User login
AUDIO: Meaningful use interoperability ‘won’t work without the Internet’
WASHINGTON – The rules for Stage 3 of the meaningful use program have been finalized by the Obama administration, despite questions about physicians’ ability to achieve “interoperability” and pleas from politicians and providers alike to delay its implementation.
Jonathan Bush, cofounder and CEO of athenahealth, said he believes interoperability will be a no-go unless data are seen as common property, and a premium is placed on the seamless transition of medical records by way of the Internet, not faxes.
Speaking about the large sums of money being spent by hospitals to comply with the government’s meaningful use requirements, Mr. Bush said, “they’re going to staff up hundreds of people who aren’t going to be able to run it. It doesn’t connect to anyone.”
In an interview at the annual Washington Ideas Forum sponsored by the Aspen Institute and The Atlantic, Mr. Bush offered his thoughts on how data could be more easily shared.
On Twitter @whitneymcknight
WASHINGTON – The rules for Stage 3 of the meaningful use program have been finalized by the Obama administration, despite questions about physicians’ ability to achieve “interoperability” and pleas from politicians and providers alike to delay its implementation.
Jonathan Bush, cofounder and CEO of athenahealth, said he believes interoperability will be a no-go unless data are seen as common property, and a premium is placed on the seamless transition of medical records by way of the Internet, not faxes.
Speaking about the large sums of money being spent by hospitals to comply with the government’s meaningful use requirements, Mr. Bush said, “they’re going to staff up hundreds of people who aren’t going to be able to run it. It doesn’t connect to anyone.”
In an interview at the annual Washington Ideas Forum sponsored by the Aspen Institute and The Atlantic, Mr. Bush offered his thoughts on how data could be more easily shared.
On Twitter @whitneymcknight
WASHINGTON – The rules for Stage 3 of the meaningful use program have been finalized by the Obama administration, despite questions about physicians’ ability to achieve “interoperability” and pleas from politicians and providers alike to delay its implementation.
Jonathan Bush, cofounder and CEO of athenahealth, said he believes interoperability will be a no-go unless data are seen as common property, and a premium is placed on the seamless transition of medical records by way of the Internet, not faxes.
Speaking about the large sums of money being spent by hospitals to comply with the government’s meaningful use requirements, Mr. Bush said, “they’re going to staff up hundreds of people who aren’t going to be able to run it. It doesn’t connect to anyone.”
In an interview at the annual Washington Ideas Forum sponsored by the Aspen Institute and The Atlantic, Mr. Bush offered his thoughts on how data could be more easily shared.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM THE WASHINGTON IDEAS FORUM
Survey: 45% order tests to avoid lawsuits
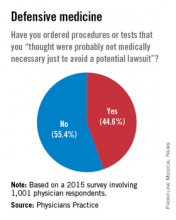
Almost 45% of physicians say that they have practiced defensive medicine, according to a survey of 1,001 physicians conducted by Physicians Practice, a practice management newspaper and website.
To be exact, 44.6% of respondents said that they had ordered tests or procedures that they “thought were probably not medically necessary just to avoid a potential lawsuit,” Physicians Practice reported in its 2015 Great American Physician Survey.
Almost 44% of the physician respondents said that they had been threatened with a malpractice lawsuit, and nearly 32% reported that they had been the defendant in such a lawsuit, the survey results showed.
Almost 45% of physicians say that they have practiced defensive medicine, according to a survey of 1,001 physicians conducted by Physicians Practice, a practice management newspaper and website.
To be exact, 44.6% of respondents said that they had ordered tests or procedures that they “thought were probably not medically necessary just to avoid a potential lawsuit,” Physicians Practice reported in its 2015 Great American Physician Survey.
Almost 44% of the physician respondents said that they had been threatened with a malpractice lawsuit, and nearly 32% reported that they had been the defendant in such a lawsuit, the survey results showed.
Almost 45% of physicians say that they have practiced defensive medicine, according to a survey of 1,001 physicians conducted by Physicians Practice, a practice management newspaper and website.
To be exact, 44.6% of respondents said that they had ordered tests or procedures that they “thought were probably not medically necessary just to avoid a potential lawsuit,” Physicians Practice reported in its 2015 Great American Physician Survey.
Almost 44% of the physician respondents said that they had been threatened with a malpractice lawsuit, and nearly 32% reported that they had been the defendant in such a lawsuit, the survey results showed.
Billing, Coding Documentation to Support Services, Minimize Risks
The electronic health record (EHR) has many benefits:
- Improved patient care;
- Improved care coordination;
- Improved diagnostics and patient outcomes;
- Increased patient participation; and
- Increased practice efficiencies and cost savings.1
EHRs also introduce risks, however. Heightened concern about EHR misuse and vulnerability elevates the level of scrutiny placed on provider documentation as it relates to billing and coding. Without clear guidelines from the Centers for Medicare and Medicaid Services (CMS) or other payers, the potential for unintentional misapplication exists. Auditor misinterpretation is also possible. Providers should utilize simple defensive documentation principles to support their services and minimize their risks.
Reason for Encounter
Under section 1862 (a)(1)(A) of the Social Security Act, the Medicare Program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).2
A payer can determine if a service is “reasonable and necessary” based on the service indication. The reason for the patient encounter, otherwise known as the chief complaint, must be evident. This can be a symptom, problem, condition, diagnosis, physician-recommended return, or another factor that necessitates the encounter.1 It cannot be inferred and must be clearly stated in the documentation. Without it, a payer may question the medical necessity of the service, especially if it involves hospital-based services in the course of which multiple specialists will see the patient on any given date. Payers are likely to deny services that cannot be easily differentiated (e.g. “no c/o”). Furthermore, payers can deny concurrent care services for the following reasons:3
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate/overlap those of the other provider without any recognizable distinction.
Providers should be specific in identifying the encounter reason, as in the following examples: “Patient seen for shortness of breath” or “Patient with COPD, feeling improved with 3L O2 NC.”
Assessment and Plan
Accurately representing patient complexity for every visit throughout the hospitalization presents its challenges. Although the problem list may not dramatically change day to day, providers must formulate an assessment of the patient’s condition with a corresponding plan of care for each encounter. Documenting problems without a corresponding plan of care does not substantiate physician participation in the management of that problem. Providing a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) minimizes the complexity and effort put forth in the encounter and could result in auditor downgrading upon documentation review.
Developing shortcuts might falsely minimize the provider’s documentation burden. An electronic documentation system might make it possible to copy previous progress notes into the current encounter to save time; however, the previously entered information could include elements that do not require reassessment during a subsequent encounter or contain information about conditions that are being managed concurrently by another specialist (e.g. CKD being managed by the nephrologist). Leaving the copied information unmodified may not accurately reflect the patient’s current condition or the care provided by the hospitalist during the current encounter. Information that is pulled forward or copied and pasted from a previous entry should be modified to demonstrate updated content and nonoverlapping care relevant to that date.
According to the Office of Inspector General (OIG), “inappropriate copy-pasting could facilitate attempts to inflate claims and duplicate or create fraudulent claims.”4
An equally problematic EHR function involves “overdocumentation,” the practice of inserting false or irrelevant documentation to create the appearance of support for billing higher level services.4 EHR technology has the ability to auto-populate fields using templates built into the system or generate extensive documentation on the basis of a single click. The OIG cautions providers to use these features carefully, because they can produce information suggesting the practitioner performed more comprehensive services than were actually rendered.4
An example is the inclusion of the same lab results more than once. Although clinicians include this information as a reference to avoid having to “find it somewhere in the chart” when it is needed—as a basis for comparison, for example—auditors mistake this as an attempt to gain credit for the daily review of the same “old” information. Including only relevant data will mitigate this concern.
Authorship
Dates and signatures are essential to each encounter. Medicare requires services provided/ordered to be authenticated by the author.5 A reviewer must be able to identify each individual who performs, documents, and bills for a service on a given date. Progress notes that fail to identify the service date or service provider will likely result in denial.
Additionally, a service is questioned when two different sets of handwriting appear on a note, yet only one signature is provided. Since the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Notes that contain an illegible signature are equally problematic. If the legibility of the signature prevents the reviewer from correctly identifying the rendering provider, the service may be denied.
CMS has instructed Medicare contractors to request a signed provider attestation before issuing a denial.5 The provider should print his/her name beside the signature or include a separate signature sheet with the requested documentation to assist the reviewer in provider identification. Stamped signatures are not acceptable under any circumstance. Medicare accepts only handwritten or electronic signatures.5
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- HealthIT.gov. Benefits of electronic health records (EHRs). Accessed August 1, 2015.
- Social Security Administration. Exclusions from coverage and Medicare as secondary payer. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered medical and other health services. Chapter 15, Section 30.E. Concurrent care. Accessed August 1, 2015.
- Department of Health and Human Services. Office of Inspector General. CMS and its contractors have adopted few program integrity practices to address vulnerabilities in EHRs. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Signature guidelines for medical review purposes. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. 1995 documentation guidelines for evaluation and management services. Accessed August 1, 2015.
The electronic health record (EHR) has many benefits:
- Improved patient care;
- Improved care coordination;
- Improved diagnostics and patient outcomes;
- Increased patient participation; and
- Increased practice efficiencies and cost savings.1
EHRs also introduce risks, however. Heightened concern about EHR misuse and vulnerability elevates the level of scrutiny placed on provider documentation as it relates to billing and coding. Without clear guidelines from the Centers for Medicare and Medicaid Services (CMS) or other payers, the potential for unintentional misapplication exists. Auditor misinterpretation is also possible. Providers should utilize simple defensive documentation principles to support their services and minimize their risks.
Reason for Encounter
Under section 1862 (a)(1)(A) of the Social Security Act, the Medicare Program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).2
A payer can determine if a service is “reasonable and necessary” based on the service indication. The reason for the patient encounter, otherwise known as the chief complaint, must be evident. This can be a symptom, problem, condition, diagnosis, physician-recommended return, or another factor that necessitates the encounter.1 It cannot be inferred and must be clearly stated in the documentation. Without it, a payer may question the medical necessity of the service, especially if it involves hospital-based services in the course of which multiple specialists will see the patient on any given date. Payers are likely to deny services that cannot be easily differentiated (e.g. “no c/o”). Furthermore, payers can deny concurrent care services for the following reasons:3
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate/overlap those of the other provider without any recognizable distinction.
Providers should be specific in identifying the encounter reason, as in the following examples: “Patient seen for shortness of breath” or “Patient with COPD, feeling improved with 3L O2 NC.”
Assessment and Plan
Accurately representing patient complexity for every visit throughout the hospitalization presents its challenges. Although the problem list may not dramatically change day to day, providers must formulate an assessment of the patient’s condition with a corresponding plan of care for each encounter. Documenting problems without a corresponding plan of care does not substantiate physician participation in the management of that problem. Providing a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) minimizes the complexity and effort put forth in the encounter and could result in auditor downgrading upon documentation review.
Developing shortcuts might falsely minimize the provider’s documentation burden. An electronic documentation system might make it possible to copy previous progress notes into the current encounter to save time; however, the previously entered information could include elements that do not require reassessment during a subsequent encounter or contain information about conditions that are being managed concurrently by another specialist (e.g. CKD being managed by the nephrologist). Leaving the copied information unmodified may not accurately reflect the patient’s current condition or the care provided by the hospitalist during the current encounter. Information that is pulled forward or copied and pasted from a previous entry should be modified to demonstrate updated content and nonoverlapping care relevant to that date.
According to the Office of Inspector General (OIG), “inappropriate copy-pasting could facilitate attempts to inflate claims and duplicate or create fraudulent claims.”4
An equally problematic EHR function involves “overdocumentation,” the practice of inserting false or irrelevant documentation to create the appearance of support for billing higher level services.4 EHR technology has the ability to auto-populate fields using templates built into the system or generate extensive documentation on the basis of a single click. The OIG cautions providers to use these features carefully, because they can produce information suggesting the practitioner performed more comprehensive services than were actually rendered.4
An example is the inclusion of the same lab results more than once. Although clinicians include this information as a reference to avoid having to “find it somewhere in the chart” when it is needed—as a basis for comparison, for example—auditors mistake this as an attempt to gain credit for the daily review of the same “old” information. Including only relevant data will mitigate this concern.
Authorship
Dates and signatures are essential to each encounter. Medicare requires services provided/ordered to be authenticated by the author.5 A reviewer must be able to identify each individual who performs, documents, and bills for a service on a given date. Progress notes that fail to identify the service date or service provider will likely result in denial.
Additionally, a service is questioned when two different sets of handwriting appear on a note, yet only one signature is provided. Since the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Notes that contain an illegible signature are equally problematic. If the legibility of the signature prevents the reviewer from correctly identifying the rendering provider, the service may be denied.
CMS has instructed Medicare contractors to request a signed provider attestation before issuing a denial.5 The provider should print his/her name beside the signature or include a separate signature sheet with the requested documentation to assist the reviewer in provider identification. Stamped signatures are not acceptable under any circumstance. Medicare accepts only handwritten or electronic signatures.5
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- HealthIT.gov. Benefits of electronic health records (EHRs). Accessed August 1, 2015.
- Social Security Administration. Exclusions from coverage and Medicare as secondary payer. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered medical and other health services. Chapter 15, Section 30.E. Concurrent care. Accessed August 1, 2015.
- Department of Health and Human Services. Office of Inspector General. CMS and its contractors have adopted few program integrity practices to address vulnerabilities in EHRs. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Signature guidelines for medical review purposes. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. 1995 documentation guidelines for evaluation and management services. Accessed August 1, 2015.
The electronic health record (EHR) has many benefits:
- Improved patient care;
- Improved care coordination;
- Improved diagnostics and patient outcomes;
- Increased patient participation; and
- Increased practice efficiencies and cost savings.1
EHRs also introduce risks, however. Heightened concern about EHR misuse and vulnerability elevates the level of scrutiny placed on provider documentation as it relates to billing and coding. Without clear guidelines from the Centers for Medicare and Medicaid Services (CMS) or other payers, the potential for unintentional misapplication exists. Auditor misinterpretation is also possible. Providers should utilize simple defensive documentation principles to support their services and minimize their risks.
Reason for Encounter
Under section 1862 (a)(1)(A) of the Social Security Act, the Medicare Program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).2
A payer can determine if a service is “reasonable and necessary” based on the service indication. The reason for the patient encounter, otherwise known as the chief complaint, must be evident. This can be a symptom, problem, condition, diagnosis, physician-recommended return, or another factor that necessitates the encounter.1 It cannot be inferred and must be clearly stated in the documentation. Without it, a payer may question the medical necessity of the service, especially if it involves hospital-based services in the course of which multiple specialists will see the patient on any given date. Payers are likely to deny services that cannot be easily differentiated (e.g. “no c/o”). Furthermore, payers can deny concurrent care services for the following reasons:3
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate/overlap those of the other provider without any recognizable distinction.
Providers should be specific in identifying the encounter reason, as in the following examples: “Patient seen for shortness of breath” or “Patient with COPD, feeling improved with 3L O2 NC.”
Assessment and Plan
Accurately representing patient complexity for every visit throughout the hospitalization presents its challenges. Although the problem list may not dramatically change day to day, providers must formulate an assessment of the patient’s condition with a corresponding plan of care for each encounter. Documenting problems without a corresponding plan of care does not substantiate physician participation in the management of that problem. Providing a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) minimizes the complexity and effort put forth in the encounter and could result in auditor downgrading upon documentation review.
Developing shortcuts might falsely minimize the provider’s documentation burden. An electronic documentation system might make it possible to copy previous progress notes into the current encounter to save time; however, the previously entered information could include elements that do not require reassessment during a subsequent encounter or contain information about conditions that are being managed concurrently by another specialist (e.g. CKD being managed by the nephrologist). Leaving the copied information unmodified may not accurately reflect the patient’s current condition or the care provided by the hospitalist during the current encounter. Information that is pulled forward or copied and pasted from a previous entry should be modified to demonstrate updated content and nonoverlapping care relevant to that date.
According to the Office of Inspector General (OIG), “inappropriate copy-pasting could facilitate attempts to inflate claims and duplicate or create fraudulent claims.”4
An equally problematic EHR function involves “overdocumentation,” the practice of inserting false or irrelevant documentation to create the appearance of support for billing higher level services.4 EHR technology has the ability to auto-populate fields using templates built into the system or generate extensive documentation on the basis of a single click. The OIG cautions providers to use these features carefully, because they can produce information suggesting the practitioner performed more comprehensive services than were actually rendered.4
An example is the inclusion of the same lab results more than once. Although clinicians include this information as a reference to avoid having to “find it somewhere in the chart” when it is needed—as a basis for comparison, for example—auditors mistake this as an attempt to gain credit for the daily review of the same “old” information. Including only relevant data will mitigate this concern.
Authorship
Dates and signatures are essential to each encounter. Medicare requires services provided/ordered to be authenticated by the author.5 A reviewer must be able to identify each individual who performs, documents, and bills for a service on a given date. Progress notes that fail to identify the service date or service provider will likely result in denial.
Additionally, a service is questioned when two different sets of handwriting appear on a note, yet only one signature is provided. Since the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Notes that contain an illegible signature are equally problematic. If the legibility of the signature prevents the reviewer from correctly identifying the rendering provider, the service may be denied.
CMS has instructed Medicare contractors to request a signed provider attestation before issuing a denial.5 The provider should print his/her name beside the signature or include a separate signature sheet with the requested documentation to assist the reviewer in provider identification. Stamped signatures are not acceptable under any circumstance. Medicare accepts only handwritten or electronic signatures.5
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- HealthIT.gov. Benefits of electronic health records (EHRs). Accessed August 1, 2015.
- Social Security Administration. Exclusions from coverage and Medicare as secondary payer. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered medical and other health services. Chapter 15, Section 30.E. Concurrent care. Accessed August 1, 2015.
- Department of Health and Human Services. Office of Inspector General. CMS and its contractors have adopted few program integrity practices to address vulnerabilities in EHRs. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Signature guidelines for medical review purposes. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. 1995 documentation guidelines for evaluation and management services. Accessed August 1, 2015.
Multistate compact could ease telemedicine licensing woes
As telemedicine hospitalists, one of the biggest challenges for Dr. Dana Giarrizzi and her staff is learning and staying updated on the many different state licensing rules.
Renewal time and dates vary, along with state requirements to become licensed and remain current, said Dr. Giarrizzi, national medical director for telehospitalist services at Eagle Hospital Physicians, based in Atlanta.
“One state renews on your birthday,” she said. Another “renews when you first activated your license. This one is every 2 years. This one requires CME. It’s hard to keep up with all the rules, and it’s costly.”
Dr. Giarrizzi believes a federal licensure process would be ideal, but she is also hopeful about state legislation in the form of the Interstate Medical Licensure Compact. The model legislation was developed by the Federation of State Medical Boards (FSMB) and aims to make it easier for telemedicine physicians to gain licenses in multiple states.
Under the legislation, physicians designate a member state as the state of principal licensure and select the other states they wish to gain licenses within. The state of principal licensure then verifies the physician’s eligibility and provides credential information to the interstate commission, which collects applicable fees and transmits the doctor’s information to the other states. Upon receipt in the additional states, the physician would be granted a license.
As of early October 2015, 11 states had enacted the compact legislation, and at least 19 states had introduced the legislation. In July, the Health Resources and Services Administration awarded the FSMB a grant to support establishment of the commission and aid with the compact’s infrastructure.
Broad support by medical associations, patients, and state leaders have quickly propelled the compact forward, said Lisa Robin, FSMB chief advocacy officer.
“I think the boards recognize the potential for telemedicine and what that can bring as far as access to health care,” Ms. Robin said. “As technologies are here – and it’s changing every day – this is a mechanism that will allow for much more efficiency and less administrative burden on the process for licensure for physicians who want to practice in multiple states.”
There have been several misconceptions tied to the compact law, Ms. Robin noted.
The compact does not change a state’s medical practice act, she stressed, nor does it create a national licensure system. In addition, the legislation does not require a physician to participate in maintenance of certification at any stage. Under the compact, approved physicians would be under the jurisdiction of the state medical board in which the patient is located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight.
The compact hopefully will reduce physicians’ frustrations and lessen administrative hassles for doctors who wish to use telehealth technologies to bring their expertise to patients across multiple states, said Dr. Reed V. Tuckson, president of the American Telemedicine Association.
“There have been several models proposed to address both of these objectives, and it appears that the Federation of State Medical Boards’ licensure model compact has emerged as the most practical and implementable of the various approaches,” Dr. Tuckson explained. “We do hope that this compact model can function efficiently and cost effectively, so that physicians are not overburdened as well-meaning organizations attempt to ensure that the public’s interests are safeguarded.”
Dr. Giarrizzi of Eagle Hospital Physicians is also optimistic about the compact.
“I am hoping this helps streamline the information,” she said. “I know it will still take time, because it is not taking away the need to go through the process, but seems more like it is just sharing the information. It will make it easier for us to cross state lines if the states we want to work in agree with this process and participate.”
On Twitter @legal_med
As telemedicine hospitalists, one of the biggest challenges for Dr. Dana Giarrizzi and her staff is learning and staying updated on the many different state licensing rules.
Renewal time and dates vary, along with state requirements to become licensed and remain current, said Dr. Giarrizzi, national medical director for telehospitalist services at Eagle Hospital Physicians, based in Atlanta.
“One state renews on your birthday,” she said. Another “renews when you first activated your license. This one is every 2 years. This one requires CME. It’s hard to keep up with all the rules, and it’s costly.”
Dr. Giarrizzi believes a federal licensure process would be ideal, but she is also hopeful about state legislation in the form of the Interstate Medical Licensure Compact. The model legislation was developed by the Federation of State Medical Boards (FSMB) and aims to make it easier for telemedicine physicians to gain licenses in multiple states.
Under the legislation, physicians designate a member state as the state of principal licensure and select the other states they wish to gain licenses within. The state of principal licensure then verifies the physician’s eligibility and provides credential information to the interstate commission, which collects applicable fees and transmits the doctor’s information to the other states. Upon receipt in the additional states, the physician would be granted a license.
As of early October 2015, 11 states had enacted the compact legislation, and at least 19 states had introduced the legislation. In July, the Health Resources and Services Administration awarded the FSMB a grant to support establishment of the commission and aid with the compact’s infrastructure.
Broad support by medical associations, patients, and state leaders have quickly propelled the compact forward, said Lisa Robin, FSMB chief advocacy officer.
“I think the boards recognize the potential for telemedicine and what that can bring as far as access to health care,” Ms. Robin said. “As technologies are here – and it’s changing every day – this is a mechanism that will allow for much more efficiency and less administrative burden on the process for licensure for physicians who want to practice in multiple states.”
There have been several misconceptions tied to the compact law, Ms. Robin noted.
The compact does not change a state’s medical practice act, she stressed, nor does it create a national licensure system. In addition, the legislation does not require a physician to participate in maintenance of certification at any stage. Under the compact, approved physicians would be under the jurisdiction of the state medical board in which the patient is located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight.
The compact hopefully will reduce physicians’ frustrations and lessen administrative hassles for doctors who wish to use telehealth technologies to bring their expertise to patients across multiple states, said Dr. Reed V. Tuckson, president of the American Telemedicine Association.
“There have been several models proposed to address both of these objectives, and it appears that the Federation of State Medical Boards’ licensure model compact has emerged as the most practical and implementable of the various approaches,” Dr. Tuckson explained. “We do hope that this compact model can function efficiently and cost effectively, so that physicians are not overburdened as well-meaning organizations attempt to ensure that the public’s interests are safeguarded.”
Dr. Giarrizzi of Eagle Hospital Physicians is also optimistic about the compact.
“I am hoping this helps streamline the information,” she said. “I know it will still take time, because it is not taking away the need to go through the process, but seems more like it is just sharing the information. It will make it easier for us to cross state lines if the states we want to work in agree with this process and participate.”
On Twitter @legal_med
As telemedicine hospitalists, one of the biggest challenges for Dr. Dana Giarrizzi and her staff is learning and staying updated on the many different state licensing rules.
Renewal time and dates vary, along with state requirements to become licensed and remain current, said Dr. Giarrizzi, national medical director for telehospitalist services at Eagle Hospital Physicians, based in Atlanta.
“One state renews on your birthday,” she said. Another “renews when you first activated your license. This one is every 2 years. This one requires CME. It’s hard to keep up with all the rules, and it’s costly.”
Dr. Giarrizzi believes a federal licensure process would be ideal, but she is also hopeful about state legislation in the form of the Interstate Medical Licensure Compact. The model legislation was developed by the Federation of State Medical Boards (FSMB) and aims to make it easier for telemedicine physicians to gain licenses in multiple states.
Under the legislation, physicians designate a member state as the state of principal licensure and select the other states they wish to gain licenses within. The state of principal licensure then verifies the physician’s eligibility and provides credential information to the interstate commission, which collects applicable fees and transmits the doctor’s information to the other states. Upon receipt in the additional states, the physician would be granted a license.
As of early October 2015, 11 states had enacted the compact legislation, and at least 19 states had introduced the legislation. In July, the Health Resources and Services Administration awarded the FSMB a grant to support establishment of the commission and aid with the compact’s infrastructure.
Broad support by medical associations, patients, and state leaders have quickly propelled the compact forward, said Lisa Robin, FSMB chief advocacy officer.
“I think the boards recognize the potential for telemedicine and what that can bring as far as access to health care,” Ms. Robin said. “As technologies are here – and it’s changing every day – this is a mechanism that will allow for much more efficiency and less administrative burden on the process for licensure for physicians who want to practice in multiple states.”
There have been several misconceptions tied to the compact law, Ms. Robin noted.
The compact does not change a state’s medical practice act, she stressed, nor does it create a national licensure system. In addition, the legislation does not require a physician to participate in maintenance of certification at any stage. Under the compact, approved physicians would be under the jurisdiction of the state medical board in which the patient is located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight.
The compact hopefully will reduce physicians’ frustrations and lessen administrative hassles for doctors who wish to use telehealth technologies to bring their expertise to patients across multiple states, said Dr. Reed V. Tuckson, president of the American Telemedicine Association.
“There have been several models proposed to address both of these objectives, and it appears that the Federation of State Medical Boards’ licensure model compact has emerged as the most practical and implementable of the various approaches,” Dr. Tuckson explained. “We do hope that this compact model can function efficiently and cost effectively, so that physicians are not overburdened as well-meaning organizations attempt to ensure that the public’s interests are safeguarded.”
Dr. Giarrizzi of Eagle Hospital Physicians is also optimistic about the compact.
“I am hoping this helps streamline the information,” she said. “I know it will still take time, because it is not taking away the need to go through the process, but seems more like it is just sharing the information. It will make it easier for us to cross state lines if the states we want to work in agree with this process and participate.”
On Twitter @legal_med
Telemedicine poses novel legal risks for doctors
Physicians who practice telemedicine have a lot to consider, including state laws, payment issues, and licensing regulations. But one overlooked area may pose the greatest risk of all: medical liability.
As the practice of telemedicine continues to grow, so do the legal risks associated with virtual care, said Dr. Joseph P. McMenamin, an emergency physician and health law defense attorney based in Richmond, Va.
“With good reason, there is a concern that as this form of care expands, claims against physicians will increase,” Dr. McMenamin said. “That’s almost inevitable, given how our society looks at litigation and how willing we are to sue our doctors. If you’re a plaintiffs’ attorney, you might be attracted to cases of this kind – partly because jurors may fear the unknown, and they may view [telemedicine] with some concern and suspicion.”
Telemedicine can fuel a wide spectrum of legal dangers, including malpractice, product liability claims, data exposure, and credentialing risks. Making matters more complicated: No uniform standard of care exists for telemedicine when it comes to medical malpractice, said René Y. Quashie, a Washington health law attorney who specializes in telemedicine and e-health practices.
“There are a lot of unanswered questions, including the prevailing standard of care,” Mr. Quashie explained. “Can we use the standard of care that we use for services provided in person for telehealth consults? Informed consent – does that process need to change? There are a lot of unanswered issues, which can only be resolved after a number of cases” are decided in the courts.
Physicians who practice telemedicine should consider legal risks associated with patient and staff privacy, inaccuracies in self-reporting, and symptoms that are more accurately diagnosed in person, said Richard F. Cahill, vice president and associate general counsel for the Doctors Company, a national medical liability insurer.
During 2007-2014, the Doctors Company had 11 claims that closed related to telemedicine, according to data provided by Mr. Cahill.
The majority of claims resulted from the remote reading of x-rays and other films by health providers, usually from home, and the remote reading of fetal monitor strips by physicians when outside of the hospital. Two of the cases were associated with attempts to diagnose a patient via telemedicine. Of the claims, six were diagnosis related, two alleged delay in treatment, two were related to improper performance of treatment, and one was associated with failure to order medication.
“The challenges of remote communications made it difficult to formulate the correct diagnosis due to limitations of radiology resolution, delayed readings of radiographs, or limits on fetal monitor strips,” said Darrell Ranum, vice president of patient safety and risk management for the Doctors Company. “Delays in treatment were closely related to delayed diagnosis. Radiologists did not receive a request for an interpretation, or they did not know that it was an emergency, so they did not provide a rapid turnaround report.”
While telemedicine claims have been low so far, a rise in the number of patient contacts, regardless of modality, may increase the risk of adverse consequences, Mr. Cahill cautioned.
“Because telemedicine is relatively new, and it takes 3-4 years for a claim to work its way through the system, we may see more cases in the future in which telemedicine is a factor,” he predicted.
Other lawsuits could arise from claims that physicians had access to telemedicine but failed to use the technology to properly treat a patient, Mr. Quashie said. Product liability claims also pose a threat, added Dr. McMenamin, who is part of the Legal Resource Team at the Robert J. Waters Center for Telehealth & e-Health Law (CTeL). Such accusations stem from equipment that malfunctioned or failed to work as indicated.
Varying credentialing rules also can trip up doctors who work virtually. Physicians at a large academic medical center, for example, could face trouble if they aren’t credentialed at the small rural hospital where a patient is located, Dr. McMenamin said. He noted that Medicare modified its telemedicine encounter rules several years ago, making it possible for rural hospitals to accept the credentialing process of the health center where the specialist is located. However, other criteria must be met for the telehealth encounter to occur.
Differing credentialing processes are challenging for doctors who practice telehealth, agreed telemedicine hospitalist Dr. Dana Giarrizzi of Eagle Hospital Physicians in Atlanta, which provides hospitalist services to hospitals and health systems nationwide via telehealth.
“The credentialing is certainly difficult at times,” Dr. Giarrizzi said. “It is a long process and sometimes requires fingerprints, taking exams, and other involved steps. It is very time consuming, and each state and certainly [each] facility can have different criteria, which makes it hard to know.”
To ensure its doctors are meeting the requirements of each facility, Eagle Hospital Physicians has its own credentialing department that works with hospitals to learn their processes and verify its physicians adhere to the rules, Dr. Giarrizzi said.
Preventing telemedicine lawsuits
To mitigate potential risks of telemedicine, doctors should clearly define protocols for use of webcams and Web-based portals and ensure such systems are secure, Mr. Cahill said. Take time to learn what constitutes the practice of medicine in each state in which doctors are delivering care, and carefully adhere to those rules, he added. Physicians also should have mechanisms in place to protect the privacy of individuals who do not want to be seen on camera, such as staff or family members.
It’s also critical to confer with malpractice insurance providers to confirm that telehealth services are covered, said Mr. Quashie, a member of the Legal Resource Team at CTeL. If telemedicine is not covered, physicians may want to buy a separate policy from another company that covers telehealth.
If physicians opt to work for a larger telemedicine company, they should check what controls the company has in place to protect them from lawsuits.
For example, national telemedicine company Teladoc has numerous safeguards in place to promote quality care and protect its doctors from claims, said Dr. Henry DePhillips, Teladoc’s chief medical officer. The company has National Committee for Quality Assurance certification, along with proprietary, evidence-based clinical practice guidelines for its physicians, a peer-review quality assurance committee, and regular data and medical reviews, Dr. DePhillips said. Teladoc is close to surpassing its 1-millionth consult and has not had a single claim filed in its history, he added.
Dr. DePhillips stressed that telemedicine is not a separate practice of medicine, and that best practices should remain the same, no matter the location.
“The bottom line is the standard of care for the diagnosis and treatment of these medical problems is the standard of care regardless whether you’re seeing the person in person, in an urgent care center, or through a secure video,” Dr. DePhillips said. “The doctor has to be able to comply with the standard of care and make a decision [about] whether that setting and that equipment at his or her disposal are adequate to make an accurate diagnosis and a medically appropriate treatment plan.”
On Twitter @legal_med
Physicians who practice telemedicine have a lot to consider, including state laws, payment issues, and licensing regulations. But one overlooked area may pose the greatest risk of all: medical liability.
As the practice of telemedicine continues to grow, so do the legal risks associated with virtual care, said Dr. Joseph P. McMenamin, an emergency physician and health law defense attorney based in Richmond, Va.
“With good reason, there is a concern that as this form of care expands, claims against physicians will increase,” Dr. McMenamin said. “That’s almost inevitable, given how our society looks at litigation and how willing we are to sue our doctors. If you’re a plaintiffs’ attorney, you might be attracted to cases of this kind – partly because jurors may fear the unknown, and they may view [telemedicine] with some concern and suspicion.”
Telemedicine can fuel a wide spectrum of legal dangers, including malpractice, product liability claims, data exposure, and credentialing risks. Making matters more complicated: No uniform standard of care exists for telemedicine when it comes to medical malpractice, said René Y. Quashie, a Washington health law attorney who specializes in telemedicine and e-health practices.
“There are a lot of unanswered questions, including the prevailing standard of care,” Mr. Quashie explained. “Can we use the standard of care that we use for services provided in person for telehealth consults? Informed consent – does that process need to change? There are a lot of unanswered issues, which can only be resolved after a number of cases” are decided in the courts.
Physicians who practice telemedicine should consider legal risks associated with patient and staff privacy, inaccuracies in self-reporting, and symptoms that are more accurately diagnosed in person, said Richard F. Cahill, vice president and associate general counsel for the Doctors Company, a national medical liability insurer.
During 2007-2014, the Doctors Company had 11 claims that closed related to telemedicine, according to data provided by Mr. Cahill.
The majority of claims resulted from the remote reading of x-rays and other films by health providers, usually from home, and the remote reading of fetal monitor strips by physicians when outside of the hospital. Two of the cases were associated with attempts to diagnose a patient via telemedicine. Of the claims, six were diagnosis related, two alleged delay in treatment, two were related to improper performance of treatment, and one was associated with failure to order medication.
“The challenges of remote communications made it difficult to formulate the correct diagnosis due to limitations of radiology resolution, delayed readings of radiographs, or limits on fetal monitor strips,” said Darrell Ranum, vice president of patient safety and risk management for the Doctors Company. “Delays in treatment were closely related to delayed diagnosis. Radiologists did not receive a request for an interpretation, or they did not know that it was an emergency, so they did not provide a rapid turnaround report.”
While telemedicine claims have been low so far, a rise in the number of patient contacts, regardless of modality, may increase the risk of adverse consequences, Mr. Cahill cautioned.
“Because telemedicine is relatively new, and it takes 3-4 years for a claim to work its way through the system, we may see more cases in the future in which telemedicine is a factor,” he predicted.
Other lawsuits could arise from claims that physicians had access to telemedicine but failed to use the technology to properly treat a patient, Mr. Quashie said. Product liability claims also pose a threat, added Dr. McMenamin, who is part of the Legal Resource Team at the Robert J. Waters Center for Telehealth & e-Health Law (CTeL). Such accusations stem from equipment that malfunctioned or failed to work as indicated.
Varying credentialing rules also can trip up doctors who work virtually. Physicians at a large academic medical center, for example, could face trouble if they aren’t credentialed at the small rural hospital where a patient is located, Dr. McMenamin said. He noted that Medicare modified its telemedicine encounter rules several years ago, making it possible for rural hospitals to accept the credentialing process of the health center where the specialist is located. However, other criteria must be met for the telehealth encounter to occur.
Differing credentialing processes are challenging for doctors who practice telehealth, agreed telemedicine hospitalist Dr. Dana Giarrizzi of Eagle Hospital Physicians in Atlanta, which provides hospitalist services to hospitals and health systems nationwide via telehealth.
“The credentialing is certainly difficult at times,” Dr. Giarrizzi said. “It is a long process and sometimes requires fingerprints, taking exams, and other involved steps. It is very time consuming, and each state and certainly [each] facility can have different criteria, which makes it hard to know.”
To ensure its doctors are meeting the requirements of each facility, Eagle Hospital Physicians has its own credentialing department that works with hospitals to learn their processes and verify its physicians adhere to the rules, Dr. Giarrizzi said.
Preventing telemedicine lawsuits
To mitigate potential risks of telemedicine, doctors should clearly define protocols for use of webcams and Web-based portals and ensure such systems are secure, Mr. Cahill said. Take time to learn what constitutes the practice of medicine in each state in which doctors are delivering care, and carefully adhere to those rules, he added. Physicians also should have mechanisms in place to protect the privacy of individuals who do not want to be seen on camera, such as staff or family members.
It’s also critical to confer with malpractice insurance providers to confirm that telehealth services are covered, said Mr. Quashie, a member of the Legal Resource Team at CTeL. If telemedicine is not covered, physicians may want to buy a separate policy from another company that covers telehealth.
If physicians opt to work for a larger telemedicine company, they should check what controls the company has in place to protect them from lawsuits.
For example, national telemedicine company Teladoc has numerous safeguards in place to promote quality care and protect its doctors from claims, said Dr. Henry DePhillips, Teladoc’s chief medical officer. The company has National Committee for Quality Assurance certification, along with proprietary, evidence-based clinical practice guidelines for its physicians, a peer-review quality assurance committee, and regular data and medical reviews, Dr. DePhillips said. Teladoc is close to surpassing its 1-millionth consult and has not had a single claim filed in its history, he added.
Dr. DePhillips stressed that telemedicine is not a separate practice of medicine, and that best practices should remain the same, no matter the location.
“The bottom line is the standard of care for the diagnosis and treatment of these medical problems is the standard of care regardless whether you’re seeing the person in person, in an urgent care center, or through a secure video,” Dr. DePhillips said. “The doctor has to be able to comply with the standard of care and make a decision [about] whether that setting and that equipment at his or her disposal are adequate to make an accurate diagnosis and a medically appropriate treatment plan.”
On Twitter @legal_med
Physicians who practice telemedicine have a lot to consider, including state laws, payment issues, and licensing regulations. But one overlooked area may pose the greatest risk of all: medical liability.
As the practice of telemedicine continues to grow, so do the legal risks associated with virtual care, said Dr. Joseph P. McMenamin, an emergency physician and health law defense attorney based in Richmond, Va.
“With good reason, there is a concern that as this form of care expands, claims against physicians will increase,” Dr. McMenamin said. “That’s almost inevitable, given how our society looks at litigation and how willing we are to sue our doctors. If you’re a plaintiffs’ attorney, you might be attracted to cases of this kind – partly because jurors may fear the unknown, and they may view [telemedicine] with some concern and suspicion.”
Telemedicine can fuel a wide spectrum of legal dangers, including malpractice, product liability claims, data exposure, and credentialing risks. Making matters more complicated: No uniform standard of care exists for telemedicine when it comes to medical malpractice, said René Y. Quashie, a Washington health law attorney who specializes in telemedicine and e-health practices.
“There are a lot of unanswered questions, including the prevailing standard of care,” Mr. Quashie explained. “Can we use the standard of care that we use for services provided in person for telehealth consults? Informed consent – does that process need to change? There are a lot of unanswered issues, which can only be resolved after a number of cases” are decided in the courts.
Physicians who practice telemedicine should consider legal risks associated with patient and staff privacy, inaccuracies in self-reporting, and symptoms that are more accurately diagnosed in person, said Richard F. Cahill, vice president and associate general counsel for the Doctors Company, a national medical liability insurer.
During 2007-2014, the Doctors Company had 11 claims that closed related to telemedicine, according to data provided by Mr. Cahill.
The majority of claims resulted from the remote reading of x-rays and other films by health providers, usually from home, and the remote reading of fetal monitor strips by physicians when outside of the hospital. Two of the cases were associated with attempts to diagnose a patient via telemedicine. Of the claims, six were diagnosis related, two alleged delay in treatment, two were related to improper performance of treatment, and one was associated with failure to order medication.
“The challenges of remote communications made it difficult to formulate the correct diagnosis due to limitations of radiology resolution, delayed readings of radiographs, or limits on fetal monitor strips,” said Darrell Ranum, vice president of patient safety and risk management for the Doctors Company. “Delays in treatment were closely related to delayed diagnosis. Radiologists did not receive a request for an interpretation, or they did not know that it was an emergency, so they did not provide a rapid turnaround report.”
While telemedicine claims have been low so far, a rise in the number of patient contacts, regardless of modality, may increase the risk of adverse consequences, Mr. Cahill cautioned.
“Because telemedicine is relatively new, and it takes 3-4 years for a claim to work its way through the system, we may see more cases in the future in which telemedicine is a factor,” he predicted.
Other lawsuits could arise from claims that physicians had access to telemedicine but failed to use the technology to properly treat a patient, Mr. Quashie said. Product liability claims also pose a threat, added Dr. McMenamin, who is part of the Legal Resource Team at the Robert J. Waters Center for Telehealth & e-Health Law (CTeL). Such accusations stem from equipment that malfunctioned or failed to work as indicated.
Varying credentialing rules also can trip up doctors who work virtually. Physicians at a large academic medical center, for example, could face trouble if they aren’t credentialed at the small rural hospital where a patient is located, Dr. McMenamin said. He noted that Medicare modified its telemedicine encounter rules several years ago, making it possible for rural hospitals to accept the credentialing process of the health center where the specialist is located. However, other criteria must be met for the telehealth encounter to occur.
Differing credentialing processes are challenging for doctors who practice telehealth, agreed telemedicine hospitalist Dr. Dana Giarrizzi of Eagle Hospital Physicians in Atlanta, which provides hospitalist services to hospitals and health systems nationwide via telehealth.
“The credentialing is certainly difficult at times,” Dr. Giarrizzi said. “It is a long process and sometimes requires fingerprints, taking exams, and other involved steps. It is very time consuming, and each state and certainly [each] facility can have different criteria, which makes it hard to know.”
To ensure its doctors are meeting the requirements of each facility, Eagle Hospital Physicians has its own credentialing department that works with hospitals to learn their processes and verify its physicians adhere to the rules, Dr. Giarrizzi said.
Preventing telemedicine lawsuits
To mitigate potential risks of telemedicine, doctors should clearly define protocols for use of webcams and Web-based portals and ensure such systems are secure, Mr. Cahill said. Take time to learn what constitutes the practice of medicine in each state in which doctors are delivering care, and carefully adhere to those rules, he added. Physicians also should have mechanisms in place to protect the privacy of individuals who do not want to be seen on camera, such as staff or family members.
It’s also critical to confer with malpractice insurance providers to confirm that telehealth services are covered, said Mr. Quashie, a member of the Legal Resource Team at CTeL. If telemedicine is not covered, physicians may want to buy a separate policy from another company that covers telehealth.
If physicians opt to work for a larger telemedicine company, they should check what controls the company has in place to protect them from lawsuits.
For example, national telemedicine company Teladoc has numerous safeguards in place to promote quality care and protect its doctors from claims, said Dr. Henry DePhillips, Teladoc’s chief medical officer. The company has National Committee for Quality Assurance certification, along with proprietary, evidence-based clinical practice guidelines for its physicians, a peer-review quality assurance committee, and regular data and medical reviews, Dr. DePhillips said. Teladoc is close to surpassing its 1-millionth consult and has not had a single claim filed in its history, he added.
Dr. DePhillips stressed that telemedicine is not a separate practice of medicine, and that best practices should remain the same, no matter the location.
“The bottom line is the standard of care for the diagnosis and treatment of these medical problems is the standard of care regardless whether you’re seeing the person in person, in an urgent care center, or through a secure video,” Dr. DePhillips said. “The doctor has to be able to comply with the standard of care and make a decision [about] whether that setting and that equipment at his or her disposal are adequate to make an accurate diagnosis and a medically appropriate treatment plan.”
On Twitter @legal_med
GAO: Physicians, hospitals struggle to achieve EHR interoperability
Physicians and health care organizations are struggling to achieve interoperability, the exchange of data between their electronic health records systems, according to a U.S. Government Accountability Office report.
The report comes as more federal lawmakers press the Obama administration to slow the start of the third stage of Meaningful Use requirements for EHRs.
The GAO interviewed 18 private companies working to enhance the interoperability of electronic health records at the request of Sen. Lamar Alexander (R-Tenn.), chair of the Senate Committee on Health, Education, Labor & Pensions.
In its report, the GAO found five key challenges that are preventing EHR interoperability:
• Insufficiencies in standards for EHR interoperability.
• Variations in states’ privacy rules.
• Difficulties in accurately matching patients’ health records.
• The costs associated with interoperability.
• A need for governance and trust among the providers and organizations using EHRs.
Many of the organizations surveyed said that the Meaningful Use requirements, passed as part of the 2009 federal stimulus and being implemented in stages, focus more on rules than on the criteria necessary to test the various systems’ ability to interoperate.
Three of the industry representatives surveyed suggested that the Obama administration should at least amend the EHR incentives law to focus on testing systems’ interoperability, while five others called for suspending or scrapping the law altogether.
“We are glad to see the GAO shining a light on the problem,” Dan Haley, Athena Health senior vice president and general counsel, said in an interview. Athena Health was not among those surveyed for the report.
“Nobody who lives and works in the 21st century can possibly dispute the proposition that information technology has the potential to vastly improve the quality and efficiency of health care delivery,” Mr. Haley noted. “Unfortunately, the Meaningful Use program, while well intentioned, has become burdened by granular requirements that impede rather than enhance care providers’ ability to maximize that potential, and do nothing to improve the interoperability of disparate technology platforms.”
Meanwhile, 116 members of the U.S. House of Representatives have signed a letter addressed to both Office of Management and Budget Director Shaun Donovan and U.S. Department of Health & Human Services Secretary Sylvia M. Burwell, asking them to delay the third stage of the law’s implementation until there’s a clearer picture of what metrics will be in the recently passed Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), which have just opened up for public comment.
“It’s time that we focus on interoperability instead of rulemaking to ensure that these products work for our nation’s providers,” Rep. Renee Ellmers (R-N.C.) said in a statement. “If the administration dives into Stage 3 prematurely, we only stand to aggravate providers and vendors who have already experienced ample challenges in meeting attestation deadlines.”
The Centers for Medicare & Medicaid Services sent the final rule for Stage 3 of Meaningful Use to the Office of Management and Budget in September. The next stage is set to take effect in 2017.
On Twitter @whitneymcknight
Physicians and health care organizations are struggling to achieve interoperability, the exchange of data between their electronic health records systems, according to a U.S. Government Accountability Office report.
The report comes as more federal lawmakers press the Obama administration to slow the start of the third stage of Meaningful Use requirements for EHRs.
The GAO interviewed 18 private companies working to enhance the interoperability of electronic health records at the request of Sen. Lamar Alexander (R-Tenn.), chair of the Senate Committee on Health, Education, Labor & Pensions.
In its report, the GAO found five key challenges that are preventing EHR interoperability:
• Insufficiencies in standards for EHR interoperability.
• Variations in states’ privacy rules.
• Difficulties in accurately matching patients’ health records.
• The costs associated with interoperability.
• A need for governance and trust among the providers and organizations using EHRs.
Many of the organizations surveyed said that the Meaningful Use requirements, passed as part of the 2009 federal stimulus and being implemented in stages, focus more on rules than on the criteria necessary to test the various systems’ ability to interoperate.
Three of the industry representatives surveyed suggested that the Obama administration should at least amend the EHR incentives law to focus on testing systems’ interoperability, while five others called for suspending or scrapping the law altogether.
“We are glad to see the GAO shining a light on the problem,” Dan Haley, Athena Health senior vice president and general counsel, said in an interview. Athena Health was not among those surveyed for the report.
“Nobody who lives and works in the 21st century can possibly dispute the proposition that information technology has the potential to vastly improve the quality and efficiency of health care delivery,” Mr. Haley noted. “Unfortunately, the Meaningful Use program, while well intentioned, has become burdened by granular requirements that impede rather than enhance care providers’ ability to maximize that potential, and do nothing to improve the interoperability of disparate technology platforms.”
Meanwhile, 116 members of the U.S. House of Representatives have signed a letter addressed to both Office of Management and Budget Director Shaun Donovan and U.S. Department of Health & Human Services Secretary Sylvia M. Burwell, asking them to delay the third stage of the law’s implementation until there’s a clearer picture of what metrics will be in the recently passed Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), which have just opened up for public comment.
“It’s time that we focus on interoperability instead of rulemaking to ensure that these products work for our nation’s providers,” Rep. Renee Ellmers (R-N.C.) said in a statement. “If the administration dives into Stage 3 prematurely, we only stand to aggravate providers and vendors who have already experienced ample challenges in meeting attestation deadlines.”
The Centers for Medicare & Medicaid Services sent the final rule for Stage 3 of Meaningful Use to the Office of Management and Budget in September. The next stage is set to take effect in 2017.
On Twitter @whitneymcknight
Physicians and health care organizations are struggling to achieve interoperability, the exchange of data between their electronic health records systems, according to a U.S. Government Accountability Office report.
The report comes as more federal lawmakers press the Obama administration to slow the start of the third stage of Meaningful Use requirements for EHRs.
The GAO interviewed 18 private companies working to enhance the interoperability of electronic health records at the request of Sen. Lamar Alexander (R-Tenn.), chair of the Senate Committee on Health, Education, Labor & Pensions.
In its report, the GAO found five key challenges that are preventing EHR interoperability:
• Insufficiencies in standards for EHR interoperability.
• Variations in states’ privacy rules.
• Difficulties in accurately matching patients’ health records.
• The costs associated with interoperability.
• A need for governance and trust among the providers and organizations using EHRs.
Many of the organizations surveyed said that the Meaningful Use requirements, passed as part of the 2009 federal stimulus and being implemented in stages, focus more on rules than on the criteria necessary to test the various systems’ ability to interoperate.
Three of the industry representatives surveyed suggested that the Obama administration should at least amend the EHR incentives law to focus on testing systems’ interoperability, while five others called for suspending or scrapping the law altogether.
“We are glad to see the GAO shining a light on the problem,” Dan Haley, Athena Health senior vice president and general counsel, said in an interview. Athena Health was not among those surveyed for the report.
“Nobody who lives and works in the 21st century can possibly dispute the proposition that information technology has the potential to vastly improve the quality and efficiency of health care delivery,” Mr. Haley noted. “Unfortunately, the Meaningful Use program, while well intentioned, has become burdened by granular requirements that impede rather than enhance care providers’ ability to maximize that potential, and do nothing to improve the interoperability of disparate technology platforms.”
Meanwhile, 116 members of the U.S. House of Representatives have signed a letter addressed to both Office of Management and Budget Director Shaun Donovan and U.S. Department of Health & Human Services Secretary Sylvia M. Burwell, asking them to delay the third stage of the law’s implementation until there’s a clearer picture of what metrics will be in the recently passed Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), which have just opened up for public comment.
“It’s time that we focus on interoperability instead of rulemaking to ensure that these products work for our nation’s providers,” Rep. Renee Ellmers (R-N.C.) said in a statement. “If the administration dives into Stage 3 prematurely, we only stand to aggravate providers and vendors who have already experienced ample challenges in meeting attestation deadlines.”
The Centers for Medicare & Medicaid Services sent the final rule for Stage 3 of Meaningful Use to the Office of Management and Budget in September. The next stage is set to take effect in 2017.
On Twitter @whitneymcknight
Hospital Groups Might Do Better Without Daytime Admission Shifts, Morning Meetings
You shouldn’t maintain things that do not deliver the value you anticipated when you first put them in place. For example, I thought Netflix streaming would be terrific, but I have used it so infrequently that it probably costs me $50 per movie or show watched. I should probably dump it.
Your hospitalist group might have some operational practices that are not as valuable as they seem and could be replaced with something better. For many groups, this might include doing away with a separate daytime admitter shift and a morning meeting to distribute the overnight admissions.
Daytime Admission Shift
My experience is that hospitalist groups with more than about five daytime doctors almost always have a day-shift person dedicated to seeing new admissions. In most cases, this procedure is implemented with the idea of reducing the stress of other day-shift doctors, who don’t have to interrupt rounds to admit a new patient. Some see a dedicated admitter as a tool to improve ED throughput, because this doctor isn’t tied up with rounds and can immediately start seeing a new admission.
I think an admitter shift does deliver both of these benefits, but its costs make it suboptimal in most settings. For example, a single admitter will impede ED throughput any time more than one new admission is waiting to be seen, and for most groups that will be much of the day. In fact, improved ED throughput is best achieved by having many hospitalists available for admissions, not just a single admitter. (There are many other factors influencing ED throughput, such as whether ED doctors simply send patients to their “floor” bed prior to being seen by a hospitalist. But for this article, I’m just considering the influence of a dedicated admitter.)
I think “silo-ing” work into different roles, such as separating rounding and admitting, makes it more difficult to ensure that each is always working productively. There are likely to be times when the admitter has little or nothing to do, even though the rounders are very busy. Or perhaps the rounders aren’t very busy, but the admitter has just been asked to admit four ED patients at the same time.
While protecting rounders from the stress of admissions is valuable, it comes at the cost of a net increase in hospitalist work, because a new doctor must get to know the patient on the day following admission. And this admitter-to-rounder handoff serves as another opportunity for errors—and probably lowers patient satisfaction.
I think most groups should consider moving the admitter shift into an additional rounder position, dividing admissions across all of the doctors working during the daytime. For example, a group that has six rounders and a separate admitter would change to seven rounders, each available to admit every seventh daytime admission. Each would bear the meaningful stress of having rounds interrupted to admit a new patient, but accepting every seventh daytime admission shouldn’t be too difficult on most days.
Don’t forget that eliminating the admitter means that the list of new patients you take on each morning will be shorter. Mornings may be a little less stressful.
A.M. Distribution
The daytime doctors at many hospitalist groups meet each morning to discuss how the new admissions from the prior night (or even the last 24 hours) will be distributed. Or perhaps one person, sometimes a nurse or clerical staff, arrives very early each day to do this.
Although it might take some careful planning, I think most groups that use this sort of morning distribution should abandon it for a better system. Consider a group in which all six daytime doctors spend an average of 20 minutes distributing patients each morning. Twenty minutes (0.33 hours) times six doctors times 365 days comes to 730 hours annually.
Assuming these doctors are compensated at typical rates, the practice is spending more than $100,000 annually just so the doctors can distribute patients each morning. On top of this, nurses and others at the hospital are usually delayed in learning which daytime hospitalist is caring for each patient. These costs seem unreasonably high.
An alternative is to develop a system by which any admitter, such as a night doctor, who will not be providing subsequent care to a patient can identify by name the doctor who will be providing that care. During the admission encounter, the admitter can tell patient/family, “Dr. Boswell will be taking over your care starting tomorrow. He’s a great guy and has been named one of Portland’s best doctors.” This seems so much better than saying, “One of my partners will be taking over tomorrow. I don’t know which of my partners it will be, but they’re all good doctors.” And Dr. Boswell’s name can be entered into the attending physician field of the EHR so that all hospital staff will know without delay.
MedAptus has recently launched software they call “Assign” that may be able to replace the morning meeting and automate assigning new admissions to each hospitalist. I haven’t seen it in operation, so I can’t speak for its effectiveness, but it might be worthwhile for some groups.
Practical Considerations
The changes I’ve described above might not be optimal for every group, and they may take meaningful work to implement. But I don’t think the difficulty of these things is the biggest barrier. The biggest barrier is probably just inertia in most cases, the same reason I’m still a Netflix streaming subscriber even though I almost never watch it. I did, however, really enjoy the Nexflix original series Lilyhammer.

You shouldn’t maintain things that do not deliver the value you anticipated when you first put them in place. For example, I thought Netflix streaming would be terrific, but I have used it so infrequently that it probably costs me $50 per movie or show watched. I should probably dump it.
Your hospitalist group might have some operational practices that are not as valuable as they seem and could be replaced with something better. For many groups, this might include doing away with a separate daytime admitter shift and a morning meeting to distribute the overnight admissions.
Daytime Admission Shift
My experience is that hospitalist groups with more than about five daytime doctors almost always have a day-shift person dedicated to seeing new admissions. In most cases, this procedure is implemented with the idea of reducing the stress of other day-shift doctors, who don’t have to interrupt rounds to admit a new patient. Some see a dedicated admitter as a tool to improve ED throughput, because this doctor isn’t tied up with rounds and can immediately start seeing a new admission.
I think an admitter shift does deliver both of these benefits, but its costs make it suboptimal in most settings. For example, a single admitter will impede ED throughput any time more than one new admission is waiting to be seen, and for most groups that will be much of the day. In fact, improved ED throughput is best achieved by having many hospitalists available for admissions, not just a single admitter. (There are many other factors influencing ED throughput, such as whether ED doctors simply send patients to their “floor” bed prior to being seen by a hospitalist. But for this article, I’m just considering the influence of a dedicated admitter.)
I think “silo-ing” work into different roles, such as separating rounding and admitting, makes it more difficult to ensure that each is always working productively. There are likely to be times when the admitter has little or nothing to do, even though the rounders are very busy. Or perhaps the rounders aren’t very busy, but the admitter has just been asked to admit four ED patients at the same time.
While protecting rounders from the stress of admissions is valuable, it comes at the cost of a net increase in hospitalist work, because a new doctor must get to know the patient on the day following admission. And this admitter-to-rounder handoff serves as another opportunity for errors—and probably lowers patient satisfaction.
I think most groups should consider moving the admitter shift into an additional rounder position, dividing admissions across all of the doctors working during the daytime. For example, a group that has six rounders and a separate admitter would change to seven rounders, each available to admit every seventh daytime admission. Each would bear the meaningful stress of having rounds interrupted to admit a new patient, but accepting every seventh daytime admission shouldn’t be too difficult on most days.
Don’t forget that eliminating the admitter means that the list of new patients you take on each morning will be shorter. Mornings may be a little less stressful.
A.M. Distribution
The daytime doctors at many hospitalist groups meet each morning to discuss how the new admissions from the prior night (or even the last 24 hours) will be distributed. Or perhaps one person, sometimes a nurse or clerical staff, arrives very early each day to do this.
Although it might take some careful planning, I think most groups that use this sort of morning distribution should abandon it for a better system. Consider a group in which all six daytime doctors spend an average of 20 minutes distributing patients each morning. Twenty minutes (0.33 hours) times six doctors times 365 days comes to 730 hours annually.
Assuming these doctors are compensated at typical rates, the practice is spending more than $100,000 annually just so the doctors can distribute patients each morning. On top of this, nurses and others at the hospital are usually delayed in learning which daytime hospitalist is caring for each patient. These costs seem unreasonably high.
An alternative is to develop a system by which any admitter, such as a night doctor, who will not be providing subsequent care to a patient can identify by name the doctor who will be providing that care. During the admission encounter, the admitter can tell patient/family, “Dr. Boswell will be taking over your care starting tomorrow. He’s a great guy and has been named one of Portland’s best doctors.” This seems so much better than saying, “One of my partners will be taking over tomorrow. I don’t know which of my partners it will be, but they’re all good doctors.” And Dr. Boswell’s name can be entered into the attending physician field of the EHR so that all hospital staff will know without delay.
MedAptus has recently launched software they call “Assign” that may be able to replace the morning meeting and automate assigning new admissions to each hospitalist. I haven’t seen it in operation, so I can’t speak for its effectiveness, but it might be worthwhile for some groups.
Practical Considerations
The changes I’ve described above might not be optimal for every group, and they may take meaningful work to implement. But I don’t think the difficulty of these things is the biggest barrier. The biggest barrier is probably just inertia in most cases, the same reason I’m still a Netflix streaming subscriber even though I almost never watch it. I did, however, really enjoy the Nexflix original series Lilyhammer.

You shouldn’t maintain things that do not deliver the value you anticipated when you first put them in place. For example, I thought Netflix streaming would be terrific, but I have used it so infrequently that it probably costs me $50 per movie or show watched. I should probably dump it.
Your hospitalist group might have some operational practices that are not as valuable as they seem and could be replaced with something better. For many groups, this might include doing away with a separate daytime admitter shift and a morning meeting to distribute the overnight admissions.
Daytime Admission Shift
My experience is that hospitalist groups with more than about five daytime doctors almost always have a day-shift person dedicated to seeing new admissions. In most cases, this procedure is implemented with the idea of reducing the stress of other day-shift doctors, who don’t have to interrupt rounds to admit a new patient. Some see a dedicated admitter as a tool to improve ED throughput, because this doctor isn’t tied up with rounds and can immediately start seeing a new admission.
I think an admitter shift does deliver both of these benefits, but its costs make it suboptimal in most settings. For example, a single admitter will impede ED throughput any time more than one new admission is waiting to be seen, and for most groups that will be much of the day. In fact, improved ED throughput is best achieved by having many hospitalists available for admissions, not just a single admitter. (There are many other factors influencing ED throughput, such as whether ED doctors simply send patients to their “floor” bed prior to being seen by a hospitalist. But for this article, I’m just considering the influence of a dedicated admitter.)
I think “silo-ing” work into different roles, such as separating rounding and admitting, makes it more difficult to ensure that each is always working productively. There are likely to be times when the admitter has little or nothing to do, even though the rounders are very busy. Or perhaps the rounders aren’t very busy, but the admitter has just been asked to admit four ED patients at the same time.
While protecting rounders from the stress of admissions is valuable, it comes at the cost of a net increase in hospitalist work, because a new doctor must get to know the patient on the day following admission. And this admitter-to-rounder handoff serves as another opportunity for errors—and probably lowers patient satisfaction.
I think most groups should consider moving the admitter shift into an additional rounder position, dividing admissions across all of the doctors working during the daytime. For example, a group that has six rounders and a separate admitter would change to seven rounders, each available to admit every seventh daytime admission. Each would bear the meaningful stress of having rounds interrupted to admit a new patient, but accepting every seventh daytime admission shouldn’t be too difficult on most days.
Don’t forget that eliminating the admitter means that the list of new patients you take on each morning will be shorter. Mornings may be a little less stressful.
A.M. Distribution
The daytime doctors at many hospitalist groups meet each morning to discuss how the new admissions from the prior night (or even the last 24 hours) will be distributed. Or perhaps one person, sometimes a nurse or clerical staff, arrives very early each day to do this.
Although it might take some careful planning, I think most groups that use this sort of morning distribution should abandon it for a better system. Consider a group in which all six daytime doctors spend an average of 20 minutes distributing patients each morning. Twenty minutes (0.33 hours) times six doctors times 365 days comes to 730 hours annually.
Assuming these doctors are compensated at typical rates, the practice is spending more than $100,000 annually just so the doctors can distribute patients each morning. On top of this, nurses and others at the hospital are usually delayed in learning which daytime hospitalist is caring for each patient. These costs seem unreasonably high.
An alternative is to develop a system by which any admitter, such as a night doctor, who will not be providing subsequent care to a patient can identify by name the doctor who will be providing that care. During the admission encounter, the admitter can tell patient/family, “Dr. Boswell will be taking over your care starting tomorrow. He’s a great guy and has been named one of Portland’s best doctors.” This seems so much better than saying, “One of my partners will be taking over tomorrow. I don’t know which of my partners it will be, but they’re all good doctors.” And Dr. Boswell’s name can be entered into the attending physician field of the EHR so that all hospital staff will know without delay.
MedAptus has recently launched software they call “Assign” that may be able to replace the morning meeting and automate assigning new admissions to each hospitalist. I haven’t seen it in operation, so I can’t speak for its effectiveness, but it might be worthwhile for some groups.
Practical Considerations
The changes I’ve described above might not be optimal for every group, and they may take meaningful work to implement. But I don’t think the difficulty of these things is the biggest barrier. The biggest barrier is probably just inertia in most cases, the same reason I’m still a Netflix streaming subscriber even though I almost never watch it. I did, however, really enjoy the Nexflix original series Lilyhammer.

ICD-10 launches nationally, changing medical billing
If you’re struck by an orca, sucked into a jet engine, or having relationship problems with your in-laws, fear not: Your doctor now has a medical diagnosis code for that.
Today, U.S. doctors, hospitals, and health insurers must start using the ICD-10, a vast new set of alphanumeric codes for describing diseases and injuries in unprecedented detail.
The transition, mandated by the federal government, has been called American health care’s Y2K moment because the codes haven’t been updated in 36 years. Doctors and hospitals are on high alert since the arcane letters and digits are key to how health care providers get paid. If they don’t use the right codes, down to the decimal, they may not be paid sufficiently – or at all.
For months, health care insiders have been venting their frustrations with the changeover, posting Halloween-themed ICD-10 office decor on social media and mocking some of the wackier codes. Among the targets: W61.33 (pecked by a chicken), Y08.01 (assault by hockey stick), and R46.1 (bizarre personal appearance).
Not to mention W56.22xA – “struck by orca” – which became the title of an illustrated book of infamous ICD-10 codes that’s sold nearly 10,000 copies, said its editor, Niko Skievaski of Madison, Wis.
“Basically everyone who works in health care interacts with this code system – it’s really the language that’s used to communicate from the clinical side to insurers,” said Skievaski, whose experience at a health information technology company helped him and colleagues come up with the book idea. “These codes, they affect everybody.”
Behind the gallows humor lies a major change in how health providers do business, albeit one that’s nearly invisible to patients.
The codes doctors now must use to diagnose patients have multiplied from about 14,000 to nearly 70,000. Hospitals use a related set of medical procedure codes, which has grown even more – from 4,000 to about 72,000.
The reason for the change? The previous set of codes, ICD-9, which were in use since 1979, didn’t reflect the complexity of modern medicine. And some of the information was wrong or obsolete.
The ICD-10 codes set a new bar for comprehensiveness. Did you break your shinbone? Your physician will need to figure out which among dozens of codes for a fractured tibia correctly identify your injury. And if you’ve eaten toxic mushrooms, there are 18 potential codes to cover you.
Government and private insurers can reject claims that aren’t specific enough, use the wrong codes, or have a mismatch between a diagnosis and procedure code.
The ICD-10 changeover will be even more complicated in four states – California, Louisiana, Maryland, and Montana – because of their antiquated billing systems. They have permission from the federal government to temporarily use the old codes, at least for their Medicaid billing, until their systems can be upgraded. California’s upgrade is expected to be completed by 2017.
In Kaiser Permanente’s 4-million member health care region in Southern California, the transition involved revamping up to 30 computer systems and training about 10,000 employees, at an estimated cost of $15 million to $25 million.
“We’re about as prepared as any region can be,” senior manager Larry Sharfstein, who has been leading the process.
A Pasadena “command center” – a term generally applied in crisis situations – has been up and running since Monday.
So how does he feel now that the big day is here?
Sharfstein laughed. “I feel older,” he said.
The ICD-10 codes used by doctors are based on the International Classification of Diseases, 10th edition, a list of medical classifications maintained by the World Health Organization. It contains codes for injuries and diseases and their causes and symptoms, along with patient complaints and socioeconomic circumstances. While health organizations have long been preparing for the transition from ICD-9, the actual changeover date was delayed several times after some physicians and provider lobbying groups said they weren’t ready.
Even with the additional time, some recent tests of the codes among early adopters nationwide resulted in about a fifth of the claims being denied because they weren’t accurate or weren’t correctly submitted, said Dr. Richard Thorp, the immediate past president of the California Medical Association.
In the small town of Paradise, Calif., 85 miles north of Sacramento, Thorp said his 18-person medical group is hoping for the best. It invested late last year in a new electronic health records system that should help with the transition. Even so, he remains skeptical that things will go smoothly.
“It’s not going to be clear for 3-6 weeks whether there are going to be payment issues,” he said.
If everything goes well, he said, “we’ll just breathe a sigh of relief and go on doing what we really want to do – which is take care of patients.”
Kaiser Health News is a nonprofit national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
If you’re struck by an orca, sucked into a jet engine, or having relationship problems with your in-laws, fear not: Your doctor now has a medical diagnosis code for that.
Today, U.S. doctors, hospitals, and health insurers must start using the ICD-10, a vast new set of alphanumeric codes for describing diseases and injuries in unprecedented detail.
The transition, mandated by the federal government, has been called American health care’s Y2K moment because the codes haven’t been updated in 36 years. Doctors and hospitals are on high alert since the arcane letters and digits are key to how health care providers get paid. If they don’t use the right codes, down to the decimal, they may not be paid sufficiently – or at all.
For months, health care insiders have been venting their frustrations with the changeover, posting Halloween-themed ICD-10 office decor on social media and mocking some of the wackier codes. Among the targets: W61.33 (pecked by a chicken), Y08.01 (assault by hockey stick), and R46.1 (bizarre personal appearance).
Not to mention W56.22xA – “struck by orca” – which became the title of an illustrated book of infamous ICD-10 codes that’s sold nearly 10,000 copies, said its editor, Niko Skievaski of Madison, Wis.
“Basically everyone who works in health care interacts with this code system – it’s really the language that’s used to communicate from the clinical side to insurers,” said Skievaski, whose experience at a health information technology company helped him and colleagues come up with the book idea. “These codes, they affect everybody.”
Behind the gallows humor lies a major change in how health providers do business, albeit one that’s nearly invisible to patients.
The codes doctors now must use to diagnose patients have multiplied from about 14,000 to nearly 70,000. Hospitals use a related set of medical procedure codes, which has grown even more – from 4,000 to about 72,000.
The reason for the change? The previous set of codes, ICD-9, which were in use since 1979, didn’t reflect the complexity of modern medicine. And some of the information was wrong or obsolete.
The ICD-10 codes set a new bar for comprehensiveness. Did you break your shinbone? Your physician will need to figure out which among dozens of codes for a fractured tibia correctly identify your injury. And if you’ve eaten toxic mushrooms, there are 18 potential codes to cover you.
Government and private insurers can reject claims that aren’t specific enough, use the wrong codes, or have a mismatch between a diagnosis and procedure code.
The ICD-10 changeover will be even more complicated in four states – California, Louisiana, Maryland, and Montana – because of their antiquated billing systems. They have permission from the federal government to temporarily use the old codes, at least for their Medicaid billing, until their systems can be upgraded. California’s upgrade is expected to be completed by 2017.
In Kaiser Permanente’s 4-million member health care region in Southern California, the transition involved revamping up to 30 computer systems and training about 10,000 employees, at an estimated cost of $15 million to $25 million.
“We’re about as prepared as any region can be,” senior manager Larry Sharfstein, who has been leading the process.
A Pasadena “command center” – a term generally applied in crisis situations – has been up and running since Monday.
So how does he feel now that the big day is here?
Sharfstein laughed. “I feel older,” he said.
The ICD-10 codes used by doctors are based on the International Classification of Diseases, 10th edition, a list of medical classifications maintained by the World Health Organization. It contains codes for injuries and diseases and their causes and symptoms, along with patient complaints and socioeconomic circumstances. While health organizations have long been preparing for the transition from ICD-9, the actual changeover date was delayed several times after some physicians and provider lobbying groups said they weren’t ready.
Even with the additional time, some recent tests of the codes among early adopters nationwide resulted in about a fifth of the claims being denied because they weren’t accurate or weren’t correctly submitted, said Dr. Richard Thorp, the immediate past president of the California Medical Association.
In the small town of Paradise, Calif., 85 miles north of Sacramento, Thorp said his 18-person medical group is hoping for the best. It invested late last year in a new electronic health records system that should help with the transition. Even so, he remains skeptical that things will go smoothly.
“It’s not going to be clear for 3-6 weeks whether there are going to be payment issues,” he said.
If everything goes well, he said, “we’ll just breathe a sigh of relief and go on doing what we really want to do – which is take care of patients.”
Kaiser Health News is a nonprofit national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
If you’re struck by an orca, sucked into a jet engine, or having relationship problems with your in-laws, fear not: Your doctor now has a medical diagnosis code for that.
Today, U.S. doctors, hospitals, and health insurers must start using the ICD-10, a vast new set of alphanumeric codes for describing diseases and injuries in unprecedented detail.
The transition, mandated by the federal government, has been called American health care’s Y2K moment because the codes haven’t been updated in 36 years. Doctors and hospitals are on high alert since the arcane letters and digits are key to how health care providers get paid. If they don’t use the right codes, down to the decimal, they may not be paid sufficiently – or at all.
For months, health care insiders have been venting their frustrations with the changeover, posting Halloween-themed ICD-10 office decor on social media and mocking some of the wackier codes. Among the targets: W61.33 (pecked by a chicken), Y08.01 (assault by hockey stick), and R46.1 (bizarre personal appearance).
Not to mention W56.22xA – “struck by orca” – which became the title of an illustrated book of infamous ICD-10 codes that’s sold nearly 10,000 copies, said its editor, Niko Skievaski of Madison, Wis.
“Basically everyone who works in health care interacts with this code system – it’s really the language that’s used to communicate from the clinical side to insurers,” said Skievaski, whose experience at a health information technology company helped him and colleagues come up with the book idea. “These codes, they affect everybody.”
Behind the gallows humor lies a major change in how health providers do business, albeit one that’s nearly invisible to patients.
The codes doctors now must use to diagnose patients have multiplied from about 14,000 to nearly 70,000. Hospitals use a related set of medical procedure codes, which has grown even more – from 4,000 to about 72,000.
The reason for the change? The previous set of codes, ICD-9, which were in use since 1979, didn’t reflect the complexity of modern medicine. And some of the information was wrong or obsolete.
The ICD-10 codes set a new bar for comprehensiveness. Did you break your shinbone? Your physician will need to figure out which among dozens of codes for a fractured tibia correctly identify your injury. And if you’ve eaten toxic mushrooms, there are 18 potential codes to cover you.
Government and private insurers can reject claims that aren’t specific enough, use the wrong codes, or have a mismatch between a diagnosis and procedure code.
The ICD-10 changeover will be even more complicated in four states – California, Louisiana, Maryland, and Montana – because of their antiquated billing systems. They have permission from the federal government to temporarily use the old codes, at least for their Medicaid billing, until their systems can be upgraded. California’s upgrade is expected to be completed by 2017.
In Kaiser Permanente’s 4-million member health care region in Southern California, the transition involved revamping up to 30 computer systems and training about 10,000 employees, at an estimated cost of $15 million to $25 million.
“We’re about as prepared as any region can be,” senior manager Larry Sharfstein, who has been leading the process.
A Pasadena “command center” – a term generally applied in crisis situations – has been up and running since Monday.
So how does he feel now that the big day is here?
Sharfstein laughed. “I feel older,” he said.
The ICD-10 codes used by doctors are based on the International Classification of Diseases, 10th edition, a list of medical classifications maintained by the World Health Organization. It contains codes for injuries and diseases and their causes and symptoms, along with patient complaints and socioeconomic circumstances. While health organizations have long been preparing for the transition from ICD-9, the actual changeover date was delayed several times after some physicians and provider lobbying groups said they weren’t ready.
Even with the additional time, some recent tests of the codes among early adopters nationwide resulted in about a fifth of the claims being denied because they weren’t accurate or weren’t correctly submitted, said Dr. Richard Thorp, the immediate past president of the California Medical Association.
In the small town of Paradise, Calif., 85 miles north of Sacramento, Thorp said his 18-person medical group is hoping for the best. It invested late last year in a new electronic health records system that should help with the transition. Even so, he remains skeptical that things will go smoothly.
“It’s not going to be clear for 3-6 weeks whether there are going to be payment issues,” he said.
If everything goes well, he said, “we’ll just breathe a sigh of relief and go on doing what we really want to do – which is take care of patients.”
Kaiser Health News is a nonprofit national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Malpractice Counsel: Cervical Spine Injury
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
U.S. injury costs topped $671 billion in 2013
Over 30 million injuries were treated in U.S. emergency departments in 2013, costing an estimated $671 billion, the Centers for Disease Control and Prevention reported.
The largest share of that cost – almost $290 billion, or about 43% – came from the 3 million persons with nonfatal injuries who were hospitalized. Costs for the 27 million people who were treated and released from emergency departments were $167 billion, which was just under 25% of the total. The lifetime cost estimate for the almost 193,000 injury-associated deaths in 2013 was over $214 billion (32%), said Curtis Florence, Ph.D., of the CDC’s National Center for Injury Prevention and Control, Atlanta, and associates.
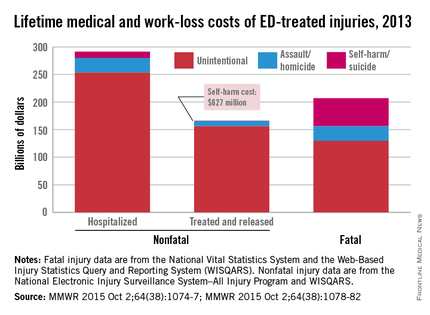
For each ED-treated injury-related death, the mean cost in terms of lost lifetime earnings and medical care provided was just over $1.1 million: Homicides cost over $1.6 million, suicides were $1.2 million each, and each unintentional injury death cost just under $1 million, they said (MMWR. 2015 Oct 2;64[38]:1074-77).
Drug poisonings, including prescription drug overdoses, accounted for the largest share of fatal injury costs (27%), followed by transportation-related deaths (23%) and firearm-related deaths (22%), Dr. Florence and associates noted.
The mean cost for each nonfatal injury (both hospitalized and treated and released from the ED) was $15,211. Self-harm injuries cost $25,121, compared with $23,034 for each assault and $14,685 for each unintentional injury (MMWR. 2015 Oct 2;64[38]:1078-82).
“Injuries cost Americans far too much money, suffering, and preventable death,” CDC Director Tom Frieden said in a written statement. “The doubling of deaths by drug poisoning, including prescription drug overdose and heroin, is particularly alarming.”
The investigators used data from the National Vital Statistics System and the Web-Based Injury Statistics Query and Reporting System (WISQARS) for injury-related deaths and the National Electronic Injury Surveillance System–All Injury Program and WISQARS for nonfatal injuries.
Over 30 million injuries were treated in U.S. emergency departments in 2013, costing an estimated $671 billion, the Centers for Disease Control and Prevention reported.
The largest share of that cost – almost $290 billion, or about 43% – came from the 3 million persons with nonfatal injuries who were hospitalized. Costs for the 27 million people who were treated and released from emergency departments were $167 billion, which was just under 25% of the total. The lifetime cost estimate for the almost 193,000 injury-associated deaths in 2013 was over $214 billion (32%), said Curtis Florence, Ph.D., of the CDC’s National Center for Injury Prevention and Control, Atlanta, and associates.
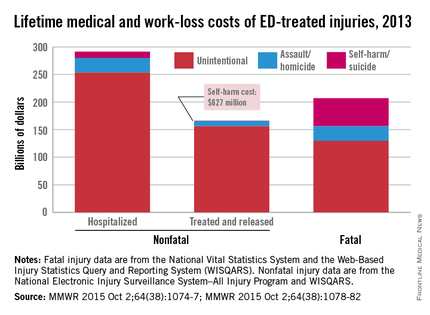
For each ED-treated injury-related death, the mean cost in terms of lost lifetime earnings and medical care provided was just over $1.1 million: Homicides cost over $1.6 million, suicides were $1.2 million each, and each unintentional injury death cost just under $1 million, they said (MMWR. 2015 Oct 2;64[38]:1074-77).
Drug poisonings, including prescription drug overdoses, accounted for the largest share of fatal injury costs (27%), followed by transportation-related deaths (23%) and firearm-related deaths (22%), Dr. Florence and associates noted.
The mean cost for each nonfatal injury (both hospitalized and treated and released from the ED) was $15,211. Self-harm injuries cost $25,121, compared with $23,034 for each assault and $14,685 for each unintentional injury (MMWR. 2015 Oct 2;64[38]:1078-82).
“Injuries cost Americans far too much money, suffering, and preventable death,” CDC Director Tom Frieden said in a written statement. “The doubling of deaths by drug poisoning, including prescription drug overdose and heroin, is particularly alarming.”
The investigators used data from the National Vital Statistics System and the Web-Based Injury Statistics Query and Reporting System (WISQARS) for injury-related deaths and the National Electronic Injury Surveillance System–All Injury Program and WISQARS for nonfatal injuries.
Over 30 million injuries were treated in U.S. emergency departments in 2013, costing an estimated $671 billion, the Centers for Disease Control and Prevention reported.
The largest share of that cost – almost $290 billion, or about 43% – came from the 3 million persons with nonfatal injuries who were hospitalized. Costs for the 27 million people who were treated and released from emergency departments were $167 billion, which was just under 25% of the total. The lifetime cost estimate for the almost 193,000 injury-associated deaths in 2013 was over $214 billion (32%), said Curtis Florence, Ph.D., of the CDC’s National Center for Injury Prevention and Control, Atlanta, and associates.
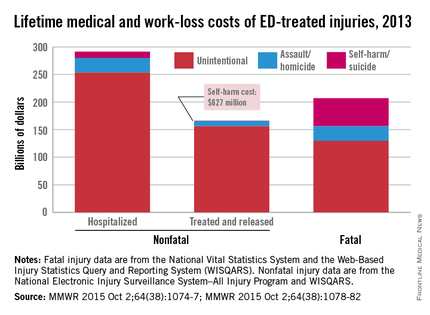
For each ED-treated injury-related death, the mean cost in terms of lost lifetime earnings and medical care provided was just over $1.1 million: Homicides cost over $1.6 million, suicides were $1.2 million each, and each unintentional injury death cost just under $1 million, they said (MMWR. 2015 Oct 2;64[38]:1074-77).
Drug poisonings, including prescription drug overdoses, accounted for the largest share of fatal injury costs (27%), followed by transportation-related deaths (23%) and firearm-related deaths (22%), Dr. Florence and associates noted.
The mean cost for each nonfatal injury (both hospitalized and treated and released from the ED) was $15,211. Self-harm injuries cost $25,121, compared with $23,034 for each assault and $14,685 for each unintentional injury (MMWR. 2015 Oct 2;64[38]:1078-82).
“Injuries cost Americans far too much money, suffering, and preventable death,” CDC Director Tom Frieden said in a written statement. “The doubling of deaths by drug poisoning, including prescription drug overdose and heroin, is particularly alarming.”
The investigators used data from the National Vital Statistics System and the Web-Based Injury Statistics Query and Reporting System (WISQARS) for injury-related deaths and the National Electronic Injury Surveillance System–All Injury Program and WISQARS for nonfatal injuries.
FROM MMWR