User login
Happy holidays from Medicare: 250,000 docs to get meaningful use penalty
About 257,000 doctors and other medical professionals, or about 50% of those eligible to participate in the electronic health record incentive program, are about to get a holiday “gift” from Medicare: a 1% reduction in Medicare pay.
The reduction will come from 2015 Medicare payments to doctors who failed to meet meaningful use requirements during a 2013 reporting period or did not receive a hardship exemption, according to the Centers for Medicare & Medicaid Services
The penalties apply to those who have not met Stage 1 of the meaningful use criteria, and given how few have attested to meeting Stage 2 so far, the number of doctors and providers being penalized could go significantly higher.
“It speaks to how hard it is” to meet the meaningful use criteria, commented Dr. Neil Skolnik, a family physician in Jenkintown, Penn. “What it’s creating is a lot of disgruntlement among physicians who aren’t meeting [meaningful use]. ... People really resent that. They are burdened by working hard to make the [EHR] work in their office and then getting a penalty. Even though they have the [EHR], they’re not meeting all the criteria. It’s a big deal. It’s really hard on people.”
Physicians continue to press CMS to reduce the 2015 attestation period for meeting meaningful use Stage 2 to 90 days, down from the current full-year requirement.
In a Dec. 15 letter to federal officials, the American College of Cardiology said it remains “unconvinced that significant numbers of [eligible professionals] and [eligible hospitals] will be able to meet the current requirements of reporting for a full year in 2015 and urge CMS and [the Office of the National Coordinator for Heath Information Technology] to adjust the 2015 reporting period to the 90 days originally afforded to [eligible professionals] and [eligible hospitals] for 2014.”
The cardiologists added that by pushing for a full-year attestation period, “CMS and ONC are setting EPs and EHs up for failure. ... It is simply too much to expect them to ... meet a full year reporting requirement, especially when coupled with implementation of the penalty phase of the federal EHR Incentive program, the value-based payment program, the Physician Quality Reporting System penalties, and ICD-10 implementation.”
About 257,000 doctors and other medical professionals, or about 50% of those eligible to participate in the electronic health record incentive program, are about to get a holiday “gift” from Medicare: a 1% reduction in Medicare pay.
The reduction will come from 2015 Medicare payments to doctors who failed to meet meaningful use requirements during a 2013 reporting period or did not receive a hardship exemption, according to the Centers for Medicare & Medicaid Services
The penalties apply to those who have not met Stage 1 of the meaningful use criteria, and given how few have attested to meeting Stage 2 so far, the number of doctors and providers being penalized could go significantly higher.
“It speaks to how hard it is” to meet the meaningful use criteria, commented Dr. Neil Skolnik, a family physician in Jenkintown, Penn. “What it’s creating is a lot of disgruntlement among physicians who aren’t meeting [meaningful use]. ... People really resent that. They are burdened by working hard to make the [EHR] work in their office and then getting a penalty. Even though they have the [EHR], they’re not meeting all the criteria. It’s a big deal. It’s really hard on people.”
Physicians continue to press CMS to reduce the 2015 attestation period for meeting meaningful use Stage 2 to 90 days, down from the current full-year requirement.
In a Dec. 15 letter to federal officials, the American College of Cardiology said it remains “unconvinced that significant numbers of [eligible professionals] and [eligible hospitals] will be able to meet the current requirements of reporting for a full year in 2015 and urge CMS and [the Office of the National Coordinator for Heath Information Technology] to adjust the 2015 reporting period to the 90 days originally afforded to [eligible professionals] and [eligible hospitals] for 2014.”
The cardiologists added that by pushing for a full-year attestation period, “CMS and ONC are setting EPs and EHs up for failure. ... It is simply too much to expect them to ... meet a full year reporting requirement, especially when coupled with implementation of the penalty phase of the federal EHR Incentive program, the value-based payment program, the Physician Quality Reporting System penalties, and ICD-10 implementation.”
About 257,000 doctors and other medical professionals, or about 50% of those eligible to participate in the electronic health record incentive program, are about to get a holiday “gift” from Medicare: a 1% reduction in Medicare pay.
The reduction will come from 2015 Medicare payments to doctors who failed to meet meaningful use requirements during a 2013 reporting period or did not receive a hardship exemption, according to the Centers for Medicare & Medicaid Services
The penalties apply to those who have not met Stage 1 of the meaningful use criteria, and given how few have attested to meeting Stage 2 so far, the number of doctors and providers being penalized could go significantly higher.
“It speaks to how hard it is” to meet the meaningful use criteria, commented Dr. Neil Skolnik, a family physician in Jenkintown, Penn. “What it’s creating is a lot of disgruntlement among physicians who aren’t meeting [meaningful use]. ... People really resent that. They are burdened by working hard to make the [EHR] work in their office and then getting a penalty. Even though they have the [EHR], they’re not meeting all the criteria. It’s a big deal. It’s really hard on people.”
Physicians continue to press CMS to reduce the 2015 attestation period for meeting meaningful use Stage 2 to 90 days, down from the current full-year requirement.
In a Dec. 15 letter to federal officials, the American College of Cardiology said it remains “unconvinced that significant numbers of [eligible professionals] and [eligible hospitals] will be able to meet the current requirements of reporting for a full year in 2015 and urge CMS and [the Office of the National Coordinator for Heath Information Technology] to adjust the 2015 reporting period to the 90 days originally afforded to [eligible professionals] and [eligible hospitals] for 2014.”
The cardiologists added that by pushing for a full-year attestation period, “CMS and ONC are setting EPs and EHs up for failure. ... It is simply too much to expect them to ... meet a full year reporting requirement, especially when coupled with implementation of the penalty phase of the federal EHR Incentive program, the value-based payment program, the Physician Quality Reporting System penalties, and ICD-10 implementation.”
Survey: Hospitals that listen to their patients make fewer errors
Hospital patients who are treated with respect by staff are less likely to experience a preventable medical error, according to a study conducted by Consumer Reports.
About a quarter of the 1,200 patients who responded to the Consumer Reports survey felt hospital staff did not treat them as adults who were involved in their own care. A third of patients felt their wishes for treatments were not respected, with a similar number reporting that hospital staff would interrupt them. Around 20% said they were not treated fairly and experienced discrimination.
Overall, patients who were unhappy with how they were treated at the hospital were two and a half times more likely to experience some sort of preventable error, such as a drug error, rehospitalization, or a hospital-acquired disease than those who were happy with their treatment. Around 440,000 deaths are attributed to medical errors every year.
“We encourage patients to speak up when they feel that their wishes are not being heard. This survey validates that doing so might actually save your life,” Lisa McGiffert, manager of Consumer Reports’ Safe Patient Project, said in a written statement.
The full report, “How Not to Get Sick(er) in the Hospital,” which includes ratings of almost 2,600 U.S. hospitals, is featured in the February 2015 issue of Consumer Reports, and at ConsumerReports.org.
Hospital patients who are treated with respect by staff are less likely to experience a preventable medical error, according to a study conducted by Consumer Reports.
About a quarter of the 1,200 patients who responded to the Consumer Reports survey felt hospital staff did not treat them as adults who were involved in their own care. A third of patients felt their wishes for treatments were not respected, with a similar number reporting that hospital staff would interrupt them. Around 20% said they were not treated fairly and experienced discrimination.
Overall, patients who were unhappy with how they were treated at the hospital were two and a half times more likely to experience some sort of preventable error, such as a drug error, rehospitalization, or a hospital-acquired disease than those who were happy with their treatment. Around 440,000 deaths are attributed to medical errors every year.
“We encourage patients to speak up when they feel that their wishes are not being heard. This survey validates that doing so might actually save your life,” Lisa McGiffert, manager of Consumer Reports’ Safe Patient Project, said in a written statement.
The full report, “How Not to Get Sick(er) in the Hospital,” which includes ratings of almost 2,600 U.S. hospitals, is featured in the February 2015 issue of Consumer Reports, and at ConsumerReports.org.
Hospital patients who are treated with respect by staff are less likely to experience a preventable medical error, according to a study conducted by Consumer Reports.
About a quarter of the 1,200 patients who responded to the Consumer Reports survey felt hospital staff did not treat them as adults who were involved in their own care. A third of patients felt their wishes for treatments were not respected, with a similar number reporting that hospital staff would interrupt them. Around 20% said they were not treated fairly and experienced discrimination.
Overall, patients who were unhappy with how they were treated at the hospital were two and a half times more likely to experience some sort of preventable error, such as a drug error, rehospitalization, or a hospital-acquired disease than those who were happy with their treatment. Around 440,000 deaths are attributed to medical errors every year.
“We encourage patients to speak up when they feel that their wishes are not being heard. This survey validates that doing so might actually save your life,” Lisa McGiffert, manager of Consumer Reports’ Safe Patient Project, said in a written statement.
The full report, “How Not to Get Sick(er) in the Hospital,” which includes ratings of almost 2,600 U.S. hospitals, is featured in the February 2015 issue of Consumer Reports, and at ConsumerReports.org.
Feds call for more transparency in reporting clinical trial results
A proposal is being floated to make clinical trial results posted to ClinicalTrials.gov more transparent, complete, and timely, regardless of whether the trial is related to an approved product.
The Department of Health & Human Services posted a proposed rule for public inspection on Nov. 19 that would expand the reporting requirements for ClinicalTrials.gov to include results on all clinical trials that are required to register on the trials database, not just results for drugs and devices that are approved, licensed, or cleared for use. It also expands data elements that are accessible and proposes more frequent updating for certain data.
Other than phase I studies of drugs and biologics and small feasibility studies of devices, trials involving drugs and devices regulated by the Food and Drug Administration would be subject to the reporting requirement under this proposal, irrespective of who is funding the study.
A separate proposal by the National Institutes of Health would apply the expanded reporting proposal to all trials funded by NIH, regardless of whether those trials would otherwise not be required to report to ClinicalTrials.gov under requirements set in the FDA Amendments Act of 2007.
“The scientific community has a disappointing track record for dissemination of clinical trial results,” NIH Deputy Director for Science, Outreach and Policy Kathy Hudson, Ph.D., and Director Dr. Francis Collins wrote in a viewpoint published in JAMA (2014 Nov. 19 [doi:10.1001/jama.2014.10716]) .
The NIH officials noted that a “recent analysis of 400 clinical studies revealed that 30% had not shared results through publication or through results reporting in ClinicalTrials.gov within 4 years of completion. This is a serious issue and the proposed rule underscores the intent of NIH to take strong action to promote timely dissemination of clinical trial results.”
Comments on the proposed rule are due within 90 days of its publication in the Federal Register on Nov. 21. The response date for comments on the NIH draft policy on reporting requirements for NIH-funded studies is Feb. 19, 2015.
A proposal is being floated to make clinical trial results posted to ClinicalTrials.gov more transparent, complete, and timely, regardless of whether the trial is related to an approved product.
The Department of Health & Human Services posted a proposed rule for public inspection on Nov. 19 that would expand the reporting requirements for ClinicalTrials.gov to include results on all clinical trials that are required to register on the trials database, not just results for drugs and devices that are approved, licensed, or cleared for use. It also expands data elements that are accessible and proposes more frequent updating for certain data.
Other than phase I studies of drugs and biologics and small feasibility studies of devices, trials involving drugs and devices regulated by the Food and Drug Administration would be subject to the reporting requirement under this proposal, irrespective of who is funding the study.
A separate proposal by the National Institutes of Health would apply the expanded reporting proposal to all trials funded by NIH, regardless of whether those trials would otherwise not be required to report to ClinicalTrials.gov under requirements set in the FDA Amendments Act of 2007.
“The scientific community has a disappointing track record for dissemination of clinical trial results,” NIH Deputy Director for Science, Outreach and Policy Kathy Hudson, Ph.D., and Director Dr. Francis Collins wrote in a viewpoint published in JAMA (2014 Nov. 19 [doi:10.1001/jama.2014.10716]) .
The NIH officials noted that a “recent analysis of 400 clinical studies revealed that 30% had not shared results through publication or through results reporting in ClinicalTrials.gov within 4 years of completion. This is a serious issue and the proposed rule underscores the intent of NIH to take strong action to promote timely dissemination of clinical trial results.”
Comments on the proposed rule are due within 90 days of its publication in the Federal Register on Nov. 21. The response date for comments on the NIH draft policy on reporting requirements for NIH-funded studies is Feb. 19, 2015.
A proposal is being floated to make clinical trial results posted to ClinicalTrials.gov more transparent, complete, and timely, regardless of whether the trial is related to an approved product.
The Department of Health & Human Services posted a proposed rule for public inspection on Nov. 19 that would expand the reporting requirements for ClinicalTrials.gov to include results on all clinical trials that are required to register on the trials database, not just results for drugs and devices that are approved, licensed, or cleared for use. It also expands data elements that are accessible and proposes more frequent updating for certain data.
Other than phase I studies of drugs and biologics and small feasibility studies of devices, trials involving drugs and devices regulated by the Food and Drug Administration would be subject to the reporting requirement under this proposal, irrespective of who is funding the study.
A separate proposal by the National Institutes of Health would apply the expanded reporting proposal to all trials funded by NIH, regardless of whether those trials would otherwise not be required to report to ClinicalTrials.gov under requirements set in the FDA Amendments Act of 2007.
“The scientific community has a disappointing track record for dissemination of clinical trial results,” NIH Deputy Director for Science, Outreach and Policy Kathy Hudson, Ph.D., and Director Dr. Francis Collins wrote in a viewpoint published in JAMA (2014 Nov. 19 [doi:10.1001/jama.2014.10716]) .
The NIH officials noted that a “recent analysis of 400 clinical studies revealed that 30% had not shared results through publication or through results reporting in ClinicalTrials.gov within 4 years of completion. This is a serious issue and the proposed rule underscores the intent of NIH to take strong action to promote timely dissemination of clinical trial results.”
Comments on the proposed rule are due within 90 days of its publication in the Federal Register on Nov. 21. The response date for comments on the NIH draft policy on reporting requirements for NIH-funded studies is Feb. 19, 2015.
Spike in Medicaid use of emergency services after expansion temporary
Concerns that Medicaid expansion could put pressure on budgets because of greater use of emergency department services may be put to rest, if California’s experience is reflected in other states.
That state’s Medicaid program saw an initial spike in usage of hospital inpatient and emergency department services; however, there was a “significant decline” in the use of these services the year after following expansion, according to the UCLA Center for Health Policy Research.
However, part of that may be tied to how California prepared for expansion, as authors notes that the research findings “suggest that early and significant investments in infrastructure and in improving the process of care delivery can effectively address some pent-up demand for health care services of previously uninsured populations. Lead author Nigel Lo, a research analyst at the center, and his colleagues note that in California, there was a Low-Income Health Program (LIHP) that served as a bridge to the state’s Medicaid expansion under the Affordable Care Act.
As the state planned to expand Medicaid services, the authors noted concern in California, not unlike elsewhere in the nation, newly eligible Medicaid enrollees “are expected to have a significant level of unmet need (pent-up demand) and disproportionately higher rates of costly emergency room visits and hospitalizations.”
But over time, those with the highest demand (defined as individuals who had previously not used county services prior to enrolling in LIHP) ultimately had usage on par with those who had the lowest demand.
High-demand LIHP enrollees in the first quarter of the program in July 2011 had 600 emergency room visits per 1,000 enrollees. By April 2013, visits dropped dramatically to 183 visits per 1,000 enrollees, a number that was relatively flat during the second full year enrolled in the LIHP program. By comparison, those with the lowest demand had 148 visits per 1,000 enrollees in July 2011 and 140 visits per 1,000 enrollees in April 2013. Hospitalization rates mirrored emergency room visits during this same period, while outpatient services were constant among all groups looked at.
In an interview, Mr. Lo said that the findings should address fears of runaway utilization. “We definitely didn’t see that,” he said. “The fact that there was no runaway utilization, I think, is really important because it implies that once they get into the system, [costs and utilization] become very predictable.”
Authors conclude that the findings have two significant implications for California and the nation.
“First, although newly eligible Medicaid enrollees have pent-up demand for care, this demand appears to decline rapidly after the first year of enrollment and becomes comparable to the demand with those with previous comprehensive coverage. Second, for the populations who were ‘pre-enrolled’ in coverage programs prior to Medicaid expansion in January 2014, much of the pent-up demand for expensive emergency room and hospital care has already been met.”
When looked at as a whole, the findings suggest that “the higher costs and utilization among newly enrolled Medicaid beneficiaries is a temporary rather than permanent phenomenon.”
Concerns that Medicaid expansion could put pressure on budgets because of greater use of emergency department services may be put to rest, if California’s experience is reflected in other states.
That state’s Medicaid program saw an initial spike in usage of hospital inpatient and emergency department services; however, there was a “significant decline” in the use of these services the year after following expansion, according to the UCLA Center for Health Policy Research.
However, part of that may be tied to how California prepared for expansion, as authors notes that the research findings “suggest that early and significant investments in infrastructure and in improving the process of care delivery can effectively address some pent-up demand for health care services of previously uninsured populations. Lead author Nigel Lo, a research analyst at the center, and his colleagues note that in California, there was a Low-Income Health Program (LIHP) that served as a bridge to the state’s Medicaid expansion under the Affordable Care Act.
As the state planned to expand Medicaid services, the authors noted concern in California, not unlike elsewhere in the nation, newly eligible Medicaid enrollees “are expected to have a significant level of unmet need (pent-up demand) and disproportionately higher rates of costly emergency room visits and hospitalizations.”
But over time, those with the highest demand (defined as individuals who had previously not used county services prior to enrolling in LIHP) ultimately had usage on par with those who had the lowest demand.
High-demand LIHP enrollees in the first quarter of the program in July 2011 had 600 emergency room visits per 1,000 enrollees. By April 2013, visits dropped dramatically to 183 visits per 1,000 enrollees, a number that was relatively flat during the second full year enrolled in the LIHP program. By comparison, those with the lowest demand had 148 visits per 1,000 enrollees in July 2011 and 140 visits per 1,000 enrollees in April 2013. Hospitalization rates mirrored emergency room visits during this same period, while outpatient services were constant among all groups looked at.
In an interview, Mr. Lo said that the findings should address fears of runaway utilization. “We definitely didn’t see that,” he said. “The fact that there was no runaway utilization, I think, is really important because it implies that once they get into the system, [costs and utilization] become very predictable.”
Authors conclude that the findings have two significant implications for California and the nation.
“First, although newly eligible Medicaid enrollees have pent-up demand for care, this demand appears to decline rapidly after the first year of enrollment and becomes comparable to the demand with those with previous comprehensive coverage. Second, for the populations who were ‘pre-enrolled’ in coverage programs prior to Medicaid expansion in January 2014, much of the pent-up demand for expensive emergency room and hospital care has already been met.”
When looked at as a whole, the findings suggest that “the higher costs and utilization among newly enrolled Medicaid beneficiaries is a temporary rather than permanent phenomenon.”
Concerns that Medicaid expansion could put pressure on budgets because of greater use of emergency department services may be put to rest, if California’s experience is reflected in other states.
That state’s Medicaid program saw an initial spike in usage of hospital inpatient and emergency department services; however, there was a “significant decline” in the use of these services the year after following expansion, according to the UCLA Center for Health Policy Research.
However, part of that may be tied to how California prepared for expansion, as authors notes that the research findings “suggest that early and significant investments in infrastructure and in improving the process of care delivery can effectively address some pent-up demand for health care services of previously uninsured populations. Lead author Nigel Lo, a research analyst at the center, and his colleagues note that in California, there was a Low-Income Health Program (LIHP) that served as a bridge to the state’s Medicaid expansion under the Affordable Care Act.
As the state planned to expand Medicaid services, the authors noted concern in California, not unlike elsewhere in the nation, newly eligible Medicaid enrollees “are expected to have a significant level of unmet need (pent-up demand) and disproportionately higher rates of costly emergency room visits and hospitalizations.”
But over time, those with the highest demand (defined as individuals who had previously not used county services prior to enrolling in LIHP) ultimately had usage on par with those who had the lowest demand.
High-demand LIHP enrollees in the first quarter of the program in July 2011 had 600 emergency room visits per 1,000 enrollees. By April 2013, visits dropped dramatically to 183 visits per 1,000 enrollees, a number that was relatively flat during the second full year enrolled in the LIHP program. By comparison, those with the lowest demand had 148 visits per 1,000 enrollees in July 2011 and 140 visits per 1,000 enrollees in April 2013. Hospitalization rates mirrored emergency room visits during this same period, while outpatient services were constant among all groups looked at.
In an interview, Mr. Lo said that the findings should address fears of runaway utilization. “We definitely didn’t see that,” he said. “The fact that there was no runaway utilization, I think, is really important because it implies that once they get into the system, [costs and utilization] become very predictable.”
Authors conclude that the findings have two significant implications for California and the nation.
“First, although newly eligible Medicaid enrollees have pent-up demand for care, this demand appears to decline rapidly after the first year of enrollment and becomes comparable to the demand with those with previous comprehensive coverage. Second, for the populations who were ‘pre-enrolled’ in coverage programs prior to Medicaid expansion in January 2014, much of the pent-up demand for expensive emergency room and hospital care has already been met.”
When looked at as a whole, the findings suggest that “the higher costs and utilization among newly enrolled Medicaid beneficiaries is a temporary rather than permanent phenomenon.”
Physicians shun Stage 2 of meaningful use
Of the 269,000 physicians and health care providers who successfully attested to Stage 1 of meaningful use, just 3,655 have successfully attested to Stage 2 and are ready to receive the incentive payment from Medicare. The Stage 2 deadline is Feb. 28.
For hospitals, the number is similarly weak: just 164 of 4,245 who successfully met the Stage 1 benchmarks have met those for Stage 2.
The totals – accurate as of the end of October – were reported Dec. 9 at a meeting of the Health IT Policy Committee, an advisory committee to the Office of the National Coordinator for Health Information Technology.
The low numbers reflect “the difficulty physicians are having in meeting the meaningful use program’s strict requirements and underlines the need for more flexibility and a shorter reporting period,” said Dr. Steven Stack, president-elect of the American Medical Association in a statement.
However, Dr. Steven Waldren, director of the Alliance for eHealth Innovation at the American Academy of Family Physicians, did not see a reason to panic yet.
“I think it’s probably fair to be nervous, but I still think we have a couple of months to actually see what happens,” Dr. Waldren said in an interview.
Dr. Waldren said several issues could affect physicians’ reporting time frames, including actually meeting Stage 2 criteria, coupled with difficulties that have been documented around implementing 2014-certified electronic health records.
“I think because of the heavy lifting, the numbers are going to be down from what we would think they should be based on this regular progression through the program,” he said.
“But I also think that we won’t know exactly what the magnitude of that decrease will be until after the February time frame.”
Of the 269,000 physicians and health care providers who successfully attested to Stage 1 of meaningful use, just 3,655 have successfully attested to Stage 2 and are ready to receive the incentive payment from Medicare. The Stage 2 deadline is Feb. 28.
For hospitals, the number is similarly weak: just 164 of 4,245 who successfully met the Stage 1 benchmarks have met those for Stage 2.
The totals – accurate as of the end of October – were reported Dec. 9 at a meeting of the Health IT Policy Committee, an advisory committee to the Office of the National Coordinator for Health Information Technology.
The low numbers reflect “the difficulty physicians are having in meeting the meaningful use program’s strict requirements and underlines the need for more flexibility and a shorter reporting period,” said Dr. Steven Stack, president-elect of the American Medical Association in a statement.
However, Dr. Steven Waldren, director of the Alliance for eHealth Innovation at the American Academy of Family Physicians, did not see a reason to panic yet.
“I think it’s probably fair to be nervous, but I still think we have a couple of months to actually see what happens,” Dr. Waldren said in an interview.
Dr. Waldren said several issues could affect physicians’ reporting time frames, including actually meeting Stage 2 criteria, coupled with difficulties that have been documented around implementing 2014-certified electronic health records.
“I think because of the heavy lifting, the numbers are going to be down from what we would think they should be based on this regular progression through the program,” he said.
“But I also think that we won’t know exactly what the magnitude of that decrease will be until after the February time frame.”
Of the 269,000 physicians and health care providers who successfully attested to Stage 1 of meaningful use, just 3,655 have successfully attested to Stage 2 and are ready to receive the incentive payment from Medicare. The Stage 2 deadline is Feb. 28.
For hospitals, the number is similarly weak: just 164 of 4,245 who successfully met the Stage 1 benchmarks have met those for Stage 2.
The totals – accurate as of the end of October – were reported Dec. 9 at a meeting of the Health IT Policy Committee, an advisory committee to the Office of the National Coordinator for Health Information Technology.
The low numbers reflect “the difficulty physicians are having in meeting the meaningful use program’s strict requirements and underlines the need for more flexibility and a shorter reporting period,” said Dr. Steven Stack, president-elect of the American Medical Association in a statement.
However, Dr. Steven Waldren, director of the Alliance for eHealth Innovation at the American Academy of Family Physicians, did not see a reason to panic yet.
“I think it’s probably fair to be nervous, but I still think we have a couple of months to actually see what happens,” Dr. Waldren said in an interview.
Dr. Waldren said several issues could affect physicians’ reporting time frames, including actually meeting Stage 2 criteria, coupled with difficulties that have been documented around implementing 2014-certified electronic health records.
“I think because of the heavy lifting, the numbers are going to be down from what we would think they should be based on this regular progression through the program,” he said.
“But I also think that we won’t know exactly what the magnitude of that decrease will be until after the February time frame.”
Court: State cannot withhold Medicaid payments for program violations
State administrators cannot withhold Medicaid payments from physicians suspected of program violations without evidence of fraud, a Texas appeals court has ruled.
Appellate judges also struck down a rule that enabled the Texas Health and Human Services Commission (THHSC) to retain seized payments after a hold is terminated to offset a possible overpayment.
Although the original plaintiffs in the case were dentists, the decision will apply to all physicians and health providers in Texas, said Donald P. “Rocky” Wilcox, vice president and general counsel for the Texas Medical Association.
“This is a really good decision,” Mr. Wilcox said in an interview. “We saw physicians, dentists, and others having a [payment] hold stay in place even after the agency said there was no more suspicion or allegation of fraud, just a dispute over whether the coding was proper.”
The case originated from a Medicaid payment hold placed on Harlingen Family Dentistry PC during a fraud investigation by the THHSC, according to Harlingen’s attorney, Jason Ray of Austin. An administrative law judge (ALJ) ruled that there was no evidence of fraud but that the dental practice may have potentially committed program violations. The ALJ allowed the payment hold to stand. Harlingen did not appeal and instead filed a separate lawsuit with another dental group that challenged the state’s authority to withhold payments in such circumstances.
A trial court ruled in favor of the state and the decision was appealed to the Texas Court of Appeals, Third District, at Austin, which overturned the decision Nov. 25. The judges said that withholding payments from health providers for alleged program violations, no matter how minor, is inconsistent with the intent of state law, which is to permit holds under instances involving Medicaid fraud or abuse.
“The fact that the challenged rules lack the due-process notice and hearing requirements that are the hallmark of legislation expressly authorizing the imposition of pre-notice payment holds bolsters our conclusion,” the judges said in their opinion.
Additionally, the appeals court revoked another rule that had allowed the state to retain Medicaid payments even after a provider had been cleared of fraud and a hold terminated. The THHSC’s right to possess funds pursuant to a payment hold for fraud depends solely on the existence of credible evidence of such fraud, the appeals court said. Once the statutory basis for imposing the hold ceases to exist, the THHSC no longer has the authority to keep the money.
In a court brief, Ann Hartley, an attorney for the Texas Attorney General’s office, argued that the state has the authority to impose a temporary payment hold when a Medicaid provider commits a program violation, whether or not fraud is alleged. The hold continues until a final determination is made as to whether, and how much, the provider has been overpaid, in which case the seized money is applied to offset or recoup overpayment or pay restitution or penalties imposed, the brief said.
Mr. Ray said that he believes the ruling will have a significant impact on health providers across the state. He oted that many medical practices and professionals have suffered because of the state’s excessive Medicaid payment holds. In a number of cases, he said, the holds resulted from accidental overbilling or paperwork errors.
“It’s a good message to government,” Mr. Ray said in an interview. “Nobody likes fraud, but they need to redirect their efforts to finding providers that are really engaged in fraud and not spend their time and effort driving good providers out of business.”
When asked to comment on this case, the THHSC did not respond to this news organization.
On Twitter @legal_med
State administrators cannot withhold Medicaid payments from physicians suspected of program violations without evidence of fraud, a Texas appeals court has ruled.
Appellate judges also struck down a rule that enabled the Texas Health and Human Services Commission (THHSC) to retain seized payments after a hold is terminated to offset a possible overpayment.
Although the original plaintiffs in the case were dentists, the decision will apply to all physicians and health providers in Texas, said Donald P. “Rocky” Wilcox, vice president and general counsel for the Texas Medical Association.
“This is a really good decision,” Mr. Wilcox said in an interview. “We saw physicians, dentists, and others having a [payment] hold stay in place even after the agency said there was no more suspicion or allegation of fraud, just a dispute over whether the coding was proper.”
The case originated from a Medicaid payment hold placed on Harlingen Family Dentistry PC during a fraud investigation by the THHSC, according to Harlingen’s attorney, Jason Ray of Austin. An administrative law judge (ALJ) ruled that there was no evidence of fraud but that the dental practice may have potentially committed program violations. The ALJ allowed the payment hold to stand. Harlingen did not appeal and instead filed a separate lawsuit with another dental group that challenged the state’s authority to withhold payments in such circumstances.
A trial court ruled in favor of the state and the decision was appealed to the Texas Court of Appeals, Third District, at Austin, which overturned the decision Nov. 25. The judges said that withholding payments from health providers for alleged program violations, no matter how minor, is inconsistent with the intent of state law, which is to permit holds under instances involving Medicaid fraud or abuse.
“The fact that the challenged rules lack the due-process notice and hearing requirements that are the hallmark of legislation expressly authorizing the imposition of pre-notice payment holds bolsters our conclusion,” the judges said in their opinion.
Additionally, the appeals court revoked another rule that had allowed the state to retain Medicaid payments even after a provider had been cleared of fraud and a hold terminated. The THHSC’s right to possess funds pursuant to a payment hold for fraud depends solely on the existence of credible evidence of such fraud, the appeals court said. Once the statutory basis for imposing the hold ceases to exist, the THHSC no longer has the authority to keep the money.
In a court brief, Ann Hartley, an attorney for the Texas Attorney General’s office, argued that the state has the authority to impose a temporary payment hold when a Medicaid provider commits a program violation, whether or not fraud is alleged. The hold continues until a final determination is made as to whether, and how much, the provider has been overpaid, in which case the seized money is applied to offset or recoup overpayment or pay restitution or penalties imposed, the brief said.
Mr. Ray said that he believes the ruling will have a significant impact on health providers across the state. He oted that many medical practices and professionals have suffered because of the state’s excessive Medicaid payment holds. In a number of cases, he said, the holds resulted from accidental overbilling or paperwork errors.
“It’s a good message to government,” Mr. Ray said in an interview. “Nobody likes fraud, but they need to redirect their efforts to finding providers that are really engaged in fraud and not spend their time and effort driving good providers out of business.”
When asked to comment on this case, the THHSC did not respond to this news organization.
On Twitter @legal_med
State administrators cannot withhold Medicaid payments from physicians suspected of program violations without evidence of fraud, a Texas appeals court has ruled.
Appellate judges also struck down a rule that enabled the Texas Health and Human Services Commission (THHSC) to retain seized payments after a hold is terminated to offset a possible overpayment.
Although the original plaintiffs in the case were dentists, the decision will apply to all physicians and health providers in Texas, said Donald P. “Rocky” Wilcox, vice president and general counsel for the Texas Medical Association.
“This is a really good decision,” Mr. Wilcox said in an interview. “We saw physicians, dentists, and others having a [payment] hold stay in place even after the agency said there was no more suspicion or allegation of fraud, just a dispute over whether the coding was proper.”
The case originated from a Medicaid payment hold placed on Harlingen Family Dentistry PC during a fraud investigation by the THHSC, according to Harlingen’s attorney, Jason Ray of Austin. An administrative law judge (ALJ) ruled that there was no evidence of fraud but that the dental practice may have potentially committed program violations. The ALJ allowed the payment hold to stand. Harlingen did not appeal and instead filed a separate lawsuit with another dental group that challenged the state’s authority to withhold payments in such circumstances.
A trial court ruled in favor of the state and the decision was appealed to the Texas Court of Appeals, Third District, at Austin, which overturned the decision Nov. 25. The judges said that withholding payments from health providers for alleged program violations, no matter how minor, is inconsistent with the intent of state law, which is to permit holds under instances involving Medicaid fraud or abuse.
“The fact that the challenged rules lack the due-process notice and hearing requirements that are the hallmark of legislation expressly authorizing the imposition of pre-notice payment holds bolsters our conclusion,” the judges said in their opinion.
Additionally, the appeals court revoked another rule that had allowed the state to retain Medicaid payments even after a provider had been cleared of fraud and a hold terminated. The THHSC’s right to possess funds pursuant to a payment hold for fraud depends solely on the existence of credible evidence of such fraud, the appeals court said. Once the statutory basis for imposing the hold ceases to exist, the THHSC no longer has the authority to keep the money.
In a court brief, Ann Hartley, an attorney for the Texas Attorney General’s office, argued that the state has the authority to impose a temporary payment hold when a Medicaid provider commits a program violation, whether or not fraud is alleged. The hold continues until a final determination is made as to whether, and how much, the provider has been overpaid, in which case the seized money is applied to offset or recoup overpayment or pay restitution or penalties imposed, the brief said.
Mr. Ray said that he believes the ruling will have a significant impact on health providers across the state. He oted that many medical practices and professionals have suffered because of the state’s excessive Medicaid payment holds. In a number of cases, he said, the holds resulted from accidental overbilling or paperwork errors.
“It’s a good message to government,” Mr. Ray said in an interview. “Nobody likes fraud, but they need to redirect their efforts to finding providers that are really engaged in fraud and not spend their time and effort driving good providers out of business.”
When asked to comment on this case, the THHSC did not respond to this news organization.
On Twitter @legal_med
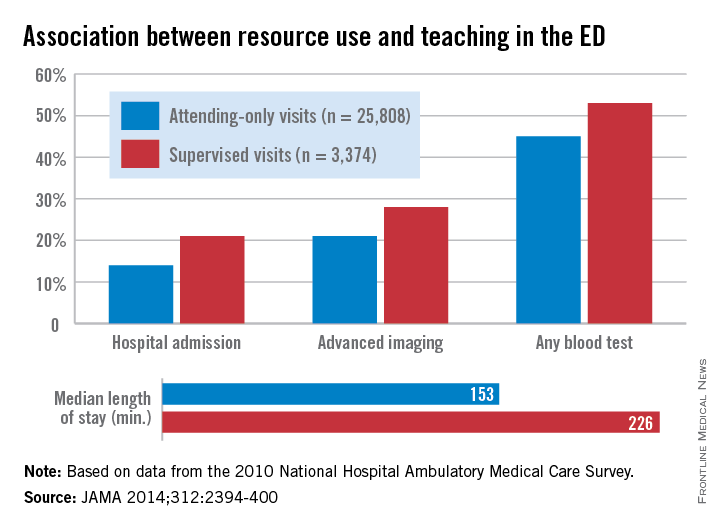
Supervised residents linked to greater ED resource use
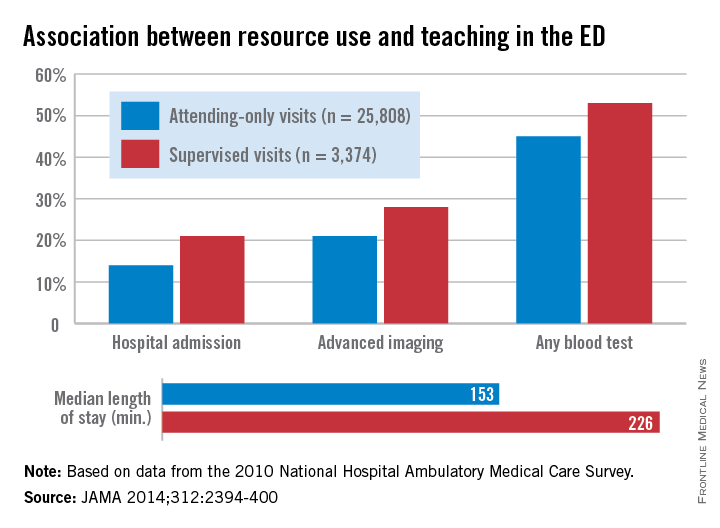
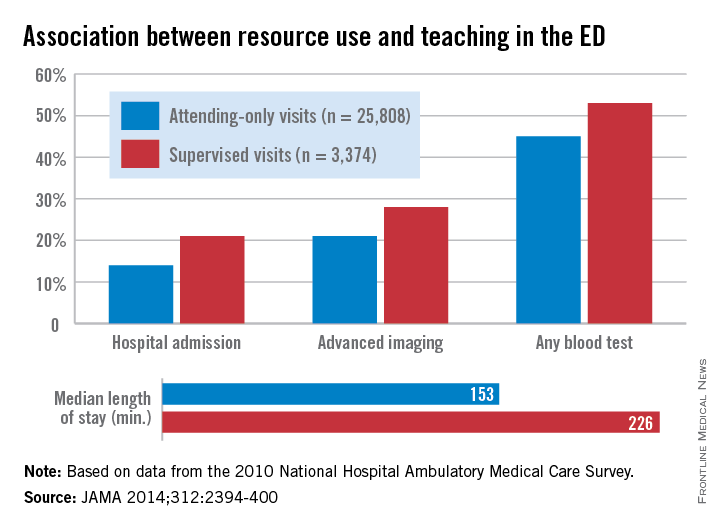
More resources are used in the emergency department when visits involve attending physicians supervising residents, according to a study published Dec. 9 in JAMA.
Compared with attending-only visits in the ED, teaching visits with residents and attendings were more likely to involve hospital admission, advanced imaging, any blood test, and a longer visit time, reported Dr. Stephen R. Pitts of Emory University, Atlanta, and his associates (JAMA 2014;312:2394-400 [doi:10.1001/jama.2014.16172]).
Data for 29,182 visits from the 2010 National Hospital Ambulatory Medical Care Survey’s ED subfile showed that 21% of teaching visits involved a hospital admission, compared with 14% of attending-only vists. Advanced imaging was used in 28% of supervised visits (21% for attending only), and any blood test was used in 53% of supervised visits vs. 45% for attending-only vists. Visits involving a resident also were longer (226 minutes), compared with attending-only visits (153 minutes), Dr. Pitts and his associates said.
“Supervised learning favors a more deliberate, reflective decision-making style than nonteaching clinical visits,” and this was shown by the “consistently higher use of several ED resources among supervised visits, even after adjustment for several other possible determinants,” they concluded.
Dr. Pitts received partial salary support for a time during the study through a contract with the U.S. Dept. of Health & Human Services. One of his associates is an emergency medicine resident and another is the director of an emergency medicine residency. No other conflicts were declared.
More resources are used in the emergency department when visits involve attending physicians supervising residents, according to a study published Dec. 9 in JAMA.
Compared with attending-only visits in the ED, teaching visits with residents and attendings were more likely to involve hospital admission, advanced imaging, any blood test, and a longer visit time, reported Dr. Stephen R. Pitts of Emory University, Atlanta, and his associates (JAMA 2014;312:2394-400 [doi:10.1001/jama.2014.16172]).
Data for 29,182 visits from the 2010 National Hospital Ambulatory Medical Care Survey’s ED subfile showed that 21% of teaching visits involved a hospital admission, compared with 14% of attending-only vists. Advanced imaging was used in 28% of supervised visits (21% for attending only), and any blood test was used in 53% of supervised visits vs. 45% for attending-only vists. Visits involving a resident also were longer (226 minutes), compared with attending-only visits (153 minutes), Dr. Pitts and his associates said.
“Supervised learning favors a more deliberate, reflective decision-making style than nonteaching clinical visits,” and this was shown by the “consistently higher use of several ED resources among supervised visits, even after adjustment for several other possible determinants,” they concluded.
Dr. Pitts received partial salary support for a time during the study through a contract with the U.S. Dept. of Health & Human Services. One of his associates is an emergency medicine resident and another is the director of an emergency medicine residency. No other conflicts were declared.
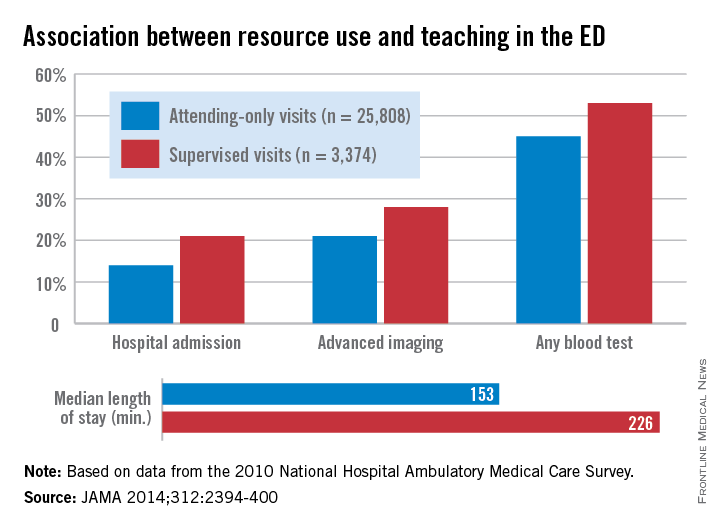
More resources are used in the emergency department when visits involve attending physicians supervising residents, according to a study published Dec. 9 in JAMA.
Compared with attending-only visits in the ED, teaching visits with residents and attendings were more likely to involve hospital admission, advanced imaging, any blood test, and a longer visit time, reported Dr. Stephen R. Pitts of Emory University, Atlanta, and his associates (JAMA 2014;312:2394-400 [doi:10.1001/jama.2014.16172]).
Data for 29,182 visits from the 2010 National Hospital Ambulatory Medical Care Survey’s ED subfile showed that 21% of teaching visits involved a hospital admission, compared with 14% of attending-only vists. Advanced imaging was used in 28% of supervised visits (21% for attending only), and any blood test was used in 53% of supervised visits vs. 45% for attending-only vists. Visits involving a resident also were longer (226 minutes), compared with attending-only visits (153 minutes), Dr. Pitts and his associates said.
“Supervised learning favors a more deliberate, reflective decision-making style than nonteaching clinical visits,” and this was shown by the “consistently higher use of several ED resources among supervised visits, even after adjustment for several other possible determinants,” they concluded.
Dr. Pitts received partial salary support for a time during the study through a contract with the U.S. Dept. of Health & Human Services. One of his associates is an emergency medicine resident and another is the director of an emergency medicine residency. No other conflicts were declared.
FROM JAMA
Reduced resident duty hours haven’t changed patient outcomes
Patient mortality and morbidity outcomes have not changed since the most recent round of reforms to medical residents’ duty hours in 2011, according to two of the first nationwide studies to assess these “improvements,” which both were published online Dec. 9 in JAMA.
In addition, one of the studies found no difference between pre-reform and post-reform scores or on pass rates for oral or written national in-training and board certification examinations.
Thus, two separate studies involving millions of hospitalized patients across the country have both found that these reforms had no discernible effect on patient care. However, both groups of researchers cautioned that their studies were observational and therefore subject to potential biases and that they covered only the first 2 years that the duty-hours reforms have been in place.
The 2011 requirements expanded on those enacted in 2003 by further restricting residents’ duty hours, in the hope of reducing medical errors attributed to exhausted residents. The hours of continuous in-hospital duty were reduced from 30 to 16 for first-year residents and to 24 for upper-year residents, and the interval between shifts was increased to at least 8 hours off for first-year residents and at least 14 hours off for upper-year residents.
“Duty hour reform is arguably one of the largest efforts ever undertaken to improve the quality and safety of patient care in teaching hospitals,” said Dr. Mitesh S. Patel of the University of Pennsylvania and the Veterans Affairs Hospital Center for Health Equity Research and Promotion, both in Philadelphia, and his associates.
They assessed 30-day mortality and readmissions among 2,790,356 Medicare patients who were treated either for acute MI, stroke, gastrointestinal bleeding, or heart failure, or who underwent general, orthopedic, or vascular surgery, at 3,104 hospitals between 2009 and 2012. The investigators found no significant associations, either positive or negative, between the reforms to residents’ duty hours and any patient outcomes. Sensitivity analyses confirmed the results of the primary data analyses.
“Our findings suggest that ... the goals of improving the quality and safety of patient care ... were not being achieved. Conversely, concerns that outcomes might actually worsen because of decreased continuity of care have not been borne out,” Dr. Patel and his associates said (JAMA 2014 Dec. 9 [doi:10.1001/jama.2014.15273]).
The investigators noted that their study was limited in that it could not take into account hospitals’ adherence to the new requirements. Their study also did not assess other outcomes such as patient safety indicators or complication rates, which “may better elucidate the relative effects of decreased resident fatigue and increased patient hand offs.” And their study couldn’t address any possible confounding effects from other concurrent policy initiatives aimed at improving care for Medicare beneficiaries, such as the Hospital Readmissions Reduction Program.
In the other study, a separate group of researchers used data from the American College of Surgeons National Surgical Quality Improvement Program to assess outcomes for 535,499 patients who underwent general surgery at 131 hospitals during the 2 years before and the 2 years after the reforms to residents’ duty hours were implemented. This included 23 teaching hospitals in which residents were involved in at least 95% of general surgeries, said Dr. Ravi Rajaram of the division of research and optimal patient care, American College of Surgeons, and the Institute for Public Health and Medicine at Northwestern University, both in Chicago, and his associates.
The reforms were not associated with any change in rates of patient mortality or serious morbidity, either in the study population as a whole or in the subgroups of high-risk and low-risk patients. They also had no effect on secondary outcomes such as surgical-site infection or sepsis. These results remained consistent across several sensitivity analyses.
Neither mean scores for in-training, written board, and oral board examinations nor pass rates for those examinations showed any significant changes during the study period.
“Moreover, first-year trainees, who were most directly affected by the 2011 reforms, did not improve their ABSITE [American Board of Surgery In-Training Examination] scores, despite presumably more free time to prepare,” Dr. Rajaram and his associates said (JAMA 2014 Dec. 9 [doi:10.1001/JAMA.2014.15277]).
They cautioned that their study assessed only the first 2 years following duty-hour reform, and “there may be differences in patient care or resident examination performance that are evident only several years after implementation and adoption of new duty-hour requirements.” In addition, a retrospective observational study such as this one could not produce the high-level evidence needed to guide policy decisions. “To that end, a national multicenter cluster-randomized trial is being conducted (the Flexibility In duty hour Requirements for Surgical Trainees [FIRST] trial), comparing current duty-hour requirements with flexible duty hours to assess the effects of this intervention on patient outcomes and resident well-being. This trial may further inform the debate of how to optimally structure postgraduate training,” they said.
The results of these two large studies are aligned with those of most previous research into the effects of duty hour requirements on patient outcomes. There is a consistent theme: a lack of a major beneficial effect.
Complex problems often demand complex answers. The goal is for the medical profession to move forward with more comprehensive and nuanced approaches to help fulfill its responsibility to provide trainees with the necessary skills to manage fatigue and allow the safest environment for quality care.
Dr. James A. Arrigh is chair of the Accreditation Council for Graduate Medical Education (ACGME) residency review committee for internal medicine. Dr. James C. Hebert is chair of the ACGME Council of Review Committee Chairs. They made these remarks in an editorial accompanying the studies.
The results of these two large studies are aligned with those of most previous research into the effects of duty hour requirements on patient outcomes. There is a consistent theme: a lack of a major beneficial effect.
Complex problems often demand complex answers. The goal is for the medical profession to move forward with more comprehensive and nuanced approaches to help fulfill its responsibility to provide trainees with the necessary skills to manage fatigue and allow the safest environment for quality care.
Dr. James A. Arrigh is chair of the Accreditation Council for Graduate Medical Education (ACGME) residency review committee for internal medicine. Dr. James C. Hebert is chair of the ACGME Council of Review Committee Chairs. They made these remarks in an editorial accompanying the studies.
The results of these two large studies are aligned with those of most previous research into the effects of duty hour requirements on patient outcomes. There is a consistent theme: a lack of a major beneficial effect.
Complex problems often demand complex answers. The goal is for the medical profession to move forward with more comprehensive and nuanced approaches to help fulfill its responsibility to provide trainees with the necessary skills to manage fatigue and allow the safest environment for quality care.
Dr. James A. Arrigh is chair of the Accreditation Council for Graduate Medical Education (ACGME) residency review committee for internal medicine. Dr. James C. Hebert is chair of the ACGME Council of Review Committee Chairs. They made these remarks in an editorial accompanying the studies.
Patient mortality and morbidity outcomes have not changed since the most recent round of reforms to medical residents’ duty hours in 2011, according to two of the first nationwide studies to assess these “improvements,” which both were published online Dec. 9 in JAMA.
In addition, one of the studies found no difference between pre-reform and post-reform scores or on pass rates for oral or written national in-training and board certification examinations.
Thus, two separate studies involving millions of hospitalized patients across the country have both found that these reforms had no discernible effect on patient care. However, both groups of researchers cautioned that their studies were observational and therefore subject to potential biases and that they covered only the first 2 years that the duty-hours reforms have been in place.
The 2011 requirements expanded on those enacted in 2003 by further restricting residents’ duty hours, in the hope of reducing medical errors attributed to exhausted residents. The hours of continuous in-hospital duty were reduced from 30 to 16 for first-year residents and to 24 for upper-year residents, and the interval between shifts was increased to at least 8 hours off for first-year residents and at least 14 hours off for upper-year residents.
“Duty hour reform is arguably one of the largest efforts ever undertaken to improve the quality and safety of patient care in teaching hospitals,” said Dr. Mitesh S. Patel of the University of Pennsylvania and the Veterans Affairs Hospital Center for Health Equity Research and Promotion, both in Philadelphia, and his associates.
They assessed 30-day mortality and readmissions among 2,790,356 Medicare patients who were treated either for acute MI, stroke, gastrointestinal bleeding, or heart failure, or who underwent general, orthopedic, or vascular surgery, at 3,104 hospitals between 2009 and 2012. The investigators found no significant associations, either positive or negative, between the reforms to residents’ duty hours and any patient outcomes. Sensitivity analyses confirmed the results of the primary data analyses.
“Our findings suggest that ... the goals of improving the quality and safety of patient care ... were not being achieved. Conversely, concerns that outcomes might actually worsen because of decreased continuity of care have not been borne out,” Dr. Patel and his associates said (JAMA 2014 Dec. 9 [doi:10.1001/jama.2014.15273]).
The investigators noted that their study was limited in that it could not take into account hospitals’ adherence to the new requirements. Their study also did not assess other outcomes such as patient safety indicators or complication rates, which “may better elucidate the relative effects of decreased resident fatigue and increased patient hand offs.” And their study couldn’t address any possible confounding effects from other concurrent policy initiatives aimed at improving care for Medicare beneficiaries, such as the Hospital Readmissions Reduction Program.
In the other study, a separate group of researchers used data from the American College of Surgeons National Surgical Quality Improvement Program to assess outcomes for 535,499 patients who underwent general surgery at 131 hospitals during the 2 years before and the 2 years after the reforms to residents’ duty hours were implemented. This included 23 teaching hospitals in which residents were involved in at least 95% of general surgeries, said Dr. Ravi Rajaram of the division of research and optimal patient care, American College of Surgeons, and the Institute for Public Health and Medicine at Northwestern University, both in Chicago, and his associates.
The reforms were not associated with any change in rates of patient mortality or serious morbidity, either in the study population as a whole or in the subgroups of high-risk and low-risk patients. They also had no effect on secondary outcomes such as surgical-site infection or sepsis. These results remained consistent across several sensitivity analyses.
Neither mean scores for in-training, written board, and oral board examinations nor pass rates for those examinations showed any significant changes during the study period.
“Moreover, first-year trainees, who were most directly affected by the 2011 reforms, did not improve their ABSITE [American Board of Surgery In-Training Examination] scores, despite presumably more free time to prepare,” Dr. Rajaram and his associates said (JAMA 2014 Dec. 9 [doi:10.1001/JAMA.2014.15277]).
They cautioned that their study assessed only the first 2 years following duty-hour reform, and “there may be differences in patient care or resident examination performance that are evident only several years after implementation and adoption of new duty-hour requirements.” In addition, a retrospective observational study such as this one could not produce the high-level evidence needed to guide policy decisions. “To that end, a national multicenter cluster-randomized trial is being conducted (the Flexibility In duty hour Requirements for Surgical Trainees [FIRST] trial), comparing current duty-hour requirements with flexible duty hours to assess the effects of this intervention on patient outcomes and resident well-being. This trial may further inform the debate of how to optimally structure postgraduate training,” they said.
Patient mortality and morbidity outcomes have not changed since the most recent round of reforms to medical residents’ duty hours in 2011, according to two of the first nationwide studies to assess these “improvements,” which both were published online Dec. 9 in JAMA.
In addition, one of the studies found no difference between pre-reform and post-reform scores or on pass rates for oral or written national in-training and board certification examinations.
Thus, two separate studies involving millions of hospitalized patients across the country have both found that these reforms had no discernible effect on patient care. However, both groups of researchers cautioned that their studies were observational and therefore subject to potential biases and that they covered only the first 2 years that the duty-hours reforms have been in place.
The 2011 requirements expanded on those enacted in 2003 by further restricting residents’ duty hours, in the hope of reducing medical errors attributed to exhausted residents. The hours of continuous in-hospital duty were reduced from 30 to 16 for first-year residents and to 24 for upper-year residents, and the interval between shifts was increased to at least 8 hours off for first-year residents and at least 14 hours off for upper-year residents.
“Duty hour reform is arguably one of the largest efforts ever undertaken to improve the quality and safety of patient care in teaching hospitals,” said Dr. Mitesh S. Patel of the University of Pennsylvania and the Veterans Affairs Hospital Center for Health Equity Research and Promotion, both in Philadelphia, and his associates.
They assessed 30-day mortality and readmissions among 2,790,356 Medicare patients who were treated either for acute MI, stroke, gastrointestinal bleeding, or heart failure, or who underwent general, orthopedic, or vascular surgery, at 3,104 hospitals between 2009 and 2012. The investigators found no significant associations, either positive or negative, between the reforms to residents’ duty hours and any patient outcomes. Sensitivity analyses confirmed the results of the primary data analyses.
“Our findings suggest that ... the goals of improving the quality and safety of patient care ... were not being achieved. Conversely, concerns that outcomes might actually worsen because of decreased continuity of care have not been borne out,” Dr. Patel and his associates said (JAMA 2014 Dec. 9 [doi:10.1001/jama.2014.15273]).
The investigators noted that their study was limited in that it could not take into account hospitals’ adherence to the new requirements. Their study also did not assess other outcomes such as patient safety indicators or complication rates, which “may better elucidate the relative effects of decreased resident fatigue and increased patient hand offs.” And their study couldn’t address any possible confounding effects from other concurrent policy initiatives aimed at improving care for Medicare beneficiaries, such as the Hospital Readmissions Reduction Program.
In the other study, a separate group of researchers used data from the American College of Surgeons National Surgical Quality Improvement Program to assess outcomes for 535,499 patients who underwent general surgery at 131 hospitals during the 2 years before and the 2 years after the reforms to residents’ duty hours were implemented. This included 23 teaching hospitals in which residents were involved in at least 95% of general surgeries, said Dr. Ravi Rajaram of the division of research and optimal patient care, American College of Surgeons, and the Institute for Public Health and Medicine at Northwestern University, both in Chicago, and his associates.
The reforms were not associated with any change in rates of patient mortality or serious morbidity, either in the study population as a whole or in the subgroups of high-risk and low-risk patients. They also had no effect on secondary outcomes such as surgical-site infection or sepsis. These results remained consistent across several sensitivity analyses.
Neither mean scores for in-training, written board, and oral board examinations nor pass rates for those examinations showed any significant changes during the study period.
“Moreover, first-year trainees, who were most directly affected by the 2011 reforms, did not improve their ABSITE [American Board of Surgery In-Training Examination] scores, despite presumably more free time to prepare,” Dr. Rajaram and his associates said (JAMA 2014 Dec. 9 [doi:10.1001/JAMA.2014.15277]).
They cautioned that their study assessed only the first 2 years following duty-hour reform, and “there may be differences in patient care or resident examination performance that are evident only several years after implementation and adoption of new duty-hour requirements.” In addition, a retrospective observational study such as this one could not produce the high-level evidence needed to guide policy decisions. “To that end, a national multicenter cluster-randomized trial is being conducted (the Flexibility In duty hour Requirements for Surgical Trainees [FIRST] trial), comparing current duty-hour requirements with flexible duty hours to assess the effects of this intervention on patient outcomes and resident well-being. This trial may further inform the debate of how to optimally structure postgraduate training,” they said.
Key clinical point: The newest (2011) reforms to resident duty hours haven’t changed patient mortality or morbidity outcomes.
Major finding: 30-day mortality and readmissions among almost 3 million Medicare patients at 3,104 hospitals did not change between 2009 and 2012.
Data source: Two observational cohort studies of millions of hospitalized adults across the country, comparing patient outcomes before with those after the 2011 reforms in duty hours for residents.
Disclosures: Dr. Patel’s study was funded in part by the National Heart, Lung, and Blood Institute, the Department of Veterans Affairs, and the Robert Wood Johnson Foundation. Dr. Rajaram’s study was supported by the Agency for Healthcare Research and Quality, the American College of Surgeons, and Merck. All of the investigators reported having no relevant financial conflicts of interest.
ONC strategic plan keeps focus on adoption, interoperability
Adoption and interoperability of electronic health records continue to be a primary focus of efforts by the Office of the National Coordinator for Health Information Technology.
“There will be a strong emphasis on interoperability,” said Dr. Karen DeSalvo, National Coordinator for Health IT, during a press conference Dec. 8 to release the updated Federal Health IT Strategic Plan 2015-2020.
Dr. DeSalvo noted that the federal government aims to make data usable across the spectrum of health care – on a one-on-one basis between doctors and patients, all the way to using Big Data to help advance population health objectives. She also emphasized a need for data to be interoperable to help individuals to become “engaged, empowered, [and] real partners in their health and health care and that is, I think an exciting frontier for all of us.”
Specific details on how ONC plans to address interoperability going forward will come with the agency’s release of its interoperability road map, expected in the early part of 2015. An overview of that road map was released earlier this year.
The plan emphasizes efforts to reach health care providers who are currently not eligible for financial incentives under the current meaningful use program.
Other goals identified in the plan include strengthening the health care delivery system; advancing the health and well-being of individuals and communities; and advancing research, scientific knowledge, and innovation.
The plan also targets technology beyond EHRs to include other types of health IT applications, such as telehealth, and calls for looking at other incentives that the 35 federal agencies who contributed to the plan can offer beyond the meaningful use program to help continue the adoption and use of health IT.
Public comments on this strategic plan are due Feb. 6, 2015.
Adoption and interoperability of electronic health records continue to be a primary focus of efforts by the Office of the National Coordinator for Health Information Technology.
“There will be a strong emphasis on interoperability,” said Dr. Karen DeSalvo, National Coordinator for Health IT, during a press conference Dec. 8 to release the updated Federal Health IT Strategic Plan 2015-2020.
Dr. DeSalvo noted that the federal government aims to make data usable across the spectrum of health care – on a one-on-one basis between doctors and patients, all the way to using Big Data to help advance population health objectives. She also emphasized a need for data to be interoperable to help individuals to become “engaged, empowered, [and] real partners in their health and health care and that is, I think an exciting frontier for all of us.”
Specific details on how ONC plans to address interoperability going forward will come with the agency’s release of its interoperability road map, expected in the early part of 2015. An overview of that road map was released earlier this year.
The plan emphasizes efforts to reach health care providers who are currently not eligible for financial incentives under the current meaningful use program.
Other goals identified in the plan include strengthening the health care delivery system; advancing the health and well-being of individuals and communities; and advancing research, scientific knowledge, and innovation.
The plan also targets technology beyond EHRs to include other types of health IT applications, such as telehealth, and calls for looking at other incentives that the 35 federal agencies who contributed to the plan can offer beyond the meaningful use program to help continue the adoption and use of health IT.
Public comments on this strategic plan are due Feb. 6, 2015.
Adoption and interoperability of electronic health records continue to be a primary focus of efforts by the Office of the National Coordinator for Health Information Technology.
“There will be a strong emphasis on interoperability,” said Dr. Karen DeSalvo, National Coordinator for Health IT, during a press conference Dec. 8 to release the updated Federal Health IT Strategic Plan 2015-2020.
Dr. DeSalvo noted that the federal government aims to make data usable across the spectrum of health care – on a one-on-one basis between doctors and patients, all the way to using Big Data to help advance population health objectives. She also emphasized a need for data to be interoperable to help individuals to become “engaged, empowered, [and] real partners in their health and health care and that is, I think an exciting frontier for all of us.”
Specific details on how ONC plans to address interoperability going forward will come with the agency’s release of its interoperability road map, expected in the early part of 2015. An overview of that road map was released earlier this year.
The plan emphasizes efforts to reach health care providers who are currently not eligible for financial incentives under the current meaningful use program.
Other goals identified in the plan include strengthening the health care delivery system; advancing the health and well-being of individuals and communities; and advancing research, scientific knowledge, and innovation.
The plan also targets technology beyond EHRs to include other types of health IT applications, such as telehealth, and calls for looking at other incentives that the 35 federal agencies who contributed to the plan can offer beyond the meaningful use program to help continue the adoption and use of health IT.
Public comments on this strategic plan are due Feb. 6, 2015.
CMS expands ability to deny provider enrollments
The Centers for Medicare & Medicaid Services is tightening scrutiny of providers enrolling in Medicare in an effort to curb fraudulent billing and keep providers with unpaid Medicare debt from reentering the program.
New rules announced Dec. 3 by the CMS strengthen the agency’s ability to deny or revoke the enrollment of entities and individuals believed to pose a program integrity risk to Medicare. The regulations come after the February 2011 revision of CMS’s enrollment policy, a revamp aimed at increasing the integrity of Medicare. Under the Dec. 3 enrollment provisions, the CMS can now:
• Deny the enrollment of providers, suppliers, and owners affiliated with an entity that has unpaid Medicare debt (existing overpayment or another form of financial obligation).
• Deny the enrollment or revoke the billing privileges of a provider or supplier if a managing employee has been convicted of certain felonies (murder, rape, assault, extortion, embezzlement, income tax evasion).
• Revoke the billing privileges of providers and suppliers who have a pattern or practice of billing for services that do not meet Medicare requirements.
The new rules will prevent individuals and entities from being able to incur substantial debt to Medicare, leave the Medicare program, and then reenroll as a new business to avoid repayment of the outstanding Medicare debt, according to the agency.
Physicians and other prospective enrollees who owe Medicare money can avoid being denied by agreeing to a CMS-approved extended repayment schedule for the entire outstanding Medicare debt or by repaying it in full.
In its final rule, the CMS acknowledged that the majority of Medicare provider enrollees submit valid claims that meet the CMS guidelines.
“A small percentage of providers and suppliers are engaging in fraudulent, wasteful, inappropriate, or abusive activities,” the agency wrote in the Federal Register. “Our provider enrollment revisions are directed at such providers and suppliers, and we believe that removing them, as necessary, from the Medicare program will only serve to benefit Medicare beneficiaries, the trust funds, the taxpayers, and the hundreds of thousands of legitimate Medicare providers and suppliers that have proven to be reliable partners of the program.”
The final rules will be published in the Federal Register Dec. 5. A preliminary version of the regulations is available on the Federal Register website.
On Twitter @legal_med
The Centers for Medicare & Medicaid Services is tightening scrutiny of providers enrolling in Medicare in an effort to curb fraudulent billing and keep providers with unpaid Medicare debt from reentering the program.
New rules announced Dec. 3 by the CMS strengthen the agency’s ability to deny or revoke the enrollment of entities and individuals believed to pose a program integrity risk to Medicare. The regulations come after the February 2011 revision of CMS’s enrollment policy, a revamp aimed at increasing the integrity of Medicare. Under the Dec. 3 enrollment provisions, the CMS can now:
• Deny the enrollment of providers, suppliers, and owners affiliated with an entity that has unpaid Medicare debt (existing overpayment or another form of financial obligation).
• Deny the enrollment or revoke the billing privileges of a provider or supplier if a managing employee has been convicted of certain felonies (murder, rape, assault, extortion, embezzlement, income tax evasion).
• Revoke the billing privileges of providers and suppliers who have a pattern or practice of billing for services that do not meet Medicare requirements.
The new rules will prevent individuals and entities from being able to incur substantial debt to Medicare, leave the Medicare program, and then reenroll as a new business to avoid repayment of the outstanding Medicare debt, according to the agency.
Physicians and other prospective enrollees who owe Medicare money can avoid being denied by agreeing to a CMS-approved extended repayment schedule for the entire outstanding Medicare debt or by repaying it in full.
In its final rule, the CMS acknowledged that the majority of Medicare provider enrollees submit valid claims that meet the CMS guidelines.
“A small percentage of providers and suppliers are engaging in fraudulent, wasteful, inappropriate, or abusive activities,” the agency wrote in the Federal Register. “Our provider enrollment revisions are directed at such providers and suppliers, and we believe that removing them, as necessary, from the Medicare program will only serve to benefit Medicare beneficiaries, the trust funds, the taxpayers, and the hundreds of thousands of legitimate Medicare providers and suppliers that have proven to be reliable partners of the program.”
The final rules will be published in the Federal Register Dec. 5. A preliminary version of the regulations is available on the Federal Register website.
On Twitter @legal_med
The Centers for Medicare & Medicaid Services is tightening scrutiny of providers enrolling in Medicare in an effort to curb fraudulent billing and keep providers with unpaid Medicare debt from reentering the program.
New rules announced Dec. 3 by the CMS strengthen the agency’s ability to deny or revoke the enrollment of entities and individuals believed to pose a program integrity risk to Medicare. The regulations come after the February 2011 revision of CMS’s enrollment policy, a revamp aimed at increasing the integrity of Medicare. Under the Dec. 3 enrollment provisions, the CMS can now:
• Deny the enrollment of providers, suppliers, and owners affiliated with an entity that has unpaid Medicare debt (existing overpayment or another form of financial obligation).
• Deny the enrollment or revoke the billing privileges of a provider or supplier if a managing employee has been convicted of certain felonies (murder, rape, assault, extortion, embezzlement, income tax evasion).
• Revoke the billing privileges of providers and suppliers who have a pattern or practice of billing for services that do not meet Medicare requirements.
The new rules will prevent individuals and entities from being able to incur substantial debt to Medicare, leave the Medicare program, and then reenroll as a new business to avoid repayment of the outstanding Medicare debt, according to the agency.
Physicians and other prospective enrollees who owe Medicare money can avoid being denied by agreeing to a CMS-approved extended repayment schedule for the entire outstanding Medicare debt or by repaying it in full.
In its final rule, the CMS acknowledged that the majority of Medicare provider enrollees submit valid claims that meet the CMS guidelines.
“A small percentage of providers and suppliers are engaging in fraudulent, wasteful, inappropriate, or abusive activities,” the agency wrote in the Federal Register. “Our provider enrollment revisions are directed at such providers and suppliers, and we believe that removing them, as necessary, from the Medicare program will only serve to benefit Medicare beneficiaries, the trust funds, the taxpayers, and the hundreds of thousands of legitimate Medicare providers and suppliers that have proven to be reliable partners of the program.”
The final rules will be published in the Federal Register Dec. 5. A preliminary version of the regulations is available on the Federal Register website.
On Twitter @legal_med