Hg | 51% | 48% | .7 | ||
| Blood pressure in patients without hypertension | n = 197 (64%) | 28 | n = 299 (61%) | 17 | |
| •Mean systolic blood pressure (mm Hg) | 145 (18) | 145 (19) | .7 | ||
| •Mean diastolic blood pressure (mm Hg) | 80 (9) | 79 (9) | .5 | ||
| •Systolic blood pressure > 150 mm Hg | 34% | 35% | .6 | ||
| •Diastolic blood pressure > 85 mm Hg | 23% | 23% | .9 | ||
| Mean cholesterol (mmol/L /mg/dL) | 6.2 (1.3) / 238 (49) | 31 | 5.4 (1.1) / 207 (42) | 17 | .0001 |
| Mean HDL (mmol/L /mg/dL) | 1.2 (0.6) / 46.5 (23.2) | 62 | 1.2 (0.4) / 46.5 (15.5) | 23 | .59 |
| Mean triglycerides (mmol /mg/dL) | 2.6 (1.5) / 226 (130) | 58 | 2.1 (1.3) / 182 (113) | 23 | .0001 |
| Patients with cardiovascular morbidity > 5 mmol/L and cholesterol >192 mg/L | 31% | ┐ | 17% | ┐ | ┐ |
| Patients without cardiovascular morbidity, smokers, and those with cholesterol/HDL ratio > 5.0 | 4% | 37 | 5% | 18 | .001 |
| Patients without cardiovascular morbidity, nonsmokers, and those with cholesterol/HDL ratio > 6.0 | 13% | ┘ | 6% | ┘ | ┘ |
| *Refers to the percentage of patients with missing data for this variable. | |||||
FIGURE
Percentage of patients with annual review (target = 75%) in 1999 (n=594)
Discussion
During 7 years of structured audit-enhanced monitoring of patients with type 2 diabetes in an academic family practice research network, the intermediate measures of diabetes care improved. In particular, the mean Hb A1c of 7.1% can be seen as a measure of good quality of care. The number of patients treated according to Dutch family practice guidelines (a process of care outcome) also increased.8
While our data were collected during normal daily care (effectiveness), the findings come close to the outcome of care under ideal trial conditions (efficacy).21 In the UK Prospective Diabetes Study (UKPDS), the median Hb A1c level for all newly diagnosed patients in the group with intensive blood glucose control over 10 years reached a comparable level of 7.0%.1 Thus, the outcome of our study approaches that achieved under trial conditions. When we analyzed patients without outcome data as poorly controlled (worst-case scenario), Hb A1c was less than 8.5% in 28%.
The trend of improvement in glycemic control could have been a result of improved overall diabetes care in the Netherlands during the study period. Data about the outcome of diabetes care in the family medicine setting in the Netherlands during the study period are scarce and, when available, are derived from other research networks. In these networks a mean Hb A1c of 7.0% to 7.6% was reached.22 Yet indicators from other studies suggest that our results were far better than outcome from usual care. Recently published data on such outcomes in family medicine in the Netherlands showed that Hb A1c, blood pressure, and lipids were measured in less than 30% of patients.23,24 Outcomes from usual care as reported in research studies appear to be strongly biased by selection and probably cannot serve as a valid reference value.
The disappointing effect on the percentage of patients who reached the target blood pressure could have resulted from evaluating the data prematurely. When the study began, the primary objective was to improve glycemic control. Shortly after the publication of the Scandinavian Simvastatin Survival Study (4S)3 and the UKPDS,12 the guidelines of the Dutch College of Family Physicians were changed8 and more attention was paid to blood pressure and lipid control. This new approach was discussed with the participating family physicians. Consequently, the target for blood pressure was revised from 160/90 mm Hg to 150/85 mm Hg and lipid-lowering therapy was tailored to each patient’s cardiovascular risk profile. The 1999 outcome with respect to blood pressure and lipid control was measured only 1 year after these changes had been announced. Nevertheless, mean diastolic blood pressure in hypertensive patients and total cholesterol and triglyceride levels decreased significantly, and more patients reached target levels for lipids in 1999 than in 1993.
Our outcome was reached through enhanced compliance to guidelines. Therefore, the outcome in 1999 was based on a larger percentage of available patients. Because the AEMS studied a dynamic group of patients, the study groups in 1993 and 1999 were not identical. Theoretically, improvement in outcome could have been reached by including more easily manageable patients. However, no patient factors such as sex, age, duration of diabetes, treatment modality, or cardiovascular morbidity were related to compliance with annual review. The higher fasting blood glucose levels in patients who were noncompliant with annual review probably reflected under-treatment rather than more severe illness status. Therefore, we are confident that the findings reflect improved overall diabetes care.
The data on process measures in this study compare favorably with those of multipractice audits of diabetes care in the United Kingdom.25-29 The high prevalence rate of 2.0% (exclusively patients with type 2 diabetes) supports the validity of our data.25-27 Among our patients, 96% had been seen at least once during the previous year. In the large studies by Khunti and Bennett, only 85% had been seen during the previous year.25,26 The mean annual compliance rate of nearly 85% with Hb A1c and blood pressure measurements in our study was high. In particular, compliance with lipid control25,26,28 and funduscopy26,28 was better in our study. In 2 longitudinal studies that used an organized care system in which feedback was provided to the participating family physicians, compliance rates in process measures of up to 75% were reported.30,31
The outcomes of this study were achieved in an academic family practice research network, with specific facilities for the proactive supervision of patients with chronic diseases. These results cannot and should not be generalized to “routine” family practice. Monitoring and feedback in routine family practice are in themselves insufficient to improve the quality of care.10 Care assessment should preferably take a more comprehensive approach in which evidence-based goals for care are formulated, care is improved to reach those goals, and care is measured to see whether those goals have been achieved.11 Our academic network provides this comprehensive approach.
The electronic Research Registration System played an important role in the audit-enhanced monitoring. In the pilot phase of the project, paper records were used. Although using paper records had clear disadvantages, one could expect to achieve similar results using such records in combination with a central electronic data bank.
Conclusions
Outcomes of diabetes care in our family research setting were comparable with those reported in randomized controlled trials. Therefore, it is possible for the management of diabetes in family practice to be efficacious. This finding should encourage more efforts by physicians in family practice to bridge the gap between efficacy and effectiveness.
Important differences remained in achieved process measures between the academic family practices. While the outcome of diabetes care in the network was favorable, the outcome of treatment was unsatisfactory in a substantial number of patients. Further implementation strategies must be developed. The differences in achieved process measures were probably unrelated to socioeconomic differences between the practice populations, since the practice pairs 1/3 and 7/10 served comparable communities and had different levels of compliance.
Our study demonstrated that a high quality of diabetes care in family practice can be achieved. Audit-enhanced monitoring, which will provide the greatest benefit to the most patients with type 2 diabetes mellitus, should be implemented as part of a quality improvement system.
ACKNOWLEDGMENTS
The authors wish to thank the family physicians and practice nurses for their continuing support and data collection.
OBJECTIVE: To assess the outcome of diabetes care in a practice-based research network after the introduction of an audit-enhanced monitoring system (AEMS).
STUDY DESIGN: An AEMS was introduced into family practices participating in the academic research network of Nijmegen University, Nijmegen, the Netherlands. One and 7 years later, a cross-sectional analysis was performed on the outcome of care in all type 2 diabetes patients under treatment by their family physicians.
POPULATION: Approximately 42,500 patients in 1993 and approximately 46,000 patients in 1999 at 10 family practices participating in the university’s academic research network.
OUTCOMES MEASURED: Targets of care were Hb A1c< 8.5% and blood pressure < 150/85 mm Hg. Targets for lipids depended on age, cardiovascular morbidity, and smoking status.
RESULTS: In 1993, 540 type 2 diabetes patients were included; in 1999, 851 such patients were included, representing a prevalence of 1.3% and 1.9%, respectively. Glycemic control improved statistically significantly by the percentage of patients with Hb A1c< 8.5% (87% vs 59%, P = .0001) and the mean Hb A1c (7.1% vs 8.2%, P = .0001) from the first to the second cohort. Mean blood pressure and the percentage of patients above the target blood pressure did not change. The mean cholesterol level (207 mg/dL vs 238 mg/dL [5.4 mmol/L vs 6.2 mmol/L], P = .0001) and the percentage of patients who met their target lipid levels (72% vs 52%, P = .001) also improved between 1993 and 1999. In addition, an increased percentage of patients attended an annual review in the past year (73% vs 84%).
CONCLUSIONS: Outcomes of diabetes care in a family practice research setting using an AEMS were comparable with those reported under randomized controlled trial conditions.
- Guidelines recommend tight metabolic control in combination with state-of-the-art management of other risk factors in order to prevent macrovascular and microvascular complications in patients with type 2 diabetes.
- The formulation of clinical guidelines alone, however, is insufficient to improve actual care.
- Monitoring and feedback with systematic follow-up of treatment targets of diabetes care in a family practice setting can produce outcomes comparable with those reported under randomized controlled trial conditions.
Recent studies have emphasized the importance of tight metabolic control in combination with state-of-the-art management of other risk factors to prevent macrovascular and microvascular complications in patients with type 2 diabetes mellitus.1-5 Guidelines for diabetes care recommend systematic monitoring of patients’ health status, including metabolic control, cardiovascular risk factors, and desired outcome of care.6-8
The formulation of clinical guidelines alone, however, is insufficient to improve actual care.9,10 Strategies to reinforce the guidelines in daily practice include monitoring the patient’s clinical condition over a given period of time, feedback to the clinician about the outcome, audit of clinical performance, academic detailing by peers, and evidence-based guidelines.10-12 Monitoring and feedback with systematic follow-up of relevant treatment targets enhanced a proactive approach to patients,13 which is a key factor for successful diabetes care.14 As large numbers of patients with type 2 diabetes are treated in family practice, it is important that target-specific monitoring fit into the overall primary care function of family practice and that it answer the needs, demands, and expectations of patients.
Since 1985, the Nijmegen University Department of Family Practice has been developing a computer-assisted practice network, the Nijmegen Academic Research Network CMR/NMP, to study chronic diseases.15,16 The objectives of this network are to support care for patients with chronic diseases and to create an optimal setting for clinical research under family practice conditions. This paper analyzes the outcome of diabetes care in the CMR/NMP 7 years after the introduction of an audit-enhanced monitoring system (AEMS).17
The aims were to assess (1) the outcome of care compared with external guideline criteria and the results of clinical trials, and (2) the relationship of outcome to process of care measures and to patient-related and practice-related factors.
Methods
Study population
Data were collected at the 10 family practices in the CMR/NMP, with 25 family physicians and a patient list of approximately 46,000 in 1999.16 All patients meeting World Health Organization criteria for the diagnosis of type 2 diabetes mellitus and under treatment by a family physician in 1993 and 1999 were included in the AEMS.15,18 Patients who were treated with insulin within 1 year of diagnosis and who continued to take it were considered to have type 1 diabetes mellitus. All other patients were regarded as type 2, regardless of current treatment. For this study we included all type 2 diabetes patients under treatment by their family physician in 1993 and 1999. Patients who had died or who had moved to another area or been admitted to a residential nursing home before the end of the year were excluded, as were those who had been newly diagnosed during the year.
Audit-enhanced monitoring system
Since 1989, data have been collected on all type 2 diabetes patients at the time of diagnosis and during all regular (quarterly) diabetes-related outpatient visits. In 1992, a structured annual review, based on guidelines from the Dutch College of Family Physicians,19 was added. Starting in 1992, monitoring has consisted of the assessment of (1) compliance with 3 monthly control visits and an annual review visit; (2) glycemic control (ie, fasting blood glucose and Hb A1c); (3) diabetes-related complications (ie, retinopathy, creatinine clearance, and foot problems); (4) cardiovascular risk factors (ie, smoking behavior, blood pressure, and lipid profile); (5) cardiovascular morbidity (ie, myocardial infarction, angina pectoris, heart failure, peripheral vascular disease, transient ischemic attack, or cerebrovascular accident). In addition, all reasons for dropping out, including cause of death, were recorded. Morbidity and causes of death were defined as in the International Classification of Health Problems in Primary Care.
To facilitate data collection, a computerized Research Registration System (RRS) was developed. The system was integrated into a standard Dutch electronic record system for family practice (Promedico, Euroned). The RRS generates templates for recording data at the quarterly or annual diabetes control visits into the patient’s electronic record. Templates guide the delivery of care and a reminder system is integrated into the RRS. Office assistants contact patients who do not come in for visits at regular intervals, both those (< 1%) who usually do not come in and those who are supposed to but fail to do so.
Family physicians sent the RRS data files to the University Department of Family Practice, where they were processed into a feedback report on process of care and outcome of care measures on 3 levels: (1) total study population; (2) practice population; (3) individual patient. Process and outcome measures were compared with external criteria based on guidelines from the Dutch College of Family Medicine and with average performance at the other practices. Feedback items were selected in consultation with the participating physicians. In this way, feedback corresponded with daily practice needs. During the project, the feedback was gradually extended from process to outcome measures. The feedback was standard to all practices.
Feedback was discussed at University Department of Family Medicine meetings, which maintained uniform registration and safeguarded the progress of the project. The feedback was also sent to every practice and participating GP. This report contained practice-level as well as physician-level data. The Figure demonstrates one way in which data are presented at the meetings and shows the percentage of patients who attended their annual diabetes control visit in the year studied.
Targets for care
Targets for care consisted of 2 elements: process and outcome measures. The key marker for process of care was compliance to the annual diabetes control visit. Key markers for desired outcome of care were (1) Hb A1c < 8.5%,19 (2) blood pressure less than 160/90 mm Hg (revised to 150/85 mm Hg in 1999),8,19 and (3) lipids in accordance with Dutch guidelines for general practice8: (a) cholesterol < 5 mmol (192 mg/dL) for patients with cardiovascular morbidity; (b) cholesterol/HDL ratio < 5.0 in smokers without cardiovascular morbidity; and (c) cholesterol/HDL < 6.0 in nonsmokers without cardiovascular morbidity. These guidelines for lipid-lowering therapy are based on sex, a life expectancy of at least 5 years, smoking status, presence of cardiovascular morbidity, total cholesterol levels, high-density lipoprotein (HDL) cholesterol levels, and triglyceride levels. If even 1 of these variables is absent, the potential value of lipid lowering cannot be determined.8
Analysis
Cross-sectional analysis was performed on the outcome of diabetes care in patients with type 2 diabetes who were treated by their family physicians in 1993 and 1999. The comparison was based on all patients who had been treated for the full calendar year in 1993 and 1999; therefore, it was based on a dynamic population. Process and outcome measures are compared using the chi-squared, unpaired t, or Mann–Whitney test, as appropriate. Results are expressed as means plus or minus standard deviations or as proportions. Multilevel analysis was performed to assess factors that contributed to the variance in compliance with the annual review and the desired glycemic level (Hb A1c < 8.5%).
Results
In 1993, 540 type 2 diabetes patients (prevalence 1.3%) were included in the AEMS. Of these, 51 had been newly diagnosed (incidence 1.2/1000); 37 had been treated by a specialist (7%); and 20 did not participate (4%). Excluding the 108 patients in the latter 3 categories left a total of 432 patients for analysis. In 1999, 851 patients were included (prevalence 1.9%). Of these, 138 had been newly diagnosed (incidence 3.0/1000); 88 had been treated by a specialist (10%); and 31 did not participate (4%). Excluding the 257 patients in those 3 categories left 594 for analysis. Table 1 shows the baseline characteristics of patients included in the analysis.
Annual review was attended by 73% of patients in 1993 and 84% of patients in 1999 (Table 2). Increased compliance was achieved at all the practices, although differences between practices remained in 1999 (Figure). Univariate analysis showed that compliance with the annual review in 1999 was related to the practice (P = .001) but not to patient factors such as sex, age, duration of diabetes, therapy regimen, or cardiovascular morbidity, even after adjusting for blood glucose levels. Patients who did not attend their annual diabetes control visit had statistically significantly higher fasting blood glucose levels than patients who did comply (8.9 mmol/L [160 mg/dL] vs 8.2 mmol [147 mg/dL], P = .03). In 1993, 59% of patients had visited an ophthalmologist in the previous 2 years versus 80% in 1999.
In 1993, Hb A1c was measured in 51% of patients with a mean of 8.2%. In 1999, compliance in measurement of Hb A1c improved to 82%, with a mean Hb A1c level of 7.1% (P = .0001, Table 3). The percentages of patients with an Hb A1c level of more than 8.5% decreased from 41% to 13% (P = .001). These outcomes were associated with changes in treatment (P = .001): a decrease in patients treated with diet only (22% in 1993 vs 13% in 1999) and with oral hypoglycemic monotherapy (45% in 1993 vs 37% in 1999); an increase in patients treated with combination therapy using 2 or more oral hypoglycemic agents (22% in 1993 vs 31% in 1999); and an increase in insulin therapy (11% in 1993 vs 19% in 1999). Univariate analysis showed that poor glycemic control (Hb A1c > 8.5%) in 1999 was related to the therapy regimen (P = .001) but not to sex, age, duration of diabetes, cardiovascular morbidity, or practice. The glycemic control in patients treated with combination therapy or insulin was poorer than in patients treated with diet only or oral hypoglycemic monotherapy, probably reflecting the fact that patients with less severe disease are managed with single agents and diet.
Compliance with measurement of blood pressure improved from 72% to 83% during the study period (Table 3). However, the percentage of patients with a systolic blood pressure below 150 mm Hg or a diastolic blood pressure below 85 mm Hg did not change between 1993 and 1999 whether patients were hypertensive or not. In hypertensive patients with type 2 diabetes, the mean diastolic blood pressure decreased from 88 mm Hg to 85 mm Hg (P = .004), but mean systolic blood pressure did not change.
The mean cholesterol level was lower in 1999 than in 1993 (6.2 vs 5.4 mmol/L; 238 mg/dL vs 207 mg/dL, P = .0001), as was the mean triglyceride level (2.54 mmol/L vs 2.07 mmol/L; 221 mg/dL vs 180 mg/dL, P = .0003). In both years, data regarding which patients could be considered for lipid-lowering therapy were available for 63% and 82%, respectively. In 1993, a far higher proportion of patients had failed to reach lipid target levels than was the case in 1999 (48% vs 28%, respectively, P = .001).
Multilevel analysis showed that paying an annual diabetes control visit (a process outcome) was related to the practice (intraclass correlation coefficient [ICC] = 0.29) but not to patient factors. Reaching the glycemic target level of Hb A1c < 8.5%, however, was not related to practice factors (ICC = 0.003).
TABLE 1
Chacteristics of type 2 diabetes patients under family physician care in 1993 and 1999
| Characteristic | 1993 (n = 432) | 1999 (n = 594) | P |
|---|---|---|---|
| Mean age (years) | 68 | 67 | .34 |
| Male, % | 38 | 44 | .06 |
| Mean duration of diabetes (years) | 6.2 | 6.7 | .08 |
| Cardiovascular morbidity,% | 31 | 27 | .08 |
| Hypertension,% | 36 | 39 | .51 |
| Mean body mass index (kg/m2) | 28.3 | 29.2 | .02 |
| NOTE: Table excludes those patients newly diagnosed during the previous year. | |||
TABLE 2
Process of care for type 2 diabetes patients under family physician care, 1993 vs 1999
| Process of care | Compliance to criterion, % (range between practices) | |
|---|---|---|
| 1993* | 1999† | |
| Any visit addressing diabetic control in past year | 97 (89–100) | 96 (91–100) |
| Annual review in past year | 73 (34–90) | 84 (64–100) |
| Visit to ophthalmologist in previous 2 years | 59 (40–79) | 80 (60–94) |
| *n = 432. | ||
| † n = 594. | ||
TABLE 3
Outcomes of care for type 2 diabetes patients under family physician care, 1993 vs 1999
| Outcome | 1993 (n = 432) | Missing* (%) | 1999 (n = 594) | Missing* (%) | P |
|---|---|---|---|---|---|
| Mean fasting glucose (mmol/L) | 8.6 (2.9) | 3 | 8.3 (2.6) | 4 | .07 |
| Mean Hb A1c (percentage) | 8.3 (2.2) | 50 | 7.1 (1.5) | 18 | .0001 |
| Hb A1c | |||||
| < 7% | 30% | 52% | ┐ | ||
| 7% to 8.5% | 29% | 35% | .001 | ||
| > 8.5% | 41% | 13% | ┘ | ||
| Blood pressure in patients with hypertension | n = 112 (36%) | 28 | n = 195(39%) | 17 | |
| •Mean systolic blood pressure (mm Hg) | 161 (19) | 158 (20) | .2 | ||
| •Mean diastolic blood pressure (mm Hg) | 88 (9) | 85 (9) | .004 | ||
| •Systolic blood pressure > 150 mm Hg | 68% | 62% | .3 | ||
| •Diastolic blood pressure > 85 mm Hg | 51% | 48% | .7 | ||
| Blood pressure in patients without hypertension | n = 197 (64%) | 28 | n = 299 (61%) | 17 | |
| •Mean systolic blood pressure (mm Hg) | 145 (18) | 145 (19) | .7 | ||
| •Mean diastolic blood pressure (mm Hg) | 80 (9) | 79 (9) | .5 | ||
| •Systolic blood pressure > 150 mm Hg | 34% | 35% | .6 | ||
| •Diastolic blood pressure > 85 mm Hg | 23% | 23% | .9 | ||
| Mean cholesterol (mmol/L /mg/dL) | 6.2 (1.3) / 238 (49) | 31 | 5.4 (1.1) / 207 (42) | 17 | .0001 |
| Mean HDL (mmol/L /mg/dL) | 1.2 (0.6) / 46.5 (23.2) | 62 | 1.2 (0.4) / 46.5 (15.5) | 23 | .59 |
| Mean triglycerides (mmol /mg/dL) | 2.6 (1.5) / 226 (130) | 58 | 2.1 (1.3) / 182 (113) | 23 | .0001 |
| Patients with cardiovascular morbidity > 5 mmol/L and cholesterol >192 mg/L | 31% | ┐ | 17% | ┐ | ┐ |
| Patients without cardiovascular morbidity, smokers, and those with cholesterol/HDL ratio > 5.0 | 4% | 37 | 5% | 18 | .001 |
| Patients without cardiovascular morbidity, nonsmokers, and those with cholesterol/HDL ratio > 6.0 | 13% | ┘ | 6% | ┘ | ┘ |
| *Refers to the percentage of patients with missing data for this variable. | |||||
FIGURE
Percentage of patients with annual review (target = 75%) in 1999 (n=594)
Discussion
During 7 years of structured audit-enhanced monitoring of patients with type 2 diabetes in an academic family practice research network, the intermediate measures of diabetes care improved. In particular, the mean Hb A1c of 7.1% can be seen as a measure of good quality of care. The number of patients treated according to Dutch family practice guidelines (a process of care outcome) also increased.8
While our data were collected during normal daily care (effectiveness), the findings come close to the outcome of care under ideal trial conditions (efficacy).21 In the UK Prospective Diabetes Study (UKPDS), the median Hb A1c level for all newly diagnosed patients in the group with intensive blood glucose control over 10 years reached a comparable level of 7.0%.1 Thus, the outcome of our study approaches that achieved under trial conditions. When we analyzed patients without outcome data as poorly controlled (worst-case scenario), Hb A1c was less than 8.5% in 28%.
The trend of improvement in glycemic control could have been a result of improved overall diabetes care in the Netherlands during the study period. Data about the outcome of diabetes care in the family medicine setting in the Netherlands during the study period are scarce and, when available, are derived from other research networks. In these networks a mean Hb A1c of 7.0% to 7.6% was reached.22 Yet indicators from other studies suggest that our results were far better than outcome from usual care. Recently published data on such outcomes in family medicine in the Netherlands showed that Hb A1c, blood pressure, and lipids were measured in less than 30% of patients.23,24 Outcomes from usual care as reported in research studies appear to be strongly biased by selection and probably cannot serve as a valid reference value.
The disappointing effect on the percentage of patients who reached the target blood pressure could have resulted from evaluating the data prematurely. When the study began, the primary objective was to improve glycemic control. Shortly after the publication of the Scandinavian Simvastatin Survival Study (4S)3 and the UKPDS,12 the guidelines of the Dutch College of Family Physicians were changed8 and more attention was paid to blood pressure and lipid control. This new approach was discussed with the participating family physicians. Consequently, the target for blood pressure was revised from 160/90 mm Hg to 150/85 mm Hg and lipid-lowering therapy was tailored to each patient’s cardiovascular risk profile. The 1999 outcome with respect to blood pressure and lipid control was measured only 1 year after these changes had been announced. Nevertheless, mean diastolic blood pressure in hypertensive patients and total cholesterol and triglyceride levels decreased significantly, and more patients reached target levels for lipids in 1999 than in 1993.
Our outcome was reached through enhanced compliance to guidelines. Therefore, the outcome in 1999 was based on a larger percentage of available patients. Because the AEMS studied a dynamic group of patients, the study groups in 1993 and 1999 were not identical. Theoretically, improvement in outcome could have been reached by including more easily manageable patients. However, no patient factors such as sex, age, duration of diabetes, treatment modality, or cardiovascular morbidity were related to compliance with annual review. The higher fasting blood glucose levels in patients who were noncompliant with annual review probably reflected under-treatment rather than more severe illness status. Therefore, we are confident that the findings reflect improved overall diabetes care.
The data on process measures in this study compare favorably with those of multipractice audits of diabetes care in the United Kingdom.25-29 The high prevalence rate of 2.0% (exclusively patients with type 2 diabetes) supports the validity of our data.25-27 Among our patients, 96% had been seen at least once during the previous year. In the large studies by Khunti and Bennett, only 85% had been seen during the previous year.25,26 The mean annual compliance rate of nearly 85% with Hb A1c and blood pressure measurements in our study was high. In particular, compliance with lipid control25,26,28 and funduscopy26,28 was better in our study. In 2 longitudinal studies that used an organized care system in which feedback was provided to the participating family physicians, compliance rates in process measures of up to 75% were reported.30,31
The outcomes of this study were achieved in an academic family practice research network, with specific facilities for the proactive supervision of patients with chronic diseases. These results cannot and should not be generalized to “routine” family practice. Monitoring and feedback in routine family practice are in themselves insufficient to improve the quality of care.10 Care assessment should preferably take a more comprehensive approach in which evidence-based goals for care are formulated, care is improved to reach those goals, and care is measured to see whether those goals have been achieved.11 Our academic network provides this comprehensive approach.
The electronic Research Registration System played an important role in the audit-enhanced monitoring. In the pilot phase of the project, paper records were used. Although using paper records had clear disadvantages, one could expect to achieve similar results using such records in combination with a central electronic data bank.
Conclusions
Outcomes of diabetes care in our family research setting were comparable with those reported in randomized controlled trials. Therefore, it is possible for the management of diabetes in family practice to be efficacious. This finding should encourage more efforts by physicians in family practice to bridge the gap between efficacy and effectiveness.
Important differences remained in achieved process measures between the academic family practices. While the outcome of diabetes care in the network was favorable, the outcome of treatment was unsatisfactory in a substantial number of patients. Further implementation strategies must be developed. The differences in achieved process measures were probably unrelated to socioeconomic differences between the practice populations, since the practice pairs 1/3 and 7/10 served comparable communities and had different levels of compliance.
Our study demonstrated that a high quality of diabetes care in family practice can be achieved. Audit-enhanced monitoring, which will provide the greatest benefit to the most patients with type 2 diabetes mellitus, should be implemented as part of a quality improvement system.
ACKNOWLEDGMENTS
The authors wish to thank the family physicians and practice nurses for their continuing support and data collection.
1. UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-53.
2. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;327:703-13.
3. Pyörälä K, Pedersen T, Klekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetes patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care 1997;20:614-20.
4. Adler AI, Stratton IM, Niel HAW, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405-12.
5. Adler AI, Stratton IM, Niel HAW, et al. Association of systolic blood pressure glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412-9.
6. American Diabetes Association. Standards of Medical Care for patients with diabetes mellitus (position statement). Diabetes Care 1999;22(suppl 1):S32-9.
7. European Diabetes Policy Group 1999. A desktop guide to type 2 diabetes mellitus. Diabet Med 1999;16:716-30.
8. Rutten GEHM, Verhoeven S, Heine RJ, et al. NHG-standaard diabetes mellitus type 2 (eerste herziening). Huisarts Wet 1999;42:67-84.Available in English at: http://www.diabetesinprimarycare.com.
9. Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of guidelines. BMJ 1999;318:527-30.
10. Grol R, Jones R. Twenty years of implementation research. Fam Pract 2000;17:S32-5.
11. Grol R. Between evidence-based practice and total quality management: the implementation of cost-effective care. Int J Qual Health Care 2000;12:297-304.
12. Thomson O’Brien MA, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. Audit and feedback: effects on professional practice and health care outcomes (Cochrane Review). In: The Cochrane Library, Issue 3, 2000. Oxford, England: Update Software.
13. Hart JT. Reactive and proactive care: a crisis. Br J Gen Pract 1990;40:4-9.
14. Greenhalgh PM. Shared care for diabetes: a systematic review. Occasional Paper 67. Royal College of General Practitioners; 1994.
15. Weel van C. Validating long-term morbidity recording. J Epidemiol Community Health 1995;49(suppl 1):29-32.
16. Weel van C, Smith H, Beasly JW. Family practice research networks: experience from three countries. J Fam Pract 2000;49:938-43.
17. Grauw de WJC, Lisdonk van de EH, Hoogen van den HJM, Weel van C. Monitoring of non-insulin dependent diabetes mellitus in general practice. Diabetes Nutr Metab 1991;4(suppl):67-71.
18. World Health Organization, Expert Committee on Diabetes Mellitus. WHO Technical Report No.727. Geneva, Switzerland: WHO; 1985.
19. Nederlands Huisartsen Genootschap. Standaard diabetes mellitus type II. Huisarts Wet 1989;32:15-8.
20. ICHPPC-2 Defined WONCA, 3rd ed. Oxford, England: Oxford University Press; 1983.
21. Weel van C, Knottnerus JA. Evidence-based interventions and comprehensive treatment. Lancet 1999;353:916-8.
22. Rutten G.H.E.M. Diabetiker-versorgung in den Nierderlanden. In: Lauterbach K, Ziegenhagen DJ. Diabetes mellitus—evidenz basierte diagnostik und therapie. Stuttgart, Germany: Schattauer; 2000;110-21.
23. Renders CM, Valk GD, Franse LV, Schellevis FG, Eijk van JThM, Wal van der G. Long-term effectiveness of a quality improvement program for patients with type 2 diabetes in general practice. Diabetes Care 2001;24:1365-70.
24. Dam van HA, Crebolder HFJM, Eijkelberg I, Nunen van M, Horst van der FG. Wegblijven van patienten met diabetes mellitus type 2—een echt probleem? Huisarts Wet 2000;43:380-4.
25. Khunti K, Baker R, Rumsey M, Lakhani M. Quality of care of patients with diabetes: collation of data from multi-practice audits of diabetes in primary care. Fam Pract 1999;16:54-9.
26. Benett IJ, Lambert C, Hinds G, Kirton C. Emerging standards for diabetes care from a city-wide primary care audit. Diabet Med 1994;11:489-92.
27. Howitt AJ, Cheales NA. Diabetes registers: a grassroots approach. BMJ 1993;307:1047-8.
28. Dunn NR, Bough P. Standards of care of diabetes patients in a typical English community. Br J Gen Pract 1996;46:401-5.
29. Turnbridge FKE, Millar JP, Schofield PJ, Spencer JA, Young G, Home PD. Diabetes care in general practice: an approach to audit of process and outcome. Br J Gen Pract 1993;34:291-5.
30. Butler CB, Smithers M, Stott N, Peters J. Audit-enhanced, districtwide primary care for people with diabetes mellitus. Eur J Gen Pract 1997;3:23-7.
31. Foulkes A, Kinmonth A, Frost S, Macdonald D. Organized personal care—an effective choice for managing diabetes in general practice. J R Coll Gen Pract 1989;39:444-7.
1. UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-53.
2. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;327:703-13.
3. Pyörälä K, Pedersen T, Klekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetes patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care 1997;20:614-20.
4. Adler AI, Stratton IM, Niel HAW, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405-12.
5. Adler AI, Stratton IM, Niel HAW, et al. Association of systolic blood pressure glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412-9.
6. American Diabetes Association. Standards of Medical Care for patients with diabetes mellitus (position statement). Diabetes Care 1999;22(suppl 1):S32-9.
7. European Diabetes Policy Group 1999. A desktop guide to type 2 diabetes mellitus. Diabet Med 1999;16:716-30.
8. Rutten GEHM, Verhoeven S, Heine RJ, et al. NHG-standaard diabetes mellitus type 2 (eerste herziening). Huisarts Wet 1999;42:67-84.Available in English at: http://www.diabetesinprimarycare.com.
9. Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of guidelines. BMJ 1999;318:527-30.
10. Grol R, Jones R. Twenty years of implementation research. Fam Pract 2000;17:S32-5.
11. Grol R. Between evidence-based practice and total quality management: the implementation of cost-effective care. Int J Qual Health Care 2000;12:297-304.
12. Thomson O’Brien MA, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. Audit and feedback: effects on professional practice and health care outcomes (Cochrane Review). In: The Cochrane Library, Issue 3, 2000. Oxford, England: Update Software.
13. Hart JT. Reactive and proactive care: a crisis. Br J Gen Pract 1990;40:4-9.
14. Greenhalgh PM. Shared care for diabetes: a systematic review. Occasional Paper 67. Royal College of General Practitioners; 1994.
15. Weel van C. Validating long-term morbidity recording. J Epidemiol Community Health 1995;49(suppl 1):29-32.
16. Weel van C, Smith H, Beasly JW. Family practice research networks: experience from three countries. J Fam Pract 2000;49:938-43.
17. Grauw de WJC, Lisdonk van de EH, Hoogen van den HJM, Weel van C. Monitoring of non-insulin dependent diabetes mellitus in general practice. Diabetes Nutr Metab 1991;4(suppl):67-71.
18. World Health Organization, Expert Committee on Diabetes Mellitus. WHO Technical Report No.727. Geneva, Switzerland: WHO; 1985.
19. Nederlands Huisartsen Genootschap. Standaard diabetes mellitus type II. Huisarts Wet 1989;32:15-8.
20. ICHPPC-2 Defined WONCA, 3rd ed. Oxford, England: Oxford University Press; 1983.
21. Weel van C, Knottnerus JA. Evidence-based interventions and comprehensive treatment. Lancet 1999;353:916-8.
22. Rutten G.H.E.M. Diabetiker-versorgung in den Nierderlanden. In: Lauterbach K, Ziegenhagen DJ. Diabetes mellitus—evidenz basierte diagnostik und therapie. Stuttgart, Germany: Schattauer; 2000;110-21.
23. Renders CM, Valk GD, Franse LV, Schellevis FG, Eijk van JThM, Wal van der G. Long-term effectiveness of a quality improvement program for patients with type 2 diabetes in general practice. Diabetes Care 2001;24:1365-70.
24. Dam van HA, Crebolder HFJM, Eijkelberg I, Nunen van M, Horst van der FG. Wegblijven van patienten met diabetes mellitus type 2—een echt probleem? Huisarts Wet 2000;43:380-4.
25. Khunti K, Baker R, Rumsey M, Lakhani M. Quality of care of patients with diabetes: collation of data from multi-practice audits of diabetes in primary care. Fam Pract 1999;16:54-9.
26. Benett IJ, Lambert C, Hinds G, Kirton C. Emerging standards for diabetes care from a city-wide primary care audit. Diabet Med 1994;11:489-92.
27. Howitt AJ, Cheales NA. Diabetes registers: a grassroots approach. BMJ 1993;307:1047-8.
28. Dunn NR, Bough P. Standards of care of diabetes patients in a typical English community. Br J Gen Pract 1996;46:401-5.
29. Turnbridge FKE, Millar JP, Schofield PJ, Spencer JA, Young G, Home PD. Diabetes care in general practice: an approach to audit of process and outcome. Br J Gen Pract 1993;34:291-5.
30. Butler CB, Smithers M, Stott N, Peters J. Audit-enhanced, districtwide primary care for people with diabetes mellitus. Eur J Gen Pract 1997;3:23-7.
31. Foulkes A, Kinmonth A, Frost S, Macdonald D. Organized personal care—an effective choice for managing diabetes in general practice. J R Coll Gen Pract 1989;39:444-7.
Are women with an unintended pregnancy less likely to breastfeed?
OBJECTIVE: To examine the association between unintended pregnancy and the initiation and duration of breastfeeding.
STUDY DESIGN: This was a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth.
POPULATION: We studied 6733 first singleton live births to US women aged 15 years to 44 years.
OUTCOMES MEASURED: Using the 1995 Institute of Medicine definitions, pregnancies were classified as intended or unintended; unintended pregnancies were further categorized as either mis-timed or unwanted. We measured initiation of breastfeeding and duration of nonexclusive breastfeeding for at least 16 weeks.
RESULTS: In this study, 51.5% of women never breastfed, 48.5% initiated breastfeeding, and 26.4% of all women continued breastfeeding for at least 16 weeks. US women with unwanted unintended pregnancies were more likely not to initiate breastfeeding (odds ratio [OR] = 1.76; 95% confidence interval [CI], 1.26-2.44) and more likely not to continue breastfeeding (OR =1.69; 95% CI, 1.12-2.55) than women with intended pregnancies. White women with unwanted unintended pregnancies were more likely not to breastfeed than those with intended ones (initiation: OR = 2.50; 95% CI, 1.54-4.05; continuation: OR = 2.56; 95% CI, 1.34-4.87). This finding was not seen for black or Hispanic women.
CONCLUSIONS: In the United States, women with unwanted pregnancies were less likely either to initiate or to continue breastfeeding than women with intended pregnancies. A strong inverse association between unwanted pregnancies and breastfeeding was observed only for white women. Education for women with unintended pregnancies may improve breastfeeding rates and subsequently, the health of women and infants.
- In the United States, women whose pregnancies were unwanted are at a higher risk of not breastfeeding than women whose pregnancies were intended.
- Future research to evaluate the importance of incorporating pregnancy intention status into patient-centered breastfeeding promotion is needed.
- For now, women with unwanted pregnancies, especially white women, should be targeted for breastfeeding counseling.
Unintended pregnancy is a significant public health issue. More than half of all pregnancies are unintended at the time of conception; approximately half of those end as births and half as induced abortions.1 Forty-eight percent of women have at least one unplanned pregnancy, and 28% of women have at least one unplanned birth during their reproductive lifetime.2 Unintended pregnancies and births are associated with numerous harmful behaviors and adverse outcomes.3,4
Breastfeeding is currently promoted as the preferred method of feeding for infants for at least 1 year because of its multiple immediate and long-term benefits for both mother and child.5,6 Yet in 1998 only 64% of US mothers were breastfeeding at the time of hospital discharge and 29% at 6 months postpartum, which is well below the Healthy People 2010 goals of 75% and 50%, respectively, for those intervals.7
We hypothesized that women with unintended pregnancies are less likely to breastfeed their infants than those with intended ones. We quantified the association between the intendedness of pregnancy at the time of conception and breastfeeding behavior, both the initiation of any breastfeeding and the continuation of nonexclusive breastfeeding for at least 16 weeks, for first singleton births to US mothers. We then explored other factors which might affect breastfeeding practices.
Methods
Study design
This study is a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth (NSFG), a periodic population-based survey conducted by the National Center for Health Statistics and the Centers for Disease Control which focuses on women’s health and pregnancy. A national probability sample of 14,000 civilian noninstitutionalized women aged 15 years to 44 years was selected from among households that responded to the 1993 National Health Interview Survey, with an oversampling of minority women. Personal interviews were conducted between January and October of 1995 with 10,847 of these women. The data were then adjusted for a response rate of 79% and weighted so that findings would reflect the US population as a whole. Full details of the NSFG survey methods are described elsewhere.8
The data set contains information on 21,332 pregnancies and 14,958 live births (Figure). After excluding multiple gestations (n=154), subsequent births to the same mother (n=7930), and neonatal adoptions or deaths (n=141), the final sample contained 6733 first singleton live births. To study the initiation of breastfeeding, women who breastfed at all were compared with those who did not. To study duration of breastfeeding, women who breastfed for 16 or more weeks were compared with those who did not. In this second set of analyses, the 1459 women who breastfed for between 0 and 16 weeks and the 33 women who were breastfeeding at the time of the interview and whose children had been born within 16 weeks of that date were excluded.
FIGURE
Study sample
Variable definitions
Pregnancies were categorized as either intended or unintended at conception, using new definitions established by the Institute of Medicine in 1995.3 Pregnancies were considered intended if a woman had stopped using birth control because she wanted to become pregnant. Unintended pregnancies were classified into 1 of 2 categories: (1) mis-timed: wanted pregnancies that occurred sooner than desired, or (2) unwanted: pregnancies that occurred while a woman was using contraception and had not ever wanted to have a(nother) baby. The 170 women who described their pregnancy intention status as “didn’t know” or “didn’t care” were excluded from analyses involving intention status as defined above. There were 2 breastfeeding outcomes in this study: (1) initiation of breastfeeding, including women who reported any breastfeeding at all, and (2) duration of non-exclusive breastfeeding for at least 16 weeks.
Maternal demographics, intrapartum and postpartum behaviors, and birth outcomes were considered as potential confounders. As missing data were imputed in the public use data file, information on each variable was complete, except where noted below. Maternal age was determined at the time of conception. Education was defined as completed years of schooling at the time of the interview. Race was categorized as white, black, Hispanic, or other. Marital status was defined as either married or not married. Socioeconomic status was measured continuously as a percentage of the 1995 poverty level. Information on prenatal care was only available for births in the last 5 years (n=1266). For the 1241 women who reported that they had received prenatal care, the mean weeks of gestation at the time of the first prenatal visit were calculated. Maternity leave was defined as the use of maternity leave, paid or unpaid, for women who were working during the pregnancy (n=3662). For those who took any leave, the mean length of that leave was calculated in weeks. The 33 women for whom data were not available and the 5 women who answered that they took 0 weeks of maternity leave were not included in this calculation. Infant variables were considered categorically: mode of delivery, either vaginal or cesarean; prematurity, birth at less than or equal to 36 weeks; and low birth weight, less than or equal to 5.5 pounds.
Statistical analysis
The statistical significance of descriptive variables was determined using 2-sample t tests and chi-square tests, with women who did not breastfeed at all as the comparison group.
To compare our results with existing literature, we calculated crude odds ratios of not breastfeeding and used chi-square tests to assess the statistical significance of these associations. The reference group was always women whose pregnancies were intended. Variables identified as potential confounders were age, race, marital status, poverty level, education, maternity leave, mode of delivery, prematurity, and low birth weight. Final logistic regression models were adjusted for those variables that changed crude odds ratios by 10% or more: age, race, marital status, poverty level, and education. Adjusted odds ratios (ORs) of not breastfeeding and 95% confidence intervals (CIs) are reported.
Effect modification was assessed by dichotomizing each of the 5 confounding variables in the following manner: teen versus 20 years or older; white versus black versus Hispanic (here, the 193 women in the sample who defined their race as other were not included); married versus unmarried; high school education or higher versus less than a high school education; and below the poverty level versus at or above the poverty level. Each stratified analysis was adjusted for the other 4 factors. Interaction terms were created and P values for heterogeneity were calculated for all logistic models. For race, an additional interaction term was created to compare white with non-white (black and Hispanic combined) women.
These data are contained on the National Survey of Family Growth Cycle 5 1995 CD-ROM, Series 23, No. 3 and were exported using SETS version 1.22a (National Center for Health Statistics, Hyattsville, MD). All analyses were performed with SAS version 6.12 (SAS Institute, Cary, NC). Odds ratios are weighted using sampling weights provided in the data set. SUDAAN version 7.5.3 was used to obtain standard errors (Research Triangle Institute, Research Triangle Park, NC).
Results
In the total sample of 6733 first singleton live births to US mothers, 3267 (48.5%) of women initiated breastfeeding, compared with 3466 (51.5%) who did not. In the entire sample, 1775 (26.4%) continued to breastfeed nonexclusively for at least 16 weeks.
The breastfeeding initiation rate was 55.9%, 37.4%, and 28.0% for women with intended, mis-timed, and unwanted pregnancies, respectively. By 16 weeks, 32.6%, 17.0%, and 15.5% of women, respectively, were still breastfeeding. For all women who breastfed, the mean number of weeks of breastfeeding was 24.4 (standard deviation = 24.9; range = < 1 week to 4.0 years). Only 3.9% of women who breastfed did so for more than 2 years.
Table 1 shows characteristics of mothers and infants by breastfeeding behavior. Women who breastfed, both initially and for at least 16 weeks, were older at conception and had had more years of education than women who did not breastfeed at all. They were more likely to be white and less likely to be black. A similar percentage of women in each group were Hispanic. Percentage of the poverty level, a proxy for socioeconomic status, was higher for those who breastfed at all, but similar for those who continued breastfeeding and those who did not breastfeed. Rates of prenatal care and mean weeks at first prenatal visit were similar in all groups. Among women who were employed during their pregnancies, almost two thirds took maternity leave, regardless of breastfeeding behavior. Mean length of maternity leave was 3.4 weeks longer among women who continued to breastfeed than among women who did not breastfeed at all. The percentage of vaginal deliveries was similar among groups. Both premature and low birth weight infants were more common among women who did not breastfeed.
The association between the intendedness of pregnancy and breastfeeding behavior is reported in Table 2. Crude odds ratios show that women with any type of unintended pregnancy were more likely not to initiate breastfeeding than women whose pregnancies were intended. Some, but not all, of this association can be attributed to confounding by demographic factors. Having an unintended pregnancy was not associated with any significant difference in the initiation of breastfeeding, after adjusting for age, race, marital status, poverty level, and education. While women with mis-timed pregnancies were as likely to initiate breastfeeding as those whose pregnancies were intended (OR = 1.03; 95% CI, 0.88-1.21), women with unwanted pregnancies were more likely not to start breastfeeding (OR = 1.76; 95% CI, 1.26-2.44).
Table 2 also describes the association between pregnancy intention status and the continuation of nonexclusive breastfeeding for at least 16 weeks. In contrast to the initiation of breastfeeding, duration of breastfeeding was affected by the intendedness of pregnancy in every comparison. Adjusted odds ratios show that women with either type of unintended pregnancy were more likely not to continue breastfeeding than those with intended ones (OR = 1.28; 95% CI, 1.06-1.54). As with breastfeeding initiation, this association is being driven by the unwanted pregnancies. Women with unwanted pregnancies were more likely not to continue breastfeeding (OR = 1.69; 95% CI, 1.12-2.55).
Each of these associations was then evaluated for effect modification. As seen in Table 3, only race was an important factor. In the total sample, 56.3% of white women, 55.4% of Hispanic women, and 24.7% of black women breastfed at all; and 41.6%, 41.2%, and 12.6% of white, Hispanic, and black women breastfed for at least 16 weeks. White women with unwanted pregnancies were more likely not to initiate breastfeeding (OR = 2.50; 95% CI, 1.54-4.05) and more likely not to continue breastfeeding (OR = 2.56; 95% CI, 1.34-4.87) than white women with intended pregnancies. These differences in breastfeeding behaviors for unwanted pregnancies were not seen for either Hispanic or black women. For each stratified analysis, a single P value for heterogeneity was calculated to compare white women with non-white women (Hispanic and black women combined). The only significant difference by race was for unwanted pregnancies. The P value for heterogeneity was 0.01 for both initiation and continuation of breastfeeding. Stratified analyses for age, marital status, education, poverty level, and year of birth showed similar odds ratios across strata and nonsignificant P values for heterogeneity in every case (analyses not shown).
TABLE 1
Characteristics of mothers and infants by breastfeeding status (n=6733)
| Characteristic | Any breastfeeding (n = 3267) | Breastfeeding for ≥ 16 weeks (n = 1775) | No breastfeeding (n = 3466) |
|---|---|---|---|
| Age (mean years, SD) | 23.5 (5.0)* | 24.0 (5.1)* | 20.5 (4.3) |
| Race (%) | |||
| White | 64.8* | 65.9* | 47.4 |
| Black | 12.8 | 10.3 | 36.6 |
| Hispanic | 18.4 | 19.1 | 14.0 |
| Other | 4.0 | 4.7 | 2.0 |
| Married (%) | 65.0* | 68.8* | 37.3 |
| Percentage of the 1995 poverty level (SD) | 320 (207)* | 235 (205)* | 246 (189) |
| Education (mean years, SD) | 13.1 (3.0)* | 13.3 (3.2)* | 11.9 (2.3) |
| Prenatal care (%)† | 98.5 | 97.4 | 97.6 |
| Mean weeks at 1st visit (SD) | 7.8 (3.9) | 7.8 (4.0) | 9.1 (5.4) |
| Maternity leave ‡ | 65.2 | 60.7 | 64.6 |
| Mean weeks (SD) | 12.2 (9.4) | 13.8 (10.8) | 10.4 (8.3) |
| Vaginal delivery (%) | 78.5 | 78.9 | 80.7 |
| Prematurity (%) | 7.4* | 6.4* | 9.9 |
| Low birth weight (%) | 4.8* | 3.9* | 9.4 |
| SD denotes standard deviation. | |||
| *P ≤ .001 in comparison with women who did not breastfeed. | |||
| † For births during 1990-1994, n=1266. | |||
| ‡ Percentage of women employed during that pregnancy, n=3662. | |||
TABLE 2
Unintended pregnancy and breastfeeding behavior in the United States
| Intendedness of pregnancy | Number breastfeeding | Number not breastfeeding | Weighted crude odds ratio of NOT breastfeeding (95% CI)* | Weighted adjusted odds ratio of NOT breastfeeding (95% CI)* † |
|---|---|---|---|---|
| Initiation of breastfeeding (any) | ||||
| Intended | 2263 | 1758 | reference | reference |
| Unintended | 924 | 1618 | 2.15 (1.91-2.43) | 1.09 (0.93-1.28) |
| Mis-timed | 822 | 1361 | 2.02 (1.79-2.29) | 1.03 (0.88-1.21) |
| Unwanted | 102 | 257 | 3.54 (2.69-4.66) | 1.76 (1.26-2.44) |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | 1304 | 1758 | reference | reference |
| Unintended | 426 | 1618 | 2.79 (2.42-3.23) | 1.28 (1.06-1.54) |
| Mis-timed | 371 | 1361 | 2.68 (2.30-3.12) | 1.22 (1.01-1.47) |
| Unwanted | 55 | 257 | 3.82 (2.69-5.42) | 1.69 (1.12-2.55) |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, race, marital status, poverty level, and education. | ||||
TABLE 3
Effect of race on unintended pregnancy and breastfeeding behavior
| Weighted adjusted odds ratio of NOT breastfeeding*† | ||||
|---|---|---|---|---|
| Intendedness of pregnancy | White (n=3661) | Hispanic (n=1063) | Black (n=1646) | |
| Initiation of breastfeeding (any) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.15 (0.93-1.42) | 0.94 (0.66-1.35) | 0.81 (0.56-1.17) | |
| Mis-timed | 1.07 (0.87-1.32) | 0.93 (0.64-1.35) | 0.78 (0.53-1.15) | |
| Unwanted | 2.50 (1.54-4.05) | 0.97 (0.55-1.70) | 0.93 (0.52-1.65) | |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.39 (1.07-1.81) | 1.08 (0.74-1.58) | 0.73 (0.44-1.20) | |
| Mis-timed | 1.29 (0.99-1.68) | 1.10 (0.76-1.60) | 0.70 (0.41-1.20) | |
| Unwanted | 2.56 (1.34-4.87) | 0.90 (0.47-1.72) | 0.78 (0.34-1.76) | |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, marital status, poverty level, and education. | ||||
Discussion
In this study of first-time US mothers, women who breastfed were demographically different from those who did not, but had relatively similar maternal behaviors and infant characteristics. After controlling for these demographic differences, having an unwanted pregnancy was associated with a lower likelihood of both initiating breastfeeding and continuing to breastfeed. In addition, race was an important effect modifier for unwanted pregnancies.
The demographic findings of this study are consistent with the current breastfeeding literature: US women who breastfeed tend to be older, white, married, well-educated, and of a higher socioeconomic status than those who do not.9 The main findings of this study are also consistent with the only other study that has examined the relationship between unintended pregnancy and breastfeeding behavior.10 A cross-sectional sample of 27,700 women who gave birth to a live baby were asked prior to postpartum discharge whether they had intended to become pregnant and their plans for breastfeeding. After controlling for education, race, Medicaid status, maternal age younger than 20, and any tobacco use during pregnancy, the authors found that women whose pregnancies were unintended were more likely not to initiate breastfeeding or to breastfeed exclusively. Adjusted odds ratios of not breastfeeding ranged from 1.10 to 1.41, depending on intention status, and all were statistically significant. In contrast to our study, a major limitation of that study was that the measured outcome was intent to breastfeed at hospital discharge, which may have differed greatly from actual breastfeeding behavior.
The interaction seen in our analysis between intention status and race is initially surprising because, in general, white and Hispanic women breastfeed at much higher rates than black women. But if a pregnancy was unwanted, white women were much less likely to breastfeed than either black or Hispanic women. Neither socioeconomic status nor educational level is the explanation, as both of these factors were controlled for in stratified analyses. Perhaps Hispanic and black women are more accepting of unintended pregnancy than white women and these results reflect cultural differences. Further studies which examine other aspects of unintended pregnancy with respect to race will help to further clarify the reasons for this finding.
Strengths and limitations
Our population-based study has several strengths. The data set provides a large national sample with excellent representation of minority women; statistical oversampling and weighting allow these data to reflect the entire national population. Adjustment of data for nonresponse lessens the risk of selection bias. Furthermore, the study sample was restricted to first births to limit the effect of previous birth experiences on postpartum behaviors. Therefore our results are generalizable to all first-time mothers in the United States.
A major limitation of our study is that information was not collected on several factors, such as substance use both during pregnancy and after birth, that might influence the relationship between pregnancy intention status and breastfeeding behavior. The work of Dye and colleagues,10 discussed above, found that prenatal tobacco, but not alcohol or drug use, was a significant confounder. Information was also not available on health service–related factors that may contribute to breastfeeding success, such as breastfeeding in the delivery room, length of hospital stay, and participation in educational programs.11
Given that data were collected for the NSFG during personal interviews at differing lengths of time after a pregnancy, inaccuracy is possible. Although the survey does not include corroboration from other sources, such as medical records or birth certificates, it is reassuring that, as an example, rates of prenatal care in our study are similar to those of other nationally reported rates for 1995 (98.1% in our study and 98.8% in National Vital Statistics Reports).12 Potential misclassification with respect to such medical outcomes as prematurity would be nondifferential and only bias odds ratios toward the null. The extended time between conception and measurement of maternal attitudes increases the uncertainty that a mother will accurately recall both her pregnancy intentions at conception and her breastfeeding practices. Women are more likely to recall a pregnancy carried to birth as intended, but this phenomenon would only bias the results if it also applied to breastfeeding practices, which is unlikely.13 While breastfeeding practices may not be exactly recalled, there is no obvious reason for differential reporting.
Conclusions
Our study has clinical implications for first-time US mothers. A recent national goal of the Institute of Medicine is that all pregnancies be planned.3 One of the many benefits of decreasing unintended pregnancy may be to increase breastfeeding rates closer to the Healthy People 2010 goals. In addition, a new hypothesis is suggested by the results of this study: Clinicians should promote breastfeeding differently for women with intended and unintended pregnancies. Future research will evaluate the importance of incorporating pregnancy intention status into patient-centered counseling. In the interim, women with unwanted pregnancies, especially white women, should be targeted for counseling, as they could benefit from breastfeeding, not just for medical reasons but for psychological and economic ones as well.
Acknowledgments
We would like to thank Larry Culpepper, MD, MPH, for his guidance.
1. Forrest JD. Unintended pregnancy among American women. Fam Plann Perspect 1987;19:76-7.
2. Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspectives 1998;30:24-9,46.-
3. Institute of Medicine Committee on Unintended Pregnancy. The best intentions: unintended pregnancy and the well-being of children and families. Washington, DC: National Academy Press, 1995.
4. Orr ST, Miller CA. Unintended pregnancy and the psychosocial well-being of pregnant women. Womens Health Issues 1997;7:38-46.
5. Institute of Medicine Subcommittee on Nutrition during Lactation. Nutrition during lactation. Washington, DC: National Academy Press, 1991.
6. American Academy of Pediatrics, Work Group on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 1997;100:1035-9.
7. US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: US Government Printing Office, November 2000.
8. Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: new data from the 1995 National Survey of Family Growth. Vital Health Stat 1997;23.19:1-114.
9. Scott JA, Binns CW. Factors associated with the initiation and duration of breastfeeding: a review of the literature. Breastfeed Rev 1999;7:5-16.
10. Dye TD, Wojtowycz MA, Aubry RH, Quade J, Kilburn H. Unintended pregnancy and breastfeeding behavior. Am J Public Health 1997;87:1709-11.
11. Kuan LW, Britto M, Decolongon J, Schoettker PJ, Atherton HD, Kotagal UR. Health system factors contributing to breastfeeding success. Pediatrics 1999;104:e28.-
12. Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: final data for 1997. Natl Vital Stat Reports 1999;47.18:1-96.
13. Petersen R, Moos MK. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues 1997;7:234-40.
OBJECTIVE: To examine the association between unintended pregnancy and the initiation and duration of breastfeeding.
STUDY DESIGN: This was a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth.
POPULATION: We studied 6733 first singleton live births to US women aged 15 years to 44 years.
OUTCOMES MEASURED: Using the 1995 Institute of Medicine definitions, pregnancies were classified as intended or unintended; unintended pregnancies were further categorized as either mis-timed or unwanted. We measured initiation of breastfeeding and duration of nonexclusive breastfeeding for at least 16 weeks.
RESULTS: In this study, 51.5% of women never breastfed, 48.5% initiated breastfeeding, and 26.4% of all women continued breastfeeding for at least 16 weeks. US women with unwanted unintended pregnancies were more likely not to initiate breastfeeding (odds ratio [OR] = 1.76; 95% confidence interval [CI], 1.26-2.44) and more likely not to continue breastfeeding (OR =1.69; 95% CI, 1.12-2.55) than women with intended pregnancies. White women with unwanted unintended pregnancies were more likely not to breastfeed than those with intended ones (initiation: OR = 2.50; 95% CI, 1.54-4.05; continuation: OR = 2.56; 95% CI, 1.34-4.87). This finding was not seen for black or Hispanic women.
CONCLUSIONS: In the United States, women with unwanted pregnancies were less likely either to initiate or to continue breastfeeding than women with intended pregnancies. A strong inverse association between unwanted pregnancies and breastfeeding was observed only for white women. Education for women with unintended pregnancies may improve breastfeeding rates and subsequently, the health of women and infants.
- In the United States, women whose pregnancies were unwanted are at a higher risk of not breastfeeding than women whose pregnancies were intended.
- Future research to evaluate the importance of incorporating pregnancy intention status into patient-centered breastfeeding promotion is needed.
- For now, women with unwanted pregnancies, especially white women, should be targeted for breastfeeding counseling.
Unintended pregnancy is a significant public health issue. More than half of all pregnancies are unintended at the time of conception; approximately half of those end as births and half as induced abortions.1 Forty-eight percent of women have at least one unplanned pregnancy, and 28% of women have at least one unplanned birth during their reproductive lifetime.2 Unintended pregnancies and births are associated with numerous harmful behaviors and adverse outcomes.3,4
Breastfeeding is currently promoted as the preferred method of feeding for infants for at least 1 year because of its multiple immediate and long-term benefits for both mother and child.5,6 Yet in 1998 only 64% of US mothers were breastfeeding at the time of hospital discharge and 29% at 6 months postpartum, which is well below the Healthy People 2010 goals of 75% and 50%, respectively, for those intervals.7
We hypothesized that women with unintended pregnancies are less likely to breastfeed their infants than those with intended ones. We quantified the association between the intendedness of pregnancy at the time of conception and breastfeeding behavior, both the initiation of any breastfeeding and the continuation of nonexclusive breastfeeding for at least 16 weeks, for first singleton births to US mothers. We then explored other factors which might affect breastfeeding practices.
Methods
Study design
This study is a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth (NSFG), a periodic population-based survey conducted by the National Center for Health Statistics and the Centers for Disease Control which focuses on women’s health and pregnancy. A national probability sample of 14,000 civilian noninstitutionalized women aged 15 years to 44 years was selected from among households that responded to the 1993 National Health Interview Survey, with an oversampling of minority women. Personal interviews were conducted between January and October of 1995 with 10,847 of these women. The data were then adjusted for a response rate of 79% and weighted so that findings would reflect the US population as a whole. Full details of the NSFG survey methods are described elsewhere.8
The data set contains information on 21,332 pregnancies and 14,958 live births (Figure). After excluding multiple gestations (n=154), subsequent births to the same mother (n=7930), and neonatal adoptions or deaths (n=141), the final sample contained 6733 first singleton live births. To study the initiation of breastfeeding, women who breastfed at all were compared with those who did not. To study duration of breastfeeding, women who breastfed for 16 or more weeks were compared with those who did not. In this second set of analyses, the 1459 women who breastfed for between 0 and 16 weeks and the 33 women who were breastfeeding at the time of the interview and whose children had been born within 16 weeks of that date were excluded.
FIGURE
Study sample
Variable definitions
Pregnancies were categorized as either intended or unintended at conception, using new definitions established by the Institute of Medicine in 1995.3 Pregnancies were considered intended if a woman had stopped using birth control because she wanted to become pregnant. Unintended pregnancies were classified into 1 of 2 categories: (1) mis-timed: wanted pregnancies that occurred sooner than desired, or (2) unwanted: pregnancies that occurred while a woman was using contraception and had not ever wanted to have a(nother) baby. The 170 women who described their pregnancy intention status as “didn’t know” or “didn’t care” were excluded from analyses involving intention status as defined above. There were 2 breastfeeding outcomes in this study: (1) initiation of breastfeeding, including women who reported any breastfeeding at all, and (2) duration of non-exclusive breastfeeding for at least 16 weeks.
Maternal demographics, intrapartum and postpartum behaviors, and birth outcomes were considered as potential confounders. As missing data were imputed in the public use data file, information on each variable was complete, except where noted below. Maternal age was determined at the time of conception. Education was defined as completed years of schooling at the time of the interview. Race was categorized as white, black, Hispanic, or other. Marital status was defined as either married or not married. Socioeconomic status was measured continuously as a percentage of the 1995 poverty level. Information on prenatal care was only available for births in the last 5 years (n=1266). For the 1241 women who reported that they had received prenatal care, the mean weeks of gestation at the time of the first prenatal visit were calculated. Maternity leave was defined as the use of maternity leave, paid or unpaid, for women who were working during the pregnancy (n=3662). For those who took any leave, the mean length of that leave was calculated in weeks. The 33 women for whom data were not available and the 5 women who answered that they took 0 weeks of maternity leave were not included in this calculation. Infant variables were considered categorically: mode of delivery, either vaginal or cesarean; prematurity, birth at less than or equal to 36 weeks; and low birth weight, less than or equal to 5.5 pounds.
Statistical analysis
The statistical significance of descriptive variables was determined using 2-sample t tests and chi-square tests, with women who did not breastfeed at all as the comparison group.
To compare our results with existing literature, we calculated crude odds ratios of not breastfeeding and used chi-square tests to assess the statistical significance of these associations. The reference group was always women whose pregnancies were intended. Variables identified as potential confounders were age, race, marital status, poverty level, education, maternity leave, mode of delivery, prematurity, and low birth weight. Final logistic regression models were adjusted for those variables that changed crude odds ratios by 10% or more: age, race, marital status, poverty level, and education. Adjusted odds ratios (ORs) of not breastfeeding and 95% confidence intervals (CIs) are reported.
Effect modification was assessed by dichotomizing each of the 5 confounding variables in the following manner: teen versus 20 years or older; white versus black versus Hispanic (here, the 193 women in the sample who defined their race as other were not included); married versus unmarried; high school education or higher versus less than a high school education; and below the poverty level versus at or above the poverty level. Each stratified analysis was adjusted for the other 4 factors. Interaction terms were created and P values for heterogeneity were calculated for all logistic models. For race, an additional interaction term was created to compare white with non-white (black and Hispanic combined) women.
These data are contained on the National Survey of Family Growth Cycle 5 1995 CD-ROM, Series 23, No. 3 and were exported using SETS version 1.22a (National Center for Health Statistics, Hyattsville, MD). All analyses were performed with SAS version 6.12 (SAS Institute, Cary, NC). Odds ratios are weighted using sampling weights provided in the data set. SUDAAN version 7.5.3 was used to obtain standard errors (Research Triangle Institute, Research Triangle Park, NC).
Results
In the total sample of 6733 first singleton live births to US mothers, 3267 (48.5%) of women initiated breastfeeding, compared with 3466 (51.5%) who did not. In the entire sample, 1775 (26.4%) continued to breastfeed nonexclusively for at least 16 weeks.
The breastfeeding initiation rate was 55.9%, 37.4%, and 28.0% for women with intended, mis-timed, and unwanted pregnancies, respectively. By 16 weeks, 32.6%, 17.0%, and 15.5% of women, respectively, were still breastfeeding. For all women who breastfed, the mean number of weeks of breastfeeding was 24.4 (standard deviation = 24.9; range = < 1 week to 4.0 years). Only 3.9% of women who breastfed did so for more than 2 years.
Table 1 shows characteristics of mothers and infants by breastfeeding behavior. Women who breastfed, both initially and for at least 16 weeks, were older at conception and had had more years of education than women who did not breastfeed at all. They were more likely to be white and less likely to be black. A similar percentage of women in each group were Hispanic. Percentage of the poverty level, a proxy for socioeconomic status, was higher for those who breastfed at all, but similar for those who continued breastfeeding and those who did not breastfeed. Rates of prenatal care and mean weeks at first prenatal visit were similar in all groups. Among women who were employed during their pregnancies, almost two thirds took maternity leave, regardless of breastfeeding behavior. Mean length of maternity leave was 3.4 weeks longer among women who continued to breastfeed than among women who did not breastfeed at all. The percentage of vaginal deliveries was similar among groups. Both premature and low birth weight infants were more common among women who did not breastfeed.
The association between the intendedness of pregnancy and breastfeeding behavior is reported in Table 2. Crude odds ratios show that women with any type of unintended pregnancy were more likely not to initiate breastfeeding than women whose pregnancies were intended. Some, but not all, of this association can be attributed to confounding by demographic factors. Having an unintended pregnancy was not associated with any significant difference in the initiation of breastfeeding, after adjusting for age, race, marital status, poverty level, and education. While women with mis-timed pregnancies were as likely to initiate breastfeeding as those whose pregnancies were intended (OR = 1.03; 95% CI, 0.88-1.21), women with unwanted pregnancies were more likely not to start breastfeeding (OR = 1.76; 95% CI, 1.26-2.44).
Table 2 also describes the association between pregnancy intention status and the continuation of nonexclusive breastfeeding for at least 16 weeks. In contrast to the initiation of breastfeeding, duration of breastfeeding was affected by the intendedness of pregnancy in every comparison. Adjusted odds ratios show that women with either type of unintended pregnancy were more likely not to continue breastfeeding than those with intended ones (OR = 1.28; 95% CI, 1.06-1.54). As with breastfeeding initiation, this association is being driven by the unwanted pregnancies. Women with unwanted pregnancies were more likely not to continue breastfeeding (OR = 1.69; 95% CI, 1.12-2.55).
Each of these associations was then evaluated for effect modification. As seen in Table 3, only race was an important factor. In the total sample, 56.3% of white women, 55.4% of Hispanic women, and 24.7% of black women breastfed at all; and 41.6%, 41.2%, and 12.6% of white, Hispanic, and black women breastfed for at least 16 weeks. White women with unwanted pregnancies were more likely not to initiate breastfeeding (OR = 2.50; 95% CI, 1.54-4.05) and more likely not to continue breastfeeding (OR = 2.56; 95% CI, 1.34-4.87) than white women with intended pregnancies. These differences in breastfeeding behaviors for unwanted pregnancies were not seen for either Hispanic or black women. For each stratified analysis, a single P value for heterogeneity was calculated to compare white women with non-white women (Hispanic and black women combined). The only significant difference by race was for unwanted pregnancies. The P value for heterogeneity was 0.01 for both initiation and continuation of breastfeeding. Stratified analyses for age, marital status, education, poverty level, and year of birth showed similar odds ratios across strata and nonsignificant P values for heterogeneity in every case (analyses not shown).
TABLE 1
Characteristics of mothers and infants by breastfeeding status (n=6733)
| Characteristic | Any breastfeeding (n = 3267) | Breastfeeding for ≥ 16 weeks (n = 1775) | No breastfeeding (n = 3466) |
|---|---|---|---|
| Age (mean years, SD) | 23.5 (5.0)* | 24.0 (5.1)* | 20.5 (4.3) |
| Race (%) | |||
| White | 64.8* | 65.9* | 47.4 |
| Black | 12.8 | 10.3 | 36.6 |
| Hispanic | 18.4 | 19.1 | 14.0 |
| Other | 4.0 | 4.7 | 2.0 |
| Married (%) | 65.0* | 68.8* | 37.3 |
| Percentage of the 1995 poverty level (SD) | 320 (207)* | 235 (205)* | 246 (189) |
| Education (mean years, SD) | 13.1 (3.0)* | 13.3 (3.2)* | 11.9 (2.3) |
| Prenatal care (%)† | 98.5 | 97.4 | 97.6 |
| Mean weeks at 1st visit (SD) | 7.8 (3.9) | 7.8 (4.0) | 9.1 (5.4) |
| Maternity leave ‡ | 65.2 | 60.7 | 64.6 |
| Mean weeks (SD) | 12.2 (9.4) | 13.8 (10.8) | 10.4 (8.3) |
| Vaginal delivery (%) | 78.5 | 78.9 | 80.7 |
| Prematurity (%) | 7.4* | 6.4* | 9.9 |
| Low birth weight (%) | 4.8* | 3.9* | 9.4 |
| SD denotes standard deviation. | |||
| *P ≤ .001 in comparison with women who did not breastfeed. | |||
| † For births during 1990-1994, n=1266. | |||
| ‡ Percentage of women employed during that pregnancy, n=3662. | |||
TABLE 2
Unintended pregnancy and breastfeeding behavior in the United States
| Intendedness of pregnancy | Number breastfeeding | Number not breastfeeding | Weighted crude odds ratio of NOT breastfeeding (95% CI)* | Weighted adjusted odds ratio of NOT breastfeeding (95% CI)* † |
|---|---|---|---|---|
| Initiation of breastfeeding (any) | ||||
| Intended | 2263 | 1758 | reference | reference |
| Unintended | 924 | 1618 | 2.15 (1.91-2.43) | 1.09 (0.93-1.28) |
| Mis-timed | 822 | 1361 | 2.02 (1.79-2.29) | 1.03 (0.88-1.21) |
| Unwanted | 102 | 257 | 3.54 (2.69-4.66) | 1.76 (1.26-2.44) |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | 1304 | 1758 | reference | reference |
| Unintended | 426 | 1618 | 2.79 (2.42-3.23) | 1.28 (1.06-1.54) |
| Mis-timed | 371 | 1361 | 2.68 (2.30-3.12) | 1.22 (1.01-1.47) |
| Unwanted | 55 | 257 | 3.82 (2.69-5.42) | 1.69 (1.12-2.55) |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, race, marital status, poverty level, and education. | ||||
TABLE 3
Effect of race on unintended pregnancy and breastfeeding behavior
| Weighted adjusted odds ratio of NOT breastfeeding*† | ||||
|---|---|---|---|---|
| Intendedness of pregnancy | White (n=3661) | Hispanic (n=1063) | Black (n=1646) | |
| Initiation of breastfeeding (any) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.15 (0.93-1.42) | 0.94 (0.66-1.35) | 0.81 (0.56-1.17) | |
| Mis-timed | 1.07 (0.87-1.32) | 0.93 (0.64-1.35) | 0.78 (0.53-1.15) | |
| Unwanted | 2.50 (1.54-4.05) | 0.97 (0.55-1.70) | 0.93 (0.52-1.65) | |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.39 (1.07-1.81) | 1.08 (0.74-1.58) | 0.73 (0.44-1.20) | |
| Mis-timed | 1.29 (0.99-1.68) | 1.10 (0.76-1.60) | 0.70 (0.41-1.20) | |
| Unwanted | 2.56 (1.34-4.87) | 0.90 (0.47-1.72) | 0.78 (0.34-1.76) | |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, marital status, poverty level, and education. | ||||
Discussion
In this study of first-time US mothers, women who breastfed were demographically different from those who did not, but had relatively similar maternal behaviors and infant characteristics. After controlling for these demographic differences, having an unwanted pregnancy was associated with a lower likelihood of both initiating breastfeeding and continuing to breastfeed. In addition, race was an important effect modifier for unwanted pregnancies.
The demographic findings of this study are consistent with the current breastfeeding literature: US women who breastfeed tend to be older, white, married, well-educated, and of a higher socioeconomic status than those who do not.9 The main findings of this study are also consistent with the only other study that has examined the relationship between unintended pregnancy and breastfeeding behavior.10 A cross-sectional sample of 27,700 women who gave birth to a live baby were asked prior to postpartum discharge whether they had intended to become pregnant and their plans for breastfeeding. After controlling for education, race, Medicaid status, maternal age younger than 20, and any tobacco use during pregnancy, the authors found that women whose pregnancies were unintended were more likely not to initiate breastfeeding or to breastfeed exclusively. Adjusted odds ratios of not breastfeeding ranged from 1.10 to 1.41, depending on intention status, and all were statistically significant. In contrast to our study, a major limitation of that study was that the measured outcome was intent to breastfeed at hospital discharge, which may have differed greatly from actual breastfeeding behavior.
The interaction seen in our analysis between intention status and race is initially surprising because, in general, white and Hispanic women breastfeed at much higher rates than black women. But if a pregnancy was unwanted, white women were much less likely to breastfeed than either black or Hispanic women. Neither socioeconomic status nor educational level is the explanation, as both of these factors were controlled for in stratified analyses. Perhaps Hispanic and black women are more accepting of unintended pregnancy than white women and these results reflect cultural differences. Further studies which examine other aspects of unintended pregnancy with respect to race will help to further clarify the reasons for this finding.
Strengths and limitations
Our population-based study has several strengths. The data set provides a large national sample with excellent representation of minority women; statistical oversampling and weighting allow these data to reflect the entire national population. Adjustment of data for nonresponse lessens the risk of selection bias. Furthermore, the study sample was restricted to first births to limit the effect of previous birth experiences on postpartum behaviors. Therefore our results are generalizable to all first-time mothers in the United States.
A major limitation of our study is that information was not collected on several factors, such as substance use both during pregnancy and after birth, that might influence the relationship between pregnancy intention status and breastfeeding behavior. The work of Dye and colleagues,10 discussed above, found that prenatal tobacco, but not alcohol or drug use, was a significant confounder. Information was also not available on health service–related factors that may contribute to breastfeeding success, such as breastfeeding in the delivery room, length of hospital stay, and participation in educational programs.11
Given that data were collected for the NSFG during personal interviews at differing lengths of time after a pregnancy, inaccuracy is possible. Although the survey does not include corroboration from other sources, such as medical records or birth certificates, it is reassuring that, as an example, rates of prenatal care in our study are similar to those of other nationally reported rates for 1995 (98.1% in our study and 98.8% in National Vital Statistics Reports).12 Potential misclassification with respect to such medical outcomes as prematurity would be nondifferential and only bias odds ratios toward the null. The extended time between conception and measurement of maternal attitudes increases the uncertainty that a mother will accurately recall both her pregnancy intentions at conception and her breastfeeding practices. Women are more likely to recall a pregnancy carried to birth as intended, but this phenomenon would only bias the results if it also applied to breastfeeding practices, which is unlikely.13 While breastfeeding practices may not be exactly recalled, there is no obvious reason for differential reporting.
Conclusions
Our study has clinical implications for first-time US mothers. A recent national goal of the Institute of Medicine is that all pregnancies be planned.3 One of the many benefits of decreasing unintended pregnancy may be to increase breastfeeding rates closer to the Healthy People 2010 goals. In addition, a new hypothesis is suggested by the results of this study: Clinicians should promote breastfeeding differently for women with intended and unintended pregnancies. Future research will evaluate the importance of incorporating pregnancy intention status into patient-centered counseling. In the interim, women with unwanted pregnancies, especially white women, should be targeted for counseling, as they could benefit from breastfeeding, not just for medical reasons but for psychological and economic ones as well.
Acknowledgments
We would like to thank Larry Culpepper, MD, MPH, for his guidance.
OBJECTIVE: To examine the association between unintended pregnancy and the initiation and duration of breastfeeding.
STUDY DESIGN: This was a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth.
POPULATION: We studied 6733 first singleton live births to US women aged 15 years to 44 years.
OUTCOMES MEASURED: Using the 1995 Institute of Medicine definitions, pregnancies were classified as intended or unintended; unintended pregnancies were further categorized as either mis-timed or unwanted. We measured initiation of breastfeeding and duration of nonexclusive breastfeeding for at least 16 weeks.
RESULTS: In this study, 51.5% of women never breastfed, 48.5% initiated breastfeeding, and 26.4% of all women continued breastfeeding for at least 16 weeks. US women with unwanted unintended pregnancies were more likely not to initiate breastfeeding (odds ratio [OR] = 1.76; 95% confidence interval [CI], 1.26-2.44) and more likely not to continue breastfeeding (OR =1.69; 95% CI, 1.12-2.55) than women with intended pregnancies. White women with unwanted unintended pregnancies were more likely not to breastfeed than those with intended ones (initiation: OR = 2.50; 95% CI, 1.54-4.05; continuation: OR = 2.56; 95% CI, 1.34-4.87). This finding was not seen for black or Hispanic women.
CONCLUSIONS: In the United States, women with unwanted pregnancies were less likely either to initiate or to continue breastfeeding than women with intended pregnancies. A strong inverse association between unwanted pregnancies and breastfeeding was observed only for white women. Education for women with unintended pregnancies may improve breastfeeding rates and subsequently, the health of women and infants.
- In the United States, women whose pregnancies were unwanted are at a higher risk of not breastfeeding than women whose pregnancies were intended.
- Future research to evaluate the importance of incorporating pregnancy intention status into patient-centered breastfeeding promotion is needed.
- For now, women with unwanted pregnancies, especially white women, should be targeted for breastfeeding counseling.
Unintended pregnancy is a significant public health issue. More than half of all pregnancies are unintended at the time of conception; approximately half of those end as births and half as induced abortions.1 Forty-eight percent of women have at least one unplanned pregnancy, and 28% of women have at least one unplanned birth during their reproductive lifetime.2 Unintended pregnancies and births are associated with numerous harmful behaviors and adverse outcomes.3,4
Breastfeeding is currently promoted as the preferred method of feeding for infants for at least 1 year because of its multiple immediate and long-term benefits for both mother and child.5,6 Yet in 1998 only 64% of US mothers were breastfeeding at the time of hospital discharge and 29% at 6 months postpartum, which is well below the Healthy People 2010 goals of 75% and 50%, respectively, for those intervals.7
We hypothesized that women with unintended pregnancies are less likely to breastfeed their infants than those with intended ones. We quantified the association between the intendedness of pregnancy at the time of conception and breastfeeding behavior, both the initiation of any breastfeeding and the continuation of nonexclusive breastfeeding for at least 16 weeks, for first singleton births to US mothers. We then explored other factors which might affect breastfeeding practices.
Methods
Study design
This study is a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth (NSFG), a periodic population-based survey conducted by the National Center for Health Statistics and the Centers for Disease Control which focuses on women’s health and pregnancy. A national probability sample of 14,000 civilian noninstitutionalized women aged 15 years to 44 years was selected from among households that responded to the 1993 National Health Interview Survey, with an oversampling of minority women. Personal interviews were conducted between January and October of 1995 with 10,847 of these women. The data were then adjusted for a response rate of 79% and weighted so that findings would reflect the US population as a whole. Full details of the NSFG survey methods are described elsewhere.8
The data set contains information on 21,332 pregnancies and 14,958 live births (Figure). After excluding multiple gestations (n=154), subsequent births to the same mother (n=7930), and neonatal adoptions or deaths (n=141), the final sample contained 6733 first singleton live births. To study the initiation of breastfeeding, women who breastfed at all were compared with those who did not. To study duration of breastfeeding, women who breastfed for 16 or more weeks were compared with those who did not. In this second set of analyses, the 1459 women who breastfed for between 0 and 16 weeks and the 33 women who were breastfeeding at the time of the interview and whose children had been born within 16 weeks of that date were excluded.
FIGURE
Study sample
Variable definitions
Pregnancies were categorized as either intended or unintended at conception, using new definitions established by the Institute of Medicine in 1995.3 Pregnancies were considered intended if a woman had stopped using birth control because she wanted to become pregnant. Unintended pregnancies were classified into 1 of 2 categories: (1) mis-timed: wanted pregnancies that occurred sooner than desired, or (2) unwanted: pregnancies that occurred while a woman was using contraception and had not ever wanted to have a(nother) baby. The 170 women who described their pregnancy intention status as “didn’t know” or “didn’t care” were excluded from analyses involving intention status as defined above. There were 2 breastfeeding outcomes in this study: (1) initiation of breastfeeding, including women who reported any breastfeeding at all, and (2) duration of non-exclusive breastfeeding for at least 16 weeks.
Maternal demographics, intrapartum and postpartum behaviors, and birth outcomes were considered as potential confounders. As missing data were imputed in the public use data file, information on each variable was complete, except where noted below. Maternal age was determined at the time of conception. Education was defined as completed years of schooling at the time of the interview. Race was categorized as white, black, Hispanic, or other. Marital status was defined as either married or not married. Socioeconomic status was measured continuously as a percentage of the 1995 poverty level. Information on prenatal care was only available for births in the last 5 years (n=1266). For the 1241 women who reported that they had received prenatal care, the mean weeks of gestation at the time of the first prenatal visit were calculated. Maternity leave was defined as the use of maternity leave, paid or unpaid, for women who were working during the pregnancy (n=3662). For those who took any leave, the mean length of that leave was calculated in weeks. The 33 women for whom data were not available and the 5 women who answered that they took 0 weeks of maternity leave were not included in this calculation. Infant variables were considered categorically: mode of delivery, either vaginal or cesarean; prematurity, birth at less than or equal to 36 weeks; and low birth weight, less than or equal to 5.5 pounds.
Statistical analysis
The statistical significance of descriptive variables was determined using 2-sample t tests and chi-square tests, with women who did not breastfeed at all as the comparison group.
To compare our results with existing literature, we calculated crude odds ratios of not breastfeeding and used chi-square tests to assess the statistical significance of these associations. The reference group was always women whose pregnancies were intended. Variables identified as potential confounders were age, race, marital status, poverty level, education, maternity leave, mode of delivery, prematurity, and low birth weight. Final logistic regression models were adjusted for those variables that changed crude odds ratios by 10% or more: age, race, marital status, poverty level, and education. Adjusted odds ratios (ORs) of not breastfeeding and 95% confidence intervals (CIs) are reported.
Effect modification was assessed by dichotomizing each of the 5 confounding variables in the following manner: teen versus 20 years or older; white versus black versus Hispanic (here, the 193 women in the sample who defined their race as other were not included); married versus unmarried; high school education or higher versus less than a high school education; and below the poverty level versus at or above the poverty level. Each stratified analysis was adjusted for the other 4 factors. Interaction terms were created and P values for heterogeneity were calculated for all logistic models. For race, an additional interaction term was created to compare white with non-white (black and Hispanic combined) women.
These data are contained on the National Survey of Family Growth Cycle 5 1995 CD-ROM, Series 23, No. 3 and were exported using SETS version 1.22a (National Center for Health Statistics, Hyattsville, MD). All analyses were performed with SAS version 6.12 (SAS Institute, Cary, NC). Odds ratios are weighted using sampling weights provided in the data set. SUDAAN version 7.5.3 was used to obtain standard errors (Research Triangle Institute, Research Triangle Park, NC).
Results
In the total sample of 6733 first singleton live births to US mothers, 3267 (48.5%) of women initiated breastfeeding, compared with 3466 (51.5%) who did not. In the entire sample, 1775 (26.4%) continued to breastfeed nonexclusively for at least 16 weeks.
The breastfeeding initiation rate was 55.9%, 37.4%, and 28.0% for women with intended, mis-timed, and unwanted pregnancies, respectively. By 16 weeks, 32.6%, 17.0%, and 15.5% of women, respectively, were still breastfeeding. For all women who breastfed, the mean number of weeks of breastfeeding was 24.4 (standard deviation = 24.9; range = < 1 week to 4.0 years). Only 3.9% of women who breastfed did so for more than 2 years.
Table 1 shows characteristics of mothers and infants by breastfeeding behavior. Women who breastfed, both initially and for at least 16 weeks, were older at conception and had had more years of education than women who did not breastfeed at all. They were more likely to be white and less likely to be black. A similar percentage of women in each group were Hispanic. Percentage of the poverty level, a proxy for socioeconomic status, was higher for those who breastfed at all, but similar for those who continued breastfeeding and those who did not breastfeed. Rates of prenatal care and mean weeks at first prenatal visit were similar in all groups. Among women who were employed during their pregnancies, almost two thirds took maternity leave, regardless of breastfeeding behavior. Mean length of maternity leave was 3.4 weeks longer among women who continued to breastfeed than among women who did not breastfeed at all. The percentage of vaginal deliveries was similar among groups. Both premature and low birth weight infants were more common among women who did not breastfeed.
The association between the intendedness of pregnancy and breastfeeding behavior is reported in Table 2. Crude odds ratios show that women with any type of unintended pregnancy were more likely not to initiate breastfeeding than women whose pregnancies were intended. Some, but not all, of this association can be attributed to confounding by demographic factors. Having an unintended pregnancy was not associated with any significant difference in the initiation of breastfeeding, after adjusting for age, race, marital status, poverty level, and education. While women with mis-timed pregnancies were as likely to initiate breastfeeding as those whose pregnancies were intended (OR = 1.03; 95% CI, 0.88-1.21), women with unwanted pregnancies were more likely not to start breastfeeding (OR = 1.76; 95% CI, 1.26-2.44).
Table 2 also describes the association between pregnancy intention status and the continuation of nonexclusive breastfeeding for at least 16 weeks. In contrast to the initiation of breastfeeding, duration of breastfeeding was affected by the intendedness of pregnancy in every comparison. Adjusted odds ratios show that women with either type of unintended pregnancy were more likely not to continue breastfeeding than those with intended ones (OR = 1.28; 95% CI, 1.06-1.54). As with breastfeeding initiation, this association is being driven by the unwanted pregnancies. Women with unwanted pregnancies were more likely not to continue breastfeeding (OR = 1.69; 95% CI, 1.12-2.55).
Each of these associations was then evaluated for effect modification. As seen in Table 3, only race was an important factor. In the total sample, 56.3% of white women, 55.4% of Hispanic women, and 24.7% of black women breastfed at all; and 41.6%, 41.2%, and 12.6% of white, Hispanic, and black women breastfed for at least 16 weeks. White women with unwanted pregnancies were more likely not to initiate breastfeeding (OR = 2.50; 95% CI, 1.54-4.05) and more likely not to continue breastfeeding (OR = 2.56; 95% CI, 1.34-4.87) than white women with intended pregnancies. These differences in breastfeeding behaviors for unwanted pregnancies were not seen for either Hispanic or black women. For each stratified analysis, a single P value for heterogeneity was calculated to compare white women with non-white women (Hispanic and black women combined). The only significant difference by race was for unwanted pregnancies. The P value for heterogeneity was 0.01 for both initiation and continuation of breastfeeding. Stratified analyses for age, marital status, education, poverty level, and year of birth showed similar odds ratios across strata and nonsignificant P values for heterogeneity in every case (analyses not shown).
TABLE 1
Characteristics of mothers and infants by breastfeeding status (n=6733)
| Characteristic | Any breastfeeding (n = 3267) | Breastfeeding for ≥ 16 weeks (n = 1775) | No breastfeeding (n = 3466) |
|---|---|---|---|
| Age (mean years, SD) | 23.5 (5.0)* | 24.0 (5.1)* | 20.5 (4.3) |
| Race (%) | |||
| White | 64.8* | 65.9* | 47.4 |
| Black | 12.8 | 10.3 | 36.6 |
| Hispanic | 18.4 | 19.1 | 14.0 |
| Other | 4.0 | 4.7 | 2.0 |
| Married (%) | 65.0* | 68.8* | 37.3 |
| Percentage of the 1995 poverty level (SD) | 320 (207)* | 235 (205)* | 246 (189) |
| Education (mean years, SD) | 13.1 (3.0)* | 13.3 (3.2)* | 11.9 (2.3) |
| Prenatal care (%)† | 98.5 | 97.4 | 97.6 |
| Mean weeks at 1st visit (SD) | 7.8 (3.9) | 7.8 (4.0) | 9.1 (5.4) |
| Maternity leave ‡ | 65.2 | 60.7 | 64.6 |
| Mean weeks (SD) | 12.2 (9.4) | 13.8 (10.8) | 10.4 (8.3) |
| Vaginal delivery (%) | 78.5 | 78.9 | 80.7 |
| Prematurity (%) | 7.4* | 6.4* | 9.9 |
| Low birth weight (%) | 4.8* | 3.9* | 9.4 |
| SD denotes standard deviation. | |||
| *P ≤ .001 in comparison with women who did not breastfeed. | |||
| † For births during 1990-1994, n=1266. | |||
| ‡ Percentage of women employed during that pregnancy, n=3662. | |||
TABLE 2
Unintended pregnancy and breastfeeding behavior in the United States
| Intendedness of pregnancy | Number breastfeeding | Number not breastfeeding | Weighted crude odds ratio of NOT breastfeeding (95% CI)* | Weighted adjusted odds ratio of NOT breastfeeding (95% CI)* † |
|---|---|---|---|---|
| Initiation of breastfeeding (any) | ||||
| Intended | 2263 | 1758 | reference | reference |
| Unintended | 924 | 1618 | 2.15 (1.91-2.43) | 1.09 (0.93-1.28) |
| Mis-timed | 822 | 1361 | 2.02 (1.79-2.29) | 1.03 (0.88-1.21) |
| Unwanted | 102 | 257 | 3.54 (2.69-4.66) | 1.76 (1.26-2.44) |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | 1304 | 1758 | reference | reference |
| Unintended | 426 | 1618 | 2.79 (2.42-3.23) | 1.28 (1.06-1.54) |
| Mis-timed | 371 | 1361 | 2.68 (2.30-3.12) | 1.22 (1.01-1.47) |
| Unwanted | 55 | 257 | 3.82 (2.69-5.42) | 1.69 (1.12-2.55) |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, race, marital status, poverty level, and education. | ||||
TABLE 3
Effect of race on unintended pregnancy and breastfeeding behavior
| Weighted adjusted odds ratio of NOT breastfeeding*† | ||||
|---|---|---|---|---|
| Intendedness of pregnancy | White (n=3661) | Hispanic (n=1063) | Black (n=1646) | |
| Initiation of breastfeeding (any) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.15 (0.93-1.42) | 0.94 (0.66-1.35) | 0.81 (0.56-1.17) | |
| Mis-timed | 1.07 (0.87-1.32) | 0.93 (0.64-1.35) | 0.78 (0.53-1.15) | |
| Unwanted | 2.50 (1.54-4.05) | 0.97 (0.55-1.70) | 0.93 (0.52-1.65) | |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.39 (1.07-1.81) | 1.08 (0.74-1.58) | 0.73 (0.44-1.20) | |
| Mis-timed | 1.29 (0.99-1.68) | 1.10 (0.76-1.60) | 0.70 (0.41-1.20) | |
| Unwanted | 2.56 (1.34-4.87) | 0.90 (0.47-1.72) | 0.78 (0.34-1.76) | |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, marital status, poverty level, and education. | ||||
Discussion
In this study of first-time US mothers, women who breastfed were demographically different from those who did not, but had relatively similar maternal behaviors and infant characteristics. After controlling for these demographic differences, having an unwanted pregnancy was associated with a lower likelihood of both initiating breastfeeding and continuing to breastfeed. In addition, race was an important effect modifier for unwanted pregnancies.
The demographic findings of this study are consistent with the current breastfeeding literature: US women who breastfeed tend to be older, white, married, well-educated, and of a higher socioeconomic status than those who do not.9 The main findings of this study are also consistent with the only other study that has examined the relationship between unintended pregnancy and breastfeeding behavior.10 A cross-sectional sample of 27,700 women who gave birth to a live baby were asked prior to postpartum discharge whether they had intended to become pregnant and their plans for breastfeeding. After controlling for education, race, Medicaid status, maternal age younger than 20, and any tobacco use during pregnancy, the authors found that women whose pregnancies were unintended were more likely not to initiate breastfeeding or to breastfeed exclusively. Adjusted odds ratios of not breastfeeding ranged from 1.10 to 1.41, depending on intention status, and all were statistically significant. In contrast to our study, a major limitation of that study was that the measured outcome was intent to breastfeed at hospital discharge, which may have differed greatly from actual breastfeeding behavior.
The interaction seen in our analysis between intention status and race is initially surprising because, in general, white and Hispanic women breastfeed at much higher rates than black women. But if a pregnancy was unwanted, white women were much less likely to breastfeed than either black or Hispanic women. Neither socioeconomic status nor educational level is the explanation, as both of these factors were controlled for in stratified analyses. Perhaps Hispanic and black women are more accepting of unintended pregnancy than white women and these results reflect cultural differences. Further studies which examine other aspects of unintended pregnancy with respect to race will help to further clarify the reasons for this finding.
Strengths and limitations
Our population-based study has several strengths. The data set provides a large national sample with excellent representation of minority women; statistical oversampling and weighting allow these data to reflect the entire national population. Adjustment of data for nonresponse lessens the risk of selection bias. Furthermore, the study sample was restricted to first births to limit the effect of previous birth experiences on postpartum behaviors. Therefore our results are generalizable to all first-time mothers in the United States.
A major limitation of our study is that information was not collected on several factors, such as substance use both during pregnancy and after birth, that might influence the relationship between pregnancy intention status and breastfeeding behavior. The work of Dye and colleagues,10 discussed above, found that prenatal tobacco, but not alcohol or drug use, was a significant confounder. Information was also not available on health service–related factors that may contribute to breastfeeding success, such as breastfeeding in the delivery room, length of hospital stay, and participation in educational programs.11
Given that data were collected for the NSFG during personal interviews at differing lengths of time after a pregnancy, inaccuracy is possible. Although the survey does not include corroboration from other sources, such as medical records or birth certificates, it is reassuring that, as an example, rates of prenatal care in our study are similar to those of other nationally reported rates for 1995 (98.1% in our study and 98.8% in National Vital Statistics Reports).12 Potential misclassification with respect to such medical outcomes as prematurity would be nondifferential and only bias odds ratios toward the null. The extended time between conception and measurement of maternal attitudes increases the uncertainty that a mother will accurately recall both her pregnancy intentions at conception and her breastfeeding practices. Women are more likely to recall a pregnancy carried to birth as intended, but this phenomenon would only bias the results if it also applied to breastfeeding practices, which is unlikely.13 While breastfeeding practices may not be exactly recalled, there is no obvious reason for differential reporting.
Conclusions
Our study has clinical implications for first-time US mothers. A recent national goal of the Institute of Medicine is that all pregnancies be planned.3 One of the many benefits of decreasing unintended pregnancy may be to increase breastfeeding rates closer to the Healthy People 2010 goals. In addition, a new hypothesis is suggested by the results of this study: Clinicians should promote breastfeeding differently for women with intended and unintended pregnancies. Future research will evaluate the importance of incorporating pregnancy intention status into patient-centered counseling. In the interim, women with unwanted pregnancies, especially white women, should be targeted for counseling, as they could benefit from breastfeeding, not just for medical reasons but for psychological and economic ones as well.
Acknowledgments
We would like to thank Larry Culpepper, MD, MPH, for his guidance.
1. Forrest JD. Unintended pregnancy among American women. Fam Plann Perspect 1987;19:76-7.
2. Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspectives 1998;30:24-9,46.-
3. Institute of Medicine Committee on Unintended Pregnancy. The best intentions: unintended pregnancy and the well-being of children and families. Washington, DC: National Academy Press, 1995.
4. Orr ST, Miller CA. Unintended pregnancy and the psychosocial well-being of pregnant women. Womens Health Issues 1997;7:38-46.
5. Institute of Medicine Subcommittee on Nutrition during Lactation. Nutrition during lactation. Washington, DC: National Academy Press, 1991.
6. American Academy of Pediatrics, Work Group on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 1997;100:1035-9.
7. US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: US Government Printing Office, November 2000.
8. Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: new data from the 1995 National Survey of Family Growth. Vital Health Stat 1997;23.19:1-114.
9. Scott JA, Binns CW. Factors associated with the initiation and duration of breastfeeding: a review of the literature. Breastfeed Rev 1999;7:5-16.
10. Dye TD, Wojtowycz MA, Aubry RH, Quade J, Kilburn H. Unintended pregnancy and breastfeeding behavior. Am J Public Health 1997;87:1709-11.
11. Kuan LW, Britto M, Decolongon J, Schoettker PJ, Atherton HD, Kotagal UR. Health system factors contributing to breastfeeding success. Pediatrics 1999;104:e28.-
12. Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: final data for 1997. Natl Vital Stat Reports 1999;47.18:1-96.
13. Petersen R, Moos MK. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues 1997;7:234-40.
1. Forrest JD. Unintended pregnancy among American women. Fam Plann Perspect 1987;19:76-7.
2. Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspectives 1998;30:24-9,46.-
3. Institute of Medicine Committee on Unintended Pregnancy. The best intentions: unintended pregnancy and the well-being of children and families. Washington, DC: National Academy Press, 1995.
4. Orr ST, Miller CA. Unintended pregnancy and the psychosocial well-being of pregnant women. Womens Health Issues 1997;7:38-46.
5. Institute of Medicine Subcommittee on Nutrition during Lactation. Nutrition during lactation. Washington, DC: National Academy Press, 1991.
6. American Academy of Pediatrics, Work Group on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 1997;100:1035-9.
7. US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: US Government Printing Office, November 2000.
8. Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: new data from the 1995 National Survey of Family Growth. Vital Health Stat 1997;23.19:1-114.
9. Scott JA, Binns CW. Factors associated with the initiation and duration of breastfeeding: a review of the literature. Breastfeed Rev 1999;7:5-16.
10. Dye TD, Wojtowycz MA, Aubry RH, Quade J, Kilburn H. Unintended pregnancy and breastfeeding behavior. Am J Public Health 1997;87:1709-11.
11. Kuan LW, Britto M, Decolongon J, Schoettker PJ, Atherton HD, Kotagal UR. Health system factors contributing to breastfeeding success. Pediatrics 1999;104:e28.-
12. Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: final data for 1997. Natl Vital Stat Reports 1999;47.18:1-96.
13. Petersen R, Moos MK. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues 1997;7:234-40.
The impact of the maternal experience with a jaundiced newborn on the breastfeeding relationship
OBJECTIVE: To examine the process by which mothers’ experiences with neonatal jaundice affects breastfeeding.
STUDY DESIGN: We used ethnographic interviews with grounded theory methodology. Audiotaped data were transcribed and analyzed for themes using ATLAS/ti qualitative data analysis software (Scientific Software Development, Berlin, Germany).
POPULATION: We studied a total of 47 Spanish- and English-speaking breastfeeding mothers of otherwise healthy infants diagnosed with neonatal jaundice.
OUTCOME MEASURED: Our outcomes were the qualitative descriptions of maternal experiences with neonatal jaundice.
RESULTS: Interactions with medical professionals emerged as the most important factor mediating the impact of neonatal jaundice on breastfeeding. Breastfeeding orders and the level of encouragement from medical professionals toward breastfeeding had the strongest effect on feeding decisions. Maternal reaction to and understanding of information from their physicians also played an important role. Guilt was common, as many mothers felt they had caused the jaundice by breastfeeding.
CONCLUSIONS: By providing accurate information and encouragement to breastfeed, medical professionals have great impact on whether a mother continues breastfeeding after her experience with neonatal jaundice. Health care providers must be aware of how mothers receive and interpret information related to jaundice to minimize maternal reactions, such as guilt, that have a negative impact on breastfeeding.
- Interactions with medical professionals emerged as the most important factor mediating the impact of the maternal experience with neonatal jaundice on breastfeeding.
- Encouragement or lack of encouragement to breastfeed plays a large role in whether women continue to breastfeed after their experience with jaundice.
- To minimize feelings of guilt and enhance maternal understanding about jaundice, health care professionals need to be aware not only of what information is given to mothers, but how mothers receive and interpret this information.
- Medical professionals must provide consistent information and ensure that mothers understand how jaundice relates to breastfeeding and the purpose of any breastfeeding instructions given during the experience.
Neonatal jaundice is the most common condition for which newborns are tested, treated, and often rehospitalized, resulting in millions of dollars of annual expenditure.1-3 Two types of jaundice are associated with breastfeeding4: early jaundice, or breastfeeding jaundice, caused by the infant receiving insufficient breast milk5,6; and breast milk jaundice, which develops later in a thriving breastfed infant and is thought to be caused by a substance in the breast milk.7,8
Diagnosis and treatment of jaundice can begin within the first few days after birth, while the breastfeeding relationship is being established. Despite the ongoing debate on the appropriate protocol for jaundice management9-11 and a wide variance in physician practice,12,13 little research has examined the effect of the jaundice experience on the newborn’s mother. The few studies to directly examine the influence of jaundice management on breastfeeding show that protocols such as maternal-infant separation for phototherapy or temporarily suspending breastfeeding are associated with a shorter duration of breastfeeding.14-16
What remains unclear is how jaundice management affects breastfeeding. Our study adds to existing knowledge by exploring the process by which the maternal experience with a jaundiced newborn affects the mother and her breastfeeding decisions. Qualitative methods, guided by grounded theory, were used because of the paucity of information on this topic and the study’s focus on process.17-19
Methods
Settings
Two distinct sites in Chicago were chosen to increase the heterogeneity of experiences: a community hospital serving a mixed-income and ethnically diverse population, and an urban teaching hospital serving primarily low-income Latino and African American patients. Breastfeeding initiation rates, tracked by the University of Illinois at Chicago breastfeeding task force, were 70% and 40%, respectively. Institutional Review Board approval was obtained from both sites.
Sample
Two purposeful sampling strategies were employed.20 Criterion sampling was used to recruit mothers, identified through medical record abstraction of all jaundiced infants, who met the following criteria: Spanish or English speaking; exclusively or partially breastfeeding at postpartum discharge; and mother of an otherwise healthy term newborn who had a serum bilirubin level of =10 mg/dL within the first month of life and received care through a study site in 1 or more of the following settings: newborn nursery, outpatient clinic, hospital ward, or home. Maximum variation sampling, which seeks heterogeneity within the sample to permit examination of common themes, was applied to achieve variation in ethnicity, language, age, parity, and jaundice treatment. Eligible mothers were invited by phone to participate in an interview. Sampling continued until data from new interviews confirmed earlier data, signifying that theoretical saturation was achieved.18
Data collection
Using the literature on hyperbilirubinemia and breastfeeding, an interview guideline was developed addressing the topics in Table 1.21 Three female ethnographers (including authors S.K.W. and P.R.H.) conducted in-depth, semi-structured interviews in women’s homes. The interviews were approximately 60 minutes in length given in either Spanish or English. Women were encouraged to lead the conversation, with ethnographers using prompts to guide the discussion toward any topics not addressed and probes to elicit detailed descriptions of the women’s experiences. Audiotaped interviews were transcribed verbatim, and edited by the ethnographer to ensure accuracy and include field notes. Spanish-language interviews were translated into English. Participants received no financial incentives.
Analysis
Interviews were carefully read by all investigators for themes, and codes were developed to represent these themes.18,22,23 A code book defining each code and listing inclusion and exclusion criteria was developed, and one investigator (S.K.W.) applied codes to the interviews using ATLAS/ti qualitative data analysis software (Scientific Software Development, Berlin, Germany). Intracoder and intercoder (with P.R.H.) agreement were determined to assure consistency of code definitions. Codes with a low level of agreement were redefined and reapplied. Coded text was retrieved and emerging themes analyzed in relation to other themes and variables. Focus was placed on comparing and contrasting women’s experiences to elicit what in the maternal experience with neonatal jaundice influenced infant feeding decisions. We also focused on women’s understanding of the information they received and the relationship between jaundice and breastfeeding.
Results
Of 69 eligible mothers, 11 declined to participate, and 13 could not be reached or scheduled for an interview. Forty-five mothers were interviewed between October 1997 and April 1998 at 2.5 to 14.5 weeks postpartum (mean = 6 weeks). Investigators attempted to hold 2 focus groups with unsuccessful show rates. Individual interviews were conducted with the 2 women who attended these sessions and analyzed with the other interviews. The 24 nonparticipants had similar demographic characteristics to women in the study.
Participants represented a range of sociodemographic and jaundice management characteristics Table 2. Mothers were predominately Latinas of Mexican descent, with a mean age of 27 years (range = 16-38 years). Women born outside the United States had lived in the US from 1 to 25 years (mean = 7 years). More than three quarters of the women lived with the father of the baby. Peak bilirubin levels of all infants ranged from 10.3 to 23.5 mg/dL; 4 infants had peak levels of >20 mg/dL and 7 had peak levels of <12 mg/dL. Thirty-nine infants experienced jaundice within the first 6 days of life, with the majority having nonhemolytic jaundice. Eight infants had breast milk jaundice with peak bilirubin levels occurring between 1 and 2 weeks of age. More than half of the multiparous women had experienced jaundice with a previous infant (n = 14) and three fourths had breastfed a previous child (n = 19).
Though each woman’s experience was unique, a pattern emerged from the women’s discussions that described a process by which their experiences affected the breastfeeding relationship. This process centered on mothers’ interactions with medical professionals during jaundice management and their internalization of the experience.
Jaundice management
Half the women described how their experiences with neonatal jaundice had directly influenced their breastfeeding decisions, positively or negatively, primarily discussing this impact in terms of the breastfeeding instructions they received. Table 3 illustrates the clear pattern seen between a maternal report of breastfeeding orders received from medical professionals and a woman’s feeding status at 2 weeks postpartum, directly after the jaundice experience. Breastfeeding orders were categorized as: continue, conflicting, supplement, suspend, and none. Regardless of parity, women’s interactions with medical professionals related to breastfeeding orders and the level of encouragement they received had the strongest influence on whether women continued to breastfeed.
Mothers exclusively breastfeeding after their experience discussed the encouragement they received from medical staff. Mothers told to continue to breastfeed felt encouraged to breastfeed frequently to help the jaundice go away. All continued to breastfeed for at least 3 weeks, none quit because of their infant’s jaundice. Mothers who returned to exclusive breastfeeding after being told to temporarily suspend breastfeeding or to supplement with formula described being encouraged not to quit breastfeeding and were reassured that their milk was good.
“Right away I wanted to stop breastfeeding, especially if it is me causing him to get that. And they were like, ‘No, no. We’re not telling you to stop. It’s good that you are breastfeeding him.’”
Women exclusively formula feeding because of their experience with jaundice shared 2 separate reasons for not resuming. The first related to not wanting to “take anymore chances” with their infant receiving insufficient milk.
“At the time she was in the hospital they told me to stop breastfeeding her. They wanted to formula feed her. They just said that they think she wasn’t getting enough. They said since they can’t measure how much she drinks that they don’t know how much she is drinking. So I decided, well, I’ll just continue formula feeding her.”
The second related to physical difficulty in reestablishing lactation.
“I breastfed my other three children. … That’s why I tried more to see if he’d latch on, but he didn’t. … Since the beginning, I had the idea that I was only going to breastfeed him, but no.”
Women who continued to supplement with formula because of their experience expressed fear that jaundice would return if they quit supplementation.
“I am still on formula now [7 weeks after experience]. The doctor said he wanted to wait until it is 3 weeks after he is released to wean down. ... I think it caused some damage for me because I am still frightened to really let go of the formula. I may be wrong and maybe it can’t come back at this stage, but I think that something could go wrong and I am still giving formula to make sure that he is getting enough.”
Although mothers whose infants did not receive phototherapy were more likely to be told to continue breastfeeding or to be given no feeding orders than mothers whose infants received phototherapy, there was not a clear pattern between feeding method at 2 weeks postpartum and form of jaundice treatment. Although a few mothers expressed concern about breastfeeding during phototherapy because of having to remove their infant from the light, no mother quit breastfeeding or began supplementing specifically because of treatment. However, many mothers discussed the strong emotional impact that blood work, phototherapy, and the mother-child separation had on them.24
The majority of mothers had prior exposure to neonatal jaundice, approximately one third through personal experience with previous children. Although a few mothers had previous experience with jaundiced infants undergoing phototherapy, only one had been told to stop breastfeeding a previous infant because of jaundice. Even though this mother was not told to stop breastfeeding her current infant, she supplemented with formula because she felt her milk was “no good.”
Maternal internalization of experience
Mothers who received breastfeeding orders to suspend or supplement, or who were given conflicting orders, repeatedly expressed confusion or discontent with these instructions. They commented on the conflict between the medical professional’s advice and their own understanding that breastfeeding was healthier for babies, and on not receiving sufficient explanation to justify changing their feeding method.
“She [doctor] just told me to stop breastfeeding because…. Actually she didn’t tell me why. Which got me confused. I remember I was thinking why did she tell me to stop breastfeeding if breast milk is better for the baby?”
Mothers also shared concerns about nipple confusion affecting their ability to exclusively breastfeed, and feeling that decisions were out of their control.
Lack of understanding about causes of jaundice and feelings of guilt over their role in the etiology were common among all women. More than one third of women expressed guilt that they had caused jaundice either during pregnancy or while breastfeeding.
“I was afraid I did something wrong... that my milk wasn’t coming in right… that I wasn’t feeding her enough or I wasn’t feeding her the right things. Or that my milk was broken ... that I wasn’t making enough or it was wrong somehow. Like it wasn’t meeting her needs.”
Several mothers also expressed belief that their infant may not have gotten jaundice if they had not started breastfeeding.
“I wonder if she would’ve started with the formula, if we would’ve started to supplement with formula from the very beginning, I wonder if it would’ve happened.”
More than half the women discussed breastfeeding as a cause of jaundice. Those women had experienced early neonatal jaundice. More than one third had a previously jaundiced infant and approximately half had previously breastfed. Those who received breastfeeding orders to suspend or supplement, or who were given conflicting orders, were much more likely to discuss breastfeeding as a cause of jaundice than were those who received no breastfeeding orders. Mothers told to continue breastfeeding were least likely to discuss breastfeeding as a cause. No pattern was evident among women by language spoken, parity, bilirubin level, jaundice treatment, or feeding at the interview.
Women’s perceptions of what it is about breastfeeding that causes jaundice related to either quantity or quality.
The causes related to the quantity of breast milk included:
- Insufficient feeding. The infant is not receiving enough breast milk because he or she is not eating enough or the mother is not feeding infant enough.
- Insufficient milk. The mother is not producing enough breast milk.
The causes related to the quality of breast milk included:
- Milk composition. The breast milk caused jaundice, often because it was not good.
- Something in milk. There is something passed through the milk to cause jaundice, such as medicine, hormones, or emotions.
Women who gave explanations for jaundice closer to a biomedical understanding of jaundice, such as insufficient fluid intake, received this information primarily from medical professionals and occasionally from family and friends. Many issues related to feelings of guilt came from their own thoughts, though they were, at times, triggered by something said by a medical professional or family member. Mothers interpreted the information, or lack of information, they received in their attempt to explain why their infant had jaundice.
“The nurse said, the baby won’t be having your breast. All the time the baby will be in the hospital he will only be given formula. Since they never explained why he was that color or anything, I thought maybe my milk was no good. That’s why they told me not to give it to him.”
Discussion
Interactions with medical professionals emerged as the most important factor mediating the impact of the maternal experience with neonatal jaundice on breastfeeding. Encouragement or lack of encouragement from health care professionals played a large role in whether women continued to breastfeed after their experience, which agrees with other findings on the influence, both positive and negative, of interactions with medical professionals on breastfeeding.25-28 Maternal understanding of and reaction to information received during jaundice management and their subsequent internalization of their experience also played a key role in mothers’ infant feeding decisions. In contrast with previous studies,14,29 no consistent pattern was seen between breastfeeding continuation and whether infants received blood work only or phototherapy. This difference may be due to our study’s inclusion of multiple settings for phototherapy and differences in the study populations. In addition, earlier studies did not include information on medical professional’s breastfeeding orders.
Limitations
Although the use of qualitative methods allowed in-depth inquiry from the mother’s perspective, it necessitated a small sample limiting generalizability. Generalizability was further limited because the women in the sample were predominately Latina, though study findings were consistent across ethnicities. Data was only collected from the mothers’ point of view, which likely differed from medical professionals’ perceptions. Limiting the sample to mothers who initiated breastfeeding may have excluded mothers who decided not to breastfeed because of a previous jaundice experience. In addition, women whose infants did not develop jaundice because of adequate early breastfeeding support were not interviewed. Careful structuring of the interview guideline and use of experienced ethnographers minimized potential threats to validity through interviewer bias. Regular team meetings to discuss data collection and analysis increased reliability.
Additional research is needed to gain further understanding of mothers’ emotional responses when faced with neonatal conditions like jaundice. While maternal guilt has been acknowledged as a potential problem arising from treatment for neonatal jaundice,4,7,8 no research has focused on the impact of this guilt on breastfeeding. How do responses like guilt influence perceptions of themselves as breastfeeding mothers and their breastfeeding decisions? The possibility that neonatal jaundice and its management may deprive future children of the opportunity to breastfeed should be examined.
Conclusions
Neonatal jaundice affects many newborns and their families. Besides the monetary cost of treatment, our study results indicate that treatment for jaundice is not completely benign; there are health and emotional costs. Medical professionals must weigh the perceived benefits of treatment decisions and feeding orders against the potential costs to the emotional well being of mothers and newly established breastfeeding relationships. To minimize guilt and enhance maternal understanding about this common condition, professionals need to be aware not only of what information is given to mothers, but how mothers receive and interpret this information. Identifying neonatal jaundice with terms such as breastfeeding jaundice and breast milk jaundice may cause maternal concerns that jaundice is a result of their decision to breastfeed. Medical professionals must provide consistent information and ensure that mothers more fully understand the causes of jaundice and how it relates to breastfeeding, as well as breastfeeding instructions during the experience. The neonatal jaundice experience provides an opportunity for medical professionals to encourage breastfeeding mothers and provide specific guidance on how to maintain a successful breastfeeding relationship.
Acknowledgments
Our study was supported by a grant from the Campus Research Board at the University of Illinois. We would like to thank the women who participated in this study and made time to share their stories with us. We would also like to thank Isabel Martinez, MPH, for her assistance with scheduling and data collection, and Nadine Peacock, PhD, Arden Handler, DrPH, and Rebecca Lipton, PhD, for their comments during the development and analysis of this project.
1. Maisels MJ, Newman TB. Jaundice in the healthy newborn: its effect on infants, families and physicians. In: Morris, Jr FH, Simmons MA, eds. The normal newborn: report of the One Hundredth Ross Conference on Pediatric Research. Columbus, Ohio: Ross Laboratories; 1991;89-98.
2. Newman TB, Easterling MJ, Goldman ES, Stevenson DK. Laboratory evaluation of jaundice in newborns: frequency, cost and yield. Am J Dis Child 1990;144:364-8.
3. Lee KS, Perlman M, Ballantyne M, Elliott I, To T. Association between duration of neonatal hospital stay and readmission rate. J Pediatr 1995;127:758-66.
4. Maisels MJ, Gifford K. Normal serum bilirubin levels in the newborn and the effect of breast-feeding. Pediatrics 1986;78:837-43.
5. Kuhr M, Paneth N. Feeding practices and early neonatal jaundice. J Pediatr Gastroenterol Nutr 1982;1:485-9.
6. Tudehope D, Bayley G, Townsend S. Breast feeding practices and severe hyperbilirubinaemia. J Paediatr Child Health 1991;27:240-4.
7. de Steuben C. Breast-feeding and jaundice: a review. J Nurse Midwifery 1992;37:59S-66S.
8. Brooten D, Brown L, Hollingsworth A, Tanis J, Bakewell-Sachs S. Breast-milk jaundice. J Obstet Gynecol Neonat Nurs 1985;14:220-3.
9. AAP Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. Practice parameter: management of hyperbilirubinemia. Pediatrics 1994;94:558-65.
10. Newman TB, Maisels MJ. Evaluation and treatment of jaundice in the term newborn: a kinder, gentler approach. Pediatrics 1992;89:809-18.
11. Oski FA. Hyperbilirubinemia in the term infant: An unjaundiced approach. Contemp Pediatr 1992;9:148-54.
12. Freed GL, Clark SJ, Sorenson J, Lohr JA, Cefalo R, Curtis P. National assessment of physicians’ breast-feeding knowledge, attitudes, training, and experience. JAMA 1995;273:472-6.
13. Gartner LM, Herrarias CT, Sebring RH. Practices patterns in neonatal hyperbilirubinemia. Pediatrics 1998;101:25-31.
14. Elander G, Lindberg T. Hospital routines in infants with hyperbilirubinemia influence the duration of breast feeding. Acta Paediatr Scand 1986;75:708-12.
15. Kemper K, Forsyth B, McCarthy P. Jaundice, terminating breastfeeding, and the vulnerable child. Pediatrics 1989;84:773-8.
16. Kemper KJ, Forsyth BW, McCarthy PL. Persistent perceptions of vulnerability following neonatal jaundice. Am J Dis Child 1990;144:239-41.
17. Glasser B, Strauss A. The discovery of grounded theory. Chicago, Ill: Aldine; 1967.
18. Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, Calif: Sage Publications; 1990.
19. Morse JM. Designing funded qualitative research. In: Denzin NK, Lincoln, YS, eds. Handbook of qualitative research. Thousand Oaks, Calif: Sage Publications; 1994;220-35.
20. Patton MQ. Qualitative evaluation and research methods. Newbury Park, Calif: Sage Publications; 1990.
21. Scrimshaw SCM, Hurtado E. Rapid assessment procedures for nutrition and primary health care: anthropological approaches to improving programme effectiveness. Tokyo: The United Nations University; 1987.
22. Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Thousand Oaks, Calif: Sage Publications; 1994.
23. Tesch R. Qualitative research: analysis types and software tools. New York: Falmar Press; 1990.
24. Hannon PR, Willis SK, Scrimshaw SC. Persistence of maternal concerns surrounding neonatal jaundice: an exploratory study. Arch Pediatr Adolesc Med 2001;155:1357-63.
25. Dermer A. Overcoming medical and social barriers to breast feeding. Am Fam Phys 1995;51:755-63.
26. Hewat RJ, Ellis DJ. Breastfeeding as a maternal-child team effort: women’s perceptions. Health Care Women Int 1984;5:437-52.
27. Raj VK, Plichta SB. The role of social support in breastfeeding promotion: a literature review. J Hum Lact 1998;14:41-5.
28. Schy DS, Maglaya CF, Mendelson SG, Race KEH, Ludwig-Beymer P. The effects of in-hospital lactation education on breastfeeding practice. J Hum Lact 1996;12:117-22.
29. James JM, Williams SD, Osborn LM. Discontinuation of breast-feeding infrequent among jaundiced neonates treated at home. Pediatrics 1993;92:153-5.
All correspondence should be addressed to Sharla K. Willis, DrPH, The Ohio State University, School of Public Health, B-209 Starling-Loving Hall, 320 West 10th Avenue, Columbus, OH 43210-1240. E-mail: [email protected].
To submit a letter to the editor on this topic, click here: [email protected]
OBJECTIVE: To examine the process by which mothers’ experiences with neonatal jaundice affects breastfeeding.
STUDY DESIGN: We used ethnographic interviews with grounded theory methodology. Audiotaped data were transcribed and analyzed for themes using ATLAS/ti qualitative data analysis software (Scientific Software Development, Berlin, Germany).
POPULATION: We studied a total of 47 Spanish- and English-speaking breastfeeding mothers of otherwise healthy infants diagnosed with neonatal jaundice.
OUTCOME MEASURED: Our outcomes were the qualitative descriptions of maternal experiences with neonatal jaundice.
RESULTS: Interactions with medical professionals emerged as the most important factor mediating the impact of neonatal jaundice on breastfeeding. Breastfeeding orders and the level of encouragement from medical professionals toward breastfeeding had the strongest effect on feeding decisions. Maternal reaction to and understanding of information from their physicians also played an important role. Guilt was common, as many mothers felt they had caused the jaundice by breastfeeding.
CONCLUSIONS: By providing accurate information and encouragement to breastfeed, medical professionals have great impact on whether a mother continues breastfeeding after her experience with neonatal jaundice. Health care providers must be aware of how mothers receive and interpret information related to jaundice to minimize maternal reactions, such as guilt, that have a negative impact on breastfeeding.
- Interactions with medical professionals emerged as the most important factor mediating the impact of the maternal experience with neonatal jaundice on breastfeeding.
- Encouragement or lack of encouragement to breastfeed plays a large role in whether women continue to breastfeed after their experience with jaundice.
- To minimize feelings of guilt and enhance maternal understanding about jaundice, health care professionals need to be aware not only of what information is given to mothers, but how mothers receive and interpret this information.
- Medical professionals must provide consistent information and ensure that mothers understand how jaundice relates to breastfeeding and the purpose of any breastfeeding instructions given during the experience.
Neonatal jaundice is the most common condition for which newborns are tested, treated, and often rehospitalized, resulting in millions of dollars of annual expenditure.1-3 Two types of jaundice are associated with breastfeeding4: early jaundice, or breastfeeding jaundice, caused by the infant receiving insufficient breast milk5,6; and breast milk jaundice, which develops later in a thriving breastfed infant and is thought to be caused by a substance in the breast milk.7,8
Diagnosis and treatment of jaundice can begin within the first few days after birth, while the breastfeeding relationship is being established. Despite the ongoing debate on the appropriate protocol for jaundice management9-11 and a wide variance in physician practice,12,13 little research has examined the effect of the jaundice experience on the newborn’s mother. The few studies to directly examine the influence of jaundice management on breastfeeding show that protocols such as maternal-infant separation for phototherapy or temporarily suspending breastfeeding are associated with a shorter duration of breastfeeding.14-16
What remains unclear is how jaundice management affects breastfeeding. Our study adds to existing knowledge by exploring the process by which the maternal experience with a jaundiced newborn affects the mother and her breastfeeding decisions. Qualitative methods, guided by grounded theory, were used because of the paucity of information on this topic and the study’s focus on process.17-19
Methods
Settings
Two distinct sites in Chicago were chosen to increase the heterogeneity of experiences: a community hospital serving a mixed-income and ethnically diverse population, and an urban teaching hospital serving primarily low-income Latino and African American patients. Breastfeeding initiation rates, tracked by the University of Illinois at Chicago breastfeeding task force, were 70% and 40%, respectively. Institutional Review Board approval was obtained from both sites.
Sample
Two purposeful sampling strategies were employed.20 Criterion sampling was used to recruit mothers, identified through medical record abstraction of all jaundiced infants, who met the following criteria: Spanish or English speaking; exclusively or partially breastfeeding at postpartum discharge; and mother of an otherwise healthy term newborn who had a serum bilirubin level of =10 mg/dL within the first month of life and received care through a study site in 1 or more of the following settings: newborn nursery, outpatient clinic, hospital ward, or home. Maximum variation sampling, which seeks heterogeneity within the sample to permit examination of common themes, was applied to achieve variation in ethnicity, language, age, parity, and jaundice treatment. Eligible mothers were invited by phone to participate in an interview. Sampling continued until data from new interviews confirmed earlier data, signifying that theoretical saturation was achieved.18
Data collection
Using the literature on hyperbilirubinemia and breastfeeding, an interview guideline was developed addressing the topics in Table 1.21 Three female ethnographers (including authors S.K.W. and P.R.H.) conducted in-depth, semi-structured interviews in women’s homes. The interviews were approximately 60 minutes in length given in either Spanish or English. Women were encouraged to lead the conversation, with ethnographers using prompts to guide the discussion toward any topics not addressed and probes to elicit detailed descriptions of the women’s experiences. Audiotaped interviews were transcribed verbatim, and edited by the ethnographer to ensure accuracy and include field notes. Spanish-language interviews were translated into English. Participants received no financial incentives.
Analysis
Interviews were carefully read by all investigators for themes, and codes were developed to represent these themes.18,22,23 A code book defining each code and listing inclusion and exclusion criteria was developed, and one investigator (S.K.W.) applied codes to the interviews using ATLAS/ti qualitative data analysis software (Scientific Software Development, Berlin, Germany). Intracoder and intercoder (with P.R.H.) agreement were determined to assure consistency of code definitions. Codes with a low level of agreement were redefined and reapplied. Coded text was retrieved and emerging themes analyzed in relation to other themes and variables. Focus was placed on comparing and contrasting women’s experiences to elicit what in the maternal experience with neonatal jaundice influenced infant feeding decisions. We also focused on women’s understanding of the information they received and the relationship between jaundice and breastfeeding.
Results
Of 69 eligible mothers, 11 declined to participate, and 13 could not be reached or scheduled for an interview. Forty-five mothers were interviewed between October 1997 and April 1998 at 2.5 to 14.5 weeks postpartum (mean = 6 weeks). Investigators attempted to hold 2 focus groups with unsuccessful show rates. Individual interviews were conducted with the 2 women who attended these sessions and analyzed with the other interviews. The 24 nonparticipants had similar demographic characteristics to women in the study.
Participants represented a range of sociodemographic and jaundice management characteristics Table 2. Mothers were predominately Latinas of Mexican descent, with a mean age of 27 years (range = 16-38 years). Women born outside the United States had lived in the US from 1 to 25 years (mean = 7 years). More than three quarters of the women lived with the father of the baby. Peak bilirubin levels of all infants ranged from 10.3 to 23.5 mg/dL; 4 infants had peak levels of >20 mg/dL and 7 had peak levels of <12 mg/dL. Thirty-nine infants experienced jaundice within the first 6 days of life, with the majority having nonhemolytic jaundice. Eight infants had breast milk jaundice with peak bilirubin levels occurring between 1 and 2 weeks of age. More than half of the multiparous women had experienced jaundice with a previous infant (n = 14) and three fourths had breastfed a previous child (n = 19).
Though each woman’s experience was unique, a pattern emerged from the women’s discussions that described a process by which their experiences affected the breastfeeding relationship. This process centered on mothers’ interactions with medical professionals during jaundice management and their internalization of the experience.
Jaundice management
Half the women described how their experiences with neonatal jaundice had directly influenced their breastfeeding decisions, positively or negatively, primarily discussing this impact in terms of the breastfeeding instructions they received. Table 3 illustrates the clear pattern seen between a maternal report of breastfeeding orders received from medical professionals and a woman’s feeding status at 2 weeks postpartum, directly after the jaundice experience. Breastfeeding orders were categorized as: continue, conflicting, supplement, suspend, and none. Regardless of parity, women’s interactions with medical professionals related to breastfeeding orders and the level of encouragement they received had the strongest influence on whether women continued to breastfeed.
Mothers exclusively breastfeeding after their experience discussed the encouragement they received from medical staff. Mothers told to continue to breastfeed felt encouraged to breastfeed frequently to help the jaundice go away. All continued to breastfeed for at least 3 weeks, none quit because of their infant’s jaundice. Mothers who returned to exclusive breastfeeding after being told to temporarily suspend breastfeeding or to supplement with formula described being encouraged not to quit breastfeeding and were reassured that their milk was good.
“Right away I wanted to stop breastfeeding, especially if it is me causing him to get that. And they were like, ‘No, no. We’re not telling you to stop. It’s good that you are breastfeeding him.’”
Women exclusively formula feeding because of their experience with jaundice shared 2 separate reasons for not resuming. The first related to not wanting to “take anymore chances” with their infant receiving insufficient milk.
“At the time she was in the hospital they told me to stop breastfeeding her. They wanted to formula feed her. They just said that they think she wasn’t getting enough. They said since they can’t measure how much she drinks that they don’t know how much she is drinking. So I decided, well, I’ll just continue formula feeding her.”
The second related to physical difficulty in reestablishing lactation.
“I breastfed my other three children. … That’s why I tried more to see if he’d latch on, but he didn’t. … Since the beginning, I had the idea that I was only going to breastfeed him, but no.”
Women who continued to supplement with formula because of their experience expressed fear that jaundice would return if they quit supplementation.
“I am still on formula now [7 weeks after experience]. The doctor said he wanted to wait until it is 3 weeks after he is released to wean down. ... I think it caused some damage for me because I am still frightened to really let go of the formula. I may be wrong and maybe it can’t come back at this stage, but I think that something could go wrong and I am still giving formula to make sure that he is getting enough.”
Although mothers whose infants did not receive phototherapy were more likely to be told to continue breastfeeding or to be given no feeding orders than mothers whose infants received phototherapy, there was not a clear pattern between feeding method at 2 weeks postpartum and form of jaundice treatment. Although a few mothers expressed concern about breastfeeding during phototherapy because of having to remove their infant from the light, no mother quit breastfeeding or began supplementing specifically because of treatment. However, many mothers discussed the strong emotional impact that blood work, phototherapy, and the mother-child separation had on them.24
The majority of mothers had prior exposure to neonatal jaundice, approximately one third through personal experience with previous children. Although a few mothers had previous experience with jaundiced infants undergoing phototherapy, only one had been told to stop breastfeeding a previous infant because of jaundice. Even though this mother was not told to stop breastfeeding her current infant, she supplemented with formula because she felt her milk was “no good.”
Maternal internalization of experience
Mothers who received breastfeeding orders to suspend or supplement, or who were given conflicting orders, repeatedly expressed confusion or discontent with these instructions. They commented on the conflict between the medical professional’s advice and their own understanding that breastfeeding was healthier for babies, and on not receiving sufficient explanation to justify changing their feeding method.
“She [doctor] just told me to stop breastfeeding because…. Actually she didn’t tell me why. Which got me confused. I remember I was thinking why did she tell me to stop breastfeeding if breast milk is better for the baby?”
Mothers also shared concerns about nipple confusion affecting their ability to exclusively breastfeed, and feeling that decisions were out of their control.
Lack of understanding about causes of jaundice and feelings of guilt over their role in the etiology were common among all women. More than one third of women expressed guilt that they had caused jaundice either during pregnancy or while breastfeeding.
“I was afraid I did something wrong... that my milk wasn’t coming in right… that I wasn’t feeding her enough or I wasn’t feeding her the right things. Or that my milk was broken ... that I wasn’t making enough or it was wrong somehow. Like it wasn’t meeting her needs.”
Several mothers also expressed belief that their infant may not have gotten jaundice if they had not started breastfeeding.
“I wonder if she would’ve started with the formula, if we would’ve started to supplement with formula from the very beginning, I wonder if it would’ve happened.”
More than half the women discussed breastfeeding as a cause of jaundice. Those women had experienced early neonatal jaundice. More than one third had a previously jaundiced infant and approximately half had previously breastfed. Those who received breastfeeding orders to suspend or supplement, or who were given conflicting orders, were much more likely to discuss breastfeeding as a cause of jaundice than were those who received no breastfeeding orders. Mothers told to continue breastfeeding were least likely to discuss breastfeeding as a cause. No pattern was evident among women by language spoken, parity, bilirubin level, jaundice treatment, or feeding at the interview.
Women’s perceptions of what it is about breastfeeding that causes jaundice related to either quantity or quality.
The causes related to the quantity of breast milk included:
- Insufficient feeding. The infant is not receiving enough breast milk because he or she is not eating enough or the mother is not feeding infant enough.
- Insufficient milk. The mother is not producing enough breast milk.
The causes related to the quality of breast milk included:
- Milk composition. The breast milk caused jaundice, often because it was not good.
- Something in milk. There is something passed through the milk to cause jaundice, such as medicine, hormones, or emotions.
Women who gave explanations for jaundice closer to a biomedical understanding of jaundice, such as insufficient fluid intake, received this information primarily from medical professionals and occasionally from family and friends. Many issues related to feelings of guilt came from their own thoughts, though they were, at times, triggered by something said by a medical professional or family member. Mothers interpreted the information, or lack of information, they received in their attempt to explain why their infant had jaundice.
“The nurse said, the baby won’t be having your breast. All the time the baby will be in the hospital he will only be given formula. Since they never explained why he was that color or anything, I thought maybe my milk was no good. That’s why they told me not to give it to him.”
Discussion
Interactions with medical professionals emerged as the most important factor mediating the impact of the maternal experience with neonatal jaundice on breastfeeding. Encouragement or lack of encouragement from health care professionals played a large role in whether women continued to breastfeed after their experience, which agrees with other findings on the influence, both positive and negative, of interactions with medical professionals on breastfeeding.25-28 Maternal understanding of and reaction to information received during jaundice management and their subsequent internalization of their experience also played a key role in mothers’ infant feeding decisions. In contrast with previous studies,14,29 no consistent pattern was seen between breastfeeding continuation and whether infants received blood work only or phototherapy. This difference may be due to our study’s inclusion of multiple settings for phototherapy and differences in the study populations. In addition, earlier studies did not include information on medical professional’s breastfeeding orders.
Limitations
Although the use of qualitative methods allowed in-depth inquiry from the mother’s perspective, it necessitated a small sample limiting generalizability. Generalizability was further limited because the women in the sample were predominately Latina, though study findings were consistent across ethnicities. Data was only collected from the mothers’ point of view, which likely differed from medical professionals’ perceptions. Limiting the sample to mothers who initiated breastfeeding may have excluded mothers who decided not to breastfeed because of a previous jaundice experience. In addition, women whose infants did not develop jaundice because of adequate early breastfeeding support were not interviewed. Careful structuring of the interview guideline and use of experienced ethnographers minimized potential threats to validity through interviewer bias. Regular team meetings to discuss data collection and analysis increased reliability.
Additional research is needed to gain further understanding of mothers’ emotional responses when faced with neonatal conditions like jaundice. While maternal guilt has been acknowledged as a potential problem arising from treatment for neonatal jaundice,4,7,8 no research has focused on the impact of this guilt on breastfeeding. How do responses like guilt influence perceptions of themselves as breastfeeding mothers and their breastfeeding decisions? The possibility that neonatal jaundice and its management may deprive future children of the opportunity to breastfeed should be examined.
Conclusions
Neonatal jaundice affects many newborns and their families. Besides the monetary cost of treatment, our study results indicate that treatment for jaundice is not completely benign; there are health and emotional costs. Medical professionals must weigh the perceived benefits of treatment decisions and feeding orders against the potential costs to the emotional well being of mothers and newly established breastfeeding relationships. To minimize guilt and enhance maternal understanding about this common condition, professionals need to be aware not only of what information is given to mothers, but how mothers receive and interpret this information. Identifying neonatal jaundice with terms such as breastfeeding jaundice and breast milk jaundice may cause maternal concerns that jaundice is a result of their decision to breastfeed. Medical professionals must provide consistent information and ensure that mothers more fully understand the causes of jaundice and how it relates to breastfeeding, as well as breastfeeding instructions during the experience. The neonatal jaundice experience provides an opportunity for medical professionals to encourage breastfeeding mothers and provide specific guidance on how to maintain a successful breastfeeding relationship.
Acknowledgments
Our study was supported by a grant from the Campus Research Board at the University of Illinois. We would like to thank the women who participated in this study and made time to share their stories with us. We would also like to thank Isabel Martinez, MPH, for her assistance with scheduling and data collection, and Nadine Peacock, PhD, Arden Handler, DrPH, and Rebecca Lipton, PhD, for their comments during the development and analysis of this project.
OBJECTIVE: To examine the process by which mothers’ experiences with neonatal jaundice affects breastfeeding.
STUDY DESIGN: We used ethnographic interviews with grounded theory methodology. Audiotaped data were transcribed and analyzed for themes using ATLAS/ti qualitative data analysis software (Scientific Software Development, Berlin, Germany).
POPULATION: We studied a total of 47 Spanish- and English-speaking breastfeeding mothers of otherwise healthy infants diagnosed with neonatal jaundice.
OUTCOME MEASURED: Our outcomes were the qualitative descriptions of maternal experiences with neonatal jaundice.
RESULTS: Interactions with medical professionals emerged as the most important factor mediating the impact of neonatal jaundice on breastfeeding. Breastfeeding orders and the level of encouragement from medical professionals toward breastfeeding had the strongest effect on feeding decisions. Maternal reaction to and understanding of information from their physicians also played an important role. Guilt was common, as many mothers felt they had caused the jaundice by breastfeeding.
CONCLUSIONS: By providing accurate information and encouragement to breastfeed, medical professionals have great impact on whether a mother continues breastfeeding after her experience with neonatal jaundice. Health care providers must be aware of how mothers receive and interpret information related to jaundice to minimize maternal reactions, such as guilt, that have a negative impact on breastfeeding.
- Interactions with medical professionals emerged as the most important factor mediating the impact of the maternal experience with neonatal jaundice on breastfeeding.
- Encouragement or lack of encouragement to breastfeed plays a large role in whether women continue to breastfeed after their experience with jaundice.
- To minimize feelings of guilt and enhance maternal understanding about jaundice, health care professionals need to be aware not only of what information is given to mothers, but how mothers receive and interpret this information.
- Medical professionals must provide consistent information and ensure that mothers understand how jaundice relates to breastfeeding and the purpose of any breastfeeding instructions given during the experience.
Neonatal jaundice is the most common condition for which newborns are tested, treated, and often rehospitalized, resulting in millions of dollars of annual expenditure.1-3 Two types of jaundice are associated with breastfeeding4: early jaundice, or breastfeeding jaundice, caused by the infant receiving insufficient breast milk5,6; and breast milk jaundice, which develops later in a thriving breastfed infant and is thought to be caused by a substance in the breast milk.7,8
Diagnosis and treatment of jaundice can begin within the first few days after birth, while the breastfeeding relationship is being established. Despite the ongoing debate on the appropriate protocol for jaundice management9-11 and a wide variance in physician practice,12,13 little research has examined the effect of the jaundice experience on the newborn’s mother. The few studies to directly examine the influence of jaundice management on breastfeeding show that protocols such as maternal-infant separation for phototherapy or temporarily suspending breastfeeding are associated with a shorter duration of breastfeeding.14-16
What remains unclear is how jaundice management affects breastfeeding. Our study adds to existing knowledge by exploring the process by which the maternal experience with a jaundiced newborn affects the mother and her breastfeeding decisions. Qualitative methods, guided by grounded theory, were used because of the paucity of information on this topic and the study’s focus on process.17-19
Methods
Settings
Two distinct sites in Chicago were chosen to increase the heterogeneity of experiences: a community hospital serving a mixed-income and ethnically diverse population, and an urban teaching hospital serving primarily low-income Latino and African American patients. Breastfeeding initiation rates, tracked by the University of Illinois at Chicago breastfeeding task force, were 70% and 40%, respectively. Institutional Review Board approval was obtained from both sites.
Sample
Two purposeful sampling strategies were employed.20 Criterion sampling was used to recruit mothers, identified through medical record abstraction of all jaundiced infants, who met the following criteria: Spanish or English speaking; exclusively or partially breastfeeding at postpartum discharge; and mother of an otherwise healthy term newborn who had a serum bilirubin level of =10 mg/dL within the first month of life and received care through a study site in 1 or more of the following settings: newborn nursery, outpatient clinic, hospital ward, or home. Maximum variation sampling, which seeks heterogeneity within the sample to permit examination of common themes, was applied to achieve variation in ethnicity, language, age, parity, and jaundice treatment. Eligible mothers were invited by phone to participate in an interview. Sampling continued until data from new interviews confirmed earlier data, signifying that theoretical saturation was achieved.18
Data collection
Using the literature on hyperbilirubinemia and breastfeeding, an interview guideline was developed addressing the topics in Table 1.21 Three female ethnographers (including authors S.K.W. and P.R.H.) conducted in-depth, semi-structured interviews in women’s homes. The interviews were approximately 60 minutes in length given in either Spanish or English. Women were encouraged to lead the conversation, with ethnographers using prompts to guide the discussion toward any topics not addressed and probes to elicit detailed descriptions of the women’s experiences. Audiotaped interviews were transcribed verbatim, and edited by the ethnographer to ensure accuracy and include field notes. Spanish-language interviews were translated into English. Participants received no financial incentives.
Analysis
Interviews were carefully read by all investigators for themes, and codes were developed to represent these themes.18,22,23 A code book defining each code and listing inclusion and exclusion criteria was developed, and one investigator (S.K.W.) applied codes to the interviews using ATLAS/ti qualitative data analysis software (Scientific Software Development, Berlin, Germany). Intracoder and intercoder (with P.R.H.) agreement were determined to assure consistency of code definitions. Codes with a low level of agreement were redefined and reapplied. Coded text was retrieved and emerging themes analyzed in relation to other themes and variables. Focus was placed on comparing and contrasting women’s experiences to elicit what in the maternal experience with neonatal jaundice influenced infant feeding decisions. We also focused on women’s understanding of the information they received and the relationship between jaundice and breastfeeding.
Results
Of 69 eligible mothers, 11 declined to participate, and 13 could not be reached or scheduled for an interview. Forty-five mothers were interviewed between October 1997 and April 1998 at 2.5 to 14.5 weeks postpartum (mean = 6 weeks). Investigators attempted to hold 2 focus groups with unsuccessful show rates. Individual interviews were conducted with the 2 women who attended these sessions and analyzed with the other interviews. The 24 nonparticipants had similar demographic characteristics to women in the study.
Participants represented a range of sociodemographic and jaundice management characteristics Table 2. Mothers were predominately Latinas of Mexican descent, with a mean age of 27 years (range = 16-38 years). Women born outside the United States had lived in the US from 1 to 25 years (mean = 7 years). More than three quarters of the women lived with the father of the baby. Peak bilirubin levels of all infants ranged from 10.3 to 23.5 mg/dL; 4 infants had peak levels of >20 mg/dL and 7 had peak levels of <12 mg/dL. Thirty-nine infants experienced jaundice within the first 6 days of life, with the majority having nonhemolytic jaundice. Eight infants had breast milk jaundice with peak bilirubin levels occurring between 1 and 2 weeks of age. More than half of the multiparous women had experienced jaundice with a previous infant (n = 14) and three fourths had breastfed a previous child (n = 19).
Though each woman’s experience was unique, a pattern emerged from the women’s discussions that described a process by which their experiences affected the breastfeeding relationship. This process centered on mothers’ interactions with medical professionals during jaundice management and their internalization of the experience.
Jaundice management
Half the women described how their experiences with neonatal jaundice had directly influenced their breastfeeding decisions, positively or negatively, primarily discussing this impact in terms of the breastfeeding instructions they received. Table 3 illustrates the clear pattern seen between a maternal report of breastfeeding orders received from medical professionals and a woman’s feeding status at 2 weeks postpartum, directly after the jaundice experience. Breastfeeding orders were categorized as: continue, conflicting, supplement, suspend, and none. Regardless of parity, women’s interactions with medical professionals related to breastfeeding orders and the level of encouragement they received had the strongest influence on whether women continued to breastfeed.
Mothers exclusively breastfeeding after their experience discussed the encouragement they received from medical staff. Mothers told to continue to breastfeed felt encouraged to breastfeed frequently to help the jaundice go away. All continued to breastfeed for at least 3 weeks, none quit because of their infant’s jaundice. Mothers who returned to exclusive breastfeeding after being told to temporarily suspend breastfeeding or to supplement with formula described being encouraged not to quit breastfeeding and were reassured that their milk was good.
“Right away I wanted to stop breastfeeding, especially if it is me causing him to get that. And they were like, ‘No, no. We’re not telling you to stop. It’s good that you are breastfeeding him.’”
Women exclusively formula feeding because of their experience with jaundice shared 2 separate reasons for not resuming. The first related to not wanting to “take anymore chances” with their infant receiving insufficient milk.
“At the time she was in the hospital they told me to stop breastfeeding her. They wanted to formula feed her. They just said that they think she wasn’t getting enough. They said since they can’t measure how much she drinks that they don’t know how much she is drinking. So I decided, well, I’ll just continue formula feeding her.”
The second related to physical difficulty in reestablishing lactation.
“I breastfed my other three children. … That’s why I tried more to see if he’d latch on, but he didn’t. … Since the beginning, I had the idea that I was only going to breastfeed him, but no.”
Women who continued to supplement with formula because of their experience expressed fear that jaundice would return if they quit supplementation.
“I am still on formula now [7 weeks after experience]. The doctor said he wanted to wait until it is 3 weeks after he is released to wean down. ... I think it caused some damage for me because I am still frightened to really let go of the formula. I may be wrong and maybe it can’t come back at this stage, but I think that something could go wrong and I am still giving formula to make sure that he is getting enough.”
Although mothers whose infants did not receive phototherapy were more likely to be told to continue breastfeeding or to be given no feeding orders than mothers whose infants received phototherapy, there was not a clear pattern between feeding method at 2 weeks postpartum and form of jaundice treatment. Although a few mothers expressed concern about breastfeeding during phototherapy because of having to remove their infant from the light, no mother quit breastfeeding or began supplementing specifically because of treatment. However, many mothers discussed the strong emotional impact that blood work, phototherapy, and the mother-child separation had on them.24
The majority of mothers had prior exposure to neonatal jaundice, approximately one third through personal experience with previous children. Although a few mothers had previous experience with jaundiced infants undergoing phototherapy, only one had been told to stop breastfeeding a previous infant because of jaundice. Even though this mother was not told to stop breastfeeding her current infant, she supplemented with formula because she felt her milk was “no good.”
Maternal internalization of experience
Mothers who received breastfeeding orders to suspend or supplement, or who were given conflicting orders, repeatedly expressed confusion or discontent with these instructions. They commented on the conflict between the medical professional’s advice and their own understanding that breastfeeding was healthier for babies, and on not receiving sufficient explanation to justify changing their feeding method.
“She [doctor] just told me to stop breastfeeding because…. Actually she didn’t tell me why. Which got me confused. I remember I was thinking why did she tell me to stop breastfeeding if breast milk is better for the baby?”
Mothers also shared concerns about nipple confusion affecting their ability to exclusively breastfeed, and feeling that decisions were out of their control.
Lack of understanding about causes of jaundice and feelings of guilt over their role in the etiology were common among all women. More than one third of women expressed guilt that they had caused jaundice either during pregnancy or while breastfeeding.
“I was afraid I did something wrong... that my milk wasn’t coming in right… that I wasn’t feeding her enough or I wasn’t feeding her the right things. Or that my milk was broken ... that I wasn’t making enough or it was wrong somehow. Like it wasn’t meeting her needs.”
Several mothers also expressed belief that their infant may not have gotten jaundice if they had not started breastfeeding.
“I wonder if she would’ve started with the formula, if we would’ve started to supplement with formula from the very beginning, I wonder if it would’ve happened.”
More than half the women discussed breastfeeding as a cause of jaundice. Those women had experienced early neonatal jaundice. More than one third had a previously jaundiced infant and approximately half had previously breastfed. Those who received breastfeeding orders to suspend or supplement, or who were given conflicting orders, were much more likely to discuss breastfeeding as a cause of jaundice than were those who received no breastfeeding orders. Mothers told to continue breastfeeding were least likely to discuss breastfeeding as a cause. No pattern was evident among women by language spoken, parity, bilirubin level, jaundice treatment, or feeding at the interview.
Women’s perceptions of what it is about breastfeeding that causes jaundice related to either quantity or quality.
The causes related to the quantity of breast milk included:
- Insufficient feeding. The infant is not receiving enough breast milk because he or she is not eating enough or the mother is not feeding infant enough.
- Insufficient milk. The mother is not producing enough breast milk.
The causes related to the quality of breast milk included:
- Milk composition. The breast milk caused jaundice, often because it was not good.
- Something in milk. There is something passed through the milk to cause jaundice, such as medicine, hormones, or emotions.
Women who gave explanations for jaundice closer to a biomedical understanding of jaundice, such as insufficient fluid intake, received this information primarily from medical professionals and occasionally from family and friends. Many issues related to feelings of guilt came from their own thoughts, though they were, at times, triggered by something said by a medical professional or family member. Mothers interpreted the information, or lack of information, they received in their attempt to explain why their infant had jaundice.
“The nurse said, the baby won’t be having your breast. All the time the baby will be in the hospital he will only be given formula. Since they never explained why he was that color or anything, I thought maybe my milk was no good. That’s why they told me not to give it to him.”
Discussion
Interactions with medical professionals emerged as the most important factor mediating the impact of the maternal experience with neonatal jaundice on breastfeeding. Encouragement or lack of encouragement from health care professionals played a large role in whether women continued to breastfeed after their experience, which agrees with other findings on the influence, both positive and negative, of interactions with medical professionals on breastfeeding.25-28 Maternal understanding of and reaction to information received during jaundice management and their subsequent internalization of their experience also played a key role in mothers’ infant feeding decisions. In contrast with previous studies,14,29 no consistent pattern was seen between breastfeeding continuation and whether infants received blood work only or phototherapy. This difference may be due to our study’s inclusion of multiple settings for phototherapy and differences in the study populations. In addition, earlier studies did not include information on medical professional’s breastfeeding orders.
Limitations
Although the use of qualitative methods allowed in-depth inquiry from the mother’s perspective, it necessitated a small sample limiting generalizability. Generalizability was further limited because the women in the sample were predominately Latina, though study findings were consistent across ethnicities. Data was only collected from the mothers’ point of view, which likely differed from medical professionals’ perceptions. Limiting the sample to mothers who initiated breastfeeding may have excluded mothers who decided not to breastfeed because of a previous jaundice experience. In addition, women whose infants did not develop jaundice because of adequate early breastfeeding support were not interviewed. Careful structuring of the interview guideline and use of experienced ethnographers minimized potential threats to validity through interviewer bias. Regular team meetings to discuss data collection and analysis increased reliability.
Additional research is needed to gain further understanding of mothers’ emotional responses when faced with neonatal conditions like jaundice. While maternal guilt has been acknowledged as a potential problem arising from treatment for neonatal jaundice,4,7,8 no research has focused on the impact of this guilt on breastfeeding. How do responses like guilt influence perceptions of themselves as breastfeeding mothers and their breastfeeding decisions? The possibility that neonatal jaundice and its management may deprive future children of the opportunity to breastfeed should be examined.
Conclusions
Neonatal jaundice affects many newborns and their families. Besides the monetary cost of treatment, our study results indicate that treatment for jaundice is not completely benign; there are health and emotional costs. Medical professionals must weigh the perceived benefits of treatment decisions and feeding orders against the potential costs to the emotional well being of mothers and newly established breastfeeding relationships. To minimize guilt and enhance maternal understanding about this common condition, professionals need to be aware not only of what information is given to mothers, but how mothers receive and interpret this information. Identifying neonatal jaundice with terms such as breastfeeding jaundice and breast milk jaundice may cause maternal concerns that jaundice is a result of their decision to breastfeed. Medical professionals must provide consistent information and ensure that mothers more fully understand the causes of jaundice and how it relates to breastfeeding, as well as breastfeeding instructions during the experience. The neonatal jaundice experience provides an opportunity for medical professionals to encourage breastfeeding mothers and provide specific guidance on how to maintain a successful breastfeeding relationship.
Acknowledgments
Our study was supported by a grant from the Campus Research Board at the University of Illinois. We would like to thank the women who participated in this study and made time to share their stories with us. We would also like to thank Isabel Martinez, MPH, for her assistance with scheduling and data collection, and Nadine Peacock, PhD, Arden Handler, DrPH, and Rebecca Lipton, PhD, for their comments during the development and analysis of this project.
1. Maisels MJ, Newman TB. Jaundice in the healthy newborn: its effect on infants, families and physicians. In: Morris, Jr FH, Simmons MA, eds. The normal newborn: report of the One Hundredth Ross Conference on Pediatric Research. Columbus, Ohio: Ross Laboratories; 1991;89-98.
2. Newman TB, Easterling MJ, Goldman ES, Stevenson DK. Laboratory evaluation of jaundice in newborns: frequency, cost and yield. Am J Dis Child 1990;144:364-8.
3. Lee KS, Perlman M, Ballantyne M, Elliott I, To T. Association between duration of neonatal hospital stay and readmission rate. J Pediatr 1995;127:758-66.
4. Maisels MJ, Gifford K. Normal serum bilirubin levels in the newborn and the effect of breast-feeding. Pediatrics 1986;78:837-43.
5. Kuhr M, Paneth N. Feeding practices and early neonatal jaundice. J Pediatr Gastroenterol Nutr 1982;1:485-9.
6. Tudehope D, Bayley G, Townsend S. Breast feeding practices and severe hyperbilirubinaemia. J Paediatr Child Health 1991;27:240-4.
7. de Steuben C. Breast-feeding and jaundice: a review. J Nurse Midwifery 1992;37:59S-66S.
8. Brooten D, Brown L, Hollingsworth A, Tanis J, Bakewell-Sachs S. Breast-milk jaundice. J Obstet Gynecol Neonat Nurs 1985;14:220-3.
9. AAP Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. Practice parameter: management of hyperbilirubinemia. Pediatrics 1994;94:558-65.
10. Newman TB, Maisels MJ. Evaluation and treatment of jaundice in the term newborn: a kinder, gentler approach. Pediatrics 1992;89:809-18.
11. Oski FA. Hyperbilirubinemia in the term infant: An unjaundiced approach. Contemp Pediatr 1992;9:148-54.
12. Freed GL, Clark SJ, Sorenson J, Lohr JA, Cefalo R, Curtis P. National assessment of physicians’ breast-feeding knowledge, attitudes, training, and experience. JAMA 1995;273:472-6.
13. Gartner LM, Herrarias CT, Sebring RH. Practices patterns in neonatal hyperbilirubinemia. Pediatrics 1998;101:25-31.
14. Elander G, Lindberg T. Hospital routines in infants with hyperbilirubinemia influence the duration of breast feeding. Acta Paediatr Scand 1986;75:708-12.
15. Kemper K, Forsyth B, McCarthy P. Jaundice, terminating breastfeeding, and the vulnerable child. Pediatrics 1989;84:773-8.
16. Kemper KJ, Forsyth BW, McCarthy PL. Persistent perceptions of vulnerability following neonatal jaundice. Am J Dis Child 1990;144:239-41.
17. Glasser B, Strauss A. The discovery of grounded theory. Chicago, Ill: Aldine; 1967.
18. Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, Calif: Sage Publications; 1990.
19. Morse JM. Designing funded qualitative research. In: Denzin NK, Lincoln, YS, eds. Handbook of qualitative research. Thousand Oaks, Calif: Sage Publications; 1994;220-35.
20. Patton MQ. Qualitative evaluation and research methods. Newbury Park, Calif: Sage Publications; 1990.
21. Scrimshaw SCM, Hurtado E. Rapid assessment procedures for nutrition and primary health care: anthropological approaches to improving programme effectiveness. Tokyo: The United Nations University; 1987.
22. Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Thousand Oaks, Calif: Sage Publications; 1994.
23. Tesch R. Qualitative research: analysis types and software tools. New York: Falmar Press; 1990.
24. Hannon PR, Willis SK, Scrimshaw SC. Persistence of maternal concerns surrounding neonatal jaundice: an exploratory study. Arch Pediatr Adolesc Med 2001;155:1357-63.
25. Dermer A. Overcoming medical and social barriers to breast feeding. Am Fam Phys 1995;51:755-63.
26. Hewat RJ, Ellis DJ. Breastfeeding as a maternal-child team effort: women’s perceptions. Health Care Women Int 1984;5:437-52.
27. Raj VK, Plichta SB. The role of social support in breastfeeding promotion: a literature review. J Hum Lact 1998;14:41-5.
28. Schy DS, Maglaya CF, Mendelson SG, Race KEH, Ludwig-Beymer P. The effects of in-hospital lactation education on breastfeeding practice. J Hum Lact 1996;12:117-22.
29. James JM, Williams SD, Osborn LM. Discontinuation of breast-feeding infrequent among jaundiced neonates treated at home. Pediatrics 1993;92:153-5.
All correspondence should be addressed to Sharla K. Willis, DrPH, The Ohio State University, School of Public Health, B-209 Starling-Loving Hall, 320 West 10th Avenue, Columbus, OH 43210-1240. E-mail: [email protected].
To submit a letter to the editor on this topic, click here: [email protected]
1. Maisels MJ, Newman TB. Jaundice in the healthy newborn: its effect on infants, families and physicians. In: Morris, Jr FH, Simmons MA, eds. The normal newborn: report of the One Hundredth Ross Conference on Pediatric Research. Columbus, Ohio: Ross Laboratories; 1991;89-98.
2. Newman TB, Easterling MJ, Goldman ES, Stevenson DK. Laboratory evaluation of jaundice in newborns: frequency, cost and yield. Am J Dis Child 1990;144:364-8.
3. Lee KS, Perlman M, Ballantyne M, Elliott I, To T. Association between duration of neonatal hospital stay and readmission rate. J Pediatr 1995;127:758-66.
4. Maisels MJ, Gifford K. Normal serum bilirubin levels in the newborn and the effect of breast-feeding. Pediatrics 1986;78:837-43.
5. Kuhr M, Paneth N. Feeding practices and early neonatal jaundice. J Pediatr Gastroenterol Nutr 1982;1:485-9.
6. Tudehope D, Bayley G, Townsend S. Breast feeding practices and severe hyperbilirubinaemia. J Paediatr Child Health 1991;27:240-4.
7. de Steuben C. Breast-feeding and jaundice: a review. J Nurse Midwifery 1992;37:59S-66S.
8. Brooten D, Brown L, Hollingsworth A, Tanis J, Bakewell-Sachs S. Breast-milk jaundice. J Obstet Gynecol Neonat Nurs 1985;14:220-3.
9. AAP Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. Practice parameter: management of hyperbilirubinemia. Pediatrics 1994;94:558-65.
10. Newman TB, Maisels MJ. Evaluation and treatment of jaundice in the term newborn: a kinder, gentler approach. Pediatrics 1992;89:809-18.
11. Oski FA. Hyperbilirubinemia in the term infant: An unjaundiced approach. Contemp Pediatr 1992;9:148-54.
12. Freed GL, Clark SJ, Sorenson J, Lohr JA, Cefalo R, Curtis P. National assessment of physicians’ breast-feeding knowledge, attitudes, training, and experience. JAMA 1995;273:472-6.
13. Gartner LM, Herrarias CT, Sebring RH. Practices patterns in neonatal hyperbilirubinemia. Pediatrics 1998;101:25-31.
14. Elander G, Lindberg T. Hospital routines in infants with hyperbilirubinemia influence the duration of breast feeding. Acta Paediatr Scand 1986;75:708-12.
15. Kemper K, Forsyth B, McCarthy P. Jaundice, terminating breastfeeding, and the vulnerable child. Pediatrics 1989;84:773-8.
16. Kemper KJ, Forsyth BW, McCarthy PL. Persistent perceptions of vulnerability following neonatal jaundice. Am J Dis Child 1990;144:239-41.
17. Glasser B, Strauss A. The discovery of grounded theory. Chicago, Ill: Aldine; 1967.
18. Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, Calif: Sage Publications; 1990.
19. Morse JM. Designing funded qualitative research. In: Denzin NK, Lincoln, YS, eds. Handbook of qualitative research. Thousand Oaks, Calif: Sage Publications; 1994;220-35.
20. Patton MQ. Qualitative evaluation and research methods. Newbury Park, Calif: Sage Publications; 1990.
21. Scrimshaw SCM, Hurtado E. Rapid assessment procedures for nutrition and primary health care: anthropological approaches to improving programme effectiveness. Tokyo: The United Nations University; 1987.
22. Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Thousand Oaks, Calif: Sage Publications; 1994.
23. Tesch R. Qualitative research: analysis types and software tools. New York: Falmar Press; 1990.
24. Hannon PR, Willis SK, Scrimshaw SC. Persistence of maternal concerns surrounding neonatal jaundice: an exploratory study. Arch Pediatr Adolesc Med 2001;155:1357-63.
25. Dermer A. Overcoming medical and social barriers to breast feeding. Am Fam Phys 1995;51:755-63.
26. Hewat RJ, Ellis DJ. Breastfeeding as a maternal-child team effort: women’s perceptions. Health Care Women Int 1984;5:437-52.
27. Raj VK, Plichta SB. The role of social support in breastfeeding promotion: a literature review. J Hum Lact 1998;14:41-5.
28. Schy DS, Maglaya CF, Mendelson SG, Race KEH, Ludwig-Beymer P. The effects of in-hospital lactation education on breastfeeding practice. J Hum Lact 1996;12:117-22.
29. James JM, Williams SD, Osborn LM. Discontinuation of breast-feeding infrequent among jaundiced neonates treated at home. Pediatrics 1993;92:153-5.
All correspondence should be addressed to Sharla K. Willis, DrPH, The Ohio State University, School of Public Health, B-209 Starling-Loving Hall, 320 West 10th Avenue, Columbus, OH 43210-1240. E-mail: [email protected].
To submit a letter to the editor on this topic, click here: [email protected]
Do Whole-Grain Oat Cereals Reduce the Need for Antihypertensive Medications and Improve Blood Pressure Control?
OBJECTIVES: Our study compared 2 whole grain oat-based cereals with 2 refined grain wheat-based cereals to determine their effects on the need for antihypertensive medications in people with high blood pressure (BP).
STUDY DESIGN: This 12-week, randomized controlled parallel-group trial with 6 weeks of voluntary follow-up was designed to investigate the antihypertensive effects of oats. After 4 weeks of baseline feeding, medication dose was maintained or reduced by half or completely throughout the middle 4 weeks of the study. In the final 4 weeks, participants continued cereal consumption; medication was adjusted according to the protocol.
POPULATION: Men and women (n = 88) being treated for hypertension with a mean baseline BP below 160/100.
OUTCOMES MEASURED: Primary study outcomes included change in SBP and DBP as well as antihypertensive medication reduction. Secondary measures included blood lipid, fasting glucose, and insulin levels and side effects related to elevated BP and increased dietary fiber intake.
RESULTS: Seventy-three percent of participants in the oats group versus 42% in the control group were able to stop or reduce their medication by half. Treatment group participants whose medication was not reduced had substantial decreases in BP. The oats group experienced a 24.2–mg/dL reduction in total cholesterol levels, a 16.2–mg/dL decrease in low-density lipoprotein cholesterol levels, and a 15.03–mg/dL drop in plasma glucose levels vs controls.
CONCLUSIONS: Results suggest that a diet containing soluble fiber–rich whole oats can significantly reduce the need for antihypertensive medication and improve BP control. Considering the lipid and glucose improvements as well, increased consumption of whole oats may significantly reduce cardiovascular disease risk.
- Whole oats, when supplemented daily, significantly reduced antihypertensive medication need and improved blood pressure control over the 12-week intervention.
- Whole oats improved blood lipid and fasting glucose levels and reduced the incidence of overall study-related side effects.
- Significantly increasing whole oat consumption may greatly reduce risk for cardiovascular disease in hypertensive patients.
Since the initial use of antihypertensive medications in the 1940s, they have been the traditional approach to treatment essential hypertension. Many of these pharmacologic agents, however, are costly and are associated with substantial adverse effects. As a result, interest has been increasing in alternative methods to prevent and treat hypertension. Clinical trials using dietary interventions for the alleviation of hypertension and observational studies have suggested that a number of foods and specific food components may exert an antihypertensive effect.1-5 Other research, however, has shown no effect.6-10 Studies specific to oats or cereal fibers have also provided mixed results. Observational studies have noted a reduction in blood pressure (BP),11 but the few clinical trials conducted to date have shown no effect.12
Selected whole grains are known to be good sources of soluble fibers. Previous research trials have demonstrated that these fibers can effectively reduce plasma insulin concentrations and provide other health benefits.13,14 Additionally, elevated insulin levels have been implicated in the etiology of hypertension.15 Based on this potential biologic mechanism and the previously inconsistent findings, we conducted a 12-week trial to evaluate the clinical effects of soluble fiber–rich whole oat cereals when added to the diet of hyperinsulinemic patients medicated for essential hypertension.
Methods
Study sample
Participants were recruited from a database of treated hypertensive patients provided by a local health maintenance organization (HealthPartners). Initial letters describing the study were mailed to 8000 potential participants. Of these, 524 people responded to the mailing and agreed to a telephone screen to determine eligibility. Among respondents, 212 passed the initial phone screening and were invited to our research clinic (Hypertension and Cholesterol Research Clinic at the University of Minnesota Medical School) for a BP screening and general physical. For inclusion in the study, average screening BP readings (2 sets of readings within 7 days) taken by our team physician could not exceed 160/100. Table 1 lists exclusion criteria. The study protocol was reviewed and approved by the University of Minnesota Human Subjects Committee of the Institutional Review Board.
Eighty-eight volunteers (45 men and 43 women) aged 33 to 67 years met all inclusion criteria and provided written informed consent. All participants had a history of essential mild or moderate hypertension (BP 120/80 to 160/100 mm Hg), and were treated with no more than 1 antihypertensive medication (excluding -adrenergic receptor blocking agents) and/or 1 diuretic medication for at least 1 month before enrollment. Eighty participants were treated with a single antihypertensive medication; 8 required an antihypertensive drug and a diuretic medication to manage their BP. Individuals taking beta blockers were excluded from the study because they often take medications prescribed for more serious cardiovascular conditions, such as cardiac arrhythmias, and medication reduction would be inappropriate under such circumstances. Participants’ primary physicians were also consulted concerning participation and study-related medication changes.
TABLE 1
EXCLUSION CRITERIA
|
Study design
This randomized controlled parallel-group trial consisted of 3 four-week phases: a Baseline Feeding phase, a Medication Reduction phase, and a Maintenance phase. Eligible individuals were stratified by baseline systolic blood pressure (SBP) (< 140 mm Hg versus 140 mm Hg) and baseline soluble fiber intake (less than 3 grams/day versus 3 to 6 grams/day). At the start of the baseline phase, participants were randomized to either an oats cereal treatment group (n = 45) or a low-fiber cereal control group (n = 43).
The cereal treatments were isocaloric and administered during all 3 phases of the study. Individuals in the oats group received a daily serving of 60 grams (approximately three fourths cup) Quaker Oatmeal (5.61 grams total dietary fiber, 3.25 grams soluble fiber, and 2.83 grams -glucans) and 77 grams (approximately one and one third cups) Quaker Oat Squares (6.07 grams total dietary fiber, 2.98 grams soluble fiber, and 2.59 grams -glucans). Individuals in the control group consumed 65 grams (0.5 cup) Malt-O-Meal Hot Wheat Cereal (2.32 grams total dietary fiber, 0.6 grams soluble fiber) and 81 grams (2 cups) Kellogg’s Crispix (1.2 grams total dietary fiber, < 0.5 grams soluble fiber).
Cereals were dispensed in unlabeled bulk containers to facilitate physician blinding. Remaining cereal was returned and weighed at each of the weekly or biweekly visits at our research clinic. Additionally, participants kept a daily cereal calendar that was reviewed by members of our research staff and used to help determine cereal compliance.
Changes in antihypertensive medication dose were implemented according to the protocol described in the Figure. Participants were asked to maintain their usual lifestyle, physical activity, dietary pattern, and body weight during the 12 weeks of the study. Individuals were invited to participate in a 6-week follow-up phase after the intervention was completed to monitor the residual BP effect after cereal consumption was discontinued.
FIGURE
MEDICATION REDUCTION PROTOCOL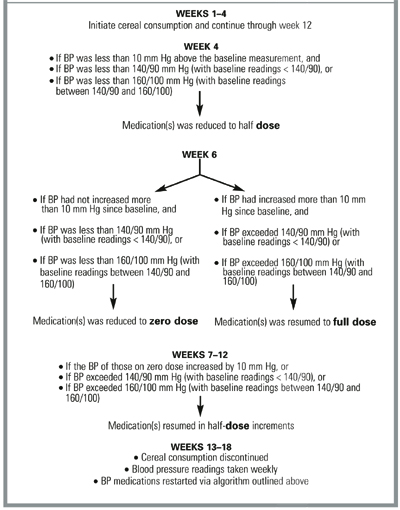
Outcomes measured
The study physician responsible for BP measurement, blood draws, and general patient examinations (described below) was unaware of the cereal group assignment. BP was measured at the clinic twice a week during the first (baseline feeding) and last (maintenance) phases of the study and weekly during the second (medication reduction) phase. Participants reported at approximately the same time of the day for all appointments. BP readings were obtained 24 hours after the last medication dose or, if the patient was unmedicated, at the same time of day as previous study BP readings and after participants had rested quietly in the seated position for at least 5 minutes in an examination room.
The study physician took all readings on the right arm, using a mercury column sphygmomanometer (Korotkoff phase V for diastolic blood pressure [DBP]). Standard cuff size was used unless upper arm circumference exceeded 31 cm, in which case a large cuff with 15 x 35–cm bladders was chosen. Measurements were repeated 4 times in 2-minute intervals. The mean of the last 3 readings was calculated and used in subsequent analyses. Baseline and final study measurements used in the analyses and reported in this paper represent the averages of the first 2 and last 2 study visits.
Preintervention and postintervention blood samples were collected into standard 6-mL serum separator tubes. Samples were analyzed within 24 hours for general chemistry and plasma lipids (total cholesterol, low-density cholesterol [LDL-C], and high-density cholesterol [HDL-C] as well as triglyceride levels) by an accredited independent laboratory and according to standard chemical methods.16
A written 42-question side effect questionnaire was administered to participants at the beginning of the baseline phase and at the end of the intervention. Participants reported the frequency with which they experienced side effects associated with increased fiber intake (eg, loose stools, flatulence) and hypertension (eg, headaches, dizziness) using a 5-item scale ranging from “never” to “very frequently” (event occurring once or several times daily). Each item of the scale was assigned a value ranging from 1 to 5. Values were tallied across all 42 questions. A final score was assigned to each participant for both time points. Mean scores by group were used in the analyses.
Participants completed a 3-day food record at baseline and at the end of the 12 weeks of intervention. Food records were examined for thoroughness by a licensed nutritionist and used to determine dietary changes. Nutrient intakes were calculated using the Nutrient Data System software (version 2.92) managed by the Nutrition Coordinating Center at the University of Minnesota School of Public Health.17
Statistics
The sample size calculation was based on a level of significance set at 0.05 and power at 80% to detect a 15% difference in medication reduction. Differences in medication reduction were determined by using the chi-square test of proportions. For continuous variables, Student’s paired and unpaired t tests were performed to determine differences within and between groups. In terms of medication reduction, logistic regression was used to adjust for potential confounders such as body weight and sodium intake. Multiple regression was employed to adjust blood lipid and glucose levels and BP findings for confounding. Because adjustment did not change the interpretation of the data, unadjusted findings are reported. The analyses of the data from this intent-to-treat population, which were determined to include all randomized patients, were conducted using the Statistical Analysis System (SAS Institute, Cary, N.C.). Results are reported as means ± SD unless noted otherwise. All P values are double sided.
Results
All the original 88 participants enrolled, all completed the 12-week trial, and all participated in the 6-week follow-up phase. Instructions to consume all dispensed cereals every day were followed well. Compliance was high for both groups (94.5% for the oat group and 92.7% for the control group) based on the amount of consumed cereal by weight. Randomization was largely effective; there were no apparent differences in baseline characteristics between each of the treatment groups (Table 2). Participants were primarily white (97%), with a mean age of 48 years (range 33 to 67 years).
BP and BP medication changes are summarized in Table 3. Among subjects in the oats group, 73% experienced a BP medication reduction during the intervention and had maintained that by the end of the study, as compared with only 42% in the control group (P < .05). Moreover, those in the oats group who did not experience a medication reduction had a 7-mm Hg decrease in SBP and a 4-mm Hg reduction in DBP. There was a small, nonsignificant change in SBP and DBP among those who did not experience a medication reduction in the control group. Medication reduction did not differ across classes of antihypertensive medication or our stratification variables of baseline soluble fiber intake or BP. Additionally, during the 6-week follow-up phase, 6 of the 18 (33%) individuals in the control group versus 22 of the 33 (67%) in the treatment group resumed taking medication.
Average BP in the oats group was lowered from 140/88 mm Hg at baseline to 134/85 mm Hg by the end of the first 4 weeks. Only the change in systolic BP was statistically significant (P < .05). Over the same 4-week period, the control group experienced a mean change of BP from 138/86 mm Hg to 136/85 mm Hg, which was not significant.
Baseline and postintervention lipid and glucose levels appear in Table 4. There were no significant modifications in any of the lipid parameters for the individuals in the control group, although there was a downward trend in all lipid measures. In the oats treatment group, mean total cholesterol (TC) concentration decreased by 31.7 mg/dL (15% drop). A similar decrease of 22.3 mg/dL (16% drop) was seen in the oats group’s average LDL-C levels. Blood glucose levels in the oats group also improved significantly (P < .01). The mean differences between post study and prestudy values (± SE) between the 2 groups, calculated for the average changes in TC, LDL-C, and glucose experienced by each of the groups, were -24.2 mg/dL (± 6.1), -16.2 mg/dL (± 4.4), and -15.03 mg/dL (± 4.3), respectively.
The frequency of dietary fiber-related and hypertension-related side effects decreased by 22% in the treatment group (Table 4). This finding was not observed in the control group. No weight changes were observed in either group, indicating that participants adjusted their diet to compensate for the addition of the cereals by substituting cereal for their standard breakfast and consuming them in place of afternoon snacks as determined by the food record inspection. Total daily energy intake (kcal/day) remained virtually unchanged when postintervention food intake was compared with intake at baseline. Participants in both groups did experience significant decreases in total fat and saturated fat intake along with significant increases in fiber (both soluble and insoluble), potassium, and calcium. The increase in total fiber intake was greater in the treatment group (P < .01) than in the control group (P < .05). In addition, the treatment group experienced a significant increase in magnesium not observed in the control group.
TABLE 2
BASELINE CHARACTERISTICS*
| Oats Group (n = 45) | Control Group (n = 43) | |
|---|---|---|
| Sex (M/F) | 23/22 | 22/21 |
| Race (% Caucasian) | 96 | 98 |
| BMI (kg/m2) | 31.2 ± 5.1 | 30.6 ± 4.7 |
| Age (years) | 48.7 ± 16.9 | 46.4 ± 15.3 |
| LDL-C (mg/dL) | 139.2 ± 29.3 | 137.7 ± 27.5 |
| HDL-C (mg/dL) | 43.1 ± 9.1 | 44.2 ± 10.2 |
| TC (mg/dL) | 211.6 ± 38.6 | 213.7 ± 42.3 |
| SBP (mm Hg) | 140 ± 16 | 138 ± 15 |
| DBP (mm Hg) | 88 ± 10 | 86 ± 9 |
| TG (mg/dL) | 185.4 ± 40.2 | 191.6 ± 41.9 |
| Insulin (μU/mL) | 16.9 ± 6.1 | 15.2 ± 5.9 |
| Soluble fiber (g) | 5.3 ± 1.6 | 4.8 ± 1.3 |
| BMI denotes body mass index; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; SD, standard deviation; TC, total cholesterol; TG, triglycerides. | ||
| * Values are means ± SD; means did not differ significantly. | ||
TABLE 3
ANTIHYPERTENSIVE MEDICATION AND BLOOD PRESSURE CHANGES BY GROUP
| Oats Group (n = 45) | Control Group (n = 43) | P * | |
|---|---|---|---|
| BP medication reduction, n (%) | 33 (73%) | 18 (42%) | <.05 |
| BP changes in those without medication reduction (post treatment, baseline)† | |||
| SBP in mm Hg | -7 ± 8 | -1 ± 9 | <.05 |
| DBP in mm Hg | -4 ± 5 | 1 ± 6 | .18 |
| BP medication resumption, n (%) | 23/33 (67%) | 6/18 (33%) | <.05 |
| *P < .05 between oats and control groups. | |||
| † Values are means ± SD. | |||
| SBP denotes systolic blood pressure; SD, standard deviation; DBP, diastolic blood pressure. | |||
TABLE 4
SECONDARY OUTCOME MEASURES BY GROUP*
| Oats Group | Control Group | |||
|---|---|---|---|---|
| Baseline | Post Study | Baseline | Post Study | |
| Total cholesterol (mg/dL) † | 211.6 ± 5.9 | 179.9 ± 5.2 | 213.7 ± 6.7 | 206.2 ± 6.5 |
| LDL cholesterol (mg/dL) † | 139.2 ± 4.5 | 116.9 ± 4.2 | 137.7 ± 4.4 | 131.6 ± 4.7 |
| HDL cholesterol (mg/dL) | 43.1 ± 1.4 | 44.6 ± 1.7 | 44.2 ± 1.6 | 43.2 ± 1.5 |
| Triglycerides (mg/dL) | 185.4 ± 6.2 | 172.6 ± 6.5 | 191.6 ± 6.4 | 184.2 ± 6.8 |
| Glucose (mg/dL) † | 118.4 ± 4.1 | 106.1 ± 4.2 | 117.1 ± 5.2 | 119.8 ± 5.5 |
| Side effects (score) † | 58.2 ± 7.2 | 47.6 ± 6.9 | 56.7 ± 8.1 | 53.4 ± 7.2 |
| Weight (kg) | 82.5 ± 5.5 | 83 ± 5.9 | 83.7 ± 5.3 | 83.4 ± 5.8 |
| * Values are means ± SEM except for body weight, which is represented as mean ± SD for all participants. | ||||
| † Indicates statistical differences between groups (change score) at P <.05. | ||||
Discussion
The results of this trial suggest that an increased consumption of soluble fiber-rich, whole-grain, oat-based cereals can significantly reduce antihypertensive medication need among patients being treated for hypertension. Of the 45 participants in the oats group, 33 experienced at least half medication reduction compared with only 18 of the 43 participants in the control group. Positive BP changes were evident during the first 4 weeks of oat cereal treatment; BP levels rose steadily during the 6-week follow-up phase.
In addition, mean BP readings in the oat group participants who did not experience a medication reduction had improved at study completion compared with baseline. A significant number of participants in the refined cereal control group experienced at least half medication reduction (18/43), a finding that might be attributed to the increase in calcium, potassium, and total dietary fiber intake8,9,18 as well as to the decreased intake of total and saturated fat.19 Additionally, during the follow-up phase, only 6 of the 18 (33%) versus 22 of the 33 (67%) in the oats group resumed taking their medication. Therefore, part of the medication reduction effect in the control group may have been the result of a greater percentage of participants who did not need their antihypertensive medication. This issue should be considered in the design of future trials.
As always, regression to the mean and the Hawthorne effect might explain some of the outcomes in this trial. However, it is likely that both increased soluble fiber and micronutrient intake explain the decrease in antihypertensive medication need observed in the treatment group. This study was designed to identify not the hypotensive effects of specific cereal components but the effects of a whole food intervention. Our findings are consistent with those of other whole-food interventions, such as the Dietary Approaches to Stop Hypertension (DASH) trial, tested in hypertensive populations.20 Nonetheless, known diet-related determinants of BP (sodium chloride, alcohol, body weight, and level of physical activity) could not explain the treatment effect because no significant differences in these variables existed between the groups.
The soluble fiber fraction of the oat-based cereal intervention is probably partially responsible for the reduction in antihypertensive medication need observed in this trial. Previous studies that tested either soluble fiber supplements or diets rich in soluble fiber have noted significant reductions in BP.21-23 Improvement in insulin sensitivity has been proposed as the pathway through which soluble fiber improves BP.24 Insulin sensitivity was not determined in this study, yet the oats treatment group experienced a significant improvement in plasma glucose levels. This finding suggests that insulin sensitivity may have been enhanced. Impaired response to insulin was recently shown to precede endothelial dysfunction and subsequent elevations in BP.25 Moreover, soluble fiber supplements and diets high in soluble fiber have been shown to improve insulin sensitivity.25-28 Other components of whole grains, such as magnesium or grain flavonoids, may also contribute to the favorable medication reduction observed in the oats group.29,30
This 12-week whole-food intervention trial was not designed to test either the long-term efficacy of oat-based cereals or the likelihood of long-term adherence to the feeding regimen. Nonetheless, a whole-grain oat-based cereal intervention might be an effective way to manage mild (type I) hypertension. The reduction in BP medication that occurred in the oats group was independent of weight change and sodium chloride and alcohol intake, suggesting that soluble fiber–rich whole grains should be added to the current dietary recommendations for people with elevated BP. Moreover, it is possible that the consumption of a diet high in soluble fiber–rich whole grains may prevent or delay the initiation of hypertension drug therapy in at-risk or borderline hypertensive patients. Based on the results from this study, physicians may be justified in recommending to their hypertensive patients a dietary regimen that includes the daily consumption of whole-grain oats (equaling 6 g of soluble fiber) in conjunction with their usual therapy. Such an intervention may be expected to yield results within 4 weeks.
Conclusions
A diet containing soluble fiber-rich whole grains can significantly reduce antihypertensive medication need and improve BP control among treated hypertensives. Combined with the reductions in blood lipids and plasma glucose, the intake of soluble fiber–rich whole oat cereals appears to be an effective nutritional approach in the reduction of cardiovascular disease risk. Future trials will need to investigate the antihypertensive effects of oats in other populations (eg, different racial groups) and determine whether reductions in BP measurements can be sustained for the long term.
Acknowledgment
The research team recognizes Anne Marie Weber-Main, PhD, for her excellent and tireless editorial contributions to this project.
1. Prisco D, Paniccia R, Bandinelli B, et al. Effect of medium-term supplementation with a moderate dose of n-3 polyunsaturated fatty acids on blood pressure in mild hypertensive patients. Thromb Res 1998;91:105-12.
2. Sanjuliani AF, de Abreu Fangundes VG, Francischetti EA. Effects of magnesium on blood pressure and intracellular ion levels of Brazilian hypertensive patients. Int J Cardiol 1996;56:177-83.
3. Fotherby MD, Potter JP. Long-term potassium supplementation lowers blood pressure in elderly hypertensive subjects. Int J Clin Pract 1997;51:219-22.
4. Griffith LE, Guyatt GH, Cook RJ, Bucher HC, Cook DJ. The influence of dietary and nondietary calcium supplementation on blood pressure: an updated meta analysis of randomized controlled trials. Am J Hypertens 1999;12:84-92.
5. Krotkiewski M. Effect of guar gum on the arterial blood pressure. Acta Med Scand 1987;222:43-9.
6. Pietinen P. Dietary fat and blood pressure. Ann Med 1994;65-8.
7. Whelton PK, Klag MJ. Magnesium and blood pressure: review of the epidemiological and clinical trial experience. Am J Cardiol 1989;63:26G-30G.
8. Barri YM, Wingo CS. The effects of potassium depletion and supplementation on blood pressure: a clinical review. Am J Med Sci 1997;314:37-40.
9. Sacks FM, Willett WC, Smith A, Brown LE, Rosner B, Moore TJ. Effect on blood pressure of potassium, calcium, and magnesium in women with low habitual intake. Hypertension 1998;31:131-8.
10. Kestin M, Moss R, Clifton PM, Nestel PJ. Comparative effects of three cereal brans on plasma lipids, blood pressure, and glucose metabolism in mildly hypercholesterolemic men. Am J Clin Nutr 1990;52:661-6.
11. Pietinen P, Rimm EB, Korhonen P, et al. Intake of dietary fiber and risk of coronary heart disease in a cohort of Finnish men. Circulation 1996;94:2720-7.
12. Swain JF, Rouse IL, Curley SB, Sacks FM. Comparison of the effects of oat bran and low-fiber wheat on serum lipoprotein levels and blood pressure. N Engl J Med 1990;322:147-52.
13. Braaten JT, Wood PJ, Scott FW, Riedel KD, Poste LM, Collins MW. Oat gum lowers glucose and insulin after an oral glucose load. Am J Clin Nutr 1991;53:1425-30.
14. Braaten JT, Scott FW, Wood PJ, et al. High beta-glucan oat bran and oat gum reduce postprandial blood glucose and insulin in subjects with and without type 2 diabetes. Diabet Med 1994;11:312-8.
15. Salonen JT, Lakka JA, Lakka HM, Valkonen VP, Everson SA, Kaplan GA. Hyperinsulinemia is associated with the incidence of hypertension and dyslipidemia in middle-aged men. Diabetes 1998;47:270-5.
16. Tietz NW, ed. Fundamentals of clinical chemistry. 3rd ed. New York, NY: Saunders; 1987.
17. Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed 1989;30:47-57.
18. He J, Klag MJ, Whelton PK, et al. Oats and buckwheat intakes and cardiovascular disease risk factors in an ethnic minority of China. Am J Clin Nutr 1995;61:366-72.
19. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24.
20. Colin PR, Chow D, Miller ER, et al. The effect of dietary patterns on blood pressure control in hypertensive patients: results from the Dietary Approaches to Stop Hypertension (DASH) trial. Am J Hypertens 2000;13:949-55.
21. Uusitupa M, Tuomilehto J, Karttunen P, Wolf E. Long term effects of guar gum on metabolic control, serum cholesterol and blood pressure in type 2 (non-insulin-dependent) diabetic patients with high blood pressure. Ann Clin Res 1984;16:126-31.
22. Landin K, Holm G, Tengborn L, Smith U. Guar gum improve insulin sensitivity, blood lipids, blood pressure, and fibrinolysis in healthy mean. Am J Clin Nutr 1992;56:1061-5.
23. Singh RB, Rastogi SS, Singh NK, Ghosh S, Gupta S, Niaz MA. Can guava fruit intake decrease blood pressure and blood lipids? J Hum Hypertens 1993;7:33-8.
24. Pins JJ, Keenan JM. Soluble fiber and hypertension. Prev Cardiol 1999;2:151-8.
25. Katakam PVG, Ujhelyi MR, Hoenig ME, Miller AW. Endothelial dysfunction precedes hypertension in diet-induced insulin resistance. Am J Physiol 1998;275:R788-R792.
26. Tagliaferro V, Cassader M, Bozzo C, et al. Moderate guar-gum addition to usual diet improves peripheral sensitivity to insulin and lipaemic profile in NIDDM. Diabet Metab 1985;11:380-5.
27. Fukagawa NK, Anderson JW, Hageman G, Young VR, Minaker KL. High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults. Am J Clin Nutr 1990;52:524-8.
28. Lovejoy J, DiGirolamo M. Habitual dietary intake and insulin sensitivity in lean and obese adults. Am J Clin Nutr 1992;55:1174-9.
29. Mizushima S, Cappuccio FP, Nichols R, Elliott P. Dietary magnesium intake and blood pressure: a qualitative overview of the observation studies. J Hum Hypertens 1998;12:447-57.
30. Wu BN, Huang YC, Wu HM, et al. A highly selective beta-1-andrenergic blocker with a partial beta-2-agonist activity derived from ferulic acid, an active component of Ligusticum wallichii Franch. J Cardiovasc Pharmacol 1998;31:750-7.
OBJECTIVES: Our study compared 2 whole grain oat-based cereals with 2 refined grain wheat-based cereals to determine their effects on the need for antihypertensive medications in people with high blood pressure (BP).
STUDY DESIGN: This 12-week, randomized controlled parallel-group trial with 6 weeks of voluntary follow-up was designed to investigate the antihypertensive effects of oats. After 4 weeks of baseline feeding, medication dose was maintained or reduced by half or completely throughout the middle 4 weeks of the study. In the final 4 weeks, participants continued cereal consumption; medication was adjusted according to the protocol.
POPULATION: Men and women (n = 88) being treated for hypertension with a mean baseline BP below 160/100.
OUTCOMES MEASURED: Primary study outcomes included change in SBP and DBP as well as antihypertensive medication reduction. Secondary measures included blood lipid, fasting glucose, and insulin levels and side effects related to elevated BP and increased dietary fiber intake.
RESULTS: Seventy-three percent of participants in the oats group versus 42% in the control group were able to stop or reduce their medication by half. Treatment group participants whose medication was not reduced had substantial decreases in BP. The oats group experienced a 24.2–mg/dL reduction in total cholesterol levels, a 16.2–mg/dL decrease in low-density lipoprotein cholesterol levels, and a 15.03–mg/dL drop in plasma glucose levels vs controls.
CONCLUSIONS: Results suggest that a diet containing soluble fiber–rich whole oats can significantly reduce the need for antihypertensive medication and improve BP control. Considering the lipid and glucose improvements as well, increased consumption of whole oats may significantly reduce cardiovascular disease risk.
- Whole oats, when supplemented daily, significantly reduced antihypertensive medication need and improved blood pressure control over the 12-week intervention.
- Whole oats improved blood lipid and fasting glucose levels and reduced the incidence of overall study-related side effects.
- Significantly increasing whole oat consumption may greatly reduce risk for cardiovascular disease in hypertensive patients.
Since the initial use of antihypertensive medications in the 1940s, they have been the traditional approach to treatment essential hypertension. Many of these pharmacologic agents, however, are costly and are associated with substantial adverse effects. As a result, interest has been increasing in alternative methods to prevent and treat hypertension. Clinical trials using dietary interventions for the alleviation of hypertension and observational studies have suggested that a number of foods and specific food components may exert an antihypertensive effect.1-5 Other research, however, has shown no effect.6-10 Studies specific to oats or cereal fibers have also provided mixed results. Observational studies have noted a reduction in blood pressure (BP),11 but the few clinical trials conducted to date have shown no effect.12
Selected whole grains are known to be good sources of soluble fibers. Previous research trials have demonstrated that these fibers can effectively reduce plasma insulin concentrations and provide other health benefits.13,14 Additionally, elevated insulin levels have been implicated in the etiology of hypertension.15 Based on this potential biologic mechanism and the previously inconsistent findings, we conducted a 12-week trial to evaluate the clinical effects of soluble fiber–rich whole oat cereals when added to the diet of hyperinsulinemic patients medicated for essential hypertension.
Methods
Study sample
Participants were recruited from a database of treated hypertensive patients provided by a local health maintenance organization (HealthPartners). Initial letters describing the study were mailed to 8000 potential participants. Of these, 524 people responded to the mailing and agreed to a telephone screen to determine eligibility. Among respondents, 212 passed the initial phone screening and were invited to our research clinic (Hypertension and Cholesterol Research Clinic at the University of Minnesota Medical School) for a BP screening and general physical. For inclusion in the study, average screening BP readings (2 sets of readings within 7 days) taken by our team physician could not exceed 160/100. Table 1 lists exclusion criteria. The study protocol was reviewed and approved by the University of Minnesota Human Subjects Committee of the Institutional Review Board.
Eighty-eight volunteers (45 men and 43 women) aged 33 to 67 years met all inclusion criteria and provided written informed consent. All participants had a history of essential mild or moderate hypertension (BP 120/80 to 160/100 mm Hg), and were treated with no more than 1 antihypertensive medication (excluding -adrenergic receptor blocking agents) and/or 1 diuretic medication for at least 1 month before enrollment. Eighty participants were treated with a single antihypertensive medication; 8 required an antihypertensive drug and a diuretic medication to manage their BP. Individuals taking beta blockers were excluded from the study because they often take medications prescribed for more serious cardiovascular conditions, such as cardiac arrhythmias, and medication reduction would be inappropriate under such circumstances. Participants’ primary physicians were also consulted concerning participation and study-related medication changes.
TABLE 1
EXCLUSION CRITERIA
|
Study design
This randomized controlled parallel-group trial consisted of 3 four-week phases: a Baseline Feeding phase, a Medication Reduction phase, and a Maintenance phase. Eligible individuals were stratified by baseline systolic blood pressure (SBP) (< 140 mm Hg versus 140 mm Hg) and baseline soluble fiber intake (less than 3 grams/day versus 3 to 6 grams/day). At the start of the baseline phase, participants were randomized to either an oats cereal treatment group (n = 45) or a low-fiber cereal control group (n = 43).
The cereal treatments were isocaloric and administered during all 3 phases of the study. Individuals in the oats group received a daily serving of 60 grams (approximately three fourths cup) Quaker Oatmeal (5.61 grams total dietary fiber, 3.25 grams soluble fiber, and 2.83 grams -glucans) and 77 grams (approximately one and one third cups) Quaker Oat Squares (6.07 grams total dietary fiber, 2.98 grams soluble fiber, and 2.59 grams -glucans). Individuals in the control group consumed 65 grams (0.5 cup) Malt-O-Meal Hot Wheat Cereal (2.32 grams total dietary fiber, 0.6 grams soluble fiber) and 81 grams (2 cups) Kellogg’s Crispix (1.2 grams total dietary fiber, < 0.5 grams soluble fiber).
Cereals were dispensed in unlabeled bulk containers to facilitate physician blinding. Remaining cereal was returned and weighed at each of the weekly or biweekly visits at our research clinic. Additionally, participants kept a daily cereal calendar that was reviewed by members of our research staff and used to help determine cereal compliance.
Changes in antihypertensive medication dose were implemented according to the protocol described in the Figure. Participants were asked to maintain their usual lifestyle, physical activity, dietary pattern, and body weight during the 12 weeks of the study. Individuals were invited to participate in a 6-week follow-up phase after the intervention was completed to monitor the residual BP effect after cereal consumption was discontinued.
FIGURE
MEDICATION REDUCTION PROTOCOL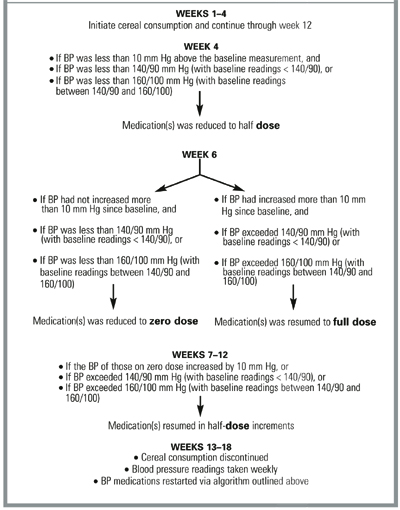
Outcomes measured
The study physician responsible for BP measurement, blood draws, and general patient examinations (described below) was unaware of the cereal group assignment. BP was measured at the clinic twice a week during the first (baseline feeding) and last (maintenance) phases of the study and weekly during the second (medication reduction) phase. Participants reported at approximately the same time of the day for all appointments. BP readings were obtained 24 hours after the last medication dose or, if the patient was unmedicated, at the same time of day as previous study BP readings and after participants had rested quietly in the seated position for at least 5 minutes in an examination room.
The study physician took all readings on the right arm, using a mercury column sphygmomanometer (Korotkoff phase V for diastolic blood pressure [DBP]). Standard cuff size was used unless upper arm circumference exceeded 31 cm, in which case a large cuff with 15 x 35–cm bladders was chosen. Measurements were repeated 4 times in 2-minute intervals. The mean of the last 3 readings was calculated and used in subsequent analyses. Baseline and final study measurements used in the analyses and reported in this paper represent the averages of the first 2 and last 2 study visits.
Preintervention and postintervention blood samples were collected into standard 6-mL serum separator tubes. Samples were analyzed within 24 hours for general chemistry and plasma lipids (total cholesterol, low-density cholesterol [LDL-C], and high-density cholesterol [HDL-C] as well as triglyceride levels) by an accredited independent laboratory and according to standard chemical methods.16
A written 42-question side effect questionnaire was administered to participants at the beginning of the baseline phase and at the end of the intervention. Participants reported the frequency with which they experienced side effects associated with increased fiber intake (eg, loose stools, flatulence) and hypertension (eg, headaches, dizziness) using a 5-item scale ranging from “never” to “very frequently” (event occurring once or several times daily). Each item of the scale was assigned a value ranging from 1 to 5. Values were tallied across all 42 questions. A final score was assigned to each participant for both time points. Mean scores by group were used in the analyses.
Participants completed a 3-day food record at baseline and at the end of the 12 weeks of intervention. Food records were examined for thoroughness by a licensed nutritionist and used to determine dietary changes. Nutrient intakes were calculated using the Nutrient Data System software (version 2.92) managed by the Nutrition Coordinating Center at the University of Minnesota School of Public Health.17
Statistics
The sample size calculation was based on a level of significance set at 0.05 and power at 80% to detect a 15% difference in medication reduction. Differences in medication reduction were determined by using the chi-square test of proportions. For continuous variables, Student’s paired and unpaired t tests were performed to determine differences within and between groups. In terms of medication reduction, logistic regression was used to adjust for potential confounders such as body weight and sodium intake. Multiple regression was employed to adjust blood lipid and glucose levels and BP findings for confounding. Because adjustment did not change the interpretation of the data, unadjusted findings are reported. The analyses of the data from this intent-to-treat population, which were determined to include all randomized patients, were conducted using the Statistical Analysis System (SAS Institute, Cary, N.C.). Results are reported as means ± SD unless noted otherwise. All P values are double sided.
Results
All the original 88 participants enrolled, all completed the 12-week trial, and all participated in the 6-week follow-up phase. Instructions to consume all dispensed cereals every day were followed well. Compliance was high for both groups (94.5% for the oat group and 92.7% for the control group) based on the amount of consumed cereal by weight. Randomization was largely effective; there were no apparent differences in baseline characteristics between each of the treatment groups (Table 2). Participants were primarily white (97%), with a mean age of 48 years (range 33 to 67 years).
BP and BP medication changes are summarized in Table 3. Among subjects in the oats group, 73% experienced a BP medication reduction during the intervention and had maintained that by the end of the study, as compared with only 42% in the control group (P < .05). Moreover, those in the oats group who did not experience a medication reduction had a 7-mm Hg decrease in SBP and a 4-mm Hg reduction in DBP. There was a small, nonsignificant change in SBP and DBP among those who did not experience a medication reduction in the control group. Medication reduction did not differ across classes of antihypertensive medication or our stratification variables of baseline soluble fiber intake or BP. Additionally, during the 6-week follow-up phase, 6 of the 18 (33%) individuals in the control group versus 22 of the 33 (67%) in the treatment group resumed taking medication.
Average BP in the oats group was lowered from 140/88 mm Hg at baseline to 134/85 mm Hg by the end of the first 4 weeks. Only the change in systolic BP was statistically significant (P < .05). Over the same 4-week period, the control group experienced a mean change of BP from 138/86 mm Hg to 136/85 mm Hg, which was not significant.
Baseline and postintervention lipid and glucose levels appear in Table 4. There were no significant modifications in any of the lipid parameters for the individuals in the control group, although there was a downward trend in all lipid measures. In the oats treatment group, mean total cholesterol (TC) concentration decreased by 31.7 mg/dL (15% drop). A similar decrease of 22.3 mg/dL (16% drop) was seen in the oats group’s average LDL-C levels. Blood glucose levels in the oats group also improved significantly (P < .01). The mean differences between post study and prestudy values (± SE) between the 2 groups, calculated for the average changes in TC, LDL-C, and glucose experienced by each of the groups, were -24.2 mg/dL (± 6.1), -16.2 mg/dL (± 4.4), and -15.03 mg/dL (± 4.3), respectively.
The frequency of dietary fiber-related and hypertension-related side effects decreased by 22% in the treatment group (Table 4). This finding was not observed in the control group. No weight changes were observed in either group, indicating that participants adjusted their diet to compensate for the addition of the cereals by substituting cereal for their standard breakfast and consuming them in place of afternoon snacks as determined by the food record inspection. Total daily energy intake (kcal/day) remained virtually unchanged when postintervention food intake was compared with intake at baseline. Participants in both groups did experience significant decreases in total fat and saturated fat intake along with significant increases in fiber (both soluble and insoluble), potassium, and calcium. The increase in total fiber intake was greater in the treatment group (P < .01) than in the control group (P < .05). In addition, the treatment group experienced a significant increase in magnesium not observed in the control group.
TABLE 2
BASELINE CHARACTERISTICS*
| Oats Group (n = 45) | Control Group (n = 43) | |
|---|---|---|
| Sex (M/F) | 23/22 | 22/21 |
| Race (% Caucasian) | 96 | 98 |
| BMI (kg/m2) | 31.2 ± 5.1 | 30.6 ± 4.7 |
| Age (years) | 48.7 ± 16.9 | 46.4 ± 15.3 |
| LDL-C (mg/dL) | 139.2 ± 29.3 | 137.7 ± 27.5 |
| HDL-C (mg/dL) | 43.1 ± 9.1 | 44.2 ± 10.2 |
| TC (mg/dL) | 211.6 ± 38.6 | 213.7 ± 42.3 |
| SBP (mm Hg) | 140 ± 16 | 138 ± 15 |
| DBP (mm Hg) | 88 ± 10 | 86 ± 9 |
| TG (mg/dL) | 185.4 ± 40.2 | 191.6 ± 41.9 |
| Insulin (μU/mL) | 16.9 ± 6.1 | 15.2 ± 5.9 |
| Soluble fiber (g) | 5.3 ± 1.6 | 4.8 ± 1.3 |
| BMI denotes body mass index; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; SD, standard deviation; TC, total cholesterol; TG, triglycerides. | ||
| * Values are means ± SD; means did not differ significantly. | ||
TABLE 3
ANTIHYPERTENSIVE MEDICATION AND BLOOD PRESSURE CHANGES BY GROUP
| Oats Group (n = 45) | Control Group (n = 43) | P * | |
|---|---|---|---|
| BP medication reduction, n (%) | 33 (73%) | 18 (42%) | <.05 |
| BP changes in those without medication reduction (post treatment, baseline)† | |||
| SBP in mm Hg | -7 ± 8 | -1 ± 9 | <.05 |
| DBP in mm Hg | -4 ± 5 | 1 ± 6 | .18 |
| BP medication resumption, n (%) | 23/33 (67%) | 6/18 (33%) | <.05 |
| *P < .05 between oats and control groups. | |||
| † Values are means ± SD. | |||
| SBP denotes systolic blood pressure; SD, standard deviation; DBP, diastolic blood pressure. | |||
TABLE 4
SECONDARY OUTCOME MEASURES BY GROUP*
| Oats Group | Control Group | |||
|---|---|---|---|---|
| Baseline | Post Study | Baseline | Post Study | |
| Total cholesterol (mg/dL) † | 211.6 ± 5.9 | 179.9 ± 5.2 | 213.7 ± 6.7 | 206.2 ± 6.5 |
| LDL cholesterol (mg/dL) † | 139.2 ± 4.5 | 116.9 ± 4.2 | 137.7 ± 4.4 | 131.6 ± 4.7 |
| HDL cholesterol (mg/dL) | 43.1 ± 1.4 | 44.6 ± 1.7 | 44.2 ± 1.6 | 43.2 ± 1.5 |
| Triglycerides (mg/dL) | 185.4 ± 6.2 | 172.6 ± 6.5 | 191.6 ± 6.4 | 184.2 ± 6.8 |
| Glucose (mg/dL) † | 118.4 ± 4.1 | 106.1 ± 4.2 | 117.1 ± 5.2 | 119.8 ± 5.5 |
| Side effects (score) † | 58.2 ± 7.2 | 47.6 ± 6.9 | 56.7 ± 8.1 | 53.4 ± 7.2 |
| Weight (kg) | 82.5 ± 5.5 | 83 ± 5.9 | 83.7 ± 5.3 | 83.4 ± 5.8 |
| * Values are means ± SEM except for body weight, which is represented as mean ± SD for all participants. | ||||
| † Indicates statistical differences between groups (change score) at P <.05. | ||||
Discussion
The results of this trial suggest that an increased consumption of soluble fiber-rich, whole-grain, oat-based cereals can significantly reduce antihypertensive medication need among patients being treated for hypertension. Of the 45 participants in the oats group, 33 experienced at least half medication reduction compared with only 18 of the 43 participants in the control group. Positive BP changes were evident during the first 4 weeks of oat cereal treatment; BP levels rose steadily during the 6-week follow-up phase.
In addition, mean BP readings in the oat group participants who did not experience a medication reduction had improved at study completion compared with baseline. A significant number of participants in the refined cereal control group experienced at least half medication reduction (18/43), a finding that might be attributed to the increase in calcium, potassium, and total dietary fiber intake8,9,18 as well as to the decreased intake of total and saturated fat.19 Additionally, during the follow-up phase, only 6 of the 18 (33%) versus 22 of the 33 (67%) in the oats group resumed taking their medication. Therefore, part of the medication reduction effect in the control group may have been the result of a greater percentage of participants who did not need their antihypertensive medication. This issue should be considered in the design of future trials.
As always, regression to the mean and the Hawthorne effect might explain some of the outcomes in this trial. However, it is likely that both increased soluble fiber and micronutrient intake explain the decrease in antihypertensive medication need observed in the treatment group. This study was designed to identify not the hypotensive effects of specific cereal components but the effects of a whole food intervention. Our findings are consistent with those of other whole-food interventions, such as the Dietary Approaches to Stop Hypertension (DASH) trial, tested in hypertensive populations.20 Nonetheless, known diet-related determinants of BP (sodium chloride, alcohol, body weight, and level of physical activity) could not explain the treatment effect because no significant differences in these variables existed between the groups.
The soluble fiber fraction of the oat-based cereal intervention is probably partially responsible for the reduction in antihypertensive medication need observed in this trial. Previous studies that tested either soluble fiber supplements or diets rich in soluble fiber have noted significant reductions in BP.21-23 Improvement in insulin sensitivity has been proposed as the pathway through which soluble fiber improves BP.24 Insulin sensitivity was not determined in this study, yet the oats treatment group experienced a significant improvement in plasma glucose levels. This finding suggests that insulin sensitivity may have been enhanced. Impaired response to insulin was recently shown to precede endothelial dysfunction and subsequent elevations in BP.25 Moreover, soluble fiber supplements and diets high in soluble fiber have been shown to improve insulin sensitivity.25-28 Other components of whole grains, such as magnesium or grain flavonoids, may also contribute to the favorable medication reduction observed in the oats group.29,30
This 12-week whole-food intervention trial was not designed to test either the long-term efficacy of oat-based cereals or the likelihood of long-term adherence to the feeding regimen. Nonetheless, a whole-grain oat-based cereal intervention might be an effective way to manage mild (type I) hypertension. The reduction in BP medication that occurred in the oats group was independent of weight change and sodium chloride and alcohol intake, suggesting that soluble fiber–rich whole grains should be added to the current dietary recommendations for people with elevated BP. Moreover, it is possible that the consumption of a diet high in soluble fiber–rich whole grains may prevent or delay the initiation of hypertension drug therapy in at-risk or borderline hypertensive patients. Based on the results from this study, physicians may be justified in recommending to their hypertensive patients a dietary regimen that includes the daily consumption of whole-grain oats (equaling 6 g of soluble fiber) in conjunction with their usual therapy. Such an intervention may be expected to yield results within 4 weeks.
Conclusions
A diet containing soluble fiber-rich whole grains can significantly reduce antihypertensive medication need and improve BP control among treated hypertensives. Combined with the reductions in blood lipids and plasma glucose, the intake of soluble fiber–rich whole oat cereals appears to be an effective nutritional approach in the reduction of cardiovascular disease risk. Future trials will need to investigate the antihypertensive effects of oats in other populations (eg, different racial groups) and determine whether reductions in BP measurements can be sustained for the long term.
Acknowledgment
The research team recognizes Anne Marie Weber-Main, PhD, for her excellent and tireless editorial contributions to this project.
OBJECTIVES: Our study compared 2 whole grain oat-based cereals with 2 refined grain wheat-based cereals to determine their effects on the need for antihypertensive medications in people with high blood pressure (BP).
STUDY DESIGN: This 12-week, randomized controlled parallel-group trial with 6 weeks of voluntary follow-up was designed to investigate the antihypertensive effects of oats. After 4 weeks of baseline feeding, medication dose was maintained or reduced by half or completely throughout the middle 4 weeks of the study. In the final 4 weeks, participants continued cereal consumption; medication was adjusted according to the protocol.
POPULATION: Men and women (n = 88) being treated for hypertension with a mean baseline BP below 160/100.
OUTCOMES MEASURED: Primary study outcomes included change in SBP and DBP as well as antihypertensive medication reduction. Secondary measures included blood lipid, fasting glucose, and insulin levels and side effects related to elevated BP and increased dietary fiber intake.
RESULTS: Seventy-three percent of participants in the oats group versus 42% in the control group were able to stop or reduce their medication by half. Treatment group participants whose medication was not reduced had substantial decreases in BP. The oats group experienced a 24.2–mg/dL reduction in total cholesterol levels, a 16.2–mg/dL decrease in low-density lipoprotein cholesterol levels, and a 15.03–mg/dL drop in plasma glucose levels vs controls.
CONCLUSIONS: Results suggest that a diet containing soluble fiber–rich whole oats can significantly reduce the need for antihypertensive medication and improve BP control. Considering the lipid and glucose improvements as well, increased consumption of whole oats may significantly reduce cardiovascular disease risk.
- Whole oats, when supplemented daily, significantly reduced antihypertensive medication need and improved blood pressure control over the 12-week intervention.
- Whole oats improved blood lipid and fasting glucose levels and reduced the incidence of overall study-related side effects.
- Significantly increasing whole oat consumption may greatly reduce risk for cardiovascular disease in hypertensive patients.
Since the initial use of antihypertensive medications in the 1940s, they have been the traditional approach to treatment essential hypertension. Many of these pharmacologic agents, however, are costly and are associated with substantial adverse effects. As a result, interest has been increasing in alternative methods to prevent and treat hypertension. Clinical trials using dietary interventions for the alleviation of hypertension and observational studies have suggested that a number of foods and specific food components may exert an antihypertensive effect.1-5 Other research, however, has shown no effect.6-10 Studies specific to oats or cereal fibers have also provided mixed results. Observational studies have noted a reduction in blood pressure (BP),11 but the few clinical trials conducted to date have shown no effect.12
Selected whole grains are known to be good sources of soluble fibers. Previous research trials have demonstrated that these fibers can effectively reduce plasma insulin concentrations and provide other health benefits.13,14 Additionally, elevated insulin levels have been implicated in the etiology of hypertension.15 Based on this potential biologic mechanism and the previously inconsistent findings, we conducted a 12-week trial to evaluate the clinical effects of soluble fiber–rich whole oat cereals when added to the diet of hyperinsulinemic patients medicated for essential hypertension.
Methods
Study sample
Participants were recruited from a database of treated hypertensive patients provided by a local health maintenance organization (HealthPartners). Initial letters describing the study were mailed to 8000 potential participants. Of these, 524 people responded to the mailing and agreed to a telephone screen to determine eligibility. Among respondents, 212 passed the initial phone screening and were invited to our research clinic (Hypertension and Cholesterol Research Clinic at the University of Minnesota Medical School) for a BP screening and general physical. For inclusion in the study, average screening BP readings (2 sets of readings within 7 days) taken by our team physician could not exceed 160/100. Table 1 lists exclusion criteria. The study protocol was reviewed and approved by the University of Minnesota Human Subjects Committee of the Institutional Review Board.
Eighty-eight volunteers (45 men and 43 women) aged 33 to 67 years met all inclusion criteria and provided written informed consent. All participants had a history of essential mild or moderate hypertension (BP 120/80 to 160/100 mm Hg), and were treated with no more than 1 antihypertensive medication (excluding -adrenergic receptor blocking agents) and/or 1 diuretic medication for at least 1 month before enrollment. Eighty participants were treated with a single antihypertensive medication; 8 required an antihypertensive drug and a diuretic medication to manage their BP. Individuals taking beta blockers were excluded from the study because they often take medications prescribed for more serious cardiovascular conditions, such as cardiac arrhythmias, and medication reduction would be inappropriate under such circumstances. Participants’ primary physicians were also consulted concerning participation and study-related medication changes.
TABLE 1
EXCLUSION CRITERIA
|
Study design
This randomized controlled parallel-group trial consisted of 3 four-week phases: a Baseline Feeding phase, a Medication Reduction phase, and a Maintenance phase. Eligible individuals were stratified by baseline systolic blood pressure (SBP) (< 140 mm Hg versus 140 mm Hg) and baseline soluble fiber intake (less than 3 grams/day versus 3 to 6 grams/day). At the start of the baseline phase, participants were randomized to either an oats cereal treatment group (n = 45) or a low-fiber cereal control group (n = 43).
The cereal treatments were isocaloric and administered during all 3 phases of the study. Individuals in the oats group received a daily serving of 60 grams (approximately three fourths cup) Quaker Oatmeal (5.61 grams total dietary fiber, 3.25 grams soluble fiber, and 2.83 grams -glucans) and 77 grams (approximately one and one third cups) Quaker Oat Squares (6.07 grams total dietary fiber, 2.98 grams soluble fiber, and 2.59 grams -glucans). Individuals in the control group consumed 65 grams (0.5 cup) Malt-O-Meal Hot Wheat Cereal (2.32 grams total dietary fiber, 0.6 grams soluble fiber) and 81 grams (2 cups) Kellogg’s Crispix (1.2 grams total dietary fiber, < 0.5 grams soluble fiber).
Cereals were dispensed in unlabeled bulk containers to facilitate physician blinding. Remaining cereal was returned and weighed at each of the weekly or biweekly visits at our research clinic. Additionally, participants kept a daily cereal calendar that was reviewed by members of our research staff and used to help determine cereal compliance.
Changes in antihypertensive medication dose were implemented according to the protocol described in the Figure. Participants were asked to maintain their usual lifestyle, physical activity, dietary pattern, and body weight during the 12 weeks of the study. Individuals were invited to participate in a 6-week follow-up phase after the intervention was completed to monitor the residual BP effect after cereal consumption was discontinued.
FIGURE
MEDICATION REDUCTION PROTOCOL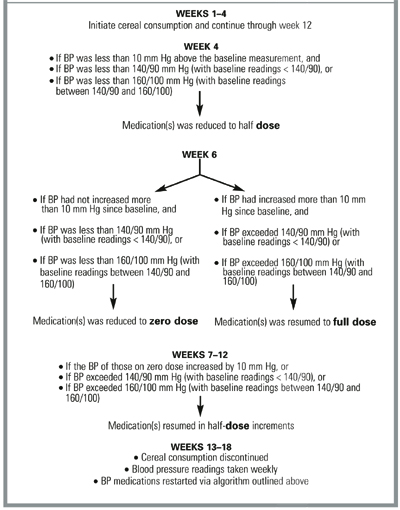
Outcomes measured
The study physician responsible for BP measurement, blood draws, and general patient examinations (described below) was unaware of the cereal group assignment. BP was measured at the clinic twice a week during the first (baseline feeding) and last (maintenance) phases of the study and weekly during the second (medication reduction) phase. Participants reported at approximately the same time of the day for all appointments. BP readings were obtained 24 hours after the last medication dose or, if the patient was unmedicated, at the same time of day as previous study BP readings and after participants had rested quietly in the seated position for at least 5 minutes in an examination room.
The study physician took all readings on the right arm, using a mercury column sphygmomanometer (Korotkoff phase V for diastolic blood pressure [DBP]). Standard cuff size was used unless upper arm circumference exceeded 31 cm, in which case a large cuff with 15 x 35–cm bladders was chosen. Measurements were repeated 4 times in 2-minute intervals. The mean of the last 3 readings was calculated and used in subsequent analyses. Baseline and final study measurements used in the analyses and reported in this paper represent the averages of the first 2 and last 2 study visits.
Preintervention and postintervention blood samples were collected into standard 6-mL serum separator tubes. Samples were analyzed within 24 hours for general chemistry and plasma lipids (total cholesterol, low-density cholesterol [LDL-C], and high-density cholesterol [HDL-C] as well as triglyceride levels) by an accredited independent laboratory and according to standard chemical methods.16
A written 42-question side effect questionnaire was administered to participants at the beginning of the baseline phase and at the end of the intervention. Participants reported the frequency with which they experienced side effects associated with increased fiber intake (eg, loose stools, flatulence) and hypertension (eg, headaches, dizziness) using a 5-item scale ranging from “never” to “very frequently” (event occurring once or several times daily). Each item of the scale was assigned a value ranging from 1 to 5. Values were tallied across all 42 questions. A final score was assigned to each participant for both time points. Mean scores by group were used in the analyses.
Participants completed a 3-day food record at baseline and at the end of the 12 weeks of intervention. Food records were examined for thoroughness by a licensed nutritionist and used to determine dietary changes. Nutrient intakes were calculated using the Nutrient Data System software (version 2.92) managed by the Nutrition Coordinating Center at the University of Minnesota School of Public Health.17
Statistics
The sample size calculation was based on a level of significance set at 0.05 and power at 80% to detect a 15% difference in medication reduction. Differences in medication reduction were determined by using the chi-square test of proportions. For continuous variables, Student’s paired and unpaired t tests were performed to determine differences within and between groups. In terms of medication reduction, logistic regression was used to adjust for potential confounders such as body weight and sodium intake. Multiple regression was employed to adjust blood lipid and glucose levels and BP findings for confounding. Because adjustment did not change the interpretation of the data, unadjusted findings are reported. The analyses of the data from this intent-to-treat population, which were determined to include all randomized patients, were conducted using the Statistical Analysis System (SAS Institute, Cary, N.C.). Results are reported as means ± SD unless noted otherwise. All P values are double sided.
Results
All the original 88 participants enrolled, all completed the 12-week trial, and all participated in the 6-week follow-up phase. Instructions to consume all dispensed cereals every day were followed well. Compliance was high for both groups (94.5% for the oat group and 92.7% for the control group) based on the amount of consumed cereal by weight. Randomization was largely effective; there were no apparent differences in baseline characteristics between each of the treatment groups (Table 2). Participants were primarily white (97%), with a mean age of 48 years (range 33 to 67 years).
BP and BP medication changes are summarized in Table 3. Among subjects in the oats group, 73% experienced a BP medication reduction during the intervention and had maintained that by the end of the study, as compared with only 42% in the control group (P < .05). Moreover, those in the oats group who did not experience a medication reduction had a 7-mm Hg decrease in SBP and a 4-mm Hg reduction in DBP. There was a small, nonsignificant change in SBP and DBP among those who did not experience a medication reduction in the control group. Medication reduction did not differ across classes of antihypertensive medication or our stratification variables of baseline soluble fiber intake or BP. Additionally, during the 6-week follow-up phase, 6 of the 18 (33%) individuals in the control group versus 22 of the 33 (67%) in the treatment group resumed taking medication.
Average BP in the oats group was lowered from 140/88 mm Hg at baseline to 134/85 mm Hg by the end of the first 4 weeks. Only the change in systolic BP was statistically significant (P < .05). Over the same 4-week period, the control group experienced a mean change of BP from 138/86 mm Hg to 136/85 mm Hg, which was not significant.
Baseline and postintervention lipid and glucose levels appear in Table 4. There were no significant modifications in any of the lipid parameters for the individuals in the control group, although there was a downward trend in all lipid measures. In the oats treatment group, mean total cholesterol (TC) concentration decreased by 31.7 mg/dL (15% drop). A similar decrease of 22.3 mg/dL (16% drop) was seen in the oats group’s average LDL-C levels. Blood glucose levels in the oats group also improved significantly (P < .01). The mean differences between post study and prestudy values (± SE) between the 2 groups, calculated for the average changes in TC, LDL-C, and glucose experienced by each of the groups, were -24.2 mg/dL (± 6.1), -16.2 mg/dL (± 4.4), and -15.03 mg/dL (± 4.3), respectively.
The frequency of dietary fiber-related and hypertension-related side effects decreased by 22% in the treatment group (Table 4). This finding was not observed in the control group. No weight changes were observed in either group, indicating that participants adjusted their diet to compensate for the addition of the cereals by substituting cereal for their standard breakfast and consuming them in place of afternoon snacks as determined by the food record inspection. Total daily energy intake (kcal/day) remained virtually unchanged when postintervention food intake was compared with intake at baseline. Participants in both groups did experience significant decreases in total fat and saturated fat intake along with significant increases in fiber (both soluble and insoluble), potassium, and calcium. The increase in total fiber intake was greater in the treatment group (P < .01) than in the control group (P < .05). In addition, the treatment group experienced a significant increase in magnesium not observed in the control group.
TABLE 2
BASELINE CHARACTERISTICS*
| Oats Group (n = 45) | Control Group (n = 43) | |
|---|---|---|
| Sex (M/F) | 23/22 | 22/21 |
| Race (% Caucasian) | 96 | 98 |
| BMI (kg/m2) | 31.2 ± 5.1 | 30.6 ± 4.7 |
| Age (years) | 48.7 ± 16.9 | 46.4 ± 15.3 |
| LDL-C (mg/dL) | 139.2 ± 29.3 | 137.7 ± 27.5 |
| HDL-C (mg/dL) | 43.1 ± 9.1 | 44.2 ± 10.2 |
| TC (mg/dL) | 211.6 ± 38.6 | 213.7 ± 42.3 |
| SBP (mm Hg) | 140 ± 16 | 138 ± 15 |
| DBP (mm Hg) | 88 ± 10 | 86 ± 9 |
| TG (mg/dL) | 185.4 ± 40.2 | 191.6 ± 41.9 |
| Insulin (μU/mL) | 16.9 ± 6.1 | 15.2 ± 5.9 |
| Soluble fiber (g) | 5.3 ± 1.6 | 4.8 ± 1.3 |
| BMI denotes body mass index; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; SD, standard deviation; TC, total cholesterol; TG, triglycerides. | ||
| * Values are means ± SD; means did not differ significantly. | ||
TABLE 3
ANTIHYPERTENSIVE MEDICATION AND BLOOD PRESSURE CHANGES BY GROUP
| Oats Group (n = 45) | Control Group (n = 43) | P * | |
|---|---|---|---|
| BP medication reduction, n (%) | 33 (73%) | 18 (42%) | <.05 |
| BP changes in those without medication reduction (post treatment, baseline)† | |||
| SBP in mm Hg | -7 ± 8 | -1 ± 9 | <.05 |
| DBP in mm Hg | -4 ± 5 | 1 ± 6 | .18 |
| BP medication resumption, n (%) | 23/33 (67%) | 6/18 (33%) | <.05 |
| *P < .05 between oats and control groups. | |||
| † Values are means ± SD. | |||
| SBP denotes systolic blood pressure; SD, standard deviation; DBP, diastolic blood pressure. | |||
TABLE 4
SECONDARY OUTCOME MEASURES BY GROUP*
| Oats Group | Control Group | |||
|---|---|---|---|---|
| Baseline | Post Study | Baseline | Post Study | |
| Total cholesterol (mg/dL) † | 211.6 ± 5.9 | 179.9 ± 5.2 | 213.7 ± 6.7 | 206.2 ± 6.5 |
| LDL cholesterol (mg/dL) † | 139.2 ± 4.5 | 116.9 ± 4.2 | 137.7 ± 4.4 | 131.6 ± 4.7 |
| HDL cholesterol (mg/dL) | 43.1 ± 1.4 | 44.6 ± 1.7 | 44.2 ± 1.6 | 43.2 ± 1.5 |
| Triglycerides (mg/dL) | 185.4 ± 6.2 | 172.6 ± 6.5 | 191.6 ± 6.4 | 184.2 ± 6.8 |
| Glucose (mg/dL) † | 118.4 ± 4.1 | 106.1 ± 4.2 | 117.1 ± 5.2 | 119.8 ± 5.5 |
| Side effects (score) † | 58.2 ± 7.2 | 47.6 ± 6.9 | 56.7 ± 8.1 | 53.4 ± 7.2 |
| Weight (kg) | 82.5 ± 5.5 | 83 ± 5.9 | 83.7 ± 5.3 | 83.4 ± 5.8 |
| * Values are means ± SEM except for body weight, which is represented as mean ± SD for all participants. | ||||
| † Indicates statistical differences between groups (change score) at P <.05. | ||||
Discussion
The results of this trial suggest that an increased consumption of soluble fiber-rich, whole-grain, oat-based cereals can significantly reduce antihypertensive medication need among patients being treated for hypertension. Of the 45 participants in the oats group, 33 experienced at least half medication reduction compared with only 18 of the 43 participants in the control group. Positive BP changes were evident during the first 4 weeks of oat cereal treatment; BP levels rose steadily during the 6-week follow-up phase.
In addition, mean BP readings in the oat group participants who did not experience a medication reduction had improved at study completion compared with baseline. A significant number of participants in the refined cereal control group experienced at least half medication reduction (18/43), a finding that might be attributed to the increase in calcium, potassium, and total dietary fiber intake8,9,18 as well as to the decreased intake of total and saturated fat.19 Additionally, during the follow-up phase, only 6 of the 18 (33%) versus 22 of the 33 (67%) in the oats group resumed taking their medication. Therefore, part of the medication reduction effect in the control group may have been the result of a greater percentage of participants who did not need their antihypertensive medication. This issue should be considered in the design of future trials.
As always, regression to the mean and the Hawthorne effect might explain some of the outcomes in this trial. However, it is likely that both increased soluble fiber and micronutrient intake explain the decrease in antihypertensive medication need observed in the treatment group. This study was designed to identify not the hypotensive effects of specific cereal components but the effects of a whole food intervention. Our findings are consistent with those of other whole-food interventions, such as the Dietary Approaches to Stop Hypertension (DASH) trial, tested in hypertensive populations.20 Nonetheless, known diet-related determinants of BP (sodium chloride, alcohol, body weight, and level of physical activity) could not explain the treatment effect because no significant differences in these variables existed between the groups.
The soluble fiber fraction of the oat-based cereal intervention is probably partially responsible for the reduction in antihypertensive medication need observed in this trial. Previous studies that tested either soluble fiber supplements or diets rich in soluble fiber have noted significant reductions in BP.21-23 Improvement in insulin sensitivity has been proposed as the pathway through which soluble fiber improves BP.24 Insulin sensitivity was not determined in this study, yet the oats treatment group experienced a significant improvement in plasma glucose levels. This finding suggests that insulin sensitivity may have been enhanced. Impaired response to insulin was recently shown to precede endothelial dysfunction and subsequent elevations in BP.25 Moreover, soluble fiber supplements and diets high in soluble fiber have been shown to improve insulin sensitivity.25-28 Other components of whole grains, such as magnesium or grain flavonoids, may also contribute to the favorable medication reduction observed in the oats group.29,30
This 12-week whole-food intervention trial was not designed to test either the long-term efficacy of oat-based cereals or the likelihood of long-term adherence to the feeding regimen. Nonetheless, a whole-grain oat-based cereal intervention might be an effective way to manage mild (type I) hypertension. The reduction in BP medication that occurred in the oats group was independent of weight change and sodium chloride and alcohol intake, suggesting that soluble fiber–rich whole grains should be added to the current dietary recommendations for people with elevated BP. Moreover, it is possible that the consumption of a diet high in soluble fiber–rich whole grains may prevent or delay the initiation of hypertension drug therapy in at-risk or borderline hypertensive patients. Based on the results from this study, physicians may be justified in recommending to their hypertensive patients a dietary regimen that includes the daily consumption of whole-grain oats (equaling 6 g of soluble fiber) in conjunction with their usual therapy. Such an intervention may be expected to yield results within 4 weeks.
Conclusions
A diet containing soluble fiber-rich whole grains can significantly reduce antihypertensive medication need and improve BP control among treated hypertensives. Combined with the reductions in blood lipids and plasma glucose, the intake of soluble fiber–rich whole oat cereals appears to be an effective nutritional approach in the reduction of cardiovascular disease risk. Future trials will need to investigate the antihypertensive effects of oats in other populations (eg, different racial groups) and determine whether reductions in BP measurements can be sustained for the long term.
Acknowledgment
The research team recognizes Anne Marie Weber-Main, PhD, for her excellent and tireless editorial contributions to this project.
1. Prisco D, Paniccia R, Bandinelli B, et al. Effect of medium-term supplementation with a moderate dose of n-3 polyunsaturated fatty acids on blood pressure in mild hypertensive patients. Thromb Res 1998;91:105-12.
2. Sanjuliani AF, de Abreu Fangundes VG, Francischetti EA. Effects of magnesium on blood pressure and intracellular ion levels of Brazilian hypertensive patients. Int J Cardiol 1996;56:177-83.
3. Fotherby MD, Potter JP. Long-term potassium supplementation lowers blood pressure in elderly hypertensive subjects. Int J Clin Pract 1997;51:219-22.
4. Griffith LE, Guyatt GH, Cook RJ, Bucher HC, Cook DJ. The influence of dietary and nondietary calcium supplementation on blood pressure: an updated meta analysis of randomized controlled trials. Am J Hypertens 1999;12:84-92.
5. Krotkiewski M. Effect of guar gum on the arterial blood pressure. Acta Med Scand 1987;222:43-9.
6. Pietinen P. Dietary fat and blood pressure. Ann Med 1994;65-8.
7. Whelton PK, Klag MJ. Magnesium and blood pressure: review of the epidemiological and clinical trial experience. Am J Cardiol 1989;63:26G-30G.
8. Barri YM, Wingo CS. The effects of potassium depletion and supplementation on blood pressure: a clinical review. Am J Med Sci 1997;314:37-40.
9. Sacks FM, Willett WC, Smith A, Brown LE, Rosner B, Moore TJ. Effect on blood pressure of potassium, calcium, and magnesium in women with low habitual intake. Hypertension 1998;31:131-8.
10. Kestin M, Moss R, Clifton PM, Nestel PJ. Comparative effects of three cereal brans on plasma lipids, blood pressure, and glucose metabolism in mildly hypercholesterolemic men. Am J Clin Nutr 1990;52:661-6.
11. Pietinen P, Rimm EB, Korhonen P, et al. Intake of dietary fiber and risk of coronary heart disease in a cohort of Finnish men. Circulation 1996;94:2720-7.
12. Swain JF, Rouse IL, Curley SB, Sacks FM. Comparison of the effects of oat bran and low-fiber wheat on serum lipoprotein levels and blood pressure. N Engl J Med 1990;322:147-52.
13. Braaten JT, Wood PJ, Scott FW, Riedel KD, Poste LM, Collins MW. Oat gum lowers glucose and insulin after an oral glucose load. Am J Clin Nutr 1991;53:1425-30.
14. Braaten JT, Scott FW, Wood PJ, et al. High beta-glucan oat bran and oat gum reduce postprandial blood glucose and insulin in subjects with and without type 2 diabetes. Diabet Med 1994;11:312-8.
15. Salonen JT, Lakka JA, Lakka HM, Valkonen VP, Everson SA, Kaplan GA. Hyperinsulinemia is associated with the incidence of hypertension and dyslipidemia in middle-aged men. Diabetes 1998;47:270-5.
16. Tietz NW, ed. Fundamentals of clinical chemistry. 3rd ed. New York, NY: Saunders; 1987.
17. Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed 1989;30:47-57.
18. He J, Klag MJ, Whelton PK, et al. Oats and buckwheat intakes and cardiovascular disease risk factors in an ethnic minority of China. Am J Clin Nutr 1995;61:366-72.
19. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24.
20. Colin PR, Chow D, Miller ER, et al. The effect of dietary patterns on blood pressure control in hypertensive patients: results from the Dietary Approaches to Stop Hypertension (DASH) trial. Am J Hypertens 2000;13:949-55.
21. Uusitupa M, Tuomilehto J, Karttunen P, Wolf E. Long term effects of guar gum on metabolic control, serum cholesterol and blood pressure in type 2 (non-insulin-dependent) diabetic patients with high blood pressure. Ann Clin Res 1984;16:126-31.
22. Landin K, Holm G, Tengborn L, Smith U. Guar gum improve insulin sensitivity, blood lipids, blood pressure, and fibrinolysis in healthy mean. Am J Clin Nutr 1992;56:1061-5.
23. Singh RB, Rastogi SS, Singh NK, Ghosh S, Gupta S, Niaz MA. Can guava fruit intake decrease blood pressure and blood lipids? J Hum Hypertens 1993;7:33-8.
24. Pins JJ, Keenan JM. Soluble fiber and hypertension. Prev Cardiol 1999;2:151-8.
25. Katakam PVG, Ujhelyi MR, Hoenig ME, Miller AW. Endothelial dysfunction precedes hypertension in diet-induced insulin resistance. Am J Physiol 1998;275:R788-R792.
26. Tagliaferro V, Cassader M, Bozzo C, et al. Moderate guar-gum addition to usual diet improves peripheral sensitivity to insulin and lipaemic profile in NIDDM. Diabet Metab 1985;11:380-5.
27. Fukagawa NK, Anderson JW, Hageman G, Young VR, Minaker KL. High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults. Am J Clin Nutr 1990;52:524-8.
28. Lovejoy J, DiGirolamo M. Habitual dietary intake and insulin sensitivity in lean and obese adults. Am J Clin Nutr 1992;55:1174-9.
29. Mizushima S, Cappuccio FP, Nichols R, Elliott P. Dietary magnesium intake and blood pressure: a qualitative overview of the observation studies. J Hum Hypertens 1998;12:447-57.
30. Wu BN, Huang YC, Wu HM, et al. A highly selective beta-1-andrenergic blocker with a partial beta-2-agonist activity derived from ferulic acid, an active component of Ligusticum wallichii Franch. J Cardiovasc Pharmacol 1998;31:750-7.
1. Prisco D, Paniccia R, Bandinelli B, et al. Effect of medium-term supplementation with a moderate dose of n-3 polyunsaturated fatty acids on blood pressure in mild hypertensive patients. Thromb Res 1998;91:105-12.
2. Sanjuliani AF, de Abreu Fangundes VG, Francischetti EA. Effects of magnesium on blood pressure and intracellular ion levels of Brazilian hypertensive patients. Int J Cardiol 1996;56:177-83.
3. Fotherby MD, Potter JP. Long-term potassium supplementation lowers blood pressure in elderly hypertensive subjects. Int J Clin Pract 1997;51:219-22.
4. Griffith LE, Guyatt GH, Cook RJ, Bucher HC, Cook DJ. The influence of dietary and nondietary calcium supplementation on blood pressure: an updated meta analysis of randomized controlled trials. Am J Hypertens 1999;12:84-92.
5. Krotkiewski M. Effect of guar gum on the arterial blood pressure. Acta Med Scand 1987;222:43-9.
6. Pietinen P. Dietary fat and blood pressure. Ann Med 1994;65-8.
7. Whelton PK, Klag MJ. Magnesium and blood pressure: review of the epidemiological and clinical trial experience. Am J Cardiol 1989;63:26G-30G.
8. Barri YM, Wingo CS. The effects of potassium depletion and supplementation on blood pressure: a clinical review. Am J Med Sci 1997;314:37-40.
9. Sacks FM, Willett WC, Smith A, Brown LE, Rosner B, Moore TJ. Effect on blood pressure of potassium, calcium, and magnesium in women with low habitual intake. Hypertension 1998;31:131-8.
10. Kestin M, Moss R, Clifton PM, Nestel PJ. Comparative effects of three cereal brans on plasma lipids, blood pressure, and glucose metabolism in mildly hypercholesterolemic men. Am J Clin Nutr 1990;52:661-6.
11. Pietinen P, Rimm EB, Korhonen P, et al. Intake of dietary fiber and risk of coronary heart disease in a cohort of Finnish men. Circulation 1996;94:2720-7.
12. Swain JF, Rouse IL, Curley SB, Sacks FM. Comparison of the effects of oat bran and low-fiber wheat on serum lipoprotein levels and blood pressure. N Engl J Med 1990;322:147-52.
13. Braaten JT, Wood PJ, Scott FW, Riedel KD, Poste LM, Collins MW. Oat gum lowers glucose and insulin after an oral glucose load. Am J Clin Nutr 1991;53:1425-30.
14. Braaten JT, Scott FW, Wood PJ, et al. High beta-glucan oat bran and oat gum reduce postprandial blood glucose and insulin in subjects with and without type 2 diabetes. Diabet Med 1994;11:312-8.
15. Salonen JT, Lakka JA, Lakka HM, Valkonen VP, Everson SA, Kaplan GA. Hyperinsulinemia is associated with the incidence of hypertension and dyslipidemia in middle-aged men. Diabetes 1998;47:270-5.
16. Tietz NW, ed. Fundamentals of clinical chemistry. 3rd ed. New York, NY: Saunders; 1987.
17. Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed 1989;30:47-57.
18. He J, Klag MJ, Whelton PK, et al. Oats and buckwheat intakes and cardiovascular disease risk factors in an ethnic minority of China. Am J Clin Nutr 1995;61:366-72.
19. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24.
20. Colin PR, Chow D, Miller ER, et al. The effect of dietary patterns on blood pressure control in hypertensive patients: results from the Dietary Approaches to Stop Hypertension (DASH) trial. Am J Hypertens 2000;13:949-55.
21. Uusitupa M, Tuomilehto J, Karttunen P, Wolf E. Long term effects of guar gum on metabolic control, serum cholesterol and blood pressure in type 2 (non-insulin-dependent) diabetic patients with high blood pressure. Ann Clin Res 1984;16:126-31.
22. Landin K, Holm G, Tengborn L, Smith U. Guar gum improve insulin sensitivity, blood lipids, blood pressure, and fibrinolysis in healthy mean. Am J Clin Nutr 1992;56:1061-5.
23. Singh RB, Rastogi SS, Singh NK, Ghosh S, Gupta S, Niaz MA. Can guava fruit intake decrease blood pressure and blood lipids? J Hum Hypertens 1993;7:33-8.
24. Pins JJ, Keenan JM. Soluble fiber and hypertension. Prev Cardiol 1999;2:151-8.
25. Katakam PVG, Ujhelyi MR, Hoenig ME, Miller AW. Endothelial dysfunction precedes hypertension in diet-induced insulin resistance. Am J Physiol 1998;275:R788-R792.
26. Tagliaferro V, Cassader M, Bozzo C, et al. Moderate guar-gum addition to usual diet improves peripheral sensitivity to insulin and lipaemic profile in NIDDM. Diabet Metab 1985;11:380-5.
27. Fukagawa NK, Anderson JW, Hageman G, Young VR, Minaker KL. High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults. Am J Clin Nutr 1990;52:524-8.
28. Lovejoy J, DiGirolamo M. Habitual dietary intake and insulin sensitivity in lean and obese adults. Am J Clin Nutr 1992;55:1174-9.
29. Mizushima S, Cappuccio FP, Nichols R, Elliott P. Dietary magnesium intake and blood pressure: a qualitative overview of the observation studies. J Hum Hypertens 1998;12:447-57.
30. Wu BN, Huang YC, Wu HM, et al. A highly selective beta-1-andrenergic blocker with a partial beta-2-agonist activity derived from ferulic acid, an active component of Ligusticum wallichii Franch. J Cardiovasc Pharmacol 1998;31:750-7.
Effect on Antibiotic Prescribing of Repeated Clinical Prompts to Use a Sore Throat Score
OBJECTIVES: Infections with group A streptococcus (GAS) occur in 10% to 20% of patients with sore throats, whereas antibiotics are prescribed 50% of the time. Clinical scoring rules can more accurately predict the likelihood of GAS infection, but whether family physicians will adopt such approaches is unclear. This study sought to determine whether repeated clinical prompts to use a scoring approach could help family physicians lower antibiotic use in patients with a sore throat.
STUDY DESIGN: Randomized trial in which physicians were assigned to use either (1) chart stickers that prompted them to calculate a score based on clinical findings and provided management recommendations linked to score totals or (2) a clinical checklist.
POPULATION: Ninety-seven family physicians in Ontario, Canada, assessed 621 children and adults with sore throat and obtained a throat swab for culture.
OUTCOMES MEASURED: (1) Unnecessary antibiotic prescriptions given to patients with a negative throat culture and (2) overall antibiotic use.
RESULTS: There were no differences between the control and intervention group in unnecessary antibiotic prescriptions (16.1% vs 20.4%, respectively, P = .29) or overall antibiotic use (27.9% vs 28.1%, P = .97). However, a number of physicians dropped out of the study; as a result, the characteristics of the physicians in the 2 groups were dissimilar in factors related to prescribing. After adjusting for these differences and patient clustering by physician, the odds ratio for the effect of the intervention on unnecessary antibiotic prescriptions was 0.76 (95% confidence interval [CI] = 0.42, 1.40) and 0.57 for overall antibiotic use (95% CI = 0.27, 1.17).
CONCLUSIONS: Chart prompts during clinical encounters to use a clinical score in the assessment of patients with a sore throat did not reduce unnecessary antibiotic prescribing by family physicians. The problems encountered in conducting this community-based intervention trial are discussed in relation to the negative result.
- Repeated chart prompts to use a clinical prediction rule for the management of children and adults with a sore throat did not help family physicians decrease unnecessary antibiotic use.
- Several problems in the conduct of this community-based intervention trial rather than a lack of the effectiveness of the intervention may have contributed to the negative result.
In the past decade, bacterial resistance to commonly used antibiotics has risen dramatically.1,2 While a number of factors have contributed to this problem, overuse of antibiotics by physicians has been implicated.3-6 An association has been demonstrated between the volume of antibiotic prescriptions and bacterial resistance at both a national4,5 and a local level.3 Where prescribing by physicians has been reduced, rates of antibiotic resistance have subsequently been observed to decline.5,6 As a result, physicians have been urged to reduce their use of antibiotics.7,8 Respiratory infections are the most common reason for the prescribing of antibiotics.9 Upper respiratory tract infections (URTIs) and pharyngitis account for 19% to 28% of all antibiotic prescriptions written by family physicians.9-11
While the use of antibiotics for URTI with sore throat is frequently debated,12-14 experts continue to recommend such treatment for group A streptococcus (GAS) infections to prevent rheumatic fever.15,16 However, only 10% to 20% of patients with a sore throat who visit a family physician have a GAS infection,17-19 whereas antibiotics are prescribed for 50% of URTIs10 and 90% of cases of tonsillitis.20 Uncertainty as to whether or not a bacterial infection is present and clinical error in estimating the likelihood of a GAS infection are associated with the unnecessary prescription of antibiotics.21,22 To address clinical uncertainty, a number of prediction rules and clinical scores have been proposed.23-30 However, physicians taught simply to generate more accurate estimates of the likelihood of a strep infection in this manner do not necessarily lower their use of antibiotics.31
We have previously shown that linking score estimates for the likelihood of a GAS infection to explicit management recommendations to take a throat swab or prescribe an antibiotic has the potential to lower antibiotic use significantly.19,32 In an observational study involving 621 children and adults, this approach would have reduced unnecessary antibiotic prescriptions by 63%.32 We also found a trend toward reduced antibiotic use when physicians were provided with an explicit reminder about the score approach.33 As a result, we hypothesized that this might also help physicians to learn to adopt the sore throat score approach. Reminders have been found to improve the delivery of preventive health services.34,35 The objective of this study was to determine whether repeated clinical prompts to community-based family physicians about the score approach could reduce unnecessary antibiotic prescriptions and lower overall antibiotic use for patients with a sore throat.
Methods
In the fall of 1998, a sample of family physicians in the province of Ontario were invited to participate in a trial to reduce antibiotic use in patients with a sore throat. Physicians who had previously participated in practice-based research projects for the College of Family Physicians of Canada and a random sample from the College’s general membership listing were contacted. Those who mailed back a reply card indicating that they wished to participate were randomized to either an intervention or a control group. The study was approved by the University of Toronto Ethics Review Committee.
Both groups of physicians received, by mail, an article describing the clinical score management approach19; a laminated pocket card summarizing the method; clinical encounter and patient consent forms; and a 1-page survey of practice characteristics. Each physician was asked to enroll 8 patients aged 3 years or older whom they believed to have a new URTI with a sore throat. No attempt was made to further define an eligible presentation to encourage physicians to enroll cases representative of their usual practice. Patients were ineligible if they had taken antibiotics during the previous week, were immunocompromised, or could not understand English. Parents were asked to provide consent for children younger than 16 years of age.
A brief standardized assessment form was completed by the physician for each patient and a throat swab was obtained. The throat swab was submitted to the physician’s local laboratory. A copy of the culture result was forwarded to the study center. Treatment decisions and the management of subsequent culture results were the responsibility of the treating physician.
In the intervention group, physicians were provided with a sticker to apply to the encounter form that listed the score management approach. The sticker contained boxes to be checked by the physicians to calculate the score total and determine appropriate management. Physicians not wishing to use the sticker were prompted on the form to write the score total in a space provided. As a result, physicians in the intervention group received repeated prompts that reminded them to use the score approach each time they completed a clinical encounter form. The control group completed a similar form but without either the sticker or the chart prompts.
The details of the clinical score approach have been previously published.19,25 Briefly, 4 clinical findings (fever > 38°C, absence of cough, tender anterior cervical adenopathy, tonsillar swelling or exudate) and age < 15 years are each assigned 1 point and totaled. One point is subtracted for age 45 years or more. Explicit recommendations for management are linked to score totals. If the score total is 1 or less, no throat swab or antibiotic is indicated. A throat swab is recommended for a score of 2 or 3 and an antibiotic only if the culture is positive. Either initiating treatment with an antibiotic or taking a throat swab is appropriate for a score of 4 or more.
The main outcome for the study was the prescription of unnecessary antibiotics, defined as a prescription for antibiotic medication given to a patient whose subsequent throat culture was negative for group A streptococcus. The secondary outcome was overall antibiotic use. The sample size was calculated to detect a 30% decrease in unnecessary antibiotic use (2-sided = 0.05, 1- = 0.90), assuming a 40% baseline prescription rate9 and a 70% negative culture rate.1719 Because groups of patients were treated by the same physician, the sample size was adjusted to take the clustered sampling design into account.36 The intraclass correlation coefficient for prescribing estimated from an earlier study was 0.07.19 Assuming an average of 5 patients assessed per physician, the sample size was estimated to be 85 physicians and 425 patients in each group.
The clinical characteristics of patients in the intervention and control groups were compared with a chi-square test for categorical variables and a t-test for continuous variables. Associations between prescription rates and the practice and demographic characteristics of the physicians were assessed and adjusted for the clustered sampling with Stata Statistical Software (Release 6, Stata Corp., College Station, Tex.). While clustering improves the efficiency of sampling by requiring participation by fewer physicians, confidence intervals that do not account for the design effect are too narrow. Multiple logistic regression was used to adjust for differences in patient and physician characteristics, taking into account the patient clusters by physician in estimating the effect of the intervention.
Results
One hundred sixty-four physicians agreed to participate and were randomized. Of these, only 97 (59.1%) completed the study and provided patient data (Figure). An equal proportion of physicians in the intervention group (40.2%) and control group (41.5%, P = .87) failed to complete the study. No significant differences were identified between the sex or age of physicians who participated and those who did not participate. Of the participating physicians, 86 (84.3%) returned surveys describing their practice settings.
Patients assessed included 692 children and adults. Of these, 71 (10.3%) were excluded because of a diagnosis of bronchitis (35), sinusitis (16), otitis media (11), or pneumonia (4) or because the patient was less than 3 years old (5). The score approach did not apply to the 4 conditions of exclusion because they involve organisms other than GAS. The remaining 621 patients in the control and intervention groups were similar in demographic and clinical characteristics as well as regarding the prevalence of GAS as documented by throat culture (Table 1). However, a diagnosis of tonsillitis, strep throat, or pharyngitis was more likely to occur in the intervention group (38.6%) than in the control group (28.9%, P = .01). These diagnoses were associated with a higher rate of antibiotic prescribing (54.8%) than were situations in which physicians recorded a URTI or other diagnosis (14.2%, P < .001).
Differences were noted in the characteristics of the treating physicians in each group when considered by patient encounter. Although there were no differences in the age or sex of individual physicians in each group, the participating physicians did not contribute equal numbers of patient encounters. The average number of patients assessed per physician was 3, ranging from a low of 1 patient contributed by some physicians to a high of 8 for others. More patient encounters in the intervention group were contributed by male physicians who had been in practice longer, who worked in smaller communities, and who reported larger practice volumes (Table 1). Physicians from small communities were more likely to diagnose strep throat, tonsillitis, or pharyngitis than were those in larger communities (45.1% vs 28.1%, respectively, P < .001), as were those with higher patient volumes (46.5% vs 30.2%, P = .003).
Certain physician practice characteristics were associated with a patient’s being more likely to receive a prescription for an unnecessary antibiotic (Table 2). For example, physicians were more likely to prescribe unnecessary antibiotics if they saw more than 150 patients per week than if they saw fewer and if they had been in practice for 20 or more years than if they had practiced for a shorter time. In addition, higher overall antibiotic use was associated with higher patient volume and with practicing in a smaller community.
There were no differences between the intervention and control groups in either unnecessary antibiotic prescriptions (20.4% vs 16.1%, respectively, P = .17) or overall antibiotic use (28.1% vs 27.9%, P = .96) (Table 1). However, while the culture reports that were needed to classify prescriptions as unnecessary were available for most (600) patients (96.6%), significantly more culture reports were missing in the control group (5.4%) than in the intervention group (1.2%, P = .007). Antibiotics were prescribed in 59% of the 17 cases with missing culture reports in the control group but for none of the 4 cases with missing culture reports in the intervention group.
Because intervention patients were more likely than controls to have been treated by physicians with higher prescribing characteristics, adjustments were made for the differing physician characteristics and diagnostic practices and for the clustering of patients by physician, using multiple logistic regression (Table 3). After adjustment, the intervention was associated with a nonsignificant reduction in unnecessary antibiotic prescriptions (odds ratio [OR] = 0.76, 95% confidence interval [CI] = 0.42, 1.40) and in overall antibiotic use (OR = 0.57, 95% CI = 0.27, 1.17).
TABLE 1
COMPARISON OF PATIENTS IN CONTROL AND INTERVENTION GROUPS
| Characteristics | Control Group (n = 317) (%) | Intervention Group (n = 304) (%) | P |
|---|---|---|---|
| Demographic Features | |||
| Mean age | 28.1 years | 27.5 years | 0.70 |
| Female | 217 (69.1)* | 198 (65.4) | 0.32 |
| Assessed October-December | 217 (68.4) | 189 (62.2) | 0.10 |
| Clinical Findings | |||
| Sore throat | 296 (93.4) | 283 (93.1) | 0.89 |
| Runny or stuffy nose | 201 (63.6) | 195 (64.4) | 0.85 |
| Cough | 206 (65.2) | 199 (65.7) | 0.90 |
| Red throat | 220 (70.3) | 207 (69.5) | 0.82 |
| Tonsillar swelling | 88 (28.0) | 90 (30.0) | 0.59 |
| Tonsillar exudate | 51 (16.3) | 51 (17.1) | 0.82 |
| Cervical adenopathy | 131 (41.7) | 127 (42.5) | 0.85 |
| Appears unwell | 81 (25.9) | 89 (29.9) | 0.27 |
| Disease | |||
| Prevalence of group A streptococcus | 50 (16.7) | 52 (17.3) | 0.83 |
| Treating Physician | |||
| Male | 152 (54.9) | 180 (75.6) | < 0.001 |
| Works in city with 25,000 population or less | 71 (26.4) | 84 (35.3) | 0.03 |
| Sees more than 150 patients/week | 39 (14.1) | 47 (20.3) | 0.06 |
| Works in solo practice | 53 (20.3) | 79 (34.4) | 0.001 |
| In practice for 20 years or more | 60 (22.8) | 69 (29.9) | 0.08 |
| Management | |||
| Diagnosis of strep throat, tonsillitis, or pharyngitis | 91 (28.9) | 117 (38.6) | 0.01 |
| Antibiotic prescribed | 88 (27.9) | 85 (28.1) | 0.96 |
| Unnecessary antibiotic | 48 (16.1) | 61 (20.4) | 0.17 |
| * Some totals < 317 in the control group and < 304 in the intervention group because data for individual items were missing. | |||
TABLE 2
ASSOCIATION BETWEEN INDIVIDUAL PHYSICIAN FACTORS* AND ANTIBIOTIC PRESCRIBING, ADJUSTING FOR THE CLUSTERING OF PATIENTS BY PHYSICIAN
| Prescribing Outcome | ||
|---|---|---|
| Physician Factor | Unnecessary Antibiotic Prescribed OR (95% CI) | Total Antibiotics Prescribed OR (95% CI) |
| Male | 1.48 (0.73, 2.99) | 1.60 (0.87, 2.94) |
| Works in city with 25,000 population or less | 1.71 (0.90, 3.24) | 2.03 (1.07, 3.85) |
| Sees more than 150 patients/week | 2.20 (1.22, 3.98) | 2.53 (1.26, 5.08) |
| Works in a solo practice | 0.65 (0.35, 1.21) | 0.53 (0.27, 1.03) |
| In practice for 20 years or more | 2.25 (1.16, 4.37) | 1.89 (0.95, 3.76) |
| *Based on 88 physicians who completed a practice survey. Not all MDs answered all questions. | ||
| CI denotes confidence interval; OR, odds ratio. | ||
TABLE 3
EFFECT OF REPEATED CHART PROMPTS ON PRESCRIBING RATES, ADJUSTING FOR PHYSICIAN FACTORS AND CLUSTERING* OF PATIENTS BY PHYSICIAN (N = 453†)
| Variable | Total Antibiotic Prescriptions (95% CI) | Unnecessary Antibiotic Prescriptions (95% CI) |
|---|---|---|
| Intervention | 0.57 (0.27, 1.17)‡ | 0.76 (0.42, 1.40) |
| Male | 1.33 (0.66, 2.68) | — |
| Practices in a city with a population of 25,000 or less | 1.58 (0.73, 3.44) | 1.13 (0.58, 2.22) |
| Sees >150 patients/week | 2.17 (0.87, 5.41) | 1.55 (0.78, 3.07) |
| Works in solo practice | 0.43 (0.18, 1.05) | — |
| In practice for 20 years or more | 1.68 (0.72, 3.92) | 2.20 (1.09, 4.43) |
| Diagnosis of strep throat, tonsillitis, or pharyngitis | 7.56 (3.89, 14.71) | 3.06 (1.66, 5.65) |
| * The average patient cluster per physician was 3 (range 1 to 8). | ||
| † Number of observations < 621 because not all physicians completed practice surveys and some who did reply left some questions unanswered. | ||
| ‡ Odds ratio. | ||
Figure
FAMILY PHYSICIANS WHO WERE CONTACTED AND WHO COMPLETED THE STUDY
Discussion
The use of repeated chart prompt reminders to family physicians to use a clinical scoring approach in the management of children and adults presenting with URTI and a sore throat did not affect unnecessary antibiotic prescriptions or overall antibiotic use. Problems encountered in conducting this community-based trial may have contributed to the negative result.
Sixty-seven (41%) physicians agreed to be randomized but failed to complete the study. These losses after randomization and the differing sizes of the patient clusters per physician led to differences in the characteristics of the treating physician between the 2 groups. Characteristics associated with higher antibiotic prescribing rates were more common in the intervention group. As a result, despite the randomized design, the 2 patient groups were not initially similar in terms of their likelihood to receive a prescription for an antibiotic. To compensate for these differences, we controlled for the different physician characteristics in the analysis. However, the large number of physician dropouts also resulted in a failure to achieve the planned sample size. As a result, the study had insufficient power to detect the effect size that had been hypothesized.
We had planned the sample size to detect a 30% decrease in unnecessary antibiotic use. The adjusted analysis produced a point estimate of a 23% decrease in unnecessary antibiotic use and a 43% decrease in overall antibiotic use. These point estimates are the same whether or not the clustering is taken into effect; however, the more appropriate clustered analysis increases the estimate for the sample variance, resulting in wider confidence intervals. Examination of the lower 95% confidence interval reveals that the study lacked sufficient power to rule out as much as a 58% reduction in unnecessary antibiotic use. Therefore, while the study failed to find a statistically significant effect from the intervention, it also did not have the power to rule out a clinically important reduction in unnecessary antibiotic use.
We gave information about the clinical scoring approach to physicians in the control group. Doing so may have reduced the study’s ability to detect an effect of the intervention. We did not include a group that had been not exposed to information because we believed that mailed information was the equivalent of “standard” care in terms of changing physician behavior. Mailed information is a common method of informing physicians about new clinical information but has a limited ability to influence clinical behavior.34 However, the rate of antibiotic prescribing in the control group was indeed somewhat lower than is generally reported in the literature.9 This finding may be compatible with volunteer bias or the Hawthorne effect. More likely, perhaps, asking the control group to complete encounter forms for multiple patients may have inadvertently reminded them about the score. As a result, the control group may have been contaminated from repeated clinical prompts.
Some problems encountered in this study have been noted by other investigators conducting community-based research in primary care.37 The difficulty of retaining community-based physicians resulted in significant losses after randomization. This situation occurred even though qualifying to be randomized required physicians to mail back a reply card indicating that they wished to participate, suggesting that they were motivated to some degree.37 In addition, they received a modest cash honorarium. Some physicians returned the package stating that circumstances had changed and they would be unable to participate. Many who initially agreed to participate failed to reply despite 3 mailed reminders. The level of dropouts did not become apparent until late in the study. In retrospect, it might have been advisable to phone physicians directly soon after randomization in order to detect problems early. Other physicians could then have been randomly selected from the general membership listing to replace those who had dropped out.
This study found that repeated reminders to physicians to use a clinical score in the management of their patients with a sore throat did not reduce unnecessary antibiotic use. The problems encountered in this community-based intervention trial may have contributed to the negative result. Studies of prescribing behavior may need to stratify physicians before randomization by characteristics, such as patient volume and experience, that are related to prescribing behavior. Including a group that received no information is probably necessary to allow the greatest chance of detecting an effect. Particular attention and resources need to be available to ensure the retention, and replacement if needed, of community-based family physicians participating in research studies.
Acknowledgments
This study was supported by a grant from the Medical Research Council of Canada, Grant No. MA-15088. Dr McIsaac’s work is supported by the Mt. Sinai Hospital and the Family Healthcare Research Unit of the Department of Family and Community Medicine, University of Toronto, Toronto, Canada. This study was conducted in conjunction with the National Research System of the College of Family Physicians of Canada. The cooperation of the Ontario Association of Medical Laboratories is gratefully acknowledged.
1. Seppälä H, Nissinen A, Järvinen H, et al. Resistance to erythromycin in group A streptococci. N Engl J Med 1992;326:292-7.
2. Chen DK, McGeer A, de Azavedo JC, Low DE. Decreased susceptibility of Streptococcus pneumoniae. to fluoroquinolones in Canada. N Engl J Med 1999;341:233-9.
3. Magee JT, Pritchard EL, Fitzgerald KA, Dunstan FDJ, Howard AJ. Antibiotic prescribing and antibiotic resistance in community practice: retrospective study, 1996-8. BMJ 1999;319:1239-40.
4. Arason VA, Kristinsson KG, Sigurdsson JA, Stefánsdóttir G, Mölstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin rate of penicillin resistant pneumococci in children? Cross sectional prevalence study. BMJ 1996;313:387-91.
5. Seppälä H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in Group A streptococci in Finland. N Engl J Med 1997;337:441-6.
6. Bass JW, Weisse ME, Plymyer MR, Murphy S, Eberly BJ. Decline of erythromycin resistance of Group A beta-hemolytic streptococci in Japan. Arch Pediatr Adolesc Med 1994;148:67-71.
7. Wise R, Hart T, Cars O, et al. Antimicrobial resistance is a major threat to public health. BMJ 1998;317:610-11.
8. Schwartz B, Bell DM, Hughes JM. Preventing the emergence of antimicrobial resistance. A call for action by clinicians, public health officials, and patients. JAMA 1997;278:944-5.
9. McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995;273:214-9.
10. Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA 1997;278:901-4.
11. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998;279:875-7.
12. Brumfit W, O’Grady F, Slator JDH. Benign streptococcal sore throat. Lancet 1959;2:419-23.
13. Little PS, Williamson I. Are antibiotics appropriate for sore throats? Costs outweigh benefits. BMJ 1994;309:1010-2.
14. Graham A, Fahey T. Sore throat: diagnostic and therapeutic dilemmas. BMJ 1999;319:173-4.
15. Dajani A, Taubert K, Ferrieri P, Peter G, Shulman S. Treatment of acute streptococcal pharyngitis and prevention of rheumatic fever: A statement for health professionals. Pediatrics 1995;96:758-64.
16. Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH. Diagnosis and management of group A streptococcal pharyngitis: a practice guideline. Clin Infect Dis 1997;25:574-83.
17. Hart WJ. Streptococcal pharyngitis. A demonstration of the inaccuracy of clinical diagnosis without culture. Can Fam Physician 1976;22:34-9.
18. Shank JC, Powell TA. A five-year experience with throat cultures. J Fam Pract 1984;18:857-63.
19. McIsaac WJ, White D, Tannenbaum D, Low DE. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. CMAJ 1998;158:75-83.
20. Touw-Otten FWMM, Johansen KS. Diagnosis, antibiotic treatment and outcome of acute tonsillitis: report of a WHO regional office for Europe study in 17 European countries. Fam Pract 1992;9:255-62.
21. Poses RM, Cebul RD, Collins M, Fager SS. The accuracy of experienced physicians’ probability estimates for patients with sore throats. Implications for decision making. JAMA 1985;254:925-9.
22. McIsaac WJ, Butler CC. Does clinical error contribute to unnecessary antibiotic use? Med Decis Making 2000;20:33-8.
23. Walsh BT, Bookheim WW, Johnson RC, Tompkins RK. Recognition of streptococcal pharyngitis in adults. Arch Intern Med 1975;135:1493-7.
24. Breese BB. A simple scorecard for the tentative diagnosis of streptococcal pharyngitis. Am J Dis Child 1977;131:514-17.
25. Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making 1981;1:239-46.
26. Fujikawa S, Ito Y. A new scoring system for diagnosis of streptopharyngitis. Jpn Circ J 1985;49:1258-61.
27. Komaroff AL, Pass TM, Aronson MD, et al. The prediction of streptococcal pharyngitis in adults. J Gen Intern Med 1986;1:1-7.
28. Hoffman S. An algorithm for a selective use of throat swabs in the diagnosis of group A streptococcal pharyngo-tonsillitis in general practice. Scand J Prim Health Care 1992;10:295-300.
29. Meland E, Digranes A, Skjærven R. Assessment of clinical features predicting streptococcal pharyngitis. Scand J Infect Dis 1993;25:177-83.
30. Dobbs F. A scoring system for predicting group A streptococcal infection. Br J Gen Pract 1996;46:461-4.
31. Poses RM, Cebul RD, Wigton RS. You can lead a horse to water: improving physicians’ knowledge of probabilities may not affect their decisions. Med Decis Making 1995;15:65-76.
32. McIsaac WJ, Goel V, To T, Low DE. The validity of a sore throat score in family practice. CMAJ 2000;163:811-5.
33. McIsaac WJ, Goel V. Effect of an explicit decision-support tool on decisions to prescribe antibiotics for sore throat. Med Decis Making 1998;18(2):220-8.
34. Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA 1995;274:700-5.
35. Rosser WW, McDowell I, Newell C. Use of reminders for prevention procedures in family medicine. CMAJ 1991;145:807-13.
36. Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ, Donner A. Evaluation of health interventions at area and organisation level. BMJ 1999;319:376-9.
37. Rogers S, Humphrey C, Nazareth I, Lister S, Tomlin Z, Haines A. Designing trials of interventions to change professional practice in primary care: lessons from an exploratory study of two change strategies. BMJ 2000;320:1580-3.
OBJECTIVES: Infections with group A streptococcus (GAS) occur in 10% to 20% of patients with sore throats, whereas antibiotics are prescribed 50% of the time. Clinical scoring rules can more accurately predict the likelihood of GAS infection, but whether family physicians will adopt such approaches is unclear. This study sought to determine whether repeated clinical prompts to use a scoring approach could help family physicians lower antibiotic use in patients with a sore throat.
STUDY DESIGN: Randomized trial in which physicians were assigned to use either (1) chart stickers that prompted them to calculate a score based on clinical findings and provided management recommendations linked to score totals or (2) a clinical checklist.
POPULATION: Ninety-seven family physicians in Ontario, Canada, assessed 621 children and adults with sore throat and obtained a throat swab for culture.
OUTCOMES MEASURED: (1) Unnecessary antibiotic prescriptions given to patients with a negative throat culture and (2) overall antibiotic use.
RESULTS: There were no differences between the control and intervention group in unnecessary antibiotic prescriptions (16.1% vs 20.4%, respectively, P = .29) or overall antibiotic use (27.9% vs 28.1%, P = .97). However, a number of physicians dropped out of the study; as a result, the characteristics of the physicians in the 2 groups were dissimilar in factors related to prescribing. After adjusting for these differences and patient clustering by physician, the odds ratio for the effect of the intervention on unnecessary antibiotic prescriptions was 0.76 (95% confidence interval [CI] = 0.42, 1.40) and 0.57 for overall antibiotic use (95% CI = 0.27, 1.17).
CONCLUSIONS: Chart prompts during clinical encounters to use a clinical score in the assessment of patients with a sore throat did not reduce unnecessary antibiotic prescribing by family physicians. The problems encountered in conducting this community-based intervention trial are discussed in relation to the negative result.
- Repeated chart prompts to use a clinical prediction rule for the management of children and adults with a sore throat did not help family physicians decrease unnecessary antibiotic use.
- Several problems in the conduct of this community-based intervention trial rather than a lack of the effectiveness of the intervention may have contributed to the negative result.
In the past decade, bacterial resistance to commonly used antibiotics has risen dramatically.1,2 While a number of factors have contributed to this problem, overuse of antibiotics by physicians has been implicated.3-6 An association has been demonstrated between the volume of antibiotic prescriptions and bacterial resistance at both a national4,5 and a local level.3 Where prescribing by physicians has been reduced, rates of antibiotic resistance have subsequently been observed to decline.5,6 As a result, physicians have been urged to reduce their use of antibiotics.7,8 Respiratory infections are the most common reason for the prescribing of antibiotics.9 Upper respiratory tract infections (URTIs) and pharyngitis account for 19% to 28% of all antibiotic prescriptions written by family physicians.9-11
While the use of antibiotics for URTI with sore throat is frequently debated,12-14 experts continue to recommend such treatment for group A streptococcus (GAS) infections to prevent rheumatic fever.15,16 However, only 10% to 20% of patients with a sore throat who visit a family physician have a GAS infection,17-19 whereas antibiotics are prescribed for 50% of URTIs10 and 90% of cases of tonsillitis.20 Uncertainty as to whether or not a bacterial infection is present and clinical error in estimating the likelihood of a GAS infection are associated with the unnecessary prescription of antibiotics.21,22 To address clinical uncertainty, a number of prediction rules and clinical scores have been proposed.23-30 However, physicians taught simply to generate more accurate estimates of the likelihood of a strep infection in this manner do not necessarily lower their use of antibiotics.31
We have previously shown that linking score estimates for the likelihood of a GAS infection to explicit management recommendations to take a throat swab or prescribe an antibiotic has the potential to lower antibiotic use significantly.19,32 In an observational study involving 621 children and adults, this approach would have reduced unnecessary antibiotic prescriptions by 63%.32 We also found a trend toward reduced antibiotic use when physicians were provided with an explicit reminder about the score approach.33 As a result, we hypothesized that this might also help physicians to learn to adopt the sore throat score approach. Reminders have been found to improve the delivery of preventive health services.34,35 The objective of this study was to determine whether repeated clinical prompts to community-based family physicians about the score approach could reduce unnecessary antibiotic prescriptions and lower overall antibiotic use for patients with a sore throat.
Methods
In the fall of 1998, a sample of family physicians in the province of Ontario were invited to participate in a trial to reduce antibiotic use in patients with a sore throat. Physicians who had previously participated in practice-based research projects for the College of Family Physicians of Canada and a random sample from the College’s general membership listing were contacted. Those who mailed back a reply card indicating that they wished to participate were randomized to either an intervention or a control group. The study was approved by the University of Toronto Ethics Review Committee.
Both groups of physicians received, by mail, an article describing the clinical score management approach19; a laminated pocket card summarizing the method; clinical encounter and patient consent forms; and a 1-page survey of practice characteristics. Each physician was asked to enroll 8 patients aged 3 years or older whom they believed to have a new URTI with a sore throat. No attempt was made to further define an eligible presentation to encourage physicians to enroll cases representative of their usual practice. Patients were ineligible if they had taken antibiotics during the previous week, were immunocompromised, or could not understand English. Parents were asked to provide consent for children younger than 16 years of age.
A brief standardized assessment form was completed by the physician for each patient and a throat swab was obtained. The throat swab was submitted to the physician’s local laboratory. A copy of the culture result was forwarded to the study center. Treatment decisions and the management of subsequent culture results were the responsibility of the treating physician.
In the intervention group, physicians were provided with a sticker to apply to the encounter form that listed the score management approach. The sticker contained boxes to be checked by the physicians to calculate the score total and determine appropriate management. Physicians not wishing to use the sticker were prompted on the form to write the score total in a space provided. As a result, physicians in the intervention group received repeated prompts that reminded them to use the score approach each time they completed a clinical encounter form. The control group completed a similar form but without either the sticker or the chart prompts.
The details of the clinical score approach have been previously published.19,25 Briefly, 4 clinical findings (fever > 38°C, absence of cough, tender anterior cervical adenopathy, tonsillar swelling or exudate) and age < 15 years are each assigned 1 point and totaled. One point is subtracted for age 45 years or more. Explicit recommendations for management are linked to score totals. If the score total is 1 or less, no throat swab or antibiotic is indicated. A throat swab is recommended for a score of 2 or 3 and an antibiotic only if the culture is positive. Either initiating treatment with an antibiotic or taking a throat swab is appropriate for a score of 4 or more.
The main outcome for the study was the prescription of unnecessary antibiotics, defined as a prescription for antibiotic medication given to a patient whose subsequent throat culture was negative for group A streptococcus. The secondary outcome was overall antibiotic use. The sample size was calculated to detect a 30% decrease in unnecessary antibiotic use (2-sided = 0.05, 1- = 0.90), assuming a 40% baseline prescription rate9 and a 70% negative culture rate.1719 Because groups of patients were treated by the same physician, the sample size was adjusted to take the clustered sampling design into account.36 The intraclass correlation coefficient for prescribing estimated from an earlier study was 0.07.19 Assuming an average of 5 patients assessed per physician, the sample size was estimated to be 85 physicians and 425 patients in each group.
The clinical characteristics of patients in the intervention and control groups were compared with a chi-square test for categorical variables and a t-test for continuous variables. Associations between prescription rates and the practice and demographic characteristics of the physicians were assessed and adjusted for the clustered sampling with Stata Statistical Software (Release 6, Stata Corp., College Station, Tex.). While clustering improves the efficiency of sampling by requiring participation by fewer physicians, confidence intervals that do not account for the design effect are too narrow. Multiple logistic regression was used to adjust for differences in patient and physician characteristics, taking into account the patient clusters by physician in estimating the effect of the intervention.
Results
One hundred sixty-four physicians agreed to participate and were randomized. Of these, only 97 (59.1%) completed the study and provided patient data (Figure). An equal proportion of physicians in the intervention group (40.2%) and control group (41.5%, P = .87) failed to complete the study. No significant differences were identified between the sex or age of physicians who participated and those who did not participate. Of the participating physicians, 86 (84.3%) returned surveys describing their practice settings.
Patients assessed included 692 children and adults. Of these, 71 (10.3%) were excluded because of a diagnosis of bronchitis (35), sinusitis (16), otitis media (11), or pneumonia (4) or because the patient was less than 3 years old (5). The score approach did not apply to the 4 conditions of exclusion because they involve organisms other than GAS. The remaining 621 patients in the control and intervention groups were similar in demographic and clinical characteristics as well as regarding the prevalence of GAS as documented by throat culture (Table 1). However, a diagnosis of tonsillitis, strep throat, or pharyngitis was more likely to occur in the intervention group (38.6%) than in the control group (28.9%, P = .01). These diagnoses were associated with a higher rate of antibiotic prescribing (54.8%) than were situations in which physicians recorded a URTI or other diagnosis (14.2%, P < .001).
Differences were noted in the characteristics of the treating physicians in each group when considered by patient encounter. Although there were no differences in the age or sex of individual physicians in each group, the participating physicians did not contribute equal numbers of patient encounters. The average number of patients assessed per physician was 3, ranging from a low of 1 patient contributed by some physicians to a high of 8 for others. More patient encounters in the intervention group were contributed by male physicians who had been in practice longer, who worked in smaller communities, and who reported larger practice volumes (Table 1). Physicians from small communities were more likely to diagnose strep throat, tonsillitis, or pharyngitis than were those in larger communities (45.1% vs 28.1%, respectively, P < .001), as were those with higher patient volumes (46.5% vs 30.2%, P = .003).
Certain physician practice characteristics were associated with a patient’s being more likely to receive a prescription for an unnecessary antibiotic (Table 2). For example, physicians were more likely to prescribe unnecessary antibiotics if they saw more than 150 patients per week than if they saw fewer and if they had been in practice for 20 or more years than if they had practiced for a shorter time. In addition, higher overall antibiotic use was associated with higher patient volume and with practicing in a smaller community.
There were no differences between the intervention and control groups in either unnecessary antibiotic prescriptions (20.4% vs 16.1%, respectively, P = .17) or overall antibiotic use (28.1% vs 27.9%, P = .96) (Table 1). However, while the culture reports that were needed to classify prescriptions as unnecessary were available for most (600) patients (96.6%), significantly more culture reports were missing in the control group (5.4%) than in the intervention group (1.2%, P = .007). Antibiotics were prescribed in 59% of the 17 cases with missing culture reports in the control group but for none of the 4 cases with missing culture reports in the intervention group.
Because intervention patients were more likely than controls to have been treated by physicians with higher prescribing characteristics, adjustments were made for the differing physician characteristics and diagnostic practices and for the clustering of patients by physician, using multiple logistic regression (Table 3). After adjustment, the intervention was associated with a nonsignificant reduction in unnecessary antibiotic prescriptions (odds ratio [OR] = 0.76, 95% confidence interval [CI] = 0.42, 1.40) and in overall antibiotic use (OR = 0.57, 95% CI = 0.27, 1.17).
TABLE 1
COMPARISON OF PATIENTS IN CONTROL AND INTERVENTION GROUPS
| Characteristics | Control Group (n = 317) (%) | Intervention Group (n = 304) (%) | P |
|---|---|---|---|
| Demographic Features | |||
| Mean age | 28.1 years | 27.5 years | 0.70 |
| Female | 217 (69.1)* | 198 (65.4) | 0.32 |
| Assessed October-December | 217 (68.4) | 189 (62.2) | 0.10 |
| Clinical Findings | |||
| Sore throat | 296 (93.4) | 283 (93.1) | 0.89 |
| Runny or stuffy nose | 201 (63.6) | 195 (64.4) | 0.85 |
| Cough | 206 (65.2) | 199 (65.7) | 0.90 |
| Red throat | 220 (70.3) | 207 (69.5) | 0.82 |
| Tonsillar swelling | 88 (28.0) | 90 (30.0) | 0.59 |
| Tonsillar exudate | 51 (16.3) | 51 (17.1) | 0.82 |
| Cervical adenopathy | 131 (41.7) | 127 (42.5) | 0.85 |
| Appears unwell | 81 (25.9) | 89 (29.9) | 0.27 |
| Disease | |||
| Prevalence of group A streptococcus | 50 (16.7) | 52 (17.3) | 0.83 |
| Treating Physician | |||
| Male | 152 (54.9) | 180 (75.6) | < 0.001 |
| Works in city with 25,000 population or less | 71 (26.4) | 84 (35.3) | 0.03 |
| Sees more than 150 patients/week | 39 (14.1) | 47 (20.3) | 0.06 |
| Works in solo practice | 53 (20.3) | 79 (34.4) | 0.001 |
| In practice for 20 years or more | 60 (22.8) | 69 (29.9) | 0.08 |
| Management | |||
| Diagnosis of strep throat, tonsillitis, or pharyngitis | 91 (28.9) | 117 (38.6) | 0.01 |
| Antibiotic prescribed | 88 (27.9) | 85 (28.1) | 0.96 |
| Unnecessary antibiotic | 48 (16.1) | 61 (20.4) | 0.17 |
| * Some totals < 317 in the control group and < 304 in the intervention group because data for individual items were missing. | |||
TABLE 2
ASSOCIATION BETWEEN INDIVIDUAL PHYSICIAN FACTORS* AND ANTIBIOTIC PRESCRIBING, ADJUSTING FOR THE CLUSTERING OF PATIENTS BY PHYSICIAN
| Prescribing Outcome | ||
|---|---|---|
| Physician Factor | Unnecessary Antibiotic Prescribed OR (95% CI) | Total Antibiotics Prescribed OR (95% CI) |
| Male | 1.48 (0.73, 2.99) | 1.60 (0.87, 2.94) |
| Works in city with 25,000 population or less | 1.71 (0.90, 3.24) | 2.03 (1.07, 3.85) |
| Sees more than 150 patients/week | 2.20 (1.22, 3.98) | 2.53 (1.26, 5.08) |
| Works in a solo practice | 0.65 (0.35, 1.21) | 0.53 (0.27, 1.03) |
| In practice for 20 years or more | 2.25 (1.16, 4.37) | 1.89 (0.95, 3.76) |
| *Based on 88 physicians who completed a practice survey. Not all MDs answered all questions. | ||
| CI denotes confidence interval; OR, odds ratio. | ||
TABLE 3
EFFECT OF REPEATED CHART PROMPTS ON PRESCRIBING RATES, ADJUSTING FOR PHYSICIAN FACTORS AND CLUSTERING* OF PATIENTS BY PHYSICIAN (N = 453†)
| Variable | Total Antibiotic Prescriptions (95% CI) | Unnecessary Antibiotic Prescriptions (95% CI) |
|---|---|---|
| Intervention | 0.57 (0.27, 1.17)‡ | 0.76 (0.42, 1.40) |
| Male | 1.33 (0.66, 2.68) | — |
| Practices in a city with a population of 25,000 or less | 1.58 (0.73, 3.44) | 1.13 (0.58, 2.22) |
| Sees >150 patients/week | 2.17 (0.87, 5.41) | 1.55 (0.78, 3.07) |
| Works in solo practice | 0.43 (0.18, 1.05) | — |
| In practice for 20 years or more | 1.68 (0.72, 3.92) | 2.20 (1.09, 4.43) |
| Diagnosis of strep throat, tonsillitis, or pharyngitis | 7.56 (3.89, 14.71) | 3.06 (1.66, 5.65) |
| * The average patient cluster per physician was 3 (range 1 to 8). | ||
| † Number of observations < 621 because not all physicians completed practice surveys and some who did reply left some questions unanswered. | ||
| ‡ Odds ratio. | ||
Figure
FAMILY PHYSICIANS WHO WERE CONTACTED AND WHO COMPLETED THE STUDY
Discussion
The use of repeated chart prompt reminders to family physicians to use a clinical scoring approach in the management of children and adults presenting with URTI and a sore throat did not affect unnecessary antibiotic prescriptions or overall antibiotic use. Problems encountered in conducting this community-based trial may have contributed to the negative result.
Sixty-seven (41%) physicians agreed to be randomized but failed to complete the study. These losses after randomization and the differing sizes of the patient clusters per physician led to differences in the characteristics of the treating physician between the 2 groups. Characteristics associated with higher antibiotic prescribing rates were more common in the intervention group. As a result, despite the randomized design, the 2 patient groups were not initially similar in terms of their likelihood to receive a prescription for an antibiotic. To compensate for these differences, we controlled for the different physician characteristics in the analysis. However, the large number of physician dropouts also resulted in a failure to achieve the planned sample size. As a result, the study had insufficient power to detect the effect size that had been hypothesized.
We had planned the sample size to detect a 30% decrease in unnecessary antibiotic use. The adjusted analysis produced a point estimate of a 23% decrease in unnecessary antibiotic use and a 43% decrease in overall antibiotic use. These point estimates are the same whether or not the clustering is taken into effect; however, the more appropriate clustered analysis increases the estimate for the sample variance, resulting in wider confidence intervals. Examination of the lower 95% confidence interval reveals that the study lacked sufficient power to rule out as much as a 58% reduction in unnecessary antibiotic use. Therefore, while the study failed to find a statistically significant effect from the intervention, it also did not have the power to rule out a clinically important reduction in unnecessary antibiotic use.
We gave information about the clinical scoring approach to physicians in the control group. Doing so may have reduced the study’s ability to detect an effect of the intervention. We did not include a group that had been not exposed to information because we believed that mailed information was the equivalent of “standard” care in terms of changing physician behavior. Mailed information is a common method of informing physicians about new clinical information but has a limited ability to influence clinical behavior.34 However, the rate of antibiotic prescribing in the control group was indeed somewhat lower than is generally reported in the literature.9 This finding may be compatible with volunteer bias or the Hawthorne effect. More likely, perhaps, asking the control group to complete encounter forms for multiple patients may have inadvertently reminded them about the score. As a result, the control group may have been contaminated from repeated clinical prompts.
Some problems encountered in this study have been noted by other investigators conducting community-based research in primary care.37 The difficulty of retaining community-based physicians resulted in significant losses after randomization. This situation occurred even though qualifying to be randomized required physicians to mail back a reply card indicating that they wished to participate, suggesting that they were motivated to some degree.37 In addition, they received a modest cash honorarium. Some physicians returned the package stating that circumstances had changed and they would be unable to participate. Many who initially agreed to participate failed to reply despite 3 mailed reminders. The level of dropouts did not become apparent until late in the study. In retrospect, it might have been advisable to phone physicians directly soon after randomization in order to detect problems early. Other physicians could then have been randomly selected from the general membership listing to replace those who had dropped out.
This study found that repeated reminders to physicians to use a clinical score in the management of their patients with a sore throat did not reduce unnecessary antibiotic use. The problems encountered in this community-based intervention trial may have contributed to the negative result. Studies of prescribing behavior may need to stratify physicians before randomization by characteristics, such as patient volume and experience, that are related to prescribing behavior. Including a group that received no information is probably necessary to allow the greatest chance of detecting an effect. Particular attention and resources need to be available to ensure the retention, and replacement if needed, of community-based family physicians participating in research studies.
Acknowledgments
This study was supported by a grant from the Medical Research Council of Canada, Grant No. MA-15088. Dr McIsaac’s work is supported by the Mt. Sinai Hospital and the Family Healthcare Research Unit of the Department of Family and Community Medicine, University of Toronto, Toronto, Canada. This study was conducted in conjunction with the National Research System of the College of Family Physicians of Canada. The cooperation of the Ontario Association of Medical Laboratories is gratefully acknowledged.
OBJECTIVES: Infections with group A streptococcus (GAS) occur in 10% to 20% of patients with sore throats, whereas antibiotics are prescribed 50% of the time. Clinical scoring rules can more accurately predict the likelihood of GAS infection, but whether family physicians will adopt such approaches is unclear. This study sought to determine whether repeated clinical prompts to use a scoring approach could help family physicians lower antibiotic use in patients with a sore throat.
STUDY DESIGN: Randomized trial in which physicians were assigned to use either (1) chart stickers that prompted them to calculate a score based on clinical findings and provided management recommendations linked to score totals or (2) a clinical checklist.
POPULATION: Ninety-seven family physicians in Ontario, Canada, assessed 621 children and adults with sore throat and obtained a throat swab for culture.
OUTCOMES MEASURED: (1) Unnecessary antibiotic prescriptions given to patients with a negative throat culture and (2) overall antibiotic use.
RESULTS: There were no differences between the control and intervention group in unnecessary antibiotic prescriptions (16.1% vs 20.4%, respectively, P = .29) or overall antibiotic use (27.9% vs 28.1%, P = .97). However, a number of physicians dropped out of the study; as a result, the characteristics of the physicians in the 2 groups were dissimilar in factors related to prescribing. After adjusting for these differences and patient clustering by physician, the odds ratio for the effect of the intervention on unnecessary antibiotic prescriptions was 0.76 (95% confidence interval [CI] = 0.42, 1.40) and 0.57 for overall antibiotic use (95% CI = 0.27, 1.17).
CONCLUSIONS: Chart prompts during clinical encounters to use a clinical score in the assessment of patients with a sore throat did not reduce unnecessary antibiotic prescribing by family physicians. The problems encountered in conducting this community-based intervention trial are discussed in relation to the negative result.
- Repeated chart prompts to use a clinical prediction rule for the management of children and adults with a sore throat did not help family physicians decrease unnecessary antibiotic use.
- Several problems in the conduct of this community-based intervention trial rather than a lack of the effectiveness of the intervention may have contributed to the negative result.
In the past decade, bacterial resistance to commonly used antibiotics has risen dramatically.1,2 While a number of factors have contributed to this problem, overuse of antibiotics by physicians has been implicated.3-6 An association has been demonstrated between the volume of antibiotic prescriptions and bacterial resistance at both a national4,5 and a local level.3 Where prescribing by physicians has been reduced, rates of antibiotic resistance have subsequently been observed to decline.5,6 As a result, physicians have been urged to reduce their use of antibiotics.7,8 Respiratory infections are the most common reason for the prescribing of antibiotics.9 Upper respiratory tract infections (URTIs) and pharyngitis account for 19% to 28% of all antibiotic prescriptions written by family physicians.9-11
While the use of antibiotics for URTI with sore throat is frequently debated,12-14 experts continue to recommend such treatment for group A streptococcus (GAS) infections to prevent rheumatic fever.15,16 However, only 10% to 20% of patients with a sore throat who visit a family physician have a GAS infection,17-19 whereas antibiotics are prescribed for 50% of URTIs10 and 90% of cases of tonsillitis.20 Uncertainty as to whether or not a bacterial infection is present and clinical error in estimating the likelihood of a GAS infection are associated with the unnecessary prescription of antibiotics.21,22 To address clinical uncertainty, a number of prediction rules and clinical scores have been proposed.23-30 However, physicians taught simply to generate more accurate estimates of the likelihood of a strep infection in this manner do not necessarily lower their use of antibiotics.31
We have previously shown that linking score estimates for the likelihood of a GAS infection to explicit management recommendations to take a throat swab or prescribe an antibiotic has the potential to lower antibiotic use significantly.19,32 In an observational study involving 621 children and adults, this approach would have reduced unnecessary antibiotic prescriptions by 63%.32 We also found a trend toward reduced antibiotic use when physicians were provided with an explicit reminder about the score approach.33 As a result, we hypothesized that this might also help physicians to learn to adopt the sore throat score approach. Reminders have been found to improve the delivery of preventive health services.34,35 The objective of this study was to determine whether repeated clinical prompts to community-based family physicians about the score approach could reduce unnecessary antibiotic prescriptions and lower overall antibiotic use for patients with a sore throat.
Methods
In the fall of 1998, a sample of family physicians in the province of Ontario were invited to participate in a trial to reduce antibiotic use in patients with a sore throat. Physicians who had previously participated in practice-based research projects for the College of Family Physicians of Canada and a random sample from the College’s general membership listing were contacted. Those who mailed back a reply card indicating that they wished to participate were randomized to either an intervention or a control group. The study was approved by the University of Toronto Ethics Review Committee.
Both groups of physicians received, by mail, an article describing the clinical score management approach19; a laminated pocket card summarizing the method; clinical encounter and patient consent forms; and a 1-page survey of practice characteristics. Each physician was asked to enroll 8 patients aged 3 years or older whom they believed to have a new URTI with a sore throat. No attempt was made to further define an eligible presentation to encourage physicians to enroll cases representative of their usual practice. Patients were ineligible if they had taken antibiotics during the previous week, were immunocompromised, or could not understand English. Parents were asked to provide consent for children younger than 16 years of age.
A brief standardized assessment form was completed by the physician for each patient and a throat swab was obtained. The throat swab was submitted to the physician’s local laboratory. A copy of the culture result was forwarded to the study center. Treatment decisions and the management of subsequent culture results were the responsibility of the treating physician.
In the intervention group, physicians were provided with a sticker to apply to the encounter form that listed the score management approach. The sticker contained boxes to be checked by the physicians to calculate the score total and determine appropriate management. Physicians not wishing to use the sticker were prompted on the form to write the score total in a space provided. As a result, physicians in the intervention group received repeated prompts that reminded them to use the score approach each time they completed a clinical encounter form. The control group completed a similar form but without either the sticker or the chart prompts.
The details of the clinical score approach have been previously published.19,25 Briefly, 4 clinical findings (fever > 38°C, absence of cough, tender anterior cervical adenopathy, tonsillar swelling or exudate) and age < 15 years are each assigned 1 point and totaled. One point is subtracted for age 45 years or more. Explicit recommendations for management are linked to score totals. If the score total is 1 or less, no throat swab or antibiotic is indicated. A throat swab is recommended for a score of 2 or 3 and an antibiotic only if the culture is positive. Either initiating treatment with an antibiotic or taking a throat swab is appropriate for a score of 4 or more.
The main outcome for the study was the prescription of unnecessary antibiotics, defined as a prescription for antibiotic medication given to a patient whose subsequent throat culture was negative for group A streptococcus. The secondary outcome was overall antibiotic use. The sample size was calculated to detect a 30% decrease in unnecessary antibiotic use (2-sided = 0.05, 1- = 0.90), assuming a 40% baseline prescription rate9 and a 70% negative culture rate.1719 Because groups of patients were treated by the same physician, the sample size was adjusted to take the clustered sampling design into account.36 The intraclass correlation coefficient for prescribing estimated from an earlier study was 0.07.19 Assuming an average of 5 patients assessed per physician, the sample size was estimated to be 85 physicians and 425 patients in each group.
The clinical characteristics of patients in the intervention and control groups were compared with a chi-square test for categorical variables and a t-test for continuous variables. Associations between prescription rates and the practice and demographic characteristics of the physicians were assessed and adjusted for the clustered sampling with Stata Statistical Software (Release 6, Stata Corp., College Station, Tex.). While clustering improves the efficiency of sampling by requiring participation by fewer physicians, confidence intervals that do not account for the design effect are too narrow. Multiple logistic regression was used to adjust for differences in patient and physician characteristics, taking into account the patient clusters by physician in estimating the effect of the intervention.
Results
One hundred sixty-four physicians agreed to participate and were randomized. Of these, only 97 (59.1%) completed the study and provided patient data (Figure). An equal proportion of physicians in the intervention group (40.2%) and control group (41.5%, P = .87) failed to complete the study. No significant differences were identified between the sex or age of physicians who participated and those who did not participate. Of the participating physicians, 86 (84.3%) returned surveys describing their practice settings.
Patients assessed included 692 children and adults. Of these, 71 (10.3%) were excluded because of a diagnosis of bronchitis (35), sinusitis (16), otitis media (11), or pneumonia (4) or because the patient was less than 3 years old (5). The score approach did not apply to the 4 conditions of exclusion because they involve organisms other than GAS. The remaining 621 patients in the control and intervention groups were similar in demographic and clinical characteristics as well as regarding the prevalence of GAS as documented by throat culture (Table 1). However, a diagnosis of tonsillitis, strep throat, or pharyngitis was more likely to occur in the intervention group (38.6%) than in the control group (28.9%, P = .01). These diagnoses were associated with a higher rate of antibiotic prescribing (54.8%) than were situations in which physicians recorded a URTI or other diagnosis (14.2%, P < .001).
Differences were noted in the characteristics of the treating physicians in each group when considered by patient encounter. Although there were no differences in the age or sex of individual physicians in each group, the participating physicians did not contribute equal numbers of patient encounters. The average number of patients assessed per physician was 3, ranging from a low of 1 patient contributed by some physicians to a high of 8 for others. More patient encounters in the intervention group were contributed by male physicians who had been in practice longer, who worked in smaller communities, and who reported larger practice volumes (Table 1). Physicians from small communities were more likely to diagnose strep throat, tonsillitis, or pharyngitis than were those in larger communities (45.1% vs 28.1%, respectively, P < .001), as were those with higher patient volumes (46.5% vs 30.2%, P = .003).
Certain physician practice characteristics were associated with a patient’s being more likely to receive a prescription for an unnecessary antibiotic (Table 2). For example, physicians were more likely to prescribe unnecessary antibiotics if they saw more than 150 patients per week than if they saw fewer and if they had been in practice for 20 or more years than if they had practiced for a shorter time. In addition, higher overall antibiotic use was associated with higher patient volume and with practicing in a smaller community.
There were no differences between the intervention and control groups in either unnecessary antibiotic prescriptions (20.4% vs 16.1%, respectively, P = .17) or overall antibiotic use (28.1% vs 27.9%, P = .96) (Table 1). However, while the culture reports that were needed to classify prescriptions as unnecessary were available for most (600) patients (96.6%), significantly more culture reports were missing in the control group (5.4%) than in the intervention group (1.2%, P = .007). Antibiotics were prescribed in 59% of the 17 cases with missing culture reports in the control group but for none of the 4 cases with missing culture reports in the intervention group.
Because intervention patients were more likely than controls to have been treated by physicians with higher prescribing characteristics, adjustments were made for the differing physician characteristics and diagnostic practices and for the clustering of patients by physician, using multiple logistic regression (Table 3). After adjustment, the intervention was associated with a nonsignificant reduction in unnecessary antibiotic prescriptions (odds ratio [OR] = 0.76, 95% confidence interval [CI] = 0.42, 1.40) and in overall antibiotic use (OR = 0.57, 95% CI = 0.27, 1.17).
TABLE 1
COMPARISON OF PATIENTS IN CONTROL AND INTERVENTION GROUPS
| Characteristics | Control Group (n = 317) (%) | Intervention Group (n = 304) (%) | P |
|---|---|---|---|
| Demographic Features | |||
| Mean age | 28.1 years | 27.5 years | 0.70 |
| Female | 217 (69.1)* | 198 (65.4) | 0.32 |
| Assessed October-December | 217 (68.4) | 189 (62.2) | 0.10 |
| Clinical Findings | |||
| Sore throat | 296 (93.4) | 283 (93.1) | 0.89 |
| Runny or stuffy nose | 201 (63.6) | 195 (64.4) | 0.85 |
| Cough | 206 (65.2) | 199 (65.7) | 0.90 |
| Red throat | 220 (70.3) | 207 (69.5) | 0.82 |
| Tonsillar swelling | 88 (28.0) | 90 (30.0) | 0.59 |
| Tonsillar exudate | 51 (16.3) | 51 (17.1) | 0.82 |
| Cervical adenopathy | 131 (41.7) | 127 (42.5) | 0.85 |
| Appears unwell | 81 (25.9) | 89 (29.9) | 0.27 |
| Disease | |||
| Prevalence of group A streptococcus | 50 (16.7) | 52 (17.3) | 0.83 |
| Treating Physician | |||
| Male | 152 (54.9) | 180 (75.6) | < 0.001 |
| Works in city with 25,000 population or less | 71 (26.4) | 84 (35.3) | 0.03 |
| Sees more than 150 patients/week | 39 (14.1) | 47 (20.3) | 0.06 |
| Works in solo practice | 53 (20.3) | 79 (34.4) | 0.001 |
| In practice for 20 years or more | 60 (22.8) | 69 (29.9) | 0.08 |
| Management | |||
| Diagnosis of strep throat, tonsillitis, or pharyngitis | 91 (28.9) | 117 (38.6) | 0.01 |
| Antibiotic prescribed | 88 (27.9) | 85 (28.1) | 0.96 |
| Unnecessary antibiotic | 48 (16.1) | 61 (20.4) | 0.17 |
| * Some totals < 317 in the control group and < 304 in the intervention group because data for individual items were missing. | |||
TABLE 2
ASSOCIATION BETWEEN INDIVIDUAL PHYSICIAN FACTORS* AND ANTIBIOTIC PRESCRIBING, ADJUSTING FOR THE CLUSTERING OF PATIENTS BY PHYSICIAN
| Prescribing Outcome | ||
|---|---|---|
| Physician Factor | Unnecessary Antibiotic Prescribed OR (95% CI) | Total Antibiotics Prescribed OR (95% CI) |
| Male | 1.48 (0.73, 2.99) | 1.60 (0.87, 2.94) |
| Works in city with 25,000 population or less | 1.71 (0.90, 3.24) | 2.03 (1.07, 3.85) |
| Sees more than 150 patients/week | 2.20 (1.22, 3.98) | 2.53 (1.26, 5.08) |
| Works in a solo practice | 0.65 (0.35, 1.21) | 0.53 (0.27, 1.03) |
| In practice for 20 years or more | 2.25 (1.16, 4.37) | 1.89 (0.95, 3.76) |
| *Based on 88 physicians who completed a practice survey. Not all MDs answered all questions. | ||
| CI denotes confidence interval; OR, odds ratio. | ||
TABLE 3
EFFECT OF REPEATED CHART PROMPTS ON PRESCRIBING RATES, ADJUSTING FOR PHYSICIAN FACTORS AND CLUSTERING* OF PATIENTS BY PHYSICIAN (N = 453†)
| Variable | Total Antibiotic Prescriptions (95% CI) | Unnecessary Antibiotic Prescriptions (95% CI) |
|---|---|---|
| Intervention | 0.57 (0.27, 1.17)‡ | 0.76 (0.42, 1.40) |
| Male | 1.33 (0.66, 2.68) | — |
| Practices in a city with a population of 25,000 or less | 1.58 (0.73, 3.44) | 1.13 (0.58, 2.22) |
| Sees >150 patients/week | 2.17 (0.87, 5.41) | 1.55 (0.78, 3.07) |
| Works in solo practice | 0.43 (0.18, 1.05) | — |
| In practice for 20 years or more | 1.68 (0.72, 3.92) | 2.20 (1.09, 4.43) |
| Diagnosis of strep throat, tonsillitis, or pharyngitis | 7.56 (3.89, 14.71) | 3.06 (1.66, 5.65) |
| * The average patient cluster per physician was 3 (range 1 to 8). | ||
| † Number of observations < 621 because not all physicians completed practice surveys and some who did reply left some questions unanswered. | ||
| ‡ Odds ratio. | ||
Figure
FAMILY PHYSICIANS WHO WERE CONTACTED AND WHO COMPLETED THE STUDY
Discussion
The use of repeated chart prompt reminders to family physicians to use a clinical scoring approach in the management of children and adults presenting with URTI and a sore throat did not affect unnecessary antibiotic prescriptions or overall antibiotic use. Problems encountered in conducting this community-based trial may have contributed to the negative result.
Sixty-seven (41%) physicians agreed to be randomized but failed to complete the study. These losses after randomization and the differing sizes of the patient clusters per physician led to differences in the characteristics of the treating physician between the 2 groups. Characteristics associated with higher antibiotic prescribing rates were more common in the intervention group. As a result, despite the randomized design, the 2 patient groups were not initially similar in terms of their likelihood to receive a prescription for an antibiotic. To compensate for these differences, we controlled for the different physician characteristics in the analysis. However, the large number of physician dropouts also resulted in a failure to achieve the planned sample size. As a result, the study had insufficient power to detect the effect size that had been hypothesized.
We had planned the sample size to detect a 30% decrease in unnecessary antibiotic use. The adjusted analysis produced a point estimate of a 23% decrease in unnecessary antibiotic use and a 43% decrease in overall antibiotic use. These point estimates are the same whether or not the clustering is taken into effect; however, the more appropriate clustered analysis increases the estimate for the sample variance, resulting in wider confidence intervals. Examination of the lower 95% confidence interval reveals that the study lacked sufficient power to rule out as much as a 58% reduction in unnecessary antibiotic use. Therefore, while the study failed to find a statistically significant effect from the intervention, it also did not have the power to rule out a clinically important reduction in unnecessary antibiotic use.
We gave information about the clinical scoring approach to physicians in the control group. Doing so may have reduced the study’s ability to detect an effect of the intervention. We did not include a group that had been not exposed to information because we believed that mailed information was the equivalent of “standard” care in terms of changing physician behavior. Mailed information is a common method of informing physicians about new clinical information but has a limited ability to influence clinical behavior.34 However, the rate of antibiotic prescribing in the control group was indeed somewhat lower than is generally reported in the literature.9 This finding may be compatible with volunteer bias or the Hawthorne effect. More likely, perhaps, asking the control group to complete encounter forms for multiple patients may have inadvertently reminded them about the score. As a result, the control group may have been contaminated from repeated clinical prompts.
Some problems encountered in this study have been noted by other investigators conducting community-based research in primary care.37 The difficulty of retaining community-based physicians resulted in significant losses after randomization. This situation occurred even though qualifying to be randomized required physicians to mail back a reply card indicating that they wished to participate, suggesting that they were motivated to some degree.37 In addition, they received a modest cash honorarium. Some physicians returned the package stating that circumstances had changed and they would be unable to participate. Many who initially agreed to participate failed to reply despite 3 mailed reminders. The level of dropouts did not become apparent until late in the study. In retrospect, it might have been advisable to phone physicians directly soon after randomization in order to detect problems early. Other physicians could then have been randomly selected from the general membership listing to replace those who had dropped out.
This study found that repeated reminders to physicians to use a clinical score in the management of their patients with a sore throat did not reduce unnecessary antibiotic use. The problems encountered in this community-based intervention trial may have contributed to the negative result. Studies of prescribing behavior may need to stratify physicians before randomization by characteristics, such as patient volume and experience, that are related to prescribing behavior. Including a group that received no information is probably necessary to allow the greatest chance of detecting an effect. Particular attention and resources need to be available to ensure the retention, and replacement if needed, of community-based family physicians participating in research studies.
Acknowledgments
This study was supported by a grant from the Medical Research Council of Canada, Grant No. MA-15088. Dr McIsaac’s work is supported by the Mt. Sinai Hospital and the Family Healthcare Research Unit of the Department of Family and Community Medicine, University of Toronto, Toronto, Canada. This study was conducted in conjunction with the National Research System of the College of Family Physicians of Canada. The cooperation of the Ontario Association of Medical Laboratories is gratefully acknowledged.
1. Seppälä H, Nissinen A, Järvinen H, et al. Resistance to erythromycin in group A streptococci. N Engl J Med 1992;326:292-7.
2. Chen DK, McGeer A, de Azavedo JC, Low DE. Decreased susceptibility of Streptococcus pneumoniae. to fluoroquinolones in Canada. N Engl J Med 1999;341:233-9.
3. Magee JT, Pritchard EL, Fitzgerald KA, Dunstan FDJ, Howard AJ. Antibiotic prescribing and antibiotic resistance in community practice: retrospective study, 1996-8. BMJ 1999;319:1239-40.
4. Arason VA, Kristinsson KG, Sigurdsson JA, Stefánsdóttir G, Mölstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin rate of penicillin resistant pneumococci in children? Cross sectional prevalence study. BMJ 1996;313:387-91.
5. Seppälä H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in Group A streptococci in Finland. N Engl J Med 1997;337:441-6.
6. Bass JW, Weisse ME, Plymyer MR, Murphy S, Eberly BJ. Decline of erythromycin resistance of Group A beta-hemolytic streptococci in Japan. Arch Pediatr Adolesc Med 1994;148:67-71.
7. Wise R, Hart T, Cars O, et al. Antimicrobial resistance is a major threat to public health. BMJ 1998;317:610-11.
8. Schwartz B, Bell DM, Hughes JM. Preventing the emergence of antimicrobial resistance. A call for action by clinicians, public health officials, and patients. JAMA 1997;278:944-5.
9. McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995;273:214-9.
10. Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA 1997;278:901-4.
11. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998;279:875-7.
12. Brumfit W, O’Grady F, Slator JDH. Benign streptococcal sore throat. Lancet 1959;2:419-23.
13. Little PS, Williamson I. Are antibiotics appropriate for sore throats? Costs outweigh benefits. BMJ 1994;309:1010-2.
14. Graham A, Fahey T. Sore throat: diagnostic and therapeutic dilemmas. BMJ 1999;319:173-4.
15. Dajani A, Taubert K, Ferrieri P, Peter G, Shulman S. Treatment of acute streptococcal pharyngitis and prevention of rheumatic fever: A statement for health professionals. Pediatrics 1995;96:758-64.
16. Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH. Diagnosis and management of group A streptococcal pharyngitis: a practice guideline. Clin Infect Dis 1997;25:574-83.
17. Hart WJ. Streptococcal pharyngitis. A demonstration of the inaccuracy of clinical diagnosis without culture. Can Fam Physician 1976;22:34-9.
18. Shank JC, Powell TA. A five-year experience with throat cultures. J Fam Pract 1984;18:857-63.
19. McIsaac WJ, White D, Tannenbaum D, Low DE. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. CMAJ 1998;158:75-83.
20. Touw-Otten FWMM, Johansen KS. Diagnosis, antibiotic treatment and outcome of acute tonsillitis: report of a WHO regional office for Europe study in 17 European countries. Fam Pract 1992;9:255-62.
21. Poses RM, Cebul RD, Collins M, Fager SS. The accuracy of experienced physicians’ probability estimates for patients with sore throats. Implications for decision making. JAMA 1985;254:925-9.
22. McIsaac WJ, Butler CC. Does clinical error contribute to unnecessary antibiotic use? Med Decis Making 2000;20:33-8.
23. Walsh BT, Bookheim WW, Johnson RC, Tompkins RK. Recognition of streptococcal pharyngitis in adults. Arch Intern Med 1975;135:1493-7.
24. Breese BB. A simple scorecard for the tentative diagnosis of streptococcal pharyngitis. Am J Dis Child 1977;131:514-17.
25. Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making 1981;1:239-46.
26. Fujikawa S, Ito Y. A new scoring system for diagnosis of streptopharyngitis. Jpn Circ J 1985;49:1258-61.
27. Komaroff AL, Pass TM, Aronson MD, et al. The prediction of streptococcal pharyngitis in adults. J Gen Intern Med 1986;1:1-7.
28. Hoffman S. An algorithm for a selective use of throat swabs in the diagnosis of group A streptococcal pharyngo-tonsillitis in general practice. Scand J Prim Health Care 1992;10:295-300.
29. Meland E, Digranes A, Skjærven R. Assessment of clinical features predicting streptococcal pharyngitis. Scand J Infect Dis 1993;25:177-83.
30. Dobbs F. A scoring system for predicting group A streptococcal infection. Br J Gen Pract 1996;46:461-4.
31. Poses RM, Cebul RD, Wigton RS. You can lead a horse to water: improving physicians’ knowledge of probabilities may not affect their decisions. Med Decis Making 1995;15:65-76.
32. McIsaac WJ, Goel V, To T, Low DE. The validity of a sore throat score in family practice. CMAJ 2000;163:811-5.
33. McIsaac WJ, Goel V. Effect of an explicit decision-support tool on decisions to prescribe antibiotics for sore throat. Med Decis Making 1998;18(2):220-8.
34. Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA 1995;274:700-5.
35. Rosser WW, McDowell I, Newell C. Use of reminders for prevention procedures in family medicine. CMAJ 1991;145:807-13.
36. Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ, Donner A. Evaluation of health interventions at area and organisation level. BMJ 1999;319:376-9.
37. Rogers S, Humphrey C, Nazareth I, Lister S, Tomlin Z, Haines A. Designing trials of interventions to change professional practice in primary care: lessons from an exploratory study of two change strategies. BMJ 2000;320:1580-3.
1. Seppälä H, Nissinen A, Järvinen H, et al. Resistance to erythromycin in group A streptococci. N Engl J Med 1992;326:292-7.
2. Chen DK, McGeer A, de Azavedo JC, Low DE. Decreased susceptibility of Streptococcus pneumoniae. to fluoroquinolones in Canada. N Engl J Med 1999;341:233-9.
3. Magee JT, Pritchard EL, Fitzgerald KA, Dunstan FDJ, Howard AJ. Antibiotic prescribing and antibiotic resistance in community practice: retrospective study, 1996-8. BMJ 1999;319:1239-40.
4. Arason VA, Kristinsson KG, Sigurdsson JA, Stefánsdóttir G, Mölstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin rate of penicillin resistant pneumococci in children? Cross sectional prevalence study. BMJ 1996;313:387-91.
5. Seppälä H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in Group A streptococci in Finland. N Engl J Med 1997;337:441-6.
6. Bass JW, Weisse ME, Plymyer MR, Murphy S, Eberly BJ. Decline of erythromycin resistance of Group A beta-hemolytic streptococci in Japan. Arch Pediatr Adolesc Med 1994;148:67-71.
7. Wise R, Hart T, Cars O, et al. Antimicrobial resistance is a major threat to public health. BMJ 1998;317:610-11.
8. Schwartz B, Bell DM, Hughes JM. Preventing the emergence of antimicrobial resistance. A call for action by clinicians, public health officials, and patients. JAMA 1997;278:944-5.
9. McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995;273:214-9.
10. Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA 1997;278:901-4.
11. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998;279:875-7.
12. Brumfit W, O’Grady F, Slator JDH. Benign streptococcal sore throat. Lancet 1959;2:419-23.
13. Little PS, Williamson I. Are antibiotics appropriate for sore throats? Costs outweigh benefits. BMJ 1994;309:1010-2.
14. Graham A, Fahey T. Sore throat: diagnostic and therapeutic dilemmas. BMJ 1999;319:173-4.
15. Dajani A, Taubert K, Ferrieri P, Peter G, Shulman S. Treatment of acute streptococcal pharyngitis and prevention of rheumatic fever: A statement for health professionals. Pediatrics 1995;96:758-64.
16. Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH. Diagnosis and management of group A streptococcal pharyngitis: a practice guideline. Clin Infect Dis 1997;25:574-83.
17. Hart WJ. Streptococcal pharyngitis. A demonstration of the inaccuracy of clinical diagnosis without culture. Can Fam Physician 1976;22:34-9.
18. Shank JC, Powell TA. A five-year experience with throat cultures. J Fam Pract 1984;18:857-63.
19. McIsaac WJ, White D, Tannenbaum D, Low DE. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. CMAJ 1998;158:75-83.
20. Touw-Otten FWMM, Johansen KS. Diagnosis, antibiotic treatment and outcome of acute tonsillitis: report of a WHO regional office for Europe study in 17 European countries. Fam Pract 1992;9:255-62.
21. Poses RM, Cebul RD, Collins M, Fager SS. The accuracy of experienced physicians’ probability estimates for patients with sore throats. Implications for decision making. JAMA 1985;254:925-9.
22. McIsaac WJ, Butler CC. Does clinical error contribute to unnecessary antibiotic use? Med Decis Making 2000;20:33-8.
23. Walsh BT, Bookheim WW, Johnson RC, Tompkins RK. Recognition of streptococcal pharyngitis in adults. Arch Intern Med 1975;135:1493-7.
24. Breese BB. A simple scorecard for the tentative diagnosis of streptococcal pharyngitis. Am J Dis Child 1977;131:514-17.
25. Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making 1981;1:239-46.
26. Fujikawa S, Ito Y. A new scoring system for diagnosis of streptopharyngitis. Jpn Circ J 1985;49:1258-61.
27. Komaroff AL, Pass TM, Aronson MD, et al. The prediction of streptococcal pharyngitis in adults. J Gen Intern Med 1986;1:1-7.
28. Hoffman S. An algorithm for a selective use of throat swabs in the diagnosis of group A streptococcal pharyngo-tonsillitis in general practice. Scand J Prim Health Care 1992;10:295-300.
29. Meland E, Digranes A, Skjærven R. Assessment of clinical features predicting streptococcal pharyngitis. Scand J Infect Dis 1993;25:177-83.
30. Dobbs F. A scoring system for predicting group A streptococcal infection. Br J Gen Pract 1996;46:461-4.
31. Poses RM, Cebul RD, Wigton RS. You can lead a horse to water: improving physicians’ knowledge of probabilities may not affect their decisions. Med Decis Making 1995;15:65-76.
32. McIsaac WJ, Goel V, To T, Low DE. The validity of a sore throat score in family practice. CMAJ 2000;163:811-5.
33. McIsaac WJ, Goel V. Effect of an explicit decision-support tool on decisions to prescribe antibiotics for sore throat. Med Decis Making 1998;18(2):220-8.
34. Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA 1995;274:700-5.
35. Rosser WW, McDowell I, Newell C. Use of reminders for prevention procedures in family medicine. CMAJ 1991;145:807-13.
36. Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ, Donner A. Evaluation of health interventions at area and organisation level. BMJ 1999;319:376-9.
37. Rogers S, Humphrey C, Nazareth I, Lister S, Tomlin Z, Haines A. Designing trials of interventions to change professional practice in primary care: lessons from an exploratory study of two change strategies. BMJ 2000;320:1580-3.
Is Roxithromycin Better than Amoxicillin in the Treatment of Acute Lower Respiratory Tract Infections in Primary Care?
OBJECTIVE: To assess the efficacy of roxithromycin relative to amoxicillin.
STUDY DESIGN: We conducted a double-blind randomized controlled trial of oral 500 mg amoxicillin 3 times per day vs oral 300 mg roxithromycin once a day for 10 days.
POPULATION: We included 196 adults who had presented to a general practitioner with lower respiratory tract infection (LRTI) and, in the physician’s opinion, needed antibiotic treatment.
OUTCOMES MEASURED: We measured clinical response after 10 and 28 days, defined in 4 ways: (1) decrease in LRTI symptoms; (2) complete absence of symptoms; (3) decrease in signs; and (4) complete absence of signs. Self-reported response included the decrease in symptoms and the time until resumption of impaired or abandoned daily activities on days 1 through 10, 21, and 27.
RESULTS: Clinical cure rates after the completion of antibiotic treatment (10 days) were not significantly different for the 2 groups. After 28 days, the roxithromycin group showed no increase in cure rate as evidenced by the decrease in symptoms, indicating a significantly lower cure rate. However, this difference did not alter physicians’ overall conclusion after complete follow-up that 90% of patients, regardless of age, had been effectively treated with either amoxicillin or roxithromycin.
CONCLUSIONS: The surplus value of roxithromycin was not confirmed. Amoxicillin remains a reliable first-choice antibiotic in the treatment of LRTI in general practice.
- Amoxicillin and roxithromycin are equally effective in the treatment of patients presenting with lower respiratory tract infections and needing antibiotic treatment.
- Most patients remain symptomatic after 10 days of treatment with either drug.
- The low incidence of atypical pathogens (Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae) in the Netherlands minimizes the potentially greater surplus value of macrolide antibiotics over amoxicillin.
Acute community-acquired lower respiratory tract infections (LRTIs) in adults include acute bronchitis, pneumonia, and infectious episodes in patients with asthma or chronic obstructive pulmonary disease (COPD). In acute bronchitis and exacerbations of COPD, the value of antibiotic therapy is doubtful; in pneumonia, however, it is widely accepted. Because distinguishing between these disease entities on clinical grounds alone is often impossible, deciding which patients would benefit from antibiotic treatment remains difficult.1-6In the Netherlands, as in the United States and Great Britain, antibiotics are prescribed for patients with acute bronchitis approximately 80% of the time.7-9
If a primary care physician (PCP) decides to treat LRTI with antibiotics, amoxicillin is the drug of first choice in the Netherlands.10-13 However, amoxicillin is not effective in infections caused by atypical organisms such as Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila, which are responsible for 1% to 50% of cases of LRTI.14-20 Roxithromycin and the newer macrolide antibiotics are recommended as drugs of choice for the empirical treatment of community-acquired pneumonia in low-risk patients in the United States and Canada21-23 because those drugs cover both typical and atypical pathogens. Amoxicillin has long proved to be a reliable drug and one to which the resistance of common respiratory tract pathogens (Streptococcus pneumoniae and Haemophilus influenzae) in the Netherlands is low.24-29
Community-based studies that evaluate treatment for LRTI are lacking. Also lacking are independent randomized controlled studies comparing amoxicillin with roxithromycin or other new macrolides for LRTI. Our double-blind randomized trial attempted to determine whether the preference for amoxicillin in the Netherlands is well founded. In the trial, patients with LRTI who in their PCP’s opinion needed antibiotic treatment were assigned to either amoxicillin or roxithromycin. We then compared the efficacy and safety of both drugs.
Methods
Eligibility criteria and baseline characteristics
Eligible study subjects were patients in the southern part of the Netherlands who presented with signs and symptoms of LRTI that their PCPs believed warranted antibiotic therapy. Table 1 lists the inclusion and exclusion criteria.
Baseline data (at day 1) were obtained to evaluate the comparability of prognostic factors between the intervention groups. The PCP performed an extensive medical history and physical examination. In addition, a sputum sample, oral washing, and nasopharyngeal swab were taken for bacteriologic examination. Venous blood samples were taken for blood chemistry, hematology, and serology (initial titers of the viral pathogens M pneumoniae and L pneumophila).
TABLE 1
CHECKLIST FOR PATIENT ELIGIBILITY
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| A: Age 18 years or older |
|
| AND | |
| B: New* or increasing cough | |
| AND | |
| C: At least 1 of the following: | |
| 1) Shortness of breath | |
| 2) Wheezing | |
| 3) Chest pain | |
| 4) Auscultation abnormalities | |
| AND | |
| D: At least 1 of the following: | |
| 1) Fever (≥ 38°C) | |
| 2) Perspiring | |
| 3) Headache | |
| 4) Myalgia | |
| AND | |
| E: Diagnosis of LRTI according to PCP and | |
| F: Antibiotics required (in PCP’s opinion) | |
| * Onset within the previous 29 days. | |
| LRTI denotes lower respiratory tract infection; PCP, primary care physician. | |
Interventions
Once the samples had been collected, patients were randomly assigned to oral treatment with either 500 mg amoxicillin 3 times daily for 10 days or 300 mg roxithromycin once daily for 10 days. A computer program using random permuted blocks of 6 prepared a randomization list for each participating center. Batches of drug packages, each provided with a unique trial code, had been sent in advance to the participating general practices. A double-dummy technique achieved blinding of patients, treating physicians, and investigators to the assigned medication. This was necessary because amoxicillin and roxithromycin have different dosing schedules (3 times a day versus once daily) and are not identical in appearance (capsule versus tablet). All capsules and tablets had identical appearance and taste. All patients received both forms of their assigned medication. Compliance with medication regimens was measured by Medical Event Monitoring Systems (MEMS), an electronic recording system that compiles the dosing history of ambulatory patients taking oral medication.30
Chest X-Rays
Every patient underwent chest x-ray. The radiographs were reassessed for the presence or absence of infiltrate by a blinded independent senior radiologist. If the first and second radiologist disagreed, a third senior radiologist made a final assessment.
Follow-up
Follow-up consultations similar to the examination on day 1 took place on days 10 and 28. During treatment (days 1 through 10) and on days 21 and 27, follow-up was supplemented by a short diary in which patients recorded their symptoms and the times at which they resumed daily activities that they had abandoned or that had been impaired.
Outcomes measured
Efficacy was assessed by comparing the groups’ clinical response on day 10 (the primary outcome measure) and day 28 and their bacteriologic response on day 10. Satisfactory clinical response was defined in 4 ways: (1) decrease in symptoms of LRTI; (2) absence of symptoms of LRTI; (3) decrease in signs of LRTI; and (4) absence of signs of LRTI. All other outcomes were regarded as unsatisfactory responses.
Self-reported symptoms and time to resolution were compared between the 2 groups on days 1 through 10, 21, and 27. The percentage of patients who had abandoned daily activities or whose participation in daily activities had been impaired by illness was followed over time. Bacteriologic cure was defined as the absence of growth of a predominant bacterial pathogen (cultured at baseline) in a sputum sample taken on day 10.
We recorded patients’ compliance rates, frequency of adverse events, and acquired bacterial resistance. Compliance was defined as the number of doses taken divided by the number of doses prescribed.
Statistical analyses
The efficacy of amoxicillin and roxithromycin was evaluated using an intention-to-treat analysis. Differences were tested using a 2-sided chi-square test ( α= 0.05). Multiple logistic regression analysis was performed to analyze the effect of differences in baseline characteristics between the randomized groups. Differences in symptoms, time to resolution of symptoms, and time to resumption of abandoned and impaired daily activities were tested in life table analyses using the Gehan test. All statistical analyses were performed with Statistical Package for the Social Sciences software, version 8.0.
Results
Patient population
From January 1998 to April 1999, 25 PCPs from 15 practices recruited 196 patients aged 18 years to 89 years. Of these patients, 99 received amoxicillin and 97 received roxithromycin (Figure 1). The 2 groups’ demographic data, signs and symptoms, comorbidities, identified pathogens, and radiographic abnormalities were similar (Table 2). Multiple logistic regression analysis showed that none of the covariables altered the effects of the study medication.
TABLE 2
FINDINGS ON PRESENTATION
| Finding | Amoxicillin Group No. (%) | Roxithromycin Group No. (%) |
|---|---|---|
| Number of Patients | 99 (51) | 97 (49) |
| Demographic Data | ||
| Ratio of men to women | 46/53 | 53/44 |
| Mean age in years (SD) | 55 (15) | 50 (16) |
| Symptoms | ||
| Recent cough in number of days | ||
| 1–7 | 34 (36) | 41 (43) |
| 8–14 | 31 (33) | 25 (26) |
| 15–28 | 22 (23) | 23 (24) |
| No recent cough | 8 (8) | 6 (6) |
| Productive cough | 77 (78) | 84 (88) |
| Dyspnea | 78 (79) | 76 (79) |
| Wheezing | 68 (69) | 61 (64) |
| Risk Factors | ||
| Cigarette smoking | 36 (36) | 29 (31) |
| Comorbidity | ||
| None | 55 (56) | 48 (52) |
| Asthma | 19 (19) | 20 (22) |
| COPD | 17 (17) | 11 (12) |
| Heart failure | 3 (3) | 4 (4) |
| Diabetes mellitus | 2 (2) | 3 (3) |
| Other | 23 (24) | 21 (23) |
| Asthma medication prescribed at start of study | 16 (16) | 13 (14) |
| Signs | ||
| Auscultation abnormalities | 93 (94) | 87 (91) |
| Body temperature 38.0°C | 25 (26) | 22 (24) |
| Infection | ||
| Mild/moderate | 91 (93) | 89 (93) |
| Severe | 7 (7) | 7 (7) |
| Laboratory Tests | ||
| CRP, median (range) | 23 (2-228) | 26 (2-312) |
| ESR, median (range) | 21 (1-104) | 19 (1-121) |
| Leukocytes, median (range) | 8.3 (3.9-19.7) | 8.4 (4.3-15.4) |
| Patients with pathogens | 45 (45) | 46 (47) |
| Chest X-Ray | ||
| Infiltrate on chest x-ray | 14 (14) | 13 (14) |
| NOTE: Values are numbers (percentages) unless otherwise stated. Percentages are based on number of patients for each variable. | ||
| COPD denotes chronic obstructive pulmonary disease; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; SD, standard deviation. | ||
FIGURE 1
DISTRIBUTION OF PATIENTS FOR EFFICACY AND SAFETY ANALYSES
Clinical cure
Early Follow-Up. The rate of clinical cure, defined as the decrease in symptoms and signs at 10 days after randomization, was high and not significantly different between both groups. Using the stricter definition of clinical cure as the complete absence of symptoms and signs led to the same conclusion. Absolute cure rates using this strict definition were low (Table 3).
Physicians discontinued treatment with the study medication in 2 cases (1 amoxicillin and 1 roxithromycin) because of unsatisfactory clinical response. Both patients recovered rapidly after alternative antibiotic treatment. In one case, the patient discontinued amoxicillin after 8 days because of rash and urticaria and recovered quickly without further treatment.
Late Follow-Up. According to the physicians’ final assessments, the rate of clinical cure at 28 days was not significantly different between the 2 groups, although the percentage of patients who showed a decrease in symptoms was significantly higher in the amoxicillin group than in the roxithromycin group (Table 3). Again, cure rates were much lower when the strict definition of cure was used. Eleven patients in the amoxicillin group and 8 in the roxithromycin group were not clinically cured after 28 days. Of these patients, 10 (5 in each group) recovered shortly thereafter or did not consult their physician again for persisting symptoms of LRTI. Nine patients (6 in the amoxicillin group, 3 in the roxithromycin group) with exacerbation of COPD slowly returned to their baseline clinical situation. Four patients (3 in the amoxicillin group, 1 in the roxithromycin group) were found to have concomitant pulmonary cancer. Curative bilobectomy was performed in one of the patients. The others received palliative treatment.
TABLE 3
CLINICAL CURE RATE AT EARLY (10-DAY) AND LATE (28-DAY) FOLLOW-UP
| Characteristic | Amoxicillin No. (%) | Roxithromycin No. (%) | Relative Risk* (CI) |
|---|---|---|---|
| Decrease in Symptoms and Signs | |||
| Day 10 | |||
| Symptoms | 84/96 (88) | 90/95 (95) | 2.38 (0.87-6.48) |
| Signs (physical examination) | 85/98 (87) | 89/95 (94) | 2.10 (0.83-5.30) |
| Day 28 | |||
| Symptoms | 91/95 (96) | 79/93 (85) | 0.28 (0.10-0.82)† |
| Signs (physical examination) | 90/96 (94) | 87/94 (93) | 0.74 (0.29-2.41) |
| Absence of Symptoms and Signs | |||
| Day 10 | |||
| Symptoms | 18/96 (19) | 22/95 (23) | 2.38 (0.87-6.48) |
| Signs (physical examination) | 68/98 (69) | 76/95 (80) | 1.53 (0.93-2.53) |
| Day 28 | |||
| Symptoms | 59/95 (62) | 50/93 (54) | 0.82 (0.58-1.15) |
| Signs (physical examination) | 82/96 (85) | 80/94 (85) | 0.98 (0.49-1.94) |
| Fever (≥38°C) gone, day 10 | 21/25 (84) | 16/22 (73) | 1.37 (0.25-7.41) |
| Cure, final conclusion by physician, day 28 | 84/95 (88) | 86/94 (91) | 1.36 (0.57-3.23) |
| NOTE: Percentages are based on number of patients for each variable. | |||
| *Risk of no cure with amoxicillin vs roxithromycin. | |||
| †P < .05. | |||
Self-reported response over time
The time before resolution of symptoms according to the patients’ diaries was similar for patients treated with amoxicillin and those treated with roxithromycin (Figures 2A and 2B). The percentage of patients who had abandoned daily activities was followed over time. At baseline, more than half of the patients in the amoxicillin group and fewer than 40% in the roxithromycin group reported that they had abandoned daily activities. At day 10, this percentage had fallen to less than 20% in both groups and to less than 10% in both groups at day 28. Differences between the amoxicillin and roxithromycin groups were not significant.
Furthermore, the patients’ diaries revealed information about the time of impaired daily activities. The percentage of patients with impaired daily activities gradually decreased in both treatment groups from approximately 75% at baseline to 30% at day 10 and 20% at day 28.
FIGURE 2
TIME TO RESOLUTION OF SYMPTOMS AS DESCRIBED IN PATIENTS’ DIARIES
Subgroup analyses
The above analyses were repeated for a group of patients aged less than 65 years and a group aged 65 years and older. The trend in cure rates was the same. No differences were found between these age groups regarding the percentage of patients with satisfactory clinical response. Furthermore, the same analyses were performed for each of the clinical diagnoses made by the PCPs at baseline (ie, pneumonia, acute bronchitis, exacerbation of asthma or COPD, and unclassified LRTI). Overall, no significant differences were found between the amoxicillin and roxithromycin groups.
Bacteriologic evaluation
Pathogens were identified in 91 patients (46%). Viruses were most frequent, followed by H (Para) influenzae, S pneumoniae, and Moraxella catarrhalis (Table 4). Bacteriologic cure was achieved in 21 of the 23 patients (91%) in the amoxicillin group and in 23 of the 27 patients (85%) in the roxithromycin group (NS, Fisher’s exact test). In 9 patients of the amoxicillin group and 8 patients of the roxithromycin group, only the sample obtained after 10 days showed the growth of a predominant bacterial pathogen (superinfection).
TABLE 4
RESPIRATORY TRACT PATHOGENS ISOLATED
| Microorganism | No. (%) |
|---|---|
| Typical Bacterial Pathogens | |
| Haemophilus (Para) influenzae | 34 (17) |
| Streptococcus pneumoniae | 12 (6) |
| Moraxella catarrhalis | 6 (3) |
| Other* | 5 (3) |
| Atypical Pathogens | |
| Mycoplasma pneumoniae | 2 (1) |
| Legionella pneumophila | 1 (0.5) |
| Viruses | |
| Influenza A | 29 (16) |
| Influenza B | 7 (4) |
| Parainfluenzae 1, 2, 3 | 7 (4) |
| Adenovirus | 5 (3) |
| Respiratory syncytial virus | 5 (3) |
| No organism (number of patients) | 122 (49) |
| * Enterobacteriaceae (n = 2), Staphylococcus aureus (n = 1), Streptococcus viridans (n = 1), Neisseria meningitidis (n = 1). | |
Safety and compliance
Thirty possible or probable adverse events were reported in 19 of 99 patients (19%) treated with amoxicillin: diarrhea (13), stomach ache (3), headache (3), and 11 other side effects, including nausea, vomiting, and rash, once each. In the roxithromycin group, 24 events were reported in 16 patients (16%): nausea (5), diarrhea (4), vomiting (4), rash (2), headache (2), and 7 others, including pruritus ani, dizziness, and mild bradycardia, once each.
Compliance with the medication regimen was high. Data from electronic monitoring were available for 160 patients (78 in the amoxicillin group, 82 in the roxithromycin group). The overall compliance rate for patients in both groups (ie, the number of doses taken divided by the number of doses prescribed) was 98%. In the amoxicillin group, the numbers of patients with less than 90% compliance in taking the tablets and capsules were 7 and 4, respectively. In the roxithromycin group, compliance in taking the tablets was at least 90% in all patients but compliance in taking the capsules was less than 90% in 6 patients.
Discussion
This community-based study shows that amoxicillin and roxithromycin are equally effective in the treatment of LRTI in the Netherlands. Clinical cure rates after 10 days of antibiotic treatment were approximately 90% in both study groups, although complete absence of symptoms was achieved in only a minority of cases. After 28 days of follow-up, cure rates remained high. The amoxicillin group had a significantly higher cure rate than the roxithromycin group as evidenced by the decrease in symptoms. However, this significant difference in favor of the amoxicillin group did not alter the PCPs’ overall conclusion after complete follow-up: that 90% of patients who received either drug had been effectively treated. Patients’ diary entries agreed with that impression.
The time to resolution of symptoms, the cumulative cure rate per day, and the influence of the illness on daily activities were not significantly different between patients treated with amoxicillin versus those given roxithromycin. Adverse events were mild and were divided evenly over both groups with the exception of diarrhea, which occurred more often in those taking amoxicillin.
In our study, complete absence of symptoms and signs after 28 days, as assessed by both physicians and patients, was achieved in only approximately half the patients. Complete remission of LRTI often takes more than 4 weeks.
Although LRTI is often managed in primary care, diagnostic and therapeutic decisions are usually based on the experiences of hospital-based specialists and on the results of trials conducted in hospital settings. Generalizing these results to primary care is of limited value, since disease in patients recruited for these studies is often at a later stage and more serious. In our trial, patients were recruited, diagnosed, and treated by PCPs in their natural setting, maintaining regular care as much as possible.
Nevertheless, generalization of our findings to everyday care may not be valid. To explore the degree of selection in our recruited patients, we compared the actual numbers of cases of LRTI in 3 practices (with a total of 9 PCPs and a total population of 13,269) with the numbers included in the present trial during 1 year of the inclusion period. Of the 463 presumably eligible patients, only 43 (9%) were actually included. This proportion is similar to that in a recent study of randomized controlled trials in primary care in which less than 10% of the eligible population were recruited for the trial.31 Included patients did not differ from other eligible patients with regard to age, clinical diagnosis, severity of illness, and need for antibiotic treatment (according to the PCPs).
Clinical studies, mostly in inpatient settings, on community-acquired pneumonia have identified causative pathogens in 50% to 69% of patients.14-17,21,23,32,33 Outpatient studies of acute bronchitis and LRTI have generally reported considerably lower percentages (16% to 44%).19,20,34-36 In our study, pathogens that presumably caused LRTI were found in 46% of patients.
Because atypical pathogens were the presumptive causative agent in only 3 cases (2 M pneumoniae, 1 L pneumophila), the potential advantage of macrolide antibiotics over amoxicillin is minimal. Furthermore, bacterial resistance to macrolide antibiotics is believed to be considerable.37,38 In Finland, bacterial resistance to erythromycin has been shown to rise quickly after an increase in the consumption of macrolide antibiotics.39 In contrast to alarming reports in the literature,14,17,22,40,41 the low incidence of M pneumoniae and L pneumophila found in the current study supports the conservative approach (ie, amoxicillin or doxycycline) to treating community-acquired LRTI in the Netherlands.
M pneumoniae occurs at high rates in 4-year to 5-year cycles.42 This timing implies that the frequency of M pneumoniae might be higher if the same study were performed 1 year later. Because most M pneumoniae infections are self-limiting and clinical cure rates of macrolide antibiotics compared with those of placebo are the same,43,44 however, this epidemiologic observation does not change the conclusions of the present study.
Compliance with medication was reliably measured and quantified by Medical Event Monitoring Systems. For both ethical and practical reasons, patients were informed about the monitoring mechanism. Their knowledge about the monitoring may have slightly increased compliance as compared with daily practice, although this assumption has not been confirmed in other studies.45,46 Furthermore, compliance with antibiotic regimens is known to be greater than compliance with chronic medication regimens.47,48
Conclusions
General practitioners frequently diagnose LRTI in general or pneumonia and acute bronchitis in particular, including infectious episodes in patients with asthma or COPD. In many cases, treatment with antibiotics follows. The results of our randomized controlled trial did not confirm the potentially greater value of roxithromycin, which is often recommended as the drug of choice for empirical treatment of community-acquired pneumonia, over amoxicillin. Because amoxicillin was as effective as roxithromycin, it remains a reliable first-choice antibiotic in the treatment of community-acquired LRTI.
Acknowledgments
The authors wish to thank the patients, general practitioners, and physicians’ assistants who participated in this study. They also thank Hans Verloop, director of the Vandra paper factory, Meer-Hoogstraten, Belgium, for donating cardboard boxes and Alexander Thissen, Josephine Asberg, and Ramon Ottenheijm for their assistance with the logistics of the study. The study was supported by a grant from the Research Institute for Extramural and Transmural Health Care, Maastricht.
1. Bartlett JG, Mundy LM. Community-acquired pneumonia. N Engl J Med 1995;333:1618-24.
2. Melbye H, Straume B, Aasebo U, Dale K. Diagnosis of pneumonia in adults in general practice. Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care. 1992;10:226-33.
3. Melbye H, Straume B, Aasebo U, Brox J. The diagnosis of adult pneumonia in general practice. The diagnostic value of history, physical examination and some blood tests. Scand J Prim Health Care. 1988;6:111-7.
4. Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination—relevant or relic? Arch Intern Med. 1999;159:1082-7.
5. Zaat JOM, Stalman WAB, Assendelft WJJ. Groaning, moaning and percussion. A systematic review on the diagnostic value of history and physical examination in patient with a suspicion of pneumonia. Huisarts Wet. 1998;41:461-9.
6. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA 1997;278:1440-5.
7. Kuyvenhoven MM, Verheij TJ, de Melker RA, van der Velden J. Antimicrobial agents in lower respiratory tract infections in Dutch general practice. Br J Gen Pract 2000;50:133-4.
8. Macfarlane J, Lewis SA, Macfarlane R, Holmes W. Contemporary use of antibiotics in 1089 adults presenting with acute lower respiratory tract illness in general practice in the UK: implications for developing management guidelines. Respir Med 1997;91:427-34.
9. Oeffinger KC, Snell LM, Foster BM, Panico KG, Archer RK. Treatment of acute bronchitis in adults. A national survey of family physicians. J Fam Pract. 1998;46:469-75.
10. Ortqvist A. Antibiotic treatment of community-acquired pneumonia in clinical practice: a European perspective. J Antimicrob Chemother 1995;35:205-12.
11. Janknegt R, Wijnands WJ, Stobberingh EE. Antibiotic policies in Dutch hospitals for the treatment of pneumonia. J Antimicrob Chemother 1994;34:431-42.
12. van der Werf GT, Smith RJA, Stewart RE, Meyboom-de Jong B. Spiegel op de huisarts: over registratie van ziekte, medicatie en verwijzingen in de geautimatiseerde huisartsenpraktijk. Groningen, the Netherlands: Disciplinegroep Huisartsgeneeskunde, University of Groningen; 1998: 1-181.
13. Stokx LJ, Foets M. Het voorschrijven van geneesmiddelen in de huisartspraktijk. Deel II [Prescribing drugs in general practice]. Utrecht: NIVEL; 1994.
14. Marrie TJ, Peeling RW, Fine MJ, Singer DE, Coley CM, Kapoor WN. Ambulatory patients with community-acquired pneumonia: the frequency of atypical agents and clinical course. Am J Med 1996;101:508-15.
15. Berntsson E, Lagergard T, Strannegard O, Trollfors B. Etiology of community-acquired pneumonia in out-patients. Eur J Clin Microbiol 1986;5:446-7.
16. Bohte R, van Furth R, van den Broek PJ. Aetiology of community-acquired pneumonia: a prospective study among adults requiring admission to hospital. Thorax 1995;50:543-7.
17. Fang GD, Fine M, Orloff J, et al. New and emerging etiologies for community-acquired pneumonia with implications for therapy. A prospective multicenter study of 359 cases. Medicine (Baltimore). 1990;69:307-16.
18. Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG. Prospective study of the aetiology and outcome of pneumonia in the community. Lancet 1987;1:671-4.
19. Jonsson JS, Sigurdsson JA, Kristinsson KG, Guthnadottir M, Magnusson S. Acute bronchitis in adults. How close do we come to its aetiology in general practice? Scand J Prim Health Care. 1997;15:156-60.
20. Macfarlane JT, Colville A, Guion A, Macfarlane RM, Rose DH. Prospective study of aetiology and outcome of adult lower-respiratory-tract infections in the community. Lancet 1993;341:511-4.
21. Niederman MS, Bass JB, Jr, Campbell GD, et al. Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. merican Thoracic Society. Medical Section of the American Lung Association. Am Rev Respir Dis. 1993;148:1418-26.
22. Mandell LA, Niederman M. Antimicrobial treatment of community acquired pneumonia in adults: a conference report. Can J Infect Dis 1993;4:25-8.
23. Marrie TJ. Community acquired pneumonia. Clin Infect Dis 1994;18:501-15.
24. Poirier R. Comparative study of clarithromycin and roxithromycin in the treatment of community-acquired pneumonia. J Antimicrob Chemother 1991;27:109-16.
25. Tilyard MW, Dovey SM. A randomized double-blind controlled trial of roxithromycin and cefaclor in the treatment of acute lower respiratory tract infections in general practice. Diagn Microbiol Infect Dis 1992;15:S97-101.
26. Zeluff BJ, Lowe P, Koornhof HJ, Gentry LO. Evaluation of roxithromycin (RU-965) versus cephradine in pneumococcal pneumonia. Eur J Clin Microbiol Infect Dis. 1988;7:69-71.
27. Schonwald S, Barsic B, Klinar I, Gunjaca M. Three-day azithromycin compared with ten-day roxithromycin treatment of atypical pneumonia. Scand J Infect Dis 1994;26:706-10.
28. Young RA, Gonzalez JP, Sorkin EM. Roxithromycin. A review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs. 1989;37:8-41.
29. de Neeling AJ, Pelt van W, Hendrix MGR, et al. Antibiotica resistentie in Nederland. Deel III: Gram-positieve bacteriën. Infect Bull. 1997;8:211-5.
30. Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Ouellette VL. How often is medication taken as prescribed? A novel assessment technique. JAMA 1989;261:3273-7.
31. Wilson S, Delaney BC, Roalfe A, et al. Randomized controlled trials in primary care: case study. BMJ 2000;321:24-7.
32. Ortqvist A, Hedlund J, Grillner L, et al. Aetiology, outcome and prognostic factors in community-acquired pneumonia requiring hospitalization. Eur Respir J 1990;3:1105-13.
33. Ortqvist A, Valtonen M, Cars O, Wahl M, Saikku P, Jean C. Oral empiric treatment of community-acquired pneumonia. A multicenter, double-blind, randomized study comparing sparfloxacin with roxithromycin. The Scandinavian Sparfloxacin Study Group. Chest. 1996;110:1499-506.
34. Boldy DA, Skidmore SJ, Ayres JG. Acute bronchitis in the community: clinical features, infective factors, changes in pulmonary function and bronchial reactivity to histamine. Respir Med 1990;84:377-85.
35. Trigg CJ, Wilks M, Herdman MJ, Clague JE, Tabaqchali S, Davies RJ. A double-blind comparison of the effects of cefaclor and amoxycillin on respiratory tract and oropharyngeal flora and clinical response in acute exacerbations of bronchitis. Respir Med 1991;85:301-8.
36. Karalus NC, Garrett JE, Lang SD, et al. Roxithromycin 150 mg bid versus amoxicillin 500 mg/clavulanic acid 125 mg tid for the treatment of lower respiratory tract infections in general practice. Infection 1995;23:S15-20.
37. Swartz MN. Use of antimicrobial agents and drug resistance. N Engl J Med 1997;337:491-2.
38. de Neeling AJ. Antibioticagebruik en het optreden van resistentie. National Institute of Public Health and the Environment/Volksgezondheid Toekomst Verkenning 1997;B3:793-800.
39. Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish Study Group for Antimicrobial Resistance. N Engl J Med. 1997;337:441-6.
40. Wood MJ. More macrolides. BMJ 1991;303:594-5.
41. Wort SJ, Rogers TR. Community acquired pneumonia in elderly people. Current British guidelines need revision. BMJ. 1998;316:1690.-
42. Bartlett JB. Management of respiratory tract infections. Baltimore, Md: Williams & Wilkins; 1997: 121.
43. King DE, Williams WC, Bishop L, Shechter A. Effectiveness of erythromycin in the treatment of acute bronchitis. J Fam Pract 1996;42:601-5.
44. Lode H, Garau J, Grassi C, et al. Treatment of community-acquired pneumonia: a randomized comparison of sparfloxacin, amoxycillin-clavulanic acid and erythromycin. Eur Respir J 1995;8:1999-2007.
45. Urquhart J. Partial compliance in cardiovascular disease: risk implications. Br J Clin Pract 1994;suppl:2-12.
46. Cramer JA, Ouelette VL, Mattson RH. Effect of microelectronic observation on compliance. Epilepsia 1990;31:617-8.
47. Favre O, Delacretaz E, Badan M, Glauser M, Waeber B. Relationship between the prescriber’s instructions and compliance with antibiotherapy in outpatients treated for an acute infectious disease. J Clin Pharmacol 1997;37:175-8.
48. Urquhart J. Role of patient compliance in clinical pharmacokinetics. A review of recent research. Clin Pharmacokinet. 1994;27:202-15.
OBJECTIVE: To assess the efficacy of roxithromycin relative to amoxicillin.
STUDY DESIGN: We conducted a double-blind randomized controlled trial of oral 500 mg amoxicillin 3 times per day vs oral 300 mg roxithromycin once a day for 10 days.
POPULATION: We included 196 adults who had presented to a general practitioner with lower respiratory tract infection (LRTI) and, in the physician’s opinion, needed antibiotic treatment.
OUTCOMES MEASURED: We measured clinical response after 10 and 28 days, defined in 4 ways: (1) decrease in LRTI symptoms; (2) complete absence of symptoms; (3) decrease in signs; and (4) complete absence of signs. Self-reported response included the decrease in symptoms and the time until resumption of impaired or abandoned daily activities on days 1 through 10, 21, and 27.
RESULTS: Clinical cure rates after the completion of antibiotic treatment (10 days) were not significantly different for the 2 groups. After 28 days, the roxithromycin group showed no increase in cure rate as evidenced by the decrease in symptoms, indicating a significantly lower cure rate. However, this difference did not alter physicians’ overall conclusion after complete follow-up that 90% of patients, regardless of age, had been effectively treated with either amoxicillin or roxithromycin.
CONCLUSIONS: The surplus value of roxithromycin was not confirmed. Amoxicillin remains a reliable first-choice antibiotic in the treatment of LRTI in general practice.
- Amoxicillin and roxithromycin are equally effective in the treatment of patients presenting with lower respiratory tract infections and needing antibiotic treatment.
- Most patients remain symptomatic after 10 days of treatment with either drug.
- The low incidence of atypical pathogens (Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae) in the Netherlands minimizes the potentially greater surplus value of macrolide antibiotics over amoxicillin.
Acute community-acquired lower respiratory tract infections (LRTIs) in adults include acute bronchitis, pneumonia, and infectious episodes in patients with asthma or chronic obstructive pulmonary disease (COPD). In acute bronchitis and exacerbations of COPD, the value of antibiotic therapy is doubtful; in pneumonia, however, it is widely accepted. Because distinguishing between these disease entities on clinical grounds alone is often impossible, deciding which patients would benefit from antibiotic treatment remains difficult.1-6In the Netherlands, as in the United States and Great Britain, antibiotics are prescribed for patients with acute bronchitis approximately 80% of the time.7-9
If a primary care physician (PCP) decides to treat LRTI with antibiotics, amoxicillin is the drug of first choice in the Netherlands.10-13 However, amoxicillin is not effective in infections caused by atypical organisms such as Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila, which are responsible for 1% to 50% of cases of LRTI.14-20 Roxithromycin and the newer macrolide antibiotics are recommended as drugs of choice for the empirical treatment of community-acquired pneumonia in low-risk patients in the United States and Canada21-23 because those drugs cover both typical and atypical pathogens. Amoxicillin has long proved to be a reliable drug and one to which the resistance of common respiratory tract pathogens (Streptococcus pneumoniae and Haemophilus influenzae) in the Netherlands is low.24-29
Community-based studies that evaluate treatment for LRTI are lacking. Also lacking are independent randomized controlled studies comparing amoxicillin with roxithromycin or other new macrolides for LRTI. Our double-blind randomized trial attempted to determine whether the preference for amoxicillin in the Netherlands is well founded. In the trial, patients with LRTI who in their PCP’s opinion needed antibiotic treatment were assigned to either amoxicillin or roxithromycin. We then compared the efficacy and safety of both drugs.
Methods
Eligibility criteria and baseline characteristics
Eligible study subjects were patients in the southern part of the Netherlands who presented with signs and symptoms of LRTI that their PCPs believed warranted antibiotic therapy. Table 1 lists the inclusion and exclusion criteria.
Baseline data (at day 1) were obtained to evaluate the comparability of prognostic factors between the intervention groups. The PCP performed an extensive medical history and physical examination. In addition, a sputum sample, oral washing, and nasopharyngeal swab were taken for bacteriologic examination. Venous blood samples were taken for blood chemistry, hematology, and serology (initial titers of the viral pathogens M pneumoniae and L pneumophila).
TABLE 1
CHECKLIST FOR PATIENT ELIGIBILITY
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| A: Age 18 years or older |
|
| AND | |
| B: New* or increasing cough | |
| AND | |
| C: At least 1 of the following: | |
| 1) Shortness of breath | |
| 2) Wheezing | |
| 3) Chest pain | |
| 4) Auscultation abnormalities | |
| AND | |
| D: At least 1 of the following: | |
| 1) Fever (≥ 38°C) | |
| 2) Perspiring | |
| 3) Headache | |
| 4) Myalgia | |
| AND | |
| E: Diagnosis of LRTI according to PCP and | |
| F: Antibiotics required (in PCP’s opinion) | |
| * Onset within the previous 29 days. | |
| LRTI denotes lower respiratory tract infection; PCP, primary care physician. | |
Interventions
Once the samples had been collected, patients were randomly assigned to oral treatment with either 500 mg amoxicillin 3 times daily for 10 days or 300 mg roxithromycin once daily for 10 days. A computer program using random permuted blocks of 6 prepared a randomization list for each participating center. Batches of drug packages, each provided with a unique trial code, had been sent in advance to the participating general practices. A double-dummy technique achieved blinding of patients, treating physicians, and investigators to the assigned medication. This was necessary because amoxicillin and roxithromycin have different dosing schedules (3 times a day versus once daily) and are not identical in appearance (capsule versus tablet). All capsules and tablets had identical appearance and taste. All patients received both forms of their assigned medication. Compliance with medication regimens was measured by Medical Event Monitoring Systems (MEMS), an electronic recording system that compiles the dosing history of ambulatory patients taking oral medication.30
Chest X-Rays
Every patient underwent chest x-ray. The radiographs were reassessed for the presence or absence of infiltrate by a blinded independent senior radiologist. If the first and second radiologist disagreed, a third senior radiologist made a final assessment.
Follow-up
Follow-up consultations similar to the examination on day 1 took place on days 10 and 28. During treatment (days 1 through 10) and on days 21 and 27, follow-up was supplemented by a short diary in which patients recorded their symptoms and the times at which they resumed daily activities that they had abandoned or that had been impaired.
Outcomes measured
Efficacy was assessed by comparing the groups’ clinical response on day 10 (the primary outcome measure) and day 28 and their bacteriologic response on day 10. Satisfactory clinical response was defined in 4 ways: (1) decrease in symptoms of LRTI; (2) absence of symptoms of LRTI; (3) decrease in signs of LRTI; and (4) absence of signs of LRTI. All other outcomes were regarded as unsatisfactory responses.
Self-reported symptoms and time to resolution were compared between the 2 groups on days 1 through 10, 21, and 27. The percentage of patients who had abandoned daily activities or whose participation in daily activities had been impaired by illness was followed over time. Bacteriologic cure was defined as the absence of growth of a predominant bacterial pathogen (cultured at baseline) in a sputum sample taken on day 10.
We recorded patients’ compliance rates, frequency of adverse events, and acquired bacterial resistance. Compliance was defined as the number of doses taken divided by the number of doses prescribed.
Statistical analyses
The efficacy of amoxicillin and roxithromycin was evaluated using an intention-to-treat analysis. Differences were tested using a 2-sided chi-square test ( α= 0.05). Multiple logistic regression analysis was performed to analyze the effect of differences in baseline characteristics between the randomized groups. Differences in symptoms, time to resolution of symptoms, and time to resumption of abandoned and impaired daily activities were tested in life table analyses using the Gehan test. All statistical analyses were performed with Statistical Package for the Social Sciences software, version 8.0.
Results
Patient population
From January 1998 to April 1999, 25 PCPs from 15 practices recruited 196 patients aged 18 years to 89 years. Of these patients, 99 received amoxicillin and 97 received roxithromycin (Figure 1). The 2 groups’ demographic data, signs and symptoms, comorbidities, identified pathogens, and radiographic abnormalities were similar (Table 2). Multiple logistic regression analysis showed that none of the covariables altered the effects of the study medication.
TABLE 2
FINDINGS ON PRESENTATION
| Finding | Amoxicillin Group No. (%) | Roxithromycin Group No. (%) |
|---|---|---|
| Number of Patients | 99 (51) | 97 (49) |
| Demographic Data | ||
| Ratio of men to women | 46/53 | 53/44 |
| Mean age in years (SD) | 55 (15) | 50 (16) |
| Symptoms | ||
| Recent cough in number of days | ||
| 1–7 | 34 (36) | 41 (43) |
| 8–14 | 31 (33) | 25 (26) |
| 15–28 | 22 (23) | 23 (24) |
| No recent cough | 8 (8) | 6 (6) |
| Productive cough | 77 (78) | 84 (88) |
| Dyspnea | 78 (79) | 76 (79) |
| Wheezing | 68 (69) | 61 (64) |
| Risk Factors | ||
| Cigarette smoking | 36 (36) | 29 (31) |
| Comorbidity | ||
| None | 55 (56) | 48 (52) |
| Asthma | 19 (19) | 20 (22) |
| COPD | 17 (17) | 11 (12) |
| Heart failure | 3 (3) | 4 (4) |
| Diabetes mellitus | 2 (2) | 3 (3) |
| Other | 23 (24) | 21 (23) |
| Asthma medication prescribed at start of study | 16 (16) | 13 (14) |
| Signs | ||
| Auscultation abnormalities | 93 (94) | 87 (91) |
| Body temperature 38.0°C | 25 (26) | 22 (24) |
| Infection | ||
| Mild/moderate | 91 (93) | 89 (93) |
| Severe | 7 (7) | 7 (7) |
| Laboratory Tests | ||
| CRP, median (range) | 23 (2-228) | 26 (2-312) |
| ESR, median (range) | 21 (1-104) | 19 (1-121) |
| Leukocytes, median (range) | 8.3 (3.9-19.7) | 8.4 (4.3-15.4) |
| Patients with pathogens | 45 (45) | 46 (47) |
| Chest X-Ray | ||
| Infiltrate on chest x-ray | 14 (14) | 13 (14) |
| NOTE: Values are numbers (percentages) unless otherwise stated. Percentages are based on number of patients for each variable. | ||
| COPD denotes chronic obstructive pulmonary disease; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; SD, standard deviation. | ||
FIGURE 1
DISTRIBUTION OF PATIENTS FOR EFFICACY AND SAFETY ANALYSES
Clinical cure
Early Follow-Up. The rate of clinical cure, defined as the decrease in symptoms and signs at 10 days after randomization, was high and not significantly different between both groups. Using the stricter definition of clinical cure as the complete absence of symptoms and signs led to the same conclusion. Absolute cure rates using this strict definition were low (Table 3).
Physicians discontinued treatment with the study medication in 2 cases (1 amoxicillin and 1 roxithromycin) because of unsatisfactory clinical response. Both patients recovered rapidly after alternative antibiotic treatment. In one case, the patient discontinued amoxicillin after 8 days because of rash and urticaria and recovered quickly without further treatment.
Late Follow-Up. According to the physicians’ final assessments, the rate of clinical cure at 28 days was not significantly different between the 2 groups, although the percentage of patients who showed a decrease in symptoms was significantly higher in the amoxicillin group than in the roxithromycin group (Table 3). Again, cure rates were much lower when the strict definition of cure was used. Eleven patients in the amoxicillin group and 8 in the roxithromycin group were not clinically cured after 28 days. Of these patients, 10 (5 in each group) recovered shortly thereafter or did not consult their physician again for persisting symptoms of LRTI. Nine patients (6 in the amoxicillin group, 3 in the roxithromycin group) with exacerbation of COPD slowly returned to their baseline clinical situation. Four patients (3 in the amoxicillin group, 1 in the roxithromycin group) were found to have concomitant pulmonary cancer. Curative bilobectomy was performed in one of the patients. The others received palliative treatment.
TABLE 3
CLINICAL CURE RATE AT EARLY (10-DAY) AND LATE (28-DAY) FOLLOW-UP
| Characteristic | Amoxicillin No. (%) | Roxithromycin No. (%) | Relative Risk* (CI) |
|---|---|---|---|
| Decrease in Symptoms and Signs | |||
| Day 10 | |||
| Symptoms | 84/96 (88) | 90/95 (95) | 2.38 (0.87-6.48) |
| Signs (physical examination) | 85/98 (87) | 89/95 (94) | 2.10 (0.83-5.30) |
| Day 28 | |||
| Symptoms | 91/95 (96) | 79/93 (85) | 0.28 (0.10-0.82)† |
| Signs (physical examination) | 90/96 (94) | 87/94 (93) | 0.74 (0.29-2.41) |
| Absence of Symptoms and Signs | |||
| Day 10 | |||
| Symptoms | 18/96 (19) | 22/95 (23) | 2.38 (0.87-6.48) |
| Signs (physical examination) | 68/98 (69) | 76/95 (80) | 1.53 (0.93-2.53) |
| Day 28 | |||
| Symptoms | 59/95 (62) | 50/93 (54) | 0.82 (0.58-1.15) |
| Signs (physical examination) | 82/96 (85) | 80/94 (85) | 0.98 (0.49-1.94) |
| Fever (≥38°C) gone, day 10 | 21/25 (84) | 16/22 (73) | 1.37 (0.25-7.41) |
| Cure, final conclusion by physician, day 28 | 84/95 (88) | 86/94 (91) | 1.36 (0.57-3.23) |
| NOTE: Percentages are based on number of patients for each variable. | |||
| *Risk of no cure with amoxicillin vs roxithromycin. | |||
| †P < .05. | |||
Self-reported response over time
The time before resolution of symptoms according to the patients’ diaries was similar for patients treated with amoxicillin and those treated with roxithromycin (Figures 2A and 2B). The percentage of patients who had abandoned daily activities was followed over time. At baseline, more than half of the patients in the amoxicillin group and fewer than 40% in the roxithromycin group reported that they had abandoned daily activities. At day 10, this percentage had fallen to less than 20% in both groups and to less than 10% in both groups at day 28. Differences between the amoxicillin and roxithromycin groups were not significant.
Furthermore, the patients’ diaries revealed information about the time of impaired daily activities. The percentage of patients with impaired daily activities gradually decreased in both treatment groups from approximately 75% at baseline to 30% at day 10 and 20% at day 28.
FIGURE 2
TIME TO RESOLUTION OF SYMPTOMS AS DESCRIBED IN PATIENTS’ DIARIES
Subgroup analyses
The above analyses were repeated for a group of patients aged less than 65 years and a group aged 65 years and older. The trend in cure rates was the same. No differences were found between these age groups regarding the percentage of patients with satisfactory clinical response. Furthermore, the same analyses were performed for each of the clinical diagnoses made by the PCPs at baseline (ie, pneumonia, acute bronchitis, exacerbation of asthma or COPD, and unclassified LRTI). Overall, no significant differences were found between the amoxicillin and roxithromycin groups.
Bacteriologic evaluation
Pathogens were identified in 91 patients (46%). Viruses were most frequent, followed by H (Para) influenzae, S pneumoniae, and Moraxella catarrhalis (Table 4). Bacteriologic cure was achieved in 21 of the 23 patients (91%) in the amoxicillin group and in 23 of the 27 patients (85%) in the roxithromycin group (NS, Fisher’s exact test). In 9 patients of the amoxicillin group and 8 patients of the roxithromycin group, only the sample obtained after 10 days showed the growth of a predominant bacterial pathogen (superinfection).
TABLE 4
RESPIRATORY TRACT PATHOGENS ISOLATED
| Microorganism | No. (%) |
|---|---|
| Typical Bacterial Pathogens | |
| Haemophilus (Para) influenzae | 34 (17) |
| Streptococcus pneumoniae | 12 (6) |
| Moraxella catarrhalis | 6 (3) |
| Other* | 5 (3) |
| Atypical Pathogens | |
| Mycoplasma pneumoniae | 2 (1) |
| Legionella pneumophila | 1 (0.5) |
| Viruses | |
| Influenza A | 29 (16) |
| Influenza B | 7 (4) |
| Parainfluenzae 1, 2, 3 | 7 (4) |
| Adenovirus | 5 (3) |
| Respiratory syncytial virus | 5 (3) |
| No organism (number of patients) | 122 (49) |
| * Enterobacteriaceae (n = 2), Staphylococcus aureus (n = 1), Streptococcus viridans (n = 1), Neisseria meningitidis (n = 1). | |
Safety and compliance
Thirty possible or probable adverse events were reported in 19 of 99 patients (19%) treated with amoxicillin: diarrhea (13), stomach ache (3), headache (3), and 11 other side effects, including nausea, vomiting, and rash, once each. In the roxithromycin group, 24 events were reported in 16 patients (16%): nausea (5), diarrhea (4), vomiting (4), rash (2), headache (2), and 7 others, including pruritus ani, dizziness, and mild bradycardia, once each.
Compliance with the medication regimen was high. Data from electronic monitoring were available for 160 patients (78 in the amoxicillin group, 82 in the roxithromycin group). The overall compliance rate for patients in both groups (ie, the number of doses taken divided by the number of doses prescribed) was 98%. In the amoxicillin group, the numbers of patients with less than 90% compliance in taking the tablets and capsules were 7 and 4, respectively. In the roxithromycin group, compliance in taking the tablets was at least 90% in all patients but compliance in taking the capsules was less than 90% in 6 patients.
Discussion
This community-based study shows that amoxicillin and roxithromycin are equally effective in the treatment of LRTI in the Netherlands. Clinical cure rates after 10 days of antibiotic treatment were approximately 90% in both study groups, although complete absence of symptoms was achieved in only a minority of cases. After 28 days of follow-up, cure rates remained high. The amoxicillin group had a significantly higher cure rate than the roxithromycin group as evidenced by the decrease in symptoms. However, this significant difference in favor of the amoxicillin group did not alter the PCPs’ overall conclusion after complete follow-up: that 90% of patients who received either drug had been effectively treated. Patients’ diary entries agreed with that impression.
The time to resolution of symptoms, the cumulative cure rate per day, and the influence of the illness on daily activities were not significantly different between patients treated with amoxicillin versus those given roxithromycin. Adverse events were mild and were divided evenly over both groups with the exception of diarrhea, which occurred more often in those taking amoxicillin.
In our study, complete absence of symptoms and signs after 28 days, as assessed by both physicians and patients, was achieved in only approximately half the patients. Complete remission of LRTI often takes more than 4 weeks.
Although LRTI is often managed in primary care, diagnostic and therapeutic decisions are usually based on the experiences of hospital-based specialists and on the results of trials conducted in hospital settings. Generalizing these results to primary care is of limited value, since disease in patients recruited for these studies is often at a later stage and more serious. In our trial, patients were recruited, diagnosed, and treated by PCPs in their natural setting, maintaining regular care as much as possible.
Nevertheless, generalization of our findings to everyday care may not be valid. To explore the degree of selection in our recruited patients, we compared the actual numbers of cases of LRTI in 3 practices (with a total of 9 PCPs and a total population of 13,269) with the numbers included in the present trial during 1 year of the inclusion period. Of the 463 presumably eligible patients, only 43 (9%) were actually included. This proportion is similar to that in a recent study of randomized controlled trials in primary care in which less than 10% of the eligible population were recruited for the trial.31 Included patients did not differ from other eligible patients with regard to age, clinical diagnosis, severity of illness, and need for antibiotic treatment (according to the PCPs).
Clinical studies, mostly in inpatient settings, on community-acquired pneumonia have identified causative pathogens in 50% to 69% of patients.14-17,21,23,32,33 Outpatient studies of acute bronchitis and LRTI have generally reported considerably lower percentages (16% to 44%).19,20,34-36 In our study, pathogens that presumably caused LRTI were found in 46% of patients.
Because atypical pathogens were the presumptive causative agent in only 3 cases (2 M pneumoniae, 1 L pneumophila), the potential advantage of macrolide antibiotics over amoxicillin is minimal. Furthermore, bacterial resistance to macrolide antibiotics is believed to be considerable.37,38 In Finland, bacterial resistance to erythromycin has been shown to rise quickly after an increase in the consumption of macrolide antibiotics.39 In contrast to alarming reports in the literature,14,17,22,40,41 the low incidence of M pneumoniae and L pneumophila found in the current study supports the conservative approach (ie, amoxicillin or doxycycline) to treating community-acquired LRTI in the Netherlands.
M pneumoniae occurs at high rates in 4-year to 5-year cycles.42 This timing implies that the frequency of M pneumoniae might be higher if the same study were performed 1 year later. Because most M pneumoniae infections are self-limiting and clinical cure rates of macrolide antibiotics compared with those of placebo are the same,43,44 however, this epidemiologic observation does not change the conclusions of the present study.
Compliance with medication was reliably measured and quantified by Medical Event Monitoring Systems. For both ethical and practical reasons, patients were informed about the monitoring mechanism. Their knowledge about the monitoring may have slightly increased compliance as compared with daily practice, although this assumption has not been confirmed in other studies.45,46 Furthermore, compliance with antibiotic regimens is known to be greater than compliance with chronic medication regimens.47,48
Conclusions
General practitioners frequently diagnose LRTI in general or pneumonia and acute bronchitis in particular, including infectious episodes in patients with asthma or COPD. In many cases, treatment with antibiotics follows. The results of our randomized controlled trial did not confirm the potentially greater value of roxithromycin, which is often recommended as the drug of choice for empirical treatment of community-acquired pneumonia, over amoxicillin. Because amoxicillin was as effective as roxithromycin, it remains a reliable first-choice antibiotic in the treatment of community-acquired LRTI.
Acknowledgments
The authors wish to thank the patients, general practitioners, and physicians’ assistants who participated in this study. They also thank Hans Verloop, director of the Vandra paper factory, Meer-Hoogstraten, Belgium, for donating cardboard boxes and Alexander Thissen, Josephine Asberg, and Ramon Ottenheijm for their assistance with the logistics of the study. The study was supported by a grant from the Research Institute for Extramural and Transmural Health Care, Maastricht.
OBJECTIVE: To assess the efficacy of roxithromycin relative to amoxicillin.
STUDY DESIGN: We conducted a double-blind randomized controlled trial of oral 500 mg amoxicillin 3 times per day vs oral 300 mg roxithromycin once a day for 10 days.
POPULATION: We included 196 adults who had presented to a general practitioner with lower respiratory tract infection (LRTI) and, in the physician’s opinion, needed antibiotic treatment.
OUTCOMES MEASURED: We measured clinical response after 10 and 28 days, defined in 4 ways: (1) decrease in LRTI symptoms; (2) complete absence of symptoms; (3) decrease in signs; and (4) complete absence of signs. Self-reported response included the decrease in symptoms and the time until resumption of impaired or abandoned daily activities on days 1 through 10, 21, and 27.
RESULTS: Clinical cure rates after the completion of antibiotic treatment (10 days) were not significantly different for the 2 groups. After 28 days, the roxithromycin group showed no increase in cure rate as evidenced by the decrease in symptoms, indicating a significantly lower cure rate. However, this difference did not alter physicians’ overall conclusion after complete follow-up that 90% of patients, regardless of age, had been effectively treated with either amoxicillin or roxithromycin.
CONCLUSIONS: The surplus value of roxithromycin was not confirmed. Amoxicillin remains a reliable first-choice antibiotic in the treatment of LRTI in general practice.
- Amoxicillin and roxithromycin are equally effective in the treatment of patients presenting with lower respiratory tract infections and needing antibiotic treatment.
- Most patients remain symptomatic after 10 days of treatment with either drug.
- The low incidence of atypical pathogens (Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae) in the Netherlands minimizes the potentially greater surplus value of macrolide antibiotics over amoxicillin.
Acute community-acquired lower respiratory tract infections (LRTIs) in adults include acute bronchitis, pneumonia, and infectious episodes in patients with asthma or chronic obstructive pulmonary disease (COPD). In acute bronchitis and exacerbations of COPD, the value of antibiotic therapy is doubtful; in pneumonia, however, it is widely accepted. Because distinguishing between these disease entities on clinical grounds alone is often impossible, deciding which patients would benefit from antibiotic treatment remains difficult.1-6In the Netherlands, as in the United States and Great Britain, antibiotics are prescribed for patients with acute bronchitis approximately 80% of the time.7-9
If a primary care physician (PCP) decides to treat LRTI with antibiotics, amoxicillin is the drug of first choice in the Netherlands.10-13 However, amoxicillin is not effective in infections caused by atypical organisms such as Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila, which are responsible for 1% to 50% of cases of LRTI.14-20 Roxithromycin and the newer macrolide antibiotics are recommended as drugs of choice for the empirical treatment of community-acquired pneumonia in low-risk patients in the United States and Canada21-23 because those drugs cover both typical and atypical pathogens. Amoxicillin has long proved to be a reliable drug and one to which the resistance of common respiratory tract pathogens (Streptococcus pneumoniae and Haemophilus influenzae) in the Netherlands is low.24-29
Community-based studies that evaluate treatment for LRTI are lacking. Also lacking are independent randomized controlled studies comparing amoxicillin with roxithromycin or other new macrolides for LRTI. Our double-blind randomized trial attempted to determine whether the preference for amoxicillin in the Netherlands is well founded. In the trial, patients with LRTI who in their PCP’s opinion needed antibiotic treatment were assigned to either amoxicillin or roxithromycin. We then compared the efficacy and safety of both drugs.
Methods
Eligibility criteria and baseline characteristics
Eligible study subjects were patients in the southern part of the Netherlands who presented with signs and symptoms of LRTI that their PCPs believed warranted antibiotic therapy. Table 1 lists the inclusion and exclusion criteria.
Baseline data (at day 1) were obtained to evaluate the comparability of prognostic factors between the intervention groups. The PCP performed an extensive medical history and physical examination. In addition, a sputum sample, oral washing, and nasopharyngeal swab were taken for bacteriologic examination. Venous blood samples were taken for blood chemistry, hematology, and serology (initial titers of the viral pathogens M pneumoniae and L pneumophila).
TABLE 1
CHECKLIST FOR PATIENT ELIGIBILITY
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| A: Age 18 years or older |
|
| AND | |
| B: New* or increasing cough | |
| AND | |
| C: At least 1 of the following: | |
| 1) Shortness of breath | |
| 2) Wheezing | |
| 3) Chest pain | |
| 4) Auscultation abnormalities | |
| AND | |
| D: At least 1 of the following: | |
| 1) Fever (≥ 38°C) | |
| 2) Perspiring | |
| 3) Headache | |
| 4) Myalgia | |
| AND | |
| E: Diagnosis of LRTI according to PCP and | |
| F: Antibiotics required (in PCP’s opinion) | |
| * Onset within the previous 29 days. | |
| LRTI denotes lower respiratory tract infection; PCP, primary care physician. | |
Interventions
Once the samples had been collected, patients were randomly assigned to oral treatment with either 500 mg amoxicillin 3 times daily for 10 days or 300 mg roxithromycin once daily for 10 days. A computer program using random permuted blocks of 6 prepared a randomization list for each participating center. Batches of drug packages, each provided with a unique trial code, had been sent in advance to the participating general practices. A double-dummy technique achieved blinding of patients, treating physicians, and investigators to the assigned medication. This was necessary because amoxicillin and roxithromycin have different dosing schedules (3 times a day versus once daily) and are not identical in appearance (capsule versus tablet). All capsules and tablets had identical appearance and taste. All patients received both forms of their assigned medication. Compliance with medication regimens was measured by Medical Event Monitoring Systems (MEMS), an electronic recording system that compiles the dosing history of ambulatory patients taking oral medication.30
Chest X-Rays
Every patient underwent chest x-ray. The radiographs were reassessed for the presence or absence of infiltrate by a blinded independent senior radiologist. If the first and second radiologist disagreed, a third senior radiologist made a final assessment.
Follow-up
Follow-up consultations similar to the examination on day 1 took place on days 10 and 28. During treatment (days 1 through 10) and on days 21 and 27, follow-up was supplemented by a short diary in which patients recorded their symptoms and the times at which they resumed daily activities that they had abandoned or that had been impaired.
Outcomes measured
Efficacy was assessed by comparing the groups’ clinical response on day 10 (the primary outcome measure) and day 28 and their bacteriologic response on day 10. Satisfactory clinical response was defined in 4 ways: (1) decrease in symptoms of LRTI; (2) absence of symptoms of LRTI; (3) decrease in signs of LRTI; and (4) absence of signs of LRTI. All other outcomes were regarded as unsatisfactory responses.
Self-reported symptoms and time to resolution were compared between the 2 groups on days 1 through 10, 21, and 27. The percentage of patients who had abandoned daily activities or whose participation in daily activities had been impaired by illness was followed over time. Bacteriologic cure was defined as the absence of growth of a predominant bacterial pathogen (cultured at baseline) in a sputum sample taken on day 10.
We recorded patients’ compliance rates, frequency of adverse events, and acquired bacterial resistance. Compliance was defined as the number of doses taken divided by the number of doses prescribed.
Statistical analyses
The efficacy of amoxicillin and roxithromycin was evaluated using an intention-to-treat analysis. Differences were tested using a 2-sided chi-square test ( α= 0.05). Multiple logistic regression analysis was performed to analyze the effect of differences in baseline characteristics between the randomized groups. Differences in symptoms, time to resolution of symptoms, and time to resumption of abandoned and impaired daily activities were tested in life table analyses using the Gehan test. All statistical analyses were performed with Statistical Package for the Social Sciences software, version 8.0.
Results
Patient population
From January 1998 to April 1999, 25 PCPs from 15 practices recruited 196 patients aged 18 years to 89 years. Of these patients, 99 received amoxicillin and 97 received roxithromycin (Figure 1). The 2 groups’ demographic data, signs and symptoms, comorbidities, identified pathogens, and radiographic abnormalities were similar (Table 2). Multiple logistic regression analysis showed that none of the covariables altered the effects of the study medication.
TABLE 2
FINDINGS ON PRESENTATION
| Finding | Amoxicillin Group No. (%) | Roxithromycin Group No. (%) |
|---|---|---|
| Number of Patients | 99 (51) | 97 (49) |
| Demographic Data | ||
| Ratio of men to women | 46/53 | 53/44 |
| Mean age in years (SD) | 55 (15) | 50 (16) |
| Symptoms | ||
| Recent cough in number of days | ||
| 1–7 | 34 (36) | 41 (43) |
| 8–14 | 31 (33) | 25 (26) |
| 15–28 | 22 (23) | 23 (24) |
| No recent cough | 8 (8) | 6 (6) |
| Productive cough | 77 (78) | 84 (88) |
| Dyspnea | 78 (79) | 76 (79) |
| Wheezing | 68 (69) | 61 (64) |
| Risk Factors | ||
| Cigarette smoking | 36 (36) | 29 (31) |
| Comorbidity | ||
| None | 55 (56) | 48 (52) |
| Asthma | 19 (19) | 20 (22) |
| COPD | 17 (17) | 11 (12) |
| Heart failure | 3 (3) | 4 (4) |
| Diabetes mellitus | 2 (2) | 3 (3) |
| Other | 23 (24) | 21 (23) |
| Asthma medication prescribed at start of study | 16 (16) | 13 (14) |
| Signs | ||
| Auscultation abnormalities | 93 (94) | 87 (91) |
| Body temperature 38.0°C | 25 (26) | 22 (24) |
| Infection | ||
| Mild/moderate | 91 (93) | 89 (93) |
| Severe | 7 (7) | 7 (7) |
| Laboratory Tests | ||
| CRP, median (range) | 23 (2-228) | 26 (2-312) |
| ESR, median (range) | 21 (1-104) | 19 (1-121) |
| Leukocytes, median (range) | 8.3 (3.9-19.7) | 8.4 (4.3-15.4) |
| Patients with pathogens | 45 (45) | 46 (47) |
| Chest X-Ray | ||
| Infiltrate on chest x-ray | 14 (14) | 13 (14) |
| NOTE: Values are numbers (percentages) unless otherwise stated. Percentages are based on number of patients for each variable. | ||
| COPD denotes chronic obstructive pulmonary disease; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; SD, standard deviation. | ||
FIGURE 1
DISTRIBUTION OF PATIENTS FOR EFFICACY AND SAFETY ANALYSES
Clinical cure
Early Follow-Up. The rate of clinical cure, defined as the decrease in symptoms and signs at 10 days after randomization, was high and not significantly different between both groups. Using the stricter definition of clinical cure as the complete absence of symptoms and signs led to the same conclusion. Absolute cure rates using this strict definition were low (Table 3).
Physicians discontinued treatment with the study medication in 2 cases (1 amoxicillin and 1 roxithromycin) because of unsatisfactory clinical response. Both patients recovered rapidly after alternative antibiotic treatment. In one case, the patient discontinued amoxicillin after 8 days because of rash and urticaria and recovered quickly without further treatment.
Late Follow-Up. According to the physicians’ final assessments, the rate of clinical cure at 28 days was not significantly different between the 2 groups, although the percentage of patients who showed a decrease in symptoms was significantly higher in the amoxicillin group than in the roxithromycin group (Table 3). Again, cure rates were much lower when the strict definition of cure was used. Eleven patients in the amoxicillin group and 8 in the roxithromycin group were not clinically cured after 28 days. Of these patients, 10 (5 in each group) recovered shortly thereafter or did not consult their physician again for persisting symptoms of LRTI. Nine patients (6 in the amoxicillin group, 3 in the roxithromycin group) with exacerbation of COPD slowly returned to their baseline clinical situation. Four patients (3 in the amoxicillin group, 1 in the roxithromycin group) were found to have concomitant pulmonary cancer. Curative bilobectomy was performed in one of the patients. The others received palliative treatment.
TABLE 3
CLINICAL CURE RATE AT EARLY (10-DAY) AND LATE (28-DAY) FOLLOW-UP
| Characteristic | Amoxicillin No. (%) | Roxithromycin No. (%) | Relative Risk* (CI) |
|---|---|---|---|
| Decrease in Symptoms and Signs | |||
| Day 10 | |||
| Symptoms | 84/96 (88) | 90/95 (95) | 2.38 (0.87-6.48) |
| Signs (physical examination) | 85/98 (87) | 89/95 (94) | 2.10 (0.83-5.30) |
| Day 28 | |||
| Symptoms | 91/95 (96) | 79/93 (85) | 0.28 (0.10-0.82)† |
| Signs (physical examination) | 90/96 (94) | 87/94 (93) | 0.74 (0.29-2.41) |
| Absence of Symptoms and Signs | |||
| Day 10 | |||
| Symptoms | 18/96 (19) | 22/95 (23) | 2.38 (0.87-6.48) |
| Signs (physical examination) | 68/98 (69) | 76/95 (80) | 1.53 (0.93-2.53) |
| Day 28 | |||
| Symptoms | 59/95 (62) | 50/93 (54) | 0.82 (0.58-1.15) |
| Signs (physical examination) | 82/96 (85) | 80/94 (85) | 0.98 (0.49-1.94) |
| Fever (≥38°C) gone, day 10 | 21/25 (84) | 16/22 (73) | 1.37 (0.25-7.41) |
| Cure, final conclusion by physician, day 28 | 84/95 (88) | 86/94 (91) | 1.36 (0.57-3.23) |
| NOTE: Percentages are based on number of patients for each variable. | |||
| *Risk of no cure with amoxicillin vs roxithromycin. | |||
| †P < .05. | |||
Self-reported response over time
The time before resolution of symptoms according to the patients’ diaries was similar for patients treated with amoxicillin and those treated with roxithromycin (Figures 2A and 2B). The percentage of patients who had abandoned daily activities was followed over time. At baseline, more than half of the patients in the amoxicillin group and fewer than 40% in the roxithromycin group reported that they had abandoned daily activities. At day 10, this percentage had fallen to less than 20% in both groups and to less than 10% in both groups at day 28. Differences between the amoxicillin and roxithromycin groups were not significant.
Furthermore, the patients’ diaries revealed information about the time of impaired daily activities. The percentage of patients with impaired daily activities gradually decreased in both treatment groups from approximately 75% at baseline to 30% at day 10 and 20% at day 28.
FIGURE 2
TIME TO RESOLUTION OF SYMPTOMS AS DESCRIBED IN PATIENTS’ DIARIES
Subgroup analyses
The above analyses were repeated for a group of patients aged less than 65 years and a group aged 65 years and older. The trend in cure rates was the same. No differences were found between these age groups regarding the percentage of patients with satisfactory clinical response. Furthermore, the same analyses were performed for each of the clinical diagnoses made by the PCPs at baseline (ie, pneumonia, acute bronchitis, exacerbation of asthma or COPD, and unclassified LRTI). Overall, no significant differences were found between the amoxicillin and roxithromycin groups.
Bacteriologic evaluation
Pathogens were identified in 91 patients (46%). Viruses were most frequent, followed by H (Para) influenzae, S pneumoniae, and Moraxella catarrhalis (Table 4). Bacteriologic cure was achieved in 21 of the 23 patients (91%) in the amoxicillin group and in 23 of the 27 patients (85%) in the roxithromycin group (NS, Fisher’s exact test). In 9 patients of the amoxicillin group and 8 patients of the roxithromycin group, only the sample obtained after 10 days showed the growth of a predominant bacterial pathogen (superinfection).
TABLE 4
RESPIRATORY TRACT PATHOGENS ISOLATED
| Microorganism | No. (%) |
|---|---|
| Typical Bacterial Pathogens | |
| Haemophilus (Para) influenzae | 34 (17) |
| Streptococcus pneumoniae | 12 (6) |
| Moraxella catarrhalis | 6 (3) |
| Other* | 5 (3) |
| Atypical Pathogens | |
| Mycoplasma pneumoniae | 2 (1) |
| Legionella pneumophila | 1 (0.5) |
| Viruses | |
| Influenza A | 29 (16) |
| Influenza B | 7 (4) |
| Parainfluenzae 1, 2, 3 | 7 (4) |
| Adenovirus | 5 (3) |
| Respiratory syncytial virus | 5 (3) |
| No organism (number of patients) | 122 (49) |
| * Enterobacteriaceae (n = 2), Staphylococcus aureus (n = 1), Streptococcus viridans (n = 1), Neisseria meningitidis (n = 1). | |
Safety and compliance
Thirty possible or probable adverse events were reported in 19 of 99 patients (19%) treated with amoxicillin: diarrhea (13), stomach ache (3), headache (3), and 11 other side effects, including nausea, vomiting, and rash, once each. In the roxithromycin group, 24 events were reported in 16 patients (16%): nausea (5), diarrhea (4), vomiting (4), rash (2), headache (2), and 7 others, including pruritus ani, dizziness, and mild bradycardia, once each.
Compliance with the medication regimen was high. Data from electronic monitoring were available for 160 patients (78 in the amoxicillin group, 82 in the roxithromycin group). The overall compliance rate for patients in both groups (ie, the number of doses taken divided by the number of doses prescribed) was 98%. In the amoxicillin group, the numbers of patients with less than 90% compliance in taking the tablets and capsules were 7 and 4, respectively. In the roxithromycin group, compliance in taking the tablets was at least 90% in all patients but compliance in taking the capsules was less than 90% in 6 patients.
Discussion
This community-based study shows that amoxicillin and roxithromycin are equally effective in the treatment of LRTI in the Netherlands. Clinical cure rates after 10 days of antibiotic treatment were approximately 90% in both study groups, although complete absence of symptoms was achieved in only a minority of cases. After 28 days of follow-up, cure rates remained high. The amoxicillin group had a significantly higher cure rate than the roxithromycin group as evidenced by the decrease in symptoms. However, this significant difference in favor of the amoxicillin group did not alter the PCPs’ overall conclusion after complete follow-up: that 90% of patients who received either drug had been effectively treated. Patients’ diary entries agreed with that impression.
The time to resolution of symptoms, the cumulative cure rate per day, and the influence of the illness on daily activities were not significantly different between patients treated with amoxicillin versus those given roxithromycin. Adverse events were mild and were divided evenly over both groups with the exception of diarrhea, which occurred more often in those taking amoxicillin.
In our study, complete absence of symptoms and signs after 28 days, as assessed by both physicians and patients, was achieved in only approximately half the patients. Complete remission of LRTI often takes more than 4 weeks.
Although LRTI is often managed in primary care, diagnostic and therapeutic decisions are usually based on the experiences of hospital-based specialists and on the results of trials conducted in hospital settings. Generalizing these results to primary care is of limited value, since disease in patients recruited for these studies is often at a later stage and more serious. In our trial, patients were recruited, diagnosed, and treated by PCPs in their natural setting, maintaining regular care as much as possible.
Nevertheless, generalization of our findings to everyday care may not be valid. To explore the degree of selection in our recruited patients, we compared the actual numbers of cases of LRTI in 3 practices (with a total of 9 PCPs and a total population of 13,269) with the numbers included in the present trial during 1 year of the inclusion period. Of the 463 presumably eligible patients, only 43 (9%) were actually included. This proportion is similar to that in a recent study of randomized controlled trials in primary care in which less than 10% of the eligible population were recruited for the trial.31 Included patients did not differ from other eligible patients with regard to age, clinical diagnosis, severity of illness, and need for antibiotic treatment (according to the PCPs).
Clinical studies, mostly in inpatient settings, on community-acquired pneumonia have identified causative pathogens in 50% to 69% of patients.14-17,21,23,32,33 Outpatient studies of acute bronchitis and LRTI have generally reported considerably lower percentages (16% to 44%).19,20,34-36 In our study, pathogens that presumably caused LRTI were found in 46% of patients.
Because atypical pathogens were the presumptive causative agent in only 3 cases (2 M pneumoniae, 1 L pneumophila), the potential advantage of macrolide antibiotics over amoxicillin is minimal. Furthermore, bacterial resistance to macrolide antibiotics is believed to be considerable.37,38 In Finland, bacterial resistance to erythromycin has been shown to rise quickly after an increase in the consumption of macrolide antibiotics.39 In contrast to alarming reports in the literature,14,17,22,40,41 the low incidence of M pneumoniae and L pneumophila found in the current study supports the conservative approach (ie, amoxicillin or doxycycline) to treating community-acquired LRTI in the Netherlands.
M pneumoniae occurs at high rates in 4-year to 5-year cycles.42 This timing implies that the frequency of M pneumoniae might be higher if the same study were performed 1 year later. Because most M pneumoniae infections are self-limiting and clinical cure rates of macrolide antibiotics compared with those of placebo are the same,43,44 however, this epidemiologic observation does not change the conclusions of the present study.
Compliance with medication was reliably measured and quantified by Medical Event Monitoring Systems. For both ethical and practical reasons, patients were informed about the monitoring mechanism. Their knowledge about the monitoring may have slightly increased compliance as compared with daily practice, although this assumption has not been confirmed in other studies.45,46 Furthermore, compliance with antibiotic regimens is known to be greater than compliance with chronic medication regimens.47,48
Conclusions
General practitioners frequently diagnose LRTI in general or pneumonia and acute bronchitis in particular, including infectious episodes in patients with asthma or COPD. In many cases, treatment with antibiotics follows. The results of our randomized controlled trial did not confirm the potentially greater value of roxithromycin, which is often recommended as the drug of choice for empirical treatment of community-acquired pneumonia, over amoxicillin. Because amoxicillin was as effective as roxithromycin, it remains a reliable first-choice antibiotic in the treatment of community-acquired LRTI.
Acknowledgments
The authors wish to thank the patients, general practitioners, and physicians’ assistants who participated in this study. They also thank Hans Verloop, director of the Vandra paper factory, Meer-Hoogstraten, Belgium, for donating cardboard boxes and Alexander Thissen, Josephine Asberg, and Ramon Ottenheijm for their assistance with the logistics of the study. The study was supported by a grant from the Research Institute for Extramural and Transmural Health Care, Maastricht.
1. Bartlett JG, Mundy LM. Community-acquired pneumonia. N Engl J Med 1995;333:1618-24.
2. Melbye H, Straume B, Aasebo U, Dale K. Diagnosis of pneumonia in adults in general practice. Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care. 1992;10:226-33.
3. Melbye H, Straume B, Aasebo U, Brox J. The diagnosis of adult pneumonia in general practice. The diagnostic value of history, physical examination and some blood tests. Scand J Prim Health Care. 1988;6:111-7.
4. Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination—relevant or relic? Arch Intern Med. 1999;159:1082-7.
5. Zaat JOM, Stalman WAB, Assendelft WJJ. Groaning, moaning and percussion. A systematic review on the diagnostic value of history and physical examination in patient with a suspicion of pneumonia. Huisarts Wet. 1998;41:461-9.
6. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA 1997;278:1440-5.
7. Kuyvenhoven MM, Verheij TJ, de Melker RA, van der Velden J. Antimicrobial agents in lower respiratory tract infections in Dutch general practice. Br J Gen Pract 2000;50:133-4.
8. Macfarlane J, Lewis SA, Macfarlane R, Holmes W. Contemporary use of antibiotics in 1089 adults presenting with acute lower respiratory tract illness in general practice in the UK: implications for developing management guidelines. Respir Med 1997;91:427-34.
9. Oeffinger KC, Snell LM, Foster BM, Panico KG, Archer RK. Treatment of acute bronchitis in adults. A national survey of family physicians. J Fam Pract. 1998;46:469-75.
10. Ortqvist A. Antibiotic treatment of community-acquired pneumonia in clinical practice: a European perspective. J Antimicrob Chemother 1995;35:205-12.
11. Janknegt R, Wijnands WJ, Stobberingh EE. Antibiotic policies in Dutch hospitals for the treatment of pneumonia. J Antimicrob Chemother 1994;34:431-42.
12. van der Werf GT, Smith RJA, Stewart RE, Meyboom-de Jong B. Spiegel op de huisarts: over registratie van ziekte, medicatie en verwijzingen in de geautimatiseerde huisartsenpraktijk. Groningen, the Netherlands: Disciplinegroep Huisartsgeneeskunde, University of Groningen; 1998: 1-181.
13. Stokx LJ, Foets M. Het voorschrijven van geneesmiddelen in de huisartspraktijk. Deel II [Prescribing drugs in general practice]. Utrecht: NIVEL; 1994.
14. Marrie TJ, Peeling RW, Fine MJ, Singer DE, Coley CM, Kapoor WN. Ambulatory patients with community-acquired pneumonia: the frequency of atypical agents and clinical course. Am J Med 1996;101:508-15.
15. Berntsson E, Lagergard T, Strannegard O, Trollfors B. Etiology of community-acquired pneumonia in out-patients. Eur J Clin Microbiol 1986;5:446-7.
16. Bohte R, van Furth R, van den Broek PJ. Aetiology of community-acquired pneumonia: a prospective study among adults requiring admission to hospital. Thorax 1995;50:543-7.
17. Fang GD, Fine M, Orloff J, et al. New and emerging etiologies for community-acquired pneumonia with implications for therapy. A prospective multicenter study of 359 cases. Medicine (Baltimore). 1990;69:307-16.
18. Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG. Prospective study of the aetiology and outcome of pneumonia in the community. Lancet 1987;1:671-4.
19. Jonsson JS, Sigurdsson JA, Kristinsson KG, Guthnadottir M, Magnusson S. Acute bronchitis in adults. How close do we come to its aetiology in general practice? Scand J Prim Health Care. 1997;15:156-60.
20. Macfarlane JT, Colville A, Guion A, Macfarlane RM, Rose DH. Prospective study of aetiology and outcome of adult lower-respiratory-tract infections in the community. Lancet 1993;341:511-4.
21. Niederman MS, Bass JB, Jr, Campbell GD, et al. Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. merican Thoracic Society. Medical Section of the American Lung Association. Am Rev Respir Dis. 1993;148:1418-26.
22. Mandell LA, Niederman M. Antimicrobial treatment of community acquired pneumonia in adults: a conference report. Can J Infect Dis 1993;4:25-8.
23. Marrie TJ. Community acquired pneumonia. Clin Infect Dis 1994;18:501-15.
24. Poirier R. Comparative study of clarithromycin and roxithromycin in the treatment of community-acquired pneumonia. J Antimicrob Chemother 1991;27:109-16.
25. Tilyard MW, Dovey SM. A randomized double-blind controlled trial of roxithromycin and cefaclor in the treatment of acute lower respiratory tract infections in general practice. Diagn Microbiol Infect Dis 1992;15:S97-101.
26. Zeluff BJ, Lowe P, Koornhof HJ, Gentry LO. Evaluation of roxithromycin (RU-965) versus cephradine in pneumococcal pneumonia. Eur J Clin Microbiol Infect Dis. 1988;7:69-71.
27. Schonwald S, Barsic B, Klinar I, Gunjaca M. Three-day azithromycin compared with ten-day roxithromycin treatment of atypical pneumonia. Scand J Infect Dis 1994;26:706-10.
28. Young RA, Gonzalez JP, Sorkin EM. Roxithromycin. A review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs. 1989;37:8-41.
29. de Neeling AJ, Pelt van W, Hendrix MGR, et al. Antibiotica resistentie in Nederland. Deel III: Gram-positieve bacteriën. Infect Bull. 1997;8:211-5.
30. Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Ouellette VL. How often is medication taken as prescribed? A novel assessment technique. JAMA 1989;261:3273-7.
31. Wilson S, Delaney BC, Roalfe A, et al. Randomized controlled trials in primary care: case study. BMJ 2000;321:24-7.
32. Ortqvist A, Hedlund J, Grillner L, et al. Aetiology, outcome and prognostic factors in community-acquired pneumonia requiring hospitalization. Eur Respir J 1990;3:1105-13.
33. Ortqvist A, Valtonen M, Cars O, Wahl M, Saikku P, Jean C. Oral empiric treatment of community-acquired pneumonia. A multicenter, double-blind, randomized study comparing sparfloxacin with roxithromycin. The Scandinavian Sparfloxacin Study Group. Chest. 1996;110:1499-506.
34. Boldy DA, Skidmore SJ, Ayres JG. Acute bronchitis in the community: clinical features, infective factors, changes in pulmonary function and bronchial reactivity to histamine. Respir Med 1990;84:377-85.
35. Trigg CJ, Wilks M, Herdman MJ, Clague JE, Tabaqchali S, Davies RJ. A double-blind comparison of the effects of cefaclor and amoxycillin on respiratory tract and oropharyngeal flora and clinical response in acute exacerbations of bronchitis. Respir Med 1991;85:301-8.
36. Karalus NC, Garrett JE, Lang SD, et al. Roxithromycin 150 mg bid versus amoxicillin 500 mg/clavulanic acid 125 mg tid for the treatment of lower respiratory tract infections in general practice. Infection 1995;23:S15-20.
37. Swartz MN. Use of antimicrobial agents and drug resistance. N Engl J Med 1997;337:491-2.
38. de Neeling AJ. Antibioticagebruik en het optreden van resistentie. National Institute of Public Health and the Environment/Volksgezondheid Toekomst Verkenning 1997;B3:793-800.
39. Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish Study Group for Antimicrobial Resistance. N Engl J Med. 1997;337:441-6.
40. Wood MJ. More macrolides. BMJ 1991;303:594-5.
41. Wort SJ, Rogers TR. Community acquired pneumonia in elderly people. Current British guidelines need revision. BMJ. 1998;316:1690.-
42. Bartlett JB. Management of respiratory tract infections. Baltimore, Md: Williams & Wilkins; 1997: 121.
43. King DE, Williams WC, Bishop L, Shechter A. Effectiveness of erythromycin in the treatment of acute bronchitis. J Fam Pract 1996;42:601-5.
44. Lode H, Garau J, Grassi C, et al. Treatment of community-acquired pneumonia: a randomized comparison of sparfloxacin, amoxycillin-clavulanic acid and erythromycin. Eur Respir J 1995;8:1999-2007.
45. Urquhart J. Partial compliance in cardiovascular disease: risk implications. Br J Clin Pract 1994;suppl:2-12.
46. Cramer JA, Ouelette VL, Mattson RH. Effect of microelectronic observation on compliance. Epilepsia 1990;31:617-8.
47. Favre O, Delacretaz E, Badan M, Glauser M, Waeber B. Relationship between the prescriber’s instructions and compliance with antibiotherapy in outpatients treated for an acute infectious disease. J Clin Pharmacol 1997;37:175-8.
48. Urquhart J. Role of patient compliance in clinical pharmacokinetics. A review of recent research. Clin Pharmacokinet. 1994;27:202-15.
1. Bartlett JG, Mundy LM. Community-acquired pneumonia. N Engl J Med 1995;333:1618-24.
2. Melbye H, Straume B, Aasebo U, Dale K. Diagnosis of pneumonia in adults in general practice. Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care. 1992;10:226-33.
3. Melbye H, Straume B, Aasebo U, Brox J. The diagnosis of adult pneumonia in general practice. The diagnostic value of history, physical examination and some blood tests. Scand J Prim Health Care. 1988;6:111-7.
4. Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination—relevant or relic? Arch Intern Med. 1999;159:1082-7.
5. Zaat JOM, Stalman WAB, Assendelft WJJ. Groaning, moaning and percussion. A systematic review on the diagnostic value of history and physical examination in patient with a suspicion of pneumonia. Huisarts Wet. 1998;41:461-9.
6. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA 1997;278:1440-5.
7. Kuyvenhoven MM, Verheij TJ, de Melker RA, van der Velden J. Antimicrobial agents in lower respiratory tract infections in Dutch general practice. Br J Gen Pract 2000;50:133-4.
8. Macfarlane J, Lewis SA, Macfarlane R, Holmes W. Contemporary use of antibiotics in 1089 adults presenting with acute lower respiratory tract illness in general practice in the UK: implications for developing management guidelines. Respir Med 1997;91:427-34.
9. Oeffinger KC, Snell LM, Foster BM, Panico KG, Archer RK. Treatment of acute bronchitis in adults. A national survey of family physicians. J Fam Pract. 1998;46:469-75.
10. Ortqvist A. Antibiotic treatment of community-acquired pneumonia in clinical practice: a European perspective. J Antimicrob Chemother 1995;35:205-12.
11. Janknegt R, Wijnands WJ, Stobberingh EE. Antibiotic policies in Dutch hospitals for the treatment of pneumonia. J Antimicrob Chemother 1994;34:431-42.
12. van der Werf GT, Smith RJA, Stewart RE, Meyboom-de Jong B. Spiegel op de huisarts: over registratie van ziekte, medicatie en verwijzingen in de geautimatiseerde huisartsenpraktijk. Groningen, the Netherlands: Disciplinegroep Huisartsgeneeskunde, University of Groningen; 1998: 1-181.
13. Stokx LJ, Foets M. Het voorschrijven van geneesmiddelen in de huisartspraktijk. Deel II [Prescribing drugs in general practice]. Utrecht: NIVEL; 1994.
14. Marrie TJ, Peeling RW, Fine MJ, Singer DE, Coley CM, Kapoor WN. Ambulatory patients with community-acquired pneumonia: the frequency of atypical agents and clinical course. Am J Med 1996;101:508-15.
15. Berntsson E, Lagergard T, Strannegard O, Trollfors B. Etiology of community-acquired pneumonia in out-patients. Eur J Clin Microbiol 1986;5:446-7.
16. Bohte R, van Furth R, van den Broek PJ. Aetiology of community-acquired pneumonia: a prospective study among adults requiring admission to hospital. Thorax 1995;50:543-7.
17. Fang GD, Fine M, Orloff J, et al. New and emerging etiologies for community-acquired pneumonia with implications for therapy. A prospective multicenter study of 359 cases. Medicine (Baltimore). 1990;69:307-16.
18. Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG. Prospective study of the aetiology and outcome of pneumonia in the community. Lancet 1987;1:671-4.
19. Jonsson JS, Sigurdsson JA, Kristinsson KG, Guthnadottir M, Magnusson S. Acute bronchitis in adults. How close do we come to its aetiology in general practice? Scand J Prim Health Care. 1997;15:156-60.
20. Macfarlane JT, Colville A, Guion A, Macfarlane RM, Rose DH. Prospective study of aetiology and outcome of adult lower-respiratory-tract infections in the community. Lancet 1993;341:511-4.
21. Niederman MS, Bass JB, Jr, Campbell GD, et al. Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. merican Thoracic Society. Medical Section of the American Lung Association. Am Rev Respir Dis. 1993;148:1418-26.
22. Mandell LA, Niederman M. Antimicrobial treatment of community acquired pneumonia in adults: a conference report. Can J Infect Dis 1993;4:25-8.
23. Marrie TJ. Community acquired pneumonia. Clin Infect Dis 1994;18:501-15.
24. Poirier R. Comparative study of clarithromycin and roxithromycin in the treatment of community-acquired pneumonia. J Antimicrob Chemother 1991;27:109-16.
25. Tilyard MW, Dovey SM. A randomized double-blind controlled trial of roxithromycin and cefaclor in the treatment of acute lower respiratory tract infections in general practice. Diagn Microbiol Infect Dis 1992;15:S97-101.
26. Zeluff BJ, Lowe P, Koornhof HJ, Gentry LO. Evaluation of roxithromycin (RU-965) versus cephradine in pneumococcal pneumonia. Eur J Clin Microbiol Infect Dis. 1988;7:69-71.
27. Schonwald S, Barsic B, Klinar I, Gunjaca M. Three-day azithromycin compared with ten-day roxithromycin treatment of atypical pneumonia. Scand J Infect Dis 1994;26:706-10.
28. Young RA, Gonzalez JP, Sorkin EM. Roxithromycin. A review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs. 1989;37:8-41.
29. de Neeling AJ, Pelt van W, Hendrix MGR, et al. Antibiotica resistentie in Nederland. Deel III: Gram-positieve bacteriën. Infect Bull. 1997;8:211-5.
30. Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Ouellette VL. How often is medication taken as prescribed? A novel assessment technique. JAMA 1989;261:3273-7.
31. Wilson S, Delaney BC, Roalfe A, et al. Randomized controlled trials in primary care: case study. BMJ 2000;321:24-7.
32. Ortqvist A, Hedlund J, Grillner L, et al. Aetiology, outcome and prognostic factors in community-acquired pneumonia requiring hospitalization. Eur Respir J 1990;3:1105-13.
33. Ortqvist A, Valtonen M, Cars O, Wahl M, Saikku P, Jean C. Oral empiric treatment of community-acquired pneumonia. A multicenter, double-blind, randomized study comparing sparfloxacin with roxithromycin. The Scandinavian Sparfloxacin Study Group. Chest. 1996;110:1499-506.
34. Boldy DA, Skidmore SJ, Ayres JG. Acute bronchitis in the community: clinical features, infective factors, changes in pulmonary function and bronchial reactivity to histamine. Respir Med 1990;84:377-85.
35. Trigg CJ, Wilks M, Herdman MJ, Clague JE, Tabaqchali S, Davies RJ. A double-blind comparison of the effects of cefaclor and amoxycillin on respiratory tract and oropharyngeal flora and clinical response in acute exacerbations of bronchitis. Respir Med 1991;85:301-8.
36. Karalus NC, Garrett JE, Lang SD, et al. Roxithromycin 150 mg bid versus amoxicillin 500 mg/clavulanic acid 125 mg tid for the treatment of lower respiratory tract infections in general practice. Infection 1995;23:S15-20.
37. Swartz MN. Use of antimicrobial agents and drug resistance. N Engl J Med 1997;337:491-2.
38. de Neeling AJ. Antibioticagebruik en het optreden van resistentie. National Institute of Public Health and the Environment/Volksgezondheid Toekomst Verkenning 1997;B3:793-800.
39. Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish Study Group for Antimicrobial Resistance. N Engl J Med. 1997;337:441-6.
40. Wood MJ. More macrolides. BMJ 1991;303:594-5.
41. Wort SJ, Rogers TR. Community acquired pneumonia in elderly people. Current British guidelines need revision. BMJ. 1998;316:1690.-
42. Bartlett JB. Management of respiratory tract infections. Baltimore, Md: Williams & Wilkins; 1997: 121.
43. King DE, Williams WC, Bishop L, Shechter A. Effectiveness of erythromycin in the treatment of acute bronchitis. J Fam Pract 1996;42:601-5.
44. Lode H, Garau J, Grassi C, et al. Treatment of community-acquired pneumonia: a randomized comparison of sparfloxacin, amoxycillin-clavulanic acid and erythromycin. Eur Respir J 1995;8:1999-2007.
45. Urquhart J. Partial compliance in cardiovascular disease: risk implications. Br J Clin Pract 1994;suppl:2-12.
46. Cramer JA, Ouelette VL, Mattson RH. Effect of microelectronic observation on compliance. Epilepsia 1990;31:617-8.
47. Favre O, Delacretaz E, Badan M, Glauser M, Waeber B. Relationship between the prescriber’s instructions and compliance with antibiotherapy in outpatients treated for an acute infectious disease. J Clin Pharmacol 1997;37:175-8.
48. Urquhart J. Role of patient compliance in clinical pharmacokinetics. A review of recent research. Clin Pharmacokinet. 1994;27:202-15.
Do Delayed Prescriptions Reduce the Use of Antibiotics for the Common Cold?
OBJECTIVE: To test the use of a delayed prescription compared with instructions to take antibiotics immediately in patients presenting to family physicians with upper respiratory tract infections (common colds).
STUDY DESIGN: Randomized controlled single-blind study.
POPULATION: Subjects were 129 patients presenting with the common cold who requested antibiotics or whose physicians thought they wanted them. All patients were in a family practice in Auckland, New Zealand, consisting of 15 physicians (9 male, 6 female) who had completed medical school between 1973 and 1992.
OUTCOMES MEASURED: Outcomes were antibiotic use (taking at least 1 dose of the antibiotic), symptom scores, and responses to the satisfaction questions asked at the end of the study.
RESULTS: Patients in the delayed-prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than were those instructed to take antibiotics immediately (89%, 95% CI, 76%-94%). Daily body temperature was higher in the immediate-prescription group. The lack of difference in the symptom score between the 2 groups suggests that there is no danger in delaying antibiotic prescriptions for the common cold.
CONCLUSIONS: Delayed prescriptions are a safe and effective means of reducing antibiotic consumption in patients with the common cold. Clarification of patient expectations for antibiotics may result in a lower prescription rate. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education.
- Delaying the prescription of antibiotics reduces antibiotic intake in patients who insist on taking antibiotics for the common cold.
- Giving a delayed prescription and asking the patient to return to the office to fill it may reduce antibiotic consumption further.
Antibiotics continue to be commonly used to treat the common cold1-3 despite longstanding doubts about their efficacy4,5 or ability to prevent complications.6 Upper respiratory tract infection (URTI) is the most common reason for a new consultation in family practice and the second most common reason for the prescribing of an antibiotic.7 Reported prescription rates for antibiotics for treating the common cold range from 17% to 60% in the United Kingdom and United States and 78% in New Zealand.1,8 Ineffective but widespread use of antibiotics is not only a poor use of health care funds but also a cause of morbidity (from adverse effects) and the development of resistant strains of bacteria.8-10
A promising technique to reduce antibiotic use is the delayed prescription. The only published randomized controlled trials of delayed prescription use examined its effect for the treatment of sore throat, acute childhood otitis media, and cough.11-13 In the sore throat study, antibiotics were used by 99% of a group given antibiotics, by 13% of a group not offered any, and 31% of a group given a prescription to be taken after 3 days if symptoms persisted. The authors of the otitis media study noted a 66% reduction of antibiotic use in the delayed-prescription group, who had more symptoms, signs, and sleepless nights than the “take-now” group. In the study with acute cough, the use of antibiotics was reduced by 55% in the group with delayed prescriptions. Our study, undertaken in winter 2000, tested the use of a delayed prescription versus instructions to take antibiotics immediately in patients presenting to general practitioners with URTIs.
Methods
The 15 family physicians (FPs) who recruited patients for this study were selected primarily from a group who had reported in a previous study that they frequently gave delayed prescriptions to patients.14 Ethical approval was given by the Auckland Ethics Committee.
Inclusion and exclusion criteria
Patients of any age were eligible if they presented to their FP with a new case of the common cold and either the FP thought the patient wanted antibiotics or the patient stated that desire. For young children, the parents indicated whether or not they wanted antibiotics. FPs were provided with the diagnostic criteria for URTI from the International Classification of Health Problems in Primary Care (ICHPPC-2), which defines an URTI as including the presence of acute inflammation of the nasal or pharyngeal mucosa in the absence of other specifically defined respiratory infection.15
Patients were excluded if they had suspected streptococcal tonsillitis, sinusitis, bronchitis, or pneumonia. Also excluded were patients with lower respiratory signs, those who needed an x-ray, those with a past history of rheumatic fever, and those who had experienced a serious illness or any antibiotic treatment in the previous 2 weeks. Throat cultures were not required. Eligible patients were invited to participate and signed an informed consent form. Ideally, the offer to join the study was to be made to consecutive patients, but this did not occur in all practices.
Interventions
The intervention group was given a prescription for antibiotics with instructions to fill it after 3 days if symptoms failed to improve. The control group received a prescription with instructions to start taking the antibiotic medication immediately. General practitioners prescribed any antibiotic that they considered most appropriate. In both groups, patients were advised to return to see their doctor if symptoms worsened.
Data collection
At recruitment, the patient’s temperature was taken and the list of symptoms was recorded in duplicate. The patient was asked to take his or her temperature daily with a digital thermometer (Assess Diagnostics Medical Industries Australia Pty. Ltd., 148-152 Regent St., Redfern NSW 2016, Australia) that was provided. Patients were given symptom checklists to complete daily for 10 days after the visit. Symptoms listed were dry cough, night cough, sneezing, sore throat, pain on inspiration, pain when coughing, hoarse voice, headache, staying home from work or unable to do normal daily tasks, unwell, diarrhea, vomiting, and nausea without vomiting. Patients were instructed to record whether they had a runny nose with clear secretions (“clear runny nose”), stuffy (blocked) nose, or runny nose with dark secretions (“colored runny nose”). Patients further checked off whether they had clear sputum only in the morning, colored sputum in the morning, clear sputum all day, or colored sputum all day.
A point was allocated for each symptom. The maximum possible score was 15.16 A study assistant telephoned all participants on day 3, day 7, and day 10 to ask about their temperature and symptoms. At the end of the study, the research assistant asked participants about their level of satisfaction with the consultation, using the questions and scoring system devised by Little et al.11 Although no data were collected about revisit rates, data were collected about the patient’s intention to visit a physician for the next cold.
Outcomes and analysis
The outcomes were antibiotic use, symptom scores, and the responses to satisfaction-related questions asked at the end of the study. Outcomes of intervention and control groups were compared on an intention-to-treat basis.17 Because of the repeated measures, the temperatures and summary scores of symptoms were determined with the general linear mixed model that uses Statistical Analysis System (SAS, Cary, N.C.), version 8, for Windows. Chi-square determinations and the Mantel-Haenszel odds ratio were performed for discrete variables using Statistical Package for the Social Sciences (SPSS), version 10, for Windows. When the final data point for continuous variables was missing, the last recorded value was analyzed as the current value. For discrete values, worst-case and best-case scenarios were performed. The sample size of 212 patients was based on a reduction from 60% of antibiotics consumed immediately to 40% in the delayed-prescription group (alpha 0.05, beta 0.2).
Allocation and masking
The unit of randomization was the patient. N.K., who was not a recruiter, generated the allocation schedule with Excel 97. Letters containing instructions for the intervention strategy pertaining to each patient or allocating the patient to the control group were placed in opaque envelopes and sealed. The study number was written on the outside of the envelope according to the randomization schedule. The envelopes were then given to the research assistant, who placed them in a large brown envelope with the consent forms and information sheets for recruiting family physicians. The recruiters opened each envelope immediately after recruitment of each patient.
Patients were told only that they would be given 1 of 2 sets of instruction about taking antibiotics for their colds. Participants read an information sheet and then completed a consent form. Thus, patients were blind to what the other group would take. The research assistant asked the participants not to tell her which instructions they had been given for taking antibiotics. If both types of blinding had been followed correctly, this study could be described as double blinded. However, because we cannot confirm the effectiveness of blinding the research assistant, we prefer to call this study single blinded. One copy of the allocation schedule was kept in the office of N.K.; another was kept by the departmental secretary.
Results
The Figure shows the trial profile summarizing participant flow. The baseline characteristics of the patients in both groups were similar (Table 1).
Patients in the delayed prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than those in the “take antibiotics now” group (89%, 95% CI, 76%-94%). The odds ratio for not using antibiotics was 0.12 (95% CI, 0.05 to 0.29) using intention-to-treat analysis. By antibiotic use, we mean that the patients consumed at least 1 dose of the antibiotic medication.
Table 2 shows the outcomes for temperature and symptom score using an intention-to-treat model. The general linear model for repeated measures found average temperature significantly higher (by 0.2°C) in the immediate antibiotic use group (P = .039) and no significant difference for the symptom score (P = .29). Reanalyzing with only collected data (without intention to treat) found no significant differences from the intention-to-treat analysis. The power to detect a difference in symptom score of 30% is 80% for an alpha of 0.05, assuming that the study gives measures of variation of the symptom score that are close to the real values. There were no significant adverse effects from taking antibiotics or not. Patients’ beliefs and intentions were not affected by the interventions (Table 3).
TABLE 1
BASELINE CHARACTERISTICS AND SYMPTOMS OF THE 2 GROUPS
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Characteristics | ||
| Number of patients | 62 | 67 |
| Male / female | 22 / 40 | 26 / 41 |
| Mean age (SD) | 27.9 years (3.1) | 23.6 years (2.7) |
| Cigarettes per day | 1.26 (0.47) | 1.17 (0.54) |
| Mean temperature (SD) | 36.9 (0.08) | 36.7 (0.08) |
| Days of illness before doctor’s visit | 4.5 (0.5) | 5.0 (0.7) |
| Total symptom score (SD) | 5.1 (0.28) | 5.4 (0.22) |
| Symptoms | ||
| Dry cough | 31 | 35 |
| Productive cough | ||
| Cough with clear sputum in morning | 8 | 5 |
| Cough with clear sputum all day | 6 | 7 |
| Cough with colored sputum in morning | 8 | 7 |
| Cough with colored sputum all day | 10 | 16 |
| Nasal symptoms | ||
| Clear rhinitis | 27 | 22 |
| Blocked or stuff nose | 21 | 26 |
| Colored runny nose | 12 | 15 |
| Night cough | 29 | 37 |
| Sneezing | 31 | 26 |
| Sore throat | 38 | 31 |
| Pain in chest on breathing in | 6 | 7 |
| Pain on coughing | 17 | 13 |
| Hoarse voice | 28 | 26 |
| Headache | 26 | 28 |
| Unwell* | 44* | 56* |
| Limitation of activities | 25 | 23 |
| Nausea | 7 | 6 |
| Vomiting | 5 | 6 |
| Diarrhea | 6 | 4 |
| * Pearson chi-square 9.134, 1 degree of freedom, P = .0025, 2 sided. | ||
| The number of patients recruited per family physician ranged from 1 to 40. | ||
| SD denotes standard deviation. | ||
TABLE 2
OUTCOMES AT BASELINE AND ON DAYS 3, 7, AND 10
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Temperature (C)* | ||
| Baseline | 36.9 (0.1) | 36.7 (0.1) |
| Day 3 | 36.4 (0.1) | 36.2 (0.1) |
| Day 7 | 36.4 (0.1) | 36.1 (0.1) |
| Day 10 | 36.3 (0.1) | 36.1 (0.1) |
| Symptom Score (1 point for each of 15 symptoms in Table 1)* | ||
| Baseline | 5.1 (0.3) | 5.4 (0.2) |
| Day 3 | 2.9 (0.2) | 3.6 (0.3) |
| Day 7 | 1.8 (0.2) | 2.0 (0.3) |
| Day 10 | 1.4 (0.2) | 1.5 (0.2) |
| *The general linear model for repeated measures found the significantly higher temperature of 0.2°C in the immediate-use antibiotic versus that in the delayed-use group (P = .039) and no significant difference for the symptom score (P = .29). | ||
TABLE 3
SATISFACTION, ATTITUDES, AND BELIEFS
| Immediate Prescription | Delayed Prescription | P | |
|---|---|---|---|
| Satisfaction with the consultation; ie, score (1+2) / (1+2+3+4) | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Doctors dealt with worries | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Likely to see doctors for next common cold | 40 / 62 (65%) | 49 / 67 (73%) | .343 † |
| Antibiotics are effective | 47 / 62 (76%) | 51 / 67 (76%) | 1.0 † |
| Importance of seeing doctor to have time off from work or school | 19 / 62 (31%) | 13 / 54 (19%) | .16 † |
| Importance of seeing doctor to explain illness to friends and family | 6 / 62 (10%) | 7 / 60 (12%) | 1.00 † |
| * Fisher’s exact test. | |||
| † Chi-square test. | |||
| 1= very satisfied; 2 = moderately satisfied; 3 = slightly satisfied; 4 = not at all satisfied. For this table, groups responding 1 and 2 have been combined and groups responding 3 and 4 have been combined. | |||
FIGURE
PROGRESS OF PATIENTS THROUGH THE TRIAL
Discussion
We believe that this is the first published randomized controlled trial of delayed prescriptions for antibiotics for the common cold. Asking patients to wait for 3 days before taking their medication reduced consumption of antibiotics from 89% to 48% (P = .0001). The 41% reduction is smaller than that found in the study by Little and colleagues11 of 1% in the take-now group and 69% in the delayed-prescription group. Patients in the UK study returned to the office in 3 days to pick up their prescription, whereas the New Zealand group received the prescription with instructions to wait 3 days before filling it. If the third day had occurred on a weekend, the patients would have had to seek assistance from an after-hours clinic, thereby incurring a direct patient charge.
Our study assessed only the effect of delayed prescriptions, whereas the study by Little and colleagues tested the combined effect of a delayed prescription and the barrier of having to return to the clinic to obtain the prescription. Furthermore, our approach may be more acceptable to a wider group of doctors and patients, although at the expense of a higher consumption rate.
The external validity (generalizability) of this study is difficult to assess. As with the study by Little and colleagues,11 the FPs had different rates of recruitment. One investigator in the current study (B.A.) kept a list of all patients who presented to him with symptoms of the common cold. Of the 44 who were potentially eligible, 4 refused to be part of the study and 10 had other medical problems (eg, heart transplant, previous lung removal) that would have made inclusion potentially hazardous. Thus, 88% of those who had a common cold and were eligible may have participated in the study.
We do not know how many patients were excluded or refused to participate; the recruiting physicians did not supply this information as requested. There was no systematic difference in symptom scores for patients of the different recruiting doctors. As with the study by Little and colleagues, the doctors found themselves too busy to enroll patients. Such problems are always an issue in general practice research.18 Little and colleagues checked the internal validity of their telephone information; therefore, we did not repeat this. In an earlier study,14 the recruiting family physicians’ preference for using delayed prescriptions may have made them more supportive of the delayed prescription than of the immediate prescription. This issue cannot be resolved, since we needed doctors who would prescribe either a delayed prescription or an immediate prescription in order to recruit enough patients.
The strength of this study lies in the blinded nature of the intervention delivery to the patient, the analysis by intention to treat, and the study’s originality. Our intervention had no impact on patients’ satisfaction, concerns, or the likelihood of seeing a doctor for next illness (Table 3). In contrast, Little11 found that antibiotic use predicted future consultations for sore throat and the belief that antibiotics were effective for sore throat.11,19 The differences may relate to the different patient symptoms and geographical differences (common cold in New Zealand versus sore throat in the UK) or the fact that all patients in our study left with a prescription. Another possible reason is that the patients knew they were participating in a study, whereas in the Little study, the instructions were more vague.11
Doctors often misinterpret patient expectations. Improving communications between patient and doctor may be central to reducing patients’ demand for antibiotics. Britten makes the claim that “all the misunderstandings were associated with lack of patients’ participation in the consultation in terms of voicing of expectations and preferences or the voicing of responses to doctors’ decisions and actions.”20 The need for delayed prescriptions had been highlighted as a solution. We know that the common cold presents no great diagnostic dilemma but can produce enormous treatment dilemmas.21 Barry believes that by changing doctors’ views and helping patients to explain what they want from the office visit may lead to changes in treatment patterns.22 We concur with Little that unless patients are very ill, general practitioners should consider exploring their concerns, explaining the natural history of their illness, and avoiding or delaying prescribing antibiotics.11
We were pleased to see a reduction of antibiotics consumed (89% to 48%). However, 48% still represents a high proportion of patients who consumed antibiotics for an illness that is most unlikely to respond to those drugs. More placebo-controlled randomized trials of antibiotics for respiratory tract infections in the primary care setting are needed. We suggest that FPs clarify patients’ expectation for antibiotics and not prescribe them unless the patient insists. For patients who expect to take antibiotics and cannot be persuaded otherwise, a delayed prescription may be the first step in educating them that these medicines are not routinely required.
Conclusions
Delayed prescriptions are a safe and effective means of reducing antibiotic use in patients with the common cold who want antibiotics. The additional barrier of asking the patient to pick up the prescription from the office if symptoms persist after 3 days may reduce antibiotic use even further. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education that antibiotics are an unnecessary treatment.
Acknowledgments
The authors acknowledge the support of the Health Research Council for funding the study, Tania Milne for data collection, and Alistair Stewart for statistical advice. The authors further thank the participating family physicians and patients for their contribution.
1. McGregor A, Dovey S, Tilyard M. Antibiotic use in upper respiratory tract infections in New Zealand. Fam Pract 1995;12:166-70.
2. Mainous AG, Hueston WJ, Clark JR. Antibiotics and upper respiratory infections: Do some folks think there is a cure for the common cold? J Fam Pract 1996;42:357-61.
3. Ochoa C, Eiros JM, Inglada L, Vallano A, Guerra L. Assessment of antibiotic prescription in acute respiratory infections in adults. The Spanish study group on antibiotic treatment. J Infect Dis 2000;41:73-80.
4. Spector SL. The common cold: current therapy and natural history. J Allergy Clin Immunol 1995;95:1133-8.
5. Arroll B, Kenealy T. Antibiotics for the common cold (Cochrane Review). The Cochrane Library, issue 4, 2000. Oxford, England: Update Software.
6. Gadomski AM. Potential interventions for preventing pneumonia among young children: lack of effect of antibiotic treatment for upper respiratory infections. Pediatr Infect Dis J 1993;12:115-20.
7. McAvoy B, Davis P, Raymont A, Gribben B. The Waikato Medical Care Survey. N Z Med J 1994;107:387-433.
8. Carrie AC, Zhanel CG. Antibacterial use in community practice: assessing quantity, indications and appropriateness and relationship to the development of resistant bacteria. Drugs 1999;57:871-81.
9. Arason VA, Kristinsson KG, Sigurdsson JA, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin resistant pneumococci in children? Cross-sectional prevalence study. BMJ 1996;313:387-91.
10. Verkatesum P, Innes JA. Antibiotic resistance in common acute respiratory pathogens. Thorax 1995;50:481-3.
11. Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmouth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ 1997;314:722-7.
12. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;322:336-42.
13. Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled trial as a strategy for managing uncomplicated respiratory tract infection in primary care. Br J Gen Pract 2001;51:200-5.
14. Arroll B, Goodyear-Smith F. General practitioners management of URTIs: when are antibiotics prescribed? N Z Med J 2000;113:493-6.
15. International Classification of Health Problems in Primary Care (ICHPPC-2). International classification of primary care. Oxford, England: Oxford University Press; 1998.
16. Kaiser L, Lew D, Hirschel B, et al. Effects of antibiotic treatment in the subset of common cold patients who have bacteria in nasopharyngeal secretions. Lancet 1996;347:1507-10.
17. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670-4.
18. McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732-3.
19. Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmouth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997;315:350-2.
20. Britten N, Stevenson FA, Barry CA, Barber N, Bradley CP. Misunderstandings in prescribing decisions in general practice. BMJ 2000;320:484-8.
21. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners and patients’ perceptions of antibiotics for sore throats. BMJ 1998;317:637-42.
22. Barry CA, Bradley CP, Britten N, Stevenson FA, Barber N. Patients’ unvoiced agendas in general practice consultations: qualitative study. BMJ 2000;320:1246-50.
OBJECTIVE: To test the use of a delayed prescription compared with instructions to take antibiotics immediately in patients presenting to family physicians with upper respiratory tract infections (common colds).
STUDY DESIGN: Randomized controlled single-blind study.
POPULATION: Subjects were 129 patients presenting with the common cold who requested antibiotics or whose physicians thought they wanted them. All patients were in a family practice in Auckland, New Zealand, consisting of 15 physicians (9 male, 6 female) who had completed medical school between 1973 and 1992.
OUTCOMES MEASURED: Outcomes were antibiotic use (taking at least 1 dose of the antibiotic), symptom scores, and responses to the satisfaction questions asked at the end of the study.
RESULTS: Patients in the delayed-prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than were those instructed to take antibiotics immediately (89%, 95% CI, 76%-94%). Daily body temperature was higher in the immediate-prescription group. The lack of difference in the symptom score between the 2 groups suggests that there is no danger in delaying antibiotic prescriptions for the common cold.
CONCLUSIONS: Delayed prescriptions are a safe and effective means of reducing antibiotic consumption in patients with the common cold. Clarification of patient expectations for antibiotics may result in a lower prescription rate. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education.
- Delaying the prescription of antibiotics reduces antibiotic intake in patients who insist on taking antibiotics for the common cold.
- Giving a delayed prescription and asking the patient to return to the office to fill it may reduce antibiotic consumption further.
Antibiotics continue to be commonly used to treat the common cold1-3 despite longstanding doubts about their efficacy4,5 or ability to prevent complications.6 Upper respiratory tract infection (URTI) is the most common reason for a new consultation in family practice and the second most common reason for the prescribing of an antibiotic.7 Reported prescription rates for antibiotics for treating the common cold range from 17% to 60% in the United Kingdom and United States and 78% in New Zealand.1,8 Ineffective but widespread use of antibiotics is not only a poor use of health care funds but also a cause of morbidity (from adverse effects) and the development of resistant strains of bacteria.8-10
A promising technique to reduce antibiotic use is the delayed prescription. The only published randomized controlled trials of delayed prescription use examined its effect for the treatment of sore throat, acute childhood otitis media, and cough.11-13 In the sore throat study, antibiotics were used by 99% of a group given antibiotics, by 13% of a group not offered any, and 31% of a group given a prescription to be taken after 3 days if symptoms persisted. The authors of the otitis media study noted a 66% reduction of antibiotic use in the delayed-prescription group, who had more symptoms, signs, and sleepless nights than the “take-now” group. In the study with acute cough, the use of antibiotics was reduced by 55% in the group with delayed prescriptions. Our study, undertaken in winter 2000, tested the use of a delayed prescription versus instructions to take antibiotics immediately in patients presenting to general practitioners with URTIs.
Methods
The 15 family physicians (FPs) who recruited patients for this study were selected primarily from a group who had reported in a previous study that they frequently gave delayed prescriptions to patients.14 Ethical approval was given by the Auckland Ethics Committee.
Inclusion and exclusion criteria
Patients of any age were eligible if they presented to their FP with a new case of the common cold and either the FP thought the patient wanted antibiotics or the patient stated that desire. For young children, the parents indicated whether or not they wanted antibiotics. FPs were provided with the diagnostic criteria for URTI from the International Classification of Health Problems in Primary Care (ICHPPC-2), which defines an URTI as including the presence of acute inflammation of the nasal or pharyngeal mucosa in the absence of other specifically defined respiratory infection.15
Patients were excluded if they had suspected streptococcal tonsillitis, sinusitis, bronchitis, or pneumonia. Also excluded were patients with lower respiratory signs, those who needed an x-ray, those with a past history of rheumatic fever, and those who had experienced a serious illness or any antibiotic treatment in the previous 2 weeks. Throat cultures were not required. Eligible patients were invited to participate and signed an informed consent form. Ideally, the offer to join the study was to be made to consecutive patients, but this did not occur in all practices.
Interventions
The intervention group was given a prescription for antibiotics with instructions to fill it after 3 days if symptoms failed to improve. The control group received a prescription with instructions to start taking the antibiotic medication immediately. General practitioners prescribed any antibiotic that they considered most appropriate. In both groups, patients were advised to return to see their doctor if symptoms worsened.
Data collection
At recruitment, the patient’s temperature was taken and the list of symptoms was recorded in duplicate. The patient was asked to take his or her temperature daily with a digital thermometer (Assess Diagnostics Medical Industries Australia Pty. Ltd., 148-152 Regent St., Redfern NSW 2016, Australia) that was provided. Patients were given symptom checklists to complete daily for 10 days after the visit. Symptoms listed were dry cough, night cough, sneezing, sore throat, pain on inspiration, pain when coughing, hoarse voice, headache, staying home from work or unable to do normal daily tasks, unwell, diarrhea, vomiting, and nausea without vomiting. Patients were instructed to record whether they had a runny nose with clear secretions (“clear runny nose”), stuffy (blocked) nose, or runny nose with dark secretions (“colored runny nose”). Patients further checked off whether they had clear sputum only in the morning, colored sputum in the morning, clear sputum all day, or colored sputum all day.
A point was allocated for each symptom. The maximum possible score was 15.16 A study assistant telephoned all participants on day 3, day 7, and day 10 to ask about their temperature and symptoms. At the end of the study, the research assistant asked participants about their level of satisfaction with the consultation, using the questions and scoring system devised by Little et al.11 Although no data were collected about revisit rates, data were collected about the patient’s intention to visit a physician for the next cold.
Outcomes and analysis
The outcomes were antibiotic use, symptom scores, and the responses to satisfaction-related questions asked at the end of the study. Outcomes of intervention and control groups were compared on an intention-to-treat basis.17 Because of the repeated measures, the temperatures and summary scores of symptoms were determined with the general linear mixed model that uses Statistical Analysis System (SAS, Cary, N.C.), version 8, for Windows. Chi-square determinations and the Mantel-Haenszel odds ratio were performed for discrete variables using Statistical Package for the Social Sciences (SPSS), version 10, for Windows. When the final data point for continuous variables was missing, the last recorded value was analyzed as the current value. For discrete values, worst-case and best-case scenarios were performed. The sample size of 212 patients was based on a reduction from 60% of antibiotics consumed immediately to 40% in the delayed-prescription group (alpha 0.05, beta 0.2).
Allocation and masking
The unit of randomization was the patient. N.K., who was not a recruiter, generated the allocation schedule with Excel 97. Letters containing instructions for the intervention strategy pertaining to each patient or allocating the patient to the control group were placed in opaque envelopes and sealed. The study number was written on the outside of the envelope according to the randomization schedule. The envelopes were then given to the research assistant, who placed them in a large brown envelope with the consent forms and information sheets for recruiting family physicians. The recruiters opened each envelope immediately after recruitment of each patient.
Patients were told only that they would be given 1 of 2 sets of instruction about taking antibiotics for their colds. Participants read an information sheet and then completed a consent form. Thus, patients were blind to what the other group would take. The research assistant asked the participants not to tell her which instructions they had been given for taking antibiotics. If both types of blinding had been followed correctly, this study could be described as double blinded. However, because we cannot confirm the effectiveness of blinding the research assistant, we prefer to call this study single blinded. One copy of the allocation schedule was kept in the office of N.K.; another was kept by the departmental secretary.
Results
The Figure shows the trial profile summarizing participant flow. The baseline characteristics of the patients in both groups were similar (Table 1).
Patients in the delayed prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than those in the “take antibiotics now” group (89%, 95% CI, 76%-94%). The odds ratio for not using antibiotics was 0.12 (95% CI, 0.05 to 0.29) using intention-to-treat analysis. By antibiotic use, we mean that the patients consumed at least 1 dose of the antibiotic medication.
Table 2 shows the outcomes for temperature and symptom score using an intention-to-treat model. The general linear model for repeated measures found average temperature significantly higher (by 0.2°C) in the immediate antibiotic use group (P = .039) and no significant difference for the symptom score (P = .29). Reanalyzing with only collected data (without intention to treat) found no significant differences from the intention-to-treat analysis. The power to detect a difference in symptom score of 30% is 80% for an alpha of 0.05, assuming that the study gives measures of variation of the symptom score that are close to the real values. There were no significant adverse effects from taking antibiotics or not. Patients’ beliefs and intentions were not affected by the interventions (Table 3).
TABLE 1
BASELINE CHARACTERISTICS AND SYMPTOMS OF THE 2 GROUPS
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Characteristics | ||
| Number of patients | 62 | 67 |
| Male / female | 22 / 40 | 26 / 41 |
| Mean age (SD) | 27.9 years (3.1) | 23.6 years (2.7) |
| Cigarettes per day | 1.26 (0.47) | 1.17 (0.54) |
| Mean temperature (SD) | 36.9 (0.08) | 36.7 (0.08) |
| Days of illness before doctor’s visit | 4.5 (0.5) | 5.0 (0.7) |
| Total symptom score (SD) | 5.1 (0.28) | 5.4 (0.22) |
| Symptoms | ||
| Dry cough | 31 | 35 |
| Productive cough | ||
| Cough with clear sputum in morning | 8 | 5 |
| Cough with clear sputum all day | 6 | 7 |
| Cough with colored sputum in morning | 8 | 7 |
| Cough with colored sputum all day | 10 | 16 |
| Nasal symptoms | ||
| Clear rhinitis | 27 | 22 |
| Blocked or stuff nose | 21 | 26 |
| Colored runny nose | 12 | 15 |
| Night cough | 29 | 37 |
| Sneezing | 31 | 26 |
| Sore throat | 38 | 31 |
| Pain in chest on breathing in | 6 | 7 |
| Pain on coughing | 17 | 13 |
| Hoarse voice | 28 | 26 |
| Headache | 26 | 28 |
| Unwell* | 44* | 56* |
| Limitation of activities | 25 | 23 |
| Nausea | 7 | 6 |
| Vomiting | 5 | 6 |
| Diarrhea | 6 | 4 |
| * Pearson chi-square 9.134, 1 degree of freedom, P = .0025, 2 sided. | ||
| The number of patients recruited per family physician ranged from 1 to 40. | ||
| SD denotes standard deviation. | ||
TABLE 2
OUTCOMES AT BASELINE AND ON DAYS 3, 7, AND 10
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Temperature (C)* | ||
| Baseline | 36.9 (0.1) | 36.7 (0.1) |
| Day 3 | 36.4 (0.1) | 36.2 (0.1) |
| Day 7 | 36.4 (0.1) | 36.1 (0.1) |
| Day 10 | 36.3 (0.1) | 36.1 (0.1) |
| Symptom Score (1 point for each of 15 symptoms in Table 1)* | ||
| Baseline | 5.1 (0.3) | 5.4 (0.2) |
| Day 3 | 2.9 (0.2) | 3.6 (0.3) |
| Day 7 | 1.8 (0.2) | 2.0 (0.3) |
| Day 10 | 1.4 (0.2) | 1.5 (0.2) |
| *The general linear model for repeated measures found the significantly higher temperature of 0.2°C in the immediate-use antibiotic versus that in the delayed-use group (P = .039) and no significant difference for the symptom score (P = .29). | ||
TABLE 3
SATISFACTION, ATTITUDES, AND BELIEFS
| Immediate Prescription | Delayed Prescription | P | |
|---|---|---|---|
| Satisfaction with the consultation; ie, score (1+2) / (1+2+3+4) | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Doctors dealt with worries | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Likely to see doctors for next common cold | 40 / 62 (65%) | 49 / 67 (73%) | .343 † |
| Antibiotics are effective | 47 / 62 (76%) | 51 / 67 (76%) | 1.0 † |
| Importance of seeing doctor to have time off from work or school | 19 / 62 (31%) | 13 / 54 (19%) | .16 † |
| Importance of seeing doctor to explain illness to friends and family | 6 / 62 (10%) | 7 / 60 (12%) | 1.00 † |
| * Fisher’s exact test. | |||
| † Chi-square test. | |||
| 1= very satisfied; 2 = moderately satisfied; 3 = slightly satisfied; 4 = not at all satisfied. For this table, groups responding 1 and 2 have been combined and groups responding 3 and 4 have been combined. | |||
FIGURE
PROGRESS OF PATIENTS THROUGH THE TRIAL
Discussion
We believe that this is the first published randomized controlled trial of delayed prescriptions for antibiotics for the common cold. Asking patients to wait for 3 days before taking their medication reduced consumption of antibiotics from 89% to 48% (P = .0001). The 41% reduction is smaller than that found in the study by Little and colleagues11 of 1% in the take-now group and 69% in the delayed-prescription group. Patients in the UK study returned to the office in 3 days to pick up their prescription, whereas the New Zealand group received the prescription with instructions to wait 3 days before filling it. If the third day had occurred on a weekend, the patients would have had to seek assistance from an after-hours clinic, thereby incurring a direct patient charge.
Our study assessed only the effect of delayed prescriptions, whereas the study by Little and colleagues tested the combined effect of a delayed prescription and the barrier of having to return to the clinic to obtain the prescription. Furthermore, our approach may be more acceptable to a wider group of doctors and patients, although at the expense of a higher consumption rate.
The external validity (generalizability) of this study is difficult to assess. As with the study by Little and colleagues,11 the FPs had different rates of recruitment. One investigator in the current study (B.A.) kept a list of all patients who presented to him with symptoms of the common cold. Of the 44 who were potentially eligible, 4 refused to be part of the study and 10 had other medical problems (eg, heart transplant, previous lung removal) that would have made inclusion potentially hazardous. Thus, 88% of those who had a common cold and were eligible may have participated in the study.
We do not know how many patients were excluded or refused to participate; the recruiting physicians did not supply this information as requested. There was no systematic difference in symptom scores for patients of the different recruiting doctors. As with the study by Little and colleagues, the doctors found themselves too busy to enroll patients. Such problems are always an issue in general practice research.18 Little and colleagues checked the internal validity of their telephone information; therefore, we did not repeat this. In an earlier study,14 the recruiting family physicians’ preference for using delayed prescriptions may have made them more supportive of the delayed prescription than of the immediate prescription. This issue cannot be resolved, since we needed doctors who would prescribe either a delayed prescription or an immediate prescription in order to recruit enough patients.
The strength of this study lies in the blinded nature of the intervention delivery to the patient, the analysis by intention to treat, and the study’s originality. Our intervention had no impact on patients’ satisfaction, concerns, or the likelihood of seeing a doctor for next illness (Table 3). In contrast, Little11 found that antibiotic use predicted future consultations for sore throat and the belief that antibiotics were effective for sore throat.11,19 The differences may relate to the different patient symptoms and geographical differences (common cold in New Zealand versus sore throat in the UK) or the fact that all patients in our study left with a prescription. Another possible reason is that the patients knew they were participating in a study, whereas in the Little study, the instructions were more vague.11
Doctors often misinterpret patient expectations. Improving communications between patient and doctor may be central to reducing patients’ demand for antibiotics. Britten makes the claim that “all the misunderstandings were associated with lack of patients’ participation in the consultation in terms of voicing of expectations and preferences or the voicing of responses to doctors’ decisions and actions.”20 The need for delayed prescriptions had been highlighted as a solution. We know that the common cold presents no great diagnostic dilemma but can produce enormous treatment dilemmas.21 Barry believes that by changing doctors’ views and helping patients to explain what they want from the office visit may lead to changes in treatment patterns.22 We concur with Little that unless patients are very ill, general practitioners should consider exploring their concerns, explaining the natural history of their illness, and avoiding or delaying prescribing antibiotics.11
We were pleased to see a reduction of antibiotics consumed (89% to 48%). However, 48% still represents a high proportion of patients who consumed antibiotics for an illness that is most unlikely to respond to those drugs. More placebo-controlled randomized trials of antibiotics for respiratory tract infections in the primary care setting are needed. We suggest that FPs clarify patients’ expectation for antibiotics and not prescribe them unless the patient insists. For patients who expect to take antibiotics and cannot be persuaded otherwise, a delayed prescription may be the first step in educating them that these medicines are not routinely required.
Conclusions
Delayed prescriptions are a safe and effective means of reducing antibiotic use in patients with the common cold who want antibiotics. The additional barrier of asking the patient to pick up the prescription from the office if symptoms persist after 3 days may reduce antibiotic use even further. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education that antibiotics are an unnecessary treatment.
Acknowledgments
The authors acknowledge the support of the Health Research Council for funding the study, Tania Milne for data collection, and Alistair Stewart for statistical advice. The authors further thank the participating family physicians and patients for their contribution.
OBJECTIVE: To test the use of a delayed prescription compared with instructions to take antibiotics immediately in patients presenting to family physicians with upper respiratory tract infections (common colds).
STUDY DESIGN: Randomized controlled single-blind study.
POPULATION: Subjects were 129 patients presenting with the common cold who requested antibiotics or whose physicians thought they wanted them. All patients were in a family practice in Auckland, New Zealand, consisting of 15 physicians (9 male, 6 female) who had completed medical school between 1973 and 1992.
OUTCOMES MEASURED: Outcomes were antibiotic use (taking at least 1 dose of the antibiotic), symptom scores, and responses to the satisfaction questions asked at the end of the study.
RESULTS: Patients in the delayed-prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than were those instructed to take antibiotics immediately (89%, 95% CI, 76%-94%). Daily body temperature was higher in the immediate-prescription group. The lack of difference in the symptom score between the 2 groups suggests that there is no danger in delaying antibiotic prescriptions for the common cold.
CONCLUSIONS: Delayed prescriptions are a safe and effective means of reducing antibiotic consumption in patients with the common cold. Clarification of patient expectations for antibiotics may result in a lower prescription rate. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education.
- Delaying the prescription of antibiotics reduces antibiotic intake in patients who insist on taking antibiotics for the common cold.
- Giving a delayed prescription and asking the patient to return to the office to fill it may reduce antibiotic consumption further.
Antibiotics continue to be commonly used to treat the common cold1-3 despite longstanding doubts about their efficacy4,5 or ability to prevent complications.6 Upper respiratory tract infection (URTI) is the most common reason for a new consultation in family practice and the second most common reason for the prescribing of an antibiotic.7 Reported prescription rates for antibiotics for treating the common cold range from 17% to 60% in the United Kingdom and United States and 78% in New Zealand.1,8 Ineffective but widespread use of antibiotics is not only a poor use of health care funds but also a cause of morbidity (from adverse effects) and the development of resistant strains of bacteria.8-10
A promising technique to reduce antibiotic use is the delayed prescription. The only published randomized controlled trials of delayed prescription use examined its effect for the treatment of sore throat, acute childhood otitis media, and cough.11-13 In the sore throat study, antibiotics were used by 99% of a group given antibiotics, by 13% of a group not offered any, and 31% of a group given a prescription to be taken after 3 days if symptoms persisted. The authors of the otitis media study noted a 66% reduction of antibiotic use in the delayed-prescription group, who had more symptoms, signs, and sleepless nights than the “take-now” group. In the study with acute cough, the use of antibiotics was reduced by 55% in the group with delayed prescriptions. Our study, undertaken in winter 2000, tested the use of a delayed prescription versus instructions to take antibiotics immediately in patients presenting to general practitioners with URTIs.
Methods
The 15 family physicians (FPs) who recruited patients for this study were selected primarily from a group who had reported in a previous study that they frequently gave delayed prescriptions to patients.14 Ethical approval was given by the Auckland Ethics Committee.
Inclusion and exclusion criteria
Patients of any age were eligible if they presented to their FP with a new case of the common cold and either the FP thought the patient wanted antibiotics or the patient stated that desire. For young children, the parents indicated whether or not they wanted antibiotics. FPs were provided with the diagnostic criteria for URTI from the International Classification of Health Problems in Primary Care (ICHPPC-2), which defines an URTI as including the presence of acute inflammation of the nasal or pharyngeal mucosa in the absence of other specifically defined respiratory infection.15
Patients were excluded if they had suspected streptococcal tonsillitis, sinusitis, bronchitis, or pneumonia. Also excluded were patients with lower respiratory signs, those who needed an x-ray, those with a past history of rheumatic fever, and those who had experienced a serious illness or any antibiotic treatment in the previous 2 weeks. Throat cultures were not required. Eligible patients were invited to participate and signed an informed consent form. Ideally, the offer to join the study was to be made to consecutive patients, but this did not occur in all practices.
Interventions
The intervention group was given a prescription for antibiotics with instructions to fill it after 3 days if symptoms failed to improve. The control group received a prescription with instructions to start taking the antibiotic medication immediately. General practitioners prescribed any antibiotic that they considered most appropriate. In both groups, patients were advised to return to see their doctor if symptoms worsened.
Data collection
At recruitment, the patient’s temperature was taken and the list of symptoms was recorded in duplicate. The patient was asked to take his or her temperature daily with a digital thermometer (Assess Diagnostics Medical Industries Australia Pty. Ltd., 148-152 Regent St., Redfern NSW 2016, Australia) that was provided. Patients were given symptom checklists to complete daily for 10 days after the visit. Symptoms listed were dry cough, night cough, sneezing, sore throat, pain on inspiration, pain when coughing, hoarse voice, headache, staying home from work or unable to do normal daily tasks, unwell, diarrhea, vomiting, and nausea without vomiting. Patients were instructed to record whether they had a runny nose with clear secretions (“clear runny nose”), stuffy (blocked) nose, or runny nose with dark secretions (“colored runny nose”). Patients further checked off whether they had clear sputum only in the morning, colored sputum in the morning, clear sputum all day, or colored sputum all day.
A point was allocated for each symptom. The maximum possible score was 15.16 A study assistant telephoned all participants on day 3, day 7, and day 10 to ask about their temperature and symptoms. At the end of the study, the research assistant asked participants about their level of satisfaction with the consultation, using the questions and scoring system devised by Little et al.11 Although no data were collected about revisit rates, data were collected about the patient’s intention to visit a physician for the next cold.
Outcomes and analysis
The outcomes were antibiotic use, symptom scores, and the responses to satisfaction-related questions asked at the end of the study. Outcomes of intervention and control groups were compared on an intention-to-treat basis.17 Because of the repeated measures, the temperatures and summary scores of symptoms were determined with the general linear mixed model that uses Statistical Analysis System (SAS, Cary, N.C.), version 8, for Windows. Chi-square determinations and the Mantel-Haenszel odds ratio were performed for discrete variables using Statistical Package for the Social Sciences (SPSS), version 10, for Windows. When the final data point for continuous variables was missing, the last recorded value was analyzed as the current value. For discrete values, worst-case and best-case scenarios were performed. The sample size of 212 patients was based on a reduction from 60% of antibiotics consumed immediately to 40% in the delayed-prescription group (alpha 0.05, beta 0.2).
Allocation and masking
The unit of randomization was the patient. N.K., who was not a recruiter, generated the allocation schedule with Excel 97. Letters containing instructions for the intervention strategy pertaining to each patient or allocating the patient to the control group were placed in opaque envelopes and sealed. The study number was written on the outside of the envelope according to the randomization schedule. The envelopes were then given to the research assistant, who placed them in a large brown envelope with the consent forms and information sheets for recruiting family physicians. The recruiters opened each envelope immediately after recruitment of each patient.
Patients were told only that they would be given 1 of 2 sets of instruction about taking antibiotics for their colds. Participants read an information sheet and then completed a consent form. Thus, patients were blind to what the other group would take. The research assistant asked the participants not to tell her which instructions they had been given for taking antibiotics. If both types of blinding had been followed correctly, this study could be described as double blinded. However, because we cannot confirm the effectiveness of blinding the research assistant, we prefer to call this study single blinded. One copy of the allocation schedule was kept in the office of N.K.; another was kept by the departmental secretary.
Results
The Figure shows the trial profile summarizing participant flow. The baseline characteristics of the patients in both groups were similar (Table 1).
Patients in the delayed prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than those in the “take antibiotics now” group (89%, 95% CI, 76%-94%). The odds ratio for not using antibiotics was 0.12 (95% CI, 0.05 to 0.29) using intention-to-treat analysis. By antibiotic use, we mean that the patients consumed at least 1 dose of the antibiotic medication.
Table 2 shows the outcomes for temperature and symptom score using an intention-to-treat model. The general linear model for repeated measures found average temperature significantly higher (by 0.2°C) in the immediate antibiotic use group (P = .039) and no significant difference for the symptom score (P = .29). Reanalyzing with only collected data (without intention to treat) found no significant differences from the intention-to-treat analysis. The power to detect a difference in symptom score of 30% is 80% for an alpha of 0.05, assuming that the study gives measures of variation of the symptom score that are close to the real values. There were no significant adverse effects from taking antibiotics or not. Patients’ beliefs and intentions were not affected by the interventions (Table 3).
TABLE 1
BASELINE CHARACTERISTICS AND SYMPTOMS OF THE 2 GROUPS
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Characteristics | ||
| Number of patients | 62 | 67 |
| Male / female | 22 / 40 | 26 / 41 |
| Mean age (SD) | 27.9 years (3.1) | 23.6 years (2.7) |
| Cigarettes per day | 1.26 (0.47) | 1.17 (0.54) |
| Mean temperature (SD) | 36.9 (0.08) | 36.7 (0.08) |
| Days of illness before doctor’s visit | 4.5 (0.5) | 5.0 (0.7) |
| Total symptom score (SD) | 5.1 (0.28) | 5.4 (0.22) |
| Symptoms | ||
| Dry cough | 31 | 35 |
| Productive cough | ||
| Cough with clear sputum in morning | 8 | 5 |
| Cough with clear sputum all day | 6 | 7 |
| Cough with colored sputum in morning | 8 | 7 |
| Cough with colored sputum all day | 10 | 16 |
| Nasal symptoms | ||
| Clear rhinitis | 27 | 22 |
| Blocked or stuff nose | 21 | 26 |
| Colored runny nose | 12 | 15 |
| Night cough | 29 | 37 |
| Sneezing | 31 | 26 |
| Sore throat | 38 | 31 |
| Pain in chest on breathing in | 6 | 7 |
| Pain on coughing | 17 | 13 |
| Hoarse voice | 28 | 26 |
| Headache | 26 | 28 |
| Unwell* | 44* | 56* |
| Limitation of activities | 25 | 23 |
| Nausea | 7 | 6 |
| Vomiting | 5 | 6 |
| Diarrhea | 6 | 4 |
| * Pearson chi-square 9.134, 1 degree of freedom, P = .0025, 2 sided. | ||
| The number of patients recruited per family physician ranged from 1 to 40. | ||
| SD denotes standard deviation. | ||
TABLE 2
OUTCOMES AT BASELINE AND ON DAYS 3, 7, AND 10
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Temperature (C)* | ||
| Baseline | 36.9 (0.1) | 36.7 (0.1) |
| Day 3 | 36.4 (0.1) | 36.2 (0.1) |
| Day 7 | 36.4 (0.1) | 36.1 (0.1) |
| Day 10 | 36.3 (0.1) | 36.1 (0.1) |
| Symptom Score (1 point for each of 15 symptoms in Table 1)* | ||
| Baseline | 5.1 (0.3) | 5.4 (0.2) |
| Day 3 | 2.9 (0.2) | 3.6 (0.3) |
| Day 7 | 1.8 (0.2) | 2.0 (0.3) |
| Day 10 | 1.4 (0.2) | 1.5 (0.2) |
| *The general linear model for repeated measures found the significantly higher temperature of 0.2°C in the immediate-use antibiotic versus that in the delayed-use group (P = .039) and no significant difference for the symptom score (P = .29). | ||
TABLE 3
SATISFACTION, ATTITUDES, AND BELIEFS
| Immediate Prescription | Delayed Prescription | P | |
|---|---|---|---|
| Satisfaction with the consultation; ie, score (1+2) / (1+2+3+4) | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Doctors dealt with worries | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Likely to see doctors for next common cold | 40 / 62 (65%) | 49 / 67 (73%) | .343 † |
| Antibiotics are effective | 47 / 62 (76%) | 51 / 67 (76%) | 1.0 † |
| Importance of seeing doctor to have time off from work or school | 19 / 62 (31%) | 13 / 54 (19%) | .16 † |
| Importance of seeing doctor to explain illness to friends and family | 6 / 62 (10%) | 7 / 60 (12%) | 1.00 † |
| * Fisher’s exact test. | |||
| † Chi-square test. | |||
| 1= very satisfied; 2 = moderately satisfied; 3 = slightly satisfied; 4 = not at all satisfied. For this table, groups responding 1 and 2 have been combined and groups responding 3 and 4 have been combined. | |||
FIGURE
PROGRESS OF PATIENTS THROUGH THE TRIAL
Discussion
We believe that this is the first published randomized controlled trial of delayed prescriptions for antibiotics for the common cold. Asking patients to wait for 3 days before taking their medication reduced consumption of antibiotics from 89% to 48% (P = .0001). The 41% reduction is smaller than that found in the study by Little and colleagues11 of 1% in the take-now group and 69% in the delayed-prescription group. Patients in the UK study returned to the office in 3 days to pick up their prescription, whereas the New Zealand group received the prescription with instructions to wait 3 days before filling it. If the third day had occurred on a weekend, the patients would have had to seek assistance from an after-hours clinic, thereby incurring a direct patient charge.
Our study assessed only the effect of delayed prescriptions, whereas the study by Little and colleagues tested the combined effect of a delayed prescription and the barrier of having to return to the clinic to obtain the prescription. Furthermore, our approach may be more acceptable to a wider group of doctors and patients, although at the expense of a higher consumption rate.
The external validity (generalizability) of this study is difficult to assess. As with the study by Little and colleagues,11 the FPs had different rates of recruitment. One investigator in the current study (B.A.) kept a list of all patients who presented to him with symptoms of the common cold. Of the 44 who were potentially eligible, 4 refused to be part of the study and 10 had other medical problems (eg, heart transplant, previous lung removal) that would have made inclusion potentially hazardous. Thus, 88% of those who had a common cold and were eligible may have participated in the study.
We do not know how many patients were excluded or refused to participate; the recruiting physicians did not supply this information as requested. There was no systematic difference in symptom scores for patients of the different recruiting doctors. As with the study by Little and colleagues, the doctors found themselves too busy to enroll patients. Such problems are always an issue in general practice research.18 Little and colleagues checked the internal validity of their telephone information; therefore, we did not repeat this. In an earlier study,14 the recruiting family physicians’ preference for using delayed prescriptions may have made them more supportive of the delayed prescription than of the immediate prescription. This issue cannot be resolved, since we needed doctors who would prescribe either a delayed prescription or an immediate prescription in order to recruit enough patients.
The strength of this study lies in the blinded nature of the intervention delivery to the patient, the analysis by intention to treat, and the study’s originality. Our intervention had no impact on patients’ satisfaction, concerns, or the likelihood of seeing a doctor for next illness (Table 3). In contrast, Little11 found that antibiotic use predicted future consultations for sore throat and the belief that antibiotics were effective for sore throat.11,19 The differences may relate to the different patient symptoms and geographical differences (common cold in New Zealand versus sore throat in the UK) or the fact that all patients in our study left with a prescription. Another possible reason is that the patients knew they were participating in a study, whereas in the Little study, the instructions were more vague.11
Doctors often misinterpret patient expectations. Improving communications between patient and doctor may be central to reducing patients’ demand for antibiotics. Britten makes the claim that “all the misunderstandings were associated with lack of patients’ participation in the consultation in terms of voicing of expectations and preferences or the voicing of responses to doctors’ decisions and actions.”20 The need for delayed prescriptions had been highlighted as a solution. We know that the common cold presents no great diagnostic dilemma but can produce enormous treatment dilemmas.21 Barry believes that by changing doctors’ views and helping patients to explain what they want from the office visit may lead to changes in treatment patterns.22 We concur with Little that unless patients are very ill, general practitioners should consider exploring their concerns, explaining the natural history of their illness, and avoiding or delaying prescribing antibiotics.11
We were pleased to see a reduction of antibiotics consumed (89% to 48%). However, 48% still represents a high proportion of patients who consumed antibiotics for an illness that is most unlikely to respond to those drugs. More placebo-controlled randomized trials of antibiotics for respiratory tract infections in the primary care setting are needed. We suggest that FPs clarify patients’ expectation for antibiotics and not prescribe them unless the patient insists. For patients who expect to take antibiotics and cannot be persuaded otherwise, a delayed prescription may be the first step in educating them that these medicines are not routinely required.
Conclusions
Delayed prescriptions are a safe and effective means of reducing antibiotic use in patients with the common cold who want antibiotics. The additional barrier of asking the patient to pick up the prescription from the office if symptoms persist after 3 days may reduce antibiotic use even further. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education that antibiotics are an unnecessary treatment.
Acknowledgments
The authors acknowledge the support of the Health Research Council for funding the study, Tania Milne for data collection, and Alistair Stewart for statistical advice. The authors further thank the participating family physicians and patients for their contribution.
1. McGregor A, Dovey S, Tilyard M. Antibiotic use in upper respiratory tract infections in New Zealand. Fam Pract 1995;12:166-70.
2. Mainous AG, Hueston WJ, Clark JR. Antibiotics and upper respiratory infections: Do some folks think there is a cure for the common cold? J Fam Pract 1996;42:357-61.
3. Ochoa C, Eiros JM, Inglada L, Vallano A, Guerra L. Assessment of antibiotic prescription in acute respiratory infections in adults. The Spanish study group on antibiotic treatment. J Infect Dis 2000;41:73-80.
4. Spector SL. The common cold: current therapy and natural history. J Allergy Clin Immunol 1995;95:1133-8.
5. Arroll B, Kenealy T. Antibiotics for the common cold (Cochrane Review). The Cochrane Library, issue 4, 2000. Oxford, England: Update Software.
6. Gadomski AM. Potential interventions for preventing pneumonia among young children: lack of effect of antibiotic treatment for upper respiratory infections. Pediatr Infect Dis J 1993;12:115-20.
7. McAvoy B, Davis P, Raymont A, Gribben B. The Waikato Medical Care Survey. N Z Med J 1994;107:387-433.
8. Carrie AC, Zhanel CG. Antibacterial use in community practice: assessing quantity, indications and appropriateness and relationship to the development of resistant bacteria. Drugs 1999;57:871-81.
9. Arason VA, Kristinsson KG, Sigurdsson JA, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin resistant pneumococci in children? Cross-sectional prevalence study. BMJ 1996;313:387-91.
10. Verkatesum P, Innes JA. Antibiotic resistance in common acute respiratory pathogens. Thorax 1995;50:481-3.
11. Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmouth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ 1997;314:722-7.
12. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;322:336-42.
13. Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled trial as a strategy for managing uncomplicated respiratory tract infection in primary care. Br J Gen Pract 2001;51:200-5.
14. Arroll B, Goodyear-Smith F. General practitioners management of URTIs: when are antibiotics prescribed? N Z Med J 2000;113:493-6.
15. International Classification of Health Problems in Primary Care (ICHPPC-2). International classification of primary care. Oxford, England: Oxford University Press; 1998.
16. Kaiser L, Lew D, Hirschel B, et al. Effects of antibiotic treatment in the subset of common cold patients who have bacteria in nasopharyngeal secretions. Lancet 1996;347:1507-10.
17. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670-4.
18. McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732-3.
19. Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmouth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997;315:350-2.
20. Britten N, Stevenson FA, Barry CA, Barber N, Bradley CP. Misunderstandings in prescribing decisions in general practice. BMJ 2000;320:484-8.
21. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners and patients’ perceptions of antibiotics for sore throats. BMJ 1998;317:637-42.
22. Barry CA, Bradley CP, Britten N, Stevenson FA, Barber N. Patients’ unvoiced agendas in general practice consultations: qualitative study. BMJ 2000;320:1246-50.
1. McGregor A, Dovey S, Tilyard M. Antibiotic use in upper respiratory tract infections in New Zealand. Fam Pract 1995;12:166-70.
2. Mainous AG, Hueston WJ, Clark JR. Antibiotics and upper respiratory infections: Do some folks think there is a cure for the common cold? J Fam Pract 1996;42:357-61.
3. Ochoa C, Eiros JM, Inglada L, Vallano A, Guerra L. Assessment of antibiotic prescription in acute respiratory infections in adults. The Spanish study group on antibiotic treatment. J Infect Dis 2000;41:73-80.
4. Spector SL. The common cold: current therapy and natural history. J Allergy Clin Immunol 1995;95:1133-8.
5. Arroll B, Kenealy T. Antibiotics for the common cold (Cochrane Review). The Cochrane Library, issue 4, 2000. Oxford, England: Update Software.
6. Gadomski AM. Potential interventions for preventing pneumonia among young children: lack of effect of antibiotic treatment for upper respiratory infections. Pediatr Infect Dis J 1993;12:115-20.
7. McAvoy B, Davis P, Raymont A, Gribben B. The Waikato Medical Care Survey. N Z Med J 1994;107:387-433.
8. Carrie AC, Zhanel CG. Antibacterial use in community practice: assessing quantity, indications and appropriateness and relationship to the development of resistant bacteria. Drugs 1999;57:871-81.
9. Arason VA, Kristinsson KG, Sigurdsson JA, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin resistant pneumococci in children? Cross-sectional prevalence study. BMJ 1996;313:387-91.
10. Verkatesum P, Innes JA. Antibiotic resistance in common acute respiratory pathogens. Thorax 1995;50:481-3.
11. Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmouth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ 1997;314:722-7.
12. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;322:336-42.
13. Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled trial as a strategy for managing uncomplicated respiratory tract infection in primary care. Br J Gen Pract 2001;51:200-5.
14. Arroll B, Goodyear-Smith F. General practitioners management of URTIs: when are antibiotics prescribed? N Z Med J 2000;113:493-6.
15. International Classification of Health Problems in Primary Care (ICHPPC-2). International classification of primary care. Oxford, England: Oxford University Press; 1998.
16. Kaiser L, Lew D, Hirschel B, et al. Effects of antibiotic treatment in the subset of common cold patients who have bacteria in nasopharyngeal secretions. Lancet 1996;347:1507-10.
17. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670-4.
18. McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732-3.
19. Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmouth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997;315:350-2.
20. Britten N, Stevenson FA, Barry CA, Barber N, Bradley CP. Misunderstandings in prescribing decisions in general practice. BMJ 2000;320:484-8.
21. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners and patients’ perceptions of antibiotics for sore throats. BMJ 1998;317:637-42.
22. Barry CA, Bradley CP, Britten N, Stevenson FA, Barber N. Patients’ unvoiced agendas in general practice consultations: qualitative study. BMJ 2000;320:1246-50.
Oat Ingestion Reduces Systolic and Diastolic Blood Pressure in Patients with Mild or Borderline Hypertension: A Pilot Trial
OBJECTIVES: We assessed the short-term antihypertensive effects of soluble fiber-rich whole oat cereals when added to a standard American diet. In addition, multiple assessments of insulin sensitivity were conducted.
STUDY DESIGN: This was a randomized, controlled, parallel-group pilot study designed to compare an oat cereal group (standardized to 5.52 g/day beta-glucan) to a low-fiber cereal control group (less than 1.0 g/day total fiber) over 6 weeks.
POPULATION: A total of 18 hypertensive and hyperinsulinemic ( ≥10 μU/mL) men and women completed the trial.
OUTCOMES MEASURED: Primary study outcomes were changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP). Secondary outcomes included blood lipid, fasting glucose, and insulin levels and side effects related to elevated blood pressure and increased dietary fiber intake.
RESULTS: The oat cereal group experienced a 7.5 mm Hg reduction in SBP (P < .01) and a 5.5 mm Hg reduction in DBP (P < .02), while there was virtually no change in either SBP or DBP in the control group. In the oat cereal group, a trend was observed for a lower total insulin response to a glucose load, suggesting improved insulin sensitivity. However, this could not be confirmed using estimates from the Bergman Minimal Model, perhaps because of our small sample size. As expected and reported in previous trials, the oats group experienced a significant reduction in both total cholesterol (9%) and low-density lipoprotein cholesterol (14%).
CONCLUSIONS: The addition of oat cereals to the normal diet of persons with hypertension significantly reduces both systolic and diastolic blood pressure. Soluble fiber-rich whole oats may be an effective dietary therapy in the prevention and adjunct treatment of hypertension.
Interest is growing in the use of nonpharmacologic methods for the prevention and management of hypertension. Specifically, the effect of dietary fiber on the incidence and treatment of hypertension has been explored. Epidemiologic studies show that the amount of dietary fiber ingested is inversely related to the incidence of hypertension as well as to systolic blood pressure (SBP) and diastolic blood pressure (DBP) in both hypertensive and normotensive patients.1–5 The results obtained from clinical trials, however, are inconsistent; some report modest blood pressure reductions after increased fiber intake,6–12 while others fail to demonstrate any effect of dietary fiber on blood pressure.13–16 Some animal trials17,18 and human trials19,20 have shown a consistent lowering of blood pressure upon consumption of larger amounts of soluble fiber, suggesting that the antihypertensive effects of fiber may be caused by the soluble fraction and that these effects may be contingent upon the intake of a sufficiently large quantity.
Hypertension often occurs in association with obesity, impaired glucose tolerance, and dyslipidemia. Hyperinsulinemia and insulin resistance are thought to be key pathogenic links among these disturbances.21–23 Studies show that soluble fiber from oats reduces both postprandial blood glucose and insulin levels.24–27 Therefore, we conducted the following pilot trial to investigate the antihypertensive and insulin-modifying effects of oat cereal supplementation in a population of mild and borderline hyperinsulinemic and hypertensive men and women.
Methods
Study protocol
The study participants in this 6-week, randomized, parallel-group, active-controlled pilot trial were recruited by means of local community screenings and mass media advertising. The study protocol was reviewed and approved by the University of Minnesota Institutional Review Board. All participants provided informed consent before official enrollment in the study. One hundred nine men and women aged 20 to 70 were screened for eligibility with a physical exam, medical history, and chemistry and lipid profile (see Table 1 for exclusion criteria). Only generally healthy, untreated hypertensives with average SBP of 130 to 160 mm Hg and DBP of 85 to 100 mm Hg and with at least 1 reading greater than 140/90 as well as moderately elevated levels of fasting insulin (≥10μU/mL) were considered for enrollment. Participants were determined to be eligible only after 2 sets of hypertensive (SBP > 130, DBP > 85) baseline blood pressure readings had been taken 7 days apart and only if all inclusion criteria were fulfilled.
Ultimately, 22 men and women were randomized to either an oat cereal treatment group (standardized to 5.52 g/day beta-glucan) or a low fiber cereal control group (<1 g/day total fiber). Four of these individuals (1 in the treatment and 3 in the control group) discontinued participation because of time constraints. Eighteen healthy, nonsmoking men and women aged 27 to 59 years (44 ± 18; mean, SD) completed the trial. Cereal treatments were isocaloric. Participants were instructed to consume all their cereal (treatment, 137 g; control, 146 g) daily for the next 6 weeks but were allowed to prepare and consume the cereal however and whenever they wished.
Cereal compliance was determined by participant self-report in a daily cereal calendar. In addition, dietary intake was reviewed both at baseline and at the end of the 6-week intervention, using 3-day food records. Side effect data were gathered from participants at baseline and the end of the intervention. Side effects were assessed via a questionnaire consisting of 21 items relating to potential side effects from increased fiber intake (eg, loose stools, flatulence) or hypertension (eg, headaches, dizziness). Participants reported the frequency at which they experienced these side effects on a scale ranging from “never” to “very frequently” (event occurring once or more per day). Each response was assigned a numerical value. Prestudy and post study averages were used in analyses.
Blood Pressure, Plasma Lipid Concentrations, Glucose Metabolism, and Insulin Sensitivity
Blood pressure was measured weekly for each participant for the duration of the study. Each participant reported to the Hypertension and Cholesterol Research Clinic located at the University of Minnesota Medical School at approximately the same time for each blood pressure reading. All readings were obtained in the morning after participants had rested quietly, seated, for at least 5 minutes in an examination room. An examiner who was blinded to the treatment groups took readings on the right arm using a mercury column sphygmomanometer (Korotkoff phase V for DBP). Standard cuff size was used unless upper arm circumference exceeded 31 cm, in which case the examiner used a large cuff with 15 x 35-cm bladders. Measurements were repeated 4 times in 2-minute intervals. The mean of the last 3 readings was calculated and used in analyses.
To determine plasma lipid concentrations (total, high-density lipoprotein [HDL], and low-density lipoprotein [LDL] cholesterol and triglycerides), pretreatment and posttreatment blood samples were drawn. A 75-g, 3-hour oral glucose-tolerance test (OGTT) was administered before and after treatment to assess participants’ glucose tolerance and insulin response. Whole blood sampling occurred at -30, 0, 30, 60, 90, 120, 150, and 180 minutes. A measure of insulin sensitivity was assessed within 48 hours after the OGTT by means of the modified frequently sampled intravenous glucose tolerance test (FSIGT).28 The glucose and insulin data derived from this test were used to calculate the insulin sensitivity index (SI) employing the minimal-model method developed by Bergman.29
Statistical methods
Reported results are expressed in terms of means ± SD or means SE. Student’s t test for independent samples was used to compare the 2 treatment groups at baseline and to compare mean change scores between the 2 groups. Additionally, area-under-the-curve analyses were performed to compare OGTT insulin curves. All analyses were performed on data from an intent-to-treat population, which included all randomized participants. Statistical tests were 2 sided, performed at the 5% level of significance, and conducted with Statistical Analysis System software (SAS Institute, Cary, N.C.).
Results
No statistically significant differences in baseline characteristics occurred between the groups, although this comparison is limited by the small sample size Table 2. LDL cholesterol and total cholesterol levels and blood pressure were somewhat higher in the treatment group. The blood pressure measurements in the treatment group resulted in an average SBP of 143 ± 3.7 mm Hg before intervention and 135 ± 2.6 mm Hg after intervention (an average of the last 2 study visits, P < .01) Table 3. No significant change in SBP was observed in the control group. A significant difference between the treatment and control groups was observed for the change in SBP (P < .02). DBP dropped from 93 ± 1.9 mm Hg to 87 ± 2.2 mm Hg after the oat fiber intervention (P = .02), with no significant change in the control group (P = .94). A borderline significant trend was noted for the change scores of DBP between groups (P = .055).
Changes in fasting insulin, insulin sensitivity (SI), and insulin curves derived from the oral glucose tolerance tests were assessed. Fasting insulin values Table 3 were taken from the OGTT (preglucose infusion values). Neither the control group (P = 1.00) nor the treatment group (P = .753) showed a significant change in fasting insulin levels. The Bergman minimal model method was used to estimate insulin sensitivity and showed no significant change in either group. Area-under-the-curve analysis of the insulin data derived from the OGTTs before and after treatment with oat cereal (Figure 1 and Figure 2) suggested a trend toward significance in terms of less insulin required to clear a glucose load (top of graphs, P = .093), with no significant changes in the control group (bottom).
Total cholesterol concentrations dropped 16.2 ± 6.3 mg/dL in the oat cereal group (P = .030), with a slight (nonsignificant) increase in the control group (P = .48). Additionally, a comparison of the changes in total cholesterol between the 2 groups revealed a significant mean difference of 21.1 ± 9.1 mg/dL (P = .035). LDL cholesterol was also reduced significantly after the oat cereal intervention by 15.8 ± 5.9 mg/dL (P = .025). The nonsignificant increase in LDL cholesterol in the control group (P = .231) combined with the significant reduction in the treatment group resulted in a significant difference between the groups after intervention (P < .015). Neither group experienced significant changes in HDL cholesterol or triglyceride concentrations.
An analysis of the side effect data showed no significant difference in the occurrence of side effects between groups. There was an overall decrease in the frequency of dietary fiber-related and hypertension-related side effects in both groups, with a more substantial reduction occurring in the oat cereal group (P = .11). Total body weight did not change significantly in either group. Additionally, both groups were very compliant (approximately 90%) in terms of cereal consumption Table 3.
Discussion
The results of this pilot study suggest that the inclusion of oats into the standard American diet of people with borderline or mild hypertension may reduce both SBP and DBP. In persons consuming 5.52 g/day of beta-glucan soluble fiber from oat cereal for 6 weeks, we found a statistically and clinically significant decrease in both SBP and DBP (7.5 mm Hg and 5.5 mm Hg, respectively) and a trend toward improved OGTT-determined insulin sensitivity. These findings warrant a large-scale clinical trial to explore further the relationship between whole-grain oat consumption and blood pressure, especially considering the limitations of this pilot study.
As with all small-scale trials, this one lacked sufficient power to detect true changes in both primary and secondary outcome variables. It is possible that regression to the mean explains at least part of the treatment effect, since participants in the oats group began the study with higher SBP, DBP, and LDL cholesterol levels than controls. In addition, it is possible that the reported blood pressure changes could have been caused by “other” undetected dietary change made by members of the oats group. Future trials will need to collect and analyze dietary data carefully; feeding trials should be considered. Such dietary analyses may indicate that certain micronutrients partially explain the hypotensive effects of whole-grain oat consumption. The DASH trial and others have consistently demonstrated that diets rich in certain micronutrients can reduce blood pressure.30,31
Soluble fiber-rich oat cereals may affect blood pressure by modulating changes in insulin metabolism. The mechanism of action is thought to involve the slowed absorption of macronutrients from the gut, resulting in a flattening of the postprandial glycemic curve.29 These lower postprandial blood glucose levels elicit a lower insulin response to accommodate its clearance from the plasma. This process may lead to improved insulin sensitivity if the lower circulating insulin levels lead eventually to upregulation of the insulin receptors in peripheral tissues. A recent animal trial demonstrated that soluble fiber feeding improved insulin sensitivity by increasing skeletal muscle plasma membrane GLUT-4 content.32 Findings in this pilot suggest that over time, oat ingestion may reduce the amount of insulin needed to clear a glucose load. However, the study was underpowered to detect significant differences in more sensitive measures of insulin resistance. The causal mechanistic relationship among whole grain oat consumption, blood pressure, and insulin resistance might be best studied using a long-term feeding study design.
Alternate mechanisms, such as attenuation in endothelial function, may have affected blood pressure responses in this study.33 Drugs specific to endothelial cell receptors mediating vasodilation are known to lower blood pressure.34 Moreover, plasma cholesterol reductions are associated with improvements in endothelium-mediated vasodilation.35,36 In addition, preliminary evidence in animals supports a direct relationship between changes in plasma cholesterol concentrations and blood pressure.37 In the present study, plasma cholesterol levels were significantly reduced in participants who ingested whole grain oat-based cereals compared to a more refined grain wheat, corn, and rice control. Thus, it is possible that the blood pressure reduction observed in the subjects consuming oats resulted in part from improved endothelial function due to a drop in plasma cholesterol. Additional research is needed to fully investigate this pathway.
From a practical standpoint, improvements in SBP and DBP such as those observed in this study would be a useful contribution to the clinical management of hypertension. The cereal feeding intervention was well tolerated. Participants were very compliant for the 6-week treatment period. Substantial improvements in blood lipids could serve as an added incentive for patients to maintain long-term compliance with feeding recommendations.18,19 Since treatment of hypertension is a lifelong process for most patients, future studies would need to assess the effectiveness of oat cereals to maintain blood pressure benefits over a longer time. Such studies may need to consider dietary options such as soluble fiber-rich fruits in addition to cereal consumption in efforts to deliver the desired quantity of soluble fiber. Future trials will have to investigate the antihypertensive effect of whole oats in other populations, such as people with diabetes, and to study not only surrogate endpoints such as blood pressure but also patient-oriented outcomes such as mortality and morbidity.
1. He J, Klag M, Whelton P, et al. Oats and buckwheat intakes and cardiovascular disease risk factors in an ethnic minority of China. Am J Clin Nutr 1995;61:366-72.
2. Lichtenstein M, Burr M, Fehily A, Yarnell J. Heart rate, employment status, and prevalent ischemic heart disease confound relation between cereal fibre intake and blood pressure. J Epidemiol Community Health 1986;40:330-3.
3. Ascherio A, Rimm E, Giovannucci E, et al. A prospective study of nutritional factors and hypertension among US men. Circulation 1992;86:1475-84.
4. Hallfrisch J, Tobin J, Muller D, Andres R. Fiber intake, age, and other coronary risk factors in men of the Baltimore Longitudinal Study (1959-1975). J Gerontol 1988;43:M64-8.
5. Ascherio A, Hennekens C, Willett W, et al. Prospective study of nutritional factors, blood pressure, and hypertension among US women. Hypertension 1996;27:1065-72.
6. Schlamowitz P, Halberg T, Warnoe O, Wilstrup F, Ryttig K. Treatment of mild to moderate hypertension with dietary fiber. Lancet 1987;2:622-3.
7. Eliasson K, Ryttig K, Hylander B, Rossner S. A dietary fiber supplement in the treatment of mild hypertension. A randomized, double-blind, placebo-controlled trial. J Hypertens 1992;10:195-9.
8. Ryttig K, Tellnes G, Haegh L, Boe E, Fagerthun H. A dietary fiber supplement and weight maintenance after weight reduction: a randomized, double-blind, placebo-controlled long-term trial. Int J Obes 1989;13:165-71.
9. Dodson P, Stephenson J, Dodson L, et al. Randomised blind controlled trial of a high fiber, low fat and low sodium dietary regimen in mild essential hypertension. J Hum Hypertens 1989;3:197-202.
10. Little P, Girling G, Hasler A, Trafford A. A controlled trial of a low sodium, low fat, high fibre diet in treated hypertensive patients: effect on antihypertensive drug requirement in clinical practice. J Hum Hypertens 1991;5:175-81.
11. Rossner S, Andersson I, Ryttig K. Effects of a dietary fiber supplement to a weight reduction program on blood pressure. Acta Med Scand 1988;223:353-7.
12. Sandstrom B, Marckmann P, Bindslev N. An eight-month controlled study of a low-fat high-fiber diet: effects on blood lipids and blood pressure in healthy young subjects. Eur J Clin Nutr 1992;46:95-109.
13. Kestin M, Moss R, Clifton P. Comparative effects of three cereal brans on plasma lipids, blood pressure, and glucose metabolism in mildly hypercholesterolemic men. Am J Clin Nutr 1990;52:661-6.
14. Swain J, Rouse I, Curley C, Sacks F. Comparison of the effects of oat bran and low-fiber wheat on serum lipoprotein levels and blood pressure. N Engl J Med 1990;322:147-52.
15. Sciarrone S, Beilin L, Rouse I, Rogers P. A factorial study of salt restriction and a low-fat/high-fibre diet in hypertensive subjects. J Hypertens 1992;10:287-98.
16. Margetts B, Beilin L, Vandongen R, Armstrong B. A randomized controlled trial of the effect of dietary fiber on blood pressure. Clin Sci 1987;72:343-50.
17. el Zein M, Areas J, Knapka J, et al. Influence of oat bran on sucrose-induced blood pressure elevations in SHR. Life Sci 1990;47:1121-8.
18. Gondal J, MacArthy P, Myers A, Preuss H. Effects of dietary sucrose and fibers on blood pressure in hypertensive rats. Clin Nephrol 1996;45:163-8.
19. Krotkiewski M. Effect of guar gum on the arterial blood pressure. Acta Med Scand 1987;222:43-9.
20. Singh R, Rastogi S, Singh N, Ghosh S, Gupta S, Niaz M. Can guava fruit intake decrease blood pressure and blood lipids? J Hum Hypertens 1993;7:33-8.
21. Weidmann P, de Courten M, Bohlen L. Insulin resistance, hyperinsulinemia and hypertension. J Hypertens 1993;11:S27-38.
22. Tuck M. Obesity, the sympathetic nervous system, and essential hypertension. Hypertension 1992;19:I67-77.
23. Sowers J. Insulin resistance, hyperinsulinemia, dyslipidemia, hypertension, and accelerated atherosclerosis. J Clin Pharmacol 1992;32:529-35.
24. Braaten J, Wood P, Scott F, Riedel K, Poste L, Collins M. Oat gum lowers glucose and insulin after an oral glucose load. Am J Clin Nutr 1991;53:1425-30.
25. Braaten J, Scott F, Wood P, et al. High ß-glucan oat bran and oat gum reduce postprandial blood glucose and insulin in subjects with and without type 2 diabetes. Diabet Med 1994;11:312-8.
26. Hallfrisch J, Scholfield D, Behall K. Diets containing soluble oat extracts improve glucose and insulin responses of moderately hypercholesterolemic men and women. Am J Clin Nutr 1995;61:379-84.
27. Fukagawa N, Anderson J, Hageman G, Young V, Minaker K. High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults. Am J Clin Nutr 1990;52:524-8.
28. Welch S, Gebhart S, Bergman R, Phillips L. Minimal model analysis of IVGTT-derived insulin sensitivity in diabetic subjects. J Clin Endocrinol Metab 1990;71:1508-18.
29. Bergman R, Ider Y, Bowden C, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol 1979;236:E667-77.
30. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial on the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24.
31. Appel LJ. The role of diet in the prevention and treatment of hypertension. Curr Atheroscler Rep 2000;2:521-8.
32. Song YJ, Sawamura M, Ikeda K, Igawa S, Yamori Y. Soluble dietary fiber improves insulin sensitivity by increasing muscle GLUT-4 content in stroke-prone spontaneously hypertensive rats. Clin Exp Pharm Physiol 2000;27:41-5.
33. Taddei S, Salvetti A. Pathogenic factors in hypertension. Endothelial Factors. Clin Exp Hypertens 1996;18:323-35.
34. Krum H, Viskoper R, Lacourciere Y, Budde B, Charlon V. The effect of an endothelium-receptor antagonist, Bosentan, on blood pressure in patients with essential hypertension. N Engl J Med 1998;338:784-90.
35. Anderson T, Meredith I, Yeung A. The effect of cholesterol-lowering and antioxidant therapy on endothelium-dependent coronary vasomotion. N Engl J Med 1995;332:488-93.
36. Vogel R, Corretti M, Plotnick G. Changes in flow-mediated brachial artery vasoactivity with lowering of desirable cholesterol levels in healthy middle-aged men. Am J Cardiol 1996;77:37-40.
37. Crago M, West S, Hoeprich K, Michaelis K, McKenzie J. Effects of hyperlipidemia on blood pressure and coronary blood flow in swine. FASEB J 1998;12:A238.-
To submit a letter to the editor on this topic, click here: [email protected].
OBJECTIVES: We assessed the short-term antihypertensive effects of soluble fiber-rich whole oat cereals when added to a standard American diet. In addition, multiple assessments of insulin sensitivity were conducted.
STUDY DESIGN: This was a randomized, controlled, parallel-group pilot study designed to compare an oat cereal group (standardized to 5.52 g/day beta-glucan) to a low-fiber cereal control group (less than 1.0 g/day total fiber) over 6 weeks.
POPULATION: A total of 18 hypertensive and hyperinsulinemic ( ≥10 μU/mL) men and women completed the trial.
OUTCOMES MEASURED: Primary study outcomes were changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP). Secondary outcomes included blood lipid, fasting glucose, and insulin levels and side effects related to elevated blood pressure and increased dietary fiber intake.
RESULTS: The oat cereal group experienced a 7.5 mm Hg reduction in SBP (P < .01) and a 5.5 mm Hg reduction in DBP (P < .02), while there was virtually no change in either SBP or DBP in the control group. In the oat cereal group, a trend was observed for a lower total insulin response to a glucose load, suggesting improved insulin sensitivity. However, this could not be confirmed using estimates from the Bergman Minimal Model, perhaps because of our small sample size. As expected and reported in previous trials, the oats group experienced a significant reduction in both total cholesterol (9%) and low-density lipoprotein cholesterol (14%).
CONCLUSIONS: The addition of oat cereals to the normal diet of persons with hypertension significantly reduces both systolic and diastolic blood pressure. Soluble fiber-rich whole oats may be an effective dietary therapy in the prevention and adjunct treatment of hypertension.
Interest is growing in the use of nonpharmacologic methods for the prevention and management of hypertension. Specifically, the effect of dietary fiber on the incidence and treatment of hypertension has been explored. Epidemiologic studies show that the amount of dietary fiber ingested is inversely related to the incidence of hypertension as well as to systolic blood pressure (SBP) and diastolic blood pressure (DBP) in both hypertensive and normotensive patients.1–5 The results obtained from clinical trials, however, are inconsistent; some report modest blood pressure reductions after increased fiber intake,6–12 while others fail to demonstrate any effect of dietary fiber on blood pressure.13–16 Some animal trials17,18 and human trials19,20 have shown a consistent lowering of blood pressure upon consumption of larger amounts of soluble fiber, suggesting that the antihypertensive effects of fiber may be caused by the soluble fraction and that these effects may be contingent upon the intake of a sufficiently large quantity.
Hypertension often occurs in association with obesity, impaired glucose tolerance, and dyslipidemia. Hyperinsulinemia and insulin resistance are thought to be key pathogenic links among these disturbances.21–23 Studies show that soluble fiber from oats reduces both postprandial blood glucose and insulin levels.24–27 Therefore, we conducted the following pilot trial to investigate the antihypertensive and insulin-modifying effects of oat cereal supplementation in a population of mild and borderline hyperinsulinemic and hypertensive men and women.
Methods
Study protocol
The study participants in this 6-week, randomized, parallel-group, active-controlled pilot trial were recruited by means of local community screenings and mass media advertising. The study protocol was reviewed and approved by the University of Minnesota Institutional Review Board. All participants provided informed consent before official enrollment in the study. One hundred nine men and women aged 20 to 70 were screened for eligibility with a physical exam, medical history, and chemistry and lipid profile (see Table 1 for exclusion criteria). Only generally healthy, untreated hypertensives with average SBP of 130 to 160 mm Hg and DBP of 85 to 100 mm Hg and with at least 1 reading greater than 140/90 as well as moderately elevated levels of fasting insulin (≥10μU/mL) were considered for enrollment. Participants were determined to be eligible only after 2 sets of hypertensive (SBP > 130, DBP > 85) baseline blood pressure readings had been taken 7 days apart and only if all inclusion criteria were fulfilled.
Ultimately, 22 men and women were randomized to either an oat cereal treatment group (standardized to 5.52 g/day beta-glucan) or a low fiber cereal control group (<1 g/day total fiber). Four of these individuals (1 in the treatment and 3 in the control group) discontinued participation because of time constraints. Eighteen healthy, nonsmoking men and women aged 27 to 59 years (44 ± 18; mean, SD) completed the trial. Cereal treatments were isocaloric. Participants were instructed to consume all their cereal (treatment, 137 g; control, 146 g) daily for the next 6 weeks but were allowed to prepare and consume the cereal however and whenever they wished.
Cereal compliance was determined by participant self-report in a daily cereal calendar. In addition, dietary intake was reviewed both at baseline and at the end of the 6-week intervention, using 3-day food records. Side effect data were gathered from participants at baseline and the end of the intervention. Side effects were assessed via a questionnaire consisting of 21 items relating to potential side effects from increased fiber intake (eg, loose stools, flatulence) or hypertension (eg, headaches, dizziness). Participants reported the frequency at which they experienced these side effects on a scale ranging from “never” to “very frequently” (event occurring once or more per day). Each response was assigned a numerical value. Prestudy and post study averages were used in analyses.
Blood Pressure, Plasma Lipid Concentrations, Glucose Metabolism, and Insulin Sensitivity
Blood pressure was measured weekly for each participant for the duration of the study. Each participant reported to the Hypertension and Cholesterol Research Clinic located at the University of Minnesota Medical School at approximately the same time for each blood pressure reading. All readings were obtained in the morning after participants had rested quietly, seated, for at least 5 minutes in an examination room. An examiner who was blinded to the treatment groups took readings on the right arm using a mercury column sphygmomanometer (Korotkoff phase V for DBP). Standard cuff size was used unless upper arm circumference exceeded 31 cm, in which case the examiner used a large cuff with 15 x 35-cm bladders. Measurements were repeated 4 times in 2-minute intervals. The mean of the last 3 readings was calculated and used in analyses.
To determine plasma lipid concentrations (total, high-density lipoprotein [HDL], and low-density lipoprotein [LDL] cholesterol and triglycerides), pretreatment and posttreatment blood samples were drawn. A 75-g, 3-hour oral glucose-tolerance test (OGTT) was administered before and after treatment to assess participants’ glucose tolerance and insulin response. Whole blood sampling occurred at -30, 0, 30, 60, 90, 120, 150, and 180 minutes. A measure of insulin sensitivity was assessed within 48 hours after the OGTT by means of the modified frequently sampled intravenous glucose tolerance test (FSIGT).28 The glucose and insulin data derived from this test were used to calculate the insulin sensitivity index (SI) employing the minimal-model method developed by Bergman.29
Statistical methods
Reported results are expressed in terms of means ± SD or means SE. Student’s t test for independent samples was used to compare the 2 treatment groups at baseline and to compare mean change scores between the 2 groups. Additionally, area-under-the-curve analyses were performed to compare OGTT insulin curves. All analyses were performed on data from an intent-to-treat population, which included all randomized participants. Statistical tests were 2 sided, performed at the 5% level of significance, and conducted with Statistical Analysis System software (SAS Institute, Cary, N.C.).
Results
No statistically significant differences in baseline characteristics occurred between the groups, although this comparison is limited by the small sample size Table 2. LDL cholesterol and total cholesterol levels and blood pressure were somewhat higher in the treatment group. The blood pressure measurements in the treatment group resulted in an average SBP of 143 ± 3.7 mm Hg before intervention and 135 ± 2.6 mm Hg after intervention (an average of the last 2 study visits, P < .01) Table 3. No significant change in SBP was observed in the control group. A significant difference between the treatment and control groups was observed for the change in SBP (P < .02). DBP dropped from 93 ± 1.9 mm Hg to 87 ± 2.2 mm Hg after the oat fiber intervention (P = .02), with no significant change in the control group (P = .94). A borderline significant trend was noted for the change scores of DBP between groups (P = .055).
Changes in fasting insulin, insulin sensitivity (SI), and insulin curves derived from the oral glucose tolerance tests were assessed. Fasting insulin values Table 3 were taken from the OGTT (preglucose infusion values). Neither the control group (P = 1.00) nor the treatment group (P = .753) showed a significant change in fasting insulin levels. The Bergman minimal model method was used to estimate insulin sensitivity and showed no significant change in either group. Area-under-the-curve analysis of the insulin data derived from the OGTTs before and after treatment with oat cereal (Figure 1 and Figure 2) suggested a trend toward significance in terms of less insulin required to clear a glucose load (top of graphs, P = .093), with no significant changes in the control group (bottom).
Total cholesterol concentrations dropped 16.2 ± 6.3 mg/dL in the oat cereal group (P = .030), with a slight (nonsignificant) increase in the control group (P = .48). Additionally, a comparison of the changes in total cholesterol between the 2 groups revealed a significant mean difference of 21.1 ± 9.1 mg/dL (P = .035). LDL cholesterol was also reduced significantly after the oat cereal intervention by 15.8 ± 5.9 mg/dL (P = .025). The nonsignificant increase in LDL cholesterol in the control group (P = .231) combined with the significant reduction in the treatment group resulted in a significant difference between the groups after intervention (P < .015). Neither group experienced significant changes in HDL cholesterol or triglyceride concentrations.
An analysis of the side effect data showed no significant difference in the occurrence of side effects between groups. There was an overall decrease in the frequency of dietary fiber-related and hypertension-related side effects in both groups, with a more substantial reduction occurring in the oat cereal group (P = .11). Total body weight did not change significantly in either group. Additionally, both groups were very compliant (approximately 90%) in terms of cereal consumption Table 3.
Discussion
The results of this pilot study suggest that the inclusion of oats into the standard American diet of people with borderline or mild hypertension may reduce both SBP and DBP. In persons consuming 5.52 g/day of beta-glucan soluble fiber from oat cereal for 6 weeks, we found a statistically and clinically significant decrease in both SBP and DBP (7.5 mm Hg and 5.5 mm Hg, respectively) and a trend toward improved OGTT-determined insulin sensitivity. These findings warrant a large-scale clinical trial to explore further the relationship between whole-grain oat consumption and blood pressure, especially considering the limitations of this pilot study.
As with all small-scale trials, this one lacked sufficient power to detect true changes in both primary and secondary outcome variables. It is possible that regression to the mean explains at least part of the treatment effect, since participants in the oats group began the study with higher SBP, DBP, and LDL cholesterol levels than controls. In addition, it is possible that the reported blood pressure changes could have been caused by “other” undetected dietary change made by members of the oats group. Future trials will need to collect and analyze dietary data carefully; feeding trials should be considered. Such dietary analyses may indicate that certain micronutrients partially explain the hypotensive effects of whole-grain oat consumption. The DASH trial and others have consistently demonstrated that diets rich in certain micronutrients can reduce blood pressure.30,31
Soluble fiber-rich oat cereals may affect blood pressure by modulating changes in insulin metabolism. The mechanism of action is thought to involve the slowed absorption of macronutrients from the gut, resulting in a flattening of the postprandial glycemic curve.29 These lower postprandial blood glucose levels elicit a lower insulin response to accommodate its clearance from the plasma. This process may lead to improved insulin sensitivity if the lower circulating insulin levels lead eventually to upregulation of the insulin receptors in peripheral tissues. A recent animal trial demonstrated that soluble fiber feeding improved insulin sensitivity by increasing skeletal muscle plasma membrane GLUT-4 content.32 Findings in this pilot suggest that over time, oat ingestion may reduce the amount of insulin needed to clear a glucose load. However, the study was underpowered to detect significant differences in more sensitive measures of insulin resistance. The causal mechanistic relationship among whole grain oat consumption, blood pressure, and insulin resistance might be best studied using a long-term feeding study design.
Alternate mechanisms, such as attenuation in endothelial function, may have affected blood pressure responses in this study.33 Drugs specific to endothelial cell receptors mediating vasodilation are known to lower blood pressure.34 Moreover, plasma cholesterol reductions are associated with improvements in endothelium-mediated vasodilation.35,36 In addition, preliminary evidence in animals supports a direct relationship between changes in plasma cholesterol concentrations and blood pressure.37 In the present study, plasma cholesterol levels were significantly reduced in participants who ingested whole grain oat-based cereals compared to a more refined grain wheat, corn, and rice control. Thus, it is possible that the blood pressure reduction observed in the subjects consuming oats resulted in part from improved endothelial function due to a drop in plasma cholesterol. Additional research is needed to fully investigate this pathway.
From a practical standpoint, improvements in SBP and DBP such as those observed in this study would be a useful contribution to the clinical management of hypertension. The cereal feeding intervention was well tolerated. Participants were very compliant for the 6-week treatment period. Substantial improvements in blood lipids could serve as an added incentive for patients to maintain long-term compliance with feeding recommendations.18,19 Since treatment of hypertension is a lifelong process for most patients, future studies would need to assess the effectiveness of oat cereals to maintain blood pressure benefits over a longer time. Such studies may need to consider dietary options such as soluble fiber-rich fruits in addition to cereal consumption in efforts to deliver the desired quantity of soluble fiber. Future trials will have to investigate the antihypertensive effect of whole oats in other populations, such as people with diabetes, and to study not only surrogate endpoints such as blood pressure but also patient-oriented outcomes such as mortality and morbidity.
OBJECTIVES: We assessed the short-term antihypertensive effects of soluble fiber-rich whole oat cereals when added to a standard American diet. In addition, multiple assessments of insulin sensitivity were conducted.
STUDY DESIGN: This was a randomized, controlled, parallel-group pilot study designed to compare an oat cereal group (standardized to 5.52 g/day beta-glucan) to a low-fiber cereal control group (less than 1.0 g/day total fiber) over 6 weeks.
POPULATION: A total of 18 hypertensive and hyperinsulinemic ( ≥10 μU/mL) men and women completed the trial.
OUTCOMES MEASURED: Primary study outcomes were changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP). Secondary outcomes included blood lipid, fasting glucose, and insulin levels and side effects related to elevated blood pressure and increased dietary fiber intake.
RESULTS: The oat cereal group experienced a 7.5 mm Hg reduction in SBP (P < .01) and a 5.5 mm Hg reduction in DBP (P < .02), while there was virtually no change in either SBP or DBP in the control group. In the oat cereal group, a trend was observed for a lower total insulin response to a glucose load, suggesting improved insulin sensitivity. However, this could not be confirmed using estimates from the Bergman Minimal Model, perhaps because of our small sample size. As expected and reported in previous trials, the oats group experienced a significant reduction in both total cholesterol (9%) and low-density lipoprotein cholesterol (14%).
CONCLUSIONS: The addition of oat cereals to the normal diet of persons with hypertension significantly reduces both systolic and diastolic blood pressure. Soluble fiber-rich whole oats may be an effective dietary therapy in the prevention and adjunct treatment of hypertension.
Interest is growing in the use of nonpharmacologic methods for the prevention and management of hypertension. Specifically, the effect of dietary fiber on the incidence and treatment of hypertension has been explored. Epidemiologic studies show that the amount of dietary fiber ingested is inversely related to the incidence of hypertension as well as to systolic blood pressure (SBP) and diastolic blood pressure (DBP) in both hypertensive and normotensive patients.1–5 The results obtained from clinical trials, however, are inconsistent; some report modest blood pressure reductions after increased fiber intake,6–12 while others fail to demonstrate any effect of dietary fiber on blood pressure.13–16 Some animal trials17,18 and human trials19,20 have shown a consistent lowering of blood pressure upon consumption of larger amounts of soluble fiber, suggesting that the antihypertensive effects of fiber may be caused by the soluble fraction and that these effects may be contingent upon the intake of a sufficiently large quantity.
Hypertension often occurs in association with obesity, impaired glucose tolerance, and dyslipidemia. Hyperinsulinemia and insulin resistance are thought to be key pathogenic links among these disturbances.21–23 Studies show that soluble fiber from oats reduces both postprandial blood glucose and insulin levels.24–27 Therefore, we conducted the following pilot trial to investigate the antihypertensive and insulin-modifying effects of oat cereal supplementation in a population of mild and borderline hyperinsulinemic and hypertensive men and women.
Methods
Study protocol
The study participants in this 6-week, randomized, parallel-group, active-controlled pilot trial were recruited by means of local community screenings and mass media advertising. The study protocol was reviewed and approved by the University of Minnesota Institutional Review Board. All participants provided informed consent before official enrollment in the study. One hundred nine men and women aged 20 to 70 were screened for eligibility with a physical exam, medical history, and chemistry and lipid profile (see Table 1 for exclusion criteria). Only generally healthy, untreated hypertensives with average SBP of 130 to 160 mm Hg and DBP of 85 to 100 mm Hg and with at least 1 reading greater than 140/90 as well as moderately elevated levels of fasting insulin (≥10μU/mL) were considered for enrollment. Participants were determined to be eligible only after 2 sets of hypertensive (SBP > 130, DBP > 85) baseline blood pressure readings had been taken 7 days apart and only if all inclusion criteria were fulfilled.
Ultimately, 22 men and women were randomized to either an oat cereal treatment group (standardized to 5.52 g/day beta-glucan) or a low fiber cereal control group (<1 g/day total fiber). Four of these individuals (1 in the treatment and 3 in the control group) discontinued participation because of time constraints. Eighteen healthy, nonsmoking men and women aged 27 to 59 years (44 ± 18; mean, SD) completed the trial. Cereal treatments were isocaloric. Participants were instructed to consume all their cereal (treatment, 137 g; control, 146 g) daily for the next 6 weeks but were allowed to prepare and consume the cereal however and whenever they wished.
Cereal compliance was determined by participant self-report in a daily cereal calendar. In addition, dietary intake was reviewed both at baseline and at the end of the 6-week intervention, using 3-day food records. Side effect data were gathered from participants at baseline and the end of the intervention. Side effects were assessed via a questionnaire consisting of 21 items relating to potential side effects from increased fiber intake (eg, loose stools, flatulence) or hypertension (eg, headaches, dizziness). Participants reported the frequency at which they experienced these side effects on a scale ranging from “never” to “very frequently” (event occurring once or more per day). Each response was assigned a numerical value. Prestudy and post study averages were used in analyses.
Blood Pressure, Plasma Lipid Concentrations, Glucose Metabolism, and Insulin Sensitivity
Blood pressure was measured weekly for each participant for the duration of the study. Each participant reported to the Hypertension and Cholesterol Research Clinic located at the University of Minnesota Medical School at approximately the same time for each blood pressure reading. All readings were obtained in the morning after participants had rested quietly, seated, for at least 5 minutes in an examination room. An examiner who was blinded to the treatment groups took readings on the right arm using a mercury column sphygmomanometer (Korotkoff phase V for DBP). Standard cuff size was used unless upper arm circumference exceeded 31 cm, in which case the examiner used a large cuff with 15 x 35-cm bladders. Measurements were repeated 4 times in 2-minute intervals. The mean of the last 3 readings was calculated and used in analyses.
To determine plasma lipid concentrations (total, high-density lipoprotein [HDL], and low-density lipoprotein [LDL] cholesterol and triglycerides), pretreatment and posttreatment blood samples were drawn. A 75-g, 3-hour oral glucose-tolerance test (OGTT) was administered before and after treatment to assess participants’ glucose tolerance and insulin response. Whole blood sampling occurred at -30, 0, 30, 60, 90, 120, 150, and 180 minutes. A measure of insulin sensitivity was assessed within 48 hours after the OGTT by means of the modified frequently sampled intravenous glucose tolerance test (FSIGT).28 The glucose and insulin data derived from this test were used to calculate the insulin sensitivity index (SI) employing the minimal-model method developed by Bergman.29
Statistical methods
Reported results are expressed in terms of means ± SD or means SE. Student’s t test for independent samples was used to compare the 2 treatment groups at baseline and to compare mean change scores between the 2 groups. Additionally, area-under-the-curve analyses were performed to compare OGTT insulin curves. All analyses were performed on data from an intent-to-treat population, which included all randomized participants. Statistical tests were 2 sided, performed at the 5% level of significance, and conducted with Statistical Analysis System software (SAS Institute, Cary, N.C.).
Results
No statistically significant differences in baseline characteristics occurred between the groups, although this comparison is limited by the small sample size Table 2. LDL cholesterol and total cholesterol levels and blood pressure were somewhat higher in the treatment group. The blood pressure measurements in the treatment group resulted in an average SBP of 143 ± 3.7 mm Hg before intervention and 135 ± 2.6 mm Hg after intervention (an average of the last 2 study visits, P < .01) Table 3. No significant change in SBP was observed in the control group. A significant difference between the treatment and control groups was observed for the change in SBP (P < .02). DBP dropped from 93 ± 1.9 mm Hg to 87 ± 2.2 mm Hg after the oat fiber intervention (P = .02), with no significant change in the control group (P = .94). A borderline significant trend was noted for the change scores of DBP between groups (P = .055).
Changes in fasting insulin, insulin sensitivity (SI), and insulin curves derived from the oral glucose tolerance tests were assessed. Fasting insulin values Table 3 were taken from the OGTT (preglucose infusion values). Neither the control group (P = 1.00) nor the treatment group (P = .753) showed a significant change in fasting insulin levels. The Bergman minimal model method was used to estimate insulin sensitivity and showed no significant change in either group. Area-under-the-curve analysis of the insulin data derived from the OGTTs before and after treatment with oat cereal (Figure 1 and Figure 2) suggested a trend toward significance in terms of less insulin required to clear a glucose load (top of graphs, P = .093), with no significant changes in the control group (bottom).
Total cholesterol concentrations dropped 16.2 ± 6.3 mg/dL in the oat cereal group (P = .030), with a slight (nonsignificant) increase in the control group (P = .48). Additionally, a comparison of the changes in total cholesterol between the 2 groups revealed a significant mean difference of 21.1 ± 9.1 mg/dL (P = .035). LDL cholesterol was also reduced significantly after the oat cereal intervention by 15.8 ± 5.9 mg/dL (P = .025). The nonsignificant increase in LDL cholesterol in the control group (P = .231) combined with the significant reduction in the treatment group resulted in a significant difference between the groups after intervention (P < .015). Neither group experienced significant changes in HDL cholesterol or triglyceride concentrations.
An analysis of the side effect data showed no significant difference in the occurrence of side effects between groups. There was an overall decrease in the frequency of dietary fiber-related and hypertension-related side effects in both groups, with a more substantial reduction occurring in the oat cereal group (P = .11). Total body weight did not change significantly in either group. Additionally, both groups were very compliant (approximately 90%) in terms of cereal consumption Table 3.
Discussion
The results of this pilot study suggest that the inclusion of oats into the standard American diet of people with borderline or mild hypertension may reduce both SBP and DBP. In persons consuming 5.52 g/day of beta-glucan soluble fiber from oat cereal for 6 weeks, we found a statistically and clinically significant decrease in both SBP and DBP (7.5 mm Hg and 5.5 mm Hg, respectively) and a trend toward improved OGTT-determined insulin sensitivity. These findings warrant a large-scale clinical trial to explore further the relationship between whole-grain oat consumption and blood pressure, especially considering the limitations of this pilot study.
As with all small-scale trials, this one lacked sufficient power to detect true changes in both primary and secondary outcome variables. It is possible that regression to the mean explains at least part of the treatment effect, since participants in the oats group began the study with higher SBP, DBP, and LDL cholesterol levels than controls. In addition, it is possible that the reported blood pressure changes could have been caused by “other” undetected dietary change made by members of the oats group. Future trials will need to collect and analyze dietary data carefully; feeding trials should be considered. Such dietary analyses may indicate that certain micronutrients partially explain the hypotensive effects of whole-grain oat consumption. The DASH trial and others have consistently demonstrated that diets rich in certain micronutrients can reduce blood pressure.30,31
Soluble fiber-rich oat cereals may affect blood pressure by modulating changes in insulin metabolism. The mechanism of action is thought to involve the slowed absorption of macronutrients from the gut, resulting in a flattening of the postprandial glycemic curve.29 These lower postprandial blood glucose levels elicit a lower insulin response to accommodate its clearance from the plasma. This process may lead to improved insulin sensitivity if the lower circulating insulin levels lead eventually to upregulation of the insulin receptors in peripheral tissues. A recent animal trial demonstrated that soluble fiber feeding improved insulin sensitivity by increasing skeletal muscle plasma membrane GLUT-4 content.32 Findings in this pilot suggest that over time, oat ingestion may reduce the amount of insulin needed to clear a glucose load. However, the study was underpowered to detect significant differences in more sensitive measures of insulin resistance. The causal mechanistic relationship among whole grain oat consumption, blood pressure, and insulin resistance might be best studied using a long-term feeding study design.
Alternate mechanisms, such as attenuation in endothelial function, may have affected blood pressure responses in this study.33 Drugs specific to endothelial cell receptors mediating vasodilation are known to lower blood pressure.34 Moreover, plasma cholesterol reductions are associated with improvements in endothelium-mediated vasodilation.35,36 In addition, preliminary evidence in animals supports a direct relationship between changes in plasma cholesterol concentrations and blood pressure.37 In the present study, plasma cholesterol levels were significantly reduced in participants who ingested whole grain oat-based cereals compared to a more refined grain wheat, corn, and rice control. Thus, it is possible that the blood pressure reduction observed in the subjects consuming oats resulted in part from improved endothelial function due to a drop in plasma cholesterol. Additional research is needed to fully investigate this pathway.
From a practical standpoint, improvements in SBP and DBP such as those observed in this study would be a useful contribution to the clinical management of hypertension. The cereal feeding intervention was well tolerated. Participants were very compliant for the 6-week treatment period. Substantial improvements in blood lipids could serve as an added incentive for patients to maintain long-term compliance with feeding recommendations.18,19 Since treatment of hypertension is a lifelong process for most patients, future studies would need to assess the effectiveness of oat cereals to maintain blood pressure benefits over a longer time. Such studies may need to consider dietary options such as soluble fiber-rich fruits in addition to cereal consumption in efforts to deliver the desired quantity of soluble fiber. Future trials will have to investigate the antihypertensive effect of whole oats in other populations, such as people with diabetes, and to study not only surrogate endpoints such as blood pressure but also patient-oriented outcomes such as mortality and morbidity.
1. He J, Klag M, Whelton P, et al. Oats and buckwheat intakes and cardiovascular disease risk factors in an ethnic minority of China. Am J Clin Nutr 1995;61:366-72.
2. Lichtenstein M, Burr M, Fehily A, Yarnell J. Heart rate, employment status, and prevalent ischemic heart disease confound relation between cereal fibre intake and blood pressure. J Epidemiol Community Health 1986;40:330-3.
3. Ascherio A, Rimm E, Giovannucci E, et al. A prospective study of nutritional factors and hypertension among US men. Circulation 1992;86:1475-84.
4. Hallfrisch J, Tobin J, Muller D, Andres R. Fiber intake, age, and other coronary risk factors in men of the Baltimore Longitudinal Study (1959-1975). J Gerontol 1988;43:M64-8.
5. Ascherio A, Hennekens C, Willett W, et al. Prospective study of nutritional factors, blood pressure, and hypertension among US women. Hypertension 1996;27:1065-72.
6. Schlamowitz P, Halberg T, Warnoe O, Wilstrup F, Ryttig K. Treatment of mild to moderate hypertension with dietary fiber. Lancet 1987;2:622-3.
7. Eliasson K, Ryttig K, Hylander B, Rossner S. A dietary fiber supplement in the treatment of mild hypertension. A randomized, double-blind, placebo-controlled trial. J Hypertens 1992;10:195-9.
8. Ryttig K, Tellnes G, Haegh L, Boe E, Fagerthun H. A dietary fiber supplement and weight maintenance after weight reduction: a randomized, double-blind, placebo-controlled long-term trial. Int J Obes 1989;13:165-71.
9. Dodson P, Stephenson J, Dodson L, et al. Randomised blind controlled trial of a high fiber, low fat and low sodium dietary regimen in mild essential hypertension. J Hum Hypertens 1989;3:197-202.
10. Little P, Girling G, Hasler A, Trafford A. A controlled trial of a low sodium, low fat, high fibre diet in treated hypertensive patients: effect on antihypertensive drug requirement in clinical practice. J Hum Hypertens 1991;5:175-81.
11. Rossner S, Andersson I, Ryttig K. Effects of a dietary fiber supplement to a weight reduction program on blood pressure. Acta Med Scand 1988;223:353-7.
12. Sandstrom B, Marckmann P, Bindslev N. An eight-month controlled study of a low-fat high-fiber diet: effects on blood lipids and blood pressure in healthy young subjects. Eur J Clin Nutr 1992;46:95-109.
13. Kestin M, Moss R, Clifton P. Comparative effects of three cereal brans on plasma lipids, blood pressure, and glucose metabolism in mildly hypercholesterolemic men. Am J Clin Nutr 1990;52:661-6.
14. Swain J, Rouse I, Curley C, Sacks F. Comparison of the effects of oat bran and low-fiber wheat on serum lipoprotein levels and blood pressure. N Engl J Med 1990;322:147-52.
15. Sciarrone S, Beilin L, Rouse I, Rogers P. A factorial study of salt restriction and a low-fat/high-fibre diet in hypertensive subjects. J Hypertens 1992;10:287-98.
16. Margetts B, Beilin L, Vandongen R, Armstrong B. A randomized controlled trial of the effect of dietary fiber on blood pressure. Clin Sci 1987;72:343-50.
17. el Zein M, Areas J, Knapka J, et al. Influence of oat bran on sucrose-induced blood pressure elevations in SHR. Life Sci 1990;47:1121-8.
18. Gondal J, MacArthy P, Myers A, Preuss H. Effects of dietary sucrose and fibers on blood pressure in hypertensive rats. Clin Nephrol 1996;45:163-8.
19. Krotkiewski M. Effect of guar gum on the arterial blood pressure. Acta Med Scand 1987;222:43-9.
20. Singh R, Rastogi S, Singh N, Ghosh S, Gupta S, Niaz M. Can guava fruit intake decrease blood pressure and blood lipids? J Hum Hypertens 1993;7:33-8.
21. Weidmann P, de Courten M, Bohlen L. Insulin resistance, hyperinsulinemia and hypertension. J Hypertens 1993;11:S27-38.
22. Tuck M. Obesity, the sympathetic nervous system, and essential hypertension. Hypertension 1992;19:I67-77.
23. Sowers J. Insulin resistance, hyperinsulinemia, dyslipidemia, hypertension, and accelerated atherosclerosis. J Clin Pharmacol 1992;32:529-35.
24. Braaten J, Wood P, Scott F, Riedel K, Poste L, Collins M. Oat gum lowers glucose and insulin after an oral glucose load. Am J Clin Nutr 1991;53:1425-30.
25. Braaten J, Scott F, Wood P, et al. High ß-glucan oat bran and oat gum reduce postprandial blood glucose and insulin in subjects with and without type 2 diabetes. Diabet Med 1994;11:312-8.
26. Hallfrisch J, Scholfield D, Behall K. Diets containing soluble oat extracts improve glucose and insulin responses of moderately hypercholesterolemic men and women. Am J Clin Nutr 1995;61:379-84.
27. Fukagawa N, Anderson J, Hageman G, Young V, Minaker K. High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults. Am J Clin Nutr 1990;52:524-8.
28. Welch S, Gebhart S, Bergman R, Phillips L. Minimal model analysis of IVGTT-derived insulin sensitivity in diabetic subjects. J Clin Endocrinol Metab 1990;71:1508-18.
29. Bergman R, Ider Y, Bowden C, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol 1979;236:E667-77.
30. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial on the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24.
31. Appel LJ. The role of diet in the prevention and treatment of hypertension. Curr Atheroscler Rep 2000;2:521-8.
32. Song YJ, Sawamura M, Ikeda K, Igawa S, Yamori Y. Soluble dietary fiber improves insulin sensitivity by increasing muscle GLUT-4 content in stroke-prone spontaneously hypertensive rats. Clin Exp Pharm Physiol 2000;27:41-5.
33. Taddei S, Salvetti A. Pathogenic factors in hypertension. Endothelial Factors. Clin Exp Hypertens 1996;18:323-35.
34. Krum H, Viskoper R, Lacourciere Y, Budde B, Charlon V. The effect of an endothelium-receptor antagonist, Bosentan, on blood pressure in patients with essential hypertension. N Engl J Med 1998;338:784-90.
35. Anderson T, Meredith I, Yeung A. The effect of cholesterol-lowering and antioxidant therapy on endothelium-dependent coronary vasomotion. N Engl J Med 1995;332:488-93.
36. Vogel R, Corretti M, Plotnick G. Changes in flow-mediated brachial artery vasoactivity with lowering of desirable cholesterol levels in healthy middle-aged men. Am J Cardiol 1996;77:37-40.
37. Crago M, West S, Hoeprich K, Michaelis K, McKenzie J. Effects of hyperlipidemia on blood pressure and coronary blood flow in swine. FASEB J 1998;12:A238.-
To submit a letter to the editor on this topic, click here: [email protected].
1. He J, Klag M, Whelton P, et al. Oats and buckwheat intakes and cardiovascular disease risk factors in an ethnic minority of China. Am J Clin Nutr 1995;61:366-72.
2. Lichtenstein M, Burr M, Fehily A, Yarnell J. Heart rate, employment status, and prevalent ischemic heart disease confound relation between cereal fibre intake and blood pressure. J Epidemiol Community Health 1986;40:330-3.
3. Ascherio A, Rimm E, Giovannucci E, et al. A prospective study of nutritional factors and hypertension among US men. Circulation 1992;86:1475-84.
4. Hallfrisch J, Tobin J, Muller D, Andres R. Fiber intake, age, and other coronary risk factors in men of the Baltimore Longitudinal Study (1959-1975). J Gerontol 1988;43:M64-8.
5. Ascherio A, Hennekens C, Willett W, et al. Prospective study of nutritional factors, blood pressure, and hypertension among US women. Hypertension 1996;27:1065-72.
6. Schlamowitz P, Halberg T, Warnoe O, Wilstrup F, Ryttig K. Treatment of mild to moderate hypertension with dietary fiber. Lancet 1987;2:622-3.
7. Eliasson K, Ryttig K, Hylander B, Rossner S. A dietary fiber supplement in the treatment of mild hypertension. A randomized, double-blind, placebo-controlled trial. J Hypertens 1992;10:195-9.
8. Ryttig K, Tellnes G, Haegh L, Boe E, Fagerthun H. A dietary fiber supplement and weight maintenance after weight reduction: a randomized, double-blind, placebo-controlled long-term trial. Int J Obes 1989;13:165-71.
9. Dodson P, Stephenson J, Dodson L, et al. Randomised blind controlled trial of a high fiber, low fat and low sodium dietary regimen in mild essential hypertension. J Hum Hypertens 1989;3:197-202.
10. Little P, Girling G, Hasler A, Trafford A. A controlled trial of a low sodium, low fat, high fibre diet in treated hypertensive patients: effect on antihypertensive drug requirement in clinical practice. J Hum Hypertens 1991;5:175-81.
11. Rossner S, Andersson I, Ryttig K. Effects of a dietary fiber supplement to a weight reduction program on blood pressure. Acta Med Scand 1988;223:353-7.
12. Sandstrom B, Marckmann P, Bindslev N. An eight-month controlled study of a low-fat high-fiber diet: effects on blood lipids and blood pressure in healthy young subjects. Eur J Clin Nutr 1992;46:95-109.
13. Kestin M, Moss R, Clifton P. Comparative effects of three cereal brans on plasma lipids, blood pressure, and glucose metabolism in mildly hypercholesterolemic men. Am J Clin Nutr 1990;52:661-6.
14. Swain J, Rouse I, Curley C, Sacks F. Comparison of the effects of oat bran and low-fiber wheat on serum lipoprotein levels and blood pressure. N Engl J Med 1990;322:147-52.
15. Sciarrone S, Beilin L, Rouse I, Rogers P. A factorial study of salt restriction and a low-fat/high-fibre diet in hypertensive subjects. J Hypertens 1992;10:287-98.
16. Margetts B, Beilin L, Vandongen R, Armstrong B. A randomized controlled trial of the effect of dietary fiber on blood pressure. Clin Sci 1987;72:343-50.
17. el Zein M, Areas J, Knapka J, et al. Influence of oat bran on sucrose-induced blood pressure elevations in SHR. Life Sci 1990;47:1121-8.
18. Gondal J, MacArthy P, Myers A, Preuss H. Effects of dietary sucrose and fibers on blood pressure in hypertensive rats. Clin Nephrol 1996;45:163-8.
19. Krotkiewski M. Effect of guar gum on the arterial blood pressure. Acta Med Scand 1987;222:43-9.
20. Singh R, Rastogi S, Singh N, Ghosh S, Gupta S, Niaz M. Can guava fruit intake decrease blood pressure and blood lipids? J Hum Hypertens 1993;7:33-8.
21. Weidmann P, de Courten M, Bohlen L. Insulin resistance, hyperinsulinemia and hypertension. J Hypertens 1993;11:S27-38.
22. Tuck M. Obesity, the sympathetic nervous system, and essential hypertension. Hypertension 1992;19:I67-77.
23. Sowers J. Insulin resistance, hyperinsulinemia, dyslipidemia, hypertension, and accelerated atherosclerosis. J Clin Pharmacol 1992;32:529-35.
24. Braaten J, Wood P, Scott F, Riedel K, Poste L, Collins M. Oat gum lowers glucose and insulin after an oral glucose load. Am J Clin Nutr 1991;53:1425-30.
25. Braaten J, Scott F, Wood P, et al. High ß-glucan oat bran and oat gum reduce postprandial blood glucose and insulin in subjects with and without type 2 diabetes. Diabet Med 1994;11:312-8.
26. Hallfrisch J, Scholfield D, Behall K. Diets containing soluble oat extracts improve glucose and insulin responses of moderately hypercholesterolemic men and women. Am J Clin Nutr 1995;61:379-84.
27. Fukagawa N, Anderson J, Hageman G, Young V, Minaker K. High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults. Am J Clin Nutr 1990;52:524-8.
28. Welch S, Gebhart S, Bergman R, Phillips L. Minimal model analysis of IVGTT-derived insulin sensitivity in diabetic subjects. J Clin Endocrinol Metab 1990;71:1508-18.
29. Bergman R, Ider Y, Bowden C, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol 1979;236:E667-77.
30. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial on the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24.
31. Appel LJ. The role of diet in the prevention and treatment of hypertension. Curr Atheroscler Rep 2000;2:521-8.
32. Song YJ, Sawamura M, Ikeda K, Igawa S, Yamori Y. Soluble dietary fiber improves insulin sensitivity by increasing muscle GLUT-4 content in stroke-prone spontaneously hypertensive rats. Clin Exp Pharm Physiol 2000;27:41-5.
33. Taddei S, Salvetti A. Pathogenic factors in hypertension. Endothelial Factors. Clin Exp Hypertens 1996;18:323-35.
34. Krum H, Viskoper R, Lacourciere Y, Budde B, Charlon V. The effect of an endothelium-receptor antagonist, Bosentan, on blood pressure in patients with essential hypertension. N Engl J Med 1998;338:784-90.
35. Anderson T, Meredith I, Yeung A. The effect of cholesterol-lowering and antioxidant therapy on endothelium-dependent coronary vasomotion. N Engl J Med 1995;332:488-93.
36. Vogel R, Corretti M, Plotnick G. Changes in flow-mediated brachial artery vasoactivity with lowering of desirable cholesterol levels in healthy middle-aged men. Am J Cardiol 1996;77:37-40.
37. Crago M, West S, Hoeprich K, Michaelis K, McKenzie J. Effects of hyperlipidemia on blood pressure and coronary blood flow in swine. FASEB J 1998;12:A238.-
To submit a letter to the editor on this topic, click here: [email protected].
Involvement of Family and Community Medicine Professionals in Community Projects
OBJECTIVES: Medical schools are being challenged to continue their excellence in education, research, and patient care while responding to the health needs of the public. The objective of our study was to determine the nature and type of community involvement of professionals in departments of family and community medicine.
STUDY DESIGN: We mailed a 24-item structured survey to a random national sample of family medicine professionals.
POPULATION: Survey recipients included 770 full-time physician and nonphysician active members of the Society of Teachers of Family Medicine.
OUTCOMES MEASURED: Our survey assessed community activities, challenges and incentives to those activities, and desired resources for working in the community.
RESULTS: A total of 446 usable surveys were returned (58% response rate). Ninety-five percent of respondents had participated in a community activity within the previous year. More male respondents precepted medical students or residents and educated faculty on topics regarding community education; more older respondents participated by sitting on community health boards or councils. Insufficient release time and lack of funding were the 2 most frequently cited barriers to community-based activities.
CONCLUSIONS: Most faculty are involved in community-related teaching and service. Reasons for low levels of research and subgroup differences, especially among women and young faculty, merit further research.
For more than 50 years academic medicine has held a privileged position in American society. Medical schools receive significant state and federal support from a variety of sources, including the National Institutes of Health, Public Health Services programs specifically developed to support medical education, the National Science Foundation, Medicare, and Medicaid.1-4 In return, academic medical centers have provided training to medical students and residents and have made significant contributions to medical research and clinical care.1,3 Recently, however, concern has been voiced about whether academic health centers have fulfilled important components of their tacit social contract with the American public, caused in part by changes in medical education financing, trends toward a competition model of health care delivery, and the erosion of trust between health care providers and patients.1,3,5-8
Foreman9 suggested changes to medical school education that would help academic health centers fulfill their reciprocal social obligation to improve the public’s health. His recommendations included integrating behavioral and population-based sciences, providing students with learning experiences in community settings where they have the opportunity to work with committed mentors, and developing a critical mass of community-based faculty who are dedicated to addressing the various needs of underserved communities and providing them with the necessary support to continue their community-based efforts. Some academic health centers, including the University of New Mexico School of Medicine, The Johns Hopkins University School of Medicine, the University of Washington School of Medicine, and the Medical College of Pennsylvania/Hahnemann School of Medicine in Philadelphia have begun to implement some of Foreman’s suggestions to strengthen social responsiveness.3,10-12
Within academic medical centers, departments of family medicine have pioneered placing medical students in community-based settings. Of the 124 medical schools that participated in the annual Liaison Committee on Medical Education survey in 1996, 69% of family practice clerkships had a community-based placement, compared with 40% for internal medicine and 25% for pediatric clerkships.13
Family practice residency programs have also striven to respond to the needs of their surrounding communities. In 1999 the Strategic Planning Working Group of the Academic Family Medicine Organization and the Association of Family Practice Residency Directors developed the following list of competencies for family practice residents to acquire during training: (1) family practice residents should understand Community-Oriented Primary Care (COPC) and the practice of population-based medicine; (2) family practice residencies should model COPC or population-based interventions within their practices; and (3) family practice graduates should be capable of recognizing community health needs, developing interventions, and assessing the outcomes.14 Several family practice residency programs, such as the one at Montefiore Medical Center in New York City have worked to address their communities’ concerns by implementing COPC.15
Less information is available on the involvement in community activities of individual family medicine professionals, which include faculty medical doctors (MDs), nonfaculty MDs, doctors of philosophy (PhDs), and master’s degree-prepared department members. The objective of our study was to determine the nature and type of community involvement of professionals in departments of family medicine. We also assessed community activities, challenges and incentives to those activities, and desired resources for working in the community. Insights into these topics increase our understanding of how personnel in academic health centers are attempting to meet the challenge of responding to the health care needs of their surrounding communities while they maintain a commitment to the traditional missions of education, research, and clinical service.
Methods
A pilot survey was sent to 25 members of the Society of Teachers of Family Medicine (STFM). Minor revisions were made according to respondents’ feedback, resulting in a 24-item, structured survey that we mailed to a national random sample of physician and nonphysician active members of STFM (N = 770). The first section of the questionnaire asked respondents a series of demographic and descriptive questions, including participants’ age, sex, ethnicity, professional effort (full or part time), length of time in their current department, and the year they completed residency or a doctoral degree. Additional information was collected on a variety of topics, including type of community-based involvement, reasons for that involvement, challenges to community-based involvement, and support or resources desired from their departments. A list of community-based activities was provided on the questionnaire, as was one write-in option Table 1. Although all activities were community-oriented, not all activities were conducted in the community.
Surveys were distributed in 2 mailings over a 6-month period with the second mailing going only to nonrespondents. Descriptive statistics consisting of percentages for categorical variables and medians for continuous, non-normally distributed variables were calculated. Univariate analyses were accomplished with the chi-square test or, in the case of non-normally distributed variables (age, years in the department, percentage of professional time spent on community-based activities), with the nonparametric Wilcoxon rank sum test.
Multiple logistic regression was used to examine the relationship between binary outcome variables and multiple explanatory variables. The logistic regression outcomes we considered were the individual types of community involvement, barriers to community involvement, and support desired. The candidate explanatory variables were chosen a priori: age, sex, degree (4 categories: master’s degree [reference group], MD degree, PhD degree, and both MD and PhD degrees), and years in department. Following the structure of the survey, analyses of barriers and desired support were restricted to those who had some type of community-based involvement in the previous year. A backward selection stepwise technique was used to build the models. Explanatory variable effects are shown as odds ratios (ORs) with 95% confidence intervals (CIs). For all analyses we used the Stata 6.0 statistical software package.16
Results
A total of 446 usable surveys were returned (58% response rate). Of these, 3 were blank and therefore unusable. Demographic characteristics indicated that respondents were representative of active STFM membership and national family medicine department faculty as reported by the Association of American Medical Colleges17Table 2.
Ninety-five percent of respondents had participated in a community-based project within the previous 12 months. Projects represented a continuum of involvement with community members. Nevertheless, much of the community-based activity was traditional in nature and included precepting medical students and residents in the community, providing clinical services at community-based sites, and conducting educational presentations in the community Table 1. When we considered only activities actually taking place within the community and excluded education about the community that took place elsewhere (the second, third, and fourth items under the heading “Any Education” in Table 1), 92% of respondents had been involved in a community-based project in the previous 12 months.
Faculty participated in community projects for several reasons, the most prevalent being personal interest or satisfaction (77%). Respondents identified insufficient time as the biggest barrier to involvement in community-based activities and noted sufficient release time as the most important form of support or resources they desired from their departments Table 3. Respondents’ academic institutions were most likely to serve urban communities (60%), followed by suburban (33%), small town (20%), and rural (16%) communities.
The association between types of community involvement and respondents’ sex, age, and professional degree was examined with logistic regression analysis. Even when controlling for degree, more men than women reported educating faculty on topics regarding community-based education and how to precept medical students or residents in community sites (OR = 2.01; 95% CI, 1.20 - 3.37; P = .008) and providing clinical care at community-based sites (OR = 1.73; 95% CI, 1.14 - 2.61; P = .009). The longer a respondent had been a member of a department, the more likely he or she was to report having served as a board, committee, or council member of a community health organization, even after controlling for age (for each 5-year interval spent in their department: OR = 1.23; 95% CI, 1.03 - 1.47; P = .023). Not surprisingly, MDs were 5.27 times more likely to report that they had precepted medical students or residents at community-based sites (95% CI, 1.29 - 21.46; P = .02) and provided medical care at community-based sites (OR = 5.35; 95% CI, 1.08 - 26.47; P = .04) than non-MD respondents. MD and PhD respondents, however, were less likely than those without such degrees to work with community members to develop and implement a research project to meet a community-identified health concern (PhDs: OR = 0.17; 95% CI, 0.04-0.84; P = .03; MDs: OR = 0.28; 95% CI, 0.07-1.09; P = .07).
We also analyzed the type of community served to determine its effect on participation in community activities. Institutions serving rural communities were more likely to have designed a community health curriculum (51% vs 36%; P = .023 by Fisher’s exact test) and to have evaluated a community-based project or program (32% vs 18%; P = .010 by Fisher’s exact test). Those serving a small town were also more likely to have evaluated a community-based project or program (30% versus 18%; P = .026 by Fisher’s exact test). Those serving urban communities were more likely to have taught students to work in a community site (58% vs 48%; P = .052 by Fisher’s exact test), to have designed a community health curriculum (43% vs 31%; P = .010 by Fisher’s exact test), and to have educated faculty on community-based education (27% vs 17%; P = .021 by Fisher’s exact test). Neither community served nor community activity, however, is mutually exclusive.
Some of the barriers to community-based activities and desired support for such work were also associated with respondents’ sex, age, and number of years in the current department. Women were 2.41 times more likely than men to report a lack of technical assistance as a barrier to community-based projects (95% CI, 1.41-4.13; P = .001). However, women were only 1.56 times (95% CI, 0.99-2.46; P = .054) more likely than men to desire technical support from their department. Men were 1.57 times (95% CI, 0.99-2.48; P = .054) more likely than women to desire help in forming relationships with the community. Increased age was associated with a decreased desire for sufficient release or protected time for community-based work. For each decade increase in age, there was a 28% reduction in the perceived need for sufficient release or protected time (OR = 0.72; 95% CI, 0.55-0.95; P = .02). Similarly, respondents who had been in their departments longer were less likely to report a need for faculty development regarding community-based activities (OR = 0.95 for each year [a 5% reduction for each additional year]; 95% CI, 0.91-0.99; P = .009).
Discussion
Advocates of community health have challenged academic institutions to more and better involvement in teaching and researching community health and providing service in the community. However, there are almost no data describing the status quo. Our study of 446 health providers who demographically mirror current STFM members and family medicine department faculty establishes a baseline of current activities. The findings support some of our beliefs, call others into question, and raise a number of specific areas for further study.
First, our results indicate that significant numbers of family medicine personnel are participating in a variety of community-based activities. Ninety-five percent of those responding reported having participated in a community education, service, or research project in the past year; 92% performed those activities in the community itself. The activities included precepting medical students and residents, providing clinical services at community-based sites, and making educational presentations in the community. Although this finding does not obviate the need for more and better services, it does suggest that faculty are fulfilling their responsibilities in this area. Less than half of our respondents participated in research, however, a finding that merits further investigation.
Second, this group of physicians and other family and community medicine personnel reported personal interest and satisfaction as the primary motivation (77%)for participating in community projects. This finding supports attempts to motivate community involvement as a personally rewarding experience. Other motivating factors were health of the community and importance to medical student and resident education.
Predictably, the most commonly perceived barrier to community service project participation was a lack of time. More release time was the most desired form of department support for surmounting that barrier. However, we found no data about release time and service. Bland and Schmitz18 have suggested that dedicating 40% of effort to research is necessary for adequate research productivity. If community service is a mission of a medical school, it seems that protecting time for community service projects would also be necessary. Further research is needed to ascertain whether schools offer faculty protected time for community service and, if so, how much is necessary or optimal.
Participation patterns, perceived barriers, and desired resources varied by age, sex, educational background, and academic rank. These factors are often interrelated and individual effects are difficult to segregate. Greater experience and time with an organization may be associated with higher status (rank), which in turn may lead to greater access to monetary and other resources, more protected time, and greater ability to allocate one’s own time. There are still more male family physicians than female, and more men have higher faculty rank. These factors may affect our findings that men were significantly more often involved in teaching other faculty about community-based education and providing care at a community or school clinic.
Among respondents who desired technical assistance, women were nearly twice as likely as men to report lack of technical assistance as a barrier (61% versus 34%) but desired technical assistance only slightly more often than men. Men reported desiring help in forming relationships with community members more often than women did; the difference approached, but did not achieve, significance. The findings are intriguing, but speculation about their implications would be based on stereotypes. Certainly further investigation is desirable.
Controlling for age, the longer the respondents had been members of their departments, the more often they participated on community health boards, committees, and organizations. Respondents who have been in their departments longer may be better established in their careers and in the community, resulting in more frequent invitations to these activities. Other explanations could include changes accompanying life stages, such as concern for assisting younger generations.
Length of employment in a particular department correlated with less reported need for faculty development around community-based activities. Since we did not attempt to ascertain respondents’ levels of expertise, we cannot interpret this finding. However, it cannot be assumed that long experience and lack of reported need necessarily reflect a high skill level.
Older respondents were less likely to desire release or supported time for their community activities. The perceived need for more time diminished by 28% with each decade of life. It may be that they have already garnered sufficient support and protected time in their institutions.
That MDs were significantly more likely than non-MDs to have precepted students and residents at community sites reflects the requirements of medical education accrediting bodies. The reason for the prevalence of research by respondents with master’s degrees and not those with terminal degrees is not known, although we surmise that at least some may have been hired specifically to conduct research. More study of the role of this small subset of respondents is warranted.
We did not examine differences in practice environments and their effect on community-based activities. University-, military-, and community-based practices have different goals, incentives, and disincentives, as do managed care and fee-for-service organizations. Furthermore, the traditional patterns of these organizations may be changing in response to interest in performance measures.19 This is another important area for investigation.
Limitations
This is a descriptive, not a definitive, study. The 58% response rate to the survey may limit the generalizability of our findings. Individuals who are involved or interested in community projects may have been more likely to return the survey, resulting in an overestimation of involvement in community-based activities. Although we do not have demographic or community involvement information about nonrespondents, our sample is demographically similar to active STFM membership and national family medicine department faculty. We provided examples of community-based activities; however, individual interpretations of what constitutes such an activity may differ. Using exploratory analyses increased the likelihood that a significant result would occur by chance. Thus, marginally significant results require further study, and those with P values between .01 and .05 should be considered hypothesis generating.
Conclusions
This descriptive study helps establish a baseline for better understanding academic physicians’ current participation in community-based activities. Although the scope of this study is narrow, it suggests that most academic faculty are providing community service and education and are deriving satisfaction from doing so.
Our results also raise a number of questions for further study. Is there enough appropriate research being done within communities to address its health needs? Should women and younger faculty receive additional support in establishing community-based activities, and if so, what kind? If women perceive technical barriers more often, why do they not report a desire for technical assistance more often? Is the difference between men and women in ease of forming community partnerships meaningful? The answers to these questions will provide a richer understanding of the ability of an academic health center to respond to the health care needs of their surrounding communities.
1. Colloton JW. Academic medicine’s changing covenant with society. Acad Med 1989;64:55-60.
2. Peabody JW. Measuring the social responsiveness of medical schools: setting the standards. Acad Med 1999;74:S59-68.
3. Schroeder SA, Zone JS, Showstack JA. Academic medicine as a public trust. JAMA 1989;262:803-12.
4. McCurdy L, Goode LD, Inui TS, et al. Fulfilling the social contract between medical schools and the public. Acad Med 1997;72:1063-70.
5. Pellegrino ED. Academic health centers and society: an ethical reflection. Acad Med 1999;74:S21-6.
6. Cohen JJ. Missions of a medical school: a North American perspective. Acad Med 1999;74:S27-30.
7. White KL, Connelly JE. The medical school’s mission and the population’s health. Ann Intern Med 1991;115:968-72.
8. Blumenthal D, Campbell EG, Weissman JS. The social missions of academic health centers. N Engl J Med 1997;337:1550-3.
9. Foreman S. Social responsibility and the academic medical center: building community-based systems for the nation’s health. Acad Med 1994;69:97-102.
10. Kaufman A. Measuring social responsiveness of medical schools: a case study from New Mexico. Acad Med 1999;74:S69-74.
11. Rubenstein HL, Franklin ED, Zarro VJ. Opportunities and challenges in educating community-responsive physicians. Am J Prev Med 1997;13:104-8.
12. Showstack J, Fein O, Ford D, et al. Health of the public: the academic response. JAMA 1992;275:2497-502.
13. Seifer SD. Recent and emerging trends in undergraduate medical education: curricular responses to a rapidly changing health care system. West J Med 1998;168:400-11.
14. Longlett SK. Community-oriented primary care: historical perspective. J Am Board Fam Pract 2001;14:54-63.
15. Strelnick AH. Integrating community oriented primary care into training and practice: a view from the Bronx. Fam Med 1986;18:205-9.
16. StataCorp 1999. Stata Statistical Software: Release 6.0 College Station, Tex: Stat Corporation.
17. Robinson L. ed. AAMC data book: statistical information related to medical schools and teaching hospitals. Washington, DC: Association of American Medical Colleges; 2000.
18. Bland CJ, Schmitz CC. Characteristics of the successful researcher and implications for faculty development. J Med Ed 1986;61:22-31.
19. Rhyne R. Bogue R. Kukulka G. Fulmer H. eds. Community-oriented primary care: health care for the 21st century. Washington, DC: American Public Health Association; 1998.
To submit a letter to the editor on this topic, click here: [email protected].
OBJECTIVES: Medical schools are being challenged to continue their excellence in education, research, and patient care while responding to the health needs of the public. The objective of our study was to determine the nature and type of community involvement of professionals in departments of family and community medicine.
STUDY DESIGN: We mailed a 24-item structured survey to a random national sample of family medicine professionals.
POPULATION: Survey recipients included 770 full-time physician and nonphysician active members of the Society of Teachers of Family Medicine.
OUTCOMES MEASURED: Our survey assessed community activities, challenges and incentives to those activities, and desired resources for working in the community.
RESULTS: A total of 446 usable surveys were returned (58% response rate). Ninety-five percent of respondents had participated in a community activity within the previous year. More male respondents precepted medical students or residents and educated faculty on topics regarding community education; more older respondents participated by sitting on community health boards or councils. Insufficient release time and lack of funding were the 2 most frequently cited barriers to community-based activities.
CONCLUSIONS: Most faculty are involved in community-related teaching and service. Reasons for low levels of research and subgroup differences, especially among women and young faculty, merit further research.
For more than 50 years academic medicine has held a privileged position in American society. Medical schools receive significant state and federal support from a variety of sources, including the National Institutes of Health, Public Health Services programs specifically developed to support medical education, the National Science Foundation, Medicare, and Medicaid.1-4 In return, academic medical centers have provided training to medical students and residents and have made significant contributions to medical research and clinical care.1,3 Recently, however, concern has been voiced about whether academic health centers have fulfilled important components of their tacit social contract with the American public, caused in part by changes in medical education financing, trends toward a competition model of health care delivery, and the erosion of trust between health care providers and patients.1,3,5-8
Foreman9 suggested changes to medical school education that would help academic health centers fulfill their reciprocal social obligation to improve the public’s health. His recommendations included integrating behavioral and population-based sciences, providing students with learning experiences in community settings where they have the opportunity to work with committed mentors, and developing a critical mass of community-based faculty who are dedicated to addressing the various needs of underserved communities and providing them with the necessary support to continue their community-based efforts. Some academic health centers, including the University of New Mexico School of Medicine, The Johns Hopkins University School of Medicine, the University of Washington School of Medicine, and the Medical College of Pennsylvania/Hahnemann School of Medicine in Philadelphia have begun to implement some of Foreman’s suggestions to strengthen social responsiveness.3,10-12
Within academic medical centers, departments of family medicine have pioneered placing medical students in community-based settings. Of the 124 medical schools that participated in the annual Liaison Committee on Medical Education survey in 1996, 69% of family practice clerkships had a community-based placement, compared with 40% for internal medicine and 25% for pediatric clerkships.13
Family practice residency programs have also striven to respond to the needs of their surrounding communities. In 1999 the Strategic Planning Working Group of the Academic Family Medicine Organization and the Association of Family Practice Residency Directors developed the following list of competencies for family practice residents to acquire during training: (1) family practice residents should understand Community-Oriented Primary Care (COPC) and the practice of population-based medicine; (2) family practice residencies should model COPC or population-based interventions within their practices; and (3) family practice graduates should be capable of recognizing community health needs, developing interventions, and assessing the outcomes.14 Several family practice residency programs, such as the one at Montefiore Medical Center in New York City have worked to address their communities’ concerns by implementing COPC.15
Less information is available on the involvement in community activities of individual family medicine professionals, which include faculty medical doctors (MDs), nonfaculty MDs, doctors of philosophy (PhDs), and master’s degree-prepared department members. The objective of our study was to determine the nature and type of community involvement of professionals in departments of family medicine. We also assessed community activities, challenges and incentives to those activities, and desired resources for working in the community. Insights into these topics increase our understanding of how personnel in academic health centers are attempting to meet the challenge of responding to the health care needs of their surrounding communities while they maintain a commitment to the traditional missions of education, research, and clinical service.
Methods
A pilot survey was sent to 25 members of the Society of Teachers of Family Medicine (STFM). Minor revisions were made according to respondents’ feedback, resulting in a 24-item, structured survey that we mailed to a national random sample of physician and nonphysician active members of STFM (N = 770). The first section of the questionnaire asked respondents a series of demographic and descriptive questions, including participants’ age, sex, ethnicity, professional effort (full or part time), length of time in their current department, and the year they completed residency or a doctoral degree. Additional information was collected on a variety of topics, including type of community-based involvement, reasons for that involvement, challenges to community-based involvement, and support or resources desired from their departments. A list of community-based activities was provided on the questionnaire, as was one write-in option Table 1. Although all activities were community-oriented, not all activities were conducted in the community.
Surveys were distributed in 2 mailings over a 6-month period with the second mailing going only to nonrespondents. Descriptive statistics consisting of percentages for categorical variables and medians for continuous, non-normally distributed variables were calculated. Univariate analyses were accomplished with the chi-square test or, in the case of non-normally distributed variables (age, years in the department, percentage of professional time spent on community-based activities), with the nonparametric Wilcoxon rank sum test.
Multiple logistic regression was used to examine the relationship between binary outcome variables and multiple explanatory variables. The logistic regression outcomes we considered were the individual types of community involvement, barriers to community involvement, and support desired. The candidate explanatory variables were chosen a priori: age, sex, degree (4 categories: master’s degree [reference group], MD degree, PhD degree, and both MD and PhD degrees), and years in department. Following the structure of the survey, analyses of barriers and desired support were restricted to those who had some type of community-based involvement in the previous year. A backward selection stepwise technique was used to build the models. Explanatory variable effects are shown as odds ratios (ORs) with 95% confidence intervals (CIs). For all analyses we used the Stata 6.0 statistical software package.16
Results
A total of 446 usable surveys were returned (58% response rate). Of these, 3 were blank and therefore unusable. Demographic characteristics indicated that respondents were representative of active STFM membership and national family medicine department faculty as reported by the Association of American Medical Colleges17Table 2.
Ninety-five percent of respondents had participated in a community-based project within the previous 12 months. Projects represented a continuum of involvement with community members. Nevertheless, much of the community-based activity was traditional in nature and included precepting medical students and residents in the community, providing clinical services at community-based sites, and conducting educational presentations in the community Table 1. When we considered only activities actually taking place within the community and excluded education about the community that took place elsewhere (the second, third, and fourth items under the heading “Any Education” in Table 1), 92% of respondents had been involved in a community-based project in the previous 12 months.
Faculty participated in community projects for several reasons, the most prevalent being personal interest or satisfaction (77%). Respondents identified insufficient time as the biggest barrier to involvement in community-based activities and noted sufficient release time as the most important form of support or resources they desired from their departments Table 3. Respondents’ academic institutions were most likely to serve urban communities (60%), followed by suburban (33%), small town (20%), and rural (16%) communities.
The association between types of community involvement and respondents’ sex, age, and professional degree was examined with logistic regression analysis. Even when controlling for degree, more men than women reported educating faculty on topics regarding community-based education and how to precept medical students or residents in community sites (OR = 2.01; 95% CI, 1.20 - 3.37; P = .008) and providing clinical care at community-based sites (OR = 1.73; 95% CI, 1.14 - 2.61; P = .009). The longer a respondent had been a member of a department, the more likely he or she was to report having served as a board, committee, or council member of a community health organization, even after controlling for age (for each 5-year interval spent in their department: OR = 1.23; 95% CI, 1.03 - 1.47; P = .023). Not surprisingly, MDs were 5.27 times more likely to report that they had precepted medical students or residents at community-based sites (95% CI, 1.29 - 21.46; P = .02) and provided medical care at community-based sites (OR = 5.35; 95% CI, 1.08 - 26.47; P = .04) than non-MD respondents. MD and PhD respondents, however, were less likely than those without such degrees to work with community members to develop and implement a research project to meet a community-identified health concern (PhDs: OR = 0.17; 95% CI, 0.04-0.84; P = .03; MDs: OR = 0.28; 95% CI, 0.07-1.09; P = .07).
We also analyzed the type of community served to determine its effect on participation in community activities. Institutions serving rural communities were more likely to have designed a community health curriculum (51% vs 36%; P = .023 by Fisher’s exact test) and to have evaluated a community-based project or program (32% vs 18%; P = .010 by Fisher’s exact test). Those serving a small town were also more likely to have evaluated a community-based project or program (30% versus 18%; P = .026 by Fisher’s exact test). Those serving urban communities were more likely to have taught students to work in a community site (58% vs 48%; P = .052 by Fisher’s exact test), to have designed a community health curriculum (43% vs 31%; P = .010 by Fisher’s exact test), and to have educated faculty on community-based education (27% vs 17%; P = .021 by Fisher’s exact test). Neither community served nor community activity, however, is mutually exclusive.
Some of the barriers to community-based activities and desired support for such work were also associated with respondents’ sex, age, and number of years in the current department. Women were 2.41 times more likely than men to report a lack of technical assistance as a barrier to community-based projects (95% CI, 1.41-4.13; P = .001). However, women were only 1.56 times (95% CI, 0.99-2.46; P = .054) more likely than men to desire technical support from their department. Men were 1.57 times (95% CI, 0.99-2.48; P = .054) more likely than women to desire help in forming relationships with the community. Increased age was associated with a decreased desire for sufficient release or protected time for community-based work. For each decade increase in age, there was a 28% reduction in the perceived need for sufficient release or protected time (OR = 0.72; 95% CI, 0.55-0.95; P = .02). Similarly, respondents who had been in their departments longer were less likely to report a need for faculty development regarding community-based activities (OR = 0.95 for each year [a 5% reduction for each additional year]; 95% CI, 0.91-0.99; P = .009).
Discussion
Advocates of community health have challenged academic institutions to more and better involvement in teaching and researching community health and providing service in the community. However, there are almost no data describing the status quo. Our study of 446 health providers who demographically mirror current STFM members and family medicine department faculty establishes a baseline of current activities. The findings support some of our beliefs, call others into question, and raise a number of specific areas for further study.
First, our results indicate that significant numbers of family medicine personnel are participating in a variety of community-based activities. Ninety-five percent of those responding reported having participated in a community education, service, or research project in the past year; 92% performed those activities in the community itself. The activities included precepting medical students and residents, providing clinical services at community-based sites, and making educational presentations in the community. Although this finding does not obviate the need for more and better services, it does suggest that faculty are fulfilling their responsibilities in this area. Less than half of our respondents participated in research, however, a finding that merits further investigation.
Second, this group of physicians and other family and community medicine personnel reported personal interest and satisfaction as the primary motivation (77%)for participating in community projects. This finding supports attempts to motivate community involvement as a personally rewarding experience. Other motivating factors were health of the community and importance to medical student and resident education.
Predictably, the most commonly perceived barrier to community service project participation was a lack of time. More release time was the most desired form of department support for surmounting that barrier. However, we found no data about release time and service. Bland and Schmitz18 have suggested that dedicating 40% of effort to research is necessary for adequate research productivity. If community service is a mission of a medical school, it seems that protecting time for community service projects would also be necessary. Further research is needed to ascertain whether schools offer faculty protected time for community service and, if so, how much is necessary or optimal.
Participation patterns, perceived barriers, and desired resources varied by age, sex, educational background, and academic rank. These factors are often interrelated and individual effects are difficult to segregate. Greater experience and time with an organization may be associated with higher status (rank), which in turn may lead to greater access to monetary and other resources, more protected time, and greater ability to allocate one’s own time. There are still more male family physicians than female, and more men have higher faculty rank. These factors may affect our findings that men were significantly more often involved in teaching other faculty about community-based education and providing care at a community or school clinic.
Among respondents who desired technical assistance, women were nearly twice as likely as men to report lack of technical assistance as a barrier (61% versus 34%) but desired technical assistance only slightly more often than men. Men reported desiring help in forming relationships with community members more often than women did; the difference approached, but did not achieve, significance. The findings are intriguing, but speculation about their implications would be based on stereotypes. Certainly further investigation is desirable.
Controlling for age, the longer the respondents had been members of their departments, the more often they participated on community health boards, committees, and organizations. Respondents who have been in their departments longer may be better established in their careers and in the community, resulting in more frequent invitations to these activities. Other explanations could include changes accompanying life stages, such as concern for assisting younger generations.
Length of employment in a particular department correlated with less reported need for faculty development around community-based activities. Since we did not attempt to ascertain respondents’ levels of expertise, we cannot interpret this finding. However, it cannot be assumed that long experience and lack of reported need necessarily reflect a high skill level.
Older respondents were less likely to desire release or supported time for their community activities. The perceived need for more time diminished by 28% with each decade of life. It may be that they have already garnered sufficient support and protected time in their institutions.
That MDs were significantly more likely than non-MDs to have precepted students and residents at community sites reflects the requirements of medical education accrediting bodies. The reason for the prevalence of research by respondents with master’s degrees and not those with terminal degrees is not known, although we surmise that at least some may have been hired specifically to conduct research. More study of the role of this small subset of respondents is warranted.
We did not examine differences in practice environments and their effect on community-based activities. University-, military-, and community-based practices have different goals, incentives, and disincentives, as do managed care and fee-for-service organizations. Furthermore, the traditional patterns of these organizations may be changing in response to interest in performance measures.19 This is another important area for investigation.
Limitations
This is a descriptive, not a definitive, study. The 58% response rate to the survey may limit the generalizability of our findings. Individuals who are involved or interested in community projects may have been more likely to return the survey, resulting in an overestimation of involvement in community-based activities. Although we do not have demographic or community involvement information about nonrespondents, our sample is demographically similar to active STFM membership and national family medicine department faculty. We provided examples of community-based activities; however, individual interpretations of what constitutes such an activity may differ. Using exploratory analyses increased the likelihood that a significant result would occur by chance. Thus, marginally significant results require further study, and those with P values between .01 and .05 should be considered hypothesis generating.
Conclusions
This descriptive study helps establish a baseline for better understanding academic physicians’ current participation in community-based activities. Although the scope of this study is narrow, it suggests that most academic faculty are providing community service and education and are deriving satisfaction from doing so.
Our results also raise a number of questions for further study. Is there enough appropriate research being done within communities to address its health needs? Should women and younger faculty receive additional support in establishing community-based activities, and if so, what kind? If women perceive technical barriers more often, why do they not report a desire for technical assistance more often? Is the difference between men and women in ease of forming community partnerships meaningful? The answers to these questions will provide a richer understanding of the ability of an academic health center to respond to the health care needs of their surrounding communities.
OBJECTIVES: Medical schools are being challenged to continue their excellence in education, research, and patient care while responding to the health needs of the public. The objective of our study was to determine the nature and type of community involvement of professionals in departments of family and community medicine.
STUDY DESIGN: We mailed a 24-item structured survey to a random national sample of family medicine professionals.
POPULATION: Survey recipients included 770 full-time physician and nonphysician active members of the Society of Teachers of Family Medicine.
OUTCOMES MEASURED: Our survey assessed community activities, challenges and incentives to those activities, and desired resources for working in the community.
RESULTS: A total of 446 usable surveys were returned (58% response rate). Ninety-five percent of respondents had participated in a community activity within the previous year. More male respondents precepted medical students or residents and educated faculty on topics regarding community education; more older respondents participated by sitting on community health boards or councils. Insufficient release time and lack of funding were the 2 most frequently cited barriers to community-based activities.
CONCLUSIONS: Most faculty are involved in community-related teaching and service. Reasons for low levels of research and subgroup differences, especially among women and young faculty, merit further research.
For more than 50 years academic medicine has held a privileged position in American society. Medical schools receive significant state and federal support from a variety of sources, including the National Institutes of Health, Public Health Services programs specifically developed to support medical education, the National Science Foundation, Medicare, and Medicaid.1-4 In return, academic medical centers have provided training to medical students and residents and have made significant contributions to medical research and clinical care.1,3 Recently, however, concern has been voiced about whether academic health centers have fulfilled important components of their tacit social contract with the American public, caused in part by changes in medical education financing, trends toward a competition model of health care delivery, and the erosion of trust between health care providers and patients.1,3,5-8
Foreman9 suggested changes to medical school education that would help academic health centers fulfill their reciprocal social obligation to improve the public’s health. His recommendations included integrating behavioral and population-based sciences, providing students with learning experiences in community settings where they have the opportunity to work with committed mentors, and developing a critical mass of community-based faculty who are dedicated to addressing the various needs of underserved communities and providing them with the necessary support to continue their community-based efforts. Some academic health centers, including the University of New Mexico School of Medicine, The Johns Hopkins University School of Medicine, the University of Washington School of Medicine, and the Medical College of Pennsylvania/Hahnemann School of Medicine in Philadelphia have begun to implement some of Foreman’s suggestions to strengthen social responsiveness.3,10-12
Within academic medical centers, departments of family medicine have pioneered placing medical students in community-based settings. Of the 124 medical schools that participated in the annual Liaison Committee on Medical Education survey in 1996, 69% of family practice clerkships had a community-based placement, compared with 40% for internal medicine and 25% for pediatric clerkships.13
Family practice residency programs have also striven to respond to the needs of their surrounding communities. In 1999 the Strategic Planning Working Group of the Academic Family Medicine Organization and the Association of Family Practice Residency Directors developed the following list of competencies for family practice residents to acquire during training: (1) family practice residents should understand Community-Oriented Primary Care (COPC) and the practice of population-based medicine; (2) family practice residencies should model COPC or population-based interventions within their practices; and (3) family practice graduates should be capable of recognizing community health needs, developing interventions, and assessing the outcomes.14 Several family practice residency programs, such as the one at Montefiore Medical Center in New York City have worked to address their communities’ concerns by implementing COPC.15
Less information is available on the involvement in community activities of individual family medicine professionals, which include faculty medical doctors (MDs), nonfaculty MDs, doctors of philosophy (PhDs), and master’s degree-prepared department members. The objective of our study was to determine the nature and type of community involvement of professionals in departments of family medicine. We also assessed community activities, challenges and incentives to those activities, and desired resources for working in the community. Insights into these topics increase our understanding of how personnel in academic health centers are attempting to meet the challenge of responding to the health care needs of their surrounding communities while they maintain a commitment to the traditional missions of education, research, and clinical service.
Methods
A pilot survey was sent to 25 members of the Society of Teachers of Family Medicine (STFM). Minor revisions were made according to respondents’ feedback, resulting in a 24-item, structured survey that we mailed to a national random sample of physician and nonphysician active members of STFM (N = 770). The first section of the questionnaire asked respondents a series of demographic and descriptive questions, including participants’ age, sex, ethnicity, professional effort (full or part time), length of time in their current department, and the year they completed residency or a doctoral degree. Additional information was collected on a variety of topics, including type of community-based involvement, reasons for that involvement, challenges to community-based involvement, and support or resources desired from their departments. A list of community-based activities was provided on the questionnaire, as was one write-in option Table 1. Although all activities were community-oriented, not all activities were conducted in the community.
Surveys were distributed in 2 mailings over a 6-month period with the second mailing going only to nonrespondents. Descriptive statistics consisting of percentages for categorical variables and medians for continuous, non-normally distributed variables were calculated. Univariate analyses were accomplished with the chi-square test or, in the case of non-normally distributed variables (age, years in the department, percentage of professional time spent on community-based activities), with the nonparametric Wilcoxon rank sum test.
Multiple logistic regression was used to examine the relationship between binary outcome variables and multiple explanatory variables. The logistic regression outcomes we considered were the individual types of community involvement, barriers to community involvement, and support desired. The candidate explanatory variables were chosen a priori: age, sex, degree (4 categories: master’s degree [reference group], MD degree, PhD degree, and both MD and PhD degrees), and years in department. Following the structure of the survey, analyses of barriers and desired support were restricted to those who had some type of community-based involvement in the previous year. A backward selection stepwise technique was used to build the models. Explanatory variable effects are shown as odds ratios (ORs) with 95% confidence intervals (CIs). For all analyses we used the Stata 6.0 statistical software package.16
Results
A total of 446 usable surveys were returned (58% response rate). Of these, 3 were blank and therefore unusable. Demographic characteristics indicated that respondents were representative of active STFM membership and national family medicine department faculty as reported by the Association of American Medical Colleges17Table 2.
Ninety-five percent of respondents had participated in a community-based project within the previous 12 months. Projects represented a continuum of involvement with community members. Nevertheless, much of the community-based activity was traditional in nature and included precepting medical students and residents in the community, providing clinical services at community-based sites, and conducting educational presentations in the community Table 1. When we considered only activities actually taking place within the community and excluded education about the community that took place elsewhere (the second, third, and fourth items under the heading “Any Education” in Table 1), 92% of respondents had been involved in a community-based project in the previous 12 months.
Faculty participated in community projects for several reasons, the most prevalent being personal interest or satisfaction (77%). Respondents identified insufficient time as the biggest barrier to involvement in community-based activities and noted sufficient release time as the most important form of support or resources they desired from their departments Table 3. Respondents’ academic institutions were most likely to serve urban communities (60%), followed by suburban (33%), small town (20%), and rural (16%) communities.
The association between types of community involvement and respondents’ sex, age, and professional degree was examined with logistic regression analysis. Even when controlling for degree, more men than women reported educating faculty on topics regarding community-based education and how to precept medical students or residents in community sites (OR = 2.01; 95% CI, 1.20 - 3.37; P = .008) and providing clinical care at community-based sites (OR = 1.73; 95% CI, 1.14 - 2.61; P = .009). The longer a respondent had been a member of a department, the more likely he or she was to report having served as a board, committee, or council member of a community health organization, even after controlling for age (for each 5-year interval spent in their department: OR = 1.23; 95% CI, 1.03 - 1.47; P = .023). Not surprisingly, MDs were 5.27 times more likely to report that they had precepted medical students or residents at community-based sites (95% CI, 1.29 - 21.46; P = .02) and provided medical care at community-based sites (OR = 5.35; 95% CI, 1.08 - 26.47; P = .04) than non-MD respondents. MD and PhD respondents, however, were less likely than those without such degrees to work with community members to develop and implement a research project to meet a community-identified health concern (PhDs: OR = 0.17; 95% CI, 0.04-0.84; P = .03; MDs: OR = 0.28; 95% CI, 0.07-1.09; P = .07).
We also analyzed the type of community served to determine its effect on participation in community activities. Institutions serving rural communities were more likely to have designed a community health curriculum (51% vs 36%; P = .023 by Fisher’s exact test) and to have evaluated a community-based project or program (32% vs 18%; P = .010 by Fisher’s exact test). Those serving a small town were also more likely to have evaluated a community-based project or program (30% versus 18%; P = .026 by Fisher’s exact test). Those serving urban communities were more likely to have taught students to work in a community site (58% vs 48%; P = .052 by Fisher’s exact test), to have designed a community health curriculum (43% vs 31%; P = .010 by Fisher’s exact test), and to have educated faculty on community-based education (27% vs 17%; P = .021 by Fisher’s exact test). Neither community served nor community activity, however, is mutually exclusive.
Some of the barriers to community-based activities and desired support for such work were also associated with respondents’ sex, age, and number of years in the current department. Women were 2.41 times more likely than men to report a lack of technical assistance as a barrier to community-based projects (95% CI, 1.41-4.13; P = .001). However, women were only 1.56 times (95% CI, 0.99-2.46; P = .054) more likely than men to desire technical support from their department. Men were 1.57 times (95% CI, 0.99-2.48; P = .054) more likely than women to desire help in forming relationships with the community. Increased age was associated with a decreased desire for sufficient release or protected time for community-based work. For each decade increase in age, there was a 28% reduction in the perceived need for sufficient release or protected time (OR = 0.72; 95% CI, 0.55-0.95; P = .02). Similarly, respondents who had been in their departments longer were less likely to report a need for faculty development regarding community-based activities (OR = 0.95 for each year [a 5% reduction for each additional year]; 95% CI, 0.91-0.99; P = .009).
Discussion
Advocates of community health have challenged academic institutions to more and better involvement in teaching and researching community health and providing service in the community. However, there are almost no data describing the status quo. Our study of 446 health providers who demographically mirror current STFM members and family medicine department faculty establishes a baseline of current activities. The findings support some of our beliefs, call others into question, and raise a number of specific areas for further study.
First, our results indicate that significant numbers of family medicine personnel are participating in a variety of community-based activities. Ninety-five percent of those responding reported having participated in a community education, service, or research project in the past year; 92% performed those activities in the community itself. The activities included precepting medical students and residents, providing clinical services at community-based sites, and making educational presentations in the community. Although this finding does not obviate the need for more and better services, it does suggest that faculty are fulfilling their responsibilities in this area. Less than half of our respondents participated in research, however, a finding that merits further investigation.
Second, this group of physicians and other family and community medicine personnel reported personal interest and satisfaction as the primary motivation (77%)for participating in community projects. This finding supports attempts to motivate community involvement as a personally rewarding experience. Other motivating factors were health of the community and importance to medical student and resident education.
Predictably, the most commonly perceived barrier to community service project participation was a lack of time. More release time was the most desired form of department support for surmounting that barrier. However, we found no data about release time and service. Bland and Schmitz18 have suggested that dedicating 40% of effort to research is necessary for adequate research productivity. If community service is a mission of a medical school, it seems that protecting time for community service projects would also be necessary. Further research is needed to ascertain whether schools offer faculty protected time for community service and, if so, how much is necessary or optimal.
Participation patterns, perceived barriers, and desired resources varied by age, sex, educational background, and academic rank. These factors are often interrelated and individual effects are difficult to segregate. Greater experience and time with an organization may be associated with higher status (rank), which in turn may lead to greater access to monetary and other resources, more protected time, and greater ability to allocate one’s own time. There are still more male family physicians than female, and more men have higher faculty rank. These factors may affect our findings that men were significantly more often involved in teaching other faculty about community-based education and providing care at a community or school clinic.
Among respondents who desired technical assistance, women were nearly twice as likely as men to report lack of technical assistance as a barrier (61% versus 34%) but desired technical assistance only slightly more often than men. Men reported desiring help in forming relationships with community members more often than women did; the difference approached, but did not achieve, significance. The findings are intriguing, but speculation about their implications would be based on stereotypes. Certainly further investigation is desirable.
Controlling for age, the longer the respondents had been members of their departments, the more often they participated on community health boards, committees, and organizations. Respondents who have been in their departments longer may be better established in their careers and in the community, resulting in more frequent invitations to these activities. Other explanations could include changes accompanying life stages, such as concern for assisting younger generations.
Length of employment in a particular department correlated with less reported need for faculty development around community-based activities. Since we did not attempt to ascertain respondents’ levels of expertise, we cannot interpret this finding. However, it cannot be assumed that long experience and lack of reported need necessarily reflect a high skill level.
Older respondents were less likely to desire release or supported time for their community activities. The perceived need for more time diminished by 28% with each decade of life. It may be that they have already garnered sufficient support and protected time in their institutions.
That MDs were significantly more likely than non-MDs to have precepted students and residents at community sites reflects the requirements of medical education accrediting bodies. The reason for the prevalence of research by respondents with master’s degrees and not those with terminal degrees is not known, although we surmise that at least some may have been hired specifically to conduct research. More study of the role of this small subset of respondents is warranted.
We did not examine differences in practice environments and their effect on community-based activities. University-, military-, and community-based practices have different goals, incentives, and disincentives, as do managed care and fee-for-service organizations. Furthermore, the traditional patterns of these organizations may be changing in response to interest in performance measures.19 This is another important area for investigation.
Limitations
This is a descriptive, not a definitive, study. The 58% response rate to the survey may limit the generalizability of our findings. Individuals who are involved or interested in community projects may have been more likely to return the survey, resulting in an overestimation of involvement in community-based activities. Although we do not have demographic or community involvement information about nonrespondents, our sample is demographically similar to active STFM membership and national family medicine department faculty. We provided examples of community-based activities; however, individual interpretations of what constitutes such an activity may differ. Using exploratory analyses increased the likelihood that a significant result would occur by chance. Thus, marginally significant results require further study, and those with P values between .01 and .05 should be considered hypothesis generating.
Conclusions
This descriptive study helps establish a baseline for better understanding academic physicians’ current participation in community-based activities. Although the scope of this study is narrow, it suggests that most academic faculty are providing community service and education and are deriving satisfaction from doing so.
Our results also raise a number of questions for further study. Is there enough appropriate research being done within communities to address its health needs? Should women and younger faculty receive additional support in establishing community-based activities, and if so, what kind? If women perceive technical barriers more often, why do they not report a desire for technical assistance more often? Is the difference between men and women in ease of forming community partnerships meaningful? The answers to these questions will provide a richer understanding of the ability of an academic health center to respond to the health care needs of their surrounding communities.
1. Colloton JW. Academic medicine’s changing covenant with society. Acad Med 1989;64:55-60.
2. Peabody JW. Measuring the social responsiveness of medical schools: setting the standards. Acad Med 1999;74:S59-68.
3. Schroeder SA, Zone JS, Showstack JA. Academic medicine as a public trust. JAMA 1989;262:803-12.
4. McCurdy L, Goode LD, Inui TS, et al. Fulfilling the social contract between medical schools and the public. Acad Med 1997;72:1063-70.
5. Pellegrino ED. Academic health centers and society: an ethical reflection. Acad Med 1999;74:S21-6.
6. Cohen JJ. Missions of a medical school: a North American perspective. Acad Med 1999;74:S27-30.
7. White KL, Connelly JE. The medical school’s mission and the population’s health. Ann Intern Med 1991;115:968-72.
8. Blumenthal D, Campbell EG, Weissman JS. The social missions of academic health centers. N Engl J Med 1997;337:1550-3.
9. Foreman S. Social responsibility and the academic medical center: building community-based systems for the nation’s health. Acad Med 1994;69:97-102.
10. Kaufman A. Measuring social responsiveness of medical schools: a case study from New Mexico. Acad Med 1999;74:S69-74.
11. Rubenstein HL, Franklin ED, Zarro VJ. Opportunities and challenges in educating community-responsive physicians. Am J Prev Med 1997;13:104-8.
12. Showstack J, Fein O, Ford D, et al. Health of the public: the academic response. JAMA 1992;275:2497-502.
13. Seifer SD. Recent and emerging trends in undergraduate medical education: curricular responses to a rapidly changing health care system. West J Med 1998;168:400-11.
14. Longlett SK. Community-oriented primary care: historical perspective. J Am Board Fam Pract 2001;14:54-63.
15. Strelnick AH. Integrating community oriented primary care into training and practice: a view from the Bronx. Fam Med 1986;18:205-9.
16. StataCorp 1999. Stata Statistical Software: Release 6.0 College Station, Tex: Stat Corporation.
17. Robinson L. ed. AAMC data book: statistical information related to medical schools and teaching hospitals. Washington, DC: Association of American Medical Colleges; 2000.
18. Bland CJ, Schmitz CC. Characteristics of the successful researcher and implications for faculty development. J Med Ed 1986;61:22-31.
19. Rhyne R. Bogue R. Kukulka G. Fulmer H. eds. Community-oriented primary care: health care for the 21st century. Washington, DC: American Public Health Association; 1998.
To submit a letter to the editor on this topic, click here: [email protected].
1. Colloton JW. Academic medicine’s changing covenant with society. Acad Med 1989;64:55-60.
2. Peabody JW. Measuring the social responsiveness of medical schools: setting the standards. Acad Med 1999;74:S59-68.
3. Schroeder SA, Zone JS, Showstack JA. Academic medicine as a public trust. JAMA 1989;262:803-12.
4. McCurdy L, Goode LD, Inui TS, et al. Fulfilling the social contract between medical schools and the public. Acad Med 1997;72:1063-70.
5. Pellegrino ED. Academic health centers and society: an ethical reflection. Acad Med 1999;74:S21-6.
6. Cohen JJ. Missions of a medical school: a North American perspective. Acad Med 1999;74:S27-30.
7. White KL, Connelly JE. The medical school’s mission and the population’s health. Ann Intern Med 1991;115:968-72.
8. Blumenthal D, Campbell EG, Weissman JS. The social missions of academic health centers. N Engl J Med 1997;337:1550-3.
9. Foreman S. Social responsibility and the academic medical center: building community-based systems for the nation’s health. Acad Med 1994;69:97-102.
10. Kaufman A. Measuring social responsiveness of medical schools: a case study from New Mexico. Acad Med 1999;74:S69-74.
11. Rubenstein HL, Franklin ED, Zarro VJ. Opportunities and challenges in educating community-responsive physicians. Am J Prev Med 1997;13:104-8.
12. Showstack J, Fein O, Ford D, et al. Health of the public: the academic response. JAMA 1992;275:2497-502.
13. Seifer SD. Recent and emerging trends in undergraduate medical education: curricular responses to a rapidly changing health care system. West J Med 1998;168:400-11.
14. Longlett SK. Community-oriented primary care: historical perspective. J Am Board Fam Pract 2001;14:54-63.
15. Strelnick AH. Integrating community oriented primary care into training and practice: a view from the Bronx. Fam Med 1986;18:205-9.
16. StataCorp 1999. Stata Statistical Software: Release 6.0 College Station, Tex: Stat Corporation.
17. Robinson L. ed. AAMC data book: statistical information related to medical schools and teaching hospitals. Washington, DC: Association of American Medical Colleges; 2000.
18. Bland CJ, Schmitz CC. Characteristics of the successful researcher and implications for faculty development. J Med Ed 1986;61:22-31.
19. Rhyne R. Bogue R. Kukulka G. Fulmer H. eds. Community-oriented primary care: health care for the 21st century. Washington, DC: American Public Health Association; 1998.
To submit a letter to the editor on this topic, click here: [email protected].
Weekly Versus Daily Dosing of Atorvastatin
Twenty-four consecutive patients of a single family physician who had achieved NCEP-II goal levels of low-density lipoprotein cholesterol (LDL-C) on a daily atorvastatin dose of 10 mg for at least 6 months were invited to switch to 20 mg weekly. Mean LDL levels for the 22 patients who completed the trial had been reduced by 43% from baseline on 10 mg daily (P < .05) and were reduced by 22% from baseline on the seventh day following the last weekly dose of 20 mg (P < .05). Total cholesterol to high-density lipoprotein cholesterol (TC/HDL-C) ratios were reduced by 31% and 17%, respectively (both P < .05) and triglycerides by 20% and 10% (both P < .05).
Atorvastatin is a potent antihyperlipidemic but is quite expensive, costing up to $700 for a 1-year supply of 10-mg tablets in retail pharmacies. Weekly dosing has the potential to lower costs and increase convenience while maintaining a similar effect on lipids. The active metabolites have a serum half-life of 11 to 57 hours,1-4 acting on a target that responds slowly to intervention. Furthermore, atorvastatin demonstrates prolonged inhibition of HMG-CoA reductase compared with other statins, presumably because of longer residence of the drug or its metabolites in the liver.5 Two abstracts of meeting presentations have reported efficacy for alternate-day dosing on small patient samples,1,2 but no reported attempts have been made to test longer dosing intervals. The purpose of this pilot study was to investigate the effect of weekly dosing of atorvastatin on patients who were currently well controlled on daily doses of the drug.
Methods
Selection of patients
Twenty-four consecutive patients presenting for routine follow-up in a private clinical practice whose LDL-C levels exceeded National Cholesterol Education Program (NCEP-II) guidelines6 on 2 occasions and who had successfully met their goals on 10 mg atorvastatin daily were offered a 12-week trial of 20 mg atorvastatin weekly. All 24 patients gave written informed consent, although one changed his mind and never altered his dosing and another experienced headaches after taking the first 20-mg dose and reverted to a regimen of 10 mg daily.
Study protocol
Study participants were instructed verbally and in writing to make no special efforts to change their lifestyle as a result of their involvement. The potential skewing effect of such efforts on research was explained. If they were already intending to alter their diet or exercise levels, this was acceptable. They were to take atorvastatin at the usual time of day on a day of the week that seemed most convenient. If they forgot a dose, it was to be taken the next day. Compliance with weekly dosing was assessed at each contact by explicit questioning. Fasting chemical and lipid profiles were available on patients’ charts; for purpose of analysis, the last profile before initiation of any statin therapy was used as the pretreatment baseline and the last profile on 10 mg atorvastatin daily as the treatment baseline. Profiles were repeated with the patient fasting on the seventh day after the last 20-mg dose before that dose was repeated.
Statistical analysis
The data were analyzed with repeated measures ANOVA followed by a Student–Newman–Kuels post hoc test to determine differences between specific treatments. Differences with a 2-tailed P value of less than .05 were considered statistically significant.
Results
Baseline characteristics
Table 1 presents the baseline characteristics of participants. The average age was 54 years (range 42 to 72 years). There were 12 men and 10 women. Thirteen subjects had comorbid conditions (9 hypertension, 4 type 2 diabetes, 1 hepatitis C, 2 coronary artery disease, and 2 tobacco use).
TABLE 1
BASELINE CHARACTERISTICS OF STUDY PARTICIPANTS
| Characteristic | Number |
|---|---|
| Male / female | 12 / 10 |
| Comorbidity | |
| Hypertension | 9 |
| Type 2 diabetes mellitus | 4 |
| Hepatitis C | 1 |
| Coronary artery disease | 2 |
| Smoking | 2 |
| Mean age in years (range) | 54 (42–72) |
Cholesterol reduction
Results for LDL-C, HDL-C, triglycerides, TC, TC/HDL-C ratio, and aspartate aminotransferase (AST) are summarized in Table 2. LDL levels fell 43% and 22%, respectively, on daily and weekly dosing; HDL-C levels were essentially unchanged; triglycerides fell 20% and 10%; TC, 33% and 16%; TC/HDL-C, 31% and 17%; and AST, 0% and 21%.
TABLE 2
RESPONSE OF LIPID PARAMETERS TO DAILY AND WEEKLY DOSING WITH ATORVASTATIN
| Pretreatment | 10 mg Daily | 20 mg Weekly | |
|---|---|---|---|
| LDL-C mg/dL | 178 | 101 *† | 138 * |
| HDL-C mg/dL | 46 | 46 | 48 |
| Triglycerides mg/dL | 174 | 139 * | 157 * |
| Total cholesterol mg/dL | 259 | 175 *† | 218 * |
| Total cholesterol/HDL-C ratio | 5.8 | 4.0 *† | 4.8 * |
| AST U/L | 28 | 28 | 22 |
| * P < .05 vs pretreatment. | |||
| † P < .05 vs 20 mg weekly. | |||
| Conversion factors: | |||
| LDL-C, HDL-C, TC: (mg/dL) x (.026) = SI mmol/L | |||
| Triglycerides: (mg/dL) x (.011) = SI mmol/L | |||
| AST denotes aspartate aminotransferase; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SI, Système Internationale. | |||
Adverse reactions
The only reported adverse reaction from doubling the dose of atorvastatin was headache in the patient who dropped out for that reason. No attempt was made to repeat the higher dose to see if this reaction was replicable. No subjects reported myalgias. The mean AST actually dropped on weekly dosing. One patient who had hepatitis C and was in clinical remission experienced a fall in pretreatment AST on daily dosing and a further reduction on weekly dosing.
Discussion
With pharmaceutical costs leading medical inflation, a current challenge for clinicians is to alter the cost-benefit ratio of prescriptions to the advantage of patients. Weekly dosing, as has recently been approved for alendronate sodium (Fosamax) and fluoxetine hydrochloride (Prozac), is one approach to this problem. In this preliminary study, weekly dosing of 20 mg atorvastatin resulted in a 22% reduction of LDL-C, measured on the seventh day after dosing. This regimen represents an approximately 80% reduction in yearly cost compared with that of a regimen of 10 mg daily.
Since this study did not investigate the pattern of LDL-C reduction in the interval between doses, further research is needed to delineate the area under the curve and the impact on clinical outcomes before conclusions may be drawn regarding the effectiveness of weekly dosing.
Acknowledgment
The author wishes to acknowledge the assistance of William Harris, PhD, in editing and statistical analysis.
1. Jafari M, et al. Efficacy of alternate day dosing with atorvastatin. ACCP annual meeting abstracts; 1999.
2. Matalka M, Ravnan M, Deedwania P. Is alternate day dosing of atorvastatin effective in managing patients with hyperlipidemia? JAAC abstracts; February 2001.
3. Cilla DD, Jr, Whitfield LR, Gibson DM, Sedman AJ, Posvar EL. Multiple-dose pharmacokinetics, pharmacodynamics, and safety of atorvastatin, an inhibitor of HMG-CoA reductase, in healthy subjects. Clin Pharmacol Ther 1996;60:687-95.
4. Posvar EL, Radulovic LL, Cilla DD, Jr, Whitfield LR, Sedman AJ. Tolerance and pharmacokinetics of single-dose atorvastatin, a potent inhibitor or HMG-CoA reductase, in healthy subjects. J Clin Pharmacol 1996;36:729-31.
5. Naoumova RP, Dunn S, Rallidis L, et al. Prolonged inhibition of cholesterol synthesis explains the efficacy of atorvastatin. J Lipid Res 1997;38:1496-500.
6. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285:2486-97.
Twenty-four consecutive patients of a single family physician who had achieved NCEP-II goal levels of low-density lipoprotein cholesterol (LDL-C) on a daily atorvastatin dose of 10 mg for at least 6 months were invited to switch to 20 mg weekly. Mean LDL levels for the 22 patients who completed the trial had been reduced by 43% from baseline on 10 mg daily (P < .05) and were reduced by 22% from baseline on the seventh day following the last weekly dose of 20 mg (P < .05). Total cholesterol to high-density lipoprotein cholesterol (TC/HDL-C) ratios were reduced by 31% and 17%, respectively (both P < .05) and triglycerides by 20% and 10% (both P < .05).
Atorvastatin is a potent antihyperlipidemic but is quite expensive, costing up to $700 for a 1-year supply of 10-mg tablets in retail pharmacies. Weekly dosing has the potential to lower costs and increase convenience while maintaining a similar effect on lipids. The active metabolites have a serum half-life of 11 to 57 hours,1-4 acting on a target that responds slowly to intervention. Furthermore, atorvastatin demonstrates prolonged inhibition of HMG-CoA reductase compared with other statins, presumably because of longer residence of the drug or its metabolites in the liver.5 Two abstracts of meeting presentations have reported efficacy for alternate-day dosing on small patient samples,1,2 but no reported attempts have been made to test longer dosing intervals. The purpose of this pilot study was to investigate the effect of weekly dosing of atorvastatin on patients who were currently well controlled on daily doses of the drug.
Methods
Selection of patients
Twenty-four consecutive patients presenting for routine follow-up in a private clinical practice whose LDL-C levels exceeded National Cholesterol Education Program (NCEP-II) guidelines6 on 2 occasions and who had successfully met their goals on 10 mg atorvastatin daily were offered a 12-week trial of 20 mg atorvastatin weekly. All 24 patients gave written informed consent, although one changed his mind and never altered his dosing and another experienced headaches after taking the first 20-mg dose and reverted to a regimen of 10 mg daily.
Study protocol
Study participants were instructed verbally and in writing to make no special efforts to change their lifestyle as a result of their involvement. The potential skewing effect of such efforts on research was explained. If they were already intending to alter their diet or exercise levels, this was acceptable. They were to take atorvastatin at the usual time of day on a day of the week that seemed most convenient. If they forgot a dose, it was to be taken the next day. Compliance with weekly dosing was assessed at each contact by explicit questioning. Fasting chemical and lipid profiles were available on patients’ charts; for purpose of analysis, the last profile before initiation of any statin therapy was used as the pretreatment baseline and the last profile on 10 mg atorvastatin daily as the treatment baseline. Profiles were repeated with the patient fasting on the seventh day after the last 20-mg dose before that dose was repeated.
Statistical analysis
The data were analyzed with repeated measures ANOVA followed by a Student–Newman–Kuels post hoc test to determine differences between specific treatments. Differences with a 2-tailed P value of less than .05 were considered statistically significant.
Results
Baseline characteristics
Table 1 presents the baseline characteristics of participants. The average age was 54 years (range 42 to 72 years). There were 12 men and 10 women. Thirteen subjects had comorbid conditions (9 hypertension, 4 type 2 diabetes, 1 hepatitis C, 2 coronary artery disease, and 2 tobacco use).
TABLE 1
BASELINE CHARACTERISTICS OF STUDY PARTICIPANTS
| Characteristic | Number |
|---|---|
| Male / female | 12 / 10 |
| Comorbidity | |
| Hypertension | 9 |
| Type 2 diabetes mellitus | 4 |
| Hepatitis C | 1 |
| Coronary artery disease | 2 |
| Smoking | 2 |
| Mean age in years (range) | 54 (42–72) |
Cholesterol reduction
Results for LDL-C, HDL-C, triglycerides, TC, TC/HDL-C ratio, and aspartate aminotransferase (AST) are summarized in Table 2. LDL levels fell 43% and 22%, respectively, on daily and weekly dosing; HDL-C levels were essentially unchanged; triglycerides fell 20% and 10%; TC, 33% and 16%; TC/HDL-C, 31% and 17%; and AST, 0% and 21%.
TABLE 2
RESPONSE OF LIPID PARAMETERS TO DAILY AND WEEKLY DOSING WITH ATORVASTATIN
| Pretreatment | 10 mg Daily | 20 mg Weekly | |
|---|---|---|---|
| LDL-C mg/dL | 178 | 101 *† | 138 * |
| HDL-C mg/dL | 46 | 46 | 48 |
| Triglycerides mg/dL | 174 | 139 * | 157 * |
| Total cholesterol mg/dL | 259 | 175 *† | 218 * |
| Total cholesterol/HDL-C ratio | 5.8 | 4.0 *† | 4.8 * |
| AST U/L | 28 | 28 | 22 |
| * P < .05 vs pretreatment. | |||
| † P < .05 vs 20 mg weekly. | |||
| Conversion factors: | |||
| LDL-C, HDL-C, TC: (mg/dL) x (.026) = SI mmol/L | |||
| Triglycerides: (mg/dL) x (.011) = SI mmol/L | |||
| AST denotes aspartate aminotransferase; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SI, Système Internationale. | |||
Adverse reactions
The only reported adverse reaction from doubling the dose of atorvastatin was headache in the patient who dropped out for that reason. No attempt was made to repeat the higher dose to see if this reaction was replicable. No subjects reported myalgias. The mean AST actually dropped on weekly dosing. One patient who had hepatitis C and was in clinical remission experienced a fall in pretreatment AST on daily dosing and a further reduction on weekly dosing.
Discussion
With pharmaceutical costs leading medical inflation, a current challenge for clinicians is to alter the cost-benefit ratio of prescriptions to the advantage of patients. Weekly dosing, as has recently been approved for alendronate sodium (Fosamax) and fluoxetine hydrochloride (Prozac), is one approach to this problem. In this preliminary study, weekly dosing of 20 mg atorvastatin resulted in a 22% reduction of LDL-C, measured on the seventh day after dosing. This regimen represents an approximately 80% reduction in yearly cost compared with that of a regimen of 10 mg daily.
Since this study did not investigate the pattern of LDL-C reduction in the interval between doses, further research is needed to delineate the area under the curve and the impact on clinical outcomes before conclusions may be drawn regarding the effectiveness of weekly dosing.
Acknowledgment
The author wishes to acknowledge the assistance of William Harris, PhD, in editing and statistical analysis.
Twenty-four consecutive patients of a single family physician who had achieved NCEP-II goal levels of low-density lipoprotein cholesterol (LDL-C) on a daily atorvastatin dose of 10 mg for at least 6 months were invited to switch to 20 mg weekly. Mean LDL levels for the 22 patients who completed the trial had been reduced by 43% from baseline on 10 mg daily (P < .05) and were reduced by 22% from baseline on the seventh day following the last weekly dose of 20 mg (P < .05). Total cholesterol to high-density lipoprotein cholesterol (TC/HDL-C) ratios were reduced by 31% and 17%, respectively (both P < .05) and triglycerides by 20% and 10% (both P < .05).
Atorvastatin is a potent antihyperlipidemic but is quite expensive, costing up to $700 for a 1-year supply of 10-mg tablets in retail pharmacies. Weekly dosing has the potential to lower costs and increase convenience while maintaining a similar effect on lipids. The active metabolites have a serum half-life of 11 to 57 hours,1-4 acting on a target that responds slowly to intervention. Furthermore, atorvastatin demonstrates prolonged inhibition of HMG-CoA reductase compared with other statins, presumably because of longer residence of the drug or its metabolites in the liver.5 Two abstracts of meeting presentations have reported efficacy for alternate-day dosing on small patient samples,1,2 but no reported attempts have been made to test longer dosing intervals. The purpose of this pilot study was to investigate the effect of weekly dosing of atorvastatin on patients who were currently well controlled on daily doses of the drug.
Methods
Selection of patients
Twenty-four consecutive patients presenting for routine follow-up in a private clinical practice whose LDL-C levels exceeded National Cholesterol Education Program (NCEP-II) guidelines6 on 2 occasions and who had successfully met their goals on 10 mg atorvastatin daily were offered a 12-week trial of 20 mg atorvastatin weekly. All 24 patients gave written informed consent, although one changed his mind and never altered his dosing and another experienced headaches after taking the first 20-mg dose and reverted to a regimen of 10 mg daily.
Study protocol
Study participants were instructed verbally and in writing to make no special efforts to change their lifestyle as a result of their involvement. The potential skewing effect of such efforts on research was explained. If they were already intending to alter their diet or exercise levels, this was acceptable. They were to take atorvastatin at the usual time of day on a day of the week that seemed most convenient. If they forgot a dose, it was to be taken the next day. Compliance with weekly dosing was assessed at each contact by explicit questioning. Fasting chemical and lipid profiles were available on patients’ charts; for purpose of analysis, the last profile before initiation of any statin therapy was used as the pretreatment baseline and the last profile on 10 mg atorvastatin daily as the treatment baseline. Profiles were repeated with the patient fasting on the seventh day after the last 20-mg dose before that dose was repeated.
Statistical analysis
The data were analyzed with repeated measures ANOVA followed by a Student–Newman–Kuels post hoc test to determine differences between specific treatments. Differences with a 2-tailed P value of less than .05 were considered statistically significant.
Results
Baseline characteristics
Table 1 presents the baseline characteristics of participants. The average age was 54 years (range 42 to 72 years). There were 12 men and 10 women. Thirteen subjects had comorbid conditions (9 hypertension, 4 type 2 diabetes, 1 hepatitis C, 2 coronary artery disease, and 2 tobacco use).
TABLE 1
BASELINE CHARACTERISTICS OF STUDY PARTICIPANTS
| Characteristic | Number |
|---|---|
| Male / female | 12 / 10 |
| Comorbidity | |
| Hypertension | 9 |
| Type 2 diabetes mellitus | 4 |
| Hepatitis C | 1 |
| Coronary artery disease | 2 |
| Smoking | 2 |
| Mean age in years (range) | 54 (42–72) |
Cholesterol reduction
Results for LDL-C, HDL-C, triglycerides, TC, TC/HDL-C ratio, and aspartate aminotransferase (AST) are summarized in Table 2. LDL levels fell 43% and 22%, respectively, on daily and weekly dosing; HDL-C levels were essentially unchanged; triglycerides fell 20% and 10%; TC, 33% and 16%; TC/HDL-C, 31% and 17%; and AST, 0% and 21%.
TABLE 2
RESPONSE OF LIPID PARAMETERS TO DAILY AND WEEKLY DOSING WITH ATORVASTATIN
| Pretreatment | 10 mg Daily | 20 mg Weekly | |
|---|---|---|---|
| LDL-C mg/dL | 178 | 101 *† | 138 * |
| HDL-C mg/dL | 46 | 46 | 48 |
| Triglycerides mg/dL | 174 | 139 * | 157 * |
| Total cholesterol mg/dL | 259 | 175 *† | 218 * |
| Total cholesterol/HDL-C ratio | 5.8 | 4.0 *† | 4.8 * |
| AST U/L | 28 | 28 | 22 |
| * P < .05 vs pretreatment. | |||
| † P < .05 vs 20 mg weekly. | |||
| Conversion factors: | |||
| LDL-C, HDL-C, TC: (mg/dL) x (.026) = SI mmol/L | |||
| Triglycerides: (mg/dL) x (.011) = SI mmol/L | |||
| AST denotes aspartate aminotransferase; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SI, Système Internationale. | |||
Adverse reactions
The only reported adverse reaction from doubling the dose of atorvastatin was headache in the patient who dropped out for that reason. No attempt was made to repeat the higher dose to see if this reaction was replicable. No subjects reported myalgias. The mean AST actually dropped on weekly dosing. One patient who had hepatitis C and was in clinical remission experienced a fall in pretreatment AST on daily dosing and a further reduction on weekly dosing.
Discussion
With pharmaceutical costs leading medical inflation, a current challenge for clinicians is to alter the cost-benefit ratio of prescriptions to the advantage of patients. Weekly dosing, as has recently been approved for alendronate sodium (Fosamax) and fluoxetine hydrochloride (Prozac), is one approach to this problem. In this preliminary study, weekly dosing of 20 mg atorvastatin resulted in a 22% reduction of LDL-C, measured on the seventh day after dosing. This regimen represents an approximately 80% reduction in yearly cost compared with that of a regimen of 10 mg daily.
Since this study did not investigate the pattern of LDL-C reduction in the interval between doses, further research is needed to delineate the area under the curve and the impact on clinical outcomes before conclusions may be drawn regarding the effectiveness of weekly dosing.
Acknowledgment
The author wishes to acknowledge the assistance of William Harris, PhD, in editing and statistical analysis.
1. Jafari M, et al. Efficacy of alternate day dosing with atorvastatin. ACCP annual meeting abstracts; 1999.
2. Matalka M, Ravnan M, Deedwania P. Is alternate day dosing of atorvastatin effective in managing patients with hyperlipidemia? JAAC abstracts; February 2001.
3. Cilla DD, Jr, Whitfield LR, Gibson DM, Sedman AJ, Posvar EL. Multiple-dose pharmacokinetics, pharmacodynamics, and safety of atorvastatin, an inhibitor of HMG-CoA reductase, in healthy subjects. Clin Pharmacol Ther 1996;60:687-95.
4. Posvar EL, Radulovic LL, Cilla DD, Jr, Whitfield LR, Sedman AJ. Tolerance and pharmacokinetics of single-dose atorvastatin, a potent inhibitor or HMG-CoA reductase, in healthy subjects. J Clin Pharmacol 1996;36:729-31.
5. Naoumova RP, Dunn S, Rallidis L, et al. Prolonged inhibition of cholesterol synthesis explains the efficacy of atorvastatin. J Lipid Res 1997;38:1496-500.
6. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285:2486-97.
1. Jafari M, et al. Efficacy of alternate day dosing with atorvastatin. ACCP annual meeting abstracts; 1999.
2. Matalka M, Ravnan M, Deedwania P. Is alternate day dosing of atorvastatin effective in managing patients with hyperlipidemia? JAAC abstracts; February 2001.
3. Cilla DD, Jr, Whitfield LR, Gibson DM, Sedman AJ, Posvar EL. Multiple-dose pharmacokinetics, pharmacodynamics, and safety of atorvastatin, an inhibitor of HMG-CoA reductase, in healthy subjects. Clin Pharmacol Ther 1996;60:687-95.
4. Posvar EL, Radulovic LL, Cilla DD, Jr, Whitfield LR, Sedman AJ. Tolerance and pharmacokinetics of single-dose atorvastatin, a potent inhibitor or HMG-CoA reductase, in healthy subjects. J Clin Pharmacol 1996;36:729-31.
5. Naoumova RP, Dunn S, Rallidis L, et al. Prolonged inhibition of cholesterol synthesis explains the efficacy of atorvastatin. J Lipid Res 1997;38:1496-500.
6. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285:2486-97.