User login
Cut Costs, Improve Quality and Patient Experience
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
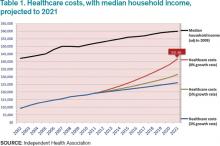
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
VIDEO: AMA president talks meaningful use, ICD-10, and Ebola
WASHINGTON – The recent deadline extensions for meaningful use attestation are encouraging, but not enough. The process must be more user-friendly and clinically meaningful.
That’s according to Dr. Robert Wah, president of the American Medical Association. Dr. Wah discussed the AMA’s concerns about meaningful use and health information technology in a video interview – including whether there is enough of a focus on interoperability of electronic health records.
He also touched on the transition to the ICD-10 code set, again questioning whether the move is clinically useful and ultimately helps improve patient care.
Recently, Dr. Karen DeSalvo, National Coordinator for Health Information Technology, was given an additional appointment as the acting assistant secretary for health to help with the effort to combat the Ebola epidemic. That caused concern among physicians that there could be a leadership vacuum at the Office of the National Coordinator at a time when so much is happening in health IT. Although it was later clarified that she would remain in charge of the effort, there are still some worries, Dr. Wah said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @aliciaault
WASHINGTON – The recent deadline extensions for meaningful use attestation are encouraging, but not enough. The process must be more user-friendly and clinically meaningful.
That’s according to Dr. Robert Wah, president of the American Medical Association. Dr. Wah discussed the AMA’s concerns about meaningful use and health information technology in a video interview – including whether there is enough of a focus on interoperability of electronic health records.
He also touched on the transition to the ICD-10 code set, again questioning whether the move is clinically useful and ultimately helps improve patient care.
Recently, Dr. Karen DeSalvo, National Coordinator for Health Information Technology, was given an additional appointment as the acting assistant secretary for health to help with the effort to combat the Ebola epidemic. That caused concern among physicians that there could be a leadership vacuum at the Office of the National Coordinator at a time when so much is happening in health IT. Although it was later clarified that she would remain in charge of the effort, there are still some worries, Dr. Wah said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @aliciaault
WASHINGTON – The recent deadline extensions for meaningful use attestation are encouraging, but not enough. The process must be more user-friendly and clinically meaningful.
That’s according to Dr. Robert Wah, president of the American Medical Association. Dr. Wah discussed the AMA’s concerns about meaningful use and health information technology in a video interview – including whether there is enough of a focus on interoperability of electronic health records.
He also touched on the transition to the ICD-10 code set, again questioning whether the move is clinically useful and ultimately helps improve patient care.
Recently, Dr. Karen DeSalvo, National Coordinator for Health Information Technology, was given an additional appointment as the acting assistant secretary for health to help with the effort to combat the Ebola epidemic. That caused concern among physicians that there could be a leadership vacuum at the Office of the National Coordinator at a time when so much is happening in health IT. Although it was later clarified that she would remain in charge of the effort, there are still some worries, Dr. Wah said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @aliciaault
VIDEO: AMA President Wah talks SGR, Medicaid parity, and IPAB
WASHINGTON – The American Medical Association is hoping – along with many other medical societies and their physician members – to convince Congress that it should repeal Medicare’s Sustainable Growth Rate formula before the end of the year.
The cost to do so is a relative bargain, and physicians have grown tired of trying to plan around a process that is predictable, yet unpredictable, according to AMA President Robert M. Wah. Why not move now, he wondered, given that there was so much progress in this Congress, including a bill that was passed by the House?
In an exclusive video interview, Dr. Wah talked about the pressing need for the SGR replacement, along with what Republican majorities in both the House and Senate in the incoming Congress might mean to physicians.
Some Republicans have said that they will press for a partial or total repeal of the Affordable Care Act. Dr. Wah touched on whether the AMA supports any part of that notion, including getting rid of the Independent Payment Advisory Board, known as the IPAB.
Dr. Wah also discussed another urgent topic: What to do about the expiring element of the ACA that gave primary care physicians who treat Medicaid patients the same rate of pay as those who serve Medicare beneficiaries. The AMA recently reiterated its position that the so-called pay bump – which ends Dec. 31 – should be extended, and that it also should include obstetricians and gynecologists, who were left out of the initial policy.
On Twitter @aliciaault
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – The American Medical Association is hoping – along with many other medical societies and their physician members – to convince Congress that it should repeal Medicare’s Sustainable Growth Rate formula before the end of the year.
The cost to do so is a relative bargain, and physicians have grown tired of trying to plan around a process that is predictable, yet unpredictable, according to AMA President Robert M. Wah. Why not move now, he wondered, given that there was so much progress in this Congress, including a bill that was passed by the House?
In an exclusive video interview, Dr. Wah talked about the pressing need for the SGR replacement, along with what Republican majorities in both the House and Senate in the incoming Congress might mean to physicians.
Some Republicans have said that they will press for a partial or total repeal of the Affordable Care Act. Dr. Wah touched on whether the AMA supports any part of that notion, including getting rid of the Independent Payment Advisory Board, known as the IPAB.
Dr. Wah also discussed another urgent topic: What to do about the expiring element of the ACA that gave primary care physicians who treat Medicaid patients the same rate of pay as those who serve Medicare beneficiaries. The AMA recently reiterated its position that the so-called pay bump – which ends Dec. 31 – should be extended, and that it also should include obstetricians and gynecologists, who were left out of the initial policy.
On Twitter @aliciaault
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – The American Medical Association is hoping – along with many other medical societies and their physician members – to convince Congress that it should repeal Medicare’s Sustainable Growth Rate formula before the end of the year.
The cost to do so is a relative bargain, and physicians have grown tired of trying to plan around a process that is predictable, yet unpredictable, according to AMA President Robert M. Wah. Why not move now, he wondered, given that there was so much progress in this Congress, including a bill that was passed by the House?
In an exclusive video interview, Dr. Wah talked about the pressing need for the SGR replacement, along with what Republican majorities in both the House and Senate in the incoming Congress might mean to physicians.
Some Republicans have said that they will press for a partial or total repeal of the Affordable Care Act. Dr. Wah touched on whether the AMA supports any part of that notion, including getting rid of the Independent Payment Advisory Board, known as the IPAB.
Dr. Wah also discussed another urgent topic: What to do about the expiring element of the ACA that gave primary care physicians who treat Medicaid patients the same rate of pay as those who serve Medicare beneficiaries. The AMA recently reiterated its position that the so-called pay bump – which ends Dec. 31 – should be extended, and that it also should include obstetricians and gynecologists, who were left out of the initial policy.
On Twitter @aliciaault
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Attorney: Be prepared for next round of HIPAA audits
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
Court: Patients can sue over HIPAA breaches
Patients can sue doctors for negligence after alleged patient privacy breaches, the Connecticut Supreme Court has ruled in a decision that could have nationwide implications.
The state’s highest court concluded that HIPAA does not preempt claims for emotional distress or negligence under state law. The ruling, published Nov. 11, sets precedence in Connecticut and is likely to encourage plaintiffs to raise similar claims in other states, according to Michael J. Kline, a New Jersey attorney who specializes in corporate and securities law.
“It’s a momentous case, and I think it’s serious for physician practices,” said Mr. Kline. “It can set the stage for plaintiffs’ attorneys within given states to [pursue] class actions for emotional distress or invasion of privacy on the grounds there was negligence” in connection to HIPAA violations.
The decision stems from a lawsuit filed by Emily Byrne v. Avery Center for Obstetrics and Gynecology P.C. in Westport, Conn. Ms. Byrne claimed that in 2004, she instructed the health center not to release her medical records to an ex-boyfriend. In 2005, the medical center was served with a subpoena by the former boyfriend requesting the plaintiff’s medical records for a paternity proceeding. The defendant did not alert Ms. Byrne about the subpoena and mailed a copy of her medical file to the probate court, according to court records.
Ms. Byrne later sued the health care center, claiming she suffered harassment and extortion threats from her ex-boyfriend because the medical records were exposed. The complaint alleged the health center engaged in negligent infliction of emotional distress and acted negligently by failing to use proper and reasonable care in protecting her medical file, including disclosing it without authorization in violation of HIPAA.
A trial court agreed with the medical practice’s contention that HIPAA precludes individual liability claims pertaining to confidentiality of medical information. The court cited well-established case law that HIPAA does not create a private right of action and requires alleged privacy violations to be raised through administrative channels. But the Connecticut Supreme Court overturned the decision, ruling that HIPAA does not preempt such negligence lawsuits.
“If Connecticut’s common law recognizes claims arising from a health care provider’s alleged breach of its duty of confidentiality in the course of complying with a subpoena, HIPAA and its implementing regulations do not preempt such claims,” judges said in their opinion. “We further conclude that, to the extent it has become the common practice for Connecticut health care providers to follow the procedures required under HIPAA in rendering services to their patients, HIPAA and its implementing regulations may be utilized to inform the standard of care applicable to such claims arising from allegations of negligence in the disclosure of patients’ medical records pursuant to a subpoena.”
The court went on to say that “the availability of such private rights of action in state courts ... do not preclude, conflict with, or complicate health care providers’ compliance with HIPAA.”
Similar decisions have been made by other courts, but the Connecticut ruling is the first state Supreme Court to issue such a ruling, Mr. Kline said.
For example, in Harmon v. Maury County, the U.S. District Court for the Middle District of Tennessee found that negligence claims founded on violation of HIPAA were not precluded because federal provisions do not completely preempt state law and expressly preserve state laws that aren’t at odds with its terms. The 2005 Tennessee case resulted from a privacy violation claim by a patient against a pharmacy manager. In another pharmacy-patient complaint, Fanean v. Rite Aid Corp. of Delaware Inc., the Superior Court of Delaware concluded that negligence claims could not be premised on a HIPAA violation, but that a common law negligence claim could be predicated upon Occupational Safety and Health Administration requirements. The 2009 opinion noted that HIPAA may act as a “guidepost” to determine the standard of care in common-law negligence claims.
The similar assertions by Connecticut judges that HIPAA does not preempt state rights and can also be used as a standard for what constitutes negligence or improper care of records is concerning for health providers, Mr. Kline said in an interview. Doctors now have to worry that inadvertent HIPAA violations may yield not only a complaint with the Office for Civil Rights, but a potential malpractice suit, as well.
“I would not be surprised if a case like this or even this case is appealed to the Supreme Court of the United States,” Mr. Kline said. “It is still a question of federal law, and what does the federal preemption mean?”
On Twitter @legal_med
Patients can sue doctors for negligence after alleged patient privacy breaches, the Connecticut Supreme Court has ruled in a decision that could have nationwide implications.
The state’s highest court concluded that HIPAA does not preempt claims for emotional distress or negligence under state law. The ruling, published Nov. 11, sets precedence in Connecticut and is likely to encourage plaintiffs to raise similar claims in other states, according to Michael J. Kline, a New Jersey attorney who specializes in corporate and securities law.
“It’s a momentous case, and I think it’s serious for physician practices,” said Mr. Kline. “It can set the stage for plaintiffs’ attorneys within given states to [pursue] class actions for emotional distress or invasion of privacy on the grounds there was negligence” in connection to HIPAA violations.
The decision stems from a lawsuit filed by Emily Byrne v. Avery Center for Obstetrics and Gynecology P.C. in Westport, Conn. Ms. Byrne claimed that in 2004, she instructed the health center not to release her medical records to an ex-boyfriend. In 2005, the medical center was served with a subpoena by the former boyfriend requesting the plaintiff’s medical records for a paternity proceeding. The defendant did not alert Ms. Byrne about the subpoena and mailed a copy of her medical file to the probate court, according to court records.
Ms. Byrne later sued the health care center, claiming she suffered harassment and extortion threats from her ex-boyfriend because the medical records were exposed. The complaint alleged the health center engaged in negligent infliction of emotional distress and acted negligently by failing to use proper and reasonable care in protecting her medical file, including disclosing it without authorization in violation of HIPAA.
A trial court agreed with the medical practice’s contention that HIPAA precludes individual liability claims pertaining to confidentiality of medical information. The court cited well-established case law that HIPAA does not create a private right of action and requires alleged privacy violations to be raised through administrative channels. But the Connecticut Supreme Court overturned the decision, ruling that HIPAA does not preempt such negligence lawsuits.
“If Connecticut’s common law recognizes claims arising from a health care provider’s alleged breach of its duty of confidentiality in the course of complying with a subpoena, HIPAA and its implementing regulations do not preempt such claims,” judges said in their opinion. “We further conclude that, to the extent it has become the common practice for Connecticut health care providers to follow the procedures required under HIPAA in rendering services to their patients, HIPAA and its implementing regulations may be utilized to inform the standard of care applicable to such claims arising from allegations of negligence in the disclosure of patients’ medical records pursuant to a subpoena.”
The court went on to say that “the availability of such private rights of action in state courts ... do not preclude, conflict with, or complicate health care providers’ compliance with HIPAA.”
Similar decisions have been made by other courts, but the Connecticut ruling is the first state Supreme Court to issue such a ruling, Mr. Kline said.
For example, in Harmon v. Maury County, the U.S. District Court for the Middle District of Tennessee found that negligence claims founded on violation of HIPAA were not precluded because federal provisions do not completely preempt state law and expressly preserve state laws that aren’t at odds with its terms. The 2005 Tennessee case resulted from a privacy violation claim by a patient against a pharmacy manager. In another pharmacy-patient complaint, Fanean v. Rite Aid Corp. of Delaware Inc., the Superior Court of Delaware concluded that negligence claims could not be premised on a HIPAA violation, but that a common law negligence claim could be predicated upon Occupational Safety and Health Administration requirements. The 2009 opinion noted that HIPAA may act as a “guidepost” to determine the standard of care in common-law negligence claims.
The similar assertions by Connecticut judges that HIPAA does not preempt state rights and can also be used as a standard for what constitutes negligence or improper care of records is concerning for health providers, Mr. Kline said in an interview. Doctors now have to worry that inadvertent HIPAA violations may yield not only a complaint with the Office for Civil Rights, but a potential malpractice suit, as well.
“I would not be surprised if a case like this or even this case is appealed to the Supreme Court of the United States,” Mr. Kline said. “It is still a question of federal law, and what does the federal preemption mean?”
On Twitter @legal_med
Patients can sue doctors for negligence after alleged patient privacy breaches, the Connecticut Supreme Court has ruled in a decision that could have nationwide implications.
The state’s highest court concluded that HIPAA does not preempt claims for emotional distress or negligence under state law. The ruling, published Nov. 11, sets precedence in Connecticut and is likely to encourage plaintiffs to raise similar claims in other states, according to Michael J. Kline, a New Jersey attorney who specializes in corporate and securities law.
“It’s a momentous case, and I think it’s serious for physician practices,” said Mr. Kline. “It can set the stage for plaintiffs’ attorneys within given states to [pursue] class actions for emotional distress or invasion of privacy on the grounds there was negligence” in connection to HIPAA violations.
The decision stems from a lawsuit filed by Emily Byrne v. Avery Center for Obstetrics and Gynecology P.C. in Westport, Conn. Ms. Byrne claimed that in 2004, she instructed the health center not to release her medical records to an ex-boyfriend. In 2005, the medical center was served with a subpoena by the former boyfriend requesting the plaintiff’s medical records for a paternity proceeding. The defendant did not alert Ms. Byrne about the subpoena and mailed a copy of her medical file to the probate court, according to court records.
Ms. Byrne later sued the health care center, claiming she suffered harassment and extortion threats from her ex-boyfriend because the medical records were exposed. The complaint alleged the health center engaged in negligent infliction of emotional distress and acted negligently by failing to use proper and reasonable care in protecting her medical file, including disclosing it without authorization in violation of HIPAA.
A trial court agreed with the medical practice’s contention that HIPAA precludes individual liability claims pertaining to confidentiality of medical information. The court cited well-established case law that HIPAA does not create a private right of action and requires alleged privacy violations to be raised through administrative channels. But the Connecticut Supreme Court overturned the decision, ruling that HIPAA does not preempt such negligence lawsuits.
“If Connecticut’s common law recognizes claims arising from a health care provider’s alleged breach of its duty of confidentiality in the course of complying with a subpoena, HIPAA and its implementing regulations do not preempt such claims,” judges said in their opinion. “We further conclude that, to the extent it has become the common practice for Connecticut health care providers to follow the procedures required under HIPAA in rendering services to their patients, HIPAA and its implementing regulations may be utilized to inform the standard of care applicable to such claims arising from allegations of negligence in the disclosure of patients’ medical records pursuant to a subpoena.”
The court went on to say that “the availability of such private rights of action in state courts ... do not preclude, conflict with, or complicate health care providers’ compliance with HIPAA.”
Similar decisions have been made by other courts, but the Connecticut ruling is the first state Supreme Court to issue such a ruling, Mr. Kline said.
For example, in Harmon v. Maury County, the U.S. District Court for the Middle District of Tennessee found that negligence claims founded on violation of HIPAA were not precluded because federal provisions do not completely preempt state law and expressly preserve state laws that aren’t at odds with its terms. The 2005 Tennessee case resulted from a privacy violation claim by a patient against a pharmacy manager. In another pharmacy-patient complaint, Fanean v. Rite Aid Corp. of Delaware Inc., the Superior Court of Delaware concluded that negligence claims could not be premised on a HIPAA violation, but that a common law negligence claim could be predicated upon Occupational Safety and Health Administration requirements. The 2009 opinion noted that HIPAA may act as a “guidepost” to determine the standard of care in common-law negligence claims.
The similar assertions by Connecticut judges that HIPAA does not preempt state rights and can also be used as a standard for what constitutes negligence or improper care of records is concerning for health providers, Mr. Kline said in an interview. Doctors now have to worry that inadvertent HIPAA violations may yield not only a complaint with the Office for Civil Rights, but a potential malpractice suit, as well.
“I would not be surprised if a case like this or even this case is appealed to the Supreme Court of the United States,” Mr. Kline said. “It is still a question of federal law, and what does the federal preemption mean?”
On Twitter @legal_med
IOM recommends social factors to include in EHRs
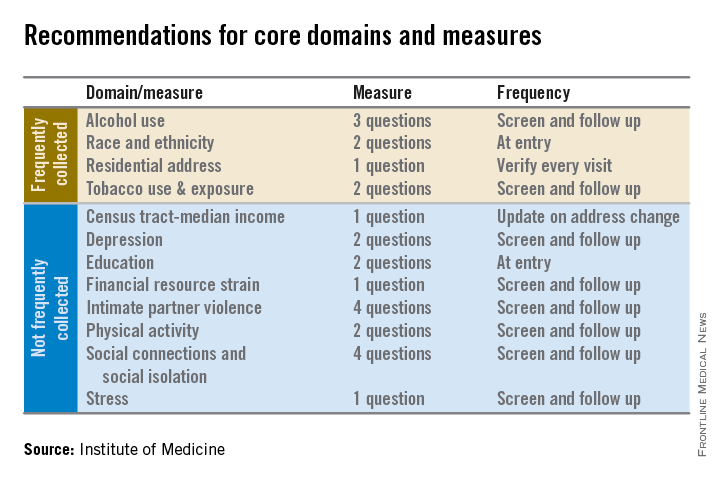
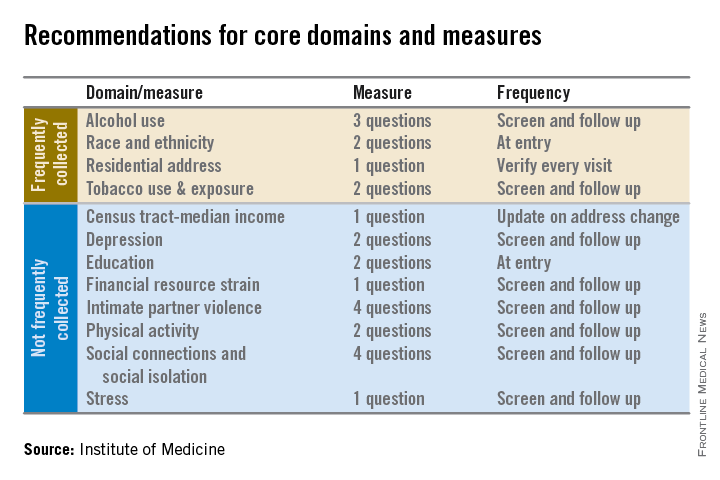
Electronic health records should be equipped to record and track 12 social and behavioral determinants of health, an Institute of Medicine committee recommended.
In addition to measures that are routinely collected now – race/ethnicity, tobacco use, alcohol use, and residential address – the committee advocated that electronic heath records (EHRs) should be able to capture:
• Educational attainment.
• Financial resource strain.
• Stress.
• Depression.
• Physical activity.
• Social isolation.
• Intimate partner violence (for women of reproductive age).
• Neighborhood median household income.
These measures can “provide crucial information about factors that influence health and the effectiveness of treatment,” collect data for researchers and policy makers, and help inform innovations that might improve health outcomes or reduce costs, according to the Nov. 13 report.
The panel aimed for what it called a “parsimonious panel of measures,” to help reduce the data collection burden for patients and health care providers, committee cochair Dr. William W. Stead, McKesson Foundation Professor of Biomedical Informatics and professor of medicine at Vanderbilt University, said during a press briefing.
The IOM report will be used by the Office of the National Coordinator for Health Information Technology (ONC) to determine what it should require from certified EHRs and from physicians who are participating in Medicare’s meaningful use incentive payment program. Physicians will be required to document social and behavioral determinants under Stage 3 of meaningful use, which begins in 2017.
Dr. Stead said that the speed of inclusion of the social and behavioral determinants in EHRs will partly be determined by whether the ONC follows the panel’s recommendations and requires them as part of meaningful use. He noted that in the past, EHR vendors and health care systems have been told by the ONC that they need to obtain certain types of information, “but then had to figure out on their own how to capture that information.
“There’s no reason why this needs to take years,” said Dr. Stead.
With the IOM recommendations, “we’re building the interoperability in from the beginning by providing a concise set of standard questions,” he said.
It will likely take less time to get the determinants into EHR packages than for health systems and physicians to figure out how to build the data collection into their workflow, Dr. Stead said.
The committee acknowledges that it will take more time during a patient encounter to collect these data. But, wrote the panel in the report, “the committee concluded that the health benefits of addressing these determinants outweigh the added burden to providers, patients, and health care systems.”
Additional recommendations in the report include:
• That the ONC’s EHR certification process be expanded to include appraisal of a vendor or product’s ability to acquire, store, transmit, and download self-reported data germane to the social and behavioral determinants of health.
• That the National Institutes of Health develops a plan for advancing research using social and behavioral determinants of health collected in electronic health records.
• That the Health & Human Services department convenes a task force within the next 3 years, and as needed thereafter, to review advances in the measurement of social and behavioral determinants and make recommendations for new standards and data elements for inclusion in electronic health records.
The committee’s work builds on draft recommendations published in April. It was sponsored by a number of federal agencies and health care foundations.
Dr. Michael E. Nelson, FCCP, comments: While physicians might agree that the recommendations of the Institute of Medicine (IOM) might enhance medical care, it is naïve to believe that this administrative burden will not make it increasingly difficult for physicians to meet Stage 3 of meaningful use should these requirements be added by the Office of the National Coordinator for Health Information Technology (ONC).

|
| Dr. Michael E. Nelson |
Assuming that EHR vendors will incorporate this information into their software, the time required to elicit and record this information is not insignificant and will put further strain on the already busy clinician.
In addition, there is a major assumption that the patient will actually provide this information willingly and that there would be implied consent to allow this information to be shared with the federal government, anonymously or otherwise.
Should the ONC adopt these recommendations from the IOM, one would hope that EHR vendors are required to add this to their software at no additional cost to physicians. Also, each question might have a button for "patient declined to answer." George Orwell might have been more prescient than credited.
Dr. Nelson is affiliated with Shawnee Mission Pulmonary Consultants in Shawnee Mission, KS.
Dr. Michael E. Nelson, FCCP, comments: While physicians might agree that the recommendations of the Institute of Medicine (IOM) might enhance medical care, it is naïve to believe that this administrative burden will not make it increasingly difficult for physicians to meet Stage 3 of meaningful use should these requirements be added by the Office of the National Coordinator for Health Information Technology (ONC).

|
| Dr. Michael E. Nelson |
Assuming that EHR vendors will incorporate this information into their software, the time required to elicit and record this information is not insignificant and will put further strain on the already busy clinician.
In addition, there is a major assumption that the patient will actually provide this information willingly and that there would be implied consent to allow this information to be shared with the federal government, anonymously or otherwise.
Should the ONC adopt these recommendations from the IOM, one would hope that EHR vendors are required to add this to their software at no additional cost to physicians. Also, each question might have a button for "patient declined to answer." George Orwell might have been more prescient than credited.
Dr. Nelson is affiliated with Shawnee Mission Pulmonary Consultants in Shawnee Mission, KS.
Dr. Michael E. Nelson, FCCP, comments: While physicians might agree that the recommendations of the Institute of Medicine (IOM) might enhance medical care, it is naïve to believe that this administrative burden will not make it increasingly difficult for physicians to meet Stage 3 of meaningful use should these requirements be added by the Office of the National Coordinator for Health Information Technology (ONC).

|
| Dr. Michael E. Nelson |
Assuming that EHR vendors will incorporate this information into their software, the time required to elicit and record this information is not insignificant and will put further strain on the already busy clinician.
In addition, there is a major assumption that the patient will actually provide this information willingly and that there would be implied consent to allow this information to be shared with the federal government, anonymously or otherwise.
Should the ONC adopt these recommendations from the IOM, one would hope that EHR vendors are required to add this to their software at no additional cost to physicians. Also, each question might have a button for "patient declined to answer." George Orwell might have been more prescient than credited.
Dr. Nelson is affiliated with Shawnee Mission Pulmonary Consultants in Shawnee Mission, KS.
Electronic health records should be equipped to record and track 12 social and behavioral determinants of health, an Institute of Medicine committee recommended.
In addition to measures that are routinely collected now – race/ethnicity, tobacco use, alcohol use, and residential address – the committee advocated that electronic heath records (EHRs) should be able to capture:
• Educational attainment.
• Financial resource strain.
• Stress.
• Depression.
• Physical activity.
• Social isolation.
• Intimate partner violence (for women of reproductive age).
• Neighborhood median household income.
These measures can “provide crucial information about factors that influence health and the effectiveness of treatment,” collect data for researchers and policy makers, and help inform innovations that might improve health outcomes or reduce costs, according to the Nov. 13 report.
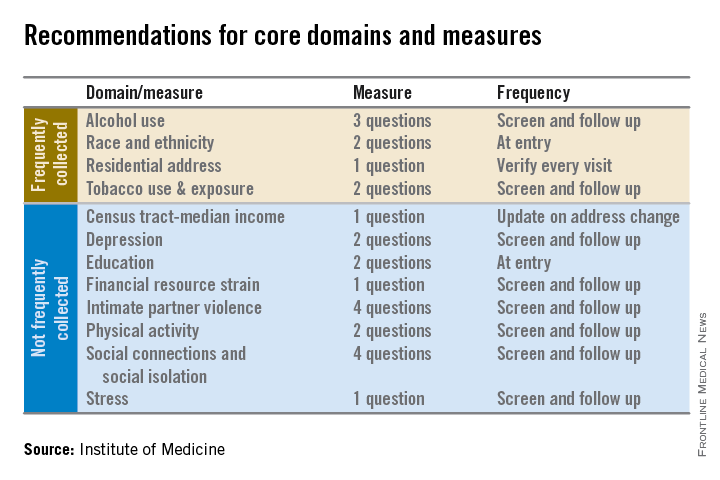
The panel aimed for what it called a “parsimonious panel of measures,” to help reduce the data collection burden for patients and health care providers, committee cochair Dr. William W. Stead, McKesson Foundation Professor of Biomedical Informatics and professor of medicine at Vanderbilt University, said during a press briefing.
The IOM report will be used by the Office of the National Coordinator for Health Information Technology (ONC) to determine what it should require from certified EHRs and from physicians who are participating in Medicare’s meaningful use incentive payment program. Physicians will be required to document social and behavioral determinants under Stage 3 of meaningful use, which begins in 2017.
Dr. Stead said that the speed of inclusion of the social and behavioral determinants in EHRs will partly be determined by whether the ONC follows the panel’s recommendations and requires them as part of meaningful use. He noted that in the past, EHR vendors and health care systems have been told by the ONC that they need to obtain certain types of information, “but then had to figure out on their own how to capture that information.
“There’s no reason why this needs to take years,” said Dr. Stead.
With the IOM recommendations, “we’re building the interoperability in from the beginning by providing a concise set of standard questions,” he said.
It will likely take less time to get the determinants into EHR packages than for health systems and physicians to figure out how to build the data collection into their workflow, Dr. Stead said.
The committee acknowledges that it will take more time during a patient encounter to collect these data. But, wrote the panel in the report, “the committee concluded that the health benefits of addressing these determinants outweigh the added burden to providers, patients, and health care systems.”
Additional recommendations in the report include:
• That the ONC’s EHR certification process be expanded to include appraisal of a vendor or product’s ability to acquire, store, transmit, and download self-reported data germane to the social and behavioral determinants of health.
• That the National Institutes of Health develops a plan for advancing research using social and behavioral determinants of health collected in electronic health records.
• That the Health & Human Services department convenes a task force within the next 3 years, and as needed thereafter, to review advances in the measurement of social and behavioral determinants and make recommendations for new standards and data elements for inclusion in electronic health records.
The committee’s work builds on draft recommendations published in April. It was sponsored by a number of federal agencies and health care foundations.
Electronic health records should be equipped to record and track 12 social and behavioral determinants of health, an Institute of Medicine committee recommended.
In addition to measures that are routinely collected now – race/ethnicity, tobacco use, alcohol use, and residential address – the committee advocated that electronic heath records (EHRs) should be able to capture:
• Educational attainment.
• Financial resource strain.
• Stress.
• Depression.
• Physical activity.
• Social isolation.
• Intimate partner violence (for women of reproductive age).
• Neighborhood median household income.
These measures can “provide crucial information about factors that influence health and the effectiveness of treatment,” collect data for researchers and policy makers, and help inform innovations that might improve health outcomes or reduce costs, according to the Nov. 13 report.
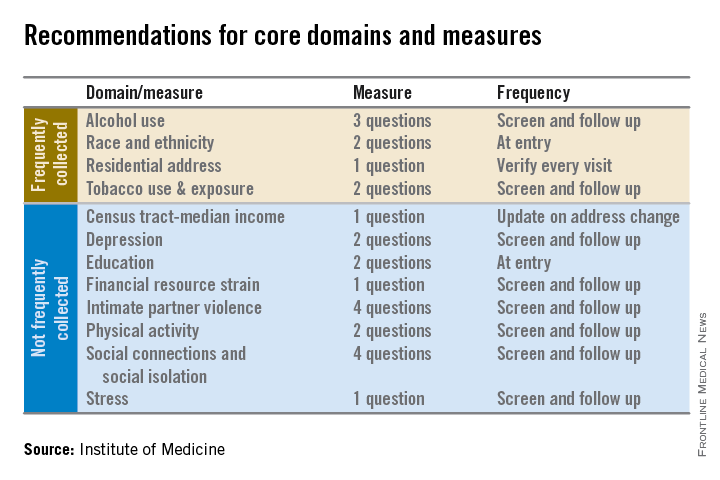
The panel aimed for what it called a “parsimonious panel of measures,” to help reduce the data collection burden for patients and health care providers, committee cochair Dr. William W. Stead, McKesson Foundation Professor of Biomedical Informatics and professor of medicine at Vanderbilt University, said during a press briefing.
The IOM report will be used by the Office of the National Coordinator for Health Information Technology (ONC) to determine what it should require from certified EHRs and from physicians who are participating in Medicare’s meaningful use incentive payment program. Physicians will be required to document social and behavioral determinants under Stage 3 of meaningful use, which begins in 2017.
Dr. Stead said that the speed of inclusion of the social and behavioral determinants in EHRs will partly be determined by whether the ONC follows the panel’s recommendations and requires them as part of meaningful use. He noted that in the past, EHR vendors and health care systems have been told by the ONC that they need to obtain certain types of information, “but then had to figure out on their own how to capture that information.
“There’s no reason why this needs to take years,” said Dr. Stead.
With the IOM recommendations, “we’re building the interoperability in from the beginning by providing a concise set of standard questions,” he said.
It will likely take less time to get the determinants into EHR packages than for health systems and physicians to figure out how to build the data collection into their workflow, Dr. Stead said.
The committee acknowledges that it will take more time during a patient encounter to collect these data. But, wrote the panel in the report, “the committee concluded that the health benefits of addressing these determinants outweigh the added burden to providers, patients, and health care systems.”
Additional recommendations in the report include:
• That the ONC’s EHR certification process be expanded to include appraisal of a vendor or product’s ability to acquire, store, transmit, and download self-reported data germane to the social and behavioral determinants of health.
• That the National Institutes of Health develops a plan for advancing research using social and behavioral determinants of health collected in electronic health records.
• That the Health & Human Services department convenes a task force within the next 3 years, and as needed thereafter, to review advances in the measurement of social and behavioral determinants and make recommendations for new standards and data elements for inclusion in electronic health records.
The committee’s work builds on draft recommendations published in April. It was sponsored by a number of federal agencies and health care foundations.
LISTEN NOW: Emergency Medicine and Hospitalist Collaboration
The focus for emergency physicians, says Dr. Heinrich, is triage and disposition. Differing incentives for hospitalists and emergency physicians can cause stress between the groups, and dialogue is needed to defray the tension, he notes. Dr. Epstein says he thinks that collaboration can be an effective tactic against becoming a “30 day readmission rule” statistic. Shared metrics, developed in partnership, can also improve patient care, he adds.
For more features, visit The Hospitalist's podcast archive.
The focus for emergency physicians, says Dr. Heinrich, is triage and disposition. Differing incentives for hospitalists and emergency physicians can cause stress between the groups, and dialogue is needed to defray the tension, he notes. Dr. Epstein says he thinks that collaboration can be an effective tactic against becoming a “30 day readmission rule” statistic. Shared metrics, developed in partnership, can also improve patient care, he adds.
For more features, visit The Hospitalist's podcast archive.
The focus for emergency physicians, says Dr. Heinrich, is triage and disposition. Differing incentives for hospitalists and emergency physicians can cause stress between the groups, and dialogue is needed to defray the tension, he notes. Dr. Epstein says he thinks that collaboration can be an effective tactic against becoming a “30 day readmission rule” statistic. Shared metrics, developed in partnership, can also improve patient care, he adds.
For more features, visit The Hospitalist's podcast archive.
HHS cuts 2015 ACA enrollment estimates by a quarter
Federal health officials expect that somewhere between 9 million and 9.9 million individuals will have obtained health insurance through the Affordable Care Act marketplaces by the end of the 2015 open enrollment period, down from a previous government estimate of 13 million.
The 9 million to 9.9 million estimate from the Health and Human Services department assumes that about 83% of individuals who purchased insurance through the marketplaces during 2014 will renew their coverage, with most of the new enrollment coming from previously uninsured individuals.
HHS released the figures just days ahead of the start of the Affordable Care Act’s (ACA’s) second open enrollment period, which runs from Nov. 15 through Feb. 15, 2015.
The Congressional Budget Office, which provides nonpartisan budget analysis for Congress, had projected in April 2014 that 13 million Americans would be insured through the ACA marketplaces by the end of the second enrollment period in February 2015.
The HHS projection is lower, according to the agency, because it assumes that fewer people who have employer-sponsored insurance will jump to the ACA marketplaces in 2015. Fewer individuals who purchased individual market insurance on their own are expected to shop on the ACA marketplaces right away, according to HHS.
Another factor is that the Congressional Budget Office made its projections in April, before the final 2014 enrollment figures were available. In the spring, HHS had said that more than 8 million people had selected plans through the ACA marketplaces, but as of October 2014, 7.1 million individuals had enrolled and were paying for coverage.
The new enrollment estimates were criticized by Republicans on Capitol Hill.
“The administration is again trying to rewrite its definition of success for the president’s signature law on the eve of Saturday’s second enrollment,” Rep. Marsha Blackburn (R-Tenn.), House Energy and Commerce Committee Vice Chairman, said in a statement. “There are still a number of important, unanswered questions, including whether or not the back end is built and if the millions of inconsistencies have been resolved.”
On Twitter @maryellenny
Federal health officials expect that somewhere between 9 million and 9.9 million individuals will have obtained health insurance through the Affordable Care Act marketplaces by the end of the 2015 open enrollment period, down from a previous government estimate of 13 million.
The 9 million to 9.9 million estimate from the Health and Human Services department assumes that about 83% of individuals who purchased insurance through the marketplaces during 2014 will renew their coverage, with most of the new enrollment coming from previously uninsured individuals.
HHS released the figures just days ahead of the start of the Affordable Care Act’s (ACA’s) second open enrollment period, which runs from Nov. 15 through Feb. 15, 2015.
The Congressional Budget Office, which provides nonpartisan budget analysis for Congress, had projected in April 2014 that 13 million Americans would be insured through the ACA marketplaces by the end of the second enrollment period in February 2015.
The HHS projection is lower, according to the agency, because it assumes that fewer people who have employer-sponsored insurance will jump to the ACA marketplaces in 2015. Fewer individuals who purchased individual market insurance on their own are expected to shop on the ACA marketplaces right away, according to HHS.
Another factor is that the Congressional Budget Office made its projections in April, before the final 2014 enrollment figures were available. In the spring, HHS had said that more than 8 million people had selected plans through the ACA marketplaces, but as of October 2014, 7.1 million individuals had enrolled and were paying for coverage.
The new enrollment estimates were criticized by Republicans on Capitol Hill.
“The administration is again trying to rewrite its definition of success for the president’s signature law on the eve of Saturday’s second enrollment,” Rep. Marsha Blackburn (R-Tenn.), House Energy and Commerce Committee Vice Chairman, said in a statement. “There are still a number of important, unanswered questions, including whether or not the back end is built and if the millions of inconsistencies have been resolved.”
On Twitter @maryellenny
Federal health officials expect that somewhere between 9 million and 9.9 million individuals will have obtained health insurance through the Affordable Care Act marketplaces by the end of the 2015 open enrollment period, down from a previous government estimate of 13 million.
The 9 million to 9.9 million estimate from the Health and Human Services department assumes that about 83% of individuals who purchased insurance through the marketplaces during 2014 will renew their coverage, with most of the new enrollment coming from previously uninsured individuals.
HHS released the figures just days ahead of the start of the Affordable Care Act’s (ACA’s) second open enrollment period, which runs from Nov. 15 through Feb. 15, 2015.
The Congressional Budget Office, which provides nonpartisan budget analysis for Congress, had projected in April 2014 that 13 million Americans would be insured through the ACA marketplaces by the end of the second enrollment period in February 2015.
The HHS projection is lower, according to the agency, because it assumes that fewer people who have employer-sponsored insurance will jump to the ACA marketplaces in 2015. Fewer individuals who purchased individual market insurance on their own are expected to shop on the ACA marketplaces right away, according to HHS.
Another factor is that the Congressional Budget Office made its projections in April, before the final 2014 enrollment figures were available. In the spring, HHS had said that more than 8 million people had selected plans through the ACA marketplaces, but as of October 2014, 7.1 million individuals had enrolled and were paying for coverage.
The new enrollment estimates were criticized by Republicans on Capitol Hill.
“The administration is again trying to rewrite its definition of success for the president’s signature law on the eve of Saturday’s second enrollment,” Rep. Marsha Blackburn (R-Tenn.), House Energy and Commerce Committee Vice Chairman, said in a statement. “There are still a number of important, unanswered questions, including whether or not the back end is built and if the millions of inconsistencies have been resolved.”
On Twitter @maryellenny
Supreme Court to hear ACA subsidy challenge
The U.S. Supreme Court has agreed to review a case challenging the legality of federal subsidies provided under the Affordable Care Act.
The Court issued the order Nov. 7, granting the plaintiffs in King v. Burwell a review of the case. The plaintiffs assert that under the ACA, only state marketplaces can issue subsidies to eligible patients.
In July, the Fourth Circuit Court of Appeals ruled against the plaintiffs, upholding the government’s ability to provide subsidies to eligible patients who purchase insurance through the 36 federally facilitated health care marketplaces.
On the same day, a limited panel of judges on the District of Columbia Circuit of the U.S. Court of Appeals ruled that the federal marketplace subsidies were not legal in a similar challenge, Halbig v. Burwell.
The government appealed, seeking a full review, which was granted in September. All 17 D.C. Circuit judges will review the case on Dec. 17.
The Supreme Court is not likely to hear King v. Burwell before that date.
On Twitter @aliciaault
The U.S. Supreme Court has agreed to review a case challenging the legality of federal subsidies provided under the Affordable Care Act.
The Court issued the order Nov. 7, granting the plaintiffs in King v. Burwell a review of the case. The plaintiffs assert that under the ACA, only state marketplaces can issue subsidies to eligible patients.
In July, the Fourth Circuit Court of Appeals ruled against the plaintiffs, upholding the government’s ability to provide subsidies to eligible patients who purchase insurance through the 36 federally facilitated health care marketplaces.
On the same day, a limited panel of judges on the District of Columbia Circuit of the U.S. Court of Appeals ruled that the federal marketplace subsidies were not legal in a similar challenge, Halbig v. Burwell.
The government appealed, seeking a full review, which was granted in September. All 17 D.C. Circuit judges will review the case on Dec. 17.
The Supreme Court is not likely to hear King v. Burwell before that date.
On Twitter @aliciaault
The U.S. Supreme Court has agreed to review a case challenging the legality of federal subsidies provided under the Affordable Care Act.
The Court issued the order Nov. 7, granting the plaintiffs in King v. Burwell a review of the case. The plaintiffs assert that under the ACA, only state marketplaces can issue subsidies to eligible patients.
In July, the Fourth Circuit Court of Appeals ruled against the plaintiffs, upholding the government’s ability to provide subsidies to eligible patients who purchase insurance through the 36 federally facilitated health care marketplaces.
On the same day, a limited panel of judges on the District of Columbia Circuit of the U.S. Court of Appeals ruled that the federal marketplace subsidies were not legal in a similar challenge, Halbig v. Burwell.
The government appealed, seeking a full review, which was granted in September. All 17 D.C. Circuit judges will review the case on Dec. 17.
The Supreme Court is not likely to hear King v. Burwell before that date.
On Twitter @aliciaault
High-risk care plans reduced ED testing, admissions
CHICAGO – Frequent flyers, patients with a history of at least five visits per year to the emergency department, might benefit from high-risk care plans, based on research from the University of Maryland health care system.
The plans are designed to improve patient safety by reducing exposure to ionizing radiation and have the additional benefit of reducing the costs of care, Dr. Leen Alblaihed, a resident physician at the university, reported at the annual meeting of the American College of Emergency Physicians.
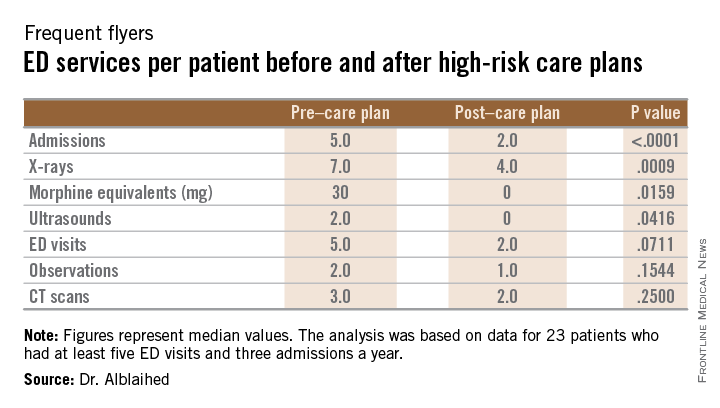
After high-risk care plans were put into the emergency physician work flow for 41 patients with a history of high emergency department utilization, unneeded tests declined. Other important outcomes were statistically significant reductions in hospitalizations and quantities of prescribed opioids.
he patients considered for the study had to have at least five ED visits and three admissions per year. Based on the electronic medical record data of the university’s two suburban medical centers, a total of 845 patients met that definition.
The high-risk care plans for the management of the 41 patients were developed by a multi-disciplinary team of case managers, emergency physicians, and hospitalists. The plans were then integrated into the physician electronic documentation and work flow.
The data analysis was based on 23 of the patients, 10 men and 13 women with a median age of 48 years, who had 6 months of data before and 6 months of data after the care plan was instituted. The primary outcome measures were a reduction in ionizing radiation. Secondary outcome measures were reductions in ED visits, hospital admissions, observation stays, and opioid prescriptions based on morphine equivalent totals.
Compared to the data before the care plan was instituted, the 23 patients had nearly half as many x-rays and CT scans and a nearly sixfold reduction in prescribing of morphine equivalents. While ED visits decreased modestly from 116 to 82, the admission rates dropped from 99 to 37 and observation stays declined from 43 to 28.
The study group had decreases in all measures after high-risk care plans. X-ray studies decreased from 202 to 106, CT scans declined from 107 to 50, and opiate prescribing decreased from 3824 mg to 675 mg in morphine equivalents.
Because the outcomes were not normally distributed, medians and interquartile ranges were analyzed using the Wilcoxon signed-rank test to compare the pre/post median values (see table).
CHICAGO – Frequent flyers, patients with a history of at least five visits per year to the emergency department, might benefit from high-risk care plans, based on research from the University of Maryland health care system.
The plans are designed to improve patient safety by reducing exposure to ionizing radiation and have the additional benefit of reducing the costs of care, Dr. Leen Alblaihed, a resident physician at the university, reported at the annual meeting of the American College of Emergency Physicians.
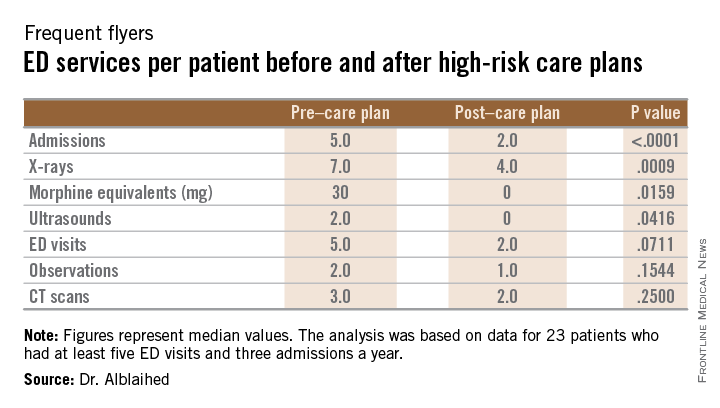
After high-risk care plans were put into the emergency physician work flow for 41 patients with a history of high emergency department utilization, unneeded tests declined. Other important outcomes were statistically significant reductions in hospitalizations and quantities of prescribed opioids.
he patients considered for the study had to have at least five ED visits and three admissions per year. Based on the electronic medical record data of the university’s two suburban medical centers, a total of 845 patients met that definition.
The high-risk care plans for the management of the 41 patients were developed by a multi-disciplinary team of case managers, emergency physicians, and hospitalists. The plans were then integrated into the physician electronic documentation and work flow.
The data analysis was based on 23 of the patients, 10 men and 13 women with a median age of 48 years, who had 6 months of data before and 6 months of data after the care plan was instituted. The primary outcome measures were a reduction in ionizing radiation. Secondary outcome measures were reductions in ED visits, hospital admissions, observation stays, and opioid prescriptions based on morphine equivalent totals.
Compared to the data before the care plan was instituted, the 23 patients had nearly half as many x-rays and CT scans and a nearly sixfold reduction in prescribing of morphine equivalents. While ED visits decreased modestly from 116 to 82, the admission rates dropped from 99 to 37 and observation stays declined from 43 to 28.
The study group had decreases in all measures after high-risk care plans. X-ray studies decreased from 202 to 106, CT scans declined from 107 to 50, and opiate prescribing decreased from 3824 mg to 675 mg in morphine equivalents.
Because the outcomes were not normally distributed, medians and interquartile ranges were analyzed using the Wilcoxon signed-rank test to compare the pre/post median values (see table).
CHICAGO – Frequent flyers, patients with a history of at least five visits per year to the emergency department, might benefit from high-risk care plans, based on research from the University of Maryland health care system.
The plans are designed to improve patient safety by reducing exposure to ionizing radiation and have the additional benefit of reducing the costs of care, Dr. Leen Alblaihed, a resident physician at the university, reported at the annual meeting of the American College of Emergency Physicians.
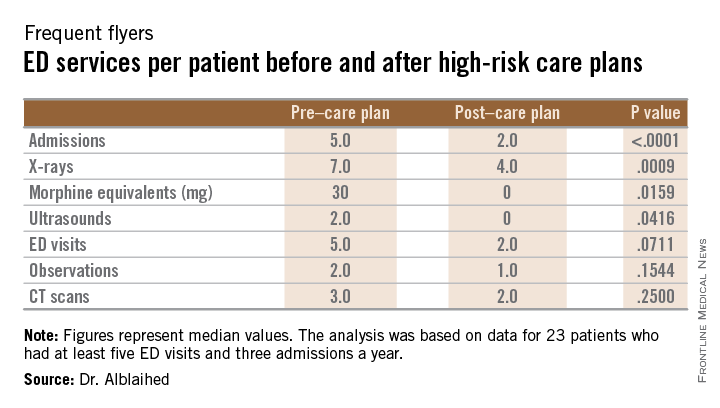
After high-risk care plans were put into the emergency physician work flow for 41 patients with a history of high emergency department utilization, unneeded tests declined. Other important outcomes were statistically significant reductions in hospitalizations and quantities of prescribed opioids.
he patients considered for the study had to have at least five ED visits and three admissions per year. Based on the electronic medical record data of the university’s two suburban medical centers, a total of 845 patients met that definition.
The high-risk care plans for the management of the 41 patients were developed by a multi-disciplinary team of case managers, emergency physicians, and hospitalists. The plans were then integrated into the physician electronic documentation and work flow.
The data analysis was based on 23 of the patients, 10 men and 13 women with a median age of 48 years, who had 6 months of data before and 6 months of data after the care plan was instituted. The primary outcome measures were a reduction in ionizing radiation. Secondary outcome measures were reductions in ED visits, hospital admissions, observation stays, and opioid prescriptions based on morphine equivalent totals.
Compared to the data before the care plan was instituted, the 23 patients had nearly half as many x-rays and CT scans and a nearly sixfold reduction in prescribing of morphine equivalents. While ED visits decreased modestly from 116 to 82, the admission rates dropped from 99 to 37 and observation stays declined from 43 to 28.
The study group had decreases in all measures after high-risk care plans. X-ray studies decreased from 202 to 106, CT scans declined from 107 to 50, and opiate prescribing decreased from 3824 mg to 675 mg in morphine equivalents.
Because the outcomes were not normally distributed, medians and interquartile ranges were analyzed using the Wilcoxon signed-rank test to compare the pre/post median values (see table).
AT ACEP14