User login
Neurodegeneration complicates psychiatric care for Parkinson’s patients
Managing depression and anxiety in Parkinson’s disease should start with a review of medications and involve multidisciplinary care, according to a recent summary of evidence.
“Depression and anxiety have a complex relationship with the disease and while the exact mechanism for this association is unknown, both disturbances occur with increased prevalence across the disease course and when present earlier in life, increase the risk of PD by about twofold,” wrote Gregory M. Pontone, MD, of Johns Hopkins University, Baltimore, and colleagues.
Randomized trials to guide treatment of anxiety and depression in patients with Parkinson’s disease (PD) are limited, the researchers noted. However, data from a longitudinal study showed that PD patients whose depression remitted spontaneously or responded to treatment were able to attain a level of function similar to that of never-depressed PD patients, Dr. Pontone and colleagues said.
The researchers offered a pair of treatment algorithms to help guide clinicians in managing depression and anxiety in PD. However, a caveat to keep in mind is that “the benefit of antidepressant medications, used for depression or anxiety, can be confounded when motor symptoms are not optimally treated,” the researchers emphasized.
For depression, the researchers advised starting with some lab work; “at a minimum we suggest checking a complete blood count, metabolic panel, TSH, B12, and folate,” they noted. They recommended an antidepressant, cognitive-behavioral therapy, or both, as a first-line treatment, such as monotherapy with selective norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors. They advised titrating the chosen monotherapy to a minimum effective dose over a 2- to 3-week period to assess response.
“We recommend continuing antidepressant therapy for at least 1 year based on literature in non-PD populations and anecdotal clinical experience. At 1 year, if not in remission, consider continuing treatment or augmenting to improve response,” the researchers said.
, and they recommended using anxiety rating scales to diagnose anxiety in PD. “Given the high prevalence of atypical anxiety syndromes in PD and their potential association with both motor and nonmotor symptoms of the disease, working with the neurologist to achieve optimal control of PD is an essential first step to alleviating anxiety,” they emphasized.
The researchers also advised addressing comorbidities, including cardiovascular disease, chronic pain, diabetes, gastrointestinal issues, hyperthyroidism, and lung disease, all of which can be associated with anxiety. Once comorbidities are addressed, they advised caution given the lack of evidence for efficacy of both pharmacologic and nonpharmacologic anxiety treatments for PD patients. However, first-tier treatment for anxiety could include monotherapy with serotonin-norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors, they said.
PD patients with depression and anxiety also may benefit from nonpharmacologic interventions, including exercise, mindfulness, relaxation therapy, and cognitive behavioral therapy the researchers said.
Although the algorithm may not differ significantly from current treatment protocols, it highlights aspects unique to PD patients, the researchers said. In particular, the algorithm shows “that interventions used for motor symptoms, for example, dopamine agonists, may be especially potent for mood in the PD population and that augmentation strategies, such as antipsychotics and lithium, may not be well tolerated given their outsized risk of adverse events in PD,” they said.
“While an article of this kind cannot hope to address the gap in knowledge on comparative efficacy between interventions, it can guide readers on the best strategies for implementation and risk mitigation in PD – essentially focusing more on effectiveness,” they concluded.
The study received no outside funding. Dr. Pontone disclosed serving as a consultant for Acadia Pharmaceuticals and Concert Pharmaceuticals.
Managing depression and anxiety in Parkinson’s disease should start with a review of medications and involve multidisciplinary care, according to a recent summary of evidence.
“Depression and anxiety have a complex relationship with the disease and while the exact mechanism for this association is unknown, both disturbances occur with increased prevalence across the disease course and when present earlier in life, increase the risk of PD by about twofold,” wrote Gregory M. Pontone, MD, of Johns Hopkins University, Baltimore, and colleagues.
Randomized trials to guide treatment of anxiety and depression in patients with Parkinson’s disease (PD) are limited, the researchers noted. However, data from a longitudinal study showed that PD patients whose depression remitted spontaneously or responded to treatment were able to attain a level of function similar to that of never-depressed PD patients, Dr. Pontone and colleagues said.
The researchers offered a pair of treatment algorithms to help guide clinicians in managing depression and anxiety in PD. However, a caveat to keep in mind is that “the benefit of antidepressant medications, used for depression or anxiety, can be confounded when motor symptoms are not optimally treated,” the researchers emphasized.
For depression, the researchers advised starting with some lab work; “at a minimum we suggest checking a complete blood count, metabolic panel, TSH, B12, and folate,” they noted. They recommended an antidepressant, cognitive-behavioral therapy, or both, as a first-line treatment, such as monotherapy with selective norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors. They advised titrating the chosen monotherapy to a minimum effective dose over a 2- to 3-week period to assess response.
“We recommend continuing antidepressant therapy for at least 1 year based on literature in non-PD populations and anecdotal clinical experience. At 1 year, if not in remission, consider continuing treatment or augmenting to improve response,” the researchers said.
, and they recommended using anxiety rating scales to diagnose anxiety in PD. “Given the high prevalence of atypical anxiety syndromes in PD and their potential association with both motor and nonmotor symptoms of the disease, working with the neurologist to achieve optimal control of PD is an essential first step to alleviating anxiety,” they emphasized.
The researchers also advised addressing comorbidities, including cardiovascular disease, chronic pain, diabetes, gastrointestinal issues, hyperthyroidism, and lung disease, all of which can be associated with anxiety. Once comorbidities are addressed, they advised caution given the lack of evidence for efficacy of both pharmacologic and nonpharmacologic anxiety treatments for PD patients. However, first-tier treatment for anxiety could include monotherapy with serotonin-norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors, they said.
PD patients with depression and anxiety also may benefit from nonpharmacologic interventions, including exercise, mindfulness, relaxation therapy, and cognitive behavioral therapy the researchers said.
Although the algorithm may not differ significantly from current treatment protocols, it highlights aspects unique to PD patients, the researchers said. In particular, the algorithm shows “that interventions used for motor symptoms, for example, dopamine agonists, may be especially potent for mood in the PD population and that augmentation strategies, such as antipsychotics and lithium, may not be well tolerated given their outsized risk of adverse events in PD,” they said.
“While an article of this kind cannot hope to address the gap in knowledge on comparative efficacy between interventions, it can guide readers on the best strategies for implementation and risk mitigation in PD – essentially focusing more on effectiveness,” they concluded.
The study received no outside funding. Dr. Pontone disclosed serving as a consultant for Acadia Pharmaceuticals and Concert Pharmaceuticals.
Managing depression and anxiety in Parkinson’s disease should start with a review of medications and involve multidisciplinary care, according to a recent summary of evidence.
“Depression and anxiety have a complex relationship with the disease and while the exact mechanism for this association is unknown, both disturbances occur with increased prevalence across the disease course and when present earlier in life, increase the risk of PD by about twofold,” wrote Gregory M. Pontone, MD, of Johns Hopkins University, Baltimore, and colleagues.
Randomized trials to guide treatment of anxiety and depression in patients with Parkinson’s disease (PD) are limited, the researchers noted. However, data from a longitudinal study showed that PD patients whose depression remitted spontaneously or responded to treatment were able to attain a level of function similar to that of never-depressed PD patients, Dr. Pontone and colleagues said.
The researchers offered a pair of treatment algorithms to help guide clinicians in managing depression and anxiety in PD. However, a caveat to keep in mind is that “the benefit of antidepressant medications, used for depression or anxiety, can be confounded when motor symptoms are not optimally treated,” the researchers emphasized.
For depression, the researchers advised starting with some lab work; “at a minimum we suggest checking a complete blood count, metabolic panel, TSH, B12, and folate,” they noted. They recommended an antidepressant, cognitive-behavioral therapy, or both, as a first-line treatment, such as monotherapy with selective norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors. They advised titrating the chosen monotherapy to a minimum effective dose over a 2- to 3-week period to assess response.
“We recommend continuing antidepressant therapy for at least 1 year based on literature in non-PD populations and anecdotal clinical experience. At 1 year, if not in remission, consider continuing treatment or augmenting to improve response,” the researchers said.
, and they recommended using anxiety rating scales to diagnose anxiety in PD. “Given the high prevalence of atypical anxiety syndromes in PD and their potential association with both motor and nonmotor symptoms of the disease, working with the neurologist to achieve optimal control of PD is an essential first step to alleviating anxiety,” they emphasized.
The researchers also advised addressing comorbidities, including cardiovascular disease, chronic pain, diabetes, gastrointestinal issues, hyperthyroidism, and lung disease, all of which can be associated with anxiety. Once comorbidities are addressed, they advised caution given the lack of evidence for efficacy of both pharmacologic and nonpharmacologic anxiety treatments for PD patients. However, first-tier treatment for anxiety could include monotherapy with serotonin-norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors, they said.
PD patients with depression and anxiety also may benefit from nonpharmacologic interventions, including exercise, mindfulness, relaxation therapy, and cognitive behavioral therapy the researchers said.
Although the algorithm may not differ significantly from current treatment protocols, it highlights aspects unique to PD patients, the researchers said. In particular, the algorithm shows “that interventions used for motor symptoms, for example, dopamine agonists, may be especially potent for mood in the PD population and that augmentation strategies, such as antipsychotics and lithium, may not be well tolerated given their outsized risk of adverse events in PD,” they said.
“While an article of this kind cannot hope to address the gap in knowledge on comparative efficacy between interventions, it can guide readers on the best strategies for implementation and risk mitigation in PD – essentially focusing more on effectiveness,” they concluded.
The study received no outside funding. Dr. Pontone disclosed serving as a consultant for Acadia Pharmaceuticals and Concert Pharmaceuticals.
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Low-dose nitrous oxide shows benefit for resistant depression
A 1-hour treatment with a low concentration of nitrous oxide, commonly known as “laughing gas,” appears to relieve symptoms of treatment-resistant major depression (TRMD), with effects lasting as long as several weeks, new research suggests.
In a trial with a crossover design, investigators randomly assigned 28 patients with severe TRMD to receive a single 1-hour inhalation of placebo or nitrous oxide once a month over a 3-month period. Participants received an inhalation of placebo; a 25% concentration of nitrous oxide; and a 50% concentration of nitrous oxide. Sessions were conducted 4 weeks apart.
Both doses of nitrous oxide were associated with substantial improvement in depressive symptoms for roughly 85% of participants. However, the 25% concentration had a lower risk for adverse effects, which included sedation, nausea, and mild dissociation, compared to the 50% concentration.
“Twenty-five percent nitrous oxide has similar efficacy, compared to 50% nitrous oxide, and reduced side effects fourfold,” lead author Peter Nagele, MD, MSc, chair and professor of anesthesia and critical care, University of Chicago, said in an interview.
“We also observed that many patients had a 2-week improvement of depressive symptoms after a nitrous oxide treatment,” said Dr. Nagele, who also is professor of psychiatry and behavioral neuroscience.
The study was published online June 9 in Science Translational Medicine.
Further refinement
A previous proof-of-principle study conducted by the same researchers demonstrated that a 1-hour inhalation of 50% nitrous oxide had rapid antidepressant effects for patients with TRMD.
The current phase 2 trial “is a follow-up study to our earlier 2015 pilot trial and was designed to further refine the dose of nitrous oxide needed for antidepressant efficacy,” Dr. Nagele said.
“An important secondary aim [of the current study] was to determine whether a lower dose – 25% – would reduce side effects, and a third aim was to determine how long the antidepressants effects last,” he explained.
To investigate, the researchers enrolled 28 patients (median [interquartile range (IQR)] age 39 years [26-68 years]; 71% women; 96% White) to have three inhalation sessions (placebo, 25%, and 50% nitrous oxide) at 4-week intervals. Twenty patients completed all three inhalation sessions, and four completed ≥1 treatment.
Participants had “sustained and refractory depressive illness,” with a mean illness lifetime duration of 17.5 years and an extensive history of antidepressant drug failure (median, 4.5 [2-10] adequate-dose/duration antidepressants).
Some patients had undergone vagus nerve stimulation, electroconvulsive therapy, or repetitive transcranial magnetic stimulation, or had received ketamine (4%, 8%, 13%, and 8%, respectively).
The primary outcome was improvement on the 21-item Hamilton Depression rating Scale (HDRS-21) score over a 2-week observation period.
‘Stronger evidence’
Compared to placebo, nitrous oxide significantly improved depressive symptoms (P = .01). There was no significant difference between the 25% and the 50% concentrations (P = .58).
The estimated difference in HDRS-21 scores between the placebo and various treatment groups are shown in the following table.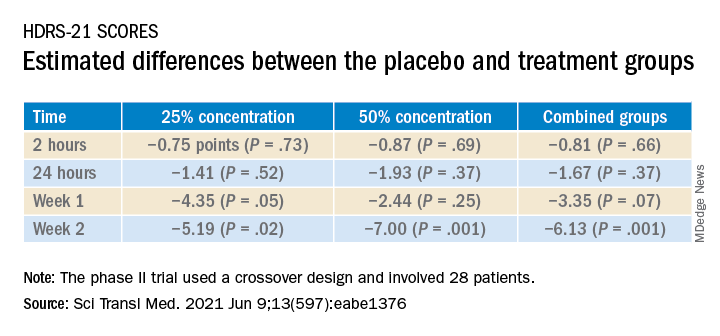
To ensure there where were carryover effects between the two doses, the researchers performed an analysis to ascertain whether order of receipt of the higher dose was related to the 2-week HDRS-21 score; they found no significant effect of trial order (P = .22).
The 20 patients who completed the entire course of treatment “experienced a clinically significant improvement in depressive symptoms from a median baseline HDRS-21 score of 20.5 (IQR, 19.0 to 25.5) to 8.5 (IQR, 2.0 to 16.0) at study completion, corresponding to a median change of −11.0 points (IQR, −3.3 to −14.0 points; P < .0001) after the 3-month study period,” the investigators noted.
The types of treatment response and improvement in depressive symptoms from baseline to study completion are listed in the table below.
There were statistically significant differences in adverse events between the two treatment doses; 47 events occurred following inhalation of the 50% concentration, compared to 11 after inhalation of the 25% concentration. There were six adverse events after inhalation of placebo (P < .0001).
“None of the adverse events were serious, and nearly all occurred either during or immediately after the treatment session and resolved within several hours,” the authors reported.
“We need to be remindful that – despite the exciting results of the study – the study was small and cannot be considered definitive evidence; as such, it is too early to advocate for the use of nitrous oxide in everyday clinical practice,” Dr. Nagele said.
Nevertheless, on the basis of the current findings, he stated.
Rapid-acting antidepressants
Commenting on the study in an interview, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit at Toronto Western Hospital, noted that the research into nitrous oxide is “part of an interest in rapid-acting antidepressants.”
Dr. McIntyre, also the chairman and executive director of the Brain and Cognition Discovery Foundation, Toronto, who was not involved with the study, found it “interesting” that “almost 20% of the sample had previously had suboptimal outcomes to ketamine and/or neurostimulation, meaning these patients had serious refractory illness, but the benefit [of nitrous oxide] was sustained at 2 weeks.”
Studies of the use of nitrous oxide for patients with bipolar depression “would be warranted, since it appears generally safe and well tolerated,” said Dr. McIntyre, director of the Depression and Bipolar Support Alliance.
The study was sponsored by an award to Dr. Nagele from the NARSAD Independent Investigator Award from the Brain and Behavior Research Foundation and an award to Dr. Nagele and other coauthors from the Taylor Family Institute for Innovative Psychiatric Research at Washington University in St. Louis. Dr. Nagele receives funding from the National Institute of Mental Health the American Foundation for Prevention of Suicide, and the Brain and Behavior Research Foundation; has received research funding and honoraria from Roche Diagnostics and Abbott Diagnostics; and has previously filed for intellectual property protection related to the use of nitrous oxide in major depression. The other authors’ disclosures are listed on the original article. Dr. McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation; speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, Eisai, Minerva, Intra-Cellular, and Abbvie. Dr. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
A 1-hour treatment with a low concentration of nitrous oxide, commonly known as “laughing gas,” appears to relieve symptoms of treatment-resistant major depression (TRMD), with effects lasting as long as several weeks, new research suggests.
In a trial with a crossover design, investigators randomly assigned 28 patients with severe TRMD to receive a single 1-hour inhalation of placebo or nitrous oxide once a month over a 3-month period. Participants received an inhalation of placebo; a 25% concentration of nitrous oxide; and a 50% concentration of nitrous oxide. Sessions were conducted 4 weeks apart.
Both doses of nitrous oxide were associated with substantial improvement in depressive symptoms for roughly 85% of participants. However, the 25% concentration had a lower risk for adverse effects, which included sedation, nausea, and mild dissociation, compared to the 50% concentration.
“Twenty-five percent nitrous oxide has similar efficacy, compared to 50% nitrous oxide, and reduced side effects fourfold,” lead author Peter Nagele, MD, MSc, chair and professor of anesthesia and critical care, University of Chicago, said in an interview.
“We also observed that many patients had a 2-week improvement of depressive symptoms after a nitrous oxide treatment,” said Dr. Nagele, who also is professor of psychiatry and behavioral neuroscience.
The study was published online June 9 in Science Translational Medicine.
Further refinement
A previous proof-of-principle study conducted by the same researchers demonstrated that a 1-hour inhalation of 50% nitrous oxide had rapid antidepressant effects for patients with TRMD.
The current phase 2 trial “is a follow-up study to our earlier 2015 pilot trial and was designed to further refine the dose of nitrous oxide needed for antidepressant efficacy,” Dr. Nagele said.
“An important secondary aim [of the current study] was to determine whether a lower dose – 25% – would reduce side effects, and a third aim was to determine how long the antidepressants effects last,” he explained.
To investigate, the researchers enrolled 28 patients (median [interquartile range (IQR)] age 39 years [26-68 years]; 71% women; 96% White) to have three inhalation sessions (placebo, 25%, and 50% nitrous oxide) at 4-week intervals. Twenty patients completed all three inhalation sessions, and four completed ≥1 treatment.
Participants had “sustained and refractory depressive illness,” with a mean illness lifetime duration of 17.5 years and an extensive history of antidepressant drug failure (median, 4.5 [2-10] adequate-dose/duration antidepressants).
Some patients had undergone vagus nerve stimulation, electroconvulsive therapy, or repetitive transcranial magnetic stimulation, or had received ketamine (4%, 8%, 13%, and 8%, respectively).
The primary outcome was improvement on the 21-item Hamilton Depression rating Scale (HDRS-21) score over a 2-week observation period.
‘Stronger evidence’
Compared to placebo, nitrous oxide significantly improved depressive symptoms (P = .01). There was no significant difference between the 25% and the 50% concentrations (P = .58).
The estimated difference in HDRS-21 scores between the placebo and various treatment groups are shown in the following table.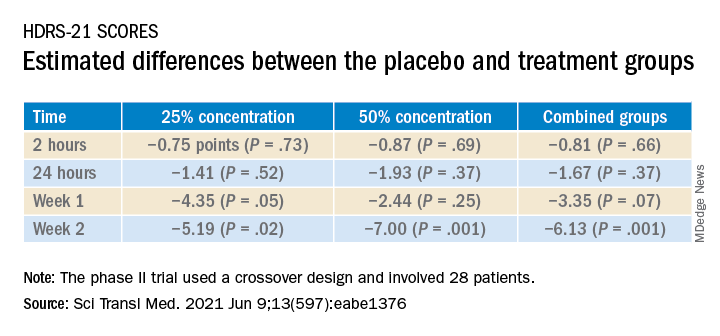
To ensure there where were carryover effects between the two doses, the researchers performed an analysis to ascertain whether order of receipt of the higher dose was related to the 2-week HDRS-21 score; they found no significant effect of trial order (P = .22).
The 20 patients who completed the entire course of treatment “experienced a clinically significant improvement in depressive symptoms from a median baseline HDRS-21 score of 20.5 (IQR, 19.0 to 25.5) to 8.5 (IQR, 2.0 to 16.0) at study completion, corresponding to a median change of −11.0 points (IQR, −3.3 to −14.0 points; P < .0001) after the 3-month study period,” the investigators noted.
The types of treatment response and improvement in depressive symptoms from baseline to study completion are listed in the table below.
There were statistically significant differences in adverse events between the two treatment doses; 47 events occurred following inhalation of the 50% concentration, compared to 11 after inhalation of the 25% concentration. There were six adverse events after inhalation of placebo (P < .0001).
“None of the adverse events were serious, and nearly all occurred either during or immediately after the treatment session and resolved within several hours,” the authors reported.
“We need to be remindful that – despite the exciting results of the study – the study was small and cannot be considered definitive evidence; as such, it is too early to advocate for the use of nitrous oxide in everyday clinical practice,” Dr. Nagele said.
Nevertheless, on the basis of the current findings, he stated.
Rapid-acting antidepressants
Commenting on the study in an interview, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit at Toronto Western Hospital, noted that the research into nitrous oxide is “part of an interest in rapid-acting antidepressants.”
Dr. McIntyre, also the chairman and executive director of the Brain and Cognition Discovery Foundation, Toronto, who was not involved with the study, found it “interesting” that “almost 20% of the sample had previously had suboptimal outcomes to ketamine and/or neurostimulation, meaning these patients had serious refractory illness, but the benefit [of nitrous oxide] was sustained at 2 weeks.”
Studies of the use of nitrous oxide for patients with bipolar depression “would be warranted, since it appears generally safe and well tolerated,” said Dr. McIntyre, director of the Depression and Bipolar Support Alliance.
The study was sponsored by an award to Dr. Nagele from the NARSAD Independent Investigator Award from the Brain and Behavior Research Foundation and an award to Dr. Nagele and other coauthors from the Taylor Family Institute for Innovative Psychiatric Research at Washington University in St. Louis. Dr. Nagele receives funding from the National Institute of Mental Health the American Foundation for Prevention of Suicide, and the Brain and Behavior Research Foundation; has received research funding and honoraria from Roche Diagnostics and Abbott Diagnostics; and has previously filed for intellectual property protection related to the use of nitrous oxide in major depression. The other authors’ disclosures are listed on the original article. Dr. McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation; speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, Eisai, Minerva, Intra-Cellular, and Abbvie. Dr. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
A 1-hour treatment with a low concentration of nitrous oxide, commonly known as “laughing gas,” appears to relieve symptoms of treatment-resistant major depression (TRMD), with effects lasting as long as several weeks, new research suggests.
In a trial with a crossover design, investigators randomly assigned 28 patients with severe TRMD to receive a single 1-hour inhalation of placebo or nitrous oxide once a month over a 3-month period. Participants received an inhalation of placebo; a 25% concentration of nitrous oxide; and a 50% concentration of nitrous oxide. Sessions were conducted 4 weeks apart.
Both doses of nitrous oxide were associated with substantial improvement in depressive symptoms for roughly 85% of participants. However, the 25% concentration had a lower risk for adverse effects, which included sedation, nausea, and mild dissociation, compared to the 50% concentration.
“Twenty-five percent nitrous oxide has similar efficacy, compared to 50% nitrous oxide, and reduced side effects fourfold,” lead author Peter Nagele, MD, MSc, chair and professor of anesthesia and critical care, University of Chicago, said in an interview.
“We also observed that many patients had a 2-week improvement of depressive symptoms after a nitrous oxide treatment,” said Dr. Nagele, who also is professor of psychiatry and behavioral neuroscience.
The study was published online June 9 in Science Translational Medicine.
Further refinement
A previous proof-of-principle study conducted by the same researchers demonstrated that a 1-hour inhalation of 50% nitrous oxide had rapid antidepressant effects for patients with TRMD.
The current phase 2 trial “is a follow-up study to our earlier 2015 pilot trial and was designed to further refine the dose of nitrous oxide needed for antidepressant efficacy,” Dr. Nagele said.
“An important secondary aim [of the current study] was to determine whether a lower dose – 25% – would reduce side effects, and a third aim was to determine how long the antidepressants effects last,” he explained.
To investigate, the researchers enrolled 28 patients (median [interquartile range (IQR)] age 39 years [26-68 years]; 71% women; 96% White) to have three inhalation sessions (placebo, 25%, and 50% nitrous oxide) at 4-week intervals. Twenty patients completed all three inhalation sessions, and four completed ≥1 treatment.
Participants had “sustained and refractory depressive illness,” with a mean illness lifetime duration of 17.5 years and an extensive history of antidepressant drug failure (median, 4.5 [2-10] adequate-dose/duration antidepressants).
Some patients had undergone vagus nerve stimulation, electroconvulsive therapy, or repetitive transcranial magnetic stimulation, or had received ketamine (4%, 8%, 13%, and 8%, respectively).
The primary outcome was improvement on the 21-item Hamilton Depression rating Scale (HDRS-21) score over a 2-week observation period.
‘Stronger evidence’
Compared to placebo, nitrous oxide significantly improved depressive symptoms (P = .01). There was no significant difference between the 25% and the 50% concentrations (P = .58).
The estimated difference in HDRS-21 scores between the placebo and various treatment groups are shown in the following table.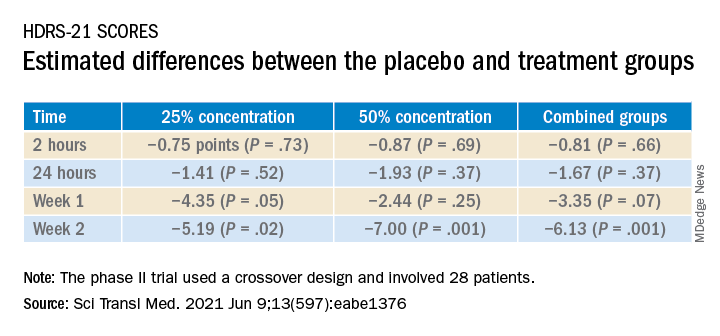
To ensure there where were carryover effects between the two doses, the researchers performed an analysis to ascertain whether order of receipt of the higher dose was related to the 2-week HDRS-21 score; they found no significant effect of trial order (P = .22).
The 20 patients who completed the entire course of treatment “experienced a clinically significant improvement in depressive symptoms from a median baseline HDRS-21 score of 20.5 (IQR, 19.0 to 25.5) to 8.5 (IQR, 2.0 to 16.0) at study completion, corresponding to a median change of −11.0 points (IQR, −3.3 to −14.0 points; P < .0001) after the 3-month study period,” the investigators noted.
The types of treatment response and improvement in depressive symptoms from baseline to study completion are listed in the table below.
There were statistically significant differences in adverse events between the two treatment doses; 47 events occurred following inhalation of the 50% concentration, compared to 11 after inhalation of the 25% concentration. There were six adverse events after inhalation of placebo (P < .0001).
“None of the adverse events were serious, and nearly all occurred either during or immediately after the treatment session and resolved within several hours,” the authors reported.
“We need to be remindful that – despite the exciting results of the study – the study was small and cannot be considered definitive evidence; as such, it is too early to advocate for the use of nitrous oxide in everyday clinical practice,” Dr. Nagele said.
Nevertheless, on the basis of the current findings, he stated.
Rapid-acting antidepressants
Commenting on the study in an interview, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit at Toronto Western Hospital, noted that the research into nitrous oxide is “part of an interest in rapid-acting antidepressants.”
Dr. McIntyre, also the chairman and executive director of the Brain and Cognition Discovery Foundation, Toronto, who was not involved with the study, found it “interesting” that “almost 20% of the sample had previously had suboptimal outcomes to ketamine and/or neurostimulation, meaning these patients had serious refractory illness, but the benefit [of nitrous oxide] was sustained at 2 weeks.”
Studies of the use of nitrous oxide for patients with bipolar depression “would be warranted, since it appears generally safe and well tolerated,” said Dr. McIntyre, director of the Depression and Bipolar Support Alliance.
The study was sponsored by an award to Dr. Nagele from the NARSAD Independent Investigator Award from the Brain and Behavior Research Foundation and an award to Dr. Nagele and other coauthors from the Taylor Family Institute for Innovative Psychiatric Research at Washington University in St. Louis. Dr. Nagele receives funding from the National Institute of Mental Health the American Foundation for Prevention of Suicide, and the Brain and Behavior Research Foundation; has received research funding and honoraria from Roche Diagnostics and Abbott Diagnostics; and has previously filed for intellectual property protection related to the use of nitrous oxide in major depression. The other authors’ disclosures are listed on the original article. Dr. McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation; speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, Eisai, Minerva, Intra-Cellular, and Abbvie. Dr. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
How a community-based program for SMI pivoted during the pandemic
For more than 70 years, Fountain House has offered a lifeline for people living with schizophrenia, bipolar disorder, major depression, and other serious mental illnesses through a community-based model of care. When he took the helm less than 2 years ago, CEO and President Ashwin Vasan, ScM, MD, PhD, wanted a greater focus on crisis-based solutions and a wider, public health approach.

That goal was put to the test in 2020, when SARS-CoV-2 shuttered all in-person activities. The nonprofit quickly rebounded, creating a digital platform, engaging with its members through online courses, face-to-face check-ins, and delivery services, and expanding partnerships to connect with individuals facing homelessness and involved in the criminal justice system. Those activities not only brought the community together – it expanded Fountain House’s footprint.
Among its membership of more than 2,000 people in New York City, about 70% connected to the digital platform. “We also enrolled more than 200 brand new members during the pandemic who had never set foot in the physical mental health “clubhouse.” They derived value as well,” Dr. Vasan said in an interview. Nationally, the program is replicated at more than 200 locations and serves about 60,000 people in almost 40 states. During the pandemic, Fountain House began formalizing affiliation opportunities with this network.
Now that the pandemic is showing signs of receding, Fountain House faces new challenges operating as a possible hybrid model. “More than three-quarters of our members say they want to continue to engage virtually as well as in person,” Dr. Vasan said. As of this writing, Fountain House is enjoying a soft reopening, slowly welcoming in-person activities. What this will look like in the coming weeks and months is a work in progress, he added. “We don’t know yet how people are going to prefer to engage.”
A role in the public policy conversation
Founded by a small group of former psychiatric patients in the late 1940s, Fountain House has since expanded from a single building in New York City to more than 300 replications in the United States and around the world. It originated the “clubhouse” model of mental health support: a community-based approach that helps members improve health, and break social and economic isolation by reclaiming social, educational, and work skills, and connecting with core services, including supportive housing and community-based primary and behavioral health care (Arts Psychother. 2012 Feb 39[1]:25-30).
Serious mental illness (SMI) is growing more pronounced as a crisis, not just in the people it affects, “but in all of the attendant and preventable social and economic crises that intersect with it, whether it’s increasing health care costs, homelessness, or criminalization,” Dr. Vasan said.
After 73 years, Fountain House is just beginning to gain relevance as a tool to help solve these intersecting public policy crises, he added.
“We’ve demonstrated through evaluation data that it reduces hospitalization rates, health care costs, reliance on emergency departments, homelessness, and recidivism to the criminal justice system,” he said. Health care costs for members are more than 20% lower than for others with mental illness, and recidivism rates among those with a criminal history are less than 5%.
Others familiar with Fountain House say the model delivers on its charge to improve quality of life for people with SMI.
It’s a great referral source for people who are under good mental health control, whether it’s therapy or a combination of therapy and medications, Robert T. London, MD, a practicing psychiatrist in New York who is not affiliated with Fountain House but has referred patients to the organization over the years, said in an interview.
“They can work with staff, learn skills regarding potential work, housekeeping, [and] social skills,” he said. One of the biggest problems facing people with SMI is they’re very isolated, Dr. London continued. “When you’re in a facility like Fountain House, you’re not isolated. You’re with fellow members, a very helpful educated staff, and you’re going to do well.” If a member is having some issues and losing touch with reality and needs to find treatment, Fountain House will provide that support.
“If you don’t have a treating person, they’re going to find you one. They’re not against traditional medical/psychiatric care,” he said.
Among those with unstable or no housing, 99% find housing within a year of joining Fountain House. While it does provide people with SMI with support to find a roof over their heads, Fountain House doesn’t necessarily fit a model of “housing first,” Stephanie Le Melle, MD, MS, director of public psychiatry education at department of psychiatry at Columbia University/New York State Psychiatric Institute, said in an interview.
“The housing first evidence-based model, as designed and implemented by Pathways to Housing program in New York in the early 90s, accepted people who were street homeless or in shelters, not involved in mental health treatment, and actively using substances into scatter-site apartments and wrapped services around them,” she said.
Dr. Le Melle, who is not affiliated with Fountain House, views it more as a supportive employment program that uses a recovery-oriented, community-based, jointly peer-run approach to engage members in vocational/educational programming. It also happens to have some supportive housing for its members, she added.
Dr. Vasan believes Fountain House could expand beyond a community model. The organization has been moving out from its history, evolving into a model that could be integrated as standard of care and standard of practice for community health, he said. Fountain House is part of Clubhouse International, an umbrella organization that received the American Psychiatric Association’s 2021 special presidential commendation award during its virtual annual meeting for the group’s use of “the evidence-based, cost-effective clubhouse model of psychosocial rehabilitation as a leading recovery resource for people living with mental illness around the world.”
How medication issues are handled
Fountain House doesn’t directly provide medication to its members. According to Dr. Vasan, psychiatric care is just one component of recovery for serious mental illness.
“We talk about Fountain House as a main vortex in a triangle of recovery. You need health care, housing, and community. The part that’s been neglected the most is community intervention, the social infrastructure for people who are deeply isolated and marginalized,” he said. “We know that people who have that infrastructure, and are stably housed, are then more likely to engage in community-based psychiatry and primary care. And in turn, people who are in stable clinical care can more durably engage in the community programming Fountain House offers.”
Health care and clinical care are changing. It’s becoming more person-centered and community based. “We need to move with the times and we have, in the last 2 decades,” he said.
Historically, Fountain House has owned and operated its own clinic in New York City. More recently, it partnered with Sun River Health and Ryan Health, two large federally qualified health center networks in New York, so that members receive access to psychiatric and medical care. It has also expanded similar partnerships with Columbia University, New York University, and other health care systems to ensure its members have access to sustainable clinical care as a part of the community conditions and resources needed to recover and thrive.
Those familiar with the organization don’t see the absence of a medication program as a negative factor. If Fountain House doesn’t provide psychiatric medications, “that tells me the patients are under control and able to function in a community setting” that focuses on rehabilitation, Dr. London said.
It’s true that psychiatric medication treatment is an essential part of a patient’s recovery journey, Dr. Le Melle said. “Treatment with medications can be done in a recovery-oriented way. However, the Fountain House model has been designed to keep these separate, and this model works well for most” of the members.
As long as members and staff are willing to collaborate with treatment providers outside of the clubhouse, when necessary, this model of separation between work and treatment can work really well, she added.
“There are some people who need a more integrated system of care. There is no ‘one size fits all’ program that can meet everyone’s needs,” said Dr. Le Melle. The absence of onsite treatment at Fountain House, to some extent “adds to the milieu and allows people to focus on other aspects of their lives besides their illness.”
This hasn’t always been the case in traditionally funded behavioral health programs, she continued. Most mental health clinics, because of fiscal structures, reimbursement, and staffing costs, focus more on psychotherapy and medication management than on other aspects of peoples’ lives, such as their recovery goals.
The bottom line is rehabilitation in medicine works – whether it’s for a mental health disorder, broken leg, arm, or stroke, Dr. London said. “Fountain House’s focus is integrating a person into society by helping them to think differently and interact socially in groups and learn some skills.”
Through cognitive-behavioral therapies, a person with mental illness can learn how to act differently. “The brain is always in a growing process where you learn and develop new ideas, make connections,” Dr. London said. “New protein molecules get created and stored; changes occur with the neurotransmitters.”
Overall, the Fountain House model is great for supporting and engaging people with serious mental illness, Dr. Le Melle said. “It provides a literal place, a community, and a safe environment that helps people to embrace their recovery journey. It is also great at supporting people in their engagement with vocational training and employment.”
Ideally, she would like Fountain House to grow and become more inclusive by engaging people who live with both mental illness and substance use.
COVID-19 changes the rules
The most difficult challenge for health care and other institutions is to keep individuals with SMI engaged and visible so that they can find access to health care and benefits – and avoid acute hospitalization or medical care. “That’s our goal, to prevent the worst effects and respond accordingly,” Dr. Vasan said.
SARS-CoV-2 forced the program to reevaluate its daily operations so that it could maintain crucial connections with its members.
Dr. Vasan and his staff immediately closed the clubhouse when COVID-19 first hit, transitioning to direct community-based services that provided one-on-one outreach, and meal, medication, and clothing delivery. “Even if people couldn’t visit our clubhouse, we wanted them to feel that sense of community connection, even if it was to drop off meals at their doorstep,” he said.
Donning personal protective equipment, his staff and interested program participants went out into the communities to do this personal outreach. At the height of pandemic in New York City, “we weren’t sure what to do,” as far as keeping safe, he admitted. Nevertheless, he believes this outreach work was lifesaving in that it kept people connected to the clubhouse.
As Fountain House worked to maintain in-person contact, it also built a digital community to keep the live community together. This wasn’t just about posting on a Facebook page – it was interactive, Dr. Vasan noted. An online group made masks for the community and sold them for people outside of Fountain House. Capacity building courses instructed members on writing resumes, looking for jobs, or filling out applications.
There’s an assumption that people with SMI lack the skills to navigate technology. Some of the hallmarks of SMI are demotivation and lack of confidence, and logging onto platforms and email can be challenging for some people, he acknowledged. Over the last 18 months, Fountain House’s virtual clubhouse proved this theory wrong, Dr. Vasan said. “There are a great number of people with serious mental illness who have basic digital skills and are already using technology, or are very eager to learn,” he said.
For the subset of members who did get discouraged by the virtual platform, Fountain House responded by giving them one-on-one home support and digital literacy training to help them stay motivated and engaged.
Fountain House also expanded partnerships during the pandemic, working with programs such as the Fortune Society to bring people with SMI from the criminal justice system into Fountain House. “We’re doing this either virtually or through outdoor, public park programs with groups such as the Times Square Alliance and Fort Greene Park Conservancy to ensure we’re meeting people where they are, at a time of a rising health crisis,” Dr. Vasan said.
Moving on to a hybrid model
At the height of the pandemic, it was easy to engage members through creative programming. People were craving socialization. Now that people are getting vaccinated and interacting inside and outside, some understandable apathy is forming toward digital platforms, Dr. Vasan said.
“The onus is on us now to look at that data and to design something new that can keep people engaged in a hybrid model,” he added.
June 14, 2021, marked Fountain House’s soft opening. “This was a big day for us, to work through the kinks,” he said. At press time, the plan was to fully reopen the clubhouse in a few weeks – if transmission and case rates stay low.
It’s unclear at this point how many people will engage with Fountain House on a daily, in-person basis. Some people might want to come to the clubhouse just a few days a week and use the online platform on other days.
“We’re doing a series of experiments to really understand what different offerings we need to make. For example, perhaps we need to have 24-7 programming on the digital platform. That way, you could access it on demand,” said Dr. Vasan. The goal is to create a menu of choices for members so that it becomes flexible and meets their needs.
Long term, Dr. Vasan hopes the digital platform will become a scalable technology. “We want this to be used not just by Fountain House, but for programs and in markets that don’t have clubhouses.” Health systems or insurance companies would benefit from software like this because it addresses one of the most difficult aspects for this population: keeping them engaged and visible to their systems, Dr. Vasan added.
“I think the most important lesson here is we’re designing for a group of people that no one designs for. No one’s paying attention to people with serious mental illness. Nor have they ever, really. Fountain House has always been their advocate and partner. It’s great that we can do this with them, and for them.”
Dr. Vasan, also an epidemiologist, serves as assistant professor of clinical population, and family health and medicine, at Columbia University. Dr. London and Dr. Le Melle have no conflicts of interest.
Two steps back, three steps forward
For some of its members, Fountain House provides more than just a sense of place. In an interview, longtime member and New York City native Rich Courage, 61, discussed his mental illness challenges and the role the organization played in reclaiming his life, leading to a new career as a counselor.
Question: What made you seek out Fountain House? Are you still a member?
Rich Courage: I’ve been a member since 2001. I was in a day program at Postgraduate, on West 36th Street. They had this huge theater program, and I was a part of that. But the program fell apart and I didn’t know what to do with myself. A friend of mine told me about Fountain House. I asked what it did, and the friend said that it puts people with mental health challenges back to life, to work, to school. I was making some art, some collages, and I heard they had an art gallery.
Seeing Fountain House, I was amazed. It was this very friendly, warm, cozy place. The staff was nice; the members were welcoming. The next thing you know it’s 2021, and here I am, a peer counselor at Fountain House. I work on “the warm line,” doing the evening shift. People call in who have crises, but a lot of them call in because they’re lonely and want someone to talk to. As a peer counselor, I don’t tell people what to do, but I do offer support. I encourage. I ask questions that enable them to figure out their own problems. And I tell stories anecdotally of people that I’ve known and about recovery.
I struggled with bad depression when I was in my 20s. My mother died, and I lost everything. Coming to Fountain House and being part of this community is unlike anything I’d ever experienced. People weren’t just sitting around and talking about their problems; they were doing something about it. They were going back to school, to work, to social engagements, and the world at large. And it wasn’t perfect or linear. It was two steps back, three steps forward.
That’s exactly what I was doing. I had a lot of self-esteem and confidence issues, and behavioral stuff. My mind was wired a certain way. I had hospitalizations; I was in psychiatric wards. I had a suicide attempt in 2006, which was nearly successful. I was feeling social, mental, and emotional pain for so long. The community has been invaluable for me. Hearing other people’s stories, being accepted, has been wonderful.
I’ve been down and now I’m up, on an upward trajectory.
Question: How else has Fountain House made a difference in your life?
RC: I’m in a Fountain House residence in a one-bedroom, and it’s the most stable housing I’ve ever had in 61 years. So I’ve gotten housing and I’ve gotten a job, which is all great, because it’s aided me in becoming a full human being. But it’s really eased my suffering and enabled me to feel some joy and have some life instead of this shadow existence that I had been living for 30 years.
Fountain House has different units, and I’ve been in the communications unit – we put out the weekly paper and handle all the mail. The unit has computers, and I was able to work on my writing. I wrote a play called "The Very Last Dance of Homeless Joe." We’ve had staged readings at Fountain House, and 200 people have seen it over 2 years. We Zoomed it through the virtual community. It was very successful. A recording of the staged reading won third place at a festival in Florida.
In September, it will be an off-Broadway show. It’s a play about the homeless, but it’s not depressing; it’s very uplifting.
Question: Did you stay connected to Fountain House during the pandemic, either through the digital community or through services they provided? What was this experience like for you?
RC: Ashwin [Vasan] had been here 6 months, and he saw the pandemic coming. During a programming meeting he said, “We need a virtual community, and we need it now.” None of us knew what Zoom was, how the mute button worked. But it’s been wonderful for me. I’m a performer, so I was able to get on to Facebook every day and post a song. Some of it was spoofs about COVID; some were dedications to members. I ended up connecting with a member in Minnesota who used to be a neighbor of mine. We had lost contact, and we reconnected through Fountain House.
Question: What would you tell someone who might need this service?
RC: We’ve partially reopened the clubhouse. In July we’ll be doing tours again. I’d say, come take a tour and see the different social, economic, housing, and educational opportunities. We have a home and garden unit that decorates the place. We have a gym, a wellness unit. But these are just things. The real heart is the people.
As a unit leader recently told me, “We’re not a clinic. We’re not a revolving door. We forge relationships with members that last in our hearts and minds for a lifetime. Even if it’s not in my job description, if there’s anything in my power that I could do to help a member ease their suffering, I will do it.”
For more than 70 years, Fountain House has offered a lifeline for people living with schizophrenia, bipolar disorder, major depression, and other serious mental illnesses through a community-based model of care. When he took the helm less than 2 years ago, CEO and President Ashwin Vasan, ScM, MD, PhD, wanted a greater focus on crisis-based solutions and a wider, public health approach.

That goal was put to the test in 2020, when SARS-CoV-2 shuttered all in-person activities. The nonprofit quickly rebounded, creating a digital platform, engaging with its members through online courses, face-to-face check-ins, and delivery services, and expanding partnerships to connect with individuals facing homelessness and involved in the criminal justice system. Those activities not only brought the community together – it expanded Fountain House’s footprint.
Among its membership of more than 2,000 people in New York City, about 70% connected to the digital platform. “We also enrolled more than 200 brand new members during the pandemic who had never set foot in the physical mental health “clubhouse.” They derived value as well,” Dr. Vasan said in an interview. Nationally, the program is replicated at more than 200 locations and serves about 60,000 people in almost 40 states. During the pandemic, Fountain House began formalizing affiliation opportunities with this network.
Now that the pandemic is showing signs of receding, Fountain House faces new challenges operating as a possible hybrid model. “More than three-quarters of our members say they want to continue to engage virtually as well as in person,” Dr. Vasan said. As of this writing, Fountain House is enjoying a soft reopening, slowly welcoming in-person activities. What this will look like in the coming weeks and months is a work in progress, he added. “We don’t know yet how people are going to prefer to engage.”
A role in the public policy conversation
Founded by a small group of former psychiatric patients in the late 1940s, Fountain House has since expanded from a single building in New York City to more than 300 replications in the United States and around the world. It originated the “clubhouse” model of mental health support: a community-based approach that helps members improve health, and break social and economic isolation by reclaiming social, educational, and work skills, and connecting with core services, including supportive housing and community-based primary and behavioral health care (Arts Psychother. 2012 Feb 39[1]:25-30).
Serious mental illness (SMI) is growing more pronounced as a crisis, not just in the people it affects, “but in all of the attendant and preventable social and economic crises that intersect with it, whether it’s increasing health care costs, homelessness, or criminalization,” Dr. Vasan said.
After 73 years, Fountain House is just beginning to gain relevance as a tool to help solve these intersecting public policy crises, he added.
“We’ve demonstrated through evaluation data that it reduces hospitalization rates, health care costs, reliance on emergency departments, homelessness, and recidivism to the criminal justice system,” he said. Health care costs for members are more than 20% lower than for others with mental illness, and recidivism rates among those with a criminal history are less than 5%.
Others familiar with Fountain House say the model delivers on its charge to improve quality of life for people with SMI.
It’s a great referral source for people who are under good mental health control, whether it’s therapy or a combination of therapy and medications, Robert T. London, MD, a practicing psychiatrist in New York who is not affiliated with Fountain House but has referred patients to the organization over the years, said in an interview.
“They can work with staff, learn skills regarding potential work, housekeeping, [and] social skills,” he said. One of the biggest problems facing people with SMI is they’re very isolated, Dr. London continued. “When you’re in a facility like Fountain House, you’re not isolated. You’re with fellow members, a very helpful educated staff, and you’re going to do well.” If a member is having some issues and losing touch with reality and needs to find treatment, Fountain House will provide that support.
“If you don’t have a treating person, they’re going to find you one. They’re not against traditional medical/psychiatric care,” he said.
Among those with unstable or no housing, 99% find housing within a year of joining Fountain House. While it does provide people with SMI with support to find a roof over their heads, Fountain House doesn’t necessarily fit a model of “housing first,” Stephanie Le Melle, MD, MS, director of public psychiatry education at department of psychiatry at Columbia University/New York State Psychiatric Institute, said in an interview.
“The housing first evidence-based model, as designed and implemented by Pathways to Housing program in New York in the early 90s, accepted people who were street homeless or in shelters, not involved in mental health treatment, and actively using substances into scatter-site apartments and wrapped services around them,” she said.
Dr. Le Melle, who is not affiliated with Fountain House, views it more as a supportive employment program that uses a recovery-oriented, community-based, jointly peer-run approach to engage members in vocational/educational programming. It also happens to have some supportive housing for its members, she added.
Dr. Vasan believes Fountain House could expand beyond a community model. The organization has been moving out from its history, evolving into a model that could be integrated as standard of care and standard of practice for community health, he said. Fountain House is part of Clubhouse International, an umbrella organization that received the American Psychiatric Association’s 2021 special presidential commendation award during its virtual annual meeting for the group’s use of “the evidence-based, cost-effective clubhouse model of psychosocial rehabilitation as a leading recovery resource for people living with mental illness around the world.”
How medication issues are handled
Fountain House doesn’t directly provide medication to its members. According to Dr. Vasan, psychiatric care is just one component of recovery for serious mental illness.
“We talk about Fountain House as a main vortex in a triangle of recovery. You need health care, housing, and community. The part that’s been neglected the most is community intervention, the social infrastructure for people who are deeply isolated and marginalized,” he said. “We know that people who have that infrastructure, and are stably housed, are then more likely to engage in community-based psychiatry and primary care. And in turn, people who are in stable clinical care can more durably engage in the community programming Fountain House offers.”
Health care and clinical care are changing. It’s becoming more person-centered and community based. “We need to move with the times and we have, in the last 2 decades,” he said.
Historically, Fountain House has owned and operated its own clinic in New York City. More recently, it partnered with Sun River Health and Ryan Health, two large federally qualified health center networks in New York, so that members receive access to psychiatric and medical care. It has also expanded similar partnerships with Columbia University, New York University, and other health care systems to ensure its members have access to sustainable clinical care as a part of the community conditions and resources needed to recover and thrive.
Those familiar with the organization don’t see the absence of a medication program as a negative factor. If Fountain House doesn’t provide psychiatric medications, “that tells me the patients are under control and able to function in a community setting” that focuses on rehabilitation, Dr. London said.
It’s true that psychiatric medication treatment is an essential part of a patient’s recovery journey, Dr. Le Melle said. “Treatment with medications can be done in a recovery-oriented way. However, the Fountain House model has been designed to keep these separate, and this model works well for most” of the members.
As long as members and staff are willing to collaborate with treatment providers outside of the clubhouse, when necessary, this model of separation between work and treatment can work really well, she added.
“There are some people who need a more integrated system of care. There is no ‘one size fits all’ program that can meet everyone’s needs,” said Dr. Le Melle. The absence of onsite treatment at Fountain House, to some extent “adds to the milieu and allows people to focus on other aspects of their lives besides their illness.”
This hasn’t always been the case in traditionally funded behavioral health programs, she continued. Most mental health clinics, because of fiscal structures, reimbursement, and staffing costs, focus more on psychotherapy and medication management than on other aspects of peoples’ lives, such as their recovery goals.
The bottom line is rehabilitation in medicine works – whether it’s for a mental health disorder, broken leg, arm, or stroke, Dr. London said. “Fountain House’s focus is integrating a person into society by helping them to think differently and interact socially in groups and learn some skills.”
Through cognitive-behavioral therapies, a person with mental illness can learn how to act differently. “The brain is always in a growing process where you learn and develop new ideas, make connections,” Dr. London said. “New protein molecules get created and stored; changes occur with the neurotransmitters.”
Overall, the Fountain House model is great for supporting and engaging people with serious mental illness, Dr. Le Melle said. “It provides a literal place, a community, and a safe environment that helps people to embrace their recovery journey. It is also great at supporting people in their engagement with vocational training and employment.”
Ideally, she would like Fountain House to grow and become more inclusive by engaging people who live with both mental illness and substance use.
COVID-19 changes the rules
The most difficult challenge for health care and other institutions is to keep individuals with SMI engaged and visible so that they can find access to health care and benefits – and avoid acute hospitalization or medical care. “That’s our goal, to prevent the worst effects and respond accordingly,” Dr. Vasan said.
SARS-CoV-2 forced the program to reevaluate its daily operations so that it could maintain crucial connections with its members.
Dr. Vasan and his staff immediately closed the clubhouse when COVID-19 first hit, transitioning to direct community-based services that provided one-on-one outreach, and meal, medication, and clothing delivery. “Even if people couldn’t visit our clubhouse, we wanted them to feel that sense of community connection, even if it was to drop off meals at their doorstep,” he said.
Donning personal protective equipment, his staff and interested program participants went out into the communities to do this personal outreach. At the height of pandemic in New York City, “we weren’t sure what to do,” as far as keeping safe, he admitted. Nevertheless, he believes this outreach work was lifesaving in that it kept people connected to the clubhouse.
As Fountain House worked to maintain in-person contact, it also built a digital community to keep the live community together. This wasn’t just about posting on a Facebook page – it was interactive, Dr. Vasan noted. An online group made masks for the community and sold them for people outside of Fountain House. Capacity building courses instructed members on writing resumes, looking for jobs, or filling out applications.
There’s an assumption that people with SMI lack the skills to navigate technology. Some of the hallmarks of SMI are demotivation and lack of confidence, and logging onto platforms and email can be challenging for some people, he acknowledged. Over the last 18 months, Fountain House’s virtual clubhouse proved this theory wrong, Dr. Vasan said. “There are a great number of people with serious mental illness who have basic digital skills and are already using technology, or are very eager to learn,” he said.
For the subset of members who did get discouraged by the virtual platform, Fountain House responded by giving them one-on-one home support and digital literacy training to help them stay motivated and engaged.
Fountain House also expanded partnerships during the pandemic, working with programs such as the Fortune Society to bring people with SMI from the criminal justice system into Fountain House. “We’re doing this either virtually or through outdoor, public park programs with groups such as the Times Square Alliance and Fort Greene Park Conservancy to ensure we’re meeting people where they are, at a time of a rising health crisis,” Dr. Vasan said.
Moving on to a hybrid model
At the height of the pandemic, it was easy to engage members through creative programming. People were craving socialization. Now that people are getting vaccinated and interacting inside and outside, some understandable apathy is forming toward digital platforms, Dr. Vasan said.
“The onus is on us now to look at that data and to design something new that can keep people engaged in a hybrid model,” he added.
June 14, 2021, marked Fountain House’s soft opening. “This was a big day for us, to work through the kinks,” he said. At press time, the plan was to fully reopen the clubhouse in a few weeks – if transmission and case rates stay low.
It’s unclear at this point how many people will engage with Fountain House on a daily, in-person basis. Some people might want to come to the clubhouse just a few days a week and use the online platform on other days.
“We’re doing a series of experiments to really understand what different offerings we need to make. For example, perhaps we need to have 24-7 programming on the digital platform. That way, you could access it on demand,” said Dr. Vasan. The goal is to create a menu of choices for members so that it becomes flexible and meets their needs.
Long term, Dr. Vasan hopes the digital platform will become a scalable technology. “We want this to be used not just by Fountain House, but for programs and in markets that don’t have clubhouses.” Health systems or insurance companies would benefit from software like this because it addresses one of the most difficult aspects for this population: keeping them engaged and visible to their systems, Dr. Vasan added.
“I think the most important lesson here is we’re designing for a group of people that no one designs for. No one’s paying attention to people with serious mental illness. Nor have they ever, really. Fountain House has always been their advocate and partner. It’s great that we can do this with them, and for them.”
Dr. Vasan, also an epidemiologist, serves as assistant professor of clinical population, and family health and medicine, at Columbia University. Dr. London and Dr. Le Melle have no conflicts of interest.
Two steps back, three steps forward
For some of its members, Fountain House provides more than just a sense of place. In an interview, longtime member and New York City native Rich Courage, 61, discussed his mental illness challenges and the role the organization played in reclaiming his life, leading to a new career as a counselor.
Question: What made you seek out Fountain House? Are you still a member?
Rich Courage: I’ve been a member since 2001. I was in a day program at Postgraduate, on West 36th Street. They had this huge theater program, and I was a part of that. But the program fell apart and I didn’t know what to do with myself. A friend of mine told me about Fountain House. I asked what it did, and the friend said that it puts people with mental health challenges back to life, to work, to school. I was making some art, some collages, and I heard they had an art gallery.
Seeing Fountain House, I was amazed. It was this very friendly, warm, cozy place. The staff was nice; the members were welcoming. The next thing you know it’s 2021, and here I am, a peer counselor at Fountain House. I work on “the warm line,” doing the evening shift. People call in who have crises, but a lot of them call in because they’re lonely and want someone to talk to. As a peer counselor, I don’t tell people what to do, but I do offer support. I encourage. I ask questions that enable them to figure out their own problems. And I tell stories anecdotally of people that I’ve known and about recovery.
I struggled with bad depression when I was in my 20s. My mother died, and I lost everything. Coming to Fountain House and being part of this community is unlike anything I’d ever experienced. People weren’t just sitting around and talking about their problems; they were doing something about it. They were going back to school, to work, to social engagements, and the world at large. And it wasn’t perfect or linear. It was two steps back, three steps forward.
That’s exactly what I was doing. I had a lot of self-esteem and confidence issues, and behavioral stuff. My mind was wired a certain way. I had hospitalizations; I was in psychiatric wards. I had a suicide attempt in 2006, which was nearly successful. I was feeling social, mental, and emotional pain for so long. The community has been invaluable for me. Hearing other people’s stories, being accepted, has been wonderful.
I’ve been down and now I’m up, on an upward trajectory.
Question: How else has Fountain House made a difference in your life?
RC: I’m in a Fountain House residence in a one-bedroom, and it’s the most stable housing I’ve ever had in 61 years. So I’ve gotten housing and I’ve gotten a job, which is all great, because it’s aided me in becoming a full human being. But it’s really eased my suffering and enabled me to feel some joy and have some life instead of this shadow existence that I had been living for 30 years.
Fountain House has different units, and I’ve been in the communications unit – we put out the weekly paper and handle all the mail. The unit has computers, and I was able to work on my writing. I wrote a play called "The Very Last Dance of Homeless Joe." We’ve had staged readings at Fountain House, and 200 people have seen it over 2 years. We Zoomed it through the virtual community. It was very successful. A recording of the staged reading won third place at a festival in Florida.
In September, it will be an off-Broadway show. It’s a play about the homeless, but it’s not depressing; it’s very uplifting.
Question: Did you stay connected to Fountain House during the pandemic, either through the digital community or through services they provided? What was this experience like for you?
RC: Ashwin [Vasan] had been here 6 months, and he saw the pandemic coming. During a programming meeting he said, “We need a virtual community, and we need it now.” None of us knew what Zoom was, how the mute button worked. But it’s been wonderful for me. I’m a performer, so I was able to get on to Facebook every day and post a song. Some of it was spoofs about COVID; some were dedications to members. I ended up connecting with a member in Minnesota who used to be a neighbor of mine. We had lost contact, and we reconnected through Fountain House.
Question: What would you tell someone who might need this service?
RC: We’ve partially reopened the clubhouse. In July we’ll be doing tours again. I’d say, come take a tour and see the different social, economic, housing, and educational opportunities. We have a home and garden unit that decorates the place. We have a gym, a wellness unit. But these are just things. The real heart is the people.
As a unit leader recently told me, “We’re not a clinic. We’re not a revolving door. We forge relationships with members that last in our hearts and minds for a lifetime. Even if it’s not in my job description, if there’s anything in my power that I could do to help a member ease their suffering, I will do it.”
For more than 70 years, Fountain House has offered a lifeline for people living with schizophrenia, bipolar disorder, major depression, and other serious mental illnesses through a community-based model of care. When he took the helm less than 2 years ago, CEO and President Ashwin Vasan, ScM, MD, PhD, wanted a greater focus on crisis-based solutions and a wider, public health approach.

That goal was put to the test in 2020, when SARS-CoV-2 shuttered all in-person activities. The nonprofit quickly rebounded, creating a digital platform, engaging with its members through online courses, face-to-face check-ins, and delivery services, and expanding partnerships to connect with individuals facing homelessness and involved in the criminal justice system. Those activities not only brought the community together – it expanded Fountain House’s footprint.
Among its membership of more than 2,000 people in New York City, about 70% connected to the digital platform. “We also enrolled more than 200 brand new members during the pandemic who had never set foot in the physical mental health “clubhouse.” They derived value as well,” Dr. Vasan said in an interview. Nationally, the program is replicated at more than 200 locations and serves about 60,000 people in almost 40 states. During the pandemic, Fountain House began formalizing affiliation opportunities with this network.
Now that the pandemic is showing signs of receding, Fountain House faces new challenges operating as a possible hybrid model. “More than three-quarters of our members say they want to continue to engage virtually as well as in person,” Dr. Vasan said. As of this writing, Fountain House is enjoying a soft reopening, slowly welcoming in-person activities. What this will look like in the coming weeks and months is a work in progress, he added. “We don’t know yet how people are going to prefer to engage.”
A role in the public policy conversation
Founded by a small group of former psychiatric patients in the late 1940s, Fountain House has since expanded from a single building in New York City to more than 300 replications in the United States and around the world. It originated the “clubhouse” model of mental health support: a community-based approach that helps members improve health, and break social and economic isolation by reclaiming social, educational, and work skills, and connecting with core services, including supportive housing and community-based primary and behavioral health care (Arts Psychother. 2012 Feb 39[1]:25-30).
Serious mental illness (SMI) is growing more pronounced as a crisis, not just in the people it affects, “but in all of the attendant and preventable social and economic crises that intersect with it, whether it’s increasing health care costs, homelessness, or criminalization,” Dr. Vasan said.
After 73 years, Fountain House is just beginning to gain relevance as a tool to help solve these intersecting public policy crises, he added.
“We’ve demonstrated through evaluation data that it reduces hospitalization rates, health care costs, reliance on emergency departments, homelessness, and recidivism to the criminal justice system,” he said. Health care costs for members are more than 20% lower than for others with mental illness, and recidivism rates among those with a criminal history are less than 5%.
Others familiar with Fountain House say the model delivers on its charge to improve quality of life for people with SMI.
It’s a great referral source for people who are under good mental health control, whether it’s therapy or a combination of therapy and medications, Robert T. London, MD, a practicing psychiatrist in New York who is not affiliated with Fountain House but has referred patients to the organization over the years, said in an interview.
“They can work with staff, learn skills regarding potential work, housekeeping, [and] social skills,” he said. One of the biggest problems facing people with SMI is they’re very isolated, Dr. London continued. “When you’re in a facility like Fountain House, you’re not isolated. You’re with fellow members, a very helpful educated staff, and you’re going to do well.” If a member is having some issues and losing touch with reality and needs to find treatment, Fountain House will provide that support.
“If you don’t have a treating person, they’re going to find you one. They’re not against traditional medical/psychiatric care,” he said.
Among those with unstable or no housing, 99% find housing within a year of joining Fountain House. While it does provide people with SMI with support to find a roof over their heads, Fountain House doesn’t necessarily fit a model of “housing first,” Stephanie Le Melle, MD, MS, director of public psychiatry education at department of psychiatry at Columbia University/New York State Psychiatric Institute, said in an interview.
“The housing first evidence-based model, as designed and implemented by Pathways to Housing program in New York in the early 90s, accepted people who were street homeless or in shelters, not involved in mental health treatment, and actively using substances into scatter-site apartments and wrapped services around them,” she said.
Dr. Le Melle, who is not affiliated with Fountain House, views it more as a supportive employment program that uses a recovery-oriented, community-based, jointly peer-run approach to engage members in vocational/educational programming. It also happens to have some supportive housing for its members, she added.
Dr. Vasan believes Fountain House could expand beyond a community model. The organization has been moving out from its history, evolving into a model that could be integrated as standard of care and standard of practice for community health, he said. Fountain House is part of Clubhouse International, an umbrella organization that received the American Psychiatric Association’s 2021 special presidential commendation award during its virtual annual meeting for the group’s use of “the evidence-based, cost-effective clubhouse model of psychosocial rehabilitation as a leading recovery resource for people living with mental illness around the world.”
How medication issues are handled
Fountain House doesn’t directly provide medication to its members. According to Dr. Vasan, psychiatric care is just one component of recovery for serious mental illness.
“We talk about Fountain House as a main vortex in a triangle of recovery. You need health care, housing, and community. The part that’s been neglected the most is community intervention, the social infrastructure for people who are deeply isolated and marginalized,” he said. “We know that people who have that infrastructure, and are stably housed, are then more likely to engage in community-based psychiatry and primary care. And in turn, people who are in stable clinical care can more durably engage in the community programming Fountain House offers.”
Health care and clinical care are changing. It’s becoming more person-centered and community based. “We need to move with the times and we have, in the last 2 decades,” he said.
Historically, Fountain House has owned and operated its own clinic in New York City. More recently, it partnered with Sun River Health and Ryan Health, two large federally qualified health center networks in New York, so that members receive access to psychiatric and medical care. It has also expanded similar partnerships with Columbia University, New York University, and other health care systems to ensure its members have access to sustainable clinical care as a part of the community conditions and resources needed to recover and thrive.
Those familiar with the organization don’t see the absence of a medication program as a negative factor. If Fountain House doesn’t provide psychiatric medications, “that tells me the patients are under control and able to function in a community setting” that focuses on rehabilitation, Dr. London said.
It’s true that psychiatric medication treatment is an essential part of a patient’s recovery journey, Dr. Le Melle said. “Treatment with medications can be done in a recovery-oriented way. However, the Fountain House model has been designed to keep these separate, and this model works well for most” of the members.
As long as members and staff are willing to collaborate with treatment providers outside of the clubhouse, when necessary, this model of separation between work and treatment can work really well, she added.
“There are some people who need a more integrated system of care. There is no ‘one size fits all’ program that can meet everyone’s needs,” said Dr. Le Melle. The absence of onsite treatment at Fountain House, to some extent “adds to the milieu and allows people to focus on other aspects of their lives besides their illness.”
This hasn’t always been the case in traditionally funded behavioral health programs, she continued. Most mental health clinics, because of fiscal structures, reimbursement, and staffing costs, focus more on psychotherapy and medication management than on other aspects of peoples’ lives, such as their recovery goals.
The bottom line is rehabilitation in medicine works – whether it’s for a mental health disorder, broken leg, arm, or stroke, Dr. London said. “Fountain House’s focus is integrating a person into society by helping them to think differently and interact socially in groups and learn some skills.”
Through cognitive-behavioral therapies, a person with mental illness can learn how to act differently. “The brain is always in a growing process where you learn and develop new ideas, make connections,” Dr. London said. “New protein molecules get created and stored; changes occur with the neurotransmitters.”
Overall, the Fountain House model is great for supporting and engaging people with serious mental illness, Dr. Le Melle said. “It provides a literal place, a community, and a safe environment that helps people to embrace their recovery journey. It is also great at supporting people in their engagement with vocational training and employment.”
Ideally, she would like Fountain House to grow and become more inclusive by engaging people who live with both mental illness and substance use.
COVID-19 changes the rules
The most difficult challenge for health care and other institutions is to keep individuals with SMI engaged and visible so that they can find access to health care and benefits – and avoid acute hospitalization or medical care. “That’s our goal, to prevent the worst effects and respond accordingly,” Dr. Vasan said.
SARS-CoV-2 forced the program to reevaluate its daily operations so that it could maintain crucial connections with its members.
Dr. Vasan and his staff immediately closed the clubhouse when COVID-19 first hit, transitioning to direct community-based services that provided one-on-one outreach, and meal, medication, and clothing delivery. “Even if people couldn’t visit our clubhouse, we wanted them to feel that sense of community connection, even if it was to drop off meals at their doorstep,” he said.
Donning personal protective equipment, his staff and interested program participants went out into the communities to do this personal outreach. At the height of pandemic in New York City, “we weren’t sure what to do,” as far as keeping safe, he admitted. Nevertheless, he believes this outreach work was lifesaving in that it kept people connected to the clubhouse.
As Fountain House worked to maintain in-person contact, it also built a digital community to keep the live community together. This wasn’t just about posting on a Facebook page – it was interactive, Dr. Vasan noted. An online group made masks for the community and sold them for people outside of Fountain House. Capacity building courses instructed members on writing resumes, looking for jobs, or filling out applications.
There’s an assumption that people with SMI lack the skills to navigate technology. Some of the hallmarks of SMI are demotivation and lack of confidence, and logging onto platforms and email can be challenging for some people, he acknowledged. Over the last 18 months, Fountain House’s virtual clubhouse proved this theory wrong, Dr. Vasan said. “There are a great number of people with serious mental illness who have basic digital skills and are already using technology, or are very eager to learn,” he said.
For the subset of members who did get discouraged by the virtual platform, Fountain House responded by giving them one-on-one home support and digital literacy training to help them stay motivated and engaged.
Fountain House also expanded partnerships during the pandemic, working with programs such as the Fortune Society to bring people with SMI from the criminal justice system into Fountain House. “We’re doing this either virtually or through outdoor, public park programs with groups such as the Times Square Alliance and Fort Greene Park Conservancy to ensure we’re meeting people where they are, at a time of a rising health crisis,” Dr. Vasan said.
Moving on to a hybrid model
At the height of the pandemic, it was easy to engage members through creative programming. People were craving socialization. Now that people are getting vaccinated and interacting inside and outside, some understandable apathy is forming toward digital platforms, Dr. Vasan said.
“The onus is on us now to look at that data and to design something new that can keep people engaged in a hybrid model,” he added.
June 14, 2021, marked Fountain House’s soft opening. “This was a big day for us, to work through the kinks,” he said. At press time, the plan was to fully reopen the clubhouse in a few weeks – if transmission and case rates stay low.
It’s unclear at this point how many people will engage with Fountain House on a daily, in-person basis. Some people might want to come to the clubhouse just a few days a week and use the online platform on other days.
“We’re doing a series of experiments to really understand what different offerings we need to make. For example, perhaps we need to have 24-7 programming on the digital platform. That way, you could access it on demand,” said Dr. Vasan. The goal is to create a menu of choices for members so that it becomes flexible and meets their needs.
Long term, Dr. Vasan hopes the digital platform will become a scalable technology. “We want this to be used not just by Fountain House, but for programs and in markets that don’t have clubhouses.” Health systems or insurance companies would benefit from software like this because it addresses one of the most difficult aspects for this population: keeping them engaged and visible to their systems, Dr. Vasan added.
“I think the most important lesson here is we’re designing for a group of people that no one designs for. No one’s paying attention to people with serious mental illness. Nor have they ever, really. Fountain House has always been their advocate and partner. It’s great that we can do this with them, and for them.”
Dr. Vasan, also an epidemiologist, serves as assistant professor of clinical population, and family health and medicine, at Columbia University. Dr. London and Dr. Le Melle have no conflicts of interest.
Two steps back, three steps forward
For some of its members, Fountain House provides more than just a sense of place. In an interview, longtime member and New York City native Rich Courage, 61, discussed his mental illness challenges and the role the organization played in reclaiming his life, leading to a new career as a counselor.
Question: What made you seek out Fountain House? Are you still a member?
Rich Courage: I’ve been a member since 2001. I was in a day program at Postgraduate, on West 36th Street. They had this huge theater program, and I was a part of that. But the program fell apart and I didn’t know what to do with myself. A friend of mine told me about Fountain House. I asked what it did, and the friend said that it puts people with mental health challenges back to life, to work, to school. I was making some art, some collages, and I heard they had an art gallery.
Seeing Fountain House, I was amazed. It was this very friendly, warm, cozy place. The staff was nice; the members were welcoming. The next thing you know it’s 2021, and here I am, a peer counselor at Fountain House. I work on “the warm line,” doing the evening shift. People call in who have crises, but a lot of them call in because they’re lonely and want someone to talk to. As a peer counselor, I don’t tell people what to do, but I do offer support. I encourage. I ask questions that enable them to figure out their own problems. And I tell stories anecdotally of people that I’ve known and about recovery.
I struggled with bad depression when I was in my 20s. My mother died, and I lost everything. Coming to Fountain House and being part of this community is unlike anything I’d ever experienced. People weren’t just sitting around and talking about their problems; they were doing something about it. They were going back to school, to work, to social engagements, and the world at large. And it wasn’t perfect or linear. It was two steps back, three steps forward.
That’s exactly what I was doing. I had a lot of self-esteem and confidence issues, and behavioral stuff. My mind was wired a certain way. I had hospitalizations; I was in psychiatric wards. I had a suicide attempt in 2006, which was nearly successful. I was feeling social, mental, and emotional pain for so long. The community has been invaluable for me. Hearing other people’s stories, being accepted, has been wonderful.
I’ve been down and now I’m up, on an upward trajectory.
Question: How else has Fountain House made a difference in your life?
RC: I’m in a Fountain House residence in a one-bedroom, and it’s the most stable housing I’ve ever had in 61 years. So I’ve gotten housing and I’ve gotten a job, which is all great, because it’s aided me in becoming a full human being. But it’s really eased my suffering and enabled me to feel some joy and have some life instead of this shadow existence that I had been living for 30 years.
Fountain House has different units, and I’ve been in the communications unit – we put out the weekly paper and handle all the mail. The unit has computers, and I was able to work on my writing. I wrote a play called "The Very Last Dance of Homeless Joe." We’ve had staged readings at Fountain House, and 200 people have seen it over 2 years. We Zoomed it through the virtual community. It was very successful. A recording of the staged reading won third place at a festival in Florida.
In September, it will be an off-Broadway show. It’s a play about the homeless, but it’s not depressing; it’s very uplifting.
Question: Did you stay connected to Fountain House during the pandemic, either through the digital community or through services they provided? What was this experience like for you?
RC: Ashwin [Vasan] had been here 6 months, and he saw the pandemic coming. During a programming meeting he said, “We need a virtual community, and we need it now.” None of us knew what Zoom was, how the mute button worked. But it’s been wonderful for me. I’m a performer, so I was able to get on to Facebook every day and post a song. Some of it was spoofs about COVID; some were dedications to members. I ended up connecting with a member in Minnesota who used to be a neighbor of mine. We had lost contact, and we reconnected through Fountain House.
Question: What would you tell someone who might need this service?
RC: We’ve partially reopened the clubhouse. In July we’ll be doing tours again. I’d say, come take a tour and see the different social, economic, housing, and educational opportunities. We have a home and garden unit that decorates the place. We have a gym, a wellness unit. But these are just things. The real heart is the people.
As a unit leader recently told me, “We’re not a clinic. We’re not a revolving door. We forge relationships with members that last in our hearts and minds for a lifetime. Even if it’s not in my job description, if there’s anything in my power that I could do to help a member ease their suffering, I will do it.”
Incorporating self-care, wellness into routines can prevent doctors’ burnout
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Schizophrenia meds a key contributor to cognitive impairment
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Child suicides drive Colorado hospital to declare state of emergency
On May 25, Jena Hausmann, CEO of Children’s Hospital Colorado, Aurora, declared a state of emergency in youth mental health in response to an astronomical increase in pediatric mental health cases, including suicide, which has overwhelmed the institution.
From April 2019 to April 2021, the demand for pediatric behavioral health treatment at the hospital system increased by 90%. In Colorado, suicide is now the number one cause of death among youth and occurs in children as young as 10 years of age.
“Now we are seeing our pediatric emergency departments and our inpatient units overrun with kids attempting suicide and suffering from other forms of major mental health illness,” Dr. Hausmann said in a press release.
“We had to draw attention to what we’re seeing in our hospital and our community on an everyday basis – an unprecedented number of suicidal children who need acute treatment for behavioral health problems – and when I say ‘unprecedented,’ I’m serious – I’ve been in pediatrics for two decades and have never seen anything like this before,” David Brumbaugh, MD, a pediatric gastroenterologist and chief medical officer for Children’s Colorado, told this news organization.
Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness, stated in an interview that she “commends the CEO of the hospital for making this announcement, because it is outrageous to see what is happening with more and more children with significant psychiatric symptoms who are not getting adequate care.”
Jenna Glover, PhD, child psychologist and director of psychology training at Children’s Hospital, said that during the past decade, there has been a steady increase in depression, anxiety, and suicide among youth in Colorado. Suicide, she added, is now the number one cause of death in youth, “so we were already in a state of crisis.” She added that COVID-19 was “the straw that broke the camel’s back.”
“In January to April of this year, behavioral health ED visits to Children’s Hospital were 72% higher than they were 2 years ago at this time,” she said. “Colorado Springs had a 145% increase for ED behavioral health visits during the first 4 months of 2021, compared to the first 4 months of 2020.”
COVID’s impact
Other problems that have been “skyrocketing” in youth are self-harm, substance use, and eating disorders. Younger children are experiencing an increase in behavioral problems, including developmental regression, such as tantrums, and problems with sleeping, toileting, and eating, Dr. Glover noted.
The youth mental health crisis has mushroomed, although social distancing requirements are now beginning to ease and we are in the “home stretch of the pandemic,” Dr. Brumbaugh said.
One possible reason “is that we took kids out of their normal routines, social circles, friendships, etc., for 12 months, and that was the limit of their physiological or mental resistance, and they got to the end of their rope,” he speculated.
Dr. Glover said, “Kids are burned out, and although they’re asking to return to their life, they don’t feel they have the resources. They feel so behind; they don’t know how to catch up.”
Dr. Brumbaugh said that there are not enough child psychiatrists to provide outpatient services or enough inpatient beds for children in crisis.
“This is an unacceptable situation. We would never allow a child with leukemia or appendicitis to go several weeks without treatment,” he said.
Community donors have come forward, enabling an anticipated 50% increase in Children’s Hospital’s mental health outpatient, inpatient, and day services by March 2022.
“On a hospital level, we are continuing to do things to expand access to care, like opening units that provide different levels of care for patients with psychiatric problems, as well as expanding into areas that are more rural,” Dr. Glover said.
However, the “blueprint is not in action yet, and a lot of money still needs to be allocated. A workforce has to be created, because there are not enough clinicians to fill these roles,” she added.
Chronic underfunding
Dr. Brumbaugh said Colorado has always had a “relatively underfunded behavioral health system for kids.” A 2021 report by
However, Dr. Glover noted that Colorado is “not exceptional.” The increased vulnerability to youth mental illness and suicide is characteristic of other mountain states, which have larger rural areas, less access to care, and increased access to guns, she said.
Mass shootings may have amped up stress levels. “For some kids, this is happening in their schools or towns, and they feel traumatized and unsafe,” Dr. Glover added.
Dr. Crawford, who is an assistant professor of psychiatry at Boston University, also pointed out that the mental health crisis in youth is not unique to Colorado.
“Throughout the country, we’ve seen these colliding pandemics – inadequate mental health resources for children and COVID-19, which exacerbated the existing mental health crisis,” she said.
“The pandemic led to an increase in telehealth services, making individual and group psychotherapy available to kids in areas that never had access to these before, which is a ‘silver lining’ of the pandemic,” Dr. Glover said.
Dr. Crawford is “encouraged that we are having more conversations about pediatric mental health, because the pandemic amplified what was already going on and made it impossible to ignore.”
Screening is essential
Screening for mental health problems should be at the top of the mind of pediatricians and other clinicians who work with children, Dr. Glover said.
“Pediatricians are in the best place to catch potentially suicidal kids, because they are more likely to see these kids than therapists,” she noted.
She suggested using a rapid screen for depression, such as the Patient Health Questionnaire-9 (PHQ-9) modified for adolescents. Parents can also fill out a PHQ-9 for younger children and even for themselves.
“Depression, anxiety, and suicidality affect the whole family, so screening for these conditions in adults will benefit the children too,” she said. Teachers should also “be aware of what depression and anxiety symptoms look like in kids, because sometimes they can manifest more as irritability,” Dr. Glover added.
Policymakers and insurers need to prioritize pediatric mental health when determining allocation of health care, said Dr. Crawford.
“Financial incentives should be provided for hospitals to want to reserve beds for psychiatric patients, and in the outpatient setting, we also need to look at the payment structure of psychiatric visits,” she added.
Many psychiatrists do not want to accept insurance because of the increased bureaucracy and low reimbursement rates of insurance companies, and families cannot afford to pay out of pocket, “so we really need to look at the insurance issue at a policy level,” Dr. Crawford said.
Dr. Brumbaugh, Dr. Glover, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
On May 25, Jena Hausmann, CEO of Children’s Hospital Colorado, Aurora, declared a state of emergency in youth mental health in response to an astronomical increase in pediatric mental health cases, including suicide, which has overwhelmed the institution.
From April 2019 to April 2021, the demand for pediatric behavioral health treatment at the hospital system increased by 90%. In Colorado, suicide is now the number one cause of death among youth and occurs in children as young as 10 years of age.
“Now we are seeing our pediatric emergency departments and our inpatient units overrun with kids attempting suicide and suffering from other forms of major mental health illness,” Dr. Hausmann said in a press release.
“We had to draw attention to what we’re seeing in our hospital and our community on an everyday basis – an unprecedented number of suicidal children who need acute treatment for behavioral health problems – and when I say ‘unprecedented,’ I’m serious – I’ve been in pediatrics for two decades and have never seen anything like this before,” David Brumbaugh, MD, a pediatric gastroenterologist and chief medical officer for Children’s Colorado, told this news organization.
Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness, stated in an interview that she “commends the CEO of the hospital for making this announcement, because it is outrageous to see what is happening with more and more children with significant psychiatric symptoms who are not getting adequate care.”
Jenna Glover, PhD, child psychologist and director of psychology training at Children’s Hospital, said that during the past decade, there has been a steady increase in depression, anxiety, and suicide among youth in Colorado. Suicide, she added, is now the number one cause of death in youth, “so we were already in a state of crisis.” She added that COVID-19 was “the straw that broke the camel’s back.”
“In January to April of this year, behavioral health ED visits to Children’s Hospital were 72% higher than they were 2 years ago at this time,” she said. “Colorado Springs had a 145% increase for ED behavioral health visits during the first 4 months of 2021, compared to the first 4 months of 2020.”
COVID’s impact
Other problems that have been “skyrocketing” in youth are self-harm, substance use, and eating disorders. Younger children are experiencing an increase in behavioral problems, including developmental regression, such as tantrums, and problems with sleeping, toileting, and eating, Dr. Glover noted.
The youth mental health crisis has mushroomed, although social distancing requirements are now beginning to ease and we are in the “home stretch of the pandemic,” Dr. Brumbaugh said.
One possible reason “is that we took kids out of their normal routines, social circles, friendships, etc., for 12 months, and that was the limit of their physiological or mental resistance, and they got to the end of their rope,” he speculated.
Dr. Glover said, “Kids are burned out, and although they’re asking to return to their life, they don’t feel they have the resources. They feel so behind; they don’t know how to catch up.”
Dr. Brumbaugh said that there are not enough child psychiatrists to provide outpatient services or enough inpatient beds for children in crisis.
“This is an unacceptable situation. We would never allow a child with leukemia or appendicitis to go several weeks without treatment,” he said.
Community donors have come forward, enabling an anticipated 50% increase in Children’s Hospital’s mental health outpatient, inpatient, and day services by March 2022.
“On a hospital level, we are continuing to do things to expand access to care, like opening units that provide different levels of care for patients with psychiatric problems, as well as expanding into areas that are more rural,” Dr. Glover said.
However, the “blueprint is not in action yet, and a lot of money still needs to be allocated. A workforce has to be created, because there are not enough clinicians to fill these roles,” she added.
Chronic underfunding
Dr. Brumbaugh said Colorado has always had a “relatively underfunded behavioral health system for kids.” A 2021 report by
However, Dr. Glover noted that Colorado is “not exceptional.” The increased vulnerability to youth mental illness and suicide is characteristic of other mountain states, which have larger rural areas, less access to care, and increased access to guns, she said.
Mass shootings may have amped up stress levels. “For some kids, this is happening in their schools or towns, and they feel traumatized and unsafe,” Dr. Glover added.
Dr. Crawford, who is an assistant professor of psychiatry at Boston University, also pointed out that the mental health crisis in youth is not unique to Colorado.
“Throughout the country, we’ve seen these colliding pandemics – inadequate mental health resources for children and COVID-19, which exacerbated the existing mental health crisis,” she said.
“The pandemic led to an increase in telehealth services, making individual and group psychotherapy available to kids in areas that never had access to these before, which is a ‘silver lining’ of the pandemic,” Dr. Glover said.
Dr. Crawford is “encouraged that we are having more conversations about pediatric mental health, because the pandemic amplified what was already going on and made it impossible to ignore.”
Screening is essential
Screening for mental health problems should be at the top of the mind of pediatricians and other clinicians who work with children, Dr. Glover said.
“Pediatricians are in the best place to catch potentially suicidal kids, because they are more likely to see these kids than therapists,” she noted.
She suggested using a rapid screen for depression, such as the Patient Health Questionnaire-9 (PHQ-9) modified for adolescents. Parents can also fill out a PHQ-9 for younger children and even for themselves.
“Depression, anxiety, and suicidality affect the whole family, so screening for these conditions in adults will benefit the children too,” she said. Teachers should also “be aware of what depression and anxiety symptoms look like in kids, because sometimes they can manifest more as irritability,” Dr. Glover added.
Policymakers and insurers need to prioritize pediatric mental health when determining allocation of health care, said Dr. Crawford.
“Financial incentives should be provided for hospitals to want to reserve beds for psychiatric patients, and in the outpatient setting, we also need to look at the payment structure of psychiatric visits,” she added.
Many psychiatrists do not want to accept insurance because of the increased bureaucracy and low reimbursement rates of insurance companies, and families cannot afford to pay out of pocket, “so we really need to look at the insurance issue at a policy level,” Dr. Crawford said.
Dr. Brumbaugh, Dr. Glover, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
On May 25, Jena Hausmann, CEO of Children’s Hospital Colorado, Aurora, declared a state of emergency in youth mental health in response to an astronomical increase in pediatric mental health cases, including suicide, which has overwhelmed the institution.
From April 2019 to April 2021, the demand for pediatric behavioral health treatment at the hospital system increased by 90%. In Colorado, suicide is now the number one cause of death among youth and occurs in children as young as 10 years of age.
“Now we are seeing our pediatric emergency departments and our inpatient units overrun with kids attempting suicide and suffering from other forms of major mental health illness,” Dr. Hausmann said in a press release.
“We had to draw attention to what we’re seeing in our hospital and our community on an everyday basis – an unprecedented number of suicidal children who need acute treatment for behavioral health problems – and when I say ‘unprecedented,’ I’m serious – I’ve been in pediatrics for two decades and have never seen anything like this before,” David Brumbaugh, MD, a pediatric gastroenterologist and chief medical officer for Children’s Colorado, told this news organization.
Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness, stated in an interview that she “commends the CEO of the hospital for making this announcement, because it is outrageous to see what is happening with more and more children with significant psychiatric symptoms who are not getting adequate care.”
Jenna Glover, PhD, child psychologist and director of psychology training at Children’s Hospital, said that during the past decade, there has been a steady increase in depression, anxiety, and suicide among youth in Colorado. Suicide, she added, is now the number one cause of death in youth, “so we were already in a state of crisis.” She added that COVID-19 was “the straw that broke the camel’s back.”
“In January to April of this year, behavioral health ED visits to Children’s Hospital were 72% higher than they were 2 years ago at this time,” she said. “Colorado Springs had a 145% increase for ED behavioral health visits during the first 4 months of 2021, compared to the first 4 months of 2020.”
COVID’s impact
Other problems that have been “skyrocketing” in youth are self-harm, substance use, and eating disorders. Younger children are experiencing an increase in behavioral problems, including developmental regression, such as tantrums, and problems with sleeping, toileting, and eating, Dr. Glover noted.
The youth mental health crisis has mushroomed, although social distancing requirements are now beginning to ease and we are in the “home stretch of the pandemic,” Dr. Brumbaugh said.
One possible reason “is that we took kids out of their normal routines, social circles, friendships, etc., for 12 months, and that was the limit of their physiological or mental resistance, and they got to the end of their rope,” he speculated.
Dr. Glover said, “Kids are burned out, and although they’re asking to return to their life, they don’t feel they have the resources. They feel so behind; they don’t know how to catch up.”
Dr. Brumbaugh said that there are not enough child psychiatrists to provide outpatient services or enough inpatient beds for children in crisis.
“This is an unacceptable situation. We would never allow a child with leukemia or appendicitis to go several weeks without treatment,” he said.
Community donors have come forward, enabling an anticipated 50% increase in Children’s Hospital’s mental health outpatient, inpatient, and day services by March 2022.
“On a hospital level, we are continuing to do things to expand access to care, like opening units that provide different levels of care for patients with psychiatric problems, as well as expanding into areas that are more rural,” Dr. Glover said.
However, the “blueprint is not in action yet, and a lot of money still needs to be allocated. A workforce has to be created, because there are not enough clinicians to fill these roles,” she added.
Chronic underfunding
Dr. Brumbaugh said Colorado has always had a “relatively underfunded behavioral health system for kids.” A 2021 report by
However, Dr. Glover noted that Colorado is “not exceptional.” The increased vulnerability to youth mental illness and suicide is characteristic of other mountain states, which have larger rural areas, less access to care, and increased access to guns, she said.
Mass shootings may have amped up stress levels. “For some kids, this is happening in their schools or towns, and they feel traumatized and unsafe,” Dr. Glover added.
Dr. Crawford, who is an assistant professor of psychiatry at Boston University, also pointed out that the mental health crisis in youth is not unique to Colorado.
“Throughout the country, we’ve seen these colliding pandemics – inadequate mental health resources for children and COVID-19, which exacerbated the existing mental health crisis,” she said.
“The pandemic led to an increase in telehealth services, making individual and group psychotherapy available to kids in areas that never had access to these before, which is a ‘silver lining’ of the pandemic,” Dr. Glover said.
Dr. Crawford is “encouraged that we are having more conversations about pediatric mental health, because the pandemic amplified what was already going on and made it impossible to ignore.”
Screening is essential
Screening for mental health problems should be at the top of the mind of pediatricians and other clinicians who work with children, Dr. Glover said.
“Pediatricians are in the best place to catch potentially suicidal kids, because they are more likely to see these kids than therapists,” she noted.
She suggested using a rapid screen for depression, such as the Patient Health Questionnaire-9 (PHQ-9) modified for adolescents. Parents can also fill out a PHQ-9 for younger children and even for themselves.
“Depression, anxiety, and suicidality affect the whole family, so screening for these conditions in adults will benefit the children too,” she said. Teachers should also “be aware of what depression and anxiety symptoms look like in kids, because sometimes they can manifest more as irritability,” Dr. Glover added.
Policymakers and insurers need to prioritize pediatric mental health when determining allocation of health care, said Dr. Crawford.
“Financial incentives should be provided for hospitals to want to reserve beds for psychiatric patients, and in the outpatient setting, we also need to look at the payment structure of psychiatric visits,” she added.
Many psychiatrists do not want to accept insurance because of the increased bureaucracy and low reimbursement rates of insurance companies, and families cannot afford to pay out of pocket, “so we really need to look at the insurance issue at a policy level,” Dr. Crawford said.
Dr. Brumbaugh, Dr. Glover, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Medical licensing questions continue to violate ADA
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
FROM JAMA
Emotional support animals help lick symptoms of depression, anxiety in serious mental illness
Use of emotional support animals (ESAs) yields quantifiable reductions in depression, anxiety, and loneliness for patients with serious mental illness (SMI) who live alone, early research suggests.
Investigators followed 11 community-dwelling adults with SMI who were paired with a shelter dog or cat for 1 year. Participants’ depression, anxiety, and loneliness were assessed at baseline and 12 months after receipt of their ESAs.
At regular home visits during the study, participants also underwent saliva testing before playing with their pets and after 10 minutes of enjoyable pet interaction to assess levels of oxytocin – a biomarker associated with bonding – as well as cortisol and alpha amylase, which are markers of stress.
Significant reductions in measures of anxiety, depression, and loneliness were found between baseline and 12 months for all participants. Moreover, there was a pattern of an increase in levels of oxytocin and a decrease in levels of cortisol after 10 minutes of ESA interaction, but the degree of change did not reach statistical significance.
“Although this was a small pilot study and the findings are correlational, rather than causal, we can nevertheless say from the self-report of this group of participants and from the data collected that having an emotional support animal was beneficial to their mental health,” lead author Janet Hoy-Gerlach, PhD, professor of social work, University of Toledo (Ohio), said in an interview.
“We feel this data is a strong justification for additional study, and we hope that it will be a catalyst for future research with larger samples and more rigorous methodology,” said Dr. Hoy-Gerlach, author of “Human-Animal Interaction: A Social Work Guide,” published by NASW Press in 2017.
The study was published online May 20 in Human Animal Interaction Bulletin.
Everyday interactions
An ESA is a “companion animal (pet) who helps to reduce disability-related impairment for a particular person through the animal’s presence and everyday interactions,” the authors wrote.
Unlike service animals, which perform specific functions, ESAs “provide benefits that fall along the same dimensions as the benefits of pets – physical, social, emotional, and psychological – and there is research supporting the role that animals can play in each of these arenas,” Dr. Hoy-Gerlach said.
ESAs require no special training. All that is needed is a letter from a medical or mental health professional “that the individual meets the definition of ‘disability’ under the Fair Housing Act and a companion animal is a needed disability-ameliorating accommodation and should be allowed in buildings that don’t ordinarily permit pets,” she noted.
There is currently no peer-reviewed research that focuses explicitly on the impact of ESAs in individuals with SMI. To investigate, the researchers turned to the Hope and Recovery Pet Program (HARP) – a community partnership of the University of Toledo, the Toledo Humane Society, and ProMedica, a large regional nonprofit Toledo-based health care system – that pairs community-living individuals who have depression and/or anxiety with shelter animals that require adoption. The program pays for pet food, supplies, and veterinary care for those unable to afford these.
Participants (n = 11; mean age, 53.67 years; 78% women) were recruited from the HARP program. Participants were required to be psychiatrically stable, have stable housing, live alone, be at risk for social isolation, have low income, be sober, and have no history of violence. Their primary diagnoses were major depressive disorder, bipolar disorder, and schizoaffective disorder (63%, 18%, and 18%, respectively).
Six participants adopted a cat, and five adopted a dog.
Prior to ESA adoption and at 12 months, participants completed the Beck Depression Inventory (BDI), the Beck Anxiety Inventory (BAI), and the UCLA Loneliness Scale Version 3.
Prior to ESA adoption and at 1, 3, 6, 9, and 12 months, saliva samples were collected from participants by researchers at the beginning of a home visit and then after 10 minutes of “focused pleasant interaction” with the ESA. The saliva was tested for oxytocin, alpha amylase, and cortisol.
Motivation, comfort, calm
The researchers found statistically significant decreases in UCLA Loneliness Scale scores from pre-ESA (mean [SD],59.20 [9.47]) to 12 months (49.90 [13.66], P = .004). The eta-squared statistic (.62) indicated a large effect size.
For 18 of the 20 items on the loneliness scale, mean values were lower after the intervention than before the intervention. Of these, four were statistically significant.
A statistically significant decrease in BDI total scores was also seen from pre-ESA to 12 months (21.09 [8.43] to 14.64 [7.03], respectively; P = .03). The eta-squared statistic (.41) indicated a large effect size.
Of the 21 items on the BDI scale, the mean value was lower for 19 after the intervention. Of these, five were statistically significant.
Similarly, a statistically significant decrease in BAI score was found from pre-ESA to 12 months (23.55 [9.81] to 17.73 [11.79], P = .049). The eta-squared statistic (.36) indicated a large effect size, although there were no statistically significant changes in individual item scores.
The researchers found “observable patterns” of decreases in cortisol and increases in oxytocin after the 10-minute enjoyable ESA interactions. The highest oxytocin increase occurred at 12 months; however, these improvements did not reach statistical significance.
Participants offered open-ended statements about the positive impact of their ESA on their mental health, Dr. Hoy-Gerlach said. “For example, they described feeling motivated to take better care of themselves because their ESA needed them. Some described feeling ‘comforted,’ distracted from symptoms, soothed, and calmed.
“There is definitely a place for ESAs, especially with mental health post pandemic, when we need all the resources that we can for those who can benefit,” she added.
Postpandemic mental health
Commenting on the study for this news organization, Christine Crawford, MD, MPH, assistant professor of psychiatry, Boston University, observed that ESAs “are not on the radar for a lot of clinicians, and a lot of clinicians don’t know about the science [supporting their use] or what an emotional support pet entails.
“ besides traditional forms of treatment, such as medication and therapy. Even a little relief is important, and having an emotional support pet is a good option,” said Dr. Crawford, associate medical director of the National Alliance on Mental Illness. She was not involved with the study.
The Kenneth A. Scott Charitable Trust provided grant funding. Dr. Hoy-Gerlach, her coauthors, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of emotional support animals (ESAs) yields quantifiable reductions in depression, anxiety, and loneliness for patients with serious mental illness (SMI) who live alone, early research suggests.
Investigators followed 11 community-dwelling adults with SMI who were paired with a shelter dog or cat for 1 year. Participants’ depression, anxiety, and loneliness were assessed at baseline and 12 months after receipt of their ESAs.
At regular home visits during the study, participants also underwent saliva testing before playing with their pets and after 10 minutes of enjoyable pet interaction to assess levels of oxytocin – a biomarker associated with bonding – as well as cortisol and alpha amylase, which are markers of stress.
Significant reductions in measures of anxiety, depression, and loneliness were found between baseline and 12 months for all participants. Moreover, there was a pattern of an increase in levels of oxytocin and a decrease in levels of cortisol after 10 minutes of ESA interaction, but the degree of change did not reach statistical significance.
“Although this was a small pilot study and the findings are correlational, rather than causal, we can nevertheless say from the self-report of this group of participants and from the data collected that having an emotional support animal was beneficial to their mental health,” lead author Janet Hoy-Gerlach, PhD, professor of social work, University of Toledo (Ohio), said in an interview.
“We feel this data is a strong justification for additional study, and we hope that it will be a catalyst for future research with larger samples and more rigorous methodology,” said Dr. Hoy-Gerlach, author of “Human-Animal Interaction: A Social Work Guide,” published by NASW Press in 2017.
The study was published online May 20 in Human Animal Interaction Bulletin.
Everyday interactions
An ESA is a “companion animal (pet) who helps to reduce disability-related impairment for a particular person through the animal’s presence and everyday interactions,” the authors wrote.
Unlike service animals, which perform specific functions, ESAs “provide benefits that fall along the same dimensions as the benefits of pets – physical, social, emotional, and psychological – and there is research supporting the role that animals can play in each of these arenas,” Dr. Hoy-Gerlach said.
ESAs require no special training. All that is needed is a letter from a medical or mental health professional “that the individual meets the definition of ‘disability’ under the Fair Housing Act and a companion animal is a needed disability-ameliorating accommodation and should be allowed in buildings that don’t ordinarily permit pets,” she noted.
There is currently no peer-reviewed research that focuses explicitly on the impact of ESAs in individuals with SMI. To investigate, the researchers turned to the Hope and Recovery Pet Program (HARP) – a community partnership of the University of Toledo, the Toledo Humane Society, and ProMedica, a large regional nonprofit Toledo-based health care system – that pairs community-living individuals who have depression and/or anxiety with shelter animals that require adoption. The program pays for pet food, supplies, and veterinary care for those unable to afford these.
Participants (n = 11; mean age, 53.67 years; 78% women) were recruited from the HARP program. Participants were required to be psychiatrically stable, have stable housing, live alone, be at risk for social isolation, have low income, be sober, and have no history of violence. Their primary diagnoses were major depressive disorder, bipolar disorder, and schizoaffective disorder (63%, 18%, and 18%, respectively).
Six participants adopted a cat, and five adopted a dog.
Prior to ESA adoption and at 12 months, participants completed the Beck Depression Inventory (BDI), the Beck Anxiety Inventory (BAI), and the UCLA Loneliness Scale Version 3.
Prior to ESA adoption and at 1, 3, 6, 9, and 12 months, saliva samples were collected from participants by researchers at the beginning of a home visit and then after 10 minutes of “focused pleasant interaction” with the ESA. The saliva was tested for oxytocin, alpha amylase, and cortisol.
Motivation, comfort, calm
The researchers found statistically significant decreases in UCLA Loneliness Scale scores from pre-ESA (mean [SD],59.20 [9.47]) to 12 months (49.90 [13.66], P = .004). The eta-squared statistic (.62) indicated a large effect size.
For 18 of the 20 items on the loneliness scale, mean values were lower after the intervention than before the intervention. Of these, four were statistically significant.
A statistically significant decrease in BDI total scores was also seen from pre-ESA to 12 months (21.09 [8.43] to 14.64 [7.03], respectively; P = .03). The eta-squared statistic (.41) indicated a large effect size.
Of the 21 items on the BDI scale, the mean value was lower for 19 after the intervention. Of these, five were statistically significant.
Similarly, a statistically significant decrease in BAI score was found from pre-ESA to 12 months (23.55 [9.81] to 17.73 [11.79], P = .049). The eta-squared statistic (.36) indicated a large effect size, although there were no statistically significant changes in individual item scores.
The researchers found “observable patterns” of decreases in cortisol and increases in oxytocin after the 10-minute enjoyable ESA interactions. The highest oxytocin increase occurred at 12 months; however, these improvements did not reach statistical significance.
Participants offered open-ended statements about the positive impact of their ESA on their mental health, Dr. Hoy-Gerlach said. “For example, they described feeling motivated to take better care of themselves because their ESA needed them. Some described feeling ‘comforted,’ distracted from symptoms, soothed, and calmed.
“There is definitely a place for ESAs, especially with mental health post pandemic, when we need all the resources that we can for those who can benefit,” she added.
Postpandemic mental health
Commenting on the study for this news organization, Christine Crawford, MD, MPH, assistant professor of psychiatry, Boston University, observed that ESAs “are not on the radar for a lot of clinicians, and a lot of clinicians don’t know about the science [supporting their use] or what an emotional support pet entails.
“ besides traditional forms of treatment, such as medication and therapy. Even a little relief is important, and having an emotional support pet is a good option,” said Dr. Crawford, associate medical director of the National Alliance on Mental Illness. She was not involved with the study.
The Kenneth A. Scott Charitable Trust provided grant funding. Dr. Hoy-Gerlach, her coauthors, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of emotional support animals (ESAs) yields quantifiable reductions in depression, anxiety, and loneliness for patients with serious mental illness (SMI) who live alone, early research suggests.
Investigators followed 11 community-dwelling adults with SMI who were paired with a shelter dog or cat for 1 year. Participants’ depression, anxiety, and loneliness were assessed at baseline and 12 months after receipt of their ESAs.
At regular home visits during the study, participants also underwent saliva testing before playing with their pets and after 10 minutes of enjoyable pet interaction to assess levels of oxytocin – a biomarker associated with bonding – as well as cortisol and alpha amylase, which are markers of stress.
Significant reductions in measures of anxiety, depression, and loneliness were found between baseline and 12 months for all participants. Moreover, there was a pattern of an increase in levels of oxytocin and a decrease in levels of cortisol after 10 minutes of ESA interaction, but the degree of change did not reach statistical significance.
“Although this was a small pilot study and the findings are correlational, rather than causal, we can nevertheless say from the self-report of this group of participants and from the data collected that having an emotional support animal was beneficial to their mental health,” lead author Janet Hoy-Gerlach, PhD, professor of social work, University of Toledo (Ohio), said in an interview.
“We feel this data is a strong justification for additional study, and we hope that it will be a catalyst for future research with larger samples and more rigorous methodology,” said Dr. Hoy-Gerlach, author of “Human-Animal Interaction: A Social Work Guide,” published by NASW Press in 2017.
The study was published online May 20 in Human Animal Interaction Bulletin.
Everyday interactions
An ESA is a “companion animal (pet) who helps to reduce disability-related impairment for a particular person through the animal’s presence and everyday interactions,” the authors wrote.
Unlike service animals, which perform specific functions, ESAs “provide benefits that fall along the same dimensions as the benefits of pets – physical, social, emotional, and psychological – and there is research supporting the role that animals can play in each of these arenas,” Dr. Hoy-Gerlach said.
ESAs require no special training. All that is needed is a letter from a medical or mental health professional “that the individual meets the definition of ‘disability’ under the Fair Housing Act and a companion animal is a needed disability-ameliorating accommodation and should be allowed in buildings that don’t ordinarily permit pets,” she noted.
There is currently no peer-reviewed research that focuses explicitly on the impact of ESAs in individuals with SMI. To investigate, the researchers turned to the Hope and Recovery Pet Program (HARP) – a community partnership of the University of Toledo, the Toledo Humane Society, and ProMedica, a large regional nonprofit Toledo-based health care system – that pairs community-living individuals who have depression and/or anxiety with shelter animals that require adoption. The program pays for pet food, supplies, and veterinary care for those unable to afford these.
Participants (n = 11; mean age, 53.67 years; 78% women) were recruited from the HARP program. Participants were required to be psychiatrically stable, have stable housing, live alone, be at risk for social isolation, have low income, be sober, and have no history of violence. Their primary diagnoses were major depressive disorder, bipolar disorder, and schizoaffective disorder (63%, 18%, and 18%, respectively).
Six participants adopted a cat, and five adopted a dog.
Prior to ESA adoption and at 12 months, participants completed the Beck Depression Inventory (BDI), the Beck Anxiety Inventory (BAI), and the UCLA Loneliness Scale Version 3.
Prior to ESA adoption and at 1, 3, 6, 9, and 12 months, saliva samples were collected from participants by researchers at the beginning of a home visit and then after 10 minutes of “focused pleasant interaction” with the ESA. The saliva was tested for oxytocin, alpha amylase, and cortisol.
Motivation, comfort, calm
The researchers found statistically significant decreases in UCLA Loneliness Scale scores from pre-ESA (mean [SD],59.20 [9.47]) to 12 months (49.90 [13.66], P = .004). The eta-squared statistic (.62) indicated a large effect size.
For 18 of the 20 items on the loneliness scale, mean values were lower after the intervention than before the intervention. Of these, four were statistically significant.
A statistically significant decrease in BDI total scores was also seen from pre-ESA to 12 months (21.09 [8.43] to 14.64 [7.03], respectively; P = .03). The eta-squared statistic (.41) indicated a large effect size.
Of the 21 items on the BDI scale, the mean value was lower for 19 after the intervention. Of these, five were statistically significant.
Similarly, a statistically significant decrease in BAI score was found from pre-ESA to 12 months (23.55 [9.81] to 17.73 [11.79], P = .049). The eta-squared statistic (.36) indicated a large effect size, although there were no statistically significant changes in individual item scores.
The researchers found “observable patterns” of decreases in cortisol and increases in oxytocin after the 10-minute enjoyable ESA interactions. The highest oxytocin increase occurred at 12 months; however, these improvements did not reach statistical significance.
Participants offered open-ended statements about the positive impact of their ESA on their mental health, Dr. Hoy-Gerlach said. “For example, they described feeling motivated to take better care of themselves because their ESA needed them. Some described feeling ‘comforted,’ distracted from symptoms, soothed, and calmed.
“There is definitely a place for ESAs, especially with mental health post pandemic, when we need all the resources that we can for those who can benefit,” she added.
Postpandemic mental health
Commenting on the study for this news organization, Christine Crawford, MD, MPH, assistant professor of psychiatry, Boston University, observed that ESAs “are not on the radar for a lot of clinicians, and a lot of clinicians don’t know about the science [supporting their use] or what an emotional support pet entails.
“ besides traditional forms of treatment, such as medication and therapy. Even a little relief is important, and having an emotional support pet is a good option,” said Dr. Crawford, associate medical director of the National Alliance on Mental Illness. She was not involved with the study.
The Kenneth A. Scott Charitable Trust provided grant funding. Dr. Hoy-Gerlach, her coauthors, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Naomi Osaka withdraws from the French Open: When athletes struggle
In 2018, when Naomi Osaka won the U.S. Open by defeating Serena Williams, the trophy ceremony was painful to watch.

Ms. Williams had argued with an umpire over a controversial call, and the ceremony began with the crowd booing. Ms. Osaka, the victor, cried while Ms. Williams comforted her and quietly assured Ms. Osaka that the crowd was not booing at her. When asked how her dream of playing against Ms. Williams compared with the reality, the new champion, looking anything but victorious, responded: “Umm, I’m gonna sort of defer from your question, I’m sorry. I know that everyone was cheering for her, and I’m sorry it had to end like this.”
It was hardly the joyous moment it should have been in this young tennis player’s life.
Ms. Osaka, now 23, entered this year’s French Open as the Women’s Tennis Association’s second-ranked player and as the highest-paid female athlete of all time. She is known for her support of Black Lives Matter. Ms. Osaka announced that she would not be attending press conferences in an Instagram post days before the competition began. “If the organizations think they can keep saying, ‘do press or you’re going to get fined,’ and continue to ignore the mental health of the athletes that are the centerpiece of their cooperation then I just gotta laugh,” Ms. Osaka posted.
She was fined $15,000 on Sunday, May 30, when she did not appear at a press conference after winning her first match. Officials noted that she would be subjected to higher fines and expulsion from the tournament if she did not attend the mandatory media briefings. On June 1, Ms. Osaka withdrew from the French Open and explained her reasons on Instagram in a post where she announced that she has been struggling with depression and social anxiety and did not mean to become a distraction for the competition.
Psychiatrists weigh in
Sue Kim, MD, a psychiatrist who both plays and watches tennis, brought up Ms. Osaka’s resignation for discussion on the Maryland Psychiatric Society’s listserv. “[Ms.] Osaka put out on social media her depression and wanted to have rules reviewed and revised by the governing body of tennis, for future occasions. I feel it is so unfortunate and unfair and I am interested in hearing your opinions.”

Yusuke Sagawa, MD, a psychiatrist and tennis fan, wrote in: “During the COVID-19 pandemic, I rekindled my interest in tennis and I followed what transpired this past weekend. Naomi Osaka is an exceptionally shy and introverted person. I have noted that her speech is somewhat akin to (for lack of a better term) ‘Valley Girl’ talk, and from reading comments on tennis-related blogs, it appears she has garnered a significant amount of hatred as a result. Most of it is along the lines of people feeling her shyness and modesty is simply a masquerade.
“I have also seen YouTube videos of her signing autographs for fans. She is cooperative and pleasant, but clearly uncomfortable around large groups of people.
“Having seen many press conferences after a match,” Dr. Sagawa continued, “tennis journalists have a penchant for asking questions that are either personal or seemingly an attempt to stir up acrimony amongst players. Whatever the case, I truly do believe that this is not some sort of ruse on her part, and I hope that people come to her defense. It is disturbing to hear the comments already coming out from the ‘big names’ in the sport that have mostly been nonsupportive. Fortunately, there have also been a number of her contemporaries who have expressed this support for her.”
In the days following Ms. Osaka’s departure from the French Open, the situation has become more complex. as it is used in these types of communications.
Maryland psychiatrist Erik Roskes, MD, wrote: “I have followed this story from a distance and what strikes me is the intermixing of athleticism – which is presumably why we watch sports – and entertainment, the money-making part of it. The athletes are both athletes and entertainers, and [Ms.] Osaka seems to be unable to fully fulfill the latter part due to her unique traits. But like many, I wonder what if this had been Michael Phelps? Is there a gender issue at play?”
Stephanie Durruthy, MD, added: “[Ms.] Osaka brings complexity to the mental health conversations. There is no one answer to her current plight, but her being a person of color cannot be minimized. She magnified the race conversation in tennis to a higher level.
“When she was new to the Grand Slam scene, her Haitian, Japanese, and Black heritage became an issue with unending curiosity.
“[Ms.] Osaka used her platform during the 2020 U.S. Open to single-handedly highlight Black Lives Matter,” Dr. Durruthy continued. “Afterward, the tennis fans could not avoid seeing her face mask. In each match, she displayed another mask depicting the name of those killed. She described on social media her fears of being a Black person in America. The biases of gender and race are well described in the sports world.”
Lindsay Crouse wrote June 1 in the New York Times: “When Naomi Osaka dropped out of the French Open, after declining to attend media interviews that she said could trigger her anxiety, she wasn’t just protecting her mental health. She was sending a message to the establishment of one of the world’s most elite sports: I will not be controlled. This was a power move – and it packed more punch coming from a young woman of color. When the system hasn’t historically stood for you, why sacrifice yourself to uphold it? Especially when you have the power to change it instead.”
Professional sports are grueling on athletes, both physically and mentally. People will speculate about Ms. Osaka’s motives for refusing to participate in the media briefings that are mandated by her contract. Some will see it as manipulative, others as the desire of a young woman struggling with anxiety and depression to push back against a system that makes few allowances for those who suffer. As psychiatrists, we see how crippling these illnesses can be and admire those who achieve at these superhuman levels, often at the expense of their own well-being.
Dr. Kim, who started the MPS listserv discussion, ended it with: “I feel bad if Naomi Osaka needs to play a mental ‘illness’ card, as opposed to mental ‘wellness’ card.”
Let’s hope that Ms. Osaka’s withdrawal from the French Open sparks more conversation about how to accommodate athletes as they endeavor to meet both the demands of their contracts and when it might be more appropriate to be flexible for those with individual struggles.
Dr. Miller is coauthor of “ Committed: The Battle Over Involuntary Psychiatric Care ” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
In 2018, when Naomi Osaka won the U.S. Open by defeating Serena Williams, the trophy ceremony was painful to watch.

Ms. Williams had argued with an umpire over a controversial call, and the ceremony began with the crowd booing. Ms. Osaka, the victor, cried while Ms. Williams comforted her and quietly assured Ms. Osaka that the crowd was not booing at her. When asked how her dream of playing against Ms. Williams compared with the reality, the new champion, looking anything but victorious, responded: “Umm, I’m gonna sort of defer from your question, I’m sorry. I know that everyone was cheering for her, and I’m sorry it had to end like this.”
It was hardly the joyous moment it should have been in this young tennis player’s life.
Ms. Osaka, now 23, entered this year’s French Open as the Women’s Tennis Association’s second-ranked player and as the highest-paid female athlete of all time. She is known for her support of Black Lives Matter. Ms. Osaka announced that she would not be attending press conferences in an Instagram post days before the competition began. “If the organizations think they can keep saying, ‘do press or you’re going to get fined,’ and continue to ignore the mental health of the athletes that are the centerpiece of their cooperation then I just gotta laugh,” Ms. Osaka posted.
She was fined $15,000 on Sunday, May 30, when she did not appear at a press conference after winning her first match. Officials noted that she would be subjected to higher fines and expulsion from the tournament if she did not attend the mandatory media briefings. On June 1, Ms. Osaka withdrew from the French Open and explained her reasons on Instagram in a post where she announced that she has been struggling with depression and social anxiety and did not mean to become a distraction for the competition.
Psychiatrists weigh in
Sue Kim, MD, a psychiatrist who both plays and watches tennis, brought up Ms. Osaka’s resignation for discussion on the Maryland Psychiatric Society’s listserv. “[Ms.] Osaka put out on social media her depression and wanted to have rules reviewed and revised by the governing body of tennis, for future occasions. I feel it is so unfortunate and unfair and I am interested in hearing your opinions.”

Yusuke Sagawa, MD, a psychiatrist and tennis fan, wrote in: “During the COVID-19 pandemic, I rekindled my interest in tennis and I followed what transpired this past weekend. Naomi Osaka is an exceptionally shy and introverted person. I have noted that her speech is somewhat akin to (for lack of a better term) ‘Valley Girl’ talk, and from reading comments on tennis-related blogs, it appears she has garnered a significant amount of hatred as a result. Most of it is along the lines of people feeling her shyness and modesty is simply a masquerade.
“I have also seen YouTube videos of her signing autographs for fans. She is cooperative and pleasant, but clearly uncomfortable around large groups of people.
“Having seen many press conferences after a match,” Dr. Sagawa continued, “tennis journalists have a penchant for asking questions that are either personal or seemingly an attempt to stir up acrimony amongst players. Whatever the case, I truly do believe that this is not some sort of ruse on her part, and I hope that people come to her defense. It is disturbing to hear the comments already coming out from the ‘big names’ in the sport that have mostly been nonsupportive. Fortunately, there have also been a number of her contemporaries who have expressed this support for her.”
In the days following Ms. Osaka’s departure from the French Open, the situation has become more complex. as it is used in these types of communications.
Maryland psychiatrist Erik Roskes, MD, wrote: “I have followed this story from a distance and what strikes me is the intermixing of athleticism – which is presumably why we watch sports – and entertainment, the money-making part of it. The athletes are both athletes and entertainers, and [Ms.] Osaka seems to be unable to fully fulfill the latter part due to her unique traits. But like many, I wonder what if this had been Michael Phelps? Is there a gender issue at play?”
Stephanie Durruthy, MD, added: “[Ms.] Osaka brings complexity to the mental health conversations. There is no one answer to her current plight, but her being a person of color cannot be minimized. She magnified the race conversation in tennis to a higher level.
“When she was new to the Grand Slam scene, her Haitian, Japanese, and Black heritage became an issue with unending curiosity.
“[Ms.] Osaka used her platform during the 2020 U.S. Open to single-handedly highlight Black Lives Matter,” Dr. Durruthy continued. “Afterward, the tennis fans could not avoid seeing her face mask. In each match, she displayed another mask depicting the name of those killed. She described on social media her fears of being a Black person in America. The biases of gender and race are well described in the sports world.”
Lindsay Crouse wrote June 1 in the New York Times: “When Naomi Osaka dropped out of the French Open, after declining to attend media interviews that she said could trigger her anxiety, she wasn’t just protecting her mental health. She was sending a message to the establishment of one of the world’s most elite sports: I will not be controlled. This was a power move – and it packed more punch coming from a young woman of color. When the system hasn’t historically stood for you, why sacrifice yourself to uphold it? Especially when you have the power to change it instead.”
Professional sports are grueling on athletes, both physically and mentally. People will speculate about Ms. Osaka’s motives for refusing to participate in the media briefings that are mandated by her contract. Some will see it as manipulative, others as the desire of a young woman struggling with anxiety and depression to push back against a system that makes few allowances for those who suffer. As psychiatrists, we see how crippling these illnesses can be and admire those who achieve at these superhuman levels, often at the expense of their own well-being.
Dr. Kim, who started the MPS listserv discussion, ended it with: “I feel bad if Naomi Osaka needs to play a mental ‘illness’ card, as opposed to mental ‘wellness’ card.”
Let’s hope that Ms. Osaka’s withdrawal from the French Open sparks more conversation about how to accommodate athletes as they endeavor to meet both the demands of their contracts and when it might be more appropriate to be flexible for those with individual struggles.
Dr. Miller is coauthor of “ Committed: The Battle Over Involuntary Psychiatric Care ” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
In 2018, when Naomi Osaka won the U.S. Open by defeating Serena Williams, the trophy ceremony was painful to watch.

Ms. Williams had argued with an umpire over a controversial call, and the ceremony began with the crowd booing. Ms. Osaka, the victor, cried while Ms. Williams comforted her and quietly assured Ms. Osaka that the crowd was not booing at her. When asked how her dream of playing against Ms. Williams compared with the reality, the new champion, looking anything but victorious, responded: “Umm, I’m gonna sort of defer from your question, I’m sorry. I know that everyone was cheering for her, and I’m sorry it had to end like this.”
It was hardly the joyous moment it should have been in this young tennis player’s life.
Ms. Osaka, now 23, entered this year’s French Open as the Women’s Tennis Association’s second-ranked player and as the highest-paid female athlete of all time. She is known for her support of Black Lives Matter. Ms. Osaka announced that she would not be attending press conferences in an Instagram post days before the competition began. “If the organizations think they can keep saying, ‘do press or you’re going to get fined,’ and continue to ignore the mental health of the athletes that are the centerpiece of their cooperation then I just gotta laugh,” Ms. Osaka posted.
She was fined $15,000 on Sunday, May 30, when she did not appear at a press conference after winning her first match. Officials noted that she would be subjected to higher fines and expulsion from the tournament if she did not attend the mandatory media briefings. On June 1, Ms. Osaka withdrew from the French Open and explained her reasons on Instagram in a post where she announced that she has been struggling with depression and social anxiety and did not mean to become a distraction for the competition.
Psychiatrists weigh in
Sue Kim, MD, a psychiatrist who both plays and watches tennis, brought up Ms. Osaka’s resignation for discussion on the Maryland Psychiatric Society’s listserv. “[Ms.] Osaka put out on social media her depression and wanted to have rules reviewed and revised by the governing body of tennis, for future occasions. I feel it is so unfortunate and unfair and I am interested in hearing your opinions.”

Yusuke Sagawa, MD, a psychiatrist and tennis fan, wrote in: “During the COVID-19 pandemic, I rekindled my interest in tennis and I followed what transpired this past weekend. Naomi Osaka is an exceptionally shy and introverted person. I have noted that her speech is somewhat akin to (for lack of a better term) ‘Valley Girl’ talk, and from reading comments on tennis-related blogs, it appears she has garnered a significant amount of hatred as a result. Most of it is along the lines of people feeling her shyness and modesty is simply a masquerade.
“I have also seen YouTube videos of her signing autographs for fans. She is cooperative and pleasant, but clearly uncomfortable around large groups of people.
“Having seen many press conferences after a match,” Dr. Sagawa continued, “tennis journalists have a penchant for asking questions that are either personal or seemingly an attempt to stir up acrimony amongst players. Whatever the case, I truly do believe that this is not some sort of ruse on her part, and I hope that people come to her defense. It is disturbing to hear the comments already coming out from the ‘big names’ in the sport that have mostly been nonsupportive. Fortunately, there have also been a number of her contemporaries who have expressed this support for her.”
In the days following Ms. Osaka’s departure from the French Open, the situation has become more complex. as it is used in these types of communications.
Maryland psychiatrist Erik Roskes, MD, wrote: “I have followed this story from a distance and what strikes me is the intermixing of athleticism – which is presumably why we watch sports – and entertainment, the money-making part of it. The athletes are both athletes and entertainers, and [Ms.] Osaka seems to be unable to fully fulfill the latter part due to her unique traits. But like many, I wonder what if this had been Michael Phelps? Is there a gender issue at play?”
Stephanie Durruthy, MD, added: “[Ms.] Osaka brings complexity to the mental health conversations. There is no one answer to her current plight, but her being a person of color cannot be minimized. She magnified the race conversation in tennis to a higher level.
“When she was new to the Grand Slam scene, her Haitian, Japanese, and Black heritage became an issue with unending curiosity.
“[Ms.] Osaka used her platform during the 2020 U.S. Open to single-handedly highlight Black Lives Matter,” Dr. Durruthy continued. “Afterward, the tennis fans could not avoid seeing her face mask. In each match, she displayed another mask depicting the name of those killed. She described on social media her fears of being a Black person in America. The biases of gender and race are well described in the sports world.”
Lindsay Crouse wrote June 1 in the New York Times: “When Naomi Osaka dropped out of the French Open, after declining to attend media interviews that she said could trigger her anxiety, she wasn’t just protecting her mental health. She was sending a message to the establishment of one of the world’s most elite sports: I will not be controlled. This was a power move – and it packed more punch coming from a young woman of color. When the system hasn’t historically stood for you, why sacrifice yourself to uphold it? Especially when you have the power to change it instead.”
Professional sports are grueling on athletes, both physically and mentally. People will speculate about Ms. Osaka’s motives for refusing to participate in the media briefings that are mandated by her contract. Some will see it as manipulative, others as the desire of a young woman struggling with anxiety and depression to push back against a system that makes few allowances for those who suffer. As psychiatrists, we see how crippling these illnesses can be and admire those who achieve at these superhuman levels, often at the expense of their own well-being.
Dr. Kim, who started the MPS listserv discussion, ended it with: “I feel bad if Naomi Osaka needs to play a mental ‘illness’ card, as opposed to mental ‘wellness’ card.”
Let’s hope that Ms. Osaka’s withdrawal from the French Open sparks more conversation about how to accommodate athletes as they endeavor to meet both the demands of their contracts and when it might be more appropriate to be flexible for those with individual struggles.
Dr. Miller is coauthor of “ Committed: The Battle Over Involuntary Psychiatric Care ” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
Psychiatric fallout from long-COVID: How to prepare
As mounting evidence points to a significant psychiatric component of COVID-19, experts are concerned about an influx of survivors presenting with persistent mental health problems and how best to prepare.
Clinicians should be aware that patients who have had COVID frequently develop psychiatric symptoms, Silvia S. Martins, MD, PhD, associate professor of epidemiology, Columbia University, New York, said in an interview.
“There should be more screening of all patients recovering from a COVID infection for anxiety, posttraumatic stress disorder, and depression, as well as referral to services, including psychotherapy, and medication as needed,” said Dr. Martins, who, along with colleagues, uncovered a high rate of these symptoms in patients who had the disease.
The COVID-19 pandemic has taken an enormous social, emotional, and public health toll. It has disrupted lives and caused stress, fear, and uncertainty about loss of health and income, not to mention forced isolation.
In addition, a significant number of patients who contract COVID-19 continue to have symptoms after the acute phase of the illness. This post-COVID, or “long-haul,” syndrome isn’t well defined; experts cite a range of symptoms that persist for weeks or months.
These ongoing symptoms can include cough, fatigue, and chronic pain, as well as psychiatric complaints. As reported by this news organization, an observational study of more than 230,000 U.S. patient health records revealed that one in three COVID-19 survivors received a psychiatric or neurologic diagnosis within 6 months of contracting the virus.
The most common psychiatric diagnoses were anxiety disorders, mood disorders, substance misuse disorders, and insomnia.
Significant symptoms even in mild cases
Another study showed that even those with mild COVID-19 may experience psychiatric symptoms independently of previous psychiatric diagnoses. Results revealed that 26% of the sample of almost 900 patients reported depression, 22% reported anxiety, and 17% reported symptoms of posttraumatic stress 2 months after testing positive for the virus. This finding is important because the majority of individuals who contract COVID-19 have a mild case.
“We saw very high levels of clinically significant depression, anxiety, and posttraumatic stress symptoms in people who had mild disease,” study investigator João Mauricio Castaldelli-Maia, MD, PhD, postdoctoral fellow, department of epidemiology, Columbia University, said in an interview.
He attributed these symptoms in part to long periods of isolation, even from relatives in the same household, in cramped spaces typical of large cities such as São Paulo.
Social isolation can have a huge impact on persons who depend on social connections and relationships, Vivian Pender, MD, president of the American Psychiatric Association and clinical professor of psychiatry, Weill Cornell Medical Center, New York, said in an interview.
“The fact that we have not been able to see our colleagues, our friends, our family, and in the case of psychiatrists, even our patients has taken a toll on everyone, and that leads to more stress, more anxiety,” she said.
National surveys show that psychiatric symptoms occur after acute COVID. One survey revealed that over 50% of 3,900 respondents who had COVID reported having at least moderate symptoms of major depression.
Unique depression subtype?
Another survey, slated for publication later this year, shows that lead investigator Roy Perlis, MD, professor of psychiatry, Harvard Medical School, Boston, said in an interview.
This might suggest a neurobiological element. Researchers are speculating as to whether lingering psychiatric problems that occur after having COVID are linked to the psychosocial impact of the disease or to pathological processes, such as inflammation, that affect the brain.
Although rates of post-COVID psychiatric symptoms vary from study to study, “they seem to be pretty enduring,” noted Faith Gunning, PhD, vice chair of research, department of psychology, Weill Cornell Medicine, who specializes in clinical neuropsychology.
“So they’re not just a brief response” to getting sick, a fact that points to the possible need for treatment, she told this news organization. “In some of the work that’s starting to emerge, it does appear that the symptoms persist, at least for a relatively large subset of individuals.”
Although depression typically affects twice as many women as men, these new surveys show that, after COVID, “that difference is not so distinct,” said Dr. Gunning.
It’s unclear why this is, but it could be cause by financial stresses that may affect men to a greater extent, she added. “There is so much we’re still learning.”
Increased suicide risk?
Other researchers, including Leo Sher, MD, professor of psychiatry, Icahn School of Medicine at Mount Sinai, and director of inpatient psychiatry, James J. Peters Veterans Affairs Medical Center, both in New York, are concerned that higher rates of psychiatric symptoms among patients with long-haul COVID raise the risk for suicidal ideation and behavior.
Studies of suicidality in COVID-19 survivors “are urgently needed,” said Dr. Sher in an article published in the Monthly Journal of the Association of Physicians.
“We need to study what factors may increase suicide risk among the COVID-19 survivors during and after the recovery. We also need to investigate whether there is a long-term increased suicide risk among COVID-19 survivors,” Dr. Sher said.
COVID-19 is not unique among viral respiratory diseases in being associated with long-term mental health problems. Research shows that survivors of the 2003 outbreak of severe acute respiratory syndrome experienced increased psychological distress that persisted for at least a year, as did patients who in 2015 had Middle East respiratory syndrome coronavirus (MERS-CoV).
Some experts believe clinicians should screen patients for mental health symptoms after the acute phase of COVID and offer early and prolonged care.
“Early mental health intervention such as psychotherapy and supportive groups could play an important role in preventing incident mental health problems for post-COVID sufferers,” said Dr. Castaldelli-Maia.
A version of this article first appeared on Medscape.com.
As mounting evidence points to a significant psychiatric component of COVID-19, experts are concerned about an influx of survivors presenting with persistent mental health problems and how best to prepare.
Clinicians should be aware that patients who have had COVID frequently develop psychiatric symptoms, Silvia S. Martins, MD, PhD, associate professor of epidemiology, Columbia University, New York, said in an interview.
“There should be more screening of all patients recovering from a COVID infection for anxiety, posttraumatic stress disorder, and depression, as well as referral to services, including psychotherapy, and medication as needed,” said Dr. Martins, who, along with colleagues, uncovered a high rate of these symptoms in patients who had the disease.
The COVID-19 pandemic has taken an enormous social, emotional, and public health toll. It has disrupted lives and caused stress, fear, and uncertainty about loss of health and income, not to mention forced isolation.
In addition, a significant number of patients who contract COVID-19 continue to have symptoms after the acute phase of the illness. This post-COVID, or “long-haul,” syndrome isn’t well defined; experts cite a range of symptoms that persist for weeks or months.
These ongoing symptoms can include cough, fatigue, and chronic pain, as well as psychiatric complaints. As reported by this news organization, an observational study of more than 230,000 U.S. patient health records revealed that one in three COVID-19 survivors received a psychiatric or neurologic diagnosis within 6 months of contracting the virus.
The most common psychiatric diagnoses were anxiety disorders, mood disorders, substance misuse disorders, and insomnia.
Significant symptoms even in mild cases
Another study showed that even those with mild COVID-19 may experience psychiatric symptoms independently of previous psychiatric diagnoses. Results revealed that 26% of the sample of almost 900 patients reported depression, 22% reported anxiety, and 17% reported symptoms of posttraumatic stress 2 months after testing positive for the virus. This finding is important because the majority of individuals who contract COVID-19 have a mild case.
“We saw very high levels of clinically significant depression, anxiety, and posttraumatic stress symptoms in people who had mild disease,” study investigator João Mauricio Castaldelli-Maia, MD, PhD, postdoctoral fellow, department of epidemiology, Columbia University, said in an interview.
He attributed these symptoms in part to long periods of isolation, even from relatives in the same household, in cramped spaces typical of large cities such as São Paulo.
Social isolation can have a huge impact on persons who depend on social connections and relationships, Vivian Pender, MD, president of the American Psychiatric Association and clinical professor of psychiatry, Weill Cornell Medical Center, New York, said in an interview.
“The fact that we have not been able to see our colleagues, our friends, our family, and in the case of psychiatrists, even our patients has taken a toll on everyone, and that leads to more stress, more anxiety,” she said.
National surveys show that psychiatric symptoms occur after acute COVID. One survey revealed that over 50% of 3,900 respondents who had COVID reported having at least moderate symptoms of major depression.
Unique depression subtype?
Another survey, slated for publication later this year, shows that lead investigator Roy Perlis, MD, professor of psychiatry, Harvard Medical School, Boston, said in an interview.
This might suggest a neurobiological element. Researchers are speculating as to whether lingering psychiatric problems that occur after having COVID are linked to the psychosocial impact of the disease or to pathological processes, such as inflammation, that affect the brain.
Although rates of post-COVID psychiatric symptoms vary from study to study, “they seem to be pretty enduring,” noted Faith Gunning, PhD, vice chair of research, department of psychology, Weill Cornell Medicine, who specializes in clinical neuropsychology.
“So they’re not just a brief response” to getting sick, a fact that points to the possible need for treatment, she told this news organization. “In some of the work that’s starting to emerge, it does appear that the symptoms persist, at least for a relatively large subset of individuals.”
Although depression typically affects twice as many women as men, these new surveys show that, after COVID, “that difference is not so distinct,” said Dr. Gunning.
It’s unclear why this is, but it could be cause by financial stresses that may affect men to a greater extent, she added. “There is so much we’re still learning.”
Increased suicide risk?
Other researchers, including Leo Sher, MD, professor of psychiatry, Icahn School of Medicine at Mount Sinai, and director of inpatient psychiatry, James J. Peters Veterans Affairs Medical Center, both in New York, are concerned that higher rates of psychiatric symptoms among patients with long-haul COVID raise the risk for suicidal ideation and behavior.
Studies of suicidality in COVID-19 survivors “are urgently needed,” said Dr. Sher in an article published in the Monthly Journal of the Association of Physicians.
“We need to study what factors may increase suicide risk among the COVID-19 survivors during and after the recovery. We also need to investigate whether there is a long-term increased suicide risk among COVID-19 survivors,” Dr. Sher said.
COVID-19 is not unique among viral respiratory diseases in being associated with long-term mental health problems. Research shows that survivors of the 2003 outbreak of severe acute respiratory syndrome experienced increased psychological distress that persisted for at least a year, as did patients who in 2015 had Middle East respiratory syndrome coronavirus (MERS-CoV).
Some experts believe clinicians should screen patients for mental health symptoms after the acute phase of COVID and offer early and prolonged care.
“Early mental health intervention such as psychotherapy and supportive groups could play an important role in preventing incident mental health problems for post-COVID sufferers,” said Dr. Castaldelli-Maia.
A version of this article first appeared on Medscape.com.
As mounting evidence points to a significant psychiatric component of COVID-19, experts are concerned about an influx of survivors presenting with persistent mental health problems and how best to prepare.
Clinicians should be aware that patients who have had COVID frequently develop psychiatric symptoms, Silvia S. Martins, MD, PhD, associate professor of epidemiology, Columbia University, New York, said in an interview.
“There should be more screening of all patients recovering from a COVID infection for anxiety, posttraumatic stress disorder, and depression, as well as referral to services, including psychotherapy, and medication as needed,” said Dr. Martins, who, along with colleagues, uncovered a high rate of these symptoms in patients who had the disease.
The COVID-19 pandemic has taken an enormous social, emotional, and public health toll. It has disrupted lives and caused stress, fear, and uncertainty about loss of health and income, not to mention forced isolation.
In addition, a significant number of patients who contract COVID-19 continue to have symptoms after the acute phase of the illness. This post-COVID, or “long-haul,” syndrome isn’t well defined; experts cite a range of symptoms that persist for weeks or months.
These ongoing symptoms can include cough, fatigue, and chronic pain, as well as psychiatric complaints. As reported by this news organization, an observational study of more than 230,000 U.S. patient health records revealed that one in three COVID-19 survivors received a psychiatric or neurologic diagnosis within 6 months of contracting the virus.
The most common psychiatric diagnoses were anxiety disorders, mood disorders, substance misuse disorders, and insomnia.
Significant symptoms even in mild cases
Another study showed that even those with mild COVID-19 may experience psychiatric symptoms independently of previous psychiatric diagnoses. Results revealed that 26% of the sample of almost 900 patients reported depression, 22% reported anxiety, and 17% reported symptoms of posttraumatic stress 2 months after testing positive for the virus. This finding is important because the majority of individuals who contract COVID-19 have a mild case.
“We saw very high levels of clinically significant depression, anxiety, and posttraumatic stress symptoms in people who had mild disease,” study investigator João Mauricio Castaldelli-Maia, MD, PhD, postdoctoral fellow, department of epidemiology, Columbia University, said in an interview.
He attributed these symptoms in part to long periods of isolation, even from relatives in the same household, in cramped spaces typical of large cities such as São Paulo.
Social isolation can have a huge impact on persons who depend on social connections and relationships, Vivian Pender, MD, president of the American Psychiatric Association and clinical professor of psychiatry, Weill Cornell Medical Center, New York, said in an interview.
“The fact that we have not been able to see our colleagues, our friends, our family, and in the case of psychiatrists, even our patients has taken a toll on everyone, and that leads to more stress, more anxiety,” she said.
National surveys show that psychiatric symptoms occur after acute COVID. One survey revealed that over 50% of 3,900 respondents who had COVID reported having at least moderate symptoms of major depression.
Unique depression subtype?
Another survey, slated for publication later this year, shows that lead investigator Roy Perlis, MD, professor of psychiatry, Harvard Medical School, Boston, said in an interview.
This might suggest a neurobiological element. Researchers are speculating as to whether lingering psychiatric problems that occur after having COVID are linked to the psychosocial impact of the disease or to pathological processes, such as inflammation, that affect the brain.
Although rates of post-COVID psychiatric symptoms vary from study to study, “they seem to be pretty enduring,” noted Faith Gunning, PhD, vice chair of research, department of psychology, Weill Cornell Medicine, who specializes in clinical neuropsychology.
“So they’re not just a brief response” to getting sick, a fact that points to the possible need for treatment, she told this news organization. “In some of the work that’s starting to emerge, it does appear that the symptoms persist, at least for a relatively large subset of individuals.”
Although depression typically affects twice as many women as men, these new surveys show that, after COVID, “that difference is not so distinct,” said Dr. Gunning.
It’s unclear why this is, but it could be cause by financial stresses that may affect men to a greater extent, she added. “There is so much we’re still learning.”
Increased suicide risk?
Other researchers, including Leo Sher, MD, professor of psychiatry, Icahn School of Medicine at Mount Sinai, and director of inpatient psychiatry, James J. Peters Veterans Affairs Medical Center, both in New York, are concerned that higher rates of psychiatric symptoms among patients with long-haul COVID raise the risk for suicidal ideation and behavior.
Studies of suicidality in COVID-19 survivors “are urgently needed,” said Dr. Sher in an article published in the Monthly Journal of the Association of Physicians.
“We need to study what factors may increase suicide risk among the COVID-19 survivors during and after the recovery. We also need to investigate whether there is a long-term increased suicide risk among COVID-19 survivors,” Dr. Sher said.
COVID-19 is not unique among viral respiratory diseases in being associated with long-term mental health problems. Research shows that survivors of the 2003 outbreak of severe acute respiratory syndrome experienced increased psychological distress that persisted for at least a year, as did patients who in 2015 had Middle East respiratory syndrome coronavirus (MERS-CoV).
Some experts believe clinicians should screen patients for mental health symptoms after the acute phase of COVID and offer early and prolonged care.
“Early mental health intervention such as psychotherapy and supportive groups could play an important role in preventing incident mental health problems for post-COVID sufferers,” said Dr. Castaldelli-Maia.
A version of this article first appeared on Medscape.com.