User login
Pharmacogenetic testing: Navigating through the confusion
Mr. J, age 30, a Black man with major depressive disorder (MDD), has been your patient for the past year. At the time of his diagnosis, Mr. J received sertraline, 100 mg/d, but had little to no improvement. During the past year, he received trials of citalopram and paroxetine, but they were not effective for his recurrent depressive symptoms and/or resulted in significant adverse effects.
During a recent visit, Mr. J asks you about “the genetic tests that help determine which medications will work.” He mentions that his brother had this testing done and that it had “worked for him,” but offers no other details. You research the different testing panels to see which test you might use. After a brief online review, you identify at least 4 different products, and are not sure which test—if any—you should consider.
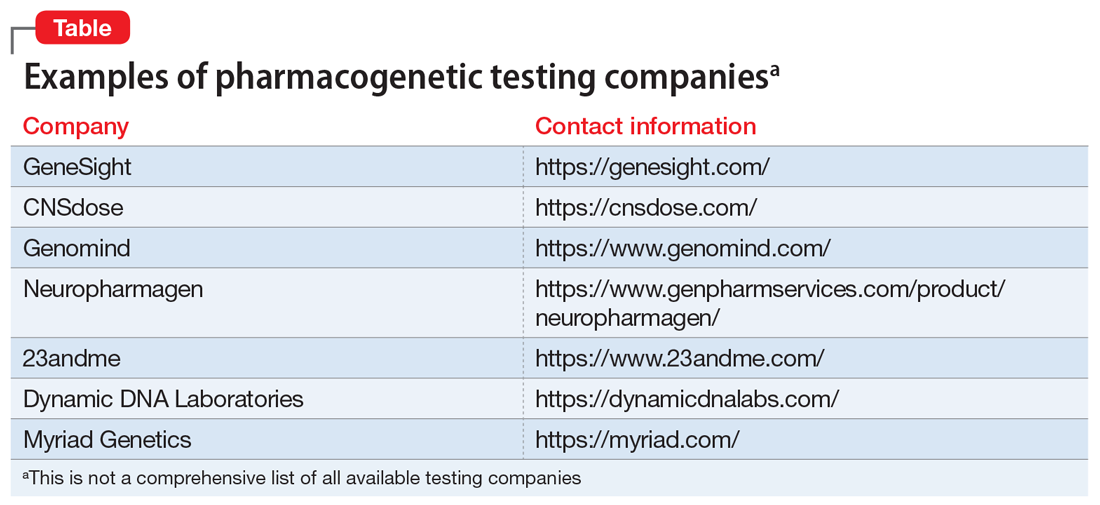
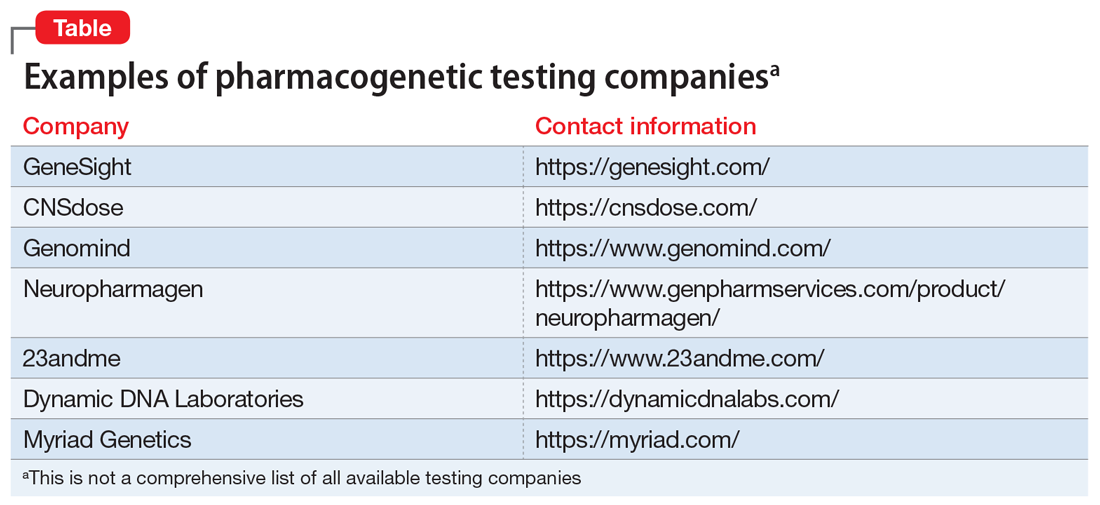
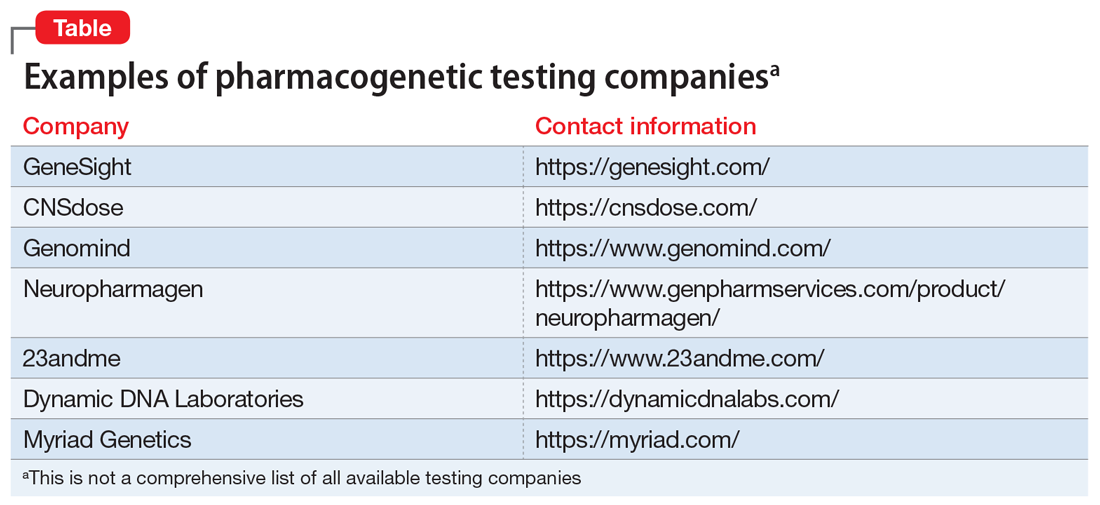
During the last few years, there has been a rise in commercial pharmacogenetic testing options, including tests available to clinicians at academic medical centers as well as direct-to-consumer testing (Table). Clinician and patient interest regarding pharmacogenetic testing in practice is often followed by the question, “Which test is best?” Although this is a logical question, providing an answer is multifactorial.1-3 Because none of the currently available tests have been compared in head-to-head clinical trials, it is nearly impossible to identify the “best” test.
In this article, we focus on the evidence-based principles that clinicians should consider when adopting pharmacogenetic testing in their practice. We discuss which genes are of most interest when prescribing psychotropic medications, the value of decision support tools, cost considerations, and patient education regarding this type of testing.
Which genes and variants should be tested?
The genes relevant to medication treatment outcomes can be broadly classified into those with pharmacokinetic vs pharmacodynamic effects. Pharmacogenes, such as those coding for the drug-metabolizing enzymes cytochrome P450 (CYP) 1A2, CYP2B6, CYP2C19, CYP2C9, CYP2D6, CYP3A4, and UDP-glucuronosyltransferase (UGT)2B1, may alter the rate at which medications are metabolized, thus varying the serum drug concentration across patients. Variants that impact the function of these enzymes are considered pharmacokinetic. Up to 40% of the variance in patients’ response to antidepressants may be due to variations in the pharmacokinetic genes.4 Alternatively, pharmacodynamic pharmacogenes impact drug action and therefore may affect the degree of receptor activation at a given drug concentration, overall drug efficacy, and/or the occurrence of medication sensitivity. These pharmacogenes may include:
- brain-derived neurotrophic factor (BDNF)
- catechol-O-methyltransferase (COMT)
- human leukocyte antigens A (HLA-A)
- serotonin receptor subtype 2 (HTR2)
- serotonin receptor subtype 2C (HTR2C)
- opioid receptor mu 1 (OPRM1)
- solute carrier family 6 member 4 (SLC6A4).
In articles previously published in
Currently, there is no standardization among commercial pharmacogenetic tests on:
- which genes to test
- which variants specific to a gene need to be included
- how the genetic data is translated to phenotype
- how the phenotype is translated to a treatment recommendation.
Continue to: Due to these factors...
Due to these factors, the FDA has advised clinicians to consult the dosing recommendations provided in a medication’s package insert for information regarding how genetic information should be used in making treatment decisions.2
The value of decision support tools
Researchers have assessed how various manufacturers’ decision support tools (DSTs) (ie, the reports the commercial testing companies send to the clinician who orders the test) agree on genotypes, predicted phenotypes, and medication recommendations.4 Overall, this research found varying levels of disagreement in the medication recommendations of the testing panels they studied, which indicates that not all tests are equivalent or interchangeable.4 Of the actionable recommendations for antidepressants, 16% were conflicting; the recommendations for fluoxetine and imipramine were most frequently in disagreement.4 Similarly, 20% of the actionable antipsychotic advice was conflicting, with the recommendations for aripiprazole and clozapine most frequently in disagreement.4 Researchers also reported a situation in which 4 testing panels agreed on the patient’s phenotyping status for CYP2C19, but the dosing recommendations provided for the CYP2C19 substrate, amitriptyline, differed.4 Thus, it is understandable why DSTs can result in confusion, and why clinicians should use testing panels with recommendations that best align with their individual practices, their patient’s needs, and FDA information.
Additionally, while the genes included on these panels vary, these testing panels also may not evaluate the same variants within a specific gene. These differences may impact the patient’s reported phenotypes and medication recommendations across DSTs. For example, the FDA has recommended HLA gene testing prior to prescribing carbamazepine. However, few of the available tests may include the HLA-B*15:02 variant, which has been associated with carbamazepine-induced severe cutaneous reactions in patients of Asian descent, and fewer may include the HLA-A*31:01 variant, for which testing is recommended prior to prescribing carbamazepine in patients of Caucasian descent.4 Additionally, some of the CYP enzymes—such as CYP2D6*17 and CYP2C19*3 variants, which may be more common in certain populations of patients who are members of ethnic or racial minority groups—may not be consistently included in the various panels. Thus, before deciding on a specific test, clinicians should understand which gene variants are relevant to their patients with regard to race and ethnicity, and key variants for specific medications. Clinicians should refer to FDA guidance and the Clinical Pharmacogenomics Implementation Consortium (CPIC) guidelines to determine the appropriate interpretations of genetic test results.1,2
Despite the disagreement in recommendations from the various testing companies, DSTs are useful and have been shown to facilitate implementation of relevant psychopharmacology dosing guidelines, assist in identifying optimal medication therapy, and improve patient outcomes. A recently published meta-analysis of randomized controlled trials (RCTs) of pharmacogenetic testing found that DSTs improved symptom remission among individuals with MDD by 70%.5 This suggests that pharmacogenetic-guided DSTs may provide superior treatment compared with treatment for DSTs were not used. However, the RCTs in this meta-analysis only included patients who had previously failed an antidepressant trial.5 Therefore, it is currently unknown at what point in care DSTs should be used, and whether they would be more beneficial if they are used when starting a new therapy, or after several trials have failed.
Consider the cost
The cost and availability of pharmacogenetic testing can be an issue when making treatment decisions, and such testing may not be covered by a patient’s insurance plan. Recently, the Centers for Medicare & Medicaid Services announced that Medicare would cover FDA-approved genomic tests that encompass broad gene panels if the evidence supports their use. Similarly, commercial insurers such as UnitedHealthcare have begun to cover some pharmacogenetic tests.6 Medicare or Medicaid plans cover some testing panels’ costs and patients do not incur any out-of-pocket costs; however, some private insurance companies require patients to pay at least a portion of the cost, and many companies offer financial assistance for patients based on income and other factors. Although financial coverage for testing has improved, patients may still face out-of-pocket costs; therefore, clinicians may need to weigh the benefits of pharmacogenetic testing vs its cost.7 Clinicians should also determine what timeline best suits their patient’s financial and clinical needs, and test accordingly.
Continue to: Patient education is critical
Patient education is critical
Although the benefits of using pharmacogenetic testing information when making certain treatment decisions is promising, it is important for both patients and clinicians to understand that test results do not always change therapy. A study on the impact of pharmacogenetic testing on clinical outcomes of patients with MDD found that 79% of patients were already prescribed medications that aligned with recommendations.8 Therefore, switching medications based on the test results of a patient who is doing well clinically is not recommended. However, DSTs may help with clinical decisions for ambiguous cases. For example, if a patient has a genotype and/or phenotype that aligns with medication recommendations, the DST might not be able to identify a better medication to use, but may be able to recommend dosing guidance to improve the tolerability of the patient’s current therapy.6 It is also important to understand that the results of such testing may have a broader use beyond the initial reason for obtaining testing, such as when prescribing a common blood thinner such as warfarin or clopidogrel. However, for many of the pharmacodynamic genes that are included in these panels, their use beyond the treatment of depression may be limited because outcome studies for pharmacodynamic pharmacogenes may vary based on psychiatric diagnosis. Regardless, it may be beneficial to securely save and store patient test results in a standardized place within the medical record for future use.
CASE CONTINUED
You work with Mr. J to help him understand the benefits and limitations associated with pharmacogenetic testing. Assuming Mr. J is comfortable with the costs of obtaining testing, you contact the testing companies you identified to determine the specific pharmacogene variants included on each of these panels, and which would be the most appropriate given his race. If the decision is made to order the testing, provide Mr. J with a copy of his testing report so that he can use this information should he need any additional pharmacotherapy in the future, and also maintain a copy in his patient records using a standardized location for easy future access. If Mr. J is not comfortable with the costs associated with the testing, find out which medication his brother is currently receiving for treatment; this information may help identify a treatment plan for Mr. J.
Impact on practice
As psychiatry continues to gain experience in using pharmacogenetic testing and DSTs to help guide treatments for depression and other disorders, clinicians need to learn about these tools and how to use an evidence-based approach to best implement them in their practice. Many academic medical centers have developed continuing education programs or consult services to help with this.9,10 Just as the choice of which medication to use may be based partly on clinician experience, so too may be which pharmacogenetic test to use.
Bottom Line
Pharmacogenetic tests have not been examined in head-to-head clinical trials, which makes it nearly impossible to identify which test is best to use. Although the testing companies’ decision support tools (DSTs) often disagree in their recommendations, research has shown that using DSTs can facilitate implementation of relevant psychopharmacology dosing guidelines, assist in identifying optimal medication therapy, and improve patient outcomes. Clinicians should use testing panels with recommendations that best align with their individual practices, their patient’s needs, and FDA information.
Related Resources
- PGx Gene-specific information tables. www.pharmgkb.org/page/pgxGeneRef
- Clinical Pharmacogenetics Implementation Consortium. https://cpicpgx.org/guidelines/
Drug Brand Names
Aripiprazole • Abilify
Carbamazepine • Tegretol
Citalopram • Celexa
Clopidogrel • Plavix
Clozapine • Clozaril
Fluoxetine • Prozac
Imipramine • Tofranil
Paroxetine • Paxil
Sertraline • Zoloft
Warfarin • Coumadin, Jantoven
1. Ellingrod, VL. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
2. Ellingrod VL. Pharmacogenomics testing: what the FDA says. Current Psychiatry. 2019;18(4):29-33.
3. Ramsey LB. Pharmacogenetic testing in children: what to test and how to use it. Current Psychiatry. 2018;17(9):30-36.
4. Bousman CA, Dunlop BW. Genotype, phenotype, and medication recommendation agreement among commercial pharmacogenetic-based decision support tools. The Pharmacogenomics Journal. 2018;18(5):613-622. doi:10.1038/s41397-018-0027-3
5. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1). doi:10.2217/pgs-2018-0142
6. Nicholson WT, Formea CM, Matey ET, et al. Considerations when applying pharmacogenomics to your practice. Mayo Clin Proc. 2021;96(1);218-230. doi:10.1016/j.mayocp.2020.03.011
7. Krebs K, Milani L. Translating pharmacogenomics into clinical decisions: do not let the perfect be the enemy of the good. Human Genomics. 2019;13(1). doi:10.1186/s40246-019-0229-z
8. Greden JF, Parikh S, Rothschild AJ, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111;59-67. doi:10.1016/j.jpsychires.2019.01.003
9. Haga SB. Integrating pharmacogenetic testing into primary care. Expert Review of Precision Medicine and Drug Development. 2017;2(6):327-336. doi:10.1080/23808993.2017.1398046
10. Ward KM, Taubman DS, Pasternak AL, et al. Teaching psychiatric pharmacogenomics effectively: evaluation of a novel interprofessional online course. J Am Coll Clin Pharm. 2021; 4:176-183.
Mr. J, age 30, a Black man with major depressive disorder (MDD), has been your patient for the past year. At the time of his diagnosis, Mr. J received sertraline, 100 mg/d, but had little to no improvement. During the past year, he received trials of citalopram and paroxetine, but they were not effective for his recurrent depressive symptoms and/or resulted in significant adverse effects.
During a recent visit, Mr. J asks you about “the genetic tests that help determine which medications will work.” He mentions that his brother had this testing done and that it had “worked for him,” but offers no other details. You research the different testing panels to see which test you might use. After a brief online review, you identify at least 4 different products, and are not sure which test—if any—you should consider.
During the last few years, there has been a rise in commercial pharmacogenetic testing options, including tests available to clinicians at academic medical centers as well as direct-to-consumer testing (Table). Clinician and patient interest regarding pharmacogenetic testing in practice is often followed by the question, “Which test is best?” Although this is a logical question, providing an answer is multifactorial.1-3 Because none of the currently available tests have been compared in head-to-head clinical trials, it is nearly impossible to identify the “best” test.
In this article, we focus on the evidence-based principles that clinicians should consider when adopting pharmacogenetic testing in their practice. We discuss which genes are of most interest when prescribing psychotropic medications, the value of decision support tools, cost considerations, and patient education regarding this type of testing.
Which genes and variants should be tested?
The genes relevant to medication treatment outcomes can be broadly classified into those with pharmacokinetic vs pharmacodynamic effects. Pharmacogenes, such as those coding for the drug-metabolizing enzymes cytochrome P450 (CYP) 1A2, CYP2B6, CYP2C19, CYP2C9, CYP2D6, CYP3A4, and UDP-glucuronosyltransferase (UGT)2B1, may alter the rate at which medications are metabolized, thus varying the serum drug concentration across patients. Variants that impact the function of these enzymes are considered pharmacokinetic. Up to 40% of the variance in patients’ response to antidepressants may be due to variations in the pharmacokinetic genes.4 Alternatively, pharmacodynamic pharmacogenes impact drug action and therefore may affect the degree of receptor activation at a given drug concentration, overall drug efficacy, and/or the occurrence of medication sensitivity. These pharmacogenes may include:
- brain-derived neurotrophic factor (BDNF)
- catechol-O-methyltransferase (COMT)
- human leukocyte antigens A (HLA-A)
- serotonin receptor subtype 2 (HTR2)
- serotonin receptor subtype 2C (HTR2C)
- opioid receptor mu 1 (OPRM1)
- solute carrier family 6 member 4 (SLC6A4).
In articles previously published in
Currently, there is no standardization among commercial pharmacogenetic tests on:
- which genes to test
- which variants specific to a gene need to be included
- how the genetic data is translated to phenotype
- how the phenotype is translated to a treatment recommendation.
Continue to: Due to these factors...
Due to these factors, the FDA has advised clinicians to consult the dosing recommendations provided in a medication’s package insert for information regarding how genetic information should be used in making treatment decisions.2
The value of decision support tools
Researchers have assessed how various manufacturers’ decision support tools (DSTs) (ie, the reports the commercial testing companies send to the clinician who orders the test) agree on genotypes, predicted phenotypes, and medication recommendations.4 Overall, this research found varying levels of disagreement in the medication recommendations of the testing panels they studied, which indicates that not all tests are equivalent or interchangeable.4 Of the actionable recommendations for antidepressants, 16% were conflicting; the recommendations for fluoxetine and imipramine were most frequently in disagreement.4 Similarly, 20% of the actionable antipsychotic advice was conflicting, with the recommendations for aripiprazole and clozapine most frequently in disagreement.4 Researchers also reported a situation in which 4 testing panels agreed on the patient’s phenotyping status for CYP2C19, but the dosing recommendations provided for the CYP2C19 substrate, amitriptyline, differed.4 Thus, it is understandable why DSTs can result in confusion, and why clinicians should use testing panels with recommendations that best align with their individual practices, their patient’s needs, and FDA information.
Additionally, while the genes included on these panels vary, these testing panels also may not evaluate the same variants within a specific gene. These differences may impact the patient’s reported phenotypes and medication recommendations across DSTs. For example, the FDA has recommended HLA gene testing prior to prescribing carbamazepine. However, few of the available tests may include the HLA-B*15:02 variant, which has been associated with carbamazepine-induced severe cutaneous reactions in patients of Asian descent, and fewer may include the HLA-A*31:01 variant, for which testing is recommended prior to prescribing carbamazepine in patients of Caucasian descent.4 Additionally, some of the CYP enzymes—such as CYP2D6*17 and CYP2C19*3 variants, which may be more common in certain populations of patients who are members of ethnic or racial minority groups—may not be consistently included in the various panels. Thus, before deciding on a specific test, clinicians should understand which gene variants are relevant to their patients with regard to race and ethnicity, and key variants for specific medications. Clinicians should refer to FDA guidance and the Clinical Pharmacogenomics Implementation Consortium (CPIC) guidelines to determine the appropriate interpretations of genetic test results.1,2
Despite the disagreement in recommendations from the various testing companies, DSTs are useful and have been shown to facilitate implementation of relevant psychopharmacology dosing guidelines, assist in identifying optimal medication therapy, and improve patient outcomes. A recently published meta-analysis of randomized controlled trials (RCTs) of pharmacogenetic testing found that DSTs improved symptom remission among individuals with MDD by 70%.5 This suggests that pharmacogenetic-guided DSTs may provide superior treatment compared with treatment for DSTs were not used. However, the RCTs in this meta-analysis only included patients who had previously failed an antidepressant trial.5 Therefore, it is currently unknown at what point in care DSTs should be used, and whether they would be more beneficial if they are used when starting a new therapy, or after several trials have failed.
Consider the cost
The cost and availability of pharmacogenetic testing can be an issue when making treatment decisions, and such testing may not be covered by a patient’s insurance plan. Recently, the Centers for Medicare & Medicaid Services announced that Medicare would cover FDA-approved genomic tests that encompass broad gene panels if the evidence supports their use. Similarly, commercial insurers such as UnitedHealthcare have begun to cover some pharmacogenetic tests.6 Medicare or Medicaid plans cover some testing panels’ costs and patients do not incur any out-of-pocket costs; however, some private insurance companies require patients to pay at least a portion of the cost, and many companies offer financial assistance for patients based on income and other factors. Although financial coverage for testing has improved, patients may still face out-of-pocket costs; therefore, clinicians may need to weigh the benefits of pharmacogenetic testing vs its cost.7 Clinicians should also determine what timeline best suits their patient’s financial and clinical needs, and test accordingly.
Continue to: Patient education is critical
Patient education is critical
Although the benefits of using pharmacogenetic testing information when making certain treatment decisions is promising, it is important for both patients and clinicians to understand that test results do not always change therapy. A study on the impact of pharmacogenetic testing on clinical outcomes of patients with MDD found that 79% of patients were already prescribed medications that aligned with recommendations.8 Therefore, switching medications based on the test results of a patient who is doing well clinically is not recommended. However, DSTs may help with clinical decisions for ambiguous cases. For example, if a patient has a genotype and/or phenotype that aligns with medication recommendations, the DST might not be able to identify a better medication to use, but may be able to recommend dosing guidance to improve the tolerability of the patient’s current therapy.6 It is also important to understand that the results of such testing may have a broader use beyond the initial reason for obtaining testing, such as when prescribing a common blood thinner such as warfarin or clopidogrel. However, for many of the pharmacodynamic genes that are included in these panels, their use beyond the treatment of depression may be limited because outcome studies for pharmacodynamic pharmacogenes may vary based on psychiatric diagnosis. Regardless, it may be beneficial to securely save and store patient test results in a standardized place within the medical record for future use.
CASE CONTINUED
You work with Mr. J to help him understand the benefits and limitations associated with pharmacogenetic testing. Assuming Mr. J is comfortable with the costs of obtaining testing, you contact the testing companies you identified to determine the specific pharmacogene variants included on each of these panels, and which would be the most appropriate given his race. If the decision is made to order the testing, provide Mr. J with a copy of his testing report so that he can use this information should he need any additional pharmacotherapy in the future, and also maintain a copy in his patient records using a standardized location for easy future access. If Mr. J is not comfortable with the costs associated with the testing, find out which medication his brother is currently receiving for treatment; this information may help identify a treatment plan for Mr. J.
Impact on practice
As psychiatry continues to gain experience in using pharmacogenetic testing and DSTs to help guide treatments for depression and other disorders, clinicians need to learn about these tools and how to use an evidence-based approach to best implement them in their practice. Many academic medical centers have developed continuing education programs or consult services to help with this.9,10 Just as the choice of which medication to use may be based partly on clinician experience, so too may be which pharmacogenetic test to use.
Bottom Line
Pharmacogenetic tests have not been examined in head-to-head clinical trials, which makes it nearly impossible to identify which test is best to use. Although the testing companies’ decision support tools (DSTs) often disagree in their recommendations, research has shown that using DSTs can facilitate implementation of relevant psychopharmacology dosing guidelines, assist in identifying optimal medication therapy, and improve patient outcomes. Clinicians should use testing panels with recommendations that best align with their individual practices, their patient’s needs, and FDA information.
Related Resources
- PGx Gene-specific information tables. www.pharmgkb.org/page/pgxGeneRef
- Clinical Pharmacogenetics Implementation Consortium. https://cpicpgx.org/guidelines/
Drug Brand Names
Aripiprazole • Abilify
Carbamazepine • Tegretol
Citalopram • Celexa
Clopidogrel • Plavix
Clozapine • Clozaril
Fluoxetine • Prozac
Imipramine • Tofranil
Paroxetine • Paxil
Sertraline • Zoloft
Warfarin • Coumadin, Jantoven
Mr. J, age 30, a Black man with major depressive disorder (MDD), has been your patient for the past year. At the time of his diagnosis, Mr. J received sertraline, 100 mg/d, but had little to no improvement. During the past year, he received trials of citalopram and paroxetine, but they were not effective for his recurrent depressive symptoms and/or resulted in significant adverse effects.
During a recent visit, Mr. J asks you about “the genetic tests that help determine which medications will work.” He mentions that his brother had this testing done and that it had “worked for him,” but offers no other details. You research the different testing panels to see which test you might use. After a brief online review, you identify at least 4 different products, and are not sure which test—if any—you should consider.
During the last few years, there has been a rise in commercial pharmacogenetic testing options, including tests available to clinicians at academic medical centers as well as direct-to-consumer testing (Table). Clinician and patient interest regarding pharmacogenetic testing in practice is often followed by the question, “Which test is best?” Although this is a logical question, providing an answer is multifactorial.1-3 Because none of the currently available tests have been compared in head-to-head clinical trials, it is nearly impossible to identify the “best” test.
In this article, we focus on the evidence-based principles that clinicians should consider when adopting pharmacogenetic testing in their practice. We discuss which genes are of most interest when prescribing psychotropic medications, the value of decision support tools, cost considerations, and patient education regarding this type of testing.
Which genes and variants should be tested?
The genes relevant to medication treatment outcomes can be broadly classified into those with pharmacokinetic vs pharmacodynamic effects. Pharmacogenes, such as those coding for the drug-metabolizing enzymes cytochrome P450 (CYP) 1A2, CYP2B6, CYP2C19, CYP2C9, CYP2D6, CYP3A4, and UDP-glucuronosyltransferase (UGT)2B1, may alter the rate at which medications are metabolized, thus varying the serum drug concentration across patients. Variants that impact the function of these enzymes are considered pharmacokinetic. Up to 40% of the variance in patients’ response to antidepressants may be due to variations in the pharmacokinetic genes.4 Alternatively, pharmacodynamic pharmacogenes impact drug action and therefore may affect the degree of receptor activation at a given drug concentration, overall drug efficacy, and/or the occurrence of medication sensitivity. These pharmacogenes may include:
- brain-derived neurotrophic factor (BDNF)
- catechol-O-methyltransferase (COMT)
- human leukocyte antigens A (HLA-A)
- serotonin receptor subtype 2 (HTR2)
- serotonin receptor subtype 2C (HTR2C)
- opioid receptor mu 1 (OPRM1)
- solute carrier family 6 member 4 (SLC6A4).
In articles previously published in
Currently, there is no standardization among commercial pharmacogenetic tests on:
- which genes to test
- which variants specific to a gene need to be included
- how the genetic data is translated to phenotype
- how the phenotype is translated to a treatment recommendation.
Continue to: Due to these factors...
Due to these factors, the FDA has advised clinicians to consult the dosing recommendations provided in a medication’s package insert for information regarding how genetic information should be used in making treatment decisions.2
The value of decision support tools
Researchers have assessed how various manufacturers’ decision support tools (DSTs) (ie, the reports the commercial testing companies send to the clinician who orders the test) agree on genotypes, predicted phenotypes, and medication recommendations.4 Overall, this research found varying levels of disagreement in the medication recommendations of the testing panels they studied, which indicates that not all tests are equivalent or interchangeable.4 Of the actionable recommendations for antidepressants, 16% were conflicting; the recommendations for fluoxetine and imipramine were most frequently in disagreement.4 Similarly, 20% of the actionable antipsychotic advice was conflicting, with the recommendations for aripiprazole and clozapine most frequently in disagreement.4 Researchers also reported a situation in which 4 testing panels agreed on the patient’s phenotyping status for CYP2C19, but the dosing recommendations provided for the CYP2C19 substrate, amitriptyline, differed.4 Thus, it is understandable why DSTs can result in confusion, and why clinicians should use testing panels with recommendations that best align with their individual practices, their patient’s needs, and FDA information.
Additionally, while the genes included on these panels vary, these testing panels also may not evaluate the same variants within a specific gene. These differences may impact the patient’s reported phenotypes and medication recommendations across DSTs. For example, the FDA has recommended HLA gene testing prior to prescribing carbamazepine. However, few of the available tests may include the HLA-B*15:02 variant, which has been associated with carbamazepine-induced severe cutaneous reactions in patients of Asian descent, and fewer may include the HLA-A*31:01 variant, for which testing is recommended prior to prescribing carbamazepine in patients of Caucasian descent.4 Additionally, some of the CYP enzymes—such as CYP2D6*17 and CYP2C19*3 variants, which may be more common in certain populations of patients who are members of ethnic or racial minority groups—may not be consistently included in the various panels. Thus, before deciding on a specific test, clinicians should understand which gene variants are relevant to their patients with regard to race and ethnicity, and key variants for specific medications. Clinicians should refer to FDA guidance and the Clinical Pharmacogenomics Implementation Consortium (CPIC) guidelines to determine the appropriate interpretations of genetic test results.1,2
Despite the disagreement in recommendations from the various testing companies, DSTs are useful and have been shown to facilitate implementation of relevant psychopharmacology dosing guidelines, assist in identifying optimal medication therapy, and improve patient outcomes. A recently published meta-analysis of randomized controlled trials (RCTs) of pharmacogenetic testing found that DSTs improved symptom remission among individuals with MDD by 70%.5 This suggests that pharmacogenetic-guided DSTs may provide superior treatment compared with treatment for DSTs were not used. However, the RCTs in this meta-analysis only included patients who had previously failed an antidepressant trial.5 Therefore, it is currently unknown at what point in care DSTs should be used, and whether they would be more beneficial if they are used when starting a new therapy, or after several trials have failed.
Consider the cost
The cost and availability of pharmacogenetic testing can be an issue when making treatment decisions, and such testing may not be covered by a patient’s insurance plan. Recently, the Centers for Medicare & Medicaid Services announced that Medicare would cover FDA-approved genomic tests that encompass broad gene panels if the evidence supports their use. Similarly, commercial insurers such as UnitedHealthcare have begun to cover some pharmacogenetic tests.6 Medicare or Medicaid plans cover some testing panels’ costs and patients do not incur any out-of-pocket costs; however, some private insurance companies require patients to pay at least a portion of the cost, and many companies offer financial assistance for patients based on income and other factors. Although financial coverage for testing has improved, patients may still face out-of-pocket costs; therefore, clinicians may need to weigh the benefits of pharmacogenetic testing vs its cost.7 Clinicians should also determine what timeline best suits their patient’s financial and clinical needs, and test accordingly.
Continue to: Patient education is critical
Patient education is critical
Although the benefits of using pharmacogenetic testing information when making certain treatment decisions is promising, it is important for both patients and clinicians to understand that test results do not always change therapy. A study on the impact of pharmacogenetic testing on clinical outcomes of patients with MDD found that 79% of patients were already prescribed medications that aligned with recommendations.8 Therefore, switching medications based on the test results of a patient who is doing well clinically is not recommended. However, DSTs may help with clinical decisions for ambiguous cases. For example, if a patient has a genotype and/or phenotype that aligns with medication recommendations, the DST might not be able to identify a better medication to use, but may be able to recommend dosing guidance to improve the tolerability of the patient’s current therapy.6 It is also important to understand that the results of such testing may have a broader use beyond the initial reason for obtaining testing, such as when prescribing a common blood thinner such as warfarin or clopidogrel. However, for many of the pharmacodynamic genes that are included in these panels, their use beyond the treatment of depression may be limited because outcome studies for pharmacodynamic pharmacogenes may vary based on psychiatric diagnosis. Regardless, it may be beneficial to securely save and store patient test results in a standardized place within the medical record for future use.
CASE CONTINUED
You work with Mr. J to help him understand the benefits and limitations associated with pharmacogenetic testing. Assuming Mr. J is comfortable with the costs of obtaining testing, you contact the testing companies you identified to determine the specific pharmacogene variants included on each of these panels, and which would be the most appropriate given his race. If the decision is made to order the testing, provide Mr. J with a copy of his testing report so that he can use this information should he need any additional pharmacotherapy in the future, and also maintain a copy in his patient records using a standardized location for easy future access. If Mr. J is not comfortable with the costs associated with the testing, find out which medication his brother is currently receiving for treatment; this information may help identify a treatment plan for Mr. J.
Impact on practice
As psychiatry continues to gain experience in using pharmacogenetic testing and DSTs to help guide treatments for depression and other disorders, clinicians need to learn about these tools and how to use an evidence-based approach to best implement them in their practice. Many academic medical centers have developed continuing education programs or consult services to help with this.9,10 Just as the choice of which medication to use may be based partly on clinician experience, so too may be which pharmacogenetic test to use.
Bottom Line
Pharmacogenetic tests have not been examined in head-to-head clinical trials, which makes it nearly impossible to identify which test is best to use. Although the testing companies’ decision support tools (DSTs) often disagree in their recommendations, research has shown that using DSTs can facilitate implementation of relevant psychopharmacology dosing guidelines, assist in identifying optimal medication therapy, and improve patient outcomes. Clinicians should use testing panels with recommendations that best align with their individual practices, their patient’s needs, and FDA information.
Related Resources
- PGx Gene-specific information tables. www.pharmgkb.org/page/pgxGeneRef
- Clinical Pharmacogenetics Implementation Consortium. https://cpicpgx.org/guidelines/
Drug Brand Names
Aripiprazole • Abilify
Carbamazepine • Tegretol
Citalopram • Celexa
Clopidogrel • Plavix
Clozapine • Clozaril
Fluoxetine • Prozac
Imipramine • Tofranil
Paroxetine • Paxil
Sertraline • Zoloft
Warfarin • Coumadin, Jantoven
1. Ellingrod, VL. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
2. Ellingrod VL. Pharmacogenomics testing: what the FDA says. Current Psychiatry. 2019;18(4):29-33.
3. Ramsey LB. Pharmacogenetic testing in children: what to test and how to use it. Current Psychiatry. 2018;17(9):30-36.
4. Bousman CA, Dunlop BW. Genotype, phenotype, and medication recommendation agreement among commercial pharmacogenetic-based decision support tools. The Pharmacogenomics Journal. 2018;18(5):613-622. doi:10.1038/s41397-018-0027-3
5. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1). doi:10.2217/pgs-2018-0142
6. Nicholson WT, Formea CM, Matey ET, et al. Considerations when applying pharmacogenomics to your practice. Mayo Clin Proc. 2021;96(1);218-230. doi:10.1016/j.mayocp.2020.03.011
7. Krebs K, Milani L. Translating pharmacogenomics into clinical decisions: do not let the perfect be the enemy of the good. Human Genomics. 2019;13(1). doi:10.1186/s40246-019-0229-z
8. Greden JF, Parikh S, Rothschild AJ, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111;59-67. doi:10.1016/j.jpsychires.2019.01.003
9. Haga SB. Integrating pharmacogenetic testing into primary care. Expert Review of Precision Medicine and Drug Development. 2017;2(6):327-336. doi:10.1080/23808993.2017.1398046
10. Ward KM, Taubman DS, Pasternak AL, et al. Teaching psychiatric pharmacogenomics effectively: evaluation of a novel interprofessional online course. J Am Coll Clin Pharm. 2021; 4:176-183.
1. Ellingrod, VL. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
2. Ellingrod VL. Pharmacogenomics testing: what the FDA says. Current Psychiatry. 2019;18(4):29-33.
3. Ramsey LB. Pharmacogenetic testing in children: what to test and how to use it. Current Psychiatry. 2018;17(9):30-36.
4. Bousman CA, Dunlop BW. Genotype, phenotype, and medication recommendation agreement among commercial pharmacogenetic-based decision support tools. The Pharmacogenomics Journal. 2018;18(5):613-622. doi:10.1038/s41397-018-0027-3
5. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1). doi:10.2217/pgs-2018-0142
6. Nicholson WT, Formea CM, Matey ET, et al. Considerations when applying pharmacogenomics to your practice. Mayo Clin Proc. 2021;96(1);218-230. doi:10.1016/j.mayocp.2020.03.011
7. Krebs K, Milani L. Translating pharmacogenomics into clinical decisions: do not let the perfect be the enemy of the good. Human Genomics. 2019;13(1). doi:10.1186/s40246-019-0229-z
8. Greden JF, Parikh S, Rothschild AJ, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111;59-67. doi:10.1016/j.jpsychires.2019.01.003
9. Haga SB. Integrating pharmacogenetic testing into primary care. Expert Review of Precision Medicine and Drug Development. 2017;2(6):327-336. doi:10.1080/23808993.2017.1398046
10. Ward KM, Taubman DS, Pasternak AL, et al. Teaching psychiatric pharmacogenomics effectively: evaluation of a novel interprofessional online course. J Am Coll Clin Pharm. 2021; 4:176-183.
How COVID-19 affects peripartum women’s mental health
The COVID-19 pandemic has had a negative impact on the mental health of people worldwide, and a disproportionate effect on peripartum women. In this article, we discuss the reasons for this disparity, review the limited literature on this topic, and suggest strategies to safeguard the mental health of peripartum women during the COVID-19 pandemic.
Catastrophic events and women’s mental health
During the peripartum period, women have increased psychosocial and physical health needs.1 In addition, women are disproportionately affected by natural disasters and catastrophic events,2 which are predictors of psychiatric symptoms during the peripartum period.3 Mass tragedies previously associated with maternal stress include wildfires, hurricanes, migrations, earthquakes, and tsunamis.4,5 For example, pregnant women who survived severe exposure during Hurricane Katrina (ie, feeling that one’s life was in danger, experiencing illness or injury to self or a family member, walking through floodwaters) in 2005 had a significantly increased risk of developing posttraumatic stress disorder (PTSD) and depression compared with pregnant women who did not have such exposure.6 After the 2011 Tōhoku earthquake and tsunami in Japan, the prevalence of psychological distress in pregnant women increased, especially among those living in the area directly affected by the tsunami.5
Epidemics and pandemics also can adversely affect peripartum women’s mental health. Studies conducted before the COVID-19 pandemic found that previous infectious disease outbreaks such as severe acute respiratory syndrome (SARS), the 2009 influenza A (H1N1) pandemic, and Zika had negative emotional impacts on pregnant women.7 Our review of the limited literature published to date suggests that COVID-19 is having similar adverse effects.
COVID-19 poses both medical and psychiatric threats
COVID-19 infection is a physical threat to pregnant women who are already vulnerable due to the hormonal and immunological changes inherent to pregnancy. A meta-analysis of 39 studies with a total of 1,316 pregnant women indicated that the most frequently reported symptoms of COVID-19 infection were cough, fever, and myalgias.8 However, COVID-19 infection during pregnancy is also associated with an increase in pregnancy complications and adverse birth outcomes.9 According to the CDC, compared with their nonpregnant counterparts, pregnant women are at greater risk for severe COVID-19 infection and adverse birth outcomes such as preterm birth.10 Pregnant women who are infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; the virus responsible for COVID-19) risk ICU admission, caesarean section, and perinatal death.8 A Swedish study of 2,682 pregnant women found an increase in preeclampsia among women who tested positive for SARS-CoV-2, a finding attributed to COVID-19’s pattern of systemic effects.11 Vertical transmission of the novel coronavirus from mother to fetus appears to be rare but possible.12
In addition to the physical dangers of becoming infected with COVID-19, the perceived threat of infection is an added source of anxiety for some peripartum women. In addition to the concerns involved in any pregnancy, COVID-19–related sources of distress for pregnant women include worrying about harm to the fetus during pregnancy, the possibility of vertical transmission, and exposures during antenatal appointments, during employment, or from a partner.8,13
The death toll from factors associated with COVID-19 adds to the mental health burden. For every person who dies of COVID-19, an estimated 9 others may develop prolonged grief or PTSD due to the loss of someone they loved.14,15 A systematic review found that PTSD in the perinatal period is associated with negative birth and child outcomes, including low birth weight and decreased rates of breastfeeding.16 The COVID-19 pandemic has disrupted human interactions, from social distancing rules and lockdowns of businesses and social activities to panic buying of grocery staples and increased economic insecurity.1 These changes have been accompanied by a rise in mental health challenges. For example, according to an August 2020 CDC survey, 40.9% of US adults reported at least 1 adverse mental or behavioral health condition, including symptoms of anxiety or depression (30.9%), symptoms of a trauma- and stressor-related disorder related to the pandemic (26.3%), and having started or increased substance use to cope with stress or emotions related to COVID-19 (13.3%).17
COVID-19–related traumas and stressors appear to affect women more than men. A study from China found that compared with men, women had significantly higher levels of self-reported pandemic-related anxiety, depression, and posttraumatic stress symptoms (PTSS).18 This trend has been observed in other parts of the world. A study conducted by the UK Office of National Statistics reported anxiety levels were 24% higher in women vs men as reflected by scores on a self-rated anxiety scale.19
Continue to: Many factors influence...
Many factors influence the disproportionate impact of COVID-19 on women in general, and peripartum women in particular (Box20-26).
Box
Factors that predispose women to increased stress during COVID-19 include an increase in child care burdens brought about by school closures and subsequent virtual schooling.20 Intimate partner violence has spiked globally during COVID-19 restrictions.24 Women also represent the majority of the health care workforce (76%) and often take on informal caregiving roles; both of these roles have seen increased burdens during the pandemic.25 Already encumbered by prepandemic gender pay inequalities, women are filing unemployment claims at a significantly increased rate compared to men.26
For women of childbearing age, the disruption of routine clinical care during COVID-19 has decreased access to reproductive health care, resulting in increases in unintended pregnancies, unsafe abortions, and deaths.20 Another source of stress for pregnant women during COVID-19 is feeling unprepared for birth because of the pandemic, a phenomenon described as “preparedness stress.”21 Visitor restriction policies and quarantines have also caused women in labor to experience birth without their support partners, which is associated with increased posttraumatic stress symptoms.22 These restrictions also may be associated with an increase in women choosing out-of-hospital births despite the increased risk of adverse outcomes.23
Psychiatric diagnoses in peripartum women
Multiple studies and meta-analyses have begun to assess the impact of the COVID-19 pandemic on maternal mental health. One meta-analysis of 8 studies conducted in 5 countries determined that COVID-19 significantly increases the risk of anxiety in women during the peripartum period.27 Results of another meta-analysis of 23 studies with >24,000 participants indicated that the prevalence of anxiety, depression, and insomnia in peripartum women was significantly higher during the pandemic than in pre-pandemic times.28
In an online survey of 4,451 pregnant women in the United States, nearly one-third of respondents reported elevated levels of pandemic-related stress as measured by the newly-developed Pandemic-Related Pregnancy Stress Scale.3 The rates were even higher among women who were already at risk for elevated stress levels, such as those who had survived abuse, those giving birth for the first time, or those experiencing high-risk pregnancies.3 Living in a pandemic “hot spot” also appeared to impact peripartum stress levels.
COVID-19 has adverse effects on women’s mental health specifically during the postpartum period. One study from a center in Italy found a high prevalence of depressive symptoms and PTSS in the postpartum period, with COVID-19–related factors playing an “indirect role” compared with prenatal experiences and other individual factors.2 A British study of mothers of infants age ≤12 months found that traveling for work, the impact of lockdown on food affordability, and having an income of less than £30,000 per year (approximately $41,000) predicted poorer mental health during the pandemic.29 Results of a study from China indicated that more than one-quarter of pregnant and postpartum women experienced depression during the pandemic, and women who worried about infection risk or missing pediatric visits were at increased risk.30
How to mitigate these risks
The increase in pandemic-related mental health concerns in the general population and specifically in peripartum women is a global health care challenge. Investing in mitigation strategies is necessary not only to address the current pandemic, but also to help prepare for the possibility of future traumatic events, such as another global pandemic.
Continue to: For pregnant women...
For pregnant women, ensuring access to outdoor space, increasing participation in healthy activities, and minimizing disruptions to prenatal care can protect against pandemic-related stress.3 Physical activity is an effective treatment for mild to moderate depressive symptoms. Because of the significant decrease in exercise among pregnant women during the pandemic, encouraging safe forms of physical activity such as online fitness classes could improve mental health outcomes for these patients.27 When counseling peripartum women, psychiatrists need to be creative in recommending fitness interventions to target mood symptoms, such as by suggesting virtual or at-home programs.
In an online survey, 118 obstetricians called for increased mental health resources for peripartum women, such as easier access to a helpline, educational videos, and mental health professionals.13 Increased screening for psychiatric disorders throughout the peripartum period can help identify women at greater risk, and advancements in telepsychiatry could help meet the increased need for psychiatric care during COVID-19. Psychiatrists and other mental health clinicians should consider reaching out to their colleagues who specialize in women’s health to establish new partnerships and create teams of multidisciplinary professionals.
Similarly, psychiatrists should familiarize themselves with telehealth services available to peripartum patients who could benefit from such services. Telehealth options can increase women’s access to peripartum care for both medical and psychiatric illnesses. Online options such as women’s support groups, parenting classes, and labor coaching seminars also represent valuable virtual tools to strengthen women’s social supports.
Women who need inpatient treatment for severe peripartum depression or anxiety might be particularly reluctant to receive this care during COVID-19 due to fears of becoming infected and of being separated from their infant and family while hospitalized. Clinicians should remain vigilant in screening peripartum women for mood disorders that might represent a danger to mothers and infants, and not allow concerns about COVID-19 to interfere with recommendations for psychiatric hospitalizations, when necessary. The creation of small, women-only inpatient behavioral units can help address this situation, especially given the possibility of frequent visits with infants and other peripartum support. Investment into such units is critical for supporting peripartum mental health, even in nonpandemic times.
What about vaccination? As of mid-May 2021, no large clinical trials of any COVID-19 vaccine that included pregnant women had been completed. However, 2 small preliminary studies suggested that the mRNA vaccines are safe and effective during pregnancy.31,32 When counseling peripartum patients on the risks and benefits, clinicians need to rely on this evidence, animal trials, and limited data from inadvertent exposures during pregnancy. While every woman will weigh the risks and benefits for her own circumstances, the CDC, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine have all stated that the mRNA vaccines should be offered to pregnant and breastfeeding individuals who are eligible for vaccination.33 Rasmussen et al33 have published a useful resource for clinicians regarding COVID-19 vaccination and pregnant women.
Continue to: Bottom Line
Bottom Line
During the COVID-19 pandemic, peripartum women have experienced increased rates of anxiety, depression, and stress. Psychiatric clinicians can help these patients by remaining vigilant in screening for psychiatric disorders, encouraging them to engage in activities to mitigate COVID-19’s adverse psychological effects, and referring them to care via telehealth and other resources as appropriate.
Related Resources
- Hu YJ, Wake M, Saffery R. Clarifying the sweeping consequences of COVID-19 in pregnant women, newborns, and children with existing cohorts. JAMA Pediatr. 2021; 75(2):117-118. doi: 10.1001/jamapediatrics.2020.2395
- Tomfohr-Madsen LM, Racine N, Giesbrecht GF, et al. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2021; 300:113912. doi: 10.1016/j.psychres.2021.113912
1. Chivers BR, Garad RM, Boyle JA, et al. Perinatal distress during COVID-19: thematic analysis of an online parenting forum. J Med Internet Res. 2020;22(9):e22002. doi: 10.2196/22002
2. Ostacoli L, Cosma S, Bevilacqua F, et al. Psychosocial factors associated with postpartum psychological distress during the Covid-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703. doi: 10.1186/s12884-020-03399-5
3. Preis H, Mahaffey B, Heiselman C, etal. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. 2020;266:113348. doi: 10.1016/j.socscimed.2020.113348
4. Olson DM, Brémault-Phillips S, King S, et al. Recent Canadian efforts to develop population-level pregnancy intervention studies to mitigate effects of natural disasters and other tragedies. J Dev Orig Health Dis. 2019;10(1):108-114. doi: 10.1017/S2040174418001113
5. Watanabe Z, Iwama N, Nishigori H, et al. Japan Environment & Children’s Study Group. Psychological distress during pregnancy in Miyagi after the Great East Japan Earthquake: the Japan Environment and Children’s Study. J Affect Disord. 2016;190:341-348. doi: 10.1016/j.jad.2015.10.024
6. Xiong X, Harville EW, Mattison DR, et al. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med. 2010;5(3):181-187. doi: 10.5055/ajdm.2010.0020
7. Brooks SK, Weston D, Greenberg N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health. 2020;189:26-36. doi: 10.1016/j.puhe.2020.09.006
8. Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):39. doi: 10.1186/s40001-020-00439-w
9. Qi M, Li X, Liu S, et al. Impact of the COVID-19 epidemic on patterns of pregnant women’s perception of threat and its relationship to mental state: a latent class analysis. PLoS One. 2020;15(10):e0239697. doi: 10.1371/journal.pone.0239697
10. Centers for Disease Control and Prevention. Investigating the impact of COVID-19 during pregnancy. Updated February 4, 2021. Accessed April 29, 2021. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19/what-cdc-is-doing.html
11. Ahlberg M, Neovius M, Saltvedt S, et al. Association of SARS-CoV-2 test status and pregnancy outcomes. JAMA. 2020;324(17):1782-1785. doi: 10.1001/jama.2020.19124
12. Ashraf MA, Keshavarz P, Hosseinpour P, et al. Coronavirus disease 2019 (COVID-19): a systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil. 2020;21(3):157-168.
13. Nanjundaswamy MH, Shiva L, Desai G, et al. COVID-19-related anxiety and concerns expressed by pregnant and postpartum women-a survey among obstetricians. Arch Womens Ment Health. 2020; 23(6):787-790. doi: 10.1007/s00737-020-01060-w
14. Verdery AM, Smith-Greenaway E, Margolis R, et al. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci U S A. 2020;117(30):17695-17701. doi: 10.1073/pnas.2007476117
15. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494. doi: 10.1001/jama.2020.19632
16. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18-31. doi: 10.1016/j.jad.2017.07.045
17. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049-1057. doi:10.15585/mmwr.mm6932a1
18. Almeida M, Shrestha AD, Stojanac D, et al. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. 2020;23(6):741-748. doi:10.1007/s00737-020-01092-2
19. Office for National Statistics. Personal and economic well-being in Great Britain: May 2020. Published May 4, 2020. Accessed April 23, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/bulletins/personalandeconomicwellbeingintheuk/may2020
20. Kuehn BM. COVID-19 halts reproductive care for millions of women. JAMA. 2020;324(15):1489. doi: 10.1001/jama.2020.19025
21. Preis H, Mahaffey B, Lobel M. Psychometric properties of the Pandemic-Related Pregnancy Stress Scale (PREPS). J Psychosom Obstet Gynaecol. 2020;41(3):191-197. doi: 10.1080/0167482X.2020.1801625
22. Hermann A, Fitelson EM, Bergink V. Meeting maternal mental health needs during the COVID-19 pandemic. JAMA Psychiatry. 2020;78(2):123-124. doi: 10.1001/jamapsychiatry.2020.1947
23. Arora KS, Mauch JT, Gibson KS. Labor and delivery visitor policies during the COVID-19 pandemic: balancing risks and benefits. JAMA. 2020;323(24):2468-2469. doi: 10.1001/jama.2020.7563
24. Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. 2020;29(13-14):2047-2049. doi: 10.1111/jocn.15296
25. Connor J, Madhavan S, Mokashi M, et al. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc Sci Med. 2020;266:113364. doi: 10.1016/j.socscimed.2020.113364
26. Scharff X, Ryley S. Breaking: some states show alarming spike in women’s share of unemployment claims. The Fuller Project. Accessed April 23, 2021. https://fullerproject.org/story/some-states-shows-alarming-spike-in-womens-share-of-unemployment-claims/
27. Hessami K, Romanelli C, Chiurazzi M, et al. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2020;1-8. doi: 10.1080/14767058.2020.1843155
28. Yan H, Ding Y, Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front Psychol. 2020;11:617001. doi: 10.3389/fpsyg.2020.617001
29. Dib S, Rougeaux E, Vázquez-Vázquez A, et al. Maternal mental health and coping during the COVID-19 lockdown in the UK: data from the COVID-19 New Mum Study. Int J Gynaecol Obstet. 2020;151(3):407-414. doi: 10.1002/ijgo.13397
30. Bo HX, Yang Y, Chen J, et al. Prevalence of depressive symptoms among Chinese pregnant and postpartum women during the COVID-19 pandemic. Psychosom Med. 2020. doi: 10.1097/PSY.0000000000000904
31. Collier AY, McMahan K, Yu J, et al. Immunogenicity of COVID-19 mRNA vaccines in pregnant and lactating women. JAMA. 2021. doi:10.1001/jama.2021.7563
32. Shanes ED, Otero S, Mithal LB, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination in pregnancy: measures of immunity and placental histopathology. Obstet Gynecol. 2021. doi: 10.1097/AOG.0000000000004457
33. Rasmussen SA, Kelley CF, Horton JP, et al. Coronavirus disease 2019 (COVID-19) vaccines and pregnancy: what obstetricians need to know. Obstet Gynecol. 2021;137(3):408-414. doi: 10.1097/AOG.0000000000004290
The COVID-19 pandemic has had a negative impact on the mental health of people worldwide, and a disproportionate effect on peripartum women. In this article, we discuss the reasons for this disparity, review the limited literature on this topic, and suggest strategies to safeguard the mental health of peripartum women during the COVID-19 pandemic.
Catastrophic events and women’s mental health
During the peripartum period, women have increased psychosocial and physical health needs.1 In addition, women are disproportionately affected by natural disasters and catastrophic events,2 which are predictors of psychiatric symptoms during the peripartum period.3 Mass tragedies previously associated with maternal stress include wildfires, hurricanes, migrations, earthquakes, and tsunamis.4,5 For example, pregnant women who survived severe exposure during Hurricane Katrina (ie, feeling that one’s life was in danger, experiencing illness or injury to self or a family member, walking through floodwaters) in 2005 had a significantly increased risk of developing posttraumatic stress disorder (PTSD) and depression compared with pregnant women who did not have such exposure.6 After the 2011 Tōhoku earthquake and tsunami in Japan, the prevalence of psychological distress in pregnant women increased, especially among those living in the area directly affected by the tsunami.5
Epidemics and pandemics also can adversely affect peripartum women’s mental health. Studies conducted before the COVID-19 pandemic found that previous infectious disease outbreaks such as severe acute respiratory syndrome (SARS), the 2009 influenza A (H1N1) pandemic, and Zika had negative emotional impacts on pregnant women.7 Our review of the limited literature published to date suggests that COVID-19 is having similar adverse effects.
COVID-19 poses both medical and psychiatric threats
COVID-19 infection is a physical threat to pregnant women who are already vulnerable due to the hormonal and immunological changes inherent to pregnancy. A meta-analysis of 39 studies with a total of 1,316 pregnant women indicated that the most frequently reported symptoms of COVID-19 infection were cough, fever, and myalgias.8 However, COVID-19 infection during pregnancy is also associated with an increase in pregnancy complications and adverse birth outcomes.9 According to the CDC, compared with their nonpregnant counterparts, pregnant women are at greater risk for severe COVID-19 infection and adverse birth outcomes such as preterm birth.10 Pregnant women who are infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; the virus responsible for COVID-19) risk ICU admission, caesarean section, and perinatal death.8 A Swedish study of 2,682 pregnant women found an increase in preeclampsia among women who tested positive for SARS-CoV-2, a finding attributed to COVID-19’s pattern of systemic effects.11 Vertical transmission of the novel coronavirus from mother to fetus appears to be rare but possible.12
In addition to the physical dangers of becoming infected with COVID-19, the perceived threat of infection is an added source of anxiety for some peripartum women. In addition to the concerns involved in any pregnancy, COVID-19–related sources of distress for pregnant women include worrying about harm to the fetus during pregnancy, the possibility of vertical transmission, and exposures during antenatal appointments, during employment, or from a partner.8,13
The death toll from factors associated with COVID-19 adds to the mental health burden. For every person who dies of COVID-19, an estimated 9 others may develop prolonged grief or PTSD due to the loss of someone they loved.14,15 A systematic review found that PTSD in the perinatal period is associated with negative birth and child outcomes, including low birth weight and decreased rates of breastfeeding.16 The COVID-19 pandemic has disrupted human interactions, from social distancing rules and lockdowns of businesses and social activities to panic buying of grocery staples and increased economic insecurity.1 These changes have been accompanied by a rise in mental health challenges. For example, according to an August 2020 CDC survey, 40.9% of US adults reported at least 1 adverse mental or behavioral health condition, including symptoms of anxiety or depression (30.9%), symptoms of a trauma- and stressor-related disorder related to the pandemic (26.3%), and having started or increased substance use to cope with stress or emotions related to COVID-19 (13.3%).17
COVID-19–related traumas and stressors appear to affect women more than men. A study from China found that compared with men, women had significantly higher levels of self-reported pandemic-related anxiety, depression, and posttraumatic stress symptoms (PTSS).18 This trend has been observed in other parts of the world. A study conducted by the UK Office of National Statistics reported anxiety levels were 24% higher in women vs men as reflected by scores on a self-rated anxiety scale.19
Continue to: Many factors influence...
Many factors influence the disproportionate impact of COVID-19 on women in general, and peripartum women in particular (Box20-26).
Box
Factors that predispose women to increased stress during COVID-19 include an increase in child care burdens brought about by school closures and subsequent virtual schooling.20 Intimate partner violence has spiked globally during COVID-19 restrictions.24 Women also represent the majority of the health care workforce (76%) and often take on informal caregiving roles; both of these roles have seen increased burdens during the pandemic.25 Already encumbered by prepandemic gender pay inequalities, women are filing unemployment claims at a significantly increased rate compared to men.26
For women of childbearing age, the disruption of routine clinical care during COVID-19 has decreased access to reproductive health care, resulting in increases in unintended pregnancies, unsafe abortions, and deaths.20 Another source of stress for pregnant women during COVID-19 is feeling unprepared for birth because of the pandemic, a phenomenon described as “preparedness stress.”21 Visitor restriction policies and quarantines have also caused women in labor to experience birth without their support partners, which is associated with increased posttraumatic stress symptoms.22 These restrictions also may be associated with an increase in women choosing out-of-hospital births despite the increased risk of adverse outcomes.23
Psychiatric diagnoses in peripartum women
Multiple studies and meta-analyses have begun to assess the impact of the COVID-19 pandemic on maternal mental health. One meta-analysis of 8 studies conducted in 5 countries determined that COVID-19 significantly increases the risk of anxiety in women during the peripartum period.27 Results of another meta-analysis of 23 studies with >24,000 participants indicated that the prevalence of anxiety, depression, and insomnia in peripartum women was significantly higher during the pandemic than in pre-pandemic times.28
In an online survey of 4,451 pregnant women in the United States, nearly one-third of respondents reported elevated levels of pandemic-related stress as measured by the newly-developed Pandemic-Related Pregnancy Stress Scale.3 The rates were even higher among women who were already at risk for elevated stress levels, such as those who had survived abuse, those giving birth for the first time, or those experiencing high-risk pregnancies.3 Living in a pandemic “hot spot” also appeared to impact peripartum stress levels.
COVID-19 has adverse effects on women’s mental health specifically during the postpartum period. One study from a center in Italy found a high prevalence of depressive symptoms and PTSS in the postpartum period, with COVID-19–related factors playing an “indirect role” compared with prenatal experiences and other individual factors.2 A British study of mothers of infants age ≤12 months found that traveling for work, the impact of lockdown on food affordability, and having an income of less than £30,000 per year (approximately $41,000) predicted poorer mental health during the pandemic.29 Results of a study from China indicated that more than one-quarter of pregnant and postpartum women experienced depression during the pandemic, and women who worried about infection risk or missing pediatric visits were at increased risk.30
How to mitigate these risks
The increase in pandemic-related mental health concerns in the general population and specifically in peripartum women is a global health care challenge. Investing in mitigation strategies is necessary not only to address the current pandemic, but also to help prepare for the possibility of future traumatic events, such as another global pandemic.
Continue to: For pregnant women...
For pregnant women, ensuring access to outdoor space, increasing participation in healthy activities, and minimizing disruptions to prenatal care can protect against pandemic-related stress.3 Physical activity is an effective treatment for mild to moderate depressive symptoms. Because of the significant decrease in exercise among pregnant women during the pandemic, encouraging safe forms of physical activity such as online fitness classes could improve mental health outcomes for these patients.27 When counseling peripartum women, psychiatrists need to be creative in recommending fitness interventions to target mood symptoms, such as by suggesting virtual or at-home programs.
In an online survey, 118 obstetricians called for increased mental health resources for peripartum women, such as easier access to a helpline, educational videos, and mental health professionals.13 Increased screening for psychiatric disorders throughout the peripartum period can help identify women at greater risk, and advancements in telepsychiatry could help meet the increased need for psychiatric care during COVID-19. Psychiatrists and other mental health clinicians should consider reaching out to their colleagues who specialize in women’s health to establish new partnerships and create teams of multidisciplinary professionals.
Similarly, psychiatrists should familiarize themselves with telehealth services available to peripartum patients who could benefit from such services. Telehealth options can increase women’s access to peripartum care for both medical and psychiatric illnesses. Online options such as women’s support groups, parenting classes, and labor coaching seminars also represent valuable virtual tools to strengthen women’s social supports.
Women who need inpatient treatment for severe peripartum depression or anxiety might be particularly reluctant to receive this care during COVID-19 due to fears of becoming infected and of being separated from their infant and family while hospitalized. Clinicians should remain vigilant in screening peripartum women for mood disorders that might represent a danger to mothers and infants, and not allow concerns about COVID-19 to interfere with recommendations for psychiatric hospitalizations, when necessary. The creation of small, women-only inpatient behavioral units can help address this situation, especially given the possibility of frequent visits with infants and other peripartum support. Investment into such units is critical for supporting peripartum mental health, even in nonpandemic times.
What about vaccination? As of mid-May 2021, no large clinical trials of any COVID-19 vaccine that included pregnant women had been completed. However, 2 small preliminary studies suggested that the mRNA vaccines are safe and effective during pregnancy.31,32 When counseling peripartum patients on the risks and benefits, clinicians need to rely on this evidence, animal trials, and limited data from inadvertent exposures during pregnancy. While every woman will weigh the risks and benefits for her own circumstances, the CDC, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine have all stated that the mRNA vaccines should be offered to pregnant and breastfeeding individuals who are eligible for vaccination.33 Rasmussen et al33 have published a useful resource for clinicians regarding COVID-19 vaccination and pregnant women.
Continue to: Bottom Line
Bottom Line
During the COVID-19 pandemic, peripartum women have experienced increased rates of anxiety, depression, and stress. Psychiatric clinicians can help these patients by remaining vigilant in screening for psychiatric disorders, encouraging them to engage in activities to mitigate COVID-19’s adverse psychological effects, and referring them to care via telehealth and other resources as appropriate.
Related Resources
- Hu YJ, Wake M, Saffery R. Clarifying the sweeping consequences of COVID-19 in pregnant women, newborns, and children with existing cohorts. JAMA Pediatr. 2021; 75(2):117-118. doi: 10.1001/jamapediatrics.2020.2395
- Tomfohr-Madsen LM, Racine N, Giesbrecht GF, et al. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2021; 300:113912. doi: 10.1016/j.psychres.2021.113912
The COVID-19 pandemic has had a negative impact on the mental health of people worldwide, and a disproportionate effect on peripartum women. In this article, we discuss the reasons for this disparity, review the limited literature on this topic, and suggest strategies to safeguard the mental health of peripartum women during the COVID-19 pandemic.
Catastrophic events and women’s mental health
During the peripartum period, women have increased psychosocial and physical health needs.1 In addition, women are disproportionately affected by natural disasters and catastrophic events,2 which are predictors of psychiatric symptoms during the peripartum period.3 Mass tragedies previously associated with maternal stress include wildfires, hurricanes, migrations, earthquakes, and tsunamis.4,5 For example, pregnant women who survived severe exposure during Hurricane Katrina (ie, feeling that one’s life was in danger, experiencing illness or injury to self or a family member, walking through floodwaters) in 2005 had a significantly increased risk of developing posttraumatic stress disorder (PTSD) and depression compared with pregnant women who did not have such exposure.6 After the 2011 Tōhoku earthquake and tsunami in Japan, the prevalence of psychological distress in pregnant women increased, especially among those living in the area directly affected by the tsunami.5
Epidemics and pandemics also can adversely affect peripartum women’s mental health. Studies conducted before the COVID-19 pandemic found that previous infectious disease outbreaks such as severe acute respiratory syndrome (SARS), the 2009 influenza A (H1N1) pandemic, and Zika had negative emotional impacts on pregnant women.7 Our review of the limited literature published to date suggests that COVID-19 is having similar adverse effects.
COVID-19 poses both medical and psychiatric threats
COVID-19 infection is a physical threat to pregnant women who are already vulnerable due to the hormonal and immunological changes inherent to pregnancy. A meta-analysis of 39 studies with a total of 1,316 pregnant women indicated that the most frequently reported symptoms of COVID-19 infection were cough, fever, and myalgias.8 However, COVID-19 infection during pregnancy is also associated with an increase in pregnancy complications and adverse birth outcomes.9 According to the CDC, compared with their nonpregnant counterparts, pregnant women are at greater risk for severe COVID-19 infection and adverse birth outcomes such as preterm birth.10 Pregnant women who are infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; the virus responsible for COVID-19) risk ICU admission, caesarean section, and perinatal death.8 A Swedish study of 2,682 pregnant women found an increase in preeclampsia among women who tested positive for SARS-CoV-2, a finding attributed to COVID-19’s pattern of systemic effects.11 Vertical transmission of the novel coronavirus from mother to fetus appears to be rare but possible.12
In addition to the physical dangers of becoming infected with COVID-19, the perceived threat of infection is an added source of anxiety for some peripartum women. In addition to the concerns involved in any pregnancy, COVID-19–related sources of distress for pregnant women include worrying about harm to the fetus during pregnancy, the possibility of vertical transmission, and exposures during antenatal appointments, during employment, or from a partner.8,13
The death toll from factors associated with COVID-19 adds to the mental health burden. For every person who dies of COVID-19, an estimated 9 others may develop prolonged grief or PTSD due to the loss of someone they loved.14,15 A systematic review found that PTSD in the perinatal period is associated with negative birth and child outcomes, including low birth weight and decreased rates of breastfeeding.16 The COVID-19 pandemic has disrupted human interactions, from social distancing rules and lockdowns of businesses and social activities to panic buying of grocery staples and increased economic insecurity.1 These changes have been accompanied by a rise in mental health challenges. For example, according to an August 2020 CDC survey, 40.9% of US adults reported at least 1 adverse mental or behavioral health condition, including symptoms of anxiety or depression (30.9%), symptoms of a trauma- and stressor-related disorder related to the pandemic (26.3%), and having started or increased substance use to cope with stress or emotions related to COVID-19 (13.3%).17
COVID-19–related traumas and stressors appear to affect women more than men. A study from China found that compared with men, women had significantly higher levels of self-reported pandemic-related anxiety, depression, and posttraumatic stress symptoms (PTSS).18 This trend has been observed in other parts of the world. A study conducted by the UK Office of National Statistics reported anxiety levels were 24% higher in women vs men as reflected by scores on a self-rated anxiety scale.19
Continue to: Many factors influence...
Many factors influence the disproportionate impact of COVID-19 on women in general, and peripartum women in particular (Box20-26).
Box
Factors that predispose women to increased stress during COVID-19 include an increase in child care burdens brought about by school closures and subsequent virtual schooling.20 Intimate partner violence has spiked globally during COVID-19 restrictions.24 Women also represent the majority of the health care workforce (76%) and often take on informal caregiving roles; both of these roles have seen increased burdens during the pandemic.25 Already encumbered by prepandemic gender pay inequalities, women are filing unemployment claims at a significantly increased rate compared to men.26
For women of childbearing age, the disruption of routine clinical care during COVID-19 has decreased access to reproductive health care, resulting in increases in unintended pregnancies, unsafe abortions, and deaths.20 Another source of stress for pregnant women during COVID-19 is feeling unprepared for birth because of the pandemic, a phenomenon described as “preparedness stress.”21 Visitor restriction policies and quarantines have also caused women in labor to experience birth without their support partners, which is associated with increased posttraumatic stress symptoms.22 These restrictions also may be associated with an increase in women choosing out-of-hospital births despite the increased risk of adverse outcomes.23
Psychiatric diagnoses in peripartum women
Multiple studies and meta-analyses have begun to assess the impact of the COVID-19 pandemic on maternal mental health. One meta-analysis of 8 studies conducted in 5 countries determined that COVID-19 significantly increases the risk of anxiety in women during the peripartum period.27 Results of another meta-analysis of 23 studies with >24,000 participants indicated that the prevalence of anxiety, depression, and insomnia in peripartum women was significantly higher during the pandemic than in pre-pandemic times.28
In an online survey of 4,451 pregnant women in the United States, nearly one-third of respondents reported elevated levels of pandemic-related stress as measured by the newly-developed Pandemic-Related Pregnancy Stress Scale.3 The rates were even higher among women who were already at risk for elevated stress levels, such as those who had survived abuse, those giving birth for the first time, or those experiencing high-risk pregnancies.3 Living in a pandemic “hot spot” also appeared to impact peripartum stress levels.
COVID-19 has adverse effects on women’s mental health specifically during the postpartum period. One study from a center in Italy found a high prevalence of depressive symptoms and PTSS in the postpartum period, with COVID-19–related factors playing an “indirect role” compared with prenatal experiences and other individual factors.2 A British study of mothers of infants age ≤12 months found that traveling for work, the impact of lockdown on food affordability, and having an income of less than £30,000 per year (approximately $41,000) predicted poorer mental health during the pandemic.29 Results of a study from China indicated that more than one-quarter of pregnant and postpartum women experienced depression during the pandemic, and women who worried about infection risk or missing pediatric visits were at increased risk.30
How to mitigate these risks
The increase in pandemic-related mental health concerns in the general population and specifically in peripartum women is a global health care challenge. Investing in mitigation strategies is necessary not only to address the current pandemic, but also to help prepare for the possibility of future traumatic events, such as another global pandemic.
Continue to: For pregnant women...
For pregnant women, ensuring access to outdoor space, increasing participation in healthy activities, and minimizing disruptions to prenatal care can protect against pandemic-related stress.3 Physical activity is an effective treatment for mild to moderate depressive symptoms. Because of the significant decrease in exercise among pregnant women during the pandemic, encouraging safe forms of physical activity such as online fitness classes could improve mental health outcomes for these patients.27 When counseling peripartum women, psychiatrists need to be creative in recommending fitness interventions to target mood symptoms, such as by suggesting virtual or at-home programs.
In an online survey, 118 obstetricians called for increased mental health resources for peripartum women, such as easier access to a helpline, educational videos, and mental health professionals.13 Increased screening for psychiatric disorders throughout the peripartum period can help identify women at greater risk, and advancements in telepsychiatry could help meet the increased need for psychiatric care during COVID-19. Psychiatrists and other mental health clinicians should consider reaching out to their colleagues who specialize in women’s health to establish new partnerships and create teams of multidisciplinary professionals.
Similarly, psychiatrists should familiarize themselves with telehealth services available to peripartum patients who could benefit from such services. Telehealth options can increase women’s access to peripartum care for both medical and psychiatric illnesses. Online options such as women’s support groups, parenting classes, and labor coaching seminars also represent valuable virtual tools to strengthen women’s social supports.
Women who need inpatient treatment for severe peripartum depression or anxiety might be particularly reluctant to receive this care during COVID-19 due to fears of becoming infected and of being separated from their infant and family while hospitalized. Clinicians should remain vigilant in screening peripartum women for mood disorders that might represent a danger to mothers and infants, and not allow concerns about COVID-19 to interfere with recommendations for psychiatric hospitalizations, when necessary. The creation of small, women-only inpatient behavioral units can help address this situation, especially given the possibility of frequent visits with infants and other peripartum support. Investment into such units is critical for supporting peripartum mental health, even in nonpandemic times.
What about vaccination? As of mid-May 2021, no large clinical trials of any COVID-19 vaccine that included pregnant women had been completed. However, 2 small preliminary studies suggested that the mRNA vaccines are safe and effective during pregnancy.31,32 When counseling peripartum patients on the risks and benefits, clinicians need to rely on this evidence, animal trials, and limited data from inadvertent exposures during pregnancy. While every woman will weigh the risks and benefits for her own circumstances, the CDC, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine have all stated that the mRNA vaccines should be offered to pregnant and breastfeeding individuals who are eligible for vaccination.33 Rasmussen et al33 have published a useful resource for clinicians regarding COVID-19 vaccination and pregnant women.
Continue to: Bottom Line
Bottom Line
During the COVID-19 pandemic, peripartum women have experienced increased rates of anxiety, depression, and stress. Psychiatric clinicians can help these patients by remaining vigilant in screening for psychiatric disorders, encouraging them to engage in activities to mitigate COVID-19’s adverse psychological effects, and referring them to care via telehealth and other resources as appropriate.
Related Resources
- Hu YJ, Wake M, Saffery R. Clarifying the sweeping consequences of COVID-19 in pregnant women, newborns, and children with existing cohorts. JAMA Pediatr. 2021; 75(2):117-118. doi: 10.1001/jamapediatrics.2020.2395
- Tomfohr-Madsen LM, Racine N, Giesbrecht GF, et al. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2021; 300:113912. doi: 10.1016/j.psychres.2021.113912
1. Chivers BR, Garad RM, Boyle JA, et al. Perinatal distress during COVID-19: thematic analysis of an online parenting forum. J Med Internet Res. 2020;22(9):e22002. doi: 10.2196/22002
2. Ostacoli L, Cosma S, Bevilacqua F, et al. Psychosocial factors associated with postpartum psychological distress during the Covid-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703. doi: 10.1186/s12884-020-03399-5
3. Preis H, Mahaffey B, Heiselman C, etal. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. 2020;266:113348. doi: 10.1016/j.socscimed.2020.113348
4. Olson DM, Brémault-Phillips S, King S, et al. Recent Canadian efforts to develop population-level pregnancy intervention studies to mitigate effects of natural disasters and other tragedies. J Dev Orig Health Dis. 2019;10(1):108-114. doi: 10.1017/S2040174418001113
5. Watanabe Z, Iwama N, Nishigori H, et al. Japan Environment & Children’s Study Group. Psychological distress during pregnancy in Miyagi after the Great East Japan Earthquake: the Japan Environment and Children’s Study. J Affect Disord. 2016;190:341-348. doi: 10.1016/j.jad.2015.10.024
6. Xiong X, Harville EW, Mattison DR, et al. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med. 2010;5(3):181-187. doi: 10.5055/ajdm.2010.0020
7. Brooks SK, Weston D, Greenberg N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health. 2020;189:26-36. doi: 10.1016/j.puhe.2020.09.006
8. Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):39. doi: 10.1186/s40001-020-00439-w
9. Qi M, Li X, Liu S, et al. Impact of the COVID-19 epidemic on patterns of pregnant women’s perception of threat and its relationship to mental state: a latent class analysis. PLoS One. 2020;15(10):e0239697. doi: 10.1371/journal.pone.0239697
10. Centers for Disease Control and Prevention. Investigating the impact of COVID-19 during pregnancy. Updated February 4, 2021. Accessed April 29, 2021. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19/what-cdc-is-doing.html
11. Ahlberg M, Neovius M, Saltvedt S, et al. Association of SARS-CoV-2 test status and pregnancy outcomes. JAMA. 2020;324(17):1782-1785. doi: 10.1001/jama.2020.19124
12. Ashraf MA, Keshavarz P, Hosseinpour P, et al. Coronavirus disease 2019 (COVID-19): a systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil. 2020;21(3):157-168.
13. Nanjundaswamy MH, Shiva L, Desai G, et al. COVID-19-related anxiety and concerns expressed by pregnant and postpartum women-a survey among obstetricians. Arch Womens Ment Health. 2020; 23(6):787-790. doi: 10.1007/s00737-020-01060-w
14. Verdery AM, Smith-Greenaway E, Margolis R, et al. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci U S A. 2020;117(30):17695-17701. doi: 10.1073/pnas.2007476117
15. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494. doi: 10.1001/jama.2020.19632
16. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18-31. doi: 10.1016/j.jad.2017.07.045
17. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049-1057. doi:10.15585/mmwr.mm6932a1
18. Almeida M, Shrestha AD, Stojanac D, et al. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. 2020;23(6):741-748. doi:10.1007/s00737-020-01092-2
19. Office for National Statistics. Personal and economic well-being in Great Britain: May 2020. Published May 4, 2020. Accessed April 23, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/bulletins/personalandeconomicwellbeingintheuk/may2020
20. Kuehn BM. COVID-19 halts reproductive care for millions of women. JAMA. 2020;324(15):1489. doi: 10.1001/jama.2020.19025
21. Preis H, Mahaffey B, Lobel M. Psychometric properties of the Pandemic-Related Pregnancy Stress Scale (PREPS). J Psychosom Obstet Gynaecol. 2020;41(3):191-197. doi: 10.1080/0167482X.2020.1801625
22. Hermann A, Fitelson EM, Bergink V. Meeting maternal mental health needs during the COVID-19 pandemic. JAMA Psychiatry. 2020;78(2):123-124. doi: 10.1001/jamapsychiatry.2020.1947
23. Arora KS, Mauch JT, Gibson KS. Labor and delivery visitor policies during the COVID-19 pandemic: balancing risks and benefits. JAMA. 2020;323(24):2468-2469. doi: 10.1001/jama.2020.7563
24. Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. 2020;29(13-14):2047-2049. doi: 10.1111/jocn.15296
25. Connor J, Madhavan S, Mokashi M, et al. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc Sci Med. 2020;266:113364. doi: 10.1016/j.socscimed.2020.113364
26. Scharff X, Ryley S. Breaking: some states show alarming spike in women’s share of unemployment claims. The Fuller Project. Accessed April 23, 2021. https://fullerproject.org/story/some-states-shows-alarming-spike-in-womens-share-of-unemployment-claims/
27. Hessami K, Romanelli C, Chiurazzi M, et al. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2020;1-8. doi: 10.1080/14767058.2020.1843155
28. Yan H, Ding Y, Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front Psychol. 2020;11:617001. doi: 10.3389/fpsyg.2020.617001
29. Dib S, Rougeaux E, Vázquez-Vázquez A, et al. Maternal mental health and coping during the COVID-19 lockdown in the UK: data from the COVID-19 New Mum Study. Int J Gynaecol Obstet. 2020;151(3):407-414. doi: 10.1002/ijgo.13397
30. Bo HX, Yang Y, Chen J, et al. Prevalence of depressive symptoms among Chinese pregnant and postpartum women during the COVID-19 pandemic. Psychosom Med. 2020. doi: 10.1097/PSY.0000000000000904
31. Collier AY, McMahan K, Yu J, et al. Immunogenicity of COVID-19 mRNA vaccines in pregnant and lactating women. JAMA. 2021. doi:10.1001/jama.2021.7563
32. Shanes ED, Otero S, Mithal LB, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination in pregnancy: measures of immunity and placental histopathology. Obstet Gynecol. 2021. doi: 10.1097/AOG.0000000000004457
33. Rasmussen SA, Kelley CF, Horton JP, et al. Coronavirus disease 2019 (COVID-19) vaccines and pregnancy: what obstetricians need to know. Obstet Gynecol. 2021;137(3):408-414. doi: 10.1097/AOG.0000000000004290
1. Chivers BR, Garad RM, Boyle JA, et al. Perinatal distress during COVID-19: thematic analysis of an online parenting forum. J Med Internet Res. 2020;22(9):e22002. doi: 10.2196/22002
2. Ostacoli L, Cosma S, Bevilacqua F, et al. Psychosocial factors associated with postpartum psychological distress during the Covid-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703. doi: 10.1186/s12884-020-03399-5
3. Preis H, Mahaffey B, Heiselman C, etal. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. 2020;266:113348. doi: 10.1016/j.socscimed.2020.113348
4. Olson DM, Brémault-Phillips S, King S, et al. Recent Canadian efforts to develop population-level pregnancy intervention studies to mitigate effects of natural disasters and other tragedies. J Dev Orig Health Dis. 2019;10(1):108-114. doi: 10.1017/S2040174418001113
5. Watanabe Z, Iwama N, Nishigori H, et al. Japan Environment & Children’s Study Group. Psychological distress during pregnancy in Miyagi after the Great East Japan Earthquake: the Japan Environment and Children’s Study. J Affect Disord. 2016;190:341-348. doi: 10.1016/j.jad.2015.10.024
6. Xiong X, Harville EW, Mattison DR, et al. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med. 2010;5(3):181-187. doi: 10.5055/ajdm.2010.0020
7. Brooks SK, Weston D, Greenberg N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health. 2020;189:26-36. doi: 10.1016/j.puhe.2020.09.006
8. Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):39. doi: 10.1186/s40001-020-00439-w
9. Qi M, Li X, Liu S, et al. Impact of the COVID-19 epidemic on patterns of pregnant women’s perception of threat and its relationship to mental state: a latent class analysis. PLoS One. 2020;15(10):e0239697. doi: 10.1371/journal.pone.0239697
10. Centers for Disease Control and Prevention. Investigating the impact of COVID-19 during pregnancy. Updated February 4, 2021. Accessed April 29, 2021. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19/what-cdc-is-doing.html
11. Ahlberg M, Neovius M, Saltvedt S, et al. Association of SARS-CoV-2 test status and pregnancy outcomes. JAMA. 2020;324(17):1782-1785. doi: 10.1001/jama.2020.19124
12. Ashraf MA, Keshavarz P, Hosseinpour P, et al. Coronavirus disease 2019 (COVID-19): a systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil. 2020;21(3):157-168.
13. Nanjundaswamy MH, Shiva L, Desai G, et al. COVID-19-related anxiety and concerns expressed by pregnant and postpartum women-a survey among obstetricians. Arch Womens Ment Health. 2020; 23(6):787-790. doi: 10.1007/s00737-020-01060-w
14. Verdery AM, Smith-Greenaway E, Margolis R, et al. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci U S A. 2020;117(30):17695-17701. doi: 10.1073/pnas.2007476117
15. Simon NM, Saxe GN, Marmar CR. Mental health disorders related to COVID-19-related deaths. JAMA. 2020;324(15):1493-1494. doi: 10.1001/jama.2020.19632
16. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18-31. doi: 10.1016/j.jad.2017.07.045
17. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049-1057. doi:10.15585/mmwr.mm6932a1
18. Almeida M, Shrestha AD, Stojanac D, et al. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. 2020;23(6):741-748. doi:10.1007/s00737-020-01092-2
19. Office for National Statistics. Personal and economic well-being in Great Britain: May 2020. Published May 4, 2020. Accessed April 23, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/bulletins/personalandeconomicwellbeingintheuk/may2020
20. Kuehn BM. COVID-19 halts reproductive care for millions of women. JAMA. 2020;324(15):1489. doi: 10.1001/jama.2020.19025
21. Preis H, Mahaffey B, Lobel M. Psychometric properties of the Pandemic-Related Pregnancy Stress Scale (PREPS). J Psychosom Obstet Gynaecol. 2020;41(3):191-197. doi: 10.1080/0167482X.2020.1801625
22. Hermann A, Fitelson EM, Bergink V. Meeting maternal mental health needs during the COVID-19 pandemic. JAMA Psychiatry. 2020;78(2):123-124. doi: 10.1001/jamapsychiatry.2020.1947
23. Arora KS, Mauch JT, Gibson KS. Labor and delivery visitor policies during the COVID-19 pandemic: balancing risks and benefits. JAMA. 2020;323(24):2468-2469. doi: 10.1001/jama.2020.7563
24. Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. 2020;29(13-14):2047-2049. doi: 10.1111/jocn.15296
25. Connor J, Madhavan S, Mokashi M, et al. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc Sci Med. 2020;266:113364. doi: 10.1016/j.socscimed.2020.113364
26. Scharff X, Ryley S. Breaking: some states show alarming spike in women’s share of unemployment claims. The Fuller Project. Accessed April 23, 2021. https://fullerproject.org/story/some-states-shows-alarming-spike-in-womens-share-of-unemployment-claims/
27. Hessami K, Romanelli C, Chiurazzi M, et al. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2020;1-8. doi: 10.1080/14767058.2020.1843155
28. Yan H, Ding Y, Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front Psychol. 2020;11:617001. doi: 10.3389/fpsyg.2020.617001
29. Dib S, Rougeaux E, Vázquez-Vázquez A, et al. Maternal mental health and coping during the COVID-19 lockdown in the UK: data from the COVID-19 New Mum Study. Int J Gynaecol Obstet. 2020;151(3):407-414. doi: 10.1002/ijgo.13397
30. Bo HX, Yang Y, Chen J, et al. Prevalence of depressive symptoms among Chinese pregnant and postpartum women during the COVID-19 pandemic. Psychosom Med. 2020. doi: 10.1097/PSY.0000000000000904
31. Collier AY, McMahan K, Yu J, et al. Immunogenicity of COVID-19 mRNA vaccines in pregnant and lactating women. JAMA. 2021. doi:10.1001/jama.2021.7563
32. Shanes ED, Otero S, Mithal LB, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination in pregnancy: measures of immunity and placental histopathology. Obstet Gynecol. 2021. doi: 10.1097/AOG.0000000000004457
33. Rasmussen SA, Kelley CF, Horton JP, et al. Coronavirus disease 2019 (COVID-19) vaccines and pregnancy: what obstetricians need to know. Obstet Gynecol. 2021;137(3):408-414. doi: 10.1097/AOG.0000000000004290
What brought me back from the brink of suicide: A physician’s story
William Lynes, MD, had a flourishing medical practice and a fulfilling family life with three children when he first attempted suicide in 1999 at age 45. By 2003, depression and two more suicide attempts led to his early retirement.
In a session at the recent virtual American Psychiatric Association (APA) 2021 annual meeting, Dr. Lynes talked about the challenges of dealing with depression while managing the stresses of a career in medicine. The session in which he spoke was called, “The Suicidal Physician: Narratives From a Physician Who Survived and the Physician Widow of One Who Did Not.”
By writing and speaking about his experiences, he says, he has been able to retain his identity as a physician and avoid obsessive thoughts about suicide. He hopes conversations like these help other physicians feel less alone and enable them to push past stigmas to get the help they need. He suspects they do. More than 600 people joined the APA session, and Dr. Lynes received dozens of thankful messages afterward.
“I love medicine, but intrinsically, the practice of medicine is stressful, and you can’t get away,” said Dr. Lynes, a retired urologist in Temecula, Calif. “As far as feedback, it made me feel like it’s something I should continue to do.”
A way to heal
For Dr. Lynes, his “downward spiral into darkness” began with a series of catastrophic medical events starting in 1998, when he came home from a family vacation in Mexico feeling unwell. He didn’t bother to do anything about it – typical of a physician, he says. Then one night he woke up shaking with chills and fever. Soon he was in the hospital with respiratory failure from septic shock.
Dr. Lynes spent 6 weeks in the intensive care unit, including 4 weeks on a ventilator. He underwent a tracheostomy. He lost 40 pounds and experienced ICU-related delirium. It was a terrifying time, he said. When he tried to return to work 10 months later, he didn’t feel as though he could function normally.
Having once been a driven doctor who worked long hours, he now doubted himself and dreaded giving patients bad news. Spontaneously, he tried to take his own life.
Afterward, he concealed what had happened from everyone except his wife and managed to resume his practice. However, he was unable to regain the enthusiasm he had once had for his work. Although he had experienced depression before, this time it was unrelenting.
He sought help from a psychiatrist, received a diagnosis of bipolar disorder, and began taking medication. Still, he struggled to fulfill his responsibilities. Then in April 2002, he had a snowboarding accident that caused multiple facial fractures and required five operations. When he returned to work this time, he felt like a failure but resisted asking colleagues for help.
A few months later, Dr. Lynes again attempted suicide, which led to another stay in the ICU and more time on a ventilator. Doctors told his family they didn’t think he would survive. When he recovered, he spent time as an inpatient in a psychiatric ward, where he received the first of a series of electroconvulsive therapy sessions. Compounding his anxiety and depression was the inability to come to terms with his life if he were not able to practice medicine.
The next fall, in September 2003, his third suicide attempt took place in his office on a weekend when no one was around. After locking the door, he looked at his reflection in the frame of his medical school diploma. The glass was cracked. “It was dark, it was black, it was cold,” he said. “I can remember seeing my reflection and thinking how disgusted I was.”
For years after that, Dr. Lynes struggled with his sense of self-worth. He hid from the medical system and dreaded doctors’ appointments. Finally in 2016, he found new meaning at a writing conference, where he met a fellow physician whose story was similar to his. She encouraged him to write about his experience. His essay was published in Annals of Internal Medicine that year. “Then I started speaking, and I feel like I’m a physician again,” he said. “That has really healed me quite a bit.”
Why physicians die by suicide
Working in health care can be extremely stressful, even in the best of times, said Michael Myers, MD, a psychiatrist at State University of New York, Brooklyn, and author of the book, “Why Physicians Die By Suicide: Lessons Learned From Their Families and Others Who Cared.”
Years of school and training culminate in a career in which demands are relentless. Societal expectations are high. Many doctors are perfectionists by nature, and physicians tend to feel intense pressure to compete for coveted positions.
Stress starts early in a medical career. A 2016 systematic review and meta-analysis of 183 studies from 43 countries showed that nearly 30% of medical students experienced symptoms of depression and that 11% reported suicidal thoughts, but only 15% sought help.
A 2015 review of 31 studies that involved residents showed that rates of depression remained close to 30% and that about three-quarters of trainees meet criteria for burnout, a type of emotional exhaustion and sense of inadequacy that can result from chronic stress at work.
The stress of medical training appears to be a direct cause of mental health struggles. Rates of depression are higher among those working to become physicians than among their peers of the same age, research shows. In addition, symptoms become more prevalent as people progress through their training.
The COVID-19 pandemic has added stress to an already stressful job. Of more than 2,300 physicians surveyed in August 2020 by the Physicians Foundation, a physicians advocacy organization, 50% indicated that they experienced excessive anger, tearfulness, or anxiety because of the way the pandemic affected their work; 30% felt hopeless or lacking purpose; and 8% had thoughts of self-harm related to the pandemic. Rates of burnout had risen from 40% in 2018 to 58%.
Those problems might be even more acute in places experiencing other types of crises. A 2020 study of 154 emergency department (ED) physicians in Libya, which is in the midst of a civil war, found that 65% were experiencing anxiety, 73% were showing signs of depression, and 68% felt emotionally exhausted.
Every story is different
It is unclear how common suicide is among physicians. One often-repeated estimate is that 300-400 physicians die by suicide each year, but no one is certain how that number was determined, said Dr. Myers, who organized the APA panel.
Studies on suicide are inconsistent, and trends are hard to pinpoint. Anecdotally, he has received just as many calls about physician suicides in the past year as he did before the pandemic started.
Every person is different, and so is every death. Sometimes, career problems have nothing to do with a physician’s suicide, Dr. Myers said. When job stress does play a role, factors are often varied and complex.
After a 35-year career as a double board certified ED physician, Matthew Seaman, MD, retired in January 2017. The same month, a patient filed a complaint against him with the Washington State medical board, which led to an investigation and a lawsuit.
The case was hard on Dr. Seaman, who had continued to work night shifts throughout his career and had won a Hero Award from the American Board of Emergency Medicine, said his wife, Linda Seaman, MD, a family practitioner in Yakima, Wash., who also spoke on the APA panel.
Dr. Seaman said that 2 years after the investigation started, her husband was growing increasingly depressed. In 2019, he testified in a deposition. She said the plaintiff’s attorney “tried every way he could to shame Matt, humiliate Matt, make him believe he was a very bad doctor.” Three days later, he died by suicide at age 62.
Looking back at the year leading up to her husband’s death, Dr. Seaman recognizes multiple obstacles that interfered with her husband’s ability to get help, including frustrating interactions with psychiatrists and the couple’s insurance company.
His identity and experience as a physician also played a role. A couple of months before he died, she tried unsuccessfully to reach his psychiatrist, whose office suggested he go to the ED. However, because he worked as an ED doctor in their small town, he wouldn’t go. Dr. Seaman suspects he was wary of the stigma.
Burnout likely set him up to cave in after decades of work on the front lines, she added. Working in the ED exposes providers to horrific, traumatic cases every day, she said. Physicians learn to suppress their own emotions to deal with what they encounter. Stuffing their feelings can lead to posttraumatic stress. “You just perform,” she said. “You learn to do that.”
A real gift
Whenever Dr. Myers hears stories about doctors who died by suicide or who have written about their mental health struggles to help others, he contacts them. One goal of his own writing and of the conference sessions he organizes is to make it easier for others to share their own stories.
“I tell them, first of all, their courage and honesty is a real gift, and they’re saving lives,” he said. “There are so many suffering doctors out there who think that they’re the only one.”
Public conversations such as those that occurred in the APA session also offer opportunities to share advice, including Dr. Myers’ recommendation that doctors be sure they have a primary care physician of their own.
Many don’t, he says, because they say they are too busy, they can treat their own symptoms, or they can self-refer to specialists when needed. But physicians don’t always recognize symptoms of depression in themselves, and when mental health problems arise, they may not seek help or treat themselves appropriately.
A primary care physician can be the first person to recognize a mental health problem and refer a patient for mental health care, said Dr. Myers, whose latest book, “Becoming a Doctors’ Doctor: A Memoir,” explores his experiences treating doctors with burnout and other mental health problems.
Whether they have a primary care doctor or not, he suggests that physicians talk to anyone they trust – a social worker, a religious leader, or a family member who can then help them find the right sort of care.
In the United States, around-the-clock help is available through the National Suicide Prevention Lifeline at 800-273-8255. A psychiatrist-run hotline specifically for physicians is available at 888-409-0141. “Reach out and get some help,” Dr. Myers said. “Just don’t do it alone.”
Dr. Lynes advocates setting boundaries between life and work. He has also benefited from writing about his experiences. A blog or a diary can help physicians process their feelings, he said. His 2016 essay marked a major turning point in his life, giving his life meaning in helping others.
“Since I wrote that article, I can’t tell you how much better I am,” he said. “Now, I’m not embarrassed to be around physicians. I actually consider myself a physician. I didn’t for many, many years. So, I’m doing pretty well.”
A version of this article first appeared on Medscape.com.
William Lynes, MD, had a flourishing medical practice and a fulfilling family life with three children when he first attempted suicide in 1999 at age 45. By 2003, depression and two more suicide attempts led to his early retirement.
In a session at the recent virtual American Psychiatric Association (APA) 2021 annual meeting, Dr. Lynes talked about the challenges of dealing with depression while managing the stresses of a career in medicine. The session in which he spoke was called, “The Suicidal Physician: Narratives From a Physician Who Survived and the Physician Widow of One Who Did Not.”
By writing and speaking about his experiences, he says, he has been able to retain his identity as a physician and avoid obsessive thoughts about suicide. He hopes conversations like these help other physicians feel less alone and enable them to push past stigmas to get the help they need. He suspects they do. More than 600 people joined the APA session, and Dr. Lynes received dozens of thankful messages afterward.
“I love medicine, but intrinsically, the practice of medicine is stressful, and you can’t get away,” said Dr. Lynes, a retired urologist in Temecula, Calif. “As far as feedback, it made me feel like it’s something I should continue to do.”
A way to heal
For Dr. Lynes, his “downward spiral into darkness” began with a series of catastrophic medical events starting in 1998, when he came home from a family vacation in Mexico feeling unwell. He didn’t bother to do anything about it – typical of a physician, he says. Then one night he woke up shaking with chills and fever. Soon he was in the hospital with respiratory failure from septic shock.
Dr. Lynes spent 6 weeks in the intensive care unit, including 4 weeks on a ventilator. He underwent a tracheostomy. He lost 40 pounds and experienced ICU-related delirium. It was a terrifying time, he said. When he tried to return to work 10 months later, he didn’t feel as though he could function normally.
Having once been a driven doctor who worked long hours, he now doubted himself and dreaded giving patients bad news. Spontaneously, he tried to take his own life.
Afterward, he concealed what had happened from everyone except his wife and managed to resume his practice. However, he was unable to regain the enthusiasm he had once had for his work. Although he had experienced depression before, this time it was unrelenting.
He sought help from a psychiatrist, received a diagnosis of bipolar disorder, and began taking medication. Still, he struggled to fulfill his responsibilities. Then in April 2002, he had a snowboarding accident that caused multiple facial fractures and required five operations. When he returned to work this time, he felt like a failure but resisted asking colleagues for help.
A few months later, Dr. Lynes again attempted suicide, which led to another stay in the ICU and more time on a ventilator. Doctors told his family they didn’t think he would survive. When he recovered, he spent time as an inpatient in a psychiatric ward, where he received the first of a series of electroconvulsive therapy sessions. Compounding his anxiety and depression was the inability to come to terms with his life if he were not able to practice medicine.
The next fall, in September 2003, his third suicide attempt took place in his office on a weekend when no one was around. After locking the door, he looked at his reflection in the frame of his medical school diploma. The glass was cracked. “It was dark, it was black, it was cold,” he said. “I can remember seeing my reflection and thinking how disgusted I was.”
For years after that, Dr. Lynes struggled with his sense of self-worth. He hid from the medical system and dreaded doctors’ appointments. Finally in 2016, he found new meaning at a writing conference, where he met a fellow physician whose story was similar to his. She encouraged him to write about his experience. His essay was published in Annals of Internal Medicine that year. “Then I started speaking, and I feel like I’m a physician again,” he said. “That has really healed me quite a bit.”
Why physicians die by suicide
Working in health care can be extremely stressful, even in the best of times, said Michael Myers, MD, a psychiatrist at State University of New York, Brooklyn, and author of the book, “Why Physicians Die By Suicide: Lessons Learned From Their Families and Others Who Cared.”
Years of school and training culminate in a career in which demands are relentless. Societal expectations are high. Many doctors are perfectionists by nature, and physicians tend to feel intense pressure to compete for coveted positions.
Stress starts early in a medical career. A 2016 systematic review and meta-analysis of 183 studies from 43 countries showed that nearly 30% of medical students experienced symptoms of depression and that 11% reported suicidal thoughts, but only 15% sought help.
A 2015 review of 31 studies that involved residents showed that rates of depression remained close to 30% and that about three-quarters of trainees meet criteria for burnout, a type of emotional exhaustion and sense of inadequacy that can result from chronic stress at work.
The stress of medical training appears to be a direct cause of mental health struggles. Rates of depression are higher among those working to become physicians than among their peers of the same age, research shows. In addition, symptoms become more prevalent as people progress through their training.
The COVID-19 pandemic has added stress to an already stressful job. Of more than 2,300 physicians surveyed in August 2020 by the Physicians Foundation, a physicians advocacy organization, 50% indicated that they experienced excessive anger, tearfulness, or anxiety because of the way the pandemic affected their work; 30% felt hopeless or lacking purpose; and 8% had thoughts of self-harm related to the pandemic. Rates of burnout had risen from 40% in 2018 to 58%.
Those problems might be even more acute in places experiencing other types of crises. A 2020 study of 154 emergency department (ED) physicians in Libya, which is in the midst of a civil war, found that 65% were experiencing anxiety, 73% were showing signs of depression, and 68% felt emotionally exhausted.
Every story is different
It is unclear how common suicide is among physicians. One often-repeated estimate is that 300-400 physicians die by suicide each year, but no one is certain how that number was determined, said Dr. Myers, who organized the APA panel.
Studies on suicide are inconsistent, and trends are hard to pinpoint. Anecdotally, he has received just as many calls about physician suicides in the past year as he did before the pandemic started.
Every person is different, and so is every death. Sometimes, career problems have nothing to do with a physician’s suicide, Dr. Myers said. When job stress does play a role, factors are often varied and complex.
After a 35-year career as a double board certified ED physician, Matthew Seaman, MD, retired in January 2017. The same month, a patient filed a complaint against him with the Washington State medical board, which led to an investigation and a lawsuit.
The case was hard on Dr. Seaman, who had continued to work night shifts throughout his career and had won a Hero Award from the American Board of Emergency Medicine, said his wife, Linda Seaman, MD, a family practitioner in Yakima, Wash., who also spoke on the APA panel.
Dr. Seaman said that 2 years after the investigation started, her husband was growing increasingly depressed. In 2019, he testified in a deposition. She said the plaintiff’s attorney “tried every way he could to shame Matt, humiliate Matt, make him believe he was a very bad doctor.” Three days later, he died by suicide at age 62.
Looking back at the year leading up to her husband’s death, Dr. Seaman recognizes multiple obstacles that interfered with her husband’s ability to get help, including frustrating interactions with psychiatrists and the couple’s insurance company.
His identity and experience as a physician also played a role. A couple of months before he died, she tried unsuccessfully to reach his psychiatrist, whose office suggested he go to the ED. However, because he worked as an ED doctor in their small town, he wouldn’t go. Dr. Seaman suspects he was wary of the stigma.
Burnout likely set him up to cave in after decades of work on the front lines, she added. Working in the ED exposes providers to horrific, traumatic cases every day, she said. Physicians learn to suppress their own emotions to deal with what they encounter. Stuffing their feelings can lead to posttraumatic stress. “You just perform,” she said. “You learn to do that.”
A real gift
Whenever Dr. Myers hears stories about doctors who died by suicide or who have written about their mental health struggles to help others, he contacts them. One goal of his own writing and of the conference sessions he organizes is to make it easier for others to share their own stories.
“I tell them, first of all, their courage and honesty is a real gift, and they’re saving lives,” he said. “There are so many suffering doctors out there who think that they’re the only one.”
Public conversations such as those that occurred in the APA session also offer opportunities to share advice, including Dr. Myers’ recommendation that doctors be sure they have a primary care physician of their own.
Many don’t, he says, because they say they are too busy, they can treat their own symptoms, or they can self-refer to specialists when needed. But physicians don’t always recognize symptoms of depression in themselves, and when mental health problems arise, they may not seek help or treat themselves appropriately.
A primary care physician can be the first person to recognize a mental health problem and refer a patient for mental health care, said Dr. Myers, whose latest book, “Becoming a Doctors’ Doctor: A Memoir,” explores his experiences treating doctors with burnout and other mental health problems.
Whether they have a primary care doctor or not, he suggests that physicians talk to anyone they trust – a social worker, a religious leader, or a family member who can then help them find the right sort of care.
In the United States, around-the-clock help is available through the National Suicide Prevention Lifeline at 800-273-8255. A psychiatrist-run hotline specifically for physicians is available at 888-409-0141. “Reach out and get some help,” Dr. Myers said. “Just don’t do it alone.”
Dr. Lynes advocates setting boundaries between life and work. He has also benefited from writing about his experiences. A blog or a diary can help physicians process their feelings, he said. His 2016 essay marked a major turning point in his life, giving his life meaning in helping others.
“Since I wrote that article, I can’t tell you how much better I am,” he said. “Now, I’m not embarrassed to be around physicians. I actually consider myself a physician. I didn’t for many, many years. So, I’m doing pretty well.”
A version of this article first appeared on Medscape.com.
William Lynes, MD, had a flourishing medical practice and a fulfilling family life with three children when he first attempted suicide in 1999 at age 45. By 2003, depression and two more suicide attempts led to his early retirement.
In a session at the recent virtual American Psychiatric Association (APA) 2021 annual meeting, Dr. Lynes talked about the challenges of dealing with depression while managing the stresses of a career in medicine. The session in which he spoke was called, “The Suicidal Physician: Narratives From a Physician Who Survived and the Physician Widow of One Who Did Not.”
By writing and speaking about his experiences, he says, he has been able to retain his identity as a physician and avoid obsessive thoughts about suicide. He hopes conversations like these help other physicians feel less alone and enable them to push past stigmas to get the help they need. He suspects they do. More than 600 people joined the APA session, and Dr. Lynes received dozens of thankful messages afterward.
“I love medicine, but intrinsically, the practice of medicine is stressful, and you can’t get away,” said Dr. Lynes, a retired urologist in Temecula, Calif. “As far as feedback, it made me feel like it’s something I should continue to do.”
A way to heal
For Dr. Lynes, his “downward spiral into darkness” began with a series of catastrophic medical events starting in 1998, when he came home from a family vacation in Mexico feeling unwell. He didn’t bother to do anything about it – typical of a physician, he says. Then one night he woke up shaking with chills and fever. Soon he was in the hospital with respiratory failure from septic shock.
Dr. Lynes spent 6 weeks in the intensive care unit, including 4 weeks on a ventilator. He underwent a tracheostomy. He lost 40 pounds and experienced ICU-related delirium. It was a terrifying time, he said. When he tried to return to work 10 months later, he didn’t feel as though he could function normally.
Having once been a driven doctor who worked long hours, he now doubted himself and dreaded giving patients bad news. Spontaneously, he tried to take his own life.
Afterward, he concealed what had happened from everyone except his wife and managed to resume his practice. However, he was unable to regain the enthusiasm he had once had for his work. Although he had experienced depression before, this time it was unrelenting.
He sought help from a psychiatrist, received a diagnosis of bipolar disorder, and began taking medication. Still, he struggled to fulfill his responsibilities. Then in April 2002, he had a snowboarding accident that caused multiple facial fractures and required five operations. When he returned to work this time, he felt like a failure but resisted asking colleagues for help.
A few months later, Dr. Lynes again attempted suicide, which led to another stay in the ICU and more time on a ventilator. Doctors told his family they didn’t think he would survive. When he recovered, he spent time as an inpatient in a psychiatric ward, where he received the first of a series of electroconvulsive therapy sessions. Compounding his anxiety and depression was the inability to come to terms with his life if he were not able to practice medicine.
The next fall, in September 2003, his third suicide attempt took place in his office on a weekend when no one was around. After locking the door, he looked at his reflection in the frame of his medical school diploma. The glass was cracked. “It was dark, it was black, it was cold,” he said. “I can remember seeing my reflection and thinking how disgusted I was.”
For years after that, Dr. Lynes struggled with his sense of self-worth. He hid from the medical system and dreaded doctors’ appointments. Finally in 2016, he found new meaning at a writing conference, where he met a fellow physician whose story was similar to his. She encouraged him to write about his experience. His essay was published in Annals of Internal Medicine that year. “Then I started speaking, and I feel like I’m a physician again,” he said. “That has really healed me quite a bit.”
Why physicians die by suicide
Working in health care can be extremely stressful, even in the best of times, said Michael Myers, MD, a psychiatrist at State University of New York, Brooklyn, and author of the book, “Why Physicians Die By Suicide: Lessons Learned From Their Families and Others Who Cared.”
Years of school and training culminate in a career in which demands are relentless. Societal expectations are high. Many doctors are perfectionists by nature, and physicians tend to feel intense pressure to compete for coveted positions.
Stress starts early in a medical career. A 2016 systematic review and meta-analysis of 183 studies from 43 countries showed that nearly 30% of medical students experienced symptoms of depression and that 11% reported suicidal thoughts, but only 15% sought help.
A 2015 review of 31 studies that involved residents showed that rates of depression remained close to 30% and that about three-quarters of trainees meet criteria for burnout, a type of emotional exhaustion and sense of inadequacy that can result from chronic stress at work.
The stress of medical training appears to be a direct cause of mental health struggles. Rates of depression are higher among those working to become physicians than among their peers of the same age, research shows. In addition, symptoms become more prevalent as people progress through their training.
The COVID-19 pandemic has added stress to an already stressful job. Of more than 2,300 physicians surveyed in August 2020 by the Physicians Foundation, a physicians advocacy organization, 50% indicated that they experienced excessive anger, tearfulness, or anxiety because of the way the pandemic affected their work; 30% felt hopeless or lacking purpose; and 8% had thoughts of self-harm related to the pandemic. Rates of burnout had risen from 40% in 2018 to 58%.
Those problems might be even more acute in places experiencing other types of crises. A 2020 study of 154 emergency department (ED) physicians in Libya, which is in the midst of a civil war, found that 65% were experiencing anxiety, 73% were showing signs of depression, and 68% felt emotionally exhausted.
Every story is different
It is unclear how common suicide is among physicians. One often-repeated estimate is that 300-400 physicians die by suicide each year, but no one is certain how that number was determined, said Dr. Myers, who organized the APA panel.
Studies on suicide are inconsistent, and trends are hard to pinpoint. Anecdotally, he has received just as many calls about physician suicides in the past year as he did before the pandemic started.
Every person is different, and so is every death. Sometimes, career problems have nothing to do with a physician’s suicide, Dr. Myers said. When job stress does play a role, factors are often varied and complex.
After a 35-year career as a double board certified ED physician, Matthew Seaman, MD, retired in January 2017. The same month, a patient filed a complaint against him with the Washington State medical board, which led to an investigation and a lawsuit.
The case was hard on Dr. Seaman, who had continued to work night shifts throughout his career and had won a Hero Award from the American Board of Emergency Medicine, said his wife, Linda Seaman, MD, a family practitioner in Yakima, Wash., who also spoke on the APA panel.
Dr. Seaman said that 2 years after the investigation started, her husband was growing increasingly depressed. In 2019, he testified in a deposition. She said the plaintiff’s attorney “tried every way he could to shame Matt, humiliate Matt, make him believe he was a very bad doctor.” Three days later, he died by suicide at age 62.
Looking back at the year leading up to her husband’s death, Dr. Seaman recognizes multiple obstacles that interfered with her husband’s ability to get help, including frustrating interactions with psychiatrists and the couple’s insurance company.
His identity and experience as a physician also played a role. A couple of months before he died, she tried unsuccessfully to reach his psychiatrist, whose office suggested he go to the ED. However, because he worked as an ED doctor in their small town, he wouldn’t go. Dr. Seaman suspects he was wary of the stigma.
Burnout likely set him up to cave in after decades of work on the front lines, she added. Working in the ED exposes providers to horrific, traumatic cases every day, she said. Physicians learn to suppress their own emotions to deal with what they encounter. Stuffing their feelings can lead to posttraumatic stress. “You just perform,” she said. “You learn to do that.”
A real gift
Whenever Dr. Myers hears stories about doctors who died by suicide or who have written about their mental health struggles to help others, he contacts them. One goal of his own writing and of the conference sessions he organizes is to make it easier for others to share their own stories.
“I tell them, first of all, their courage and honesty is a real gift, and they’re saving lives,” he said. “There are so many suffering doctors out there who think that they’re the only one.”
Public conversations such as those that occurred in the APA session also offer opportunities to share advice, including Dr. Myers’ recommendation that doctors be sure they have a primary care physician of their own.
Many don’t, he says, because they say they are too busy, they can treat their own symptoms, or they can self-refer to specialists when needed. But physicians don’t always recognize symptoms of depression in themselves, and when mental health problems arise, they may not seek help or treat themselves appropriately.
A primary care physician can be the first person to recognize a mental health problem and refer a patient for mental health care, said Dr. Myers, whose latest book, “Becoming a Doctors’ Doctor: A Memoir,” explores his experiences treating doctors with burnout and other mental health problems.
Whether they have a primary care doctor or not, he suggests that physicians talk to anyone they trust – a social worker, a religious leader, or a family member who can then help them find the right sort of care.
In the United States, around-the-clock help is available through the National Suicide Prevention Lifeline at 800-273-8255. A psychiatrist-run hotline specifically for physicians is available at 888-409-0141. “Reach out and get some help,” Dr. Myers said. “Just don’t do it alone.”
Dr. Lynes advocates setting boundaries between life and work. He has also benefited from writing about his experiences. A blog or a diary can help physicians process their feelings, he said. His 2016 essay marked a major turning point in his life, giving his life meaning in helping others.
“Since I wrote that article, I can’t tell you how much better I am,” he said. “Now, I’m not embarrassed to be around physicians. I actually consider myself a physician. I didn’t for many, many years. So, I’m doing pretty well.”
A version of this article first appeared on Medscape.com.
APA, AMA, others move to stop insurer from overturning mental health claims ruling
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
No-cancel culture: How telehealth is making it easier to keep that therapy session
When the COVID-19 pandemic forced behavioral health providers to stop seeing patients in person and instead hold therapy sessions remotely, the switch produced an unintended, positive consequence: Fewer patients skipped appointments.
That had long been a problem in mental health care. Some outpatient programs previously had no-show rates as high as 60%, according to several studies.
Only 9% of psychiatrists reported that all patients kept their appointments before the pandemic, according to an American Psychiatric Association report. Once providers switched to telepsychiatry, that number increased to 32%.
Not only that, but providers and patients say teletherapy has largely been an effective lifeline for people struggling with anxiety, depression, and other psychological issues during an extraordinarily difficult time, even though it created a new set of challenges.
Many providers say they plan to continue offering teletherapy after the pandemic. Some states are making permanent the temporary pandemic rules that allow providers to be reimbursed at the same rates as for in-person visits, which is welcome news to practitioners who take patients’ insurance.
“We are in a mental health crisis right now, so more people are struggling and may be more open to accessing services,” said psychologist Allison Dempsey, PhD, associate professor at University of Colorado at Denver, Aurora. “It’s much easier to connect from your living room.”
The problem for patients who didn’t show up was often as simple as a canceled ride, said Jody Long, a clinical social worker who studied the 60% rate of no-shows or late cancellations at the University of Tennessee Health Science Center psychiatric clinic in Memphis.
But sometimes it was the health problem itself. Mr. Long remembers seeing a first-time patient drive around the parking lot and then exit. The patient later called and told Mr. Long, “I just could not get out of the car; please forgive me and reschedule me.”
Mr. Long, now an assistant professor at Jacksonville (Ala.) State University, said that incident changed his perspective. “I realized when you’re having panic attacks or anxiety attacks or suffering from major depressive disorder, it’s hard,” he said. “It’s like you have built up these walls for protection and then all of a sudden you’re having to let these walls down.”
Absences strain providers whose bosses set billing and productivity expectations and those in private practice who lose billable hours, said Dr. Dempsey, who directs a program to provide mental health care for families of babies with serious medical complications. Psychotherapists often overbooked patients with the expectation that some would not show up.
Now Dr. Dempsey and colleagues no longer need to overbook. When patients don’t show up, staffers can sometimes contact a patient right away and hold the session. Other times, they can reschedule them for later that day or a different day.
And telepsychiatry performs as well as, if not better than, face-to-face delivery of mental health services, according to a World Journal of Psychiatry review of 452 studies.
Virtual visits can also save patients money, because they might not need to travel, take time off work, or pay for child care, said Jay Shore, MD, MPH, chairperson of the American Psychiatric Association’s telepsychiatry committee and a psychiatrist at the University of Colorado.
Dr. Shore started examining the potential of video conferencing to reach rural patients in the late ’90s and concluded that patients and providers can virtually build rapport, which he said is fundamental for effective therapy and medicine management.
But before the pandemic, almost 64% of psychiatrists had never used telehealth, according to the psychiatric association. Amid widespread skepticism, providers then had to do “10 years of implementations in 10 days,” said Dr. Shore, who has consulted with Dr. Dempsey and other providers.
Dr. Dempsey and colleagues faced a steep learning curve. She said she recently held a video therapy session with a mother who “seemed very out of it” before disappearing from the screen while her baby was crying.
She wondered if the patient’s exit was related to the stress of new motherhood or “something more concerning,” like addiction. She thinks she might have better understood the woman’s condition had they been in the same room. The patient called Dr. Dempsey’s team that night and told them she had relapsed into drug use and been taken to the emergency room. The mental health providers directed her to a treatment program, Dr. Dempsey said.
“We spent a lot of time reviewing what happened with that case and thinking about what we need to do differently,” Dr. Dempsey said.
Providers now routinely ask for the name of someone to call if they lose a connection and can no longer reach the patient.
In another session, Dr. Dempsey noticed that a patient seemed guarded and saw her partner hovering in the background. She said she worried about the possibility of domestic violence or “some other form of controlling behavior.”
In such cases, Dr. Dempsey called after the appointments or sent the patients secure messages to their online health portal. She asked if they felt safe and suggested they talk in person.
Such inability to maintain privacy remains a concern.
In a Walmart parking lot recently, psychologist Kristy Keefe, PsyD, of Western Illinois University, Macomb, heard a patient talking with her therapist from her car. Dr. Keefe said she wondered if the patient “had no other safe place to go to.”
To avoid that scenario, Dr. Keefe does 30-minute consultations with patients before their first telehealth appointment. She asks if they have space to talk where no one can overhear them and makes sure they have sufficient internet access and know how to use video conferencing.
To ensure that she, too, was prepared, Dr. Keefe upgraded her WiFi router, purchased two white-noise machines to drown out her conversations, and placed a stop sign on her door during appointments so her 5-year-old son knew she was seeing patients.
Dr. Keefe concluded that audio alone sometimes works better than video, which often lags. Over the phone, she and her psychology students “got really sensitive to tone fluctuations” in a patient’s voice and were better able to “pick up the emotion” than with video conferencing.
With those telehealth visits, her 20% no-show rate evaporated.
Kate Barnes, a 29-year-old middle school teacher in Fayetteville, Ark., who struggles with anxiety and depression, also has found visits easier by phone than by Zoom, because she doesn’t feel like a spotlight is on her.
“I can focus more on what I want to say,” she said.
In one of Dr. Keefe’s video sessions, though, a patient reached out, touched the camera and started to cry as she said how appreciative she was that someone was there, Dr. Keefe recalled.
“I am so very thankful that they had something in this terrible time of loss and trauma and isolation,” said Dr. Keefe.
Demand for mental health services will likely continue even after the lifting of all COVID restrictions. according to data from the U.S. Census Bureau and the National Health Interview Survey.
“That is not going to go away with snapping our fingers,” Dr. Dempsey said.
After the pandemic, Dr. Shore said, providers should review data from the past year and determine when virtual care or in-person care is more effective. He also said the health care industry needs to work to bridge the digital divide that exists because of lack of access to devices and broadband internet.
Even though Ms. Barnes said she did not see teletherapy as less effective than in-person therapy, she would like to return to seeing her therapist in person.
“When you are in person with someone, you can pick up on their body language better,” she said. “It’s a lot harder over a video call to do that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
When the COVID-19 pandemic forced behavioral health providers to stop seeing patients in person and instead hold therapy sessions remotely, the switch produced an unintended, positive consequence: Fewer patients skipped appointments.
That had long been a problem in mental health care. Some outpatient programs previously had no-show rates as high as 60%, according to several studies.
Only 9% of psychiatrists reported that all patients kept their appointments before the pandemic, according to an American Psychiatric Association report. Once providers switched to telepsychiatry, that number increased to 32%.
Not only that, but providers and patients say teletherapy has largely been an effective lifeline for people struggling with anxiety, depression, and other psychological issues during an extraordinarily difficult time, even though it created a new set of challenges.
Many providers say they plan to continue offering teletherapy after the pandemic. Some states are making permanent the temporary pandemic rules that allow providers to be reimbursed at the same rates as for in-person visits, which is welcome news to practitioners who take patients’ insurance.
“We are in a mental health crisis right now, so more people are struggling and may be more open to accessing services,” said psychologist Allison Dempsey, PhD, associate professor at University of Colorado at Denver, Aurora. “It’s much easier to connect from your living room.”
The problem for patients who didn’t show up was often as simple as a canceled ride, said Jody Long, a clinical social worker who studied the 60% rate of no-shows or late cancellations at the University of Tennessee Health Science Center psychiatric clinic in Memphis.
But sometimes it was the health problem itself. Mr. Long remembers seeing a first-time patient drive around the parking lot and then exit. The patient later called and told Mr. Long, “I just could not get out of the car; please forgive me and reschedule me.”
Mr. Long, now an assistant professor at Jacksonville (Ala.) State University, said that incident changed his perspective. “I realized when you’re having panic attacks or anxiety attacks or suffering from major depressive disorder, it’s hard,” he said. “It’s like you have built up these walls for protection and then all of a sudden you’re having to let these walls down.”
Absences strain providers whose bosses set billing and productivity expectations and those in private practice who lose billable hours, said Dr. Dempsey, who directs a program to provide mental health care for families of babies with serious medical complications. Psychotherapists often overbooked patients with the expectation that some would not show up.
Now Dr. Dempsey and colleagues no longer need to overbook. When patients don’t show up, staffers can sometimes contact a patient right away and hold the session. Other times, they can reschedule them for later that day or a different day.
And telepsychiatry performs as well as, if not better than, face-to-face delivery of mental health services, according to a World Journal of Psychiatry review of 452 studies.
Virtual visits can also save patients money, because they might not need to travel, take time off work, or pay for child care, said Jay Shore, MD, MPH, chairperson of the American Psychiatric Association’s telepsychiatry committee and a psychiatrist at the University of Colorado.
Dr. Shore started examining the potential of video conferencing to reach rural patients in the late ’90s and concluded that patients and providers can virtually build rapport, which he said is fundamental for effective therapy and medicine management.
But before the pandemic, almost 64% of psychiatrists had never used telehealth, according to the psychiatric association. Amid widespread skepticism, providers then had to do “10 years of implementations in 10 days,” said Dr. Shore, who has consulted with Dr. Dempsey and other providers.
Dr. Dempsey and colleagues faced a steep learning curve. She said she recently held a video therapy session with a mother who “seemed very out of it” before disappearing from the screen while her baby was crying.
She wondered if the patient’s exit was related to the stress of new motherhood or “something more concerning,” like addiction. She thinks she might have better understood the woman’s condition had they been in the same room. The patient called Dr. Dempsey’s team that night and told them she had relapsed into drug use and been taken to the emergency room. The mental health providers directed her to a treatment program, Dr. Dempsey said.
“We spent a lot of time reviewing what happened with that case and thinking about what we need to do differently,” Dr. Dempsey said.
Providers now routinely ask for the name of someone to call if they lose a connection and can no longer reach the patient.
In another session, Dr. Dempsey noticed that a patient seemed guarded and saw her partner hovering in the background. She said she worried about the possibility of domestic violence or “some other form of controlling behavior.”
In such cases, Dr. Dempsey called after the appointments or sent the patients secure messages to their online health portal. She asked if they felt safe and suggested they talk in person.
Such inability to maintain privacy remains a concern.
In a Walmart parking lot recently, psychologist Kristy Keefe, PsyD, of Western Illinois University, Macomb, heard a patient talking with her therapist from her car. Dr. Keefe said she wondered if the patient “had no other safe place to go to.”
To avoid that scenario, Dr. Keefe does 30-minute consultations with patients before their first telehealth appointment. She asks if they have space to talk where no one can overhear them and makes sure they have sufficient internet access and know how to use video conferencing.
To ensure that she, too, was prepared, Dr. Keefe upgraded her WiFi router, purchased two white-noise machines to drown out her conversations, and placed a stop sign on her door during appointments so her 5-year-old son knew she was seeing patients.
Dr. Keefe concluded that audio alone sometimes works better than video, which often lags. Over the phone, she and her psychology students “got really sensitive to tone fluctuations” in a patient’s voice and were better able to “pick up the emotion” than with video conferencing.
With those telehealth visits, her 20% no-show rate evaporated.
Kate Barnes, a 29-year-old middle school teacher in Fayetteville, Ark., who struggles with anxiety and depression, also has found visits easier by phone than by Zoom, because she doesn’t feel like a spotlight is on her.
“I can focus more on what I want to say,” she said.
In one of Dr. Keefe’s video sessions, though, a patient reached out, touched the camera and started to cry as she said how appreciative she was that someone was there, Dr. Keefe recalled.
“I am so very thankful that they had something in this terrible time of loss and trauma and isolation,” said Dr. Keefe.
Demand for mental health services will likely continue even after the lifting of all COVID restrictions. according to data from the U.S. Census Bureau and the National Health Interview Survey.
“That is not going to go away with snapping our fingers,” Dr. Dempsey said.
After the pandemic, Dr. Shore said, providers should review data from the past year and determine when virtual care or in-person care is more effective. He also said the health care industry needs to work to bridge the digital divide that exists because of lack of access to devices and broadband internet.
Even though Ms. Barnes said she did not see teletherapy as less effective than in-person therapy, she would like to return to seeing her therapist in person.
“When you are in person with someone, you can pick up on their body language better,” she said. “It’s a lot harder over a video call to do that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
When the COVID-19 pandemic forced behavioral health providers to stop seeing patients in person and instead hold therapy sessions remotely, the switch produced an unintended, positive consequence: Fewer patients skipped appointments.
That had long been a problem in mental health care. Some outpatient programs previously had no-show rates as high as 60%, according to several studies.
Only 9% of psychiatrists reported that all patients kept their appointments before the pandemic, according to an American Psychiatric Association report. Once providers switched to telepsychiatry, that number increased to 32%.
Not only that, but providers and patients say teletherapy has largely been an effective lifeline for people struggling with anxiety, depression, and other psychological issues during an extraordinarily difficult time, even though it created a new set of challenges.
Many providers say they plan to continue offering teletherapy after the pandemic. Some states are making permanent the temporary pandemic rules that allow providers to be reimbursed at the same rates as for in-person visits, which is welcome news to practitioners who take patients’ insurance.
“We are in a mental health crisis right now, so more people are struggling and may be more open to accessing services,” said psychologist Allison Dempsey, PhD, associate professor at University of Colorado at Denver, Aurora. “It’s much easier to connect from your living room.”
The problem for patients who didn’t show up was often as simple as a canceled ride, said Jody Long, a clinical social worker who studied the 60% rate of no-shows or late cancellations at the University of Tennessee Health Science Center psychiatric clinic in Memphis.
But sometimes it was the health problem itself. Mr. Long remembers seeing a first-time patient drive around the parking lot and then exit. The patient later called and told Mr. Long, “I just could not get out of the car; please forgive me and reschedule me.”
Mr. Long, now an assistant professor at Jacksonville (Ala.) State University, said that incident changed his perspective. “I realized when you’re having panic attacks or anxiety attacks or suffering from major depressive disorder, it’s hard,” he said. “It’s like you have built up these walls for protection and then all of a sudden you’re having to let these walls down.”
Absences strain providers whose bosses set billing and productivity expectations and those in private practice who lose billable hours, said Dr. Dempsey, who directs a program to provide mental health care for families of babies with serious medical complications. Psychotherapists often overbooked patients with the expectation that some would not show up.
Now Dr. Dempsey and colleagues no longer need to overbook. When patients don’t show up, staffers can sometimes contact a patient right away and hold the session. Other times, they can reschedule them for later that day or a different day.
And telepsychiatry performs as well as, if not better than, face-to-face delivery of mental health services, according to a World Journal of Psychiatry review of 452 studies.
Virtual visits can also save patients money, because they might not need to travel, take time off work, or pay for child care, said Jay Shore, MD, MPH, chairperson of the American Psychiatric Association’s telepsychiatry committee and a psychiatrist at the University of Colorado.
Dr. Shore started examining the potential of video conferencing to reach rural patients in the late ’90s and concluded that patients and providers can virtually build rapport, which he said is fundamental for effective therapy and medicine management.
But before the pandemic, almost 64% of psychiatrists had never used telehealth, according to the psychiatric association. Amid widespread skepticism, providers then had to do “10 years of implementations in 10 days,” said Dr. Shore, who has consulted with Dr. Dempsey and other providers.
Dr. Dempsey and colleagues faced a steep learning curve. She said she recently held a video therapy session with a mother who “seemed very out of it” before disappearing from the screen while her baby was crying.
She wondered if the patient’s exit was related to the stress of new motherhood or “something more concerning,” like addiction. She thinks she might have better understood the woman’s condition had they been in the same room. The patient called Dr. Dempsey’s team that night and told them she had relapsed into drug use and been taken to the emergency room. The mental health providers directed her to a treatment program, Dr. Dempsey said.
“We spent a lot of time reviewing what happened with that case and thinking about what we need to do differently,” Dr. Dempsey said.
Providers now routinely ask for the name of someone to call if they lose a connection and can no longer reach the patient.
In another session, Dr. Dempsey noticed that a patient seemed guarded and saw her partner hovering in the background. She said she worried about the possibility of domestic violence or “some other form of controlling behavior.”
In such cases, Dr. Dempsey called after the appointments or sent the patients secure messages to their online health portal. She asked if they felt safe and suggested they talk in person.
Such inability to maintain privacy remains a concern.
In a Walmart parking lot recently, psychologist Kristy Keefe, PsyD, of Western Illinois University, Macomb, heard a patient talking with her therapist from her car. Dr. Keefe said she wondered if the patient “had no other safe place to go to.”
To avoid that scenario, Dr. Keefe does 30-minute consultations with patients before their first telehealth appointment. She asks if they have space to talk where no one can overhear them and makes sure they have sufficient internet access and know how to use video conferencing.
To ensure that she, too, was prepared, Dr. Keefe upgraded her WiFi router, purchased two white-noise machines to drown out her conversations, and placed a stop sign on her door during appointments so her 5-year-old son knew she was seeing patients.
Dr. Keefe concluded that audio alone sometimes works better than video, which often lags. Over the phone, she and her psychology students “got really sensitive to tone fluctuations” in a patient’s voice and were better able to “pick up the emotion” than with video conferencing.
With those telehealth visits, her 20% no-show rate evaporated.
Kate Barnes, a 29-year-old middle school teacher in Fayetteville, Ark., who struggles with anxiety and depression, also has found visits easier by phone than by Zoom, because she doesn’t feel like a spotlight is on her.
“I can focus more on what I want to say,” she said.
In one of Dr. Keefe’s video sessions, though, a patient reached out, touched the camera and started to cry as she said how appreciative she was that someone was there, Dr. Keefe recalled.
“I am so very thankful that they had something in this terrible time of loss and trauma and isolation,” said Dr. Keefe.
Demand for mental health services will likely continue even after the lifting of all COVID restrictions. according to data from the U.S. Census Bureau and the National Health Interview Survey.
“That is not going to go away with snapping our fingers,” Dr. Dempsey said.
After the pandemic, Dr. Shore said, providers should review data from the past year and determine when virtual care or in-person care is more effective. He also said the health care industry needs to work to bridge the digital divide that exists because of lack of access to devices and broadband internet.
Even though Ms. Barnes said she did not see teletherapy as less effective than in-person therapy, she would like to return to seeing her therapist in person.
“When you are in person with someone, you can pick up on their body language better,” she said. “It’s a lot harder over a video call to do that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Young adults with epilepsy face higher mental illness risks
Young adults with epilepsy experience higher rates of anxiety, depression, and suicidality, compared with their counterparts in the general population, a new study shows.
The findings, based on a study of 144 young adults with epilepsy (YAWE), was published recently in Epilepsy & Behavior.
“People with epilepsy (PWE) are at a significantly higher risk of experiencing mental health difficulties, compared with healthy controls and individuals with other [long-term conditions] such as asthma and diabetes,” according to Rachel Batchelor, MSc, and Michelle D. Taylor, PhD, of the University of London (England) in Surrey.
Young adulthood, which encompasses people aged 18-25 years, has been identified as “a peak age of onset for anxiety and depression,” but mental health in young adults with epilepsy in particular has not been well studied, they wrote.
The survey measured current mental health symptoms, including anxiety, depression, and suicidality, as well as sociodemographic and epilepsy-related factors, coping strategies, and social support (Epilepsy Behav. 2021 May;118:107911. doi: 10.1016/j.yebeh.2021.107911).
The average age of the respondents was 21.6 years, 61% were female, and 88% were of White British ethnicity. A total of 88 participants were single, 48 were in a relationship, and 8 were married or engaged. About one-third (38%) worked full-time, and 28.5% were full-time university students, 18.8% worked part-time, and 8.3% were unemployed and not students. The average age of seizure onset was 12.4 years.
Overall, 116 (80.6%) of the survey respondents met the criteria for anxiety, 110 (76.4%) for depression, and 51 (35.4%) for suicidality.
Ratings of all three of these conditions were significantly higher in females, compared with males, the researchers noted. Anxiety, depression, and suicidality also were rated higher for individuals who waited more than 1 year vs. less than 1 year for an epilepsy diagnosis from the time of seizure onset, for those suffering from anti-seizure medication side effects vs. no side effects, and for those with comorbid conditions vs. no comorbid conditions.
Avoidant-focused coping strategies were positively correlated with anxiety, depression, and suicidality, while problem-focused coping and meaning-focused coping were negatively correlated, the researchers said. In addition, those who reported greater levels of support from friends had lower rates of anxiety and depression, and those who reported greater levels of support from family had lower rates of suicidality.
The study findings were limited by several factors, including the relatively homogenous population, and the absence of data on current anxiety and depression medications and additional professional support, the researchers noted.
However, the results extend the research on mental health in people with epilepsy, and the study is the first known to focus on the young adult population with epilepsy, they said.
“The high rates of anxiety, depression, and suicidality underscore the need for better integration of mental health provision into epilepsy care,” the researchers wrote. “While it would be premature to base recommendations for treating anxiety, depression, and suicidality in YAWE on the current study, investigating the efficacy of psychological interventions (for example, [acceptance and commitment therapy], [compassion-focused therapy], peer support, and family-based [therapy]) designed to address the psychosocial variables shown to independently predict mental health outcomes in YAWE would be worthy future research avenues,” they concluded.
The study received no outside funding, and the researchers disclosed no financial conflicts.
Young adults with epilepsy experience higher rates of anxiety, depression, and suicidality, compared with their counterparts in the general population, a new study shows.
The findings, based on a study of 144 young adults with epilepsy (YAWE), was published recently in Epilepsy & Behavior.
“People with epilepsy (PWE) are at a significantly higher risk of experiencing mental health difficulties, compared with healthy controls and individuals with other [long-term conditions] such as asthma and diabetes,” according to Rachel Batchelor, MSc, and Michelle D. Taylor, PhD, of the University of London (England) in Surrey.
Young adulthood, which encompasses people aged 18-25 years, has been identified as “a peak age of onset for anxiety and depression,” but mental health in young adults with epilepsy in particular has not been well studied, they wrote.
The survey measured current mental health symptoms, including anxiety, depression, and suicidality, as well as sociodemographic and epilepsy-related factors, coping strategies, and social support (Epilepsy Behav. 2021 May;118:107911. doi: 10.1016/j.yebeh.2021.107911).
The average age of the respondents was 21.6 years, 61% were female, and 88% were of White British ethnicity. A total of 88 participants were single, 48 were in a relationship, and 8 were married or engaged. About one-third (38%) worked full-time, and 28.5% were full-time university students, 18.8% worked part-time, and 8.3% were unemployed and not students. The average age of seizure onset was 12.4 years.
Overall, 116 (80.6%) of the survey respondents met the criteria for anxiety, 110 (76.4%) for depression, and 51 (35.4%) for suicidality.
Ratings of all three of these conditions were significantly higher in females, compared with males, the researchers noted. Anxiety, depression, and suicidality also were rated higher for individuals who waited more than 1 year vs. less than 1 year for an epilepsy diagnosis from the time of seizure onset, for those suffering from anti-seizure medication side effects vs. no side effects, and for those with comorbid conditions vs. no comorbid conditions.
Avoidant-focused coping strategies were positively correlated with anxiety, depression, and suicidality, while problem-focused coping and meaning-focused coping were negatively correlated, the researchers said. In addition, those who reported greater levels of support from friends had lower rates of anxiety and depression, and those who reported greater levels of support from family had lower rates of suicidality.
The study findings were limited by several factors, including the relatively homogenous population, and the absence of data on current anxiety and depression medications and additional professional support, the researchers noted.
However, the results extend the research on mental health in people with epilepsy, and the study is the first known to focus on the young adult population with epilepsy, they said.
“The high rates of anxiety, depression, and suicidality underscore the need for better integration of mental health provision into epilepsy care,” the researchers wrote. “While it would be premature to base recommendations for treating anxiety, depression, and suicidality in YAWE on the current study, investigating the efficacy of psychological interventions (for example, [acceptance and commitment therapy], [compassion-focused therapy], peer support, and family-based [therapy]) designed to address the psychosocial variables shown to independently predict mental health outcomes in YAWE would be worthy future research avenues,” they concluded.
The study received no outside funding, and the researchers disclosed no financial conflicts.
Young adults with epilepsy experience higher rates of anxiety, depression, and suicidality, compared with their counterparts in the general population, a new study shows.
The findings, based on a study of 144 young adults with epilepsy (YAWE), was published recently in Epilepsy & Behavior.
“People with epilepsy (PWE) are at a significantly higher risk of experiencing mental health difficulties, compared with healthy controls and individuals with other [long-term conditions] such as asthma and diabetes,” according to Rachel Batchelor, MSc, and Michelle D. Taylor, PhD, of the University of London (England) in Surrey.
Young adulthood, which encompasses people aged 18-25 years, has been identified as “a peak age of onset for anxiety and depression,” but mental health in young adults with epilepsy in particular has not been well studied, they wrote.
The survey measured current mental health symptoms, including anxiety, depression, and suicidality, as well as sociodemographic and epilepsy-related factors, coping strategies, and social support (Epilepsy Behav. 2021 May;118:107911. doi: 10.1016/j.yebeh.2021.107911).
The average age of the respondents was 21.6 years, 61% were female, and 88% were of White British ethnicity. A total of 88 participants were single, 48 were in a relationship, and 8 were married or engaged. About one-third (38%) worked full-time, and 28.5% were full-time university students, 18.8% worked part-time, and 8.3% were unemployed and not students. The average age of seizure onset was 12.4 years.
Overall, 116 (80.6%) of the survey respondents met the criteria for anxiety, 110 (76.4%) for depression, and 51 (35.4%) for suicidality.
Ratings of all three of these conditions were significantly higher in females, compared with males, the researchers noted. Anxiety, depression, and suicidality also were rated higher for individuals who waited more than 1 year vs. less than 1 year for an epilepsy diagnosis from the time of seizure onset, for those suffering from anti-seizure medication side effects vs. no side effects, and for those with comorbid conditions vs. no comorbid conditions.
Avoidant-focused coping strategies were positively correlated with anxiety, depression, and suicidality, while problem-focused coping and meaning-focused coping were negatively correlated, the researchers said. In addition, those who reported greater levels of support from friends had lower rates of anxiety and depression, and those who reported greater levels of support from family had lower rates of suicidality.
The study findings were limited by several factors, including the relatively homogenous population, and the absence of data on current anxiety and depression medications and additional professional support, the researchers noted.
However, the results extend the research on mental health in people with epilepsy, and the study is the first known to focus on the young adult population with epilepsy, they said.
“The high rates of anxiety, depression, and suicidality underscore the need for better integration of mental health provision into epilepsy care,” the researchers wrote. “While it would be premature to base recommendations for treating anxiety, depression, and suicidality in YAWE on the current study, investigating the efficacy of psychological interventions (for example, [acceptance and commitment therapy], [compassion-focused therapy], peer support, and family-based [therapy]) designed to address the psychosocial variables shown to independently predict mental health outcomes in YAWE would be worthy future research avenues,” they concluded.
The study received no outside funding, and the researchers disclosed no financial conflicts.
FROM EPILEPSY & BEHAVIOR
Psychosis, depression tied to neurodegeneration in Parkinson’s
Depression and psychosis are significantly associated with neuronal loss and gliosis – but not with Lewy body scores – in Parkinson’s disease, data from analyses of the brains of 175 patients suggest.
Previous research has suggested a link between neuronal loss and depression in Parkinson’s disease (PD) but the impact of Lewy bodies has not been well studied, Nicole Mercado Fischer, MPH, of Johns Hopkins University, Baltimore, and colleagues wrote.
Evaluating Lewy body scores and neuronal loss/gliosis in the substantia nigra pars compacta (SN) and locus coeruleus (LC) could increase understanding of pathophysiology in PD, they said.
In a study published in the American Journal of Geriatric Psychiatry, the researchers analyzed the brains of 175 individuals with a primary diagnosis of PD.
A total of 98 participants had diagnoses of psychosis, 88 had depression, and 55 had anxiety. The average age of onset for PD was 62.4 years; 67.4% of the subjects were male, and 97.8% were White. The mean duration of illness was 16 years, and the average age at death was 78 years.
Psychosis was significantly associated with severe neuronal loss and gliosis in both the LC and SN (P = .048 and P = .042, respectively). Depression was significantly associated with severe neuronal loss in the SN (P = .042) but not in the LC. Anxiety was not associated with severe neuronal loss in either brain region. These results remained significant after a multivariate analysis, the researchers noted. However, Lewy body scores were not associated with any neuropsychiatric symptom, and severity of neuronal loss and gliosis was not correlated with Lewy body scores.
The study findings were limited by several factors, including the retrospective design and inability to collect pathology data for all patients, the researchers noted. Also, in some cases, the collection of clinical data and observation of brain tissue pathology took place years apart, and the researchers did not assess medication records.
However, the results were strengthened by the large sample size and “further support the notion that in vivo clinical symptoms of PD are either not caused by Lewy body pathology or that the relationship is confounded by the time of autopsy,” they said. and eventually by using new functional imaging techniques in vivo.”
The researchers had no financial conflicts to disclose. Two coauthors were supported in part by the National Institutes of Health.
Depression and psychosis are significantly associated with neuronal loss and gliosis – but not with Lewy body scores – in Parkinson’s disease, data from analyses of the brains of 175 patients suggest.
Previous research has suggested a link between neuronal loss and depression in Parkinson’s disease (PD) but the impact of Lewy bodies has not been well studied, Nicole Mercado Fischer, MPH, of Johns Hopkins University, Baltimore, and colleagues wrote.
Evaluating Lewy body scores and neuronal loss/gliosis in the substantia nigra pars compacta (SN) and locus coeruleus (LC) could increase understanding of pathophysiology in PD, they said.
In a study published in the American Journal of Geriatric Psychiatry, the researchers analyzed the brains of 175 individuals with a primary diagnosis of PD.
A total of 98 participants had diagnoses of psychosis, 88 had depression, and 55 had anxiety. The average age of onset for PD was 62.4 years; 67.4% of the subjects were male, and 97.8% were White. The mean duration of illness was 16 years, and the average age at death was 78 years.
Psychosis was significantly associated with severe neuronal loss and gliosis in both the LC and SN (P = .048 and P = .042, respectively). Depression was significantly associated with severe neuronal loss in the SN (P = .042) but not in the LC. Anxiety was not associated with severe neuronal loss in either brain region. These results remained significant after a multivariate analysis, the researchers noted. However, Lewy body scores were not associated with any neuropsychiatric symptom, and severity of neuronal loss and gliosis was not correlated with Lewy body scores.
The study findings were limited by several factors, including the retrospective design and inability to collect pathology data for all patients, the researchers noted. Also, in some cases, the collection of clinical data and observation of brain tissue pathology took place years apart, and the researchers did not assess medication records.
However, the results were strengthened by the large sample size and “further support the notion that in vivo clinical symptoms of PD are either not caused by Lewy body pathology or that the relationship is confounded by the time of autopsy,” they said. and eventually by using new functional imaging techniques in vivo.”
The researchers had no financial conflicts to disclose. Two coauthors were supported in part by the National Institutes of Health.
Depression and psychosis are significantly associated with neuronal loss and gliosis – but not with Lewy body scores – in Parkinson’s disease, data from analyses of the brains of 175 patients suggest.
Previous research has suggested a link between neuronal loss and depression in Parkinson’s disease (PD) but the impact of Lewy bodies has not been well studied, Nicole Mercado Fischer, MPH, of Johns Hopkins University, Baltimore, and colleagues wrote.
Evaluating Lewy body scores and neuronal loss/gliosis in the substantia nigra pars compacta (SN) and locus coeruleus (LC) could increase understanding of pathophysiology in PD, they said.
In a study published in the American Journal of Geriatric Psychiatry, the researchers analyzed the brains of 175 individuals with a primary diagnosis of PD.
A total of 98 participants had diagnoses of psychosis, 88 had depression, and 55 had anxiety. The average age of onset for PD was 62.4 years; 67.4% of the subjects were male, and 97.8% were White. The mean duration of illness was 16 years, and the average age at death was 78 years.
Psychosis was significantly associated with severe neuronal loss and gliosis in both the LC and SN (P = .048 and P = .042, respectively). Depression was significantly associated with severe neuronal loss in the SN (P = .042) but not in the LC. Anxiety was not associated with severe neuronal loss in either brain region. These results remained significant after a multivariate analysis, the researchers noted. However, Lewy body scores were not associated with any neuropsychiatric symptom, and severity of neuronal loss and gliosis was not correlated with Lewy body scores.
The study findings were limited by several factors, including the retrospective design and inability to collect pathology data for all patients, the researchers noted. Also, in some cases, the collection of clinical data and observation of brain tissue pathology took place years apart, and the researchers did not assess medication records.
However, the results were strengthened by the large sample size and “further support the notion that in vivo clinical symptoms of PD are either not caused by Lewy body pathology or that the relationship is confounded by the time of autopsy,” they said. and eventually by using new functional imaging techniques in vivo.”
The researchers had no financial conflicts to disclose. Two coauthors were supported in part by the National Institutes of Health.
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Prevalence of psychiatric disorders higher in adult cerebral palsy patients
Adults with cerebral palsy, especially those with intellectual disabilities, are significantly more likely to be diagnosed with a psychiatric disorder, compared with the general population, a review of seven datasets shows.
The body of literature on psychiatric issues in children with cerebral palsy (CP) is increasing, but population-based studies of psychiatric issues in adults with CP have been limited in number and in scope. Most of those studies focus mainly on anxiety and depression, rather than on other issues such as psychosis or schizophrenia, Carly A. McMorris, PhD, of the University of Calgary (Alta.) and colleagues wrote.
In a retrospective, cross-sectional study published in Research in Developmental Disabilities, the researchers reviewed information from five health data sets, one registry, and census data for adults aged 18-64 years with a CP diagnosis living in Ontario, including those with and without diagnosed intellectual disabilities (ID) and a comparison group of individuals in the general population. The researchers examined the proportion of individuals with a psychiatric disorder in each of four groups: total CP, CP without ID, CP with ID, and the general population.
The study participants included 9,388 individuals with CP, 4,767 individuals with CP and ID, and a general population of 2,757,744 individuals. About half of the participants were male, and at least 85% lived in urban areas.
Overall, compared with the general population group, over a 2-year period (33.7 % vs. 24.7%). Also, the CP group was more than twice as likely to be diagnosed with a psychotic disorder, schizophrenia, personality disorder, or bipolar disorder, compared with the general population. Individuals with CP were significantly more likely to suffer from mood or affective disorders, and depression and anxiety disorders, compared with the general population, but less likely to suffer from substance use disorders.
When the data were assessed by ID status, disorders such as psychotic disorders, bipolar disorders, and schizophrenia were six times more common among individuals with CP and ID, compared with the general population (adjusted prevalence ratios, 6.26 and 6.46, respectively).
Individuals with CP and ID also had a notably higher prevalence of bipolar disorder (confidence interval, 2.06-2.89) and personality disorder, compared with the general population (aPR, 2.44 and 4.22, respectively), but this subgroup also was less likely than the general population to engage in substance use (aPR, 0.44).
The study findings were limited by several factors, including the absence of universal definitions for some of the conditions studied, potential misclassification of ID, the inclusion of data on specific psychiatric diagnoses but not elevated symptoms, and by the challenges of diagnosing psychiatric disorders in individuals with ID, the researchers noted.
However, “the present study contributes important information to the existing literature, highlighting that psychiatric issues are common in adults with CP, similar to what has been reported in children and youth,” they said. “Further research is needed to determine the validity and reliability of mental health assessment measures for this population, the efficacy of evidence-based psychotherapeutic approaches ... and the underlying causes or mechanisms of psychiatric issues in individuals with CP.”
The findings also highlight the need for health care clinicians to screen for psychiatric issues in CP patients, they said.
The study was supported in part by the Province of Ontario research grants and the Institute for Clinical Evaluative Sciences, funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The researchers had no disclosures.
Adults with cerebral palsy, especially those with intellectual disabilities, are significantly more likely to be diagnosed with a psychiatric disorder, compared with the general population, a review of seven datasets shows.
The body of literature on psychiatric issues in children with cerebral palsy (CP) is increasing, but population-based studies of psychiatric issues in adults with CP have been limited in number and in scope. Most of those studies focus mainly on anxiety and depression, rather than on other issues such as psychosis or schizophrenia, Carly A. McMorris, PhD, of the University of Calgary (Alta.) and colleagues wrote.
In a retrospective, cross-sectional study published in Research in Developmental Disabilities, the researchers reviewed information from five health data sets, one registry, and census data for adults aged 18-64 years with a CP diagnosis living in Ontario, including those with and without diagnosed intellectual disabilities (ID) and a comparison group of individuals in the general population. The researchers examined the proportion of individuals with a psychiatric disorder in each of four groups: total CP, CP without ID, CP with ID, and the general population.
The study participants included 9,388 individuals with CP, 4,767 individuals with CP and ID, and a general population of 2,757,744 individuals. About half of the participants were male, and at least 85% lived in urban areas.
Overall, compared with the general population group, over a 2-year period (33.7 % vs. 24.7%). Also, the CP group was more than twice as likely to be diagnosed with a psychotic disorder, schizophrenia, personality disorder, or bipolar disorder, compared with the general population. Individuals with CP were significantly more likely to suffer from mood or affective disorders, and depression and anxiety disorders, compared with the general population, but less likely to suffer from substance use disorders.
When the data were assessed by ID status, disorders such as psychotic disorders, bipolar disorders, and schizophrenia were six times more common among individuals with CP and ID, compared with the general population (adjusted prevalence ratios, 6.26 and 6.46, respectively).
Individuals with CP and ID also had a notably higher prevalence of bipolar disorder (confidence interval, 2.06-2.89) and personality disorder, compared with the general population (aPR, 2.44 and 4.22, respectively), but this subgroup also was less likely than the general population to engage in substance use (aPR, 0.44).
The study findings were limited by several factors, including the absence of universal definitions for some of the conditions studied, potential misclassification of ID, the inclusion of data on specific psychiatric diagnoses but not elevated symptoms, and by the challenges of diagnosing psychiatric disorders in individuals with ID, the researchers noted.
However, “the present study contributes important information to the existing literature, highlighting that psychiatric issues are common in adults with CP, similar to what has been reported in children and youth,” they said. “Further research is needed to determine the validity and reliability of mental health assessment measures for this population, the efficacy of evidence-based psychotherapeutic approaches ... and the underlying causes or mechanisms of psychiatric issues in individuals with CP.”
The findings also highlight the need for health care clinicians to screen for psychiatric issues in CP patients, they said.
The study was supported in part by the Province of Ontario research grants and the Institute for Clinical Evaluative Sciences, funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The researchers had no disclosures.
Adults with cerebral palsy, especially those with intellectual disabilities, are significantly more likely to be diagnosed with a psychiatric disorder, compared with the general population, a review of seven datasets shows.
The body of literature on psychiatric issues in children with cerebral palsy (CP) is increasing, but population-based studies of psychiatric issues in adults with CP have been limited in number and in scope. Most of those studies focus mainly on anxiety and depression, rather than on other issues such as psychosis or schizophrenia, Carly A. McMorris, PhD, of the University of Calgary (Alta.) and colleagues wrote.
In a retrospective, cross-sectional study published in Research in Developmental Disabilities, the researchers reviewed information from five health data sets, one registry, and census data for adults aged 18-64 years with a CP diagnosis living in Ontario, including those with and without diagnosed intellectual disabilities (ID) and a comparison group of individuals in the general population. The researchers examined the proportion of individuals with a psychiatric disorder in each of four groups: total CP, CP without ID, CP with ID, and the general population.
The study participants included 9,388 individuals with CP, 4,767 individuals with CP and ID, and a general population of 2,757,744 individuals. About half of the participants were male, and at least 85% lived in urban areas.
Overall, compared with the general population group, over a 2-year period (33.7 % vs. 24.7%). Also, the CP group was more than twice as likely to be diagnosed with a psychotic disorder, schizophrenia, personality disorder, or bipolar disorder, compared with the general population. Individuals with CP were significantly more likely to suffer from mood or affective disorders, and depression and anxiety disorders, compared with the general population, but less likely to suffer from substance use disorders.
When the data were assessed by ID status, disorders such as psychotic disorders, bipolar disorders, and schizophrenia were six times more common among individuals with CP and ID, compared with the general population (adjusted prevalence ratios, 6.26 and 6.46, respectively).
Individuals with CP and ID also had a notably higher prevalence of bipolar disorder (confidence interval, 2.06-2.89) and personality disorder, compared with the general population (aPR, 2.44 and 4.22, respectively), but this subgroup also was less likely than the general population to engage in substance use (aPR, 0.44).
The study findings were limited by several factors, including the absence of universal definitions for some of the conditions studied, potential misclassification of ID, the inclusion of data on specific psychiatric diagnoses but not elevated symptoms, and by the challenges of diagnosing psychiatric disorders in individuals with ID, the researchers noted.
However, “the present study contributes important information to the existing literature, highlighting that psychiatric issues are common in adults with CP, similar to what has been reported in children and youth,” they said. “Further research is needed to determine the validity and reliability of mental health assessment measures for this population, the efficacy of evidence-based psychotherapeutic approaches ... and the underlying causes or mechanisms of psychiatric issues in individuals with CP.”
The findings also highlight the need for health care clinicians to screen for psychiatric issues in CP patients, they said.
The study was supported in part by the Province of Ontario research grants and the Institute for Clinical Evaluative Sciences, funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The researchers had no disclosures.
FROM RESEARCH IN DEVELOPMENTAL DISABILITIES
Two key suicide risk factors identified in borderline personality disorder
Feelings of chronic emptiness and self-injury have been identified as two key risk factors for suicide attempts (SAs) in patients with borderline personality disorder (BPD), a new cross-sectional, nationally representative study suggests.
The findings also show lifetime and past-year SAs are common among patients with BPD, even when excluding self-injurious behaviors.
The results suggest that in addition to asking patients about self-harm during suicide risk screenings and assessments, clinicians should query them about “longstanding” feelings of emptiness, study investigator Carlos M. Grilo, PhD, professor of psychiatry and psychology, Yale University, New Haven, Conn., said in an interview.
Although related, chronic emptiness “is distinct and goes beyond feelings of sadness, loneliness, and hopelessness,” explained Dr. Grilo. he said.
The study was published online May 11 in JAMA Network Open.
Filling a research gap
While BPD and other psychiatric disorders are associated with suicide, the authors noted there is a “dearth of epidemiological research” examining the link between BPD and suicide.
Criteria for BPD diagnosis requires any five of the following criteria: relationships, affective instability, abandonment fear, anger, identity disturbance, emptiness, disassociation/paranoia, self-injurious behavior, and impulsivity, along with social-occupation dysfunction.
To determine SA risk with specific BPD diagnostic criteria, the investigators examined data on 36,309 individuals who participated in the third wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III), conducted from 2012 to 2013.
During computer-assisted, face-to-face interviews, study participants answered questions based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) of the National Institute on Alcohol Abuse and Alcoholism.
This structured interview assesses a range of DSM-5–defined psychiatric disorders and their criteria. In addition to BPD, the AUDADIS-5 generates diagnoses for mood disorders, anxiety disorders, posttraumatic stress disorder, substance use disorders, antisocial personality disorder, schizotypal disorder, and conduct disorder.
During the interviews, respondents were asked if they had ever attempted suicide. For those who had, interviewers recorded the total number of lifetime attempts.
Participants also answered questions about childhood maltreatment including physical neglect, emotional neglect, physical abuse, emotional abuse, and sexual abuse by parents or caregivers and other adverse events occurring before the age of 18.
Childhood trauma common
Patients with BPD frequently report a history of childhood trauma, noted Dr. Grilo, adding that such trauma is associated with self-harm and suicide attempts. Sociodemographic information, including age, sex, and ethnicity/race, education level, and income, was also gathered.
Investigators examined data on suicide attempts using relatively stringent coding that required serious dysfunction in at least five BPD criteria.
Using this definition, investigators found the lifetime SA prevalence in patients with BPD was 30.4%, and 3.2% for past-year SAs. This compared with a rate of 3.7% for lifetime SAs and 0.2% for past-year SAs in those without a BPD diagnosis.
The authors examined SA rates using diagnostic codes in the NESARC-III that required seriously impaired function in only 1 or 2 BPD criteria. Rates were higher using the 5-criteria definition.
When the researchers excluded the BPD criterion of self-injurious behavior, the prevalence was 28.1% for lifetime and 3.0% for past-year SAs among the BPD group, with corresponding rates of 3.8% and 0.2% in those without a BPD diagnosis.
It’s important to look at this, said Dr. Grilo, as some patients with BPD who engage in self-harm have suicidal intent while others don’t.
“We tested whether BPD had heightened risk for suicide attempts if we eliminated the self-injurious criterion and we found that heightened risk was still there,” he explained.
Looking at individual criteria for BPD, a model that adjusted for sociodemographic characteristics, other psychiatric disorders, age at BPD onset, and history of childhood adverse events uncovered two criteria that were significantly associated with increased odds of SAs.
One was emptiness. For lifetime suicide attempts, the adjusted odds ratio (aOR) was 1.58 (95% confidence interval, 1.16-2.14) and for past-year attempts, the aOR was 1.99 (95% CI, 1.08-3.66).
The second was self-injurious behavior. For lifetime attempts, the aOR was 24.28 (95% CI, 16.83-32.03) and for past-year attempts, the aOR was 19.32 (95% CI, 5.22-71.58).
In a model in which all BPD-specific criteria were entered while excluding self-injurious behavior, the aORs for emptiness were 1.66 (95% CI, 1.23-2.24) for lifetime suicide attempts and 2.45 (95% CI, 1.18-5.08) for past year attempts.
Unlike another recent study that included more than 700 treatment-seeking patients with BPD who were followed for 10 years, the current study did not show significant associations with SAs for two other BPD criteria – identity disturbance and frantic attempts to avoid abandonment.
Dr. Grilo explained this might be because the earlier study included treatment-seeking patients instead of community cases, or because of differences in assessment interviews or other factors.
‘Compelling evidence’
“Our epidemiological sample has much broader generalizability and fewer potential confounds than the clinical treatment-seeking sample,” said Dr. Grilo.
However, he noted that the two studies “converge strongly and provide compelling evidence that BPD is associated with substantially heightened risk for suicide attempts over the lifetime.”
The two studies “also converge in finding that the presence of symptoms such as repeated self-harm and feelings of chronic emptiness are also associated with risk for suicide attempts.”
The new findings highlight the need to ask potentially at-risk patients about feelings of emptiness as well as self-injurious behaviors. Clinicians could, for example, ask: “Have you often felt like your life had no purpose or meaning?” or “Have you often felt empty inside?”
Limitations of the study include reliance on retrospective self-reports and use of lay interviewers, although these interviewers were trained and had an average of 5 years of experience conducting health-related surveys.
Although the study included a representative sample of U.S. adults, the sample did not include groups known to have high rates of suicide and self-harm behaviors, such as institutionalized, incarcerated, or homeless individuals.
In addition, the study did not evaluate severity and duration of BPD, although the authors noted they did adjust for age at BPD onset, this did not alter the findings.
Often misdiagnosed
Commenting on the study, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, and past-president, American Psychiatric Association, and an expert on BPD, had high praise for the research.
BPD is often misdiagnosed, Dr. Oldham said in an interview. Many patients seek help from primary care doctors who may label the symptoms as an anxiety disorder or a mood disorder, he said.
Although medications can help treat some BPD symptoms, “the primary, core evidence-based treatment for BPD is psychotherapy,” said Dr. Oldham, who some years ago helped develop evidence-based practice guidelines for BPD.
“It’s a clear and very well-designed study, and I don’t see any major limitations or problems with it,” he said. “The authors kept their focus rigorously on their goals and they used really careful methodology.”
He noted the “huge” numbers of patients included in the data and the relatively large percentage of men (43.7%).
“There’s a general belief that it’s mostly females who have BPD, but that’s not true; it’s females who come to treatment,” said Dr. Oldham.
Requiring that all five criteria lead to seriously impaired functioning “is a much more rigorous diagnostic methodology” than requiring only one or two criteria to lead to such impairment, said Dr. Oldham. “This is really important” and makes it “a much stronger study.”
The finding that self-harm behavior was linked to suicide attempts isn’t that surprising as this association has been well documented, but the finding that chronic emptiness is also predictive of future suicide attempts “is news,” said Dr. Oldham.
“We have not paid enough attention to this criterion in the clinical world or in the research world.”
Dr. Oldham said one patient with BPD gave him an ideal metaphor for emptiness. “She said it’s like there’s just nobody home. Think of it as an empty house that may look fine on the outside but you go inside and nobody lives there; there’s no furniture; no favorite things; no photos; no possessions.”
The authors have “important messages we need to pay attention to, and the main one is to explore this sense of chronic ‘nobody home’ emptiness,” said Dr. Oldham.
Dr. Grilo has reported receiving research grants from the National Institutes of Health; serving as a consultant for Sunovion and Weight Watchers; receiving honoraria for lectures, continuing medical education activities, and presentations at scientific conferences; and receiving royalties from Guilford Press and Taylor & Francis, all outside the submitted work.
A version of this article first appeared on Medscape.com.
Feelings of chronic emptiness and self-injury have been identified as two key risk factors for suicide attempts (SAs) in patients with borderline personality disorder (BPD), a new cross-sectional, nationally representative study suggests.
The findings also show lifetime and past-year SAs are common among patients with BPD, even when excluding self-injurious behaviors.
The results suggest that in addition to asking patients about self-harm during suicide risk screenings and assessments, clinicians should query them about “longstanding” feelings of emptiness, study investigator Carlos M. Grilo, PhD, professor of psychiatry and psychology, Yale University, New Haven, Conn., said in an interview.
Although related, chronic emptiness “is distinct and goes beyond feelings of sadness, loneliness, and hopelessness,” explained Dr. Grilo. he said.
The study was published online May 11 in JAMA Network Open.
Filling a research gap
While BPD and other psychiatric disorders are associated with suicide, the authors noted there is a “dearth of epidemiological research” examining the link between BPD and suicide.
Criteria for BPD diagnosis requires any five of the following criteria: relationships, affective instability, abandonment fear, anger, identity disturbance, emptiness, disassociation/paranoia, self-injurious behavior, and impulsivity, along with social-occupation dysfunction.
To determine SA risk with specific BPD diagnostic criteria, the investigators examined data on 36,309 individuals who participated in the third wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III), conducted from 2012 to 2013.
During computer-assisted, face-to-face interviews, study participants answered questions based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) of the National Institute on Alcohol Abuse and Alcoholism.
This structured interview assesses a range of DSM-5–defined psychiatric disorders and their criteria. In addition to BPD, the AUDADIS-5 generates diagnoses for mood disorders, anxiety disorders, posttraumatic stress disorder, substance use disorders, antisocial personality disorder, schizotypal disorder, and conduct disorder.
During the interviews, respondents were asked if they had ever attempted suicide. For those who had, interviewers recorded the total number of lifetime attempts.
Participants also answered questions about childhood maltreatment including physical neglect, emotional neglect, physical abuse, emotional abuse, and sexual abuse by parents or caregivers and other adverse events occurring before the age of 18.
Childhood trauma common
Patients with BPD frequently report a history of childhood trauma, noted Dr. Grilo, adding that such trauma is associated with self-harm and suicide attempts. Sociodemographic information, including age, sex, and ethnicity/race, education level, and income, was also gathered.
Investigators examined data on suicide attempts using relatively stringent coding that required serious dysfunction in at least five BPD criteria.
Using this definition, investigators found the lifetime SA prevalence in patients with BPD was 30.4%, and 3.2% for past-year SAs. This compared with a rate of 3.7% for lifetime SAs and 0.2% for past-year SAs in those without a BPD diagnosis.
The authors examined SA rates using diagnostic codes in the NESARC-III that required seriously impaired function in only 1 or 2 BPD criteria. Rates were higher using the 5-criteria definition.
When the researchers excluded the BPD criterion of self-injurious behavior, the prevalence was 28.1% for lifetime and 3.0% for past-year SAs among the BPD group, with corresponding rates of 3.8% and 0.2% in those without a BPD diagnosis.
It’s important to look at this, said Dr. Grilo, as some patients with BPD who engage in self-harm have suicidal intent while others don’t.
“We tested whether BPD had heightened risk for suicide attempts if we eliminated the self-injurious criterion and we found that heightened risk was still there,” he explained.
Looking at individual criteria for BPD, a model that adjusted for sociodemographic characteristics, other psychiatric disorders, age at BPD onset, and history of childhood adverse events uncovered two criteria that were significantly associated with increased odds of SAs.
One was emptiness. For lifetime suicide attempts, the adjusted odds ratio (aOR) was 1.58 (95% confidence interval, 1.16-2.14) and for past-year attempts, the aOR was 1.99 (95% CI, 1.08-3.66).
The second was self-injurious behavior. For lifetime attempts, the aOR was 24.28 (95% CI, 16.83-32.03) and for past-year attempts, the aOR was 19.32 (95% CI, 5.22-71.58).
In a model in which all BPD-specific criteria were entered while excluding self-injurious behavior, the aORs for emptiness were 1.66 (95% CI, 1.23-2.24) for lifetime suicide attempts and 2.45 (95% CI, 1.18-5.08) for past year attempts.
Unlike another recent study that included more than 700 treatment-seeking patients with BPD who were followed for 10 years, the current study did not show significant associations with SAs for two other BPD criteria – identity disturbance and frantic attempts to avoid abandonment.
Dr. Grilo explained this might be because the earlier study included treatment-seeking patients instead of community cases, or because of differences in assessment interviews or other factors.
‘Compelling evidence’
“Our epidemiological sample has much broader generalizability and fewer potential confounds than the clinical treatment-seeking sample,” said Dr. Grilo.
However, he noted that the two studies “converge strongly and provide compelling evidence that BPD is associated with substantially heightened risk for suicide attempts over the lifetime.”
The two studies “also converge in finding that the presence of symptoms such as repeated self-harm and feelings of chronic emptiness are also associated with risk for suicide attempts.”
The new findings highlight the need to ask potentially at-risk patients about feelings of emptiness as well as self-injurious behaviors. Clinicians could, for example, ask: “Have you often felt like your life had no purpose or meaning?” or “Have you often felt empty inside?”
Limitations of the study include reliance on retrospective self-reports and use of lay interviewers, although these interviewers were trained and had an average of 5 years of experience conducting health-related surveys.
Although the study included a representative sample of U.S. adults, the sample did not include groups known to have high rates of suicide and self-harm behaviors, such as institutionalized, incarcerated, or homeless individuals.
In addition, the study did not evaluate severity and duration of BPD, although the authors noted they did adjust for age at BPD onset, this did not alter the findings.
Often misdiagnosed
Commenting on the study, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, and past-president, American Psychiatric Association, and an expert on BPD, had high praise for the research.
BPD is often misdiagnosed, Dr. Oldham said in an interview. Many patients seek help from primary care doctors who may label the symptoms as an anxiety disorder or a mood disorder, he said.
Although medications can help treat some BPD symptoms, “the primary, core evidence-based treatment for BPD is psychotherapy,” said Dr. Oldham, who some years ago helped develop evidence-based practice guidelines for BPD.
“It’s a clear and very well-designed study, and I don’t see any major limitations or problems with it,” he said. “The authors kept their focus rigorously on their goals and they used really careful methodology.”
He noted the “huge” numbers of patients included in the data and the relatively large percentage of men (43.7%).
“There’s a general belief that it’s mostly females who have BPD, but that’s not true; it’s females who come to treatment,” said Dr. Oldham.
Requiring that all five criteria lead to seriously impaired functioning “is a much more rigorous diagnostic methodology” than requiring only one or two criteria to lead to such impairment, said Dr. Oldham. “This is really important” and makes it “a much stronger study.”
The finding that self-harm behavior was linked to suicide attempts isn’t that surprising as this association has been well documented, but the finding that chronic emptiness is also predictive of future suicide attempts “is news,” said Dr. Oldham.
“We have not paid enough attention to this criterion in the clinical world or in the research world.”
Dr. Oldham said one patient with BPD gave him an ideal metaphor for emptiness. “She said it’s like there’s just nobody home. Think of it as an empty house that may look fine on the outside but you go inside and nobody lives there; there’s no furniture; no favorite things; no photos; no possessions.”
The authors have “important messages we need to pay attention to, and the main one is to explore this sense of chronic ‘nobody home’ emptiness,” said Dr. Oldham.
Dr. Grilo has reported receiving research grants from the National Institutes of Health; serving as a consultant for Sunovion and Weight Watchers; receiving honoraria for lectures, continuing medical education activities, and presentations at scientific conferences; and receiving royalties from Guilford Press and Taylor & Francis, all outside the submitted work.
A version of this article first appeared on Medscape.com.
Feelings of chronic emptiness and self-injury have been identified as two key risk factors for suicide attempts (SAs) in patients with borderline personality disorder (BPD), a new cross-sectional, nationally representative study suggests.
The findings also show lifetime and past-year SAs are common among patients with BPD, even when excluding self-injurious behaviors.
The results suggest that in addition to asking patients about self-harm during suicide risk screenings and assessments, clinicians should query them about “longstanding” feelings of emptiness, study investigator Carlos M. Grilo, PhD, professor of psychiatry and psychology, Yale University, New Haven, Conn., said in an interview.
Although related, chronic emptiness “is distinct and goes beyond feelings of sadness, loneliness, and hopelessness,” explained Dr. Grilo. he said.
The study was published online May 11 in JAMA Network Open.
Filling a research gap
While BPD and other psychiatric disorders are associated with suicide, the authors noted there is a “dearth of epidemiological research” examining the link between BPD and suicide.
Criteria for BPD diagnosis requires any five of the following criteria: relationships, affective instability, abandonment fear, anger, identity disturbance, emptiness, disassociation/paranoia, self-injurious behavior, and impulsivity, along with social-occupation dysfunction.
To determine SA risk with specific BPD diagnostic criteria, the investigators examined data on 36,309 individuals who participated in the third wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III), conducted from 2012 to 2013.
During computer-assisted, face-to-face interviews, study participants answered questions based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) of the National Institute on Alcohol Abuse and Alcoholism.
This structured interview assesses a range of DSM-5–defined psychiatric disorders and their criteria. In addition to BPD, the AUDADIS-5 generates diagnoses for mood disorders, anxiety disorders, posttraumatic stress disorder, substance use disorders, antisocial personality disorder, schizotypal disorder, and conduct disorder.
During the interviews, respondents were asked if they had ever attempted suicide. For those who had, interviewers recorded the total number of lifetime attempts.
Participants also answered questions about childhood maltreatment including physical neglect, emotional neglect, physical abuse, emotional abuse, and sexual abuse by parents or caregivers and other adverse events occurring before the age of 18.
Childhood trauma common
Patients with BPD frequently report a history of childhood trauma, noted Dr. Grilo, adding that such trauma is associated with self-harm and suicide attempts. Sociodemographic information, including age, sex, and ethnicity/race, education level, and income, was also gathered.
Investigators examined data on suicide attempts using relatively stringent coding that required serious dysfunction in at least five BPD criteria.
Using this definition, investigators found the lifetime SA prevalence in patients with BPD was 30.4%, and 3.2% for past-year SAs. This compared with a rate of 3.7% for lifetime SAs and 0.2% for past-year SAs in those without a BPD diagnosis.
The authors examined SA rates using diagnostic codes in the NESARC-III that required seriously impaired function in only 1 or 2 BPD criteria. Rates were higher using the 5-criteria definition.
When the researchers excluded the BPD criterion of self-injurious behavior, the prevalence was 28.1% for lifetime and 3.0% for past-year SAs among the BPD group, with corresponding rates of 3.8% and 0.2% in those without a BPD diagnosis.
It’s important to look at this, said Dr. Grilo, as some patients with BPD who engage in self-harm have suicidal intent while others don’t.
“We tested whether BPD had heightened risk for suicide attempts if we eliminated the self-injurious criterion and we found that heightened risk was still there,” he explained.
Looking at individual criteria for BPD, a model that adjusted for sociodemographic characteristics, other psychiatric disorders, age at BPD onset, and history of childhood adverse events uncovered two criteria that were significantly associated with increased odds of SAs.
One was emptiness. For lifetime suicide attempts, the adjusted odds ratio (aOR) was 1.58 (95% confidence interval, 1.16-2.14) and for past-year attempts, the aOR was 1.99 (95% CI, 1.08-3.66).
The second was self-injurious behavior. For lifetime attempts, the aOR was 24.28 (95% CI, 16.83-32.03) and for past-year attempts, the aOR was 19.32 (95% CI, 5.22-71.58).
In a model in which all BPD-specific criteria were entered while excluding self-injurious behavior, the aORs for emptiness were 1.66 (95% CI, 1.23-2.24) for lifetime suicide attempts and 2.45 (95% CI, 1.18-5.08) for past year attempts.
Unlike another recent study that included more than 700 treatment-seeking patients with BPD who were followed for 10 years, the current study did not show significant associations with SAs for two other BPD criteria – identity disturbance and frantic attempts to avoid abandonment.
Dr. Grilo explained this might be because the earlier study included treatment-seeking patients instead of community cases, or because of differences in assessment interviews or other factors.
‘Compelling evidence’
“Our epidemiological sample has much broader generalizability and fewer potential confounds than the clinical treatment-seeking sample,” said Dr. Grilo.
However, he noted that the two studies “converge strongly and provide compelling evidence that BPD is associated with substantially heightened risk for suicide attempts over the lifetime.”
The two studies “also converge in finding that the presence of symptoms such as repeated self-harm and feelings of chronic emptiness are also associated with risk for suicide attempts.”
The new findings highlight the need to ask potentially at-risk patients about feelings of emptiness as well as self-injurious behaviors. Clinicians could, for example, ask: “Have you often felt like your life had no purpose or meaning?” or “Have you often felt empty inside?”
Limitations of the study include reliance on retrospective self-reports and use of lay interviewers, although these interviewers were trained and had an average of 5 years of experience conducting health-related surveys.
Although the study included a representative sample of U.S. adults, the sample did not include groups known to have high rates of suicide and self-harm behaviors, such as institutionalized, incarcerated, or homeless individuals.
In addition, the study did not evaluate severity and duration of BPD, although the authors noted they did adjust for age at BPD onset, this did not alter the findings.
Often misdiagnosed
Commenting on the study, John M. Oldham, MD, Distinguished Emeritus Professor, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, and past-president, American Psychiatric Association, and an expert on BPD, had high praise for the research.
BPD is often misdiagnosed, Dr. Oldham said in an interview. Many patients seek help from primary care doctors who may label the symptoms as an anxiety disorder or a mood disorder, he said.
Although medications can help treat some BPD symptoms, “the primary, core evidence-based treatment for BPD is psychotherapy,” said Dr. Oldham, who some years ago helped develop evidence-based practice guidelines for BPD.
“It’s a clear and very well-designed study, and I don’t see any major limitations or problems with it,” he said. “The authors kept their focus rigorously on their goals and they used really careful methodology.”
He noted the “huge” numbers of patients included in the data and the relatively large percentage of men (43.7%).
“There’s a general belief that it’s mostly females who have BPD, but that’s not true; it’s females who come to treatment,” said Dr. Oldham.
Requiring that all five criteria lead to seriously impaired functioning “is a much more rigorous diagnostic methodology” than requiring only one or two criteria to lead to such impairment, said Dr. Oldham. “This is really important” and makes it “a much stronger study.”
The finding that self-harm behavior was linked to suicide attempts isn’t that surprising as this association has been well documented, but the finding that chronic emptiness is also predictive of future suicide attempts “is news,” said Dr. Oldham.
“We have not paid enough attention to this criterion in the clinical world or in the research world.”
Dr. Oldham said one patient with BPD gave him an ideal metaphor for emptiness. “She said it’s like there’s just nobody home. Think of it as an empty house that may look fine on the outside but you go inside and nobody lives there; there’s no furniture; no favorite things; no photos; no possessions.”
The authors have “important messages we need to pay attention to, and the main one is to explore this sense of chronic ‘nobody home’ emptiness,” said Dr. Oldham.
Dr. Grilo has reported receiving research grants from the National Institutes of Health; serving as a consultant for Sunovion and Weight Watchers; receiving honoraria for lectures, continuing medical education activities, and presentations at scientific conferences; and receiving royalties from Guilford Press and Taylor & Francis, all outside the submitted work.
A version of this article first appeared on Medscape.com.
HHS to inject billions into mental health, substance use disorders
The U.S. Department of Health and Human Services will inject billions of dollars into programs designed to address mental health and substance use disorders, including $3 billion released to states as of May 18, said federal officials.
The American Rescue Plan, a COVID-relief package signed into law in March, contained the money, which will be divided equally between the Community Mental Health Services Block Grant Program and the Substance Abuse Prevention and Treatment Block Grant Program, said Tom Coderre, Acting Assistant Secretary for Mental Health and Substance Use, in a call with reporters.
The award amounts will vary by state.
The mental health program helps states and territories provide services for children with serious emotional issues and adults with serious mental illness.
The substance use program provides money to plan, implement, and evaluate prevention, intervention, treatment, and recovery services.
, which fueled an increase in anxiety, depression, and overdose, said Assistant Secretary for Health Rachel Levine, MD, on the call.
“We know multiple stressors during the pandemic – isolation, sickness, grief, job loss, food instability, and loss of routines – have devastated many Americans and presented the unprecedented behavioral health challenges across the nation,” said Dr. Levine.
The HHS also announced that it is re-establishing a Behavioral Health Coordinating Council (BHCC). Dr. Levine and Mr. Coderre will serve as cochairs of the Council, which will coordinate action-oriented approaches to addressing the HHS’s behavioral health efforts.
However, in 2014, the U.S. Government Accountability Office criticized the BHCC for only focusing on the HHS, and noted the lack of coordination across the federal government’s various efforts to address mental health.
‘A huge step forward’
The American Psychiatric Association welcomed the new money and the return of the council.
“In the wake of the pandemic an unprecedented, and as of yet untold, number of Americans are faced with mental health and substance use disorders, particularly in communities impacted by structural racism,” said APA President Vivian Pender, MD, in a statement. “With the creation of this Council and this investment in mental health, the administration is taking a huge step forward.”
APA CEO and Medical Director Saul Levin, MD, MPA, added: “This Council has great potential to ease the challenges we face as we begin to recover from the pandemic’s impact on our society, and [the] APA looks forward to assisting in their efforts.”
HHS Secretary Xavier Becerra noted in a statement that the COVID-19 pandemic “has made clear the need to invest resources in our nation’s mental health and address the inequities that still exist around behavioral health care.” He added, “This national problem calls for department-wide coordination to address the issue.”
Dr. Levine said the Council “will assure the right prioritization and guidelines are in place to provide pathways to prevention, intervention, treatment, and recovery services.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Health and Human Services will inject billions of dollars into programs designed to address mental health and substance use disorders, including $3 billion released to states as of May 18, said federal officials.
The American Rescue Plan, a COVID-relief package signed into law in March, contained the money, which will be divided equally between the Community Mental Health Services Block Grant Program and the Substance Abuse Prevention and Treatment Block Grant Program, said Tom Coderre, Acting Assistant Secretary for Mental Health and Substance Use, in a call with reporters.
The award amounts will vary by state.
The mental health program helps states and territories provide services for children with serious emotional issues and adults with serious mental illness.
The substance use program provides money to plan, implement, and evaluate prevention, intervention, treatment, and recovery services.
, which fueled an increase in anxiety, depression, and overdose, said Assistant Secretary for Health Rachel Levine, MD, on the call.
“We know multiple stressors during the pandemic – isolation, sickness, grief, job loss, food instability, and loss of routines – have devastated many Americans and presented the unprecedented behavioral health challenges across the nation,” said Dr. Levine.
The HHS also announced that it is re-establishing a Behavioral Health Coordinating Council (BHCC). Dr. Levine and Mr. Coderre will serve as cochairs of the Council, which will coordinate action-oriented approaches to addressing the HHS’s behavioral health efforts.
However, in 2014, the U.S. Government Accountability Office criticized the BHCC for only focusing on the HHS, and noted the lack of coordination across the federal government’s various efforts to address mental health.
‘A huge step forward’
The American Psychiatric Association welcomed the new money and the return of the council.
“In the wake of the pandemic an unprecedented, and as of yet untold, number of Americans are faced with mental health and substance use disorders, particularly in communities impacted by structural racism,” said APA President Vivian Pender, MD, in a statement. “With the creation of this Council and this investment in mental health, the administration is taking a huge step forward.”
APA CEO and Medical Director Saul Levin, MD, MPA, added: “This Council has great potential to ease the challenges we face as we begin to recover from the pandemic’s impact on our society, and [the] APA looks forward to assisting in their efforts.”
HHS Secretary Xavier Becerra noted in a statement that the COVID-19 pandemic “has made clear the need to invest resources in our nation’s mental health and address the inequities that still exist around behavioral health care.” He added, “This national problem calls for department-wide coordination to address the issue.”
Dr. Levine said the Council “will assure the right prioritization and guidelines are in place to provide pathways to prevention, intervention, treatment, and recovery services.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Health and Human Services will inject billions of dollars into programs designed to address mental health and substance use disorders, including $3 billion released to states as of May 18, said federal officials.
The American Rescue Plan, a COVID-relief package signed into law in March, contained the money, which will be divided equally between the Community Mental Health Services Block Grant Program and the Substance Abuse Prevention and Treatment Block Grant Program, said Tom Coderre, Acting Assistant Secretary for Mental Health and Substance Use, in a call with reporters.
The award amounts will vary by state.
The mental health program helps states and territories provide services for children with serious emotional issues and adults with serious mental illness.
The substance use program provides money to plan, implement, and evaluate prevention, intervention, treatment, and recovery services.
, which fueled an increase in anxiety, depression, and overdose, said Assistant Secretary for Health Rachel Levine, MD, on the call.
“We know multiple stressors during the pandemic – isolation, sickness, grief, job loss, food instability, and loss of routines – have devastated many Americans and presented the unprecedented behavioral health challenges across the nation,” said Dr. Levine.
The HHS also announced that it is re-establishing a Behavioral Health Coordinating Council (BHCC). Dr. Levine and Mr. Coderre will serve as cochairs of the Council, which will coordinate action-oriented approaches to addressing the HHS’s behavioral health efforts.
However, in 2014, the U.S. Government Accountability Office criticized the BHCC for only focusing on the HHS, and noted the lack of coordination across the federal government’s various efforts to address mental health.
‘A huge step forward’
The American Psychiatric Association welcomed the new money and the return of the council.
“In the wake of the pandemic an unprecedented, and as of yet untold, number of Americans are faced with mental health and substance use disorders, particularly in communities impacted by structural racism,” said APA President Vivian Pender, MD, in a statement. “With the creation of this Council and this investment in mental health, the administration is taking a huge step forward.”
APA CEO and Medical Director Saul Levin, MD, MPA, added: “This Council has great potential to ease the challenges we face as we begin to recover from the pandemic’s impact on our society, and [the] APA looks forward to assisting in their efforts.”
HHS Secretary Xavier Becerra noted in a statement that the COVID-19 pandemic “has made clear the need to invest resources in our nation’s mental health and address the inequities that still exist around behavioral health care.” He added, “This national problem calls for department-wide coordination to address the issue.”
Dr. Levine said the Council “will assure the right prioritization and guidelines are in place to provide pathways to prevention, intervention, treatment, and recovery services.”
A version of this article first appeared on Medscape.com.