User login
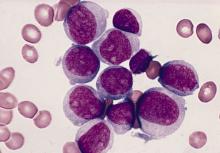
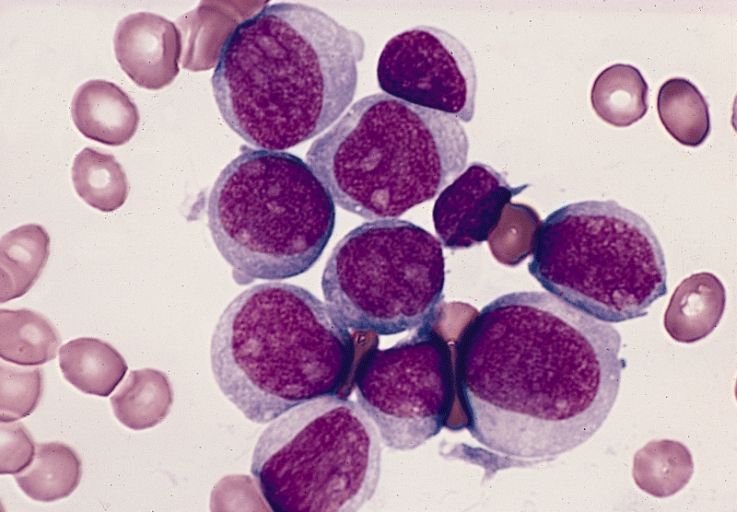
Pediatric AML: Gemtuzumab ozogamicin prior to allo-HCT increases risk for veno-occlusive disease
Key clinical point: Prior treatment with gemtuzumab ozogamicin (GO) before allogeneic hematopoietic cell transplantation (allo-HCT) in pediatric patients with acute myeloid leukemia (AML) increased risk for veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS) but did not affect survival.
Major finding: Compared with nonexposure, exposure to GO was associated with increased risk for VOD/SOS at 100 days (odds ratio, 2.26; P = .004). However, posttransplant overall survival (P = .43), disease-free survival (P = .20), relapse (P = .32), and nonrelapse mortality (P = .51) did not differ in patients with or without prior GO treatment.
Study details: Findings are from retrospective assessment of pediatric patients with AML who received myeloablative allo-HCT between 2008 and 2011 with (n=148) or without (n=348) prior GO treatment.
Disclosures: This study was funded by Pfizer. D Chirnomas, CJ Hoang, and FR Loberiza Jr declared being current/former employees of and/or had equity ownership in Pfizer. Other authors declared no conflicts of interest.
Source: Duncan C et al. Pediatr Blood Cancer. 2021 Apr 19. doi: 10.1002/pbc.29067.
Key clinical point: Prior treatment with gemtuzumab ozogamicin (GO) before allogeneic hematopoietic cell transplantation (allo-HCT) in pediatric patients with acute myeloid leukemia (AML) increased risk for veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS) but did not affect survival.
Major finding: Compared with nonexposure, exposure to GO was associated with increased risk for VOD/SOS at 100 days (odds ratio, 2.26; P = .004). However, posttransplant overall survival (P = .43), disease-free survival (P = .20), relapse (P = .32), and nonrelapse mortality (P = .51) did not differ in patients with or without prior GO treatment.
Study details: Findings are from retrospective assessment of pediatric patients with AML who received myeloablative allo-HCT between 2008 and 2011 with (n=148) or without (n=348) prior GO treatment.
Disclosures: This study was funded by Pfizer. D Chirnomas, CJ Hoang, and FR Loberiza Jr declared being current/former employees of and/or had equity ownership in Pfizer. Other authors declared no conflicts of interest.
Source: Duncan C et al. Pediatr Blood Cancer. 2021 Apr 19. doi: 10.1002/pbc.29067.
Key clinical point: Prior treatment with gemtuzumab ozogamicin (GO) before allogeneic hematopoietic cell transplantation (allo-HCT) in pediatric patients with acute myeloid leukemia (AML) increased risk for veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS) but did not affect survival.
Major finding: Compared with nonexposure, exposure to GO was associated with increased risk for VOD/SOS at 100 days (odds ratio, 2.26; P = .004). However, posttransplant overall survival (P = .43), disease-free survival (P = .20), relapse (P = .32), and nonrelapse mortality (P = .51) did not differ in patients with or without prior GO treatment.
Study details: Findings are from retrospective assessment of pediatric patients with AML who received myeloablative allo-HCT between 2008 and 2011 with (n=148) or without (n=348) prior GO treatment.
Disclosures: This study was funded by Pfizer. D Chirnomas, CJ Hoang, and FR Loberiza Jr declared being current/former employees of and/or had equity ownership in Pfizer. Other authors declared no conflicts of interest.
Source: Duncan C et al. Pediatr Blood Cancer. 2021 Apr 19. doi: 10.1002/pbc.29067.
De novo AML: Data spanning 4 decades show significant improvement in outcomes
Key clinical point: Survival outcomes have improved significantly in patients with de novo acute myeloid leukemia (AML) over a 4-decade period from 1980 to 2017; however, least improvement was observed in patients aged 70 years or older.
Major finding: Overall, 5-year survival increased from 9% during 1980-1989 to 15% in 1990-1999, 22% in 2000-2009, and 28% in 2010-2017 (all P less than .001). However, improvement in 5-year survival was poorest in patients aged 70 years or older with 1% in 1980-1989 to 5% in 2010-2017.
Study details: Findings are from a U.S. population-based study that evaluated 29,107 patients from the Surveillance, Epidemiology, and End Results registries, who were diagnosed with de novo AML between 1980 and 2017.
Disclosures: No funding source was identified. Some investigators including the lead author reported personal fees, research funding, honoraria, or other support from various pharmaceutical companies.
Source: Sasaki K et al. Cancer. 2021 Apr 5. doi: 10.1002/cncr.33458.
Key clinical point: Survival outcomes have improved significantly in patients with de novo acute myeloid leukemia (AML) over a 4-decade period from 1980 to 2017; however, least improvement was observed in patients aged 70 years or older.
Major finding: Overall, 5-year survival increased from 9% during 1980-1989 to 15% in 1990-1999, 22% in 2000-2009, and 28% in 2010-2017 (all P less than .001). However, improvement in 5-year survival was poorest in patients aged 70 years or older with 1% in 1980-1989 to 5% in 2010-2017.
Study details: Findings are from a U.S. population-based study that evaluated 29,107 patients from the Surveillance, Epidemiology, and End Results registries, who were diagnosed with de novo AML between 1980 and 2017.
Disclosures: No funding source was identified. Some investigators including the lead author reported personal fees, research funding, honoraria, or other support from various pharmaceutical companies.
Source: Sasaki K et al. Cancer. 2021 Apr 5. doi: 10.1002/cncr.33458.
Key clinical point: Survival outcomes have improved significantly in patients with de novo acute myeloid leukemia (AML) over a 4-decade period from 1980 to 2017; however, least improvement was observed in patients aged 70 years or older.
Major finding: Overall, 5-year survival increased from 9% during 1980-1989 to 15% in 1990-1999, 22% in 2000-2009, and 28% in 2010-2017 (all P less than .001). However, improvement in 5-year survival was poorest in patients aged 70 years or older with 1% in 1980-1989 to 5% in 2010-2017.
Study details: Findings are from a U.S. population-based study that evaluated 29,107 patients from the Surveillance, Epidemiology, and End Results registries, who were diagnosed with de novo AML between 1980 and 2017.
Disclosures: No funding source was identified. Some investigators including the lead author reported personal fees, research funding, honoraria, or other support from various pharmaceutical companies.
Source: Sasaki K et al. Cancer. 2021 Apr 5. doi: 10.1002/cncr.33458.
Clinical Edge Journal Scan Commentary: AML May 2021
Two recently published studies added to our knowledge on the clinical benefit of gemtuzumab in patients with AML. The first study by Bouvier A et al demonstrated no survival benefit with the addition of gemtuzumab in patients with intermediate risk AML. The second study by Duncan et al was a retrospective study by the CIBMTR. That study demonstrated increased risk of VOD in pediatric patients who received gemtuzmab. However, overall survival and event free survival was similar in both groups. These results highlight the need for increased awareness post-transplant for the possibility of VOD, and also reduces concern regarding overall survival for patients receiving gemtuzumab.
Another study by the EBMT (Debaja et al) evaluated factors affecting the outcome of patients with AML receiving a second allogeneic HCT. Outcome was worse for patients not in CR and those with a short time from allo-HCT. Overall survival was similar for patients receiving a MUD or haploidentical donor. Two year overall survival was 31% vs. 29% for patients receiving MUD vs. haploidentical allo-HCT. This study clearly expands options for patients receiving a second allo-HCT. In addition, a prior study by EBMT demonstrated no difference in overall survival between patients receiving same vs. different vs. haplo donor.
Finally, a large study by the CIBMTR (Percival et al) demonstrated that in AML patients, achieving CRi and having persistent MRD prior to transplantation were associated with worse outcome compared to CR with no evidence of MRD. The adjusted 5 year survival for patient with CR/MRD-ve, CR/MRD+ve, CRi/MRD-ve and CRi/MRD+ve was 52%, 37%, 44% and 34% respectively.
Two recently published studies added to our knowledge on the clinical benefit of gemtuzumab in patients with AML. The first study by Bouvier A et al demonstrated no survival benefit with the addition of gemtuzumab in patients with intermediate risk AML. The second study by Duncan et al was a retrospective study by the CIBMTR. That study demonstrated increased risk of VOD in pediatric patients who received gemtuzmab. However, overall survival and event free survival was similar in both groups. These results highlight the need for increased awareness post-transplant for the possibility of VOD, and also reduces concern regarding overall survival for patients receiving gemtuzumab.
Another study by the EBMT (Debaja et al) evaluated factors affecting the outcome of patients with AML receiving a second allogeneic HCT. Outcome was worse for patients not in CR and those with a short time from allo-HCT. Overall survival was similar for patients receiving a MUD or haploidentical donor. Two year overall survival was 31% vs. 29% for patients receiving MUD vs. haploidentical allo-HCT. This study clearly expands options for patients receiving a second allo-HCT. In addition, a prior study by EBMT demonstrated no difference in overall survival between patients receiving same vs. different vs. haplo donor.
Finally, a large study by the CIBMTR (Percival et al) demonstrated that in AML patients, achieving CRi and having persistent MRD prior to transplantation were associated with worse outcome compared to CR with no evidence of MRD. The adjusted 5 year survival for patient with CR/MRD-ve, CR/MRD+ve, CRi/MRD-ve and CRi/MRD+ve was 52%, 37%, 44% and 34% respectively.
Two recently published studies added to our knowledge on the clinical benefit of gemtuzumab in patients with AML. The first study by Bouvier A et al demonstrated no survival benefit with the addition of gemtuzumab in patients with intermediate risk AML. The second study by Duncan et al was a retrospective study by the CIBMTR. That study demonstrated increased risk of VOD in pediatric patients who received gemtuzmab. However, overall survival and event free survival was similar in both groups. These results highlight the need for increased awareness post-transplant for the possibility of VOD, and also reduces concern regarding overall survival for patients receiving gemtuzumab.
Another study by the EBMT (Debaja et al) evaluated factors affecting the outcome of patients with AML receiving a second allogeneic HCT. Outcome was worse for patients not in CR and those with a short time from allo-HCT. Overall survival was similar for patients receiving a MUD or haploidentical donor. Two year overall survival was 31% vs. 29% for patients receiving MUD vs. haploidentical allo-HCT. This study clearly expands options for patients receiving a second allo-HCT. In addition, a prior study by EBMT demonstrated no difference in overall survival between patients receiving same vs. different vs. haplo donor.
Finally, a large study by the CIBMTR (Percival et al) demonstrated that in AML patients, achieving CRi and having persistent MRD prior to transplantation were associated with worse outcome compared to CR with no evidence of MRD. The adjusted 5 year survival for patient with CR/MRD-ve, CR/MRD+ve, CRi/MRD-ve and CRi/MRD+ve was 52%, 37%, 44% and 34% respectively.
Pediatric cancer survivors at risk for opioid misuse
Survivors of childhood cancers are at increased risk for prescription opioid misuse compared with their peers, a review of a claims database revealed.
Among more than 8,000 patients age 21 or younger who had completed treatment for hematologic, central nervous system, bone, or gonadal cancers, survivors were significantly more likely than were their peers to have an opioid prescription, longer duration of prescription, and higher daily doses of opioids, and to have opioid prescriptions overlapping for a week or more, reported Xu Ji, PhD, of Emory University in Atlanta.
Teenage and young adult patients were at higher risk than were patients younger than 12, and the risk was highest among patients who had been treated for bone malignancies, as well as those who had undergone any hematopoietic stem cell transplant.
“These findings suggest that health care providers who regularly see survivors should explore nonopioid options to help prevent opioid misuse, and screen for potential misuse in those who actually receive opioids,” she said in an oral abstract presented during the annual meeting of the American Society of Pediatric Hematology/Oncology.
“This is a really important topic, and something that’s probably been underinvestigated and underexplored in our patient population,” said session comoderator Sheri Spunt, MD, Endowed Professor of Pediatric Cancer at Stanford (Calif.) University.
Database review
Dr. Ji and colleagues used the IBM MarketScan Commercial Claims and Encounters database from 2009 to 2018 to examine prescription opioid use, potential misuse, and substance use disorders in pediatric cancer survivors in the first year after completion of therapy, and to identify factors associated with risk for misuse or substance use disorders. Specifically, the period of interest was the first year after completion of all treatments, including surgery, chemotherapy, radiation, and stem cell transplant (Abstract 2015).
They looked at deidentified records on any opioid prescription and for treatment of any opioid use or substance use disorder (alcohol, psychotherapeutic drugs, marijuana, or illicit drug use disorders).
They defined indicators of potential misuse as either prescriptions for long-acting or extended-release opioids for acute pain conditions; opioid and benzodiazepine prescriptions overlapping by a week or more; opioid prescriptions overlapping by a week or more; high daily opioid dosage (prescribed daily dose of 100 or greater morphine milligram equivalent [MME]; and/or opioid dose escalation (an increase of at least 50% in mean MMEs per month twice consecutively within 1 year).
They compared outcomes between a total of 8,635 survivors and 44,175 controls, matched on a 1:5 basis with survivors by age, sex, and region, and continuous enrollment during the 1-year posttherapy period.
In each of three age categories – 0 to 11 years, 12 to 17 years, and 18 years and older – survivors were significantly more likely to have received an opioid prescription, at 15% for the youngest survivors vs. 2% of controls, 25% vs. 8% for 12- to 17-year-olds, and 28% vs. 12% for those 18 and older (P < .01 for all three comparisons).
Survivors were also significantly more likely to have any indicator of potential misuse (1.6% vs. 0.1%, 4.6% vs. 0.5%, and 7.4% vs. 1.2%, respectively, P < .001 for all) and both the youngest and oldest groups (but not 12- to 17-year-olds) were significantly more like to have opioid or substance use disorder (0.4% vs. 0% for 0-11 years, 5.76% vs. 4.2% for 18 years and older, P < .001 for both).
Among patients with any opioid prescription, survivors were significantly more likely than were controls of any age to have indicators for potential misuse. For example, 13% of survivors aged 18 years and older had prescriptions for high opioid doses, compared with 5% of controls, and 12% had prescription overlap, vs. 2%.
Compared with patients with leukemia, patients treated for bone malignancies had a 6% greater risk for having any indicator of misuse, while patients with other malignancies were at slightly lower risk for misuse than those who completed leukemia therapy.
Patients who received any stem cell transplant had an 8.4% greater risk for misuse compared with patients who had surgery only.
Opioids pre- and posttreatment?
“Being someone who takes care of a lot of bone cancer patients, I do see patients with these issues,” Dr. Spunt said.
Audience member Jack H. Staddon, MD, PhD, of the Billings (Montana) Clinic, noted the possibility that opioid use during treatment may have been carried on into the posttreatment period, and asked whether use of narcotics during treatment was an independent risk factor for posttreatment narcotic use or misuse.
The researchers plan to investigate this question in future studies, Dr. Ji replied.
They did not report a study funding source. Dr. Ji and coauthors and Dr. Staddon reported no relevant disclosures.
Survivors of childhood cancers are at increased risk for prescription opioid misuse compared with their peers, a review of a claims database revealed.
Among more than 8,000 patients age 21 or younger who had completed treatment for hematologic, central nervous system, bone, or gonadal cancers, survivors were significantly more likely than were their peers to have an opioid prescription, longer duration of prescription, and higher daily doses of opioids, and to have opioid prescriptions overlapping for a week or more, reported Xu Ji, PhD, of Emory University in Atlanta.
Teenage and young adult patients were at higher risk than were patients younger than 12, and the risk was highest among patients who had been treated for bone malignancies, as well as those who had undergone any hematopoietic stem cell transplant.
“These findings suggest that health care providers who regularly see survivors should explore nonopioid options to help prevent opioid misuse, and screen for potential misuse in those who actually receive opioids,” she said in an oral abstract presented during the annual meeting of the American Society of Pediatric Hematology/Oncology.
“This is a really important topic, and something that’s probably been underinvestigated and underexplored in our patient population,” said session comoderator Sheri Spunt, MD, Endowed Professor of Pediatric Cancer at Stanford (Calif.) University.
Database review
Dr. Ji and colleagues used the IBM MarketScan Commercial Claims and Encounters database from 2009 to 2018 to examine prescription opioid use, potential misuse, and substance use disorders in pediatric cancer survivors in the first year after completion of therapy, and to identify factors associated with risk for misuse or substance use disorders. Specifically, the period of interest was the first year after completion of all treatments, including surgery, chemotherapy, radiation, and stem cell transplant (Abstract 2015).
They looked at deidentified records on any opioid prescription and for treatment of any opioid use or substance use disorder (alcohol, psychotherapeutic drugs, marijuana, or illicit drug use disorders).
They defined indicators of potential misuse as either prescriptions for long-acting or extended-release opioids for acute pain conditions; opioid and benzodiazepine prescriptions overlapping by a week or more; opioid prescriptions overlapping by a week or more; high daily opioid dosage (prescribed daily dose of 100 or greater morphine milligram equivalent [MME]; and/or opioid dose escalation (an increase of at least 50% in mean MMEs per month twice consecutively within 1 year).
They compared outcomes between a total of 8,635 survivors and 44,175 controls, matched on a 1:5 basis with survivors by age, sex, and region, and continuous enrollment during the 1-year posttherapy period.
In each of three age categories – 0 to 11 years, 12 to 17 years, and 18 years and older – survivors were significantly more likely to have received an opioid prescription, at 15% for the youngest survivors vs. 2% of controls, 25% vs. 8% for 12- to 17-year-olds, and 28% vs. 12% for those 18 and older (P < .01 for all three comparisons).
Survivors were also significantly more likely to have any indicator of potential misuse (1.6% vs. 0.1%, 4.6% vs. 0.5%, and 7.4% vs. 1.2%, respectively, P < .001 for all) and both the youngest and oldest groups (but not 12- to 17-year-olds) were significantly more like to have opioid or substance use disorder (0.4% vs. 0% for 0-11 years, 5.76% vs. 4.2% for 18 years and older, P < .001 for both).
Among patients with any opioid prescription, survivors were significantly more likely than were controls of any age to have indicators for potential misuse. For example, 13% of survivors aged 18 years and older had prescriptions for high opioid doses, compared with 5% of controls, and 12% had prescription overlap, vs. 2%.
Compared with patients with leukemia, patients treated for bone malignancies had a 6% greater risk for having any indicator of misuse, while patients with other malignancies were at slightly lower risk for misuse than those who completed leukemia therapy.
Patients who received any stem cell transplant had an 8.4% greater risk for misuse compared with patients who had surgery only.
Opioids pre- and posttreatment?
“Being someone who takes care of a lot of bone cancer patients, I do see patients with these issues,” Dr. Spunt said.
Audience member Jack H. Staddon, MD, PhD, of the Billings (Montana) Clinic, noted the possibility that opioid use during treatment may have been carried on into the posttreatment period, and asked whether use of narcotics during treatment was an independent risk factor for posttreatment narcotic use or misuse.
The researchers plan to investigate this question in future studies, Dr. Ji replied.
They did not report a study funding source. Dr. Ji and coauthors and Dr. Staddon reported no relevant disclosures.
Survivors of childhood cancers are at increased risk for prescription opioid misuse compared with their peers, a review of a claims database revealed.
Among more than 8,000 patients age 21 or younger who had completed treatment for hematologic, central nervous system, bone, or gonadal cancers, survivors were significantly more likely than were their peers to have an opioid prescription, longer duration of prescription, and higher daily doses of opioids, and to have opioid prescriptions overlapping for a week or more, reported Xu Ji, PhD, of Emory University in Atlanta.
Teenage and young adult patients were at higher risk than were patients younger than 12, and the risk was highest among patients who had been treated for bone malignancies, as well as those who had undergone any hematopoietic stem cell transplant.
“These findings suggest that health care providers who regularly see survivors should explore nonopioid options to help prevent opioid misuse, and screen for potential misuse in those who actually receive opioids,” she said in an oral abstract presented during the annual meeting of the American Society of Pediatric Hematology/Oncology.
“This is a really important topic, and something that’s probably been underinvestigated and underexplored in our patient population,” said session comoderator Sheri Spunt, MD, Endowed Professor of Pediatric Cancer at Stanford (Calif.) University.
Database review
Dr. Ji and colleagues used the IBM MarketScan Commercial Claims and Encounters database from 2009 to 2018 to examine prescription opioid use, potential misuse, and substance use disorders in pediatric cancer survivors in the first year after completion of therapy, and to identify factors associated with risk for misuse or substance use disorders. Specifically, the period of interest was the first year after completion of all treatments, including surgery, chemotherapy, radiation, and stem cell transplant (Abstract 2015).
They looked at deidentified records on any opioid prescription and for treatment of any opioid use or substance use disorder (alcohol, psychotherapeutic drugs, marijuana, or illicit drug use disorders).
They defined indicators of potential misuse as either prescriptions for long-acting or extended-release opioids for acute pain conditions; opioid and benzodiazepine prescriptions overlapping by a week or more; opioid prescriptions overlapping by a week or more; high daily opioid dosage (prescribed daily dose of 100 or greater morphine milligram equivalent [MME]; and/or opioid dose escalation (an increase of at least 50% in mean MMEs per month twice consecutively within 1 year).
They compared outcomes between a total of 8,635 survivors and 44,175 controls, matched on a 1:5 basis with survivors by age, sex, and region, and continuous enrollment during the 1-year posttherapy period.
In each of three age categories – 0 to 11 years, 12 to 17 years, and 18 years and older – survivors were significantly more likely to have received an opioid prescription, at 15% for the youngest survivors vs. 2% of controls, 25% vs. 8% for 12- to 17-year-olds, and 28% vs. 12% for those 18 and older (P < .01 for all three comparisons).
Survivors were also significantly more likely to have any indicator of potential misuse (1.6% vs. 0.1%, 4.6% vs. 0.5%, and 7.4% vs. 1.2%, respectively, P < .001 for all) and both the youngest and oldest groups (but not 12- to 17-year-olds) were significantly more like to have opioid or substance use disorder (0.4% vs. 0% for 0-11 years, 5.76% vs. 4.2% for 18 years and older, P < .001 for both).
Among patients with any opioid prescription, survivors were significantly more likely than were controls of any age to have indicators for potential misuse. For example, 13% of survivors aged 18 years and older had prescriptions for high opioid doses, compared with 5% of controls, and 12% had prescription overlap, vs. 2%.
Compared with patients with leukemia, patients treated for bone malignancies had a 6% greater risk for having any indicator of misuse, while patients with other malignancies were at slightly lower risk for misuse than those who completed leukemia therapy.
Patients who received any stem cell transplant had an 8.4% greater risk for misuse compared with patients who had surgery only.
Opioids pre- and posttreatment?
“Being someone who takes care of a lot of bone cancer patients, I do see patients with these issues,” Dr. Spunt said.
Audience member Jack H. Staddon, MD, PhD, of the Billings (Montana) Clinic, noted the possibility that opioid use during treatment may have been carried on into the posttreatment period, and asked whether use of narcotics during treatment was an independent risk factor for posttreatment narcotic use or misuse.
The researchers plan to investigate this question in future studies, Dr. Ji replied.
They did not report a study funding source. Dr. Ji and coauthors and Dr. Staddon reported no relevant disclosures.
FROM 2021 ASPHO CONFERENCE
Mitochondrial DNA predicts survival in pediatric acute myeloid leukemia
Mitochondrial DNA (mtDNA) copy number alterations are known to occur in acute myeloid leukemia (AML), however their biological significance has not been well studied. Pediatric AML has a distinct biology, different from adults, and with heterogeneous clinical outcomes, the biological basis of which are not well understood, according to researchers Shilpi Chaudhary, PhD, of the All India Institute of Medical Sciences, New Delhi, and colleagues.
Their analysis of 123 pediatric patients with AML found that mtDNA copy number was an independent predictor of aggressive disease, lower event-free survival, and overall survival, according to a report published in Mitochondrion.
In an attempt to find the biological factors involved in the increased mtDNA copy numbers and their effect on the development and aggressiveness of pediatric AML, the researchers studied the regulation and significance of mtDNA copy number in pediatric AML patients using quantitative real time–polymerase chain reaction, as well as in vitro studies. For patients, results were correlated with clinical outcomes.
Mitochondrial biogenesis genes (TFAM, POLG, POLRMT) and two regulator of mitochondrial biogenesis, MYC and PGC1A, were also assessed, according to Dr. Chaudhary and colleagues.
Predictive results
MtDNA copy number was significantly higher in patients, compared with controls (P < .001) and was found to be an independent predictor of aggressive disease (P = .006), lower event-free survival (P = .033), and overall survival (P = .007).
TFAM, POLG & POLRMT and ND3 were also found to be significantly up-regulated in patients, compared with controls as was the expression of the mitochondrial biogenesis regulator MYC (P < .001). However, correlation analysis showed that mtDNA copy number was not associated with the expression of these genes.
In contrast, PGC1A expression was not significantly different in patients, compared with controls overall, although there was a subset of patients whose PGC1A expression was extremely high, according to the researchers.
Importantly, however, in the subset of patients with high PGC1A expression (n = 28), mtDNA copy number had a positive correlation with PGC1A expression (P = .013). On the other hand, among patients with low MYC expression (n = 27), there was no correlation of mtDNA copy number with either PGC1A or MYC expression.
These results were corroborated in in vitro studies, where treatment with the inhibitor tigecycline led to a significant decrease in expression of MYC (P < .001), TFAM (P = .037) and ND3 (P = .010) but resulted in no significant change in mtDNA copy number (P = .23) or expression of PGC1A (P = .10).
Therapeutic candidate?
In contrast to the case of MYC, in vitro PGC1A inhibition significantly reduced mtDNA copy number in along with expression of TFAM and even expression of POLG and POLRMT at higher concentration.
“This observation is in line with our finding in patient samples as well that PGC1A expression positively correlated with mtDNA copy number, more so in patients with higher PGC1A expression,” the researchers stated.
“This makes it plausible to infer that PGC1A may have a possible role in enhancing mtDNA copy number in AML patients, likely independent of MYC,” they added. “Therefore, a strategy of designing therapeutics using already approved inhibitors targeting PGC1A may be an exciting area of therapeutic intervention.”
The authors reported that they have no competing financial conflicts of interests.
Mitochondrial DNA (mtDNA) copy number alterations are known to occur in acute myeloid leukemia (AML), however their biological significance has not been well studied. Pediatric AML has a distinct biology, different from adults, and with heterogeneous clinical outcomes, the biological basis of which are not well understood, according to researchers Shilpi Chaudhary, PhD, of the All India Institute of Medical Sciences, New Delhi, and colleagues.
Their analysis of 123 pediatric patients with AML found that mtDNA copy number was an independent predictor of aggressive disease, lower event-free survival, and overall survival, according to a report published in Mitochondrion.
In an attempt to find the biological factors involved in the increased mtDNA copy numbers and their effect on the development and aggressiveness of pediatric AML, the researchers studied the regulation and significance of mtDNA copy number in pediatric AML patients using quantitative real time–polymerase chain reaction, as well as in vitro studies. For patients, results were correlated with clinical outcomes.
Mitochondrial biogenesis genes (TFAM, POLG, POLRMT) and two regulator of mitochondrial biogenesis, MYC and PGC1A, were also assessed, according to Dr. Chaudhary and colleagues.
Predictive results
MtDNA copy number was significantly higher in patients, compared with controls (P < .001) and was found to be an independent predictor of aggressive disease (P = .006), lower event-free survival (P = .033), and overall survival (P = .007).
TFAM, POLG & POLRMT and ND3 were also found to be significantly up-regulated in patients, compared with controls as was the expression of the mitochondrial biogenesis regulator MYC (P < .001). However, correlation analysis showed that mtDNA copy number was not associated with the expression of these genes.
In contrast, PGC1A expression was not significantly different in patients, compared with controls overall, although there was a subset of patients whose PGC1A expression was extremely high, according to the researchers.
Importantly, however, in the subset of patients with high PGC1A expression (n = 28), mtDNA copy number had a positive correlation with PGC1A expression (P = .013). On the other hand, among patients with low MYC expression (n = 27), there was no correlation of mtDNA copy number with either PGC1A or MYC expression.
These results were corroborated in in vitro studies, where treatment with the inhibitor tigecycline led to a significant decrease in expression of MYC (P < .001), TFAM (P = .037) and ND3 (P = .010) but resulted in no significant change in mtDNA copy number (P = .23) or expression of PGC1A (P = .10).
Therapeutic candidate?
In contrast to the case of MYC, in vitro PGC1A inhibition significantly reduced mtDNA copy number in along with expression of TFAM and even expression of POLG and POLRMT at higher concentration.
“This observation is in line with our finding in patient samples as well that PGC1A expression positively correlated with mtDNA copy number, more so in patients with higher PGC1A expression,” the researchers stated.
“This makes it plausible to infer that PGC1A may have a possible role in enhancing mtDNA copy number in AML patients, likely independent of MYC,” they added. “Therefore, a strategy of designing therapeutics using already approved inhibitors targeting PGC1A may be an exciting area of therapeutic intervention.”
The authors reported that they have no competing financial conflicts of interests.
Mitochondrial DNA (mtDNA) copy number alterations are known to occur in acute myeloid leukemia (AML), however their biological significance has not been well studied. Pediatric AML has a distinct biology, different from adults, and with heterogeneous clinical outcomes, the biological basis of which are not well understood, according to researchers Shilpi Chaudhary, PhD, of the All India Institute of Medical Sciences, New Delhi, and colleagues.
Their analysis of 123 pediatric patients with AML found that mtDNA copy number was an independent predictor of aggressive disease, lower event-free survival, and overall survival, according to a report published in Mitochondrion.
In an attempt to find the biological factors involved in the increased mtDNA copy numbers and their effect on the development and aggressiveness of pediatric AML, the researchers studied the regulation and significance of mtDNA copy number in pediatric AML patients using quantitative real time–polymerase chain reaction, as well as in vitro studies. For patients, results were correlated with clinical outcomes.
Mitochondrial biogenesis genes (TFAM, POLG, POLRMT) and two regulator of mitochondrial biogenesis, MYC and PGC1A, were also assessed, according to Dr. Chaudhary and colleagues.
Predictive results
MtDNA copy number was significantly higher in patients, compared with controls (P < .001) and was found to be an independent predictor of aggressive disease (P = .006), lower event-free survival (P = .033), and overall survival (P = .007).
TFAM, POLG & POLRMT and ND3 were also found to be significantly up-regulated in patients, compared with controls as was the expression of the mitochondrial biogenesis regulator MYC (P < .001). However, correlation analysis showed that mtDNA copy number was not associated with the expression of these genes.
In contrast, PGC1A expression was not significantly different in patients, compared with controls overall, although there was a subset of patients whose PGC1A expression was extremely high, according to the researchers.
Importantly, however, in the subset of patients with high PGC1A expression (n = 28), mtDNA copy number had a positive correlation with PGC1A expression (P = .013). On the other hand, among patients with low MYC expression (n = 27), there was no correlation of mtDNA copy number with either PGC1A or MYC expression.
These results were corroborated in in vitro studies, where treatment with the inhibitor tigecycline led to a significant decrease in expression of MYC (P < .001), TFAM (P = .037) and ND3 (P = .010) but resulted in no significant change in mtDNA copy number (P = .23) or expression of PGC1A (P = .10).
Therapeutic candidate?
In contrast to the case of MYC, in vitro PGC1A inhibition significantly reduced mtDNA copy number in along with expression of TFAM and even expression of POLG and POLRMT at higher concentration.
“This observation is in line with our finding in patient samples as well that PGC1A expression positively correlated with mtDNA copy number, more so in patients with higher PGC1A expression,” the researchers stated.
“This makes it plausible to infer that PGC1A may have a possible role in enhancing mtDNA copy number in AML patients, likely independent of MYC,” they added. “Therefore, a strategy of designing therapeutics using already approved inhibitors targeting PGC1A may be an exciting area of therapeutic intervention.”
The authors reported that they have no competing financial conflicts of interests.
FROM MITOCHONDRION
Predicting outcomes in therapy-related AML
Therapy-related acute myeloid leukemia (t-AML) occurs as a complication of chemotherapy and/or radiotherapy for previous cancer or for nonmalignant disorders, with an estimated prevalence of 10%-15% of all AML cases, according to Ram Vasudevan Nampoothiri, MD, and colleagues at the Princess Margaret Cancer Center, University of Toronto.
Dr. Nampoothiri and colleagues performed a retrospective study of 68 patients with t-AML who underwent hematopoietic stem cell transplantation (HSCT) at their institution. They found significant predictors of reduced overall survival, including chromosomal rearrangements, induction regimens, donor type, patient performance status, and the type of graft-versus-host disease (GVHD) prophylaxis the patients received, as reported in Hematology/Oncology and Stem Cell Therapy.
Some populations benefit
Among the 68 patients studied, a total of 59.9% were women; and the median age was 56.5 years. All patients were analyzed for prior malignancy, therapy, time to diagnosis of t-AML, transplant details, relapse-free survival, overall survival, and predictors of outcomes.
At 2 years, the cumulative incidence of relapse, nonrelapse mortality, relapse-free survival, and overall survival were 17.9%, 34.5%, 47.6%, and 49.3%, respectively. Overall, acute and chronic GVHD occurred in 39 (57.4%) and 23 (33.8%) patients, respectively, according to the researchers.
The significant predictors of reduced overall survival were the presence of the 11q23 chromosomal rearrangement (hazard ratio, 3.24), use of induction regimens other than fludarabine, cytarabine, idarubicin, and granulocyte colony-stimulating factor or 7 + 3 (HR, 3.65), use of haploidentical donors (HR, 3.48), an Eastern Cooperative Oncology Group performance status of 2 or higher (HR, 5.83), and use of cyclosporine A–methotrexate as GVHD prophylaxis (HR, 2.41).
The researchers also found that a significant decrease in survival was seen with an increasing number of any of these prognostic factors.
A growing need
The incidence of t-AML is increasing because of longer life expectancy of the general population and also because of the improved survival of patients treated with chemotherapy and/or radiation for prior malignancies, according to the researchers.
They concluded that, even with this increasing prevalence and normally poor prognosis, “patients of t-AML having good-risk karyotypes, good performance status, and having HLA-matched donors have favorable outcomes after allo-HSCT.”
The authors reported that they had no competing financial interests.
Therapy-related acute myeloid leukemia (t-AML) occurs as a complication of chemotherapy and/or radiotherapy for previous cancer or for nonmalignant disorders, with an estimated prevalence of 10%-15% of all AML cases, according to Ram Vasudevan Nampoothiri, MD, and colleagues at the Princess Margaret Cancer Center, University of Toronto.
Dr. Nampoothiri and colleagues performed a retrospective study of 68 patients with t-AML who underwent hematopoietic stem cell transplantation (HSCT) at their institution. They found significant predictors of reduced overall survival, including chromosomal rearrangements, induction regimens, donor type, patient performance status, and the type of graft-versus-host disease (GVHD) prophylaxis the patients received, as reported in Hematology/Oncology and Stem Cell Therapy.
Some populations benefit
Among the 68 patients studied, a total of 59.9% were women; and the median age was 56.5 years. All patients were analyzed for prior malignancy, therapy, time to diagnosis of t-AML, transplant details, relapse-free survival, overall survival, and predictors of outcomes.
At 2 years, the cumulative incidence of relapse, nonrelapse mortality, relapse-free survival, and overall survival were 17.9%, 34.5%, 47.6%, and 49.3%, respectively. Overall, acute and chronic GVHD occurred in 39 (57.4%) and 23 (33.8%) patients, respectively, according to the researchers.
The significant predictors of reduced overall survival were the presence of the 11q23 chromosomal rearrangement (hazard ratio, 3.24), use of induction regimens other than fludarabine, cytarabine, idarubicin, and granulocyte colony-stimulating factor or 7 + 3 (HR, 3.65), use of haploidentical donors (HR, 3.48), an Eastern Cooperative Oncology Group performance status of 2 or higher (HR, 5.83), and use of cyclosporine A–methotrexate as GVHD prophylaxis (HR, 2.41).
The researchers also found that a significant decrease in survival was seen with an increasing number of any of these prognostic factors.
A growing need
The incidence of t-AML is increasing because of longer life expectancy of the general population and also because of the improved survival of patients treated with chemotherapy and/or radiation for prior malignancies, according to the researchers.
They concluded that, even with this increasing prevalence and normally poor prognosis, “patients of t-AML having good-risk karyotypes, good performance status, and having HLA-matched donors have favorable outcomes after allo-HSCT.”
The authors reported that they had no competing financial interests.
Therapy-related acute myeloid leukemia (t-AML) occurs as a complication of chemotherapy and/or radiotherapy for previous cancer or for nonmalignant disorders, with an estimated prevalence of 10%-15% of all AML cases, according to Ram Vasudevan Nampoothiri, MD, and colleagues at the Princess Margaret Cancer Center, University of Toronto.
Dr. Nampoothiri and colleagues performed a retrospective study of 68 patients with t-AML who underwent hematopoietic stem cell transplantation (HSCT) at their institution. They found significant predictors of reduced overall survival, including chromosomal rearrangements, induction regimens, donor type, patient performance status, and the type of graft-versus-host disease (GVHD) prophylaxis the patients received, as reported in Hematology/Oncology and Stem Cell Therapy.
Some populations benefit
Among the 68 patients studied, a total of 59.9% were women; and the median age was 56.5 years. All patients were analyzed for prior malignancy, therapy, time to diagnosis of t-AML, transplant details, relapse-free survival, overall survival, and predictors of outcomes.
At 2 years, the cumulative incidence of relapse, nonrelapse mortality, relapse-free survival, and overall survival were 17.9%, 34.5%, 47.6%, and 49.3%, respectively. Overall, acute and chronic GVHD occurred in 39 (57.4%) and 23 (33.8%) patients, respectively, according to the researchers.
The significant predictors of reduced overall survival were the presence of the 11q23 chromosomal rearrangement (hazard ratio, 3.24), use of induction regimens other than fludarabine, cytarabine, idarubicin, and granulocyte colony-stimulating factor or 7 + 3 (HR, 3.65), use of haploidentical donors (HR, 3.48), an Eastern Cooperative Oncology Group performance status of 2 or higher (HR, 5.83), and use of cyclosporine A–methotrexate as GVHD prophylaxis (HR, 2.41).
The researchers also found that a significant decrease in survival was seen with an increasing number of any of these prognostic factors.
A growing need
The incidence of t-AML is increasing because of longer life expectancy of the general population and also because of the improved survival of patients treated with chemotherapy and/or radiation for prior malignancies, according to the researchers.
They concluded that, even with this increasing prevalence and normally poor prognosis, “patients of t-AML having good-risk karyotypes, good performance status, and having HLA-matched donors have favorable outcomes after allo-HSCT.”
The authors reported that they had no competing financial interests.
FROM HEMATOLOGY/ONCOLOGY AND STEM CELL THERAPY
Clinical Edge Commentary: AML April 2021
In a study by Trembely et al. sponsored by Pfizer, an indirect comparison of both studies was performed using a simulated treatment comparison to account for differences in patient characteristics. As expected, the overall response rates were higher in the venetoclax study compared to the glasdegib study (48% vs. 24%), but overall survival was similar (hazard ratio 0.75 vs. HR 0.46). This study demonstrates again that CR/CRi cannot be used as a surrogate endpoint for survival in AML. In addition, with the negative study of V-LDAC vs. LDAC and the improved overall survival of the combination of azacytidine + venetoclax (Aza-ven) vs. azacitdine, the current standard of care of newly diagnosed patients with AML unbale to tolerate intensive chemotherapy is Aza-ven and V-LDAC is rarely used.
The success of Aza-ven is not without side effects. This was demonstrated recently in a retrospective study by Feld et al. In that study 72 patients with newly diagnosed AML (26), relapsed refractory AML (39) and MDS (7) received azacitdine + venetoclax. The main side effect was myelosuppression with only 15% of patients who were transfusion dependent become transfusion independent. In addition, 46% of patients had a neutropenic fever and 43.7% of patients requiring admission. Most patients (54.9%) required treatment interruption and 35.2% stopped venetoclax for toxicity.
This study highlighted that the optimal dose and frequency of venetoclax remains unclear. A shorted duration or lower dose of venetoclax maybe more ideal, however that may lead to less efficacy. In addition, bone marrow evaluation to assess for cellularity on D21 to D28 of the first cycle may help guide dose adjustments. Finally with the high CR/CRi rates in AML and short duration of response further studies are ongoing to further define molecular abnormalities that may refine prognosis or guide therapy. Two of those studies recently reported identified a prognostic and possible therapeutic role for both EZH2 and the PI3 kinase mTOR pathway.
In a study by Trembely et al. sponsored by Pfizer, an indirect comparison of both studies was performed using a simulated treatment comparison to account for differences in patient characteristics. As expected, the overall response rates were higher in the venetoclax study compared to the glasdegib study (48% vs. 24%), but overall survival was similar (hazard ratio 0.75 vs. HR 0.46). This study demonstrates again that CR/CRi cannot be used as a surrogate endpoint for survival in AML. In addition, with the negative study of V-LDAC vs. LDAC and the improved overall survival of the combination of azacytidine + venetoclax (Aza-ven) vs. azacitdine, the current standard of care of newly diagnosed patients with AML unbale to tolerate intensive chemotherapy is Aza-ven and V-LDAC is rarely used.
The success of Aza-ven is not without side effects. This was demonstrated recently in a retrospective study by Feld et al. In that study 72 patients with newly diagnosed AML (26), relapsed refractory AML (39) and MDS (7) received azacitdine + venetoclax. The main side effect was myelosuppression with only 15% of patients who were transfusion dependent become transfusion independent. In addition, 46% of patients had a neutropenic fever and 43.7% of patients requiring admission. Most patients (54.9%) required treatment interruption and 35.2% stopped venetoclax for toxicity.
This study highlighted that the optimal dose and frequency of venetoclax remains unclear. A shorted duration or lower dose of venetoclax maybe more ideal, however that may lead to less efficacy. In addition, bone marrow evaluation to assess for cellularity on D21 to D28 of the first cycle may help guide dose adjustments. Finally with the high CR/CRi rates in AML and short duration of response further studies are ongoing to further define molecular abnormalities that may refine prognosis or guide therapy. Two of those studies recently reported identified a prognostic and possible therapeutic role for both EZH2 and the PI3 kinase mTOR pathway.
In a study by Trembely et al. sponsored by Pfizer, an indirect comparison of both studies was performed using a simulated treatment comparison to account for differences in patient characteristics. As expected, the overall response rates were higher in the venetoclax study compared to the glasdegib study (48% vs. 24%), but overall survival was similar (hazard ratio 0.75 vs. HR 0.46). This study demonstrates again that CR/CRi cannot be used as a surrogate endpoint for survival in AML. In addition, with the negative study of V-LDAC vs. LDAC and the improved overall survival of the combination of azacytidine + venetoclax (Aza-ven) vs. azacitdine, the current standard of care of newly diagnosed patients with AML unbale to tolerate intensive chemotherapy is Aza-ven and V-LDAC is rarely used.
The success of Aza-ven is not without side effects. This was demonstrated recently in a retrospective study by Feld et al. In that study 72 patients with newly diagnosed AML (26), relapsed refractory AML (39) and MDS (7) received azacitdine + venetoclax. The main side effect was myelosuppression with only 15% of patients who were transfusion dependent become transfusion independent. In addition, 46% of patients had a neutropenic fever and 43.7% of patients requiring admission. Most patients (54.9%) required treatment interruption and 35.2% stopped venetoclax for toxicity.
This study highlighted that the optimal dose and frequency of venetoclax remains unclear. A shorted duration or lower dose of venetoclax maybe more ideal, however that may lead to less efficacy. In addition, bone marrow evaluation to assess for cellularity on D21 to D28 of the first cycle may help guide dose adjustments. Finally with the high CR/CRi rates in AML and short duration of response further studies are ongoing to further define molecular abnormalities that may refine prognosis or guide therapy. Two of those studies recently reported identified a prognostic and possible therapeutic role for both EZH2 and the PI3 kinase mTOR pathway.
Bone marrow cells contribute to AML disease environment
Key clinical point: Bone marrow stromal cells in patients with myelodysplastic syndromes and acute myeloid leukemia showed a reduced frequency of colony forming unit-fibroblasts.
Major finding: The frequencies of positive/positive bone marrow stromal cells were significantly lower in AML patient samples compared to healthy individuals and MDS bone marrow samples. The median cell numbers of bone marrow stromal cells in diagnostic samples were 3,200 for healthy samples, 476 for MDS samples, and 70 for AML samples.
Study details: The data come from bone marrow samples in AML patients, MDS patients, and healthy donors.
Disclosures: The study was supported in part by Projekt DEAL and the Deutsche Forschungsgemeinschaft SFB 1243 for projects A09 and the FOR2033 project B3, as well as the Deutsche Jose Carreras Leukämie Stiftung. The researchers had no financial conflicts to disclose.
Source: Weickert M-T et al. Sci Rep. 2021 Mar 15. doi: 10.1038/s41598-021-85122-8.
Key clinical point: Bone marrow stromal cells in patients with myelodysplastic syndromes and acute myeloid leukemia showed a reduced frequency of colony forming unit-fibroblasts.
Major finding: The frequencies of positive/positive bone marrow stromal cells were significantly lower in AML patient samples compared to healthy individuals and MDS bone marrow samples. The median cell numbers of bone marrow stromal cells in diagnostic samples were 3,200 for healthy samples, 476 for MDS samples, and 70 for AML samples.
Study details: The data come from bone marrow samples in AML patients, MDS patients, and healthy donors.
Disclosures: The study was supported in part by Projekt DEAL and the Deutsche Forschungsgemeinschaft SFB 1243 for projects A09 and the FOR2033 project B3, as well as the Deutsche Jose Carreras Leukämie Stiftung. The researchers had no financial conflicts to disclose.
Source: Weickert M-T et al. Sci Rep. 2021 Mar 15. doi: 10.1038/s41598-021-85122-8.
Key clinical point: Bone marrow stromal cells in patients with myelodysplastic syndromes and acute myeloid leukemia showed a reduced frequency of colony forming unit-fibroblasts.
Major finding: The frequencies of positive/positive bone marrow stromal cells were significantly lower in AML patient samples compared to healthy individuals and MDS bone marrow samples. The median cell numbers of bone marrow stromal cells in diagnostic samples were 3,200 for healthy samples, 476 for MDS samples, and 70 for AML samples.
Study details: The data come from bone marrow samples in AML patients, MDS patients, and healthy donors.
Disclosures: The study was supported in part by Projekt DEAL and the Deutsche Forschungsgemeinschaft SFB 1243 for projects A09 and the FOR2033 project B3, as well as the Deutsche Jose Carreras Leukämie Stiftung. The researchers had no financial conflicts to disclose.
Source: Weickert M-T et al. Sci Rep. 2021 Mar 15. doi: 10.1038/s41598-021-85122-8.
Transfusion reliance remains after AML treatment with VEN and HMA
Key clinical point: Treatment with a combination of venetoclax (VEN) and hypomethylating agents (HMA) may be an option for younger AML patients, but myelosuppression was a concern, and 43.7% of treated patients were hospitalized for a treatment-related adverse event.
Major finding: In the 26 newly-diagnosed AML patients, the complete remission rate was 53.8%, but only 38.5% in the 39 relapsed/refractory patients; however, 70% remained dependent on red blood cell transfusion and 58.6% remained dependent on platelet transfusion during and after treatment.
Study details: The data come from 65 patients with acute myeloid leukemia and 7 patients with myelodysplastic syndrome who were treated with a combination of VEN and HMA.
Disclosures: The study’s corresponding author was supported by the National Institutes of Health and the National Cancer Institute. Lead author Dr. Feld had no financial conflicts to disclose.
Source: Feld J et al. Hemasphere. 2021 Mar 9. doi: 10.1097/HS9.0000000000000549.
Key clinical point: Treatment with a combination of venetoclax (VEN) and hypomethylating agents (HMA) may be an option for younger AML patients, but myelosuppression was a concern, and 43.7% of treated patients were hospitalized for a treatment-related adverse event.
Major finding: In the 26 newly-diagnosed AML patients, the complete remission rate was 53.8%, but only 38.5% in the 39 relapsed/refractory patients; however, 70% remained dependent on red blood cell transfusion and 58.6% remained dependent on platelet transfusion during and after treatment.
Study details: The data come from 65 patients with acute myeloid leukemia and 7 patients with myelodysplastic syndrome who were treated with a combination of VEN and HMA.
Disclosures: The study’s corresponding author was supported by the National Institutes of Health and the National Cancer Institute. Lead author Dr. Feld had no financial conflicts to disclose.
Source: Feld J et al. Hemasphere. 2021 Mar 9. doi: 10.1097/HS9.0000000000000549.
Key clinical point: Treatment with a combination of venetoclax (VEN) and hypomethylating agents (HMA) may be an option for younger AML patients, but myelosuppression was a concern, and 43.7% of treated patients were hospitalized for a treatment-related adverse event.
Major finding: In the 26 newly-diagnosed AML patients, the complete remission rate was 53.8%, but only 38.5% in the 39 relapsed/refractory patients; however, 70% remained dependent on red blood cell transfusion and 58.6% remained dependent on platelet transfusion during and after treatment.
Study details: The data come from 65 patients with acute myeloid leukemia and 7 patients with myelodysplastic syndrome who were treated with a combination of VEN and HMA.
Disclosures: The study’s corresponding author was supported by the National Institutes of Health and the National Cancer Institute. Lead author Dr. Feld had no financial conflicts to disclose.
Source: Feld J et al. Hemasphere. 2021 Mar 9. doi: 10.1097/HS9.0000000000000549.
Loss of tumor suppressor may drive cytarabine resistance in AML
Key clinical point: Mutations promoting loss of function in the histone methyltransferase EZH2 are relatively rare but may promote chemoresistance to the treatment agent cytarabine in patients with acute myeloid leukemia.
Major finding: In cell lines and in patient samples, AML patients, loss of function of EZH2 fostered resistance to cytarabine; the EZH2 mutation was present in 4% of AML patients at diagnosis; low expression of EZH2 mRNA was correlated with poor overall survival and relapse-free survival.
Study details: The data come from a combination of patient samples, in vivo and in vitro patient-derived xenografts, and haematopeoietic cell lines, and included 25 patients with an EZH2 mutation at the time of diagnosis.
Disclosures: The study was supported by Projekt DEAL. The researchers had no financial conflicts to disclose.
Source: Kempf JM et al. Sci Rep. 2021 Mar 12. doi: 10.1038/s41598-021-84708-6.
Key clinical point: Mutations promoting loss of function in the histone methyltransferase EZH2 are relatively rare but may promote chemoresistance to the treatment agent cytarabine in patients with acute myeloid leukemia.
Major finding: In cell lines and in patient samples, AML patients, loss of function of EZH2 fostered resistance to cytarabine; the EZH2 mutation was present in 4% of AML patients at diagnosis; low expression of EZH2 mRNA was correlated with poor overall survival and relapse-free survival.
Study details: The data come from a combination of patient samples, in vivo and in vitro patient-derived xenografts, and haematopeoietic cell lines, and included 25 patients with an EZH2 mutation at the time of diagnosis.
Disclosures: The study was supported by Projekt DEAL. The researchers had no financial conflicts to disclose.
Source: Kempf JM et al. Sci Rep. 2021 Mar 12. doi: 10.1038/s41598-021-84708-6.
Key clinical point: Mutations promoting loss of function in the histone methyltransferase EZH2 are relatively rare but may promote chemoresistance to the treatment agent cytarabine in patients with acute myeloid leukemia.
Major finding: In cell lines and in patient samples, AML patients, loss of function of EZH2 fostered resistance to cytarabine; the EZH2 mutation was present in 4% of AML patients at diagnosis; low expression of EZH2 mRNA was correlated with poor overall survival and relapse-free survival.
Study details: The data come from a combination of patient samples, in vivo and in vitro patient-derived xenografts, and haematopeoietic cell lines, and included 25 patients with an EZH2 mutation at the time of diagnosis.
Disclosures: The study was supported by Projekt DEAL. The researchers had no financial conflicts to disclose.
Source: Kempf JM et al. Sci Rep. 2021 Mar 12. doi: 10.1038/s41598-021-84708-6.