User login
Repeat MRI not useful in suspected axial spondyloarthritis
Patients with chronic back pain suspected of having axial spondyloarthritis (axSpA) should not undergo follow-up MRI of the sacroiliac joint (MRI-SI) within a year if they had a negative baseline MRI-SI, according to investigators.
It is very unlikely that a follow-up MRI-SI will yield new results, reported Pauline A. Bakker, MD, of the department of rheumatology at Leiden University Medical Centre, the Netherlands, and her colleagues.
Since gender and HLA-B27 status were closely associated with MRI-SI positivity, these factors should be considered when deciding to repeat an MRI-SI.
“Over the last decade, MRI rapidly gained ground and proved to be an important imaging technique in the diagnostic process of [nonradiographic] axial spondyloarthritis,” the investigators wrote in Arthritis and Rheumatology. “It has been shown that MRI can detect the early inflammatory stages of sacroiliitis months to years before structural damage can be detected on a conventional radiograph.”
Although MRI represents a diagnostic leap forward, questions of clinical application remain. “For example… if an MRI is completely normal and there is still a clinical suspicion of axSpA, should the MRI be repeated? And if so, after what period of follow-up? Or does this not contribute to the diagnostic process?”
To answer these questions, the investigators observed the “evolution of MRI lesions over a 3-month and 1-year time frame” in patients with early chronic back pain and suspected axSpA.
The prospective study involved 188 patients from the Spondyloarthritis Caught Early (SPACE) cohort. The authors commented that this is “an ideal cohort… since it includes a population of patients with back pain of short duration referred to rheumatologists with a suspicion of SpA [but without the mandatory presence of a single or multiple SpA features].”
Enrolled patients had chronic back pain lasting between 3 months and 2 years, with onset beginning between 16 and 45 years of age. Each underwent physical examination (including evaluation of other SpA features), MRI and radiographs of the sacroiliac joints, and HLA-B27 testing. If patients fulfilled axSpA criteria or had possible axSpA (at least one SpA feature), then they proceeded into the follow-up phase of the study, which included repeat MRI-SI at 3 months and 1 year.
Among enrolled patients, slightly more than one-third were male, almost half were HLA-B27 positive, and about three-quarters had Assessment of Spondyloarthritis International Society–defined inflammatory back pain. Mean age was 31 years; 31 (16.5%) patients were MRI-SI positive.
Of patients that were MRI-SI positive at baseline, 11.1% and 37.9% had a negative MRI-SI at 3 months and 1 year, respectively. The authors noted that this change “was partly induced by the start of anti-TNF [tumor necrosis factor] therapy.” In patients who were MRI-SI negative at baseline, 4.3% and 7.2% were positive at 3 months and 1 year, respectively.
“A very small percentage of patients become positive… which indicates that the usefulness of repeating an MRI-SI in the diagnostic process after 3 months or 1 year is very limited,” the authors wrote.
Gender and HLA-B27 status were independently associated with a positive MRI-SI at any point in time. About 43% of HLA-B27-positive men had a positive MRI-SI, compared with just 7% of HLA-B27-negative women. The investigators advised that these associations be considered when deciding upon repeat MRI-SI.
“If a clinical suspicion [of axSpA] remains [for example, a patient develops other SpA features] it might be worthwhile to consider redoing an MRI in HLA-B27 positive patients,” the investigators wrote. “Likewise, there is a statistically significant difference between male and female patients with a negative baseline MRI, namely that in male patients more often a positive MRI at follow-up is seen [difference: 12% in men, 3% in women].”
The researchers reported having no conflicts of interest.
SOURCE: Bakker PA et al. Arthritis Rheumatol. 2018 Sep 11. doi: 10.1002/art.40718.
Patients with chronic back pain suspected of having axial spondyloarthritis (axSpA) should not undergo follow-up MRI of the sacroiliac joint (MRI-SI) within a year if they had a negative baseline MRI-SI, according to investigators.
It is very unlikely that a follow-up MRI-SI will yield new results, reported Pauline A. Bakker, MD, of the department of rheumatology at Leiden University Medical Centre, the Netherlands, and her colleagues.
Since gender and HLA-B27 status were closely associated with MRI-SI positivity, these factors should be considered when deciding to repeat an MRI-SI.
“Over the last decade, MRI rapidly gained ground and proved to be an important imaging technique in the diagnostic process of [nonradiographic] axial spondyloarthritis,” the investigators wrote in Arthritis and Rheumatology. “It has been shown that MRI can detect the early inflammatory stages of sacroiliitis months to years before structural damage can be detected on a conventional radiograph.”
Although MRI represents a diagnostic leap forward, questions of clinical application remain. “For example… if an MRI is completely normal and there is still a clinical suspicion of axSpA, should the MRI be repeated? And if so, after what period of follow-up? Or does this not contribute to the diagnostic process?”
To answer these questions, the investigators observed the “evolution of MRI lesions over a 3-month and 1-year time frame” in patients with early chronic back pain and suspected axSpA.
The prospective study involved 188 patients from the Spondyloarthritis Caught Early (SPACE) cohort. The authors commented that this is “an ideal cohort… since it includes a population of patients with back pain of short duration referred to rheumatologists with a suspicion of SpA [but without the mandatory presence of a single or multiple SpA features].”
Enrolled patients had chronic back pain lasting between 3 months and 2 years, with onset beginning between 16 and 45 years of age. Each underwent physical examination (including evaluation of other SpA features), MRI and radiographs of the sacroiliac joints, and HLA-B27 testing. If patients fulfilled axSpA criteria or had possible axSpA (at least one SpA feature), then they proceeded into the follow-up phase of the study, which included repeat MRI-SI at 3 months and 1 year.
Among enrolled patients, slightly more than one-third were male, almost half were HLA-B27 positive, and about three-quarters had Assessment of Spondyloarthritis International Society–defined inflammatory back pain. Mean age was 31 years; 31 (16.5%) patients were MRI-SI positive.
Of patients that were MRI-SI positive at baseline, 11.1% and 37.9% had a negative MRI-SI at 3 months and 1 year, respectively. The authors noted that this change “was partly induced by the start of anti-TNF [tumor necrosis factor] therapy.” In patients who were MRI-SI negative at baseline, 4.3% and 7.2% were positive at 3 months and 1 year, respectively.
“A very small percentage of patients become positive… which indicates that the usefulness of repeating an MRI-SI in the diagnostic process after 3 months or 1 year is very limited,” the authors wrote.
Gender and HLA-B27 status were independently associated with a positive MRI-SI at any point in time. About 43% of HLA-B27-positive men had a positive MRI-SI, compared with just 7% of HLA-B27-negative women. The investigators advised that these associations be considered when deciding upon repeat MRI-SI.
“If a clinical suspicion [of axSpA] remains [for example, a patient develops other SpA features] it might be worthwhile to consider redoing an MRI in HLA-B27 positive patients,” the investigators wrote. “Likewise, there is a statistically significant difference between male and female patients with a negative baseline MRI, namely that in male patients more often a positive MRI at follow-up is seen [difference: 12% in men, 3% in women].”
The researchers reported having no conflicts of interest.
SOURCE: Bakker PA et al. Arthritis Rheumatol. 2018 Sep 11. doi: 10.1002/art.40718.
Patients with chronic back pain suspected of having axial spondyloarthritis (axSpA) should not undergo follow-up MRI of the sacroiliac joint (MRI-SI) within a year if they had a negative baseline MRI-SI, according to investigators.
It is very unlikely that a follow-up MRI-SI will yield new results, reported Pauline A. Bakker, MD, of the department of rheumatology at Leiden University Medical Centre, the Netherlands, and her colleagues.
Since gender and HLA-B27 status were closely associated with MRI-SI positivity, these factors should be considered when deciding to repeat an MRI-SI.
“Over the last decade, MRI rapidly gained ground and proved to be an important imaging technique in the diagnostic process of [nonradiographic] axial spondyloarthritis,” the investigators wrote in Arthritis and Rheumatology. “It has been shown that MRI can detect the early inflammatory stages of sacroiliitis months to years before structural damage can be detected on a conventional radiograph.”
Although MRI represents a diagnostic leap forward, questions of clinical application remain. “For example… if an MRI is completely normal and there is still a clinical suspicion of axSpA, should the MRI be repeated? And if so, after what period of follow-up? Or does this not contribute to the diagnostic process?”
To answer these questions, the investigators observed the “evolution of MRI lesions over a 3-month and 1-year time frame” in patients with early chronic back pain and suspected axSpA.
The prospective study involved 188 patients from the Spondyloarthritis Caught Early (SPACE) cohort. The authors commented that this is “an ideal cohort… since it includes a population of patients with back pain of short duration referred to rheumatologists with a suspicion of SpA [but without the mandatory presence of a single or multiple SpA features].”
Enrolled patients had chronic back pain lasting between 3 months and 2 years, with onset beginning between 16 and 45 years of age. Each underwent physical examination (including evaluation of other SpA features), MRI and radiographs of the sacroiliac joints, and HLA-B27 testing. If patients fulfilled axSpA criteria or had possible axSpA (at least one SpA feature), then they proceeded into the follow-up phase of the study, which included repeat MRI-SI at 3 months and 1 year.
Among enrolled patients, slightly more than one-third were male, almost half were HLA-B27 positive, and about three-quarters had Assessment of Spondyloarthritis International Society–defined inflammatory back pain. Mean age was 31 years; 31 (16.5%) patients were MRI-SI positive.
Of patients that were MRI-SI positive at baseline, 11.1% and 37.9% had a negative MRI-SI at 3 months and 1 year, respectively. The authors noted that this change “was partly induced by the start of anti-TNF [tumor necrosis factor] therapy.” In patients who were MRI-SI negative at baseline, 4.3% and 7.2% were positive at 3 months and 1 year, respectively.
“A very small percentage of patients become positive… which indicates that the usefulness of repeating an MRI-SI in the diagnostic process after 3 months or 1 year is very limited,” the authors wrote.
Gender and HLA-B27 status were independently associated with a positive MRI-SI at any point in time. About 43% of HLA-B27-positive men had a positive MRI-SI, compared with just 7% of HLA-B27-negative women. The investigators advised that these associations be considered when deciding upon repeat MRI-SI.
“If a clinical suspicion [of axSpA] remains [for example, a patient develops other SpA features] it might be worthwhile to consider redoing an MRI in HLA-B27 positive patients,” the investigators wrote. “Likewise, there is a statistically significant difference between male and female patients with a negative baseline MRI, namely that in male patients more often a positive MRI at follow-up is seen [difference: 12% in men, 3% in women].”
The researchers reported having no conflicts of interest.
SOURCE: Bakker PA et al. Arthritis Rheumatol. 2018 Sep 11. doi: 10.1002/art.40718.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Major finding: In patients who had a negative baseline MRI of the sacroiliac joints, the maximum likelihood of a follow-up MRI being positive was 7%.
Study details: A prospective study involving 188 patients (from the Spondyloarthritis Caught Early cohort) with early chronic back pain suspected of axial spondyloarthritis.
Disclosures: The researchers reported having no financial disclosures.
Source: Bakker PA et al. Arthritis Rheumatol. 2018 Sep 11. doi: 10.1002/art.40718.
Infliximab biosimilar only moderately less expensive in Medicare Part D
The infliximab-dyyb biosimilar was only moderately less expensive than the originator infliximab product Remicade in the United States in 2017 under Medicare Part D, an analysis shows.
Infliximab-dyyb (Inflectra) cost 18% less than infliximab, with an annual cost exceeding $14,000 in an analysis published online Sept. 4 in JAMA by Jinoos Yazdany, MD, of the division of rheumatology at the University of California, San Francisco, and her coauthors.
However, “without biosimilar gap discounts in 2017, beneficiaries would have paid more than $5,100 for infliximab-dyyb, or nearly $1,700 more in projected out-of-pocket costs than infliximab,” Dr. Yazdany and her coauthors wrote.
Biologics represent only 2% of U.S. prescriptions but made up 38% of drug spending in 2015 and accounted for 70% of growth in drug spending from 2010 to 2015, according to Dr. Yazdany and her colleagues.
Biologics for rheumatoid arthritis (RA) cost more than $14,000 per year, and in 2015, 3 were among the top 15 drugs in terms of Medicare expenditures, they added.
While biosimilars are supposed to increase competition and lower prices, it’s an open question whether they actually reduce out-of-pocket expenditures for the 43 million individuals with drug benefits under Medicare Part D.
That uncertainty is due in part to the complex cost-sharing design of Part D, which includes an initial deductible, a coverage phase, a coverage gap, and catastrophic coverage.
In 2017, the plan included an initial $400 deductible, followed by the coverage phase, in which the patient paid 25% of drug costs. In the coverage gap, which started at $3,700 in total drug costs, the patient’s share of drug costs increased to 40% for biologics, and 51% for biosimilars. In the catastrophic coverage phase, triggered when out-of-pocket costs exceeded $4,950, the patient was responsible for 5% of drug costs.
“Currently, beneficiaries receive a 50% manufacturer discount during the gap for brand-name drugs and biologics, but not for biosimilars,” Dr. Yazdany and her coauthors said in the report.
To evaluate cost-sharing for infliximab-dyyb, which in 2016 became the first available RA biosimilar, the authors analyzed data for all Part D plans in the June 2017 Medicare Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information Files.
Out of 2,547 plans, only 10% covered the biosimilar, while 96% covered infliximab, the authors found.
The mean total cost of infliximab-dyyb was “modestly lower,” they reported. Eight-week prescription costs were $2,185 for infliximab-dyyb versus $2,667 for infliximab, while annual costs were $14,202 for the biosimilar and $17,335 for infliximab.
However, all plans required coinsurance cost-sharing for the biosimilar, they said. The mean coinsurance rate was 26.6% of the total drug cost for the biosimilar and 28.4% for infliximab.
For beneficiaries, projected annual out-of-pocket costs without the gap discount were $5,118 for infliximab-dyyb and $3,432 for infliximab, the researchers said.
Biosimilar gap discounts are set to start in 2019, according to the authors. However, they said those discounts may not substantially reduce out-of-pocket costs for Part D beneficiaries because of the high price of infliximab-dyyb and a coinsurance cost-sharing rate similar to that of infliximab.
“Further policies are needed to address affordability and access to specialty drugs,” Dr. Yazdany and her coauthors concluded.
The study was funded in part by grants from the Agency for Healthcare Research and Quality, the Robert L. Kroc Endowed Chair in Rheumatic and Connective Tissue Diseases, and other sources. Dr. Yazdany reported receiving an independent investigator award from Pfizer. Her coauthors reported no conflict of interest disclosures.
The infliximab-dyyb biosimilar was only moderately less expensive than the originator infliximab product Remicade in the United States in 2017 under Medicare Part D, an analysis shows.
Infliximab-dyyb (Inflectra) cost 18% less than infliximab, with an annual cost exceeding $14,000 in an analysis published online Sept. 4 in JAMA by Jinoos Yazdany, MD, of the division of rheumatology at the University of California, San Francisco, and her coauthors.
However, “without biosimilar gap discounts in 2017, beneficiaries would have paid more than $5,100 for infliximab-dyyb, or nearly $1,700 more in projected out-of-pocket costs than infliximab,” Dr. Yazdany and her coauthors wrote.
Biologics represent only 2% of U.S. prescriptions but made up 38% of drug spending in 2015 and accounted for 70% of growth in drug spending from 2010 to 2015, according to Dr. Yazdany and her colleagues.
Biologics for rheumatoid arthritis (RA) cost more than $14,000 per year, and in 2015, 3 were among the top 15 drugs in terms of Medicare expenditures, they added.
While biosimilars are supposed to increase competition and lower prices, it’s an open question whether they actually reduce out-of-pocket expenditures for the 43 million individuals with drug benefits under Medicare Part D.
That uncertainty is due in part to the complex cost-sharing design of Part D, which includes an initial deductible, a coverage phase, a coverage gap, and catastrophic coverage.
In 2017, the plan included an initial $400 deductible, followed by the coverage phase, in which the patient paid 25% of drug costs. In the coverage gap, which started at $3,700 in total drug costs, the patient’s share of drug costs increased to 40% for biologics, and 51% for biosimilars. In the catastrophic coverage phase, triggered when out-of-pocket costs exceeded $4,950, the patient was responsible for 5% of drug costs.
“Currently, beneficiaries receive a 50% manufacturer discount during the gap for brand-name drugs and biologics, but not for biosimilars,” Dr. Yazdany and her coauthors said in the report.
To evaluate cost-sharing for infliximab-dyyb, which in 2016 became the first available RA biosimilar, the authors analyzed data for all Part D plans in the June 2017 Medicare Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information Files.
Out of 2,547 plans, only 10% covered the biosimilar, while 96% covered infliximab, the authors found.
The mean total cost of infliximab-dyyb was “modestly lower,” they reported. Eight-week prescription costs were $2,185 for infliximab-dyyb versus $2,667 for infliximab, while annual costs were $14,202 for the biosimilar and $17,335 for infliximab.
However, all plans required coinsurance cost-sharing for the biosimilar, they said. The mean coinsurance rate was 26.6% of the total drug cost for the biosimilar and 28.4% for infliximab.
For beneficiaries, projected annual out-of-pocket costs without the gap discount were $5,118 for infliximab-dyyb and $3,432 for infliximab, the researchers said.
Biosimilar gap discounts are set to start in 2019, according to the authors. However, they said those discounts may not substantially reduce out-of-pocket costs for Part D beneficiaries because of the high price of infliximab-dyyb and a coinsurance cost-sharing rate similar to that of infliximab.
“Further policies are needed to address affordability and access to specialty drugs,” Dr. Yazdany and her coauthors concluded.
The study was funded in part by grants from the Agency for Healthcare Research and Quality, the Robert L. Kroc Endowed Chair in Rheumatic and Connective Tissue Diseases, and other sources. Dr. Yazdany reported receiving an independent investigator award from Pfizer. Her coauthors reported no conflict of interest disclosures.
The infliximab-dyyb biosimilar was only moderately less expensive than the originator infliximab product Remicade in the United States in 2017 under Medicare Part D, an analysis shows.
Infliximab-dyyb (Inflectra) cost 18% less than infliximab, with an annual cost exceeding $14,000 in an analysis published online Sept. 4 in JAMA by Jinoos Yazdany, MD, of the division of rheumatology at the University of California, San Francisco, and her coauthors.
However, “without biosimilar gap discounts in 2017, beneficiaries would have paid more than $5,100 for infliximab-dyyb, or nearly $1,700 more in projected out-of-pocket costs than infliximab,” Dr. Yazdany and her coauthors wrote.
Biologics represent only 2% of U.S. prescriptions but made up 38% of drug spending in 2015 and accounted for 70% of growth in drug spending from 2010 to 2015, according to Dr. Yazdany and her colleagues.
Biologics for rheumatoid arthritis (RA) cost more than $14,000 per year, and in 2015, 3 were among the top 15 drugs in terms of Medicare expenditures, they added.
While biosimilars are supposed to increase competition and lower prices, it’s an open question whether they actually reduce out-of-pocket expenditures for the 43 million individuals with drug benefits under Medicare Part D.
That uncertainty is due in part to the complex cost-sharing design of Part D, which includes an initial deductible, a coverage phase, a coverage gap, and catastrophic coverage.
In 2017, the plan included an initial $400 deductible, followed by the coverage phase, in which the patient paid 25% of drug costs. In the coverage gap, which started at $3,700 in total drug costs, the patient’s share of drug costs increased to 40% for biologics, and 51% for biosimilars. In the catastrophic coverage phase, triggered when out-of-pocket costs exceeded $4,950, the patient was responsible for 5% of drug costs.
“Currently, beneficiaries receive a 50% manufacturer discount during the gap for brand-name drugs and biologics, but not for biosimilars,” Dr. Yazdany and her coauthors said in the report.
To evaluate cost-sharing for infliximab-dyyb, which in 2016 became the first available RA biosimilar, the authors analyzed data for all Part D plans in the June 2017 Medicare Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information Files.
Out of 2,547 plans, only 10% covered the biosimilar, while 96% covered infliximab, the authors found.
The mean total cost of infliximab-dyyb was “modestly lower,” they reported. Eight-week prescription costs were $2,185 for infliximab-dyyb versus $2,667 for infliximab, while annual costs were $14,202 for the biosimilar and $17,335 for infliximab.
However, all plans required coinsurance cost-sharing for the biosimilar, they said. The mean coinsurance rate was 26.6% of the total drug cost for the biosimilar and 28.4% for infliximab.
For beneficiaries, projected annual out-of-pocket costs without the gap discount were $5,118 for infliximab-dyyb and $3,432 for infliximab, the researchers said.
Biosimilar gap discounts are set to start in 2019, according to the authors. However, they said those discounts may not substantially reduce out-of-pocket costs for Part D beneficiaries because of the high price of infliximab-dyyb and a coinsurance cost-sharing rate similar to that of infliximab.
“Further policies are needed to address affordability and access to specialty drugs,” Dr. Yazdany and her coauthors concluded.
The study was funded in part by grants from the Agency for Healthcare Research and Quality, the Robert L. Kroc Endowed Chair in Rheumatic and Connective Tissue Diseases, and other sources. Dr. Yazdany reported receiving an independent investigator award from Pfizer. Her coauthors reported no conflict of interest disclosures.
FROM JAMA
Key clinical point:
Major finding: Infliximab-dyyb was 18% less costly than infliximab, with an annual cost exceeding $14,000.
Study details: Analysis of data for 2,547 Part D plans in the June 2017 Medicare Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information Files.
Disclosures: The study was funded in part by grants from the Agency for Healthcare Research and Quality, the Robert L. Kroc Endowed Chair in Rheumatic and Connective Tissue Diseases, and other sources. One author reported receiving an independent investigator award from Pfizer.
Source: Yazdany J et al. JAMA. 2018;320(9):931-3.
Diclofenac’s cardiovascular risk confirmed in novel Nordic study
Those beginning diclofenac had a 50% increased 30-day risk for a composite outcome of major adverse cardiovascular events (MACE) compared with individuals who didn’t initiate an NSAID or acetaminophen (95% confidence interval for incidence rate ratio, 1.4-1.7).
The risk was still significantly elevated when the study’s first author, Morten Schmidt, MD, and his colleagues compared diclofenac initiation with beginning other NSAIDs or acetaminophen. Compared with those starting ibuprofen or acetaminophen, the MACE risk was elevated 20% in diclofenac initiators (95% CI, 1.1-1.3 for both). Initiating diclofenac was associated with 30% greater risk for MACE compared with initiating naproxen (95% CI, 1.1-1.5).
“Diclofenac is the most frequently used NSAID in low-, middle-, and high-income countries and is available over the counter in most countries; therefore, its cardiovascular risk profile is of major clinical and public health importance,” wrote Dr. Schmidt and his coauthors.
In all, the study included 1,370,832 individuals who initiated diclofenac, 3,878,454 ibuprofen initiators, 291,490 naproxen initiators, and 764,781 acetaminophen initiators. Those starting diclofenac were compared with those starting other medications, and with 1,303,209 individuals who sought health care but did not start one of the medications.
The researchers used the longstanding and complete Danish health registry system to their advantage in designing a cohort trial that was modeled to resemble a clinical trial. For each month, beginning in 1996 and continuing through 2016, Dr. Schmidt and his collaborators assembled propensity-matched cohorts of individuals to compare each study group. The study design achieved many of the aims of a clinical trial while working within the ethical constraints of studying medications now known to elevate cardiovascular risk.
For each 30-day period, the investigators were then able to track and compare cardiovascular outcomes for each group. Each month, data for a new cohort were collected, beginning a new “clinical trial.” Individuals could be included in more than one month’s worth of “trial” data as long as they continued to meet inclusion criteria.
The completeness of Danish health data meant that the researchers were confident in data about comorbidities, other prescription medications, and outcomes.
Dr. Schmidt and his colleagues performed subgroup and sensitivity analyses to look at the extent to which preexisting risks for cardiovascular disease mediated MACE risk on diclofenac initiation. They found that diclofenac initiators in the highest risk group had up to 40 excess cardiovascular events per year – about half of them fatal – that were attributable to starting the medication. Although that group had the highest absolute risk, however, “the relative risks were highest in those with the lowest baseline risk,” wrote the investigators.
In addition to looking at rates of MACE, secondary outcomes for the study included evaluating the association between medication use or non-use and each individual component of the composite primary outcome. These included first-time occurrences of the nonfatal endpoints of atrial fibrillation or flutter, ischemic (but not hemorrhagic) stroke, heart failure, and myocardial infarction. Cardiac death was death from any cardiac cause.
“Supporting use of a combined endpoint, event rates consistently increased for all individual outcomes” for diclofenac initiators compared with those who did not start an NSAID, wrote Dr. Schmidt and his colleagues.
Individuals were excluded if they had known cardiovascular, kidney, liver, or ulcer disease, and if they had malignancy or serious mental health diagnoses such as dementia or schizophrenia. Participants, aged a mean 48-56 years, had to be at least 18 years of age and could not have filled a prescription for an NSAID within the previous 12 months. Men made up 36.6%-46.3% of the cohorts.
Dr. Schmidt, of Aarhus (Denmark) University, and his collaborators said that in comparison with other NSAIDs, the short half-life of diclofenac means that a supratherapeutic plasma concentration of diclofenac soon after initiation achieves not just cyclooxygenase-2 (COX-2), but also COX-1 inhibition. However, after those high levels fall, patients taking diclofenac spend a substantial period of time with unopposed COX-2 inhibition, a state that is known to be prothrombotic, and also associated with blood pressure elevation, atherogenesis, and worsening of heart failure.
Diclofenac and ibuprofen had similar gastrointestinal bleeding risks, and both medications were associated with a higher risk of bleeding than were ibuprofen, acetaminophen, or no medication.
“Comparing diclofenac initiation with no NSAID initiation, the consistency between our results and those of previous meta-analyses of both trial and observational data provides strong evidence to guide clinical decision making,” said Dr. Schmidt and his coauthors.
“Considering its cardiovascular and gastrointestinal risks, however, there is little justification to initiate diclofenac treatment before other traditional NSAIDs,” noted the investigators. “It is time to acknowledge the potential health risk of diclofenac and to reduce its use.”
The study was funded by the Department of Clinical Epidemiology Research Foundation, University of Aarhus, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
SOURCE: Schmidt M et al. BMJ 2018;362:k3426
Those beginning diclofenac had a 50% increased 30-day risk for a composite outcome of major adverse cardiovascular events (MACE) compared with individuals who didn’t initiate an NSAID or acetaminophen (95% confidence interval for incidence rate ratio, 1.4-1.7).
The risk was still significantly elevated when the study’s first author, Morten Schmidt, MD, and his colleagues compared diclofenac initiation with beginning other NSAIDs or acetaminophen. Compared with those starting ibuprofen or acetaminophen, the MACE risk was elevated 20% in diclofenac initiators (95% CI, 1.1-1.3 for both). Initiating diclofenac was associated with 30% greater risk for MACE compared with initiating naproxen (95% CI, 1.1-1.5).
“Diclofenac is the most frequently used NSAID in low-, middle-, and high-income countries and is available over the counter in most countries; therefore, its cardiovascular risk profile is of major clinical and public health importance,” wrote Dr. Schmidt and his coauthors.
In all, the study included 1,370,832 individuals who initiated diclofenac, 3,878,454 ibuprofen initiators, 291,490 naproxen initiators, and 764,781 acetaminophen initiators. Those starting diclofenac were compared with those starting other medications, and with 1,303,209 individuals who sought health care but did not start one of the medications.
The researchers used the longstanding and complete Danish health registry system to their advantage in designing a cohort trial that was modeled to resemble a clinical trial. For each month, beginning in 1996 and continuing through 2016, Dr. Schmidt and his collaborators assembled propensity-matched cohorts of individuals to compare each study group. The study design achieved many of the aims of a clinical trial while working within the ethical constraints of studying medications now known to elevate cardiovascular risk.
For each 30-day period, the investigators were then able to track and compare cardiovascular outcomes for each group. Each month, data for a new cohort were collected, beginning a new “clinical trial.” Individuals could be included in more than one month’s worth of “trial” data as long as they continued to meet inclusion criteria.
The completeness of Danish health data meant that the researchers were confident in data about comorbidities, other prescription medications, and outcomes.
Dr. Schmidt and his colleagues performed subgroup and sensitivity analyses to look at the extent to which preexisting risks for cardiovascular disease mediated MACE risk on diclofenac initiation. They found that diclofenac initiators in the highest risk group had up to 40 excess cardiovascular events per year – about half of them fatal – that were attributable to starting the medication. Although that group had the highest absolute risk, however, “the relative risks were highest in those with the lowest baseline risk,” wrote the investigators.
In addition to looking at rates of MACE, secondary outcomes for the study included evaluating the association between medication use or non-use and each individual component of the composite primary outcome. These included first-time occurrences of the nonfatal endpoints of atrial fibrillation or flutter, ischemic (but not hemorrhagic) stroke, heart failure, and myocardial infarction. Cardiac death was death from any cardiac cause.
“Supporting use of a combined endpoint, event rates consistently increased for all individual outcomes” for diclofenac initiators compared with those who did not start an NSAID, wrote Dr. Schmidt and his colleagues.
Individuals were excluded if they had known cardiovascular, kidney, liver, or ulcer disease, and if they had malignancy or serious mental health diagnoses such as dementia or schizophrenia. Participants, aged a mean 48-56 years, had to be at least 18 years of age and could not have filled a prescription for an NSAID within the previous 12 months. Men made up 36.6%-46.3% of the cohorts.
Dr. Schmidt, of Aarhus (Denmark) University, and his collaborators said that in comparison with other NSAIDs, the short half-life of diclofenac means that a supratherapeutic plasma concentration of diclofenac soon after initiation achieves not just cyclooxygenase-2 (COX-2), but also COX-1 inhibition. However, after those high levels fall, patients taking diclofenac spend a substantial period of time with unopposed COX-2 inhibition, a state that is known to be prothrombotic, and also associated with blood pressure elevation, atherogenesis, and worsening of heart failure.
Diclofenac and ibuprofen had similar gastrointestinal bleeding risks, and both medications were associated with a higher risk of bleeding than were ibuprofen, acetaminophen, or no medication.
“Comparing diclofenac initiation with no NSAID initiation, the consistency between our results and those of previous meta-analyses of both trial and observational data provides strong evidence to guide clinical decision making,” said Dr. Schmidt and his coauthors.
“Considering its cardiovascular and gastrointestinal risks, however, there is little justification to initiate diclofenac treatment before other traditional NSAIDs,” noted the investigators. “It is time to acknowledge the potential health risk of diclofenac and to reduce its use.”
The study was funded by the Department of Clinical Epidemiology Research Foundation, University of Aarhus, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
SOURCE: Schmidt M et al. BMJ 2018;362:k3426
Those beginning diclofenac had a 50% increased 30-day risk for a composite outcome of major adverse cardiovascular events (MACE) compared with individuals who didn’t initiate an NSAID or acetaminophen (95% confidence interval for incidence rate ratio, 1.4-1.7).
The risk was still significantly elevated when the study’s first author, Morten Schmidt, MD, and his colleagues compared diclofenac initiation with beginning other NSAIDs or acetaminophen. Compared with those starting ibuprofen or acetaminophen, the MACE risk was elevated 20% in diclofenac initiators (95% CI, 1.1-1.3 for both). Initiating diclofenac was associated with 30% greater risk for MACE compared with initiating naproxen (95% CI, 1.1-1.5).
“Diclofenac is the most frequently used NSAID in low-, middle-, and high-income countries and is available over the counter in most countries; therefore, its cardiovascular risk profile is of major clinical and public health importance,” wrote Dr. Schmidt and his coauthors.
In all, the study included 1,370,832 individuals who initiated diclofenac, 3,878,454 ibuprofen initiators, 291,490 naproxen initiators, and 764,781 acetaminophen initiators. Those starting diclofenac were compared with those starting other medications, and with 1,303,209 individuals who sought health care but did not start one of the medications.
The researchers used the longstanding and complete Danish health registry system to their advantage in designing a cohort trial that was modeled to resemble a clinical trial. For each month, beginning in 1996 and continuing through 2016, Dr. Schmidt and his collaborators assembled propensity-matched cohorts of individuals to compare each study group. The study design achieved many of the aims of a clinical trial while working within the ethical constraints of studying medications now known to elevate cardiovascular risk.
For each 30-day period, the investigators were then able to track and compare cardiovascular outcomes for each group. Each month, data for a new cohort were collected, beginning a new “clinical trial.” Individuals could be included in more than one month’s worth of “trial” data as long as they continued to meet inclusion criteria.
The completeness of Danish health data meant that the researchers were confident in data about comorbidities, other prescription medications, and outcomes.
Dr. Schmidt and his colleagues performed subgroup and sensitivity analyses to look at the extent to which preexisting risks for cardiovascular disease mediated MACE risk on diclofenac initiation. They found that diclofenac initiators in the highest risk group had up to 40 excess cardiovascular events per year – about half of them fatal – that were attributable to starting the medication. Although that group had the highest absolute risk, however, “the relative risks were highest in those with the lowest baseline risk,” wrote the investigators.
In addition to looking at rates of MACE, secondary outcomes for the study included evaluating the association between medication use or non-use and each individual component of the composite primary outcome. These included first-time occurrences of the nonfatal endpoints of atrial fibrillation or flutter, ischemic (but not hemorrhagic) stroke, heart failure, and myocardial infarction. Cardiac death was death from any cardiac cause.
“Supporting use of a combined endpoint, event rates consistently increased for all individual outcomes” for diclofenac initiators compared with those who did not start an NSAID, wrote Dr. Schmidt and his colleagues.
Individuals were excluded if they had known cardiovascular, kidney, liver, or ulcer disease, and if they had malignancy or serious mental health diagnoses such as dementia or schizophrenia. Participants, aged a mean 48-56 years, had to be at least 18 years of age and could not have filled a prescription for an NSAID within the previous 12 months. Men made up 36.6%-46.3% of the cohorts.
Dr. Schmidt, of Aarhus (Denmark) University, and his collaborators said that in comparison with other NSAIDs, the short half-life of diclofenac means that a supratherapeutic plasma concentration of diclofenac soon after initiation achieves not just cyclooxygenase-2 (COX-2), but also COX-1 inhibition. However, after those high levels fall, patients taking diclofenac spend a substantial period of time with unopposed COX-2 inhibition, a state that is known to be prothrombotic, and also associated with blood pressure elevation, atherogenesis, and worsening of heart failure.
Diclofenac and ibuprofen had similar gastrointestinal bleeding risks, and both medications were associated with a higher risk of bleeding than were ibuprofen, acetaminophen, or no medication.
“Comparing diclofenac initiation with no NSAID initiation, the consistency between our results and those of previous meta-analyses of both trial and observational data provides strong evidence to guide clinical decision making,” said Dr. Schmidt and his coauthors.
“Considering its cardiovascular and gastrointestinal risks, however, there is little justification to initiate diclofenac treatment before other traditional NSAIDs,” noted the investigators. “It is time to acknowledge the potential health risk of diclofenac and to reduce its use.”
The study was funded by the Department of Clinical Epidemiology Research Foundation, University of Aarhus, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
SOURCE: Schmidt M et al. BMJ 2018;362:k3426
FROM BMJ
Key clinical point: Those starting diclofenac had increased risk for cardiovascular events or cardiac death.
Major finding: Risk for major adverse cardiovascular events was increased by 50% compared with noninitiators.
Study details: Retrospective propensity-matched cohort study using national databases and registries.
Disclosures: The study was supported by the Department of Clinical Epidemiology Research Foundation of the University of Aarhus, Denmark, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
Source: Schmidt M et al. BMJ 2018;362:k3426.
AS inflammatory back pain criteria fall short in PsA
Established criteria for identifying inflammatory back pain in people with ankylosing spondylitis do not perform well in identifying axial involvement in people with psoriatic arthritis and neither does clinical judgment, a study shows.
There’s reason to believe that the natural history of patients with psoriatic arthritis (PsA) who have axial disease could differ from those without it, and there are differences in how well criteria that are currently used to identify inflammatory back pain (IBP) in people with ankylosing spondylitis (AS) perform in people with PsA, study first author Kristy S. Yap, MBBS, and her colleagues at the University of Toronto Psoriatic Arthritis Clinic wrote in Annals of the Rheumatic Diseases.
“Axial involvement in PsA is a marker of disease severity, and those with axial disease often have worse outcomes, compared with peripheral arthritis alone,” they wrote.
This is backed up by European League Against Rheumatism recommendations that advise clinicians to consider prescribing tumor necrosis factor inhibitors for people with PsA who have active axial involvement.
“Thus, an important question when evaluating a patient with PsA is to determine if axial PsA is present,” they wrote, noting that it was currently unclear whether the three sets of criteria that exist for defining inflammatory back pain in AS – Calin, Rudwaleit, and Assessment of Spondyloarthritis International Society (ASAS) – were useful for screening for axial involvement in people with PsA.
The researchers therefore set out to determine the agreement between rheumatologist judgment of the presence of IBP as well as the presence of IBP according to the three criteria in 171 patients with PsA (52% male, average age 46.6 years), 96 of whom reported chronic back pain, including 65 with IBP and 31 with nonspecific back pain.
Radiology data from these patients showed that 27 with baseline x-rays fulfilled the New York radiographic criteria for AS, and 45 had radiographic sacroiliitis not satisfying NY criteria (excluding grade 1) and/or syndesmophytes. Nine out of 31 patients with no axial disease on x-ray had evidence of axial disease on MRI. Eighteen out of 54 patients had axial involvement without back pain.
Results showed that agreement (kappa coefficient) between rheumatologist judgment of IBP and IBP criteria in patients with back pain was moderate and was highest for the Calin criteria (0.70; 95% confidence interval, 0.56-0.85), followed by the ASAS criteria (0.61; 95% CI, 0.46-0.76) and the Rudwaleit criteria (0.59; 95% CI, 0.44-0.74).
When x-ray or MRI change was considered “gold standard” for axial involvement for all patients, the specificity was high for rheumatologist judgment of IBP as well as Calin, Rudwaleit, and ASAS criteria, but their sensitivity was low, the researchers reported.
When the investigators compared positive likelihood ratios (LRs) for the presence of back pain, the Rudwaleit criteria (2.17) performed the best in ruling in axial disease, whereas the LRs were 1.75 for Calin and 1.86 for ASAS criteria. Rheumatologist-reported back pain (0.68) performed the best for ruling out axial disease when comparing negative LRs.
“The low positive LRs of the Calin, Rudwaleit, and ASAS criteria as well as that of rheumatologist report of back pain or judgment of IBP for [axial] PsA defined as any axial radiological change found in our study suggests that none of these criteria performed well in detecting axial disease in patients with PsA,” the study authors wrote.
The authors also conducted an exploratory analysis within patients with PsA with back involvement (defined by x-rays or MRI) and compared those with back pain (n = 36) or without (n = 18). The back pain group had a significantly higher Bath Ankylosing Spondylitis Disease Activity Index score (5.72 vs. 4.27), a finding that the authors said they expected because it is a patient-reported measure.
The back pain group also had a lower prevalence of human leukocyte antigen-B*38 (2.78 vs. 27.78), a finding that the authors said was interesting but would need to be replicated in future studies.
The prevalence of HLA-B*27, HLA-B*08, and HLA-C*06 was similar between patients with and without back pain, indicating “that the two groups are largely similar and hence, for the purpose of defining axial disease in PsA, symptoms (back pain) may not be important.”
“The findings of this study suggest that rheumatologist-judged IBP or the criteria for IBP developed for AS may not perform well when ascertaining axial involvement in PsA,” the study authors concluded.
“Moreover, patients with axial radiological changes without back pain were similar to those with back pain. ... In order to stratify patients with poorer prognosis, rheumatologists should consider conducting axial imaging in all patients with PsA regardless of the presence or the nature of back pain,” they added.
The study was funded by the University of Toronto Psoriatic Arthritis Program, which is supported by the Krembil Foundation.
SOURCE: Yap KS et al. Ann Rheum Dis. 2018 Aug 4. doi: 10.1136/annrheumdis-2018-213334.
Identifying psoriatic arthritis with axial disease (AxPsA) is important because it changes the treatment selection and also may be associated with a more severe disease course. In a recent paper by Yap et al, the investigators underscore the challenges in identifying the prevalence of axial disease in PsA. Many of our patients with PsA report back pain at some point in their disease course, and as the rheumatologist, we must grapple with whether their symptoms represent inflammatory disease that requires a change in therapy.
In this study, the authors examined the correlation of three definitions of inflammatory back pain (IBP) with both the rheumatologist’s assessment of whether the patient has IBP and with the presence of imaging findings such as x-ray or MRI abnormalities in the sacroiliac joints or lumbar spine. Of the 171 patients studied, 38% were reported to have IBP per the rheumatologist, 18% were thought to have noninflammatory back pain, and 32% had imaging findings consistent with AxSpA. The agreement between the rheumatologist and the inflammatory back pain criteria was reasonable (kappa 0.6-0.7). Rheumatologists and IBP criteria had moderate sensitivity (0.73-0.82) for having x-ray or MRI changes consistent with axial disease but low specificity (0.33-0.46). Surprisingly, HLA markers were not good markers of having axial disease in this population, aside from HLA-B38, which was protective but relatively uncommon.
The bottom line is that using IBP criteria or our general gestalt is still not as good as getting appropriate imaging and further underscores the potential need to screen patients with PsA, particularly those reporting back pain, for axial involvement.
Alexis R. Ogdie, MD, is director of the Penn Psoriatic Arthritis Clinic at the University of Pennsylvania, Philadelphia, and is a member of the steering committee for the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Identifying psoriatic arthritis with axial disease (AxPsA) is important because it changes the treatment selection and also may be associated with a more severe disease course. In a recent paper by Yap et al, the investigators underscore the challenges in identifying the prevalence of axial disease in PsA. Many of our patients with PsA report back pain at some point in their disease course, and as the rheumatologist, we must grapple with whether their symptoms represent inflammatory disease that requires a change in therapy.
In this study, the authors examined the correlation of three definitions of inflammatory back pain (IBP) with both the rheumatologist’s assessment of whether the patient has IBP and with the presence of imaging findings such as x-ray or MRI abnormalities in the sacroiliac joints or lumbar spine. Of the 171 patients studied, 38% were reported to have IBP per the rheumatologist, 18% were thought to have noninflammatory back pain, and 32% had imaging findings consistent with AxSpA. The agreement between the rheumatologist and the inflammatory back pain criteria was reasonable (kappa 0.6-0.7). Rheumatologists and IBP criteria had moderate sensitivity (0.73-0.82) for having x-ray or MRI changes consistent with axial disease but low specificity (0.33-0.46). Surprisingly, HLA markers were not good markers of having axial disease in this population, aside from HLA-B38, which was protective but relatively uncommon.
The bottom line is that using IBP criteria or our general gestalt is still not as good as getting appropriate imaging and further underscores the potential need to screen patients with PsA, particularly those reporting back pain, for axial involvement.
Alexis R. Ogdie, MD, is director of the Penn Psoriatic Arthritis Clinic at the University of Pennsylvania, Philadelphia, and is a member of the steering committee for the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Identifying psoriatic arthritis with axial disease (AxPsA) is important because it changes the treatment selection and also may be associated with a more severe disease course. In a recent paper by Yap et al, the investigators underscore the challenges in identifying the prevalence of axial disease in PsA. Many of our patients with PsA report back pain at some point in their disease course, and as the rheumatologist, we must grapple with whether their symptoms represent inflammatory disease that requires a change in therapy.
In this study, the authors examined the correlation of three definitions of inflammatory back pain (IBP) with both the rheumatologist’s assessment of whether the patient has IBP and with the presence of imaging findings such as x-ray or MRI abnormalities in the sacroiliac joints or lumbar spine. Of the 171 patients studied, 38% were reported to have IBP per the rheumatologist, 18% were thought to have noninflammatory back pain, and 32% had imaging findings consistent with AxSpA. The agreement between the rheumatologist and the inflammatory back pain criteria was reasonable (kappa 0.6-0.7). Rheumatologists and IBP criteria had moderate sensitivity (0.73-0.82) for having x-ray or MRI changes consistent with axial disease but low specificity (0.33-0.46). Surprisingly, HLA markers were not good markers of having axial disease in this population, aside from HLA-B38, which was protective but relatively uncommon.
The bottom line is that using IBP criteria or our general gestalt is still not as good as getting appropriate imaging and further underscores the potential need to screen patients with PsA, particularly those reporting back pain, for axial involvement.
Alexis R. Ogdie, MD, is director of the Penn Psoriatic Arthritis Clinic at the University of Pennsylvania, Philadelphia, and is a member of the steering committee for the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Established criteria for identifying inflammatory back pain in people with ankylosing spondylitis do not perform well in identifying axial involvement in people with psoriatic arthritis and neither does clinical judgment, a study shows.
There’s reason to believe that the natural history of patients with psoriatic arthritis (PsA) who have axial disease could differ from those without it, and there are differences in how well criteria that are currently used to identify inflammatory back pain (IBP) in people with ankylosing spondylitis (AS) perform in people with PsA, study first author Kristy S. Yap, MBBS, and her colleagues at the University of Toronto Psoriatic Arthritis Clinic wrote in Annals of the Rheumatic Diseases.
“Axial involvement in PsA is a marker of disease severity, and those with axial disease often have worse outcomes, compared with peripheral arthritis alone,” they wrote.
This is backed up by European League Against Rheumatism recommendations that advise clinicians to consider prescribing tumor necrosis factor inhibitors for people with PsA who have active axial involvement.
“Thus, an important question when evaluating a patient with PsA is to determine if axial PsA is present,” they wrote, noting that it was currently unclear whether the three sets of criteria that exist for defining inflammatory back pain in AS – Calin, Rudwaleit, and Assessment of Spondyloarthritis International Society (ASAS) – were useful for screening for axial involvement in people with PsA.
The researchers therefore set out to determine the agreement between rheumatologist judgment of the presence of IBP as well as the presence of IBP according to the three criteria in 171 patients with PsA (52% male, average age 46.6 years), 96 of whom reported chronic back pain, including 65 with IBP and 31 with nonspecific back pain.
Radiology data from these patients showed that 27 with baseline x-rays fulfilled the New York radiographic criteria for AS, and 45 had radiographic sacroiliitis not satisfying NY criteria (excluding grade 1) and/or syndesmophytes. Nine out of 31 patients with no axial disease on x-ray had evidence of axial disease on MRI. Eighteen out of 54 patients had axial involvement without back pain.
Results showed that agreement (kappa coefficient) between rheumatologist judgment of IBP and IBP criteria in patients with back pain was moderate and was highest for the Calin criteria (0.70; 95% confidence interval, 0.56-0.85), followed by the ASAS criteria (0.61; 95% CI, 0.46-0.76) and the Rudwaleit criteria (0.59; 95% CI, 0.44-0.74).
When x-ray or MRI change was considered “gold standard” for axial involvement for all patients, the specificity was high for rheumatologist judgment of IBP as well as Calin, Rudwaleit, and ASAS criteria, but their sensitivity was low, the researchers reported.
When the investigators compared positive likelihood ratios (LRs) for the presence of back pain, the Rudwaleit criteria (2.17) performed the best in ruling in axial disease, whereas the LRs were 1.75 for Calin and 1.86 for ASAS criteria. Rheumatologist-reported back pain (0.68) performed the best for ruling out axial disease when comparing negative LRs.
“The low positive LRs of the Calin, Rudwaleit, and ASAS criteria as well as that of rheumatologist report of back pain or judgment of IBP for [axial] PsA defined as any axial radiological change found in our study suggests that none of these criteria performed well in detecting axial disease in patients with PsA,” the study authors wrote.
The authors also conducted an exploratory analysis within patients with PsA with back involvement (defined by x-rays or MRI) and compared those with back pain (n = 36) or without (n = 18). The back pain group had a significantly higher Bath Ankylosing Spondylitis Disease Activity Index score (5.72 vs. 4.27), a finding that the authors said they expected because it is a patient-reported measure.
The back pain group also had a lower prevalence of human leukocyte antigen-B*38 (2.78 vs. 27.78), a finding that the authors said was interesting but would need to be replicated in future studies.
The prevalence of HLA-B*27, HLA-B*08, and HLA-C*06 was similar between patients with and without back pain, indicating “that the two groups are largely similar and hence, for the purpose of defining axial disease in PsA, symptoms (back pain) may not be important.”
“The findings of this study suggest that rheumatologist-judged IBP or the criteria for IBP developed for AS may not perform well when ascertaining axial involvement in PsA,” the study authors concluded.
“Moreover, patients with axial radiological changes without back pain were similar to those with back pain. ... In order to stratify patients with poorer prognosis, rheumatologists should consider conducting axial imaging in all patients with PsA regardless of the presence or the nature of back pain,” they added.
The study was funded by the University of Toronto Psoriatic Arthritis Program, which is supported by the Krembil Foundation.
SOURCE: Yap KS et al. Ann Rheum Dis. 2018 Aug 4. doi: 10.1136/annrheumdis-2018-213334.
Established criteria for identifying inflammatory back pain in people with ankylosing spondylitis do not perform well in identifying axial involvement in people with psoriatic arthritis and neither does clinical judgment, a study shows.
There’s reason to believe that the natural history of patients with psoriatic arthritis (PsA) who have axial disease could differ from those without it, and there are differences in how well criteria that are currently used to identify inflammatory back pain (IBP) in people with ankylosing spondylitis (AS) perform in people with PsA, study first author Kristy S. Yap, MBBS, and her colleagues at the University of Toronto Psoriatic Arthritis Clinic wrote in Annals of the Rheumatic Diseases.
“Axial involvement in PsA is a marker of disease severity, and those with axial disease often have worse outcomes, compared with peripheral arthritis alone,” they wrote.
This is backed up by European League Against Rheumatism recommendations that advise clinicians to consider prescribing tumor necrosis factor inhibitors for people with PsA who have active axial involvement.
“Thus, an important question when evaluating a patient with PsA is to determine if axial PsA is present,” they wrote, noting that it was currently unclear whether the three sets of criteria that exist for defining inflammatory back pain in AS – Calin, Rudwaleit, and Assessment of Spondyloarthritis International Society (ASAS) – were useful for screening for axial involvement in people with PsA.
The researchers therefore set out to determine the agreement between rheumatologist judgment of the presence of IBP as well as the presence of IBP according to the three criteria in 171 patients with PsA (52% male, average age 46.6 years), 96 of whom reported chronic back pain, including 65 with IBP and 31 with nonspecific back pain.
Radiology data from these patients showed that 27 with baseline x-rays fulfilled the New York radiographic criteria for AS, and 45 had radiographic sacroiliitis not satisfying NY criteria (excluding grade 1) and/or syndesmophytes. Nine out of 31 patients with no axial disease on x-ray had evidence of axial disease on MRI. Eighteen out of 54 patients had axial involvement without back pain.
Results showed that agreement (kappa coefficient) between rheumatologist judgment of IBP and IBP criteria in patients with back pain was moderate and was highest for the Calin criteria (0.70; 95% confidence interval, 0.56-0.85), followed by the ASAS criteria (0.61; 95% CI, 0.46-0.76) and the Rudwaleit criteria (0.59; 95% CI, 0.44-0.74).
When x-ray or MRI change was considered “gold standard” for axial involvement for all patients, the specificity was high for rheumatologist judgment of IBP as well as Calin, Rudwaleit, and ASAS criteria, but their sensitivity was low, the researchers reported.
When the investigators compared positive likelihood ratios (LRs) for the presence of back pain, the Rudwaleit criteria (2.17) performed the best in ruling in axial disease, whereas the LRs were 1.75 for Calin and 1.86 for ASAS criteria. Rheumatologist-reported back pain (0.68) performed the best for ruling out axial disease when comparing negative LRs.
“The low positive LRs of the Calin, Rudwaleit, and ASAS criteria as well as that of rheumatologist report of back pain or judgment of IBP for [axial] PsA defined as any axial radiological change found in our study suggests that none of these criteria performed well in detecting axial disease in patients with PsA,” the study authors wrote.
The authors also conducted an exploratory analysis within patients with PsA with back involvement (defined by x-rays or MRI) and compared those with back pain (n = 36) or without (n = 18). The back pain group had a significantly higher Bath Ankylosing Spondylitis Disease Activity Index score (5.72 vs. 4.27), a finding that the authors said they expected because it is a patient-reported measure.
The back pain group also had a lower prevalence of human leukocyte antigen-B*38 (2.78 vs. 27.78), a finding that the authors said was interesting but would need to be replicated in future studies.
The prevalence of HLA-B*27, HLA-B*08, and HLA-C*06 was similar between patients with and without back pain, indicating “that the two groups are largely similar and hence, for the purpose of defining axial disease in PsA, symptoms (back pain) may not be important.”
“The findings of this study suggest that rheumatologist-judged IBP or the criteria for IBP developed for AS may not perform well when ascertaining axial involvement in PsA,” the study authors concluded.
“Moreover, patients with axial radiological changes without back pain were similar to those with back pain. ... In order to stratify patients with poorer prognosis, rheumatologists should consider conducting axial imaging in all patients with PsA regardless of the presence or the nature of back pain,” they added.
The study was funded by the University of Toronto Psoriatic Arthritis Program, which is supported by the Krembil Foundation.
SOURCE: Yap KS et al. Ann Rheum Dis. 2018 Aug 4. doi: 10.1136/annrheumdis-2018-213334.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point:
Major finding: Agreement as measured by kappa coefficient between rheumatologist judgment of inflammatory back pain and IBP criteria in patients with back pain was moderate and was highest for the Calin criteria (0.70; 95% confidence interval, 0.56-0.85), followed by the ASAS criteria (0.61; 95% CI, 0.46-0.76) and the Rudwaleit criteria (0.59; 95% CI, 0.44-0.74).
Study details: Prospectively collected data from 171 patients attending a PsA clinic
Disclosures: The study was funded by the University of Toronto Psoriatic Arthritis Program, which is supported by the Krembil Foundation.
Source: Yap KS et al. Ann Rheum Dis. 2018 Aug 4. doi: 10.1136/annrheumdis-2018-213334.
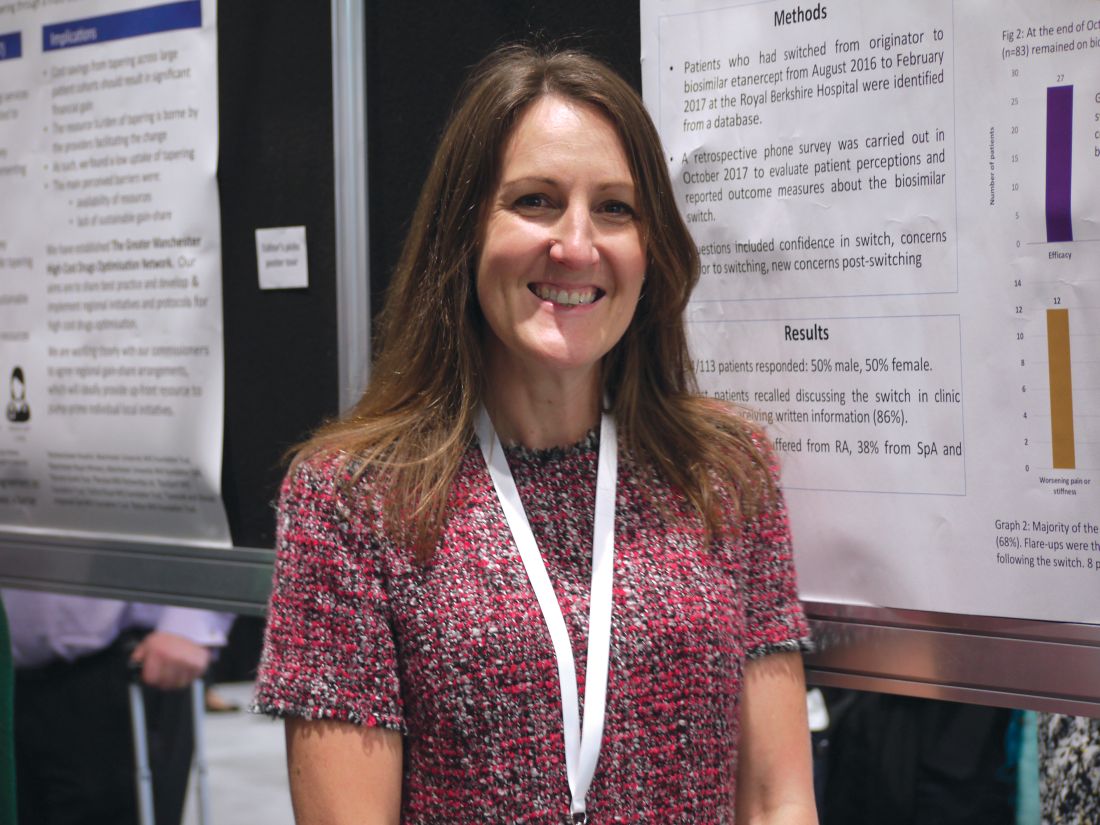
Biosimilar switch accepted by most rheumatic disease patients
LIVERPOOL, ENGLAND – , although the biosimilar they are being switched to may be important, according to data from three separate poster presentations at the British Society for Rheumatology annual conference.
Of 35 patients who expressed concerns about the switch, most (n = 27) were concerned about the efficacy of the biosimilar, with others were mainly concerned about safety (n = 5), side effects (n = 3), or other factors (n = 5).
“This is the population of patients we were worried about, because we had got them on a drug that had finally worked for them,” poster presenter Joanne Kitchen, MBChB, said in an interview.
“It’s hard enough to get on the biologic, and we were concerned about whether they would lose response. ... There wasn’t a lot of evidence about if they didn’t respond and we switched back, would it still work for them,” explained Dr. Kitchen, a consultant rheumatologist who works at the Royal Berkshire Hospital in Reading, England.
Biosimilar etanercept became available in the United Kingdom in April 2016, and many rheumatology centers had to make the switch to its use at the behest of their health trusts in a cost-saving effort. The switch at the Royal Berkshire occurred in August 2016, and Dr. Kitchen explained that prior to the switch, letters were sent out to inform patients, who were then seen in the clinic. There also was an understanding between the medical team and the patients that, if things did not work out, patients could switch back to the originator etanercept.
Between August 2016 and February 2017, 113 patients had switched to biosimilar etanercept for their rheumatoid arthritis (RA), spondyloarthritis, or psoriatic arthritis.
Although worsening joint pain or stiffness (n = 12) or increased fatigue (n = 4) were reported by some patients, the fact that 88% of those who responded to the survey in October 2017 were still taking the drug 6-12 months after initiation suggests that these side effects were minor or manageable. Adherence to medication was not checked, however, which might have been a factor in any flare ups.
Medication changes occurred for four patients who switched back to originator etanercept, three to an alternative biologic, and four who discontinued biologics.
Other adverse effects reported by patients were more painful injections (n = 5), infections (n = 2), and others incidents such as individual cases of rash and headache in the remainder.
“We know our biologic costs are incrementally increasing, but it’s still very hard for some patients to get onto these drugs,” Dr. Kitchen said. She hopes that with the cost-savings being made from the switch, it could help with negotiations to lower the threshold at which patients become eligible for biologic/biosimilar use, thus enabling more patients in need to be treated.
“I think these data have given confidence that patients can switch onto a biosimilar, and that the real-world experience matches what we’re seeing in trials,” Dr. Kitchen said. “We haven’t had a negative experience, and that’s what patients and we were worried about.”
In a separate poster presentation, Kavina Shah, MBBS, and her associates from Northwick Park Hospital, London, reported their experience of switching 115 patients with RA from etanercept to the biosimilar Benepali between January and June 2017.
They conducted a prospective study in which patients were offered an education session and then attended a clinic appointment set up to manage the switch. Patients were assessed by various objective and subjective means before and 4 months after the switch.
Dr. Shah and her associates found that 43% of patients were pleased with the switch. Part of the reason patients might have been happy with the switch was the easier mode of administration, they observed: “Patients commented on the easier technique and less manual dexterity required.”
However, almost a quarter (23%) of patients were not happy with the switch, with others being indifferent (7%) or unsure (8%).
Patients were also asked how they felt their RA was after the switch, and 75% responded that it was no different, 11% said it had improved, and 17% said it was worse.
The mean Disease Activity Score in 28 joints (DAS28) values were significantly lower in patients after the switch than before (2.66 vs. 2.97; P = .0019). “This could be explained by the lower levels of immunogenicity with Benepali,” Dr. Shah and her coauthors wrote on their poster. Alternatively, it could be an artifact introduced by lower rates of anxiety at follow-up, they said.
There were also statistically nonsignificant improvements in health assessment questionnaire (HAQ) and European Quality of Life-5 Dimensions (EQ-5D) scores.
Taken together, these findings are “reassuring,” Dr. Shah and her associates noted, and “should positively encourage clinicians and patients to switch to biosimilars in order to optimize the cost saving to the NHS.”
Not all biosimilar switches may go as smoothly as switching from TNF inhibitors, as Muhammad K. Nisar, MBBS, reported in another poster presentation at the conference. Dr. Nisar, a consultant rheumatologist for Luton (England) and Dunstable Hospital University Trust, reported his center’s experience of switching patients on rituximab (Rituxan) to biosimilar rituximab (Truxima).
Of 44 patients who were established on rituximab, 39 were eligible to make the switch. Four patients had stopped taking rituximab before the switch took place and one patient remained on the originator. As of October 2017, 24 (61.5%) of patients had actually made the switch.
“All were happy to switch after receiving a letter and having the opportunity to contact if necessary,” Dr. Nisar reported. “At group level there were no major differences in disease outcomes and 80% reported no issues.”
However, five (20%) patients developed a severe serum sickness reaction early on with loss of efficacy. This happened in the first week after the second dose of the biosimilar was given, Dr. Nisar explained. No obvious reason could be found, but two patients required emergency hospital treatment within 24 hours.
“Our experience of switching rituximab patients is certainly not as smooth as it was for infliximab or and etanercept,” Dr. Nisar said. While he said “they support routine switching from originator to biosimilar,” he noted that “close monitoring is required, certainly in the first week of dose administration.”
All authors had nothing to disclose.
SOURCES: Hoque T et al. Rheumatology. 2018 Apr 25;57(Suppl. 3):key075.296. Shah K et al. Rheumatology. 2018 Apr 25;57(Suppl. 3):key075.456. Nisar MK. Rheumatology. 2018 Apr 1;57(Suppl. 3):key075.516.
LIVERPOOL, ENGLAND – , although the biosimilar they are being switched to may be important, according to data from three separate poster presentations at the British Society for Rheumatology annual conference.
Of 35 patients who expressed concerns about the switch, most (n = 27) were concerned about the efficacy of the biosimilar, with others were mainly concerned about safety (n = 5), side effects (n = 3), or other factors (n = 5).
“This is the population of patients we were worried about, because we had got them on a drug that had finally worked for them,” poster presenter Joanne Kitchen, MBChB, said in an interview.
“It’s hard enough to get on the biologic, and we were concerned about whether they would lose response. ... There wasn’t a lot of evidence about if they didn’t respond and we switched back, would it still work for them,” explained Dr. Kitchen, a consultant rheumatologist who works at the Royal Berkshire Hospital in Reading, England.
Biosimilar etanercept became available in the United Kingdom in April 2016, and many rheumatology centers had to make the switch to its use at the behest of their health trusts in a cost-saving effort. The switch at the Royal Berkshire occurred in August 2016, and Dr. Kitchen explained that prior to the switch, letters were sent out to inform patients, who were then seen in the clinic. There also was an understanding between the medical team and the patients that, if things did not work out, patients could switch back to the originator etanercept.
Between August 2016 and February 2017, 113 patients had switched to biosimilar etanercept for their rheumatoid arthritis (RA), spondyloarthritis, or psoriatic arthritis.
Although worsening joint pain or stiffness (n = 12) or increased fatigue (n = 4) were reported by some patients, the fact that 88% of those who responded to the survey in October 2017 were still taking the drug 6-12 months after initiation suggests that these side effects were minor or manageable. Adherence to medication was not checked, however, which might have been a factor in any flare ups.
Medication changes occurred for four patients who switched back to originator etanercept, three to an alternative biologic, and four who discontinued biologics.
Other adverse effects reported by patients were more painful injections (n = 5), infections (n = 2), and others incidents such as individual cases of rash and headache in the remainder.
“We know our biologic costs are incrementally increasing, but it’s still very hard for some patients to get onto these drugs,” Dr. Kitchen said. She hopes that with the cost-savings being made from the switch, it could help with negotiations to lower the threshold at which patients become eligible for biologic/biosimilar use, thus enabling more patients in need to be treated.
“I think these data have given confidence that patients can switch onto a biosimilar, and that the real-world experience matches what we’re seeing in trials,” Dr. Kitchen said. “We haven’t had a negative experience, and that’s what patients and we were worried about.”
In a separate poster presentation, Kavina Shah, MBBS, and her associates from Northwick Park Hospital, London, reported their experience of switching 115 patients with RA from etanercept to the biosimilar Benepali between January and June 2017.
They conducted a prospective study in which patients were offered an education session and then attended a clinic appointment set up to manage the switch. Patients were assessed by various objective and subjective means before and 4 months after the switch.
Dr. Shah and her associates found that 43% of patients were pleased with the switch. Part of the reason patients might have been happy with the switch was the easier mode of administration, they observed: “Patients commented on the easier technique and less manual dexterity required.”
However, almost a quarter (23%) of patients were not happy with the switch, with others being indifferent (7%) or unsure (8%).
Patients were also asked how they felt their RA was after the switch, and 75% responded that it was no different, 11% said it had improved, and 17% said it was worse.
The mean Disease Activity Score in 28 joints (DAS28) values were significantly lower in patients after the switch than before (2.66 vs. 2.97; P = .0019). “This could be explained by the lower levels of immunogenicity with Benepali,” Dr. Shah and her coauthors wrote on their poster. Alternatively, it could be an artifact introduced by lower rates of anxiety at follow-up, they said.
There were also statistically nonsignificant improvements in health assessment questionnaire (HAQ) and European Quality of Life-5 Dimensions (EQ-5D) scores.
Taken together, these findings are “reassuring,” Dr. Shah and her associates noted, and “should positively encourage clinicians and patients to switch to biosimilars in order to optimize the cost saving to the NHS.”
Not all biosimilar switches may go as smoothly as switching from TNF inhibitors, as Muhammad K. Nisar, MBBS, reported in another poster presentation at the conference. Dr. Nisar, a consultant rheumatologist for Luton (England) and Dunstable Hospital University Trust, reported his center’s experience of switching patients on rituximab (Rituxan) to biosimilar rituximab (Truxima).
Of 44 patients who were established on rituximab, 39 were eligible to make the switch. Four patients had stopped taking rituximab before the switch took place and one patient remained on the originator. As of October 2017, 24 (61.5%) of patients had actually made the switch.
“All were happy to switch after receiving a letter and having the opportunity to contact if necessary,” Dr. Nisar reported. “At group level there were no major differences in disease outcomes and 80% reported no issues.”
However, five (20%) patients developed a severe serum sickness reaction early on with loss of efficacy. This happened in the first week after the second dose of the biosimilar was given, Dr. Nisar explained. No obvious reason could be found, but two patients required emergency hospital treatment within 24 hours.
“Our experience of switching rituximab patients is certainly not as smooth as it was for infliximab or and etanercept,” Dr. Nisar said. While he said “they support routine switching from originator to biosimilar,” he noted that “close monitoring is required, certainly in the first week of dose administration.”
All authors had nothing to disclose.
SOURCES: Hoque T et al. Rheumatology. 2018 Apr 25;57(Suppl. 3):key075.296. Shah K et al. Rheumatology. 2018 Apr 25;57(Suppl. 3):key075.456. Nisar MK. Rheumatology. 2018 Apr 1;57(Suppl. 3):key075.516.
LIVERPOOL, ENGLAND – , although the biosimilar they are being switched to may be important, according to data from three separate poster presentations at the British Society for Rheumatology annual conference.
Of 35 patients who expressed concerns about the switch, most (n = 27) were concerned about the efficacy of the biosimilar, with others were mainly concerned about safety (n = 5), side effects (n = 3), or other factors (n = 5).
“This is the population of patients we were worried about, because we had got them on a drug that had finally worked for them,” poster presenter Joanne Kitchen, MBChB, said in an interview.
“It’s hard enough to get on the biologic, and we were concerned about whether they would lose response. ... There wasn’t a lot of evidence about if they didn’t respond and we switched back, would it still work for them,” explained Dr. Kitchen, a consultant rheumatologist who works at the Royal Berkshire Hospital in Reading, England.
Biosimilar etanercept became available in the United Kingdom in April 2016, and many rheumatology centers had to make the switch to its use at the behest of their health trusts in a cost-saving effort. The switch at the Royal Berkshire occurred in August 2016, and Dr. Kitchen explained that prior to the switch, letters were sent out to inform patients, who were then seen in the clinic. There also was an understanding between the medical team and the patients that, if things did not work out, patients could switch back to the originator etanercept.
Between August 2016 and February 2017, 113 patients had switched to biosimilar etanercept for their rheumatoid arthritis (RA), spondyloarthritis, or psoriatic arthritis.
Although worsening joint pain or stiffness (n = 12) or increased fatigue (n = 4) were reported by some patients, the fact that 88% of those who responded to the survey in October 2017 were still taking the drug 6-12 months after initiation suggests that these side effects were minor or manageable. Adherence to medication was not checked, however, which might have been a factor in any flare ups.
Medication changes occurred for four patients who switched back to originator etanercept, three to an alternative biologic, and four who discontinued biologics.
Other adverse effects reported by patients were more painful injections (n = 5), infections (n = 2), and others incidents such as individual cases of rash and headache in the remainder.
“We know our biologic costs are incrementally increasing, but it’s still very hard for some patients to get onto these drugs,” Dr. Kitchen said. She hopes that with the cost-savings being made from the switch, it could help with negotiations to lower the threshold at which patients become eligible for biologic/biosimilar use, thus enabling more patients in need to be treated.
“I think these data have given confidence that patients can switch onto a biosimilar, and that the real-world experience matches what we’re seeing in trials,” Dr. Kitchen said. “We haven’t had a negative experience, and that’s what patients and we were worried about.”
In a separate poster presentation, Kavina Shah, MBBS, and her associates from Northwick Park Hospital, London, reported their experience of switching 115 patients with RA from etanercept to the biosimilar Benepali between January and June 2017.
They conducted a prospective study in which patients were offered an education session and then attended a clinic appointment set up to manage the switch. Patients were assessed by various objective and subjective means before and 4 months after the switch.
Dr. Shah and her associates found that 43% of patients were pleased with the switch. Part of the reason patients might have been happy with the switch was the easier mode of administration, they observed: “Patients commented on the easier technique and less manual dexterity required.”
However, almost a quarter (23%) of patients were not happy with the switch, with others being indifferent (7%) or unsure (8%).
Patients were also asked how they felt their RA was after the switch, and 75% responded that it was no different, 11% said it had improved, and 17% said it was worse.
The mean Disease Activity Score in 28 joints (DAS28) values were significantly lower in patients after the switch than before (2.66 vs. 2.97; P = .0019). “This could be explained by the lower levels of immunogenicity with Benepali,” Dr. Shah and her coauthors wrote on their poster. Alternatively, it could be an artifact introduced by lower rates of anxiety at follow-up, they said.
There were also statistically nonsignificant improvements in health assessment questionnaire (HAQ) and European Quality of Life-5 Dimensions (EQ-5D) scores.
Taken together, these findings are “reassuring,” Dr. Shah and her associates noted, and “should positively encourage clinicians and patients to switch to biosimilars in order to optimize the cost saving to the NHS.”
Not all biosimilar switches may go as smoothly as switching from TNF inhibitors, as Muhammad K. Nisar, MBBS, reported in another poster presentation at the conference. Dr. Nisar, a consultant rheumatologist for Luton (England) and Dunstable Hospital University Trust, reported his center’s experience of switching patients on rituximab (Rituxan) to biosimilar rituximab (Truxima).
Of 44 patients who were established on rituximab, 39 were eligible to make the switch. Four patients had stopped taking rituximab before the switch took place and one patient remained on the originator. As of October 2017, 24 (61.5%) of patients had actually made the switch.
“All were happy to switch after receiving a letter and having the opportunity to contact if necessary,” Dr. Nisar reported. “At group level there were no major differences in disease outcomes and 80% reported no issues.”
However, five (20%) patients developed a severe serum sickness reaction early on with loss of efficacy. This happened in the first week after the second dose of the biosimilar was given, Dr. Nisar explained. No obvious reason could be found, but two patients required emergency hospital treatment within 24 hours.
“Our experience of switching rituximab patients is certainly not as smooth as it was for infliximab or and etanercept,” Dr. Nisar said. While he said “they support routine switching from originator to biosimilar,” he noted that “close monitoring is required, certainly in the first week of dose administration.”
All authors had nothing to disclose.
SOURCES: Hoque T et al. Rheumatology. 2018 Apr 25;57(Suppl. 3):key075.296. Shah K et al. Rheumatology. 2018 Apr 25;57(Suppl. 3):key075.456. Nisar MK. Rheumatology. 2018 Apr 1;57(Suppl. 3):key075.516.
REPORTING FROM BSR 2018
Ankylosing spondylitis progression slowed when NSAIDs added to TNFi
AMSTERDAM – When combined with a tumor necrosis factor inhibitor, NSAIDs provide protection against long-term radiographic progression in patients with ankylosing spondylitis, according to an analysis of more than 500 patients presented at the European Congress of Rheumatology.
Relative to TNFi alone, the addition of NSAIDs of any type provided protection at 4 years against radiographic progression as measured with the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS). However, the protection associated with adding celecoxib was significant at 2 years and greater than that of adding nonselective NSAIDs at 4 years.
These data were drawn from 519 patients participating in the Prospective Study of Ankylosing Spondylitis study. All patients in this analysis were followed for at least 4 years. Radiographs were obtained every 6 months.
Although the study was a retrospective analysis of prospectively collected data, Dr. Gensler explained that control of variables such as disease and symptom duration with a technique called causal interference modeling “allows simulation of a randomized, controlled trial with observational data.”
Whether measured at 2 or 4 years, the reductions in mSASSS score for TNFi use versus no TNFi use were modest and did not reach statistical significance. However, exposure to NSAIDs plus TNFi did reach significance at 4 years, and the effect was dose dependent when patients taking a low-dose NSAID, defined as less than 50% of the index dose, were compared with those taking a higher dose. In this study, 70% were on chronic NSAID therapy, and these patients were divided relatively evenly between those on a low-dose or high-dose regimen.
At 2 years, relative radiographic protection for TNFi plus NSAIDs was not significantly greater than with TNFi alone, but at 4 years the median mSASSS score was 1.24 points lower (P less than .001) in those receiving low-dose NSAIDs, and 3.31 points lower (P less than .001) in those receiving high-dose NSAIDs.
In the subgroup of patients taking high-dose NSAIDs, the protection from progression was greatest among those receiving the selective COX2-inhibitor celecoxib. In these, the median 3.98 points lower mSASSS score (P less than .001) was already significant at 2 years. At 4 years, the median mSASSS score in those receiving TNFi plus celecoxib was 4.69 points lower (P less than .001).
Further evaluation suggested that the benefit from celecoxib plus TNFi was not just additive but synergistic, according to Dr. Gensler. She reported that neither TNFi nor celecoxib alone provided radiographic protection at 2 or 4 years.
Despite the modeling strategy employed to reduce the effect of bias, Dr. Gensler acknowledged that residual confounding is still possible. But she contended that “a large effect [from a such a variable] would be required to negate the findings.”
One of the messages from this study is that “not all NSAIDs are alike,” Dr. Gensler said. “Despite this, when I sit with a patient across from me, I will still treat the patient based on symptoms and disease activity first, though perhaps choose to be more NSAID selective if this is warranted and feasible.”
The next steps for research include a randomized, controlled trial combining TNFi and varying NSAIDs or different doses, Dr. Gensler said. In addition, “the development of newer imaging modalities will allow us to answer these questions in a more feasible time frame.”
The study was not industry funded. Dr. Gensler reported financial relationships with Amgen, AbbVie, Janssen, Eli Lilly, Novartis, and UCB.
SOURCE: Gensler L et al. Ann Rheum Dis. 2018;77(Suppl 2):148. Abstract OP0198.
AMSTERDAM – When combined with a tumor necrosis factor inhibitor, NSAIDs provide protection against long-term radiographic progression in patients with ankylosing spondylitis, according to an analysis of more than 500 patients presented at the European Congress of Rheumatology.
Relative to TNFi alone, the addition of NSAIDs of any type provided protection at 4 years against radiographic progression as measured with the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS). However, the protection associated with adding celecoxib was significant at 2 years and greater than that of adding nonselective NSAIDs at 4 years.
These data were drawn from 519 patients participating in the Prospective Study of Ankylosing Spondylitis study. All patients in this analysis were followed for at least 4 years. Radiographs were obtained every 6 months.
Although the study was a retrospective analysis of prospectively collected data, Dr. Gensler explained that control of variables such as disease and symptom duration with a technique called causal interference modeling “allows simulation of a randomized, controlled trial with observational data.”
Whether measured at 2 or 4 years, the reductions in mSASSS score for TNFi use versus no TNFi use were modest and did not reach statistical significance. However, exposure to NSAIDs plus TNFi did reach significance at 4 years, and the effect was dose dependent when patients taking a low-dose NSAID, defined as less than 50% of the index dose, were compared with those taking a higher dose. In this study, 70% were on chronic NSAID therapy, and these patients were divided relatively evenly between those on a low-dose or high-dose regimen.
At 2 years, relative radiographic protection for TNFi plus NSAIDs was not significantly greater than with TNFi alone, but at 4 years the median mSASSS score was 1.24 points lower (P less than .001) in those receiving low-dose NSAIDs, and 3.31 points lower (P less than .001) in those receiving high-dose NSAIDs.
In the subgroup of patients taking high-dose NSAIDs, the protection from progression was greatest among those receiving the selective COX2-inhibitor celecoxib. In these, the median 3.98 points lower mSASSS score (P less than .001) was already significant at 2 years. At 4 years, the median mSASSS score in those receiving TNFi plus celecoxib was 4.69 points lower (P less than .001).
Further evaluation suggested that the benefit from celecoxib plus TNFi was not just additive but synergistic, according to Dr. Gensler. She reported that neither TNFi nor celecoxib alone provided radiographic protection at 2 or 4 years.
Despite the modeling strategy employed to reduce the effect of bias, Dr. Gensler acknowledged that residual confounding is still possible. But she contended that “a large effect [from a such a variable] would be required to negate the findings.”
One of the messages from this study is that “not all NSAIDs are alike,” Dr. Gensler said. “Despite this, when I sit with a patient across from me, I will still treat the patient based on symptoms and disease activity first, though perhaps choose to be more NSAID selective if this is warranted and feasible.”
The next steps for research include a randomized, controlled trial combining TNFi and varying NSAIDs or different doses, Dr. Gensler said. In addition, “the development of newer imaging modalities will allow us to answer these questions in a more feasible time frame.”
The study was not industry funded. Dr. Gensler reported financial relationships with Amgen, AbbVie, Janssen, Eli Lilly, Novartis, and UCB.
SOURCE: Gensler L et al. Ann Rheum Dis. 2018;77(Suppl 2):148. Abstract OP0198.
AMSTERDAM – When combined with a tumor necrosis factor inhibitor, NSAIDs provide protection against long-term radiographic progression in patients with ankylosing spondylitis, according to an analysis of more than 500 patients presented at the European Congress of Rheumatology.
Relative to TNFi alone, the addition of NSAIDs of any type provided protection at 4 years against radiographic progression as measured with the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS). However, the protection associated with adding celecoxib was significant at 2 years and greater than that of adding nonselective NSAIDs at 4 years.
These data were drawn from 519 patients participating in the Prospective Study of Ankylosing Spondylitis study. All patients in this analysis were followed for at least 4 years. Radiographs were obtained every 6 months.
Although the study was a retrospective analysis of prospectively collected data, Dr. Gensler explained that control of variables such as disease and symptom duration with a technique called causal interference modeling “allows simulation of a randomized, controlled trial with observational data.”
Whether measured at 2 or 4 years, the reductions in mSASSS score for TNFi use versus no TNFi use were modest and did not reach statistical significance. However, exposure to NSAIDs plus TNFi did reach significance at 4 years, and the effect was dose dependent when patients taking a low-dose NSAID, defined as less than 50% of the index dose, were compared with those taking a higher dose. In this study, 70% were on chronic NSAID therapy, and these patients were divided relatively evenly between those on a low-dose or high-dose regimen.
At 2 years, relative radiographic protection for TNFi plus NSAIDs was not significantly greater than with TNFi alone, but at 4 years the median mSASSS score was 1.24 points lower (P less than .001) in those receiving low-dose NSAIDs, and 3.31 points lower (P less than .001) in those receiving high-dose NSAIDs.
In the subgroup of patients taking high-dose NSAIDs, the protection from progression was greatest among those receiving the selective COX2-inhibitor celecoxib. In these, the median 3.98 points lower mSASSS score (P less than .001) was already significant at 2 years. At 4 years, the median mSASSS score in those receiving TNFi plus celecoxib was 4.69 points lower (P less than .001).
Further evaluation suggested that the benefit from celecoxib plus TNFi was not just additive but synergistic, according to Dr. Gensler. She reported that neither TNFi nor celecoxib alone provided radiographic protection at 2 or 4 years.
Despite the modeling strategy employed to reduce the effect of bias, Dr. Gensler acknowledged that residual confounding is still possible. But she contended that “a large effect [from a such a variable] would be required to negate the findings.”
One of the messages from this study is that “not all NSAIDs are alike,” Dr. Gensler said. “Despite this, when I sit with a patient across from me, I will still treat the patient based on symptoms and disease activity first, though perhaps choose to be more NSAID selective if this is warranted and feasible.”
The next steps for research include a randomized, controlled trial combining TNFi and varying NSAIDs or different doses, Dr. Gensler said. In addition, “the development of newer imaging modalities will allow us to answer these questions in a more feasible time frame.”
The study was not industry funded. Dr. Gensler reported financial relationships with Amgen, AbbVie, Janssen, Eli Lilly, Novartis, and UCB.
SOURCE: Gensler L et al. Ann Rheum Dis. 2018;77(Suppl 2):148. Abstract OP0198.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Ankylosing spondylitis patients have less progression on a TNFi when they also receive an NSAID, especially celecoxib.
Major finding: At 4 years, the mSASSS score was 4.69 points (P less than .0001) lower on TNFi with celecoxib than on TNFi alone.
Study details: Retrospective study with causal interference modeling.
Disclosures: The study was not industry funded. Dr. Gensler reported financial relationships with Amgen, AbbVie, Janssen, Eli Lilly, Novartis, and UCB.
Source: Gensler L et al. Ann Rheum Dis. 2018;77(Suppl 2):148. Abstract OP0198.
Biologics improve axial spondyloarthritis patients’ work performance
LIVERPOOL, ENGLAND – Biologic therapy for axial spondyloarthritis can improve individuals’ work productivity and decrease the extent that the disease impairs overall work and overall activity, new data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis have shown.
A variety of work outcomes on the Work Productivity and Impairment Specific Health Problem (WPAI-SHP) questionnaire improved to a significantly greater extent with biologics use than without. Presenteeism, or working while sick, improved by a mean of –9.4%. Overall work impairment reduced by 13.9%, and overall activity impairment decreased by 19.2%. There was no great effect on absenteeism, however, with a mean difference in improvement of –1.5% between the groups.
“Research into this chronic condition has shown that it has detrimental impact on one’s ability to work,” she added. People may take sick leave and be less productive at work, which can have a psychological effect and cause worry about job loss.
While there is “strong evidence” to show that biologic therapy can improve disease activity in those with axSpA, there is equivocal evidence on whether it has any effect on work outcomes, explained Dr. Shim, a physiotherapist and a postdoctoral research fellow in the Epidemiology Group at the University of Aberdeen (Scotland).
The British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) started recruiting patients with axSpA from 84 centers across the United Kingdom in 2012 and there are now more than 2,500 participants included in the register. Similar to other biologics registers run under the auspices of the British Society for Rheumatology, the BSRBR-AS consists of two cohorts of patients, one who are about to start biologic therapy (with Enbrel [etanercept], Humira [adalimumab], or Cimzia [certolizumab pegol]) and one not receiving biologics.
The current analysis of 577 participants included 161 who had been treated with biologics and 416 who had not. Dr. Shim pointed out that people treated with biologics were younger (42 vs. 47 years), had shorter disease duration (7.7 vs. 12.3 years), and were more likely to be smokers (21% vs. 11%) than were those who had not taken biologics. Biologics-treated patients also had higher mean baseline disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (5.8 vs. 3.3), poorer function as measured by the Bath Ankylosing Spondylitis Functional Index (5.4 vs. 2.7), and worse overall Bath Ankylosing Spondylitis Global status scores (6.7 vs. 3.2).
“That’s the reason why they are given biologic therapy in the first place,” Dr. Shim said. To even out these differences, the investigators used propensity score matching before assessing work outcomes with the WPAI-SHP questionnaire. This consists of four components that are assessed in the last 7 days: absenteeism, presenteeism, overall work impairments (a combination of absenteeism and presenteeism), and overall activity impairment.
At recruitment, the investigators found that patients who later received biologics had greater impairment in work outcomes than did patients who later did not receive biologics. Patients who went on to receive biologics reported more absenteeism (13.0% vs. 3.0%), presenteeism (41.5% vs. 19.9%), overall work impairment (43.3% vs. 20.6%), and overall activity impairment (59.9% vs. 32.5%).
“Despite the improvements that we observed, there is still substantial unmet need, in the sense that people in the biologic therapy group are still experiencing significantly higher work impairments, compared to people in the nonbiologic therapy group,” Dr. Shim said. She added that, ideally, there should be no work impairment at all.
Dr. Shim and her associates combined the new BSRBR-AS findings with data from four prior randomized, controlled studies that met criteria for a meta-analysis. The results showed a mean difference between biologic and nonbiologic treatment of –5.35 on presenteeism, –11.20 on overall work impairment, and –12.13 on overall activity impairment. Again, there was little overall effect on absenteeism, with a mean difference of 0.84 between the groups.
The apparent lack of effect of biologic treatment on absenteeism could be from several reasons, one being that absenteeism was reportedly low in the BSRBR-AS and in other studies. Also, there is some evidence that presenteeism precedes absenteeism. The type of work done or number of allowed sick days may also play a role, Dr. Shim suggested.
“Work is a very important economic and social outcome,” Dr. Shim said. “We propose that future work should look into the assessment of work outcomes as standard measures,” in order to generate a greater evidence base around pharmacologic and nonpharmacologic approaches to improve work outcomes.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn has received function from AbbVie, Pfizer, and UCB. Dr. Shim reported that she had no conflicts of interest in relation to her presentation.
SOURCE: Shim J et al. Rheumatology. 2018;57[Suppl. 3]:key075.181.
LIVERPOOL, ENGLAND – Biologic therapy for axial spondyloarthritis can improve individuals’ work productivity and decrease the extent that the disease impairs overall work and overall activity, new data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis have shown.
A variety of work outcomes on the Work Productivity and Impairment Specific Health Problem (WPAI-SHP) questionnaire improved to a significantly greater extent with biologics use than without. Presenteeism, or working while sick, improved by a mean of –9.4%. Overall work impairment reduced by 13.9%, and overall activity impairment decreased by 19.2%. There was no great effect on absenteeism, however, with a mean difference in improvement of –1.5% between the groups.
“Research into this chronic condition has shown that it has detrimental impact on one’s ability to work,” she added. People may take sick leave and be less productive at work, which can have a psychological effect and cause worry about job loss.
While there is “strong evidence” to show that biologic therapy can improve disease activity in those with axSpA, there is equivocal evidence on whether it has any effect on work outcomes, explained Dr. Shim, a physiotherapist and a postdoctoral research fellow in the Epidemiology Group at the University of Aberdeen (Scotland).
The British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) started recruiting patients with axSpA from 84 centers across the United Kingdom in 2012 and there are now more than 2,500 participants included in the register. Similar to other biologics registers run under the auspices of the British Society for Rheumatology, the BSRBR-AS consists of two cohorts of patients, one who are about to start biologic therapy (with Enbrel [etanercept], Humira [adalimumab], or Cimzia [certolizumab pegol]) and one not receiving biologics.
The current analysis of 577 participants included 161 who had been treated with biologics and 416 who had not. Dr. Shim pointed out that people treated with biologics were younger (42 vs. 47 years), had shorter disease duration (7.7 vs. 12.3 years), and were more likely to be smokers (21% vs. 11%) than were those who had not taken biologics. Biologics-treated patients also had higher mean baseline disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (5.8 vs. 3.3), poorer function as measured by the Bath Ankylosing Spondylitis Functional Index (5.4 vs. 2.7), and worse overall Bath Ankylosing Spondylitis Global status scores (6.7 vs. 3.2).
“That’s the reason why they are given biologic therapy in the first place,” Dr. Shim said. To even out these differences, the investigators used propensity score matching before assessing work outcomes with the WPAI-SHP questionnaire. This consists of four components that are assessed in the last 7 days: absenteeism, presenteeism, overall work impairments (a combination of absenteeism and presenteeism), and overall activity impairment.
At recruitment, the investigators found that patients who later received biologics had greater impairment in work outcomes than did patients who later did not receive biologics. Patients who went on to receive biologics reported more absenteeism (13.0% vs. 3.0%), presenteeism (41.5% vs. 19.9%), overall work impairment (43.3% vs. 20.6%), and overall activity impairment (59.9% vs. 32.5%).
“Despite the improvements that we observed, there is still substantial unmet need, in the sense that people in the biologic therapy group are still experiencing significantly higher work impairments, compared to people in the nonbiologic therapy group,” Dr. Shim said. She added that, ideally, there should be no work impairment at all.
Dr. Shim and her associates combined the new BSRBR-AS findings with data from four prior randomized, controlled studies that met criteria for a meta-analysis. The results showed a mean difference between biologic and nonbiologic treatment of –5.35 on presenteeism, –11.20 on overall work impairment, and –12.13 on overall activity impairment. Again, there was little overall effect on absenteeism, with a mean difference of 0.84 between the groups.
The apparent lack of effect of biologic treatment on absenteeism could be from several reasons, one being that absenteeism was reportedly low in the BSRBR-AS and in other studies. Also, there is some evidence that presenteeism precedes absenteeism. The type of work done or number of allowed sick days may also play a role, Dr. Shim suggested.
“Work is a very important economic and social outcome,” Dr. Shim said. “We propose that future work should look into the assessment of work outcomes as standard measures,” in order to generate a greater evidence base around pharmacologic and nonpharmacologic approaches to improve work outcomes.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn has received function from AbbVie, Pfizer, and UCB. Dr. Shim reported that she had no conflicts of interest in relation to her presentation.
SOURCE: Shim J et al. Rheumatology. 2018;57[Suppl. 3]:key075.181.
LIVERPOOL, ENGLAND – Biologic therapy for axial spondyloarthritis can improve individuals’ work productivity and decrease the extent that the disease impairs overall work and overall activity, new data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis have shown.
A variety of work outcomes on the Work Productivity and Impairment Specific Health Problem (WPAI-SHP) questionnaire improved to a significantly greater extent with biologics use than without. Presenteeism, or working while sick, improved by a mean of –9.4%. Overall work impairment reduced by 13.9%, and overall activity impairment decreased by 19.2%. There was no great effect on absenteeism, however, with a mean difference in improvement of –1.5% between the groups.
“Research into this chronic condition has shown that it has detrimental impact on one’s ability to work,” she added. People may take sick leave and be less productive at work, which can have a psychological effect and cause worry about job loss.
While there is “strong evidence” to show that biologic therapy can improve disease activity in those with axSpA, there is equivocal evidence on whether it has any effect on work outcomes, explained Dr. Shim, a physiotherapist and a postdoctoral research fellow in the Epidemiology Group at the University of Aberdeen (Scotland).
The British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) started recruiting patients with axSpA from 84 centers across the United Kingdom in 2012 and there are now more than 2,500 participants included in the register. Similar to other biologics registers run under the auspices of the British Society for Rheumatology, the BSRBR-AS consists of two cohorts of patients, one who are about to start biologic therapy (with Enbrel [etanercept], Humira [adalimumab], or Cimzia [certolizumab pegol]) and one not receiving biologics.
The current analysis of 577 participants included 161 who had been treated with biologics and 416 who had not. Dr. Shim pointed out that people treated with biologics were younger (42 vs. 47 years), had shorter disease duration (7.7 vs. 12.3 years), and were more likely to be smokers (21% vs. 11%) than were those who had not taken biologics. Biologics-treated patients also had higher mean baseline disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (5.8 vs. 3.3), poorer function as measured by the Bath Ankylosing Spondylitis Functional Index (5.4 vs. 2.7), and worse overall Bath Ankylosing Spondylitis Global status scores (6.7 vs. 3.2).
“That’s the reason why they are given biologic therapy in the first place,” Dr. Shim said. To even out these differences, the investigators used propensity score matching before assessing work outcomes with the WPAI-SHP questionnaire. This consists of four components that are assessed in the last 7 days: absenteeism, presenteeism, overall work impairments (a combination of absenteeism and presenteeism), and overall activity impairment.
At recruitment, the investigators found that patients who later received biologics had greater impairment in work outcomes than did patients who later did not receive biologics. Patients who went on to receive biologics reported more absenteeism (13.0% vs. 3.0%), presenteeism (41.5% vs. 19.9%), overall work impairment (43.3% vs. 20.6%), and overall activity impairment (59.9% vs. 32.5%).
“Despite the improvements that we observed, there is still substantial unmet need, in the sense that people in the biologic therapy group are still experiencing significantly higher work impairments, compared to people in the nonbiologic therapy group,” Dr. Shim said. She added that, ideally, there should be no work impairment at all.
Dr. Shim and her associates combined the new BSRBR-AS findings with data from four prior randomized, controlled studies that met criteria for a meta-analysis. The results showed a mean difference between biologic and nonbiologic treatment of –5.35 on presenteeism, –11.20 on overall work impairment, and –12.13 on overall activity impairment. Again, there was little overall effect on absenteeism, with a mean difference of 0.84 between the groups.
The apparent lack of effect of biologic treatment on absenteeism could be from several reasons, one being that absenteeism was reportedly low in the BSRBR-AS and in other studies. Also, there is some evidence that presenteeism precedes absenteeism. The type of work done or number of allowed sick days may also play a role, Dr. Shim suggested.
“Work is a very important economic and social outcome,” Dr. Shim said. “We propose that future work should look into the assessment of work outcomes as standard measures,” in order to generate a greater evidence base around pharmacologic and nonpharmacologic approaches to improve work outcomes.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn has received function from AbbVie, Pfizer, and UCB. Dr. Shim reported that she had no conflicts of interest in relation to her presentation.
SOURCE: Shim J et al. Rheumatology. 2018;57[Suppl. 3]:key075.181.
REPORTING FROM RHEUMATOLOGY 2018
Key clinical point: Treatment with biologic therapy led to improved work outcomes to a greater extent over time than in patients who did not take biologics.
Major finding: Presenteeism improved by a mean of –9.4%, overall work impairment reduced by 13.9%, and overall activity impairment decreased by 19.2%.
Study details: 577 patients registered in BSRBR-AS (the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis).
Disclosures: The BSRBR-AS is funded by the British Society for Rheumatology, which in turn has received function from AbbVie, Pfizer, and UCB. Dr. Shim reported that she has no conflicts of interest in relation to her presentation.
Source: Shim J et al. Rheumatology. 2018;57(Suppl. 3):key075.181.
Observational data can’t answer question of inhibiting ankylosing spondylitis progression
AMSTERDAM – The attempt to determine whether biologics such as tumor necrosis factor inhibitors (TNFi) inhibit progression of ankylosing spondylitis has been pursued with observational studies, but these types of studies will never definitively answer the question, according to Robert B.M. Landewé, MD, PhD, professor of rheumatology at the University of Amsterdam.
“The methodology is sensitive to a lot of measurement error, making the results spurious,” Dr. Landewé said in an interview, recapping remarks he made in a presentation at the European Congress of Rheumatology.
This was disappointing to many investigators, including several speaking in the same symposium where Dr. Landewé made his remarks. Randomized, controlled trials that employ serial radiographs to document changes in ankylosing spondylitis are expensive, making observational studies an attractive surrogate, but Dr. Landewé said such studies are associated with an inherent risk of residual confounding.
In addition, he believes the effect size of biologics on progression, if it exists at all, is likely to be subtle. In the observational studies that have concluded that there is protection, complicated statistical analyses have been typically employed to produce a significant finding.
Observational studies do have hypothesis-generating value, according to Dr. Landewé, but he cautioned that they produce “more questions than answers.” He also emphasized that the inflammation-related progression that leads to bone growth in ankylosing spondylitis is different than it is in the destructive inflammatory diseases, such as rheumatoid arthritis, where the issue is bone loss.
It is rational to assume that effective anti-inflammatory therapy would prevent progression of inflammatory diseases, but Dr. Landewé said in his presentation that this is the type of bias that undermines the value of observational studies for reaching objective conclusions. Unlike the results of a registered randomized, controlled trial, which will be known to be consistent or not with the underlying hypothesis, there is a strong risk that data in an observational study will be reworked until they produce the desired result.
AMSTERDAM – The attempt to determine whether biologics such as tumor necrosis factor inhibitors (TNFi) inhibit progression of ankylosing spondylitis has been pursued with observational studies, but these types of studies will never definitively answer the question, according to Robert B.M. Landewé, MD, PhD, professor of rheumatology at the University of Amsterdam.
“The methodology is sensitive to a lot of measurement error, making the results spurious,” Dr. Landewé said in an interview, recapping remarks he made in a presentation at the European Congress of Rheumatology.
This was disappointing to many investigators, including several speaking in the same symposium where Dr. Landewé made his remarks. Randomized, controlled trials that employ serial radiographs to document changes in ankylosing spondylitis are expensive, making observational studies an attractive surrogate, but Dr. Landewé said such studies are associated with an inherent risk of residual confounding.
In addition, he believes the effect size of biologics on progression, if it exists at all, is likely to be subtle. In the observational studies that have concluded that there is protection, complicated statistical analyses have been typically employed to produce a significant finding.
Observational studies do have hypothesis-generating value, according to Dr. Landewé, but he cautioned that they produce “more questions than answers.” He also emphasized that the inflammation-related progression that leads to bone growth in ankylosing spondylitis is different than it is in the destructive inflammatory diseases, such as rheumatoid arthritis, where the issue is bone loss.
It is rational to assume that effective anti-inflammatory therapy would prevent progression of inflammatory diseases, but Dr. Landewé said in his presentation that this is the type of bias that undermines the value of observational studies for reaching objective conclusions. Unlike the results of a registered randomized, controlled trial, which will be known to be consistent or not with the underlying hypothesis, there is a strong risk that data in an observational study will be reworked until they produce the desired result.
AMSTERDAM – The attempt to determine whether biologics such as tumor necrosis factor inhibitors (TNFi) inhibit progression of ankylosing spondylitis has been pursued with observational studies, but these types of studies will never definitively answer the question, according to Robert B.M. Landewé, MD, PhD, professor of rheumatology at the University of Amsterdam.
“The methodology is sensitive to a lot of measurement error, making the results spurious,” Dr. Landewé said in an interview, recapping remarks he made in a presentation at the European Congress of Rheumatology.
This was disappointing to many investigators, including several speaking in the same symposium where Dr. Landewé made his remarks. Randomized, controlled trials that employ serial radiographs to document changes in ankylosing spondylitis are expensive, making observational studies an attractive surrogate, but Dr. Landewé said such studies are associated with an inherent risk of residual confounding.
In addition, he believes the effect size of biologics on progression, if it exists at all, is likely to be subtle. In the observational studies that have concluded that there is protection, complicated statistical analyses have been typically employed to produce a significant finding.
Observational studies do have hypothesis-generating value, according to Dr. Landewé, but he cautioned that they produce “more questions than answers.” He also emphasized that the inflammation-related progression that leads to bone growth in ankylosing spondylitis is different than it is in the destructive inflammatory diseases, such as rheumatoid arthritis, where the issue is bone loss.
It is rational to assume that effective anti-inflammatory therapy would prevent progression of inflammatory diseases, but Dr. Landewé said in his presentation that this is the type of bias that undermines the value of observational studies for reaching objective conclusions. Unlike the results of a registered randomized, controlled trial, which will be known to be consistent or not with the underlying hypothesis, there is a strong risk that data in an observational study will be reworked until they produce the desired result.
REPORTING FROM THE EULAR 2018 CONGRESS
TNF inhibitor may protect against axSpA sacroiliac joint progression
AMSTERDAM – In patients with axial spondyloarthritis, new evidence presented at the European Congress of Rheumatology associated tumor necrosis factor inhibitor therapy with prevention of sacroiliac joint progression.
“We already know that biologics can decelerate progression in the spine. The goal of this analysis was to determine whether there is also reduced risk of progression in the sacroiliac joints,” reported Valeria Rios-Rodríguez, MD, of Charité University Clinic in Berlin.
The patients were drawn from the ESTHER trial (Evidence-based Stimulation Trial With Human rFSH in Europe and Rest of World 1), which established the efficacy of the tumor necrosis factor (TNF) inhibitor etanercept over sulfasalazine in patients with early axSpA (Ann Rheum Dis. 2011 Jul;70:590-6). In ESTHER, all patients not in remission after 1 year continued on or were switched to maintenance etanercept. These patients provided the basis for Dr. Rios-Rodriguez and her colleagues’ analysis.
In this study of patients who remained on therapy, two blinded and experienced readers scored the radiographs for sacroiliac joint damage. A standardized modified New York grading system was employed. In addition, blinded readers graded MRI scans with the Berlin MRI Scoring System for inflammatory changes. Only 35% of patients had radiographic axSpA at baseline, reflecting the fact that ESTHER enrolled patients with early-stage axSpA.
A variety of factors were evaluated for their association with progression, including age, symptom duration, treatment duration, and HLA-B27 positivity. Of these factors, elevated C-reactive protein, defined as more than 5 mg/L, and the presence of sacroiliac joint osteitis on MRI emerged as predictive factors on univariate analysis.
“Evaluated with two different analyses, both of these factors were found to be independently associated with radiographic progression,” Dr. Rios-Rodriguez said. However, she reiterated that these factors were meaningful only at year 2 and 4 when progression was seen.
“Our results show a deceleration of progression of structural damage in sacroiliac joints in patients under long-term TNF inhibitor therapy. These findings match the deceleration of spine progression observed in previous studies under similar conditions,” she said, noting that the predictors for structural damage in sacroiliac joints identified in this study are similar to the ones identified for the progression in the spine.
“To our knowledge, our data on sacroiliac joints is unique and will continue to be so in the coming years,” she said.
Pfizer provided funding for the study. Dr. Rios-Rodriguez reported financial relationships with AbbVie and Novartis.
SOURCE: Rios-Rodriguez V et al. Ann Rheum Dis. 2018;77(Suppl 2):62-3. Abstract OP0025.
AMSTERDAM – In patients with axial spondyloarthritis, new evidence presented at the European Congress of Rheumatology associated tumor necrosis factor inhibitor therapy with prevention of sacroiliac joint progression.
“We already know that biologics can decelerate progression in the spine. The goal of this analysis was to determine whether there is also reduced risk of progression in the sacroiliac joints,” reported Valeria Rios-Rodríguez, MD, of Charité University Clinic in Berlin.
The patients were drawn from the ESTHER trial (Evidence-based Stimulation Trial With Human rFSH in Europe and Rest of World 1), which established the efficacy of the tumor necrosis factor (TNF) inhibitor etanercept over sulfasalazine in patients with early axSpA (Ann Rheum Dis. 2011 Jul;70:590-6). In ESTHER, all patients not in remission after 1 year continued on or were switched to maintenance etanercept. These patients provided the basis for Dr. Rios-Rodriguez and her colleagues’ analysis.
In this study of patients who remained on therapy, two blinded and experienced readers scored the radiographs for sacroiliac joint damage. A standardized modified New York grading system was employed. In addition, blinded readers graded MRI scans with the Berlin MRI Scoring System for inflammatory changes. Only 35% of patients had radiographic axSpA at baseline, reflecting the fact that ESTHER enrolled patients with early-stage axSpA.
A variety of factors were evaluated for their association with progression, including age, symptom duration, treatment duration, and HLA-B27 positivity. Of these factors, elevated C-reactive protein, defined as more than 5 mg/L, and the presence of sacroiliac joint osteitis on MRI emerged as predictive factors on univariate analysis.
“Evaluated with two different analyses, both of these factors were found to be independently associated with radiographic progression,” Dr. Rios-Rodriguez said. However, she reiterated that these factors were meaningful only at year 2 and 4 when progression was seen.
“Our results show a deceleration of progression of structural damage in sacroiliac joints in patients under long-term TNF inhibitor therapy. These findings match the deceleration of spine progression observed in previous studies under similar conditions,” she said, noting that the predictors for structural damage in sacroiliac joints identified in this study are similar to the ones identified for the progression in the spine.
“To our knowledge, our data on sacroiliac joints is unique and will continue to be so in the coming years,” she said.
Pfizer provided funding for the study. Dr. Rios-Rodriguez reported financial relationships with AbbVie and Novartis.
SOURCE: Rios-Rodriguez V et al. Ann Rheum Dis. 2018;77(Suppl 2):62-3. Abstract OP0025.
AMSTERDAM – In patients with axial spondyloarthritis, new evidence presented at the European Congress of Rheumatology associated tumor necrosis factor inhibitor therapy with prevention of sacroiliac joint progression.
“We already know that biologics can decelerate progression in the spine. The goal of this analysis was to determine whether there is also reduced risk of progression in the sacroiliac joints,” reported Valeria Rios-Rodríguez, MD, of Charité University Clinic in Berlin.
The patients were drawn from the ESTHER trial (Evidence-based Stimulation Trial With Human rFSH in Europe and Rest of World 1), which established the efficacy of the tumor necrosis factor (TNF) inhibitor etanercept over sulfasalazine in patients with early axSpA (Ann Rheum Dis. 2011 Jul;70:590-6). In ESTHER, all patients not in remission after 1 year continued on or were switched to maintenance etanercept. These patients provided the basis for Dr. Rios-Rodriguez and her colleagues’ analysis.
In this study of patients who remained on therapy, two blinded and experienced readers scored the radiographs for sacroiliac joint damage. A standardized modified New York grading system was employed. In addition, blinded readers graded MRI scans with the Berlin MRI Scoring System for inflammatory changes. Only 35% of patients had radiographic axSpA at baseline, reflecting the fact that ESTHER enrolled patients with early-stage axSpA.
A variety of factors were evaluated for their association with progression, including age, symptom duration, treatment duration, and HLA-B27 positivity. Of these factors, elevated C-reactive protein, defined as more than 5 mg/L, and the presence of sacroiliac joint osteitis on MRI emerged as predictive factors on univariate analysis.
“Evaluated with two different analyses, both of these factors were found to be independently associated with radiographic progression,” Dr. Rios-Rodriguez said. However, she reiterated that these factors were meaningful only at year 2 and 4 when progression was seen.
“Our results show a deceleration of progression of structural damage in sacroiliac joints in patients under long-term TNF inhibitor therapy. These findings match the deceleration of spine progression observed in previous studies under similar conditions,” she said, noting that the predictors for structural damage in sacroiliac joints identified in this study are similar to the ones identified for the progression in the spine.
“To our knowledge, our data on sacroiliac joints is unique and will continue to be so in the coming years,” she said.
Pfizer provided funding for the study. Dr. Rios-Rodriguez reported financial relationships with AbbVie and Novartis.
SOURCE: Rios-Rodriguez V et al. Ann Rheum Dis. 2018;77(Suppl 2):62-3. Abstract OP0025.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point:
Major finding: Sacroiliac joint progression was seen in 18% of patients at year 2, 4.1% at year 4, and 0% at year 6.
Study details: A post hoc analysis of a subset of 42 patients in the randomized ESTHER trial.
Disclosures: Pfizer provided funding for the study. Dr. Rios-Rodriguez reported financial relationships with AbbVie and Novartis.
Source: Rios-Rodriguez V et al. Ann Rheum Dis. 2018;77(Suppl 2):62-3. Abstract OP0025.
Ankylosing spondylitis diagnosis linked to self-harm attempts
AMSTERDAM – There is an increased relative risk of deliberate self-harm that results in emergency treatment among individuals newly diagnosed with ankylosing spondylitis, according to the results of a large, Canadian population-based study.
A diagnosis of ankylosing spondylitis was associated with a 59% increased risk of deliberate self-harm, compared with no diagnosis (HR = 1.59, 95% CI, 1.16-2.21). While the risk of deliberate self-harm in patients diagnosed with rheumatoid arthritis (RA) was initially elevated, the association was not significant after adjustment for confounding factors (HR = 1.08, 95% CI, 0.87-1.34).
These findings call for heightened awareness among clinicians, study investigator Nigil Haroon, MD, PhD, said in an interview at the European Congress of Rheumatology. “Depression is generally well known to be increased in patients with chronic diseases, especially so with chronic inflammatory rheumatic diseases like ankylosing spondylitis and rheumatoid arthritis,” he said. This may in turn be linked to increased cases of deliberate self-harm, but there have been few studies to determine if this is the case, he said, which may be because it is a relatively rare event in routine clinical practice.
Dr. Haroon, who runs a specialist clinic in ankylosing spondylitis in Toronto, has seen the long-term effects of chronic pain, lack of social support, and inability to sleep on patients’ mood first hand. This is what drove him and other colleagues at the University of Toronto and University Health Network to look at the possibility that this could be linked to an increased risk for depression and perhaps deliberate self-harm among newly diagnosed patients.
To try to estimate the risk, they obtained administrative data on more than 100,000 individuals diagnosed with ankylosing spondylitis or RA in the province of Ontario, Canada, between 2002 and 2014. Excluding those with a history of mental illness or a prior self-harm attempt resulted in the creation of two cohorts of patients – 13,964 with ankylosing spondylitis and 53,240 with RA. Indviduals in these two cohorts were then matched, 4:1, to similar controls in the general population.
The average age of those diagnosed with ankylosing spondylitis was 46 years and of those with RA was 57 years, with more males than females in the ankylosing spondylitis group (57% vs. 43%) and more females than males in the RA group (67% vs. 33%).
The main outcome assessed was the first episode of intentional self-injury or self-poisoning that required emergency treatment that occurred after the diagnosis of ankylosing spondylitis or RA.
Overall, there were 69 deliberate self-harm attempts recorded in the ankylosing spondylitis patient group, compared with 131 attempts in the non-ankylosing spondylitis group. In the RA patient group, there were 129 attempts, and 372 attempts in the non-RA group.
Poisoning was “by far the most common modality” used to intentionally self-harm, used by 67% of patients with ankylosing spondylitis and by 81% of those with RA, Dr. Haroon reported. Contact with a sharp object was the second most common method used to deliberately self-harm by 30% of ankylosing spondylitis patients and 16% of RA patients.
Most (70%) patients were discharged following emergency treatment for a deliberate self-harm attempt, with around 15% of ankylosing spondylitis and 22% of RA patients requiring hospital admission.
“For any chronic disease there is a potential for depression to settle, and we should identify [patients] early, even at the primary care levels itself and try to address it,” Dr. Haroon advised. It’s important to spend time and to develop a good rapport with your patients, he added, which can help them open up and talk about their mood.
The work was funded by the Division of Rheumatology Pfizer Research Chair, University of Toronto. Dr. Haroon reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Kuriya B et al. Ann Rheum Dis. 2018;77(Suppl 2):195. Abstract OP0296.
AMSTERDAM – There is an increased relative risk of deliberate self-harm that results in emergency treatment among individuals newly diagnosed with ankylosing spondylitis, according to the results of a large, Canadian population-based study.
A diagnosis of ankylosing spondylitis was associated with a 59% increased risk of deliberate self-harm, compared with no diagnosis (HR = 1.59, 95% CI, 1.16-2.21). While the risk of deliberate self-harm in patients diagnosed with rheumatoid arthritis (RA) was initially elevated, the association was not significant after adjustment for confounding factors (HR = 1.08, 95% CI, 0.87-1.34).
These findings call for heightened awareness among clinicians, study investigator Nigil Haroon, MD, PhD, said in an interview at the European Congress of Rheumatology. “Depression is generally well known to be increased in patients with chronic diseases, especially so with chronic inflammatory rheumatic diseases like ankylosing spondylitis and rheumatoid arthritis,” he said. This may in turn be linked to increased cases of deliberate self-harm, but there have been few studies to determine if this is the case, he said, which may be because it is a relatively rare event in routine clinical practice.
Dr. Haroon, who runs a specialist clinic in ankylosing spondylitis in Toronto, has seen the long-term effects of chronic pain, lack of social support, and inability to sleep on patients’ mood first hand. This is what drove him and other colleagues at the University of Toronto and University Health Network to look at the possibility that this could be linked to an increased risk for depression and perhaps deliberate self-harm among newly diagnosed patients.
To try to estimate the risk, they obtained administrative data on more than 100,000 individuals diagnosed with ankylosing spondylitis or RA in the province of Ontario, Canada, between 2002 and 2014. Excluding those with a history of mental illness or a prior self-harm attempt resulted in the creation of two cohorts of patients – 13,964 with ankylosing spondylitis and 53,240 with RA. Indviduals in these two cohorts were then matched, 4:1, to similar controls in the general population.
The average age of those diagnosed with ankylosing spondylitis was 46 years and of those with RA was 57 years, with more males than females in the ankylosing spondylitis group (57% vs. 43%) and more females than males in the RA group (67% vs. 33%).
The main outcome assessed was the first episode of intentional self-injury or self-poisoning that required emergency treatment that occurred after the diagnosis of ankylosing spondylitis or RA.
Overall, there were 69 deliberate self-harm attempts recorded in the ankylosing spondylitis patient group, compared with 131 attempts in the non-ankylosing spondylitis group. In the RA patient group, there were 129 attempts, and 372 attempts in the non-RA group.
Poisoning was “by far the most common modality” used to intentionally self-harm, used by 67% of patients with ankylosing spondylitis and by 81% of those with RA, Dr. Haroon reported. Contact with a sharp object was the second most common method used to deliberately self-harm by 30% of ankylosing spondylitis patients and 16% of RA patients.
Most (70%) patients were discharged following emergency treatment for a deliberate self-harm attempt, with around 15% of ankylosing spondylitis and 22% of RA patients requiring hospital admission.
“For any chronic disease there is a potential for depression to settle, and we should identify [patients] early, even at the primary care levels itself and try to address it,” Dr. Haroon advised. It’s important to spend time and to develop a good rapport with your patients, he added, which can help them open up and talk about their mood.
The work was funded by the Division of Rheumatology Pfizer Research Chair, University of Toronto. Dr. Haroon reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Kuriya B et al. Ann Rheum Dis. 2018;77(Suppl 2):195. Abstract OP0296.
AMSTERDAM – There is an increased relative risk of deliberate self-harm that results in emergency treatment among individuals newly diagnosed with ankylosing spondylitis, according to the results of a large, Canadian population-based study.
A diagnosis of ankylosing spondylitis was associated with a 59% increased risk of deliberate self-harm, compared with no diagnosis (HR = 1.59, 95% CI, 1.16-2.21). While the risk of deliberate self-harm in patients diagnosed with rheumatoid arthritis (RA) was initially elevated, the association was not significant after adjustment for confounding factors (HR = 1.08, 95% CI, 0.87-1.34).
These findings call for heightened awareness among clinicians, study investigator Nigil Haroon, MD, PhD, said in an interview at the European Congress of Rheumatology. “Depression is generally well known to be increased in patients with chronic diseases, especially so with chronic inflammatory rheumatic diseases like ankylosing spondylitis and rheumatoid arthritis,” he said. This may in turn be linked to increased cases of deliberate self-harm, but there have been few studies to determine if this is the case, he said, which may be because it is a relatively rare event in routine clinical practice.
Dr. Haroon, who runs a specialist clinic in ankylosing spondylitis in Toronto, has seen the long-term effects of chronic pain, lack of social support, and inability to sleep on patients’ mood first hand. This is what drove him and other colleagues at the University of Toronto and University Health Network to look at the possibility that this could be linked to an increased risk for depression and perhaps deliberate self-harm among newly diagnosed patients.
To try to estimate the risk, they obtained administrative data on more than 100,000 individuals diagnosed with ankylosing spondylitis or RA in the province of Ontario, Canada, between 2002 and 2014. Excluding those with a history of mental illness or a prior self-harm attempt resulted in the creation of two cohorts of patients – 13,964 with ankylosing spondylitis and 53,240 with RA. Indviduals in these two cohorts were then matched, 4:1, to similar controls in the general population.
The average age of those diagnosed with ankylosing spondylitis was 46 years and of those with RA was 57 years, with more males than females in the ankylosing spondylitis group (57% vs. 43%) and more females than males in the RA group (67% vs. 33%).
The main outcome assessed was the first episode of intentional self-injury or self-poisoning that required emergency treatment that occurred after the diagnosis of ankylosing spondylitis or RA.
Overall, there were 69 deliberate self-harm attempts recorded in the ankylosing spondylitis patient group, compared with 131 attempts in the non-ankylosing spondylitis group. In the RA patient group, there were 129 attempts, and 372 attempts in the non-RA group.
Poisoning was “by far the most common modality” used to intentionally self-harm, used by 67% of patients with ankylosing spondylitis and by 81% of those with RA, Dr. Haroon reported. Contact with a sharp object was the second most common method used to deliberately self-harm by 30% of ankylosing spondylitis patients and 16% of RA patients.
Most (70%) patients were discharged following emergency treatment for a deliberate self-harm attempt, with around 15% of ankylosing spondylitis and 22% of RA patients requiring hospital admission.
“For any chronic disease there is a potential for depression to settle, and we should identify [patients] early, even at the primary care levels itself and try to address it,” Dr. Haroon advised. It’s important to spend time and to develop a good rapport with your patients, he added, which can help them open up and talk about their mood.
The work was funded by the Division of Rheumatology Pfizer Research Chair, University of Toronto. Dr. Haroon reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Kuriya B et al. Ann Rheum Dis. 2018;77(Suppl 2):195. Abstract OP0296.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Major finding: Newly-diagnosed individuals with ankylosing spondylitis are more likely to attempt self harm than those without the diagnosis (HR = 1.59, 95% CI, 1.16-2.21).
Study details: Population-based study of 13,964 individuals with ankylosing spondylitis, 53,240 individuals with RA, and matched controls from the general population.
Disclosures: The work was funded by the Division of Rheumatology Pfizer Research Chair, University of Toronto. Dr. Haroon reported having no relevant financial disclosures.
Source: Kuriya B et al. Ann Rheum Dis. 2018;77(Suppl 2):195. Abstract OP0296.