User login
Clinicians slow to implement lipid-lowering guidelines: GOULD registry
Among patients with atherosclerotic cardiovascular disease (ASCVD), 2 years after release of treat-to-target guidelines from the American Heart Association and the European Society of Cardiology and European Atherosclerosis Society, most patients with LDL cholesterol higher than 70 mg/dL did not receive intensification of therapy, and two-thirds continued to have LDL levels above that level, according to a prospective registry study.
Both guidelines recommend driving LDL-C levels to 50% or below of baseline levels; results from the Getting to an Improved Understanding of Low-Density Lipoprotein Cholesterol and Dyslipidemia Management (GOULD) registry suggest this is rarely achieved. “Unfortunately it’s not a total surprise, but it’s disappointing,” said Christopher Cannon, MD, the study’s lead author.
“Therapeutic inertia seems to be the rule in clinical practice,” said Jennifer G. Robinson, MD, MPH, who was asked to comment on the study. Dr. Robinson is professor epidemiology and cardiology at the University of Iowa, Iowa City.
“This is yet another disappointing reminder of how we are failing our patients. Lipid lowering is one of the safest, most effective ways to prevent cardiovascular disease, and yet we are falling short. We have the tools in our toolkit to achieve guideline-based lipid lowering goals, but we just aren’t using them,” said Ann Marie Navar, MD, PhD, associate professor of cardiology at the University of Texas, Dallas.
Patients hesitant
Changes in practice following guidelines can often be slow, but in this case may have been complicated by the fact that statins have a reputation for causing side effects, so some patients may be refusing treatment based on what they’ve seen on the Internet. Even though the study looked at all lipid-lowering agents, the misinformation around statins may be spilling over, according to Dr. Cannon. “There’s in general so much misinformation around COVID and every other topic in the world. That makes people question what is real [about] anything,” said Dr. Cannon, a cardiologist at Brigham and Women’s hospital and professor of medicine at Harvard Medical School, both in Boston.
Patient characteristics may partly explain slow uptake. “Clinicians may not think further LDL-C lowering is a high enough priority in terms of potential benefit for a given patient in light of the effort being expended to take care of all their other issues and chronic health problems. If the clinician does bring it up to the patient, there may be barriers in terms of additional medication burden, cost, or acquisition issues,” said Dr. Robinson.
The answer may be better evidence and a more personalized approach. Clinical trials that explore defined patient populations could convince patients of a benefit, and payers to reimburse, according to Dr. Robinson.
Changing guidance
Another complication is that both the guidelines and the field are rapidly changing. The 2013 AHA guidelines did not include a treatment to goal and focused instead on use of high-dose statins. But the 2018 update reversed course after randomized studies demonstrated a benefit to treating to target. The researchers found no increase in the frequency of treating to target after the release of the 2018 guidelines. “Publication and announcement of guidelines doesn’t mean that people are getting treated better. We really have to implement them,” said Dr. Cannon.
On a positive note, the GOULD researchers found high acceptance of the new proprotein convertase subtilisin/kexin type 9 serine protease (PCSK9) inhibitors, with over 90% of patients continuing those medications after 2 years. “That’s nice and high. If people do get onto the very intensive lipid-lowing therapies, they tend to stay on them,” said Dr. Cannon.
What’s next
Still, the lack of intensification is concerning, and the findings led to some consternation in Twitter exchanges, said Dr. Cannon. “People posted ‘Well, what do we do now?’ ” Dr. Cannon’s team is addressing the issue with an algorithm-based risk management program with prospective enrollment. They have conducted educational webinars and provided site-specific reports on LDL status among patients at each center compared to others, and hope that information will improve compliance. In 2020, the group published an interim analysis of the first 5,000 enrollees, and Dr. Cannon expects to finish that study by the end of the year.
Dr. Navar agreed that physicians need to do a better job of testing LDL-C levels after treatment to identify patients who require more aggressive therapy. That can be deferred in some primary prevention patients with high LDL-C but normal particle numbers as measured with ApoB. “But in those at high risk for disease and those with established CVD who are not at goal, as long as they don’t have a life-limiting condition, we should always up-titrate therapy. It’s one of the safest, most effective ways to lower cardiovascular risk,” said Dr. Navar.
Key study results
The prospective study included 5,006 patients at 119 centers with a mean age of 68 years. About 40% were women, and 86.1% were White. All had ASCVD and LDL levels of at least 70 mg/dL. After 2 years, 17% had undergone intensification of lipid-lowering therapy (LLT). Among patients with LDL-C levels ≥ 100 mg/dL, 22% underwent LLT intensification, compared with 14% of patients with LDL-C levels of 70-99 mg/dL.
The vast majority, 92%, of patients who underwent LLT via addition of PCSK9 inhibitors were still taking the drug after 2 years.
Three-quarters (3,768) had lipid level measurements at least once during follow-up, and median LDL-C levels dropped from 120 to 95 mg/dL in the ≥100-mg/dL cohort (P < .001), and from 82 to 77 mg/dL in the 70- to 99-mg/dL cohort (P <. 001). There was no significant difference in the median values in the patients on PCSK9 inhibitors.
In all, 21% of the ≥100-mg/dL cohort achieved LDL-C levels <70 mg/dL at 2 years, versus 34% in the 77- to 99-mg/dL cohort and 52% of patients taking PCSK9 inhibitors.
Patients seen at teaching hospitals were more likely to undergo LLT intensification compared to nonteaching hospitals (25% versus 17%; P < .001), as were those where lipid protocols were in place (22% versus 15%; P < .001), and those treated in cardiology (22%) compared to treatment in internal or family medicine (12%; P <.001). The study was published online June 16 in JAMA Cardiology.
Dr. Cannon, Dr. Navar, and Dr. Robinson disclosed ties with Amgen, which funded the study, and other companies.
Among patients with atherosclerotic cardiovascular disease (ASCVD), 2 years after release of treat-to-target guidelines from the American Heart Association and the European Society of Cardiology and European Atherosclerosis Society, most patients with LDL cholesterol higher than 70 mg/dL did not receive intensification of therapy, and two-thirds continued to have LDL levels above that level, according to a prospective registry study.
Both guidelines recommend driving LDL-C levels to 50% or below of baseline levels; results from the Getting to an Improved Understanding of Low-Density Lipoprotein Cholesterol and Dyslipidemia Management (GOULD) registry suggest this is rarely achieved. “Unfortunately it’s not a total surprise, but it’s disappointing,” said Christopher Cannon, MD, the study’s lead author.
“Therapeutic inertia seems to be the rule in clinical practice,” said Jennifer G. Robinson, MD, MPH, who was asked to comment on the study. Dr. Robinson is professor epidemiology and cardiology at the University of Iowa, Iowa City.
“This is yet another disappointing reminder of how we are failing our patients. Lipid lowering is one of the safest, most effective ways to prevent cardiovascular disease, and yet we are falling short. We have the tools in our toolkit to achieve guideline-based lipid lowering goals, but we just aren’t using them,” said Ann Marie Navar, MD, PhD, associate professor of cardiology at the University of Texas, Dallas.
Patients hesitant
Changes in practice following guidelines can often be slow, but in this case may have been complicated by the fact that statins have a reputation for causing side effects, so some patients may be refusing treatment based on what they’ve seen on the Internet. Even though the study looked at all lipid-lowering agents, the misinformation around statins may be spilling over, according to Dr. Cannon. “There’s in general so much misinformation around COVID and every other topic in the world. That makes people question what is real [about] anything,” said Dr. Cannon, a cardiologist at Brigham and Women’s hospital and professor of medicine at Harvard Medical School, both in Boston.
Patient characteristics may partly explain slow uptake. “Clinicians may not think further LDL-C lowering is a high enough priority in terms of potential benefit for a given patient in light of the effort being expended to take care of all their other issues and chronic health problems. If the clinician does bring it up to the patient, there may be barriers in terms of additional medication burden, cost, or acquisition issues,” said Dr. Robinson.
The answer may be better evidence and a more personalized approach. Clinical trials that explore defined patient populations could convince patients of a benefit, and payers to reimburse, according to Dr. Robinson.
Changing guidance
Another complication is that both the guidelines and the field are rapidly changing. The 2013 AHA guidelines did not include a treatment to goal and focused instead on use of high-dose statins. But the 2018 update reversed course after randomized studies demonstrated a benefit to treating to target. The researchers found no increase in the frequency of treating to target after the release of the 2018 guidelines. “Publication and announcement of guidelines doesn’t mean that people are getting treated better. We really have to implement them,” said Dr. Cannon.
On a positive note, the GOULD researchers found high acceptance of the new proprotein convertase subtilisin/kexin type 9 serine protease (PCSK9) inhibitors, with over 90% of patients continuing those medications after 2 years. “That’s nice and high. If people do get onto the very intensive lipid-lowing therapies, they tend to stay on them,” said Dr. Cannon.
What’s next
Still, the lack of intensification is concerning, and the findings led to some consternation in Twitter exchanges, said Dr. Cannon. “People posted ‘Well, what do we do now?’ ” Dr. Cannon’s team is addressing the issue with an algorithm-based risk management program with prospective enrollment. They have conducted educational webinars and provided site-specific reports on LDL status among patients at each center compared to others, and hope that information will improve compliance. In 2020, the group published an interim analysis of the first 5,000 enrollees, and Dr. Cannon expects to finish that study by the end of the year.
Dr. Navar agreed that physicians need to do a better job of testing LDL-C levels after treatment to identify patients who require more aggressive therapy. That can be deferred in some primary prevention patients with high LDL-C but normal particle numbers as measured with ApoB. “But in those at high risk for disease and those with established CVD who are not at goal, as long as they don’t have a life-limiting condition, we should always up-titrate therapy. It’s one of the safest, most effective ways to lower cardiovascular risk,” said Dr. Navar.
Key study results
The prospective study included 5,006 patients at 119 centers with a mean age of 68 years. About 40% were women, and 86.1% were White. All had ASCVD and LDL levels of at least 70 mg/dL. After 2 years, 17% had undergone intensification of lipid-lowering therapy (LLT). Among patients with LDL-C levels ≥ 100 mg/dL, 22% underwent LLT intensification, compared with 14% of patients with LDL-C levels of 70-99 mg/dL.
The vast majority, 92%, of patients who underwent LLT via addition of PCSK9 inhibitors were still taking the drug after 2 years.
Three-quarters (3,768) had lipid level measurements at least once during follow-up, and median LDL-C levels dropped from 120 to 95 mg/dL in the ≥100-mg/dL cohort (P < .001), and from 82 to 77 mg/dL in the 70- to 99-mg/dL cohort (P <. 001). There was no significant difference in the median values in the patients on PCSK9 inhibitors.
In all, 21% of the ≥100-mg/dL cohort achieved LDL-C levels <70 mg/dL at 2 years, versus 34% in the 77- to 99-mg/dL cohort and 52% of patients taking PCSK9 inhibitors.
Patients seen at teaching hospitals were more likely to undergo LLT intensification compared to nonteaching hospitals (25% versus 17%; P < .001), as were those where lipid protocols were in place (22% versus 15%; P < .001), and those treated in cardiology (22%) compared to treatment in internal or family medicine (12%; P <.001). The study was published online June 16 in JAMA Cardiology.
Dr. Cannon, Dr. Navar, and Dr. Robinson disclosed ties with Amgen, which funded the study, and other companies.
Among patients with atherosclerotic cardiovascular disease (ASCVD), 2 years after release of treat-to-target guidelines from the American Heart Association and the European Society of Cardiology and European Atherosclerosis Society, most patients with LDL cholesterol higher than 70 mg/dL did not receive intensification of therapy, and two-thirds continued to have LDL levels above that level, according to a prospective registry study.
Both guidelines recommend driving LDL-C levels to 50% or below of baseline levels; results from the Getting to an Improved Understanding of Low-Density Lipoprotein Cholesterol and Dyslipidemia Management (GOULD) registry suggest this is rarely achieved. “Unfortunately it’s not a total surprise, but it’s disappointing,” said Christopher Cannon, MD, the study’s lead author.
“Therapeutic inertia seems to be the rule in clinical practice,” said Jennifer G. Robinson, MD, MPH, who was asked to comment on the study. Dr. Robinson is professor epidemiology and cardiology at the University of Iowa, Iowa City.
“This is yet another disappointing reminder of how we are failing our patients. Lipid lowering is one of the safest, most effective ways to prevent cardiovascular disease, and yet we are falling short. We have the tools in our toolkit to achieve guideline-based lipid lowering goals, but we just aren’t using them,” said Ann Marie Navar, MD, PhD, associate professor of cardiology at the University of Texas, Dallas.
Patients hesitant
Changes in practice following guidelines can often be slow, but in this case may have been complicated by the fact that statins have a reputation for causing side effects, so some patients may be refusing treatment based on what they’ve seen on the Internet. Even though the study looked at all lipid-lowering agents, the misinformation around statins may be spilling over, according to Dr. Cannon. “There’s in general so much misinformation around COVID and every other topic in the world. That makes people question what is real [about] anything,” said Dr. Cannon, a cardiologist at Brigham and Women’s hospital and professor of medicine at Harvard Medical School, both in Boston.
Patient characteristics may partly explain slow uptake. “Clinicians may not think further LDL-C lowering is a high enough priority in terms of potential benefit for a given patient in light of the effort being expended to take care of all their other issues and chronic health problems. If the clinician does bring it up to the patient, there may be barriers in terms of additional medication burden, cost, or acquisition issues,” said Dr. Robinson.
The answer may be better evidence and a more personalized approach. Clinical trials that explore defined patient populations could convince patients of a benefit, and payers to reimburse, according to Dr. Robinson.
Changing guidance
Another complication is that both the guidelines and the field are rapidly changing. The 2013 AHA guidelines did not include a treatment to goal and focused instead on use of high-dose statins. But the 2018 update reversed course after randomized studies demonstrated a benefit to treating to target. The researchers found no increase in the frequency of treating to target after the release of the 2018 guidelines. “Publication and announcement of guidelines doesn’t mean that people are getting treated better. We really have to implement them,” said Dr. Cannon.
On a positive note, the GOULD researchers found high acceptance of the new proprotein convertase subtilisin/kexin type 9 serine protease (PCSK9) inhibitors, with over 90% of patients continuing those medications after 2 years. “That’s nice and high. If people do get onto the very intensive lipid-lowing therapies, they tend to stay on them,” said Dr. Cannon.
What’s next
Still, the lack of intensification is concerning, and the findings led to some consternation in Twitter exchanges, said Dr. Cannon. “People posted ‘Well, what do we do now?’ ” Dr. Cannon’s team is addressing the issue with an algorithm-based risk management program with prospective enrollment. They have conducted educational webinars and provided site-specific reports on LDL status among patients at each center compared to others, and hope that information will improve compliance. In 2020, the group published an interim analysis of the first 5,000 enrollees, and Dr. Cannon expects to finish that study by the end of the year.
Dr. Navar agreed that physicians need to do a better job of testing LDL-C levels after treatment to identify patients who require more aggressive therapy. That can be deferred in some primary prevention patients with high LDL-C but normal particle numbers as measured with ApoB. “But in those at high risk for disease and those with established CVD who are not at goal, as long as they don’t have a life-limiting condition, we should always up-titrate therapy. It’s one of the safest, most effective ways to lower cardiovascular risk,” said Dr. Navar.
Key study results
The prospective study included 5,006 patients at 119 centers with a mean age of 68 years. About 40% were women, and 86.1% were White. All had ASCVD and LDL levels of at least 70 mg/dL. After 2 years, 17% had undergone intensification of lipid-lowering therapy (LLT). Among patients with LDL-C levels ≥ 100 mg/dL, 22% underwent LLT intensification, compared with 14% of patients with LDL-C levels of 70-99 mg/dL.
The vast majority, 92%, of patients who underwent LLT via addition of PCSK9 inhibitors were still taking the drug after 2 years.
Three-quarters (3,768) had lipid level measurements at least once during follow-up, and median LDL-C levels dropped from 120 to 95 mg/dL in the ≥100-mg/dL cohort (P < .001), and from 82 to 77 mg/dL in the 70- to 99-mg/dL cohort (P <. 001). There was no significant difference in the median values in the patients on PCSK9 inhibitors.
In all, 21% of the ≥100-mg/dL cohort achieved LDL-C levels <70 mg/dL at 2 years, versus 34% in the 77- to 99-mg/dL cohort and 52% of patients taking PCSK9 inhibitors.
Patients seen at teaching hospitals were more likely to undergo LLT intensification compared to nonteaching hospitals (25% versus 17%; P < .001), as were those where lipid protocols were in place (22% versus 15%; P < .001), and those treated in cardiology (22%) compared to treatment in internal or family medicine (12%; P <.001). The study was published online June 16 in JAMA Cardiology.
Dr. Cannon, Dr. Navar, and Dr. Robinson disclosed ties with Amgen, which funded the study, and other companies.
FROM JAMA CARDIOLOGY
No overall statin effect seen on dementia, cognition in ASPREE analysis
Statin therapy likely didn’t lead to dementia or even mild cognitive impairment (MCI) in older patients taking the drugs for cardiovascular (CV) primary prevention in a post hoc analysis of a trial that required normal cognitive ability for entry.
Nor did statins, whether lipophilic or hydrophilic, appear to influence changes in cognition or affect separate domains of mental performance, such as memory, language ability, or executive function, over the trial’s follow-up, which averaged almost 5 years.
Although such findings aren’t novel – they are consistent with observations from a number of earlier studies – the new analysis included a possible signal for a statin association with new-onset dementia in a subgroup of more than 18,000 patients. Researchers attribute the retrospective finding, from a trial not designed to explore the issue, to confounding or chance.
Still, the adjusted risk for dementia seemed to go up by a third among statin users who at baseline placed in the lowest quartile for cognitive function, based on a composite test score, in the ASPREE trial, a test of primary-prevention low-dose aspirin in patients 65 or older. The better the baseline cognitive score by quartile, the lower the risk for dementia ( interaction P < .001).
The bottom-quartile association of statins with dementia was driven by new diagnoses of Alzheimer’s disease, as opposed to the study’s other “mixed presentation” dementia subtype, wrote the authors of analysis, published June 21, 2021, in the Journal of the American College of Cardiology), led by Zhen Zhou, PhD, Menzies Institute for Medical Research, University of Tasmania, Hobart, Australia.
“I wouldn’t overinterpret that,” said senior author Mark R. Nelson, MBBS, PhD, of the same institution. Indeed, it should be “reassuring” for physicians prescribing statins to older patients that there was no overall statin effect on cognition or new-onset dementia, he said in an interview.
“This is a post hoc analysis within a dataset, although a very-high-quality dataset, it must be said.” The patients were prospectively followed for a range of cognition domains, and the results were adjudicated, Dr. Nelson observed. Although the question of statins and dementia risk is thought to be largely settled, the analysis “was just too tempting not to do.”
On the basis of the current analysis and the bulk of preceding evidence, “lipid lowering in the short term does not appear to result in improvement or deterioration of cognition irrespective of baseline LDL cholesterol levels and medication used,” Christie M. Ballantyne, MD, and Vijay Nambi, MD, PhD, both from Baylor College of Medicine, Houston, wrote in an accompanying editorial.
The current study “provides additional information that the lipo- or hydrophilicity of the statin does not affect changes in cognition. However, the potential increased risk for Alzheimer’s disease, especially among patients with baseline cognitive impairment, requires further investigation.”
The current analysis is reassuring that the likelihood of such statin effects on cognition “is vanishingly small,” Neil J. Stone MD, Northwestern University, Chicago, said in an interview. In fact, its primary finding of no such association “best summarizes what we know in 2021 about statin therapy” after exploration of the issue in a number of prospective trials and systematic reviews, said Dr. Stone, who was not a coauthor on the report.
The observed interaction between statin use and baseline neurocognitive ability “is hypothesis raising at best. It should be explored in randomized, controlled trials that can look at this question in an unbiased manner,” he agreed.
If patients believe or suspect that a statin is causing symptoms that suggest cognitive dysfunction, “what they really need to do is to stop it for 3 weeks and check out other causes. And in rechallenging, the guidelines say, if they think that it’s causing a memory problem that occurs anecdotally, then they can be given another statin, usually, which doesn’t cause it.”
ASPREE compared daily low-dose aspirin with placebo in a community-based older population numbering about 19,000 in Australia and the United States. Patients were initially without known CV disease, dementia, or physical disabilities. It did not randomize patients by statin therapy.
Of note, entry to the trial required a score of at least 78 on the Modified Mini-Mental State Examination (3MS), corresponding to normal cognition.
Aspirin showed no significant benefit for disability-free survival, an endpoint that included death and dementia, or CV events over a median of 4.7 years. It was associated with slightly more cases of major hemorrhage, as previously reported.
A subsequent ASPREE analysis suggested that the aspirin had no effect on risks of mild cognitive impairment, cognitive decline, or dementia.
Of the 18,846 patients in the current post hoc analysis, the average age of the patients was 74 years, and 56.4% were women; 31.3% were taking statins at baseline. The incidence of dementia per 1,000 person-years for those taking statins in comparison with those not taking statins was 6.91 and 6.48, respectively. Any cognitive changes were tracked by the 3MS and three other validated tests in different domains of cognition, with results contributing to the composite score.
The corresponding incidence of dementia considered probable Alzheimer’s disease was 2.97 and 2.65 for those receiving versus not receiving statins, respectively. The incidence of dementia with mixed presentation was 3.94 and 3.84, respectively.
There were no significant differences in risk for dementia overall or for either dementia subtype in multivariate analyses. Adjustments included demographics, CV lifestyle risk factors, family medical history, including dementia, ASPREE randomization group, and individual scores on the four tests of cognition.
Results for development of MCI mirrored those for dementia, as did results stratified for baseline lipids and for use of lipophilic statins, such as atorvastatin or simvastatin versus hydrophilic statins, including pravastatin and rosuvastatin.
Significant interactions were observed between composite cognitive scores and statin therapy at baseline; as scores increased, indicating better cognitive performance, the risks for dementia and its subtypes went down. Statins were associated with incident dementia at the lowest cognitive performance quartile.
That association is probably a function of the cohort’s advanced age, Dr. Nelson said. “If you get into old age, and you’ve got high cognitive scores, you’ve probably got protective factors. That’s how I would interpret that.”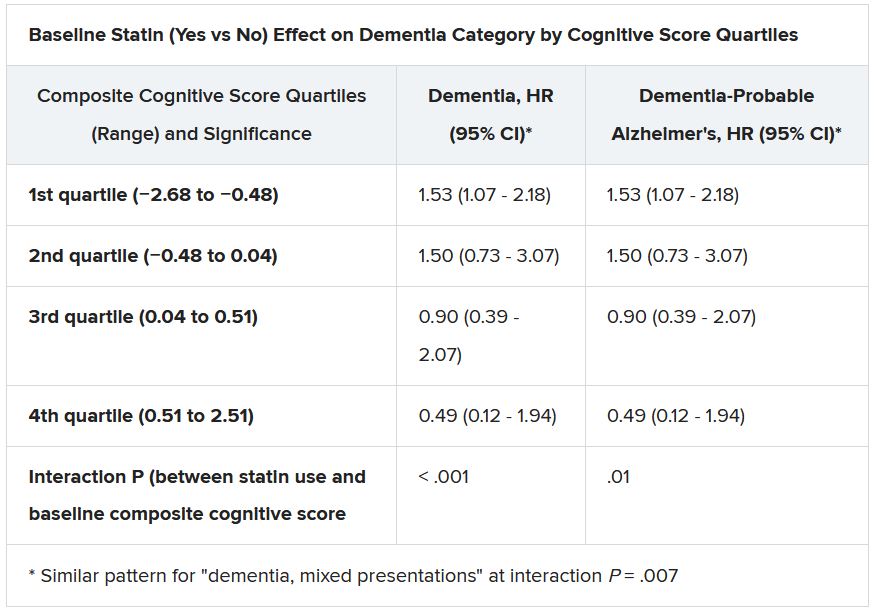
Dr. Ballantyne and Dr. Nambi also emphasized the difficulties of controlling for potential biases even with extensive covariate adjustments. The statin dosages at which patients were treated were not part of the analysis, “and achieved LDL [cholesterol levels over the study period were not known,” they wrote.
“Furthermore, patients who were treated with statins were more likely to have diabetes, hypertension, chronic kidney disease, and obesity, all of which are known to increase risk for cognitive decline, and, as might have been predicted, statin users therefore had significantly lower scores for global cognition and episodic memory.”
Dr. Nelson pointed to an ongoing prospective atorvastatin trial that includes dementia in its primary endpoint and should be “the definitive study.” STAREE (Statin Therapy for Reducing Events in the Elderly) is running throughout Australia with a projected enrollment of 18,000 and primary completion by the end of 2022. “We’ve already enrolled 8,000 patients.”
Less far along is the PREVENTABLE (Pragmatic Evaluation of Events and Benefits of Lipid-Lowering in Older Adults) trial, based in the United States and also randomizing to atorvastatin or placebo, that will have an estimated 20,000 older patients and completion in 5 years. The primary endpoint is new dementia or persistent disability.
Both trials “are powered to enable firm conclusions concerning any statin effects,” said Dr. Ballantyne and Dr. Nambi. “In the meantime, practicing clinicians can have confidence and share with their patients that short-term lipid-lowering therapy in older patients, including with statins, is unlikely to have a major impact on cognition.”
ASPREE was supported by grants from the U.S. National Institute on Aging and the National Cancer Institute and the National Health and Medical Research Council of Australia, by Monash University, and by the Victorian Cancer Agency. Dr. Nelson reported receiving honoraria from Sanofi and Amgen; support from Bayer for ASPREE; and grant support for STAREE. Disclosures for the other authors are in the report. Dr. Ballantyne disclosed grant and research support from Abbott Diagnostic, Akcea, Amgen, Esperion, Ionis, Novartis, Regeneron, and Roche Diagnostics; and consulting for Abbott Diagnostics, Althera, Amarin, Amgen, Arrowhead, AstraZeneca, Corvidia, Denka Seiken, Esperion, Genentech, Gilead, Matinas BioPharma, New Amsterdam, Novartis, Novo Nordisk, Pfizer, Regeneron, Roche Diagnostics, and Sanofi-Synthelabo. Dr. Nambi is a coinvestigator on a provisional patent along with Baylor College of Medicine and Roche on the use of biomarkers to predict heart failure, and a site principal investigator for studies sponsored by Amgen and Merck. Dr. Stone had no disclosures.
A version of this article first appeared on Medscape.com.
Statin therapy likely didn’t lead to dementia or even mild cognitive impairment (MCI) in older patients taking the drugs for cardiovascular (CV) primary prevention in a post hoc analysis of a trial that required normal cognitive ability for entry.
Nor did statins, whether lipophilic or hydrophilic, appear to influence changes in cognition or affect separate domains of mental performance, such as memory, language ability, or executive function, over the trial’s follow-up, which averaged almost 5 years.
Although such findings aren’t novel – they are consistent with observations from a number of earlier studies – the new analysis included a possible signal for a statin association with new-onset dementia in a subgroup of more than 18,000 patients. Researchers attribute the retrospective finding, from a trial not designed to explore the issue, to confounding or chance.
Still, the adjusted risk for dementia seemed to go up by a third among statin users who at baseline placed in the lowest quartile for cognitive function, based on a composite test score, in the ASPREE trial, a test of primary-prevention low-dose aspirin in patients 65 or older. The better the baseline cognitive score by quartile, the lower the risk for dementia ( interaction P < .001).
The bottom-quartile association of statins with dementia was driven by new diagnoses of Alzheimer’s disease, as opposed to the study’s other “mixed presentation” dementia subtype, wrote the authors of analysis, published June 21, 2021, in the Journal of the American College of Cardiology), led by Zhen Zhou, PhD, Menzies Institute for Medical Research, University of Tasmania, Hobart, Australia.
“I wouldn’t overinterpret that,” said senior author Mark R. Nelson, MBBS, PhD, of the same institution. Indeed, it should be “reassuring” for physicians prescribing statins to older patients that there was no overall statin effect on cognition or new-onset dementia, he said in an interview.
“This is a post hoc analysis within a dataset, although a very-high-quality dataset, it must be said.” The patients were prospectively followed for a range of cognition domains, and the results were adjudicated, Dr. Nelson observed. Although the question of statins and dementia risk is thought to be largely settled, the analysis “was just too tempting not to do.”
On the basis of the current analysis and the bulk of preceding evidence, “lipid lowering in the short term does not appear to result in improvement or deterioration of cognition irrespective of baseline LDL cholesterol levels and medication used,” Christie M. Ballantyne, MD, and Vijay Nambi, MD, PhD, both from Baylor College of Medicine, Houston, wrote in an accompanying editorial.
The current study “provides additional information that the lipo- or hydrophilicity of the statin does not affect changes in cognition. However, the potential increased risk for Alzheimer’s disease, especially among patients with baseline cognitive impairment, requires further investigation.”
The current analysis is reassuring that the likelihood of such statin effects on cognition “is vanishingly small,” Neil J. Stone MD, Northwestern University, Chicago, said in an interview. In fact, its primary finding of no such association “best summarizes what we know in 2021 about statin therapy” after exploration of the issue in a number of prospective trials and systematic reviews, said Dr. Stone, who was not a coauthor on the report.
The observed interaction between statin use and baseline neurocognitive ability “is hypothesis raising at best. It should be explored in randomized, controlled trials that can look at this question in an unbiased manner,” he agreed.
If patients believe or suspect that a statin is causing symptoms that suggest cognitive dysfunction, “what they really need to do is to stop it for 3 weeks and check out other causes. And in rechallenging, the guidelines say, if they think that it’s causing a memory problem that occurs anecdotally, then they can be given another statin, usually, which doesn’t cause it.”
ASPREE compared daily low-dose aspirin with placebo in a community-based older population numbering about 19,000 in Australia and the United States. Patients were initially without known CV disease, dementia, or physical disabilities. It did not randomize patients by statin therapy.
Of note, entry to the trial required a score of at least 78 on the Modified Mini-Mental State Examination (3MS), corresponding to normal cognition.
Aspirin showed no significant benefit for disability-free survival, an endpoint that included death and dementia, or CV events over a median of 4.7 years. It was associated with slightly more cases of major hemorrhage, as previously reported.
A subsequent ASPREE analysis suggested that the aspirin had no effect on risks of mild cognitive impairment, cognitive decline, or dementia.
Of the 18,846 patients in the current post hoc analysis, the average age of the patients was 74 years, and 56.4% were women; 31.3% were taking statins at baseline. The incidence of dementia per 1,000 person-years for those taking statins in comparison with those not taking statins was 6.91 and 6.48, respectively. Any cognitive changes were tracked by the 3MS and three other validated tests in different domains of cognition, with results contributing to the composite score.
The corresponding incidence of dementia considered probable Alzheimer’s disease was 2.97 and 2.65 for those receiving versus not receiving statins, respectively. The incidence of dementia with mixed presentation was 3.94 and 3.84, respectively.
There were no significant differences in risk for dementia overall or for either dementia subtype in multivariate analyses. Adjustments included demographics, CV lifestyle risk factors, family medical history, including dementia, ASPREE randomization group, and individual scores on the four tests of cognition.
Results for development of MCI mirrored those for dementia, as did results stratified for baseline lipids and for use of lipophilic statins, such as atorvastatin or simvastatin versus hydrophilic statins, including pravastatin and rosuvastatin.
Significant interactions were observed between composite cognitive scores and statin therapy at baseline; as scores increased, indicating better cognitive performance, the risks for dementia and its subtypes went down. Statins were associated with incident dementia at the lowest cognitive performance quartile.
That association is probably a function of the cohort’s advanced age, Dr. Nelson said. “If you get into old age, and you’ve got high cognitive scores, you’ve probably got protective factors. That’s how I would interpret that.”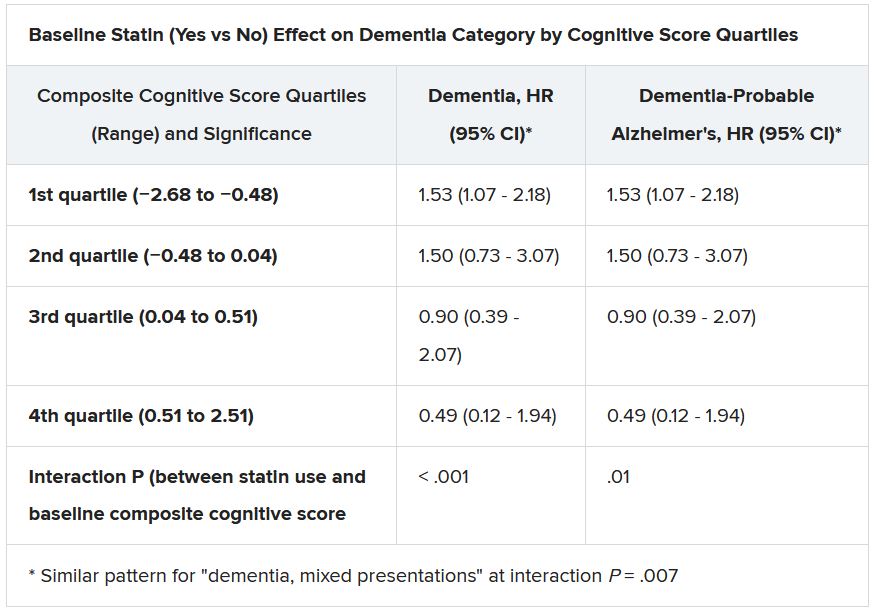
Dr. Ballantyne and Dr. Nambi also emphasized the difficulties of controlling for potential biases even with extensive covariate adjustments. The statin dosages at which patients were treated were not part of the analysis, “and achieved LDL [cholesterol levels over the study period were not known,” they wrote.
“Furthermore, patients who were treated with statins were more likely to have diabetes, hypertension, chronic kidney disease, and obesity, all of which are known to increase risk for cognitive decline, and, as might have been predicted, statin users therefore had significantly lower scores for global cognition and episodic memory.”
Dr. Nelson pointed to an ongoing prospective atorvastatin trial that includes dementia in its primary endpoint and should be “the definitive study.” STAREE (Statin Therapy for Reducing Events in the Elderly) is running throughout Australia with a projected enrollment of 18,000 and primary completion by the end of 2022. “We’ve already enrolled 8,000 patients.”
Less far along is the PREVENTABLE (Pragmatic Evaluation of Events and Benefits of Lipid-Lowering in Older Adults) trial, based in the United States and also randomizing to atorvastatin or placebo, that will have an estimated 20,000 older patients and completion in 5 years. The primary endpoint is new dementia or persistent disability.
Both trials “are powered to enable firm conclusions concerning any statin effects,” said Dr. Ballantyne and Dr. Nambi. “In the meantime, practicing clinicians can have confidence and share with their patients that short-term lipid-lowering therapy in older patients, including with statins, is unlikely to have a major impact on cognition.”
ASPREE was supported by grants from the U.S. National Institute on Aging and the National Cancer Institute and the National Health and Medical Research Council of Australia, by Monash University, and by the Victorian Cancer Agency. Dr. Nelson reported receiving honoraria from Sanofi and Amgen; support from Bayer for ASPREE; and grant support for STAREE. Disclosures for the other authors are in the report. Dr. Ballantyne disclosed grant and research support from Abbott Diagnostic, Akcea, Amgen, Esperion, Ionis, Novartis, Regeneron, and Roche Diagnostics; and consulting for Abbott Diagnostics, Althera, Amarin, Amgen, Arrowhead, AstraZeneca, Corvidia, Denka Seiken, Esperion, Genentech, Gilead, Matinas BioPharma, New Amsterdam, Novartis, Novo Nordisk, Pfizer, Regeneron, Roche Diagnostics, and Sanofi-Synthelabo. Dr. Nambi is a coinvestigator on a provisional patent along with Baylor College of Medicine and Roche on the use of biomarkers to predict heart failure, and a site principal investigator for studies sponsored by Amgen and Merck. Dr. Stone had no disclosures.
A version of this article first appeared on Medscape.com.
Statin therapy likely didn’t lead to dementia or even mild cognitive impairment (MCI) in older patients taking the drugs for cardiovascular (CV) primary prevention in a post hoc analysis of a trial that required normal cognitive ability for entry.
Nor did statins, whether lipophilic or hydrophilic, appear to influence changes in cognition or affect separate domains of mental performance, such as memory, language ability, or executive function, over the trial’s follow-up, which averaged almost 5 years.
Although such findings aren’t novel – they are consistent with observations from a number of earlier studies – the new analysis included a possible signal for a statin association with new-onset dementia in a subgroup of more than 18,000 patients. Researchers attribute the retrospective finding, from a trial not designed to explore the issue, to confounding or chance.
Still, the adjusted risk for dementia seemed to go up by a third among statin users who at baseline placed in the lowest quartile for cognitive function, based on a composite test score, in the ASPREE trial, a test of primary-prevention low-dose aspirin in patients 65 or older. The better the baseline cognitive score by quartile, the lower the risk for dementia ( interaction P < .001).
The bottom-quartile association of statins with dementia was driven by new diagnoses of Alzheimer’s disease, as opposed to the study’s other “mixed presentation” dementia subtype, wrote the authors of analysis, published June 21, 2021, in the Journal of the American College of Cardiology), led by Zhen Zhou, PhD, Menzies Institute for Medical Research, University of Tasmania, Hobart, Australia.
“I wouldn’t overinterpret that,” said senior author Mark R. Nelson, MBBS, PhD, of the same institution. Indeed, it should be “reassuring” for physicians prescribing statins to older patients that there was no overall statin effect on cognition or new-onset dementia, he said in an interview.
“This is a post hoc analysis within a dataset, although a very-high-quality dataset, it must be said.” The patients were prospectively followed for a range of cognition domains, and the results were adjudicated, Dr. Nelson observed. Although the question of statins and dementia risk is thought to be largely settled, the analysis “was just too tempting not to do.”
On the basis of the current analysis and the bulk of preceding evidence, “lipid lowering in the short term does not appear to result in improvement or deterioration of cognition irrespective of baseline LDL cholesterol levels and medication used,” Christie M. Ballantyne, MD, and Vijay Nambi, MD, PhD, both from Baylor College of Medicine, Houston, wrote in an accompanying editorial.
The current study “provides additional information that the lipo- or hydrophilicity of the statin does not affect changes in cognition. However, the potential increased risk for Alzheimer’s disease, especially among patients with baseline cognitive impairment, requires further investigation.”
The current analysis is reassuring that the likelihood of such statin effects on cognition “is vanishingly small,” Neil J. Stone MD, Northwestern University, Chicago, said in an interview. In fact, its primary finding of no such association “best summarizes what we know in 2021 about statin therapy” after exploration of the issue in a number of prospective trials and systematic reviews, said Dr. Stone, who was not a coauthor on the report.
The observed interaction between statin use and baseline neurocognitive ability “is hypothesis raising at best. It should be explored in randomized, controlled trials that can look at this question in an unbiased manner,” he agreed.
If patients believe or suspect that a statin is causing symptoms that suggest cognitive dysfunction, “what they really need to do is to stop it for 3 weeks and check out other causes. And in rechallenging, the guidelines say, if they think that it’s causing a memory problem that occurs anecdotally, then they can be given another statin, usually, which doesn’t cause it.”
ASPREE compared daily low-dose aspirin with placebo in a community-based older population numbering about 19,000 in Australia and the United States. Patients were initially without known CV disease, dementia, or physical disabilities. It did not randomize patients by statin therapy.
Of note, entry to the trial required a score of at least 78 on the Modified Mini-Mental State Examination (3MS), corresponding to normal cognition.
Aspirin showed no significant benefit for disability-free survival, an endpoint that included death and dementia, or CV events over a median of 4.7 years. It was associated with slightly more cases of major hemorrhage, as previously reported.
A subsequent ASPREE analysis suggested that the aspirin had no effect on risks of mild cognitive impairment, cognitive decline, or dementia.
Of the 18,846 patients in the current post hoc analysis, the average age of the patients was 74 years, and 56.4% were women; 31.3% were taking statins at baseline. The incidence of dementia per 1,000 person-years for those taking statins in comparison with those not taking statins was 6.91 and 6.48, respectively. Any cognitive changes were tracked by the 3MS and three other validated tests in different domains of cognition, with results contributing to the composite score.
The corresponding incidence of dementia considered probable Alzheimer’s disease was 2.97 and 2.65 for those receiving versus not receiving statins, respectively. The incidence of dementia with mixed presentation was 3.94 and 3.84, respectively.
There were no significant differences in risk for dementia overall or for either dementia subtype in multivariate analyses. Adjustments included demographics, CV lifestyle risk factors, family medical history, including dementia, ASPREE randomization group, and individual scores on the four tests of cognition.
Results for development of MCI mirrored those for dementia, as did results stratified for baseline lipids and for use of lipophilic statins, such as atorvastatin or simvastatin versus hydrophilic statins, including pravastatin and rosuvastatin.
Significant interactions were observed between composite cognitive scores and statin therapy at baseline; as scores increased, indicating better cognitive performance, the risks for dementia and its subtypes went down. Statins were associated with incident dementia at the lowest cognitive performance quartile.
That association is probably a function of the cohort’s advanced age, Dr. Nelson said. “If you get into old age, and you’ve got high cognitive scores, you’ve probably got protective factors. That’s how I would interpret that.”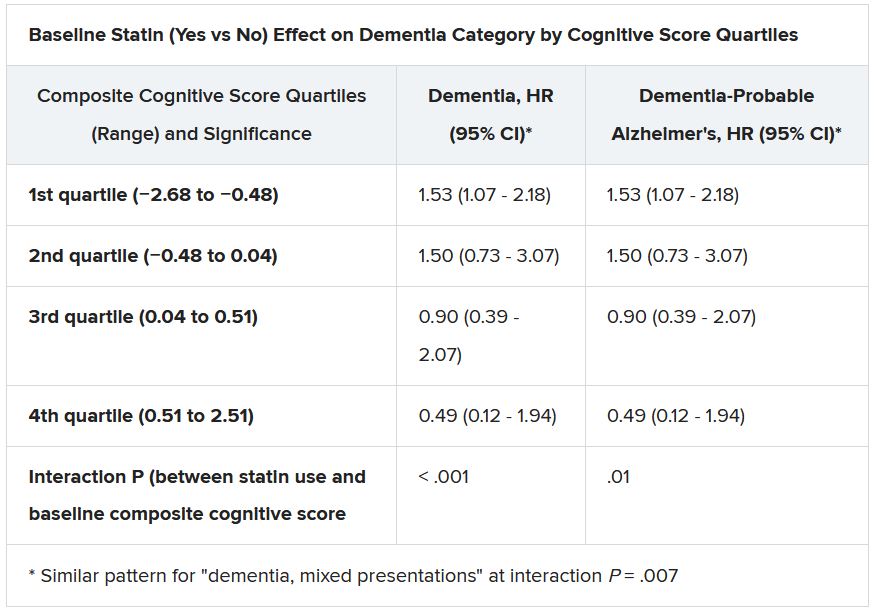
Dr. Ballantyne and Dr. Nambi also emphasized the difficulties of controlling for potential biases even with extensive covariate adjustments. The statin dosages at which patients were treated were not part of the analysis, “and achieved LDL [cholesterol levels over the study period were not known,” they wrote.
“Furthermore, patients who were treated with statins were more likely to have diabetes, hypertension, chronic kidney disease, and obesity, all of which are known to increase risk for cognitive decline, and, as might have been predicted, statin users therefore had significantly lower scores for global cognition and episodic memory.”
Dr. Nelson pointed to an ongoing prospective atorvastatin trial that includes dementia in its primary endpoint and should be “the definitive study.” STAREE (Statin Therapy for Reducing Events in the Elderly) is running throughout Australia with a projected enrollment of 18,000 and primary completion by the end of 2022. “We’ve already enrolled 8,000 patients.”
Less far along is the PREVENTABLE (Pragmatic Evaluation of Events and Benefits of Lipid-Lowering in Older Adults) trial, based in the United States and also randomizing to atorvastatin or placebo, that will have an estimated 20,000 older patients and completion in 5 years. The primary endpoint is new dementia or persistent disability.
Both trials “are powered to enable firm conclusions concerning any statin effects,” said Dr. Ballantyne and Dr. Nambi. “In the meantime, practicing clinicians can have confidence and share with their patients that short-term lipid-lowering therapy in older patients, including with statins, is unlikely to have a major impact on cognition.”
ASPREE was supported by grants from the U.S. National Institute on Aging and the National Cancer Institute and the National Health and Medical Research Council of Australia, by Monash University, and by the Victorian Cancer Agency. Dr. Nelson reported receiving honoraria from Sanofi and Amgen; support from Bayer for ASPREE; and grant support for STAREE. Disclosures for the other authors are in the report. Dr. Ballantyne disclosed grant and research support from Abbott Diagnostic, Akcea, Amgen, Esperion, Ionis, Novartis, Regeneron, and Roche Diagnostics; and consulting for Abbott Diagnostics, Althera, Amarin, Amgen, Arrowhead, AstraZeneca, Corvidia, Denka Seiken, Esperion, Genentech, Gilead, Matinas BioPharma, New Amsterdam, Novartis, Novo Nordisk, Pfizer, Regeneron, Roche Diagnostics, and Sanofi-Synthelabo. Dr. Nambi is a coinvestigator on a provisional patent along with Baylor College of Medicine and Roche on the use of biomarkers to predict heart failure, and a site principal investigator for studies sponsored by Amgen and Merck. Dr. Stone had no disclosures.
A version of this article first appeared on Medscape.com.
Bariatric surgery’s cardiovascular benefit extends to 7 years
Patients with obesity who had bariatric surgery had a lower risk of having a major adverse cardiovascular event (MACE) or dying from all causes during a median 7-year follow-up, compared with similar patients who did not undergo surgery.
These findings, from a province-wide retrospective cohort study from Quebec, follow two recent, slightly shorter similar trials.
Now we need a large randomized clinical trial (RCT), experts say, to definitively establish cardiovascular and mortality benefits in people with obesity who have metabolic/bariatric surgery. And such a trial is just beginning.
Philippe Bouchard, MD, a general surgery resident from McGill University in Montreal presented the Quebec study in a top papers session at the annual meeting of the American Society for Metabolic & Bariatric Surgery.
The findings showed that, among obese patients with metabolic syndrome, bariatric/metabolic surgery is associated with a sustained decrease in the incidence of MACE and all-cause mortality of at least 5 years, Dr. Bouchard said.
“The results of this population-based observational study should be validated in randomized controlled trials,” he concluded.
In the meantime, “we believe our study adds to the body of evidence in mainly two ways,” Dr. Bouchard told this news organization in an email.
It has a longer follow-up than recent observational studies, “a median of 7 years, compared to 3.9 years in a study from the Cleveland Clinic, and 4.6 years in one from Ontario, he said.
“This allows us to [estimate] an absolute risk reduction of MACE of 5.11% at 10 years,” he added. This is a smaller risk reduction than the roughly 40% risk reduction seen in the other two studies, possibly because of selection bias, Dr. Bouchard speculated.
“Second, most of the larger cohorts are heavily weighted on Roux-en-Y gastric bypass,” he continued. In contrast, their study included diverse procedures, including sleeve gastrectomy, duodenal switch, and adjustable gastric banding.
“Given the rise in popularity of a derivative of the duodenal switch – the single-anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADi-S) – we believe this information is timely and relevant to clinicians,” Dr. Bouchard said.
RCT on the subject is coming
“I totally agree that we need a large randomized controlled trial of bariatric surgery versus optimal medical therapy to conclusively establish” the impact of bariatric surgery on cardiovascular outcomes, said the assigned discussant, Mehran Anvari, MD. And their research group is just about to begin one.
In the absence of RCT data, clinicians “may currently not refer [eligible] patients for bariatric surgery because of the high risk they pose,” said Dr. Anvari, professor and director of the Centre for Minimal Access Surgery of McMaster University, Hamilton, Ont., and senior author in the Ontario study.
Furthermore, an important point is that the current trial extended the follow-up to 7 years, he told this news organization in an email.
That study included patients with diabetes and hypertension, he added, whereas his group included patients with a history of cardiovascular disease and/or heart failure.
“We hope these studies encourage general practitioners and cardiologists to consider bariatric surgery as a viable treatment option to prevent and reduce the risk of MACE in the obese patients [body mass index >35 kg/m2] with significant cardiovascular disease,” he said.
“We have embarked on a pilot RCT among bariatric centers of excellence in Ontario,” Dr. Anvari added, which showed the feasibility and safety of such a study.
He estimates that the RCT will need to recruit 2,000 patients to demonstrate the safety and effectiveness of bariatric surgery in reducing MACE and cardiac and all-cause mortality among patients with existing cardiovascular disease.
This “will require international collaboration,” he added, “and our group is currently establishing collaboration with sites in North America, Europe, and Australia to conduct such a study.”
Patients matched for age, sex, number of comorbidities
Quebec has a single public health care system that covers the cost of bariatric surgery for eligible patients; that is, those with a BMI greater than 35 kg/m2 and comorbidities or a BMI greater than 40 kg/m2.
Using this provincial health care database, which covers over 97% of the population, the researchers identified 3,637 patients with diabetes and/or hypertension who had bariatric surgery during 2007-2012.
They matched the surgery patients with 5,420 control patients with obesity who lived in the same geographic region and had a similar age, sex, and number of Charlson Comorbidity Index comorbidities, but did not undergo bariatric surgery.
The patients had a mean age of 50 and 64% were women.
Half had zero to one comorbidities, a quarter had two comorbidities, and another quarter had at least three comorbidities.
Most patients in the surgery group had type 2 diabetes (70%) and 50% had hypertension, whereas in the control group, most patients had hypertension (82%) and 41% had diabetes.
The most common type of bariatric surgery was adjustable gastric banding (42% of patients), followed by duodenal switch (24%), sleeve gastrectomy (23%), and Roux-en-Y gastric bypass (11%).
The primary outcome was the incidence of MACE, defined as coronary artery events (including myocardial infarction, percutaneous coronary intervention, and coronary artery bypass graft), stroke, heart failure, and all-cause mortality,
After a median follow-up of 7-11 years, fewer patients in the surgical group than in the control group had MACE (20% vs. 25%) or died from all causes (4.1% vs. 6.3%, both statistically significant at P < .01)
Similarly, significantly fewer patients in the surgical group than in the control group had a coronary artery event or heart failure (each P < .01).
However, there were no significant between-group difference in the rate of stroke, possibly because of the small number of strokes.
The risk of MACE was 17% lower in the group that had bariatric surgery than in the control group (adjusted hazard ratio, 0.83; 95% confidence interval, 0.78-0.89), after adjusting for age, sex, and number of comorbidities.
In subgroup analysis, patients who had adjustable gastric banding, Roux-en-Y gastric bypass, or duodenal switch had a significantly lower risk of MACE than control patients.
The risk of MACE was similar in patients who had sleeve gastrectomy and in control patients.
However, these subgroup results need to be interpreted with caution since the surgery and control patients in each surgery type subgroup were not matched for age, sex, and comorbidities, said Dr. Bouchard.
He acknowledged that study limitations include a lack of information about the patients’ BMI, weight, medications, and glycemic control (hemoglobin A1c).
Dr. Bouchard and Dr. Anvari have no relevant financial disclosures.
Patients with obesity who had bariatric surgery had a lower risk of having a major adverse cardiovascular event (MACE) or dying from all causes during a median 7-year follow-up, compared with similar patients who did not undergo surgery.
These findings, from a province-wide retrospective cohort study from Quebec, follow two recent, slightly shorter similar trials.
Now we need a large randomized clinical trial (RCT), experts say, to definitively establish cardiovascular and mortality benefits in people with obesity who have metabolic/bariatric surgery. And such a trial is just beginning.
Philippe Bouchard, MD, a general surgery resident from McGill University in Montreal presented the Quebec study in a top papers session at the annual meeting of the American Society for Metabolic & Bariatric Surgery.
The findings showed that, among obese patients with metabolic syndrome, bariatric/metabolic surgery is associated with a sustained decrease in the incidence of MACE and all-cause mortality of at least 5 years, Dr. Bouchard said.
“The results of this population-based observational study should be validated in randomized controlled trials,” he concluded.
In the meantime, “we believe our study adds to the body of evidence in mainly two ways,” Dr. Bouchard told this news organization in an email.
It has a longer follow-up than recent observational studies, “a median of 7 years, compared to 3.9 years in a study from the Cleveland Clinic, and 4.6 years in one from Ontario, he said.
“This allows us to [estimate] an absolute risk reduction of MACE of 5.11% at 10 years,” he added. This is a smaller risk reduction than the roughly 40% risk reduction seen in the other two studies, possibly because of selection bias, Dr. Bouchard speculated.
“Second, most of the larger cohorts are heavily weighted on Roux-en-Y gastric bypass,” he continued. In contrast, their study included diverse procedures, including sleeve gastrectomy, duodenal switch, and adjustable gastric banding.
“Given the rise in popularity of a derivative of the duodenal switch – the single-anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADi-S) – we believe this information is timely and relevant to clinicians,” Dr. Bouchard said.
RCT on the subject is coming
“I totally agree that we need a large randomized controlled trial of bariatric surgery versus optimal medical therapy to conclusively establish” the impact of bariatric surgery on cardiovascular outcomes, said the assigned discussant, Mehran Anvari, MD. And their research group is just about to begin one.
In the absence of RCT data, clinicians “may currently not refer [eligible] patients for bariatric surgery because of the high risk they pose,” said Dr. Anvari, professor and director of the Centre for Minimal Access Surgery of McMaster University, Hamilton, Ont., and senior author in the Ontario study.
Furthermore, an important point is that the current trial extended the follow-up to 7 years, he told this news organization in an email.
That study included patients with diabetes and hypertension, he added, whereas his group included patients with a history of cardiovascular disease and/or heart failure.
“We hope these studies encourage general practitioners and cardiologists to consider bariatric surgery as a viable treatment option to prevent and reduce the risk of MACE in the obese patients [body mass index >35 kg/m2] with significant cardiovascular disease,” he said.
“We have embarked on a pilot RCT among bariatric centers of excellence in Ontario,” Dr. Anvari added, which showed the feasibility and safety of such a study.
He estimates that the RCT will need to recruit 2,000 patients to demonstrate the safety and effectiveness of bariatric surgery in reducing MACE and cardiac and all-cause mortality among patients with existing cardiovascular disease.
This “will require international collaboration,” he added, “and our group is currently establishing collaboration with sites in North America, Europe, and Australia to conduct such a study.”
Patients matched for age, sex, number of comorbidities
Quebec has a single public health care system that covers the cost of bariatric surgery for eligible patients; that is, those with a BMI greater than 35 kg/m2 and comorbidities or a BMI greater than 40 kg/m2.
Using this provincial health care database, which covers over 97% of the population, the researchers identified 3,637 patients with diabetes and/or hypertension who had bariatric surgery during 2007-2012.
They matched the surgery patients with 5,420 control patients with obesity who lived in the same geographic region and had a similar age, sex, and number of Charlson Comorbidity Index comorbidities, but did not undergo bariatric surgery.
The patients had a mean age of 50 and 64% were women.
Half had zero to one comorbidities, a quarter had two comorbidities, and another quarter had at least three comorbidities.
Most patients in the surgery group had type 2 diabetes (70%) and 50% had hypertension, whereas in the control group, most patients had hypertension (82%) and 41% had diabetes.
The most common type of bariatric surgery was adjustable gastric banding (42% of patients), followed by duodenal switch (24%), sleeve gastrectomy (23%), and Roux-en-Y gastric bypass (11%).
The primary outcome was the incidence of MACE, defined as coronary artery events (including myocardial infarction, percutaneous coronary intervention, and coronary artery bypass graft), stroke, heart failure, and all-cause mortality,
After a median follow-up of 7-11 years, fewer patients in the surgical group than in the control group had MACE (20% vs. 25%) or died from all causes (4.1% vs. 6.3%, both statistically significant at P < .01)
Similarly, significantly fewer patients in the surgical group than in the control group had a coronary artery event or heart failure (each P < .01).
However, there were no significant between-group difference in the rate of stroke, possibly because of the small number of strokes.
The risk of MACE was 17% lower in the group that had bariatric surgery than in the control group (adjusted hazard ratio, 0.83; 95% confidence interval, 0.78-0.89), after adjusting for age, sex, and number of comorbidities.
In subgroup analysis, patients who had adjustable gastric banding, Roux-en-Y gastric bypass, or duodenal switch had a significantly lower risk of MACE than control patients.
The risk of MACE was similar in patients who had sleeve gastrectomy and in control patients.
However, these subgroup results need to be interpreted with caution since the surgery and control patients in each surgery type subgroup were not matched for age, sex, and comorbidities, said Dr. Bouchard.
He acknowledged that study limitations include a lack of information about the patients’ BMI, weight, medications, and glycemic control (hemoglobin A1c).
Dr. Bouchard and Dr. Anvari have no relevant financial disclosures.
Patients with obesity who had bariatric surgery had a lower risk of having a major adverse cardiovascular event (MACE) or dying from all causes during a median 7-year follow-up, compared with similar patients who did not undergo surgery.
These findings, from a province-wide retrospective cohort study from Quebec, follow two recent, slightly shorter similar trials.
Now we need a large randomized clinical trial (RCT), experts say, to definitively establish cardiovascular and mortality benefits in people with obesity who have metabolic/bariatric surgery. And such a trial is just beginning.
Philippe Bouchard, MD, a general surgery resident from McGill University in Montreal presented the Quebec study in a top papers session at the annual meeting of the American Society for Metabolic & Bariatric Surgery.
The findings showed that, among obese patients with metabolic syndrome, bariatric/metabolic surgery is associated with a sustained decrease in the incidence of MACE and all-cause mortality of at least 5 years, Dr. Bouchard said.
“The results of this population-based observational study should be validated in randomized controlled trials,” he concluded.
In the meantime, “we believe our study adds to the body of evidence in mainly two ways,” Dr. Bouchard told this news organization in an email.
It has a longer follow-up than recent observational studies, “a median of 7 years, compared to 3.9 years in a study from the Cleveland Clinic, and 4.6 years in one from Ontario, he said.
“This allows us to [estimate] an absolute risk reduction of MACE of 5.11% at 10 years,” he added. This is a smaller risk reduction than the roughly 40% risk reduction seen in the other two studies, possibly because of selection bias, Dr. Bouchard speculated.
“Second, most of the larger cohorts are heavily weighted on Roux-en-Y gastric bypass,” he continued. In contrast, their study included diverse procedures, including sleeve gastrectomy, duodenal switch, and adjustable gastric banding.
“Given the rise in popularity of a derivative of the duodenal switch – the single-anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADi-S) – we believe this information is timely and relevant to clinicians,” Dr. Bouchard said.
RCT on the subject is coming
“I totally agree that we need a large randomized controlled trial of bariatric surgery versus optimal medical therapy to conclusively establish” the impact of bariatric surgery on cardiovascular outcomes, said the assigned discussant, Mehran Anvari, MD. And their research group is just about to begin one.
In the absence of RCT data, clinicians “may currently not refer [eligible] patients for bariatric surgery because of the high risk they pose,” said Dr. Anvari, professor and director of the Centre for Minimal Access Surgery of McMaster University, Hamilton, Ont., and senior author in the Ontario study.
Furthermore, an important point is that the current trial extended the follow-up to 7 years, he told this news organization in an email.
That study included patients with diabetes and hypertension, he added, whereas his group included patients with a history of cardiovascular disease and/or heart failure.
“We hope these studies encourage general practitioners and cardiologists to consider bariatric surgery as a viable treatment option to prevent and reduce the risk of MACE in the obese patients [body mass index >35 kg/m2] with significant cardiovascular disease,” he said.
“We have embarked on a pilot RCT among bariatric centers of excellence in Ontario,” Dr. Anvari added, which showed the feasibility and safety of such a study.
He estimates that the RCT will need to recruit 2,000 patients to demonstrate the safety and effectiveness of bariatric surgery in reducing MACE and cardiac and all-cause mortality among patients with existing cardiovascular disease.
This “will require international collaboration,” he added, “and our group is currently establishing collaboration with sites in North America, Europe, and Australia to conduct such a study.”
Patients matched for age, sex, number of comorbidities
Quebec has a single public health care system that covers the cost of bariatric surgery for eligible patients; that is, those with a BMI greater than 35 kg/m2 and comorbidities or a BMI greater than 40 kg/m2.
Using this provincial health care database, which covers over 97% of the population, the researchers identified 3,637 patients with diabetes and/or hypertension who had bariatric surgery during 2007-2012.
They matched the surgery patients with 5,420 control patients with obesity who lived in the same geographic region and had a similar age, sex, and number of Charlson Comorbidity Index comorbidities, but did not undergo bariatric surgery.
The patients had a mean age of 50 and 64% were women.
Half had zero to one comorbidities, a quarter had two comorbidities, and another quarter had at least three comorbidities.
Most patients in the surgery group had type 2 diabetes (70%) and 50% had hypertension, whereas in the control group, most patients had hypertension (82%) and 41% had diabetes.
The most common type of bariatric surgery was adjustable gastric banding (42% of patients), followed by duodenal switch (24%), sleeve gastrectomy (23%), and Roux-en-Y gastric bypass (11%).
The primary outcome was the incidence of MACE, defined as coronary artery events (including myocardial infarction, percutaneous coronary intervention, and coronary artery bypass graft), stroke, heart failure, and all-cause mortality,
After a median follow-up of 7-11 years, fewer patients in the surgical group than in the control group had MACE (20% vs. 25%) or died from all causes (4.1% vs. 6.3%, both statistically significant at P < .01)
Similarly, significantly fewer patients in the surgical group than in the control group had a coronary artery event or heart failure (each P < .01).
However, there were no significant between-group difference in the rate of stroke, possibly because of the small number of strokes.
The risk of MACE was 17% lower in the group that had bariatric surgery than in the control group (adjusted hazard ratio, 0.83; 95% confidence interval, 0.78-0.89), after adjusting for age, sex, and number of comorbidities.
In subgroup analysis, patients who had adjustable gastric banding, Roux-en-Y gastric bypass, or duodenal switch had a significantly lower risk of MACE than control patients.
The risk of MACE was similar in patients who had sleeve gastrectomy and in control patients.
However, these subgroup results need to be interpreted with caution since the surgery and control patients in each surgery type subgroup were not matched for age, sex, and comorbidities, said Dr. Bouchard.
He acknowledged that study limitations include a lack of information about the patients’ BMI, weight, medications, and glycemic control (hemoglobin A1c).
Dr. Bouchard and Dr. Anvari have no relevant financial disclosures.
FROM ASMBS 2021
Healthy with obesity? The latest study casts doubt
compared with people without obesity and or adverse metabolic profiles, new research suggests.
The latest data on this controversial subject come from an analysis of nearly 400,000 people in the U.K. Biobank. Although the data also showed that metabolically healthy obesity poses less risk than “metabolically unhealthy” obesity, the risk of progression from healthy to unhealthy within 3-5 years was high.
“People with metabolically healthy obesity are not ‘healthy’ as they are at higher risk of atherosclerotic cardiovascular disease [ASCVD], heart failure, and respiratory diseases, compared with nonobese people with a normal metabolic profile. As such, weight management could be beneficial to all people with obesity irrespective of metabolic profile,” Ziyi Zhou and colleagues wrote in their report, published June 10, 2021, in Diabetologia.
Moreover, they advised avoiding the term metabolically healthy obesity entirely in clinical medicine “as it is misleading, and different strategies for risk stratification should be explored.”
In interviews, two experts provided somewhat different takes on the study and the overall subject.
‘Lifestyle should be explored with every single patient regardless of their weight’
Yoni Freedhoff, MD, medical director of the Bariatric Medical Institute, Ottawa, said “clinicians and patients need to be aware that obesity increases a person’s risk of various medical problems, and in turn this might lead to more frequent screening. This increased screening might be analogous to that of a person with a strong familial history of cancer who of course we would never describe as being ‘unhealthy’ as a consequence of their increased risk.”
In addition to screening, “lifestyle should be explored with every single patient regardless of their weight, and if a person’s weight is not affecting their health or their quality of life, a clinician need only let the patient know that, were they to want to discuss weight management options in the future, that they’d be there for them,” said Dr. Freedhoff.
‘Metabolically healthy obesity’ has had many definitions
Matthias Schulze, DrPH, head of the molecular epidemiology at the German Institute of Human Nutrition, Potsdam, and professor at the University of Potsdam, pointed out that the way metabolically healthy obesity is defined and the outcomes assessed make a difference.
In the current study, the term is defined as having a body mass index of at least 30 kg/m2 and at least four of six metabolically healthy criteria: blood pressure, C-reactive protein, triacylglycerols, LDL cholesterol, HDL cholesterol, and hemoglobin A1c.
In May 2021, Dr. Schulze and associates reported in JAMA Network Open on a different definition that they found to identify individuals who do not have an increased risk of cardiovascular disease death and total mortality. Interestingly, they also used the U.K. Biobank as their validation cohort.
“We derived a new definition of metabolic health ... that is different from those used in [the current] article. Importantly, we included a measure of body fat distribution, waist-to-hip ratio. On the other side, we investigated only mortality outcomes and we can therefore not exclude the possibility that other outcomes may still be related. [For example], a higher diabetes risk may still be present among those we have defined as having metabolically healthy obesity.”
Dr. Schulze also said that several previous studies and meta-analyses have suggested that “previous common definitions of metabolically healthy obesity do not identify a subgroup without risk, or being at risk comparable to normal-weight metabolically healthy. Thus, this study confirms this conclusion. [But] this doesn’t rule out that there are better ways of defining subgroups.”
Clinically, he said “given that we investigated only mortality, we cannot conclude that our ‘metabolically healthy obesity’ group doesn’t require intervention.”
Higher rates of diabetes, ASCVD, heart failure, death
The current population-based study included 381,363 U.K. Biobank participants who were followed up for a median 11.2 years. Overall, about 55% did not have obesity or metabolic abnormalities, 9% had metabolically healthy obesity, 20% were metabolically unhealthy but did not have obesity, and 16% had metabolically unhealthy obesity as defined by the investigators.
The investigators adjusted the data for several potential confounders, including age, sex, ethnicity, education, socioeconomic status, smoking status, physical activity, and dietary factors.
Compared with individuals without obesity or metabolic abnormalities, those with metabolically healthy obesity had significantly higher rates of incident diabetes (hazard ratio, 4.32), ASCVD (HR, 1.18), myocardial infarction (HR, 1.23), stroke (HR, 1.10), heart failure (HR, 1.76), respiratory diseases (HR, 1.28), and chronic obstructive pulmonary disease (HR, 1.19).
In general, rates of cardiovascular and respiratory outcomes were highest in metabolically unhealthy obesity, followed by those without obesity but with metabolic abnormalities and those with metabolically healthy obesity. However, for incident and fatal heart failure and incident respiratory diseases, those with metabolically healthy obesity had higher rates than did those without obesity but with metabolic abnormalities.
Compared with those without obesity or metabolic abnormalities, those with metabolically healthy obesity had significantly higher all-cause mortality rates (HR, 1.22). And, compared with those without obesity (regardless of metabolic status) at baseline, those with metabolically healthy obesity were significantly more likely to have diabetes (HR, 2.06), heart failure (HR, 1.6), and respiratory diseases (HR, 1.2), but not ASCVD. The association was also significant for all-cause and heart failure mortality (HR, 1.12 and 1.44, respectively), but not for other causes of death.
Progression from metabolically healthy to unhealthy is common
Among 8,512 participants for whom longitudinal data were available for a median of 4.4 years, half of those with metabolically healthy obesity remained in that category, 20% no longer had obesity, and more than a quarter transitioned to metabolically unhealthy obesity. Compared with those without obesity or metabolic abnormalities throughout, those who transitioned from metabolically healthy to metabolically unhealthy had significantly higher rates of incident ASCVD (HR, 2.46) and all-cause mortality (HR, 3.07).
But those who remained in the metabolically healthy obesity category throughout did not have significantly increased risks for the adverse outcomes measured.
Ms. Zhou and colleagues noted that the data demonstrate heterogeneity among people with obesity, which offers the potential to stratify risk based on prognosis. For example, “people with [metabolically unhealthy obesity] were at a higher risk of mortality and morbidity than everyone else, and thus they should be prioritized for intervention.”
However, they add, “Obesity is associated with a wide range of diseases, and using a single label or categorical risk algorithm is unlikely to be effective compared with prediction algorithms based on disease-specific and continuous risk markers.”
Ms. Zhou has no disclosures. One coauthor has relationships with numerous pharmaceutical companies; the rest have none. Dr. Freedhoff has served as a director, officer, partner, employee, adviser, consultant, or trustee for the Bariatric Medical Institute and Constant Health. He is a speaker or a member of a speakers bureau for Obesity Canada and Novo Nordisk, received research grant from Novo Nordisk, and received income of at least $250 from WebMD, CTV, and Random House. Dr/ Schulze has received grants from German Federal Ministry of Education and Research.
compared with people without obesity and or adverse metabolic profiles, new research suggests.
The latest data on this controversial subject come from an analysis of nearly 400,000 people in the U.K. Biobank. Although the data also showed that metabolically healthy obesity poses less risk than “metabolically unhealthy” obesity, the risk of progression from healthy to unhealthy within 3-5 years was high.
“People with metabolically healthy obesity are not ‘healthy’ as they are at higher risk of atherosclerotic cardiovascular disease [ASCVD], heart failure, and respiratory diseases, compared with nonobese people with a normal metabolic profile. As such, weight management could be beneficial to all people with obesity irrespective of metabolic profile,” Ziyi Zhou and colleagues wrote in their report, published June 10, 2021, in Diabetologia.
Moreover, they advised avoiding the term metabolically healthy obesity entirely in clinical medicine “as it is misleading, and different strategies for risk stratification should be explored.”
In interviews, two experts provided somewhat different takes on the study and the overall subject.
‘Lifestyle should be explored with every single patient regardless of their weight’
Yoni Freedhoff, MD, medical director of the Bariatric Medical Institute, Ottawa, said “clinicians and patients need to be aware that obesity increases a person’s risk of various medical problems, and in turn this might lead to more frequent screening. This increased screening might be analogous to that of a person with a strong familial history of cancer who of course we would never describe as being ‘unhealthy’ as a consequence of their increased risk.”
In addition to screening, “lifestyle should be explored with every single patient regardless of their weight, and if a person’s weight is not affecting their health or their quality of life, a clinician need only let the patient know that, were they to want to discuss weight management options in the future, that they’d be there for them,” said Dr. Freedhoff.
‘Metabolically healthy obesity’ has had many definitions
Matthias Schulze, DrPH, head of the molecular epidemiology at the German Institute of Human Nutrition, Potsdam, and professor at the University of Potsdam, pointed out that the way metabolically healthy obesity is defined and the outcomes assessed make a difference.
In the current study, the term is defined as having a body mass index of at least 30 kg/m2 and at least four of six metabolically healthy criteria: blood pressure, C-reactive protein, triacylglycerols, LDL cholesterol, HDL cholesterol, and hemoglobin A1c.
In May 2021, Dr. Schulze and associates reported in JAMA Network Open on a different definition that they found to identify individuals who do not have an increased risk of cardiovascular disease death and total mortality. Interestingly, they also used the U.K. Biobank as their validation cohort.
“We derived a new definition of metabolic health ... that is different from those used in [the current] article. Importantly, we included a measure of body fat distribution, waist-to-hip ratio. On the other side, we investigated only mortality outcomes and we can therefore not exclude the possibility that other outcomes may still be related. [For example], a higher diabetes risk may still be present among those we have defined as having metabolically healthy obesity.”
Dr. Schulze also said that several previous studies and meta-analyses have suggested that “previous common definitions of metabolically healthy obesity do not identify a subgroup without risk, or being at risk comparable to normal-weight metabolically healthy. Thus, this study confirms this conclusion. [But] this doesn’t rule out that there are better ways of defining subgroups.”
Clinically, he said “given that we investigated only mortality, we cannot conclude that our ‘metabolically healthy obesity’ group doesn’t require intervention.”
Higher rates of diabetes, ASCVD, heart failure, death
The current population-based study included 381,363 U.K. Biobank participants who were followed up for a median 11.2 years. Overall, about 55% did not have obesity or metabolic abnormalities, 9% had metabolically healthy obesity, 20% were metabolically unhealthy but did not have obesity, and 16% had metabolically unhealthy obesity as defined by the investigators.
The investigators adjusted the data for several potential confounders, including age, sex, ethnicity, education, socioeconomic status, smoking status, physical activity, and dietary factors.
Compared with individuals without obesity or metabolic abnormalities, those with metabolically healthy obesity had significantly higher rates of incident diabetes (hazard ratio, 4.32), ASCVD (HR, 1.18), myocardial infarction (HR, 1.23), stroke (HR, 1.10), heart failure (HR, 1.76), respiratory diseases (HR, 1.28), and chronic obstructive pulmonary disease (HR, 1.19).
In general, rates of cardiovascular and respiratory outcomes were highest in metabolically unhealthy obesity, followed by those without obesity but with metabolic abnormalities and those with metabolically healthy obesity. However, for incident and fatal heart failure and incident respiratory diseases, those with metabolically healthy obesity had higher rates than did those without obesity but with metabolic abnormalities.
Compared with those without obesity or metabolic abnormalities, those with metabolically healthy obesity had significantly higher all-cause mortality rates (HR, 1.22). And, compared with those without obesity (regardless of metabolic status) at baseline, those with metabolically healthy obesity were significantly more likely to have diabetes (HR, 2.06), heart failure (HR, 1.6), and respiratory diseases (HR, 1.2), but not ASCVD. The association was also significant for all-cause and heart failure mortality (HR, 1.12 and 1.44, respectively), but not for other causes of death.
Progression from metabolically healthy to unhealthy is common
Among 8,512 participants for whom longitudinal data were available for a median of 4.4 years, half of those with metabolically healthy obesity remained in that category, 20% no longer had obesity, and more than a quarter transitioned to metabolically unhealthy obesity. Compared with those without obesity or metabolic abnormalities throughout, those who transitioned from metabolically healthy to metabolically unhealthy had significantly higher rates of incident ASCVD (HR, 2.46) and all-cause mortality (HR, 3.07).
But those who remained in the metabolically healthy obesity category throughout did not have significantly increased risks for the adverse outcomes measured.
Ms. Zhou and colleagues noted that the data demonstrate heterogeneity among people with obesity, which offers the potential to stratify risk based on prognosis. For example, “people with [metabolically unhealthy obesity] were at a higher risk of mortality and morbidity than everyone else, and thus they should be prioritized for intervention.”
However, they add, “Obesity is associated with a wide range of diseases, and using a single label or categorical risk algorithm is unlikely to be effective compared with prediction algorithms based on disease-specific and continuous risk markers.”
Ms. Zhou has no disclosures. One coauthor has relationships with numerous pharmaceutical companies; the rest have none. Dr. Freedhoff has served as a director, officer, partner, employee, adviser, consultant, or trustee for the Bariatric Medical Institute and Constant Health. He is a speaker or a member of a speakers bureau for Obesity Canada and Novo Nordisk, received research grant from Novo Nordisk, and received income of at least $250 from WebMD, CTV, and Random House. Dr/ Schulze has received grants from German Federal Ministry of Education and Research.
compared with people without obesity and or adverse metabolic profiles, new research suggests.
The latest data on this controversial subject come from an analysis of nearly 400,000 people in the U.K. Biobank. Although the data also showed that metabolically healthy obesity poses less risk than “metabolically unhealthy” obesity, the risk of progression from healthy to unhealthy within 3-5 years was high.
“People with metabolically healthy obesity are not ‘healthy’ as they are at higher risk of atherosclerotic cardiovascular disease [ASCVD], heart failure, and respiratory diseases, compared with nonobese people with a normal metabolic profile. As such, weight management could be beneficial to all people with obesity irrespective of metabolic profile,” Ziyi Zhou and colleagues wrote in their report, published June 10, 2021, in Diabetologia.
Moreover, they advised avoiding the term metabolically healthy obesity entirely in clinical medicine “as it is misleading, and different strategies for risk stratification should be explored.”
In interviews, two experts provided somewhat different takes on the study and the overall subject.
‘Lifestyle should be explored with every single patient regardless of their weight’
Yoni Freedhoff, MD, medical director of the Bariatric Medical Institute, Ottawa, said “clinicians and patients need to be aware that obesity increases a person’s risk of various medical problems, and in turn this might lead to more frequent screening. This increased screening might be analogous to that of a person with a strong familial history of cancer who of course we would never describe as being ‘unhealthy’ as a consequence of their increased risk.”
In addition to screening, “lifestyle should be explored with every single patient regardless of their weight, and if a person’s weight is not affecting their health or their quality of life, a clinician need only let the patient know that, were they to want to discuss weight management options in the future, that they’d be there for them,” said Dr. Freedhoff.
‘Metabolically healthy obesity’ has had many definitions
Matthias Schulze, DrPH, head of the molecular epidemiology at the German Institute of Human Nutrition, Potsdam, and professor at the University of Potsdam, pointed out that the way metabolically healthy obesity is defined and the outcomes assessed make a difference.
In the current study, the term is defined as having a body mass index of at least 30 kg/m2 and at least four of six metabolically healthy criteria: blood pressure, C-reactive protein, triacylglycerols, LDL cholesterol, HDL cholesterol, and hemoglobin A1c.
In May 2021, Dr. Schulze and associates reported in JAMA Network Open on a different definition that they found to identify individuals who do not have an increased risk of cardiovascular disease death and total mortality. Interestingly, they also used the U.K. Biobank as their validation cohort.
“We derived a new definition of metabolic health ... that is different from those used in [the current] article. Importantly, we included a measure of body fat distribution, waist-to-hip ratio. On the other side, we investigated only mortality outcomes and we can therefore not exclude the possibility that other outcomes may still be related. [For example], a higher diabetes risk may still be present among those we have defined as having metabolically healthy obesity.”
Dr. Schulze also said that several previous studies and meta-analyses have suggested that “previous common definitions of metabolically healthy obesity do not identify a subgroup without risk, or being at risk comparable to normal-weight metabolically healthy. Thus, this study confirms this conclusion. [But] this doesn’t rule out that there are better ways of defining subgroups.”
Clinically, he said “given that we investigated only mortality, we cannot conclude that our ‘metabolically healthy obesity’ group doesn’t require intervention.”
Higher rates of diabetes, ASCVD, heart failure, death
The current population-based study included 381,363 U.K. Biobank participants who were followed up for a median 11.2 years. Overall, about 55% did not have obesity or metabolic abnormalities, 9% had metabolically healthy obesity, 20% were metabolically unhealthy but did not have obesity, and 16% had metabolically unhealthy obesity as defined by the investigators.
The investigators adjusted the data for several potential confounders, including age, sex, ethnicity, education, socioeconomic status, smoking status, physical activity, and dietary factors.
Compared with individuals without obesity or metabolic abnormalities, those with metabolically healthy obesity had significantly higher rates of incident diabetes (hazard ratio, 4.32), ASCVD (HR, 1.18), myocardial infarction (HR, 1.23), stroke (HR, 1.10), heart failure (HR, 1.76), respiratory diseases (HR, 1.28), and chronic obstructive pulmonary disease (HR, 1.19).
In general, rates of cardiovascular and respiratory outcomes were highest in metabolically unhealthy obesity, followed by those without obesity but with metabolic abnormalities and those with metabolically healthy obesity. However, for incident and fatal heart failure and incident respiratory diseases, those with metabolically healthy obesity had higher rates than did those without obesity but with metabolic abnormalities.
Compared with those without obesity or metabolic abnormalities, those with metabolically healthy obesity had significantly higher all-cause mortality rates (HR, 1.22). And, compared with those without obesity (regardless of metabolic status) at baseline, those with metabolically healthy obesity were significantly more likely to have diabetes (HR, 2.06), heart failure (HR, 1.6), and respiratory diseases (HR, 1.2), but not ASCVD. The association was also significant for all-cause and heart failure mortality (HR, 1.12 and 1.44, respectively), but not for other causes of death.
Progression from metabolically healthy to unhealthy is common
Among 8,512 participants for whom longitudinal data were available for a median of 4.4 years, half of those with metabolically healthy obesity remained in that category, 20% no longer had obesity, and more than a quarter transitioned to metabolically unhealthy obesity. Compared with those without obesity or metabolic abnormalities throughout, those who transitioned from metabolically healthy to metabolically unhealthy had significantly higher rates of incident ASCVD (HR, 2.46) and all-cause mortality (HR, 3.07).
But those who remained in the metabolically healthy obesity category throughout did not have significantly increased risks for the adverse outcomes measured.
Ms. Zhou and colleagues noted that the data demonstrate heterogeneity among people with obesity, which offers the potential to stratify risk based on prognosis. For example, “people with [metabolically unhealthy obesity] were at a higher risk of mortality and morbidity than everyone else, and thus they should be prioritized for intervention.”
However, they add, “Obesity is associated with a wide range of diseases, and using a single label or categorical risk algorithm is unlikely to be effective compared with prediction algorithms based on disease-specific and continuous risk markers.”
Ms. Zhou has no disclosures. One coauthor has relationships with numerous pharmaceutical companies; the rest have none. Dr. Freedhoff has served as a director, officer, partner, employee, adviser, consultant, or trustee for the Bariatric Medical Institute and Constant Health. He is a speaker or a member of a speakers bureau for Obesity Canada and Novo Nordisk, received research grant from Novo Nordisk, and received income of at least $250 from WebMD, CTV, and Random House. Dr/ Schulze has received grants from German Federal Ministry of Education and Research.
FROM DIABETOLOGIA
Simple risk assessment predicts post-PCI ischemic events
A patient’s risk for ischemic events, but not bleeding, after percutaneous coronary intervention (PCI) can be predicted simply based on whether they have one or more guideline-based standardized risk criteria, a large-scale real-world analysis suggests.
Haoyu Wang, MD, and colleagues showed that having at least one high-risk feature, as outlined in the 2018 European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) Guidelines on Myocardial Revascularization, was associated with an increased risk for target vessel failure by 48% and for a patient-oriented composite outcome by 44%.
Moreover, they showed that implantation of at least three stents and the presence of diabetes and diffuse multivessel disease were the only high-risk features from the guidelines that were independent predictors of the two outcomes.
The study of more than 10,000 PCI patients also showed that determining whether patients were at high bleeding risk (HBR) did not modify their ischemic risk.
This, said Dr. Wang, from the National Center for Cardiovascular Diseases, Fuwai Hospital, Beijing, underscores the importance of applying the high ischemic risk (HIR) criteria from the ESC/EACTS guidelines when tailoring dual antiplatelet therapy (DAPT).
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress on June 2, and published online in the Journal of Atherosclerosis and Thrombosis.
Dr. Wang told theheart.org | Medscape Cardiology that they conducted the study to determine which – HIR or HBR – is “most important to balance when treating patients undergoing PCI and then having dual antiplatelet therapy.”
The results showed that when patients have both a HIR and HBR, it is the ESC/EACTS guideline HIR criteria that have “a higher impact” than the bleeding risk, and that this can be “used to guide our choice of the duration of dual anti-platelet therapy.”
“Maybe we can extend, or use more potent, P2Y12 inhibitors” in those situations, he said.
S. Lale Tokgözoglu, MD, PhD, professor of cardiology, Hacettepe University, Ankara, Turkey, who was not involved in the study, said the HIR assessment “performed well,” adding that the HBR score might have been expected to attenuate its “prognostic advantage.”
She told this news organization that the results “are interesting since previous observations have suggested that Asian patients may be more prone to medication side effects and bleeding.”
These findings emphasize the importance of assessing HIR in daily PCI practice and confirm that it “performs well in different populations in real life,” added Dr. Tokgözoglu, a former president of the EAS.
The ESC/EACTS guidelines aimed to standardize the definition of HIR, Dr. Wang said during the presentation.
They set out 10 high-risk features for ischemic events for patients undergoing revascularization, which included patient medical history, comorbid conditions, and the characteristics of the PCI procedure.
Although the goals of the criteria are to inform decision-making and stimulate research, Dr. Wang said that their “prevalence and prognostic association with clinical outcomes are yet to be established in real-world PCI practice.”
Alongside, the Predicting Bleeding Complication in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score was developed to predict out-of-hospital bleeding in patients receiving DAPT after stent implantation.
Although a PRECISE-DAPT score of at least 25 constitutes a patient at high bleeding risk, Dr. Wang pointed out that such patients are typically also at risk for ischemic events after PCI, and it is “unclear” whether being at HBR modifies this risk.
To investigate further, they used the prospective, real-world Fuwai PCI registry to collate an all-comer patient population with unselected use of drug-eluting stents at the National Center for Cardiovascular Diseases at Fuwai Hospital.
They excluded individuals who were treated with balloon angioplasty alone, bioresorbable scaffolds, or bare metal stents, leaving a total population of 10,167 patients who were treated in 2013.
In that cohort, 5,149 patients (50.6%) met at least one risk criterion from the ESC/EACTS guidelines (HIR patients) and 5,018 (49.4%) met none of the risk criteria (non-HIR patients).
The most common criteria were implantation of at least three stents (23.5%); total stent length greater than 60 mm (20.2%); diffuse multivessel disease, especially in diabetic patients (18.5%); and a history of ST-segment elevation myocardial infarction (13.9%).
HIR patients were significantly older than non-HIR patients (average age, 58.86 vs. 57.77 years; P < .001), were more likely to have diabetes mellitus (42.6% vs. 16.9%; P < .001); and were more likely to have already had a myocardial infarction (32.2% vs. 5.2%; P < .001).
HIR patients also had higher average PRECISE-ADAPT scores than those without HIR (11.22 vs. 9.94; P < .001), and were conversely less likely to have the left anterior descending artery as the target vessel than non-HIR patients (86.0% vs. 94.6%; P < .001).
Cox regression analysis taking into account a range of patient and clinical factors revealed that HIR patients were significantly more likely than their non-HIR counterparts to experience target vessel failure (hazard ratio, 1.48; 95% confidence interval, 1.25-1.74; P < .001).
They were also significantly more likely to have a patient-oriented composite outcome, defined as all-cause death, any myocardial infarction, or any revascularization (HR, 1.44; 95% CI, 1.28-1.63; P < .001).
There was also a significantly higher risk for cardiac death in HIR than in non-HIR patients (HR, 1.95; 95% CI, 1.16-3.29; P = .012).
However, there was no significant association between HIR status and clinically relevant bleeding (HR, 0.84; 95% CI, 0.66-1.06; P = .143).
When the researchers looked at individual ischemic risk features, they found that, on fully adjusted analyses, only two were independent predictors of target vessel failure and the patient-oriented composite outcome.
Having at least three stents implanted was significantly associated with target vessel failure (HR, 1.36; 95% CI, 1.02-1.80; P = .038), and borderline significantly associated with the patient oriented composite outcome (HR, 1.23; 95% CI, 1.00-1.53; P = .056).
Diffuse multivessel disease, especially in diabetic patients, was significantly associated with both target vessel failure (HR, 1.24; 95% CI, 1.02-1.51; P = .035) and with the patient-oriented composite outcome (HR, 1.20; 95% CI, 1.04-1.39; P = .012).
Neither risk feature was significantly associated with clinically relevant bleeding, Dr. Wang noted.
Stratifying the patients by HBR status, the team found that rates of target vessel failure, the patient-oriented composite outcome, cardiac death, myocardial infarction, and definite/probable stent thrombosis were higher in patients with both HIR and HBR than those with neither HIR nor HBR (P < .001).
Further stratifying patients by PRECISE-ADAPT scores – 10 or less indicating very low risk, 11-17 indicating low risk, 18-24 indicating moderate risk, and at least 25 indicating high risk – showed that HIR features had a consistent effect on ischemic and bleeding outcomes, regardless of bleeding risk.
No funding declared. No relevant financial relationships declared.
A version of this article first appeared on Medscape.com.
A patient’s risk for ischemic events, but not bleeding, after percutaneous coronary intervention (PCI) can be predicted simply based on whether they have one or more guideline-based standardized risk criteria, a large-scale real-world analysis suggests.
Haoyu Wang, MD, and colleagues showed that having at least one high-risk feature, as outlined in the 2018 European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) Guidelines on Myocardial Revascularization, was associated with an increased risk for target vessel failure by 48% and for a patient-oriented composite outcome by 44%.
Moreover, they showed that implantation of at least three stents and the presence of diabetes and diffuse multivessel disease were the only high-risk features from the guidelines that were independent predictors of the two outcomes.
The study of more than 10,000 PCI patients also showed that determining whether patients were at high bleeding risk (HBR) did not modify their ischemic risk.
This, said Dr. Wang, from the National Center for Cardiovascular Diseases, Fuwai Hospital, Beijing, underscores the importance of applying the high ischemic risk (HIR) criteria from the ESC/EACTS guidelines when tailoring dual antiplatelet therapy (DAPT).
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress on June 2, and published online in the Journal of Atherosclerosis and Thrombosis.
Dr. Wang told theheart.org | Medscape Cardiology that they conducted the study to determine which – HIR or HBR – is “most important to balance when treating patients undergoing PCI and then having dual antiplatelet therapy.”
The results showed that when patients have both a HIR and HBR, it is the ESC/EACTS guideline HIR criteria that have “a higher impact” than the bleeding risk, and that this can be “used to guide our choice of the duration of dual anti-platelet therapy.”
“Maybe we can extend, or use more potent, P2Y12 inhibitors” in those situations, he said.
S. Lale Tokgözoglu, MD, PhD, professor of cardiology, Hacettepe University, Ankara, Turkey, who was not involved in the study, said the HIR assessment “performed well,” adding that the HBR score might have been expected to attenuate its “prognostic advantage.”
She told this news organization that the results “are interesting since previous observations have suggested that Asian patients may be more prone to medication side effects and bleeding.”
These findings emphasize the importance of assessing HIR in daily PCI practice and confirm that it “performs well in different populations in real life,” added Dr. Tokgözoglu, a former president of the EAS.
The ESC/EACTS guidelines aimed to standardize the definition of HIR, Dr. Wang said during the presentation.
They set out 10 high-risk features for ischemic events for patients undergoing revascularization, which included patient medical history, comorbid conditions, and the characteristics of the PCI procedure.
Although the goals of the criteria are to inform decision-making and stimulate research, Dr. Wang said that their “prevalence and prognostic association with clinical outcomes are yet to be established in real-world PCI practice.”
Alongside, the Predicting Bleeding Complication in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score was developed to predict out-of-hospital bleeding in patients receiving DAPT after stent implantation.
Although a PRECISE-DAPT score of at least 25 constitutes a patient at high bleeding risk, Dr. Wang pointed out that such patients are typically also at risk for ischemic events after PCI, and it is “unclear” whether being at HBR modifies this risk.
To investigate further, they used the prospective, real-world Fuwai PCI registry to collate an all-comer patient population with unselected use of drug-eluting stents at the National Center for Cardiovascular Diseases at Fuwai Hospital.
They excluded individuals who were treated with balloon angioplasty alone, bioresorbable scaffolds, or bare metal stents, leaving a total population of 10,167 patients who were treated in 2013.
In that cohort, 5,149 patients (50.6%) met at least one risk criterion from the ESC/EACTS guidelines (HIR patients) and 5,018 (49.4%) met none of the risk criteria (non-HIR patients).
The most common criteria were implantation of at least three stents (23.5%); total stent length greater than 60 mm (20.2%); diffuse multivessel disease, especially in diabetic patients (18.5%); and a history of ST-segment elevation myocardial infarction (13.9%).
HIR patients were significantly older than non-HIR patients (average age, 58.86 vs. 57.77 years; P < .001), were more likely to have diabetes mellitus (42.6% vs. 16.9%; P < .001); and were more likely to have already had a myocardial infarction (32.2% vs. 5.2%; P < .001).
HIR patients also had higher average PRECISE-ADAPT scores than those without HIR (11.22 vs. 9.94; P < .001), and were conversely less likely to have the left anterior descending artery as the target vessel than non-HIR patients (86.0% vs. 94.6%; P < .001).
Cox regression analysis taking into account a range of patient and clinical factors revealed that HIR patients were significantly more likely than their non-HIR counterparts to experience target vessel failure (hazard ratio, 1.48; 95% confidence interval, 1.25-1.74; P < .001).
They were also significantly more likely to have a patient-oriented composite outcome, defined as all-cause death, any myocardial infarction, or any revascularization (HR, 1.44; 95% CI, 1.28-1.63; P < .001).
There was also a significantly higher risk for cardiac death in HIR than in non-HIR patients (HR, 1.95; 95% CI, 1.16-3.29; P = .012).
However, there was no significant association between HIR status and clinically relevant bleeding (HR, 0.84; 95% CI, 0.66-1.06; P = .143).
When the researchers looked at individual ischemic risk features, they found that, on fully adjusted analyses, only two were independent predictors of target vessel failure and the patient-oriented composite outcome.
Having at least three stents implanted was significantly associated with target vessel failure (HR, 1.36; 95% CI, 1.02-1.80; P = .038), and borderline significantly associated with the patient oriented composite outcome (HR, 1.23; 95% CI, 1.00-1.53; P = .056).
Diffuse multivessel disease, especially in diabetic patients, was significantly associated with both target vessel failure (HR, 1.24; 95% CI, 1.02-1.51; P = .035) and with the patient-oriented composite outcome (HR, 1.20; 95% CI, 1.04-1.39; P = .012).
Neither risk feature was significantly associated with clinically relevant bleeding, Dr. Wang noted.
Stratifying the patients by HBR status, the team found that rates of target vessel failure, the patient-oriented composite outcome, cardiac death, myocardial infarction, and definite/probable stent thrombosis were higher in patients with both HIR and HBR than those with neither HIR nor HBR (P < .001).
Further stratifying patients by PRECISE-ADAPT scores – 10 or less indicating very low risk, 11-17 indicating low risk, 18-24 indicating moderate risk, and at least 25 indicating high risk – showed that HIR features had a consistent effect on ischemic and bleeding outcomes, regardless of bleeding risk.
No funding declared. No relevant financial relationships declared.
A version of this article first appeared on Medscape.com.
A patient’s risk for ischemic events, but not bleeding, after percutaneous coronary intervention (PCI) can be predicted simply based on whether they have one or more guideline-based standardized risk criteria, a large-scale real-world analysis suggests.
Haoyu Wang, MD, and colleagues showed that having at least one high-risk feature, as outlined in the 2018 European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) Guidelines on Myocardial Revascularization, was associated with an increased risk for target vessel failure by 48% and for a patient-oriented composite outcome by 44%.
Moreover, they showed that implantation of at least three stents and the presence of diabetes and diffuse multivessel disease were the only high-risk features from the guidelines that were independent predictors of the two outcomes.
The study of more than 10,000 PCI patients also showed that determining whether patients were at high bleeding risk (HBR) did not modify their ischemic risk.
This, said Dr. Wang, from the National Center for Cardiovascular Diseases, Fuwai Hospital, Beijing, underscores the importance of applying the high ischemic risk (HIR) criteria from the ESC/EACTS guidelines when tailoring dual antiplatelet therapy (DAPT).
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress on June 2, and published online in the Journal of Atherosclerosis and Thrombosis.
Dr. Wang told theheart.org | Medscape Cardiology that they conducted the study to determine which – HIR or HBR – is “most important to balance when treating patients undergoing PCI and then having dual antiplatelet therapy.”
The results showed that when patients have both a HIR and HBR, it is the ESC/EACTS guideline HIR criteria that have “a higher impact” than the bleeding risk, and that this can be “used to guide our choice of the duration of dual anti-platelet therapy.”
“Maybe we can extend, or use more potent, P2Y12 inhibitors” in those situations, he said.
S. Lale Tokgözoglu, MD, PhD, professor of cardiology, Hacettepe University, Ankara, Turkey, who was not involved in the study, said the HIR assessment “performed well,” adding that the HBR score might have been expected to attenuate its “prognostic advantage.”
She told this news organization that the results “are interesting since previous observations have suggested that Asian patients may be more prone to medication side effects and bleeding.”
These findings emphasize the importance of assessing HIR in daily PCI practice and confirm that it “performs well in different populations in real life,” added Dr. Tokgözoglu, a former president of the EAS.
The ESC/EACTS guidelines aimed to standardize the definition of HIR, Dr. Wang said during the presentation.
They set out 10 high-risk features for ischemic events for patients undergoing revascularization, which included patient medical history, comorbid conditions, and the characteristics of the PCI procedure.
Although the goals of the criteria are to inform decision-making and stimulate research, Dr. Wang said that their “prevalence and prognostic association with clinical outcomes are yet to be established in real-world PCI practice.”
Alongside, the Predicting Bleeding Complication in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score was developed to predict out-of-hospital bleeding in patients receiving DAPT after stent implantation.
Although a PRECISE-DAPT score of at least 25 constitutes a patient at high bleeding risk, Dr. Wang pointed out that such patients are typically also at risk for ischemic events after PCI, and it is “unclear” whether being at HBR modifies this risk.
To investigate further, they used the prospective, real-world Fuwai PCI registry to collate an all-comer patient population with unselected use of drug-eluting stents at the National Center for Cardiovascular Diseases at Fuwai Hospital.
They excluded individuals who were treated with balloon angioplasty alone, bioresorbable scaffolds, or bare metal stents, leaving a total population of 10,167 patients who were treated in 2013.
In that cohort, 5,149 patients (50.6%) met at least one risk criterion from the ESC/EACTS guidelines (HIR patients) and 5,018 (49.4%) met none of the risk criteria (non-HIR patients).
The most common criteria were implantation of at least three stents (23.5%); total stent length greater than 60 mm (20.2%); diffuse multivessel disease, especially in diabetic patients (18.5%); and a history of ST-segment elevation myocardial infarction (13.9%).
HIR patients were significantly older than non-HIR patients (average age, 58.86 vs. 57.77 years; P < .001), were more likely to have diabetes mellitus (42.6% vs. 16.9%; P < .001); and were more likely to have already had a myocardial infarction (32.2% vs. 5.2%; P < .001).
HIR patients also had higher average PRECISE-ADAPT scores than those without HIR (11.22 vs. 9.94; P < .001), and were conversely less likely to have the left anterior descending artery as the target vessel than non-HIR patients (86.0% vs. 94.6%; P < .001).
Cox regression analysis taking into account a range of patient and clinical factors revealed that HIR patients were significantly more likely than their non-HIR counterparts to experience target vessel failure (hazard ratio, 1.48; 95% confidence interval, 1.25-1.74; P < .001).
They were also significantly more likely to have a patient-oriented composite outcome, defined as all-cause death, any myocardial infarction, or any revascularization (HR, 1.44; 95% CI, 1.28-1.63; P < .001).
There was also a significantly higher risk for cardiac death in HIR than in non-HIR patients (HR, 1.95; 95% CI, 1.16-3.29; P = .012).
However, there was no significant association between HIR status and clinically relevant bleeding (HR, 0.84; 95% CI, 0.66-1.06; P = .143).
When the researchers looked at individual ischemic risk features, they found that, on fully adjusted analyses, only two were independent predictors of target vessel failure and the patient-oriented composite outcome.
Having at least three stents implanted was significantly associated with target vessel failure (HR, 1.36; 95% CI, 1.02-1.80; P = .038), and borderline significantly associated with the patient oriented composite outcome (HR, 1.23; 95% CI, 1.00-1.53; P = .056).
Diffuse multivessel disease, especially in diabetic patients, was significantly associated with both target vessel failure (HR, 1.24; 95% CI, 1.02-1.51; P = .035) and with the patient-oriented composite outcome (HR, 1.20; 95% CI, 1.04-1.39; P = .012).
Neither risk feature was significantly associated with clinically relevant bleeding, Dr. Wang noted.
Stratifying the patients by HBR status, the team found that rates of target vessel failure, the patient-oriented composite outcome, cardiac death, myocardial infarction, and definite/probable stent thrombosis were higher in patients with both HIR and HBR than those with neither HIR nor HBR (P < .001).
Further stratifying patients by PRECISE-ADAPT scores – 10 or less indicating very low risk, 11-17 indicating low risk, 18-24 indicating moderate risk, and at least 25 indicating high risk – showed that HIR features had a consistent effect on ischemic and bleeding outcomes, regardless of bleeding risk.
No funding declared. No relevant financial relationships declared.
A version of this article first appeared on Medscape.com.
Eat two fruits a day, ward off diabetes?
A new study supports the recommendation of eating two servings of fruit a day for health benefits – in this case a lower risk of diabetes.
Adults who ate two servings of fruit a day had 36% lower odds of developing diabetes within 5 years compared to those who ate less than a half serving of fruit a day, after adjusting for confounders, in a population-based Australian study.
The findings by Nicola P. Bondonno, PhD, and colleagues, based on data from the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab), were published online June 2 in the Journal of Clinical Endocrinology & Metabolism.
The study also showed that a higher fruit intake was associated with higher insulin sensitivity and lower pancreatic beta-cell function in a dose-response manner.
And a higher intake of apples – but not citrus fruit or bananas, the two other fruits studied – was associated with lower post-load serum insulin levels.
“This indicates that people who consumed more fruit [especially apples] had to produce less insulin to lower their blood glucose levels,” Dr. Bondonno, from the Institute for Nutrition Research, Edith Cowan University, Perth, Australia, explained in a statement from the Endocrine Society.
“This is important since high levels of circulating insulin (hyperinsulinemia) can damage blood vessels” and this is “related not only to diabetes, but also to high blood pressure, obesity, and heart disease,” she observed.
Fruit juice doesn’t have same effect
The study supports the recommendation of the Australian Dietary Guidelines – 2 servings of fruit a day, where one serving is 150 grams, which corresponds to a medium-sized apple, orange, or banana – Dr. Bondonno clarified in an email.
However, fruit juice was not associated with better glucose or insulin levels, or lower risk of diabetes, possibly because of its relatively high glycemic load and fewer beneficial fibers, the researchers speculate; added data suggest that even juice with added fiber does not trigger satiety.
The study findings “support encouragement of the consumption of whole fruits, but not fruit juice, to preserve insulin sensitivity and mitigate [type 2 diabetes] risk,” Dr. Bondonno and colleagues summarize.
“Promoting a healthy diet and lifestyle which includes the consumption of popular fruits such as apples, bananas, and oranges, with widespread geographical availability, may lower [type 2 diabetes] incidence,” they conclude.
Lower 5-year odds of diabetes
It is not clear how eating fruit may confer protection against developing diabetes, the researchers write.
They aimed to examine how consumption of total fruit, individual fruit, and fruit juice is related to glucose tolerance, insulin sensitivity, and incident diabetes at 5 years and 12 years in participants in the nationally representative AusDiab study.
They identified 7,675 adults aged 25 and older without diabetes who had undergone blood tests and completed a food frequency questionnaire in 1999-2000.
Participants had indicated how often they ate 10 different types of fruit, any type of fruit juice, and other foods on a scale of 0 (never) to 10 (three or more times/day).
Researchers divided participants into quartiles based on their median fruit consumption: 62 (range 0-95) g/day, 122 (95-162) g/day, 230 (162-283) g/day, and 372 (283-961) g/day.
The most commonly consumed fruit was apples (23% of total fruit intake), followed by bananas (20%) and citrus fruit (18%). Other fruits each accounted for less than 8% of total fruit intake, so they were not studied separately.
Participants in each quartile had a similar mean age (54 years) and body mass index (27 kg/m2).
However, compared with participants in quartile 1 (low fruit intake), those in quartiles 3 and 4 (moderate and high fruit intakes, respectively) were more likely to be female, do at least 150 minutes of physical activity a week, and less likely to smoke. They also ate more vegetables and less red meat and processed meat, but they consumed more sugar.
Of 4,674 participants who had 5-year follow-up, 179 participants developed diabetes.
Compared to participants with a low fruit intake (quartile 1), those with a moderate fruit intake (quartile 3) had a 36% lower odds of developing diabetes within 5 years (odds ratio, 0.64; 95% confidence interval, 0.44-0.92) after adjusting for age, sex, physical activity, education, socioeconomic status, income, body mass index, smoking, cardiovascular disease, parental history of diabetes, and consumption of alcohol, vegetables, red meat, processed meat, and calories.
Of the 3,518 participants with 12-year follow-up, 247 participants had diabetes, but there were no significant associations between fruit consumption and this longer-term risk of diabetes, possibly due to the small number of participants and events.
The study was supported by grants from the National Health and Medical Research Council of Australia and the National Heart Foundation of Australia. Dr. Bondonno has reported no relevant financial disclosures. Disclosures of the other authors are listed with the article.
A version of this article first appeared on Medscape.com.
A new study supports the recommendation of eating two servings of fruit a day for health benefits – in this case a lower risk of diabetes.
Adults who ate two servings of fruit a day had 36% lower odds of developing diabetes within 5 years compared to those who ate less than a half serving of fruit a day, after adjusting for confounders, in a population-based Australian study.
The findings by Nicola P. Bondonno, PhD, and colleagues, based on data from the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab), were published online June 2 in the Journal of Clinical Endocrinology & Metabolism.
The study also showed that a higher fruit intake was associated with higher insulin sensitivity and lower pancreatic beta-cell function in a dose-response manner.
And a higher intake of apples – but not citrus fruit or bananas, the two other fruits studied – was associated with lower post-load serum insulin levels.
“This indicates that people who consumed more fruit [especially apples] had to produce less insulin to lower their blood glucose levels,” Dr. Bondonno, from the Institute for Nutrition Research, Edith Cowan University, Perth, Australia, explained in a statement from the Endocrine Society.
“This is important since high levels of circulating insulin (hyperinsulinemia) can damage blood vessels” and this is “related not only to diabetes, but also to high blood pressure, obesity, and heart disease,” she observed.
Fruit juice doesn’t have same effect
The study supports the recommendation of the Australian Dietary Guidelines – 2 servings of fruit a day, where one serving is 150 grams, which corresponds to a medium-sized apple, orange, or banana – Dr. Bondonno clarified in an email.
However, fruit juice was not associated with better glucose or insulin levels, or lower risk of diabetes, possibly because of its relatively high glycemic load and fewer beneficial fibers, the researchers speculate; added data suggest that even juice with added fiber does not trigger satiety.
The study findings “support encouragement of the consumption of whole fruits, but not fruit juice, to preserve insulin sensitivity and mitigate [type 2 diabetes] risk,” Dr. Bondonno and colleagues summarize.
“Promoting a healthy diet and lifestyle which includes the consumption of popular fruits such as apples, bananas, and oranges, with widespread geographical availability, may lower [type 2 diabetes] incidence,” they conclude.
Lower 5-year odds of diabetes
It is not clear how eating fruit may confer protection against developing diabetes, the researchers write.
They aimed to examine how consumption of total fruit, individual fruit, and fruit juice is related to glucose tolerance, insulin sensitivity, and incident diabetes at 5 years and 12 years in participants in the nationally representative AusDiab study.
They identified 7,675 adults aged 25 and older without diabetes who had undergone blood tests and completed a food frequency questionnaire in 1999-2000.
Participants had indicated how often they ate 10 different types of fruit, any type of fruit juice, and other foods on a scale of 0 (never) to 10 (three or more times/day).
Researchers divided participants into quartiles based on their median fruit consumption: 62 (range 0-95) g/day, 122 (95-162) g/day, 230 (162-283) g/day, and 372 (283-961) g/day.
The most commonly consumed fruit was apples (23% of total fruit intake), followed by bananas (20%) and citrus fruit (18%). Other fruits each accounted for less than 8% of total fruit intake, so they were not studied separately.
Participants in each quartile had a similar mean age (54 years) and body mass index (27 kg/m2).
However, compared with participants in quartile 1 (low fruit intake), those in quartiles 3 and 4 (moderate and high fruit intakes, respectively) were more likely to be female, do at least 150 minutes of physical activity a week, and less likely to smoke. They also ate more vegetables and less red meat and processed meat, but they consumed more sugar.
Of 4,674 participants who had 5-year follow-up, 179 participants developed diabetes.
Compared to participants with a low fruit intake (quartile 1), those with a moderate fruit intake (quartile 3) had a 36% lower odds of developing diabetes within 5 years (odds ratio, 0.64; 95% confidence interval, 0.44-0.92) after adjusting for age, sex, physical activity, education, socioeconomic status, income, body mass index, smoking, cardiovascular disease, parental history of diabetes, and consumption of alcohol, vegetables, red meat, processed meat, and calories.
Of the 3,518 participants with 12-year follow-up, 247 participants had diabetes, but there were no significant associations between fruit consumption and this longer-term risk of diabetes, possibly due to the small number of participants and events.
The study was supported by grants from the National Health and Medical Research Council of Australia and the National Heart Foundation of Australia. Dr. Bondonno has reported no relevant financial disclosures. Disclosures of the other authors are listed with the article.
A version of this article first appeared on Medscape.com.
A new study supports the recommendation of eating two servings of fruit a day for health benefits – in this case a lower risk of diabetes.
Adults who ate two servings of fruit a day had 36% lower odds of developing diabetes within 5 years compared to those who ate less than a half serving of fruit a day, after adjusting for confounders, in a population-based Australian study.
The findings by Nicola P. Bondonno, PhD, and colleagues, based on data from the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab), were published online June 2 in the Journal of Clinical Endocrinology & Metabolism.
The study also showed that a higher fruit intake was associated with higher insulin sensitivity and lower pancreatic beta-cell function in a dose-response manner.
And a higher intake of apples – but not citrus fruit or bananas, the two other fruits studied – was associated with lower post-load serum insulin levels.
“This indicates that people who consumed more fruit [especially apples] had to produce less insulin to lower their blood glucose levels,” Dr. Bondonno, from the Institute for Nutrition Research, Edith Cowan University, Perth, Australia, explained in a statement from the Endocrine Society.
“This is important since high levels of circulating insulin (hyperinsulinemia) can damage blood vessels” and this is “related not only to diabetes, but also to high blood pressure, obesity, and heart disease,” she observed.
Fruit juice doesn’t have same effect
The study supports the recommendation of the Australian Dietary Guidelines – 2 servings of fruit a day, where one serving is 150 grams, which corresponds to a medium-sized apple, orange, or banana – Dr. Bondonno clarified in an email.
However, fruit juice was not associated with better glucose or insulin levels, or lower risk of diabetes, possibly because of its relatively high glycemic load and fewer beneficial fibers, the researchers speculate; added data suggest that even juice with added fiber does not trigger satiety.
The study findings “support encouragement of the consumption of whole fruits, but not fruit juice, to preserve insulin sensitivity and mitigate [type 2 diabetes] risk,” Dr. Bondonno and colleagues summarize.
“Promoting a healthy diet and lifestyle which includes the consumption of popular fruits such as apples, bananas, and oranges, with widespread geographical availability, may lower [type 2 diabetes] incidence,” they conclude.
Lower 5-year odds of diabetes
It is not clear how eating fruit may confer protection against developing diabetes, the researchers write.
They aimed to examine how consumption of total fruit, individual fruit, and fruit juice is related to glucose tolerance, insulin sensitivity, and incident diabetes at 5 years and 12 years in participants in the nationally representative AusDiab study.
They identified 7,675 adults aged 25 and older without diabetes who had undergone blood tests and completed a food frequency questionnaire in 1999-2000.
Participants had indicated how often they ate 10 different types of fruit, any type of fruit juice, and other foods on a scale of 0 (never) to 10 (three or more times/day).
Researchers divided participants into quartiles based on their median fruit consumption: 62 (range 0-95) g/day, 122 (95-162) g/day, 230 (162-283) g/day, and 372 (283-961) g/day.
The most commonly consumed fruit was apples (23% of total fruit intake), followed by bananas (20%) and citrus fruit (18%). Other fruits each accounted for less than 8% of total fruit intake, so they were not studied separately.
Participants in each quartile had a similar mean age (54 years) and body mass index (27 kg/m2).
However, compared with participants in quartile 1 (low fruit intake), those in quartiles 3 and 4 (moderate and high fruit intakes, respectively) were more likely to be female, do at least 150 minutes of physical activity a week, and less likely to smoke. They also ate more vegetables and less red meat and processed meat, but they consumed more sugar.
Of 4,674 participants who had 5-year follow-up, 179 participants developed diabetes.
Compared to participants with a low fruit intake (quartile 1), those with a moderate fruit intake (quartile 3) had a 36% lower odds of developing diabetes within 5 years (odds ratio, 0.64; 95% confidence interval, 0.44-0.92) after adjusting for age, sex, physical activity, education, socioeconomic status, income, body mass index, smoking, cardiovascular disease, parental history of diabetes, and consumption of alcohol, vegetables, red meat, processed meat, and calories.
Of the 3,518 participants with 12-year follow-up, 247 participants had diabetes, but there were no significant associations between fruit consumption and this longer-term risk of diabetes, possibly due to the small number of participants and events.
The study was supported by grants from the National Health and Medical Research Council of Australia and the National Heart Foundation of Australia. Dr. Bondonno has reported no relevant financial disclosures. Disclosures of the other authors are listed with the article.
A version of this article first appeared on Medscape.com.
‘Twincretin’ meets primary endpoints in five pivotal diabetes trials
The investigational, novel, injected once-weekly “twincretin” tirzepatide met its primary efficacy endpoint of significantly cutting hemoglobin A1c as well as its secondary weight-loss endpoint in patients with type 2 diabetes when compared with control patients in top-line results from each of five discrete pivotal trials.
The company developing tirzepatide, Lilly, announced these results in a series of four press releases issued during December 2020–May 2021. Scientific reports on the outcomes from four of these trials are scheduled during the American Diabetes Association’s Scientific Sessions being held virtually in late June 2021, with results from the fifth on track for a report during the annual meeting of the European Association for the Study of Diabetes in September 2021.
Tirzepatide is a “twincretin” because it combines in a single molecule two different gut-hormone activities. It works as both a glucagonlike peptide–1 receptor agonist (GLP-1 RA) and as an agent that mimics the glucose-dependent insulinotropic polypeptide (GIP).
While diabetologists qualified their comments on these results because of the limited scope and format of the five reports to date, they also expressed enthusiasm over what the press releases said.
Results give hope
“It’s quite exciting, but of course we would like to go by the data that’s presented” at upcoming meetings, commented Robert A. Gabbay, MD, PhD, chief science and medical officer of the American Diabetes Association in Arlington, Va. “The idea of GLP-1 and GIP activities working together has been out there for a while, but without any therapeutic options that leverage this,” he said in an interview.
“The preliminary results give us hope that tirzepatide will be a very effective glucose-lowering agent, perhaps the most effective among all options currently available, including insulin,” commented Ildiko Lingvay, MD, a diabetologist and professor at the University of Texas Southwestern Medical Center, Dallas. “Tirzepatide might have the added benefit of clinically meaningful weight loss,” and “the adverse event profile seems to be in line with what we are accustomed to with the GLP-1 RA class. I look forward to seeing the full results. Tirzepatide promises to be a great addition for type 2 diabetes,” Dr. Lingvay said in an interview.
A rare head-to-head against semaglutide
The five phase 3, randomized controlled trials described by Lilly in its four press releases all belong to the SURPASS series of studies for this agent. Perhaps the most intriguing of the five were results from SURPASS-2, announced in a release on March 4. This trial randomized 1,879 patients from the United States or any of seven other countries to 40 weeks of open-label treatment with one of three different dosages of tirzepatide administered by injection once weekly, or to the control group that received a weekly 1-mg injection of semaglutide (Ozempic), the highest dosage approved for controlling glycemia in patients with type 2 diabetes at the time the study launched.
In SURPASS-2 all three tested dosages of tirzepatide led to a significantly larger reduction, from baseline in A1c, compared with semaglutide, after 40 weeks, according to the Lilly release. Each of the three tirzepatide dosages also led to significantly greater weight loss from baseline, compared with semaglutide, and significantly greater percentages of patients who achieved an A1c of less than 7%, compared with semaglutide.
As an example, the highest tested tirzepatide dosage of 15 mg weekly led to an average A1c reduction from baseline of 2.46% and an average weight loss from baseline of 12.4 kg; 92% of patients achieved an A1c of less than 7%, and 51% had their A1c fall below 5.7% which indicates completely normalization of glycemic control. By comparison, the patients randomized to treatment with semaglutide had an average 1.86% reduction in their A1c level from baseline and a 6.2-kg average cut in body weight from baseline; 81% achieved an A1c of less than 7%, and 20% reached an A1c of less than 5.7%.
There are caveats
While these findings are notable as a rare example of an industry-sponsored head-to-head comparison of two new agents, the study comes with a few important asterisks.
First, it was open label, a curious limitation given that both agents are delivered by the same delivery method and schedule. “I cannot conclude based on this study that tirzepatide is superior because it was open label,” commented Anastassia Amaro, MD, medical director of Penn Metabolic Medicine at the University of Pennsylvania, Philadelphia.
“The gold standard is the double-blind study. An open-label design is a limitation,” agreed Dr. Gabbay.
A second caveat is that the Food and Drug Administration recently approved a higher dosage of semaglutide (2.4 g once/week) for treating overweight or obesity in patients with type 2 diabetes and in those without diabetes but a different weight-related condition such as hypertension of hypercholesterolemia. This means that the tested comparator dosage of 1 mg/week is no longer the maximum that most patients treated with semaglutide for glycemic control can receive.
“The inevitable question” about this comparison study is “what about a higher semaglutide dose,” and how might tirzepatide perform relative to that, said Dr. Gabbay. The recently approved higher dosage of semaglutide “adds an interesting wrinkle.”
Lilly has launched a series of studies testing tirzepatide as a treatment for overweight or obesity in people without diabetes, but the results are not expected until sometime in 2022 or 2023.
And there’s a third caveat: Semaglutide has already shown its value for cardiovascular risk reduction in patients with type 2 diabetes in the SUSTAIN 6 trial with nearly 3,300 randomized patients followed for 2 years and reported in 2016. The cardiovascular outcomes trial for tirzepatide, SURPASS-CVOT with more than 12,000 patients with type 2 diabetes, is underway but its results are not expected until 2024.
Despite these important limitations, a blinded comparison of tirzepatide and higher-dose semaglutide is unlikely, Dr. Amaro predicted. “It’s not worth the expense,” she said in an interview. A more likely scenario will be that, if tirzepatide enters the U.S. market, decisions on whether to treat patients with it or semaglutide will pivot on factors like the cost for treatment to individual patients based on their insurance coverage and tolerability, suggested both Dr. Amaro and Dr. Gabbay. “Physicians will need to develop a sense for tirzepatide: Do patients tolerate it and are they happy using it?” Dr. Amaro said.
Tirzepatide versus insulin, or on top of insulin
The other four trials in patients with type 2 diabetes reported by Lilly in releases included SURPASS-1, which randomized 478 patients to treatment with tirzepatide or placebo as monotherapy; SURPASS-3, which randomized 1,444 patients to tirzepatide or insulin degludec (Tresiba) on top of background treatment with metformin; SURPASS-4, which randomized 2,002 patients with high cardiovascular disease risk to treatment with tirzepatide or insulin glargine (Lantus) on top of background treatment with one to three different oral drugs; and SURPASS-5, which randomized 475 patients to treatment with tirzepatide or placebo on top of background treatment with insulin glargine and optional addition of metformin. Altogether, the five trials randomized nearly 6,300 patients.
The studies that compared tirzepatide against two different types of insulin, and the third that tested tirzepatide on top of insulin glargine, are especially notable. “It’s good to see that the combination [of tirzepatide and insulin glargine] works without causing major adverse events,” said Dr. Amaro.
“These are fair and helpful comparisons. I applaud Lilly for doing the right kind of comparisons,” said Dr. Gabbay.
In total, the five studies “provide evidence that tirzepatide will be effective at all stages of type 2 diabetes and can safely be used in combination with other glucose-lowering agents, including insulin,” said Dr. Lingvay. The studies with active comparator agents “allow us to compare tirzepatide’s efficacy against established therapies.”
The SURPASS trials were sponsored by Lilly, which is developing tirzepatide. Dr. Gabbay had no relevant disclosures. Dr. Lingvay has received research funds, consulting and advisory fees, or other support from Lilly as well as from several other companies including Novo Nordisk, which markets semaglutide (Ozempic) and insulin degludec (Tresiba), and Sanofi, which markets insulin glargine (Lantus). Dr. Amaro has received research funding from Lilly and from Fractyl, and has been a consultant to and received research funding from Novo Nordisk.
The investigational, novel, injected once-weekly “twincretin” tirzepatide met its primary efficacy endpoint of significantly cutting hemoglobin A1c as well as its secondary weight-loss endpoint in patients with type 2 diabetes when compared with control patients in top-line results from each of five discrete pivotal trials.
The company developing tirzepatide, Lilly, announced these results in a series of four press releases issued during December 2020–May 2021. Scientific reports on the outcomes from four of these trials are scheduled during the American Diabetes Association’s Scientific Sessions being held virtually in late June 2021, with results from the fifth on track for a report during the annual meeting of the European Association for the Study of Diabetes in September 2021.
Tirzepatide is a “twincretin” because it combines in a single molecule two different gut-hormone activities. It works as both a glucagonlike peptide–1 receptor agonist (GLP-1 RA) and as an agent that mimics the glucose-dependent insulinotropic polypeptide (GIP).
While diabetologists qualified their comments on these results because of the limited scope and format of the five reports to date, they also expressed enthusiasm over what the press releases said.
Results give hope
“It’s quite exciting, but of course we would like to go by the data that’s presented” at upcoming meetings, commented Robert A. Gabbay, MD, PhD, chief science and medical officer of the American Diabetes Association in Arlington, Va. “The idea of GLP-1 and GIP activities working together has been out there for a while, but without any therapeutic options that leverage this,” he said in an interview.
“The preliminary results give us hope that tirzepatide will be a very effective glucose-lowering agent, perhaps the most effective among all options currently available, including insulin,” commented Ildiko Lingvay, MD, a diabetologist and professor at the University of Texas Southwestern Medical Center, Dallas. “Tirzepatide might have the added benefit of clinically meaningful weight loss,” and “the adverse event profile seems to be in line with what we are accustomed to with the GLP-1 RA class. I look forward to seeing the full results. Tirzepatide promises to be a great addition for type 2 diabetes,” Dr. Lingvay said in an interview.
A rare head-to-head against semaglutide
The five phase 3, randomized controlled trials described by Lilly in its four press releases all belong to the SURPASS series of studies for this agent. Perhaps the most intriguing of the five were results from SURPASS-2, announced in a release on March 4. This trial randomized 1,879 patients from the United States or any of seven other countries to 40 weeks of open-label treatment with one of three different dosages of tirzepatide administered by injection once weekly, or to the control group that received a weekly 1-mg injection of semaglutide (Ozempic), the highest dosage approved for controlling glycemia in patients with type 2 diabetes at the time the study launched.
In SURPASS-2 all three tested dosages of tirzepatide led to a significantly larger reduction, from baseline in A1c, compared with semaglutide, after 40 weeks, according to the Lilly release. Each of the three tirzepatide dosages also led to significantly greater weight loss from baseline, compared with semaglutide, and significantly greater percentages of patients who achieved an A1c of less than 7%, compared with semaglutide.
As an example, the highest tested tirzepatide dosage of 15 mg weekly led to an average A1c reduction from baseline of 2.46% and an average weight loss from baseline of 12.4 kg; 92% of patients achieved an A1c of less than 7%, and 51% had their A1c fall below 5.7% which indicates completely normalization of glycemic control. By comparison, the patients randomized to treatment with semaglutide had an average 1.86% reduction in their A1c level from baseline and a 6.2-kg average cut in body weight from baseline; 81% achieved an A1c of less than 7%, and 20% reached an A1c of less than 5.7%.
There are caveats
While these findings are notable as a rare example of an industry-sponsored head-to-head comparison of two new agents, the study comes with a few important asterisks.
First, it was open label, a curious limitation given that both agents are delivered by the same delivery method and schedule. “I cannot conclude based on this study that tirzepatide is superior because it was open label,” commented Anastassia Amaro, MD, medical director of Penn Metabolic Medicine at the University of Pennsylvania, Philadelphia.
“The gold standard is the double-blind study. An open-label design is a limitation,” agreed Dr. Gabbay.
A second caveat is that the Food and Drug Administration recently approved a higher dosage of semaglutide (2.4 g once/week) for treating overweight or obesity in patients with type 2 diabetes and in those without diabetes but a different weight-related condition such as hypertension of hypercholesterolemia. This means that the tested comparator dosage of 1 mg/week is no longer the maximum that most patients treated with semaglutide for glycemic control can receive.
“The inevitable question” about this comparison study is “what about a higher semaglutide dose,” and how might tirzepatide perform relative to that, said Dr. Gabbay. The recently approved higher dosage of semaglutide “adds an interesting wrinkle.”
Lilly has launched a series of studies testing tirzepatide as a treatment for overweight or obesity in people without diabetes, but the results are not expected until sometime in 2022 or 2023.
And there’s a third caveat: Semaglutide has already shown its value for cardiovascular risk reduction in patients with type 2 diabetes in the SUSTAIN 6 trial with nearly 3,300 randomized patients followed for 2 years and reported in 2016. The cardiovascular outcomes trial for tirzepatide, SURPASS-CVOT with more than 12,000 patients with type 2 diabetes, is underway but its results are not expected until 2024.
Despite these important limitations, a blinded comparison of tirzepatide and higher-dose semaglutide is unlikely, Dr. Amaro predicted. “It’s not worth the expense,” she said in an interview. A more likely scenario will be that, if tirzepatide enters the U.S. market, decisions on whether to treat patients with it or semaglutide will pivot on factors like the cost for treatment to individual patients based on their insurance coverage and tolerability, suggested both Dr. Amaro and Dr. Gabbay. “Physicians will need to develop a sense for tirzepatide: Do patients tolerate it and are they happy using it?” Dr. Amaro said.
Tirzepatide versus insulin, or on top of insulin
The other four trials in patients with type 2 diabetes reported by Lilly in releases included SURPASS-1, which randomized 478 patients to treatment with tirzepatide or placebo as monotherapy; SURPASS-3, which randomized 1,444 patients to tirzepatide or insulin degludec (Tresiba) on top of background treatment with metformin; SURPASS-4, which randomized 2,002 patients with high cardiovascular disease risk to treatment with tirzepatide or insulin glargine (Lantus) on top of background treatment with one to three different oral drugs; and SURPASS-5, which randomized 475 patients to treatment with tirzepatide or placebo on top of background treatment with insulin glargine and optional addition of metformin. Altogether, the five trials randomized nearly 6,300 patients.
The studies that compared tirzepatide against two different types of insulin, and the third that tested tirzepatide on top of insulin glargine, are especially notable. “It’s good to see that the combination [of tirzepatide and insulin glargine] works without causing major adverse events,” said Dr. Amaro.
“These are fair and helpful comparisons. I applaud Lilly for doing the right kind of comparisons,” said Dr. Gabbay.
In total, the five studies “provide evidence that tirzepatide will be effective at all stages of type 2 diabetes and can safely be used in combination with other glucose-lowering agents, including insulin,” said Dr. Lingvay. The studies with active comparator agents “allow us to compare tirzepatide’s efficacy against established therapies.”
The SURPASS trials were sponsored by Lilly, which is developing tirzepatide. Dr. Gabbay had no relevant disclosures. Dr. Lingvay has received research funds, consulting and advisory fees, or other support from Lilly as well as from several other companies including Novo Nordisk, which markets semaglutide (Ozempic) and insulin degludec (Tresiba), and Sanofi, which markets insulin glargine (Lantus). Dr. Amaro has received research funding from Lilly and from Fractyl, and has been a consultant to and received research funding from Novo Nordisk.
The investigational, novel, injected once-weekly “twincretin” tirzepatide met its primary efficacy endpoint of significantly cutting hemoglobin A1c as well as its secondary weight-loss endpoint in patients with type 2 diabetes when compared with control patients in top-line results from each of five discrete pivotal trials.
The company developing tirzepatide, Lilly, announced these results in a series of four press releases issued during December 2020–May 2021. Scientific reports on the outcomes from four of these trials are scheduled during the American Diabetes Association’s Scientific Sessions being held virtually in late June 2021, with results from the fifth on track for a report during the annual meeting of the European Association for the Study of Diabetes in September 2021.
Tirzepatide is a “twincretin” because it combines in a single molecule two different gut-hormone activities. It works as both a glucagonlike peptide–1 receptor agonist (GLP-1 RA) and as an agent that mimics the glucose-dependent insulinotropic polypeptide (GIP).
While diabetologists qualified their comments on these results because of the limited scope and format of the five reports to date, they also expressed enthusiasm over what the press releases said.
Results give hope
“It’s quite exciting, but of course we would like to go by the data that’s presented” at upcoming meetings, commented Robert A. Gabbay, MD, PhD, chief science and medical officer of the American Diabetes Association in Arlington, Va. “The idea of GLP-1 and GIP activities working together has been out there for a while, but without any therapeutic options that leverage this,” he said in an interview.
“The preliminary results give us hope that tirzepatide will be a very effective glucose-lowering agent, perhaps the most effective among all options currently available, including insulin,” commented Ildiko Lingvay, MD, a diabetologist and professor at the University of Texas Southwestern Medical Center, Dallas. “Tirzepatide might have the added benefit of clinically meaningful weight loss,” and “the adverse event profile seems to be in line with what we are accustomed to with the GLP-1 RA class. I look forward to seeing the full results. Tirzepatide promises to be a great addition for type 2 diabetes,” Dr. Lingvay said in an interview.
A rare head-to-head against semaglutide
The five phase 3, randomized controlled trials described by Lilly in its four press releases all belong to the SURPASS series of studies for this agent. Perhaps the most intriguing of the five were results from SURPASS-2, announced in a release on March 4. This trial randomized 1,879 patients from the United States or any of seven other countries to 40 weeks of open-label treatment with one of three different dosages of tirzepatide administered by injection once weekly, or to the control group that received a weekly 1-mg injection of semaglutide (Ozempic), the highest dosage approved for controlling glycemia in patients with type 2 diabetes at the time the study launched.
In SURPASS-2 all three tested dosages of tirzepatide led to a significantly larger reduction, from baseline in A1c, compared with semaglutide, after 40 weeks, according to the Lilly release. Each of the three tirzepatide dosages also led to significantly greater weight loss from baseline, compared with semaglutide, and significantly greater percentages of patients who achieved an A1c of less than 7%, compared with semaglutide.
As an example, the highest tested tirzepatide dosage of 15 mg weekly led to an average A1c reduction from baseline of 2.46% and an average weight loss from baseline of 12.4 kg; 92% of patients achieved an A1c of less than 7%, and 51% had their A1c fall below 5.7% which indicates completely normalization of glycemic control. By comparison, the patients randomized to treatment with semaglutide had an average 1.86% reduction in their A1c level from baseline and a 6.2-kg average cut in body weight from baseline; 81% achieved an A1c of less than 7%, and 20% reached an A1c of less than 5.7%.
There are caveats
While these findings are notable as a rare example of an industry-sponsored head-to-head comparison of two new agents, the study comes with a few important asterisks.
First, it was open label, a curious limitation given that both agents are delivered by the same delivery method and schedule. “I cannot conclude based on this study that tirzepatide is superior because it was open label,” commented Anastassia Amaro, MD, medical director of Penn Metabolic Medicine at the University of Pennsylvania, Philadelphia.
“The gold standard is the double-blind study. An open-label design is a limitation,” agreed Dr. Gabbay.
A second caveat is that the Food and Drug Administration recently approved a higher dosage of semaglutide (2.4 g once/week) for treating overweight or obesity in patients with type 2 diabetes and in those without diabetes but a different weight-related condition such as hypertension of hypercholesterolemia. This means that the tested comparator dosage of 1 mg/week is no longer the maximum that most patients treated with semaglutide for glycemic control can receive.
“The inevitable question” about this comparison study is “what about a higher semaglutide dose,” and how might tirzepatide perform relative to that, said Dr. Gabbay. The recently approved higher dosage of semaglutide “adds an interesting wrinkle.”
Lilly has launched a series of studies testing tirzepatide as a treatment for overweight or obesity in people without diabetes, but the results are not expected until sometime in 2022 or 2023.
And there’s a third caveat: Semaglutide has already shown its value for cardiovascular risk reduction in patients with type 2 diabetes in the SUSTAIN 6 trial with nearly 3,300 randomized patients followed for 2 years and reported in 2016. The cardiovascular outcomes trial for tirzepatide, SURPASS-CVOT with more than 12,000 patients with type 2 diabetes, is underway but its results are not expected until 2024.
Despite these important limitations, a blinded comparison of tirzepatide and higher-dose semaglutide is unlikely, Dr. Amaro predicted. “It’s not worth the expense,” she said in an interview. A more likely scenario will be that, if tirzepatide enters the U.S. market, decisions on whether to treat patients with it or semaglutide will pivot on factors like the cost for treatment to individual patients based on their insurance coverage and tolerability, suggested both Dr. Amaro and Dr. Gabbay. “Physicians will need to develop a sense for tirzepatide: Do patients tolerate it and are they happy using it?” Dr. Amaro said.
Tirzepatide versus insulin, or on top of insulin
The other four trials in patients with type 2 diabetes reported by Lilly in releases included SURPASS-1, which randomized 478 patients to treatment with tirzepatide or placebo as monotherapy; SURPASS-3, which randomized 1,444 patients to tirzepatide or insulin degludec (Tresiba) on top of background treatment with metformin; SURPASS-4, which randomized 2,002 patients with high cardiovascular disease risk to treatment with tirzepatide or insulin glargine (Lantus) on top of background treatment with one to three different oral drugs; and SURPASS-5, which randomized 475 patients to treatment with tirzepatide or placebo on top of background treatment with insulin glargine and optional addition of metformin. Altogether, the five trials randomized nearly 6,300 patients.
The studies that compared tirzepatide against two different types of insulin, and the third that tested tirzepatide on top of insulin glargine, are especially notable. “It’s good to see that the combination [of tirzepatide and insulin glargine] works without causing major adverse events,” said Dr. Amaro.
“These are fair and helpful comparisons. I applaud Lilly for doing the right kind of comparisons,” said Dr. Gabbay.
In total, the five studies “provide evidence that tirzepatide will be effective at all stages of type 2 diabetes and can safely be used in combination with other glucose-lowering agents, including insulin,” said Dr. Lingvay. The studies with active comparator agents “allow us to compare tirzepatide’s efficacy against established therapies.”
The SURPASS trials were sponsored by Lilly, which is developing tirzepatide. Dr. Gabbay had no relevant disclosures. Dr. Lingvay has received research funds, consulting and advisory fees, or other support from Lilly as well as from several other companies including Novo Nordisk, which markets semaglutide (Ozempic) and insulin degludec (Tresiba), and Sanofi, which markets insulin glargine (Lantus). Dr. Amaro has received research funding from Lilly and from Fractyl, and has been a consultant to and received research funding from Novo Nordisk.
Are left atrial thrombi that defy preprocedure anticoagulation predictable?
Three or more weeks of oral anticoagulation (OAC) sometimes isn’t up to the job of clearing any potentially embolic left atrial (LA) thrombi before procedures like cardioversion or catheter ablation in patients with atrial fibrillation (AF). Such OAC-defiant LA thrombi aren’t common, nor are they rare enough to ignore, suggests a new meta-analysis that might also have identified features that predispose to them.
Such predictors of LA clots that persist despite OAC could potentially guide selective use of transesophageal echocardiography (TEE) instead of more routine policies to either use or not use TEE for thrombus rule-out before rhythm-control procedures, researchers propose.
Their prevalence was about 2.7% among the study’s more than 14,000 patients who received at least 3 weeks of OAC with either vitamin K antagonists (VKA) or direct oral anticoagulants (DOAC) before undergoing TEE.
But OAC-resistant LA thrombi were two- to four-times as common in patients with than without certain features, including AF other than paroxysmal and higher CHADS2 and CHA2DS2-VASc stroke risk-stratification scores.
“TEE imaging in select patients at an elevated risk of LA thrombus, despite anticoagulation status, may be a reasonable approach to minimize the risk of thromboembolic complications following cardioversion or catheter ablation,” propose the study’s authors, led by Antony Lurie, BMSC, Population Health Research Institute, Hamilton, Ont. Their report was published in the June 15 issue of the Journal of the American College of Cardiology.
Guidelines don’t encourage TEE before cardioversion in patients who have been on OAC for at least 3 weeks, the group notes, and policies on TEE use before AF ablation vary widely regardless of anticoagulation status.
The current study suggests that 3 weeks of OAC isn’t enough for a substantial number of patients, who might be put at thromboembolic risk if TEE were to be skipped before rhythm-control procedures.
Conversely, many patients unlikely to have LA thrombi get preprocedure TEE anyway. That can happen “irrespective of how long they’ve been anticoagulated, their pattern of atrial fibrillation, or their stroke risk,” senior author Jorge A. Wong, MD, MPH, Population Health Research Institute and McMaster University, Hamilton, Ont., told this news organization.
But “TEE is an invasive imaging modality, so it is associated with small element of risk.” The current study, Dr. Wong said, points to potential risk-stratification tools clinicians might use to guide more selective TEE screening.
“At sites where TEEs are done all the time for patients undergoing ablation, one could use several of these risk markers to perhaps tailor use of TEE in individuals,” Dr. Wong said. “For example, in people with paroxysmal atrial fibrillation, we found that the risk of left atrial appendage clot was approximately 1% or less.” Screening by TEE might reasonably be avoided in such patients.
“Fortunately, continued oral anticoagulation already yields low peri-procedural stroke rates,” observes an accompanying editorial from Paulus Kirchhof, MD, and Christoph Sinning, MD, from the University Heart & Vascular Center and German Centre of Cardiovascular Research, Hamburg.
“Based on this new analysis of existing data, a risk-based use of TEE imaging in anticoagulated patients could enable further improvement in the safe delivery of rhythm control interventions in patients with AF,” the editorialists agree.
The meta-analysis covered 10 prospective and 25 retrospective studies with a total of 14,653 patients that reported whether LA thrombus was present in patients with AF or atrial flutter (AFL) who underwent TEE after at least 3 weeks of VKA or DOAC therapy. Reports for 30 of the studies identified patients by rhythm-control procedure, and the remaining five didn’t specify TEE indications.
The weighted mean prevalence of LA thrombus at TEE was 2.73% (95% confidence interval, 1.95%-3.80%). The finding was not significantly changed in separate sensitivity analyses, the report says, including one limited to studies with low risk of bias and others excluding patients with valvular AF, interrupted OAC, heparin bridging, or subtherapeutic anticoagulation, respectively.
Patients treated with VKA and DOACs showed similar prevalences of LA thrombi, with means of 2.80% and 3.12%, respectively (P = .674). The prevalence was significantly higher in patients:
- with nonparoxysmal than with paroxysmal AF/AFL (4.81% vs. 1.03%; P < .001)
- undergoing cardioversion than ablation (5.55% vs. 1.65; P < .001)
- with CHA2DS2-VASc scores of at least 3 than with scores of 2 or less (6.31% vs. 1.06%; P < .001).
A limitation of the study, observe Dr. Kirchhof and Dr. Sinning, “is that all patients had a clinical indication for a TEE, which might be a selection bias. When a thrombus was found on TEE, clinical judgment led to postponing of the procedure,” thereby avoiding potential thromboembolism.
“Thus, the paper cannot demonstrate that presence of a thrombus on TEE is related to peri-procedural ischemic stroke,” they write.
The literature puts the risk for stroke or systemic embolism at well under 1% for patients anticoagulated with either VKA or DOACs for at least 3 weeks prior to cardioversion, in contrast to the nearly 3% prevalence of LA appendage thrombus by TEE in the current analysis, Dr. Wong observed.
“So we’re seeing a lot more left atrial appendage thrombus than we would see stroke,” but there wasn’t a way to determine whether that increases the stroke risk, he agreed.Dr. Wong, Dr. Lurie, and the other authors report no relevant conflicts. Dr. Kirchhof discloses receiving partial support “from several drug and device companies active in atrial fibrillation” and to being listed as inventor on two AF-related patents held by the University of Birmingham. Dr. Sinning reports no relevant relationships.
A version of this article first appeared on Medscape.com.
Three or more weeks of oral anticoagulation (OAC) sometimes isn’t up to the job of clearing any potentially embolic left atrial (LA) thrombi before procedures like cardioversion or catheter ablation in patients with atrial fibrillation (AF). Such OAC-defiant LA thrombi aren’t common, nor are they rare enough to ignore, suggests a new meta-analysis that might also have identified features that predispose to them.
Such predictors of LA clots that persist despite OAC could potentially guide selective use of transesophageal echocardiography (TEE) instead of more routine policies to either use or not use TEE for thrombus rule-out before rhythm-control procedures, researchers propose.
Their prevalence was about 2.7% among the study’s more than 14,000 patients who received at least 3 weeks of OAC with either vitamin K antagonists (VKA) or direct oral anticoagulants (DOAC) before undergoing TEE.
But OAC-resistant LA thrombi were two- to four-times as common in patients with than without certain features, including AF other than paroxysmal and higher CHADS2 and CHA2DS2-VASc stroke risk-stratification scores.
“TEE imaging in select patients at an elevated risk of LA thrombus, despite anticoagulation status, may be a reasonable approach to minimize the risk of thromboembolic complications following cardioversion or catheter ablation,” propose the study’s authors, led by Antony Lurie, BMSC, Population Health Research Institute, Hamilton, Ont. Their report was published in the June 15 issue of the Journal of the American College of Cardiology.
Guidelines don’t encourage TEE before cardioversion in patients who have been on OAC for at least 3 weeks, the group notes, and policies on TEE use before AF ablation vary widely regardless of anticoagulation status.
The current study suggests that 3 weeks of OAC isn’t enough for a substantial number of patients, who might be put at thromboembolic risk if TEE were to be skipped before rhythm-control procedures.
Conversely, many patients unlikely to have LA thrombi get preprocedure TEE anyway. That can happen “irrespective of how long they’ve been anticoagulated, their pattern of atrial fibrillation, or their stroke risk,” senior author Jorge A. Wong, MD, MPH, Population Health Research Institute and McMaster University, Hamilton, Ont., told this news organization.
But “TEE is an invasive imaging modality, so it is associated with small element of risk.” The current study, Dr. Wong said, points to potential risk-stratification tools clinicians might use to guide more selective TEE screening.
“At sites where TEEs are done all the time for patients undergoing ablation, one could use several of these risk markers to perhaps tailor use of TEE in individuals,” Dr. Wong said. “For example, in people with paroxysmal atrial fibrillation, we found that the risk of left atrial appendage clot was approximately 1% or less.” Screening by TEE might reasonably be avoided in such patients.
“Fortunately, continued oral anticoagulation already yields low peri-procedural stroke rates,” observes an accompanying editorial from Paulus Kirchhof, MD, and Christoph Sinning, MD, from the University Heart & Vascular Center and German Centre of Cardiovascular Research, Hamburg.
“Based on this new analysis of existing data, a risk-based use of TEE imaging in anticoagulated patients could enable further improvement in the safe delivery of rhythm control interventions in patients with AF,” the editorialists agree.
The meta-analysis covered 10 prospective and 25 retrospective studies with a total of 14,653 patients that reported whether LA thrombus was present in patients with AF or atrial flutter (AFL) who underwent TEE after at least 3 weeks of VKA or DOAC therapy. Reports for 30 of the studies identified patients by rhythm-control procedure, and the remaining five didn’t specify TEE indications.
The weighted mean prevalence of LA thrombus at TEE was 2.73% (95% confidence interval, 1.95%-3.80%). The finding was not significantly changed in separate sensitivity analyses, the report says, including one limited to studies with low risk of bias and others excluding patients with valvular AF, interrupted OAC, heparin bridging, or subtherapeutic anticoagulation, respectively.
Patients treated with VKA and DOACs showed similar prevalences of LA thrombi, with means of 2.80% and 3.12%, respectively (P = .674). The prevalence was significantly higher in patients:
- with nonparoxysmal than with paroxysmal AF/AFL (4.81% vs. 1.03%; P < .001)
- undergoing cardioversion than ablation (5.55% vs. 1.65; P < .001)
- with CHA2DS2-VASc scores of at least 3 than with scores of 2 or less (6.31% vs. 1.06%; P < .001).
A limitation of the study, observe Dr. Kirchhof and Dr. Sinning, “is that all patients had a clinical indication for a TEE, which might be a selection bias. When a thrombus was found on TEE, clinical judgment led to postponing of the procedure,” thereby avoiding potential thromboembolism.
“Thus, the paper cannot demonstrate that presence of a thrombus on TEE is related to peri-procedural ischemic stroke,” they write.
The literature puts the risk for stroke or systemic embolism at well under 1% for patients anticoagulated with either VKA or DOACs for at least 3 weeks prior to cardioversion, in contrast to the nearly 3% prevalence of LA appendage thrombus by TEE in the current analysis, Dr. Wong observed.
“So we’re seeing a lot more left atrial appendage thrombus than we would see stroke,” but there wasn’t a way to determine whether that increases the stroke risk, he agreed.Dr. Wong, Dr. Lurie, and the other authors report no relevant conflicts. Dr. Kirchhof discloses receiving partial support “from several drug and device companies active in atrial fibrillation” and to being listed as inventor on two AF-related patents held by the University of Birmingham. Dr. Sinning reports no relevant relationships.
A version of this article first appeared on Medscape.com.
Three or more weeks of oral anticoagulation (OAC) sometimes isn’t up to the job of clearing any potentially embolic left atrial (LA) thrombi before procedures like cardioversion or catheter ablation in patients with atrial fibrillation (AF). Such OAC-defiant LA thrombi aren’t common, nor are they rare enough to ignore, suggests a new meta-analysis that might also have identified features that predispose to them.
Such predictors of LA clots that persist despite OAC could potentially guide selective use of transesophageal echocardiography (TEE) instead of more routine policies to either use or not use TEE for thrombus rule-out before rhythm-control procedures, researchers propose.
Their prevalence was about 2.7% among the study’s more than 14,000 patients who received at least 3 weeks of OAC with either vitamin K antagonists (VKA) or direct oral anticoagulants (DOAC) before undergoing TEE.
But OAC-resistant LA thrombi were two- to four-times as common in patients with than without certain features, including AF other than paroxysmal and higher CHADS2 and CHA2DS2-VASc stroke risk-stratification scores.
“TEE imaging in select patients at an elevated risk of LA thrombus, despite anticoagulation status, may be a reasonable approach to minimize the risk of thromboembolic complications following cardioversion or catheter ablation,” propose the study’s authors, led by Antony Lurie, BMSC, Population Health Research Institute, Hamilton, Ont. Their report was published in the June 15 issue of the Journal of the American College of Cardiology.
Guidelines don’t encourage TEE before cardioversion in patients who have been on OAC for at least 3 weeks, the group notes, and policies on TEE use before AF ablation vary widely regardless of anticoagulation status.
The current study suggests that 3 weeks of OAC isn’t enough for a substantial number of patients, who might be put at thromboembolic risk if TEE were to be skipped before rhythm-control procedures.
Conversely, many patients unlikely to have LA thrombi get preprocedure TEE anyway. That can happen “irrespective of how long they’ve been anticoagulated, their pattern of atrial fibrillation, or their stroke risk,” senior author Jorge A. Wong, MD, MPH, Population Health Research Institute and McMaster University, Hamilton, Ont., told this news organization.
But “TEE is an invasive imaging modality, so it is associated with small element of risk.” The current study, Dr. Wong said, points to potential risk-stratification tools clinicians might use to guide more selective TEE screening.
“At sites where TEEs are done all the time for patients undergoing ablation, one could use several of these risk markers to perhaps tailor use of TEE in individuals,” Dr. Wong said. “For example, in people with paroxysmal atrial fibrillation, we found that the risk of left atrial appendage clot was approximately 1% or less.” Screening by TEE might reasonably be avoided in such patients.
“Fortunately, continued oral anticoagulation already yields low peri-procedural stroke rates,” observes an accompanying editorial from Paulus Kirchhof, MD, and Christoph Sinning, MD, from the University Heart & Vascular Center and German Centre of Cardiovascular Research, Hamburg.
“Based on this new analysis of existing data, a risk-based use of TEE imaging in anticoagulated patients could enable further improvement in the safe delivery of rhythm control interventions in patients with AF,” the editorialists agree.
The meta-analysis covered 10 prospective and 25 retrospective studies with a total of 14,653 patients that reported whether LA thrombus was present in patients with AF or atrial flutter (AFL) who underwent TEE after at least 3 weeks of VKA or DOAC therapy. Reports for 30 of the studies identified patients by rhythm-control procedure, and the remaining five didn’t specify TEE indications.
The weighted mean prevalence of LA thrombus at TEE was 2.73% (95% confidence interval, 1.95%-3.80%). The finding was not significantly changed in separate sensitivity analyses, the report says, including one limited to studies with low risk of bias and others excluding patients with valvular AF, interrupted OAC, heparin bridging, or subtherapeutic anticoagulation, respectively.
Patients treated with VKA and DOACs showed similar prevalences of LA thrombi, with means of 2.80% and 3.12%, respectively (P = .674). The prevalence was significantly higher in patients:
- with nonparoxysmal than with paroxysmal AF/AFL (4.81% vs. 1.03%; P < .001)
- undergoing cardioversion than ablation (5.55% vs. 1.65; P < .001)
- with CHA2DS2-VASc scores of at least 3 than with scores of 2 or less (6.31% vs. 1.06%; P < .001).
A limitation of the study, observe Dr. Kirchhof and Dr. Sinning, “is that all patients had a clinical indication for a TEE, which might be a selection bias. When a thrombus was found on TEE, clinical judgment led to postponing of the procedure,” thereby avoiding potential thromboembolism.
“Thus, the paper cannot demonstrate that presence of a thrombus on TEE is related to peri-procedural ischemic stroke,” they write.
The literature puts the risk for stroke or systemic embolism at well under 1% for patients anticoagulated with either VKA or DOACs for at least 3 weeks prior to cardioversion, in contrast to the nearly 3% prevalence of LA appendage thrombus by TEE in the current analysis, Dr. Wong observed.
“So we’re seeing a lot more left atrial appendage thrombus than we would see stroke,” but there wasn’t a way to determine whether that increases the stroke risk, he agreed.Dr. Wong, Dr. Lurie, and the other authors report no relevant conflicts. Dr. Kirchhof discloses receiving partial support “from several drug and device companies active in atrial fibrillation” and to being listed as inventor on two AF-related patents held by the University of Birmingham. Dr. Sinning reports no relevant relationships.
A version of this article first appeared on Medscape.com.
AHA: Physical activity best first-line for high BP, cholesterol
The optimal first step to address mild to moderately elevated blood pressure and cholesterol in otherwise healthy adults is a “prescription” to sit less and move more, the American Heart Association says in a new scientific statement.
“The current American Heart Association guidelines for diagnosing high blood pressure and cholesterol recognize that otherwise healthy individuals with mildly or moderately elevated levels of these cardiovascular risk factors should actively attempt to reduce these risks,” Bethany Barone Gibbs, PhD, chair of the statement writing group, said in an AHA news release.
“The first treatment strategy for many of these patients should be healthy lifestyle changes beginning with increasing physical activity,” said Dr. Gibbs, from the University of Pittsburgh.
The 12-page AHA scientific statement – Physical Activity as a Critical Component of First-Line Treatment for Elevated Blood Pressure or Cholesterol: Who, What, and How? – was published online June 2 in Hypertension.
Every little bit helps
According to the AHA, about 21% of American adults have systolic blood pressure between 120 and 139 mm Hg, or diastolic blood pressure between 80 and 89 mm Hg, which meets the criteria for lifestyle-only treatment for elevated BP outlined in the American College of Cardiology (ACC)/AHA high blood pressure guideline.
In addition, about 28% of American adults have LDL cholesterol above 70 mg/dL and otherwise meet the low-risk criteria for heart disease or stroke. These individuals would meet the criteria for lifestyle-only treatment outlined in the 2018 ACC/AHA cholesterol treatment guidelines, which include increased physical activity, weight loss, better diet, smoking cessation, and moderating alcohol intake.
“Of the recommended lifestyle changes, increasing physical activity has extensive benefits, including improving both blood pressure and blood cholesterol, that are comparable, superior, or complementary to other healthy lifestyle changes,” the writing group says.
“Physical activity assessment and prescription are an excellent lifestyle behavior treatment option for all patients, including for the large population of mild-moderate-risk patients with elevated blood pressure and blood cholesterol,” they note.
Research has shown that increasing physical activity can lead to clinically meaningful 3 or 4 mm Hg reductions in systolic and diastolic blood pressure, and 3 to 6 mg/dL decreases in LDL cholesterol, the authors point out.
Previous evidence also shows that physically active people have a 21% lower risk of developing cardiovascular disease and a 36% lower risk for death from cardiovascular diseases than those who are not physically active.
Physical activity also has benefits beyond heart health, including a lower risk for some cancers; improved bone, brain, and mental health; and better sleep, they note.
The U.S. Department of Health and Human Services 2018 physical activity guidelines advise Americans to log 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous aerobic activity each week and to participate in two or more weekly strength training sessions.
However, there is no minimum amount of time to receive benefits from physical activity.
“Every little bit of activity is better than none. Even small initial increases of 5 to 10 minutes a day can yield health benefits,” Dr. Gibbs said.
Translational advice for clinicians
The AHA statement encourages clinicians to ask patients about their physical activity at every interaction; provide ideas and resources to help patients improve and sustain regular life-long physical activity; and encourage and celebrate small increases in activity, such as walking more or taking the stairs, to help with motivation.
“In our world where physical activity is increasingly engineered out of our lives and the overwhelming default is to sit – and even more so now as the nation and the world is practicing quarantine and isolation to reduce the spread of coronavirus – the message that we must be relentless in our pursuit to ‘sit less and move more’ throughout the day is more important than ever,” said Dr. Gibbs.
The statement was prepared by a volunteer writing group on behalf of the AHA Council on Lifestyle and Cardiometabolic Health; the Council on Cardiovascular and Stroke Nursing; and the Council on Clinical Cardiology.
This research had no commercial funding. A list of disclosures for the writing group is available with the original article.
A version of this article first appeared on Medscape.com.
The optimal first step to address mild to moderately elevated blood pressure and cholesterol in otherwise healthy adults is a “prescription” to sit less and move more, the American Heart Association says in a new scientific statement.
“The current American Heart Association guidelines for diagnosing high blood pressure and cholesterol recognize that otherwise healthy individuals with mildly or moderately elevated levels of these cardiovascular risk factors should actively attempt to reduce these risks,” Bethany Barone Gibbs, PhD, chair of the statement writing group, said in an AHA news release.
“The first treatment strategy for many of these patients should be healthy lifestyle changes beginning with increasing physical activity,” said Dr. Gibbs, from the University of Pittsburgh.
The 12-page AHA scientific statement – Physical Activity as a Critical Component of First-Line Treatment for Elevated Blood Pressure or Cholesterol: Who, What, and How? – was published online June 2 in Hypertension.
Every little bit helps
According to the AHA, about 21% of American adults have systolic blood pressure between 120 and 139 mm Hg, or diastolic blood pressure between 80 and 89 mm Hg, which meets the criteria for lifestyle-only treatment for elevated BP outlined in the American College of Cardiology (ACC)/AHA high blood pressure guideline.
In addition, about 28% of American adults have LDL cholesterol above 70 mg/dL and otherwise meet the low-risk criteria for heart disease or stroke. These individuals would meet the criteria for lifestyle-only treatment outlined in the 2018 ACC/AHA cholesterol treatment guidelines, which include increased physical activity, weight loss, better diet, smoking cessation, and moderating alcohol intake.
“Of the recommended lifestyle changes, increasing physical activity has extensive benefits, including improving both blood pressure and blood cholesterol, that are comparable, superior, or complementary to other healthy lifestyle changes,” the writing group says.
“Physical activity assessment and prescription are an excellent lifestyle behavior treatment option for all patients, including for the large population of mild-moderate-risk patients with elevated blood pressure and blood cholesterol,” they note.
Research has shown that increasing physical activity can lead to clinically meaningful 3 or 4 mm Hg reductions in systolic and diastolic blood pressure, and 3 to 6 mg/dL decreases in LDL cholesterol, the authors point out.
Previous evidence also shows that physically active people have a 21% lower risk of developing cardiovascular disease and a 36% lower risk for death from cardiovascular diseases than those who are not physically active.
Physical activity also has benefits beyond heart health, including a lower risk for some cancers; improved bone, brain, and mental health; and better sleep, they note.
The U.S. Department of Health and Human Services 2018 physical activity guidelines advise Americans to log 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous aerobic activity each week and to participate in two or more weekly strength training sessions.
However, there is no minimum amount of time to receive benefits from physical activity.
“Every little bit of activity is better than none. Even small initial increases of 5 to 10 minutes a day can yield health benefits,” Dr. Gibbs said.
Translational advice for clinicians
The AHA statement encourages clinicians to ask patients about their physical activity at every interaction; provide ideas and resources to help patients improve and sustain regular life-long physical activity; and encourage and celebrate small increases in activity, such as walking more or taking the stairs, to help with motivation.
“In our world where physical activity is increasingly engineered out of our lives and the overwhelming default is to sit – and even more so now as the nation and the world is practicing quarantine and isolation to reduce the spread of coronavirus – the message that we must be relentless in our pursuit to ‘sit less and move more’ throughout the day is more important than ever,” said Dr. Gibbs.
The statement was prepared by a volunteer writing group on behalf of the AHA Council on Lifestyle and Cardiometabolic Health; the Council on Cardiovascular and Stroke Nursing; and the Council on Clinical Cardiology.
This research had no commercial funding. A list of disclosures for the writing group is available with the original article.
A version of this article first appeared on Medscape.com.
The optimal first step to address mild to moderately elevated blood pressure and cholesterol in otherwise healthy adults is a “prescription” to sit less and move more, the American Heart Association says in a new scientific statement.
“The current American Heart Association guidelines for diagnosing high blood pressure and cholesterol recognize that otherwise healthy individuals with mildly or moderately elevated levels of these cardiovascular risk factors should actively attempt to reduce these risks,” Bethany Barone Gibbs, PhD, chair of the statement writing group, said in an AHA news release.
“The first treatment strategy for many of these patients should be healthy lifestyle changes beginning with increasing physical activity,” said Dr. Gibbs, from the University of Pittsburgh.
The 12-page AHA scientific statement – Physical Activity as a Critical Component of First-Line Treatment for Elevated Blood Pressure or Cholesterol: Who, What, and How? – was published online June 2 in Hypertension.
Every little bit helps
According to the AHA, about 21% of American adults have systolic blood pressure between 120 and 139 mm Hg, or diastolic blood pressure between 80 and 89 mm Hg, which meets the criteria for lifestyle-only treatment for elevated BP outlined in the American College of Cardiology (ACC)/AHA high blood pressure guideline.
In addition, about 28% of American adults have LDL cholesterol above 70 mg/dL and otherwise meet the low-risk criteria for heart disease or stroke. These individuals would meet the criteria for lifestyle-only treatment outlined in the 2018 ACC/AHA cholesterol treatment guidelines, which include increased physical activity, weight loss, better diet, smoking cessation, and moderating alcohol intake.
“Of the recommended lifestyle changes, increasing physical activity has extensive benefits, including improving both blood pressure and blood cholesterol, that are comparable, superior, or complementary to other healthy lifestyle changes,” the writing group says.
“Physical activity assessment and prescription are an excellent lifestyle behavior treatment option for all patients, including for the large population of mild-moderate-risk patients with elevated blood pressure and blood cholesterol,” they note.
Research has shown that increasing physical activity can lead to clinically meaningful 3 or 4 mm Hg reductions in systolic and diastolic blood pressure, and 3 to 6 mg/dL decreases in LDL cholesterol, the authors point out.
Previous evidence also shows that physically active people have a 21% lower risk of developing cardiovascular disease and a 36% lower risk for death from cardiovascular diseases than those who are not physically active.
Physical activity also has benefits beyond heart health, including a lower risk for some cancers; improved bone, brain, and mental health; and better sleep, they note.
The U.S. Department of Health and Human Services 2018 physical activity guidelines advise Americans to log 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous aerobic activity each week and to participate in two or more weekly strength training sessions.
However, there is no minimum amount of time to receive benefits from physical activity.
“Every little bit of activity is better than none. Even small initial increases of 5 to 10 minutes a day can yield health benefits,” Dr. Gibbs said.
Translational advice for clinicians
The AHA statement encourages clinicians to ask patients about their physical activity at every interaction; provide ideas and resources to help patients improve and sustain regular life-long physical activity; and encourage and celebrate small increases in activity, such as walking more or taking the stairs, to help with motivation.
“In our world where physical activity is increasingly engineered out of our lives and the overwhelming default is to sit – and even more so now as the nation and the world is practicing quarantine and isolation to reduce the spread of coronavirus – the message that we must be relentless in our pursuit to ‘sit less and move more’ throughout the day is more important than ever,” said Dr. Gibbs.
The statement was prepared by a volunteer writing group on behalf of the AHA Council on Lifestyle and Cardiometabolic Health; the Council on Cardiovascular and Stroke Nursing; and the Council on Clinical Cardiology.
This research had no commercial funding. A list of disclosures for the writing group is available with the original article.
A version of this article first appeared on Medscape.com.
LDCT lung cancer screening may ID aortic stenosis risk
says new research published in Annals of Internal Medicine.
Aortic stenosis is one of the most common valve disease problems and is characterized by the narrowing of the aortic valve opening, according to the American Heart Association. The condition impedes the delivery of blood from the heart to the body.
Researchers found that LDCT, which according to the Centers for Disease Control and Prevention is the only recommended screening test for lung cancer, also can be used to identify aortic valve calcification – a condition in which calcium deposits form on the aortic valve, narrowing it.
Since cardiovascular events and lung cancer are known to have the same modifiable risk factors, people screened for lung cancer could also be diagnosed with cardiovascular diseases, the authors noted in their paper.
Furthermore, a 2019 study published in the Journal of Thoracic Imaging found that LDCT can be useful for identifying not just lung cancer, but the early stages of chronic obstructive pulmonary disease and coronary artery disease.
“LDCT has been described as useful for identifying the early stages of chronic obstructive pulmonary disease and coronary artery disease, but it can also [screen for] calcified aortic valve [which corresponds] with the risk of severe aortic stenosis,” study author Marcin Fijalkowski, MD, PhD, of the Medical University of Gdansk, said in an interview. “This additional evaluation is not time-consuming and is easy to perform.”
Methods and results
For the study, Dr. Fijalkowski and his colleagues examined data from 6,631 people between the ages of 50 and 80 years of age with a smoking history of 30 or more pack-years. The group was enrolled in the MOLTEST BIS lung cancer screening program between 2016 and 2018, which assessed the usefulness of LDCT performed during lung cancer screening in determining the degree of aortic valve calcification as an additional finding. The researchers arbitrarily determined a calcium score of 900 as a cutoff point indicating a positive test result. Positive patients were sent for an echocardiogram for confirmation of diagnosis.
Aortic valve calcification was identified in 869 patients, 13.1% of the group. Sixty-eight participants, which is about 8% of this group, were identified as having a calcium score of 900 at least and were referred for echocardiography to confirm these results. Of this group, 0.5% were diagnosed with at least moderate aortic stenosis after receiving an echocardiogram. About 55% of the participants with this condition were unaware of their valvular heart disease, including 23% with a severe form of the disease.
Study identified patients who had not been aware of disease
Dr. Fijalkowski said while he was not surprised by the findings, he was surprised that the study may have saved some of the participants’ lives.
“We were expecting the same degree of calcification of aortic valve and correlation with aortic stenosis severity, but what surprised us was that half of diagnosed patients were not aware of disease,” he said. “This additional finding was lifesaving.”
In the paper, the authors noted that cardiology societies do not yet recognize LDCT as a diagnostic tool for aortic stenosis. Based on their findings, they propose that aortic valve calcification become a routine assessment procedure in the LDCT protocol for lung cancer screening.
Findings are ‘important’ but not practice changing
Salim S. Virani, MD, FACC, who was not involved in the study, said this new research is important.
The analyses were done well and push the needle further in a direction that suggests “when we are doing imaging for one reason, we should use the totality of information that we have available,” he noted.
“I mean, if you are looking at a lung nodule, if you see an aortic valve that’s very calcified, then it should prompt you to at least ask the patient about some symptoms related to that,” Dr. Virani explained.
However, he said more research is needed on a larger population before LDCT can be considered a diagnostic tool for aortic stenosis.
“I think we have to understand that this study was done in a very specific group of patients,” said Dr. Virani, professor in the sections of cardiology and cardiovascular research at Baylor College of Medicine, Houston. “If you were to do it in a population that was much younger, with much lower risk of even lung cancer, then the yield of a CT to pick up aortic stenosis would be lower.”
Before any practice changes are made regarding LDCT and the diagnosis of aortic stenosis, there needs to be more research on how many people in the general population are getting non–cardiology-related chest imaging and then come up with a population-based metric as to what calcium score cutoff could be used, he said.
Dr. Fijalkowski said he believes the results of his study will encourage physicians to focus not only on pulmonary nodules but also to look for additional things such as aortic valve calcification.
The experts did not disclose any relevant financial relationships.
says new research published in Annals of Internal Medicine.
Aortic stenosis is one of the most common valve disease problems and is characterized by the narrowing of the aortic valve opening, according to the American Heart Association. The condition impedes the delivery of blood from the heart to the body.
Researchers found that LDCT, which according to the Centers for Disease Control and Prevention is the only recommended screening test for lung cancer, also can be used to identify aortic valve calcification – a condition in which calcium deposits form on the aortic valve, narrowing it.
Since cardiovascular events and lung cancer are known to have the same modifiable risk factors, people screened for lung cancer could also be diagnosed with cardiovascular diseases, the authors noted in their paper.
Furthermore, a 2019 study published in the Journal of Thoracic Imaging found that LDCT can be useful for identifying not just lung cancer, but the early stages of chronic obstructive pulmonary disease and coronary artery disease.
“LDCT has been described as useful for identifying the early stages of chronic obstructive pulmonary disease and coronary artery disease, but it can also [screen for] calcified aortic valve [which corresponds] with the risk of severe aortic stenosis,” study author Marcin Fijalkowski, MD, PhD, of the Medical University of Gdansk, said in an interview. “This additional evaluation is not time-consuming and is easy to perform.”
Methods and results
For the study, Dr. Fijalkowski and his colleagues examined data from 6,631 people between the ages of 50 and 80 years of age with a smoking history of 30 or more pack-years. The group was enrolled in the MOLTEST BIS lung cancer screening program between 2016 and 2018, which assessed the usefulness of LDCT performed during lung cancer screening in determining the degree of aortic valve calcification as an additional finding. The researchers arbitrarily determined a calcium score of 900 as a cutoff point indicating a positive test result. Positive patients were sent for an echocardiogram for confirmation of diagnosis.
Aortic valve calcification was identified in 869 patients, 13.1% of the group. Sixty-eight participants, which is about 8% of this group, were identified as having a calcium score of 900 at least and were referred for echocardiography to confirm these results. Of this group, 0.5% were diagnosed with at least moderate aortic stenosis after receiving an echocardiogram. About 55% of the participants with this condition were unaware of their valvular heart disease, including 23% with a severe form of the disease.
Study identified patients who had not been aware of disease
Dr. Fijalkowski said while he was not surprised by the findings, he was surprised that the study may have saved some of the participants’ lives.
“We were expecting the same degree of calcification of aortic valve and correlation with aortic stenosis severity, but what surprised us was that half of diagnosed patients were not aware of disease,” he said. “This additional finding was lifesaving.”
In the paper, the authors noted that cardiology societies do not yet recognize LDCT as a diagnostic tool for aortic stenosis. Based on their findings, they propose that aortic valve calcification become a routine assessment procedure in the LDCT protocol for lung cancer screening.
Findings are ‘important’ but not practice changing
Salim S. Virani, MD, FACC, who was not involved in the study, said this new research is important.
The analyses were done well and push the needle further in a direction that suggests “when we are doing imaging for one reason, we should use the totality of information that we have available,” he noted.
“I mean, if you are looking at a lung nodule, if you see an aortic valve that’s very calcified, then it should prompt you to at least ask the patient about some symptoms related to that,” Dr. Virani explained.
However, he said more research is needed on a larger population before LDCT can be considered a diagnostic tool for aortic stenosis.
“I think we have to understand that this study was done in a very specific group of patients,” said Dr. Virani, professor in the sections of cardiology and cardiovascular research at Baylor College of Medicine, Houston. “If you were to do it in a population that was much younger, with much lower risk of even lung cancer, then the yield of a CT to pick up aortic stenosis would be lower.”
Before any practice changes are made regarding LDCT and the diagnosis of aortic stenosis, there needs to be more research on how many people in the general population are getting non–cardiology-related chest imaging and then come up with a population-based metric as to what calcium score cutoff could be used, he said.
Dr. Fijalkowski said he believes the results of his study will encourage physicians to focus not only on pulmonary nodules but also to look for additional things such as aortic valve calcification.
The experts did not disclose any relevant financial relationships.
says new research published in Annals of Internal Medicine.
Aortic stenosis is one of the most common valve disease problems and is characterized by the narrowing of the aortic valve opening, according to the American Heart Association. The condition impedes the delivery of blood from the heart to the body.
Researchers found that LDCT, which according to the Centers for Disease Control and Prevention is the only recommended screening test for lung cancer, also can be used to identify aortic valve calcification – a condition in which calcium deposits form on the aortic valve, narrowing it.
Since cardiovascular events and lung cancer are known to have the same modifiable risk factors, people screened for lung cancer could also be diagnosed with cardiovascular diseases, the authors noted in their paper.
Furthermore, a 2019 study published in the Journal of Thoracic Imaging found that LDCT can be useful for identifying not just lung cancer, but the early stages of chronic obstructive pulmonary disease and coronary artery disease.
“LDCT has been described as useful for identifying the early stages of chronic obstructive pulmonary disease and coronary artery disease, but it can also [screen for] calcified aortic valve [which corresponds] with the risk of severe aortic stenosis,” study author Marcin Fijalkowski, MD, PhD, of the Medical University of Gdansk, said in an interview. “This additional evaluation is not time-consuming and is easy to perform.”
Methods and results
For the study, Dr. Fijalkowski and his colleagues examined data from 6,631 people between the ages of 50 and 80 years of age with a smoking history of 30 or more pack-years. The group was enrolled in the MOLTEST BIS lung cancer screening program between 2016 and 2018, which assessed the usefulness of LDCT performed during lung cancer screening in determining the degree of aortic valve calcification as an additional finding. The researchers arbitrarily determined a calcium score of 900 as a cutoff point indicating a positive test result. Positive patients were sent for an echocardiogram for confirmation of diagnosis.
Aortic valve calcification was identified in 869 patients, 13.1% of the group. Sixty-eight participants, which is about 8% of this group, were identified as having a calcium score of 900 at least and were referred for echocardiography to confirm these results. Of this group, 0.5% were diagnosed with at least moderate aortic stenosis after receiving an echocardiogram. About 55% of the participants with this condition were unaware of their valvular heart disease, including 23% with a severe form of the disease.
Study identified patients who had not been aware of disease
Dr. Fijalkowski said while he was not surprised by the findings, he was surprised that the study may have saved some of the participants’ lives.
“We were expecting the same degree of calcification of aortic valve and correlation with aortic stenosis severity, but what surprised us was that half of diagnosed patients were not aware of disease,” he said. “This additional finding was lifesaving.”
In the paper, the authors noted that cardiology societies do not yet recognize LDCT as a diagnostic tool for aortic stenosis. Based on their findings, they propose that aortic valve calcification become a routine assessment procedure in the LDCT protocol for lung cancer screening.
Findings are ‘important’ but not practice changing
Salim S. Virani, MD, FACC, who was not involved in the study, said this new research is important.
The analyses were done well and push the needle further in a direction that suggests “when we are doing imaging for one reason, we should use the totality of information that we have available,” he noted.
“I mean, if you are looking at a lung nodule, if you see an aortic valve that’s very calcified, then it should prompt you to at least ask the patient about some symptoms related to that,” Dr. Virani explained.
However, he said more research is needed on a larger population before LDCT can be considered a diagnostic tool for aortic stenosis.
“I think we have to understand that this study was done in a very specific group of patients,” said Dr. Virani, professor in the sections of cardiology and cardiovascular research at Baylor College of Medicine, Houston. “If you were to do it in a population that was much younger, with much lower risk of even lung cancer, then the yield of a CT to pick up aortic stenosis would be lower.”
Before any practice changes are made regarding LDCT and the diagnosis of aortic stenosis, there needs to be more research on how many people in the general population are getting non–cardiology-related chest imaging and then come up with a population-based metric as to what calcium score cutoff could be used, he said.
Dr. Fijalkowski said he believes the results of his study will encourage physicians to focus not only on pulmonary nodules but also to look for additional things such as aortic valve calcification.
The experts did not disclose any relevant financial relationships.
FROM ANNALS OF INTERNAL MEDICINE