User login
Rash, Reaction, or Red Flag?
1. The patient had just recovered from a sore throat and noticed discrete red nodules, which eventually coalesced into a single large edematous plaque over the right anterior tibia. The deep intradermal and subdermal edema is exquisitely tender to touch, considerably warmer than the surrounding skin, and highly blanchable.
Diagnosis: Erythema nodosum is a reactive form of septal panniculitis with many potential triggers. Notable triggers include Crohn disease flares and use of drugs such as sulfa, gold salts, and oral contraceptives. Several infections have been identified as triggers, including strep, mycoplasma, and campylobacter, as well as deep fungal infections (histoplasmosis, blastomycosis, coccidioidomycosis, and sporotrichosis). More unusual causes include pregnancy and diseases such as sarcoidosis, tuberculosis, Behçet disease, and leukemia/lymphoma.
For more information, see “Painful Lesion Hasn’t Responded to Antibiotics.” Clin Rev. 2015;25(11):10,12.
For the next photograph, proceed to the next page >>
2. A 16-year-old high school student joins her friends in a 2K run one morning. The next day, her shins are so painful she can hardly walk. She applied ice packs to her legs, using elastic bandages to hold them in place until the ice cubes melt. As her legs rewarm, a rash appears where the ice packs contacted the skin.
Diagnosis: This condition is urticarial in nature—albeit an unusual form, triggered by cold. Though it appears counterintuitive, cold uriticaria typically appears only on rewarming of the affected area and is marked by the sudden appearance of “welts” or “hives” that usually clear (with or without treatment) within hours.
Uncomplicated urticaria resolves without leaving any signs (eg, purpura, ecchymosis) that might otherwise suggest the presence of a vasculitic component, such as that seen with lupus or other autoimmune diseases. Blanchability on digital pressure is one way to confirm benignancy, since blood tends to leak from vessels damaged by vasculitis, emptying into the surrounding interstitial spaces and presenting as nonblanchable petechiae, purpura, or ecchymosis. The relatively benign nature of this patient’s urticaria was also suggested by additional history taking, in which she denied having fever, malaise, or arthralgia. These are all symptoms we might have seen with more serious underlying causes.
Cold urticaria is one of the so-called physical urticarias, a group that includes urticaria caused by vibration, pressure, heat, sun, and even exposure to water. Thought to comprise up to 20% of all urticarias, the physical urticarias occur most frequently in persons ages 17 to 40. Dermatographism is the most common form, occurring in the linear track of a vigorous scratch as a wheal that manifests rapidly, lasts a few minutes, then disappears without a trace. Its presence is purposely sought by the examiner to confirm the diagnosis of urticaria (most often the chronic idiopathic variety).
For more information, see “Inexperienced runner develops leg rash.” Clin Rev. 2012;22(8):W3
For the next photograph, proceed to the next page >>
Source: PhotoStock-Israel / Science Source
3. Typically manifesting with edema, pruritus, warmth, and tenderness, this lesion is usually associated with a history of recent trauma or pharyngitis followed by malaise, chills, and high fever. The lesion is usually raised with a clear line of demarcation at the edge.
Diagnosis: Erysipelas, an acute infection of the skin and subcutaneous tissue, is caused by beta-hemolytic streptococci invading tissues via a disruption to the skin barrier. Streptococcus strains are susceptible to penicillin and 99.5% are susceptible to clindamycin. Associated comorbidities in erysipelas include diabetes mellitus, as well as hypertension, chronic venous insufficiency, and other cardiovascular diseases.
For more information, see “Painful rash on face.” J Fam Pract. 2010;59(8):459-462.
For the next photograph, proceed to the next page >>
Source: CDC Public Health Image Library.
4. This patient presented with a red, expanding rash on the lateral aspect of the left thigh. Affecting any part of the body, this illness may present with fever, chills, sweats, muscle aches, fatigue, nausea and joint pain. Some patients have a rash or Bell’s palsy.
Diagnosis: Lyme disease, caused by B. burgdorferi bacteria, is transmitted to humans through the bite of infected Ixodes ticks. Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, infection can spread to joints, the heart, and the nervous system.
Because its symptoms mimic many other diseases, diagnosing Lyme disease can be difficult. The diagnosis is based on symptoms, physical findings, eg, rash, and the possibility of exposure to infected ticks; laboratory testing is helpful if used correctly and performed with validated methods.
Treatment choice depends on the whether the disease is early or late. Most cases of early Lyme disease can be treated successfully with a few weeks of antibiotics.
For more information, see “Lyme Disease Presents Differently in Men and Women.”
1. The patient had just recovered from a sore throat and noticed discrete red nodules, which eventually coalesced into a single large edematous plaque over the right anterior tibia. The deep intradermal and subdermal edema is exquisitely tender to touch, considerably warmer than the surrounding skin, and highly blanchable.
Diagnosis: Erythema nodosum is a reactive form of septal panniculitis with many potential triggers. Notable triggers include Crohn disease flares and use of drugs such as sulfa, gold salts, and oral contraceptives. Several infections have been identified as triggers, including strep, mycoplasma, and campylobacter, as well as deep fungal infections (histoplasmosis, blastomycosis, coccidioidomycosis, and sporotrichosis). More unusual causes include pregnancy and diseases such as sarcoidosis, tuberculosis, Behçet disease, and leukemia/lymphoma.
For more information, see “Painful Lesion Hasn’t Responded to Antibiotics.” Clin Rev. 2015;25(11):10,12.
For the next photograph, proceed to the next page >>
2. A 16-year-old high school student joins her friends in a 2K run one morning. The next day, her shins are so painful she can hardly walk. She applied ice packs to her legs, using elastic bandages to hold them in place until the ice cubes melt. As her legs rewarm, a rash appears where the ice packs contacted the skin.
Diagnosis: This condition is urticarial in nature—albeit an unusual form, triggered by cold. Though it appears counterintuitive, cold uriticaria typically appears only on rewarming of the affected area and is marked by the sudden appearance of “welts” or “hives” that usually clear (with or without treatment) within hours.
Uncomplicated urticaria resolves without leaving any signs (eg, purpura, ecchymosis) that might otherwise suggest the presence of a vasculitic component, such as that seen with lupus or other autoimmune diseases. Blanchability on digital pressure is one way to confirm benignancy, since blood tends to leak from vessels damaged by vasculitis, emptying into the surrounding interstitial spaces and presenting as nonblanchable petechiae, purpura, or ecchymosis. The relatively benign nature of this patient’s urticaria was also suggested by additional history taking, in which she denied having fever, malaise, or arthralgia. These are all symptoms we might have seen with more serious underlying causes.
Cold urticaria is one of the so-called physical urticarias, a group that includes urticaria caused by vibration, pressure, heat, sun, and even exposure to water. Thought to comprise up to 20% of all urticarias, the physical urticarias occur most frequently in persons ages 17 to 40. Dermatographism is the most common form, occurring in the linear track of a vigorous scratch as a wheal that manifests rapidly, lasts a few minutes, then disappears without a trace. Its presence is purposely sought by the examiner to confirm the diagnosis of urticaria (most often the chronic idiopathic variety).
For more information, see “Inexperienced runner develops leg rash.” Clin Rev. 2012;22(8):W3
For the next photograph, proceed to the next page >>
Source: PhotoStock-Israel / Science Source
3. Typically manifesting with edema, pruritus, warmth, and tenderness, this lesion is usually associated with a history of recent trauma or pharyngitis followed by malaise, chills, and high fever. The lesion is usually raised with a clear line of demarcation at the edge.
Diagnosis: Erysipelas, an acute infection of the skin and subcutaneous tissue, is caused by beta-hemolytic streptococci invading tissues via a disruption to the skin barrier. Streptococcus strains are susceptible to penicillin and 99.5% are susceptible to clindamycin. Associated comorbidities in erysipelas include diabetes mellitus, as well as hypertension, chronic venous insufficiency, and other cardiovascular diseases.
For more information, see “Painful rash on face.” J Fam Pract. 2010;59(8):459-462.
For the next photograph, proceed to the next page >>
Source: CDC Public Health Image Library.
4. This patient presented with a red, expanding rash on the lateral aspect of the left thigh. Affecting any part of the body, this illness may present with fever, chills, sweats, muscle aches, fatigue, nausea and joint pain. Some patients have a rash or Bell’s palsy.
Diagnosis: Lyme disease, caused by B. burgdorferi bacteria, is transmitted to humans through the bite of infected Ixodes ticks. Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, infection can spread to joints, the heart, and the nervous system.
Because its symptoms mimic many other diseases, diagnosing Lyme disease can be difficult. The diagnosis is based on symptoms, physical findings, eg, rash, and the possibility of exposure to infected ticks; laboratory testing is helpful if used correctly and performed with validated methods.
Treatment choice depends on the whether the disease is early or late. Most cases of early Lyme disease can be treated successfully with a few weeks of antibiotics.
For more information, see “Lyme Disease Presents Differently in Men and Women.”
1. The patient had just recovered from a sore throat and noticed discrete red nodules, which eventually coalesced into a single large edematous plaque over the right anterior tibia. The deep intradermal and subdermal edema is exquisitely tender to touch, considerably warmer than the surrounding skin, and highly blanchable.
Diagnosis: Erythema nodosum is a reactive form of septal panniculitis with many potential triggers. Notable triggers include Crohn disease flares and use of drugs such as sulfa, gold salts, and oral contraceptives. Several infections have been identified as triggers, including strep, mycoplasma, and campylobacter, as well as deep fungal infections (histoplasmosis, blastomycosis, coccidioidomycosis, and sporotrichosis). More unusual causes include pregnancy and diseases such as sarcoidosis, tuberculosis, Behçet disease, and leukemia/lymphoma.
For more information, see “Painful Lesion Hasn’t Responded to Antibiotics.” Clin Rev. 2015;25(11):10,12.
For the next photograph, proceed to the next page >>
2. A 16-year-old high school student joins her friends in a 2K run one morning. The next day, her shins are so painful she can hardly walk. She applied ice packs to her legs, using elastic bandages to hold them in place until the ice cubes melt. As her legs rewarm, a rash appears where the ice packs contacted the skin.
Diagnosis: This condition is urticarial in nature—albeit an unusual form, triggered by cold. Though it appears counterintuitive, cold uriticaria typically appears only on rewarming of the affected area and is marked by the sudden appearance of “welts” or “hives” that usually clear (with or without treatment) within hours.
Uncomplicated urticaria resolves without leaving any signs (eg, purpura, ecchymosis) that might otherwise suggest the presence of a vasculitic component, such as that seen with lupus or other autoimmune diseases. Blanchability on digital pressure is one way to confirm benignancy, since blood tends to leak from vessels damaged by vasculitis, emptying into the surrounding interstitial spaces and presenting as nonblanchable petechiae, purpura, or ecchymosis. The relatively benign nature of this patient’s urticaria was also suggested by additional history taking, in which she denied having fever, malaise, or arthralgia. These are all symptoms we might have seen with more serious underlying causes.
Cold urticaria is one of the so-called physical urticarias, a group that includes urticaria caused by vibration, pressure, heat, sun, and even exposure to water. Thought to comprise up to 20% of all urticarias, the physical urticarias occur most frequently in persons ages 17 to 40. Dermatographism is the most common form, occurring in the linear track of a vigorous scratch as a wheal that manifests rapidly, lasts a few minutes, then disappears without a trace. Its presence is purposely sought by the examiner to confirm the diagnosis of urticaria (most often the chronic idiopathic variety).
For more information, see “Inexperienced runner develops leg rash.” Clin Rev. 2012;22(8):W3
For the next photograph, proceed to the next page >>
Source: PhotoStock-Israel / Science Source
3. Typically manifesting with edema, pruritus, warmth, and tenderness, this lesion is usually associated with a history of recent trauma or pharyngitis followed by malaise, chills, and high fever. The lesion is usually raised with a clear line of demarcation at the edge.
Diagnosis: Erysipelas, an acute infection of the skin and subcutaneous tissue, is caused by beta-hemolytic streptococci invading tissues via a disruption to the skin barrier. Streptococcus strains are susceptible to penicillin and 99.5% are susceptible to clindamycin. Associated comorbidities in erysipelas include diabetes mellitus, as well as hypertension, chronic venous insufficiency, and other cardiovascular diseases.
For more information, see “Painful rash on face.” J Fam Pract. 2010;59(8):459-462.
For the next photograph, proceed to the next page >>
Source: CDC Public Health Image Library.
4. This patient presented with a red, expanding rash on the lateral aspect of the left thigh. Affecting any part of the body, this illness may present with fever, chills, sweats, muscle aches, fatigue, nausea and joint pain. Some patients have a rash or Bell’s palsy.
Diagnosis: Lyme disease, caused by B. burgdorferi bacteria, is transmitted to humans through the bite of infected Ixodes ticks. Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, infection can spread to joints, the heart, and the nervous system.
Because its symptoms mimic many other diseases, diagnosing Lyme disease can be difficult. The diagnosis is based on symptoms, physical findings, eg, rash, and the possibility of exposure to infected ticks; laboratory testing is helpful if used correctly and performed with validated methods.
Treatment choice depends on the whether the disease is early or late. Most cases of early Lyme disease can be treated successfully with a few weeks of antibiotics.
For more information, see “Lyme Disease Presents Differently in Men and Women.”
Say Ahh…
Credit: These cases were adapted from Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013. You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: usatinemedia.com.
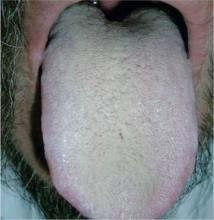
1. A painless white, thick lesion with fissuring had been on the side of this 57-year-old man’s tongue for the past 7 months. The patient drinks two to three beers in the evening and smokes one pack of cigarettes a day.
Diagnosis: This patient was given a diagnosis of leukoplakia and the biopsy indicated that the lesion was premalignant. The World Health Organization defines leukoplakia as “white plaques of questionable risk” in cases where other known diseases that don’t carry an increased risk for cancer have been excluded. For all types of leukoplakia, the risk of malignant transformation is approximately 1%, with a much higher risk associated with leukoplakias that contain red spots and/or rough spots.
For more information, read “White patch on tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
2. This nonhealing painful lesion on the side of her tongue had increased in size recently, and the patient, a 56-year-old homeless woman, was worried because her dad had died from oral cancer. She had smoked since she was 11 and acknowledged being a heavy drinker.
Diagnosis: A punch biopsy revealed that the patient had a squamous cell carcinoma. Fully two-thirds of oropharyngeal cancers (OPCs) will present with advanced disease at the time of diagnosis. Ninety percent of OPCs are of the squamous cell type. Reports in the literature suggest that clinicians may be missing early disease by not conducting thorough soft-tissue examinations on a routine basis. However, the fact that more than 35% of patients do not see a dentist on a routine basis likely contributes to the diagnostic delay. The 5-year survival rate for OPC is 62% for whites and 42% for blacks.
Tobacco use is the major risk factor for OPC and is implicated in approximately 75% of cases. Alcohol use is also a major risk factor. The combined use of tobacco and alcohol increases the risk of OPC far more than either alone. Human papillomavirus (especially HPV 16) is a newly recognized major risk factor for carcinomas affecting the lingual and palatine tonsils.
For more information, read “Lesion on side of tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
3. A 58-year-old man sought care for painful sores that had been in his mouth, on and off, for a year. The ulcers erupted on his tongue, gums, buccal mucosa, and inner lips, making it painful to eat. The patient was not taking any medications.
Diagnosis: The clinician recognized his condition as recurrent aphthous ulcers with giant ulcers. Aphthous ulcers are painful ulcerations in the mouth, which can be single, multiple, occasional, or recurrent. These ulcers can be small or large but are uniformly painful and may interfere with eating, speaking, and swallowing.
For more information, read “Lesions on tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
4. A 60-year-old man, smelling of alcohol and tobacco, complained of a black discoloration of his tongue and occasional gagging sensation. He smoked one to 2 packs of cigarettes and drank 6 to 8 beers daily. On physical exam, his teeth were stained and his tongue shows elongated papillae with brown discoloration.
Diagnosis: This patient had a black hairy tongue (BHT), poor oral hygiene, and tobacco and alcohol addiction. BHT is a benign disorder of the tongue characterized by abnormally hypertrophied and elongated filiform papillae on the surface of the tongue. In addition, there is defective desquamation of the papillae on the dorsal tongue, resulting in a hair-like appearance. These papillae, which are normally about 1 mm in length, may become as long as 12 mm. The elongated filiform papillae can then collect debris, bacteria, fungus, or other foreign materials.
For more information, read “Discoloration of the tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
5. A 5-year-old girl had a temperature of 102.4°F, a sore throat, and a red tongue with prominent papillae. The posterior pharynx was also erythematous with slight exudate visible. The anterior cervical lymph nodes were mildly tender and somewhat enlarged, and no rashes were noted.
Diagnosis: The child had a strawberry tongue and scarlet fever caused by strep pharyngitis. The tongue had prominent papillae along with erythema, making it resemble a strawberry. Strawberry tongue is most commonly seen in children with scarlet fever or Kawasaki disease. Strawberry tongue usually develops within the first 2 to 3 days of illness. A white or yellowish coating usually precedes the classic red tongue with white papillae.
For more information, read “Papillae on tongue.” J Fam Pract. 2014.
Credit: These cases were adapted from Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013. You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: usatinemedia.com.
1. A painless white, thick lesion with fissuring had been on the side of this 57-year-old man’s tongue for the past 7 months. The patient drinks two to three beers in the evening and smokes one pack of cigarettes a day.
Diagnosis: This patient was given a diagnosis of leukoplakia and the biopsy indicated that the lesion was premalignant. The World Health Organization defines leukoplakia as “white plaques of questionable risk” in cases where other known diseases that don’t carry an increased risk for cancer have been excluded. For all types of leukoplakia, the risk of malignant transformation is approximately 1%, with a much higher risk associated with leukoplakias that contain red spots and/or rough spots.
For more information, read “White patch on tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
2. This nonhealing painful lesion on the side of her tongue had increased in size recently, and the patient, a 56-year-old homeless woman, was worried because her dad had died from oral cancer. She had smoked since she was 11 and acknowledged being a heavy drinker.
Diagnosis: A punch biopsy revealed that the patient had a squamous cell carcinoma. Fully two-thirds of oropharyngeal cancers (OPCs) will present with advanced disease at the time of diagnosis. Ninety percent of OPCs are of the squamous cell type. Reports in the literature suggest that clinicians may be missing early disease by not conducting thorough soft-tissue examinations on a routine basis. However, the fact that more than 35% of patients do not see a dentist on a routine basis likely contributes to the diagnostic delay. The 5-year survival rate for OPC is 62% for whites and 42% for blacks.
Tobacco use is the major risk factor for OPC and is implicated in approximately 75% of cases. Alcohol use is also a major risk factor. The combined use of tobacco and alcohol increases the risk of OPC far more than either alone. Human papillomavirus (especially HPV 16) is a newly recognized major risk factor for carcinomas affecting the lingual and palatine tonsils.
For more information, read “Lesion on side of tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
3. A 58-year-old man sought care for painful sores that had been in his mouth, on and off, for a year. The ulcers erupted on his tongue, gums, buccal mucosa, and inner lips, making it painful to eat. The patient was not taking any medications.
Diagnosis: The clinician recognized his condition as recurrent aphthous ulcers with giant ulcers. Aphthous ulcers are painful ulcerations in the mouth, which can be single, multiple, occasional, or recurrent. These ulcers can be small or large but are uniformly painful and may interfere with eating, speaking, and swallowing.
For more information, read “Lesions on tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
4. A 60-year-old man, smelling of alcohol and tobacco, complained of a black discoloration of his tongue and occasional gagging sensation. He smoked one to 2 packs of cigarettes and drank 6 to 8 beers daily. On physical exam, his teeth were stained and his tongue shows elongated papillae with brown discoloration.
Diagnosis: This patient had a black hairy tongue (BHT), poor oral hygiene, and tobacco and alcohol addiction. BHT is a benign disorder of the tongue characterized by abnormally hypertrophied and elongated filiform papillae on the surface of the tongue. In addition, there is defective desquamation of the papillae on the dorsal tongue, resulting in a hair-like appearance. These papillae, which are normally about 1 mm in length, may become as long as 12 mm. The elongated filiform papillae can then collect debris, bacteria, fungus, or other foreign materials.
For more information, read “Discoloration of the tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
5. A 5-year-old girl had a temperature of 102.4°F, a sore throat, and a red tongue with prominent papillae. The posterior pharynx was also erythematous with slight exudate visible. The anterior cervical lymph nodes were mildly tender and somewhat enlarged, and no rashes were noted.
Diagnosis: The child had a strawberry tongue and scarlet fever caused by strep pharyngitis. The tongue had prominent papillae along with erythema, making it resemble a strawberry. Strawberry tongue is most commonly seen in children with scarlet fever or Kawasaki disease. Strawberry tongue usually develops within the first 2 to 3 days of illness. A white or yellowish coating usually precedes the classic red tongue with white papillae.
For more information, read “Papillae on tongue.” J Fam Pract. 2014.
Credit: These cases were adapted from Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013. You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: usatinemedia.com.
1. A painless white, thick lesion with fissuring had been on the side of this 57-year-old man’s tongue for the past 7 months. The patient drinks two to three beers in the evening and smokes one pack of cigarettes a day.
Diagnosis: This patient was given a diagnosis of leukoplakia and the biopsy indicated that the lesion was premalignant. The World Health Organization defines leukoplakia as “white plaques of questionable risk” in cases where other known diseases that don’t carry an increased risk for cancer have been excluded. For all types of leukoplakia, the risk of malignant transformation is approximately 1%, with a much higher risk associated with leukoplakias that contain red spots and/or rough spots.
For more information, read “White patch on tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
2. This nonhealing painful lesion on the side of her tongue had increased in size recently, and the patient, a 56-year-old homeless woman, was worried because her dad had died from oral cancer. She had smoked since she was 11 and acknowledged being a heavy drinker.
Diagnosis: A punch biopsy revealed that the patient had a squamous cell carcinoma. Fully two-thirds of oropharyngeal cancers (OPCs) will present with advanced disease at the time of diagnosis. Ninety percent of OPCs are of the squamous cell type. Reports in the literature suggest that clinicians may be missing early disease by not conducting thorough soft-tissue examinations on a routine basis. However, the fact that more than 35% of patients do not see a dentist on a routine basis likely contributes to the diagnostic delay. The 5-year survival rate for OPC is 62% for whites and 42% for blacks.
Tobacco use is the major risk factor for OPC and is implicated in approximately 75% of cases. Alcohol use is also a major risk factor. The combined use of tobacco and alcohol increases the risk of OPC far more than either alone. Human papillomavirus (especially HPV 16) is a newly recognized major risk factor for carcinomas affecting the lingual and palatine tonsils.
For more information, read “Lesion on side of tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
3. A 58-year-old man sought care for painful sores that had been in his mouth, on and off, for a year. The ulcers erupted on his tongue, gums, buccal mucosa, and inner lips, making it painful to eat. The patient was not taking any medications.
Diagnosis: The clinician recognized his condition as recurrent aphthous ulcers with giant ulcers. Aphthous ulcers are painful ulcerations in the mouth, which can be single, multiple, occasional, or recurrent. These ulcers can be small or large but are uniformly painful and may interfere with eating, speaking, and swallowing.
For more information, read “Lesions on tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
4. A 60-year-old man, smelling of alcohol and tobacco, complained of a black discoloration of his tongue and occasional gagging sensation. He smoked one to 2 packs of cigarettes and drank 6 to 8 beers daily. On physical exam, his teeth were stained and his tongue shows elongated papillae with brown discoloration.
Diagnosis: This patient had a black hairy tongue (BHT), poor oral hygiene, and tobacco and alcohol addiction. BHT is a benign disorder of the tongue characterized by abnormally hypertrophied and elongated filiform papillae on the surface of the tongue. In addition, there is defective desquamation of the papillae on the dorsal tongue, resulting in a hair-like appearance. These papillae, which are normally about 1 mm in length, may become as long as 12 mm. The elongated filiform papillae can then collect debris, bacteria, fungus, or other foreign materials.
For more information, read “Discoloration of the tongue.” J Fam Pract. 2014.
For the next photograph, proceed to the next page >>
5. A 5-year-old girl had a temperature of 102.4°F, a sore throat, and a red tongue with prominent papillae. The posterior pharynx was also erythematous with slight exudate visible. The anterior cervical lymph nodes were mildly tender and somewhat enlarged, and no rashes were noted.
Diagnosis: The child had a strawberry tongue and scarlet fever caused by strep pharyngitis. The tongue had prominent papillae along with erythema, making it resemble a strawberry. Strawberry tongue is most commonly seen in children with scarlet fever or Kawasaki disease. Strawberry tongue usually develops within the first 2 to 3 days of illness. A white or yellowish coating usually precedes the classic red tongue with white papillae.
For more information, read “Papillae on tongue.” J Fam Pract. 2014.
More Than Skin Deep
1. About a year ago, this 40-year-old man developed scaling on the distal one-third of his thumbnail. The condition began to worsen, leaving most of his thumb covered by thick adherent white scales on a pinkish base with sharply defined margins. The adjacent thumbnail has focal areas of pitting in the nail plate, as well as yellowish discoloration on the distal edge.
Diagnosis: The most likely diagnosis is psoriasis, which can manifest with localized involvement.
For more information, see “Thumb: Scaling with Pitted Nail Plate.” Clin Rev. 2013 March;23(3):11.
For the next photograph, proceed to the next page >>
2. A 10-year-old girl has had patches of dry skin appearing and disappearing on her arms, legs, and neck for years. Recently manifested on her extensor forearm is an annular, distinctly salmon-pink plaque with a tenacious white scale. Scaly areas are observed in both postauricular sulci; several tiny pits are seen on her fingernails.
Diagnosis: It would be difficult to imagine a more clear-cut case of psoriasis, not only manifesting with a classic plaque on the extensor forearm but also with corroboratory stigmata behind the ears and classic fingernail pits.
It’s helpful to know that psoriasis affects almost 3% of the white population in the United States, meaning that you will see it with considerable frequency. It would also help if you knew the diagnosis can be corroborated by identification of other, lesser known features.
For more information, see “Girl, 10, Asks Tough Questions About Skin Problem.” Clin Rev. 2015;25(8):W2.
For the next photograph, proceed to the next page >>
3. A 62-year-old woman complained bitterly of itching on the soles of both feet. Both insteps are covered with discrete, confluent papules and tiny pustules on an erythematous and hyperpigmented (brown), sharply demarcated, and highly symmetrical base. No such lesions appear elsewhere.
Diagnosis: Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
For more information, see “Pruritic Rash on Both Soles.” Clin Rev. 2012 Jan;22(1).
For the next photograph, proceed to the next page >>
4. The patient presented with fiery red, burned looking skin covering ≥90% of the skin surface and shedding in large "sheets" instead of smaller scales. He was monitored for fever, systemic symptoms, and multiorgan dysfunction.
Photo courtesy of Peter A. Lio, MD, and Alisa McQueen, MD
Diagnosis: This patient was given a diagnosis of erythrodermic psoriasis. This form of psoriasis can be life-threatening.
For more information, see “Derm emergencies— detecting early signs of trouble.” J Fam Pract. 2012 February;61(2):71-78.
For the next photograph, proceed to the next page >>
5. This 18-year-old patient had multiple, erythematous papules and plaques with a fine scale over her face, neck, trunk, and lower legs. She noted that the eruption had developed after a sore throat 2 weeks earlier and that it was itchy.
Photos courtesy of David A. Boyd, MD
Diagnosis: Guttate psoriasis was diagnosed in this patient based on her history and physical exam, a throat culture that was positive for group A beta-hemolytic streptococci, and blood work that showed an elevated antistreptolysin O titer. Further confirmation was obtained via punch biopsy.
Guttate psoriasis is a fairly uncommon form of psoriasis, affecting approximately 2% of patients with psoriasis.1 It is characterized by the abrupt onset of pruritic, salmon-pink 1- to 10-mm droplike lesions with fine scale that may spread to the face, but spare the palms and soles. It’s uncommon for this sub-type of psoriasis to involve the nails.
Guttate psoriasis affects individuals younger than 30; there appears to be no gender predilection.2 The rash usually appears 2 to 3 weeks after an upper respiratory group A beta-hemolytic streptococci infection. Although less common, there have also been reports of guttate psoriasis associated with perianal streptococcal disease.2
1. Habif TP. Clinical Dermatology. 4th ed. St. Louis, Mo: Mosby; 2004;209-239
2. Honig PJ. Guttate psoriasis associated with perianal streptococcal disease. J Pediatr. 1988;113:1037-1039.
For more information, see “Teen with a diffuse erythematous, pruritic eruption.” J Fam Pract. 2011 January;60(1):37-39.
1. About a year ago, this 40-year-old man developed scaling on the distal one-third of his thumbnail. The condition began to worsen, leaving most of his thumb covered by thick adherent white scales on a pinkish base with sharply defined margins. The adjacent thumbnail has focal areas of pitting in the nail plate, as well as yellowish discoloration on the distal edge.
Diagnosis: The most likely diagnosis is psoriasis, which can manifest with localized involvement.
For more information, see “Thumb: Scaling with Pitted Nail Plate.” Clin Rev. 2013 March;23(3):11.
For the next photograph, proceed to the next page >>
2. A 10-year-old girl has had patches of dry skin appearing and disappearing on her arms, legs, and neck for years. Recently manifested on her extensor forearm is an annular, distinctly salmon-pink plaque with a tenacious white scale. Scaly areas are observed in both postauricular sulci; several tiny pits are seen on her fingernails.
Diagnosis: It would be difficult to imagine a more clear-cut case of psoriasis, not only manifesting with a classic plaque on the extensor forearm but also with corroboratory stigmata behind the ears and classic fingernail pits.
It’s helpful to know that psoriasis affects almost 3% of the white population in the United States, meaning that you will see it with considerable frequency. It would also help if you knew the diagnosis can be corroborated by identification of other, lesser known features.
For more information, see “Girl, 10, Asks Tough Questions About Skin Problem.” Clin Rev. 2015;25(8):W2.
For the next photograph, proceed to the next page >>
3. A 62-year-old woman complained bitterly of itching on the soles of both feet. Both insteps are covered with discrete, confluent papules and tiny pustules on an erythematous and hyperpigmented (brown), sharply demarcated, and highly symmetrical base. No such lesions appear elsewhere.
Diagnosis: Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
For more information, see “Pruritic Rash on Both Soles.” Clin Rev. 2012 Jan;22(1).
For the next photograph, proceed to the next page >>
4. The patient presented with fiery red, burned looking skin covering ≥90% of the skin surface and shedding in large "sheets" instead of smaller scales. He was monitored for fever, systemic symptoms, and multiorgan dysfunction.
Photo courtesy of Peter A. Lio, MD, and Alisa McQueen, MD
Diagnosis: This patient was given a diagnosis of erythrodermic psoriasis. This form of psoriasis can be life-threatening.
For more information, see “Derm emergencies— detecting early signs of trouble.” J Fam Pract. 2012 February;61(2):71-78.
For the next photograph, proceed to the next page >>
5. This 18-year-old patient had multiple, erythematous papules and plaques with a fine scale over her face, neck, trunk, and lower legs. She noted that the eruption had developed after a sore throat 2 weeks earlier and that it was itchy.
Photos courtesy of David A. Boyd, MD
Diagnosis: Guttate psoriasis was diagnosed in this patient based on her history and physical exam, a throat culture that was positive for group A beta-hemolytic streptococci, and blood work that showed an elevated antistreptolysin O titer. Further confirmation was obtained via punch biopsy.
Guttate psoriasis is a fairly uncommon form of psoriasis, affecting approximately 2% of patients with psoriasis.1 It is characterized by the abrupt onset of pruritic, salmon-pink 1- to 10-mm droplike lesions with fine scale that may spread to the face, but spare the palms and soles. It’s uncommon for this sub-type of psoriasis to involve the nails.
Guttate psoriasis affects individuals younger than 30; there appears to be no gender predilection.2 The rash usually appears 2 to 3 weeks after an upper respiratory group A beta-hemolytic streptococci infection. Although less common, there have also been reports of guttate psoriasis associated with perianal streptococcal disease.2
1. Habif TP. Clinical Dermatology. 4th ed. St. Louis, Mo: Mosby; 2004;209-239
2. Honig PJ. Guttate psoriasis associated with perianal streptococcal disease. J Pediatr. 1988;113:1037-1039.
For more information, see “Teen with a diffuse erythematous, pruritic eruption.” J Fam Pract. 2011 January;60(1):37-39.
1. About a year ago, this 40-year-old man developed scaling on the distal one-third of his thumbnail. The condition began to worsen, leaving most of his thumb covered by thick adherent white scales on a pinkish base with sharply defined margins. The adjacent thumbnail has focal areas of pitting in the nail plate, as well as yellowish discoloration on the distal edge.
Diagnosis: The most likely diagnosis is psoriasis, which can manifest with localized involvement.
For more information, see “Thumb: Scaling with Pitted Nail Plate.” Clin Rev. 2013 March;23(3):11.
For the next photograph, proceed to the next page >>
2. A 10-year-old girl has had patches of dry skin appearing and disappearing on her arms, legs, and neck for years. Recently manifested on her extensor forearm is an annular, distinctly salmon-pink plaque with a tenacious white scale. Scaly areas are observed in both postauricular sulci; several tiny pits are seen on her fingernails.
Diagnosis: It would be difficult to imagine a more clear-cut case of psoriasis, not only manifesting with a classic plaque on the extensor forearm but also with corroboratory stigmata behind the ears and classic fingernail pits.
It’s helpful to know that psoriasis affects almost 3% of the white population in the United States, meaning that you will see it with considerable frequency. It would also help if you knew the diagnosis can be corroborated by identification of other, lesser known features.
For more information, see “Girl, 10, Asks Tough Questions About Skin Problem.” Clin Rev. 2015;25(8):W2.
For the next photograph, proceed to the next page >>
3. A 62-year-old woman complained bitterly of itching on the soles of both feet. Both insteps are covered with discrete, confluent papules and tiny pustules on an erythematous and hyperpigmented (brown), sharply demarcated, and highly symmetrical base. No such lesions appear elsewhere.
Diagnosis: Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
For more information, see “Pruritic Rash on Both Soles.” Clin Rev. 2012 Jan;22(1).
For the next photograph, proceed to the next page >>
4. The patient presented with fiery red, burned looking skin covering ≥90% of the skin surface and shedding in large "sheets" instead of smaller scales. He was monitored for fever, systemic symptoms, and multiorgan dysfunction.
Photo courtesy of Peter A. Lio, MD, and Alisa McQueen, MD
Diagnosis: This patient was given a diagnosis of erythrodermic psoriasis. This form of psoriasis can be life-threatening.
For more information, see “Derm emergencies— detecting early signs of trouble.” J Fam Pract. 2012 February;61(2):71-78.
For the next photograph, proceed to the next page >>
5. This 18-year-old patient had multiple, erythematous papules and plaques with a fine scale over her face, neck, trunk, and lower legs. She noted that the eruption had developed after a sore throat 2 weeks earlier and that it was itchy.
Photos courtesy of David A. Boyd, MD
Diagnosis: Guttate psoriasis was diagnosed in this patient based on her history and physical exam, a throat culture that was positive for group A beta-hemolytic streptococci, and blood work that showed an elevated antistreptolysin O titer. Further confirmation was obtained via punch biopsy.
Guttate psoriasis is a fairly uncommon form of psoriasis, affecting approximately 2% of patients with psoriasis.1 It is characterized by the abrupt onset of pruritic, salmon-pink 1- to 10-mm droplike lesions with fine scale that may spread to the face, but spare the palms and soles. It’s uncommon for this sub-type of psoriasis to involve the nails.
Guttate psoriasis affects individuals younger than 30; there appears to be no gender predilection.2 The rash usually appears 2 to 3 weeks after an upper respiratory group A beta-hemolytic streptococci infection. Although less common, there have also been reports of guttate psoriasis associated with perianal streptococcal disease.2
1. Habif TP. Clinical Dermatology. 4th ed. St. Louis, Mo: Mosby; 2004;209-239
2. Honig PJ. Guttate psoriasis associated with perianal streptococcal disease. J Pediatr. 1988;113:1037-1039.
For more information, see “Teen with a diffuse erythematous, pruritic eruption.” J Fam Pract. 2011 January;60(1):37-39.
Derm Morphology, Part 2
1. Flat, distinct, discolored area usually less than 1 cm wide without change in skin texture or thickness.
Diagnosis: Macule
For more information on this case, see “Could Lesion Become a Pain in the Neck?” Clin Rev. 2015;25(7):W1
For the next photograph, proceed to the next page >>
2. Solid or cystic raised area less than 1 cm wide.
Diagnosis: Papule
For more information on this case, see “Irritated and Downright Painful.” Clin Rev. 2014;24(11):W3.
For the next photograph, proceed to the next page >>
3. Collection of pus in any part of the body typically accompanied by swelling and inflammation.
Diagnosis: Skin abscesses/Boils
For more information on this case, see “What Actually Qualifies as a ‘Boil’?” Clin Rev. 2013;23(8):W4.
For the next photograph, proceed to the next page >>
4. Resulting from chronic irritation from conditions like eczema or from continuous rubbing or scratching, the skin becomes thickened and leathery.
Diagnosis: Lichenification
For more information on Figure 4a, see “Leg Lesion Represents a Vicious Cycle.” Clin Rev. 2012;22(12):W5.
1. Flat, distinct, discolored area usually less than 1 cm wide without change in skin texture or thickness.
Diagnosis: Macule
For more information on this case, see “Could Lesion Become a Pain in the Neck?” Clin Rev. 2015;25(7):W1
For the next photograph, proceed to the next page >>
2. Solid or cystic raised area less than 1 cm wide.
Diagnosis: Papule
For more information on this case, see “Irritated and Downright Painful.” Clin Rev. 2014;24(11):W3.
For the next photograph, proceed to the next page >>
3. Collection of pus in any part of the body typically accompanied by swelling and inflammation.
Diagnosis: Skin abscesses/Boils
For more information on this case, see “What Actually Qualifies as a ‘Boil’?” Clin Rev. 2013;23(8):W4.
For the next photograph, proceed to the next page >>
4. Resulting from chronic irritation from conditions like eczema or from continuous rubbing or scratching, the skin becomes thickened and leathery.
Diagnosis: Lichenification
For more information on Figure 4a, see “Leg Lesion Represents a Vicious Cycle.” Clin Rev. 2012;22(12):W5.
1. Flat, distinct, discolored area usually less than 1 cm wide without change in skin texture or thickness.
Diagnosis: Macule
For more information on this case, see “Could Lesion Become a Pain in the Neck?” Clin Rev. 2015;25(7):W1
For the next photograph, proceed to the next page >>
2. Solid or cystic raised area less than 1 cm wide.
Diagnosis: Papule
For more information on this case, see “Irritated and Downright Painful.” Clin Rev. 2014;24(11):W3.
For the next photograph, proceed to the next page >>
3. Collection of pus in any part of the body typically accompanied by swelling and inflammation.
Diagnosis: Skin abscesses/Boils
For more information on this case, see “What Actually Qualifies as a ‘Boil’?” Clin Rev. 2013;23(8):W4.
For the next photograph, proceed to the next page >>
4. Resulting from chronic irritation from conditions like eczema or from continuous rubbing or scratching, the skin becomes thickened and leathery.
Diagnosis: Lichenification
For more information on Figure 4a, see “Leg Lesion Represents a Vicious Cycle.” Clin Rev. 2012;22(12):W5.
Derm Morphology, Part 1
1. Raised, often itchy, red bumps on the surface of the skin, usually from an allergic reaction.
Diagnosis: Hives/Wheals
For more information on this case, see “Inexperienced runner develops leg rash.” Clin Rev. 2012;22(8):W3.
For the next photograph, proceed to the next page >>
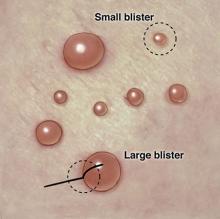
2. Large and small clear-fluid-filled blisters.
Diagnosis: Bullae/Vesicles
For more information, see “High-Yield Biopsy Technique for Subepidermal Blisters.” Cutis. 2015 April;95(ISSUE):4.
For the next photograph, proceed to the next page >>
3. Small, inflamed, pus-filled, blister-like lesions on the skin surface, commonly found in acne.
Diagnosis: Pustules
For more information on this case, see “Neonatal and Infantile Acne Vulgaris: An Update.” Cutis. 2014 July;94(1):13-16.
For the next photograph, proceed to the next page >>
4. Solid or cystic raised bumps wider than 1 cm but less than 2 cm.
Diagnosis: Nodules
For more information on this case, see “Lesion Has Doubled in Size in Two Weeks.” Clin Rev. 2009;19(10):2.
1. Raised, often itchy, red bumps on the surface of the skin, usually from an allergic reaction.
Diagnosis: Hives/Wheals
For more information on this case, see “Inexperienced runner develops leg rash.” Clin Rev. 2012;22(8):W3.
For the next photograph, proceed to the next page >>
2. Large and small clear-fluid-filled blisters.
Diagnosis: Bullae/Vesicles
For more information, see “High-Yield Biopsy Technique for Subepidermal Blisters.” Cutis. 2015 April;95(ISSUE):4.
For the next photograph, proceed to the next page >>
3. Small, inflamed, pus-filled, blister-like lesions on the skin surface, commonly found in acne.
Diagnosis: Pustules
For more information on this case, see “Neonatal and Infantile Acne Vulgaris: An Update.” Cutis. 2014 July;94(1):13-16.
For the next photograph, proceed to the next page >>
4. Solid or cystic raised bumps wider than 1 cm but less than 2 cm.
Diagnosis: Nodules
For more information on this case, see “Lesion Has Doubled in Size in Two Weeks.” Clin Rev. 2009;19(10):2.
1. Raised, often itchy, red bumps on the surface of the skin, usually from an allergic reaction.
Diagnosis: Hives/Wheals
For more information on this case, see “Inexperienced runner develops leg rash.” Clin Rev. 2012;22(8):W3.
For the next photograph, proceed to the next page >>
2. Large and small clear-fluid-filled blisters.
Diagnosis: Bullae/Vesicles
For more information, see “High-Yield Biopsy Technique for Subepidermal Blisters.” Cutis. 2015 April;95(ISSUE):4.
For the next photograph, proceed to the next page >>
3. Small, inflamed, pus-filled, blister-like lesions on the skin surface, commonly found in acne.
Diagnosis: Pustules
For more information on this case, see “Neonatal and Infantile Acne Vulgaris: An Update.” Cutis. 2014 July;94(1):13-16.
For the next photograph, proceed to the next page >>
4. Solid or cystic raised bumps wider than 1 cm but less than 2 cm.
Diagnosis: Nodules
For more information on this case, see “Lesion Has Doubled in Size in Two Weeks.” Clin Rev. 2009;19(10):2.
Earaches Visualized
1. A 30-year-old woman complained of drainage from her ear for the past three months. She admitted that her hearing was diminished in that ear. She had a history of recurrent ear infections since childhood.
Photo courtesy of Vladimir Zlinsky, MD, in Roy F. Sullivan, PhD. Audiology Forum: video otoscopy, www.rcsullivan.com. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Cholesteatoma, similar to an epidermal inclusion cyst in the skin, produces keratinaceous material that fills the middle ear, causing hearing loss and otorrhea.
For more information, see “Diminished hearing.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
2. A 2-year-old child was brought for a well-child exam two months after an episode of acute otitis media. He appeared healthy and was meeting all of his developmental milestones. An otoscopic examination revealed air-fluid levels in the right ear.
Photo courtesy of Frank Miller, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Otitis media with effusion, which is a characterized by fluid in the middle ear in a patient without signs or symptoms of an acute ear infection. The most common problem, present in more than half of patients, is mild hearing loss. This is usually identified when parents express concern regarding their child’s behavior, performance at school, or language development. The absence of signs and symptoms of acute illness assists in differentiating OME from AOM.
For more information, see “Air-fluid levels in ear.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
3. A 15-month-old boy was brought in with a two-day history of fever, irritability, and frequent tugging on his left ear. The week before, he had nasal congestion, cough, and rhinorrhea. On otoscopy, his left tympanic membrane (TM) appeared erythematous, cloudy, and bulging. The TM failed to move on pneumatic otoscopy.
Photo courtesy of William Clark, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Acute otitis media, which is characterized by middle-ear effusion in a patient with signs and symptoms of acute illness (eg, fever, irritability, otalgia).
For more information, see “Ear pain in baby.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
4. A 72-year-old man sought treatment for an earache in his left ear. He said that the pain began when he got a new “in the canal” hearing aid for his left ear a month earlier.
Photo courtesy of Dr. Roy F. Sullivan. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Acute otitis externa, secondary to ear canal damage done by using the new hearing aid, caused the viscous purulent discharge and narrowing of the ear canal.
For more information, see “Earache.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
5. Parents brought their 3-year-old daughter to an urgent care facility because she had been crying all day. The child was irritable, had scant otorrhea, and had been pulling on her right ear.
Photo courtesy of William Clark, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Otoscopy revealed an erythematous, swollen external auditory canal and a foreign object. The parents reported that their child had been playing with a toy beaded necklace when she started crying. The patient was referred to an otolaryngologist, who removed the bead using an operating microscope for visualization. She evaluated the child for a co-existing otitis externa and decided that the external canal was markedly inflamed and probably infected.
For more information, see “Object in ear.” J Fam Pract. 2013.
1. A 30-year-old woman complained of drainage from her ear for the past three months. She admitted that her hearing was diminished in that ear. She had a history of recurrent ear infections since childhood.
Photo courtesy of Vladimir Zlinsky, MD, in Roy F. Sullivan, PhD. Audiology Forum: video otoscopy, www.rcsullivan.com. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Cholesteatoma, similar to an epidermal inclusion cyst in the skin, produces keratinaceous material that fills the middle ear, causing hearing loss and otorrhea.
For more information, see “Diminished hearing.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
2. A 2-year-old child was brought for a well-child exam two months after an episode of acute otitis media. He appeared healthy and was meeting all of his developmental milestones. An otoscopic examination revealed air-fluid levels in the right ear.
Photo courtesy of Frank Miller, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Otitis media with effusion, which is a characterized by fluid in the middle ear in a patient without signs or symptoms of an acute ear infection. The most common problem, present in more than half of patients, is mild hearing loss. This is usually identified when parents express concern regarding their child’s behavior, performance at school, or language development. The absence of signs and symptoms of acute illness assists in differentiating OME from AOM.
For more information, see “Air-fluid levels in ear.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
3. A 15-month-old boy was brought in with a two-day history of fever, irritability, and frequent tugging on his left ear. The week before, he had nasal congestion, cough, and rhinorrhea. On otoscopy, his left tympanic membrane (TM) appeared erythematous, cloudy, and bulging. The TM failed to move on pneumatic otoscopy.
Photo courtesy of William Clark, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Acute otitis media, which is characterized by middle-ear effusion in a patient with signs and symptoms of acute illness (eg, fever, irritability, otalgia).
For more information, see “Ear pain in baby.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
4. A 72-year-old man sought treatment for an earache in his left ear. He said that the pain began when he got a new “in the canal” hearing aid for his left ear a month earlier.
Photo courtesy of Dr. Roy F. Sullivan. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Acute otitis externa, secondary to ear canal damage done by using the new hearing aid, caused the viscous purulent discharge and narrowing of the ear canal.
For more information, see “Earache.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
5. Parents brought their 3-year-old daughter to an urgent care facility because she had been crying all day. The child was irritable, had scant otorrhea, and had been pulling on her right ear.
Photo courtesy of William Clark, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Otoscopy revealed an erythematous, swollen external auditory canal and a foreign object. The parents reported that their child had been playing with a toy beaded necklace when she started crying. The patient was referred to an otolaryngologist, who removed the bead using an operating microscope for visualization. She evaluated the child for a co-existing otitis externa and decided that the external canal was markedly inflamed and probably infected.
For more information, see “Object in ear.” J Fam Pract. 2013.
1. A 30-year-old woman complained of drainage from her ear for the past three months. She admitted that her hearing was diminished in that ear. She had a history of recurrent ear infections since childhood.
Photo courtesy of Vladimir Zlinsky, MD, in Roy F. Sullivan, PhD. Audiology Forum: video otoscopy, www.rcsullivan.com. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Cholesteatoma, similar to an epidermal inclusion cyst in the skin, produces keratinaceous material that fills the middle ear, causing hearing loss and otorrhea.
For more information, see “Diminished hearing.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
2. A 2-year-old child was brought for a well-child exam two months after an episode of acute otitis media. He appeared healthy and was meeting all of his developmental milestones. An otoscopic examination revealed air-fluid levels in the right ear.
Photo courtesy of Frank Miller, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Otitis media with effusion, which is a characterized by fluid in the middle ear in a patient without signs or symptoms of an acute ear infection. The most common problem, present in more than half of patients, is mild hearing loss. This is usually identified when parents express concern regarding their child’s behavior, performance at school, or language development. The absence of signs and symptoms of acute illness assists in differentiating OME from AOM.
For more information, see “Air-fluid levels in ear.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
3. A 15-month-old boy was brought in with a two-day history of fever, irritability, and frequent tugging on his left ear. The week before, he had nasal congestion, cough, and rhinorrhea. On otoscopy, his left tympanic membrane (TM) appeared erythematous, cloudy, and bulging. The TM failed to move on pneumatic otoscopy.
Photo courtesy of William Clark, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Acute otitis media, which is characterized by middle-ear effusion in a patient with signs and symptoms of acute illness (eg, fever, irritability, otalgia).
For more information, see “Ear pain in baby.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
4. A 72-year-old man sought treatment for an earache in his left ear. He said that the pain began when he got a new “in the canal” hearing aid for his left ear a month earlier.
Photo courtesy of Dr. Roy F. Sullivan. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Acute otitis externa, secondary to ear canal damage done by using the new hearing aid, caused the viscous purulent discharge and narrowing of the ear canal.
For more information, see “Earache.” J Fam Pract. 2013.
For the next photograph, proceed to the next page >>
5. Parents brought their 3-year-old daughter to an urgent care facility because she had been crying all day. The child was irritable, had scant otorrhea, and had been pulling on her right ear.
Photo courtesy of William Clark, MD. Reprinted from The Color Atlas of Family Medicine. 2nd ed.
Diagnosis: Otoscopy revealed an erythematous, swollen external auditory canal and a foreign object. The parents reported that their child had been playing with a toy beaded necklace when she started crying. The patient was referred to an otolaryngologist, who removed the bead using an operating microscope for visualization. She evaluated the child for a co-existing otitis externa and decided that the external canal was markedly inflamed and probably infected.
For more information, see “Object in ear.” J Fam Pract. 2013.
Nail the Genetic Disorder
1. The patient has a long-standing pruritic rash. Flat, slightly elevated, greasy brown papules are scattered on the chest, abdomen, and upper back, with mild surrounding erythema. The fingernails are deformed, with longitudinal red streaks and ridges and v-shaped notching of the free margin.
Reprinted with permission from Cutis. 2003;72:124-126.
Diagnosis: Darier disease (DD) or Darier-White disease is a rare genetic skin disorder caused by mutations of the ATP2A2 gene, located on the long arm of chromosome 12 at position 24,11.1,2 This genetic mutation is inherited as an autosomal dominant trait with complete penetrance. DD affects men and women equally, with progressive skin signs of interfamilial and intrafamilial variability.3 Skin manifestations occur from late childhood to early adulthood and are typical during adolescence.3 Acute flare-ups can be triggered by heat, perspiration, sunlight, ultraviolet B exposure, stress, or certain medications (in particular, lithium).2 DD is not contagious.2
1. Creamer D, Barker J, Kerdel FA. Papular and papulosquamous dermatoses. In: Acute Adult Dermatology: Diagnosis and Management (A Colour Handbook). London, UK: Manson Publishing Ltd; 2011:48.
2. Kelly EB. Darier disease (DAR). In: Encyclopedia of Human Genetics and Disease. Santa Barbara, CA: ABC-CLIO; 2013:186-187.
3. Ringpfeil F. Dermatologic disorders. In: NORD Guide to Rare Disorders. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:101.
For more information on this case, see “Man, 45, With Greasy Rash and Deformed Nails.” Clin Rev. 2014;24(1):38,40-41
For the next photograph, proceed to the next page >>
2. Six months ago, this 36-year-old man’s left fourth finger began to bother him. He’s tried topical antibiotics, colloidal silver solution, and two different oral antibiotics. None have relieved the pain, which is severe enough to interfere with daily activity—particularly his job, which requires extensive computer time.
Diagnosis: “Infection” is only one potential cause of redness, swelling, increased warmth, and localized pain. Classically termed rubor, tumor, calor, and dolor, these are indicators of inflammation, which can occur in many conditions besides “infection.” In the case described, a simple hangnail was incompletely removed, leaving a shard of nail that then dug into the perionychial skin as it grew out. This set into motion a healing process that could not proceed to resolution, because the tissue was re-injured every time the finger struck the computer keyboard. This not only caused the wound to get stuck in a certain phase of healing (angioneogenesis) but also prevented completion of the process.
For more information on this case, see “Red and Swollen Doesn’t Mean “Infection.” Clin Rev. 2014;24(6):W1.
For the next photograph, proceed to the next page >>
3. A 25-year-old man presents with what he describes as a “fungal infection” of the fingernails that he’s had since birth. The nails are uniformly thickened and dystrophic, without significant discoloration. The patient’s palms and soles are hyperkeratotic, and the upper anterior legs are covered by a folliculocentric papular hyperkeratosis reminiscent of a coarse keratosis pilaris.
Diagnosis: Pachyonychia congenita (PC) is a rare condition that represents a mutation of keratin genes and is usually of autosomal dominant inheritance. First described by Muller in 1904, it was eventually categorized into one of two types: type I, MIM 167200, also known as Jadassohn-Lewandowsky, the most common type, and type II, MIM 167210, also known as Jackson-Lawler, with slightly different features. Today, a more common view is that no such divisions exist—only variations of PC that exhibit overlapping features.
For more information on this case, see “A fingernail "infection" present since birth.” Clin Rev. 2013;23(4):W6.
For the next photograph, proceed to the next page >>
4. Usually apparent at birth, this disorder may manifest with abnormal or missing nails. Characteristic nail changes include triangular lunulae and, most prominently on the thumb and index fingers, hypoplasia. Also apparent are orthopedic changes (particularly affecting the knees and elbows), renal disease, and glaucoma.
Reprinted with permission from Cutis. 2000;66:71, 75-76.
Diagnosis: The osteo-onychodysplasia, or nail-patella syndrome, is an autosomal dominant disorder. Studies have linked the syndrome to chromosome 9q34 and identified point mutations in the LMX1B gene.4 Other kindreds have been linked to chromosome 17q21-22.5 Prenatal diagnosis is possible, including noninvasive prenatal diagnosis using ultrasonography. Because of the risk for glaucoma, all family members should be screened by an ophthalmologist.6
4. Seri M, Melchionda S, Dreyer S, et al. Identification of LMX1B gene point mutations in Italian patients affected with nail-patella syndrome. Int J Mol Med. 1999;4:285-290.
5. Mangino M, Sanchez O, Torrente I, et al. Localization of a gene for familial patella aplasia-hypoplasia (PTLAH) to chromosome 17q21-22. Am J Hum Genetics. 1999;65:441-447.
6. Lichter PR, Richards JE, Downs CA, et al. Cosegregation of open-angle glaucoma and the nail-patella syndrome. Am J Ophthalmol. 1997;124:506-515.
For more information on this case, see “What Is Your Diagnosis? Nail-Patella Syndrome.” Cutis. 2000;66:71, 75-76.
1. The patient has a long-standing pruritic rash. Flat, slightly elevated, greasy brown papules are scattered on the chest, abdomen, and upper back, with mild surrounding erythema. The fingernails are deformed, with longitudinal red streaks and ridges and v-shaped notching of the free margin.
Reprinted with permission from Cutis. 2003;72:124-126.
Diagnosis: Darier disease (DD) or Darier-White disease is a rare genetic skin disorder caused by mutations of the ATP2A2 gene, located on the long arm of chromosome 12 at position 24,11.1,2 This genetic mutation is inherited as an autosomal dominant trait with complete penetrance. DD affects men and women equally, with progressive skin signs of interfamilial and intrafamilial variability.3 Skin manifestations occur from late childhood to early adulthood and are typical during adolescence.3 Acute flare-ups can be triggered by heat, perspiration, sunlight, ultraviolet B exposure, stress, or certain medications (in particular, lithium).2 DD is not contagious.2
1. Creamer D, Barker J, Kerdel FA. Papular and papulosquamous dermatoses. In: Acute Adult Dermatology: Diagnosis and Management (A Colour Handbook). London, UK: Manson Publishing Ltd; 2011:48.
2. Kelly EB. Darier disease (DAR). In: Encyclopedia of Human Genetics and Disease. Santa Barbara, CA: ABC-CLIO; 2013:186-187.
3. Ringpfeil F. Dermatologic disorders. In: NORD Guide to Rare Disorders. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:101.
For more information on this case, see “Man, 45, With Greasy Rash and Deformed Nails.” Clin Rev. 2014;24(1):38,40-41
For the next photograph, proceed to the next page >>
2. Six months ago, this 36-year-old man’s left fourth finger began to bother him. He’s tried topical antibiotics, colloidal silver solution, and two different oral antibiotics. None have relieved the pain, which is severe enough to interfere with daily activity—particularly his job, which requires extensive computer time.
Diagnosis: “Infection” is only one potential cause of redness, swelling, increased warmth, and localized pain. Classically termed rubor, tumor, calor, and dolor, these are indicators of inflammation, which can occur in many conditions besides “infection.” In the case described, a simple hangnail was incompletely removed, leaving a shard of nail that then dug into the perionychial skin as it grew out. This set into motion a healing process that could not proceed to resolution, because the tissue was re-injured every time the finger struck the computer keyboard. This not only caused the wound to get stuck in a certain phase of healing (angioneogenesis) but also prevented completion of the process.
For more information on this case, see “Red and Swollen Doesn’t Mean “Infection.” Clin Rev. 2014;24(6):W1.
For the next photograph, proceed to the next page >>
3. A 25-year-old man presents with what he describes as a “fungal infection” of the fingernails that he’s had since birth. The nails are uniformly thickened and dystrophic, without significant discoloration. The patient’s palms and soles are hyperkeratotic, and the upper anterior legs are covered by a folliculocentric papular hyperkeratosis reminiscent of a coarse keratosis pilaris.
Diagnosis: Pachyonychia congenita (PC) is a rare condition that represents a mutation of keratin genes and is usually of autosomal dominant inheritance. First described by Muller in 1904, it was eventually categorized into one of two types: type I, MIM 167200, also known as Jadassohn-Lewandowsky, the most common type, and type II, MIM 167210, also known as Jackson-Lawler, with slightly different features. Today, a more common view is that no such divisions exist—only variations of PC that exhibit overlapping features.
For more information on this case, see “A fingernail "infection" present since birth.” Clin Rev. 2013;23(4):W6.
For the next photograph, proceed to the next page >>
4. Usually apparent at birth, this disorder may manifest with abnormal or missing nails. Characteristic nail changes include triangular lunulae and, most prominently on the thumb and index fingers, hypoplasia. Also apparent are orthopedic changes (particularly affecting the knees and elbows), renal disease, and glaucoma.
Reprinted with permission from Cutis. 2000;66:71, 75-76.
Diagnosis: The osteo-onychodysplasia, or nail-patella syndrome, is an autosomal dominant disorder. Studies have linked the syndrome to chromosome 9q34 and identified point mutations in the LMX1B gene.4 Other kindreds have been linked to chromosome 17q21-22.5 Prenatal diagnosis is possible, including noninvasive prenatal diagnosis using ultrasonography. Because of the risk for glaucoma, all family members should be screened by an ophthalmologist.6
4. Seri M, Melchionda S, Dreyer S, et al. Identification of LMX1B gene point mutations in Italian patients affected with nail-patella syndrome. Int J Mol Med. 1999;4:285-290.
5. Mangino M, Sanchez O, Torrente I, et al. Localization of a gene for familial patella aplasia-hypoplasia (PTLAH) to chromosome 17q21-22. Am J Hum Genetics. 1999;65:441-447.
6. Lichter PR, Richards JE, Downs CA, et al. Cosegregation of open-angle glaucoma and the nail-patella syndrome. Am J Ophthalmol. 1997;124:506-515.
For more information on this case, see “What Is Your Diagnosis? Nail-Patella Syndrome.” Cutis. 2000;66:71, 75-76.
1. The patient has a long-standing pruritic rash. Flat, slightly elevated, greasy brown papules are scattered on the chest, abdomen, and upper back, with mild surrounding erythema. The fingernails are deformed, with longitudinal red streaks and ridges and v-shaped notching of the free margin.
Reprinted with permission from Cutis. 2003;72:124-126.
Diagnosis: Darier disease (DD) or Darier-White disease is a rare genetic skin disorder caused by mutations of the ATP2A2 gene, located on the long arm of chromosome 12 at position 24,11.1,2 This genetic mutation is inherited as an autosomal dominant trait with complete penetrance. DD affects men and women equally, with progressive skin signs of interfamilial and intrafamilial variability.3 Skin manifestations occur from late childhood to early adulthood and are typical during adolescence.3 Acute flare-ups can be triggered by heat, perspiration, sunlight, ultraviolet B exposure, stress, or certain medications (in particular, lithium).2 DD is not contagious.2
1. Creamer D, Barker J, Kerdel FA. Papular and papulosquamous dermatoses. In: Acute Adult Dermatology: Diagnosis and Management (A Colour Handbook). London, UK: Manson Publishing Ltd; 2011:48.
2. Kelly EB. Darier disease (DAR). In: Encyclopedia of Human Genetics and Disease. Santa Barbara, CA: ABC-CLIO; 2013:186-187.
3. Ringpfeil F. Dermatologic disorders. In: NORD Guide to Rare Disorders. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:101.
For more information on this case, see “Man, 45, With Greasy Rash and Deformed Nails.” Clin Rev. 2014;24(1):38,40-41
For the next photograph, proceed to the next page >>
2. Six months ago, this 36-year-old man’s left fourth finger began to bother him. He’s tried topical antibiotics, colloidal silver solution, and two different oral antibiotics. None have relieved the pain, which is severe enough to interfere with daily activity—particularly his job, which requires extensive computer time.
Diagnosis: “Infection” is only one potential cause of redness, swelling, increased warmth, and localized pain. Classically termed rubor, tumor, calor, and dolor, these are indicators of inflammation, which can occur in many conditions besides “infection.” In the case described, a simple hangnail was incompletely removed, leaving a shard of nail that then dug into the perionychial skin as it grew out. This set into motion a healing process that could not proceed to resolution, because the tissue was re-injured every time the finger struck the computer keyboard. This not only caused the wound to get stuck in a certain phase of healing (angioneogenesis) but also prevented completion of the process.
For more information on this case, see “Red and Swollen Doesn’t Mean “Infection.” Clin Rev. 2014;24(6):W1.
For the next photograph, proceed to the next page >>
3. A 25-year-old man presents with what he describes as a “fungal infection” of the fingernails that he’s had since birth. The nails are uniformly thickened and dystrophic, without significant discoloration. The patient’s palms and soles are hyperkeratotic, and the upper anterior legs are covered by a folliculocentric papular hyperkeratosis reminiscent of a coarse keratosis pilaris.
Diagnosis: Pachyonychia congenita (PC) is a rare condition that represents a mutation of keratin genes and is usually of autosomal dominant inheritance. First described by Muller in 1904, it was eventually categorized into one of two types: type I, MIM 167200, also known as Jadassohn-Lewandowsky, the most common type, and type II, MIM 167210, also known as Jackson-Lawler, with slightly different features. Today, a more common view is that no such divisions exist—only variations of PC that exhibit overlapping features.
For more information on this case, see “A fingernail "infection" present since birth.” Clin Rev. 2013;23(4):W6.
For the next photograph, proceed to the next page >>
4. Usually apparent at birth, this disorder may manifest with abnormal or missing nails. Characteristic nail changes include triangular lunulae and, most prominently on the thumb and index fingers, hypoplasia. Also apparent are orthopedic changes (particularly affecting the knees and elbows), renal disease, and glaucoma.
Reprinted with permission from Cutis. 2000;66:71, 75-76.
Diagnosis: The osteo-onychodysplasia, or nail-patella syndrome, is an autosomal dominant disorder. Studies have linked the syndrome to chromosome 9q34 and identified point mutations in the LMX1B gene.4 Other kindreds have been linked to chromosome 17q21-22.5 Prenatal diagnosis is possible, including noninvasive prenatal diagnosis using ultrasonography. Because of the risk for glaucoma, all family members should be screened by an ophthalmologist.6
4. Seri M, Melchionda S, Dreyer S, et al. Identification of LMX1B gene point mutations in Italian patients affected with nail-patella syndrome. Int J Mol Med. 1999;4:285-290.
5. Mangino M, Sanchez O, Torrente I, et al. Localization of a gene for familial patella aplasia-hypoplasia (PTLAH) to chromosome 17q21-22. Am J Hum Genetics. 1999;65:441-447.
6. Lichter PR, Richards JE, Downs CA, et al. Cosegregation of open-angle glaucoma and the nail-patella syndrome. Am J Ophthalmol. 1997;124:506-515.
For more information on this case, see “What Is Your Diagnosis? Nail-Patella Syndrome.” Cutis. 2000;66:71, 75-76.
Will the Real Tinea Please Stand Up …
1. The patient’s original lesion is dark brown, macular, and ovoid. An additional 15 to 20 oval, papulosquamous lesions are seen elsewhere on her trunk. These are widely scattered, hyperpigmented, and have scaly centers. The long axes of her oval back lesions are parallel with natural lines of cleavage in the skin.
Diagnosis: Pityriasis rosea, which is commonly seen in patients ages 10 to 35 and is about twice as likely to occur in women as in men.
The so-called herald patch appears initially, in a majority of cases, as a salmon-pink patch that can become as large as 5 to 10 cm, on the trunk or arms. The smaller oval lesions begin to appear within a week or two, averaging 1 to 2 cm in diameter; most display the characteristic “centripetal” scaling, clearly sparing the lesions’ periphery and serving as an essentially pathognomic finding.
On darker-skinned patients, the lesions (including the herald patch) will tend to be brown to black. The examiner must then look for the other characteristic aspects of PR, including the oval (as opposed to round) shape, the long axes of which will often parallel the skin tension lines on the back to produce what is termed the “Christmas tree pattern.”
For more information on this case, see “All of Her Friends Say She Has Ringworm.” Clin Rev. 2013;23(2).
For the next photograph, proceed to the next page >>
2. A man has had an asymptomatic rash for several weeks. Prior to its appearance, he was diagnosed with strep throat and treated with amoxicillin. The rash is quite striking: brightly erythematous, with annular margins on which the skin is red. But just behind the advancing margin is a parallel band of scaling.
Diagnosis: Erythema annulare centrifugum (EAC), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis. EAC lesions can be large, appear in multiples, and spare only palms and soles. EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
For more information on this case, see “Is A Common Illness The Cause of This Man's Rash?” Clin Rev. 2011;21(12).
For the next photograph, proceed to the next page >>
3. For two months, an 8-year-old girl has had a mildly tender and markedly pruritic rash on her right lower leg. Physical exam reveals concentric annular lesions on the affected leg. The central areas demonstrate a bruised appearance that does not resolve with diascopy.
Image courtesy of Robert Brodell, MD; reprinted from The Journal of Family Practice (2014;63:395-396).
Diagnosis: Tinea corporis was confirmed by the results of a potassium hydroxide (KOH) preparation showing septate hyphae. A periodic acid-Schiff (PAS) stain performed on the previous biopsy specimen revealed septate hyphae in the stratum corneum that were not apparent on the original hematoxylin and eosin (H&E) stained sections.
Dermatophyte infections of the skin are known as tinea corporis or “ringworm.” Ringworm fungi belong to 3 genera, Microsporum, Trichophyton, and Epidermophyton. These infections occur at any age and are more common in warmer climates.1 The classic lesion is an annular scaly patch, sometimes with the concentric rings, as seen in our patient. The bruising was almost certainly caused by rubbing and scratching.
1. Shrum JP, Millikan LE, Bataineh O. Superficial fungal infections in the tropics. Dermatol Clin. 1994;12:687-693.
For more information on this case, see “Young girl with lower leg rash.” J Fam Pract. 2014;63(7):395-396.
For the next photograph, proceed to the next page >>
4. For three months (since the long, cold winter), this man has had very itchy lesions on his legs that he often scratches vigorously. He is not atopic and has no new pets, but he does admit to being “addicted” to sitting in his new hot tub. Examination of the patient’s legs, particularly his calves, shows discrete and confluent round, scaly plaques of a striking reddish orange hue.
Diagnosis: Nummular eczema (NE), an extremely common condition, especially in older men with dry skin made drier by bathing habits, swimming, or use of hot tubs. But many cases appear without these conditions, causing much conjecture about potential triggers, such as contact versus irritant dermatitis. Indeed, the multiplicity of topical medications applied by this patient was probably making things worse, as is often the case. NE typically manifests acutely, but can persist for months. If need be, a 4-mm punch biopsy will rule out the other suspects in the differential diagnosis.
For more information on this case, see “Family Thinks Man has Worms.” Clin Rev. 2010;20(8):6.
1. The patient’s original lesion is dark brown, macular, and ovoid. An additional 15 to 20 oval, papulosquamous lesions are seen elsewhere on her trunk. These are widely scattered, hyperpigmented, and have scaly centers. The long axes of her oval back lesions are parallel with natural lines of cleavage in the skin.
Diagnosis: Pityriasis rosea, which is commonly seen in patients ages 10 to 35 and is about twice as likely to occur in women as in men.
The so-called herald patch appears initially, in a majority of cases, as a salmon-pink patch that can become as large as 5 to 10 cm, on the trunk or arms. The smaller oval lesions begin to appear within a week or two, averaging 1 to 2 cm in diameter; most display the characteristic “centripetal” scaling, clearly sparing the lesions’ periphery and serving as an essentially pathognomic finding.
On darker-skinned patients, the lesions (including the herald patch) will tend to be brown to black. The examiner must then look for the other characteristic aspects of PR, including the oval (as opposed to round) shape, the long axes of which will often parallel the skin tension lines on the back to produce what is termed the “Christmas tree pattern.”
For more information on this case, see “All of Her Friends Say She Has Ringworm.” Clin Rev. 2013;23(2).
For the next photograph, proceed to the next page >>
2. A man has had an asymptomatic rash for several weeks. Prior to its appearance, he was diagnosed with strep throat and treated with amoxicillin. The rash is quite striking: brightly erythematous, with annular margins on which the skin is red. But just behind the advancing margin is a parallel band of scaling.
Diagnosis: Erythema annulare centrifugum (EAC), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis. EAC lesions can be large, appear in multiples, and spare only palms and soles. EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
For more information on this case, see “Is A Common Illness The Cause of This Man's Rash?” Clin Rev. 2011;21(12).
For the next photograph, proceed to the next page >>
3. For two months, an 8-year-old girl has had a mildly tender and markedly pruritic rash on her right lower leg. Physical exam reveals concentric annular lesions on the affected leg. The central areas demonstrate a bruised appearance that does not resolve with diascopy.
Image courtesy of Robert Brodell, MD; reprinted from The Journal of Family Practice (2014;63:395-396).
Diagnosis: Tinea corporis was confirmed by the results of a potassium hydroxide (KOH) preparation showing septate hyphae. A periodic acid-Schiff (PAS) stain performed on the previous biopsy specimen revealed septate hyphae in the stratum corneum that were not apparent on the original hematoxylin and eosin (H&E) stained sections.
Dermatophyte infections of the skin are known as tinea corporis or “ringworm.” Ringworm fungi belong to 3 genera, Microsporum, Trichophyton, and Epidermophyton. These infections occur at any age and are more common in warmer climates.1 The classic lesion is an annular scaly patch, sometimes with the concentric rings, as seen in our patient. The bruising was almost certainly caused by rubbing and scratching.
1. Shrum JP, Millikan LE, Bataineh O. Superficial fungal infections in the tropics. Dermatol Clin. 1994;12:687-693.
For more information on this case, see “Young girl with lower leg rash.” J Fam Pract. 2014;63(7):395-396.
For the next photograph, proceed to the next page >>
4. For three months (since the long, cold winter), this man has had very itchy lesions on his legs that he often scratches vigorously. He is not atopic and has no new pets, but he does admit to being “addicted” to sitting in his new hot tub. Examination of the patient’s legs, particularly his calves, shows discrete and confluent round, scaly plaques of a striking reddish orange hue.
Diagnosis: Nummular eczema (NE), an extremely common condition, especially in older men with dry skin made drier by bathing habits, swimming, or use of hot tubs. But many cases appear without these conditions, causing much conjecture about potential triggers, such as contact versus irritant dermatitis. Indeed, the multiplicity of topical medications applied by this patient was probably making things worse, as is often the case. NE typically manifests acutely, but can persist for months. If need be, a 4-mm punch biopsy will rule out the other suspects in the differential diagnosis.
For more information on this case, see “Family Thinks Man has Worms.” Clin Rev. 2010;20(8):6.
1. The patient’s original lesion is dark brown, macular, and ovoid. An additional 15 to 20 oval, papulosquamous lesions are seen elsewhere on her trunk. These are widely scattered, hyperpigmented, and have scaly centers. The long axes of her oval back lesions are parallel with natural lines of cleavage in the skin.
Diagnosis: Pityriasis rosea, which is commonly seen in patients ages 10 to 35 and is about twice as likely to occur in women as in men.
The so-called herald patch appears initially, in a majority of cases, as a salmon-pink patch that can become as large as 5 to 10 cm, on the trunk or arms. The smaller oval lesions begin to appear within a week or two, averaging 1 to 2 cm in diameter; most display the characteristic “centripetal” scaling, clearly sparing the lesions’ periphery and serving as an essentially pathognomic finding.
On darker-skinned patients, the lesions (including the herald patch) will tend to be brown to black. The examiner must then look for the other characteristic aspects of PR, including the oval (as opposed to round) shape, the long axes of which will often parallel the skin tension lines on the back to produce what is termed the “Christmas tree pattern.”
For more information on this case, see “All of Her Friends Say She Has Ringworm.” Clin Rev. 2013;23(2).
For the next photograph, proceed to the next page >>
2. A man has had an asymptomatic rash for several weeks. Prior to its appearance, he was diagnosed with strep throat and treated with amoxicillin. The rash is quite striking: brightly erythematous, with annular margins on which the skin is red. But just behind the advancing margin is a parallel band of scaling.
Diagnosis: Erythema annulare centrifugum (EAC), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis. EAC lesions can be large, appear in multiples, and spare only palms and soles. EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
For more information on this case, see “Is A Common Illness The Cause of This Man's Rash?” Clin Rev. 2011;21(12).
For the next photograph, proceed to the next page >>
3. For two months, an 8-year-old girl has had a mildly tender and markedly pruritic rash on her right lower leg. Physical exam reveals concentric annular lesions on the affected leg. The central areas demonstrate a bruised appearance that does not resolve with diascopy.
Image courtesy of Robert Brodell, MD; reprinted from The Journal of Family Practice (2014;63:395-396).
Diagnosis: Tinea corporis was confirmed by the results of a potassium hydroxide (KOH) preparation showing septate hyphae. A periodic acid-Schiff (PAS) stain performed on the previous biopsy specimen revealed septate hyphae in the stratum corneum that were not apparent on the original hematoxylin and eosin (H&E) stained sections.
Dermatophyte infections of the skin are known as tinea corporis or “ringworm.” Ringworm fungi belong to 3 genera, Microsporum, Trichophyton, and Epidermophyton. These infections occur at any age and are more common in warmer climates.1 The classic lesion is an annular scaly patch, sometimes with the concentric rings, as seen in our patient. The bruising was almost certainly caused by rubbing and scratching.
1. Shrum JP, Millikan LE, Bataineh O. Superficial fungal infections in the tropics. Dermatol Clin. 1994;12:687-693.
For more information on this case, see “Young girl with lower leg rash.” J Fam Pract. 2014;63(7):395-396.
For the next photograph, proceed to the next page >>
4. For three months (since the long, cold winter), this man has had very itchy lesions on his legs that he often scratches vigorously. He is not atopic and has no new pets, but he does admit to being “addicted” to sitting in his new hot tub. Examination of the patient’s legs, particularly his calves, shows discrete and confluent round, scaly plaques of a striking reddish orange hue.
Diagnosis: Nummular eczema (NE), an extremely common condition, especially in older men with dry skin made drier by bathing habits, swimming, or use of hot tubs. But many cases appear without these conditions, causing much conjecture about potential triggers, such as contact versus irritant dermatitis. Indeed, the multiplicity of topical medications applied by this patient was probably making things worse, as is often the case. NE typically manifests acutely, but can persist for months. If need be, a 4-mm punch biopsy will rule out the other suspects in the differential diagnosis.
For more information on this case, see “Family Thinks Man has Worms.” Clin Rev. 2010;20(8):6.
About Face
1. Papulosquamous skin disease marked by a history of waxing and waning in severity and scaling in perinasal area manifested in this patient.
Diagnosis: Seborrheic dermatitis presenting as erythema with scaling on the perinasal and perioral area. Similar to rosacea, seborrheic dermatitis is a chronic and relapsing erythematous rash with well-demarcated erythematous patches, papules, or plaques; however, unlike rosacea, the distribution varies from minimal asymptomatic scaliness of the scalp to more widespread involvement (eg, scalp, ears, upper aspect of the trunk, intertriginous areas). Also, although macular erythema and scaling involving the perinasal area may be seen in either rosacea or seborrheic dermatitis, a greasy quality to the scales and involvement of other sites such as the scalp, retroauricular skin, and eyebrows suggest a diagnosis of seborrheic dermatitis
Read more about seborrheic dermatitis at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
For the next photograph, proceed to the next page >>
2. The patient had a painful, erythematous skin rash over the bridge of her nose, spreading to the malar area, eyelids, and forehead.
Diagnosis: Erysipelas is an acute superficial cellulitis with lymphatic involvement. It is characterized by the abrupt onset of a warm, erythematous rash with a sharply demarcated, indurated, elevated margin. There are no suppurative foci; sometimes, however, there are bullae or vesicles.
In facial “butterfly” erysipelas (which this patient had), the plaques may involve the eyelids, cheeks, nose, and forehead. Upon palpation, the skin is hot and tender. As the process develops, the color becomes a dark, fiery red and vesicles appear at the advancing border and over the surface. Associated regional lymphadenopathy may be present. There is no necrosis.1
Read more about erysipelas at Painful rash on face. J Fam Pract. 2010 August;59(8):459-462.
For the next photograph, proceed to the next page >>
3. Shortly after she started taking Bikram yoga classes, this 30-year-old patient developed inflammatory papules and pustules. Her symptoms worsened after each 1-hour session. On physical exam, there were erythematous, inflammatory papules and pustules concentrated on her forehead. No comedones were present.
Diagnosis: Rosacea, an inflammatory condition of the skin that typically affects the convex portions of the central face. This chronic cutaneous disorder usually starts after age 30 in both men and women, and is more prevalent in those with fairer skin.2 In fact, an epidemiologic study showed the prevalence to be as high as 10% in the Swedish population.3 The condition, which is not life threatening, can be controlled, although not cured. Its effect on appearance may have a negative impact on a patient’s quality of life.
Read more about Rosacea at Pustular eruption on face. J Fam Pract. 2010 July;59(7):399-401.
For the next photograph, proceed to the next page >>
4. Erythematous papules, papulovesicles, and plaques appeared on sun-exposed surfaces of the skin.
Diagnosis: Polymorphous light eruption (PMLE) manifesting as erythematous papules over the cheek and dorsal aspect of the nose. Similarities between PMLE and rosacea include exacerbation by sun exposure and a higher prevalence in fair-skinned individuals.4 Also, in both conditions erythematous papules appear on the face and may be pruritic and in some instances painful; however, unlike rosacea, which is chronic, PMLE tends to be intermittent and recurrent, typically occurring in the spring and early summer months.
Read more about PMLE at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
For the next photograph, proceed to the next page >>
5. This patient presented with isolated, grouped, and multiple erythematous to violaceous papules, plaques, or nodules, in an asymmetric distribution.
Diagnosis: B-cell neoplasms with skin involvement can present as primary cutaneous lymphomas or as secondary processes, including specific infiltrates of nodal or extranodal lymphoma or leukemia.5 B-cell lymphomas involving the skin have a distinct clinical appearance, presenting as isolated, grouped, or multiple erythematous to violaceous papules, plaques, or nodules, usually in an asymmetric distribution. B-cell lymphoproliferative diseases simulating rosacea are extremely rare.5 Nevertheless, B-cell lymphoma mimicking rhinophyma has been documented in the literature.5-11
Read more about B-cell neoplasms at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
Figures 1, 4, 5 reprinted with permission from Cutis. 2014;94(1):39-45; photographs for Figures 4 and 5 courtesy of Marc Silverstein, MD. Figure 2 reprinted with permission from J Fam Pract. 2010 August;59(8):459-462; photograph courtesy of Felix B. Chang, MD. Figure 3 reprinted courtesy of J Fam Pract. 2010 July;59(7):399-401; photograph courtesy of Nikki N. Kim, MD, Heather W. Wickless, MD, MPH.
REFERENCES
1. Chang F, Lopes A. Erysipelas. In: Domino FJ, ed. The 5-Minute Clinical Consult 2008. 16th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2008:448–449.
2. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad Dermatol Venereol. 2005;19:273-285.
3. Berg M, Liden S. An epidemiological study of rosacea. Acta Derm Venereol. 1989;69:419-423.
4. Tutrone WD. Polymorphic light eruption. Dermatol Ther. 2003;16:28-39.
5. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148:824-831.
6. Moulonguet I, Ghnassia M, Molina T, et al. Miliarial-type perifollicular B-cell pseudolymphoma (lymphocytoma cutis): a misleading eruption in two women. J Cutan Pathol. 2012;39:1016-1021.
7. Soon CW, Pincus LB, Ai WZ, et al. Acneiform presentation of primary cutaneous follicle center lymphoma. J Am Acad Dermatol. 2011;65:887-889.
8. Rosmaninho A, Alves R, Lima M, et al. Red nose: primary cutaneous marginal zone B-cell lymphoma. Leuk Res.2010;34:682-684.
9. Ogden S, Coulson IH. B-cell lymphoma mimicking rhinophyma. Clin Exp Dermatol. 2008;33:213-214.
10. Seward JL, Malone JC, Callen JP. Rhinophymalike swelling in an 86-year-old woman. Primary cutaneous B-cell lymphoma of the nose. Arch Dermatol. 2004;140:751-756.
11. Colvin JH, Lamerson CL, Cualing H, et al. Cutaneous lymphoplasmacytoid lymphoma (immunocytoma) with Waldenström’s macroglobulinemia mimicking rosacea. J Am Acad Dermatol. 2003;49:1159-1162.
1. Papulosquamous skin disease marked by a history of waxing and waning in severity and scaling in perinasal area manifested in this patient.
Diagnosis: Seborrheic dermatitis presenting as erythema with scaling on the perinasal and perioral area. Similar to rosacea, seborrheic dermatitis is a chronic and relapsing erythematous rash with well-demarcated erythematous patches, papules, or plaques; however, unlike rosacea, the distribution varies from minimal asymptomatic scaliness of the scalp to more widespread involvement (eg, scalp, ears, upper aspect of the trunk, intertriginous areas). Also, although macular erythema and scaling involving the perinasal area may be seen in either rosacea or seborrheic dermatitis, a greasy quality to the scales and involvement of other sites such as the scalp, retroauricular skin, and eyebrows suggest a diagnosis of seborrheic dermatitis
Read more about seborrheic dermatitis at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
For the next photograph, proceed to the next page >>
2. The patient had a painful, erythematous skin rash over the bridge of her nose, spreading to the malar area, eyelids, and forehead.
Diagnosis: Erysipelas is an acute superficial cellulitis with lymphatic involvement. It is characterized by the abrupt onset of a warm, erythematous rash with a sharply demarcated, indurated, elevated margin. There are no suppurative foci; sometimes, however, there are bullae or vesicles.
In facial “butterfly” erysipelas (which this patient had), the plaques may involve the eyelids, cheeks, nose, and forehead. Upon palpation, the skin is hot and tender. As the process develops, the color becomes a dark, fiery red and vesicles appear at the advancing border and over the surface. Associated regional lymphadenopathy may be present. There is no necrosis.1
Read more about erysipelas at Painful rash on face. J Fam Pract. 2010 August;59(8):459-462.
For the next photograph, proceed to the next page >>
3. Shortly after she started taking Bikram yoga classes, this 30-year-old patient developed inflammatory papules and pustules. Her symptoms worsened after each 1-hour session. On physical exam, there were erythematous, inflammatory papules and pustules concentrated on her forehead. No comedones were present.
Diagnosis: Rosacea, an inflammatory condition of the skin that typically affects the convex portions of the central face. This chronic cutaneous disorder usually starts after age 30 in both men and women, and is more prevalent in those with fairer skin.2 In fact, an epidemiologic study showed the prevalence to be as high as 10% in the Swedish population.3 The condition, which is not life threatening, can be controlled, although not cured. Its effect on appearance may have a negative impact on a patient’s quality of life.
Read more about Rosacea at Pustular eruption on face. J Fam Pract. 2010 July;59(7):399-401.
For the next photograph, proceed to the next page >>
4. Erythematous papules, papulovesicles, and plaques appeared on sun-exposed surfaces of the skin.
Diagnosis: Polymorphous light eruption (PMLE) manifesting as erythematous papules over the cheek and dorsal aspect of the nose. Similarities between PMLE and rosacea include exacerbation by sun exposure and a higher prevalence in fair-skinned individuals.4 Also, in both conditions erythematous papules appear on the face and may be pruritic and in some instances painful; however, unlike rosacea, which is chronic, PMLE tends to be intermittent and recurrent, typically occurring in the spring and early summer months.
Read more about PMLE at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
For the next photograph, proceed to the next page >>
5. This patient presented with isolated, grouped, and multiple erythematous to violaceous papules, plaques, or nodules, in an asymmetric distribution.
Diagnosis: B-cell neoplasms with skin involvement can present as primary cutaneous lymphomas or as secondary processes, including specific infiltrates of nodal or extranodal lymphoma or leukemia.5 B-cell lymphomas involving the skin have a distinct clinical appearance, presenting as isolated, grouped, or multiple erythematous to violaceous papules, plaques, or nodules, usually in an asymmetric distribution. B-cell lymphoproliferative diseases simulating rosacea are extremely rare.5 Nevertheless, B-cell lymphoma mimicking rhinophyma has been documented in the literature.5-11
Read more about B-cell neoplasms at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
Figures 1, 4, 5 reprinted with permission from Cutis. 2014;94(1):39-45; photographs for Figures 4 and 5 courtesy of Marc Silverstein, MD. Figure 2 reprinted with permission from J Fam Pract. 2010 August;59(8):459-462; photograph courtesy of Felix B. Chang, MD. Figure 3 reprinted courtesy of J Fam Pract. 2010 July;59(7):399-401; photograph courtesy of Nikki N. Kim, MD, Heather W. Wickless, MD, MPH.
REFERENCES
1. Chang F, Lopes A. Erysipelas. In: Domino FJ, ed. The 5-Minute Clinical Consult 2008. 16th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2008:448–449.
2. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad Dermatol Venereol. 2005;19:273-285.
3. Berg M, Liden S. An epidemiological study of rosacea. Acta Derm Venereol. 1989;69:419-423.
4. Tutrone WD. Polymorphic light eruption. Dermatol Ther. 2003;16:28-39.
5. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148:824-831.
6. Moulonguet I, Ghnassia M, Molina T, et al. Miliarial-type perifollicular B-cell pseudolymphoma (lymphocytoma cutis): a misleading eruption in two women. J Cutan Pathol. 2012;39:1016-1021.
7. Soon CW, Pincus LB, Ai WZ, et al. Acneiform presentation of primary cutaneous follicle center lymphoma. J Am Acad Dermatol. 2011;65:887-889.
8. Rosmaninho A, Alves R, Lima M, et al. Red nose: primary cutaneous marginal zone B-cell lymphoma. Leuk Res.2010;34:682-684.
9. Ogden S, Coulson IH. B-cell lymphoma mimicking rhinophyma. Clin Exp Dermatol. 2008;33:213-214.
10. Seward JL, Malone JC, Callen JP. Rhinophymalike swelling in an 86-year-old woman. Primary cutaneous B-cell lymphoma of the nose. Arch Dermatol. 2004;140:751-756.
11. Colvin JH, Lamerson CL, Cualing H, et al. Cutaneous lymphoplasmacytoid lymphoma (immunocytoma) with Waldenström’s macroglobulinemia mimicking rosacea. J Am Acad Dermatol. 2003;49:1159-1162.
1. Papulosquamous skin disease marked by a history of waxing and waning in severity and scaling in perinasal area manifested in this patient.
Diagnosis: Seborrheic dermatitis presenting as erythema with scaling on the perinasal and perioral area. Similar to rosacea, seborrheic dermatitis is a chronic and relapsing erythematous rash with well-demarcated erythematous patches, papules, or plaques; however, unlike rosacea, the distribution varies from minimal asymptomatic scaliness of the scalp to more widespread involvement (eg, scalp, ears, upper aspect of the trunk, intertriginous areas). Also, although macular erythema and scaling involving the perinasal area may be seen in either rosacea or seborrheic dermatitis, a greasy quality to the scales and involvement of other sites such as the scalp, retroauricular skin, and eyebrows suggest a diagnosis of seborrheic dermatitis
Read more about seborrheic dermatitis at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
For the next photograph, proceed to the next page >>
2. The patient had a painful, erythematous skin rash over the bridge of her nose, spreading to the malar area, eyelids, and forehead.
Diagnosis: Erysipelas is an acute superficial cellulitis with lymphatic involvement. It is characterized by the abrupt onset of a warm, erythematous rash with a sharply demarcated, indurated, elevated margin. There are no suppurative foci; sometimes, however, there are bullae or vesicles.
In facial “butterfly” erysipelas (which this patient had), the plaques may involve the eyelids, cheeks, nose, and forehead. Upon palpation, the skin is hot and tender. As the process develops, the color becomes a dark, fiery red and vesicles appear at the advancing border and over the surface. Associated regional lymphadenopathy may be present. There is no necrosis.1
Read more about erysipelas at Painful rash on face. J Fam Pract. 2010 August;59(8):459-462.
For the next photograph, proceed to the next page >>
3. Shortly after she started taking Bikram yoga classes, this 30-year-old patient developed inflammatory papules and pustules. Her symptoms worsened after each 1-hour session. On physical exam, there were erythematous, inflammatory papules and pustules concentrated on her forehead. No comedones were present.
Diagnosis: Rosacea, an inflammatory condition of the skin that typically affects the convex portions of the central face. This chronic cutaneous disorder usually starts after age 30 in both men and women, and is more prevalent in those with fairer skin.2 In fact, an epidemiologic study showed the prevalence to be as high as 10% in the Swedish population.3 The condition, which is not life threatening, can be controlled, although not cured. Its effect on appearance may have a negative impact on a patient’s quality of life.
Read more about Rosacea at Pustular eruption on face. J Fam Pract. 2010 July;59(7):399-401.
For the next photograph, proceed to the next page >>
4. Erythematous papules, papulovesicles, and plaques appeared on sun-exposed surfaces of the skin.
Diagnosis: Polymorphous light eruption (PMLE) manifesting as erythematous papules over the cheek and dorsal aspect of the nose. Similarities between PMLE and rosacea include exacerbation by sun exposure and a higher prevalence in fair-skinned individuals.4 Also, in both conditions erythematous papules appear on the face and may be pruritic and in some instances painful; however, unlike rosacea, which is chronic, PMLE tends to be intermittent and recurrent, typically occurring in the spring and early summer months.
Read more about PMLE at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
For the next photograph, proceed to the next page >>
5. This patient presented with isolated, grouped, and multiple erythematous to violaceous papules, plaques, or nodules, in an asymmetric distribution.
Diagnosis: B-cell neoplasms with skin involvement can present as primary cutaneous lymphomas or as secondary processes, including specific infiltrates of nodal or extranodal lymphoma or leukemia.5 B-cell lymphomas involving the skin have a distinct clinical appearance, presenting as isolated, grouped, or multiple erythematous to violaceous papules, plaques, or nodules, usually in an asymmetric distribution. B-cell lymphoproliferative diseases simulating rosacea are extremely rare.5 Nevertheless, B-cell lymphoma mimicking rhinophyma has been documented in the literature.5-11
Read more about B-cell neoplasms at The great mimickers of rosacea. Cutis. 2014;94(1):39-45.
Figures 1, 4, 5 reprinted with permission from Cutis. 2014;94(1):39-45; photographs for Figures 4 and 5 courtesy of Marc Silverstein, MD. Figure 2 reprinted with permission from J Fam Pract. 2010 August;59(8):459-462; photograph courtesy of Felix B. Chang, MD. Figure 3 reprinted courtesy of J Fam Pract. 2010 July;59(7):399-401; photograph courtesy of Nikki N. Kim, MD, Heather W. Wickless, MD, MPH.
REFERENCES
1. Chang F, Lopes A. Erysipelas. In: Domino FJ, ed. The 5-Minute Clinical Consult 2008. 16th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2008:448–449.
2. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad Dermatol Venereol. 2005;19:273-285.
3. Berg M, Liden S. An epidemiological study of rosacea. Acta Derm Venereol. 1989;69:419-423.
4. Tutrone WD. Polymorphic light eruption. Dermatol Ther. 2003;16:28-39.
5. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148:824-831.
6. Moulonguet I, Ghnassia M, Molina T, et al. Miliarial-type perifollicular B-cell pseudolymphoma (lymphocytoma cutis): a misleading eruption in two women. J Cutan Pathol. 2012;39:1016-1021.
7. Soon CW, Pincus LB, Ai WZ, et al. Acneiform presentation of primary cutaneous follicle center lymphoma. J Am Acad Dermatol. 2011;65:887-889.
8. Rosmaninho A, Alves R, Lima M, et al. Red nose: primary cutaneous marginal zone B-cell lymphoma. Leuk Res.2010;34:682-684.
9. Ogden S, Coulson IH. B-cell lymphoma mimicking rhinophyma. Clin Exp Dermatol. 2008;33:213-214.
10. Seward JL, Malone JC, Callen JP. Rhinophymalike swelling in an 86-year-old woman. Primary cutaneous B-cell lymphoma of the nose. Arch Dermatol. 2004;140:751-756.
11. Colvin JH, Lamerson CL, Cualing H, et al. Cutaneous lymphoplasmacytoid lymphoma (immunocytoma) with Waldenström’s macroglobulinemia mimicking rosacea. J Am Acad Dermatol. 2003;49:1159-1162.