User login
Serum testosterone and estradiol levels associated with current asthma in women
possibly explaining in part the different prevalence of asthma in men and women, according to the findings of a large cross-sectional population based study.
Yueh-Ying Han, PhD, of the Children’s Hospital of Pittsburgh and colleagues investigated the role of free testosterone and estradiol levels and current asthma among adults. The impact of obesity on that association was also examined. The investigators analyzed data from 7,615 adults (3,953 men and 3,662 women) who participated in the 2013-2014 and 2015-2016 U.S. National Health and Nutrition Examination Survey. The data included health interviews, examination components, and laboratory tests on each patient. Serum samples were analyzed by the division of laboratory sciences of the Centers for Disease Control and Prevention. Logistic regression was used for the multivariable analysis of sex hormone levels (as quartiles) and current asthma, and the analysis was done separately on men and women. Pregnant women were excluded, in addition to individuals with incomplete data. The exclusions tended to be Hispanic, former smokers, lower income, and lacking private insurance. The overall prevalence of current asthma in the sample was 9% (6% in men and 13% in women).
Three models were generated based on serum levels in women and in men.
For model 1 (unadjusted for estradiol), women whose serum testosterone levels were in the second and fourth quartiles had 30%-45% significantly lower odds of having current asthma than those whose serum testosterone level was in the lowest quartile. Among men, those whose serum testosterone levels were in the second and fourth quartiles had 12%-13% lower odds for current asthma.
For model 2 (unadjusted for free testosterone), women whose serum estradiol levels were in the third quartile had 34% significantly lower odds of having current asthma than those whose estradiol levels were in the lowest quartile. The findings were similar for men, that is, those whose serum estradiol levels were in the third quartile had 30% lower odds for having asthma, compared with those with in the lowest quartile.
For model 3 (a multivariable model including serum levels of both estradiol and free testosterone), women whose serum testosterone levels were in the second and fourth quartiles had 30% and 44% lower odds of current asthma than those whose serum testosterone levels were in the lowest quartile. But in this multivariable model, the association between serum estradiol and current asthma was not significant. Among men (models 1-3), the magnitude of the estimated effect of serum testosterone and serum estradiol on current asthma was similar to that observed in female participants, but neither serum testosterone nor serum estradiol was significantly associated with current asthma.
The investigators then analyzed the impact of obesity on the relationship between serum hormone levels and obesity. Obesity was defined as body mass index equal to or greater than 30 kg/m2. A total of 1,370 men and 1,653 women were included in this analysis. In multivariable analyses of the obese participants, adjustment without (model 1) and with (model 3) serum estradiol, serum free-testosterone levels in the highest (fourth) quartile were significantly associated with reduced odds of asthma in obese women. In multivariable analyses without (model 2) and with (model 3), serum estradiol levels above the first quartile were significantly associated with reduced odds of current asthma in obese women.
In contrast to the results in obese women, neither serum free testosterone nor serum estradiol was significantly associated with current asthma in obese men or nonobese women.
Dr. Han and coauthors suggested a possible mechanism of the role of sex hormones in asthma. “Androgens such as testosterone may reduce innate and adaptive immune responses, while estrogen and progesterone may enhance T-helper cell type 2 allergic airway inflammation.”
They concluded: “We found that elevated serum levels of both free testosterone and estradiol were significantly associated with reduced odds of asthma in obese women, and that elevated levels of serum estradiol were significantly associated with reduced odds of asthma in nonobese men. Our findings further suggest that sex steroid hormones play a role in known sex differences in asthma among adults.”
One coauthor has received research materials from Merck and GlaxoSmithKline (inhaled steroids), as well as Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in National Institutes for Health–funded studies, unrelated to the current work. The other authors reported no conflicts of interest.
SOURCE: Han Y-Y et al. J Respir Crit Care Med. 2019 Sep 16. doi: 10.1164/rccm.201905-0996OC.
possibly explaining in part the different prevalence of asthma in men and women, according to the findings of a large cross-sectional population based study.
Yueh-Ying Han, PhD, of the Children’s Hospital of Pittsburgh and colleagues investigated the role of free testosterone and estradiol levels and current asthma among adults. The impact of obesity on that association was also examined. The investigators analyzed data from 7,615 adults (3,953 men and 3,662 women) who participated in the 2013-2014 and 2015-2016 U.S. National Health and Nutrition Examination Survey. The data included health interviews, examination components, and laboratory tests on each patient. Serum samples were analyzed by the division of laboratory sciences of the Centers for Disease Control and Prevention. Logistic regression was used for the multivariable analysis of sex hormone levels (as quartiles) and current asthma, and the analysis was done separately on men and women. Pregnant women were excluded, in addition to individuals with incomplete data. The exclusions tended to be Hispanic, former smokers, lower income, and lacking private insurance. The overall prevalence of current asthma in the sample was 9% (6% in men and 13% in women).
Three models were generated based on serum levels in women and in men.
For model 1 (unadjusted for estradiol), women whose serum testosterone levels were in the second and fourth quartiles had 30%-45% significantly lower odds of having current asthma than those whose serum testosterone level was in the lowest quartile. Among men, those whose serum testosterone levels were in the second and fourth quartiles had 12%-13% lower odds for current asthma.
For model 2 (unadjusted for free testosterone), women whose serum estradiol levels were in the third quartile had 34% significantly lower odds of having current asthma than those whose estradiol levels were in the lowest quartile. The findings were similar for men, that is, those whose serum estradiol levels were in the third quartile had 30% lower odds for having asthma, compared with those with in the lowest quartile.
For model 3 (a multivariable model including serum levels of both estradiol and free testosterone), women whose serum testosterone levels were in the second and fourth quartiles had 30% and 44% lower odds of current asthma than those whose serum testosterone levels were in the lowest quartile. But in this multivariable model, the association between serum estradiol and current asthma was not significant. Among men (models 1-3), the magnitude of the estimated effect of serum testosterone and serum estradiol on current asthma was similar to that observed in female participants, but neither serum testosterone nor serum estradiol was significantly associated with current asthma.
The investigators then analyzed the impact of obesity on the relationship between serum hormone levels and obesity. Obesity was defined as body mass index equal to or greater than 30 kg/m2. A total of 1,370 men and 1,653 women were included in this analysis. In multivariable analyses of the obese participants, adjustment without (model 1) and with (model 3) serum estradiol, serum free-testosterone levels in the highest (fourth) quartile were significantly associated with reduced odds of asthma in obese women. In multivariable analyses without (model 2) and with (model 3), serum estradiol levels above the first quartile were significantly associated with reduced odds of current asthma in obese women.
In contrast to the results in obese women, neither serum free testosterone nor serum estradiol was significantly associated with current asthma in obese men or nonobese women.
Dr. Han and coauthors suggested a possible mechanism of the role of sex hormones in asthma. “Androgens such as testosterone may reduce innate and adaptive immune responses, while estrogen and progesterone may enhance T-helper cell type 2 allergic airway inflammation.”
They concluded: “We found that elevated serum levels of both free testosterone and estradiol were significantly associated with reduced odds of asthma in obese women, and that elevated levels of serum estradiol were significantly associated with reduced odds of asthma in nonobese men. Our findings further suggest that sex steroid hormones play a role in known sex differences in asthma among adults.”
One coauthor has received research materials from Merck and GlaxoSmithKline (inhaled steroids), as well as Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in National Institutes for Health–funded studies, unrelated to the current work. The other authors reported no conflicts of interest.
SOURCE: Han Y-Y et al. J Respir Crit Care Med. 2019 Sep 16. doi: 10.1164/rccm.201905-0996OC.
possibly explaining in part the different prevalence of asthma in men and women, according to the findings of a large cross-sectional population based study.
Yueh-Ying Han, PhD, of the Children’s Hospital of Pittsburgh and colleagues investigated the role of free testosterone and estradiol levels and current asthma among adults. The impact of obesity on that association was also examined. The investigators analyzed data from 7,615 adults (3,953 men and 3,662 women) who participated in the 2013-2014 and 2015-2016 U.S. National Health and Nutrition Examination Survey. The data included health interviews, examination components, and laboratory tests on each patient. Serum samples were analyzed by the division of laboratory sciences of the Centers for Disease Control and Prevention. Logistic regression was used for the multivariable analysis of sex hormone levels (as quartiles) and current asthma, and the analysis was done separately on men and women. Pregnant women were excluded, in addition to individuals with incomplete data. The exclusions tended to be Hispanic, former smokers, lower income, and lacking private insurance. The overall prevalence of current asthma in the sample was 9% (6% in men and 13% in women).
Three models were generated based on serum levels in women and in men.
For model 1 (unadjusted for estradiol), women whose serum testosterone levels were in the second and fourth quartiles had 30%-45% significantly lower odds of having current asthma than those whose serum testosterone level was in the lowest quartile. Among men, those whose serum testosterone levels were in the second and fourth quartiles had 12%-13% lower odds for current asthma.
For model 2 (unadjusted for free testosterone), women whose serum estradiol levels were in the third quartile had 34% significantly lower odds of having current asthma than those whose estradiol levels were in the lowest quartile. The findings were similar for men, that is, those whose serum estradiol levels were in the third quartile had 30% lower odds for having asthma, compared with those with in the lowest quartile.
For model 3 (a multivariable model including serum levels of both estradiol and free testosterone), women whose serum testosterone levels were in the second and fourth quartiles had 30% and 44% lower odds of current asthma than those whose serum testosterone levels were in the lowest quartile. But in this multivariable model, the association between serum estradiol and current asthma was not significant. Among men (models 1-3), the magnitude of the estimated effect of serum testosterone and serum estradiol on current asthma was similar to that observed in female participants, but neither serum testosterone nor serum estradiol was significantly associated with current asthma.
The investigators then analyzed the impact of obesity on the relationship between serum hormone levels and obesity. Obesity was defined as body mass index equal to or greater than 30 kg/m2. A total of 1,370 men and 1,653 women were included in this analysis. In multivariable analyses of the obese participants, adjustment without (model 1) and with (model 3) serum estradiol, serum free-testosterone levels in the highest (fourth) quartile were significantly associated with reduced odds of asthma in obese women. In multivariable analyses without (model 2) and with (model 3), serum estradiol levels above the first quartile were significantly associated with reduced odds of current asthma in obese women.
In contrast to the results in obese women, neither serum free testosterone nor serum estradiol was significantly associated with current asthma in obese men or nonobese women.
Dr. Han and coauthors suggested a possible mechanism of the role of sex hormones in asthma. “Androgens such as testosterone may reduce innate and adaptive immune responses, while estrogen and progesterone may enhance T-helper cell type 2 allergic airway inflammation.”
They concluded: “We found that elevated serum levels of both free testosterone and estradiol were significantly associated with reduced odds of asthma in obese women, and that elevated levels of serum estradiol were significantly associated with reduced odds of asthma in nonobese men. Our findings further suggest that sex steroid hormones play a role in known sex differences in asthma among adults.”
One coauthor has received research materials from Merck and GlaxoSmithKline (inhaled steroids), as well as Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in National Institutes for Health–funded studies, unrelated to the current work. The other authors reported no conflicts of interest.
SOURCE: Han Y-Y et al. J Respir Crit Care Med. 2019 Sep 16. doi: 10.1164/rccm.201905-0996OC.
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
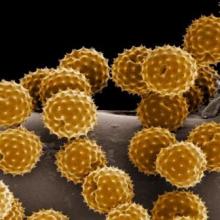
Allergy immunotherapy may modify asthma severity progression
The use of a grass-based allergy immunotherapy (AIT) lowered the risk of progression from milder to more severe asthma, according to the results of a large, real-world, industry-sponsored, observational study.
The researchers analyzed a cohort of 1,739,440 patients aged 12 years and older using 2005-2014 data from a statutory health insurance database in Germany. From this population, 39,167 individuals aged 14 years or older were classified as having incident asthma during the observation period and were included in the study.
The severity of asthma was classified according to the treatment steps recommended by the Global Initiative for Asthma (GINA).
Among these, 4,111 patients (10.5%) received AIT. AIT use was associated with a significantly decreased likelihood of asthma progression from GINA step 1 to step 3 (hazard ratio, 0.87; 95% confidence interval, 0.80‐0.95) and GINA step 3 to step 4 (HR, 0.66; 95% CI, 0.60‐0.74).
Medications for GINA step 2 (3.5%) and GINA step 5 (0.03%) were rarely prescribed, so the researchers could not analyze the transition between GINA steps 1 and 2, step 2 and 3, and step 4 and 5.
A total of 8,726 patients had at least one transition between GINA steps 1, 3, or 4, and 1,085 had two transitions, though not all 39,167 patients were under risk of severity progression into all GINA steps, according to the authors.
The findings are consistent with earlier studies that indicate grass-based immunotherapy can effectively treat asthma symptoms and potentially asthma progression (J Allergy Clin Immuno. 2012;129[3];717-25; J Allergy Clin Immunol. 2018;141[2]:529‐38).
“This study indicates that AIT may modify the course of asthma. Our study supports the assumption that treatment with AIT may prevent the progression from mild to more severe asthma,” the authors concluded.
The study was financially supported by ALK‐Abelló; several of the authors were also employees of or received funding from the company.
SOURCE: Schmitt J et al. Allergy. 2019. doi: 10.1111/all.14020.
The use of a grass-based allergy immunotherapy (AIT) lowered the risk of progression from milder to more severe asthma, according to the results of a large, real-world, industry-sponsored, observational study.
The researchers analyzed a cohort of 1,739,440 patients aged 12 years and older using 2005-2014 data from a statutory health insurance database in Germany. From this population, 39,167 individuals aged 14 years or older were classified as having incident asthma during the observation period and were included in the study.
The severity of asthma was classified according to the treatment steps recommended by the Global Initiative for Asthma (GINA).
Among these, 4,111 patients (10.5%) received AIT. AIT use was associated with a significantly decreased likelihood of asthma progression from GINA step 1 to step 3 (hazard ratio, 0.87; 95% confidence interval, 0.80‐0.95) and GINA step 3 to step 4 (HR, 0.66; 95% CI, 0.60‐0.74).
Medications for GINA step 2 (3.5%) and GINA step 5 (0.03%) were rarely prescribed, so the researchers could not analyze the transition between GINA steps 1 and 2, step 2 and 3, and step 4 and 5.
A total of 8,726 patients had at least one transition between GINA steps 1, 3, or 4, and 1,085 had two transitions, though not all 39,167 patients were under risk of severity progression into all GINA steps, according to the authors.
The findings are consistent with earlier studies that indicate grass-based immunotherapy can effectively treat asthma symptoms and potentially asthma progression (J Allergy Clin Immuno. 2012;129[3];717-25; J Allergy Clin Immunol. 2018;141[2]:529‐38).
“This study indicates that AIT may modify the course of asthma. Our study supports the assumption that treatment with AIT may prevent the progression from mild to more severe asthma,” the authors concluded.
The study was financially supported by ALK‐Abelló; several of the authors were also employees of or received funding from the company.
SOURCE: Schmitt J et al. Allergy. 2019. doi: 10.1111/all.14020.
The use of a grass-based allergy immunotherapy (AIT) lowered the risk of progression from milder to more severe asthma, according to the results of a large, real-world, industry-sponsored, observational study.
The researchers analyzed a cohort of 1,739,440 patients aged 12 years and older using 2005-2014 data from a statutory health insurance database in Germany. From this population, 39,167 individuals aged 14 years or older were classified as having incident asthma during the observation period and were included in the study.
The severity of asthma was classified according to the treatment steps recommended by the Global Initiative for Asthma (GINA).
Among these, 4,111 patients (10.5%) received AIT. AIT use was associated with a significantly decreased likelihood of asthma progression from GINA step 1 to step 3 (hazard ratio, 0.87; 95% confidence interval, 0.80‐0.95) and GINA step 3 to step 4 (HR, 0.66; 95% CI, 0.60‐0.74).
Medications for GINA step 2 (3.5%) and GINA step 5 (0.03%) were rarely prescribed, so the researchers could not analyze the transition between GINA steps 1 and 2, step 2 and 3, and step 4 and 5.
A total of 8,726 patients had at least one transition between GINA steps 1, 3, or 4, and 1,085 had two transitions, though not all 39,167 patients were under risk of severity progression into all GINA steps, according to the authors.
The findings are consistent with earlier studies that indicate grass-based immunotherapy can effectively treat asthma symptoms and potentially asthma progression (J Allergy Clin Immuno. 2012;129[3];717-25; J Allergy Clin Immunol. 2018;141[2]:529‐38).
“This study indicates that AIT may modify the course of asthma. Our study supports the assumption that treatment with AIT may prevent the progression from mild to more severe asthma,” the authors concluded.
The study was financially supported by ALK‐Abelló; several of the authors were also employees of or received funding from the company.
SOURCE: Schmitt J et al. Allergy. 2019. doi: 10.1111/all.14020.
FROM ALLERGY
Step-up therapy with glucocorticoids benefits black children with asthma
based on data from 280 children aged 5-11 years with at least one grandparent identified as black.
Previous studies have suggested that long-acting beta2-agonists (LABAs) may be more effective for patients with poorly controlled asthma, but such step-up therapy has not been well studied in black patients, wrote Michael E. Wechsler, MD, of National Jewish Health, Denver, and colleagues.
In a study published in the New England Journal of Medicine, the researchers reported results of two parallel BARD (Best African American Response to Asthma Drugs) trials conducted at nine centers between January 2014 and March 2016 of individuals with poorly controlled asthma. One trial included 280 children aged 5-11 years (average age, 8.5 years); the second trial included adolescents aged 12 years and older and adults (average age, 37 years) who had family backgrounds that were similar to those of the children.
The researchers randomized the children to four groups to compare the following protocols: doubling the dose of a glucocorticoid (fluticasone propionate) to a dose of 100 mcg, twice daily (the double-fluticasone group); doubling the dose of fluticasone to 100 mcg and adding 50 mcg of the LABA salmeterol (the salmeterol/double-fluticasone group); quintupling the dose of fluticasone to 250 mcg (the quintuple-fluticasone group); or quintupling the dose of fluticasone to 250 mcg and adding 50 mcg of salmeterol (the salmeterol/quintuple-fluticasone group). The trial consisted of a four-way crossover design with each treatment period lasting 14 weeks.
The primary outcome was a composite measure including asthma exacerbations, asthma control days, and percentage of predicted forced expiratory volume in the first second at the end of each treatment.
Overall, a superior response occurred in 53% of the salmeterol/double-fluticasone group, 41% of the double-fluticasone group, 43% of the salmeterol/quintuple fluticasone group, and 47% of the quintuple-fluticasone group.
The superior response was 46% for both groups when the researchers compared a quintupled dose of fluticasone propionate (250 mcg) with a two step–up strategy of adding salmeterol at a dose of 50 mcg and increasing the dose of fluticasone to 100 mcg.
“In contrast to black adults and white persons of all ages, almost half the children who had at least one grandparent who identified as black and who had poorly controlled asthma had a superior response to an increased dose of an inhaled glucocorticoid over the addition of a LABA,” Dr. Wechsler and coauthors wrote. No more than 12% of the children in any treatment group did not have a superior response. No significant differences in reports of respiratory tract infections or pneumonia were seen between the groups. Children younger than 8 years showed a decrease in the ratio of urinary cortisol to creatinine with an increased dose of inhaled glucocorticoids.
In the adolescent and adult study using the same treatment protocols, 20%-25% of patients did not have a differential outcome between treatments. “In adolescents and adults, the addition of a LABA was more likely to produce superior responses than increasing the dose of an inhaled glucocorticoid,” Dr. Wechsler and coauthors wrote.
The study findings were limited by several factors, including the inability to assess long-term effects on growth and inability to detect biomarkers associated with responses to specific therapies, the researchers noted. However, the results suggest that black children with poorly controlled asthma can benefit from additional inhaled glucocorticoids, and larger studies are needed to identify the best treatment for this patient population.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Wechsler reported relationships with companies including AstraZeneca, Equillium, Genentech, GlaxoSmithKline, Mylan, Novartis, Regeneron, resTORbio, Sanofi, and others. Coauthors identified relationships with numerous pharmaceutical companies.
SOURCE: Wechsler ME et al. N Engl J Med. 2019 Sep 25. doi: 10.1056/NEJMoa1905560.
based on data from 280 children aged 5-11 years with at least one grandparent identified as black.
Previous studies have suggested that long-acting beta2-agonists (LABAs) may be more effective for patients with poorly controlled asthma, but such step-up therapy has not been well studied in black patients, wrote Michael E. Wechsler, MD, of National Jewish Health, Denver, and colleagues.
In a study published in the New England Journal of Medicine, the researchers reported results of two parallel BARD (Best African American Response to Asthma Drugs) trials conducted at nine centers between January 2014 and March 2016 of individuals with poorly controlled asthma. One trial included 280 children aged 5-11 years (average age, 8.5 years); the second trial included adolescents aged 12 years and older and adults (average age, 37 years) who had family backgrounds that were similar to those of the children.
The researchers randomized the children to four groups to compare the following protocols: doubling the dose of a glucocorticoid (fluticasone propionate) to a dose of 100 mcg, twice daily (the double-fluticasone group); doubling the dose of fluticasone to 100 mcg and adding 50 mcg of the LABA salmeterol (the salmeterol/double-fluticasone group); quintupling the dose of fluticasone to 250 mcg (the quintuple-fluticasone group); or quintupling the dose of fluticasone to 250 mcg and adding 50 mcg of salmeterol (the salmeterol/quintuple-fluticasone group). The trial consisted of a four-way crossover design with each treatment period lasting 14 weeks.
The primary outcome was a composite measure including asthma exacerbations, asthma control days, and percentage of predicted forced expiratory volume in the first second at the end of each treatment.
Overall, a superior response occurred in 53% of the salmeterol/double-fluticasone group, 41% of the double-fluticasone group, 43% of the salmeterol/quintuple fluticasone group, and 47% of the quintuple-fluticasone group.
The superior response was 46% for both groups when the researchers compared a quintupled dose of fluticasone propionate (250 mcg) with a two step–up strategy of adding salmeterol at a dose of 50 mcg and increasing the dose of fluticasone to 100 mcg.
“In contrast to black adults and white persons of all ages, almost half the children who had at least one grandparent who identified as black and who had poorly controlled asthma had a superior response to an increased dose of an inhaled glucocorticoid over the addition of a LABA,” Dr. Wechsler and coauthors wrote. No more than 12% of the children in any treatment group did not have a superior response. No significant differences in reports of respiratory tract infections or pneumonia were seen between the groups. Children younger than 8 years showed a decrease in the ratio of urinary cortisol to creatinine with an increased dose of inhaled glucocorticoids.
In the adolescent and adult study using the same treatment protocols, 20%-25% of patients did not have a differential outcome between treatments. “In adolescents and adults, the addition of a LABA was more likely to produce superior responses than increasing the dose of an inhaled glucocorticoid,” Dr. Wechsler and coauthors wrote.
The study findings were limited by several factors, including the inability to assess long-term effects on growth and inability to detect biomarkers associated with responses to specific therapies, the researchers noted. However, the results suggest that black children with poorly controlled asthma can benefit from additional inhaled glucocorticoids, and larger studies are needed to identify the best treatment for this patient population.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Wechsler reported relationships with companies including AstraZeneca, Equillium, Genentech, GlaxoSmithKline, Mylan, Novartis, Regeneron, resTORbio, Sanofi, and others. Coauthors identified relationships with numerous pharmaceutical companies.
SOURCE: Wechsler ME et al. N Engl J Med. 2019 Sep 25. doi: 10.1056/NEJMoa1905560.
based on data from 280 children aged 5-11 years with at least one grandparent identified as black.
Previous studies have suggested that long-acting beta2-agonists (LABAs) may be more effective for patients with poorly controlled asthma, but such step-up therapy has not been well studied in black patients, wrote Michael E. Wechsler, MD, of National Jewish Health, Denver, and colleagues.
In a study published in the New England Journal of Medicine, the researchers reported results of two parallel BARD (Best African American Response to Asthma Drugs) trials conducted at nine centers between January 2014 and March 2016 of individuals with poorly controlled asthma. One trial included 280 children aged 5-11 years (average age, 8.5 years); the second trial included adolescents aged 12 years and older and adults (average age, 37 years) who had family backgrounds that were similar to those of the children.
The researchers randomized the children to four groups to compare the following protocols: doubling the dose of a glucocorticoid (fluticasone propionate) to a dose of 100 mcg, twice daily (the double-fluticasone group); doubling the dose of fluticasone to 100 mcg and adding 50 mcg of the LABA salmeterol (the salmeterol/double-fluticasone group); quintupling the dose of fluticasone to 250 mcg (the quintuple-fluticasone group); or quintupling the dose of fluticasone to 250 mcg and adding 50 mcg of salmeterol (the salmeterol/quintuple-fluticasone group). The trial consisted of a four-way crossover design with each treatment period lasting 14 weeks.
The primary outcome was a composite measure including asthma exacerbations, asthma control days, and percentage of predicted forced expiratory volume in the first second at the end of each treatment.
Overall, a superior response occurred in 53% of the salmeterol/double-fluticasone group, 41% of the double-fluticasone group, 43% of the salmeterol/quintuple fluticasone group, and 47% of the quintuple-fluticasone group.
The superior response was 46% for both groups when the researchers compared a quintupled dose of fluticasone propionate (250 mcg) with a two step–up strategy of adding salmeterol at a dose of 50 mcg and increasing the dose of fluticasone to 100 mcg.
“In contrast to black adults and white persons of all ages, almost half the children who had at least one grandparent who identified as black and who had poorly controlled asthma had a superior response to an increased dose of an inhaled glucocorticoid over the addition of a LABA,” Dr. Wechsler and coauthors wrote. No more than 12% of the children in any treatment group did not have a superior response. No significant differences in reports of respiratory tract infections or pneumonia were seen between the groups. Children younger than 8 years showed a decrease in the ratio of urinary cortisol to creatinine with an increased dose of inhaled glucocorticoids.
In the adolescent and adult study using the same treatment protocols, 20%-25% of patients did not have a differential outcome between treatments. “In adolescents and adults, the addition of a LABA was more likely to produce superior responses than increasing the dose of an inhaled glucocorticoid,” Dr. Wechsler and coauthors wrote.
The study findings were limited by several factors, including the inability to assess long-term effects on growth and inability to detect biomarkers associated with responses to specific therapies, the researchers noted. However, the results suggest that black children with poorly controlled asthma can benefit from additional inhaled glucocorticoids, and larger studies are needed to identify the best treatment for this patient population.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Wechsler reported relationships with companies including AstraZeneca, Equillium, Genentech, GlaxoSmithKline, Mylan, Novartis, Regeneron, resTORbio, Sanofi, and others. Coauthors identified relationships with numerous pharmaceutical companies.
SOURCE: Wechsler ME et al. N Engl J Med. 2019 Sep 25. doi: 10.1056/NEJMoa1905560.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Black children with poorly controlled asthma had a superior response to stepped increases in inhaled glucocorticoids, compared with stepped increases in long-acting beta2-agonists.
Major finding: A total of 46% of black children with poorly controlled asthma improved when inhaled glucocorticoids were increased.
Study details: The data come from the BARD trials, a pair of prospective, randomized, double-blind trials including 280 children aged 5-11 years with at least one grandparent identified as black and 294 adolescents and adults who had family backgrounds that were similar to the children.
Disclosures: The study was supported by the National Heart, Lung, and Blood Institute. Dr. Wechsler reported relationships with companies including AstraZeneca, Equillium, Genentech, GlaxoSmithKline, Mylan, Novartis, Regeneron, resTORbio, Sanofi, and others. Coauthors identified relationships with numerous pharmaceutical companies.
Source: Wechsler ME et al. N Engl J Med. 2019 Sep 25. doi: 10.1056/NEJMoa1905560.
Wildfire smoke has acute cardiorespiratory impact, but long-term effects still under study
The 2019 wildfire season is underway in many locales across the United States, exposing millions of individuals to smoky conditions that will have health consequences ranging from stinging eyes to scratchy throats to a trip to the ED for asthma or chronic obstructive pulmonary disease (COPD) exacerbation. Questions about long-term health impacts are on the minds of many, including physicians and their patients who live with cardiorespiratory conditions.

John R. Balmes, MD, a pulmonologist at the University of California, San Francisco, and an expert on the respiratory and cardiovascular effects of air pollutants, suggested that the best available published literature points to “pretty strong evidence for acute effects of wildfire smoke on respiratory health, meaning people with preexisting asthma and COPD are at risk for exacerbations, and probably for respiratory tract infections as well.” He said, “It’s a little less clear, but there’s good biological plausibility for increased risk of respiratory tract infections because when your alveolar macrophages are overloaded with carbon particles that are toxic to those cells, they don’t function as well as a first line of defense against bacterial infection, for example.”
The new normal of wildfires
Warmer, drier summers in recent years in the western United States and many other regions, attributed by climate experts to global climate change, have produced catastrophic wildfires (PNAS;2016 Oct 18;113[42]11770-5; Science 2006 Aug 18;313:940-3). The Camp Fire in Northern California broke out in November 2018, took the lives of at least 85 people, and cost more than $16 billion in damage. Smoke from that blaze reached hazardous levels in San Francisco, Sacramento, Fresno, and many other smaller towns. Other forest fires in that year caused heavy smoke conditions in Portland, Seattle, Vancouver, and Anchorage. Such events are expected to be repeated often in the coming years (Int J Environ Res Public Health. 2019 Jul 6;16[13]).

Wildfire smoke can contain a wide range of substances, chemicals, and gases with known and unknown cardiorespiratory implications. “Smoke is composed primarily of carbon dioxide, water vapor, carbon monoxide, particulate matter, hydrocarbons and other organic chemicals, nitrogen oxides, trace minerals and several thousand other compounds,” according to the U.S. Environmental Protection Agency (Wildfire smoke: A guide for public health officials 2019. Washington, D.C.: EPA, 2019). The EPA report noted, “Particles with diameters less than 10 mcm (particulate matter, or PM10) can be inhaled into the lungs and affect the lungs, heart, and blood vessels. The smallest particles, those less than 2.5 mcm in diameter (PM2.5), are the greatest risk to public health because they can reach deep into the lungs and may even make it into the bloodstream.”
Research on health impact
In early June of 2008, Wayne Cascio, MD, awoke in his Greenville, N.C., home to the stench of smoke emanating from a large peat fire burning some 65 miles away. By the time he reached the parking lot at East Carolina University in Greenville to begin his workday as chief of cardiology, the haze of smoke had thickened to the point where he could only see a few feet in front of him.
Over the next several weeks, the fire scorched 41,000 acres and produced haze and air pollution that far exceeded National Ambient Air Quality Standards for particulate matter and blanketed rural communities in the state’s eastern region. The price tag for management of the blaze reached $20 million. Because of his interest in the health effects of wildfire smoke and because of his relationship with investigators at the EPA, Dr. Cascio initiated an epidemiology study to investigate the effects of exposure on cardiorespiratory outcomes in the population affected by the fire (Environ Health Perspect. 2011 Oct;119[10]:1415-20).
By combining satellite data with syndromic surveillance drawn from hospital records in 41 counties contained in the North Carolina Disease Event Tracking and Epidemiologic Collection Tool, he and his colleagues found that exposure to the peat wildfire smoke led to increases in the cumulative risk ratio for asthma (relative risk, 1.65), chronic obstructive pulmonary disease (RR, 1.73), and pneumonia and acute bronchitis (RR, 1.59). ED visits related to cardiopulmonary symptoms and heart failure also were significantly increased (RR, 1.23 and 1.37, respectively). “That was really the first study to strongly identify a cardiac endpoint related to wildfire smoke exposure,” said Dr. Cascio, who now directs the EPA’s National Health and Environmental Effects Research Laboratory. “It really pointed out how little we knew about the health effects of wildfire up until that time.”
Those early findings have been replicated in subsequent research about the acute health effects of exposure to wildfire smoke, which contains PM2.5 and other toxic substances from structures, electronic devices, and automobiles destroyed in the path of flames, including heavy metals and asbestos. Most of the work has focused on smoke-related cardiovascular and respiratory ED visits and hospitalizations.
A study of the 2008 California wildfire impact on ED visits accounted for ozone levels in addition to PM2.5 in the smoke. During the active fire periods, PM2.5 was significantly associated with exacerbations of asthma and COPD and these effects remained after controlling for ozone levels. PM2.5 inhalation during the wildfires was associated with increased risk of an ED visit for asthma (RR, 1.112; 95% confidence interval, 1.087-1.138) for a 10 mcg/m3 increase in PM2.5 and COPD (RR, 1.05; 95% CI, 1.019-1.0825), as well as for combined respiratory visits (RR, 1.035; 95% CI, 1.023-1.046) (Environ Int. 2109 Aug;129:291-8).
Researchers who evaluated the health impacts of wildfires in California during the 2015 fire season found an increase in all-cause cardiovascular and respiratory ED visits, especially among those aged 65 years and older during smoke days. The population-based study included 1,196,233 ED visits during May 1–Sept. 30 that year. PM2.5 concentrations were categorized as light, medium, or dense. Relative risk rose with the amount of smoke in the air. Rates of all-cause cardiovascular ED visits were elevated across levels of smoke density, with the greatest increase on dense smoke days and among those aged 65 years or older (RR,1.15; 95% CI, 1.09-1.22). All-cause cerebrovascular visits were associated with dense smoke days, especially among those aged 65 years and older (RR, 1.22; 95% CI, 1.00-1.49). Respiratory conditions also were increased on dense smoke days (RR, 1.18; 95% CI, 1.08-1.28) (J Am Heart Assoc. 2018 Apr 11;7:e007492. doi: 10.1161/JAHA.117.007492).
Long-term effects unknown
When it comes to the long-term effects of wildfire smoke on human health outcomes, much less is known. In a recent literature review, Colleen E. Reid, PhD, and Melissa May Maestas, PhD, found only one study that investigated long-term respiratory health impacts of wildfire smoke, and only a few studies that have estimated future health impacts of wildfires under likely climate change scenarios (Curr Opin Pulm Med. 2019 Mar;25:179-87).
“We know that there are immediate respiratory health effects from wildfire smoke,” said Dr. Reid of the department of geography at the University of Colorado Boulder. “What’s less known is everything else. That’s challenging, because people want to know about the long-term health effects.”
Evidence from the scientific literature suggests that exposure to air pollution adversely affects cardiovascular health, but whether exposure to wildfire smoke confers a similar risk is less clear. “Until just a few years ago we haven’t been able to study wildfire exposure measures on a large scale,” said EPA scientist Ana G. Rappold, PhD, a statistician there in the environmental public health division of the National Health and Environmental Effects Research Laboratory. “It’s also hard to predict wildfires, so it’s hard to plan for an epidemiologic study if you don’t know where they’re going to occur.”
Dr. Rappold and colleagues examined cardiopulmonary hospitalizations among adults aged 65 years and older in 692 U.S. counties within 200 km of 123 large wildfires during 2008-2010 (Environ Health Perspect. 2019;127[3]:37006. doi: 10.1289/EHP3860). They observed that an increased risk of PM2.5-related cardiopulmonary hospitalizations was similar on smoke and nonsmoke days across multiple lags and exposure metrics, while risk for asthma-related hospitalizations was higher during smoke days. “One hypothesis is that this was an older study population, so naturally if you’re inhaling smoke, the first organ that’s impacted in an older population is the lungs,” Dr. Rappold said. “If you go to the hospital for asthma, wheezing, or bronchitis, you are taken out of the risk pool for cardiovascular and other diseases. That could explain why in other studies we don’t see a clear cardiovascular signal as we have for air pollution studies in general. Another aspect to this study is, the exposure metric was PM2.5, but smoke contains many other components, particularly gases, which are respiratory irritants. It could be that this triggers a higher risk for respiratory [effects] than regular episodes of high PM2.5 exposure, just because of the additional gases that people are exposed to.”
Another complicating factor is the paucity of data about solutions to long-term exposure to wildfire smoke. “If you’re impacted by high-exposure levels for 60 days, that is not something we have experienced before,” Dr. Rappold noted. “What are the solutions for that community? What works? Can we show that by implementing community-level resilience plans with HEPA [high-efficiency particulate air] filters or other interventions, do the overall outcomes improve? Doctors are the first ones to talk with their patients about their symptoms and about how to take care of their conditions. They can clearly make a difference in emphasizing reducing exposures in a way that fits their patients individually, either reducing the amount of time spent outside, the duration of exposure, and the level of exposure. Maybe change activities based on the intensity of exposure. Don’t go for a run outside when it’s smoky, because your ventilation rate is higher and you will breathe in more smoke. Become aware of those things.”
Advising vulnerable patients
While research in this field advances, the unforgiving wildfire season looms, assuring more destruction of property and threats to cardiorespiratory health. “There are a lot of questions that research will have an opportunity to address as we go forward, including the utility and the benefit of N95 masks, the utility of HEPA filters used in the house, and even with HVAC [heating, ventilation, and air conditioning] systems,” Dr. Cascio said. “Can we really clean up the indoor air well enough to protect us from wildfire smoke?”
The way he sees it, the time is ripe for clinicians and officials in public and private practice settings to refine how they distribute information to people living in areas affected by wildfire smoke. “We can’t force people do anything, but at least if they’re informed, then they understand they can make an informed decision about how they might want to affect what they do that would limit their exposure,” he said. “As a patient, my health care system sends text and email messages to me. So, why couldn’t the hospital send out a text message or an email to all of the patients with COPD, coronary disease, and heart failure when an area is impacted by smoke, saying, ‘Check your air quality and take action if air quality is poor?’ Physicians don’t have time to do this kind of education in the office for all of their patients. I know that from experience. But if one were to only focus on those at highest risk, and encourage them to follow our guidelines, which might include doing HEPA filter treatment in the home, we probably would reduce the number of clinical events in a cost-effective way.”
The 2019 wildfire season is underway in many locales across the United States, exposing millions of individuals to smoky conditions that will have health consequences ranging from stinging eyes to scratchy throats to a trip to the ED for asthma or chronic obstructive pulmonary disease (COPD) exacerbation. Questions about long-term health impacts are on the minds of many, including physicians and their patients who live with cardiorespiratory conditions.

John R. Balmes, MD, a pulmonologist at the University of California, San Francisco, and an expert on the respiratory and cardiovascular effects of air pollutants, suggested that the best available published literature points to “pretty strong evidence for acute effects of wildfire smoke on respiratory health, meaning people with preexisting asthma and COPD are at risk for exacerbations, and probably for respiratory tract infections as well.” He said, “It’s a little less clear, but there’s good biological plausibility for increased risk of respiratory tract infections because when your alveolar macrophages are overloaded with carbon particles that are toxic to those cells, they don’t function as well as a first line of defense against bacterial infection, for example.”
The new normal of wildfires
Warmer, drier summers in recent years in the western United States and many other regions, attributed by climate experts to global climate change, have produced catastrophic wildfires (PNAS;2016 Oct 18;113[42]11770-5; Science 2006 Aug 18;313:940-3). The Camp Fire in Northern California broke out in November 2018, took the lives of at least 85 people, and cost more than $16 billion in damage. Smoke from that blaze reached hazardous levels in San Francisco, Sacramento, Fresno, and many other smaller towns. Other forest fires in that year caused heavy smoke conditions in Portland, Seattle, Vancouver, and Anchorage. Such events are expected to be repeated often in the coming years (Int J Environ Res Public Health. 2019 Jul 6;16[13]).

Wildfire smoke can contain a wide range of substances, chemicals, and gases with known and unknown cardiorespiratory implications. “Smoke is composed primarily of carbon dioxide, water vapor, carbon monoxide, particulate matter, hydrocarbons and other organic chemicals, nitrogen oxides, trace minerals and several thousand other compounds,” according to the U.S. Environmental Protection Agency (Wildfire smoke: A guide for public health officials 2019. Washington, D.C.: EPA, 2019). The EPA report noted, “Particles with diameters less than 10 mcm (particulate matter, or PM10) can be inhaled into the lungs and affect the lungs, heart, and blood vessels. The smallest particles, those less than 2.5 mcm in diameter (PM2.5), are the greatest risk to public health because they can reach deep into the lungs and may even make it into the bloodstream.”
Research on health impact
In early June of 2008, Wayne Cascio, MD, awoke in his Greenville, N.C., home to the stench of smoke emanating from a large peat fire burning some 65 miles away. By the time he reached the parking lot at East Carolina University in Greenville to begin his workday as chief of cardiology, the haze of smoke had thickened to the point where he could only see a few feet in front of him.
Over the next several weeks, the fire scorched 41,000 acres and produced haze and air pollution that far exceeded National Ambient Air Quality Standards for particulate matter and blanketed rural communities in the state’s eastern region. The price tag for management of the blaze reached $20 million. Because of his interest in the health effects of wildfire smoke and because of his relationship with investigators at the EPA, Dr. Cascio initiated an epidemiology study to investigate the effects of exposure on cardiorespiratory outcomes in the population affected by the fire (Environ Health Perspect. 2011 Oct;119[10]:1415-20).
By combining satellite data with syndromic surveillance drawn from hospital records in 41 counties contained in the North Carolina Disease Event Tracking and Epidemiologic Collection Tool, he and his colleagues found that exposure to the peat wildfire smoke led to increases in the cumulative risk ratio for asthma (relative risk, 1.65), chronic obstructive pulmonary disease (RR, 1.73), and pneumonia and acute bronchitis (RR, 1.59). ED visits related to cardiopulmonary symptoms and heart failure also were significantly increased (RR, 1.23 and 1.37, respectively). “That was really the first study to strongly identify a cardiac endpoint related to wildfire smoke exposure,” said Dr. Cascio, who now directs the EPA’s National Health and Environmental Effects Research Laboratory. “It really pointed out how little we knew about the health effects of wildfire up until that time.”
Those early findings have been replicated in subsequent research about the acute health effects of exposure to wildfire smoke, which contains PM2.5 and other toxic substances from structures, electronic devices, and automobiles destroyed in the path of flames, including heavy metals and asbestos. Most of the work has focused on smoke-related cardiovascular and respiratory ED visits and hospitalizations.
A study of the 2008 California wildfire impact on ED visits accounted for ozone levels in addition to PM2.5 in the smoke. During the active fire periods, PM2.5 was significantly associated with exacerbations of asthma and COPD and these effects remained after controlling for ozone levels. PM2.5 inhalation during the wildfires was associated with increased risk of an ED visit for asthma (RR, 1.112; 95% confidence interval, 1.087-1.138) for a 10 mcg/m3 increase in PM2.5 and COPD (RR, 1.05; 95% CI, 1.019-1.0825), as well as for combined respiratory visits (RR, 1.035; 95% CI, 1.023-1.046) (Environ Int. 2109 Aug;129:291-8).
Researchers who evaluated the health impacts of wildfires in California during the 2015 fire season found an increase in all-cause cardiovascular and respiratory ED visits, especially among those aged 65 years and older during smoke days. The population-based study included 1,196,233 ED visits during May 1–Sept. 30 that year. PM2.5 concentrations were categorized as light, medium, or dense. Relative risk rose with the amount of smoke in the air. Rates of all-cause cardiovascular ED visits were elevated across levels of smoke density, with the greatest increase on dense smoke days and among those aged 65 years or older (RR,1.15; 95% CI, 1.09-1.22). All-cause cerebrovascular visits were associated with dense smoke days, especially among those aged 65 years and older (RR, 1.22; 95% CI, 1.00-1.49). Respiratory conditions also were increased on dense smoke days (RR, 1.18; 95% CI, 1.08-1.28) (J Am Heart Assoc. 2018 Apr 11;7:e007492. doi: 10.1161/JAHA.117.007492).
Long-term effects unknown
When it comes to the long-term effects of wildfire smoke on human health outcomes, much less is known. In a recent literature review, Colleen E. Reid, PhD, and Melissa May Maestas, PhD, found only one study that investigated long-term respiratory health impacts of wildfire smoke, and only a few studies that have estimated future health impacts of wildfires under likely climate change scenarios (Curr Opin Pulm Med. 2019 Mar;25:179-87).
“We know that there are immediate respiratory health effects from wildfire smoke,” said Dr. Reid of the department of geography at the University of Colorado Boulder. “What’s less known is everything else. That’s challenging, because people want to know about the long-term health effects.”
Evidence from the scientific literature suggests that exposure to air pollution adversely affects cardiovascular health, but whether exposure to wildfire smoke confers a similar risk is less clear. “Until just a few years ago we haven’t been able to study wildfire exposure measures on a large scale,” said EPA scientist Ana G. Rappold, PhD, a statistician there in the environmental public health division of the National Health and Environmental Effects Research Laboratory. “It’s also hard to predict wildfires, so it’s hard to plan for an epidemiologic study if you don’t know where they’re going to occur.”
Dr. Rappold and colleagues examined cardiopulmonary hospitalizations among adults aged 65 years and older in 692 U.S. counties within 200 km of 123 large wildfires during 2008-2010 (Environ Health Perspect. 2019;127[3]:37006. doi: 10.1289/EHP3860). They observed that an increased risk of PM2.5-related cardiopulmonary hospitalizations was similar on smoke and nonsmoke days across multiple lags and exposure metrics, while risk for asthma-related hospitalizations was higher during smoke days. “One hypothesis is that this was an older study population, so naturally if you’re inhaling smoke, the first organ that’s impacted in an older population is the lungs,” Dr. Rappold said. “If you go to the hospital for asthma, wheezing, or bronchitis, you are taken out of the risk pool for cardiovascular and other diseases. That could explain why in other studies we don’t see a clear cardiovascular signal as we have for air pollution studies in general. Another aspect to this study is, the exposure metric was PM2.5, but smoke contains many other components, particularly gases, which are respiratory irritants. It could be that this triggers a higher risk for respiratory [effects] than regular episodes of high PM2.5 exposure, just because of the additional gases that people are exposed to.”
Another complicating factor is the paucity of data about solutions to long-term exposure to wildfire smoke. “If you’re impacted by high-exposure levels for 60 days, that is not something we have experienced before,” Dr. Rappold noted. “What are the solutions for that community? What works? Can we show that by implementing community-level resilience plans with HEPA [high-efficiency particulate air] filters or other interventions, do the overall outcomes improve? Doctors are the first ones to talk with their patients about their symptoms and about how to take care of their conditions. They can clearly make a difference in emphasizing reducing exposures in a way that fits their patients individually, either reducing the amount of time spent outside, the duration of exposure, and the level of exposure. Maybe change activities based on the intensity of exposure. Don’t go for a run outside when it’s smoky, because your ventilation rate is higher and you will breathe in more smoke. Become aware of those things.”
Advising vulnerable patients
While research in this field advances, the unforgiving wildfire season looms, assuring more destruction of property and threats to cardiorespiratory health. “There are a lot of questions that research will have an opportunity to address as we go forward, including the utility and the benefit of N95 masks, the utility of HEPA filters used in the house, and even with HVAC [heating, ventilation, and air conditioning] systems,” Dr. Cascio said. “Can we really clean up the indoor air well enough to protect us from wildfire smoke?”
The way he sees it, the time is ripe for clinicians and officials in public and private practice settings to refine how they distribute information to people living in areas affected by wildfire smoke. “We can’t force people do anything, but at least if they’re informed, then they understand they can make an informed decision about how they might want to affect what they do that would limit their exposure,” he said. “As a patient, my health care system sends text and email messages to me. So, why couldn’t the hospital send out a text message or an email to all of the patients with COPD, coronary disease, and heart failure when an area is impacted by smoke, saying, ‘Check your air quality and take action if air quality is poor?’ Physicians don’t have time to do this kind of education in the office for all of their patients. I know that from experience. But if one were to only focus on those at highest risk, and encourage them to follow our guidelines, which might include doing HEPA filter treatment in the home, we probably would reduce the number of clinical events in a cost-effective way.”
The 2019 wildfire season is underway in many locales across the United States, exposing millions of individuals to smoky conditions that will have health consequences ranging from stinging eyes to scratchy throats to a trip to the ED for asthma or chronic obstructive pulmonary disease (COPD) exacerbation. Questions about long-term health impacts are on the minds of many, including physicians and their patients who live with cardiorespiratory conditions.

John R. Balmes, MD, a pulmonologist at the University of California, San Francisco, and an expert on the respiratory and cardiovascular effects of air pollutants, suggested that the best available published literature points to “pretty strong evidence for acute effects of wildfire smoke on respiratory health, meaning people with preexisting asthma and COPD are at risk for exacerbations, and probably for respiratory tract infections as well.” He said, “It’s a little less clear, but there’s good biological plausibility for increased risk of respiratory tract infections because when your alveolar macrophages are overloaded with carbon particles that are toxic to those cells, they don’t function as well as a first line of defense against bacterial infection, for example.”
The new normal of wildfires
Warmer, drier summers in recent years in the western United States and many other regions, attributed by climate experts to global climate change, have produced catastrophic wildfires (PNAS;2016 Oct 18;113[42]11770-5; Science 2006 Aug 18;313:940-3). The Camp Fire in Northern California broke out in November 2018, took the lives of at least 85 people, and cost more than $16 billion in damage. Smoke from that blaze reached hazardous levels in San Francisco, Sacramento, Fresno, and many other smaller towns. Other forest fires in that year caused heavy smoke conditions in Portland, Seattle, Vancouver, and Anchorage. Such events are expected to be repeated often in the coming years (Int J Environ Res Public Health. 2019 Jul 6;16[13]).

Wildfire smoke can contain a wide range of substances, chemicals, and gases with known and unknown cardiorespiratory implications. “Smoke is composed primarily of carbon dioxide, water vapor, carbon monoxide, particulate matter, hydrocarbons and other organic chemicals, nitrogen oxides, trace minerals and several thousand other compounds,” according to the U.S. Environmental Protection Agency (Wildfire smoke: A guide for public health officials 2019. Washington, D.C.: EPA, 2019). The EPA report noted, “Particles with diameters less than 10 mcm (particulate matter, or PM10) can be inhaled into the lungs and affect the lungs, heart, and blood vessels. The smallest particles, those less than 2.5 mcm in diameter (PM2.5), are the greatest risk to public health because they can reach deep into the lungs and may even make it into the bloodstream.”
Research on health impact
In early June of 2008, Wayne Cascio, MD, awoke in his Greenville, N.C., home to the stench of smoke emanating from a large peat fire burning some 65 miles away. By the time he reached the parking lot at East Carolina University in Greenville to begin his workday as chief of cardiology, the haze of smoke had thickened to the point where he could only see a few feet in front of him.
Over the next several weeks, the fire scorched 41,000 acres and produced haze and air pollution that far exceeded National Ambient Air Quality Standards for particulate matter and blanketed rural communities in the state’s eastern region. The price tag for management of the blaze reached $20 million. Because of his interest in the health effects of wildfire smoke and because of his relationship with investigators at the EPA, Dr. Cascio initiated an epidemiology study to investigate the effects of exposure on cardiorespiratory outcomes in the population affected by the fire (Environ Health Perspect. 2011 Oct;119[10]:1415-20).
By combining satellite data with syndromic surveillance drawn from hospital records in 41 counties contained in the North Carolina Disease Event Tracking and Epidemiologic Collection Tool, he and his colleagues found that exposure to the peat wildfire smoke led to increases in the cumulative risk ratio for asthma (relative risk, 1.65), chronic obstructive pulmonary disease (RR, 1.73), and pneumonia and acute bronchitis (RR, 1.59). ED visits related to cardiopulmonary symptoms and heart failure also were significantly increased (RR, 1.23 and 1.37, respectively). “That was really the first study to strongly identify a cardiac endpoint related to wildfire smoke exposure,” said Dr. Cascio, who now directs the EPA’s National Health and Environmental Effects Research Laboratory. “It really pointed out how little we knew about the health effects of wildfire up until that time.”
Those early findings have been replicated in subsequent research about the acute health effects of exposure to wildfire smoke, which contains PM2.5 and other toxic substances from structures, electronic devices, and automobiles destroyed in the path of flames, including heavy metals and asbestos. Most of the work has focused on smoke-related cardiovascular and respiratory ED visits and hospitalizations.
A study of the 2008 California wildfire impact on ED visits accounted for ozone levels in addition to PM2.5 in the smoke. During the active fire periods, PM2.5 was significantly associated with exacerbations of asthma and COPD and these effects remained after controlling for ozone levels. PM2.5 inhalation during the wildfires was associated with increased risk of an ED visit for asthma (RR, 1.112; 95% confidence interval, 1.087-1.138) for a 10 mcg/m3 increase in PM2.5 and COPD (RR, 1.05; 95% CI, 1.019-1.0825), as well as for combined respiratory visits (RR, 1.035; 95% CI, 1.023-1.046) (Environ Int. 2109 Aug;129:291-8).
Researchers who evaluated the health impacts of wildfires in California during the 2015 fire season found an increase in all-cause cardiovascular and respiratory ED visits, especially among those aged 65 years and older during smoke days. The population-based study included 1,196,233 ED visits during May 1–Sept. 30 that year. PM2.5 concentrations were categorized as light, medium, or dense. Relative risk rose with the amount of smoke in the air. Rates of all-cause cardiovascular ED visits were elevated across levels of smoke density, with the greatest increase on dense smoke days and among those aged 65 years or older (RR,1.15; 95% CI, 1.09-1.22). All-cause cerebrovascular visits were associated with dense smoke days, especially among those aged 65 years and older (RR, 1.22; 95% CI, 1.00-1.49). Respiratory conditions also were increased on dense smoke days (RR, 1.18; 95% CI, 1.08-1.28) (J Am Heart Assoc. 2018 Apr 11;7:e007492. doi: 10.1161/JAHA.117.007492).
Long-term effects unknown
When it comes to the long-term effects of wildfire smoke on human health outcomes, much less is known. In a recent literature review, Colleen E. Reid, PhD, and Melissa May Maestas, PhD, found only one study that investigated long-term respiratory health impacts of wildfire smoke, and only a few studies that have estimated future health impacts of wildfires under likely climate change scenarios (Curr Opin Pulm Med. 2019 Mar;25:179-87).
“We know that there are immediate respiratory health effects from wildfire smoke,” said Dr. Reid of the department of geography at the University of Colorado Boulder. “What’s less known is everything else. That’s challenging, because people want to know about the long-term health effects.”
Evidence from the scientific literature suggests that exposure to air pollution adversely affects cardiovascular health, but whether exposure to wildfire smoke confers a similar risk is less clear. “Until just a few years ago we haven’t been able to study wildfire exposure measures on a large scale,” said EPA scientist Ana G. Rappold, PhD, a statistician there in the environmental public health division of the National Health and Environmental Effects Research Laboratory. “It’s also hard to predict wildfires, so it’s hard to plan for an epidemiologic study if you don’t know where they’re going to occur.”
Dr. Rappold and colleagues examined cardiopulmonary hospitalizations among adults aged 65 years and older in 692 U.S. counties within 200 km of 123 large wildfires during 2008-2010 (Environ Health Perspect. 2019;127[3]:37006. doi: 10.1289/EHP3860). They observed that an increased risk of PM2.5-related cardiopulmonary hospitalizations was similar on smoke and nonsmoke days across multiple lags and exposure metrics, while risk for asthma-related hospitalizations was higher during smoke days. “One hypothesis is that this was an older study population, so naturally if you’re inhaling smoke, the first organ that’s impacted in an older population is the lungs,” Dr. Rappold said. “If you go to the hospital for asthma, wheezing, or bronchitis, you are taken out of the risk pool for cardiovascular and other diseases. That could explain why in other studies we don’t see a clear cardiovascular signal as we have for air pollution studies in general. Another aspect to this study is, the exposure metric was PM2.5, but smoke contains many other components, particularly gases, which are respiratory irritants. It could be that this triggers a higher risk for respiratory [effects] than regular episodes of high PM2.5 exposure, just because of the additional gases that people are exposed to.”
Another complicating factor is the paucity of data about solutions to long-term exposure to wildfire smoke. “If you’re impacted by high-exposure levels for 60 days, that is not something we have experienced before,” Dr. Rappold noted. “What are the solutions for that community? What works? Can we show that by implementing community-level resilience plans with HEPA [high-efficiency particulate air] filters or other interventions, do the overall outcomes improve? Doctors are the first ones to talk with their patients about their symptoms and about how to take care of their conditions. They can clearly make a difference in emphasizing reducing exposures in a way that fits their patients individually, either reducing the amount of time spent outside, the duration of exposure, and the level of exposure. Maybe change activities based on the intensity of exposure. Don’t go for a run outside when it’s smoky, because your ventilation rate is higher and you will breathe in more smoke. Become aware of those things.”
Advising vulnerable patients
While research in this field advances, the unforgiving wildfire season looms, assuring more destruction of property and threats to cardiorespiratory health. “There are a lot of questions that research will have an opportunity to address as we go forward, including the utility and the benefit of N95 masks, the utility of HEPA filters used in the house, and even with HVAC [heating, ventilation, and air conditioning] systems,” Dr. Cascio said. “Can we really clean up the indoor air well enough to protect us from wildfire smoke?”
The way he sees it, the time is ripe for clinicians and officials in public and private practice settings to refine how they distribute information to people living in areas affected by wildfire smoke. “We can’t force people do anything, but at least if they’re informed, then they understand they can make an informed decision about how they might want to affect what they do that would limit their exposure,” he said. “As a patient, my health care system sends text and email messages to me. So, why couldn’t the hospital send out a text message or an email to all of the patients with COPD, coronary disease, and heart failure when an area is impacted by smoke, saying, ‘Check your air quality and take action if air quality is poor?’ Physicians don’t have time to do this kind of education in the office for all of their patients. I know that from experience. But if one were to only focus on those at highest risk, and encourage them to follow our guidelines, which might include doing HEPA filter treatment in the home, we probably would reduce the number of clinical events in a cost-effective way.”
FDA approves mepolizumab for severe eosinophilic asthma in younger kids
according to a release from GlaxoSmithKline, which developed the drug. This is the first targeted biologic approved for this condition in this age group.
The approval is supported by both an open-label study in children aged 6-11 years and evidence from other trials conducted in adults and adolescents. The 52-week, long-term study in these younger patients investigated pharmacokinetics, pharmacodynamics, and safety, the last of which was shown to be similar to that seen in older patients.
Hypersensitivity reactions, such as anaphylaxis, rash, and bronchospasm, have been associated with mepolizumab. It should not be used to treat acute bronchospasm or status asthmaticus, nor should systemic or inhaled corticosteroids be stopped abruptly after initiating mepolizumab treatment. Common adverse events include headache, injection-site reactions, back pain, and fatigue. Injection site reactions (such as pain, erythema, and itching) occurred in 8% of mepolizumab patients treated with 100 mg of the drug versus 3% of placebo patients.
The monoclonal antibody targeting interleukin-5 was first approved for severe eosinophilic asthma in 2015 for ages 12 years and older and in ages 6 years and older in the European Union in August 2018. It inhibits IL-5 from binding to eosinophils, which reduces the presence of eosinophils in blood without completely eliminating them.
according to a release from GlaxoSmithKline, which developed the drug. This is the first targeted biologic approved for this condition in this age group.
The approval is supported by both an open-label study in children aged 6-11 years and evidence from other trials conducted in adults and adolescents. The 52-week, long-term study in these younger patients investigated pharmacokinetics, pharmacodynamics, and safety, the last of which was shown to be similar to that seen in older patients.
Hypersensitivity reactions, such as anaphylaxis, rash, and bronchospasm, have been associated with mepolizumab. It should not be used to treat acute bronchospasm or status asthmaticus, nor should systemic or inhaled corticosteroids be stopped abruptly after initiating mepolizumab treatment. Common adverse events include headache, injection-site reactions, back pain, and fatigue. Injection site reactions (such as pain, erythema, and itching) occurred in 8% of mepolizumab patients treated with 100 mg of the drug versus 3% of placebo patients.
The monoclonal antibody targeting interleukin-5 was first approved for severe eosinophilic asthma in 2015 for ages 12 years and older and in ages 6 years and older in the European Union in August 2018. It inhibits IL-5 from binding to eosinophils, which reduces the presence of eosinophils in blood without completely eliminating them.
according to a release from GlaxoSmithKline, which developed the drug. This is the first targeted biologic approved for this condition in this age group.
The approval is supported by both an open-label study in children aged 6-11 years and evidence from other trials conducted in adults and adolescents. The 52-week, long-term study in these younger patients investigated pharmacokinetics, pharmacodynamics, and safety, the last of which was shown to be similar to that seen in older patients.
Hypersensitivity reactions, such as anaphylaxis, rash, and bronchospasm, have been associated with mepolizumab. It should not be used to treat acute bronchospasm or status asthmaticus, nor should systemic or inhaled corticosteroids be stopped abruptly after initiating mepolizumab treatment. Common adverse events include headache, injection-site reactions, back pain, and fatigue. Injection site reactions (such as pain, erythema, and itching) occurred in 8% of mepolizumab patients treated with 100 mg of the drug versus 3% of placebo patients.
The monoclonal antibody targeting interleukin-5 was first approved for severe eosinophilic asthma in 2015 for ages 12 years and older and in ages 6 years and older in the European Union in August 2018. It inhibits IL-5 from binding to eosinophils, which reduces the presence of eosinophils in blood without completely eliminating them.
Asthma hospitalization in kids linked with doubled migraine incidence
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
REPORTING FROM AHS 2019
PCPs play role in identifying severe, difficult-to-treat asthma
ORLANDO – Clinicians at the primary care level should learn to distinguish the difference between severe and difficult-to-treat asthma to help facilitate referral to an asthma care specialist, according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
Care providers are seeing patients with severe asthma at their primary care practice, whether they realize it or not, and should therefore learn to recognize and diagnose these patients even if they are not directly treating them for asthma, said Michelle R. Dickens, MSN, RN, FNP-C, AE-C, a nurse practitioner at Ferrell-Duncan Clinic department of allergy, asthma, and immunology in Springfield, Mo., said in her presentation.
“There’s still a lot we can do to get the ball rolling,” Ms. Dickens said. “While you may not be prescribing some of these newer biologics and some of the high-level, $30,000-a-year medications for your asthmatic, you still have a role in this in identifying them and helping us to get to where they need to be.”
Ms. Dickens noted that patients may not even disclose their asthma history with their primary care provider if it is not the reason for the office visit. “Because asthma can be such an episodic disease, it’s not right on the top of their radar,” she said. “They have bigger issues they want to talk about with you, and they forget to mention the asthma part.”
Under Global Initiative for Asthma (GINA) criteria, severe asthma is defined as poorly controlled asthma even after patients demonstrate adherence and good technique. However, before diagnosing a patient with severe asthma, clinicians should first rule out whether the patient has asthma that is difficult to treat, said Ms. Dickens. Difficult-to-treat asthma is characterized by inadequate dosing of medication, noncompliance with medication dose (“spreading out” the medication), poor technique when self-administering the medication, and comorbid conditions. It is also possible that difficult-to-treat asthma is not well controlled because the asthma was misdiagnosed and is actually another condition, she added.
If a patient has difficult-to-treat asthma, ensure they are adhering to the therapy, using proper technique, and that the medicine is being administered at the proper dose. Using Expert Panel Report 3 (EPR-3) and Global Initiative for Asthma (GINA) guidelines, clinicians should maximize the treatment for a patient with severe asthma based on the stepwise approach outlined in the guidelines, and referring out to an asthma specialist for add-on therapy or stepping up therapy when indicated.
Researchers are beginning to explore the genotypes, phenotypes, and endotypes of asthma to learn more about severe asthma and potentially identify asthma subtypes, said Ms. Dickens. “We’re not there yet, but we are learning a little bit about why certain patients have certain types of asthma,” she said.
The Severe Asthma Research Program has found three clusters of likely severe asthma candidates: those with classic childhood asthma onset, those who have asthma with chronic obstructive pulmonary disease (COPD), and patients with both obesity and asthma characterized by “high impairment but mildly abnormal lung function.” Clinicians can use spirometry, complete blood count with differential, total immunoglobulin E, body mass index, allergy testing, and exhaled nitric oxide with these data and biomarkers to gain a better idea of a patient’s asthma situation.
Referrals to an asthma specialist should be considered if a patient experiences a life-threatening exacerbation, is not responding to therapy, has an unusual presentation of asthma symptoms, has comorbid conditions, or needs additional testing or additional education. Patients who are at step 2 or higher in EPR-3 guidelines and ready to move to step 3 and are under 4 years of age, and patients who are 5 years or older at step 4 of therapy or higher should be referred to an asthma specialist. “I think the younger the patient and the more severe the [symptoms], the more likely you should be referring to a specialist,” said Ms. Dickens.
Ms. Dickens reports no relevant financial disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO – Clinicians at the primary care level should learn to distinguish the difference between severe and difficult-to-treat asthma to help facilitate referral to an asthma care specialist, according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
Care providers are seeing patients with severe asthma at their primary care practice, whether they realize it or not, and should therefore learn to recognize and diagnose these patients even if they are not directly treating them for asthma, said Michelle R. Dickens, MSN, RN, FNP-C, AE-C, a nurse practitioner at Ferrell-Duncan Clinic department of allergy, asthma, and immunology in Springfield, Mo., said in her presentation.
“There’s still a lot we can do to get the ball rolling,” Ms. Dickens said. “While you may not be prescribing some of these newer biologics and some of the high-level, $30,000-a-year medications for your asthmatic, you still have a role in this in identifying them and helping us to get to where they need to be.”
Ms. Dickens noted that patients may not even disclose their asthma history with their primary care provider if it is not the reason for the office visit. “Because asthma can be such an episodic disease, it’s not right on the top of their radar,” she said. “They have bigger issues they want to talk about with you, and they forget to mention the asthma part.”
Under Global Initiative for Asthma (GINA) criteria, severe asthma is defined as poorly controlled asthma even after patients demonstrate adherence and good technique. However, before diagnosing a patient with severe asthma, clinicians should first rule out whether the patient has asthma that is difficult to treat, said Ms. Dickens. Difficult-to-treat asthma is characterized by inadequate dosing of medication, noncompliance with medication dose (“spreading out” the medication), poor technique when self-administering the medication, and comorbid conditions. It is also possible that difficult-to-treat asthma is not well controlled because the asthma was misdiagnosed and is actually another condition, she added.
If a patient has difficult-to-treat asthma, ensure they are adhering to the therapy, using proper technique, and that the medicine is being administered at the proper dose. Using Expert Panel Report 3 (EPR-3) and Global Initiative for Asthma (GINA) guidelines, clinicians should maximize the treatment for a patient with severe asthma based on the stepwise approach outlined in the guidelines, and referring out to an asthma specialist for add-on therapy or stepping up therapy when indicated.
Researchers are beginning to explore the genotypes, phenotypes, and endotypes of asthma to learn more about severe asthma and potentially identify asthma subtypes, said Ms. Dickens. “We’re not there yet, but we are learning a little bit about why certain patients have certain types of asthma,” she said.
The Severe Asthma Research Program has found three clusters of likely severe asthma candidates: those with classic childhood asthma onset, those who have asthma with chronic obstructive pulmonary disease (COPD), and patients with both obesity and asthma characterized by “high impairment but mildly abnormal lung function.” Clinicians can use spirometry, complete blood count with differential, total immunoglobulin E, body mass index, allergy testing, and exhaled nitric oxide with these data and biomarkers to gain a better idea of a patient’s asthma situation.
Referrals to an asthma specialist should be considered if a patient experiences a life-threatening exacerbation, is not responding to therapy, has an unusual presentation of asthma symptoms, has comorbid conditions, or needs additional testing or additional education. Patients who are at step 2 or higher in EPR-3 guidelines and ready to move to step 3 and are under 4 years of age, and patients who are 5 years or older at step 4 of therapy or higher should be referred to an asthma specialist. “I think the younger the patient and the more severe the [symptoms], the more likely you should be referring to a specialist,” said Ms. Dickens.
Ms. Dickens reports no relevant financial disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO – Clinicians at the primary care level should learn to distinguish the difference between severe and difficult-to-treat asthma to help facilitate referral to an asthma care specialist, according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
Care providers are seeing patients with severe asthma at their primary care practice, whether they realize it or not, and should therefore learn to recognize and diagnose these patients even if they are not directly treating them for asthma, said Michelle R. Dickens, MSN, RN, FNP-C, AE-C, a nurse practitioner at Ferrell-Duncan Clinic department of allergy, asthma, and immunology in Springfield, Mo., said in her presentation.
“There’s still a lot we can do to get the ball rolling,” Ms. Dickens said. “While you may not be prescribing some of these newer biologics and some of the high-level, $30,000-a-year medications for your asthmatic, you still have a role in this in identifying them and helping us to get to where they need to be.”
Ms. Dickens noted that patients may not even disclose their asthma history with their primary care provider if it is not the reason for the office visit. “Because asthma can be such an episodic disease, it’s not right on the top of their radar,” she said. “They have bigger issues they want to talk about with you, and they forget to mention the asthma part.”
Under Global Initiative for Asthma (GINA) criteria, severe asthma is defined as poorly controlled asthma even after patients demonstrate adherence and good technique. However, before diagnosing a patient with severe asthma, clinicians should first rule out whether the patient has asthma that is difficult to treat, said Ms. Dickens. Difficult-to-treat asthma is characterized by inadequate dosing of medication, noncompliance with medication dose (“spreading out” the medication), poor technique when self-administering the medication, and comorbid conditions. It is also possible that difficult-to-treat asthma is not well controlled because the asthma was misdiagnosed and is actually another condition, she added.
If a patient has difficult-to-treat asthma, ensure they are adhering to the therapy, using proper technique, and that the medicine is being administered at the proper dose. Using Expert Panel Report 3 (EPR-3) and Global Initiative for Asthma (GINA) guidelines, clinicians should maximize the treatment for a patient with severe asthma based on the stepwise approach outlined in the guidelines, and referring out to an asthma specialist for add-on therapy or stepping up therapy when indicated.
Researchers are beginning to explore the genotypes, phenotypes, and endotypes of asthma to learn more about severe asthma and potentially identify asthma subtypes, said Ms. Dickens. “We’re not there yet, but we are learning a little bit about why certain patients have certain types of asthma,” she said.
The Severe Asthma Research Program has found three clusters of likely severe asthma candidates: those with classic childhood asthma onset, those who have asthma with chronic obstructive pulmonary disease (COPD), and patients with both obesity and asthma characterized by “high impairment but mildly abnormal lung function.” Clinicians can use spirometry, complete blood count with differential, total immunoglobulin E, body mass index, allergy testing, and exhaled nitric oxide with these data and biomarkers to gain a better idea of a patient’s asthma situation.
Referrals to an asthma specialist should be considered if a patient experiences a life-threatening exacerbation, is not responding to therapy, has an unusual presentation of asthma symptoms, has comorbid conditions, or needs additional testing or additional education. Patients who are at step 2 or higher in EPR-3 guidelines and ready to move to step 3 and are under 4 years of age, and patients who are 5 years or older at step 4 of therapy or higher should be referred to an asthma specialist. “I think the younger the patient and the more severe the [symptoms], the more likely you should be referring to a specialist,” said Ms. Dickens.
Ms. Dickens reports no relevant financial disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM CARPS 2019
Patient and family education of asthma management is critical
ORLANDO – according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
“Every contact with them is a teachable moment,” Mary Lou Hayden, RN, MS, FNP-BC, AE-C, a board-certified nurse practitioner and asthma educator, said in her presentation. “You want to make sure you’re involving the important people in their lives to help them.”
Education for asthma includes teaching patients and their families the difference between long-term control and reliever medications; the proper timing and technique with the medications, as well as the importance of adherence; how to recognize and avoid triggers for asthma; how to self-monitor their asthma and control the disease; and when to seek medication care, she said.
“We review their inhaler technique every time they come in,” she added.
According to the American Lung Association, patients learn in visual, auditory, and kinesthetic styles. Teaching patients in a kinesthetic style by actually showing the patient how to take the medication through example will help the patient learn through feeling, or muscle memory. This also method works even if patients do not have the medication with them at the time, said Ms. Hayden.
“Let’s say, you don’t have [the medication], but you prescribe it,” she said. “When they come back, tell them to bring their bag of medications and make sure you go back through because if they can kinesthetically use it correctly, they’ve already mastered the visual and the auditory piece.
Written action plans are also important to successful asthma management. The plan should be tailored to the patient’s disease severity, loss of control, and include information like the peak expiratory flow and medication types, dosages, and frequencies. The action plan should also be available at home, daycare, and school. “You want them to know how to recognize their symptoms, what to do about their symptoms, and when to contact you or go to urgent care or [the emergency room],” said Ms. Hayden.
To simplify the plan, Ms. Hayden recommended zoning actions based on color, like the asthma action plan provided by the American Academy of Allergy, Asthma & Immunology. The AAAAI plan uses traffic colors to signify how well controlled a patient’s asthma is, with green indicating well-controlled disease, yellow denoting worsening asthma, and red indicating that the asthma needs to be treated right away.
Action plans should also address a patient’s health literacy level and culture. “Think about who’s going to be using it,” said Ms. Hayden.
The goal of asthma therapy is to prevent chronic or problematic symptoms, lower use of short-acting beta-agonists, maintain good pulmonary function, normalize activity levels at school and work, prevent exacerbations and hospitalizations, and meet the patient’s expectations, as well as those of their family. “If you’re thinking only severe patients have exacerbations that are near fatal or fatal, that’s not true,” she said. It’s “very common for somebody with a very mild and intermittent asthma to go to severe in a very short period of time.”
When properly implemented, patient education is performed at the time of diagnosis, is done according to a plan, is integrated into care, reinforces important information, improves adherence, is individualized to the patient and addresses their needs, and builds a partnership between provider and patient.
“We really are thinking of the team concept: us, the patient and the important people the patient’s lives, and other clinicians that might be involved with other diseases to care for the patient,” said Ms. Hayden.
Ms. Hayden reports no relevant conflicts of interest. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO – according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
“Every contact with them is a teachable moment,” Mary Lou Hayden, RN, MS, FNP-BC, AE-C, a board-certified nurse practitioner and asthma educator, said in her presentation. “You want to make sure you’re involving the important people in their lives to help them.”
Education for asthma includes teaching patients and their families the difference between long-term control and reliever medications; the proper timing and technique with the medications, as well as the importance of adherence; how to recognize and avoid triggers for asthma; how to self-monitor their asthma and control the disease; and when to seek medication care, she said.
“We review their inhaler technique every time they come in,” she added.
According to the American Lung Association, patients learn in visual, auditory, and kinesthetic styles. Teaching patients in a kinesthetic style by actually showing the patient how to take the medication through example will help the patient learn through feeling, or muscle memory. This also method works even if patients do not have the medication with them at the time, said Ms. Hayden.
“Let’s say, you don’t have [the medication], but you prescribe it,” she said. “When they come back, tell them to bring their bag of medications and make sure you go back through because if they can kinesthetically use it correctly, they’ve already mastered the visual and the auditory piece.
Written action plans are also important to successful asthma management. The plan should be tailored to the patient’s disease severity, loss of control, and include information like the peak expiratory flow and medication types, dosages, and frequencies. The action plan should also be available at home, daycare, and school. “You want them to know how to recognize their symptoms, what to do about their symptoms, and when to contact you or go to urgent care or [the emergency room],” said Ms. Hayden.
To simplify the plan, Ms. Hayden recommended zoning actions based on color, like the asthma action plan provided by the American Academy of Allergy, Asthma & Immunology. The AAAAI plan uses traffic colors to signify how well controlled a patient’s asthma is, with green indicating well-controlled disease, yellow denoting worsening asthma, and red indicating that the asthma needs to be treated right away.
Action plans should also address a patient’s health literacy level and culture. “Think about who’s going to be using it,” said Ms. Hayden.
The goal of asthma therapy is to prevent chronic or problematic symptoms, lower use of short-acting beta-agonists, maintain good pulmonary function, normalize activity levels at school and work, prevent exacerbations and hospitalizations, and meet the patient’s expectations, as well as those of their family. “If you’re thinking only severe patients have exacerbations that are near fatal or fatal, that’s not true,” she said. It’s “very common for somebody with a very mild and intermittent asthma to go to severe in a very short period of time.”
When properly implemented, patient education is performed at the time of diagnosis, is done according to a plan, is integrated into care, reinforces important information, improves adherence, is individualized to the patient and addresses their needs, and builds a partnership between provider and patient.
“We really are thinking of the team concept: us, the patient and the important people the patient’s lives, and other clinicians that might be involved with other diseases to care for the patient,” said Ms. Hayden.
Ms. Hayden reports no relevant conflicts of interest. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO – according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
“Every contact with them is a teachable moment,” Mary Lou Hayden, RN, MS, FNP-BC, AE-C, a board-certified nurse practitioner and asthma educator, said in her presentation. “You want to make sure you’re involving the important people in their lives to help them.”
Education for asthma includes teaching patients and their families the difference between long-term control and reliever medications; the proper timing and technique with the medications, as well as the importance of adherence; how to recognize and avoid triggers for asthma; how to self-monitor their asthma and control the disease; and when to seek medication care, she said.
“We review their inhaler technique every time they come in,” she added.
According to the American Lung Association, patients learn in visual, auditory, and kinesthetic styles. Teaching patients in a kinesthetic style by actually showing the patient how to take the medication through example will help the patient learn through feeling, or muscle memory. This also method works even if patients do not have the medication with them at the time, said Ms. Hayden.
“Let’s say, you don’t have [the medication], but you prescribe it,” she said. “When they come back, tell them to bring their bag of medications and make sure you go back through because if they can kinesthetically use it correctly, they’ve already mastered the visual and the auditory piece.
Written action plans are also important to successful asthma management. The plan should be tailored to the patient’s disease severity, loss of control, and include information like the peak expiratory flow and medication types, dosages, and frequencies. The action plan should also be available at home, daycare, and school. “You want them to know how to recognize their symptoms, what to do about their symptoms, and when to contact you or go to urgent care or [the emergency room],” said Ms. Hayden.
To simplify the plan, Ms. Hayden recommended zoning actions based on color, like the asthma action plan provided by the American Academy of Allergy, Asthma & Immunology. The AAAAI plan uses traffic colors to signify how well controlled a patient’s asthma is, with green indicating well-controlled disease, yellow denoting worsening asthma, and red indicating that the asthma needs to be treated right away.
Action plans should also address a patient’s health literacy level and culture. “Think about who’s going to be using it,” said Ms. Hayden.
The goal of asthma therapy is to prevent chronic or problematic symptoms, lower use of short-acting beta-agonists, maintain good pulmonary function, normalize activity levels at school and work, prevent exacerbations and hospitalizations, and meet the patient’s expectations, as well as those of their family. “If you’re thinking only severe patients have exacerbations that are near fatal or fatal, that’s not true,” she said. It’s “very common for somebody with a very mild and intermittent asthma to go to severe in a very short period of time.”
When properly implemented, patient education is performed at the time of diagnosis, is done according to a plan, is integrated into care, reinforces important information, improves adherence, is individualized to the patient and addresses their needs, and builds a partnership between provider and patient.
“We really are thinking of the team concept: us, the patient and the important people the patient’s lives, and other clinicians that might be involved with other diseases to care for the patient,” said Ms. Hayden.
Ms. Hayden reports no relevant conflicts of interest. Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM CARPS 2019
Short-course azithromycin no benefit in pediatric asthma admissions
SEATTLE – Adding a 3-day course of azithromycin to treatment regimens of children hospitalized with asthma did not shorten length of stay or bring other benefits in a randomized, blinded trial of more than 150 youngsters at The Children’s Hospital at Montefiore, New York.
In recent years, some pediatricians at Montefiore had begun giving short-course azithromycin to hospitalized children who were not recovering as quickly as they had hoped, spurred by outpatient reports of reduced exacerbations and other benefits with long-term azithromycin (e.g., Lancet. 2017 Aug 12;390(10095):659-68).
“We had no evidence for doing that at all” in the hospital, and it might be going on elsewhere, said senior investigator Alyssa Silver, MD, assistant professor of pediatrics at Montefiore and Albert Einstein College of Medicine, New York. She and her colleagues, including primary investigator Lindsey Douglas, MD, assistant professor of pediatrics at the Icahn School of Medicine at Mount Sinai, New York, took a closer look.
The negative results mean that “we can stop doing this, giving kids unnecessary things. Word is starting to get out” at Montefiore. “People are not using it as much,” she said at Pediatric Hospital Medicine, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The team had expected azithromycin to shorten length of stay (LOS) by about half a day, due to its anti-inflammatory effects, but that’s not what was found when they randomized 80 children aged 4-12 years with persistent asthma to oral azithromycin 10 mg/kg per day for 3 days within 12 hours of admission, and 79 to placebo.
LOS was 1.86 days in the placebo arm, and 1.69 days in the azithromycin group (P = .23). One placebo child was transferred to the pediatric ICU, versus none in the azithromycin arm (P = .50). The study was stopped short of its 214 subject enrollment goal because of futility, but even so, it was well powered to detect a difference in LOS, the primary outcome, Dr. Silver said.
At 1 week phone follow-up, 7 placebo children and 11 in the azithromycin arm had persistent asthma symptoms (P = .42), and 1 placebo child and 2 azithromycin children had been readmitted (P greater than .99). There were no differences in days of school missed, or work days missed among parents and guardians.
At one month, 23 placebo and 18 azithromycin children had persistent asthma symptoms (P = .5); 7 placebo and 6 azithromycin children had returned to the ED (P = .75).
In short, “we really found no difference” with short-course azithromycin. “Clinicians should consider [these] data before prescribing azithromycin [to] children hospitalized with asthma,” Dr. Silver and her team concluded.
Subjects were an average of about 7 years old, and about two-thirds were boys. They were not on azithromycin or other antibiotics prior to admission. About half had been admitted in the previous year, and about a quarter had at least one previous pediatric ICU admission. Over two-thirds had been on daily asthma medications. There were about 2 days of symptoms prior to admission.
There was no external funding, and Dr. Silver had no disclosures.
SEATTLE – Adding a 3-day course of azithromycin to treatment regimens of children hospitalized with asthma did not shorten length of stay or bring other benefits in a randomized, blinded trial of more than 150 youngsters at The Children’s Hospital at Montefiore, New York.
In recent years, some pediatricians at Montefiore had begun giving short-course azithromycin to hospitalized children who were not recovering as quickly as they had hoped, spurred by outpatient reports of reduced exacerbations and other benefits with long-term azithromycin (e.g., Lancet. 2017 Aug 12;390(10095):659-68).
“We had no evidence for doing that at all” in the hospital, and it might be going on elsewhere, said senior investigator Alyssa Silver, MD, assistant professor of pediatrics at Montefiore and Albert Einstein College of Medicine, New York. She and her colleagues, including primary investigator Lindsey Douglas, MD, assistant professor of pediatrics at the Icahn School of Medicine at Mount Sinai, New York, took a closer look.
The negative results mean that “we can stop doing this, giving kids unnecessary things. Word is starting to get out” at Montefiore. “People are not using it as much,” she said at Pediatric Hospital Medicine, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The team had expected azithromycin to shorten length of stay (LOS) by about half a day, due to its anti-inflammatory effects, but that’s not what was found when they randomized 80 children aged 4-12 years with persistent asthma to oral azithromycin 10 mg/kg per day for 3 days within 12 hours of admission, and 79 to placebo.
LOS was 1.86 days in the placebo arm, and 1.69 days in the azithromycin group (P = .23). One placebo child was transferred to the pediatric ICU, versus none in the azithromycin arm (P = .50). The study was stopped short of its 214 subject enrollment goal because of futility, but even so, it was well powered to detect a difference in LOS, the primary outcome, Dr. Silver said.
At 1 week phone follow-up, 7 placebo children and 11 in the azithromycin arm had persistent asthma symptoms (P = .42), and 1 placebo child and 2 azithromycin children had been readmitted (P greater than .99). There were no differences in days of school missed, or work days missed among parents and guardians.
At one month, 23 placebo and 18 azithromycin children had persistent asthma symptoms (P = .5); 7 placebo and 6 azithromycin children had returned to the ED (P = .75).
In short, “we really found no difference” with short-course azithromycin. “Clinicians should consider [these] data before prescribing azithromycin [to] children hospitalized with asthma,” Dr. Silver and her team concluded.
Subjects were an average of about 7 years old, and about two-thirds were boys. They were not on azithromycin or other antibiotics prior to admission. About half had been admitted in the previous year, and about a quarter had at least one previous pediatric ICU admission. Over two-thirds had been on daily asthma medications. There were about 2 days of symptoms prior to admission.
There was no external funding, and Dr. Silver had no disclosures.
SEATTLE – Adding a 3-day course of azithromycin to treatment regimens of children hospitalized with asthma did not shorten length of stay or bring other benefits in a randomized, blinded trial of more than 150 youngsters at The Children’s Hospital at Montefiore, New York.
In recent years, some pediatricians at Montefiore had begun giving short-course azithromycin to hospitalized children who were not recovering as quickly as they had hoped, spurred by outpatient reports of reduced exacerbations and other benefits with long-term azithromycin (e.g., Lancet. 2017 Aug 12;390(10095):659-68).
“We had no evidence for doing that at all” in the hospital, and it might be going on elsewhere, said senior investigator Alyssa Silver, MD, assistant professor of pediatrics at Montefiore and Albert Einstein College of Medicine, New York. She and her colleagues, including primary investigator Lindsey Douglas, MD, assistant professor of pediatrics at the Icahn School of Medicine at Mount Sinai, New York, took a closer look.
The negative results mean that “we can stop doing this, giving kids unnecessary things. Word is starting to get out” at Montefiore. “People are not using it as much,” she said at Pediatric Hospital Medicine, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The team had expected azithromycin to shorten length of stay (LOS) by about half a day, due to its anti-inflammatory effects, but that’s not what was found when they randomized 80 children aged 4-12 years with persistent asthma to oral azithromycin 10 mg/kg per day for 3 days within 12 hours of admission, and 79 to placebo.
LOS was 1.86 days in the placebo arm, and 1.69 days in the azithromycin group (P = .23). One placebo child was transferred to the pediatric ICU, versus none in the azithromycin arm (P = .50). The study was stopped short of its 214 subject enrollment goal because of futility, but even so, it was well powered to detect a difference in LOS, the primary outcome, Dr. Silver said.
At 1 week phone follow-up, 7 placebo children and 11 in the azithromycin arm had persistent asthma symptoms (P = .42), and 1 placebo child and 2 azithromycin children had been readmitted (P greater than .99). There were no differences in days of school missed, or work days missed among parents and guardians.
At one month, 23 placebo and 18 azithromycin children had persistent asthma symptoms (P = .5); 7 placebo and 6 azithromycin children had returned to the ED (P = .75).
In short, “we really found no difference” with short-course azithromycin. “Clinicians should consider [these] data before prescribing azithromycin [to] children hospitalized with asthma,” Dr. Silver and her team concluded.
Subjects were an average of about 7 years old, and about two-thirds were boys. They were not on azithromycin or other antibiotics prior to admission. About half had been admitted in the previous year, and about a quarter had at least one previous pediatric ICU admission. Over two-thirds had been on daily asthma medications. There were about 2 days of symptoms prior to admission.
There was no external funding, and Dr. Silver had no disclosures.
REPORTING FROM PHM 2019
Best inhaler for COPD is the one the patient will use
ORLANDO –
That’s according to Gabriel Ortiz, MPAS, PA-C, DFAAPA, a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
There are several treatment options available in inhaler form for patients with COPD, including short-acting and long-acting beta2-agonists (SABA/LABA), short-acting and long-acting antimuscarinics (SAMA/LAMA), combination therapy, and triple therapy. But education and training on how to use an inhaler is also important, Mr. Ortiz said in his presentation.
Providers should help a patient choose an inhaler they are most likely to use. “It’s difficult to actuate and inhale, so there’s a lot of education that goes into that,” said Mr. Ortiz, of Pediatric Pulmonary Services in El Paso, Texas. “What we do for our patients is, we educate them, we tell them to demonstrate it, then bring [the] inhaler back on the next visit and demonstrate to us every time.”
“Make sure that they demonstrate because, as patients get older, they may lose their ability to actuate and inhale,” he added.
Adherence to therapy should also be considered before changing from a current therapy, he added. Mr. Ortiz described a scenario in which a prescription was filled, but because of the cost, the patient reduced the dose by half to make the therapy last longer.
“We could be the best providers in the world, prescribing the best medication in the world. If the medication doesn’t get to where we need it, it’s not going to help anybody,” he said.
Providers should also use nonpharmacological treatments to prevent or keep COPD from progressing. Smoking cessation is key to reducing the risk of developing COPD, and it is not clear whether e-cigarettes aid in smoking cessation, despite companies that market these products making that claim. “We have a huge e-cigarette epidemic here,” he said.
Instead, Mr. Ortiz recommended identifying which patients are current tobacco users, encouraging them to quit, determining whether the patient is willing to make a commitment to cut down on tobacco use or stop entirely, helping draft a quit plan and obtaining intra- and extratreatment social support for smoking cessation, and scheduling follow-up. Providers should discuss smoking cessation at each visit, and it may take multiple visits before a patient is willing to consider quitting, he said.
Another measure providers can take is making sure patients with COPD have received influenza and pneumococcal vaccinations because this can lower the risk of respiratory tract infections. Physical activity, training in exercise, nutritional support, and pulmonary rehabilitation can improve their health status, dyspnea, and exercise tolerance. While C-level evidence shows education alone is not effective according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, providers working with patients through self-management interventions have been shown to improve health status and decrease COPD-related hospitalizations.
Oxygen therapy has been effective for patients with severe resting chronic hypoxia and improves survival, said Mr. Ortiz. For patients who gradually decline in health despite treatment, palliative, hospice, and end-of-life care may be an option. “Remember that as acute exacerbations continue, that increases the risk of death,” he said. “We want to try and prevent [those] exacerbations and improve quality of life.”
During follow-up visits, providers should continue performing spirometry tests annually to measure decline in forced expiratory volume in 1 second, information on symptoms that have presented since the previous visit, details of any exacerbations that occurred, and current smoking status. When making decisions to adjust therapy, providers should examine the effectiveness of the current regimen and consider the dose of prescribed medications, whether the patient is adhering to the regimen, inhaler technique, and any side effects.
Mr. Ortiz reports also being a paid employee for Thermo Fisher, a biotechnology product development company based in Waltham, Mass. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO –
That’s according to Gabriel Ortiz, MPAS, PA-C, DFAAPA, a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
There are several treatment options available in inhaler form for patients with COPD, including short-acting and long-acting beta2-agonists (SABA/LABA), short-acting and long-acting antimuscarinics (SAMA/LAMA), combination therapy, and triple therapy. But education and training on how to use an inhaler is also important, Mr. Ortiz said in his presentation.
Providers should help a patient choose an inhaler they are most likely to use. “It’s difficult to actuate and inhale, so there’s a lot of education that goes into that,” said Mr. Ortiz, of Pediatric Pulmonary Services in El Paso, Texas. “What we do for our patients is, we educate them, we tell them to demonstrate it, then bring [the] inhaler back on the next visit and demonstrate to us every time.”
“Make sure that they demonstrate because, as patients get older, they may lose their ability to actuate and inhale,” he added.
Adherence to therapy should also be considered before changing from a current therapy, he added. Mr. Ortiz described a scenario in which a prescription was filled, but because of the cost, the patient reduced the dose by half to make the therapy last longer.
“We could be the best providers in the world, prescribing the best medication in the world. If the medication doesn’t get to where we need it, it’s not going to help anybody,” he said.
Providers should also use nonpharmacological treatments to prevent or keep COPD from progressing. Smoking cessation is key to reducing the risk of developing COPD, and it is not clear whether e-cigarettes aid in smoking cessation, despite companies that market these products making that claim. “We have a huge e-cigarette epidemic here,” he said.
Instead, Mr. Ortiz recommended identifying which patients are current tobacco users, encouraging them to quit, determining whether the patient is willing to make a commitment to cut down on tobacco use or stop entirely, helping draft a quit plan and obtaining intra- and extratreatment social support for smoking cessation, and scheduling follow-up. Providers should discuss smoking cessation at each visit, and it may take multiple visits before a patient is willing to consider quitting, he said.
Another measure providers can take is making sure patients with COPD have received influenza and pneumococcal vaccinations because this can lower the risk of respiratory tract infections. Physical activity, training in exercise, nutritional support, and pulmonary rehabilitation can improve their health status, dyspnea, and exercise tolerance. While C-level evidence shows education alone is not effective according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, providers working with patients through self-management interventions have been shown to improve health status and decrease COPD-related hospitalizations.
Oxygen therapy has been effective for patients with severe resting chronic hypoxia and improves survival, said Mr. Ortiz. For patients who gradually decline in health despite treatment, palliative, hospice, and end-of-life care may be an option. “Remember that as acute exacerbations continue, that increases the risk of death,” he said. “We want to try and prevent [those] exacerbations and improve quality of life.”
During follow-up visits, providers should continue performing spirometry tests annually to measure decline in forced expiratory volume in 1 second, information on symptoms that have presented since the previous visit, details of any exacerbations that occurred, and current smoking status. When making decisions to adjust therapy, providers should examine the effectiveness of the current regimen and consider the dose of prescribed medications, whether the patient is adhering to the regimen, inhaler technique, and any side effects.
Mr. Ortiz reports also being a paid employee for Thermo Fisher, a biotechnology product development company based in Waltham, Mass. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO –
That’s according to Gabriel Ortiz, MPAS, PA-C, DFAAPA, a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
There are several treatment options available in inhaler form for patients with COPD, including short-acting and long-acting beta2-agonists (SABA/LABA), short-acting and long-acting antimuscarinics (SAMA/LAMA), combination therapy, and triple therapy. But education and training on how to use an inhaler is also important, Mr. Ortiz said in his presentation.
Providers should help a patient choose an inhaler they are most likely to use. “It’s difficult to actuate and inhale, so there’s a lot of education that goes into that,” said Mr. Ortiz, of Pediatric Pulmonary Services in El Paso, Texas. “What we do for our patients is, we educate them, we tell them to demonstrate it, then bring [the] inhaler back on the next visit and demonstrate to us every time.”
“Make sure that they demonstrate because, as patients get older, they may lose their ability to actuate and inhale,” he added.
Adherence to therapy should also be considered before changing from a current therapy, he added. Mr. Ortiz described a scenario in which a prescription was filled, but because of the cost, the patient reduced the dose by half to make the therapy last longer.
“We could be the best providers in the world, prescribing the best medication in the world. If the medication doesn’t get to where we need it, it’s not going to help anybody,” he said.
Providers should also use nonpharmacological treatments to prevent or keep COPD from progressing. Smoking cessation is key to reducing the risk of developing COPD, and it is not clear whether e-cigarettes aid in smoking cessation, despite companies that market these products making that claim. “We have a huge e-cigarette epidemic here,” he said.
Instead, Mr. Ortiz recommended identifying which patients are current tobacco users, encouraging them to quit, determining whether the patient is willing to make a commitment to cut down on tobacco use or stop entirely, helping draft a quit plan and obtaining intra- and extratreatment social support for smoking cessation, and scheduling follow-up. Providers should discuss smoking cessation at each visit, and it may take multiple visits before a patient is willing to consider quitting, he said.
Another measure providers can take is making sure patients with COPD have received influenza and pneumococcal vaccinations because this can lower the risk of respiratory tract infections. Physical activity, training in exercise, nutritional support, and pulmonary rehabilitation can improve their health status, dyspnea, and exercise tolerance. While C-level evidence shows education alone is not effective according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, providers working with patients through self-management interventions have been shown to improve health status and decrease COPD-related hospitalizations.
Oxygen therapy has been effective for patients with severe resting chronic hypoxia and improves survival, said Mr. Ortiz. For patients who gradually decline in health despite treatment, palliative, hospice, and end-of-life care may be an option. “Remember that as acute exacerbations continue, that increases the risk of death,” he said. “We want to try and prevent [those] exacerbations and improve quality of life.”
During follow-up visits, providers should continue performing spirometry tests annually to measure decline in forced expiratory volume in 1 second, information on symptoms that have presented since the previous visit, details of any exacerbations that occurred, and current smoking status. When making decisions to adjust therapy, providers should examine the effectiveness of the current regimen and consider the dose of prescribed medications, whether the patient is adhering to the regimen, inhaler technique, and any side effects.
Mr. Ortiz reports also being a paid employee for Thermo Fisher, a biotechnology product development company based in Waltham, Mass. Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM CARPS 2019