User login
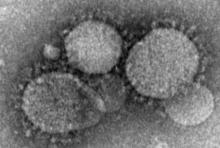
Health care workers at risk for mild MERS-CoV infections
Health care workers directly caring for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) are more highly predisposed to contracting the virus, but in a milder form than that of their patients, thus making it difficult to diagnose and treat.
In a study published in Emerging Infectious Diseases, health care professionals (HCP) from the King Faisal Specialist Hospital and Research Centre in Riyadh, Saudi Arabia, were examined to determine their likelihood for getting MERS-CoV based on their proximity to patients who already had it.
“Healthcare settings are important amplifiers of transmission,” explained the investigators, led by Basem M. Alraddadi, MD. “Current MERS-CoV infection control recommendations are based on experience with other viruses rather than on a complete understanding of the epidemiology of MERS-CoV transmission.”
Dr. Alraddadi and his coinvestigators identified 363 HCP, all of whom would be placed into one of three cohorts based on the department in which they worked most extensively: the Medical Intensive Care Unit (MICU), the emergency department (ED), and the neurology unit. A total of 292 HCP were ultimately enrolled in the study: 131 in MICU, 127 in ED, and 34 in neurology. After 9 subjects were excluded because of unavailability of serum specimens, 128 MICU, 122 ED, and 33 neurology unit workers remained.
While none of the neurology unit workers contracted the virus, 15 MICU workers (11.7%) and 5 ED workers (4.1%) did, for a total of 20 out of the 250 subjects in those two cohorts (8%). Radiology technicians were the most susceptible, as 5 of 17 (29.4%) got the virus, followed by 13 of 138 nurses (9.4%), 1 of 31 respiratory therapists (3.2%), and 1 of 41 physicians (2.4%).
“HCP who reported always covering their nose and mouth with either a medical mask or N95 respirator had lower risk for infection than did HCP reporting not always or never doing so, [while] those who reported always using N95 respirators for direct patient contact were less likely to be seropositive, a trend that approached statistical significance (P = .07),” the authors noted.
The most frequent symptoms reported by those surveyed were muscle pain, fevers, headaches, dry cough, and shortness of breath. In the 20-case HCP sample, however, 12 subjects (60%) only had mild illness while 3 (15%) were asymptomatic, making it very hard to diagnose and treat their infection. Three subjects (15%) had severe illness, while another two (10%) had moderate illness, meaning they were admitted to hospital but did not require any mechanical ventilation.
“Our study did not identify strong associations with underlying chronic illnesses, most likely because the prevalence of such conditions was low ([less than] 10%) in this population, [but] HCPs with a history of smoking had a risk for infection almost 3 times that of nonsmokers,” the authors wrote (Emerg Infect Dis. 2016 Nov. doi: 10.3201/eid2211.160920).
The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. Dr. Alraddadi and his coauthors did not report any disclosures.
Health care workers directly caring for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) are more highly predisposed to contracting the virus, but in a milder form than that of their patients, thus making it difficult to diagnose and treat.
In a study published in Emerging Infectious Diseases, health care professionals (HCP) from the King Faisal Specialist Hospital and Research Centre in Riyadh, Saudi Arabia, were examined to determine their likelihood for getting MERS-CoV based on their proximity to patients who already had it.
“Healthcare settings are important amplifiers of transmission,” explained the investigators, led by Basem M. Alraddadi, MD. “Current MERS-CoV infection control recommendations are based on experience with other viruses rather than on a complete understanding of the epidemiology of MERS-CoV transmission.”
Dr. Alraddadi and his coinvestigators identified 363 HCP, all of whom would be placed into one of three cohorts based on the department in which they worked most extensively: the Medical Intensive Care Unit (MICU), the emergency department (ED), and the neurology unit. A total of 292 HCP were ultimately enrolled in the study: 131 in MICU, 127 in ED, and 34 in neurology. After 9 subjects were excluded because of unavailability of serum specimens, 128 MICU, 122 ED, and 33 neurology unit workers remained.
While none of the neurology unit workers contracted the virus, 15 MICU workers (11.7%) and 5 ED workers (4.1%) did, for a total of 20 out of the 250 subjects in those two cohorts (8%). Radiology technicians were the most susceptible, as 5 of 17 (29.4%) got the virus, followed by 13 of 138 nurses (9.4%), 1 of 31 respiratory therapists (3.2%), and 1 of 41 physicians (2.4%).
“HCP who reported always covering their nose and mouth with either a medical mask or N95 respirator had lower risk for infection than did HCP reporting not always or never doing so, [while] those who reported always using N95 respirators for direct patient contact were less likely to be seropositive, a trend that approached statistical significance (P = .07),” the authors noted.
The most frequent symptoms reported by those surveyed were muscle pain, fevers, headaches, dry cough, and shortness of breath. In the 20-case HCP sample, however, 12 subjects (60%) only had mild illness while 3 (15%) were asymptomatic, making it very hard to diagnose and treat their infection. Three subjects (15%) had severe illness, while another two (10%) had moderate illness, meaning they were admitted to hospital but did not require any mechanical ventilation.
“Our study did not identify strong associations with underlying chronic illnesses, most likely because the prevalence of such conditions was low ([less than] 10%) in this population, [but] HCPs with a history of smoking had a risk for infection almost 3 times that of nonsmokers,” the authors wrote (Emerg Infect Dis. 2016 Nov. doi: 10.3201/eid2211.160920).
The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. Dr. Alraddadi and his coauthors did not report any disclosures.
Health care workers directly caring for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) are more highly predisposed to contracting the virus, but in a milder form than that of their patients, thus making it difficult to diagnose and treat.
In a study published in Emerging Infectious Diseases, health care professionals (HCP) from the King Faisal Specialist Hospital and Research Centre in Riyadh, Saudi Arabia, were examined to determine their likelihood for getting MERS-CoV based on their proximity to patients who already had it.
“Healthcare settings are important amplifiers of transmission,” explained the investigators, led by Basem M. Alraddadi, MD. “Current MERS-CoV infection control recommendations are based on experience with other viruses rather than on a complete understanding of the epidemiology of MERS-CoV transmission.”
Dr. Alraddadi and his coinvestigators identified 363 HCP, all of whom would be placed into one of three cohorts based on the department in which they worked most extensively: the Medical Intensive Care Unit (MICU), the emergency department (ED), and the neurology unit. A total of 292 HCP were ultimately enrolled in the study: 131 in MICU, 127 in ED, and 34 in neurology. After 9 subjects were excluded because of unavailability of serum specimens, 128 MICU, 122 ED, and 33 neurology unit workers remained.
While none of the neurology unit workers contracted the virus, 15 MICU workers (11.7%) and 5 ED workers (4.1%) did, for a total of 20 out of the 250 subjects in those two cohorts (8%). Radiology technicians were the most susceptible, as 5 of 17 (29.4%) got the virus, followed by 13 of 138 nurses (9.4%), 1 of 31 respiratory therapists (3.2%), and 1 of 41 physicians (2.4%).
“HCP who reported always covering their nose and mouth with either a medical mask or N95 respirator had lower risk for infection than did HCP reporting not always or never doing so, [while] those who reported always using N95 respirators for direct patient contact were less likely to be seropositive, a trend that approached statistical significance (P = .07),” the authors noted.
The most frequent symptoms reported by those surveyed were muscle pain, fevers, headaches, dry cough, and shortness of breath. In the 20-case HCP sample, however, 12 subjects (60%) only had mild illness while 3 (15%) were asymptomatic, making it very hard to diagnose and treat their infection. Three subjects (15%) had severe illness, while another two (10%) had moderate illness, meaning they were admitted to hospital but did not require any mechanical ventilation.
“Our study did not identify strong associations with underlying chronic illnesses, most likely because the prevalence of such conditions was low ([less than] 10%) in this population, [but] HCPs with a history of smoking had a risk for infection almost 3 times that of nonsmokers,” the authors wrote (Emerg Infect Dis. 2016 Nov. doi: 10.3201/eid2211.160920).
The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. Dr. Alraddadi and his coauthors did not report any disclosures.
Key clinical point:
Major finding: Among workers who actually treated MERS-CoV patients, 20 out of 250 (8%) contracted the virus, while none of the clerical staff or patient transporters did.
Data source: Retrospective, single-center study of 363 health care personnel during May-June 2014.
Disclosures: The Ministry of Health of Saudi Arabia and the Centers for Disease Control and Prevention funded the study. The authors reported no financial disclosures.
Pembrolizumab ‘new standard of care’ in advanced PD-L1-rich NSCLC
COPENHAGEN – Chalk up another one for immunotherapy: the PD-1 checkpoint inhibitor pembrolizumab cut the risk of disease progression or death in half among select patients with non–small cell lung cancer (NSCLC), compared with standard platinum doublet chemotherapy, in the first-line setting.
Among 305 patients with non–small cell lung cancers with 50% or greater expression of the programmed death ligand 1 (PD-L1), median progression-free survival (PFS) for patients treated with pembrolizumab (Keytruda) was 10.3 months, compared with 6 months for patients assigned to receive platinum-based chemotherapy at the investigators discretion (hazard ratio, 0.50, P less than .001), reported Martin Reck, MD, from the department of thoracic oncology at the Lung Clinic Grosshansdorf, in Germany.
Results of the KEYNOTE-024 study were also published online in the New England Journal of Medicine (2016 Oct 9. doi: 10.1056/NEJMoa1606774). Approximately 23%-30% of patients with advanced non–small cell lung cancers have tumors that express PD-L1 on the membrane of at least 50% of tumor cells, making them attractive targets for pembrolizumab, which is a monoclonal antibody directed against programmed death 1 (PD-1). Pembrolizumab disengages the brake on the immune system caused by the interaction of receptor PD-1 with the PD-L1 and PD-L2 ligands.
The study was conducted to compare upfront pembrolizumab with platinum-based chemotherapy in patients with newly diagnosed advanced NSCLC that did not carry targetable EGFR-activating mutations or ALK translocations.
A total of 305 patients from 16 countries with untreated stage IV NSCLC, good performance status, and tumors with a 50% or greater expression of PD-L1 were enrolled and randomized to either pembrolizumab 200 mg intravenously every 3 weeks for up to 2 years. Or four to six cycles of platinum-doublet chemotherapy at the investigator’s discretion. The combinations included carboplatin plus pemetrexed, cisplatin plus pemetrexed, carboplatin plus gemcitabine, cisplatin plus gemcitabine, or carboplatin plus paclitaxel.
At a median follow-up of 11.2 months, 48.1% of patients assigned to pembrolizumab were still on treatment, as were 10% of those assigned to standard chemotherapy.
As noted before, PFS, the primary endpoint, was significantly better with pembrolizumab, as was the secondary endpoint of overall survival at 6 months. In all, 80% of patients treated with pembrolizumab were still alive at 6 months, compared with 72% of patients on chemotherapy (HR, 0.60; P = .005).
The confirmed response rate was also higher in the pembrolizumab arm, at 44.8% vs. 27.8%(P = .0011), and the median duration of response was longer (not reached vs. 6.3 months). There were six complete responses in the pembrolizumab arm.
Pembrolizumab also demonstrated a generally more favorable safety profile, with adverse events of any grade occurring in 73.4% of patients, compared with 90% of those treated with chemotherapy.
Grade 3 or 4 adverse events and treatment-related deaths were also lower in the pembrolizumab arm, at 26.6% vs. 53.3%.
Jean-Charles Soria, MD, chair of drug development at Gustave Roussy Cancer Center in Paris, the invited discussant, noted that the “45% objective response rate in first-line non–small cell lung cancer is unheard of, and is achieved with a monotherapy.”
“Pembrolizumab clearly leads to a higher objective response, a longer duration of response, a lower frequency of adverse events, better PFS, better OS, compared to chemotherapy.”
“We have, probably, a new standard of care” for patients with high PD-L1 expression and no targetable mutations,” he said.
COPENHAGEN – Chalk up another one for immunotherapy: the PD-1 checkpoint inhibitor pembrolizumab cut the risk of disease progression or death in half among select patients with non–small cell lung cancer (NSCLC), compared with standard platinum doublet chemotherapy, in the first-line setting.
Among 305 patients with non–small cell lung cancers with 50% or greater expression of the programmed death ligand 1 (PD-L1), median progression-free survival (PFS) for patients treated with pembrolizumab (Keytruda) was 10.3 months, compared with 6 months for patients assigned to receive platinum-based chemotherapy at the investigators discretion (hazard ratio, 0.50, P less than .001), reported Martin Reck, MD, from the department of thoracic oncology at the Lung Clinic Grosshansdorf, in Germany.
Results of the KEYNOTE-024 study were also published online in the New England Journal of Medicine (2016 Oct 9. doi: 10.1056/NEJMoa1606774). Approximately 23%-30% of patients with advanced non–small cell lung cancers have tumors that express PD-L1 on the membrane of at least 50% of tumor cells, making them attractive targets for pembrolizumab, which is a monoclonal antibody directed against programmed death 1 (PD-1). Pembrolizumab disengages the brake on the immune system caused by the interaction of receptor PD-1 with the PD-L1 and PD-L2 ligands.
The study was conducted to compare upfront pembrolizumab with platinum-based chemotherapy in patients with newly diagnosed advanced NSCLC that did not carry targetable EGFR-activating mutations or ALK translocations.
A total of 305 patients from 16 countries with untreated stage IV NSCLC, good performance status, and tumors with a 50% or greater expression of PD-L1 were enrolled and randomized to either pembrolizumab 200 mg intravenously every 3 weeks for up to 2 years. Or four to six cycles of platinum-doublet chemotherapy at the investigator’s discretion. The combinations included carboplatin plus pemetrexed, cisplatin plus pemetrexed, carboplatin plus gemcitabine, cisplatin plus gemcitabine, or carboplatin plus paclitaxel.
At a median follow-up of 11.2 months, 48.1% of patients assigned to pembrolizumab were still on treatment, as were 10% of those assigned to standard chemotherapy.
As noted before, PFS, the primary endpoint, was significantly better with pembrolizumab, as was the secondary endpoint of overall survival at 6 months. In all, 80% of patients treated with pembrolizumab were still alive at 6 months, compared with 72% of patients on chemotherapy (HR, 0.60; P = .005).
The confirmed response rate was also higher in the pembrolizumab arm, at 44.8% vs. 27.8%(P = .0011), and the median duration of response was longer (not reached vs. 6.3 months). There were six complete responses in the pembrolizumab arm.
Pembrolizumab also demonstrated a generally more favorable safety profile, with adverse events of any grade occurring in 73.4% of patients, compared with 90% of those treated with chemotherapy.
Grade 3 or 4 adverse events and treatment-related deaths were also lower in the pembrolizumab arm, at 26.6% vs. 53.3%.
Jean-Charles Soria, MD, chair of drug development at Gustave Roussy Cancer Center in Paris, the invited discussant, noted that the “45% objective response rate in first-line non–small cell lung cancer is unheard of, and is achieved with a monotherapy.”
“Pembrolizumab clearly leads to a higher objective response, a longer duration of response, a lower frequency of adverse events, better PFS, better OS, compared to chemotherapy.”
“We have, probably, a new standard of care” for patients with high PD-L1 expression and no targetable mutations,” he said.
COPENHAGEN – Chalk up another one for immunotherapy: the PD-1 checkpoint inhibitor pembrolizumab cut the risk of disease progression or death in half among select patients with non–small cell lung cancer (NSCLC), compared with standard platinum doublet chemotherapy, in the first-line setting.
Among 305 patients with non–small cell lung cancers with 50% or greater expression of the programmed death ligand 1 (PD-L1), median progression-free survival (PFS) for patients treated with pembrolizumab (Keytruda) was 10.3 months, compared with 6 months for patients assigned to receive platinum-based chemotherapy at the investigators discretion (hazard ratio, 0.50, P less than .001), reported Martin Reck, MD, from the department of thoracic oncology at the Lung Clinic Grosshansdorf, in Germany.
Results of the KEYNOTE-024 study were also published online in the New England Journal of Medicine (2016 Oct 9. doi: 10.1056/NEJMoa1606774). Approximately 23%-30% of patients with advanced non–small cell lung cancers have tumors that express PD-L1 on the membrane of at least 50% of tumor cells, making them attractive targets for pembrolizumab, which is a monoclonal antibody directed against programmed death 1 (PD-1). Pembrolizumab disengages the brake on the immune system caused by the interaction of receptor PD-1 with the PD-L1 and PD-L2 ligands.
The study was conducted to compare upfront pembrolizumab with platinum-based chemotherapy in patients with newly diagnosed advanced NSCLC that did not carry targetable EGFR-activating mutations or ALK translocations.
A total of 305 patients from 16 countries with untreated stage IV NSCLC, good performance status, and tumors with a 50% or greater expression of PD-L1 were enrolled and randomized to either pembrolizumab 200 mg intravenously every 3 weeks for up to 2 years. Or four to six cycles of platinum-doublet chemotherapy at the investigator’s discretion. The combinations included carboplatin plus pemetrexed, cisplatin plus pemetrexed, carboplatin plus gemcitabine, cisplatin plus gemcitabine, or carboplatin plus paclitaxel.
At a median follow-up of 11.2 months, 48.1% of patients assigned to pembrolizumab were still on treatment, as were 10% of those assigned to standard chemotherapy.
As noted before, PFS, the primary endpoint, was significantly better with pembrolizumab, as was the secondary endpoint of overall survival at 6 months. In all, 80% of patients treated with pembrolizumab were still alive at 6 months, compared with 72% of patients on chemotherapy (HR, 0.60; P = .005).
The confirmed response rate was also higher in the pembrolizumab arm, at 44.8% vs. 27.8%(P = .0011), and the median duration of response was longer (not reached vs. 6.3 months). There were six complete responses in the pembrolizumab arm.
Pembrolizumab also demonstrated a generally more favorable safety profile, with adverse events of any grade occurring in 73.4% of patients, compared with 90% of those treated with chemotherapy.
Grade 3 or 4 adverse events and treatment-related deaths were also lower in the pembrolizumab arm, at 26.6% vs. 53.3%.
Jean-Charles Soria, MD, chair of drug development at Gustave Roussy Cancer Center in Paris, the invited discussant, noted that the “45% objective response rate in first-line non–small cell lung cancer is unheard of, and is achieved with a monotherapy.”
“Pembrolizumab clearly leads to a higher objective response, a longer duration of response, a lower frequency of adverse events, better PFS, better OS, compared to chemotherapy.”
“We have, probably, a new standard of care” for patients with high PD-L1 expression and no targetable mutations,” he said.
AT ESMO 2016
Key clinical point: Pembrolizumab was superior to chemotherapy in stage IV NSCLC with PD-L1 expression of 50% or more.
Major finding: The hazard ratio for progression-free survival was 0.50 for pembrolizumab vs. platinum-based chemotherapy.
Data source: Randomized phase III trial in 305 patients with untreated stage IV NSCLC with 50% or more of tumor cells expressing PD-L1
Disclosures: The study was sponsored by Merck, Sharp & Dohme. Dr. Reck and Dr. Soria disclosed financial relationships (consulting/honoraria, research funding, etc.) with several companies, but not Merck.
Patients with stage 1 NSCLC more likely to die of other causes in short term
Patients with stage 1 non–small cell lung cancer who underwent resection with intent to cure were more likely, over the short term, to die of other causes, investigators reported.
“Non–cancer-specific mortality represents a significant competing event for lung cancer–specific mortality, with an increasing impact as age increases,” Takashi Eguchi, MD, and his associates at Memorial Sloan Kettering Cancer Center, New York wrote (J Clin Oncol. 2016 Oct 10. doi: 10.1200/JCO.2016.69.0834).
“These findings can provide patients with more accurate information on survivorship on the basis of their individual preoperative status, and help determine patients’ optimal treatment options.”
The study included 2,186 patients who underwent curative-intent resection of stage 1 non-small cell lung cancer at Memorial Sloan Kettering between 2000 and 2011. The cumulative 5-year lung cancer death rate was 10.4%, but rose with age from 7.5% among patients younger than 65 years to 13.2% among patients who were at least 75 years old. Cumulative 5-year rates of mortality not due to cancer were lower, at 5.3% overall, 1.8% in the youngest cohort, and 9% in the oldest cohort. But a competing risk analysis of the entire cohort showed that non–cancer-specific cumulative mortality was higher than mortality from lung cancer for up to 1.5 years after resection, the investigators found. Furthermore, patients who were at least 75 years old were more likely to die of causes other than cancer for up to 2.5 years after surgery.
In the multivariable analysis, low predicted postoperative diffusing capacity of lung for carbon monoxide (DCLO) independently predicted severe morbidity (P less than .001), 1-year mortality (P less than .001), and non–cancer-specific mortality (P less than .001), the researchers said. These findings reflect prior work linking low DCLO with obstructive, restrictive, and pulmonary vascular disease, chronic heart failure, and poor postoperative outcomes, they noted.
Senior author Prasad S. Adusumilli, MD, provided funding. Dr. Eguchi and Dr. Adusumilli had no relevant financial disclosures.
Patients with stage 1 non–small cell lung cancer who underwent resection with intent to cure were more likely, over the short term, to die of other causes, investigators reported.
“Non–cancer-specific mortality represents a significant competing event for lung cancer–specific mortality, with an increasing impact as age increases,” Takashi Eguchi, MD, and his associates at Memorial Sloan Kettering Cancer Center, New York wrote (J Clin Oncol. 2016 Oct 10. doi: 10.1200/JCO.2016.69.0834).
“These findings can provide patients with more accurate information on survivorship on the basis of their individual preoperative status, and help determine patients’ optimal treatment options.”
The study included 2,186 patients who underwent curative-intent resection of stage 1 non-small cell lung cancer at Memorial Sloan Kettering between 2000 and 2011. The cumulative 5-year lung cancer death rate was 10.4%, but rose with age from 7.5% among patients younger than 65 years to 13.2% among patients who were at least 75 years old. Cumulative 5-year rates of mortality not due to cancer were lower, at 5.3% overall, 1.8% in the youngest cohort, and 9% in the oldest cohort. But a competing risk analysis of the entire cohort showed that non–cancer-specific cumulative mortality was higher than mortality from lung cancer for up to 1.5 years after resection, the investigators found. Furthermore, patients who were at least 75 years old were more likely to die of causes other than cancer for up to 2.5 years after surgery.
In the multivariable analysis, low predicted postoperative diffusing capacity of lung for carbon monoxide (DCLO) independently predicted severe morbidity (P less than .001), 1-year mortality (P less than .001), and non–cancer-specific mortality (P less than .001), the researchers said. These findings reflect prior work linking low DCLO with obstructive, restrictive, and pulmonary vascular disease, chronic heart failure, and poor postoperative outcomes, they noted.
Senior author Prasad S. Adusumilli, MD, provided funding. Dr. Eguchi and Dr. Adusumilli had no relevant financial disclosures.
Patients with stage 1 non–small cell lung cancer who underwent resection with intent to cure were more likely, over the short term, to die of other causes, investigators reported.
“Non–cancer-specific mortality represents a significant competing event for lung cancer–specific mortality, with an increasing impact as age increases,” Takashi Eguchi, MD, and his associates at Memorial Sloan Kettering Cancer Center, New York wrote (J Clin Oncol. 2016 Oct 10. doi: 10.1200/JCO.2016.69.0834).
“These findings can provide patients with more accurate information on survivorship on the basis of their individual preoperative status, and help determine patients’ optimal treatment options.”
The study included 2,186 patients who underwent curative-intent resection of stage 1 non-small cell lung cancer at Memorial Sloan Kettering between 2000 and 2011. The cumulative 5-year lung cancer death rate was 10.4%, but rose with age from 7.5% among patients younger than 65 years to 13.2% among patients who were at least 75 years old. Cumulative 5-year rates of mortality not due to cancer were lower, at 5.3% overall, 1.8% in the youngest cohort, and 9% in the oldest cohort. But a competing risk analysis of the entire cohort showed that non–cancer-specific cumulative mortality was higher than mortality from lung cancer for up to 1.5 years after resection, the investigators found. Furthermore, patients who were at least 75 years old were more likely to die of causes other than cancer for up to 2.5 years after surgery.
In the multivariable analysis, low predicted postoperative diffusing capacity of lung for carbon monoxide (DCLO) independently predicted severe morbidity (P less than .001), 1-year mortality (P less than .001), and non–cancer-specific mortality (P less than .001), the researchers said. These findings reflect prior work linking low DCLO with obstructive, restrictive, and pulmonary vascular disease, chronic heart failure, and poor postoperative outcomes, they noted.
Senior author Prasad S. Adusumilli, MD, provided funding. Dr. Eguchi and Dr. Adusumilli had no relevant financial disclosures.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Patients with resected stage 1 non-small cell lung cancer are more likely to die of other causes in the short term. Major finding: The non–cancer-specific cumulative incidence of death was higher than CID from lung cancer for up to 1.5 years after resection.
Data source: A single-center competing risk analysis of 2,186 patients who underwent curative-intent resection for stage 1 non–small cell lung cancer.
Disclosures: Senior author Prasad Adusumilli, MD, provided funding. Dr. Eguchi and Dr. Adusumilli had no relevant financial disclosures.
Lung cryobiopsies could reduce need for surgical biopsy
LONDON – The vast majority of surgical lung biopsies currently used to diagnose interstitial lung diseases (ILDs) could be avoided, suggests research presented at the annual congress of the European Respiratory Society.
During an oral presentation, Benjamin Bondue, MD, of Hopital Erasme, Brussels, presented the preliminary results of a Belgian prospective study evaluating the role of transbronchial lung cryobiopsies in 24 patients with undefined ILD treated at three participating centers.
Cryobiopsies were found to have a diagnostic yield of 79%, meaning that patients might be able to avoid undergoing a more invasive surgical removal of tissue in many cases. Compared with surgical biopsy, cryobiopsies offered the potential advantage of lower morbidity and shorter hospitalization time, Dr. Bondue said. He reported that patients needed to stay in hospital just 1.2 days after the procedure in the study.
“Our data also show that there is some benefit of surgical lung biopsy after cryobiopsy if we identify an NSIP [nonspecific interstitial pneumonia] pattern or idiopathic conditions, or if we cannot obtain a clear pathological diagnosis,” he reported. Acknowledging the study was small and conducted in a single center, he said the use of cryobiopsies following surgical biopsy might be worth further study.
Transbronchial lung cryobiopsy is a relatively new technique that uses a cryoprobe inserted down through a bronchoscope about 1-2 cm from the thoracic wall. Once in place, the probe is cooled for between 3 and 6 seconds, lung tissue freezes to the probe, and the probe and bronchoscope are removed together. This method allows for larger samples of tissue to be taken than does traditional transbronchial biopsy, which involves using large forceps to obtain tissue samples (Respirology. 2014;19:645-54).
In the Belgian study, Dr. Bondue noted that a Fogarty balloon was used to control any bleeding and that four transbronchial lung cryobiopsies were obtained from two different segments of the same lobe of a patient’s lungs. All biopsies were then analyzed by an expert pathologist in ILDs, and reviewed by two other expert pathologists when needed. The mean sample size obtained was 16 mm2.
The patients included in the study had undergone chest X-ray and had inconclusive findings in the majority (84%) of cases. They then had the option to undergo cryobiopsy or surgical lung biopsy, with the latter performed following discussion among a multidisciplinary team’s members.
Following cryobiopsy, 16 of the 24 patients – who were a mean age of 62 years, and over half of whom were past (56%) or current (12%) smokers – were diagnosed with a specific pattern of ILD not due to NSIP. Of the 16 cases, 6 were due to hypersensitive pneumonitis, 4 were due to interstitial pulmonary fibrosis, and 2 were due to sarcoidosis. The other four cases included patients with one of the following conditions: adenocarcinoma, desquamative interstitial pneumonia, eosinophilic pneumonia, and amyloidosis.
Six of the 24 cases were defined as NSIP, with 2 reclassified as definite and 1 as probable hypersensitive pneumonitis, after discussion within the multidisciplinary team.
Five patients – three who had been diagnosed with NSIP and two who had been given no pathological diagnosis after cryobiopsy – underwent surgical lung biopsy. Of these, following the surgical biopsies, only one patient was considered to have NSIP and the other four were eventually diagnosed with interstitial pulmonary fibrosis.
In terms of safety, five patients experienced pneumothorax, two patients required chest drainage, two needed simple aspiration and one underwent observation. In the majority of cases, patients experienced mild bleeding, with only one patient having experienced severe bleeding. During this study, none of the participants experienced significant chest pain, acute exacerbations, or infections, and none of them died.
Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
LONDON – The vast majority of surgical lung biopsies currently used to diagnose interstitial lung diseases (ILDs) could be avoided, suggests research presented at the annual congress of the European Respiratory Society.
During an oral presentation, Benjamin Bondue, MD, of Hopital Erasme, Brussels, presented the preliminary results of a Belgian prospective study evaluating the role of transbronchial lung cryobiopsies in 24 patients with undefined ILD treated at three participating centers.
Cryobiopsies were found to have a diagnostic yield of 79%, meaning that patients might be able to avoid undergoing a more invasive surgical removal of tissue in many cases. Compared with surgical biopsy, cryobiopsies offered the potential advantage of lower morbidity and shorter hospitalization time, Dr. Bondue said. He reported that patients needed to stay in hospital just 1.2 days after the procedure in the study.
“Our data also show that there is some benefit of surgical lung biopsy after cryobiopsy if we identify an NSIP [nonspecific interstitial pneumonia] pattern or idiopathic conditions, or if we cannot obtain a clear pathological diagnosis,” he reported. Acknowledging the study was small and conducted in a single center, he said the use of cryobiopsies following surgical biopsy might be worth further study.
Transbronchial lung cryobiopsy is a relatively new technique that uses a cryoprobe inserted down through a bronchoscope about 1-2 cm from the thoracic wall. Once in place, the probe is cooled for between 3 and 6 seconds, lung tissue freezes to the probe, and the probe and bronchoscope are removed together. This method allows for larger samples of tissue to be taken than does traditional transbronchial biopsy, which involves using large forceps to obtain tissue samples (Respirology. 2014;19:645-54).
In the Belgian study, Dr. Bondue noted that a Fogarty balloon was used to control any bleeding and that four transbronchial lung cryobiopsies were obtained from two different segments of the same lobe of a patient’s lungs. All biopsies were then analyzed by an expert pathologist in ILDs, and reviewed by two other expert pathologists when needed. The mean sample size obtained was 16 mm2.
The patients included in the study had undergone chest X-ray and had inconclusive findings in the majority (84%) of cases. They then had the option to undergo cryobiopsy or surgical lung biopsy, with the latter performed following discussion among a multidisciplinary team’s members.
Following cryobiopsy, 16 of the 24 patients – who were a mean age of 62 years, and over half of whom were past (56%) or current (12%) smokers – were diagnosed with a specific pattern of ILD not due to NSIP. Of the 16 cases, 6 were due to hypersensitive pneumonitis, 4 were due to interstitial pulmonary fibrosis, and 2 were due to sarcoidosis. The other four cases included patients with one of the following conditions: adenocarcinoma, desquamative interstitial pneumonia, eosinophilic pneumonia, and amyloidosis.
Six of the 24 cases were defined as NSIP, with 2 reclassified as definite and 1 as probable hypersensitive pneumonitis, after discussion within the multidisciplinary team.
Five patients – three who had been diagnosed with NSIP and two who had been given no pathological diagnosis after cryobiopsy – underwent surgical lung biopsy. Of these, following the surgical biopsies, only one patient was considered to have NSIP and the other four were eventually diagnosed with interstitial pulmonary fibrosis.
In terms of safety, five patients experienced pneumothorax, two patients required chest drainage, two needed simple aspiration and one underwent observation. In the majority of cases, patients experienced mild bleeding, with only one patient having experienced severe bleeding. During this study, none of the participants experienced significant chest pain, acute exacerbations, or infections, and none of them died.
Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
LONDON – The vast majority of surgical lung biopsies currently used to diagnose interstitial lung diseases (ILDs) could be avoided, suggests research presented at the annual congress of the European Respiratory Society.
During an oral presentation, Benjamin Bondue, MD, of Hopital Erasme, Brussels, presented the preliminary results of a Belgian prospective study evaluating the role of transbronchial lung cryobiopsies in 24 patients with undefined ILD treated at three participating centers.
Cryobiopsies were found to have a diagnostic yield of 79%, meaning that patients might be able to avoid undergoing a more invasive surgical removal of tissue in many cases. Compared with surgical biopsy, cryobiopsies offered the potential advantage of lower morbidity and shorter hospitalization time, Dr. Bondue said. He reported that patients needed to stay in hospital just 1.2 days after the procedure in the study.
“Our data also show that there is some benefit of surgical lung biopsy after cryobiopsy if we identify an NSIP [nonspecific interstitial pneumonia] pattern or idiopathic conditions, or if we cannot obtain a clear pathological diagnosis,” he reported. Acknowledging the study was small and conducted in a single center, he said the use of cryobiopsies following surgical biopsy might be worth further study.
Transbronchial lung cryobiopsy is a relatively new technique that uses a cryoprobe inserted down through a bronchoscope about 1-2 cm from the thoracic wall. Once in place, the probe is cooled for between 3 and 6 seconds, lung tissue freezes to the probe, and the probe and bronchoscope are removed together. This method allows for larger samples of tissue to be taken than does traditional transbronchial biopsy, which involves using large forceps to obtain tissue samples (Respirology. 2014;19:645-54).
In the Belgian study, Dr. Bondue noted that a Fogarty balloon was used to control any bleeding and that four transbronchial lung cryobiopsies were obtained from two different segments of the same lobe of a patient’s lungs. All biopsies were then analyzed by an expert pathologist in ILDs, and reviewed by two other expert pathologists when needed. The mean sample size obtained was 16 mm2.
The patients included in the study had undergone chest X-ray and had inconclusive findings in the majority (84%) of cases. They then had the option to undergo cryobiopsy or surgical lung biopsy, with the latter performed following discussion among a multidisciplinary team’s members.
Following cryobiopsy, 16 of the 24 patients – who were a mean age of 62 years, and over half of whom were past (56%) or current (12%) smokers – were diagnosed with a specific pattern of ILD not due to NSIP. Of the 16 cases, 6 were due to hypersensitive pneumonitis, 4 were due to interstitial pulmonary fibrosis, and 2 were due to sarcoidosis. The other four cases included patients with one of the following conditions: adenocarcinoma, desquamative interstitial pneumonia, eosinophilic pneumonia, and amyloidosis.
Six of the 24 cases were defined as NSIP, with 2 reclassified as definite and 1 as probable hypersensitive pneumonitis, after discussion within the multidisciplinary team.
Five patients – three who had been diagnosed with NSIP and two who had been given no pathological diagnosis after cryobiopsy – underwent surgical lung biopsy. Of these, following the surgical biopsies, only one patient was considered to have NSIP and the other four were eventually diagnosed with interstitial pulmonary fibrosis.
In terms of safety, five patients experienced pneumothorax, two patients required chest drainage, two needed simple aspiration and one underwent observation. In the majority of cases, patients experienced mild bleeding, with only one patient having experienced severe bleeding. During this study, none of the participants experienced significant chest pain, acute exacerbations, or infections, and none of them died.
Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
AT THE ERS CONGRESS 2016 LONDON
Key clinical point: Transbronchial lung cryobiopsies are useful for the diagnosis of interstitial lung diseases and could help avoid surgical lung biopsies.
Major finding: Transbronchial lung cryobiopsy had a diagnostic yield of 79%.
Data source: Single-center study of 24 patients with interstitial lung diseases who underwent transbronchial lung cryobiopsies, surgical lung biopsies, or both.
Disclosures: Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
Steroids could reduce death rate for TB patients with acute respiratory failure
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Key clinical point: Corticosteroids used in combination with anti-TB treatment appeared to lower 90-day mortality in TB patients with ARF.
Major finding: Reduced 90-day mortality was associated with corticosteroid use (odds ratio, 0.47; 95% CI, 0.22-0.98; P = .049).
Data source: A retrospective cohort study of 124 patients admitted to intensive care units with TB and ARF in a single Korean center from 1989 to 2014.
Disclosures: The investigators reported no outside funding or conflicts of interest.
Cerebral protection in TAVI reduces ischemic brain lesions
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Key clinical point: In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions.
Major finding: At 2 days, the number of new brain lesions was markedly lower in the filter group than in the control group (8 vs. 16), as was the lesion volume (466 mm vs. 800 mm).
Data source: A prospective single-center randomized clinical trial involving 100 patients undergoing TAVI for severe aortic stenosis.
Disclosures: This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
NSCLC survival comparable with accelerated and conventional RT
BOSTON – Patients with stage II or III non–small-cell lung cancer with comorbidities that make them poor candidates for surgery or chemotherapy may still benefit from accelerated hypofractionated radiation, an interim analysis of a randomized trial suggests.
Among 48 patients followed for a median of 24 months, there were no statistical differences in either overall survival (OS) or progression-free survival between patients with stage II or III NSCLC and poor performance status treated with either conventional radiation delivered over 6 weeks, or image-guided radiation therapy (IGRT) delivered over 3 weeks, reported Puneeth Iyengar, MD, PhD, of the University of Texas Southwestern in Dallas.
“There is limited grade 3-5 toxicity, and as importantly, and more important to patients, is that the treatment time is cut in half and may be acceptable to the patient as well as to the treating physician,” he added.
The investigators are hopeful that the study, when completed, will “change the paradigm of how we treat these patients who can’t receive the standard-of-care treatment.”
The UT Southwestern investigators had previously shown in a phase I dose-escalation study that treating patients with 60 Gy delivered in 15 fractions instead of the conventional 30 fractions did not increase treatment-related toxicity,
In the current study, they explored the question of whether accelerated hypofractionated radiation therapy could improve survival in a difficult-to-treat population.
They have enrolled to date 60 patients with stage II or III NSCLC and Zubrod performance status of 2 or greater.
In arm A, 28 patients were assigned to receive conventional radiation at total doses of 60 to 66 Gy delivered in 30-33 fractions of 2 Gy each, In arm B, 32 patients were assigned to receive a total dose of 60 Gy delivered in 15 fractions of 4 Gy each.
The median age was 68 in both arms. The male-to-female ratio was equal in arm A, but 4:1 in arm B, The distribution of tumor types was equally weighted in each arm, with squamous cell carcinomas accounting for 53% of lesions, and adenocarcinomas accounting for the remainder.
Among all 60 patients, 53 presented with stage III disease, and 7 with stage II.
Of the 60 patients, 48 had follow-up sufficient for interim evaluation, and of this group, 27 (56%) were alive at last follow-up.
Median OS on Kaplan-Meier analysis was 11.5 months, with no statistical differences between the groups (per-group rates were not shown), Median PFS was 14 months, also with no statistical differences.
There were three deaths from hypoxia possibly related to radiation, two in the conventional fractionation arm, and one in the IGRT, accelerated fractionation arm. There were 10 grade 3 radiation-associated toxicities in arm A, and 6 in Arm B. There were no grade 4 toxicities in either group.
George Rodrigues, MD, of London (Ontario) Health Sciences Center, who moderated the briefing, said that in addition to patients with poor performance status, there are some patients who simply do not want to undergo chemotherapy, and for these patients the efficacy, low side effects, and convenience of accelerated fractionation radiation therapy may prove to be a good treatment option.
BOSTON – Patients with stage II or III non–small-cell lung cancer with comorbidities that make them poor candidates for surgery or chemotherapy may still benefit from accelerated hypofractionated radiation, an interim analysis of a randomized trial suggests.
Among 48 patients followed for a median of 24 months, there were no statistical differences in either overall survival (OS) or progression-free survival between patients with stage II or III NSCLC and poor performance status treated with either conventional radiation delivered over 6 weeks, or image-guided radiation therapy (IGRT) delivered over 3 weeks, reported Puneeth Iyengar, MD, PhD, of the University of Texas Southwestern in Dallas.
“There is limited grade 3-5 toxicity, and as importantly, and more important to patients, is that the treatment time is cut in half and may be acceptable to the patient as well as to the treating physician,” he added.
The investigators are hopeful that the study, when completed, will “change the paradigm of how we treat these patients who can’t receive the standard-of-care treatment.”
The UT Southwestern investigators had previously shown in a phase I dose-escalation study that treating patients with 60 Gy delivered in 15 fractions instead of the conventional 30 fractions did not increase treatment-related toxicity,
In the current study, they explored the question of whether accelerated hypofractionated radiation therapy could improve survival in a difficult-to-treat population.
They have enrolled to date 60 patients with stage II or III NSCLC and Zubrod performance status of 2 or greater.
In arm A, 28 patients were assigned to receive conventional radiation at total doses of 60 to 66 Gy delivered in 30-33 fractions of 2 Gy each, In arm B, 32 patients were assigned to receive a total dose of 60 Gy delivered in 15 fractions of 4 Gy each.
The median age was 68 in both arms. The male-to-female ratio was equal in arm A, but 4:1 in arm B, The distribution of tumor types was equally weighted in each arm, with squamous cell carcinomas accounting for 53% of lesions, and adenocarcinomas accounting for the remainder.
Among all 60 patients, 53 presented with stage III disease, and 7 with stage II.
Of the 60 patients, 48 had follow-up sufficient for interim evaluation, and of this group, 27 (56%) were alive at last follow-up.
Median OS on Kaplan-Meier analysis was 11.5 months, with no statistical differences between the groups (per-group rates were not shown), Median PFS was 14 months, also with no statistical differences.
There were three deaths from hypoxia possibly related to radiation, two in the conventional fractionation arm, and one in the IGRT, accelerated fractionation arm. There were 10 grade 3 radiation-associated toxicities in arm A, and 6 in Arm B. There were no grade 4 toxicities in either group.
George Rodrigues, MD, of London (Ontario) Health Sciences Center, who moderated the briefing, said that in addition to patients with poor performance status, there are some patients who simply do not want to undergo chemotherapy, and for these patients the efficacy, low side effects, and convenience of accelerated fractionation radiation therapy may prove to be a good treatment option.
BOSTON – Patients with stage II or III non–small-cell lung cancer with comorbidities that make them poor candidates for surgery or chemotherapy may still benefit from accelerated hypofractionated radiation, an interim analysis of a randomized trial suggests.
Among 48 patients followed for a median of 24 months, there were no statistical differences in either overall survival (OS) or progression-free survival between patients with stage II or III NSCLC and poor performance status treated with either conventional radiation delivered over 6 weeks, or image-guided radiation therapy (IGRT) delivered over 3 weeks, reported Puneeth Iyengar, MD, PhD, of the University of Texas Southwestern in Dallas.
“There is limited grade 3-5 toxicity, and as importantly, and more important to patients, is that the treatment time is cut in half and may be acceptable to the patient as well as to the treating physician,” he added.
The investigators are hopeful that the study, when completed, will “change the paradigm of how we treat these patients who can’t receive the standard-of-care treatment.”
The UT Southwestern investigators had previously shown in a phase I dose-escalation study that treating patients with 60 Gy delivered in 15 fractions instead of the conventional 30 fractions did not increase treatment-related toxicity,
In the current study, they explored the question of whether accelerated hypofractionated radiation therapy could improve survival in a difficult-to-treat population.
They have enrolled to date 60 patients with stage II or III NSCLC and Zubrod performance status of 2 or greater.
In arm A, 28 patients were assigned to receive conventional radiation at total doses of 60 to 66 Gy delivered in 30-33 fractions of 2 Gy each, In arm B, 32 patients were assigned to receive a total dose of 60 Gy delivered in 15 fractions of 4 Gy each.
The median age was 68 in both arms. The male-to-female ratio was equal in arm A, but 4:1 in arm B, The distribution of tumor types was equally weighted in each arm, with squamous cell carcinomas accounting for 53% of lesions, and adenocarcinomas accounting for the remainder.
Among all 60 patients, 53 presented with stage III disease, and 7 with stage II.
Of the 60 patients, 48 had follow-up sufficient for interim evaluation, and of this group, 27 (56%) were alive at last follow-up.
Median OS on Kaplan-Meier analysis was 11.5 months, with no statistical differences between the groups (per-group rates were not shown), Median PFS was 14 months, also with no statistical differences.
There were three deaths from hypoxia possibly related to radiation, two in the conventional fractionation arm, and one in the IGRT, accelerated fractionation arm. There were 10 grade 3 radiation-associated toxicities in arm A, and 6 in Arm B. There were no grade 4 toxicities in either group.
George Rodrigues, MD, of London (Ontario) Health Sciences Center, who moderated the briefing, said that in addition to patients with poor performance status, there are some patients who simply do not want to undergo chemotherapy, and for these patients the efficacy, low side effects, and convenience of accelerated fractionation radiation therapy may prove to be a good treatment option.
Key clinical point: Accelerated hypofractionated radiation therapy offers survival and safety comparable to that of conventional radiation in non–small-cell lung cancer in half the time.
Major finding: There were no differences in overall or progression-free survival among patients with NSCLC treated with either accelerated or conventional fractionation radiation.
Data source: Interim analysis of randomized phase III trial in 48 of 60 evaluable patients with stage II or III NSCLC and poor performance status.
Disclosures: UT Southwestern Medical Center, Dallas, sponsored the trial. Dr. Iyengar and Dr. Rodrigues reported having no conflicts of interest.
Has mystery of exercise-intolerant chronic thromboembolic disease been solved?
The pathophysiology of exercise intolerance in chronic thromboembolic disease (CTED) and mechanism of improvement after pulmonary endarterectomy have not been well understood, but researchers in the Netherlands have identified those key clinical characteristics of exercise intolerance as well as the mechanisms to response of treatment.
This is the first study to identify the pathophysiology of the exercise intolerance—abnormal pulmonary vascular response—and the underlying mechanism for the pulmonary improvement, Coen van Kan, MD, of Our Lady’s Hospital in Amsterdam and colleagues at the University of Amsterdam reported in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152[3]:763-71).
“Our observations point to a hampered pulmonary vascular response and decreased ventilatory efficiency as underlying pathophysiological mechanisms to explain the exercise limitation observed in patients with CTED,” Dr. van Kan and colleagues wrote. “The clinically significant symptomatic improvement after surgery was shown to be related to significant improvements in both circulatory and ventilatory responses indicative for an improved right ventricle stroke volume during exercise and ventilatory efficiency.”
The researchers studied 14 patients with symptomatic CTED but with normal pulmonary pressures at rest. The patients underwent cardiopulmonary exercise testing (CPET) during right heart catheterization and then had noninvasive CPET 1 year later. During exercise the study subjects showed four features of abnormal pulmonary vascular responses:
• Steep mean pulmonary artery pressure/cardiac output (2.7 mm Hg/min per L).
• Low pulmonary vascular compliance (2.8 mL/mm Hg).
• Mean pulmonary artery pressure (mPAP)/cardiac output slope correlated with dead space ventilation (r = 0.586; P = .028).
• Ventilatory equivalents for carbon dioxide slope (r = 0.580; P = .030).
After screening for exercise-induced pulmonary hypertension, nine patients went on to have pulmonary endarterectomy (three patients had mPAP within normal limits during exercise and hence were not candidates, while two others declined surgery). All nine patients who had surgery survived, and a year afterward, their New York Heart Association functional class scores had improved from class II or II to class I in all patients. “Also, mean peak workload and mean oxygen consumption peak had increased, and the improvements observed tended to reach statistical significance,” Dr. van Kan and colleagues said.
After catheterization, improvement in exercise capacity was related to restoration of right ventricle stroke volume response, as measured by oxygen pulse improvement from 11.7 to 13.3 (P = .027) and heart rate response from 80.9 to 72 (P = .003); and a decrease in ventilatory equivalents for carbon dioxide slope from 38.2 to 32.8 (P = .014).
Dr. van Kan and coauthors had no financial relationships to disclose.
By studying subjects with symptomatic chronic thromboembolic disease and normal pulmonary pressures, Dr. van Kan and colleagues “cleverly opted to study an interesting group,” Robert B. Cameron, MD, of the University of California, Los Angeles, said in his invited commentary.

|
Dr. Robert B. Cameron |
“Logically, this patient group, representing potentially early pathophysiologic CTED, could reveal more pathophysiologic information about mechanisms active during the development of chronic thromboembolic pulmonary hypertension than would be seen in patients with more end-stage disease,” Dr. Cameron said (J Thorac Cardiovasc Surg. 2016;152[3]:771-2).
The early physiologic changes in patients with CTED that Dr. van Kan and colleagues reported on may make it possible to detect chronic thromboembolic pulmonary hypertension and intervene before advance disease sets in, Dr. Cameron said. “Surgical mortality may decrease to very-low levels simply from early surgical intervention,” he said.
Although the retrospective design is a limitation of the study, “these data improve our understanding of CTED and motivate all surgeons to promote prospective trials evaluating these findings and early intervention in a disease that is notoriously difficult to understand and treat,” Dr. Cameron said.
Dr. Cameron had no financial relationships to disclose.
By studying subjects with symptomatic chronic thromboembolic disease and normal pulmonary pressures, Dr. van Kan and colleagues “cleverly opted to study an interesting group,” Robert B. Cameron, MD, of the University of California, Los Angeles, said in his invited commentary.

|
Dr. Robert B. Cameron |
“Logically, this patient group, representing potentially early pathophysiologic CTED, could reveal more pathophysiologic information about mechanisms active during the development of chronic thromboembolic pulmonary hypertension than would be seen in patients with more end-stage disease,” Dr. Cameron said (J Thorac Cardiovasc Surg. 2016;152[3]:771-2).
The early physiologic changes in patients with CTED that Dr. van Kan and colleagues reported on may make it possible to detect chronic thromboembolic pulmonary hypertension and intervene before advance disease sets in, Dr. Cameron said. “Surgical mortality may decrease to very-low levels simply from early surgical intervention,” he said.
Although the retrospective design is a limitation of the study, “these data improve our understanding of CTED and motivate all surgeons to promote prospective trials evaluating these findings and early intervention in a disease that is notoriously difficult to understand and treat,” Dr. Cameron said.
Dr. Cameron had no financial relationships to disclose.
By studying subjects with symptomatic chronic thromboembolic disease and normal pulmonary pressures, Dr. van Kan and colleagues “cleverly opted to study an interesting group,” Robert B. Cameron, MD, of the University of California, Los Angeles, said in his invited commentary.

|
Dr. Robert B. Cameron |
“Logically, this patient group, representing potentially early pathophysiologic CTED, could reveal more pathophysiologic information about mechanisms active during the development of chronic thromboembolic pulmonary hypertension than would be seen in patients with more end-stage disease,” Dr. Cameron said (J Thorac Cardiovasc Surg. 2016;152[3]:771-2).
The early physiologic changes in patients with CTED that Dr. van Kan and colleagues reported on may make it possible to detect chronic thromboembolic pulmonary hypertension and intervene before advance disease sets in, Dr. Cameron said. “Surgical mortality may decrease to very-low levels simply from early surgical intervention,” he said.
Although the retrospective design is a limitation of the study, “these data improve our understanding of CTED and motivate all surgeons to promote prospective trials evaluating these findings and early intervention in a disease that is notoriously difficult to understand and treat,” Dr. Cameron said.
Dr. Cameron had no financial relationships to disclose.
The pathophysiology of exercise intolerance in chronic thromboembolic disease (CTED) and mechanism of improvement after pulmonary endarterectomy have not been well understood, but researchers in the Netherlands have identified those key clinical characteristics of exercise intolerance as well as the mechanisms to response of treatment.
This is the first study to identify the pathophysiology of the exercise intolerance—abnormal pulmonary vascular response—and the underlying mechanism for the pulmonary improvement, Coen van Kan, MD, of Our Lady’s Hospital in Amsterdam and colleagues at the University of Amsterdam reported in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152[3]:763-71).
“Our observations point to a hampered pulmonary vascular response and decreased ventilatory efficiency as underlying pathophysiological mechanisms to explain the exercise limitation observed in patients with CTED,” Dr. van Kan and colleagues wrote. “The clinically significant symptomatic improvement after surgery was shown to be related to significant improvements in both circulatory and ventilatory responses indicative for an improved right ventricle stroke volume during exercise and ventilatory efficiency.”
The researchers studied 14 patients with symptomatic CTED but with normal pulmonary pressures at rest. The patients underwent cardiopulmonary exercise testing (CPET) during right heart catheterization and then had noninvasive CPET 1 year later. During exercise the study subjects showed four features of abnormal pulmonary vascular responses:
• Steep mean pulmonary artery pressure/cardiac output (2.7 mm Hg/min per L).
• Low pulmonary vascular compliance (2.8 mL/mm Hg).
• Mean pulmonary artery pressure (mPAP)/cardiac output slope correlated with dead space ventilation (r = 0.586; P = .028).
• Ventilatory equivalents for carbon dioxide slope (r = 0.580; P = .030).
After screening for exercise-induced pulmonary hypertension, nine patients went on to have pulmonary endarterectomy (three patients had mPAP within normal limits during exercise and hence were not candidates, while two others declined surgery). All nine patients who had surgery survived, and a year afterward, their New York Heart Association functional class scores had improved from class II or II to class I in all patients. “Also, mean peak workload and mean oxygen consumption peak had increased, and the improvements observed tended to reach statistical significance,” Dr. van Kan and colleagues said.
After catheterization, improvement in exercise capacity was related to restoration of right ventricle stroke volume response, as measured by oxygen pulse improvement from 11.7 to 13.3 (P = .027) and heart rate response from 80.9 to 72 (P = .003); and a decrease in ventilatory equivalents for carbon dioxide slope from 38.2 to 32.8 (P = .014).
Dr. van Kan and coauthors had no financial relationships to disclose.
The pathophysiology of exercise intolerance in chronic thromboembolic disease (CTED) and mechanism of improvement after pulmonary endarterectomy have not been well understood, but researchers in the Netherlands have identified those key clinical characteristics of exercise intolerance as well as the mechanisms to response of treatment.
This is the first study to identify the pathophysiology of the exercise intolerance—abnormal pulmonary vascular response—and the underlying mechanism for the pulmonary improvement, Coen van Kan, MD, of Our Lady’s Hospital in Amsterdam and colleagues at the University of Amsterdam reported in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152[3]:763-71).
“Our observations point to a hampered pulmonary vascular response and decreased ventilatory efficiency as underlying pathophysiological mechanisms to explain the exercise limitation observed in patients with CTED,” Dr. van Kan and colleagues wrote. “The clinically significant symptomatic improvement after surgery was shown to be related to significant improvements in both circulatory and ventilatory responses indicative for an improved right ventricle stroke volume during exercise and ventilatory efficiency.”
The researchers studied 14 patients with symptomatic CTED but with normal pulmonary pressures at rest. The patients underwent cardiopulmonary exercise testing (CPET) during right heart catheterization and then had noninvasive CPET 1 year later. During exercise the study subjects showed four features of abnormal pulmonary vascular responses:
• Steep mean pulmonary artery pressure/cardiac output (2.7 mm Hg/min per L).
• Low pulmonary vascular compliance (2.8 mL/mm Hg).
• Mean pulmonary artery pressure (mPAP)/cardiac output slope correlated with dead space ventilation (r = 0.586; P = .028).
• Ventilatory equivalents for carbon dioxide slope (r = 0.580; P = .030).
After screening for exercise-induced pulmonary hypertension, nine patients went on to have pulmonary endarterectomy (three patients had mPAP within normal limits during exercise and hence were not candidates, while two others declined surgery). All nine patients who had surgery survived, and a year afterward, their New York Heart Association functional class scores had improved from class II or II to class I in all patients. “Also, mean peak workload and mean oxygen consumption peak had increased, and the improvements observed tended to reach statistical significance,” Dr. van Kan and colleagues said.
After catheterization, improvement in exercise capacity was related to restoration of right ventricle stroke volume response, as measured by oxygen pulse improvement from 11.7 to 13.3 (P = .027) and heart rate response from 80.9 to 72 (P = .003); and a decrease in ventilatory equivalents for carbon dioxide slope from 38.2 to 32.8 (P = .014).
Dr. van Kan and coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: This study identifies key clinical features of the pathophysiology of exercise intolerance in chronic thromboembolic disease (CTED) as well and the mechanisms of responses to treatment that have not been well understood .
Major finding: Exercise intolerance may result from an abnormal pulmonary vascular response and decreased ventilatory efficiency, while pulmonary endarterectomy restores right ventricle stroke volume response and ventilatory efficiency.
Data source: Fourteen subjects with exercise-intolerant CTED but normal pulmonary pressure underwent cardiopulmonary exercise testing (CPET) during right heart catheterization and noninvasive CPET 1 year later.
Disclosures: Dr. van Kan and coauthors had no financial relationships to disclose.
Simtuzumab did not help IPF patients
LONDON – Despite very promising activity in animal models of idiopathic pulmonary fibrosis (IPF), a monoclonal antibody targeted at an enzyme considered to be important to collagen cross-linking did not produce any improvement in progression-free survival (PFS), according to results of a multicenter study presented at the annual congress of the European Respiratory Society.
“This was such a negative study, there is no point in doing another,” reported Ganesh Raghu, MD, director of the Pulmonary Fibrosis Program at the University of Washington Medical Center, Seattle.
The focus of this study was simtuzumab, a monoclonal antibody targeted at lysyl oxidase like 2 (LOXL2), an enzyme which catalyzes a step in the formation of collagen crosslinks, which are thought to be important in fibrosis formation. Simtuzumab has been entered into clinical trials for treatment of several forms of fibrosis, including fibrosis in the liver.
“In animal models, simtuzumab has demonstrated efficacy in reducing fibrosis when administered prior to fibrosis formation or after the process has already begun,” Dr. Raghu explained. He said a large trial was initiated in IPF because the agent seemed so promising and because a large study was thought to be the best strategy to arrive at a definitive answer regarding safety and efficacy.
The drug was found safe but not effective. The independent data monitoring and safety committee terminated the trial early for futility.
In the study, 544 IPF patients were randomized to 125 mg simtuzumab or placebo administered subcutaneously once weekly. The primary endpoint was PFS, but there were a large number of secondary endpoints including hospitalization for progressive disease, change in 6-minute walk distance (6MWD), and overall survival.
For the endpoint of PFS, “there was absolutely no difference” between the groups receiving simtuzumab or placebo. When the patients were stratified for demonstrating above or below median expression of LOXL2, which was a prespecified analysis for the trial, there was still no difference between groups. Even when those in the top quarter percentile of LOXL2 expression were compared with those with less [expression of the enzyme], there was still “absolutely no difference.”
There was also no significant evidence of benefit for simtuzumab observed on key secondary endpoints, such as overall survival. When patients were stratified by baseline lung function as expressed by percentage of predicted forced expiratory volume in 1 second (FEV1), there was no signal of benefit for those with severe, moderate, or mild impairment.
One criticism of this study raised after the presentation was that patients with 26% or greater of predicted FEV1 were permitted into the study. It was suggested that such patients would be expected to already have a high degree of fibrosis and therefore would be less likely to benefit from an antifibrosis therapy. Dr. Raghu acknowledged this criticism, but he said it was important to include patients with advanced disease in order to generate an adequate event rate. Even with inclusion of patients with severe lung impairment, the mortality rate was less than 10%.
He concluded that there was no signal of benefit even among those with the greatest expression of the target.
“We absolutely need better markers for IPF,” Dr. Raghu maintained. While other members of the LOXL family of enzymes may still prove to be valuable markers of IPF risk and targets of therapy, these data appear to rule out a therapeutic role for blocking LOXL2.
Dr. Raghu is a consultant for Boehringer Ingelheim, Biogen, FibroGen, Gilead, Janssen, MedImmune, Promedior, Sanofi-Aventis, and Veracyte.
LONDON – Despite very promising activity in animal models of idiopathic pulmonary fibrosis (IPF), a monoclonal antibody targeted at an enzyme considered to be important to collagen cross-linking did not produce any improvement in progression-free survival (PFS), according to results of a multicenter study presented at the annual congress of the European Respiratory Society.
“This was such a negative study, there is no point in doing another,” reported Ganesh Raghu, MD, director of the Pulmonary Fibrosis Program at the University of Washington Medical Center, Seattle.
The focus of this study was simtuzumab, a monoclonal antibody targeted at lysyl oxidase like 2 (LOXL2), an enzyme which catalyzes a step in the formation of collagen crosslinks, which are thought to be important in fibrosis formation. Simtuzumab has been entered into clinical trials for treatment of several forms of fibrosis, including fibrosis in the liver.
“In animal models, simtuzumab has demonstrated efficacy in reducing fibrosis when administered prior to fibrosis formation or after the process has already begun,” Dr. Raghu explained. He said a large trial was initiated in IPF because the agent seemed so promising and because a large study was thought to be the best strategy to arrive at a definitive answer regarding safety and efficacy.
The drug was found safe but not effective. The independent data monitoring and safety committee terminated the trial early for futility.
In the study, 544 IPF patients were randomized to 125 mg simtuzumab or placebo administered subcutaneously once weekly. The primary endpoint was PFS, but there were a large number of secondary endpoints including hospitalization for progressive disease, change in 6-minute walk distance (6MWD), and overall survival.
For the endpoint of PFS, “there was absolutely no difference” between the groups receiving simtuzumab or placebo. When the patients were stratified for demonstrating above or below median expression of LOXL2, which was a prespecified analysis for the trial, there was still no difference between groups. Even when those in the top quarter percentile of LOXL2 expression were compared with those with less [expression of the enzyme], there was still “absolutely no difference.”
There was also no significant evidence of benefit for simtuzumab observed on key secondary endpoints, such as overall survival. When patients were stratified by baseline lung function as expressed by percentage of predicted forced expiratory volume in 1 second (FEV1), there was no signal of benefit for those with severe, moderate, or mild impairment.
One criticism of this study raised after the presentation was that patients with 26% or greater of predicted FEV1 were permitted into the study. It was suggested that such patients would be expected to already have a high degree of fibrosis and therefore would be less likely to benefit from an antifibrosis therapy. Dr. Raghu acknowledged this criticism, but he said it was important to include patients with advanced disease in order to generate an adequate event rate. Even with inclusion of patients with severe lung impairment, the mortality rate was less than 10%.
He concluded that there was no signal of benefit even among those with the greatest expression of the target.
“We absolutely need better markers for IPF,” Dr. Raghu maintained. While other members of the LOXL family of enzymes may still prove to be valuable markers of IPF risk and targets of therapy, these data appear to rule out a therapeutic role for blocking LOXL2.
Dr. Raghu is a consultant for Boehringer Ingelheim, Biogen, FibroGen, Gilead, Janssen, MedImmune, Promedior, Sanofi-Aventis, and Veracyte.
LONDON – Despite very promising activity in animal models of idiopathic pulmonary fibrosis (IPF), a monoclonal antibody targeted at an enzyme considered to be important to collagen cross-linking did not produce any improvement in progression-free survival (PFS), according to results of a multicenter study presented at the annual congress of the European Respiratory Society.
“This was such a negative study, there is no point in doing another,” reported Ganesh Raghu, MD, director of the Pulmonary Fibrosis Program at the University of Washington Medical Center, Seattle.
The focus of this study was simtuzumab, a monoclonal antibody targeted at lysyl oxidase like 2 (LOXL2), an enzyme which catalyzes a step in the formation of collagen crosslinks, which are thought to be important in fibrosis formation. Simtuzumab has been entered into clinical trials for treatment of several forms of fibrosis, including fibrosis in the liver.
“In animal models, simtuzumab has demonstrated efficacy in reducing fibrosis when administered prior to fibrosis formation or after the process has already begun,” Dr. Raghu explained. He said a large trial was initiated in IPF because the agent seemed so promising and because a large study was thought to be the best strategy to arrive at a definitive answer regarding safety and efficacy.
The drug was found safe but not effective. The independent data monitoring and safety committee terminated the trial early for futility.
In the study, 544 IPF patients were randomized to 125 mg simtuzumab or placebo administered subcutaneously once weekly. The primary endpoint was PFS, but there were a large number of secondary endpoints including hospitalization for progressive disease, change in 6-minute walk distance (6MWD), and overall survival.
For the endpoint of PFS, “there was absolutely no difference” between the groups receiving simtuzumab or placebo. When the patients were stratified for demonstrating above or below median expression of LOXL2, which was a prespecified analysis for the trial, there was still no difference between groups. Even when those in the top quarter percentile of LOXL2 expression were compared with those with less [expression of the enzyme], there was still “absolutely no difference.”
There was also no significant evidence of benefit for simtuzumab observed on key secondary endpoints, such as overall survival. When patients were stratified by baseline lung function as expressed by percentage of predicted forced expiratory volume in 1 second (FEV1), there was no signal of benefit for those with severe, moderate, or mild impairment.
One criticism of this study raised after the presentation was that patients with 26% or greater of predicted FEV1 were permitted into the study. It was suggested that such patients would be expected to already have a high degree of fibrosis and therefore would be less likely to benefit from an antifibrosis therapy. Dr. Raghu acknowledged this criticism, but he said it was important to include patients with advanced disease in order to generate an adequate event rate. Even with inclusion of patients with severe lung impairment, the mortality rate was less than 10%.
He concluded that there was no signal of benefit even among those with the greatest expression of the target.
“We absolutely need better markers for IPF,” Dr. Raghu maintained. While other members of the LOXL family of enzymes may still prove to be valuable markers of IPF risk and targets of therapy, these data appear to rule out a therapeutic role for blocking LOXL2.
Dr. Raghu is a consultant for Boehringer Ingelheim, Biogen, FibroGen, Gilead, Janssen, MedImmune, Promedior, Sanofi-Aventis, and Veracyte.
AT THE ERS CONGRESS 2016
Key clinical point: A large multicenter trial with simtuzumab in idiopathic pulmonary fibrosis failed to generate a hint of benefit.
Major finding: In this study, efficacy was not seen even in those with high expression of the simtuzumab target, lysyl oxidase like 2 (LOXL2).
Data source: Phase II multicenter, placebo-controlled trial.
Disclosures: Dr. Raghu is a consultant for Boehringer Ingelheim, Biogen, FibroGen, Gilead, Janssen, MedImmune, Promedior, Sanofi-Aventis, and Veracyte.
New anticancer drugs linked to increased costs, life expectancy
New anticancer drugs are often expensive and have been accompanied by large increases in the cost of medical treatment, but they also are associated with gains in life expectancy, according to an analysis of Medicare data published online.
Investigators looked at four different types of cancer – breast, kidney, lung, and chronic myeloid leukemia (CML) – over two time periods: 1996-2000 and 2007-2011. Patients treated for CML during 2007-2011 had the largest increases in both average lifetime medical cost ($142,000) and months of life gained (22.1) over those treated during 1996-2000, reported David H. Howard, PhD, of Emory University, Atlanta, and his associates.
Breast cancer patients had the next-largest increases: 13.2 months of life expectancy and $72,000 in lifetime medical cost for those who received physician-administered intravenous drugs. For breast cancer patients who received only oral drugs, the increases were 2 months of life and $9,000 in lifetime cost, they noted.
Patients with kidney cancer had an average life-expectancy increase of 7.9 months and a cost increase of $45,000, but those estimates don’t fully reflect the effect of several oral drugs that were introduced after 2007 but did not come into widespread use during the entire study period, Dr. Howard and his associates noted (Health Aff. 2016 Sep 7;35[9]:1581-7).
Lung cancer patients experienced the smallest changes between the two time periods, with an increase in life expectancy of 3.9 months for those who received physician-administered anticancer drugs and a lifetime medical cost increase of $23,000. Patients with lung cancer who did not receive such drugs had increases of 0.7 months of life expectancy and $4,000 in lifetime medical costs.
The researchers used data from the Surveillance, Epidemiology, and End Results–Medicare database, and all costs are adjusted to 2012 dollars. Data collection was supported by the California Department of Health and funding for the study was provided by Pfizer. Three of Dr. Howard’s five coinvestigators are Pfizer employees.
New anticancer drugs are often expensive and have been accompanied by large increases in the cost of medical treatment, but they also are associated with gains in life expectancy, according to an analysis of Medicare data published online.
Investigators looked at four different types of cancer – breast, kidney, lung, and chronic myeloid leukemia (CML) – over two time periods: 1996-2000 and 2007-2011. Patients treated for CML during 2007-2011 had the largest increases in both average lifetime medical cost ($142,000) and months of life gained (22.1) over those treated during 1996-2000, reported David H. Howard, PhD, of Emory University, Atlanta, and his associates.
Breast cancer patients had the next-largest increases: 13.2 months of life expectancy and $72,000 in lifetime medical cost for those who received physician-administered intravenous drugs. For breast cancer patients who received only oral drugs, the increases were 2 months of life and $9,000 in lifetime cost, they noted.
Patients with kidney cancer had an average life-expectancy increase of 7.9 months and a cost increase of $45,000, but those estimates don’t fully reflect the effect of several oral drugs that were introduced after 2007 but did not come into widespread use during the entire study period, Dr. Howard and his associates noted (Health Aff. 2016 Sep 7;35[9]:1581-7).
Lung cancer patients experienced the smallest changes between the two time periods, with an increase in life expectancy of 3.9 months for those who received physician-administered anticancer drugs and a lifetime medical cost increase of $23,000. Patients with lung cancer who did not receive such drugs had increases of 0.7 months of life expectancy and $4,000 in lifetime medical costs.
The researchers used data from the Surveillance, Epidemiology, and End Results–Medicare database, and all costs are adjusted to 2012 dollars. Data collection was supported by the California Department of Health and funding for the study was provided by Pfizer. Three of Dr. Howard’s five coinvestigators are Pfizer employees.
New anticancer drugs are often expensive and have been accompanied by large increases in the cost of medical treatment, but they also are associated with gains in life expectancy, according to an analysis of Medicare data published online.
Investigators looked at four different types of cancer – breast, kidney, lung, and chronic myeloid leukemia (CML) – over two time periods: 1996-2000 and 2007-2011. Patients treated for CML during 2007-2011 had the largest increases in both average lifetime medical cost ($142,000) and months of life gained (22.1) over those treated during 1996-2000, reported David H. Howard, PhD, of Emory University, Atlanta, and his associates.
Breast cancer patients had the next-largest increases: 13.2 months of life expectancy and $72,000 in lifetime medical cost for those who received physician-administered intravenous drugs. For breast cancer patients who received only oral drugs, the increases were 2 months of life and $9,000 in lifetime cost, they noted.
Patients with kidney cancer had an average life-expectancy increase of 7.9 months and a cost increase of $45,000, but those estimates don’t fully reflect the effect of several oral drugs that were introduced after 2007 but did not come into widespread use during the entire study period, Dr. Howard and his associates noted (Health Aff. 2016 Sep 7;35[9]:1581-7).
Lung cancer patients experienced the smallest changes between the two time periods, with an increase in life expectancy of 3.9 months for those who received physician-administered anticancer drugs and a lifetime medical cost increase of $23,000. Patients with lung cancer who did not receive such drugs had increases of 0.7 months of life expectancy and $4,000 in lifetime medical costs.
The researchers used data from the Surveillance, Epidemiology, and End Results–Medicare database, and all costs are adjusted to 2012 dollars. Data collection was supported by the California Department of Health and funding for the study was provided by Pfizer. Three of Dr. Howard’s five coinvestigators are Pfizer employees.
FROM HEALTH AFFAIRS