User login
HFSA: Next-generation LVAD meets survival goal
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: A next-generation left ventricular assist device, HeartMate 3, met its 6-month survival goal to receive CE mark approval in Europe.
Major finding: The advanced heart failure patients who received the HeartMate 3 LVAD had a 92% survival rate after 6 months.
Data source: A prospective series of 50 patients enrolled at 10 centers in six countries.
Disclosures: The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
Lives saved with lower systolic BP: SPRINT trial
Deaths were reduced by nearly one-quarter when systolic blood pressure was treated to a target of 120 rather than 140 mm Hg, according to a large NIH-sponsored study comparing standard blood pressure treatment with more-intensive lowering of systolic blood pressure. The lower blood pressure group also saw a 30% reduction in the composite primary composite endpoint of cardiovascular events, stroke, and cardiovascular death.
The magnitude of the effect of the lower blood pressure target prompted the study’s data safety monitoring board to end the study early, said officials from several National Institutes of Health agencies at a telebriefing. The study was unblinded in August 2015, and a full report of the primary outcome measures will come in a paper due out by the end of the year, they said.
The Systolic Blood Pressure Intervention Trial, or SPRINT, is a 100-site trial that enrolled more than 9,300 people in the United States and Puerto Rico aged at least 50 years with high blood pressure and at risk for cardiovascular disease; those with diabetes were excluded. Patients were randomized to a standard treatment target of 140 mm Hg or less, or to a more intensive 120 mm Hg.
SPRINT participants received evidence-based treatment with a variety of antihypertensives, with the intervention arm requiring an average of almost three medications, compared with just under two for the less-intensive treatment arm.
Against a backdrop of uncertainty in the literature about what the target systolic blood pressure should be for those with hypertension and at risk for cardiovascular events or kidney disease, the study provides compelling evidence that more-aggressive blood pressure lowering is important. “More-intensive management of blood pressure can save lives,” said Dr. Gary Gibbons, director of the National Heart, Lung, and Blood Institute. This is good news, he said, since about one in three Americans has high blood pressure, and only about half of those 70 million currently have their blood pressure under control.
Dr. Jackson T. Wright Jr., SPRINT study lead and director of the clinical hypertension program at Case Western Reserve University in Cleveland, also emphasized that intensive blood pressure management can prevent the cardiovascular complications of hypertension. Though subgroup analysis is ongoing, the effect seems robust and consistent across age groups, sex, and ethnicity, he said. SPRINT, he said, also “offers an excellent opportunity to examine the tolerability and safety of the lower target.” The first look at the safety data shows that the more-intensive treatment is well tolerated, though data analysis is ongoing, he said.
Dr. Suzanne Oparil, director of the vascular biology and hypertension program at the University of Alabama-Birmingham, said, “This is a time of enlightenment.” The previous absence of compelling data played a part in the debate surrounding blood pressure levels that should be used in guidance documents, and Dr. Gibbons and Dr. Wright both emphasized that they would expect the forthcoming primary outcomes paper to have an impact on guideline-writing bodies. Dr. Wright said, however, “We are not providing guidance for providers or patients right now. The study was just unblinded a little less than 3 weeks ago.”
In 2014, the group of experts who had constituted the JNC 8 panel, a team assembled in 2008 by NHLBI to update official U.S. hypertension management guidelines, set the target blood pressure for the general population aged 60 years or older to less than 150/90 mm Hg, a major break from long-standing practice to treat such patients to a target systolic pressure of less than 140 mm Hg (JAMA. 2014;311[5]:507-20). These guidelines, released after SPRINT began, remain controversial.
The SPRINT MIND trial, tracking the relationship between systolic blood pressure and cognitive impairment or dementia, is ongoing. The study is also still collecting data about kidney function in study participants.
The study was funded by the National Institutes of Health. Two drug companies, Takeda and Arbor, provided some medication for the trial.
On Twitter @karioakes
Deaths were reduced by nearly one-quarter when systolic blood pressure was treated to a target of 120 rather than 140 mm Hg, according to a large NIH-sponsored study comparing standard blood pressure treatment with more-intensive lowering of systolic blood pressure. The lower blood pressure group also saw a 30% reduction in the composite primary composite endpoint of cardiovascular events, stroke, and cardiovascular death.
The magnitude of the effect of the lower blood pressure target prompted the study’s data safety monitoring board to end the study early, said officials from several National Institutes of Health agencies at a telebriefing. The study was unblinded in August 2015, and a full report of the primary outcome measures will come in a paper due out by the end of the year, they said.
The Systolic Blood Pressure Intervention Trial, or SPRINT, is a 100-site trial that enrolled more than 9,300 people in the United States and Puerto Rico aged at least 50 years with high blood pressure and at risk for cardiovascular disease; those with diabetes were excluded. Patients were randomized to a standard treatment target of 140 mm Hg or less, or to a more intensive 120 mm Hg.
SPRINT participants received evidence-based treatment with a variety of antihypertensives, with the intervention arm requiring an average of almost three medications, compared with just under two for the less-intensive treatment arm.
Against a backdrop of uncertainty in the literature about what the target systolic blood pressure should be for those with hypertension and at risk for cardiovascular events or kidney disease, the study provides compelling evidence that more-aggressive blood pressure lowering is important. “More-intensive management of blood pressure can save lives,” said Dr. Gary Gibbons, director of the National Heart, Lung, and Blood Institute. This is good news, he said, since about one in three Americans has high blood pressure, and only about half of those 70 million currently have their blood pressure under control.
Dr. Jackson T. Wright Jr., SPRINT study lead and director of the clinical hypertension program at Case Western Reserve University in Cleveland, also emphasized that intensive blood pressure management can prevent the cardiovascular complications of hypertension. Though subgroup analysis is ongoing, the effect seems robust and consistent across age groups, sex, and ethnicity, he said. SPRINT, he said, also “offers an excellent opportunity to examine the tolerability and safety of the lower target.” The first look at the safety data shows that the more-intensive treatment is well tolerated, though data analysis is ongoing, he said.
Dr. Suzanne Oparil, director of the vascular biology and hypertension program at the University of Alabama-Birmingham, said, “This is a time of enlightenment.” The previous absence of compelling data played a part in the debate surrounding blood pressure levels that should be used in guidance documents, and Dr. Gibbons and Dr. Wright both emphasized that they would expect the forthcoming primary outcomes paper to have an impact on guideline-writing bodies. Dr. Wright said, however, “We are not providing guidance for providers or patients right now. The study was just unblinded a little less than 3 weeks ago.”
In 2014, the group of experts who had constituted the JNC 8 panel, a team assembled in 2008 by NHLBI to update official U.S. hypertension management guidelines, set the target blood pressure for the general population aged 60 years or older to less than 150/90 mm Hg, a major break from long-standing practice to treat such patients to a target systolic pressure of less than 140 mm Hg (JAMA. 2014;311[5]:507-20). These guidelines, released after SPRINT began, remain controversial.
The SPRINT MIND trial, tracking the relationship between systolic blood pressure and cognitive impairment or dementia, is ongoing. The study is also still collecting data about kidney function in study participants.
The study was funded by the National Institutes of Health. Two drug companies, Takeda and Arbor, provided some medication for the trial.
On Twitter @karioakes
Deaths were reduced by nearly one-quarter when systolic blood pressure was treated to a target of 120 rather than 140 mm Hg, according to a large NIH-sponsored study comparing standard blood pressure treatment with more-intensive lowering of systolic blood pressure. The lower blood pressure group also saw a 30% reduction in the composite primary composite endpoint of cardiovascular events, stroke, and cardiovascular death.
The magnitude of the effect of the lower blood pressure target prompted the study’s data safety monitoring board to end the study early, said officials from several National Institutes of Health agencies at a telebriefing. The study was unblinded in August 2015, and a full report of the primary outcome measures will come in a paper due out by the end of the year, they said.
The Systolic Blood Pressure Intervention Trial, or SPRINT, is a 100-site trial that enrolled more than 9,300 people in the United States and Puerto Rico aged at least 50 years with high blood pressure and at risk for cardiovascular disease; those with diabetes were excluded. Patients were randomized to a standard treatment target of 140 mm Hg or less, or to a more intensive 120 mm Hg.
SPRINT participants received evidence-based treatment with a variety of antihypertensives, with the intervention arm requiring an average of almost three medications, compared with just under two for the less-intensive treatment arm.
Against a backdrop of uncertainty in the literature about what the target systolic blood pressure should be for those with hypertension and at risk for cardiovascular events or kidney disease, the study provides compelling evidence that more-aggressive blood pressure lowering is important. “More-intensive management of blood pressure can save lives,” said Dr. Gary Gibbons, director of the National Heart, Lung, and Blood Institute. This is good news, he said, since about one in three Americans has high blood pressure, and only about half of those 70 million currently have their blood pressure under control.
Dr. Jackson T. Wright Jr., SPRINT study lead and director of the clinical hypertension program at Case Western Reserve University in Cleveland, also emphasized that intensive blood pressure management can prevent the cardiovascular complications of hypertension. Though subgroup analysis is ongoing, the effect seems robust and consistent across age groups, sex, and ethnicity, he said. SPRINT, he said, also “offers an excellent opportunity to examine the tolerability and safety of the lower target.” The first look at the safety data shows that the more-intensive treatment is well tolerated, though data analysis is ongoing, he said.
Dr. Suzanne Oparil, director of the vascular biology and hypertension program at the University of Alabama-Birmingham, said, “This is a time of enlightenment.” The previous absence of compelling data played a part in the debate surrounding blood pressure levels that should be used in guidance documents, and Dr. Gibbons and Dr. Wright both emphasized that they would expect the forthcoming primary outcomes paper to have an impact on guideline-writing bodies. Dr. Wright said, however, “We are not providing guidance for providers or patients right now. The study was just unblinded a little less than 3 weeks ago.”
In 2014, the group of experts who had constituted the JNC 8 panel, a team assembled in 2008 by NHLBI to update official U.S. hypertension management guidelines, set the target blood pressure for the general population aged 60 years or older to less than 150/90 mm Hg, a major break from long-standing practice to treat such patients to a target systolic pressure of less than 140 mm Hg (JAMA. 2014;311[5]:507-20). These guidelines, released after SPRINT began, remain controversial.
The SPRINT MIND trial, tracking the relationship between systolic blood pressure and cognitive impairment or dementia, is ongoing. The study is also still collecting data about kidney function in study participants.
The study was funded by the National Institutes of Health. Two drug companies, Takeda and Arbor, provided some medication for the trial.
On Twitter @karioakes
FROM AN NHLBI TELEBRIEFING
Right-side mini-AVR an option for frail patients
Many patients with aortic valve disease still undergo conventional aortic valve replacement (AVR) with standard full sternotomy or seek out alternative treatments like transcatheter aortic valve insertion (TAVI). But a minimally invasive approach that uses a sutureless prostheses may reduce operation times and put AVR within reach of more frail patients.
Investigators from G. Pasquinucci Heart Hospital in Massa, Italy, reported on 593 patients who had AVR through right anterior minithoracotomy (RAMT) over 10 years at their institution (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.06.045). In 302 of the patients, the researchers used a sutureless or rapidly implantable biological prosthesis.
“More surgeons should enrich their armamentarium by RAMT AVR,” lead author Dr. Mattia Glauber and his coauthors said. “Sutureless prostheses can increase adoption of RAMT AVR.”
The authors acknowledged that minimally invasive approaches to AVR, including partial sternotomy, require longer operation times than open surgery despite reduced aortic cross-clamping and cardiopulmonary bypass times, but have resulted in better outcomes and lower death rates.
A new generation of aortic valve prostheses, including sutureless devices, have emerged in an attempt to further reduce operative times and improve outcomes, so the Italian investigators designed their study to compare early and midterm outcomes after minimally invasive AVR using sutured and sutureless repair at their institution between 2004 and 2014.
In 302 (50.9%) patients, sutureless or rapidly implantable biological prosthesis was used, 23 (3.9%) had a mechanical prosthesis, and the remainder received a conventional biological prosthesis.
The investigators determined patients were suitable for RAMT if CT scan showed specific anatomic features, including rightward positioning of the ascending aorta at the level of the main pulmonary artery. Once the sutureless prostheses became available in 2011, every patient undergoing AVR via RAMT was considered a potential candidate, although the investigators decided that patients with type 1 and 2 bicuspid aortic valves without raphe and asymmetric aortic root were not suitable for the sutureless approach.
The subgroup that underwent sutureless repair tended to be older and sicker than the overall study population and had a higher prevalence of tricuspid aortic valve and aortic stenosis, a slightly higher body mass index, and a higher propensity to be obese. The sutureless subgroup also had fewer smokers.
Cardiopulmonary bypass time averaged 88 minutes and aortic cross-clamping times 55 minutes in the sutureless subgroup vs. 107 and 74 minutes, respectively, in the overall RAMT study subgroup.
The death before discharge rate of patients who had RAMT repair was 1%, and the 30-day in-hospital death rate was 1.5%. Overall, 97% of patients who had RAMT did not require reoperation at 5 years.
Between the sutured and sutureless subgroups, hospital and intensive care unit lengths of stay were similar, as were bleeding rates and in-hospital mortality. One measure in which the two subgroups deviated was prolonged ICU stay – a rate of 11.3% in the sutureless subgroup and 6.6% in the sutured subgroup.
“To the best of our knowledge, this is the largest up-to-date single-center experience on minimally invasive AVR through RAMT,” Dr. Glauber and coauthors said. “Our data along with earlier reports confirm that minimally invasive AVR through RAMT is safe and reproducible. It is associated with low perioperative mortality and morbidity.”
Dr. Glauber and coauthor Dr. Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
“Have we found the end of the road, and the future for isolated AVR is made up of RAMT with sutureless AVR?” asks Dr. Patrick M. McCarthy, chief of cardiac surgery at Northwestern University Feinberg School of Medicine in Chicago, in his invited commentary (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.007). “The cardiology literature serves as a reality check.”
He noted that results from the NOTION Trial of transaortic valve replacement (TAVR) vs. surgical AVR (J Am Coll Cardiol. 2015;65:2184-94) had 30-day results similar to the G. Pasquinucci Heart Hospital results. However, 34% in the TAVR group in NOTION needed pacemakers, and 16% had moderate or greater valvular regurgitation and higher rates of dyspnea.

|
Dr. Patrick M. McCarthy |
Right anterior minithoracotomy is different from other minimally invasive approaches, Dr. McCarthy said. “It’s more of a tunnel down to the aortic valve which is why patient selection based on anatomic factors determined by preoperative CT scan (which is an unnecessary expense for hemisternotomy) is so important,” he said.
The evolution of TAVR is still in the early stage, so the “flaws” involved in the approach can yet be eliminated, “but the message that TAVR outcomes today are still very different than [surgical] AVR in low-risk patients, the type that have a minimally invasive AVR, may be lost on many readers,” Dr. McCarthy said.
For isolated aortic stenosis, the era of minimally invasive procedures that involve bypass, cross-clamping and a difficult surgical approach may be fading, he said. “The handwriting is on the wall, or in the journals in this case.”
Dr. McCarthy disclosed relationships with Edwards Lifesciences and Abbott Vascular. He is the inventor of the Edwards MC3 Ring and dETlogix Ring and coinventor of the IMR ETlogix Ring.
“Have we found the end of the road, and the future for isolated AVR is made up of RAMT with sutureless AVR?” asks Dr. Patrick M. McCarthy, chief of cardiac surgery at Northwestern University Feinberg School of Medicine in Chicago, in his invited commentary (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.007). “The cardiology literature serves as a reality check.”
He noted that results from the NOTION Trial of transaortic valve replacement (TAVR) vs. surgical AVR (J Am Coll Cardiol. 2015;65:2184-94) had 30-day results similar to the G. Pasquinucci Heart Hospital results. However, 34% in the TAVR group in NOTION needed pacemakers, and 16% had moderate or greater valvular regurgitation and higher rates of dyspnea.

|
Dr. Patrick M. McCarthy |
Right anterior minithoracotomy is different from other minimally invasive approaches, Dr. McCarthy said. “It’s more of a tunnel down to the aortic valve which is why patient selection based on anatomic factors determined by preoperative CT scan (which is an unnecessary expense for hemisternotomy) is so important,” he said.
The evolution of TAVR is still in the early stage, so the “flaws” involved in the approach can yet be eliminated, “but the message that TAVR outcomes today are still very different than [surgical] AVR in low-risk patients, the type that have a minimally invasive AVR, may be lost on many readers,” Dr. McCarthy said.
For isolated aortic stenosis, the era of minimally invasive procedures that involve bypass, cross-clamping and a difficult surgical approach may be fading, he said. “The handwriting is on the wall, or in the journals in this case.”
Dr. McCarthy disclosed relationships with Edwards Lifesciences and Abbott Vascular. He is the inventor of the Edwards MC3 Ring and dETlogix Ring and coinventor of the IMR ETlogix Ring.
“Have we found the end of the road, and the future for isolated AVR is made up of RAMT with sutureless AVR?” asks Dr. Patrick M. McCarthy, chief of cardiac surgery at Northwestern University Feinberg School of Medicine in Chicago, in his invited commentary (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.007). “The cardiology literature serves as a reality check.”
He noted that results from the NOTION Trial of transaortic valve replacement (TAVR) vs. surgical AVR (J Am Coll Cardiol. 2015;65:2184-94) had 30-day results similar to the G. Pasquinucci Heart Hospital results. However, 34% in the TAVR group in NOTION needed pacemakers, and 16% had moderate or greater valvular regurgitation and higher rates of dyspnea.

|
Dr. Patrick M. McCarthy |
Right anterior minithoracotomy is different from other minimally invasive approaches, Dr. McCarthy said. “It’s more of a tunnel down to the aortic valve which is why patient selection based on anatomic factors determined by preoperative CT scan (which is an unnecessary expense for hemisternotomy) is so important,” he said.
The evolution of TAVR is still in the early stage, so the “flaws” involved in the approach can yet be eliminated, “but the message that TAVR outcomes today are still very different than [surgical] AVR in low-risk patients, the type that have a minimally invasive AVR, may be lost on many readers,” Dr. McCarthy said.
For isolated aortic stenosis, the era of minimally invasive procedures that involve bypass, cross-clamping and a difficult surgical approach may be fading, he said. “The handwriting is on the wall, or in the journals in this case.”
Dr. McCarthy disclosed relationships with Edwards Lifesciences and Abbott Vascular. He is the inventor of the Edwards MC3 Ring and dETlogix Ring and coinventor of the IMR ETlogix Ring.
Many patients with aortic valve disease still undergo conventional aortic valve replacement (AVR) with standard full sternotomy or seek out alternative treatments like transcatheter aortic valve insertion (TAVI). But a minimally invasive approach that uses a sutureless prostheses may reduce operation times and put AVR within reach of more frail patients.
Investigators from G. Pasquinucci Heart Hospital in Massa, Italy, reported on 593 patients who had AVR through right anterior minithoracotomy (RAMT) over 10 years at their institution (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.06.045). In 302 of the patients, the researchers used a sutureless or rapidly implantable biological prosthesis.
“More surgeons should enrich their armamentarium by RAMT AVR,” lead author Dr. Mattia Glauber and his coauthors said. “Sutureless prostheses can increase adoption of RAMT AVR.”
The authors acknowledged that minimally invasive approaches to AVR, including partial sternotomy, require longer operation times than open surgery despite reduced aortic cross-clamping and cardiopulmonary bypass times, but have resulted in better outcomes and lower death rates.
A new generation of aortic valve prostheses, including sutureless devices, have emerged in an attempt to further reduce operative times and improve outcomes, so the Italian investigators designed their study to compare early and midterm outcomes after minimally invasive AVR using sutured and sutureless repair at their institution between 2004 and 2014.
In 302 (50.9%) patients, sutureless or rapidly implantable biological prosthesis was used, 23 (3.9%) had a mechanical prosthesis, and the remainder received a conventional biological prosthesis.
The investigators determined patients were suitable for RAMT if CT scan showed specific anatomic features, including rightward positioning of the ascending aorta at the level of the main pulmonary artery. Once the sutureless prostheses became available in 2011, every patient undergoing AVR via RAMT was considered a potential candidate, although the investigators decided that patients with type 1 and 2 bicuspid aortic valves without raphe and asymmetric aortic root were not suitable for the sutureless approach.
The subgroup that underwent sutureless repair tended to be older and sicker than the overall study population and had a higher prevalence of tricuspid aortic valve and aortic stenosis, a slightly higher body mass index, and a higher propensity to be obese. The sutureless subgroup also had fewer smokers.
Cardiopulmonary bypass time averaged 88 minutes and aortic cross-clamping times 55 minutes in the sutureless subgroup vs. 107 and 74 minutes, respectively, in the overall RAMT study subgroup.
The death before discharge rate of patients who had RAMT repair was 1%, and the 30-day in-hospital death rate was 1.5%. Overall, 97% of patients who had RAMT did not require reoperation at 5 years.
Between the sutured and sutureless subgroups, hospital and intensive care unit lengths of stay were similar, as were bleeding rates and in-hospital mortality. One measure in which the two subgroups deviated was prolonged ICU stay – a rate of 11.3% in the sutureless subgroup and 6.6% in the sutured subgroup.
“To the best of our knowledge, this is the largest up-to-date single-center experience on minimally invasive AVR through RAMT,” Dr. Glauber and coauthors said. “Our data along with earlier reports confirm that minimally invasive AVR through RAMT is safe and reproducible. It is associated with low perioperative mortality and morbidity.”
Dr. Glauber and coauthor Dr. Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
Many patients with aortic valve disease still undergo conventional aortic valve replacement (AVR) with standard full sternotomy or seek out alternative treatments like transcatheter aortic valve insertion (TAVI). But a minimally invasive approach that uses a sutureless prostheses may reduce operation times and put AVR within reach of more frail patients.
Investigators from G. Pasquinucci Heart Hospital in Massa, Italy, reported on 593 patients who had AVR through right anterior minithoracotomy (RAMT) over 10 years at their institution (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.06.045). In 302 of the patients, the researchers used a sutureless or rapidly implantable biological prosthesis.
“More surgeons should enrich their armamentarium by RAMT AVR,” lead author Dr. Mattia Glauber and his coauthors said. “Sutureless prostheses can increase adoption of RAMT AVR.”
The authors acknowledged that minimally invasive approaches to AVR, including partial sternotomy, require longer operation times than open surgery despite reduced aortic cross-clamping and cardiopulmonary bypass times, but have resulted in better outcomes and lower death rates.
A new generation of aortic valve prostheses, including sutureless devices, have emerged in an attempt to further reduce operative times and improve outcomes, so the Italian investigators designed their study to compare early and midterm outcomes after minimally invasive AVR using sutured and sutureless repair at their institution between 2004 and 2014.
In 302 (50.9%) patients, sutureless or rapidly implantable biological prosthesis was used, 23 (3.9%) had a mechanical prosthesis, and the remainder received a conventional biological prosthesis.
The investigators determined patients were suitable for RAMT if CT scan showed specific anatomic features, including rightward positioning of the ascending aorta at the level of the main pulmonary artery. Once the sutureless prostheses became available in 2011, every patient undergoing AVR via RAMT was considered a potential candidate, although the investigators decided that patients with type 1 and 2 bicuspid aortic valves without raphe and asymmetric aortic root were not suitable for the sutureless approach.
The subgroup that underwent sutureless repair tended to be older and sicker than the overall study population and had a higher prevalence of tricuspid aortic valve and aortic stenosis, a slightly higher body mass index, and a higher propensity to be obese. The sutureless subgroup also had fewer smokers.
Cardiopulmonary bypass time averaged 88 minutes and aortic cross-clamping times 55 minutes in the sutureless subgroup vs. 107 and 74 minutes, respectively, in the overall RAMT study subgroup.
The death before discharge rate of patients who had RAMT repair was 1%, and the 30-day in-hospital death rate was 1.5%. Overall, 97% of patients who had RAMT did not require reoperation at 5 years.
Between the sutured and sutureless subgroups, hospital and intensive care unit lengths of stay were similar, as were bleeding rates and in-hospital mortality. One measure in which the two subgroups deviated was prolonged ICU stay – a rate of 11.3% in the sutureless subgroup and 6.6% in the sutured subgroup.
“To the best of our knowledge, this is the largest up-to-date single-center experience on minimally invasive AVR through RAMT,” Dr. Glauber and coauthors said. “Our data along with earlier reports confirm that minimally invasive AVR through RAMT is safe and reproducible. It is associated with low perioperative mortality and morbidity.”
Dr. Glauber and coauthor Dr. Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Aortic valve replacement through right anterior minithoracotomy provides excellent outcomes. Sutureless prostheses facilitate mini-AVR.
Major finding: Study subjects had a survival rate of 95% at 31.5 months follow-up on average, and operative times were significantly shorter with sutureless prostheses, compared with sutured prostheses.
Data source: A retrospective, observational cohort study with prospective data collection on 593 patients who had right anterior minithoracotomy for AVR at a single institution over a 10-yar period.
Disclosures: Study coauthors Mattia Glauber and Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
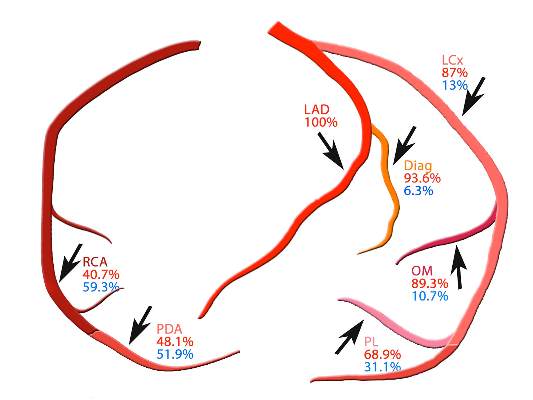
SYNTAX: Early CABG results with arterial grafts similar to venous in matched groups
While single-center studies have supported the advantages of multiple arterial grafts over venous grafts in coronary artery bypass surgery, an analysis of patients in the international and multicenter SYNTAX trial has shown that, on propensity matching, rates of cardiac events and death are actually similar between the two groups.
These findings of the SYNTAX investigators, led by Dr. Catalina Parasca of Erasmus University in Rotterdam, the Netherlands, were published online in the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j.jtcvs.2015.05.010).
The SYNTAX trial compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with left main or three-vessel coronary artery disease (Lancet. 2013;381[9867]:629-38).
In the latest report, the SYNTAX investigators found that patients in unmatched groups who received arterial grafts in addition to an arterial graft of the left anterior descending artery (LAD) had noticeably lower rates of death and a composite endpoint of death-stroke-MI than did those who received a second venous graft. However, when the researchers applied propensity matching, the outcomes between the two groups were similar.
Because large randomized trials have yet to prove the superiority of multiarterial grafts, the adoption rate has been low, Dr. Parasca and colleagues said. “The objective of this study was to assess the effect of using a second arterial graft on 5-year outcomes in patients who underwent CABG in the SYNTAX trial and registry,” they said.
They looked at 1,322 SYNTAX trial patients who had CABG with 5-year follow-up. In unmatched groups, the safety endpoint of the death-stroke-MI composite was 13.3% in the multiarterial group vs. 18.7% in the vein graft group. Although the incidence of stroke, MI, and graft occlusion was similar between the unmatched groups, the second-graft arterial group had a higher revascularization rate at 5 years, 12.6% vs. 9.6%, mainly due to repeat PCI. The element of the composite where the two unmatched groups deviated was the all-cause death rate at 5 years: 8.9% in the second-graft arterial group and 13.1% in the venous group.
However, when the investigators applied propensity matching, the differences between the two groups were insignificant.
“The results of the present study must be seen in the light of a multicenter CABG cohort with complex coronary disease, where revascularization was performed according to surgeon’s personal experience and local practices,” Dr. Parasca and coauthors noted. “The result was a high heterogeneity of CABG techniques, which shows different understanding of the best ‘graft-target match’ across centers.”
While the SYNTAX analysis demonstrates the variation in patient selection and operator technique with regard to arterial revascularization typical of a multicenter study, “extended follow-up beyond 5 years is required to estimate its impact on long-term outcomes,” Dr. Parasca and colleagues said.
Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.
That arterial grafts are a better long-term match in coronary bypass surgery has been a tenet in cardiac surgery, but multiple factors have prevented their more widespread acceptance, Dr. Davis C. Drinkwater Jr. said in his invited commentary (J Thorac Cardiovasc Surg. 2015.doi:10.1016/j.jtcvs.2015.06.014). Concerns about sternal wound healing, particularly in diabetic or obese patients, as well as the alternative generally good early and mid-term results in multivessel coronary artery disease using the left internal thoracic artery to LAD accompanied by saphenous vein grafts, have made surgeons hesitant to take up the approach more readily, said Dr. Drinkwater of Frist Cardiology, Tristar Centennial Medical Center, Nashville, Tenn.
The SYNTAX investigators’ main finding of no survival advantage among the matched groups at 5 years is in line with most reports comparing patency between arterial and venous grafts, “requiring between 5- and 10-year follow-up to show a divergence,” Dr. Drinkwater said.
He pointed out that the patients who had second arterial grafts in the unmatched group were younger and healthier – the average age was 62 years, and 27% of them had previous heart attacks, compared with 66 years of age and a heart attack rate of 35.6% in the venous graft group – and that may explain the higher reintervention rate in the former group. Another factor may be the younger and healthier patients had longer cardiopulmonary bypass and aortic cross clamp times despite a greater percentage having undergone the off-pump technique.
“This counterintuitive information underscores an inherent weakness of this multicenter trial that is without surgical randomization into the two arterial groups, and with potentially varied surgical experience using nonstandardized technical and management protocols,” Dr. Drinkwater said. “This is in stark contrast to the previous and well accepted single high-volume-center reports of the benefits of using multiple arterial bypass grafts.”
Because the report points out the technical challenges of achieving complete revascularization with multiple arterial grafting at “the early” interval of up to 5 years, the authors may be inappropriately discouraging centers that do not currently offer multiarterial grafting from embracing it, Dr. Drinkwater concluded.
He had no disclosures to report.
That arterial grafts are a better long-term match in coronary bypass surgery has been a tenet in cardiac surgery, but multiple factors have prevented their more widespread acceptance, Dr. Davis C. Drinkwater Jr. said in his invited commentary (J Thorac Cardiovasc Surg. 2015.doi:10.1016/j.jtcvs.2015.06.014). Concerns about sternal wound healing, particularly in diabetic or obese patients, as well as the alternative generally good early and mid-term results in multivessel coronary artery disease using the left internal thoracic artery to LAD accompanied by saphenous vein grafts, have made surgeons hesitant to take up the approach more readily, said Dr. Drinkwater of Frist Cardiology, Tristar Centennial Medical Center, Nashville, Tenn.
The SYNTAX investigators’ main finding of no survival advantage among the matched groups at 5 years is in line with most reports comparing patency between arterial and venous grafts, “requiring between 5- and 10-year follow-up to show a divergence,” Dr. Drinkwater said.
He pointed out that the patients who had second arterial grafts in the unmatched group were younger and healthier – the average age was 62 years, and 27% of them had previous heart attacks, compared with 66 years of age and a heart attack rate of 35.6% in the venous graft group – and that may explain the higher reintervention rate in the former group. Another factor may be the younger and healthier patients had longer cardiopulmonary bypass and aortic cross clamp times despite a greater percentage having undergone the off-pump technique.
“This counterintuitive information underscores an inherent weakness of this multicenter trial that is without surgical randomization into the two arterial groups, and with potentially varied surgical experience using nonstandardized technical and management protocols,” Dr. Drinkwater said. “This is in stark contrast to the previous and well accepted single high-volume-center reports of the benefits of using multiple arterial bypass grafts.”
Because the report points out the technical challenges of achieving complete revascularization with multiple arterial grafting at “the early” interval of up to 5 years, the authors may be inappropriately discouraging centers that do not currently offer multiarterial grafting from embracing it, Dr. Drinkwater concluded.
He had no disclosures to report.
That arterial grafts are a better long-term match in coronary bypass surgery has been a tenet in cardiac surgery, but multiple factors have prevented their more widespread acceptance, Dr. Davis C. Drinkwater Jr. said in his invited commentary (J Thorac Cardiovasc Surg. 2015.doi:10.1016/j.jtcvs.2015.06.014). Concerns about sternal wound healing, particularly in diabetic or obese patients, as well as the alternative generally good early and mid-term results in multivessel coronary artery disease using the left internal thoracic artery to LAD accompanied by saphenous vein grafts, have made surgeons hesitant to take up the approach more readily, said Dr. Drinkwater of Frist Cardiology, Tristar Centennial Medical Center, Nashville, Tenn.
The SYNTAX investigators’ main finding of no survival advantage among the matched groups at 5 years is in line with most reports comparing patency between arterial and venous grafts, “requiring between 5- and 10-year follow-up to show a divergence,” Dr. Drinkwater said.
He pointed out that the patients who had second arterial grafts in the unmatched group were younger and healthier – the average age was 62 years, and 27% of them had previous heart attacks, compared with 66 years of age and a heart attack rate of 35.6% in the venous graft group – and that may explain the higher reintervention rate in the former group. Another factor may be the younger and healthier patients had longer cardiopulmonary bypass and aortic cross clamp times despite a greater percentage having undergone the off-pump technique.
“This counterintuitive information underscores an inherent weakness of this multicenter trial that is without surgical randomization into the two arterial groups, and with potentially varied surgical experience using nonstandardized technical and management protocols,” Dr. Drinkwater said. “This is in stark contrast to the previous and well accepted single high-volume-center reports of the benefits of using multiple arterial bypass grafts.”
Because the report points out the technical challenges of achieving complete revascularization with multiple arterial grafting at “the early” interval of up to 5 years, the authors may be inappropriately discouraging centers that do not currently offer multiarterial grafting from embracing it, Dr. Drinkwater concluded.
He had no disclosures to report.
While single-center studies have supported the advantages of multiple arterial grafts over venous grafts in coronary artery bypass surgery, an analysis of patients in the international and multicenter SYNTAX trial has shown that, on propensity matching, rates of cardiac events and death are actually similar between the two groups.
These findings of the SYNTAX investigators, led by Dr. Catalina Parasca of Erasmus University in Rotterdam, the Netherlands, were published online in the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j.jtcvs.2015.05.010).
The SYNTAX trial compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with left main or three-vessel coronary artery disease (Lancet. 2013;381[9867]:629-38).
In the latest report, the SYNTAX investigators found that patients in unmatched groups who received arterial grafts in addition to an arterial graft of the left anterior descending artery (LAD) had noticeably lower rates of death and a composite endpoint of death-stroke-MI than did those who received a second venous graft. However, when the researchers applied propensity matching, the outcomes between the two groups were similar.
Because large randomized trials have yet to prove the superiority of multiarterial grafts, the adoption rate has been low, Dr. Parasca and colleagues said. “The objective of this study was to assess the effect of using a second arterial graft on 5-year outcomes in patients who underwent CABG in the SYNTAX trial and registry,” they said.
They looked at 1,322 SYNTAX trial patients who had CABG with 5-year follow-up. In unmatched groups, the safety endpoint of the death-stroke-MI composite was 13.3% in the multiarterial group vs. 18.7% in the vein graft group. Although the incidence of stroke, MI, and graft occlusion was similar between the unmatched groups, the second-graft arterial group had a higher revascularization rate at 5 years, 12.6% vs. 9.6%, mainly due to repeat PCI. The element of the composite where the two unmatched groups deviated was the all-cause death rate at 5 years: 8.9% in the second-graft arterial group and 13.1% in the venous group.
However, when the investigators applied propensity matching, the differences between the two groups were insignificant.
“The results of the present study must be seen in the light of a multicenter CABG cohort with complex coronary disease, where revascularization was performed according to surgeon’s personal experience and local practices,” Dr. Parasca and coauthors noted. “The result was a high heterogeneity of CABG techniques, which shows different understanding of the best ‘graft-target match’ across centers.”
While the SYNTAX analysis demonstrates the variation in patient selection and operator technique with regard to arterial revascularization typical of a multicenter study, “extended follow-up beyond 5 years is required to estimate its impact on long-term outcomes,” Dr. Parasca and colleagues said.
Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.
While single-center studies have supported the advantages of multiple arterial grafts over venous grafts in coronary artery bypass surgery, an analysis of patients in the international and multicenter SYNTAX trial has shown that, on propensity matching, rates of cardiac events and death are actually similar between the two groups.
These findings of the SYNTAX investigators, led by Dr. Catalina Parasca of Erasmus University in Rotterdam, the Netherlands, were published online in the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j.jtcvs.2015.05.010).
The SYNTAX trial compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with left main or three-vessel coronary artery disease (Lancet. 2013;381[9867]:629-38).
In the latest report, the SYNTAX investigators found that patients in unmatched groups who received arterial grafts in addition to an arterial graft of the left anterior descending artery (LAD) had noticeably lower rates of death and a composite endpoint of death-stroke-MI than did those who received a second venous graft. However, when the researchers applied propensity matching, the outcomes between the two groups were similar.
Because large randomized trials have yet to prove the superiority of multiarterial grafts, the adoption rate has been low, Dr. Parasca and colleagues said. “The objective of this study was to assess the effect of using a second arterial graft on 5-year outcomes in patients who underwent CABG in the SYNTAX trial and registry,” they said.
They looked at 1,322 SYNTAX trial patients who had CABG with 5-year follow-up. In unmatched groups, the safety endpoint of the death-stroke-MI composite was 13.3% in the multiarterial group vs. 18.7% in the vein graft group. Although the incidence of stroke, MI, and graft occlusion was similar between the unmatched groups, the second-graft arterial group had a higher revascularization rate at 5 years, 12.6% vs. 9.6%, mainly due to repeat PCI. The element of the composite where the two unmatched groups deviated was the all-cause death rate at 5 years: 8.9% in the second-graft arterial group and 13.1% in the venous group.
However, when the investigators applied propensity matching, the differences between the two groups were insignificant.
“The results of the present study must be seen in the light of a multicenter CABG cohort with complex coronary disease, where revascularization was performed according to surgeon’s personal experience and local practices,” Dr. Parasca and coauthors noted. “The result was a high heterogeneity of CABG techniques, which shows different understanding of the best ‘graft-target match’ across centers.”
While the SYNTAX analysis demonstrates the variation in patient selection and operator technique with regard to arterial revascularization typical of a multicenter study, “extended follow-up beyond 5 years is required to estimate its impact on long-term outcomes,” Dr. Parasca and colleagues said.
Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Surgeons should choose arterial grafts for multigraft coronary artery bypass surgery when feasible.
Major finding: Patients who received multiple arterial graft had significantly lower rates of death and other problems than did those who received venous grafts in unmatched groups, but results were similar between propensity matched groups.
Data source: Registry of 1,322 patients who had 5-year follow-up after coronary artery bypass surgery within the SYNTAX trial.
Disclosures: Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.
Heart failure readmission-reducing device debuts slowly
In an era when rehospitalization of patients with heart failure for episodes of acute decompensation has become a top target for reduction in the U.S. health care system via Medicare’s Readmissions Reduction Program CardioMEMS looks like the tool that every U.S. health care system and medical center has dreamed of having.
A wireless and battery-less implanted device, CardioMEMS guides management of stage III heart failure patients by allowing daily monitoring of patients’ pulmonary-artery pressure (PAP). Using these measures to fine-tune patient treatment with diuretics and vasodilators led to a statistically significant and clinically meaningful 37% relative reduction in heart failure rehospitalizations over an average 15-month follow-up, based on results from CardioMEMS’ pivotal U.S. trial as well as from subsequent secondary analyses. All-cause mortality was reduced and patients’ quality of life improved. And device-driven therapy yielded these benefits equally well in patients with either preserved or reduced left ventricular function as well as in a variety of other subgroups including patients with cardiac resynchronization devices or implantable cardioverter defibrillators, chronic obstructive pulmonary disease, chronic kidney disease, atrial fibrillation, pulmonary hypertension, or a history of myocardial infarction.
Yet in the first year after CardioMEMS received Food and Drug Administration approval and came onto the U.S. market, the device has taken a strikingly slow path into routine heart failure practice, according to heart failure cardiologists at several U.S. centers. A representative of St. Jude, the company that markets CardioMEMS, saidin July that sales of the device during the first half of 2015 had involved more than 200 U.S. customers and slightly surpassed earlier expectations, and the company now anticipated full 2015 sales to run roughly 25% ahead of projections made at the start of this year. Despite that, the company’s second quarter report acknowledged the challenges that CardioMEMS faced during its first year on the U.S. market.
Numbers show a slow rollout
“I belong to a consortium of academic heart failure physicians who come from many of the major U.S. academic medical centers, and a recent straw poll of the members showed that close to no one was using it [CardioMEMS] on a regular basis, and the majority said they were not yet using it at all or in the process of starting their program,” said Dr. Javed Butler, a heart failure specialist who is professor of medicine, chief of cardiology, and codirector of the Stony Brook (N.Y.) University Heart Center.
At Stony Brook, no heart failure patient had received the device as of July 2015, although Dr. Butler said that his program’s use of CardioMEMS will probably start soon. Cardiologists at a handful of other U.S. centers report similarly slow starts.
At Massachusetts General Hospital (MGH) in Boston not a single patient has received CardioMEMS, though the heart failure staff there hopes to soon launch pilot use in 10 patients, said Dr. Kimberly A. Parks, associate director of the resynchronization and advanced cardiac therapeutics program. At the University of Colorado Hospital in Aurora, three patients have received the device since their first implant in the late winter, and the program is now on track to place devices in another one or two patients each month, said Dr. Natasha L. Altman, a cardiologist who heads the center’s CardioMEMS program. At Brigham and Women’s Hospital in Boston, which participated in the CHAMPION (CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients) pivotal trial that led to CardioMEMS approval, so far a “handful, fewer than 10 patients” received the device since marketing began, said Dr. Akshay S. Desai, associate director of Brigham Cardiovascular Consultants. Even at Ohio State’s Wexner Medical Center in Columbus, the program run by Dr. William T. Abraham, coprincipal investigator for CHAMPION, a relatively modest number of roughly 50 patients had received CardioMEMS in routine practice since the first patient received a device there in June 2014 following the FDA’s approval, Dr. Abraham said in an interview.
Contrasting with this level of use is the substantial number of patients who meet the CHAMPION enrollment criteria of New York Heart Association class III heart failure and a heart failure hospitalization within the prior year. Experts estimate that throughout the United States this group must number at least a half-million patients, and at the level of individual medical centers that provide advanced heart failure care, the numbers likely reach several hundred patients at each site.
Several challenges slow CardioMEMS implantation
Why such a slow start for what seems to be such an attractive device that clinicians uniformly praise for having a strong evidence base in CHAMPION and a compelling medical rationale? The answer seems multifactorial, including the need to convince skeptical hospital administrators and insurance payers to provide and pay for the device and follow-up care, a requirement to ramp up the patient-monitoring and management infrastructure, and the challenge of transitioning a relatively complex therapeutic formula from a successful clinical trial model into routine care.
“If this was a pill that you could prescribe to patients at hospital discharge, people would jump on it. But CardioMEMS is not as simple as prescribing a pill. There are a lot of logistical issues that make it very difficult,” said Stony Brook’s Dr. Butler in an interview.
This sentiment was shared not only by other cardiologists but also by St. Jude itself, as a company spokesman itemized several challenges the company encountered once it began trying to sell CardioMEMS commercially. “Developing the market for CardioMEMS will continue to take time,” said the St. Jude staffer during a July webcast on the company’s second-quarter 2015 performance. CardioMEMS’ sales were affected by the need to educate multiple constituencies, satisfy new-technology review committees, address reimbursement, access capital budgets, and create consensus among disparate stakeholders, the webcast said. In addition, the early St. Jude experience selling CardioMEMS showed that once a new customer signs a contract, “we find that customers tend to introduce CardioMEMS ... [on] a pilot basis to gain experience with the technology and the reimbursement process.”
First is the challenge of selling a hospital’s administrative leadership on making an upfront capital investment in CardioMEMS equipment, giving the green light to performing procedures that just about break even relative to reimbursement, and then waiting to recoup the initial expenditure and perhaps make some money in the long term by avoiding readmissions and cutting lengths of stay. According to an analysis run by Dr. Parks of MGH, based on the CHAMPION results, for every 10 patients managed using CardioMEMS for 6 months, a center could expect to prevent nearly 15 patient-days in the hospital.
“Our administration is in support, but skeptical; I think that’s why it’s been slow to start,” said Dr. Parks. “The biggest limitation is the upfront cost of the device, and it’s not clear that the reimbursement will allow you to break even” when putting in devices, she said in an interview. “You could justify this by saying you’ll reduce hospitalizations, but the first impression from our administrators was that we were already doing a pretty good job limiting rehospitalizations so why do we need to add this?” The MGH leadership and clinicians eventually agreed on a plan to start the program with 10 implants and then analyze the results to decide if it makes sense to continue. Dr. Parks said she and her colleagues hope to have their first 10 patients implanted with a CardioMEMS before the end of this year.
Another hurdle at MGH was setting up the infrastructure so that a nurse could monitor patients and set in motion the alerts and treatment changes designed to normalize PAP normalized when it falls out of the target range. “It’s a lot of work to put the system in place to manage the devices,” Dr. Parks noted.
Dr. Butler echoed both these challenges. “You need to convince the hospital administrators and make a case based on the cost savings [later on during ongoing management] rather than positive revenue when you do the procedure. If you can expect future cost savings it’s a viable case to make, but a more difficult case to make,” he said. “You also take on the liability of monitoring patients” long term. “If you can follow several hundred patients there may be enough [follow-up] interventions to pay the salaries of staff ” who monitor the patients, but it is very difficult if you have a nurse who is monitoring five patients,” he said. Another issue complicating the economics is that the physicians who supervise monitoring are mostly not the same ones who performed the CardioMEMS placement procedure and received the procedure’s reimbursement. “These are the system barriers that are out there,” Dr. Butler said.
Dr. Altman in Colorado faced a different challenge. “We had good buy-in from our administration. Everyone is interested in reducing rehospitalizations so the administrators were very supportive. The major roadblock has been insurers. Medicare covers it, but so far Colorado Medicaid and several private insurers do not,” Dr. Altman said in an interview. The inconsistent pattern of insurance coverage has already meant that some heart failure patients in her program who were good clinical candidates for CardioMEMS could not receive the device. “I’ve had at least six or seven good candidates, but only three received the device because of insurance reimbursement issues,” she said.
But Dr. Altman expressed optimism that the coverage situation would improve as more programs start using CarioMEMS and insurers grow more familiar with daily PAP monitoring of heart failure patients. She noted that a new CardioMEMS program will soon start at a second Denver-based medical center, and she expressed confidence that ongoing pressure from physicians and administrators at both institutions will change the mind of officials at Colorado’s Medicaid program to provide reimbursement, and once that happens she expects the private insurers will change their policies as well.
To Dr. Abraham at Ohio State, one of the developers of the concept of using an implanted PAP monitor to guide management of heart failure patients, CardioMEMS slow take off is not surprising. “It provides physicians with daily information on a patient’s hemodynamics, which is something they never had before except in the catheterization laboratory, intensive care unit or cardiac care unit. Managing patients based on hemodynamics even in the absence of worsening signs and symptoms is a paradigm shift. It takes time to adopt new things.” He noted that most hospitals and health systems already have in place case managers or nurse navigators who run systems that have relied on the insensitive parameters of signs, symptoms, and patients’ weights. The same infrastructure should be able to fairly easily switch to focusing instead on PAP, said Dr. Abraham, professor and director of cardiovascular medicine at Wexner Medical Center.
He acknowledged that the upfront capital cost required to start a CardioMEMS program can poses a financial barrier at many U.S. centers, but once that start-up price is paid the actual implantation into each patient comes close to breaking even with existing reimbursements and the system should eventually result in a return on the investment in the form of reduced readmissions and keeping patients stable, he said. Dr. Abraham suggested that the possibility also exists that maintaining better stability in patients with class III heart failure and preventing episodes of acute decompensation through better-titrated fluid-volume control could produce a long-term change in the natural history of these patients, whose disease historically has been marked by progression to class IV heart failure and the eventual need for a left ventricular assist device, heart transplant, and death. Although this potential impact of refined treatment based on daily PAP monitoring remains to be proven, a secondary analysis from CHAMPION showing a 57% relative reduction in all-cause mortality over an average of 17 months of follow-up that Dr. Abraham reported at the American College of Cardiology annual meeting in March
The hurdle of routine practice
Transitioning CardioMEMS from its successful research track record to everyday clinical practice may pose the trickiest barrier of all. The consensus among heart failure experts seems to be that the best approach to do this successfully is to start slow, focus on the most rational patients within the broad enrollment criteria used in CHAMPION, and then gradually expand from that presuming the first wave of results from routine use at a particular site look similar to those from the trial.
“The next big question for PAP monitoring is can we replicate the trial’s success in routine practice? Can this be scaled up?” said Dr. Desai from Brigham and Women’s. “We’re still learning how to identify the right patients, the ones who’ll benefit,”
“The two types of patients we are primarily implanting now are those with classic class III heart failure who were hospitalized during the past 12 months and now are hospitalized again and are right in front of us. They are the lowest-hanging fruit because they are in the hospital today,” said Dr. Abraham. “The second group are the patients who come into the clinic complaining about their symptoms. What we are not yet doing is calling in all patients” with stage III heart failure and a history of at least one hospitalization.”
Other groups are taking a much more selective approach. Dr. Altman and her colleagues in Denver are only targeting patients who have been hospitalized at least twice within the past year, and more specifically patients recently rehospitalized within 30 days of their prior hospitalization. They are also focusing on patients expected to have a high level of compliance with the daily data-collection demands of PAP monitoring and the need to regularly adjust their medication dosages after receiving call backs from their clinicians. This criteria means that they are ruling out patients with a history of substance abuse, she said.
She also noted the need to tailor the target PAP to the specific clinical status of individual patients. Patients with mitral regurgitation, for example, will have a higher “normal” diastolic PAP and hence require a somewhat different target for stability maintenance. “You need to understand each patient’s baseline pressures and adjust their medications based on that,” Dr. Altman said.
“In real life patients tend to be older and sicker, so their benefit may be even greater than what was seen in CHAMPION, but perhaps the results will also be diluted because of comorbidities like renal failure or chronic obstructive pulmonary disease,” said Dr. Butler, although post hoc subanalyses of CHAMPION data showed that these comorbidities did not blunt the positive impact of PAP-guided treatment. “I don’t know if I’ll be successful in selecting the right patients, and whether my interventions in real life will produce the same good outcomes” seen in CHAMPION. “We’ll select patients who are close to the CHAMPION criteria, but not patients on dialysis [who were excluded from CHAMPION]; we’ll select patients with a modest degree of comorbidity and reasonable expected survival,” Dr. Butler said.
“If you had a drug that reduced rehospitalization rates it would be pretty clear how to proceed, but in this case it is not the device that reduces readmissions, it just gives you data and you need to act on the data,” Dr. Butler added. He acknowledged that the CHAMPION investigators used a relatively simple, straightforward management algorithm for patients whose PAP fell out of the target range, such as a diastolic PAP greater than 20 mm Hg or less than 8 mm Hg. The first management step is to raise or reduce the patient’s diuretic dosage, and if that fails to quickly normalize PAP the next step is to adjust the vasodilator dosage.
Managing patients in CHAMPION was “not totally an art” but neither was it “totally a science,” Dr. Butler said. Managing patients based on daily data collected using a CardioMEMS device will “require a little finesse,” he said. “It’s not straight science.”
Programs that have already used PAP monitoring on a routine basis, like those in Denver and at Brigham and Women’s, consider their experience too small in size and short in duration to draw any substantive conclusions regarding their success compared with the CHAMPION results. But Dr. Abraham, whose program has now placed CardioMEMS routinely in a few dozen patients and followed them for as long as a year, said that in his center’s patients the device and management system has produced outcomes that roughly match what he saw in the pivotal trial.
“The ongoing concern is that what was achieved in the CHAMPION trial may not be what is achieved in routine practice,” said Dr. Desai. The care that patients received in the trial is “a little of a black box,” he said, and during the FDA’s approval process some reviewers raised concerns that patients in the active-treatment arm simply received more intensive surveillance, although this concern eventually resolved. “There is not a lot of skepticism” among clinicians about this treatment, but there is uncertainly about exactly whom are the best patients to treat and whether their responses be as good as in CHAMPION, Dr. Desai said in an interview.
“The proof [of efficacy] will be in each individual center’s experience” using CardioMEMS, Dr. Altman said.
CHAMPION was initially funded by CardioMEMS, which then was acquired by St. Jude which is the company marketing the CardioMEMS device and associated hardware. Dr. Butler said that he had no current relevant disclosures, although in the past he had been a consultant to CardioMEMS (prior to its acquisition by St. Jude). Dr. Parks and Dr. Altman had no disclosures. Dr. Desai has been a consultant to and has received honoraria as a speaker on behalf of CardioMEMS and St. Jude. Dr. Abraham has been a consultant to CardioMEMS and St. Jude, was co-principal investigator on the CHAMPION trial, and is the principal investigator on a new St. Jude-funded trial studying CardioMEMS.
On Twitter @mitchelzoler
In an era when rehospitalization of patients with heart failure for episodes of acute decompensation has become a top target for reduction in the U.S. health care system via Medicare’s Readmissions Reduction Program CardioMEMS looks like the tool that every U.S. health care system and medical center has dreamed of having.
A wireless and battery-less implanted device, CardioMEMS guides management of stage III heart failure patients by allowing daily monitoring of patients’ pulmonary-artery pressure (PAP). Using these measures to fine-tune patient treatment with diuretics and vasodilators led to a statistically significant and clinically meaningful 37% relative reduction in heart failure rehospitalizations over an average 15-month follow-up, based on results from CardioMEMS’ pivotal U.S. trial as well as from subsequent secondary analyses. All-cause mortality was reduced and patients’ quality of life improved. And device-driven therapy yielded these benefits equally well in patients with either preserved or reduced left ventricular function as well as in a variety of other subgroups including patients with cardiac resynchronization devices or implantable cardioverter defibrillators, chronic obstructive pulmonary disease, chronic kidney disease, atrial fibrillation, pulmonary hypertension, or a history of myocardial infarction.
Yet in the first year after CardioMEMS received Food and Drug Administration approval and came onto the U.S. market, the device has taken a strikingly slow path into routine heart failure practice, according to heart failure cardiologists at several U.S. centers. A representative of St. Jude, the company that markets CardioMEMS, saidin July that sales of the device during the first half of 2015 had involved more than 200 U.S. customers and slightly surpassed earlier expectations, and the company now anticipated full 2015 sales to run roughly 25% ahead of projections made at the start of this year. Despite that, the company’s second quarter report acknowledged the challenges that CardioMEMS faced during its first year on the U.S. market.
Numbers show a slow rollout
“I belong to a consortium of academic heart failure physicians who come from many of the major U.S. academic medical centers, and a recent straw poll of the members showed that close to no one was using it [CardioMEMS] on a regular basis, and the majority said they were not yet using it at all or in the process of starting their program,” said Dr. Javed Butler, a heart failure specialist who is professor of medicine, chief of cardiology, and codirector of the Stony Brook (N.Y.) University Heart Center.
At Stony Brook, no heart failure patient had received the device as of July 2015, although Dr. Butler said that his program’s use of CardioMEMS will probably start soon. Cardiologists at a handful of other U.S. centers report similarly slow starts.
At Massachusetts General Hospital (MGH) in Boston not a single patient has received CardioMEMS, though the heart failure staff there hopes to soon launch pilot use in 10 patients, said Dr. Kimberly A. Parks, associate director of the resynchronization and advanced cardiac therapeutics program. At the University of Colorado Hospital in Aurora, three patients have received the device since their first implant in the late winter, and the program is now on track to place devices in another one or two patients each month, said Dr. Natasha L. Altman, a cardiologist who heads the center’s CardioMEMS program. At Brigham and Women’s Hospital in Boston, which participated in the CHAMPION (CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients) pivotal trial that led to CardioMEMS approval, so far a “handful, fewer than 10 patients” received the device since marketing began, said Dr. Akshay S. Desai, associate director of Brigham Cardiovascular Consultants. Even at Ohio State’s Wexner Medical Center in Columbus, the program run by Dr. William T. Abraham, coprincipal investigator for CHAMPION, a relatively modest number of roughly 50 patients had received CardioMEMS in routine practice since the first patient received a device there in June 2014 following the FDA’s approval, Dr. Abraham said in an interview.
Contrasting with this level of use is the substantial number of patients who meet the CHAMPION enrollment criteria of New York Heart Association class III heart failure and a heart failure hospitalization within the prior year. Experts estimate that throughout the United States this group must number at least a half-million patients, and at the level of individual medical centers that provide advanced heart failure care, the numbers likely reach several hundred patients at each site.
Several challenges slow CardioMEMS implantation
Why such a slow start for what seems to be such an attractive device that clinicians uniformly praise for having a strong evidence base in CHAMPION and a compelling medical rationale? The answer seems multifactorial, including the need to convince skeptical hospital administrators and insurance payers to provide and pay for the device and follow-up care, a requirement to ramp up the patient-monitoring and management infrastructure, and the challenge of transitioning a relatively complex therapeutic formula from a successful clinical trial model into routine care.
“If this was a pill that you could prescribe to patients at hospital discharge, people would jump on it. But CardioMEMS is not as simple as prescribing a pill. There are a lot of logistical issues that make it very difficult,” said Stony Brook’s Dr. Butler in an interview.
This sentiment was shared not only by other cardiologists but also by St. Jude itself, as a company spokesman itemized several challenges the company encountered once it began trying to sell CardioMEMS commercially. “Developing the market for CardioMEMS will continue to take time,” said the St. Jude staffer during a July webcast on the company’s second-quarter 2015 performance. CardioMEMS’ sales were affected by the need to educate multiple constituencies, satisfy new-technology review committees, address reimbursement, access capital budgets, and create consensus among disparate stakeholders, the webcast said. In addition, the early St. Jude experience selling CardioMEMS showed that once a new customer signs a contract, “we find that customers tend to introduce CardioMEMS ... [on] a pilot basis to gain experience with the technology and the reimbursement process.”
First is the challenge of selling a hospital’s administrative leadership on making an upfront capital investment in CardioMEMS equipment, giving the green light to performing procedures that just about break even relative to reimbursement, and then waiting to recoup the initial expenditure and perhaps make some money in the long term by avoiding readmissions and cutting lengths of stay. According to an analysis run by Dr. Parks of MGH, based on the CHAMPION results, for every 10 patients managed using CardioMEMS for 6 months, a center could expect to prevent nearly 15 patient-days in the hospital.
“Our administration is in support, but skeptical; I think that’s why it’s been slow to start,” said Dr. Parks. “The biggest limitation is the upfront cost of the device, and it’s not clear that the reimbursement will allow you to break even” when putting in devices, she said in an interview. “You could justify this by saying you’ll reduce hospitalizations, but the first impression from our administrators was that we were already doing a pretty good job limiting rehospitalizations so why do we need to add this?” The MGH leadership and clinicians eventually agreed on a plan to start the program with 10 implants and then analyze the results to decide if it makes sense to continue. Dr. Parks said she and her colleagues hope to have their first 10 patients implanted with a CardioMEMS before the end of this year.
Another hurdle at MGH was setting up the infrastructure so that a nurse could monitor patients and set in motion the alerts and treatment changes designed to normalize PAP normalized when it falls out of the target range. “It’s a lot of work to put the system in place to manage the devices,” Dr. Parks noted.
Dr. Butler echoed both these challenges. “You need to convince the hospital administrators and make a case based on the cost savings [later on during ongoing management] rather than positive revenue when you do the procedure. If you can expect future cost savings it’s a viable case to make, but a more difficult case to make,” he said. “You also take on the liability of monitoring patients” long term. “If you can follow several hundred patients there may be enough [follow-up] interventions to pay the salaries of staff ” who monitor the patients, but it is very difficult if you have a nurse who is monitoring five patients,” he said. Another issue complicating the economics is that the physicians who supervise monitoring are mostly not the same ones who performed the CardioMEMS placement procedure and received the procedure’s reimbursement. “These are the system barriers that are out there,” Dr. Butler said.
Dr. Altman in Colorado faced a different challenge. “We had good buy-in from our administration. Everyone is interested in reducing rehospitalizations so the administrators were very supportive. The major roadblock has been insurers. Medicare covers it, but so far Colorado Medicaid and several private insurers do not,” Dr. Altman said in an interview. The inconsistent pattern of insurance coverage has already meant that some heart failure patients in her program who were good clinical candidates for CardioMEMS could not receive the device. “I’ve had at least six or seven good candidates, but only three received the device because of insurance reimbursement issues,” she said.
But Dr. Altman expressed optimism that the coverage situation would improve as more programs start using CarioMEMS and insurers grow more familiar with daily PAP monitoring of heart failure patients. She noted that a new CardioMEMS program will soon start at a second Denver-based medical center, and she expressed confidence that ongoing pressure from physicians and administrators at both institutions will change the mind of officials at Colorado’s Medicaid program to provide reimbursement, and once that happens she expects the private insurers will change their policies as well.
To Dr. Abraham at Ohio State, one of the developers of the concept of using an implanted PAP monitor to guide management of heart failure patients, CardioMEMS slow take off is not surprising. “It provides physicians with daily information on a patient’s hemodynamics, which is something they never had before except in the catheterization laboratory, intensive care unit or cardiac care unit. Managing patients based on hemodynamics even in the absence of worsening signs and symptoms is a paradigm shift. It takes time to adopt new things.” He noted that most hospitals and health systems already have in place case managers or nurse navigators who run systems that have relied on the insensitive parameters of signs, symptoms, and patients’ weights. The same infrastructure should be able to fairly easily switch to focusing instead on PAP, said Dr. Abraham, professor and director of cardiovascular medicine at Wexner Medical Center.
He acknowledged that the upfront capital cost required to start a CardioMEMS program can poses a financial barrier at many U.S. centers, but once that start-up price is paid the actual implantation into each patient comes close to breaking even with existing reimbursements and the system should eventually result in a return on the investment in the form of reduced readmissions and keeping patients stable, he said. Dr. Abraham suggested that the possibility also exists that maintaining better stability in patients with class III heart failure and preventing episodes of acute decompensation through better-titrated fluid-volume control could produce a long-term change in the natural history of these patients, whose disease historically has been marked by progression to class IV heart failure and the eventual need for a left ventricular assist device, heart transplant, and death. Although this potential impact of refined treatment based on daily PAP monitoring remains to be proven, a secondary analysis from CHAMPION showing a 57% relative reduction in all-cause mortality over an average of 17 months of follow-up that Dr. Abraham reported at the American College of Cardiology annual meeting in March
The hurdle of routine practice
Transitioning CardioMEMS from its successful research track record to everyday clinical practice may pose the trickiest barrier of all. The consensus among heart failure experts seems to be that the best approach to do this successfully is to start slow, focus on the most rational patients within the broad enrollment criteria used in CHAMPION, and then gradually expand from that presuming the first wave of results from routine use at a particular site look similar to those from the trial.
“The next big question for PAP monitoring is can we replicate the trial’s success in routine practice? Can this be scaled up?” said Dr. Desai from Brigham and Women’s. “We’re still learning how to identify the right patients, the ones who’ll benefit,”
“The two types of patients we are primarily implanting now are those with classic class III heart failure who were hospitalized during the past 12 months and now are hospitalized again and are right in front of us. They are the lowest-hanging fruit because they are in the hospital today,” said Dr. Abraham. “The second group are the patients who come into the clinic complaining about their symptoms. What we are not yet doing is calling in all patients” with stage III heart failure and a history of at least one hospitalization.”
Other groups are taking a much more selective approach. Dr. Altman and her colleagues in Denver are only targeting patients who have been hospitalized at least twice within the past year, and more specifically patients recently rehospitalized within 30 days of their prior hospitalization. They are also focusing on patients expected to have a high level of compliance with the daily data-collection demands of PAP monitoring and the need to regularly adjust their medication dosages after receiving call backs from their clinicians. This criteria means that they are ruling out patients with a history of substance abuse, she said.
She also noted the need to tailor the target PAP to the specific clinical status of individual patients. Patients with mitral regurgitation, for example, will have a higher “normal” diastolic PAP and hence require a somewhat different target for stability maintenance. “You need to understand each patient’s baseline pressures and adjust their medications based on that,” Dr. Altman said.
“In real life patients tend to be older and sicker, so their benefit may be even greater than what was seen in CHAMPION, but perhaps the results will also be diluted because of comorbidities like renal failure or chronic obstructive pulmonary disease,” said Dr. Butler, although post hoc subanalyses of CHAMPION data showed that these comorbidities did not blunt the positive impact of PAP-guided treatment. “I don’t know if I’ll be successful in selecting the right patients, and whether my interventions in real life will produce the same good outcomes” seen in CHAMPION. “We’ll select patients who are close to the CHAMPION criteria, but not patients on dialysis [who were excluded from CHAMPION]; we’ll select patients with a modest degree of comorbidity and reasonable expected survival,” Dr. Butler said.
“If you had a drug that reduced rehospitalization rates it would be pretty clear how to proceed, but in this case it is not the device that reduces readmissions, it just gives you data and you need to act on the data,” Dr. Butler added. He acknowledged that the CHAMPION investigators used a relatively simple, straightforward management algorithm for patients whose PAP fell out of the target range, such as a diastolic PAP greater than 20 mm Hg or less than 8 mm Hg. The first management step is to raise or reduce the patient’s diuretic dosage, and if that fails to quickly normalize PAP the next step is to adjust the vasodilator dosage.
Managing patients in CHAMPION was “not totally an art” but neither was it “totally a science,” Dr. Butler said. Managing patients based on daily data collected using a CardioMEMS device will “require a little finesse,” he said. “It’s not straight science.”
Programs that have already used PAP monitoring on a routine basis, like those in Denver and at Brigham and Women’s, consider their experience too small in size and short in duration to draw any substantive conclusions regarding their success compared with the CHAMPION results. But Dr. Abraham, whose program has now placed CardioMEMS routinely in a few dozen patients and followed them for as long as a year, said that in his center’s patients the device and management system has produced outcomes that roughly match what he saw in the pivotal trial.
“The ongoing concern is that what was achieved in the CHAMPION trial may not be what is achieved in routine practice,” said Dr. Desai. The care that patients received in the trial is “a little of a black box,” he said, and during the FDA’s approval process some reviewers raised concerns that patients in the active-treatment arm simply received more intensive surveillance, although this concern eventually resolved. “There is not a lot of skepticism” among clinicians about this treatment, but there is uncertainly about exactly whom are the best patients to treat and whether their responses be as good as in CHAMPION, Dr. Desai said in an interview.
“The proof [of efficacy] will be in each individual center’s experience” using CardioMEMS, Dr. Altman said.
CHAMPION was initially funded by CardioMEMS, which then was acquired by St. Jude which is the company marketing the CardioMEMS device and associated hardware. Dr. Butler said that he had no current relevant disclosures, although in the past he had been a consultant to CardioMEMS (prior to its acquisition by St. Jude). Dr. Parks and Dr. Altman had no disclosures. Dr. Desai has been a consultant to and has received honoraria as a speaker on behalf of CardioMEMS and St. Jude. Dr. Abraham has been a consultant to CardioMEMS and St. Jude, was co-principal investigator on the CHAMPION trial, and is the principal investigator on a new St. Jude-funded trial studying CardioMEMS.
On Twitter @mitchelzoler
In an era when rehospitalization of patients with heart failure for episodes of acute decompensation has become a top target for reduction in the U.S. health care system via Medicare’s Readmissions Reduction Program CardioMEMS looks like the tool that every U.S. health care system and medical center has dreamed of having.
A wireless and battery-less implanted device, CardioMEMS guides management of stage III heart failure patients by allowing daily monitoring of patients’ pulmonary-artery pressure (PAP). Using these measures to fine-tune patient treatment with diuretics and vasodilators led to a statistically significant and clinically meaningful 37% relative reduction in heart failure rehospitalizations over an average 15-month follow-up, based on results from CardioMEMS’ pivotal U.S. trial as well as from subsequent secondary analyses. All-cause mortality was reduced and patients’ quality of life improved. And device-driven therapy yielded these benefits equally well in patients with either preserved or reduced left ventricular function as well as in a variety of other subgroups including patients with cardiac resynchronization devices or implantable cardioverter defibrillators, chronic obstructive pulmonary disease, chronic kidney disease, atrial fibrillation, pulmonary hypertension, or a history of myocardial infarction.
Yet in the first year after CardioMEMS received Food and Drug Administration approval and came onto the U.S. market, the device has taken a strikingly slow path into routine heart failure practice, according to heart failure cardiologists at several U.S. centers. A representative of St. Jude, the company that markets CardioMEMS, saidin July that sales of the device during the first half of 2015 had involved more than 200 U.S. customers and slightly surpassed earlier expectations, and the company now anticipated full 2015 sales to run roughly 25% ahead of projections made at the start of this year. Despite that, the company’s second quarter report acknowledged the challenges that CardioMEMS faced during its first year on the U.S. market.
Numbers show a slow rollout
“I belong to a consortium of academic heart failure physicians who come from many of the major U.S. academic medical centers, and a recent straw poll of the members showed that close to no one was using it [CardioMEMS] on a regular basis, and the majority said they were not yet using it at all or in the process of starting their program,” said Dr. Javed Butler, a heart failure specialist who is professor of medicine, chief of cardiology, and codirector of the Stony Brook (N.Y.) University Heart Center.
At Stony Brook, no heart failure patient had received the device as of July 2015, although Dr. Butler said that his program’s use of CardioMEMS will probably start soon. Cardiologists at a handful of other U.S. centers report similarly slow starts.
At Massachusetts General Hospital (MGH) in Boston not a single patient has received CardioMEMS, though the heart failure staff there hopes to soon launch pilot use in 10 patients, said Dr. Kimberly A. Parks, associate director of the resynchronization and advanced cardiac therapeutics program. At the University of Colorado Hospital in Aurora, three patients have received the device since their first implant in the late winter, and the program is now on track to place devices in another one or two patients each month, said Dr. Natasha L. Altman, a cardiologist who heads the center’s CardioMEMS program. At Brigham and Women’s Hospital in Boston, which participated in the CHAMPION (CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients) pivotal trial that led to CardioMEMS approval, so far a “handful, fewer than 10 patients” received the device since marketing began, said Dr. Akshay S. Desai, associate director of Brigham Cardiovascular Consultants. Even at Ohio State’s Wexner Medical Center in Columbus, the program run by Dr. William T. Abraham, coprincipal investigator for CHAMPION, a relatively modest number of roughly 50 patients had received CardioMEMS in routine practice since the first patient received a device there in June 2014 following the FDA’s approval, Dr. Abraham said in an interview.
Contrasting with this level of use is the substantial number of patients who meet the CHAMPION enrollment criteria of New York Heart Association class III heart failure and a heart failure hospitalization within the prior year. Experts estimate that throughout the United States this group must number at least a half-million patients, and at the level of individual medical centers that provide advanced heart failure care, the numbers likely reach several hundred patients at each site.
Several challenges slow CardioMEMS implantation
Why such a slow start for what seems to be such an attractive device that clinicians uniformly praise for having a strong evidence base in CHAMPION and a compelling medical rationale? The answer seems multifactorial, including the need to convince skeptical hospital administrators and insurance payers to provide and pay for the device and follow-up care, a requirement to ramp up the patient-monitoring and management infrastructure, and the challenge of transitioning a relatively complex therapeutic formula from a successful clinical trial model into routine care.
“If this was a pill that you could prescribe to patients at hospital discharge, people would jump on it. But CardioMEMS is not as simple as prescribing a pill. There are a lot of logistical issues that make it very difficult,” said Stony Brook’s Dr. Butler in an interview.
This sentiment was shared not only by other cardiologists but also by St. Jude itself, as a company spokesman itemized several challenges the company encountered once it began trying to sell CardioMEMS commercially. “Developing the market for CardioMEMS will continue to take time,” said the St. Jude staffer during a July webcast on the company’s second-quarter 2015 performance. CardioMEMS’ sales were affected by the need to educate multiple constituencies, satisfy new-technology review committees, address reimbursement, access capital budgets, and create consensus among disparate stakeholders, the webcast said. In addition, the early St. Jude experience selling CardioMEMS showed that once a new customer signs a contract, “we find that customers tend to introduce CardioMEMS ... [on] a pilot basis to gain experience with the technology and the reimbursement process.”
First is the challenge of selling a hospital’s administrative leadership on making an upfront capital investment in CardioMEMS equipment, giving the green light to performing procedures that just about break even relative to reimbursement, and then waiting to recoup the initial expenditure and perhaps make some money in the long term by avoiding readmissions and cutting lengths of stay. According to an analysis run by Dr. Parks of MGH, based on the CHAMPION results, for every 10 patients managed using CardioMEMS for 6 months, a center could expect to prevent nearly 15 patient-days in the hospital.
“Our administration is in support, but skeptical; I think that’s why it’s been slow to start,” said Dr. Parks. “The biggest limitation is the upfront cost of the device, and it’s not clear that the reimbursement will allow you to break even” when putting in devices, she said in an interview. “You could justify this by saying you’ll reduce hospitalizations, but the first impression from our administrators was that we were already doing a pretty good job limiting rehospitalizations so why do we need to add this?” The MGH leadership and clinicians eventually agreed on a plan to start the program with 10 implants and then analyze the results to decide if it makes sense to continue. Dr. Parks said she and her colleagues hope to have their first 10 patients implanted with a CardioMEMS before the end of this year.
Another hurdle at MGH was setting up the infrastructure so that a nurse could monitor patients and set in motion the alerts and treatment changes designed to normalize PAP normalized when it falls out of the target range. “It’s a lot of work to put the system in place to manage the devices,” Dr. Parks noted.
Dr. Butler echoed both these challenges. “You need to convince the hospital administrators and make a case based on the cost savings [later on during ongoing management] rather than positive revenue when you do the procedure. If you can expect future cost savings it’s a viable case to make, but a more difficult case to make,” he said. “You also take on the liability of monitoring patients” long term. “If you can follow several hundred patients there may be enough [follow-up] interventions to pay the salaries of staff ” who monitor the patients, but it is very difficult if you have a nurse who is monitoring five patients,” he said. Another issue complicating the economics is that the physicians who supervise monitoring are mostly not the same ones who performed the CardioMEMS placement procedure and received the procedure’s reimbursement. “These are the system barriers that are out there,” Dr. Butler said.
Dr. Altman in Colorado faced a different challenge. “We had good buy-in from our administration. Everyone is interested in reducing rehospitalizations so the administrators were very supportive. The major roadblock has been insurers. Medicare covers it, but so far Colorado Medicaid and several private insurers do not,” Dr. Altman said in an interview. The inconsistent pattern of insurance coverage has already meant that some heart failure patients in her program who were good clinical candidates for CardioMEMS could not receive the device. “I’ve had at least six or seven good candidates, but only three received the device because of insurance reimbursement issues,” she said.
But Dr. Altman expressed optimism that the coverage situation would improve as more programs start using CarioMEMS and insurers grow more familiar with daily PAP monitoring of heart failure patients. She noted that a new CardioMEMS program will soon start at a second Denver-based medical center, and she expressed confidence that ongoing pressure from physicians and administrators at both institutions will change the mind of officials at Colorado’s Medicaid program to provide reimbursement, and once that happens she expects the private insurers will change their policies as well.
To Dr. Abraham at Ohio State, one of the developers of the concept of using an implanted PAP monitor to guide management of heart failure patients, CardioMEMS slow take off is not surprising. “It provides physicians with daily information on a patient’s hemodynamics, which is something they never had before except in the catheterization laboratory, intensive care unit or cardiac care unit. Managing patients based on hemodynamics even in the absence of worsening signs and symptoms is a paradigm shift. It takes time to adopt new things.” He noted that most hospitals and health systems already have in place case managers or nurse navigators who run systems that have relied on the insensitive parameters of signs, symptoms, and patients’ weights. The same infrastructure should be able to fairly easily switch to focusing instead on PAP, said Dr. Abraham, professor and director of cardiovascular medicine at Wexner Medical Center.
He acknowledged that the upfront capital cost required to start a CardioMEMS program can poses a financial barrier at many U.S. centers, but once that start-up price is paid the actual implantation into each patient comes close to breaking even with existing reimbursements and the system should eventually result in a return on the investment in the form of reduced readmissions and keeping patients stable, he said. Dr. Abraham suggested that the possibility also exists that maintaining better stability in patients with class III heart failure and preventing episodes of acute decompensation through better-titrated fluid-volume control could produce a long-term change in the natural history of these patients, whose disease historically has been marked by progression to class IV heart failure and the eventual need for a left ventricular assist device, heart transplant, and death. Although this potential impact of refined treatment based on daily PAP monitoring remains to be proven, a secondary analysis from CHAMPION showing a 57% relative reduction in all-cause mortality over an average of 17 months of follow-up that Dr. Abraham reported at the American College of Cardiology annual meeting in March
The hurdle of routine practice
Transitioning CardioMEMS from its successful research track record to everyday clinical practice may pose the trickiest barrier of all. The consensus among heart failure experts seems to be that the best approach to do this successfully is to start slow, focus on the most rational patients within the broad enrollment criteria used in CHAMPION, and then gradually expand from that presuming the first wave of results from routine use at a particular site look similar to those from the trial.
“The next big question for PAP monitoring is can we replicate the trial’s success in routine practice? Can this be scaled up?” said Dr. Desai from Brigham and Women’s. “We’re still learning how to identify the right patients, the ones who’ll benefit,”
“The two types of patients we are primarily implanting now are those with classic class III heart failure who were hospitalized during the past 12 months and now are hospitalized again and are right in front of us. They are the lowest-hanging fruit because they are in the hospital today,” said Dr. Abraham. “The second group are the patients who come into the clinic complaining about their symptoms. What we are not yet doing is calling in all patients” with stage III heart failure and a history of at least one hospitalization.”
Other groups are taking a much more selective approach. Dr. Altman and her colleagues in Denver are only targeting patients who have been hospitalized at least twice within the past year, and more specifically patients recently rehospitalized within 30 days of their prior hospitalization. They are also focusing on patients expected to have a high level of compliance with the daily data-collection demands of PAP monitoring and the need to regularly adjust their medication dosages after receiving call backs from their clinicians. This criteria means that they are ruling out patients with a history of substance abuse, she said.
She also noted the need to tailor the target PAP to the specific clinical status of individual patients. Patients with mitral regurgitation, for example, will have a higher “normal” diastolic PAP and hence require a somewhat different target for stability maintenance. “You need to understand each patient’s baseline pressures and adjust their medications based on that,” Dr. Altman said.
“In real life patients tend to be older and sicker, so their benefit may be even greater than what was seen in CHAMPION, but perhaps the results will also be diluted because of comorbidities like renal failure or chronic obstructive pulmonary disease,” said Dr. Butler, although post hoc subanalyses of CHAMPION data showed that these comorbidities did not blunt the positive impact of PAP-guided treatment. “I don’t know if I’ll be successful in selecting the right patients, and whether my interventions in real life will produce the same good outcomes” seen in CHAMPION. “We’ll select patients who are close to the CHAMPION criteria, but not patients on dialysis [who were excluded from CHAMPION]; we’ll select patients with a modest degree of comorbidity and reasonable expected survival,” Dr. Butler said.
“If you had a drug that reduced rehospitalization rates it would be pretty clear how to proceed, but in this case it is not the device that reduces readmissions, it just gives you data and you need to act on the data,” Dr. Butler added. He acknowledged that the CHAMPION investigators used a relatively simple, straightforward management algorithm for patients whose PAP fell out of the target range, such as a diastolic PAP greater than 20 mm Hg or less than 8 mm Hg. The first management step is to raise or reduce the patient’s diuretic dosage, and if that fails to quickly normalize PAP the next step is to adjust the vasodilator dosage.
Managing patients in CHAMPION was “not totally an art” but neither was it “totally a science,” Dr. Butler said. Managing patients based on daily data collected using a CardioMEMS device will “require a little finesse,” he said. “It’s not straight science.”
Programs that have already used PAP monitoring on a routine basis, like those in Denver and at Brigham and Women’s, consider their experience too small in size and short in duration to draw any substantive conclusions regarding their success compared with the CHAMPION results. But Dr. Abraham, whose program has now placed CardioMEMS routinely in a few dozen patients and followed them for as long as a year, said that in his center’s patients the device and management system has produced outcomes that roughly match what he saw in the pivotal trial.
“The ongoing concern is that what was achieved in the CHAMPION trial may not be what is achieved in routine practice,” said Dr. Desai. The care that patients received in the trial is “a little of a black box,” he said, and during the FDA’s approval process some reviewers raised concerns that patients in the active-treatment arm simply received more intensive surveillance, although this concern eventually resolved. “There is not a lot of skepticism” among clinicians about this treatment, but there is uncertainly about exactly whom are the best patients to treat and whether their responses be as good as in CHAMPION, Dr. Desai said in an interview.
“The proof [of efficacy] will be in each individual center’s experience” using CardioMEMS, Dr. Altman said.
CHAMPION was initially funded by CardioMEMS, which then was acquired by St. Jude which is the company marketing the CardioMEMS device and associated hardware. Dr. Butler said that he had no current relevant disclosures, although in the past he had been a consultant to CardioMEMS (prior to its acquisition by St. Jude). Dr. Parks and Dr. Altman had no disclosures. Dr. Desai has been a consultant to and has received honoraria as a speaker on behalf of CardioMEMS and St. Jude. Dr. Abraham has been a consultant to CardioMEMS and St. Jude, was co-principal investigator on the CHAMPION trial, and is the principal investigator on a new St. Jude-funded trial studying CardioMEMS.
On Twitter @mitchelzoler
ACC to launch registries for atrial fibrillation treatments
The American College of Cardiology (ACC) will launch two registries to track the outcomes of treatments for atrial fibrillation, the medical society announced today.
The LAAO Registry will capture data on left atrial appendage occlusion procedures to assess real-world procedural indications and outcomes, as well as short- and long-term safety.
The AFib Ablation Registry will assess the prevalence, demographics, acute management, and outcomes of patients undergoing atrial fibrillation ablation procedures. This registry’s data will support the development of evidence-based guidelines and quality metrics for atrial fibrillation treatments that will improve outcomes, according to the ACC.
“With a growing prevalence of atrial fibrillation and growing options for treatment and stroke prevention in AFib patients, the ACC saw a need for real-world data to track and evaluate the use of these new technologies,” said Dr. Kim A. Williams Sr., ACC president.
The American College of Cardiology (ACC) will launch two registries to track the outcomes of treatments for atrial fibrillation, the medical society announced today.
The LAAO Registry will capture data on left atrial appendage occlusion procedures to assess real-world procedural indications and outcomes, as well as short- and long-term safety.
The AFib Ablation Registry will assess the prevalence, demographics, acute management, and outcomes of patients undergoing atrial fibrillation ablation procedures. This registry’s data will support the development of evidence-based guidelines and quality metrics for atrial fibrillation treatments that will improve outcomes, according to the ACC.
“With a growing prevalence of atrial fibrillation and growing options for treatment and stroke prevention in AFib patients, the ACC saw a need for real-world data to track and evaluate the use of these new technologies,” said Dr. Kim A. Williams Sr., ACC president.
The American College of Cardiology (ACC) will launch two registries to track the outcomes of treatments for atrial fibrillation, the medical society announced today.
The LAAO Registry will capture data on left atrial appendage occlusion procedures to assess real-world procedural indications and outcomes, as well as short- and long-term safety.
The AFib Ablation Registry will assess the prevalence, demographics, acute management, and outcomes of patients undergoing atrial fibrillation ablation procedures. This registry’s data will support the development of evidence-based guidelines and quality metrics for atrial fibrillation treatments that will improve outcomes, according to the ACC.
“With a growing prevalence of atrial fibrillation and growing options for treatment and stroke prevention in AFib patients, the ACC saw a need for real-world data to track and evaluate the use of these new technologies,” said Dr. Kim A. Williams Sr., ACC president.
‘David technique’ may enhance aortic repair
Many techniques for repair of aortic dissection have evolved, but no trials have compared those techniques to determine which is the best. However, a study team has attempted to evaluate a surgical approach (the “David technique”) that includes three specific steps – no aortic cross clamp, the use of deep hypothermic circulatory arrest (DHCA), and the antegrade resumption of cardiopulmonary bypass. They found that this approach yielded significantly better long-term outcomes than did other approaches tried.
The study investigators, led by Dr. Jennifer S. Lawton of Washington University in St. Louis, reported their findings in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.03.023]). “We hypothesized that a surgical strategy to prevent cross-clamp injury or false lumen pressurization would be associated with reduced morbidity, mortality, persistent false lumen patency, and improved survival,” Dr. Lawton and her coauthors wrote. “This study was designed to determine the differences in outcomes between operative techniques.”
The study evaluated 196 patients who had surgery for acute type A aortic dissection over 17 years. Group 1, which comprised 49 patients, had the operation according to the protocol that involved the three specific steps, as Dr. Tirone David of the University of Toronto first reported in 1999 (Ann. Thorac. Surg. 1999;67:1999-2001) — the “David technique,” as the study authors called it. Group 2 consisted of patients whose repair involved a variety of techniques, including one or two steps of the David technique but not all three.
Study endpoints were 30-day mortality rate, postoperative adverse events, presence of a false aortic lumen, and overall survival, the latter defined as the time from the date of surgery to the date or death or last follow-up. The evaluation included examination of patients’ latest CT scan or MRI that was at least 6 months after the operation for false lumen, but only 78 patients had imaging at that interval.
Patients in Group 1 had a higher rate of persistent false lumen – 74% vs. 68% in Group 2. Thirty-day mortality was 6.1% in Group 1 and 15.7% in Group 2, but Dr. Lawton and her coauthors said this difference was not statistically significant.
Survival rates at 1, 5 and 10 years among both groups were “consistent with published ranges,” the authors said. At 5 years, the predicted survival was 86% for Group 1 and 56% for Group 2; and at 10 years, 72% and 37% respectively.
The study authors acknowledged the controversy that surrounds the use of retrograde resumption of cardiopulmonary bypass after replacement of the ascending aorta and that there’s no consensus on which method is best for resuming cardiopulmonary bypass after repair of a type A aortic dissection.
The study also found no difference in the incidence of false lumen between the two groups, but again, this is a source of controversy. “Persistence of a false lumen following repair for type A aortic dissection has been reported to be associated with poor prognosis and reduced long-term survival,” Dr. Lawton and her colleagues said.
“Others have reported a patent false lumen was not an independent predictor of late reoperation, but was a predictor of aortic growth following repair of type A aortic dissection.”
The study authors said one limit of their findings is its retrospective nature, but they also said that a prospective, randomized trial would be difficult to conduct.
None of the study coauthors had any relationships to disclose. They presented their original data at the American Association for Thoracic Surgery Aortic Symposium, April 24-25, 2014, in New York.
Whether or not to use a cross-clamp in type A aortic dissection repair is a critical question, but a major concern of this study was the wide variability of techniques used in the comparison group, Dr. Richard J. Shemin said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.04.038]). “The variety of approaches attests to the lack of institutional agreement on the surgical principles tested in the study,” he said. “The large variety of techniques in the control group makes the comparison and interpretation of this study difficult.”
“There are more questions to consider from this study than answers derived from the data about the clamp strategy,” he said
But, Dr. Shemin said, using the cross-clamp with axillary antegrade perfusion is “not a major issue.” And the use of clamping during the cooling period can save overall cardiac arrest time during the operation.
“If one does use femoral cannulation, then not applying the cross-clamp until achieving circulatory arrest is prudent,” he said. “With axillary cannulation, one achieves antegrade perfusion so early cross-clamping can be safely performed with the advantages of saving operative time.”
The clamp site must be inspected during circulatory arrest. Antegrade cerebral perfusion is proven to be an excellent technique and is facilitated by right axillary cannulation, Dr. Shemin said. “Most importantly, establishing antegrade CPB [cardiopulmonary bypass] perfusion after circulatory arrest is mandatory in all cases to minimize distal aorta trauma,” he said.
Dr. Richard J. Shemin is a cardiothoracic surgeon at UCLA Medical Center, Santa Monica, Calif.
Whether or not to use a cross-clamp in type A aortic dissection repair is a critical question, but a major concern of this study was the wide variability of techniques used in the comparison group, Dr. Richard J. Shemin said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.04.038]). “The variety of approaches attests to the lack of institutional agreement on the surgical principles tested in the study,” he said. “The large variety of techniques in the control group makes the comparison and interpretation of this study difficult.”
“There are more questions to consider from this study than answers derived from the data about the clamp strategy,” he said
But, Dr. Shemin said, using the cross-clamp with axillary antegrade perfusion is “not a major issue.” And the use of clamping during the cooling period can save overall cardiac arrest time during the operation.
“If one does use femoral cannulation, then not applying the cross-clamp until achieving circulatory arrest is prudent,” he said. “With axillary cannulation, one achieves antegrade perfusion so early cross-clamping can be safely performed with the advantages of saving operative time.”
The clamp site must be inspected during circulatory arrest. Antegrade cerebral perfusion is proven to be an excellent technique and is facilitated by right axillary cannulation, Dr. Shemin said. “Most importantly, establishing antegrade CPB [cardiopulmonary bypass] perfusion after circulatory arrest is mandatory in all cases to minimize distal aorta trauma,” he said.
Dr. Richard J. Shemin is a cardiothoracic surgeon at UCLA Medical Center, Santa Monica, Calif.
Whether or not to use a cross-clamp in type A aortic dissection repair is a critical question, but a major concern of this study was the wide variability of techniques used in the comparison group, Dr. Richard J. Shemin said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.04.038]). “The variety of approaches attests to the lack of institutional agreement on the surgical principles tested in the study,” he said. “The large variety of techniques in the control group makes the comparison and interpretation of this study difficult.”
“There are more questions to consider from this study than answers derived from the data about the clamp strategy,” he said
But, Dr. Shemin said, using the cross-clamp with axillary antegrade perfusion is “not a major issue.” And the use of clamping during the cooling period can save overall cardiac arrest time during the operation.
“If one does use femoral cannulation, then not applying the cross-clamp until achieving circulatory arrest is prudent,” he said. “With axillary cannulation, one achieves antegrade perfusion so early cross-clamping can be safely performed with the advantages of saving operative time.”
The clamp site must be inspected during circulatory arrest. Antegrade cerebral perfusion is proven to be an excellent technique and is facilitated by right axillary cannulation, Dr. Shemin said. “Most importantly, establishing antegrade CPB [cardiopulmonary bypass] perfusion after circulatory arrest is mandatory in all cases to minimize distal aorta trauma,” he said.
Dr. Richard J. Shemin is a cardiothoracic surgeon at UCLA Medical Center, Santa Monica, Calif.
Many techniques for repair of aortic dissection have evolved, but no trials have compared those techniques to determine which is the best. However, a study team has attempted to evaluate a surgical approach (the “David technique”) that includes three specific steps – no aortic cross clamp, the use of deep hypothermic circulatory arrest (DHCA), and the antegrade resumption of cardiopulmonary bypass. They found that this approach yielded significantly better long-term outcomes than did other approaches tried.
The study investigators, led by Dr. Jennifer S. Lawton of Washington University in St. Louis, reported their findings in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.03.023]). “We hypothesized that a surgical strategy to prevent cross-clamp injury or false lumen pressurization would be associated with reduced morbidity, mortality, persistent false lumen patency, and improved survival,” Dr. Lawton and her coauthors wrote. “This study was designed to determine the differences in outcomes between operative techniques.”
The study evaluated 196 patients who had surgery for acute type A aortic dissection over 17 years. Group 1, which comprised 49 patients, had the operation according to the protocol that involved the three specific steps, as Dr. Tirone David of the University of Toronto first reported in 1999 (Ann. Thorac. Surg. 1999;67:1999-2001) — the “David technique,” as the study authors called it. Group 2 consisted of patients whose repair involved a variety of techniques, including one or two steps of the David technique but not all three.
Study endpoints were 30-day mortality rate, postoperative adverse events, presence of a false aortic lumen, and overall survival, the latter defined as the time from the date of surgery to the date or death or last follow-up. The evaluation included examination of patients’ latest CT scan or MRI that was at least 6 months after the operation for false lumen, but only 78 patients had imaging at that interval.
Patients in Group 1 had a higher rate of persistent false lumen – 74% vs. 68% in Group 2. Thirty-day mortality was 6.1% in Group 1 and 15.7% in Group 2, but Dr. Lawton and her coauthors said this difference was not statistically significant.
Survival rates at 1, 5 and 10 years among both groups were “consistent with published ranges,” the authors said. At 5 years, the predicted survival was 86% for Group 1 and 56% for Group 2; and at 10 years, 72% and 37% respectively.
The study authors acknowledged the controversy that surrounds the use of retrograde resumption of cardiopulmonary bypass after replacement of the ascending aorta and that there’s no consensus on which method is best for resuming cardiopulmonary bypass after repair of a type A aortic dissection.
The study also found no difference in the incidence of false lumen between the two groups, but again, this is a source of controversy. “Persistence of a false lumen following repair for type A aortic dissection has been reported to be associated with poor prognosis and reduced long-term survival,” Dr. Lawton and her colleagues said.
“Others have reported a patent false lumen was not an independent predictor of late reoperation, but was a predictor of aortic growth following repair of type A aortic dissection.”
The study authors said one limit of their findings is its retrospective nature, but they also said that a prospective, randomized trial would be difficult to conduct.
None of the study coauthors had any relationships to disclose. They presented their original data at the American Association for Thoracic Surgery Aortic Symposium, April 24-25, 2014, in New York.
Many techniques for repair of aortic dissection have evolved, but no trials have compared those techniques to determine which is the best. However, a study team has attempted to evaluate a surgical approach (the “David technique”) that includes three specific steps – no aortic cross clamp, the use of deep hypothermic circulatory arrest (DHCA), and the antegrade resumption of cardiopulmonary bypass. They found that this approach yielded significantly better long-term outcomes than did other approaches tried.
The study investigators, led by Dr. Jennifer S. Lawton of Washington University in St. Louis, reported their findings in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.03.023]). “We hypothesized that a surgical strategy to prevent cross-clamp injury or false lumen pressurization would be associated with reduced morbidity, mortality, persistent false lumen patency, and improved survival,” Dr. Lawton and her coauthors wrote. “This study was designed to determine the differences in outcomes between operative techniques.”
The study evaluated 196 patients who had surgery for acute type A aortic dissection over 17 years. Group 1, which comprised 49 patients, had the operation according to the protocol that involved the three specific steps, as Dr. Tirone David of the University of Toronto first reported in 1999 (Ann. Thorac. Surg. 1999;67:1999-2001) — the “David technique,” as the study authors called it. Group 2 consisted of patients whose repair involved a variety of techniques, including one or two steps of the David technique but not all three.
Study endpoints were 30-day mortality rate, postoperative adverse events, presence of a false aortic lumen, and overall survival, the latter defined as the time from the date of surgery to the date or death or last follow-up. The evaluation included examination of patients’ latest CT scan or MRI that was at least 6 months after the operation for false lumen, but only 78 patients had imaging at that interval.
Patients in Group 1 had a higher rate of persistent false lumen – 74% vs. 68% in Group 2. Thirty-day mortality was 6.1% in Group 1 and 15.7% in Group 2, but Dr. Lawton and her coauthors said this difference was not statistically significant.
Survival rates at 1, 5 and 10 years among both groups were “consistent with published ranges,” the authors said. At 5 years, the predicted survival was 86% for Group 1 and 56% for Group 2; and at 10 years, 72% and 37% respectively.
The study authors acknowledged the controversy that surrounds the use of retrograde resumption of cardiopulmonary bypass after replacement of the ascending aorta and that there’s no consensus on which method is best for resuming cardiopulmonary bypass after repair of a type A aortic dissection.
The study also found no difference in the incidence of false lumen between the two groups, but again, this is a source of controversy. “Persistence of a false lumen following repair for type A aortic dissection has been reported to be associated with poor prognosis and reduced long-term survival,” Dr. Lawton and her colleagues said.
“Others have reported a patent false lumen was not an independent predictor of late reoperation, but was a predictor of aortic growth following repair of type A aortic dissection.”
The study authors said one limit of their findings is its retrospective nature, but they also said that a prospective, randomized trial would be difficult to conduct.
None of the study coauthors had any relationships to disclose. They presented their original data at the American Association for Thoracic Surgery Aortic Symposium, April 24-25, 2014, in New York.
Key clinical point: An operation to repair type A aortic dissection that involves three specific steps achieves better outcomes than do other surgical approaches.
Major finding: Survival rates at 5 years were 86% for the group that had operations in which the surgeons used the three specific steps vs. 56% for the other group.
Data source: Retrospective analysis of single-center population of 146 patients who had repairs for type A aortic dissection.
Disclosures: None of the study coauthors had any relationships to disclose.
Talent: Too much or too little depends on the kind of team
Talent facilitates team performance, but only up to a point, depending on the type of team. For highly interdependent teams, there is a threshold where the benefits of more talent decrease and eventually become detrimental rather than beneficial, according to an analysis of five studies performed by Roderick I. Swaab and his colleagues.
Surveys across industries and countries show that organizations consider talent attraction is their top priority, presumably based on the belief that more talent is better and the relationship between talent and team performance is linear and monotonic, they stated in Psychological Science (2014;25:1581-91)
The researchers analyzed the results of five studies they performed to investigate this relationship, comparing the impact of talent on team performance in the highly interdependent sports soccer (World Cup performance) and basketball (NBA), compared with the less interdependent sport of baseball (MLB).
In the case of soccer, team performance data were based on the average Fédération Internationale de Football Association (FIFA) rankings of national teams during the 2010 and 2014 World Cup qualification periods. Top talent was assessed by dividing the team’s numbers of players in each national team active in one of the world’s elite clubs divided by the total number of players on the national team.
In the case of the NBA, top talent was determined using the individual players’ estimated wins added (EWA) as determined over a 10-year period (2002-2012), with an index determining whether a player was in the top one-third (1) or not (0). Team performance was measured using each team’s end-of-year win percentage.
For baseball, top talent was determined using a player’s wins above replacement statistic (WAR), which is the number of wins a player contributes relative to a freely available minor-league player. Team performance was measured using each team’s win percentage.
In their results, basketball and soccer, the two most interdependent of the three sports, both showed a significant quadratic effect in which top talent benefited performance only up to a point, after which the marginal benefit of talent decreased and turned negative.
These results were in contrast to those seen with baseball. “As we predicted, the effect of top talent never turned negative in baseball, a sport in which task interdependence is relatively low. Thus there was no too-much-talent effect in baseball unlike in football [soccer] and basketball” according to the researchers.
“We predict that the too-much-talent effect will be found in other organizational contexts as well,” they added.
“Just as a colony of high-performing chickens competing for dominance suffers decrements in overall egg production and increases in bird mortality, teams with too much talent appear to divert attention away from coordination as team members peck at each other in their attempts to establish intergroup standing. In many cases, too much talent can be the seed of failure,” Mr. Swaab and his colleagues concluded.
The authors all declared that they had no conflicts of interest relative to the paper.
Mr. Swaab and his colleagues hypothesized the “too-much-talent effect” and found that talent often facilitates team performance, but only up to a point. They report that the relationship between talent and performance is not linear and monotonic. In contrast, they found that the relationship in football and basketball eventually turns negative (Psychol. Science 2014;25;1581-91). We have all heard the phrase, “There is no ‘I’ in team,” and it is clear that in certain sports, a team is necessary. No single cyclist can win the Tour de France without a strong team of support, and a soccer striker who is arrogant and feels he or she can score alone will fail to pass to the open teammate time and time again. We have all seen this strategy fail to result in a win. In contrast, one role of the midfielder in soccer is to provide selfless service to the striker – for the benefit of the team.
The cardiothoracic surgery world that we all work in can benefit from the findings reported by Swaab and colleagues. The individual with the “talent” in the cardiothoracic surgery realm – the skilled surgeon – may not be the best at building teams that work well together, and putting together several talented surgeons does not make an outstanding surgical team. Surgeons are not trained to be leaders, team builders, or to model collaborative behavior. A good leader requires emotional intelligence to be aware of others around her and of the successes and failures of the team. Lynda Gratton and Tamara J. Erickson found that the most productive, innovative teams were led by people who were both task- and relationship-oriented and that these leaders changed their style during the project (Eight Ways to Build Collaborative Teams, Harvard Bushiness Review, November 2007). Their findings were similar to those reported by Mr. Swaab and his colleagues in that they also found that the greater the proportion of highly educated specialists on a team, the more likely the team is to disintegrate into unproductive conflicts.
If we wish to establish world-renowned service lines or surgical programs, we would be well served by understanding that a great team requires collaboration, cohesion, and diversity. Diversity not only in talent but also in background and experiences. In addition, surgeon leaders cannot score all of the goals alone; they need an integrated, cohesive, diverse, and collaborative team to provide excellent patient care.
Dr. Jennifer S. Lawton is a professor of surgery at the division of cardiothoracic surgery, Washington University, St. Louis. She is also an associate medical editor for Vascular Specialist.
Mr. Swaab and his colleagues hypothesized the “too-much-talent effect” and found that talent often facilitates team performance, but only up to a point. They report that the relationship between talent and performance is not linear and monotonic. In contrast, they found that the relationship in football and basketball eventually turns negative (Psychol. Science 2014;25;1581-91). We have all heard the phrase, “There is no ‘I’ in team,” and it is clear that in certain sports, a team is necessary. No single cyclist can win the Tour de France without a strong team of support, and a soccer striker who is arrogant and feels he or she can score alone will fail to pass to the open teammate time and time again. We have all seen this strategy fail to result in a win. In contrast, one role of the midfielder in soccer is to provide selfless service to the striker – for the benefit of the team.
The cardiothoracic surgery world that we all work in can benefit from the findings reported by Swaab and colleagues. The individual with the “talent” in the cardiothoracic surgery realm – the skilled surgeon – may not be the best at building teams that work well together, and putting together several talented surgeons does not make an outstanding surgical team. Surgeons are not trained to be leaders, team builders, or to model collaborative behavior. A good leader requires emotional intelligence to be aware of others around her and of the successes and failures of the team. Lynda Gratton and Tamara J. Erickson found that the most productive, innovative teams were led by people who were both task- and relationship-oriented and that these leaders changed their style during the project (Eight Ways to Build Collaborative Teams, Harvard Bushiness Review, November 2007). Their findings were similar to those reported by Mr. Swaab and his colleagues in that they also found that the greater the proportion of highly educated specialists on a team, the more likely the team is to disintegrate into unproductive conflicts.
If we wish to establish world-renowned service lines or surgical programs, we would be well served by understanding that a great team requires collaboration, cohesion, and diversity. Diversity not only in talent but also in background and experiences. In addition, surgeon leaders cannot score all of the goals alone; they need an integrated, cohesive, diverse, and collaborative team to provide excellent patient care.
Dr. Jennifer S. Lawton is a professor of surgery at the division of cardiothoracic surgery, Washington University, St. Louis. She is also an associate medical editor for Vascular Specialist.
Mr. Swaab and his colleagues hypothesized the “too-much-talent effect” and found that talent often facilitates team performance, but only up to a point. They report that the relationship between talent and performance is not linear and monotonic. In contrast, they found that the relationship in football and basketball eventually turns negative (Psychol. Science 2014;25;1581-91). We have all heard the phrase, “There is no ‘I’ in team,” and it is clear that in certain sports, a team is necessary. No single cyclist can win the Tour de France without a strong team of support, and a soccer striker who is arrogant and feels he or she can score alone will fail to pass to the open teammate time and time again. We have all seen this strategy fail to result in a win. In contrast, one role of the midfielder in soccer is to provide selfless service to the striker – for the benefit of the team.
The cardiothoracic surgery world that we all work in can benefit from the findings reported by Swaab and colleagues. The individual with the “talent” in the cardiothoracic surgery realm – the skilled surgeon – may not be the best at building teams that work well together, and putting together several talented surgeons does not make an outstanding surgical team. Surgeons are not trained to be leaders, team builders, or to model collaborative behavior. A good leader requires emotional intelligence to be aware of others around her and of the successes and failures of the team. Lynda Gratton and Tamara J. Erickson found that the most productive, innovative teams were led by people who were both task- and relationship-oriented and that these leaders changed their style during the project (Eight Ways to Build Collaborative Teams, Harvard Bushiness Review, November 2007). Their findings were similar to those reported by Mr. Swaab and his colleagues in that they also found that the greater the proportion of highly educated specialists on a team, the more likely the team is to disintegrate into unproductive conflicts.
If we wish to establish world-renowned service lines or surgical programs, we would be well served by understanding that a great team requires collaboration, cohesion, and diversity. Diversity not only in talent but also in background and experiences. In addition, surgeon leaders cannot score all of the goals alone; they need an integrated, cohesive, diverse, and collaborative team to provide excellent patient care.
Dr. Jennifer S. Lawton is a professor of surgery at the division of cardiothoracic surgery, Washington University, St. Louis. She is also an associate medical editor for Vascular Specialist.
Talent facilitates team performance, but only up to a point, depending on the type of team. For highly interdependent teams, there is a threshold where the benefits of more talent decrease and eventually become detrimental rather than beneficial, according to an analysis of five studies performed by Roderick I. Swaab and his colleagues.
Surveys across industries and countries show that organizations consider talent attraction is their top priority, presumably based on the belief that more talent is better and the relationship between talent and team performance is linear and monotonic, they stated in Psychological Science (2014;25:1581-91)
The researchers analyzed the results of five studies they performed to investigate this relationship, comparing the impact of talent on team performance in the highly interdependent sports soccer (World Cup performance) and basketball (NBA), compared with the less interdependent sport of baseball (MLB).
In the case of soccer, team performance data were based on the average Fédération Internationale de Football Association (FIFA) rankings of national teams during the 2010 and 2014 World Cup qualification periods. Top talent was assessed by dividing the team’s numbers of players in each national team active in one of the world’s elite clubs divided by the total number of players on the national team.
In the case of the NBA, top talent was determined using the individual players’ estimated wins added (EWA) as determined over a 10-year period (2002-2012), with an index determining whether a player was in the top one-third (1) or not (0). Team performance was measured using each team’s end-of-year win percentage.
For baseball, top talent was determined using a player’s wins above replacement statistic (WAR), which is the number of wins a player contributes relative to a freely available minor-league player. Team performance was measured using each team’s win percentage.
In their results, basketball and soccer, the two most interdependent of the three sports, both showed a significant quadratic effect in which top talent benefited performance only up to a point, after which the marginal benefit of talent decreased and turned negative.
These results were in contrast to those seen with baseball. “As we predicted, the effect of top talent never turned negative in baseball, a sport in which task interdependence is relatively low. Thus there was no too-much-talent effect in baseball unlike in football [soccer] and basketball” according to the researchers.
“We predict that the too-much-talent effect will be found in other organizational contexts as well,” they added.
“Just as a colony of high-performing chickens competing for dominance suffers decrements in overall egg production and increases in bird mortality, teams with too much talent appear to divert attention away from coordination as team members peck at each other in their attempts to establish intergroup standing. In many cases, too much talent can be the seed of failure,” Mr. Swaab and his colleagues concluded.
The authors all declared that they had no conflicts of interest relative to the paper.
Talent facilitates team performance, but only up to a point, depending on the type of team. For highly interdependent teams, there is a threshold where the benefits of more talent decrease and eventually become detrimental rather than beneficial, according to an analysis of five studies performed by Roderick I. Swaab and his colleagues.
Surveys across industries and countries show that organizations consider talent attraction is their top priority, presumably based on the belief that more talent is better and the relationship between talent and team performance is linear and monotonic, they stated in Psychological Science (2014;25:1581-91)
The researchers analyzed the results of five studies they performed to investigate this relationship, comparing the impact of talent on team performance in the highly interdependent sports soccer (World Cup performance) and basketball (NBA), compared with the less interdependent sport of baseball (MLB).
In the case of soccer, team performance data were based on the average Fédération Internationale de Football Association (FIFA) rankings of national teams during the 2010 and 2014 World Cup qualification periods. Top talent was assessed by dividing the team’s numbers of players in each national team active in one of the world’s elite clubs divided by the total number of players on the national team.
In the case of the NBA, top talent was determined using the individual players’ estimated wins added (EWA) as determined over a 10-year period (2002-2012), with an index determining whether a player was in the top one-third (1) or not (0). Team performance was measured using each team’s end-of-year win percentage.
For baseball, top talent was determined using a player’s wins above replacement statistic (WAR), which is the number of wins a player contributes relative to a freely available minor-league player. Team performance was measured using each team’s win percentage.
In their results, basketball and soccer, the two most interdependent of the three sports, both showed a significant quadratic effect in which top talent benefited performance only up to a point, after which the marginal benefit of talent decreased and turned negative.
These results were in contrast to those seen with baseball. “As we predicted, the effect of top talent never turned negative in baseball, a sport in which task interdependence is relatively low. Thus there was no too-much-talent effect in baseball unlike in football [soccer] and basketball” according to the researchers.
“We predict that the too-much-talent effect will be found in other organizational contexts as well,” they added.
“Just as a colony of high-performing chickens competing for dominance suffers decrements in overall egg production and increases in bird mortality, teams with too much talent appear to divert attention away from coordination as team members peck at each other in their attempts to establish intergroup standing. In many cases, too much talent can be the seed of failure,” Mr. Swaab and his colleagues concluded.
The authors all declared that they had no conflicts of interest relative to the paper.
FROM PSYCHOLOGICAL SCIENCE
Key clinical point: Talent facilitates team performance, but it’s only up to a point, depending on the type of team.
Major finding: For highly interdependent teams, there is a threshold where the benefits of more talent decrease and eventually become detrimental rather than beneficial.
Data source: Five studies compared the impact of talent on team performance in the highly interdependent sports soccer (World Cup performance) and basketball (NBA), compared with the less interdependent sport of baseball (MLB)
Disclosures: The authors of the study reported no relevant disclosures.
CABG costs more in patients with diabetes
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
FROM JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The percentage of CABG patients with diabetes increased from 7% in the 1970s to 37% in the 2000s. The risk/benefit ratio warrants greater use of bilateral mammary arteries except in obese women with diabetes.
Major finding: Diabetic patients had significantly worse outcomes than nondiabetics with regard to hospital death, deep sternal wound infections, strokes, and renal failure as well as hospital stay and costs.
Data source: A retrospective analysis of a prospective database of patients undergoing first-time CABG at the Cleveland Clinic from 1972 to 2011.
Disclosures: The authors reported that they had no relevant conflicts of interest.
SVS: Cryoallografts, NAIS best to reconstruct infected aortic grafts
CHICAGO – Neoaortoiliac system reconstruction or cryopreserved allografts should be used first-line to replace infected aortic endografts, followed by antibiotic-soaked prosthetic grafts, according to a review of 206 cases from vascular surgery centers across the United States.
In the study, 75 patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Forty-nine of the 92 (53%) patients reconstructed with antibiotic-soaked prosthetic grafts also made it to 5 years, while two of 19 (11%) reconstructed with untreated prosthetic grafts survived that long.
The cases were reconstructed inline. The index procedure had been endovascular aortic repair (EVAR) in 165, and thoracic EVAR (TEVAR) in 21, with a better 5-year survival for the EVAR group. Another 11 patients had extra-anatomic reconstruction after initial EVAR, and their 5-year survival was comparable to inline reconstruction at about 50% overall. Nine other patients were managed medically; the majority died soon after being diagnosed with an infected graft.
“Clinicians should have a high index of suspicion to diagnose symptomatic postop EVAR and TEVAR patients with graft infection, especially in those patients with chronic infections or contaminated index procedures. NAIS and cryopreserved allografts require longer procedure times” – about 500 minutes versus about 350 minutes for prosthetic grafts – “but offer improved survival, while prosthetics soaked in antibiotic do better than prosthetic grafts alone,” said lead investigator Dr. Audra Duncan, professor of surgery at the Mayo Clinic in Rochester, Minn.
Patients were treated at the Mayo Clinic, the Cleveland Clinic in Ohio, Johns Hopkins University in Baltimore, the University of California, Los Angeles, and 15 other vascular centers around the country during 2004-2014. They were 68 years old on average, and 78% were men. Comorbidities included hypertension in 84%, smoking in 58%, and renal insufficiency in 30%.
On multivariate analysis, chronic infection, polymicrobial infection, and prosthetic reconstruction, among other things, predicted mortality after reconstruction.
Graft infections were primarily polymicrobial and fungal, and were diagnosed a mean of 716 days after the initial implant, generally by CT. Symptoms included pain in 66%, mostly in the back and abdomen, and fever and chills, also in 66%. Streptococcus, Escherichia coli, and both methicillin-sensitive and -resistant Staphylococcus aureus were among the most commonly isolated organisms. No particular type of graft seemed more likely to get infected.
The sources of infection are unknown, but index procedures were complicated by urinary tract, groin, and other infections in about one-third of patients. About one-third also had interval procedures, including endoleak intervention. About 14% of patients were thought to have had a contaminated index procedure.
Patients stayed in the hospital a mean of 24 days after reconstruction. Early complications included persistent sepsis in 27 patients, myocardial infarction in 9, recurrent infection in 9, and pneumonia in 8. Mortality at 30 days was 11%.
Nineteen replacement grafts – mostly unsoaked Dacron – were explanted after a mean of 540 days. Persistent sepsis after reconstruction was associated with unsoaked Dacron and polytetrafluoroethylene (PTFE) grafts.
To prevent graft infections, Mayo patients “take an antibiotic for any invasive procedure,” including dental work. “I am not sure we have data to support that, but it is something we do,” Dr. Duncan said.
Dr. Duncan has no relevant disclosures.
CHICAGO – Neoaortoiliac system reconstruction or cryopreserved allografts should be used first-line to replace infected aortic endografts, followed by antibiotic-soaked prosthetic grafts, according to a review of 206 cases from vascular surgery centers across the United States.
In the study, 75 patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Forty-nine of the 92 (53%) patients reconstructed with antibiotic-soaked prosthetic grafts also made it to 5 years, while two of 19 (11%) reconstructed with untreated prosthetic grafts survived that long.
The cases were reconstructed inline. The index procedure had been endovascular aortic repair (EVAR) in 165, and thoracic EVAR (TEVAR) in 21, with a better 5-year survival for the EVAR group. Another 11 patients had extra-anatomic reconstruction after initial EVAR, and their 5-year survival was comparable to inline reconstruction at about 50% overall. Nine other patients were managed medically; the majority died soon after being diagnosed with an infected graft.
“Clinicians should have a high index of suspicion to diagnose symptomatic postop EVAR and TEVAR patients with graft infection, especially in those patients with chronic infections or contaminated index procedures. NAIS and cryopreserved allografts require longer procedure times” – about 500 minutes versus about 350 minutes for prosthetic grafts – “but offer improved survival, while prosthetics soaked in antibiotic do better than prosthetic grafts alone,” said lead investigator Dr. Audra Duncan, professor of surgery at the Mayo Clinic in Rochester, Minn.
Patients were treated at the Mayo Clinic, the Cleveland Clinic in Ohio, Johns Hopkins University in Baltimore, the University of California, Los Angeles, and 15 other vascular centers around the country during 2004-2014. They were 68 years old on average, and 78% were men. Comorbidities included hypertension in 84%, smoking in 58%, and renal insufficiency in 30%.
On multivariate analysis, chronic infection, polymicrobial infection, and prosthetic reconstruction, among other things, predicted mortality after reconstruction.
Graft infections were primarily polymicrobial and fungal, and were diagnosed a mean of 716 days after the initial implant, generally by CT. Symptoms included pain in 66%, mostly in the back and abdomen, and fever and chills, also in 66%. Streptococcus, Escherichia coli, and both methicillin-sensitive and -resistant Staphylococcus aureus were among the most commonly isolated organisms. No particular type of graft seemed more likely to get infected.
The sources of infection are unknown, but index procedures were complicated by urinary tract, groin, and other infections in about one-third of patients. About one-third also had interval procedures, including endoleak intervention. About 14% of patients were thought to have had a contaminated index procedure.
Patients stayed in the hospital a mean of 24 days after reconstruction. Early complications included persistent sepsis in 27 patients, myocardial infarction in 9, recurrent infection in 9, and pneumonia in 8. Mortality at 30 days was 11%.
Nineteen replacement grafts – mostly unsoaked Dacron – were explanted after a mean of 540 days. Persistent sepsis after reconstruction was associated with unsoaked Dacron and polytetrafluoroethylene (PTFE) grafts.
To prevent graft infections, Mayo patients “take an antibiotic for any invasive procedure,” including dental work. “I am not sure we have data to support that, but it is something we do,” Dr. Duncan said.
Dr. Duncan has no relevant disclosures.
CHICAGO – Neoaortoiliac system reconstruction or cryopreserved allografts should be used first-line to replace infected aortic endografts, followed by antibiotic-soaked prosthetic grafts, according to a review of 206 cases from vascular surgery centers across the United States.
In the study, 75 patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Forty-nine of the 92 (53%) patients reconstructed with antibiotic-soaked prosthetic grafts also made it to 5 years, while two of 19 (11%) reconstructed with untreated prosthetic grafts survived that long.
The cases were reconstructed inline. The index procedure had been endovascular aortic repair (EVAR) in 165, and thoracic EVAR (TEVAR) in 21, with a better 5-year survival for the EVAR group. Another 11 patients had extra-anatomic reconstruction after initial EVAR, and their 5-year survival was comparable to inline reconstruction at about 50% overall. Nine other patients were managed medically; the majority died soon after being diagnosed with an infected graft.
“Clinicians should have a high index of suspicion to diagnose symptomatic postop EVAR and TEVAR patients with graft infection, especially in those patients with chronic infections or contaminated index procedures. NAIS and cryopreserved allografts require longer procedure times” – about 500 minutes versus about 350 minutes for prosthetic grafts – “but offer improved survival, while prosthetics soaked in antibiotic do better than prosthetic grafts alone,” said lead investigator Dr. Audra Duncan, professor of surgery at the Mayo Clinic in Rochester, Minn.
Patients were treated at the Mayo Clinic, the Cleveland Clinic in Ohio, Johns Hopkins University in Baltimore, the University of California, Los Angeles, and 15 other vascular centers around the country during 2004-2014. They were 68 years old on average, and 78% were men. Comorbidities included hypertension in 84%, smoking in 58%, and renal insufficiency in 30%.
On multivariate analysis, chronic infection, polymicrobial infection, and prosthetic reconstruction, among other things, predicted mortality after reconstruction.
Graft infections were primarily polymicrobial and fungal, and were diagnosed a mean of 716 days after the initial implant, generally by CT. Symptoms included pain in 66%, mostly in the back and abdomen, and fever and chills, also in 66%. Streptococcus, Escherichia coli, and both methicillin-sensitive and -resistant Staphylococcus aureus were among the most commonly isolated organisms. No particular type of graft seemed more likely to get infected.
The sources of infection are unknown, but index procedures were complicated by urinary tract, groin, and other infections in about one-third of patients. About one-third also had interval procedures, including endoleak intervention. About 14% of patients were thought to have had a contaminated index procedure.
Patients stayed in the hospital a mean of 24 days after reconstruction. Early complications included persistent sepsis in 27 patients, myocardial infarction in 9, recurrent infection in 9, and pneumonia in 8. Mortality at 30 days was 11%.
Nineteen replacement grafts – mostly unsoaked Dacron – were explanted after a mean of 540 days. Persistent sepsis after reconstruction was associated with unsoaked Dacron and polytetrafluoroethylene (PTFE) grafts.
To prevent graft infections, Mayo patients “take an antibiotic for any invasive procedure,” including dental work. “I am not sure we have data to support that, but it is something we do,” Dr. Duncan said.
Dr. Duncan has no relevant disclosures.
AT THE 2015 VASCULAR ANNUAL MEETING
Key clinical point: Neoaortoiliac system reconstruction or cryopreserved allografts perform best in replacing infected aortic endografts, but if you have to use prosthetics, use ones soaked in antibiotics.
Major finding: Seventy-five patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Two of 19 (11%) patients reconstructed with untreated prosthetic grafts survived that long.
Data source: Review of 206 patients at 19 vascular surgery centers in the United States.
Disclosures: The lead investigator has no relevant disclosures.