User login
Axial SpA diagnostic strategies need not be sex-specific
AMSTERDAM – Imaging and a positive HLA-B27 test are effective tools for early diagnosis of axial spondyloarthritis in both men and women, according to data from a study of 719 patients with chronic back pain reported at the European Congress of Rheumatology.
Data from previous studies have shown greater severity of axial spondyloarthritis (axSpA) in men, but gender differences at first presentation of the disease have not been well studied, noted Dr. Augusta Ortolan of the University of Padova (Italy) and her colleagues.
The researchers analyzed baseline data from 444 women and 275 men in the Spondyloarthritis Caught Early (SPACE) cohort, which included patients with chronic back pain that had lasted 3 months to 2 years. The patients were younger than 45 years at the onset of symptoms.
Overall, 53% of men and 35% of women were diagnosed with axSpA. The duration of symptoms was similar between genders, but the average age at diagnosis was significantly younger for men, compared with women (27 years vs. 30 years; P = .021). A positive HLA-B27 test was more common among men with axSpA than among women with axSpA (80% vs. 60%; P less than .001).
Similarly, the presence of axial spondyloarthritis features on imaging was greater among men with axSpA than women with axSpA (78% vs. 64%; P = .007).
Dr. Ortolan said in an interview that she was somewhat surprised by the findings. “I probably expected to see more differences between male and female patients,” she said. “Although it has been demonstrated that the proportion of men to women is more balanced in axial spondyloarthritis in general [nearly 1:1] as compared to the more advanced stages of the disease [known as ankylosing spondylitis or radiographic axial spondyloarthritis, where the male-to-female ratio is around 3:1], there is a tendency to believe that spondyloarthritis in females is rarer or at least more difficult to detect,” she said. “In fact, the study does not completely contradict this belief as we found that from our chronic back pain population, males are twice as likely to be diagnosed. However, all in all, they do not present so much differently than women,” she noted.
The take home message is for clinicians to examine all features that may lead to a diagnosis of axSpA in patients regardless of gender, Dr. Ortolan said. The study results showing that HLA-B27 and imaging are strongly associated with axSpA diagnosis in both genders in a multivariate analysis, which suggests that clinicians do not need to adopt different diagnostic strategies, she said.
The study findings were the result of a cross-sectional approach that was based on an examination of baseline data, Dr. Ortolan noted. “However, it would be really interesting to see what happens in the long term: Do these gender differences tend to increase? Does the disease have a different long-term impact in men and women? Should we treat them differently? These are open questions that need to be addressed in the future,” she said.
Dr. Ortolan and her colleagues had no relevant disclosures.
Mitchel L. Zoler contributed to this story.
SOURCE: Ortolan A et al. Ann Rheum Dis. 2018;77(Suppl 2):207-8. Abstract OP0323.
AMSTERDAM – Imaging and a positive HLA-B27 test are effective tools for early diagnosis of axial spondyloarthritis in both men and women, according to data from a study of 719 patients with chronic back pain reported at the European Congress of Rheumatology.
Data from previous studies have shown greater severity of axial spondyloarthritis (axSpA) in men, but gender differences at first presentation of the disease have not been well studied, noted Dr. Augusta Ortolan of the University of Padova (Italy) and her colleagues.
The researchers analyzed baseline data from 444 women and 275 men in the Spondyloarthritis Caught Early (SPACE) cohort, which included patients with chronic back pain that had lasted 3 months to 2 years. The patients were younger than 45 years at the onset of symptoms.
Overall, 53% of men and 35% of women were diagnosed with axSpA. The duration of symptoms was similar between genders, but the average age at diagnosis was significantly younger for men, compared with women (27 years vs. 30 years; P = .021). A positive HLA-B27 test was more common among men with axSpA than among women with axSpA (80% vs. 60%; P less than .001).
Similarly, the presence of axial spondyloarthritis features on imaging was greater among men with axSpA than women with axSpA (78% vs. 64%; P = .007).
Dr. Ortolan said in an interview that she was somewhat surprised by the findings. “I probably expected to see more differences between male and female patients,” she said. “Although it has been demonstrated that the proportion of men to women is more balanced in axial spondyloarthritis in general [nearly 1:1] as compared to the more advanced stages of the disease [known as ankylosing spondylitis or radiographic axial spondyloarthritis, where the male-to-female ratio is around 3:1], there is a tendency to believe that spondyloarthritis in females is rarer or at least more difficult to detect,” she said. “In fact, the study does not completely contradict this belief as we found that from our chronic back pain population, males are twice as likely to be diagnosed. However, all in all, they do not present so much differently than women,” she noted.
The take home message is for clinicians to examine all features that may lead to a diagnosis of axSpA in patients regardless of gender, Dr. Ortolan said. The study results showing that HLA-B27 and imaging are strongly associated with axSpA diagnosis in both genders in a multivariate analysis, which suggests that clinicians do not need to adopt different diagnostic strategies, she said.
The study findings were the result of a cross-sectional approach that was based on an examination of baseline data, Dr. Ortolan noted. “However, it would be really interesting to see what happens in the long term: Do these gender differences tend to increase? Does the disease have a different long-term impact in men and women? Should we treat them differently? These are open questions that need to be addressed in the future,” she said.
Dr. Ortolan and her colleagues had no relevant disclosures.
Mitchel L. Zoler contributed to this story.
SOURCE: Ortolan A et al. Ann Rheum Dis. 2018;77(Suppl 2):207-8. Abstract OP0323.
AMSTERDAM – Imaging and a positive HLA-B27 test are effective tools for early diagnosis of axial spondyloarthritis in both men and women, according to data from a study of 719 patients with chronic back pain reported at the European Congress of Rheumatology.
Data from previous studies have shown greater severity of axial spondyloarthritis (axSpA) in men, but gender differences at first presentation of the disease have not been well studied, noted Dr. Augusta Ortolan of the University of Padova (Italy) and her colleagues.
The researchers analyzed baseline data from 444 women and 275 men in the Spondyloarthritis Caught Early (SPACE) cohort, which included patients with chronic back pain that had lasted 3 months to 2 years. The patients were younger than 45 years at the onset of symptoms.
Overall, 53% of men and 35% of women were diagnosed with axSpA. The duration of symptoms was similar between genders, but the average age at diagnosis was significantly younger for men, compared with women (27 years vs. 30 years; P = .021). A positive HLA-B27 test was more common among men with axSpA than among women with axSpA (80% vs. 60%; P less than .001).
Similarly, the presence of axial spondyloarthritis features on imaging was greater among men with axSpA than women with axSpA (78% vs. 64%; P = .007).
Dr. Ortolan said in an interview that she was somewhat surprised by the findings. “I probably expected to see more differences between male and female patients,” she said. “Although it has been demonstrated that the proportion of men to women is more balanced in axial spondyloarthritis in general [nearly 1:1] as compared to the more advanced stages of the disease [known as ankylosing spondylitis or radiographic axial spondyloarthritis, where the male-to-female ratio is around 3:1], there is a tendency to believe that spondyloarthritis in females is rarer or at least more difficult to detect,” she said. “In fact, the study does not completely contradict this belief as we found that from our chronic back pain population, males are twice as likely to be diagnosed. However, all in all, they do not present so much differently than women,” she noted.
The take home message is for clinicians to examine all features that may lead to a diagnosis of axSpA in patients regardless of gender, Dr. Ortolan said. The study results showing that HLA-B27 and imaging are strongly associated with axSpA diagnosis in both genders in a multivariate analysis, which suggests that clinicians do not need to adopt different diagnostic strategies, she said.
The study findings were the result of a cross-sectional approach that was based on an examination of baseline data, Dr. Ortolan noted. “However, it would be really interesting to see what happens in the long term: Do these gender differences tend to increase? Does the disease have a different long-term impact in men and women? Should we treat them differently? These are open questions that need to be addressed in the future,” she said.
Dr. Ortolan and her colleagues had no relevant disclosures.
Mitchel L. Zoler contributed to this story.
SOURCE: Ortolan A et al. Ann Rheum Dis. 2018;77(Suppl 2):207-8. Abstract OP0323.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Although there are clear sex differences in early axSpA, HLA-B27 and imaging are key elements for a diagnosis of axSpA in both sexes.
Major finding: The presence of axSpA features on imaging was greater among men with axSpA than women with axSpA (78% vs. 64%; P = .007).
Study details: A cross-sectional study of baseline data from 444 women and 275 men in the Spondyloarthritis Caught Early (SPACE) cohort.
Disclosures: Dr. Ortolan and her colleagues had no relevant disclosures.
Source: Ortolan A et al. Ann Rheum Dis. 2018;77(Suppl 2):207-8. Abstract OP0323.
EULAR scientific program highlights spectrum of translational research
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
Eye-opening findings cast spondyloarthritis in new light, expert says
SANDESTIN, FLA. – Recent findings have led to eye-opening results in the axial spondyloarthritis (SpA) field, including a surprisingly high number of patients with inflammatory back pain who don’t progress to the disease, healthy people who develop SpA-like details on imaging, and significant gender differences in the efficacy of biologic therapy, said Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego.
The findings could lead clinicians to see the disease differently and consult with patients in new ways, he said.
Just over 20% of the patients progressed to SpA within 5 years, and about 30% over 15 years. But after 5 years, the condition resolved in over 30% of patients – and after 15 years, it resolved in almost half.
In about 5% of patients, symptoms persisted but the condition remained unidentified.
“A lot of people with inflammatory back pain, it doesn’t continue to be an issue – this goes out a decade and a half,” Dr. Kavanaugh said. “I was surprised with this. I would have guess that over this many years, more people would have developed ankylosing spondylitis, but they don’t.”
He said that clinicians should cite this information in their discussions with patients. They should review their case and evaluate spinal symptoms, but let them know that the condition might not progress and might not be permanent.
“I would use this information and say, ‘Well you’re having inflammatory back pain, but let’s go review things,’ ” he said. “ ‘If you don’t have the true spondyloarthropathy or ankylosing spondylitis now, there’s a chance that this will go away. It’s almost 50-50, or we still don’t know what it is even if you’re having some symptoms (after 15 years).’ ”
Other important findings underscore the need for a complete clinical picture rather than just findings on imaging for an axial SpA diagnosis, Dr. Kavanaugh said. Researchers examined MRI images of new military recruits who were healthy with no back pain (Rheumatology [Oxford]. 2018 Mar 1;57[3]:508-13). They found that 23% of them at baseline – and 37% after strenuous training – had MRI findings that would qualify as positive for spondyloarthritis by Assessment of Spondyloarthritis international Society criteria. But they wouldn’t meet the definition of disease.
More recent findings showed similar results in imaging of healthy runners and hockey players (Arthritis Rheumatol. 2018 May;70[5]:736-45), with 30%-40% of them having MRI findings that would be considered positive on ASAS, Dr. Kavanaugh said.
“These were just people who were out stressing their joints,” he said. “We were super excited at the start of having MRI because now we can look and evaluate the activity within a joint. But I think, like everything, we have to take it with a little bit of caution. Just in and of itself, without the clinical picture, it does not diagnose axial spondyloarthropathy.”
In another recent study, women with axial SpA were found to have significantly lower responses over time than men with axial SpA (J Rheumatol. 2018 Feb;45[2]:195-201). Dr. Kavanaugh said that there might be some selection bias because of the higher male prevalence of disease but said the findings were noteworthy, especially in light of findings in animal models suggesting gender differences in disease expression and response to treatment.
“I think this is fascinating,” he said. “I think there’s a lot more to come for this.”
Dr. Kavanaugh reported financial relationships with AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Gilead, Genentech, Novartis, Pfizer, and other companies.
SANDESTIN, FLA. – Recent findings have led to eye-opening results in the axial spondyloarthritis (SpA) field, including a surprisingly high number of patients with inflammatory back pain who don’t progress to the disease, healthy people who develop SpA-like details on imaging, and significant gender differences in the efficacy of biologic therapy, said Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego.
The findings could lead clinicians to see the disease differently and consult with patients in new ways, he said.
Just over 20% of the patients progressed to SpA within 5 years, and about 30% over 15 years. But after 5 years, the condition resolved in over 30% of patients – and after 15 years, it resolved in almost half.
In about 5% of patients, symptoms persisted but the condition remained unidentified.
“A lot of people with inflammatory back pain, it doesn’t continue to be an issue – this goes out a decade and a half,” Dr. Kavanaugh said. “I was surprised with this. I would have guess that over this many years, more people would have developed ankylosing spondylitis, but they don’t.”
He said that clinicians should cite this information in their discussions with patients. They should review their case and evaluate spinal symptoms, but let them know that the condition might not progress and might not be permanent.
“I would use this information and say, ‘Well you’re having inflammatory back pain, but let’s go review things,’ ” he said. “ ‘If you don’t have the true spondyloarthropathy or ankylosing spondylitis now, there’s a chance that this will go away. It’s almost 50-50, or we still don’t know what it is even if you’re having some symptoms (after 15 years).’ ”
Other important findings underscore the need for a complete clinical picture rather than just findings on imaging for an axial SpA diagnosis, Dr. Kavanaugh said. Researchers examined MRI images of new military recruits who were healthy with no back pain (Rheumatology [Oxford]. 2018 Mar 1;57[3]:508-13). They found that 23% of them at baseline – and 37% after strenuous training – had MRI findings that would qualify as positive for spondyloarthritis by Assessment of Spondyloarthritis international Society criteria. But they wouldn’t meet the definition of disease.
More recent findings showed similar results in imaging of healthy runners and hockey players (Arthritis Rheumatol. 2018 May;70[5]:736-45), with 30%-40% of them having MRI findings that would be considered positive on ASAS, Dr. Kavanaugh said.
“These were just people who were out stressing their joints,” he said. “We were super excited at the start of having MRI because now we can look and evaluate the activity within a joint. But I think, like everything, we have to take it with a little bit of caution. Just in and of itself, without the clinical picture, it does not diagnose axial spondyloarthropathy.”
In another recent study, women with axial SpA were found to have significantly lower responses over time than men with axial SpA (J Rheumatol. 2018 Feb;45[2]:195-201). Dr. Kavanaugh said that there might be some selection bias because of the higher male prevalence of disease but said the findings were noteworthy, especially in light of findings in animal models suggesting gender differences in disease expression and response to treatment.
“I think this is fascinating,” he said. “I think there’s a lot more to come for this.”
Dr. Kavanaugh reported financial relationships with AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Gilead, Genentech, Novartis, Pfizer, and other companies.
SANDESTIN, FLA. – Recent findings have led to eye-opening results in the axial spondyloarthritis (SpA) field, including a surprisingly high number of patients with inflammatory back pain who don’t progress to the disease, healthy people who develop SpA-like details on imaging, and significant gender differences in the efficacy of biologic therapy, said Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego.
The findings could lead clinicians to see the disease differently and consult with patients in new ways, he said.
Just over 20% of the patients progressed to SpA within 5 years, and about 30% over 15 years. But after 5 years, the condition resolved in over 30% of patients – and after 15 years, it resolved in almost half.
In about 5% of patients, symptoms persisted but the condition remained unidentified.
“A lot of people with inflammatory back pain, it doesn’t continue to be an issue – this goes out a decade and a half,” Dr. Kavanaugh said. “I was surprised with this. I would have guess that over this many years, more people would have developed ankylosing spondylitis, but they don’t.”
He said that clinicians should cite this information in their discussions with patients. They should review their case and evaluate spinal symptoms, but let them know that the condition might not progress and might not be permanent.
“I would use this information and say, ‘Well you’re having inflammatory back pain, but let’s go review things,’ ” he said. “ ‘If you don’t have the true spondyloarthropathy or ankylosing spondylitis now, there’s a chance that this will go away. It’s almost 50-50, or we still don’t know what it is even if you’re having some symptoms (after 15 years).’ ”
Other important findings underscore the need for a complete clinical picture rather than just findings on imaging for an axial SpA diagnosis, Dr. Kavanaugh said. Researchers examined MRI images of new military recruits who were healthy with no back pain (Rheumatology [Oxford]. 2018 Mar 1;57[3]:508-13). They found that 23% of them at baseline – and 37% after strenuous training – had MRI findings that would qualify as positive for spondyloarthritis by Assessment of Spondyloarthritis international Society criteria. But they wouldn’t meet the definition of disease.
More recent findings showed similar results in imaging of healthy runners and hockey players (Arthritis Rheumatol. 2018 May;70[5]:736-45), with 30%-40% of them having MRI findings that would be considered positive on ASAS, Dr. Kavanaugh said.
“These were just people who were out stressing their joints,” he said. “We were super excited at the start of having MRI because now we can look and evaluate the activity within a joint. But I think, like everything, we have to take it with a little bit of caution. Just in and of itself, without the clinical picture, it does not diagnose axial spondyloarthropathy.”
In another recent study, women with axial SpA were found to have significantly lower responses over time than men with axial SpA (J Rheumatol. 2018 Feb;45[2]:195-201). Dr. Kavanaugh said that there might be some selection bias because of the higher male prevalence of disease but said the findings were noteworthy, especially in light of findings in animal models suggesting gender differences in disease expression and response to treatment.
“I think this is fascinating,” he said. “I think there’s a lot more to come for this.”
Dr. Kavanaugh reported financial relationships with AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Gilead, Genentech, Novartis, Pfizer, and other companies.
EXPERT ANALYSIS FROM CCR 18
Comorbid spondyloarthritis and fibromyalgia lower response to TNF inhibitors
LIVERPOOL, ENGLAND – Individuals with axial spondyloarthritis (axSpA) who have comorbid fibromyalgia do respond to biologic therapy but at a seemingly lower rate if they have a high symptom score during early assessments.
Data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) showed that participants with axSpA who were starting biologic therapy with a tumor necrosis factor inhibitor (TNFi) for the first time also had worse disease activity at baseline if they met fibromyalgia research criteria than if they did not.
“The issue of fibromyalgia as a comorbidity in axial SpA has been the subject of current considerable interest,” said Dr. Macfarlane, who is Clinical Chair in Epidemiology at the University of Aberdeen (Scotland), where the BSRBR-AS is run. This is for several reasons: “One is the challenge of identifying patients with axial SpA who have comorbid fibromyalgia.
“The second is the concern that comorbid fibromyalgia may have an effect on disease indices such as BASDAI [Bath Ankylosing Spondylitis Disease Activity Index],” Dr. Macfarlane observed.
This leads to the third issue: “Are patients with comorbid fibromyalgia inappropriately receiving biological therapy, and how do they respond if they do receive it?”
Previous data from the BSRBR-AS have shown that approximately one in five patients with axSpA meet research criteria for fibromyalgia (Arthritis Rheumatol. 2017;69:2144-50) and that the prevalence of the comorbidity was higher in those who met Assessment of SpondyloArthritis International Society imaging criteria and lower in those who only met clinical criteria (25% vs. 10%).
The current aims of the study presented by Dr. Macfarlane were to first quantify the extent to which meeting fibromyalgia criteria was associated with higher measures of disease activity and impact, and then to see if meeting these criteria was associated with a poorer response to first use of a TNFi.
In order to find out, Dr. Macfarlane and his associates examined data from the prospective BSRBR-AS, which has been running since 2012. The BSRBR-AS recruits patients with ASAS-confirmed axSpA who are newly starting biologics from 83 U.K. centers.
At recruitment and at 3 months, patients starting biologic treatment undergo several assessments, which since 2015 has included research criteria for fibromyalgia (J Rheumatol. 2011;38:1113–22). The latter incorporate a Widespread Pain Index rated 0-19 and a Symptom Severity Scale rated 0-12 and cover items such as fatigue and waking up unrefreshed, and the presence of lower abdominal pain or headaches.
To date, around 1,750 participants in the BSRBR-AS have completed the fibromyalgia criteria, Dr. Macfarlane said.
Across the board, baseline measures of disease activity were lower in patients who met the fibromyalgia criteria versus those who did not. This included the BASDAI and the Bath Ankylosing Spondylitis Functional Index, where scores were approximately 6.5 and 4.5 for each measure.
“Quality of life was significantly lower in those who were fibromyalgia positive,” Dr. Macfarlane said. Indeed, whatever the measure used, from the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) Scale to the general EuroQoL Quality of Life Scale, there were significant differences between those who did and did not meet fibromyalgia criteria. There were also higher scores for depression, anxiety, poorer-quality sleep, and higher levels of fatigue.
Patients treated with TNFi therapy showed improvement in both BASDAI and ASQoL scores regardless of whether they met fibromyalgia criteria, but crucially, the responses were still lower and significantly different from those without fibromyalgia.
An ASAS20 response to TNFi therapy was met by “slightly fewer” patients who met the fibromyalgia criteria than by those who did not at all follow-up points: at 3 months (about 35% vs. 45%), 6 months (about 58% vs. 61%), and 12 months (about 60% vs. 62%).
A high score on the Symptom Severity Scale but not the Widespread Pain Index of the fibromyalgia criteria was associated with a lower response to TNFi therapy at 3 months. “Such patients may benefit from the use of TNFi and nonpharmacological therapy,” Dr. Macfarlane said.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
SOURCE: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
LIVERPOOL, ENGLAND – Individuals with axial spondyloarthritis (axSpA) who have comorbid fibromyalgia do respond to biologic therapy but at a seemingly lower rate if they have a high symptom score during early assessments.
Data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) showed that participants with axSpA who were starting biologic therapy with a tumor necrosis factor inhibitor (TNFi) for the first time also had worse disease activity at baseline if they met fibromyalgia research criteria than if they did not.
“The issue of fibromyalgia as a comorbidity in axial SpA has been the subject of current considerable interest,” said Dr. Macfarlane, who is Clinical Chair in Epidemiology at the University of Aberdeen (Scotland), where the BSRBR-AS is run. This is for several reasons: “One is the challenge of identifying patients with axial SpA who have comorbid fibromyalgia.
“The second is the concern that comorbid fibromyalgia may have an effect on disease indices such as BASDAI [Bath Ankylosing Spondylitis Disease Activity Index],” Dr. Macfarlane observed.
This leads to the third issue: “Are patients with comorbid fibromyalgia inappropriately receiving biological therapy, and how do they respond if they do receive it?”
Previous data from the BSRBR-AS have shown that approximately one in five patients with axSpA meet research criteria for fibromyalgia (Arthritis Rheumatol. 2017;69:2144-50) and that the prevalence of the comorbidity was higher in those who met Assessment of SpondyloArthritis International Society imaging criteria and lower in those who only met clinical criteria (25% vs. 10%).
The current aims of the study presented by Dr. Macfarlane were to first quantify the extent to which meeting fibromyalgia criteria was associated with higher measures of disease activity and impact, and then to see if meeting these criteria was associated with a poorer response to first use of a TNFi.
In order to find out, Dr. Macfarlane and his associates examined data from the prospective BSRBR-AS, which has been running since 2012. The BSRBR-AS recruits patients with ASAS-confirmed axSpA who are newly starting biologics from 83 U.K. centers.
At recruitment and at 3 months, patients starting biologic treatment undergo several assessments, which since 2015 has included research criteria for fibromyalgia (J Rheumatol. 2011;38:1113–22). The latter incorporate a Widespread Pain Index rated 0-19 and a Symptom Severity Scale rated 0-12 and cover items such as fatigue and waking up unrefreshed, and the presence of lower abdominal pain or headaches.
To date, around 1,750 participants in the BSRBR-AS have completed the fibromyalgia criteria, Dr. Macfarlane said.
Across the board, baseline measures of disease activity were lower in patients who met the fibromyalgia criteria versus those who did not. This included the BASDAI and the Bath Ankylosing Spondylitis Functional Index, where scores were approximately 6.5 and 4.5 for each measure.
“Quality of life was significantly lower in those who were fibromyalgia positive,” Dr. Macfarlane said. Indeed, whatever the measure used, from the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) Scale to the general EuroQoL Quality of Life Scale, there were significant differences between those who did and did not meet fibromyalgia criteria. There were also higher scores for depression, anxiety, poorer-quality sleep, and higher levels of fatigue.
Patients treated with TNFi therapy showed improvement in both BASDAI and ASQoL scores regardless of whether they met fibromyalgia criteria, but crucially, the responses were still lower and significantly different from those without fibromyalgia.
An ASAS20 response to TNFi therapy was met by “slightly fewer” patients who met the fibromyalgia criteria than by those who did not at all follow-up points: at 3 months (about 35% vs. 45%), 6 months (about 58% vs. 61%), and 12 months (about 60% vs. 62%).
A high score on the Symptom Severity Scale but not the Widespread Pain Index of the fibromyalgia criteria was associated with a lower response to TNFi therapy at 3 months. “Such patients may benefit from the use of TNFi and nonpharmacological therapy,” Dr. Macfarlane said.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
SOURCE: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
LIVERPOOL, ENGLAND – Individuals with axial spondyloarthritis (axSpA) who have comorbid fibromyalgia do respond to biologic therapy but at a seemingly lower rate if they have a high symptom score during early assessments.
Data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) showed that participants with axSpA who were starting biologic therapy with a tumor necrosis factor inhibitor (TNFi) for the first time also had worse disease activity at baseline if they met fibromyalgia research criteria than if they did not.
“The issue of fibromyalgia as a comorbidity in axial SpA has been the subject of current considerable interest,” said Dr. Macfarlane, who is Clinical Chair in Epidemiology at the University of Aberdeen (Scotland), where the BSRBR-AS is run. This is for several reasons: “One is the challenge of identifying patients with axial SpA who have comorbid fibromyalgia.
“The second is the concern that comorbid fibromyalgia may have an effect on disease indices such as BASDAI [Bath Ankylosing Spondylitis Disease Activity Index],” Dr. Macfarlane observed.
This leads to the third issue: “Are patients with comorbid fibromyalgia inappropriately receiving biological therapy, and how do they respond if they do receive it?”
Previous data from the BSRBR-AS have shown that approximately one in five patients with axSpA meet research criteria for fibromyalgia (Arthritis Rheumatol. 2017;69:2144-50) and that the prevalence of the comorbidity was higher in those who met Assessment of SpondyloArthritis International Society imaging criteria and lower in those who only met clinical criteria (25% vs. 10%).
The current aims of the study presented by Dr. Macfarlane were to first quantify the extent to which meeting fibromyalgia criteria was associated with higher measures of disease activity and impact, and then to see if meeting these criteria was associated with a poorer response to first use of a TNFi.
In order to find out, Dr. Macfarlane and his associates examined data from the prospective BSRBR-AS, which has been running since 2012. The BSRBR-AS recruits patients with ASAS-confirmed axSpA who are newly starting biologics from 83 U.K. centers.
At recruitment and at 3 months, patients starting biologic treatment undergo several assessments, which since 2015 has included research criteria for fibromyalgia (J Rheumatol. 2011;38:1113–22). The latter incorporate a Widespread Pain Index rated 0-19 and a Symptom Severity Scale rated 0-12 and cover items such as fatigue and waking up unrefreshed, and the presence of lower abdominal pain or headaches.
To date, around 1,750 participants in the BSRBR-AS have completed the fibromyalgia criteria, Dr. Macfarlane said.
Across the board, baseline measures of disease activity were lower in patients who met the fibromyalgia criteria versus those who did not. This included the BASDAI and the Bath Ankylosing Spondylitis Functional Index, where scores were approximately 6.5 and 4.5 for each measure.
“Quality of life was significantly lower in those who were fibromyalgia positive,” Dr. Macfarlane said. Indeed, whatever the measure used, from the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) Scale to the general EuroQoL Quality of Life Scale, there were significant differences between those who did and did not meet fibromyalgia criteria. There were also higher scores for depression, anxiety, poorer-quality sleep, and higher levels of fatigue.
Patients treated with TNFi therapy showed improvement in both BASDAI and ASQoL scores regardless of whether they met fibromyalgia criteria, but crucially, the responses were still lower and significantly different from those without fibromyalgia.
An ASAS20 response to TNFi therapy was met by “slightly fewer” patients who met the fibromyalgia criteria than by those who did not at all follow-up points: at 3 months (about 35% vs. 45%), 6 months (about 58% vs. 61%), and 12 months (about 60% vs. 62%).
A high score on the Symptom Severity Scale but not the Widespread Pain Index of the fibromyalgia criteria was associated with a lower response to TNFi therapy at 3 months. “Such patients may benefit from the use of TNFi and nonpharmacological therapy,” Dr. Macfarlane said.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
SOURCE: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
REPORTING FROM RHEUMATOLOGY 2018
Key clinical point: Comorbid axial spondyloarthritis and fibromyalgia are associated with a lower response to biologic therapy.
Major finding: About 35% vs. 45% of patients who did and did not meet research criteria for fibromyalgia had an ASAS20 response at 3 months.
Study details: Data on 1,750 participants of the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS).
Disclosures: The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
Source: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
Physical therapy, exercise still relevant for ankylosing spondylitis
CAMBRIDGE, MASS. – , according to Angelo Papachristos, an advanced physiotherapist at St. Michaels Hospital in Toronto.
Speaking in an education session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Mr. Papachristos said that therapy should be introduced at diagnosis, individualized, and constantly reevaluated.
“There is no one recommendation,” he said. “Therapy should be monitored and adjusted over time depending on how the patient responds.”
Mr. Papachristos drew attention to two portions of recommendations from the American College of Sports Medicine (ACSM).
First, that scientific evidence demonstrates that the beneficial effects of exercise are indisputable and that the benefits far outweigh the risks.
Second, that a program of regular exercise that includes cardiorespiratory, resistance, flexibility, and neuromotor aspects to improve and maintain fitness and health is essential for most adults.
How much exercise to prescribe and when to introduce exercise remains a question.
The ACSM recommends moderate-intensity cardiovascular exercise for 30 minutes or more each day or 150 minutes per week, resistance training, neuromotor exercise, and flexibility training at least twice each week.
In a 2011 literature review published in Arthritis Care & Research, researchers analyzed 12 studies (826 total patients) to find out if exercise had actual potential for patients with ankylosing spondylitis. They used three criteria: whether the programs were designed using ACSM recommendations, if/how physiological responses were measured, and whether adherence to programs was monitored.
Of the 12 trials, 5 included cardiovascular exercise, 5 included strength training, 11 included flexibility, and 4 reported program adherence.
Only one trial met ACSM recommendations for intensity, duration, frequency, and length of exercise period. That trial showed the greatest improvement in aerobic capacity (Arthritis Car Res. 2011 Apr;63[4]:597-603).
“The literature isn’t impressive,” said Mr. Papachristos. “But, that’s because it isn’t uniform. No specific protocol is being followed.”
He compared what he believes is happening with what he believes to be a better alternative.
What he calls the hit-them-with-everything approach includes diagnosis, NSAIDs, biologics, smoking cessation at the same time as exercise that includes posture, swimming, strength, and aerobic conditioning. According to Mr. Papachristos, this approach can lead to patient burnout.
Indeed, research from 2010 published in the Journal of Rheumatology showed that 40% of patients with ankylosing spondylitis said that exercise takes too much time, 60% said that exercise is hard work, 60% reported being fatigued by exercise, and 20% said that their family members did not encourage exercise (J Rheumatol. 2010 Mar 1. doi: 10.3899/jrheum.090655).
To combat burnout and improve patient outcomes, Mr. Papachristos suggested an alternative approach whereby patients would begin with diagnosis and medication, but disease education and a baseline fitness assessment would also be a priority. The first 6-9 months following diagnosis would then be used to evaluate a patient’s home and work/school ergonomic situation to assess needs. During this time, the patient would be introduced to basic exercises for range of motion and flexibility. Throughout this approach, the patient would be consistently reevaluated and, if appropriate, would slowly ramp up exercise efforts. At 12 months, the patients could graduate to core cervical and lumbar strength before reaching cardiovascular and sports recreation at 12-18 months following diagnosis.
Mr. Papachristos concluded that the coordination between physical therapist, primary care provider, and rheumatologist is of the utmost importance.
“It’s just like anything else – if we’re all on the same page, it’s better for the patient,” he said. “Patients should be encouraged on lifestyle and wellness management with the goal of lifelong regular exercise.”
Mr. Papachristos reported having no disclosures.
CAMBRIDGE, MASS. – , according to Angelo Papachristos, an advanced physiotherapist at St. Michaels Hospital in Toronto.
Speaking in an education session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Mr. Papachristos said that therapy should be introduced at diagnosis, individualized, and constantly reevaluated.
“There is no one recommendation,” he said. “Therapy should be monitored and adjusted over time depending on how the patient responds.”
Mr. Papachristos drew attention to two portions of recommendations from the American College of Sports Medicine (ACSM).
First, that scientific evidence demonstrates that the beneficial effects of exercise are indisputable and that the benefits far outweigh the risks.
Second, that a program of regular exercise that includes cardiorespiratory, resistance, flexibility, and neuromotor aspects to improve and maintain fitness and health is essential for most adults.
How much exercise to prescribe and when to introduce exercise remains a question.
The ACSM recommends moderate-intensity cardiovascular exercise for 30 minutes or more each day or 150 minutes per week, resistance training, neuromotor exercise, and flexibility training at least twice each week.
In a 2011 literature review published in Arthritis Care & Research, researchers analyzed 12 studies (826 total patients) to find out if exercise had actual potential for patients with ankylosing spondylitis. They used three criteria: whether the programs were designed using ACSM recommendations, if/how physiological responses were measured, and whether adherence to programs was monitored.
Of the 12 trials, 5 included cardiovascular exercise, 5 included strength training, 11 included flexibility, and 4 reported program adherence.
Only one trial met ACSM recommendations for intensity, duration, frequency, and length of exercise period. That trial showed the greatest improvement in aerobic capacity (Arthritis Car Res. 2011 Apr;63[4]:597-603).
“The literature isn’t impressive,” said Mr. Papachristos. “But, that’s because it isn’t uniform. No specific protocol is being followed.”
He compared what he believes is happening with what he believes to be a better alternative.
What he calls the hit-them-with-everything approach includes diagnosis, NSAIDs, biologics, smoking cessation at the same time as exercise that includes posture, swimming, strength, and aerobic conditioning. According to Mr. Papachristos, this approach can lead to patient burnout.
Indeed, research from 2010 published in the Journal of Rheumatology showed that 40% of patients with ankylosing spondylitis said that exercise takes too much time, 60% said that exercise is hard work, 60% reported being fatigued by exercise, and 20% said that their family members did not encourage exercise (J Rheumatol. 2010 Mar 1. doi: 10.3899/jrheum.090655).
To combat burnout and improve patient outcomes, Mr. Papachristos suggested an alternative approach whereby patients would begin with diagnosis and medication, but disease education and a baseline fitness assessment would also be a priority. The first 6-9 months following diagnosis would then be used to evaluate a patient’s home and work/school ergonomic situation to assess needs. During this time, the patient would be introduced to basic exercises for range of motion and flexibility. Throughout this approach, the patient would be consistently reevaluated and, if appropriate, would slowly ramp up exercise efforts. At 12 months, the patients could graduate to core cervical and lumbar strength before reaching cardiovascular and sports recreation at 12-18 months following diagnosis.
Mr. Papachristos concluded that the coordination between physical therapist, primary care provider, and rheumatologist is of the utmost importance.
“It’s just like anything else – if we’re all on the same page, it’s better for the patient,” he said. “Patients should be encouraged on lifestyle and wellness management with the goal of lifelong regular exercise.”
Mr. Papachristos reported having no disclosures.
CAMBRIDGE, MASS. – , according to Angelo Papachristos, an advanced physiotherapist at St. Michaels Hospital in Toronto.
Speaking in an education session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Mr. Papachristos said that therapy should be introduced at diagnosis, individualized, and constantly reevaluated.
“There is no one recommendation,” he said. “Therapy should be monitored and adjusted over time depending on how the patient responds.”
Mr. Papachristos drew attention to two portions of recommendations from the American College of Sports Medicine (ACSM).
First, that scientific evidence demonstrates that the beneficial effects of exercise are indisputable and that the benefits far outweigh the risks.
Second, that a program of regular exercise that includes cardiorespiratory, resistance, flexibility, and neuromotor aspects to improve and maintain fitness and health is essential for most adults.
How much exercise to prescribe and when to introduce exercise remains a question.
The ACSM recommends moderate-intensity cardiovascular exercise for 30 minutes or more each day or 150 minutes per week, resistance training, neuromotor exercise, and flexibility training at least twice each week.
In a 2011 literature review published in Arthritis Care & Research, researchers analyzed 12 studies (826 total patients) to find out if exercise had actual potential for patients with ankylosing spondylitis. They used three criteria: whether the programs were designed using ACSM recommendations, if/how physiological responses were measured, and whether adherence to programs was monitored.
Of the 12 trials, 5 included cardiovascular exercise, 5 included strength training, 11 included flexibility, and 4 reported program adherence.
Only one trial met ACSM recommendations for intensity, duration, frequency, and length of exercise period. That trial showed the greatest improvement in aerobic capacity (Arthritis Car Res. 2011 Apr;63[4]:597-603).
“The literature isn’t impressive,” said Mr. Papachristos. “But, that’s because it isn’t uniform. No specific protocol is being followed.”
He compared what he believes is happening with what he believes to be a better alternative.
What he calls the hit-them-with-everything approach includes diagnosis, NSAIDs, biologics, smoking cessation at the same time as exercise that includes posture, swimming, strength, and aerobic conditioning. According to Mr. Papachristos, this approach can lead to patient burnout.
Indeed, research from 2010 published in the Journal of Rheumatology showed that 40% of patients with ankylosing spondylitis said that exercise takes too much time, 60% said that exercise is hard work, 60% reported being fatigued by exercise, and 20% said that their family members did not encourage exercise (J Rheumatol. 2010 Mar 1. doi: 10.3899/jrheum.090655).
To combat burnout and improve patient outcomes, Mr. Papachristos suggested an alternative approach whereby patients would begin with diagnosis and medication, but disease education and a baseline fitness assessment would also be a priority. The first 6-9 months following diagnosis would then be used to evaluate a patient’s home and work/school ergonomic situation to assess needs. During this time, the patient would be introduced to basic exercises for range of motion and flexibility. Throughout this approach, the patient would be consistently reevaluated and, if appropriate, would slowly ramp up exercise efforts. At 12 months, the patients could graduate to core cervical and lumbar strength before reaching cardiovascular and sports recreation at 12-18 months following diagnosis.
Mr. Papachristos concluded that the coordination between physical therapist, primary care provider, and rheumatologist is of the utmost importance.
“It’s just like anything else – if we’re all on the same page, it’s better for the patient,” he said. “Patients should be encouraged on lifestyle and wellness management with the goal of lifelong regular exercise.”
Mr. Papachristos reported having no disclosures.
REPORTING FROM SPARTAN
Certolizumab pegol shows promise for nr-axSpA treatment
Certolizumab pegol was effective at treating nonradiographic axial spondyloarthritis, the first drug to show positive results with the disease, according to topline data from a phase 3, placebo-controlled trial.
After 52 weeks, 47.2% of adult nonradiographic axial spondyloarthritis (nr-axSpA) patients within the C-AXSPAND trial who received certolizumab pegol (Cimzia) achieved at least a 2-point improvement on their Ankylosing Spondylitis Disease Activity Score, compared with 7.0% of nr-axSpA patients who received a placebo. In addition, patients who received certolizumab pegol also met the Assessment of Spondyloarthritis International Society criteria of 40% response after 12 weeks.
“People living with nr-axSpA frequently face delayed or incorrect diagnosis, and currently, in the U.S., there are no FDA-approved options to treat this condition. The C-AXSPAND study results provide important insights into the potential of Cimzia as an effective and durable treatment option for these patients,” Atul Deodhar, MD, professor of medicine at Oregon Health and Science University, Portland, and a lead investigator of the study, said in an announcement from certolizumab’s manufacturer, UCB.
Certolizumab pegol is currently indicated for the treatment of moderate to severe RA, active psoriatic arthritis, and active ankylosing spondylitis, as well as for the reduction of Crohn’s disease symptoms. The most common adverse events in RA, psoriatic arthritis, and ankylosing spondylitis are upper respiratory tract infection, headache, hypertension, nasopharyngitis, back pain, pyrexia, pharyngitis, and rash.
Certolizumab pegol was effective at treating nonradiographic axial spondyloarthritis, the first drug to show positive results with the disease, according to topline data from a phase 3, placebo-controlled trial.
After 52 weeks, 47.2% of adult nonradiographic axial spondyloarthritis (nr-axSpA) patients within the C-AXSPAND trial who received certolizumab pegol (Cimzia) achieved at least a 2-point improvement on their Ankylosing Spondylitis Disease Activity Score, compared with 7.0% of nr-axSpA patients who received a placebo. In addition, patients who received certolizumab pegol also met the Assessment of Spondyloarthritis International Society criteria of 40% response after 12 weeks.
“People living with nr-axSpA frequently face delayed or incorrect diagnosis, and currently, in the U.S., there are no FDA-approved options to treat this condition. The C-AXSPAND study results provide important insights into the potential of Cimzia as an effective and durable treatment option for these patients,” Atul Deodhar, MD, professor of medicine at Oregon Health and Science University, Portland, and a lead investigator of the study, said in an announcement from certolizumab’s manufacturer, UCB.
Certolizumab pegol is currently indicated for the treatment of moderate to severe RA, active psoriatic arthritis, and active ankylosing spondylitis, as well as for the reduction of Crohn’s disease symptoms. The most common adverse events in RA, psoriatic arthritis, and ankylosing spondylitis are upper respiratory tract infection, headache, hypertension, nasopharyngitis, back pain, pyrexia, pharyngitis, and rash.
Certolizumab pegol was effective at treating nonradiographic axial spondyloarthritis, the first drug to show positive results with the disease, according to topline data from a phase 3, placebo-controlled trial.
After 52 weeks, 47.2% of adult nonradiographic axial spondyloarthritis (nr-axSpA) patients within the C-AXSPAND trial who received certolizumab pegol (Cimzia) achieved at least a 2-point improvement on their Ankylosing Spondylitis Disease Activity Score, compared with 7.0% of nr-axSpA patients who received a placebo. In addition, patients who received certolizumab pegol also met the Assessment of Spondyloarthritis International Society criteria of 40% response after 12 weeks.
“People living with nr-axSpA frequently face delayed or incorrect diagnosis, and currently, in the U.S., there are no FDA-approved options to treat this condition. The C-AXSPAND study results provide important insights into the potential of Cimzia as an effective and durable treatment option for these patients,” Atul Deodhar, MD, professor of medicine at Oregon Health and Science University, Portland, and a lead investigator of the study, said in an announcement from certolizumab’s manufacturer, UCB.
Certolizumab pegol is currently indicated for the treatment of moderate to severe RA, active psoriatic arthritis, and active ankylosing spondylitis, as well as for the reduction of Crohn’s disease symptoms. The most common adverse events in RA, psoriatic arthritis, and ankylosing spondylitis are upper respiratory tract infection, headache, hypertension, nasopharyngitis, back pain, pyrexia, pharyngitis, and rash.
MACE risk similar across arthritis subtypes
Rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis were linked to similarly increased risks of major adverse cardiovascular events in a large population-based cohort study.
Inflammation itself drives this relationship and “adequate control of disease activity is needed to lower cardiovascular risk,” wrote Kim Lauper, MD, of Geneva University Hospitals, and her coinvestigators.
Major adverse cardiovascular events (MACE) also were significantly associated with traditional cardiovascular risk factors such as smoking, hypertension, and hyperlipidemia, “stressing the importance of [their] detection and management,” the researchers wrote in Arthritis Care and Research.
Previous studies linked inflammatory arthritis to a 40%-50% increase in risk of cardiovascular events, such as MI and acute coronary syndrome. Inflammatory arthritis also increases the risk of cerebrovascular disease, and traditional cardiovascular risk factors alone do not explain these associations, the researchers noted. Mounting data suggest that inflammation underlies the pathogenesis of atherosclerosis. Other studies have documented the cardioprotective effect of disease-modifying antirheumatic drugs (DMARDs) in patients with rheumatoid arthritis and psoriasis.
Dr. Lauper and her coinvestigators examined the prevalence and incidence of MACE, including MI, transient or permanent cerebrovascular events, or cardiovascular deaths among patients with rheumatoid arthritis, psoriatic arthritis, or spondyloarthritis. The 5,315 patients in the study were part of the Swiss Clinical Quality Management registry, which longitudinally tracks individuals throughout Switzerland who receive biologic DMARDs.
The investigators also asked rheumatologists to supply missing data and used a questionnaire to survey patients about cardiovascular events and associated risk factors. These efforts produced more than 66,000 patient-years of follow-up data, more than half of which were for rheumatoid arthritis and less than 10,000 of which were for psoriatic arthritis.
For every 1,000 patient-years, there were 2.7 MACE for rheumatoid arthritis, 1.4 MACE for axial spondyloarthritis, and 1.4 MACE for psoriatic arthritis. Patients with rheumatoid arthritis tended to be older, which explained most of their excess risk of MACE, the researchers said. Controlling for age only, MACE incidence rate ratios were 1.16 for spondyloarthritis (P = .52) and 0.75 for psoriatic arthritis (P = .34).
The analysis of prevalent MACE included more than 5,000 patients. Nonfatal MACE had affected 4.8% of patients with rheumatoid arthritis, 2.2% of patients with axial spondyloarthritis, and 2.9% of patients with psoriatic arthritis (P less than .001). Once again, differences among groups were not significant after researchers controlled for the older age of the rheumatoid arthritis patients.
Among all patients, independent risk factors for MACE included older age (P less than .001), disease duration (P = .002), male gender (P less than .001), family history of MACE (P = .03), personal history of hyperlipidemia (P less than .001), and hypertension (P = .04). In contrast, there was no link between MACE and use of NSAIDs. “Similarly, a recent Taiwanese nationwide study did not find an increase in coronary disease in patients taking etoricoxib or celecoxib after adjustment for gender, age, comorbidities, hypertension, hyperlipidemia, and DMARDs,” the researchers wrote.Dr. Lauper reported having no conflicts of interest. The senior author and two coinvestigators disclosed ties to Roche, Abbvie, Pfizer, and several other pharmaceutical companies.
SOURCE: Lauper K et al. Arthritis Care Res. 2018 Apr 2. doi: 10.1002/acr.23567.
Rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis were linked to similarly increased risks of major adverse cardiovascular events in a large population-based cohort study.
Inflammation itself drives this relationship and “adequate control of disease activity is needed to lower cardiovascular risk,” wrote Kim Lauper, MD, of Geneva University Hospitals, and her coinvestigators.
Major adverse cardiovascular events (MACE) also were significantly associated with traditional cardiovascular risk factors such as smoking, hypertension, and hyperlipidemia, “stressing the importance of [their] detection and management,” the researchers wrote in Arthritis Care and Research.
Previous studies linked inflammatory arthritis to a 40%-50% increase in risk of cardiovascular events, such as MI and acute coronary syndrome. Inflammatory arthritis also increases the risk of cerebrovascular disease, and traditional cardiovascular risk factors alone do not explain these associations, the researchers noted. Mounting data suggest that inflammation underlies the pathogenesis of atherosclerosis. Other studies have documented the cardioprotective effect of disease-modifying antirheumatic drugs (DMARDs) in patients with rheumatoid arthritis and psoriasis.
Dr. Lauper and her coinvestigators examined the prevalence and incidence of MACE, including MI, transient or permanent cerebrovascular events, or cardiovascular deaths among patients with rheumatoid arthritis, psoriatic arthritis, or spondyloarthritis. The 5,315 patients in the study were part of the Swiss Clinical Quality Management registry, which longitudinally tracks individuals throughout Switzerland who receive biologic DMARDs.
The investigators also asked rheumatologists to supply missing data and used a questionnaire to survey patients about cardiovascular events and associated risk factors. These efforts produced more than 66,000 patient-years of follow-up data, more than half of which were for rheumatoid arthritis and less than 10,000 of which were for psoriatic arthritis.
For every 1,000 patient-years, there were 2.7 MACE for rheumatoid arthritis, 1.4 MACE for axial spondyloarthritis, and 1.4 MACE for psoriatic arthritis. Patients with rheumatoid arthritis tended to be older, which explained most of their excess risk of MACE, the researchers said. Controlling for age only, MACE incidence rate ratios were 1.16 for spondyloarthritis (P = .52) and 0.75 for psoriatic arthritis (P = .34).
The analysis of prevalent MACE included more than 5,000 patients. Nonfatal MACE had affected 4.8% of patients with rheumatoid arthritis, 2.2% of patients with axial spondyloarthritis, and 2.9% of patients with psoriatic arthritis (P less than .001). Once again, differences among groups were not significant after researchers controlled for the older age of the rheumatoid arthritis patients.
Among all patients, independent risk factors for MACE included older age (P less than .001), disease duration (P = .002), male gender (P less than .001), family history of MACE (P = .03), personal history of hyperlipidemia (P less than .001), and hypertension (P = .04). In contrast, there was no link between MACE and use of NSAIDs. “Similarly, a recent Taiwanese nationwide study did not find an increase in coronary disease in patients taking etoricoxib or celecoxib after adjustment for gender, age, comorbidities, hypertension, hyperlipidemia, and DMARDs,” the researchers wrote.Dr. Lauper reported having no conflicts of interest. The senior author and two coinvestigators disclosed ties to Roche, Abbvie, Pfizer, and several other pharmaceutical companies.
SOURCE: Lauper K et al. Arthritis Care Res. 2018 Apr 2. doi: 10.1002/acr.23567.
Rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis were linked to similarly increased risks of major adverse cardiovascular events in a large population-based cohort study.
Inflammation itself drives this relationship and “adequate control of disease activity is needed to lower cardiovascular risk,” wrote Kim Lauper, MD, of Geneva University Hospitals, and her coinvestigators.
Major adverse cardiovascular events (MACE) also were significantly associated with traditional cardiovascular risk factors such as smoking, hypertension, and hyperlipidemia, “stressing the importance of [their] detection and management,” the researchers wrote in Arthritis Care and Research.
Previous studies linked inflammatory arthritis to a 40%-50% increase in risk of cardiovascular events, such as MI and acute coronary syndrome. Inflammatory arthritis also increases the risk of cerebrovascular disease, and traditional cardiovascular risk factors alone do not explain these associations, the researchers noted. Mounting data suggest that inflammation underlies the pathogenesis of atherosclerosis. Other studies have documented the cardioprotective effect of disease-modifying antirheumatic drugs (DMARDs) in patients with rheumatoid arthritis and psoriasis.
Dr. Lauper and her coinvestigators examined the prevalence and incidence of MACE, including MI, transient or permanent cerebrovascular events, or cardiovascular deaths among patients with rheumatoid arthritis, psoriatic arthritis, or spondyloarthritis. The 5,315 patients in the study were part of the Swiss Clinical Quality Management registry, which longitudinally tracks individuals throughout Switzerland who receive biologic DMARDs.
The investigators also asked rheumatologists to supply missing data and used a questionnaire to survey patients about cardiovascular events and associated risk factors. These efforts produced more than 66,000 patient-years of follow-up data, more than half of which were for rheumatoid arthritis and less than 10,000 of which were for psoriatic arthritis.
For every 1,000 patient-years, there were 2.7 MACE for rheumatoid arthritis, 1.4 MACE for axial spondyloarthritis, and 1.4 MACE for psoriatic arthritis. Patients with rheumatoid arthritis tended to be older, which explained most of their excess risk of MACE, the researchers said. Controlling for age only, MACE incidence rate ratios were 1.16 for spondyloarthritis (P = .52) and 0.75 for psoriatic arthritis (P = .34).
The analysis of prevalent MACE included more than 5,000 patients. Nonfatal MACE had affected 4.8% of patients with rheumatoid arthritis, 2.2% of patients with axial spondyloarthritis, and 2.9% of patients with psoriatic arthritis (P less than .001). Once again, differences among groups were not significant after researchers controlled for the older age of the rheumatoid arthritis patients.
Among all patients, independent risk factors for MACE included older age (P less than .001), disease duration (P = .002), male gender (P less than .001), family history of MACE (P = .03), personal history of hyperlipidemia (P less than .001), and hypertension (P = .04). In contrast, there was no link between MACE and use of NSAIDs. “Similarly, a recent Taiwanese nationwide study did not find an increase in coronary disease in patients taking etoricoxib or celecoxib after adjustment for gender, age, comorbidities, hypertension, hyperlipidemia, and DMARDs,” the researchers wrote.Dr. Lauper reported having no conflicts of interest. The senior author and two coinvestigators disclosed ties to Roche, Abbvie, Pfizer, and several other pharmaceutical companies.
SOURCE: Lauper K et al. Arthritis Care Res. 2018 Apr 2. doi: 10.1002/acr.23567.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: Risk of major adverse cardiovascular events (MACE) was similar for patients with rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis.
Major finding: For every 1,000 patient-years, there were 2.7 MACE for rheumatoid arthritis, 1.4 MACE for axial spondyloarthritis, and 1.4 MACE for psoriatic arthritis. The older age of patients with rheumatoid arthritis explained most of their elevated absolute risk.
Study details: Population-based cohort study of 5,315 patients.
Disclosures: Dr. Lauper reported having no conflicts of interest. The senior author and two coinvestigators disclosed ties to Roche, Abbvie, Pfizer, and several other pharmaceutical companies.
Source: Lauper K et al. Arthritis Care Res. 2018 Apr 2. doi: 10.1002/acr.23567.
Reassurance for women taking certolizumab during pregnancy
according to results of a new study.
Megan E.B. Clowse, MD, of Duke University Medical Center, Durham, N.C., and her coauthors reported on a prospective and retrospective analysis of data from 528 pregnancies – including 10 twin pregnancies – in which the mother was exposed to the anti–tumor necrosis factor (anti-TNF) drug certolizumab during pregnancy.
There were 459 (85.3%) live births, 47 (8.7%) miscarriages, 27 (5%) elective abortions, and five (0.9%) stillbirths, figures that are similar to those seen in the general population. Among the singleton births, 11.7% were low birth weight, which the authors noted was slightly higher than the frequency observed in the general population but was in line with previous reports with TNF inhibitors.
Two cases of neonatal death were reported. One occurred in one member of a female twin pair, born at 25 weeks, who succumbed to brain damage and pneumoperitoneum. The other was also in female twins, born at 27 weeks, in which one of the pair was born with a heart defect and died during surgery for an unspecified infection of the intestines, the authors reported in Arthritis & Rheumatology.
The study noted eight (1.7%) reports of congenital malformations in the infants born alive, including accessory auricle, polydactyly, hydronephrosis, cerebral ventricle dilatation, and congenital heart disease.
Four cases were in infants whose mothers had rheumatoid arthritis, one in an infant whose mother had ankylosing spondylitis, and three in infants whose mothers had Crohn’s disease (CD).
In five cases, the women were exposed to certolizumab at least in the first trimester, in four they were exposed at least in the second trimester, and in five cases, the women were exposed at least during the third trimester of pregnancy.
“The teratologist review concluded no temporal association with CZP [certolizumab] exposure for the case of hydronephrosis, owing to evidence of anomalies on ultrasound prior to initiation of medication (during the third trimester); the possibility of an association could not be ruled out for the cases of anal fistula, accessory auricle, vesicoureteric reflux, talipes, and congenital heart disease,” the researchers wrote.
Twenty-two women (4.2%) had serious infections during pregnancy, which was in line with the frequency of serious infections reported in patients taking certolizumab.
Among the live births, nearly half (44.5%) reported certolizumab exposure during all three trimesters, 81.2% reported exposure at least during the first trimester, and 29.2% were exposed during the first trimester only.
“More women with rheumatic diseases than CD had first-trimester–only or first- and second-trimester exposure to CZP, reflecting the differing clinical practice between CD and rheumatic diseases,” the authors wrote. “Spontaneous disease improvement in women with IBD [inflammatory bowel disease] during pregnancy is less likely, compared to RA and other rheumatic diseases, and many patients may require treatment throughout pregnancy; thus, potentially reducing the risk of adverse outcomes, such as spontaneous miscarriage, premature birth, low birth weight, small gestational age.”
The authors commented that, despite increasing evidence of the safety of TNF inhibitors during pregnancy – recent systematic reviews and meta-analyses have found no link to adverse outcomes with anti-TNF exposure during the first trimester – patients and physicians still have had concerns about their use.
“This analysis of prospective pregnancy reports from the UCB Pharma safety database represents the largest published cohort of pregnant women exposed to an anti-TNF for the management of chronic inflammatory diseases,” the authors wrote. “It addresses the need for new and detailed studies on the impact of drug exposure during pregnancy and supports the conclusion that CZP exposure in utero does not appear to increase the risk of major congenital malformations or fetal loss.”
However, they acknowledged the lack of an untreated control group and said this meant a formal statistical analysis was not possible. They also noted that outcomes data were not available for about one-third of the entire cohort of 1,137 women whose pregnancies were exposed to certolizumab.
“However, these data are reassuring for women of childbearing age affected by chronic inflammatory diseases who need an anti-TNF to control their condition and wish to become or are pregnant during CZP treatment,” they wrote.
The study was funded by UCB Pharma. One author was a contractor for, and three were employees of, UCB Pharma. Six authors declared grants, consulting fees, and other remuneration from pharmaceutical companies, including UCB Pharma.
SOURCE: Clowse MEB et al. Arthritis & Rheumatology. 2018 Apr 5. doi: 10.1002/art.40508.
according to results of a new study.
Megan E.B. Clowse, MD, of Duke University Medical Center, Durham, N.C., and her coauthors reported on a prospective and retrospective analysis of data from 528 pregnancies – including 10 twin pregnancies – in which the mother was exposed to the anti–tumor necrosis factor (anti-TNF) drug certolizumab during pregnancy.
There were 459 (85.3%) live births, 47 (8.7%) miscarriages, 27 (5%) elective abortions, and five (0.9%) stillbirths, figures that are similar to those seen in the general population. Among the singleton births, 11.7% were low birth weight, which the authors noted was slightly higher than the frequency observed in the general population but was in line with previous reports with TNF inhibitors.
Two cases of neonatal death were reported. One occurred in one member of a female twin pair, born at 25 weeks, who succumbed to brain damage and pneumoperitoneum. The other was also in female twins, born at 27 weeks, in which one of the pair was born with a heart defect and died during surgery for an unspecified infection of the intestines, the authors reported in Arthritis & Rheumatology.
The study noted eight (1.7%) reports of congenital malformations in the infants born alive, including accessory auricle, polydactyly, hydronephrosis, cerebral ventricle dilatation, and congenital heart disease.
Four cases were in infants whose mothers had rheumatoid arthritis, one in an infant whose mother had ankylosing spondylitis, and three in infants whose mothers had Crohn’s disease (CD).
In five cases, the women were exposed to certolizumab at least in the first trimester, in four they were exposed at least in the second trimester, and in five cases, the women were exposed at least during the third trimester of pregnancy.
“The teratologist review concluded no temporal association with CZP [certolizumab] exposure for the case of hydronephrosis, owing to evidence of anomalies on ultrasound prior to initiation of medication (during the third trimester); the possibility of an association could not be ruled out for the cases of anal fistula, accessory auricle, vesicoureteric reflux, talipes, and congenital heart disease,” the researchers wrote.
Twenty-two women (4.2%) had serious infections during pregnancy, which was in line with the frequency of serious infections reported in patients taking certolizumab.
Among the live births, nearly half (44.5%) reported certolizumab exposure during all three trimesters, 81.2% reported exposure at least during the first trimester, and 29.2% were exposed during the first trimester only.
“More women with rheumatic diseases than CD had first-trimester–only or first- and second-trimester exposure to CZP, reflecting the differing clinical practice between CD and rheumatic diseases,” the authors wrote. “Spontaneous disease improvement in women with IBD [inflammatory bowel disease] during pregnancy is less likely, compared to RA and other rheumatic diseases, and many patients may require treatment throughout pregnancy; thus, potentially reducing the risk of adverse outcomes, such as spontaneous miscarriage, premature birth, low birth weight, small gestational age.”
The authors commented that, despite increasing evidence of the safety of TNF inhibitors during pregnancy – recent systematic reviews and meta-analyses have found no link to adverse outcomes with anti-TNF exposure during the first trimester – patients and physicians still have had concerns about their use.
“This analysis of prospective pregnancy reports from the UCB Pharma safety database represents the largest published cohort of pregnant women exposed to an anti-TNF for the management of chronic inflammatory diseases,” the authors wrote. “It addresses the need for new and detailed studies on the impact of drug exposure during pregnancy and supports the conclusion that CZP exposure in utero does not appear to increase the risk of major congenital malformations or fetal loss.”
However, they acknowledged the lack of an untreated control group and said this meant a formal statistical analysis was not possible. They also noted that outcomes data were not available for about one-third of the entire cohort of 1,137 women whose pregnancies were exposed to certolizumab.
“However, these data are reassuring for women of childbearing age affected by chronic inflammatory diseases who need an anti-TNF to control their condition and wish to become or are pregnant during CZP treatment,” they wrote.
The study was funded by UCB Pharma. One author was a contractor for, and three were employees of, UCB Pharma. Six authors declared grants, consulting fees, and other remuneration from pharmaceutical companies, including UCB Pharma.
SOURCE: Clowse MEB et al. Arthritis & Rheumatology. 2018 Apr 5. doi: 10.1002/art.40508.
according to results of a new study.
Megan E.B. Clowse, MD, of Duke University Medical Center, Durham, N.C., and her coauthors reported on a prospective and retrospective analysis of data from 528 pregnancies – including 10 twin pregnancies – in which the mother was exposed to the anti–tumor necrosis factor (anti-TNF) drug certolizumab during pregnancy.
There were 459 (85.3%) live births, 47 (8.7%) miscarriages, 27 (5%) elective abortions, and five (0.9%) stillbirths, figures that are similar to those seen in the general population. Among the singleton births, 11.7% were low birth weight, which the authors noted was slightly higher than the frequency observed in the general population but was in line with previous reports with TNF inhibitors.
Two cases of neonatal death were reported. One occurred in one member of a female twin pair, born at 25 weeks, who succumbed to brain damage and pneumoperitoneum. The other was also in female twins, born at 27 weeks, in which one of the pair was born with a heart defect and died during surgery for an unspecified infection of the intestines, the authors reported in Arthritis & Rheumatology.
The study noted eight (1.7%) reports of congenital malformations in the infants born alive, including accessory auricle, polydactyly, hydronephrosis, cerebral ventricle dilatation, and congenital heart disease.
Four cases were in infants whose mothers had rheumatoid arthritis, one in an infant whose mother had ankylosing spondylitis, and three in infants whose mothers had Crohn’s disease (CD).
In five cases, the women were exposed to certolizumab at least in the first trimester, in four they were exposed at least in the second trimester, and in five cases, the women were exposed at least during the third trimester of pregnancy.
“The teratologist review concluded no temporal association with CZP [certolizumab] exposure for the case of hydronephrosis, owing to evidence of anomalies on ultrasound prior to initiation of medication (during the third trimester); the possibility of an association could not be ruled out for the cases of anal fistula, accessory auricle, vesicoureteric reflux, talipes, and congenital heart disease,” the researchers wrote.
Twenty-two women (4.2%) had serious infections during pregnancy, which was in line with the frequency of serious infections reported in patients taking certolizumab.
Among the live births, nearly half (44.5%) reported certolizumab exposure during all three trimesters, 81.2% reported exposure at least during the first trimester, and 29.2% were exposed during the first trimester only.
“More women with rheumatic diseases than CD had first-trimester–only or first- and second-trimester exposure to CZP, reflecting the differing clinical practice between CD and rheumatic diseases,” the authors wrote. “Spontaneous disease improvement in women with IBD [inflammatory bowel disease] during pregnancy is less likely, compared to RA and other rheumatic diseases, and many patients may require treatment throughout pregnancy; thus, potentially reducing the risk of adverse outcomes, such as spontaneous miscarriage, premature birth, low birth weight, small gestational age.”
The authors commented that, despite increasing evidence of the safety of TNF inhibitors during pregnancy – recent systematic reviews and meta-analyses have found no link to adverse outcomes with anti-TNF exposure during the first trimester – patients and physicians still have had concerns about their use.
“This analysis of prospective pregnancy reports from the UCB Pharma safety database represents the largest published cohort of pregnant women exposed to an anti-TNF for the management of chronic inflammatory diseases,” the authors wrote. “It addresses the need for new and detailed studies on the impact of drug exposure during pregnancy and supports the conclusion that CZP exposure in utero does not appear to increase the risk of major congenital malformations or fetal loss.”
However, they acknowledged the lack of an untreated control group and said this meant a formal statistical analysis was not possible. They also noted that outcomes data were not available for about one-third of the entire cohort of 1,137 women whose pregnancies were exposed to certolizumab.
“However, these data are reassuring for women of childbearing age affected by chronic inflammatory diseases who need an anti-TNF to control their condition and wish to become or are pregnant during CZP treatment,” they wrote.
The study was funded by UCB Pharma. One author was a contractor for, and three were employees of, UCB Pharma. Six authors declared grants, consulting fees, and other remuneration from pharmaceutical companies, including UCB Pharma.
SOURCE: Clowse MEB et al. Arthritis & Rheumatology. 2018 Apr 5. doi: 10.1002/art.40508.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Certolizumab use during pregnancy does not appear to increase the risk of congenital malformations.
Major finding: The incidence of fetal death and congenital malformations in certolizumab-exposed pregnancies is similar to that in the general population.
Study details: A prospective and retrospective analysis of data from 528 certolizumab-exposed pregnancies.
Disclosures: The study was funded by UCB Pharma. One author was a contractor for UCB Pharma, and three were employees of, UCB Pharma. Six authors declared grants, consulting fees, and other remuneration from pharmaceutical companies, including UCB Pharma.
Source: Clowse MEB et al. Arthritis & Rheumatology. 2018 Apr 5. doi: 10.1002/art.40508
TB in 2017: Good news and bad news
according to the Centers for Disease Control and Prevention.
Those new lows – TB incidence of 2.8 per 100,000 persons and 9,093 new cases – continue a downward trend that started in 1993, but the current rate of decline is much lower than the threshold needed to eliminate TB by the year 2100, Rebekah J. Stewart and her associates at the CDC’s Division of Tuberculosis Elimination, Atlanta, wrote in the Morbidity and Mortality Weekly Report.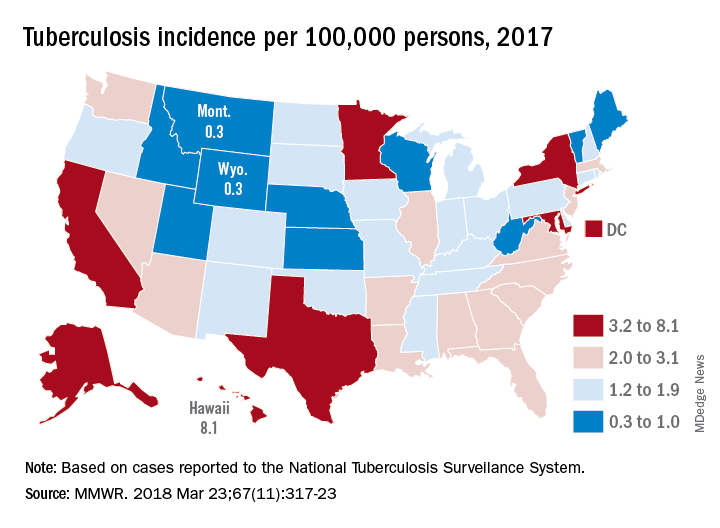
Geographically, at least, the states with populations at the highest risk are Hawaii, which had a TB incidence of 8.1 per 100,000 persons in 2017, and Alaska, with an incidence of 7.0 per 100,000. California and the District of Columbia were next, each with an incidence of 5.2. The states with the lowest rates were Montana and Wyoming at 0.3 per 100,000, the investigators reported, based on data from the National Tuberculosis Surveillance System as of Feb. 12, 2018.
Groups most affected by TB include persons housed in congregate settings – homeless shelters, long-term care facilities, and correctional facilities – and those from countries that have high TB prevalence. Overall incidence for non–U.S. born residents was 14.6 per 100,000 in 2017, compared with 1.0 for the native born, with large discrepancies seen between U.S. and non–U.S. born blacks (2.8 vs. 22.0), native Hawaiian/Pacific Islanders (6.5 vs. 21.0), and Asians (2.0 vs. 27.0), Ms. Stewart and her associates said.
“Increased support of global TB elimination efforts would help to reduce global … prevalence, thereby indirectly reducing the incidence of reactivation TB in the United States among non–U.S. born persons from higher-prevalence countries,” they wrote.
The issue of global action on TB was addressed by the Forum of International Respiratory Societies in a statement recognizing World TB Day (March 24). “TB is the world’s most common infectious disease killer, yet is identifiable, treatable and preventable; what is missing is the political will to dedicate the resources necessary to eradicate it, once and for all,” said Dean E. Schraufnagel, MD, the organization’s executive director.
SOURCE: Stewart RJ et al. MMWR 2018 Mar 23;67(11):317-23.
according to the Centers for Disease Control and Prevention.
Those new lows – TB incidence of 2.8 per 100,000 persons and 9,093 new cases – continue a downward trend that started in 1993, but the current rate of decline is much lower than the threshold needed to eliminate TB by the year 2100, Rebekah J. Stewart and her associates at the CDC’s Division of Tuberculosis Elimination, Atlanta, wrote in the Morbidity and Mortality Weekly Report.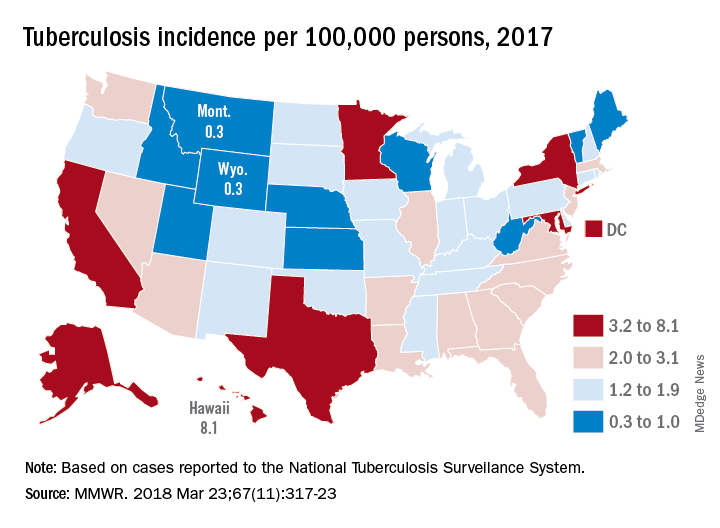
Geographically, at least, the states with populations at the highest risk are Hawaii, which had a TB incidence of 8.1 per 100,000 persons in 2017, and Alaska, with an incidence of 7.0 per 100,000. California and the District of Columbia were next, each with an incidence of 5.2. The states with the lowest rates were Montana and Wyoming at 0.3 per 100,000, the investigators reported, based on data from the National Tuberculosis Surveillance System as of Feb. 12, 2018.
Groups most affected by TB include persons housed in congregate settings – homeless shelters, long-term care facilities, and correctional facilities – and those from countries that have high TB prevalence. Overall incidence for non–U.S. born residents was 14.6 per 100,000 in 2017, compared with 1.0 for the native born, with large discrepancies seen between U.S. and non–U.S. born blacks (2.8 vs. 22.0), native Hawaiian/Pacific Islanders (6.5 vs. 21.0), and Asians (2.0 vs. 27.0), Ms. Stewart and her associates said.
“Increased support of global TB elimination efforts would help to reduce global … prevalence, thereby indirectly reducing the incidence of reactivation TB in the United States among non–U.S. born persons from higher-prevalence countries,” they wrote.
The issue of global action on TB was addressed by the Forum of International Respiratory Societies in a statement recognizing World TB Day (March 24). “TB is the world’s most common infectious disease killer, yet is identifiable, treatable and preventable; what is missing is the political will to dedicate the resources necessary to eradicate it, once and for all,” said Dean E. Schraufnagel, MD, the organization’s executive director.
SOURCE: Stewart RJ et al. MMWR 2018 Mar 23;67(11):317-23.
according to the Centers for Disease Control and Prevention.
Those new lows – TB incidence of 2.8 per 100,000 persons and 9,093 new cases – continue a downward trend that started in 1993, but the current rate of decline is much lower than the threshold needed to eliminate TB by the year 2100, Rebekah J. Stewart and her associates at the CDC’s Division of Tuberculosis Elimination, Atlanta, wrote in the Morbidity and Mortality Weekly Report.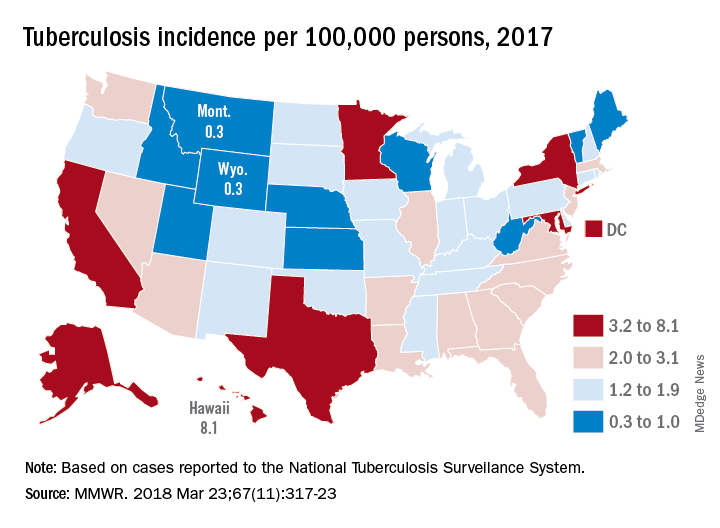
Geographically, at least, the states with populations at the highest risk are Hawaii, which had a TB incidence of 8.1 per 100,000 persons in 2017, and Alaska, with an incidence of 7.0 per 100,000. California and the District of Columbia were next, each with an incidence of 5.2. The states with the lowest rates were Montana and Wyoming at 0.3 per 100,000, the investigators reported, based on data from the National Tuberculosis Surveillance System as of Feb. 12, 2018.
Groups most affected by TB include persons housed in congregate settings – homeless shelters, long-term care facilities, and correctional facilities – and those from countries that have high TB prevalence. Overall incidence for non–U.S. born residents was 14.6 per 100,000 in 2017, compared with 1.0 for the native born, with large discrepancies seen between U.S. and non–U.S. born blacks (2.8 vs. 22.0), native Hawaiian/Pacific Islanders (6.5 vs. 21.0), and Asians (2.0 vs. 27.0), Ms. Stewart and her associates said.
“Increased support of global TB elimination efforts would help to reduce global … prevalence, thereby indirectly reducing the incidence of reactivation TB in the United States among non–U.S. born persons from higher-prevalence countries,” they wrote.
The issue of global action on TB was addressed by the Forum of International Respiratory Societies in a statement recognizing World TB Day (March 24). “TB is the world’s most common infectious disease killer, yet is identifiable, treatable and preventable; what is missing is the political will to dedicate the resources necessary to eradicate it, once and for all,” said Dean E. Schraufnagel, MD, the organization’s executive director.
SOURCE: Stewart RJ et al. MMWR 2018 Mar 23;67(11):317-23.
FROM MMWR
Axial SpA disease activity remains mostly stable throughout pregnancy
, according to results of a prospective study.
“In the largest prospective study to date exploring disease activity during pregnancy in women with axSpA, we found that the majority experienced stable, low disease activity,” Kristin Ursin, MD, of the Trondheim (Norway) University Hospital and her associates wrote in Rheumatology. “In accordance with two previous studies, we found a small increase in disease activity in the second trimester.”
All women in the study fulfilled the Assessment of SpondyloArthritis International Society criteria for axSpA and had seven clinic visits throughout their pregnancy: one before conception, one at each trimester, another at 6 weeks, and two visits 6 and 12 months after delivery. No differentiation was made between women with radiographic or nonradiographic axSpA. At each visit, patients’ disease activity was determined using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), which is calculated based on six patient factors scored from 1 to 10, including: fatigue, back pain, peripheral joint pain and swelling, localized tenderness, duration of morning stiffness, and severity of morning stiffness. A disease score of 4 is commonly used to define active disease. Disease activity was also assessed by measuring C-reactive protein (CRP). Women’s function and health was also assessed using the Bath Ankylosing Spondylitis Functional Index (BASFI), scored similarly to the BASDAI, and the RAND-36 questionnaire to assess general health.
The research team found that, across the span of pregnancy, axSpA disease activity was relatively low and consistent throughout the study. But there was a significant relationship between disease activity and time (P = .029) in which disease activity was highest during the second trimester and proved to be significantly higher than 6 weeks after giving birth (mean BASDAI 3.97 vs. 3.46, P = .005). In fact, 45% of women had active disease in their second trimester (BASDAI of 4 or greater). But among women with data from the second trimester and 6 weeks post partum, 42% had a decrease in BASDAI score of 1 or more, and 22% had an equivalent increase. CRP values remained low and stable throughout the study.
Like the BASDAI scores, physical function and well being seemed to correlate with later time points during pregnancy. The lowest level of physical functioning for most women was during the second and third trimesters, and those periods were significantly worse than 6 weeks after giving birth (mean BASFI of 3.2 during the second trimester and 3.6 during the third vs. 2.6 at 6 weeks post partum). Similarly, patients reported overall worse general health during the second and third trimesters, compared with 6 weeks after giving birth, based on RAND-36 scores (mean physical functioning score of 63.1 in the second trimester and 54.5 in the third vs. 71.0 at 6 weeks post partum).
Use of nonbiologic medications remained relatively stable during pregnancy, while biologic disease-modifying antirheumatic drug (DMARD) use (all tumor necrosis factor [TNF] inhibitors) dropped significantly when pregnancy was confirmed. About 20% used NSAIDs during pregnancy, except for during the third trimester when use decreased to 8%. Prednisolone use remained stable at 5%-8%. A total of 11% had used synthetic DMARDs prior to pregnancy, and this rate stayed at 10%-16% during the three trimesters. Overall, 44% had used a biologic DMARD (TNF inhibitor) prior to pregnancy, but this declined sharply to 6% during the first trimester and 1% in the third.
The main limitations of the study included not having data from all of the women for all the time points. In fact, only 22% were included prior to conceiving, which could suggest that women with low disease activity were less likely to visit their rheumatologist, thereby biasing the sample toward an overestimated disease activity at preconception that could have potentially hidden a “more evident deterioration between the preconception visit and the second trimester,” the authors said.
“Future research on pregnancy in women with axSpA should differentiate between subgroups of the disease and aim to include objective assessment of inflammation.”
The study was funded by the Research Fund of the Norwegian Organization for People With Rheumatic Diseases. None of the authors had any conflicts of interest to declare.
SOURCE: Ursin K et al. Rheumatology. 2018 Mar 14. doi: 10.1093/rheumatology/key047.
, according to results of a prospective study.
“In the largest prospective study to date exploring disease activity during pregnancy in women with axSpA, we found that the majority experienced stable, low disease activity,” Kristin Ursin, MD, of the Trondheim (Norway) University Hospital and her associates wrote in Rheumatology. “In accordance with two previous studies, we found a small increase in disease activity in the second trimester.”
All women in the study fulfilled the Assessment of SpondyloArthritis International Society criteria for axSpA and had seven clinic visits throughout their pregnancy: one before conception, one at each trimester, another at 6 weeks, and two visits 6 and 12 months after delivery. No differentiation was made between women with radiographic or nonradiographic axSpA. At each visit, patients’ disease activity was determined using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), which is calculated based on six patient factors scored from 1 to 10, including: fatigue, back pain, peripheral joint pain and swelling, localized tenderness, duration of morning stiffness, and severity of morning stiffness. A disease score of 4 is commonly used to define active disease. Disease activity was also assessed by measuring C-reactive protein (CRP). Women’s function and health was also assessed using the Bath Ankylosing Spondylitis Functional Index (BASFI), scored similarly to the BASDAI, and the RAND-36 questionnaire to assess general health.
The research team found that, across the span of pregnancy, axSpA disease activity was relatively low and consistent throughout the study. But there was a significant relationship between disease activity and time (P = .029) in which disease activity was highest during the second trimester and proved to be significantly higher than 6 weeks after giving birth (mean BASDAI 3.97 vs. 3.46, P = .005). In fact, 45% of women had active disease in their second trimester (BASDAI of 4 or greater). But among women with data from the second trimester and 6 weeks post partum, 42% had a decrease in BASDAI score of 1 or more, and 22% had an equivalent increase. CRP values remained low and stable throughout the study.
Like the BASDAI scores, physical function and well being seemed to correlate with later time points during pregnancy. The lowest level of physical functioning for most women was during the second and third trimesters, and those periods were significantly worse than 6 weeks after giving birth (mean BASFI of 3.2 during the second trimester and 3.6 during the third vs. 2.6 at 6 weeks post partum). Similarly, patients reported overall worse general health during the second and third trimesters, compared with 6 weeks after giving birth, based on RAND-36 scores (mean physical functioning score of 63.1 in the second trimester and 54.5 in the third vs. 71.0 at 6 weeks post partum).
Use of nonbiologic medications remained relatively stable during pregnancy, while biologic disease-modifying antirheumatic drug (DMARD) use (all tumor necrosis factor [TNF] inhibitors) dropped significantly when pregnancy was confirmed. About 20% used NSAIDs during pregnancy, except for during the third trimester when use decreased to 8%. Prednisolone use remained stable at 5%-8%. A total of 11% had used synthetic DMARDs prior to pregnancy, and this rate stayed at 10%-16% during the three trimesters. Overall, 44% had used a biologic DMARD (TNF inhibitor) prior to pregnancy, but this declined sharply to 6% during the first trimester and 1% in the third.
The main limitations of the study included not having data from all of the women for all the time points. In fact, only 22% were included prior to conceiving, which could suggest that women with low disease activity were less likely to visit their rheumatologist, thereby biasing the sample toward an overestimated disease activity at preconception that could have potentially hidden a “more evident deterioration between the preconception visit and the second trimester,” the authors said.
“Future research on pregnancy in women with axSpA should differentiate between subgroups of the disease and aim to include objective assessment of inflammation.”
The study was funded by the Research Fund of the Norwegian Organization for People With Rheumatic Diseases. None of the authors had any conflicts of interest to declare.
SOURCE: Ursin K et al. Rheumatology. 2018 Mar 14. doi: 10.1093/rheumatology/key047.
, according to results of a prospective study.
“In the largest prospective study to date exploring disease activity during pregnancy in women with axSpA, we found that the majority experienced stable, low disease activity,” Kristin Ursin, MD, of the Trondheim (Norway) University Hospital and her associates wrote in Rheumatology. “In accordance with two previous studies, we found a small increase in disease activity in the second trimester.”
All women in the study fulfilled the Assessment of SpondyloArthritis International Society criteria for axSpA and had seven clinic visits throughout their pregnancy: one before conception, one at each trimester, another at 6 weeks, and two visits 6 and 12 months after delivery. No differentiation was made between women with radiographic or nonradiographic axSpA. At each visit, patients’ disease activity was determined using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), which is calculated based on six patient factors scored from 1 to 10, including: fatigue, back pain, peripheral joint pain and swelling, localized tenderness, duration of morning stiffness, and severity of morning stiffness. A disease score of 4 is commonly used to define active disease. Disease activity was also assessed by measuring C-reactive protein (CRP). Women’s function and health was also assessed using the Bath Ankylosing Spondylitis Functional Index (BASFI), scored similarly to the BASDAI, and the RAND-36 questionnaire to assess general health.
The research team found that, across the span of pregnancy, axSpA disease activity was relatively low and consistent throughout the study. But there was a significant relationship between disease activity and time (P = .029) in which disease activity was highest during the second trimester and proved to be significantly higher than 6 weeks after giving birth (mean BASDAI 3.97 vs. 3.46, P = .005). In fact, 45% of women had active disease in their second trimester (BASDAI of 4 or greater). But among women with data from the second trimester and 6 weeks post partum, 42% had a decrease in BASDAI score of 1 or more, and 22% had an equivalent increase. CRP values remained low and stable throughout the study.
Like the BASDAI scores, physical function and well being seemed to correlate with later time points during pregnancy. The lowest level of physical functioning for most women was during the second and third trimesters, and those periods were significantly worse than 6 weeks after giving birth (mean BASFI of 3.2 during the second trimester and 3.6 during the third vs. 2.6 at 6 weeks post partum). Similarly, patients reported overall worse general health during the second and third trimesters, compared with 6 weeks after giving birth, based on RAND-36 scores (mean physical functioning score of 63.1 in the second trimester and 54.5 in the third vs. 71.0 at 6 weeks post partum).
Use of nonbiologic medications remained relatively stable during pregnancy, while biologic disease-modifying antirheumatic drug (DMARD) use (all tumor necrosis factor [TNF] inhibitors) dropped significantly when pregnancy was confirmed. About 20% used NSAIDs during pregnancy, except for during the third trimester when use decreased to 8%. Prednisolone use remained stable at 5%-8%. A total of 11% had used synthetic DMARDs prior to pregnancy, and this rate stayed at 10%-16% during the three trimesters. Overall, 44% had used a biologic DMARD (TNF inhibitor) prior to pregnancy, but this declined sharply to 6% during the first trimester and 1% in the third.
The main limitations of the study included not having data from all of the women for all the time points. In fact, only 22% were included prior to conceiving, which could suggest that women with low disease activity were less likely to visit their rheumatologist, thereby biasing the sample toward an overestimated disease activity at preconception that could have potentially hidden a “more evident deterioration between the preconception visit and the second trimester,” the authors said.
“Future research on pregnancy in women with axSpA should differentiate between subgroups of the disease and aim to include objective assessment of inflammation.”
The study was funded by the Research Fund of the Norwegian Organization for People With Rheumatic Diseases. None of the authors had any conflicts of interest to declare.
SOURCE: Ursin K et al. Rheumatology. 2018 Mar 14. doi: 10.1093/rheumatology/key047.
FROM RHEUMATOLOGY
Key clinical point: Higher disease activity and lower physical well being correspond with late stage pregnancy.
Major finding: Disease activity appears to be highest in the second trimester, compared with 6 weeks post partum (mean BASDAI 3.97 vs. 3.46, P = .005).
Study details: A prospective study of 179 pregnancies in 166 Norwegian women with axSpA from a Norwegian health registry between 2006 and 2016.
Disclosures: The study was funded by the Research Fund of the Norwegian Organization for People With Rheumatic Diseases. None of the authors had any conflicts of interest to declare.
Source: Ursin K et al. Rheumatology. 2018 Mar 14. doi: 10.1093/rheumatology/key047.