User login
Gene mutation status impacts overall survival in acute myeloid leukemia
Key clinical point: Gene set variation analysis (GSVA) showed that the PI3K-Akt-mTOR pathway was positively related to FLT3-ITD mutation.
Major finding: In patients with acute myeloid leukemia, expression of RPS6KA1 and AP2M1 were predictors of chemoresistance and overall survival.
Study details: The data come from four genetic data sets: GSE6891, GSE10358, GSE15434, and GSE61804 of patients with acute myeloid leukemia.
Disclosures: The study was supported by the Young & Middle-aged Medical Key Talents Training Project of Wuhan. The researchers had no financial conflicts to disclose.
Source: Yu D-H et al. Front Cell Dev Biol. 2021 Feb 26. doi: 10.3389/fcell.2021.641629.
Key clinical point: Gene set variation analysis (GSVA) showed that the PI3K-Akt-mTOR pathway was positively related to FLT3-ITD mutation.
Major finding: In patients with acute myeloid leukemia, expression of RPS6KA1 and AP2M1 were predictors of chemoresistance and overall survival.
Study details: The data come from four genetic data sets: GSE6891, GSE10358, GSE15434, and GSE61804 of patients with acute myeloid leukemia.
Disclosures: The study was supported by the Young & Middle-aged Medical Key Talents Training Project of Wuhan. The researchers had no financial conflicts to disclose.
Source: Yu D-H et al. Front Cell Dev Biol. 2021 Feb 26. doi: 10.3389/fcell.2021.641629.
Key clinical point: Gene set variation analysis (GSVA) showed that the PI3K-Akt-mTOR pathway was positively related to FLT3-ITD mutation.
Major finding: In patients with acute myeloid leukemia, expression of RPS6KA1 and AP2M1 were predictors of chemoresistance and overall survival.
Study details: The data come from four genetic data sets: GSE6891, GSE10358, GSE15434, and GSE61804 of patients with acute myeloid leukemia.
Disclosures: The study was supported by the Young & Middle-aged Medical Key Talents Training Project of Wuhan. The researchers had no financial conflicts to disclose.
Source: Yu D-H et al. Front Cell Dev Biol. 2021 Feb 26. doi: 10.3389/fcell.2021.641629.
Glasdegib and venetoclax show similar success for AML
Key clinical point: For AML patients unable to undergo intensive chemotherapy, glasdegib and venetoclax were similarly effective, each in combination with low-dose cytarabine.
Major finding: Overall response rates were higher in the venetoclax study compared to the glasdegib study (48% vs. 24%), but overall survival was similar (hazard ratio 0.75 vs. HR 0.46).
Study details: The data come an indirect comparison of studies of each treatment: the BRIGHT AML 1003 GLAS+LDAC trial, and the VIALE-C VEN+LDAC trial.
Disclosures: The study was sponsored by Pfizer. Several researchers are Pfizer employees and lead author Dr. Tremblay served as a paid consultant to Pfizer during the study.
Source: Tremblay G et al. J Comp Eff Res. 2021 Mar 18. doi: 10.2217/cer-2020-0280.
Key clinical point: For AML patients unable to undergo intensive chemotherapy, glasdegib and venetoclax were similarly effective, each in combination with low-dose cytarabine.
Major finding: Overall response rates were higher in the venetoclax study compared to the glasdegib study (48% vs. 24%), but overall survival was similar (hazard ratio 0.75 vs. HR 0.46).
Study details: The data come an indirect comparison of studies of each treatment: the BRIGHT AML 1003 GLAS+LDAC trial, and the VIALE-C VEN+LDAC trial.
Disclosures: The study was sponsored by Pfizer. Several researchers are Pfizer employees and lead author Dr. Tremblay served as a paid consultant to Pfizer during the study.
Source: Tremblay G et al. J Comp Eff Res. 2021 Mar 18. doi: 10.2217/cer-2020-0280.
Key clinical point: For AML patients unable to undergo intensive chemotherapy, glasdegib and venetoclax were similarly effective, each in combination with low-dose cytarabine.
Major finding: Overall response rates were higher in the venetoclax study compared to the glasdegib study (48% vs. 24%), but overall survival was similar (hazard ratio 0.75 vs. HR 0.46).
Study details: The data come an indirect comparison of studies of each treatment: the BRIGHT AML 1003 GLAS+LDAC trial, and the VIALE-C VEN+LDAC trial.
Disclosures: The study was sponsored by Pfizer. Several researchers are Pfizer employees and lead author Dr. Tremblay served as a paid consultant to Pfizer during the study.
Source: Tremblay G et al. J Comp Eff Res. 2021 Mar 18. doi: 10.2217/cer-2020-0280.
Venetoclax succeeds for AML remission in untreated older patients
Key clinical point: Venetoclax combination therapy was safe and effective in older adults with acute myeloid leukemia who had not been previously treated.
Major finding: A total of 12 patients achieved complete remission, and another 4 patients achieved complete remission with incomplete blood recovery, with a median response duration of 8.9 months; however, response duration dropped to 4.6 months for patients with adverse cytogenetic risk.
Study details: The data come from 19 consecutive patients with a median age of 77 years and previously untreated AML who received venetoclax combination therapy at a single center; 12 of these received a starting dose of 400 mg daily, 4 received 200 mg, and 3 patients received 100 mg.
Disclosures: The study was supported by the Ligue Nationale Contre le Cancer, and the association Laurette Fugain. The researchers had no financial conflicts to disclose.
Source: Vazquez R et al. Blood Cancer J. 2021 Mar 19. doi: 10.1038/s41408-021-00448-w.
Key clinical point: Venetoclax combination therapy was safe and effective in older adults with acute myeloid leukemia who had not been previously treated.
Major finding: A total of 12 patients achieved complete remission, and another 4 patients achieved complete remission with incomplete blood recovery, with a median response duration of 8.9 months; however, response duration dropped to 4.6 months for patients with adverse cytogenetic risk.
Study details: The data come from 19 consecutive patients with a median age of 77 years and previously untreated AML who received venetoclax combination therapy at a single center; 12 of these received a starting dose of 400 mg daily, 4 received 200 mg, and 3 patients received 100 mg.
Disclosures: The study was supported by the Ligue Nationale Contre le Cancer, and the association Laurette Fugain. The researchers had no financial conflicts to disclose.
Source: Vazquez R et al. Blood Cancer J. 2021 Mar 19. doi: 10.1038/s41408-021-00448-w.
Key clinical point: Venetoclax combination therapy was safe and effective in older adults with acute myeloid leukemia who had not been previously treated.
Major finding: A total of 12 patients achieved complete remission, and another 4 patients achieved complete remission with incomplete blood recovery, with a median response duration of 8.9 months; however, response duration dropped to 4.6 months for patients with adverse cytogenetic risk.
Study details: The data come from 19 consecutive patients with a median age of 77 years and previously untreated AML who received venetoclax combination therapy at a single center; 12 of these received a starting dose of 400 mg daily, 4 received 200 mg, and 3 patients received 100 mg.
Disclosures: The study was supported by the Ligue Nationale Contre le Cancer, and the association Laurette Fugain. The researchers had no financial conflicts to disclose.
Source: Vazquez R et al. Blood Cancer J. 2021 Mar 19. doi: 10.1038/s41408-021-00448-w.
Green tea extract promotes immune system function in older AML patients
Key clinical point: Green tea extract was safely tolerated and associated with improved immune modulation regardless of tumor burden in older acute myeloid leukemia patients on low-dose chemotherapy.
Major finding: After 30 days, older adults with acute myeloid leukemia who consumed green tea extract showed an increase in total and CD8+ T cells, perforin+/granzyme B+ natural killer cells, monocytes, and classical monocytes.
Study details: The data come from 10 patients aged 60 years and older with acute myeloid leukemia with myelodysplasia-related changes (AML-MRC) who received two capsules of green tea extract for a 1,000-mg daily dose for at least 6 months.
Disclosures: The study was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico, the Fundação de Amparo à Pesquisa do Estado de São Paulo, and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior. The researchers had no financial conflicts to disclose.
Source: Calgarotto AK et al. Integr Cancer Ther. 2021 Mar 23. doi:10.1177/15347354211002647.
Key clinical point: Green tea extract was safely tolerated and associated with improved immune modulation regardless of tumor burden in older acute myeloid leukemia patients on low-dose chemotherapy.
Major finding: After 30 days, older adults with acute myeloid leukemia who consumed green tea extract showed an increase in total and CD8+ T cells, perforin+/granzyme B+ natural killer cells, monocytes, and classical monocytes.
Study details: The data come from 10 patients aged 60 years and older with acute myeloid leukemia with myelodysplasia-related changes (AML-MRC) who received two capsules of green tea extract for a 1,000-mg daily dose for at least 6 months.
Disclosures: The study was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico, the Fundação de Amparo à Pesquisa do Estado de São Paulo, and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior. The researchers had no financial conflicts to disclose.
Source: Calgarotto AK et al. Integr Cancer Ther. 2021 Mar 23. doi:10.1177/15347354211002647.
Key clinical point: Green tea extract was safely tolerated and associated with improved immune modulation regardless of tumor burden in older acute myeloid leukemia patients on low-dose chemotherapy.
Major finding: After 30 days, older adults with acute myeloid leukemia who consumed green tea extract showed an increase in total and CD8+ T cells, perforin+/granzyme B+ natural killer cells, monocytes, and classical monocytes.
Study details: The data come from 10 patients aged 60 years and older with acute myeloid leukemia with myelodysplasia-related changes (AML-MRC) who received two capsules of green tea extract for a 1,000-mg daily dose for at least 6 months.
Disclosures: The study was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico, the Fundação de Amparo à Pesquisa do Estado de São Paulo, and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior. The researchers had no financial conflicts to disclose.
Source: Calgarotto AK et al. Integr Cancer Ther. 2021 Mar 23. doi:10.1177/15347354211002647.
Early tumor cell response predicts AML treatment success
Key clinical point: Treatment regimen was a key factor in survival rates among adults with acute myeloid leukemia, and patients with high responsiveness of tumor cells in vitro showed stronger response to chemotherapy.
Major finding: Patients with high sensitivity to daunorubicin showed a good response to anthracycline‐based therapy; by contrast, patients who received daunorubicin during induction chemotherapy as part of standard clinical care, but who did not sensitivity to it, responded poorly to treatment,
Study details: The data come from a retrospective analysis of survival rates in 127 adults with acute myeloid leukemia.
Disclosures: The study was funded by the Russian Science Foundation and the Russian State Budget Project of ICBFM SB RAS. The researchers had no financial conflicts to disclose.
Source: Kolesnikova MA et al. Cancer Rep. 2021 Mar 6. doi: 10.1002/cnr2.1362.
Key clinical point: Treatment regimen was a key factor in survival rates among adults with acute myeloid leukemia, and patients with high responsiveness of tumor cells in vitro showed stronger response to chemotherapy.
Major finding: Patients with high sensitivity to daunorubicin showed a good response to anthracycline‐based therapy; by contrast, patients who received daunorubicin during induction chemotherapy as part of standard clinical care, but who did not sensitivity to it, responded poorly to treatment,
Study details: The data come from a retrospective analysis of survival rates in 127 adults with acute myeloid leukemia.
Disclosures: The study was funded by the Russian Science Foundation and the Russian State Budget Project of ICBFM SB RAS. The researchers had no financial conflicts to disclose.
Source: Kolesnikova MA et al. Cancer Rep. 2021 Mar 6. doi: 10.1002/cnr2.1362.
Key clinical point: Treatment regimen was a key factor in survival rates among adults with acute myeloid leukemia, and patients with high responsiveness of tumor cells in vitro showed stronger response to chemotherapy.
Major finding: Patients with high sensitivity to daunorubicin showed a good response to anthracycline‐based therapy; by contrast, patients who received daunorubicin during induction chemotherapy as part of standard clinical care, but who did not sensitivity to it, responded poorly to treatment,
Study details: The data come from a retrospective analysis of survival rates in 127 adults with acute myeloid leukemia.
Disclosures: The study was funded by the Russian Science Foundation and the Russian State Budget Project of ICBFM SB RAS. The researchers had no financial conflicts to disclose.
Source: Kolesnikova MA et al. Cancer Rep. 2021 Mar 6. doi: 10.1002/cnr2.1362.
Rural AML patients fare as well as urban patients for survival and treatment
Key clinical point: No significant differences were seen between urban and rural acute myeloid leukemia patients with regard to overall survival or progression to hematopoietic cell transplantation.
Major finding: Overall survival at one year was 47.9% between the groups (45% for rural and 49% for urban). In addition, the proportions of patients with cytogenetic risk factors and who went on to hematopoietic cell transplantation (HCT) were not significantly different between the two groups.
Study details: The data come from a retrospective study of 163 acute myeloid leukemia patients diagnosed at a single center between September 2015 and December 2019, 42% of whom lived in a rural area at the time of diagnosis.
Disclosures: The study received no outside funding. Lead author Dr. Isaac had no financial conflicts to disclose.
Source: Isaac KM et al. Cancer Rep 2021 Mar 9. doi: 10.1002/cnr2.1354.
Key clinical point: No significant differences were seen between urban and rural acute myeloid leukemia patients with regard to overall survival or progression to hematopoietic cell transplantation.
Major finding: Overall survival at one year was 47.9% between the groups (45% for rural and 49% for urban). In addition, the proportions of patients with cytogenetic risk factors and who went on to hematopoietic cell transplantation (HCT) were not significantly different between the two groups.
Study details: The data come from a retrospective study of 163 acute myeloid leukemia patients diagnosed at a single center between September 2015 and December 2019, 42% of whom lived in a rural area at the time of diagnosis.
Disclosures: The study received no outside funding. Lead author Dr. Isaac had no financial conflicts to disclose.
Source: Isaac KM et al. Cancer Rep 2021 Mar 9. doi: 10.1002/cnr2.1354.
Key clinical point: No significant differences were seen between urban and rural acute myeloid leukemia patients with regard to overall survival or progression to hematopoietic cell transplantation.
Major finding: Overall survival at one year was 47.9% between the groups (45% for rural and 49% for urban). In addition, the proportions of patients with cytogenetic risk factors and who went on to hematopoietic cell transplantation (HCT) were not significantly different between the two groups.
Study details: The data come from a retrospective study of 163 acute myeloid leukemia patients diagnosed at a single center between September 2015 and December 2019, 42% of whom lived in a rural area at the time of diagnosis.
Disclosures: The study received no outside funding. Lead author Dr. Isaac had no financial conflicts to disclose.
Source: Isaac KM et al. Cancer Rep 2021 Mar 9. doi: 10.1002/cnr2.1354.
Risk factors predict graft failure in pediatric acute leukemia patients
Researchers developed a predictive score for the risk of graft failure in patients with acute leukemia who underwent allogeneic hematopoietic stem cell transplantation (aHSCT) with ex vivo T-cell depletion. T-cell depletion is performed in an effort to prevent subsequent graft-versus-host disease (GVHD) after transplant.
The risk score was based on patient age and the T-lymphocyte population pre-aHSCT with 1 point of risk possible in each category. Patients with 1 point had a graft failure risk of 5% and 13% if they had 2 points, according to the results of the study presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Graft failure is a potentially severe complication in patients treated with aHSCT, but there are few studies analyzing risk factors when ex vivo T-cell depletion is used, Ivan López Torija of the Hospital Infantil Universitario Niño Jesús, Madrid, and colleagues noted in their presentation, which won the Best Young Poster Abstract Award at the meeting.
The researchers assessed 148 pediatric patients (64% boys) with acute leukemia who underwent allogeneic HSCT from haploidentical donors using ex vivo T-cell depletion between 2005 and 2020. About 53% of the patients were diagnosed with acute lymphoblastic leukemia, the rest with acute myeloid leukemia. The donor mean age was 40 years, and all transplant patients received toxicity reduction conditioning based on fludarabine busulfan and thiotepa.
Predictive results
Multivariate analysis showed that T-cell count (CD3+/CD8+ ≥ 350/mL: hazard ratio, 2,6; P = .01) and patient age (less than 9 years: HR; 5.0; P = .04) were associated with graft failure. A risk score was established using these results and based on patient age and T lymphocyte pre-aHSCT with 1 point each for each increased risk category. Patients with 1 point had a graft failure risk of 5% and a risk of 13% if they had 2 points.
However, in this particular population, with a mean follow up of 4 years, the overall survival rate was 60%, with no significant differences seen between patients that presented graft failure and those without graft failure.
“Patient age and pretransplant number of CD3+/CD8+ are associated with [graft failure] in pediatric patients with acute leukemia undergoing ex vivo T-cell–depleted haploidentical transplantation. These findings highlight the importance of preexisting cellular immunity in the transplant recipient and support T-cell population analysis as part of a pretransplant working program,” the researchers concluded.
The authors reported that they had no disclosures.
Researchers developed a predictive score for the risk of graft failure in patients with acute leukemia who underwent allogeneic hematopoietic stem cell transplantation (aHSCT) with ex vivo T-cell depletion. T-cell depletion is performed in an effort to prevent subsequent graft-versus-host disease (GVHD) after transplant.
The risk score was based on patient age and the T-lymphocyte population pre-aHSCT with 1 point of risk possible in each category. Patients with 1 point had a graft failure risk of 5% and 13% if they had 2 points, according to the results of the study presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Graft failure is a potentially severe complication in patients treated with aHSCT, but there are few studies analyzing risk factors when ex vivo T-cell depletion is used, Ivan López Torija of the Hospital Infantil Universitario Niño Jesús, Madrid, and colleagues noted in their presentation, which won the Best Young Poster Abstract Award at the meeting.
The researchers assessed 148 pediatric patients (64% boys) with acute leukemia who underwent allogeneic HSCT from haploidentical donors using ex vivo T-cell depletion between 2005 and 2020. About 53% of the patients were diagnosed with acute lymphoblastic leukemia, the rest with acute myeloid leukemia. The donor mean age was 40 years, and all transplant patients received toxicity reduction conditioning based on fludarabine busulfan and thiotepa.
Predictive results
Multivariate analysis showed that T-cell count (CD3+/CD8+ ≥ 350/mL: hazard ratio, 2,6; P = .01) and patient age (less than 9 years: HR; 5.0; P = .04) were associated with graft failure. A risk score was established using these results and based on patient age and T lymphocyte pre-aHSCT with 1 point each for each increased risk category. Patients with 1 point had a graft failure risk of 5% and a risk of 13% if they had 2 points.
However, in this particular population, with a mean follow up of 4 years, the overall survival rate was 60%, with no significant differences seen between patients that presented graft failure and those without graft failure.
“Patient age and pretransplant number of CD3+/CD8+ are associated with [graft failure] in pediatric patients with acute leukemia undergoing ex vivo T-cell–depleted haploidentical transplantation. These findings highlight the importance of preexisting cellular immunity in the transplant recipient and support T-cell population analysis as part of a pretransplant working program,” the researchers concluded.
The authors reported that they had no disclosures.
Researchers developed a predictive score for the risk of graft failure in patients with acute leukemia who underwent allogeneic hematopoietic stem cell transplantation (aHSCT) with ex vivo T-cell depletion. T-cell depletion is performed in an effort to prevent subsequent graft-versus-host disease (GVHD) after transplant.
The risk score was based on patient age and the T-lymphocyte population pre-aHSCT with 1 point of risk possible in each category. Patients with 1 point had a graft failure risk of 5% and 13% if they had 2 points, according to the results of the study presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Graft failure is a potentially severe complication in patients treated with aHSCT, but there are few studies analyzing risk factors when ex vivo T-cell depletion is used, Ivan López Torija of the Hospital Infantil Universitario Niño Jesús, Madrid, and colleagues noted in their presentation, which won the Best Young Poster Abstract Award at the meeting.
The researchers assessed 148 pediatric patients (64% boys) with acute leukemia who underwent allogeneic HSCT from haploidentical donors using ex vivo T-cell depletion between 2005 and 2020. About 53% of the patients were diagnosed with acute lymphoblastic leukemia, the rest with acute myeloid leukemia. The donor mean age was 40 years, and all transplant patients received toxicity reduction conditioning based on fludarabine busulfan and thiotepa.
Predictive results
Multivariate analysis showed that T-cell count (CD3+/CD8+ ≥ 350/mL: hazard ratio, 2,6; P = .01) and patient age (less than 9 years: HR; 5.0; P = .04) were associated with graft failure. A risk score was established using these results and based on patient age and T lymphocyte pre-aHSCT with 1 point each for each increased risk category. Patients with 1 point had a graft failure risk of 5% and a risk of 13% if they had 2 points.
However, in this particular population, with a mean follow up of 4 years, the overall survival rate was 60%, with no significant differences seen between patients that presented graft failure and those without graft failure.
“Patient age and pretransplant number of CD3+/CD8+ are associated with [graft failure] in pediatric patients with acute leukemia undergoing ex vivo T-cell–depleted haploidentical transplantation. These findings highlight the importance of preexisting cellular immunity in the transplant recipient and support T-cell population analysis as part of a pretransplant working program,” the researchers concluded.
The authors reported that they had no disclosures.
FROM EBMT 2021
Omidubicel improves on umbilical cord blood transplants
Omidubicel, an investigational enriched umbilical cord blood product being developed by Gamida Cell for transplantation in patients with blood cancers, appears to have some advantages over standard umbilical cord blood.
The results come from a global phase 3 trial (NCT02730299) presented at the annual meeting of the European Society for Blood and Bone Marrow Transplantation.
“Transplantation with omidubicel, compared to standard cord blood transplantation, results in faster hematopoietic recovery, fewer infections, and fewer days in hospital,” said coinvestigator Guillermo F. Sanz, MD, PhD, from the Hospital Universitari i Politècnic la Fe in Valencia, Spain.
“Omidubicel should be considered as the new standard of care for patients eligible for umbilical cord blood transplantation,” Dr. Sanz concluded.
Zachariah DeFilipp, MD, from Mass General Cancer Center in Boston, a hematopoietic stem cell transplantation specialist who was not involved in the study, said in an interview that “omidubicel significantly improves the engraftment after transplant, as compared to standard cord blood transplant. For patients that lack an HLA-matched donor, this approach can help overcome the prolonged cytopenias that occur with standard cord blood transplants in adults.”
Gamida Cell plans to submit these data for approval of omidubicel by the Food and Drug Administration in the fourth quarter of 2021.
Omidubicel is also being evaluated in a phase 1/2 clinical study in patients with severe aplastic anemia (NCT03173937).
Expanding possibilities
Although umbilical cord blood stem cell grafts come from a readily available source and show greater tolerance across HLA barriers than other sources (such as bone marrow), the relatively low dose of stem cells in each unit results in delayed hematopoietic recovery, increased transplant-related morbidity and mortality, and longer hospitalizations, Dr. Sanz said.
Omidubicel consists of two cryopreserved fractions from a single cord blood unit. The product contains both noncultured CD133-negative cells, including T cells, and CD133-positive cells that are then expanded ex vivo for 21 days in the presence of nicotinamide.
“Nicotinamide increases stem and progenitor cells, inhibits differentiation and increases migration, bone marrow homing, and engraftment efficiency while preserving cellular functionality and phenotype,” Dr. Sanz explained during his presentation.
In an earlier phase 1/2 trial in 36 patients with high-risk hematologic malignancies, omidubicel was associated with hematopoietic engraftment lasting at least 10 years.
Details of phase 3 trial results
The global phase 3 trial was conducted in 125 patients (aged 13-65 years) with high-risk malignancies, including acute myeloid and lymphoblastic leukemias, myelodysplastic syndrome, chronic myeloid leukemia, lymphomas, and rare leukemias. These patients were all eligible for allogeneic stem cell transplantation but did not have matched donors.
Patients were randomly assigned to receive hematopoietic reconstitution with either omidubicel (n = 52) or standard cord blood (n = 58).
At 42 days of follow-up, the median time to neutrophil engraftment in the intention-to-treat (ITT) population, the primary endpoint, was 12 days with omidubicel versus 22 days with standard cord blood (P < .001).
In the as-treated population – the 108 patients who actually received omidubicel or standard cord blood – median time to engraftment was 10.0 versus 20.5 days, respectively (P < .001).
Rates of neutrophil engraftment at 42 days were 96% with omidubicel versus 89% with standard cord blood.
The secondary endpoint of time-to-platelet engraftment in the ITT population also favored omidubicel, with a cumulative day 42 incidence rate of 55%, compared with 35% with standard cord blood (P = .028).
In the as-treated population, median times to platelet engraftment were 37 days and 50 days, respectively (P = .023). The cumulative rates of platelet engraftment at 100 days of follow-up were 83% and 73%, respectively.
The incidence of grade 2 or 3 bacterial or invasive fungal infections by day 100 in the ITT population was 37% among patients who received omidubicel, compared with 57% for patients who received standard cord blood (P = .027). Viral infections occurred in 10% versus 26% of patients, respectively.
The incidence of acute graft versus host disease at day 100 was similar between treatment groups, and there was no significant difference at 1 year.
Relapse and nonrelapse mortality rates, as well as disease-free and overall survival rates also did not differ between groups.
In the first 100 days post transplant, patients who received omidubicel were alive and out of the hospital for a median of 60.5 days, compared with 48 days for patients who received standard cord blood (P = .005).
The study was funded by Gamida Cell. Dr. Sanz reported receiving research funding from the company and several others, and consulting fees, honoraria, speakers bureau activity, and travel expenses from other companies. Dr. DeFilipp reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Omidubicel, an investigational enriched umbilical cord blood product being developed by Gamida Cell for transplantation in patients with blood cancers, appears to have some advantages over standard umbilical cord blood.
The results come from a global phase 3 trial (NCT02730299) presented at the annual meeting of the European Society for Blood and Bone Marrow Transplantation.
“Transplantation with omidubicel, compared to standard cord blood transplantation, results in faster hematopoietic recovery, fewer infections, and fewer days in hospital,” said coinvestigator Guillermo F. Sanz, MD, PhD, from the Hospital Universitari i Politècnic la Fe in Valencia, Spain.
“Omidubicel should be considered as the new standard of care for patients eligible for umbilical cord blood transplantation,” Dr. Sanz concluded.
Zachariah DeFilipp, MD, from Mass General Cancer Center in Boston, a hematopoietic stem cell transplantation specialist who was not involved in the study, said in an interview that “omidubicel significantly improves the engraftment after transplant, as compared to standard cord blood transplant. For patients that lack an HLA-matched donor, this approach can help overcome the prolonged cytopenias that occur with standard cord blood transplants in adults.”
Gamida Cell plans to submit these data for approval of omidubicel by the Food and Drug Administration in the fourth quarter of 2021.
Omidubicel is also being evaluated in a phase 1/2 clinical study in patients with severe aplastic anemia (NCT03173937).
Expanding possibilities
Although umbilical cord blood stem cell grafts come from a readily available source and show greater tolerance across HLA barriers than other sources (such as bone marrow), the relatively low dose of stem cells in each unit results in delayed hematopoietic recovery, increased transplant-related morbidity and mortality, and longer hospitalizations, Dr. Sanz said.
Omidubicel consists of two cryopreserved fractions from a single cord blood unit. The product contains both noncultured CD133-negative cells, including T cells, and CD133-positive cells that are then expanded ex vivo for 21 days in the presence of nicotinamide.
“Nicotinamide increases stem and progenitor cells, inhibits differentiation and increases migration, bone marrow homing, and engraftment efficiency while preserving cellular functionality and phenotype,” Dr. Sanz explained during his presentation.
In an earlier phase 1/2 trial in 36 patients with high-risk hematologic malignancies, omidubicel was associated with hematopoietic engraftment lasting at least 10 years.
Details of phase 3 trial results
The global phase 3 trial was conducted in 125 patients (aged 13-65 years) with high-risk malignancies, including acute myeloid and lymphoblastic leukemias, myelodysplastic syndrome, chronic myeloid leukemia, lymphomas, and rare leukemias. These patients were all eligible for allogeneic stem cell transplantation but did not have matched donors.
Patients were randomly assigned to receive hematopoietic reconstitution with either omidubicel (n = 52) or standard cord blood (n = 58).
At 42 days of follow-up, the median time to neutrophil engraftment in the intention-to-treat (ITT) population, the primary endpoint, was 12 days with omidubicel versus 22 days with standard cord blood (P < .001).
In the as-treated population – the 108 patients who actually received omidubicel or standard cord blood – median time to engraftment was 10.0 versus 20.5 days, respectively (P < .001).
Rates of neutrophil engraftment at 42 days were 96% with omidubicel versus 89% with standard cord blood.
The secondary endpoint of time-to-platelet engraftment in the ITT population also favored omidubicel, with a cumulative day 42 incidence rate of 55%, compared with 35% with standard cord blood (P = .028).
In the as-treated population, median times to platelet engraftment were 37 days and 50 days, respectively (P = .023). The cumulative rates of platelet engraftment at 100 days of follow-up were 83% and 73%, respectively.
The incidence of grade 2 or 3 bacterial or invasive fungal infections by day 100 in the ITT population was 37% among patients who received omidubicel, compared with 57% for patients who received standard cord blood (P = .027). Viral infections occurred in 10% versus 26% of patients, respectively.
The incidence of acute graft versus host disease at day 100 was similar between treatment groups, and there was no significant difference at 1 year.
Relapse and nonrelapse mortality rates, as well as disease-free and overall survival rates also did not differ between groups.
In the first 100 days post transplant, patients who received omidubicel were alive and out of the hospital for a median of 60.5 days, compared with 48 days for patients who received standard cord blood (P = .005).
The study was funded by Gamida Cell. Dr. Sanz reported receiving research funding from the company and several others, and consulting fees, honoraria, speakers bureau activity, and travel expenses from other companies. Dr. DeFilipp reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Omidubicel, an investigational enriched umbilical cord blood product being developed by Gamida Cell for transplantation in patients with blood cancers, appears to have some advantages over standard umbilical cord blood.
The results come from a global phase 3 trial (NCT02730299) presented at the annual meeting of the European Society for Blood and Bone Marrow Transplantation.
“Transplantation with omidubicel, compared to standard cord blood transplantation, results in faster hematopoietic recovery, fewer infections, and fewer days in hospital,” said coinvestigator Guillermo F. Sanz, MD, PhD, from the Hospital Universitari i Politècnic la Fe in Valencia, Spain.
“Omidubicel should be considered as the new standard of care for patients eligible for umbilical cord blood transplantation,” Dr. Sanz concluded.
Zachariah DeFilipp, MD, from Mass General Cancer Center in Boston, a hematopoietic stem cell transplantation specialist who was not involved in the study, said in an interview that “omidubicel significantly improves the engraftment after transplant, as compared to standard cord blood transplant. For patients that lack an HLA-matched donor, this approach can help overcome the prolonged cytopenias that occur with standard cord blood transplants in adults.”
Gamida Cell plans to submit these data for approval of omidubicel by the Food and Drug Administration in the fourth quarter of 2021.
Omidubicel is also being evaluated in a phase 1/2 clinical study in patients with severe aplastic anemia (NCT03173937).
Expanding possibilities
Although umbilical cord blood stem cell grafts come from a readily available source and show greater tolerance across HLA barriers than other sources (such as bone marrow), the relatively low dose of stem cells in each unit results in delayed hematopoietic recovery, increased transplant-related morbidity and mortality, and longer hospitalizations, Dr. Sanz said.
Omidubicel consists of two cryopreserved fractions from a single cord blood unit. The product contains both noncultured CD133-negative cells, including T cells, and CD133-positive cells that are then expanded ex vivo for 21 days in the presence of nicotinamide.
“Nicotinamide increases stem and progenitor cells, inhibits differentiation and increases migration, bone marrow homing, and engraftment efficiency while preserving cellular functionality and phenotype,” Dr. Sanz explained during his presentation.
In an earlier phase 1/2 trial in 36 patients with high-risk hematologic malignancies, omidubicel was associated with hematopoietic engraftment lasting at least 10 years.
Details of phase 3 trial results
The global phase 3 trial was conducted in 125 patients (aged 13-65 years) with high-risk malignancies, including acute myeloid and lymphoblastic leukemias, myelodysplastic syndrome, chronic myeloid leukemia, lymphomas, and rare leukemias. These patients were all eligible for allogeneic stem cell transplantation but did not have matched donors.
Patients were randomly assigned to receive hematopoietic reconstitution with either omidubicel (n = 52) or standard cord blood (n = 58).
At 42 days of follow-up, the median time to neutrophil engraftment in the intention-to-treat (ITT) population, the primary endpoint, was 12 days with omidubicel versus 22 days with standard cord blood (P < .001).
In the as-treated population – the 108 patients who actually received omidubicel or standard cord blood – median time to engraftment was 10.0 versus 20.5 days, respectively (P < .001).
Rates of neutrophil engraftment at 42 days were 96% with omidubicel versus 89% with standard cord blood.
The secondary endpoint of time-to-platelet engraftment in the ITT population also favored omidubicel, with a cumulative day 42 incidence rate of 55%, compared with 35% with standard cord blood (P = .028).
In the as-treated population, median times to platelet engraftment were 37 days and 50 days, respectively (P = .023). The cumulative rates of platelet engraftment at 100 days of follow-up were 83% and 73%, respectively.
The incidence of grade 2 or 3 bacterial or invasive fungal infections by day 100 in the ITT population was 37% among patients who received omidubicel, compared with 57% for patients who received standard cord blood (P = .027). Viral infections occurred in 10% versus 26% of patients, respectively.
The incidence of acute graft versus host disease at day 100 was similar between treatment groups, and there was no significant difference at 1 year.
Relapse and nonrelapse mortality rates, as well as disease-free and overall survival rates also did not differ between groups.
In the first 100 days post transplant, patients who received omidubicel were alive and out of the hospital for a median of 60.5 days, compared with 48 days for patients who received standard cord blood (P = .005).
The study was funded by Gamida Cell. Dr. Sanz reported receiving research funding from the company and several others, and consulting fees, honoraria, speakers bureau activity, and travel expenses from other companies. Dr. DeFilipp reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Don’t delay: Cancer patients need both doses of COVID vaccine
The new findings, which are soon to be published as a preprint, cast doubt on the current U.K. policy of delaying the second dose of the vaccine.
Delaying the second dose can leave most patients with cancer wholly or partially unprotected, according to the researchers. Moreover, such a delay has implications for transmission of SARS-CoV-2 in the cancer patient’s environs as well as for the evolution of virus variants that could be of concern, the researchers concluded.
The data come from a British study that included 151 patients with cancer and 54 healthy control persons. All participants received the COVID-19 mRNA BNT162b2 vaccine (Pfizer-BioNTech).
This vaccine requires two doses. The first few participants in this study were given the second dose 21 days after they had received the first dose, but then national guidelines changed, and the remaining participants had to wait 12 weeks to receive their second dose.
The researchers reported that, among health controls, the immune efficacy of the first dose was very high (97% efficacious). By contrast, among patients with solid tumors, the immune efficacy of a single dose was strikingly low (39%), and it was even lower in patients with hematologic malignancies (13%).
The second dose of vaccine greatly and rapidly increased the immune efficacy in patients with solid tumors (95% within 2 weeks of receiving the second dose), the researchers added.
Too few patients with hematologic cancers had received the second dose before the study ended for clear conclusions to be drawn. Nevertheless, the available data suggest that 50% of patients with hematologic cancers who had received the booster at day 21 were seropositive at 5 weeks vs. only 8% of those who had not received the booster.
“Our data provide the first real-world evidence of immune efficacy following one dose of the Pfizer vaccine in immunocompromised patient populations [and] clearly show that the poor one-dose efficacy in cancer patients can be rescued with an early booster at day 21,” commented senior author Sheeba Irshad, MD, senior clinical lecturer, King’s College London.
“Based on our findings, we would recommend an urgent review of the vaccine strategy for clinically extremely vulnerable groups. Until then, it is important that cancer patients continue to observe all public health measures in place, such as social distancing and shielding when attending hospitals, even after vaccination,” Dr. Irshad added.
The paper, with first author Leticia Monin-Aldama, PhD, is scheduled to appear on the preprint server medRxiv. It has not undergone peer review. The paper was distributed to journalists, with comments from experts not involved in the study, by the UK Science Media Centre.
These data are “of immediate importance” to patients with cancer, commented Shoba Amarnath, PhD, Newcastle University research fellow, Laboratory of T-cell Regulation, Newcastle University Center for Cancer, Newcastle upon Tyne, England.
“These findings are consistent with our understanding. … We know that the immune system within cancer patients is compromised as compared to healthy controls,” Dr. Amarnath said. “The data in the study support the notion that, in solid cancer patients, a considerable delay in second dose will extend the period when cancer patients are at risk of SARS-CoV-2 infection.”
Although more data are required, “this study does raise the issue of whether patients with cancer, other diseases, or those undergoing therapies that affect the body’s immune response should be fast-tracked for their second vaccine dose,” commented Lawrence Young, PhD, professor of molecular oncology and director of the Warwick Cancer Research Center, University of Warwick, Coventry, England.
Stephen Evans, MSc, professor of pharmacoepidemiology, London School of Hygiene and Tropical Medicine, underlined that the study is “essentially” observational and “inevitable limitations must be taken into account.
“Nevertheless, these results do suggest that the vaccines may well not protect those patients with cancer as well as those without cancer,” Mr. Evans said. He added that it is “important that this population continues to observe all COVID-19–associated measures, such as social distancing and shielding when attending hospitals, even after vaccination.”
Study details
Previous studies have shown that some patients with cancer have prolonged responses to SARS-CoV-2 infection, with ongoing immune dysregulation, inefficient seroconversion, and prolonged viral shedding.
There are few data, however, on how these patients respond to COVID-19 vaccination. The authors point out that, among the 18,860 individuals who received the Pfizer vaccine during its development trials, “none with an active oncological diagnosis was included.”
To investigate this issue, they launched the SARS-CoV-2 for Cancer Patients (SOAP-02) study.
The 151 patients with cancer who participated in this study were mostly elderly, the authors noted (75% were older than 65 years; the median age was 73 years). The majority (63%) had solid-tumor malignancies. Of those, 8% had late-stage disease and had been living with their cancer for more than 24 months.
The healthy control persons were vaccine-eligible primary health care workers who were not age matched to the cancer patients.
All participants received the first dose of vaccine; 31 (of 151) patients with cancer and 16 (of 54) healthy control persons received the second dose on day 21.
The remaining participants were scheduled to receive their second dose 12 weeks later (after the study ended), in line with the changes in the national guidelines.
The team reported that, approximately 21 days after receiving the first vaccine dose, the immune efficacy of the vaccine was estimated to be 97% among healthy control persons vs. 39% for patients with solid tumors and only 13% for those with hematologic malignancies (P < .0001 for both).
T-cell responses, as assessed via interferon-gamma and/or interleukin-2 production, were observed in 82% of healthy control persons, 71% of patients with solid tumors, and 50% of those with hematologic cancers.
Vaccine boosting at day 21 resulted in immune efficacy of 100% for healthy control persons and 95% for patients with solid tumors. In contrast, only 43% of those who did not receive the second dose were seropositive 2 weeks later.
Further analysis suggested that participants who did not have a serologic response were “spread evenly” across different cancer types, but the reduced responses were more frequent among patients who had received the vaccine within 15 days of cancer treatment, especially chemotherapy, and had undergone intensive treatments.
The SOAP study is sponsored by King’s College London and Guy’s and St. Thomas Trust Foundation NHS Trust. It is funded from grants from the KCL Charity, Cancer Research UK, and program grants from Breast Cancer Now. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The new findings, which are soon to be published as a preprint, cast doubt on the current U.K. policy of delaying the second dose of the vaccine.
Delaying the second dose can leave most patients with cancer wholly or partially unprotected, according to the researchers. Moreover, such a delay has implications for transmission of SARS-CoV-2 in the cancer patient’s environs as well as for the evolution of virus variants that could be of concern, the researchers concluded.
The data come from a British study that included 151 patients with cancer and 54 healthy control persons. All participants received the COVID-19 mRNA BNT162b2 vaccine (Pfizer-BioNTech).
This vaccine requires two doses. The first few participants in this study were given the second dose 21 days after they had received the first dose, but then national guidelines changed, and the remaining participants had to wait 12 weeks to receive their second dose.
The researchers reported that, among health controls, the immune efficacy of the first dose was very high (97% efficacious). By contrast, among patients with solid tumors, the immune efficacy of a single dose was strikingly low (39%), and it was even lower in patients with hematologic malignancies (13%).
The second dose of vaccine greatly and rapidly increased the immune efficacy in patients with solid tumors (95% within 2 weeks of receiving the second dose), the researchers added.
Too few patients with hematologic cancers had received the second dose before the study ended for clear conclusions to be drawn. Nevertheless, the available data suggest that 50% of patients with hematologic cancers who had received the booster at day 21 were seropositive at 5 weeks vs. only 8% of those who had not received the booster.
“Our data provide the first real-world evidence of immune efficacy following one dose of the Pfizer vaccine in immunocompromised patient populations [and] clearly show that the poor one-dose efficacy in cancer patients can be rescued with an early booster at day 21,” commented senior author Sheeba Irshad, MD, senior clinical lecturer, King’s College London.
“Based on our findings, we would recommend an urgent review of the vaccine strategy for clinically extremely vulnerable groups. Until then, it is important that cancer patients continue to observe all public health measures in place, such as social distancing and shielding when attending hospitals, even after vaccination,” Dr. Irshad added.
The paper, with first author Leticia Monin-Aldama, PhD, is scheduled to appear on the preprint server medRxiv. It has not undergone peer review. The paper was distributed to journalists, with comments from experts not involved in the study, by the UK Science Media Centre.
These data are “of immediate importance” to patients with cancer, commented Shoba Amarnath, PhD, Newcastle University research fellow, Laboratory of T-cell Regulation, Newcastle University Center for Cancer, Newcastle upon Tyne, England.
“These findings are consistent with our understanding. … We know that the immune system within cancer patients is compromised as compared to healthy controls,” Dr. Amarnath said. “The data in the study support the notion that, in solid cancer patients, a considerable delay in second dose will extend the period when cancer patients are at risk of SARS-CoV-2 infection.”
Although more data are required, “this study does raise the issue of whether patients with cancer, other diseases, or those undergoing therapies that affect the body’s immune response should be fast-tracked for their second vaccine dose,” commented Lawrence Young, PhD, professor of molecular oncology and director of the Warwick Cancer Research Center, University of Warwick, Coventry, England.
Stephen Evans, MSc, professor of pharmacoepidemiology, London School of Hygiene and Tropical Medicine, underlined that the study is “essentially” observational and “inevitable limitations must be taken into account.
“Nevertheless, these results do suggest that the vaccines may well not protect those patients with cancer as well as those without cancer,” Mr. Evans said. He added that it is “important that this population continues to observe all COVID-19–associated measures, such as social distancing and shielding when attending hospitals, even after vaccination.”
Study details
Previous studies have shown that some patients with cancer have prolonged responses to SARS-CoV-2 infection, with ongoing immune dysregulation, inefficient seroconversion, and prolonged viral shedding.
There are few data, however, on how these patients respond to COVID-19 vaccination. The authors point out that, among the 18,860 individuals who received the Pfizer vaccine during its development trials, “none with an active oncological diagnosis was included.”
To investigate this issue, they launched the SARS-CoV-2 for Cancer Patients (SOAP-02) study.
The 151 patients with cancer who participated in this study were mostly elderly, the authors noted (75% were older than 65 years; the median age was 73 years). The majority (63%) had solid-tumor malignancies. Of those, 8% had late-stage disease and had been living with their cancer for more than 24 months.
The healthy control persons were vaccine-eligible primary health care workers who were not age matched to the cancer patients.
All participants received the first dose of vaccine; 31 (of 151) patients with cancer and 16 (of 54) healthy control persons received the second dose on day 21.
The remaining participants were scheduled to receive their second dose 12 weeks later (after the study ended), in line with the changes in the national guidelines.
The team reported that, approximately 21 days after receiving the first vaccine dose, the immune efficacy of the vaccine was estimated to be 97% among healthy control persons vs. 39% for patients with solid tumors and only 13% for those with hematologic malignancies (P < .0001 for both).
T-cell responses, as assessed via interferon-gamma and/or interleukin-2 production, were observed in 82% of healthy control persons, 71% of patients with solid tumors, and 50% of those with hematologic cancers.
Vaccine boosting at day 21 resulted in immune efficacy of 100% for healthy control persons and 95% for patients with solid tumors. In contrast, only 43% of those who did not receive the second dose were seropositive 2 weeks later.
Further analysis suggested that participants who did not have a serologic response were “spread evenly” across different cancer types, but the reduced responses were more frequent among patients who had received the vaccine within 15 days of cancer treatment, especially chemotherapy, and had undergone intensive treatments.
The SOAP study is sponsored by King’s College London and Guy’s and St. Thomas Trust Foundation NHS Trust. It is funded from grants from the KCL Charity, Cancer Research UK, and program grants from Breast Cancer Now. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The new findings, which are soon to be published as a preprint, cast doubt on the current U.K. policy of delaying the second dose of the vaccine.
Delaying the second dose can leave most patients with cancer wholly or partially unprotected, according to the researchers. Moreover, such a delay has implications for transmission of SARS-CoV-2 in the cancer patient’s environs as well as for the evolution of virus variants that could be of concern, the researchers concluded.
The data come from a British study that included 151 patients with cancer and 54 healthy control persons. All participants received the COVID-19 mRNA BNT162b2 vaccine (Pfizer-BioNTech).
This vaccine requires two doses. The first few participants in this study were given the second dose 21 days after they had received the first dose, but then national guidelines changed, and the remaining participants had to wait 12 weeks to receive their second dose.
The researchers reported that, among health controls, the immune efficacy of the first dose was very high (97% efficacious). By contrast, among patients with solid tumors, the immune efficacy of a single dose was strikingly low (39%), and it was even lower in patients with hematologic malignancies (13%).
The second dose of vaccine greatly and rapidly increased the immune efficacy in patients with solid tumors (95% within 2 weeks of receiving the second dose), the researchers added.
Too few patients with hematologic cancers had received the second dose before the study ended for clear conclusions to be drawn. Nevertheless, the available data suggest that 50% of patients with hematologic cancers who had received the booster at day 21 were seropositive at 5 weeks vs. only 8% of those who had not received the booster.
“Our data provide the first real-world evidence of immune efficacy following one dose of the Pfizer vaccine in immunocompromised patient populations [and] clearly show that the poor one-dose efficacy in cancer patients can be rescued with an early booster at day 21,” commented senior author Sheeba Irshad, MD, senior clinical lecturer, King’s College London.
“Based on our findings, we would recommend an urgent review of the vaccine strategy for clinically extremely vulnerable groups. Until then, it is important that cancer patients continue to observe all public health measures in place, such as social distancing and shielding when attending hospitals, even after vaccination,” Dr. Irshad added.
The paper, with first author Leticia Monin-Aldama, PhD, is scheduled to appear on the preprint server medRxiv. It has not undergone peer review. The paper was distributed to journalists, with comments from experts not involved in the study, by the UK Science Media Centre.
These data are “of immediate importance” to patients with cancer, commented Shoba Amarnath, PhD, Newcastle University research fellow, Laboratory of T-cell Regulation, Newcastle University Center for Cancer, Newcastle upon Tyne, England.
“These findings are consistent with our understanding. … We know that the immune system within cancer patients is compromised as compared to healthy controls,” Dr. Amarnath said. “The data in the study support the notion that, in solid cancer patients, a considerable delay in second dose will extend the period when cancer patients are at risk of SARS-CoV-2 infection.”
Although more data are required, “this study does raise the issue of whether patients with cancer, other diseases, or those undergoing therapies that affect the body’s immune response should be fast-tracked for their second vaccine dose,” commented Lawrence Young, PhD, professor of molecular oncology and director of the Warwick Cancer Research Center, University of Warwick, Coventry, England.
Stephen Evans, MSc, professor of pharmacoepidemiology, London School of Hygiene and Tropical Medicine, underlined that the study is “essentially” observational and “inevitable limitations must be taken into account.
“Nevertheless, these results do suggest that the vaccines may well not protect those patients with cancer as well as those without cancer,” Mr. Evans said. He added that it is “important that this population continues to observe all COVID-19–associated measures, such as social distancing and shielding when attending hospitals, even after vaccination.”
Study details
Previous studies have shown that some patients with cancer have prolonged responses to SARS-CoV-2 infection, with ongoing immune dysregulation, inefficient seroconversion, and prolonged viral shedding.
There are few data, however, on how these patients respond to COVID-19 vaccination. The authors point out that, among the 18,860 individuals who received the Pfizer vaccine during its development trials, “none with an active oncological diagnosis was included.”
To investigate this issue, they launched the SARS-CoV-2 for Cancer Patients (SOAP-02) study.
The 151 patients with cancer who participated in this study were mostly elderly, the authors noted (75% were older than 65 years; the median age was 73 years). The majority (63%) had solid-tumor malignancies. Of those, 8% had late-stage disease and had been living with their cancer for more than 24 months.
The healthy control persons were vaccine-eligible primary health care workers who were not age matched to the cancer patients.
All participants received the first dose of vaccine; 31 (of 151) patients with cancer and 16 (of 54) healthy control persons received the second dose on day 21.
The remaining participants were scheduled to receive their second dose 12 weeks later (after the study ended), in line with the changes in the national guidelines.
The team reported that, approximately 21 days after receiving the first vaccine dose, the immune efficacy of the vaccine was estimated to be 97% among healthy control persons vs. 39% for patients with solid tumors and only 13% for those with hematologic malignancies (P < .0001 for both).
T-cell responses, as assessed via interferon-gamma and/or interleukin-2 production, were observed in 82% of healthy control persons, 71% of patients with solid tumors, and 50% of those with hematologic cancers.
Vaccine boosting at day 21 resulted in immune efficacy of 100% for healthy control persons and 95% for patients with solid tumors. In contrast, only 43% of those who did not receive the second dose were seropositive 2 weeks later.
Further analysis suggested that participants who did not have a serologic response were “spread evenly” across different cancer types, but the reduced responses were more frequent among patients who had received the vaccine within 15 days of cancer treatment, especially chemotherapy, and had undergone intensive treatments.
The SOAP study is sponsored by King’s College London and Guy’s and St. Thomas Trust Foundation NHS Trust. It is funded from grants from the KCL Charity, Cancer Research UK, and program grants from Breast Cancer Now. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
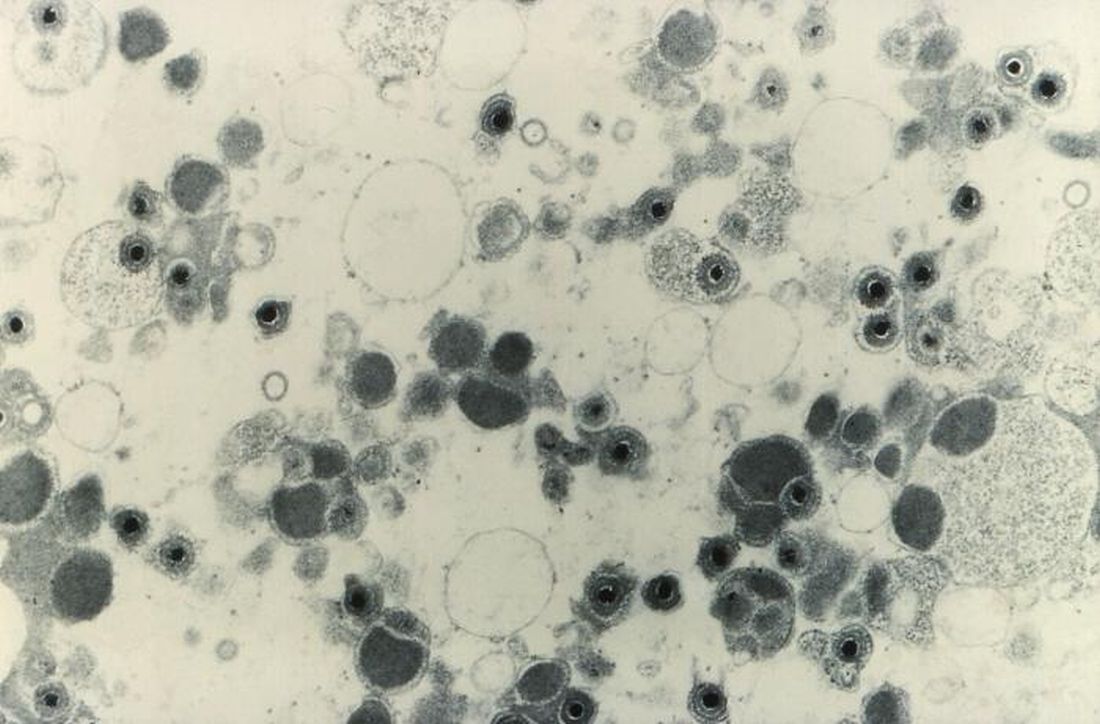
Maribavir seen as superior to other antivirals for CMV clearance post transplant
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
FROM TCT 2021