User login
Noninfectious Penile Lesions
1. A 26-year-old man presents with a penile lesion that has existed at least 10 years without significant change and with no attendant symptoms. The lesion consists of four 1-to-1.5-mm soft, compressible purple papules, in aggregate measuring about 8 mm. No other lesions are seen on the genitals or on the body.

Diagnosis: The lesion proved to be angiokeratoma of Fordyce, a totally benign lesion. This type of angiokeratoma is ectatic, thin-walled vessels in the superficial dermis, with overlying epidermal hyperplasia that forms secondary to normal friction. When they are seen on the scrotum, vulva, or penis, they are usually referred to as angiokeratoma of Fordyce, a type of localized angiokeratoma, other types of which can appear on the legs or hands.
These totally benign lesions must be distinguished from generalized types of angiokeratomata, such as those seen in Fabry disease (angiokeratoma corporis diffusum), an inheritable metabolic disorder. With our patient’s history, his lesion was clearly benign.
Had his lesion been new or changing in any substantive way, additional testing, including a biopsy, might have been necessary to rule out entities such as squamous cell carcinoma (which is almost unknown in circumcised patients), condyloma, melanoma, the aforementioned Kaposi’s sarcoma, or even angiosarcoma.
For more information, see “Skin is skin, no matter the location.” Clinician Reviews. 2013 June;23(6):W5.
2. A 59-year-old uncircumcised man presents with a phimotic foreskin, which cannot be retracted without pain. Only a tiny opening remains through which the patient can urinate (with difficulty). The surface of the foreskin is atrophic, dry, and shiny with focal areas of purpura but little, if any, redness or swelling.

Diagnosis: This patient’s condition is lichen sclerosus, also called balanitis xerotica obliterans (BXO), a diagnosis of sufficient obscurity to almost guarantee initial misdiagnosis as “yeast infection” or “herpes.” One treatment failure after another eventually leads to referral to a provider familiar with BXO, which is the male version of lichen sclerosus et atrophicus (LS&A) and usually affects the glans, foreskin, and distal shaft.
The causes of these conditions are as yet unknown. However, much is known about how they present, how they look under a microscope, and how to treat them.
Treatment entails use of the most powerful topical steroid ointments, which are so effective that they have completely replaced previous treatment options (eg, testosterone ointment). While a cure is unlikely, control is a realistic goal.
BXO, as in this case, can also cause urinary obstruction, both from the overlying foreskin and from actual meatal stenosis. This is why advanced cases need referral to urology for possible circumcision. As with many penile diagnoses (eg, squamous cell carcinoma or condyloma), BXO is far more common in the uncircumcised.
For more information, see “Man has very uncomfortable problem.” Clinician Reviews. 2012 September;22(9):W4.
3. A 31-year-old man has a relatively asymptomatic penile rash that has repeatedly manifested and resolved over a period of months. A round, papulosquamous, bright pink patch on the distal right shaft of his circumcised penis measures > 3 cm in diameter and has a shiny appearance with slightly irregular margins. A similar rash is seen behind both ears, in the umbilicus, and patches of dandruff are noted. Despite good health, he has been under a great deal of stress recently.

Diagnosis: Seborrheic dermatitis (SD), also known as seborrhea, is an extremely common chronic papulosquamous disorder patterned on the sebum-rich areas of the scalp, face, and trunk. Although not directly caused by the highly lipophilic commensal yeast Malassezia furfur, it does appear to be related to increases in the number of those organisms, as well as to immunologic abnormalities and increased production of sebum. It can range from a mild scaly rash to whole-body erythroderma and can affect an astonishing range of areas, including the genitals.
SD, especially in this case, represents the perfect example of the need to “look elsewhere” for clues when confronted with a mysterious rash. Patients can certainly have more than one dermatologic diagnosis at a time, but a single explanation is considerably more likely and should therefore be sought. In this case, corroboration for the diagnosis of SD was readily found by looking for it in its known locations.
In this case, treatment comprised a combination of oxiconazole lotion and 2.5% hydrocortisone cream. Many other combinations have been used successfully, including pimecrolimus or tacrolimus combined with ketoconazole cream.
Whatever is used, a cure will not be forthcoming, since the condition is almost always chronic. The main value of an accurate diagnosis in such a case lies in easing the patient’s mind regarding the terrible diseases he doesn’t have.
For more information, see “Relatively Asymptomatic, but Still Problematic." Clinician Reviews. 2014 April;24(4):15-16.
4. This circumscribed inflammatory plaque on the glans penis of allegedly > 20 years' duration was refractory to circumcision and local treatment. Because of unresponsiveness of the lesion to circumcision and focal steroid infiltration, repeated biopsies were performed.

Diagnosis: One biopsy again showed the features of a plasmacellular inflammation, while the other finally revealed the histopathologic features of erythroplasia of Queyrat (carcinoma in situ or Bowen's disease of the glans penis). We assume that either the former biopsy specimens were taken from a plasma cell-rich reactive infiltrate around the neoplastic lesion, or that carcinoma in situ may have arisen due to the chronic inflammation of Zoon's balanitis plasmacellularis. Radiotherapy was performed with good clinical response and subsequent histopathologic proof of complete remission of the lesion.
For more information, see “Bowen's Disease of the Glans Penis (Erythroplasia of Queyrat) in Plasma Cell Balanitis.” Cutis. 2000 June;65(6):395-398.
1. A 26-year-old man presents with a penile lesion that has existed at least 10 years without significant change and with no attendant symptoms. The lesion consists of four 1-to-1.5-mm soft, compressible purple papules, in aggregate measuring about 8 mm. No other lesions are seen on the genitals or on the body.

Diagnosis: The lesion proved to be angiokeratoma of Fordyce, a totally benign lesion. This type of angiokeratoma is ectatic, thin-walled vessels in the superficial dermis, with overlying epidermal hyperplasia that forms secondary to normal friction. When they are seen on the scrotum, vulva, or penis, they are usually referred to as angiokeratoma of Fordyce, a type of localized angiokeratoma, other types of which can appear on the legs or hands.
These totally benign lesions must be distinguished from generalized types of angiokeratomata, such as those seen in Fabry disease (angiokeratoma corporis diffusum), an inheritable metabolic disorder. With our patient’s history, his lesion was clearly benign.
Had his lesion been new or changing in any substantive way, additional testing, including a biopsy, might have been necessary to rule out entities such as squamous cell carcinoma (which is almost unknown in circumcised patients), condyloma, melanoma, the aforementioned Kaposi’s sarcoma, or even angiosarcoma.
For more information, see “Skin is skin, no matter the location.” Clinician Reviews. 2013 June;23(6):W5.
2. A 59-year-old uncircumcised man presents with a phimotic foreskin, which cannot be retracted without pain. Only a tiny opening remains through which the patient can urinate (with difficulty). The surface of the foreskin is atrophic, dry, and shiny with focal areas of purpura but little, if any, redness or swelling.

Diagnosis: This patient’s condition is lichen sclerosus, also called balanitis xerotica obliterans (BXO), a diagnosis of sufficient obscurity to almost guarantee initial misdiagnosis as “yeast infection” or “herpes.” One treatment failure after another eventually leads to referral to a provider familiar with BXO, which is the male version of lichen sclerosus et atrophicus (LS&A) and usually affects the glans, foreskin, and distal shaft.
The causes of these conditions are as yet unknown. However, much is known about how they present, how they look under a microscope, and how to treat them.
Treatment entails use of the most powerful topical steroid ointments, which are so effective that they have completely replaced previous treatment options (eg, testosterone ointment). While a cure is unlikely, control is a realistic goal.
BXO, as in this case, can also cause urinary obstruction, both from the overlying foreskin and from actual meatal stenosis. This is why advanced cases need referral to urology for possible circumcision. As with many penile diagnoses (eg, squamous cell carcinoma or condyloma), BXO is far more common in the uncircumcised.
For more information, see “Man has very uncomfortable problem.” Clinician Reviews. 2012 September;22(9):W4.
3. A 31-year-old man has a relatively asymptomatic penile rash that has repeatedly manifested and resolved over a period of months. A round, papulosquamous, bright pink patch on the distal right shaft of his circumcised penis measures > 3 cm in diameter and has a shiny appearance with slightly irregular margins. A similar rash is seen behind both ears, in the umbilicus, and patches of dandruff are noted. Despite good health, he has been under a great deal of stress recently.

Diagnosis: Seborrheic dermatitis (SD), also known as seborrhea, is an extremely common chronic papulosquamous disorder patterned on the sebum-rich areas of the scalp, face, and trunk. Although not directly caused by the highly lipophilic commensal yeast Malassezia furfur, it does appear to be related to increases in the number of those organisms, as well as to immunologic abnormalities and increased production of sebum. It can range from a mild scaly rash to whole-body erythroderma and can affect an astonishing range of areas, including the genitals.
SD, especially in this case, represents the perfect example of the need to “look elsewhere” for clues when confronted with a mysterious rash. Patients can certainly have more than one dermatologic diagnosis at a time, but a single explanation is considerably more likely and should therefore be sought. In this case, corroboration for the diagnosis of SD was readily found by looking for it in its known locations.
In this case, treatment comprised a combination of oxiconazole lotion and 2.5% hydrocortisone cream. Many other combinations have been used successfully, including pimecrolimus or tacrolimus combined with ketoconazole cream.
Whatever is used, a cure will not be forthcoming, since the condition is almost always chronic. The main value of an accurate diagnosis in such a case lies in easing the patient’s mind regarding the terrible diseases he doesn’t have.
For more information, see “Relatively Asymptomatic, but Still Problematic." Clinician Reviews. 2014 April;24(4):15-16.
4. This circumscribed inflammatory plaque on the glans penis of allegedly > 20 years' duration was refractory to circumcision and local treatment. Because of unresponsiveness of the lesion to circumcision and focal steroid infiltration, repeated biopsies were performed.

Diagnosis: One biopsy again showed the features of a plasmacellular inflammation, while the other finally revealed the histopathologic features of erythroplasia of Queyrat (carcinoma in situ or Bowen's disease of the glans penis). We assume that either the former biopsy specimens were taken from a plasma cell-rich reactive infiltrate around the neoplastic lesion, or that carcinoma in situ may have arisen due to the chronic inflammation of Zoon's balanitis plasmacellularis. Radiotherapy was performed with good clinical response and subsequent histopathologic proof of complete remission of the lesion.
For more information, see “Bowen's Disease of the Glans Penis (Erythroplasia of Queyrat) in Plasma Cell Balanitis.” Cutis. 2000 June;65(6):395-398.
1. A 26-year-old man presents with a penile lesion that has existed at least 10 years without significant change and with no attendant symptoms. The lesion consists of four 1-to-1.5-mm soft, compressible purple papules, in aggregate measuring about 8 mm. No other lesions are seen on the genitals or on the body.

Diagnosis: The lesion proved to be angiokeratoma of Fordyce, a totally benign lesion. This type of angiokeratoma is ectatic, thin-walled vessels in the superficial dermis, with overlying epidermal hyperplasia that forms secondary to normal friction. When they are seen on the scrotum, vulva, or penis, they are usually referred to as angiokeratoma of Fordyce, a type of localized angiokeratoma, other types of which can appear on the legs or hands.
These totally benign lesions must be distinguished from generalized types of angiokeratomata, such as those seen in Fabry disease (angiokeratoma corporis diffusum), an inheritable metabolic disorder. With our patient’s history, his lesion was clearly benign.
Had his lesion been new or changing in any substantive way, additional testing, including a biopsy, might have been necessary to rule out entities such as squamous cell carcinoma (which is almost unknown in circumcised patients), condyloma, melanoma, the aforementioned Kaposi’s sarcoma, or even angiosarcoma.
For more information, see “Skin is skin, no matter the location.” Clinician Reviews. 2013 June;23(6):W5.
2. A 59-year-old uncircumcised man presents with a phimotic foreskin, which cannot be retracted without pain. Only a tiny opening remains through which the patient can urinate (with difficulty). The surface of the foreskin is atrophic, dry, and shiny with focal areas of purpura but little, if any, redness or swelling.

Diagnosis: This patient’s condition is lichen sclerosus, also called balanitis xerotica obliterans (BXO), a diagnosis of sufficient obscurity to almost guarantee initial misdiagnosis as “yeast infection” or “herpes.” One treatment failure after another eventually leads to referral to a provider familiar with BXO, which is the male version of lichen sclerosus et atrophicus (LS&A) and usually affects the glans, foreskin, and distal shaft.
The causes of these conditions are as yet unknown. However, much is known about how they present, how they look under a microscope, and how to treat them.
Treatment entails use of the most powerful topical steroid ointments, which are so effective that they have completely replaced previous treatment options (eg, testosterone ointment). While a cure is unlikely, control is a realistic goal.
BXO, as in this case, can also cause urinary obstruction, both from the overlying foreskin and from actual meatal stenosis. This is why advanced cases need referral to urology for possible circumcision. As with many penile diagnoses (eg, squamous cell carcinoma or condyloma), BXO is far more common in the uncircumcised.
For more information, see “Man has very uncomfortable problem.” Clinician Reviews. 2012 September;22(9):W4.
3. A 31-year-old man has a relatively asymptomatic penile rash that has repeatedly manifested and resolved over a period of months. A round, papulosquamous, bright pink patch on the distal right shaft of his circumcised penis measures > 3 cm in diameter and has a shiny appearance with slightly irregular margins. A similar rash is seen behind both ears, in the umbilicus, and patches of dandruff are noted. Despite good health, he has been under a great deal of stress recently.

Diagnosis: Seborrheic dermatitis (SD), also known as seborrhea, is an extremely common chronic papulosquamous disorder patterned on the sebum-rich areas of the scalp, face, and trunk. Although not directly caused by the highly lipophilic commensal yeast Malassezia furfur, it does appear to be related to increases in the number of those organisms, as well as to immunologic abnormalities and increased production of sebum. It can range from a mild scaly rash to whole-body erythroderma and can affect an astonishing range of areas, including the genitals.
SD, especially in this case, represents the perfect example of the need to “look elsewhere” for clues when confronted with a mysterious rash. Patients can certainly have more than one dermatologic diagnosis at a time, but a single explanation is considerably more likely and should therefore be sought. In this case, corroboration for the diagnosis of SD was readily found by looking for it in its known locations.
In this case, treatment comprised a combination of oxiconazole lotion and 2.5% hydrocortisone cream. Many other combinations have been used successfully, including pimecrolimus or tacrolimus combined with ketoconazole cream.
Whatever is used, a cure will not be forthcoming, since the condition is almost always chronic. The main value of an accurate diagnosis in such a case lies in easing the patient’s mind regarding the terrible diseases he doesn’t have.
For more information, see “Relatively Asymptomatic, but Still Problematic." Clinician Reviews. 2014 April;24(4):15-16.
4. This circumscribed inflammatory plaque on the glans penis of allegedly > 20 years' duration was refractory to circumcision and local treatment. Because of unresponsiveness of the lesion to circumcision and focal steroid infiltration, repeated biopsies were performed.

Diagnosis: One biopsy again showed the features of a plasmacellular inflammation, while the other finally revealed the histopathologic features of erythroplasia of Queyrat (carcinoma in situ or Bowen's disease of the glans penis). We assume that either the former biopsy specimens were taken from a plasma cell-rich reactive infiltrate around the neoplastic lesion, or that carcinoma in situ may have arisen due to the chronic inflammation of Zoon's balanitis plasmacellularis. Radiotherapy was performed with good clinical response and subsequent histopathologic proof of complete remission of the lesion.
For more information, see “Bowen's Disease of the Glans Penis (Erythroplasia of Queyrat) in Plasma Cell Balanitis.” Cutis. 2000 June;65(6):395-398.
Shingles Strikes With a Vengeance
1. A 16-year-old girl presents with a rash manifesting several weeks ago that became enlarged and more symptomatic after she applied hydrogen peroxide and scrubbed with antibacterial soap. Large, annular, honey-colored crusts are focally located around the left eye, and faint pinkness is noted peripherally around the lesions. Modest but palpable adenopathy is detected in the pretragal and submental nodal areas.
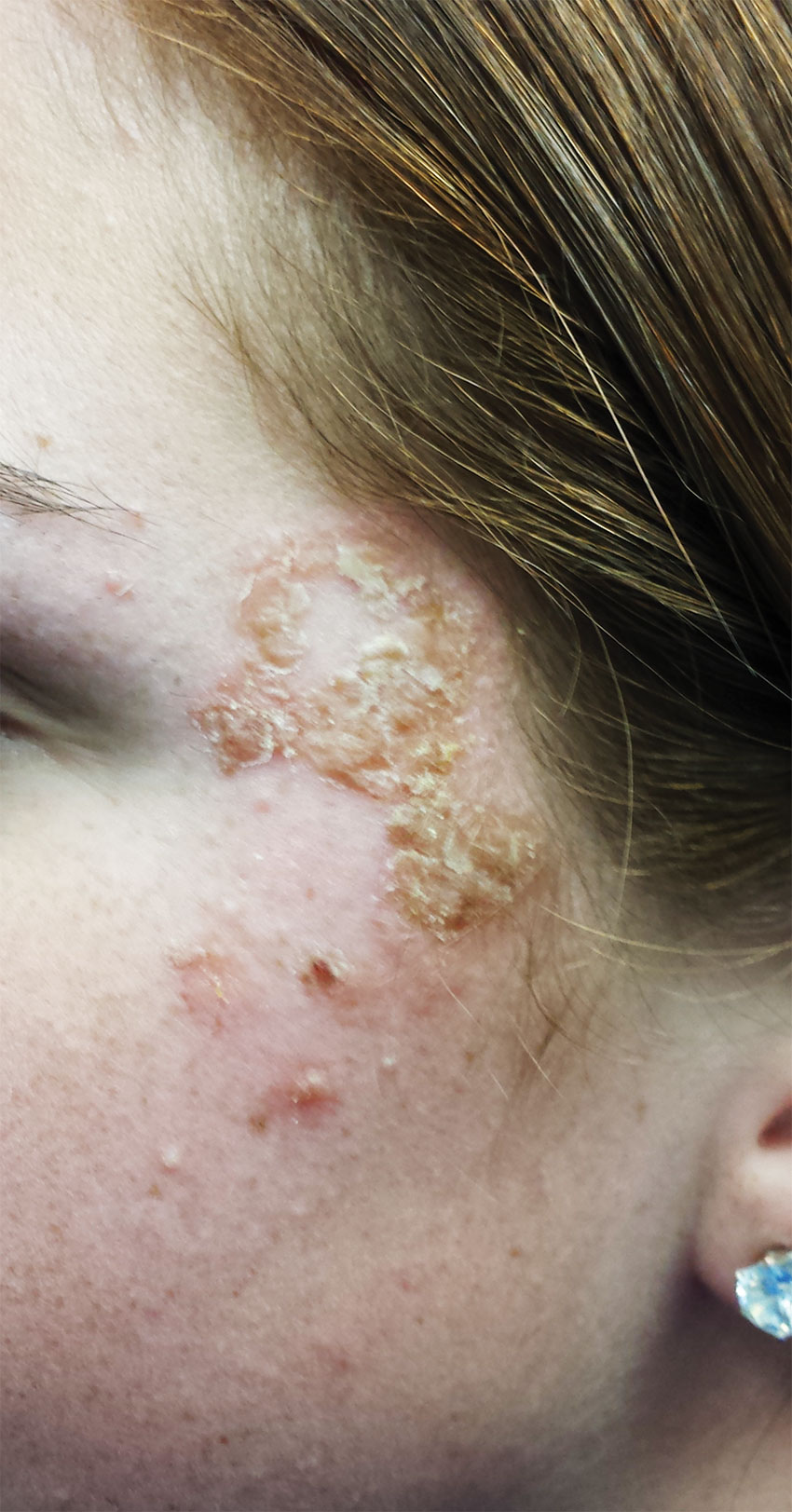
Diagnosis: Impetigo has also been called impetiginized dermatitis because it almost always starts with minor breaks in the skin as a result of conditions such as eczema, acne, contact dermatitis, or insect bite. Thus provided with access to deeper portions of the epithelial surface, bacterial organisms that normally cause no problems on intact skin are able to create the minor but annoying condition we call impetigo. Rarely associated with morbidity, it tends to resolve in two to three weeks at most, even without treatment.
For more information, see “Is It Ringworm, Herpes— Or Something Else Entirely?” Clinician Reviews. 2014;24(11):8-9.
2. A 38-year-old man presents with an itchy, blistery rash that usually appears in the summer, getting worse each year. The lesions are collections of vesicles with faint underlying erythema that crisscross his legs in linear configurations. Smaller but similar lesions are scattered over his arms and trunk.

Diagnosis: The rash produced by poison ivy exposure can be severe and can last six weeks or more without treatment. Poison ivy is not contagious, cannot be spread by scratching, and (despite its name) is not poisonous in any way. The number of poison ivy plants has doubled in the past 50 years and is expected to double again within 20 years. The potency of the plant’s allergen is also expected to increase. The patient (height, 6’3”; weight, > 300 lb) was treated with a 60-mg IM injection of triamcinolone, a two-week, 40-mg taper of prednisone, and twice-daily application of betamethasone cream. This, of course, followed a discussion of the risks versus benefits of such a course of action.
For more information, see “He Tried So Hard to Avoid It … .” Clinician Reviews. 2015 July;25(7):W2.
3. For several months, a 69-year-old woman has had a rash around her eyes. It is terribly symptomatic, burning and itching regardless of any type of OTC treatment. She finally requests referral to dermatology from her primary care provider.

Diagnosis: Eyelid dermatitis, or irritant contact dermatitis, is an extremely common complaint, and this patient’s history is quite typical: The worse the problem gets, the more attempts the patient makes to relieve symptoms.
When this patient presented to dermatology, she was applying six different products (all OTC) to the affected areas. None helped, and in fact, most seemed to worsen the problem. Even if one had helped, she would never have known which. But desperation drives patients to do irrational things, especially when the problem is out in the open for the whole world to see.
For more information, see “The Eyes Have It, and It Itches Like Crazy.” Clinician Reviews. 2015;25(9):W1.
4. A 58-year-old man seeks care for burning in his right eye and a skin eruption on his forehead and scalp with progressive worsening over the past 10 days. The patient has decreased vision in his right eye, as well as fever, chills, photophobia, and headache. A physical exam reveals vesicles on an erythematous base on his right scalp, forehead, upper and lower eyelids, dorsum of his nose, and cheek distributed along the ophthalmic branch of the trigeminal nerve.

Diagnosis: Herpes zoster ophthalmicus, confirmed by an ophthalmologic exam. This serious condition has been linked to reactivation of the varicella-zoster virus (VZV) within the trigeminal ganglion. Primary infection with VZV results in varicella (chickenpox), whereas reactivation of a latent VZV infection within the sensory ganglia is known as herpes zoster.
For more information, see “Painful rash on face.” J Fam Pract. 2015;64(11):E1-E3.
RELATED ARTICLE
Jacobsen E, Hull CE. “Herpes Zoster Infection.” Clinician Reviews. 2013;23(8):42-49.
1. A 16-year-old girl presents with a rash manifesting several weeks ago that became enlarged and more symptomatic after she applied hydrogen peroxide and scrubbed with antibacterial soap. Large, annular, honey-colored crusts are focally located around the left eye, and faint pinkness is noted peripherally around the lesions. Modest but palpable adenopathy is detected in the pretragal and submental nodal areas.
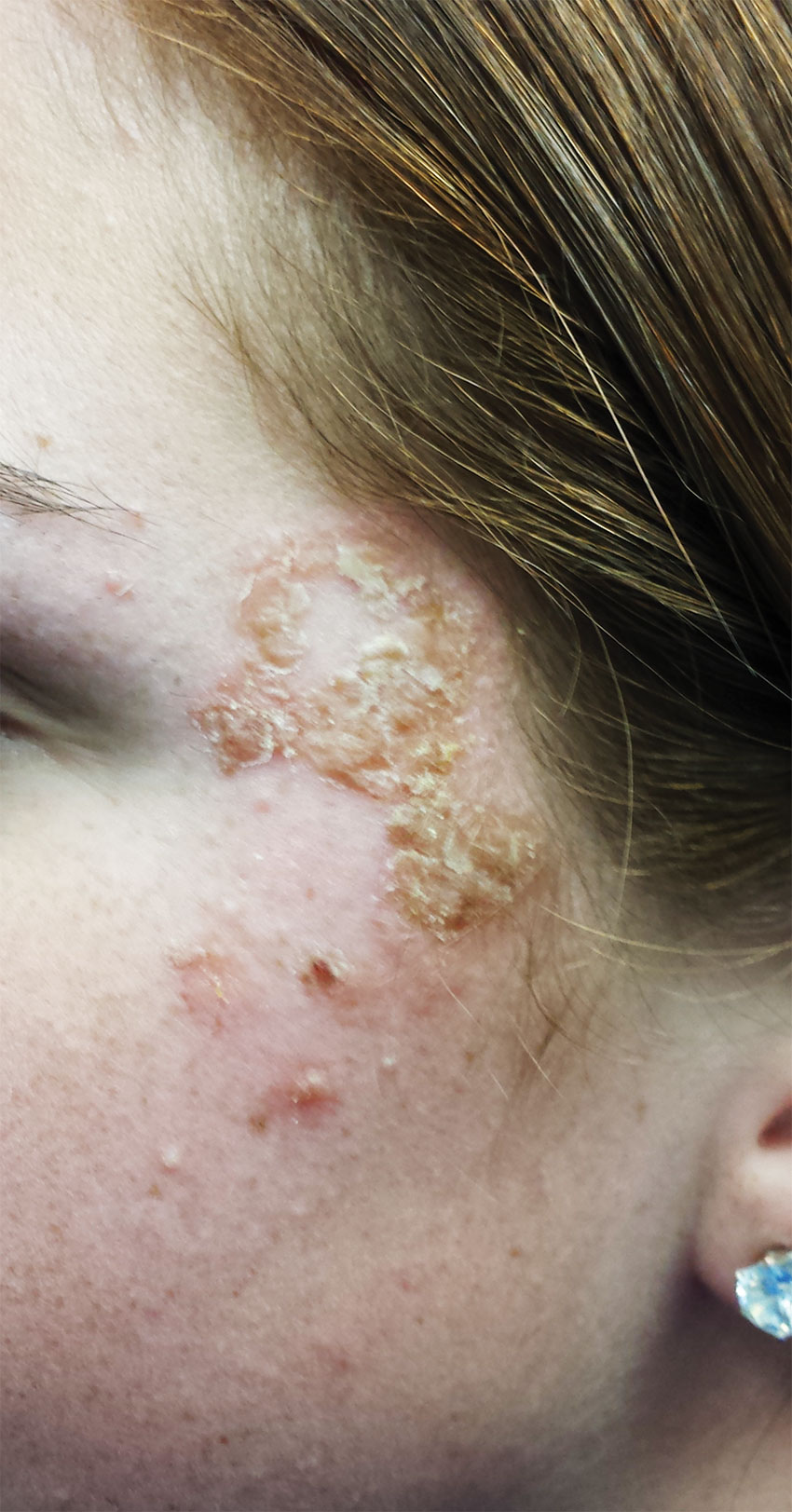
Diagnosis: Impetigo has also been called impetiginized dermatitis because it almost always starts with minor breaks in the skin as a result of conditions such as eczema, acne, contact dermatitis, or insect bite. Thus provided with access to deeper portions of the epithelial surface, bacterial organisms that normally cause no problems on intact skin are able to create the minor but annoying condition we call impetigo. Rarely associated with morbidity, it tends to resolve in two to three weeks at most, even without treatment.
For more information, see “Is It Ringworm, Herpes— Or Something Else Entirely?” Clinician Reviews. 2014;24(11):8-9.
2. A 38-year-old man presents with an itchy, blistery rash that usually appears in the summer, getting worse each year. The lesions are collections of vesicles with faint underlying erythema that crisscross his legs in linear configurations. Smaller but similar lesions are scattered over his arms and trunk.

Diagnosis: The rash produced by poison ivy exposure can be severe and can last six weeks or more without treatment. Poison ivy is not contagious, cannot be spread by scratching, and (despite its name) is not poisonous in any way. The number of poison ivy plants has doubled in the past 50 years and is expected to double again within 20 years. The potency of the plant’s allergen is also expected to increase. The patient (height, 6’3”; weight, > 300 lb) was treated with a 60-mg IM injection of triamcinolone, a two-week, 40-mg taper of prednisone, and twice-daily application of betamethasone cream. This, of course, followed a discussion of the risks versus benefits of such a course of action.
For more information, see “He Tried So Hard to Avoid It … .” Clinician Reviews. 2015 July;25(7):W2.
3. For several months, a 69-year-old woman has had a rash around her eyes. It is terribly symptomatic, burning and itching regardless of any type of OTC treatment. She finally requests referral to dermatology from her primary care provider.

Diagnosis: Eyelid dermatitis, or irritant contact dermatitis, is an extremely common complaint, and this patient’s history is quite typical: The worse the problem gets, the more attempts the patient makes to relieve symptoms.
When this patient presented to dermatology, she was applying six different products (all OTC) to the affected areas. None helped, and in fact, most seemed to worsen the problem. Even if one had helped, she would never have known which. But desperation drives patients to do irrational things, especially when the problem is out in the open for the whole world to see.
For more information, see “The Eyes Have It, and It Itches Like Crazy.” Clinician Reviews. 2015;25(9):W1.
4. A 58-year-old man seeks care for burning in his right eye and a skin eruption on his forehead and scalp with progressive worsening over the past 10 days. The patient has decreased vision in his right eye, as well as fever, chills, photophobia, and headache. A physical exam reveals vesicles on an erythematous base on his right scalp, forehead, upper and lower eyelids, dorsum of his nose, and cheek distributed along the ophthalmic branch of the trigeminal nerve.

Diagnosis: Herpes zoster ophthalmicus, confirmed by an ophthalmologic exam. This serious condition has been linked to reactivation of the varicella-zoster virus (VZV) within the trigeminal ganglion. Primary infection with VZV results in varicella (chickenpox), whereas reactivation of a latent VZV infection within the sensory ganglia is known as herpes zoster.
For more information, see “Painful rash on face.” J Fam Pract. 2015;64(11):E1-E3.
RELATED ARTICLE
Jacobsen E, Hull CE. “Herpes Zoster Infection.” Clinician Reviews. 2013;23(8):42-49.
1. A 16-year-old girl presents with a rash manifesting several weeks ago that became enlarged and more symptomatic after she applied hydrogen peroxide and scrubbed with antibacterial soap. Large, annular, honey-colored crusts are focally located around the left eye, and faint pinkness is noted peripherally around the lesions. Modest but palpable adenopathy is detected in the pretragal and submental nodal areas.
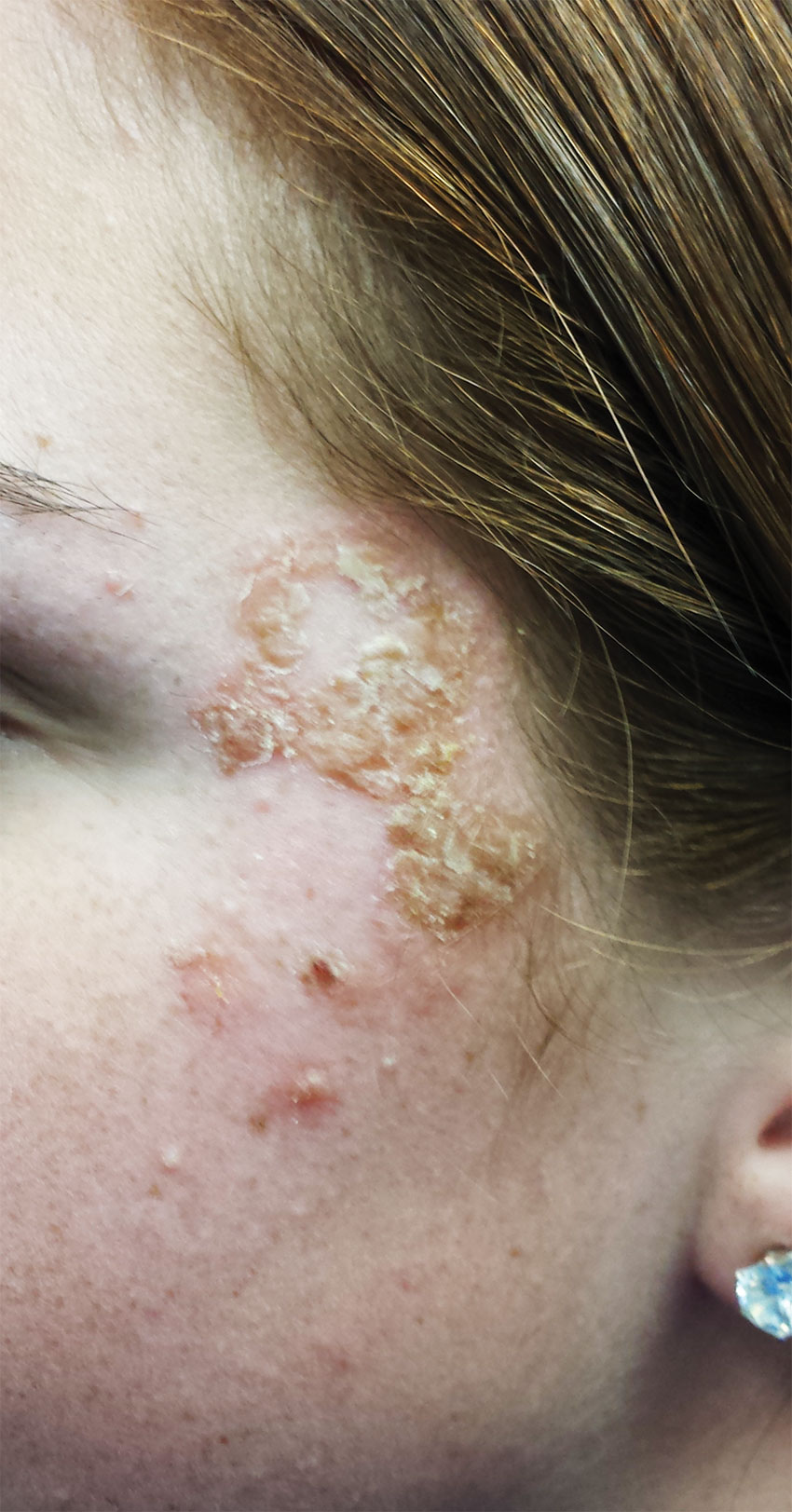
Diagnosis: Impetigo has also been called impetiginized dermatitis because it almost always starts with minor breaks in the skin as a result of conditions such as eczema, acne, contact dermatitis, or insect bite. Thus provided with access to deeper portions of the epithelial surface, bacterial organisms that normally cause no problems on intact skin are able to create the minor but annoying condition we call impetigo. Rarely associated with morbidity, it tends to resolve in two to three weeks at most, even without treatment.
For more information, see “Is It Ringworm, Herpes— Or Something Else Entirely?” Clinician Reviews. 2014;24(11):8-9.
2. A 38-year-old man presents with an itchy, blistery rash that usually appears in the summer, getting worse each year. The lesions are collections of vesicles with faint underlying erythema that crisscross his legs in linear configurations. Smaller but similar lesions are scattered over his arms and trunk.

Diagnosis: The rash produced by poison ivy exposure can be severe and can last six weeks or more without treatment. Poison ivy is not contagious, cannot be spread by scratching, and (despite its name) is not poisonous in any way. The number of poison ivy plants has doubled in the past 50 years and is expected to double again within 20 years. The potency of the plant’s allergen is also expected to increase. The patient (height, 6’3”; weight, > 300 lb) was treated with a 60-mg IM injection of triamcinolone, a two-week, 40-mg taper of prednisone, and twice-daily application of betamethasone cream. This, of course, followed a discussion of the risks versus benefits of such a course of action.
For more information, see “He Tried So Hard to Avoid It … .” Clinician Reviews. 2015 July;25(7):W2.
3. For several months, a 69-year-old woman has had a rash around her eyes. It is terribly symptomatic, burning and itching regardless of any type of OTC treatment. She finally requests referral to dermatology from her primary care provider.

Diagnosis: Eyelid dermatitis, or irritant contact dermatitis, is an extremely common complaint, and this patient’s history is quite typical: The worse the problem gets, the more attempts the patient makes to relieve symptoms.
When this patient presented to dermatology, she was applying six different products (all OTC) to the affected areas. None helped, and in fact, most seemed to worsen the problem. Even if one had helped, she would never have known which. But desperation drives patients to do irrational things, especially when the problem is out in the open for the whole world to see.
For more information, see “The Eyes Have It, and It Itches Like Crazy.” Clinician Reviews. 2015;25(9):W1.
4. A 58-year-old man seeks care for burning in his right eye and a skin eruption on his forehead and scalp with progressive worsening over the past 10 days. The patient has decreased vision in his right eye, as well as fever, chills, photophobia, and headache. A physical exam reveals vesicles on an erythematous base on his right scalp, forehead, upper and lower eyelids, dorsum of his nose, and cheek distributed along the ophthalmic branch of the trigeminal nerve.

Diagnosis: Herpes zoster ophthalmicus, confirmed by an ophthalmologic exam. This serious condition has been linked to reactivation of the varicella-zoster virus (VZV) within the trigeminal ganglion. Primary infection with VZV results in varicella (chickenpox), whereas reactivation of a latent VZV infection within the sensory ganglia is known as herpes zoster.
For more information, see “Painful rash on face.” J Fam Pract. 2015;64(11):E1-E3.
RELATED ARTICLE
Jacobsen E, Hull CE. “Herpes Zoster Infection.” Clinician Reviews. 2013;23(8):42-49.
Give a Hand
1. A 45-year-old construction worker accidentally fell 20 ft from a scaffolding. He is unable to flex or extend his right wrist due to pain. Examination of the wrist shows a moderate amount of soft-tissue swelling with moderate tenderness along the base of the first metacarpal.

Diagnosis: The radiograph shows an acute, comminuted fracture of the scaphoid bone. The patient was placed in a thumb spica splint and sling. He was instructed to follow up in one to two days with the hand surgeon who was on call, with anticipation of subsequent open reduction and internal fixation.
For more information, see “Construction Worker Falls From Scaffolding.” Clinician Reviews. 2013;23(11):15.
2. A 90-year-old man “just passed out” in his yard, landing in an ant nest. He experiences bilateral wrist pain, presumably from multiple ant bites. Both wrists are tender; range of motion causes tenderness. Inspection demonstrates mild to moderate circumferential swelling with several raised, reddened bumps.

Diagnosis: The radiograph shows some osteopenia and significant vascular calcifications. Of note, there is a fracture of the styloid process of the radius, extending slightly to the joint space. The patient was placed in a splint and orthopedic referral was obtained.
Wrist Pain After a Fall. Clinician Reviews. 2012;22(9):22.
3. The middorsal aspect of a 48-year-old woman’s right hand was accidentally caught in a metal door as it was being shut. Examination shows mild to moderate soft tissue swelling and some early bruising. There is extreme tenderness over the fourth and fifth metacarpal bones. Although limited by swelling, she can flex her fingers somewhat.

Diagnosis: The radiograph shows a comminuted fracture of the proximal fifth phalanx. Soft tissue swelling is noted as well. The patient’s hand was splinted, and arrangements for outpatient orthopedic follow-up were made.
For more information, see “Hand Slammed in Door.” Clinician Reviews. 2013 May;23(5):20.
4. A trauma patient arrives in your facility after a motor vehicle collision. His right hand and wrist appear to be moderately swollen, and he has been placed in a splint.

Diagnosis: The radiograph shows a slightly displaced fracture of the distal fourth metacarpal head. No other injuries are present.
The patient’s hand was left in the splint, and orthopedic evaluation was obtained.
For more information, see “Secondary Survey of Trauma Patient.” Clinician Reviews. 2015;25(12):10,35.
1. A 45-year-old construction worker accidentally fell 20 ft from a scaffolding. He is unable to flex or extend his right wrist due to pain. Examination of the wrist shows a moderate amount of soft-tissue swelling with moderate tenderness along the base of the first metacarpal.

Diagnosis: The radiograph shows an acute, comminuted fracture of the scaphoid bone. The patient was placed in a thumb spica splint and sling. He was instructed to follow up in one to two days with the hand surgeon who was on call, with anticipation of subsequent open reduction and internal fixation.
For more information, see “Construction Worker Falls From Scaffolding.” Clinician Reviews. 2013;23(11):15.
2. A 90-year-old man “just passed out” in his yard, landing in an ant nest. He experiences bilateral wrist pain, presumably from multiple ant bites. Both wrists are tender; range of motion causes tenderness. Inspection demonstrates mild to moderate circumferential swelling with several raised, reddened bumps.

Diagnosis: The radiograph shows some osteopenia and significant vascular calcifications. Of note, there is a fracture of the styloid process of the radius, extending slightly to the joint space. The patient was placed in a splint and orthopedic referral was obtained.
Wrist Pain After a Fall. Clinician Reviews. 2012;22(9):22.
3. The middorsal aspect of a 48-year-old woman’s right hand was accidentally caught in a metal door as it was being shut. Examination shows mild to moderate soft tissue swelling and some early bruising. There is extreme tenderness over the fourth and fifth metacarpal bones. Although limited by swelling, she can flex her fingers somewhat.

Diagnosis: The radiograph shows a comminuted fracture of the proximal fifth phalanx. Soft tissue swelling is noted as well. The patient’s hand was splinted, and arrangements for outpatient orthopedic follow-up were made.
For more information, see “Hand Slammed in Door.” Clinician Reviews. 2013 May;23(5):20.
4. A trauma patient arrives in your facility after a motor vehicle collision. His right hand and wrist appear to be moderately swollen, and he has been placed in a splint.

Diagnosis: The radiograph shows a slightly displaced fracture of the distal fourth metacarpal head. No other injuries are present.
The patient’s hand was left in the splint, and orthopedic evaluation was obtained.
For more information, see “Secondary Survey of Trauma Patient.” Clinician Reviews. 2015;25(12):10,35.
1. A 45-year-old construction worker accidentally fell 20 ft from a scaffolding. He is unable to flex or extend his right wrist due to pain. Examination of the wrist shows a moderate amount of soft-tissue swelling with moderate tenderness along the base of the first metacarpal.

Diagnosis: The radiograph shows an acute, comminuted fracture of the scaphoid bone. The patient was placed in a thumb spica splint and sling. He was instructed to follow up in one to two days with the hand surgeon who was on call, with anticipation of subsequent open reduction and internal fixation.
For more information, see “Construction Worker Falls From Scaffolding.” Clinician Reviews. 2013;23(11):15.
2. A 90-year-old man “just passed out” in his yard, landing in an ant nest. He experiences bilateral wrist pain, presumably from multiple ant bites. Both wrists are tender; range of motion causes tenderness. Inspection demonstrates mild to moderate circumferential swelling with several raised, reddened bumps.

Diagnosis: The radiograph shows some osteopenia and significant vascular calcifications. Of note, there is a fracture of the styloid process of the radius, extending slightly to the joint space. The patient was placed in a splint and orthopedic referral was obtained.
Wrist Pain After a Fall. Clinician Reviews. 2012;22(9):22.
3. The middorsal aspect of a 48-year-old woman’s right hand was accidentally caught in a metal door as it was being shut. Examination shows mild to moderate soft tissue swelling and some early bruising. There is extreme tenderness over the fourth and fifth metacarpal bones. Although limited by swelling, she can flex her fingers somewhat.

Diagnosis: The radiograph shows a comminuted fracture of the proximal fifth phalanx. Soft tissue swelling is noted as well. The patient’s hand was splinted, and arrangements for outpatient orthopedic follow-up were made.
For more information, see “Hand Slammed in Door.” Clinician Reviews. 2013 May;23(5):20.
4. A trauma patient arrives in your facility after a motor vehicle collision. His right hand and wrist appear to be moderately swollen, and he has been placed in a splint.

Diagnosis: The radiograph shows a slightly displaced fracture of the distal fourth metacarpal head. No other injuries are present.
The patient’s hand was left in the splint, and orthopedic evaluation was obtained.
For more information, see “Secondary Survey of Trauma Patient.” Clinician Reviews. 2015;25(12):10,35.
These Patients Knee’d Your Help
1. A 23-year-old man is brought in after being hit by a car. There is a moderate amount of soft tissue swelling around the knee, with limited flexion and extension due to pain. He can wiggle his toes, and there appears to be no neurovascular compromise.
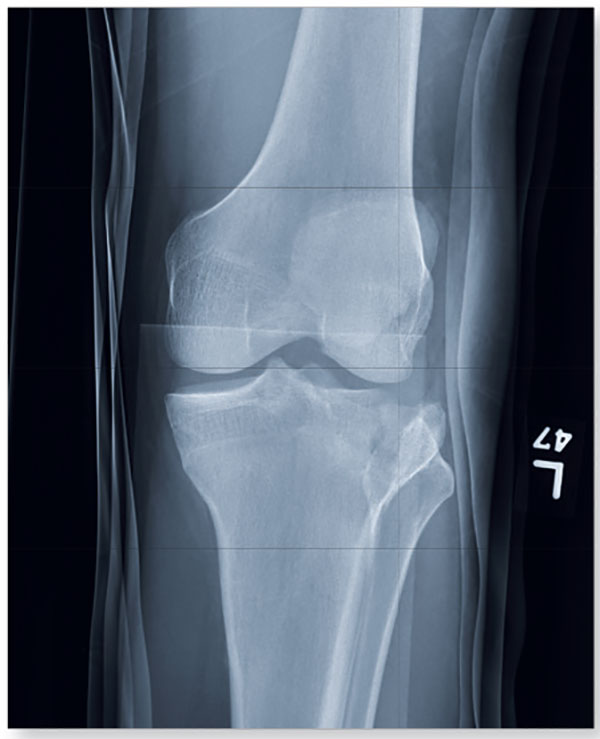
Diagnosis: The image shows a comminuted and depressed fracture of the lateral tibial plateau. It is depressed approximately 6 to 7 mm. The patient was admitted, and orthopedic consultation was obtained. The patient subsequently underwent an open reduction and internal fixation of the fracture.
For more information, see “Clipped by an Oncoming Car.” Clinician Reviews. 2014;24(6):23,36.
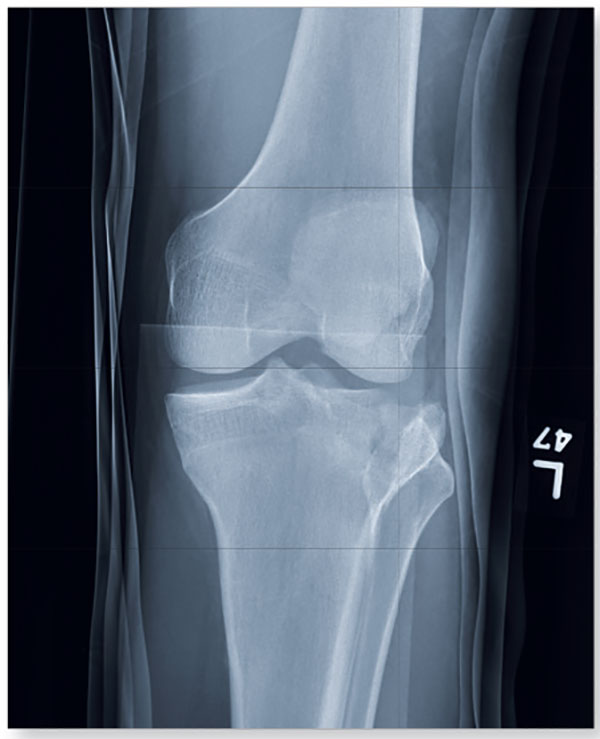
2. A 20-year-old man presents after his car was broadsided by another vehicle. His air bag deployed, and the patient now complains of right-sided chest wall pain and right knee pain. Inspection of his right knee shows some joint deformity, with mild swelling and moderate tenderness. The patient is unable to perform flexion with his right knee. Good distal pulses are present, and sensation is intact.

Diagnosis: The radiograph demonstrates lateral dislocation of the patella, with no evidence of an acute fracture in any surrounding bones. The patella was easily reduced in the emergency department, and the patient was placed in a knee immobilizer. Orthopedic consultation was obtained.
For more information, see “Chest Wall and Knee Pain Following Motor Vehicle Collision.” Clinician Reviews. 2013;23(1):8.
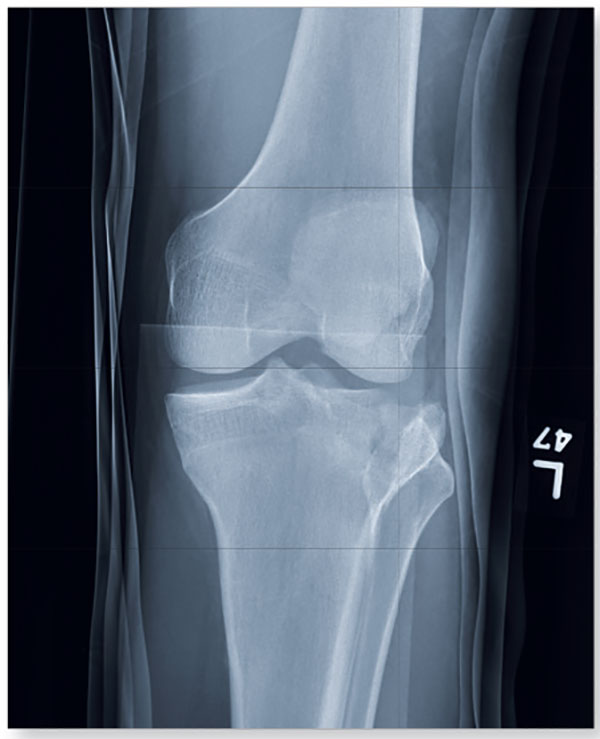
3. A 70-year-old woman presents for evaluation of right knee pain secondary to a fall. When she tripped and fell, all her weight landed on her right knee; she says it is now “extremely painful” to bear weight on that leg. Inspection of her right knee shows no obvious deformity, but a moderate amount of swelling and limited range of motion. She also has moderate tenderness circumferentially around the knee. There is additional swelling and mild bruising on both the medial and lateral aspects of the right ankle.

Diagnosis: The radiograph has several findings, one of which is a nondisplaced proximal fibula fracture. In addition, there is a moderate suprapatellar joint effusion. The patient also has fairly advanced tricompartment degenerative arthrosis. (To review, the tricompartment comprises all three anatomic areas of the knee: the patellofemoral, lateral tibiofemoral, and medial tibiofemoral joints.) The patient was placed in a knee immobilizer, and orthopedic evaluation was coordinated.
For more information, see “In Middle of Trip, Woman Falls.” Clinician Reviews. 2016;26(6):20,53.
4. A 28-year-old man is brought to you by EMS for evaluation after a motor vehicle accident. The patient was an unrestrained driver in a truck that went off the road into a ditch. The paramedics state that he was partially ejected, with his left leg caught in the window. He complains of back and left leg pain. Primary survey shows no obvious injury. Secondary survey reveals moderate swelling and decreased range of motion in the left knee. Good distal pulses are present.

Diagnosis: The radiograph shows that the distal femur is medially dislocated relative to the tibial plateau. In addition, the patella is laterally dislocated. No obvious fractures are evident. Such injuries are typically associated with significant ligament injuries, especially of the medial collateral ligament (MCL), lateral collateral ligament (LCL), and anterior cruciate ligament (ACL). Orthopedics was consulted for reduction of the dislocation and further workup (including MRI of the knee).
For more information, see “Driver Partially Ejected From Vehicle.” Clinician Reviews. 2015;25(7):20,27.
1. A 23-year-old man is brought in after being hit by a car. There is a moderate amount of soft tissue swelling around the knee, with limited flexion and extension due to pain. He can wiggle his toes, and there appears to be no neurovascular compromise.
Diagnosis: The image shows a comminuted and depressed fracture of the lateral tibial plateau. It is depressed approximately 6 to 7 mm. The patient was admitted, and orthopedic consultation was obtained. The patient subsequently underwent an open reduction and internal fixation of the fracture.
For more information, see “Clipped by an Oncoming Car.” Clinician Reviews. 2014;24(6):23,36.
2. A 20-year-old man presents after his car was broadsided by another vehicle. His air bag deployed, and the patient now complains of right-sided chest wall pain and right knee pain. Inspection of his right knee shows some joint deformity, with mild swelling and moderate tenderness. The patient is unable to perform flexion with his right knee. Good distal pulses are present, and sensation is intact.

Diagnosis: The radiograph demonstrates lateral dislocation of the patella, with no evidence of an acute fracture in any surrounding bones. The patella was easily reduced in the emergency department, and the patient was placed in a knee immobilizer. Orthopedic consultation was obtained.
For more information, see “Chest Wall and Knee Pain Following Motor Vehicle Collision.” Clinician Reviews. 2013;23(1):8.
3. A 70-year-old woman presents for evaluation of right knee pain secondary to a fall. When she tripped and fell, all her weight landed on her right knee; she says it is now “extremely painful” to bear weight on that leg. Inspection of her right knee shows no obvious deformity, but a moderate amount of swelling and limited range of motion. She also has moderate tenderness circumferentially around the knee. There is additional swelling and mild bruising on both the medial and lateral aspects of the right ankle.

Diagnosis: The radiograph has several findings, one of which is a nondisplaced proximal fibula fracture. In addition, there is a moderate suprapatellar joint effusion. The patient also has fairly advanced tricompartment degenerative arthrosis. (To review, the tricompartment comprises all three anatomic areas of the knee: the patellofemoral, lateral tibiofemoral, and medial tibiofemoral joints.) The patient was placed in a knee immobilizer, and orthopedic evaluation was coordinated.
For more information, see “In Middle of Trip, Woman Falls.” Clinician Reviews. 2016;26(6):20,53.
4. A 28-year-old man is brought to you by EMS for evaluation after a motor vehicle accident. The patient was an unrestrained driver in a truck that went off the road into a ditch. The paramedics state that he was partially ejected, with his left leg caught in the window. He complains of back and left leg pain. Primary survey shows no obvious injury. Secondary survey reveals moderate swelling and decreased range of motion in the left knee. Good distal pulses are present.

Diagnosis: The radiograph shows that the distal femur is medially dislocated relative to the tibial plateau. In addition, the patella is laterally dislocated. No obvious fractures are evident. Such injuries are typically associated with significant ligament injuries, especially of the medial collateral ligament (MCL), lateral collateral ligament (LCL), and anterior cruciate ligament (ACL). Orthopedics was consulted for reduction of the dislocation and further workup (including MRI of the knee).
For more information, see “Driver Partially Ejected From Vehicle.” Clinician Reviews. 2015;25(7):20,27.
1. A 23-year-old man is brought in after being hit by a car. There is a moderate amount of soft tissue swelling around the knee, with limited flexion and extension due to pain. He can wiggle his toes, and there appears to be no neurovascular compromise.
Diagnosis: The image shows a comminuted and depressed fracture of the lateral tibial plateau. It is depressed approximately 6 to 7 mm. The patient was admitted, and orthopedic consultation was obtained. The patient subsequently underwent an open reduction and internal fixation of the fracture.
For more information, see “Clipped by an Oncoming Car.” Clinician Reviews. 2014;24(6):23,36.
2. A 20-year-old man presents after his car was broadsided by another vehicle. His air bag deployed, and the patient now complains of right-sided chest wall pain and right knee pain. Inspection of his right knee shows some joint deformity, with mild swelling and moderate tenderness. The patient is unable to perform flexion with his right knee. Good distal pulses are present, and sensation is intact.

Diagnosis: The radiograph demonstrates lateral dislocation of the patella, with no evidence of an acute fracture in any surrounding bones. The patella was easily reduced in the emergency department, and the patient was placed in a knee immobilizer. Orthopedic consultation was obtained.
For more information, see “Chest Wall and Knee Pain Following Motor Vehicle Collision.” Clinician Reviews. 2013;23(1):8.
3. A 70-year-old woman presents for evaluation of right knee pain secondary to a fall. When she tripped and fell, all her weight landed on her right knee; she says it is now “extremely painful” to bear weight on that leg. Inspection of her right knee shows no obvious deformity, but a moderate amount of swelling and limited range of motion. She also has moderate tenderness circumferentially around the knee. There is additional swelling and mild bruising on both the medial and lateral aspects of the right ankle.

Diagnosis: The radiograph has several findings, one of which is a nondisplaced proximal fibula fracture. In addition, there is a moderate suprapatellar joint effusion. The patient also has fairly advanced tricompartment degenerative arthrosis. (To review, the tricompartment comprises all three anatomic areas of the knee: the patellofemoral, lateral tibiofemoral, and medial tibiofemoral joints.) The patient was placed in a knee immobilizer, and orthopedic evaluation was coordinated.
For more information, see “In Middle of Trip, Woman Falls.” Clinician Reviews. 2016;26(6):20,53.
4. A 28-year-old man is brought to you by EMS for evaluation after a motor vehicle accident. The patient was an unrestrained driver in a truck that went off the road into a ditch. The paramedics state that he was partially ejected, with his left leg caught in the window. He complains of back and left leg pain. Primary survey shows no obvious injury. Secondary survey reveals moderate swelling and decreased range of motion in the left knee. Good distal pulses are present.

Diagnosis: The radiograph shows that the distal femur is medially dislocated relative to the tibial plateau. In addition, the patella is laterally dislocated. No obvious fractures are evident. Such injuries are typically associated with significant ligament injuries, especially of the medial collateral ligament (MCL), lateral collateral ligament (LCL), and anterior cruciate ligament (ACL). Orthopedics was consulted for reduction of the dislocation and further workup (including MRI of the knee).
For more information, see “Driver Partially Ejected From Vehicle.” Clinician Reviews. 2015;25(7):20,27.
Itch, Scratch, Ad Infinitum, Part 2
1. A 25-year-old woman reports anogenital itching, burning, and redness, present for 3 months. She says she developed a yeast infection after antibiotic therapy for a dental infection. The yeast infection was treated with terconazole, which resulted in immediate severe burning, redness, and swelling. Clobetasol cream used twice daily also caused burning, so she discontinued it. Her symptoms improved when she tried cool soaks and applied topical benzocaine gel as a local anesthetic.

Diagnosis: Irritant contact dermatitis (as opposed to allergic contact dermatitis) associated with the use of terconazole and clobetasol. This was followed by allergic contact dermatitis in association with benzocaine. Treatment consists of withdrawal of benzocaine, reinitiation of cool soaks, and a switch to clobetasol ointment rather than cream. Nighttime sedation enables the patient to sleep through the itching and gradually allows her skin to heal.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
2. This 13-year-old presents with sudden-onset vulvar pain and sores. The child developed a sore throat and low-grade fever 3 days earlier, with vulvar pain and vulvar dysuria the next day. Oral acyclovir was prescribed for herpes simplex virus infection, but the girl’s condition has not improved. She claims sexual abstinence, and her mother believes her.

Diagnosis: Vulvar aphthae, believed to be of hyperimmune origin, are often precipitated by a viral syndrome. They are most common in girls aged 9 to 18 years.
Aphthae are uncommon and under-recognized on the vulva. Genital aphthae are usually much larger than oral aphthae. Most patients are mistakenly evaluated and treated for sexually transmitted infection, but the large, well-demarcated, painful, nonindurated, deep nature of the ulcer is pathognomonic for an aphthous ulcer.
Recommended treatment is prednisone 40 mg/day plus hydrocodone in usual doses of 5/325, one or two tablets every 4 to 6 hours, as needed; topical petroleum jelly (especially before urination); and sitz baths. When the patient returns one week later, she is much improved.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
3. A 36-year-old woman reports introital itching, vulvar dysuria, and superficial dyspareunia that have lasted 6 months. Apparent on physical examination are redness of the vestibule, medial labia minora, and vaginal walls, with edema of the surrounding skin and yellowish, copious vaginal secretions at the introitus. Lab tests for chlamydia, trichomonas, and gonorrhea are returned as normal.

Diagnosis: Desquamative inflammatory vaginitis (DIV) is described as noninfectious inflammatory vaginitis in a setting of normal estrogen and absence of skin disease of the mucous membranes of the vagina. The condition is characterized by an increase in white blood cells and parabasal cells and absent lactobacilli, with relatively high vaginal pH. DIV is thought to represent an inflammatory dermatosis of the vaginal epithelium. Although some clinicians believe that DIV is actually lichen planus, the latter exhibits erosions as well as redness, nearly always affects the mouth and the vulva, and produces remarkable scarring. DIV does not erode, affect any other skin surfaces, or scar.
Treatment for DIV consists of clindamycin vaginal cream, 1/2 to 1 full applicator nightly, with a weekly oral fluconazole tablet (200 mg is more easily covered by insurance) to prevent secondary candidiasis. Schedule a follow-up visit in one month.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
4. A 43-year-old woman reports a “recalcitrant yeast infection” of the vulva, with itching and irritation. She is overweight and diabetic, with mild stress incontinence. Physical examination reveals a fairly well-demarcated red, rough plaque on the vulva and labiocrural folds, with satellite red papules and peripheral peeling. Similar plaques occur in the gluteal cleft, umbilicus, and axillae as well as under the breasts. A fungal preparation of the vagina and skin is negative.

Diagnosis: Of the several morphologic types of psoriasis, anogenital psoriasis is most often of the inverse pattern. Inverse psoriasis preferentially affects skin folds and is frequently mistaken for (and often initially superinfected with) candidiasis. Scale is thin and unapparent, and there often is a shiny, glazed appearance to the skin. Tiny satellite lesions are often visible as well. A skin biopsy of inverse psoriasis often is not diagnostic, showing only nonspecific psoriasiform dermatitis; this does not disprove psoriasis.
Psoriasis is a systemic condition and is associated with metabolic syndrome, carrying an increased risk for overweight, hypertension, diabetes, and cardiovascular disease. Management of these conditions is very important in the overall treatment of the patient.
The recommended treatment is clobetasol ointment applied to the skin folds, along with continuation of the topical miconazole cream. A week later, the patient’s condition is remarkably improved, and her biopsy shows psoriasiform dermatitis. The potency of her corticosteroid was reduced by switching to desonide cream, sparingly applied daily.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
1. A 25-year-old woman reports anogenital itching, burning, and redness, present for 3 months. She says she developed a yeast infection after antibiotic therapy for a dental infection. The yeast infection was treated with terconazole, which resulted in immediate severe burning, redness, and swelling. Clobetasol cream used twice daily also caused burning, so she discontinued it. Her symptoms improved when she tried cool soaks and applied topical benzocaine gel as a local anesthetic.

Diagnosis: Irritant contact dermatitis (as opposed to allergic contact dermatitis) associated with the use of terconazole and clobetasol. This was followed by allergic contact dermatitis in association with benzocaine. Treatment consists of withdrawal of benzocaine, reinitiation of cool soaks, and a switch to clobetasol ointment rather than cream. Nighttime sedation enables the patient to sleep through the itching and gradually allows her skin to heal.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
2. This 13-year-old presents with sudden-onset vulvar pain and sores. The child developed a sore throat and low-grade fever 3 days earlier, with vulvar pain and vulvar dysuria the next day. Oral acyclovir was prescribed for herpes simplex virus infection, but the girl’s condition has not improved. She claims sexual abstinence, and her mother believes her.

Diagnosis: Vulvar aphthae, believed to be of hyperimmune origin, are often precipitated by a viral syndrome. They are most common in girls aged 9 to 18 years.
Aphthae are uncommon and under-recognized on the vulva. Genital aphthae are usually much larger than oral aphthae. Most patients are mistakenly evaluated and treated for sexually transmitted infection, but the large, well-demarcated, painful, nonindurated, deep nature of the ulcer is pathognomonic for an aphthous ulcer.
Recommended treatment is prednisone 40 mg/day plus hydrocodone in usual doses of 5/325, one or two tablets every 4 to 6 hours, as needed; topical petroleum jelly (especially before urination); and sitz baths. When the patient returns one week later, she is much improved.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
3. A 36-year-old woman reports introital itching, vulvar dysuria, and superficial dyspareunia that have lasted 6 months. Apparent on physical examination are redness of the vestibule, medial labia minora, and vaginal walls, with edema of the surrounding skin and yellowish, copious vaginal secretions at the introitus. Lab tests for chlamydia, trichomonas, and gonorrhea are returned as normal.

Diagnosis: Desquamative inflammatory vaginitis (DIV) is described as noninfectious inflammatory vaginitis in a setting of normal estrogen and absence of skin disease of the mucous membranes of the vagina. The condition is characterized by an increase in white blood cells and parabasal cells and absent lactobacilli, with relatively high vaginal pH. DIV is thought to represent an inflammatory dermatosis of the vaginal epithelium. Although some clinicians believe that DIV is actually lichen planus, the latter exhibits erosions as well as redness, nearly always affects the mouth and the vulva, and produces remarkable scarring. DIV does not erode, affect any other skin surfaces, or scar.
Treatment for DIV consists of clindamycin vaginal cream, 1/2 to 1 full applicator nightly, with a weekly oral fluconazole tablet (200 mg is more easily covered by insurance) to prevent secondary candidiasis. Schedule a follow-up visit in one month.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
4. A 43-year-old woman reports a “recalcitrant yeast infection” of the vulva, with itching and irritation. She is overweight and diabetic, with mild stress incontinence. Physical examination reveals a fairly well-demarcated red, rough plaque on the vulva and labiocrural folds, with satellite red papules and peripheral peeling. Similar plaques occur in the gluteal cleft, umbilicus, and axillae as well as under the breasts. A fungal preparation of the vagina and skin is negative.

Diagnosis: Of the several morphologic types of psoriasis, anogenital psoriasis is most often of the inverse pattern. Inverse psoriasis preferentially affects skin folds and is frequently mistaken for (and often initially superinfected with) candidiasis. Scale is thin and unapparent, and there often is a shiny, glazed appearance to the skin. Tiny satellite lesions are often visible as well. A skin biopsy of inverse psoriasis often is not diagnostic, showing only nonspecific psoriasiform dermatitis; this does not disprove psoriasis.
Psoriasis is a systemic condition and is associated with metabolic syndrome, carrying an increased risk for overweight, hypertension, diabetes, and cardiovascular disease. Management of these conditions is very important in the overall treatment of the patient.
The recommended treatment is clobetasol ointment applied to the skin folds, along with continuation of the topical miconazole cream. A week later, the patient’s condition is remarkably improved, and her biopsy shows psoriasiform dermatitis. The potency of her corticosteroid was reduced by switching to desonide cream, sparingly applied daily.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
1. A 25-year-old woman reports anogenital itching, burning, and redness, present for 3 months. She says she developed a yeast infection after antibiotic therapy for a dental infection. The yeast infection was treated with terconazole, which resulted in immediate severe burning, redness, and swelling. Clobetasol cream used twice daily also caused burning, so she discontinued it. Her symptoms improved when she tried cool soaks and applied topical benzocaine gel as a local anesthetic.

Diagnosis: Irritant contact dermatitis (as opposed to allergic contact dermatitis) associated with the use of terconazole and clobetasol. This was followed by allergic contact dermatitis in association with benzocaine. Treatment consists of withdrawal of benzocaine, reinitiation of cool soaks, and a switch to clobetasol ointment rather than cream. Nighttime sedation enables the patient to sleep through the itching and gradually allows her skin to heal.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
2. This 13-year-old presents with sudden-onset vulvar pain and sores. The child developed a sore throat and low-grade fever 3 days earlier, with vulvar pain and vulvar dysuria the next day. Oral acyclovir was prescribed for herpes simplex virus infection, but the girl’s condition has not improved. She claims sexual abstinence, and her mother believes her.

Diagnosis: Vulvar aphthae, believed to be of hyperimmune origin, are often precipitated by a viral syndrome. They are most common in girls aged 9 to 18 years.
Aphthae are uncommon and under-recognized on the vulva. Genital aphthae are usually much larger than oral aphthae. Most patients are mistakenly evaluated and treated for sexually transmitted infection, but the large, well-demarcated, painful, nonindurated, deep nature of the ulcer is pathognomonic for an aphthous ulcer.
Recommended treatment is prednisone 40 mg/day plus hydrocodone in usual doses of 5/325, one or two tablets every 4 to 6 hours, as needed; topical petroleum jelly (especially before urination); and sitz baths. When the patient returns one week later, she is much improved.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
3. A 36-year-old woman reports introital itching, vulvar dysuria, and superficial dyspareunia that have lasted 6 months. Apparent on physical examination are redness of the vestibule, medial labia minora, and vaginal walls, with edema of the surrounding skin and yellowish, copious vaginal secretions at the introitus. Lab tests for chlamydia, trichomonas, and gonorrhea are returned as normal.

Diagnosis: Desquamative inflammatory vaginitis (DIV) is described as noninfectious inflammatory vaginitis in a setting of normal estrogen and absence of skin disease of the mucous membranes of the vagina. The condition is characterized by an increase in white blood cells and parabasal cells and absent lactobacilli, with relatively high vaginal pH. DIV is thought to represent an inflammatory dermatosis of the vaginal epithelium. Although some clinicians believe that DIV is actually lichen planus, the latter exhibits erosions as well as redness, nearly always affects the mouth and the vulva, and produces remarkable scarring. DIV does not erode, affect any other skin surfaces, or scar.
Treatment for DIV consists of clindamycin vaginal cream, 1/2 to 1 full applicator nightly, with a weekly oral fluconazole tablet (200 mg is more easily covered by insurance) to prevent secondary candidiasis. Schedule a follow-up visit in one month.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
4. A 43-year-old woman reports a “recalcitrant yeast infection” of the vulva, with itching and irritation. She is overweight and diabetic, with mild stress incontinence. Physical examination reveals a fairly well-demarcated red, rough plaque on the vulva and labiocrural folds, with satellite red papules and peripheral peeling. Similar plaques occur in the gluteal cleft, umbilicus, and axillae as well as under the breasts. A fungal preparation of the vagina and skin is negative.

Diagnosis: Of the several morphologic types of psoriasis, anogenital psoriasis is most often of the inverse pattern. Inverse psoriasis preferentially affects skin folds and is frequently mistaken for (and often initially superinfected with) candidiasis. Scale is thin and unapparent, and there often is a shiny, glazed appearance to the skin. Tiny satellite lesions are often visible as well. A skin biopsy of inverse psoriasis often is not diagnostic, showing only nonspecific psoriasiform dermatitis; this does not disprove psoriasis.
Psoriasis is a systemic condition and is associated with metabolic syndrome, carrying an increased risk for overweight, hypertension, diabetes, and cardiovascular disease. Management of these conditions is very important in the overall treatment of the patient.
The recommended treatment is clobetasol ointment applied to the skin folds, along with continuation of the topical miconazole cream. A week later, the patient’s condition is remarkably improved, and her biopsy shows psoriasiform dermatitis. The potency of her corticosteroid was reduced by switching to desonide cream, sparingly applied daily.
For more information on this case, see “Chronic vulvar irritation, itching, and pain. What is the diagnosis?” OBG Manag. 2014;26(6):30-37.
Congenital craniofacial deformities
1. This youngster is being followed for symptoms related to his right-sided cranial asymmetry noted at birth, including neurologic impairment (sensorineural hearing loss and visual problems including strabismus) and breathing problems; developmental delay and/or intellectual disability; and hydrocephalus. The hands and feet are normal.
Source: By Michael L. Kaufman at the English language Wikipedia, CC BY-SA 3.0
Diagnosis: Craniosynostosis, also known as acrocephalosyndactyly, is a condition in which the skull sutures close prematurely. This can cause pressure to build up inside the head and skull or facial bones, leading to a misshapen head and distinctive facial features—ocular hypertelorism, proptosis, midface hypoplasia, small beaked nose, and prognathism—and occasionally abnormal fingers and toes.
Mutations of the FGFR gene, which regulates the fibroblast growth factor receptor protein, are responsible for the eight disorders comprising the FGFR-related craniosynostosis spectrum. The protein plays an important role in bone growth, particularly during embryonic development. For example, this protein signals certain immature cells in the developing embryo to become bone cells in the head, hands, feet, and other tissues.
For more information, see Robin NH, MD, Falk MJ, Haldeman-Englert CR. FGFR-related craniosynostosis syndromes. In: GeneReviews® [Internet]. Pagon RA, Adam MP, Ardinger HH, et al, eds. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
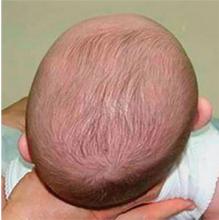
2. This infant presents with a misshapen cranium, most notably the flattened area on the posterior right side. His history includes limited passive neck rotation at birth, preferential head orientation, supine sleep position, and lower activity level.
Source: Wikimedia Commons; By Medical advises - http://larece.ru/?p=27115, CC BY-SA 3.0
Diagnosis: Plagiocephaly, literally means "oblique head" (from the Greek "plagio" for oblique and "cephale" for head). The incidence in infants at 7 to 12 weeks of age is estimated to be 46.6%. Of all infants with plagiocephaly, 63.2% are affected on the right side and 78.3% have a mild form.
For more information, see “Helmets for Positional Skull Deformities: A Good Idea or Not?” Clin Rev. 2015;25(2):16,18.
For the next photograph, proceed to the next page >>
3. An adolescent patient presents with marked facial asymmetry, present since birth. The auricular tissue on the left side is malformed; on the right side, low set. The right midface is underdeveloped with micrognathia and chin deviation, resulting in malocclusion.
Source: Wikimedia Commons
Diagnosis: Craniofacial microsomia, possibly caused by bleeding in the temporal area during gestation, describes a spectrum of cranial and facial abnormalities. After Down syndrome, it is the most common congenital syndrome, occurring in approximately 1 in 3,500 to 4,500 live births. In about two-thirds of cases, abnormalities differ from one side to the other.
These individuals typically demonstrate one-sided maxillary or mandibular hypoplasia, which can cause dental problems and difficulties with feeding and speech. In cases of severe mandibular hypoplasia, breathing may also be affected.
Abnormalities affecting one or both ears may range from preauricular tags to an underdeveloped or absent external ear or a closed or absent ear canal; these patients may experience hearing loss. Microphthalmia, occurring less frequently, may result in vision loss.
For more information, see Heike CL, Luquetti DV, Hing AV. Craniofacial microsomia overview. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
4. A 4-month-old boy is brought in by his mother for evaluation of a “birthmark” on his forehead that has become more prominent with time. The child complains a bit when the lesion is touched.
His mother gives a history of a normal full-term pregnancy with an uneventful delivery. Other than the skin lesion, there have been no other known problems with the child’s health.
Diagnosis: Most first-year medical students could tell you this was a case of an infantile hemangioma—but within the past five years, the categorization and treatment of hemangiomas have changed rapidly.
Hemangiomas are benign and usually self-involuting vascular tumors. They are distinct from the family of permanent congenital vascular lesions, such as port wine stains. About 80% occur on the face or neck and more commonly in females. Those that occur near the skin’s surface tend to be bright red, while those of deeper origin are more bluish. Hemangiomas can also manifest in extracutaneous areas (eg, the liver); these are usually detected via imaging.
For more information, see “A New Approach to “Birthmarks” Clin Rev. 2016;26(3):W1.
RELATED ARTICLE:
Infantile Hemangiomas Increasing, Linked to Prematurity, Low Birth Weight Bruce Jancin, Family Practice News Digital Network
1. This youngster is being followed for symptoms related to his right-sided cranial asymmetry noted at birth, including neurologic impairment (sensorineural hearing loss and visual problems including strabismus) and breathing problems; developmental delay and/or intellectual disability; and hydrocephalus. The hands and feet are normal.
Source: By Michael L. Kaufman at the English language Wikipedia, CC BY-SA 3.0
Diagnosis: Craniosynostosis, also known as acrocephalosyndactyly, is a condition in which the skull sutures close prematurely. This can cause pressure to build up inside the head and skull or facial bones, leading to a misshapen head and distinctive facial features—ocular hypertelorism, proptosis, midface hypoplasia, small beaked nose, and prognathism—and occasionally abnormal fingers and toes.
Mutations of the FGFR gene, which regulates the fibroblast growth factor receptor protein, are responsible for the eight disorders comprising the FGFR-related craniosynostosis spectrum. The protein plays an important role in bone growth, particularly during embryonic development. For example, this protein signals certain immature cells in the developing embryo to become bone cells in the head, hands, feet, and other tissues.
For more information, see Robin NH, MD, Falk MJ, Haldeman-Englert CR. FGFR-related craniosynostosis syndromes. In: GeneReviews® [Internet]. Pagon RA, Adam MP, Ardinger HH, et al, eds. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
2. This infant presents with a misshapen cranium, most notably the flattened area on the posterior right side. His history includes limited passive neck rotation at birth, preferential head orientation, supine sleep position, and lower activity level.
Source: Wikimedia Commons; By Medical advises - http://larece.ru/?p=27115, CC BY-SA 3.0
Diagnosis: Plagiocephaly, literally means "oblique head" (from the Greek "plagio" for oblique and "cephale" for head). The incidence in infants at 7 to 12 weeks of age is estimated to be 46.6%. Of all infants with plagiocephaly, 63.2% are affected on the right side and 78.3% have a mild form.
For more information, see “Helmets for Positional Skull Deformities: A Good Idea or Not?” Clin Rev. 2015;25(2):16,18.
For the next photograph, proceed to the next page >>
3. An adolescent patient presents with marked facial asymmetry, present since birth. The auricular tissue on the left side is malformed; on the right side, low set. The right midface is underdeveloped with micrognathia and chin deviation, resulting in malocclusion.
Source: Wikimedia Commons
Diagnosis: Craniofacial microsomia, possibly caused by bleeding in the temporal area during gestation, describes a spectrum of cranial and facial abnormalities. After Down syndrome, it is the most common congenital syndrome, occurring in approximately 1 in 3,500 to 4,500 live births. In about two-thirds of cases, abnormalities differ from one side to the other.
These individuals typically demonstrate one-sided maxillary or mandibular hypoplasia, which can cause dental problems and difficulties with feeding and speech. In cases of severe mandibular hypoplasia, breathing may also be affected.
Abnormalities affecting one or both ears may range from preauricular tags to an underdeveloped or absent external ear or a closed or absent ear canal; these patients may experience hearing loss. Microphthalmia, occurring less frequently, may result in vision loss.
For more information, see Heike CL, Luquetti DV, Hing AV. Craniofacial microsomia overview. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
4. A 4-month-old boy is brought in by his mother for evaluation of a “birthmark” on his forehead that has become more prominent with time. The child complains a bit when the lesion is touched.
His mother gives a history of a normal full-term pregnancy with an uneventful delivery. Other than the skin lesion, there have been no other known problems with the child’s health.
Diagnosis: Most first-year medical students could tell you this was a case of an infantile hemangioma—but within the past five years, the categorization and treatment of hemangiomas have changed rapidly.
Hemangiomas are benign and usually self-involuting vascular tumors. They are distinct from the family of permanent congenital vascular lesions, such as port wine stains. About 80% occur on the face or neck and more commonly in females. Those that occur near the skin’s surface tend to be bright red, while those of deeper origin are more bluish. Hemangiomas can also manifest in extracutaneous areas (eg, the liver); these are usually detected via imaging.
For more information, see “A New Approach to “Birthmarks” Clin Rev. 2016;26(3):W1.
RELATED ARTICLE:
Infantile Hemangiomas Increasing, Linked to Prematurity, Low Birth Weight Bruce Jancin, Family Practice News Digital Network
1. This youngster is being followed for symptoms related to his right-sided cranial asymmetry noted at birth, including neurologic impairment (sensorineural hearing loss and visual problems including strabismus) and breathing problems; developmental delay and/or intellectual disability; and hydrocephalus. The hands and feet are normal.
Source: By Michael L. Kaufman at the English language Wikipedia, CC BY-SA 3.0
Diagnosis: Craniosynostosis, also known as acrocephalosyndactyly, is a condition in which the skull sutures close prematurely. This can cause pressure to build up inside the head and skull or facial bones, leading to a misshapen head and distinctive facial features—ocular hypertelorism, proptosis, midface hypoplasia, small beaked nose, and prognathism—and occasionally abnormal fingers and toes.
Mutations of the FGFR gene, which regulates the fibroblast growth factor receptor protein, are responsible for the eight disorders comprising the FGFR-related craniosynostosis spectrum. The protein plays an important role in bone growth, particularly during embryonic development. For example, this protein signals certain immature cells in the developing embryo to become bone cells in the head, hands, feet, and other tissues.
For more information, see Robin NH, MD, Falk MJ, Haldeman-Englert CR. FGFR-related craniosynostosis syndromes. In: GeneReviews® [Internet]. Pagon RA, Adam MP, Ardinger HH, et al, eds. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
2. This infant presents with a misshapen cranium, most notably the flattened area on the posterior right side. His history includes limited passive neck rotation at birth, preferential head orientation, supine sleep position, and lower activity level.
Source: Wikimedia Commons; By Medical advises - http://larece.ru/?p=27115, CC BY-SA 3.0
Diagnosis: Plagiocephaly, literally means "oblique head" (from the Greek "plagio" for oblique and "cephale" for head). The incidence in infants at 7 to 12 weeks of age is estimated to be 46.6%. Of all infants with plagiocephaly, 63.2% are affected on the right side and 78.3% have a mild form.
For more information, see “Helmets for Positional Skull Deformities: A Good Idea or Not?” Clin Rev. 2015;25(2):16,18.
For the next photograph, proceed to the next page >>
3. An adolescent patient presents with marked facial asymmetry, present since birth. The auricular tissue on the left side is malformed; on the right side, low set. The right midface is underdeveloped with micrognathia and chin deviation, resulting in malocclusion.
Source: Wikimedia Commons
Diagnosis: Craniofacial microsomia, possibly caused by bleeding in the temporal area during gestation, describes a spectrum of cranial and facial abnormalities. After Down syndrome, it is the most common congenital syndrome, occurring in approximately 1 in 3,500 to 4,500 live births. In about two-thirds of cases, abnormalities differ from one side to the other.
These individuals typically demonstrate one-sided maxillary or mandibular hypoplasia, which can cause dental problems and difficulties with feeding and speech. In cases of severe mandibular hypoplasia, breathing may also be affected.
Abnormalities affecting one or both ears may range from preauricular tags to an underdeveloped or absent external ear or a closed or absent ear canal; these patients may experience hearing loss. Microphthalmia, occurring less frequently, may result in vision loss.
For more information, see Heike CL, Luquetti DV, Hing AV. Craniofacial microsomia overview. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
4. A 4-month-old boy is brought in by his mother for evaluation of a “birthmark” on his forehead that has become more prominent with time. The child complains a bit when the lesion is touched.
His mother gives a history of a normal full-term pregnancy with an uneventful delivery. Other than the skin lesion, there have been no other known problems with the child’s health.
Diagnosis: Most first-year medical students could tell you this was a case of an infantile hemangioma—but within the past five years, the categorization and treatment of hemangiomas have changed rapidly.
Hemangiomas are benign and usually self-involuting vascular tumors. They are distinct from the family of permanent congenital vascular lesions, such as port wine stains. About 80% occur on the face or neck and more commonly in females. Those that occur near the skin’s surface tend to be bright red, while those of deeper origin are more bluish. Hemangiomas can also manifest in extracutaneous areas (eg, the liver); these are usually detected via imaging.
For more information, see “A New Approach to “Birthmarks” Clin Rev. 2016;26(3):W1.
RELATED ARTICLE:
Infantile Hemangiomas Increasing, Linked to Prematurity, Low Birth Weight Bruce Jancin, Family Practice News Digital Network
Bone Ache and Stiffness
1. This patient presented with rapid onset of severe pain in the MTP joint of the great toe accompanied swelling, redness, and fever. The pain was most severe in the first two to 24 hours and peaked within 24 hours. The history was remarkable for a trauma to the toe and a first-degree relative who had experienced the same symptoms. The patient admitted to drinking alcohol regularly.
Diagnosis: A presumptive diagnosis of gout may be acceptable in a patient with the classic presentation: rapid onset of severe pain in a swollen, erythematous joint (classically described in Latin as calor, rubor, dolor, et tumor) and symptoms peaking within 24 hours. The presence of tophi is pathognomonic for chronic tophaceous gout. In cases of questionable or unusual manifestation of gout, however, various imaging techniques and crystal visualization may be indicated.
For more information, see “Gout: A Clinical Overview.” Clin Rev. 2011;21(7):29-35.
For the next photograph, proceed to the next page >>
2. A 75-year-old woman presented to her family physician (FP) with pain in both hands. She said that she’d had the pain for a year and that it got worse with cold weather and better with ibuprofen.
Diagnosis: Osteoarthritis (OA) was diagnosed after noting Heberden’s nodes and Bouchard’s nodes at the distal and proximal interphalangeal joints, respectively. Arthritis is the most common cause of disability in the United States. Twenty-one million adults have functional limitations because of arthritis. Fifty percent of adults ages 65 years or older have been given an arthritis diagnosis. The most commonly affected joints are the knees, hips, hands (distal and proximal interphalangeal joints), and spine. If the diagnosis is uncertain, plain x-rays can often differentiate between OA and other forms of arthritis.
For more information, read “Hand pain.” J Fam Pract. 2015.
Photo courtesy of Dr. Richard Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
For the next photograph, proceed to the next page >>
3. A 45-year-old man with longstanding psoriasis began experiencing finger pain and swelling. The patient, who had a history of hepatitis C, noted that his fingernails had recently begun crumbling and his fingers were stiff in the morning.
Diagnosis: Psoriatic arthritis (with dactylitis and significant distal interphalangeal joint [DIP] involvement) was diagnosed in both hands, but the left hand was worse. The condition of the patient’s nails was not surprising, given that almost all patients with psoriatic arthritis have nail involvement. Radiographs of the patient’s hands showed periarticular erosions and new bone formation. There was also telescoping of the third DIP joint.
For more information, read “Finger pain and swelling.” J Fam Pract. 2015.
Photo courtesy of Ricardo Zuniga-Montes, MD; text courtesy of Richard P. Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
For the next photograph, proceed to the next page >>
4. A 62-year-old woman was concerned about her fingers, which weren’t straight. She’d had increasing pain in both hands (specifically the metacarpophalangeal [MCP] joints) over the past 2 years. Her fingers were stiff in the morning, but she was able to gain some relief with ibuprofen and naproxen. On physical exam, her fingers had an ulnar deviation and there was swelling of the MCP joints on both hands.
Diagnosis: Rheumatoid arthritis (RA) was diagnosed, based on the patient’s bilateral MCP joint swelling, ulnar deviation, and morning stiffness. Patients with RA initially experience swelling and stiffness in their wrists, as well as their MCP and metatarsophalangeal joints. Later, the larger joints are affected. When RA is advanced, severe destruction and subluxation occur.
“Crooked fingers.” J Fam Pract. 2015.
Photo courtesy of Dr. Richard Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
1. This patient presented with rapid onset of severe pain in the MTP joint of the great toe accompanied swelling, redness, and fever. The pain was most severe in the first two to 24 hours and peaked within 24 hours. The history was remarkable for a trauma to the toe and a first-degree relative who had experienced the same symptoms. The patient admitted to drinking alcohol regularly.
Diagnosis: A presumptive diagnosis of gout may be acceptable in a patient with the classic presentation: rapid onset of severe pain in a swollen, erythematous joint (classically described in Latin as calor, rubor, dolor, et tumor) and symptoms peaking within 24 hours. The presence of tophi is pathognomonic for chronic tophaceous gout. In cases of questionable or unusual manifestation of gout, however, various imaging techniques and crystal visualization may be indicated.
For more information, see “Gout: A Clinical Overview.” Clin Rev. 2011;21(7):29-35.
For the next photograph, proceed to the next page >>
2. A 75-year-old woman presented to her family physician (FP) with pain in both hands. She said that she’d had the pain for a year and that it got worse with cold weather and better with ibuprofen.
Diagnosis: Osteoarthritis (OA) was diagnosed after noting Heberden’s nodes and Bouchard’s nodes at the distal and proximal interphalangeal joints, respectively. Arthritis is the most common cause of disability in the United States. Twenty-one million adults have functional limitations because of arthritis. Fifty percent of adults ages 65 years or older have been given an arthritis diagnosis. The most commonly affected joints are the knees, hips, hands (distal and proximal interphalangeal joints), and spine. If the diagnosis is uncertain, plain x-rays can often differentiate between OA and other forms of arthritis.
For more information, read “Hand pain.” J Fam Pract. 2015.
Photo courtesy of Dr. Richard Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
For the next photograph, proceed to the next page >>
3. A 45-year-old man with longstanding psoriasis began experiencing finger pain and swelling. The patient, who had a history of hepatitis C, noted that his fingernails had recently begun crumbling and his fingers were stiff in the morning.
Diagnosis: Psoriatic arthritis (with dactylitis and significant distal interphalangeal joint [DIP] involvement) was diagnosed in both hands, but the left hand was worse. The condition of the patient’s nails was not surprising, given that almost all patients with psoriatic arthritis have nail involvement. Radiographs of the patient’s hands showed periarticular erosions and new bone formation. There was also telescoping of the third DIP joint.
For more information, read “Finger pain and swelling.” J Fam Pract. 2015.
Photo courtesy of Ricardo Zuniga-Montes, MD; text courtesy of Richard P. Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
For the next photograph, proceed to the next page >>
4. A 62-year-old woman was concerned about her fingers, which weren’t straight. She’d had increasing pain in both hands (specifically the metacarpophalangeal [MCP] joints) over the past 2 years. Her fingers were stiff in the morning, but she was able to gain some relief with ibuprofen and naproxen. On physical exam, her fingers had an ulnar deviation and there was swelling of the MCP joints on both hands.
Diagnosis: Rheumatoid arthritis (RA) was diagnosed, based on the patient’s bilateral MCP joint swelling, ulnar deviation, and morning stiffness. Patients with RA initially experience swelling and stiffness in their wrists, as well as their MCP and metatarsophalangeal joints. Later, the larger joints are affected. When RA is advanced, severe destruction and subluxation occur.
“Crooked fingers.” J Fam Pract. 2015.
Photo courtesy of Dr. Richard Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
1. This patient presented with rapid onset of severe pain in the MTP joint of the great toe accompanied swelling, redness, and fever. The pain was most severe in the first two to 24 hours and peaked within 24 hours. The history was remarkable for a trauma to the toe and a first-degree relative who had experienced the same symptoms. The patient admitted to drinking alcohol regularly.
Diagnosis: A presumptive diagnosis of gout may be acceptable in a patient with the classic presentation: rapid onset of severe pain in a swollen, erythematous joint (classically described in Latin as calor, rubor, dolor, et tumor) and symptoms peaking within 24 hours. The presence of tophi is pathognomonic for chronic tophaceous gout. In cases of questionable or unusual manifestation of gout, however, various imaging techniques and crystal visualization may be indicated.
For more information, see “Gout: A Clinical Overview.” Clin Rev. 2011;21(7):29-35.
For the next photograph, proceed to the next page >>
2. A 75-year-old woman presented to her family physician (FP) with pain in both hands. She said that she’d had the pain for a year and that it got worse with cold weather and better with ibuprofen.
Diagnosis: Osteoarthritis (OA) was diagnosed after noting Heberden’s nodes and Bouchard’s nodes at the distal and proximal interphalangeal joints, respectively. Arthritis is the most common cause of disability in the United States. Twenty-one million adults have functional limitations because of arthritis. Fifty percent of adults ages 65 years or older have been given an arthritis diagnosis. The most commonly affected joints are the knees, hips, hands (distal and proximal interphalangeal joints), and spine. If the diagnosis is uncertain, plain x-rays can often differentiate between OA and other forms of arthritis.
For more information, read “Hand pain.” J Fam Pract. 2015.
Photo courtesy of Dr. Richard Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
For the next photograph, proceed to the next page >>
3. A 45-year-old man with longstanding psoriasis began experiencing finger pain and swelling. The patient, who had a history of hepatitis C, noted that his fingernails had recently begun crumbling and his fingers were stiff in the morning.
Diagnosis: Psoriatic arthritis (with dactylitis and significant distal interphalangeal joint [DIP] involvement) was diagnosed in both hands, but the left hand was worse. The condition of the patient’s nails was not surprising, given that almost all patients with psoriatic arthritis have nail involvement. Radiographs of the patient’s hands showed periarticular erosions and new bone formation. There was also telescoping of the third DIP joint.
For more information, read “Finger pain and swelling.” J Fam Pract. 2015.
Photo courtesy of Ricardo Zuniga-Montes, MD; text courtesy of Richard P. Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
For the next photograph, proceed to the next page >>
4. A 62-year-old woman was concerned about her fingers, which weren’t straight. She’d had increasing pain in both hands (specifically the metacarpophalangeal [MCP] joints) over the past 2 years. Her fingers were stiff in the morning, but she was able to gain some relief with ibuprofen and naproxen. On physical exam, her fingers had an ulnar deviation and there was swelling of the MCP joints on both hands.
Diagnosis: Rheumatoid arthritis (RA) was diagnosed, based on the patient’s bilateral MCP joint swelling, ulnar deviation, and morning stiffness. Patients with RA initially experience swelling and stiffness in their wrists, as well as their MCP and metatarsophalangeal joints. Later, the larger joints are affected. When RA is advanced, severe destruction and subluxation occur.
“Crooked fingers.” J Fam Pract. 2015.
Photo courtesy of Dr. Richard Usatine, MD. The case was adapted with permission from Chumley H, Usatine R. Arthritis overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:562-568.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Itch, scratch, ad infinitum
1. A 62-year-old woman reports anogenital itching with pain on scratching and has developed introital dyspareunia. Physical exam reveals a well-demarcated white plaque of thickened, crinkled skin. A wet mount shows parabasal cells and no lactobacilli.
Diagnosis: Lichen sclerosus is a skin disease found most often on the vulva of postmenopausal women, although it also can affect prepubertal children and reproductive-age women. Lichen sclerosus is multifactorial in pathogenesis, including prominent autoimmune factors, local environmental factors, and genetic predisposition.1
Although there is no cure for lichen sclerosus, the symptoms and clinical abnormalities usually can be well managed with ultra-potent topical corticosteroids. However, scarring and architectural changes are not reversible. Moreover, poorly controlled lichen sclerosus exhibits malignant transformation on anogenital skin in about 3% of affected patients.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
2. A 34-year-old patient reports excruciating itching, with disruption of daily activities and sleep. She has been treated for candidiasis on multiple occasions, but her wet mount and confirmatory culture are negative. Physical exam reveals a pink, lichenified plaque with excoriation.
Diagnosis: Lichen simplex chronicus (formerly called squamous hyperplasia or hyperplastic dystrophy, and also known as eczema, neurodermatitis, or localized atopic dermatitis) occurs when irritation from any cause produces itching in a predisposed person. The subsequent scratching and rubbing both produce the rash and exacerbate the irritation that drives the itching, even after the original cause is gone. The rubbing and scratching perpetuate the irritation and itching, producing the “itch-scratch” cycle.
The appearance of lichen simplex chronicus is produced by rubbing (where the skin thickens and lichenifies) or scratching (where the skin becomes red with linear erosions, called excoriations, caused by fingernails).
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
3. A 36-year-old has a history of chronic yeast infection with introital burning, discharge, and dyspareunia. She is otherwise healthy, except for irritable bowel syndrome and fibromyalgia. A mild patchy redness appears on the vestibule and surrounding modified mucous membranes. Gentle probing triggers exquisite pain in the vestibule, with slight extension to the labia minora. Lactobacilli are abundant.
Diagnosis: Vulvodynia is a genital pain syndrome defined as sensations of chronic burning, irritation, rawness, and soreness in the absence of objective disease and infection that could explain the discomfort. Vulvodynia occurs in approximately 7% to 8% of women.
Vulvodynia generally is believed to be a multifactorial symptom, occurring as a result of pelvic floor dysfunction and neuropathic pain, with anxiety/depression issues exacerbating symptoms. Some recent studies have shown the presence of biochemical mediators of inflammation in the absence of clinical and histologic inflammation. Discomfort often is worsened by infections or the application of common irritants (creams, panty liners, soaps, some topical anesthetics). Estrogen deficiency is another common exacerbating factor.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
4. A 73-year-old patient has longstanding introital itching and rawness, with dyspareunia. Topical estradiol cream intravaginally three times weekly with weekly fluconazole has not helped. The physical reveals deep red patches and erosions of the vestibule and anterior mucosal membranes, with loss of the labia minora. An oral exam shows deep redness of the gingivae and erosions of the buccal mucosae, with surrounding white, lacy papules.
Diagnosis: After correlating the vulvar and oral findings, you make a diagnosis of lichen planus. Erosive multimucosal lichen planus is a disease of cell-mediated immunity that overwhelmingly affects menopausal women. The most common surfaces involved are the mouth, vagina, rectal mucosa, and vulva; usually, at least two surfaces are affected. The esophagus, extra-auditory canals, nasal mucosa, and eyes also can be involved. Dry, extragenital skin usually is not affected in the setting of erosive vulvovaginal lichen planus.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
1. A 62-year-old woman reports anogenital itching with pain on scratching and has developed introital dyspareunia. Physical exam reveals a well-demarcated white plaque of thickened, crinkled skin. A wet mount shows parabasal cells and no lactobacilli.
Diagnosis: Lichen sclerosus is a skin disease found most often on the vulva of postmenopausal women, although it also can affect prepubertal children and reproductive-age women. Lichen sclerosus is multifactorial in pathogenesis, including prominent autoimmune factors, local environmental factors, and genetic predisposition.1
Although there is no cure for lichen sclerosus, the symptoms and clinical abnormalities usually can be well managed with ultra-potent topical corticosteroids. However, scarring and architectural changes are not reversible. Moreover, poorly controlled lichen sclerosus exhibits malignant transformation on anogenital skin in about 3% of affected patients.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
2. A 34-year-old patient reports excruciating itching, with disruption of daily activities and sleep. She has been treated for candidiasis on multiple occasions, but her wet mount and confirmatory culture are negative. Physical exam reveals a pink, lichenified plaque with excoriation.
Diagnosis: Lichen simplex chronicus (formerly called squamous hyperplasia or hyperplastic dystrophy, and also known as eczema, neurodermatitis, or localized atopic dermatitis) occurs when irritation from any cause produces itching in a predisposed person. The subsequent scratching and rubbing both produce the rash and exacerbate the irritation that drives the itching, even after the original cause is gone. The rubbing and scratching perpetuate the irritation and itching, producing the “itch-scratch” cycle.
The appearance of lichen simplex chronicus is produced by rubbing (where the skin thickens and lichenifies) or scratching (where the skin becomes red with linear erosions, called excoriations, caused by fingernails).
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
3. A 36-year-old has a history of chronic yeast infection with introital burning, discharge, and dyspareunia. She is otherwise healthy, except for irritable bowel syndrome and fibromyalgia. A mild patchy redness appears on the vestibule and surrounding modified mucous membranes. Gentle probing triggers exquisite pain in the vestibule, with slight extension to the labia minora. Lactobacilli are abundant.
Diagnosis: Vulvodynia is a genital pain syndrome defined as sensations of chronic burning, irritation, rawness, and soreness in the absence of objective disease and infection that could explain the discomfort. Vulvodynia occurs in approximately 7% to 8% of women.
Vulvodynia generally is believed to be a multifactorial symptom, occurring as a result of pelvic floor dysfunction and neuropathic pain, with anxiety/depression issues exacerbating symptoms. Some recent studies have shown the presence of biochemical mediators of inflammation in the absence of clinical and histologic inflammation. Discomfort often is worsened by infections or the application of common irritants (creams, panty liners, soaps, some topical anesthetics). Estrogen deficiency is another common exacerbating factor.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
4. A 73-year-old patient has longstanding introital itching and rawness, with dyspareunia. Topical estradiol cream intravaginally three times weekly with weekly fluconazole has not helped. The physical reveals deep red patches and erosions of the vestibule and anterior mucosal membranes, with loss of the labia minora. An oral exam shows deep redness of the gingivae and erosions of the buccal mucosae, with surrounding white, lacy papules.
Diagnosis: After correlating the vulvar and oral findings, you make a diagnosis of lichen planus. Erosive multimucosal lichen planus is a disease of cell-mediated immunity that overwhelmingly affects menopausal women. The most common surfaces involved are the mouth, vagina, rectal mucosa, and vulva; usually, at least two surfaces are affected. The esophagus, extra-auditory canals, nasal mucosa, and eyes also can be involved. Dry, extragenital skin usually is not affected in the setting of erosive vulvovaginal lichen planus.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
1. A 62-year-old woman reports anogenital itching with pain on scratching and has developed introital dyspareunia. Physical exam reveals a well-demarcated white plaque of thickened, crinkled skin. A wet mount shows parabasal cells and no lactobacilli.
Diagnosis: Lichen sclerosus is a skin disease found most often on the vulva of postmenopausal women, although it also can affect prepubertal children and reproductive-age women. Lichen sclerosus is multifactorial in pathogenesis, including prominent autoimmune factors, local environmental factors, and genetic predisposition.1
Although there is no cure for lichen sclerosus, the symptoms and clinical abnormalities usually can be well managed with ultra-potent topical corticosteroids. However, scarring and architectural changes are not reversible. Moreover, poorly controlled lichen sclerosus exhibits malignant transformation on anogenital skin in about 3% of affected patients.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
2. A 34-year-old patient reports excruciating itching, with disruption of daily activities and sleep. She has been treated for candidiasis on multiple occasions, but her wet mount and confirmatory culture are negative. Physical exam reveals a pink, lichenified plaque with excoriation.
Diagnosis: Lichen simplex chronicus (formerly called squamous hyperplasia or hyperplastic dystrophy, and also known as eczema, neurodermatitis, or localized atopic dermatitis) occurs when irritation from any cause produces itching in a predisposed person. The subsequent scratching and rubbing both produce the rash and exacerbate the irritation that drives the itching, even after the original cause is gone. The rubbing and scratching perpetuate the irritation and itching, producing the “itch-scratch” cycle.
The appearance of lichen simplex chronicus is produced by rubbing (where the skin thickens and lichenifies) or scratching (where the skin becomes red with linear erosions, called excoriations, caused by fingernails).
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
3. A 36-year-old has a history of chronic yeast infection with introital burning, discharge, and dyspareunia. She is otherwise healthy, except for irritable bowel syndrome and fibromyalgia. A mild patchy redness appears on the vestibule and surrounding modified mucous membranes. Gentle probing triggers exquisite pain in the vestibule, with slight extension to the labia minora. Lactobacilli are abundant.
Diagnosis: Vulvodynia is a genital pain syndrome defined as sensations of chronic burning, irritation, rawness, and soreness in the absence of objective disease and infection that could explain the discomfort. Vulvodynia occurs in approximately 7% to 8% of women.
Vulvodynia generally is believed to be a multifactorial symptom, occurring as a result of pelvic floor dysfunction and neuropathic pain, with anxiety/depression issues exacerbating symptoms. Some recent studies have shown the presence of biochemical mediators of inflammation in the absence of clinical and histologic inflammation. Discomfort often is worsened by infections or the application of common irritants (creams, panty liners, soaps, some topical anesthetics). Estrogen deficiency is another common exacerbating factor.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
For the next photograph, proceed to the next page >>
4. A 73-year-old patient has longstanding introital itching and rawness, with dyspareunia. Topical estradiol cream intravaginally three times weekly with weekly fluconazole has not helped. The physical reveals deep red patches and erosions of the vestibule and anterior mucosal membranes, with loss of the labia minora. An oral exam shows deep redness of the gingivae and erosions of the buccal mucosae, with surrounding white, lacy papules.
Diagnosis: After correlating the vulvar and oral findings, you make a diagnosis of lichen planus. Erosive multimucosal lichen planus is a disease of cell-mediated immunity that overwhelmingly affects menopausal women. The most common surfaces involved are the mouth, vagina, rectal mucosa, and vulva; usually, at least two surfaces are affected. The esophagus, extra-auditory canals, nasal mucosa, and eyes also can be involved. Dry, extragenital skin usually is not affected in the setting of erosive vulvovaginal lichen planus.
For more information on this case, see “Chronic vulvar symptoms and dermatologic disruptions: How to make the correct diagnosis.” OBG Manag. 2014;26(5):30-49.
A Case of Nerves
1. After several years of progressively worsening symptoms, starting with intermittent muscular rigidity and spasms in the lower back, this patient now has stiff leg muscles (more pronounced on the right side). On exam, she demonstrates a slow, stiff manner of walking and lordosis of the lower spine.
Diagnosis: Moersch-Woltman syndrome, or stiff person syndrome, is a rare acquired neurologic disorder, affecting both men and women of any age; most, however, are women. Thought to be an autoimmune disorder, this syndrome may localized to one area of the body or may be widespread, and rapidly progressive, including the body, brain stem, and spinal cord. If untreated, the patient may have difficulty walking and performing activities of daily living.
For more information, see “Stiff Person Syndrome.”
For the next photograph, proceed to the next page >>
2. This patient lost control of her eye and eyelid rather suddenly and then noticed difficulty swallowing and slurred speech. She is now experiencing limb weakness that worsens as the day progresses.
Diagnosis: Myasthenia gravis is a chronic autoimmune disease characterized by varying degrees of weakness of the skeletal muscles of the body. Muscles that control eye and eyelid movement, facial expression, chewing, talking, and swallowing are often, but not always, involved in the disorder. The muscles that control breathing and neck and limb movements may also be affected.
For more information, see “Test Accurately Diagnoses Myasthenia Gravis.” Neurology Reviews. 2016;24(3):36.
For the next photograph, proceed to the next page >>
3. After a night out on the town, this patient is concerned that something is wrong, and it’s not the splitting headache: He is unable to extend his right wrist, thumb, or fingers in the pronated position. Furthermore, the radial and dorsal skin is numb. During the history, he reports that he fell asleep sitting upright with his arm over the back of a chair.
Diagnosis: Radial neuropathy, or Saturday night palsy, is typically produced by direct, prolonged pressure on the radial nerve. The nerve is especially susceptible as it spirals around the midportion of the humerus, in this case by allowing the hard edge of a chair back to compress it all night long. Although alcohol and drugs are usually implicated, radial palsy can also result from fracturing the humerus, leaning on crutches, or from long-term constriction of the wrist (tight watch or bracelet).
For more information, see “9.19 Radial Neuropathy (Saturday Night Palsy).”
For the next photograph, proceed to the next page >>
4. The patient reports spontaneous severe pain near his right shoulder, unrelated to any trauma. Two weeks later, the shoulder protrudes in a winglike position on the upper back, made more apparent when the same side arm pushes against resistance. He has limited ability to lift that arm above his head.
Diagnosis: Winged scapula injury is due to dysfunction of the anterior serratus muscle, which is supplied by the injury-prone long thoracic nerve.
Damage can be caused by a contusion or blunt trauma of the shoulder, traction of the neck, and sometimes a viral illness. Paralysis of the serratus anterior muscle has been well documented among athletes and laborers. To identify an injury, the patient stands facing a wall from about two feet away and then pushes against the wall with flat palms at waist level. Conservative treatment is often recommended; if after 6-24 months if there is no recovery, patients become candidates for corrective surgery.
For more information, see “Scapular winging: anatomical review, diagnosis, and treatments.” Curr Rev Musculoskelet Med. 2008;1(1):1-11.
Related article
For more on peripheral neuropathies, see “An easy approach to evaluating peripheral neuropathy.” J Fam Pract. 2006 October;55(10):853-861.
Photographs courtesy of Ashley Owens and Alexander Orban. They are included for illustration only and do not represent actual cases.
1. After several years of progressively worsening symptoms, starting with intermittent muscular rigidity and spasms in the lower back, this patient now has stiff leg muscles (more pronounced on the right side). On exam, she demonstrates a slow, stiff manner of walking and lordosis of the lower spine.
Diagnosis: Moersch-Woltman syndrome, or stiff person syndrome, is a rare acquired neurologic disorder, affecting both men and women of any age; most, however, are women. Thought to be an autoimmune disorder, this syndrome may localized to one area of the body or may be widespread, and rapidly progressive, including the body, brain stem, and spinal cord. If untreated, the patient may have difficulty walking and performing activities of daily living.
For more information, see “Stiff Person Syndrome.”
For the next photograph, proceed to the next page >>
2. This patient lost control of her eye and eyelid rather suddenly and then noticed difficulty swallowing and slurred speech. She is now experiencing limb weakness that worsens as the day progresses.
Diagnosis: Myasthenia gravis is a chronic autoimmune disease characterized by varying degrees of weakness of the skeletal muscles of the body. Muscles that control eye and eyelid movement, facial expression, chewing, talking, and swallowing are often, but not always, involved in the disorder. The muscles that control breathing and neck and limb movements may also be affected.
For more information, see “Test Accurately Diagnoses Myasthenia Gravis.” Neurology Reviews. 2016;24(3):36.
For the next photograph, proceed to the next page >>
3. After a night out on the town, this patient is concerned that something is wrong, and it’s not the splitting headache: He is unable to extend his right wrist, thumb, or fingers in the pronated position. Furthermore, the radial and dorsal skin is numb. During the history, he reports that he fell asleep sitting upright with his arm over the back of a chair.
Diagnosis: Radial neuropathy, or Saturday night palsy, is typically produced by direct, prolonged pressure on the radial nerve. The nerve is especially susceptible as it spirals around the midportion of the humerus, in this case by allowing the hard edge of a chair back to compress it all night long. Although alcohol and drugs are usually implicated, radial palsy can also result from fracturing the humerus, leaning on crutches, or from long-term constriction of the wrist (tight watch or bracelet).
For more information, see “9.19 Radial Neuropathy (Saturday Night Palsy).”
For the next photograph, proceed to the next page >>
4. The patient reports spontaneous severe pain near his right shoulder, unrelated to any trauma. Two weeks later, the shoulder protrudes in a winglike position on the upper back, made more apparent when the same side arm pushes against resistance. He has limited ability to lift that arm above his head.
Diagnosis: Winged scapula injury is due to dysfunction of the anterior serratus muscle, which is supplied by the injury-prone long thoracic nerve.
Damage can be caused by a contusion or blunt trauma of the shoulder, traction of the neck, and sometimes a viral illness. Paralysis of the serratus anterior muscle has been well documented among athletes and laborers. To identify an injury, the patient stands facing a wall from about two feet away and then pushes against the wall with flat palms at waist level. Conservative treatment is often recommended; if after 6-24 months if there is no recovery, patients become candidates for corrective surgery.
For more information, see “Scapular winging: anatomical review, diagnosis, and treatments.” Curr Rev Musculoskelet Med. 2008;1(1):1-11.
Related article
For more on peripheral neuropathies, see “An easy approach to evaluating peripheral neuropathy.” J Fam Pract. 2006 October;55(10):853-861.
Photographs courtesy of Ashley Owens and Alexander Orban. They are included for illustration only and do not represent actual cases.
1. After several years of progressively worsening symptoms, starting with intermittent muscular rigidity and spasms in the lower back, this patient now has stiff leg muscles (more pronounced on the right side). On exam, she demonstrates a slow, stiff manner of walking and lordosis of the lower spine.
Diagnosis: Moersch-Woltman syndrome, or stiff person syndrome, is a rare acquired neurologic disorder, affecting both men and women of any age; most, however, are women. Thought to be an autoimmune disorder, this syndrome may localized to one area of the body or may be widespread, and rapidly progressive, including the body, brain stem, and spinal cord. If untreated, the patient may have difficulty walking and performing activities of daily living.
For more information, see “Stiff Person Syndrome.”
For the next photograph, proceed to the next page >>
2. This patient lost control of her eye and eyelid rather suddenly and then noticed difficulty swallowing and slurred speech. She is now experiencing limb weakness that worsens as the day progresses.
Diagnosis: Myasthenia gravis is a chronic autoimmune disease characterized by varying degrees of weakness of the skeletal muscles of the body. Muscles that control eye and eyelid movement, facial expression, chewing, talking, and swallowing are often, but not always, involved in the disorder. The muscles that control breathing and neck and limb movements may also be affected.
For more information, see “Test Accurately Diagnoses Myasthenia Gravis.” Neurology Reviews. 2016;24(3):36.
For the next photograph, proceed to the next page >>
3. After a night out on the town, this patient is concerned that something is wrong, and it’s not the splitting headache: He is unable to extend his right wrist, thumb, or fingers in the pronated position. Furthermore, the radial and dorsal skin is numb. During the history, he reports that he fell asleep sitting upright with his arm over the back of a chair.
Diagnosis: Radial neuropathy, or Saturday night palsy, is typically produced by direct, prolonged pressure on the radial nerve. The nerve is especially susceptible as it spirals around the midportion of the humerus, in this case by allowing the hard edge of a chair back to compress it all night long. Although alcohol and drugs are usually implicated, radial palsy can also result from fracturing the humerus, leaning on crutches, or from long-term constriction of the wrist (tight watch or bracelet).
For more information, see “9.19 Radial Neuropathy (Saturday Night Palsy).”
For the next photograph, proceed to the next page >>
4. The patient reports spontaneous severe pain near his right shoulder, unrelated to any trauma. Two weeks later, the shoulder protrudes in a winglike position on the upper back, made more apparent when the same side arm pushes against resistance. He has limited ability to lift that arm above his head.
Diagnosis: Winged scapula injury is due to dysfunction of the anterior serratus muscle, which is supplied by the injury-prone long thoracic nerve.
Damage can be caused by a contusion or blunt trauma of the shoulder, traction of the neck, and sometimes a viral illness. Paralysis of the serratus anterior muscle has been well documented among athletes and laborers. To identify an injury, the patient stands facing a wall from about two feet away and then pushes against the wall with flat palms at waist level. Conservative treatment is often recommended; if after 6-24 months if there is no recovery, patients become candidates for corrective surgery.
For more information, see “Scapular winging: anatomical review, diagnosis, and treatments.” Curr Rev Musculoskelet Med. 2008;1(1):1-11.
Related article
For more on peripheral neuropathies, see “An easy approach to evaluating peripheral neuropathy.” J Fam Pract. 2006 October;55(10):853-861.
Photographs courtesy of Ashley Owens and Alexander Orban. They are included for illustration only and do not represent actual cases.
The Great Masquerader
1. Several weeks ago, this 56-year-old man noticed numerous asymptomatic round macules and papules on his palms and soles, many with scaly peripheral margins. Similar lesions are noted on the penile corona and glans. There is a faint but definite morbiliform, blanchable pink rash covering most of the patient’s trunk, taking on a “shawl” distribution across the shoulders. The patient is exclusively homosexual and recently engaged in high-risk sexual activity.

| 
|
Diagnosis: It would be hard to imagine a more classic example of secondary syphilis than was seen in this case, occurring in a patient so obviously at risk. But it’s only “obvious” if you’re ready and aware of how syphilis manifests. It also helps if you understand how common it is and who’s likely to get it.
TAKE-HOME LEARNING POINTS
• Palmar and plantar rashes are unusual and should prompt the examiner to expand the history and physical.
• Secondary syphilis, though uncommon, is far from rare, especially among gay men engaging in high-risk sexual behavior.
• It’s common for the patient to deny the appearance of the chancre of primary syphilis, and such a lesion would be long gone by the time those of secondary syphilis manifest.
• Conditions involving the skin should be seen by a dermatology provider, regardless of location. This includes diseases of the skin, hair, nails, oral mucosa, genitals, feet, or palms. One potential exception is the eye itself, though most diseases “of the eye” are, in reality, diseases of the periocular skin—and belong with a dermatology provider.
For more information on this case, see “When There’s More to the Story ….” Clin Rev. 2013;12;2013(12):W2.
For the next photograph, proceed to the next page >>
2. First appearing a month ago, this rash was first confined to the patient’s abdomen and subsequently spread. The blanchable, erythematous papules and nodules are fairly dense, uniformly covering most of his skin but sparing face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations. More than 10 years ago, the patient was diagnosed with HIV, which is well controlled with medication. Homosexually active, he denies having any new contacts.
Diagnosis: This case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
For more information on this case, see “Unusual Cause for Asymptomatic Rash.” Clin Rev. 2013;23(9):W6.
For the next photograph, proceed to the next page >>
3. A 43-year-old man presented with a rapidly enlarging ulcerated nodule on the right ankle with a necrotic and crusted center. He also had multiple red-brown papules on the trunk and extremities. Some of these lesions had central erosions, while others had surface scale. He was known to be HIV positive but had no lymphadenopathy.
Diagnosis: Lues maligna is used to describe a rare noduloulcerative form of secondary syphilis.1 It was first described in 18592 and has been associated with other disorders such as diabetes mellitus3 and chronic alcoholism.4 Patients usually are gravely ill and develop polymorphic ulcerating lesions. Facial and scalp involvement are common, but patients typically do not have palmoplantar involvement in conventional presentations of secondary syphilis.
…The patient’s rapid plasma reagin titer at the time of the fourth biopsy was 1:256, and appropriate treatment with penicillin resulted in complete clearance of the lesions in 3 to 4 weeks.
For more information on this case, see “Rapidly Enlarging Noduloulcerative Lesions.” Cutis. 2014;94(3):E20-E22.
Photograph and case description courtesy of Cutis. 2014;94(3):E20-E22.
Related article
Man, 54, With Delusions and Seizures
2011;21(4):20, 22, 24
1. Several weeks ago, this 56-year-old man noticed numerous asymptomatic round macules and papules on his palms and soles, many with scaly peripheral margins. Similar lesions are noted on the penile corona and glans. There is a faint but definite morbiliform, blanchable pink rash covering most of the patient’s trunk, taking on a “shawl” distribution across the shoulders. The patient is exclusively homosexual and recently engaged in high-risk sexual activity.

| 
|
Diagnosis: It would be hard to imagine a more classic example of secondary syphilis than was seen in this case, occurring in a patient so obviously at risk. But it’s only “obvious” if you’re ready and aware of how syphilis manifests. It also helps if you understand how common it is and who’s likely to get it.
TAKE-HOME LEARNING POINTS
• Palmar and plantar rashes are unusual and should prompt the examiner to expand the history and physical.
• Secondary syphilis, though uncommon, is far from rare, especially among gay men engaging in high-risk sexual behavior.
• It’s common for the patient to deny the appearance of the chancre of primary syphilis, and such a lesion would be long gone by the time those of secondary syphilis manifest.
• Conditions involving the skin should be seen by a dermatology provider, regardless of location. This includes diseases of the skin, hair, nails, oral mucosa, genitals, feet, or palms. One potential exception is the eye itself, though most diseases “of the eye” are, in reality, diseases of the periocular skin—and belong with a dermatology provider.
For more information on this case, see “When There’s More to the Story ….” Clin Rev. 2013;12;2013(12):W2.
For the next photograph, proceed to the next page >>
2. First appearing a month ago, this rash was first confined to the patient’s abdomen and subsequently spread. The blanchable, erythematous papules and nodules are fairly dense, uniformly covering most of his skin but sparing face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations. More than 10 years ago, the patient was diagnosed with HIV, which is well controlled with medication. Homosexually active, he denies having any new contacts.
Diagnosis: This case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
For more information on this case, see “Unusual Cause for Asymptomatic Rash.” Clin Rev. 2013;23(9):W6.
For the next photograph, proceed to the next page >>
3. A 43-year-old man presented with a rapidly enlarging ulcerated nodule on the right ankle with a necrotic and crusted center. He also had multiple red-brown papules on the trunk and extremities. Some of these lesions had central erosions, while others had surface scale. He was known to be HIV positive but had no lymphadenopathy.
Diagnosis: Lues maligna is used to describe a rare noduloulcerative form of secondary syphilis.1 It was first described in 18592 and has been associated with other disorders such as diabetes mellitus3 and chronic alcoholism.4 Patients usually are gravely ill and develop polymorphic ulcerating lesions. Facial and scalp involvement are common, but patients typically do not have palmoplantar involvement in conventional presentations of secondary syphilis.
…The patient’s rapid plasma reagin titer at the time of the fourth biopsy was 1:256, and appropriate treatment with penicillin resulted in complete clearance of the lesions in 3 to 4 weeks.
For more information on this case, see “Rapidly Enlarging Noduloulcerative Lesions.” Cutis. 2014;94(3):E20-E22.
Photograph and case description courtesy of Cutis. 2014;94(3):E20-E22.
Related article
Man, 54, With Delusions and Seizures
2011;21(4):20, 22, 24
1. Several weeks ago, this 56-year-old man noticed numerous asymptomatic round macules and papules on his palms and soles, many with scaly peripheral margins. Similar lesions are noted on the penile corona and glans. There is a faint but definite morbiliform, blanchable pink rash covering most of the patient’s trunk, taking on a “shawl” distribution across the shoulders. The patient is exclusively homosexual and recently engaged in high-risk sexual activity.

| 
|
Diagnosis: It would be hard to imagine a more classic example of secondary syphilis than was seen in this case, occurring in a patient so obviously at risk. But it’s only “obvious” if you’re ready and aware of how syphilis manifests. It also helps if you understand how common it is and who’s likely to get it.
TAKE-HOME LEARNING POINTS
• Palmar and plantar rashes are unusual and should prompt the examiner to expand the history and physical.
• Secondary syphilis, though uncommon, is far from rare, especially among gay men engaging in high-risk sexual behavior.
• It’s common for the patient to deny the appearance of the chancre of primary syphilis, and such a lesion would be long gone by the time those of secondary syphilis manifest.
• Conditions involving the skin should be seen by a dermatology provider, regardless of location. This includes diseases of the skin, hair, nails, oral mucosa, genitals, feet, or palms. One potential exception is the eye itself, though most diseases “of the eye” are, in reality, diseases of the periocular skin—and belong with a dermatology provider.
For more information on this case, see “When There’s More to the Story ….” Clin Rev. 2013;12;2013(12):W2.
For the next photograph, proceed to the next page >>
2. First appearing a month ago, this rash was first confined to the patient’s abdomen and subsequently spread. The blanchable, erythematous papules and nodules are fairly dense, uniformly covering most of his skin but sparing face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations. More than 10 years ago, the patient was diagnosed with HIV, which is well controlled with medication. Homosexually active, he denies having any new contacts.
Diagnosis: This case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
For more information on this case, see “Unusual Cause for Asymptomatic Rash.” Clin Rev. 2013;23(9):W6.
For the next photograph, proceed to the next page >>
3. A 43-year-old man presented with a rapidly enlarging ulcerated nodule on the right ankle with a necrotic and crusted center. He also had multiple red-brown papules on the trunk and extremities. Some of these lesions had central erosions, while others had surface scale. He was known to be HIV positive but had no lymphadenopathy.
Diagnosis: Lues maligna is used to describe a rare noduloulcerative form of secondary syphilis.1 It was first described in 18592 and has been associated with other disorders such as diabetes mellitus3 and chronic alcoholism.4 Patients usually are gravely ill and develop polymorphic ulcerating lesions. Facial and scalp involvement are common, but patients typically do not have palmoplantar involvement in conventional presentations of secondary syphilis.
…The patient’s rapid plasma reagin titer at the time of the fourth biopsy was 1:256, and appropriate treatment with penicillin resulted in complete clearance of the lesions in 3 to 4 weeks.
For more information on this case, see “Rapidly Enlarging Noduloulcerative Lesions.” Cutis. 2014;94(3):E20-E22.
Photograph and case description courtesy of Cutis. 2014;94(3):E20-E22.
Related article
Man, 54, With Delusions and Seizures
2011;21(4):20, 22, 24