User login
Point/Counterpoint: Mechanical vs. biological mitral valve for 50-year-old with rheumatic disease
Mechanical valve is the best choice
BY THORALF M. SUNDT III, M.D.
It’s not very sexy to talk about mechanical valves, but the reasons for placing a mechanical valve in a 50-year-old patient with rheumatic disease are obvious: Mechanical valves provide outstanding hemodynamics, they are beautifully engineered devices, their durability is beyond question, and, importantly, there’s no survival advantage to a biological prosthesis although one incurs the penalty of reoperation, which in a 50-year-old is going to be inevitable.
While this patient will have to continue on anticoagulation therapy with a mechanical valve, many patients who receive a biological valve, especially those with rheumatic disease, need anticoagulation for atrial fibrillation anyway. One can argue that a maze procedure might convert them to sinus rhythm, but this is least reproducible in the subset of patients with rheumatic disease. What’s more, the American Heart Association/American College of Cardiology Guideline for the Management of Patients With Valvular Heart Disease states that a mechanical prosthesis is reasonable for aortic or mitral valve replacement in patients aged 60 and younger with no contraindication to anticoagulation.
The fact that you have to use Coumadin (warfarin, Bristol-Myers Squibb), is not a condemnation of the mechanical valve; it just means we need to get smarter and better about how we manage anticoagulation in people with these prostheses.
While neither option is desirable, surprisingly morbidity with mechanical and biological valves is not demonstrably different. Stroke, embolic events, and bleeding complications have been found to be similar in numerous studies including a recent one authored by Dr. Vinay Badhwar and colleagues. Among 469 patients aged 65 years or younger who received a bileaflet mechanical prostheses or tissue valves, researchers found nearly identical rates of bleeding and thromboembolic complications when the anticoagulation was closely monitored (Ann. Thorac. Surg. 2012;93:748-53) Indeed, they even identified a mortality benefit among those with mechanical valves.
It’s also worth noting that the risk of anticoagulation-related complications is higher when the patient’s INR (international normalized ratio) is poorly controlled; up to 60% of INR values are outside the therapeutic range when thromboembolic complications occur. One can anticipate home INR testing and home management as ways to help patients stay within therapeutic range and reduce these risks. If the issue is anticoagulation, let’s improve it.
In summary, if you implant a biological valve in a 50-year-old patient, I guarantee that patient is going to be back for a reoperation and the prosthesis is going to deteriorate. For the surgeon, a biological valve can be an annuity of sorts. The mechanical valve has a clear advantage in durability, especially in younger patients.
Neither one is perfect, but there is no difference in morbidity between the two. A tissue prosthesis just buys you a reoperation – maybe valve-in-valve transcatheter valve. Maybe.
Dr. Sundt is chief of the division of cardiac surgery, Massachusetts General Hospital, Harvard Medical School, Boston. He is an adviser to Thrasos Innovation, but has no relevant relationships to disclose.
Why biological valve is the better choice
BY ANELECHI C. ANYANWU, M.D.
The reality is that whether you implant a mechanical or biological valve for mitral regurgitation, neither is good. The survival is poor. The half-life or median survival of a patient after either valve is about 15-20 years. The death rates are about 3% per year. The morbidity is high whether you have mechanical or biological valve, and none of them are good mitral substitutes.
Yet the biological valve is often a reasonable choice for a 50-year-old patient, despite studies that have shown a higher reoperation rate and decreased survival rate after biological mitral valve repair when compared to mechanical valve implantation in patients aged 65 and younger. But those study results may be skewed.
Dr. Tsuyoshi Kaneko and colleagues at Brigham and Women’s Hospital, Boston, showed that survival at about 20 years was much better with the mechanical valve. (J. Thorac. Cardiovasc. Surg. 2014;147:117-26). However, the difference in survival is greatest immediately after surgery. By 1 year the survival difference between mechanical valve and a tissue valve was more than 10%.
Why is this? I would argue this is a function of patient selection. We know in the United States that a patient with no insurance or low socioeconomic status does poorly compared to one who does have insurance. With a mechanical valve, they can thrombose; but with a biological valve, if they don’t take care of their health, of course they can die early. The reality is surgeons tend to use biological valves in patients of lower socioeconomic status and those with questionable compliance. None of these factors were considered in the propensity matching used in this study.
Dr. Joanna Chikwe and colleagues at Mount Sinai recently compared outcomes in several thousand patients who underwent biological or mechanical mitral valve replacement in New York State (JAMA 2015:323:1435-42). They found no survival difference in the first 30 or 90 days after surgery, or even at 15 years among patients aged 50-69 years. Indeed, a critical review of any study that has shown a survival advantage of the mechanical valve would find that the advantage occurred within the first few months after surgery, making it likely that such differences are due to patient selection, or other systematic bias, rather than a prostheses effect.
Mayo Clinic investigators, including Dr. Thoralf M. Sundt III, reported that among a cohort that received a mechanical valve, with an average age of 65 years, 16% had had a stroke at 5 years, compared with 8% of the biological valve group (J. Am. Coll. Cardiol. 2008;51:1203-11). You can only imagine what would happen at 10 or 20 years. They followed the data out to 10 years for thromboembolic events; that rate was 30% in the mechanical valve group. They concluded, “the mechanical valve is the least desirable correction of mitral regurgitation.”
As for managing anticoagulation, the literature provides no evidence that self-testing is superior to clinic testing. A trial published in the New England Journal of Medicine involving more than 2,000 patients, 700 of whom had a mechanical valve, showed a higher rate of stroke in patients who were randomized to home-INR monitoring compared with INR in the clinic. (N. Engl. J. Med. 2010;363:1608-20). Self-testing did not delay the time to first stroke, bleeding, or death.
Anticoagulation can be problematic if the patient needs to undergo another operation or medical procedure later, especially on an emergent basis. If the patient with a mechanical valve stops anticoagulation for even a short period of time, the risk of valve thrombosis is great. A patient with a biological valve can stop anticoagulation for a week or more without any consequence.
Finally, I relate the story of a man who could not bear the clicking sound of his mechanical valve. He asked for a new valve, but the surgeon would not take his request seriously. The man was taking drugs and started treatment for posttraumatic stress disorder. After 3 years, he killed himself. How many times have we sat down and talked to patients about what the clicking sound can do to them? Why don’t we make more of this? The patient should be given more choice.
Dr. Anyanwu is with the department of cardiac surgery, Mount Sinai Medical Center, New York. He has no relationships to disclose.
Mechanical valve is the best choice
BY THORALF M. SUNDT III, M.D.
It’s not very sexy to talk about mechanical valves, but the reasons for placing a mechanical valve in a 50-year-old patient with rheumatic disease are obvious: Mechanical valves provide outstanding hemodynamics, they are beautifully engineered devices, their durability is beyond question, and, importantly, there’s no survival advantage to a biological prosthesis although one incurs the penalty of reoperation, which in a 50-year-old is going to be inevitable.
While this patient will have to continue on anticoagulation therapy with a mechanical valve, many patients who receive a biological valve, especially those with rheumatic disease, need anticoagulation for atrial fibrillation anyway. One can argue that a maze procedure might convert them to sinus rhythm, but this is least reproducible in the subset of patients with rheumatic disease. What’s more, the American Heart Association/American College of Cardiology Guideline for the Management of Patients With Valvular Heart Disease states that a mechanical prosthesis is reasonable for aortic or mitral valve replacement in patients aged 60 and younger with no contraindication to anticoagulation.
The fact that you have to use Coumadin (warfarin, Bristol-Myers Squibb), is not a condemnation of the mechanical valve; it just means we need to get smarter and better about how we manage anticoagulation in people with these prostheses.
While neither option is desirable, surprisingly morbidity with mechanical and biological valves is not demonstrably different. Stroke, embolic events, and bleeding complications have been found to be similar in numerous studies including a recent one authored by Dr. Vinay Badhwar and colleagues. Among 469 patients aged 65 years or younger who received a bileaflet mechanical prostheses or tissue valves, researchers found nearly identical rates of bleeding and thromboembolic complications when the anticoagulation was closely monitored (Ann. Thorac. Surg. 2012;93:748-53) Indeed, they even identified a mortality benefit among those with mechanical valves.
It’s also worth noting that the risk of anticoagulation-related complications is higher when the patient’s INR (international normalized ratio) is poorly controlled; up to 60% of INR values are outside the therapeutic range when thromboembolic complications occur. One can anticipate home INR testing and home management as ways to help patients stay within therapeutic range and reduce these risks. If the issue is anticoagulation, let’s improve it.
In summary, if you implant a biological valve in a 50-year-old patient, I guarantee that patient is going to be back for a reoperation and the prosthesis is going to deteriorate. For the surgeon, a biological valve can be an annuity of sorts. The mechanical valve has a clear advantage in durability, especially in younger patients.
Neither one is perfect, but there is no difference in morbidity between the two. A tissue prosthesis just buys you a reoperation – maybe valve-in-valve transcatheter valve. Maybe.
Dr. Sundt is chief of the division of cardiac surgery, Massachusetts General Hospital, Harvard Medical School, Boston. He is an adviser to Thrasos Innovation, but has no relevant relationships to disclose.
Why biological valve is the better choice
BY ANELECHI C. ANYANWU, M.D.
The reality is that whether you implant a mechanical or biological valve for mitral regurgitation, neither is good. The survival is poor. The half-life or median survival of a patient after either valve is about 15-20 years. The death rates are about 3% per year. The morbidity is high whether you have mechanical or biological valve, and none of them are good mitral substitutes.
Yet the biological valve is often a reasonable choice for a 50-year-old patient, despite studies that have shown a higher reoperation rate and decreased survival rate after biological mitral valve repair when compared to mechanical valve implantation in patients aged 65 and younger. But those study results may be skewed.
Dr. Tsuyoshi Kaneko and colleagues at Brigham and Women’s Hospital, Boston, showed that survival at about 20 years was much better with the mechanical valve. (J. Thorac. Cardiovasc. Surg. 2014;147:117-26). However, the difference in survival is greatest immediately after surgery. By 1 year the survival difference between mechanical valve and a tissue valve was more than 10%.
Why is this? I would argue this is a function of patient selection. We know in the United States that a patient with no insurance or low socioeconomic status does poorly compared to one who does have insurance. With a mechanical valve, they can thrombose; but with a biological valve, if they don’t take care of their health, of course they can die early. The reality is surgeons tend to use biological valves in patients of lower socioeconomic status and those with questionable compliance. None of these factors were considered in the propensity matching used in this study.
Dr. Joanna Chikwe and colleagues at Mount Sinai recently compared outcomes in several thousand patients who underwent biological or mechanical mitral valve replacement in New York State (JAMA 2015:323:1435-42). They found no survival difference in the first 30 or 90 days after surgery, or even at 15 years among patients aged 50-69 years. Indeed, a critical review of any study that has shown a survival advantage of the mechanical valve would find that the advantage occurred within the first few months after surgery, making it likely that such differences are due to patient selection, or other systematic bias, rather than a prostheses effect.
Mayo Clinic investigators, including Dr. Thoralf M. Sundt III, reported that among a cohort that received a mechanical valve, with an average age of 65 years, 16% had had a stroke at 5 years, compared with 8% of the biological valve group (J. Am. Coll. Cardiol. 2008;51:1203-11). You can only imagine what would happen at 10 or 20 years. They followed the data out to 10 years for thromboembolic events; that rate was 30% in the mechanical valve group. They concluded, “the mechanical valve is the least desirable correction of mitral regurgitation.”
As for managing anticoagulation, the literature provides no evidence that self-testing is superior to clinic testing. A trial published in the New England Journal of Medicine involving more than 2,000 patients, 700 of whom had a mechanical valve, showed a higher rate of stroke in patients who were randomized to home-INR monitoring compared with INR in the clinic. (N. Engl. J. Med. 2010;363:1608-20). Self-testing did not delay the time to first stroke, bleeding, or death.
Anticoagulation can be problematic if the patient needs to undergo another operation or medical procedure later, especially on an emergent basis. If the patient with a mechanical valve stops anticoagulation for even a short period of time, the risk of valve thrombosis is great. A patient with a biological valve can stop anticoagulation for a week or more without any consequence.
Finally, I relate the story of a man who could not bear the clicking sound of his mechanical valve. He asked for a new valve, but the surgeon would not take his request seriously. The man was taking drugs and started treatment for posttraumatic stress disorder. After 3 years, he killed himself. How many times have we sat down and talked to patients about what the clicking sound can do to them? Why don’t we make more of this? The patient should be given more choice.
Dr. Anyanwu is with the department of cardiac surgery, Mount Sinai Medical Center, New York. He has no relationships to disclose.
Mechanical valve is the best choice
BY THORALF M. SUNDT III, M.D.
It’s not very sexy to talk about mechanical valves, but the reasons for placing a mechanical valve in a 50-year-old patient with rheumatic disease are obvious: Mechanical valves provide outstanding hemodynamics, they are beautifully engineered devices, their durability is beyond question, and, importantly, there’s no survival advantage to a biological prosthesis although one incurs the penalty of reoperation, which in a 50-year-old is going to be inevitable.
While this patient will have to continue on anticoagulation therapy with a mechanical valve, many patients who receive a biological valve, especially those with rheumatic disease, need anticoagulation for atrial fibrillation anyway. One can argue that a maze procedure might convert them to sinus rhythm, but this is least reproducible in the subset of patients with rheumatic disease. What’s more, the American Heart Association/American College of Cardiology Guideline for the Management of Patients With Valvular Heart Disease states that a mechanical prosthesis is reasonable for aortic or mitral valve replacement in patients aged 60 and younger with no contraindication to anticoagulation.
The fact that you have to use Coumadin (warfarin, Bristol-Myers Squibb), is not a condemnation of the mechanical valve; it just means we need to get smarter and better about how we manage anticoagulation in people with these prostheses.
While neither option is desirable, surprisingly morbidity with mechanical and biological valves is not demonstrably different. Stroke, embolic events, and bleeding complications have been found to be similar in numerous studies including a recent one authored by Dr. Vinay Badhwar and colleagues. Among 469 patients aged 65 years or younger who received a bileaflet mechanical prostheses or tissue valves, researchers found nearly identical rates of bleeding and thromboembolic complications when the anticoagulation was closely monitored (Ann. Thorac. Surg. 2012;93:748-53) Indeed, they even identified a mortality benefit among those with mechanical valves.
It’s also worth noting that the risk of anticoagulation-related complications is higher when the patient’s INR (international normalized ratio) is poorly controlled; up to 60% of INR values are outside the therapeutic range when thromboembolic complications occur. One can anticipate home INR testing and home management as ways to help patients stay within therapeutic range and reduce these risks. If the issue is anticoagulation, let’s improve it.
In summary, if you implant a biological valve in a 50-year-old patient, I guarantee that patient is going to be back for a reoperation and the prosthesis is going to deteriorate. For the surgeon, a biological valve can be an annuity of sorts. The mechanical valve has a clear advantage in durability, especially in younger patients.
Neither one is perfect, but there is no difference in morbidity between the two. A tissue prosthesis just buys you a reoperation – maybe valve-in-valve transcatheter valve. Maybe.
Dr. Sundt is chief of the division of cardiac surgery, Massachusetts General Hospital, Harvard Medical School, Boston. He is an adviser to Thrasos Innovation, but has no relevant relationships to disclose.
Why biological valve is the better choice
BY ANELECHI C. ANYANWU, M.D.
The reality is that whether you implant a mechanical or biological valve for mitral regurgitation, neither is good. The survival is poor. The half-life or median survival of a patient after either valve is about 15-20 years. The death rates are about 3% per year. The morbidity is high whether you have mechanical or biological valve, and none of them are good mitral substitutes.
Yet the biological valve is often a reasonable choice for a 50-year-old patient, despite studies that have shown a higher reoperation rate and decreased survival rate after biological mitral valve repair when compared to mechanical valve implantation in patients aged 65 and younger. But those study results may be skewed.
Dr. Tsuyoshi Kaneko and colleagues at Brigham and Women’s Hospital, Boston, showed that survival at about 20 years was much better with the mechanical valve. (J. Thorac. Cardiovasc. Surg. 2014;147:117-26). However, the difference in survival is greatest immediately after surgery. By 1 year the survival difference between mechanical valve and a tissue valve was more than 10%.
Why is this? I would argue this is a function of patient selection. We know in the United States that a patient with no insurance or low socioeconomic status does poorly compared to one who does have insurance. With a mechanical valve, they can thrombose; but with a biological valve, if they don’t take care of their health, of course they can die early. The reality is surgeons tend to use biological valves in patients of lower socioeconomic status and those with questionable compliance. None of these factors were considered in the propensity matching used in this study.
Dr. Joanna Chikwe and colleagues at Mount Sinai recently compared outcomes in several thousand patients who underwent biological or mechanical mitral valve replacement in New York State (JAMA 2015:323:1435-42). They found no survival difference in the first 30 or 90 days after surgery, or even at 15 years among patients aged 50-69 years. Indeed, a critical review of any study that has shown a survival advantage of the mechanical valve would find that the advantage occurred within the first few months after surgery, making it likely that such differences are due to patient selection, or other systematic bias, rather than a prostheses effect.
Mayo Clinic investigators, including Dr. Thoralf M. Sundt III, reported that among a cohort that received a mechanical valve, with an average age of 65 years, 16% had had a stroke at 5 years, compared with 8% of the biological valve group (J. Am. Coll. Cardiol. 2008;51:1203-11). You can only imagine what would happen at 10 or 20 years. They followed the data out to 10 years for thromboembolic events; that rate was 30% in the mechanical valve group. They concluded, “the mechanical valve is the least desirable correction of mitral regurgitation.”
As for managing anticoagulation, the literature provides no evidence that self-testing is superior to clinic testing. A trial published in the New England Journal of Medicine involving more than 2,000 patients, 700 of whom had a mechanical valve, showed a higher rate of stroke in patients who were randomized to home-INR monitoring compared with INR in the clinic. (N. Engl. J. Med. 2010;363:1608-20). Self-testing did not delay the time to first stroke, bleeding, or death.
Anticoagulation can be problematic if the patient needs to undergo another operation or medical procedure later, especially on an emergent basis. If the patient with a mechanical valve stops anticoagulation for even a short period of time, the risk of valve thrombosis is great. A patient with a biological valve can stop anticoagulation for a week or more without any consequence.
Finally, I relate the story of a man who could not bear the clicking sound of his mechanical valve. He asked for a new valve, but the surgeon would not take his request seriously. The man was taking drugs and started treatment for posttraumatic stress disorder. After 3 years, he killed himself. How many times have we sat down and talked to patients about what the clicking sound can do to them? Why don’t we make more of this? The patient should be given more choice.
Dr. Anyanwu is with the department of cardiac surgery, Mount Sinai Medical Center, New York. He has no relationships to disclose.
The ‘threats and obstacles’ facing TMVR
NEW YORK – What if correcting secondary mitral regurgitation doesn’t improve patients’ lives or helps them live longer? What if results of the COAPT trial of the MitraClip (Abbott Vascular) repair for mitral regurgitation are negative or inconclusive? What if transcatheter mitral valve repair works too well?
The answers to these questions could determine the future landscape of transcatheter mitral valve replacement (TMVR) for mitral regurgitation (MR) and the prosthetics in various stages of clinical and preclinical investigation, Dr. Michael Mack of Baylor University said at the 2015 Mitral Valve Conclave, which was sponsored by the American Association for Thoracic Surgery.
Dr. Mack reviewed the first four transcatheter mitral valve replacement devices approved for early feasibility studies in the United States, noting that “it has become a very crowded field very quickly,” especially when one considers that only between 20 and 50 TMVR procedures have been done worldwide up until now.
For the makers of the devices, it is becoming a potentially perilous field as well. Replacement, Dr. Mack said, does meet a “large clinical unmet need” in that it can completely correct mitral regurgitation better than valve repair.
“But what are the challenges for transcatheter mitral valve replacement and why isn’t this going to be the same as TAVR (transcatheter aortic valve replacement) all over again?” he said. “Unlike aortic stenosis, there is not a single cause of mitral regurgitation. In addition, it has never even been definitively proven that correcting MR helps prolong survival and improve quality of life.”
Another obstacle for TMVR is that delivery of the device into the mitral valve is more complex than doing so in the aortic valve. “The seating and the anchoring of the valve is more complex,” Dr. Mack said. “Based on the profile of the device, left ventricular outflow tract obstruction can be an issue, and perivalvular leak may carry more import here because mitral perivalvular leaks have the potential to cause hemololysis.”
He reviewed the four systems cleared for early feasibility studies.
CardiAQ (CardiAQ Valve Technologies), a porcine pericardial valve, has been implanted in eight patients worldwide and last month received Food and Drug Administration (FDA) approval for early feasibility study in 20 U.S. patients: 10 by a transfemoral approach and 10 by a transapical approach.
Tendyne Bioprosthetic Mitral Valve (Tendyne Holdings), a trileaflet porcine pericardium, also has been implanted in eight patients worldwide and was used for the first time in the United States last month by Dr. Wes Pederson and colleagues at the Minneapolis Heart Institute.
FORTIS (Edwards Lifesciences), a bovine pericardium valve, has been implanted in early feasibility trials in Europe and has been approved for an early feasibility trial of 15 patients in the United States.
Tiara (Neovasc), a D-shaped bovine pericardium valve, received FDA approval last year for the TIARA-I early feasibility trial in the United States (NCT02276547). The trial will enroll up to 30 patients worldwide.
At least five other TMVR devices are in preclinical studies, Dr. Mack said. These emerging devices face “threats and obstacles” as they move through the pipeline – a number of “what ifs,” Dr. Mack said.
“What if you can’t prove that correcting secondary mitral regurgitation makes a difference? What are the repercussions of the COAPT Trial (NCT01626079) of the MitraClip if it is positive and shows that correcting mitral regurgitation does make a difference? Does completely correcting mitral regurgitation then really make a difference? What if transcatheter mitral valve repair works too well?” (COAPT stands for Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation). “With the excellent safety profile of MitraClip, it may be hard to justify TMVR,” he said.
Dr. Mack noted that MitraClip for mitral valve repair has “a superb safety profile.” He added, “How do you choose what patients should be treated by a mitral valve replacement vs. a MitraClip by a transfemoral venous approach that enables them to go home the next day?”
The early feasibility trials of TMVR devices may point a way to answers.
Dr. Mack has received research grants from Edwards Lifesciences. He is a principal investigator in the ongoing COAPT Trial, which is sponsored by EVALVE with the collaboration of Abbott Vascular.
NEW YORK – What if correcting secondary mitral regurgitation doesn’t improve patients’ lives or helps them live longer? What if results of the COAPT trial of the MitraClip (Abbott Vascular) repair for mitral regurgitation are negative or inconclusive? What if transcatheter mitral valve repair works too well?
The answers to these questions could determine the future landscape of transcatheter mitral valve replacement (TMVR) for mitral regurgitation (MR) and the prosthetics in various stages of clinical and preclinical investigation, Dr. Michael Mack of Baylor University said at the 2015 Mitral Valve Conclave, which was sponsored by the American Association for Thoracic Surgery.
Dr. Mack reviewed the first four transcatheter mitral valve replacement devices approved for early feasibility studies in the United States, noting that “it has become a very crowded field very quickly,” especially when one considers that only between 20 and 50 TMVR procedures have been done worldwide up until now.
For the makers of the devices, it is becoming a potentially perilous field as well. Replacement, Dr. Mack said, does meet a “large clinical unmet need” in that it can completely correct mitral regurgitation better than valve repair.
“But what are the challenges for transcatheter mitral valve replacement and why isn’t this going to be the same as TAVR (transcatheter aortic valve replacement) all over again?” he said. “Unlike aortic stenosis, there is not a single cause of mitral regurgitation. In addition, it has never even been definitively proven that correcting MR helps prolong survival and improve quality of life.”
Another obstacle for TMVR is that delivery of the device into the mitral valve is more complex than doing so in the aortic valve. “The seating and the anchoring of the valve is more complex,” Dr. Mack said. “Based on the profile of the device, left ventricular outflow tract obstruction can be an issue, and perivalvular leak may carry more import here because mitral perivalvular leaks have the potential to cause hemololysis.”
He reviewed the four systems cleared for early feasibility studies.
CardiAQ (CardiAQ Valve Technologies), a porcine pericardial valve, has been implanted in eight patients worldwide and last month received Food and Drug Administration (FDA) approval for early feasibility study in 20 U.S. patients: 10 by a transfemoral approach and 10 by a transapical approach.
Tendyne Bioprosthetic Mitral Valve (Tendyne Holdings), a trileaflet porcine pericardium, also has been implanted in eight patients worldwide and was used for the first time in the United States last month by Dr. Wes Pederson and colleagues at the Minneapolis Heart Institute.
FORTIS (Edwards Lifesciences), a bovine pericardium valve, has been implanted in early feasibility trials in Europe and has been approved for an early feasibility trial of 15 patients in the United States.
Tiara (Neovasc), a D-shaped bovine pericardium valve, received FDA approval last year for the TIARA-I early feasibility trial in the United States (NCT02276547). The trial will enroll up to 30 patients worldwide.
At least five other TMVR devices are in preclinical studies, Dr. Mack said. These emerging devices face “threats and obstacles” as they move through the pipeline – a number of “what ifs,” Dr. Mack said.
“What if you can’t prove that correcting secondary mitral regurgitation makes a difference? What are the repercussions of the COAPT Trial (NCT01626079) of the MitraClip if it is positive and shows that correcting mitral regurgitation does make a difference? Does completely correcting mitral regurgitation then really make a difference? What if transcatheter mitral valve repair works too well?” (COAPT stands for Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation). “With the excellent safety profile of MitraClip, it may be hard to justify TMVR,” he said.
Dr. Mack noted that MitraClip for mitral valve repair has “a superb safety profile.” He added, “How do you choose what patients should be treated by a mitral valve replacement vs. a MitraClip by a transfemoral venous approach that enables them to go home the next day?”
The early feasibility trials of TMVR devices may point a way to answers.
Dr. Mack has received research grants from Edwards Lifesciences. He is a principal investigator in the ongoing COAPT Trial, which is sponsored by EVALVE with the collaboration of Abbott Vascular.
NEW YORK – What if correcting secondary mitral regurgitation doesn’t improve patients’ lives or helps them live longer? What if results of the COAPT trial of the MitraClip (Abbott Vascular) repair for mitral regurgitation are negative or inconclusive? What if transcatheter mitral valve repair works too well?
The answers to these questions could determine the future landscape of transcatheter mitral valve replacement (TMVR) for mitral regurgitation (MR) and the prosthetics in various stages of clinical and preclinical investigation, Dr. Michael Mack of Baylor University said at the 2015 Mitral Valve Conclave, which was sponsored by the American Association for Thoracic Surgery.
Dr. Mack reviewed the first four transcatheter mitral valve replacement devices approved for early feasibility studies in the United States, noting that “it has become a very crowded field very quickly,” especially when one considers that only between 20 and 50 TMVR procedures have been done worldwide up until now.
For the makers of the devices, it is becoming a potentially perilous field as well. Replacement, Dr. Mack said, does meet a “large clinical unmet need” in that it can completely correct mitral regurgitation better than valve repair.
“But what are the challenges for transcatheter mitral valve replacement and why isn’t this going to be the same as TAVR (transcatheter aortic valve replacement) all over again?” he said. “Unlike aortic stenosis, there is not a single cause of mitral regurgitation. In addition, it has never even been definitively proven that correcting MR helps prolong survival and improve quality of life.”
Another obstacle for TMVR is that delivery of the device into the mitral valve is more complex than doing so in the aortic valve. “The seating and the anchoring of the valve is more complex,” Dr. Mack said. “Based on the profile of the device, left ventricular outflow tract obstruction can be an issue, and perivalvular leak may carry more import here because mitral perivalvular leaks have the potential to cause hemololysis.”
He reviewed the four systems cleared for early feasibility studies.
CardiAQ (CardiAQ Valve Technologies), a porcine pericardial valve, has been implanted in eight patients worldwide and last month received Food and Drug Administration (FDA) approval for early feasibility study in 20 U.S. patients: 10 by a transfemoral approach and 10 by a transapical approach.
Tendyne Bioprosthetic Mitral Valve (Tendyne Holdings), a trileaflet porcine pericardium, also has been implanted in eight patients worldwide and was used for the first time in the United States last month by Dr. Wes Pederson and colleagues at the Minneapolis Heart Institute.
FORTIS (Edwards Lifesciences), a bovine pericardium valve, has been implanted in early feasibility trials in Europe and has been approved for an early feasibility trial of 15 patients in the United States.
Tiara (Neovasc), a D-shaped bovine pericardium valve, received FDA approval last year for the TIARA-I early feasibility trial in the United States (NCT02276547). The trial will enroll up to 30 patients worldwide.
At least five other TMVR devices are in preclinical studies, Dr. Mack said. These emerging devices face “threats and obstacles” as they move through the pipeline – a number of “what ifs,” Dr. Mack said.
“What if you can’t prove that correcting secondary mitral regurgitation makes a difference? What are the repercussions of the COAPT Trial (NCT01626079) of the MitraClip if it is positive and shows that correcting mitral regurgitation does make a difference? Does completely correcting mitral regurgitation then really make a difference? What if transcatheter mitral valve repair works too well?” (COAPT stands for Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation). “With the excellent safety profile of MitraClip, it may be hard to justify TMVR,” he said.
Dr. Mack noted that MitraClip for mitral valve repair has “a superb safety profile.” He added, “How do you choose what patients should be treated by a mitral valve replacement vs. a MitraClip by a transfemoral venous approach that enables them to go home the next day?”
The early feasibility trials of TMVR devices may point a way to answers.
Dr. Mack has received research grants from Edwards Lifesciences. He is a principal investigator in the ongoing COAPT Trial, which is sponsored by EVALVE with the collaboration of Abbott Vascular.
EXPERT ANALYSIS FROM THE 2015 MITRAL VALVE CONCLAVE
AATS: Spare the aortic valve when possible during aortic root replacements
SEATTLE – Aortic valve–sparing procedures have better outcomes than Bentall procedures with biologic or mechanical valves, according to a review of 1,187 aortic root cases at the University of Toronto.
“If the aortic valve can be spared, AVS [aortic valve–sparing] procedures should be considered for patients undergoing aortic root replacement,” concluded the investigators, led by Dr. Maral Ouzounian, a cardiovascular surgeon at the university.
The team reviewed surgical outcomes there from 1990 to 2010; 282 patients had AVS procedures, 562 had Bentall procedures with biologic valve replacements (b-Bentall); and 343 had Bentalls with mechanical valve replacements (m-Bentall). About 7.5% of AVS patients had bicuspid aortic valves, versus 67.6% in the b-Bentall group and 51.7% in the m-Bentall group.
To control for confounders, patients were matched into 185 triads based on age, year of surgery, and stage of heart failure. The surgeries were all elective; patients with endocarditis or aortic dissections were excluded from the analysis.
Early postoperative outcomes and overall long-term survival were similar between the groups, with about 80% of patients in all three alive at 15-year follow-up.
However, AVS procedures had better long-term freedom from cardiac death (95% at 15 years versus 93% in the b-Bentall and 90% in the m-Bentall groups). Also, AVS patients had lower rates of anticoagulant-related hemorrhages, compared with m-Bentall patients (3.2% versus 17.8%), and lower rates of structural valve deterioration (0% versus 6.5%) and reoperations (6.5% versus 13.5%) than b-Bentall patients. The differences were statistically significant.
About 5% of AVS patients had previous cardiac surgery, versus 12.4% in the b-Bentall and 36.2% in the m-Bentall groups. AVS patients were more likely to have Marfan syndrome, and about 8% of AVS patients had preoperative ejection fractions below 40%, versus 9.3% in the b-Bentall and 13% in the m-Bentall groups. There were no between-group differences in the rates of concomitant coronary bypass or mitral valve surgery. Patients were about 50 years old on average, and about 80% were men.
“In Toronto, we are quite aggressive with valve-sparing operations. We believe in this operation, so whenever we can spare the valve, we do.” Although valve-sparing procedures have become more common in large, high-volume surgery centers over the past 20 years, “community surgeons in small-volume centers are still much more likely to do a Bentall because of the complexity of AVS operations and the art it takes to get it right,” Dr. Ouzounian said at the annual meeting of the American Association for Thoracic Surgery.
Previous investigations have found benefits for AVS procedures, as well. One concluded that “there is no significant difference in terms of re-operation between patients, who presented with [bicuspid or tricuspid aortic valves]. Re-operation rates are higher for patients who presented with severe [aortic regurgitation], but these rates do not reach statistical significance. Hence, root replacement with aortic valve sparing should be offered even in the presence of a” bicuspid aortic valve or severe aortic regurgitation (Eur. J. Cardiothorac. Surg. 2010;38:515-22).
Dr. Ouzounian said she has no disclosures.
SEATTLE – Aortic valve–sparing procedures have better outcomes than Bentall procedures with biologic or mechanical valves, according to a review of 1,187 aortic root cases at the University of Toronto.
“If the aortic valve can be spared, AVS [aortic valve–sparing] procedures should be considered for patients undergoing aortic root replacement,” concluded the investigators, led by Dr. Maral Ouzounian, a cardiovascular surgeon at the university.
The team reviewed surgical outcomes there from 1990 to 2010; 282 patients had AVS procedures, 562 had Bentall procedures with biologic valve replacements (b-Bentall); and 343 had Bentalls with mechanical valve replacements (m-Bentall). About 7.5% of AVS patients had bicuspid aortic valves, versus 67.6% in the b-Bentall group and 51.7% in the m-Bentall group.
To control for confounders, patients were matched into 185 triads based on age, year of surgery, and stage of heart failure. The surgeries were all elective; patients with endocarditis or aortic dissections were excluded from the analysis.
Early postoperative outcomes and overall long-term survival were similar between the groups, with about 80% of patients in all three alive at 15-year follow-up.
However, AVS procedures had better long-term freedom from cardiac death (95% at 15 years versus 93% in the b-Bentall and 90% in the m-Bentall groups). Also, AVS patients had lower rates of anticoagulant-related hemorrhages, compared with m-Bentall patients (3.2% versus 17.8%), and lower rates of structural valve deterioration (0% versus 6.5%) and reoperations (6.5% versus 13.5%) than b-Bentall patients. The differences were statistically significant.
About 5% of AVS patients had previous cardiac surgery, versus 12.4% in the b-Bentall and 36.2% in the m-Bentall groups. AVS patients were more likely to have Marfan syndrome, and about 8% of AVS patients had preoperative ejection fractions below 40%, versus 9.3% in the b-Bentall and 13% in the m-Bentall groups. There were no between-group differences in the rates of concomitant coronary bypass or mitral valve surgery. Patients were about 50 years old on average, and about 80% were men.
“In Toronto, we are quite aggressive with valve-sparing operations. We believe in this operation, so whenever we can spare the valve, we do.” Although valve-sparing procedures have become more common in large, high-volume surgery centers over the past 20 years, “community surgeons in small-volume centers are still much more likely to do a Bentall because of the complexity of AVS operations and the art it takes to get it right,” Dr. Ouzounian said at the annual meeting of the American Association for Thoracic Surgery.
Previous investigations have found benefits for AVS procedures, as well. One concluded that “there is no significant difference in terms of re-operation between patients, who presented with [bicuspid or tricuspid aortic valves]. Re-operation rates are higher for patients who presented with severe [aortic regurgitation], but these rates do not reach statistical significance. Hence, root replacement with aortic valve sparing should be offered even in the presence of a” bicuspid aortic valve or severe aortic regurgitation (Eur. J. Cardiothorac. Surg. 2010;38:515-22).
Dr. Ouzounian said she has no disclosures.
SEATTLE – Aortic valve–sparing procedures have better outcomes than Bentall procedures with biologic or mechanical valves, according to a review of 1,187 aortic root cases at the University of Toronto.
“If the aortic valve can be spared, AVS [aortic valve–sparing] procedures should be considered for patients undergoing aortic root replacement,” concluded the investigators, led by Dr. Maral Ouzounian, a cardiovascular surgeon at the university.
The team reviewed surgical outcomes there from 1990 to 2010; 282 patients had AVS procedures, 562 had Bentall procedures with biologic valve replacements (b-Bentall); and 343 had Bentalls with mechanical valve replacements (m-Bentall). About 7.5% of AVS patients had bicuspid aortic valves, versus 67.6% in the b-Bentall group and 51.7% in the m-Bentall group.
To control for confounders, patients were matched into 185 triads based on age, year of surgery, and stage of heart failure. The surgeries were all elective; patients with endocarditis or aortic dissections were excluded from the analysis.
Early postoperative outcomes and overall long-term survival were similar between the groups, with about 80% of patients in all three alive at 15-year follow-up.
However, AVS procedures had better long-term freedom from cardiac death (95% at 15 years versus 93% in the b-Bentall and 90% in the m-Bentall groups). Also, AVS patients had lower rates of anticoagulant-related hemorrhages, compared with m-Bentall patients (3.2% versus 17.8%), and lower rates of structural valve deterioration (0% versus 6.5%) and reoperations (6.5% versus 13.5%) than b-Bentall patients. The differences were statistically significant.
About 5% of AVS patients had previous cardiac surgery, versus 12.4% in the b-Bentall and 36.2% in the m-Bentall groups. AVS patients were more likely to have Marfan syndrome, and about 8% of AVS patients had preoperative ejection fractions below 40%, versus 9.3% in the b-Bentall and 13% in the m-Bentall groups. There were no between-group differences in the rates of concomitant coronary bypass or mitral valve surgery. Patients were about 50 years old on average, and about 80% were men.
“In Toronto, we are quite aggressive with valve-sparing operations. We believe in this operation, so whenever we can spare the valve, we do.” Although valve-sparing procedures have become more common in large, high-volume surgery centers over the past 20 years, “community surgeons in small-volume centers are still much more likely to do a Bentall because of the complexity of AVS operations and the art it takes to get it right,” Dr. Ouzounian said at the annual meeting of the American Association for Thoracic Surgery.
Previous investigations have found benefits for AVS procedures, as well. One concluded that “there is no significant difference in terms of re-operation between patients, who presented with [bicuspid or tricuspid aortic valves]. Re-operation rates are higher for patients who presented with severe [aortic regurgitation], but these rates do not reach statistical significance. Hence, root replacement with aortic valve sparing should be offered even in the presence of a” bicuspid aortic valve or severe aortic regurgitation (Eur. J. Cardiothorac. Surg. 2010;38:515-22).
Dr. Ouzounian said she has no disclosures.
AT THE AATS ANNUAL MEETING
Key clinical point: Your patients will do better with aortic valve–sparing procedures.
Major finding: Aortic valve–sparing procedures are associated with improved long-term freedom from cardiac death (95% at 15 years) when compared with Bentall procedures with biologic valves (93% freedom from cardiac death at 15 years) or mechanical valves (90% freedom at 15 years).
Data source: Review of 1,187 aortic root replacements at the University of Toronto.
Disclosures: The lead investigator has no disclosures.
AATS: No postpneumonectomy survival benefit in adding radiation to chemotherapy for NSCLC
SEATTLE – Adding radiotherapy to neoadjuvant chemotherapy does not improve long-term survival after pneumonectomy for non–small cell lung cancer, according to a Turkish investigation of 140 patients.
In the study, 100 (71.4%) patients had two to six cycles of platinum-based chemotherapy at least 3 weeks before surgery; 40 (28.6%) others underwent the same regimen with the addition of radiotherapy dosed at 45-66 Gy 6-8 weeks before surgery.
Five-year survival was 48% in the chemotherapy group and 50% in the chemoradiation group, an insignificant difference (P = .7).
“Chemotherapy before surgery is definitely beneficial, but I think we will get rid of the radiotherapy” in patients with operable tumors, said lead investigator Dr. Cengiz Gebitekin, professor and head of thoracic surgery at Uludag University in Bursa, Turkey.
“It does not provide any survival benefit,” and it might cause harm, he noted, adding that “the benefit of neoadjuvant treatment comes from the chemotherapy.”
The chemoradiation group showed a tendency toward tumor down-staging and higher complete response rates, but also a trend toward more radiation-induced tissue damage. The rate of bronchopleural fistula was 3% in the chemotherapy group and 5% in the chemoradiation group, although the difference was not significant. Even so, “some of these patients had pneumonectomies because of lung damage from the radiotherapy,” Dr. Gebitekin said at the annual meeting of the American Association for Thoracic Surgery.
It’s uncertain why radiation didn’t improve survival. The investigators excluded patients with known metastases or other malignancies, but it’s possible that some patients had occult metastases that had spread beyond the field of their localized neoadjuvant radiation, he said.
The patients were treated between 2000 and 2013 at Uludag University, Istanbul University, and Zurich University Hospital. They were 55 years old on average, and 84% were men.
About 40% of patients in both the chemotherapy and chemoradiation groups had right pneumonectomies; the rest had left pneumonectomies. Bronchopleural fistulas and other comorbidities were more common after right pneumonectomies, but not significantly so.
Seven patients (5%) in the chemotherapy group but none in the chemoradiation group died within 90 days of surgery.
About 32% of chemotherapy patients and 28% of chemoradiation patients (P = .6) developed major morbidities following surgery, including arrhythmias, pneumonia, empyema, and other problems.
Staples were used to close the bronchus in almost all patients, with the stump covered with live tissue in about 70%.
The majority of patients had stage IIb or IIIa disease on postop staging; postop staging was the only factor predictive of long-term survival, with higher-stage patients doing worse.
Dr. Gebitekin said that he had no relevant disclosures.
SEATTLE – Adding radiotherapy to neoadjuvant chemotherapy does not improve long-term survival after pneumonectomy for non–small cell lung cancer, according to a Turkish investigation of 140 patients.
In the study, 100 (71.4%) patients had two to six cycles of platinum-based chemotherapy at least 3 weeks before surgery; 40 (28.6%) others underwent the same regimen with the addition of radiotherapy dosed at 45-66 Gy 6-8 weeks before surgery.
Five-year survival was 48% in the chemotherapy group and 50% in the chemoradiation group, an insignificant difference (P = .7).
“Chemotherapy before surgery is definitely beneficial, but I think we will get rid of the radiotherapy” in patients with operable tumors, said lead investigator Dr. Cengiz Gebitekin, professor and head of thoracic surgery at Uludag University in Bursa, Turkey.
“It does not provide any survival benefit,” and it might cause harm, he noted, adding that “the benefit of neoadjuvant treatment comes from the chemotherapy.”
The chemoradiation group showed a tendency toward tumor down-staging and higher complete response rates, but also a trend toward more radiation-induced tissue damage. The rate of bronchopleural fistula was 3% in the chemotherapy group and 5% in the chemoradiation group, although the difference was not significant. Even so, “some of these patients had pneumonectomies because of lung damage from the radiotherapy,” Dr. Gebitekin said at the annual meeting of the American Association for Thoracic Surgery.
It’s uncertain why radiation didn’t improve survival. The investigators excluded patients with known metastases or other malignancies, but it’s possible that some patients had occult metastases that had spread beyond the field of their localized neoadjuvant radiation, he said.
The patients were treated between 2000 and 2013 at Uludag University, Istanbul University, and Zurich University Hospital. They were 55 years old on average, and 84% were men.
About 40% of patients in both the chemotherapy and chemoradiation groups had right pneumonectomies; the rest had left pneumonectomies. Bronchopleural fistulas and other comorbidities were more common after right pneumonectomies, but not significantly so.
Seven patients (5%) in the chemotherapy group but none in the chemoradiation group died within 90 days of surgery.
About 32% of chemotherapy patients and 28% of chemoradiation patients (P = .6) developed major morbidities following surgery, including arrhythmias, pneumonia, empyema, and other problems.
Staples were used to close the bronchus in almost all patients, with the stump covered with live tissue in about 70%.
The majority of patients had stage IIb or IIIa disease on postop staging; postop staging was the only factor predictive of long-term survival, with higher-stage patients doing worse.
Dr. Gebitekin said that he had no relevant disclosures.
SEATTLE – Adding radiotherapy to neoadjuvant chemotherapy does not improve long-term survival after pneumonectomy for non–small cell lung cancer, according to a Turkish investigation of 140 patients.
In the study, 100 (71.4%) patients had two to six cycles of platinum-based chemotherapy at least 3 weeks before surgery; 40 (28.6%) others underwent the same regimen with the addition of radiotherapy dosed at 45-66 Gy 6-8 weeks before surgery.
Five-year survival was 48% in the chemotherapy group and 50% in the chemoradiation group, an insignificant difference (P = .7).
“Chemotherapy before surgery is definitely beneficial, but I think we will get rid of the radiotherapy” in patients with operable tumors, said lead investigator Dr. Cengiz Gebitekin, professor and head of thoracic surgery at Uludag University in Bursa, Turkey.
“It does not provide any survival benefit,” and it might cause harm, he noted, adding that “the benefit of neoadjuvant treatment comes from the chemotherapy.”
The chemoradiation group showed a tendency toward tumor down-staging and higher complete response rates, but also a trend toward more radiation-induced tissue damage. The rate of bronchopleural fistula was 3% in the chemotherapy group and 5% in the chemoradiation group, although the difference was not significant. Even so, “some of these patients had pneumonectomies because of lung damage from the radiotherapy,” Dr. Gebitekin said at the annual meeting of the American Association for Thoracic Surgery.
It’s uncertain why radiation didn’t improve survival. The investigators excluded patients with known metastases or other malignancies, but it’s possible that some patients had occult metastases that had spread beyond the field of their localized neoadjuvant radiation, he said.
The patients were treated between 2000 and 2013 at Uludag University, Istanbul University, and Zurich University Hospital. They were 55 years old on average, and 84% were men.
About 40% of patients in both the chemotherapy and chemoradiation groups had right pneumonectomies; the rest had left pneumonectomies. Bronchopleural fistulas and other comorbidities were more common after right pneumonectomies, but not significantly so.
Seven patients (5%) in the chemotherapy group but none in the chemoradiation group died within 90 days of surgery.
About 32% of chemotherapy patients and 28% of chemoradiation patients (P = .6) developed major morbidities following surgery, including arrhythmias, pneumonia, empyema, and other problems.
Staples were used to close the bronchus in almost all patients, with the stump covered with live tissue in about 70%.
The majority of patients had stage IIb or IIIa disease on postop staging; postop staging was the only factor predictive of long-term survival, with higher-stage patients doing worse.
Dr. Gebitekin said that he had no relevant disclosures.
AT THE AATS ANNUAL MEETING
Key clinical point: Limit neoadjuvant treatment to chemotherapy for non–small cell lung cancer patients.
Major finding: About half of patients were alive 5 years after pneumonectomies for lung cancer, whether they had neoadjuvant chemotherapy or chemoradiation.
Data source: Retrospective study of 140 pneumonectomy patients.
Disclosures: Dr. Gebitekin had no disclosures.
AATS: Avoid mass ligation of the thoracic duct during esophagectomy
SEATTLE – Thoracic duct ligation did not seem to prevent chylothorax in a review of 827 esophagectomy cases at Brigham and Women’s Hospital in Boston.
In fact, chylothorax was most likely in patients who had mass ligation of the duct and its surrounding soft tissue, instead of ligation of simply the duct itself.
The results are surprising because ligation is actually meant to prevent chylothorax, but “it didn’t serve that purpose,” said lead investigator Dr. Yifan Zheng, a clinical research fellow at the hospital.
Results have been mixed in previous studies of ligation, with some finding benefit for preventing chylothorax but others not. With contradictory evidence, some surgeons – including some in the Brigham and Women’s review, which covered 11 years of data – opt for routine ligation, while others don’t, Dr. Zheng said at the annual meeting of the American Association for Thoracic Surgery.
At this point, “if you see the thoracic duct and you have concerns about ductal injury, your best bet is to ligate the duct directly. We observed in our series that there is a significantly higher incidence of chylothorax” with mass ligation, she said.
Of the 827 esophagectomies, 635 were performed without thoracic duct ligation; 33 (5.2%) cases developed postop chylothorax. Among the 56 cases with explicit identification and ligation of the thoracic duct alone, chylothorax developed in four (7.1%). There were 136 esophagectomies with mass ligation; 27 (19.9%) developed chylothorax (P = .0314).
The majority of the ligations were performed during open procedures. Mass ligations were mostly done with surgical sutures, while clips were used for direct ductal ligations. It’s likely that surgeons opted for direct ligation when they could see the duct and mass ligation when they could not.
Esophagectomy patients in the study were largely the same, so it’s unclear why some were ligated but others were not. About 75% in both groups had adenocarcinomas, most of which were in the distal esophagus or gastroesophageal junction. About half of the ligated group had preop chemoradiation, versus about 60% in the nonligated group.
Patients who developed postop chyle leaks were also similar, whether or not they were ligated. Most had adenocarcinomas in the distal esophagus or gastroesophageal junction, and the majority had received neoadjuvant therapy. “It’s unlikely that operative approach influenced the development of chylothorax,” Dr. Zheng said.
Both ligated and nonligated patients responded well to chylothorax management. Of the 64 total cases, 28 were successfully treated by thoracic duct embolization and 20 were successfully treated by operative thoracic duct ligation. In 10 cases, thoracic duct embolization was attempted but unsuccessful and all were successfully treated with operative ligation. Six cases were managed with chest tube drainage and total parenteral nutrition. It is possible that patients were ligated because they appeared during surgery to be at risk for postop chylothorax, which would help explain the findings.
It also is possible, however, that ligation itself – especially mass ligation – increases the risk. “The thoracic duct is a high-pressure system, so [blocking it] could create a pressure buildup and a potential leak,” Dr. Zheng said. That might be especially true with mass ligation, when both the thoracic duct and its tributaries are tied off.
Dr. Zheng said that she had no relevant disclosures.
SEATTLE – Thoracic duct ligation did not seem to prevent chylothorax in a review of 827 esophagectomy cases at Brigham and Women’s Hospital in Boston.
In fact, chylothorax was most likely in patients who had mass ligation of the duct and its surrounding soft tissue, instead of ligation of simply the duct itself.
The results are surprising because ligation is actually meant to prevent chylothorax, but “it didn’t serve that purpose,” said lead investigator Dr. Yifan Zheng, a clinical research fellow at the hospital.
Results have been mixed in previous studies of ligation, with some finding benefit for preventing chylothorax but others not. With contradictory evidence, some surgeons – including some in the Brigham and Women’s review, which covered 11 years of data – opt for routine ligation, while others don’t, Dr. Zheng said at the annual meeting of the American Association for Thoracic Surgery.
At this point, “if you see the thoracic duct and you have concerns about ductal injury, your best bet is to ligate the duct directly. We observed in our series that there is a significantly higher incidence of chylothorax” with mass ligation, she said.
Of the 827 esophagectomies, 635 were performed without thoracic duct ligation; 33 (5.2%) cases developed postop chylothorax. Among the 56 cases with explicit identification and ligation of the thoracic duct alone, chylothorax developed in four (7.1%). There were 136 esophagectomies with mass ligation; 27 (19.9%) developed chylothorax (P = .0314).
The majority of the ligations were performed during open procedures. Mass ligations were mostly done with surgical sutures, while clips were used for direct ductal ligations. It’s likely that surgeons opted for direct ligation when they could see the duct and mass ligation when they could not.
Esophagectomy patients in the study were largely the same, so it’s unclear why some were ligated but others were not. About 75% in both groups had adenocarcinomas, most of which were in the distal esophagus or gastroesophageal junction. About half of the ligated group had preop chemoradiation, versus about 60% in the nonligated group.
Patients who developed postop chyle leaks were also similar, whether or not they were ligated. Most had adenocarcinomas in the distal esophagus or gastroesophageal junction, and the majority had received neoadjuvant therapy. “It’s unlikely that operative approach influenced the development of chylothorax,” Dr. Zheng said.
Both ligated and nonligated patients responded well to chylothorax management. Of the 64 total cases, 28 were successfully treated by thoracic duct embolization and 20 were successfully treated by operative thoracic duct ligation. In 10 cases, thoracic duct embolization was attempted but unsuccessful and all were successfully treated with operative ligation. Six cases were managed with chest tube drainage and total parenteral nutrition. It is possible that patients were ligated because they appeared during surgery to be at risk for postop chylothorax, which would help explain the findings.
It also is possible, however, that ligation itself – especially mass ligation – increases the risk. “The thoracic duct is a high-pressure system, so [blocking it] could create a pressure buildup and a potential leak,” Dr. Zheng said. That might be especially true with mass ligation, when both the thoracic duct and its tributaries are tied off.
Dr. Zheng said that she had no relevant disclosures.
SEATTLE – Thoracic duct ligation did not seem to prevent chylothorax in a review of 827 esophagectomy cases at Brigham and Women’s Hospital in Boston.
In fact, chylothorax was most likely in patients who had mass ligation of the duct and its surrounding soft tissue, instead of ligation of simply the duct itself.
The results are surprising because ligation is actually meant to prevent chylothorax, but “it didn’t serve that purpose,” said lead investigator Dr. Yifan Zheng, a clinical research fellow at the hospital.
Results have been mixed in previous studies of ligation, with some finding benefit for preventing chylothorax but others not. With contradictory evidence, some surgeons – including some in the Brigham and Women’s review, which covered 11 years of data – opt for routine ligation, while others don’t, Dr. Zheng said at the annual meeting of the American Association for Thoracic Surgery.
At this point, “if you see the thoracic duct and you have concerns about ductal injury, your best bet is to ligate the duct directly. We observed in our series that there is a significantly higher incidence of chylothorax” with mass ligation, she said.
Of the 827 esophagectomies, 635 were performed without thoracic duct ligation; 33 (5.2%) cases developed postop chylothorax. Among the 56 cases with explicit identification and ligation of the thoracic duct alone, chylothorax developed in four (7.1%). There were 136 esophagectomies with mass ligation; 27 (19.9%) developed chylothorax (P = .0314).
The majority of the ligations were performed during open procedures. Mass ligations were mostly done with surgical sutures, while clips were used for direct ductal ligations. It’s likely that surgeons opted for direct ligation when they could see the duct and mass ligation when they could not.
Esophagectomy patients in the study were largely the same, so it’s unclear why some were ligated but others were not. About 75% in both groups had adenocarcinomas, most of which were in the distal esophagus or gastroesophageal junction. About half of the ligated group had preop chemoradiation, versus about 60% in the nonligated group.
Patients who developed postop chyle leaks were also similar, whether or not they were ligated. Most had adenocarcinomas in the distal esophagus or gastroesophageal junction, and the majority had received neoadjuvant therapy. “It’s unlikely that operative approach influenced the development of chylothorax,” Dr. Zheng said.
Both ligated and nonligated patients responded well to chylothorax management. Of the 64 total cases, 28 were successfully treated by thoracic duct embolization and 20 were successfully treated by operative thoracic duct ligation. In 10 cases, thoracic duct embolization was attempted but unsuccessful and all were successfully treated with operative ligation. Six cases were managed with chest tube drainage and total parenteral nutrition. It is possible that patients were ligated because they appeared during surgery to be at risk for postop chylothorax, which would help explain the findings.
It also is possible, however, that ligation itself – especially mass ligation – increases the risk. “The thoracic duct is a high-pressure system, so [blocking it] could create a pressure buildup and a potential leak,” Dr. Zheng said. That might be especially true with mass ligation, when both the thoracic duct and its tributaries are tied off.
Dr. Zheng said that she had no relevant disclosures.
AT THE AATS ANNUAL MEETING
Key clinical point: Mass thoracic duct ligation increases the risk of postop chylothorax.
Major finding: Of 827 esophagectomies, 635 were performed without thoracic duct ligation; 33 (5.2%) cases developed postop chylothorax. Among 56 cases with explicit identification and ligation of the thoracic duct alone, four (7.1%) developed chylothorax. There were 136 esophagectomies with mass ligation; 27 (19.9%) developed chylothorax (P = .0314).
Data source: Review of 827 esophagectomy cases at Brigham and Women’s Hospital in Boston.
Disclosures: The lead investigator had no disclosures.
Cardiac surgeons defy guidelines for severe disease
Although expert committees spend hours developing guidelines for best practices, clinicians on the front line of care can be somewhat hesitant to adopt them, as a recent study evaluating the use of guidelines for treatment of heart attack patients at three major cardiothoracic centers in London revealed.
The study, published in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.10.110]) , found that surgeons more often than not flaunted the Joint European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) guidelines that call for a multidisciplinary “Heart Team” to discuss each case of severe coronary artery disease before treatment.
The investigators looked at January-to-June periods in 2010 (before the guidelines) and 2012 (after the guidelines had been in place for 18 months) and found identical 17% rates of multidisciplinary team discussions before treatment. Both samples involved patients who had percutaneous coronary interventions (PCI). The 621 cases in the 2010 sample and 686 cases in the 2012 group comprise “a significant proportion of the coronary revascularization workload” of the National Health Service (NHS) hospitals in London, Dr. Martin T. Yates of St. George’s Hospital, University of London, and coauthors reported. The other participating centers were Barts Health NHS Trust and King College Hospital.
The ESC/EACTS guidelines (Eur. Heart J. 2010;31:2501-55) determined that PCI at the same catheterization session as the diagnostic angiogram and elective PCI are inappropriate for patients with severe coronary artery disease, defined as proximal left-anterior descending, left-main stem or three-vessel disease. The guidelines state that these patients should be considered for surgery first.
In a previous single-center study a year after the guidelines were adopted, Dr. Yates and his colleagues reported that almost a third of all elective PCI (29%) were carried out on patients who may have benefited more from coronary artery bypass grafting (CABG) (J. Thorac. Cardiovasc. Surg. 2014;147:606-10). Of those cases, the multidisciplinary team again discussed only 17% of cases before PCI.
Dr. Yates and his colleagues intimated that the rush to PCI might be circumventing in-depth discussions about more appropriate CABG for patients with severe coronary artery disease. “Furthermore, despite the guidelines suggesting that ad hoc PCI is inappropriate in the elective setting, this practice continues,” they said. “Although this is convenient for the patient and more cost effective, it does not allow time for Heart Team discussions prior to intervention.”
In the current study, the 2010 group included 187 patients with severe coronary artery disease who had treatment without a multidisciplinary team consultation, and less than half (44%) achieved complete revascularization. The 2012 group included 225 patients with severe heart disease, and precisely half achieved complete revascularization.
In both groups, a considerable majority of patients with three-vessel disease had PCI without the multidisciplinary team discussion: 76% in 2010 and 64% in 2012.
Dr. Yates and his associates noted that this is not a problem specific to London cardiac centers. They cited variations in the use of PCI and CABG in a large study of the New York State Registry, which showed that only 53% of patients suitable for CABG, according to the American College of Cardiology/American Heart Association guidelines, actually had the procedure (Circulation 2010;121:267-75). They cited similar results in a Canadian study (CMAJ 2012;184;179-86).
One way to get cardiac surgeons to adhere to guidelines is to tie payment to treatment – an approach that may work better in the United States than in Canada or the United Kingdom. “This may be easier to implement in countries with payment linked to insurance systems as opposed to those with a nationalized service,” Dr. Yates and his associates wrote.
The authors reported no financial disclosures.
Gathering evidence over recent years has shown that multidisciplinary teams can improve overall outcomes in many clinical scenarios, Dr. M. Sertac Cicek said in his commentary (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.008]). He cited a 2012 study that showed an 18% lower mortality at 5 years when multidisciplinary teams got involved in the treatment of breast cancer, compared with cases that did not involve team consultation (BMJ 2012;344:e2718).

|
Dr. M. Sertac Cicek |
Cardiovascular disease is a specialty that demands teamwork, but controversy still surrounds the role of surgery vs. PCI for patients with severe coronary disease, despite the evidence supporting CABG as the “gold standard,” Dr. Cicek said. The data presented by Dr. Yates and his colleagues, Dr. Cicek said, “simply confirm once again how far we are away from providing the optimal care to our patients, raising the question: ‘Are guidelines there to be disrespected?’ ”
A key factor in implementing the multidisciplinary approach involves educating patients and accepting them as members of the heart team during decision-making, Dr. Cicek noted. “It seems increasingly evident that multidisciplinary teams clearly strengthen our ability to provide higher quality and more efficient care; so much so that it may not come as surprise to anyone in the practice if in the very near future practicing ‘medicine without teamwork’ were declared and added to the Seven [Social] Sins of Mahatma Gandhi as the eighth [social] sin,” Dr. Cicek wrote.
Dr. Cicek is professor of cardiovascular surgery at the Anadolu Medical Center in Kocaeli, Turkey.
Gathering evidence over recent years has shown that multidisciplinary teams can improve overall outcomes in many clinical scenarios, Dr. M. Sertac Cicek said in his commentary (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.008]). He cited a 2012 study that showed an 18% lower mortality at 5 years when multidisciplinary teams got involved in the treatment of breast cancer, compared with cases that did not involve team consultation (BMJ 2012;344:e2718).

|
Dr. M. Sertac Cicek |
Cardiovascular disease is a specialty that demands teamwork, but controversy still surrounds the role of surgery vs. PCI for patients with severe coronary disease, despite the evidence supporting CABG as the “gold standard,” Dr. Cicek said. The data presented by Dr. Yates and his colleagues, Dr. Cicek said, “simply confirm once again how far we are away from providing the optimal care to our patients, raising the question: ‘Are guidelines there to be disrespected?’ ”
A key factor in implementing the multidisciplinary approach involves educating patients and accepting them as members of the heart team during decision-making, Dr. Cicek noted. “It seems increasingly evident that multidisciplinary teams clearly strengthen our ability to provide higher quality and more efficient care; so much so that it may not come as surprise to anyone in the practice if in the very near future practicing ‘medicine without teamwork’ were declared and added to the Seven [Social] Sins of Mahatma Gandhi as the eighth [social] sin,” Dr. Cicek wrote.
Dr. Cicek is professor of cardiovascular surgery at the Anadolu Medical Center in Kocaeli, Turkey.
Gathering evidence over recent years has shown that multidisciplinary teams can improve overall outcomes in many clinical scenarios, Dr. M. Sertac Cicek said in his commentary (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.008]). He cited a 2012 study that showed an 18% lower mortality at 5 years when multidisciplinary teams got involved in the treatment of breast cancer, compared with cases that did not involve team consultation (BMJ 2012;344:e2718).

|
Dr. M. Sertac Cicek |
Cardiovascular disease is a specialty that demands teamwork, but controversy still surrounds the role of surgery vs. PCI for patients with severe coronary disease, despite the evidence supporting CABG as the “gold standard,” Dr. Cicek said. The data presented by Dr. Yates and his colleagues, Dr. Cicek said, “simply confirm once again how far we are away from providing the optimal care to our patients, raising the question: ‘Are guidelines there to be disrespected?’ ”
A key factor in implementing the multidisciplinary approach involves educating patients and accepting them as members of the heart team during decision-making, Dr. Cicek noted. “It seems increasingly evident that multidisciplinary teams clearly strengthen our ability to provide higher quality and more efficient care; so much so that it may not come as surprise to anyone in the practice if in the very near future practicing ‘medicine without teamwork’ were declared and added to the Seven [Social] Sins of Mahatma Gandhi as the eighth [social] sin,” Dr. Cicek wrote.
Dr. Cicek is professor of cardiovascular surgery at the Anadolu Medical Center in Kocaeli, Turkey.
Although expert committees spend hours developing guidelines for best practices, clinicians on the front line of care can be somewhat hesitant to adopt them, as a recent study evaluating the use of guidelines for treatment of heart attack patients at three major cardiothoracic centers in London revealed.
The study, published in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.10.110]) , found that surgeons more often than not flaunted the Joint European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) guidelines that call for a multidisciplinary “Heart Team” to discuss each case of severe coronary artery disease before treatment.
The investigators looked at January-to-June periods in 2010 (before the guidelines) and 2012 (after the guidelines had been in place for 18 months) and found identical 17% rates of multidisciplinary team discussions before treatment. Both samples involved patients who had percutaneous coronary interventions (PCI). The 621 cases in the 2010 sample and 686 cases in the 2012 group comprise “a significant proportion of the coronary revascularization workload” of the National Health Service (NHS) hospitals in London, Dr. Martin T. Yates of St. George’s Hospital, University of London, and coauthors reported. The other participating centers were Barts Health NHS Trust and King College Hospital.
The ESC/EACTS guidelines (Eur. Heart J. 2010;31:2501-55) determined that PCI at the same catheterization session as the diagnostic angiogram and elective PCI are inappropriate for patients with severe coronary artery disease, defined as proximal left-anterior descending, left-main stem or three-vessel disease. The guidelines state that these patients should be considered for surgery first.
In a previous single-center study a year after the guidelines were adopted, Dr. Yates and his colleagues reported that almost a third of all elective PCI (29%) were carried out on patients who may have benefited more from coronary artery bypass grafting (CABG) (J. Thorac. Cardiovasc. Surg. 2014;147:606-10). Of those cases, the multidisciplinary team again discussed only 17% of cases before PCI.
Dr. Yates and his colleagues intimated that the rush to PCI might be circumventing in-depth discussions about more appropriate CABG for patients with severe coronary artery disease. “Furthermore, despite the guidelines suggesting that ad hoc PCI is inappropriate in the elective setting, this practice continues,” they said. “Although this is convenient for the patient and more cost effective, it does not allow time for Heart Team discussions prior to intervention.”
In the current study, the 2010 group included 187 patients with severe coronary artery disease who had treatment without a multidisciplinary team consultation, and less than half (44%) achieved complete revascularization. The 2012 group included 225 patients with severe heart disease, and precisely half achieved complete revascularization.
In both groups, a considerable majority of patients with three-vessel disease had PCI without the multidisciplinary team discussion: 76% in 2010 and 64% in 2012.
Dr. Yates and his associates noted that this is not a problem specific to London cardiac centers. They cited variations in the use of PCI and CABG in a large study of the New York State Registry, which showed that only 53% of patients suitable for CABG, according to the American College of Cardiology/American Heart Association guidelines, actually had the procedure (Circulation 2010;121:267-75). They cited similar results in a Canadian study (CMAJ 2012;184;179-86).
One way to get cardiac surgeons to adhere to guidelines is to tie payment to treatment – an approach that may work better in the United States than in Canada or the United Kingdom. “This may be easier to implement in countries with payment linked to insurance systems as opposed to those with a nationalized service,” Dr. Yates and his associates wrote.
The authors reported no financial disclosures.
Although expert committees spend hours developing guidelines for best practices, clinicians on the front line of care can be somewhat hesitant to adopt them, as a recent study evaluating the use of guidelines for treatment of heart attack patients at three major cardiothoracic centers in London revealed.
The study, published in the Journal of Thoracic and Cardiovascular Surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.10.110]) , found that surgeons more often than not flaunted the Joint European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) guidelines that call for a multidisciplinary “Heart Team” to discuss each case of severe coronary artery disease before treatment.
The investigators looked at January-to-June periods in 2010 (before the guidelines) and 2012 (after the guidelines had been in place for 18 months) and found identical 17% rates of multidisciplinary team discussions before treatment. Both samples involved patients who had percutaneous coronary interventions (PCI). The 621 cases in the 2010 sample and 686 cases in the 2012 group comprise “a significant proportion of the coronary revascularization workload” of the National Health Service (NHS) hospitals in London, Dr. Martin T. Yates of St. George’s Hospital, University of London, and coauthors reported. The other participating centers were Barts Health NHS Trust and King College Hospital.
The ESC/EACTS guidelines (Eur. Heart J. 2010;31:2501-55) determined that PCI at the same catheterization session as the diagnostic angiogram and elective PCI are inappropriate for patients with severe coronary artery disease, defined as proximal left-anterior descending, left-main stem or three-vessel disease. The guidelines state that these patients should be considered for surgery first.
In a previous single-center study a year after the guidelines were adopted, Dr. Yates and his colleagues reported that almost a third of all elective PCI (29%) were carried out on patients who may have benefited more from coronary artery bypass grafting (CABG) (J. Thorac. Cardiovasc. Surg. 2014;147:606-10). Of those cases, the multidisciplinary team again discussed only 17% of cases before PCI.
Dr. Yates and his colleagues intimated that the rush to PCI might be circumventing in-depth discussions about more appropriate CABG for patients with severe coronary artery disease. “Furthermore, despite the guidelines suggesting that ad hoc PCI is inappropriate in the elective setting, this practice continues,” they said. “Although this is convenient for the patient and more cost effective, it does not allow time for Heart Team discussions prior to intervention.”
In the current study, the 2010 group included 187 patients with severe coronary artery disease who had treatment without a multidisciplinary team consultation, and less than half (44%) achieved complete revascularization. The 2012 group included 225 patients with severe heart disease, and precisely half achieved complete revascularization.
In both groups, a considerable majority of patients with three-vessel disease had PCI without the multidisciplinary team discussion: 76% in 2010 and 64% in 2012.
Dr. Yates and his associates noted that this is not a problem specific to London cardiac centers. They cited variations in the use of PCI and CABG in a large study of the New York State Registry, which showed that only 53% of patients suitable for CABG, according to the American College of Cardiology/American Heart Association guidelines, actually had the procedure (Circulation 2010;121:267-75). They cited similar results in a Canadian study (CMAJ 2012;184;179-86).
One way to get cardiac surgeons to adhere to guidelines is to tie payment to treatment – an approach that may work better in the United States than in Canada or the United Kingdom. “This may be easier to implement in countries with payment linked to insurance systems as opposed to those with a nationalized service,” Dr. Yates and his associates wrote.
The authors reported no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Cardiac surgeons at three London hospitals complied poorly with clinical guidelines for managing patients with severe coronary artery disease.
Major finding: Only 17% of patients with severe coronary artery disease were subjects of multidisciplinary discussions before treatment in periods before and after treatment guidelines, and most were likely to have percutaneous coronary intervention rather than the recommended surgical revascularization.
Data source: Surgical patients were from the Central Cardiac Audit Database; PCI patients were from the British Cardiovascular Intervention Society database.
Disclosures: The authors reported no financial disclosures.
NOTION: TAVI has edge in patients at low surgical risk
PARIS – The writing is on the wall: 2-year results of the NOTION* trial suggest that transcatheter aortic valve replacement is the future – and already in selected cases, the present – preferred therapy for aortic stenosis in patients at low surgical risk.
NOTION was a multicenter, prospective, nonblinded, randomized trial, the first-ever study to compare less-invasive transcatheter aortic valve implantation (TAVI, also called transcatheter aortic valve replacement, or TAVR) and traditional surgical aortic valve replacement (SAVR) in a truly low-surgical-risk population. The 280 participants had a median Society of Thoracic Surgeons score of 3 and no major comorbid conditions.
At 2 years’ follow-up, the TAVI group had significantly larger valve orifice areas and lower gradients, along with lower rates of life-threatening bleeding, cardiogenic stroke, and severe kidney injury than did the SAVR group. Moreover, the TAVI group showed a strong favorable trend in terms of the primary composite endpoint comprising all-cause mortality, MI, or stroke, although the advantage didn’t achieve statistical significance because of the relatively small study size, Dr. Lars Søndergaard said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Longer-term data on durability and more randomized controlled trials are needed before we adopt routine use of TAVI in low-risk patients, but I think it’s reasonable to offer TAVI in selected low-risk patients today,” concluded Dr. Søndergaard of the University of Copenhagen.
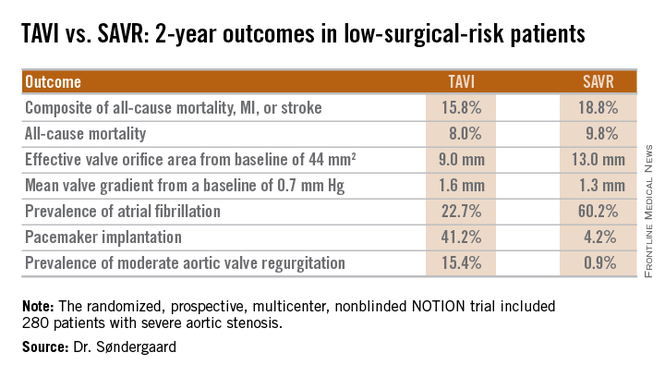
Session cochair Dr. William Wijns noted that NOTION, which utilized Medtronics’ self-expanding CoreValve for TAVI, began in 2009 and thus used an early iteration of the device. One might reasonably expect that the study results would be substantially more strongly in favor of TAVI had the contemporary version of the CoreValve been employed, observed Dr. Wijns, codirector of the cardiovascular center in Aalst, Belgium.
Dr. Søndergaard concurred. While the prevalence of moderate aortic regurgitation at 2 years in the TAVI arm of NOTION was 15.4%, in part because the valves were routinely placed under echocardiographic guidance, current-generation TAVI valves placed under CT guidance have a 1%-5% rate of moderate regurgitation. And while 41% of the TAVI group in NOTION had a pacemaker at 2 years, other studies show the rate drops to roughly 10% with the newest version of the CoreValve.
Dr. Søndergaard and coinvestigators plan to follow the NOTION participants for 10 years, issuing periodic updates. That’s a welcome development because patients at low surgical risk constitute the largest portion of those with significant aortic stenosis. Many of them are young enough that they should have a substantial remaining lifespan after aortic valve replacement, so it will be important to establish TAVI’s long-term durability.
The NOTION trial was funded by the Danish Heart Foundation. Dr. Søndergaard reported having no financial conflicts.
*Correction, 6/1/2015: An earlier version of this article misstated the name of the NOTION trial.
PARIS – The writing is on the wall: 2-year results of the NOTION* trial suggest that transcatheter aortic valve replacement is the future – and already in selected cases, the present – preferred therapy for aortic stenosis in patients at low surgical risk.
NOTION was a multicenter, prospective, nonblinded, randomized trial, the first-ever study to compare less-invasive transcatheter aortic valve implantation (TAVI, also called transcatheter aortic valve replacement, or TAVR) and traditional surgical aortic valve replacement (SAVR) in a truly low-surgical-risk population. The 280 participants had a median Society of Thoracic Surgeons score of 3 and no major comorbid conditions.
At 2 years’ follow-up, the TAVI group had significantly larger valve orifice areas and lower gradients, along with lower rates of life-threatening bleeding, cardiogenic stroke, and severe kidney injury than did the SAVR group. Moreover, the TAVI group showed a strong favorable trend in terms of the primary composite endpoint comprising all-cause mortality, MI, or stroke, although the advantage didn’t achieve statistical significance because of the relatively small study size, Dr. Lars Søndergaard said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Longer-term data on durability and more randomized controlled trials are needed before we adopt routine use of TAVI in low-risk patients, but I think it’s reasonable to offer TAVI in selected low-risk patients today,” concluded Dr. Søndergaard of the University of Copenhagen.
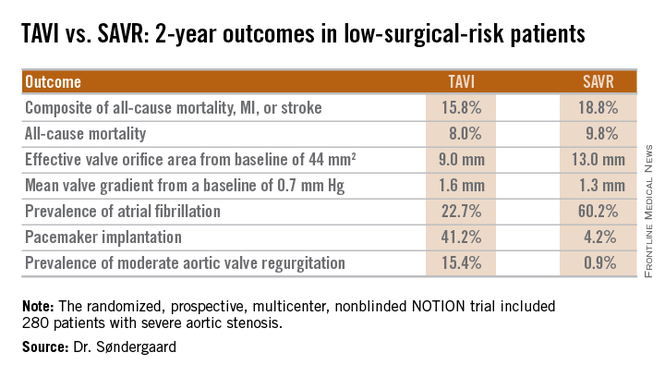
Session cochair Dr. William Wijns noted that NOTION, which utilized Medtronics’ self-expanding CoreValve for TAVI, began in 2009 and thus used an early iteration of the device. One might reasonably expect that the study results would be substantially more strongly in favor of TAVI had the contemporary version of the CoreValve been employed, observed Dr. Wijns, codirector of the cardiovascular center in Aalst, Belgium.
Dr. Søndergaard concurred. While the prevalence of moderate aortic regurgitation at 2 years in the TAVI arm of NOTION was 15.4%, in part because the valves were routinely placed under echocardiographic guidance, current-generation TAVI valves placed under CT guidance have a 1%-5% rate of moderate regurgitation. And while 41% of the TAVI group in NOTION had a pacemaker at 2 years, other studies show the rate drops to roughly 10% with the newest version of the CoreValve.
Dr. Søndergaard and coinvestigators plan to follow the NOTION participants for 10 years, issuing periodic updates. That’s a welcome development because patients at low surgical risk constitute the largest portion of those with significant aortic stenosis. Many of them are young enough that they should have a substantial remaining lifespan after aortic valve replacement, so it will be important to establish TAVI’s long-term durability.
The NOTION trial was funded by the Danish Heart Foundation. Dr. Søndergaard reported having no financial conflicts.
*Correction, 6/1/2015: An earlier version of this article misstated the name of the NOTION trial.
PARIS – The writing is on the wall: 2-year results of the NOTION* trial suggest that transcatheter aortic valve replacement is the future – and already in selected cases, the present – preferred therapy for aortic stenosis in patients at low surgical risk.
NOTION was a multicenter, prospective, nonblinded, randomized trial, the first-ever study to compare less-invasive transcatheter aortic valve implantation (TAVI, also called transcatheter aortic valve replacement, or TAVR) and traditional surgical aortic valve replacement (SAVR) in a truly low-surgical-risk population. The 280 participants had a median Society of Thoracic Surgeons score of 3 and no major comorbid conditions.
At 2 years’ follow-up, the TAVI group had significantly larger valve orifice areas and lower gradients, along with lower rates of life-threatening bleeding, cardiogenic stroke, and severe kidney injury than did the SAVR group. Moreover, the TAVI group showed a strong favorable trend in terms of the primary composite endpoint comprising all-cause mortality, MI, or stroke, although the advantage didn’t achieve statistical significance because of the relatively small study size, Dr. Lars Søndergaard said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Longer-term data on durability and more randomized controlled trials are needed before we adopt routine use of TAVI in low-risk patients, but I think it’s reasonable to offer TAVI in selected low-risk patients today,” concluded Dr. Søndergaard of the University of Copenhagen.
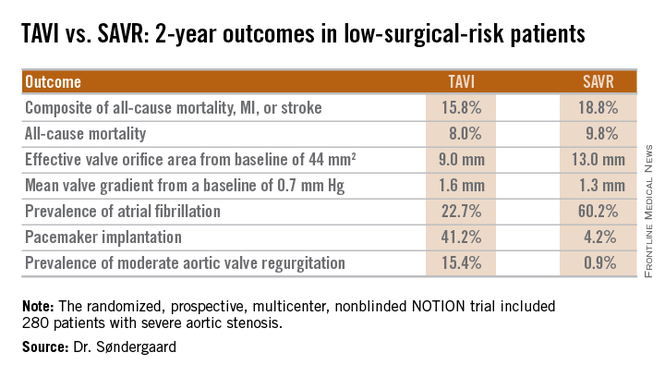
Session cochair Dr. William Wijns noted that NOTION, which utilized Medtronics’ self-expanding CoreValve for TAVI, began in 2009 and thus used an early iteration of the device. One might reasonably expect that the study results would be substantially more strongly in favor of TAVI had the contemporary version of the CoreValve been employed, observed Dr. Wijns, codirector of the cardiovascular center in Aalst, Belgium.
Dr. Søndergaard concurred. While the prevalence of moderate aortic regurgitation at 2 years in the TAVI arm of NOTION was 15.4%, in part because the valves were routinely placed under echocardiographic guidance, current-generation TAVI valves placed under CT guidance have a 1%-5% rate of moderate regurgitation. And while 41% of the TAVI group in NOTION had a pacemaker at 2 years, other studies show the rate drops to roughly 10% with the newest version of the CoreValve.
Dr. Søndergaard and coinvestigators plan to follow the NOTION participants for 10 years, issuing periodic updates. That’s a welcome development because patients at low surgical risk constitute the largest portion of those with significant aortic stenosis. Many of them are young enough that they should have a substantial remaining lifespan after aortic valve replacement, so it will be important to establish TAVI’s long-term durability.
The NOTION trial was funded by the Danish Heart Foundation. Dr. Søndergaard reported having no financial conflicts.
*Correction, 6/1/2015: An earlier version of this article misstated the name of the NOTION trial.
AT EUROPCR
Key clinical point: At 2 years, outcomes of TAVI look as good as and in some domains better than outcomes of surgical aortic valve replacement in low-surgical-risk patients.
Major finding: The 2-year composite outcome of all-cause mortality, MI, or stroke occurred in 15.8% of the TAVI group compared with 18.8% of surgically treated patients.
Data source: The randomized, prospective, multicenter, nonblinded NOTION trial includes 280 low-surgical-risk patients with severe aortic stenosis.
Disclosures: The NOTION trial was sponsored by the Danish Heart Foundation. The presenter reported having no financial conflicts.
Stricter DVT prophylaxis guidelines needed for cardiac and vascular surgery
Cardiac and vascular surgery patients should receive deep vein thrombosis (DVT) prophylaxis before and after surgery, say researchers who found a high incidence of postoperative DVT in these patients compared to general surgery patients.
The retrospective study of 2,669,772 surgery patients from the American College of Surgeons National Surgical Quality Improvement Program database found that 18,670 patients developed a DVT within 30 days of the operation.
The incidence of DVT according to the type of surgery was 2% for cardiac surgery, 0.99% for vascular surgery and 0.66% for general surgery, reported Dr. Faisal Aziz and his colleagues at Pennsylvania State University (Ann. Vasc. Surg. 2015; 29: 661-9).
Vascular surgery patients were at 1.5 times the risk of a postop DVT and cardiac surgery patients were at 3 times the risk compared with general surgery patients, a significant difference.
Preoperative factors associated with increased risk of developing DVT in the postoperative period included inpatient admission status (OR 7.8), general anesthesia (OR 2), and dyspnea at rest (OR 5).
“Despite the fact that most arterial surgery operations involve administration of therapeutic doses of anticoagulation therapy during the operations, incidence of postoperative DVT is high in these patients,” the study authors wrote.
“Intraoperative anticoagulation is not protective against development of DVT in the postoperative period” they said.
“Physicians should ensure adequate DVT prophylaxis in postoperative vascular surgery and cardiac surgery patients, according to established evidence based guidelines,” they concluded.
The authors did not report any financial disclosures.
Cardiac and vascular surgery patients should receive deep vein thrombosis (DVT) prophylaxis before and after surgery, say researchers who found a high incidence of postoperative DVT in these patients compared to general surgery patients.
The retrospective study of 2,669,772 surgery patients from the American College of Surgeons National Surgical Quality Improvement Program database found that 18,670 patients developed a DVT within 30 days of the operation.
The incidence of DVT according to the type of surgery was 2% for cardiac surgery, 0.99% for vascular surgery and 0.66% for general surgery, reported Dr. Faisal Aziz and his colleagues at Pennsylvania State University (Ann. Vasc. Surg. 2015; 29: 661-9).
Vascular surgery patients were at 1.5 times the risk of a postop DVT and cardiac surgery patients were at 3 times the risk compared with general surgery patients, a significant difference.
Preoperative factors associated with increased risk of developing DVT in the postoperative period included inpatient admission status (OR 7.8), general anesthesia (OR 2), and dyspnea at rest (OR 5).
“Despite the fact that most arterial surgery operations involve administration of therapeutic doses of anticoagulation therapy during the operations, incidence of postoperative DVT is high in these patients,” the study authors wrote.
“Intraoperative anticoagulation is not protective against development of DVT in the postoperative period” they said.
“Physicians should ensure adequate DVT prophylaxis in postoperative vascular surgery and cardiac surgery patients, according to established evidence based guidelines,” they concluded.
The authors did not report any financial disclosures.
Cardiac and vascular surgery patients should receive deep vein thrombosis (DVT) prophylaxis before and after surgery, say researchers who found a high incidence of postoperative DVT in these patients compared to general surgery patients.
The retrospective study of 2,669,772 surgery patients from the American College of Surgeons National Surgical Quality Improvement Program database found that 18,670 patients developed a DVT within 30 days of the operation.
The incidence of DVT according to the type of surgery was 2% for cardiac surgery, 0.99% for vascular surgery and 0.66% for general surgery, reported Dr. Faisal Aziz and his colleagues at Pennsylvania State University (Ann. Vasc. Surg. 2015; 29: 661-9).
Vascular surgery patients were at 1.5 times the risk of a postop DVT and cardiac surgery patients were at 3 times the risk compared with general surgery patients, a significant difference.
Preoperative factors associated with increased risk of developing DVT in the postoperative period included inpatient admission status (OR 7.8), general anesthesia (OR 2), and dyspnea at rest (OR 5).
“Despite the fact that most arterial surgery operations involve administration of therapeutic doses of anticoagulation therapy during the operations, incidence of postoperative DVT is high in these patients,” the study authors wrote.
“Intraoperative anticoagulation is not protective against development of DVT in the postoperative period” they said.
“Physicians should ensure adequate DVT prophylaxis in postoperative vascular surgery and cardiac surgery patients, according to established evidence based guidelines,” they concluded.
The authors did not report any financial disclosures.
FROM ANNALS OF VASCULAR SURGERY
Key clinical point: Intraoperative anticoagulation alone does not prevent DVT in patients undergoing vascular and cardiac surgery.
Major finding: The incidence of DVT according to the type of surgery was 2% for cardiac surgery, 0.99% for vascular surgery and 0.66% for general surgery.
Data source: Retrospective study of 2,669,772 surgery patients from the American College of Surgeons National Surgical Quality Improvement Program database.
Disclosures: The authors did not report any financial disclosures.
Ultrasound accurately predicts trauma thoracotomy survival
SAN DIEGO – The few trauma patients who will survive a high-risk thoracotomy procedure for cardiac arrest can be predicted by the presence of cardiac motion as detected by a quick and inexpensive bedside ultrasound, a prospective study conducted at a level I trauma center showed.
Focused assessment with sonography in trauma (FAST) was 100% sensitive and 62% specific in predicting those who would survive or be eligible for organ donation after receiving a resuscitative thoracotomy for traumatic cardiac arrest, said Dr. Kenji Inaba of the department of surgery at the University of Southern California Medical Center in Los Angeles.
Resuscitative thoracotomy, said Dr. Inaba, is a salvage procedure performed after cardiac arrest. It is a “high-risk, resource-intensive procedure, with a low quantitative yield. And yet, patients do survive.” Previous retrospective studies found that of those receiving resuscitative thoracotomy for traumatic arrest, 7.4% survived, with more than 90% of survivors retaining neurologic function; an additional 4.2% of recipients were potentially eligible for organ donation. Thus, a tool to identify potential survivors among those who present in post-traumatic cardiac arrest would help avoid unnecessary use of a procedure with such risks and resource burdens.
FAST, an inexpensive procedure that is standard for other indications in trauma, has been effective in identifying potential survivors in thoracotomy for nontrauma cardiac arrests, Dr. Inaba said at the annual meeting of the American Surgical Association.
The technique “has near-universal availability, can be performed immediately at the bedside without moving the patient, and yields real-time results with no radiation involved,” he said.
For the current prospective study, the specific aim was to examine the ability of FAST to differentiate survivors and potential organ donors from those who would not survive resuscitative thoracotomy among those presenting in traumatic cardiac arrest. Dr. Inaba and his associates examined the predictive value of cardiac motion and the presence of pericardial fluid for survival, as well as the adequacy of the FAST study for each patient.
The single-center study, conducted from 2010 to 2014, enrolled 187 patients (mean age, 31; 84.5% male) presenting in traumatic arrest who received resuscitative thoracotomy in the emergency department and also received a FAST. The scans were performed by emergency medicine residents under direct faculty supervision. Of the 187 patients studied, 6 (3.2%) survived, 3 (1.6%) became organ donors, and 178 (95.2%) died but were not organ donor eligible.
Cardiac motion was detected by FAST in 54 (28.9%) individuals in the total study population; among these were all nine of the survivors and donors, yielding a sensitivity of 100% and a specificity of 73.7% for survival (P < .001). All 16 of the patients with pericardial fluid detected by FAST died, as did all 7 patients in whom the study was deemed inadequate. Put simply, Dr. Inaba said, “no cardiac motion equals no survival.”
If thoracotomies had been performed only on patients in the study group who had cardiac motion on FAST, more than half of the unsuccessful resuscitative thoracotomies would have been avoided, Dr. Inaba noted. The study, he said, has particular application for lower-volume trauma centers, which must carefully weigh the prolonged use of limited resources required in a resuscitative thoracotomy.
Dr. David Spain, chief of trauma and critical care surgery at Stanford (Calif.) University, asked whether the study captured the mechanism of injury. Though the study did not do so, said Dr. Inaba, he and his colleagues realized that a subset of patients who went immediately to the operating room were not included in the study, a potential limitation. This group of patients included those with a penetrating cardiac injury – a possible reason, he said, why no patients among the survivors had a cardiac injury.
The authors reported no relevant financial disclosures.
SAN DIEGO – The few trauma patients who will survive a high-risk thoracotomy procedure for cardiac arrest can be predicted by the presence of cardiac motion as detected by a quick and inexpensive bedside ultrasound, a prospective study conducted at a level I trauma center showed.
Focused assessment with sonography in trauma (FAST) was 100% sensitive and 62% specific in predicting those who would survive or be eligible for organ donation after receiving a resuscitative thoracotomy for traumatic cardiac arrest, said Dr. Kenji Inaba of the department of surgery at the University of Southern California Medical Center in Los Angeles.
Resuscitative thoracotomy, said Dr. Inaba, is a salvage procedure performed after cardiac arrest. It is a “high-risk, resource-intensive procedure, with a low quantitative yield. And yet, patients do survive.” Previous retrospective studies found that of those receiving resuscitative thoracotomy for traumatic arrest, 7.4% survived, with more than 90% of survivors retaining neurologic function; an additional 4.2% of recipients were potentially eligible for organ donation. Thus, a tool to identify potential survivors among those who present in post-traumatic cardiac arrest would help avoid unnecessary use of a procedure with such risks and resource burdens.
FAST, an inexpensive procedure that is standard for other indications in trauma, has been effective in identifying potential survivors in thoracotomy for nontrauma cardiac arrests, Dr. Inaba said at the annual meeting of the American Surgical Association.
The technique “has near-universal availability, can be performed immediately at the bedside without moving the patient, and yields real-time results with no radiation involved,” he said.
For the current prospective study, the specific aim was to examine the ability of FAST to differentiate survivors and potential organ donors from those who would not survive resuscitative thoracotomy among those presenting in traumatic cardiac arrest. Dr. Inaba and his associates examined the predictive value of cardiac motion and the presence of pericardial fluid for survival, as well as the adequacy of the FAST study for each patient.
The single-center study, conducted from 2010 to 2014, enrolled 187 patients (mean age, 31; 84.5% male) presenting in traumatic arrest who received resuscitative thoracotomy in the emergency department and also received a FAST. The scans were performed by emergency medicine residents under direct faculty supervision. Of the 187 patients studied, 6 (3.2%) survived, 3 (1.6%) became organ donors, and 178 (95.2%) died but were not organ donor eligible.
Cardiac motion was detected by FAST in 54 (28.9%) individuals in the total study population; among these were all nine of the survivors and donors, yielding a sensitivity of 100% and a specificity of 73.7% for survival (P < .001). All 16 of the patients with pericardial fluid detected by FAST died, as did all 7 patients in whom the study was deemed inadequate. Put simply, Dr. Inaba said, “no cardiac motion equals no survival.”
If thoracotomies had been performed only on patients in the study group who had cardiac motion on FAST, more than half of the unsuccessful resuscitative thoracotomies would have been avoided, Dr. Inaba noted. The study, he said, has particular application for lower-volume trauma centers, which must carefully weigh the prolonged use of limited resources required in a resuscitative thoracotomy.
Dr. David Spain, chief of trauma and critical care surgery at Stanford (Calif.) University, asked whether the study captured the mechanism of injury. Though the study did not do so, said Dr. Inaba, he and his colleagues realized that a subset of patients who went immediately to the operating room were not included in the study, a potential limitation. This group of patients included those with a penetrating cardiac injury – a possible reason, he said, why no patients among the survivors had a cardiac injury.
The authors reported no relevant financial disclosures.
SAN DIEGO – The few trauma patients who will survive a high-risk thoracotomy procedure for cardiac arrest can be predicted by the presence of cardiac motion as detected by a quick and inexpensive bedside ultrasound, a prospective study conducted at a level I trauma center showed.
Focused assessment with sonography in trauma (FAST) was 100% sensitive and 62% specific in predicting those who would survive or be eligible for organ donation after receiving a resuscitative thoracotomy for traumatic cardiac arrest, said Dr. Kenji Inaba of the department of surgery at the University of Southern California Medical Center in Los Angeles.
Resuscitative thoracotomy, said Dr. Inaba, is a salvage procedure performed after cardiac arrest. It is a “high-risk, resource-intensive procedure, with a low quantitative yield. And yet, patients do survive.” Previous retrospective studies found that of those receiving resuscitative thoracotomy for traumatic arrest, 7.4% survived, with more than 90% of survivors retaining neurologic function; an additional 4.2% of recipients were potentially eligible for organ donation. Thus, a tool to identify potential survivors among those who present in post-traumatic cardiac arrest would help avoid unnecessary use of a procedure with such risks and resource burdens.
FAST, an inexpensive procedure that is standard for other indications in trauma, has been effective in identifying potential survivors in thoracotomy for nontrauma cardiac arrests, Dr. Inaba said at the annual meeting of the American Surgical Association.
The technique “has near-universal availability, can be performed immediately at the bedside without moving the patient, and yields real-time results with no radiation involved,” he said.
For the current prospective study, the specific aim was to examine the ability of FAST to differentiate survivors and potential organ donors from those who would not survive resuscitative thoracotomy among those presenting in traumatic cardiac arrest. Dr. Inaba and his associates examined the predictive value of cardiac motion and the presence of pericardial fluid for survival, as well as the adequacy of the FAST study for each patient.
The single-center study, conducted from 2010 to 2014, enrolled 187 patients (mean age, 31; 84.5% male) presenting in traumatic arrest who received resuscitative thoracotomy in the emergency department and also received a FAST. The scans were performed by emergency medicine residents under direct faculty supervision. Of the 187 patients studied, 6 (3.2%) survived, 3 (1.6%) became organ donors, and 178 (95.2%) died but were not organ donor eligible.
Cardiac motion was detected by FAST in 54 (28.9%) individuals in the total study population; among these were all nine of the survivors and donors, yielding a sensitivity of 100% and a specificity of 73.7% for survival (P < .001). All 16 of the patients with pericardial fluid detected by FAST died, as did all 7 patients in whom the study was deemed inadequate. Put simply, Dr. Inaba said, “no cardiac motion equals no survival.”
If thoracotomies had been performed only on patients in the study group who had cardiac motion on FAST, more than half of the unsuccessful resuscitative thoracotomies would have been avoided, Dr. Inaba noted. The study, he said, has particular application for lower-volume trauma centers, which must carefully weigh the prolonged use of limited resources required in a resuscitative thoracotomy.
Dr. David Spain, chief of trauma and critical care surgery at Stanford (Calif.) University, asked whether the study captured the mechanism of injury. Though the study did not do so, said Dr. Inaba, he and his colleagues realized that a subset of patients who went immediately to the operating room were not included in the study, a potential limitation. This group of patients included those with a penetrating cardiac injury – a possible reason, he said, why no patients among the survivors had a cardiac injury.
The authors reported no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Trauma arrest victims who will survive resuscitative thoracotomy can be predicted using focused assessment with sonography in trauma.
Major findings: FAST was 100% sensitive for detecting survivors after resuscitative thoracotomy for traumatic cardiac arrest.
Data source: A prospective series of 187 trauma patients in cardiac arrest undergoing resuscitative thoracotomy from 2010 to 2014 at a level I trauma center.
Disclosures: The authors reported no relevant financial disclosures.
AATS: Simplified mitral valve repair effective in children with Marfan’s
NEW YORK – A simplified surgical approach that uses an adult-sized, basic ring annuloplasty with a complete edge-to-edge leaflet repair has been found to yield good outcomes in a group of children with connective tissue disorders like Marfan syndrome and Loeys-Dietz syndrome and mitral regurgitation, based on an evaluation of the technique at four centers.
Cardiac surgeons employed the simplified operation in 18 patients under age 18 (median age 8.2 years) and found that after 2.4 years of follow-up, no patients required another operation for mitral regurgitation, reported Dr. Luca Vricella, pediatrics director, pediatric cardiac surgery and heart transplantation, John Hopkins University, Baltimore.
The patients underwent the simplified mitral valve repair at Johns Hopkins Pediatric Cardiac Surgery in Baltimore and Orlando; Duke University School of Medicine in Durham, N.C.; and University of Pavia Medical School in Italy.
These young patients can be challenging to operate on because of skeletal abnormalities and marginal pulmonary reserve, Dr. Vricella said at the meeting sponsored by the American Association for Thoracic Surgery. Of the 18 children in the study, 15 had Marfan syndrome, a genetic disorder that commonly affects the heart valves and aorta. “The most common mode of early presentation of mitral valve pathology, from a morphological standpoint, is that mitral regurgitation is often characterized as severe bileaflet prolapse and annular and left ventricular dilation,” Dr. Vricella said.
The simplified technique involves an approach through an atriotomy and placing an adult-sized annuloplasty ring in the valve. The next step is to place an Alfieri stitch, named for the Italian cardiac surgeon Dr. Ottavio Alfieri, with a braided suture in the middle of the valve, which opposes the leaflet “very effectively,” Dr. Vricella said.
In the study group, all 18 patients had severe bileaflet prolapse and severe mitral regurgitation of grade 4 or higher, but all patients also had normal ejection fraction, Dr. Vricella said. One infant was being considered for a heart transplant.
The operation was achieved in isolation in less than an hour. Five patients underwent simultaneous valve-sparing aortic root replacement, one of whom died (one of two deaths in a larger 300-plus group of both adults and children who had valve-sparing aortic root repair). No other complications were reported among the 18-patient group. Median length of stay in the hospital was 9 days.
After the operation, all patients had significant reductions in mitral regurgitation. After 2.4 years, 94% of survivors maintained mild regurgitation or better without stenosis. Entering the study, the median left ventricular end-diastolic diameter (LVEDD) score of all patients was 4.9 (range 2.1-11.9), but at 2.4 years after the operation the median LVEDD score had regressed to 1.3 (range –0.51-4.3).
“In pediatric patients with severe mitral regurgitation and connective tissue disorders, a simplified repair can result in intermediate-term competency without systolic anterior motion and with no mitral stenosis,” Dr. Vricella said. “We’ve been pleasantly surprised in seeing this reduction in left ventricular enlargement, and particularly in this group of patients in which you may need to have a longer plant time, simplifying things so you don’t have to intervene on the subvalvular annuloplasty.”
NEW YORK – A simplified surgical approach that uses an adult-sized, basic ring annuloplasty with a complete edge-to-edge leaflet repair has been found to yield good outcomes in a group of children with connective tissue disorders like Marfan syndrome and Loeys-Dietz syndrome and mitral regurgitation, based on an evaluation of the technique at four centers.
Cardiac surgeons employed the simplified operation in 18 patients under age 18 (median age 8.2 years) and found that after 2.4 years of follow-up, no patients required another operation for mitral regurgitation, reported Dr. Luca Vricella, pediatrics director, pediatric cardiac surgery and heart transplantation, John Hopkins University, Baltimore.
The patients underwent the simplified mitral valve repair at Johns Hopkins Pediatric Cardiac Surgery in Baltimore and Orlando; Duke University School of Medicine in Durham, N.C.; and University of Pavia Medical School in Italy.
These young patients can be challenging to operate on because of skeletal abnormalities and marginal pulmonary reserve, Dr. Vricella said at the meeting sponsored by the American Association for Thoracic Surgery. Of the 18 children in the study, 15 had Marfan syndrome, a genetic disorder that commonly affects the heart valves and aorta. “The most common mode of early presentation of mitral valve pathology, from a morphological standpoint, is that mitral regurgitation is often characterized as severe bileaflet prolapse and annular and left ventricular dilation,” Dr. Vricella said.
The simplified technique involves an approach through an atriotomy and placing an adult-sized annuloplasty ring in the valve. The next step is to place an Alfieri stitch, named for the Italian cardiac surgeon Dr. Ottavio Alfieri, with a braided suture in the middle of the valve, which opposes the leaflet “very effectively,” Dr. Vricella said.
In the study group, all 18 patients had severe bileaflet prolapse and severe mitral regurgitation of grade 4 or higher, but all patients also had normal ejection fraction, Dr. Vricella said. One infant was being considered for a heart transplant.
The operation was achieved in isolation in less than an hour. Five patients underwent simultaneous valve-sparing aortic root replacement, one of whom died (one of two deaths in a larger 300-plus group of both adults and children who had valve-sparing aortic root repair). No other complications were reported among the 18-patient group. Median length of stay in the hospital was 9 days.
After the operation, all patients had significant reductions in mitral regurgitation. After 2.4 years, 94% of survivors maintained mild regurgitation or better without stenosis. Entering the study, the median left ventricular end-diastolic diameter (LVEDD) score of all patients was 4.9 (range 2.1-11.9), but at 2.4 years after the operation the median LVEDD score had regressed to 1.3 (range –0.51-4.3).
“In pediatric patients with severe mitral regurgitation and connective tissue disorders, a simplified repair can result in intermediate-term competency without systolic anterior motion and with no mitral stenosis,” Dr. Vricella said. “We’ve been pleasantly surprised in seeing this reduction in left ventricular enlargement, and particularly in this group of patients in which you may need to have a longer plant time, simplifying things so you don’t have to intervene on the subvalvular annuloplasty.”
NEW YORK – A simplified surgical approach that uses an adult-sized, basic ring annuloplasty with a complete edge-to-edge leaflet repair has been found to yield good outcomes in a group of children with connective tissue disorders like Marfan syndrome and Loeys-Dietz syndrome and mitral regurgitation, based on an evaluation of the technique at four centers.
Cardiac surgeons employed the simplified operation in 18 patients under age 18 (median age 8.2 years) and found that after 2.4 years of follow-up, no patients required another operation for mitral regurgitation, reported Dr. Luca Vricella, pediatrics director, pediatric cardiac surgery and heart transplantation, John Hopkins University, Baltimore.
The patients underwent the simplified mitral valve repair at Johns Hopkins Pediatric Cardiac Surgery in Baltimore and Orlando; Duke University School of Medicine in Durham, N.C.; and University of Pavia Medical School in Italy.
These young patients can be challenging to operate on because of skeletal abnormalities and marginal pulmonary reserve, Dr. Vricella said at the meeting sponsored by the American Association for Thoracic Surgery. Of the 18 children in the study, 15 had Marfan syndrome, a genetic disorder that commonly affects the heart valves and aorta. “The most common mode of early presentation of mitral valve pathology, from a morphological standpoint, is that mitral regurgitation is often characterized as severe bileaflet prolapse and annular and left ventricular dilation,” Dr. Vricella said.
The simplified technique involves an approach through an atriotomy and placing an adult-sized annuloplasty ring in the valve. The next step is to place an Alfieri stitch, named for the Italian cardiac surgeon Dr. Ottavio Alfieri, with a braided suture in the middle of the valve, which opposes the leaflet “very effectively,” Dr. Vricella said.
In the study group, all 18 patients had severe bileaflet prolapse and severe mitral regurgitation of grade 4 or higher, but all patients also had normal ejection fraction, Dr. Vricella said. One infant was being considered for a heart transplant.
The operation was achieved in isolation in less than an hour. Five patients underwent simultaneous valve-sparing aortic root replacement, one of whom died (one of two deaths in a larger 300-plus group of both adults and children who had valve-sparing aortic root repair). No other complications were reported among the 18-patient group. Median length of stay in the hospital was 9 days.
After the operation, all patients had significant reductions in mitral regurgitation. After 2.4 years, 94% of survivors maintained mild regurgitation or better without stenosis. Entering the study, the median left ventricular end-diastolic diameter (LVEDD) score of all patients was 4.9 (range 2.1-11.9), but at 2.4 years after the operation the median LVEDD score had regressed to 1.3 (range –0.51-4.3).
“In pediatric patients with severe mitral regurgitation and connective tissue disorders, a simplified repair can result in intermediate-term competency without systolic anterior motion and with no mitral stenosis,” Dr. Vricella said. “We’ve been pleasantly surprised in seeing this reduction in left ventricular enlargement, and particularly in this group of patients in which you may need to have a longer plant time, simplifying things so you don’t have to intervene on the subvalvular annuloplasty.”
AT THE 2015 MITRAL VALVE CONCLAVE
Key clinical point: A simplified approach for mitral valve repair resulted in good outcomes in a group of children with connective tissue disorders.
Major finding: All 18 children in the study avoided reoperation after mitral valve repair.
Data source: A small trial involving 18 patients at four hospitals.
Disclosures: Dr. Vricella had no relevant relationships to disclose.