User login
Real-world CAS results in Medicare patients not up to trial standards
The presence of competing risks and overall lower levels of provider proficiency appeared to limit the benefits of carotid artery stenting in Medicare beneficiaries, according to the results of a large retrospective cohort study of the Centers for Medicare & Medicaid Services CAS database (2005-2009).
Periprocedural mortality was more than twice the rate in this patient population than in those earlier patients those involved in the pivotal CREST and SAPPHIRE clinical trials, according to a report published online Jan. 12 in JAMA Neurology [doi:10.1001/jamaneurol.2014.3638].
“The higher risk of periprocedural complications and the burden of competing risks owing to age and comorbidity burden must be carefully considered when deciding between carotid stenosis treatments for Medicare beneficiaries,” according to Jessica J. Jalbert, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, Boston, and her colleagues.
Over 22,000 patients were assessed in the study. The mean patient age was just over 76 years, 60.5% were men, and 94% were white. Approximately half were symptomatic, 91.2% were at high surgical risk, and 97.4% had carotid stenosis of at least 70%.
Almost 80% of the patients undergoing carotid artery stenting (CAS) met the SAPPHIRE trial indications and about half met at least one of the SAPPHIRE criteria for high surgical risk.
In the mean follow-up of approximately 2 years, mortality risks exceeded one-third for patients who were 80 years of age or older (41.5% mortality risk), symptomatic (37.3% risk), at high surgical risk with symptomatic carotid stenosis of at least 50% (37.3% risk), or admitted nonelectively (36.2% risk). In addition, among asymptomatic patients, mortality after the periprocedural period exceeded one-third for patients at least 80 years old.
Of particular concern, few of these Medicare beneficiaries undergoing CAS as per the National Coverage Determinations were treated by providers with proficiency levels similar to those required in the clinical trials. This is a potential problem because lower annual volume and early operator experience are associated with increased periprocedural mortality, the authors wrote.
CAS was performed primarily by male physicians (98.4%), specializing in cardiology (52.9%), practicing within a group (79.4%), and residing in the South (42.5%). The mean number of past-year CAS procedures performed was only 13.9 for physicians and 29.8 for hospitals. This translated to more than 80% of the physicians not meeting the minimum CAS volume requirements and/or minimum complication rates of the SAPPHIRE trial, and more than 90% not meeting the requirements of the CREST trial.
“Our results may support concerns about the limited generalizability of [randomized clinical trial] findings,” the researchers stated.
“Real-world observational studies comparing CAS, carotid endarterectomy, and medical management are needed to determine the performance of carotid stenosis treatment options for Medicare beneficiaries,” Dr. Jalbert and her colleagues concluded.
The authors reported no relevant disclosures. The study was funded by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services.
The presence of competing risks and overall lower levels of provider proficiency appeared to limit the benefits of carotid artery stenting in Medicare beneficiaries, according to the results of a large retrospective cohort study of the Centers for Medicare & Medicaid Services CAS database (2005-2009).
Periprocedural mortality was more than twice the rate in this patient population than in those earlier patients those involved in the pivotal CREST and SAPPHIRE clinical trials, according to a report published online Jan. 12 in JAMA Neurology [doi:10.1001/jamaneurol.2014.3638].
“The higher risk of periprocedural complications and the burden of competing risks owing to age and comorbidity burden must be carefully considered when deciding between carotid stenosis treatments for Medicare beneficiaries,” according to Jessica J. Jalbert, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, Boston, and her colleagues.
Over 22,000 patients were assessed in the study. The mean patient age was just over 76 years, 60.5% were men, and 94% were white. Approximately half were symptomatic, 91.2% were at high surgical risk, and 97.4% had carotid stenosis of at least 70%.
Almost 80% of the patients undergoing carotid artery stenting (CAS) met the SAPPHIRE trial indications and about half met at least one of the SAPPHIRE criteria for high surgical risk.
In the mean follow-up of approximately 2 years, mortality risks exceeded one-third for patients who were 80 years of age or older (41.5% mortality risk), symptomatic (37.3% risk), at high surgical risk with symptomatic carotid stenosis of at least 50% (37.3% risk), or admitted nonelectively (36.2% risk). In addition, among asymptomatic patients, mortality after the periprocedural period exceeded one-third for patients at least 80 years old.
Of particular concern, few of these Medicare beneficiaries undergoing CAS as per the National Coverage Determinations were treated by providers with proficiency levels similar to those required in the clinical trials. This is a potential problem because lower annual volume and early operator experience are associated with increased periprocedural mortality, the authors wrote.
CAS was performed primarily by male physicians (98.4%), specializing in cardiology (52.9%), practicing within a group (79.4%), and residing in the South (42.5%). The mean number of past-year CAS procedures performed was only 13.9 for physicians and 29.8 for hospitals. This translated to more than 80% of the physicians not meeting the minimum CAS volume requirements and/or minimum complication rates of the SAPPHIRE trial, and more than 90% not meeting the requirements of the CREST trial.
“Our results may support concerns about the limited generalizability of [randomized clinical trial] findings,” the researchers stated.
“Real-world observational studies comparing CAS, carotid endarterectomy, and medical management are needed to determine the performance of carotid stenosis treatment options for Medicare beneficiaries,” Dr. Jalbert and her colleagues concluded.
The authors reported no relevant disclosures. The study was funded by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services.
The presence of competing risks and overall lower levels of provider proficiency appeared to limit the benefits of carotid artery stenting in Medicare beneficiaries, according to the results of a large retrospective cohort study of the Centers for Medicare & Medicaid Services CAS database (2005-2009).
Periprocedural mortality was more than twice the rate in this patient population than in those earlier patients those involved in the pivotal CREST and SAPPHIRE clinical trials, according to a report published online Jan. 12 in JAMA Neurology [doi:10.1001/jamaneurol.2014.3638].
“The higher risk of periprocedural complications and the burden of competing risks owing to age and comorbidity burden must be carefully considered when deciding between carotid stenosis treatments for Medicare beneficiaries,” according to Jessica J. Jalbert, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, Boston, and her colleagues.
Over 22,000 patients were assessed in the study. The mean patient age was just over 76 years, 60.5% were men, and 94% were white. Approximately half were symptomatic, 91.2% were at high surgical risk, and 97.4% had carotid stenosis of at least 70%.
Almost 80% of the patients undergoing carotid artery stenting (CAS) met the SAPPHIRE trial indications and about half met at least one of the SAPPHIRE criteria for high surgical risk.
In the mean follow-up of approximately 2 years, mortality risks exceeded one-third for patients who were 80 years of age or older (41.5% mortality risk), symptomatic (37.3% risk), at high surgical risk with symptomatic carotid stenosis of at least 50% (37.3% risk), or admitted nonelectively (36.2% risk). In addition, among asymptomatic patients, mortality after the periprocedural period exceeded one-third for patients at least 80 years old.
Of particular concern, few of these Medicare beneficiaries undergoing CAS as per the National Coverage Determinations were treated by providers with proficiency levels similar to those required in the clinical trials. This is a potential problem because lower annual volume and early operator experience are associated with increased periprocedural mortality, the authors wrote.
CAS was performed primarily by male physicians (98.4%), specializing in cardiology (52.9%), practicing within a group (79.4%), and residing in the South (42.5%). The mean number of past-year CAS procedures performed was only 13.9 for physicians and 29.8 for hospitals. This translated to more than 80% of the physicians not meeting the minimum CAS volume requirements and/or minimum complication rates of the SAPPHIRE trial, and more than 90% not meeting the requirements of the CREST trial.
“Our results may support concerns about the limited generalizability of [randomized clinical trial] findings,” the researchers stated.
“Real-world observational studies comparing CAS, carotid endarterectomy, and medical management are needed to determine the performance of carotid stenosis treatment options for Medicare beneficiaries,” Dr. Jalbert and her colleagues concluded.
The authors reported no relevant disclosures. The study was funded by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services.
FROM JAMA NEUROLOGY
Key clinical point: Mortality risks exceeded one-third for patients who were 80 years of age or older, symptomatic, at high surgical risk with symptomatic carotid stenosis of at least 50%, or admitted nonelectively.
Major finding: More than 80% of the physicians performing CAS in the real world did not meet the minimum CAS volume requirements and/or minimum complication rates of the SAPPPHIRE trial.
Data source: Data were obtained from a large retrospective cohort study of the Centers for Medicare and Medicaid Services CAS database (2005-2009).
Disclosures: The authors reported no relevant disclosures.
Risk factors identified for the 1 in 500 likely to require postoperative CPR
PHOENIX – Pneumonia, dehydration, and septicemia topped the list of risk factors associated with the need for cardiopulmonary resuscitation during hospitalization for a major surgical procedure in 1 in 500 patients, a retrospective analysis found.
The large sample studied shows that having emergency rather than elective surgery, being older, being African American, and lacking health insurance were also associated with greater odds of needing CPR in this cohort, Dr. Ashima Das of Rainbow Children’s Hospital in Cleveland reported.
A review of 12,631,502 patient records found in the 2009 and 2010 National Inpatient Sample showed that 0.2% of all major surgery patients between 18 and 64 years went into cardiac arrest during their surgical hospitalization. Patients with postoperative pneumonia were at 3.05 (95% confidence interval = 2.75-3.39, P < .0001) times higher risk for needing CPR; meanwhile, major surgery patients with postoperative dehydration or other fluid and electrolyte disruptions faced an increased risk of 3.50 (95% CI = 3.18-3.85, P < .0001), Dr. Das reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Septicemia posed a 2.60 greater risk (95% CI = 2.34-2.86, P < .0001). The odds ratio of needing CPR for patients with coagulopathy was 2.54 (95% CI = 2.30-2.81, P < .0001).
Dr. Das and her colleagues found that 80% of the 23,858 surgical procedures performed in patients who also needed CPR were emergent rather than elective. Patients’ risk of cardiac arrest increased by 1.02 ( 95% CI = 1.01-1.03, P < .0001) with every year of age, while African Americans had a slightly higher risk of needing CPR, compared with whites (OR, 1.51; 95% CI = 1.35-1.68; P < .0001), as did the uninsured, compared with the insured (P < .0001).
The authors of this study said they had no relevant financial disclosures.
On Twitter @whitneymcknight
PHOENIX – Pneumonia, dehydration, and septicemia topped the list of risk factors associated with the need for cardiopulmonary resuscitation during hospitalization for a major surgical procedure in 1 in 500 patients, a retrospective analysis found.
The large sample studied shows that having emergency rather than elective surgery, being older, being African American, and lacking health insurance were also associated with greater odds of needing CPR in this cohort, Dr. Ashima Das of Rainbow Children’s Hospital in Cleveland reported.
A review of 12,631,502 patient records found in the 2009 and 2010 National Inpatient Sample showed that 0.2% of all major surgery patients between 18 and 64 years went into cardiac arrest during their surgical hospitalization. Patients with postoperative pneumonia were at 3.05 (95% confidence interval = 2.75-3.39, P < .0001) times higher risk for needing CPR; meanwhile, major surgery patients with postoperative dehydration or other fluid and electrolyte disruptions faced an increased risk of 3.50 (95% CI = 3.18-3.85, P < .0001), Dr. Das reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Septicemia posed a 2.60 greater risk (95% CI = 2.34-2.86, P < .0001). The odds ratio of needing CPR for patients with coagulopathy was 2.54 (95% CI = 2.30-2.81, P < .0001).
Dr. Das and her colleagues found that 80% of the 23,858 surgical procedures performed in patients who also needed CPR were emergent rather than elective. Patients’ risk of cardiac arrest increased by 1.02 ( 95% CI = 1.01-1.03, P < .0001) with every year of age, while African Americans had a slightly higher risk of needing CPR, compared with whites (OR, 1.51; 95% CI = 1.35-1.68; P < .0001), as did the uninsured, compared with the insured (P < .0001).
The authors of this study said they had no relevant financial disclosures.
On Twitter @whitneymcknight
PHOENIX – Pneumonia, dehydration, and septicemia topped the list of risk factors associated with the need for cardiopulmonary resuscitation during hospitalization for a major surgical procedure in 1 in 500 patients, a retrospective analysis found.
The large sample studied shows that having emergency rather than elective surgery, being older, being African American, and lacking health insurance were also associated with greater odds of needing CPR in this cohort, Dr. Ashima Das of Rainbow Children’s Hospital in Cleveland reported.
A review of 12,631,502 patient records found in the 2009 and 2010 National Inpatient Sample showed that 0.2% of all major surgery patients between 18 and 64 years went into cardiac arrest during their surgical hospitalization. Patients with postoperative pneumonia were at 3.05 (95% confidence interval = 2.75-3.39, P < .0001) times higher risk for needing CPR; meanwhile, major surgery patients with postoperative dehydration or other fluid and electrolyte disruptions faced an increased risk of 3.50 (95% CI = 3.18-3.85, P < .0001), Dr. Das reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Septicemia posed a 2.60 greater risk (95% CI = 2.34-2.86, P < .0001). The odds ratio of needing CPR for patients with coagulopathy was 2.54 (95% CI = 2.30-2.81, P < .0001).
Dr. Das and her colleagues found that 80% of the 23,858 surgical procedures performed in patients who also needed CPR were emergent rather than elective. Patients’ risk of cardiac arrest increased by 1.02 ( 95% CI = 1.01-1.03, P < .0001) with every year of age, while African Americans had a slightly higher risk of needing CPR, compared with whites (OR, 1.51; 95% CI = 1.35-1.68; P < .0001), as did the uninsured, compared with the insured (P < .0001).
The authors of this study said they had no relevant financial disclosures.
On Twitter @whitneymcknight
AT THE CRITICAL CARE CONGRESS
Key clinical point: Risk modification for certain patient populations undergoing major surgical procedures may help reduce the rates of associated CPR.
Major finding: One in 500 patients who had a major surgical procedure required cardiopulmonary resuscitation.
Data source: A retrospective analysis of 12,631,502 patient records from the 2009-2010 Nationwide Inpatient Sample, identifying several risk factors for cardiac arrest occurring during a surgical hospitalization.
Disclosures: The authors of this study said they had no relevant financial disclosures.
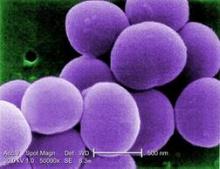
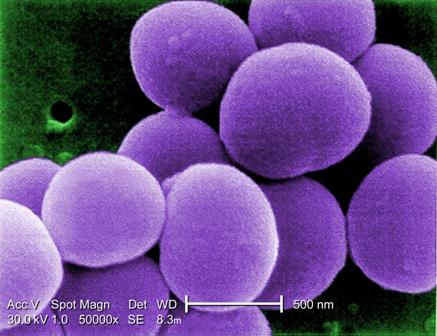
Bundled intervention tackles S. aureus SSIs
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
AT IDWEEK 2014
Key clinical point: Implementing a bundled intervention reduced S. aureus SSIs and could reduce patient morbidity and costs.
Major finding: The pooled S. aureus SSI rate decreased from 0.36% to 0.20% (rate ratio, 0.58).
Data source: A multicenter quasi-experimental effectiveness study of 42,534 procedures.
Disclosures: The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
VTE risk models target a formidable surgery foe
CHICAGO – Implementation of preoperative venous thromboembolism prophylaxis requires a highly individualized approach and a little boost from information technology, one expert suggested.
“What may not be appreciated by some vascular surgeons is that for certain procedures we do, our patients actually have a high VTE [venous thromboembolism] risk. I know people think, ‘We use heparin, so our patients aren’t at high risk,’ but they actually are,” Dr. Melina Kibbe said at a symposium on vascular surgery sponsored by Northwestern University.
The VTE risk is 4.2% for open thoracoabdominal aortic aneurysm repair and 2.2% for thoracic endovascular aortic repair in the American College of Surgeons National Surgical Quality Improvement Program database. That may be an underestimation, however, because the NSQIP database captures only symptomatic events documented by imaging and those events occurring in the first 30 days after surgery.
Smaller studies looking at the problem prospectively suggest the VTE risk is closer to 2%-12% after open aortic surgery and 5.3% after endovascular aortic repair, she said.
Add to that the U.S. Surgeon General’s 2008 call to action to prevent VTE and the Institute of Medicine’s stance that failure to provide VTE prophylaxis qualifies as a medical error, and it would be tempting for vascular surgeons to prescribe pharmacologic prophylaxis for all of their patients, or at least do so based on the type of procedure.
“But VTE formation is really secondary to patient-specific and procedure-related factors,” said Dr. Kibbe, a professor of vascular surgery at Northwestern University in Chicago.
She highlighted five current VTE risk assessment models (RAMs) and the potential returns when RAMs are incorporated into clinical decision support systems.
• Kucher model. One of the earlier and most straightforward RAMs is the Kucher model. It assessed eight weighted risk factors (advanced age, obesity, bed rest, hormone replacement therapy/oral contraceptives, major surgery, cancer, prior VTE, and hypercoagulability) and provided surgeons with electronic alerts regarding prophylaxis.
VTE rates dropped from 8.2% to 4.9% in the high-risk category (score ≥ 4) with the use of the simple physician reminders (N. Engl. J. Med. 2005;352:969-77). Prospective validation showed that VTE increased proportionally with higher scores, Dr. Kibbe said. On the other hand, the model lacked sensitivity at low VTE risk, because 20% of patients with a score of 4 or less actually had VTEs.
“So, while it was simple, it only works well for the high-risk category,” she said.
• Rogers model. One of the most vigorously studied and developed RAMs is the Rogers model (J. Am. Coll. Surg. 2007;204:1211-21). It identified 15 variables (including lab values, patient characteristics, disease states, work relative-value unit, and type of operation) that were independently associated with VTE formation among 183,609 patients undergoing general, vascular, or thoracic procedures at 142 Veterans Health Administration and private hospitals. Each variable is assigned a value from 0 to 9 and added together to create a Rogers score.
Validation showed that VTE risk correlates with the Rogers score, rising from 0.11% for patients with a low score (< 7) to 1.32% for those with a high score (> 10), Dr. Kibbe said. Criticisms of the model are that it is complex, VTE incidence in the entire cohort was low at just 0.63%, the type of VTE prophylaxis used was unclear, and the model lacks prospective validation in a vascular surgery cohort.
• Caprini model. The most commonly used RAM is the 2005 Caprini model (Dis. Mon. 2005;51:70-8), which assigns a weighted score based on more than 30 VTE risk factors compiled by the authors. It has been prospectively validated in numerous studies and shown to accurately stratify 30-day VTE risk at 0.5% for patients at very low risk, 1.5% for low risk, 3% for moderate risk, and 6% for high risk.
The Caprini model, however, was not developed with the same rigor as the Rogers RAM, some of the risk factors have been shown not to be a risk for VTE, and it is complex, Dr. Kibbe observed.
• Pannucci model. The Pannucci model was created specifically to counteract the complexity of the Rogers and Caprini RAMs and incorporates only seven risk factors (personal history of VTE, current cancer, age ≥ 60 years, body mass index ≥ 40 kg/m2, male sex, sepsis/septic shock/systemic inflammatory response syndrome, and family history of VTE) into a weighted index for 90-day VTE risk (Chest 2014;145:567-73). The model was developed using a statewide database and a derivation cohort made up of 20% vascular surgery patients.
Both the derivation and validation cohorts identified an 18-fold variation in VTE risk from the lowest- to highest-risk surgical population, showing that the model stratifies patients correctly. Further prospective validation is needed, Dr. Kibbe said.
• Scarborough model. Finally, in an attempt to develop a RAM specific to vascular surgery patients, Dr. John Scarborough and colleagues examined 6,035 patients undergoing open AAA repair in the NSQIP database. The 30-day VTE rate was 2.4% for the entire cohort. Eight independent perioperative risk factors were identified and used to create a nonweighted scoring system (J. Am. Coll. Surg. 2012;214:620-6).
Overall, 65% of patients had 0-1 risk factor and a VTE incidence of 1.5%, while 15% had 3 or more risk factors and a VTE incidence of 6.1%. The Scarborough model has good risk stratification, Dr. Kibbe said, but it is limited by the aforementioned criticisms regarding the NSQIP database, and it also needs prospective validation.
“We all know that proper VTE prophylaxis is very important for our patients; but we need mechanisms by which the attention given to this need for prophylaxis, which is a lot, is turned into proper implementation,” she said.
For Dr. Kibbe and her colleagues, proper implementation meant developing a RAM that was incorporated into the electronic medical record system for all surgical patients at the Jesse Brown VA Medical Center in Chicago. Clinicians were prompted to complete the RAM upon placing orders for preanesthesia testing clearance, and the clinical decision support system would provide a recommended prophylaxis regimen and easily selected electronic orders that could be signed.
A pre- and postimplementation analysis involving 400 consecutive patients revealed an 82% increase in patients with preoperative VTE prophylaxis ordered (22% vs. 40%), a 75% decrease in inappropriate cancellation of orders more than 12 hours before surgery (37% vs. 9%), and a nearly sevenfold increase in the number of patients receiving pharmacologic and mechanical prophylaxis (5% vs. 32%), she said. There was an 80% and 36% decline in DVT rates at 30 and 90 days postoperative, but event rates were too low to detect a significant difference (J. Vasc. Surg. 2010;51:648-54).
Dr. Kibbe reported having no financial disclosures.
CHICAGO – Implementation of preoperative venous thromboembolism prophylaxis requires a highly individualized approach and a little boost from information technology, one expert suggested.
“What may not be appreciated by some vascular surgeons is that for certain procedures we do, our patients actually have a high VTE [venous thromboembolism] risk. I know people think, ‘We use heparin, so our patients aren’t at high risk,’ but they actually are,” Dr. Melina Kibbe said at a symposium on vascular surgery sponsored by Northwestern University.
The VTE risk is 4.2% for open thoracoabdominal aortic aneurysm repair and 2.2% for thoracic endovascular aortic repair in the American College of Surgeons National Surgical Quality Improvement Program database. That may be an underestimation, however, because the NSQIP database captures only symptomatic events documented by imaging and those events occurring in the first 30 days after surgery.
Smaller studies looking at the problem prospectively suggest the VTE risk is closer to 2%-12% after open aortic surgery and 5.3% after endovascular aortic repair, she said.
Add to that the U.S. Surgeon General’s 2008 call to action to prevent VTE and the Institute of Medicine’s stance that failure to provide VTE prophylaxis qualifies as a medical error, and it would be tempting for vascular surgeons to prescribe pharmacologic prophylaxis for all of their patients, or at least do so based on the type of procedure.
“But VTE formation is really secondary to patient-specific and procedure-related factors,” said Dr. Kibbe, a professor of vascular surgery at Northwestern University in Chicago.
She highlighted five current VTE risk assessment models (RAMs) and the potential returns when RAMs are incorporated into clinical decision support systems.
• Kucher model. One of the earlier and most straightforward RAMs is the Kucher model. It assessed eight weighted risk factors (advanced age, obesity, bed rest, hormone replacement therapy/oral contraceptives, major surgery, cancer, prior VTE, and hypercoagulability) and provided surgeons with electronic alerts regarding prophylaxis.
VTE rates dropped from 8.2% to 4.9% in the high-risk category (score ≥ 4) with the use of the simple physician reminders (N. Engl. J. Med. 2005;352:969-77). Prospective validation showed that VTE increased proportionally with higher scores, Dr. Kibbe said. On the other hand, the model lacked sensitivity at low VTE risk, because 20% of patients with a score of 4 or less actually had VTEs.
“So, while it was simple, it only works well for the high-risk category,” she said.
• Rogers model. One of the most vigorously studied and developed RAMs is the Rogers model (J. Am. Coll. Surg. 2007;204:1211-21). It identified 15 variables (including lab values, patient characteristics, disease states, work relative-value unit, and type of operation) that were independently associated with VTE formation among 183,609 patients undergoing general, vascular, or thoracic procedures at 142 Veterans Health Administration and private hospitals. Each variable is assigned a value from 0 to 9 and added together to create a Rogers score.
Validation showed that VTE risk correlates with the Rogers score, rising from 0.11% for patients with a low score (< 7) to 1.32% for those with a high score (> 10), Dr. Kibbe said. Criticisms of the model are that it is complex, VTE incidence in the entire cohort was low at just 0.63%, the type of VTE prophylaxis used was unclear, and the model lacks prospective validation in a vascular surgery cohort.
• Caprini model. The most commonly used RAM is the 2005 Caprini model (Dis. Mon. 2005;51:70-8), which assigns a weighted score based on more than 30 VTE risk factors compiled by the authors. It has been prospectively validated in numerous studies and shown to accurately stratify 30-day VTE risk at 0.5% for patients at very low risk, 1.5% for low risk, 3% for moderate risk, and 6% for high risk.
The Caprini model, however, was not developed with the same rigor as the Rogers RAM, some of the risk factors have been shown not to be a risk for VTE, and it is complex, Dr. Kibbe observed.
• Pannucci model. The Pannucci model was created specifically to counteract the complexity of the Rogers and Caprini RAMs and incorporates only seven risk factors (personal history of VTE, current cancer, age ≥ 60 years, body mass index ≥ 40 kg/m2, male sex, sepsis/septic shock/systemic inflammatory response syndrome, and family history of VTE) into a weighted index for 90-day VTE risk (Chest 2014;145:567-73). The model was developed using a statewide database and a derivation cohort made up of 20% vascular surgery patients.
Both the derivation and validation cohorts identified an 18-fold variation in VTE risk from the lowest- to highest-risk surgical population, showing that the model stratifies patients correctly. Further prospective validation is needed, Dr. Kibbe said.
• Scarborough model. Finally, in an attempt to develop a RAM specific to vascular surgery patients, Dr. John Scarborough and colleagues examined 6,035 patients undergoing open AAA repair in the NSQIP database. The 30-day VTE rate was 2.4% for the entire cohort. Eight independent perioperative risk factors were identified and used to create a nonweighted scoring system (J. Am. Coll. Surg. 2012;214:620-6).
Overall, 65% of patients had 0-1 risk factor and a VTE incidence of 1.5%, while 15% had 3 or more risk factors and a VTE incidence of 6.1%. The Scarborough model has good risk stratification, Dr. Kibbe said, but it is limited by the aforementioned criticisms regarding the NSQIP database, and it also needs prospective validation.
“We all know that proper VTE prophylaxis is very important for our patients; but we need mechanisms by which the attention given to this need for prophylaxis, which is a lot, is turned into proper implementation,” she said.
For Dr. Kibbe and her colleagues, proper implementation meant developing a RAM that was incorporated into the electronic medical record system for all surgical patients at the Jesse Brown VA Medical Center in Chicago. Clinicians were prompted to complete the RAM upon placing orders for preanesthesia testing clearance, and the clinical decision support system would provide a recommended prophylaxis regimen and easily selected electronic orders that could be signed.
A pre- and postimplementation analysis involving 400 consecutive patients revealed an 82% increase in patients with preoperative VTE prophylaxis ordered (22% vs. 40%), a 75% decrease in inappropriate cancellation of orders more than 12 hours before surgery (37% vs. 9%), and a nearly sevenfold increase in the number of patients receiving pharmacologic and mechanical prophylaxis (5% vs. 32%), she said. There was an 80% and 36% decline in DVT rates at 30 and 90 days postoperative, but event rates were too low to detect a significant difference (J. Vasc. Surg. 2010;51:648-54).
Dr. Kibbe reported having no financial disclosures.
CHICAGO – Implementation of preoperative venous thromboembolism prophylaxis requires a highly individualized approach and a little boost from information technology, one expert suggested.
“What may not be appreciated by some vascular surgeons is that for certain procedures we do, our patients actually have a high VTE [venous thromboembolism] risk. I know people think, ‘We use heparin, so our patients aren’t at high risk,’ but they actually are,” Dr. Melina Kibbe said at a symposium on vascular surgery sponsored by Northwestern University.
The VTE risk is 4.2% for open thoracoabdominal aortic aneurysm repair and 2.2% for thoracic endovascular aortic repair in the American College of Surgeons National Surgical Quality Improvement Program database. That may be an underestimation, however, because the NSQIP database captures only symptomatic events documented by imaging and those events occurring in the first 30 days after surgery.
Smaller studies looking at the problem prospectively suggest the VTE risk is closer to 2%-12% after open aortic surgery and 5.3% after endovascular aortic repair, she said.
Add to that the U.S. Surgeon General’s 2008 call to action to prevent VTE and the Institute of Medicine’s stance that failure to provide VTE prophylaxis qualifies as a medical error, and it would be tempting for vascular surgeons to prescribe pharmacologic prophylaxis for all of their patients, or at least do so based on the type of procedure.
“But VTE formation is really secondary to patient-specific and procedure-related factors,” said Dr. Kibbe, a professor of vascular surgery at Northwestern University in Chicago.
She highlighted five current VTE risk assessment models (RAMs) and the potential returns when RAMs are incorporated into clinical decision support systems.
• Kucher model. One of the earlier and most straightforward RAMs is the Kucher model. It assessed eight weighted risk factors (advanced age, obesity, bed rest, hormone replacement therapy/oral contraceptives, major surgery, cancer, prior VTE, and hypercoagulability) and provided surgeons with electronic alerts regarding prophylaxis.
VTE rates dropped from 8.2% to 4.9% in the high-risk category (score ≥ 4) with the use of the simple physician reminders (N. Engl. J. Med. 2005;352:969-77). Prospective validation showed that VTE increased proportionally with higher scores, Dr. Kibbe said. On the other hand, the model lacked sensitivity at low VTE risk, because 20% of patients with a score of 4 or less actually had VTEs.
“So, while it was simple, it only works well for the high-risk category,” she said.
• Rogers model. One of the most vigorously studied and developed RAMs is the Rogers model (J. Am. Coll. Surg. 2007;204:1211-21). It identified 15 variables (including lab values, patient characteristics, disease states, work relative-value unit, and type of operation) that were independently associated with VTE formation among 183,609 patients undergoing general, vascular, or thoracic procedures at 142 Veterans Health Administration and private hospitals. Each variable is assigned a value from 0 to 9 and added together to create a Rogers score.
Validation showed that VTE risk correlates with the Rogers score, rising from 0.11% for patients with a low score (< 7) to 1.32% for those with a high score (> 10), Dr. Kibbe said. Criticisms of the model are that it is complex, VTE incidence in the entire cohort was low at just 0.63%, the type of VTE prophylaxis used was unclear, and the model lacks prospective validation in a vascular surgery cohort.
• Caprini model. The most commonly used RAM is the 2005 Caprini model (Dis. Mon. 2005;51:70-8), which assigns a weighted score based on more than 30 VTE risk factors compiled by the authors. It has been prospectively validated in numerous studies and shown to accurately stratify 30-day VTE risk at 0.5% for patients at very low risk, 1.5% for low risk, 3% for moderate risk, and 6% for high risk.
The Caprini model, however, was not developed with the same rigor as the Rogers RAM, some of the risk factors have been shown not to be a risk for VTE, and it is complex, Dr. Kibbe observed.
• Pannucci model. The Pannucci model was created specifically to counteract the complexity of the Rogers and Caprini RAMs and incorporates only seven risk factors (personal history of VTE, current cancer, age ≥ 60 years, body mass index ≥ 40 kg/m2, male sex, sepsis/septic shock/systemic inflammatory response syndrome, and family history of VTE) into a weighted index for 90-day VTE risk (Chest 2014;145:567-73). The model was developed using a statewide database and a derivation cohort made up of 20% vascular surgery patients.
Both the derivation and validation cohorts identified an 18-fold variation in VTE risk from the lowest- to highest-risk surgical population, showing that the model stratifies patients correctly. Further prospective validation is needed, Dr. Kibbe said.
• Scarborough model. Finally, in an attempt to develop a RAM specific to vascular surgery patients, Dr. John Scarborough and colleagues examined 6,035 patients undergoing open AAA repair in the NSQIP database. The 30-day VTE rate was 2.4% for the entire cohort. Eight independent perioperative risk factors were identified and used to create a nonweighted scoring system (J. Am. Coll. Surg. 2012;214:620-6).
Overall, 65% of patients had 0-1 risk factor and a VTE incidence of 1.5%, while 15% had 3 or more risk factors and a VTE incidence of 6.1%. The Scarborough model has good risk stratification, Dr. Kibbe said, but it is limited by the aforementioned criticisms regarding the NSQIP database, and it also needs prospective validation.
“We all know that proper VTE prophylaxis is very important for our patients; but we need mechanisms by which the attention given to this need for prophylaxis, which is a lot, is turned into proper implementation,” she said.
For Dr. Kibbe and her colleagues, proper implementation meant developing a RAM that was incorporated into the electronic medical record system for all surgical patients at the Jesse Brown VA Medical Center in Chicago. Clinicians were prompted to complete the RAM upon placing orders for preanesthesia testing clearance, and the clinical decision support system would provide a recommended prophylaxis regimen and easily selected electronic orders that could be signed.
A pre- and postimplementation analysis involving 400 consecutive patients revealed an 82% increase in patients with preoperative VTE prophylaxis ordered (22% vs. 40%), a 75% decrease in inappropriate cancellation of orders more than 12 hours before surgery (37% vs. 9%), and a nearly sevenfold increase in the number of patients receiving pharmacologic and mechanical prophylaxis (5% vs. 32%), she said. There was an 80% and 36% decline in DVT rates at 30 and 90 days postoperative, but event rates were too low to detect a significant difference (J. Vasc. Surg. 2010;51:648-54).
Dr. Kibbe reported having no financial disclosures.
AT THE NORTHWESTERN VASCULAR SYMPOSIUM
ICD lead extraction complication rates warrant surgical backup
CHICAGO– Transvenous lead extraction was associated with a significant risk of urgent cardiac surgery and mortality in a real-world cohort of patients undergoing procedures across a wide spectrum of centers and operators.
Among the 11,304 extractions, the major complication rate was 2.3% and mortality rate 0.9%.
While the complication rate was in line with previously published single-center registry data, the mortality rate was more than twice that reported in recent single-center studies from high-volume centers (0.9% vs. 0.4%), Dr. Nitesh Sood reported at the American Heart Association annual scientific sessions.
Of the 98 perioperative deaths, 18 occurred during the lead extraction procedure.
Another 41 patients (16%) required urgent cardiac surgery, of whom 14 (34%) died during or in the immediate postoperative period after surgery.
“Thus, while overall rate of major complications remains low, there exists a significant risk of urgent cardiac surgery and mortality during transvenous lead extractions [TLE] performed in the ‘real world.’ Appropriate training of all personnel involved and optimal cardiothoracic surgical back-up at centers performing TLE is imperative,” Dr. Sood of the Southcoast Health System, Fall River, Mass., concluded.
The analysis is the largest real-world cohort of TLE involving 11,304 patients with an implantable cardioverter defibrillator (ICD) in the American College of Cardiology Foundation’s National Cardiovascular Data Registry (NCDR) ICD Registry with lead extraction data submitted between April 2010 and July 2012. Major complication was a combined endpoint of major operative complications, postoperative or in-hospital mortality, as defined by the NCDR ICD Registry.
The 258 complications included 62 cardiac arrests, 55 pericardial tamponades, 47 pneumothoraces, and 40 cardiac perforations.
In multivariate analysis, significant predictors of any complication were female sex (adjusted odds ratio, 1.46), heart failure admission vs. lead extraction admission (OR, 2.6), noncardiac admission vs. lead extraction admission (OR, 2.4), lead-only procedure vs. extraction during generator change/upgrade (OR, 1.76), age of lead (OR, 1.08), and clinical status requiring lead replacement (OR, 2.2). Dr. Sood reported.
Among lead characteristics, multivariate predictors of major perioperative complications included at least three concurrent leads extracted (OR, 2.13), longer implant duration (OR, 1.13), flat coil design vs. round (OR, 2.68), greater proximal coil surface area (OR, 1.04), and dislodgement of other leads during extraction (OR, 3.97), he noted.
CHICAGO– Transvenous lead extraction was associated with a significant risk of urgent cardiac surgery and mortality in a real-world cohort of patients undergoing procedures across a wide spectrum of centers and operators.
Among the 11,304 extractions, the major complication rate was 2.3% and mortality rate 0.9%.
While the complication rate was in line with previously published single-center registry data, the mortality rate was more than twice that reported in recent single-center studies from high-volume centers (0.9% vs. 0.4%), Dr. Nitesh Sood reported at the American Heart Association annual scientific sessions.
Of the 98 perioperative deaths, 18 occurred during the lead extraction procedure.
Another 41 patients (16%) required urgent cardiac surgery, of whom 14 (34%) died during or in the immediate postoperative period after surgery.
“Thus, while overall rate of major complications remains low, there exists a significant risk of urgent cardiac surgery and mortality during transvenous lead extractions [TLE] performed in the ‘real world.’ Appropriate training of all personnel involved and optimal cardiothoracic surgical back-up at centers performing TLE is imperative,” Dr. Sood of the Southcoast Health System, Fall River, Mass., concluded.
The analysis is the largest real-world cohort of TLE involving 11,304 patients with an implantable cardioverter defibrillator (ICD) in the American College of Cardiology Foundation’s National Cardiovascular Data Registry (NCDR) ICD Registry with lead extraction data submitted between April 2010 and July 2012. Major complication was a combined endpoint of major operative complications, postoperative or in-hospital mortality, as defined by the NCDR ICD Registry.
The 258 complications included 62 cardiac arrests, 55 pericardial tamponades, 47 pneumothoraces, and 40 cardiac perforations.
In multivariate analysis, significant predictors of any complication were female sex (adjusted odds ratio, 1.46), heart failure admission vs. lead extraction admission (OR, 2.6), noncardiac admission vs. lead extraction admission (OR, 2.4), lead-only procedure vs. extraction during generator change/upgrade (OR, 1.76), age of lead (OR, 1.08), and clinical status requiring lead replacement (OR, 2.2). Dr. Sood reported.
Among lead characteristics, multivariate predictors of major perioperative complications included at least three concurrent leads extracted (OR, 2.13), longer implant duration (OR, 1.13), flat coil design vs. round (OR, 2.68), greater proximal coil surface area (OR, 1.04), and dislodgement of other leads during extraction (OR, 3.97), he noted.
CHICAGO– Transvenous lead extraction was associated with a significant risk of urgent cardiac surgery and mortality in a real-world cohort of patients undergoing procedures across a wide spectrum of centers and operators.
Among the 11,304 extractions, the major complication rate was 2.3% and mortality rate 0.9%.
While the complication rate was in line with previously published single-center registry data, the mortality rate was more than twice that reported in recent single-center studies from high-volume centers (0.9% vs. 0.4%), Dr. Nitesh Sood reported at the American Heart Association annual scientific sessions.
Of the 98 perioperative deaths, 18 occurred during the lead extraction procedure.
Another 41 patients (16%) required urgent cardiac surgery, of whom 14 (34%) died during or in the immediate postoperative period after surgery.
“Thus, while overall rate of major complications remains low, there exists a significant risk of urgent cardiac surgery and mortality during transvenous lead extractions [TLE] performed in the ‘real world.’ Appropriate training of all personnel involved and optimal cardiothoracic surgical back-up at centers performing TLE is imperative,” Dr. Sood of the Southcoast Health System, Fall River, Mass., concluded.
The analysis is the largest real-world cohort of TLE involving 11,304 patients with an implantable cardioverter defibrillator (ICD) in the American College of Cardiology Foundation’s National Cardiovascular Data Registry (NCDR) ICD Registry with lead extraction data submitted between April 2010 and July 2012. Major complication was a combined endpoint of major operative complications, postoperative or in-hospital mortality, as defined by the NCDR ICD Registry.
The 258 complications included 62 cardiac arrests, 55 pericardial tamponades, 47 pneumothoraces, and 40 cardiac perforations.
In multivariate analysis, significant predictors of any complication were female sex (adjusted odds ratio, 1.46), heart failure admission vs. lead extraction admission (OR, 2.6), noncardiac admission vs. lead extraction admission (OR, 2.4), lead-only procedure vs. extraction during generator change/upgrade (OR, 1.76), age of lead (OR, 1.08), and clinical status requiring lead replacement (OR, 2.2). Dr. Sood reported.
Among lead characteristics, multivariate predictors of major perioperative complications included at least three concurrent leads extracted (OR, 2.13), longer implant duration (OR, 1.13), flat coil design vs. round (OR, 2.68), greater proximal coil surface area (OR, 1.04), and dislodgement of other leads during extraction (OR, 3.97), he noted.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Appropriate training and optimal cardiothoracic surgical backup is necessary at all centers performing lead extractions, because of a significant risk of urgent cardiac surgery and death.
Major finding: The major complication rate was 2.3% and mortality rate 0.9%.
Data source: Retrospective analysis of 11,304 patients with transvenous lead extraction in the NCDR ICD Registry.
Disclosures: The study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry. Dr. Sood reported having no financial disclosures. Three coauthors reported relationships with device makers.
Endoscopic mucosal resection proves effective, durable for Barrett’s-associated neoplasia
Complete endoscopic mucosal resection is an effective, durable, and relatively safe treatment for Barrett’s esophagus with high-grade dysplasia, findings from a series of 107 patients suggest.
A particular benefit of endoscopic mucosal resection is that it provides large and intact tissue specimens that allow for accurate staging, according to a report by Dr. Vani J.A. Konda of the University of Chicago and her colleagues in the December issue of Clinical Gastroenterology and Hepatology (doi:10.1016/j.cgh.2014.04.010).
Based on an intention-to-treat analysis, the approach resulted in complete eradication of Barrett’s esophagus in 86 of the 107 patients (80%) who were referred to the Center for Endoscopic Research and Therapeutics at the University of Chicago between August 2003 and December 2012 for Barrett’s esophagus with suspected high-grade dysplasia or intramucosal carcinoma. Based on a per-protocol analysis, the approach resulted in complete eradication in 79 of 80 patients (98.8%), the investigators reported.
Endoscopic mucosal resection resulted in a change in the diagnosis in 27 cases (25.2%), which were upstaged based on assessment of the resection specimens. Four of the cases in which the diagnosis was changed were initially diagnosed as high-grade dysplasia on biopsy and were found on endoscopic mucosal resection to have evidence of submucosal invasion, they said.
Patients included in the series had a mean lesion length of 3.6 cm. All patients underwent complete endoscopic mucosal resection performed on an outpatient basis by a single endoscopist and were followed through January 2014 for a median of 33 months. Most (78.5%) were treated using the cap-assisted technique, while 8.4% were treated using band ligation, 2.8% were treated using a mixed band ligation and cap technique, and 11.2% were treated using an injection-assisted, free-hand technique. Two patients with suspected submucosal invasion underwent a combination of endoscopic submucosal dissection and endoscopic mucosal resection.
Esophageal strictures occurred in 44 patients (41.1%) and 40 were symptomatic; strictures required an average of 2.3 dilations. Symptomatic dysphagia developed in 37.3% of patients, and perforations occurred in two patients, suggesting a need for surgical back-up for patients undergoing endoscopic mucosal resection, the investigators said.High-grade dysplasia and intramucosal carcinoma each recurred in one patient, and both were treated successfully with endoscopic mucosal resection, they reported.
At the most recent analysis, 53 of 74 patients (71.6%) in a durability cohort were in complete remission from intestinal metaplasia, and all were in complete remission from high-grade dysplasia or intramucosal carcinoma, they noted.
Endoscopic therapy is now preferred over esophagectomy in most cases of Barrett’s esophagus with high-grade dysplasia or intramucosal carcinoma, and the current findings show that complete endoscopic mucosal resection is an effective and durable method to treat Barrett’s-associated neoplasia, the investigators concluded, adding that the results support the replacement of esophagectomy by endoscopic therapy for the condition.
“The most commonly encountered complication of esophageal stricture formation can be addressed with endoscopic dilation,” the investigators said.
However, long-term outcomes, particularly in those with advanced pathology who undergo endoscopic management, are still needed, as is an improved understanding of the behavior of the disease following treatment with specific modalities in order to optimize endoscopic therapy, they added.
This study was supported by the Francis L. Lederer Foundation. The authors reported having no disclosures.
Localized treatments aimed at the eradication of dysplasia, early cancer, and surrounding mucosa in Barrett’s esophagus have been a major advancement in gastroenterology. Although radiofrequency ablation (RFA) has become the procedure of choice, debate exists regarding the role of other mucosal extirpative procedures. The work by Dr. Konda and her colleagues gives life to another proposed procedure, complete endoscopic mucosal resection (EMR) of dysplastic and Barrett’s mucosa. In this study, complete EMR led to results comparable with previous reports on RFA (Gastroenterology 2013;145:96-104). EMR also has theoretical advantages over RFA, including avoidance of promoting protumorigenic mutations and clonal expansion in remaining mucosa (Am. J. Gastroenterol. 2013;108:1584-92).

|
| Dr. David A. Katzka |
EMR, like RFA, however, is not risk free; perforations occurred in three patients (one during dilation) and 38% developed symptomatic strictures. Furthermore, the endoscopic skill required to complete this protocol also necessitated expertise in cap technique, band ligation, injection-assisted free-hand technique, focal RFA, and endoscopic submucosal dissection. In other words, performing complete EMR is for a select group of endoscopic intensivists only. Unfortunately, endoscopic eradication of Barrett’s mucosa remains a procedure that is betwixt and between. It is between the mucosal and submucosal layer but is betwixt because of limitations on the depth of penetration of RFA (around 0.7 mm) and EMR (Dig. Dis. 2009;26:280-4) needed to eradicate the elusive Barrett’s stem cell, coupled with the increasing chance of esophageal stricture formation with these deeper levels of injury. Nevertheless, work such as this from Dr. Konda and her colleagues allows us to continue to claim at least a partial victory over Barrett’s dysplasia. It is hoped that with future techniques, we may come up with a “kinder” and easier method of removing all Barrett’s mucosa without the provocation of a substantial fibrotic reaction of the remaining esophageal wall.
Dr. David A. Katzka is in the department of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn. He has no conflicts of interest.
Localized treatments aimed at the eradication of dysplasia, early cancer, and surrounding mucosa in Barrett’s esophagus have been a major advancement in gastroenterology. Although radiofrequency ablation (RFA) has become the procedure of choice, debate exists regarding the role of other mucosal extirpative procedures. The work by Dr. Konda and her colleagues gives life to another proposed procedure, complete endoscopic mucosal resection (EMR) of dysplastic and Barrett’s mucosa. In this study, complete EMR led to results comparable with previous reports on RFA (Gastroenterology 2013;145:96-104). EMR also has theoretical advantages over RFA, including avoidance of promoting protumorigenic mutations and clonal expansion in remaining mucosa (Am. J. Gastroenterol. 2013;108:1584-92).

|
| Dr. David A. Katzka |
EMR, like RFA, however, is not risk free; perforations occurred in three patients (one during dilation) and 38% developed symptomatic strictures. Furthermore, the endoscopic skill required to complete this protocol also necessitated expertise in cap technique, band ligation, injection-assisted free-hand technique, focal RFA, and endoscopic submucosal dissection. In other words, performing complete EMR is for a select group of endoscopic intensivists only. Unfortunately, endoscopic eradication of Barrett’s mucosa remains a procedure that is betwixt and between. It is between the mucosal and submucosal layer but is betwixt because of limitations on the depth of penetration of RFA (around 0.7 mm) and EMR (Dig. Dis. 2009;26:280-4) needed to eradicate the elusive Barrett’s stem cell, coupled with the increasing chance of esophageal stricture formation with these deeper levels of injury. Nevertheless, work such as this from Dr. Konda and her colleagues allows us to continue to claim at least a partial victory over Barrett’s dysplasia. It is hoped that with future techniques, we may come up with a “kinder” and easier method of removing all Barrett’s mucosa without the provocation of a substantial fibrotic reaction of the remaining esophageal wall.
Dr. David A. Katzka is in the department of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn. He has no conflicts of interest.
Localized treatments aimed at the eradication of dysplasia, early cancer, and surrounding mucosa in Barrett’s esophagus have been a major advancement in gastroenterology. Although radiofrequency ablation (RFA) has become the procedure of choice, debate exists regarding the role of other mucosal extirpative procedures. The work by Dr. Konda and her colleagues gives life to another proposed procedure, complete endoscopic mucosal resection (EMR) of dysplastic and Barrett’s mucosa. In this study, complete EMR led to results comparable with previous reports on RFA (Gastroenterology 2013;145:96-104). EMR also has theoretical advantages over RFA, including avoidance of promoting protumorigenic mutations and clonal expansion in remaining mucosa (Am. J. Gastroenterol. 2013;108:1584-92).

|
| Dr. David A. Katzka |
EMR, like RFA, however, is not risk free; perforations occurred in three patients (one during dilation) and 38% developed symptomatic strictures. Furthermore, the endoscopic skill required to complete this protocol also necessitated expertise in cap technique, band ligation, injection-assisted free-hand technique, focal RFA, and endoscopic submucosal dissection. In other words, performing complete EMR is for a select group of endoscopic intensivists only. Unfortunately, endoscopic eradication of Barrett’s mucosa remains a procedure that is betwixt and between. It is between the mucosal and submucosal layer but is betwixt because of limitations on the depth of penetration of RFA (around 0.7 mm) and EMR (Dig. Dis. 2009;26:280-4) needed to eradicate the elusive Barrett’s stem cell, coupled with the increasing chance of esophageal stricture formation with these deeper levels of injury. Nevertheless, work such as this from Dr. Konda and her colleagues allows us to continue to claim at least a partial victory over Barrett’s dysplasia. It is hoped that with future techniques, we may come up with a “kinder” and easier method of removing all Barrett’s mucosa without the provocation of a substantial fibrotic reaction of the remaining esophageal wall.
Dr. David A. Katzka is in the department of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn. He has no conflicts of interest.
Complete endoscopic mucosal resection is an effective, durable, and relatively safe treatment for Barrett’s esophagus with high-grade dysplasia, findings from a series of 107 patients suggest.
A particular benefit of endoscopic mucosal resection is that it provides large and intact tissue specimens that allow for accurate staging, according to a report by Dr. Vani J.A. Konda of the University of Chicago and her colleagues in the December issue of Clinical Gastroenterology and Hepatology (doi:10.1016/j.cgh.2014.04.010).
Based on an intention-to-treat analysis, the approach resulted in complete eradication of Barrett’s esophagus in 86 of the 107 patients (80%) who were referred to the Center for Endoscopic Research and Therapeutics at the University of Chicago between August 2003 and December 2012 for Barrett’s esophagus with suspected high-grade dysplasia or intramucosal carcinoma. Based on a per-protocol analysis, the approach resulted in complete eradication in 79 of 80 patients (98.8%), the investigators reported.
Endoscopic mucosal resection resulted in a change in the diagnosis in 27 cases (25.2%), which were upstaged based on assessment of the resection specimens. Four of the cases in which the diagnosis was changed were initially diagnosed as high-grade dysplasia on biopsy and were found on endoscopic mucosal resection to have evidence of submucosal invasion, they said.
Patients included in the series had a mean lesion length of 3.6 cm. All patients underwent complete endoscopic mucosal resection performed on an outpatient basis by a single endoscopist and were followed through January 2014 for a median of 33 months. Most (78.5%) were treated using the cap-assisted technique, while 8.4% were treated using band ligation, 2.8% were treated using a mixed band ligation and cap technique, and 11.2% were treated using an injection-assisted, free-hand technique. Two patients with suspected submucosal invasion underwent a combination of endoscopic submucosal dissection and endoscopic mucosal resection.
Esophageal strictures occurred in 44 patients (41.1%) and 40 were symptomatic; strictures required an average of 2.3 dilations. Symptomatic dysphagia developed in 37.3% of patients, and perforations occurred in two patients, suggesting a need for surgical back-up for patients undergoing endoscopic mucosal resection, the investigators said.High-grade dysplasia and intramucosal carcinoma each recurred in one patient, and both were treated successfully with endoscopic mucosal resection, they reported.
At the most recent analysis, 53 of 74 patients (71.6%) in a durability cohort were in complete remission from intestinal metaplasia, and all were in complete remission from high-grade dysplasia or intramucosal carcinoma, they noted.
Endoscopic therapy is now preferred over esophagectomy in most cases of Barrett’s esophagus with high-grade dysplasia or intramucosal carcinoma, and the current findings show that complete endoscopic mucosal resection is an effective and durable method to treat Barrett’s-associated neoplasia, the investigators concluded, adding that the results support the replacement of esophagectomy by endoscopic therapy for the condition.
“The most commonly encountered complication of esophageal stricture formation can be addressed with endoscopic dilation,” the investigators said.
However, long-term outcomes, particularly in those with advanced pathology who undergo endoscopic management, are still needed, as is an improved understanding of the behavior of the disease following treatment with specific modalities in order to optimize endoscopic therapy, they added.
This study was supported by the Francis L. Lederer Foundation. The authors reported having no disclosures.
Complete endoscopic mucosal resection is an effective, durable, and relatively safe treatment for Barrett’s esophagus with high-grade dysplasia, findings from a series of 107 patients suggest.
A particular benefit of endoscopic mucosal resection is that it provides large and intact tissue specimens that allow for accurate staging, according to a report by Dr. Vani J.A. Konda of the University of Chicago and her colleagues in the December issue of Clinical Gastroenterology and Hepatology (doi:10.1016/j.cgh.2014.04.010).
Based on an intention-to-treat analysis, the approach resulted in complete eradication of Barrett’s esophagus in 86 of the 107 patients (80%) who were referred to the Center for Endoscopic Research and Therapeutics at the University of Chicago between August 2003 and December 2012 for Barrett’s esophagus with suspected high-grade dysplasia or intramucosal carcinoma. Based on a per-protocol analysis, the approach resulted in complete eradication in 79 of 80 patients (98.8%), the investigators reported.
Endoscopic mucosal resection resulted in a change in the diagnosis in 27 cases (25.2%), which were upstaged based on assessment of the resection specimens. Four of the cases in which the diagnosis was changed were initially diagnosed as high-grade dysplasia on biopsy and were found on endoscopic mucosal resection to have evidence of submucosal invasion, they said.
Patients included in the series had a mean lesion length of 3.6 cm. All patients underwent complete endoscopic mucosal resection performed on an outpatient basis by a single endoscopist and were followed through January 2014 for a median of 33 months. Most (78.5%) were treated using the cap-assisted technique, while 8.4% were treated using band ligation, 2.8% were treated using a mixed band ligation and cap technique, and 11.2% were treated using an injection-assisted, free-hand technique. Two patients with suspected submucosal invasion underwent a combination of endoscopic submucosal dissection and endoscopic mucosal resection.
Esophageal strictures occurred in 44 patients (41.1%) and 40 were symptomatic; strictures required an average of 2.3 dilations. Symptomatic dysphagia developed in 37.3% of patients, and perforations occurred in two patients, suggesting a need for surgical back-up for patients undergoing endoscopic mucosal resection, the investigators said.High-grade dysplasia and intramucosal carcinoma each recurred in one patient, and both were treated successfully with endoscopic mucosal resection, they reported.
At the most recent analysis, 53 of 74 patients (71.6%) in a durability cohort were in complete remission from intestinal metaplasia, and all were in complete remission from high-grade dysplasia or intramucosal carcinoma, they noted.
Endoscopic therapy is now preferred over esophagectomy in most cases of Barrett’s esophagus with high-grade dysplasia or intramucosal carcinoma, and the current findings show that complete endoscopic mucosal resection is an effective and durable method to treat Barrett’s-associated neoplasia, the investigators concluded, adding that the results support the replacement of esophagectomy by endoscopic therapy for the condition.
“The most commonly encountered complication of esophageal stricture formation can be addressed with endoscopic dilation,” the investigators said.
However, long-term outcomes, particularly in those with advanced pathology who undergo endoscopic management, are still needed, as is an improved understanding of the behavior of the disease following treatment with specific modalities in order to optimize endoscopic therapy, they added.
This study was supported by the Francis L. Lederer Foundation. The authors reported having no disclosures.
Key clinical point: Endoscopic therapy should replace esophagectomy for Barrett’s-associated neoplasia.
Major finding: Barrett’s esophagus was completely eradicated in 86 of 107 patients (80%) on intention-to-treat analysis.
Data source: A series of 107 cases.
Disclosures: This study was supported by the Francis L. Lederer Foundation. The authors reported having no disclosures.
Vascular surgeons have better outcomes for aneurysm repair, endarterectomy
SAN FRANCISCO – Patients undergoing carotid endarterectomy and open abdominal aortic aneurysm repair are less likely to have complications and die if their surgeon is a vascular specialist, according to a study reported at the annual clinical congress of the American College of Surgeons.
“We feel that carotid endarterectomy and open triple-A repair performed by a vascular surgeon is an independent predictor of improved morbidity and mortality. Hospitals should consider utilizing this specialty-specific information to identify potential quality improvement initiatives,” recommended lead investigator Dr. Carla C. Moreira, a surgeon in the division of vascular and endovascular surgery, Boston Medical Center.
She and her colleagues analyzed data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP), assessing outcomes for 94,029 patients who underwent open vascular procedures between 2006 and 2012. Some 8% had abdominal aneurysm repairs, 57% had carotid endarterectomies, and 35% had lower-extremity bypasses.
Overall, 94% of the procedures were performed by vascular surgeons, while the rest were performed by other types of surgeons (including cardiac surgeons because their numbers were too small to tease out, according to Dr. Moreira).
Results showed that for patients undergoing abdominal aneurysm repair, the unadjusted rate of 30-day mortality did not differ significantly by surgeon specialty. However, in multivariate, propensity-matched analysis, the odds of complications were reduced by half when the repair was done by a vascular surgeon as compared with some other type of surgeon (odds ratio, 0.50).
Patients undergoing carotid endarterectomy had a lower unadjusted mortality if the operation was performed by a vascular surgeon (0.7% vs. 1.0%), although the difference was no longer significant after multivariate adjustment. However, they had significantly lower adjusted odds of complications (odds ratio, 0.62).
For patients undergoing lower-extremity bypass, neither the rate of mortality nor the odds of complications differed significantly by surgeon specialty.
An analysis of temporal trends showed that the proportions of all eligible patients undergoing open abdominal aneurysm repair and lower-extremity bypass during the study period fell, regardless of surgeon type, whereas the proportion of eligible patients undergoing carotid endarterectomies remained stable. “I think this is reflective likely of the penetration of endovascular procedures when it comes to the treatment of abdominal aneurysm and lower-extremity peripheral arterial disease, as compared to carotid disease,” speculated Dr. Moreira, who disclosed that she had no relevant conflicts of interest.
Session moderator Dr. Peter K. Henke, associate chair of research, department of surgery, and Leland Ira Doan Professor of Vascular Surgery at the University of Michigan in Ann Arbor, asked whether the findings have implications for surgeon training.
“Our results were different from what has been previously published for open aneurysm repair. I think that open aneurysm repair is probably becoming more and more specialized in terms that more and more, you are going to see just vascular surgeons performing it as compared to other specialties, especially as I have shown that there is a decreasing number of general surgeons being exposed to open vascular procedures,” Dr. Moreira replied. “So I think this [speaks] to individual surgeons and their individual experience with triple-A repair. Our data does show that general surgeons who are performing these procedures are doing a good job because there is not a difference in outcome at least in terms of mortality. But as the easy triple-A repairs go away, I think it’s going to push the procedure to be done more by specialized surgeons.”
In an interview, Dr. Henke commented, “I think it has been alluded to in other studies and other reports in the literature, but this study brings to the forefront the fact that overall numbers of open vascular procedures are less and less, so the surgeons performing those procedures need to be specialists. And I’d say within the U.S. anyway, most practitioners who do vascular procedures are vascular surgeons or cardiovascularly trained, as compared with general surgeons. I suspect that some of the general surgeons who are still doing these procedures may be at a place where they are the only ones who can do it or there are no vascular specialists there.
“The other issue that this study may impact, as more of these reports come out, is hospital credentialing, because hospital credentialing of surgeons really determines what they can and cannot do at that hospital,” he added. “So as more hospital credentialing boards see this type of data, I think they will limit open vascular procedures to vascular specialists who have had training in vascular disease.”
SAN FRANCISCO – Patients undergoing carotid endarterectomy and open abdominal aortic aneurysm repair are less likely to have complications and die if their surgeon is a vascular specialist, according to a study reported at the annual clinical congress of the American College of Surgeons.
“We feel that carotid endarterectomy and open triple-A repair performed by a vascular surgeon is an independent predictor of improved morbidity and mortality. Hospitals should consider utilizing this specialty-specific information to identify potential quality improvement initiatives,” recommended lead investigator Dr. Carla C. Moreira, a surgeon in the division of vascular and endovascular surgery, Boston Medical Center.
She and her colleagues analyzed data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP), assessing outcomes for 94,029 patients who underwent open vascular procedures between 2006 and 2012. Some 8% had abdominal aneurysm repairs, 57% had carotid endarterectomies, and 35% had lower-extremity bypasses.
Overall, 94% of the procedures were performed by vascular surgeons, while the rest were performed by other types of surgeons (including cardiac surgeons because their numbers were too small to tease out, according to Dr. Moreira).
Results showed that for patients undergoing abdominal aneurysm repair, the unadjusted rate of 30-day mortality did not differ significantly by surgeon specialty. However, in multivariate, propensity-matched analysis, the odds of complications were reduced by half when the repair was done by a vascular surgeon as compared with some other type of surgeon (odds ratio, 0.50).
Patients undergoing carotid endarterectomy had a lower unadjusted mortality if the operation was performed by a vascular surgeon (0.7% vs. 1.0%), although the difference was no longer significant after multivariate adjustment. However, they had significantly lower adjusted odds of complications (odds ratio, 0.62).
For patients undergoing lower-extremity bypass, neither the rate of mortality nor the odds of complications differed significantly by surgeon specialty.
An analysis of temporal trends showed that the proportions of all eligible patients undergoing open abdominal aneurysm repair and lower-extremity bypass during the study period fell, regardless of surgeon type, whereas the proportion of eligible patients undergoing carotid endarterectomies remained stable. “I think this is reflective likely of the penetration of endovascular procedures when it comes to the treatment of abdominal aneurysm and lower-extremity peripheral arterial disease, as compared to carotid disease,” speculated Dr. Moreira, who disclosed that she had no relevant conflicts of interest.
Session moderator Dr. Peter K. Henke, associate chair of research, department of surgery, and Leland Ira Doan Professor of Vascular Surgery at the University of Michigan in Ann Arbor, asked whether the findings have implications for surgeon training.
“Our results were different from what has been previously published for open aneurysm repair. I think that open aneurysm repair is probably becoming more and more specialized in terms that more and more, you are going to see just vascular surgeons performing it as compared to other specialties, especially as I have shown that there is a decreasing number of general surgeons being exposed to open vascular procedures,” Dr. Moreira replied. “So I think this [speaks] to individual surgeons and their individual experience with triple-A repair. Our data does show that general surgeons who are performing these procedures are doing a good job because there is not a difference in outcome at least in terms of mortality. But as the easy triple-A repairs go away, I think it’s going to push the procedure to be done more by specialized surgeons.”
In an interview, Dr. Henke commented, “I think it has been alluded to in other studies and other reports in the literature, but this study brings to the forefront the fact that overall numbers of open vascular procedures are less and less, so the surgeons performing those procedures need to be specialists. And I’d say within the U.S. anyway, most practitioners who do vascular procedures are vascular surgeons or cardiovascularly trained, as compared with general surgeons. I suspect that some of the general surgeons who are still doing these procedures may be at a place where they are the only ones who can do it or there are no vascular specialists there.
“The other issue that this study may impact, as more of these reports come out, is hospital credentialing, because hospital credentialing of surgeons really determines what they can and cannot do at that hospital,” he added. “So as more hospital credentialing boards see this type of data, I think they will limit open vascular procedures to vascular specialists who have had training in vascular disease.”
SAN FRANCISCO – Patients undergoing carotid endarterectomy and open abdominal aortic aneurysm repair are less likely to have complications and die if their surgeon is a vascular specialist, according to a study reported at the annual clinical congress of the American College of Surgeons.
“We feel that carotid endarterectomy and open triple-A repair performed by a vascular surgeon is an independent predictor of improved morbidity and mortality. Hospitals should consider utilizing this specialty-specific information to identify potential quality improvement initiatives,” recommended lead investigator Dr. Carla C. Moreira, a surgeon in the division of vascular and endovascular surgery, Boston Medical Center.
She and her colleagues analyzed data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP), assessing outcomes for 94,029 patients who underwent open vascular procedures between 2006 and 2012. Some 8% had abdominal aneurysm repairs, 57% had carotid endarterectomies, and 35% had lower-extremity bypasses.
Overall, 94% of the procedures were performed by vascular surgeons, while the rest were performed by other types of surgeons (including cardiac surgeons because their numbers were too small to tease out, according to Dr. Moreira).
Results showed that for patients undergoing abdominal aneurysm repair, the unadjusted rate of 30-day mortality did not differ significantly by surgeon specialty. However, in multivariate, propensity-matched analysis, the odds of complications were reduced by half when the repair was done by a vascular surgeon as compared with some other type of surgeon (odds ratio, 0.50).
Patients undergoing carotid endarterectomy had a lower unadjusted mortality if the operation was performed by a vascular surgeon (0.7% vs. 1.0%), although the difference was no longer significant after multivariate adjustment. However, they had significantly lower adjusted odds of complications (odds ratio, 0.62).
For patients undergoing lower-extremity bypass, neither the rate of mortality nor the odds of complications differed significantly by surgeon specialty.
An analysis of temporal trends showed that the proportions of all eligible patients undergoing open abdominal aneurysm repair and lower-extremity bypass during the study period fell, regardless of surgeon type, whereas the proportion of eligible patients undergoing carotid endarterectomies remained stable. “I think this is reflective likely of the penetration of endovascular procedures when it comes to the treatment of abdominal aneurysm and lower-extremity peripheral arterial disease, as compared to carotid disease,” speculated Dr. Moreira, who disclosed that she had no relevant conflicts of interest.
Session moderator Dr. Peter K. Henke, associate chair of research, department of surgery, and Leland Ira Doan Professor of Vascular Surgery at the University of Michigan in Ann Arbor, asked whether the findings have implications for surgeon training.
“Our results were different from what has been previously published for open aneurysm repair. I think that open aneurysm repair is probably becoming more and more specialized in terms that more and more, you are going to see just vascular surgeons performing it as compared to other specialties, especially as I have shown that there is a decreasing number of general surgeons being exposed to open vascular procedures,” Dr. Moreira replied. “So I think this [speaks] to individual surgeons and their individual experience with triple-A repair. Our data does show that general surgeons who are performing these procedures are doing a good job because there is not a difference in outcome at least in terms of mortality. But as the easy triple-A repairs go away, I think it’s going to push the procedure to be done more by specialized surgeons.”
In an interview, Dr. Henke commented, “I think it has been alluded to in other studies and other reports in the literature, but this study brings to the forefront the fact that overall numbers of open vascular procedures are less and less, so the surgeons performing those procedures need to be specialists. And I’d say within the U.S. anyway, most practitioners who do vascular procedures are vascular surgeons or cardiovascularly trained, as compared with general surgeons. I suspect that some of the general surgeons who are still doing these procedures may be at a place where they are the only ones who can do it or there are no vascular specialists there.
“The other issue that this study may impact, as more of these reports come out, is hospital credentialing, because hospital credentialing of surgeons really determines what they can and cannot do at that hospital,” he added. “So as more hospital credentialing boards see this type of data, I think they will limit open vascular procedures to vascular specialists who have had training in vascular disease.”
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients undergoing certain open vascular procedures have better outcomes when operated on by vascular surgeons.
Major finding: Vascular surgeons achieved lower rates of morbidity and mortality in cases of open abdominal aneurysm repair and carotid endarterectomy.
Data source: An analysis of NSQIP data for 94,029 patients undergoing open vascular procedures.
Disclosures: Dr. Moreira disclosed that she had no relevant conflicts of interest.
Bicuspid valve surgical management in rapid flux
CHICAGO – Surgical management of leaky bicuspid valves is rapidly evolving from replacement to repair of any purely insufficient bicuspid valve with enough leaflet surface area.
“We’re coming to the point like with mitral valves 20 years ago, that we don’t have to replace every blessed bicuspid valve. We can repair a lot of these valves,” Dr. Joseph Bavaria, vice chief of cardiovascular surgery, University of Pennsylvania, Philadelphia, said.
A valve-sparing root procedure in a patient with bicuspid aortic valve (BAV) disease and aortic insufficiency (AI) provides excellent results, no matter if the aortic root is abnormal or not. Many patients with BAV, however, have leaky valves without a root aneurysm.
Thus, the “great dilemma” facing surgeons now is whether they can continue to justify doing a root procedure, which is a much bigger operation, when the root is normal diameter, Dr. Bavaria said at Heart Valve Summit 2014.
“It may be inappropriate in today’s world to take a normal physiological valve and just take it out and consign someone who’s in their 30s and 40s to a mechanical or bioprosthetic valve for life,” he said in an interview. “That has anticoagulation issues, structural deterioration issues, infection issues.”
The alternative is a valve repair operation, but that’s complicated by the growing understanding that BAV AI has three distinct phenotypic presentations:
• BAV with AI with relatively normal root diameters.
• BAV with AI and relatively normal root diameters, with an ascending aortic aneurysm.
• BAV with AI and root dilation.
“The problem we have is there’s probably a different therapeutic procedure for each of these three presentations,” Dr. Bavaria said.
The goals for any bicuspid repair are to equalize the free margin lengths with plication or resection of the redundant leaflet, reduce the annulus by 10%-15%, and stabilize it with either reimplantation or a subannular technique, and to increase the height of the free margin, if the leaflet belly falls below the annular plane.
In the university’s current surgical management algorithm, patients who have an aortic annulus dilated to 28 mm or more undergo root reimplantation if they have an aneurysmal root or receive external annuloplasty rings plus a valve repair if their aortic annulus is dilated and they have a nonaneurysmal root. The Dacron ring is placed subcoronary and subannular and is generally sized 5-7 mm larger than the desired end-procedural annular diameter, he said.
For patients with a normal aortic annulus (27 mm or less), root reimplantation or remodeling is used for those with an aneurysmal root, while subcommissural annuloplasty is reserved only for those with a normal aortic annulus and a nonaneurysmal root.
Subcommissural annuloplasty had been used for many BAV patients with AI who were candidates for repair, but emerging data over the last 2 years from Dr. Bavaria’s group (Annals Thor. Surg. 2014;97:1227-34) and others show it results in a lot of midterm failures and reoperations, compared with root reimplantation. Some groups continue to use this procedure routinely, but “It doesn’t work,” Dr. Bavaria said.
His team recently compared postoperative outcomes among BAV repairs and the more commonly performed tricuspid repair between 2004 and 2014. Overall, the outcomes were the same between the two groups including mortality, stroke, freedom from AI grade +1, and aortic reoperation for bleeding (P = NS). Notably, all 41 BAV patients required concomitant primary leaflet repair, compared with only 7% of the 99 patients who underwent tricuspid valve repair (P < .01), he said.
Dr. Bavaria reported consultant fees and honoraria from St. Jude Medical and research grants from Edwards Lifesciences and Sorin Group.
CHICAGO – Surgical management of leaky bicuspid valves is rapidly evolving from replacement to repair of any purely insufficient bicuspid valve with enough leaflet surface area.
“We’re coming to the point like with mitral valves 20 years ago, that we don’t have to replace every blessed bicuspid valve. We can repair a lot of these valves,” Dr. Joseph Bavaria, vice chief of cardiovascular surgery, University of Pennsylvania, Philadelphia, said.
A valve-sparing root procedure in a patient with bicuspid aortic valve (BAV) disease and aortic insufficiency (AI) provides excellent results, no matter if the aortic root is abnormal or not. Many patients with BAV, however, have leaky valves without a root aneurysm.
Thus, the “great dilemma” facing surgeons now is whether they can continue to justify doing a root procedure, which is a much bigger operation, when the root is normal diameter, Dr. Bavaria said at Heart Valve Summit 2014.
“It may be inappropriate in today’s world to take a normal physiological valve and just take it out and consign someone who’s in their 30s and 40s to a mechanical or bioprosthetic valve for life,” he said in an interview. “That has anticoagulation issues, structural deterioration issues, infection issues.”
The alternative is a valve repair operation, but that’s complicated by the growing understanding that BAV AI has three distinct phenotypic presentations:
• BAV with AI with relatively normal root diameters.
• BAV with AI and relatively normal root diameters, with an ascending aortic aneurysm.
• BAV with AI and root dilation.
“The problem we have is there’s probably a different therapeutic procedure for each of these three presentations,” Dr. Bavaria said.
The goals for any bicuspid repair are to equalize the free margin lengths with plication or resection of the redundant leaflet, reduce the annulus by 10%-15%, and stabilize it with either reimplantation or a subannular technique, and to increase the height of the free margin, if the leaflet belly falls below the annular plane.
In the university’s current surgical management algorithm, patients who have an aortic annulus dilated to 28 mm or more undergo root reimplantation if they have an aneurysmal root or receive external annuloplasty rings plus a valve repair if their aortic annulus is dilated and they have a nonaneurysmal root. The Dacron ring is placed subcoronary and subannular and is generally sized 5-7 mm larger than the desired end-procedural annular diameter, he said.
For patients with a normal aortic annulus (27 mm or less), root reimplantation or remodeling is used for those with an aneurysmal root, while subcommissural annuloplasty is reserved only for those with a normal aortic annulus and a nonaneurysmal root.
Subcommissural annuloplasty had been used for many BAV patients with AI who were candidates for repair, but emerging data over the last 2 years from Dr. Bavaria’s group (Annals Thor. Surg. 2014;97:1227-34) and others show it results in a lot of midterm failures and reoperations, compared with root reimplantation. Some groups continue to use this procedure routinely, but “It doesn’t work,” Dr. Bavaria said.
His team recently compared postoperative outcomes among BAV repairs and the more commonly performed tricuspid repair between 2004 and 2014. Overall, the outcomes were the same between the two groups including mortality, stroke, freedom from AI grade +1, and aortic reoperation for bleeding (P = NS). Notably, all 41 BAV patients required concomitant primary leaflet repair, compared with only 7% of the 99 patients who underwent tricuspid valve repair (P < .01), he said.
Dr. Bavaria reported consultant fees and honoraria from St. Jude Medical and research grants from Edwards Lifesciences and Sorin Group.
CHICAGO – Surgical management of leaky bicuspid valves is rapidly evolving from replacement to repair of any purely insufficient bicuspid valve with enough leaflet surface area.
“We’re coming to the point like with mitral valves 20 years ago, that we don’t have to replace every blessed bicuspid valve. We can repair a lot of these valves,” Dr. Joseph Bavaria, vice chief of cardiovascular surgery, University of Pennsylvania, Philadelphia, said.
A valve-sparing root procedure in a patient with bicuspid aortic valve (BAV) disease and aortic insufficiency (AI) provides excellent results, no matter if the aortic root is abnormal or not. Many patients with BAV, however, have leaky valves without a root aneurysm.
Thus, the “great dilemma” facing surgeons now is whether they can continue to justify doing a root procedure, which is a much bigger operation, when the root is normal diameter, Dr. Bavaria said at Heart Valve Summit 2014.
“It may be inappropriate in today’s world to take a normal physiological valve and just take it out and consign someone who’s in their 30s and 40s to a mechanical or bioprosthetic valve for life,” he said in an interview. “That has anticoagulation issues, structural deterioration issues, infection issues.”
The alternative is a valve repair operation, but that’s complicated by the growing understanding that BAV AI has three distinct phenotypic presentations:
• BAV with AI with relatively normal root diameters.
• BAV with AI and relatively normal root diameters, with an ascending aortic aneurysm.
• BAV with AI and root dilation.
“The problem we have is there’s probably a different therapeutic procedure for each of these three presentations,” Dr. Bavaria said.
The goals for any bicuspid repair are to equalize the free margin lengths with plication or resection of the redundant leaflet, reduce the annulus by 10%-15%, and stabilize it with either reimplantation or a subannular technique, and to increase the height of the free margin, if the leaflet belly falls below the annular plane.
In the university’s current surgical management algorithm, patients who have an aortic annulus dilated to 28 mm or more undergo root reimplantation if they have an aneurysmal root or receive external annuloplasty rings plus a valve repair if their aortic annulus is dilated and they have a nonaneurysmal root. The Dacron ring is placed subcoronary and subannular and is generally sized 5-7 mm larger than the desired end-procedural annular diameter, he said.
For patients with a normal aortic annulus (27 mm or less), root reimplantation or remodeling is used for those with an aneurysmal root, while subcommissural annuloplasty is reserved only for those with a normal aortic annulus and a nonaneurysmal root.
Subcommissural annuloplasty had been used for many BAV patients with AI who were candidates for repair, but emerging data over the last 2 years from Dr. Bavaria’s group (Annals Thor. Surg. 2014;97:1227-34) and others show it results in a lot of midterm failures and reoperations, compared with root reimplantation. Some groups continue to use this procedure routinely, but “It doesn’t work,” Dr. Bavaria said.
His team recently compared postoperative outcomes among BAV repairs and the more commonly performed tricuspid repair between 2004 and 2014. Overall, the outcomes were the same between the two groups including mortality, stroke, freedom from AI grade +1, and aortic reoperation for bleeding (P = NS). Notably, all 41 BAV patients required concomitant primary leaflet repair, compared with only 7% of the 99 patients who underwent tricuspid valve repair (P < .01), he said.
Dr. Bavaria reported consultant fees and honoraria from St. Jude Medical and research grants from Edwards Lifesciences and Sorin Group.
EXPERT OPINION FROM HEART VALVE SUMMIT 2014
VIDEO: EMR reminder reduces unnecessary transfusions
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
Spotlight falls on rising levels of tricuspid valve surgery
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2014