User login
Rectal pressure
Upon examination, the family physician (FP) noted an external hemorrhoid. The patient indicated that she’d had large hemorrhoids during her last pregnancy. Hemorrhoids are cushions of highly vascular structures found within the submucosa of the anal canal. They become pathologic when swollen or inflamed.
There are 3 hemorrhoidal cushions in the anal canal and they have several functions, including maintaining fecal continence by engorging with blood and closing the anal canal and protecting the anal sphincter during defecation. Hemorrhoidal tissue provides important sensory information, enabling the differentiation between solid, liquid, and gas and subsequent decision to evacuate. External hemorrhoids arise distal to the dentate line. They are covered by stratified squamous epithelium and receive somatic sensory innervation from the inferior rectal nerve.
Patients with hemorrhoids should be encouraged to increase dietary fiber and/or add a fiber supplement to reduce severity and duration of symptoms. In this case, the FP encouraged the patient to take in adequate amounts of fluid and increase her dietary fiber. He also prescribed a stool softener because of the patient's history of constipation. Since the hemorrhoid was external, no suppositories were prescribed. Also, the FP did not recommend sitz baths because of a lack of data supporting their use.
Photo and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Hemorrhoids. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:414-418.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Upon examination, the family physician (FP) noted an external hemorrhoid. The patient indicated that she’d had large hemorrhoids during her last pregnancy. Hemorrhoids are cushions of highly vascular structures found within the submucosa of the anal canal. They become pathologic when swollen or inflamed.
There are 3 hemorrhoidal cushions in the anal canal and they have several functions, including maintaining fecal continence by engorging with blood and closing the anal canal and protecting the anal sphincter during defecation. Hemorrhoidal tissue provides important sensory information, enabling the differentiation between solid, liquid, and gas and subsequent decision to evacuate. External hemorrhoids arise distal to the dentate line. They are covered by stratified squamous epithelium and receive somatic sensory innervation from the inferior rectal nerve.
Patients with hemorrhoids should be encouraged to increase dietary fiber and/or add a fiber supplement to reduce severity and duration of symptoms. In this case, the FP encouraged the patient to take in adequate amounts of fluid and increase her dietary fiber. He also prescribed a stool softener because of the patient's history of constipation. Since the hemorrhoid was external, no suppositories were prescribed. Also, the FP did not recommend sitz baths because of a lack of data supporting their use.
Photo and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Hemorrhoids. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:414-418.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Upon examination, the family physician (FP) noted an external hemorrhoid. The patient indicated that she’d had large hemorrhoids during her last pregnancy. Hemorrhoids are cushions of highly vascular structures found within the submucosa of the anal canal. They become pathologic when swollen or inflamed.
There are 3 hemorrhoidal cushions in the anal canal and they have several functions, including maintaining fecal continence by engorging with blood and closing the anal canal and protecting the anal sphincter during defecation. Hemorrhoidal tissue provides important sensory information, enabling the differentiation between solid, liquid, and gas and subsequent decision to evacuate. External hemorrhoids arise distal to the dentate line. They are covered by stratified squamous epithelium and receive somatic sensory innervation from the inferior rectal nerve.
Patients with hemorrhoids should be encouraged to increase dietary fiber and/or add a fiber supplement to reduce severity and duration of symptoms. In this case, the FP encouraged the patient to take in adequate amounts of fluid and increase her dietary fiber. He also prescribed a stool softener because of the patient's history of constipation. Since the hemorrhoid was external, no suppositories were prescribed. Also, the FP did not recommend sitz baths because of a lack of data supporting their use.
Photo and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Hemorrhoids. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:414-418.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Hands with erythematous patches

This patient had erythropoietic protoporphyria (EPP), a metabolic disease caused by a deficiency in ferrochelatase enzyme activity. Approximately 25% of patients develop hepatobiliary disease, which may be the only manifestation of the disease. EPP most commonly occurs in children ages 2 through 5, but diagnosis can be delayed until adulthood if a patient’s symptoms are mild or do not affect the skin.
Photosensitivity with a stinging or burning sensation on sun-exposed areas distinguishes EPP from other porphyrias. With repeated sun exposure, the affected areas can develop a waxy thickening with shallow linear or elliptical scars that make the skin look older. Blisters, erosions, and crusting can manifest with prolonged sun exposure.
EPP lesions could resemble contact dermatitis, porphyria cutanea tarda, dyshidrotic eczema, solar urticarial, or hydroa vacciniforme. Suspicion of EPP should be high when a patient presents with photosensitivity. Patients with EPP will have an elevated erythrocyte protoporphyrin level and elevated levels of protoporphyrins in feces. Liver enzymes should be ordered to evaluate for hepatobiliary disease.
Our patient began taking beta-carotene supplements to reduce photosensitivity, and tacrolimus 0.1% ointment to treat the lesions on his hands. He also used over-the-counter zinc oxide sun block and skin moisturizer, and reduced his exposure to the sun for several months. The patient saw improvement in his disease, with no further blistering or ulcerations.
Adapted from: Kasper DA, Centilli M, Silverton K. Photo Rounds: erythematous patches on the hands. J Fam Pract. 2012;61:101-104.

This patient had erythropoietic protoporphyria (EPP), a metabolic disease caused by a deficiency in ferrochelatase enzyme activity. Approximately 25% of patients develop hepatobiliary disease, which may be the only manifestation of the disease. EPP most commonly occurs in children ages 2 through 5, but diagnosis can be delayed until adulthood if a patient’s symptoms are mild or do not affect the skin.
Photosensitivity with a stinging or burning sensation on sun-exposed areas distinguishes EPP from other porphyrias. With repeated sun exposure, the affected areas can develop a waxy thickening with shallow linear or elliptical scars that make the skin look older. Blisters, erosions, and crusting can manifest with prolonged sun exposure.
EPP lesions could resemble contact dermatitis, porphyria cutanea tarda, dyshidrotic eczema, solar urticarial, or hydroa vacciniforme. Suspicion of EPP should be high when a patient presents with photosensitivity. Patients with EPP will have an elevated erythrocyte protoporphyrin level and elevated levels of protoporphyrins in feces. Liver enzymes should be ordered to evaluate for hepatobiliary disease.
Our patient began taking beta-carotene supplements to reduce photosensitivity, and tacrolimus 0.1% ointment to treat the lesions on his hands. He also used over-the-counter zinc oxide sun block and skin moisturizer, and reduced his exposure to the sun for several months. The patient saw improvement in his disease, with no further blistering or ulcerations.
Adapted from: Kasper DA, Centilli M, Silverton K. Photo Rounds: erythematous patches on the hands. J Fam Pract. 2012;61:101-104.

This patient had erythropoietic protoporphyria (EPP), a metabolic disease caused by a deficiency in ferrochelatase enzyme activity. Approximately 25% of patients develop hepatobiliary disease, which may be the only manifestation of the disease. EPP most commonly occurs in children ages 2 through 5, but diagnosis can be delayed until adulthood if a patient’s symptoms are mild or do not affect the skin.
Photosensitivity with a stinging or burning sensation on sun-exposed areas distinguishes EPP from other porphyrias. With repeated sun exposure, the affected areas can develop a waxy thickening with shallow linear or elliptical scars that make the skin look older. Blisters, erosions, and crusting can manifest with prolonged sun exposure.
EPP lesions could resemble contact dermatitis, porphyria cutanea tarda, dyshidrotic eczema, solar urticarial, or hydroa vacciniforme. Suspicion of EPP should be high when a patient presents with photosensitivity. Patients with EPP will have an elevated erythrocyte protoporphyrin level and elevated levels of protoporphyrins in feces. Liver enzymes should be ordered to evaluate for hepatobiliary disease.
Our patient began taking beta-carotene supplements to reduce photosensitivity, and tacrolimus 0.1% ointment to treat the lesions on his hands. He also used over-the-counter zinc oxide sun block and skin moisturizer, and reduced his exposure to the sun for several months. The patient saw improvement in his disease, with no further blistering or ulcerations.
Adapted from: Kasper DA, Centilli M, Silverton K. Photo Rounds: erythematous patches on the hands. J Fam Pract. 2012;61:101-104.
Blood-tinged diarrhea
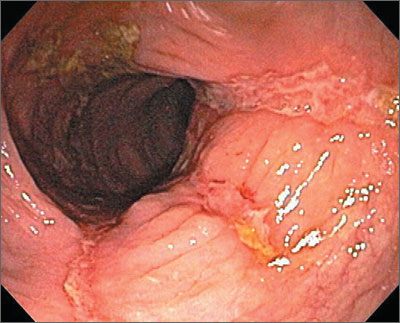
The colonoscopy revealed deep longitudinal ulcers and normal-appearing tissue in between—indicative of Crohn’s disease. The biopsies clinched the diagnosis, as the tissue in between the ulcers was normal. (Crohn’s disease often skips areas, whereas ulcerative colitis is diffuse.)
Symptoms in patients with Crohn’s disease depend on the location of the disease. Patients become symptomatic when lesions are extensive or distal (eg, colitis), systemic inflammatory reaction is present, or when disease is complicated by stricture, abscess, or fistula. Gross blood and mucus in the stool are less frequent than in ulcerative colitis and systemic symptoms, extracolonic features, pain, perineal disease, and obstruction are more common. There is no relationship between symptoms and anatomic damage.
Treatment for mild to moderate disease includes: oral aminosalicylates (ASAs), topical mesalamine, or topical steroids. An oral 5-ASA agent can be a prodrug (eg, sulfasalazine, 2-6 g/day), a drug with a pH-dependent coating (eg, Asacol, 2.4-4.8 g/day), or a slow-release agent (Pentasa, 2-4 g/day).
Patients with Crohn’s disease are also treated with nutritional therapy. Treatment for mild to moderate active ileocolic Crohn’s disease includes oral budesonide or prednisone if distal colonic disease is present. For patients who do not tolerate steroids or in cases where steroids are ineffective, biologic therapy with infliximab, adalimumab, or certolizumab pegol is appropriate. Methotrexate (up to 25 mg/week) is also effective. Patients with weight loss or strictures may benefit from early introduction of a biologic or immunomodulator therapy.
In this case, the gastroenterologist initially treated the patient with oral prednisone. He subsequently talked with her about other systemic therapies.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Inflammatory bowel disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:405-413.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The colonoscopy revealed deep longitudinal ulcers and normal-appearing tissue in between—indicative of Crohn’s disease. The biopsies clinched the diagnosis, as the tissue in between the ulcers was normal. (Crohn’s disease often skips areas, whereas ulcerative colitis is diffuse.)
Symptoms in patients with Crohn’s disease depend on the location of the disease. Patients become symptomatic when lesions are extensive or distal (eg, colitis), systemic inflammatory reaction is present, or when disease is complicated by stricture, abscess, or fistula. Gross blood and mucus in the stool are less frequent than in ulcerative colitis and systemic symptoms, extracolonic features, pain, perineal disease, and obstruction are more common. There is no relationship between symptoms and anatomic damage.
Treatment for mild to moderate disease includes: oral aminosalicylates (ASAs), topical mesalamine, or topical steroids. An oral 5-ASA agent can be a prodrug (eg, sulfasalazine, 2-6 g/day), a drug with a pH-dependent coating (eg, Asacol, 2.4-4.8 g/day), or a slow-release agent (Pentasa, 2-4 g/day).
Patients with Crohn’s disease are also treated with nutritional therapy. Treatment for mild to moderate active ileocolic Crohn’s disease includes oral budesonide or prednisone if distal colonic disease is present. For patients who do not tolerate steroids or in cases where steroids are ineffective, biologic therapy with infliximab, adalimumab, or certolizumab pegol is appropriate. Methotrexate (up to 25 mg/week) is also effective. Patients with weight loss or strictures may benefit from early introduction of a biologic or immunomodulator therapy.
In this case, the gastroenterologist initially treated the patient with oral prednisone. He subsequently talked with her about other systemic therapies.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Inflammatory bowel disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:405-413.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The colonoscopy revealed deep longitudinal ulcers and normal-appearing tissue in between—indicative of Crohn’s disease. The biopsies clinched the diagnosis, as the tissue in between the ulcers was normal. (Crohn’s disease often skips areas, whereas ulcerative colitis is diffuse.)
Symptoms in patients with Crohn’s disease depend on the location of the disease. Patients become symptomatic when lesions are extensive or distal (eg, colitis), systemic inflammatory reaction is present, or when disease is complicated by stricture, abscess, or fistula. Gross blood and mucus in the stool are less frequent than in ulcerative colitis and systemic symptoms, extracolonic features, pain, perineal disease, and obstruction are more common. There is no relationship between symptoms and anatomic damage.
Treatment for mild to moderate disease includes: oral aminosalicylates (ASAs), topical mesalamine, or topical steroids. An oral 5-ASA agent can be a prodrug (eg, sulfasalazine, 2-6 g/day), a drug with a pH-dependent coating (eg, Asacol, 2.4-4.8 g/day), or a slow-release agent (Pentasa, 2-4 g/day).
Patients with Crohn’s disease are also treated with nutritional therapy. Treatment for mild to moderate active ileocolic Crohn’s disease includes oral budesonide or prednisone if distal colonic disease is present. For patients who do not tolerate steroids or in cases where steroids are ineffective, biologic therapy with infliximab, adalimumab, or certolizumab pegol is appropriate. Methotrexate (up to 25 mg/week) is also effective. Patients with weight loss or strictures may benefit from early introduction of a biologic or immunomodulator therapy.
In this case, the gastroenterologist initially treated the patient with oral prednisone. He subsequently talked with her about other systemic therapies.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Inflammatory bowel disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:405-413.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
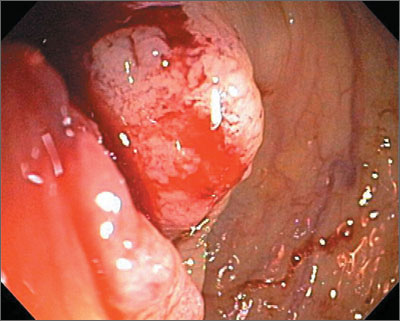
Episodic rectal bleeding
The FP made a clinical diagnosis of ulcerative colitis that was confirmed by colonoscopic biopsy.
Inflammatory bowel disease (IBD) includes ulcerative colitis (UC) and Crohn’s disease. The intestinal inflammation in UC is usually confined to the mucosa and affects the rectum with or without parts or the entire colon (pancolitis) in an uninterrupted pattern. In Crohn’s disease, inflammation is often transmural and affects primarily the ileum and colon, often discontinuously. However, Crohn’s disease can affect the entire GI tract from mouth to anus.
There is a predilection for IBD in those of Jewish ancestry (especially Ashkenazi Jews) followed in order by non-Jewish whites and African Americans, Hispanics, and Asians.
UC is classified by severity based on the clinical picture and results of endoscopy; treatment is based on disease classification.
○ Mild: Less than 4 stools per day, with or without blood, no signs of systemic toxicity, and a normal erythrocyte sedimentation rate (ESR).
○ Moderate: More than 4 stools per day but with minimal signs of toxicity.
○ Severe: More than 6 bloody stools per day, and evidence of toxicity is demonstrated by fever, tachycardia, anemia, and elevated ESR.
○ Fulminant: Patient may have more than 10 bowel movements daily, continuous bleeding, toxicity, abdominal tenderness and distention, a blood transfusion requirement, and colonic dilation on abdominal plain films.
Treatment for mild to moderate distal disease includes: oral aminosalicylates (ASAs), topical mesalamine, or topical steroids. An oral 5-ASA agent can be a prodrug (eg, sulfasalazine, 2 - 6 g/day), a drug with a pH-dependent coating (eg, Asacol, 2.4 - 4.8 g/day), or a slow-release agent (Pentasa, 2 - 4 g/day). Mesalamine suppositories (1 g/day) are the best way to induce remission in patients with proctitis. Rectal suppositories or enemas should also be used to improve medication delivery when treating active distal colitis, and a combination of oral and rectal mesalamine is better than monotherapy to stop rectal bleeding.
Up to 75% of patients will show clinical improvement with 2 g/day of 5-ASA and a similar percentage will maintain remission with doses of 1.5 to 4 g/day.
In this case, the patient’s physician started him on sulfasalazine and referred him to a gastroenterologist.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Inflammatory bowel disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:405-413.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP made a clinical diagnosis of ulcerative colitis that was confirmed by colonoscopic biopsy.
Inflammatory bowel disease (IBD) includes ulcerative colitis (UC) and Crohn’s disease. The intestinal inflammation in UC is usually confined to the mucosa and affects the rectum with or without parts or the entire colon (pancolitis) in an uninterrupted pattern. In Crohn’s disease, inflammation is often transmural and affects primarily the ileum and colon, often discontinuously. However, Crohn’s disease can affect the entire GI tract from mouth to anus.
There is a predilection for IBD in those of Jewish ancestry (especially Ashkenazi Jews) followed in order by non-Jewish whites and African Americans, Hispanics, and Asians.
UC is classified by severity based on the clinical picture and results of endoscopy; treatment is based on disease classification.
○ Mild: Less than 4 stools per day, with or without blood, no signs of systemic toxicity, and a normal erythrocyte sedimentation rate (ESR).
○ Moderate: More than 4 stools per day but with minimal signs of toxicity.
○ Severe: More than 6 bloody stools per day, and evidence of toxicity is demonstrated by fever, tachycardia, anemia, and elevated ESR.
○ Fulminant: Patient may have more than 10 bowel movements daily, continuous bleeding, toxicity, abdominal tenderness and distention, a blood transfusion requirement, and colonic dilation on abdominal plain films.
Treatment for mild to moderate distal disease includes: oral aminosalicylates (ASAs), topical mesalamine, or topical steroids. An oral 5-ASA agent can be a prodrug (eg, sulfasalazine, 2 - 6 g/day), a drug with a pH-dependent coating (eg, Asacol, 2.4 - 4.8 g/day), or a slow-release agent (Pentasa, 2 - 4 g/day). Mesalamine suppositories (1 g/day) are the best way to induce remission in patients with proctitis. Rectal suppositories or enemas should also be used to improve medication delivery when treating active distal colitis, and a combination of oral and rectal mesalamine is better than monotherapy to stop rectal bleeding.
Up to 75% of patients will show clinical improvement with 2 g/day of 5-ASA and a similar percentage will maintain remission with doses of 1.5 to 4 g/day.
In this case, the patient’s physician started him on sulfasalazine and referred him to a gastroenterologist.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Inflammatory bowel disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:405-413.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP made a clinical diagnosis of ulcerative colitis that was confirmed by colonoscopic biopsy.
Inflammatory bowel disease (IBD) includes ulcerative colitis (UC) and Crohn’s disease. The intestinal inflammation in UC is usually confined to the mucosa and affects the rectum with or without parts or the entire colon (pancolitis) in an uninterrupted pattern. In Crohn’s disease, inflammation is often transmural and affects primarily the ileum and colon, often discontinuously. However, Crohn’s disease can affect the entire GI tract from mouth to anus.
There is a predilection for IBD in those of Jewish ancestry (especially Ashkenazi Jews) followed in order by non-Jewish whites and African Americans, Hispanics, and Asians.
UC is classified by severity based on the clinical picture and results of endoscopy; treatment is based on disease classification.
○ Mild: Less than 4 stools per day, with or without blood, no signs of systemic toxicity, and a normal erythrocyte sedimentation rate (ESR).
○ Moderate: More than 4 stools per day but with minimal signs of toxicity.
○ Severe: More than 6 bloody stools per day, and evidence of toxicity is demonstrated by fever, tachycardia, anemia, and elevated ESR.
○ Fulminant: Patient may have more than 10 bowel movements daily, continuous bleeding, toxicity, abdominal tenderness and distention, a blood transfusion requirement, and colonic dilation on abdominal plain films.
Treatment for mild to moderate distal disease includes: oral aminosalicylates (ASAs), topical mesalamine, or topical steroids. An oral 5-ASA agent can be a prodrug (eg, sulfasalazine, 2 - 6 g/day), a drug with a pH-dependent coating (eg, Asacol, 2.4 - 4.8 g/day), or a slow-release agent (Pentasa, 2 - 4 g/day). Mesalamine suppositories (1 g/day) are the best way to induce remission in patients with proctitis. Rectal suppositories or enemas should also be used to improve medication delivery when treating active distal colitis, and a combination of oral and rectal mesalamine is better than monotherapy to stop rectal bleeding.
Up to 75% of patients will show clinical improvement with 2 g/day of 5-ASA and a similar percentage will maintain remission with doses of 1.5 to 4 g/day.
In this case, the patient’s physician started him on sulfasalazine and referred him to a gastroenterologist.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Inflammatory bowel disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:405-413.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
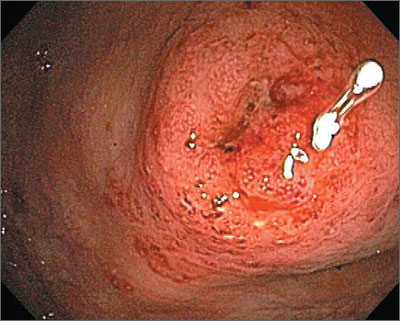
Rectal bleeding
A biopsy was obtained and pathology confirmed adenocarcinoma, the most common type of colon cancer. Colon cancer is the third most common cancer in both men and women in the United States, second only to lung cancer as a cause of death.
The diagnosis of colon cancer is sometimes made following a positive screening test (eg, digital rectal examination, fecal occult blood test, sigmoidoscopy, colonoscopy, or barium enema). For patients who have signs and symptoms suggestive of colon cancer, the confirmative diagnostic test most commonly performed is colonoscopy with biopsy.
Colonoscopy allows direct visualization of the lesion, examination of the entire large bowel for synchronous and metachronous lesions, and collection of tissue for histologic diagnosis.
In this case, the patient underwent a partial colectomy. Examination of the liver, pelvis, hemidiaphragm, and full length of the colon during surgery showed no metastases. Despite the large size of the primary tumor, pathology indicated that it was confined to the bowel wall with invasion into the muscularis propia (Duke B). Other tests and computed tomography imaging showed no evidence of metastases or lymph node involvement.
The patient decided not to take the adjuvant chemotherapy and recovered from his surgery. He agreed to have screening colonoscopy on a frequent and regular basis along with monitoring of his blood for post-treatment carcinoembryonic antigen levels.
Photo Courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Wang B. Colon cancer. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:399-404.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
A biopsy was obtained and pathology confirmed adenocarcinoma, the most common type of colon cancer. Colon cancer is the third most common cancer in both men and women in the United States, second only to lung cancer as a cause of death.
The diagnosis of colon cancer is sometimes made following a positive screening test (eg, digital rectal examination, fecal occult blood test, sigmoidoscopy, colonoscopy, or barium enema). For patients who have signs and symptoms suggestive of colon cancer, the confirmative diagnostic test most commonly performed is colonoscopy with biopsy.
Colonoscopy allows direct visualization of the lesion, examination of the entire large bowel for synchronous and metachronous lesions, and collection of tissue for histologic diagnosis.
In this case, the patient underwent a partial colectomy. Examination of the liver, pelvis, hemidiaphragm, and full length of the colon during surgery showed no metastases. Despite the large size of the primary tumor, pathology indicated that it was confined to the bowel wall with invasion into the muscularis propia (Duke B). Other tests and computed tomography imaging showed no evidence of metastases or lymph node involvement.
The patient decided not to take the adjuvant chemotherapy and recovered from his surgery. He agreed to have screening colonoscopy on a frequent and regular basis along with monitoring of his blood for post-treatment carcinoembryonic antigen levels.
Photo Courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Wang B. Colon cancer. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:399-404.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
A biopsy was obtained and pathology confirmed adenocarcinoma, the most common type of colon cancer. Colon cancer is the third most common cancer in both men and women in the United States, second only to lung cancer as a cause of death.
The diagnosis of colon cancer is sometimes made following a positive screening test (eg, digital rectal examination, fecal occult blood test, sigmoidoscopy, colonoscopy, or barium enema). For patients who have signs and symptoms suggestive of colon cancer, the confirmative diagnostic test most commonly performed is colonoscopy with biopsy.
Colonoscopy allows direct visualization of the lesion, examination of the entire large bowel for synchronous and metachronous lesions, and collection of tissue for histologic diagnosis.
In this case, the patient underwent a partial colectomy. Examination of the liver, pelvis, hemidiaphragm, and full length of the colon during surgery showed no metastases. Despite the large size of the primary tumor, pathology indicated that it was confined to the bowel wall with invasion into the muscularis propia (Duke B). Other tests and computed tomography imaging showed no evidence of metastases or lymph node involvement.
The patient decided not to take the adjuvant chemotherapy and recovered from his surgery. He agreed to have screening colonoscopy on a frequent and regular basis along with monitoring of his blood for post-treatment carcinoembryonic antigen levels.
Photo Courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Wang B. Colon cancer. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:399-404.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
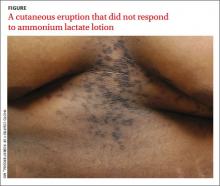
Cutaneous eruption on chest and back
A 22-year-old African American man sought care at our clinic for an asymptomatic, “dirty-looking” rash on the epigastrium that had expanded and thickened over the previous 2 years. The rash hadn’t responded to scrubbing with soap and water, ammonium lactate lotion 12% BID, or over-the-counter moisturizing lotions.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Confluent and reticulated papillomatosis
This patient was given a diagnosis of confluent and reticulated papillomatosis (CRP) based on the clinical presentation.
Although this condition is uncommon,1 we see it at least once a month in our dermatology clinic. CRP is characterized by centrally confluent and peripherally reticulated scaly brown plaques and papules that are cosmetically disfiguring.1
CRP usually is asymptomatic2 and primarily affects young adults—especially teenagers.3 It occurs in both males and females3 and it commonly occurs on the trunk.1,2
CRP is believed to be a disorder of keratinization. Malassezia furfur may induce CRP’s hyperproliferative epidermal changes, but systemic treatment that eliminates this organism does not clear CRP.3
Differential diagnosis includes acanthosis nigricans
Acanthosis nigricans (AN) shares similar “dirty” brown, confluent textural plaques, as well as nonspecific acanthosis and papillomatosis on histopathologic examination. However, AN affects flexural areas, whereas CRP typically is found on the epigastrium, central chest, and central back.1,2
Tinea versicolor (TV) and CRP are both brown in color, and occur in a similar distribution on the central back and chest.4 However, in contrast to the fine perifollicular scaling seen in TV, CRP is associated with textural, confluent plaques. TV also can be distinguished by its pathognomonic “spaghetti and meatball” pattern of hyphae and spores on potassium hydroxide (KOH) preparation; KOH will be negative in patients with CRP. When a presumed case of TV does not respond to antifungal therapy, CRP should be considered.1
Making the diagnosis
A CRP diagnosis is made based on clinical presentation. The eruption usually begins as verrucous papules in the inframammary or epigastric region that enlarge to 4 to 5 mm in diameter and coalesce to form a confluent plaque with a peripheral reticulated pattern. CRP can extend over the back, chest, and abdomen to the neck, shoulders, and gluteal cleft. CRP does not affect the oral mucosa and rarely involves flexural areas.2 Although most cases are asymptomatic, mild pruritus may occur.1,2
A skin biopsy rarely is necessary for making a CRP diagnosis, but histopathologic findings include papillomatosis, hyperkeratosis, variable acanthosis, follicular plugging, and sparse dermal inflammation.1,3
Antibiotics usually clear this rash
Systemic antibiotics, most commonly minocycline 100 mg twice daily for 30 days or doxycycline 100 mg twice daily for 30 days, are safe and effective for CRP.1,5 Sometimes treatment is extended for as long as 6 months. Although CRP usually responds to minocycline or doxycycline, it is believed that this is the result of these drugs’ anti-inflammatory—rather than antibiotic—properties.1,2,5 Azithromycin is an effective alternative therapy.2,5
There is a high rate of recurrence of CRP in patients after systemic antibiotics are discontinued.2 Uniform responses to treatment and retreatment of flares have solidified the belief that antibiotics are an effective suppressive if not curative therapy, despite a lack of randomized controlled trials.5
Our patient was treated with minocycline 100 mg BID. After 1 month, the rash had improved by 70%. In 3 months it was completely clear and the treatment was discontinued.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
1. Davis MD, Weenig RH, Camilleri MJ. Confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteria. Br J Dermatol. 2006;154:287-293.
2. Scheinfeld N. Confluent and reticulated papillomatosis: a review of the literature. Am J Clin Dermatol. 2006;7: 305-313.
3. Tamraz H, Raffoul M, Kurban M, et al. Confluent and reticulated papillomatosis: clinical and histopathological study of 10 cases from Lebanon. J Eur Acad Dermatol Venereol. 2013;27:e119-e123.
4. Hudacek KD, Haque MS, Hochberg AL, et al. An unusual variant of confluent and reticulated papillomatosis masquerading as tinea versicolor. Arch Dermatol. 2012;148:505-508.
5. Jang HS, Oh CK, Cha JH, et al. Six cases of confluent and reticulated papillomatosis alleviated by various antibiotics. J Am Acad Dermatol. 2001;44:652-655.
A 22-year-old African American man sought care at our clinic for an asymptomatic, “dirty-looking” rash on the epigastrium that had expanded and thickened over the previous 2 years. The rash hadn’t responded to scrubbing with soap and water, ammonium lactate lotion 12% BID, or over-the-counter moisturizing lotions.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Confluent and reticulated papillomatosis
This patient was given a diagnosis of confluent and reticulated papillomatosis (CRP) based on the clinical presentation.
Although this condition is uncommon,1 we see it at least once a month in our dermatology clinic. CRP is characterized by centrally confluent and peripherally reticulated scaly brown plaques and papules that are cosmetically disfiguring.1
CRP usually is asymptomatic2 and primarily affects young adults—especially teenagers.3 It occurs in both males and females3 and it commonly occurs on the trunk.1,2
CRP is believed to be a disorder of keratinization. Malassezia furfur may induce CRP’s hyperproliferative epidermal changes, but systemic treatment that eliminates this organism does not clear CRP.3
Differential diagnosis includes acanthosis nigricans
Acanthosis nigricans (AN) shares similar “dirty” brown, confluent textural plaques, as well as nonspecific acanthosis and papillomatosis on histopathologic examination. However, AN affects flexural areas, whereas CRP typically is found on the epigastrium, central chest, and central back.1,2
Tinea versicolor (TV) and CRP are both brown in color, and occur in a similar distribution on the central back and chest.4 However, in contrast to the fine perifollicular scaling seen in TV, CRP is associated with textural, confluent plaques. TV also can be distinguished by its pathognomonic “spaghetti and meatball” pattern of hyphae and spores on potassium hydroxide (KOH) preparation; KOH will be negative in patients with CRP. When a presumed case of TV does not respond to antifungal therapy, CRP should be considered.1
Making the diagnosis
A CRP diagnosis is made based on clinical presentation. The eruption usually begins as verrucous papules in the inframammary or epigastric region that enlarge to 4 to 5 mm in diameter and coalesce to form a confluent plaque with a peripheral reticulated pattern. CRP can extend over the back, chest, and abdomen to the neck, shoulders, and gluteal cleft. CRP does not affect the oral mucosa and rarely involves flexural areas.2 Although most cases are asymptomatic, mild pruritus may occur.1,2
A skin biopsy rarely is necessary for making a CRP diagnosis, but histopathologic findings include papillomatosis, hyperkeratosis, variable acanthosis, follicular plugging, and sparse dermal inflammation.1,3
Antibiotics usually clear this rash
Systemic antibiotics, most commonly minocycline 100 mg twice daily for 30 days or doxycycline 100 mg twice daily for 30 days, are safe and effective for CRP.1,5 Sometimes treatment is extended for as long as 6 months. Although CRP usually responds to minocycline or doxycycline, it is believed that this is the result of these drugs’ anti-inflammatory—rather than antibiotic—properties.1,2,5 Azithromycin is an effective alternative therapy.2,5
There is a high rate of recurrence of CRP in patients after systemic antibiotics are discontinued.2 Uniform responses to treatment and retreatment of flares have solidified the belief that antibiotics are an effective suppressive if not curative therapy, despite a lack of randomized controlled trials.5
Our patient was treated with minocycline 100 mg BID. After 1 month, the rash had improved by 70%. In 3 months it was completely clear and the treatment was discontinued.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
A 22-year-old African American man sought care at our clinic for an asymptomatic, “dirty-looking” rash on the epigastrium that had expanded and thickened over the previous 2 years. The rash hadn’t responded to scrubbing with soap and water, ammonium lactate lotion 12% BID, or over-the-counter moisturizing lotions.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Confluent and reticulated papillomatosis
This patient was given a diagnosis of confluent and reticulated papillomatosis (CRP) based on the clinical presentation.
Although this condition is uncommon,1 we see it at least once a month in our dermatology clinic. CRP is characterized by centrally confluent and peripherally reticulated scaly brown plaques and papules that are cosmetically disfiguring.1
CRP usually is asymptomatic2 and primarily affects young adults—especially teenagers.3 It occurs in both males and females3 and it commonly occurs on the trunk.1,2
CRP is believed to be a disorder of keratinization. Malassezia furfur may induce CRP’s hyperproliferative epidermal changes, but systemic treatment that eliminates this organism does not clear CRP.3
Differential diagnosis includes acanthosis nigricans
Acanthosis nigricans (AN) shares similar “dirty” brown, confluent textural plaques, as well as nonspecific acanthosis and papillomatosis on histopathologic examination. However, AN affects flexural areas, whereas CRP typically is found on the epigastrium, central chest, and central back.1,2
Tinea versicolor (TV) and CRP are both brown in color, and occur in a similar distribution on the central back and chest.4 However, in contrast to the fine perifollicular scaling seen in TV, CRP is associated with textural, confluent plaques. TV also can be distinguished by its pathognomonic “spaghetti and meatball” pattern of hyphae and spores on potassium hydroxide (KOH) preparation; KOH will be negative in patients with CRP. When a presumed case of TV does not respond to antifungal therapy, CRP should be considered.1
Making the diagnosis
A CRP diagnosis is made based on clinical presentation. The eruption usually begins as verrucous papules in the inframammary or epigastric region that enlarge to 4 to 5 mm in diameter and coalesce to form a confluent plaque with a peripheral reticulated pattern. CRP can extend over the back, chest, and abdomen to the neck, shoulders, and gluteal cleft. CRP does not affect the oral mucosa and rarely involves flexural areas.2 Although most cases are asymptomatic, mild pruritus may occur.1,2
A skin biopsy rarely is necessary for making a CRP diagnosis, but histopathologic findings include papillomatosis, hyperkeratosis, variable acanthosis, follicular plugging, and sparse dermal inflammation.1,3
Antibiotics usually clear this rash
Systemic antibiotics, most commonly minocycline 100 mg twice daily for 30 days or doxycycline 100 mg twice daily for 30 days, are safe and effective for CRP.1,5 Sometimes treatment is extended for as long as 6 months. Although CRP usually responds to minocycline or doxycycline, it is believed that this is the result of these drugs’ anti-inflammatory—rather than antibiotic—properties.1,2,5 Azithromycin is an effective alternative therapy.2,5
There is a high rate of recurrence of CRP in patients after systemic antibiotics are discontinued.2 Uniform responses to treatment and retreatment of flares have solidified the belief that antibiotics are an effective suppressive if not curative therapy, despite a lack of randomized controlled trials.5
Our patient was treated with minocycline 100 mg BID. After 1 month, the rash had improved by 70%. In 3 months it was completely clear and the treatment was discontinued.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
1. Davis MD, Weenig RH, Camilleri MJ. Confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteria. Br J Dermatol. 2006;154:287-293.
2. Scheinfeld N. Confluent and reticulated papillomatosis: a review of the literature. Am J Clin Dermatol. 2006;7: 305-313.
3. Tamraz H, Raffoul M, Kurban M, et al. Confluent and reticulated papillomatosis: clinical and histopathological study of 10 cases from Lebanon. J Eur Acad Dermatol Venereol. 2013;27:e119-e123.
4. Hudacek KD, Haque MS, Hochberg AL, et al. An unusual variant of confluent and reticulated papillomatosis masquerading as tinea versicolor. Arch Dermatol. 2012;148:505-508.
5. Jang HS, Oh CK, Cha JH, et al. Six cases of confluent and reticulated papillomatosis alleviated by various antibiotics. J Am Acad Dermatol. 2001;44:652-655.
1. Davis MD, Weenig RH, Camilleri MJ. Confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteria. Br J Dermatol. 2006;154:287-293.
2. Scheinfeld N. Confluent and reticulated papillomatosis: a review of the literature. Am J Clin Dermatol. 2006;7: 305-313.
3. Tamraz H, Raffoul M, Kurban M, et al. Confluent and reticulated papillomatosis: clinical and histopathological study of 10 cases from Lebanon. J Eur Acad Dermatol Venereol. 2013;27:e119-e123.
4. Hudacek KD, Haque MS, Hochberg AL, et al. An unusual variant of confluent and reticulated papillomatosis masquerading as tinea versicolor. Arch Dermatol. 2012;148:505-508.
5. Jang HS, Oh CK, Cha JH, et al. Six cases of confluent and reticulated papillomatosis alleviated by various antibiotics. J Am Acad Dermatol. 2001;44:652-655.
Copper ring around cornea
The FP suspected that the patient had a Kayser-Fleischer ring around the edge of the cornea. The ring is the color of copper and is caused by copper deposition. The FP ordered serum ceruloplasmin because she suspected Wilson disease as the cause of the eye finding, the fatigue, and the abnormal liver function tests.
The patient’s serum ceruloplasmin was markedly low, so a 24-hour urine copper test was ordered and that came back elevated. This established the diagnosis of Wilson disease and the patient was referred to Gastroenterology for management.
Wilson disease is an autosomal recessive disease that results in defective copper transport and copper toxicity. Copper is deposited in the liver and brain, resulting in liver disease, cirrhosis, and various neurologic abnormalities. Neurologic manifestations include fatigue, behavior changes, tremors, and difficulty walking or swallowing. Gastrointestinal symptoms can include nausea, abdominal pain, and jaundice.
Treatment involves the chelation of copper using either penicillamine or trientine. Once the copper level is sufficiently reduced, the patient is placed on zinc acetate for maintenance therapy.
In this case, the patient was started on penicillamine. When she was unable to tolerate that, her medication was switched to trientine. Over time her fatigue improved and her liver function tests normalized.
Photo courtesy of Marc Solioz. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Mathia A. Liver disease. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:377-385.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP suspected that the patient had a Kayser-Fleischer ring around the edge of the cornea. The ring is the color of copper and is caused by copper deposition. The FP ordered serum ceruloplasmin because she suspected Wilson disease as the cause of the eye finding, the fatigue, and the abnormal liver function tests.
The patient’s serum ceruloplasmin was markedly low, so a 24-hour urine copper test was ordered and that came back elevated. This established the diagnosis of Wilson disease and the patient was referred to Gastroenterology for management.
Wilson disease is an autosomal recessive disease that results in defective copper transport and copper toxicity. Copper is deposited in the liver and brain, resulting in liver disease, cirrhosis, and various neurologic abnormalities. Neurologic manifestations include fatigue, behavior changes, tremors, and difficulty walking or swallowing. Gastrointestinal symptoms can include nausea, abdominal pain, and jaundice.
Treatment involves the chelation of copper using either penicillamine or trientine. Once the copper level is sufficiently reduced, the patient is placed on zinc acetate for maintenance therapy.
In this case, the patient was started on penicillamine. When she was unable to tolerate that, her medication was switched to trientine. Over time her fatigue improved and her liver function tests normalized.
Photo courtesy of Marc Solioz. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Mathia A. Liver disease. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:377-385.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The FP suspected that the patient had a Kayser-Fleischer ring around the edge of the cornea. The ring is the color of copper and is caused by copper deposition. The FP ordered serum ceruloplasmin because she suspected Wilson disease as the cause of the eye finding, the fatigue, and the abnormal liver function tests.
The patient’s serum ceruloplasmin was markedly low, so a 24-hour urine copper test was ordered and that came back elevated. This established the diagnosis of Wilson disease and the patient was referred to Gastroenterology for management.
Wilson disease is an autosomal recessive disease that results in defective copper transport and copper toxicity. Copper is deposited in the liver and brain, resulting in liver disease, cirrhosis, and various neurologic abnormalities. Neurologic manifestations include fatigue, behavior changes, tremors, and difficulty walking or swallowing. Gastrointestinal symptoms can include nausea, abdominal pain, and jaundice.
Treatment involves the chelation of copper using either penicillamine or trientine. Once the copper level is sufficiently reduced, the patient is placed on zinc acetate for maintenance therapy.
In this case, the patient was started on penicillamine. When she was unable to tolerate that, her medication was switched to trientine. Over time her fatigue improved and her liver function tests normalized.
Photo courtesy of Marc Solioz. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Mathia A. Liver disease. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:377-385.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Episodic abdominal pain
The ultrasound confirmed the presence of gallstones, with obvious shadowing of the sound waves behind the gallstones. Gallstones are inorganic masses (usually composed of cholesterol) that form in the gallbladder or bile duct. They are formed by concretion (joining together of adjacent parts and hardening) or accretion (growth by addition or adherence of parts normally separated) of normal and/or abnormal bile constituents. Autopsy data suggest 20% of women and 8% of men have gallstones.
In this case, the FP referred the patient to General Surgery for laparoscopic cholecystectomy. She also counseled the patient on the importance of weight loss through eating a low-fat diet and exercising.
Image courtesy of Jeff Russell, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Gallstones. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:386-392.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The ultrasound confirmed the presence of gallstones, with obvious shadowing of the sound waves behind the gallstones. Gallstones are inorganic masses (usually composed of cholesterol) that form in the gallbladder or bile duct. They are formed by concretion (joining together of adjacent parts and hardening) or accretion (growth by addition or adherence of parts normally separated) of normal and/or abnormal bile constituents. Autopsy data suggest 20% of women and 8% of men have gallstones.
In this case, the FP referred the patient to General Surgery for laparoscopic cholecystectomy. She also counseled the patient on the importance of weight loss through eating a low-fat diet and exercising.
Image courtesy of Jeff Russell, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Gallstones. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:386-392.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
The ultrasound confirmed the presence of gallstones, with obvious shadowing of the sound waves behind the gallstones. Gallstones are inorganic masses (usually composed of cholesterol) that form in the gallbladder or bile duct. They are formed by concretion (joining together of adjacent parts and hardening) or accretion (growth by addition or adherence of parts normally separated) of normal and/or abnormal bile constituents. Autopsy data suggest 20% of women and 8% of men have gallstones.
In this case, the FP referred the patient to General Surgery for laparoscopic cholecystectomy. She also counseled the patient on the importance of weight loss through eating a low-fat diet and exercising.
Image courtesy of Jeff Russell, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Gallstones. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:386-392.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Jaundice and pruritus
Laboratory testing revealed elevated liver enzymes, particularly serum alkaline phosphatase and γ-glutamyl-transpeptidase, and positive antinuclear and antimitochondrial antibodies. A liver biopsy confirmed primary biliary cirrhosis.
Primary biliary cirrhosis is a disease of unknown etiology characterized by inflammatory destruction of the small bile ducts and gradual liver cirrhosis. It is much more common in women than men (9:1 ratio).
Regardless of the histologic stage of their cirrhosis or their eventual need for liver transplantation, patients with primary biliary cirrhosis typically are treated with ursodeoxycholic acid, 13 to 15 mg/kg/d. It is given with food 2 to 4 times a day. In a meta-analysis of 7 trials, ursodeoxycholic acid significantly reduced the incidence of liver transplantation. Bile acid sequestrants such as cholestyramine can be used to treat pruritus. This patient was treated with ursodeoxycholic acid and cholestyramine, which relieved her symptoms and improved her liver function test results.
Photo courtesy of Javid Ghandehari, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Mathia A. Liver disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:377-385.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Laboratory testing revealed elevated liver enzymes, particularly serum alkaline phosphatase and γ-glutamyl-transpeptidase, and positive antinuclear and antimitochondrial antibodies. A liver biopsy confirmed primary biliary cirrhosis.
Primary biliary cirrhosis is a disease of unknown etiology characterized by inflammatory destruction of the small bile ducts and gradual liver cirrhosis. It is much more common in women than men (9:1 ratio).
Regardless of the histologic stage of their cirrhosis or their eventual need for liver transplantation, patients with primary biliary cirrhosis typically are treated with ursodeoxycholic acid, 13 to 15 mg/kg/d. It is given with food 2 to 4 times a day. In a meta-analysis of 7 trials, ursodeoxycholic acid significantly reduced the incidence of liver transplantation. Bile acid sequestrants such as cholestyramine can be used to treat pruritus. This patient was treated with ursodeoxycholic acid and cholestyramine, which relieved her symptoms and improved her liver function test results.
Photo courtesy of Javid Ghandehari, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Mathia A. Liver disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:377-385.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Laboratory testing revealed elevated liver enzymes, particularly serum alkaline phosphatase and γ-glutamyl-transpeptidase, and positive antinuclear and antimitochondrial antibodies. A liver biopsy confirmed primary biliary cirrhosis.
Primary biliary cirrhosis is a disease of unknown etiology characterized by inflammatory destruction of the small bile ducts and gradual liver cirrhosis. It is much more common in women than men (9:1 ratio).
Regardless of the histologic stage of their cirrhosis or their eventual need for liver transplantation, patients with primary biliary cirrhosis typically are treated with ursodeoxycholic acid, 13 to 15 mg/kg/d. It is given with food 2 to 4 times a day. In a meta-analysis of 7 trials, ursodeoxycholic acid significantly reduced the incidence of liver transplantation. Bile acid sequestrants such as cholestyramine can be used to treat pruritus. This patient was treated with ursodeoxycholic acid and cholestyramine, which relieved her symptoms and improved her liver function test results.
Photo courtesy of Javid Ghandehari, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M, Mathia A. Liver disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:377-385.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Epigastric pain
Endoscopy revealed a pyloric ulcer and an erosion of the mucosa. Biopsies showed the presence of Helicobacter pylori.
Peptic ulcer disease (PUD) is characterized by a break in the mucosal lining of the stomach or duodenum secondary to pepsin and gastric acid secretion; this damage is greater than 5 mm in size and the depth reaches the submucosal layer. Note that duodenal ulcers are virtually never malignant and do not require biopsy. However, gastric ulcers (including the pylorus) should be biopsied because 3% to 5% of benign-appearing gastric ulcers prove to be malignant.
The goals of treatment of active H pylori-associated ulcers are to relieve dyspeptic symptoms, promote ulcer healing, and eradicate H pylori infection. Eradication of H pylori is better than drug therapy for duodenal ulcer healing and greatly reduces the incidence of recurrence from 67% to 6% in patients with duodenal ulcers and from 59% to 4% in patients with gastric ulcers.
Four drug combinations currently provide the best results and consist of 2 general combinations: (a) a proton-pump inhibitor (PPI), amoxicillin, clarithromycin, metronidazole/tinidazole given either sequentially or concomitantly, or (b) a PPI, a bismuth, tetracycline HCL, and metronidazole/tinidazole.
In this case, the physician prescribed combination “a” and the patient’s symptoms resolved completely.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Azhary H, Smith M. Peptic ulcer disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 365-370.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Endoscopy revealed a pyloric ulcer and an erosion of the mucosa. Biopsies showed the presence of Helicobacter pylori.
Peptic ulcer disease (PUD) is characterized by a break in the mucosal lining of the stomach or duodenum secondary to pepsin and gastric acid secretion; this damage is greater than 5 mm in size and the depth reaches the submucosal layer. Note that duodenal ulcers are virtually never malignant and do not require biopsy. However, gastric ulcers (including the pylorus) should be biopsied because 3% to 5% of benign-appearing gastric ulcers prove to be malignant.
The goals of treatment of active H pylori-associated ulcers are to relieve dyspeptic symptoms, promote ulcer healing, and eradicate H pylori infection. Eradication of H pylori is better than drug therapy for duodenal ulcer healing and greatly reduces the incidence of recurrence from 67% to 6% in patients with duodenal ulcers and from 59% to 4% in patients with gastric ulcers.
Four drug combinations currently provide the best results and consist of 2 general combinations: (a) a proton-pump inhibitor (PPI), amoxicillin, clarithromycin, metronidazole/tinidazole given either sequentially or concomitantly, or (b) a PPI, a bismuth, tetracycline HCL, and metronidazole/tinidazole.
In this case, the physician prescribed combination “a” and the patient’s symptoms resolved completely.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Azhary H, Smith M. Peptic ulcer disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 365-370.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/
Endoscopy revealed a pyloric ulcer and an erosion of the mucosa. Biopsies showed the presence of Helicobacter pylori.
Peptic ulcer disease (PUD) is characterized by a break in the mucosal lining of the stomach or duodenum secondary to pepsin and gastric acid secretion; this damage is greater than 5 mm in size and the depth reaches the submucosal layer. Note that duodenal ulcers are virtually never malignant and do not require biopsy. However, gastric ulcers (including the pylorus) should be biopsied because 3% to 5% of benign-appearing gastric ulcers prove to be malignant.
The goals of treatment of active H pylori-associated ulcers are to relieve dyspeptic symptoms, promote ulcer healing, and eradicate H pylori infection. Eradication of H pylori is better than drug therapy for duodenal ulcer healing and greatly reduces the incidence of recurrence from 67% to 6% in patients with duodenal ulcers and from 59% to 4% in patients with gastric ulcers.
Four drug combinations currently provide the best results and consist of 2 general combinations: (a) a proton-pump inhibitor (PPI), amoxicillin, clarithromycin, metronidazole/tinidazole given either sequentially or concomitantly, or (b) a PPI, a bismuth, tetracycline HCL, and metronidazole/tinidazole.
In this case, the physician prescribed combination “a” and the patient’s symptoms resolved completely.
Photo courtesy of Marvin Derezin, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Azhary H, Smith M. Peptic ulcer disease. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 365-370.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/