User login
Abdominal pain

|
Many Ascaris lumbricoides roundworms were seen in the resected bowel of this patient with bowel obstruction. A lumbricoides is a common parasite in Africa and Central America, especially where the drinking water is not clean. Although less common in the United States, it is found in tropical and subtropical areas, including the southeastern rural United States.
When fertilized eggs of A lumbricoides are ingested, they enter the circulation through the intestinal mucosa, travel to the lungs, climb to the pharynx, are swallowed, and finally find a “home” in the small intestine. If detected before there are complications, A lumbricoides can be treated with a single oral dose of either albendazole 400 mg or mebendazole 500 mg. In endemic areas outside of the United States, there are some public health programs that administer albendazole or mebendazole to at-risk children and adults every 3 to 6 months.
The patient described here recovered from her surgery. She and her family were all treated prophylactically with mebendazole to eradicate any remaining roundworms.
Photo courtesy of James L. Fishback, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Chumley H. Intestinal worms and parasites. In: Usatine R, Smith M, Mayeaux EJ, et al. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:916-920.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

|
Many Ascaris lumbricoides roundworms were seen in the resected bowel of this patient with bowel obstruction. A lumbricoides is a common parasite in Africa and Central America, especially where the drinking water is not clean. Although less common in the United States, it is found in tropical and subtropical areas, including the southeastern rural United States.
When fertilized eggs of A lumbricoides are ingested, they enter the circulation through the intestinal mucosa, travel to the lungs, climb to the pharynx, are swallowed, and finally find a “home” in the small intestine. If detected before there are complications, A lumbricoides can be treated with a single oral dose of either albendazole 400 mg or mebendazole 500 mg. In endemic areas outside of the United States, there are some public health programs that administer albendazole or mebendazole to at-risk children and adults every 3 to 6 months.
The patient described here recovered from her surgery. She and her family were all treated prophylactically with mebendazole to eradicate any remaining roundworms.
Photo courtesy of James L. Fishback, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Chumley H. Intestinal worms and parasites. In: Usatine R, Smith M, Mayeaux EJ, et al. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:916-920.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

|
Many Ascaris lumbricoides roundworms were seen in the resected bowel of this patient with bowel obstruction. A lumbricoides is a common parasite in Africa and Central America, especially where the drinking water is not clean. Although less common in the United States, it is found in tropical and subtropical areas, including the southeastern rural United States.
When fertilized eggs of A lumbricoides are ingested, they enter the circulation through the intestinal mucosa, travel to the lungs, climb to the pharynx, are swallowed, and finally find a “home” in the small intestine. If detected before there are complications, A lumbricoides can be treated with a single oral dose of either albendazole 400 mg or mebendazole 500 mg. In endemic areas outside of the United States, there are some public health programs that administer albendazole or mebendazole to at-risk children and adults every 3 to 6 months.
The patient described here recovered from her surgery. She and her family were all treated prophylactically with mebendazole to eradicate any remaining roundworms.
Photo courtesy of James L. Fishback, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Chumley H. Intestinal worms and parasites. In: Usatine R, Smith M, Mayeaux EJ, et al. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:916-920.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Anal itching

The FP detected adult worms and ova of Enterobius vermicularis. Pinworms are acquired through the oral route when hands that have been in contact with contaminated objects are placed in the mouth. This can happen when kids play together in a sand box.
In this case, the young boy was treated with a single dose of chewable 100 mg mebendazole and his symptoms resolved. The parent was told to repeat the mebendazole dose in 2 weeks to increase the long-term cure rate.
If the tape test had been negative, the FP could have chosen to treat empirically, since mebendazole is a safe medication. Another option would have been to have the parent apply the scotch tape to the boy’s perianal area first thing in the morning and bring the tape back to the office. (The yield is higher in the morning.)
Photo courtesy of James L. Fishback, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Chumley H. Intestinal worms and parasites. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:916-920.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The FP detected adult worms and ova of Enterobius vermicularis. Pinworms are acquired through the oral route when hands that have been in contact with contaminated objects are placed in the mouth. This can happen when kids play together in a sand box.
In this case, the young boy was treated with a single dose of chewable 100 mg mebendazole and his symptoms resolved. The parent was told to repeat the mebendazole dose in 2 weeks to increase the long-term cure rate.
If the tape test had been negative, the FP could have chosen to treat empirically, since mebendazole is a safe medication. Another option would have been to have the parent apply the scotch tape to the boy’s perianal area first thing in the morning and bring the tape back to the office. (The yield is higher in the morning.)
Photo courtesy of James L. Fishback, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Chumley H. Intestinal worms and parasites. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:916-920.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The FP detected adult worms and ova of Enterobius vermicularis. Pinworms are acquired through the oral route when hands that have been in contact with contaminated objects are placed in the mouth. This can happen when kids play together in a sand box.
In this case, the young boy was treated with a single dose of chewable 100 mg mebendazole and his symptoms resolved. The parent was told to repeat the mebendazole dose in 2 weeks to increase the long-term cure rate.
If the tape test had been negative, the FP could have chosen to treat empirically, since mebendazole is a safe medication. Another option would have been to have the parent apply the scotch tape to the boy’s perianal area first thing in the morning and bring the tape back to the office. (The yield is higher in the morning.)
Photo courtesy of James L. Fishback, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Chumley H. Intestinal worms and parasites. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:916-920.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Painless cutaneous nodules
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 46-YEAR-OLD MAN came into our family medicine clinic because he wanted a few “lumps” removed from his left medial elbow and the back of his right thigh and knee. He indicated that he’d had the painless lesions for a long time, but that recently they’d started bothering him because they were getting caught on his clothes.
Other than these lesions, his past medical, social, and surgical histories were unremarkable. He indicated that his mother and 3 of his 5 siblings had similar lesions.
On physical exam, the patient had multiple nontender, soft, pedunculated, and relatively mobile nodules in different sizes (FIGURE 1A). There were also a few well-circumscribed and light brown patches on his left medial elbow (FIGURE 1B), the back of his right thigh, and his upper back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is an autosomal dominant multisystem disorder affecting about one in 3000 people.1-3 The NF1 gene is on chromosome 17q11.2, which encodes for neurofibromin protein.2,3 About half of these patients demonstrate a spontaneous mutation.1-5 Clinical features include cutaneous, subcutaneous, skeletal, peripheral, and central nervous systems abnormalities.
3 common features
Neurofibroma is the hallmark of NF1. Cutaneous and subcutaneous neurofibromas are benign peripheral nerve sheath tumors consisting of Schwann cells, fibroblasts, peripheral cells, mast cells, axons, and blood vessels.1-5 Neurofibromas usually develop when patients are in their late teens; they are often painless.
Café-au-lait spots are well-circumscribed, evenly pigmented, light to dark brown macules and/or patches with an average size of 2 to 5 cm (FIGURE 1B). Up to 10% of the general population may have one or 2 café-au-lait spots with no other abnormalities.6 Patients with NF1 will have 6 or more.1
Skin fold freckling is the most specific feature in patients with NF1. This freckling usually occurs in the axilla and groin regions when patients are between 3 and 5 years of age. The freckles are typically small, with an average size of 1 to 3 mm.
Other less common clinical features of NF1 include plexiform neurofibroma, skeletal abnormalities (short stature, scoliosis, long bone dysplasia, and osteopenia/ osteoporosis), Lisch nodules (iris hamartomas), neurocognitive deficits, cardiovascular abnormalities, and optic pathway gliomas.1-5
FIGURE 1
Widespread cutaneous nodules with hyperpigmented patches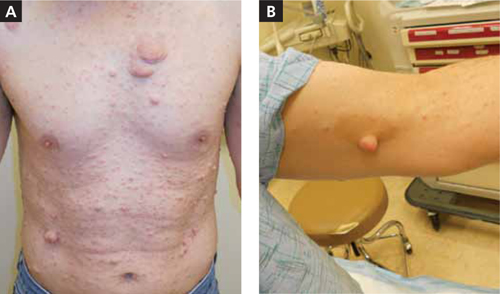
Is it neurofibromatosis type 1, or one of these 4 conditions?
Consider these conditions in the differential diagnosis of a patient who presents with soft, pedunculated nodules:
- Segmental/mosaic NF1 occurs as a result of NF1 somatic gene mutation. Clinical manifestations (pigmentary changes, tumor growths, or both) are limited to one or more body segments.3 The extent of the body parts affected depends on the time of the mutation in embryonic development.
- Neurofibromatosis 2 (NF2) is an autosomal dominant disease affecting one in 25,000 individuals.2 The characteristic feature is bilateral vestibular schwannomas.4,5 Other clinical features include meningiomas, schwannomas, gliomas, neurofibromas, and posterior subcapsular lens opacity. Café-au-lait spots are less common in NF2 than in NF1; only about one-third of NF2 patients have them.6
- Schwannomatosis is a disease with multiple subcutaneous, peripheral nerve, and spinal schwannomas.4,5 Patients do not have the vestibular schwannomas or the ophthalmologic features of NF2.
- Lipomatosis is an autosomal dominant disease featuring multiple lipomas on the trunk, proximal thighs, and distal arms. Depending on the location, the lipomas can be tender to touch. Biopsy may be necessary to differentiate lipomas from neurofibromas and schwannomas.
Diagnosis hinges on 2 of these 7 criteria
For adult patients, the diagnosis is clinical and straightforward. At least 2 of the following criteria should be present for the diagnosis:1-6
- 6 or more café-au-lait spots
- axillary or inguinal freckling
- 2 or more neurofibromas
- a first-degree relative with NF1
- 2 or more Lisch nodules
- a distinctive osseous lesion
- optic pathway glioma.
The diagnosis in youngsters, especially those younger than 8 years, can be difficult and may require genetic testing. Genetic testing is also recommended for individuals with a single sign, or with variant disorders.3 Genetic counseling and testing are also recommended in preimplantation and prenatal situations.3 Biopsy of the cutaneous and subcutaneous lesions for diagnostic purposes is not usually recommended.1-5
Management is challenging as there is no definitive treatment
The effect of NF1 on patients’ lives is significant. Management usually requires a multidisciplinary approach led by a primary care physician.3 To date, there is no definitive treatment for NF1.
Removal of symptomatic cutaneous and subcutaneous lesions is recommended; however, the recurrence rate is high1-3 (strength of recommendation [SOR]: B). About 10% of patients with NF1 will develop a malignant nerve sheath tumor, which usually arises from preexisting plexiform neurofibromas.1-4 Surgical excision with clear margins is the goal of treatment.2
A good outcome for my patient
The nodules on the patient’s medial elbow and the back of his thigh and knee were excised. The pathology confirmed the diagnosis. There was no malignant transformation.
CORRESPONDENCE Morteza Khodaee, MD, MPH, AFW Family Medicine Clinic, 3055 Roslyn Street, Denver, CO 80238; [email protected]
1. Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133.
2. Ferner RE. The neurofibromatoses. Pract Neurol. 2010;10:82-93.
3. Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1-14.
4. Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44:81-88.
5. Gerber PA, Antal AS, Neumann NJ, et al. Neurofibromatosis. Eur J Med Res. 2009;14:102-105.
6. Shah KN. The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am. 2010;57:1131-1153.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 46-YEAR-OLD MAN came into our family medicine clinic because he wanted a few “lumps” removed from his left medial elbow and the back of his right thigh and knee. He indicated that he’d had the painless lesions for a long time, but that recently they’d started bothering him because they were getting caught on his clothes.
Other than these lesions, his past medical, social, and surgical histories were unremarkable. He indicated that his mother and 3 of his 5 siblings had similar lesions.
On physical exam, the patient had multiple nontender, soft, pedunculated, and relatively mobile nodules in different sizes (FIGURE 1A). There were also a few well-circumscribed and light brown patches on his left medial elbow (FIGURE 1B), the back of his right thigh, and his upper back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is an autosomal dominant multisystem disorder affecting about one in 3000 people.1-3 The NF1 gene is on chromosome 17q11.2, which encodes for neurofibromin protein.2,3 About half of these patients demonstrate a spontaneous mutation.1-5 Clinical features include cutaneous, subcutaneous, skeletal, peripheral, and central nervous systems abnormalities.
3 common features
Neurofibroma is the hallmark of NF1. Cutaneous and subcutaneous neurofibromas are benign peripheral nerve sheath tumors consisting of Schwann cells, fibroblasts, peripheral cells, mast cells, axons, and blood vessels.1-5 Neurofibromas usually develop when patients are in their late teens; they are often painless.
Café-au-lait spots are well-circumscribed, evenly pigmented, light to dark brown macules and/or patches with an average size of 2 to 5 cm (FIGURE 1B). Up to 10% of the general population may have one or 2 café-au-lait spots with no other abnormalities.6 Patients with NF1 will have 6 or more.1
Skin fold freckling is the most specific feature in patients with NF1. This freckling usually occurs in the axilla and groin regions when patients are between 3 and 5 years of age. The freckles are typically small, with an average size of 1 to 3 mm.
Other less common clinical features of NF1 include plexiform neurofibroma, skeletal abnormalities (short stature, scoliosis, long bone dysplasia, and osteopenia/ osteoporosis), Lisch nodules (iris hamartomas), neurocognitive deficits, cardiovascular abnormalities, and optic pathway gliomas.1-5
FIGURE 1
Widespread cutaneous nodules with hyperpigmented patches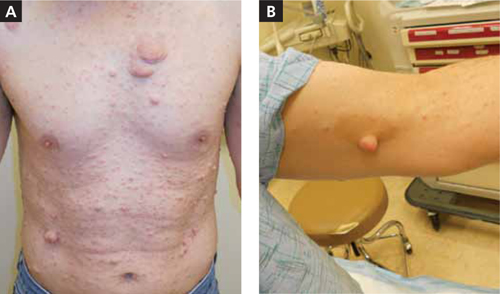
Is it neurofibromatosis type 1, or one of these 4 conditions?
Consider these conditions in the differential diagnosis of a patient who presents with soft, pedunculated nodules:
- Segmental/mosaic NF1 occurs as a result of NF1 somatic gene mutation. Clinical manifestations (pigmentary changes, tumor growths, or both) are limited to one or more body segments.3 The extent of the body parts affected depends on the time of the mutation in embryonic development.
- Neurofibromatosis 2 (NF2) is an autosomal dominant disease affecting one in 25,000 individuals.2 The characteristic feature is bilateral vestibular schwannomas.4,5 Other clinical features include meningiomas, schwannomas, gliomas, neurofibromas, and posterior subcapsular lens opacity. Café-au-lait spots are less common in NF2 than in NF1; only about one-third of NF2 patients have them.6
- Schwannomatosis is a disease with multiple subcutaneous, peripheral nerve, and spinal schwannomas.4,5 Patients do not have the vestibular schwannomas or the ophthalmologic features of NF2.
- Lipomatosis is an autosomal dominant disease featuring multiple lipomas on the trunk, proximal thighs, and distal arms. Depending on the location, the lipomas can be tender to touch. Biopsy may be necessary to differentiate lipomas from neurofibromas and schwannomas.
Diagnosis hinges on 2 of these 7 criteria
For adult patients, the diagnosis is clinical and straightforward. At least 2 of the following criteria should be present for the diagnosis:1-6
- 6 or more café-au-lait spots
- axillary or inguinal freckling
- 2 or more neurofibromas
- a first-degree relative with NF1
- 2 or more Lisch nodules
- a distinctive osseous lesion
- optic pathway glioma.
The diagnosis in youngsters, especially those younger than 8 years, can be difficult and may require genetic testing. Genetic testing is also recommended for individuals with a single sign, or with variant disorders.3 Genetic counseling and testing are also recommended in preimplantation and prenatal situations.3 Biopsy of the cutaneous and subcutaneous lesions for diagnostic purposes is not usually recommended.1-5
Management is challenging as there is no definitive treatment
The effect of NF1 on patients’ lives is significant. Management usually requires a multidisciplinary approach led by a primary care physician.3 To date, there is no definitive treatment for NF1.
Removal of symptomatic cutaneous and subcutaneous lesions is recommended; however, the recurrence rate is high1-3 (strength of recommendation [SOR]: B). About 10% of patients with NF1 will develop a malignant nerve sheath tumor, which usually arises from preexisting plexiform neurofibromas.1-4 Surgical excision with clear margins is the goal of treatment.2
A good outcome for my patient
The nodules on the patient’s medial elbow and the back of his thigh and knee were excised. The pathology confirmed the diagnosis. There was no malignant transformation.
CORRESPONDENCE Morteza Khodaee, MD, MPH, AFW Family Medicine Clinic, 3055 Roslyn Street, Denver, CO 80238; [email protected]
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 46-YEAR-OLD MAN came into our family medicine clinic because he wanted a few “lumps” removed from his left medial elbow and the back of his right thigh and knee. He indicated that he’d had the painless lesions for a long time, but that recently they’d started bothering him because they were getting caught on his clothes.
Other than these lesions, his past medical, social, and surgical histories were unremarkable. He indicated that his mother and 3 of his 5 siblings had similar lesions.
On physical exam, the patient had multiple nontender, soft, pedunculated, and relatively mobile nodules in different sizes (FIGURE 1A). There were also a few well-circumscribed and light brown patches on his left medial elbow (FIGURE 1B), the back of his right thigh, and his upper back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is an autosomal dominant multisystem disorder affecting about one in 3000 people.1-3 The NF1 gene is on chromosome 17q11.2, which encodes for neurofibromin protein.2,3 About half of these patients demonstrate a spontaneous mutation.1-5 Clinical features include cutaneous, subcutaneous, skeletal, peripheral, and central nervous systems abnormalities.
3 common features
Neurofibroma is the hallmark of NF1. Cutaneous and subcutaneous neurofibromas are benign peripheral nerve sheath tumors consisting of Schwann cells, fibroblasts, peripheral cells, mast cells, axons, and blood vessels.1-5 Neurofibromas usually develop when patients are in their late teens; they are often painless.
Café-au-lait spots are well-circumscribed, evenly pigmented, light to dark brown macules and/or patches with an average size of 2 to 5 cm (FIGURE 1B). Up to 10% of the general population may have one or 2 café-au-lait spots with no other abnormalities.6 Patients with NF1 will have 6 or more.1
Skin fold freckling is the most specific feature in patients with NF1. This freckling usually occurs in the axilla and groin regions when patients are between 3 and 5 years of age. The freckles are typically small, with an average size of 1 to 3 mm.
Other less common clinical features of NF1 include plexiform neurofibroma, skeletal abnormalities (short stature, scoliosis, long bone dysplasia, and osteopenia/ osteoporosis), Lisch nodules (iris hamartomas), neurocognitive deficits, cardiovascular abnormalities, and optic pathway gliomas.1-5
FIGURE 1
Widespread cutaneous nodules with hyperpigmented patches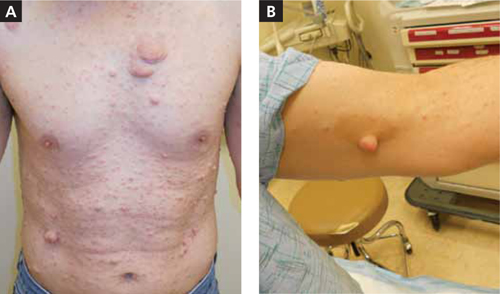
Is it neurofibromatosis type 1, or one of these 4 conditions?
Consider these conditions in the differential diagnosis of a patient who presents with soft, pedunculated nodules:
- Segmental/mosaic NF1 occurs as a result of NF1 somatic gene mutation. Clinical manifestations (pigmentary changes, tumor growths, or both) are limited to one or more body segments.3 The extent of the body parts affected depends on the time of the mutation in embryonic development.
- Neurofibromatosis 2 (NF2) is an autosomal dominant disease affecting one in 25,000 individuals.2 The characteristic feature is bilateral vestibular schwannomas.4,5 Other clinical features include meningiomas, schwannomas, gliomas, neurofibromas, and posterior subcapsular lens opacity. Café-au-lait spots are less common in NF2 than in NF1; only about one-third of NF2 patients have them.6
- Schwannomatosis is a disease with multiple subcutaneous, peripheral nerve, and spinal schwannomas.4,5 Patients do not have the vestibular schwannomas or the ophthalmologic features of NF2.
- Lipomatosis is an autosomal dominant disease featuring multiple lipomas on the trunk, proximal thighs, and distal arms. Depending on the location, the lipomas can be tender to touch. Biopsy may be necessary to differentiate lipomas from neurofibromas and schwannomas.
Diagnosis hinges on 2 of these 7 criteria
For adult patients, the diagnosis is clinical and straightforward. At least 2 of the following criteria should be present for the diagnosis:1-6
- 6 or more café-au-lait spots
- axillary or inguinal freckling
- 2 or more neurofibromas
- a first-degree relative with NF1
- 2 or more Lisch nodules
- a distinctive osseous lesion
- optic pathway glioma.
The diagnosis in youngsters, especially those younger than 8 years, can be difficult and may require genetic testing. Genetic testing is also recommended for individuals with a single sign, or with variant disorders.3 Genetic counseling and testing are also recommended in preimplantation and prenatal situations.3 Biopsy of the cutaneous and subcutaneous lesions for diagnostic purposes is not usually recommended.1-5
Management is challenging as there is no definitive treatment
The effect of NF1 on patients’ lives is significant. Management usually requires a multidisciplinary approach led by a primary care physician.3 To date, there is no definitive treatment for NF1.
Removal of symptomatic cutaneous and subcutaneous lesions is recommended; however, the recurrence rate is high1-3 (strength of recommendation [SOR]: B). About 10% of patients with NF1 will develop a malignant nerve sheath tumor, which usually arises from preexisting plexiform neurofibromas.1-4 Surgical excision with clear margins is the goal of treatment.2
A good outcome for my patient
The nodules on the patient’s medial elbow and the back of his thigh and knee were excised. The pathology confirmed the diagnosis. There was no malignant transformation.
CORRESPONDENCE Morteza Khodaee, MD, MPH, AFW Family Medicine Clinic, 3055 Roslyn Street, Denver, CO 80238; [email protected]
1. Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133.
2. Ferner RE. The neurofibromatoses. Pract Neurol. 2010;10:82-93.
3. Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1-14.
4. Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44:81-88.
5. Gerber PA, Antal AS, Neumann NJ, et al. Neurofibromatosis. Eur J Med Res. 2009;14:102-105.
6. Shah KN. The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am. 2010;57:1131-1153.
1. Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133.
2. Ferner RE. The neurofibromatoses. Pract Neurol. 2010;10:82-93.
3. Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1-14.
4. Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44:81-88.
5. Gerber PA, Antal AS, Neumann NJ, et al. Neurofibromatosis. Eur J Med Res. 2009;14:102-105.
6. Shah KN. The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am. 2010;57:1131-1153.
Black toes

|
The family physician diagnosed peripheral arterial disease. PAD is an important factor leading to lower extremity amputation in patients with diabetes. Thirty percent of patients with diabetes who have an absent pedal pulse will have some degree of coronary artery disease.
PAD manifests in the lower extremity in 2 ways: macro- and microvascular diseases. Risk factors such as hypercholesteremia, hyperlipidemia, and hypertension are often associated with patients with PAD and, therefore, poor wound healing.
Dry, black eschar commonly begins distally at the extremities. There is a clear demarcation between healthy tissue and necrotic tissue. Pain may be present, and trauma is the most common etiology. Pulses may be nonpalpable. Smoking is commonly associated with this problem. Associated trophic skin changes include absent pedal hair and thin shiny skin.
Even in the presence of a palpable pulse, noninvasive studies (eg, arterial Doppler and pulse volume recordings) are important for baseline assessment of the patient’s blood flow. An angiogram is required to evaluate the possibility of revascularization. Radiographs may be necessary to rule out osteomyelitis.
This patient was admitted for IV antibiotics and revascularization was performed. Subsequently, the toes were partially amputated and the wounds healed without complication. Physicians attempted to help the patient to quit smoking, but were unsuccessful.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: La Fontaine J, Shibuya, N. Dry gangrene. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:912-913.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

|
The family physician diagnosed peripheral arterial disease. PAD is an important factor leading to lower extremity amputation in patients with diabetes. Thirty percent of patients with diabetes who have an absent pedal pulse will have some degree of coronary artery disease.
PAD manifests in the lower extremity in 2 ways: macro- and microvascular diseases. Risk factors such as hypercholesteremia, hyperlipidemia, and hypertension are often associated with patients with PAD and, therefore, poor wound healing.
Dry, black eschar commonly begins distally at the extremities. There is a clear demarcation between healthy tissue and necrotic tissue. Pain may be present, and trauma is the most common etiology. Pulses may be nonpalpable. Smoking is commonly associated with this problem. Associated trophic skin changes include absent pedal hair and thin shiny skin.
Even in the presence of a palpable pulse, noninvasive studies (eg, arterial Doppler and pulse volume recordings) are important for baseline assessment of the patient’s blood flow. An angiogram is required to evaluate the possibility of revascularization. Radiographs may be necessary to rule out osteomyelitis.
This patient was admitted for IV antibiotics and revascularization was performed. Subsequently, the toes were partially amputated and the wounds healed without complication. Physicians attempted to help the patient to quit smoking, but were unsuccessful.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: La Fontaine J, Shibuya, N. Dry gangrene. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:912-913.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

|
The family physician diagnosed peripheral arterial disease. PAD is an important factor leading to lower extremity amputation in patients with diabetes. Thirty percent of patients with diabetes who have an absent pedal pulse will have some degree of coronary artery disease.
PAD manifests in the lower extremity in 2 ways: macro- and microvascular diseases. Risk factors such as hypercholesteremia, hyperlipidemia, and hypertension are often associated with patients with PAD and, therefore, poor wound healing.
Dry, black eschar commonly begins distally at the extremities. There is a clear demarcation between healthy tissue and necrotic tissue. Pain may be present, and trauma is the most common etiology. Pulses may be nonpalpable. Smoking is commonly associated with this problem. Associated trophic skin changes include absent pedal hair and thin shiny skin.
Even in the presence of a palpable pulse, noninvasive studies (eg, arterial Doppler and pulse volume recordings) are important for baseline assessment of the patient’s blood flow. An angiogram is required to evaluate the possibility of revascularization. Radiographs may be necessary to rule out osteomyelitis.
This patient was admitted for IV antibiotics and revascularization was performed. Subsequently, the toes were partially amputated and the wounds healed without complication. Physicians attempted to help the patient to quit smoking, but were unsuccessful.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: La Fontaine J, Shibuya, N. Dry gangrene. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:912-913.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Swollen foot

| 
| 
|
| FIGURE 1 | FIGURE 2 | FIGURE 3 |
The appearance of the patient’s foot (FIGURE 1) prompted the physician to order a radiograph (FIGURE 2), which revealed midfoot osteopenia—an early sign of acute Charcot arthropathy. The incidence of Charcot arthropathy in diabetes ranges from 0.1% to 5%. Untreated Charcot foot may lead to a rockerbottom foot (FIGURE 3), which in turn leads to increased plantar pressure in the neuropathic foot. This cascade will result in ulceration and possible amputation. Charcot arthropathy is a gradual destruction of the joint in patients with neurosensory loss. Its most common presentation is in the diabetic neuropathic patient. Clinical features include a red, hot, swollen foot with neurosensory loss. The pathogenesis is unknown.
Radiographs are imperative for diagnosis. Usually, radiographs show arch collapse within the joints of the midfoot (tarsometatarsal joints). Radiographs can also show erosions and cystic degeneration of the tarsometatarsal joints. When infection is suspected, other imaging modalities such as a bone scan and magnetic resonance imaging may be ordered, but are often inconclusive because of the difficulty differentiating cellulitis, osteomyelitis, and Charcot arthropathy.
If osteomyelitis is suspected, bone cultures and bone biopsy are recommended. Cultures need to be taken during the bone biopsy so that the suspected infected bone can be visualized for accurate sampling.
Off-loading pressure from the foot is the standard of care. The total contact cast is most effective, and it covers the toes for protection. Other methods that are used include the removable cast boot, crutches, and a wheelchair.
If foot care is not optimized, a plantar ulcer can form under the Charcot’s joints. The bones will take approximately 4 to 5 months to heal in the presence of neuropathy. Oral antibiotics are not indicated unless infection is suspected. If deformity develops, custom-molded shoes and insoles must be ordered to prevent plantar ulcers that can lead to amputation.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photos courtesy of Javier La Fontaine, DPM. This case was adapted from: La Fontaine J, Shibuya, N. Charcot arthropathy. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:909-911.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

| 
| 
|
| FIGURE 1 | FIGURE 2 | FIGURE 3 |
The appearance of the patient’s foot (FIGURE 1) prompted the physician to order a radiograph (FIGURE 2), which revealed midfoot osteopenia—an early sign of acute Charcot arthropathy. The incidence of Charcot arthropathy in diabetes ranges from 0.1% to 5%. Untreated Charcot foot may lead to a rockerbottom foot (FIGURE 3), which in turn leads to increased plantar pressure in the neuropathic foot. This cascade will result in ulceration and possible amputation. Charcot arthropathy is a gradual destruction of the joint in patients with neurosensory loss. Its most common presentation is in the diabetic neuropathic patient. Clinical features include a red, hot, swollen foot with neurosensory loss. The pathogenesis is unknown.
Radiographs are imperative for diagnosis. Usually, radiographs show arch collapse within the joints of the midfoot (tarsometatarsal joints). Radiographs can also show erosions and cystic degeneration of the tarsometatarsal joints. When infection is suspected, other imaging modalities such as a bone scan and magnetic resonance imaging may be ordered, but are often inconclusive because of the difficulty differentiating cellulitis, osteomyelitis, and Charcot arthropathy.
If osteomyelitis is suspected, bone cultures and bone biopsy are recommended. Cultures need to be taken during the bone biopsy so that the suspected infected bone can be visualized for accurate sampling.
Off-loading pressure from the foot is the standard of care. The total contact cast is most effective, and it covers the toes for protection. Other methods that are used include the removable cast boot, crutches, and a wheelchair.
If foot care is not optimized, a plantar ulcer can form under the Charcot’s joints. The bones will take approximately 4 to 5 months to heal in the presence of neuropathy. Oral antibiotics are not indicated unless infection is suspected. If deformity develops, custom-molded shoes and insoles must be ordered to prevent plantar ulcers that can lead to amputation.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photos courtesy of Javier La Fontaine, DPM. This case was adapted from: La Fontaine J, Shibuya, N. Charcot arthropathy. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:909-911.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

| 
| 
|
| FIGURE 1 | FIGURE 2 | FIGURE 3 |
The appearance of the patient’s foot (FIGURE 1) prompted the physician to order a radiograph (FIGURE 2), which revealed midfoot osteopenia—an early sign of acute Charcot arthropathy. The incidence of Charcot arthropathy in diabetes ranges from 0.1% to 5%. Untreated Charcot foot may lead to a rockerbottom foot (FIGURE 3), which in turn leads to increased plantar pressure in the neuropathic foot. This cascade will result in ulceration and possible amputation. Charcot arthropathy is a gradual destruction of the joint in patients with neurosensory loss. Its most common presentation is in the diabetic neuropathic patient. Clinical features include a red, hot, swollen foot with neurosensory loss. The pathogenesis is unknown.
Radiographs are imperative for diagnosis. Usually, radiographs show arch collapse within the joints of the midfoot (tarsometatarsal joints). Radiographs can also show erosions and cystic degeneration of the tarsometatarsal joints. When infection is suspected, other imaging modalities such as a bone scan and magnetic resonance imaging may be ordered, but are often inconclusive because of the difficulty differentiating cellulitis, osteomyelitis, and Charcot arthropathy.
If osteomyelitis is suspected, bone cultures and bone biopsy are recommended. Cultures need to be taken during the bone biopsy so that the suspected infected bone can be visualized for accurate sampling.
Off-loading pressure from the foot is the standard of care. The total contact cast is most effective, and it covers the toes for protection. Other methods that are used include the removable cast boot, crutches, and a wheelchair.
If foot care is not optimized, a plantar ulcer can form under the Charcot’s joints. The bones will take approximately 4 to 5 months to heal in the presence of neuropathy. Oral antibiotics are not indicated unless infection is suspected. If deformity develops, custom-molded shoes and insoles must be ordered to prevent plantar ulcers that can lead to amputation.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photos courtesy of Javier La Fontaine, DPM. This case was adapted from: La Fontaine J, Shibuya, N. Charcot arthropathy. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:909-911.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Foot ulcer

The family physician made a diagnosis of neuropathic ulceration based upon the clinical findings. Neuropathy causes approximately 50% of diabetic foot ulcers. Having diabetic neuropathy alone makes a patient 1.7 times more likely to develop foot ulceration. Patients with diabetic neuropathy combined with pedal deformity are 12.1 times more likely to develop ulceration. The mechanism of injury is commonly described as moderate pressure with repetitive trauma.
Overall 15% of people with diabetes will experience a foot ulcer during their lifetime, and 15% of these will have osteomyelitis. Foot ulcers can develop in any location of the foot but are more common under the metatarsal heads, hallux, heel, or other weight-bearing areas. Foot ulcers may also result from poorly fitting footwear, which creates excessive pressure, friction, or irritation.
Neuropathic ulcers often have a red, granular base with surrounding hyperkeratosis with white, macerated margins. The ulcer is most commonly found under the metatarsal heads, but it can also be present in the distal and plantar aspects of the toes. Cultures are only indicated if infection is suspected. Swab cultures are not reliable. Curettage of the base of the wound may be more reliable. Radiographs may identify a foreign body, or underlying osteomyelitis. A biopsy may be necessary to rule out a suspected malignancy.
Off-loading pressure from the foot is the standard of care. Multiple devices (eg, removable cast boot, surgical shoes, and wedge shoes) are used for off-loading; however, a total contact cast is the gold standard. Serial tissue debridement should be performed weekly to biweekly to maintain minimal bacterial load, low pressure surrounding the ulcer, and a metabolically active wound base.
If no improvement in the ulcer is noticed in 4 weeks, the ulcer should be considered a chronic wound, and adjunctive therapy (eg, growth factors) must be considered.
In this case, the primary physician referred the patient to a podiatrist, who immediately off-loaded the foot with a total contact cast. The patient’s ulcer healed in one month and he was subsequently fitted with orthopedic shoes.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Javier La Fontaine, DPM. This case was adapted from: La Fontaine J, Shibuya, N. Neuropathic ulcer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:907-908.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The family physician made a diagnosis of neuropathic ulceration based upon the clinical findings. Neuropathy causes approximately 50% of diabetic foot ulcers. Having diabetic neuropathy alone makes a patient 1.7 times more likely to develop foot ulceration. Patients with diabetic neuropathy combined with pedal deformity are 12.1 times more likely to develop ulceration. The mechanism of injury is commonly described as moderate pressure with repetitive trauma.
Overall 15% of people with diabetes will experience a foot ulcer during their lifetime, and 15% of these will have osteomyelitis. Foot ulcers can develop in any location of the foot but are more common under the metatarsal heads, hallux, heel, or other weight-bearing areas. Foot ulcers may also result from poorly fitting footwear, which creates excessive pressure, friction, or irritation.
Neuropathic ulcers often have a red, granular base with surrounding hyperkeratosis with white, macerated margins. The ulcer is most commonly found under the metatarsal heads, but it can also be present in the distal and plantar aspects of the toes. Cultures are only indicated if infection is suspected. Swab cultures are not reliable. Curettage of the base of the wound may be more reliable. Radiographs may identify a foreign body, or underlying osteomyelitis. A biopsy may be necessary to rule out a suspected malignancy.
Off-loading pressure from the foot is the standard of care. Multiple devices (eg, removable cast boot, surgical shoes, and wedge shoes) are used for off-loading; however, a total contact cast is the gold standard. Serial tissue debridement should be performed weekly to biweekly to maintain minimal bacterial load, low pressure surrounding the ulcer, and a metabolically active wound base.
If no improvement in the ulcer is noticed in 4 weeks, the ulcer should be considered a chronic wound, and adjunctive therapy (eg, growth factors) must be considered.
In this case, the primary physician referred the patient to a podiatrist, who immediately off-loaded the foot with a total contact cast. The patient’s ulcer healed in one month and he was subsequently fitted with orthopedic shoes.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Javier La Fontaine, DPM. This case was adapted from: La Fontaine J, Shibuya, N. Neuropathic ulcer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:907-908.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The family physician made a diagnosis of neuropathic ulceration based upon the clinical findings. Neuropathy causes approximately 50% of diabetic foot ulcers. Having diabetic neuropathy alone makes a patient 1.7 times more likely to develop foot ulceration. Patients with diabetic neuropathy combined with pedal deformity are 12.1 times more likely to develop ulceration. The mechanism of injury is commonly described as moderate pressure with repetitive trauma.
Overall 15% of people with diabetes will experience a foot ulcer during their lifetime, and 15% of these will have osteomyelitis. Foot ulcers can develop in any location of the foot but are more common under the metatarsal heads, hallux, heel, or other weight-bearing areas. Foot ulcers may also result from poorly fitting footwear, which creates excessive pressure, friction, or irritation.
Neuropathic ulcers often have a red, granular base with surrounding hyperkeratosis with white, macerated margins. The ulcer is most commonly found under the metatarsal heads, but it can also be present in the distal and plantar aspects of the toes. Cultures are only indicated if infection is suspected. Swab cultures are not reliable. Curettage of the base of the wound may be more reliable. Radiographs may identify a foreign body, or underlying osteomyelitis. A biopsy may be necessary to rule out a suspected malignancy.
Off-loading pressure from the foot is the standard of care. Multiple devices (eg, removable cast boot, surgical shoes, and wedge shoes) are used for off-loading; however, a total contact cast is the gold standard. Serial tissue debridement should be performed weekly to biweekly to maintain minimal bacterial load, low pressure surrounding the ulcer, and a metabolically active wound base.
If no improvement in the ulcer is noticed in 4 weeks, the ulcer should be considered a chronic wound, and adjunctive therapy (eg, growth factors) must be considered.
In this case, the primary physician referred the patient to a podiatrist, who immediately off-loaded the foot with a total contact cast. The patient’s ulcer healed in one month and he was subsequently fitted with orthopedic shoes.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Javier La Fontaine, DPM. This case was adapted from: La Fontaine J, Shibuya, N. Neuropathic ulcer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:907-908.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Stubborn hand rash
A 24-YEAR-OLD MAN sought care at our primary care clinic for a stubborn rash that had come on gradually and grown to cover much of his left hand. The rash itched and after much scratching, it began to crack and enlarge. The patient denied any trauma to the hand, but said that the rash was now mildly painful.
The patient indicated that he’d applied a topical antifungal agent to his hand and that the lesion initially shrunk. However, after he stopped using the cream, the rash flared again. He denied any similar lesions on his body, but did note that he occasionally suffered from athlete’s foot. The patient said that he did not wear any rings or gloves regularly. He also denied excessive hand washing.
On examination, I noted a well-circumscribed, dry, flaky, erythematous plaque that extended to the base of each of his 4 fingers (FIGURE 1A). One of the extensions continued to the dorsal side of the middle finger; this area was raised, scaly, and had a scab (FIGURE 1B). The webbing of the fingers was also involved, but the nails were spared.
FIGURE 1
Pruritic rash extends to the dorsal side of the middle finger
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tinea manuum
This patient was given a diagnosis of tinea manuum, also known as two feet-one hand syndrome, a dermatophyte infection. The patient was initially treating his rash appropriately with the topical antifungal, but failed to treat his concomitant tinea pedis.
The infection is believed to be spread from the feet to the hand by scratching, as tinea pedis or onychomycosis of the toenails precede infection of the hand.1 Whether one is right-handed or left-handed does not appear to play a role in which hand is affected.2,3 However, the hand used to scratch or pick the feet is usually the hand that becomes involved.3,4 The condition is more common in men and it tends to develop at an earlier age in patients who work with their hands.3
Tinea manuum is rare, with occurrence rates ranging from 0.3% to 0.7% of those with superficial fungal infections.5 The true culprit in two feet-one hand syndrome are the feet. Unlike tinea manuum, tinea pedis is the most common fungal skin infection in North America and Europe.6 The most common agents isolated in tinea pedis are Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum.7
The condition presents in one of 4 ways
The differential for two feet-one hand syndrome includes contact dermatitis, an Id reaction (autoeczematization), cellulitis, or a herpetic lesion.2,8
Tinea pedis generally presents in one of 4 ways:1
- Classic ringworm features an erythematous, scaly, well-circumscribed rash on the feet.
- Interdigital tinea pedis has toe web involvement, often between the fourth and fifth toes. It can transition between dry and scaly to soft, soggy, and macerated. Skin may become white and fissures may arise. Pruritus is often worse after the toes dry.
- Moccasin type (plantar hyperkeratotic tinea pedis) features a fine white silvery scale that often covers the entire sole. Skin may be pink and itch. The dorsum of the feet is not usually involved.
- Acute vesicular tinea pedis is a highly inflammatory infection with vesicles that may coalesce into bullae. It likely stems from a chronic infection and is more common when occlusive shoes are worn.
Do a skin scraping
Diagnosis can be easily made with a good history and physical and a potassium hydroxide test. If a scraping from the hand proves to be fungal, a thorough inspection of the feet should be undertaken, as tinea manuum alone is uncommon.
Tx is the same for feet and hand
Topical antifungals such as terbinafine, clotrimazole, or ketoconazole are first-line therapy for the feet and hand.9 Consider oral antifungals if the affected area is large, the patient doesn’t respond to topical therapy, or the patient is immunocompromised.9,10
When oral therapy is initiated for tinea manuum, one week of itraconazole (200 mg twice daily for 7 days) has been shown to be as effective as 2 weeks of oral terbinafine (250 mg daily for 14 days).10
Oral therapy worked for my patient
In light of the patient’s previous failure with topical therapy, he was reluctant to try this approach again. After a normal hepatic panel, I started him on a 2-week course of oral terbinafine 250 mg daily. (Terbinafine was available at our clinic pharmacy, while itraconazole was not). Follow-up at one month showed no sign of previous infection.
CORRESPONDENCE LT Michael Crandall, MD, Department of Dermatology, Naval Medical Center San Diego, 34800 Bob Wilson Drive, San Diego, CA 92134; [email protected]
1. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 5th ed. Philadelphia, Pa: Mosby/Elsevier; 2010:491–540.
2. Wilson M, Bender S, Lynfield Y, et al. Two feet-one hand syndrome. J Am Podiatr Med Assoc. 1988;78:250-253.
3. Daniel CR 3rd, Gupta AK, Daniel MP, et al. Two feet-one hand syndrome: a retrospective multicenter survey. Int J Dermatol. 1997;36:658-660.
4. Park BC, Lee SJ, Kim do W, et al. Molecular identification of mycologic correlation in patients with concomitant tinea pedis and tinea manuum infection. Arch Dermatol. 2009;145:205-207.
5. Zhan P, Ge YP, Lu XL, et al. A case-control analysis and laboratory study of the two feet-one hand syndrome in two dermatology hospitals in China. Clin Exp Dermatol. 2010;35:468-472.
6. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin: tinea capitis and tinea barbae. J Am Acad Dermatol. 1996;34(2 pt 1):290-294.
7. Geary RJ, Lucky AW. Tinea pedis in children presenting as unilateral inflammatory lesions of the sole. Pediatr Dermatol. 1999;16:255-258.
8. Sweeney SM, Wiss K, Mallory SB. Inflammatory tinea pedis/manuum masquerading as bacterial cellulitis. Arch Pediatr Adolesc Med. 2002;156:1149-1152.
9. Gupta AK, Cooper EA. Update in antifungal therapy of dermatophytosis. Mycopathologia. 2008;166:353-367.
10. Gupta AK, De Doncker P, Degreef H. Tinea manus treated with 1-week itraconazole vs. terbinafine. Int J Dermatol. 2000;39:529-531.
A 24-YEAR-OLD MAN sought care at our primary care clinic for a stubborn rash that had come on gradually and grown to cover much of his left hand. The rash itched and after much scratching, it began to crack and enlarge. The patient denied any trauma to the hand, but said that the rash was now mildly painful.
The patient indicated that he’d applied a topical antifungal agent to his hand and that the lesion initially shrunk. However, after he stopped using the cream, the rash flared again. He denied any similar lesions on his body, but did note that he occasionally suffered from athlete’s foot. The patient said that he did not wear any rings or gloves regularly. He also denied excessive hand washing.
On examination, I noted a well-circumscribed, dry, flaky, erythematous plaque that extended to the base of each of his 4 fingers (FIGURE 1A). One of the extensions continued to the dorsal side of the middle finger; this area was raised, scaly, and had a scab (FIGURE 1B). The webbing of the fingers was also involved, but the nails were spared.
FIGURE 1
Pruritic rash extends to the dorsal side of the middle finger
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tinea manuum
This patient was given a diagnosis of tinea manuum, also known as two feet-one hand syndrome, a dermatophyte infection. The patient was initially treating his rash appropriately with the topical antifungal, but failed to treat his concomitant tinea pedis.
The infection is believed to be spread from the feet to the hand by scratching, as tinea pedis or onychomycosis of the toenails precede infection of the hand.1 Whether one is right-handed or left-handed does not appear to play a role in which hand is affected.2,3 However, the hand used to scratch or pick the feet is usually the hand that becomes involved.3,4 The condition is more common in men and it tends to develop at an earlier age in patients who work with their hands.3
Tinea manuum is rare, with occurrence rates ranging from 0.3% to 0.7% of those with superficial fungal infections.5 The true culprit in two feet-one hand syndrome are the feet. Unlike tinea manuum, tinea pedis is the most common fungal skin infection in North America and Europe.6 The most common agents isolated in tinea pedis are Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum.7
The condition presents in one of 4 ways
The differential for two feet-one hand syndrome includes contact dermatitis, an Id reaction (autoeczematization), cellulitis, or a herpetic lesion.2,8
Tinea pedis generally presents in one of 4 ways:1
- Classic ringworm features an erythematous, scaly, well-circumscribed rash on the feet.
- Interdigital tinea pedis has toe web involvement, often between the fourth and fifth toes. It can transition between dry and scaly to soft, soggy, and macerated. Skin may become white and fissures may arise. Pruritus is often worse after the toes dry.
- Moccasin type (plantar hyperkeratotic tinea pedis) features a fine white silvery scale that often covers the entire sole. Skin may be pink and itch. The dorsum of the feet is not usually involved.
- Acute vesicular tinea pedis is a highly inflammatory infection with vesicles that may coalesce into bullae. It likely stems from a chronic infection and is more common when occlusive shoes are worn.
Do a skin scraping
Diagnosis can be easily made with a good history and physical and a potassium hydroxide test. If a scraping from the hand proves to be fungal, a thorough inspection of the feet should be undertaken, as tinea manuum alone is uncommon.
Tx is the same for feet and hand
Topical antifungals such as terbinafine, clotrimazole, or ketoconazole are first-line therapy for the feet and hand.9 Consider oral antifungals if the affected area is large, the patient doesn’t respond to topical therapy, or the patient is immunocompromised.9,10
When oral therapy is initiated for tinea manuum, one week of itraconazole (200 mg twice daily for 7 days) has been shown to be as effective as 2 weeks of oral terbinafine (250 mg daily for 14 days).10
Oral therapy worked for my patient
In light of the patient’s previous failure with topical therapy, he was reluctant to try this approach again. After a normal hepatic panel, I started him on a 2-week course of oral terbinafine 250 mg daily. (Terbinafine was available at our clinic pharmacy, while itraconazole was not). Follow-up at one month showed no sign of previous infection.
CORRESPONDENCE LT Michael Crandall, MD, Department of Dermatology, Naval Medical Center San Diego, 34800 Bob Wilson Drive, San Diego, CA 92134; [email protected]
A 24-YEAR-OLD MAN sought care at our primary care clinic for a stubborn rash that had come on gradually and grown to cover much of his left hand. The rash itched and after much scratching, it began to crack and enlarge. The patient denied any trauma to the hand, but said that the rash was now mildly painful.
The patient indicated that he’d applied a topical antifungal agent to his hand and that the lesion initially shrunk. However, after he stopped using the cream, the rash flared again. He denied any similar lesions on his body, but did note that he occasionally suffered from athlete’s foot. The patient said that he did not wear any rings or gloves regularly. He also denied excessive hand washing.
On examination, I noted a well-circumscribed, dry, flaky, erythematous plaque that extended to the base of each of his 4 fingers (FIGURE 1A). One of the extensions continued to the dorsal side of the middle finger; this area was raised, scaly, and had a scab (FIGURE 1B). The webbing of the fingers was also involved, but the nails were spared.
FIGURE 1
Pruritic rash extends to the dorsal side of the middle finger
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tinea manuum
This patient was given a diagnosis of tinea manuum, also known as two feet-one hand syndrome, a dermatophyte infection. The patient was initially treating his rash appropriately with the topical antifungal, but failed to treat his concomitant tinea pedis.
The infection is believed to be spread from the feet to the hand by scratching, as tinea pedis or onychomycosis of the toenails precede infection of the hand.1 Whether one is right-handed or left-handed does not appear to play a role in which hand is affected.2,3 However, the hand used to scratch or pick the feet is usually the hand that becomes involved.3,4 The condition is more common in men and it tends to develop at an earlier age in patients who work with their hands.3
Tinea manuum is rare, with occurrence rates ranging from 0.3% to 0.7% of those with superficial fungal infections.5 The true culprit in two feet-one hand syndrome are the feet. Unlike tinea manuum, tinea pedis is the most common fungal skin infection in North America and Europe.6 The most common agents isolated in tinea pedis are Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum.7
The condition presents in one of 4 ways
The differential for two feet-one hand syndrome includes contact dermatitis, an Id reaction (autoeczematization), cellulitis, or a herpetic lesion.2,8
Tinea pedis generally presents in one of 4 ways:1
- Classic ringworm features an erythematous, scaly, well-circumscribed rash on the feet.
- Interdigital tinea pedis has toe web involvement, often between the fourth and fifth toes. It can transition between dry and scaly to soft, soggy, and macerated. Skin may become white and fissures may arise. Pruritus is often worse after the toes dry.
- Moccasin type (plantar hyperkeratotic tinea pedis) features a fine white silvery scale that often covers the entire sole. Skin may be pink and itch. The dorsum of the feet is not usually involved.
- Acute vesicular tinea pedis is a highly inflammatory infection with vesicles that may coalesce into bullae. It likely stems from a chronic infection and is more common when occlusive shoes are worn.
Do a skin scraping
Diagnosis can be easily made with a good history and physical and a potassium hydroxide test. If a scraping from the hand proves to be fungal, a thorough inspection of the feet should be undertaken, as tinea manuum alone is uncommon.
Tx is the same for feet and hand
Topical antifungals such as terbinafine, clotrimazole, or ketoconazole are first-line therapy for the feet and hand.9 Consider oral antifungals if the affected area is large, the patient doesn’t respond to topical therapy, or the patient is immunocompromised.9,10
When oral therapy is initiated for tinea manuum, one week of itraconazole (200 mg twice daily for 7 days) has been shown to be as effective as 2 weeks of oral terbinafine (250 mg daily for 14 days).10
Oral therapy worked for my patient
In light of the patient’s previous failure with topical therapy, he was reluctant to try this approach again. After a normal hepatic panel, I started him on a 2-week course of oral terbinafine 250 mg daily. (Terbinafine was available at our clinic pharmacy, while itraconazole was not). Follow-up at one month showed no sign of previous infection.
CORRESPONDENCE LT Michael Crandall, MD, Department of Dermatology, Naval Medical Center San Diego, 34800 Bob Wilson Drive, San Diego, CA 92134; [email protected]
1. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 5th ed. Philadelphia, Pa: Mosby/Elsevier; 2010:491–540.
2. Wilson M, Bender S, Lynfield Y, et al. Two feet-one hand syndrome. J Am Podiatr Med Assoc. 1988;78:250-253.
3. Daniel CR 3rd, Gupta AK, Daniel MP, et al. Two feet-one hand syndrome: a retrospective multicenter survey. Int J Dermatol. 1997;36:658-660.
4. Park BC, Lee SJ, Kim do W, et al. Molecular identification of mycologic correlation in patients with concomitant tinea pedis and tinea manuum infection. Arch Dermatol. 2009;145:205-207.
5. Zhan P, Ge YP, Lu XL, et al. A case-control analysis and laboratory study of the two feet-one hand syndrome in two dermatology hospitals in China. Clin Exp Dermatol. 2010;35:468-472.
6. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin: tinea capitis and tinea barbae. J Am Acad Dermatol. 1996;34(2 pt 1):290-294.
7. Geary RJ, Lucky AW. Tinea pedis in children presenting as unilateral inflammatory lesions of the sole. Pediatr Dermatol. 1999;16:255-258.
8. Sweeney SM, Wiss K, Mallory SB. Inflammatory tinea pedis/manuum masquerading as bacterial cellulitis. Arch Pediatr Adolesc Med. 2002;156:1149-1152.
9. Gupta AK, Cooper EA. Update in antifungal therapy of dermatophytosis. Mycopathologia. 2008;166:353-367.
10. Gupta AK, De Doncker P, Degreef H. Tinea manus treated with 1-week itraconazole vs. terbinafine. Int J Dermatol. 2000;39:529-531.
1. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 5th ed. Philadelphia, Pa: Mosby/Elsevier; 2010:491–540.
2. Wilson M, Bender S, Lynfield Y, et al. Two feet-one hand syndrome. J Am Podiatr Med Assoc. 1988;78:250-253.
3. Daniel CR 3rd, Gupta AK, Daniel MP, et al. Two feet-one hand syndrome: a retrospective multicenter survey. Int J Dermatol. 1997;36:658-660.
4. Park BC, Lee SJ, Kim do W, et al. Molecular identification of mycologic correlation in patients with concomitant tinea pedis and tinea manuum infection. Arch Dermatol. 2009;145:205-207.
5. Zhan P, Ge YP, Lu XL, et al. A case-control analysis and laboratory study of the two feet-one hand syndrome in two dermatology hospitals in China. Clin Exp Dermatol. 2010;35:468-472.
6. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin: tinea capitis and tinea barbae. J Am Acad Dermatol. 1996;34(2 pt 1):290-294.
7. Geary RJ, Lucky AW. Tinea pedis in children presenting as unilateral inflammatory lesions of the sole. Pediatr Dermatol. 1999;16:255-258.
8. Sweeney SM, Wiss K, Mallory SB. Inflammatory tinea pedis/manuum masquerading as bacterial cellulitis. Arch Pediatr Adolesc Med. 2002;156:1149-1152.
9. Gupta AK, Cooper EA. Update in antifungal therapy of dermatophytosis. Mycopathologia. 2008;166:353-367.
10. Gupta AK, De Doncker P, Degreef H. Tinea manus treated with 1-week itraconazole vs. terbinafine. Int J Dermatol. 2000;39:529-531.
Rash on buttocks

The patient was given a diagnosis of seabather’s eruption (SBE), also called seabather’s dermatitis or sea lice. SBE is an intensely itchy papular-erythematous dermatitis that can develop after an individual has been swimming in the ocean.
Planula larvae of the scyphomadusae Linuche unguiculata—commonly known as the thimble jellyfish—are to blame for this form of dermatitis. L unguiculata are most frequently found in the waters of the Caribbean, Gulf of Mexico, southern United States, and South America. Cases of SBE are most common in the spring and summer months, peaking in May. Those at highest risk include children, people with a history of SBE, and water sports enthusiasts (eg, surfers).
SBE usually resolves spontaneously within a week or 2. If treatment is necessary, start with topical corticosteroids and oral antihistamines. If this proves insufficient, move on to oral corticosteroids. To minimize risk, swimmers should remove their bathing suits and shower as soon as possible after leaving the water.
In this case, the physician advised the patient to take diphenhydramine (Benadryl) and the itching went away.
Adapted from: Monckton R, Fagan B, Frayne DJ, et al. Photo Rounds: Pruritic erythematous maculopapular rash. J Fam Pract. 2011;60:613-615.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The patient was given a diagnosis of seabather’s eruption (SBE), also called seabather’s dermatitis or sea lice. SBE is an intensely itchy papular-erythematous dermatitis that can develop after an individual has been swimming in the ocean.
Planula larvae of the scyphomadusae Linuche unguiculata—commonly known as the thimble jellyfish—are to blame for this form of dermatitis. L unguiculata are most frequently found in the waters of the Caribbean, Gulf of Mexico, southern United States, and South America. Cases of SBE are most common in the spring and summer months, peaking in May. Those at highest risk include children, people with a history of SBE, and water sports enthusiasts (eg, surfers).
SBE usually resolves spontaneously within a week or 2. If treatment is necessary, start with topical corticosteroids and oral antihistamines. If this proves insufficient, move on to oral corticosteroids. To minimize risk, swimmers should remove their bathing suits and shower as soon as possible after leaving the water.
In this case, the physician advised the patient to take diphenhydramine (Benadryl) and the itching went away.
Adapted from: Monckton R, Fagan B, Frayne DJ, et al. Photo Rounds: Pruritic erythematous maculopapular rash. J Fam Pract. 2011;60:613-615.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The patient was given a diagnosis of seabather’s eruption (SBE), also called seabather’s dermatitis or sea lice. SBE is an intensely itchy papular-erythematous dermatitis that can develop after an individual has been swimming in the ocean.
Planula larvae of the scyphomadusae Linuche unguiculata—commonly known as the thimble jellyfish—are to blame for this form of dermatitis. L unguiculata are most frequently found in the waters of the Caribbean, Gulf of Mexico, southern United States, and South America. Cases of SBE are most common in the spring and summer months, peaking in May. Those at highest risk include children, people with a history of SBE, and water sports enthusiasts (eg, surfers).
SBE usually resolves spontaneously within a week or 2. If treatment is necessary, start with topical corticosteroids and oral antihistamines. If this proves insufficient, move on to oral corticosteroids. To minimize risk, swimmers should remove their bathing suits and shower as soon as possible after leaving the water.
In this case, the physician advised the patient to take diphenhydramine (Benadryl) and the itching went away.
Adapted from: Monckton R, Fagan B, Frayne DJ, et al. Photo Rounds: Pruritic erythematous maculopapular rash. J Fam Pract. 2011;60:613-615.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Toe deformity

| 
|
| FIGURE 1 | FIGURE 2 |
The family physician (FP) diagnosed a single hammertoe deformity (FIGURES 1 and 2). Hammertoe deformity is the most common digital deformity, and it can affect up to 60% of adults. The second digit is most commonly affected. Conservative measures include:
- change in shoes
- padding to limit shearing force from shoes
- splinting (in an early, flexible hammertoe)
- steroid injection into the metatarsophalangeal (MTP) joint for a patient who complains of joint pain secondary to early-stage osteoarthritis or capsulitis. (However, avoid excessive steroid injections, as these can result in further damage of the capsule and worsening of the deformity)
- custom-made orthoses to slow down the progression of the deformity if it is caused by biomechanical factors
- resting, nonsteroidal anti-inflammatory drugs, and ice for an inflamed joint and/or shoe irritation.
In this case, the patient was referred to a podiatrist, who fused her proximal interphalangeal joint and released her extensor tendon and dorsal capsule at the MTP joint to reduce the deformity. The plantar plate was also repaired.
The patient started protective ambulation with a surgical shoe on the third postoperative day. An internal fixation wire, which was used to fixate the fusion site, was removed 4 weeks later.
The patient returned to work and her regular activities within 6 weeks of the operation. Based on her history and the findings at surgery, it appeared that she had a rupture of the plantar plate from overuse, which resulted in a hammertoe deformity of her second digit.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Images courtesy of Naohiro Shibuya, DPM. This case was adapted from: Shibuya N, Fontaine J. Hammertoe deformities. Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:900-903.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

| 
|
| FIGURE 1 | FIGURE 2 |
The family physician (FP) diagnosed a single hammertoe deformity (FIGURES 1 and 2). Hammertoe deformity is the most common digital deformity, and it can affect up to 60% of adults. The second digit is most commonly affected. Conservative measures include:
- change in shoes
- padding to limit shearing force from shoes
- splinting (in an early, flexible hammertoe)
- steroid injection into the metatarsophalangeal (MTP) joint for a patient who complains of joint pain secondary to early-stage osteoarthritis or capsulitis. (However, avoid excessive steroid injections, as these can result in further damage of the capsule and worsening of the deformity)
- custom-made orthoses to slow down the progression of the deformity if it is caused by biomechanical factors
- resting, nonsteroidal anti-inflammatory drugs, and ice for an inflamed joint and/or shoe irritation.
In this case, the patient was referred to a podiatrist, who fused her proximal interphalangeal joint and released her extensor tendon and dorsal capsule at the MTP joint to reduce the deformity. The plantar plate was also repaired.
The patient started protective ambulation with a surgical shoe on the third postoperative day. An internal fixation wire, which was used to fixate the fusion site, was removed 4 weeks later.
The patient returned to work and her regular activities within 6 weeks of the operation. Based on her history and the findings at surgery, it appeared that she had a rupture of the plantar plate from overuse, which resulted in a hammertoe deformity of her second digit.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Images courtesy of Naohiro Shibuya, DPM. This case was adapted from: Shibuya N, Fontaine J. Hammertoe deformities. Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:900-903.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

| 
|
| FIGURE 1 | FIGURE 2 |
The family physician (FP) diagnosed a single hammertoe deformity (FIGURES 1 and 2). Hammertoe deformity is the most common digital deformity, and it can affect up to 60% of adults. The second digit is most commonly affected. Conservative measures include:
- change in shoes
- padding to limit shearing force from shoes
- splinting (in an early, flexible hammertoe)
- steroid injection into the metatarsophalangeal (MTP) joint for a patient who complains of joint pain secondary to early-stage osteoarthritis or capsulitis. (However, avoid excessive steroid injections, as these can result in further damage of the capsule and worsening of the deformity)
- custom-made orthoses to slow down the progression of the deformity if it is caused by biomechanical factors
- resting, nonsteroidal anti-inflammatory drugs, and ice for an inflamed joint and/or shoe irritation.
In this case, the patient was referred to a podiatrist, who fused her proximal interphalangeal joint and released her extensor tendon and dorsal capsule at the MTP joint to reduce the deformity. The plantar plate was also repaired.
The patient started protective ambulation with a surgical shoe on the third postoperative day. An internal fixation wire, which was used to fixate the fusion site, was removed 4 weeks later.
The patient returned to work and her regular activities within 6 weeks of the operation. Based on her history and the findings at surgery, it appeared that she had a rupture of the plantar plate from overuse, which resulted in a hammertoe deformity of her second digit.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Images courtesy of Naohiro Shibuya, DPM. This case was adapted from: Shibuya N, Fontaine J. Hammertoe deformities. Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:900-903.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Hard swelling on toe

The FP diagnosed a hard corn secondary to the hammer-toe deformity. Corns can be seen on a non-weight-bearing surface, such as the dorsal proximal interphalangeal joints in patients with hammer-toe deformity. It is often referred to as a hard corn in that location. Corns in the interdigital spaces (commonly in the fourth space) are referred to as a soft corns. Corns are often slightly hyperpigmented (or normal in color) and are usually well demarcated. The lesion may have a hard or soft nucleus upon debridement.
Common associated signs include: prominent underlying bony structure, gross deformity of the foot (eg, cavus [high-arch] foot deformity, flatfoot deformity, bunion deformity, or lesser digital deformity), decreased ankle dorsiflexion, and an overall decrease in pedal joint range of motion.
The FP debrided the dead hyperkeratotic skin with a #10 scalpel blade. He then recommended that the patient use a pumice stone on a regular basis to keep the corn from regrowing. He discussed the possibility of surgery to correct the underlying hammertoe deformity. The patient, however, was not ready to undergo surgery but said she would consider it if the corn recurred.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photos courtesy of Naohiro Shibuya, DPM. This case was adapted from: Shibuya N, Fontaine J. Calluses and corns. Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:892-895.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The FP diagnosed a hard corn secondary to the hammer-toe deformity. Corns can be seen on a non-weight-bearing surface, such as the dorsal proximal interphalangeal joints in patients with hammer-toe deformity. It is often referred to as a hard corn in that location. Corns in the interdigital spaces (commonly in the fourth space) are referred to as a soft corns. Corns are often slightly hyperpigmented (or normal in color) and are usually well demarcated. The lesion may have a hard or soft nucleus upon debridement.
Common associated signs include: prominent underlying bony structure, gross deformity of the foot (eg, cavus [high-arch] foot deformity, flatfoot deformity, bunion deformity, or lesser digital deformity), decreased ankle dorsiflexion, and an overall decrease in pedal joint range of motion.
The FP debrided the dead hyperkeratotic skin with a #10 scalpel blade. He then recommended that the patient use a pumice stone on a regular basis to keep the corn from regrowing. He discussed the possibility of surgery to correct the underlying hammertoe deformity. The patient, however, was not ready to undergo surgery but said she would consider it if the corn recurred.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photos courtesy of Naohiro Shibuya, DPM. This case was adapted from: Shibuya N, Fontaine J. Calluses and corns. Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:892-895.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The FP diagnosed a hard corn secondary to the hammer-toe deformity. Corns can be seen on a non-weight-bearing surface, such as the dorsal proximal interphalangeal joints in patients with hammer-toe deformity. It is often referred to as a hard corn in that location. Corns in the interdigital spaces (commonly in the fourth space) are referred to as a soft corns. Corns are often slightly hyperpigmented (or normal in color) and are usually well demarcated. The lesion may have a hard or soft nucleus upon debridement.
Common associated signs include: prominent underlying bony structure, gross deformity of the foot (eg, cavus [high-arch] foot deformity, flatfoot deformity, bunion deformity, or lesser digital deformity), decreased ankle dorsiflexion, and an overall decrease in pedal joint range of motion.
The FP debrided the dead hyperkeratotic skin with a #10 scalpel blade. He then recommended that the patient use a pumice stone on a regular basis to keep the corn from regrowing. He discussed the possibility of surgery to correct the underlying hammertoe deformity. The patient, however, was not ready to undergo surgery but said she would consider it if the corn recurred.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photos courtesy of Naohiro Shibuya, DPM. This case was adapted from: Shibuya N, Fontaine J. Calluses and corns. Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:892-895.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link: