User login
Enteral contrast did not add diagnostic benefit in suspected appendicitis
Enteral contrast did not augment the accuracy of computed tomography in appendectomy patients, compared with intravenous contrast CT alone, according to a large multihospital study published in Annals of Surgery.
"Enteral contrast should be eliminated in IV-enhanced CT scans performed for suspected appendicitis," said Dr. Frederick Drake at the University of Washington Medical Center in Seattle and his associates. "We conclude that IV contrast alone is sufficient for the diagnosis of appendicitis in a wide variety of hospitals, outside of tertiary centers and strict research protocols."
The investigators studied 9,047 adults who underwent nonelective appendectomies at 56 hospitals in the state of Washington during a 2-year period. Patients were identified through the Surgical Care Outcomes and Assessment Program (SCOAP), which is based on direct reviews of clinical records and captures more than 85% of nonelective appendectomies performed in the state, the researchers said (Ann. Surg. 2014;260:311-6).
The primary outcome measure was concordance between a patient’s final pathology and the final radiologic report, they said.
Almost 90% of patients underwent CT before surgery. Among these patients, 54% received only IV contrast and 28.5% received both IV and enteral contrast, said the investigators. After controlling for age, sex, comorbidities, weight, hospital type, and perforation, they found no significant difference in concordance rates for IV-only contrast versus IV with enteral contrast (odds ratio, 0.95; 95% confidence interval, 0.72-1.25). Pathology and radiographic findings correlated in 90% of patients who received IV and enteral contrast, and in 90.4% of patients who received only IV contrast, they added, noting that eliminating enteral contrast could improve patients’ safety and comfort, and the efficiency of emergency departments.
The Life Discovery Fund of Washington State, the Agency for Healthcare Research and Quality, and the National Institutes of Health funded the research. The authors reported having no conflicts of interest.
Enteral contrast did not augment the accuracy of computed tomography in appendectomy patients, compared with intravenous contrast CT alone, according to a large multihospital study published in Annals of Surgery.
"Enteral contrast should be eliminated in IV-enhanced CT scans performed for suspected appendicitis," said Dr. Frederick Drake at the University of Washington Medical Center in Seattle and his associates. "We conclude that IV contrast alone is sufficient for the diagnosis of appendicitis in a wide variety of hospitals, outside of tertiary centers and strict research protocols."
The investigators studied 9,047 adults who underwent nonelective appendectomies at 56 hospitals in the state of Washington during a 2-year period. Patients were identified through the Surgical Care Outcomes and Assessment Program (SCOAP), which is based on direct reviews of clinical records and captures more than 85% of nonelective appendectomies performed in the state, the researchers said (Ann. Surg. 2014;260:311-6).
The primary outcome measure was concordance between a patient’s final pathology and the final radiologic report, they said.
Almost 90% of patients underwent CT before surgery. Among these patients, 54% received only IV contrast and 28.5% received both IV and enteral contrast, said the investigators. After controlling for age, sex, comorbidities, weight, hospital type, and perforation, they found no significant difference in concordance rates for IV-only contrast versus IV with enteral contrast (odds ratio, 0.95; 95% confidence interval, 0.72-1.25). Pathology and radiographic findings correlated in 90% of patients who received IV and enteral contrast, and in 90.4% of patients who received only IV contrast, they added, noting that eliminating enteral contrast could improve patients’ safety and comfort, and the efficiency of emergency departments.
The Life Discovery Fund of Washington State, the Agency for Healthcare Research and Quality, and the National Institutes of Health funded the research. The authors reported having no conflicts of interest.
Enteral contrast did not augment the accuracy of computed tomography in appendectomy patients, compared with intravenous contrast CT alone, according to a large multihospital study published in Annals of Surgery.
"Enteral contrast should be eliminated in IV-enhanced CT scans performed for suspected appendicitis," said Dr. Frederick Drake at the University of Washington Medical Center in Seattle and his associates. "We conclude that IV contrast alone is sufficient for the diagnosis of appendicitis in a wide variety of hospitals, outside of tertiary centers and strict research protocols."
The investigators studied 9,047 adults who underwent nonelective appendectomies at 56 hospitals in the state of Washington during a 2-year period. Patients were identified through the Surgical Care Outcomes and Assessment Program (SCOAP), which is based on direct reviews of clinical records and captures more than 85% of nonelective appendectomies performed in the state, the researchers said (Ann. Surg. 2014;260:311-6).
The primary outcome measure was concordance between a patient’s final pathology and the final radiologic report, they said.
Almost 90% of patients underwent CT before surgery. Among these patients, 54% received only IV contrast and 28.5% received both IV and enteral contrast, said the investigators. After controlling for age, sex, comorbidities, weight, hospital type, and perforation, they found no significant difference in concordance rates for IV-only contrast versus IV with enteral contrast (odds ratio, 0.95; 95% confidence interval, 0.72-1.25). Pathology and radiographic findings correlated in 90% of patients who received IV and enteral contrast, and in 90.4% of patients who received only IV contrast, they added, noting that eliminating enteral contrast could improve patients’ safety and comfort, and the efficiency of emergency departments.
The Life Discovery Fund of Washington State, the Agency for Healthcare Research and Quality, and the National Institutes of Health funded the research. The authors reported having no conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Enteral contrast is not of additional diagnostic benefit in appendectomy patients undergoing intravenous contrast computed tomography.
Major finding: After adjustment for age, sex, comorbidities, weight, hospital type, and perforation, there was no significant difference in rates of pathologic and radiologic concordance for patients who underwent IV-only contrast CT versus IV and enteral contrast CT (odds ratio, 0.95; 95% confidence interval, 0.72-1.25).
Data Source: Prospective cohort study of 9,047 adults who underwent nonelective appendectomies at 56 hospitals in the state of Washington between Jan. 1, 2010, and Dec. 31, 2011.
Disclosures: The Life Discovery Fund of Washington State, the Agency for Healthcare Research and Quality, and the National Institutes of Health funded the research. The authors reported having no conflicts of interest.
Laparoscopy found effective alternative to open IBD surgery
In an urban colorectal surgery department, a near-doubling in the proportion of surgical procedures performed laparoscopically accompanied significant declines in both severe postoperative morbidity and conversions to laparotomy, in a 14-year, single-hospital study reported in Annals of Surgery.
"This study demonstrated that a laparoscopic approach is a safe and effective alternative to open surgery" for management of inflammatory bowel disease (IBD), wrote Dr. León Maggiori and his associates at the Assistance Publique-Hôpitaux de Paris.
"Associated postoperative morbidity was comparable to reported rates after open approach," the researchers added.
Dr. Maggiori and his associates studied 790 consecutive intestinal resections for IBD performed on 633 patients between June 1998 and July 2012. About two-thirds of the procedures were for Crohn’s disease, and one-third were for ulcerative colitis, the investigators said (Ann. Surg. 2014;260:305-10). The proportion of laparoscopically performed procedures rose from 42% to 80% during the study period (P less than .001), and the trend occurred both for Crohn’s and for ulcerative colitis cases, they added.
As surgeons accrued experience, the rate of complex cases performed laparoscopically also approximately doubled (from 16% to 33%; P less than .023), the researchers said. Furthermore, the mean adjusted risk of conversion to open surgery fell significantly (from 18% to 6%; P less than .001), as did the rate of severe postoperative morbidity (from 14% to 8%; P less than .001).
In all, 12% of laparoscopic cases required conversion, most often because of abscesses or fistulas found during surgery or difficulty dissecting adhesions, the investigators said. Thirteen percent of laparoscopies led to severe postoperative morbidity, defined as Clavien-Dindo grade 3 or 4 complications, they added. The single postoperative death occurred in a patient who developed peritonitis and septic shock 3 days after laparoscopic colectomy with ileosigmoidostomy, the researchers said.
The hospital now uses laparoscopy as the standard approach for surgical management of IBD, except in cases of complicated acute colitis, Dr. Maggiori and his associates said.
The limited number of straight open surgical cases meant that they could not directly be compared with laparoscopy, said the investigators, adding that they lacked data on long-term outcomes because many patients underwent surgery in 2008 or later.
The Association François Aupetit partially funded the study. The authors reported having no conflicts of interest.
In an urban colorectal surgery department, a near-doubling in the proportion of surgical procedures performed laparoscopically accompanied significant declines in both severe postoperative morbidity and conversions to laparotomy, in a 14-year, single-hospital study reported in Annals of Surgery.
"This study demonstrated that a laparoscopic approach is a safe and effective alternative to open surgery" for management of inflammatory bowel disease (IBD), wrote Dr. León Maggiori and his associates at the Assistance Publique-Hôpitaux de Paris.
"Associated postoperative morbidity was comparable to reported rates after open approach," the researchers added.
Dr. Maggiori and his associates studied 790 consecutive intestinal resections for IBD performed on 633 patients between June 1998 and July 2012. About two-thirds of the procedures were for Crohn’s disease, and one-third were for ulcerative colitis, the investigators said (Ann. Surg. 2014;260:305-10). The proportion of laparoscopically performed procedures rose from 42% to 80% during the study period (P less than .001), and the trend occurred both for Crohn’s and for ulcerative colitis cases, they added.
As surgeons accrued experience, the rate of complex cases performed laparoscopically also approximately doubled (from 16% to 33%; P less than .023), the researchers said. Furthermore, the mean adjusted risk of conversion to open surgery fell significantly (from 18% to 6%; P less than .001), as did the rate of severe postoperative morbidity (from 14% to 8%; P less than .001).
In all, 12% of laparoscopic cases required conversion, most often because of abscesses or fistulas found during surgery or difficulty dissecting adhesions, the investigators said. Thirteen percent of laparoscopies led to severe postoperative morbidity, defined as Clavien-Dindo grade 3 or 4 complications, they added. The single postoperative death occurred in a patient who developed peritonitis and septic shock 3 days after laparoscopic colectomy with ileosigmoidostomy, the researchers said.
The hospital now uses laparoscopy as the standard approach for surgical management of IBD, except in cases of complicated acute colitis, Dr. Maggiori and his associates said.
The limited number of straight open surgical cases meant that they could not directly be compared with laparoscopy, said the investigators, adding that they lacked data on long-term outcomes because many patients underwent surgery in 2008 or later.
The Association François Aupetit partially funded the study. The authors reported having no conflicts of interest.
In an urban colorectal surgery department, a near-doubling in the proportion of surgical procedures performed laparoscopically accompanied significant declines in both severe postoperative morbidity and conversions to laparotomy, in a 14-year, single-hospital study reported in Annals of Surgery.
"This study demonstrated that a laparoscopic approach is a safe and effective alternative to open surgery" for management of inflammatory bowel disease (IBD), wrote Dr. León Maggiori and his associates at the Assistance Publique-Hôpitaux de Paris.
"Associated postoperative morbidity was comparable to reported rates after open approach," the researchers added.
Dr. Maggiori and his associates studied 790 consecutive intestinal resections for IBD performed on 633 patients between June 1998 and July 2012. About two-thirds of the procedures were for Crohn’s disease, and one-third were for ulcerative colitis, the investigators said (Ann. Surg. 2014;260:305-10). The proportion of laparoscopically performed procedures rose from 42% to 80% during the study period (P less than .001), and the trend occurred both for Crohn’s and for ulcerative colitis cases, they added.
As surgeons accrued experience, the rate of complex cases performed laparoscopically also approximately doubled (from 16% to 33%; P less than .023), the researchers said. Furthermore, the mean adjusted risk of conversion to open surgery fell significantly (from 18% to 6%; P less than .001), as did the rate of severe postoperative morbidity (from 14% to 8%; P less than .001).
In all, 12% of laparoscopic cases required conversion, most often because of abscesses or fistulas found during surgery or difficulty dissecting adhesions, the investigators said. Thirteen percent of laparoscopies led to severe postoperative morbidity, defined as Clavien-Dindo grade 3 or 4 complications, they added. The single postoperative death occurred in a patient who developed peritonitis and septic shock 3 days after laparoscopic colectomy with ileosigmoidostomy, the researchers said.
The hospital now uses laparoscopy as the standard approach for surgical management of IBD, except in cases of complicated acute colitis, Dr. Maggiori and his associates said.
The limited number of straight open surgical cases meant that they could not directly be compared with laparoscopy, said the investigators, adding that they lacked data on long-term outcomes because many patients underwent surgery in 2008 or later.
The Association François Aupetit partially funded the study. The authors reported having no conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Laparoscopic approaches are becoming standard for the surgical management of inflammatory bowel disease (IBD), except in cases of complicated acute colitis.
Major finding: The proportion of IBD procedures performed laparoscopically increased from 42% to 80% (P less than .001). The rate of complex laparoscopies also increased (P = .023), while the mean adjusted risks of conversion and severe postoperative morbidity dropped (P less than .001 for both).
Data source: Prospective analysis of 790 consecutive resections for IBD performed during a 14-year period, including 574 (73%) laparoscopic procedures.
Disclosures: The Association François Aupetit partially funded the study. The authors reported having no conflicts of interest.
Prevention program led to steep drop in postop pneumonia cases
A quality improvement program cut postoperative pneumonia rates by 43.6%, investigators reported July 23 in JAMA Surgery.
The small, single-center retrospective cohort study is the first to present long-term findings for such a program, said Dr. Hadiza Kazaure at Stanford (Calif.) University and her associates.
The program, which investigators started at a Stanford-affiliated Veterans Affairs hospital, included coughing and deep-breathing exercises with incentive spirometry, a twice-daily oral chlorhexidine hygiene, ambulation with pain control, elevating the head of the bed by 30 degrees and sitting for meals, educating surgical nursing staff about their roles in preventing pneumonia, and automating physician orders for pneumonia prevention, the researchers said (JAMA Surg. 2014 July 23 [doi:10.1001/jamasurg.2014.1216]).
The investigators calculated postimplementation rates of ward-acquired pneumonia in all noncardiac, unventilated surgical patients in the 5 years after the program started, they said.
Among 4,099 hospitalized patients who were at risk, 18 (0.44%) developed postoperative pneumonia, a 43.6% drop from the preprogram rate of 0.78%, the investigators reported.
By comparison, the postintervention rate for the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) was 582% higher than that of the VA hospital for 2008-2012. By achieving the VA hospital program’s results, the hospitals in the ACS-NSQIP could save about $280 million, Dr. Kazaure and her associates said.
The database abstraction methods used to choose patients were validated, but nonetheless could have caused selection errors. Also, few patients developed pneumonia, which kept the investigators from tracking trends over time on the ward, they said. "Based on published data, we used a national average of $46,400 cost of care per postoperative pneumonia case to estimate potential cost savings in our analyses," they added. "The validity of cost estimates in this study to individual hospitals must be considered because geographic variation in cost of care is well established."
The authors reported no funding sources or conflicts of interest.
The "remarkably low" baseline rate of postoperative pneumonia "calls into question the adequacy of detection and reporting of pneumonia" on the surgical ward, making findings "of somewhat less consequence," Dr. Catherine Lewis said.
"Moreover, the authors’ program was implemented and evaluated over a period in which there was an ongoing shift from open to laparoscopic or robotic surgical techniques, which has been shown to significantly decrease the rates of postoperative pneumonia, particularly in colorectal and prostate operations," she said.
The authors did not examine whether changes in patient care or surgical technique affected postoperative pneumonia rates, Dr. Lewis noted. She pointed to other research showing that using a neuraxial blockade instead of general anesthesia led to a significant drop in postoperative pneumonia, as did using selective nasogastric decompression (Ann. Intern. Med. 2006;144:596-608).
Previously, the authors of the current study reported that postoperative non–ventilator-associated pneumonia rates did not change after they started their program, Dr. Lewis said. The number of ward cases decreased, but the number of non–ventilator-associated pneumonia intensive care unit cases increased, so the decrease could reflect redistribution in the location of patients, she said.
But the authors also deserved praise for developing and starting a relatively cost- and time-efficient quality improvement measure, Dr. Lewis added. She said that such programs could increase awareness and education among health care providers who care for patients after surgery.
Dr. Lewis specializes in general, critical care, and trauma surgery at the University of California, Los Angeles. The remarks were excerpted from her invited editorial accompanying Dr. Kazaure’s report (JAMA Surg. 2014 July 23 [doi:10.1001/jamasurg.2014.1249]).
The "remarkably low" baseline rate of postoperative pneumonia "calls into question the adequacy of detection and reporting of pneumonia" on the surgical ward, making findings "of somewhat less consequence," Dr. Catherine Lewis said.
"Moreover, the authors’ program was implemented and evaluated over a period in which there was an ongoing shift from open to laparoscopic or robotic surgical techniques, which has been shown to significantly decrease the rates of postoperative pneumonia, particularly in colorectal and prostate operations," she said.
The authors did not examine whether changes in patient care or surgical technique affected postoperative pneumonia rates, Dr. Lewis noted. She pointed to other research showing that using a neuraxial blockade instead of general anesthesia led to a significant drop in postoperative pneumonia, as did using selective nasogastric decompression (Ann. Intern. Med. 2006;144:596-608).
Previously, the authors of the current study reported that postoperative non–ventilator-associated pneumonia rates did not change after they started their program, Dr. Lewis said. The number of ward cases decreased, but the number of non–ventilator-associated pneumonia intensive care unit cases increased, so the decrease could reflect redistribution in the location of patients, she said.
But the authors also deserved praise for developing and starting a relatively cost- and time-efficient quality improvement measure, Dr. Lewis added. She said that such programs could increase awareness and education among health care providers who care for patients after surgery.
Dr. Lewis specializes in general, critical care, and trauma surgery at the University of California, Los Angeles. The remarks were excerpted from her invited editorial accompanying Dr. Kazaure’s report (JAMA Surg. 2014 July 23 [doi:10.1001/jamasurg.2014.1249]).
The "remarkably low" baseline rate of postoperative pneumonia "calls into question the adequacy of detection and reporting of pneumonia" on the surgical ward, making findings "of somewhat less consequence," Dr. Catherine Lewis said.
"Moreover, the authors’ program was implemented and evaluated over a period in which there was an ongoing shift from open to laparoscopic or robotic surgical techniques, which has been shown to significantly decrease the rates of postoperative pneumonia, particularly in colorectal and prostate operations," she said.
The authors did not examine whether changes in patient care or surgical technique affected postoperative pneumonia rates, Dr. Lewis noted. She pointed to other research showing that using a neuraxial blockade instead of general anesthesia led to a significant drop in postoperative pneumonia, as did using selective nasogastric decompression (Ann. Intern. Med. 2006;144:596-608).
Previously, the authors of the current study reported that postoperative non–ventilator-associated pneumonia rates did not change after they started their program, Dr. Lewis said. The number of ward cases decreased, but the number of non–ventilator-associated pneumonia intensive care unit cases increased, so the decrease could reflect redistribution in the location of patients, she said.
But the authors also deserved praise for developing and starting a relatively cost- and time-efficient quality improvement measure, Dr. Lewis added. She said that such programs could increase awareness and education among health care providers who care for patients after surgery.
Dr. Lewis specializes in general, critical care, and trauma surgery at the University of California, Los Angeles. The remarks were excerpted from her invited editorial accompanying Dr. Kazaure’s report (JAMA Surg. 2014 July 23 [doi:10.1001/jamasurg.2014.1249]).
A quality improvement program cut postoperative pneumonia rates by 43.6%, investigators reported July 23 in JAMA Surgery.
The small, single-center retrospective cohort study is the first to present long-term findings for such a program, said Dr. Hadiza Kazaure at Stanford (Calif.) University and her associates.
The program, which investigators started at a Stanford-affiliated Veterans Affairs hospital, included coughing and deep-breathing exercises with incentive spirometry, a twice-daily oral chlorhexidine hygiene, ambulation with pain control, elevating the head of the bed by 30 degrees and sitting for meals, educating surgical nursing staff about their roles in preventing pneumonia, and automating physician orders for pneumonia prevention, the researchers said (JAMA Surg. 2014 July 23 [doi:10.1001/jamasurg.2014.1216]).
The investigators calculated postimplementation rates of ward-acquired pneumonia in all noncardiac, unventilated surgical patients in the 5 years after the program started, they said.
Among 4,099 hospitalized patients who were at risk, 18 (0.44%) developed postoperative pneumonia, a 43.6% drop from the preprogram rate of 0.78%, the investigators reported.
By comparison, the postintervention rate for the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) was 582% higher than that of the VA hospital for 2008-2012. By achieving the VA hospital program’s results, the hospitals in the ACS-NSQIP could save about $280 million, Dr. Kazaure and her associates said.
The database abstraction methods used to choose patients were validated, but nonetheless could have caused selection errors. Also, few patients developed pneumonia, which kept the investigators from tracking trends over time on the ward, they said. "Based on published data, we used a national average of $46,400 cost of care per postoperative pneumonia case to estimate potential cost savings in our analyses," they added. "The validity of cost estimates in this study to individual hospitals must be considered because geographic variation in cost of care is well established."
The authors reported no funding sources or conflicts of interest.
A quality improvement program cut postoperative pneumonia rates by 43.6%, investigators reported July 23 in JAMA Surgery.
The small, single-center retrospective cohort study is the first to present long-term findings for such a program, said Dr. Hadiza Kazaure at Stanford (Calif.) University and her associates.
The program, which investigators started at a Stanford-affiliated Veterans Affairs hospital, included coughing and deep-breathing exercises with incentive spirometry, a twice-daily oral chlorhexidine hygiene, ambulation with pain control, elevating the head of the bed by 30 degrees and sitting for meals, educating surgical nursing staff about their roles in preventing pneumonia, and automating physician orders for pneumonia prevention, the researchers said (JAMA Surg. 2014 July 23 [doi:10.1001/jamasurg.2014.1216]).
The investigators calculated postimplementation rates of ward-acquired pneumonia in all noncardiac, unventilated surgical patients in the 5 years after the program started, they said.
Among 4,099 hospitalized patients who were at risk, 18 (0.44%) developed postoperative pneumonia, a 43.6% drop from the preprogram rate of 0.78%, the investigators reported.
By comparison, the postintervention rate for the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) was 582% higher than that of the VA hospital for 2008-2012. By achieving the VA hospital program’s results, the hospitals in the ACS-NSQIP could save about $280 million, Dr. Kazaure and her associates said.
The database abstraction methods used to choose patients were validated, but nonetheless could have caused selection errors. Also, few patients developed pneumonia, which kept the investigators from tracking trends over time on the ward, they said. "Based on published data, we used a national average of $46,400 cost of care per postoperative pneumonia case to estimate potential cost savings in our analyses," they added. "The validity of cost estimates in this study to individual hospitals must be considered because geographic variation in cost of care is well established."
The authors reported no funding sources or conflicts of interest.
FROM JAMA SURGERY
Key clinical point: Cost-effective quality improvement programs can potentially prevent postoperative pneumonia in unventilated patients.
Major finding: Among 4,099 hospitalized patients at risk between 2008 and 2012, 18 (0.44%) developed postoperative pneumonia, a 43.6% decrease from the preintervention rate of 0.78%.
Data source: Retrospective cohort study of all noncardiac surgical patients who acquired postoperative pneumonia on a Veterans Affairs hospital ward from 2008 to 2012.
Disclosures: The authors reported no funding sources or conflicts of interest.
Survival benefit from contralateral prophylactic mastectomy small
The absolute 20-year survival benefit from contralateral prophylactic mastectomy stands at less than 1%, regardless of age, estrogen receptor status, and cancer stage, a decision analysis demonstrated.
"Long-term survival in women with unilateral breast cancer treated with or without CPM depends upon several factors, including mortality of the primary breast cancer, risk of CBC [contralateral breast cancer], stage and mortality of the CBC, and the individual patient’s overall life expectancy," wrote Dr. Pamela R. Portschy of the University of Minnesota, Minneapolis.
The report was published July 16 in the Journal of the National Cancer Institute.
"Prospective randomized trials comparing CPM with no CPM are not feasible. Retrospective studies evaluating a potential survival benefit with CPM are limited by short follow-up, potential selection bias, and lack of important clinical information," noted Dr. Portschy and her associates.
They limited their analysis to women with stage I and II breast cancer without BRCA mutations. They developed a Markov model to simulate survival outcomes among those who did and did not have contralateral prophylactic mastectomy (CPM), and they used published studies to estimate probabilities for developing CBC, dying from CBC, dying from primary breast cancer, and age-specific mortality rates. Data were extracted from numerous sources including Surveillance, Epidemiology, and End Results (SEER), the Early Breast Cancer Trialists’ Collaborative Group, and the Oregon State Cancer Registry.
The researchers estimated the 20-year overall survival and life expectancy, but not quality of life or cost, and their analysis considered variation in age, estrogen receptor status, and cancer stage (J. Natl. Cancer Inst. 2014 July 16 [doi:10.1093/jnci/dju160]).
The predicted life expectancy gain from CPM ranged from .13 to .59 years for women with stage I breast cancer, and .08 to .29 years for those with stage II breast cancer. CPM conferred a life expectancy benefit among younger women and among those who had stage I and estrogen receptor–positive disease. "The potential benefit of CPM was consistently lower for patients with stage II breast cancer because of the worse prognosis associated with the primary breast cancer," the researchers wrote. "Similarly, the potential benefits of CPM are more modest for older women because they have relatively fewer years remaining of [life expectancy]."
Dr. Portschy and her associates could not identify any cohort of women that had a greater than 1% absolute survival difference at 20 years. In fact, the predicted 20-year survival differences ranged from .56 to .94% for women with stage I breast cancer and .36 to .61% for those with stage II breast cancer.
The researchers acknowledged limitations of the study, including the fact that the results "do not apply to BRCA gene mutation carriers with unilateral breast cancer who have a cumulative 10-year risk of CBC of approximately 30% to 40%," they wrote. "The outcomes of this analysis were limited to overall and disease-specific survival; we did not evaluate other important outcomes such as surgical complications and quality of life. Also, we assumed the mortality of CBC was the same as the mortality of the index cancer reported by SEER."
They also noted that survival is not the only potential benefit of a cancer risk reduction strategy. "Effects on cancer-related anxiety, cosmesis, and self-image are also important in the decision-making process," they wrote. "For some women, the negative impact of CPM on quality of life may outweigh a potential survival benefit. For others who are very anxious about CBC, CPM may result in a psychological benefit even if survival benefits are minimal."
They concluded that the survival estimates from their Markov model "may be useful for physicians and breast cancer patients to arrive at evidence-based informed decisions regarding CPM. Moreover, the use of accurate and easily understood decision aids may reverse some of the mastectomy trends recently observed in the United States."
The researchers stated that they had no relevant financial conflicts to disclose.
The decision of whether or not to undergo a contralateral prophylactic mastectomy after being treated for breast cancer is a difficult one for many women. The goal of such aggressive therapy is to lower the likelihood of a second primary carcinoma. The downsides are operative risk, impairment of the woman’s self-image, and short-term and long-term morbidities.
This is a well done analysis from an experienced group of investigators and is based on the currently available data. Given the JNCI audience, we shall refrain from niggling points about modeling. Rather, we will stick to the big picture and clinical implications. Although the survival benefit from CPM is small as demonstrated in this model, it is greater than zero, which suggests that for some patients even that small gain may be enough to make it a not unreasonable choice.
From a societal perspective, which was not addressed by Portschy et al., the associated costs of CPM, including the procedure, its complications, reconstruction, and perhaps psychotherapy, may outweigh the modest benefit CPM provides. The small denominator of the cost-effectiveness ratio, were one to be calculated, would imply that the ratio would be very high, making CPM a suboptimal use of health care dollars. Further, we suspect that adding quality of life to the analysis would diminish the benefit and well might turn it into a net harm, in particular for patients with high concern for negative impact of CPM on cosmesis, self image, and morbidity. However, in a fraction of patients who are very troubled by a 0.7% risk of a second, contralateral cancer, CPM might provide an acceptable benefit. The balance between harm and benefit depends on the patient’s preferences and highlights the importance of capturing the patient’s values and expectations before considering CPM.
Of course, these conclusions are based on analysis of women who are at average risk for a contralateral second primary. In women at substantially higher risk (based either on family history or genetics), the benefit of CPM might be far greater, and CPM might be a good choice for the patient or for society.
Dr. Stephen G. Pauker and Dr. Mohamed Alseiari are with the division of clinical decision making in the department of medicine at Tufts Medical Center, Boston. They reported no relevant financial conflicts. This was excerpted from an editorial (J. Natl. Cancer Inst. 2014 July 16 [doi:10.1093/jnci/dju175]).
The decision of whether or not to undergo a contralateral prophylactic mastectomy after being treated for breast cancer is a difficult one for many women. The goal of such aggressive therapy is to lower the likelihood of a second primary carcinoma. The downsides are operative risk, impairment of the woman’s self-image, and short-term and long-term morbidities.
This is a well done analysis from an experienced group of investigators and is based on the currently available data. Given the JNCI audience, we shall refrain from niggling points about modeling. Rather, we will stick to the big picture and clinical implications. Although the survival benefit from CPM is small as demonstrated in this model, it is greater than zero, which suggests that for some patients even that small gain may be enough to make it a not unreasonable choice.
From a societal perspective, which was not addressed by Portschy et al., the associated costs of CPM, including the procedure, its complications, reconstruction, and perhaps psychotherapy, may outweigh the modest benefit CPM provides. The small denominator of the cost-effectiveness ratio, were one to be calculated, would imply that the ratio would be very high, making CPM a suboptimal use of health care dollars. Further, we suspect that adding quality of life to the analysis would diminish the benefit and well might turn it into a net harm, in particular for patients with high concern for negative impact of CPM on cosmesis, self image, and morbidity. However, in a fraction of patients who are very troubled by a 0.7% risk of a second, contralateral cancer, CPM might provide an acceptable benefit. The balance between harm and benefit depends on the patient’s preferences and highlights the importance of capturing the patient’s values and expectations before considering CPM.
Of course, these conclusions are based on analysis of women who are at average risk for a contralateral second primary. In women at substantially higher risk (based either on family history or genetics), the benefit of CPM might be far greater, and CPM might be a good choice for the patient or for society.
Dr. Stephen G. Pauker and Dr. Mohamed Alseiari are with the division of clinical decision making in the department of medicine at Tufts Medical Center, Boston. They reported no relevant financial conflicts. This was excerpted from an editorial (J. Natl. Cancer Inst. 2014 July 16 [doi:10.1093/jnci/dju175]).
The decision of whether or not to undergo a contralateral prophylactic mastectomy after being treated for breast cancer is a difficult one for many women. The goal of such aggressive therapy is to lower the likelihood of a second primary carcinoma. The downsides are operative risk, impairment of the woman’s self-image, and short-term and long-term morbidities.
This is a well done analysis from an experienced group of investigators and is based on the currently available data. Given the JNCI audience, we shall refrain from niggling points about modeling. Rather, we will stick to the big picture and clinical implications. Although the survival benefit from CPM is small as demonstrated in this model, it is greater than zero, which suggests that for some patients even that small gain may be enough to make it a not unreasonable choice.
From a societal perspective, which was not addressed by Portschy et al., the associated costs of CPM, including the procedure, its complications, reconstruction, and perhaps psychotherapy, may outweigh the modest benefit CPM provides. The small denominator of the cost-effectiveness ratio, were one to be calculated, would imply that the ratio would be very high, making CPM a suboptimal use of health care dollars. Further, we suspect that adding quality of life to the analysis would diminish the benefit and well might turn it into a net harm, in particular for patients with high concern for negative impact of CPM on cosmesis, self image, and morbidity. However, in a fraction of patients who are very troubled by a 0.7% risk of a second, contralateral cancer, CPM might provide an acceptable benefit. The balance between harm and benefit depends on the patient’s preferences and highlights the importance of capturing the patient’s values and expectations before considering CPM.
Of course, these conclusions are based on analysis of women who are at average risk for a contralateral second primary. In women at substantially higher risk (based either on family history or genetics), the benefit of CPM might be far greater, and CPM might be a good choice for the patient or for society.
Dr. Stephen G. Pauker and Dr. Mohamed Alseiari are with the division of clinical decision making in the department of medicine at Tufts Medical Center, Boston. They reported no relevant financial conflicts. This was excerpted from an editorial (J. Natl. Cancer Inst. 2014 July 16 [doi:10.1093/jnci/dju175]).
The absolute 20-year survival benefit from contralateral prophylactic mastectomy stands at less than 1%, regardless of age, estrogen receptor status, and cancer stage, a decision analysis demonstrated.
"Long-term survival in women with unilateral breast cancer treated with or without CPM depends upon several factors, including mortality of the primary breast cancer, risk of CBC [contralateral breast cancer], stage and mortality of the CBC, and the individual patient’s overall life expectancy," wrote Dr. Pamela R. Portschy of the University of Minnesota, Minneapolis.
The report was published July 16 in the Journal of the National Cancer Institute.
"Prospective randomized trials comparing CPM with no CPM are not feasible. Retrospective studies evaluating a potential survival benefit with CPM are limited by short follow-up, potential selection bias, and lack of important clinical information," noted Dr. Portschy and her associates.
They limited their analysis to women with stage I and II breast cancer without BRCA mutations. They developed a Markov model to simulate survival outcomes among those who did and did not have contralateral prophylactic mastectomy (CPM), and they used published studies to estimate probabilities for developing CBC, dying from CBC, dying from primary breast cancer, and age-specific mortality rates. Data were extracted from numerous sources including Surveillance, Epidemiology, and End Results (SEER), the Early Breast Cancer Trialists’ Collaborative Group, and the Oregon State Cancer Registry.
The researchers estimated the 20-year overall survival and life expectancy, but not quality of life or cost, and their analysis considered variation in age, estrogen receptor status, and cancer stage (J. Natl. Cancer Inst. 2014 July 16 [doi:10.1093/jnci/dju160]).
The predicted life expectancy gain from CPM ranged from .13 to .59 years for women with stage I breast cancer, and .08 to .29 years for those with stage II breast cancer. CPM conferred a life expectancy benefit among younger women and among those who had stage I and estrogen receptor–positive disease. "The potential benefit of CPM was consistently lower for patients with stage II breast cancer because of the worse prognosis associated with the primary breast cancer," the researchers wrote. "Similarly, the potential benefits of CPM are more modest for older women because they have relatively fewer years remaining of [life expectancy]."
Dr. Portschy and her associates could not identify any cohort of women that had a greater than 1% absolute survival difference at 20 years. In fact, the predicted 20-year survival differences ranged from .56 to .94% for women with stage I breast cancer and .36 to .61% for those with stage II breast cancer.
The researchers acknowledged limitations of the study, including the fact that the results "do not apply to BRCA gene mutation carriers with unilateral breast cancer who have a cumulative 10-year risk of CBC of approximately 30% to 40%," they wrote. "The outcomes of this analysis were limited to overall and disease-specific survival; we did not evaluate other important outcomes such as surgical complications and quality of life. Also, we assumed the mortality of CBC was the same as the mortality of the index cancer reported by SEER."
They also noted that survival is not the only potential benefit of a cancer risk reduction strategy. "Effects on cancer-related anxiety, cosmesis, and self-image are also important in the decision-making process," they wrote. "For some women, the negative impact of CPM on quality of life may outweigh a potential survival benefit. For others who are very anxious about CBC, CPM may result in a psychological benefit even if survival benefits are minimal."
They concluded that the survival estimates from their Markov model "may be useful for physicians and breast cancer patients to arrive at evidence-based informed decisions regarding CPM. Moreover, the use of accurate and easily understood decision aids may reverse some of the mastectomy trends recently observed in the United States."
The researchers stated that they had no relevant financial conflicts to disclose.
The absolute 20-year survival benefit from contralateral prophylactic mastectomy stands at less than 1%, regardless of age, estrogen receptor status, and cancer stage, a decision analysis demonstrated.
"Long-term survival in women with unilateral breast cancer treated with or without CPM depends upon several factors, including mortality of the primary breast cancer, risk of CBC [contralateral breast cancer], stage and mortality of the CBC, and the individual patient’s overall life expectancy," wrote Dr. Pamela R. Portschy of the University of Minnesota, Minneapolis.
The report was published July 16 in the Journal of the National Cancer Institute.
"Prospective randomized trials comparing CPM with no CPM are not feasible. Retrospective studies evaluating a potential survival benefit with CPM are limited by short follow-up, potential selection bias, and lack of important clinical information," noted Dr. Portschy and her associates.
They limited their analysis to women with stage I and II breast cancer without BRCA mutations. They developed a Markov model to simulate survival outcomes among those who did and did not have contralateral prophylactic mastectomy (CPM), and they used published studies to estimate probabilities for developing CBC, dying from CBC, dying from primary breast cancer, and age-specific mortality rates. Data were extracted from numerous sources including Surveillance, Epidemiology, and End Results (SEER), the Early Breast Cancer Trialists’ Collaborative Group, and the Oregon State Cancer Registry.
The researchers estimated the 20-year overall survival and life expectancy, but not quality of life or cost, and their analysis considered variation in age, estrogen receptor status, and cancer stage (J. Natl. Cancer Inst. 2014 July 16 [doi:10.1093/jnci/dju160]).
The predicted life expectancy gain from CPM ranged from .13 to .59 years for women with stage I breast cancer, and .08 to .29 years for those with stage II breast cancer. CPM conferred a life expectancy benefit among younger women and among those who had stage I and estrogen receptor–positive disease. "The potential benefit of CPM was consistently lower for patients with stage II breast cancer because of the worse prognosis associated with the primary breast cancer," the researchers wrote. "Similarly, the potential benefits of CPM are more modest for older women because they have relatively fewer years remaining of [life expectancy]."
Dr. Portschy and her associates could not identify any cohort of women that had a greater than 1% absolute survival difference at 20 years. In fact, the predicted 20-year survival differences ranged from .56 to .94% for women with stage I breast cancer and .36 to .61% for those with stage II breast cancer.
The researchers acknowledged limitations of the study, including the fact that the results "do not apply to BRCA gene mutation carriers with unilateral breast cancer who have a cumulative 10-year risk of CBC of approximately 30% to 40%," they wrote. "The outcomes of this analysis were limited to overall and disease-specific survival; we did not evaluate other important outcomes such as surgical complications and quality of life. Also, we assumed the mortality of CBC was the same as the mortality of the index cancer reported by SEER."
They also noted that survival is not the only potential benefit of a cancer risk reduction strategy. "Effects on cancer-related anxiety, cosmesis, and self-image are also important in the decision-making process," they wrote. "For some women, the negative impact of CPM on quality of life may outweigh a potential survival benefit. For others who are very anxious about CBC, CPM may result in a psychological benefit even if survival benefits are minimal."
They concluded that the survival estimates from their Markov model "may be useful for physicians and breast cancer patients to arrive at evidence-based informed decisions regarding CPM. Moreover, the use of accurate and easily understood decision aids may reverse some of the mastectomy trends recently observed in the United States."
The researchers stated that they had no relevant financial conflicts to disclose.
FROM THE JOURNAL OF THE NATIONAL CANCER INSTITUTE
Key clinical point: The long-term survival benefit of contralateral prophylactic mastectomy is small.
Major Finding: The absolute 20-year survival benefit from contralateral prophylactic mastectomy was less than 1% among all age groups, regardless of estrogen receptor status and cancer stage.
Data Source: Results from a Markov model designed to simulate 20-year survival outcomes among those who did and did not have CPM, with considerations for variation in age, estrogen receptor status, and cancer stage.
Disclosures: The researchers disclosed no relevant financial conflicts.
Hypoglycemia common after bariatric surgery
SAN FRANCISCO – Hypoglycemic episodes were common and largely unnoticed after bariatric surgery, a controlled study of 45 patients found.
During a 3-day period of "normal living," symptomatic hypoglycemias occurred in 22% of 15 patients after gastric bypass surgery, 20% of 15 patients after biliopancreatic diversion with duodenal switch, and in none of 15 obese, nondiabetic control patients matched to the surgical patients by body mass index.
Continuous glucose monitoring showed that patients in both postsurgery groups spent significant amounts of time in hypoglycemia, Dr. Niclas Abrahamsson and his associates reported at the annual scientific session of the American Diabetes Association.
After gastric bypass, patients averaged 42 minutes per day with glucose levels lower than 3.3 mmol/L and 21 minutes per day with levels lower than 2.8 mmol/L. After duodenal switch surgery, patients averaged 85 minutes per day with glucose levels lower than 3.3 mmol/L and 39 minutes per day with levels lower than 2.8 mmol/L. No patients in the control group had glucose levels that low, reported Dr. Abrahamsson of the University of Uppsala, Sweden.
"We were very surprised that they had so many hypoglycemic episodes, especially since the controls had none," he said. Patients were unaware of approximately 80% of the hypoglycemic episodes, he added.
"The clinical significance should be that one should be alert to any hypoglycemia symptoms," Dr. Abrahamsson said.
Patients in the post–duodenal switch group had the lowest mean glucose level (4.6 mmol/L) and mean hemoglobin A1c level (29 mmol/mol), compared with the post–gastric bypass group (mean glucose 5.3 mmol/L and HbA1c 36 mmol/mol) and the control group (mean glucose 5.9 mmol/L and HbA1c 38 mmol/mol).
Glucose curves on continuous monitoring were more variable in the post–gastric bypass group, compared with controls, and less variable in the post–duodenal switch group, compared with controls. That difference between the two surgical groups probably relates to the different glucose absorption capabilities after surgery, he suggested.
Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
On Twitter @sherryboschert
The finding that patients with recent duodenal switch surgery spent 85 minutes per day with hypoglycemia, compared with 42 minutes per 24 hours for patients in the gastric bypass group, is quite alarming. Although these hypoglycemias were largely unnoticed, we know that hypoglycemia can affect brain function, cognition, and motor function.

|
|
The problem with continuous glucose monitoring is that it’s a research tool, but it’s not very practical to be doing in every single patient who’s had a gastric bypass surgery. The problem with doing blood glucose measurement is that it’s a snapshot and you can potentially miss hypoglycemia. So, this has a lot of clinical implications as to how we investigate such patients.
This study has safety and legal implications for things like driving and operating machinery and raises questions of how we can best manage patients in terms of mitigating the effects of hypoglycemia. I think it opens up a whole area of questions at which we need to look.
I think this study will change my practice. It has opened my eyes. I was quite shocked at the data. At my center, we don’t tend to do many duodenal switches. We do many more sleeve gastrectomies than the bypass procedures. But, certainly, following a bypass procedure, I will be much more cognizant of the potential for hypoglycemia and caution our patients regarding driving and about monitoring their sugars closely following the procedure.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the University of Warwick, England. These comments are excerpted from an interview at the meeting. Dr. Barber reported having no financial disclosures.
The finding that patients with recent duodenal switch surgery spent 85 minutes per day with hypoglycemia, compared with 42 minutes per 24 hours for patients in the gastric bypass group, is quite alarming. Although these hypoglycemias were largely unnoticed, we know that hypoglycemia can affect brain function, cognition, and motor function.

|
|
The problem with continuous glucose monitoring is that it’s a research tool, but it’s not very practical to be doing in every single patient who’s had a gastric bypass surgery. The problem with doing blood glucose measurement is that it’s a snapshot and you can potentially miss hypoglycemia. So, this has a lot of clinical implications as to how we investigate such patients.
This study has safety and legal implications for things like driving and operating machinery and raises questions of how we can best manage patients in terms of mitigating the effects of hypoglycemia. I think it opens up a whole area of questions at which we need to look.
I think this study will change my practice. It has opened my eyes. I was quite shocked at the data. At my center, we don’t tend to do many duodenal switches. We do many more sleeve gastrectomies than the bypass procedures. But, certainly, following a bypass procedure, I will be much more cognizant of the potential for hypoglycemia and caution our patients regarding driving and about monitoring their sugars closely following the procedure.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the University of Warwick, England. These comments are excerpted from an interview at the meeting. Dr. Barber reported having no financial disclosures.
The finding that patients with recent duodenal switch surgery spent 85 minutes per day with hypoglycemia, compared with 42 minutes per 24 hours for patients in the gastric bypass group, is quite alarming. Although these hypoglycemias were largely unnoticed, we know that hypoglycemia can affect brain function, cognition, and motor function.

|
|
The problem with continuous glucose monitoring is that it’s a research tool, but it’s not very practical to be doing in every single patient who’s had a gastric bypass surgery. The problem with doing blood glucose measurement is that it’s a snapshot and you can potentially miss hypoglycemia. So, this has a lot of clinical implications as to how we investigate such patients.
This study has safety and legal implications for things like driving and operating machinery and raises questions of how we can best manage patients in terms of mitigating the effects of hypoglycemia. I think it opens up a whole area of questions at which we need to look.
I think this study will change my practice. It has opened my eyes. I was quite shocked at the data. At my center, we don’t tend to do many duodenal switches. We do many more sleeve gastrectomies than the bypass procedures. But, certainly, following a bypass procedure, I will be much more cognizant of the potential for hypoglycemia and caution our patients regarding driving and about monitoring their sugars closely following the procedure.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the University of Warwick, England. These comments are excerpted from an interview at the meeting. Dr. Barber reported having no financial disclosures.
SAN FRANCISCO – Hypoglycemic episodes were common and largely unnoticed after bariatric surgery, a controlled study of 45 patients found.
During a 3-day period of "normal living," symptomatic hypoglycemias occurred in 22% of 15 patients after gastric bypass surgery, 20% of 15 patients after biliopancreatic diversion with duodenal switch, and in none of 15 obese, nondiabetic control patients matched to the surgical patients by body mass index.
Continuous glucose monitoring showed that patients in both postsurgery groups spent significant amounts of time in hypoglycemia, Dr. Niclas Abrahamsson and his associates reported at the annual scientific session of the American Diabetes Association.
After gastric bypass, patients averaged 42 minutes per day with glucose levels lower than 3.3 mmol/L and 21 minutes per day with levels lower than 2.8 mmol/L. After duodenal switch surgery, patients averaged 85 minutes per day with glucose levels lower than 3.3 mmol/L and 39 minutes per day with levels lower than 2.8 mmol/L. No patients in the control group had glucose levels that low, reported Dr. Abrahamsson of the University of Uppsala, Sweden.
"We were very surprised that they had so many hypoglycemic episodes, especially since the controls had none," he said. Patients were unaware of approximately 80% of the hypoglycemic episodes, he added.
"The clinical significance should be that one should be alert to any hypoglycemia symptoms," Dr. Abrahamsson said.
Patients in the post–duodenal switch group had the lowest mean glucose level (4.6 mmol/L) and mean hemoglobin A1c level (29 mmol/mol), compared with the post–gastric bypass group (mean glucose 5.3 mmol/L and HbA1c 36 mmol/mol) and the control group (mean glucose 5.9 mmol/L and HbA1c 38 mmol/mol).
Glucose curves on continuous monitoring were more variable in the post–gastric bypass group, compared with controls, and less variable in the post–duodenal switch group, compared with controls. That difference between the two surgical groups probably relates to the different glucose absorption capabilities after surgery, he suggested.
Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
On Twitter @sherryboschert
SAN FRANCISCO – Hypoglycemic episodes were common and largely unnoticed after bariatric surgery, a controlled study of 45 patients found.
During a 3-day period of "normal living," symptomatic hypoglycemias occurred in 22% of 15 patients after gastric bypass surgery, 20% of 15 patients after biliopancreatic diversion with duodenal switch, and in none of 15 obese, nondiabetic control patients matched to the surgical patients by body mass index.
Continuous glucose monitoring showed that patients in both postsurgery groups spent significant amounts of time in hypoglycemia, Dr. Niclas Abrahamsson and his associates reported at the annual scientific session of the American Diabetes Association.
After gastric bypass, patients averaged 42 minutes per day with glucose levels lower than 3.3 mmol/L and 21 minutes per day with levels lower than 2.8 mmol/L. After duodenal switch surgery, patients averaged 85 minutes per day with glucose levels lower than 3.3 mmol/L and 39 minutes per day with levels lower than 2.8 mmol/L. No patients in the control group had glucose levels that low, reported Dr. Abrahamsson of the University of Uppsala, Sweden.
"We were very surprised that they had so many hypoglycemic episodes, especially since the controls had none," he said. Patients were unaware of approximately 80% of the hypoglycemic episodes, he added.
"The clinical significance should be that one should be alert to any hypoglycemia symptoms," Dr. Abrahamsson said.
Patients in the post–duodenal switch group had the lowest mean glucose level (4.6 mmol/L) and mean hemoglobin A1c level (29 mmol/mol), compared with the post–gastric bypass group (mean glucose 5.3 mmol/L and HbA1c 36 mmol/mol) and the control group (mean glucose 5.9 mmol/L and HbA1c 38 mmol/mol).
Glucose curves on continuous monitoring were more variable in the post–gastric bypass group, compared with controls, and less variable in the post–duodenal switch group, compared with controls. That difference between the two surgical groups probably relates to the different glucose absorption capabilities after surgery, he suggested.
Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSION
Key clinical point: Be alert for frequent hypoglycemia after bariatric surgery.
Major finding: Patients averaged 42 minutes/day in hypoglycemia after gastric bypass surgery or 85 minutes/day after biliopancreatic diversion with duodenal switch, compared with no hypoglycemia in controls.
Data source: A prospective study of continuous glucose monitoring during 3 days of normal living in 15 patients after gastric bypass, 15 patients after duodenal switch surgery, and 15 matched obese control patients.
Disclosures: Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
Obesity malpractice claims up 64%, study shows
Obesity-related lawsuits against health providers are on the rise, according to a claims analysis by national medical liability insurer The Doctors Company. Claims associated with obesity totaled 415 between 2007 and 2012, an increase of 64% in the number of such lawsuits from the period between 1992 and 2002.
The increase "is not at all surprising, as obesity itself has increased a great deal in the population," said Dr. Neil Skolnik, associate director of the family practice residency program at Abington (Pa.) Memorial Hospital. "We’re going to see that reflected in malpractice suits."
The Doctors Company study analyzed 415 obesity-related claims from 2007 through 2012 and compared them with a previous analysis of claims from 1992 to 2002. The most recent suits involved instances such as a 290-pound patient who had complications following a gastric bypass surgery, a 325-pound patient with hypertension and diabetes who died after a physician did not diagnose myocardial infarction and pneumonia, and a 350-pound patient with nerve damage that resulted from improper positioning on a treatment table. Twenty-five percent of the patients involved in the claims died, according to the study, published on The Doctors Company website in May.
Orthopedists were the top specialty sued for obesity-related claims, followed by family physicians, anesthesiologists, plastic surgeons, general surgeons, and internists.
Family physicians may be sued more often than some other specialties because of their interaction with patients who develop conditions associated with obesity over time, said Paul Nagle, director of physician patient safety for The Doctors Company.
"Family medicine physicians can be at risk due to the latent risk of obesity," he said in an interview. "If a patient’s weight gradually increases, what is a family medicine physician doing to monitor the weight and the potentially resulting medical issues, including diabetes, hypertension, cardiac, vascular, joint, or pulmonary health issues?"
Communicating clearly with obese patients early is essential to avoid obesity-related claims, said Liz Brott, regional vice president, risk resource for ProAssurance, a national medical liability insurer.
"It’s extremely important as far as communicating with them about what to expect from procedures or treatment," she said in an interview. "You don’t want to leave this to your staff to communicate. [It should be] the physician sitting down, one-on-one, whether it’s the primary care physician or the surgeon. There should be appropriate communication by the physician."
Ms. Brott said ProAssurance has handled obesity-related claims continually, but their numbers do not show a dramatic rise. In her experience, obesity claims against surgeons related to bariatric procedures are most common, she said.
Along with informed consent, physicians also may want to consider an informed refusal approach for noncompliant patients, Mr. Nagle said. This refers to informing patients about how obesity impacts their overall health and/or a specific health issue and having patients sign a document stating that they were advised but chose not to follow recommendations.
"This may reduce any claims that you did not address and warn of obesity’s impact," he said.
Physicians should also document all activity related to weight interventions and conversations with patients about weight education and guidance, he added
The analysis is a reminder that obesity is a serious disease that has its own direct complications, as well as acting as a catalyst for related conditions, said Dr. Skolnik, who is also a professor of family medicine at Temple University in Philadelphia.
"The overriding theme here is obesity is an area to which patients are paying increasing attention and to which lawyers also must be paying increasing attention," he said. "It’s an area that should be addressed directly and with sensitivity to the often emotional issues that go along with addressing weight issues."
Obesity-related lawsuits against health providers are on the rise, according to a claims analysis by national medical liability insurer The Doctors Company. Claims associated with obesity totaled 415 between 2007 and 2012, an increase of 64% in the number of such lawsuits from the period between 1992 and 2002.
The increase "is not at all surprising, as obesity itself has increased a great deal in the population," said Dr. Neil Skolnik, associate director of the family practice residency program at Abington (Pa.) Memorial Hospital. "We’re going to see that reflected in malpractice suits."
The Doctors Company study analyzed 415 obesity-related claims from 2007 through 2012 and compared them with a previous analysis of claims from 1992 to 2002. The most recent suits involved instances such as a 290-pound patient who had complications following a gastric bypass surgery, a 325-pound patient with hypertension and diabetes who died after a physician did not diagnose myocardial infarction and pneumonia, and a 350-pound patient with nerve damage that resulted from improper positioning on a treatment table. Twenty-five percent of the patients involved in the claims died, according to the study, published on The Doctors Company website in May.
Orthopedists were the top specialty sued for obesity-related claims, followed by family physicians, anesthesiologists, plastic surgeons, general surgeons, and internists.
Family physicians may be sued more often than some other specialties because of their interaction with patients who develop conditions associated with obesity over time, said Paul Nagle, director of physician patient safety for The Doctors Company.
"Family medicine physicians can be at risk due to the latent risk of obesity," he said in an interview. "If a patient’s weight gradually increases, what is a family medicine physician doing to monitor the weight and the potentially resulting medical issues, including diabetes, hypertension, cardiac, vascular, joint, or pulmonary health issues?"
Communicating clearly with obese patients early is essential to avoid obesity-related claims, said Liz Brott, regional vice president, risk resource for ProAssurance, a national medical liability insurer.
"It’s extremely important as far as communicating with them about what to expect from procedures or treatment," she said in an interview. "You don’t want to leave this to your staff to communicate. [It should be] the physician sitting down, one-on-one, whether it’s the primary care physician or the surgeon. There should be appropriate communication by the physician."
Ms. Brott said ProAssurance has handled obesity-related claims continually, but their numbers do not show a dramatic rise. In her experience, obesity claims against surgeons related to bariatric procedures are most common, she said.
Along with informed consent, physicians also may want to consider an informed refusal approach for noncompliant patients, Mr. Nagle said. This refers to informing patients about how obesity impacts their overall health and/or a specific health issue and having patients sign a document stating that they were advised but chose not to follow recommendations.
"This may reduce any claims that you did not address and warn of obesity’s impact," he said.
Physicians should also document all activity related to weight interventions and conversations with patients about weight education and guidance, he added
The analysis is a reminder that obesity is a serious disease that has its own direct complications, as well as acting as a catalyst for related conditions, said Dr. Skolnik, who is also a professor of family medicine at Temple University in Philadelphia.
"The overriding theme here is obesity is an area to which patients are paying increasing attention and to which lawyers also must be paying increasing attention," he said. "It’s an area that should be addressed directly and with sensitivity to the often emotional issues that go along with addressing weight issues."
Obesity-related lawsuits against health providers are on the rise, according to a claims analysis by national medical liability insurer The Doctors Company. Claims associated with obesity totaled 415 between 2007 and 2012, an increase of 64% in the number of such lawsuits from the period between 1992 and 2002.
The increase "is not at all surprising, as obesity itself has increased a great deal in the population," said Dr. Neil Skolnik, associate director of the family practice residency program at Abington (Pa.) Memorial Hospital. "We’re going to see that reflected in malpractice suits."
The Doctors Company study analyzed 415 obesity-related claims from 2007 through 2012 and compared them with a previous analysis of claims from 1992 to 2002. The most recent suits involved instances such as a 290-pound patient who had complications following a gastric bypass surgery, a 325-pound patient with hypertension and diabetes who died after a physician did not diagnose myocardial infarction and pneumonia, and a 350-pound patient with nerve damage that resulted from improper positioning on a treatment table. Twenty-five percent of the patients involved in the claims died, according to the study, published on The Doctors Company website in May.
Orthopedists were the top specialty sued for obesity-related claims, followed by family physicians, anesthesiologists, plastic surgeons, general surgeons, and internists.
Family physicians may be sued more often than some other specialties because of their interaction with patients who develop conditions associated with obesity over time, said Paul Nagle, director of physician patient safety for The Doctors Company.
"Family medicine physicians can be at risk due to the latent risk of obesity," he said in an interview. "If a patient’s weight gradually increases, what is a family medicine physician doing to monitor the weight and the potentially resulting medical issues, including diabetes, hypertension, cardiac, vascular, joint, or pulmonary health issues?"
Communicating clearly with obese patients early is essential to avoid obesity-related claims, said Liz Brott, regional vice president, risk resource for ProAssurance, a national medical liability insurer.
"It’s extremely important as far as communicating with them about what to expect from procedures or treatment," she said in an interview. "You don’t want to leave this to your staff to communicate. [It should be] the physician sitting down, one-on-one, whether it’s the primary care physician or the surgeon. There should be appropriate communication by the physician."
Ms. Brott said ProAssurance has handled obesity-related claims continually, but their numbers do not show a dramatic rise. In her experience, obesity claims against surgeons related to bariatric procedures are most common, she said.
Along with informed consent, physicians also may want to consider an informed refusal approach for noncompliant patients, Mr. Nagle said. This refers to informing patients about how obesity impacts their overall health and/or a specific health issue and having patients sign a document stating that they were advised but chose not to follow recommendations.
"This may reduce any claims that you did not address and warn of obesity’s impact," he said.
Physicians should also document all activity related to weight interventions and conversations with patients about weight education and guidance, he added
The analysis is a reminder that obesity is a serious disease that has its own direct complications, as well as acting as a catalyst for related conditions, said Dr. Skolnik, who is also a professor of family medicine at Temple University in Philadelphia.
"The overriding theme here is obesity is an area to which patients are paying increasing attention and to which lawyers also must be paying increasing attention," he said. "It’s an area that should be addressed directly and with sensitivity to the often emotional issues that go along with addressing weight issues."
Initial cholecystectomy bests standard approach for suspected common duct stone
For patients at intermediate risk for having a common duct stone, initial cholecystectomy resulted in a shorter hospital stay, fewer invasive procedures, and no increase in morbidity, compared with the standard approach of doing a common duct exploration via endoscopic ultrasound followed by (if indicated) endoscopic retrograde cholangiopancreatography and cholecystectomy, according to a report published online July 8 in JAMA.
At present there are no specific guidelines as to the initial treatment approach for patients who present to the emergency department with suspected choledocholithiasis and who are at intermediate risk for retaining a common duct stone. In contrast, guidelines recommend initial laparoscopic cholecystectomy for patients at low risk for a retained common duct stone and preoperative endoscopic retrograde cholangiopancreatography (ERCP) followed by cholecystectomy for those at high risk, said Dr. Pouya Iranmanesh of the divisions of digestive surgery and transplant surgery, Geneva University Hospital, and his associates.
They performed a single-center randomized clinical trial comparing these two approaches in 100 intermediate-risk patients who presented to the emergency department during a 2-year period with sudden abdominal pain in the right upper quadrant and/or epigastric region, which was associated with elevated liver enzymes and the presence of a gallstone on ultrasound. Patients were included in the study whether they had associated acute cholecystitis or not and were randomly assigned to undergo either initial emergency laparoscopic cholecystectomy with intraoperative cholangiogram (50 patients) or initial common duct ultrasound exploration followed by (if indicated) ERCP and cholecystectomy (50 control subjects).
The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71). In particular, the number of endoscopic ultrasounds was only 10 in the initial-cholecystectomy group, compared with 54 in the control group. All 50 patients in the control group (100%) underwent at least one common duct investigation exclusive of the intraoperative cholangiogram, compared with only 20 patients (40%) in the initial-cholecystectomy group, the investigators reported (JAMA 2014 July 8 [doi:10.1001/jama.2014.7587]).
The two study groups had similar rates of conversion to laparotomy, similar operation times, a similar number of failed intraoperative cholangiograms, and similar results on quality of life measures at 1 month and 6 months after hospital discharge. The rates of complications (8% vs 14%) and of severe complications (4% vs 8%) were approximately twice as high in the control group as in the initial-cholecystectomy group.
Since 30 (60%) of the patients in the initial-cholecystectomy group never needed any common duct investigation, it follows that many intermediate-risk patients in real-world practice are undergoing unnecessary common duct procedures. A policy of performing a cholecystectomy first ensures that only patients who retain common duct stones will undergo such invasive procedures, Dr. Iranmanesh and his associates said.
Dr. Iranmanesh and his associates reported no relevant financial disclosures.
For patients at intermediate risk for having a common duct stone, initial cholecystectomy resulted in a shorter hospital stay, fewer invasive procedures, and no increase in morbidity, compared with the standard approach of doing a common duct exploration via endoscopic ultrasound followed by (if indicated) endoscopic retrograde cholangiopancreatography and cholecystectomy, according to a report published online July 8 in JAMA.
At present there are no specific guidelines as to the initial treatment approach for patients who present to the emergency department with suspected choledocholithiasis and who are at intermediate risk for retaining a common duct stone. In contrast, guidelines recommend initial laparoscopic cholecystectomy for patients at low risk for a retained common duct stone and preoperative endoscopic retrograde cholangiopancreatography (ERCP) followed by cholecystectomy for those at high risk, said Dr. Pouya Iranmanesh of the divisions of digestive surgery and transplant surgery, Geneva University Hospital, and his associates.
They performed a single-center randomized clinical trial comparing these two approaches in 100 intermediate-risk patients who presented to the emergency department during a 2-year period with sudden abdominal pain in the right upper quadrant and/or epigastric region, which was associated with elevated liver enzymes and the presence of a gallstone on ultrasound. Patients were included in the study whether they had associated acute cholecystitis or not and were randomly assigned to undergo either initial emergency laparoscopic cholecystectomy with intraoperative cholangiogram (50 patients) or initial common duct ultrasound exploration followed by (if indicated) ERCP and cholecystectomy (50 control subjects).
The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71). In particular, the number of endoscopic ultrasounds was only 10 in the initial-cholecystectomy group, compared with 54 in the control group. All 50 patients in the control group (100%) underwent at least one common duct investigation exclusive of the intraoperative cholangiogram, compared with only 20 patients (40%) in the initial-cholecystectomy group, the investigators reported (JAMA 2014 July 8 [doi:10.1001/jama.2014.7587]).
The two study groups had similar rates of conversion to laparotomy, similar operation times, a similar number of failed intraoperative cholangiograms, and similar results on quality of life measures at 1 month and 6 months after hospital discharge. The rates of complications (8% vs 14%) and of severe complications (4% vs 8%) were approximately twice as high in the control group as in the initial-cholecystectomy group.
Since 30 (60%) of the patients in the initial-cholecystectomy group never needed any common duct investigation, it follows that many intermediate-risk patients in real-world practice are undergoing unnecessary common duct procedures. A policy of performing a cholecystectomy first ensures that only patients who retain common duct stones will undergo such invasive procedures, Dr. Iranmanesh and his associates said.
Dr. Iranmanesh and his associates reported no relevant financial disclosures.
For patients at intermediate risk for having a common duct stone, initial cholecystectomy resulted in a shorter hospital stay, fewer invasive procedures, and no increase in morbidity, compared with the standard approach of doing a common duct exploration via endoscopic ultrasound followed by (if indicated) endoscopic retrograde cholangiopancreatography and cholecystectomy, according to a report published online July 8 in JAMA.
At present there are no specific guidelines as to the initial treatment approach for patients who present to the emergency department with suspected choledocholithiasis and who are at intermediate risk for retaining a common duct stone. In contrast, guidelines recommend initial laparoscopic cholecystectomy for patients at low risk for a retained common duct stone and preoperative endoscopic retrograde cholangiopancreatography (ERCP) followed by cholecystectomy for those at high risk, said Dr. Pouya Iranmanesh of the divisions of digestive surgery and transplant surgery, Geneva University Hospital, and his associates.
They performed a single-center randomized clinical trial comparing these two approaches in 100 intermediate-risk patients who presented to the emergency department during a 2-year period with sudden abdominal pain in the right upper quadrant and/or epigastric region, which was associated with elevated liver enzymes and the presence of a gallstone on ultrasound. Patients were included in the study whether they had associated acute cholecystitis or not and were randomly assigned to undergo either initial emergency laparoscopic cholecystectomy with intraoperative cholangiogram (50 patients) or initial common duct ultrasound exploration followed by (if indicated) ERCP and cholecystectomy (50 control subjects).
The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71). In particular, the number of endoscopic ultrasounds was only 10 in the initial-cholecystectomy group, compared with 54 in the control group. All 50 patients in the control group (100%) underwent at least one common duct investigation exclusive of the intraoperative cholangiogram, compared with only 20 patients (40%) in the initial-cholecystectomy group, the investigators reported (JAMA 2014 July 8 [doi:10.1001/jama.2014.7587]).
The two study groups had similar rates of conversion to laparotomy, similar operation times, a similar number of failed intraoperative cholangiograms, and similar results on quality of life measures at 1 month and 6 months after hospital discharge. The rates of complications (8% vs 14%) and of severe complications (4% vs 8%) were approximately twice as high in the control group as in the initial-cholecystectomy group.
Since 30 (60%) of the patients in the initial-cholecystectomy group never needed any common duct investigation, it follows that many intermediate-risk patients in real-world practice are undergoing unnecessary common duct procedures. A policy of performing a cholecystectomy first ensures that only patients who retain common duct stones will undergo such invasive procedures, Dr. Iranmanesh and his associates said.
Dr. Iranmanesh and his associates reported no relevant financial disclosures.
FROM JAMA
Key clinical point: Initial cholecystectomy for patients at intermediate risk for common duct stone results in shorter hospital stays and fewer invasive procedures.
Major finding: The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71).
Data source: A single-center randomized clinical trial comparing 50 patients who had initial cholecystectomy with 50 who had common duct exploration followed by ERCP and cholecystectomy; follow-up was done at 1 and 6 months.
Disclosures: Dr. Iranmanesh and his associates reported no relevant financial conflicts of interest.
Initial cholecystectomy bests standard approach for suspected common duct stone
For patients at intermediate risk for having a common duct stone, initial cholecystectomy resulted in a shorter hospital stay, fewer invasive procedures, and no increase in morbidity, compared with the standard approach of doing a common duct exploration via endoscopic ultrasound followed by (if indicated) endoscopic retrograde cholangiopancreatography and cholecystectomy, according to a report published online July 8 in JAMA.
At present there are no specific guidelines as to the initial treatment approach for patients who present to the emergency department with suspected choledocholithiasis and who are at intermediate risk for retaining a common duct stone. In contrast, guidelines recommend initial laparoscopic cholecystectomy for patients at low risk for a retained common duct stone and preoperative endoscopic retrograde cholangiopancreatography (ERCP) followed by cholecystectomy for those at high risk, said Dr. Pouya Iranmanesh of the divisions of digestive surgery and transplant surgery, Geneva University Hospital, and his associates.
They performed a single-center randomized clinical trial comparing these two approaches in 100 intermediate-risk patients who presented to the emergency department during a 2-year period with sudden abdominal pain in the right upper quadrant and/or epigastric region, which was associated with elevated liver enzymes and the presence of a gallstone on ultrasound. Patients were included in the study whether they had associated acute cholecystitis or not and were randomly assigned to undergo either initial emergency laparoscopic cholecystectomy with intraoperative cholangiogram (50 patients) or initial common duct ultrasound exploration followed by (if indicated) ERCP and cholecystectomy (50 control subjects).
The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71). In particular, the number of endoscopic ultrasounds was only 10 in the initial-cholecystectomy group, compared with 54 in the control group. All 50 patients in the control group (100%) underwent at least one common duct investigation exclusive of the intraoperative cholangiogram, compared with only 20 patients (40%) in the initial-cholecystectomy group, the investigators reported (JAMA 2014 July 8 [doi:10.1001/jama.2014.7587]).
The two study groups had similar rates of conversion to laparotomy, similar operation times, a similar number of failed intraoperative cholangiograms, and similar results on quality of life measures at 1 month and 6 months after hospital discharge. The rates of complications (8% vs 14%) and of severe complications (4% vs 8%) were approximately twice as high in the control group as in the initial-cholecystectomy group.
Since 30 (60%) of the patients in the initial-cholecystectomy group never needed any common duct investigation, it follows that many intermediate-risk patients in real-world practice are undergoing unnecessary common duct procedures. A policy of performing a cholecystectomy first ensures that only patients who retain common duct stones will undergo such invasive procedures, Dr. Iranmanesh and his associates said.
Dr. Iranmanesh and his associates reported no relevant financial disclosures.
For patients at intermediate risk for having a common duct stone, initial cholecystectomy resulted in a shorter hospital stay, fewer invasive procedures, and no increase in morbidity, compared with the standard approach of doing a common duct exploration via endoscopic ultrasound followed by (if indicated) endoscopic retrograde cholangiopancreatography and cholecystectomy, according to a report published online July 8 in JAMA.
At present there are no specific guidelines as to the initial treatment approach for patients who present to the emergency department with suspected choledocholithiasis and who are at intermediate risk for retaining a common duct stone. In contrast, guidelines recommend initial laparoscopic cholecystectomy for patients at low risk for a retained common duct stone and preoperative endoscopic retrograde cholangiopancreatography (ERCP) followed by cholecystectomy for those at high risk, said Dr. Pouya Iranmanesh of the divisions of digestive surgery and transplant surgery, Geneva University Hospital, and his associates.
They performed a single-center randomized clinical trial comparing these two approaches in 100 intermediate-risk patients who presented to the emergency department during a 2-year period with sudden abdominal pain in the right upper quadrant and/or epigastric region, which was associated with elevated liver enzymes and the presence of a gallstone on ultrasound. Patients were included in the study whether they had associated acute cholecystitis or not and were randomly assigned to undergo either initial emergency laparoscopic cholecystectomy with intraoperative cholangiogram (50 patients) or initial common duct ultrasound exploration followed by (if indicated) ERCP and cholecystectomy (50 control subjects).
The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71). In particular, the number of endoscopic ultrasounds was only 10 in the initial-cholecystectomy group, compared with 54 in the control group. All 50 patients in the control group (100%) underwent at least one common duct investigation exclusive of the intraoperative cholangiogram, compared with only 20 patients (40%) in the initial-cholecystectomy group, the investigators reported (JAMA 2014 July 8 [doi:10.1001/jama.2014.7587]).
The two study groups had similar rates of conversion to laparotomy, similar operation times, a similar number of failed intraoperative cholangiograms, and similar results on quality of life measures at 1 month and 6 months after hospital discharge. The rates of complications (8% vs 14%) and of severe complications (4% vs 8%) were approximately twice as high in the control group as in the initial-cholecystectomy group.
Since 30 (60%) of the patients in the initial-cholecystectomy group never needed any common duct investigation, it follows that many intermediate-risk patients in real-world practice are undergoing unnecessary common duct procedures. A policy of performing a cholecystectomy first ensures that only patients who retain common duct stones will undergo such invasive procedures, Dr. Iranmanesh and his associates said.
Dr. Iranmanesh and his associates reported no relevant financial disclosures.
For patients at intermediate risk for having a common duct stone, initial cholecystectomy resulted in a shorter hospital stay, fewer invasive procedures, and no increase in morbidity, compared with the standard approach of doing a common duct exploration via endoscopic ultrasound followed by (if indicated) endoscopic retrograde cholangiopancreatography and cholecystectomy, according to a report published online July 8 in JAMA.
At present there are no specific guidelines as to the initial treatment approach for patients who present to the emergency department with suspected choledocholithiasis and who are at intermediate risk for retaining a common duct stone. In contrast, guidelines recommend initial laparoscopic cholecystectomy for patients at low risk for a retained common duct stone and preoperative endoscopic retrograde cholangiopancreatography (ERCP) followed by cholecystectomy for those at high risk, said Dr. Pouya Iranmanesh of the divisions of digestive surgery and transplant surgery, Geneva University Hospital, and his associates.
They performed a single-center randomized clinical trial comparing these two approaches in 100 intermediate-risk patients who presented to the emergency department during a 2-year period with sudden abdominal pain in the right upper quadrant and/or epigastric region, which was associated with elevated liver enzymes and the presence of a gallstone on ultrasound. Patients were included in the study whether they had associated acute cholecystitis or not and were randomly assigned to undergo either initial emergency laparoscopic cholecystectomy with intraoperative cholangiogram (50 patients) or initial common duct ultrasound exploration followed by (if indicated) ERCP and cholecystectomy (50 control subjects).
The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71). In particular, the number of endoscopic ultrasounds was only 10 in the initial-cholecystectomy group, compared with 54 in the control group. All 50 patients in the control group (100%) underwent at least one common duct investigation exclusive of the intraoperative cholangiogram, compared with only 20 patients (40%) in the initial-cholecystectomy group, the investigators reported (JAMA 2014 July 8 [doi:10.1001/jama.2014.7587]).
The two study groups had similar rates of conversion to laparotomy, similar operation times, a similar number of failed intraoperative cholangiograms, and similar results on quality of life measures at 1 month and 6 months after hospital discharge. The rates of complications (8% vs 14%) and of severe complications (4% vs 8%) were approximately twice as high in the control group as in the initial-cholecystectomy group.
Since 30 (60%) of the patients in the initial-cholecystectomy group never needed any common duct investigation, it follows that many intermediate-risk patients in real-world practice are undergoing unnecessary common duct procedures. A policy of performing a cholecystectomy first ensures that only patients who retain common duct stones will undergo such invasive procedures, Dr. Iranmanesh and his associates said.
Dr. Iranmanesh and his associates reported no relevant financial disclosures.
FROM JAMA
Key clinical point: Initial cholecystectomy for patients at intermediate risk for common duct stone results in shorter hospital stays and fewer invasive procedures.
Major finding: The median length of hospital stay was significantly shorter for the initial-cholecystectomy group (5 days) than for the control group (8 days), and the total number of procedures (endoscopic ultrasounds, magnetic resonance cholangiopancreatographies, and ERCPs) also was significantly smaller (25 vs. 71).
Data source: A single-center randomized clinical trial comparing 50 patients who had initial cholecystectomy with 50 who had common duct exploration followed by ERCP and cholecystectomy; follow-up was done at 1 and 6 months.
Disclosures: Dr. Iranmanesh and his associates reported no relevant financial conflicts of interest.
Reoperative bariatric surgery yields low complication rates, substantial weight loss at 1 year
CHICAGO – Reoperative bariatric surgery has impressively low major morbidity and mortality, substantial 1-year weight loss, and a high rate of resolution of the common obesity-linked comorbid conditions, according to an analysis of a large national database.
These data demonstrate that outcomes after contemporary reoperative bariatric surgery are better than believed by insurance carriers, who often deny coverage for these procedures because of a misperception that complication rates are high and benefits uncertain, Dr. Ranjan Sudan said at the annual Digestive Disease Week.
"I think that these data need to get out there to the stakeholders," added Dr. Sudan, a bariatric surgeon and a digestive disorders specialist who is vice chair of education in the department of surgery at Duke University, Durham, N.C.
He presented an analysis of outcomes after reoperative surgery that was carried out by a task force of the American Society for Metabolic and Bariatric Surgery. He and his coinvestigators reviewed all 451,485 bariatric surgery operations entered into the society’s prospective database during a 5-year period ending in spring 2012. The procedures were performed by 1,029 participating surgeons at 709 U.S. hospitals.
The focus of this analysis was on the 6.3% of operations that were reoperations. A total of 70% of the reoperations were corrective operations, essentially redos of the same type of procedure performed initially. The other 30% were conversion procedures, as when a patient who had a gastric band procedure on the first go-round subsequently was converted to a Roux-en-Y gastric bypass or sleeve procedure.
The mean length of stay for primary bariatric operations was 1.78 days, compared with 2.04 days for reoperative corrective procedures and 2.86 days for conversion operations.
The 30-day incidence of serious adverse events, such as leaks, bleeding, or pulmonary embolism, was 1.61% for primary procedures, nearly identical at 1.66% for corrective reoperations, and 3.26% for conversion procedures. The 1-year rate of serious adverse events was 1.87% for primary bariatric operations, 1.9% for corrective procedures, and 3.61% for conversions.
The mortality rate in patients undergoing a primary operation was 0.10% at 30 days and 0.17% at 1 year. Among patients who underwent reoperative bariatric surgery, the 30-day and 1-year mortality rates were 0.14% and 0.26%, respectively.
"Most bariatric surgery patients do not need reoperations. It’s gratifying to see that among those who do, the severe complication rates were low and acceptable and comorbidities often resolved [see chart]," Dr. Sudan declared.
The 1-year rate of excess weight loss following reoperative surgery averaged 36%.
Discussant Dr. Alfons Pomp liked what he saw from the registry.
"Your data show just how good we as bariatric surgeons are to operate on these surgically difficult, very obese, and seriously ill patients, mostly laparoscopically, and get pretty amazing results," commented Dr. Pomp, professor of surgery and chief of GI metabolic and bariatric surgery at Cornell University in New York.
The registry study was funded by Covidien. Dr. Sudan reported having no financial conflicts of interest.
CHICAGO – Reoperative bariatric surgery has impressively low major morbidity and mortality, substantial 1-year weight loss, and a high rate of resolution of the common obesity-linked comorbid conditions, according to an analysis of a large national database.
These data demonstrate that outcomes after contemporary reoperative bariatric surgery are better than believed by insurance carriers, who often deny coverage for these procedures because of a misperception that complication rates are high and benefits uncertain, Dr. Ranjan Sudan said at the annual Digestive Disease Week.
"I think that these data need to get out there to the stakeholders," added Dr. Sudan, a bariatric surgeon and a digestive disorders specialist who is vice chair of education in the department of surgery at Duke University, Durham, N.C.
He presented an analysis of outcomes after reoperative surgery that was carried out by a task force of the American Society for Metabolic and Bariatric Surgery. He and his coinvestigators reviewed all 451,485 bariatric surgery operations entered into the society’s prospective database during a 5-year period ending in spring 2012. The procedures were performed by 1,029 participating surgeons at 709 U.S. hospitals.
The focus of this analysis was on the 6.3% of operations that were reoperations. A total of 70% of the reoperations were corrective operations, essentially redos of the same type of procedure performed initially. The other 30% were conversion procedures, as when a patient who had a gastric band procedure on the first go-round subsequently was converted to a Roux-en-Y gastric bypass or sleeve procedure.
The mean length of stay for primary bariatric operations was 1.78 days, compared with 2.04 days for reoperative corrective procedures and 2.86 days for conversion operations.
The 30-day incidence of serious adverse events, such as leaks, bleeding, or pulmonary embolism, was 1.61% for primary procedures, nearly identical at 1.66% for corrective reoperations, and 3.26% for conversion procedures. The 1-year rate of serious adverse events was 1.87% for primary bariatric operations, 1.9% for corrective procedures, and 3.61% for conversions.
The mortality rate in patients undergoing a primary operation was 0.10% at 30 days and 0.17% at 1 year. Among patients who underwent reoperative bariatric surgery, the 30-day and 1-year mortality rates were 0.14% and 0.26%, respectively.
"Most bariatric surgery patients do not need reoperations. It’s gratifying to see that among those who do, the severe complication rates were low and acceptable and comorbidities often resolved [see chart]," Dr. Sudan declared.
The 1-year rate of excess weight loss following reoperative surgery averaged 36%.
Discussant Dr. Alfons Pomp liked what he saw from the registry.
"Your data show just how good we as bariatric surgeons are to operate on these surgically difficult, very obese, and seriously ill patients, mostly laparoscopically, and get pretty amazing results," commented Dr. Pomp, professor of surgery and chief of GI metabolic and bariatric surgery at Cornell University in New York.
The registry study was funded by Covidien. Dr. Sudan reported having no financial conflicts of interest.
CHICAGO – Reoperative bariatric surgery has impressively low major morbidity and mortality, substantial 1-year weight loss, and a high rate of resolution of the common obesity-linked comorbid conditions, according to an analysis of a large national database.
These data demonstrate that outcomes after contemporary reoperative bariatric surgery are better than believed by insurance carriers, who often deny coverage for these procedures because of a misperception that complication rates are high and benefits uncertain, Dr. Ranjan Sudan said at the annual Digestive Disease Week.
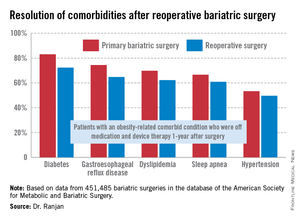
"I think that these data need to get out there to the stakeholders," added Dr. Sudan, a bariatric surgeon and a digestive disorders specialist who is vice chair of education in the department of surgery at Duke University, Durham, N.C.
He presented an analysis of outcomes after reoperative surgery that was carried out by a task force of the American Society for Metabolic and Bariatric Surgery. He and his coinvestigators reviewed all 451,485 bariatric surgery operations entered into the society’s prospective database during a 5-year period ending in spring 2012. The procedures were performed by 1,029 participating surgeons at 709 U.S. hospitals.
The focus of this analysis was on the 6.3% of operations that were reoperations. A total of 70% of the reoperations were corrective operations, essentially redos of the same type of procedure performed initially. The other 30% were conversion procedures, as when a patient who had a gastric band procedure on the first go-round subsequently was converted to a Roux-en-Y gastric bypass or sleeve procedure.
The mean length of stay for primary bariatric operations was 1.78 days, compared with 2.04 days for reoperative corrective procedures and 2.86 days for conversion operations.
The 30-day incidence of serious adverse events, such as leaks, bleeding, or pulmonary embolism, was 1.61% for primary procedures, nearly identical at 1.66% for corrective reoperations, and 3.26% for conversion procedures. The 1-year rate of serious adverse events was 1.87% for primary bariatric operations, 1.9% for corrective procedures, and 3.61% for conversions.
The mortality rate in patients undergoing a primary operation was 0.10% at 30 days and 0.17% at 1 year. Among patients who underwent reoperative bariatric surgery, the 30-day and 1-year mortality rates were 0.14% and 0.26%, respectively.
"Most bariatric surgery patients do not need reoperations. It’s gratifying to see that among those who do, the severe complication rates were low and acceptable and comorbidities often resolved [see chart]," Dr. Sudan declared.
The 1-year rate of excess weight loss following reoperative surgery averaged 36%.
Discussant Dr. Alfons Pomp liked what he saw from the registry.
"Your data show just how good we as bariatric surgeons are to operate on these surgically difficult, very obese, and seriously ill patients, mostly laparoscopically, and get pretty amazing results," commented Dr. Pomp, professor of surgery and chief of GI metabolic and bariatric surgery at Cornell University in New York.
The registry study was funded by Covidien. Dr. Sudan reported having no financial conflicts of interest.
AT DDW 2014
Key clinical point: Reoperative bariatric surgery is considerably safer than previously recognized outside the specialist surgical community. The 1-year excess weight loss is substantial, and common obesity-related comorbidities often resolve.
Major finding: Mortality rates at 30 days and 1-year following reoperative bariatric surgery were just 0.14% and 0. 26%, with an average excess weight loss of 36%at 1 year.
Data source: This was an analysis of more than 450,000 consecutive bariatric surgery operations entered into a prospective national database. Reoperations accounted for 6.3% of the procedures.
Disclosures: The study was funded by Covidien. The presenter reported having no financial conflicts.
SSTI guidelines stress diagnostic skill, careful treatment
New practice guidelines on skin and soft tissue infections from the Infectious Diseases Society of America stress careful clinical attention to the type of infection, the epidemiological setting in which the infection occurred, the health status of the patient, and the selection and dosage of the most appropriate treatment agents.
The guidelines, published online June 18 in Clinical Infectious Diseases (doi:10.1093/cid/ciu296), update those issued by IDSA in 2005 and cover everything from preventing infections caused by animal bites in healthy hosts to life-threatening infections in immunocompromised patients. They also emphasize accurate identification of pathogens, stressing that clinical presentations can be very similar.
"This is not one of those guidelines that boils complex issues down to a choice between a couple of different drugs or combinations of drugs," said Dr. Dennis Stevens of the Department of Veterans Affairs in Boise, Idaho, the guidelines’ lead author. "Skin and soft tissue infections [SSTIs] have multiple causes and different presentations, depending upon the immune status of the host. Here it’s much more complicated and really requires an astute physician to consider a number of things."
The guidelines, drafted by a 10-member panel, offer a novel algorithm for management of nonpurulent and purulent infections that aims to define a pathway for mild, moderate, and severe infections in each category. For example, no antibiotic is recommended for a purulent infection – only incision and drainage – if the patient has no signs of systemic involvement.
For moderate cases of purulent infection with some systemic involvement, incision and drainage should be followed by culture and sensitivity testing, the guidelines say, listing two antibiotics, trimethoprim-sulfamethoxazole and doxycycline, as appropriate for empiric treatment, while trimethoprim-sulfamethoxazole is recommended if the pathogen is found to be methicillin-resistant Staphylococcus aureus (MRSA) and dicloxacillin or cephalexin if it is methicillin-susceptible S. aureus (MSSA).
The purpose of the algorithm, expressed in the guidelines in chart form, "is to make the physician think," Dr. Stevens said in an interview. "There is a huge move to try and monitor antibiotic stewardship to prevent resistance, and we’re just trying to get the clinician to think of tier 1, tier 2, and tier 3 approaches, depending not only on the bug, but on how sick the patient is. Instead of a knee-jerk approach treating everybody with highly expensive IV antibiotics, [the algorithm] provides a clear pathway to treat appropriately."
In people with an abscess who have failed antibiotic treatment, are immunocompromised, or have fever and elevated white blood cell counts or other evidence of severe infection, "we’re not going to gamble," Dr. Stevens said, adding that the guidelines recommend prompt treatment using "an antibiotic that gets all of these organisms, including resistant ones." Newly approved agents dalbavancin and tedizolid are effective in treating SSTIs caused by MRSA, the guidelines note.
The guidelines are intended for use by clinicians in emergency departments, family practice, internal medicine, general surgery, orthopedics, gynecology, dermatology, infectious disease, and oncology.
Another algorithm charted in the guidelines covers wound infections following surgeries, which can involve multiple pathogens. The algorithm provides simple clinical clues as to which require antibiotics, a simple opening of the suture line, "or a full-court press for the kind of devastating infections that occur within the first 48 hours," Dr. Stevens said. Additional recommendations address infections that can occur in individuals receiving treatment for cancer or receiving immunosuppressant medications, or those who have had an organ transplant or who have HIV/AIDS.
Immunocompromised patients, Dr. Stevens said, are among the most challenging to treat because they may have a history of extensive antibiotic exposure, are likely to have infections with resistant bacteria, and often see involvement with fungal and parasitic agents that might be considered innocuous in normal individuals. "This is the first time physicians will have some decent guidelines about how to approach the problem of skin and soft tissue infections in these kinds of patients," he noted.
The guidelines’ development was funded by the IDSA. Dr. Stevens reported no conflicts of interest. Panel member Alan L. Bisno disclosed receiving honoraria from UpToDate, while five other members – Dr. Henry F. Chambers, Dr. E. Patchen Dellinger, Dr. Ellie J. C. Goldstein, Dr. Sherwood L. Gorbach, and Dr. Sheldon L. Kaplan – disclosed financial relationships with pharmaceutical manufacturers.
Skin and soft tissue infections are one of the most common causes for patient evaluation in emergency departments and are common reasons for consultations by surgeons. SSTIs occur across a broad continuum of severity and often require only antimicrobial therapy (such as cellulitis), but they may be fulminate and life-threatening necrotizing infections that require aggressive surgical intervention. The guidelines provided by a distinguished group of clinicians from the Infectious Diseases Society of America provide an excellent organizational framework to understand this heterogenous collection of infections and provide a meaningful structure to direct management.
Several points in these guidelines deserve emphasis. First, considerable discussion in the guidelines has focused on the immunocompromised patient with SSTIs, and appropriately so. A broader consideration might have been to also include those patients with health care-associated exposure in addition to clinical immunosuppression. About 40 million hospitalizations occur annually in the United State, which makes over 3 million patients within 30 days of discharge. A larger number of patients have had recent antibiotic exposure. About 1.5 million patients are in chronic care facilities and nearly 500,000 are receiving chronic hemodialysis. Accordingly, immunocompromised and health care-associated patient exposures require that assumptions about the microbiology of SSTIs have "sensitivity" to the resistant pathogens (such as MRSA) not traditionally typical of community-acquired infections.
Second, the guidelines refer to the use of Gram stains for directing antimicrobial therapy. Although the Gram stain does not have the high-technology flare of contemporary health care, it remains a useful tool in differentiating pathogens, especially in necrotizing SSTIs.
Of the major microbiological presentations of necrotizing SSTIs, Streptococcus pyogenes is a gram-positive cocci in chains, Staphylococcus aureus is a gram-positive cocci in clusters, Clostridium perfringens is a gram-positive rod, and polymicrobial infections will have an assortment of different morphologic and gram-staining characteristics in identified bacteria. Aeromonas hydrophilia and Vibrio vulnificus will appear as gram-negative rods in those necrotizing SSTIs associated with fresh or salt-water recreational exposure. The Gram stain provides immediate direction for therapy when culture results will often be too late for a meaningful impact on patient care. Unfortunately, many hospitals have abandoned the use of Gram stains for clinical specimens.
Finally, prompt diagnosis of necrotizing SSTIs is essential. A cause of potentially preventable morbidity and deaths is a delay in the recognition of necrotizing SSTIs and the need for urgent surgical debridement. Necrotizing SSTIs are common issues in medicolegal actions because of the issue of failure to make the timely diagnosis. The hallmark of necrotizing SSTIs is pain out of proportion to the inciting injury. Trivial cutaneous injuries that are associated with an advancing perimeter of palpable tenderness and induration are necrotizing SSTIs until proven otherwise. Importantly, S. pyogenes in particular is associated with "metastatic" infection. Patients with soft-tissue contusions, joint effusions, and even fractures may have blood-borne streptococcal contamination of the injury site and yield a necrotizing infection without any cutaneous source of microbial contamination.
Because monitoring the progression of SSTIs is so important in differentiating necrotizing infections, I would only take to task the recommendation for the use of corticosteroids in treatment of cellulitic infections. Pharmacologic immunosuppression of the patient with an active SSTI in the interest of providing symptomatic relief compromises the clinical evaluation of disease progression.
In summary, the guidelines and the two algorithms for managing community-acquired and surgical incision infections are very useful for providing surgical clinicians direction in patient management. The increased incidence of S. aureus-associated necrotizing SSTIs and the emergence of community-associated MRSA over the last 20 years indicate that this is a dynamic area with changing characteristics. The changing pattern of pathogens and antimicrobial choices require a more frequent updating of these important guidelines for patient management.
Dr. Donald E. Fry is an ACS Fellow, executive vice-president for clinical outcomes management of MPA Inc. of Chicago, adjunct professor of surgery at the Northwestern University in Chicago, and professor emeritus of surgery at the University of New Mexico. He is a fellow of the Infectious Diseases Society of America, a past president of the Surgical Infection Society, and associate editor of the journal Surgical Infections.
Skin and soft tissue infections are one of the most common causes for patient evaluation in emergency departments and are common reasons for consultations by surgeons. SSTIs occur across a broad continuum of severity and often require only antimicrobial therapy (such as cellulitis), but they may be fulminate and life-threatening necrotizing infections that require aggressive surgical intervention. The guidelines provided by a distinguished group of clinicians from the Infectious Diseases Society of America provide an excellent organizational framework to understand this heterogenous collection of infections and provide a meaningful structure to direct management.
Several points in these guidelines deserve emphasis. First, considerable discussion in the guidelines has focused on the immunocompromised patient with SSTIs, and appropriately so. A broader consideration might have been to also include those patients with health care-associated exposure in addition to clinical immunosuppression. About 40 million hospitalizations occur annually in the United State, which makes over 3 million patients within 30 days of discharge. A larger number of patients have had recent antibiotic exposure. About 1.5 million patients are in chronic care facilities and nearly 500,000 are receiving chronic hemodialysis. Accordingly, immunocompromised and health care-associated patient exposures require that assumptions about the microbiology of SSTIs have "sensitivity" to the resistant pathogens (such as MRSA) not traditionally typical of community-acquired infections.
Second, the guidelines refer to the use of Gram stains for directing antimicrobial therapy. Although the Gram stain does not have the high-technology flare of contemporary health care, it remains a useful tool in differentiating pathogens, especially in necrotizing SSTIs.
Of the major microbiological presentations of necrotizing SSTIs, Streptococcus pyogenes is a gram-positive cocci in chains, Staphylococcus aureus is a gram-positive cocci in clusters, Clostridium perfringens is a gram-positive rod, and polymicrobial infections will have an assortment of different morphologic and gram-staining characteristics in identified bacteria. Aeromonas hydrophilia and Vibrio vulnificus will appear as gram-negative rods in those necrotizing SSTIs associated with fresh or salt-water recreational exposure. The Gram stain provides immediate direction for therapy when culture results will often be too late for a meaningful impact on patient care. Unfortunately, many hospitals have abandoned the use of Gram stains for clinical specimens.
Finally, prompt diagnosis of necrotizing SSTIs is essential. A cause of potentially preventable morbidity and deaths is a delay in the recognition of necrotizing SSTIs and the need for urgent surgical debridement. Necrotizing SSTIs are common issues in medicolegal actions because of the issue of failure to make the timely diagnosis. The hallmark of necrotizing SSTIs is pain out of proportion to the inciting injury. Trivial cutaneous injuries that are associated with an advancing perimeter of palpable tenderness and induration are necrotizing SSTIs until proven otherwise. Importantly, S. pyogenes in particular is associated with "metastatic" infection. Patients with soft-tissue contusions, joint effusions, and even fractures may have blood-borne streptococcal contamination of the injury site and yield a necrotizing infection without any cutaneous source of microbial contamination.
Because monitoring the progression of SSTIs is so important in differentiating necrotizing infections, I would only take to task the recommendation for the use of corticosteroids in treatment of cellulitic infections. Pharmacologic immunosuppression of the patient with an active SSTI in the interest of providing symptomatic relief compromises the clinical evaluation of disease progression.
In summary, the guidelines and the two algorithms for managing community-acquired and surgical incision infections are very useful for providing surgical clinicians direction in patient management. The increased incidence of S. aureus-associated necrotizing SSTIs and the emergence of community-associated MRSA over the last 20 years indicate that this is a dynamic area with changing characteristics. The changing pattern of pathogens and antimicrobial choices require a more frequent updating of these important guidelines for patient management.
Dr. Donald E. Fry is an ACS Fellow, executive vice-president for clinical outcomes management of MPA Inc. of Chicago, adjunct professor of surgery at the Northwestern University in Chicago, and professor emeritus of surgery at the University of New Mexico. He is a fellow of the Infectious Diseases Society of America, a past president of the Surgical Infection Society, and associate editor of the journal Surgical Infections.
Skin and soft tissue infections are one of the most common causes for patient evaluation in emergency departments and are common reasons for consultations by surgeons. SSTIs occur across a broad continuum of severity and often require only antimicrobial therapy (such as cellulitis), but they may be fulminate and life-threatening necrotizing infections that require aggressive surgical intervention. The guidelines provided by a distinguished group of clinicians from the Infectious Diseases Society of America provide an excellent organizational framework to understand this heterogenous collection of infections and provide a meaningful structure to direct management.
Several points in these guidelines deserve emphasis. First, considerable discussion in the guidelines has focused on the immunocompromised patient with SSTIs, and appropriately so. A broader consideration might have been to also include those patients with health care-associated exposure in addition to clinical immunosuppression. About 40 million hospitalizations occur annually in the United State, which makes over 3 million patients within 30 days of discharge. A larger number of patients have had recent antibiotic exposure. About 1.5 million patients are in chronic care facilities and nearly 500,000 are receiving chronic hemodialysis. Accordingly, immunocompromised and health care-associated patient exposures require that assumptions about the microbiology of SSTIs have "sensitivity" to the resistant pathogens (such as MRSA) not traditionally typical of community-acquired infections.
Second, the guidelines refer to the use of Gram stains for directing antimicrobial therapy. Although the Gram stain does not have the high-technology flare of contemporary health care, it remains a useful tool in differentiating pathogens, especially in necrotizing SSTIs.
Of the major microbiological presentations of necrotizing SSTIs, Streptococcus pyogenes is a gram-positive cocci in chains, Staphylococcus aureus is a gram-positive cocci in clusters, Clostridium perfringens is a gram-positive rod, and polymicrobial infections will have an assortment of different morphologic and gram-staining characteristics in identified bacteria. Aeromonas hydrophilia and Vibrio vulnificus will appear as gram-negative rods in those necrotizing SSTIs associated with fresh or salt-water recreational exposure. The Gram stain provides immediate direction for therapy when culture results will often be too late for a meaningful impact on patient care. Unfortunately, many hospitals have abandoned the use of Gram stains for clinical specimens.
Finally, prompt diagnosis of necrotizing SSTIs is essential. A cause of potentially preventable morbidity and deaths is a delay in the recognition of necrotizing SSTIs and the need for urgent surgical debridement. Necrotizing SSTIs are common issues in medicolegal actions because of the issue of failure to make the timely diagnosis. The hallmark of necrotizing SSTIs is pain out of proportion to the inciting injury. Trivial cutaneous injuries that are associated with an advancing perimeter of palpable tenderness and induration are necrotizing SSTIs until proven otherwise. Importantly, S. pyogenes in particular is associated with "metastatic" infection. Patients with soft-tissue contusions, joint effusions, and even fractures may have blood-borne streptococcal contamination of the injury site and yield a necrotizing infection without any cutaneous source of microbial contamination.
Because monitoring the progression of SSTIs is so important in differentiating necrotizing infections, I would only take to task the recommendation for the use of corticosteroids in treatment of cellulitic infections. Pharmacologic immunosuppression of the patient with an active SSTI in the interest of providing symptomatic relief compromises the clinical evaluation of disease progression.
In summary, the guidelines and the two algorithms for managing community-acquired and surgical incision infections are very useful for providing surgical clinicians direction in patient management. The increased incidence of S. aureus-associated necrotizing SSTIs and the emergence of community-associated MRSA over the last 20 years indicate that this is a dynamic area with changing characteristics. The changing pattern of pathogens and antimicrobial choices require a more frequent updating of these important guidelines for patient management.
Dr. Donald E. Fry is an ACS Fellow, executive vice-president for clinical outcomes management of MPA Inc. of Chicago, adjunct professor of surgery at the Northwestern University in Chicago, and professor emeritus of surgery at the University of New Mexico. He is a fellow of the Infectious Diseases Society of America, a past president of the Surgical Infection Society, and associate editor of the journal Surgical Infections.
New practice guidelines on skin and soft tissue infections from the Infectious Diseases Society of America stress careful clinical attention to the type of infection, the epidemiological setting in which the infection occurred, the health status of the patient, and the selection and dosage of the most appropriate treatment agents.
The guidelines, published online June 18 in Clinical Infectious Diseases (doi:10.1093/cid/ciu296), update those issued by IDSA in 2005 and cover everything from preventing infections caused by animal bites in healthy hosts to life-threatening infections in immunocompromised patients. They also emphasize accurate identification of pathogens, stressing that clinical presentations can be very similar.
"This is not one of those guidelines that boils complex issues down to a choice between a couple of different drugs or combinations of drugs," said Dr. Dennis Stevens of the Department of Veterans Affairs in Boise, Idaho, the guidelines’ lead author. "Skin and soft tissue infections [SSTIs] have multiple causes and different presentations, depending upon the immune status of the host. Here it’s much more complicated and really requires an astute physician to consider a number of things."
The guidelines, drafted by a 10-member panel, offer a novel algorithm for management of nonpurulent and purulent infections that aims to define a pathway for mild, moderate, and severe infections in each category. For example, no antibiotic is recommended for a purulent infection – only incision and drainage – if the patient has no signs of systemic involvement.
For moderate cases of purulent infection with some systemic involvement, incision and drainage should be followed by culture and sensitivity testing, the guidelines say, listing two antibiotics, trimethoprim-sulfamethoxazole and doxycycline, as appropriate for empiric treatment, while trimethoprim-sulfamethoxazole is recommended if the pathogen is found to be methicillin-resistant Staphylococcus aureus (MRSA) and dicloxacillin or cephalexin if it is methicillin-susceptible S. aureus (MSSA).
The purpose of the algorithm, expressed in the guidelines in chart form, "is to make the physician think," Dr. Stevens said in an interview. "There is a huge move to try and monitor antibiotic stewardship to prevent resistance, and we’re just trying to get the clinician to think of tier 1, tier 2, and tier 3 approaches, depending not only on the bug, but on how sick the patient is. Instead of a knee-jerk approach treating everybody with highly expensive IV antibiotics, [the algorithm] provides a clear pathway to treat appropriately."
In people with an abscess who have failed antibiotic treatment, are immunocompromised, or have fever and elevated white blood cell counts or other evidence of severe infection, "we’re not going to gamble," Dr. Stevens said, adding that the guidelines recommend prompt treatment using "an antibiotic that gets all of these organisms, including resistant ones." Newly approved agents dalbavancin and tedizolid are effective in treating SSTIs caused by MRSA, the guidelines note.
The guidelines are intended for use by clinicians in emergency departments, family practice, internal medicine, general surgery, orthopedics, gynecology, dermatology, infectious disease, and oncology.
Another algorithm charted in the guidelines covers wound infections following surgeries, which can involve multiple pathogens. The algorithm provides simple clinical clues as to which require antibiotics, a simple opening of the suture line, "or a full-court press for the kind of devastating infections that occur within the first 48 hours," Dr. Stevens said. Additional recommendations address infections that can occur in individuals receiving treatment for cancer or receiving immunosuppressant medications, or those who have had an organ transplant or who have HIV/AIDS.
Immunocompromised patients, Dr. Stevens said, are among the most challenging to treat because they may have a history of extensive antibiotic exposure, are likely to have infections with resistant bacteria, and often see involvement with fungal and parasitic agents that might be considered innocuous in normal individuals. "This is the first time physicians will have some decent guidelines about how to approach the problem of skin and soft tissue infections in these kinds of patients," he noted.
The guidelines’ development was funded by the IDSA. Dr. Stevens reported no conflicts of interest. Panel member Alan L. Bisno disclosed receiving honoraria from UpToDate, while five other members – Dr. Henry F. Chambers, Dr. E. Patchen Dellinger, Dr. Ellie J. C. Goldstein, Dr. Sherwood L. Gorbach, and Dr. Sheldon L. Kaplan – disclosed financial relationships with pharmaceutical manufacturers.
New practice guidelines on skin and soft tissue infections from the Infectious Diseases Society of America stress careful clinical attention to the type of infection, the epidemiological setting in which the infection occurred, the health status of the patient, and the selection and dosage of the most appropriate treatment agents.
The guidelines, published online June 18 in Clinical Infectious Diseases (doi:10.1093/cid/ciu296), update those issued by IDSA in 2005 and cover everything from preventing infections caused by animal bites in healthy hosts to life-threatening infections in immunocompromised patients. They also emphasize accurate identification of pathogens, stressing that clinical presentations can be very similar.
"This is not one of those guidelines that boils complex issues down to a choice between a couple of different drugs or combinations of drugs," said Dr. Dennis Stevens of the Department of Veterans Affairs in Boise, Idaho, the guidelines’ lead author. "Skin and soft tissue infections [SSTIs] have multiple causes and different presentations, depending upon the immune status of the host. Here it’s much more complicated and really requires an astute physician to consider a number of things."
The guidelines, drafted by a 10-member panel, offer a novel algorithm for management of nonpurulent and purulent infections that aims to define a pathway for mild, moderate, and severe infections in each category. For example, no antibiotic is recommended for a purulent infection – only incision and drainage – if the patient has no signs of systemic involvement.
For moderate cases of purulent infection with some systemic involvement, incision and drainage should be followed by culture and sensitivity testing, the guidelines say, listing two antibiotics, trimethoprim-sulfamethoxazole and doxycycline, as appropriate for empiric treatment, while trimethoprim-sulfamethoxazole is recommended if the pathogen is found to be methicillin-resistant Staphylococcus aureus (MRSA) and dicloxacillin or cephalexin if it is methicillin-susceptible S. aureus (MSSA).
The purpose of the algorithm, expressed in the guidelines in chart form, "is to make the physician think," Dr. Stevens said in an interview. "There is a huge move to try and monitor antibiotic stewardship to prevent resistance, and we’re just trying to get the clinician to think of tier 1, tier 2, and tier 3 approaches, depending not only on the bug, but on how sick the patient is. Instead of a knee-jerk approach treating everybody with highly expensive IV antibiotics, [the algorithm] provides a clear pathway to treat appropriately."
In people with an abscess who have failed antibiotic treatment, are immunocompromised, or have fever and elevated white blood cell counts or other evidence of severe infection, "we’re not going to gamble," Dr. Stevens said, adding that the guidelines recommend prompt treatment using "an antibiotic that gets all of these organisms, including resistant ones." Newly approved agents dalbavancin and tedizolid are effective in treating SSTIs caused by MRSA, the guidelines note.
The guidelines are intended for use by clinicians in emergency departments, family practice, internal medicine, general surgery, orthopedics, gynecology, dermatology, infectious disease, and oncology.
Another algorithm charted in the guidelines covers wound infections following surgeries, which can involve multiple pathogens. The algorithm provides simple clinical clues as to which require antibiotics, a simple opening of the suture line, "or a full-court press for the kind of devastating infections that occur within the first 48 hours," Dr. Stevens said. Additional recommendations address infections that can occur in individuals receiving treatment for cancer or receiving immunosuppressant medications, or those who have had an organ transplant or who have HIV/AIDS.
Immunocompromised patients, Dr. Stevens said, are among the most challenging to treat because they may have a history of extensive antibiotic exposure, are likely to have infections with resistant bacteria, and often see involvement with fungal and parasitic agents that might be considered innocuous in normal individuals. "This is the first time physicians will have some decent guidelines about how to approach the problem of skin and soft tissue infections in these kinds of patients," he noted.
The guidelines’ development was funded by the IDSA. Dr. Stevens reported no conflicts of interest. Panel member Alan L. Bisno disclosed receiving honoraria from UpToDate, while five other members – Dr. Henry F. Chambers, Dr. E. Patchen Dellinger, Dr. Ellie J. C. Goldstein, Dr. Sherwood L. Gorbach, and Dr. Sheldon L. Kaplan – disclosed financial relationships with pharmaceutical manufacturers.
FROM CLINICAL INFECTIOUS DISEASES