User login
Combined ablation–mitral surgery safe for atrial fib
NEW YORK – Patients with both mitral valve regurgitation and atrial fibrillation who undergo concurrent mitral valve surgery and surgical ablation are more than twice as likely to be free of AF a year after surgery than are their counterparts who have mitral valve surgery alone, according to results of a randomized trial.
“About a quarter to a half of our your patients coming for mitral valve surgery also have AF,” Dr. A. Marc Gillinov said at the 2015 Mitral Valve Conclave sponsored by the American Association for Thoracic Surgery. “A great mitral valve repair is your first priority, but you also want to treat the AF.” Currently, cardiac surgeons perform concurrent mitral valve surgery and surgical ablation about 60% of the time in patients eligible for both procedures, he said.
The American College of Cardiology/American Health Association Guidelines state that surgical ablation in patients with AF having cardiac surgery for other indications is “reasonable” – “not very strong language,” he noted, and the level of evidence for concurrent procedures is C.
That led the Cardiothoracic Surgical Trials Network to pursue the clinical trial. The investigators randomized 260 patients with persistent or long-standing persistent atrial fibrillation who needed mitral valve surgery to also undergo either surgical ablation (133) or no ablation (127). The primary endpoint was freedom from AF at both 6 months and 12 months as assessed by 3-day Holter monitoring.
Almost two-thirds (63%) of patients in the ablation group were free from atrial fibrillation at both 6 and 12 months, compared with 29% of those who had mitral valve surgery only, a highly significant difference. Dr. Gillinov described the trial population as “tougher patients” with persistent AF whose average age was around 70 years, and most had organic mitral valve regurgitation.
Results were similar whether the patients underwent pulmonary vein isolation or biatrial maze procedure (61% and 66%, respectively). One-year mortality was 6.8% in the ablation group and 8.7% in the control group, reported Dr. Gillinov, who is surgical director of the Center for Atrial Fibrillation at Cleveland Clinic.
The trial found no significant differences between the ablation and nonablation groups in major cardiac or cerebrovascular adverse events, overall serious adverse events, or hospital readmissions. The results were published prior to the Dr. Gillinov’s presentation (N. Engl. J. Med. 2015;372:1399-409).
These results debunk findings from a survey a few years ago that found cardiac surgeons avoided doing surgical ablation during mitral valve surgery because it makes the operation too complex, requires longer pump times, and raises the risk of surgery, said Dr. Gillinov. “Does ablation improve rhythm control? Yes. Does ablation increase risk? No. Does ablation improve clinical outcomes? It probably does,” he said.
The trial had some limitations, Dr. Gillinov said. Its endpoint was not a clinical outcome, although looking at stroke risk or mortality would have required thousands of patients. Also, 20% of patients did not have follow-up with the 3-day Holter test. However, previous studies have shown a strong association between surgical ablation and a reduced risk of stroke. When Dr. Jolanda Kluin of Utrecht (the Netherlands) University asked if a patient would be better off with AF or a pacemaker, Dr. Gillinov replied, “I think it’s better to have an AV sequential rhythm, but the truth is no one can answer that question without clinical data.”
The bottom line is, “if you have a patient who’s having mitral valve surgery who also has AF, do an ablation,” he said.
The study was supported by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov disclosed relationships with AtriCure, Medtronic, Edwards Lifesciences, On-X Life Technologies, Abbott, Tendyne, and Clear Catheter.
NEW YORK – Patients with both mitral valve regurgitation and atrial fibrillation who undergo concurrent mitral valve surgery and surgical ablation are more than twice as likely to be free of AF a year after surgery than are their counterparts who have mitral valve surgery alone, according to results of a randomized trial.
“About a quarter to a half of our your patients coming for mitral valve surgery also have AF,” Dr. A. Marc Gillinov said at the 2015 Mitral Valve Conclave sponsored by the American Association for Thoracic Surgery. “A great mitral valve repair is your first priority, but you also want to treat the AF.” Currently, cardiac surgeons perform concurrent mitral valve surgery and surgical ablation about 60% of the time in patients eligible for both procedures, he said.
The American College of Cardiology/American Health Association Guidelines state that surgical ablation in patients with AF having cardiac surgery for other indications is “reasonable” – “not very strong language,” he noted, and the level of evidence for concurrent procedures is C.
That led the Cardiothoracic Surgical Trials Network to pursue the clinical trial. The investigators randomized 260 patients with persistent or long-standing persistent atrial fibrillation who needed mitral valve surgery to also undergo either surgical ablation (133) or no ablation (127). The primary endpoint was freedom from AF at both 6 months and 12 months as assessed by 3-day Holter monitoring.
Almost two-thirds (63%) of patients in the ablation group were free from atrial fibrillation at both 6 and 12 months, compared with 29% of those who had mitral valve surgery only, a highly significant difference. Dr. Gillinov described the trial population as “tougher patients” with persistent AF whose average age was around 70 years, and most had organic mitral valve regurgitation.
Results were similar whether the patients underwent pulmonary vein isolation or biatrial maze procedure (61% and 66%, respectively). One-year mortality was 6.8% in the ablation group and 8.7% in the control group, reported Dr. Gillinov, who is surgical director of the Center for Atrial Fibrillation at Cleveland Clinic.
The trial found no significant differences between the ablation and nonablation groups in major cardiac or cerebrovascular adverse events, overall serious adverse events, or hospital readmissions. The results were published prior to the Dr. Gillinov’s presentation (N. Engl. J. Med. 2015;372:1399-409).
These results debunk findings from a survey a few years ago that found cardiac surgeons avoided doing surgical ablation during mitral valve surgery because it makes the operation too complex, requires longer pump times, and raises the risk of surgery, said Dr. Gillinov. “Does ablation improve rhythm control? Yes. Does ablation increase risk? No. Does ablation improve clinical outcomes? It probably does,” he said.
The trial had some limitations, Dr. Gillinov said. Its endpoint was not a clinical outcome, although looking at stroke risk or mortality would have required thousands of patients. Also, 20% of patients did not have follow-up with the 3-day Holter test. However, previous studies have shown a strong association between surgical ablation and a reduced risk of stroke. When Dr. Jolanda Kluin of Utrecht (the Netherlands) University asked if a patient would be better off with AF or a pacemaker, Dr. Gillinov replied, “I think it’s better to have an AV sequential rhythm, but the truth is no one can answer that question without clinical data.”
The bottom line is, “if you have a patient who’s having mitral valve surgery who also has AF, do an ablation,” he said.
The study was supported by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov disclosed relationships with AtriCure, Medtronic, Edwards Lifesciences, On-X Life Technologies, Abbott, Tendyne, and Clear Catheter.
NEW YORK – Patients with both mitral valve regurgitation and atrial fibrillation who undergo concurrent mitral valve surgery and surgical ablation are more than twice as likely to be free of AF a year after surgery than are their counterparts who have mitral valve surgery alone, according to results of a randomized trial.
“About a quarter to a half of our your patients coming for mitral valve surgery also have AF,” Dr. A. Marc Gillinov said at the 2015 Mitral Valve Conclave sponsored by the American Association for Thoracic Surgery. “A great mitral valve repair is your first priority, but you also want to treat the AF.” Currently, cardiac surgeons perform concurrent mitral valve surgery and surgical ablation about 60% of the time in patients eligible for both procedures, he said.
The American College of Cardiology/American Health Association Guidelines state that surgical ablation in patients with AF having cardiac surgery for other indications is “reasonable” – “not very strong language,” he noted, and the level of evidence for concurrent procedures is C.
That led the Cardiothoracic Surgical Trials Network to pursue the clinical trial. The investigators randomized 260 patients with persistent or long-standing persistent atrial fibrillation who needed mitral valve surgery to also undergo either surgical ablation (133) or no ablation (127). The primary endpoint was freedom from AF at both 6 months and 12 months as assessed by 3-day Holter monitoring.
Almost two-thirds (63%) of patients in the ablation group were free from atrial fibrillation at both 6 and 12 months, compared with 29% of those who had mitral valve surgery only, a highly significant difference. Dr. Gillinov described the trial population as “tougher patients” with persistent AF whose average age was around 70 years, and most had organic mitral valve regurgitation.
Results were similar whether the patients underwent pulmonary vein isolation or biatrial maze procedure (61% and 66%, respectively). One-year mortality was 6.8% in the ablation group and 8.7% in the control group, reported Dr. Gillinov, who is surgical director of the Center for Atrial Fibrillation at Cleveland Clinic.
The trial found no significant differences between the ablation and nonablation groups in major cardiac or cerebrovascular adverse events, overall serious adverse events, or hospital readmissions. The results were published prior to the Dr. Gillinov’s presentation (N. Engl. J. Med. 2015;372:1399-409).
These results debunk findings from a survey a few years ago that found cardiac surgeons avoided doing surgical ablation during mitral valve surgery because it makes the operation too complex, requires longer pump times, and raises the risk of surgery, said Dr. Gillinov. “Does ablation improve rhythm control? Yes. Does ablation increase risk? No. Does ablation improve clinical outcomes? It probably does,” he said.
The trial had some limitations, Dr. Gillinov said. Its endpoint was not a clinical outcome, although looking at stroke risk or mortality would have required thousands of patients. Also, 20% of patients did not have follow-up with the 3-day Holter test. However, previous studies have shown a strong association between surgical ablation and a reduced risk of stroke. When Dr. Jolanda Kluin of Utrecht (the Netherlands) University asked if a patient would be better off with AF or a pacemaker, Dr. Gillinov replied, “I think it’s better to have an AV sequential rhythm, but the truth is no one can answer that question without clinical data.”
The bottom line is, “if you have a patient who’s having mitral valve surgery who also has AF, do an ablation,” he said.
The study was supported by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov disclosed relationships with AtriCure, Medtronic, Edwards Lifesciences, On-X Life Technologies, Abbott, Tendyne, and Clear Catheter.
AT THE 2015 MITRAL VALVE CONCLAVE
Key clinical point: Patients with atrial fibrillation who have mitral valve surgery would benefit from surgical ablation at the same time.
Major finding: People with AF who had surgical ablation along with mitral valve surgery were more than twice as likely to be free of AF afterwards than were those who had mitral valve surgery only (63.2% vs. 29.4%).
Data source: A clinical trial in 260 patients with AF undergoing mitral valve surgery that randomized 127 to mitral valve surgery alone and 133 to mitral valve surgery with surgical ablation.
Disclosures: The study was supported by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov disclosed relationships with AtriCure, Medtronic, Edwards Lifesciences, On-X Life Technologies, Abbott, Tendyne, and Clear Catheter.
CABG costs more in patients with diabetes
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
FROM JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The percentage of CABG patients with diabetes increased from 7% in the 1970s to 37% in the 2000s. The risk/benefit ratio warrants greater use of bilateral mammary arteries except in obese women with diabetes.
Major finding: Diabetic patients had significantly worse outcomes than nondiabetics with regard to hospital death, deep sternal wound infections, strokes, and renal failure as well as hospital stay and costs.
Data source: A retrospective analysis of a prospective database of patients undergoing first-time CABG at the Cleveland Clinic from 1972 to 2011.
Disclosures: The authors reported that they had no relevant conflicts of interest.
Dicloxacillin may cut INR levels in warfarin users
The antibiotic dicloxacillin appears to markedly decrease INR levels in patients taking warfarin, reducing the mean INR to subtherapeutic ranges in the majority who take both drugs concomitantly, according to a research letter to the editor published online July 20 in JAMA.
Adverse interactions between warfarin and other drugs are often suspected, but solid data are lacking. Case reports have suggested that the commonly used antibiotic dicloxacillin reduces warfarin’s anticoagulant effects, but no studies have examined the issue, said Anton Pottegård, Ph.D., of the department of clinical pharmacology, University of Southern Denmark, Odense, and his associates (JAMA 2015;314:296-7).
To further investigate that possibility, the investigators analyzed information in an anticoagulant database covering 7,400 patients treated by three outpatient clinics and 50 general practitioners during a 15-year period. They focused on weekly INR levels recorded for 236 patients (median age, 68 years), most of whom took warfarin because of atrial fibrillation or heart valve replacement.
The mean INR level before dicloxacillin exposure was 2.59, compared with 1.97 after dicloxacillin exposure (P < .001). A total of 144 patients (61%) had subtherapeutic INR levels (< 2.0) during the 2-4 weeks following a course of dicloxacillin, Dr. Pottegård and his associates said.
A similar but less drastic decrease was observed among the 64 patients taking a different anticoagulant, phenprocoumon, who were given dicloxacillin. Mean INR levels dropped from 2.61 before exposure to 2.30 afterward (P = .003), and 41% of the group had subtherapeutic INR levels after taking the antibiotic.
No sponsor was reported for this study. Dr. Pottegård and his associates reported having no relevant financial disclosures.
The antibiotic dicloxacillin appears to markedly decrease INR levels in patients taking warfarin, reducing the mean INR to subtherapeutic ranges in the majority who take both drugs concomitantly, according to a research letter to the editor published online July 20 in JAMA.
Adverse interactions between warfarin and other drugs are often suspected, but solid data are lacking. Case reports have suggested that the commonly used antibiotic dicloxacillin reduces warfarin’s anticoagulant effects, but no studies have examined the issue, said Anton Pottegård, Ph.D., of the department of clinical pharmacology, University of Southern Denmark, Odense, and his associates (JAMA 2015;314:296-7).
To further investigate that possibility, the investigators analyzed information in an anticoagulant database covering 7,400 patients treated by three outpatient clinics and 50 general practitioners during a 15-year period. They focused on weekly INR levels recorded for 236 patients (median age, 68 years), most of whom took warfarin because of atrial fibrillation or heart valve replacement.
The mean INR level before dicloxacillin exposure was 2.59, compared with 1.97 after dicloxacillin exposure (P < .001). A total of 144 patients (61%) had subtherapeutic INR levels (< 2.0) during the 2-4 weeks following a course of dicloxacillin, Dr. Pottegård and his associates said.
A similar but less drastic decrease was observed among the 64 patients taking a different anticoagulant, phenprocoumon, who were given dicloxacillin. Mean INR levels dropped from 2.61 before exposure to 2.30 afterward (P = .003), and 41% of the group had subtherapeutic INR levels after taking the antibiotic.
No sponsor was reported for this study. Dr. Pottegård and his associates reported having no relevant financial disclosures.
The antibiotic dicloxacillin appears to markedly decrease INR levels in patients taking warfarin, reducing the mean INR to subtherapeutic ranges in the majority who take both drugs concomitantly, according to a research letter to the editor published online July 20 in JAMA.
Adverse interactions between warfarin and other drugs are often suspected, but solid data are lacking. Case reports have suggested that the commonly used antibiotic dicloxacillin reduces warfarin’s anticoagulant effects, but no studies have examined the issue, said Anton Pottegård, Ph.D., of the department of clinical pharmacology, University of Southern Denmark, Odense, and his associates (JAMA 2015;314:296-7).
To further investigate that possibility, the investigators analyzed information in an anticoagulant database covering 7,400 patients treated by three outpatient clinics and 50 general practitioners during a 15-year period. They focused on weekly INR levels recorded for 236 patients (median age, 68 years), most of whom took warfarin because of atrial fibrillation or heart valve replacement.
The mean INR level before dicloxacillin exposure was 2.59, compared with 1.97 after dicloxacillin exposure (P < .001). A total of 144 patients (61%) had subtherapeutic INR levels (< 2.0) during the 2-4 weeks following a course of dicloxacillin, Dr. Pottegård and his associates said.
A similar but less drastic decrease was observed among the 64 patients taking a different anticoagulant, phenprocoumon, who were given dicloxacillin. Mean INR levels dropped from 2.61 before exposure to 2.30 afterward (P = .003), and 41% of the group had subtherapeutic INR levels after taking the antibiotic.
No sponsor was reported for this study. Dr. Pottegård and his associates reported having no relevant financial disclosures.
FROM JAMA
Key clinical point: The antibiotic dicloxacillin appears to markedly decrease INR levels in patients using warfarin.
Major finding: 144 patients taking warfarin (61%) had subtherapeutic international normalized ratio levels during the 2-4 weeks following a course of dicloxacillin.
Data source: An analysis of INR levels before and after antibiotic use from a Danish database of 7,400 patients taking anticoagulants.
Disclosures: No sponsor was reported for this study. Dr. Pottegard and his associates reported having no relevant financial disclosures.
Transcatheter mitral valve-in-valve implantation advantageous in failed bioprosthetic valves
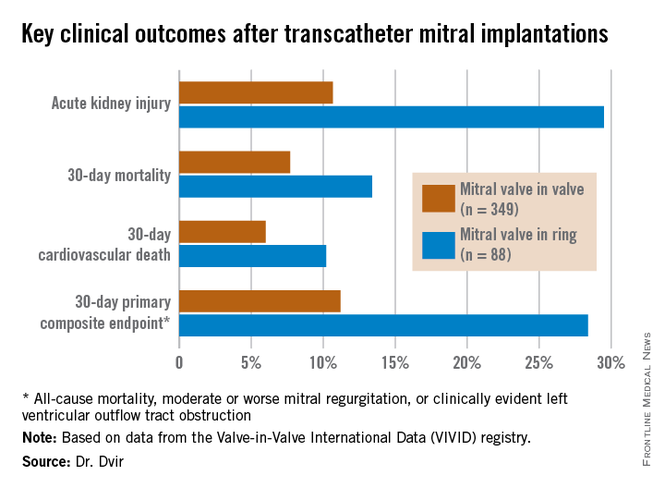
PARIS – Transcatheter mitral valve-in-valve procedures in patients with a failed bioprosthetic mitral valve provide superior clinical results, compared with valve-in-ring implantations, according to the latest data from the VIVID registry.
“Obviously, these results have numerous implications for the interventional community: for surgeons, who employ bioprostheses and rings, and for the cardiovascular industry that designs transcatheter strategies for mitral valve and ring implantations,” Dr. Danny Dvir said in presenting the VIVID update at the annual congress of the European Association of Percutaneous Cardiovascular Interventio
Bioprosthetic rather than mechanical valves are increasingly popular in open-heart valve replacement operations because they avoid the need for lifelong oral anticoagulation. But over time bioprosthetic valves often fail. And that event creates a need for a high-risk, repeat open surgery or a far less invasive transcatheter valve replacement.
Lots of data are available regarding the effectiveness and limitations of transcatheter aortic valve-in-valve procedures in patients with failed bioprosthetic aortic valves, including a previous report from the VIVID (Valve-in-Valve International Data registry) by Dr. Dvir and coworkers (JAMA 2014;312:162-70). However, very little data exist about the effectiveness of mitral valve-in-valve and valve-in-ring procedures, noted Dr. Dvir of St. Paul’s Hospital and the University of British Columbia, Vancouver.
The VIVID registry is drawn from 94 sites on six continents. Dr. Dvir presented an analysis of 437 transcatheter mitral implantations in patients with failed bioprosthetic valves. The study population consisted of 349 patients with mitral valve-in-valve (VIV) and 88 with valve-in-ring (VIR) procedures.
The average Society of Thoracic Surgeons (STS) score was 12.9. “This is one of the highest-risk groups of patients that you’ll ever see,” the cardiologist commented.
Mitral regurgitation was the mechanism of bioprosthetic valve failure in 45% of cases, stenosis in 23%, and a combination of the two in the remainder. The median time from placement of the initial bioprosthetic valve to the transcatheter VIV or VIR procedure was 9 years.
Transcatheter access for the mitral VIV or VIR was transapical in 79% of cases, directly through the left atrium in 2.5%, and by the increasingly popular transseptal route in the remainder. The median follow-up post procedure was 408 days.
Mitral VIV procedures looked significantly better from the standpoint of procedural characteristics. Moderate or severe mitral regurgitation was present at the conclusion of the procedure in 2.6% of patients undergoing mitral VIV, compared with 14.8% who had a VIR procedure.
“We were a bit shocked to see that difference between the two groups,” Dr. Dvir said.
Implantation of a small surgical valve of 25 mm or less was the major independent predictor of having an elevated gradient post procedure, with an adjusted odds ratio of 3.7.
In addition, the mean valve area was 1.99 cm2 in the VIV group vs. 2.33 cm2 in the VIR group. Postinflation was employed in 3.2% of the VIV group, compared with 22.7% of the VIR group. Left ventricular outflow tract obstruction – a potentially fatal complication – occurred in 2.6% of the mitral VIV group and was significantly more common at 8% in the VIR group.
Mitral VIR procedures were associated with markedly worse clinical outcomes. Highlighting the 11.2% rate of the 30-day primary composite endpoint in the mitral VIV group, Dr. Dvir commented, “I must say, I think that is a very reasonable number given that we’re talking about a very high–risk group of patients. For this group of patients having a very high STS score, reaching good results in 30 days in the mitral valve-in-valve group is a good signal for the regulatory groups and for the community that this is a good procedure.”
In contrast, the 28.4% rate of the composite endpoint in the VIR group “is a big disappointment; almost one-third of patients undergoing mitral valve in ring experience the composite adverse event endpoint at 30 days. There is an issue there,” he added.
Dr. Dvir reported having no relevant financial conflicts.
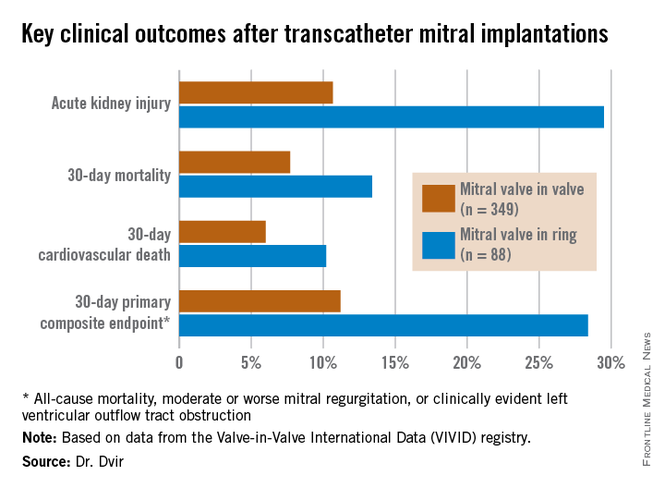
PARIS – Transcatheter mitral valve-in-valve procedures in patients with a failed bioprosthetic mitral valve provide superior clinical results, compared with valve-in-ring implantations, according to the latest data from the VIVID registry.
“Obviously, these results have numerous implications for the interventional community: for surgeons, who employ bioprostheses and rings, and for the cardiovascular industry that designs transcatheter strategies for mitral valve and ring implantations,” Dr. Danny Dvir said in presenting the VIVID update at the annual congress of the European Association of Percutaneous Cardiovascular Interventio
Bioprosthetic rather than mechanical valves are increasingly popular in open-heart valve replacement operations because they avoid the need for lifelong oral anticoagulation. But over time bioprosthetic valves often fail. And that event creates a need for a high-risk, repeat open surgery or a far less invasive transcatheter valve replacement.
Lots of data are available regarding the effectiveness and limitations of transcatheter aortic valve-in-valve procedures in patients with failed bioprosthetic aortic valves, including a previous report from the VIVID (Valve-in-Valve International Data registry) by Dr. Dvir and coworkers (JAMA 2014;312:162-70). However, very little data exist about the effectiveness of mitral valve-in-valve and valve-in-ring procedures, noted Dr. Dvir of St. Paul’s Hospital and the University of British Columbia, Vancouver.
The VIVID registry is drawn from 94 sites on six continents. Dr. Dvir presented an analysis of 437 transcatheter mitral implantations in patients with failed bioprosthetic valves. The study population consisted of 349 patients with mitral valve-in-valve (VIV) and 88 with valve-in-ring (VIR) procedures.
The average Society of Thoracic Surgeons (STS) score was 12.9. “This is one of the highest-risk groups of patients that you’ll ever see,” the cardiologist commented.
Mitral regurgitation was the mechanism of bioprosthetic valve failure in 45% of cases, stenosis in 23%, and a combination of the two in the remainder. The median time from placement of the initial bioprosthetic valve to the transcatheter VIV or VIR procedure was 9 years.
Transcatheter access for the mitral VIV or VIR was transapical in 79% of cases, directly through the left atrium in 2.5%, and by the increasingly popular transseptal route in the remainder. The median follow-up post procedure was 408 days.
Mitral VIV procedures looked significantly better from the standpoint of procedural characteristics. Moderate or severe mitral regurgitation was present at the conclusion of the procedure in 2.6% of patients undergoing mitral VIV, compared with 14.8% who had a VIR procedure.
“We were a bit shocked to see that difference between the two groups,” Dr. Dvir said.
Implantation of a small surgical valve of 25 mm or less was the major independent predictor of having an elevated gradient post procedure, with an adjusted odds ratio of 3.7.
In addition, the mean valve area was 1.99 cm2 in the VIV group vs. 2.33 cm2 in the VIR group. Postinflation was employed in 3.2% of the VIV group, compared with 22.7% of the VIR group. Left ventricular outflow tract obstruction – a potentially fatal complication – occurred in 2.6% of the mitral VIV group and was significantly more common at 8% in the VIR group.
Mitral VIR procedures were associated with markedly worse clinical outcomes. Highlighting the 11.2% rate of the 30-day primary composite endpoint in the mitral VIV group, Dr. Dvir commented, “I must say, I think that is a very reasonable number given that we’re talking about a very high–risk group of patients. For this group of patients having a very high STS score, reaching good results in 30 days in the mitral valve-in-valve group is a good signal for the regulatory groups and for the community that this is a good procedure.”
In contrast, the 28.4% rate of the composite endpoint in the VIR group “is a big disappointment; almost one-third of patients undergoing mitral valve in ring experience the composite adverse event endpoint at 30 days. There is an issue there,” he added.
Dr. Dvir reported having no relevant financial conflicts.
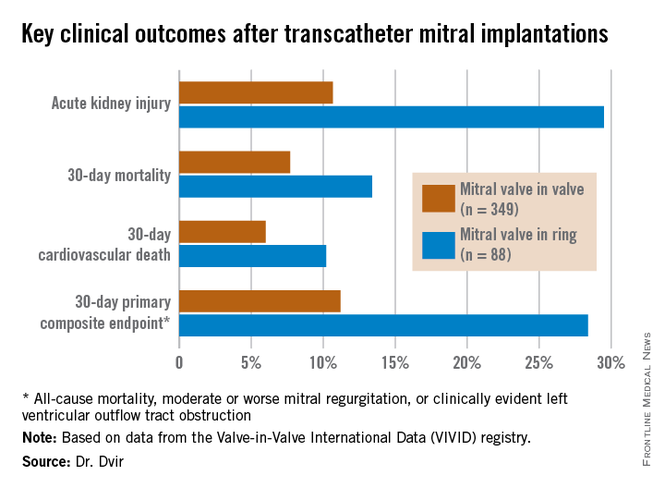
PARIS – Transcatheter mitral valve-in-valve procedures in patients with a failed bioprosthetic mitral valve provide superior clinical results, compared with valve-in-ring implantations, according to the latest data from the VIVID registry.
“Obviously, these results have numerous implications for the interventional community: for surgeons, who employ bioprostheses and rings, and for the cardiovascular industry that designs transcatheter strategies for mitral valve and ring implantations,” Dr. Danny Dvir said in presenting the VIVID update at the annual congress of the European Association of Percutaneous Cardiovascular Interventio
Bioprosthetic rather than mechanical valves are increasingly popular in open-heart valve replacement operations because they avoid the need for lifelong oral anticoagulation. But over time bioprosthetic valves often fail. And that event creates a need for a high-risk, repeat open surgery or a far less invasive transcatheter valve replacement.
Lots of data are available regarding the effectiveness and limitations of transcatheter aortic valve-in-valve procedures in patients with failed bioprosthetic aortic valves, including a previous report from the VIVID (Valve-in-Valve International Data registry) by Dr. Dvir and coworkers (JAMA 2014;312:162-70). However, very little data exist about the effectiveness of mitral valve-in-valve and valve-in-ring procedures, noted Dr. Dvir of St. Paul’s Hospital and the University of British Columbia, Vancouver.
The VIVID registry is drawn from 94 sites on six continents. Dr. Dvir presented an analysis of 437 transcatheter mitral implantations in patients with failed bioprosthetic valves. The study population consisted of 349 patients with mitral valve-in-valve (VIV) and 88 with valve-in-ring (VIR) procedures.
The average Society of Thoracic Surgeons (STS) score was 12.9. “This is one of the highest-risk groups of patients that you’ll ever see,” the cardiologist commented.
Mitral regurgitation was the mechanism of bioprosthetic valve failure in 45% of cases, stenosis in 23%, and a combination of the two in the remainder. The median time from placement of the initial bioprosthetic valve to the transcatheter VIV or VIR procedure was 9 years.
Transcatheter access for the mitral VIV or VIR was transapical in 79% of cases, directly through the left atrium in 2.5%, and by the increasingly popular transseptal route in the remainder. The median follow-up post procedure was 408 days.
Mitral VIV procedures looked significantly better from the standpoint of procedural characteristics. Moderate or severe mitral regurgitation was present at the conclusion of the procedure in 2.6% of patients undergoing mitral VIV, compared with 14.8% who had a VIR procedure.
“We were a bit shocked to see that difference between the two groups,” Dr. Dvir said.
Implantation of a small surgical valve of 25 mm or less was the major independent predictor of having an elevated gradient post procedure, with an adjusted odds ratio of 3.7.
In addition, the mean valve area was 1.99 cm2 in the VIV group vs. 2.33 cm2 in the VIR group. Postinflation was employed in 3.2% of the VIV group, compared with 22.7% of the VIR group. Left ventricular outflow tract obstruction – a potentially fatal complication – occurred in 2.6% of the mitral VIV group and was significantly more common at 8% in the VIR group.
Mitral VIR procedures were associated with markedly worse clinical outcomes. Highlighting the 11.2% rate of the 30-day primary composite endpoint in the mitral VIV group, Dr. Dvir commented, “I must say, I think that is a very reasonable number given that we’re talking about a very high–risk group of patients. For this group of patients having a very high STS score, reaching good results in 30 days in the mitral valve-in-valve group is a good signal for the regulatory groups and for the community that this is a good procedure.”
In contrast, the 28.4% rate of the composite endpoint in the VIR group “is a big disappointment; almost one-third of patients undergoing mitral valve in ring experience the composite adverse event endpoint at 30 days. There is an issue there,” he added.
Dr. Dvir reported having no relevant financial conflicts.
AT EuroPCR 2015
Key clinical point: Transcatheter mitral valve-in-valve procedures for very high surgical risk patients with a failed bioprosthetic valve yield far superior outcomes, compared with mitral valve-in-ring procedures.
Major finding: The 30-day composite adverse outcome rate comprised of death, moderate or severe mitral regurgitation, or clinically evident left ventricular outflow tract obstruction occurred in 11.2% of patients who underwent a transcatheter mitral valve-in-valve procedure, compared with 28.4% of those with a transcatheter valve-in-ring procedure.
Data source: The ongoing VIVID registry includes patients on six continents undergoing transcatheter implantation of aortic, mitral, and/or tricuspid valves after failure of an earlier bioprosthetic valve.
Disclosures: The presenter reported having no relevant financial conflicts.
SVS: Cryoallografts, NAIS best to reconstruct infected aortic grafts
CHICAGO – Neoaortoiliac system reconstruction or cryopreserved allografts should be used first-line to replace infected aortic endografts, followed by antibiotic-soaked prosthetic grafts, according to a review of 206 cases from vascular surgery centers across the United States.
In the study, 75 patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Forty-nine of the 92 (53%) patients reconstructed with antibiotic-soaked prosthetic grafts also made it to 5 years, while two of 19 (11%) reconstructed with untreated prosthetic grafts survived that long.
The cases were reconstructed inline. The index procedure had been endovascular aortic repair (EVAR) in 165, and thoracic EVAR (TEVAR) in 21, with a better 5-year survival for the EVAR group. Another 11 patients had extra-anatomic reconstruction after initial EVAR, and their 5-year survival was comparable to inline reconstruction at about 50% overall. Nine other patients were managed medically; the majority died soon after being diagnosed with an infected graft.
“Clinicians should have a high index of suspicion to diagnose symptomatic postop EVAR and TEVAR patients with graft infection, especially in those patients with chronic infections or contaminated index procedures. NAIS and cryopreserved allografts require longer procedure times” – about 500 minutes versus about 350 minutes for prosthetic grafts – “but offer improved survival, while prosthetics soaked in antibiotic do better than prosthetic grafts alone,” said lead investigator Dr. Audra Duncan, professor of surgery at the Mayo Clinic in Rochester, Minn.
Patients were treated at the Mayo Clinic, the Cleveland Clinic in Ohio, Johns Hopkins University in Baltimore, the University of California, Los Angeles, and 15 other vascular centers around the country during 2004-2014. They were 68 years old on average, and 78% were men. Comorbidities included hypertension in 84%, smoking in 58%, and renal insufficiency in 30%.
On multivariate analysis, chronic infection, polymicrobial infection, and prosthetic reconstruction, among other things, predicted mortality after reconstruction.
Graft infections were primarily polymicrobial and fungal, and were diagnosed a mean of 716 days after the initial implant, generally by CT. Symptoms included pain in 66%, mostly in the back and abdomen, and fever and chills, also in 66%. Streptococcus, Escherichia coli, and both methicillin-sensitive and -resistant Staphylococcus aureus were among the most commonly isolated organisms. No particular type of graft seemed more likely to get infected.
The sources of infection are unknown, but index procedures were complicated by urinary tract, groin, and other infections in about one-third of patients. About one-third also had interval procedures, including endoleak intervention. About 14% of patients were thought to have had a contaminated index procedure.
Patients stayed in the hospital a mean of 24 days after reconstruction. Early complications included persistent sepsis in 27 patients, myocardial infarction in 9, recurrent infection in 9, and pneumonia in 8. Mortality at 30 days was 11%.
Nineteen replacement grafts – mostly unsoaked Dacron – were explanted after a mean of 540 days. Persistent sepsis after reconstruction was associated with unsoaked Dacron and polytetrafluoroethylene (PTFE) grafts.
To prevent graft infections, Mayo patients “take an antibiotic for any invasive procedure,” including dental work. “I am not sure we have data to support that, but it is something we do,” Dr. Duncan said.
Dr. Duncan has no relevant disclosures.
CHICAGO – Neoaortoiliac system reconstruction or cryopreserved allografts should be used first-line to replace infected aortic endografts, followed by antibiotic-soaked prosthetic grafts, according to a review of 206 cases from vascular surgery centers across the United States.
In the study, 75 patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Forty-nine of the 92 (53%) patients reconstructed with antibiotic-soaked prosthetic grafts also made it to 5 years, while two of 19 (11%) reconstructed with untreated prosthetic grafts survived that long.
The cases were reconstructed inline. The index procedure had been endovascular aortic repair (EVAR) in 165, and thoracic EVAR (TEVAR) in 21, with a better 5-year survival for the EVAR group. Another 11 patients had extra-anatomic reconstruction after initial EVAR, and their 5-year survival was comparable to inline reconstruction at about 50% overall. Nine other patients were managed medically; the majority died soon after being diagnosed with an infected graft.
“Clinicians should have a high index of suspicion to diagnose symptomatic postop EVAR and TEVAR patients with graft infection, especially in those patients with chronic infections or contaminated index procedures. NAIS and cryopreserved allografts require longer procedure times” – about 500 minutes versus about 350 minutes for prosthetic grafts – “but offer improved survival, while prosthetics soaked in antibiotic do better than prosthetic grafts alone,” said lead investigator Dr. Audra Duncan, professor of surgery at the Mayo Clinic in Rochester, Minn.
Patients were treated at the Mayo Clinic, the Cleveland Clinic in Ohio, Johns Hopkins University in Baltimore, the University of California, Los Angeles, and 15 other vascular centers around the country during 2004-2014. They were 68 years old on average, and 78% were men. Comorbidities included hypertension in 84%, smoking in 58%, and renal insufficiency in 30%.
On multivariate analysis, chronic infection, polymicrobial infection, and prosthetic reconstruction, among other things, predicted mortality after reconstruction.
Graft infections were primarily polymicrobial and fungal, and were diagnosed a mean of 716 days after the initial implant, generally by CT. Symptoms included pain in 66%, mostly in the back and abdomen, and fever and chills, also in 66%. Streptococcus, Escherichia coli, and both methicillin-sensitive and -resistant Staphylococcus aureus were among the most commonly isolated organisms. No particular type of graft seemed more likely to get infected.
The sources of infection are unknown, but index procedures were complicated by urinary tract, groin, and other infections in about one-third of patients. About one-third also had interval procedures, including endoleak intervention. About 14% of patients were thought to have had a contaminated index procedure.
Patients stayed in the hospital a mean of 24 days after reconstruction. Early complications included persistent sepsis in 27 patients, myocardial infarction in 9, recurrent infection in 9, and pneumonia in 8. Mortality at 30 days was 11%.
Nineteen replacement grafts – mostly unsoaked Dacron – were explanted after a mean of 540 days. Persistent sepsis after reconstruction was associated with unsoaked Dacron and polytetrafluoroethylene (PTFE) grafts.
To prevent graft infections, Mayo patients “take an antibiotic for any invasive procedure,” including dental work. “I am not sure we have data to support that, but it is something we do,” Dr. Duncan said.
Dr. Duncan has no relevant disclosures.
CHICAGO – Neoaortoiliac system reconstruction or cryopreserved allografts should be used first-line to replace infected aortic endografts, followed by antibiotic-soaked prosthetic grafts, according to a review of 206 cases from vascular surgery centers across the United States.
In the study, 75 patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Forty-nine of the 92 (53%) patients reconstructed with antibiotic-soaked prosthetic grafts also made it to 5 years, while two of 19 (11%) reconstructed with untreated prosthetic grafts survived that long.
The cases were reconstructed inline. The index procedure had been endovascular aortic repair (EVAR) in 165, and thoracic EVAR (TEVAR) in 21, with a better 5-year survival for the EVAR group. Another 11 patients had extra-anatomic reconstruction after initial EVAR, and their 5-year survival was comparable to inline reconstruction at about 50% overall. Nine other patients were managed medically; the majority died soon after being diagnosed with an infected graft.
“Clinicians should have a high index of suspicion to diagnose symptomatic postop EVAR and TEVAR patients with graft infection, especially in those patients with chronic infections or contaminated index procedures. NAIS and cryopreserved allografts require longer procedure times” – about 500 minutes versus about 350 minutes for prosthetic grafts – “but offer improved survival, while prosthetics soaked in antibiotic do better than prosthetic grafts alone,” said lead investigator Dr. Audra Duncan, professor of surgery at the Mayo Clinic in Rochester, Minn.
Patients were treated at the Mayo Clinic, the Cleveland Clinic in Ohio, Johns Hopkins University in Baltimore, the University of California, Los Angeles, and 15 other vascular centers around the country during 2004-2014. They were 68 years old on average, and 78% were men. Comorbidities included hypertension in 84%, smoking in 58%, and renal insufficiency in 30%.
On multivariate analysis, chronic infection, polymicrobial infection, and prosthetic reconstruction, among other things, predicted mortality after reconstruction.
Graft infections were primarily polymicrobial and fungal, and were diagnosed a mean of 716 days after the initial implant, generally by CT. Symptoms included pain in 66%, mostly in the back and abdomen, and fever and chills, also in 66%. Streptococcus, Escherichia coli, and both methicillin-sensitive and -resistant Staphylococcus aureus were among the most commonly isolated organisms. No particular type of graft seemed more likely to get infected.
The sources of infection are unknown, but index procedures were complicated by urinary tract, groin, and other infections in about one-third of patients. About one-third also had interval procedures, including endoleak intervention. About 14% of patients were thought to have had a contaminated index procedure.
Patients stayed in the hospital a mean of 24 days after reconstruction. Early complications included persistent sepsis in 27 patients, myocardial infarction in 9, recurrent infection in 9, and pneumonia in 8. Mortality at 30 days was 11%.
Nineteen replacement grafts – mostly unsoaked Dacron – were explanted after a mean of 540 days. Persistent sepsis after reconstruction was associated with unsoaked Dacron and polytetrafluoroethylene (PTFE) grafts.
To prevent graft infections, Mayo patients “take an antibiotic for any invasive procedure,” including dental work. “I am not sure we have data to support that, but it is something we do,” Dr. Duncan said.
Dr. Duncan has no relevant disclosures.
AT THE 2015 VASCULAR ANNUAL MEETING
Key clinical point: Neoaortoiliac system reconstruction or cryopreserved allografts perform best in replacing infected aortic endografts, but if you have to use prosthetics, use ones soaked in antibiotics.
Major finding: Seventy-five patients had cryoallograft reconstruction, mostly cryoartery, or neoaortoiliac system (NAIS) reconstruction with femoral vein; 53 (71%) were alive at 5 years. Two of 19 (11%) patients reconstructed with untreated prosthetic grafts survived that long.
Data source: Review of 206 patients at 19 vascular surgery centers in the United States.
Disclosures: The lead investigator has no relevant disclosures.
EUROPCR: New technology shows early promise for transcatheter tricuspid valve repair
PARIS – Early highly preliminary results from the first-in-human study of percutaneous repair of a failing tricuspid valve indicate that the transcatheter procedure appears safe, durable, and effective – at least through the first 6 months.
“Even though the one-grade reduction of tricuspid regurgitation on color Doppler flow imaging is modest, the impact in terms of clinical improvement seems very encouraging and warrants pursuing this innovative technique,” Dr. Jean-Michel Juliard said in presenting the early findings at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The three-country, prospective, single-arm study is aimed at winning European regulatory approval for 4tech Cardio’s TriCinch System. The study includes 24 patients with severe functional tricuspid regurgitation. Dr. Juliard, a cardiologist at Bichat Hospital in Paris, presented 6-month follow-up data on two patients and 3-month follow-up for a third.
First, a bit about the procedure. It’s conducted under general anesthesia and relies upon transesophageal and intracardiac echocardiographic guidance. The objectives are to reduce the effective cross-sectional valve area by diminishing the septo-lateral dimension of the tricuspid annulus diameter, restore tricuspid valve leaflet coaptation, and relieve symptoms.
The 4tech delivery system consists of two parts. To begin, a guidewire is placed in the right coronary artery, a 24-French sheath is introduced via the right femoral vein, and an exchange guidewire is positioned in the right ventricular apex. The first part of the delivery system is then inserted in order to place an anchor on the tricuspid valve annulus in the vicinity of the antero-posterior commissure.
“This is probably the most difficult part of the whole procedure,” according to Dr. Juliard. “It is done using intracoronary and transesophageal echo guidance.”
Once the anchor is well positioned, the second part of the system is advanced, locked into the first part, and tension is applied under echocardiographic control in order to implant a nitinol self-expanding stent in the inferior vena cava. As soon as traction is applied, the tricuspid regurgitation decreases. Once the correction process is completed, the TriCinch delivery system and venous introducers are removed. For study purposes, dosing of diuretics remained unchanged post procedure.
In the first 6 months, the tricuspid septo-lateral distance improved from 52 to 42 mm in one patient and from 45 to 40 mm in another. A third patient had improvement from 43 to 34 mm at 3 months of follow-up.
In terms of clinical improvement, two patients went from New York Heart Association functional class III to class II, and another went from class III to class I. Six-minute walk distance increased from a baseline of 320 m to 367 m at 6 months of follow-up in one patient and from 400 m to 750 m in another, with a 3-month improvement from 160 to 280 m in the third patient.
Serial imaging studies showed device stability over time, with no migration and no stent thrombosis.
In response to an audience question, Dr. Juliard conceded that at this early stage in the development of the procedure, the placebo effect can’t be ruled out as a possible explanation for the observed strong clinical improvement despite what he conceded was “very modest” reduction in tricuspid regurgitation. Time will tell.
“I hope it is not a placebo effect, but as we maintain the same dose of diuretics, it does seem that the patients feel better,” he added.
The rationale for developing a transcatheter solution to functional tricuspid regurgitation, especially one that’s compatible with concomitant transcatheter mitral valve procedures, as the TriCinch System is intended to be, lies in the wealth of evidence that tricuspid regurgitation is associated with increased mortality, substantial morbidity, and severely impaired quality of life due to the need for repeated hospitalizations. Surgery for patients with tricuspid regurgitation is often extremely high risk because affected patients typically have right ventricular dysfunction, pulmonary hypertension, and/or previous valve surgery.
The ongoing study is funded by 4tech Cardio. Dr. Juliard reported having no financial conflicts.
PARIS – Early highly preliminary results from the first-in-human study of percutaneous repair of a failing tricuspid valve indicate that the transcatheter procedure appears safe, durable, and effective – at least through the first 6 months.
“Even though the one-grade reduction of tricuspid regurgitation on color Doppler flow imaging is modest, the impact in terms of clinical improvement seems very encouraging and warrants pursuing this innovative technique,” Dr. Jean-Michel Juliard said in presenting the early findings at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The three-country, prospective, single-arm study is aimed at winning European regulatory approval for 4tech Cardio’s TriCinch System. The study includes 24 patients with severe functional tricuspid regurgitation. Dr. Juliard, a cardiologist at Bichat Hospital in Paris, presented 6-month follow-up data on two patients and 3-month follow-up for a third.
First, a bit about the procedure. It’s conducted under general anesthesia and relies upon transesophageal and intracardiac echocardiographic guidance. The objectives are to reduce the effective cross-sectional valve area by diminishing the septo-lateral dimension of the tricuspid annulus diameter, restore tricuspid valve leaflet coaptation, and relieve symptoms.
The 4tech delivery system consists of two parts. To begin, a guidewire is placed in the right coronary artery, a 24-French sheath is introduced via the right femoral vein, and an exchange guidewire is positioned in the right ventricular apex. The first part of the delivery system is then inserted in order to place an anchor on the tricuspid valve annulus in the vicinity of the antero-posterior commissure.
“This is probably the most difficult part of the whole procedure,” according to Dr. Juliard. “It is done using intracoronary and transesophageal echo guidance.”
Once the anchor is well positioned, the second part of the system is advanced, locked into the first part, and tension is applied under echocardiographic control in order to implant a nitinol self-expanding stent in the inferior vena cava. As soon as traction is applied, the tricuspid regurgitation decreases. Once the correction process is completed, the TriCinch delivery system and venous introducers are removed. For study purposes, dosing of diuretics remained unchanged post procedure.
In the first 6 months, the tricuspid septo-lateral distance improved from 52 to 42 mm in one patient and from 45 to 40 mm in another. A third patient had improvement from 43 to 34 mm at 3 months of follow-up.
In terms of clinical improvement, two patients went from New York Heart Association functional class III to class II, and another went from class III to class I. Six-minute walk distance increased from a baseline of 320 m to 367 m at 6 months of follow-up in one patient and from 400 m to 750 m in another, with a 3-month improvement from 160 to 280 m in the third patient.
Serial imaging studies showed device stability over time, with no migration and no stent thrombosis.
In response to an audience question, Dr. Juliard conceded that at this early stage in the development of the procedure, the placebo effect can’t be ruled out as a possible explanation for the observed strong clinical improvement despite what he conceded was “very modest” reduction in tricuspid regurgitation. Time will tell.
“I hope it is not a placebo effect, but as we maintain the same dose of diuretics, it does seem that the patients feel better,” he added.
The rationale for developing a transcatheter solution to functional tricuspid regurgitation, especially one that’s compatible with concomitant transcatheter mitral valve procedures, as the TriCinch System is intended to be, lies in the wealth of evidence that tricuspid regurgitation is associated with increased mortality, substantial morbidity, and severely impaired quality of life due to the need for repeated hospitalizations. Surgery for patients with tricuspid regurgitation is often extremely high risk because affected patients typically have right ventricular dysfunction, pulmonary hypertension, and/or previous valve surgery.
The ongoing study is funded by 4tech Cardio. Dr. Juliard reported having no financial conflicts.
PARIS – Early highly preliminary results from the first-in-human study of percutaneous repair of a failing tricuspid valve indicate that the transcatheter procedure appears safe, durable, and effective – at least through the first 6 months.
“Even though the one-grade reduction of tricuspid regurgitation on color Doppler flow imaging is modest, the impact in terms of clinical improvement seems very encouraging and warrants pursuing this innovative technique,” Dr. Jean-Michel Juliard said in presenting the early findings at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The three-country, prospective, single-arm study is aimed at winning European regulatory approval for 4tech Cardio’s TriCinch System. The study includes 24 patients with severe functional tricuspid regurgitation. Dr. Juliard, a cardiologist at Bichat Hospital in Paris, presented 6-month follow-up data on two patients and 3-month follow-up for a third.
First, a bit about the procedure. It’s conducted under general anesthesia and relies upon transesophageal and intracardiac echocardiographic guidance. The objectives are to reduce the effective cross-sectional valve area by diminishing the septo-lateral dimension of the tricuspid annulus diameter, restore tricuspid valve leaflet coaptation, and relieve symptoms.
The 4tech delivery system consists of two parts. To begin, a guidewire is placed in the right coronary artery, a 24-French sheath is introduced via the right femoral vein, and an exchange guidewire is positioned in the right ventricular apex. The first part of the delivery system is then inserted in order to place an anchor on the tricuspid valve annulus in the vicinity of the antero-posterior commissure.
“This is probably the most difficult part of the whole procedure,” according to Dr. Juliard. “It is done using intracoronary and transesophageal echo guidance.”
Once the anchor is well positioned, the second part of the system is advanced, locked into the first part, and tension is applied under echocardiographic control in order to implant a nitinol self-expanding stent in the inferior vena cava. As soon as traction is applied, the tricuspid regurgitation decreases. Once the correction process is completed, the TriCinch delivery system and venous introducers are removed. For study purposes, dosing of diuretics remained unchanged post procedure.
In the first 6 months, the tricuspid septo-lateral distance improved from 52 to 42 mm in one patient and from 45 to 40 mm in another. A third patient had improvement from 43 to 34 mm at 3 months of follow-up.
In terms of clinical improvement, two patients went from New York Heart Association functional class III to class II, and another went from class III to class I. Six-minute walk distance increased from a baseline of 320 m to 367 m at 6 months of follow-up in one patient and from 400 m to 750 m in another, with a 3-month improvement from 160 to 280 m in the third patient.
Serial imaging studies showed device stability over time, with no migration and no stent thrombosis.
In response to an audience question, Dr. Juliard conceded that at this early stage in the development of the procedure, the placebo effect can’t be ruled out as a possible explanation for the observed strong clinical improvement despite what he conceded was “very modest” reduction in tricuspid regurgitation. Time will tell.
“I hope it is not a placebo effect, but as we maintain the same dose of diuretics, it does seem that the patients feel better,” he added.
The rationale for developing a transcatheter solution to functional tricuspid regurgitation, especially one that’s compatible with concomitant transcatheter mitral valve procedures, as the TriCinch System is intended to be, lies in the wealth of evidence that tricuspid regurgitation is associated with increased mortality, substantial morbidity, and severely impaired quality of life due to the need for repeated hospitalizations. Surgery for patients with tricuspid regurgitation is often extremely high risk because affected patients typically have right ventricular dysfunction, pulmonary hypertension, and/or previous valve surgery.
The ongoing study is funded by 4tech Cardio. Dr. Juliard reported having no financial conflicts.
AT EUROPCR 2015
Key clinical point: A novel technology for transcatheter repair of a failing tricuspid valve shows early promise of safety and efficacy.
Major finding: At 3-6 months of follow-up, the first three participants in a first-in-human study of percutaneous tricuspid valve repair show substantial clinical benefits.
Data source: This is a prospective, three-center, nonrandomized, single-arm study of a novel percutaneous therapy in 24 patients with severe functional tricuspid regurgitation.
Disclosures: This ongoing study is funded by 4tech Cardio. The presenter reported having no financial conflicts.
ZEUS: Second-generation DES with 30 days DAPT best in bleeding-risk patients
PARIS – The use of a second-generation zotarolimus-eluting coronary stent rather than a bare metal stent in conjunction with 30 days of dual antiplatelet therapy (DAPT) in patients deemed at high bleeding risk results in lower 1-year rates of major adverse cardiovascular events and stent thrombosis, according to a prespecified analysis of the ZEUS trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Asked if the ZEUS results mean it’s time to take bare-metal stents (BMS) out of the cupboard and get rid of them, the study presenter, Dr. Marco Valgimigli, replied “I did so already.”
ZEUS (Zotarolimus-Eluting Endeavor Sprint Stent in Uncertain DES Candidates Study) was an open-label, prospective study in which 1,606 patients undergoing urgent or emergent percutaneous coronary intervention were randomized to a thin-strut BMS or the zotarolimus-eluting Endeavor Sprint stent, a second-generation hydrophilic polymer-based device that, uniquely, elutes 100% of the drug within the first 2 weeks. All participants were placed on an intended 30-day regimen of DAPT. The study was conducted in four European countries, explained Dr. Valgimigli of Erasmus University in Rotterdam.
This prespecified analysis focused on the 828 patients with one or more factors placing them at high bleeding risk, since the use of a drug-eluting stent (DES) with a 30-day DAPT protocol hadn’t been adequately studied in that setting, the cardiologist noted.
High bleeding risk was defined by one or more of the following: age greater than 80, being on oral anticoagulation therapy, a prior bleeding event, need for corticosteroid or NSAID therapy, known anemia, or a bleeding diathesis; 47% of study participants had more than one of these criteria.
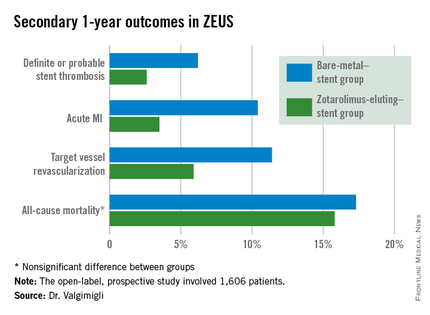
The primary study endpoint was the composite of all-cause mortality, acute MI, or target vessel revascularization through 1 year of follow-up. The rate was 29% in the BMS group, compared with 22.6% in the DES group, for a highly significant 26% relative risk reduction.
The zotarolimus-eluting stent group also fared significantly better in terms of stent thrombosis and the other prespecified secondary endpoints.
Asked how the ZEUS findings have affected his own clinical practice, Dr. Valgimigli replied, “My stent of choice in patients at high bleeding risk is a second-generation DES. Since there aren’t data showing a specific second-generation DES is preferable, basically whatever I have I implant.”
He sticks to the 30-day DAPT regimen featured in the ZEUS protocol except under specific circumstances, which were allowed under the protocol. One involves staged PCI procedures, in which case the 30 days of DAPT begins after the last stent is implanted, even though the patient has been on DAPT in the interim. The other circumstance where he goes beyond 30 days of DAPT in a patient on a second-generation DES is if an ischemic event occurs down the road: “That patient is put back on DAPT and left there,” he said.
In response to another question, Dr. Valgimigli said he doesn’t believe the lower stent thrombosis rate seen in the Endeavor Sprint group in ZEUS is unique to that stent.
“If you look at any BMS versus DES study, taking the first-generation DES out of the picture, it’s quite clear that the second-generation DES are much safer than a BMS,” according to the cardiologist.
The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. Dr. Valgimigli serves as a consultant to and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
PARIS – The use of a second-generation zotarolimus-eluting coronary stent rather than a bare metal stent in conjunction with 30 days of dual antiplatelet therapy (DAPT) in patients deemed at high bleeding risk results in lower 1-year rates of major adverse cardiovascular events and stent thrombosis, according to a prespecified analysis of the ZEUS trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Asked if the ZEUS results mean it’s time to take bare-metal stents (BMS) out of the cupboard and get rid of them, the study presenter, Dr. Marco Valgimigli, replied “I did so already.”
ZEUS (Zotarolimus-Eluting Endeavor Sprint Stent in Uncertain DES Candidates Study) was an open-label, prospective study in which 1,606 patients undergoing urgent or emergent percutaneous coronary intervention were randomized to a thin-strut BMS or the zotarolimus-eluting Endeavor Sprint stent, a second-generation hydrophilic polymer-based device that, uniquely, elutes 100% of the drug within the first 2 weeks. All participants were placed on an intended 30-day regimen of DAPT. The study was conducted in four European countries, explained Dr. Valgimigli of Erasmus University in Rotterdam.
This prespecified analysis focused on the 828 patients with one or more factors placing them at high bleeding risk, since the use of a drug-eluting stent (DES) with a 30-day DAPT protocol hadn’t been adequately studied in that setting, the cardiologist noted.
High bleeding risk was defined by one or more of the following: age greater than 80, being on oral anticoagulation therapy, a prior bleeding event, need for corticosteroid or NSAID therapy, known anemia, or a bleeding diathesis; 47% of study participants had more than one of these criteria.
The primary study endpoint was the composite of all-cause mortality, acute MI, or target vessel revascularization through 1 year of follow-up. The rate was 29% in the BMS group, compared with 22.6% in the DES group, for a highly significant 26% relative risk reduction.
The zotarolimus-eluting stent group also fared significantly better in terms of stent thrombosis and the other prespecified secondary endpoints.
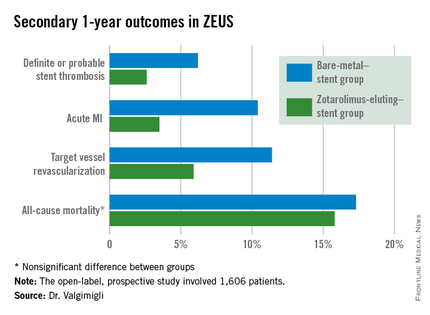
Asked how the ZEUS findings have affected his own clinical practice, Dr. Valgimigli replied, “My stent of choice in patients at high bleeding risk is a second-generation DES. Since there aren’t data showing a specific second-generation DES is preferable, basically whatever I have I implant.”
He sticks to the 30-day DAPT regimen featured in the ZEUS protocol except under specific circumstances, which were allowed under the protocol. One involves staged PCI procedures, in which case the 30 days of DAPT begins after the last stent is implanted, even though the patient has been on DAPT in the interim. The other circumstance where he goes beyond 30 days of DAPT in a patient on a second-generation DES is if an ischemic event occurs down the road: “That patient is put back on DAPT and left there,” he said.
In response to another question, Dr. Valgimigli said he doesn’t believe the lower stent thrombosis rate seen in the Endeavor Sprint group in ZEUS is unique to that stent.
“If you look at any BMS versus DES study, taking the first-generation DES out of the picture, it’s quite clear that the second-generation DES are much safer than a BMS,” according to the cardiologist.
The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. Dr. Valgimigli serves as a consultant to and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
PARIS – The use of a second-generation zotarolimus-eluting coronary stent rather than a bare metal stent in conjunction with 30 days of dual antiplatelet therapy (DAPT) in patients deemed at high bleeding risk results in lower 1-year rates of major adverse cardiovascular events and stent thrombosis, according to a prespecified analysis of the ZEUS trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Asked if the ZEUS results mean it’s time to take bare-metal stents (BMS) out of the cupboard and get rid of them, the study presenter, Dr. Marco Valgimigli, replied “I did so already.”
ZEUS (Zotarolimus-Eluting Endeavor Sprint Stent in Uncertain DES Candidates Study) was an open-label, prospective study in which 1,606 patients undergoing urgent or emergent percutaneous coronary intervention were randomized to a thin-strut BMS or the zotarolimus-eluting Endeavor Sprint stent, a second-generation hydrophilic polymer-based device that, uniquely, elutes 100% of the drug within the first 2 weeks. All participants were placed on an intended 30-day regimen of DAPT. The study was conducted in four European countries, explained Dr. Valgimigli of Erasmus University in Rotterdam.
This prespecified analysis focused on the 828 patients with one or more factors placing them at high bleeding risk, since the use of a drug-eluting stent (DES) with a 30-day DAPT protocol hadn’t been adequately studied in that setting, the cardiologist noted.
High bleeding risk was defined by one or more of the following: age greater than 80, being on oral anticoagulation therapy, a prior bleeding event, need for corticosteroid or NSAID therapy, known anemia, or a bleeding diathesis; 47% of study participants had more than one of these criteria.
The primary study endpoint was the composite of all-cause mortality, acute MI, or target vessel revascularization through 1 year of follow-up. The rate was 29% in the BMS group, compared with 22.6% in the DES group, for a highly significant 26% relative risk reduction.
The zotarolimus-eluting stent group also fared significantly better in terms of stent thrombosis and the other prespecified secondary endpoints.
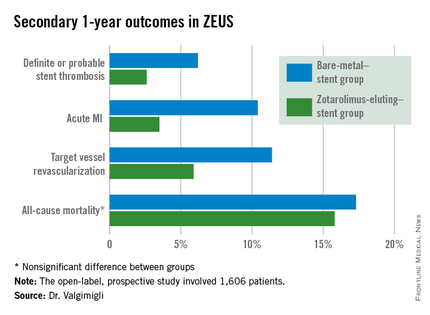
Asked how the ZEUS findings have affected his own clinical practice, Dr. Valgimigli replied, “My stent of choice in patients at high bleeding risk is a second-generation DES. Since there aren’t data showing a specific second-generation DES is preferable, basically whatever I have I implant.”
He sticks to the 30-day DAPT regimen featured in the ZEUS protocol except under specific circumstances, which were allowed under the protocol. One involves staged PCI procedures, in which case the 30 days of DAPT begins after the last stent is implanted, even though the patient has been on DAPT in the interim. The other circumstance where he goes beyond 30 days of DAPT in a patient on a second-generation DES is if an ischemic event occurs down the road: “That patient is put back on DAPT and left there,” he said.
In response to another question, Dr. Valgimigli said he doesn’t believe the lower stent thrombosis rate seen in the Endeavor Sprint group in ZEUS is unique to that stent.
“If you look at any BMS versus DES study, taking the first-generation DES out of the picture, it’s quite clear that the second-generation DES are much safer than a BMS,” according to the cardiologist.
The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. Dr. Valgimigli serves as a consultant to and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
AT EUROPCR 2015
Key clinical point: High bleeding risk patients fare significantly better with a second-generation drug-eluting stent and 30 days of dual antiplatelet therapy than with a bare-metal stent.
Major finding: The 1-year incidence of major adverse cardiovascular events was 29.6% in high bleeding risk patients who received a bare-metal stent and 22.6% in those who got a second-generation zotarolimus-eluting stent with 30 days of dual antiplatelet therapy.
Data source: This was a prespecified analysis of 828 high bleeding risk patients randomized to a bare-metal stent or a second-generation zotarolimus-eluting stent in conjunction with 30 days of DAPT and then followed prospectively for 1 year.
Disclosures: The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. The presenter serves as a consultant and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
Bivalirudin in STEMI has low real-world stent thrombosis rate
PARIS – Antithrombotic therapy with bivalirudin for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction may have been unfairly tarnished as having a high stent thrombosis rate, according to a large, prospective, observational cohort study.
A new analysis from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) showed similarly low stent thrombosis rates within 30 days following primary PCI for STEMI regardless of whether the antithrombotic regimen involved bivalirudin (Angiomax), heparin only, or a glycoprotein IIb/IIIa inhibitor, Dr. Per Grimfjard reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The SCAAR analysis captured all STEMI patients undergoing primary PCI in Sweden from 2007 through mid-2014. These data reflect real-world interventional practice in Sweden and elsewhere, where bivalirudin is typically administered in a prolonged infusion to protect against early stent thrombosis. In contrast, the randomized trials that linked bivalirudin to high stent thrombosis rates featured protocols in which the drug was stopped immediately after the procedure, noted Dr. Grimfjard, an interventional cardiologist at Uppsala (Sweden) University.
“These are nationwide Swedish numbers, and they are complete. We think the numbers are reassuring in that respect,” he said.
Session chair Dr. Andreas Baumbach said the Swedish data are consistent with his own experience in using bivalirudin in primary PCI for STEMI.
“The headline last year was that bivalirudin has a high stent thrombosis rate. It made the newspapers everywhere. But we never saw that, and we always thought that the difference might be in how we used the drug. There’s a new headline now, that this high stent thrombosis rate is not seen in clinical practice. The practice differs from the randomized trials, and the outcomes differ as well,” observed Dr. Baumbach, professor of interventional cardiology at the University of Bristol (England).
In SCAAR, the 30-day rate of definite, angiographically proven stent thrombosis was 0.84% in 16,860 bivalirudin-treated patients, 0.94% in 3,182 who got heparin only, and 0.83% in 11,216 glycoprotein IIb/IIIa inhibitor recipients. These numeric differences weren’t statistically significant.
All-cause mortality 1 year post-PCI was 9.1% in patients with no stent thrombosis, 16.1% in those who experienced stent thrombosis within 1 day post PCI, and 23.0% in those whose stent thrombosis occurred on days 2-30. Dr. Grimfjard speculated that the explanation for the numerically higher 1-year all-cause mortality rate in patients whose stent thrombosis occurred on days 2-30 as opposed to day 0-1 is probably that they were more likely to have left the hospital when stent thrombosis occurred. That would translate to a longer time to repeat revascularization, hence a larger MI, more heart failure and arrhythmia, and thus a higher long-term risk of death.
Several audience members commented that they weren’t sure what to make of the observational Swedish data because of the looming presence of several potential confounders. For one, clinical practice trends changed considerably during the 7-year time frame of the study, as evidenced by the fact that the use of drug-eluting stents was far more common in bivalirudin-treated patients than in the glycoprotein IIb/IIIa inhibitor group. Also, Swedish cardiologists who put their STEMI patients on bivalirudin were more likely to utilize the more modern radial artery access in performing primary PCI; their practice may have differed from their colleagues’ in other, unrecorded ways as well, it was noted.
Dr. Grimfjard reported having no financial conflicts regarding the study, which was conducted free of commercial support.
PARIS – Antithrombotic therapy with bivalirudin for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction may have been unfairly tarnished as having a high stent thrombosis rate, according to a large, prospective, observational cohort study.
A new analysis from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) showed similarly low stent thrombosis rates within 30 days following primary PCI for STEMI regardless of whether the antithrombotic regimen involved bivalirudin (Angiomax), heparin only, or a glycoprotein IIb/IIIa inhibitor, Dr. Per Grimfjard reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The SCAAR analysis captured all STEMI patients undergoing primary PCI in Sweden from 2007 through mid-2014. These data reflect real-world interventional practice in Sweden and elsewhere, where bivalirudin is typically administered in a prolonged infusion to protect against early stent thrombosis. In contrast, the randomized trials that linked bivalirudin to high stent thrombosis rates featured protocols in which the drug was stopped immediately after the procedure, noted Dr. Grimfjard, an interventional cardiologist at Uppsala (Sweden) University.
“These are nationwide Swedish numbers, and they are complete. We think the numbers are reassuring in that respect,” he said.
Session chair Dr. Andreas Baumbach said the Swedish data are consistent with his own experience in using bivalirudin in primary PCI for STEMI.
“The headline last year was that bivalirudin has a high stent thrombosis rate. It made the newspapers everywhere. But we never saw that, and we always thought that the difference might be in how we used the drug. There’s a new headline now, that this high stent thrombosis rate is not seen in clinical practice. The practice differs from the randomized trials, and the outcomes differ as well,” observed Dr. Baumbach, professor of interventional cardiology at the University of Bristol (England).
In SCAAR, the 30-day rate of definite, angiographically proven stent thrombosis was 0.84% in 16,860 bivalirudin-treated patients, 0.94% in 3,182 who got heparin only, and 0.83% in 11,216 glycoprotein IIb/IIIa inhibitor recipients. These numeric differences weren’t statistically significant.
All-cause mortality 1 year post-PCI was 9.1% in patients with no stent thrombosis, 16.1% in those who experienced stent thrombosis within 1 day post PCI, and 23.0% in those whose stent thrombosis occurred on days 2-30. Dr. Grimfjard speculated that the explanation for the numerically higher 1-year all-cause mortality rate in patients whose stent thrombosis occurred on days 2-30 as opposed to day 0-1 is probably that they were more likely to have left the hospital when stent thrombosis occurred. That would translate to a longer time to repeat revascularization, hence a larger MI, more heart failure and arrhythmia, and thus a higher long-term risk of death.
Several audience members commented that they weren’t sure what to make of the observational Swedish data because of the looming presence of several potential confounders. For one, clinical practice trends changed considerably during the 7-year time frame of the study, as evidenced by the fact that the use of drug-eluting stents was far more common in bivalirudin-treated patients than in the glycoprotein IIb/IIIa inhibitor group. Also, Swedish cardiologists who put their STEMI patients on bivalirudin were more likely to utilize the more modern radial artery access in performing primary PCI; their practice may have differed from their colleagues’ in other, unrecorded ways as well, it was noted.
Dr. Grimfjard reported having no financial conflicts regarding the study, which was conducted free of commercial support.
PARIS – Antithrombotic therapy with bivalirudin for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction may have been unfairly tarnished as having a high stent thrombosis rate, according to a large, prospective, observational cohort study.
A new analysis from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) showed similarly low stent thrombosis rates within 30 days following primary PCI for STEMI regardless of whether the antithrombotic regimen involved bivalirudin (Angiomax), heparin only, or a glycoprotein IIb/IIIa inhibitor, Dr. Per Grimfjard reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The SCAAR analysis captured all STEMI patients undergoing primary PCI in Sweden from 2007 through mid-2014. These data reflect real-world interventional practice in Sweden and elsewhere, where bivalirudin is typically administered in a prolonged infusion to protect against early stent thrombosis. In contrast, the randomized trials that linked bivalirudin to high stent thrombosis rates featured protocols in which the drug was stopped immediately after the procedure, noted Dr. Grimfjard, an interventional cardiologist at Uppsala (Sweden) University.
“These are nationwide Swedish numbers, and they are complete. We think the numbers are reassuring in that respect,” he said.
Session chair Dr. Andreas Baumbach said the Swedish data are consistent with his own experience in using bivalirudin in primary PCI for STEMI.
“The headline last year was that bivalirudin has a high stent thrombosis rate. It made the newspapers everywhere. But we never saw that, and we always thought that the difference might be in how we used the drug. There’s a new headline now, that this high stent thrombosis rate is not seen in clinical practice. The practice differs from the randomized trials, and the outcomes differ as well,” observed Dr. Baumbach, professor of interventional cardiology at the University of Bristol (England).
In SCAAR, the 30-day rate of definite, angiographically proven stent thrombosis was 0.84% in 16,860 bivalirudin-treated patients, 0.94% in 3,182 who got heparin only, and 0.83% in 11,216 glycoprotein IIb/IIIa inhibitor recipients. These numeric differences weren’t statistically significant.
All-cause mortality 1 year post-PCI was 9.1% in patients with no stent thrombosis, 16.1% in those who experienced stent thrombosis within 1 day post PCI, and 23.0% in those whose stent thrombosis occurred on days 2-30. Dr. Grimfjard speculated that the explanation for the numerically higher 1-year all-cause mortality rate in patients whose stent thrombosis occurred on days 2-30 as opposed to day 0-1 is probably that they were more likely to have left the hospital when stent thrombosis occurred. That would translate to a longer time to repeat revascularization, hence a larger MI, more heart failure and arrhythmia, and thus a higher long-term risk of death.
Several audience members commented that they weren’t sure what to make of the observational Swedish data because of the looming presence of several potential confounders. For one, clinical practice trends changed considerably during the 7-year time frame of the study, as evidenced by the fact that the use of drug-eluting stents was far more common in bivalirudin-treated patients than in the glycoprotein IIb/IIIa inhibitor group. Also, Swedish cardiologists who put their STEMI patients on bivalirudin were more likely to utilize the more modern radial artery access in performing primary PCI; their practice may have differed from their colleagues’ in other, unrecorded ways as well, it was noted.
Dr. Grimfjard reported having no financial conflicts regarding the study, which was conducted free of commercial support.
AT EUROPCR 2015
Key clinical point: The 30-day incidence of stent thrombosis following primary PCI in a large, real-world STEMI population was reassuringly low regardless of the antithrombotic regimen.
Major finding: The stent thrombosis rate within 30 days after primary PCI for STEMI was 0.84% in patients who received bivalirudin for antithrombotic therapy, 0.94% with heparin only, and 0.83% with a glycoprotein IIb/IIIa inhibitor in this real-world nationwide Swedish registry.
Data source: A prospective observational cohort study which included all patients who underwent primary PCI for STEMI in Sweden during 2007-2014.
Disclosures: The presenter reported having no financial conflicts regarding the study, which was conducted free of commercial support.
Reports of TAVI leaflet thickening downplayed – for now
PARIS – Thought leaders in interventional cardiology have been quick to throw cold water on recent reports of valve leaflet thickening and abnormal leaflet motion being detected in roughly 10% of patients after transcatheter aortic valve implantation (TAVI) or surgical aortic valve replacement.
“The take home message for the interventional community is there is no need for clinicians to modify their practice in relation to patient selection, TAVI implantation, or follow-up protocols. Specifically, there is no role for systematic CT or transesophageal echocardiographic follow-up of asymptomatic TAVI patients because they’re not at clinical risk, and these additional procedures carry risk in themselves,” Dr. Bernard Prendergast said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Whilst there is room here for speculation and conjecture, I think most of us are confident that some of these findings may represent imaging artifact or reflect the natural history of biological valve leaflets, which has never been examined in such detail in the past,” added Dr. Prendergast, director of the cardiac structural intervention program at Guys and St. Thomas’ Hospital in London and cochair of the special EuroPCR session devoted to the emerging data on valve leaflet abnormalities.
The session featured three separate studies totaling 345 patients who underwent sophisticated, high-resolution 4D CT imaging or transesophageal echocardiography 5 days or more following TAVI or, less frequently, after surgical aortic valve replacement. Roughly 10% of patients showed a spectrum of leaflet abnormalities: thickening, mildly impaired motion, and/or thin films believed to be thrombi.
The leaflet abnormalities weren’t associated with any particular valve. And, as was emphasized by Dr. Prendergast and other speakers, to date these abnormalities haven’t been associated with a single case of stroke, systemic embolism, or valve failure.
Indeed, more than 100,000 TAVI procedures have been performed worldwide, and stroke rates in contemporary randomized trials and large registries are in the 1%-2% range. That’s better than with surgical valve replacement, Dr. Prendergast observed.
“Nowadays we can see much more than we could in the past, when we worked with 2D echocardiography,” observed discussant Dr. Jeroen J. Bax, professor of cardiology and director of noninvasive cardiology imaging at Leiden (the Netherlands) University Medical Center. “We see things that we do not completely understand. We could say that technology has outpaced our clinical understanding. But although we see things, at the moment there is no consequence in terms of hemodynamic performance or clinical outcomes. And this phenomenon of leaflet thickening has been occurring with surgical aortic valve replacement for many, many years and we simply didn’t realize it.”
Dr. Franz-Josef Neumann, who led one of the three studies, reported that 4D CT on day 5 post TAVI revealed leaflet abnormalities, all completely asymptomatic, in 16 of 154 patients. Two-thirds of the study population were on dual antiplatelet therapy at the time, the rest on a single antiplatelet agent. Dual antiplatelet therapy didn’t protect against leaflet thickening or other abnormalities.
All 16 affected patients were placed on an oral vitamin K antagonist with a target international normalized ratio (INR) of 2.5-3.5. To date, 11 of the 16 have undergone follow-up high-resolution CT after a median of 77 days. The leaflet thickening was resolved in all instances, according to Dr. Neumann, medical director of the department of cardiology and angiology at the University of Freiburg (Germany).
Dr. Raj R. Makkar presented a study of 125 patients who underwent high-resolution imaging after TAVI. Importantly, none of those who were on warfarin as part of their post-TAVI regimen developed leaflet abnormalities.
But he cautioned his colleagues against overreacting to the studies he and Dr. Neumann presented by placing all of their TAVI patients on an oral anticoagulant. He noted that the current TAVI population is elderly and laden with many comorbid conditions, placing them at high risk for bleeding complications.
There is at present no standard, guideline-recommended antiplatelet/antithrombotic regimen for before, during, or after TAVI. Working out the optimal protective drug regimen in this population is now a priority in light of the leaflet abnormality findings, but it will take time and require careful study, said Dr. Makkar, associate director of the Cedars Sinai Heart Institute in Los Angeles.
“Everyone is talking about anticoagulation as the imminent solution. But I want to emphasize that it comes with a price in terms of bleeding. These images are beautiful in terms of spatial resolution, but we must resist our temptation while the industry works on designing less thrombogenic valves,” the cardiologist added.
Discussant Dr. Christoph K. Naber confessed he was “stunned” by the images of leaflet abnormalities.
“Although we haven’t seen any clinical consequences, we have to keep in mind that the group of patients is still small. We have very good experience with TAVI; it has saved the lives of many patients. We know it’s a very good therapy. But if we believe we can go further and offer it to younger, lower-risk patients who will have their device for a longer time, then we should take the time and money to understand what is going on here and what consequences it could have. It’s something we should closely watch, especially if we want to extend the indication,” said Dr. Naber, director of the department of cardiology and angiology at the Contilia Cardiovascular Center in Essen, Germany.
He disclosed that he serves as a consultant to Abbott Vascular, Biotronik, Medtronic, and The Medicines Company. Dr. Makkar has received research grants from Edwards Lifesciences, St. Jude Medical, and Boston Scientific. Dr. Prendergast is on the speakers’ bureau for Edwards Lifesciences.
PARIS – Thought leaders in interventional cardiology have been quick to throw cold water on recent reports of valve leaflet thickening and abnormal leaflet motion being detected in roughly 10% of patients after transcatheter aortic valve implantation (TAVI) or surgical aortic valve replacement.
“The take home message for the interventional community is there is no need for clinicians to modify their practice in relation to patient selection, TAVI implantation, or follow-up protocols. Specifically, there is no role for systematic CT or transesophageal echocardiographic follow-up of asymptomatic TAVI patients because they’re not at clinical risk, and these additional procedures carry risk in themselves,” Dr. Bernard Prendergast said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Whilst there is room here for speculation and conjecture, I think most of us are confident that some of these findings may represent imaging artifact or reflect the natural history of biological valve leaflets, which has never been examined in such detail in the past,” added Dr. Prendergast, director of the cardiac structural intervention program at Guys and St. Thomas’ Hospital in London and cochair of the special EuroPCR session devoted to the emerging data on valve leaflet abnormalities.
The session featured three separate studies totaling 345 patients who underwent sophisticated, high-resolution 4D CT imaging or transesophageal echocardiography 5 days or more following TAVI or, less frequently, after surgical aortic valve replacement. Roughly 10% of patients showed a spectrum of leaflet abnormalities: thickening, mildly impaired motion, and/or thin films believed to be thrombi.
The leaflet abnormalities weren’t associated with any particular valve. And, as was emphasized by Dr. Prendergast and other speakers, to date these abnormalities haven’t been associated with a single case of stroke, systemic embolism, or valve failure.
Indeed, more than 100,000 TAVI procedures have been performed worldwide, and stroke rates in contemporary randomized trials and large registries are in the 1%-2% range. That’s better than with surgical valve replacement, Dr. Prendergast observed.
“Nowadays we can see much more than we could in the past, when we worked with 2D echocardiography,” observed discussant Dr. Jeroen J. Bax, professor of cardiology and director of noninvasive cardiology imaging at Leiden (the Netherlands) University Medical Center. “We see things that we do not completely understand. We could say that technology has outpaced our clinical understanding. But although we see things, at the moment there is no consequence in terms of hemodynamic performance or clinical outcomes. And this phenomenon of leaflet thickening has been occurring with surgical aortic valve replacement for many, many years and we simply didn’t realize it.”
Dr. Franz-Josef Neumann, who led one of the three studies, reported that 4D CT on day 5 post TAVI revealed leaflet abnormalities, all completely asymptomatic, in 16 of 154 patients. Two-thirds of the study population were on dual antiplatelet therapy at the time, the rest on a single antiplatelet agent. Dual antiplatelet therapy didn’t protect against leaflet thickening or other abnormalities.
All 16 affected patients were placed on an oral vitamin K antagonist with a target international normalized ratio (INR) of 2.5-3.5. To date, 11 of the 16 have undergone follow-up high-resolution CT after a median of 77 days. The leaflet thickening was resolved in all instances, according to Dr. Neumann, medical director of the department of cardiology and angiology at the University of Freiburg (Germany).
Dr. Raj R. Makkar presented a study of 125 patients who underwent high-resolution imaging after TAVI. Importantly, none of those who were on warfarin as part of their post-TAVI regimen developed leaflet abnormalities.
But he cautioned his colleagues against overreacting to the studies he and Dr. Neumann presented by placing all of their TAVI patients on an oral anticoagulant. He noted that the current TAVI population is elderly and laden with many comorbid conditions, placing them at high risk for bleeding complications.
There is at present no standard, guideline-recommended antiplatelet/antithrombotic regimen for before, during, or after TAVI. Working out the optimal protective drug regimen in this population is now a priority in light of the leaflet abnormality findings, but it will take time and require careful study, said Dr. Makkar, associate director of the Cedars Sinai Heart Institute in Los Angeles.
“Everyone is talking about anticoagulation as the imminent solution. But I want to emphasize that it comes with a price in terms of bleeding. These images are beautiful in terms of spatial resolution, but we must resist our temptation while the industry works on designing less thrombogenic valves,” the cardiologist added.
Discussant Dr. Christoph K. Naber confessed he was “stunned” by the images of leaflet abnormalities.
“Although we haven’t seen any clinical consequences, we have to keep in mind that the group of patients is still small. We have very good experience with TAVI; it has saved the lives of many patients. We know it’s a very good therapy. But if we believe we can go further and offer it to younger, lower-risk patients who will have their device for a longer time, then we should take the time and money to understand what is going on here and what consequences it could have. It’s something we should closely watch, especially if we want to extend the indication,” said Dr. Naber, director of the department of cardiology and angiology at the Contilia Cardiovascular Center in Essen, Germany.
He disclosed that he serves as a consultant to Abbott Vascular, Biotronik, Medtronic, and The Medicines Company. Dr. Makkar has received research grants from Edwards Lifesciences, St. Jude Medical, and Boston Scientific. Dr. Prendergast is on the speakers’ bureau for Edwards Lifesciences.
PARIS – Thought leaders in interventional cardiology have been quick to throw cold water on recent reports of valve leaflet thickening and abnormal leaflet motion being detected in roughly 10% of patients after transcatheter aortic valve implantation (TAVI) or surgical aortic valve replacement.
“The take home message for the interventional community is there is no need for clinicians to modify their practice in relation to patient selection, TAVI implantation, or follow-up protocols. Specifically, there is no role for systematic CT or transesophageal echocardiographic follow-up of asymptomatic TAVI patients because they’re not at clinical risk, and these additional procedures carry risk in themselves,” Dr. Bernard Prendergast said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Whilst there is room here for speculation and conjecture, I think most of us are confident that some of these findings may represent imaging artifact or reflect the natural history of biological valve leaflets, which has never been examined in such detail in the past,” added Dr. Prendergast, director of the cardiac structural intervention program at Guys and St. Thomas’ Hospital in London and cochair of the special EuroPCR session devoted to the emerging data on valve leaflet abnormalities.
The session featured three separate studies totaling 345 patients who underwent sophisticated, high-resolution 4D CT imaging or transesophageal echocardiography 5 days or more following TAVI or, less frequently, after surgical aortic valve replacement. Roughly 10% of patients showed a spectrum of leaflet abnormalities: thickening, mildly impaired motion, and/or thin films believed to be thrombi.
The leaflet abnormalities weren’t associated with any particular valve. And, as was emphasized by Dr. Prendergast and other speakers, to date these abnormalities haven’t been associated with a single case of stroke, systemic embolism, or valve failure.
Indeed, more than 100,000 TAVI procedures have been performed worldwide, and stroke rates in contemporary randomized trials and large registries are in the 1%-2% range. That’s better than with surgical valve replacement, Dr. Prendergast observed.
“Nowadays we can see much more than we could in the past, when we worked with 2D echocardiography,” observed discussant Dr. Jeroen J. Bax, professor of cardiology and director of noninvasive cardiology imaging at Leiden (the Netherlands) University Medical Center. “We see things that we do not completely understand. We could say that technology has outpaced our clinical understanding. But although we see things, at the moment there is no consequence in terms of hemodynamic performance or clinical outcomes. And this phenomenon of leaflet thickening has been occurring with surgical aortic valve replacement for many, many years and we simply didn’t realize it.”
Dr. Franz-Josef Neumann, who led one of the three studies, reported that 4D CT on day 5 post TAVI revealed leaflet abnormalities, all completely asymptomatic, in 16 of 154 patients. Two-thirds of the study population were on dual antiplatelet therapy at the time, the rest on a single antiplatelet agent. Dual antiplatelet therapy didn’t protect against leaflet thickening or other abnormalities.
All 16 affected patients were placed on an oral vitamin K antagonist with a target international normalized ratio (INR) of 2.5-3.5. To date, 11 of the 16 have undergone follow-up high-resolution CT after a median of 77 days. The leaflet thickening was resolved in all instances, according to Dr. Neumann, medical director of the department of cardiology and angiology at the University of Freiburg (Germany).
Dr. Raj R. Makkar presented a study of 125 patients who underwent high-resolution imaging after TAVI. Importantly, none of those who were on warfarin as part of their post-TAVI regimen developed leaflet abnormalities.
But he cautioned his colleagues against overreacting to the studies he and Dr. Neumann presented by placing all of their TAVI patients on an oral anticoagulant. He noted that the current TAVI population is elderly and laden with many comorbid conditions, placing them at high risk for bleeding complications.
There is at present no standard, guideline-recommended antiplatelet/antithrombotic regimen for before, during, or after TAVI. Working out the optimal protective drug regimen in this population is now a priority in light of the leaflet abnormality findings, but it will take time and require careful study, said Dr. Makkar, associate director of the Cedars Sinai Heart Institute in Los Angeles.
“Everyone is talking about anticoagulation as the imminent solution. But I want to emphasize that it comes with a price in terms of bleeding. These images are beautiful in terms of spatial resolution, but we must resist our temptation while the industry works on designing less thrombogenic valves,” the cardiologist added.
Discussant Dr. Christoph K. Naber confessed he was “stunned” by the images of leaflet abnormalities.
“Although we haven’t seen any clinical consequences, we have to keep in mind that the group of patients is still small. We have very good experience with TAVI; it has saved the lives of many patients. We know it’s a very good therapy. But if we believe we can go further and offer it to younger, lower-risk patients who will have their device for a longer time, then we should take the time and money to understand what is going on here and what consequences it could have. It’s something we should closely watch, especially if we want to extend the indication,” said Dr. Naber, director of the department of cardiology and angiology at the Contilia Cardiovascular Center in Essen, Germany.
He disclosed that he serves as a consultant to Abbott Vascular, Biotronik, Medtronic, and The Medicines Company. Dr. Makkar has received research grants from Edwards Lifesciences, St. Jude Medical, and Boston Scientific. Dr. Prendergast is on the speakers’ bureau for Edwards Lifesciences.
EXPERT ANALYSIS FROM EUROPCR
Post-CABG stroke risk same with one or two clamps
When performing on-pump coronary artery bypass grafting (CABG), cardiac surgeons can control very few factors to reduce the risk of stroke – with the exception of which method of aortic manipulation they use. Debate and controversy, however, have surrounded which aortic manipulation technique is best: single- or double-clamp occlusion.
A large retrospective study of almost 8,500 patients who had CABG at the Mayo Clinic in Rochester, Minn., over a 17-year period showed that, while use of the single-aortic cross-clamp (SC) technique steadily increased, the risk of stroke is virtually the same as it is with the partial aortic cross-clamp (PC), or double cross-clamp, technique. The study authors, led by Dr. Juan C. Araque, published their results online in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.04.010]).
“It is intuitive that less aortic manipulation would result in less risk of stroke,” Dr. Araque and colleagues said, but even off-pump CABG, which requires no aortic manipulation, is not without stroke risk.
“It is conceivable that there is some inherent risk of stroke associated with any cardiac operation, and that risk may increase with manipulation of the ascending aortic with the aortic cross clamp,” they wrote. “Our data would suggest, however, that the risk does not increase further with the additional aortic manipulation of the partial occlusion clamp.”
The study comes on the heels of a 2008 meta-analysis that found no benefit of SC in comparison to PC (Interact. Cardiovasc. Thorac. Surg. 2008;7:500-3), while another study in 2011 suggested that less aortic manipulation carried a significantly lower stroke risk (Heart Lung Circ. 2011;20:318-24).
The Mayo study evaluated the SC technique in 2,051 patients and PC in 6,446 patients who had isolated on-pump CABG between 1993 and 2010. The rate of stroke was 1.2% in the SC group and 1.5% among those who had PC. In two propensity-matched cohorts of 1,333 patients each, the stroke rate was 1.2% in each group. The investigators used the Society of Thoracic Surgeons’ risk calculator variables to create the propensity-matched cohorts.
The study group excluded high-risk patients, including those who had off-pump operations or previous cardiac surgeries or required replacement of a cross clamp during an unplanned operation.
The goal of the study was not to compare outcomes with the off-pump technique. “It is only to bring attention to the associated non-zero stroke rate with both techniques,” Dr. Araque and colleagues said.
Their findings are significant because on-pump CABG is the preferred operation of cardiac surgeons, accounting for more than 80% of the CABG operations in the SYNTAX study (N. Engl. J. Med. 2009;360:961-72). “The ‘anaortic’ off-pump technique may be a more specialized technique, representing less than 15% of operations in one large series,” Dr. Araque and coauthors said.
They acknowledged a few limitations resulting from the observational nature of the study, including that surgeons may have missed some strokes because they did not use a routine, standardized procedure for evaluating stroke signs along with the lack of documented assessment of the descending aorta. But they also stated that the large number of patients in the study, along with the use of propensity matching, addresses some of the bias inherent in an observational study.
The study authors disclosed no relationships.
“A randomized trial is needed to answer the question, ‘Can CABG [coronary artery bypass grafting] be safely performed with either one or two aortic clamps in all patients?’ ” Dr. Jennifer S. Lawton said in her invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.05.002]).
Dr. Lawton acknowledged the positions that advocates of both techniques have staked out: advocates of the single-clamp (SC) technique prefer the ability to perform the proximal anastomoses without the added space constraints and reduced visibility of the partial clamp and moving heart; proponents of the partial-clamp (PC) method cite advantages in the ability to determine graft length with the full heart and the likelihood to reanimate the heart earlier to reduce the risk of a heart attack.
The PC technique required longer cardiopulmonary bypass time, 88.2 minutes vs. 73.7 minutes, but the SC group had longer cross-clamp times, 54.5. vs. 50.7 minutes. “The longer clamp time did not alter the outcomes reported (stroke and mortality) – although specific outcomes of myocardial injury including need for inotropes, troponin levels, myocardial infarction, etc. were not reported,” Dr. Lawton said. “Thus, the question for the surgeon is, ‘What is more important, the brain or the heart?’ ”
The results from Dr. Araque’s study “are valuable” because of the large patient cohort and the suggestion that “the use of a second clamp is not likely to significantly alter outcomes of stroke and mortality,” she wrote.
But their study leaves a few questions remaining, Dr. Lawton said. “What is the best treatment of high-risk patients who may benefit from limited aortic manipulation the most? Can two clamps be safely applied to all types of aortas? And does the risk of dissection go up with the use of two clamps?”
Although a randomized trial would be difficult because of the low risk of stroke in on-pump CABG, such a trial could answer those questions if it involved routine epiaortic ultrasound, Dr. Lawton said.
Dr. Lawton is professor of surgery in the division of cardiothoracic surgery at Washington University, St. Louis.
“A randomized trial is needed to answer the question, ‘Can CABG [coronary artery bypass grafting] be safely performed with either one or two aortic clamps in all patients?’ ” Dr. Jennifer S. Lawton said in her invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.05.002]).
Dr. Lawton acknowledged the positions that advocates of both techniques have staked out: advocates of the single-clamp (SC) technique prefer the ability to perform the proximal anastomoses without the added space constraints and reduced visibility of the partial clamp and moving heart; proponents of the partial-clamp (PC) method cite advantages in the ability to determine graft length with the full heart and the likelihood to reanimate the heart earlier to reduce the risk of a heart attack.
The PC technique required longer cardiopulmonary bypass time, 88.2 minutes vs. 73.7 minutes, but the SC group had longer cross-clamp times, 54.5. vs. 50.7 minutes. “The longer clamp time did not alter the outcomes reported (stroke and mortality) – although specific outcomes of myocardial injury including need for inotropes, troponin levels, myocardial infarction, etc. were not reported,” Dr. Lawton said. “Thus, the question for the surgeon is, ‘What is more important, the brain or the heart?’ ”
The results from Dr. Araque’s study “are valuable” because of the large patient cohort and the suggestion that “the use of a second clamp is not likely to significantly alter outcomes of stroke and mortality,” she wrote.
But their study leaves a few questions remaining, Dr. Lawton said. “What is the best treatment of high-risk patients who may benefit from limited aortic manipulation the most? Can two clamps be safely applied to all types of aortas? And does the risk of dissection go up with the use of two clamps?”
Although a randomized trial would be difficult because of the low risk of stroke in on-pump CABG, such a trial could answer those questions if it involved routine epiaortic ultrasound, Dr. Lawton said.
Dr. Lawton is professor of surgery in the division of cardiothoracic surgery at Washington University, St. Louis.
“A randomized trial is needed to answer the question, ‘Can CABG [coronary artery bypass grafting] be safely performed with either one or two aortic clamps in all patients?’ ” Dr. Jennifer S. Lawton said in her invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.05.002]).
Dr. Lawton acknowledged the positions that advocates of both techniques have staked out: advocates of the single-clamp (SC) technique prefer the ability to perform the proximal anastomoses without the added space constraints and reduced visibility of the partial clamp and moving heart; proponents of the partial-clamp (PC) method cite advantages in the ability to determine graft length with the full heart and the likelihood to reanimate the heart earlier to reduce the risk of a heart attack.
The PC technique required longer cardiopulmonary bypass time, 88.2 minutes vs. 73.7 minutes, but the SC group had longer cross-clamp times, 54.5. vs. 50.7 minutes. “The longer clamp time did not alter the outcomes reported (stroke and mortality) – although specific outcomes of myocardial injury including need for inotropes, troponin levels, myocardial infarction, etc. were not reported,” Dr. Lawton said. “Thus, the question for the surgeon is, ‘What is more important, the brain or the heart?’ ”
The results from Dr. Araque’s study “are valuable” because of the large patient cohort and the suggestion that “the use of a second clamp is not likely to significantly alter outcomes of stroke and mortality,” she wrote.
But their study leaves a few questions remaining, Dr. Lawton said. “What is the best treatment of high-risk patients who may benefit from limited aortic manipulation the most? Can two clamps be safely applied to all types of aortas? And does the risk of dissection go up with the use of two clamps?”
Although a randomized trial would be difficult because of the low risk of stroke in on-pump CABG, such a trial could answer those questions if it involved routine epiaortic ultrasound, Dr. Lawton said.
Dr. Lawton is professor of surgery in the division of cardiothoracic surgery at Washington University, St. Louis.
When performing on-pump coronary artery bypass grafting (CABG), cardiac surgeons can control very few factors to reduce the risk of stroke – with the exception of which method of aortic manipulation they use. Debate and controversy, however, have surrounded which aortic manipulation technique is best: single- or double-clamp occlusion.
A large retrospective study of almost 8,500 patients who had CABG at the Mayo Clinic in Rochester, Minn., over a 17-year period showed that, while use of the single-aortic cross-clamp (SC) technique steadily increased, the risk of stroke is virtually the same as it is with the partial aortic cross-clamp (PC), or double cross-clamp, technique. The study authors, led by Dr. Juan C. Araque, published their results online in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.04.010]).
“It is intuitive that less aortic manipulation would result in less risk of stroke,” Dr. Araque and colleagues said, but even off-pump CABG, which requires no aortic manipulation, is not without stroke risk.
“It is conceivable that there is some inherent risk of stroke associated with any cardiac operation, and that risk may increase with manipulation of the ascending aortic with the aortic cross clamp,” they wrote. “Our data would suggest, however, that the risk does not increase further with the additional aortic manipulation of the partial occlusion clamp.”
The study comes on the heels of a 2008 meta-analysis that found no benefit of SC in comparison to PC (Interact. Cardiovasc. Thorac. Surg. 2008;7:500-3), while another study in 2011 suggested that less aortic manipulation carried a significantly lower stroke risk (Heart Lung Circ. 2011;20:318-24).
The Mayo study evaluated the SC technique in 2,051 patients and PC in 6,446 patients who had isolated on-pump CABG between 1993 and 2010. The rate of stroke was 1.2% in the SC group and 1.5% among those who had PC. In two propensity-matched cohorts of 1,333 patients each, the stroke rate was 1.2% in each group. The investigators used the Society of Thoracic Surgeons’ risk calculator variables to create the propensity-matched cohorts.
The study group excluded high-risk patients, including those who had off-pump operations or previous cardiac surgeries or required replacement of a cross clamp during an unplanned operation.
The goal of the study was not to compare outcomes with the off-pump technique. “It is only to bring attention to the associated non-zero stroke rate with both techniques,” Dr. Araque and colleagues said.
Their findings are significant because on-pump CABG is the preferred operation of cardiac surgeons, accounting for more than 80% of the CABG operations in the SYNTAX study (N. Engl. J. Med. 2009;360:961-72). “The ‘anaortic’ off-pump technique may be a more specialized technique, representing less than 15% of operations in one large series,” Dr. Araque and coauthors said.
They acknowledged a few limitations resulting from the observational nature of the study, including that surgeons may have missed some strokes because they did not use a routine, standardized procedure for evaluating stroke signs along with the lack of documented assessment of the descending aorta. But they also stated that the large number of patients in the study, along with the use of propensity matching, addresses some of the bias inherent in an observational study.
The study authors disclosed no relationships.
When performing on-pump coronary artery bypass grafting (CABG), cardiac surgeons can control very few factors to reduce the risk of stroke – with the exception of which method of aortic manipulation they use. Debate and controversy, however, have surrounded which aortic manipulation technique is best: single- or double-clamp occlusion.
A large retrospective study of almost 8,500 patients who had CABG at the Mayo Clinic in Rochester, Minn., over a 17-year period showed that, while use of the single-aortic cross-clamp (SC) technique steadily increased, the risk of stroke is virtually the same as it is with the partial aortic cross-clamp (PC), or double cross-clamp, technique. The study authors, led by Dr. Juan C. Araque, published their results online in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.04.010]).
“It is intuitive that less aortic manipulation would result in less risk of stroke,” Dr. Araque and colleagues said, but even off-pump CABG, which requires no aortic manipulation, is not without stroke risk.
“It is conceivable that there is some inherent risk of stroke associated with any cardiac operation, and that risk may increase with manipulation of the ascending aortic with the aortic cross clamp,” they wrote. “Our data would suggest, however, that the risk does not increase further with the additional aortic manipulation of the partial occlusion clamp.”
The study comes on the heels of a 2008 meta-analysis that found no benefit of SC in comparison to PC (Interact. Cardiovasc. Thorac. Surg. 2008;7:500-3), while another study in 2011 suggested that less aortic manipulation carried a significantly lower stroke risk (Heart Lung Circ. 2011;20:318-24).
The Mayo study evaluated the SC technique in 2,051 patients and PC in 6,446 patients who had isolated on-pump CABG between 1993 and 2010. The rate of stroke was 1.2% in the SC group and 1.5% among those who had PC. In two propensity-matched cohorts of 1,333 patients each, the stroke rate was 1.2% in each group. The investigators used the Society of Thoracic Surgeons’ risk calculator variables to create the propensity-matched cohorts.
The study group excluded high-risk patients, including those who had off-pump operations or previous cardiac surgeries or required replacement of a cross clamp during an unplanned operation.
The goal of the study was not to compare outcomes with the off-pump technique. “It is only to bring attention to the associated non-zero stroke rate with both techniques,” Dr. Araque and colleagues said.
Their findings are significant because on-pump CABG is the preferred operation of cardiac surgeons, accounting for more than 80% of the CABG operations in the SYNTAX study (N. Engl. J. Med. 2009;360:961-72). “The ‘anaortic’ off-pump technique may be a more specialized technique, representing less than 15% of operations in one large series,” Dr. Araque and coauthors said.
They acknowledged a few limitations resulting from the observational nature of the study, including that surgeons may have missed some strokes because they did not use a routine, standardized procedure for evaluating stroke signs along with the lack of documented assessment of the descending aorta. But they also stated that the large number of patients in the study, along with the use of propensity matching, addresses some of the bias inherent in an observational study.
The study authors disclosed no relationships.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Two different approaches to aortic manipulation that surgeons use during on-pump coronary artery bypass graft surgery – single and double cross-clamp techniques – had similar rates of postoperative stroke.
Major finding: The single cross-clamp group had a stroke rate of 1.2% within 30 days of the operation, compared with 1.5% in the double cross-clamp group in unmatched cohorts.
Data source: Retrospective analysis of 8,497 patients treated with isolated on-pump coronary artery bypass grafting from 1993 to 2010.
Disclosures: The study authors reported having no financial disclosures.