User login
3 court cases to watch in 2015
Pay close attention to the outcomes of three cases winding their way through the courts this summer, legal experts advise.
On deck are cases that could reshape Stark Law, the Anti-kickback Statute, and the 60-day federal overpayment rule. Decisions on these cases could affect billing practices and practices arrangements, as well as federal reporting obligations. Below is a selection of critical health law cases facing doctors and how they might impact practice.
1. Council for Urological Interests v. Sylvia Burwell et al.
Summary: This case centers on whether the federal Stark Law can prevent physicians from referring patients to hospitals to which the physicians lease equipment, among other things. In 2008, the U.S. Department of Health & Human Services (HHS) issued regulations that effectively prohibit physicians who lease medical equipment to hospitals from referring their Medicare patients to these same hospitals for outpatient care involving that equipment. The regulation prohibits physicians from charging hospitals for the leased equipment on a per-use basis, or a “per-click” basis as it is commonly known. In 2009, the Council for Urological Interests – a nonprofit corporation owned by urologists – sued, claiming the text and legislative history of the Stark Law preclude the HHS from enforcing the per-click ban. The regulation limits the ability of physicians who own joint ventures to refer their patients to receive services under these arrangements, the plaintiffs said. A district court ruled in favor of the HHS, and the Council appealed. A spokeswoman for the U.S. Department of Justice declined to comment for this story.
Case status: In June 2015, the U.S. Court of Appeals for the District of Columbia Circuit ruled that the HHS must reconsider its per-click referral ban. The court suggested that the agency may have misconstrued the legislative history of the Stark Law in order to enact the rule.
Why doctors should care: The ultimate outcome of the case will determine whether or not physicians can engage in per-click leases under Stark Law, said Chicago health law attorney Ericka L. Adler.
“When HHS changed the regulations to no longer allow the per-click arrangement where physicians were self-referring, it caused a lot of deals to be undone,” Ms. Adler said in an interview. “[Certainly], these lease arrangements could, in many cases, be restructured to look more like normal leases and meet the Stark equipment lease exception, but in some cases it created hardships, such as in rural areas.”
Reconsideration of the regulation could mean that the HHS creates more appropriate carve-outs to the rule, Ms. Adler noted.
In the meantime, the appeals court ruling means the per-click ban cannot be enforced while the government reconsiders, which is a positive development for physicians, said Washington health law attorney Thomas L. Mills, who represented the Council for Urological Interests.
“CMS’ permitting per-click leases to non–physician-owned companies while banning them for physician-owned entities made no sense, particularly when the medical procedure is not susceptible to overuse,” Mr. Mills said in an interview. “Perhaps more importantly, the [appeals] decision is a victory for the rule of law. It shows that CMS does not have carte blanche to disadvantage physicians by steering control of the implements of their practices to less important participants in the health care delivery system. ... Physicians should be free to band together to purchase the equipment they believe will provide the most effective treatment for their patients, instead of being forced to rely on the arbitrary procurement decisions of hospitals.”
2. United States v. Continuum Health Partners Inc.
Summary: The federal government contends that three hospitals failed to return overpayments to Medicaid in violation of an Affordable Care Act requirement that they be reported and repaid within 60 days of identification. The government alleges that because of a computer glitch, three hospitals that are operated by Continuum Health Partners Inc., billed both the government and a managed care organization (MCO) for the same services. After the New York State Comptroller’s Office alerted Continuum to a possible overbilling, Continuum conducted an internal investigation and allegedly found 900 potentially improper Medicaid claims totaling $1 million, according to court documents. The government claims that Continuum failed to repay the overpayments within 60 days and instead repaid only “small batches” of the affected claims over the next 2 years. Continuum argues that the hospitals did not knowingly conceal the overpayments from the government and that the overbillings had not been officially identified. Rather, Continuum argues there is only evidence that administrators discussed potential overpayments. The “mere notice of a potential overpayment does not give rise to an established duty until 60 days after the overpayment is identified,” Continuum said in court documents. Attorneys for the government and for Continuum did not return messages seeking comment.
Case status: The case is before the U.S. District Court for the Southern District of New York.
Why doctors should care: The Continuum case will provide significant guidance to health providers about the ACA 60-day overpayment rule, said Houston health law attorney Micheal E. Clark, who chairs the America Bar Association Health Law Section. As it stands, the federal rule is somewhat unclear, leading to confusion for doctors about their reporting obligations, he said.
“The agency hasn’t really defined what is ‘knowing,’ what is reasonable knowledge of a known overpayment,” Mr. Clark said in an interview. “It’s a gray area. [The ruling] will be very informative about what this is actually going to mean.”
3. Ameritox v. Millennium Laboratories
Summary: Ameritox revolves around whether a laboratory’s giveaway of urine specimen cups to physicians amounted to an illegal kickback. In 2012, lab testing company Ameritox sued Millennium in a Florida district court alleging that Millennium harmed its business by giving the urine cups to doctors in violation of the Stark Law. Physicians used the cups – which have chemically activated strips that contain patient information – to monitor patients’ use of pain medications. Millennium unlawfully obtained physician referrals through free cup agreements, according to Ameritox’s complaint. A federal jury found Millennium had violated the Stark Law as well as the Anti-Kickback Statute by providing the free cups in exchange for referrals and Ameritox was awarded $11 million. Attorneys for both parties did not return messages seeking comment.
Case status: Millennium appealed, and the case is before the 11th U.S. Circuit Court of Appeals. The federal Justice Department has weighed in on the side of Ameritox, arguing that the cup giveaway violated Stark Law and the Anti-Kickback Statute.
Why doctors should care: The Ameritox case makes it clear that doctors should never accept free point-of-care testing cups or similar medical equipment from a lab, said health law attorney Adrienne Dresevic of Southfield, Mich. The case also highlights the broad spectrum of “remuneration,” when it comes to free items or services to doctors, she noted. Under the Anti-Kickback Statute, remuneration refers to the transfer of anything of value, directly or indirectly, overtly or covertly, in cash or in kind.
“The takeaways in Ameritox are applicable to other relationships, such as in the radiology realm,” Ms. Dresevic said in an interview. “Physicians should closely scrutinize any free items or services offered to them to ensure it falls within the exception to what is considered ‘remuneration.’ ”
Exceptions to remuneration could include payments that are a return on an investment interest, such as a dividend or interest income. However, physicians should ensure they are familiar with all exceptions to the law before entering into such agreements, experts advise.
The Ameritox case is important for physicians because more laboratories are approaching doctors with various “arrangements,” and touting that the arrangements are compliant with federal regulations, Ms. Dresevic added. Many doctors are taking the labs’ word for the arrangements’ legality, leading to serious legal risk.
“Physicians need to know how to look beyond what the laboratory representative is presenting to them and make their own determinations, sometimes with the help of health care counsel, regarding the legality of a particular arrangement,” she said.
On Twitter @legal_med
Pay close attention to the outcomes of three cases winding their way through the courts this summer, legal experts advise.
On deck are cases that could reshape Stark Law, the Anti-kickback Statute, and the 60-day federal overpayment rule. Decisions on these cases could affect billing practices and practices arrangements, as well as federal reporting obligations. Below is a selection of critical health law cases facing doctors and how they might impact practice.
1. Council for Urological Interests v. Sylvia Burwell et al.
Summary: This case centers on whether the federal Stark Law can prevent physicians from referring patients to hospitals to which the physicians lease equipment, among other things. In 2008, the U.S. Department of Health & Human Services (HHS) issued regulations that effectively prohibit physicians who lease medical equipment to hospitals from referring their Medicare patients to these same hospitals for outpatient care involving that equipment. The regulation prohibits physicians from charging hospitals for the leased equipment on a per-use basis, or a “per-click” basis as it is commonly known. In 2009, the Council for Urological Interests – a nonprofit corporation owned by urologists – sued, claiming the text and legislative history of the Stark Law preclude the HHS from enforcing the per-click ban. The regulation limits the ability of physicians who own joint ventures to refer their patients to receive services under these arrangements, the plaintiffs said. A district court ruled in favor of the HHS, and the Council appealed. A spokeswoman for the U.S. Department of Justice declined to comment for this story.
Case status: In June 2015, the U.S. Court of Appeals for the District of Columbia Circuit ruled that the HHS must reconsider its per-click referral ban. The court suggested that the agency may have misconstrued the legislative history of the Stark Law in order to enact the rule.
Why doctors should care: The ultimate outcome of the case will determine whether or not physicians can engage in per-click leases under Stark Law, said Chicago health law attorney Ericka L. Adler.
“When HHS changed the regulations to no longer allow the per-click arrangement where physicians were self-referring, it caused a lot of deals to be undone,” Ms. Adler said in an interview. “[Certainly], these lease arrangements could, in many cases, be restructured to look more like normal leases and meet the Stark equipment lease exception, but in some cases it created hardships, such as in rural areas.”
Reconsideration of the regulation could mean that the HHS creates more appropriate carve-outs to the rule, Ms. Adler noted.
In the meantime, the appeals court ruling means the per-click ban cannot be enforced while the government reconsiders, which is a positive development for physicians, said Washington health law attorney Thomas L. Mills, who represented the Council for Urological Interests.
“CMS’ permitting per-click leases to non–physician-owned companies while banning them for physician-owned entities made no sense, particularly when the medical procedure is not susceptible to overuse,” Mr. Mills said in an interview. “Perhaps more importantly, the [appeals] decision is a victory for the rule of law. It shows that CMS does not have carte blanche to disadvantage physicians by steering control of the implements of their practices to less important participants in the health care delivery system. ... Physicians should be free to band together to purchase the equipment they believe will provide the most effective treatment for their patients, instead of being forced to rely on the arbitrary procurement decisions of hospitals.”
2. United States v. Continuum Health Partners Inc.
Summary: The federal government contends that three hospitals failed to return overpayments to Medicaid in violation of an Affordable Care Act requirement that they be reported and repaid within 60 days of identification. The government alleges that because of a computer glitch, three hospitals that are operated by Continuum Health Partners Inc., billed both the government and a managed care organization (MCO) for the same services. After the New York State Comptroller’s Office alerted Continuum to a possible overbilling, Continuum conducted an internal investigation and allegedly found 900 potentially improper Medicaid claims totaling $1 million, according to court documents. The government claims that Continuum failed to repay the overpayments within 60 days and instead repaid only “small batches” of the affected claims over the next 2 years. Continuum argues that the hospitals did not knowingly conceal the overpayments from the government and that the overbillings had not been officially identified. Rather, Continuum argues there is only evidence that administrators discussed potential overpayments. The “mere notice of a potential overpayment does not give rise to an established duty until 60 days after the overpayment is identified,” Continuum said in court documents. Attorneys for the government and for Continuum did not return messages seeking comment.
Case status: The case is before the U.S. District Court for the Southern District of New York.
Why doctors should care: The Continuum case will provide significant guidance to health providers about the ACA 60-day overpayment rule, said Houston health law attorney Micheal E. Clark, who chairs the America Bar Association Health Law Section. As it stands, the federal rule is somewhat unclear, leading to confusion for doctors about their reporting obligations, he said.
“The agency hasn’t really defined what is ‘knowing,’ what is reasonable knowledge of a known overpayment,” Mr. Clark said in an interview. “It’s a gray area. [The ruling] will be very informative about what this is actually going to mean.”
3. Ameritox v. Millennium Laboratories
Summary: Ameritox revolves around whether a laboratory’s giveaway of urine specimen cups to physicians amounted to an illegal kickback. In 2012, lab testing company Ameritox sued Millennium in a Florida district court alleging that Millennium harmed its business by giving the urine cups to doctors in violation of the Stark Law. Physicians used the cups – which have chemically activated strips that contain patient information – to monitor patients’ use of pain medications. Millennium unlawfully obtained physician referrals through free cup agreements, according to Ameritox’s complaint. A federal jury found Millennium had violated the Stark Law as well as the Anti-Kickback Statute by providing the free cups in exchange for referrals and Ameritox was awarded $11 million. Attorneys for both parties did not return messages seeking comment.
Case status: Millennium appealed, and the case is before the 11th U.S. Circuit Court of Appeals. The federal Justice Department has weighed in on the side of Ameritox, arguing that the cup giveaway violated Stark Law and the Anti-Kickback Statute.
Why doctors should care: The Ameritox case makes it clear that doctors should never accept free point-of-care testing cups or similar medical equipment from a lab, said health law attorney Adrienne Dresevic of Southfield, Mich. The case also highlights the broad spectrum of “remuneration,” when it comes to free items or services to doctors, she noted. Under the Anti-Kickback Statute, remuneration refers to the transfer of anything of value, directly or indirectly, overtly or covertly, in cash or in kind.
“The takeaways in Ameritox are applicable to other relationships, such as in the radiology realm,” Ms. Dresevic said in an interview. “Physicians should closely scrutinize any free items or services offered to them to ensure it falls within the exception to what is considered ‘remuneration.’ ”
Exceptions to remuneration could include payments that are a return on an investment interest, such as a dividend or interest income. However, physicians should ensure they are familiar with all exceptions to the law before entering into such agreements, experts advise.
The Ameritox case is important for physicians because more laboratories are approaching doctors with various “arrangements,” and touting that the arrangements are compliant with federal regulations, Ms. Dresevic added. Many doctors are taking the labs’ word for the arrangements’ legality, leading to serious legal risk.
“Physicians need to know how to look beyond what the laboratory representative is presenting to them and make their own determinations, sometimes with the help of health care counsel, regarding the legality of a particular arrangement,” she said.
On Twitter @legal_med
Pay close attention to the outcomes of three cases winding their way through the courts this summer, legal experts advise.
On deck are cases that could reshape Stark Law, the Anti-kickback Statute, and the 60-day federal overpayment rule. Decisions on these cases could affect billing practices and practices arrangements, as well as federal reporting obligations. Below is a selection of critical health law cases facing doctors and how they might impact practice.
1. Council for Urological Interests v. Sylvia Burwell et al.
Summary: This case centers on whether the federal Stark Law can prevent physicians from referring patients to hospitals to which the physicians lease equipment, among other things. In 2008, the U.S. Department of Health & Human Services (HHS) issued regulations that effectively prohibit physicians who lease medical equipment to hospitals from referring their Medicare patients to these same hospitals for outpatient care involving that equipment. The regulation prohibits physicians from charging hospitals for the leased equipment on a per-use basis, or a “per-click” basis as it is commonly known. In 2009, the Council for Urological Interests – a nonprofit corporation owned by urologists – sued, claiming the text and legislative history of the Stark Law preclude the HHS from enforcing the per-click ban. The regulation limits the ability of physicians who own joint ventures to refer their patients to receive services under these arrangements, the plaintiffs said. A district court ruled in favor of the HHS, and the Council appealed. A spokeswoman for the U.S. Department of Justice declined to comment for this story.
Case status: In June 2015, the U.S. Court of Appeals for the District of Columbia Circuit ruled that the HHS must reconsider its per-click referral ban. The court suggested that the agency may have misconstrued the legislative history of the Stark Law in order to enact the rule.
Why doctors should care: The ultimate outcome of the case will determine whether or not physicians can engage in per-click leases under Stark Law, said Chicago health law attorney Ericka L. Adler.
“When HHS changed the regulations to no longer allow the per-click arrangement where physicians were self-referring, it caused a lot of deals to be undone,” Ms. Adler said in an interview. “[Certainly], these lease arrangements could, in many cases, be restructured to look more like normal leases and meet the Stark equipment lease exception, but in some cases it created hardships, such as in rural areas.”
Reconsideration of the regulation could mean that the HHS creates more appropriate carve-outs to the rule, Ms. Adler noted.
In the meantime, the appeals court ruling means the per-click ban cannot be enforced while the government reconsiders, which is a positive development for physicians, said Washington health law attorney Thomas L. Mills, who represented the Council for Urological Interests.
“CMS’ permitting per-click leases to non–physician-owned companies while banning them for physician-owned entities made no sense, particularly when the medical procedure is not susceptible to overuse,” Mr. Mills said in an interview. “Perhaps more importantly, the [appeals] decision is a victory for the rule of law. It shows that CMS does not have carte blanche to disadvantage physicians by steering control of the implements of their practices to less important participants in the health care delivery system. ... Physicians should be free to band together to purchase the equipment they believe will provide the most effective treatment for their patients, instead of being forced to rely on the arbitrary procurement decisions of hospitals.”
2. United States v. Continuum Health Partners Inc.
Summary: The federal government contends that three hospitals failed to return overpayments to Medicaid in violation of an Affordable Care Act requirement that they be reported and repaid within 60 days of identification. The government alleges that because of a computer glitch, three hospitals that are operated by Continuum Health Partners Inc., billed both the government and a managed care organization (MCO) for the same services. After the New York State Comptroller’s Office alerted Continuum to a possible overbilling, Continuum conducted an internal investigation and allegedly found 900 potentially improper Medicaid claims totaling $1 million, according to court documents. The government claims that Continuum failed to repay the overpayments within 60 days and instead repaid only “small batches” of the affected claims over the next 2 years. Continuum argues that the hospitals did not knowingly conceal the overpayments from the government and that the overbillings had not been officially identified. Rather, Continuum argues there is only evidence that administrators discussed potential overpayments. The “mere notice of a potential overpayment does not give rise to an established duty until 60 days after the overpayment is identified,” Continuum said in court documents. Attorneys for the government and for Continuum did not return messages seeking comment.
Case status: The case is before the U.S. District Court for the Southern District of New York.
Why doctors should care: The Continuum case will provide significant guidance to health providers about the ACA 60-day overpayment rule, said Houston health law attorney Micheal E. Clark, who chairs the America Bar Association Health Law Section. As it stands, the federal rule is somewhat unclear, leading to confusion for doctors about their reporting obligations, he said.
“The agency hasn’t really defined what is ‘knowing,’ what is reasonable knowledge of a known overpayment,” Mr. Clark said in an interview. “It’s a gray area. [The ruling] will be very informative about what this is actually going to mean.”
3. Ameritox v. Millennium Laboratories
Summary: Ameritox revolves around whether a laboratory’s giveaway of urine specimen cups to physicians amounted to an illegal kickback. In 2012, lab testing company Ameritox sued Millennium in a Florida district court alleging that Millennium harmed its business by giving the urine cups to doctors in violation of the Stark Law. Physicians used the cups – which have chemically activated strips that contain patient information – to monitor patients’ use of pain medications. Millennium unlawfully obtained physician referrals through free cup agreements, according to Ameritox’s complaint. A federal jury found Millennium had violated the Stark Law as well as the Anti-Kickback Statute by providing the free cups in exchange for referrals and Ameritox was awarded $11 million. Attorneys for both parties did not return messages seeking comment.
Case status: Millennium appealed, and the case is before the 11th U.S. Circuit Court of Appeals. The federal Justice Department has weighed in on the side of Ameritox, arguing that the cup giveaway violated Stark Law and the Anti-Kickback Statute.
Why doctors should care: The Ameritox case makes it clear that doctors should never accept free point-of-care testing cups or similar medical equipment from a lab, said health law attorney Adrienne Dresevic of Southfield, Mich. The case also highlights the broad spectrum of “remuneration,” when it comes to free items or services to doctors, she noted. Under the Anti-Kickback Statute, remuneration refers to the transfer of anything of value, directly or indirectly, overtly or covertly, in cash or in kind.
“The takeaways in Ameritox are applicable to other relationships, such as in the radiology realm,” Ms. Dresevic said in an interview. “Physicians should closely scrutinize any free items or services offered to them to ensure it falls within the exception to what is considered ‘remuneration.’ ”
Exceptions to remuneration could include payments that are a return on an investment interest, such as a dividend or interest income. However, physicians should ensure they are familiar with all exceptions to the law before entering into such agreements, experts advise.
The Ameritox case is important for physicians because more laboratories are approaching doctors with various “arrangements,” and touting that the arrangements are compliant with federal regulations, Ms. Dresevic added. Many doctors are taking the labs’ word for the arrangements’ legality, leading to serious legal risk.
“Physicians need to know how to look beyond what the laboratory representative is presenting to them and make their own determinations, sometimes with the help of health care counsel, regarding the legality of a particular arrangement,” she said.
On Twitter @legal_med
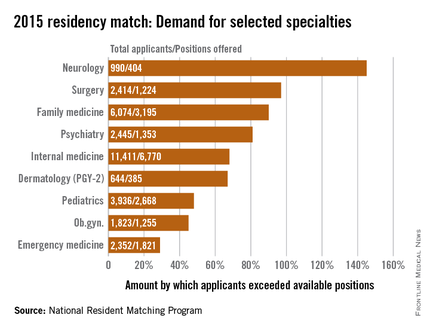
Which specialties are sitting at residents’ popular table?
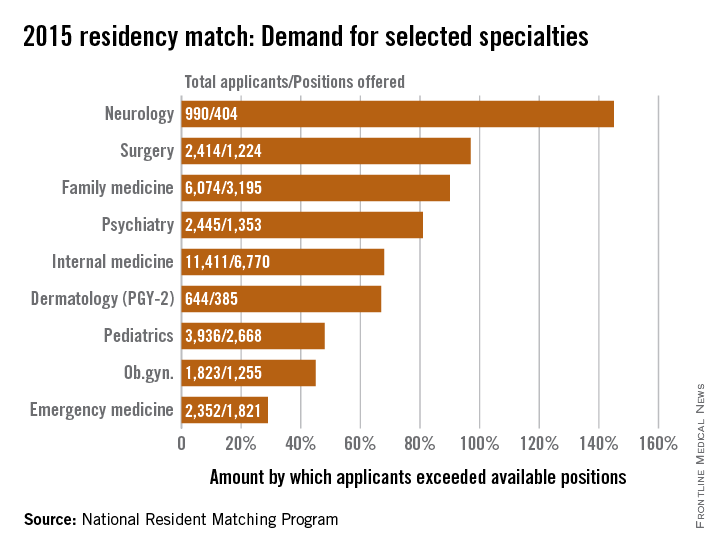
Demand for residency positions exceeded supply for all 47 specialties included in the 2015 residency match, but some specialties were more in demand than others.
Sheer weight of numbers gives the largest specialty, internal medicine, the largest demand – 11,411 total applicants – and the biggest difference between that demand and the number of PGY-1 positions offered: 6,770 slots, leaving 4,641 new doctors to settle for another specialty, according to data from the National Resident Matching Program (NRMP).
There is, however, more than one way to look at Match supply and demand. By doing a little math to take specialty size out of the equation, neurology gets a lot more popular. With 990 residents vying for just 404 positions, the total number of neurology applicants exceeded successful ones by 145%, compared with 68% for internal medicine. Also moving ahead of IM were surgery (97%), family medicine (90%), and psychiatry (81%).
Among the smallest subspecialties – those with less than 100 positions to fill – the demand becomes even more impressive. Radiation oncology had a rate of 600%, while pediatrics-primary put up a rate of 978%. The top of the demand heap, however, is occupied by medicine–preventive medicine, which had 94 applicants for just 7 available slots, according to the NRMP, which means that the number of applicants topped the number accepted by 1,243%.
The total PGY-1 numbers for 2015 look like this: 52,860 applicants filled 27,293 residency positions, so the number of total applicants exceeded those accepted by 94%. Think of it this way: For every residency applicant who matched in 2015, there was nearly one complete applicant who didn’t.
Demand for residency positions exceeded supply for all 47 specialties included in the 2015 residency match, but some specialties were more in demand than others.
Sheer weight of numbers gives the largest specialty, internal medicine, the largest demand – 11,411 total applicants – and the biggest difference between that demand and the number of PGY-1 positions offered: 6,770 slots, leaving 4,641 new doctors to settle for another specialty, according to data from the National Resident Matching Program (NRMP).
There is, however, more than one way to look at Match supply and demand. By doing a little math to take specialty size out of the equation, neurology gets a lot more popular. With 990 residents vying for just 404 positions, the total number of neurology applicants exceeded successful ones by 145%, compared with 68% for internal medicine. Also moving ahead of IM were surgery (97%), family medicine (90%), and psychiatry (81%).
Among the smallest subspecialties – those with less than 100 positions to fill – the demand becomes even more impressive. Radiation oncology had a rate of 600%, while pediatrics-primary put up a rate of 978%. The top of the demand heap, however, is occupied by medicine–preventive medicine, which had 94 applicants for just 7 available slots, according to the NRMP, which means that the number of applicants topped the number accepted by 1,243%.
The total PGY-1 numbers for 2015 look like this: 52,860 applicants filled 27,293 residency positions, so the number of total applicants exceeded those accepted by 94%. Think of it this way: For every residency applicant who matched in 2015, there was nearly one complete applicant who didn’t.
Demand for residency positions exceeded supply for all 47 specialties included in the 2015 residency match, but some specialties were more in demand than others.
Sheer weight of numbers gives the largest specialty, internal medicine, the largest demand – 11,411 total applicants – and the biggest difference between that demand and the number of PGY-1 positions offered: 6,770 slots, leaving 4,641 new doctors to settle for another specialty, according to data from the National Resident Matching Program (NRMP).
There is, however, more than one way to look at Match supply and demand. By doing a little math to take specialty size out of the equation, neurology gets a lot more popular. With 990 residents vying for just 404 positions, the total number of neurology applicants exceeded successful ones by 145%, compared with 68% for internal medicine. Also moving ahead of IM were surgery (97%), family medicine (90%), and psychiatry (81%).
Among the smallest subspecialties – those with less than 100 positions to fill – the demand becomes even more impressive. Radiation oncology had a rate of 600%, while pediatrics-primary put up a rate of 978%. The top of the demand heap, however, is occupied by medicine–preventive medicine, which had 94 applicants for just 7 available slots, according to the NRMP, which means that the number of applicants topped the number accepted by 1,243%.
The total PGY-1 numbers for 2015 look like this: 52,860 applicants filled 27,293 residency positions, so the number of total applicants exceeded those accepted by 94%. Think of it this way: For every residency applicant who matched in 2015, there was nearly one complete applicant who didn’t.
21st Century Cures bill passes House
The House has overwhemingly passed the 21st Century Cures Act, H.R. 6, a broad piece of legislation aimed at streamlining the approval process for medical drugs and devices.
The bill, passed by a 344-77 vote on July 10, also aims to spur innovation in biomedical research and to boost funding to the National Institutes of Health.
Changes made prior to the bill’s introduction to the House floor raised the ire of some legislators and included a reduction in NIH funding and the inclusion of Hyde Amendment language that prohibits the use of federal funds for abortions except in the case of rape, incest, or to save the life of the mother. The bill as it stands is not expected to be picked up in the Senate, which is expected to craft its own legislation.
“I am concerned that the very goal of this legislation set out to achieve, to encourage biomedical innovation and the development of new treatment and cures is undermined somewhat by the reduction in funding for NIH from $10 billion to $8.75 billion,” House Energy and Commerce Committee Ranking Member Frank Pallone, D-N.J., said during the floor debate on July 9.
Despite the concerns over the changes to the bill, support for the bill was overwhelmingly voiced throughout the debate.
“It is time now that we as a nation got serious about curing the major diseases – not treating the diseases, but curing the major diseases – that are affecting this country and affecting us personally,” said House Republican Doctors’ Caucus Chairman Phil Roe, R-Tenn. “I am more passionate about this bill and excited about passing the 21st Century Cures bill than anything I have voted on since I have been in the Congress.”
The House has overwhemingly passed the 21st Century Cures Act, H.R. 6, a broad piece of legislation aimed at streamlining the approval process for medical drugs and devices.
The bill, passed by a 344-77 vote on July 10, also aims to spur innovation in biomedical research and to boost funding to the National Institutes of Health.
Changes made prior to the bill’s introduction to the House floor raised the ire of some legislators and included a reduction in NIH funding and the inclusion of Hyde Amendment language that prohibits the use of federal funds for abortions except in the case of rape, incest, or to save the life of the mother. The bill as it stands is not expected to be picked up in the Senate, which is expected to craft its own legislation.
“I am concerned that the very goal of this legislation set out to achieve, to encourage biomedical innovation and the development of new treatment and cures is undermined somewhat by the reduction in funding for NIH from $10 billion to $8.75 billion,” House Energy and Commerce Committee Ranking Member Frank Pallone, D-N.J., said during the floor debate on July 9.
Despite the concerns over the changes to the bill, support for the bill was overwhelmingly voiced throughout the debate.
“It is time now that we as a nation got serious about curing the major diseases – not treating the diseases, but curing the major diseases – that are affecting this country and affecting us personally,” said House Republican Doctors’ Caucus Chairman Phil Roe, R-Tenn. “I am more passionate about this bill and excited about passing the 21st Century Cures bill than anything I have voted on since I have been in the Congress.”
The House has overwhemingly passed the 21st Century Cures Act, H.R. 6, a broad piece of legislation aimed at streamlining the approval process for medical drugs and devices.
The bill, passed by a 344-77 vote on July 10, also aims to spur innovation in biomedical research and to boost funding to the National Institutes of Health.
Changes made prior to the bill’s introduction to the House floor raised the ire of some legislators and included a reduction in NIH funding and the inclusion of Hyde Amendment language that prohibits the use of federal funds for abortions except in the case of rape, incest, or to save the life of the mother. The bill as it stands is not expected to be picked up in the Senate, which is expected to craft its own legislation.
“I am concerned that the very goal of this legislation set out to achieve, to encourage biomedical innovation and the development of new treatment and cures is undermined somewhat by the reduction in funding for NIH from $10 billion to $8.75 billion,” House Energy and Commerce Committee Ranking Member Frank Pallone, D-N.J., said during the floor debate on July 9.
Despite the concerns over the changes to the bill, support for the bill was overwhelmingly voiced throughout the debate.
“It is time now that we as a nation got serious about curing the major diseases – not treating the diseases, but curing the major diseases – that are affecting this country and affecting us personally,” said House Republican Doctors’ Caucus Chairman Phil Roe, R-Tenn. “I am more passionate about this bill and excited about passing the 21st Century Cures bill than anything I have voted on since I have been in the Congress.”
Fee schedule update includes advance care planning, PQRS changes
Physicians are praising a new proposal by the Centers for Medicare & Medicaid Services to pay for end-of-life counseling as part of a sweeping draft of updates to its 2016 physician payment schedule.
The proposed fee schedule – the first since repeal of the Sustainable Growth Rate (SGR) formula and enactment of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – includes modifications to reimbursement policies, changes to misvalued codes, and updates to quality performance metrics for physicians who participate in the Physician Quality Reporting System (PQRS).
As part of the proposal, released on July 8, two new advance care planning codes would be created to pay physicians for time discussing patient options for advance directives. The first code would cover an initial 30 minutes of the doctors’ time, and the second would cover additional 30-minute blocks as necessary.
Dr. Andrew W. Gurman, president-elect of the American Medical Association, said the proposed rule affirms the need to support conversations between doctors and patients about end-of-life wishes before critical medical events occur. The AMA Current Procedural Terminology (CPT) Editorial Panel and the AMA Relative Value Update Committee (RUC) created the new CPT codes and recommended the associated payments for calendar year 2015.
“This is a patient-centered policy intended to support a careful planning process that is assisted by a physician or other qualified health care professional,” Dr. Gurman said in a statement. “This issue has been mischaracterized in the past and it is time to facilitate patient choices about advance care planning decisions.”
The American College of Physicians (ACP) applauded inclusion of the advance care planning codes, calling it an important step to improve care for Medicare patients with serious illnesses.
“The nation’s physicians believe that conversations among physicians, patients, and loved ones is the standard of care,” ACP President Dr. Wayne J. Riley said in a statement. “The College is pleased that CMS has recognized what the medical community is doing to address the needs and requests made by patients and their loved ones.”
CMS’ proposal also includes updates to the PQRS, the federal program that provides incentive payments to eligible professionals and group practices that report data on quality measures for covered services and/or participate in a qualified clinical data registry (QCDR). The proposal would establish criteria for satisfactory reporting similar to that of previous years, including the general reporting of nine measures covering three National Quality Strategy domains.
Eligible professionals and practices who do not report on PQRS standards in 2016 will see their 2018 Medicare pay cut by 2%. The proposed fee schedule also would eliminate measures that are topped out, duplicative, or are being replaced with more robust measures. If the proposal is finalized, 300 total measures in the PQRS program are slated for 2016.
The proposed fee schedule also would modify the the Medicare Shared Savings Program (MSSP) by:
• Allowing participants to add or delete a measure if it no longer aligns with updated clinical practice or causes patient harm.
• Clarifying how PQRS-eligible professionals participating within an ACO can meet PQRS requirements when their ACO satisfactorily reports quality measures.
• Amending the definition of primary care services to include claims submitted by certain teaching hospitals and excluding those submitted by skilled nursing facilities.
The proposed fee schedule also addresses telemedicine services. CMS says it will pay for telemedicine if the treatment is on the list of approved Medicare telehealth services, and if:
• the service is furnished via an interactive telecommunications system.
• The service is furnished by a physician or authorized practitioner.
• The service is furnished to an eligible telehealth patient.
• The patient receiving the service must be located in a telehealth originating site.
If these conditions are met, Medicare will pay a facility fee to the originating site and make separates payment to the distant site health provider furnishing the service.
CMS is also proposing payment changes for certain specialty services based on codes determined to be misvalued. Specifically, physicians who practice radiation therapy, radiation oncology, and gastroenterology would experience significant decreases to payments for services that they frequently furnish as a result of widespread revisions to the Relative Value Unit (RVU) structure used to establish such codes. Other specialties, such as pathology, would experience significant increases to payments for similar reasons, CMS states. The modifications are a result of an initiative to review misvalued codes and establish new and revised codes.
Meanwhile, CMS is seeking feedback on several components of MACRA, including the definition of clinical practice improvement activities and input on how to define a physician-focused payment model. The agency is also asking for feedback on whether to expand the Comprehensive Primary Care Initiative, a 4-year multipayer pilot that aims to strengthen primary care by offering population-based care management fees and shared savings opportunities to participating health providers.
The proposed rule will be published in the Federal Register on July 15; comments will be accepted through Sept. 8.
On Twitter @legal_med
Physicians are praising a new proposal by the Centers for Medicare & Medicaid Services to pay for end-of-life counseling as part of a sweeping draft of updates to its 2016 physician payment schedule.
The proposed fee schedule – the first since repeal of the Sustainable Growth Rate (SGR) formula and enactment of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – includes modifications to reimbursement policies, changes to misvalued codes, and updates to quality performance metrics for physicians who participate in the Physician Quality Reporting System (PQRS).
As part of the proposal, released on July 8, two new advance care planning codes would be created to pay physicians for time discussing patient options for advance directives. The first code would cover an initial 30 minutes of the doctors’ time, and the second would cover additional 30-minute blocks as necessary.
Dr. Andrew W. Gurman, president-elect of the American Medical Association, said the proposed rule affirms the need to support conversations between doctors and patients about end-of-life wishes before critical medical events occur. The AMA Current Procedural Terminology (CPT) Editorial Panel and the AMA Relative Value Update Committee (RUC) created the new CPT codes and recommended the associated payments for calendar year 2015.
“This is a patient-centered policy intended to support a careful planning process that is assisted by a physician or other qualified health care professional,” Dr. Gurman said in a statement. “This issue has been mischaracterized in the past and it is time to facilitate patient choices about advance care planning decisions.”
The American College of Physicians (ACP) applauded inclusion of the advance care planning codes, calling it an important step to improve care for Medicare patients with serious illnesses.
“The nation’s physicians believe that conversations among physicians, patients, and loved ones is the standard of care,” ACP President Dr. Wayne J. Riley said in a statement. “The College is pleased that CMS has recognized what the medical community is doing to address the needs and requests made by patients and their loved ones.”
CMS’ proposal also includes updates to the PQRS, the federal program that provides incentive payments to eligible professionals and group practices that report data on quality measures for covered services and/or participate in a qualified clinical data registry (QCDR). The proposal would establish criteria for satisfactory reporting similar to that of previous years, including the general reporting of nine measures covering three National Quality Strategy domains.
Eligible professionals and practices who do not report on PQRS standards in 2016 will see their 2018 Medicare pay cut by 2%. The proposed fee schedule also would eliminate measures that are topped out, duplicative, or are being replaced with more robust measures. If the proposal is finalized, 300 total measures in the PQRS program are slated for 2016.
The proposed fee schedule also would modify the the Medicare Shared Savings Program (MSSP) by:
• Allowing participants to add or delete a measure if it no longer aligns with updated clinical practice or causes patient harm.
• Clarifying how PQRS-eligible professionals participating within an ACO can meet PQRS requirements when their ACO satisfactorily reports quality measures.
• Amending the definition of primary care services to include claims submitted by certain teaching hospitals and excluding those submitted by skilled nursing facilities.
The proposed fee schedule also addresses telemedicine services. CMS says it will pay for telemedicine if the treatment is on the list of approved Medicare telehealth services, and if:
• the service is furnished via an interactive telecommunications system.
• The service is furnished by a physician or authorized practitioner.
• The service is furnished to an eligible telehealth patient.
• The patient receiving the service must be located in a telehealth originating site.
If these conditions are met, Medicare will pay a facility fee to the originating site and make separates payment to the distant site health provider furnishing the service.
CMS is also proposing payment changes for certain specialty services based on codes determined to be misvalued. Specifically, physicians who practice radiation therapy, radiation oncology, and gastroenterology would experience significant decreases to payments for services that they frequently furnish as a result of widespread revisions to the Relative Value Unit (RVU) structure used to establish such codes. Other specialties, such as pathology, would experience significant increases to payments for similar reasons, CMS states. The modifications are a result of an initiative to review misvalued codes and establish new and revised codes.
Meanwhile, CMS is seeking feedback on several components of MACRA, including the definition of clinical practice improvement activities and input on how to define a physician-focused payment model. The agency is also asking for feedback on whether to expand the Comprehensive Primary Care Initiative, a 4-year multipayer pilot that aims to strengthen primary care by offering population-based care management fees and shared savings opportunities to participating health providers.
The proposed rule will be published in the Federal Register on July 15; comments will be accepted through Sept. 8.
On Twitter @legal_med
Physicians are praising a new proposal by the Centers for Medicare & Medicaid Services to pay for end-of-life counseling as part of a sweeping draft of updates to its 2016 physician payment schedule.
The proposed fee schedule – the first since repeal of the Sustainable Growth Rate (SGR) formula and enactment of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – includes modifications to reimbursement policies, changes to misvalued codes, and updates to quality performance metrics for physicians who participate in the Physician Quality Reporting System (PQRS).
As part of the proposal, released on July 8, two new advance care planning codes would be created to pay physicians for time discussing patient options for advance directives. The first code would cover an initial 30 minutes of the doctors’ time, and the second would cover additional 30-minute blocks as necessary.
Dr. Andrew W. Gurman, president-elect of the American Medical Association, said the proposed rule affirms the need to support conversations between doctors and patients about end-of-life wishes before critical medical events occur. The AMA Current Procedural Terminology (CPT) Editorial Panel and the AMA Relative Value Update Committee (RUC) created the new CPT codes and recommended the associated payments for calendar year 2015.
“This is a patient-centered policy intended to support a careful planning process that is assisted by a physician or other qualified health care professional,” Dr. Gurman said in a statement. “This issue has been mischaracterized in the past and it is time to facilitate patient choices about advance care planning decisions.”
The American College of Physicians (ACP) applauded inclusion of the advance care planning codes, calling it an important step to improve care for Medicare patients with serious illnesses.
“The nation’s physicians believe that conversations among physicians, patients, and loved ones is the standard of care,” ACP President Dr. Wayne J. Riley said in a statement. “The College is pleased that CMS has recognized what the medical community is doing to address the needs and requests made by patients and their loved ones.”
CMS’ proposal also includes updates to the PQRS, the federal program that provides incentive payments to eligible professionals and group practices that report data on quality measures for covered services and/or participate in a qualified clinical data registry (QCDR). The proposal would establish criteria for satisfactory reporting similar to that of previous years, including the general reporting of nine measures covering three National Quality Strategy domains.
Eligible professionals and practices who do not report on PQRS standards in 2016 will see their 2018 Medicare pay cut by 2%. The proposed fee schedule also would eliminate measures that are topped out, duplicative, or are being replaced with more robust measures. If the proposal is finalized, 300 total measures in the PQRS program are slated for 2016.
The proposed fee schedule also would modify the the Medicare Shared Savings Program (MSSP) by:
• Allowing participants to add or delete a measure if it no longer aligns with updated clinical practice or causes patient harm.
• Clarifying how PQRS-eligible professionals participating within an ACO can meet PQRS requirements when their ACO satisfactorily reports quality measures.
• Amending the definition of primary care services to include claims submitted by certain teaching hospitals and excluding those submitted by skilled nursing facilities.
The proposed fee schedule also addresses telemedicine services. CMS says it will pay for telemedicine if the treatment is on the list of approved Medicare telehealth services, and if:
• the service is furnished via an interactive telecommunications system.
• The service is furnished by a physician or authorized practitioner.
• The service is furnished to an eligible telehealth patient.
• The patient receiving the service must be located in a telehealth originating site.
If these conditions are met, Medicare will pay a facility fee to the originating site and make separates payment to the distant site health provider furnishing the service.
CMS is also proposing payment changes for certain specialty services based on codes determined to be misvalued. Specifically, physicians who practice radiation therapy, radiation oncology, and gastroenterology would experience significant decreases to payments for services that they frequently furnish as a result of widespread revisions to the Relative Value Unit (RVU) structure used to establish such codes. Other specialties, such as pathology, would experience significant increases to payments for similar reasons, CMS states. The modifications are a result of an initiative to review misvalued codes and establish new and revised codes.
Meanwhile, CMS is seeking feedback on several components of MACRA, including the definition of clinical practice improvement activities and input on how to define a physician-focused payment model. The agency is also asking for feedback on whether to expand the Comprehensive Primary Care Initiative, a 4-year multipayer pilot that aims to strengthen primary care by offering population-based care management fees and shared savings opportunities to participating health providers.
The proposed rule will be published in the Federal Register on July 15; comments will be accepted through Sept. 8.
On Twitter @legal_med
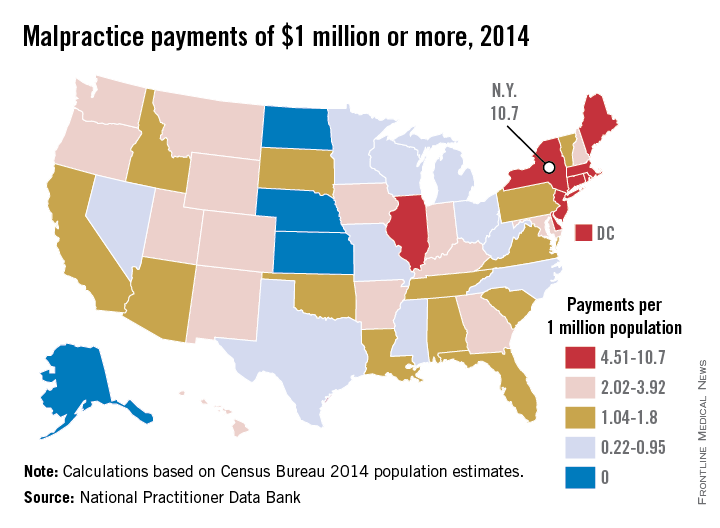
Where are the really big malpractice awards?
Everything may be bigger in Texas, but New York is the biggest in at least one area: large medical malpractice payments. New York had more than three times as many $1 million–plus malpractice awards as any other state in 2014, according to data from the National Practitioner Data Bank.
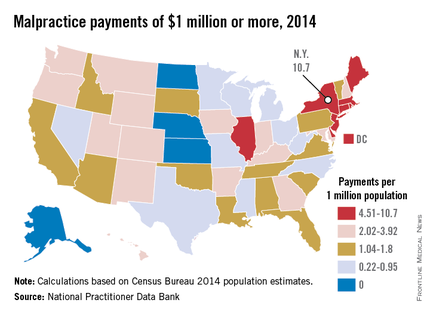
New York physicians had 210 malpractice payments of $1 million or more reported to the NPDB last year, compared with 61 for Illinois, the next-highest state. Rounding out the top five were Massachusetts with 49, followed by California with 43 and New Jersey with 41, the NPDB data show.
After taking population into account, New York was still the leader with 10.66 large awards per million residents. Next in this category was the New England trio of Rhode Island, which had 9.42 such payments per 1 million population; Massachusetts (7.26); and Connecticut (6.39).
In 2014, there were four states that had no malpractice payments of at least $1 million reported to the NPDB: Alaska, Kansas, North Dakota, and Nebraska, with Kansas having the largest population. In states with at least one $1 million–plus malpractice payment, Texas physicians had the lowest rate per million population, 0.22 – just 6 awards from a population of 27 million.
Everything may be bigger in Texas, but New York is the biggest in at least one area: large medical malpractice payments. New York had more than three times as many $1 million–plus malpractice awards as any other state in 2014, according to data from the National Practitioner Data Bank.
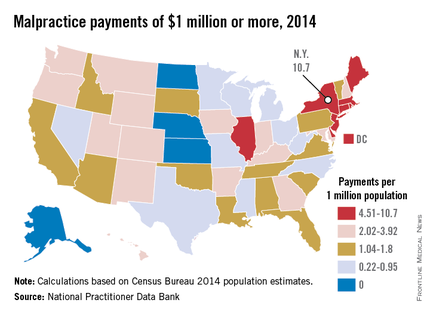
New York physicians had 210 malpractice payments of $1 million or more reported to the NPDB last year, compared with 61 for Illinois, the next-highest state. Rounding out the top five were Massachusetts with 49, followed by California with 43 and New Jersey with 41, the NPDB data show.
After taking population into account, New York was still the leader with 10.66 large awards per million residents. Next in this category was the New England trio of Rhode Island, which had 9.42 such payments per 1 million population; Massachusetts (7.26); and Connecticut (6.39).
In 2014, there were four states that had no malpractice payments of at least $1 million reported to the NPDB: Alaska, Kansas, North Dakota, and Nebraska, with Kansas having the largest population. In states with at least one $1 million–plus malpractice payment, Texas physicians had the lowest rate per million population, 0.22 – just 6 awards from a population of 27 million.
Everything may be bigger in Texas, but New York is the biggest in at least one area: large medical malpractice payments. New York had more than three times as many $1 million–plus malpractice awards as any other state in 2014, according to data from the National Practitioner Data Bank.
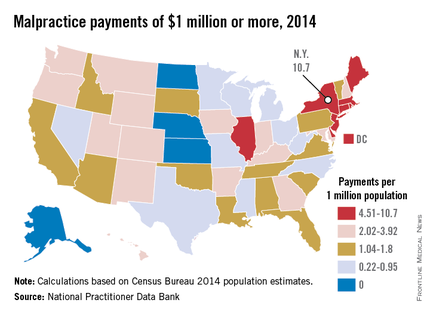
New York physicians had 210 malpractice payments of $1 million or more reported to the NPDB last year, compared with 61 for Illinois, the next-highest state. Rounding out the top five were Massachusetts with 49, followed by California with 43 and New Jersey with 41, the NPDB data show.
After taking population into account, New York was still the leader with 10.66 large awards per million residents. Next in this category was the New England trio of Rhode Island, which had 9.42 such payments per 1 million population; Massachusetts (7.26); and Connecticut (6.39).
In 2014, there were four states that had no malpractice payments of at least $1 million reported to the NPDB: Alaska, Kansas, North Dakota, and Nebraska, with Kansas having the largest population. In states with at least one $1 million–plus malpractice payment, Texas physicians had the lowest rate per million population, 0.22 – just 6 awards from a population of 27 million.
LISTEN NOW: Hospitalist, Edwin Lopez, PA-C, on Post-Acute Care in the U.S. Health System
Edwin Lopez, PA-C, of St. Elizabeth Hospital in Enumclaw, Wash., offers his views on post-acute care in the U.S. health system, and how his work as a hospitalist has expanded to the nursing home across the street.
Edwin Lopez, PA-C, of St. Elizabeth Hospital in Enumclaw, Wash., offers his views on post-acute care in the U.S. health system, and how his work as a hospitalist has expanded to the nursing home across the street.
Edwin Lopez, PA-C, of St. Elizabeth Hospital in Enumclaw, Wash., offers his views on post-acute care in the U.S. health system, and how his work as a hospitalist has expanded to the nursing home across the street.
CMS pledges flexibility during first year of ICD-10
Physicians will have a year to learn how to properly code under ICD-10 before facing potential penalties or withheld payments, according to a joint announcement from the Centers for Medicare & Medicaid Services and the American Medical Association.
During that first year using the new coding system, Medicare will not deny claims based solely on the specificity of diagnosis codes, provided they are in the appropriate family of ICD-10 codes. However, physicians still will not be able to use ICD-9 codes after Sept. 30, 2015.
“This means that Medicare will not deny payment for these unintentional errors as practices become accustomed to ICD-10 coding,” Dr. Steven Stack, AMA president, wrote in a blog post on the AMA website. “This transition period will give physicians and their practice teams time to get up to speed on the more complicated code set.”
Similarly, physicians will not face penalties under the Physician Quality Reporting System, the value-based modifier, or the meaningful use program based on the specificity of diagnosis codes if the appropriate family of ICD-10 codes are used, according to the AMA. Finally, if a Medicare contractor is unable to process a claim due to coding issues, CMS will authorize an advance payment to the physician.
CMS also plans to create an ICD-10 coordination center and appoint an ombudsman to answer questions about claims submission using ICD-10.
“With easy-to-use tools, a new ICD-10 ombudsman, and added flexibility in our claims audit and quality reporting process, CMS is committed to working with the physician community to work through this transition.” Andy Slavitt, CMS Acting Administrator, said in a statement.
Physicians will have a year to learn how to properly code under ICD-10 before facing potential penalties or withheld payments, according to a joint announcement from the Centers for Medicare & Medicaid Services and the American Medical Association.
During that first year using the new coding system, Medicare will not deny claims based solely on the specificity of diagnosis codes, provided they are in the appropriate family of ICD-10 codes. However, physicians still will not be able to use ICD-9 codes after Sept. 30, 2015.
“This means that Medicare will not deny payment for these unintentional errors as practices become accustomed to ICD-10 coding,” Dr. Steven Stack, AMA president, wrote in a blog post on the AMA website. “This transition period will give physicians and their practice teams time to get up to speed on the more complicated code set.”
Similarly, physicians will not face penalties under the Physician Quality Reporting System, the value-based modifier, or the meaningful use program based on the specificity of diagnosis codes if the appropriate family of ICD-10 codes are used, according to the AMA. Finally, if a Medicare contractor is unable to process a claim due to coding issues, CMS will authorize an advance payment to the physician.
CMS also plans to create an ICD-10 coordination center and appoint an ombudsman to answer questions about claims submission using ICD-10.
“With easy-to-use tools, a new ICD-10 ombudsman, and added flexibility in our claims audit and quality reporting process, CMS is committed to working with the physician community to work through this transition.” Andy Slavitt, CMS Acting Administrator, said in a statement.
Physicians will have a year to learn how to properly code under ICD-10 before facing potential penalties or withheld payments, according to a joint announcement from the Centers for Medicare & Medicaid Services and the American Medical Association.
During that first year using the new coding system, Medicare will not deny claims based solely on the specificity of diagnosis codes, provided they are in the appropriate family of ICD-10 codes. However, physicians still will not be able to use ICD-9 codes after Sept. 30, 2015.
“This means that Medicare will not deny payment for these unintentional errors as practices become accustomed to ICD-10 coding,” Dr. Steven Stack, AMA president, wrote in a blog post on the AMA website. “This transition period will give physicians and their practice teams time to get up to speed on the more complicated code set.”
Similarly, physicians will not face penalties under the Physician Quality Reporting System, the value-based modifier, or the meaningful use program based on the specificity of diagnosis codes if the appropriate family of ICD-10 codes are used, according to the AMA. Finally, if a Medicare contractor is unable to process a claim due to coding issues, CMS will authorize an advance payment to the physician.
CMS also plans to create an ICD-10 coordination center and appoint an ombudsman to answer questions about claims submission using ICD-10.
“With easy-to-use tools, a new ICD-10 ombudsman, and added flexibility in our claims audit and quality reporting process, CMS is committed to working with the physician community to work through this transition.” Andy Slavitt, CMS Acting Administrator, said in a statement.
Survey: Most health care organizations had a recent security breach
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
More than two-thirds of health care organizations responding to a survey have experienced a significant and recent security event, according to the Health Information and Management Systems Society (HIMSS).
The single largest source of significant security incidents were negligent insiders, defined as well-meaning individuals who unwittingly caused a breach. However, 64% of respondents reported that their organization had been the victim of an attack from an external actor – usually an online scam artist. The results are part of the 2015 HIMSS Cybersecurity Survey, which polled 297 health care leaders and information security officers.
Most of the security incidents resulted in limited disruption of IT systems with limited impact on clinical care, according to the report. The majority of respondents said security incidents were detected within 24 hours of occurrence, “approximately 20% of these security incidents ultimately resulted in loss of patient, financial, or operational data.”
While security breaches may seem like an IT issue, Jennifer Horowitz, senior director of research at HIMSS, said physicians need to be aware of what they can do to help keep their systems secure.
“This is a rapidly changing environment and I think that physicians also need ... to do their part: adhering to the security policies and protocols as their organization,” Ms. Horowitz said in an interivew, highlighting particularly that physicians need to be aware of potential phishing scams sent via email that could comprompise data security.
CMS considers easing two-midnight rule for hospital stays
Medicare officials are proposing to ease the requirements of the so-called two-midnight rule governing how the agency pays for short hospital stays, deferring more to the medical judgment of the admitting physician.
For stays in which the physician expects the patient to need less than two midnights of hospital care for procedures not on the inpatient only list or listed as a national exception, “an inpatient submission would be payable under Medicare Part A on a case-by-case basis based on the judgment of the admitting physician. The documentation in the medical record must support that an inpatient admission is necessary, and is subject to medical review,” officials at the Centers for Medicare & Medicaid Services wrote in a fact sheet.
The change is included in the proposed annual update to the Hospital Outpatient Prospective Payment System. The proposed rule is scheduled to be published July 8 in the Federal Register, but was made available online July 1.
It would be “rare and unusual for a beneficiary to require inpatient hospital admission for a minor surgical procedure or other treatment in the hospital that is expected to keep him or her in the hospital for a period of time that is only a few hours and does not span at least overnight,” CMS added.
Medicare’s payment policy would not change when hospital stays span two midnights or longer, the agency said.
The proposal comes after extensive input from physicians and hospitals, as well as the results of “probe and educate” audits. Currently, CMS policy states that stays of at least two midnights are generally paid under Medicare Part A, while stays that are expected to be shorter are classified as outpatient stays and are paid under Medicare Part B.
Enforcement for this two-midnight policy would also shift under the proposal. Quality improvement organizations (QIOs) rather than Medicare administrative contractors (MACs) or recovery auditors would conduct first-line medical reviews of providers submitting claims for inpatient admissions. Recovery auditors will conduct reviews for those hospitals that have consistently high denial rates based on QIO patient status review outcomes.
“QIOs have a significant history of collaborating with hospitals and other stakeholders to ensure high quality care for beneficiaries,” CMS stated.
Overall, the proposed Hospital Outpatient Prospective Payment System update is expected to result in a –0.2% adjustment for hospital payments in 2016, which includes a 2.7% projected hospital market basket increase minus adjustments for multifactor productivity and other required cuts.
Medicare officials are proposing to ease the requirements of the so-called two-midnight rule governing how the agency pays for short hospital stays, deferring more to the medical judgment of the admitting physician.
For stays in which the physician expects the patient to need less than two midnights of hospital care for procedures not on the inpatient only list or listed as a national exception, “an inpatient submission would be payable under Medicare Part A on a case-by-case basis based on the judgment of the admitting physician. The documentation in the medical record must support that an inpatient admission is necessary, and is subject to medical review,” officials at the Centers for Medicare & Medicaid Services wrote in a fact sheet.
The change is included in the proposed annual update to the Hospital Outpatient Prospective Payment System. The proposed rule is scheduled to be published July 8 in the Federal Register, but was made available online July 1.
It would be “rare and unusual for a beneficiary to require inpatient hospital admission for a minor surgical procedure or other treatment in the hospital that is expected to keep him or her in the hospital for a period of time that is only a few hours and does not span at least overnight,” CMS added.
Medicare’s payment policy would not change when hospital stays span two midnights or longer, the agency said.
The proposal comes after extensive input from physicians and hospitals, as well as the results of “probe and educate” audits. Currently, CMS policy states that stays of at least two midnights are generally paid under Medicare Part A, while stays that are expected to be shorter are classified as outpatient stays and are paid under Medicare Part B.
Enforcement for this two-midnight policy would also shift under the proposal. Quality improvement organizations (QIOs) rather than Medicare administrative contractors (MACs) or recovery auditors would conduct first-line medical reviews of providers submitting claims for inpatient admissions. Recovery auditors will conduct reviews for those hospitals that have consistently high denial rates based on QIO patient status review outcomes.
“QIOs have a significant history of collaborating with hospitals and other stakeholders to ensure high quality care for beneficiaries,” CMS stated.
Overall, the proposed Hospital Outpatient Prospective Payment System update is expected to result in a –0.2% adjustment for hospital payments in 2016, which includes a 2.7% projected hospital market basket increase minus adjustments for multifactor productivity and other required cuts.
Medicare officials are proposing to ease the requirements of the so-called two-midnight rule governing how the agency pays for short hospital stays, deferring more to the medical judgment of the admitting physician.
For stays in which the physician expects the patient to need less than two midnights of hospital care for procedures not on the inpatient only list or listed as a national exception, “an inpatient submission would be payable under Medicare Part A on a case-by-case basis based on the judgment of the admitting physician. The documentation in the medical record must support that an inpatient admission is necessary, and is subject to medical review,” officials at the Centers for Medicare & Medicaid Services wrote in a fact sheet.
The change is included in the proposed annual update to the Hospital Outpatient Prospective Payment System. The proposed rule is scheduled to be published July 8 in the Federal Register, but was made available online July 1.
It would be “rare and unusual for a beneficiary to require inpatient hospital admission for a minor surgical procedure or other treatment in the hospital that is expected to keep him or her in the hospital for a period of time that is only a few hours and does not span at least overnight,” CMS added.
Medicare’s payment policy would not change when hospital stays span two midnights or longer, the agency said.
The proposal comes after extensive input from physicians and hospitals, as well as the results of “probe and educate” audits. Currently, CMS policy states that stays of at least two midnights are generally paid under Medicare Part A, while stays that are expected to be shorter are classified as outpatient stays and are paid under Medicare Part B.
Enforcement for this two-midnight policy would also shift under the proposal. Quality improvement organizations (QIOs) rather than Medicare administrative contractors (MACs) or recovery auditors would conduct first-line medical reviews of providers submitting claims for inpatient admissions. Recovery auditors will conduct reviews for those hospitals that have consistently high denial rates based on QIO patient status review outcomes.
“QIOs have a significant history of collaborating with hospitals and other stakeholders to ensure high quality care for beneficiaries,” CMS stated.
Overall, the proposed Hospital Outpatient Prospective Payment System update is expected to result in a –0.2% adjustment for hospital payments in 2016, which includes a 2.7% projected hospital market basket increase minus adjustments for multifactor productivity and other required cuts.
Hospital Medicine's Old Practices Become New Again
The musty collections of National Geographic magazines once found in so many basements are largely gone. Replacing them are dusty sets of the Advisory Board binders and booklets found in hospital administration offices around the country. I think the same principle drives the impulse to collect both publications—the idea that they contain worthwhile information that one day will be reviewed. But I think it’s more likely they will be ignored until it is time to move and someone has to decide what to do with the painfully heavy pile of paper.
Lots of old and largely forgotten things are making a comeback in healthcare. I suppose this is always happening, but I sense we’re now experiencing more of this than usual. It’s a renaissance of sorts.
I first heard about fecal transplant for Clostridium difficile infection (instilling a “better” microbiome in the hope of realizing many benefits) about six or eight years ago. Although I was sure this was a new idea, my retired internist father told me this had been around when he was in training. Wikipedia says that four Colorado surgeons published a paper about it in 1958 and that the Chinese were doing this 1,600 years ago.
PCPs Visit Hospitalized Patients
Writing in the NEJM earlier this year, Goroll and Hunt proposed that primary care physicians visit their hospitalized patients in the role of consultant while the hospitalist remains attending. As they note, this idea surfaced as soon as the hospitalist model began taking hold. Back then, we usually referred to it as a “social visit” by the PCP. Anecdotal experience from my work with hundreds of hospitalist groups tells me that such visits have all but disappeared. But nearly every such PCP visit on a patient I’ve cared for has seemed worthwhile; in many cases, these hospital calls simply reassure a nervous patient or family member, and occasionally they ensure that the PCP and I arrive at a more effective plan of care than we might otherwise.
Perhaps new forms of healthcare reimbursement, accountable care, and population health may make “continuity visits” economically viable for PCPs. Wouldn’t it be interesting if PCP visits to hospitalized patients and hospitalist visits to outpatients, such as those occurring in a pre-op clinic or a skilled nursing facility, become commonplace? The trick in all of this will be to ensure the right amount of overlap, or shared visits, between PCP and hospitalist without expensive duplication of effort or errors stemming from too many cooks in the kitchen.
Post-Hospital Follow-Up Schedules
When I began practicing as a hospitalist in the 1980s, doctors routinely wrote orders similar to this one: “Have patient follow up with Dr. Smith (PCP or specialist) in 1-2 weeks.” The unit secretary or other hospital clerical staff would contact the physician’s office to schedule the appointment, and the patient would leave the hospital with a written reminder in hand. My sense is that nearly all hospitals had been doing this for decades; somehow this practice has nearly disappeared over the last 10-20 years, however, and I sometimes hear this old practice discussed as a new idea.
I think making sure the patient has a follow-up appointment in hand when leaving the hospital is likely good for clinical outcomes, readmissions, and patient satisfaction. In my view, it is hardly worth lots of research to prove the benefit of what should be a relatively low-cost intervention. Why not just have providers write orders detailing follow-up with a specific doctor or clinic and a timeframe, and have unit secretaries communicate with outpatient clinics to schedule the appointments and ensure that the details are provided to the patient, maybe via an EHR-generated after visit summary? Seems pretty easy, right?
Turns out it isn’t easy at all for most hospitals. Lots of energetic hospitalists have taken on a project like this, only to run into so many brick walls. One hospitalist told me recently that the unit secretary’s labor union at her hospital refused to allow it. So some hospitals have turned to a single person, or a small group of people, who make appointments for all hospital patients. Some hospitalist groups have one of their own staff make appointments for hospitalist patients. This relieves the unit secretaries of the task but requires additional funding for the salaries of these people.
Maybe, at some time not so far off, EHRs will be so user-friendly and patients/families so accustomed to using them that it will be common for patients/families to arrange the appointments on their own. It could even be a required step—a hard stop—in the discharge process.
Whatever emerges as the most common method of making these appointments, I think it is safe to say this old practice will become “new” and common within the next few years.
Multidisciplinary Rounds
While working as an orderly in the 1970s, I would often visit with the nurses in their break room. When a doctor arrived to make rounds on the floor, the RN would jump up, stub out her cigarette, and round with the doctor. I sometimes tagged along as an observer. The nurse let the doctor know just how the patient had been doing and provided test results and any other relevant information the doctor might need. The doctor would provide orders, and sometimes the nurse wrote them into the chart (think of today’s medical scribes). Although their interaction was much less collaborative than is typical today, they did ask lots of questions of one another to clarify ambiguities.
I think these 1970s caregivers were doing effective multidisciplinary rounds. But by the late 1980s or so, as both doctor and nurse became busier, they stopped rounding together.
I smile when I hear descriptions of this “new” idea of doctor and nurse (and often other caregivers) rounding together. Today’s hospital culture is less hierarchical than the 1970s, though some would say it still has a ways to go, so teamwork and multidisciplinary rounds may yield more benefit than decades ago. But the idea of rounding together certainly isn’t new.
As we try to figure out the best way to thrive in a rapidly changing healthcare environment, we may find value in returning to the old ways of doing some things.

The musty collections of National Geographic magazines once found in so many basements are largely gone. Replacing them are dusty sets of the Advisory Board binders and booklets found in hospital administration offices around the country. I think the same principle drives the impulse to collect both publications—the idea that they contain worthwhile information that one day will be reviewed. But I think it’s more likely they will be ignored until it is time to move and someone has to decide what to do with the painfully heavy pile of paper.
Lots of old and largely forgotten things are making a comeback in healthcare. I suppose this is always happening, but I sense we’re now experiencing more of this than usual. It’s a renaissance of sorts.
I first heard about fecal transplant for Clostridium difficile infection (instilling a “better” microbiome in the hope of realizing many benefits) about six or eight years ago. Although I was sure this was a new idea, my retired internist father told me this had been around when he was in training. Wikipedia says that four Colorado surgeons published a paper about it in 1958 and that the Chinese were doing this 1,600 years ago.
PCPs Visit Hospitalized Patients
Writing in the NEJM earlier this year, Goroll and Hunt proposed that primary care physicians visit their hospitalized patients in the role of consultant while the hospitalist remains attending. As they note, this idea surfaced as soon as the hospitalist model began taking hold. Back then, we usually referred to it as a “social visit” by the PCP. Anecdotal experience from my work with hundreds of hospitalist groups tells me that such visits have all but disappeared. But nearly every such PCP visit on a patient I’ve cared for has seemed worthwhile; in many cases, these hospital calls simply reassure a nervous patient or family member, and occasionally they ensure that the PCP and I arrive at a more effective plan of care than we might otherwise.
Perhaps new forms of healthcare reimbursement, accountable care, and population health may make “continuity visits” economically viable for PCPs. Wouldn’t it be interesting if PCP visits to hospitalized patients and hospitalist visits to outpatients, such as those occurring in a pre-op clinic or a skilled nursing facility, become commonplace? The trick in all of this will be to ensure the right amount of overlap, or shared visits, between PCP and hospitalist without expensive duplication of effort or errors stemming from too many cooks in the kitchen.
Post-Hospital Follow-Up Schedules
When I began practicing as a hospitalist in the 1980s, doctors routinely wrote orders similar to this one: “Have patient follow up with Dr. Smith (PCP or specialist) in 1-2 weeks.” The unit secretary or other hospital clerical staff would contact the physician’s office to schedule the appointment, and the patient would leave the hospital with a written reminder in hand. My sense is that nearly all hospitals had been doing this for decades; somehow this practice has nearly disappeared over the last 10-20 years, however, and I sometimes hear this old practice discussed as a new idea.
I think making sure the patient has a follow-up appointment in hand when leaving the hospital is likely good for clinical outcomes, readmissions, and patient satisfaction. In my view, it is hardly worth lots of research to prove the benefit of what should be a relatively low-cost intervention. Why not just have providers write orders detailing follow-up with a specific doctor or clinic and a timeframe, and have unit secretaries communicate with outpatient clinics to schedule the appointments and ensure that the details are provided to the patient, maybe via an EHR-generated after visit summary? Seems pretty easy, right?
Turns out it isn’t easy at all for most hospitals. Lots of energetic hospitalists have taken on a project like this, only to run into so many brick walls. One hospitalist told me recently that the unit secretary’s labor union at her hospital refused to allow it. So some hospitals have turned to a single person, or a small group of people, who make appointments for all hospital patients. Some hospitalist groups have one of their own staff make appointments for hospitalist patients. This relieves the unit secretaries of the task but requires additional funding for the salaries of these people.
Maybe, at some time not so far off, EHRs will be so user-friendly and patients/families so accustomed to using them that it will be common for patients/families to arrange the appointments on their own. It could even be a required step—a hard stop—in the discharge process.
Whatever emerges as the most common method of making these appointments, I think it is safe to say this old practice will become “new” and common within the next few years.
Multidisciplinary Rounds
While working as an orderly in the 1970s, I would often visit with the nurses in their break room. When a doctor arrived to make rounds on the floor, the RN would jump up, stub out her cigarette, and round with the doctor. I sometimes tagged along as an observer. The nurse let the doctor know just how the patient had been doing and provided test results and any other relevant information the doctor might need. The doctor would provide orders, and sometimes the nurse wrote them into the chart (think of today’s medical scribes). Although their interaction was much less collaborative than is typical today, they did ask lots of questions of one another to clarify ambiguities.
I think these 1970s caregivers were doing effective multidisciplinary rounds. But by the late 1980s or so, as both doctor and nurse became busier, they stopped rounding together.
I smile when I hear descriptions of this “new” idea of doctor and nurse (and often other caregivers) rounding together. Today’s hospital culture is less hierarchical than the 1970s, though some would say it still has a ways to go, so teamwork and multidisciplinary rounds may yield more benefit than decades ago. But the idea of rounding together certainly isn’t new.
As we try to figure out the best way to thrive in a rapidly changing healthcare environment, we may find value in returning to the old ways of doing some things.

The musty collections of National Geographic magazines once found in so many basements are largely gone. Replacing them are dusty sets of the Advisory Board binders and booklets found in hospital administration offices around the country. I think the same principle drives the impulse to collect both publications—the idea that they contain worthwhile information that one day will be reviewed. But I think it’s more likely they will be ignored until it is time to move and someone has to decide what to do with the painfully heavy pile of paper.
Lots of old and largely forgotten things are making a comeback in healthcare. I suppose this is always happening, but I sense we’re now experiencing more of this than usual. It’s a renaissance of sorts.
I first heard about fecal transplant for Clostridium difficile infection (instilling a “better” microbiome in the hope of realizing many benefits) about six or eight years ago. Although I was sure this was a new idea, my retired internist father told me this had been around when he was in training. Wikipedia says that four Colorado surgeons published a paper about it in 1958 and that the Chinese were doing this 1,600 years ago.
PCPs Visit Hospitalized Patients
Writing in the NEJM earlier this year, Goroll and Hunt proposed that primary care physicians visit their hospitalized patients in the role of consultant while the hospitalist remains attending. As they note, this idea surfaced as soon as the hospitalist model began taking hold. Back then, we usually referred to it as a “social visit” by the PCP. Anecdotal experience from my work with hundreds of hospitalist groups tells me that such visits have all but disappeared. But nearly every such PCP visit on a patient I’ve cared for has seemed worthwhile; in many cases, these hospital calls simply reassure a nervous patient or family member, and occasionally they ensure that the PCP and I arrive at a more effective plan of care than we might otherwise.
Perhaps new forms of healthcare reimbursement, accountable care, and population health may make “continuity visits” economically viable for PCPs. Wouldn’t it be interesting if PCP visits to hospitalized patients and hospitalist visits to outpatients, such as those occurring in a pre-op clinic or a skilled nursing facility, become commonplace? The trick in all of this will be to ensure the right amount of overlap, or shared visits, between PCP and hospitalist without expensive duplication of effort or errors stemming from too many cooks in the kitchen.
Post-Hospital Follow-Up Schedules
When I began practicing as a hospitalist in the 1980s, doctors routinely wrote orders similar to this one: “Have patient follow up with Dr. Smith (PCP or specialist) in 1-2 weeks.” The unit secretary or other hospital clerical staff would contact the physician’s office to schedule the appointment, and the patient would leave the hospital with a written reminder in hand. My sense is that nearly all hospitals had been doing this for decades; somehow this practice has nearly disappeared over the last 10-20 years, however, and I sometimes hear this old practice discussed as a new idea.
I think making sure the patient has a follow-up appointment in hand when leaving the hospital is likely good for clinical outcomes, readmissions, and patient satisfaction. In my view, it is hardly worth lots of research to prove the benefit of what should be a relatively low-cost intervention. Why not just have providers write orders detailing follow-up with a specific doctor or clinic and a timeframe, and have unit secretaries communicate with outpatient clinics to schedule the appointments and ensure that the details are provided to the patient, maybe via an EHR-generated after visit summary? Seems pretty easy, right?
Turns out it isn’t easy at all for most hospitals. Lots of energetic hospitalists have taken on a project like this, only to run into so many brick walls. One hospitalist told me recently that the unit secretary’s labor union at her hospital refused to allow it. So some hospitals have turned to a single person, or a small group of people, who make appointments for all hospital patients. Some hospitalist groups have one of their own staff make appointments for hospitalist patients. This relieves the unit secretaries of the task but requires additional funding for the salaries of these people.
Maybe, at some time not so far off, EHRs will be so user-friendly and patients/families so accustomed to using them that it will be common for patients/families to arrange the appointments on their own. It could even be a required step—a hard stop—in the discharge process.
Whatever emerges as the most common method of making these appointments, I think it is safe to say this old practice will become “new” and common within the next few years.
Multidisciplinary Rounds
While working as an orderly in the 1970s, I would often visit with the nurses in their break room. When a doctor arrived to make rounds on the floor, the RN would jump up, stub out her cigarette, and round with the doctor. I sometimes tagged along as an observer. The nurse let the doctor know just how the patient had been doing and provided test results and any other relevant information the doctor might need. The doctor would provide orders, and sometimes the nurse wrote them into the chart (think of today’s medical scribes). Although their interaction was much less collaborative than is typical today, they did ask lots of questions of one another to clarify ambiguities.
I think these 1970s caregivers were doing effective multidisciplinary rounds. But by the late 1980s or so, as both doctor and nurse became busier, they stopped rounding together.
I smile when I hear descriptions of this “new” idea of doctor and nurse (and often other caregivers) rounding together. Today’s hospital culture is less hierarchical than the 1970s, though some would say it still has a ways to go, so teamwork and multidisciplinary rounds may yield more benefit than decades ago. But the idea of rounding together certainly isn’t new.
As we try to figure out the best way to thrive in a rapidly changing healthcare environment, we may find value in returning to the old ways of doing some things.