User login
NHLBI expert panel issues guideline on sickle cell disease
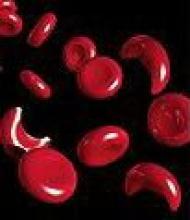
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
FROM JAMA
Major finding: The two most widely available disease-modifying therapies for SCD, hydroxyurea and long-term transfusions, are underused, in large part because no evidence-based treatment protocols have been devised until now.
Data source: A review of the literature and compilation of management guidelines "to assist health care professionals in the management of common issues of sickle cell disease."
Disclosures: The National Heart, Lung, and Blood Institute sponsored the development of this guideline. All expert panel members served voluntarily. Many reported numerous ties to industry sources.
Risk of multidrug-resistant gram-negative infections rose 1% per day of hospitalization
WASHINGTON – With each day of hospitalization, the risk rises by 1% for contracting an infection with a gram-negative, multidrug-resistant organism, based on results from a single-hospital retrospective study.
While conventional wisdom holds that infection risk increases with duration of hospitalization, the study is the first to quantify the potential risk of contracting a multidrug-resistant infection based on length of stay. And while the results may not be applicable to all patients at all hospitals, the findings do give clinicians a sense of the risk posed by a prolonged stay, according to John A. Bosso, Pharm.D., a professor in the College of Pharmacy at the Medical University of South Carolina, Charleston.
Dr. Bosso and his colleagues focused on gram-negative organisms because a colleague had compiled data for 949 episodes of documented gram-negative infections that occurred between 1998 and 2011 at the university hospital. A statement issued at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy noted that the Centers for Disease Control and Prevention has estimated that on any given day, 1 in 25 hospitalized patients has at least one health care–associated infection, and about a third of these are caused by gram-negative bacteria.
The study defined drug-resistant organisms as those that did not respond to treatment with one or more agents in three or more antibiotic classes. The five classes of antibiotics used in the cases studied included aminoglycosides, penicillins, cephalosporins, fluoroquinolones, and folic acid inhibitors. The largest percentage of isolates (38%) was taken from patients with blood stream infections; 29% had pneumonia, 23% had surgical site infections, 6% had urinary tract infections, and 4% had other infections.
Of the 949 organisms reviewed, 251 (26%) were determined to be multidrug resistant.
Ultimately, the type of infection was found to be unrelated to whether a patient had a multidrug-resistant infection. Certain pathogens were more likely to be multidrug resistant. About 56% of Enterobacter isolates, for example, were multidrug resistant as compared with 20% of all other organisms. Alternatively, Pseudomonas isolates were 44% less likely than other isolates to be multidrug resistant.
Length of stay seemed to have the greatest impact on contracting multidrug-resistant strains of gram-negative organisms, with risk maximizing at 10 days of hospitalization. Each day of hospitalization increased the likelihood of multidrug resistance by 1%, Dr. Bosso said.
The researchers were unable to determine the proportion of patients who were already colonized with a multidrug-resistant strain at admission from those who acquired their infections while hospitalized, said Dr. Bosso.
Dr. Bosso reported no financial conflicts of interest.
On Twitter @aliciaault
WASHINGTON – With each day of hospitalization, the risk rises by 1% for contracting an infection with a gram-negative, multidrug-resistant organism, based on results from a single-hospital retrospective study.
While conventional wisdom holds that infection risk increases with duration of hospitalization, the study is the first to quantify the potential risk of contracting a multidrug-resistant infection based on length of stay. And while the results may not be applicable to all patients at all hospitals, the findings do give clinicians a sense of the risk posed by a prolonged stay, according to John A. Bosso, Pharm.D., a professor in the College of Pharmacy at the Medical University of South Carolina, Charleston.
Dr. Bosso and his colleagues focused on gram-negative organisms because a colleague had compiled data for 949 episodes of documented gram-negative infections that occurred between 1998 and 2011 at the university hospital. A statement issued at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy noted that the Centers for Disease Control and Prevention has estimated that on any given day, 1 in 25 hospitalized patients has at least one health care–associated infection, and about a third of these are caused by gram-negative bacteria.
The study defined drug-resistant organisms as those that did not respond to treatment with one or more agents in three or more antibiotic classes. The five classes of antibiotics used in the cases studied included aminoglycosides, penicillins, cephalosporins, fluoroquinolones, and folic acid inhibitors. The largest percentage of isolates (38%) was taken from patients with blood stream infections; 29% had pneumonia, 23% had surgical site infections, 6% had urinary tract infections, and 4% had other infections.
Of the 949 organisms reviewed, 251 (26%) were determined to be multidrug resistant.
Ultimately, the type of infection was found to be unrelated to whether a patient had a multidrug-resistant infection. Certain pathogens were more likely to be multidrug resistant. About 56% of Enterobacter isolates, for example, were multidrug resistant as compared with 20% of all other organisms. Alternatively, Pseudomonas isolates were 44% less likely than other isolates to be multidrug resistant.
Length of stay seemed to have the greatest impact on contracting multidrug-resistant strains of gram-negative organisms, with risk maximizing at 10 days of hospitalization. Each day of hospitalization increased the likelihood of multidrug resistance by 1%, Dr. Bosso said.
The researchers were unable to determine the proportion of patients who were already colonized with a multidrug-resistant strain at admission from those who acquired their infections while hospitalized, said Dr. Bosso.
Dr. Bosso reported no financial conflicts of interest.
On Twitter @aliciaault
WASHINGTON – With each day of hospitalization, the risk rises by 1% for contracting an infection with a gram-negative, multidrug-resistant organism, based on results from a single-hospital retrospective study.
While conventional wisdom holds that infection risk increases with duration of hospitalization, the study is the first to quantify the potential risk of contracting a multidrug-resistant infection based on length of stay. And while the results may not be applicable to all patients at all hospitals, the findings do give clinicians a sense of the risk posed by a prolonged stay, according to John A. Bosso, Pharm.D., a professor in the College of Pharmacy at the Medical University of South Carolina, Charleston.
Dr. Bosso and his colleagues focused on gram-negative organisms because a colleague had compiled data for 949 episodes of documented gram-negative infections that occurred between 1998 and 2011 at the university hospital. A statement issued at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy noted that the Centers for Disease Control and Prevention has estimated that on any given day, 1 in 25 hospitalized patients has at least one health care–associated infection, and about a third of these are caused by gram-negative bacteria.
The study defined drug-resistant organisms as those that did not respond to treatment with one or more agents in three or more antibiotic classes. The five classes of antibiotics used in the cases studied included aminoglycosides, penicillins, cephalosporins, fluoroquinolones, and folic acid inhibitors. The largest percentage of isolates (38%) was taken from patients with blood stream infections; 29% had pneumonia, 23% had surgical site infections, 6% had urinary tract infections, and 4% had other infections.
Of the 949 organisms reviewed, 251 (26%) were determined to be multidrug resistant.
Ultimately, the type of infection was found to be unrelated to whether a patient had a multidrug-resistant infection. Certain pathogens were more likely to be multidrug resistant. About 56% of Enterobacter isolates, for example, were multidrug resistant as compared with 20% of all other organisms. Alternatively, Pseudomonas isolates were 44% less likely than other isolates to be multidrug resistant.
Length of stay seemed to have the greatest impact on contracting multidrug-resistant strains of gram-negative organisms, with risk maximizing at 10 days of hospitalization. Each day of hospitalization increased the likelihood of multidrug resistance by 1%, Dr. Bosso said.
The researchers were unable to determine the proportion of patients who were already colonized with a multidrug-resistant strain at admission from those who acquired their infections while hospitalized, said Dr. Bosso.
Dr. Bosso reported no financial conflicts of interest.
On Twitter @aliciaault
AT ICAAC 2014
Key clinical point: Risk of multidrug-resistant gram-negative infections rise with length of stay.
Major finding: With each day of hospitalization, the risk of a multidrug resistant gram-negative infection rose by 1%.
Data source: A single-hospital review of 949 documented cases of gram-negative infections from 1998 to 2011.
Disclosures: The authors reported no financial conflicts.
Vagal nerve blockade effects on morbid obesity warrant further study
Intra-abdominal vagal nerve blockade to treat morbid obesity didn’t meet prespecified efficacy objectives in the randomized, double-blind ReCharge study, but treated patients did experience significantly greater weight loss than did those who underwent a sham procedure.
Mean excess weight loss was 24.4% (9.2% of initial body weight loss) in 162 patients who had a body mass index of 40-45 kg/m2 or 35-40 kg/m2 plus one or more obesity-related conditions, who underwent vagal nerve block therapy, compared with 15.9% (6% of initial body weight loss) in 77 patients in the sham group, for a mean between-group difference of 8.5 percentage points.
The difference was statistically significant, but it was less than the prespecified 10-point superiority margin, Dr. Sayeed Ikramuddin of the University of Minnesota, Minneapolis, and colleagues reported online Sept. 2 in JAMA.
At 12 months, 20% or more excess weight loss was achieved by 52% of patients in the vagal nerve block group, compared with 32% of patients in the sham procedure group. A total of 25% or more excess weight loss was achieved by 38% and 23% of patients in the groups, respectively, the investigators said (JAMA 2014;312:915-22).
Patients in the treatment group experienced more heartburn and dyspepsia, abdominal and other nonspecific pain, dysphagia, nausea, and eructation or belching than those in the control group. But these side effects were generally mild or moderate in severity. Serious adverse events associated with vagal nerve blockade occurred in 3.7% of treatment group patients, which was well below the 15% upper threshold for safety in the trial.
Additional study is needed to compare vagal nerve block with other obesity treatments, and to assess long-term durability and safety of the procedure, the investigators concluded.
This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
The findings suggest that vagal nerve blockade has little to offer when compared with other treatments for morbid obesity, according to Dr. David E. Arterburn and Dr. David P. Fisher.
The treatment does not appear to be much more effective than an intensive lifestyle program, which in one study was shown to be associated with an 8.6% weight loss. Also, other procedures – including adjustable gastric banding, Roux-en-Y gastric bypass, and vertical sleeve gastrectomy – are associated with excess weight loss of between 50% and 68%, and thus are "clearly more effective for initial weight loss than vagal nerve blockade," Dr. Arterburn and Dr. Fisher wrote in an editorial (JAMA 2014;312:898-9).
The clinically important 8.6% rate of serious adverse events associated with intra-abdominal surgery and vagal nerve blockade in the study is also of concern, as are costs, which were not addressed by the authors, they noted.
"Although vagal nerve blockade therapy is an innovative approach, it does not appear to be a sustained, effective treatment for severe obesity," Dr. Arterburn and Dr. Fisher concluded.
Dr. Arterburn is with Group Health Research Institute, Seattle. He reported receiving institutional grants from the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Department of Veterans Affairs, and the Informed Medical Decisions Foundation, and receiving payment for travel expenses from the Informed Medical Decisions Foundation. Dr. Fisher is with the Permanente Medical Group, Kaiser Permanente Northern California, Bariatric Surgery Center, Richmond, Calif. He reported receiving institutional grants from the National Institutes of Health.
The findings suggest that vagal nerve blockade has little to offer when compared with other treatments for morbid obesity, according to Dr. David E. Arterburn and Dr. David P. Fisher.
The treatment does not appear to be much more effective than an intensive lifestyle program, which in one study was shown to be associated with an 8.6% weight loss. Also, other procedures – including adjustable gastric banding, Roux-en-Y gastric bypass, and vertical sleeve gastrectomy – are associated with excess weight loss of between 50% and 68%, and thus are "clearly more effective for initial weight loss than vagal nerve blockade," Dr. Arterburn and Dr. Fisher wrote in an editorial (JAMA 2014;312:898-9).
The clinically important 8.6% rate of serious adverse events associated with intra-abdominal surgery and vagal nerve blockade in the study is also of concern, as are costs, which were not addressed by the authors, they noted.
"Although vagal nerve blockade therapy is an innovative approach, it does not appear to be a sustained, effective treatment for severe obesity," Dr. Arterburn and Dr. Fisher concluded.
Dr. Arterburn is with Group Health Research Institute, Seattle. He reported receiving institutional grants from the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Department of Veterans Affairs, and the Informed Medical Decisions Foundation, and receiving payment for travel expenses from the Informed Medical Decisions Foundation. Dr. Fisher is with the Permanente Medical Group, Kaiser Permanente Northern California, Bariatric Surgery Center, Richmond, Calif. He reported receiving institutional grants from the National Institutes of Health.
The findings suggest that vagal nerve blockade has little to offer when compared with other treatments for morbid obesity, according to Dr. David E. Arterburn and Dr. David P. Fisher.
The treatment does not appear to be much more effective than an intensive lifestyle program, which in one study was shown to be associated with an 8.6% weight loss. Also, other procedures – including adjustable gastric banding, Roux-en-Y gastric bypass, and vertical sleeve gastrectomy – are associated with excess weight loss of between 50% and 68%, and thus are "clearly more effective for initial weight loss than vagal nerve blockade," Dr. Arterburn and Dr. Fisher wrote in an editorial (JAMA 2014;312:898-9).
The clinically important 8.6% rate of serious adverse events associated with intra-abdominal surgery and vagal nerve blockade in the study is also of concern, as are costs, which were not addressed by the authors, they noted.
"Although vagal nerve blockade therapy is an innovative approach, it does not appear to be a sustained, effective treatment for severe obesity," Dr. Arterburn and Dr. Fisher concluded.
Dr. Arterburn is with Group Health Research Institute, Seattle. He reported receiving institutional grants from the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Department of Veterans Affairs, and the Informed Medical Decisions Foundation, and receiving payment for travel expenses from the Informed Medical Decisions Foundation. Dr. Fisher is with the Permanente Medical Group, Kaiser Permanente Northern California, Bariatric Surgery Center, Richmond, Calif. He reported receiving institutional grants from the National Institutes of Health.
Intra-abdominal vagal nerve blockade to treat morbid obesity didn’t meet prespecified efficacy objectives in the randomized, double-blind ReCharge study, but treated patients did experience significantly greater weight loss than did those who underwent a sham procedure.
Mean excess weight loss was 24.4% (9.2% of initial body weight loss) in 162 patients who had a body mass index of 40-45 kg/m2 or 35-40 kg/m2 plus one or more obesity-related conditions, who underwent vagal nerve block therapy, compared with 15.9% (6% of initial body weight loss) in 77 patients in the sham group, for a mean between-group difference of 8.5 percentage points.
The difference was statistically significant, but it was less than the prespecified 10-point superiority margin, Dr. Sayeed Ikramuddin of the University of Minnesota, Minneapolis, and colleagues reported online Sept. 2 in JAMA.
At 12 months, 20% or more excess weight loss was achieved by 52% of patients in the vagal nerve block group, compared with 32% of patients in the sham procedure group. A total of 25% or more excess weight loss was achieved by 38% and 23% of patients in the groups, respectively, the investigators said (JAMA 2014;312:915-22).
Patients in the treatment group experienced more heartburn and dyspepsia, abdominal and other nonspecific pain, dysphagia, nausea, and eructation or belching than those in the control group. But these side effects were generally mild or moderate in severity. Serious adverse events associated with vagal nerve blockade occurred in 3.7% of treatment group patients, which was well below the 15% upper threshold for safety in the trial.
Additional study is needed to compare vagal nerve block with other obesity treatments, and to assess long-term durability and safety of the procedure, the investigators concluded.
This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
Intra-abdominal vagal nerve blockade to treat morbid obesity didn’t meet prespecified efficacy objectives in the randomized, double-blind ReCharge study, but treated patients did experience significantly greater weight loss than did those who underwent a sham procedure.
Mean excess weight loss was 24.4% (9.2% of initial body weight loss) in 162 patients who had a body mass index of 40-45 kg/m2 or 35-40 kg/m2 plus one or more obesity-related conditions, who underwent vagal nerve block therapy, compared with 15.9% (6% of initial body weight loss) in 77 patients in the sham group, for a mean between-group difference of 8.5 percentage points.
The difference was statistically significant, but it was less than the prespecified 10-point superiority margin, Dr. Sayeed Ikramuddin of the University of Minnesota, Minneapolis, and colleagues reported online Sept. 2 in JAMA.
At 12 months, 20% or more excess weight loss was achieved by 52% of patients in the vagal nerve block group, compared with 32% of patients in the sham procedure group. A total of 25% or more excess weight loss was achieved by 38% and 23% of patients in the groups, respectively, the investigators said (JAMA 2014;312:915-22).
Patients in the treatment group experienced more heartburn and dyspepsia, abdominal and other nonspecific pain, dysphagia, nausea, and eructation or belching than those in the control group. But these side effects were generally mild or moderate in severity. Serious adverse events associated with vagal nerve blockade occurred in 3.7% of treatment group patients, which was well below the 15% upper threshold for safety in the trial.
Additional study is needed to compare vagal nerve block with other obesity treatments, and to assess long-term durability and safety of the procedure, the investigators concluded.
This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
FROM JAMA
Major finding: At 12 months, 20% or more excess weight loss was achieved by 52% and 32% of patients in the treatment and control groups, respectively.
Data source: The randomized, double-blind ReCharge Study involving 239 patients.
Disclosures: This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
Sleeve gastrectomy replacing other bariatric surgery
Sleeve gastrectomy appears to be replacing other types of bariatric surgery in Michigan, even among subgroups of patients in whom its use is controversial, according to a Research Letter to the Editor published in the Sept. 3 issue of JAMA.
To examine time trends in the use of various bariatric procedures, investigators reviewed the medical records of 43,732 adults who had bariatric surgery and were enrolled in a statewide database between June 2006 and December 2013. They found that the relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, which represents an increase of 61%, said Dr. Bradley N. Reames of the department of surgery and the Center for Healthcare Outcomes and Policy, University of Michigan, Ann Arbor, and his associates.
At the same time, the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%, they said (JAMA 2014;312:959-61).
"Moreover, despite controversy regarding the optimal procedure for patients with gastroesophageal reflux disease and type 2 diabetes, sleeve gastrectomy has become the predominant procedure in both groups," Dr. Reames and his associates said.
The long-term outcomes after sleeve gastrectomy are not yet clear, so this trend "may reflect the favorable perioperative safety profile and emerging evidence of successful weight loss at 2-3 years after" the procedure, they added.
Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
Sleeve gastrectomy appears to be replacing other types of bariatric surgery in Michigan, even among subgroups of patients in whom its use is controversial, according to a Research Letter to the Editor published in the Sept. 3 issue of JAMA.
To examine time trends in the use of various bariatric procedures, investigators reviewed the medical records of 43,732 adults who had bariatric surgery and were enrolled in a statewide database between June 2006 and December 2013. They found that the relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, which represents an increase of 61%, said Dr. Bradley N. Reames of the department of surgery and the Center for Healthcare Outcomes and Policy, University of Michigan, Ann Arbor, and his associates.
At the same time, the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%, they said (JAMA 2014;312:959-61).
"Moreover, despite controversy regarding the optimal procedure for patients with gastroesophageal reflux disease and type 2 diabetes, sleeve gastrectomy has become the predominant procedure in both groups," Dr. Reames and his associates said.
The long-term outcomes after sleeve gastrectomy are not yet clear, so this trend "may reflect the favorable perioperative safety profile and emerging evidence of successful weight loss at 2-3 years after" the procedure, they added.
Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
Sleeve gastrectomy appears to be replacing other types of bariatric surgery in Michigan, even among subgroups of patients in whom its use is controversial, according to a Research Letter to the Editor published in the Sept. 3 issue of JAMA.
To examine time trends in the use of various bariatric procedures, investigators reviewed the medical records of 43,732 adults who had bariatric surgery and were enrolled in a statewide database between June 2006 and December 2013. They found that the relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, which represents an increase of 61%, said Dr. Bradley N. Reames of the department of surgery and the Center for Healthcare Outcomes and Policy, University of Michigan, Ann Arbor, and his associates.
At the same time, the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%, they said (JAMA 2014;312:959-61).
"Moreover, despite controversy regarding the optimal procedure for patients with gastroesophageal reflux disease and type 2 diabetes, sleeve gastrectomy has become the predominant procedure in both groups," Dr. Reames and his associates said.
The long-term outcomes after sleeve gastrectomy are not yet clear, so this trend "may reflect the favorable perioperative safety profile and emerging evidence of successful weight loss at 2-3 years after" the procedure, they added.
Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
FROM JAMA
Major finding: The relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, while the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%.
Data Source: An analysis of data regarding 43,732 adults who had bariatric surgery and were registered in a statewide database in Michigan between 2006 and 2013.
Disclosures: Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
Successful bariatric surgery also may improve urinary incontinence
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
AT AUGS/IUGA 2014
Key clinical point: Obese women who report urinary incontinence may experience improvement or even resolution of symptoms after bariatric surgery.
Major finding: About one-quarter of the 772 severely obese women who reported having urinary incontinence before undergoing bariatric surgery had complete remission of urinary incontinence 3 years after surgery.
Data source: The frequency of urinary incontinence symptoms at baseline and for up to 3 years after bariatric surgery was evaluated in a substudy of 1,565 severely obese women who were enrolled in a multicenter, longitudinal cohort study based on self-administered questionnaires.
Disclosures: The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
Permacol shows low recurrence rates for hernia repair, even in high-risk patients
The collagen-based Permacol surgical implant is safe and feasible for incisional and ventral hernia repair, according to the authors of a study that found hernia recurrence probabilities of 5.8%, 16.6%, and 31.0% at 1, 2, and 3 years, respectively.
Retrospective data from 343 patients with 213 incisional and 130 ventral hernias, treated with the cross-linked porcine collagen product, showed open surgery was associated with a significantly higher rate of recurrence than laparoscopic surgery at 12 months (7.7% vs. 2.5%, P = .047).
Mesh location also affected recurrence rates at 12 months, with onlay (suprafascial) repair associated with an 18.9% recurrence rate, compared with 2.4% for underlay (subfascial, intraperitoneal) repair. But wound classification, wound infection, and seromas did not impact the risk of recurrence at 12 or 24 months (Int. J. Surg. 2014;12:296-303).
Dr. Bipan Chand of the Loyola Center for Metabolic Surgery and Bariatric Care, Loyola University, and colleagues described the study as the largest retrospective multinational study to date evaluating outcomes from hernia repair using Permacol.
"Despite an initially enthusiastic adoption [of collagen-based prosthetics] by the surgical community, clinical data supporting product safety and efficacy and proper indication is needed," the authors wrote.
"The use of biologics is still controversial in class III (contaminated) and IV (infected) wounds and fields with increased collagenase due to potential accelerated breakdown of the collagen-based materials in these more hostile environments and limited evidence of long-term efficacy under those conditions."
At the time of surgery, 8.2% of patients had class III wounds and 6.4% had class IV.
Researchers observed a 1-year hernia recurrence rate of 7.4% in clean wounds and 4.5% in dirty wounds, compared with another study using a non–cross-linked biologic that recorded recurrence rates of 39% in dirty wounds and 5% in clean wounds after 1 year.
There was a 15.2% rate of wound infection and a 19% incidence of seroma. In addition, there was a 3.2% incidence of hematoma and a 0.9% incidence of fistula. One patient required reoperation to remove the mesh, which the authors said was procedure related.
Biologic mesh such as Permacol includes an intact extracellular matrix that supports tissue incorporation, revascularization, and cell repopulation that may also help to clear bacterial contamination, the authors reported.
"Permacol surgical implant was shown to be safe and feasible with low rates of postoperative morbidity even in patients with higher risk of failure," the researchers wrote.
"We recommend optimizing controllable patient conditions, performing these complex operations on an elective basis, reducing the bioburden of the wound, and reapproximating the fascial midline while utilizing Permacol surgical implant as reinforcement."
The study was sponsored and funded by Covidien, who also provided editorial support. Most authors declared a range of honoraria, consultancies, lecture fees, and travel support, including from Covidien.
The collagen-based Permacol surgical implant is safe and feasible for incisional and ventral hernia repair, according to the authors of a study that found hernia recurrence probabilities of 5.8%, 16.6%, and 31.0% at 1, 2, and 3 years, respectively.
Retrospective data from 343 patients with 213 incisional and 130 ventral hernias, treated with the cross-linked porcine collagen product, showed open surgery was associated with a significantly higher rate of recurrence than laparoscopic surgery at 12 months (7.7% vs. 2.5%, P = .047).
Mesh location also affected recurrence rates at 12 months, with onlay (suprafascial) repair associated with an 18.9% recurrence rate, compared with 2.4% for underlay (subfascial, intraperitoneal) repair. But wound classification, wound infection, and seromas did not impact the risk of recurrence at 12 or 24 months (Int. J. Surg. 2014;12:296-303).
Dr. Bipan Chand of the Loyola Center for Metabolic Surgery and Bariatric Care, Loyola University, and colleagues described the study as the largest retrospective multinational study to date evaluating outcomes from hernia repair using Permacol.
"Despite an initially enthusiastic adoption [of collagen-based prosthetics] by the surgical community, clinical data supporting product safety and efficacy and proper indication is needed," the authors wrote.
"The use of biologics is still controversial in class III (contaminated) and IV (infected) wounds and fields with increased collagenase due to potential accelerated breakdown of the collagen-based materials in these more hostile environments and limited evidence of long-term efficacy under those conditions."
At the time of surgery, 8.2% of patients had class III wounds and 6.4% had class IV.
Researchers observed a 1-year hernia recurrence rate of 7.4% in clean wounds and 4.5% in dirty wounds, compared with another study using a non–cross-linked biologic that recorded recurrence rates of 39% in dirty wounds and 5% in clean wounds after 1 year.
There was a 15.2% rate of wound infection and a 19% incidence of seroma. In addition, there was a 3.2% incidence of hematoma and a 0.9% incidence of fistula. One patient required reoperation to remove the mesh, which the authors said was procedure related.
Biologic mesh such as Permacol includes an intact extracellular matrix that supports tissue incorporation, revascularization, and cell repopulation that may also help to clear bacterial contamination, the authors reported.
"Permacol surgical implant was shown to be safe and feasible with low rates of postoperative morbidity even in patients with higher risk of failure," the researchers wrote.
"We recommend optimizing controllable patient conditions, performing these complex operations on an elective basis, reducing the bioburden of the wound, and reapproximating the fascial midline while utilizing Permacol surgical implant as reinforcement."
The study was sponsored and funded by Covidien, who also provided editorial support. Most authors declared a range of honoraria, consultancies, lecture fees, and travel support, including from Covidien.
The collagen-based Permacol surgical implant is safe and feasible for incisional and ventral hernia repair, according to the authors of a study that found hernia recurrence probabilities of 5.8%, 16.6%, and 31.0% at 1, 2, and 3 years, respectively.
Retrospective data from 343 patients with 213 incisional and 130 ventral hernias, treated with the cross-linked porcine collagen product, showed open surgery was associated with a significantly higher rate of recurrence than laparoscopic surgery at 12 months (7.7% vs. 2.5%, P = .047).
Mesh location also affected recurrence rates at 12 months, with onlay (suprafascial) repair associated with an 18.9% recurrence rate, compared with 2.4% for underlay (subfascial, intraperitoneal) repair. But wound classification, wound infection, and seromas did not impact the risk of recurrence at 12 or 24 months (Int. J. Surg. 2014;12:296-303).
Dr. Bipan Chand of the Loyola Center for Metabolic Surgery and Bariatric Care, Loyola University, and colleagues described the study as the largest retrospective multinational study to date evaluating outcomes from hernia repair using Permacol.
"Despite an initially enthusiastic adoption [of collagen-based prosthetics] by the surgical community, clinical data supporting product safety and efficacy and proper indication is needed," the authors wrote.
"The use of biologics is still controversial in class III (contaminated) and IV (infected) wounds and fields with increased collagenase due to potential accelerated breakdown of the collagen-based materials in these more hostile environments and limited evidence of long-term efficacy under those conditions."
At the time of surgery, 8.2% of patients had class III wounds and 6.4% had class IV.
Researchers observed a 1-year hernia recurrence rate of 7.4% in clean wounds and 4.5% in dirty wounds, compared with another study using a non–cross-linked biologic that recorded recurrence rates of 39% in dirty wounds and 5% in clean wounds after 1 year.
There was a 15.2% rate of wound infection and a 19% incidence of seroma. In addition, there was a 3.2% incidence of hematoma and a 0.9% incidence of fistula. One patient required reoperation to remove the mesh, which the authors said was procedure related.
Biologic mesh such as Permacol includes an intact extracellular matrix that supports tissue incorporation, revascularization, and cell repopulation that may also help to clear bacterial contamination, the authors reported.
"Permacol surgical implant was shown to be safe and feasible with low rates of postoperative morbidity even in patients with higher risk of failure," the researchers wrote.
"We recommend optimizing controllable patient conditions, performing these complex operations on an elective basis, reducing the bioburden of the wound, and reapproximating the fascial midline while utilizing Permacol surgical implant as reinforcement."
The study was sponsored and funded by Covidien, who also provided editorial support. Most authors declared a range of honoraria, consultancies, lecture fees, and travel support, including from Covidien.
FROM INTERNATIONAL JOURNAL OF SURGERY
Key clinical point: For hernia repair, consider utilizing Permacol surgical implant in cases where controllable patient conditions can be optimized and the bioburden of the wound can be reduced.
Major finding: The cross-linked porcine collagen surgical implant Permacol is associated with hernia recurrence probabilities of 5.8%, 16.6%, and 31.0% at 1, 2, and 3 years, respectively.
Data source: A retrospective, multinational cohort study
Disclosures: The study was sponsored and funded by Covidien, who also provided editorial support. Most authors declared a range of honoraria, consultancies, lecture fees, and travel support, including from Covidien.
Postbariatric cholecystectomy most common among Roux-en-Y patients
The overall rate of cholecystectomy after weight loss surgery is low, but it is more likely to occur among patients who experience excessive weight loss following their procedure and those who undergo laparoscopic Roux-en-Y gastric bypass.
Analysis of prospective data from 1,398 patients undergoing bariatric surgery showed an overall cholecystectomy rate of 7.8% over a median follow-up of 49 months, with the frequency higher in the first 6 months, according to data published in Surgery for Obesity and Related Diseases.
Cholecystectomy rates were significantly higher among individuals who underwent laparoscopic Roux-en-Y gastric bypass (LRYGB), compared with those who received a laparoscopic adjustable gastric band (LAGB) or laparoscopic sleeve gastrectomy (LSG) (10.6% vs. 2.9% vs. 3.5%, P = .001).
"Although the LRYGB was the procedure associated with the highest rate of cholecystectomy, the present study found that this relationship was due to the superior %EWL [percent excess weight loss] associated with this procedure, compared with the LAGB and LSG procedures," wrote the late Dr. Victor B. Tsirline of Northwestern Memorial Hospital, and his colleagues.
Patients who lost more than a quarter of their weight within 3 months of surgery showed significantly higher rates of cholecystectomy, and there was a 25% increase in cholecystectomy per 10% of excess weight loss within the first 3 months after weight loss surgery, although this association was only significant among patients treated with gastric bypass (Surg. Obes. Relat. Dis. 2014;10:313-21).
There were statistically significant differences in cholecystectomy rates performed by the three surgeons involved, although again, this was only in patients who had undergone gastric bypass, and researchers said this could be partly attributed to the fact that one surgeon saw a greater proportion of revision patients.
Researchers also noted an interaction with race, as black patients had significantly lower rates of cholecystectomy, compared with white patients (2.2% vs. 8.9%, P = .0001), and Native American patients showed the highest rates of all (65%).
This study found no difference in cholecystectomy rates between patients taking ursodiol and those who weren’t.
Rapid weight loss after bariatric surgery is associated with an increased risk of gallstones, and routine cholecystectomy at the time of bariatric surgery has been the subject of considerable debate.
Those in favor argue that it prevents the morbidity of symptomatic cholelithiasis and avoids the risk of duct stones which can be difficult to treat after gastric bypass.
However opponents say routine cholecystectomy would prolong hospital stays, lengthen operating times, and potentially increase complication rates, when the use of ursodiol after weight loss surgery has been shown to decrease the frequency of gallstones.
"The findings of the present study indicate that a conservative approach to cholecystectomy, rather than prophylactic cholecystectomy, is warranted, because only 7.8% of patients developed symptomatic gallbladder disease within 4 years on average," researchers wrote.
"Furthermore, there are technical advantages of delayed cholecystectomy that stem from reduced intra-abdominal fat content and decreased liver size secondary to weight loss."
There were no conflicts of interest declared.
The overall rate of cholecystectomy after weight loss surgery is low, but it is more likely to occur among patients who experience excessive weight loss following their procedure and those who undergo laparoscopic Roux-en-Y gastric bypass.
Analysis of prospective data from 1,398 patients undergoing bariatric surgery showed an overall cholecystectomy rate of 7.8% over a median follow-up of 49 months, with the frequency higher in the first 6 months, according to data published in Surgery for Obesity and Related Diseases.
Cholecystectomy rates were significantly higher among individuals who underwent laparoscopic Roux-en-Y gastric bypass (LRYGB), compared with those who received a laparoscopic adjustable gastric band (LAGB) or laparoscopic sleeve gastrectomy (LSG) (10.6% vs. 2.9% vs. 3.5%, P = .001).
"Although the LRYGB was the procedure associated with the highest rate of cholecystectomy, the present study found that this relationship was due to the superior %EWL [percent excess weight loss] associated with this procedure, compared with the LAGB and LSG procedures," wrote the late Dr. Victor B. Tsirline of Northwestern Memorial Hospital, and his colleagues.
Patients who lost more than a quarter of their weight within 3 months of surgery showed significantly higher rates of cholecystectomy, and there was a 25% increase in cholecystectomy per 10% of excess weight loss within the first 3 months after weight loss surgery, although this association was only significant among patients treated with gastric bypass (Surg. Obes. Relat. Dis. 2014;10:313-21).
There were statistically significant differences in cholecystectomy rates performed by the three surgeons involved, although again, this was only in patients who had undergone gastric bypass, and researchers said this could be partly attributed to the fact that one surgeon saw a greater proportion of revision patients.
Researchers also noted an interaction with race, as black patients had significantly lower rates of cholecystectomy, compared with white patients (2.2% vs. 8.9%, P = .0001), and Native American patients showed the highest rates of all (65%).
This study found no difference in cholecystectomy rates between patients taking ursodiol and those who weren’t.
Rapid weight loss after bariatric surgery is associated with an increased risk of gallstones, and routine cholecystectomy at the time of bariatric surgery has been the subject of considerable debate.
Those in favor argue that it prevents the morbidity of symptomatic cholelithiasis and avoids the risk of duct stones which can be difficult to treat after gastric bypass.
However opponents say routine cholecystectomy would prolong hospital stays, lengthen operating times, and potentially increase complication rates, when the use of ursodiol after weight loss surgery has been shown to decrease the frequency of gallstones.
"The findings of the present study indicate that a conservative approach to cholecystectomy, rather than prophylactic cholecystectomy, is warranted, because only 7.8% of patients developed symptomatic gallbladder disease within 4 years on average," researchers wrote.
"Furthermore, there are technical advantages of delayed cholecystectomy that stem from reduced intra-abdominal fat content and decreased liver size secondary to weight loss."
There were no conflicts of interest declared.
The overall rate of cholecystectomy after weight loss surgery is low, but it is more likely to occur among patients who experience excessive weight loss following their procedure and those who undergo laparoscopic Roux-en-Y gastric bypass.
Analysis of prospective data from 1,398 patients undergoing bariatric surgery showed an overall cholecystectomy rate of 7.8% over a median follow-up of 49 months, with the frequency higher in the first 6 months, according to data published in Surgery for Obesity and Related Diseases.
Cholecystectomy rates were significantly higher among individuals who underwent laparoscopic Roux-en-Y gastric bypass (LRYGB), compared with those who received a laparoscopic adjustable gastric band (LAGB) or laparoscopic sleeve gastrectomy (LSG) (10.6% vs. 2.9% vs. 3.5%, P = .001).
"Although the LRYGB was the procedure associated with the highest rate of cholecystectomy, the present study found that this relationship was due to the superior %EWL [percent excess weight loss] associated with this procedure, compared with the LAGB and LSG procedures," wrote the late Dr. Victor B. Tsirline of Northwestern Memorial Hospital, and his colleagues.
Patients who lost more than a quarter of their weight within 3 months of surgery showed significantly higher rates of cholecystectomy, and there was a 25% increase in cholecystectomy per 10% of excess weight loss within the first 3 months after weight loss surgery, although this association was only significant among patients treated with gastric bypass (Surg. Obes. Relat. Dis. 2014;10:313-21).
There were statistically significant differences in cholecystectomy rates performed by the three surgeons involved, although again, this was only in patients who had undergone gastric bypass, and researchers said this could be partly attributed to the fact that one surgeon saw a greater proportion of revision patients.
Researchers also noted an interaction with race, as black patients had significantly lower rates of cholecystectomy, compared with white patients (2.2% vs. 8.9%, P = .0001), and Native American patients showed the highest rates of all (65%).
This study found no difference in cholecystectomy rates between patients taking ursodiol and those who weren’t.
Rapid weight loss after bariatric surgery is associated with an increased risk of gallstones, and routine cholecystectomy at the time of bariatric surgery has been the subject of considerable debate.
Those in favor argue that it prevents the morbidity of symptomatic cholelithiasis and avoids the risk of duct stones which can be difficult to treat after gastric bypass.
However opponents say routine cholecystectomy would prolong hospital stays, lengthen operating times, and potentially increase complication rates, when the use of ursodiol after weight loss surgery has been shown to decrease the frequency of gallstones.
"The findings of the present study indicate that a conservative approach to cholecystectomy, rather than prophylactic cholecystectomy, is warranted, because only 7.8% of patients developed symptomatic gallbladder disease within 4 years on average," researchers wrote.
"Furthermore, there are technical advantages of delayed cholecystectomy that stem from reduced intra-abdominal fat content and decreased liver size secondary to weight loss."
There were no conflicts of interest declared.
FROM SURGERY FOR OBESITY AND RELATED DISEASES
Key clinical point: Prophylactic cholecystectomy may not be necessary in bariatric surgery since few of patients develop symptomatic gallbladder disease.
Major finding: The overall rate of cholecystectomy after weight loss surgery is 7.8% but the incidence is greater with laparoscopic Roux-en-Y gastric bypass and among patients who lose more than 25% of their weight in the first 3 months after surgery.
Data source: Analysis of prospective data from 1,398 patients undergoing bariatric surgery.
Disclosures: No relevant conflicts of interest disclosed.
Medical consultation rates for surgical cases vary
The use of inpatient medical consultations for hospitalized surgical patients was found to vary by hospital, but consultations didn’t appear to have much of an impact on risk-adjusted 30-day mortality rates, a study found.
Rates of medical consultations varied from 50% to 91% among 91,684 patients undergoing colectomy and from 36% to 90% among 339,319 patients undergoing total hip replacements, a retrospective study found.
The variation was most dramatic for patients undergoing colectomy who did not have complications, among whom rates of inpatient medical consultation ranged from 47% to 79% between hospitals, Dr. Lena M. Chen and her associates reported. For patients undergoing colectomy who did have complications, 90%-95% received medical consultations.
Similarly, variation in the use of medical consultation for patients getting total hip replacement was wider for those without complications (36%-87%), compared with patients with complications (89%-94%).
The results highlight the fact that there’s no consensus on when and how to best provide medical consultation for hospitalized surgical patients. "Wide variation in medical consultation use – particularly among patients without complications – suggests that understanding when medical consultations provide value will be important as hospitals seek to increase their efficiency under bundled payments," wrote Dr. Chen of the University of Michigan, Ann Arbor (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.3376]).
She and her associates analyzed Medicare claims data and American Hospital Association data on patients aged 65-99 years who underwent colectomy at 930 hospitals or total hip replacement at 1,589 hospitals in 2007-2010. These are 2 of the top 10 procedures performed on Medicare patients, and total hip replacement is included in the Centers for Medicare & Medicaid Services bundled payment demonstration project, the authors noted.
At least one medical consultant saw 69% of patients undergoing colectomy and 63% of patients getting a total hip replacement. Among patients who got consultations, colectomy patients saw consultants a median of nine times, and hip replacement patients saw consultants a median of three times.
Colectomy patients most often saw general medicine consultants (50%), followed by cardiologists (28%), oncologists (25%), or gastroenterologists (22%). Among patients receiving total hip replacement, 53% had a general medicine consultation, and the most common specialist consultations were for physical medicine and rehabilitation (11%) or cardiology (8%).
Approximately a third of hip replacement patients were "comanaged" by surgeons and medical consultants, defined by records of a claim for evaluation and management by a medicine physician on at least 70% of inpatient days.
It seems logical to assume that extra care from nonsurgical physicians should improve outcomes for some surgical patients, but an exploratory analysis of the data found that risk-adjusted 30-day mortality rates were not significantly different between hospitals with the greatest or least use of medical consultations, Dr. Chen reported. The 30-day mortality rate for colectomy patients was 5% at hospitals in the lowest quintile of medical consultations and 6% at hospitals in the highest quintile. The results for total hip replacement were similar.
Greater use of medical consultation was associated with a significantly greater likelihood of having at least one postoperative complication, affecting 24% of colectomy patients at hospitals in the lowest quintile of consultations and 28% at hospitals in the highest quintile. The results for total hip replacement were similar.
The National Institute of Aging and a University of Michigan McCubed grant funded the study. Dr. Chen reported having no relevant financial disclosures. One of her coinvestigators owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
On Twitter @sherryboschert
Dr. Chen’s findings that rates of medical consultation varied widely for surgical patients without complications complement a 2010 study by Dr. Gulshan Sharma and his associates that found 35% of patients hospitalized for a common surgical procedure were comanaged by medicine physicians (Arch. Intern. Med. 2010;170:363-8).
"I agree [with Dr. Chen] that understanding the ‘value’ of medical consultation is an important next step, especially in low-risk patients undergoing elective surgery," Dr. Sharma commented in an article accompanying Dr. Chen’s study (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.1499]).
Comanagement may benefit patients by increasing the use of evidence-based treatments or reducing the time to surgery, postoperative complications, the need for ICU care, the length of stay, and readmission rates, among other possibilities. But there are possible downsides, too, including potential confusion among caregivers, more complicated decision making, lack of "ownership" of problems, or added costs, he noted.
Hospitals with the greatest use of medical consultation in Dr. Chen’s study had higher risk-adjusted rates of 30-day mortality and complications, compared with hospitals with the least use of medical consultation (though the difference in mortality was not statistically significant). "Is there a potential harm associated with medical consultation?" Dr. Sharma asked.
"There is no one fit for all" hospitals, he wrote. Institutional data on quality and cost should drive decisions on the routine use of medical consultation. The practice of mandating comanagement of all surgical patients "should be discouraged," Dr. Sharma said. "During preoperative evaluation, patients with comorbid conditions and those at significant risk of postoperative complications should be considered for medical comanagement."
Dr. Sharma is director of the division of pulmonary critical care and sleep medicine at the University of Texas Medical Branch, Galveston. He reported having no relevant financial disclosures.
Dr. Chen’s findings that rates of medical consultation varied widely for surgical patients without complications complement a 2010 study by Dr. Gulshan Sharma and his associates that found 35% of patients hospitalized for a common surgical procedure were comanaged by medicine physicians (Arch. Intern. Med. 2010;170:363-8).
"I agree [with Dr. Chen] that understanding the ‘value’ of medical consultation is an important next step, especially in low-risk patients undergoing elective surgery," Dr. Sharma commented in an article accompanying Dr. Chen’s study (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.1499]).
Comanagement may benefit patients by increasing the use of evidence-based treatments or reducing the time to surgery, postoperative complications, the need for ICU care, the length of stay, and readmission rates, among other possibilities. But there are possible downsides, too, including potential confusion among caregivers, more complicated decision making, lack of "ownership" of problems, or added costs, he noted.
Hospitals with the greatest use of medical consultation in Dr. Chen’s study had higher risk-adjusted rates of 30-day mortality and complications, compared with hospitals with the least use of medical consultation (though the difference in mortality was not statistically significant). "Is there a potential harm associated with medical consultation?" Dr. Sharma asked.
"There is no one fit for all" hospitals, he wrote. Institutional data on quality and cost should drive decisions on the routine use of medical consultation. The practice of mandating comanagement of all surgical patients "should be discouraged," Dr. Sharma said. "During preoperative evaluation, patients with comorbid conditions and those at significant risk of postoperative complications should be considered for medical comanagement."
Dr. Sharma is director of the division of pulmonary critical care and sleep medicine at the University of Texas Medical Branch, Galveston. He reported having no relevant financial disclosures.
Dr. Chen’s findings that rates of medical consultation varied widely for surgical patients without complications complement a 2010 study by Dr. Gulshan Sharma and his associates that found 35% of patients hospitalized for a common surgical procedure were comanaged by medicine physicians (Arch. Intern. Med. 2010;170:363-8).
"I agree [with Dr. Chen] that understanding the ‘value’ of medical consultation is an important next step, especially in low-risk patients undergoing elective surgery," Dr. Sharma commented in an article accompanying Dr. Chen’s study (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.1499]).
Comanagement may benefit patients by increasing the use of evidence-based treatments or reducing the time to surgery, postoperative complications, the need for ICU care, the length of stay, and readmission rates, among other possibilities. But there are possible downsides, too, including potential confusion among caregivers, more complicated decision making, lack of "ownership" of problems, or added costs, he noted.
Hospitals with the greatest use of medical consultation in Dr. Chen’s study had higher risk-adjusted rates of 30-day mortality and complications, compared with hospitals with the least use of medical consultation (though the difference in mortality was not statistically significant). "Is there a potential harm associated with medical consultation?" Dr. Sharma asked.
"There is no one fit for all" hospitals, he wrote. Institutional data on quality and cost should drive decisions on the routine use of medical consultation. The practice of mandating comanagement of all surgical patients "should be discouraged," Dr. Sharma said. "During preoperative evaluation, patients with comorbid conditions and those at significant risk of postoperative complications should be considered for medical comanagement."
Dr. Sharma is director of the division of pulmonary critical care and sleep medicine at the University of Texas Medical Branch, Galveston. He reported having no relevant financial disclosures.
The use of inpatient medical consultations for hospitalized surgical patients was found to vary by hospital, but consultations didn’t appear to have much of an impact on risk-adjusted 30-day mortality rates, a study found.
Rates of medical consultations varied from 50% to 91% among 91,684 patients undergoing colectomy and from 36% to 90% among 339,319 patients undergoing total hip replacements, a retrospective study found.
The variation was most dramatic for patients undergoing colectomy who did not have complications, among whom rates of inpatient medical consultation ranged from 47% to 79% between hospitals, Dr. Lena M. Chen and her associates reported. For patients undergoing colectomy who did have complications, 90%-95% received medical consultations.
Similarly, variation in the use of medical consultation for patients getting total hip replacement was wider for those without complications (36%-87%), compared with patients with complications (89%-94%).
The results highlight the fact that there’s no consensus on when and how to best provide medical consultation for hospitalized surgical patients. "Wide variation in medical consultation use – particularly among patients without complications – suggests that understanding when medical consultations provide value will be important as hospitals seek to increase their efficiency under bundled payments," wrote Dr. Chen of the University of Michigan, Ann Arbor (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.3376]).
She and her associates analyzed Medicare claims data and American Hospital Association data on patients aged 65-99 years who underwent colectomy at 930 hospitals or total hip replacement at 1,589 hospitals in 2007-2010. These are 2 of the top 10 procedures performed on Medicare patients, and total hip replacement is included in the Centers for Medicare & Medicaid Services bundled payment demonstration project, the authors noted.
At least one medical consultant saw 69% of patients undergoing colectomy and 63% of patients getting a total hip replacement. Among patients who got consultations, colectomy patients saw consultants a median of nine times, and hip replacement patients saw consultants a median of three times.
Colectomy patients most often saw general medicine consultants (50%), followed by cardiologists (28%), oncologists (25%), or gastroenterologists (22%). Among patients receiving total hip replacement, 53% had a general medicine consultation, and the most common specialist consultations were for physical medicine and rehabilitation (11%) or cardiology (8%).
Approximately a third of hip replacement patients were "comanaged" by surgeons and medical consultants, defined by records of a claim for evaluation and management by a medicine physician on at least 70% of inpatient days.
It seems logical to assume that extra care from nonsurgical physicians should improve outcomes for some surgical patients, but an exploratory analysis of the data found that risk-adjusted 30-day mortality rates were not significantly different between hospitals with the greatest or least use of medical consultations, Dr. Chen reported. The 30-day mortality rate for colectomy patients was 5% at hospitals in the lowest quintile of medical consultations and 6% at hospitals in the highest quintile. The results for total hip replacement were similar.
Greater use of medical consultation was associated with a significantly greater likelihood of having at least one postoperative complication, affecting 24% of colectomy patients at hospitals in the lowest quintile of consultations and 28% at hospitals in the highest quintile. The results for total hip replacement were similar.
The National Institute of Aging and a University of Michigan McCubed grant funded the study. Dr. Chen reported having no relevant financial disclosures. One of her coinvestigators owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
On Twitter @sherryboschert
The use of inpatient medical consultations for hospitalized surgical patients was found to vary by hospital, but consultations didn’t appear to have much of an impact on risk-adjusted 30-day mortality rates, a study found.
Rates of medical consultations varied from 50% to 91% among 91,684 patients undergoing colectomy and from 36% to 90% among 339,319 patients undergoing total hip replacements, a retrospective study found.
The variation was most dramatic for patients undergoing colectomy who did not have complications, among whom rates of inpatient medical consultation ranged from 47% to 79% between hospitals, Dr. Lena M. Chen and her associates reported. For patients undergoing colectomy who did have complications, 90%-95% received medical consultations.
Similarly, variation in the use of medical consultation for patients getting total hip replacement was wider for those without complications (36%-87%), compared with patients with complications (89%-94%).
The results highlight the fact that there’s no consensus on when and how to best provide medical consultation for hospitalized surgical patients. "Wide variation in medical consultation use – particularly among patients without complications – suggests that understanding when medical consultations provide value will be important as hospitals seek to increase their efficiency under bundled payments," wrote Dr. Chen of the University of Michigan, Ann Arbor (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.3376]).
She and her associates analyzed Medicare claims data and American Hospital Association data on patients aged 65-99 years who underwent colectomy at 930 hospitals or total hip replacement at 1,589 hospitals in 2007-2010. These are 2 of the top 10 procedures performed on Medicare patients, and total hip replacement is included in the Centers for Medicare & Medicaid Services bundled payment demonstration project, the authors noted.
At least one medical consultant saw 69% of patients undergoing colectomy and 63% of patients getting a total hip replacement. Among patients who got consultations, colectomy patients saw consultants a median of nine times, and hip replacement patients saw consultants a median of three times.
Colectomy patients most often saw general medicine consultants (50%), followed by cardiologists (28%), oncologists (25%), or gastroenterologists (22%). Among patients receiving total hip replacement, 53% had a general medicine consultation, and the most common specialist consultations were for physical medicine and rehabilitation (11%) or cardiology (8%).
Approximately a third of hip replacement patients were "comanaged" by surgeons and medical consultants, defined by records of a claim for evaluation and management by a medicine physician on at least 70% of inpatient days.
It seems logical to assume that extra care from nonsurgical physicians should improve outcomes for some surgical patients, but an exploratory analysis of the data found that risk-adjusted 30-day mortality rates were not significantly different between hospitals with the greatest or least use of medical consultations, Dr. Chen reported. The 30-day mortality rate for colectomy patients was 5% at hospitals in the lowest quintile of medical consultations and 6% at hospitals in the highest quintile. The results for total hip replacement were similar.
Greater use of medical consultation was associated with a significantly greater likelihood of having at least one postoperative complication, affecting 24% of colectomy patients at hospitals in the lowest quintile of consultations and 28% at hospitals in the highest quintile. The results for total hip replacement were similar.
The National Institute of Aging and a University of Michigan McCubed grant funded the study. Dr. Chen reported having no relevant financial disclosures. One of her coinvestigators owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
On Twitter @sherryboschert
FROM JAMA INTERNAL MEDICINE
Key clinical point: In the era of bundled payments for episodes of care, consider when and how medical consultation for surgical patients is helpful.
Major finding: Use of medical consultations ranged from 50%-91% for colectomies and 36%-90% for total hip replacements.
Data source: A retrospective study of Medicare data on 431,003 older adults undergoing colectomy or total hip replacement in 2007-2010.
Disclosures: Dr. Chen reported having no financial disclosures. One of her associates owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
Long-term benefits shown after gastric banding
SAN FRANCISCO – The greater benefits of laparoscopic gastric banding surgery compared with medical treatment for obese patients were maintained for up to 17 years in a study of data on 1,490 patients.
The 527 obese patients (with or without diabetes) who underwent laparoscopic banding were significantly less likely to die of cardiovascular or noncardiovascular causes and were less likely to develop new cases of type 2 diabetes or cardiovascular disease, compared with the 963 nonsurgery patients, Dr. Antonio E. Pontiroli and his associates reported at the annual scientific sessions of the American Diabetes Association.
Patients underwent laparoscopic banding surgery or were seen for a first visit for medical therapy in 1995-2001, and were followed for 11-17 years, through September 2012.
Three percent of the surgery group and 10% of the nonsurgery group died during follow-up, reported Dr. Pontiroli, chair of internal medicine at Università Degli Studi de Milano and San Paolo Hospital, Milan.
To track morbidity, the investigators analyzed records to see which patients got "exemptions" for specific diseases, an Italian government system in which development of a chronic disease exempts someone from having to pay for exams or treatments for that disease. Any exemption obtained after the first surgical or medical visit was considered a proxy of new disease.
New exemptions were granted to 25% in the surgery group and 42% in the nonsurgery group.
Subset analyses divided 385 surgery patients based on the presence or absence of diabetes, and matched the subgroups separately with 681 nonsurgery patients by sex, age, blood pressure, and body mass index.
In the matched comparisons, 3% of the surgery group and 10% of the nonsurgery group died, and exemptions were granted to 22% of the surgery group and 28% of the nonsurgery group, which were statistically significant differences in the intention-to-treat analyses.
Patients in the surgery group were 66% less likely to die than the nonsurgery patients. Patients without diabetes at the first visit were 67% less likely to die than matched nonsurgery patients, and those with diabetes at the first visit were 56% less likely to die compared with matched nonsurgery patients.
Cardiovascular disease, noncardiovascular disease, or neoplasia were significantly less likely to be the causes of death in the surgery group compared with the nonsurgery group. The surgery group recorded significantly fewer hospitalizations during follow-up (120) than the nonsurgery group (273).
New cases of cardiovascular disease (defined by exemptions) appeared in 13% of the surgery group and 22% of the nonsurgery group. In the matched subgroups, 13% who underwent surgery and 18% in the nonsurgery group developed cardiovascular disease.
Among patients without diabetes at baseline, 5% of 454 in the surgery group and 10% of 724 in the nonsurgery group developed diabetes during follow-up. In the subset analysis of matched patients without diabetes at baseline, 4% of 333 in the surgery group and 9% in the nonsurgery group developed diabetes.
The investigators plan another data assessment in 2017 to confirm these long-term findings. Similar studies are needed for other bariatric surgery techniques, he suggested.
Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
On Twitter @sherryboschert
This is a very interesting study. It was a long-term study, over 17 years, of patients who’d had gastric banding in Milan, looking at development of cardiovascular disease, type 2 diabetes, and death. It is reassuring that there did appear to be favorable outcomes.
There clearly are limitations to the study. The researchers only looked at banding; they didn’t look at sleeve gastrectomies or gastric bypass. The study is specifically related to banding. The comparisons with medical therapies didn’t really define the medical therapies. We’d obviously need details on what they were comparing and whether there are subgroup analyses that could be done.
Nonetheless, they did show that there’s a significant improvement in death rates, cardiovascular death, all-cause death, development of type 2 diabetes, and new cases of cardiovascular disease both in the whole population and in the matched groups. I think these are useful data that are kind of reassuring.
The other thing I would mention: Although bariatric surgery has been done for many years now, it’s really only over the last 10-15 years that the numbers of surgeries have increased hugely. It will be interesting to see the outcomes of the most current cohort over the next 10-15 years.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the Warwick Medical School, Coventry, England. He gave these comments in an interview at the meeting. Dr. Barber reported having no financial disclosures.
This is a very interesting study. It was a long-term study, over 17 years, of patients who’d had gastric banding in Milan, looking at development of cardiovascular disease, type 2 diabetes, and death. It is reassuring that there did appear to be favorable outcomes.
There clearly are limitations to the study. The researchers only looked at banding; they didn’t look at sleeve gastrectomies or gastric bypass. The study is specifically related to banding. The comparisons with medical therapies didn’t really define the medical therapies. We’d obviously need details on what they were comparing and whether there are subgroup analyses that could be done.
Nonetheless, they did show that there’s a significant improvement in death rates, cardiovascular death, all-cause death, development of type 2 diabetes, and new cases of cardiovascular disease both in the whole population and in the matched groups. I think these are useful data that are kind of reassuring.
The other thing I would mention: Although bariatric surgery has been done for many years now, it’s really only over the last 10-15 years that the numbers of surgeries have increased hugely. It will be interesting to see the outcomes of the most current cohort over the next 10-15 years.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the Warwick Medical School, Coventry, England. He gave these comments in an interview at the meeting. Dr. Barber reported having no financial disclosures.
This is a very interesting study. It was a long-term study, over 17 years, of patients who’d had gastric banding in Milan, looking at development of cardiovascular disease, type 2 diabetes, and death. It is reassuring that there did appear to be favorable outcomes.
There clearly are limitations to the study. The researchers only looked at banding; they didn’t look at sleeve gastrectomies or gastric bypass. The study is specifically related to banding. The comparisons with medical therapies didn’t really define the medical therapies. We’d obviously need details on what they were comparing and whether there are subgroup analyses that could be done.
Nonetheless, they did show that there’s a significant improvement in death rates, cardiovascular death, all-cause death, development of type 2 diabetes, and new cases of cardiovascular disease both in the whole population and in the matched groups. I think these are useful data that are kind of reassuring.
The other thing I would mention: Although bariatric surgery has been done for many years now, it’s really only over the last 10-15 years that the numbers of surgeries have increased hugely. It will be interesting to see the outcomes of the most current cohort over the next 10-15 years.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the Warwick Medical School, Coventry, England. He gave these comments in an interview at the meeting. Dr. Barber reported having no financial disclosures.
SAN FRANCISCO – The greater benefits of laparoscopic gastric banding surgery compared with medical treatment for obese patients were maintained for up to 17 years in a study of data on 1,490 patients.
The 527 obese patients (with or without diabetes) who underwent laparoscopic banding were significantly less likely to die of cardiovascular or noncardiovascular causes and were less likely to develop new cases of type 2 diabetes or cardiovascular disease, compared with the 963 nonsurgery patients, Dr. Antonio E. Pontiroli and his associates reported at the annual scientific sessions of the American Diabetes Association.
Patients underwent laparoscopic banding surgery or were seen for a first visit for medical therapy in 1995-2001, and were followed for 11-17 years, through September 2012.
Three percent of the surgery group and 10% of the nonsurgery group died during follow-up, reported Dr. Pontiroli, chair of internal medicine at Università Degli Studi de Milano and San Paolo Hospital, Milan.
To track morbidity, the investigators analyzed records to see which patients got "exemptions" for specific diseases, an Italian government system in which development of a chronic disease exempts someone from having to pay for exams or treatments for that disease. Any exemption obtained after the first surgical or medical visit was considered a proxy of new disease.
New exemptions were granted to 25% in the surgery group and 42% in the nonsurgery group.
Subset analyses divided 385 surgery patients based on the presence or absence of diabetes, and matched the subgroups separately with 681 nonsurgery patients by sex, age, blood pressure, and body mass index.
In the matched comparisons, 3% of the surgery group and 10% of the nonsurgery group died, and exemptions were granted to 22% of the surgery group and 28% of the nonsurgery group, which were statistically significant differences in the intention-to-treat analyses.
Patients in the surgery group were 66% less likely to die than the nonsurgery patients. Patients without diabetes at the first visit were 67% less likely to die than matched nonsurgery patients, and those with diabetes at the first visit were 56% less likely to die compared with matched nonsurgery patients.
Cardiovascular disease, noncardiovascular disease, or neoplasia were significantly less likely to be the causes of death in the surgery group compared with the nonsurgery group. The surgery group recorded significantly fewer hospitalizations during follow-up (120) than the nonsurgery group (273).
New cases of cardiovascular disease (defined by exemptions) appeared in 13% of the surgery group and 22% of the nonsurgery group. In the matched subgroups, 13% who underwent surgery and 18% in the nonsurgery group developed cardiovascular disease.
Among patients without diabetes at baseline, 5% of 454 in the surgery group and 10% of 724 in the nonsurgery group developed diabetes during follow-up. In the subset analysis of matched patients without diabetes at baseline, 4% of 333 in the surgery group and 9% in the nonsurgery group developed diabetes.
The investigators plan another data assessment in 2017 to confirm these long-term findings. Similar studies are needed for other bariatric surgery techniques, he suggested.
Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
On Twitter @sherryboschert
SAN FRANCISCO – The greater benefits of laparoscopic gastric banding surgery compared with medical treatment for obese patients were maintained for up to 17 years in a study of data on 1,490 patients.
The 527 obese patients (with or without diabetes) who underwent laparoscopic banding were significantly less likely to die of cardiovascular or noncardiovascular causes and were less likely to develop new cases of type 2 diabetes or cardiovascular disease, compared with the 963 nonsurgery patients, Dr. Antonio E. Pontiroli and his associates reported at the annual scientific sessions of the American Diabetes Association.
Patients underwent laparoscopic banding surgery or were seen for a first visit for medical therapy in 1995-2001, and were followed for 11-17 years, through September 2012.
Three percent of the surgery group and 10% of the nonsurgery group died during follow-up, reported Dr. Pontiroli, chair of internal medicine at Università Degli Studi de Milano and San Paolo Hospital, Milan.
To track morbidity, the investigators analyzed records to see which patients got "exemptions" for specific diseases, an Italian government system in which development of a chronic disease exempts someone from having to pay for exams or treatments for that disease. Any exemption obtained after the first surgical or medical visit was considered a proxy of new disease.
New exemptions were granted to 25% in the surgery group and 42% in the nonsurgery group.
Subset analyses divided 385 surgery patients based on the presence or absence of diabetes, and matched the subgroups separately with 681 nonsurgery patients by sex, age, blood pressure, and body mass index.
In the matched comparisons, 3% of the surgery group and 10% of the nonsurgery group died, and exemptions were granted to 22% of the surgery group and 28% of the nonsurgery group, which were statistically significant differences in the intention-to-treat analyses.
Patients in the surgery group were 66% less likely to die than the nonsurgery patients. Patients without diabetes at the first visit were 67% less likely to die than matched nonsurgery patients, and those with diabetes at the first visit were 56% less likely to die compared with matched nonsurgery patients.
Cardiovascular disease, noncardiovascular disease, or neoplasia were significantly less likely to be the causes of death in the surgery group compared with the nonsurgery group. The surgery group recorded significantly fewer hospitalizations during follow-up (120) than the nonsurgery group (273).
New cases of cardiovascular disease (defined by exemptions) appeared in 13% of the surgery group and 22% of the nonsurgery group. In the matched subgroups, 13% who underwent surgery and 18% in the nonsurgery group developed cardiovascular disease.
Among patients without diabetes at baseline, 5% of 454 in the surgery group and 10% of 724 in the nonsurgery group developed diabetes during follow-up. In the subset analysis of matched patients without diabetes at baseline, 4% of 333 in the surgery group and 9% in the nonsurgery group developed diabetes.
The investigators plan another data assessment in 2017 to confirm these long-term findings. Similar studies are needed for other bariatric surgery techniques, he suggested.
Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Gastric banding produced significant benefits in 17 years of follow-up.
Major finding: Obese patients treated with gastric banding were 66% less likely to die, compared with those who received medical therapy.
Data source: An intent-to-treat analysis of data on 1,490 obese patients treated at four Italian centers.
Disclosures: Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
Guideline adjusts perioperative cardiac care in noncardiac surgery
A new clinical practice guideline on cardiovascular evaluation and management of patients undergoing noncardiac surgery adds some clarity around the controversial issue of beta-blocker therapy and updates other aspects of care.
If a patient on beta-blocker medication needs noncardiac surgery, continue the beta-blocker, because there is no evidence of harm from doing so; but you risk doing harm if the drug is stopped, according to the new guideline from the American College of Cardiology (ACC) and the American Heart Association (AHA).
Surgeons will be happy to hear that, said Dr. Lee A. Fleisher, the chair of the guideline-writing committee, because that conforms to one of the Surgical Care Improvement Project’s National Measures.
For patients at elevated risk of a cardiovascular event during noncardiac surgery who are not already on beta-blocker therapy, however, the new guideline steps back from the organization’s 2009 position that beta-blockers not be started, and says instead that it’s not unreasonable to start the drug, with a caveat. Be very cautious and start the drug early enough before surgery that you can titrate it to avoid causing hypotension or a low heart rate.
"Make sure that you’re giving the right amount and monitoring their blood pressure and heart rate," Dr. Fleisher, chair of the guideline writing committee, said in an interview. "Really think once, twice, and thrice about starting a protocol," added Dr. Fleisher, the Robert D. Dripps Professor of Anesthesiology and Critical Care at the University of Pennsylvania, Philadelphia.
The ACC and AHA commissioned a committee to review the evidence for and against beta-blockers in patients undergoing noncardiac surgery. A separate writing committee then considered the evidence review committee’s report, reviewed the literature on other aspects of perioperative care for noncardiac surgery, and compiled a 102-page guideline with a 59-page executive summary.
The "2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery" will be published online on the ACC and AHA websites.
Dr. Fleisher described other highlights of the new guideline pertinent to cardiologists, primary care physicians, or surgeons. For the first time, palliative care has been added as an option that may come out of the preoperative evaluation, he said. Patient categories of high risk and intermediate risk have been lumped together as having "elevated" risk for simplicity’s sake because recommendations for the two separate categories were so similar.
The guideline now endorses two tools to choose from for preoperative risk assessments: the Revised Cardiac Risk Index (RCRI), and the National Surgical Quality Improvement Project risk calculator. "There have been a lot of comments that [the NSQIP] is a very useful tool to have shared decision-making conversations with patients," he said.
Another change applies to patients who receive second- or third-generation coronary stents. Instead of a wait of a year after stent implantation to perform noncardiac surgery, a 6-month wait may be reasonable if the risks of delaying noncardiac surgery outweigh the risks of interrupting dual-antiplatelet therapy for the noncardiac surgery.
In addition, the guideline incorporates findings from the recent POISE-2 study to say that aspirin can be stopped and clonidine is not useful in patients without stents undergoing noncardiac surgery (N. Engl. J. Med. 2014;370:1494-503).
A new statement in the guideline about troponin says to check troponin in high-risk patients with signs or symptoms of trouble but not to include troponin in routine screening.
The recommendations on beta-blockers, however, address the most controversial topic in the guideline, Dr. Fleisher said. "There is a lot of confusing evidence" on the use of beta-blockers, "so we’ve tried to clarify as much as we can."
The ACC and AHA funded the work of the committees. Dr. Fleisher reported having no financial disclosures.
On Twitter @sherryboschert
A new clinical practice guideline on cardiovascular evaluation and management of patients undergoing noncardiac surgery adds some clarity around the controversial issue of beta-blocker therapy and updates other aspects of care.
If a patient on beta-blocker medication needs noncardiac surgery, continue the beta-blocker, because there is no evidence of harm from doing so; but you risk doing harm if the drug is stopped, according to the new guideline from the American College of Cardiology (ACC) and the American Heart Association (AHA).
Surgeons will be happy to hear that, said Dr. Lee A. Fleisher, the chair of the guideline-writing committee, because that conforms to one of the Surgical Care Improvement Project’s National Measures.
For patients at elevated risk of a cardiovascular event during noncardiac surgery who are not already on beta-blocker therapy, however, the new guideline steps back from the organization’s 2009 position that beta-blockers not be started, and says instead that it’s not unreasonable to start the drug, with a caveat. Be very cautious and start the drug early enough before surgery that you can titrate it to avoid causing hypotension or a low heart rate.
"Make sure that you’re giving the right amount and monitoring their blood pressure and heart rate," Dr. Fleisher, chair of the guideline writing committee, said in an interview. "Really think once, twice, and thrice about starting a protocol," added Dr. Fleisher, the Robert D. Dripps Professor of Anesthesiology and Critical Care at the University of Pennsylvania, Philadelphia.
The ACC and AHA commissioned a committee to review the evidence for and against beta-blockers in patients undergoing noncardiac surgery. A separate writing committee then considered the evidence review committee’s report, reviewed the literature on other aspects of perioperative care for noncardiac surgery, and compiled a 102-page guideline with a 59-page executive summary.
The "2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery" will be published online on the ACC and AHA websites.
Dr. Fleisher described other highlights of the new guideline pertinent to cardiologists, primary care physicians, or surgeons. For the first time, palliative care has been added as an option that may come out of the preoperative evaluation, he said. Patient categories of high risk and intermediate risk have been lumped together as having "elevated" risk for simplicity’s sake because recommendations for the two separate categories were so similar.
The guideline now endorses two tools to choose from for preoperative risk assessments: the Revised Cardiac Risk Index (RCRI), and the National Surgical Quality Improvement Project risk calculator. "There have been a lot of comments that [the NSQIP] is a very useful tool to have shared decision-making conversations with patients," he said.
Another change applies to patients who receive second- or third-generation coronary stents. Instead of a wait of a year after stent implantation to perform noncardiac surgery, a 6-month wait may be reasonable if the risks of delaying noncardiac surgery outweigh the risks of interrupting dual-antiplatelet therapy for the noncardiac surgery.
In addition, the guideline incorporates findings from the recent POISE-2 study to say that aspirin can be stopped and clonidine is not useful in patients without stents undergoing noncardiac surgery (N. Engl. J. Med. 2014;370:1494-503).
A new statement in the guideline about troponin says to check troponin in high-risk patients with signs or symptoms of trouble but not to include troponin in routine screening.
The recommendations on beta-blockers, however, address the most controversial topic in the guideline, Dr. Fleisher said. "There is a lot of confusing evidence" on the use of beta-blockers, "so we’ve tried to clarify as much as we can."
The ACC and AHA funded the work of the committees. Dr. Fleisher reported having no financial disclosures.
On Twitter @sherryboschert
A new clinical practice guideline on cardiovascular evaluation and management of patients undergoing noncardiac surgery adds some clarity around the controversial issue of beta-blocker therapy and updates other aspects of care.
If a patient on beta-blocker medication needs noncardiac surgery, continue the beta-blocker, because there is no evidence of harm from doing so; but you risk doing harm if the drug is stopped, according to the new guideline from the American College of Cardiology (ACC) and the American Heart Association (AHA).
Surgeons will be happy to hear that, said Dr. Lee A. Fleisher, the chair of the guideline-writing committee, because that conforms to one of the Surgical Care Improvement Project’s National Measures.
For patients at elevated risk of a cardiovascular event during noncardiac surgery who are not already on beta-blocker therapy, however, the new guideline steps back from the organization’s 2009 position that beta-blockers not be started, and says instead that it’s not unreasonable to start the drug, with a caveat. Be very cautious and start the drug early enough before surgery that you can titrate it to avoid causing hypotension or a low heart rate.
"Make sure that you’re giving the right amount and monitoring their blood pressure and heart rate," Dr. Fleisher, chair of the guideline writing committee, said in an interview. "Really think once, twice, and thrice about starting a protocol," added Dr. Fleisher, the Robert D. Dripps Professor of Anesthesiology and Critical Care at the University of Pennsylvania, Philadelphia.
The ACC and AHA commissioned a committee to review the evidence for and against beta-blockers in patients undergoing noncardiac surgery. A separate writing committee then considered the evidence review committee’s report, reviewed the literature on other aspects of perioperative care for noncardiac surgery, and compiled a 102-page guideline with a 59-page executive summary.
The "2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery" will be published online on the ACC and AHA websites.
Dr. Fleisher described other highlights of the new guideline pertinent to cardiologists, primary care physicians, or surgeons. For the first time, palliative care has been added as an option that may come out of the preoperative evaluation, he said. Patient categories of high risk and intermediate risk have been lumped together as having "elevated" risk for simplicity’s sake because recommendations for the two separate categories were so similar.
The guideline now endorses two tools to choose from for preoperative risk assessments: the Revised Cardiac Risk Index (RCRI), and the National Surgical Quality Improvement Project risk calculator. "There have been a lot of comments that [the NSQIP] is a very useful tool to have shared decision-making conversations with patients," he said.
Another change applies to patients who receive second- or third-generation coronary stents. Instead of a wait of a year after stent implantation to perform noncardiac surgery, a 6-month wait may be reasonable if the risks of delaying noncardiac surgery outweigh the risks of interrupting dual-antiplatelet therapy for the noncardiac surgery.
In addition, the guideline incorporates findings from the recent POISE-2 study to say that aspirin can be stopped and clonidine is not useful in patients without stents undergoing noncardiac surgery (N. Engl. J. Med. 2014;370:1494-503).
A new statement in the guideline about troponin says to check troponin in high-risk patients with signs or symptoms of trouble but not to include troponin in routine screening.
The recommendations on beta-blockers, however, address the most controversial topic in the guideline, Dr. Fleisher said. "There is a lot of confusing evidence" on the use of beta-blockers, "so we’ve tried to clarify as much as we can."
The ACC and AHA funded the work of the committees. Dr. Fleisher reported having no financial disclosures.
On Twitter @sherryboschert