User login
Gene therapy regimen for XSCID shows rapid results in newly diagnosed infants
ATLANTA – A new approach to gene therapy produced rapid T cell reconstruction and normal markers of B-cell and natural killer (NK)-cell function in newly diagnosed infants with X-linked Severe Combined Immunodeficiency (XSCID), according to initial results from a phase 1/2 trial.
Researchers used a regimen of safety-modified lentiviral vector plus reduced-exposure busulfan conditioning in seven newly diagnosed infants and found that it was well tolerated in all patients and quickly improved T-cell immunity in five of seven patients.
Initial gene therapy trials used a mouse vector without busulfan conditioning. These trials produced T-cell correction but were unable to restore B-cell function, NK-cell function, or myeloid-cell function. As a result, patients continued to experience viral infections and required monthly, life-long intravenous immunoglobulin infusions, Dr. Mamcarz said.
The phase 1/2 multicenter safety and efficacy study tested the gene therapy regimen for the first time in seven newly diagnosed infants. The regimen involved transducing purified bone marrow CD34+ cells with the lentiviral vector, which was generated by a stable producer cell line and then cryopreserved. The busulfan was given as two single daily doses, which were tailored based on patient age and weight.
In total, seven patients have been treated and all tolerated the low-dose busulfan chemotherapy well. Five patients had normal numbers of previously defective cells (T cells, B cells, and NK cells) and were taken off protective isolation and prophylactic medications. Those infants appear to have functioning immune systems, Dr. Mamcarz said. One infant has stopped monthly intravenous immunoglobulin infusions and has received normal pediatric vaccines, but responses have not yet been tested.
For the two infants who did not show responses, one is early in the trial and there is not yet adequate follow-up data to assess the immune system reconstitution, Dr. Mamcarz said.
The other infant had high levels of maternal T cell engraftment, severe neutropenia, and ongoing cytomegalovirus infection, resulting in delayed and partial T-cell reconstitution. The researchers sought to boost the patient’s immunity through an infusion of corrected cells – without busulfan – at 1 year after receiving the initial therapy. Three months after the second treatment, the infant has normal functioning of T cells and NK cells, but he is not yet engrafting B cells, Dr. Mamcarz said.
Overall, there was no evidence of vector-mediated effects on blood formation, Dr. Mamcarz reported.
The ultimate evaluation of the efficacy of the trial would be to assess vaccine responses in the infants treated with gene therapy, she said.
The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
[email protected]
SOURCE: Mamcarz E et al. Abstract 523.
ATLANTA – A new approach to gene therapy produced rapid T cell reconstruction and normal markers of B-cell and natural killer (NK)-cell function in newly diagnosed infants with X-linked Severe Combined Immunodeficiency (XSCID), according to initial results from a phase 1/2 trial.
Researchers used a regimen of safety-modified lentiviral vector plus reduced-exposure busulfan conditioning in seven newly diagnosed infants and found that it was well tolerated in all patients and quickly improved T-cell immunity in five of seven patients.
Initial gene therapy trials used a mouse vector without busulfan conditioning. These trials produced T-cell correction but were unable to restore B-cell function, NK-cell function, or myeloid-cell function. As a result, patients continued to experience viral infections and required monthly, life-long intravenous immunoglobulin infusions, Dr. Mamcarz said.
The phase 1/2 multicenter safety and efficacy study tested the gene therapy regimen for the first time in seven newly diagnosed infants. The regimen involved transducing purified bone marrow CD34+ cells with the lentiviral vector, which was generated by a stable producer cell line and then cryopreserved. The busulfan was given as two single daily doses, which were tailored based on patient age and weight.
In total, seven patients have been treated and all tolerated the low-dose busulfan chemotherapy well. Five patients had normal numbers of previously defective cells (T cells, B cells, and NK cells) and were taken off protective isolation and prophylactic medications. Those infants appear to have functioning immune systems, Dr. Mamcarz said. One infant has stopped monthly intravenous immunoglobulin infusions and has received normal pediatric vaccines, but responses have not yet been tested.
For the two infants who did not show responses, one is early in the trial and there is not yet adequate follow-up data to assess the immune system reconstitution, Dr. Mamcarz said.
The other infant had high levels of maternal T cell engraftment, severe neutropenia, and ongoing cytomegalovirus infection, resulting in delayed and partial T-cell reconstitution. The researchers sought to boost the patient’s immunity through an infusion of corrected cells – without busulfan – at 1 year after receiving the initial therapy. Three months after the second treatment, the infant has normal functioning of T cells and NK cells, but he is not yet engrafting B cells, Dr. Mamcarz said.
Overall, there was no evidence of vector-mediated effects on blood formation, Dr. Mamcarz reported.
The ultimate evaluation of the efficacy of the trial would be to assess vaccine responses in the infants treated with gene therapy, she said.
The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
[email protected]
SOURCE: Mamcarz E et al. Abstract 523.
ATLANTA – A new approach to gene therapy produced rapid T cell reconstruction and normal markers of B-cell and natural killer (NK)-cell function in newly diagnosed infants with X-linked Severe Combined Immunodeficiency (XSCID), according to initial results from a phase 1/2 trial.
Researchers used a regimen of safety-modified lentiviral vector plus reduced-exposure busulfan conditioning in seven newly diagnosed infants and found that it was well tolerated in all patients and quickly improved T-cell immunity in five of seven patients.
Initial gene therapy trials used a mouse vector without busulfan conditioning. These trials produced T-cell correction but were unable to restore B-cell function, NK-cell function, or myeloid-cell function. As a result, patients continued to experience viral infections and required monthly, life-long intravenous immunoglobulin infusions, Dr. Mamcarz said.
The phase 1/2 multicenter safety and efficacy study tested the gene therapy regimen for the first time in seven newly diagnosed infants. The regimen involved transducing purified bone marrow CD34+ cells with the lentiviral vector, which was generated by a stable producer cell line and then cryopreserved. The busulfan was given as two single daily doses, which were tailored based on patient age and weight.
In total, seven patients have been treated and all tolerated the low-dose busulfan chemotherapy well. Five patients had normal numbers of previously defective cells (T cells, B cells, and NK cells) and were taken off protective isolation and prophylactic medications. Those infants appear to have functioning immune systems, Dr. Mamcarz said. One infant has stopped monthly intravenous immunoglobulin infusions and has received normal pediatric vaccines, but responses have not yet been tested.
For the two infants who did not show responses, one is early in the trial and there is not yet adequate follow-up data to assess the immune system reconstitution, Dr. Mamcarz said.
The other infant had high levels of maternal T cell engraftment, severe neutropenia, and ongoing cytomegalovirus infection, resulting in delayed and partial T-cell reconstitution. The researchers sought to boost the patient’s immunity through an infusion of corrected cells – without busulfan – at 1 year after receiving the initial therapy. Three months after the second treatment, the infant has normal functioning of T cells and NK cells, but he is not yet engrafting B cells, Dr. Mamcarz said.
Overall, there was no evidence of vector-mediated effects on blood formation, Dr. Mamcarz reported.
The ultimate evaluation of the efficacy of the trial would be to assess vaccine responses in the infants treated with gene therapy, she said.
The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
[email protected]
SOURCE: Mamcarz E et al. Abstract 523.
REPORTING FROM ASH 2017
Key clinical point:
Major finding: In total, five of seven infants with XSCID had normal functioning of T cells, B cells, and NK cells.
Study details: A phase 1/2 multicenter study of seven infants with newly diagnosed XSCID.
Disclosures: The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
Source: Mamcarz E et al. Abstract 523.
Cyclophosphamide after transplant reduced GVHD in myeloma patients
Post-transplantation cyclophosphamide may help decrease the rate of nonrelapse mortality and graft-versus-host disease (GVHD) in patients who have undergone allogeneic blood or marrow transplantation, according to new findings published in Biology of Blood and Marrow Transplantation.
Even though it is a potentially curative option for patients with poor-risk hematologic malignancies, allogeneic blood or marrow transplantation (alloBMT) has not been commonly used in multiple myeloma because of its association with high nonrelapse mortality and high relapse rates. However, the use of post-transplantation cyclophosphamide (PTCy) in this study led to low rates of both acute and chronic GVHD, which translated to low rates of nonrelapse mortality and maintenance of long-term remissions in a subset of patients with multiple myeloma treated at Johns Hopkins Hospital, Baltimore.
“The favorable toxicity profile of alloBMT using PTCy in patients with MM offers the potential to further explore the use of post-transplantation strategies to improve disease control,” wrote Nilanjan Ghosh, MD, of the Levine Cancer Institute, Charlotte, N.C., and his colleagues.
The researchers examined outcomes of 39 patients with multiple myeloma who underwent bone marrow or peripheral blood alloBMT from HLA-matched related/unrelated or haploidentical related donors after either myeloablative or nonmyeloablative conditioning.
Patients who underwent myeloablative conditioning received PTCy 50 mg/kg per day (given intravenously on days 3 and 4 after alloBMT) as GVHD prophylaxis, while those who received nonmyeloablative conditioning received PTCy (same dose and schedule) and additional immunosuppression with mycophenolate mofetil 15 mg/kg (orally two to three times daily, up to 1,000 mg/dose on days 4-35 after transplantation).
At a median follow-up of 10.3 years following alloBMT, 23% of the cohort remained alive and without any evidence of disease. The median overall survival was 4.4 years. The 5-year survival probability was 49% (95% confidence interval, 32%-67%) and 10-year survival probability was 43% (95% CI, 29%-62%).
Following transplantation, 10 (26%) patients achieved a complete response, 8 (21%) had a very good partial response, 6 (15%) had a partial response, and 15 (38%) had progressive disease, the investigators reported (Biol Blood Marrow Transplant. 2017 Nov;23[11]:1903-9).
Among the 36 patients with evidence of donor engraftment, the cumulative incidences of grade 2-4 and grade 3 and 4 acute GVHD were 0.41 (95% CI, 0.25-0.57) and 0.08 (95% CI, 0.01-0.16), respectively. For chronic GVHD, the cumulative incidence was 0.13 (95% CI, 0.02-0.23), and the median time to development was 109 days after alloBMT.
The median progression-free survival was 12 months (95% CI, 7.6-40), and the estimated cumulative incidence of relapse was 0.46 (95% CI, 0.3-0.62) at 1 year and 0.56 (95% CI, 0.41-0.72) at 2 years.
In univariate analysis, achievement of a complete response following alloBMT correlated with overall survival. Factors such as the intensity of the alloBMT conditioning regimen, stem cell source, age, and disease response before alloBMT did not appear to impact overall survival.
“Given the low incidence of GVHD and [nonrelapse mortality] in our study, it is possible that post-transplantation maintenance therapies can be used to improve diseases control,” Dr. Ghosh and his associates wrote. “Emerging data suggest that many anticancer agents may be more active after alloBMT than before transplantation.”
The study was funded in part by grants from the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Post-transplantation cyclophosphamide may help decrease the rate of nonrelapse mortality and graft-versus-host disease (GVHD) in patients who have undergone allogeneic blood or marrow transplantation, according to new findings published in Biology of Blood and Marrow Transplantation.
Even though it is a potentially curative option for patients with poor-risk hematologic malignancies, allogeneic blood or marrow transplantation (alloBMT) has not been commonly used in multiple myeloma because of its association with high nonrelapse mortality and high relapse rates. However, the use of post-transplantation cyclophosphamide (PTCy) in this study led to low rates of both acute and chronic GVHD, which translated to low rates of nonrelapse mortality and maintenance of long-term remissions in a subset of patients with multiple myeloma treated at Johns Hopkins Hospital, Baltimore.
“The favorable toxicity profile of alloBMT using PTCy in patients with MM offers the potential to further explore the use of post-transplantation strategies to improve disease control,” wrote Nilanjan Ghosh, MD, of the Levine Cancer Institute, Charlotte, N.C., and his colleagues.
The researchers examined outcomes of 39 patients with multiple myeloma who underwent bone marrow or peripheral blood alloBMT from HLA-matched related/unrelated or haploidentical related donors after either myeloablative or nonmyeloablative conditioning.
Patients who underwent myeloablative conditioning received PTCy 50 mg/kg per day (given intravenously on days 3 and 4 after alloBMT) as GVHD prophylaxis, while those who received nonmyeloablative conditioning received PTCy (same dose and schedule) and additional immunosuppression with mycophenolate mofetil 15 mg/kg (orally two to three times daily, up to 1,000 mg/dose on days 4-35 after transplantation).
At a median follow-up of 10.3 years following alloBMT, 23% of the cohort remained alive and without any evidence of disease. The median overall survival was 4.4 years. The 5-year survival probability was 49% (95% confidence interval, 32%-67%) and 10-year survival probability was 43% (95% CI, 29%-62%).
Following transplantation, 10 (26%) patients achieved a complete response, 8 (21%) had a very good partial response, 6 (15%) had a partial response, and 15 (38%) had progressive disease, the investigators reported (Biol Blood Marrow Transplant. 2017 Nov;23[11]:1903-9).
Among the 36 patients with evidence of donor engraftment, the cumulative incidences of grade 2-4 and grade 3 and 4 acute GVHD were 0.41 (95% CI, 0.25-0.57) and 0.08 (95% CI, 0.01-0.16), respectively. For chronic GVHD, the cumulative incidence was 0.13 (95% CI, 0.02-0.23), and the median time to development was 109 days after alloBMT.
The median progression-free survival was 12 months (95% CI, 7.6-40), and the estimated cumulative incidence of relapse was 0.46 (95% CI, 0.3-0.62) at 1 year and 0.56 (95% CI, 0.41-0.72) at 2 years.
In univariate analysis, achievement of a complete response following alloBMT correlated with overall survival. Factors such as the intensity of the alloBMT conditioning regimen, stem cell source, age, and disease response before alloBMT did not appear to impact overall survival.
“Given the low incidence of GVHD and [nonrelapse mortality] in our study, it is possible that post-transplantation maintenance therapies can be used to improve diseases control,” Dr. Ghosh and his associates wrote. “Emerging data suggest that many anticancer agents may be more active after alloBMT than before transplantation.”
The study was funded in part by grants from the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Post-transplantation cyclophosphamide may help decrease the rate of nonrelapse mortality and graft-versus-host disease (GVHD) in patients who have undergone allogeneic blood or marrow transplantation, according to new findings published in Biology of Blood and Marrow Transplantation.
Even though it is a potentially curative option for patients with poor-risk hematologic malignancies, allogeneic blood or marrow transplantation (alloBMT) has not been commonly used in multiple myeloma because of its association with high nonrelapse mortality and high relapse rates. However, the use of post-transplantation cyclophosphamide (PTCy) in this study led to low rates of both acute and chronic GVHD, which translated to low rates of nonrelapse mortality and maintenance of long-term remissions in a subset of patients with multiple myeloma treated at Johns Hopkins Hospital, Baltimore.
“The favorable toxicity profile of alloBMT using PTCy in patients with MM offers the potential to further explore the use of post-transplantation strategies to improve disease control,” wrote Nilanjan Ghosh, MD, of the Levine Cancer Institute, Charlotte, N.C., and his colleagues.
The researchers examined outcomes of 39 patients with multiple myeloma who underwent bone marrow or peripheral blood alloBMT from HLA-matched related/unrelated or haploidentical related donors after either myeloablative or nonmyeloablative conditioning.
Patients who underwent myeloablative conditioning received PTCy 50 mg/kg per day (given intravenously on days 3 and 4 after alloBMT) as GVHD prophylaxis, while those who received nonmyeloablative conditioning received PTCy (same dose and schedule) and additional immunosuppression with mycophenolate mofetil 15 mg/kg (orally two to three times daily, up to 1,000 mg/dose on days 4-35 after transplantation).
At a median follow-up of 10.3 years following alloBMT, 23% of the cohort remained alive and without any evidence of disease. The median overall survival was 4.4 years. The 5-year survival probability was 49% (95% confidence interval, 32%-67%) and 10-year survival probability was 43% (95% CI, 29%-62%).
Following transplantation, 10 (26%) patients achieved a complete response, 8 (21%) had a very good partial response, 6 (15%) had a partial response, and 15 (38%) had progressive disease, the investigators reported (Biol Blood Marrow Transplant. 2017 Nov;23[11]:1903-9).
Among the 36 patients with evidence of donor engraftment, the cumulative incidences of grade 2-4 and grade 3 and 4 acute GVHD were 0.41 (95% CI, 0.25-0.57) and 0.08 (95% CI, 0.01-0.16), respectively. For chronic GVHD, the cumulative incidence was 0.13 (95% CI, 0.02-0.23), and the median time to development was 109 days after alloBMT.
The median progression-free survival was 12 months (95% CI, 7.6-40), and the estimated cumulative incidence of relapse was 0.46 (95% CI, 0.3-0.62) at 1 year and 0.56 (95% CI, 0.41-0.72) at 2 years.
In univariate analysis, achievement of a complete response following alloBMT correlated with overall survival. Factors such as the intensity of the alloBMT conditioning regimen, stem cell source, age, and disease response before alloBMT did not appear to impact overall survival.
“Given the low incidence of GVHD and [nonrelapse mortality] in our study, it is possible that post-transplantation maintenance therapies can be used to improve diseases control,” Dr. Ghosh and his associates wrote. “Emerging data suggest that many anticancer agents may be more active after alloBMT than before transplantation.”
The study was funded in part by grants from the National Institutes of Health. The researchers reported having no relevant financial disclosures.
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
Key clinical point:
Major finding: At 10.3 years following alloBMT, 16 of 39 (23%) of patients were alive and free of disease. Median overall survival was 4.4 years.
Data source: A single-institution series involving 39 patients with multiple myeloma who underwent alloBMT and received post-transplantation cyclophosphamide.
Disclosures: The study was funded in part by grants from the National Institutes of Health. The researchers reported having no relevant financial disclosures.
FDA addresses cell-based regenerative medicine in comprehensive new policy
The Food and Drug Administration has announced a new policy that addresses the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
“The framework – outlined in a suite of four guidance documents – builds upon the FDA’s existing risk-based regulatory approach to more clearly describe what products are regulated as drugs, devices, and/or biological products,” the FDA announced in a statement released on Nov. 16.
He added: “This is no longer the stuff of science fiction. This is the practical promise of modern applications of regenerative medicine.” But, while advances have benefited many patients, he referred to a small number of “unscrupulous actors” that have provided treatments that have harmed patients, which is why stricter FDA enforcement is needed.
Clarification of the existing regulations will “promote responsible and flexible regulation that leverages science to advance public health,” Dr. Gottlieb said during a media briefing held by the FDA to discuss the new framework.
During the briefing, in response to a question concerning adipose tissue injections and their associated risks, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, explained that the guidance documents will clearly delineate when adipose tissue will be classified as a structural tissue and a stem cell product. If a provider is purveying dangerous products, the FDA can “when necessary, undertake seizures, ask for injunctions, and in some cases when it has been determined that certain violations have occurred even criminal actions can be taken,” he said.
Earlier this year, a report of three patients who had severe visual loss after treatment with intravitreal injections of autologous adipose tissue for age-related macular degeneration was published (N Engl J Med. 2017;376:1047-53).
The new framework is composed of two final guidance documents and two draft guidance documents. The first final guidance document provides details about regulations concerning cell and tissue-based products and when those products are subject to regulation in surgical procedures. The second final guidance document elaborates on the definition of “minimal manipulation” and “homologous use” with the hopes of clarifying what products are subject to regulation. These documents will also explain how the FDA will provide a framework for premarket authorization for cell-based regenerative products.
One draft guidance outlines the FDA’s plan to simplify and expedite the application of the regulatory requirements for devices used in relation to regenerative medicine advanced therapies; the second draft guidance outlines the expedited programs that may be available to sponsors of regenerative therapies.
The Food and Drug Administration has announced a new policy that addresses the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
“The framework – outlined in a suite of four guidance documents – builds upon the FDA’s existing risk-based regulatory approach to more clearly describe what products are regulated as drugs, devices, and/or biological products,” the FDA announced in a statement released on Nov. 16.
He added: “This is no longer the stuff of science fiction. This is the practical promise of modern applications of regenerative medicine.” But, while advances have benefited many patients, he referred to a small number of “unscrupulous actors” that have provided treatments that have harmed patients, which is why stricter FDA enforcement is needed.
Clarification of the existing regulations will “promote responsible and flexible regulation that leverages science to advance public health,” Dr. Gottlieb said during a media briefing held by the FDA to discuss the new framework.
During the briefing, in response to a question concerning adipose tissue injections and their associated risks, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, explained that the guidance documents will clearly delineate when adipose tissue will be classified as a structural tissue and a stem cell product. If a provider is purveying dangerous products, the FDA can “when necessary, undertake seizures, ask for injunctions, and in some cases when it has been determined that certain violations have occurred even criminal actions can be taken,” he said.
Earlier this year, a report of three patients who had severe visual loss after treatment with intravitreal injections of autologous adipose tissue for age-related macular degeneration was published (N Engl J Med. 2017;376:1047-53).
The new framework is composed of two final guidance documents and two draft guidance documents. The first final guidance document provides details about regulations concerning cell and tissue-based products and when those products are subject to regulation in surgical procedures. The second final guidance document elaborates on the definition of “minimal manipulation” and “homologous use” with the hopes of clarifying what products are subject to regulation. These documents will also explain how the FDA will provide a framework for premarket authorization for cell-based regenerative products.
One draft guidance outlines the FDA’s plan to simplify and expedite the application of the regulatory requirements for devices used in relation to regenerative medicine advanced therapies; the second draft guidance outlines the expedited programs that may be available to sponsors of regenerative therapies.
The Food and Drug Administration has announced a new policy that addresses the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
“The framework – outlined in a suite of four guidance documents – builds upon the FDA’s existing risk-based regulatory approach to more clearly describe what products are regulated as drugs, devices, and/or biological products,” the FDA announced in a statement released on Nov. 16.
He added: “This is no longer the stuff of science fiction. This is the practical promise of modern applications of regenerative medicine.” But, while advances have benefited many patients, he referred to a small number of “unscrupulous actors” that have provided treatments that have harmed patients, which is why stricter FDA enforcement is needed.
Clarification of the existing regulations will “promote responsible and flexible regulation that leverages science to advance public health,” Dr. Gottlieb said during a media briefing held by the FDA to discuss the new framework.
During the briefing, in response to a question concerning adipose tissue injections and their associated risks, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, explained that the guidance documents will clearly delineate when adipose tissue will be classified as a structural tissue and a stem cell product. If a provider is purveying dangerous products, the FDA can “when necessary, undertake seizures, ask for injunctions, and in some cases when it has been determined that certain violations have occurred even criminal actions can be taken,” he said.
Earlier this year, a report of three patients who had severe visual loss after treatment with intravitreal injections of autologous adipose tissue for age-related macular degeneration was published (N Engl J Med. 2017;376:1047-53).
The new framework is composed of two final guidance documents and two draft guidance documents. The first final guidance document provides details about regulations concerning cell and tissue-based products and when those products are subject to regulation in surgical procedures. The second final guidance document elaborates on the definition of “minimal manipulation” and “homologous use” with the hopes of clarifying what products are subject to regulation. These documents will also explain how the FDA will provide a framework for premarket authorization for cell-based regenerative products.
One draft guidance outlines the FDA’s plan to simplify and expedite the application of the regulatory requirements for devices used in relation to regenerative medicine advanced therapies; the second draft guidance outlines the expedited programs that may be available to sponsors of regenerative therapies.
FROM an FDA MEDIA BRIEFING
FDA approves letermovir for CMV prophylaxis
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
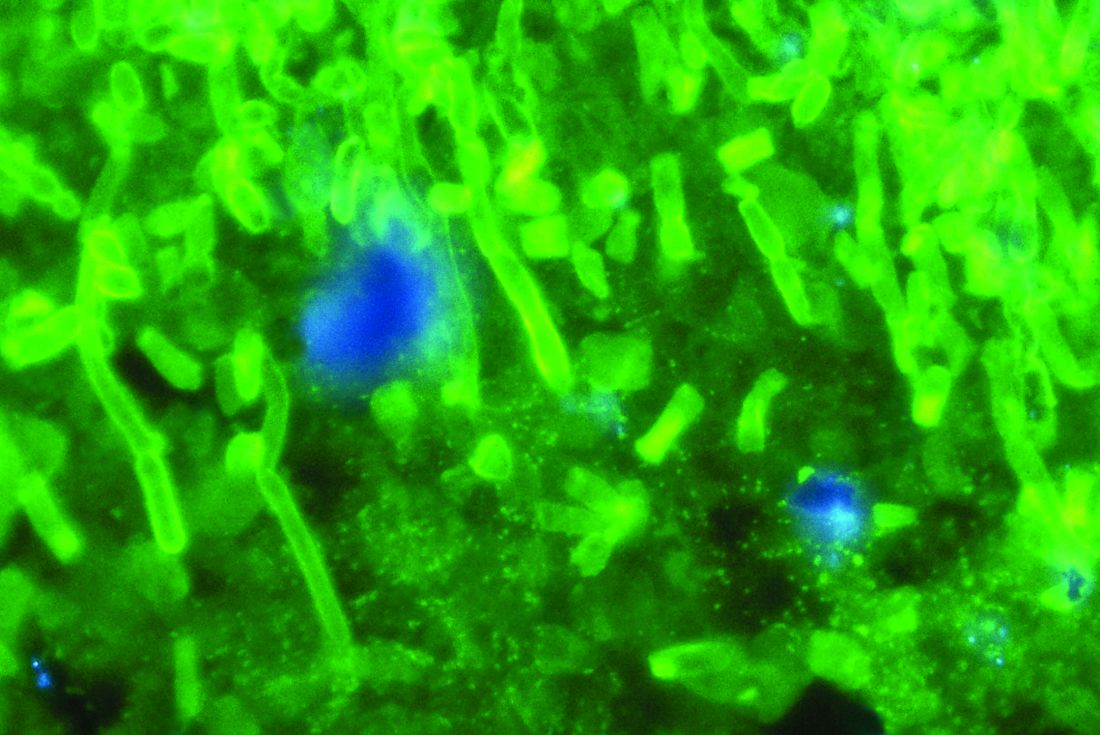
Anidulafungin effectively treated invasive pediatric candidiasis in open-label trial
SAN DIEGO – The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in a single-arm, multicenter, open-label trial of 47 children aged 2-17 years.
The overall global response rate of 72% resembled that from the prior adult registry study (76%), Emmanuel Roilides, MD, PhD, and his associates reported in a poster presented at an annual scientific meeting on infectious diseases.
At 6-week follow-up, two patients (4%) had relapsed, both with Candida parapsilosis, which was more resistant to treatment with anidulafungin (Eraxis) than other Candida species, the researchers reported. Treating the children with 3.0 mg/kg anidulafungin on day 1, followed by 1.5 mg/kg every 24 hours, yielded similar pharmacokinetics as the 200/100 mg regimen used in adults. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%), which also reflected findings in adults, the investigators said. Five patients (10%) developed at least one severe treatment-emergent adverse event, including neutropenia, gastrointestinal hemorrhage, increased hepatic transaminases, hyponatremia, and myalgia. The study (NCT00761267) is ongoing and continues to recruit patients in 11 states in the United States and nine other countries, with final top-line results expected in 2019.
Although rates of invasive candidiasis appear to be decreasing in children overall, the population at risk is expanding, experts have noted. Relevant guidelines from the Infectious Disease Society of America and the European Society of Clinical Microbiology and Infectious Diseases list amphotericin B, echinocandins, and azoles as treatment options, but these recommendations are extrapolated mainly from adult studies, noted Dr. Roilides, who is a pediatric infectious disease specialist at Aristotle University School of Health Sciences and Hippokration General Hospital in Thessaloniki, Greece.
To better characterize the safety and efficacy of anidulafungin in children, the researchers enrolled patients up to 17 years of age who had signs and symptoms of invasive candidiasis and Candida cultured from a normally sterile site. Patients received intravenous anidulafungin (3 mg/kg on day 1, followed by 1.5 mg/kg every 24 hours) for at least 10 days, after which they could switch to oral fluconazole. Treatment continued for at least 14 days after blood cultures were negative and signs and symptoms resolved.
At interim data cutoff in October 2016, patients were exposed to anidulafungin for a median of 11.5 days (range, 1-28 days). Among 47 patients who received at least one dose of anidulafungin, about two-thirds were male, about 70% were white, and the average age was 8 years (standard deviation, 4.7 years). Rates of global success – a combination of clinical and microbiological response – were 82% in patients up to 5 years old and 67% in older children. Children whose baseline neutrophil count was at least 500 per mm3 had a 78% global response rate versus 50% among those with more severe neutropenia. C. parapsilosis had higher minimum inhibitory concentrations than other Candida species, and in vitro susceptibility rates of 85% for C. parapsilosis versus 100% for other species.
All patients experienced at least one treatment-emergent adverse effect. In addition to diarrhea, vomiting, and pyrexia, adverse events affecting more than 10% of patients included epistaxis (17%), headache (15%), and abdominal pain (13%). Half of patients switched to oral fluconazole. Four patients stopped treatment because of vomiting, generalized pruritus, or increased transaminases. A total of 15% of patients died, although no deaths were considered treatment related. The patient who stopped treatment because of pruritus later died of septic shock secondary to invasive candidiasis, despite having started treatment with fluconazole and micafungin, the investigators reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Nearly all patients had bloodstream infections, and catheters also cultured positive in more than two-thirds of cases, the researchers said. Many patients had multiple risk factors for infection such as central venous catheters, broad-spectrum antibiotic therapy, total parenteral nutrition, and chemotherapy. Cultures were most often positive for Candida albicans (38%), followed by C. parapsilosis (26%) and C. tropicalis (13%).
Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
SAN DIEGO – The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in a single-arm, multicenter, open-label trial of 47 children aged 2-17 years.
The overall global response rate of 72% resembled that from the prior adult registry study (76%), Emmanuel Roilides, MD, PhD, and his associates reported in a poster presented at an annual scientific meeting on infectious diseases.
At 6-week follow-up, two patients (4%) had relapsed, both with Candida parapsilosis, which was more resistant to treatment with anidulafungin (Eraxis) than other Candida species, the researchers reported. Treating the children with 3.0 mg/kg anidulafungin on day 1, followed by 1.5 mg/kg every 24 hours, yielded similar pharmacokinetics as the 200/100 mg regimen used in adults. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%), which also reflected findings in adults, the investigators said. Five patients (10%) developed at least one severe treatment-emergent adverse event, including neutropenia, gastrointestinal hemorrhage, increased hepatic transaminases, hyponatremia, and myalgia. The study (NCT00761267) is ongoing and continues to recruit patients in 11 states in the United States and nine other countries, with final top-line results expected in 2019.
Although rates of invasive candidiasis appear to be decreasing in children overall, the population at risk is expanding, experts have noted. Relevant guidelines from the Infectious Disease Society of America and the European Society of Clinical Microbiology and Infectious Diseases list amphotericin B, echinocandins, and azoles as treatment options, but these recommendations are extrapolated mainly from adult studies, noted Dr. Roilides, who is a pediatric infectious disease specialist at Aristotle University School of Health Sciences and Hippokration General Hospital in Thessaloniki, Greece.
To better characterize the safety and efficacy of anidulafungin in children, the researchers enrolled patients up to 17 years of age who had signs and symptoms of invasive candidiasis and Candida cultured from a normally sterile site. Patients received intravenous anidulafungin (3 mg/kg on day 1, followed by 1.5 mg/kg every 24 hours) for at least 10 days, after which they could switch to oral fluconazole. Treatment continued for at least 14 days after blood cultures were negative and signs and symptoms resolved.
At interim data cutoff in October 2016, patients were exposed to anidulafungin for a median of 11.5 days (range, 1-28 days). Among 47 patients who received at least one dose of anidulafungin, about two-thirds were male, about 70% were white, and the average age was 8 years (standard deviation, 4.7 years). Rates of global success – a combination of clinical and microbiological response – were 82% in patients up to 5 years old and 67% in older children. Children whose baseline neutrophil count was at least 500 per mm3 had a 78% global response rate versus 50% among those with more severe neutropenia. C. parapsilosis had higher minimum inhibitory concentrations than other Candida species, and in vitro susceptibility rates of 85% for C. parapsilosis versus 100% for other species.
All patients experienced at least one treatment-emergent adverse effect. In addition to diarrhea, vomiting, and pyrexia, adverse events affecting more than 10% of patients included epistaxis (17%), headache (15%), and abdominal pain (13%). Half of patients switched to oral fluconazole. Four patients stopped treatment because of vomiting, generalized pruritus, or increased transaminases. A total of 15% of patients died, although no deaths were considered treatment related. The patient who stopped treatment because of pruritus later died of septic shock secondary to invasive candidiasis, despite having started treatment with fluconazole and micafungin, the investigators reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Nearly all patients had bloodstream infections, and catheters also cultured positive in more than two-thirds of cases, the researchers said. Many patients had multiple risk factors for infection such as central venous catheters, broad-spectrum antibiotic therapy, total parenteral nutrition, and chemotherapy. Cultures were most often positive for Candida albicans (38%), followed by C. parapsilosis (26%) and C. tropicalis (13%).
Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
SAN DIEGO – The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in a single-arm, multicenter, open-label trial of 47 children aged 2-17 years.
The overall global response rate of 72% resembled that from the prior adult registry study (76%), Emmanuel Roilides, MD, PhD, and his associates reported in a poster presented at an annual scientific meeting on infectious diseases.
At 6-week follow-up, two patients (4%) had relapsed, both with Candida parapsilosis, which was more resistant to treatment with anidulafungin (Eraxis) than other Candida species, the researchers reported. Treating the children with 3.0 mg/kg anidulafungin on day 1, followed by 1.5 mg/kg every 24 hours, yielded similar pharmacokinetics as the 200/100 mg regimen used in adults. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%), which also reflected findings in adults, the investigators said. Five patients (10%) developed at least one severe treatment-emergent adverse event, including neutropenia, gastrointestinal hemorrhage, increased hepatic transaminases, hyponatremia, and myalgia. The study (NCT00761267) is ongoing and continues to recruit patients in 11 states in the United States and nine other countries, with final top-line results expected in 2019.
Although rates of invasive candidiasis appear to be decreasing in children overall, the population at risk is expanding, experts have noted. Relevant guidelines from the Infectious Disease Society of America and the European Society of Clinical Microbiology and Infectious Diseases list amphotericin B, echinocandins, and azoles as treatment options, but these recommendations are extrapolated mainly from adult studies, noted Dr. Roilides, who is a pediatric infectious disease specialist at Aristotle University School of Health Sciences and Hippokration General Hospital in Thessaloniki, Greece.
To better characterize the safety and efficacy of anidulafungin in children, the researchers enrolled patients up to 17 years of age who had signs and symptoms of invasive candidiasis and Candida cultured from a normally sterile site. Patients received intravenous anidulafungin (3 mg/kg on day 1, followed by 1.5 mg/kg every 24 hours) for at least 10 days, after which they could switch to oral fluconazole. Treatment continued for at least 14 days after blood cultures were negative and signs and symptoms resolved.
At interim data cutoff in October 2016, patients were exposed to anidulafungin for a median of 11.5 days (range, 1-28 days). Among 47 patients who received at least one dose of anidulafungin, about two-thirds were male, about 70% were white, and the average age was 8 years (standard deviation, 4.7 years). Rates of global success – a combination of clinical and microbiological response – were 82% in patients up to 5 years old and 67% in older children. Children whose baseline neutrophil count was at least 500 per mm3 had a 78% global response rate versus 50% among those with more severe neutropenia. C. parapsilosis had higher minimum inhibitory concentrations than other Candida species, and in vitro susceptibility rates of 85% for C. parapsilosis versus 100% for other species.
All patients experienced at least one treatment-emergent adverse effect. In addition to diarrhea, vomiting, and pyrexia, adverse events affecting more than 10% of patients included epistaxis (17%), headache (15%), and abdominal pain (13%). Half of patients switched to oral fluconazole. Four patients stopped treatment because of vomiting, generalized pruritus, or increased transaminases. A total of 15% of patients died, although no deaths were considered treatment related. The patient who stopped treatment because of pruritus later died of septic shock secondary to invasive candidiasis, despite having started treatment with fluconazole and micafungin, the investigators reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Nearly all patients had bloodstream infections, and catheters also cultured positive in more than two-thirds of cases, the researchers said. Many patients had multiple risk factors for infection such as central venous catheters, broad-spectrum antibiotic therapy, total parenteral nutrition, and chemotherapy. Cultures were most often positive for Candida albicans (38%), followed by C. parapsilosis (26%) and C. tropicalis (13%).
Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
AT IDWEEK 2017
Key clinical point: The intravenous echinocandin anidulafungin effectively treated invasive candidiasis in children, with a safety profile resembling what has been previously reported for adults.
Major finding: The overall global response rate was 72%. The most common treatment-emergent adverse effects included diarrhea (23%), vomiting (23%), and fever (19%). Five patients (10%) developed at least one severe treatment-emergent adverse event.
Data source: A multicenter, single-arm, open-label study of 47 patients aged 2-17 years.
Disclosures: Pfizer makes anidulafungin and sponsored the study. Dr. Roilides disclosed research grants and advisory relationships with Pfizer, Astellas, Gilead, and Merck.
Tocilizumab looks promising for corticosteroid refractory anti-PD-1-related adverse events
CHICAGO – Tocilizumab may be a therapeutic option for steroid-refractory immune-related adverse events that are secondary to PD-1 blockade, according to findings from a review of patients treated with nivolumab for various malignancies.
Of 87 patients who were treated with the PD-1 inhibitor between April 2015 and October 2016, 34 received tocilizumab for high-grade immune-related adverse events (irAEs) that were refractory to corticosteroids. Of those, 27 experienced clinical improvement, which was defined as documentation of symptom resolution or hospital discharge within 7 days, Aparna Hegde, MD, of East Carolina University, Greenville, N.C., reported at the Chicago Multidisciplinary Symposium in Thoracic Oncology.
The median time to discharge was 4 days, and no adverse effect on median overall survival was seen between those who received tocilizumab and those who did not (6.1 vs, 6.7 months, respectively), Dr. Hegde said.
There was, however, a trend toward inferior overall survival in patients who required more than one dose of tocilizumab, but the difference was not statistically significant (hazard ratio, 1.72), she noted.
“Immune checkpoint inhibitors are associated with an unprecedented clinical benefit in patients with lung cancer. However, they are also associated with a unique spectrum of immune-mediated adverse events. While the standard of care for initial management of these adverse events is corticosteroids, the management of steroid-refractory events is poorly defined,” she said, adding that data from randomized trials on which consensus guidelines could be based are lacking.
At East Carolina University, a significant proportion of patients treated with PD-1 inhibitors were presenting with systemic inflammatory response syndrome (SIRS)-like symptoms and immune-related organ toxicities similar to what has been described in cytokine release syndrome, Dr. Hegde said.
Such symptoms have also been reported with other types of immune therapy, such as CAR T-cell therapy and bispecific T-cell receptor–engaging antibodies in hematologic malignancies, she noted.
“In our experience, when we treated these patients with tocilizumab, which is an [anti-interleukin-6] receptor monoclonal antibody, we saw dramatic and rapid responses, not only in the SIRS symptoms, but also in other immune-related organ toxicities. Therefore, we adopted the use of tocilizumab as our standard treatment for high-grade immune-related adverse events,” she said, explaining that it has been well documented that interleukin (IL)-6 levels increase during cytokine release syndrome and are mediators of inflammation, suggesting that blocking IL-6 may treat irAEs without compromising the efficacy of immune therapy.
The current study was undertaken to look more closely at the responses to tocilizumab and to assess overall survival in those who received tocilizumab.
Study participants were being prospectively followed as part of another ongoing study looking at the relationship between systemic inflammation and cancer-related symptom burden. Most (77) were being treated for lung cancer and 10 had other types of malignancy. They received nivolumab at a dose of 3 mg/kg (or a flat dose of 240 mg after September 2016) every 2 weeks, and received tocilizumab at a dose of 4 mg/kg given over 1 hour. Those with grade 3 or 4 irAEs also received supportive care and corticosteroids. Median follow-up was 10.6 months.
C-reactive protein (CRP), a reliable surrogate marker of IL-6, was drawn at the first nivolumab infusion and before each subsequent infusion as part of the study in which the patients were enrolled, and for the current analysis was measured in relation to irAEs.
Significant reductions were seen in CRP levels after tocilizumab treatment; similar responses have been described in cytokine release syndrome, Dr. Hegde noted.
“Tocilizumab is a therapeutic option for management of immune-related adverse events in patients who are already on corticosteroids. CRP may be of clinical utility in detecting immune-related adverse events as well as monitoring the response to tocilizumab,” she said, adding that the current analysis is limited by the small patient number, single-center setting, use of tocilizumab outside of a clinical trial setting, and short follow-up.
Therefore, the findings require confirmation in multicenter randomized trials to determine “the definitive utility of tocilizumab, as well as CRP as an accompanying biomarker in the management of high-grade steroid refractory immune-related adverse events.”
Heather Wakelee, MD, an invited discussant at the symposium, commended Dr. Hegde and her colleagues for “coming up with a novel idea about how to treat [irAEs],” but also stressed the need for further study.
“This is a novel agent that has the potential ability to manage toxicity, and that’s important, because when you get beyond the steroids that we use as a first-line approach ... there’s not a whole lot else. We definitely have a clear unmet need,” said Dr. Wakelee of Stanford (Calif.) University.
However, she stressed that the approach must be evaluated in multicenter randomized trials “before we can be widely discussing this as a good thing to be doing.”
Dr. Hegde reported having no disclosures. Dr. Wakelee has been the institutional principal investigator for studies of nivolumab, tocilizumab, and other agents. She has consulted for Peregrine, ACEA, Pfizer, Helsinn, Genentech/Roche, Clovis, and Lilly, and received research/grant support from Clovis, Exelixis, AstraZeneca/Medimmune, Genentech/Roche, BMS, Gilead, Novartis, Xcovery, Pfizer, Celgene, Gilead, Pharmacyclics, and Lilly.
CHICAGO – Tocilizumab may be a therapeutic option for steroid-refractory immune-related adverse events that are secondary to PD-1 blockade, according to findings from a review of patients treated with nivolumab for various malignancies.
Of 87 patients who were treated with the PD-1 inhibitor between April 2015 and October 2016, 34 received tocilizumab for high-grade immune-related adverse events (irAEs) that were refractory to corticosteroids. Of those, 27 experienced clinical improvement, which was defined as documentation of symptom resolution or hospital discharge within 7 days, Aparna Hegde, MD, of East Carolina University, Greenville, N.C., reported at the Chicago Multidisciplinary Symposium in Thoracic Oncology.
The median time to discharge was 4 days, and no adverse effect on median overall survival was seen between those who received tocilizumab and those who did not (6.1 vs, 6.7 months, respectively), Dr. Hegde said.
There was, however, a trend toward inferior overall survival in patients who required more than one dose of tocilizumab, but the difference was not statistically significant (hazard ratio, 1.72), she noted.
“Immune checkpoint inhibitors are associated with an unprecedented clinical benefit in patients with lung cancer. However, they are also associated with a unique spectrum of immune-mediated adverse events. While the standard of care for initial management of these adverse events is corticosteroids, the management of steroid-refractory events is poorly defined,” she said, adding that data from randomized trials on which consensus guidelines could be based are lacking.
At East Carolina University, a significant proportion of patients treated with PD-1 inhibitors were presenting with systemic inflammatory response syndrome (SIRS)-like symptoms and immune-related organ toxicities similar to what has been described in cytokine release syndrome, Dr. Hegde said.
Such symptoms have also been reported with other types of immune therapy, such as CAR T-cell therapy and bispecific T-cell receptor–engaging antibodies in hematologic malignancies, she noted.
“In our experience, when we treated these patients with tocilizumab, which is an [anti-interleukin-6] receptor monoclonal antibody, we saw dramatic and rapid responses, not only in the SIRS symptoms, but also in other immune-related organ toxicities. Therefore, we adopted the use of tocilizumab as our standard treatment for high-grade immune-related adverse events,” she said, explaining that it has been well documented that interleukin (IL)-6 levels increase during cytokine release syndrome and are mediators of inflammation, suggesting that blocking IL-6 may treat irAEs without compromising the efficacy of immune therapy.
The current study was undertaken to look more closely at the responses to tocilizumab and to assess overall survival in those who received tocilizumab.
Study participants were being prospectively followed as part of another ongoing study looking at the relationship between systemic inflammation and cancer-related symptom burden. Most (77) were being treated for lung cancer and 10 had other types of malignancy. They received nivolumab at a dose of 3 mg/kg (or a flat dose of 240 mg after September 2016) every 2 weeks, and received tocilizumab at a dose of 4 mg/kg given over 1 hour. Those with grade 3 or 4 irAEs also received supportive care and corticosteroids. Median follow-up was 10.6 months.
C-reactive protein (CRP), a reliable surrogate marker of IL-6, was drawn at the first nivolumab infusion and before each subsequent infusion as part of the study in which the patients were enrolled, and for the current analysis was measured in relation to irAEs.
Significant reductions were seen in CRP levels after tocilizumab treatment; similar responses have been described in cytokine release syndrome, Dr. Hegde noted.
“Tocilizumab is a therapeutic option for management of immune-related adverse events in patients who are already on corticosteroids. CRP may be of clinical utility in detecting immune-related adverse events as well as monitoring the response to tocilizumab,” she said, adding that the current analysis is limited by the small patient number, single-center setting, use of tocilizumab outside of a clinical trial setting, and short follow-up.
Therefore, the findings require confirmation in multicenter randomized trials to determine “the definitive utility of tocilizumab, as well as CRP as an accompanying biomarker in the management of high-grade steroid refractory immune-related adverse events.”
Heather Wakelee, MD, an invited discussant at the symposium, commended Dr. Hegde and her colleagues for “coming up with a novel idea about how to treat [irAEs],” but also stressed the need for further study.
“This is a novel agent that has the potential ability to manage toxicity, and that’s important, because when you get beyond the steroids that we use as a first-line approach ... there’s not a whole lot else. We definitely have a clear unmet need,” said Dr. Wakelee of Stanford (Calif.) University.
However, she stressed that the approach must be evaluated in multicenter randomized trials “before we can be widely discussing this as a good thing to be doing.”
Dr. Hegde reported having no disclosures. Dr. Wakelee has been the institutional principal investigator for studies of nivolumab, tocilizumab, and other agents. She has consulted for Peregrine, ACEA, Pfizer, Helsinn, Genentech/Roche, Clovis, and Lilly, and received research/grant support from Clovis, Exelixis, AstraZeneca/Medimmune, Genentech/Roche, BMS, Gilead, Novartis, Xcovery, Pfizer, Celgene, Gilead, Pharmacyclics, and Lilly.
CHICAGO – Tocilizumab may be a therapeutic option for steroid-refractory immune-related adverse events that are secondary to PD-1 blockade, according to findings from a review of patients treated with nivolumab for various malignancies.
Of 87 patients who were treated with the PD-1 inhibitor between April 2015 and October 2016, 34 received tocilizumab for high-grade immune-related adverse events (irAEs) that were refractory to corticosteroids. Of those, 27 experienced clinical improvement, which was defined as documentation of symptom resolution or hospital discharge within 7 days, Aparna Hegde, MD, of East Carolina University, Greenville, N.C., reported at the Chicago Multidisciplinary Symposium in Thoracic Oncology.
The median time to discharge was 4 days, and no adverse effect on median overall survival was seen between those who received tocilizumab and those who did not (6.1 vs, 6.7 months, respectively), Dr. Hegde said.
There was, however, a trend toward inferior overall survival in patients who required more than one dose of tocilizumab, but the difference was not statistically significant (hazard ratio, 1.72), she noted.
“Immune checkpoint inhibitors are associated with an unprecedented clinical benefit in patients with lung cancer. However, they are also associated with a unique spectrum of immune-mediated adverse events. While the standard of care for initial management of these adverse events is corticosteroids, the management of steroid-refractory events is poorly defined,” she said, adding that data from randomized trials on which consensus guidelines could be based are lacking.
At East Carolina University, a significant proportion of patients treated with PD-1 inhibitors were presenting with systemic inflammatory response syndrome (SIRS)-like symptoms and immune-related organ toxicities similar to what has been described in cytokine release syndrome, Dr. Hegde said.
Such symptoms have also been reported with other types of immune therapy, such as CAR T-cell therapy and bispecific T-cell receptor–engaging antibodies in hematologic malignancies, she noted.
“In our experience, when we treated these patients with tocilizumab, which is an [anti-interleukin-6] receptor monoclonal antibody, we saw dramatic and rapid responses, not only in the SIRS symptoms, but also in other immune-related organ toxicities. Therefore, we adopted the use of tocilizumab as our standard treatment for high-grade immune-related adverse events,” she said, explaining that it has been well documented that interleukin (IL)-6 levels increase during cytokine release syndrome and are mediators of inflammation, suggesting that blocking IL-6 may treat irAEs without compromising the efficacy of immune therapy.
The current study was undertaken to look more closely at the responses to tocilizumab and to assess overall survival in those who received tocilizumab.
Study participants were being prospectively followed as part of another ongoing study looking at the relationship between systemic inflammation and cancer-related symptom burden. Most (77) were being treated for lung cancer and 10 had other types of malignancy. They received nivolumab at a dose of 3 mg/kg (or a flat dose of 240 mg after September 2016) every 2 weeks, and received tocilizumab at a dose of 4 mg/kg given over 1 hour. Those with grade 3 or 4 irAEs also received supportive care and corticosteroids. Median follow-up was 10.6 months.
C-reactive protein (CRP), a reliable surrogate marker of IL-6, was drawn at the first nivolumab infusion and before each subsequent infusion as part of the study in which the patients were enrolled, and for the current analysis was measured in relation to irAEs.
Significant reductions were seen in CRP levels after tocilizumab treatment; similar responses have been described in cytokine release syndrome, Dr. Hegde noted.
“Tocilizumab is a therapeutic option for management of immune-related adverse events in patients who are already on corticosteroids. CRP may be of clinical utility in detecting immune-related adverse events as well as monitoring the response to tocilizumab,” she said, adding that the current analysis is limited by the small patient number, single-center setting, use of tocilizumab outside of a clinical trial setting, and short follow-up.
Therefore, the findings require confirmation in multicenter randomized trials to determine “the definitive utility of tocilizumab, as well as CRP as an accompanying biomarker in the management of high-grade steroid refractory immune-related adverse events.”
Heather Wakelee, MD, an invited discussant at the symposium, commended Dr. Hegde and her colleagues for “coming up with a novel idea about how to treat [irAEs],” but also stressed the need for further study.
“This is a novel agent that has the potential ability to manage toxicity, and that’s important, because when you get beyond the steroids that we use as a first-line approach ... there’s not a whole lot else. We definitely have a clear unmet need,” said Dr. Wakelee of Stanford (Calif.) University.
However, she stressed that the approach must be evaluated in multicenter randomized trials “before we can be widely discussing this as a good thing to be doing.”
Dr. Hegde reported having no disclosures. Dr. Wakelee has been the institutional principal investigator for studies of nivolumab, tocilizumab, and other agents. She has consulted for Peregrine, ACEA, Pfizer, Helsinn, Genentech/Roche, Clovis, and Lilly, and received research/grant support from Clovis, Exelixis, AstraZeneca/Medimmune, Genentech/Roche, BMS, Gilead, Novartis, Xcovery, Pfizer, Celgene, Gilead, Pharmacyclics, and Lilly.
AT A SYMPOSIUM IN THORACIC ONCOLOGY
Key clinical point:
Major finding: Twenty-seven of 34 patients treated with tocilizumab experienced clinical improvement.
Data source: A review of 87 patients.
Disclosures: Dr. Hegde reported having no disclosures. Dr. Wakelee has been the institutional principal investigator for studies of nivolumab, tocilizumab, and other agents. She has consulted for Peregrine, ACEA, Pfizer, Helsinn, Genentech/Roche, Clovis, and Lilly, and received research/grant support from Clovis, Exelixis, AstraZeneca/Medimmune, Genentech/Roche, BMS, Gilead, Novartis, Xcovery, Pfizer, Celgene, Gilead, Pharmacyclics, and Lilly.
Off-the-shelf T cells used to treat viral infections after HSCT
One-size-fits-all T cells designed to recognize and mount an immune response against five common viral pathogens may help to reduce the incidence of severe viral infections and treatment-related deaths in patients who have undergone hematopoietic stem cell transplants (HSCT), investigators reported.
Among 37 evaluable patients who had undergone an allogeneic HSCT, a single infusion of banked virus-specific T cells (VSTs) directed against adenovirus, BK virus, cytomegalovirus (CMV), Epstein-Barr virus (EBV), and human herpesvirus 6 (HHV-6) was associated with a 92% cumulative complete or partial response rate, reported Ifigeneia Tzannou, MD, and her colleagues from Baylor College of Medicine in Houston.
“Although a randomized trial will be required to definitively assess the value of banked VSTs, this study strongly suggests that off-the-shelf, multiple-virus–directed VSTs are a safe and effective broad-spectrum approach to treat severe viral infections after HSCT. These VSTs can be rapidly and cost effectively produced in scalable quantities with excellent long-term stability, which facilitates the broad implementation of this therapy,” they wrote in the Journal of Clinical Oncology (2017 Aug 7. doi: 10.1200/JCO.2017.73.0655).
Although adoptive transfer of VSTs derived from donor stem cells has been shown to protect patients against viral pathogens, the technique is hampered by costs, complexity, the time-consuming manufacturing process, and the need for seropositive donors, Dr. Tzannou and her colleagues pointed out.
“One way to overcome these limitations and to supply antiviral protection to recipients of allogeneic HSCT would be to prepare and cryopreserve banks of VST lines from healthy seropositive donors, which would be available for immediate use as an off-the-shelf product,” they wrote.
They tested this concept in a phase 2 clinical trial in 38 patients with a total of 45 infections.
A single infusion was associated with cumulative complete and partial responses rates of 71% in 7 patients with adenoviral infections, 100% in 16 patients with BK virus infections, 94% in 17 patients with CMV infections, 100% for 2 patients with EBV infections, and 67% for 3 patients with HHV-6 infections.
Seven of the 38 patients received VSTs for two viral infections, and all patients had viral control after a single infusion. All cases of CMV, adenovirus, and EBV infections were cleared from serum. One patient with HHV-6 encephalitis had complete resolution of encephalitis after one infusion and resolution of hemorrhagic cystitis after a second infusion; 14 patients with BK virus–associated hemorrhagic cystitis had clinical improvement or resolution of disease.
The infusions were delivered safely. After infusion, one patient developed recurrent grade 3 gastrointestinal graft versus host disease (GVHD) after a rapid corticosteroid taper, three patients had recurrent grade 1 or 2 skin GVHD, and two patients had de novo skin GVHD. Of the five cases of skin GVHD, four resolved with the administration of topical treatments and one with the reinstitution of corticosteroids after a taper.
“More widespread and earlier use of this modality could minimize both drug-related and virus-associated complications and thereby decrease treatment-related mortality in recipients of allogeneic HSCT,” the investigators wrote.
The study was supported by the National Heart, Lung, and Blood Institute; Conquer Cancer Foundation; and Dan L. Duncan Comprehensive Cancer Center. Dr. Tzannou disclosed having a consulting or advisory role with ViraCyte, and several coauthors reported financial ties with various companies.
One-size-fits-all T cells designed to recognize and mount an immune response against five common viral pathogens may help to reduce the incidence of severe viral infections and treatment-related deaths in patients who have undergone hematopoietic stem cell transplants (HSCT), investigators reported.
Among 37 evaluable patients who had undergone an allogeneic HSCT, a single infusion of banked virus-specific T cells (VSTs) directed against adenovirus, BK virus, cytomegalovirus (CMV), Epstein-Barr virus (EBV), and human herpesvirus 6 (HHV-6) was associated with a 92% cumulative complete or partial response rate, reported Ifigeneia Tzannou, MD, and her colleagues from Baylor College of Medicine in Houston.
“Although a randomized trial will be required to definitively assess the value of banked VSTs, this study strongly suggests that off-the-shelf, multiple-virus–directed VSTs are a safe and effective broad-spectrum approach to treat severe viral infections after HSCT. These VSTs can be rapidly and cost effectively produced in scalable quantities with excellent long-term stability, which facilitates the broad implementation of this therapy,” they wrote in the Journal of Clinical Oncology (2017 Aug 7. doi: 10.1200/JCO.2017.73.0655).
Although adoptive transfer of VSTs derived from donor stem cells has been shown to protect patients against viral pathogens, the technique is hampered by costs, complexity, the time-consuming manufacturing process, and the need for seropositive donors, Dr. Tzannou and her colleagues pointed out.
“One way to overcome these limitations and to supply antiviral protection to recipients of allogeneic HSCT would be to prepare and cryopreserve banks of VST lines from healthy seropositive donors, which would be available for immediate use as an off-the-shelf product,” they wrote.
They tested this concept in a phase 2 clinical trial in 38 patients with a total of 45 infections.
A single infusion was associated with cumulative complete and partial responses rates of 71% in 7 patients with adenoviral infections, 100% in 16 patients with BK virus infections, 94% in 17 patients with CMV infections, 100% for 2 patients with EBV infections, and 67% for 3 patients with HHV-6 infections.
Seven of the 38 patients received VSTs for two viral infections, and all patients had viral control after a single infusion. All cases of CMV, adenovirus, and EBV infections were cleared from serum. One patient with HHV-6 encephalitis had complete resolution of encephalitis after one infusion and resolution of hemorrhagic cystitis after a second infusion; 14 patients with BK virus–associated hemorrhagic cystitis had clinical improvement or resolution of disease.
The infusions were delivered safely. After infusion, one patient developed recurrent grade 3 gastrointestinal graft versus host disease (GVHD) after a rapid corticosteroid taper, three patients had recurrent grade 1 or 2 skin GVHD, and two patients had de novo skin GVHD. Of the five cases of skin GVHD, four resolved with the administration of topical treatments and one with the reinstitution of corticosteroids after a taper.
“More widespread and earlier use of this modality could minimize both drug-related and virus-associated complications and thereby decrease treatment-related mortality in recipients of allogeneic HSCT,” the investigators wrote.
The study was supported by the National Heart, Lung, and Blood Institute; Conquer Cancer Foundation; and Dan L. Duncan Comprehensive Cancer Center. Dr. Tzannou disclosed having a consulting or advisory role with ViraCyte, and several coauthors reported financial ties with various companies.
One-size-fits-all T cells designed to recognize and mount an immune response against five common viral pathogens may help to reduce the incidence of severe viral infections and treatment-related deaths in patients who have undergone hematopoietic stem cell transplants (HSCT), investigators reported.
Among 37 evaluable patients who had undergone an allogeneic HSCT, a single infusion of banked virus-specific T cells (VSTs) directed against adenovirus, BK virus, cytomegalovirus (CMV), Epstein-Barr virus (EBV), and human herpesvirus 6 (HHV-6) was associated with a 92% cumulative complete or partial response rate, reported Ifigeneia Tzannou, MD, and her colleagues from Baylor College of Medicine in Houston.
“Although a randomized trial will be required to definitively assess the value of banked VSTs, this study strongly suggests that off-the-shelf, multiple-virus–directed VSTs are a safe and effective broad-spectrum approach to treat severe viral infections after HSCT. These VSTs can be rapidly and cost effectively produced in scalable quantities with excellent long-term stability, which facilitates the broad implementation of this therapy,” they wrote in the Journal of Clinical Oncology (2017 Aug 7. doi: 10.1200/JCO.2017.73.0655).
Although adoptive transfer of VSTs derived from donor stem cells has been shown to protect patients against viral pathogens, the technique is hampered by costs, complexity, the time-consuming manufacturing process, and the need for seropositive donors, Dr. Tzannou and her colleagues pointed out.
“One way to overcome these limitations and to supply antiviral protection to recipients of allogeneic HSCT would be to prepare and cryopreserve banks of VST lines from healthy seropositive donors, which would be available for immediate use as an off-the-shelf product,” they wrote.
They tested this concept in a phase 2 clinical trial in 38 patients with a total of 45 infections.
A single infusion was associated with cumulative complete and partial responses rates of 71% in 7 patients with adenoviral infections, 100% in 16 patients with BK virus infections, 94% in 17 patients with CMV infections, 100% for 2 patients with EBV infections, and 67% for 3 patients with HHV-6 infections.
Seven of the 38 patients received VSTs for two viral infections, and all patients had viral control after a single infusion. All cases of CMV, adenovirus, and EBV infections were cleared from serum. One patient with HHV-6 encephalitis had complete resolution of encephalitis after one infusion and resolution of hemorrhagic cystitis after a second infusion; 14 patients with BK virus–associated hemorrhagic cystitis had clinical improvement or resolution of disease.
The infusions were delivered safely. After infusion, one patient developed recurrent grade 3 gastrointestinal graft versus host disease (GVHD) after a rapid corticosteroid taper, three patients had recurrent grade 1 or 2 skin GVHD, and two patients had de novo skin GVHD. Of the five cases of skin GVHD, four resolved with the administration of topical treatments and one with the reinstitution of corticosteroids after a taper.
“More widespread and earlier use of this modality could minimize both drug-related and virus-associated complications and thereby decrease treatment-related mortality in recipients of allogeneic HSCT,” the investigators wrote.
The study was supported by the National Heart, Lung, and Blood Institute; Conquer Cancer Foundation; and Dan L. Duncan Comprehensive Cancer Center. Dr. Tzannou disclosed having a consulting or advisory role with ViraCyte, and several coauthors reported financial ties with various companies.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Off-the-shelf virus-specific T-cell preparations can effectively treat infections following HSCT.
Major finding: Banked T cells directed against five common viruses were associated with a 92% cumulative partial or complete response rate.
Data source: Phase 2 clinical trial in 38 patients with viral infections following HSCT.
Disclosures: The study was supported by the National Heart, Lung, and Blood Institute; Conquer Cancer Foundation; and Dan L. Duncan Comprehensive Cancer Center. Dr. Tzannou disclosed having a consulting or advisory role with ViraCyte, and several coauthors reported financial ties with various companies.
ALLOZITHRO trial: HSCT patients fared worse with azithromycin
Administration of azithromycin beginning at the time of conditioning in patients undergoing allogeneic hematopoietic stem cell transplant resulted in worse airflow decline–free survival than did placebo, according to findings from the randomized ALLOZITHRO trial.
The 2-year airflow decline–free survival rate was 32.8% in 243 patients who received 250 mg of azithromycin for 2 years, compared with 41.3% in 237 who received placebo (hazard ratio, 1.3), Anne Bergeron, MD, of Hopital Saint-Louis, Paris, and her colleagues reported in the Aug. 8 issue of JAMA.
Further, of 22 patients who experienced bronchiolitis obliterans syndrome, 15 were in the azithromycin group, compared with 7 in the placebo group, and 2-year mortality was increased in the azithromycin group (56.6% vs. 70.1%; hazard ratio, 1.5) the investigators noted (JAMA. 2017 Aug 8;318[6]:557-66. doi: 10.1001/jama.2017.9938).
A post hoc analysis showed that the 2-year cumulative incidence of hematological relapse was 33.5% with azithromycin vs. 22.3% with placebo; the trial was terminated early because of this unexpected finding.
Although prior studies have suggested that azithromycin may reduce the incidence of post–lung transplant bronchiolitis obliterans syndrome, which has been shown to increase morbidity and mortality after allogeneic HSCT, the findings of this parallel-group trial conducted in 19 French transplant centers between February 2014 and August 2015 showed a decrease in survival and an increase in hematological relapse at 2 years with azithromycin vs. placebo. The findings, however, are limited by several factors – including the trial’s early termination – and require further study, particularly of the potential for harm related to relapse, the investigators concluded.
The ALLOZITHRO trial (NCT01959100) was funded by the French Cancer Institute, Oxygene, and SFGM-TC Capucine. Dr. Bergeron reported receiving unrestricted research grant funding for the trial from the French Ministry of Health, SFGM-TC Capucine association, and SOS Oxygene; receiving speaker fees from Merck, Gilead, and Pfizer; and serving on the advisory board of Merck.
Administration of azithromycin beginning at the time of conditioning in patients undergoing allogeneic hematopoietic stem cell transplant resulted in worse airflow decline–free survival than did placebo, according to findings from the randomized ALLOZITHRO trial.
The 2-year airflow decline–free survival rate was 32.8% in 243 patients who received 250 mg of azithromycin for 2 years, compared with 41.3% in 237 who received placebo (hazard ratio, 1.3), Anne Bergeron, MD, of Hopital Saint-Louis, Paris, and her colleagues reported in the Aug. 8 issue of JAMA.
Further, of 22 patients who experienced bronchiolitis obliterans syndrome, 15 were in the azithromycin group, compared with 7 in the placebo group, and 2-year mortality was increased in the azithromycin group (56.6% vs. 70.1%; hazard ratio, 1.5) the investigators noted (JAMA. 2017 Aug 8;318[6]:557-66. doi: 10.1001/jama.2017.9938).
A post hoc analysis showed that the 2-year cumulative incidence of hematological relapse was 33.5% with azithromycin vs. 22.3% with placebo; the trial was terminated early because of this unexpected finding.
Although prior studies have suggested that azithromycin may reduce the incidence of post–lung transplant bronchiolitis obliterans syndrome, which has been shown to increase morbidity and mortality after allogeneic HSCT, the findings of this parallel-group trial conducted in 19 French transplant centers between February 2014 and August 2015 showed a decrease in survival and an increase in hematological relapse at 2 years with azithromycin vs. placebo. The findings, however, are limited by several factors – including the trial’s early termination – and require further study, particularly of the potential for harm related to relapse, the investigators concluded.
The ALLOZITHRO trial (NCT01959100) was funded by the French Cancer Institute, Oxygene, and SFGM-TC Capucine. Dr. Bergeron reported receiving unrestricted research grant funding for the trial from the French Ministry of Health, SFGM-TC Capucine association, and SOS Oxygene; receiving speaker fees from Merck, Gilead, and Pfizer; and serving on the advisory board of Merck.
Administration of azithromycin beginning at the time of conditioning in patients undergoing allogeneic hematopoietic stem cell transplant resulted in worse airflow decline–free survival than did placebo, according to findings from the randomized ALLOZITHRO trial.
The 2-year airflow decline–free survival rate was 32.8% in 243 patients who received 250 mg of azithromycin for 2 years, compared with 41.3% in 237 who received placebo (hazard ratio, 1.3), Anne Bergeron, MD, of Hopital Saint-Louis, Paris, and her colleagues reported in the Aug. 8 issue of JAMA.
Further, of 22 patients who experienced bronchiolitis obliterans syndrome, 15 were in the azithromycin group, compared with 7 in the placebo group, and 2-year mortality was increased in the azithromycin group (56.6% vs. 70.1%; hazard ratio, 1.5) the investigators noted (JAMA. 2017 Aug 8;318[6]:557-66. doi: 10.1001/jama.2017.9938).
A post hoc analysis showed that the 2-year cumulative incidence of hematological relapse was 33.5% with azithromycin vs. 22.3% with placebo; the trial was terminated early because of this unexpected finding.
Although prior studies have suggested that azithromycin may reduce the incidence of post–lung transplant bronchiolitis obliterans syndrome, which has been shown to increase morbidity and mortality after allogeneic HSCT, the findings of this parallel-group trial conducted in 19 French transplant centers between February 2014 and August 2015 showed a decrease in survival and an increase in hematological relapse at 2 years with azithromycin vs. placebo. The findings, however, are limited by several factors – including the trial’s early termination – and require further study, particularly of the potential for harm related to relapse, the investigators concluded.
The ALLOZITHRO trial (NCT01959100) was funded by the French Cancer Institute, Oxygene, and SFGM-TC Capucine. Dr. Bergeron reported receiving unrestricted research grant funding for the trial from the French Ministry of Health, SFGM-TC Capucine association, and SOS Oxygene; receiving speaker fees from Merck, Gilead, and Pfizer; and serving on the advisory board of Merck.
FROM JAMA
Key clinical point:
Major finding: The 2-year airflow decline–free survival rates were 32.8% and 41.3% in the azithromycin and placebo groups, respectively (hazard ratio, 1.3).
Data source: The randomized, placebo-controlled ALLOZITHRO trial of 480 patients.
Disclosures: The ALLOZITHRO trial was funded by the French Cancer Institute, Oxygene, and SFGM-TC Capucine. Dr. Bergeron reported receiving unrestricted research grant funding for the trial from the French Ministry of Health, SFGM-TC Capucine association, and SOS Oxygene; receiving speaker fees from Merck, Gilead, and Pfizer; and serving on the advisory board of Merck.
Alopecia may be permanent in one in four pediatric HSCT patients
CHICAGO – Late dermatologic manifestations in children who have received hematopoietic stem cell transplants may be more common than previously thought, according to results of a new study.
Johanna Song, MD, and her collaborators reported that, in their prospective pediatric study, 25% of patients had permanent alopecia and 16% had psoriasis, noting that late nonmalignant skin effects of hematopoietic stem cell transplantation (HSCT) have been studied primarily retrospectively, and in adults. Vitiligo and nail changes were also seen.
In a poster presentation at the World Congress of Dermatology, Dr. Song and her colleagues noted that these figures are higher than the previously reported pediatric rates of 1.7% for vitiligo and 15.6% for permanent alopecia. “Early recognition of these late effects can facilitate prompt and appropriate treatment, if desired,” they said.
The single-center, cross-sectional cohort study tracked pediatric patients over an 18-month period and included patients who were at least 1 year post allogeneic HSCT and had not relapsed. Patients who were not English speaking were excluded.
The median age of the 85 patients enrolled in the study was 13.8 years, and participants were a median of 3.6 years post transplant at the time of enrollment. The study’s analysis attempted to determine which patient, transplant, and disease factors might be associated with the late nonmalignant skin changes, according to Dr. Song, a resident dermatologist at Harvard University, Boston, and her colleagues.
Most – 52– of the patients (61.2%) had hematologic malignancies; 12 patients (14.1%) received their transplant for bone marrow failure, and 11 patients (12.5%) had immunodeficiency. Three patients (3.5%) received HSCT for other malignancies, and seven (8.2%) for nonmalignant diseases.
Diffuse hair thinning was seen in 13 (62%) of the 21 patients who had alopecia, while 11 (52%) of the patients with alopecia had an androgenetic hair loss pattern. Chronic graft versus host disease (GVHD), skin chronic GVHD, a HSCT regimen that included busulfan conditioning, and a family history of early male-pattern alopecia were all significantly associated with post-HSCT permanent alopecia (P less than .05 for all).
The patients with androgenetic alopecia may be experiencing an accelerated time course of a condition to which they are already genetically disposed, noted Dr. Song and her colleagues.
Psoriasis was commonly seen on the scalp, affecting 11 of the 14 patients with psoriasis (79%), and involved the face in five of the patients (36%). Just one patient had psoriasis elsewhere on the body. There was a nonsignificant trend towards human leukocyte antigen mismatch among patients who had psoriasis. Although “psoriasis may be a marker of persistent immune dysregulation,” the investigators said, they did not identify any associated risk factors that would point toward this mechanism in their analysis.
Twelve patients (14%) had vitiligo, with halo nevi seen in four of these patients. Children who were younger than age 10 years and those who received their transplant for primary immunodeficiency were significantly more likely to have vitiligo (P less than .05 for both). Specific possible mechanisms triggering vitiligo could include thymic dysfunction resulting in loss of self-tolerance, and donor alloreactivity against the patient’s host antigens, according to the authors.
Nail changes such as pterygium and nail pitting, ridging, or thickening were seen in just five patients, all of whom had chronic GVHD of the skin. “Nail changes are likely a result of persistent inflammation and immune dysregulation from chronic GVHD,” said Dr. Song.
These late effects “can significantly impact patients’ quality of life,” according to the authors, who called for larger studies that follow pediatric HSCT patients longitudinally, beginning before the transplant – and for more investigation into the pathogenesis of specific late effects.
Dr. Song reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Late dermatologic manifestations in children who have received hematopoietic stem cell transplants may be more common than previously thought, according to results of a new study.
Johanna Song, MD, and her collaborators reported that, in their prospective pediatric study, 25% of patients had permanent alopecia and 16% had psoriasis, noting that late nonmalignant skin effects of hematopoietic stem cell transplantation (HSCT) have been studied primarily retrospectively, and in adults. Vitiligo and nail changes were also seen.
In a poster presentation at the World Congress of Dermatology, Dr. Song and her colleagues noted that these figures are higher than the previously reported pediatric rates of 1.7% for vitiligo and 15.6% for permanent alopecia. “Early recognition of these late effects can facilitate prompt and appropriate treatment, if desired,” they said.
The single-center, cross-sectional cohort study tracked pediatric patients over an 18-month period and included patients who were at least 1 year post allogeneic HSCT and had not relapsed. Patients who were not English speaking were excluded.
The median age of the 85 patients enrolled in the study was 13.8 years, and participants were a median of 3.6 years post transplant at the time of enrollment. The study’s analysis attempted to determine which patient, transplant, and disease factors might be associated with the late nonmalignant skin changes, according to Dr. Song, a resident dermatologist at Harvard University, Boston, and her colleagues.
Most – 52– of the patients (61.2%) had hematologic malignancies; 12 patients (14.1%) received their transplant for bone marrow failure, and 11 patients (12.5%) had immunodeficiency. Three patients (3.5%) received HSCT for other malignancies, and seven (8.2%) for nonmalignant diseases.
Diffuse hair thinning was seen in 13 (62%) of the 21 patients who had alopecia, while 11 (52%) of the patients with alopecia had an androgenetic hair loss pattern. Chronic graft versus host disease (GVHD), skin chronic GVHD, a HSCT regimen that included busulfan conditioning, and a family history of early male-pattern alopecia were all significantly associated with post-HSCT permanent alopecia (P less than .05 for all).
The patients with androgenetic alopecia may be experiencing an accelerated time course of a condition to which they are already genetically disposed, noted Dr. Song and her colleagues.
Psoriasis was commonly seen on the scalp, affecting 11 of the 14 patients with psoriasis (79%), and involved the face in five of the patients (36%). Just one patient had psoriasis elsewhere on the body. There was a nonsignificant trend towards human leukocyte antigen mismatch among patients who had psoriasis. Although “psoriasis may be a marker of persistent immune dysregulation,” the investigators said, they did not identify any associated risk factors that would point toward this mechanism in their analysis.
Twelve patients (14%) had vitiligo, with halo nevi seen in four of these patients. Children who were younger than age 10 years and those who received their transplant for primary immunodeficiency were significantly more likely to have vitiligo (P less than .05 for both). Specific possible mechanisms triggering vitiligo could include thymic dysfunction resulting in loss of self-tolerance, and donor alloreactivity against the patient’s host antigens, according to the authors.
Nail changes such as pterygium and nail pitting, ridging, or thickening were seen in just five patients, all of whom had chronic GVHD of the skin. “Nail changes are likely a result of persistent inflammation and immune dysregulation from chronic GVHD,” said Dr. Song.
These late effects “can significantly impact patients’ quality of life,” according to the authors, who called for larger studies that follow pediatric HSCT patients longitudinally, beginning before the transplant – and for more investigation into the pathogenesis of specific late effects.
Dr. Song reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Late dermatologic manifestations in children who have received hematopoietic stem cell transplants may be more common than previously thought, according to results of a new study.
Johanna Song, MD, and her collaborators reported that, in their prospective pediatric study, 25% of patients had permanent alopecia and 16% had psoriasis, noting that late nonmalignant skin effects of hematopoietic stem cell transplantation (HSCT) have been studied primarily retrospectively, and in adults. Vitiligo and nail changes were also seen.
In a poster presentation at the World Congress of Dermatology, Dr. Song and her colleagues noted that these figures are higher than the previously reported pediatric rates of 1.7% for vitiligo and 15.6% for permanent alopecia. “Early recognition of these late effects can facilitate prompt and appropriate treatment, if desired,” they said.
The single-center, cross-sectional cohort study tracked pediatric patients over an 18-month period and included patients who were at least 1 year post allogeneic HSCT and had not relapsed. Patients who were not English speaking were excluded.
The median age of the 85 patients enrolled in the study was 13.8 years, and participants were a median of 3.6 years post transplant at the time of enrollment. The study’s analysis attempted to determine which patient, transplant, and disease factors might be associated with the late nonmalignant skin changes, according to Dr. Song, a resident dermatologist at Harvard University, Boston, and her colleagues.
Most – 52– of the patients (61.2%) had hematologic malignancies; 12 patients (14.1%) received their transplant for bone marrow failure, and 11 patients (12.5%) had immunodeficiency. Three patients (3.5%) received HSCT for other malignancies, and seven (8.2%) for nonmalignant diseases.
Diffuse hair thinning was seen in 13 (62%) of the 21 patients who had alopecia, while 11 (52%) of the patients with alopecia had an androgenetic hair loss pattern. Chronic graft versus host disease (GVHD), skin chronic GVHD, a HSCT regimen that included busulfan conditioning, and a family history of early male-pattern alopecia were all significantly associated with post-HSCT permanent alopecia (P less than .05 for all).
The patients with androgenetic alopecia may be experiencing an accelerated time course of a condition to which they are already genetically disposed, noted Dr. Song and her colleagues.
Psoriasis was commonly seen on the scalp, affecting 11 of the 14 patients with psoriasis (79%), and involved the face in five of the patients (36%). Just one patient had psoriasis elsewhere on the body. There was a nonsignificant trend towards human leukocyte antigen mismatch among patients who had psoriasis. Although “psoriasis may be a marker of persistent immune dysregulation,” the investigators said, they did not identify any associated risk factors that would point toward this mechanism in their analysis.
Twelve patients (14%) had vitiligo, with halo nevi seen in four of these patients. Children who were younger than age 10 years and those who received their transplant for primary immunodeficiency were significantly more likely to have vitiligo (P less than .05 for both). Specific possible mechanisms triggering vitiligo could include thymic dysfunction resulting in loss of self-tolerance, and donor alloreactivity against the patient’s host antigens, according to the authors.
Nail changes such as pterygium and nail pitting, ridging, or thickening were seen in just five patients, all of whom had chronic GVHD of the skin. “Nail changes are likely a result of persistent inflammation and immune dysregulation from chronic GVHD,” said Dr. Song.
These late effects “can significantly impact patients’ quality of life,” according to the authors, who called for larger studies that follow pediatric HSCT patients longitudinally, beginning before the transplant – and for more investigation into the pathogenesis of specific late effects.
Dr. Song reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
AT WCPD 2017
Key clinical point:
Major finding: Permanent alopecia was seen in 25% of patients, and 16% had psoriasis a median of 3.6 years after transplant.
Data source: A single-center prospective study of 85 children in routine post-HSCT follow-up.
Disclosures: Dr. Song reported no conflicts of interest.
Ibrutinib becomes first FDA-approved treatment for chronic GVHD
Ibrutinib (Imbruvica) added another notch on its indications belt with its Aug. 2 approval by the U.S. Food and Drug Administration for the treatment of adult patients with chronic graft versus host disease (cGVHD) after failure of one or more lines of systemic therapy.
The new indication makes ibrutinib the first FDA-approved therapy for the treatment of cGVHD, according to an FDA press release.
Ibrutinib’s other approved indications include chronic lymphocytic leukemia/small lymphocytic lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma with 17p deletion, Waldenström’s macroglobulinemia, marginal zone lymphoma, and mantle cell lymphoma, according to a press release from the FDA.
The recommended dose of ibrutinib for cGVHD is 420 mg (three 140 mg capsules once daily). Prescribing information is available on the FDA website.
Imbruvica is manufactured by Pharmacyclics.
[email protected]
On Twitter @maryjodales
Ibrutinib (Imbruvica) added another notch on its indications belt with its Aug. 2 approval by the U.S. Food and Drug Administration for the treatment of adult patients with chronic graft versus host disease (cGVHD) after failure of one or more lines of systemic therapy.
The new indication makes ibrutinib the first FDA-approved therapy for the treatment of cGVHD, according to an FDA press release.
Ibrutinib’s other approved indications include chronic lymphocytic leukemia/small lymphocytic lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma with 17p deletion, Waldenström’s macroglobulinemia, marginal zone lymphoma, and mantle cell lymphoma, according to a press release from the FDA.
The recommended dose of ibrutinib for cGVHD is 420 mg (three 140 mg capsules once daily). Prescribing information is available on the FDA website.
Imbruvica is manufactured by Pharmacyclics.
[email protected]
On Twitter @maryjodales
Ibrutinib (Imbruvica) added another notch on its indications belt with its Aug. 2 approval by the U.S. Food and Drug Administration for the treatment of adult patients with chronic graft versus host disease (cGVHD) after failure of one or more lines of systemic therapy.
The new indication makes ibrutinib the first FDA-approved therapy for the treatment of cGVHD, according to an FDA press release.
Ibrutinib’s other approved indications include chronic lymphocytic leukemia/small lymphocytic lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma with 17p deletion, Waldenström’s macroglobulinemia, marginal zone lymphoma, and mantle cell lymphoma, according to a press release from the FDA.
The recommended dose of ibrutinib for cGVHD is 420 mg (three 140 mg capsules once daily). Prescribing information is available on the FDA website.
Imbruvica is manufactured by Pharmacyclics.
[email protected]
On Twitter @maryjodales