User login
ICD-10 Medical Coding System Likely to Improve Documentation, Reimbursement
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
Post-Acute Patient Care Offers Opportunities for Non-Physicians
More than in the inpatient setting, post-acute care offers opportunities for nurse practitioners and physician assistants to play important clinical and administrative roles. Physician assistant (PA) Edwin Lopez, PA-C, is chief of an eight-member HM group—four doctors, four PAs—that provides coverage at St. Elizabeth, a rural critical access hospital in Enumclaw, Wash., population 10,669, and in the 80-bed SNF located across the street. Lopez was recruited to establish the HM group “in the shadow of Mt. Rainier” about eight years ago, at a time when the hospital’s parent, CHI Franciscan Health System, was trying to rebuild its quality and reputation while planning a new building.
He succeeded, dramatically improving its performance on HCAHPS surveys and other metrics; however, hospital readmissions then emerged as an issue.
“I began to realize, with our little facility’s large population of elderly patients with multiple chronic problems—typically the highest cohort for readmissions—all the gains we had made could be lost if we didn’t do something about this problem,” Lopez says. “I ran the numbers and found that the nursing home across the street readmitted 35% of patients discharged from our hospital.”
It took a year to get the larger system’s approval, but Lopez’s hospitalist group manages all the patients transferred to the nearby nursing home, with daily visits by the doctor and/or PA on duty.
“We started the program in January 2014, and, in one year, readmissions went from 35% down to 7%,” he says. “We developed culturally from the very beginning as a PA/MD collaborative model. The doctor doesn’t need to see the more routine patients with more common conditions but instead is freed up to focus on higher-acuity, more complex patients.”
In Dr. Tollman’s opinion, physician extenders “own” the post-acute realm, because of the demand for their care.
“There just aren’t going to be enough doctors for all of the patients who need to be seen,” he says, “and the amount of money for this care isn’t enough for these facilities to employ groups of doctors.”
Emily Rosenbaum, PA-C, works for Northwest Community Healthcare in Arlington Heights, Ill. She is the lone PA working with eight physician hospitalists. Much of her work is in a rehabilitation facility across the street from Northwest Community Hospital.
“I see all of the new admissions, although under my scope of practice I can’t bill for the initial visit. But I do the follow-ups, see patients that have been in rehab for 30 days or less, and put out [clinical] fires in the facility,” she says.
Rosenbaum works at the hospital part of her day taking care of acute patients, then works with the hospitalist assigned to the rehabilitation facility.
“It’s easier for me to go back and forth and keep my finger on the patients’ pulse,” she says. “As there are more demands on doctors on the acute side, it’s natural for the NP and PA to step up and take a larger role on the post-acute side.”
More than in the inpatient setting, post-acute care offers opportunities for nurse practitioners and physician assistants to play important clinical and administrative roles. Physician assistant (PA) Edwin Lopez, PA-C, is chief of an eight-member HM group—four doctors, four PAs—that provides coverage at St. Elizabeth, a rural critical access hospital in Enumclaw, Wash., population 10,669, and in the 80-bed SNF located across the street. Lopez was recruited to establish the HM group “in the shadow of Mt. Rainier” about eight years ago, at a time when the hospital’s parent, CHI Franciscan Health System, was trying to rebuild its quality and reputation while planning a new building.
He succeeded, dramatically improving its performance on HCAHPS surveys and other metrics; however, hospital readmissions then emerged as an issue.
“I began to realize, with our little facility’s large population of elderly patients with multiple chronic problems—typically the highest cohort for readmissions—all the gains we had made could be lost if we didn’t do something about this problem,” Lopez says. “I ran the numbers and found that the nursing home across the street readmitted 35% of patients discharged from our hospital.”
It took a year to get the larger system’s approval, but Lopez’s hospitalist group manages all the patients transferred to the nearby nursing home, with daily visits by the doctor and/or PA on duty.
“We started the program in January 2014, and, in one year, readmissions went from 35% down to 7%,” he says. “We developed culturally from the very beginning as a PA/MD collaborative model. The doctor doesn’t need to see the more routine patients with more common conditions but instead is freed up to focus on higher-acuity, more complex patients.”
In Dr. Tollman’s opinion, physician extenders “own” the post-acute realm, because of the demand for their care.
“There just aren’t going to be enough doctors for all of the patients who need to be seen,” he says, “and the amount of money for this care isn’t enough for these facilities to employ groups of doctors.”
Emily Rosenbaum, PA-C, works for Northwest Community Healthcare in Arlington Heights, Ill. She is the lone PA working with eight physician hospitalists. Much of her work is in a rehabilitation facility across the street from Northwest Community Hospital.
“I see all of the new admissions, although under my scope of practice I can’t bill for the initial visit. But I do the follow-ups, see patients that have been in rehab for 30 days or less, and put out [clinical] fires in the facility,” she says.
Rosenbaum works at the hospital part of her day taking care of acute patients, then works with the hospitalist assigned to the rehabilitation facility.
“It’s easier for me to go back and forth and keep my finger on the patients’ pulse,” she says. “As there are more demands on doctors on the acute side, it’s natural for the NP and PA to step up and take a larger role on the post-acute side.”
More than in the inpatient setting, post-acute care offers opportunities for nurse practitioners and physician assistants to play important clinical and administrative roles. Physician assistant (PA) Edwin Lopez, PA-C, is chief of an eight-member HM group—four doctors, four PAs—that provides coverage at St. Elizabeth, a rural critical access hospital in Enumclaw, Wash., population 10,669, and in the 80-bed SNF located across the street. Lopez was recruited to establish the HM group “in the shadow of Mt. Rainier” about eight years ago, at a time when the hospital’s parent, CHI Franciscan Health System, was trying to rebuild its quality and reputation while planning a new building.
He succeeded, dramatically improving its performance on HCAHPS surveys and other metrics; however, hospital readmissions then emerged as an issue.
“I began to realize, with our little facility’s large population of elderly patients with multiple chronic problems—typically the highest cohort for readmissions—all the gains we had made could be lost if we didn’t do something about this problem,” Lopez says. “I ran the numbers and found that the nursing home across the street readmitted 35% of patients discharged from our hospital.”
It took a year to get the larger system’s approval, but Lopez’s hospitalist group manages all the patients transferred to the nearby nursing home, with daily visits by the doctor and/or PA on duty.
“We started the program in January 2014, and, in one year, readmissions went from 35% down to 7%,” he says. “We developed culturally from the very beginning as a PA/MD collaborative model. The doctor doesn’t need to see the more routine patients with more common conditions but instead is freed up to focus on higher-acuity, more complex patients.”
In Dr. Tollman’s opinion, physician extenders “own” the post-acute realm, because of the demand for their care.
“There just aren’t going to be enough doctors for all of the patients who need to be seen,” he says, “and the amount of money for this care isn’t enough for these facilities to employ groups of doctors.”
Emily Rosenbaum, PA-C, works for Northwest Community Healthcare in Arlington Heights, Ill. She is the lone PA working with eight physician hospitalists. Much of her work is in a rehabilitation facility across the street from Northwest Community Hospital.
“I see all of the new admissions, although under my scope of practice I can’t bill for the initial visit. But I do the follow-ups, see patients that have been in rehab for 30 days or less, and put out [clinical] fires in the facility,” she says.
Rosenbaum works at the hospital part of her day taking care of acute patients, then works with the hospitalist assigned to the rehabilitation facility.
“It’s easier for me to go back and forth and keep my finger on the patients’ pulse,” she says. “As there are more demands on doctors on the acute side, it’s natural for the NP and PA to step up and take a larger role on the post-acute side.”
11 Things Gastroenterologists Think Hospitalists Need to Know
So many symptoms that are staples of gastroenterology—chest pain, nausea, diarrhea—are mainstay causes for hospitalization that it might be worth fine-tuning how well you handle patients with gastroenterology disorders.
The Hospitalist asked several gastroenterologists for their guidance on better care and their suggestions for correcting some common mistakes that they encounter. Here are their tips:
1 Fluid resuscitation is crucial for pancreatitis patients.
It’s very important to rehydrate these patients within the first 24 hours, because those who remain underhydrated can have a worse prognosis, says Robert Coben, MD, academic coordinator for the Gastroentestinal Fellowship Program at Thomas Jefferson University Hospital in Philadelphia. On occasion, physicians are reluctant to give extra fluids to these patients, he says, particularly if they have heart failure or suffer kidney problems. A 70-kg patient should be receiving about 200 cc per hour, he notes.
“Sometimes we’ll walk in the room and they’re getting 80 cc an hour,” Dr. Coben says.
“These patients…need to be flooded with fluids,” says Rajeev Jain, MD, chief of gastroenterology at Presbyterian Hospital of Dallas, partner at Texas Digestive Disease Consultants, and chair of the Practice Management and Economics Committee of the American Gastroenterological Association. “We’re talking sometimes liters and liters of IV normal saline or lactated Ringer’s (solution) in a 24-hour period.”1
Marcelo Vela, MD, a gastroenterologist and hepatologist at the Mayo Clinic in Scottsdale, Ariz., and an associate editor with Clinical Gastroenterology and Hepatology, says Ringer’s solution is a better choice than normal saline.2
“If you’re going to start IV fluids on somebody who’s coming in with acute pancreatitis, Ringer’s solution has been shown to be superior to saline in randomized controlled trials,” Dr. Vela says. “It reduces systemic inflammation.”
2 Gastrointestinal bleeding decisions
When inpatients have gastrointestinal bleeding, the hospitalist often has to assess its severity and make the call on whether a patient needs the ICU.
“The most important thing for that is obviously the vital signs,” says John Pandolfino, MD, chief of the division of medicine–gastroenterology and hepatology at Northwestern University Feinberg School of Medicine in Chicago. “If people are tachycardic and they’re not responding to hydration and blood transfusion, that usually means it’s a pretty active bleed and they need to go to the intensive care unit. If you have somebody who’s GI bleeding and they’re coagulopathic (i.e., they’re on anti-coagulation because they have a valve and they need anti-coagulation or they have cancer or bad cardiovascular disease), those are the people that you should have a low threshold for sending to the intensive care unit with a GI bleed; those are the people who are at a very high mortality [risk].”
He added that those with an ulcer, with a visible vessel, are at a high-risk of a rebleed and should spend some time in the ICU.
“Those people should be evaluated in the intensive care unit for at least 24 hours, maybe even 72 hours,” Dr. Pandolfino says, “and they should have IV PPI [proton pump inhibitor] therapy.”
3 Endoscopy has very low yield for diagnosis of reflux.
“Endoscopy has good yield for mucosa abnormalities on inspection of the esophageal mucosa, but it does not give you a diagnosis of reflux, especially on patients who have already been treated with a PPI,” says Prakash Gyawali, MD, MRCP, professor of gastroenterology at Washington University in St. Louis, Mo. “So, usually, in those settings, obtaining a consult or trying to decide exactly what you’re looking for to explain the symptoms has better yield than an endoscopy.”
Sometimes a pH study is needed, but that has to be planned, because patients may have to be taken off of a PPI in advance. That means those studies are not easy to set up in the hospital and might best be arranged by the gastroenterologist, Dr. Gyawali says.
4 In cases of acute diarrhea, order a stool sample right away.
That will help guide care from the gastroenterologist, if and when the gastroenterologist is called in, Dr. Pandolfino says.
“One of the things that is frustrating for the gastroenterologist is that we get called initially, but really the hospitalist should be getting stool studies, and they should have at least a very good idea of what they need from us,” he says. “Because, really, endoscopy is not usually needed very often in diagnosis of acute diarrhea.”
Broad-range stool studies, a good history and physical, and examining labs for a possible chronic inflammatory process or anemia are good ways to begin to assess patients with diarrhea, he says. Clostridium difficile colitis has to be considered as well, Dr. Pandolfino says.
Endoscopy is more helpful in evaluating acute diarrhea in those with bloody diarrhea suspected of having inflammatory bowel disease or an infectious diarrhea but on whom cultures have come back negative. For those with compromised immune systems, endoscopy could be done earlier, as well.
“So for us, I think we really need to get into the picture a little bit after the patient has been brought into the hospital and the stool study is negative, unless they’re an immune-compromised patient,” Dr. Pandolfino says.
5 When—and how—to test the stool.
If a patient develops diarrhea while already in the hospital, the only stool test needed is C. diff.
“They shouldn’t be developing a viral diarrhea, they shouldn’t be developing an infectious diarrhea—let’s say, from E. coli or Salmonella—unless they literally developed it a couple hours after getting in,” Dr. Jain says. “It should either be C. diff or a side effect of some medication. … We don’t need to spend the extra money, which is of low-value care to send for OVA and parasites, or bacterial pathogens and so forth.”
Dr. Jain says he thinks such testing is being done more appropriately of late.
“But I still will see multiple stool tests sent on somebody who’s been in the hospital for a week and then develops diarrhea,” he explains.
6 Gastroenterologists do not need to be consulted for every C. diff infection.
“I think that we really should get involved when patients are either not responding or when they’re very ill,” Dr. Pandolfino says.
Hospitalists should consider whether patients are on antibiotics or a PPI and whether or not they need to stay on those medications. Also, medications that slow motility (i.e., loperamide) should be avoided, if possible.
“We don’t want it to linger,” Dr. Pandolfino says. “One of the basic mechanisms of how we get rid of pathogens is to expel them with diarrhea.
“But you certainly don’t want the patient to be uncomfortable to the point where they’re having 20 to 30 bowel movements a day.”
In non-severe patients who have some diarrhea, abdominal pain, nausea, and vomiting—but are able to keep food down—the specialists might not have to be called in, and patients can just be treated with oral metronidazole or oral vancomycin fairly simply, he says.
For those who seem severely ill with a dilating colon, are in nearly a septic state, and have very severe diarrhea, the gastroenterologist should probably be called in, he says.

7 For patients with a possible GI bleed and black stools, do an exam before calling in the gastroenterologist.
The exam should determine what the stool color is and whether it is heme-positive, and the patient’s blood count should be evaluated, Dr. Coben says.
Frequently, “the consultant’s the one who ends up doing the rectal exam and checking that,” he says. “Sometimes we find that [the patient is] really not bleeding,” and it was just a case of a hospitalist taking the patient’s word that they were bleeding.
Being on iron therapy or taking Pepto-Bismol can turn the stool black, and the stool might not really be black; colors can sometimes be open to interpretation.
But he cautions that colon cancer could be the cause for a GI bleed.
“We’ve had it happen a few times where this occurred,” he says. “The patient was discharged, and they really didn’t get proper follow-up, and it ended up that they had a colon cancer. It kind of delayed that diagnosis. So I think you have to be aware of [the fact that], especially in somebody over the age of 40 or 50, if they have an iron-deficiency, anemia, or heme-positive stool, the first thing you really need to exclude is a colon cancer.”
8 Minimize CT scans in early evaluation and management of acute pancreatitis patients.
“The reason for that is they tend to be intravascularly volume-depleted,” Dr. Jain says. “So [with] the IV contrast, there’s an increased risk of developing kidney failure. It’s also been associated with increased risk of necrotizing pancreatitis.”
Dr. Jain notes that when he is consulted on this kind of patient, he will order a sonogram. If it doesn’t show gallstones, and there’s no clear reason for the pancreatitis, he will want a CT scan, but he will wait a few days until the patient is fluid-resuscitated.
Dr. Jain says that this is a problem more often seen in the ED—where 90% of patients with acute pancreatitis have already gotten the CT scan—and less so among hospitalists, but it’s still worth the reminder.
A CT scan right away is justified to rule out something such as a perforation, but not in the case of classic symptoms of acute pancreatitis, he adds.
9 Actively bleeding patients?
It’s smart to give patients a unit of packed red blood cells more quickly if they’re actively bleeding. Even over just one hour is OK, Dr. Jain says.
“Even if they have underlying heart failure, if they’re volume-depleted, they need that volume,” Dr. Jain explains. “Sometimes you’ll see that it takes eight hours to get two units of blood in. That’s inadequate.”
Another point worth a reminder, he says: Two large-bore peripheral IV’s are “much, much better” than a central or PICC line to deliver IV fluid resuscitation.
“Sometimes hospitalists order barium studies because these can be done the same day, whereas with endoscopy, patients need to be put on a schedule and have to be NPO [nothing by mouth] overnight.” —Prakash Gyawali, MD, MRCP
10 Don’t be too quick to order barium studies, especially in patients with dysphagia.
“The problem with that is it takes much longer to do an endoscopy if barium is put in the esophagus, because we usually wait until the barium clears,” Dr. Gyawali says. “And inpatient evaluation of new-onset dysphagia should be endoscopy first, and not barium, because biopsies need to be taken to rule out eosinophilic esophagitis.
“Sometimes hospitalists order barium studies because these can be done the same day, whereas with endoscopy, patients need to be put on a schedule and have to be NPO [nothing by mouth] overnight.”
11 Gastric-emptying studies should be outpatient.
Gastric-emptying studies are often better done when patients are not in a hospital, experts say, because they might be on medications that would interfere with the study.
“A common issue, not just among hospitalists but also gastroenterologists, is that patients may be on a bunch of medicines that would affect stomach-emptying while they are in-house for some other problem,” Dr. Gyawali says. “A lot of times, these patients with pain may get narcotics. They may be on medicines to prevent them from throwing up. … And all of these will slow down gastric emptying.”
With an abnormal test result, “you are left to decide whether that is a real abnormality or whether the medicines the patients were on impacted the abnormality.”
If emptying was significantly prolonged, the test may have some value, “but then it probably will need to be corroborated with symptoms and with endoscopic findings.”
Thomas Collins is a freelance writer in South Florida.
References
- Warndorf MG, Kurtzman JT, Bartel MJ, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9(8):705-709.
- Wu BU, Hwang JQ, Gardner TH, et al. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9(8):710-717.
So many symptoms that are staples of gastroenterology—chest pain, nausea, diarrhea—are mainstay causes for hospitalization that it might be worth fine-tuning how well you handle patients with gastroenterology disorders.
The Hospitalist asked several gastroenterologists for their guidance on better care and their suggestions for correcting some common mistakes that they encounter. Here are their tips:
1 Fluid resuscitation is crucial for pancreatitis patients.
It’s very important to rehydrate these patients within the first 24 hours, because those who remain underhydrated can have a worse prognosis, says Robert Coben, MD, academic coordinator for the Gastroentestinal Fellowship Program at Thomas Jefferson University Hospital in Philadelphia. On occasion, physicians are reluctant to give extra fluids to these patients, he says, particularly if they have heart failure or suffer kidney problems. A 70-kg patient should be receiving about 200 cc per hour, he notes.
“Sometimes we’ll walk in the room and they’re getting 80 cc an hour,” Dr. Coben says.
“These patients…need to be flooded with fluids,” says Rajeev Jain, MD, chief of gastroenterology at Presbyterian Hospital of Dallas, partner at Texas Digestive Disease Consultants, and chair of the Practice Management and Economics Committee of the American Gastroenterological Association. “We’re talking sometimes liters and liters of IV normal saline or lactated Ringer’s (solution) in a 24-hour period.”1
Marcelo Vela, MD, a gastroenterologist and hepatologist at the Mayo Clinic in Scottsdale, Ariz., and an associate editor with Clinical Gastroenterology and Hepatology, says Ringer’s solution is a better choice than normal saline.2
“If you’re going to start IV fluids on somebody who’s coming in with acute pancreatitis, Ringer’s solution has been shown to be superior to saline in randomized controlled trials,” Dr. Vela says. “It reduces systemic inflammation.”
2 Gastrointestinal bleeding decisions
When inpatients have gastrointestinal bleeding, the hospitalist often has to assess its severity and make the call on whether a patient needs the ICU.
“The most important thing for that is obviously the vital signs,” says John Pandolfino, MD, chief of the division of medicine–gastroenterology and hepatology at Northwestern University Feinberg School of Medicine in Chicago. “If people are tachycardic and they’re not responding to hydration and blood transfusion, that usually means it’s a pretty active bleed and they need to go to the intensive care unit. If you have somebody who’s GI bleeding and they’re coagulopathic (i.e., they’re on anti-coagulation because they have a valve and they need anti-coagulation or they have cancer or bad cardiovascular disease), those are the people that you should have a low threshold for sending to the intensive care unit with a GI bleed; those are the people who are at a very high mortality [risk].”
He added that those with an ulcer, with a visible vessel, are at a high-risk of a rebleed and should spend some time in the ICU.
“Those people should be evaluated in the intensive care unit for at least 24 hours, maybe even 72 hours,” Dr. Pandolfino says, “and they should have IV PPI [proton pump inhibitor] therapy.”
3 Endoscopy has very low yield for diagnosis of reflux.
“Endoscopy has good yield for mucosa abnormalities on inspection of the esophageal mucosa, but it does not give you a diagnosis of reflux, especially on patients who have already been treated with a PPI,” says Prakash Gyawali, MD, MRCP, professor of gastroenterology at Washington University in St. Louis, Mo. “So, usually, in those settings, obtaining a consult or trying to decide exactly what you’re looking for to explain the symptoms has better yield than an endoscopy.”
Sometimes a pH study is needed, but that has to be planned, because patients may have to be taken off of a PPI in advance. That means those studies are not easy to set up in the hospital and might best be arranged by the gastroenterologist, Dr. Gyawali says.
4 In cases of acute diarrhea, order a stool sample right away.
That will help guide care from the gastroenterologist, if and when the gastroenterologist is called in, Dr. Pandolfino says.
“One of the things that is frustrating for the gastroenterologist is that we get called initially, but really the hospitalist should be getting stool studies, and they should have at least a very good idea of what they need from us,” he says. “Because, really, endoscopy is not usually needed very often in diagnosis of acute diarrhea.”
Broad-range stool studies, a good history and physical, and examining labs for a possible chronic inflammatory process or anemia are good ways to begin to assess patients with diarrhea, he says. Clostridium difficile colitis has to be considered as well, Dr. Pandolfino says.
Endoscopy is more helpful in evaluating acute diarrhea in those with bloody diarrhea suspected of having inflammatory bowel disease or an infectious diarrhea but on whom cultures have come back negative. For those with compromised immune systems, endoscopy could be done earlier, as well.
“So for us, I think we really need to get into the picture a little bit after the patient has been brought into the hospital and the stool study is negative, unless they’re an immune-compromised patient,” Dr. Pandolfino says.
5 When—and how—to test the stool.
If a patient develops diarrhea while already in the hospital, the only stool test needed is C. diff.
“They shouldn’t be developing a viral diarrhea, they shouldn’t be developing an infectious diarrhea—let’s say, from E. coli or Salmonella—unless they literally developed it a couple hours after getting in,” Dr. Jain says. “It should either be C. diff or a side effect of some medication. … We don’t need to spend the extra money, which is of low-value care to send for OVA and parasites, or bacterial pathogens and so forth.”
Dr. Jain says he thinks such testing is being done more appropriately of late.
“But I still will see multiple stool tests sent on somebody who’s been in the hospital for a week and then develops diarrhea,” he explains.
6 Gastroenterologists do not need to be consulted for every C. diff infection.
“I think that we really should get involved when patients are either not responding or when they’re very ill,” Dr. Pandolfino says.
Hospitalists should consider whether patients are on antibiotics or a PPI and whether or not they need to stay on those medications. Also, medications that slow motility (i.e., loperamide) should be avoided, if possible.
“We don’t want it to linger,” Dr. Pandolfino says. “One of the basic mechanisms of how we get rid of pathogens is to expel them with diarrhea.
“But you certainly don’t want the patient to be uncomfortable to the point where they’re having 20 to 30 bowel movements a day.”
In non-severe patients who have some diarrhea, abdominal pain, nausea, and vomiting—but are able to keep food down—the specialists might not have to be called in, and patients can just be treated with oral metronidazole or oral vancomycin fairly simply, he says.
For those who seem severely ill with a dilating colon, are in nearly a septic state, and have very severe diarrhea, the gastroenterologist should probably be called in, he says.

7 For patients with a possible GI bleed and black stools, do an exam before calling in the gastroenterologist.
The exam should determine what the stool color is and whether it is heme-positive, and the patient’s blood count should be evaluated, Dr. Coben says.
Frequently, “the consultant’s the one who ends up doing the rectal exam and checking that,” he says. “Sometimes we find that [the patient is] really not bleeding,” and it was just a case of a hospitalist taking the patient’s word that they were bleeding.
Being on iron therapy or taking Pepto-Bismol can turn the stool black, and the stool might not really be black; colors can sometimes be open to interpretation.
But he cautions that colon cancer could be the cause for a GI bleed.
“We’ve had it happen a few times where this occurred,” he says. “The patient was discharged, and they really didn’t get proper follow-up, and it ended up that they had a colon cancer. It kind of delayed that diagnosis. So I think you have to be aware of [the fact that], especially in somebody over the age of 40 or 50, if they have an iron-deficiency, anemia, or heme-positive stool, the first thing you really need to exclude is a colon cancer.”
8 Minimize CT scans in early evaluation and management of acute pancreatitis patients.
“The reason for that is they tend to be intravascularly volume-depleted,” Dr. Jain says. “So [with] the IV contrast, there’s an increased risk of developing kidney failure. It’s also been associated with increased risk of necrotizing pancreatitis.”
Dr. Jain notes that when he is consulted on this kind of patient, he will order a sonogram. If it doesn’t show gallstones, and there’s no clear reason for the pancreatitis, he will want a CT scan, but he will wait a few days until the patient is fluid-resuscitated.
Dr. Jain says that this is a problem more often seen in the ED—where 90% of patients with acute pancreatitis have already gotten the CT scan—and less so among hospitalists, but it’s still worth the reminder.
A CT scan right away is justified to rule out something such as a perforation, but not in the case of classic symptoms of acute pancreatitis, he adds.
9 Actively bleeding patients?
It’s smart to give patients a unit of packed red blood cells more quickly if they’re actively bleeding. Even over just one hour is OK, Dr. Jain says.
“Even if they have underlying heart failure, if they’re volume-depleted, they need that volume,” Dr. Jain explains. “Sometimes you’ll see that it takes eight hours to get two units of blood in. That’s inadequate.”
Another point worth a reminder, he says: Two large-bore peripheral IV’s are “much, much better” than a central or PICC line to deliver IV fluid resuscitation.
“Sometimes hospitalists order barium studies because these can be done the same day, whereas with endoscopy, patients need to be put on a schedule and have to be NPO [nothing by mouth] overnight.” —Prakash Gyawali, MD, MRCP
10 Don’t be too quick to order barium studies, especially in patients with dysphagia.
“The problem with that is it takes much longer to do an endoscopy if barium is put in the esophagus, because we usually wait until the barium clears,” Dr. Gyawali says. “And inpatient evaluation of new-onset dysphagia should be endoscopy first, and not barium, because biopsies need to be taken to rule out eosinophilic esophagitis.
“Sometimes hospitalists order barium studies because these can be done the same day, whereas with endoscopy, patients need to be put on a schedule and have to be NPO [nothing by mouth] overnight.”
11 Gastric-emptying studies should be outpatient.
Gastric-emptying studies are often better done when patients are not in a hospital, experts say, because they might be on medications that would interfere with the study.
“A common issue, not just among hospitalists but also gastroenterologists, is that patients may be on a bunch of medicines that would affect stomach-emptying while they are in-house for some other problem,” Dr. Gyawali says. “A lot of times, these patients with pain may get narcotics. They may be on medicines to prevent them from throwing up. … And all of these will slow down gastric emptying.”
With an abnormal test result, “you are left to decide whether that is a real abnormality or whether the medicines the patients were on impacted the abnormality.”
If emptying was significantly prolonged, the test may have some value, “but then it probably will need to be corroborated with symptoms and with endoscopic findings.”
Thomas Collins is a freelance writer in South Florida.
References
- Warndorf MG, Kurtzman JT, Bartel MJ, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9(8):705-709.
- Wu BU, Hwang JQ, Gardner TH, et al. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9(8):710-717.
So many symptoms that are staples of gastroenterology—chest pain, nausea, diarrhea—are mainstay causes for hospitalization that it might be worth fine-tuning how well you handle patients with gastroenterology disorders.
The Hospitalist asked several gastroenterologists for their guidance on better care and their suggestions for correcting some common mistakes that they encounter. Here are their tips:
1 Fluid resuscitation is crucial for pancreatitis patients.
It’s very important to rehydrate these patients within the first 24 hours, because those who remain underhydrated can have a worse prognosis, says Robert Coben, MD, academic coordinator for the Gastroentestinal Fellowship Program at Thomas Jefferson University Hospital in Philadelphia. On occasion, physicians are reluctant to give extra fluids to these patients, he says, particularly if they have heart failure or suffer kidney problems. A 70-kg patient should be receiving about 200 cc per hour, he notes.
“Sometimes we’ll walk in the room and they’re getting 80 cc an hour,” Dr. Coben says.
“These patients…need to be flooded with fluids,” says Rajeev Jain, MD, chief of gastroenterology at Presbyterian Hospital of Dallas, partner at Texas Digestive Disease Consultants, and chair of the Practice Management and Economics Committee of the American Gastroenterological Association. “We’re talking sometimes liters and liters of IV normal saline or lactated Ringer’s (solution) in a 24-hour period.”1
Marcelo Vela, MD, a gastroenterologist and hepatologist at the Mayo Clinic in Scottsdale, Ariz., and an associate editor with Clinical Gastroenterology and Hepatology, says Ringer’s solution is a better choice than normal saline.2
“If you’re going to start IV fluids on somebody who’s coming in with acute pancreatitis, Ringer’s solution has been shown to be superior to saline in randomized controlled trials,” Dr. Vela says. “It reduces systemic inflammation.”
2 Gastrointestinal bleeding decisions
When inpatients have gastrointestinal bleeding, the hospitalist often has to assess its severity and make the call on whether a patient needs the ICU.
“The most important thing for that is obviously the vital signs,” says John Pandolfino, MD, chief of the division of medicine–gastroenterology and hepatology at Northwestern University Feinberg School of Medicine in Chicago. “If people are tachycardic and they’re not responding to hydration and blood transfusion, that usually means it’s a pretty active bleed and they need to go to the intensive care unit. If you have somebody who’s GI bleeding and they’re coagulopathic (i.e., they’re on anti-coagulation because they have a valve and they need anti-coagulation or they have cancer or bad cardiovascular disease), those are the people that you should have a low threshold for sending to the intensive care unit with a GI bleed; those are the people who are at a very high mortality [risk].”
He added that those with an ulcer, with a visible vessel, are at a high-risk of a rebleed and should spend some time in the ICU.
“Those people should be evaluated in the intensive care unit for at least 24 hours, maybe even 72 hours,” Dr. Pandolfino says, “and they should have IV PPI [proton pump inhibitor] therapy.”
3 Endoscopy has very low yield for diagnosis of reflux.
“Endoscopy has good yield for mucosa abnormalities on inspection of the esophageal mucosa, but it does not give you a diagnosis of reflux, especially on patients who have already been treated with a PPI,” says Prakash Gyawali, MD, MRCP, professor of gastroenterology at Washington University in St. Louis, Mo. “So, usually, in those settings, obtaining a consult or trying to decide exactly what you’re looking for to explain the symptoms has better yield than an endoscopy.”
Sometimes a pH study is needed, but that has to be planned, because patients may have to be taken off of a PPI in advance. That means those studies are not easy to set up in the hospital and might best be arranged by the gastroenterologist, Dr. Gyawali says.
4 In cases of acute diarrhea, order a stool sample right away.
That will help guide care from the gastroenterologist, if and when the gastroenterologist is called in, Dr. Pandolfino says.
“One of the things that is frustrating for the gastroenterologist is that we get called initially, but really the hospitalist should be getting stool studies, and they should have at least a very good idea of what they need from us,” he says. “Because, really, endoscopy is not usually needed very often in diagnosis of acute diarrhea.”
Broad-range stool studies, a good history and physical, and examining labs for a possible chronic inflammatory process or anemia are good ways to begin to assess patients with diarrhea, he says. Clostridium difficile colitis has to be considered as well, Dr. Pandolfino says.
Endoscopy is more helpful in evaluating acute diarrhea in those with bloody diarrhea suspected of having inflammatory bowel disease or an infectious diarrhea but on whom cultures have come back negative. For those with compromised immune systems, endoscopy could be done earlier, as well.
“So for us, I think we really need to get into the picture a little bit after the patient has been brought into the hospital and the stool study is negative, unless they’re an immune-compromised patient,” Dr. Pandolfino says.
5 When—and how—to test the stool.
If a patient develops diarrhea while already in the hospital, the only stool test needed is C. diff.
“They shouldn’t be developing a viral diarrhea, they shouldn’t be developing an infectious diarrhea—let’s say, from E. coli or Salmonella—unless they literally developed it a couple hours after getting in,” Dr. Jain says. “It should either be C. diff or a side effect of some medication. … We don’t need to spend the extra money, which is of low-value care to send for OVA and parasites, or bacterial pathogens and so forth.”
Dr. Jain says he thinks such testing is being done more appropriately of late.
“But I still will see multiple stool tests sent on somebody who’s been in the hospital for a week and then develops diarrhea,” he explains.
6 Gastroenterologists do not need to be consulted for every C. diff infection.
“I think that we really should get involved when patients are either not responding or when they’re very ill,” Dr. Pandolfino says.
Hospitalists should consider whether patients are on antibiotics or a PPI and whether or not they need to stay on those medications. Also, medications that slow motility (i.e., loperamide) should be avoided, if possible.
“We don’t want it to linger,” Dr. Pandolfino says. “One of the basic mechanisms of how we get rid of pathogens is to expel them with diarrhea.
“But you certainly don’t want the patient to be uncomfortable to the point where they’re having 20 to 30 bowel movements a day.”
In non-severe patients who have some diarrhea, abdominal pain, nausea, and vomiting—but are able to keep food down—the specialists might not have to be called in, and patients can just be treated with oral metronidazole or oral vancomycin fairly simply, he says.
For those who seem severely ill with a dilating colon, are in nearly a septic state, and have very severe diarrhea, the gastroenterologist should probably be called in, he says.

7 For patients with a possible GI bleed and black stools, do an exam before calling in the gastroenterologist.
The exam should determine what the stool color is and whether it is heme-positive, and the patient’s blood count should be evaluated, Dr. Coben says.
Frequently, “the consultant’s the one who ends up doing the rectal exam and checking that,” he says. “Sometimes we find that [the patient is] really not bleeding,” and it was just a case of a hospitalist taking the patient’s word that they were bleeding.
Being on iron therapy or taking Pepto-Bismol can turn the stool black, and the stool might not really be black; colors can sometimes be open to interpretation.
But he cautions that colon cancer could be the cause for a GI bleed.
“We’ve had it happen a few times where this occurred,” he says. “The patient was discharged, and they really didn’t get proper follow-up, and it ended up that they had a colon cancer. It kind of delayed that diagnosis. So I think you have to be aware of [the fact that], especially in somebody over the age of 40 or 50, if they have an iron-deficiency, anemia, or heme-positive stool, the first thing you really need to exclude is a colon cancer.”
8 Minimize CT scans in early evaluation and management of acute pancreatitis patients.
“The reason for that is they tend to be intravascularly volume-depleted,” Dr. Jain says. “So [with] the IV contrast, there’s an increased risk of developing kidney failure. It’s also been associated with increased risk of necrotizing pancreatitis.”
Dr. Jain notes that when he is consulted on this kind of patient, he will order a sonogram. If it doesn’t show gallstones, and there’s no clear reason for the pancreatitis, he will want a CT scan, but he will wait a few days until the patient is fluid-resuscitated.
Dr. Jain says that this is a problem more often seen in the ED—where 90% of patients with acute pancreatitis have already gotten the CT scan—and less so among hospitalists, but it’s still worth the reminder.
A CT scan right away is justified to rule out something such as a perforation, but not in the case of classic symptoms of acute pancreatitis, he adds.
9 Actively bleeding patients?
It’s smart to give patients a unit of packed red blood cells more quickly if they’re actively bleeding. Even over just one hour is OK, Dr. Jain says.
“Even if they have underlying heart failure, if they’re volume-depleted, they need that volume,” Dr. Jain explains. “Sometimes you’ll see that it takes eight hours to get two units of blood in. That’s inadequate.”
Another point worth a reminder, he says: Two large-bore peripheral IV’s are “much, much better” than a central or PICC line to deliver IV fluid resuscitation.
“Sometimes hospitalists order barium studies because these can be done the same day, whereas with endoscopy, patients need to be put on a schedule and have to be NPO [nothing by mouth] overnight.” —Prakash Gyawali, MD, MRCP
10 Don’t be too quick to order barium studies, especially in patients with dysphagia.
“The problem with that is it takes much longer to do an endoscopy if barium is put in the esophagus, because we usually wait until the barium clears,” Dr. Gyawali says. “And inpatient evaluation of new-onset dysphagia should be endoscopy first, and not barium, because biopsies need to be taken to rule out eosinophilic esophagitis.
“Sometimes hospitalists order barium studies because these can be done the same day, whereas with endoscopy, patients need to be put on a schedule and have to be NPO [nothing by mouth] overnight.”
11 Gastric-emptying studies should be outpatient.
Gastric-emptying studies are often better done when patients are not in a hospital, experts say, because they might be on medications that would interfere with the study.
“A common issue, not just among hospitalists but also gastroenterologists, is that patients may be on a bunch of medicines that would affect stomach-emptying while they are in-house for some other problem,” Dr. Gyawali says. “A lot of times, these patients with pain may get narcotics. They may be on medicines to prevent them from throwing up. … And all of these will slow down gastric emptying.”
With an abnormal test result, “you are left to decide whether that is a real abnormality or whether the medicines the patients were on impacted the abnormality.”
If emptying was significantly prolonged, the test may have some value, “but then it probably will need to be corroborated with symptoms and with endoscopic findings.”
Thomas Collins is a freelance writer in South Florida.
References
- Warndorf MG, Kurtzman JT, Bartel MJ, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9(8):705-709.
- Wu BU, Hwang JQ, Gardner TH, et al. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9(8):710-717.
CMS improves Open Payments system, but not enough
Improvements to the Open Payments reporting system are welcome, but don’t go far enough.
That was the message from the American Medical Association upon the July 1 release of another round of data in the financial disclosure system created by the Affordable Care Act.
CMS “has improved our interface for both collecting and reporting this data about compensation and other payments between drug and medical device manufacturers and physicians and teaching hospitals,” Dr. Shantanu Agrawal, CMS deputy administrator and director of the Center for Program Integrity, said in a statement.
“While we appreciate the efforts of the Centers for Medicare & Medicaid Services to verify the data submitted by industry, the complicated and cumbersome process for physicians to register to review their data and seek correction of any inaccuracies continues to hinder their participation in the validation process,” the AMA said in a statement.
Dr. David O. Barbe, a family physician in Mountain Grove, Mo., noted that “the ability to navigate [Open Payments] has substantially improved since the first iteration of this. You can get around the website pretty well. ... You can sort the data. You can search on individuals. You can sort it by large amounts, either by individual physician or by payer.”
However, the approach used still makes it extremely difficult for determining the validity and accuracy of the information that is being presented, said Dr. Barbe, a member of the AMA Board of Trustees.
“I am looking at one physician here who has 511 total transactions,” he said. “There is no way that that physician can legitimately validate or even refute those transactions. I can’t imagine what the record-keeping would be like if he were to attempt to track 511 transactions from industry over the course of the year.”
The complexity of tracking all those data could be the reason so few transactions have been disputed. In 2014, CMS reported data on 10.8 million general payments to physicians and teaching hospitals; 1,732 were transactions disputed. In 2013, data were reported on 4.1 million general payments, with 880 disputed. The value of general payments rose to $2.6 billion ($5.1 million disputed) from $972 million (nearly $2 million disputed).
Open Payments captured payments to 607,000 physicians and to 1,121 teaching hospitals made by 1,444 companies in 2014, up from 470,000 physicians and 1,019 teaching hospitals receiving payments from 1,347 companies in 2013.
But Dr. Barbe said that his primary complaint remains that the information comes without any context and really doesn’t convey any useful information. They’re just data.
“To suppose that because he has a lot of transactions, that means there’s some kind of illicit or nefarious relationship that the physician has with industry, I think is also not necessarily a conclusion one can draw.”
Improvements to the Open Payments reporting system are welcome, but don’t go far enough.
That was the message from the American Medical Association upon the July 1 release of another round of data in the financial disclosure system created by the Affordable Care Act.
CMS “has improved our interface for both collecting and reporting this data about compensation and other payments between drug and medical device manufacturers and physicians and teaching hospitals,” Dr. Shantanu Agrawal, CMS deputy administrator and director of the Center for Program Integrity, said in a statement.
“While we appreciate the efforts of the Centers for Medicare & Medicaid Services to verify the data submitted by industry, the complicated and cumbersome process for physicians to register to review their data and seek correction of any inaccuracies continues to hinder their participation in the validation process,” the AMA said in a statement.
Dr. David O. Barbe, a family physician in Mountain Grove, Mo., noted that “the ability to navigate [Open Payments] has substantially improved since the first iteration of this. You can get around the website pretty well. ... You can sort the data. You can search on individuals. You can sort it by large amounts, either by individual physician or by payer.”
However, the approach used still makes it extremely difficult for determining the validity and accuracy of the information that is being presented, said Dr. Barbe, a member of the AMA Board of Trustees.
“I am looking at one physician here who has 511 total transactions,” he said. “There is no way that that physician can legitimately validate or even refute those transactions. I can’t imagine what the record-keeping would be like if he were to attempt to track 511 transactions from industry over the course of the year.”
The complexity of tracking all those data could be the reason so few transactions have been disputed. In 2014, CMS reported data on 10.8 million general payments to physicians and teaching hospitals; 1,732 were transactions disputed. In 2013, data were reported on 4.1 million general payments, with 880 disputed. The value of general payments rose to $2.6 billion ($5.1 million disputed) from $972 million (nearly $2 million disputed).
Open Payments captured payments to 607,000 physicians and to 1,121 teaching hospitals made by 1,444 companies in 2014, up from 470,000 physicians and 1,019 teaching hospitals receiving payments from 1,347 companies in 2013.
But Dr. Barbe said that his primary complaint remains that the information comes without any context and really doesn’t convey any useful information. They’re just data.
“To suppose that because he has a lot of transactions, that means there’s some kind of illicit or nefarious relationship that the physician has with industry, I think is also not necessarily a conclusion one can draw.”
Improvements to the Open Payments reporting system are welcome, but don’t go far enough.
That was the message from the American Medical Association upon the July 1 release of another round of data in the financial disclosure system created by the Affordable Care Act.
CMS “has improved our interface for both collecting and reporting this data about compensation and other payments between drug and medical device manufacturers and physicians and teaching hospitals,” Dr. Shantanu Agrawal, CMS deputy administrator and director of the Center for Program Integrity, said in a statement.
“While we appreciate the efforts of the Centers for Medicare & Medicaid Services to verify the data submitted by industry, the complicated and cumbersome process for physicians to register to review their data and seek correction of any inaccuracies continues to hinder their participation in the validation process,” the AMA said in a statement.
Dr. David O. Barbe, a family physician in Mountain Grove, Mo., noted that “the ability to navigate [Open Payments] has substantially improved since the first iteration of this. You can get around the website pretty well. ... You can sort the data. You can search on individuals. You can sort it by large amounts, either by individual physician or by payer.”
However, the approach used still makes it extremely difficult for determining the validity and accuracy of the information that is being presented, said Dr. Barbe, a member of the AMA Board of Trustees.
“I am looking at one physician here who has 511 total transactions,” he said. “There is no way that that physician can legitimately validate or even refute those transactions. I can’t imagine what the record-keeping would be like if he were to attempt to track 511 transactions from industry over the course of the year.”
The complexity of tracking all those data could be the reason so few transactions have been disputed. In 2014, CMS reported data on 10.8 million general payments to physicians and teaching hospitals; 1,732 were transactions disputed. In 2013, data were reported on 4.1 million general payments, with 880 disputed. The value of general payments rose to $2.6 billion ($5.1 million disputed) from $972 million (nearly $2 million disputed).
Open Payments captured payments to 607,000 physicians and to 1,121 teaching hospitals made by 1,444 companies in 2014, up from 470,000 physicians and 1,019 teaching hospitals receiving payments from 1,347 companies in 2013.
But Dr. Barbe said that his primary complaint remains that the information comes without any context and really doesn’t convey any useful information. They’re just data.
“To suppose that because he has a lot of transactions, that means there’s some kind of illicit or nefarious relationship that the physician has with industry, I think is also not necessarily a conclusion one can draw.”
LISTEN NOW: Hospitalist Manya Gupta on Choosing Wisely
Excerpt of our interviews with Choosing Wisely, hospitalist Manya Gupta, MD, an assistant professor in the department of internal medicine of Rush University Medical Center in Chicago, discusses an example of a Choosing Wisely program.
Excerpt of our interviews with Choosing Wisely, hospitalist Manya Gupta, MD, an assistant professor in the department of internal medicine of Rush University Medical Center in Chicago, discusses an example of a Choosing Wisely program.
Excerpt of our interviews with Choosing Wisely, hospitalist Manya Gupta, MD, an assistant professor in the department of internal medicine of Rush University Medical Center in Chicago, discusses an example of a Choosing Wisely program.
LISTEN NOW: Hospitalist Lisa Shieh on Choosing Wisely
Excerpt of our interviews with Choosing Wisely, Lisa Shieh, MD, PhD, of Stanford University School of Medicine, discusses an example of a Choosing Wisely program.
Excerpt of our interviews with Choosing Wisely, Lisa Shieh, MD, PhD, of Stanford University School of Medicine, discusses an example of a Choosing Wisely program.
Excerpt of our interviews with Choosing Wisely, Lisa Shieh, MD, PhD, of Stanford University School of Medicine, discusses an example of a Choosing Wisely program.
LISTEN NOW: Gregory Seymann, MD, on Choosing Wisely
Gregory Seymann, MD, discusses a Choosing Wisely program.
Gregory Seymann, MD, discusses a Choosing Wisely program.
Gregory Seymann, MD, discusses a Choosing Wisely program.
Malpractice Counsel
Acute Coronary Syndromes
A 53-year-old obese man presented to the ED complaining of pain in his chest, bilateral jaw, and back. He stated that his symptoms had started the previous evening and had increased in severity the morning of presentation. He denied any change in breathing, or any nausea or vomiting. The patient’s medical history was significant for hypertension and chronic back pain. Regarding his social history, the patient noted that he smoked one pack of cigarettes per day; he denied alcohol use.
On physical examination, the patient’s weight was 350 lb, and he was profusely diaphoretic. Vital signs were remarkable for an elevated blood pressure (BP) of 214/106 mm Hg; respiratory rate (RR), heart rate (HR), temperature (T), and oxygen saturation were normal. The head, eyes, ears, nose, and throat examination was normal, and there was no jugular venous distention. The lung and heart examinations were also normal, and the abdominal examination was unremarkable. The patient had 2+ pitting edema in his lower extremities, which he said had been present for the past few weeks. The back examination was unremarkable, and the neurological examination was completely normal, including deep tendon reflexes.
Because of the presence of chest and back pain and history of hypertension, the EP ordered a computed tomography (CT) scan of the chest with intravenous (IV) contrast to rule out aortic dissection. He also administered 0.2 mg of clonidine orally for the elevated BP. Approximately 20 minutes later, the patient was given 2 mg morphine IV for the back pain and another 0.2 mg of clonidine orally. The elevated BP responded to the clonidine, and the patient stated he was feeling better.
The CT scan of the chest was interpreted by radiology services as normal. The patient was then administered 325 mg of aspirin by mouth. Since the EP’s hospital did not have facilities for cardiac catheterization, the EP consulted with a physician at another facility regarding a possible transfer. The consulted physician did not accept the patient for transfer, but instead recommended keeping the patient at the EP’s institution for observation and continuing treatment for the elevated BP and pain. The EP agreed, and diagnosed the patient with a hypertensive emergency and a flare-up of his chronic back pain.
In the ED, the patient’s BP decreased to near normal levels, and he was feeling much improved. Approximately 5.5 hours after his arrival to the ED, he was admitted to a monitored bed under the care of a hospitalist.
A few hours later, the patient began to complain of burning in the epigastric area; analgesics and nitroglycerin were administered and a repeat ECG was ordered. A second troponin level, drawn approximately 6 hours after the original, was found to be significantly elevated. The repeat ECG demonstrated sinus tachycardia with ST-segment depression.
The hospitalist was concerned about an acute coronary syndrome (ACS) and attempted to make contact with the other facility to transfer the patient for an emergent cardiac catheterization. The consulted physician agreed to accept the patient and recommended starting an IV heparin drip and giving clopidogrel bisulfate (Plavix). While arranging for the transfer, the patient suffered a cardiac arrest; resuscitation attempts were unsuccessful.
The family of the patient sued the hospital, the EP, and the hospitalist, alleging the EP failed to recognize that the initial ECG and elevated troponin level were suggestive of an ACS. They also complained that the morphine, oxygen, nitroglycerin, and aspirin were not started in a timely manner. In addition, the family claimed the decedent should have been immediately transferred to another facility because the defendant’s hospital could not perform cardiac catheterization. They further alleged that the hospitalist failed to perform an independent evaluation of the patient and also failed to obtain a repeat 12-lead ECG sooner. Lastly, the plaintiffs claimed that the hospital’s nursing staff was negligent in failing to provide nursing care for 3 hours prior to the patient being found unresponsive.
The defendant EP asserted that the initial ECG was nondiagnostic and that the initial troponin level, while elevated, was nonspecific. He argued the ED evaluation and care provided was appropriate. Following trial, a defense verdict was returned.
Discussion
Fortunately, the jury ruled correctly in this case. Acute coronary sydromes can be some of the most challenging medical conditions to evaluate and manage in the ED. The EP’s initial cardiac workup and evaluation for a possible acute thoracic aortic dissection were appropriate—an acute thoracic aortic dissection is a true cardiovascular emergency. After interpreting the initial ECG as nondiagnostic (specifically, to rule out evidence of ST-segment elevation, myocardial infarction [MI], or STEMI), obtaining the contrast CT scan of the chest emergently was critically important. This patient had multiple risk factors for aortic dissection: he was a male between the ages of 50 and 55 years old (the mean age for proximal thoracic aortic dissection); he had a history of hypertension; and he was experiencing chest and back pain.1
Once an acute aortic dissection was excluded, focusing on a cardiac etiology, as the EP did, was appropriate. The only criticism is that this patient probably should have been managed with an IV antihypertensive agent to allow for a more controlled BP reduction; this, however, does not seem to have played any role in the patient’s ultimate outcome.
Acute coronary syndromes are a dynamic process and progress over time. The EP was clearly concerned about an ACS very early in the case, as evidenced by his attempt to transfer the patient to a facility with specialized cardiac capabilities. After not being able to do so, the most appropriate next step was his admission of the patient to a monitored bed with serial cardiac enzymes and ECGs. It is well known that initial evaluation of both ECG and cardiac enzymes can be normal early on in an ACS. Patients with a normal or nonspecific ECG have a 1% to 5% incidence of MI and a 4% to 23% incidence of unstable angina.2
This patient ultimately experienced a non-ST-segment elevation myocardial infarction (NSTEMI). However, this diagnosis did not become evident until several hours after the patient’s admission to the hospital. It is unfortunate the physician consulted by the EP at the onset did not agree to accept this patient. This patient’s best chance for survival was at a facility capable of percutaneous coronary intervention.
Serotonin Syndrome
| A 20-year-old man was brought to the ED by his friends for concerns of an overdose. Just prior to arrival, the patient reportedly drank the entire contents of a bottle of cough medicine containing dextromethorphan. His friends reported the patient had been depressed lately, but was otherwise in good health. The patient was not known to abuse alcohol or use illicit drugs. The EP was unable to obtain any history from the patient, who was extremely agitated and yelling frequently. A review of the hospital records revealed the patient had been admitted a few months prior for a suicide attempt. On physical examination, the patient’s vital signs were: pulse, 126 beats/minute; BP, 144/92 mm Hg, RR 22 breaths/minute; and T, 100.6˚F. Oxygen saturation was 99% on room air. The patient was diaphoretic, agitated, and only able to provide one-word answers between screaming episodes. His pupils were mildly dilated but reactive. The cardiac examination revealed a tachycardic rate with a normal rhythm, and no murmurs, rubs, or gallops. The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender, without guarding or rebound. The patient would not cooperate for a neurological examination, but was found to be moving all four extremities with good strength. He was noted to have myoclonus. The EP immediately called the Poison Control Center for advice about treatment. In the meantime, laboratory studies were drawn, including an alcohol level, acetaminophen level, salicylate level, and a urine drug screen. A 12-lead ECG demonstrated a sinus tachycardia with a normal axis. The patient was given IV lorazepam to treat the agitation. The patient’s alcohol, acetaminophen, and salicylate levels were all negative. The EP attempted to transfer the patient to another facility with a higher level of care, but unfortunately, the patient went into cardiac arrest and died in the ED. An autopsy showed that the patient died from serotonin syndrome as a result of acute dextromethorphan and selegiline toxicity. It was later discovered that the patient had been prescribed selegiline as an antidepressant following his recent hospitalization for the suicide attempt. Unfortunately, this information was not available in the records from his previous presentation or from the patient or his friends during the history taking. The patient’s family sued the EP for failing to diagnose serotonin syndrome. They argued the patient did not die from a suicide, but rather from serotonin syndrome. The EP contended the patient had deliberately combined the two drugs to commit suicide. Both parties argued application of the state’s “dead man’s statute” (also known as a “dead man’s act” or “dead man’s rule”). Following trial, a defense verdict was returned. Discussion Serotonin syndrome (or serotonin toxicity) is a drug-induced syndrome characterized by a cluster of dose-related adverse effects due to increased serotonin concentrations in the central nervous system.1 Severe toxicity, as seen in this case, usually occurs only when two or more serotonergic drugs (even when each is at therapeutic dose) are combined. One of the drugs is usually a monoamine oxidase inhibitor (MAOI).1 While selegiline is used primarily as an adjunct treatment for Parkinson disease, it is also used to treat depression, attention deficit and hyperactivity disorder, and Alzheimer disease. Its primary mechanism of action is as an irreversible inhibitor of MAO. Dextromethorphan is used primarily as an antitussive (cough suppressant). It is also used recreationally for its reported effects as a hallucinogen. Its mechanism of action occurs through several effects, one of which is as a nonselective serotonin reuptake inhibitor (NSRI). Although the label on all NSRIs clearly states this medication should not be taken with MAOIs (ie, selegiline), few lay people know the mechanism of action of their medications. The patient in this case took a combination of medications that are known to cause severe serotonin toxicity. It is unclear whether or not he was aware of the dangers associated with combining these two medications. The classic triad of clinical features of serotonin syndrome are neuromuscular excitation (eg, clonus, hyperreflexia, myoclonus, rigidity); autonomic nervous system excitation (eg, hyperthermia, tachycardia); and altered mental status (eg, agitation, confusion).1 The onset of symptoms typically occurs within a few hours of ingestion. Serotonin syndrome can be confused with neuroleptic malignant syndrome (NMS), but there are three key differentiating features: (1) In NMS, symptom onset is slow, usually over days, not hours; (2) extrapyramidal features and rigidity are much more prominent in NMS; and (3) clonus is usually pronounced and easily elicited (especially with ankle dorsiflexion) in serotonin syndrome, but minimal to absent in NMS.1 The initial treatment of serotonin syndrome involves symptomatic care and discontinuation of all serotonergic drugs.2 Benzodiazepines can be used for muscle relaxation and treatment of agitation. All patients with serotonin syndrome require hospital admission, and those with severe toxicity should be admitted to an intensive care unit. Cyproheptadine is the most effective antiserotonergic agent, but it is only available in oral formulation. Chlorpromazine IV has also been used to treat serotonin syndrome, but resulting hypotension is a drawback.1 Approximately 25% of patients with severe serotonin toxicity require intubation and mechanical ventilation. Most patients show dramatic improvement within 24 hours of symptom onset.2 Regarding the dead man statute, according to Cornell University Law School, this statute states that in a civil action, a party with an interest in the litigation may not testify against a dead party about communications with the dead party. This is a state statute and therefore the exact wording varies from state to state. The Federal Rules of Evidence does not contain a dead man’s statute. |
Reference - Acute Coronary Syndromes
- Pacini D, Di Marco L, Fortuna D, et al. Acute aortic dissection: epidemiology and outcomes. Int J Cardiol. 2013;167(6):2806-2812.
- Hollander JE, Diercks DB. Acute coronary syndromes: acute myocardial infarction and unstable angina. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:367.
Reference - Serotonin Syndrome
- Buckley NA, Dawson AH, Isbister GK. Serotonin Syndrome. BMJ. 2014;348:g1626.
- Mills KC, Bora KM. Atypical antidepressants, serotonin reuptake inhibitors, and serotonin syndrome. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:1202.
Acute Coronary Syndromes
A 53-year-old obese man presented to the ED complaining of pain in his chest, bilateral jaw, and back. He stated that his symptoms had started the previous evening and had increased in severity the morning of presentation. He denied any change in breathing, or any nausea or vomiting. The patient’s medical history was significant for hypertension and chronic back pain. Regarding his social history, the patient noted that he smoked one pack of cigarettes per day; he denied alcohol use.
On physical examination, the patient’s weight was 350 lb, and he was profusely diaphoretic. Vital signs were remarkable for an elevated blood pressure (BP) of 214/106 mm Hg; respiratory rate (RR), heart rate (HR), temperature (T), and oxygen saturation were normal. The head, eyes, ears, nose, and throat examination was normal, and there was no jugular venous distention. The lung and heart examinations were also normal, and the abdominal examination was unremarkable. The patient had 2+ pitting edema in his lower extremities, which he said had been present for the past few weeks. The back examination was unremarkable, and the neurological examination was completely normal, including deep tendon reflexes.
Because of the presence of chest and back pain and history of hypertension, the EP ordered a computed tomography (CT) scan of the chest with intravenous (IV) contrast to rule out aortic dissection. He also administered 0.2 mg of clonidine orally for the elevated BP. Approximately 20 minutes later, the patient was given 2 mg morphine IV for the back pain and another 0.2 mg of clonidine orally. The elevated BP responded to the clonidine, and the patient stated he was feeling better.
The CT scan of the chest was interpreted by radiology services as normal. The patient was then administered 325 mg of aspirin by mouth. Since the EP’s hospital did not have facilities for cardiac catheterization, the EP consulted with a physician at another facility regarding a possible transfer. The consulted physician did not accept the patient for transfer, but instead recommended keeping the patient at the EP’s institution for observation and continuing treatment for the elevated BP and pain. The EP agreed, and diagnosed the patient with a hypertensive emergency and a flare-up of his chronic back pain.
In the ED, the patient’s BP decreased to near normal levels, and he was feeling much improved. Approximately 5.5 hours after his arrival to the ED, he was admitted to a monitored bed under the care of a hospitalist.
A few hours later, the patient began to complain of burning in the epigastric area; analgesics and nitroglycerin were administered and a repeat ECG was ordered. A second troponin level, drawn approximately 6 hours after the original, was found to be significantly elevated. The repeat ECG demonstrated sinus tachycardia with ST-segment depression.
The hospitalist was concerned about an acute coronary syndrome (ACS) and attempted to make contact with the other facility to transfer the patient for an emergent cardiac catheterization. The consulted physician agreed to accept the patient and recommended starting an IV heparin drip and giving clopidogrel bisulfate (Plavix). While arranging for the transfer, the patient suffered a cardiac arrest; resuscitation attempts were unsuccessful.
The family of the patient sued the hospital, the EP, and the hospitalist, alleging the EP failed to recognize that the initial ECG and elevated troponin level were suggestive of an ACS. They also complained that the morphine, oxygen, nitroglycerin, and aspirin were not started in a timely manner. In addition, the family claimed the decedent should have been immediately transferred to another facility because the defendant’s hospital could not perform cardiac catheterization. They further alleged that the hospitalist failed to perform an independent evaluation of the patient and also failed to obtain a repeat 12-lead ECG sooner. Lastly, the plaintiffs claimed that the hospital’s nursing staff was negligent in failing to provide nursing care for 3 hours prior to the patient being found unresponsive.
The defendant EP asserted that the initial ECG was nondiagnostic and that the initial troponin level, while elevated, was nonspecific. He argued the ED evaluation and care provided was appropriate. Following trial, a defense verdict was returned.
Discussion
Fortunately, the jury ruled correctly in this case. Acute coronary sydromes can be some of the most challenging medical conditions to evaluate and manage in the ED. The EP’s initial cardiac workup and evaluation for a possible acute thoracic aortic dissection were appropriate—an acute thoracic aortic dissection is a true cardiovascular emergency. After interpreting the initial ECG as nondiagnostic (specifically, to rule out evidence of ST-segment elevation, myocardial infarction [MI], or STEMI), obtaining the contrast CT scan of the chest emergently was critically important. This patient had multiple risk factors for aortic dissection: he was a male between the ages of 50 and 55 years old (the mean age for proximal thoracic aortic dissection); he had a history of hypertension; and he was experiencing chest and back pain.1
Once an acute aortic dissection was excluded, focusing on a cardiac etiology, as the EP did, was appropriate. The only criticism is that this patient probably should have been managed with an IV antihypertensive agent to allow for a more controlled BP reduction; this, however, does not seem to have played any role in the patient’s ultimate outcome.
Acute coronary syndromes are a dynamic process and progress over time. The EP was clearly concerned about an ACS very early in the case, as evidenced by his attempt to transfer the patient to a facility with specialized cardiac capabilities. After not being able to do so, the most appropriate next step was his admission of the patient to a monitored bed with serial cardiac enzymes and ECGs. It is well known that initial evaluation of both ECG and cardiac enzymes can be normal early on in an ACS. Patients with a normal or nonspecific ECG have a 1% to 5% incidence of MI and a 4% to 23% incidence of unstable angina.2
This patient ultimately experienced a non-ST-segment elevation myocardial infarction (NSTEMI). However, this diagnosis did not become evident until several hours after the patient’s admission to the hospital. It is unfortunate the physician consulted by the EP at the onset did not agree to accept this patient. This patient’s best chance for survival was at a facility capable of percutaneous coronary intervention.
Serotonin Syndrome
| A 20-year-old man was brought to the ED by his friends for concerns of an overdose. Just prior to arrival, the patient reportedly drank the entire contents of a bottle of cough medicine containing dextromethorphan. His friends reported the patient had been depressed lately, but was otherwise in good health. The patient was not known to abuse alcohol or use illicit drugs. The EP was unable to obtain any history from the patient, who was extremely agitated and yelling frequently. A review of the hospital records revealed the patient had been admitted a few months prior for a suicide attempt. On physical examination, the patient’s vital signs were: pulse, 126 beats/minute; BP, 144/92 mm Hg, RR 22 breaths/minute; and T, 100.6˚F. Oxygen saturation was 99% on room air. The patient was diaphoretic, agitated, and only able to provide one-word answers between screaming episodes. His pupils were mildly dilated but reactive. The cardiac examination revealed a tachycardic rate with a normal rhythm, and no murmurs, rubs, or gallops. The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender, without guarding or rebound. The patient would not cooperate for a neurological examination, but was found to be moving all four extremities with good strength. He was noted to have myoclonus. The EP immediately called the Poison Control Center for advice about treatment. In the meantime, laboratory studies were drawn, including an alcohol level, acetaminophen level, salicylate level, and a urine drug screen. A 12-lead ECG demonstrated a sinus tachycardia with a normal axis. The patient was given IV lorazepam to treat the agitation. The patient’s alcohol, acetaminophen, and salicylate levels were all negative. The EP attempted to transfer the patient to another facility with a higher level of care, but unfortunately, the patient went into cardiac arrest and died in the ED. An autopsy showed that the patient died from serotonin syndrome as a result of acute dextromethorphan and selegiline toxicity. It was later discovered that the patient had been prescribed selegiline as an antidepressant following his recent hospitalization for the suicide attempt. Unfortunately, this information was not available in the records from his previous presentation or from the patient or his friends during the history taking. The patient’s family sued the EP for failing to diagnose serotonin syndrome. They argued the patient did not die from a suicide, but rather from serotonin syndrome. The EP contended the patient had deliberately combined the two drugs to commit suicide. Both parties argued application of the state’s “dead man’s statute” (also known as a “dead man’s act” or “dead man’s rule”). Following trial, a defense verdict was returned. Discussion Serotonin syndrome (or serotonin toxicity) is a drug-induced syndrome characterized by a cluster of dose-related adverse effects due to increased serotonin concentrations in the central nervous system.1 Severe toxicity, as seen in this case, usually occurs only when two or more serotonergic drugs (even when each is at therapeutic dose) are combined. One of the drugs is usually a monoamine oxidase inhibitor (MAOI).1 While selegiline is used primarily as an adjunct treatment for Parkinson disease, it is also used to treat depression, attention deficit and hyperactivity disorder, and Alzheimer disease. Its primary mechanism of action is as an irreversible inhibitor of MAO. Dextromethorphan is used primarily as an antitussive (cough suppressant). It is also used recreationally for its reported effects as a hallucinogen. Its mechanism of action occurs through several effects, one of which is as a nonselective serotonin reuptake inhibitor (NSRI). Although the label on all NSRIs clearly states this medication should not be taken with MAOIs (ie, selegiline), few lay people know the mechanism of action of their medications. The patient in this case took a combination of medications that are known to cause severe serotonin toxicity. It is unclear whether or not he was aware of the dangers associated with combining these two medications. The classic triad of clinical features of serotonin syndrome are neuromuscular excitation (eg, clonus, hyperreflexia, myoclonus, rigidity); autonomic nervous system excitation (eg, hyperthermia, tachycardia); and altered mental status (eg, agitation, confusion).1 The onset of symptoms typically occurs within a few hours of ingestion. Serotonin syndrome can be confused with neuroleptic malignant syndrome (NMS), but there are three key differentiating features: (1) In NMS, symptom onset is slow, usually over days, not hours; (2) extrapyramidal features and rigidity are much more prominent in NMS; and (3) clonus is usually pronounced and easily elicited (especially with ankle dorsiflexion) in serotonin syndrome, but minimal to absent in NMS.1 The initial treatment of serotonin syndrome involves symptomatic care and discontinuation of all serotonergic drugs.2 Benzodiazepines can be used for muscle relaxation and treatment of agitation. All patients with serotonin syndrome require hospital admission, and those with severe toxicity should be admitted to an intensive care unit. Cyproheptadine is the most effective antiserotonergic agent, but it is only available in oral formulation. Chlorpromazine IV has also been used to treat serotonin syndrome, but resulting hypotension is a drawback.1 Approximately 25% of patients with severe serotonin toxicity require intubation and mechanical ventilation. Most patients show dramatic improvement within 24 hours of symptom onset.2 Regarding the dead man statute, according to Cornell University Law School, this statute states that in a civil action, a party with an interest in the litigation may not testify against a dead party about communications with the dead party. This is a state statute and therefore the exact wording varies from state to state. The Federal Rules of Evidence does not contain a dead man’s statute. |
Acute Coronary Syndromes
A 53-year-old obese man presented to the ED complaining of pain in his chest, bilateral jaw, and back. He stated that his symptoms had started the previous evening and had increased in severity the morning of presentation. He denied any change in breathing, or any nausea or vomiting. The patient’s medical history was significant for hypertension and chronic back pain. Regarding his social history, the patient noted that he smoked one pack of cigarettes per day; he denied alcohol use.
On physical examination, the patient’s weight was 350 lb, and he was profusely diaphoretic. Vital signs were remarkable for an elevated blood pressure (BP) of 214/106 mm Hg; respiratory rate (RR), heart rate (HR), temperature (T), and oxygen saturation were normal. The head, eyes, ears, nose, and throat examination was normal, and there was no jugular venous distention. The lung and heart examinations were also normal, and the abdominal examination was unremarkable. The patient had 2+ pitting edema in his lower extremities, which he said had been present for the past few weeks. The back examination was unremarkable, and the neurological examination was completely normal, including deep tendon reflexes.
Because of the presence of chest and back pain and history of hypertension, the EP ordered a computed tomography (CT) scan of the chest with intravenous (IV) contrast to rule out aortic dissection. He also administered 0.2 mg of clonidine orally for the elevated BP. Approximately 20 minutes later, the patient was given 2 mg morphine IV for the back pain and another 0.2 mg of clonidine orally. The elevated BP responded to the clonidine, and the patient stated he was feeling better.
The CT scan of the chest was interpreted by radiology services as normal. The patient was then administered 325 mg of aspirin by mouth. Since the EP’s hospital did not have facilities for cardiac catheterization, the EP consulted with a physician at another facility regarding a possible transfer. The consulted physician did not accept the patient for transfer, but instead recommended keeping the patient at the EP’s institution for observation and continuing treatment for the elevated BP and pain. The EP agreed, and diagnosed the patient with a hypertensive emergency and a flare-up of his chronic back pain.
In the ED, the patient’s BP decreased to near normal levels, and he was feeling much improved. Approximately 5.5 hours after his arrival to the ED, he was admitted to a monitored bed under the care of a hospitalist.
A few hours later, the patient began to complain of burning in the epigastric area; analgesics and nitroglycerin were administered and a repeat ECG was ordered. A second troponin level, drawn approximately 6 hours after the original, was found to be significantly elevated. The repeat ECG demonstrated sinus tachycardia with ST-segment depression.
The hospitalist was concerned about an acute coronary syndrome (ACS) and attempted to make contact with the other facility to transfer the patient for an emergent cardiac catheterization. The consulted physician agreed to accept the patient and recommended starting an IV heparin drip and giving clopidogrel bisulfate (Plavix). While arranging for the transfer, the patient suffered a cardiac arrest; resuscitation attempts were unsuccessful.
The family of the patient sued the hospital, the EP, and the hospitalist, alleging the EP failed to recognize that the initial ECG and elevated troponin level were suggestive of an ACS. They also complained that the morphine, oxygen, nitroglycerin, and aspirin were not started in a timely manner. In addition, the family claimed the decedent should have been immediately transferred to another facility because the defendant’s hospital could not perform cardiac catheterization. They further alleged that the hospitalist failed to perform an independent evaluation of the patient and also failed to obtain a repeat 12-lead ECG sooner. Lastly, the plaintiffs claimed that the hospital’s nursing staff was negligent in failing to provide nursing care for 3 hours prior to the patient being found unresponsive.
The defendant EP asserted that the initial ECG was nondiagnostic and that the initial troponin level, while elevated, was nonspecific. He argued the ED evaluation and care provided was appropriate. Following trial, a defense verdict was returned.
Discussion
Fortunately, the jury ruled correctly in this case. Acute coronary sydromes can be some of the most challenging medical conditions to evaluate and manage in the ED. The EP’s initial cardiac workup and evaluation for a possible acute thoracic aortic dissection were appropriate—an acute thoracic aortic dissection is a true cardiovascular emergency. After interpreting the initial ECG as nondiagnostic (specifically, to rule out evidence of ST-segment elevation, myocardial infarction [MI], or STEMI), obtaining the contrast CT scan of the chest emergently was critically important. This patient had multiple risk factors for aortic dissection: he was a male between the ages of 50 and 55 years old (the mean age for proximal thoracic aortic dissection); he had a history of hypertension; and he was experiencing chest and back pain.1
Once an acute aortic dissection was excluded, focusing on a cardiac etiology, as the EP did, was appropriate. The only criticism is that this patient probably should have been managed with an IV antihypertensive agent to allow for a more controlled BP reduction; this, however, does not seem to have played any role in the patient’s ultimate outcome.
Acute coronary syndromes are a dynamic process and progress over time. The EP was clearly concerned about an ACS very early in the case, as evidenced by his attempt to transfer the patient to a facility with specialized cardiac capabilities. After not being able to do so, the most appropriate next step was his admission of the patient to a monitored bed with serial cardiac enzymes and ECGs. It is well known that initial evaluation of both ECG and cardiac enzymes can be normal early on in an ACS. Patients with a normal or nonspecific ECG have a 1% to 5% incidence of MI and a 4% to 23% incidence of unstable angina.2
This patient ultimately experienced a non-ST-segment elevation myocardial infarction (NSTEMI). However, this diagnosis did not become evident until several hours after the patient’s admission to the hospital. It is unfortunate the physician consulted by the EP at the onset did not agree to accept this patient. This patient’s best chance for survival was at a facility capable of percutaneous coronary intervention.
Serotonin Syndrome
| A 20-year-old man was brought to the ED by his friends for concerns of an overdose. Just prior to arrival, the patient reportedly drank the entire contents of a bottle of cough medicine containing dextromethorphan. His friends reported the patient had been depressed lately, but was otherwise in good health. The patient was not known to abuse alcohol or use illicit drugs. The EP was unable to obtain any history from the patient, who was extremely agitated and yelling frequently. A review of the hospital records revealed the patient had been admitted a few months prior for a suicide attempt. On physical examination, the patient’s vital signs were: pulse, 126 beats/minute; BP, 144/92 mm Hg, RR 22 breaths/minute; and T, 100.6˚F. Oxygen saturation was 99% on room air. The patient was diaphoretic, agitated, and only able to provide one-word answers between screaming episodes. His pupils were mildly dilated but reactive. The cardiac examination revealed a tachycardic rate with a normal rhythm, and no murmurs, rubs, or gallops. The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender, without guarding or rebound. The patient would not cooperate for a neurological examination, but was found to be moving all four extremities with good strength. He was noted to have myoclonus. The EP immediately called the Poison Control Center for advice about treatment. In the meantime, laboratory studies were drawn, including an alcohol level, acetaminophen level, salicylate level, and a urine drug screen. A 12-lead ECG demonstrated a sinus tachycardia with a normal axis. The patient was given IV lorazepam to treat the agitation. The patient’s alcohol, acetaminophen, and salicylate levels were all negative. The EP attempted to transfer the patient to another facility with a higher level of care, but unfortunately, the patient went into cardiac arrest and died in the ED. An autopsy showed that the patient died from serotonin syndrome as a result of acute dextromethorphan and selegiline toxicity. It was later discovered that the patient had been prescribed selegiline as an antidepressant following his recent hospitalization for the suicide attempt. Unfortunately, this information was not available in the records from his previous presentation or from the patient or his friends during the history taking. The patient’s family sued the EP for failing to diagnose serotonin syndrome. They argued the patient did not die from a suicide, but rather from serotonin syndrome. The EP contended the patient had deliberately combined the two drugs to commit suicide. Both parties argued application of the state’s “dead man’s statute” (also known as a “dead man’s act” or “dead man’s rule”). Following trial, a defense verdict was returned. Discussion Serotonin syndrome (or serotonin toxicity) is a drug-induced syndrome characterized by a cluster of dose-related adverse effects due to increased serotonin concentrations in the central nervous system.1 Severe toxicity, as seen in this case, usually occurs only when two or more serotonergic drugs (even when each is at therapeutic dose) are combined. One of the drugs is usually a monoamine oxidase inhibitor (MAOI).1 While selegiline is used primarily as an adjunct treatment for Parkinson disease, it is also used to treat depression, attention deficit and hyperactivity disorder, and Alzheimer disease. Its primary mechanism of action is as an irreversible inhibitor of MAO. Dextromethorphan is used primarily as an antitussive (cough suppressant). It is also used recreationally for its reported effects as a hallucinogen. Its mechanism of action occurs through several effects, one of which is as a nonselective serotonin reuptake inhibitor (NSRI). Although the label on all NSRIs clearly states this medication should not be taken with MAOIs (ie, selegiline), few lay people know the mechanism of action of their medications. The patient in this case took a combination of medications that are known to cause severe serotonin toxicity. It is unclear whether or not he was aware of the dangers associated with combining these two medications. The classic triad of clinical features of serotonin syndrome are neuromuscular excitation (eg, clonus, hyperreflexia, myoclonus, rigidity); autonomic nervous system excitation (eg, hyperthermia, tachycardia); and altered mental status (eg, agitation, confusion).1 The onset of symptoms typically occurs within a few hours of ingestion. Serotonin syndrome can be confused with neuroleptic malignant syndrome (NMS), but there are three key differentiating features: (1) In NMS, symptom onset is slow, usually over days, not hours; (2) extrapyramidal features and rigidity are much more prominent in NMS; and (3) clonus is usually pronounced and easily elicited (especially with ankle dorsiflexion) in serotonin syndrome, but minimal to absent in NMS.1 The initial treatment of serotonin syndrome involves symptomatic care and discontinuation of all serotonergic drugs.2 Benzodiazepines can be used for muscle relaxation and treatment of agitation. All patients with serotonin syndrome require hospital admission, and those with severe toxicity should be admitted to an intensive care unit. Cyproheptadine is the most effective antiserotonergic agent, but it is only available in oral formulation. Chlorpromazine IV has also been used to treat serotonin syndrome, but resulting hypotension is a drawback.1 Approximately 25% of patients with severe serotonin toxicity require intubation and mechanical ventilation. Most patients show dramatic improvement within 24 hours of symptom onset.2 Regarding the dead man statute, according to Cornell University Law School, this statute states that in a civil action, a party with an interest in the litigation may not testify against a dead party about communications with the dead party. This is a state statute and therefore the exact wording varies from state to state. The Federal Rules of Evidence does not contain a dead man’s statute. |
Reference - Acute Coronary Syndromes
- Pacini D, Di Marco L, Fortuna D, et al. Acute aortic dissection: epidemiology and outcomes. Int J Cardiol. 2013;167(6):2806-2812.
- Hollander JE, Diercks DB. Acute coronary syndromes: acute myocardial infarction and unstable angina. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:367.
Reference - Serotonin Syndrome
- Buckley NA, Dawson AH, Isbister GK. Serotonin Syndrome. BMJ. 2014;348:g1626.
- Mills KC, Bora KM. Atypical antidepressants, serotonin reuptake inhibitors, and serotonin syndrome. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:1202.
Reference - Acute Coronary Syndromes
- Pacini D, Di Marco L, Fortuna D, et al. Acute aortic dissection: epidemiology and outcomes. Int J Cardiol. 2013;167(6):2806-2812.
- Hollander JE, Diercks DB. Acute coronary syndromes: acute myocardial infarction and unstable angina. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:367.
Reference - Serotonin Syndrome
- Buckley NA, Dawson AH, Isbister GK. Serotonin Syndrome. BMJ. 2014;348:g1626.
- Mills KC, Bora KM. Atypical antidepressants, serotonin reuptake inhibitors, and serotonin syndrome. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:1202.
Vermont leads the way in marketplace enrollment
Vermont enrolled the highest percentage of potential enrollees for the Health Insurance Marketplace in 2015, while Hawaii enrolled the lowest percentage, according to an analysis from the Kaiser Family Foundation.
Enrollment in Vermont’s state-based marketplace as of March 31 was 34,923 – which works out to 77% of the estimated potential population of 45,000. The state with the next-highest enrollment was Florida, with 57% of the potential population, then Maine at 55%, Pennsylvania at 48%, and Delaware at 47%, Kaiser reported.
Hawaii had a marketplace enrollment of 8,200 out of an estimated potential population of 55,000, or 15%, as of March 31. Just ahead of Hawaii were Iowa (17%), Minnesota (19%), South Dakota (19%), and Ohio (20%).
Vermont, Hawaii, and Minnesota have state-based marketplaces, while those in Florida, Maine, Pennsylvania, South Dakota, and Ohio are federally facilitated. Delaware and Iowa have state-partnership marketplaces.
Number-crunching reveals that the 14 state-based marketplaces have the highest average enrollment at 35.6%, followed by the 27 federally facilitated marketplaces at 34.1%, the 7 state partnerships at 33%, and the 3 states with federally supported marketplaces at 28.3%, according to the Kaiser data, which come from the March 31, 2015 Effectuated Enrollment Snapshot from the Centers for Medicare & Medicaid Services and analysis based on 2014 Medicaid eligibility levels and the 2014 Current Population Survey.
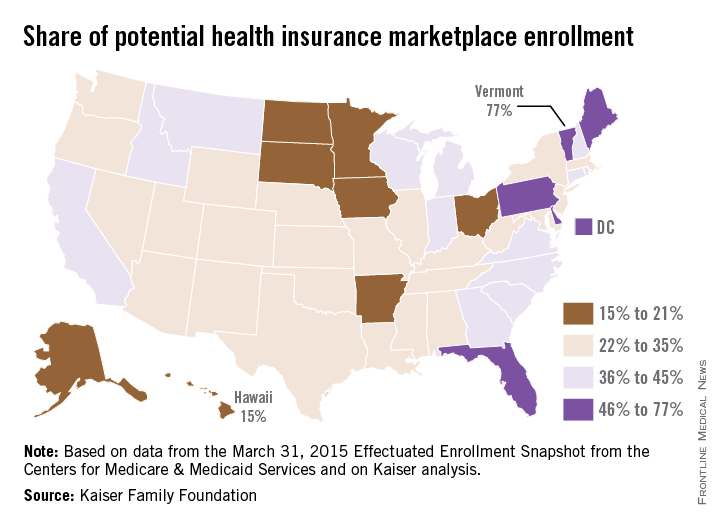
Vermont enrolled the highest percentage of potential enrollees for the Health Insurance Marketplace in 2015, while Hawaii enrolled the lowest percentage, according to an analysis from the Kaiser Family Foundation.
Enrollment in Vermont’s state-based marketplace as of March 31 was 34,923 – which works out to 77% of the estimated potential population of 45,000. The state with the next-highest enrollment was Florida, with 57% of the potential population, then Maine at 55%, Pennsylvania at 48%, and Delaware at 47%, Kaiser reported.
Hawaii had a marketplace enrollment of 8,200 out of an estimated potential population of 55,000, or 15%, as of March 31. Just ahead of Hawaii were Iowa (17%), Minnesota (19%), South Dakota (19%), and Ohio (20%).
Vermont, Hawaii, and Minnesota have state-based marketplaces, while those in Florida, Maine, Pennsylvania, South Dakota, and Ohio are federally facilitated. Delaware and Iowa have state-partnership marketplaces.
Number-crunching reveals that the 14 state-based marketplaces have the highest average enrollment at 35.6%, followed by the 27 federally facilitated marketplaces at 34.1%, the 7 state partnerships at 33%, and the 3 states with federally supported marketplaces at 28.3%, according to the Kaiser data, which come from the March 31, 2015 Effectuated Enrollment Snapshot from the Centers for Medicare & Medicaid Services and analysis based on 2014 Medicaid eligibility levels and the 2014 Current Population Survey.
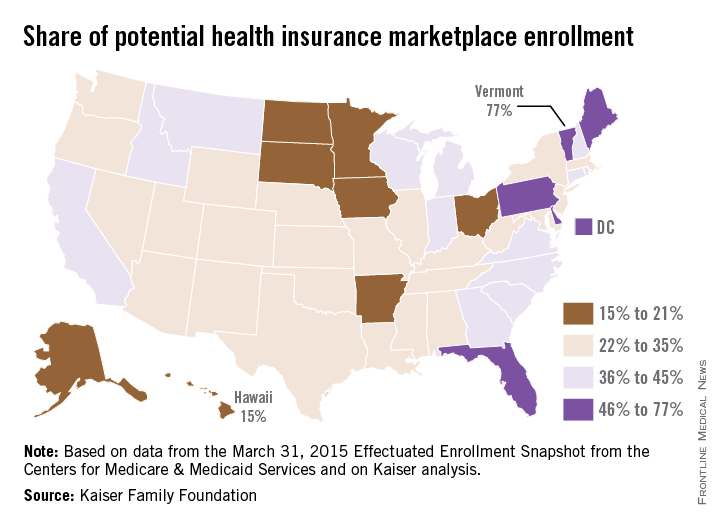
Vermont enrolled the highest percentage of potential enrollees for the Health Insurance Marketplace in 2015, while Hawaii enrolled the lowest percentage, according to an analysis from the Kaiser Family Foundation.
Enrollment in Vermont’s state-based marketplace as of March 31 was 34,923 – which works out to 77% of the estimated potential population of 45,000. The state with the next-highest enrollment was Florida, with 57% of the potential population, then Maine at 55%, Pennsylvania at 48%, and Delaware at 47%, Kaiser reported.
Hawaii had a marketplace enrollment of 8,200 out of an estimated potential population of 55,000, or 15%, as of March 31. Just ahead of Hawaii were Iowa (17%), Minnesota (19%), South Dakota (19%), and Ohio (20%).
Vermont, Hawaii, and Minnesota have state-based marketplaces, while those in Florida, Maine, Pennsylvania, South Dakota, and Ohio are federally facilitated. Delaware and Iowa have state-partnership marketplaces.
Number-crunching reveals that the 14 state-based marketplaces have the highest average enrollment at 35.6%, followed by the 27 federally facilitated marketplaces at 34.1%, the 7 state partnerships at 33%, and the 3 states with federally supported marketplaces at 28.3%, according to the Kaiser data, which come from the March 31, 2015 Effectuated Enrollment Snapshot from the Centers for Medicare & Medicaid Services and analysis based on 2014 Medicaid eligibility levels and the 2014 Current Population Survey.
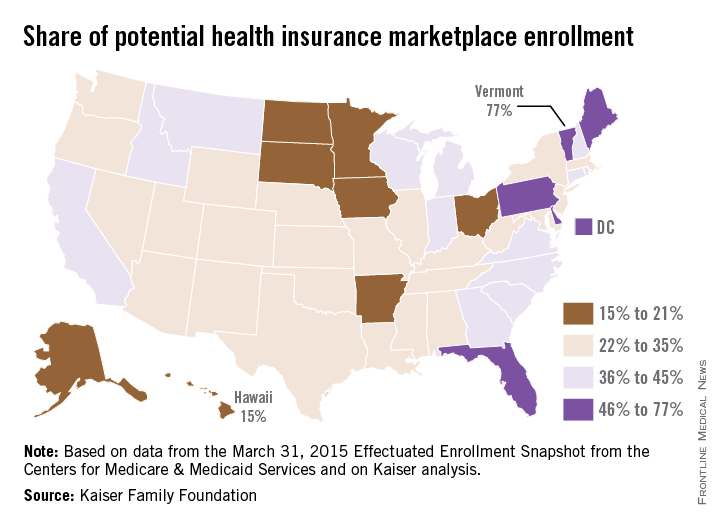
Supreme Court upholds use of federal subsidies under ACA
In a decision that keeps the Affordable Care Act intact, the U.S. Supreme Court has upheld the use of federal subsidies under the health law in states that have not created state-run marketplaces.
With a 6-3 vote in favor of the Obama administration, justices ruled that residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance, based on the high court’s interpretation of ACA language.
In their opinion, justices said the context and structure of the act’s language compel the conclusion that tax credits are available for insurance purchased on any exchange created under the law. The credits are necessary for the federal exchanges to function like their state exchange counterparts, the high court stated, and to avoid calamitous results that Congress intended to avoid.
“When read in context, the phrase ‘an exchange established by the state’ [in the ACA], is properly viewed as ambiguous,” the majority justices said. “The phrase may be limited in its reach to state exchanges. But it could also refer to all exchanges – both state and federal – for purposes of the tax credits. If a state chooses not to follow the directive to establish an exchange, the Act tells [HHS] to establish ‘such exchange.’ By using the words ‘such exchange,’ the Act indicates that state and federal exchanges should be the same.”
President Obama quickly praised the decision, calling it a win for the nation and a testament to the law’s value.
“The Court upheld a critical part of this law; the part that’s made it easier for Americans to afford health insurance, regardless of where you live,” President Obama said during a press conference. The ruling “is a victory to hardworking Americans all across this country whose lives will continue to become more secure in a changing economy because of this law.”
Supporters for the plaintiff issued sharp criticism of the decision and the ACA itself.
The “ruling is deeply disappointing, but it does not change the fact that Obamacare is a fundamentally flawed law,” House Ways and Means Committee Chair Paul Ryan (R-Wisc.) said in a statement. “It’s increasing health care costs, reducing coverage choices, and weighing down our economy. We need a system that makes coverage more affordable and puts patients – not Washington – in charge of health care decisions.”
Former Arkansas Gov. Mike Huckabee, a 2016 Republican presidential candidate, went a step farther, calling the Supreme Court decision “an out-of-control act of judicial tyranny.”
“Our Founding Fathers didn’t create a “do-over” provision in our Constitution that allows unelected Supreme Court justices the power to circumvent Congress and rewrite bad laws,” Mr. Huckabee said in a statement.
Meanwhile, the American Medial Association and other physician leaders expressed relief at the decision, stressing that millions of patients can now continue to access necessary health care.
“The subsidies upheld today help patients afford health insurance so they can see a doctor when they need one and not have to wait until a small health problem becomes a crisis,” AMA President Steven J. Stack said in a statement. “The subsidies provide patients with peace of mind that they will not risk bankruptcy should they become seriously ill or injured and experience catastrophic health care costs.”
The closely watched case was heard before the Supreme Court on March 4, and analysts had issued mixed predictions about how justices would find. The case centered on a handful of words in the ACA’s language that states tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argued the language did not mention the federal exchange and that subsidies should be available only for purchases through state exchanges.
However, the Supreme Court countered this interpretation, arguing that such a reading would destabilize the individual insurance market in any state with a federal exchange, and likely create the death spirals that Congress designed the law to avoid.
“Under petitioners’ reading … one of the Act’s three major reforms – the tax credits – would not apply. And a second major reform – the coverage requirement – would not apply in a meaningful way, because so many individuals would be exempt from the requirement without the tax credits. If petitioners are right, therefore, only one of the Act’s three major reforms would apply in states with a federal exchange. … It is implausible that Congress meant the Act to operate in this manner,” the majority justices wrote in their decision.
Justice Antonin Scalia, Justice Clarence Thomas, and Justice Samuel Alito Jr. disagreed. The dissenters accused the majority of failing to interpret the ACA and instead rewriting the law as they saw fit.
“Words no longer have meaning if an exchange that is not established by a state is ‘established by the state,’ ” Justice Scalia wrote in his dissent. “It is hard to come up with a clearer way to limit tax credits to state exchanges than to use the words ‘established by the state. And it is hard to come up with a reason to include the words ‘by the state’ other than the purpose of limiting credits to state exchanges.”
Justice Scalia and his fellow dissenters added that normal rules of interpretation don’t appear to apply to a Court that yields always to the overriding principle of saving the ACA.
“Having transformed two major parts of the law, the Court today has turned its attention to a third,” Justice Scalia wrote. “The Act that Congress passed makes tax credits available only on an ‘exchange established by the state.’ This Court, however, concludes that this limitation would prevent the rest of the Act from working as well as hoped. So it rewrites the law to make tax credits available everywhere. We should start calling this law SCOTUScare.”
On Twitter @legal_med
This story was updated 6/25/2015.
In a decision that keeps the Affordable Care Act intact, the U.S. Supreme Court has upheld the use of federal subsidies under the health law in states that have not created state-run marketplaces.
With a 6-3 vote in favor of the Obama administration, justices ruled that residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance, based on the high court’s interpretation of ACA language.
In their opinion, justices said the context and structure of the act’s language compel the conclusion that tax credits are available for insurance purchased on any exchange created under the law. The credits are necessary for the federal exchanges to function like their state exchange counterparts, the high court stated, and to avoid calamitous results that Congress intended to avoid.
“When read in context, the phrase ‘an exchange established by the state’ [in the ACA], is properly viewed as ambiguous,” the majority justices said. “The phrase may be limited in its reach to state exchanges. But it could also refer to all exchanges – both state and federal – for purposes of the tax credits. If a state chooses not to follow the directive to establish an exchange, the Act tells [HHS] to establish ‘such exchange.’ By using the words ‘such exchange,’ the Act indicates that state and federal exchanges should be the same.”
President Obama quickly praised the decision, calling it a win for the nation and a testament to the law’s value.
“The Court upheld a critical part of this law; the part that’s made it easier for Americans to afford health insurance, regardless of where you live,” President Obama said during a press conference. The ruling “is a victory to hardworking Americans all across this country whose lives will continue to become more secure in a changing economy because of this law.”
Supporters for the plaintiff issued sharp criticism of the decision and the ACA itself.
The “ruling is deeply disappointing, but it does not change the fact that Obamacare is a fundamentally flawed law,” House Ways and Means Committee Chair Paul Ryan (R-Wisc.) said in a statement. “It’s increasing health care costs, reducing coverage choices, and weighing down our economy. We need a system that makes coverage more affordable and puts patients – not Washington – in charge of health care decisions.”
Former Arkansas Gov. Mike Huckabee, a 2016 Republican presidential candidate, went a step farther, calling the Supreme Court decision “an out-of-control act of judicial tyranny.”
“Our Founding Fathers didn’t create a “do-over” provision in our Constitution that allows unelected Supreme Court justices the power to circumvent Congress and rewrite bad laws,” Mr. Huckabee said in a statement.
Meanwhile, the American Medial Association and other physician leaders expressed relief at the decision, stressing that millions of patients can now continue to access necessary health care.
“The subsidies upheld today help patients afford health insurance so they can see a doctor when they need one and not have to wait until a small health problem becomes a crisis,” AMA President Steven J. Stack said in a statement. “The subsidies provide patients with peace of mind that they will not risk bankruptcy should they become seriously ill or injured and experience catastrophic health care costs.”
The closely watched case was heard before the Supreme Court on March 4, and analysts had issued mixed predictions about how justices would find. The case centered on a handful of words in the ACA’s language that states tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argued the language did not mention the federal exchange and that subsidies should be available only for purchases through state exchanges.
However, the Supreme Court countered this interpretation, arguing that such a reading would destabilize the individual insurance market in any state with a federal exchange, and likely create the death spirals that Congress designed the law to avoid.
“Under petitioners’ reading … one of the Act’s three major reforms – the tax credits – would not apply. And a second major reform – the coverage requirement – would not apply in a meaningful way, because so many individuals would be exempt from the requirement without the tax credits. If petitioners are right, therefore, only one of the Act’s three major reforms would apply in states with a federal exchange. … It is implausible that Congress meant the Act to operate in this manner,” the majority justices wrote in their decision.
Justice Antonin Scalia, Justice Clarence Thomas, and Justice Samuel Alito Jr. disagreed. The dissenters accused the majority of failing to interpret the ACA and instead rewriting the law as they saw fit.
“Words no longer have meaning if an exchange that is not established by a state is ‘established by the state,’ ” Justice Scalia wrote in his dissent. “It is hard to come up with a clearer way to limit tax credits to state exchanges than to use the words ‘established by the state. And it is hard to come up with a reason to include the words ‘by the state’ other than the purpose of limiting credits to state exchanges.”
Justice Scalia and his fellow dissenters added that normal rules of interpretation don’t appear to apply to a Court that yields always to the overriding principle of saving the ACA.
“Having transformed two major parts of the law, the Court today has turned its attention to a third,” Justice Scalia wrote. “The Act that Congress passed makes tax credits available only on an ‘exchange established by the state.’ This Court, however, concludes that this limitation would prevent the rest of the Act from working as well as hoped. So it rewrites the law to make tax credits available everywhere. We should start calling this law SCOTUScare.”
On Twitter @legal_med
This story was updated 6/25/2015.
In a decision that keeps the Affordable Care Act intact, the U.S. Supreme Court has upheld the use of federal subsidies under the health law in states that have not created state-run marketplaces.
With a 6-3 vote in favor of the Obama administration, justices ruled that residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance, based on the high court’s interpretation of ACA language.
In their opinion, justices said the context and structure of the act’s language compel the conclusion that tax credits are available for insurance purchased on any exchange created under the law. The credits are necessary for the federal exchanges to function like their state exchange counterparts, the high court stated, and to avoid calamitous results that Congress intended to avoid.
“When read in context, the phrase ‘an exchange established by the state’ [in the ACA], is properly viewed as ambiguous,” the majority justices said. “The phrase may be limited in its reach to state exchanges. But it could also refer to all exchanges – both state and federal – for purposes of the tax credits. If a state chooses not to follow the directive to establish an exchange, the Act tells [HHS] to establish ‘such exchange.’ By using the words ‘such exchange,’ the Act indicates that state and federal exchanges should be the same.”
President Obama quickly praised the decision, calling it a win for the nation and a testament to the law’s value.
“The Court upheld a critical part of this law; the part that’s made it easier for Americans to afford health insurance, regardless of where you live,” President Obama said during a press conference. The ruling “is a victory to hardworking Americans all across this country whose lives will continue to become more secure in a changing economy because of this law.”
Supporters for the plaintiff issued sharp criticism of the decision and the ACA itself.
The “ruling is deeply disappointing, but it does not change the fact that Obamacare is a fundamentally flawed law,” House Ways and Means Committee Chair Paul Ryan (R-Wisc.) said in a statement. “It’s increasing health care costs, reducing coverage choices, and weighing down our economy. We need a system that makes coverage more affordable and puts patients – not Washington – in charge of health care decisions.”
Former Arkansas Gov. Mike Huckabee, a 2016 Republican presidential candidate, went a step farther, calling the Supreme Court decision “an out-of-control act of judicial tyranny.”
“Our Founding Fathers didn’t create a “do-over” provision in our Constitution that allows unelected Supreme Court justices the power to circumvent Congress and rewrite bad laws,” Mr. Huckabee said in a statement.
Meanwhile, the American Medial Association and other physician leaders expressed relief at the decision, stressing that millions of patients can now continue to access necessary health care.
“The subsidies upheld today help patients afford health insurance so they can see a doctor when they need one and not have to wait until a small health problem becomes a crisis,” AMA President Steven J. Stack said in a statement. “The subsidies provide patients with peace of mind that they will not risk bankruptcy should they become seriously ill or injured and experience catastrophic health care costs.”
The closely watched case was heard before the Supreme Court on March 4, and analysts had issued mixed predictions about how justices would find. The case centered on a handful of words in the ACA’s language that states tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argued the language did not mention the federal exchange and that subsidies should be available only for purchases through state exchanges.
However, the Supreme Court countered this interpretation, arguing that such a reading would destabilize the individual insurance market in any state with a federal exchange, and likely create the death spirals that Congress designed the law to avoid.
“Under petitioners’ reading … one of the Act’s three major reforms – the tax credits – would not apply. And a second major reform – the coverage requirement – would not apply in a meaningful way, because so many individuals would be exempt from the requirement without the tax credits. If petitioners are right, therefore, only one of the Act’s three major reforms would apply in states with a federal exchange. … It is implausible that Congress meant the Act to operate in this manner,” the majority justices wrote in their decision.
Justice Antonin Scalia, Justice Clarence Thomas, and Justice Samuel Alito Jr. disagreed. The dissenters accused the majority of failing to interpret the ACA and instead rewriting the law as they saw fit.
“Words no longer have meaning if an exchange that is not established by a state is ‘established by the state,’ ” Justice Scalia wrote in his dissent. “It is hard to come up with a clearer way to limit tax credits to state exchanges than to use the words ‘established by the state. And it is hard to come up with a reason to include the words ‘by the state’ other than the purpose of limiting credits to state exchanges.”
Justice Scalia and his fellow dissenters added that normal rules of interpretation don’t appear to apply to a Court that yields always to the overriding principle of saving the ACA.
“Having transformed two major parts of the law, the Court today has turned its attention to a third,” Justice Scalia wrote. “The Act that Congress passed makes tax credits available only on an ‘exchange established by the state.’ This Court, however, concludes that this limitation would prevent the rest of the Act from working as well as hoped. So it rewrites the law to make tax credits available everywhere. We should start calling this law SCOTUScare.”
On Twitter @legal_med
This story was updated 6/25/2015.