User login
Tardive dyskinesia is theme of awards competition for early career psychiatrists
Important advances in neuroscience and clinical psychiatry have been achieved in recent years, but there are significant gaps in knowledge and much that we don’t understand about the brain and behavior. Further advances depend on cultivating and supporting a new generation of dedicated basic science and clinical investigators. While there is a compelling need to attract, recruit, and encourage talented individuals to pursue scholarly interests, competing life and career demands often prove daunting.
The theme of the competition this year concerning tardive dyskinesia is timely and consistent with the mission of NMSIS to promote knowledge on neurologic side effects of antipsychotic drugs. Tardive dyskinesia can have a negative impact on the social, psychological, and physical well-being of patients; it remains a legacy of past treatment with antipsychotics; it is an increasing concern among an ever widening population of patients receiving even newer antipsychotics; and there are now two Food and Drug Administration–approved treatments for the disorder. Early career psychiatrists may have had limited instruction on tardive dyskinesia, which has not received prominent attention in curricular programs in recent years. Thus, in addition to supporting scholarly work and research experience, the 2018 Promising Scholars Award Program aims to promote knowledge and skills in managing patients with tardive dyskinesia.
Specific learning objectives are:
- Participants will learn the steps necessary to prepare a scientific manuscript for publication.
- Participants will review comments by expert referees and learn to incorporate and respond to the peer review process.
- Participants will review the evidence related to the diagnosis and treatment of tardive dyskinesia.
- Participants will be introduced to the spectrum of educational and networking opportunities at the Institute for Psychiatric Services conference.
In the past, this program was very popular and gained national recognition among psychiatric trainees. Numerous submitted papers were accepted for publication in peer-reviewed journals after the competition was completed.
Instructions for manuscript preparation are:
- First author must be a student, resident, or fellow.
- Papers should address specific issues related to the theme of tardive dyskinesia and be no longer than 15 double-spaced typed pages in length (excluding references and illustrations).
- Literature reviews, case reports, or studies that are original and newly developed or recently published are acceptable.
- Reviews and feedback will be provided by a panel of academic psychiatrists.
- Papers will be judged on relevance to tardive dyskinesia, originality, scholarship, scientific rigor, valid methodology, clinical significance, and organization.
To participate, papers and curriculum vitae of the first author must be submitted by July 1, 2018, to Dianne Daugherty by email at [email protected]. Winners will be announced by Aug. 10, 2018. For additional information, write to [email protected] or visit www.mhaus.org/nmsis/about-us/what-is-nmsis.
Dr. Caroff, professor of psychiatry, Corporal Michael J. Crescenz VA Medical Center and at the University of Pennsylvania, both in Philadelphia, is director of the NMSIS. He served as consultant to Neurocrine Biosciences and Teva Pharmaceutical Industries, and receives research grant funding from Neurocrine Biosciences.
Important advances in neuroscience and clinical psychiatry have been achieved in recent years, but there are significant gaps in knowledge and much that we don’t understand about the brain and behavior. Further advances depend on cultivating and supporting a new generation of dedicated basic science and clinical investigators. While there is a compelling need to attract, recruit, and encourage talented individuals to pursue scholarly interests, competing life and career demands often prove daunting.
The theme of the competition this year concerning tardive dyskinesia is timely and consistent with the mission of NMSIS to promote knowledge on neurologic side effects of antipsychotic drugs. Tardive dyskinesia can have a negative impact on the social, psychological, and physical well-being of patients; it remains a legacy of past treatment with antipsychotics; it is an increasing concern among an ever widening population of patients receiving even newer antipsychotics; and there are now two Food and Drug Administration–approved treatments for the disorder. Early career psychiatrists may have had limited instruction on tardive dyskinesia, which has not received prominent attention in curricular programs in recent years. Thus, in addition to supporting scholarly work and research experience, the 2018 Promising Scholars Award Program aims to promote knowledge and skills in managing patients with tardive dyskinesia.
Specific learning objectives are:
- Participants will learn the steps necessary to prepare a scientific manuscript for publication.
- Participants will review comments by expert referees and learn to incorporate and respond to the peer review process.
- Participants will review the evidence related to the diagnosis and treatment of tardive dyskinesia.
- Participants will be introduced to the spectrum of educational and networking opportunities at the Institute for Psychiatric Services conference.
In the past, this program was very popular and gained national recognition among psychiatric trainees. Numerous submitted papers were accepted for publication in peer-reviewed journals after the competition was completed.
Instructions for manuscript preparation are:
- First author must be a student, resident, or fellow.
- Papers should address specific issues related to the theme of tardive dyskinesia and be no longer than 15 double-spaced typed pages in length (excluding references and illustrations).
- Literature reviews, case reports, or studies that are original and newly developed or recently published are acceptable.
- Reviews and feedback will be provided by a panel of academic psychiatrists.
- Papers will be judged on relevance to tardive dyskinesia, originality, scholarship, scientific rigor, valid methodology, clinical significance, and organization.
To participate, papers and curriculum vitae of the first author must be submitted by July 1, 2018, to Dianne Daugherty by email at [email protected]. Winners will be announced by Aug. 10, 2018. For additional information, write to [email protected] or visit www.mhaus.org/nmsis/about-us/what-is-nmsis.
Dr. Caroff, professor of psychiatry, Corporal Michael J. Crescenz VA Medical Center and at the University of Pennsylvania, both in Philadelphia, is director of the NMSIS. He served as consultant to Neurocrine Biosciences and Teva Pharmaceutical Industries, and receives research grant funding from Neurocrine Biosciences.
Important advances in neuroscience and clinical psychiatry have been achieved in recent years, but there are significant gaps in knowledge and much that we don’t understand about the brain and behavior. Further advances depend on cultivating and supporting a new generation of dedicated basic science and clinical investigators. While there is a compelling need to attract, recruit, and encourage talented individuals to pursue scholarly interests, competing life and career demands often prove daunting.
The theme of the competition this year concerning tardive dyskinesia is timely and consistent with the mission of NMSIS to promote knowledge on neurologic side effects of antipsychotic drugs. Tardive dyskinesia can have a negative impact on the social, psychological, and physical well-being of patients; it remains a legacy of past treatment with antipsychotics; it is an increasing concern among an ever widening population of patients receiving even newer antipsychotics; and there are now two Food and Drug Administration–approved treatments for the disorder. Early career psychiatrists may have had limited instruction on tardive dyskinesia, which has not received prominent attention in curricular programs in recent years. Thus, in addition to supporting scholarly work and research experience, the 2018 Promising Scholars Award Program aims to promote knowledge and skills in managing patients with tardive dyskinesia.
Specific learning objectives are:
- Participants will learn the steps necessary to prepare a scientific manuscript for publication.
- Participants will review comments by expert referees and learn to incorporate and respond to the peer review process.
- Participants will review the evidence related to the diagnosis and treatment of tardive dyskinesia.
- Participants will be introduced to the spectrum of educational and networking opportunities at the Institute for Psychiatric Services conference.
In the past, this program was very popular and gained national recognition among psychiatric trainees. Numerous submitted papers were accepted for publication in peer-reviewed journals after the competition was completed.
Instructions for manuscript preparation are:
- First author must be a student, resident, or fellow.
- Papers should address specific issues related to the theme of tardive dyskinesia and be no longer than 15 double-spaced typed pages in length (excluding references and illustrations).
- Literature reviews, case reports, or studies that are original and newly developed or recently published are acceptable.
- Reviews and feedback will be provided by a panel of academic psychiatrists.
- Papers will be judged on relevance to tardive dyskinesia, originality, scholarship, scientific rigor, valid methodology, clinical significance, and organization.
To participate, papers and curriculum vitae of the first author must be submitted by July 1, 2018, to Dianne Daugherty by email at [email protected]. Winners will be announced by Aug. 10, 2018. For additional information, write to [email protected] or visit www.mhaus.org/nmsis/about-us/what-is-nmsis.
Dr. Caroff, professor of psychiatry, Corporal Michael J. Crescenz VA Medical Center and at the University of Pennsylvania, both in Philadelphia, is director of the NMSIS. He served as consultant to Neurocrine Biosciences and Teva Pharmaceutical Industries, and receives research grant funding from Neurocrine Biosciences.
Career Choices: Community mental health in an urban/public setting
Editor’s note : Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Cornel Stanciu, MD, talked with Mufida Wadhwania, MD. Dr. Wadhwania is an adult psychiatrist practicing in an urban/public setting in metro Atlanta, Georgia, at DeKalb Community Service Board. She manages a variety of uninsured and underinsured patients in an outpatient setting.
Dr. Stanciu: What attracted you to practice community mental health in an urban-public setting?
Dr. Wadhwania: A high portion of the population here has no health insurance, and hence there is a great need in the community. The psychopathology severity is high, so one can see a wide range of disorders. One can also build on the skill to pull together resources, such as linking patients to community resources and patient assistance programs, finding food banks, and finding ways to secure stable housing. There is continuity of care, and when a staff member leaves the agency, patients are linked to the next provider in an adequate time frame so that the patient’s quality of care is not compromised. The new provider is also given notification so that he or she is aware of the transfer of the patient and is able to review the chart in advance.
Along with medication management, we also provide psychotherapy. We utilize a single electronic health record (EHR) throughout the agency and we are able to contribute to changes in the EHR to make it more user-friendly. We have monthly journal club meetings and meetings with other staff members to review and discuss the progress of our organization. There are also numerous online resources through which we can keep ourselves updated with current research and earn CME. Some of the providers at our agency have academic affiliations, and hence there are opportunities to teach medical students and residents who rotate at some of our sites.
Dr. Stanciu: What are some of the more prevalent disorders you encounter?
Dr. Wadhwania: We see a wide range of disorders, such as affective disorders, schizophrenia, and comorbid disorders, specifically comorbid substance use disorders. So we encounter a high number of chronic mental illnesses.
Continue to: What are some challenges in working with this population?
Dr. Stanciu: What are some challenges in working with this population?
Dr. Wadhwania: Based on the high volume of patients we encounter, the resources available in the community are limited. But this challenges us to be creative and maximize what we have available to create new resources, such as having on-site case managers rather than just in the community, and building psychosocial rehabilitation programs near our various clinics for the patients to bring them the best care possible. Other challenges include a lack of education on and awareness of mental illness; there is still a lot of stigma surrounding mental illness in the community.
Dr. Stanciu: How would you describe your experience working in this setting?
Dr. Wadhwania: It’s a very rewarding experience, as you get to be creative, and patients appreciate your efforts. We use a patient-centered approach, and we work as a team. Each team member brings in a unique set of skills, and we bounce ideas off each other. There is a sense of satisfaction when you help people who don’t have easy access to health care. Finally, in a setting like this, young psychiatrists are able to gain more opportunities earlier than they would while working in other settings.
Continue to: How did you career path prepare you to work in such a challenging setting?
Dr. Stanciu: How did your career path prepare you to work in such a challenging setting?
Dr. Wadhwania: While at East Carolina University
Dr. Stanciu: How would you describe a psychiatric physician who is well-suited for such a setting?
Dr. Wadhwania: A perfect fit would be someone who is able to harness and build resources for the patients in the community and in the practice and wants to continue to build that skill. This individual is someone who is a team player, is flexible, and has a high professional frustration tolerance. The physician’s main aim would be to serve, and his or her mission would not be monetarily driven.
Continue to: What is the typical reimbursement model for your practice, and do you run into difficulties with health insurance providers in this setting?
Dr. Stanciu: What is the typical reimbursement model for your practice, and do you run into difficulties with health insurance providers in this setting?
Dr. Wadhwania: Approximately 40% of the patients we treat have no health insurance, and approximately 60% have Medicaid or managed Medicaid or Medicare. There is no burden of health insurance. Full-time employees are salaried, and part-time employees are compensated on an hourly model. There is also an incentive bonus system based on quality and productivity.
Dr. Stanciu: What model does your clinic use to overcome the shortage of services?
Dr. Wadhwania: There are approximately 37 medical staff members in the agency, most of whom are MDs, but this group also includes nurse practitioners and clinical nurse specialists, so there is no shortage within our agency. We do contract for telepsychiatry services, but because our agency’s clinics are located throughout the county, most of our patients have easy access to any one of our clinics. We have a number of social workers, therapists, nurses, case managers, and pharmacists. We have a crisis center where unstable patients who require admission to an inpatient unit can be admitted; we also are able to refer patients directly to other inpatient psychiatric units. Our agency also has an addiction clinic and a residential substance abuse program catering specifically to patients with substance use disorders. We have educational, therapeutic, and behavioral support services, including residential services, for patients who have developmental disabilities. Our agency also has residential services for patients who are homeless or have a lower income and would benefit from support in a residential setting.
Our therapists are able to refer patients to state-contracted Assertive Community Treatment teams that serve our county. We are also able to set up intensive case management for patients in the community, as well as other community support services, peer support programs, and psychosocial rehabilitation programs.
Continue to: What advice do you have for early career psychiatrists and trainees who are contemplating working in an urban-public setting?
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating working in an urban-public setting?
Dr. Wadhwania: First of all, realize that there are many misconceptions about serving in the public sector, such as there is no access to new medications, etc. It is important to establish whether public sector service is “in your heart.” You need to learn the organization’s philosophy, mission, and vision, and figure out whether these views align with yours. Getting to know the leadership and how they value psychiatrists and other staff members is also very important. Also, make sure that there are opportunities for you to become a leader in the organization, that there is room for growth, and that it’s a stable organization.
Editor’s note : Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Cornel Stanciu, MD, talked with Mufida Wadhwania, MD. Dr. Wadhwania is an adult psychiatrist practicing in an urban/public setting in metro Atlanta, Georgia, at DeKalb Community Service Board. She manages a variety of uninsured and underinsured patients in an outpatient setting.
Dr. Stanciu: What attracted you to practice community mental health in an urban-public setting?
Dr. Wadhwania: A high portion of the population here has no health insurance, and hence there is a great need in the community. The psychopathology severity is high, so one can see a wide range of disorders. One can also build on the skill to pull together resources, such as linking patients to community resources and patient assistance programs, finding food banks, and finding ways to secure stable housing. There is continuity of care, and when a staff member leaves the agency, patients are linked to the next provider in an adequate time frame so that the patient’s quality of care is not compromised. The new provider is also given notification so that he or she is aware of the transfer of the patient and is able to review the chart in advance.
Along with medication management, we also provide psychotherapy. We utilize a single electronic health record (EHR) throughout the agency and we are able to contribute to changes in the EHR to make it more user-friendly. We have monthly journal club meetings and meetings with other staff members to review and discuss the progress of our organization. There are also numerous online resources through which we can keep ourselves updated with current research and earn CME. Some of the providers at our agency have academic affiliations, and hence there are opportunities to teach medical students and residents who rotate at some of our sites.
Dr. Stanciu: What are some of the more prevalent disorders you encounter?
Dr. Wadhwania: We see a wide range of disorders, such as affective disorders, schizophrenia, and comorbid disorders, specifically comorbid substance use disorders. So we encounter a high number of chronic mental illnesses.
Continue to: What are some challenges in working with this population?
Dr. Stanciu: What are some challenges in working with this population?
Dr. Wadhwania: Based on the high volume of patients we encounter, the resources available in the community are limited. But this challenges us to be creative and maximize what we have available to create new resources, such as having on-site case managers rather than just in the community, and building psychosocial rehabilitation programs near our various clinics for the patients to bring them the best care possible. Other challenges include a lack of education on and awareness of mental illness; there is still a lot of stigma surrounding mental illness in the community.
Dr. Stanciu: How would you describe your experience working in this setting?
Dr. Wadhwania: It’s a very rewarding experience, as you get to be creative, and patients appreciate your efforts. We use a patient-centered approach, and we work as a team. Each team member brings in a unique set of skills, and we bounce ideas off each other. There is a sense of satisfaction when you help people who don’t have easy access to health care. Finally, in a setting like this, young psychiatrists are able to gain more opportunities earlier than they would while working in other settings.
Continue to: How did you career path prepare you to work in such a challenging setting?
Dr. Stanciu: How did your career path prepare you to work in such a challenging setting?
Dr. Wadhwania: While at East Carolina University
Dr. Stanciu: How would you describe a psychiatric physician who is well-suited for such a setting?
Dr. Wadhwania: A perfect fit would be someone who is able to harness and build resources for the patients in the community and in the practice and wants to continue to build that skill. This individual is someone who is a team player, is flexible, and has a high professional frustration tolerance. The physician’s main aim would be to serve, and his or her mission would not be monetarily driven.
Continue to: What is the typical reimbursement model for your practice, and do you run into difficulties with health insurance providers in this setting?
Dr. Stanciu: What is the typical reimbursement model for your practice, and do you run into difficulties with health insurance providers in this setting?
Dr. Wadhwania: Approximately 40% of the patients we treat have no health insurance, and approximately 60% have Medicaid or managed Medicaid or Medicare. There is no burden of health insurance. Full-time employees are salaried, and part-time employees are compensated on an hourly model. There is also an incentive bonus system based on quality and productivity.
Dr. Stanciu: What model does your clinic use to overcome the shortage of services?
Dr. Wadhwania: There are approximately 37 medical staff members in the agency, most of whom are MDs, but this group also includes nurse practitioners and clinical nurse specialists, so there is no shortage within our agency. We do contract for telepsychiatry services, but because our agency’s clinics are located throughout the county, most of our patients have easy access to any one of our clinics. We have a number of social workers, therapists, nurses, case managers, and pharmacists. We have a crisis center where unstable patients who require admission to an inpatient unit can be admitted; we also are able to refer patients directly to other inpatient psychiatric units. Our agency also has an addiction clinic and a residential substance abuse program catering specifically to patients with substance use disorders. We have educational, therapeutic, and behavioral support services, including residential services, for patients who have developmental disabilities. Our agency also has residential services for patients who are homeless or have a lower income and would benefit from support in a residential setting.
Our therapists are able to refer patients to state-contracted Assertive Community Treatment teams that serve our county. We are also able to set up intensive case management for patients in the community, as well as other community support services, peer support programs, and psychosocial rehabilitation programs.
Continue to: What advice do you have for early career psychiatrists and trainees who are contemplating working in an urban-public setting?
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating working in an urban-public setting?
Dr. Wadhwania: First of all, realize that there are many misconceptions about serving in the public sector, such as there is no access to new medications, etc. It is important to establish whether public sector service is “in your heart.” You need to learn the organization’s philosophy, mission, and vision, and figure out whether these views align with yours. Getting to know the leadership and how they value psychiatrists and other staff members is also very important. Also, make sure that there are opportunities for you to become a leader in the organization, that there is room for growth, and that it’s a stable organization.
Editor’s note : Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Cornel Stanciu, MD, talked with Mufida Wadhwania, MD. Dr. Wadhwania is an adult psychiatrist practicing in an urban/public setting in metro Atlanta, Georgia, at DeKalb Community Service Board. She manages a variety of uninsured and underinsured patients in an outpatient setting.
Dr. Stanciu: What attracted you to practice community mental health in an urban-public setting?
Dr. Wadhwania: A high portion of the population here has no health insurance, and hence there is a great need in the community. The psychopathology severity is high, so one can see a wide range of disorders. One can also build on the skill to pull together resources, such as linking patients to community resources and patient assistance programs, finding food banks, and finding ways to secure stable housing. There is continuity of care, and when a staff member leaves the agency, patients are linked to the next provider in an adequate time frame so that the patient’s quality of care is not compromised. The new provider is also given notification so that he or she is aware of the transfer of the patient and is able to review the chart in advance.
Along with medication management, we also provide psychotherapy. We utilize a single electronic health record (EHR) throughout the agency and we are able to contribute to changes in the EHR to make it more user-friendly. We have monthly journal club meetings and meetings with other staff members to review and discuss the progress of our organization. There are also numerous online resources through which we can keep ourselves updated with current research and earn CME. Some of the providers at our agency have academic affiliations, and hence there are opportunities to teach medical students and residents who rotate at some of our sites.
Dr. Stanciu: What are some of the more prevalent disorders you encounter?
Dr. Wadhwania: We see a wide range of disorders, such as affective disorders, schizophrenia, and comorbid disorders, specifically comorbid substance use disorders. So we encounter a high number of chronic mental illnesses.
Continue to: What are some challenges in working with this population?
Dr. Stanciu: What are some challenges in working with this population?
Dr. Wadhwania: Based on the high volume of patients we encounter, the resources available in the community are limited. But this challenges us to be creative and maximize what we have available to create new resources, such as having on-site case managers rather than just in the community, and building psychosocial rehabilitation programs near our various clinics for the patients to bring them the best care possible. Other challenges include a lack of education on and awareness of mental illness; there is still a lot of stigma surrounding mental illness in the community.
Dr. Stanciu: How would you describe your experience working in this setting?
Dr. Wadhwania: It’s a very rewarding experience, as you get to be creative, and patients appreciate your efforts. We use a patient-centered approach, and we work as a team. Each team member brings in a unique set of skills, and we bounce ideas off each other. There is a sense of satisfaction when you help people who don’t have easy access to health care. Finally, in a setting like this, young psychiatrists are able to gain more opportunities earlier than they would while working in other settings.
Continue to: How did you career path prepare you to work in such a challenging setting?
Dr. Stanciu: How did your career path prepare you to work in such a challenging setting?
Dr. Wadhwania: While at East Carolina University
Dr. Stanciu: How would you describe a psychiatric physician who is well-suited for such a setting?
Dr. Wadhwania: A perfect fit would be someone who is able to harness and build resources for the patients in the community and in the practice and wants to continue to build that skill. This individual is someone who is a team player, is flexible, and has a high professional frustration tolerance. The physician’s main aim would be to serve, and his or her mission would not be monetarily driven.
Continue to: What is the typical reimbursement model for your practice, and do you run into difficulties with health insurance providers in this setting?
Dr. Stanciu: What is the typical reimbursement model for your practice, and do you run into difficulties with health insurance providers in this setting?
Dr. Wadhwania: Approximately 40% of the patients we treat have no health insurance, and approximately 60% have Medicaid or managed Medicaid or Medicare. There is no burden of health insurance. Full-time employees are salaried, and part-time employees are compensated on an hourly model. There is also an incentive bonus system based on quality and productivity.
Dr. Stanciu: What model does your clinic use to overcome the shortage of services?
Dr. Wadhwania: There are approximately 37 medical staff members in the agency, most of whom are MDs, but this group also includes nurse practitioners and clinical nurse specialists, so there is no shortage within our agency. We do contract for telepsychiatry services, but because our agency’s clinics are located throughout the county, most of our patients have easy access to any one of our clinics. We have a number of social workers, therapists, nurses, case managers, and pharmacists. We have a crisis center where unstable patients who require admission to an inpatient unit can be admitted; we also are able to refer patients directly to other inpatient psychiatric units. Our agency also has an addiction clinic and a residential substance abuse program catering specifically to patients with substance use disorders. We have educational, therapeutic, and behavioral support services, including residential services, for patients who have developmental disabilities. Our agency also has residential services for patients who are homeless or have a lower income and would benefit from support in a residential setting.
Our therapists are able to refer patients to state-contracted Assertive Community Treatment teams that serve our county. We are also able to set up intensive case management for patients in the community, as well as other community support services, peer support programs, and psychosocial rehabilitation programs.
Continue to: What advice do you have for early career psychiatrists and trainees who are contemplating working in an urban-public setting?
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating working in an urban-public setting?
Dr. Wadhwania: First of all, realize that there are many misconceptions about serving in the public sector, such as there is no access to new medications, etc. It is important to establish whether public sector service is “in your heart.” You need to learn the organization’s philosophy, mission, and vision, and figure out whether these views align with yours. Getting to know the leadership and how they value psychiatrists and other staff members is also very important. Also, make sure that there are opportunities for you to become a leader in the organization, that there is room for growth, and that it’s a stable organization.
Career Choices: Consultation-liaison psychiatry
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Cornel Stanciu, MD, talked with Peter Ganpat, MD, a consultation-liaison (C-L) psychiatrist at Florida Hospital, where he provides guidance to various medical specialties on managing acute and chronic mental illness and substance use disorders. In addition, he also is the medical director for the repetitive transcranial magnetic stimulation service and staffs the inpatient unit.
Dr. Stanciu: What made you choose to become a C-L psychiatrist?
Dr. Ganpat: In my opinion, C-L is the most challenging area of psychiatry because not only are you thinking along the realms of a psychiatrist, but you’re also considering the viewpoint of the other subspecialties at the same time. For me, it brings together my medical background with my passion for psychiatry, and the patients I see daily allow for this incorporation.
Dr. Stanciu: How did your career path prepare you to become a C-L psychiatrist?
Dr. Ganpat: My career path was unique in that I completed a family medicine residency, and then immediately pursued training in psychiatry. Some may consider this as “overkill” for C-L, but as I’ve come to learn, this background grants me a level of understanding and confidence to step in when dealing with a complex case and lend a hand to the consulting physician beyond psychiatry. I do not feel a fellowship is required to practice C-L psychiatry. However, a psychosomatic fellowship will definitely provide the experience needed for this career path, and also will enable one to get a second American Board of Psychiatry and Neurology board certification.
Dr. Stanciu: What types of clinical conditions are you asked to provide input on managing, and how do you find working alongside other specialties?
Dr. Ganpat: I have been managing the full breadth of psychiatry, and in some cases I also provide medical management. Practicing in a metropolitan area with a high influx of tourists also brings in unique cultural cases. The level of respect that the other specialties give is impressive, because they have now seen what a C-L psychiatrist can do. Their performance scores also have improved as a result of my involvement. They greatly appreciate my efforts to shed light on cases or assist with the ever-challenging patient whose psychiatric complexity impedes care.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Ganpat: The perfect candidate for this role should be capable of abstract as well as objective thinking. Having a good understanding of the other medical specialties and being able to solve problems is essential, because often it isn’t a clear-cut picture. It is imperative for the C-L psychiatrist to have sound teaching abilities and to be able to educate and communicate his (her) reasoning to the consulting team. It also is important to be well-versed in the psychiatric manifestations of various medical disorders and the psychiatric iatrogenesis of widely used prescription medications.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Ganpat: I think the largest challenge that I have encountered is the lack of resources. Substance abuse is a major problem here, especially opioids, and there are limited community resources for these patients, so they wind up in the hospital.
Dr. Stanciu: What are the disadvantages of C-L compared with other branches of psychiatry?
Dr. Ganpat: There isn’t much continuity of care with C-L psychiatry over the long run, but you do get to see patients improve during the duration of their hospitalization, which is very rewarding.
Dr. Stanciu: What is the typical reimbursement model for a C-L psychiatrist, and have you run into difficulties with insurance providers in this setting?
Dr. Ganpat: The reimbursement model varies from one system to the next. The common model is to bill just as any other hospital service would, based on the time or level of complexity. Obviously, the more consults you have, the more billing is generated. Most insurance carriers recognize this and so I haven’t had much of an issue with reimbursement, although some unexpected problems may arise.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a C-L career?
Dr. Ganpat: If you enjoy working in the hospital and interfacing with other specialties, then consider C-L psychiatry. It is challenging but intellectually stimulating. Make sure you request a C-L rotation during your training, because the Accreditation Council for Graduate Medical Education requires it during a psychiatric residency.
Dr. Stanciu: What is the future outlook of C-L?
Dr. Ganpat: There is a shortage of C-L psychiatrists because >50% of practicing psychiatrists are in private practice in an outpatient setting. Because access to psychiatric care outside of a hospital setting is an issue, and much care is being driven to hospitals, there will be an increasing need for C-L psychiatrists.
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Cornel Stanciu, MD, talked with Peter Ganpat, MD, a consultation-liaison (C-L) psychiatrist at Florida Hospital, where he provides guidance to various medical specialties on managing acute and chronic mental illness and substance use disorders. In addition, he also is the medical director for the repetitive transcranial magnetic stimulation service and staffs the inpatient unit.
Dr. Stanciu: What made you choose to become a C-L psychiatrist?
Dr. Ganpat: In my opinion, C-L is the most challenging area of psychiatry because not only are you thinking along the realms of a psychiatrist, but you’re also considering the viewpoint of the other subspecialties at the same time. For me, it brings together my medical background with my passion for psychiatry, and the patients I see daily allow for this incorporation.
Dr. Stanciu: How did your career path prepare you to become a C-L psychiatrist?
Dr. Ganpat: My career path was unique in that I completed a family medicine residency, and then immediately pursued training in psychiatry. Some may consider this as “overkill” for C-L, but as I’ve come to learn, this background grants me a level of understanding and confidence to step in when dealing with a complex case and lend a hand to the consulting physician beyond psychiatry. I do not feel a fellowship is required to practice C-L psychiatry. However, a psychosomatic fellowship will definitely provide the experience needed for this career path, and also will enable one to get a second American Board of Psychiatry and Neurology board certification.
Dr. Stanciu: What types of clinical conditions are you asked to provide input on managing, and how do you find working alongside other specialties?
Dr. Ganpat: I have been managing the full breadth of psychiatry, and in some cases I also provide medical management. Practicing in a metropolitan area with a high influx of tourists also brings in unique cultural cases. The level of respect that the other specialties give is impressive, because they have now seen what a C-L psychiatrist can do. Their performance scores also have improved as a result of my involvement. They greatly appreciate my efforts to shed light on cases or assist with the ever-challenging patient whose psychiatric complexity impedes care.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Ganpat: The perfect candidate for this role should be capable of abstract as well as objective thinking. Having a good understanding of the other medical specialties and being able to solve problems is essential, because often it isn’t a clear-cut picture. It is imperative for the C-L psychiatrist to have sound teaching abilities and to be able to educate and communicate his (her) reasoning to the consulting team. It also is important to be well-versed in the psychiatric manifestations of various medical disorders and the psychiatric iatrogenesis of widely used prescription medications.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Ganpat: I think the largest challenge that I have encountered is the lack of resources. Substance abuse is a major problem here, especially opioids, and there are limited community resources for these patients, so they wind up in the hospital.
Dr. Stanciu: What are the disadvantages of C-L compared with other branches of psychiatry?
Dr. Ganpat: There isn’t much continuity of care with C-L psychiatry over the long run, but you do get to see patients improve during the duration of their hospitalization, which is very rewarding.
Dr. Stanciu: What is the typical reimbursement model for a C-L psychiatrist, and have you run into difficulties with insurance providers in this setting?
Dr. Ganpat: The reimbursement model varies from one system to the next. The common model is to bill just as any other hospital service would, based on the time or level of complexity. Obviously, the more consults you have, the more billing is generated. Most insurance carriers recognize this and so I haven’t had much of an issue with reimbursement, although some unexpected problems may arise.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a C-L career?
Dr. Ganpat: If you enjoy working in the hospital and interfacing with other specialties, then consider C-L psychiatry. It is challenging but intellectually stimulating. Make sure you request a C-L rotation during your training, because the Accreditation Council for Graduate Medical Education requires it during a psychiatric residency.
Dr. Stanciu: What is the future outlook of C-L?
Dr. Ganpat: There is a shortage of C-L psychiatrists because >50% of practicing psychiatrists are in private practice in an outpatient setting. Because access to psychiatric care outside of a hospital setting is an issue, and much care is being driven to hospitals, there will be an increasing need for C-L psychiatrists.
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Cornel Stanciu, MD, talked with Peter Ganpat, MD, a consultation-liaison (C-L) psychiatrist at Florida Hospital, where he provides guidance to various medical specialties on managing acute and chronic mental illness and substance use disorders. In addition, he also is the medical director for the repetitive transcranial magnetic stimulation service and staffs the inpatient unit.
Dr. Stanciu: What made you choose to become a C-L psychiatrist?
Dr. Ganpat: In my opinion, C-L is the most challenging area of psychiatry because not only are you thinking along the realms of a psychiatrist, but you’re also considering the viewpoint of the other subspecialties at the same time. For me, it brings together my medical background with my passion for psychiatry, and the patients I see daily allow for this incorporation.
Dr. Stanciu: How did your career path prepare you to become a C-L psychiatrist?
Dr. Ganpat: My career path was unique in that I completed a family medicine residency, and then immediately pursued training in psychiatry. Some may consider this as “overkill” for C-L, but as I’ve come to learn, this background grants me a level of understanding and confidence to step in when dealing with a complex case and lend a hand to the consulting physician beyond psychiatry. I do not feel a fellowship is required to practice C-L psychiatry. However, a psychosomatic fellowship will definitely provide the experience needed for this career path, and also will enable one to get a second American Board of Psychiatry and Neurology board certification.
Dr. Stanciu: What types of clinical conditions are you asked to provide input on managing, and how do you find working alongside other specialties?
Dr. Ganpat: I have been managing the full breadth of psychiatry, and in some cases I also provide medical management. Practicing in a metropolitan area with a high influx of tourists also brings in unique cultural cases. The level of respect that the other specialties give is impressive, because they have now seen what a C-L psychiatrist can do. Their performance scores also have improved as a result of my involvement. They greatly appreciate my efforts to shed light on cases or assist with the ever-challenging patient whose psychiatric complexity impedes care.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Ganpat: The perfect candidate for this role should be capable of abstract as well as objective thinking. Having a good understanding of the other medical specialties and being able to solve problems is essential, because often it isn’t a clear-cut picture. It is imperative for the C-L psychiatrist to have sound teaching abilities and to be able to educate and communicate his (her) reasoning to the consulting team. It also is important to be well-versed in the psychiatric manifestations of various medical disorders and the psychiatric iatrogenesis of widely used prescription medications.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Ganpat: I think the largest challenge that I have encountered is the lack of resources. Substance abuse is a major problem here, especially opioids, and there are limited community resources for these patients, so they wind up in the hospital.
Dr. Stanciu: What are the disadvantages of C-L compared with other branches of psychiatry?
Dr. Ganpat: There isn’t much continuity of care with C-L psychiatry over the long run, but you do get to see patients improve during the duration of their hospitalization, which is very rewarding.
Dr. Stanciu: What is the typical reimbursement model for a C-L psychiatrist, and have you run into difficulties with insurance providers in this setting?
Dr. Ganpat: The reimbursement model varies from one system to the next. The common model is to bill just as any other hospital service would, based on the time or level of complexity. Obviously, the more consults you have, the more billing is generated. Most insurance carriers recognize this and so I haven’t had much of an issue with reimbursement, although some unexpected problems may arise.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a C-L career?
Dr. Ganpat: If you enjoy working in the hospital and interfacing with other specialties, then consider C-L psychiatry. It is challenging but intellectually stimulating. Make sure you request a C-L rotation during your training, because the Accreditation Council for Graduate Medical Education requires it during a psychiatric residency.
Dr. Stanciu: What is the future outlook of C-L?
Dr. Ganpat: There is a shortage of C-L psychiatrists because >50% of practicing psychiatrists are in private practice in an outpatient setting. Because access to psychiatric care outside of a hospital setting is an issue, and much care is being driven to hospitals, there will be an increasing need for C-L psychiatrists.
A trainee’s path to fighting addiction
When I came to this country, even before my current residency, I launched my addiction psychiatry career by researching nicotine addiction in schizophrenia patients. Those early experiences gave me a greater understanding of the health concerns and life experiences of people with addictions – and those more likely to develop them.
So imagine my excitement when I first became acquainted with the American Academy of Addiction Psychiatry (AAAP). I first learned about the AAAP, its mission, and activities at the 2017 American Psychiatric Association’s annual meeting in San Diego.
Getting in and involved
After returning to New York, I took those next steps and joined up, which opened the AAAP gates so I could receive its newsletters and submission calls, gain access to resources such as The American Journal on Addictions, survey the various joinable task forces, as well as discover who might be available to me as a mentor as part of the AAAP’s mentor-mentee program.
Sometime during my third-year residency training, I received a member-email advertising the AAAP 28th Annual Meeting and Scientific Symposium, and soon after that, received another email calling for research submissions to be presented there, as well as an invitation to apply for a trainee travel scholarship that would defray the cost for and allow its fellows to attend the meeting in San Diego. That alone was enticing enough to apply. But even more enticing was the opportunity to showcase the addiction work I had been doing during my residency, as well as to meet other members at various levels of the AAAP to determine whether I wanted to become more involved.
Pursuing experiences
I did not think twice about applying for the poster presentation and the travel scholarship. The AAAP’s online application forms for both were easy to understand and very well structured, which greatly helped me with filling out and formatting my applications. Taking the initiative toward even these first AAAP offerings brought more positive echoes. I was thrilled when the poster I proposed was accepted, mostly because it would give me the chance to present my recent addiction psych work from a higher platform. A few weeks later, I was thrilled again when I received an AAAP email congratulating me on being awarded the San Diego 28th annual meeting travel scholarship, which would waive the annual membership and conference registration fees, in addition to defraying my travel costs. Pacific breezes, here I come. And there I went. (Thanks to my extremely supportive training director, who first nominated me for the award.)
On the ground at 2017 AAAP
The 28th AAAP annual meeting opened on a balmy December Thursday, and that’s the day I arrived. I attended many addiction workshops and symposiums, which featured premier figures in addiction psychiatry. Of the numerous trainee-specific events I attended, the most informative was the “Fellowship Forum: Exploring the Field of Addiction Psychiatry.” At this forum, I learned the true benefits of doing an addiction psychiatry fellowship, while meeting many of the fellowship program directors of top institutions. Having them all under one “roof” made it easy to compare and contrast the specific training they offered.
Then came what were, for me, major highlights of the AAAP 2017. After I delivered my poster presentation and shared my research, I was able to receive very close, constructive feedback from the field’s most experienced professionals. And, finally, I met my AAAP mentors face to face: Dr. Amy Yule of Harvard Medical School, Boston; Dr. Thomas Penders, of East Carolina University, Greenville, N.C.; and Dr. Cornel Stanciu of Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
One AAAP trainee’s takeaways
All AAAP trainees, fellows, presenters leave the meeting with their own conclusions, but my biggest takeaways were:
- Regarding barriers to buprenorphine, emerging research supports similar efficacy for long-acting injectable naltrexone.
- Various protocols for rapid implementation of naltrexone are being used, and these allow for smoother transition and shorter “washout” periods.
- We should not overlook the effects of tobacco use in our patient population – and should address it aggressively, regardless of psychiatric comorbidities.
- The cannabinoid CBD receptors that exist on the dopamine pathway strengthen and complicate their relationship with psychosis.
- , especially in rural and remote settings. The body of evidence supporting its efficacy is expanding.
- Synthetic cannabinoids are prevalent, and toxidromes exist – yet, trainees are not current on these.
The challenges facing those of us dedicated to fighting addiction have never been greater. I would urge more trainees and psychiatrists to join the AAAP in light of the opioid crisis and the potential fallout tied to marijuana legalization. I am grateful to have the opportunity to join my colleagues in this fight. Becoming part of the AAAP has led to a highly rewarding, career-enriching experience.
This article was updated 1/17/17.
Dr. Ahmed is a third-year resident in the department of psychiatry at Nassau University Medical Center, East Meadow, New York. Besides addiction psychiatry, his interests include public social psychiatry, health care policy, health disparities, and mental health stigma. Dr. Ahmed is a member of the American Psychiatric Association, the American Society of Clinical Psychopharmacology, and the American Association for Social Psychiatry.
When I came to this country, even before my current residency, I launched my addiction psychiatry career by researching nicotine addiction in schizophrenia patients. Those early experiences gave me a greater understanding of the health concerns and life experiences of people with addictions – and those more likely to develop them.
So imagine my excitement when I first became acquainted with the American Academy of Addiction Psychiatry (AAAP). I first learned about the AAAP, its mission, and activities at the 2017 American Psychiatric Association’s annual meeting in San Diego.
Getting in and involved
After returning to New York, I took those next steps and joined up, which opened the AAAP gates so I could receive its newsletters and submission calls, gain access to resources such as The American Journal on Addictions, survey the various joinable task forces, as well as discover who might be available to me as a mentor as part of the AAAP’s mentor-mentee program.
Sometime during my third-year residency training, I received a member-email advertising the AAAP 28th Annual Meeting and Scientific Symposium, and soon after that, received another email calling for research submissions to be presented there, as well as an invitation to apply for a trainee travel scholarship that would defray the cost for and allow its fellows to attend the meeting in San Diego. That alone was enticing enough to apply. But even more enticing was the opportunity to showcase the addiction work I had been doing during my residency, as well as to meet other members at various levels of the AAAP to determine whether I wanted to become more involved.
Pursuing experiences
I did not think twice about applying for the poster presentation and the travel scholarship. The AAAP’s online application forms for both were easy to understand and very well structured, which greatly helped me with filling out and formatting my applications. Taking the initiative toward even these first AAAP offerings brought more positive echoes. I was thrilled when the poster I proposed was accepted, mostly because it would give me the chance to present my recent addiction psych work from a higher platform. A few weeks later, I was thrilled again when I received an AAAP email congratulating me on being awarded the San Diego 28th annual meeting travel scholarship, which would waive the annual membership and conference registration fees, in addition to defraying my travel costs. Pacific breezes, here I come. And there I went. (Thanks to my extremely supportive training director, who first nominated me for the award.)
On the ground at 2017 AAAP
The 28th AAAP annual meeting opened on a balmy December Thursday, and that’s the day I arrived. I attended many addiction workshops and symposiums, which featured premier figures in addiction psychiatry. Of the numerous trainee-specific events I attended, the most informative was the “Fellowship Forum: Exploring the Field of Addiction Psychiatry.” At this forum, I learned the true benefits of doing an addiction psychiatry fellowship, while meeting many of the fellowship program directors of top institutions. Having them all under one “roof” made it easy to compare and contrast the specific training they offered.
Then came what were, for me, major highlights of the AAAP 2017. After I delivered my poster presentation and shared my research, I was able to receive very close, constructive feedback from the field’s most experienced professionals. And, finally, I met my AAAP mentors face to face: Dr. Amy Yule of Harvard Medical School, Boston; Dr. Thomas Penders, of East Carolina University, Greenville, N.C.; and Dr. Cornel Stanciu of Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
One AAAP trainee’s takeaways
All AAAP trainees, fellows, presenters leave the meeting with their own conclusions, but my biggest takeaways were:
- Regarding barriers to buprenorphine, emerging research supports similar efficacy for long-acting injectable naltrexone.
- Various protocols for rapid implementation of naltrexone are being used, and these allow for smoother transition and shorter “washout” periods.
- We should not overlook the effects of tobacco use in our patient population – and should address it aggressively, regardless of psychiatric comorbidities.
- The cannabinoid CBD receptors that exist on the dopamine pathway strengthen and complicate their relationship with psychosis.
- , especially in rural and remote settings. The body of evidence supporting its efficacy is expanding.
- Synthetic cannabinoids are prevalent, and toxidromes exist – yet, trainees are not current on these.
The challenges facing those of us dedicated to fighting addiction have never been greater. I would urge more trainees and psychiatrists to join the AAAP in light of the opioid crisis and the potential fallout tied to marijuana legalization. I am grateful to have the opportunity to join my colleagues in this fight. Becoming part of the AAAP has led to a highly rewarding, career-enriching experience.
This article was updated 1/17/17.
Dr. Ahmed is a third-year resident in the department of psychiatry at Nassau University Medical Center, East Meadow, New York. Besides addiction psychiatry, his interests include public social psychiatry, health care policy, health disparities, and mental health stigma. Dr. Ahmed is a member of the American Psychiatric Association, the American Society of Clinical Psychopharmacology, and the American Association for Social Psychiatry.
When I came to this country, even before my current residency, I launched my addiction psychiatry career by researching nicotine addiction in schizophrenia patients. Those early experiences gave me a greater understanding of the health concerns and life experiences of people with addictions – and those more likely to develop them.
So imagine my excitement when I first became acquainted with the American Academy of Addiction Psychiatry (AAAP). I first learned about the AAAP, its mission, and activities at the 2017 American Psychiatric Association’s annual meeting in San Diego.
Getting in and involved
After returning to New York, I took those next steps and joined up, which opened the AAAP gates so I could receive its newsletters and submission calls, gain access to resources such as The American Journal on Addictions, survey the various joinable task forces, as well as discover who might be available to me as a mentor as part of the AAAP’s mentor-mentee program.
Sometime during my third-year residency training, I received a member-email advertising the AAAP 28th Annual Meeting and Scientific Symposium, and soon after that, received another email calling for research submissions to be presented there, as well as an invitation to apply for a trainee travel scholarship that would defray the cost for and allow its fellows to attend the meeting in San Diego. That alone was enticing enough to apply. But even more enticing was the opportunity to showcase the addiction work I had been doing during my residency, as well as to meet other members at various levels of the AAAP to determine whether I wanted to become more involved.
Pursuing experiences
I did not think twice about applying for the poster presentation and the travel scholarship. The AAAP’s online application forms for both were easy to understand and very well structured, which greatly helped me with filling out and formatting my applications. Taking the initiative toward even these first AAAP offerings brought more positive echoes. I was thrilled when the poster I proposed was accepted, mostly because it would give me the chance to present my recent addiction psych work from a higher platform. A few weeks later, I was thrilled again when I received an AAAP email congratulating me on being awarded the San Diego 28th annual meeting travel scholarship, which would waive the annual membership and conference registration fees, in addition to defraying my travel costs. Pacific breezes, here I come. And there I went. (Thanks to my extremely supportive training director, who first nominated me for the award.)
On the ground at 2017 AAAP
The 28th AAAP annual meeting opened on a balmy December Thursday, and that’s the day I arrived. I attended many addiction workshops and symposiums, which featured premier figures in addiction psychiatry. Of the numerous trainee-specific events I attended, the most informative was the “Fellowship Forum: Exploring the Field of Addiction Psychiatry.” At this forum, I learned the true benefits of doing an addiction psychiatry fellowship, while meeting many of the fellowship program directors of top institutions. Having them all under one “roof” made it easy to compare and contrast the specific training they offered.
Then came what were, for me, major highlights of the AAAP 2017. After I delivered my poster presentation and shared my research, I was able to receive very close, constructive feedback from the field’s most experienced professionals. And, finally, I met my AAAP mentors face to face: Dr. Amy Yule of Harvard Medical School, Boston; Dr. Thomas Penders, of East Carolina University, Greenville, N.C.; and Dr. Cornel Stanciu of Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
One AAAP trainee’s takeaways
All AAAP trainees, fellows, presenters leave the meeting with their own conclusions, but my biggest takeaways were:
- Regarding barriers to buprenorphine, emerging research supports similar efficacy for long-acting injectable naltrexone.
- Various protocols for rapid implementation of naltrexone are being used, and these allow for smoother transition and shorter “washout” periods.
- We should not overlook the effects of tobacco use in our patient population – and should address it aggressively, regardless of psychiatric comorbidities.
- The cannabinoid CBD receptors that exist on the dopamine pathway strengthen and complicate their relationship with psychosis.
- , especially in rural and remote settings. The body of evidence supporting its efficacy is expanding.
- Synthetic cannabinoids are prevalent, and toxidromes exist – yet, trainees are not current on these.
The challenges facing those of us dedicated to fighting addiction have never been greater. I would urge more trainees and psychiatrists to join the AAAP in light of the opioid crisis and the potential fallout tied to marijuana legalization. I am grateful to have the opportunity to join my colleagues in this fight. Becoming part of the AAAP has led to a highly rewarding, career-enriching experience.
This article was updated 1/17/17.
Dr. Ahmed is a third-year resident in the department of psychiatry at Nassau University Medical Center, East Meadow, New York. Besides addiction psychiatry, his interests include public social psychiatry, health care policy, health disparities, and mental health stigma. Dr. Ahmed is a member of the American Psychiatric Association, the American Society of Clinical Psychopharmacology, and the American Association for Social Psychiatry.
Career Choices: State hospital psychiatry
Editor’s note: Career Choices is a new feature of Residents’ Voices. It features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths. Future installments will feature interviews with psychiatrists who have focused their careers on consultation-liaison psychiatry, academic psychiatry, rural psychiatry, and other career paths.
In this first Career Choices, Cornel Stanciu, MD, talked with Samantha Gnanasegaram, MD, a state hospital psychiatrist at New Hampshire Hospital, where she treats severe and chronic mental illness and testifies in various court proceedings.
Dr. Stanciu: What made you choose to become a state hospital psychiatrist?
Dr. Gnanasegaram: When I started thinking about career options after residency, I knew I wanted to start my career in a facility where I could be challenged, remain up-to-date with the most current evidence-based literature, and have the support and mentorship of seasoned psychiatrists in the field. The opportunity to work under the auspices of a great academic institution with the “bread and butter” of psychiatry reminds me every day why I chose the field in the first place. The often chronic and sometimes refractory cases I encounter daily are extremely thought-provoking, and they motivate me to think and pursue more complex management options. [This setting] also enables me to work closely as [part of] an interdisciplinary team with nursing, social work, and recreational and occupational therapy in ensuring these individuals get the best care and aftercare plans.
We often forget that psychosis often takes weeks to respond [to treatment]. Unfortunately, often in private hospitals, the longer stays that are necessary for patient care are not always possible, leading to premature psychotropic changes and discharge. In this setting, I am able to practice medicine based on what is best for the patient from an evidence-based standpoint. Additionally, being in the state system also allows me to learn first-hand and work closely with the legal system in this state and to testify in various settings to ensure my patients get the best possible care.
Dr. Stanciu: How did your career path prepare you to become a state hospital psychiatrist?
Dr. Gnanasegaram: During my residency, I had exposure to the affiliated state psychiatric hospital and spent some time on various units, each geared toward different patient populations. I also became very familiar with a wide range of psychotropics, ranging from first-line to second- and third-tier medications, as well as off-label. The ECT exposure as well as Crisis Prevention Institute training in how to deal with violent and aggressive individuals certainly added extra layers to my proficiency.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Gnanasegaram: This setting is great for someone who likes to be challenged and stay current with literature. Furthermore, this is a great setting for those who are comfortable with the use of medications such as [clozapine] and long-acting injectables, and procedures such as ECT. Additionally, an ideal candidate is someone who understands the chronicity and complexity of mental illness, and has the patience to follow the course and does not rush to make drastic changes or panics at the first sign of a patient taking a step back.
A good candidate also should be comfortable with medical comorbidities, because severe mental illness often leads to poor self-care, diabetes, hypertension, etc., and should be able to work effectively in a team setting and interact with other specialties. State hospital physicians need to be cognizant of outpatient resources available to prevent decompensation in the community and not only focus on acute stabilization. Additionally, this is a great setting for those who enjoy working in an interdisciplinary team and learning from the expertise of different members of a treatment team.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Gnanasegaram: When I started, the biggest challenge was learning about the differences in practice and legislature in a different state, because all states vary in their involuntary commitment laws, process, and ability to institute forced medications. Learning this as well as how they apply to my practice occurred quicker than I anticipated. As I started practicing, I became more proficient in being able to incorporate the resources I have available.
Dr. Stanciu: What are the disadvantages compared with other branches of psychiatry?
Dr. Gnanasegaram: This is a subjective question. Some physicians may desire a rapid turnaround of patients, which is not always the case in state psychiatric hospitals. Even at discharge, some patients may have low-functioning baselines, requiring guardianship and/or placement in a more supervised setting to ensure they receive the care they need. It is also important to realize these are primarily not voluntary patients, but rather patients committed here involuntarily for treatment due to impaired insight and judgment. At times, the acuity can be high, but the potential for violence is mitigated through comprehensive risk assessments, staff training, and prevention strategies to help ensure patient and staff safety.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a state hospital career?
Dr. Gnanasegaram: I would recommend seeking exposure to working in a state psychiatric hospital early in your training so you can see the daily routine and protocol. It would help to obtain mentorship from a state hospital psychiatrist in the state where you intend to work. Ask as many questions as needed and seek their insight into the challenges and benefits of working there. During training, it’s important to familiarize yourself with managing difficult and refractory cases, and don’t shy away from challenging patients. The next step would be to apply for a position of interest to interview and learn more about the facility and the staff that you will be working with.
Dr. Stanciu: How important is the academic affiliation?
Dr. Gnanasegaram: Very important. Especially during the early phase of your career, it is important to have at your fingertips senior mentors and to be involved in the conferences and CME activities offered. This ensures good quality measures in patient care. The academic affiliation helps keep you up-to-date with advancements and maintains an atmosphere that fosters ongoing learning and the best possible care for your patients. Working with trainees at various levels, such as medical students, residents, and fellows, allows you to maintain an evidence-based practice approach as well as share your knowledge and experience with those in training. Being in this academic setting, you also have the opportunity for involvement in research activities and publications.
Editor’s note: Career Choices is a new feature of Residents’ Voices. It features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths. Future installments will feature interviews with psychiatrists who have focused their careers on consultation-liaison psychiatry, academic psychiatry, rural psychiatry, and other career paths.
In this first Career Choices, Cornel Stanciu, MD, talked with Samantha Gnanasegaram, MD, a state hospital psychiatrist at New Hampshire Hospital, where she treats severe and chronic mental illness and testifies in various court proceedings.
Dr. Stanciu: What made you choose to become a state hospital psychiatrist?
Dr. Gnanasegaram: When I started thinking about career options after residency, I knew I wanted to start my career in a facility where I could be challenged, remain up-to-date with the most current evidence-based literature, and have the support and mentorship of seasoned psychiatrists in the field. The opportunity to work under the auspices of a great academic institution with the “bread and butter” of psychiatry reminds me every day why I chose the field in the first place. The often chronic and sometimes refractory cases I encounter daily are extremely thought-provoking, and they motivate me to think and pursue more complex management options. [This setting] also enables me to work closely as [part of] an interdisciplinary team with nursing, social work, and recreational and occupational therapy in ensuring these individuals get the best care and aftercare plans.
We often forget that psychosis often takes weeks to respond [to treatment]. Unfortunately, often in private hospitals, the longer stays that are necessary for patient care are not always possible, leading to premature psychotropic changes and discharge. In this setting, I am able to practice medicine based on what is best for the patient from an evidence-based standpoint. Additionally, being in the state system also allows me to learn first-hand and work closely with the legal system in this state and to testify in various settings to ensure my patients get the best possible care.
Dr. Stanciu: How did your career path prepare you to become a state hospital psychiatrist?
Dr. Gnanasegaram: During my residency, I had exposure to the affiliated state psychiatric hospital and spent some time on various units, each geared toward different patient populations. I also became very familiar with a wide range of psychotropics, ranging from first-line to second- and third-tier medications, as well as off-label. The ECT exposure as well as Crisis Prevention Institute training in how to deal with violent and aggressive individuals certainly added extra layers to my proficiency.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Gnanasegaram: This setting is great for someone who likes to be challenged and stay current with literature. Furthermore, this is a great setting for those who are comfortable with the use of medications such as [clozapine] and long-acting injectables, and procedures such as ECT. Additionally, an ideal candidate is someone who understands the chronicity and complexity of mental illness, and has the patience to follow the course and does not rush to make drastic changes or panics at the first sign of a patient taking a step back.
A good candidate also should be comfortable with medical comorbidities, because severe mental illness often leads to poor self-care, diabetes, hypertension, etc., and should be able to work effectively in a team setting and interact with other specialties. State hospital physicians need to be cognizant of outpatient resources available to prevent decompensation in the community and not only focus on acute stabilization. Additionally, this is a great setting for those who enjoy working in an interdisciplinary team and learning from the expertise of different members of a treatment team.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Gnanasegaram: When I started, the biggest challenge was learning about the differences in practice and legislature in a different state, because all states vary in their involuntary commitment laws, process, and ability to institute forced medications. Learning this as well as how they apply to my practice occurred quicker than I anticipated. As I started practicing, I became more proficient in being able to incorporate the resources I have available.
Dr. Stanciu: What are the disadvantages compared with other branches of psychiatry?
Dr. Gnanasegaram: This is a subjective question. Some physicians may desire a rapid turnaround of patients, which is not always the case in state psychiatric hospitals. Even at discharge, some patients may have low-functioning baselines, requiring guardianship and/or placement in a more supervised setting to ensure they receive the care they need. It is also important to realize these are primarily not voluntary patients, but rather patients committed here involuntarily for treatment due to impaired insight and judgment. At times, the acuity can be high, but the potential for violence is mitigated through comprehensive risk assessments, staff training, and prevention strategies to help ensure patient and staff safety.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a state hospital career?
Dr. Gnanasegaram: I would recommend seeking exposure to working in a state psychiatric hospital early in your training so you can see the daily routine and protocol. It would help to obtain mentorship from a state hospital psychiatrist in the state where you intend to work. Ask as many questions as needed and seek their insight into the challenges and benefits of working there. During training, it’s important to familiarize yourself with managing difficult and refractory cases, and don’t shy away from challenging patients. The next step would be to apply for a position of interest to interview and learn more about the facility and the staff that you will be working with.
Dr. Stanciu: How important is the academic affiliation?
Dr. Gnanasegaram: Very important. Especially during the early phase of your career, it is important to have at your fingertips senior mentors and to be involved in the conferences and CME activities offered. This ensures good quality measures in patient care. The academic affiliation helps keep you up-to-date with advancements and maintains an atmosphere that fosters ongoing learning and the best possible care for your patients. Working with trainees at various levels, such as medical students, residents, and fellows, allows you to maintain an evidence-based practice approach as well as share your knowledge and experience with those in training. Being in this academic setting, you also have the opportunity for involvement in research activities and publications.
Editor’s note: Career Choices is a new feature of Residents’ Voices. It features a psychiatry resident/fellow interviewing a psychiatrist about why he (she) has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths. Future installments will feature interviews with psychiatrists who have focused their careers on consultation-liaison psychiatry, academic psychiatry, rural psychiatry, and other career paths.
In this first Career Choices, Cornel Stanciu, MD, talked with Samantha Gnanasegaram, MD, a state hospital psychiatrist at New Hampshire Hospital, where she treats severe and chronic mental illness and testifies in various court proceedings.
Dr. Stanciu: What made you choose to become a state hospital psychiatrist?
Dr. Gnanasegaram: When I started thinking about career options after residency, I knew I wanted to start my career in a facility where I could be challenged, remain up-to-date with the most current evidence-based literature, and have the support and mentorship of seasoned psychiatrists in the field. The opportunity to work under the auspices of a great academic institution with the “bread and butter” of psychiatry reminds me every day why I chose the field in the first place. The often chronic and sometimes refractory cases I encounter daily are extremely thought-provoking, and they motivate me to think and pursue more complex management options. [This setting] also enables me to work closely as [part of] an interdisciplinary team with nursing, social work, and recreational and occupational therapy in ensuring these individuals get the best care and aftercare plans.
We often forget that psychosis often takes weeks to respond [to treatment]. Unfortunately, often in private hospitals, the longer stays that are necessary for patient care are not always possible, leading to premature psychotropic changes and discharge. In this setting, I am able to practice medicine based on what is best for the patient from an evidence-based standpoint. Additionally, being in the state system also allows me to learn first-hand and work closely with the legal system in this state and to testify in various settings to ensure my patients get the best possible care.
Dr. Stanciu: How did your career path prepare you to become a state hospital psychiatrist?
Dr. Gnanasegaram: During my residency, I had exposure to the affiliated state psychiatric hospital and spent some time on various units, each geared toward different patient populations. I also became very familiar with a wide range of psychotropics, ranging from first-line to second- and third-tier medications, as well as off-label. The ECT exposure as well as Crisis Prevention Institute training in how to deal with violent and aggressive individuals certainly added extra layers to my proficiency.
Dr. Stanciu: How would you describe a physician who is well-suited for such a setting?
Dr. Gnanasegaram: This setting is great for someone who likes to be challenged and stay current with literature. Furthermore, this is a great setting for those who are comfortable with the use of medications such as [clozapine] and long-acting injectables, and procedures such as ECT. Additionally, an ideal candidate is someone who understands the chronicity and complexity of mental illness, and has the patience to follow the course and does not rush to make drastic changes or panics at the first sign of a patient taking a step back.
A good candidate also should be comfortable with medical comorbidities, because severe mental illness often leads to poor self-care, diabetes, hypertension, etc., and should be able to work effectively in a team setting and interact with other specialties. State hospital physicians need to be cognizant of outpatient resources available to prevent decompensation in the community and not only focus on acute stabilization. Additionally, this is a great setting for those who enjoy working in an interdisciplinary team and learning from the expertise of different members of a treatment team.
Dr. Stanciu: What challenges and surprises did you encounter when you first began to practice in this setting?
Dr. Gnanasegaram: When I started, the biggest challenge was learning about the differences in practice and legislature in a different state, because all states vary in their involuntary commitment laws, process, and ability to institute forced medications. Learning this as well as how they apply to my practice occurred quicker than I anticipated. As I started practicing, I became more proficient in being able to incorporate the resources I have available.
Dr. Stanciu: What are the disadvantages compared with other branches of psychiatry?
Dr. Gnanasegaram: This is a subjective question. Some physicians may desire a rapid turnaround of patients, which is not always the case in state psychiatric hospitals. Even at discharge, some patients may have low-functioning baselines, requiring guardianship and/or placement in a more supervised setting to ensure they receive the care they need. It is also important to realize these are primarily not voluntary patients, but rather patients committed here involuntarily for treatment due to impaired insight and judgment. At times, the acuity can be high, but the potential for violence is mitigated through comprehensive risk assessments, staff training, and prevention strategies to help ensure patient and staff safety.
Dr. Stanciu: What advice do you have for early career psychiatrists and trainees who are contemplating a state hospital career?
Dr. Gnanasegaram: I would recommend seeking exposure to working in a state psychiatric hospital early in your training so you can see the daily routine and protocol. It would help to obtain mentorship from a state hospital psychiatrist in the state where you intend to work. Ask as many questions as needed and seek their insight into the challenges and benefits of working there. During training, it’s important to familiarize yourself with managing difficult and refractory cases, and don’t shy away from challenging patients. The next step would be to apply for a position of interest to interview and learn more about the facility and the staff that you will be working with.
Dr. Stanciu: How important is the academic affiliation?
Dr. Gnanasegaram: Very important. Especially during the early phase of your career, it is important to have at your fingertips senior mentors and to be involved in the conferences and CME activities offered. This ensures good quality measures in patient care. The academic affiliation helps keep you up-to-date with advancements and maintains an atmosphere that fosters ongoing learning and the best possible care for your patients. Working with trainees at various levels, such as medical students, residents, and fellows, allows you to maintain an evidence-based practice approach as well as share your knowledge and experience with those in training. Being in this academic setting, you also have the opportunity for involvement in research activities and publications.
Call for Applications
Dr. Henry Nasrallah, Editor-in-Chief of Current Psychiatry, and Chair of the Department of Psychiatry and Behavioral Neuroscience at Saint Louis University, invites PGY-4 residents who will complete their training in June 2018 to consider applying for a full-time faculty position, which is a mix of student mental health at the university and supervision of the resident's outpatient clinic.
Those interested can email Dr. Nasrallah directly at [email protected] and include a CV.
Dr. Henry Nasrallah, Editor-in-Chief of Current Psychiatry, and Chair of the Department of Psychiatry and Behavioral Neuroscience at Saint Louis University, invites PGY-4 residents who will complete their training in June 2018 to consider applying for a full-time faculty position, which is a mix of student mental health at the university and supervision of the resident's outpatient clinic.
Those interested can email Dr. Nasrallah directly at [email protected] and include a CV.
Dr. Henry Nasrallah, Editor-in-Chief of Current Psychiatry, and Chair of the Department of Psychiatry and Behavioral Neuroscience at Saint Louis University, invites PGY-4 residents who will complete their training in June 2018 to consider applying for a full-time faculty position, which is a mix of student mental health at the university and supervision of the resident's outpatient clinic.
Those interested can email Dr. Nasrallah directly at [email protected] and include a CV.
The art of psychopharmacology: Avoiding medication changes and slowing down
As physicians, we are cognizant of the importance of patient-centered care, active listening, empathy, and patience—the so-called “hidden curriculum of medicine.”1 However, our attempts to centralize these concepts may be overshadowed by the deeply rooted drive to treat and fix. At times, we are simply treating uncertainty, whether it be diagnostic uncertainty or the uncertainty arising from clinical responses and outcomes that are far from binary. Definitive actions, such as adding medications or altering dosages, may appear to both patients and physicians to be a step closer to a “cure.” However, watchful waiting, re-evaluation, and accepting uncertainty are the true skills of effective care.
Be savvy about psychopharmacology
Psychotropics can take weeks to months to reach their full potential, and have varying responses and adverse effects. Beware of changing regimens prematurely, and keep in mind basic, yet crucial, pharmacokinetic concepts (eg, 4 to 5 half-lives to reach steady state, variations in metabolism). Receptor binding and dosing heuristics are notably common in psychiatry. Although such concepts are important to grasp, there is no one-size-fits-all rule. The brain simply does not possess the heart’s machine-like, linear functioning. Therefore, targeting individual parts (ie, receptors) will not equate to fixing the whole organ systematically or predictably.
Is the patient truly treatment-resistant?
Even the best treatment regimen has no clinical benefit if the patient cannot afford the prescription or does not take the medication. If cost is an impediment, switch from brand name drugs to generic formulations or to older medications in the same class. Before declaring the patient “treatment-resistant” and making medication changes, assess for compliance. This may require assistance from collateral informants. Ask family members to count the number of pills remaining in the bottle, and call the pharmacy to find out the last refill dates. If the patient exhibits a partial response to what should be a therapeutic dose, consider obtaining drug plasma levels to rule out rapid metabolism before deeming the medication trial a failure.2
Medications as liabilities
Overreliance on medications can result in the medications becoming liabilities. The polypharmacy problem is not unique to psychiatry.3 However, psychiatric patients may be more likely to inadvertently use medications in a maladaptive manner and disrupt the fundamental goals of long-term care. Avoid making medication adjustments in response to a patient’s life stressors and normative situational reactions. Doing so is a disservice to patients, because we are robbing them of chances to develop necessary coping skills and defenses. This can be overtly damaging in certain patient populations, such as those with borderline personality disorder, who may use medication adjustments as a crutch during crises.4
Treat the patient, not yourself
We physicians mean well in prescribing evidence-based treatments; however, if the symptoms or adverse effects are not bothersome or cause functional impairment, we risk losing sight of the patient’s goals in treatment and imposing our own instead. Displacing the treatment focus can alienate the patient, harm the therapeutic alliance, and result in “pill fatigue.” For example, we may be tempted to treat antipsychotic-induced tardive dyskinesia, even if the patient is not concerned about abnormal movements. Although we see this adverse effect
Change does not happen overnight
Picking a treatment option out of a lineup of choices, à la UWorld questions, does not always translate into patients agreeing with the suggested treatment, let alone the idea of receiving treatment at all. Motivational interviewing is our chance to shine in such situations and the reason why we are physicians, rather than answer-picking bots. Patients cannot change if they are not ready. However, we should be ready to roll with resistance while looking for signs of readiness to change. We must accept that it may take a week, a month, a year, or even longer for patients to align with our plan of action. The only futile decision is deeming our efforts as futile while discounting the benefits of incremental care.
1. Hafferty FW, Gaufberg EH, O’Donnell JF. The role of the hidden curriculum in “on doctoring” courses. AMA J Ethics. 2015;17(2):130-139.
2. Horvitz-Lennon M, Mattke S, Predmore Z, et al. The role of antipsychotic plasma levels in the treatment of schizophrenia. Am J Psychiatry. 2017;174(5):421-426.
3. Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818-1831.
4. Gunderson JG. The emergence of a generalist model to meet public health needs for patients with borderline personality disorder. Am J Psychiatry. 2016;173(5):452-458.
5. Kikkert MJ, Schene AH, Koeter MW, et al. Medication adherence in schizophrenia: exploring patients’, carers’ and professionals’ views. Schizophr Bull. 2005;32(4):786-794.
As physicians, we are cognizant of the importance of patient-centered care, active listening, empathy, and patience—the so-called “hidden curriculum of medicine.”1 However, our attempts to centralize these concepts may be overshadowed by the deeply rooted drive to treat and fix. At times, we are simply treating uncertainty, whether it be diagnostic uncertainty or the uncertainty arising from clinical responses and outcomes that are far from binary. Definitive actions, such as adding medications or altering dosages, may appear to both patients and physicians to be a step closer to a “cure.” However, watchful waiting, re-evaluation, and accepting uncertainty are the true skills of effective care.
Be savvy about psychopharmacology
Psychotropics can take weeks to months to reach their full potential, and have varying responses and adverse effects. Beware of changing regimens prematurely, and keep in mind basic, yet crucial, pharmacokinetic concepts (eg, 4 to 5 half-lives to reach steady state, variations in metabolism). Receptor binding and dosing heuristics are notably common in psychiatry. Although such concepts are important to grasp, there is no one-size-fits-all rule. The brain simply does not possess the heart’s machine-like, linear functioning. Therefore, targeting individual parts (ie, receptors) will not equate to fixing the whole organ systematically or predictably.
Is the patient truly treatment-resistant?
Even the best treatment regimen has no clinical benefit if the patient cannot afford the prescription or does not take the medication. If cost is an impediment, switch from brand name drugs to generic formulations or to older medications in the same class. Before declaring the patient “treatment-resistant” and making medication changes, assess for compliance. This may require assistance from collateral informants. Ask family members to count the number of pills remaining in the bottle, and call the pharmacy to find out the last refill dates. If the patient exhibits a partial response to what should be a therapeutic dose, consider obtaining drug plasma levels to rule out rapid metabolism before deeming the medication trial a failure.2
Medications as liabilities
Overreliance on medications can result in the medications becoming liabilities. The polypharmacy problem is not unique to psychiatry.3 However, psychiatric patients may be more likely to inadvertently use medications in a maladaptive manner and disrupt the fundamental goals of long-term care. Avoid making medication adjustments in response to a patient’s life stressors and normative situational reactions. Doing so is a disservice to patients, because we are robbing them of chances to develop necessary coping skills and defenses. This can be overtly damaging in certain patient populations, such as those with borderline personality disorder, who may use medication adjustments as a crutch during crises.4
Treat the patient, not yourself
We physicians mean well in prescribing evidence-based treatments; however, if the symptoms or adverse effects are not bothersome or cause functional impairment, we risk losing sight of the patient’s goals in treatment and imposing our own instead. Displacing the treatment focus can alienate the patient, harm the therapeutic alliance, and result in “pill fatigue.” For example, we may be tempted to treat antipsychotic-induced tardive dyskinesia, even if the patient is not concerned about abnormal movements. Although we see this adverse effect
Change does not happen overnight
Picking a treatment option out of a lineup of choices, à la UWorld questions, does not always translate into patients agreeing with the suggested treatment, let alone the idea of receiving treatment at all. Motivational interviewing is our chance to shine in such situations and the reason why we are physicians, rather than answer-picking bots. Patients cannot change if they are not ready. However, we should be ready to roll with resistance while looking for signs of readiness to change. We must accept that it may take a week, a month, a year, or even longer for patients to align with our plan of action. The only futile decision is deeming our efforts as futile while discounting the benefits of incremental care.
As physicians, we are cognizant of the importance of patient-centered care, active listening, empathy, and patience—the so-called “hidden curriculum of medicine.”1 However, our attempts to centralize these concepts may be overshadowed by the deeply rooted drive to treat and fix. At times, we are simply treating uncertainty, whether it be diagnostic uncertainty or the uncertainty arising from clinical responses and outcomes that are far from binary. Definitive actions, such as adding medications or altering dosages, may appear to both patients and physicians to be a step closer to a “cure.” However, watchful waiting, re-evaluation, and accepting uncertainty are the true skills of effective care.
Be savvy about psychopharmacology
Psychotropics can take weeks to months to reach their full potential, and have varying responses and adverse effects. Beware of changing regimens prematurely, and keep in mind basic, yet crucial, pharmacokinetic concepts (eg, 4 to 5 half-lives to reach steady state, variations in metabolism). Receptor binding and dosing heuristics are notably common in psychiatry. Although such concepts are important to grasp, there is no one-size-fits-all rule. The brain simply does not possess the heart’s machine-like, linear functioning. Therefore, targeting individual parts (ie, receptors) will not equate to fixing the whole organ systematically or predictably.
Is the patient truly treatment-resistant?
Even the best treatment regimen has no clinical benefit if the patient cannot afford the prescription or does not take the medication. If cost is an impediment, switch from brand name drugs to generic formulations or to older medications in the same class. Before declaring the patient “treatment-resistant” and making medication changes, assess for compliance. This may require assistance from collateral informants. Ask family members to count the number of pills remaining in the bottle, and call the pharmacy to find out the last refill dates. If the patient exhibits a partial response to what should be a therapeutic dose, consider obtaining drug plasma levels to rule out rapid metabolism before deeming the medication trial a failure.2
Medications as liabilities
Overreliance on medications can result in the medications becoming liabilities. The polypharmacy problem is not unique to psychiatry.3 However, psychiatric patients may be more likely to inadvertently use medications in a maladaptive manner and disrupt the fundamental goals of long-term care. Avoid making medication adjustments in response to a patient’s life stressors and normative situational reactions. Doing so is a disservice to patients, because we are robbing them of chances to develop necessary coping skills and defenses. This can be overtly damaging in certain patient populations, such as those with borderline personality disorder, who may use medication adjustments as a crutch during crises.4
Treat the patient, not yourself
We physicians mean well in prescribing evidence-based treatments; however, if the symptoms or adverse effects are not bothersome or cause functional impairment, we risk losing sight of the patient’s goals in treatment and imposing our own instead. Displacing the treatment focus can alienate the patient, harm the therapeutic alliance, and result in “pill fatigue.” For example, we may be tempted to treat antipsychotic-induced tardive dyskinesia, even if the patient is not concerned about abnormal movements. Although we see this adverse effect
Change does not happen overnight
Picking a treatment option out of a lineup of choices, à la UWorld questions, does not always translate into patients agreeing with the suggested treatment, let alone the idea of receiving treatment at all. Motivational interviewing is our chance to shine in such situations and the reason why we are physicians, rather than answer-picking bots. Patients cannot change if they are not ready. However, we should be ready to roll with resistance while looking for signs of readiness to change. We must accept that it may take a week, a month, a year, or even longer for patients to align with our plan of action. The only futile decision is deeming our efforts as futile while discounting the benefits of incremental care.
1. Hafferty FW, Gaufberg EH, O’Donnell JF. The role of the hidden curriculum in “on doctoring” courses. AMA J Ethics. 2015;17(2):130-139.
2. Horvitz-Lennon M, Mattke S, Predmore Z, et al. The role of antipsychotic plasma levels in the treatment of schizophrenia. Am J Psychiatry. 2017;174(5):421-426.
3. Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818-1831.
4. Gunderson JG. The emergence of a generalist model to meet public health needs for patients with borderline personality disorder. Am J Psychiatry. 2016;173(5):452-458.
5. Kikkert MJ, Schene AH, Koeter MW, et al. Medication adherence in schizophrenia: exploring patients’, carers’ and professionals’ views. Schizophr Bull. 2005;32(4):786-794.
1. Hafferty FW, Gaufberg EH, O’Donnell JF. The role of the hidden curriculum in “on doctoring” courses. AMA J Ethics. 2015;17(2):130-139.
2. Horvitz-Lennon M, Mattke S, Predmore Z, et al. The role of antipsychotic plasma levels in the treatment of schizophrenia. Am J Psychiatry. 2017;174(5):421-426.
3. Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818-1831.
4. Gunderson JG. The emergence of a generalist model to meet public health needs for patients with borderline personality disorder. Am J Psychiatry. 2016;173(5):452-458.
5. Kikkert MJ, Schene AH, Koeter MW, et al. Medication adherence in schizophrenia: exploring patients’, carers’ and professionals’ views. Schizophr Bull. 2005;32(4):786-794.
Personal models of illness
Cognitive reappraisal is a top-down emotional regulation skill associated with resilience – the capacity to adaptively overcome adversity.
A person with this ability, also known as cognitive flexibility or reframing, monitors negative thoughts or situations and intentionally changes the way he or she views them. This reframing can involve retaining a positive outlook, trying to create meaning from a difficult situation, or finding ways to exert control over specific circumstances (Front Behav Neurosci. 2013 Feb 15;7:10). Some individuals cope with their mental illness by creating their own models of their illness (Achieving Cultural Competency: A Case-Based Approach to Training Health Professionals, Hoboken, N.J.: Wiley-Blackwell Publishing, 2009).
Creating a model of illness is a type of reframing to help explain what’s happening to an individual by placing the locus of control either inside our ourselves, adjacent, or far away and uncontrollable. Depending on the model, there might be choice that results in action taken to face the mental illness. Sometimes, there is surrender, either to the illness or the treatment.
In one of my weekly phone conversations with my mother in Texas, she told me that Ricardo, the husband of close family friend, had sunk into a deep depression to the point where he could no longer leave the house for work. Ricardo is an unauthorized immigrant, having crossed the border from Mexico into Texas 17 years ago with his wife and 2-year-old son. He lives a story common to many families in Texas: two undocumented parents working in local businesses, one child with a DACA (Deferred Action for Childhood Arrivals) permit and their second child born in the United States, all assimilated into American culture. With Ricardo’s descent into personal darkness, their American dream was fraying. Family and neighbors were gossiping about what could have happened – had Ricardo gotten into trouble with drugs and alcohol? Perhaps his wife had bewitched him; perhaps this was a godly test that only prayer could overcome.
I called his wife to see if I could offer her help navigating the local mental health system. She recounted a story of severe depression, and, most worryingly, a recent self-aborted hanging. Because of cultural beliefs, stigma of mental illness, and his immigration status, Ricardo would not call the local mental health authority for assessment and treatment.
So I made a trip to Texas to see Ricardo as a friend and psychiatrist, despite not quite knowing how to navigate the moral and legal ambiguity of this situation. I could at least offer a comprehensive psychiatric assessment and provide him with some understanding of his illness to help guide his decisions. My conversation with Ricardo found a man helpless and confused as to how and why he lost all drive, energy, and desire to live. We spoke about his and my understanding of depression. I tried to help Ricardo by shifting his perception of his illness from fear of an unknown specter to the idea that his current state of mind could be attributed to a treatable brain disease.
The trip to Texas was also an opportunity to see my older brother’s newly purchased home. This was a serious achievement, following 2 years where he had lived with our parents to save money for a down payment. He had initially been forced to live at home because of legal consequences related to his struggles with addiction and depression, both backdrops to his life as a devoted math teacher. In the car ride to his new house, he told me about his twice weekly, state-mandated addiction counseling group sessions. He has benefited from the instruction to fill his sober time with positive forces, telling me that he could not have bought his house and started working a second, part-time job without his sobriety.
Yet, he disagrees when the counselor tells his class that addiction is a disease that compromises his free will, and compared to his peers, he has less control over his mind when exposed to alcohol. He says it’s a mixed message – be proactive and take control over a new sober life, but be careful, your brain is too weak and diseased to ever have a healthy relationship with alcohol.
I was affected when he told me that he was afraid to ever drink again; that he cannot trust himself. He is afraid to fail and lose the life he is building for himself. Now he lives in conflict between two models of his illness: the determinism of addiction versus free will to overcome his abusive relationship with alcohol. To overcome this conflict, he has surrendered himself to a self-designed treatment program, working two jobs to fill his days and nights, and guarantee fatigue and sleep by the end of the day. No time to think or drink; just time to work and sleep.
The night before I flew to Texas, I had an overnight call in the emergency department. I encountered a young woman whom I’ll call Laura. She was in her mid 30s with HIV/AIDS with a CD4 count of less than 30, and had not taken medication for her HIV in years. Mostly, she lived in and out of hospitals, both psychiatric and medical wards. I was called to assess her suicidal ideation with a stated plan to slip and fall in her shower in order to hit her head and die. She was cachectic, tired, withdrawn, disheveled, buried under a heap of blankets.
Our interview was an awkward dance around why she could not and would not take medications for either her HIV/AIDS or posttraumatic stress disorder and depression. No money, no transport, intermittently homeless, no desire to live nor a future to live for.
In our conversation, I searched for reasons for Laura to live, and she countered with reasons why it was easier to die. It was a level of apathy I have encountered with other severely ill AIDS patients – the brain is so immunocompromised and muddled, the body so tired, the spirit so damaged. Her three children living with a sister had lost their potency as motivation to desire recovery of her physical and mental health. I doubted the active nature of her suicidality, and her apathy and physical deterioration made me question her ability to act on a plan. Nonetheless, I admitted Laura to the psychiatric unit for safety. Two weeks later, I learned she had died in hospital of AIDS-related sepsis. She had 10 days of treatment on the psychiatric unit with no movement in her depressive symptoms and apathy. Eventually, she physically crashed and was sent to the ICU, where she died.
As psychiatrists, we create our own models of what mental illness and treatments are, and we apply some version of the model to each patient. With the concepts of cultural psychiatry and therapeutic alliance, we learn to work within our patients’ models of disease to enhance their response to treatment. My initial reaction to Laura’s death was surprise, fear, and guilt that maybe I had missed a pressing medical issue that contributed to her death. Then I just felt resigned to her death, probably as she did. She told me in the emergency department she was set on dying, and her actions, well before this last admission, had indirectly ensured an early death. We psychiatrists feel failure when we are unable to prevent a suicide. What was Laura’s death: Was it a suicide by apathy that a psychiatrist could have prevented? Or just an expected complication of an untreated chronic illness? Many residents had done their job by admitting her again and again for either psychiatric or medical illness. Yet none of us could understand why she refused to treat her HIV/AIDS, and none of us was able to address the model she had created of her illness. Her model, that her HIV was a death sentence, was anathema to our training.
Because of that dissonance, it was difficult to understand her narrative, let alone find a way to help her reframe it. Her model of illness was misunderstood by a wide swathe of medical professionals, and together we were unable to tailor a treatment to her needs. Since, I’ve worked to reframe her death in my own mind as a way to better understand models of illness, learning from her as well as from my brother and my friend Ricardo. Both the patient’s and physician’s conceptualization of illness affects prognosis of whether to surrender to a treatment or the illness. As psychiatrists, we must strive to understand all models of illness, so we can plan and implement our treatment intervention accordingly.
I asked my friend from home and my brother for their permission and sent them this piece to make sure they approved. I changed certain details about Ricardo’s story to protect his identity. With my brother, there was no way to change his identity, but he was touched and happy to be included. I also changed key facts about the patient I called Laura.
Dr. Posada is a third-year resident in the psychiatry and behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, and health disparities, and she plans to pursue a fellowship in consult liaison psychiatry.
Cognitive reappraisal is a top-down emotional regulation skill associated with resilience – the capacity to adaptively overcome adversity.
A person with this ability, also known as cognitive flexibility or reframing, monitors negative thoughts or situations and intentionally changes the way he or she views them. This reframing can involve retaining a positive outlook, trying to create meaning from a difficult situation, or finding ways to exert control over specific circumstances (Front Behav Neurosci. 2013 Feb 15;7:10). Some individuals cope with their mental illness by creating their own models of their illness (Achieving Cultural Competency: A Case-Based Approach to Training Health Professionals, Hoboken, N.J.: Wiley-Blackwell Publishing, 2009).
Creating a model of illness is a type of reframing to help explain what’s happening to an individual by placing the locus of control either inside our ourselves, adjacent, or far away and uncontrollable. Depending on the model, there might be choice that results in action taken to face the mental illness. Sometimes, there is surrender, either to the illness or the treatment.
In one of my weekly phone conversations with my mother in Texas, she told me that Ricardo, the husband of close family friend, had sunk into a deep depression to the point where he could no longer leave the house for work. Ricardo is an unauthorized immigrant, having crossed the border from Mexico into Texas 17 years ago with his wife and 2-year-old son. He lives a story common to many families in Texas: two undocumented parents working in local businesses, one child with a DACA (Deferred Action for Childhood Arrivals) permit and their second child born in the United States, all assimilated into American culture. With Ricardo’s descent into personal darkness, their American dream was fraying. Family and neighbors were gossiping about what could have happened – had Ricardo gotten into trouble with drugs and alcohol? Perhaps his wife had bewitched him; perhaps this was a godly test that only prayer could overcome.
I called his wife to see if I could offer her help navigating the local mental health system. She recounted a story of severe depression, and, most worryingly, a recent self-aborted hanging. Because of cultural beliefs, stigma of mental illness, and his immigration status, Ricardo would not call the local mental health authority for assessment and treatment.
So I made a trip to Texas to see Ricardo as a friend and psychiatrist, despite not quite knowing how to navigate the moral and legal ambiguity of this situation. I could at least offer a comprehensive psychiatric assessment and provide him with some understanding of his illness to help guide his decisions. My conversation with Ricardo found a man helpless and confused as to how and why he lost all drive, energy, and desire to live. We spoke about his and my understanding of depression. I tried to help Ricardo by shifting his perception of his illness from fear of an unknown specter to the idea that his current state of mind could be attributed to a treatable brain disease.
The trip to Texas was also an opportunity to see my older brother’s newly purchased home. This was a serious achievement, following 2 years where he had lived with our parents to save money for a down payment. He had initially been forced to live at home because of legal consequences related to his struggles with addiction and depression, both backdrops to his life as a devoted math teacher. In the car ride to his new house, he told me about his twice weekly, state-mandated addiction counseling group sessions. He has benefited from the instruction to fill his sober time with positive forces, telling me that he could not have bought his house and started working a second, part-time job without his sobriety.
Yet, he disagrees when the counselor tells his class that addiction is a disease that compromises his free will, and compared to his peers, he has less control over his mind when exposed to alcohol. He says it’s a mixed message – be proactive and take control over a new sober life, but be careful, your brain is too weak and diseased to ever have a healthy relationship with alcohol.
I was affected when he told me that he was afraid to ever drink again; that he cannot trust himself. He is afraid to fail and lose the life he is building for himself. Now he lives in conflict between two models of his illness: the determinism of addiction versus free will to overcome his abusive relationship with alcohol. To overcome this conflict, he has surrendered himself to a self-designed treatment program, working two jobs to fill his days and nights, and guarantee fatigue and sleep by the end of the day. No time to think or drink; just time to work and sleep.
The night before I flew to Texas, I had an overnight call in the emergency department. I encountered a young woman whom I’ll call Laura. She was in her mid 30s with HIV/AIDS with a CD4 count of less than 30, and had not taken medication for her HIV in years. Mostly, she lived in and out of hospitals, both psychiatric and medical wards. I was called to assess her suicidal ideation with a stated plan to slip and fall in her shower in order to hit her head and die. She was cachectic, tired, withdrawn, disheveled, buried under a heap of blankets.
Our interview was an awkward dance around why she could not and would not take medications for either her HIV/AIDS or posttraumatic stress disorder and depression. No money, no transport, intermittently homeless, no desire to live nor a future to live for.
In our conversation, I searched for reasons for Laura to live, and she countered with reasons why it was easier to die. It was a level of apathy I have encountered with other severely ill AIDS patients – the brain is so immunocompromised and muddled, the body so tired, the spirit so damaged. Her three children living with a sister had lost their potency as motivation to desire recovery of her physical and mental health. I doubted the active nature of her suicidality, and her apathy and physical deterioration made me question her ability to act on a plan. Nonetheless, I admitted Laura to the psychiatric unit for safety. Two weeks later, I learned she had died in hospital of AIDS-related sepsis. She had 10 days of treatment on the psychiatric unit with no movement in her depressive symptoms and apathy. Eventually, she physically crashed and was sent to the ICU, where she died.
As psychiatrists, we create our own models of what mental illness and treatments are, and we apply some version of the model to each patient. With the concepts of cultural psychiatry and therapeutic alliance, we learn to work within our patients’ models of disease to enhance their response to treatment. My initial reaction to Laura’s death was surprise, fear, and guilt that maybe I had missed a pressing medical issue that contributed to her death. Then I just felt resigned to her death, probably as she did. She told me in the emergency department she was set on dying, and her actions, well before this last admission, had indirectly ensured an early death. We psychiatrists feel failure when we are unable to prevent a suicide. What was Laura’s death: Was it a suicide by apathy that a psychiatrist could have prevented? Or just an expected complication of an untreated chronic illness? Many residents had done their job by admitting her again and again for either psychiatric or medical illness. Yet none of us could understand why she refused to treat her HIV/AIDS, and none of us was able to address the model she had created of her illness. Her model, that her HIV was a death sentence, was anathema to our training.
Because of that dissonance, it was difficult to understand her narrative, let alone find a way to help her reframe it. Her model of illness was misunderstood by a wide swathe of medical professionals, and together we were unable to tailor a treatment to her needs. Since, I’ve worked to reframe her death in my own mind as a way to better understand models of illness, learning from her as well as from my brother and my friend Ricardo. Both the patient’s and physician’s conceptualization of illness affects prognosis of whether to surrender to a treatment or the illness. As psychiatrists, we must strive to understand all models of illness, so we can plan and implement our treatment intervention accordingly.
I asked my friend from home and my brother for their permission and sent them this piece to make sure they approved. I changed certain details about Ricardo’s story to protect his identity. With my brother, there was no way to change his identity, but he was touched and happy to be included. I also changed key facts about the patient I called Laura.
Dr. Posada is a third-year resident in the psychiatry and behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, and health disparities, and she plans to pursue a fellowship in consult liaison psychiatry.
Cognitive reappraisal is a top-down emotional regulation skill associated with resilience – the capacity to adaptively overcome adversity.
A person with this ability, also known as cognitive flexibility or reframing, monitors negative thoughts or situations and intentionally changes the way he or she views them. This reframing can involve retaining a positive outlook, trying to create meaning from a difficult situation, or finding ways to exert control over specific circumstances (Front Behav Neurosci. 2013 Feb 15;7:10). Some individuals cope with their mental illness by creating their own models of their illness (Achieving Cultural Competency: A Case-Based Approach to Training Health Professionals, Hoboken, N.J.: Wiley-Blackwell Publishing, 2009).
Creating a model of illness is a type of reframing to help explain what’s happening to an individual by placing the locus of control either inside our ourselves, adjacent, or far away and uncontrollable. Depending on the model, there might be choice that results in action taken to face the mental illness. Sometimes, there is surrender, either to the illness or the treatment.
In one of my weekly phone conversations with my mother in Texas, she told me that Ricardo, the husband of close family friend, had sunk into a deep depression to the point where he could no longer leave the house for work. Ricardo is an unauthorized immigrant, having crossed the border from Mexico into Texas 17 years ago with his wife and 2-year-old son. He lives a story common to many families in Texas: two undocumented parents working in local businesses, one child with a DACA (Deferred Action for Childhood Arrivals) permit and their second child born in the United States, all assimilated into American culture. With Ricardo’s descent into personal darkness, their American dream was fraying. Family and neighbors were gossiping about what could have happened – had Ricardo gotten into trouble with drugs and alcohol? Perhaps his wife had bewitched him; perhaps this was a godly test that only prayer could overcome.
I called his wife to see if I could offer her help navigating the local mental health system. She recounted a story of severe depression, and, most worryingly, a recent self-aborted hanging. Because of cultural beliefs, stigma of mental illness, and his immigration status, Ricardo would not call the local mental health authority for assessment and treatment.
So I made a trip to Texas to see Ricardo as a friend and psychiatrist, despite not quite knowing how to navigate the moral and legal ambiguity of this situation. I could at least offer a comprehensive psychiatric assessment and provide him with some understanding of his illness to help guide his decisions. My conversation with Ricardo found a man helpless and confused as to how and why he lost all drive, energy, and desire to live. We spoke about his and my understanding of depression. I tried to help Ricardo by shifting his perception of his illness from fear of an unknown specter to the idea that his current state of mind could be attributed to a treatable brain disease.
The trip to Texas was also an opportunity to see my older brother’s newly purchased home. This was a serious achievement, following 2 years where he had lived with our parents to save money for a down payment. He had initially been forced to live at home because of legal consequences related to his struggles with addiction and depression, both backdrops to his life as a devoted math teacher. In the car ride to his new house, he told me about his twice weekly, state-mandated addiction counseling group sessions. He has benefited from the instruction to fill his sober time with positive forces, telling me that he could not have bought his house and started working a second, part-time job without his sobriety.
Yet, he disagrees when the counselor tells his class that addiction is a disease that compromises his free will, and compared to his peers, he has less control over his mind when exposed to alcohol. He says it’s a mixed message – be proactive and take control over a new sober life, but be careful, your brain is too weak and diseased to ever have a healthy relationship with alcohol.
I was affected when he told me that he was afraid to ever drink again; that he cannot trust himself. He is afraid to fail and lose the life he is building for himself. Now he lives in conflict between two models of his illness: the determinism of addiction versus free will to overcome his abusive relationship with alcohol. To overcome this conflict, he has surrendered himself to a self-designed treatment program, working two jobs to fill his days and nights, and guarantee fatigue and sleep by the end of the day. No time to think or drink; just time to work and sleep.
The night before I flew to Texas, I had an overnight call in the emergency department. I encountered a young woman whom I’ll call Laura. She was in her mid 30s with HIV/AIDS with a CD4 count of less than 30, and had not taken medication for her HIV in years. Mostly, she lived in and out of hospitals, both psychiatric and medical wards. I was called to assess her suicidal ideation with a stated plan to slip and fall in her shower in order to hit her head and die. She was cachectic, tired, withdrawn, disheveled, buried under a heap of blankets.
Our interview was an awkward dance around why she could not and would not take medications for either her HIV/AIDS or posttraumatic stress disorder and depression. No money, no transport, intermittently homeless, no desire to live nor a future to live for.
In our conversation, I searched for reasons for Laura to live, and she countered with reasons why it was easier to die. It was a level of apathy I have encountered with other severely ill AIDS patients – the brain is so immunocompromised and muddled, the body so tired, the spirit so damaged. Her three children living with a sister had lost their potency as motivation to desire recovery of her physical and mental health. I doubted the active nature of her suicidality, and her apathy and physical deterioration made me question her ability to act on a plan. Nonetheless, I admitted Laura to the psychiatric unit for safety. Two weeks later, I learned she had died in hospital of AIDS-related sepsis. She had 10 days of treatment on the psychiatric unit with no movement in her depressive symptoms and apathy. Eventually, she physically crashed and was sent to the ICU, where she died.
As psychiatrists, we create our own models of what mental illness and treatments are, and we apply some version of the model to each patient. With the concepts of cultural psychiatry and therapeutic alliance, we learn to work within our patients’ models of disease to enhance their response to treatment. My initial reaction to Laura’s death was surprise, fear, and guilt that maybe I had missed a pressing medical issue that contributed to her death. Then I just felt resigned to her death, probably as she did. She told me in the emergency department she was set on dying, and her actions, well before this last admission, had indirectly ensured an early death. We psychiatrists feel failure when we are unable to prevent a suicide. What was Laura’s death: Was it a suicide by apathy that a psychiatrist could have prevented? Or just an expected complication of an untreated chronic illness? Many residents had done their job by admitting her again and again for either psychiatric or medical illness. Yet none of us could understand why she refused to treat her HIV/AIDS, and none of us was able to address the model she had created of her illness. Her model, that her HIV was a death sentence, was anathema to our training.
Because of that dissonance, it was difficult to understand her narrative, let alone find a way to help her reframe it. Her model of illness was misunderstood by a wide swathe of medical professionals, and together we were unable to tailor a treatment to her needs. Since, I’ve worked to reframe her death in my own mind as a way to better understand models of illness, learning from her as well as from my brother and my friend Ricardo. Both the patient’s and physician’s conceptualization of illness affects prognosis of whether to surrender to a treatment or the illness. As psychiatrists, we must strive to understand all models of illness, so we can plan and implement our treatment intervention accordingly.
I asked my friend from home and my brother for their permission and sent them this piece to make sure they approved. I changed certain details about Ricardo’s story to protect his identity. With my brother, there was no way to change his identity, but he was touched and happy to be included. I also changed key facts about the patient I called Laura.
Dr. Posada is a third-year resident in the psychiatry and behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, and health disparities, and she plans to pursue a fellowship in consult liaison psychiatry.
Breaking bad news
As psychiatrists, we do not often encounter situations in which we need to inform patients and their families that they have a life-threatening diagnosis. Nonetheless, on the rare occasions when we work with such patients, new psychiatrists may find their clinical skills challenged. Breaking bad news remains an aspect of clinical training that is often overlooked by medical schools.
Here I present a case that illustrates the challenges residents and medical students face when they need to deliver bad news and review the current literature on how to present patients with this type of information.
Case
Bizarre behavior, difficult diagnosis
Mr. C, age 59, with a 1-year history of major depressive disorder, was brought to the emergency department by his wife for worsening depression and disorganized behavior over the course of 3 weeks. Mr. C had obsessive thoughts about arranging things in symmetrical patterns, difficulty sleeping, loss of appetite, and anhedonia. His wife reported that his bizarre, disorganized behavior further intensified in the previous week; he was urinating on the rug, rubbing his genitals against the bathroom counter, staring into space without moving for prolonged periods of time, and arranging his food in symmetrical patterns. Mr. C has no reported substance use or suicidal or homicidal ideation.
Strategies for delivering bad news
Initially, I struggled when I realized I would have to deliver the news of this potentially life-threatening diagnosis to the patient and his wife because I had not received any training on how to do so. However, I took time to look into the literature and used the skills that we as psychiatrists have, including empathy, listening, and validation. My experience with Mr. C and his family made me realize that delivering bad news with empathy and being involved in the struggle that follows can make a significant difference to their suffering.
There are various models and techniques for breaking bad news to patients. Two of the most commonly used models in the oncology setting are the SPIKES (Set up, Perception, Interview, Knowledge, Emotions, Strategize and Summarize) model (Table 12) and Kaye’s model (Table 23).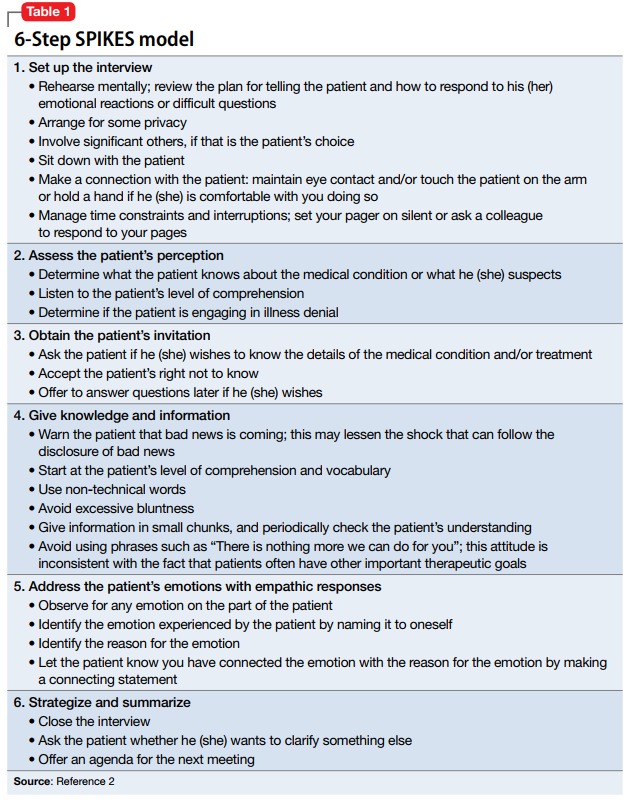
A clinician’s attitude and communication skills play a crucial role in how well patients and family members cope when they receive bad news. When delivering bad news:
- Choose a setting with adequate privacy, use simple language that distills medical facts into appreciable pieces of information, and give the recipients ample space and time to process the implications. Doing so will foster better understanding and facilitate their acceptance of the bad news.
- Although physicians can rarely appreciate the patient’s feelings at a personal level, make every effort to validate their thoughts and offer emotional support. In such situations, it is often appropriate to move closer to the recipient and make brief physical gestures, such as laying a hand on the shoulder, which might comfort them.
- In the aftermath of such encounters, it is important to remain active in the patient’s emotional journey and available for further clarification, which can mitigate uncertainties and facilitate the difficult process of coming to terms with new realities.4,5
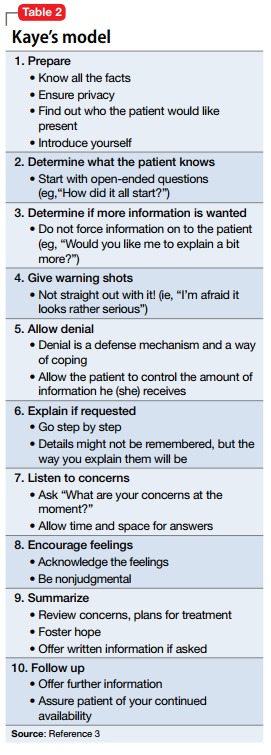
1. Munjal S, Pahlajani S, Baxi A, et al. Delayed diagnosis of glioblastoma multiforme presenting with atypical psychiatric symptoms. Prim Care Companion CNS Disord. 2016;18(6). doi: 10.4088/PCC.16l01972.
2. Baile WF, Buckman R, Lenzi R, et al. SPIKES-a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302-311.
3. Kaye P. Breaking bad news: a 10 step approach. Northampton, MA: EPL Publications; 1995.
4. Chaturvedi SK, Chandra PS. Breaking bad news-issues important for psychiatrists. Asian J Psychiatr. 2010;3(2):87-89.
5. VandeKieft GK. Breaking bad news. Am Fam Physician. 2001;64(12):1975-1978.
As psychiatrists, we do not often encounter situations in which we need to inform patients and their families that they have a life-threatening diagnosis. Nonetheless, on the rare occasions when we work with such patients, new psychiatrists may find their clinical skills challenged. Breaking bad news remains an aspect of clinical training that is often overlooked by medical schools.
Here I present a case that illustrates the challenges residents and medical students face when they need to deliver bad news and review the current literature on how to present patients with this type of information.
Case
Bizarre behavior, difficult diagnosis
Mr. C, age 59, with a 1-year history of major depressive disorder, was brought to the emergency department by his wife for worsening depression and disorganized behavior over the course of 3 weeks. Mr. C had obsessive thoughts about arranging things in symmetrical patterns, difficulty sleeping, loss of appetite, and anhedonia. His wife reported that his bizarre, disorganized behavior further intensified in the previous week; he was urinating on the rug, rubbing his genitals against the bathroom counter, staring into space without moving for prolonged periods of time, and arranging his food in symmetrical patterns. Mr. C has no reported substance use or suicidal or homicidal ideation.
Strategies for delivering bad news
Initially, I struggled when I realized I would have to deliver the news of this potentially life-threatening diagnosis to the patient and his wife because I had not received any training on how to do so. However, I took time to look into the literature and used the skills that we as psychiatrists have, including empathy, listening, and validation. My experience with Mr. C and his family made me realize that delivering bad news with empathy and being involved in the struggle that follows can make a significant difference to their suffering.
There are various models and techniques for breaking bad news to patients. Two of the most commonly used models in the oncology setting are the SPIKES (Set up, Perception, Interview, Knowledge, Emotions, Strategize and Summarize) model (Table 12) and Kaye’s model (Table 23).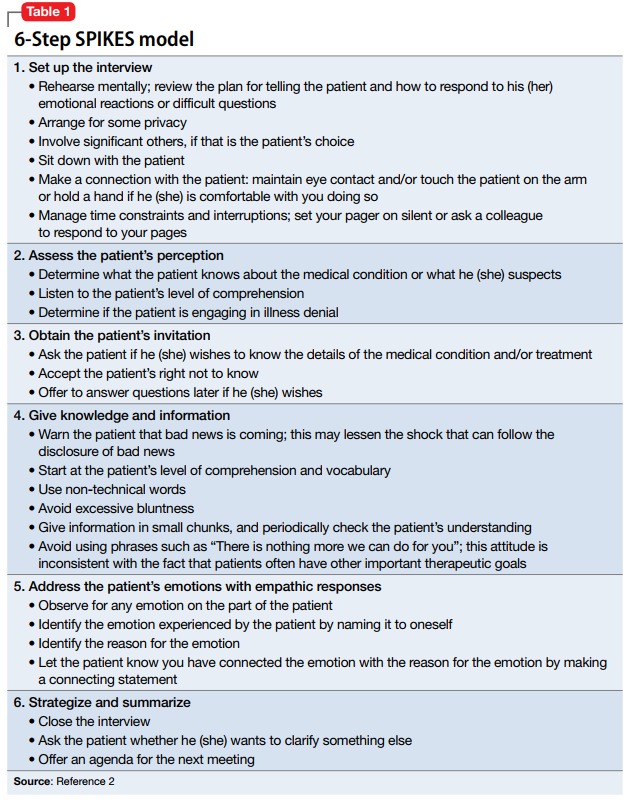
A clinician’s attitude and communication skills play a crucial role in how well patients and family members cope when they receive bad news. When delivering bad news:
- Choose a setting with adequate privacy, use simple language that distills medical facts into appreciable pieces of information, and give the recipients ample space and time to process the implications. Doing so will foster better understanding and facilitate their acceptance of the bad news.
- Although physicians can rarely appreciate the patient’s feelings at a personal level, make every effort to validate their thoughts and offer emotional support. In such situations, it is often appropriate to move closer to the recipient and make brief physical gestures, such as laying a hand on the shoulder, which might comfort them.
- In the aftermath of such encounters, it is important to remain active in the patient’s emotional journey and available for further clarification, which can mitigate uncertainties and facilitate the difficult process of coming to terms with new realities.4,5
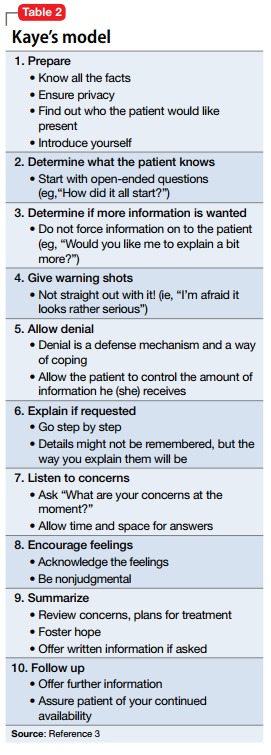
As psychiatrists, we do not often encounter situations in which we need to inform patients and their families that they have a life-threatening diagnosis. Nonetheless, on the rare occasions when we work with such patients, new psychiatrists may find their clinical skills challenged. Breaking bad news remains an aspect of clinical training that is often overlooked by medical schools.
Here I present a case that illustrates the challenges residents and medical students face when they need to deliver bad news and review the current literature on how to present patients with this type of information.
Case
Bizarre behavior, difficult diagnosis
Mr. C, age 59, with a 1-year history of major depressive disorder, was brought to the emergency department by his wife for worsening depression and disorganized behavior over the course of 3 weeks. Mr. C had obsessive thoughts about arranging things in symmetrical patterns, difficulty sleeping, loss of appetite, and anhedonia. His wife reported that his bizarre, disorganized behavior further intensified in the previous week; he was urinating on the rug, rubbing his genitals against the bathroom counter, staring into space without moving for prolonged periods of time, and arranging his food in symmetrical patterns. Mr. C has no reported substance use or suicidal or homicidal ideation.
Strategies for delivering bad news
Initially, I struggled when I realized I would have to deliver the news of this potentially life-threatening diagnosis to the patient and his wife because I had not received any training on how to do so. However, I took time to look into the literature and used the skills that we as psychiatrists have, including empathy, listening, and validation. My experience with Mr. C and his family made me realize that delivering bad news with empathy and being involved in the struggle that follows can make a significant difference to their suffering.
There are various models and techniques for breaking bad news to patients. Two of the most commonly used models in the oncology setting are the SPIKES (Set up, Perception, Interview, Knowledge, Emotions, Strategize and Summarize) model (Table 12) and Kaye’s model (Table 23).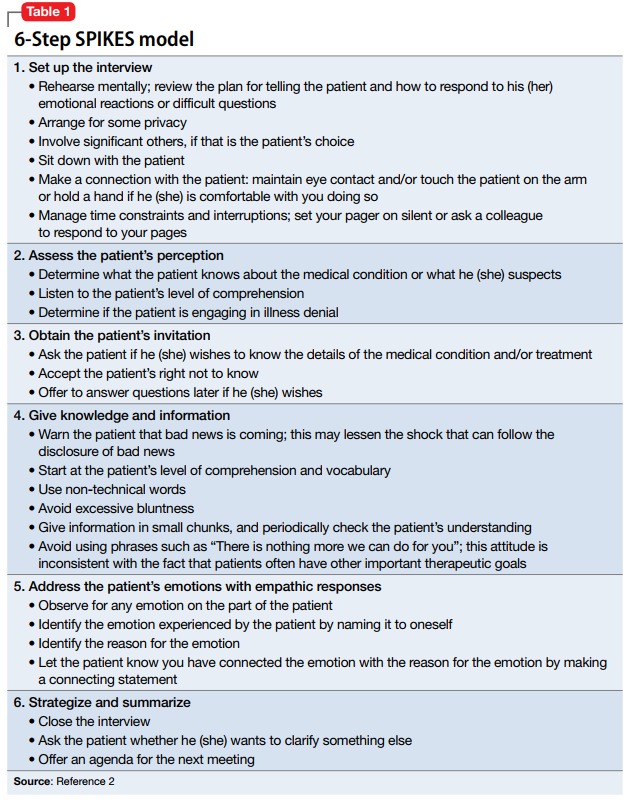
A clinician’s attitude and communication skills play a crucial role in how well patients and family members cope when they receive bad news. When delivering bad news:
- Choose a setting with adequate privacy, use simple language that distills medical facts into appreciable pieces of information, and give the recipients ample space and time to process the implications. Doing so will foster better understanding and facilitate their acceptance of the bad news.
- Although physicians can rarely appreciate the patient’s feelings at a personal level, make every effort to validate their thoughts and offer emotional support. In such situations, it is often appropriate to move closer to the recipient and make brief physical gestures, such as laying a hand on the shoulder, which might comfort them.
- In the aftermath of such encounters, it is important to remain active in the patient’s emotional journey and available for further clarification, which can mitigate uncertainties and facilitate the difficult process of coming to terms with new realities.4,5
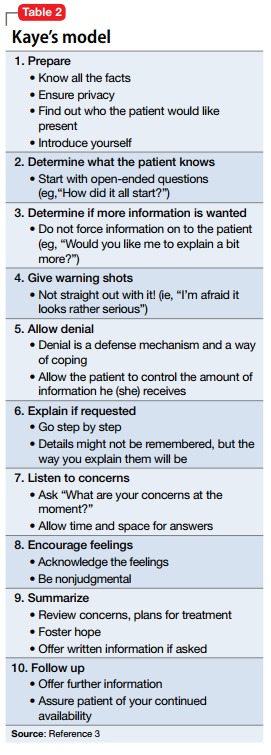
1. Munjal S, Pahlajani S, Baxi A, et al. Delayed diagnosis of glioblastoma multiforme presenting with atypical psychiatric symptoms. Prim Care Companion CNS Disord. 2016;18(6). doi: 10.4088/PCC.16l01972.
2. Baile WF, Buckman R, Lenzi R, et al. SPIKES-a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302-311.
3. Kaye P. Breaking bad news: a 10 step approach. Northampton, MA: EPL Publications; 1995.
4. Chaturvedi SK, Chandra PS. Breaking bad news-issues important for psychiatrists. Asian J Psychiatr. 2010;3(2):87-89.
5. VandeKieft GK. Breaking bad news. Am Fam Physician. 2001;64(12):1975-1978.
1. Munjal S, Pahlajani S, Baxi A, et al. Delayed diagnosis of glioblastoma multiforme presenting with atypical psychiatric symptoms. Prim Care Companion CNS Disord. 2016;18(6). doi: 10.4088/PCC.16l01972.
2. Baile WF, Buckman R, Lenzi R, et al. SPIKES-a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302-311.
3. Kaye P. Breaking bad news: a 10 step approach. Northampton, MA: EPL Publications; 1995.
4. Chaturvedi SK, Chandra PS. Breaking bad news-issues important for psychiatrists. Asian J Psychiatr. 2010;3(2):87-89.
5. VandeKieft GK. Breaking bad news. Am Fam Physician. 2001;64(12):1975-1978.
Do you talk about marijuana with your patients?
Do you talk about marijuana with your patients?
In medical school, I had a roommate. He was a smart law school graduate, good looking, outgoing, had lots of friends, was funny, and he was a great cook.
I should tell you another thing about my friend: He was a heavy, daily user of marijuana.
I believe that most of us, at a certain point of our lives, have met someone like my friend. The combination of a high-stress lifestyle, high self-expectations, and lack of appropriate skills to tackle life’s obstacles when encountered with failure frequently leads to addiction or a behavioral problem. In most cases, that will cause a pathological relationship with an outside substance or stimuli (Internet overuse/shopping too much/overeating or drinking, and so on).
Living a life filled with severe trauma and pain, especially at a developmental stage, often leads to an addiction. We frequently see people escape to the sweet narcotic-induced sleep via opioid abuse. On the other hand, for people who did not suffer trauma and are highly functional, marijuana offers a means of emotional detachment from pain, in its different form, and existential depression. That is the main benefit my patients who live with marijuana addiction get.
My friend serves as a rather stereotypical – and some may say – subjective, simplistic example of what is becoming more and more common in our society. I’m willing to bet that a good number of clinicians who read this have a similar example in mind.
With its intoxication state perceived as benign and the limited medicinal advantages, marijuana rapidly is gaining more and more legitimacy in the eyes of the general public (Addict Behav. 2008 Mar;33:397-411), (Monitoring the Future: National Results on Drug Use: 1975-2016). The risk of addiction is perceived as negligible and often nonexistent.
Almost no one knows about the potential risk of addiction (around 9%) (Drug Alcohol Depend. 2011;115:120-30). No one knows about about tolerance and withdrawal states – or about the real risk of psychosis (N Engl J Med. 2014 Jun 5;370:2219-27) or about the possible risk of schizophrenia in vulnerable populations (Schizophr Res. 2016 Mar;171:[1-3]:62-7). No one talks about the fact that it’s often used with tobacco. (How many times have you been told during history taking that a patient doesn’t smoke tobacco, only to find that in drug history he smokes 3-5 joints with tobacco daily?)
[polldaddy:9796432]
Throughout my journey in the psychiatric world (studying and working on three different continents) another typical marijuana user is the patient living with chronic mental illness. My Israeli mentor often complained about not having a single “clean” patient with schizophrenia anymore. I now see the same phenomena in Philadelphia and was also exposed to the same reality in Europe during medical school.
As physicians, and especially as psychiatrists, I believe we are obligated to educate our patients by telling them about the risks in their behaviors. Educating patients about marijuana in today’s atmosphere can be a very important preventive measure, and awareness is an important step toward change.
The current generation of psychiatrists is dealing with an opioid epidemic. Let’s educate ourselves and our patients so this current epidemic won’t be followed by another, severe cannabis epidemic.
Dr. Shilo is a second-year PGY in the department of psychiatry at Einstein Medical Center, Philadelphia.
Do you talk about marijuana with your patients?
In medical school, I had a roommate. He was a smart law school graduate, good looking, outgoing, had lots of friends, was funny, and he was a great cook.
I should tell you another thing about my friend: He was a heavy, daily user of marijuana.
I believe that most of us, at a certain point of our lives, have met someone like my friend. The combination of a high-stress lifestyle, high self-expectations, and lack of appropriate skills to tackle life’s obstacles when encountered with failure frequently leads to addiction or a behavioral problem. In most cases, that will cause a pathological relationship with an outside substance or stimuli (Internet overuse/shopping too much/overeating or drinking, and so on).
Living a life filled with severe trauma and pain, especially at a developmental stage, often leads to an addiction. We frequently see people escape to the sweet narcotic-induced sleep via opioid abuse. On the other hand, for people who did not suffer trauma and are highly functional, marijuana offers a means of emotional detachment from pain, in its different form, and existential depression. That is the main benefit my patients who live with marijuana addiction get.
My friend serves as a rather stereotypical – and some may say – subjective, simplistic example of what is becoming more and more common in our society. I’m willing to bet that a good number of clinicians who read this have a similar example in mind.
With its intoxication state perceived as benign and the limited medicinal advantages, marijuana rapidly is gaining more and more legitimacy in the eyes of the general public (Addict Behav. 2008 Mar;33:397-411), (Monitoring the Future: National Results on Drug Use: 1975-2016). The risk of addiction is perceived as negligible and often nonexistent.
Almost no one knows about the potential risk of addiction (around 9%) (Drug Alcohol Depend. 2011;115:120-30). No one knows about about tolerance and withdrawal states – or about the real risk of psychosis (N Engl J Med. 2014 Jun 5;370:2219-27) or about the possible risk of schizophrenia in vulnerable populations (Schizophr Res. 2016 Mar;171:[1-3]:62-7). No one talks about the fact that it’s often used with tobacco. (How many times have you been told during history taking that a patient doesn’t smoke tobacco, only to find that in drug history he smokes 3-5 joints with tobacco daily?)
[polldaddy:9796432]
Throughout my journey in the psychiatric world (studying and working on three different continents) another typical marijuana user is the patient living with chronic mental illness. My Israeli mentor often complained about not having a single “clean” patient with schizophrenia anymore. I now see the same phenomena in Philadelphia and was also exposed to the same reality in Europe during medical school.
As physicians, and especially as psychiatrists, I believe we are obligated to educate our patients by telling them about the risks in their behaviors. Educating patients about marijuana in today’s atmosphere can be a very important preventive measure, and awareness is an important step toward change.
The current generation of psychiatrists is dealing with an opioid epidemic. Let’s educate ourselves and our patients so this current epidemic won’t be followed by another, severe cannabis epidemic.
Dr. Shilo is a second-year PGY in the department of psychiatry at Einstein Medical Center, Philadelphia.
Do you talk about marijuana with your patients?
In medical school, I had a roommate. He was a smart law school graduate, good looking, outgoing, had lots of friends, was funny, and he was a great cook.
I should tell you another thing about my friend: He was a heavy, daily user of marijuana.
I believe that most of us, at a certain point of our lives, have met someone like my friend. The combination of a high-stress lifestyle, high self-expectations, and lack of appropriate skills to tackle life’s obstacles when encountered with failure frequently leads to addiction or a behavioral problem. In most cases, that will cause a pathological relationship with an outside substance or stimuli (Internet overuse/shopping too much/overeating or drinking, and so on).
Living a life filled with severe trauma and pain, especially at a developmental stage, often leads to an addiction. We frequently see people escape to the sweet narcotic-induced sleep via opioid abuse. On the other hand, for people who did not suffer trauma and are highly functional, marijuana offers a means of emotional detachment from pain, in its different form, and existential depression. That is the main benefit my patients who live with marijuana addiction get.
My friend serves as a rather stereotypical – and some may say – subjective, simplistic example of what is becoming more and more common in our society. I’m willing to bet that a good number of clinicians who read this have a similar example in mind.
With its intoxication state perceived as benign and the limited medicinal advantages, marijuana rapidly is gaining more and more legitimacy in the eyes of the general public (Addict Behav. 2008 Mar;33:397-411), (Monitoring the Future: National Results on Drug Use: 1975-2016). The risk of addiction is perceived as negligible and often nonexistent.
Almost no one knows about the potential risk of addiction (around 9%) (Drug Alcohol Depend. 2011;115:120-30). No one knows about about tolerance and withdrawal states – or about the real risk of psychosis (N Engl J Med. 2014 Jun 5;370:2219-27) or about the possible risk of schizophrenia in vulnerable populations (Schizophr Res. 2016 Mar;171:[1-3]:62-7). No one talks about the fact that it’s often used with tobacco. (How many times have you been told during history taking that a patient doesn’t smoke tobacco, only to find that in drug history he smokes 3-5 joints with tobacco daily?)
[polldaddy:9796432]
Throughout my journey in the psychiatric world (studying and working on three different continents) another typical marijuana user is the patient living with chronic mental illness. My Israeli mentor often complained about not having a single “clean” patient with schizophrenia anymore. I now see the same phenomena in Philadelphia and was also exposed to the same reality in Europe during medical school.
As physicians, and especially as psychiatrists, I believe we are obligated to educate our patients by telling them about the risks in their behaviors. Educating patients about marijuana in today’s atmosphere can be a very important preventive measure, and awareness is an important step toward change.
The current generation of psychiatrists is dealing with an opioid epidemic. Let’s educate ourselves and our patients so this current epidemic won’t be followed by another, severe cannabis epidemic.
Dr. Shilo is a second-year PGY in the department of psychiatry at Einstein Medical Center, Philadelphia.