User login
Proinflammatory diet linked to colorectal cancer testing positive for Fusobacterium nucleatum
Diets promoting colonic inflammation were associated with a greater risk of colorectal carcinomas containing Fusobacterium nucleatum bacteria, according to a report in the October issue of Clinical Gastroenterology and Hepatology.
Courtesy American Gastroenterological Association
Proinflammatory diets were not linked to heightened risk for colon cancers without these bacteria, reported Li Liu, MD, PhD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston. “These findings indicate that diet-induced intestinal inflammation alters the gut microbiome to contribute to colorectal carcinogenesis,” they wrote. “Nutritional interventions might be used in precision medicine and cancer prevention.”
Intestinal inflammation, a risk factor for colorectal cancer, is associated with high levels of circulating interleukin 6, C-reactive protein, and tumor necrosis factor–receptor superfamily member 1B. Colonic inflammation impairs the mucosal barrier and alters immune cell responses, which affects the composition of colonic microbiota. Among these, F. nucleatum is known to potentiate colorectal tumors and is associated with proximal tumor location, other tumor features, and cancer progression and chemoresistance.
For the study, the investigators examined self-reported data from more than 124,000 individuals followed for 28 years as part of the Nurses’ Health Study and the Health Professionals Follow-Up Study. They calculated average dietary patterns based on the empiric dietary inflammatory pattern (EDIP) score, which sums weighted intake scores for 18 foods (such as red and processed meat, coffee, tea, and leafy green or dark yellow vegetables) that are known to affect plasma levels of interleukin 6, C-reactive protein, tumor necrosis factor–receptor superfamily member 1B, and tumor necrosis factor alpha–receptor 2. A higher EDIP score denotes a more inflammatory diet.
During the 28-year follow-up period, 951 individuals developed colorectal carcinomas that were tested with a polymerase chain reaction assay for F. nucleatum DNA. A total of 115 tumors tested positive for F. nucleatum. After the researchers controlled for potential confounders, individuals whose EDIP scores were in the highest tertile were significantly more likely to develop F. nucleatum–positive colorectal cancer than were those who scored in the lowest tertile (adjusted hazard ratio, 1.63; 95% confidence interval, 1.03 to 2.58; P = .03). This differential association “appeared to be stronger in proximal colon cancer than in distal colon and rectal cancer,” the researchers said.
More than 90% of individuals in this study were non-Hispanic white, the researchers noted. Tumor tissue was not available from all cases of colorectal cancer and a fairly small number of cases tested positive for tumor F. nucleatum. Nonetheless, the findings suggest that an inflammatory diet could help amplify gut microbiota involved in tumorigenesis, they said. Pending confirmatory studies, they recommended an anti-inflammatory diet with high intake of green leafy vegetables, dark yellow vegetables, coffee, and tea, and with low intake of red meat, processed meat, refined grain, and sugary beverages. They also recommended studying whether F. nucleatum tumor or stool tests could help personalize dietary interventions.
Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
SOURCE: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.
The underlying reasons colorectal cancer (CRC) develops are unknown, but they likely include a complex interaction between genetics and environmental exposures. Recent studies have highlighted important links between diet, the intestinal microbiota, and CRC development and progression.
Liu et al. used the Nurses’ Health Study and Health Professionals Follow-Up Study cohorts to extend our understanding of the relationship between diet, the intestinal microbiota, and CRC. They utilized validated food frequency questionnaires obtained every 4 years and formalin-fixed paraffin embedded CRC tissue samples collected from 951 individuals. They calculated an empiric dietary inflammatory pattern (EDIP) score, which correlates components of the diet with plasma inflammatory markers. After adjusting for confounders, they found high EDIP scores were significantly associated with Fusobacterium nucleatum–positive CRC, but not with F. nucleatum–negative CRC. In addition, they demonstrated this association was stronger for proximal compared with distal CRC. Their findings suggest an inflammatory diet may interact with the intestinal microbiota to promote the development of CRC and they provide a preliminary recommendation to minimize intake of potentially harmful foods (i.e., red meat, processed meat, refined grains, etc.). Despite the intriguing results, the authors do recognize limitations including the small number of cases with F. nucleatum present (n = 115) and the homogeneous cohort (90% non-Hispanic whites), which may limit generalizability.
As clinicians, we should continue strongly advocating for CRC screening and, based on these findings, may consider dietary recommendations to reduce intake of potentially harmful foods. Further research will be needed to confirm these findings in additional cohorts and to clarify the molecular interactions between dietary components, intestinal microbiota, and development of CRC.
Rajesh R. Shah, MD, is assistant professor of gastroenterology, department of internal medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
The underlying reasons colorectal cancer (CRC) develops are unknown, but they likely include a complex interaction between genetics and environmental exposures. Recent studies have highlighted important links between diet, the intestinal microbiota, and CRC development and progression.
Liu et al. used the Nurses’ Health Study and Health Professionals Follow-Up Study cohorts to extend our understanding of the relationship between diet, the intestinal microbiota, and CRC. They utilized validated food frequency questionnaires obtained every 4 years and formalin-fixed paraffin embedded CRC tissue samples collected from 951 individuals. They calculated an empiric dietary inflammatory pattern (EDIP) score, which correlates components of the diet with plasma inflammatory markers. After adjusting for confounders, they found high EDIP scores were significantly associated with Fusobacterium nucleatum–positive CRC, but not with F. nucleatum–negative CRC. In addition, they demonstrated this association was stronger for proximal compared with distal CRC. Their findings suggest an inflammatory diet may interact with the intestinal microbiota to promote the development of CRC and they provide a preliminary recommendation to minimize intake of potentially harmful foods (i.e., red meat, processed meat, refined grains, etc.). Despite the intriguing results, the authors do recognize limitations including the small number of cases with F. nucleatum present (n = 115) and the homogeneous cohort (90% non-Hispanic whites), which may limit generalizability.
As clinicians, we should continue strongly advocating for CRC screening and, based on these findings, may consider dietary recommendations to reduce intake of potentially harmful foods. Further research will be needed to confirm these findings in additional cohorts and to clarify the molecular interactions between dietary components, intestinal microbiota, and development of CRC.
Rajesh R. Shah, MD, is assistant professor of gastroenterology, department of internal medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
The underlying reasons colorectal cancer (CRC) develops are unknown, but they likely include a complex interaction between genetics and environmental exposures. Recent studies have highlighted important links between diet, the intestinal microbiota, and CRC development and progression.
Liu et al. used the Nurses’ Health Study and Health Professionals Follow-Up Study cohorts to extend our understanding of the relationship between diet, the intestinal microbiota, and CRC. They utilized validated food frequency questionnaires obtained every 4 years and formalin-fixed paraffin embedded CRC tissue samples collected from 951 individuals. They calculated an empiric dietary inflammatory pattern (EDIP) score, which correlates components of the diet with plasma inflammatory markers. After adjusting for confounders, they found high EDIP scores were significantly associated with Fusobacterium nucleatum–positive CRC, but not with F. nucleatum–negative CRC. In addition, they demonstrated this association was stronger for proximal compared with distal CRC. Their findings suggest an inflammatory diet may interact with the intestinal microbiota to promote the development of CRC and they provide a preliminary recommendation to minimize intake of potentially harmful foods (i.e., red meat, processed meat, refined grains, etc.). Despite the intriguing results, the authors do recognize limitations including the small number of cases with F. nucleatum present (n = 115) and the homogeneous cohort (90% non-Hispanic whites), which may limit generalizability.
As clinicians, we should continue strongly advocating for CRC screening and, based on these findings, may consider dietary recommendations to reduce intake of potentially harmful foods. Further research will be needed to confirm these findings in additional cohorts and to clarify the molecular interactions between dietary components, intestinal microbiota, and development of CRC.
Rajesh R. Shah, MD, is assistant professor of gastroenterology, department of internal medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Diets promoting colonic inflammation were associated with a greater risk of colorectal carcinomas containing Fusobacterium nucleatum bacteria, according to a report in the October issue of Clinical Gastroenterology and Hepatology.
Courtesy American Gastroenterological Association
Proinflammatory diets were not linked to heightened risk for colon cancers without these bacteria, reported Li Liu, MD, PhD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston. “These findings indicate that diet-induced intestinal inflammation alters the gut microbiome to contribute to colorectal carcinogenesis,” they wrote. “Nutritional interventions might be used in precision medicine and cancer prevention.”
Intestinal inflammation, a risk factor for colorectal cancer, is associated with high levels of circulating interleukin 6, C-reactive protein, and tumor necrosis factor–receptor superfamily member 1B. Colonic inflammation impairs the mucosal barrier and alters immune cell responses, which affects the composition of colonic microbiota. Among these, F. nucleatum is known to potentiate colorectal tumors and is associated with proximal tumor location, other tumor features, and cancer progression and chemoresistance.
For the study, the investigators examined self-reported data from more than 124,000 individuals followed for 28 years as part of the Nurses’ Health Study and the Health Professionals Follow-Up Study. They calculated average dietary patterns based on the empiric dietary inflammatory pattern (EDIP) score, which sums weighted intake scores for 18 foods (such as red and processed meat, coffee, tea, and leafy green or dark yellow vegetables) that are known to affect plasma levels of interleukin 6, C-reactive protein, tumor necrosis factor–receptor superfamily member 1B, and tumor necrosis factor alpha–receptor 2. A higher EDIP score denotes a more inflammatory diet.
During the 28-year follow-up period, 951 individuals developed colorectal carcinomas that were tested with a polymerase chain reaction assay for F. nucleatum DNA. A total of 115 tumors tested positive for F. nucleatum. After the researchers controlled for potential confounders, individuals whose EDIP scores were in the highest tertile were significantly more likely to develop F. nucleatum–positive colorectal cancer than were those who scored in the lowest tertile (adjusted hazard ratio, 1.63; 95% confidence interval, 1.03 to 2.58; P = .03). This differential association “appeared to be stronger in proximal colon cancer than in distal colon and rectal cancer,” the researchers said.
More than 90% of individuals in this study were non-Hispanic white, the researchers noted. Tumor tissue was not available from all cases of colorectal cancer and a fairly small number of cases tested positive for tumor F. nucleatum. Nonetheless, the findings suggest that an inflammatory diet could help amplify gut microbiota involved in tumorigenesis, they said. Pending confirmatory studies, they recommended an anti-inflammatory diet with high intake of green leafy vegetables, dark yellow vegetables, coffee, and tea, and with low intake of red meat, processed meat, refined grain, and sugary beverages. They also recommended studying whether F. nucleatum tumor or stool tests could help personalize dietary interventions.
Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
SOURCE: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.
Diets promoting colonic inflammation were associated with a greater risk of colorectal carcinomas containing Fusobacterium nucleatum bacteria, according to a report in the October issue of Clinical Gastroenterology and Hepatology.
Courtesy American Gastroenterological Association
Proinflammatory diets were not linked to heightened risk for colon cancers without these bacteria, reported Li Liu, MD, PhD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston. “These findings indicate that diet-induced intestinal inflammation alters the gut microbiome to contribute to colorectal carcinogenesis,” they wrote. “Nutritional interventions might be used in precision medicine and cancer prevention.”
Intestinal inflammation, a risk factor for colorectal cancer, is associated with high levels of circulating interleukin 6, C-reactive protein, and tumor necrosis factor–receptor superfamily member 1B. Colonic inflammation impairs the mucosal barrier and alters immune cell responses, which affects the composition of colonic microbiota. Among these, F. nucleatum is known to potentiate colorectal tumors and is associated with proximal tumor location, other tumor features, and cancer progression and chemoresistance.
For the study, the investigators examined self-reported data from more than 124,000 individuals followed for 28 years as part of the Nurses’ Health Study and the Health Professionals Follow-Up Study. They calculated average dietary patterns based on the empiric dietary inflammatory pattern (EDIP) score, which sums weighted intake scores for 18 foods (such as red and processed meat, coffee, tea, and leafy green or dark yellow vegetables) that are known to affect plasma levels of interleukin 6, C-reactive protein, tumor necrosis factor–receptor superfamily member 1B, and tumor necrosis factor alpha–receptor 2. A higher EDIP score denotes a more inflammatory diet.
During the 28-year follow-up period, 951 individuals developed colorectal carcinomas that were tested with a polymerase chain reaction assay for F. nucleatum DNA. A total of 115 tumors tested positive for F. nucleatum. After the researchers controlled for potential confounders, individuals whose EDIP scores were in the highest tertile were significantly more likely to develop F. nucleatum–positive colorectal cancer than were those who scored in the lowest tertile (adjusted hazard ratio, 1.63; 95% confidence interval, 1.03 to 2.58; P = .03). This differential association “appeared to be stronger in proximal colon cancer than in distal colon and rectal cancer,” the researchers said.
More than 90% of individuals in this study were non-Hispanic white, the researchers noted. Tumor tissue was not available from all cases of colorectal cancer and a fairly small number of cases tested positive for tumor F. nucleatum. Nonetheless, the findings suggest that an inflammatory diet could help amplify gut microbiota involved in tumorigenesis, they said. Pending confirmatory studies, they recommended an anti-inflammatory diet with high intake of green leafy vegetables, dark yellow vegetables, coffee, and tea, and with low intake of red meat, processed meat, refined grain, and sugary beverages. They also recommended studying whether F. nucleatum tumor or stool tests could help personalize dietary interventions.
Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
SOURCE: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A proinflammatory diet was associated with a significantly increased risk for colorectal cancer testing positive for Fusobacterium nucleatum.
Major finding: Dietary scores in the highest inflammatory tertile correlated with significantly increased risk (HR, 1.63; P = .03).
Study details: Longitudinal study of self-reported dietary patterns and cancers among 124,433 individuals with 28 years of follow-up.
Disclosures: Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
Source: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.
U.S. perspective: Euro hypertension guidelines look a lot like ours
MUNICH – The “overwhelming impression” that Paul K. Whelton, MD, has of the newly revised hypertension diagnosis and management guidelines of the European Society of Cardiology is their similarity to hypertension guidelines released by the American College of Cardiology and American Heart Association in November 2017.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We both recommend the same treatment target, of less than 130/80 mm Hg,” noted Dr. Whelton, professor at Tulane University in New Orleans, although the European guidelines (Euro J Cardiology. 2018 Sep 1; 39[33]:3021-104) put more qualifications on this target and specify treating to no lower than 130 mm Hg systolic pressure in patients who are at least 65 years old as well as in patients with chronic kidney disease at any age. In a video interview, Dr. Whelton also cited areas of disagreement, such as how patients with an untreated blood pressure of 130-139 mm Hg are classified (high normal in the European guidelines, stage 1 hypertension in the U.S. guidelines), and whether initial drug monotherapy is a reasonable treatment strategy (U.S. says yes, Europe says no).
Dr. Whelton noted that recent modeling studies have documented the potential public health benefits from following the diagnosis and management approaches set forth in the 2017 U.S. guidelines (J Am Coll Cardiol. 2018 May;71[19]:e127-e248). For example, an analysis based on data collected by the U.S. National Health and Nutrition Examination Survey during 2013-2016 showed that following the 2017 guidelines for diagnosing and treating hypertension would have resulted in prevention of more than twice the number of cardiovascular disease events nationally as compared with application of the prior, 2014 U.S. hypertension guideline (JAMA. 2014 Feb 5;311[5]:507-20): 610,000 events prevented, compared with 270,000 events prevented. The same study showed that the 2017 guidelines would have nearly doubled the number of all-cause deaths prevented, with 334,000 deaths prevented, compared with 177,000 prevented by applying the 2014 guidelines (JAMA Cardiology. 2018 July;3[7]:572-81).
Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – The “overwhelming impression” that Paul K. Whelton, MD, has of the newly revised hypertension diagnosis and management guidelines of the European Society of Cardiology is their similarity to hypertension guidelines released by the American College of Cardiology and American Heart Association in November 2017.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We both recommend the same treatment target, of less than 130/80 mm Hg,” noted Dr. Whelton, professor at Tulane University in New Orleans, although the European guidelines (Euro J Cardiology. 2018 Sep 1; 39[33]:3021-104) put more qualifications on this target and specify treating to no lower than 130 mm Hg systolic pressure in patients who are at least 65 years old as well as in patients with chronic kidney disease at any age. In a video interview, Dr. Whelton also cited areas of disagreement, such as how patients with an untreated blood pressure of 130-139 mm Hg are classified (high normal in the European guidelines, stage 1 hypertension in the U.S. guidelines), and whether initial drug monotherapy is a reasonable treatment strategy (U.S. says yes, Europe says no).
Dr. Whelton noted that recent modeling studies have documented the potential public health benefits from following the diagnosis and management approaches set forth in the 2017 U.S. guidelines (J Am Coll Cardiol. 2018 May;71[19]:e127-e248). For example, an analysis based on data collected by the U.S. National Health and Nutrition Examination Survey during 2013-2016 showed that following the 2017 guidelines for diagnosing and treating hypertension would have resulted in prevention of more than twice the number of cardiovascular disease events nationally as compared with application of the prior, 2014 U.S. hypertension guideline (JAMA. 2014 Feb 5;311[5]:507-20): 610,000 events prevented, compared with 270,000 events prevented. The same study showed that the 2017 guidelines would have nearly doubled the number of all-cause deaths prevented, with 334,000 deaths prevented, compared with 177,000 prevented by applying the 2014 guidelines (JAMA Cardiology. 2018 July;3[7]:572-81).
Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – The “overwhelming impression” that Paul K. Whelton, MD, has of the newly revised hypertension diagnosis and management guidelines of the European Society of Cardiology is their similarity to hypertension guidelines released by the American College of Cardiology and American Heart Association in November 2017.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We both recommend the same treatment target, of less than 130/80 mm Hg,” noted Dr. Whelton, professor at Tulane University in New Orleans, although the European guidelines (Euro J Cardiology. 2018 Sep 1; 39[33]:3021-104) put more qualifications on this target and specify treating to no lower than 130 mm Hg systolic pressure in patients who are at least 65 years old as well as in patients with chronic kidney disease at any age. In a video interview, Dr. Whelton also cited areas of disagreement, such as how patients with an untreated blood pressure of 130-139 mm Hg are classified (high normal in the European guidelines, stage 1 hypertension in the U.S. guidelines), and whether initial drug monotherapy is a reasonable treatment strategy (U.S. says yes, Europe says no).
Dr. Whelton noted that recent modeling studies have documented the potential public health benefits from following the diagnosis and management approaches set forth in the 2017 U.S. guidelines (J Am Coll Cardiol. 2018 May;71[19]:e127-e248). For example, an analysis based on data collected by the U.S. National Health and Nutrition Examination Survey during 2013-2016 showed that following the 2017 guidelines for diagnosing and treating hypertension would have resulted in prevention of more than twice the number of cardiovascular disease events nationally as compared with application of the prior, 2014 U.S. hypertension guideline (JAMA. 2014 Feb 5;311[5]:507-20): 610,000 events prevented, compared with 270,000 events prevented. The same study showed that the 2017 guidelines would have nearly doubled the number of all-cause deaths prevented, with 334,000 deaths prevented, compared with 177,000 prevented by applying the 2014 guidelines (JAMA Cardiology. 2018 July;3[7]:572-81).
Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM THE ESC CONGRESS 2018
New Euro hypertension guidelines target most adults to less than 130/80 mm Hg
MUNICH – The European Society of Cardiology joined other international cardiology groups in endorsing lower targets for blood pressure treatment and lower pressure thresholds for starting drug treatment in its revised hypertension diagnosis and management guidelines released in August during the Society’s annual congress here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Provided that treatment is well tolerated, treated blood pressure should be targeted to 130/80 mm Hg or lower in most patients,” Giuseppe Mancia, MD, said as he and his colleagues presented the new guidelines at the annual congress of the European Society of Cardiology.
Although the new European guidelines further buttress this more aggressive approach to blood pressure management that first appeared almost a year ago in U.S. guidelines from the American College of Cardiology and the American Heart Association, an approach that remains controversial among U.S. primary care physicians, the European strategy (Eur Heart J. 2018 Sep 1;39[33]:3021-104) was generally more cautious than the broader endorsement of lower blood pressure goals advanced by the U.S. recommendations (J Am Coll Cardiol. 2018 May;71[19]:e127-e248).
In the European approach, “the first objective is to treat to less than 140/90 mm Hg. If this is well tolerated, then treat to less than 130/80 mm Hg in most patients,” said Dr. Mancia, cochair of the European writing panel. Further pressure reductions to less than 130/80 mm Hg are usually harder, the incremental benefit from further reduction is less than when pressures first fall below 140/90 mm Hg, and the evidence for incremental benefit of any size from further pressure reduction is less strong for certain key patient subgroups: people at least 80 years old, and patients with diabetes, chronic kidney disease, or coronary artery disease, said Dr. Mancia, an emeritus professor at the University of Milan.
“The consistency between two major guidelines is important, but there are differences that may look subtle but are not subtle,” he said in a video interview. “If a patient gets to less than 140 mm Hg, the doctor should not think that’s a failure; it’s a very important result.”
One striking example of how the two guidelines differ on treatment targets is for people at least 80 years old. The overall blood pressure threshold for starting drug treatment in patients this age in the European guidelines is 160/90 mm Hg, although it remains at 140/90 for people aged 65-79 years old “provided that treatment is well tolerated” and the patients are “fit.” The 2017 U.S. guidelines, by contrast, say that considering drug treatment for everyone with a pressure at or above 130/80 mm Hg is a class I recommendation regardless of age as long as the person is “noninstitutionalized, ambulatory, [and] community-dwelling.” Once an older patient of any age, 65 years or older, starts drug treatment to reduce blood pressure, the European guidelines allow for treating to a target systolic blood pressure of 130-139 mm Hg as long as the regimen is well tolerated, and the guidelines say that a diastolic pressure target of less than 80 mm Hg should be considered for all adults regardless of age.
The new European guidelines also define adults with an untreated pressure of 130-139/85-89 mm Hg as “high normal,” rather than the “stage 1 hypertension” designation given to people with pressures of 130-139/80-89 mm Hg in the U.S. guidelines. Robert M. Carey, MD, vice chair of the U.S. guidelines panel, minimized this as a “semantic” difference, and he highlighted that management of people with pressures in this range is roughly similar in the two sets of recommendations. “The name is different, but treatment is the same,” Dr. Carey said.
The European guidelines call for initial lifestyle interventions, followed by drug treatment “that may be considered” for patients who have “very-high” cardiovascular risk because of established cardiovascular disease, especially coronary artery disease, and detail the specific clinical conditions that fall into the very-high-risk category. The U.S. guidelines say that stage 1 hypertension patients should get lifestyle interventions, followed by drug treatment for the roughly 30% of patients in this category who score at least a 10% 10-year risk on the American College of Cardiology’s Atherosclerotic Cardiovascular Disease Risk Estimator Plus.The new European guidelines are a “validation” of the ACC/AHA 2017 guidelines, commented Dr. Carey, a professor of medicine at the University of Virginia in Charlottesville. “Overall, we’re delighted to have these two major groups” agree, he said in an interview. “There is a tremendous amount of concurrence.”
Other areas of agreement between the two guidelines include their emphasis on careful and repeated blood pressure measurement, including out-of-office measurement, before settling on a diagnosis of hypertension; systematic assessment of possible masked or white-coat hypertension in selected people; and frequent use of combined drug treatment including initiation of a dual-drug, single-pill regimen when starting drug treatment and aggressive follow-up by adding a third drug when needed. However, in another divergence the U.S. guidelines give a much stronger endorsement to starting treatment with monotherapy, a strategy the European guidelines scrapped.
Dr. Carey also noted that the European endorsement of three antihypertensives formulated into a single pill for patients who need more than two drugs would be difficult for American clinicians to follow as virtually no such formulations are approved for U.S. use.
Dr. Mancini has received honoraria from Boehringer Ingelheim, CVRx, Daiichi Sankyo, Ferrer, Medtronic, Menarini, Merck, Novartis, Recordati, and Servier. Dr. Williams has been a consultant to Novartis, Relypsa, and Vascular Dynamics, and he has spoken on behalf of Boehringer Ingelheim, Daiichi Sankyo, Novartis, and Servier. Dr. Carey and Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – The European Society of Cardiology joined other international cardiology groups in endorsing lower targets for blood pressure treatment and lower pressure thresholds for starting drug treatment in its revised hypertension diagnosis and management guidelines released in August during the Society’s annual congress here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Provided that treatment is well tolerated, treated blood pressure should be targeted to 130/80 mm Hg or lower in most patients,” Giuseppe Mancia, MD, said as he and his colleagues presented the new guidelines at the annual congress of the European Society of Cardiology.
Although the new European guidelines further buttress this more aggressive approach to blood pressure management that first appeared almost a year ago in U.S. guidelines from the American College of Cardiology and the American Heart Association, an approach that remains controversial among U.S. primary care physicians, the European strategy (Eur Heart J. 2018 Sep 1;39[33]:3021-104) was generally more cautious than the broader endorsement of lower blood pressure goals advanced by the U.S. recommendations (J Am Coll Cardiol. 2018 May;71[19]:e127-e248).
In the European approach, “the first objective is to treat to less than 140/90 mm Hg. If this is well tolerated, then treat to less than 130/80 mm Hg in most patients,” said Dr. Mancia, cochair of the European writing panel. Further pressure reductions to less than 130/80 mm Hg are usually harder, the incremental benefit from further reduction is less than when pressures first fall below 140/90 mm Hg, and the evidence for incremental benefit of any size from further pressure reduction is less strong for certain key patient subgroups: people at least 80 years old, and patients with diabetes, chronic kidney disease, or coronary artery disease, said Dr. Mancia, an emeritus professor at the University of Milan.
“The consistency between two major guidelines is important, but there are differences that may look subtle but are not subtle,” he said in a video interview. “If a patient gets to less than 140 mm Hg, the doctor should not think that’s a failure; it’s a very important result.”
One striking example of how the two guidelines differ on treatment targets is for people at least 80 years old. The overall blood pressure threshold for starting drug treatment in patients this age in the European guidelines is 160/90 mm Hg, although it remains at 140/90 for people aged 65-79 years old “provided that treatment is well tolerated” and the patients are “fit.” The 2017 U.S. guidelines, by contrast, say that considering drug treatment for everyone with a pressure at or above 130/80 mm Hg is a class I recommendation regardless of age as long as the person is “noninstitutionalized, ambulatory, [and] community-dwelling.” Once an older patient of any age, 65 years or older, starts drug treatment to reduce blood pressure, the European guidelines allow for treating to a target systolic blood pressure of 130-139 mm Hg as long as the regimen is well tolerated, and the guidelines say that a diastolic pressure target of less than 80 mm Hg should be considered for all adults regardless of age.
The new European guidelines also define adults with an untreated pressure of 130-139/85-89 mm Hg as “high normal,” rather than the “stage 1 hypertension” designation given to people with pressures of 130-139/80-89 mm Hg in the U.S. guidelines. Robert M. Carey, MD, vice chair of the U.S. guidelines panel, minimized this as a “semantic” difference, and he highlighted that management of people with pressures in this range is roughly similar in the two sets of recommendations. “The name is different, but treatment is the same,” Dr. Carey said.
The European guidelines call for initial lifestyle interventions, followed by drug treatment “that may be considered” for patients who have “very-high” cardiovascular risk because of established cardiovascular disease, especially coronary artery disease, and detail the specific clinical conditions that fall into the very-high-risk category. The U.S. guidelines say that stage 1 hypertension patients should get lifestyle interventions, followed by drug treatment for the roughly 30% of patients in this category who score at least a 10% 10-year risk on the American College of Cardiology’s Atherosclerotic Cardiovascular Disease Risk Estimator Plus.The new European guidelines are a “validation” of the ACC/AHA 2017 guidelines, commented Dr. Carey, a professor of medicine at the University of Virginia in Charlottesville. “Overall, we’re delighted to have these two major groups” agree, he said in an interview. “There is a tremendous amount of concurrence.”
Other areas of agreement between the two guidelines include their emphasis on careful and repeated blood pressure measurement, including out-of-office measurement, before settling on a diagnosis of hypertension; systematic assessment of possible masked or white-coat hypertension in selected people; and frequent use of combined drug treatment including initiation of a dual-drug, single-pill regimen when starting drug treatment and aggressive follow-up by adding a third drug when needed. However, in another divergence the U.S. guidelines give a much stronger endorsement to starting treatment with monotherapy, a strategy the European guidelines scrapped.
Dr. Carey also noted that the European endorsement of three antihypertensives formulated into a single pill for patients who need more than two drugs would be difficult for American clinicians to follow as virtually no such formulations are approved for U.S. use.
Dr. Mancini has received honoraria from Boehringer Ingelheim, CVRx, Daiichi Sankyo, Ferrer, Medtronic, Menarini, Merck, Novartis, Recordati, and Servier. Dr. Williams has been a consultant to Novartis, Relypsa, and Vascular Dynamics, and he has spoken on behalf of Boehringer Ingelheim, Daiichi Sankyo, Novartis, and Servier. Dr. Carey and Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – The European Society of Cardiology joined other international cardiology groups in endorsing lower targets for blood pressure treatment and lower pressure thresholds for starting drug treatment in its revised hypertension diagnosis and management guidelines released in August during the Society’s annual congress here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Provided that treatment is well tolerated, treated blood pressure should be targeted to 130/80 mm Hg or lower in most patients,” Giuseppe Mancia, MD, said as he and his colleagues presented the new guidelines at the annual congress of the European Society of Cardiology.
Although the new European guidelines further buttress this more aggressive approach to blood pressure management that first appeared almost a year ago in U.S. guidelines from the American College of Cardiology and the American Heart Association, an approach that remains controversial among U.S. primary care physicians, the European strategy (Eur Heart J. 2018 Sep 1;39[33]:3021-104) was generally more cautious than the broader endorsement of lower blood pressure goals advanced by the U.S. recommendations (J Am Coll Cardiol. 2018 May;71[19]:e127-e248).
In the European approach, “the first objective is to treat to less than 140/90 mm Hg. If this is well tolerated, then treat to less than 130/80 mm Hg in most patients,” said Dr. Mancia, cochair of the European writing panel. Further pressure reductions to less than 130/80 mm Hg are usually harder, the incremental benefit from further reduction is less than when pressures first fall below 140/90 mm Hg, and the evidence for incremental benefit of any size from further pressure reduction is less strong for certain key patient subgroups: people at least 80 years old, and patients with diabetes, chronic kidney disease, or coronary artery disease, said Dr. Mancia, an emeritus professor at the University of Milan.
“The consistency between two major guidelines is important, but there are differences that may look subtle but are not subtle,” he said in a video interview. “If a patient gets to less than 140 mm Hg, the doctor should not think that’s a failure; it’s a very important result.”
One striking example of how the two guidelines differ on treatment targets is for people at least 80 years old. The overall blood pressure threshold for starting drug treatment in patients this age in the European guidelines is 160/90 mm Hg, although it remains at 140/90 for people aged 65-79 years old “provided that treatment is well tolerated” and the patients are “fit.” The 2017 U.S. guidelines, by contrast, say that considering drug treatment for everyone with a pressure at or above 130/80 mm Hg is a class I recommendation regardless of age as long as the person is “noninstitutionalized, ambulatory, [and] community-dwelling.” Once an older patient of any age, 65 years or older, starts drug treatment to reduce blood pressure, the European guidelines allow for treating to a target systolic blood pressure of 130-139 mm Hg as long as the regimen is well tolerated, and the guidelines say that a diastolic pressure target of less than 80 mm Hg should be considered for all adults regardless of age.
The new European guidelines also define adults with an untreated pressure of 130-139/85-89 mm Hg as “high normal,” rather than the “stage 1 hypertension” designation given to people with pressures of 130-139/80-89 mm Hg in the U.S. guidelines. Robert M. Carey, MD, vice chair of the U.S. guidelines panel, minimized this as a “semantic” difference, and he highlighted that management of people with pressures in this range is roughly similar in the two sets of recommendations. “The name is different, but treatment is the same,” Dr. Carey said.
The European guidelines call for initial lifestyle interventions, followed by drug treatment “that may be considered” for patients who have “very-high” cardiovascular risk because of established cardiovascular disease, especially coronary artery disease, and detail the specific clinical conditions that fall into the very-high-risk category. The U.S. guidelines say that stage 1 hypertension patients should get lifestyle interventions, followed by drug treatment for the roughly 30% of patients in this category who score at least a 10% 10-year risk on the American College of Cardiology’s Atherosclerotic Cardiovascular Disease Risk Estimator Plus.The new European guidelines are a “validation” of the ACC/AHA 2017 guidelines, commented Dr. Carey, a professor of medicine at the University of Virginia in Charlottesville. “Overall, we’re delighted to have these two major groups” agree, he said in an interview. “There is a tremendous amount of concurrence.”
Other areas of agreement between the two guidelines include their emphasis on careful and repeated blood pressure measurement, including out-of-office measurement, before settling on a diagnosis of hypertension; systematic assessment of possible masked or white-coat hypertension in selected people; and frequent use of combined drug treatment including initiation of a dual-drug, single-pill regimen when starting drug treatment and aggressive follow-up by adding a third drug when needed. However, in another divergence the U.S. guidelines give a much stronger endorsement to starting treatment with monotherapy, a strategy the European guidelines scrapped.
Dr. Carey also noted that the European endorsement of three antihypertensives formulated into a single pill for patients who need more than two drugs would be difficult for American clinicians to follow as virtually no such formulations are approved for U.S. use.
Dr. Mancini has received honoraria from Boehringer Ingelheim, CVRx, Daiichi Sankyo, Ferrer, Medtronic, Menarini, Merck, Novartis, Recordati, and Servier. Dr. Williams has been a consultant to Novartis, Relypsa, and Vascular Dynamics, and he has spoken on behalf of Boehringer Ingelheim, Daiichi Sankyo, Novartis, and Servier. Dr. Carey and Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM THE ESC CONGRESS 2018
Pediatric hypertension linked to troubling MRI changes
CHICAGO – There’s another reason to worry about hypertension in children: cognitive decline later in life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In a pilot study, Marc Lande, MD, a professor of pediatric nephrology at the University of Rochester (N.Y.), and his colleagues found similar to what’s found in adults with cognitive impairment from hypertension.
The work is ongoing, but it helps explain the subtle deficits on cognitive testing that have been previously demonstrated in children with hypertension.
“The fact that we are finding anything at this very early stage of disease is striking and somewhat bothersome. The hope is that, by improving blood pressure in children, you can improve subsequent cognition and maybe even delay the onset of dementia further down the road,” Dr. Lande said.
For now, the findings underscore the need to diagnose and manage hypertension in children, but there might be additional treatment implications in the future, especially if blood pressure targets are found that ameliorate the problem.
Dr. Lande explained the issues and the emerging evidence in a video interview at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
CHICAGO – There’s another reason to worry about hypertension in children: cognitive decline later in life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In a pilot study, Marc Lande, MD, a professor of pediatric nephrology at the University of Rochester (N.Y.), and his colleagues found similar to what’s found in adults with cognitive impairment from hypertension.
The work is ongoing, but it helps explain the subtle deficits on cognitive testing that have been previously demonstrated in children with hypertension.
“The fact that we are finding anything at this very early stage of disease is striking and somewhat bothersome. The hope is that, by improving blood pressure in children, you can improve subsequent cognition and maybe even delay the onset of dementia further down the road,” Dr. Lande said.
For now, the findings underscore the need to diagnose and manage hypertension in children, but there might be additional treatment implications in the future, especially if blood pressure targets are found that ameliorate the problem.
Dr. Lande explained the issues and the emerging evidence in a video interview at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
CHICAGO – There’s another reason to worry about hypertension in children: cognitive decline later in life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In a pilot study, Marc Lande, MD, a professor of pediatric nephrology at the University of Rochester (N.Y.), and his colleagues found similar to what’s found in adults with cognitive impairment from hypertension.
The work is ongoing, but it helps explain the subtle deficits on cognitive testing that have been previously demonstrated in children with hypertension.
“The fact that we are finding anything at this very early stage of disease is striking and somewhat bothersome. The hope is that, by improving blood pressure in children, you can improve subsequent cognition and maybe even delay the onset of dementia further down the road,” Dr. Lande said.
For now, the findings underscore the need to diagnose and manage hypertension in children, but there might be additional treatment implications in the future, especially if blood pressure targets are found that ameliorate the problem.
Dr. Lande explained the issues and the emerging evidence in a video interview at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
REPORTING FROM JOINT HYPERTENSION 2018
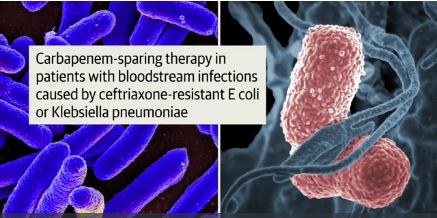
Piperacillin-tazobactam fails to outperform meropenem in bloodstream infections
A new study finds that piperacillin-tazobactam doesn’t improve mortality compared to meropenem in patients with ceftriaxone-resistant blood poisoning caused by E. coli or K. pneumoniae. The findings were so striking that the study was ended early.

Courtesy: JAMA
“These findings do not support use of piperacillin-tazobactam in this setting,” wrote the authors. The report was published Sept. 11 in JAMA (2018;320[10]:984-94.)
According to the Centers for Disease Control and Prevention, an estimated 1,700 deaths in the United States in 2011 were caused by gram-negative bacteria that produce extended-spectrum beta-lactamase enzymes.
While carbapenems such as meropenem (Merrem) are “regarded as the treatment of choice for serious infections,” the MERINO trial (NCT02176122) authors wrote, their rising use could lead to drug resistance.
One alternate option is to embrace beta-lactam/beta-lactamase inhibitors such as piperacillin-tazobactam (Zosyn), the researchers noted, but research has produced conflicting results.
Piperacillin-tazobactam is an injected penicillin antibiotic used to treat conditions such as severe pneumonia, complicated urinary tract infections and complicated skin and soft tissue infections.
For the new study, researchers led by Patrick N. A. Harris, MBBS, of the University of Queensland, randomly assigned 188 patients to intravenous piperacillin-tazobactam (4.5 g every 6 hours) and 191 patients to meropenem (1 g every 8 hours) for 4-14 days, depending on clinician’s preference. (12 other patients did not continue with the study after initial randomization due to factors such as errors).
All patients were adults and had at least one blood test showing they were positive for E. coli or K. pneumoniae. They all had to be nonsusceptible to ceftriaxone (Rocephin) but susceptible to piperacillin-tazobactam.
The study was ceased prior to enrollment because of the risk of harm. Interim findings suggested the study was unlikely to show higher effectiveness for piperacillin-tazobactam
The primary analysis included 379 patients (mean age 67 years, 48% were women), and the primary outcome analysis included 378 patients.
A total of 23 (12.3%) of 187 patients in the piperacillin-tazobactam group died by 30 days compared to 7 (3.7%) of 191 in the meropenem group (risk difference: 8.6%, P = .90 for noninferiority).
By day 4, 68% of the piperacillin-tazobactam group and 75% of the meropenem group achieved clinical and microbiological resolution.
Serious adverse effects other than death were rare, occurring in around 3% of the piperacillin-tazobactam group and nearly 2% of the meropenem group.
The researchers note various limitations, including the unblinded nature of the study and the fact that it’s not known if extended or continuous infusions of piperacillin-tazobactam would boost the drug’s effectiveness. They also note that delays resulted in some patients initially receiving treatment with one of the study’s two drugs before being randomized to the other.
The study authors caution that it’s not clear if newer beta-lactam/beta-lactamase inhibitors agents such as ceftolozane-tazobactam or ceftazidime-avibactam may be effective in this population.
The study was funded by the University of Queensland, Australian Society for Antimicrobials, International Society for Chemotherapy, and National University Hospital Singapore. Various organizations funded the researchers and the study’s whole-genome sequencing. The study authors report various disclosures, including funding from drugmakers such as Pfizer, maker of Zosyn (through its subsidiary Wyeth) and Merrem.
SOURCE: Harris PNA et al. JAMA 2018 Sep 11;320[10]:984-94. doi: 10.1001/jama.2018.12163.
There may be no greater present-day antibiotic resistance threat than the prospect of nonsusceptibility developing among patients with blood poisoning who receive carbapenems for infections caused by E. coli or K. pneumonia. New antibiotics are being developed and researchers are taking a second look at existing drugs.
The new study aims to shed light on the effectiveness of piperacillin-tazobactam in this population compared to carbapenems. Surprisingly, the researchers failed to show a mortality benefit for the drug vs. meropenem. What now? Future research could shed light on newer beta-lactam/beta-lactamase inhibitors, and studies may also offer insight into alternatives such as short-term antibiotic therapy. The upcoming availability of electronic decision support tools may be helpful, and it remains important to prevent infections in the first place.
This commentary was taken from an editorial by Mary K. Hayden, MD, and Sarah Y. Won, MD, MPH, of Rush University Medical Center (JAMA 2018 Sep 11;320[10]:979-81). Dr. Hayden reports research funding from Colorox and serving as an investigator on research products that received product support from Sage Corporation, Molnlycke, Clorox, OpGen and Medline.
There may be no greater present-day antibiotic resistance threat than the prospect of nonsusceptibility developing among patients with blood poisoning who receive carbapenems for infections caused by E. coli or K. pneumonia. New antibiotics are being developed and researchers are taking a second look at existing drugs.
The new study aims to shed light on the effectiveness of piperacillin-tazobactam in this population compared to carbapenems. Surprisingly, the researchers failed to show a mortality benefit for the drug vs. meropenem. What now? Future research could shed light on newer beta-lactam/beta-lactamase inhibitors, and studies may also offer insight into alternatives such as short-term antibiotic therapy. The upcoming availability of electronic decision support tools may be helpful, and it remains important to prevent infections in the first place.
This commentary was taken from an editorial by Mary K. Hayden, MD, and Sarah Y. Won, MD, MPH, of Rush University Medical Center (JAMA 2018 Sep 11;320[10]:979-81). Dr. Hayden reports research funding from Colorox and serving as an investigator on research products that received product support from Sage Corporation, Molnlycke, Clorox, OpGen and Medline.
There may be no greater present-day antibiotic resistance threat than the prospect of nonsusceptibility developing among patients with blood poisoning who receive carbapenems for infections caused by E. coli or K. pneumonia. New antibiotics are being developed and researchers are taking a second look at existing drugs.
The new study aims to shed light on the effectiveness of piperacillin-tazobactam in this population compared to carbapenems. Surprisingly, the researchers failed to show a mortality benefit for the drug vs. meropenem. What now? Future research could shed light on newer beta-lactam/beta-lactamase inhibitors, and studies may also offer insight into alternatives such as short-term antibiotic therapy. The upcoming availability of electronic decision support tools may be helpful, and it remains important to prevent infections in the first place.
This commentary was taken from an editorial by Mary K. Hayden, MD, and Sarah Y. Won, MD, MPH, of Rush University Medical Center (JAMA 2018 Sep 11;320[10]:979-81). Dr. Hayden reports research funding from Colorox and serving as an investigator on research products that received product support from Sage Corporation, Molnlycke, Clorox, OpGen and Medline.
A new study finds that piperacillin-tazobactam doesn’t improve mortality compared to meropenem in patients with ceftriaxone-resistant blood poisoning caused by E. coli or K. pneumoniae. The findings were so striking that the study was ended early.

Courtesy: JAMA
“These findings do not support use of piperacillin-tazobactam in this setting,” wrote the authors. The report was published Sept. 11 in JAMA (2018;320[10]:984-94.)
According to the Centers for Disease Control and Prevention, an estimated 1,700 deaths in the United States in 2011 were caused by gram-negative bacteria that produce extended-spectrum beta-lactamase enzymes.
While carbapenems such as meropenem (Merrem) are “regarded as the treatment of choice for serious infections,” the MERINO trial (NCT02176122) authors wrote, their rising use could lead to drug resistance.
One alternate option is to embrace beta-lactam/beta-lactamase inhibitors such as piperacillin-tazobactam (Zosyn), the researchers noted, but research has produced conflicting results.
Piperacillin-tazobactam is an injected penicillin antibiotic used to treat conditions such as severe pneumonia, complicated urinary tract infections and complicated skin and soft tissue infections.
For the new study, researchers led by Patrick N. A. Harris, MBBS, of the University of Queensland, randomly assigned 188 patients to intravenous piperacillin-tazobactam (4.5 g every 6 hours) and 191 patients to meropenem (1 g every 8 hours) for 4-14 days, depending on clinician’s preference. (12 other patients did not continue with the study after initial randomization due to factors such as errors).
All patients were adults and had at least one blood test showing they were positive for E. coli or K. pneumoniae. They all had to be nonsusceptible to ceftriaxone (Rocephin) but susceptible to piperacillin-tazobactam.
The study was ceased prior to enrollment because of the risk of harm. Interim findings suggested the study was unlikely to show higher effectiveness for piperacillin-tazobactam
The primary analysis included 379 patients (mean age 67 years, 48% were women), and the primary outcome analysis included 378 patients.
A total of 23 (12.3%) of 187 patients in the piperacillin-tazobactam group died by 30 days compared to 7 (3.7%) of 191 in the meropenem group (risk difference: 8.6%, P = .90 for noninferiority).
By day 4, 68% of the piperacillin-tazobactam group and 75% of the meropenem group achieved clinical and microbiological resolution.
Serious adverse effects other than death were rare, occurring in around 3% of the piperacillin-tazobactam group and nearly 2% of the meropenem group.
The researchers note various limitations, including the unblinded nature of the study and the fact that it’s not known if extended or continuous infusions of piperacillin-tazobactam would boost the drug’s effectiveness. They also note that delays resulted in some patients initially receiving treatment with one of the study’s two drugs before being randomized to the other.
The study authors caution that it’s not clear if newer beta-lactam/beta-lactamase inhibitors agents such as ceftolozane-tazobactam or ceftazidime-avibactam may be effective in this population.
The study was funded by the University of Queensland, Australian Society for Antimicrobials, International Society for Chemotherapy, and National University Hospital Singapore. Various organizations funded the researchers and the study’s whole-genome sequencing. The study authors report various disclosures, including funding from drugmakers such as Pfizer, maker of Zosyn (through its subsidiary Wyeth) and Merrem.
SOURCE: Harris PNA et al. JAMA 2018 Sep 11;320[10]:984-94. doi: 10.1001/jama.2018.12163.
A new study finds that piperacillin-tazobactam doesn’t improve mortality compared to meropenem in patients with ceftriaxone-resistant blood poisoning caused by E. coli or K. pneumoniae. The findings were so striking that the study was ended early.

Courtesy: JAMA
“These findings do not support use of piperacillin-tazobactam in this setting,” wrote the authors. The report was published Sept. 11 in JAMA (2018;320[10]:984-94.)
According to the Centers for Disease Control and Prevention, an estimated 1,700 deaths in the United States in 2011 were caused by gram-negative bacteria that produce extended-spectrum beta-lactamase enzymes.
While carbapenems such as meropenem (Merrem) are “regarded as the treatment of choice for serious infections,” the MERINO trial (NCT02176122) authors wrote, their rising use could lead to drug resistance.
One alternate option is to embrace beta-lactam/beta-lactamase inhibitors such as piperacillin-tazobactam (Zosyn), the researchers noted, but research has produced conflicting results.
Piperacillin-tazobactam is an injected penicillin antibiotic used to treat conditions such as severe pneumonia, complicated urinary tract infections and complicated skin and soft tissue infections.
For the new study, researchers led by Patrick N. A. Harris, MBBS, of the University of Queensland, randomly assigned 188 patients to intravenous piperacillin-tazobactam (4.5 g every 6 hours) and 191 patients to meropenem (1 g every 8 hours) for 4-14 days, depending on clinician’s preference. (12 other patients did not continue with the study after initial randomization due to factors such as errors).
All patients were adults and had at least one blood test showing they were positive for E. coli or K. pneumoniae. They all had to be nonsusceptible to ceftriaxone (Rocephin) but susceptible to piperacillin-tazobactam.
The study was ceased prior to enrollment because of the risk of harm. Interim findings suggested the study was unlikely to show higher effectiveness for piperacillin-tazobactam
The primary analysis included 379 patients (mean age 67 years, 48% were women), and the primary outcome analysis included 378 patients.
A total of 23 (12.3%) of 187 patients in the piperacillin-tazobactam group died by 30 days compared to 7 (3.7%) of 191 in the meropenem group (risk difference: 8.6%, P = .90 for noninferiority).
By day 4, 68% of the piperacillin-tazobactam group and 75% of the meropenem group achieved clinical and microbiological resolution.
Serious adverse effects other than death were rare, occurring in around 3% of the piperacillin-tazobactam group and nearly 2% of the meropenem group.
The researchers note various limitations, including the unblinded nature of the study and the fact that it’s not known if extended or continuous infusions of piperacillin-tazobactam would boost the drug’s effectiveness. They also note that delays resulted in some patients initially receiving treatment with one of the study’s two drugs before being randomized to the other.
The study authors caution that it’s not clear if newer beta-lactam/beta-lactamase inhibitors agents such as ceftolozane-tazobactam or ceftazidime-avibactam may be effective in this population.
The study was funded by the University of Queensland, Australian Society for Antimicrobials, International Society for Chemotherapy, and National University Hospital Singapore. Various organizations funded the researchers and the study’s whole-genome sequencing. The study authors report various disclosures, including funding from drugmakers such as Pfizer, maker of Zosyn (through its subsidiary Wyeth) and Merrem.
SOURCE: Harris PNA et al. JAMA 2018 Sep 11;320[10]:984-94. doi: 10.1001/jama.2018.12163.
FROM JAMA
Key clinical point: Piperacillin-tazobactam isn’t a superior alternative to meropenem in patients with ceftriaxone-resistant blood poisoning caused by E. coli or K. pneumoniae.
Major finding: By 30 days, 12% of patients in the piperacillin-tazobactam group died compared to 4% of the meropenem group.
Study details: Unblinded, randomized, noninferiority trial of 379 patients with bloodstream infection caused by ceftriaxone-nonsusceptible E. coli or K. pneumoniae who received piperacillin-tazobactam (n=188) or meropenem (n = 191).
Disclosures: The study was funded by the University of Queensland, Australian Society for Antimicrobials, International Society for Chemotherapy, and National University Hospital Singapore. Various organizations funded the researchers and the study’s whole-genome sequencing. The study authors report various disclosures.
Source: Harris PNA et al. JAMA 2018 Sep 11. doi: 10.1001/jama.2018.12163.
Plan to ‘Learn by Doing’ at the CHEST Annual Meeting 2018
Don’t miss the CHEST Annual Meeting 2018 in San Antonio, Oct 6-10. Watch as CHEST 2018 Program Chair David A. Schulman, MD, MPH, FCCP, walks you through the vision of this year’s meeting. View complete details at chestmeeting.chestnet.org.
Don’t miss the CHEST Annual Meeting 2018 in San Antonio, Oct 6-10. Watch as CHEST 2018 Program Chair David A. Schulman, MD, MPH, FCCP, walks you through the vision of this year’s meeting. View complete details at chestmeeting.chestnet.org.
Don’t miss the CHEST Annual Meeting 2018 in San Antonio, Oct 6-10. Watch as CHEST 2018 Program Chair David A. Schulman, MD, MPH, FCCP, walks you through the vision of this year’s meeting. View complete details at chestmeeting.chestnet.org.
Avatrombopag cut procedure-related transfusions in patients with thrombocytopenia, chronic liver disease
Once-daily treatment with the oral second-generation thrombopoietin agonist avatrombopag (Doptelet) significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures, according to the results of two international, randomized, double-blind, phase III, placebo-controlled trials reported in the September issue of Gastroenterology.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia, versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group, versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
These results led the Food and Drug Administration to approve avatrombopag in May 2018 under its priority review process. The novel therapy “may be a safe and effective alternative to platelet transfusions” that could simplify the clinical management of patients with chronic liver disease and thrombocytopenia, Norah Terrault, MD, MPH, and her associates wrote in Gastroenterology.
The ADAPT-1 study included 231 patients, while ADAPT-2 included 204 patients. In each trial, patients were randomized on a 2:1 basis to receive oral avatrombopag or placebo once daily for 5 consecutive days. Patients in the intervention arms received 60 mg avatrombopag if their baseline platelet count was less than 40 x 109 per liter, and 40 mg if their baseline platelet count was 40-50 x 109 per liter. Procedures were scheduled for 10-13 days after treatment initiation.
“Platelet counts increased by [treatment] day 4, peaked at days 10-13, and then returned to baseline levels by day 35,” the researchers reported. Among ADAPT-1 patients with low baseline counts, 69% of avatrombopag recipients reached a prespecified target of at least 50 x 109 platelets per liter on their procedure day, versus 4% of placebo recipients (P less than .0001). Corresponding proportions in ADAPT-2 were 67% and 7%, respectively (P less than .0001). Among patients with higher baseline counts, 88% and 20% achieved the target, respectively, in ADAPT-1 (P less than .0001), as did 93% versus 39%, respectively, in ADAPT-2 (P less than .0001).
Avatrombopag and placebo produced similar rates of treatment-emergent adverse events. These most often consisted of abdominal pain, dyspepsia, nausea, pyrexia, dizziness, and headache. Only three avatrombopag patients developed platelet counts above 200 x 109 per liter, and they all remained asymptomatic, the investigators said.
Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, Bristol-Myers Squibb, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
SOURCE: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
Thrombocytopenia in cirrhosis is frequent and multifactorial and includes sequestration in the spleen, reduced liver-derived thrombopoietin, bone marrow toxicity, and autoimmunity towards platelets. Severe thrombocytopenia (less than 50/nL) is rare in cirrhotic patients, but when it occurs may prevent required procedures from being performed or require platelet transfusions, which are associated with significant risks.
Previous attempts to increase platelets in cirrhotic patients with thrombopoietin agonists were halted because of increased frequency of portal vein thrombosis and hepatic decompensation.
Now avatrombopag has been specifically licensed with a 5-day regimen to increase platelets prior to elective interventions in severely thrombocytopenic (less than 50/nL) patients with chronic liver disease with a seemingly better safety profile than earlier treatments and good efficacy. The patient groups studied in the licensing trial had slightly milder but not significantly different liver disease, compared with those in the eltrombopag studies. The key difference was a pretreatment requirement of a portal vein flow of more than 10 cm/sec prior to enrollment, which likely reduced the risk of portal vein thrombosis. It is important that providers ready to use avatrombopag are aware of this.
Importantly, no data are currently available for patients with a Model for End-Stage Liver Disease score greater than 24, and very limited data are available for patients with Child B and Child C cirrhosis.
Given this limitation, careful judgment will be needed; a pretreatment portal vein flow may be advisable, though not a label requirement.
An observational study, NCT03554759, in patients with chronic liver disease and thrombocytopenia is ongoing and will further confirm the likely safety of avatrombopag.
Hans L. Tillmann, MD, is a clinical associate professor, East Carolina University, Greenville, and staff physician, Greenville (N.C.) VA Health Care Center. He has no relevant conflicts of interest.
Thrombocytopenia in cirrhosis is frequent and multifactorial and includes sequestration in the spleen, reduced liver-derived thrombopoietin, bone marrow toxicity, and autoimmunity towards platelets. Severe thrombocytopenia (less than 50/nL) is rare in cirrhotic patients, but when it occurs may prevent required procedures from being performed or require platelet transfusions, which are associated with significant risks.
Previous attempts to increase platelets in cirrhotic patients with thrombopoietin agonists were halted because of increased frequency of portal vein thrombosis and hepatic decompensation.
Now avatrombopag has been specifically licensed with a 5-day regimen to increase platelets prior to elective interventions in severely thrombocytopenic (less than 50/nL) patients with chronic liver disease with a seemingly better safety profile than earlier treatments and good efficacy. The patient groups studied in the licensing trial had slightly milder but not significantly different liver disease, compared with those in the eltrombopag studies. The key difference was a pretreatment requirement of a portal vein flow of more than 10 cm/sec prior to enrollment, which likely reduced the risk of portal vein thrombosis. It is important that providers ready to use avatrombopag are aware of this.
Importantly, no data are currently available for patients with a Model for End-Stage Liver Disease score greater than 24, and very limited data are available for patients with Child B and Child C cirrhosis.
Given this limitation, careful judgment will be needed; a pretreatment portal vein flow may be advisable, though not a label requirement.
An observational study, NCT03554759, in patients with chronic liver disease and thrombocytopenia is ongoing and will further confirm the likely safety of avatrombopag.
Hans L. Tillmann, MD, is a clinical associate professor, East Carolina University, Greenville, and staff physician, Greenville (N.C.) VA Health Care Center. He has no relevant conflicts of interest.
Thrombocytopenia in cirrhosis is frequent and multifactorial and includes sequestration in the spleen, reduced liver-derived thrombopoietin, bone marrow toxicity, and autoimmunity towards platelets. Severe thrombocytopenia (less than 50/nL) is rare in cirrhotic patients, but when it occurs may prevent required procedures from being performed or require platelet transfusions, which are associated with significant risks.
Previous attempts to increase platelets in cirrhotic patients with thrombopoietin agonists were halted because of increased frequency of portal vein thrombosis and hepatic decompensation.
Now avatrombopag has been specifically licensed with a 5-day regimen to increase platelets prior to elective interventions in severely thrombocytopenic (less than 50/nL) patients with chronic liver disease with a seemingly better safety profile than earlier treatments and good efficacy. The patient groups studied in the licensing trial had slightly milder but not significantly different liver disease, compared with those in the eltrombopag studies. The key difference was a pretreatment requirement of a portal vein flow of more than 10 cm/sec prior to enrollment, which likely reduced the risk of portal vein thrombosis. It is important that providers ready to use avatrombopag are aware of this.
Importantly, no data are currently available for patients with a Model for End-Stage Liver Disease score greater than 24, and very limited data are available for patients with Child B and Child C cirrhosis.
Given this limitation, careful judgment will be needed; a pretreatment portal vein flow may be advisable, though not a label requirement.
An observational study, NCT03554759, in patients with chronic liver disease and thrombocytopenia is ongoing and will further confirm the likely safety of avatrombopag.
Hans L. Tillmann, MD, is a clinical associate professor, East Carolina University, Greenville, and staff physician, Greenville (N.C.) VA Health Care Center. He has no relevant conflicts of interest.
Once-daily treatment with the oral second-generation thrombopoietin agonist avatrombopag (Doptelet) significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures, according to the results of two international, randomized, double-blind, phase III, placebo-controlled trials reported in the September issue of Gastroenterology.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia, versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group, versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
These results led the Food and Drug Administration to approve avatrombopag in May 2018 under its priority review process. The novel therapy “may be a safe and effective alternative to platelet transfusions” that could simplify the clinical management of patients with chronic liver disease and thrombocytopenia, Norah Terrault, MD, MPH, and her associates wrote in Gastroenterology.
The ADAPT-1 study included 231 patients, while ADAPT-2 included 204 patients. In each trial, patients were randomized on a 2:1 basis to receive oral avatrombopag or placebo once daily for 5 consecutive days. Patients in the intervention arms received 60 mg avatrombopag if their baseline platelet count was less than 40 x 109 per liter, and 40 mg if their baseline platelet count was 40-50 x 109 per liter. Procedures were scheduled for 10-13 days after treatment initiation.
“Platelet counts increased by [treatment] day 4, peaked at days 10-13, and then returned to baseline levels by day 35,” the researchers reported. Among ADAPT-1 patients with low baseline counts, 69% of avatrombopag recipients reached a prespecified target of at least 50 x 109 platelets per liter on their procedure day, versus 4% of placebo recipients (P less than .0001). Corresponding proportions in ADAPT-2 were 67% and 7%, respectively (P less than .0001). Among patients with higher baseline counts, 88% and 20% achieved the target, respectively, in ADAPT-1 (P less than .0001), as did 93% versus 39%, respectively, in ADAPT-2 (P less than .0001).
Avatrombopag and placebo produced similar rates of treatment-emergent adverse events. These most often consisted of abdominal pain, dyspepsia, nausea, pyrexia, dizziness, and headache. Only three avatrombopag patients developed platelet counts above 200 x 109 per liter, and they all remained asymptomatic, the investigators said.
Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, Bristol-Myers Squibb, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
SOURCE: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
Once-daily treatment with the oral second-generation thrombopoietin agonist avatrombopag (Doptelet) significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures, according to the results of two international, randomized, double-blind, phase III, placebo-controlled trials reported in the September issue of Gastroenterology.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia, versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group, versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
These results led the Food and Drug Administration to approve avatrombopag in May 2018 under its priority review process. The novel therapy “may be a safe and effective alternative to platelet transfusions” that could simplify the clinical management of patients with chronic liver disease and thrombocytopenia, Norah Terrault, MD, MPH, and her associates wrote in Gastroenterology.
The ADAPT-1 study included 231 patients, while ADAPT-2 included 204 patients. In each trial, patients were randomized on a 2:1 basis to receive oral avatrombopag or placebo once daily for 5 consecutive days. Patients in the intervention arms received 60 mg avatrombopag if their baseline platelet count was less than 40 x 109 per liter, and 40 mg if their baseline platelet count was 40-50 x 109 per liter. Procedures were scheduled for 10-13 days after treatment initiation.
“Platelet counts increased by [treatment] day 4, peaked at days 10-13, and then returned to baseline levels by day 35,” the researchers reported. Among ADAPT-1 patients with low baseline counts, 69% of avatrombopag recipients reached a prespecified target of at least 50 x 109 platelets per liter on their procedure day, versus 4% of placebo recipients (P less than .0001). Corresponding proportions in ADAPT-2 were 67% and 7%, respectively (P less than .0001). Among patients with higher baseline counts, 88% and 20% achieved the target, respectively, in ADAPT-1 (P less than .0001), as did 93% versus 39%, respectively, in ADAPT-2 (P less than .0001).
Avatrombopag and placebo produced similar rates of treatment-emergent adverse events. These most often consisted of abdominal pain, dyspepsia, nausea, pyrexia, dizziness, and headache. Only three avatrombopag patients developed platelet counts above 200 x 109 per liter, and they all remained asymptomatic, the investigators said.
Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, Bristol-Myers Squibb, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
SOURCE: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
FROM GASTROENTEROLOGY
Key clinical point: Once-daily treatment with oral avatrombopag significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures.
Major finding: In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
Study details: ADAPT-1 and ADAPT-2, international, randomized, double-blind, placebo-controlled, phase III trials.
Disclosures: Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, BMS, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
Source: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
ASCEND: Aspirin, fish oil flop in diabetes
MUNICH – In a double blow to the current, widespread routine use of low-dose aspirin and fish oil supplements for primary cardiovascular prevention in patients with diabetes, neither treatment provided any net clinical benefit in the massive, long-term ASCEND study, investigators reported at the annual congress of the European Society of Cardiology.
And, in yet another bitter pill to swallow, low-dose aspirin failed to reduce the incidence of GI cancer or any other type of cancer, compared with placebo in the study. Earlier, nondefinitive meta-analyses of much smaller randomized trials had raised the possibility of a roughly 30% reduction in the incidence of colorectal cancer in long-time users, said Jane Armitage, MD, professor of clinical trials and epidemiology at the University of Oxford (England).
“We saw no suggestion of an anticancer effect emerging over time,” Dr. Armitage said. “We did see a significant reduction in the risk of vascular events but also an increase in major bleeding such that the absolute benefits from avoiding a serious vascular event were largely counterbalanced by increased risk of bleeding. And there was no subgroup in which we could clearly define that the benefit outweighs the risk,” she added in a video interview.
ASCEND (A Study of Cardiovascular Events in Diabetes) was a randomized, blinded trial in which 15,480 U.K. patients with diabetes and no known cardiovascular disease were placed on 100 mg/day of enteric-coated aspirin or placebo and 1 g/day of omega-3 fatty acids in capsule form or placebo in a 2 x 2 factorial design and followed prospectively for a mean of 7.4 years.
The study was undertaken because, even though the value of low-dose aspirin for secondary prevention is supported by strong evidence, the medication’s value for primary prevention in patients with diabetes has long been uncertain. American Diabetes Association guidelines give a Grade C recommendation to consideration of low-dose aspirin as a primary prevention strategy in patients with diabetes having a 10-year cardiovascular risk estimated at 10% or greater.
The primary efficacy endpoint in ASCEND was the occurrence of a first serious vascular event, defined as MI, stroke, transient ischemic attack, or death from any vascular cause other than intracranial hemorrhage. The rate was 8.5% in the aspirin group and 9.6% with placebo, for a statistically significant 12% relative risk reduction. However, the rate of the primary composite safety endpoint, comprising intracranial hemorrhage, GI bleeding, sight-threatening bleeding in the eye, or other bleeding serious enough to entail a trip to the hospital, was 4.1% in the aspirin group and 3.2% with placebo, a 29% increase in risk.
Aspirin reduced the absolute risk of a serious vascular event by 1.1%, compared with placebo, while boosting the risk of major bleeding by an absolute 0.9% – essentially a wash. The number needed to treat to avoid a serious vascular event was 91 patients, with 112 being the number needed to cause a major bleeding event. The risk of major bleeding rose with increasing baseline 5-year vascular event risk.
ASCEND provided no support for a recent report suggesting the benefit of low-dose aspirin for cardioprotection is largely confined to individuals weighing less than 70 kg (Lancet. 2018; 392:387-99); in fact, the opposite appeared to be true, according to Dr. Armitage.
The incidence of cancer of the GI tract was 2.0% in both study arms. The overall cancer rate was 11.6% in the aspirin arm and 11.5% with placebo. Additional follow-up focused on cancer is planned for 5 and 10 years after the end of ASCEND in order to examine the possibility of a delayed anticancer effect, she added.
Dr. Armitage said one reason aspirin may have failed to show a significant net benefit was the high rate of background cardioprotective medication usage, especially statins and antihypertensive drugs.
“I think if your diabetes is well managed and you’ve got your other risk factors under control, you have to consider very carefully whether or not, for you, the benefits of aspirin outweigh the risks,” she concluded.
Cardiologists respond
ASCEND’s two designated discussants, both cardiologists, took a more positive view of the results than Dr. Armitage, who isn’t a cardiologist.
Sigrun Halvorsen, MD, professor of cardiology at the University of Oslo, noted that most ASCEND participants were at relatively low cardiovascular risk, with an event rate of about 1.3% per year. She indicated that she’d like to see more data on higher-risk individuals before excluding any role for aspirin in primary cardiovascular prevention in patients with diabetes.
“Serious vascular events and bleeding are not necessarily equally weighted,” she added. “Most major bleeds in ASCEND were GI bleeds, and these can be largely prevented by PPIs [proton pump inhibitors], in contrast to death and stroke, which are irreversible events.”
“I think this study could be interpreted more favorably,” agreed Christopher P. Cannon, MD, professor of medicine at Harvard Medical School, Boston. “Bleeds are reversible, but MIs and whatnot are not.”
Fish oil flounders in ASCEND
Louise Bowman, MD, also at the University of Oxford, presented the ASCEND fish oil findings. Over an average of 7.4 years, omega-3 fatty acid supplementation had no effect on the rate of serious vascular events, no effect on cancer, no impact on all-cause or cause-specific mortality, and raised no safety issues in patients with diabetes. She argued that current guidelines recommending fish oil supplements for cardiovascular prevention should be reconsidered.
“Certainly there doesn’t seem to be any justification for the use of this dose of omega-3 fatty acids – 1 g/day – for the prevention of cardiovascular disease,” Dr. Bowman said.
However, Dr. Cannon saw a sliver of hope within the ASCEND findings. One component of the serious vascular event composite endpoint – vascular death – occurred in 2.4% of the fish oil group and 2.9% of placebo-treated controls, for a statistically significant 19% relative risk reduction. It could be a fluke, given that none of the other vascular endpoints followed suit. But physicians and patients won’t have to wait long to find out. Another randomized trial of low-dose fish oil supplements for primary cardiovascular prevention – the nearly 26,000-patient VITAL trial – is due to report later in 2018.
In addition, two major, randomized trials of higher-dose fish oil supplementation for secondary prevention are ongoing. The roughly 8,000-patient REDUCE-IT trial is expected to report results later this year, and the STRENGTH trial, featuring more than 13,000 patients, should be completed in 2020. Both studies are heavily loaded with diabetes patients, Dr. Cannon noted.
Simultaneous with presentation of the ASCEND results at the ESC congress, the study was published online at the New England Journal of Medicine website (doi: 10.1056/NEJMoa1804988 and doi: 10.1056/NEJMoa1804989).
The ASCEND study was funded by the British Heart Foundation and the U.K. Medical Research Council with support provided by Abbott Laboratories, Bayer, Mylan, and Solvay. Dr. Armitage and Dr. Bowman reported receiving research grants from the Medicines Company, Bayer, and Mylan. Dr. Halvorsen reported no financial conflicts. Dr. Cannon reported serving as a consultant to roughly a dozen pharmaceutical companies, including the Amarin Corporation, which markets a fish oil supplement and sponsored the REDUCE-IT trial.
MUNICH – In a double blow to the current, widespread routine use of low-dose aspirin and fish oil supplements for primary cardiovascular prevention in patients with diabetes, neither treatment provided any net clinical benefit in the massive, long-term ASCEND study, investigators reported at the annual congress of the European Society of Cardiology.
And, in yet another bitter pill to swallow, low-dose aspirin failed to reduce the incidence of GI cancer or any other type of cancer, compared with placebo in the study. Earlier, nondefinitive meta-analyses of much smaller randomized trials had raised the possibility of a roughly 30% reduction in the incidence of colorectal cancer in long-time users, said Jane Armitage, MD, professor of clinical trials and epidemiology at the University of Oxford (England).
“We saw no suggestion of an anticancer effect emerging over time,” Dr. Armitage said. “We did see a significant reduction in the risk of vascular events but also an increase in major bleeding such that the absolute benefits from avoiding a serious vascular event were largely counterbalanced by increased risk of bleeding. And there was no subgroup in which we could clearly define that the benefit outweighs the risk,” she added in a video interview.
ASCEND (A Study of Cardiovascular Events in Diabetes) was a randomized, blinded trial in which 15,480 U.K. patients with diabetes and no known cardiovascular disease were placed on 100 mg/day of enteric-coated aspirin or placebo and 1 g/day of omega-3 fatty acids in capsule form or placebo in a 2 x 2 factorial design and followed prospectively for a mean of 7.4 years.
The study was undertaken because, even though the value of low-dose aspirin for secondary prevention is supported by strong evidence, the medication’s value for primary prevention in patients with diabetes has long been uncertain. American Diabetes Association guidelines give a Grade C recommendation to consideration of low-dose aspirin as a primary prevention strategy in patients with diabetes having a 10-year cardiovascular risk estimated at 10% or greater.
The primary efficacy endpoint in ASCEND was the occurrence of a first serious vascular event, defined as MI, stroke, transient ischemic attack, or death from any vascular cause other than intracranial hemorrhage. The rate was 8.5% in the aspirin group and 9.6% with placebo, for a statistically significant 12% relative risk reduction. However, the rate of the primary composite safety endpoint, comprising intracranial hemorrhage, GI bleeding, sight-threatening bleeding in the eye, or other bleeding serious enough to entail a trip to the hospital, was 4.1% in the aspirin group and 3.2% with placebo, a 29% increase in risk.
Aspirin reduced the absolute risk of a serious vascular event by 1.1%, compared with placebo, while boosting the risk of major bleeding by an absolute 0.9% – essentially a wash. The number needed to treat to avoid a serious vascular event was 91 patients, with 112 being the number needed to cause a major bleeding event. The risk of major bleeding rose with increasing baseline 5-year vascular event risk.
ASCEND provided no support for a recent report suggesting the benefit of low-dose aspirin for cardioprotection is largely confined to individuals weighing less than 70 kg (Lancet. 2018; 392:387-99); in fact, the opposite appeared to be true, according to Dr. Armitage.
The incidence of cancer of the GI tract was 2.0% in both study arms. The overall cancer rate was 11.6% in the aspirin arm and 11.5% with placebo. Additional follow-up focused on cancer is planned for 5 and 10 years after the end of ASCEND in order to examine the possibility of a delayed anticancer effect, she added.
Dr. Armitage said one reason aspirin may have failed to show a significant net benefit was the high rate of background cardioprotective medication usage, especially statins and antihypertensive drugs.
“I think if your diabetes is well managed and you’ve got your other risk factors under control, you have to consider very carefully whether or not, for you, the benefits of aspirin outweigh the risks,” she concluded.
Cardiologists respond
ASCEND’s two designated discussants, both cardiologists, took a more positive view of the results than Dr. Armitage, who isn’t a cardiologist.
Sigrun Halvorsen, MD, professor of cardiology at the University of Oslo, noted that most ASCEND participants were at relatively low cardiovascular risk, with an event rate of about 1.3% per year. She indicated that she’d like to see more data on higher-risk individuals before excluding any role for aspirin in primary cardiovascular prevention in patients with diabetes.
“Serious vascular events and bleeding are not necessarily equally weighted,” she added. “Most major bleeds in ASCEND were GI bleeds, and these can be largely prevented by PPIs [proton pump inhibitors], in contrast to death and stroke, which are irreversible events.”
“I think this study could be interpreted more favorably,” agreed Christopher P. Cannon, MD, professor of medicine at Harvard Medical School, Boston. “Bleeds are reversible, but MIs and whatnot are not.”
Fish oil flounders in ASCEND
Louise Bowman, MD, also at the University of Oxford, presented the ASCEND fish oil findings. Over an average of 7.4 years, omega-3 fatty acid supplementation had no effect on the rate of serious vascular events, no effect on cancer, no impact on all-cause or cause-specific mortality, and raised no safety issues in patients with diabetes. She argued that current guidelines recommending fish oil supplements for cardiovascular prevention should be reconsidered.
“Certainly there doesn’t seem to be any justification for the use of this dose of omega-3 fatty acids – 1 g/day – for the prevention of cardiovascular disease,” Dr. Bowman said.
However, Dr. Cannon saw a sliver of hope within the ASCEND findings. One component of the serious vascular event composite endpoint – vascular death – occurred in 2.4% of the fish oil group and 2.9% of placebo-treated controls, for a statistically significant 19% relative risk reduction. It could be a fluke, given that none of the other vascular endpoints followed suit. But physicians and patients won’t have to wait long to find out. Another randomized trial of low-dose fish oil supplements for primary cardiovascular prevention – the nearly 26,000-patient VITAL trial – is due to report later in 2018.
In addition, two major, randomized trials of higher-dose fish oil supplementation for secondary prevention are ongoing. The roughly 8,000-patient REDUCE-IT trial is expected to report results later this year, and the STRENGTH trial, featuring more than 13,000 patients, should be completed in 2020. Both studies are heavily loaded with diabetes patients, Dr. Cannon noted.
Simultaneous with presentation of the ASCEND results at the ESC congress, the study was published online at the New England Journal of Medicine website (doi: 10.1056/NEJMoa1804988 and doi: 10.1056/NEJMoa1804989).
The ASCEND study was funded by the British Heart Foundation and the U.K. Medical Research Council with support provided by Abbott Laboratories, Bayer, Mylan, and Solvay. Dr. Armitage and Dr. Bowman reported receiving research grants from the Medicines Company, Bayer, and Mylan. Dr. Halvorsen reported no financial conflicts. Dr. Cannon reported serving as a consultant to roughly a dozen pharmaceutical companies, including the Amarin Corporation, which markets a fish oil supplement and sponsored the REDUCE-IT trial.
MUNICH – In a double blow to the current, widespread routine use of low-dose aspirin and fish oil supplements for primary cardiovascular prevention in patients with diabetes, neither treatment provided any net clinical benefit in the massive, long-term ASCEND study, investigators reported at the annual congress of the European Society of Cardiology.
And, in yet another bitter pill to swallow, low-dose aspirin failed to reduce the incidence of GI cancer or any other type of cancer, compared with placebo in the study. Earlier, nondefinitive meta-analyses of much smaller randomized trials had raised the possibility of a roughly 30% reduction in the incidence of colorectal cancer in long-time users, said Jane Armitage, MD, professor of clinical trials and epidemiology at the University of Oxford (England).
“We saw no suggestion of an anticancer effect emerging over time,” Dr. Armitage said. “We did see a significant reduction in the risk of vascular events but also an increase in major bleeding such that the absolute benefits from avoiding a serious vascular event were largely counterbalanced by increased risk of bleeding. And there was no subgroup in which we could clearly define that the benefit outweighs the risk,” she added in a video interview.
ASCEND (A Study of Cardiovascular Events in Diabetes) was a randomized, blinded trial in which 15,480 U.K. patients with diabetes and no known cardiovascular disease were placed on 100 mg/day of enteric-coated aspirin or placebo and 1 g/day of omega-3 fatty acids in capsule form or placebo in a 2 x 2 factorial design and followed prospectively for a mean of 7.4 years.
The study was undertaken because, even though the value of low-dose aspirin for secondary prevention is supported by strong evidence, the medication’s value for primary prevention in patients with diabetes has long been uncertain. American Diabetes Association guidelines give a Grade C recommendation to consideration of low-dose aspirin as a primary prevention strategy in patients with diabetes having a 10-year cardiovascular risk estimated at 10% or greater.
The primary efficacy endpoint in ASCEND was the occurrence of a first serious vascular event, defined as MI, stroke, transient ischemic attack, or death from any vascular cause other than intracranial hemorrhage. The rate was 8.5% in the aspirin group and 9.6% with placebo, for a statistically significant 12% relative risk reduction. However, the rate of the primary composite safety endpoint, comprising intracranial hemorrhage, GI bleeding, sight-threatening bleeding in the eye, or other bleeding serious enough to entail a trip to the hospital, was 4.1% in the aspirin group and 3.2% with placebo, a 29% increase in risk.
Aspirin reduced the absolute risk of a serious vascular event by 1.1%, compared with placebo, while boosting the risk of major bleeding by an absolute 0.9% – essentially a wash. The number needed to treat to avoid a serious vascular event was 91 patients, with 112 being the number needed to cause a major bleeding event. The risk of major bleeding rose with increasing baseline 5-year vascular event risk.
ASCEND provided no support for a recent report suggesting the benefit of low-dose aspirin for cardioprotection is largely confined to individuals weighing less than 70 kg (Lancet. 2018; 392:387-99); in fact, the opposite appeared to be true, according to Dr. Armitage.
The incidence of cancer of the GI tract was 2.0% in both study arms. The overall cancer rate was 11.6% in the aspirin arm and 11.5% with placebo. Additional follow-up focused on cancer is planned for 5 and 10 years after the end of ASCEND in order to examine the possibility of a delayed anticancer effect, she added.
Dr. Armitage said one reason aspirin may have failed to show a significant net benefit was the high rate of background cardioprotective medication usage, especially statins and antihypertensive drugs.
“I think if your diabetes is well managed and you’ve got your other risk factors under control, you have to consider very carefully whether or not, for you, the benefits of aspirin outweigh the risks,” she concluded.
Cardiologists respond
ASCEND’s two designated discussants, both cardiologists, took a more positive view of the results than Dr. Armitage, who isn’t a cardiologist.
Sigrun Halvorsen, MD, professor of cardiology at the University of Oslo, noted that most ASCEND participants were at relatively low cardiovascular risk, with an event rate of about 1.3% per year. She indicated that she’d like to see more data on higher-risk individuals before excluding any role for aspirin in primary cardiovascular prevention in patients with diabetes.
“Serious vascular events and bleeding are not necessarily equally weighted,” she added. “Most major bleeds in ASCEND were GI bleeds, and these can be largely prevented by PPIs [proton pump inhibitors], in contrast to death and stroke, which are irreversible events.”
“I think this study could be interpreted more favorably,” agreed Christopher P. Cannon, MD, professor of medicine at Harvard Medical School, Boston. “Bleeds are reversible, but MIs and whatnot are not.”
Fish oil flounders in ASCEND
Louise Bowman, MD, also at the University of Oxford, presented the ASCEND fish oil findings. Over an average of 7.4 years, omega-3 fatty acid supplementation had no effect on the rate of serious vascular events, no effect on cancer, no impact on all-cause or cause-specific mortality, and raised no safety issues in patients with diabetes. She argued that current guidelines recommending fish oil supplements for cardiovascular prevention should be reconsidered.
“Certainly there doesn’t seem to be any justification for the use of this dose of omega-3 fatty acids – 1 g/day – for the prevention of cardiovascular disease,” Dr. Bowman said.
However, Dr. Cannon saw a sliver of hope within the ASCEND findings. One component of the serious vascular event composite endpoint – vascular death – occurred in 2.4% of the fish oil group and 2.9% of placebo-treated controls, for a statistically significant 19% relative risk reduction. It could be a fluke, given that none of the other vascular endpoints followed suit. But physicians and patients won’t have to wait long to find out. Another randomized trial of low-dose fish oil supplements for primary cardiovascular prevention – the nearly 26,000-patient VITAL trial – is due to report later in 2018.
In addition, two major, randomized trials of higher-dose fish oil supplementation for secondary prevention are ongoing. The roughly 8,000-patient REDUCE-IT trial is expected to report results later this year, and the STRENGTH trial, featuring more than 13,000 patients, should be completed in 2020. Both studies are heavily loaded with diabetes patients, Dr. Cannon noted.
Simultaneous with presentation of the ASCEND results at the ESC congress, the study was published online at the New England Journal of Medicine website (doi: 10.1056/NEJMoa1804988 and doi: 10.1056/NEJMoa1804989).
The ASCEND study was funded by the British Heart Foundation and the U.K. Medical Research Council with support provided by Abbott Laboratories, Bayer, Mylan, and Solvay. Dr. Armitage and Dr. Bowman reported receiving research grants from the Medicines Company, Bayer, and Mylan. Dr. Halvorsen reported no financial conflicts. Dr. Cannon reported serving as a consultant to roughly a dozen pharmaceutical companies, including the Amarin Corporation, which markets a fish oil supplement and sponsored the REDUCE-IT trial.
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point:
Major finding: Low-dose aspirin reduced the risk of serious vascular events by 12% versus placebo, but boosted major bleeding events by 29%.
Study details: This prospective, randomized trial included 15,480 patients with diabetes without known cardiovascular disease who were randomized to 100 mg/day of enteric-coated aspirin or placebo and 1 g/day of omega-3 fatty acids or placebo and followed for a mean of 7.4 years.
Disclosures: The study was funded by the British Heart Foundation and the U.K. Medical Research Council with support provided by Abbott Laboratories, Bayer, Mylan, and Solvay. The presenters reported receiving research grants from the Medicines Company, Bayer, and Mylan.
Lorcaserin shows CV safety in CAMELLIA-TIMI 61
MUNICH – Lorcaserin is the first weight-loss drug proven to have cardiovascular safety, Erin A. Bohula, MD, DPhil, told Mitchel L. Zoler in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bohula reported on the results of the CAMELLIA-TIMI 61 trial, which was designed to evaluate the cardiovascular safety of the weight-loss drug lorcaserin in more than 10,000 patients. She presented the data at the annual congress of the European Society of Cardiology.
In CAMELLIA-TIMI 61, the primary safety endpoint, a composite of cardiovascular death, MI, or stroke, was nearly identical between patients on lorcaserin and those given placebo, 2% and 2.1% per year, at P less than .001 for noninferiority. Similarly, the primary efficacy outcome comprising heart failure, hospitalization for unstable angina, and coronary revascularization, was very close between the treated and placebo patients, occurring in 4.1% and 4.2% per year, respectively.
In addition, “there was a sustained weight loss, more than with lifestyle alone or lifestyle plus placebo, which at its peak was about 3 kg. With that there were small, but significant, reductions in heart rate, blood pressure, triglycerides, and hemoglobin A1c, and there was a significant reduction in new-onset diabetes.”
“Overall, there’s not a lot of use of pharmacologic agents for weight loss in the United States, and a lot of that is based on fear of the historical experience, which is that they were not safe. I suspect that having a drug that is proven safe will now lead people to reach for a pharmacologic agent like lorcaserin,” said Dr. Bohula, a cardiologist at of Brigham and Women’s Hospital and an investigator at the TIMI study group.
MUNICH – Lorcaserin is the first weight-loss drug proven to have cardiovascular safety, Erin A. Bohula, MD, DPhil, told Mitchel L. Zoler in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bohula reported on the results of the CAMELLIA-TIMI 61 trial, which was designed to evaluate the cardiovascular safety of the weight-loss drug lorcaserin in more than 10,000 patients. She presented the data at the annual congress of the European Society of Cardiology.
In CAMELLIA-TIMI 61, the primary safety endpoint, a composite of cardiovascular death, MI, or stroke, was nearly identical between patients on lorcaserin and those given placebo, 2% and 2.1% per year, at P less than .001 for noninferiority. Similarly, the primary efficacy outcome comprising heart failure, hospitalization for unstable angina, and coronary revascularization, was very close between the treated and placebo patients, occurring in 4.1% and 4.2% per year, respectively.
In addition, “there was a sustained weight loss, more than with lifestyle alone or lifestyle plus placebo, which at its peak was about 3 kg. With that there were small, but significant, reductions in heart rate, blood pressure, triglycerides, and hemoglobin A1c, and there was a significant reduction in new-onset diabetes.”
“Overall, there’s not a lot of use of pharmacologic agents for weight loss in the United States, and a lot of that is based on fear of the historical experience, which is that they were not safe. I suspect that having a drug that is proven safe will now lead people to reach for a pharmacologic agent like lorcaserin,” said Dr. Bohula, a cardiologist at of Brigham and Women’s Hospital and an investigator at the TIMI study group.
MUNICH – Lorcaserin is the first weight-loss drug proven to have cardiovascular safety, Erin A. Bohula, MD, DPhil, told Mitchel L. Zoler in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bohula reported on the results of the CAMELLIA-TIMI 61 trial, which was designed to evaluate the cardiovascular safety of the weight-loss drug lorcaserin in more than 10,000 patients. She presented the data at the annual congress of the European Society of Cardiology.
In CAMELLIA-TIMI 61, the primary safety endpoint, a composite of cardiovascular death, MI, or stroke, was nearly identical between patients on lorcaserin and those given placebo, 2% and 2.1% per year, at P less than .001 for noninferiority. Similarly, the primary efficacy outcome comprising heart failure, hospitalization for unstable angina, and coronary revascularization, was very close between the treated and placebo patients, occurring in 4.1% and 4.2% per year, respectively.
In addition, “there was a sustained weight loss, more than with lifestyle alone or lifestyle plus placebo, which at its peak was about 3 kg. With that there were small, but significant, reductions in heart rate, blood pressure, triglycerides, and hemoglobin A1c, and there was a significant reduction in new-onset diabetes.”
“Overall, there’s not a lot of use of pharmacologic agents for weight loss in the United States, and a lot of that is based on fear of the historical experience, which is that they were not safe. I suspect that having a drug that is proven safe will now lead people to reach for a pharmacologic agent like lorcaserin,” said Dr. Bohula, a cardiologist at of Brigham and Women’s Hospital and an investigator at the TIMI study group.
Lorcaserin shows CV safety in CAMELLIA-TIMI 61
Erin A. Bohula, MD, DPhil, told Mitchel L. Zoler in an interview.
Dr. Bohula reported on the results of the CAMELLIA-TIMI 61 trial, which was designed to evaluate the cardiovascular safety of the weight-loss drug lorcaserin in more than 10,000 patients. She presented the data at the annual congress of the European Society of Cardiology.
In CAMELLIA-TIMI 61, the primary safety endpoint, a composite of cardiovascular death, MI, or stroke, was nearly identical between patients on lorcaserin and those given placebo, 2% and 2.1% per year, at P less than .001 for noninferiority. Similarly, the primary efficacy outcome comprising heart failure, hospitalization for unstable angina, and coronary revascularization, was very close between the treated and placebo patients, occurring in 4.1% and 4.2% per year, respectively.
In addition, “there was a sustained weight loss, more than with lifestyle alone or lifestyle plus placebo, which at its peak was about 3 kg. With that there were small, but significant, reductions in heart rate, blood pressure, triglycerides, and hemoglobin A1c, and there was a significant reduction in new-onset diabetes.”
“Overall, there’s not a lot of use of pharmacologic agents for weight loss in the United States, and a lot of that is based on fear of the historical experience, which is that they were not safe. I suspect that having a drug that is proven safe will now lead people to reach for a pharmacologic agent like lorcaserin,” said Dr. Bohula, a cardiologist at of Brigham and Women’s Hospital and an investigator at the TIMI study group.
The AGA Obesity Practice Guide provides physicians with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at https://www.gastro.org/practice-guidance/practice-updates/obesity-practice-guide.
Erin A. Bohula, MD, DPhil, told Mitchel L. Zoler in an interview.
Dr. Bohula reported on the results of the CAMELLIA-TIMI 61 trial, which was designed to evaluate the cardiovascular safety of the weight-loss drug lorcaserin in more than 10,000 patients. She presented the data at the annual congress of the European Society of Cardiology.
In CAMELLIA-TIMI 61, the primary safety endpoint, a composite of cardiovascular death, MI, or stroke, was nearly identical between patients on lorcaserin and those given placebo, 2% and 2.1% per year, at P less than .001 for noninferiority. Similarly, the primary efficacy outcome comprising heart failure, hospitalization for unstable angina, and coronary revascularization, was very close between the treated and placebo patients, occurring in 4.1% and 4.2% per year, respectively.
In addition, “there was a sustained weight loss, more than with lifestyle alone or lifestyle plus placebo, which at its peak was about 3 kg. With that there were small, but significant, reductions in heart rate, blood pressure, triglycerides, and hemoglobin A1c, and there was a significant reduction in new-onset diabetes.”
“Overall, there’s not a lot of use of pharmacologic agents for weight loss in the United States, and a lot of that is based on fear of the historical experience, which is that they were not safe. I suspect that having a drug that is proven safe will now lead people to reach for a pharmacologic agent like lorcaserin,” said Dr. Bohula, a cardiologist at of Brigham and Women’s Hospital and an investigator at the TIMI study group.
The AGA Obesity Practice Guide provides physicians with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at https://www.gastro.org/practice-guidance/practice-updates/obesity-practice-guide.
Erin A. Bohula, MD, DPhil, told Mitchel L. Zoler in an interview.
Dr. Bohula reported on the results of the CAMELLIA-TIMI 61 trial, which was designed to evaluate the cardiovascular safety of the weight-loss drug lorcaserin in more than 10,000 patients. She presented the data at the annual congress of the European Society of Cardiology.
In CAMELLIA-TIMI 61, the primary safety endpoint, a composite of cardiovascular death, MI, or stroke, was nearly identical between patients on lorcaserin and those given placebo, 2% and 2.1% per year, at P less than .001 for noninferiority. Similarly, the primary efficacy outcome comprising heart failure, hospitalization for unstable angina, and coronary revascularization, was very close between the treated and placebo patients, occurring in 4.1% and 4.2% per year, respectively.
In addition, “there was a sustained weight loss, more than with lifestyle alone or lifestyle plus placebo, which at its peak was about 3 kg. With that there were small, but significant, reductions in heart rate, blood pressure, triglycerides, and hemoglobin A1c, and there was a significant reduction in new-onset diabetes.”
“Overall, there’s not a lot of use of pharmacologic agents for weight loss in the United States, and a lot of that is based on fear of the historical experience, which is that they were not safe. I suspect that having a drug that is proven safe will now lead people to reach for a pharmacologic agent like lorcaserin,” said Dr. Bohula, a cardiologist at of Brigham and Women’s Hospital and an investigator at the TIMI study group.
The AGA Obesity Practice Guide provides physicians with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at https://www.gastro.org/practice-guidance/practice-updates/obesity-practice-guide.
REPORTING FROM THE ESC CONGRESS 2018