User login
VIDEO: Hybrid thoracoscopic and transcatheter ablation of persistent AF
SEATTLE – The presentation of the late-breaking HISTORIC-AF Trial by Dr. Claudio Muneretto and his colleagues “is a very interesting one, which brings to the table a very different approach of hybrid procedures to treat stand-alone atrial fibrillation,” said Dr. Niv Ad of Inova Heart and Vascular Institute, Falls Church, Va.
Dr. Ad gave his comments in a video interview at the annual meeting of the American Association for Thoracic Surgery.
In his assessment, Dr. Ad noted that such studies are useful and can stimulate discussion, even if he would prefer a prospective, comparative study of all procedures. “I hope someday we can create an algorithm where everything has a place: catheter ablation, hybrid procedures where you do catheter ablation and surgical procedure together or in stage, and the stand-alone Maze procedure on pump,” Dr. Ad said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – The presentation of the late-breaking HISTORIC-AF Trial by Dr. Claudio Muneretto and his colleagues “is a very interesting one, which brings to the table a very different approach of hybrid procedures to treat stand-alone atrial fibrillation,” said Dr. Niv Ad of Inova Heart and Vascular Institute, Falls Church, Va.
Dr. Ad gave his comments in a video interview at the annual meeting of the American Association for Thoracic Surgery.
In his assessment, Dr. Ad noted that such studies are useful and can stimulate discussion, even if he would prefer a prospective, comparative study of all procedures. “I hope someday we can create an algorithm where everything has a place: catheter ablation, hybrid procedures where you do catheter ablation and surgical procedure together or in stage, and the stand-alone Maze procedure on pump,” Dr. Ad said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – The presentation of the late-breaking HISTORIC-AF Trial by Dr. Claudio Muneretto and his colleagues “is a very interesting one, which brings to the table a very different approach of hybrid procedures to treat stand-alone atrial fibrillation,” said Dr. Niv Ad of Inova Heart and Vascular Institute, Falls Church, Va.
Dr. Ad gave his comments in a video interview at the annual meeting of the American Association for Thoracic Surgery.
In his assessment, Dr. Ad noted that such studies are useful and can stimulate discussion, even if he would prefer a prospective, comparative study of all procedures. “I hope someday we can create an algorithm where everything has a place: catheter ablation, hybrid procedures where you do catheter ablation and surgical procedure together or in stage, and the stand-alone Maze procedure on pump,” Dr. Ad said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AATS ANNUAL MEETING
VIDEO: Esophagectomy outcomes better in hospitals that handle complex cases
SEATTLE – Hospitals that perform at least one nongastric conduit esophageal reconstruction per year have half the esophagectomy mortality of hospitals that do not, according to a review by the Mayo Clinic in Rochester, Minn., of 11,211 esophagectomies in the Nationwide Inpatient Sample database from 2000 to 2011.
“There is tremendous variation in outcome after esophagectomy, and some advocate for regionalization to high-volume hospitals,” the investigators said. The findings suggest that case complexity could be one of the things that help define which hospitals do it best, they added.
The study seems to confirm that hospital case volume makes a difference in surgical outcomes, said Dr. Nabil Rizk, a thoracic surgeon at Memorial Sloan-Kettering Cancer Center in New York.
Dr. Rizk, a discussant on the paper at the American Association for Thoracic Surgery annual meeting, explained how the study fits into regionalization trends, but also shared his concerns about the work in an interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – Hospitals that perform at least one nongastric conduit esophageal reconstruction per year have half the esophagectomy mortality of hospitals that do not, according to a review by the Mayo Clinic in Rochester, Minn., of 11,211 esophagectomies in the Nationwide Inpatient Sample database from 2000 to 2011.
“There is tremendous variation in outcome after esophagectomy, and some advocate for regionalization to high-volume hospitals,” the investigators said. The findings suggest that case complexity could be one of the things that help define which hospitals do it best, they added.
The study seems to confirm that hospital case volume makes a difference in surgical outcomes, said Dr. Nabil Rizk, a thoracic surgeon at Memorial Sloan-Kettering Cancer Center in New York.
Dr. Rizk, a discussant on the paper at the American Association for Thoracic Surgery annual meeting, explained how the study fits into regionalization trends, but also shared his concerns about the work in an interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – Hospitals that perform at least one nongastric conduit esophageal reconstruction per year have half the esophagectomy mortality of hospitals that do not, according to a review by the Mayo Clinic in Rochester, Minn., of 11,211 esophagectomies in the Nationwide Inpatient Sample database from 2000 to 2011.
“There is tremendous variation in outcome after esophagectomy, and some advocate for regionalization to high-volume hospitals,” the investigators said. The findings suggest that case complexity could be one of the things that help define which hospitals do it best, they added.
The study seems to confirm that hospital case volume makes a difference in surgical outcomes, said Dr. Nabil Rizk, a thoracic surgeon at Memorial Sloan-Kettering Cancer Center in New York.
Dr. Rizk, a discussant on the paper at the American Association for Thoracic Surgery annual meeting, explained how the study fits into regionalization trends, but also shared his concerns about the work in an interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AATS ANNUAL MEETING
VIDEO: Cardiosphere-derived cells improve outcomes in hypoplastic left heart syndrome
SEATTLE – Autologous stem cell therapy improves surgery outcomes in children with hypoplastic left heart syndrome, according to the results of a small prospective trial from Okayama University in Japan.
The investigators cultured cardiosphere-derived cells (CDCs) – cardiac progenitor cells – from right atrium samples taken during stage 2 or 3 surgical palliations in seven HLHS children. A month later, they injected 300,000 CDCs/kg into the children’s coronary arteries by catheter, with each child getting cells cultured from their own tissue.
The cells seemed to jump-start the intrinsic regenerative properties of very young hearts. At 30 months follow-up, right ventricular mass and ejection fractions were about 10% greater in CDC treated patients compared to seven controls. Treated children also had better growth.
It’s possible the technique could help older children, too, and even adults, said lead investigator Dr. Shunji Sano, professor and chairman of the department of cardiovascular surgery at Okayama. He explained the work, its implications, and the next phase of research in an interview at the annual meeting of the American Association for Thoracic Surgery.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – Autologous stem cell therapy improves surgery outcomes in children with hypoplastic left heart syndrome, according to the results of a small prospective trial from Okayama University in Japan.
The investigators cultured cardiosphere-derived cells (CDCs) – cardiac progenitor cells – from right atrium samples taken during stage 2 or 3 surgical palliations in seven HLHS children. A month later, they injected 300,000 CDCs/kg into the children’s coronary arteries by catheter, with each child getting cells cultured from their own tissue.
The cells seemed to jump-start the intrinsic regenerative properties of very young hearts. At 30 months follow-up, right ventricular mass and ejection fractions were about 10% greater in CDC treated patients compared to seven controls. Treated children also had better growth.
It’s possible the technique could help older children, too, and even adults, said lead investigator Dr. Shunji Sano, professor and chairman of the department of cardiovascular surgery at Okayama. He explained the work, its implications, and the next phase of research in an interview at the annual meeting of the American Association for Thoracic Surgery.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – Autologous stem cell therapy improves surgery outcomes in children with hypoplastic left heart syndrome, according to the results of a small prospective trial from Okayama University in Japan.
The investigators cultured cardiosphere-derived cells (CDCs) – cardiac progenitor cells – from right atrium samples taken during stage 2 or 3 surgical palliations in seven HLHS children. A month later, they injected 300,000 CDCs/kg into the children’s coronary arteries by catheter, with each child getting cells cultured from their own tissue.
The cells seemed to jump-start the intrinsic regenerative properties of very young hearts. At 30 months follow-up, right ventricular mass and ejection fractions were about 10% greater in CDC treated patients compared to seven controls. Treated children also had better growth.
It’s possible the technique could help older children, too, and even adults, said lead investigator Dr. Shunji Sano, professor and chairman of the department of cardiovascular surgery at Okayama. He explained the work, its implications, and the next phase of research in an interview at the annual meeting of the American Association for Thoracic Surgery.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AATS ANNUAL MEETING
VIDEO: Less tricuspid regurgitation seen with Sano shunt in Norwood procedures
SEATTLE – Sano shunts outperform Blalock-Taussig shunts for Norwood procedures in neonates with hypoplastic left heart syndrome, according to a research registry study of 322 patients at the Cleveland Clinic and elsewhere.
The 166 newborns who had Sano shunts were matched to 166 who had Blalock-Taussig (BT) shunts.
“For comparable neonates with HLHS [hypoplastic left heart syndrome] undergoing Norwood operations, Sano offers better late survival [more than 3 years], less late tricuspid regurgitation, and perhaps less late right ventricular dysfunction than BT,” the investigators concluded.
Even so, Dr. Richard Ohye, professor of cardiac surgery at the University of Michigan, Ann Arbor, said the jury is still out on which shunt is best. He explained why in an interview at the American Association for Thoracic Surgery annual meeting. He also shared tips on shunt selection and explained a novel technique he has developed for doing a Sano shunt with a smaller hole in the right ventricle.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – Sano shunts outperform Blalock-Taussig shunts for Norwood procedures in neonates with hypoplastic left heart syndrome, according to a research registry study of 322 patients at the Cleveland Clinic and elsewhere.
The 166 newborns who had Sano shunts were matched to 166 who had Blalock-Taussig (BT) shunts.
“For comparable neonates with HLHS [hypoplastic left heart syndrome] undergoing Norwood operations, Sano offers better late survival [more than 3 years], less late tricuspid regurgitation, and perhaps less late right ventricular dysfunction than BT,” the investigators concluded.
Even so, Dr. Richard Ohye, professor of cardiac surgery at the University of Michigan, Ann Arbor, said the jury is still out on which shunt is best. He explained why in an interview at the American Association for Thoracic Surgery annual meeting. He also shared tips on shunt selection and explained a novel technique he has developed for doing a Sano shunt with a smaller hole in the right ventricle.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SEATTLE – Sano shunts outperform Blalock-Taussig shunts for Norwood procedures in neonates with hypoplastic left heart syndrome, according to a research registry study of 322 patients at the Cleveland Clinic and elsewhere.
The 166 newborns who had Sano shunts were matched to 166 who had Blalock-Taussig (BT) shunts.
“For comparable neonates with HLHS [hypoplastic left heart syndrome] undergoing Norwood operations, Sano offers better late survival [more than 3 years], less late tricuspid regurgitation, and perhaps less late right ventricular dysfunction than BT,” the investigators concluded.
Even so, Dr. Richard Ohye, professor of cardiac surgery at the University of Michigan, Ann Arbor, said the jury is still out on which shunt is best. He explained why in an interview at the American Association for Thoracic Surgery annual meeting. He also shared tips on shunt selection and explained a novel technique he has developed for doing a Sano shunt with a smaller hole in the right ventricle.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AATS ANNUAL MEETING
Linking registries, databases may reduce surgical site infections
Surveillance of cardiac surgical site infections (SSIs) improved significantly when registry and infection control surveillance data were linked with electronic health records, a retrospective analysis showed.
Over the course of a 47-month period starting in 2011, Vaidehi Nayar of the Children’s Hospital of Philadelphia and her coinvestigators launched a quality improvement initiative at their institution that linked administrative databases with their clinical registry, allowing caregivers to more accurately monitor and assess SSIs and provide more effective adjudication and treatments thereafter. The investigators chose to link their hospital’s electronic health record (EHR) billing information and reporting from the infection surveillance database for the National Healthcare Safety Network with data from the Society of Thoracic Surgeons Congenital Heart Surgery Database (STS-CHSD).
To further facilitate the flow and interpretation of data, the investigators used a visualization tool to analyze the STS-CHSD for case ascertainment; to resolve discrepancies among STS-CHSD, infection surveillance, and billing SSI cases; and to assess the impact of the hospital’s quality improvement protocols. These protocols consisted of wound alert reports from the EHR, bedside reviews for SSI adjudication, inpatient and outpatient SSI prevention bundles, prophylactic antibiotic dosing changes, removal of steroids from the bypass circuit, and biller education on SSIs.
Control charts in the data visualization tool allowed for statistical monitoring of SSI rate changes, and SSI case discrepancies across the databases were reviewed to ensure that differences were the result of variations in SSI reporting criteria for each database, not inaccurate surveillance population ascertainment or inaccurate SSI identification, according to Ms. Nayar and her colleagues,
“Workflow changes, including the wound alert report and bedside reviews, facilitated communication among providers and improved adjudication of suspected SSIs,” she said in presenting the J. Maxwell Chamberlain Memorial Paper for Congenital Heart Surgery at the annual meeting of the Society of Thoracic Surgeons in San Diego earlier this year.
In total, 156 SSIs were identified via the STS-CHSD, 79 via the infection surveillance database, and 433 via billing. There was a significant decrease in the rolling 12-month SSI rate from 2.48% (21/848 in January 2013) to 0.76% (11/1,442 in January 2014), based on the STS-CHSD data, although Ms. Nayar pointed out that this decline could not definitely be attributed to reporting improvements or to the specific quality improvement initiatives that were implemented. Ms. Nayar also explained that there was a “general improvement in reporting, as shown by the stark drop in billing” and “a general alignment of all three data sources.”
“Accurate assessment of morbidity data, including [SSIs], has implications for public reporting, benchmarking, assessment of [quality improvement] impact, and possible denial of payments,” said Ms. Nayar. “In summary, we achieved our two simultaneous goals of improving SSI reporting – or decreasing the data errors – and decreasing SSI incidents by improving overall patient care.”
During discussion, Ms. Nayar elaborated on the study’s generalizability and potential application to other facets of congenital heart disease treatments, saying that such application is, in fact, possible.
“Yes, this is very generalizable, but one key important fact is relevant: As long as there is a source of truth for case ascertainment, this methodology can be used in several different areas,” she explained. “For example, we are currently working at our institution to integrate and link the [Pediatric Cardiac Critical Care Consortium] database to be able to better monitor any critical care–related morbidity information and ultimately use similar methodology to assess the impact of outcomes in the critical care field.”
Ms. Nayar said that she did not have any relevant financial conflicts of interest to disclose.
This study demonstrates dramatically different surgical site infection (SSI) rates for the same patient cohort as detected by three different surveillance methods: hospital billing (derived from the electronic health records), a surgical database, and a tracking system developed by the Centers for Disease Control and Prevention.
On the low end, 79 SSIs were reported by one system, 156 by another, and 433 by the third method – a more than fivefold discrepancy. The authors developed a technique to reconcile the three systems and then evaluated a variety of interventions designed to reduce the SSI rate. As a result of this initiative, the quality of event reporting was improved (with greater agreement between reporting methods) and the rate of SSIs was reduced.
The implications of this report are sobering and should be of great interest to all surgeons and hospital administrators for several reasons. First and fundamentally, the report suggests that widely used reporting systems may be inaccurate and produce conflicting results. Since the results of these reports are used to assess and modify clinical practice, this is very disturbing. Additionally, the results may be used by payers as a basis for financial reward (or penalty) and therefore must be accurate. Finally, exposure of the use of erroneous information as the source data for billing may render an institution vulnerable to civil and criminal penalties. For all of these reasons, the present report should prompt self-assessment by all institutions, if it has not already been undertaken.
Dr. Robert Jaquiss is associate medical editor for congenital heart disease for Thoracic Surgery News.
This study demonstrates dramatically different surgical site infection (SSI) rates for the same patient cohort as detected by three different surveillance methods: hospital billing (derived from the electronic health records), a surgical database, and a tracking system developed by the Centers for Disease Control and Prevention.
On the low end, 79 SSIs were reported by one system, 156 by another, and 433 by the third method – a more than fivefold discrepancy. The authors developed a technique to reconcile the three systems and then evaluated a variety of interventions designed to reduce the SSI rate. As a result of this initiative, the quality of event reporting was improved (with greater agreement between reporting methods) and the rate of SSIs was reduced.
The implications of this report are sobering and should be of great interest to all surgeons and hospital administrators for several reasons. First and fundamentally, the report suggests that widely used reporting systems may be inaccurate and produce conflicting results. Since the results of these reports are used to assess and modify clinical practice, this is very disturbing. Additionally, the results may be used by payers as a basis for financial reward (or penalty) and therefore must be accurate. Finally, exposure of the use of erroneous information as the source data for billing may render an institution vulnerable to civil and criminal penalties. For all of these reasons, the present report should prompt self-assessment by all institutions, if it has not already been undertaken.
Dr. Robert Jaquiss is associate medical editor for congenital heart disease for Thoracic Surgery News.
This study demonstrates dramatically different surgical site infection (SSI) rates for the same patient cohort as detected by three different surveillance methods: hospital billing (derived from the electronic health records), a surgical database, and a tracking system developed by the Centers for Disease Control and Prevention.
On the low end, 79 SSIs were reported by one system, 156 by another, and 433 by the third method – a more than fivefold discrepancy. The authors developed a technique to reconcile the three systems and then evaluated a variety of interventions designed to reduce the SSI rate. As a result of this initiative, the quality of event reporting was improved (with greater agreement between reporting methods) and the rate of SSIs was reduced.
The implications of this report are sobering and should be of great interest to all surgeons and hospital administrators for several reasons. First and fundamentally, the report suggests that widely used reporting systems may be inaccurate and produce conflicting results. Since the results of these reports are used to assess and modify clinical practice, this is very disturbing. Additionally, the results may be used by payers as a basis for financial reward (or penalty) and therefore must be accurate. Finally, exposure of the use of erroneous information as the source data for billing may render an institution vulnerable to civil and criminal penalties. For all of these reasons, the present report should prompt self-assessment by all institutions, if it has not already been undertaken.
Dr. Robert Jaquiss is associate medical editor for congenital heart disease for Thoracic Surgery News.
Surveillance of cardiac surgical site infections (SSIs) improved significantly when registry and infection control surveillance data were linked with electronic health records, a retrospective analysis showed.
Over the course of a 47-month period starting in 2011, Vaidehi Nayar of the Children’s Hospital of Philadelphia and her coinvestigators launched a quality improvement initiative at their institution that linked administrative databases with their clinical registry, allowing caregivers to more accurately monitor and assess SSIs and provide more effective adjudication and treatments thereafter. The investigators chose to link their hospital’s electronic health record (EHR) billing information and reporting from the infection surveillance database for the National Healthcare Safety Network with data from the Society of Thoracic Surgeons Congenital Heart Surgery Database (STS-CHSD).
To further facilitate the flow and interpretation of data, the investigators used a visualization tool to analyze the STS-CHSD for case ascertainment; to resolve discrepancies among STS-CHSD, infection surveillance, and billing SSI cases; and to assess the impact of the hospital’s quality improvement protocols. These protocols consisted of wound alert reports from the EHR, bedside reviews for SSI adjudication, inpatient and outpatient SSI prevention bundles, prophylactic antibiotic dosing changes, removal of steroids from the bypass circuit, and biller education on SSIs.
Control charts in the data visualization tool allowed for statistical monitoring of SSI rate changes, and SSI case discrepancies across the databases were reviewed to ensure that differences were the result of variations in SSI reporting criteria for each database, not inaccurate surveillance population ascertainment or inaccurate SSI identification, according to Ms. Nayar and her colleagues,
“Workflow changes, including the wound alert report and bedside reviews, facilitated communication among providers and improved adjudication of suspected SSIs,” she said in presenting the J. Maxwell Chamberlain Memorial Paper for Congenital Heart Surgery at the annual meeting of the Society of Thoracic Surgeons in San Diego earlier this year.
In total, 156 SSIs were identified via the STS-CHSD, 79 via the infection surveillance database, and 433 via billing. There was a significant decrease in the rolling 12-month SSI rate from 2.48% (21/848 in January 2013) to 0.76% (11/1,442 in January 2014), based on the STS-CHSD data, although Ms. Nayar pointed out that this decline could not definitely be attributed to reporting improvements or to the specific quality improvement initiatives that were implemented. Ms. Nayar also explained that there was a “general improvement in reporting, as shown by the stark drop in billing” and “a general alignment of all three data sources.”
“Accurate assessment of morbidity data, including [SSIs], has implications for public reporting, benchmarking, assessment of [quality improvement] impact, and possible denial of payments,” said Ms. Nayar. “In summary, we achieved our two simultaneous goals of improving SSI reporting – or decreasing the data errors – and decreasing SSI incidents by improving overall patient care.”
During discussion, Ms. Nayar elaborated on the study’s generalizability and potential application to other facets of congenital heart disease treatments, saying that such application is, in fact, possible.
“Yes, this is very generalizable, but one key important fact is relevant: As long as there is a source of truth for case ascertainment, this methodology can be used in several different areas,” she explained. “For example, we are currently working at our institution to integrate and link the [Pediatric Cardiac Critical Care Consortium] database to be able to better monitor any critical care–related morbidity information and ultimately use similar methodology to assess the impact of outcomes in the critical care field.”
Ms. Nayar said that she did not have any relevant financial conflicts of interest to disclose.
Surveillance of cardiac surgical site infections (SSIs) improved significantly when registry and infection control surveillance data were linked with electronic health records, a retrospective analysis showed.
Over the course of a 47-month period starting in 2011, Vaidehi Nayar of the Children’s Hospital of Philadelphia and her coinvestigators launched a quality improvement initiative at their institution that linked administrative databases with their clinical registry, allowing caregivers to more accurately monitor and assess SSIs and provide more effective adjudication and treatments thereafter. The investigators chose to link their hospital’s electronic health record (EHR) billing information and reporting from the infection surveillance database for the National Healthcare Safety Network with data from the Society of Thoracic Surgeons Congenital Heart Surgery Database (STS-CHSD).
To further facilitate the flow and interpretation of data, the investigators used a visualization tool to analyze the STS-CHSD for case ascertainment; to resolve discrepancies among STS-CHSD, infection surveillance, and billing SSI cases; and to assess the impact of the hospital’s quality improvement protocols. These protocols consisted of wound alert reports from the EHR, bedside reviews for SSI adjudication, inpatient and outpatient SSI prevention bundles, prophylactic antibiotic dosing changes, removal of steroids from the bypass circuit, and biller education on SSIs.
Control charts in the data visualization tool allowed for statistical monitoring of SSI rate changes, and SSI case discrepancies across the databases were reviewed to ensure that differences were the result of variations in SSI reporting criteria for each database, not inaccurate surveillance population ascertainment or inaccurate SSI identification, according to Ms. Nayar and her colleagues,
“Workflow changes, including the wound alert report and bedside reviews, facilitated communication among providers and improved adjudication of suspected SSIs,” she said in presenting the J. Maxwell Chamberlain Memorial Paper for Congenital Heart Surgery at the annual meeting of the Society of Thoracic Surgeons in San Diego earlier this year.
In total, 156 SSIs were identified via the STS-CHSD, 79 via the infection surveillance database, and 433 via billing. There was a significant decrease in the rolling 12-month SSI rate from 2.48% (21/848 in January 2013) to 0.76% (11/1,442 in January 2014), based on the STS-CHSD data, although Ms. Nayar pointed out that this decline could not definitely be attributed to reporting improvements or to the specific quality improvement initiatives that were implemented. Ms. Nayar also explained that there was a “general improvement in reporting, as shown by the stark drop in billing” and “a general alignment of all three data sources.”
“Accurate assessment of morbidity data, including [SSIs], has implications for public reporting, benchmarking, assessment of [quality improvement] impact, and possible denial of payments,” said Ms. Nayar. “In summary, we achieved our two simultaneous goals of improving SSI reporting – or decreasing the data errors – and decreasing SSI incidents by improving overall patient care.”
During discussion, Ms. Nayar elaborated on the study’s generalizability and potential application to other facets of congenital heart disease treatments, saying that such application is, in fact, possible.
“Yes, this is very generalizable, but one key important fact is relevant: As long as there is a source of truth for case ascertainment, this methodology can be used in several different areas,” she explained. “For example, we are currently working at our institution to integrate and link the [Pediatric Cardiac Critical Care Consortium] database to be able to better monitor any critical care–related morbidity information and ultimately use similar methodology to assess the impact of outcomes in the critical care field.”
Ms. Nayar said that she did not have any relevant financial conflicts of interest to disclose.
Key clinical point: Linking registry and infection control data with a hospital’s electronic health records can significantly improve surveillance of SSIs, as the linkage allows for improved visualization abilities, communication within and between departments, facilitated adjudication of SSIs, and improved assessment of quality improvement initiatives to prevent further SSIs.
Major finding: Over the 47-month study period, 156 SSIs were identified via the STS-CHSD, 79 via the infection surveillance database, and 433 via billing. The rolling 12-month SSI rate based on the STS-CHSD decreased from 2.48% (21/848) to 0.76% (11/1,442).
Data source: A retrospective analysis of 668 cases in the STS-CHSD database over the course of 47 months.
Disclosures: Ms. Nayar reported that she had no relevant financial conflicts.
Three-dimensional models show superiority of nanoparticles in mesothelioma
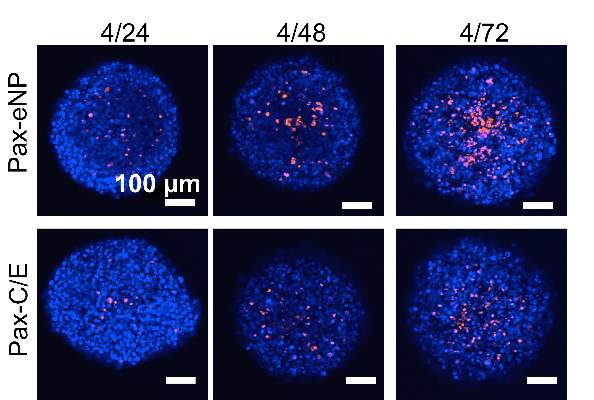
Malignant mesothelioma poses a significant challenge for clinicians because of its ability to resist chemotherapy, but the use of three-dimensional tumor spheroid models has shown that local administration of paclitaxel in a nanoparticle platform achieved better tumor penetration than conventional paclitaxel therapy, investigators reported. The study is in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Dr. Hongyi Lei of Brigham and Women’s Hospital, Boston, and his colleagues used the in vitro mesothelioma spheroid model because two-dimensional in vitro monolayer cell culture experiments do not replicate the superior efficacy of paclitaxel-loaded expansile nanoparticles (Pax-eNPs), suggesting that Pax-eNPs utilize a unique drug delivery mechanism.
The study observed that spheroids treated with Pax-eNP showed increased drug penetration and a 38-fold higher intraspheroidal drug concentration at 24 hours than that of paclitaxel dissolved in Cremophor EL/ethanol (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2015.02.020]).
The researchers said their findings showed that three-dimensional spheroid models “are valuable tools for investigating cytotoxic mechanisms and nanoparticle-tumor interactions, particularly given the costs and limitations of in vivo animal studies.” Their findings were first presented at the 94th Annual Meeting of the American Association of Thoracic Surgery last year in Toronto.
Despite advances of nanoparticle-based drug delivery systems, difficulties in evaluating the effectiveness of these drugs in local chemotherapy have hindered their adoption in the clinic. Studies of the same agent utilizing in vitro vs. in vivo methods have shown conflicting results.
The observation that Pax-eNP treatment of intraperitoneal mesothelioma significantly improved survival in lab animals in vivo compared to conventional paclitaxel led to the use of the three-dimensional spheroid model. Dr. Lei and colleagues called this revelation “striking” because Pax-eNP exposure of the identical mesothelioma tumor cells plated as a two-dimensional monolayer in vitro demonstrated equal or worse results. “This suggested that eNP may be more effective at penetration and/or persistence within multicellular tumors and led to the use of a 3-D tumor spheroid mode,” they said.
“Given the high cost and limitations of in vivo animal studies, spheroid models may present a clinically relevant platform for screening novel pharmaceuticals and unique drug-delivery systems during the preclinical phase,” the researchers indicated.
They also investigated spheroid cytotoxicity in a clinic-like setting following a 4-hour, high-dose (1,000 ng/mL) paclitaxel exposure via conventional and eNP vehicles. They found that Pax-eNP exposure led to greater tumor cytotoxicity at 72 hours, and that cytotoxicity continued seven days later because Pax-eNPs rapidly enter the tumor spheroid and remain intracellular, slowly releasing the drug.
“The prolonged drug release mechanism that pH-triggered Pax-eNP uses appears to be unique, leading to markedly higher intraspheroidal drug delivery, prolonged intratumoral drug release and superior antitumor efficacy,” the investigators concluded. The authors had no disclosures.
“While this study contributes greatly to the body of knowledge available regarding potential treatment strategies for malignant mesothelioma, one might argue that the more important impact of this paper relates to the successful implementation of an unconventional tumor model,” Dr. Mara B. Antonoff wrote in her invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi: 10.1016/j.jtcvs.2015.02.015].
The investigators’ earlier studies noted the limitations of the two-dimensional cell monolayer for in vitro experiments, but Dr. Antonoff acknowledged their quest for a solution that was more cost-effective than animal models and better approximated in vivo biological actions of the drug.

|
Dr. Mara B. Antonoff |
However, she noted the three-dimensional models “are not without limits, either.” Widespread adoption is limited because of the time and expertise involved in spheroid formation. “Nonetheless, it is clear that such models are a huge improvement over our current in vitro models,” she wrote.
Among the limits of the three-dimensional spheroid model she pointed out are that it lacks the multiple cell types typical in an actual tumor and quantitative assessment of the results can be difficult.
But the spheroid model does enhance the ability to screen novel drugs and drug-delivery systems, she wrote. “This timely and well-constructed study provides a foundation upon which we may build our knowledge of chemotherapeutic delivery mechanisms, while setting an outstanding example, and perhaps a new standard, for in vitro methodology,” she wrote.
Dr. Antonoff is a clinical instructor at University of Texas M.D. Anderson Cancer Center in Houston.
“While this study contributes greatly to the body of knowledge available regarding potential treatment strategies for malignant mesothelioma, one might argue that the more important impact of this paper relates to the successful implementation of an unconventional tumor model,” Dr. Mara B. Antonoff wrote in her invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi: 10.1016/j.jtcvs.2015.02.015].
The investigators’ earlier studies noted the limitations of the two-dimensional cell monolayer for in vitro experiments, but Dr. Antonoff acknowledged their quest for a solution that was more cost-effective than animal models and better approximated in vivo biological actions of the drug.

|
Dr. Mara B. Antonoff |
However, she noted the three-dimensional models “are not without limits, either.” Widespread adoption is limited because of the time and expertise involved in spheroid formation. “Nonetheless, it is clear that such models are a huge improvement over our current in vitro models,” she wrote.
Among the limits of the three-dimensional spheroid model she pointed out are that it lacks the multiple cell types typical in an actual tumor and quantitative assessment of the results can be difficult.
But the spheroid model does enhance the ability to screen novel drugs and drug-delivery systems, she wrote. “This timely and well-constructed study provides a foundation upon which we may build our knowledge of chemotherapeutic delivery mechanisms, while setting an outstanding example, and perhaps a new standard, for in vitro methodology,” she wrote.
Dr. Antonoff is a clinical instructor at University of Texas M.D. Anderson Cancer Center in Houston.
“While this study contributes greatly to the body of knowledge available regarding potential treatment strategies for malignant mesothelioma, one might argue that the more important impact of this paper relates to the successful implementation of an unconventional tumor model,” Dr. Mara B. Antonoff wrote in her invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi: 10.1016/j.jtcvs.2015.02.015].
The investigators’ earlier studies noted the limitations of the two-dimensional cell monolayer for in vitro experiments, but Dr. Antonoff acknowledged their quest for a solution that was more cost-effective than animal models and better approximated in vivo biological actions of the drug.

|
Dr. Mara B. Antonoff |
However, she noted the three-dimensional models “are not without limits, either.” Widespread adoption is limited because of the time and expertise involved in spheroid formation. “Nonetheless, it is clear that such models are a huge improvement over our current in vitro models,” she wrote.
Among the limits of the three-dimensional spheroid model she pointed out are that it lacks the multiple cell types typical in an actual tumor and quantitative assessment of the results can be difficult.
But the spheroid model does enhance the ability to screen novel drugs and drug-delivery systems, she wrote. “This timely and well-constructed study provides a foundation upon which we may build our knowledge of chemotherapeutic delivery mechanisms, while setting an outstanding example, and perhaps a new standard, for in vitro methodology,” she wrote.
Dr. Antonoff is a clinical instructor at University of Texas M.D. Anderson Cancer Center in Houston.
Malignant mesothelioma poses a significant challenge for clinicians because of its ability to resist chemotherapy, but the use of three-dimensional tumor spheroid models has shown that local administration of paclitaxel in a nanoparticle platform achieved better tumor penetration than conventional paclitaxel therapy, investigators reported. The study is in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Dr. Hongyi Lei of Brigham and Women’s Hospital, Boston, and his colleagues used the in vitro mesothelioma spheroid model because two-dimensional in vitro monolayer cell culture experiments do not replicate the superior efficacy of paclitaxel-loaded expansile nanoparticles (Pax-eNPs), suggesting that Pax-eNPs utilize a unique drug delivery mechanism.
The study observed that spheroids treated with Pax-eNP showed increased drug penetration and a 38-fold higher intraspheroidal drug concentration at 24 hours than that of paclitaxel dissolved in Cremophor EL/ethanol (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2015.02.020]).
The researchers said their findings showed that three-dimensional spheroid models “are valuable tools for investigating cytotoxic mechanisms and nanoparticle-tumor interactions, particularly given the costs and limitations of in vivo animal studies.” Their findings were first presented at the 94th Annual Meeting of the American Association of Thoracic Surgery last year in Toronto.
Despite advances of nanoparticle-based drug delivery systems, difficulties in evaluating the effectiveness of these drugs in local chemotherapy have hindered their adoption in the clinic. Studies of the same agent utilizing in vitro vs. in vivo methods have shown conflicting results.
The observation that Pax-eNP treatment of intraperitoneal mesothelioma significantly improved survival in lab animals in vivo compared to conventional paclitaxel led to the use of the three-dimensional spheroid model. Dr. Lei and colleagues called this revelation “striking” because Pax-eNP exposure of the identical mesothelioma tumor cells plated as a two-dimensional monolayer in vitro demonstrated equal or worse results. “This suggested that eNP may be more effective at penetration and/or persistence within multicellular tumors and led to the use of a 3-D tumor spheroid mode,” they said.
“Given the high cost and limitations of in vivo animal studies, spheroid models may present a clinically relevant platform for screening novel pharmaceuticals and unique drug-delivery systems during the preclinical phase,” the researchers indicated.
They also investigated spheroid cytotoxicity in a clinic-like setting following a 4-hour, high-dose (1,000 ng/mL) paclitaxel exposure via conventional and eNP vehicles. They found that Pax-eNP exposure led to greater tumor cytotoxicity at 72 hours, and that cytotoxicity continued seven days later because Pax-eNPs rapidly enter the tumor spheroid and remain intracellular, slowly releasing the drug.
“The prolonged drug release mechanism that pH-triggered Pax-eNP uses appears to be unique, leading to markedly higher intraspheroidal drug delivery, prolonged intratumoral drug release and superior antitumor efficacy,” the investigators concluded. The authors had no disclosures.
Malignant mesothelioma poses a significant challenge for clinicians because of its ability to resist chemotherapy, but the use of three-dimensional tumor spheroid models has shown that local administration of paclitaxel in a nanoparticle platform achieved better tumor penetration than conventional paclitaxel therapy, investigators reported. The study is in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Dr. Hongyi Lei of Brigham and Women’s Hospital, Boston, and his colleagues used the in vitro mesothelioma spheroid model because two-dimensional in vitro monolayer cell culture experiments do not replicate the superior efficacy of paclitaxel-loaded expansile nanoparticles (Pax-eNPs), suggesting that Pax-eNPs utilize a unique drug delivery mechanism.
The study observed that spheroids treated with Pax-eNP showed increased drug penetration and a 38-fold higher intraspheroidal drug concentration at 24 hours than that of paclitaxel dissolved in Cremophor EL/ethanol (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2015.02.020]).
The researchers said their findings showed that three-dimensional spheroid models “are valuable tools for investigating cytotoxic mechanisms and nanoparticle-tumor interactions, particularly given the costs and limitations of in vivo animal studies.” Their findings were first presented at the 94th Annual Meeting of the American Association of Thoracic Surgery last year in Toronto.
Despite advances of nanoparticle-based drug delivery systems, difficulties in evaluating the effectiveness of these drugs in local chemotherapy have hindered their adoption in the clinic. Studies of the same agent utilizing in vitro vs. in vivo methods have shown conflicting results.
The observation that Pax-eNP treatment of intraperitoneal mesothelioma significantly improved survival in lab animals in vivo compared to conventional paclitaxel led to the use of the three-dimensional spheroid model. Dr. Lei and colleagues called this revelation “striking” because Pax-eNP exposure of the identical mesothelioma tumor cells plated as a two-dimensional monolayer in vitro demonstrated equal or worse results. “This suggested that eNP may be more effective at penetration and/or persistence within multicellular tumors and led to the use of a 3-D tumor spheroid mode,” they said.
“Given the high cost and limitations of in vivo animal studies, spheroid models may present a clinically relevant platform for screening novel pharmaceuticals and unique drug-delivery systems during the preclinical phase,” the researchers indicated.
They also investigated spheroid cytotoxicity in a clinic-like setting following a 4-hour, high-dose (1,000 ng/mL) paclitaxel exposure via conventional and eNP vehicles. They found that Pax-eNP exposure led to greater tumor cytotoxicity at 72 hours, and that cytotoxicity continued seven days later because Pax-eNPs rapidly enter the tumor spheroid and remain intracellular, slowly releasing the drug.
“The prolonged drug release mechanism that pH-triggered Pax-eNP uses appears to be unique, leading to markedly higher intraspheroidal drug delivery, prolonged intratumoral drug release and superior antitumor efficacy,” the investigators concluded. The authors had no disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Three-dimensional spheroid models, as opposed to monolayer cell cultures, are valuable tools for predicting the efficacy of nanoparticle-tumor interactions in malignant mesothelioma.
Major finding: There was increased drug penetration and a 38-fold higher drug concentration 24 hours after human malignant mesothelioma spheroids were treated with paclitaxel-loaded expansile nanoparticles, compared to conventional drug delivery.
Data source: A study of a mesothelioma spheroid model comparing treatment with Pax-eNP and paclitaxel dissolved in Cremophor EL/ethanol.
Disclosures: This work was supported by the Brigham and Women’s Hospital International Mesothelioma Program, National Science Foundation and Boston University’s Nanomedicine Program and Cross-Disciplinary Training in Nanotechnology for Cancer, and the Zhujiang Hospital (Guangzhou, China) Scholarship Program. The authors had no relevant disclosures.
Biopsy bests HCRT for lung fibrosis, has risks
Surgical lung biopsy performs well and is relatively safe for evaluating suspected interstitial lung diseases, but may be especially helpful in confirming the diagnosis and directing the treatment of patients with idiopathic pulmonary fibrosis with atypical signs and symptoms, researchers have found.
In patients with immune disorders or severe respiratory dysfunction, or on mechanical ventilation, clinicians should weigh the diagnostic benefits of surgical lung biopsy (SLB) against its potential risks, according to a systematic review and meta-analysis of 23 studies published between 2000 and 2014, comprising 2,148 patients. Dr. Qian Han of the Guangzhou Institute of Respiratory Disease in China led the investigative team. The findings were published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
The meta-analysis focused on diagnostic yield of biopsy samples and postbiopsy mortality within 90 days of surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.057). The mean age of patients across the studies ranged from 36 to 62 years. The population of the meta-analysis included 1,632 (76%) who had undergone video-assisted thoracic surgery (VATS) and 268 (12.5%) who had open-lung biopsy.
Slightly more than one third (33.5%) of diagnoses involved idiopathic pulmonary fibrosis, followed by nonspecific interstitial pneumonia (12%), hypersensitivity pneumonitis (9.6%), cryptogenic organizing pneumonia (7.5%), sarcoidosis (6.8%), and connective tissue disease related to interstitial lung disease (4%).
The median diagnostic yield across all studies was 95%, ranging from 42% to 100% depending on the study. One study showed a diagnostic yield below 70%. Eight studies showed that the biopsy influenced a change in the treatment plan 42%-90% of the time. In the entire meta-analysis, treatment plans were altered for 59.5% of patients who received a specific diagnosis and in 55.2% of those without a definitive diagnosis.
“These results suggested that an alteration in treatment may not be directed by a definitive histological diagnosis and nonspecific histological results could also be useful in clinical practice,” Dr. Han said.
Eleven of the studies used CT guidance to obtain biopsies without a preference to lobe, but two studies predisposed to the right lobes had diagnostic yields of 84% and 94%. One study avoided the lingual or middle lobe, with a diagnostic yield of 97%, and another focused on the lingular lobe only, with a 100% yield. Two studies showed that biopsy samples from lingual or middle lobes had the same diagnostic yield as did those from other lobes.
With regard to diagnostic performance based on biopsy numbers, one study showed that multiple biopsies may increase the diagnostic yield. Twelve studies obtained one to three samples, and among them eight studies suggested one sample containing both lesion and normal tissue was sufficient to represent pathological changes. One study showed that multiple biopsies may increase diagnostic yield.
Of the 16 studies that provided sufficient data on mortality rates, the pooled 30- and 90-day mortality rates were 2.2% (95% CI 1.0-4.0%) and 3.4% (95% CI 1.8-5.5%), respectively. The composite postoperative mortality rate was 3.6% (95% CI 2.1%-5.5%).
In their discussion, Dr. Han and colleagues addressed the controversy surrounding lingual vs. middle lobe biopsy by noting that high-resolution CT (HRCT) can be valuable in identifying the appropriate biopsy location. While multiple studies supported the effectiveness of only one biopsy as long as it contained both normal and abnormal tissue, the researchers pointed out that future studies evaluating biopsy samples would do well to evaluate biopsy number combined with sample size.
HRCT, while highly specific, may be less sensitive than SLB in the diagnosis of idiopathic pulmonary fibrosis, they found. Two studies the meta-analysis looked at compared the diagnostic yield between SLB and HRCT; SLB finally diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease. “These findings suggested that HRCT, albeit highly specific, is less sensitive in the diagnosis of IPF, therefore necessitating the utility of SLB in the diagnosis of these HRCT-omitted cases,” Dr. Han said.
On the safety issue, while studies that excluded patients on mechanical ventilation reported lower mortality rates and two studies identified ventilator dependence as an independent risk factor for mortality, the investigators reported that the higher mortality rates were probably the result of a sicker patient population rather than the SLB procedure itself. They wrote that to “indiscreetly refuse” to perform SLB in these patients is “overcautious and inappropriate” given the benefits of SLB in validating diagnoses and influencing treatment plans.
Dr. Han and his colleagues reported having no relevant disclosures.
The role of surgical biopsy in the high-risk population with interstitial lung disease is well suited for surgical review because thoracic surgeons must weigh the risks, including potential mortality, and benefits when discussion options with patients and families, Dr. Katie S. Nason noted in her invited editorial commentary.

|
Dr. Katie S. Nason |
Current guidelines suggest that SLB is no longer essential for diagnosis of idiopathic pulmonary fibrosis and they now consider an HRCT scan showing unusual interstitial pneumonia (UIP) sufficient for diagnosis. “However, in the absence of diagnostic imaging criteria for UIP, specifically honeycombing, surgical lung biopsy with interpretation by an expert pathologist is necessary and should be performed to further define patients with possible UIP,” Dr. Nason wrote. “Comprehensive application of this approach will delineate circumstances in which a surgical biopsy will be more informative than an HRCT scan as well as when a surgical biopsy is not necessary.”
She called for a multi-institutional, international registry to collect and better understand data on the diagnostic yield and mortality after SLB for interstitial lung disease.
Dr. Nason is an assistant professor of cardiothoracic surgery at the University of Pittsburgh.
The role of surgical biopsy in the high-risk population with interstitial lung disease is well suited for surgical review because thoracic surgeons must weigh the risks, including potential mortality, and benefits when discussion options with patients and families, Dr. Katie S. Nason noted in her invited editorial commentary.

|
Dr. Katie S. Nason |
Current guidelines suggest that SLB is no longer essential for diagnosis of idiopathic pulmonary fibrosis and they now consider an HRCT scan showing unusual interstitial pneumonia (UIP) sufficient for diagnosis. “However, in the absence of diagnostic imaging criteria for UIP, specifically honeycombing, surgical lung biopsy with interpretation by an expert pathologist is necessary and should be performed to further define patients with possible UIP,” Dr. Nason wrote. “Comprehensive application of this approach will delineate circumstances in which a surgical biopsy will be more informative than an HRCT scan as well as when a surgical biopsy is not necessary.”
She called for a multi-institutional, international registry to collect and better understand data on the diagnostic yield and mortality after SLB for interstitial lung disease.
Dr. Nason is an assistant professor of cardiothoracic surgery at the University of Pittsburgh.
The role of surgical biopsy in the high-risk population with interstitial lung disease is well suited for surgical review because thoracic surgeons must weigh the risks, including potential mortality, and benefits when discussion options with patients and families, Dr. Katie S. Nason noted in her invited editorial commentary.

|
Dr. Katie S. Nason |
Current guidelines suggest that SLB is no longer essential for diagnosis of idiopathic pulmonary fibrosis and they now consider an HRCT scan showing unusual interstitial pneumonia (UIP) sufficient for diagnosis. “However, in the absence of diagnostic imaging criteria for UIP, specifically honeycombing, surgical lung biopsy with interpretation by an expert pathologist is necessary and should be performed to further define patients with possible UIP,” Dr. Nason wrote. “Comprehensive application of this approach will delineate circumstances in which a surgical biopsy will be more informative than an HRCT scan as well as when a surgical biopsy is not necessary.”
She called for a multi-institutional, international registry to collect and better understand data on the diagnostic yield and mortality after SLB for interstitial lung disease.
Dr. Nason is an assistant professor of cardiothoracic surgery at the University of Pittsburgh.
Surgical lung biopsy performs well and is relatively safe for evaluating suspected interstitial lung diseases, but may be especially helpful in confirming the diagnosis and directing the treatment of patients with idiopathic pulmonary fibrosis with atypical signs and symptoms, researchers have found.
In patients with immune disorders or severe respiratory dysfunction, or on mechanical ventilation, clinicians should weigh the diagnostic benefits of surgical lung biopsy (SLB) against its potential risks, according to a systematic review and meta-analysis of 23 studies published between 2000 and 2014, comprising 2,148 patients. Dr. Qian Han of the Guangzhou Institute of Respiratory Disease in China led the investigative team. The findings were published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
The meta-analysis focused on diagnostic yield of biopsy samples and postbiopsy mortality within 90 days of surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.057). The mean age of patients across the studies ranged from 36 to 62 years. The population of the meta-analysis included 1,632 (76%) who had undergone video-assisted thoracic surgery (VATS) and 268 (12.5%) who had open-lung biopsy.
Slightly more than one third (33.5%) of diagnoses involved idiopathic pulmonary fibrosis, followed by nonspecific interstitial pneumonia (12%), hypersensitivity pneumonitis (9.6%), cryptogenic organizing pneumonia (7.5%), sarcoidosis (6.8%), and connective tissue disease related to interstitial lung disease (4%).
The median diagnostic yield across all studies was 95%, ranging from 42% to 100% depending on the study. One study showed a diagnostic yield below 70%. Eight studies showed that the biopsy influenced a change in the treatment plan 42%-90% of the time. In the entire meta-analysis, treatment plans were altered for 59.5% of patients who received a specific diagnosis and in 55.2% of those without a definitive diagnosis.
“These results suggested that an alteration in treatment may not be directed by a definitive histological diagnosis and nonspecific histological results could also be useful in clinical practice,” Dr. Han said.
Eleven of the studies used CT guidance to obtain biopsies without a preference to lobe, but two studies predisposed to the right lobes had diagnostic yields of 84% and 94%. One study avoided the lingual or middle lobe, with a diagnostic yield of 97%, and another focused on the lingular lobe only, with a 100% yield. Two studies showed that biopsy samples from lingual or middle lobes had the same diagnostic yield as did those from other lobes.
With regard to diagnostic performance based on biopsy numbers, one study showed that multiple biopsies may increase the diagnostic yield. Twelve studies obtained one to three samples, and among them eight studies suggested one sample containing both lesion and normal tissue was sufficient to represent pathological changes. One study showed that multiple biopsies may increase diagnostic yield.
Of the 16 studies that provided sufficient data on mortality rates, the pooled 30- and 90-day mortality rates were 2.2% (95% CI 1.0-4.0%) and 3.4% (95% CI 1.8-5.5%), respectively. The composite postoperative mortality rate was 3.6% (95% CI 2.1%-5.5%).
In their discussion, Dr. Han and colleagues addressed the controversy surrounding lingual vs. middle lobe biopsy by noting that high-resolution CT (HRCT) can be valuable in identifying the appropriate biopsy location. While multiple studies supported the effectiveness of only one biopsy as long as it contained both normal and abnormal tissue, the researchers pointed out that future studies evaluating biopsy samples would do well to evaluate biopsy number combined with sample size.
HRCT, while highly specific, may be less sensitive than SLB in the diagnosis of idiopathic pulmonary fibrosis, they found. Two studies the meta-analysis looked at compared the diagnostic yield between SLB and HRCT; SLB finally diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease. “These findings suggested that HRCT, albeit highly specific, is less sensitive in the diagnosis of IPF, therefore necessitating the utility of SLB in the diagnosis of these HRCT-omitted cases,” Dr. Han said.
On the safety issue, while studies that excluded patients on mechanical ventilation reported lower mortality rates and two studies identified ventilator dependence as an independent risk factor for mortality, the investigators reported that the higher mortality rates were probably the result of a sicker patient population rather than the SLB procedure itself. They wrote that to “indiscreetly refuse” to perform SLB in these patients is “overcautious and inappropriate” given the benefits of SLB in validating diagnoses and influencing treatment plans.
Dr. Han and his colleagues reported having no relevant disclosures.
Surgical lung biopsy performs well and is relatively safe for evaluating suspected interstitial lung diseases, but may be especially helpful in confirming the diagnosis and directing the treatment of patients with idiopathic pulmonary fibrosis with atypical signs and symptoms, researchers have found.
In patients with immune disorders or severe respiratory dysfunction, or on mechanical ventilation, clinicians should weigh the diagnostic benefits of surgical lung biopsy (SLB) against its potential risks, according to a systematic review and meta-analysis of 23 studies published between 2000 and 2014, comprising 2,148 patients. Dr. Qian Han of the Guangzhou Institute of Respiratory Disease in China led the investigative team. The findings were published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
The meta-analysis focused on diagnostic yield of biopsy samples and postbiopsy mortality within 90 days of surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.057). The mean age of patients across the studies ranged from 36 to 62 years. The population of the meta-analysis included 1,632 (76%) who had undergone video-assisted thoracic surgery (VATS) and 268 (12.5%) who had open-lung biopsy.
Slightly more than one third (33.5%) of diagnoses involved idiopathic pulmonary fibrosis, followed by nonspecific interstitial pneumonia (12%), hypersensitivity pneumonitis (9.6%), cryptogenic organizing pneumonia (7.5%), sarcoidosis (6.8%), and connective tissue disease related to interstitial lung disease (4%).
The median diagnostic yield across all studies was 95%, ranging from 42% to 100% depending on the study. One study showed a diagnostic yield below 70%. Eight studies showed that the biopsy influenced a change in the treatment plan 42%-90% of the time. In the entire meta-analysis, treatment plans were altered for 59.5% of patients who received a specific diagnosis and in 55.2% of those without a definitive diagnosis.
“These results suggested that an alteration in treatment may not be directed by a definitive histological diagnosis and nonspecific histological results could also be useful in clinical practice,” Dr. Han said.
Eleven of the studies used CT guidance to obtain biopsies without a preference to lobe, but two studies predisposed to the right lobes had diagnostic yields of 84% and 94%. One study avoided the lingual or middle lobe, with a diagnostic yield of 97%, and another focused on the lingular lobe only, with a 100% yield. Two studies showed that biopsy samples from lingual or middle lobes had the same diagnostic yield as did those from other lobes.
With regard to diagnostic performance based on biopsy numbers, one study showed that multiple biopsies may increase the diagnostic yield. Twelve studies obtained one to three samples, and among them eight studies suggested one sample containing both lesion and normal tissue was sufficient to represent pathological changes. One study showed that multiple biopsies may increase diagnostic yield.
Of the 16 studies that provided sufficient data on mortality rates, the pooled 30- and 90-day mortality rates were 2.2% (95% CI 1.0-4.0%) and 3.4% (95% CI 1.8-5.5%), respectively. The composite postoperative mortality rate was 3.6% (95% CI 2.1%-5.5%).
In their discussion, Dr. Han and colleagues addressed the controversy surrounding lingual vs. middle lobe biopsy by noting that high-resolution CT (HRCT) can be valuable in identifying the appropriate biopsy location. While multiple studies supported the effectiveness of only one biopsy as long as it contained both normal and abnormal tissue, the researchers pointed out that future studies evaluating biopsy samples would do well to evaluate biopsy number combined with sample size.
HRCT, while highly specific, may be less sensitive than SLB in the diagnosis of idiopathic pulmonary fibrosis, they found. Two studies the meta-analysis looked at compared the diagnostic yield between SLB and HRCT; SLB finally diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease. “These findings suggested that HRCT, albeit highly specific, is less sensitive in the diagnosis of IPF, therefore necessitating the utility of SLB in the diagnosis of these HRCT-omitted cases,” Dr. Han said.
On the safety issue, while studies that excluded patients on mechanical ventilation reported lower mortality rates and two studies identified ventilator dependence as an independent risk factor for mortality, the investigators reported that the higher mortality rates were probably the result of a sicker patient population rather than the SLB procedure itself. They wrote that to “indiscreetly refuse” to perform SLB in these patients is “overcautious and inappropriate” given the benefits of SLB in validating diagnoses and influencing treatment plans.
Dr. Han and his colleagues reported having no relevant disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Surgical lung biopsy is helpful to confirm interstitial lung disease in patients with unique signs and symptoms, but the benefit of SLB should be balanced against the risks in patients with more severe disease.
Major finding: In two studies that compared the diagnostic yield between SLB and HRCT; SLB diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease.
Data source: Meta-analysis of 23 studies published between 2000 and 2014 and involving 2,148 patients.
Disclosures: The National Natural Science Foundation of China Young Investigator Funding supported the work. The investigators reported having no conflicts of interest.
Stenting before CABG linked to higher mortality for diabetic patients
Since the debut of drug-eluting stents, more high-risk patient groups, namely diabetic patients, have undergone coronary stenting as opposed to coronary artery bypass grafting (CABG) as an option to open blocked arteries; however, diabetic patients with stents who go on to have CABG have significantly higher 5-year death rates than do unstented diabetics who undergo CABG, according to a study published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
A review of 7,005 CABG procedures performed from 1996 to 2007 at Mercy St. Vincent Medical Center in Toledo, Ohio, found that diabetic patients with triple-vessel disease and a prior percutaneous coronary intervention with stenting (PCI-S) who underwent CABG had a 39% greater risk of death within 5 years of the operation. The findings are significant, according to Dr. Victor Nauffal and his colleagues at the American University of Beirut, because increasing numbers of patients with coronary stents are referred for CABG (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.051).
Previous studies have linked prior stenting to an increased risk of bleeding and stent thrombosis during CABG, so having a better understanding of anticoagulation during the operation and the timing of the surgery after stenting could decrease complications. Investigations of the long-term outcomes of patients with stents who have CABG, however, have been lacking. This study investigated the premise that diabetics with triple-vessel disease and a stent had poorer outcomes because of endothelial dysfunction and the increased strain that triple-vessel disease places on the heart.
After exclusions, the final study population comprised 1,583 diabetic patients with concomitant triple-vessel disease, 202 (12.8%) of whom had coronary stents. The study defined triple-vessel disease as blockages of 50% or more in all three native coronary vessels or left main artery plus right coronary artery disease.
Early mortality rates – death within 30 days of the procedure – were similar between the two groups: 3.3% overall, 3% in the prior-PCI group, and 3.3% in the no-PCI group; therefore, prior PCI was not a predictor of early mortality.
Five-year cumulative survival was 78.5% in the no-PCI group, compared with 74.8% in the PCI group. When adjusting for a variety of clinical variables before CABG, stenting was associated with a 39% greater mortality at 5 years. The investigators accounted for the emergence of drug-eluting stents during the 10-year study period but found that they did not contribute significantly to overall outcomes.
The cause of death was known for 81.7% (282 of 345) of the deaths in the overall cohort, with 5-year cardiac deaths higher in the PCI-S group: 8.4% vs. 7.5% for the no-PCI group. “Notably, 100% of PCI-S cardiac mortality was categorized as coronary heart disease related compared to 89.3% (92/103) of cardiac mortality in the no-PCI group,” Dr. Nauffal and his associates said.
Careful patient selection for CABG is in order for diabetics with triple-vessel disease, particularly those with a prior stent, the authors advised. “An early team-based approach including a cardiologist and cardiac surgeon should be implemented for optimal revascularization strategy selection in diabetics with triple-vessel disease and for close medical follow-up of those higher risk CABG patients with history of intracoronary stents,” Dr. Nauffal and his colleagues concluded.
The Johns Hopkins Murex Research Award supported Dr. Nauffal. The authors had no other relevant disclosures.
Because diabetes affects vascular physiology and can lead to multivessel disease, surgical revascularization vs. percutaneous coronary intervention has proved more successful in diabetic patients, Dr. Paul Kurlansky said in his invited commentary. However, “the potential impact of newer generation drug-eluting stents on improving these results remains to be seen,” he wrote (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.02.007).
Comparing CABG and PCI in diabetic patients has been challenging for a variety of reasons, including the nuances of clinical judgment and different techniques. “It is in this gray zone of clinical ambiguity that many if not most patients actually reside,” he said, giving credit to Dr. Nauffal and colleagues for trying to address this ambiguity.

|
Dr. Paul Kurlansky |
The study data, however, had many limitations, Dr. Kurlansky said. The authors could not specify indications for stent deployment, disease severity at the time of stenting and the choice of procedure among them. “An equally plausible hypothesis might therefore suggest that the appropriate need for prior stenting identified a subset of patients with more aggressive disease who therefore succumbed at an earlier age,” he said.
CABG that utilizes the internal mammary artery has been linked to enhanced physiologic properties that promote vasodilatation, inhibit thrombosis and atherosclerosis, and support the health of the vascular endothelium, he noted. In the diabetic patient, these properties may enhance the ability of CABG to address not only arterial blockages, but also the underlying physiology of atherosclerosis. “With the rising tide of diabetic vasculopathy, it will become increasingly important to consider both clinical utility and underlying physiology in navigating the uncertain path to optimal patient care,” Dr. Kurlansky wrote.
Dr. Kurlansky is with the department of surgery at Columbia University, New York.
Because diabetes affects vascular physiology and can lead to multivessel disease, surgical revascularization vs. percutaneous coronary intervention has proved more successful in diabetic patients, Dr. Paul Kurlansky said in his invited commentary. However, “the potential impact of newer generation drug-eluting stents on improving these results remains to be seen,” he wrote (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.02.007).
Comparing CABG and PCI in diabetic patients has been challenging for a variety of reasons, including the nuances of clinical judgment and different techniques. “It is in this gray zone of clinical ambiguity that many if not most patients actually reside,” he said, giving credit to Dr. Nauffal and colleagues for trying to address this ambiguity.

|
Dr. Paul Kurlansky |
The study data, however, had many limitations, Dr. Kurlansky said. The authors could not specify indications for stent deployment, disease severity at the time of stenting and the choice of procedure among them. “An equally plausible hypothesis might therefore suggest that the appropriate need for prior stenting identified a subset of patients with more aggressive disease who therefore succumbed at an earlier age,” he said.
CABG that utilizes the internal mammary artery has been linked to enhanced physiologic properties that promote vasodilatation, inhibit thrombosis and atherosclerosis, and support the health of the vascular endothelium, he noted. In the diabetic patient, these properties may enhance the ability of CABG to address not only arterial blockages, but also the underlying physiology of atherosclerosis. “With the rising tide of diabetic vasculopathy, it will become increasingly important to consider both clinical utility and underlying physiology in navigating the uncertain path to optimal patient care,” Dr. Kurlansky wrote.
Dr. Kurlansky is with the department of surgery at Columbia University, New York.
Because diabetes affects vascular physiology and can lead to multivessel disease, surgical revascularization vs. percutaneous coronary intervention has proved more successful in diabetic patients, Dr. Paul Kurlansky said in his invited commentary. However, “the potential impact of newer generation drug-eluting stents on improving these results remains to be seen,” he wrote (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.02.007).
Comparing CABG and PCI in diabetic patients has been challenging for a variety of reasons, including the nuances of clinical judgment and different techniques. “It is in this gray zone of clinical ambiguity that many if not most patients actually reside,” he said, giving credit to Dr. Nauffal and colleagues for trying to address this ambiguity.

|
Dr. Paul Kurlansky |
The study data, however, had many limitations, Dr. Kurlansky said. The authors could not specify indications for stent deployment, disease severity at the time of stenting and the choice of procedure among them. “An equally plausible hypothesis might therefore suggest that the appropriate need for prior stenting identified a subset of patients with more aggressive disease who therefore succumbed at an earlier age,” he said.
CABG that utilizes the internal mammary artery has been linked to enhanced physiologic properties that promote vasodilatation, inhibit thrombosis and atherosclerosis, and support the health of the vascular endothelium, he noted. In the diabetic patient, these properties may enhance the ability of CABG to address not only arterial blockages, but also the underlying physiology of atherosclerosis. “With the rising tide of diabetic vasculopathy, it will become increasingly important to consider both clinical utility and underlying physiology in navigating the uncertain path to optimal patient care,” Dr. Kurlansky wrote.
Dr. Kurlansky is with the department of surgery at Columbia University, New York.
Since the debut of drug-eluting stents, more high-risk patient groups, namely diabetic patients, have undergone coronary stenting as opposed to coronary artery bypass grafting (CABG) as an option to open blocked arteries; however, diabetic patients with stents who go on to have CABG have significantly higher 5-year death rates than do unstented diabetics who undergo CABG, according to a study published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
A review of 7,005 CABG procedures performed from 1996 to 2007 at Mercy St. Vincent Medical Center in Toledo, Ohio, found that diabetic patients with triple-vessel disease and a prior percutaneous coronary intervention with stenting (PCI-S) who underwent CABG had a 39% greater risk of death within 5 years of the operation. The findings are significant, according to Dr. Victor Nauffal and his colleagues at the American University of Beirut, because increasing numbers of patients with coronary stents are referred for CABG (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.051).
Previous studies have linked prior stenting to an increased risk of bleeding and stent thrombosis during CABG, so having a better understanding of anticoagulation during the operation and the timing of the surgery after stenting could decrease complications. Investigations of the long-term outcomes of patients with stents who have CABG, however, have been lacking. This study investigated the premise that diabetics with triple-vessel disease and a stent had poorer outcomes because of endothelial dysfunction and the increased strain that triple-vessel disease places on the heart.
After exclusions, the final study population comprised 1,583 diabetic patients with concomitant triple-vessel disease, 202 (12.8%) of whom had coronary stents. The study defined triple-vessel disease as blockages of 50% or more in all three native coronary vessels or left main artery plus right coronary artery disease.
Early mortality rates – death within 30 days of the procedure – were similar between the two groups: 3.3% overall, 3% in the prior-PCI group, and 3.3% in the no-PCI group; therefore, prior PCI was not a predictor of early mortality.
Five-year cumulative survival was 78.5% in the no-PCI group, compared with 74.8% in the PCI group. When adjusting for a variety of clinical variables before CABG, stenting was associated with a 39% greater mortality at 5 years. The investigators accounted for the emergence of drug-eluting stents during the 10-year study period but found that they did not contribute significantly to overall outcomes.
The cause of death was known for 81.7% (282 of 345) of the deaths in the overall cohort, with 5-year cardiac deaths higher in the PCI-S group: 8.4% vs. 7.5% for the no-PCI group. “Notably, 100% of PCI-S cardiac mortality was categorized as coronary heart disease related compared to 89.3% (92/103) of cardiac mortality in the no-PCI group,” Dr. Nauffal and his associates said.
Careful patient selection for CABG is in order for diabetics with triple-vessel disease, particularly those with a prior stent, the authors advised. “An early team-based approach including a cardiologist and cardiac surgeon should be implemented for optimal revascularization strategy selection in diabetics with triple-vessel disease and for close medical follow-up of those higher risk CABG patients with history of intracoronary stents,” Dr. Nauffal and his colleagues concluded.
The Johns Hopkins Murex Research Award supported Dr. Nauffal. The authors had no other relevant disclosures.
Since the debut of drug-eluting stents, more high-risk patient groups, namely diabetic patients, have undergone coronary stenting as opposed to coronary artery bypass grafting (CABG) as an option to open blocked arteries; however, diabetic patients with stents who go on to have CABG have significantly higher 5-year death rates than do unstented diabetics who undergo CABG, according to a study published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
A review of 7,005 CABG procedures performed from 1996 to 2007 at Mercy St. Vincent Medical Center in Toledo, Ohio, found that diabetic patients with triple-vessel disease and a prior percutaneous coronary intervention with stenting (PCI-S) who underwent CABG had a 39% greater risk of death within 5 years of the operation. The findings are significant, according to Dr. Victor Nauffal and his colleagues at the American University of Beirut, because increasing numbers of patients with coronary stents are referred for CABG (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.051).
Previous studies have linked prior stenting to an increased risk of bleeding and stent thrombosis during CABG, so having a better understanding of anticoagulation during the operation and the timing of the surgery after stenting could decrease complications. Investigations of the long-term outcomes of patients with stents who have CABG, however, have been lacking. This study investigated the premise that diabetics with triple-vessel disease and a stent had poorer outcomes because of endothelial dysfunction and the increased strain that triple-vessel disease places on the heart.
After exclusions, the final study population comprised 1,583 diabetic patients with concomitant triple-vessel disease, 202 (12.8%) of whom had coronary stents. The study defined triple-vessel disease as blockages of 50% or more in all three native coronary vessels or left main artery plus right coronary artery disease.
Early mortality rates – death within 30 days of the procedure – were similar between the two groups: 3.3% overall, 3% in the prior-PCI group, and 3.3% in the no-PCI group; therefore, prior PCI was not a predictor of early mortality.
Five-year cumulative survival was 78.5% in the no-PCI group, compared with 74.8% in the PCI group. When adjusting for a variety of clinical variables before CABG, stenting was associated with a 39% greater mortality at 5 years. The investigators accounted for the emergence of drug-eluting stents during the 10-year study period but found that they did not contribute significantly to overall outcomes.
The cause of death was known for 81.7% (282 of 345) of the deaths in the overall cohort, with 5-year cardiac deaths higher in the PCI-S group: 8.4% vs. 7.5% for the no-PCI group. “Notably, 100% of PCI-S cardiac mortality was categorized as coronary heart disease related compared to 89.3% (92/103) of cardiac mortality in the no-PCI group,” Dr. Nauffal and his associates said.
Careful patient selection for CABG is in order for diabetics with triple-vessel disease, particularly those with a prior stent, the authors advised. “An early team-based approach including a cardiologist and cardiac surgeon should be implemented for optimal revascularization strategy selection in diabetics with triple-vessel disease and for close medical follow-up of those higher risk CABG patients with history of intracoronary stents,” Dr. Nauffal and his colleagues concluded.
The Johns Hopkins Murex Research Award supported Dr. Nauffal. The authors had no other relevant disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Diabetic triple vessel–disease patients with prior percutaneous coronary intervention stenting (PCI-S) have poorer long-term outcomes after coronary artery bypass grafting than do patients who had no prior PCI-S.
Major finding: After adjusting for preoperative clinical characteristics and other factors, prior PCI-S was associated with 39% increased risk of mortality 5 years after surgery. Further adjustment for date of surgery or operative parameters did not alter the association.
Data source: Single-center review of 7,005 CABG cases performed from 1996 to 2007.
Disclosures: The Johns Hopkins Murex Research Award supported the lead author. The authors had no other relevant disclosures.
Guidelines for adults with congenital heart disease note changing landscape
New recommendations from the American Heart Association focus on the treatment of people older than age 40 years with congenital heart disease (CHD), a population that was believed to number about 850,000 in the year 2000 and is estimated to increase 5% each year.
“This improved longevity is leading to increased use of the medical system for both routine and episodic care, and caregivers need to be prepared to diagnose, follow-up, and treat the older adult with congenital heart disease,” authors led by Dr. Ami B. Bhatt wrote in a scientific statement published online April 20, 2015 in Circulation. “The predictable natural progression of CHD entities and sequelae of previous interventions must now be treated in the setting of late complications, acquired cardiac disease, multiorgan effects of lifelong processes, and the unrelenting process of aging. Despite the advances in this field, death rates in the population from 20 to [more than] 70 years of age may be twice to 7 times higher for the [adults] with CHD population than for their peers.”
Intended as a complement to the 2008 American College of Cardiology/AHA guidelines for ACHD (Circulation 2008;118:e714-833), the new recommendations cover the diagnosis and management of CHD in adults over the age of 40 years to summarize what is currently known “and to outline areas in which additional knowledge is critical to their care.” The scientific statement is limited to structural CHD, including coronary artery anomalies and aortopathy associated with bicuspid aortic valve disease (Circulation 2015 April 20; doi:10.1161/CIR.0000000000000204).
Working on behalf of the American Heart Association Council on Clinical Cardiology, Dr. Bhatt, who directs the adult congenital heart disease program at Massachusetts General Hospital, Boston, and her coauthors emphasized that the exposure to cardiovascular risk factors among ACHD patients is “no less problematic than with the non-CHD population. The ACHD individual may have abnormal myocardial substrate, abnormal cardiovascular physiology, abnormal anatomy, or any combination of the 3. The adverse impact of superimposed cardiovascular risk factors may well be amplified in this group, who also may already be at risk for systemic ventricular dysfunction, rhythm disturbances, and heart failure.”
In an interview, Dr. Bhatt noted that the ACHD population is distinct from both the pediatric and young adult populations with CHD and has many interactions with the health care system outside of adult congenital cardiac visits. “Therefore, this statement is written to serve as a reference for the many caregivers who will increasingly come across this population in their practice,” she said. “This includes general adult and pediatric cardiologists, electrophysiologists, interventionalists (percutaneous and surgical), cardiac imagers, as well as primary care physicians, hospitalists, and emergency medicine colleagues who need to understand and easily reference the issues and clinical challenges pertinent to this segment of the CHD population.”
The statement addresses diagnosis and management of late presentation of native disease, evolving long-term complications in disease diagnosed and/or intervened upon in childhood, and the additional burden of multiorgan dysfunction and acquired cardiovascular disease with age. Special attention is given to noncardiac involvement, including hepatic and renal disease screening and management, issues of aging including cognitive decline and sexual dysfunction, and challenging populations including those with coronary artery anomalies or superimposed pulmonary hypertension. The statement includes thorough discussions of diagnostic imaging, arrhythmia management, and surgical options in the older adult.
Among the issues addressed in the statement:
• Patient medical records, especially cardiac catheterization reports, should be obtained from primary sources. “This allow[s] comprehensive evaluation of these patients,” the authors wrote. They also emphasized the importance of multidisciplinary care when needed, in a medical center where other illnesses can be managed in a setting that also is knowledgeable about CHD.
• Psychosocial screening should be part of routine care of ACHD patients. This includes a team approach involving physicians, advanced practice nurses, physician assistants, psychologists, and social workers.
• Physical activity is encouraged. Sedentary lifestyle is a risk factor for many older adults with CHD. Cardiopulmonary exercise testing can be used in ACHD patients to help physicians create an individualized exercise plan. Research demonstrates that a structured regimen can improve exercise tolerance in this population.
• Sexual activity is reasonable for most ACHD patients. Exceptions include those who have decompensated or advanced heart failure, severe and/or significantly symptomatic valvular disease, or uncontrolled arrhythmias. Counseling must be provided by health care providers and “is useful to assist in resumption of sexual activity [especially] after an acute cardiac event, new cardiovascular disease diagnosis, or [implantable cardioverter defibrillator] implantation.”
• Many men with ACHD can take erectile dysfunction drugs as long as they are not taking nitrates and as long as their condition does not preclude sexual activity. However, “the effectiveness of phosphodiesterase type 5 inhibitors has not been established in the presence of severe ventricular outflow tract obstruction.”
• The use of hormone replacement therapy by women with ACHD must consider the risk for thromboembolic disease as well as the severity of menopausal symptoms. “For example, women with Fontan surgery have a high risk of venous thromboembolism and should avoid HRT, whereas women with [tetralogy of Fallot] repair and good RV function have a low risk and could probably receive HRT for symptoms,” the authors wrote.
The statement also includes recommendations for clinicians treating ACHD patients regarding screening for and management of concomitant lung, kidney, or liver disease. For example, it recommends serial evaluation of liver function for all patients with a history of previous palliation with the Fontan procedure and routine assessment of renal function for all adults with moderate-to-complex CHD.
The information provided in the AHA statement is based on scientific research and combined clinical experience from longitudinal care, Dr. Bhatt said in the interview. “The authors engaged in a truly multidisciplinary effort as pediatric and adult cardiologists, cardiac subspecialists, radiologists, and surgeons worked together to create a document to assist caregivers in meeting the needs of this challenging and growing population,” she said. “Importantly, by sharing the clinical trajectory of the older adult with CHD, the authors hope this statement and future versions will inform pediatric and young adult care and research as we strive to together improve lifelong care in congenital heart disease.”
Five of the coauthors disclosed relevant financial relationships. Dr. Michael C. Earing has received honoraria from Actelion Pharmaceuticals. Dr. Elyse Foster has received a research grant from Abbott Vascular and is a consultant or advisory board member for Gilead. Dr. Brian B. Ghoshhajra is a consultant or advisory board member for Siemens Healthcare. Dr. Seema Mital is a consultant or advisory board member for Novartis. Dr. Zian H. Tseng has received honoraria from Biotronik. The remaining authors reported having no relevant financial disclosures.
On Twitter @dougbrunk
Diagnosis and treatment of congenital heart disease has improved dramatically over the last 5 decades, such that there is a growing population of adults with CHD. By some estimates, there are over a million adults with CHD and the population is growing by 5% per year. Despite the significant improvement in outcomes in children with CHD, there are significant sequelae of underlying CHD and necessary repairs that affect adults with CHD (ACHD). Common problems include arrhythmias, heart failure, sudden death, premature mortality, and complications related to other affected organs, such as hepatic or renal dysfunction. While understanding of these issues in ACHD patients as a whole is increasing steadily, most ACHD patients are young adults, thus the understanding of how CHD will impact older adults is less clear. Many of the issues related to CHD would be expected to progressively worsen through the lifespan, such that arrhythmias and heart failure may be even more prevalent in older adults, yet due to the underlying CHD may not respond to treatment in the ways expected in other adults with acquired cardiovascular disease. Additionally, the impact of comorbid diseases commonly encountered in older adults on underlying CHD will add a layer of complexity to both the CHD and the other comorbid diseases.

|
| Dr. Karen Stout |
The scientific statement from Dr. Bhatt and her colleagues is a comprehensive, detailed discussion of the issues anticipated in older adults with CHD. The statement reviews the breadth of issues in older adults with CHD, beginning with CHD-related complications that occur regardless of the specific type of CHD and followed by a discussion on issues of specific types of CHD, such as transposition of the great arteries and shunt lesions. They discuss both unoperated and operated CHD in the older adult. An important part of the document is the sections reviewing the acquired cardiovascular risks and diseases in the ACHD patient and the noncardiac issues that are important in older adults with CHD.
Throughout the document, there is an overarching theme that ACHD cardiology expertise is needed in the care of these patients. There also is a call to arms that more data are needed to better care for these patients, and that we must develop registries and larger clinical trials to improve outcomes for these patients.
Dr. Karen K. Stout is a cardiologist and professor of medicine at the University of Washington, Seattle.
Diagnosis and treatment of congenital heart disease has improved dramatically over the last 5 decades, such that there is a growing population of adults with CHD. By some estimates, there are over a million adults with CHD and the population is growing by 5% per year. Despite the significant improvement in outcomes in children with CHD, there are significant sequelae of underlying CHD and necessary repairs that affect adults with CHD (ACHD). Common problems include arrhythmias, heart failure, sudden death, premature mortality, and complications related to other affected organs, such as hepatic or renal dysfunction. While understanding of these issues in ACHD patients as a whole is increasing steadily, most ACHD patients are young adults, thus the understanding of how CHD will impact older adults is less clear. Many of the issues related to CHD would be expected to progressively worsen through the lifespan, such that arrhythmias and heart failure may be even more prevalent in older adults, yet due to the underlying CHD may not respond to treatment in the ways expected in other adults with acquired cardiovascular disease. Additionally, the impact of comorbid diseases commonly encountered in older adults on underlying CHD will add a layer of complexity to both the CHD and the other comorbid diseases.

|
| Dr. Karen Stout |
The scientific statement from Dr. Bhatt and her colleagues is a comprehensive, detailed discussion of the issues anticipated in older adults with CHD. The statement reviews the breadth of issues in older adults with CHD, beginning with CHD-related complications that occur regardless of the specific type of CHD and followed by a discussion on issues of specific types of CHD, such as transposition of the great arteries and shunt lesions. They discuss both unoperated and operated CHD in the older adult. An important part of the document is the sections reviewing the acquired cardiovascular risks and diseases in the ACHD patient and the noncardiac issues that are important in older adults with CHD.
Throughout the document, there is an overarching theme that ACHD cardiology expertise is needed in the care of these patients. There also is a call to arms that more data are needed to better care for these patients, and that we must develop registries and larger clinical trials to improve outcomes for these patients.
Dr. Karen K. Stout is a cardiologist and professor of medicine at the University of Washington, Seattle.
Diagnosis and treatment of congenital heart disease has improved dramatically over the last 5 decades, such that there is a growing population of adults with CHD. By some estimates, there are over a million adults with CHD and the population is growing by 5% per year. Despite the significant improvement in outcomes in children with CHD, there are significant sequelae of underlying CHD and necessary repairs that affect adults with CHD (ACHD). Common problems include arrhythmias, heart failure, sudden death, premature mortality, and complications related to other affected organs, such as hepatic or renal dysfunction. While understanding of these issues in ACHD patients as a whole is increasing steadily, most ACHD patients are young adults, thus the understanding of how CHD will impact older adults is less clear. Many of the issues related to CHD would be expected to progressively worsen through the lifespan, such that arrhythmias and heart failure may be even more prevalent in older adults, yet due to the underlying CHD may not respond to treatment in the ways expected in other adults with acquired cardiovascular disease. Additionally, the impact of comorbid diseases commonly encountered in older adults on underlying CHD will add a layer of complexity to both the CHD and the other comorbid diseases.

|
| Dr. Karen Stout |
The scientific statement from Dr. Bhatt and her colleagues is a comprehensive, detailed discussion of the issues anticipated in older adults with CHD. The statement reviews the breadth of issues in older adults with CHD, beginning with CHD-related complications that occur regardless of the specific type of CHD and followed by a discussion on issues of specific types of CHD, such as transposition of the great arteries and shunt lesions. They discuss both unoperated and operated CHD in the older adult. An important part of the document is the sections reviewing the acquired cardiovascular risks and diseases in the ACHD patient and the noncardiac issues that are important in older adults with CHD.
Throughout the document, there is an overarching theme that ACHD cardiology expertise is needed in the care of these patients. There also is a call to arms that more data are needed to better care for these patients, and that we must develop registries and larger clinical trials to improve outcomes for these patients.
Dr. Karen K. Stout is a cardiologist and professor of medicine at the University of Washington, Seattle.
New recommendations from the American Heart Association focus on the treatment of people older than age 40 years with congenital heart disease (CHD), a population that was believed to number about 850,000 in the year 2000 and is estimated to increase 5% each year.
“This improved longevity is leading to increased use of the medical system for both routine and episodic care, and caregivers need to be prepared to diagnose, follow-up, and treat the older adult with congenital heart disease,” authors led by Dr. Ami B. Bhatt wrote in a scientific statement published online April 20, 2015 in Circulation. “The predictable natural progression of CHD entities and sequelae of previous interventions must now be treated in the setting of late complications, acquired cardiac disease, multiorgan effects of lifelong processes, and the unrelenting process of aging. Despite the advances in this field, death rates in the population from 20 to [more than] 70 years of age may be twice to 7 times higher for the [adults] with CHD population than for their peers.”
Intended as a complement to the 2008 American College of Cardiology/AHA guidelines for ACHD (Circulation 2008;118:e714-833), the new recommendations cover the diagnosis and management of CHD in adults over the age of 40 years to summarize what is currently known “and to outline areas in which additional knowledge is critical to their care.” The scientific statement is limited to structural CHD, including coronary artery anomalies and aortopathy associated with bicuspid aortic valve disease (Circulation 2015 April 20; doi:10.1161/CIR.0000000000000204).
Working on behalf of the American Heart Association Council on Clinical Cardiology, Dr. Bhatt, who directs the adult congenital heart disease program at Massachusetts General Hospital, Boston, and her coauthors emphasized that the exposure to cardiovascular risk factors among ACHD patients is “no less problematic than with the non-CHD population. The ACHD individual may have abnormal myocardial substrate, abnormal cardiovascular physiology, abnormal anatomy, or any combination of the 3. The adverse impact of superimposed cardiovascular risk factors may well be amplified in this group, who also may already be at risk for systemic ventricular dysfunction, rhythm disturbances, and heart failure.”
In an interview, Dr. Bhatt noted that the ACHD population is distinct from both the pediatric and young adult populations with CHD and has many interactions with the health care system outside of adult congenital cardiac visits. “Therefore, this statement is written to serve as a reference for the many caregivers who will increasingly come across this population in their practice,” she said. “This includes general adult and pediatric cardiologists, electrophysiologists, interventionalists (percutaneous and surgical), cardiac imagers, as well as primary care physicians, hospitalists, and emergency medicine colleagues who need to understand and easily reference the issues and clinical challenges pertinent to this segment of the CHD population.”
The statement addresses diagnosis and management of late presentation of native disease, evolving long-term complications in disease diagnosed and/or intervened upon in childhood, and the additional burden of multiorgan dysfunction and acquired cardiovascular disease with age. Special attention is given to noncardiac involvement, including hepatic and renal disease screening and management, issues of aging including cognitive decline and sexual dysfunction, and challenging populations including those with coronary artery anomalies or superimposed pulmonary hypertension. The statement includes thorough discussions of diagnostic imaging, arrhythmia management, and surgical options in the older adult.
Among the issues addressed in the statement:
• Patient medical records, especially cardiac catheterization reports, should be obtained from primary sources. “This allow[s] comprehensive evaluation of these patients,” the authors wrote. They also emphasized the importance of multidisciplinary care when needed, in a medical center where other illnesses can be managed in a setting that also is knowledgeable about CHD.
• Psychosocial screening should be part of routine care of ACHD patients. This includes a team approach involving physicians, advanced practice nurses, physician assistants, psychologists, and social workers.
• Physical activity is encouraged. Sedentary lifestyle is a risk factor for many older adults with CHD. Cardiopulmonary exercise testing can be used in ACHD patients to help physicians create an individualized exercise plan. Research demonstrates that a structured regimen can improve exercise tolerance in this population.
• Sexual activity is reasonable for most ACHD patients. Exceptions include those who have decompensated or advanced heart failure, severe and/or significantly symptomatic valvular disease, or uncontrolled arrhythmias. Counseling must be provided by health care providers and “is useful to assist in resumption of sexual activity [especially] after an acute cardiac event, new cardiovascular disease diagnosis, or [implantable cardioverter defibrillator] implantation.”
• Many men with ACHD can take erectile dysfunction drugs as long as they are not taking nitrates and as long as their condition does not preclude sexual activity. However, “the effectiveness of phosphodiesterase type 5 inhibitors has not been established in the presence of severe ventricular outflow tract obstruction.”
• The use of hormone replacement therapy by women with ACHD must consider the risk for thromboembolic disease as well as the severity of menopausal symptoms. “For example, women with Fontan surgery have a high risk of venous thromboembolism and should avoid HRT, whereas women with [tetralogy of Fallot] repair and good RV function have a low risk and could probably receive HRT for symptoms,” the authors wrote.
The statement also includes recommendations for clinicians treating ACHD patients regarding screening for and management of concomitant lung, kidney, or liver disease. For example, it recommends serial evaluation of liver function for all patients with a history of previous palliation with the Fontan procedure and routine assessment of renal function for all adults with moderate-to-complex CHD.
The information provided in the AHA statement is based on scientific research and combined clinical experience from longitudinal care, Dr. Bhatt said in the interview. “The authors engaged in a truly multidisciplinary effort as pediatric and adult cardiologists, cardiac subspecialists, radiologists, and surgeons worked together to create a document to assist caregivers in meeting the needs of this challenging and growing population,” she said. “Importantly, by sharing the clinical trajectory of the older adult with CHD, the authors hope this statement and future versions will inform pediatric and young adult care and research as we strive to together improve lifelong care in congenital heart disease.”
Five of the coauthors disclosed relevant financial relationships. Dr. Michael C. Earing has received honoraria from Actelion Pharmaceuticals. Dr. Elyse Foster has received a research grant from Abbott Vascular and is a consultant or advisory board member for Gilead. Dr. Brian B. Ghoshhajra is a consultant or advisory board member for Siemens Healthcare. Dr. Seema Mital is a consultant or advisory board member for Novartis. Dr. Zian H. Tseng has received honoraria from Biotronik. The remaining authors reported having no relevant financial disclosures.
On Twitter @dougbrunk
New recommendations from the American Heart Association focus on the treatment of people older than age 40 years with congenital heart disease (CHD), a population that was believed to number about 850,000 in the year 2000 and is estimated to increase 5% each year.
“This improved longevity is leading to increased use of the medical system for both routine and episodic care, and caregivers need to be prepared to diagnose, follow-up, and treat the older adult with congenital heart disease,” authors led by Dr. Ami B. Bhatt wrote in a scientific statement published online April 20, 2015 in Circulation. “The predictable natural progression of CHD entities and sequelae of previous interventions must now be treated in the setting of late complications, acquired cardiac disease, multiorgan effects of lifelong processes, and the unrelenting process of aging. Despite the advances in this field, death rates in the population from 20 to [more than] 70 years of age may be twice to 7 times higher for the [adults] with CHD population than for their peers.”
Intended as a complement to the 2008 American College of Cardiology/AHA guidelines for ACHD (Circulation 2008;118:e714-833), the new recommendations cover the diagnosis and management of CHD in adults over the age of 40 years to summarize what is currently known “and to outline areas in which additional knowledge is critical to their care.” The scientific statement is limited to structural CHD, including coronary artery anomalies and aortopathy associated with bicuspid aortic valve disease (Circulation 2015 April 20; doi:10.1161/CIR.0000000000000204).
Working on behalf of the American Heart Association Council on Clinical Cardiology, Dr. Bhatt, who directs the adult congenital heart disease program at Massachusetts General Hospital, Boston, and her coauthors emphasized that the exposure to cardiovascular risk factors among ACHD patients is “no less problematic than with the non-CHD population. The ACHD individual may have abnormal myocardial substrate, abnormal cardiovascular physiology, abnormal anatomy, or any combination of the 3. The adverse impact of superimposed cardiovascular risk factors may well be amplified in this group, who also may already be at risk for systemic ventricular dysfunction, rhythm disturbances, and heart failure.”
In an interview, Dr. Bhatt noted that the ACHD population is distinct from both the pediatric and young adult populations with CHD and has many interactions with the health care system outside of adult congenital cardiac visits. “Therefore, this statement is written to serve as a reference for the many caregivers who will increasingly come across this population in their practice,” she said. “This includes general adult and pediatric cardiologists, electrophysiologists, interventionalists (percutaneous and surgical), cardiac imagers, as well as primary care physicians, hospitalists, and emergency medicine colleagues who need to understand and easily reference the issues and clinical challenges pertinent to this segment of the CHD population.”
The statement addresses diagnosis and management of late presentation of native disease, evolving long-term complications in disease diagnosed and/or intervened upon in childhood, and the additional burden of multiorgan dysfunction and acquired cardiovascular disease with age. Special attention is given to noncardiac involvement, including hepatic and renal disease screening and management, issues of aging including cognitive decline and sexual dysfunction, and challenging populations including those with coronary artery anomalies or superimposed pulmonary hypertension. The statement includes thorough discussions of diagnostic imaging, arrhythmia management, and surgical options in the older adult.
Among the issues addressed in the statement:
• Patient medical records, especially cardiac catheterization reports, should be obtained from primary sources. “This allow[s] comprehensive evaluation of these patients,” the authors wrote. They also emphasized the importance of multidisciplinary care when needed, in a medical center where other illnesses can be managed in a setting that also is knowledgeable about CHD.
• Psychosocial screening should be part of routine care of ACHD patients. This includes a team approach involving physicians, advanced practice nurses, physician assistants, psychologists, and social workers.
• Physical activity is encouraged. Sedentary lifestyle is a risk factor for many older adults with CHD. Cardiopulmonary exercise testing can be used in ACHD patients to help physicians create an individualized exercise plan. Research demonstrates that a structured regimen can improve exercise tolerance in this population.
• Sexual activity is reasonable for most ACHD patients. Exceptions include those who have decompensated or advanced heart failure, severe and/or significantly symptomatic valvular disease, or uncontrolled arrhythmias. Counseling must be provided by health care providers and “is useful to assist in resumption of sexual activity [especially] after an acute cardiac event, new cardiovascular disease diagnosis, or [implantable cardioverter defibrillator] implantation.”
• Many men with ACHD can take erectile dysfunction drugs as long as they are not taking nitrates and as long as their condition does not preclude sexual activity. However, “the effectiveness of phosphodiesterase type 5 inhibitors has not been established in the presence of severe ventricular outflow tract obstruction.”
• The use of hormone replacement therapy by women with ACHD must consider the risk for thromboembolic disease as well as the severity of menopausal symptoms. “For example, women with Fontan surgery have a high risk of venous thromboembolism and should avoid HRT, whereas women with [tetralogy of Fallot] repair and good RV function have a low risk and could probably receive HRT for symptoms,” the authors wrote.
The statement also includes recommendations for clinicians treating ACHD patients regarding screening for and management of concomitant lung, kidney, or liver disease. For example, it recommends serial evaluation of liver function for all patients with a history of previous palliation with the Fontan procedure and routine assessment of renal function for all adults with moderate-to-complex CHD.
The information provided in the AHA statement is based on scientific research and combined clinical experience from longitudinal care, Dr. Bhatt said in the interview. “The authors engaged in a truly multidisciplinary effort as pediatric and adult cardiologists, cardiac subspecialists, radiologists, and surgeons worked together to create a document to assist caregivers in meeting the needs of this challenging and growing population,” she said. “Importantly, by sharing the clinical trajectory of the older adult with CHD, the authors hope this statement and future versions will inform pediatric and young adult care and research as we strive to together improve lifelong care in congenital heart disease.”
Five of the coauthors disclosed relevant financial relationships. Dr. Michael C. Earing has received honoraria from Actelion Pharmaceuticals. Dr. Elyse Foster has received a research grant from Abbott Vascular and is a consultant or advisory board member for Gilead. Dr. Brian B. Ghoshhajra is a consultant or advisory board member for Siemens Healthcare. Dr. Seema Mital is a consultant or advisory board member for Novartis. Dr. Zian H. Tseng has received honoraria from Biotronik. The remaining authors reported having no relevant financial disclosures.
On Twitter @dougbrunk
FROM CIRCULATION
Ablation during mitral valve surgery offers up mixed results
SAN DIEGO – Surgical ablation of atrial fibrillation at the time of mitral valve surgery provides significantly greater rhythm control than mitral valve surgery alone, a study showed.
Freedom from atrial fibrillation (AF) at both 6 months and 1 year was 63% in patients undergoing mitral valve surgery (MVS) plus ablation and 29% in those undergoing MVS alone, a statistically significant difference.
However, patients who had ablation plus MVS were 2.5 times more likely to have a permanent pacemaker implanted than were those who had MVS alone, at 21.5% and 8.1%, respectively, also a significant difference.
Ablation did not increase mortality or major adverse cardiac or cerebrovascular events, Dr. A. Marc Gillinov said at the annual meeting of the American College of Cardiology.
Preoperative AF is present in up to 50% of patients undergoing mitral valve operations and is associated with an increased risk of death and stroke.
The study enrolled 260 relatively elderly patients (mean age 69 years) with AF that was persistent (non–self-terminating for at least 7 days) or long-standing persistent (continuous for at least a year), in addition to mitral valve disease. A total of 133 patients were randomly assigned to MVS plus ablation and 127 to MVS alone. The ablation group was further randomized to pulmonary vein isolation or a biatrial maze procedure; all underwent closure of the left atrial appendage.
There was no significant difference in freedom from AF at 6 months and 1 year between patients who had pulmonary vein isolation or a biatrial maze procedure, at 61% and 66%, respectively, said Dr. Gillinov, a cardiac surgeon at Cleveland Clinic.
One-year mortality was similar among all patients undergoing MVS plus ablation vs. MVS alone, at 6.8% and 8.7%.
The two groups also had similar Short Form-12 questionnaire scores for physical function and mental function, although AF occurring at least once daily was significantly less common with ablation, at 19.8%, compared with 45.2% in the MVS-alone patients, he said.
The heart rhythm endpoint was “stringent,” with 3-day Holter monitors obtained at both 6 and 12 months and repeat ablation procedures and death considered treatment failures, Dr. Gillinov said.
He acknowledged that 20% of patients did not have data for the primary endpoint and that the endpoint was not a clinical one, but said a trial with mortality or stroke as the endpoint would require more than 1,000 patients and many years follow-up.
Regarding whether ablation should now be performed routinely, “the glass is half full or half empty,” remarked discussant Dr. Bernard Gersh of Mayo Clinic in Rochester, Minn. “On one hand, you have shown less atrial fibrillation [with ablation], but no effect on quality of life, and the price to be paid was a higher rate of pacemaker implantation,” he said.
The pacemaker implantation rate was higher than expected – 17% in-hospital – and does represent a potential cost, but he would routinely do a maze procedure, Dr. Gillinov said.
Discussant Dr. Alice Jacobs of the Cardiovascular Center at Boston Medical Center, said she expected Dr. Gillinov to say the procedure should not be used in everyone given the lack of benefit in stroke, probably because they tied off the left atrium appendage, and the increase in pacemaker implantations.
About half of the pacemaker implantations were due to atrioventricular block, possibly a consequence of the valve surgery, and one-third to sinus-node dysfunction, which is common in elderly patients, Dr. Gillinov explained.
The study was funded by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov reported serving as a consultant/speaker for AtriCure, Medtronic, On-X, Edwards, and Tendyne; research funding from St. Jude Medical; an equity interest in Clear Catheter; and that his institution receives royalties from AtriCure for a left atrial appendage occlusion device.
SAN DIEGO – Surgical ablation of atrial fibrillation at the time of mitral valve surgery provides significantly greater rhythm control than mitral valve surgery alone, a study showed.
Freedom from atrial fibrillation (AF) at both 6 months and 1 year was 63% in patients undergoing mitral valve surgery (MVS) plus ablation and 29% in those undergoing MVS alone, a statistically significant difference.
However, patients who had ablation plus MVS were 2.5 times more likely to have a permanent pacemaker implanted than were those who had MVS alone, at 21.5% and 8.1%, respectively, also a significant difference.
Ablation did not increase mortality or major adverse cardiac or cerebrovascular events, Dr. A. Marc Gillinov said at the annual meeting of the American College of Cardiology.
Preoperative AF is present in up to 50% of patients undergoing mitral valve operations and is associated with an increased risk of death and stroke.
The study enrolled 260 relatively elderly patients (mean age 69 years) with AF that was persistent (non–self-terminating for at least 7 days) or long-standing persistent (continuous for at least a year), in addition to mitral valve disease. A total of 133 patients were randomly assigned to MVS plus ablation and 127 to MVS alone. The ablation group was further randomized to pulmonary vein isolation or a biatrial maze procedure; all underwent closure of the left atrial appendage.
There was no significant difference in freedom from AF at 6 months and 1 year between patients who had pulmonary vein isolation or a biatrial maze procedure, at 61% and 66%, respectively, said Dr. Gillinov, a cardiac surgeon at Cleveland Clinic.
One-year mortality was similar among all patients undergoing MVS plus ablation vs. MVS alone, at 6.8% and 8.7%.
The two groups also had similar Short Form-12 questionnaire scores for physical function and mental function, although AF occurring at least once daily was significantly less common with ablation, at 19.8%, compared with 45.2% in the MVS-alone patients, he said.
The heart rhythm endpoint was “stringent,” with 3-day Holter monitors obtained at both 6 and 12 months and repeat ablation procedures and death considered treatment failures, Dr. Gillinov said.
He acknowledged that 20% of patients did not have data for the primary endpoint and that the endpoint was not a clinical one, but said a trial with mortality or stroke as the endpoint would require more than 1,000 patients and many years follow-up.
Regarding whether ablation should now be performed routinely, “the glass is half full or half empty,” remarked discussant Dr. Bernard Gersh of Mayo Clinic in Rochester, Minn. “On one hand, you have shown less atrial fibrillation [with ablation], but no effect on quality of life, and the price to be paid was a higher rate of pacemaker implantation,” he said.
The pacemaker implantation rate was higher than expected – 17% in-hospital – and does represent a potential cost, but he would routinely do a maze procedure, Dr. Gillinov said.
Discussant Dr. Alice Jacobs of the Cardiovascular Center at Boston Medical Center, said she expected Dr. Gillinov to say the procedure should not be used in everyone given the lack of benefit in stroke, probably because they tied off the left atrium appendage, and the increase in pacemaker implantations.
About half of the pacemaker implantations were due to atrioventricular block, possibly a consequence of the valve surgery, and one-third to sinus-node dysfunction, which is common in elderly patients, Dr. Gillinov explained.
The study was funded by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov reported serving as a consultant/speaker for AtriCure, Medtronic, On-X, Edwards, and Tendyne; research funding from St. Jude Medical; an equity interest in Clear Catheter; and that his institution receives royalties from AtriCure for a left atrial appendage occlusion device.
SAN DIEGO – Surgical ablation of atrial fibrillation at the time of mitral valve surgery provides significantly greater rhythm control than mitral valve surgery alone, a study showed.
Freedom from atrial fibrillation (AF) at both 6 months and 1 year was 63% in patients undergoing mitral valve surgery (MVS) plus ablation and 29% in those undergoing MVS alone, a statistically significant difference.
However, patients who had ablation plus MVS were 2.5 times more likely to have a permanent pacemaker implanted than were those who had MVS alone, at 21.5% and 8.1%, respectively, also a significant difference.
Ablation did not increase mortality or major adverse cardiac or cerebrovascular events, Dr. A. Marc Gillinov said at the annual meeting of the American College of Cardiology.
Preoperative AF is present in up to 50% of patients undergoing mitral valve operations and is associated with an increased risk of death and stroke.
The study enrolled 260 relatively elderly patients (mean age 69 years) with AF that was persistent (non–self-terminating for at least 7 days) or long-standing persistent (continuous for at least a year), in addition to mitral valve disease. A total of 133 patients were randomly assigned to MVS plus ablation and 127 to MVS alone. The ablation group was further randomized to pulmonary vein isolation or a biatrial maze procedure; all underwent closure of the left atrial appendage.
There was no significant difference in freedom from AF at 6 months and 1 year between patients who had pulmonary vein isolation or a biatrial maze procedure, at 61% and 66%, respectively, said Dr. Gillinov, a cardiac surgeon at Cleveland Clinic.
One-year mortality was similar among all patients undergoing MVS plus ablation vs. MVS alone, at 6.8% and 8.7%.
The two groups also had similar Short Form-12 questionnaire scores for physical function and mental function, although AF occurring at least once daily was significantly less common with ablation, at 19.8%, compared with 45.2% in the MVS-alone patients, he said.
The heart rhythm endpoint was “stringent,” with 3-day Holter monitors obtained at both 6 and 12 months and repeat ablation procedures and death considered treatment failures, Dr. Gillinov said.
He acknowledged that 20% of patients did not have data for the primary endpoint and that the endpoint was not a clinical one, but said a trial with mortality or stroke as the endpoint would require more than 1,000 patients and many years follow-up.
Regarding whether ablation should now be performed routinely, “the glass is half full or half empty,” remarked discussant Dr. Bernard Gersh of Mayo Clinic in Rochester, Minn. “On one hand, you have shown less atrial fibrillation [with ablation], but no effect on quality of life, and the price to be paid was a higher rate of pacemaker implantation,” he said.
The pacemaker implantation rate was higher than expected – 17% in-hospital – and does represent a potential cost, but he would routinely do a maze procedure, Dr. Gillinov said.
Discussant Dr. Alice Jacobs of the Cardiovascular Center at Boston Medical Center, said she expected Dr. Gillinov to say the procedure should not be used in everyone given the lack of benefit in stroke, probably because they tied off the left atrium appendage, and the increase in pacemaker implantations.
About half of the pacemaker implantations were due to atrioventricular block, possibly a consequence of the valve surgery, and one-third to sinus-node dysfunction, which is common in elderly patients, Dr. Gillinov explained.
The study was funded by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov reported serving as a consultant/speaker for AtriCure, Medtronic, On-X, Edwards, and Tendyne; research funding from St. Jude Medical; an equity interest in Clear Catheter; and that his institution receives royalties from AtriCure for a left atrial appendage occlusion device.
AT ACC 15
Key clinical point: Surgical ablation of atrial fibrillation during mitral valve surgery decreases AF at 6 months and 1 year, but increases pacemaker implantations.
Major finding: Freedom from AF at both 6 months and 1 year was 63% with mitral valve surgery plus ablation and 29% for MVS alone.
Data source: Prospective, randomized study in 260 patients with persistent or longstanding persistent AF who required mitral valve surgery.
Disclosures: The study was funded by the National Institutes of Health and the Canadian Institutes of Health Research. Dr. Gillinov reported serving as a consultant/speaker for AtriCure, Medtronic, On-X, Edwards, and Tendyne; research funding from St. Jude Medical; an equity interest in Clear Catheter; and that his institution receives royalties from AtriCure for a left atrial appendage occlusion device.