User login
Concerns over discretion, efficacy lead teen females to use emergency contraception
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
FROM THE JOURNAL OF PEDIATRIC AND ADOLESCENT GYNECOLOGY
Key clinical point: 65% of adolescent females who were interviewed incorrectly believed that emergency contraception is 90%-99% effective.
Major finding: Adolescents who use emergency contraception prefer it over nonemergent contraception because it is perceived as easy to use and a more private alternative.
Study details: A study of 28 interviews of adolescent females who self-reported emergency contraception use.
Disclosures: The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
Source: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
Trump administration rule erodes ACA contraceptive mandate
More employers can opt out of providing contraception coverage to their employees under final regulations from the Trump administration that narrow the Affordable Care Act’s contraceptive mandate.
The two regulations, released Nov. 7, allow an expanded group of employers and insurers to get out of covering contraception methods by objecting on either religious or moral grounds.
The first rule broadens exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. The second rule protects nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions apply to institutions of education, issuers, and individuals, but not to governmental entities.
When first proposed in 2017, Trump administration officials said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” The U.S. Department of Health & Human Services estimates that the rules, which take effect in January 2019, will affect no more than 200 employers.
The American College of Obstetricians and Gynecologists expressed concern that the final rules will restrict patient access to meaningful contraceptive methods and will erode decades of progress in increasing women’s reproductive autonomy and restrict patient access to contraception.
“Women, families and our nation all benefit from seamless, affordable access to contraception,” ACOG President Lisa M. Hollier, MD, said in a statement. “Contraception improves women’s health and well-being, reduces unintended pregnancy, enables pregnancy spacing for safer pregnancies and deliveries, and empowers women’s engagement in the workforce and economic self-sufficiency. A woman’s employer should not determine whether or not she has this access.”
Marjorie Dannenfelser, president of Susan B. Anthony List, an anti-abortion group, praised the final rules, calling them needed protections from the burdensome Obama-era ACA abortifacient drug mandate.
“President Trump and HHS Secretary Azar delivered a huge victory for conscience rights and religious liberty in America,” Ms. Dannenfelser said in a statement. “No longer will Catholic nuns who care for the elderly poor be forced by the government to provide abortion-inducing drugs in their health care plans. Not only that, moral objectors such as Susan B. Anthony List, will also no longer have to pay for life-ending drugs that are antithetical to their mission and for which we have argued there is certainly no compelling state interest.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
Under the approved regulations, employers or insurers can stop their coverage of contraceptive services if they have religious beliefs or moral convictions against covering birth control. Exempted entities and individuals also can choose to cover some, but not all, contraceptive services, depending on their specific religious or moral objection, according to an HHS fact sheet.
The agency emphasized that the regulations leave in place government programs that provide free or subsidized contraceptive coverage to low-income women, such as through community health centers, and that the rules do not ban any employer from covering contraceptives.
The regulations become effective 60 days after they are published in the Federal Register.
More employers can opt out of providing contraception coverage to their employees under final regulations from the Trump administration that narrow the Affordable Care Act’s contraceptive mandate.
The two regulations, released Nov. 7, allow an expanded group of employers and insurers to get out of covering contraception methods by objecting on either religious or moral grounds.
The first rule broadens exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. The second rule protects nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions apply to institutions of education, issuers, and individuals, but not to governmental entities.
When first proposed in 2017, Trump administration officials said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” The U.S. Department of Health & Human Services estimates that the rules, which take effect in January 2019, will affect no more than 200 employers.
The American College of Obstetricians and Gynecologists expressed concern that the final rules will restrict patient access to meaningful contraceptive methods and will erode decades of progress in increasing women’s reproductive autonomy and restrict patient access to contraception.
“Women, families and our nation all benefit from seamless, affordable access to contraception,” ACOG President Lisa M. Hollier, MD, said in a statement. “Contraception improves women’s health and well-being, reduces unintended pregnancy, enables pregnancy spacing for safer pregnancies and deliveries, and empowers women’s engagement in the workforce and economic self-sufficiency. A woman’s employer should not determine whether or not she has this access.”
Marjorie Dannenfelser, president of Susan B. Anthony List, an anti-abortion group, praised the final rules, calling them needed protections from the burdensome Obama-era ACA abortifacient drug mandate.
“President Trump and HHS Secretary Azar delivered a huge victory for conscience rights and religious liberty in America,” Ms. Dannenfelser said in a statement. “No longer will Catholic nuns who care for the elderly poor be forced by the government to provide abortion-inducing drugs in their health care plans. Not only that, moral objectors such as Susan B. Anthony List, will also no longer have to pay for life-ending drugs that are antithetical to their mission and for which we have argued there is certainly no compelling state interest.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
Under the approved regulations, employers or insurers can stop their coverage of contraceptive services if they have religious beliefs or moral convictions against covering birth control. Exempted entities and individuals also can choose to cover some, but not all, contraceptive services, depending on their specific religious or moral objection, according to an HHS fact sheet.
The agency emphasized that the regulations leave in place government programs that provide free or subsidized contraceptive coverage to low-income women, such as through community health centers, and that the rules do not ban any employer from covering contraceptives.
The regulations become effective 60 days after they are published in the Federal Register.
More employers can opt out of providing contraception coverage to their employees under final regulations from the Trump administration that narrow the Affordable Care Act’s contraceptive mandate.
The two regulations, released Nov. 7, allow an expanded group of employers and insurers to get out of covering contraception methods by objecting on either religious or moral grounds.
The first rule broadens exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. The second rule protects nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions apply to institutions of education, issuers, and individuals, but not to governmental entities.
When first proposed in 2017, Trump administration officials said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” The U.S. Department of Health & Human Services estimates that the rules, which take effect in January 2019, will affect no more than 200 employers.
The American College of Obstetricians and Gynecologists expressed concern that the final rules will restrict patient access to meaningful contraceptive methods and will erode decades of progress in increasing women’s reproductive autonomy and restrict patient access to contraception.
“Women, families and our nation all benefit from seamless, affordable access to contraception,” ACOG President Lisa M. Hollier, MD, said in a statement. “Contraception improves women’s health and well-being, reduces unintended pregnancy, enables pregnancy spacing for safer pregnancies and deliveries, and empowers women’s engagement in the workforce and economic self-sufficiency. A woman’s employer should not determine whether or not she has this access.”
Marjorie Dannenfelser, president of Susan B. Anthony List, an anti-abortion group, praised the final rules, calling them needed protections from the burdensome Obama-era ACA abortifacient drug mandate.
“President Trump and HHS Secretary Azar delivered a huge victory for conscience rights and religious liberty in America,” Ms. Dannenfelser said in a statement. “No longer will Catholic nuns who care for the elderly poor be forced by the government to provide abortion-inducing drugs in their health care plans. Not only that, moral objectors such as Susan B. Anthony List, will also no longer have to pay for life-ending drugs that are antithetical to their mission and for which we have argued there is certainly no compelling state interest.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
Under the approved regulations, employers or insurers can stop their coverage of contraceptive services if they have religious beliefs or moral convictions against covering birth control. Exempted entities and individuals also can choose to cover some, but not all, contraceptive services, depending on their specific religious or moral objection, according to an HHS fact sheet.
The agency emphasized that the regulations leave in place government programs that provide free or subsidized contraceptive coverage to low-income women, such as through community health centers, and that the rules do not ban any employer from covering contraceptives.
The regulations become effective 60 days after they are published in the Federal Register.
Single-dose zoliflodacin successfully treats uncomplicated urogenital gonorrhea
A new antibiotic successfully treated uncomplicated urogenital and rectal gonococcal infections, but was not as effective as ceftriaxone in treating pharyngeal infections, according to the results of a randomized, phase 2 study.
About 96% of patients with infection at urogenital sites had microbiologic cure with zoliflodacin, a novel antimicrobial agent that inhibits DNA biosynthesis. The cure rate was 100% for rectal infections, but was just 50%-82% for pharyngeal infections, though few participants in this study had infection at either of those sites.
The study investigators, led by Stephanie N. Taylor, MD, professor of medicine and microbiology at Louisiana State University, New Orleans, wrote that the need for new antimicrobial agents has been underscored by reports of multidrug-resistant Neisseria gonorrhoeae and the possibility of untreatable gonorrhea.
“This phase 2 trial creates equipoise for larger, more definitive studies of zoliflodacin,” Dr. Taylor and her coauthors wrote in the New England Journal of Medicine.
At this point, N. gonorrhoeae has developed resistance to every recommended antibiotic class, including cephalosporins and macrolides, they added.
Zoliflodacin (ETX0914) is an antimicrobial that has received fast-track designation from the Food and Drug Administration specifically for development as an oral treatment for gonococcal infections, the authors noted.
“The mechanism of action of zoliflodacin differs from currently available therapies in that it inhibits microbial biosynthesis by arresting the cleaved covalent gyrase complex and the formation of fused circular DNA required for biosynthesis,” they wrote.
Dr. Taylor and her colleagues studied single 2- and 3-gram doses of zoliflodacin in comparison with 500 mg of intramuscular ceftriaxone in 181 patients with uncomplicated urogenital gonorrhea enrolled in the open-label, randomized, phase 2 study between November 2014 and December 2015.
A total of 141 patients included in the microbiologic intention-to-treat analysis had confirmed positive urethral or cervical cultures. Cures were seen in 55 of 57 infections treated with 2 grams (96%) and 54 of 56 treated with 3 grams (96%) of zoliflodacin, and in 28 of 28 infections (100%) treated with ceftriaxone.
Of 15 confirmed rectal infections, 100% were cured, including 12 treated with zoliflodacin at 2 or 3 grams and 3 treated with ceftriaxone. Of 23 confirmed pharyngeal infections, cures were seen in 4 of 8 (50%) treated with 2 grams of zoliflodacin and 9 of 11 (82%) treated with 3 grams, compared with 4 of 4 cured (100%) with ceftriaxone.
That suggests zoliflodacin was not as effective as ceftriaxone in treating pharyngeal gonorrhea, which is generally considered more difficult to treat than infections at other sites, according to Dr. Taylor and her coauthors.
“Currently, this limitation has not curtailed recommendations for the use of drugs such as spectinomycin or fluoroquinolones for the treatment of gonorrhea,” they wrote.
The study was funded by the National Institutes of Health and Entasis Therapeutics. Dr. Taylor reported grants from the NIH during the study, and other disclosures related to a variety of pharma companies. Her coauthors reported disclosures related to AstraZeneca (parent company of Entasis, which is developing zoliflodacin) and other pharmaceutical companies.
SOURCE: Taylor SN et al. N Engl J Med. 2018 Nov 7; 379:1835-45.
This study represents a “step forward” in identifying new antimicrobial treatment options for patients with gonorrhea, according to Susan Blank, MD, and Demetre C. Daskalakis, MD.
“Given the challenges in clinical follow-up in this patient population, the single-dose regimen is promising,” Dr. Blank and Dr. Daskalakis wrote in a editorial.
While zoliflodacin has the potential to be an effective treatment for gonorrhea, its activity needs to be better defined, particularly in key anatomical sites of infection such as the pharynx, where limited activity was observed.
Progression of resistance of Neisseria gonorrhoeae is an “ever-present concern” given the history of the organism, the authors wrote.
“We are facing the real danger of multidrug-resistant, nearly untreatable gonorrhea,” they wrote. “To avoid untreatable cases of this high-incidence infection, we need to advance diagnostic technology and develop treatments with different mechanisms of action.”
Dr. Blank and Dr. Daskalakis are with the division of disease control in the New York City Department of Health and Mental Hygiene. Their editorial appears in the New England Journal of Medicine . Both reported having no conflicts of interest.
This study represents a “step forward” in identifying new antimicrobial treatment options for patients with gonorrhea, according to Susan Blank, MD, and Demetre C. Daskalakis, MD.
“Given the challenges in clinical follow-up in this patient population, the single-dose regimen is promising,” Dr. Blank and Dr. Daskalakis wrote in a editorial.
While zoliflodacin has the potential to be an effective treatment for gonorrhea, its activity needs to be better defined, particularly in key anatomical sites of infection such as the pharynx, where limited activity was observed.
Progression of resistance of Neisseria gonorrhoeae is an “ever-present concern” given the history of the organism, the authors wrote.
“We are facing the real danger of multidrug-resistant, nearly untreatable gonorrhea,” they wrote. “To avoid untreatable cases of this high-incidence infection, we need to advance diagnostic technology and develop treatments with different mechanisms of action.”
Dr. Blank and Dr. Daskalakis are with the division of disease control in the New York City Department of Health and Mental Hygiene. Their editorial appears in the New England Journal of Medicine . Both reported having no conflicts of interest.
This study represents a “step forward” in identifying new antimicrobial treatment options for patients with gonorrhea, according to Susan Blank, MD, and Demetre C. Daskalakis, MD.
“Given the challenges in clinical follow-up in this patient population, the single-dose regimen is promising,” Dr. Blank and Dr. Daskalakis wrote in a editorial.
While zoliflodacin has the potential to be an effective treatment for gonorrhea, its activity needs to be better defined, particularly in key anatomical sites of infection such as the pharynx, where limited activity was observed.
Progression of resistance of Neisseria gonorrhoeae is an “ever-present concern” given the history of the organism, the authors wrote.
“We are facing the real danger of multidrug-resistant, nearly untreatable gonorrhea,” they wrote. “To avoid untreatable cases of this high-incidence infection, we need to advance diagnostic technology and develop treatments with different mechanisms of action.”
Dr. Blank and Dr. Daskalakis are with the division of disease control in the New York City Department of Health and Mental Hygiene. Their editorial appears in the New England Journal of Medicine . Both reported having no conflicts of interest.
A new antibiotic successfully treated uncomplicated urogenital and rectal gonococcal infections, but was not as effective as ceftriaxone in treating pharyngeal infections, according to the results of a randomized, phase 2 study.
About 96% of patients with infection at urogenital sites had microbiologic cure with zoliflodacin, a novel antimicrobial agent that inhibits DNA biosynthesis. The cure rate was 100% for rectal infections, but was just 50%-82% for pharyngeal infections, though few participants in this study had infection at either of those sites.
The study investigators, led by Stephanie N. Taylor, MD, professor of medicine and microbiology at Louisiana State University, New Orleans, wrote that the need for new antimicrobial agents has been underscored by reports of multidrug-resistant Neisseria gonorrhoeae and the possibility of untreatable gonorrhea.
“This phase 2 trial creates equipoise for larger, more definitive studies of zoliflodacin,” Dr. Taylor and her coauthors wrote in the New England Journal of Medicine.
At this point, N. gonorrhoeae has developed resistance to every recommended antibiotic class, including cephalosporins and macrolides, they added.
Zoliflodacin (ETX0914) is an antimicrobial that has received fast-track designation from the Food and Drug Administration specifically for development as an oral treatment for gonococcal infections, the authors noted.
“The mechanism of action of zoliflodacin differs from currently available therapies in that it inhibits microbial biosynthesis by arresting the cleaved covalent gyrase complex and the formation of fused circular DNA required for biosynthesis,” they wrote.
Dr. Taylor and her colleagues studied single 2- and 3-gram doses of zoliflodacin in comparison with 500 mg of intramuscular ceftriaxone in 181 patients with uncomplicated urogenital gonorrhea enrolled in the open-label, randomized, phase 2 study between November 2014 and December 2015.
A total of 141 patients included in the microbiologic intention-to-treat analysis had confirmed positive urethral or cervical cultures. Cures were seen in 55 of 57 infections treated with 2 grams (96%) and 54 of 56 treated with 3 grams (96%) of zoliflodacin, and in 28 of 28 infections (100%) treated with ceftriaxone.
Of 15 confirmed rectal infections, 100% were cured, including 12 treated with zoliflodacin at 2 or 3 grams and 3 treated with ceftriaxone. Of 23 confirmed pharyngeal infections, cures were seen in 4 of 8 (50%) treated with 2 grams of zoliflodacin and 9 of 11 (82%) treated with 3 grams, compared with 4 of 4 cured (100%) with ceftriaxone.
That suggests zoliflodacin was not as effective as ceftriaxone in treating pharyngeal gonorrhea, which is generally considered more difficult to treat than infections at other sites, according to Dr. Taylor and her coauthors.
“Currently, this limitation has not curtailed recommendations for the use of drugs such as spectinomycin or fluoroquinolones for the treatment of gonorrhea,” they wrote.
The study was funded by the National Institutes of Health and Entasis Therapeutics. Dr. Taylor reported grants from the NIH during the study, and other disclosures related to a variety of pharma companies. Her coauthors reported disclosures related to AstraZeneca (parent company of Entasis, which is developing zoliflodacin) and other pharmaceutical companies.
SOURCE: Taylor SN et al. N Engl J Med. 2018 Nov 7; 379:1835-45.
A new antibiotic successfully treated uncomplicated urogenital and rectal gonococcal infections, but was not as effective as ceftriaxone in treating pharyngeal infections, according to the results of a randomized, phase 2 study.
About 96% of patients with infection at urogenital sites had microbiologic cure with zoliflodacin, a novel antimicrobial agent that inhibits DNA biosynthesis. The cure rate was 100% for rectal infections, but was just 50%-82% for pharyngeal infections, though few participants in this study had infection at either of those sites.
The study investigators, led by Stephanie N. Taylor, MD, professor of medicine and microbiology at Louisiana State University, New Orleans, wrote that the need for new antimicrobial agents has been underscored by reports of multidrug-resistant Neisseria gonorrhoeae and the possibility of untreatable gonorrhea.
“This phase 2 trial creates equipoise for larger, more definitive studies of zoliflodacin,” Dr. Taylor and her coauthors wrote in the New England Journal of Medicine.
At this point, N. gonorrhoeae has developed resistance to every recommended antibiotic class, including cephalosporins and macrolides, they added.
Zoliflodacin (ETX0914) is an antimicrobial that has received fast-track designation from the Food and Drug Administration specifically for development as an oral treatment for gonococcal infections, the authors noted.
“The mechanism of action of zoliflodacin differs from currently available therapies in that it inhibits microbial biosynthesis by arresting the cleaved covalent gyrase complex and the formation of fused circular DNA required for biosynthesis,” they wrote.
Dr. Taylor and her colleagues studied single 2- and 3-gram doses of zoliflodacin in comparison with 500 mg of intramuscular ceftriaxone in 181 patients with uncomplicated urogenital gonorrhea enrolled in the open-label, randomized, phase 2 study between November 2014 and December 2015.
A total of 141 patients included in the microbiologic intention-to-treat analysis had confirmed positive urethral or cervical cultures. Cures were seen in 55 of 57 infections treated with 2 grams (96%) and 54 of 56 treated with 3 grams (96%) of zoliflodacin, and in 28 of 28 infections (100%) treated with ceftriaxone.
Of 15 confirmed rectal infections, 100% were cured, including 12 treated with zoliflodacin at 2 or 3 grams and 3 treated with ceftriaxone. Of 23 confirmed pharyngeal infections, cures were seen in 4 of 8 (50%) treated with 2 grams of zoliflodacin and 9 of 11 (82%) treated with 3 grams, compared with 4 of 4 cured (100%) with ceftriaxone.
That suggests zoliflodacin was not as effective as ceftriaxone in treating pharyngeal gonorrhea, which is generally considered more difficult to treat than infections at other sites, according to Dr. Taylor and her coauthors.
“Currently, this limitation has not curtailed recommendations for the use of drugs such as spectinomycin or fluoroquinolones for the treatment of gonorrhea,” they wrote.
The study was funded by the National Institutes of Health and Entasis Therapeutics. Dr. Taylor reported grants from the NIH during the study, and other disclosures related to a variety of pharma companies. Her coauthors reported disclosures related to AstraZeneca (parent company of Entasis, which is developing zoliflodacin) and other pharmaceutical companies.
SOURCE: Taylor SN et al. N Engl J Med. 2018 Nov 7; 379:1835-45.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Cure rates of 96% and 100% were reported for urethral/cervical and rectal infections, respectively, and ranged from 50% to 82% in pharyngeal infections.
Study details: A randomized, open-label, phase 2 study including 181 patients with uncomplicated urogenital gonorrhea who received zoliflodacin or ceftriaxone.
Disclosures: The study authors reported disclosures related to AstraZeneca (parent company of Entasis Therapeutics, which is developing zoliflodacin) and other pharmaceutical companies.
Source: Taylor SN et al. N Engl J Med. 2018 Nov 7; 379:1835-45.
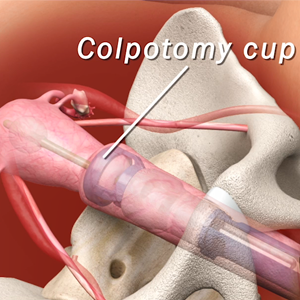
Rate of sling removal 9 years after MUS for SUI over 3%
a British study found.
Ipek Gurol-Urganci, PhD, of the London School of Hygiene and Tropical Medicine, and her coauthors said their study comes as a result of safety concerns around the procedure, which resulted in a suspension of the operation in the United Kingdom.
“There is concern about problems that some women experience following MUS insertion, including pain, dyspareunia, persistent urinary incontinence, and exposure or erosion. However, there is little randomized, clinical trial evidence on these longer-term outcomes,” they wrote in JAMA, noting that an estimated 250,000 MUS operations were performed in 2010 in the United States.
The current study involved 95,057 women in England who underwent an MUS insertion procedure for SUI for the first time in a National Health Service hospital between 2006 and 2015. Overall, 60,194 of the women had a retropubic insertion and 34,863 had a transobturator insertion.
At 9 years after the initial insertion, the mesh was removed in 3.3% of women. The risk of removal was higher for women who had a retropubic insertion (3.6%), compared with those who had a transobturator insertion (2.7%).
“The risk of a removal was about 30% lower if the mesh sling had been inserted via the transobturator route, which may be explained by the removal of transobturator sling being a more complicated procedure,” Dr. Gurol-Urganci and her associates noted.
Mesh sling removal risk decreased with age, with the risk at 4.4% for women aged 18-39 years, compared with 2.1% in women aged 70 years and older at 9 years after insertion.
The authors wrote that the risks of removal and any reoperation (mesh removal and/or reoperation for SUI) were higher among women from a white racial/ethnic background. However, it was not possible to “disentangle explanations” for these possible differences in risk seen with patient characteristics, which ranged from higher morbidity to differences in the reasons for surgery.
Results also showed that the risk of reoperation was 4.5% at 9 years after the initial insertion, and was slightly higher for a transobturator insertion at 5.3%, compared with 4.1% for a retropubic insertion.
The risk of any reoperation, including mesh removal and/or reoperation for SUI, following the initial MUS insertion was 6.9% at 9 years (95% confidence interval, 6.7%-7.1%), but no statistically significant difference was observed between retropubic and transobturator insertion.
“The present results demonstrate that removal and reoperation risks were associated with the insertion route and patient factors,” Dr. Gurol-Urganci and her associates wrote.
“These findings may guide women and their surgeons when making decisions about surgical treatment of stress urinary incontinence,” they concluded.
The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas.
SOURCE: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
a British study found.
Ipek Gurol-Urganci, PhD, of the London School of Hygiene and Tropical Medicine, and her coauthors said their study comes as a result of safety concerns around the procedure, which resulted in a suspension of the operation in the United Kingdom.
“There is concern about problems that some women experience following MUS insertion, including pain, dyspareunia, persistent urinary incontinence, and exposure or erosion. However, there is little randomized, clinical trial evidence on these longer-term outcomes,” they wrote in JAMA, noting that an estimated 250,000 MUS operations were performed in 2010 in the United States.
The current study involved 95,057 women in England who underwent an MUS insertion procedure for SUI for the first time in a National Health Service hospital between 2006 and 2015. Overall, 60,194 of the women had a retropubic insertion and 34,863 had a transobturator insertion.
At 9 years after the initial insertion, the mesh was removed in 3.3% of women. The risk of removal was higher for women who had a retropubic insertion (3.6%), compared with those who had a transobturator insertion (2.7%).
“The risk of a removal was about 30% lower if the mesh sling had been inserted via the transobturator route, which may be explained by the removal of transobturator sling being a more complicated procedure,” Dr. Gurol-Urganci and her associates noted.
Mesh sling removal risk decreased with age, with the risk at 4.4% for women aged 18-39 years, compared with 2.1% in women aged 70 years and older at 9 years after insertion.
The authors wrote that the risks of removal and any reoperation (mesh removal and/or reoperation for SUI) were higher among women from a white racial/ethnic background. However, it was not possible to “disentangle explanations” for these possible differences in risk seen with patient characteristics, which ranged from higher morbidity to differences in the reasons for surgery.
Results also showed that the risk of reoperation was 4.5% at 9 years after the initial insertion, and was slightly higher for a transobturator insertion at 5.3%, compared with 4.1% for a retropubic insertion.
The risk of any reoperation, including mesh removal and/or reoperation for SUI, following the initial MUS insertion was 6.9% at 9 years (95% confidence interval, 6.7%-7.1%), but no statistically significant difference was observed between retropubic and transobturator insertion.
“The present results demonstrate that removal and reoperation risks were associated with the insertion route and patient factors,” Dr. Gurol-Urganci and her associates wrote.
“These findings may guide women and their surgeons when making decisions about surgical treatment of stress urinary incontinence,” they concluded.
The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas.
SOURCE: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
a British study found.
Ipek Gurol-Urganci, PhD, of the London School of Hygiene and Tropical Medicine, and her coauthors said their study comes as a result of safety concerns around the procedure, which resulted in a suspension of the operation in the United Kingdom.
“There is concern about problems that some women experience following MUS insertion, including pain, dyspareunia, persistent urinary incontinence, and exposure or erosion. However, there is little randomized, clinical trial evidence on these longer-term outcomes,” they wrote in JAMA, noting that an estimated 250,000 MUS operations were performed in 2010 in the United States.
The current study involved 95,057 women in England who underwent an MUS insertion procedure for SUI for the first time in a National Health Service hospital between 2006 and 2015. Overall, 60,194 of the women had a retropubic insertion and 34,863 had a transobturator insertion.
At 9 years after the initial insertion, the mesh was removed in 3.3% of women. The risk of removal was higher for women who had a retropubic insertion (3.6%), compared with those who had a transobturator insertion (2.7%).
“The risk of a removal was about 30% lower if the mesh sling had been inserted via the transobturator route, which may be explained by the removal of transobturator sling being a more complicated procedure,” Dr. Gurol-Urganci and her associates noted.
Mesh sling removal risk decreased with age, with the risk at 4.4% for women aged 18-39 years, compared with 2.1% in women aged 70 years and older at 9 years after insertion.
The authors wrote that the risks of removal and any reoperation (mesh removal and/or reoperation for SUI) were higher among women from a white racial/ethnic background. However, it was not possible to “disentangle explanations” for these possible differences in risk seen with patient characteristics, which ranged from higher morbidity to differences in the reasons for surgery.
Results also showed that the risk of reoperation was 4.5% at 9 years after the initial insertion, and was slightly higher for a transobturator insertion at 5.3%, compared with 4.1% for a retropubic insertion.
The risk of any reoperation, including mesh removal and/or reoperation for SUI, following the initial MUS insertion was 6.9% at 9 years (95% confidence interval, 6.7%-7.1%), but no statistically significant difference was observed between retropubic and transobturator insertion.
“The present results demonstrate that removal and reoperation risks were associated with the insertion route and patient factors,” Dr. Gurol-Urganci and her associates wrote.
“These findings may guide women and their surgeons when making decisions about surgical treatment of stress urinary incontinence,” they concluded.
The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas.
SOURCE: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
FROM JAMA
Key clinical point: The findings of this study may inform decision making when choosing treatment for stress urinary incontinence.
Major finding: Within 9 years of a mesh insertion for stress urinary incontinence, the rate of sling removal was 3.3% and the rate of reoperation was 4.5%.
Study details: A prospective, observational study examining long-term mesh removal and reoperations in over 95,000 women who underwent midurethral mesh operations for stress urinary incontinence between 2006 and 2015.
Disclosures: The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas Pharma.
Source: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
Yoga feasible, provides modest benefits for women with urinary incontinence
according to Alison J. Huang, MD, of the University of California, San Francisco, and her associates.
In a small study published in the American Journal of Obstetrics and Gynecology, 28 women enrolled in a 3-month yoga intervention program and 28 were enrolled in a control program consisting of nonspecific muscle stretching and strengthening. The mean age was 65 years, baseline urinary incontinence was 3.5 episodes/day, and 37 women had urgency-predominant incontinence.
Of those who completed the study, 89% of 27 patients in the yoga group attended at least 80% of classes, compared with 87% in the control group; over 90% of women in the yoga group completed at least 9 home practice hours.
Overall incontinence frequency was reduced by 76% in the yoga group and by 56% in the control group. Incontinence caused by stress was significantly reduced in the yoga group, compared with the control group (61% vs. 35%; P = .045), but the rate of incontinence caused by urgency did not noticeably differ. A total of 48 nonserious adverse events were reported over the 3-month period (23 in the yoga and 25 in the control group), but none were associated with either yoga or control treatment.
“Yoga may be useful for incontinent women in the community who lack access to incontinence specialists, are unable to use clinical therapies, or wish to enhance conventional care. Since yoga can be practiced in a group setting without continuous supervision by health care specialists, it offers a potentially cost-effective, community-based self-management strategy for incontinence, provided that it can be taught with appropriate attention to safety and to patients’ clinical needs,” the authors noted.
The study was supported with grants from the National Center for Complementary and Integrative Medicine and the UCSF Osher Center for Integrative Medicine’s Bradley fund. One of the authors received a grant from the National Institute of Diabetes and Digestive and Kidney Disorders. Two study authors reported receiving funding from Pfizer and Astellas to conduct research unrelated to the current study.
SOURCE: Huang AJ et al. Am J Obstet Gynecol. 2018 Oct 26. doi: 10.1016/j.ajog.2018.10.031.
according to Alison J. Huang, MD, of the University of California, San Francisco, and her associates.
In a small study published in the American Journal of Obstetrics and Gynecology, 28 women enrolled in a 3-month yoga intervention program and 28 were enrolled in a control program consisting of nonspecific muscle stretching and strengthening. The mean age was 65 years, baseline urinary incontinence was 3.5 episodes/day, and 37 women had urgency-predominant incontinence.
Of those who completed the study, 89% of 27 patients in the yoga group attended at least 80% of classes, compared with 87% in the control group; over 90% of women in the yoga group completed at least 9 home practice hours.
Overall incontinence frequency was reduced by 76% in the yoga group and by 56% in the control group. Incontinence caused by stress was significantly reduced in the yoga group, compared with the control group (61% vs. 35%; P = .045), but the rate of incontinence caused by urgency did not noticeably differ. A total of 48 nonserious adverse events were reported over the 3-month period (23 in the yoga and 25 in the control group), but none were associated with either yoga or control treatment.
“Yoga may be useful for incontinent women in the community who lack access to incontinence specialists, are unable to use clinical therapies, or wish to enhance conventional care. Since yoga can be practiced in a group setting without continuous supervision by health care specialists, it offers a potentially cost-effective, community-based self-management strategy for incontinence, provided that it can be taught with appropriate attention to safety and to patients’ clinical needs,” the authors noted.
The study was supported with grants from the National Center for Complementary and Integrative Medicine and the UCSF Osher Center for Integrative Medicine’s Bradley fund. One of the authors received a grant from the National Institute of Diabetes and Digestive and Kidney Disorders. Two study authors reported receiving funding from Pfizer and Astellas to conduct research unrelated to the current study.
SOURCE: Huang AJ et al. Am J Obstet Gynecol. 2018 Oct 26. doi: 10.1016/j.ajog.2018.10.031.
according to Alison J. Huang, MD, of the University of California, San Francisco, and her associates.
In a small study published in the American Journal of Obstetrics and Gynecology, 28 women enrolled in a 3-month yoga intervention program and 28 were enrolled in a control program consisting of nonspecific muscle stretching and strengthening. The mean age was 65 years, baseline urinary incontinence was 3.5 episodes/day, and 37 women had urgency-predominant incontinence.
Of those who completed the study, 89% of 27 patients in the yoga group attended at least 80% of classes, compared with 87% in the control group; over 90% of women in the yoga group completed at least 9 home practice hours.
Overall incontinence frequency was reduced by 76% in the yoga group and by 56% in the control group. Incontinence caused by stress was significantly reduced in the yoga group, compared with the control group (61% vs. 35%; P = .045), but the rate of incontinence caused by urgency did not noticeably differ. A total of 48 nonserious adverse events were reported over the 3-month period (23 in the yoga and 25 in the control group), but none were associated with either yoga or control treatment.
“Yoga may be useful for incontinent women in the community who lack access to incontinence specialists, are unable to use clinical therapies, or wish to enhance conventional care. Since yoga can be practiced in a group setting without continuous supervision by health care specialists, it offers a potentially cost-effective, community-based self-management strategy for incontinence, provided that it can be taught with appropriate attention to safety and to patients’ clinical needs,” the authors noted.
The study was supported with grants from the National Center for Complementary and Integrative Medicine and the UCSF Osher Center for Integrative Medicine’s Bradley fund. One of the authors received a grant from the National Institute of Diabetes and Digestive and Kidney Disorders. Two study authors reported receiving funding from Pfizer and Astellas to conduct research unrelated to the current study.
SOURCE: Huang AJ et al. Am J Obstet Gynecol. 2018 Oct 26. doi: 10.1016/j.ajog.2018.10.031.
FROM THE AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Are patients more satisfied with combination or monotherapy for hirsutism in PCOS?
EXPERT COMMENTARY
Ezeh and colleagues conducted a retrospective analysis to evaluate the effectiveness of long-term combination suppressive therapy on hirsutism, acne, and menstrual disturbances in patients with PCOS and to identify the elements that could predict therapeutic response.
Details of the study
This chart review examined data from 200 nondiabetic patients with PCOS who presented between October 1987 and June 2002. PCOS diagnosis was based on the National Institutes of Health (NIH) 1990 criteria. During the initial visit, patients underwent a detailed medical history and physical exam, including a modified Ferriman-Gallwey hirsutism score and hormonal evaluation.
Treatment regimens. Patients were treated with suppressive therapy that consisted of an oral contraceptive (OC) (35 µg ethinyl estradiol plus 1 mg ethynodiol diacetate), an antiandrogen (spironolactone 200 mg/day), or a combination of these drugs. They were followed every 4 to 12 months (mean follow-up time, 34.2 months; range, 6–155 months), and subjective therapy response was assessed from medical records and by improvements in hirsutism scores.
Study findings. The 138 patients treated with combination suppressive therapy reported higher rates of subjective improvement in hirsutism compared with patients treated with other regimens (89.9% vs 72.0%, P<.0001). They also had a significant objective reduction in their modified Ferriman-Gallwey hirsutism score (6.0 vs 3.2; P = .0001). The combination therapy was superior to either regimen alone; the response to therapy for symptom resolution took at least 6 months and continued for up to 60 months of combination suppressive therapy.
Adding electrolysis treatment to the combination regimen resulted in improved patient satisfaction, but the differences were not significant. Patients’ satisfaction with the therapeutic response could be predicted from their pretreatment hirsutism scores or circulating sex hormone–binding globulin levels.
Study strengths and weaknesses
The study’s major strengths are the large number of patients included, the uniformity of criteria for diagnosis, and the prolonged follow-up. This is one of the few studies to report the impact of therapy on health-related quality of life in patients with PCOS and to assess response to therapy with use of objective measures, such as changes in the modified Ferriman-Gallwey score.
However, the criteria used to diagnose PCOS—the NIH 1990 criteria—currently are used less commonly than the Rotterdam 2003 criteria, and they are less inclusive for the diagnosis of PCOS.
The OC pill formulation used in this study contained the progestogen ethynodiol diacetate, which is not used routinely in modern clinical practice. In addition, the majority of patients were non-Hispanic white, which limits extrapolating these findings to other races and ethnicities.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
This retrospective study offers Level II evidence confirming the superiority of a combined OC plus spironolactone (compared with either agent alone) in the treatment of hirsutism in women with PCOS. In addition, this study emphasizes the importance of using combination suppressive therapy for at least 6 months to see a clinical response. Electrolysis may be helpful to patients especially during the initial 6 months of suppressive treatment. Finally, spironolactone alone could be reserved for cases in which OCs are contraindicated in women not interested in becoming pregnant.
In our practice, we treat patients with hirsutism using OC pills containing the progestogen levonorgestrel plus spironolactone at a lower dose of 100 mg/day, since patients treated with higher spironolactone doses report irregular bleeding and fatigue.
--ELIE HOBEIKA, MD, AND BERT SCOCCIA, MD
EXPERT COMMENTARY
Ezeh and colleagues conducted a retrospective analysis to evaluate the effectiveness of long-term combination suppressive therapy on hirsutism, acne, and menstrual disturbances in patients with PCOS and to identify the elements that could predict therapeutic response.
Details of the study
This chart review examined data from 200 nondiabetic patients with PCOS who presented between October 1987 and June 2002. PCOS diagnosis was based on the National Institutes of Health (NIH) 1990 criteria. During the initial visit, patients underwent a detailed medical history and physical exam, including a modified Ferriman-Gallwey hirsutism score and hormonal evaluation.
Treatment regimens. Patients were treated with suppressive therapy that consisted of an oral contraceptive (OC) (35 µg ethinyl estradiol plus 1 mg ethynodiol diacetate), an antiandrogen (spironolactone 200 mg/day), or a combination of these drugs. They were followed every 4 to 12 months (mean follow-up time, 34.2 months; range, 6–155 months), and subjective therapy response was assessed from medical records and by improvements in hirsutism scores.
Study findings. The 138 patients treated with combination suppressive therapy reported higher rates of subjective improvement in hirsutism compared with patients treated with other regimens (89.9% vs 72.0%, P<.0001). They also had a significant objective reduction in their modified Ferriman-Gallwey hirsutism score (6.0 vs 3.2; P = .0001). The combination therapy was superior to either regimen alone; the response to therapy for symptom resolution took at least 6 months and continued for up to 60 months of combination suppressive therapy.
Adding electrolysis treatment to the combination regimen resulted in improved patient satisfaction, but the differences were not significant. Patients’ satisfaction with the therapeutic response could be predicted from their pretreatment hirsutism scores or circulating sex hormone–binding globulin levels.
Study strengths and weaknesses
The study’s major strengths are the large number of patients included, the uniformity of criteria for diagnosis, and the prolonged follow-up. This is one of the few studies to report the impact of therapy on health-related quality of life in patients with PCOS and to assess response to therapy with use of objective measures, such as changes in the modified Ferriman-Gallwey score.
However, the criteria used to diagnose PCOS—the NIH 1990 criteria—currently are used less commonly than the Rotterdam 2003 criteria, and they are less inclusive for the diagnosis of PCOS.
The OC pill formulation used in this study contained the progestogen ethynodiol diacetate, which is not used routinely in modern clinical practice. In addition, the majority of patients were non-Hispanic white, which limits extrapolating these findings to other races and ethnicities.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
This retrospective study offers Level II evidence confirming the superiority of a combined OC plus spironolactone (compared with either agent alone) in the treatment of hirsutism in women with PCOS. In addition, this study emphasizes the importance of using combination suppressive therapy for at least 6 months to see a clinical response. Electrolysis may be helpful to patients especially during the initial 6 months of suppressive treatment. Finally, spironolactone alone could be reserved for cases in which OCs are contraindicated in women not interested in becoming pregnant.
In our practice, we treat patients with hirsutism using OC pills containing the progestogen levonorgestrel plus spironolactone at a lower dose of 100 mg/day, since patients treated with higher spironolactone doses report irregular bleeding and fatigue.
--ELIE HOBEIKA, MD, AND BERT SCOCCIA, MD
EXPERT COMMENTARY
Ezeh and colleagues conducted a retrospective analysis to evaluate the effectiveness of long-term combination suppressive therapy on hirsutism, acne, and menstrual disturbances in patients with PCOS and to identify the elements that could predict therapeutic response.
Details of the study
This chart review examined data from 200 nondiabetic patients with PCOS who presented between October 1987 and June 2002. PCOS diagnosis was based on the National Institutes of Health (NIH) 1990 criteria. During the initial visit, patients underwent a detailed medical history and physical exam, including a modified Ferriman-Gallwey hirsutism score and hormonal evaluation.
Treatment regimens. Patients were treated with suppressive therapy that consisted of an oral contraceptive (OC) (35 µg ethinyl estradiol plus 1 mg ethynodiol diacetate), an antiandrogen (spironolactone 200 mg/day), or a combination of these drugs. They were followed every 4 to 12 months (mean follow-up time, 34.2 months; range, 6–155 months), and subjective therapy response was assessed from medical records and by improvements in hirsutism scores.
Study findings. The 138 patients treated with combination suppressive therapy reported higher rates of subjective improvement in hirsutism compared with patients treated with other regimens (89.9% vs 72.0%, P<.0001). They also had a significant objective reduction in their modified Ferriman-Gallwey hirsutism score (6.0 vs 3.2; P = .0001). The combination therapy was superior to either regimen alone; the response to therapy for symptom resolution took at least 6 months and continued for up to 60 months of combination suppressive therapy.
Adding electrolysis treatment to the combination regimen resulted in improved patient satisfaction, but the differences were not significant. Patients’ satisfaction with the therapeutic response could be predicted from their pretreatment hirsutism scores or circulating sex hormone–binding globulin levels.
Study strengths and weaknesses
The study’s major strengths are the large number of patients included, the uniformity of criteria for diagnosis, and the prolonged follow-up. This is one of the few studies to report the impact of therapy on health-related quality of life in patients with PCOS and to assess response to therapy with use of objective measures, such as changes in the modified Ferriman-Gallwey score.
However, the criteria used to diagnose PCOS—the NIH 1990 criteria—currently are used less commonly than the Rotterdam 2003 criteria, and they are less inclusive for the diagnosis of PCOS.
The OC pill formulation used in this study contained the progestogen ethynodiol diacetate, which is not used routinely in modern clinical practice. In addition, the majority of patients were non-Hispanic white, which limits extrapolating these findings to other races and ethnicities.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
This retrospective study offers Level II evidence confirming the superiority of a combined OC plus spironolactone (compared with either agent alone) in the treatment of hirsutism in women with PCOS. In addition, this study emphasizes the importance of using combination suppressive therapy for at least 6 months to see a clinical response. Electrolysis may be helpful to patients especially during the initial 6 months of suppressive treatment. Finally, spironolactone alone could be reserved for cases in which OCs are contraindicated in women not interested in becoming pregnant.
In our practice, we treat patients with hirsutism using OC pills containing the progestogen levonorgestrel plus spironolactone at a lower dose of 100 mg/day, since patients treated with higher spironolactone doses report irregular bleeding and fatigue.
--ELIE HOBEIKA, MD, AND BERT SCOCCIA, MD
The art of manipulation: Simplifying hysterectomy by preparing the learner

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
- Vaginal and bilateral thigh removal of a transobturator sling
- Morcellation at the time of vaginal hysterectomy
- Surgical management of non-tubal ectopic pregnancies
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
- Vaginal and bilateral thigh removal of a transobturator sling
- Morcellation at the time of vaginal hysterectomy
- Surgical management of non-tubal ectopic pregnancies
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
- Vaginal and bilateral thigh removal of a transobturator sling
- Morcellation at the time of vaginal hysterectomy
- Surgical management of non-tubal ectopic pregnancies
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
This video is brought to you by
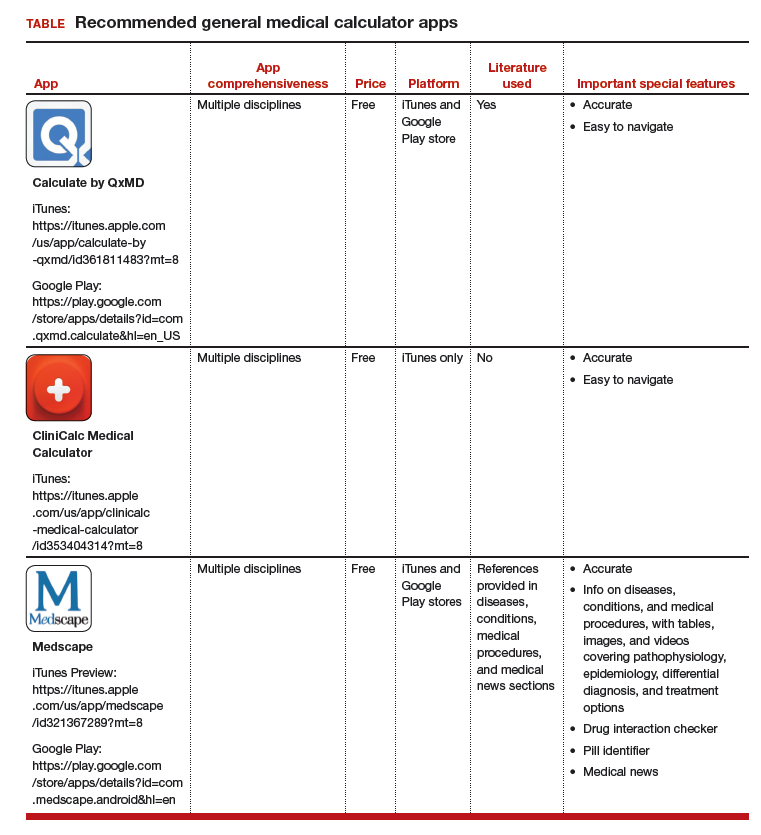
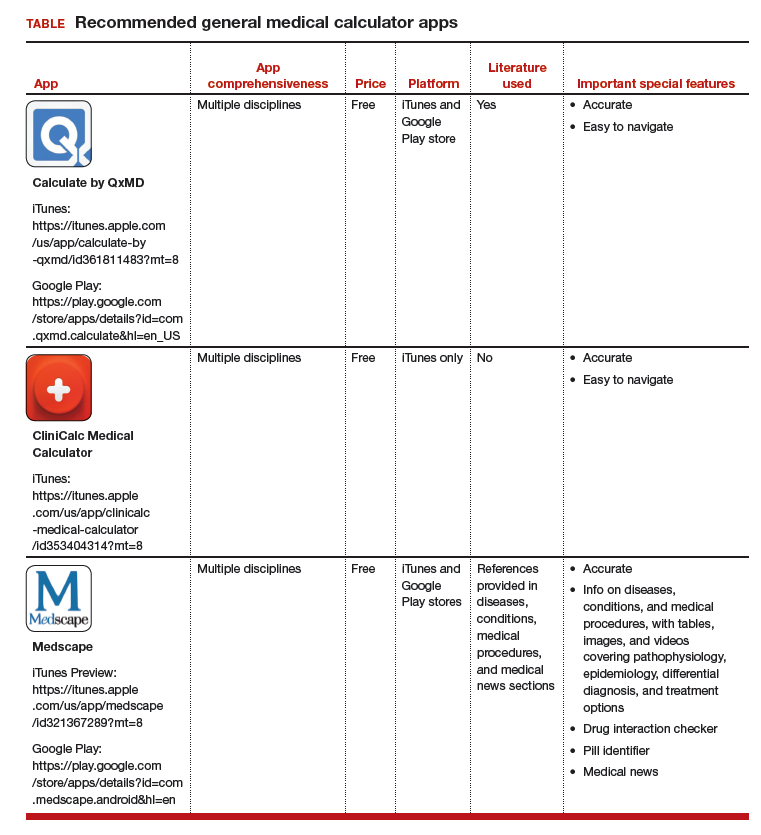
Medical calculator apps allow point of care, rapid decision-making
The most useful applications (apps) for health care professionals and students? Medical calculator apps (along with drug reference and disease diagnosis apps), according to surveys of clinicians and students.1,2 The utility of calculator apps to these groups is not surprising; calculator apps fall in the category of clinical decision-making apps, which also includes decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, laboratory test ordering, laboratory test interpretation, and medical exams.3 Calculator apps obviously save time as most health care providers have not memorized the many medical formulas and do not have computational speed. I have previously discussed other, more ObGyn-specific calculators, such as due date calculators.4,5 In this App Review column, however, I would like to highlight 3 general calculator apps: Calculate by QxMD, CliniCalc Medical Calculator, and Medscape. Researchers found all 3 apps 100% accurate and contained the most functions desired by internists.6 The apps are available at no cost and include many unique calculators. My colleagues and I actually used Calculate by QxMD to verify calculations in a previous study.7
A clinical example for how to apply calculators in practice is as follows: A multiparous patient at term has undergone an unscheduled cesarean delivery for arrest of dilation and intra-amniotic infection. You need to decide if the patient requires anti‑coagulants for deep venous thrombosis (DVT) prophylaxis and her necessary daily dose for gentamicin for postpartum infection prophylaxis. You can use Medscape’s body mass index (BMI) calculator to find out that this patient’s BMI is 45 kg/m2 and that DVT prophylaxis is in fact indicated. You also can use QxMD’s ideal body weight calculator to get the patient’s weight and determine the appropriate daily dose for gentamicin.
The TABLE provides more information on the apps, with its inclusions based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).7
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67.
2. Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012;12:121.
3. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39:356-364.
4. Chen KT. Three good apps for calculating the date of delivery. OBG Manag. 2017;29:45-46.
5. Chen KT. ACOG app and applets: tools to augment your practice. OBG Manag. 2018;30:41-42.
6. Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res. 2014;16:e32.
7. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
The most useful applications (apps) for health care professionals and students? Medical calculator apps (along with drug reference and disease diagnosis apps), according to surveys of clinicians and students.1,2 The utility of calculator apps to these groups is not surprising; calculator apps fall in the category of clinical decision-making apps, which also includes decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, laboratory test ordering, laboratory test interpretation, and medical exams.3 Calculator apps obviously save time as most health care providers have not memorized the many medical formulas and do not have computational speed. I have previously discussed other, more ObGyn-specific calculators, such as due date calculators.4,5 In this App Review column, however, I would like to highlight 3 general calculator apps: Calculate by QxMD, CliniCalc Medical Calculator, and Medscape. Researchers found all 3 apps 100% accurate and contained the most functions desired by internists.6 The apps are available at no cost and include many unique calculators. My colleagues and I actually used Calculate by QxMD to verify calculations in a previous study.7
A clinical example for how to apply calculators in practice is as follows: A multiparous patient at term has undergone an unscheduled cesarean delivery for arrest of dilation and intra-amniotic infection. You need to decide if the patient requires anti‑coagulants for deep venous thrombosis (DVT) prophylaxis and her necessary daily dose for gentamicin for postpartum infection prophylaxis. You can use Medscape’s body mass index (BMI) calculator to find out that this patient’s BMI is 45 kg/m2 and that DVT prophylaxis is in fact indicated. You also can use QxMD’s ideal body weight calculator to get the patient’s weight and determine the appropriate daily dose for gentamicin.
The TABLE provides more information on the apps, with its inclusions based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).7
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The most useful applications (apps) for health care professionals and students? Medical calculator apps (along with drug reference and disease diagnosis apps), according to surveys of clinicians and students.1,2 The utility of calculator apps to these groups is not surprising; calculator apps fall in the category of clinical decision-making apps, which also includes decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, laboratory test ordering, laboratory test interpretation, and medical exams.3 Calculator apps obviously save time as most health care providers have not memorized the many medical formulas and do not have computational speed. I have previously discussed other, more ObGyn-specific calculators, such as due date calculators.4,5 In this App Review column, however, I would like to highlight 3 general calculator apps: Calculate by QxMD, CliniCalc Medical Calculator, and Medscape. Researchers found all 3 apps 100% accurate and contained the most functions desired by internists.6 The apps are available at no cost and include many unique calculators. My colleagues and I actually used Calculate by QxMD to verify calculations in a previous study.7
A clinical example for how to apply calculators in practice is as follows: A multiparous patient at term has undergone an unscheduled cesarean delivery for arrest of dilation and intra-amniotic infection. You need to decide if the patient requires anti‑coagulants for deep venous thrombosis (DVT) prophylaxis and her necessary daily dose for gentamicin for postpartum infection prophylaxis. You can use Medscape’s body mass index (BMI) calculator to find out that this patient’s BMI is 45 kg/m2 and that DVT prophylaxis is in fact indicated. You also can use QxMD’s ideal body weight calculator to get the patient’s weight and determine the appropriate daily dose for gentamicin.
The TABLE provides more information on the apps, with its inclusions based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).7
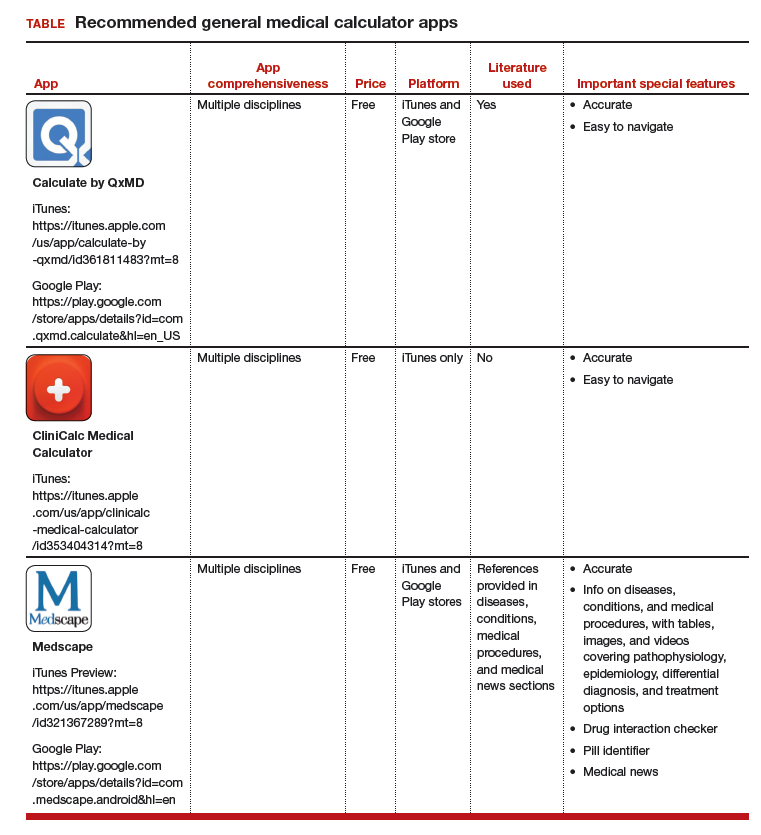
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67.
2. Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012;12:121.
3. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39:356-364.
4. Chen KT. Three good apps for calculating the date of delivery. OBG Manag. 2017;29:45-46.
5. Chen KT. ACOG app and applets: tools to augment your practice. OBG Manag. 2018;30:41-42.
6. Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res. 2014;16:e32.
7. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
1. Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67.
2. Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012;12:121.
3. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39:356-364.
4. Chen KT. Three good apps for calculating the date of delivery. OBG Manag. 2017;29:45-46.
5. Chen KT. ACOG app and applets: tools to augment your practice. OBG Manag. 2018;30:41-42.
6. Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res. 2014;16:e32.
7. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
ACOG: First gynecologist visit between ages 13 and 15
The American College of Obstetricians and Gynecologists (ACOG) recommends that girls receive their first reproductive health visit between the ages of 13 and 15 years to discuss healthy relationships in addition to general reproductive health, according to a new committee opinion.
The recommendation, published online Oct. 24, emphasizes that such early visits provide opportunities for ob.gyns. to educate teenage girls and their guardians about age-appropriate health issues, such as sexual relationships, dating violence, and sexual coercion. Between the ages of 13 years and 15 years is an ideal window because middle school is a time that some adolescents develop their first romantic and sexual relationships (Obstet Gynecol. 2018; 132[5]:1317-18 doi: 10.1097/AOG.0000000000002946).
“Creating a nonjudgmental environment and educating staff on the unique concerns of adolescents are helpful ways to provide effective and appropriate care to this group of patients,” the authors wrote.
Ob.gyns. can use the early meeting to discuss key aspects of a healthy relationship with patients, including communication, self-respect, and mutual respect, while helping adolescents identify the characteristics of an unhealthy relationships such as dishonesty, intimidation, disrespect, and abuse, according to the opinion. As part of the discussion, ob.gyns. also may counsel patients to define their current relationship and their expectations for future relationships. Both relationships with and without sexual intimacy should be discussed, the opinion advises.
The recommendation reminds health care professionals to be mindful of federal and state confidentiality laws and that they be aware of mandatory reporting laws when intimate partner violence, teen dating violence, or statutory rape is suspected. In addition, the opinion notes that pregnant and parenting adolescents; lesbian, gay, bisexual, transgender, queer, or questioning (LGBTQ) individuals; and adolescents with physical and mental disabilities are at particular risk of disparities in the health care system.
“The promotion of healthy relationships in these groups requires the obstetrician-gynecologist to be aware of the unique barriers and hurdles to sexual and nonsexual expression, as well as to health care,” the opinion states. “Interventions to promote healthy relationships and a strong sexual health framework are more effective when started early and can affect indicators of long-term individual health and public health.”
The American College of Obstetricians and Gynecologists recommends that the first reproductive health visit occur between the ages of 13 and 15, and I agree with them. Often patients attending this appointment don’t have physical complaints, and we can focus on prevention and education. The visit can be about building the provider-patient relationship and may serve to ease fears and develop trust before visits for problem management.
There are a number of important health education topics to cover from puberty and menses to confidentiality and minor-access laws. Because many young people will begin to initiate romantic relationships during middle school, the topic of healthy relationships is critical. Unhealthy relationships, in their many forms, can have far reaching impacts on a young person’s health and wellness. For years, we’ve been talking with young people about preventing STIs or preventing unwanted pregnancy, but we’ve spent less energy working towards something.
I’m excited to see these recommendations and look forward to helping my younger patients think through relationships as important aspects of life and health, what they want from them, and how they can work towards them.
Melissa Kottke , MD is an obstetrician-gynecologist specializing in family planning and adolescent reproductive health at Emory University in Atlanta.
The American College of Obstetricians and Gynecologists recommends that the first reproductive health visit occur between the ages of 13 and 15, and I agree with them. Often patients attending this appointment don’t have physical complaints, and we can focus on prevention and education. The visit can be about building the provider-patient relationship and may serve to ease fears and develop trust before visits for problem management.
There are a number of important health education topics to cover from puberty and menses to confidentiality and minor-access laws. Because many young people will begin to initiate romantic relationships during middle school, the topic of healthy relationships is critical. Unhealthy relationships, in their many forms, can have far reaching impacts on a young person’s health and wellness. For years, we’ve been talking with young people about preventing STIs or preventing unwanted pregnancy, but we’ve spent less energy working towards something.
I’m excited to see these recommendations and look forward to helping my younger patients think through relationships as important aspects of life and health, what they want from them, and how they can work towards them.
Melissa Kottke , MD is an obstetrician-gynecologist specializing in family planning and adolescent reproductive health at Emory University in Atlanta.
The American College of Obstetricians and Gynecologists recommends that the first reproductive health visit occur between the ages of 13 and 15, and I agree with them. Often patients attending this appointment don’t have physical complaints, and we can focus on prevention and education. The visit can be about building the provider-patient relationship and may serve to ease fears and develop trust before visits for problem management.
There are a number of important health education topics to cover from puberty and menses to confidentiality and minor-access laws. Because many young people will begin to initiate romantic relationships during middle school, the topic of healthy relationships is critical. Unhealthy relationships, in their many forms, can have far reaching impacts on a young person’s health and wellness. For years, we’ve been talking with young people about preventing STIs or preventing unwanted pregnancy, but we’ve spent less energy working towards something.
I’m excited to see these recommendations and look forward to helping my younger patients think through relationships as important aspects of life and health, what they want from them, and how they can work towards them.
Melissa Kottke , MD is an obstetrician-gynecologist specializing in family planning and adolescent reproductive health at Emory University in Atlanta.
The American College of Obstetricians and Gynecologists (ACOG) recommends that girls receive their first reproductive health visit between the ages of 13 and 15 years to discuss healthy relationships in addition to general reproductive health, according to a new committee opinion.
The recommendation, published online Oct. 24, emphasizes that such early visits provide opportunities for ob.gyns. to educate teenage girls and their guardians about age-appropriate health issues, such as sexual relationships, dating violence, and sexual coercion. Between the ages of 13 years and 15 years is an ideal window because middle school is a time that some adolescents develop their first romantic and sexual relationships (Obstet Gynecol. 2018; 132[5]:1317-18 doi: 10.1097/AOG.0000000000002946).
“Creating a nonjudgmental environment and educating staff on the unique concerns of adolescents are helpful ways to provide effective and appropriate care to this group of patients,” the authors wrote.
Ob.gyns. can use the early meeting to discuss key aspects of a healthy relationship with patients, including communication, self-respect, and mutual respect, while helping adolescents identify the characteristics of an unhealthy relationships such as dishonesty, intimidation, disrespect, and abuse, according to the opinion. As part of the discussion, ob.gyns. also may counsel patients to define their current relationship and their expectations for future relationships. Both relationships with and without sexual intimacy should be discussed, the opinion advises.
The recommendation reminds health care professionals to be mindful of federal and state confidentiality laws and that they be aware of mandatory reporting laws when intimate partner violence, teen dating violence, or statutory rape is suspected. In addition, the opinion notes that pregnant and parenting adolescents; lesbian, gay, bisexual, transgender, queer, or questioning (LGBTQ) individuals; and adolescents with physical and mental disabilities are at particular risk of disparities in the health care system.
“The promotion of healthy relationships in these groups requires the obstetrician-gynecologist to be aware of the unique barriers and hurdles to sexual and nonsexual expression, as well as to health care,” the opinion states. “Interventions to promote healthy relationships and a strong sexual health framework are more effective when started early and can affect indicators of long-term individual health and public health.”
The American College of Obstetricians and Gynecologists (ACOG) recommends that girls receive their first reproductive health visit between the ages of 13 and 15 years to discuss healthy relationships in addition to general reproductive health, according to a new committee opinion.
The recommendation, published online Oct. 24, emphasizes that such early visits provide opportunities for ob.gyns. to educate teenage girls and their guardians about age-appropriate health issues, such as sexual relationships, dating violence, and sexual coercion. Between the ages of 13 years and 15 years is an ideal window because middle school is a time that some adolescents develop their first romantic and sexual relationships (Obstet Gynecol. 2018; 132[5]:1317-18 doi: 10.1097/AOG.0000000000002946).
“Creating a nonjudgmental environment and educating staff on the unique concerns of adolescents are helpful ways to provide effective and appropriate care to this group of patients,” the authors wrote.
Ob.gyns. can use the early meeting to discuss key aspects of a healthy relationship with patients, including communication, self-respect, and mutual respect, while helping adolescents identify the characteristics of an unhealthy relationships such as dishonesty, intimidation, disrespect, and abuse, according to the opinion. As part of the discussion, ob.gyns. also may counsel patients to define their current relationship and their expectations for future relationships. Both relationships with and without sexual intimacy should be discussed, the opinion advises.
The recommendation reminds health care professionals to be mindful of federal and state confidentiality laws and that they be aware of mandatory reporting laws when intimate partner violence, teen dating violence, or statutory rape is suspected. In addition, the opinion notes that pregnant and parenting adolescents; lesbian, gay, bisexual, transgender, queer, or questioning (LGBTQ) individuals; and adolescents with physical and mental disabilities are at particular risk of disparities in the health care system.
“The promotion of healthy relationships in these groups requires the obstetrician-gynecologist to be aware of the unique barriers and hurdles to sexual and nonsexual expression, as well as to health care,” the opinion states. “Interventions to promote healthy relationships and a strong sexual health framework are more effective when started early and can affect indicators of long-term individual health and public health.”
FROM OBSTETRICS & GYNECOLOGY
VTE risk after gynecologic surgery lower with laparoscopic procedures
according to a study published in Obstetrics & Gynecology.

The retrospective cohort study looked at data from 37,485 patients who underwent 43,751 gynecologic surgical procedures, including hysterectomy and myomectomy, at two tertiary care academic hospitals.
Overall, 96 patients (0.2%) were diagnosed with postoperative venous thromboembolism. However patients who underwent laparoscopic or vaginal surgery had a significant 78% and 93% lower risk of venous thromboembolism, respectively, than those who underwent laparotomy, even after adjusting for potential confounders such as age, cancer, race, pharmacologic thromboprophylaxis, and surgical time.
The incidence of postoperative thromboembolism was significantly higher among patients undergoing gynecologic surgery for cancer (1.1%). The incidence among those undergoing surgery for benign indications was only 0.2%, and the highest incidence was among patients with cancer who underwent laparotomy (2.2%).
“This study adds to data demonstrating that venous thromboembolism is rare in gynecologic surgery, particularly when a patient undergoes a minimally invasive procedure for benign indications,” wrote Dr. Elisa M. Jorgensen of Beth Israel Deaconess Medical Center, and her coauthors.
Among the 8,273 patients who underwent a hysterectomy, there were 55 cases of venous thromboembolism – representing an 0.7% incidence. However patients who underwent laparotomy had a 1% incidence of postoperative venous thromboembolism, while those who underwent laparoscopic hysterectomy had an 0.3% incidence and those who underwent vaginal hysterectomy had an 0.1% incidence.
Laparotomy was the most common mode of surgery for hysterectomy – accounting for 57% of operations – while 34% were laparoscopic and 9% were vaginal.
However, the authors noted that the use of laparoscopy increased and laparotomy declined over the 9 years of the study. In 2006, 12% of hysterectomies were laparoscopic, compared with 55% in 2015, while over that same period the percentage of laparotomies dropped from 74% to 41%, and the percentage of vaginal procedures declined from 14% to 4%.
“Because current practice guidelines do not account for mode of surgery, we find them to be insufficient for the modern gynecologic surgeon to counsel patients on their individual venous thromboembolism risk or to make ideal decisions regarding selection of thromboprophylaxis,” Dr. Jorgenson and her associates wrote.
Only 5 patients of the 2,851 who underwent myomectomy developed postoperative VTE – an overall incidence of 0.2% – and the authors said numbers were too small to analyze. Vaginal or hysteroscopic myomectomy was the most common surgical method, accounting for 62% of procedures, compared with 23% for laparotomies and 15% for laparoscopies.
More than 90% of patients who experienced postoperative thromboembolism had received some form of thromboprophylaxis before surgery, either mechanical, pharmacologic, or both. In comparison, only 55% of the group who didn’t experience thromboembolism had received thromboprophylaxis.
“The high rate of prophylaxis among patients who developed postoperative venous thromboembolism may reflect surgeons’ abilities to preoperatively identify patients at increased risk, guiding appropriate selection of thromboprophylaxis,” Dr. Jorgenson and her associates wrote.
Addressing the study’s limitations, the authors noted that they were not able to capture data on patients’ body mass index and also were unable to account for patients who might have been diagnosed and treated for postoperative VTE at other hospitals.
No conflicts of interest were declared.
SOURCE: Jorgensen EM et al. Obstet Gynecol. 2018 Nov;132:1275-84.
The aim of this study was to determine the 3-month postoperative incidence of venous thromboembolism among patients undergoing gynecologic surgery. The study also addressed the mode of surgery to allow a comparison between laparotomy and minimally invasive approaches.
Postoperative VTE was defined as deep venous thrombosis of the lower extremities, pulmonary embolism, or both that occurred within 90 days of surgery. A key component of the study was that clinically recognized VTEs that required treatment with anticoagulation, vena caval filter, or both were included.
The study evaluated 43,751 gynecological cases among 37,485 patients. As expected, 59% of the cases were classified as vaginal surgery, 24% were laparoscopic cases, and 17% of the cases were laparotomies.
Of the 8,273 hysterectomies, 57% were via an abdominal approach, 34% were laparoscopic, and 9 were vaginal cases.
Overall, 0.2% of patients were diagnosed with a VTE. As expected, the greatest incidence of VTE was in patients with cancer who underwent a laparotomy. Those with a VTE were significantly more likely to have had an inpatient stay (longer than 24 hours), a cancer diagnosis, a longer surgical time, and an American Society of Anesthesiologists score of 3 or more. They also were older (mean age 56 years vs. 44 years). Of note, 20% of the VTE group identified as black.
Among patients who had a hysterectomy, there were VTEs in 0.7%: 1% in the laparotomy group, 0.3% in the laparoscopic group, and only 0.1% in the vaginal hysterectomy group.
It is interesting to note that 91% of the patients diagnosed with a VTE did received preoperative VTE prophylaxis. The authors noted that the high rate of prophylaxis may have reflected the surgeon’s ability to identify patients who are at high risk.
The authors recognized that the current guidelines do not stratify VTE risk based on the mode of surgery. Further, they noted that low-risk patients undergoing low-risk surgery may be receiving pharmacologic VTE prophylaxis, thus placing these patients at risk for complications related to such therapy.
This paper by Jorgensen et al. should remind us that VTE prophylaxis should be individualized. Patients may not fit nicely into boxes on our EMR; each clinical decision should be made for each patient and for each clinical scenario. The surgeon’s responsibility is to adopt the evidence-based guidelines that serve each individual patient’s unique risk/benefit profile.
David M. Jaspan, DO, is director of minimally invasive and pelvic surgery and chairman of the department of obstetrics and gynecology at the Einstein Medical Center in Philadelphia. Dr. Jaspan, who was asked to comment on the Jorgenson et al. article, said he had no relevant financial disclosures.
The aim of this study was to determine the 3-month postoperative incidence of venous thromboembolism among patients undergoing gynecologic surgery. The study also addressed the mode of surgery to allow a comparison between laparotomy and minimally invasive approaches.
Postoperative VTE was defined as deep venous thrombosis of the lower extremities, pulmonary embolism, or both that occurred within 90 days of surgery. A key component of the study was that clinically recognized VTEs that required treatment with anticoagulation, vena caval filter, or both were included.
The study evaluated 43,751 gynecological cases among 37,485 patients. As expected, 59% of the cases were classified as vaginal surgery, 24% were laparoscopic cases, and 17% of the cases were laparotomies.
Of the 8,273 hysterectomies, 57% were via an abdominal approach, 34% were laparoscopic, and 9 were vaginal cases.
Overall, 0.2% of patients were diagnosed with a VTE. As expected, the greatest incidence of VTE was in patients with cancer who underwent a laparotomy. Those with a VTE were significantly more likely to have had an inpatient stay (longer than 24 hours), a cancer diagnosis, a longer surgical time, and an American Society of Anesthesiologists score of 3 or more. They also were older (mean age 56 years vs. 44 years). Of note, 20% of the VTE group identified as black.
Among patients who had a hysterectomy, there were VTEs in 0.7%: 1% in the laparotomy group, 0.3% in the laparoscopic group, and only 0.1% in the vaginal hysterectomy group.
It is interesting to note that 91% of the patients diagnosed with a VTE did received preoperative VTE prophylaxis. The authors noted that the high rate of prophylaxis may have reflected the surgeon’s ability to identify patients who are at high risk.
The authors recognized that the current guidelines do not stratify VTE risk based on the mode of surgery. Further, they noted that low-risk patients undergoing low-risk surgery may be receiving pharmacologic VTE prophylaxis, thus placing these patients at risk for complications related to such therapy.
This paper by Jorgensen et al. should remind us that VTE prophylaxis should be individualized. Patients may not fit nicely into boxes on our EMR; each clinical decision should be made for each patient and for each clinical scenario. The surgeon’s responsibility is to adopt the evidence-based guidelines that serve each individual patient’s unique risk/benefit profile.
David M. Jaspan, DO, is director of minimally invasive and pelvic surgery and chairman of the department of obstetrics and gynecology at the Einstein Medical Center in Philadelphia. Dr. Jaspan, who was asked to comment on the Jorgenson et al. article, said he had no relevant financial disclosures.
The aim of this study was to determine the 3-month postoperative incidence of venous thromboembolism among patients undergoing gynecologic surgery. The study also addressed the mode of surgery to allow a comparison between laparotomy and minimally invasive approaches.
Postoperative VTE was defined as deep venous thrombosis of the lower extremities, pulmonary embolism, or both that occurred within 90 days of surgery. A key component of the study was that clinically recognized VTEs that required treatment with anticoagulation, vena caval filter, or both were included.
The study evaluated 43,751 gynecological cases among 37,485 patients. As expected, 59% of the cases were classified as vaginal surgery, 24% were laparoscopic cases, and 17% of the cases were laparotomies.
Of the 8,273 hysterectomies, 57% were via an abdominal approach, 34% were laparoscopic, and 9 were vaginal cases.
Overall, 0.2% of patients were diagnosed with a VTE. As expected, the greatest incidence of VTE was in patients with cancer who underwent a laparotomy. Those with a VTE were significantly more likely to have had an inpatient stay (longer than 24 hours), a cancer diagnosis, a longer surgical time, and an American Society of Anesthesiologists score of 3 or more. They also were older (mean age 56 years vs. 44 years). Of note, 20% of the VTE group identified as black.
Among patients who had a hysterectomy, there were VTEs in 0.7%: 1% in the laparotomy group, 0.3% in the laparoscopic group, and only 0.1% in the vaginal hysterectomy group.
It is interesting to note that 91% of the patients diagnosed with a VTE did received preoperative VTE prophylaxis. The authors noted that the high rate of prophylaxis may have reflected the surgeon’s ability to identify patients who are at high risk.
The authors recognized that the current guidelines do not stratify VTE risk based on the mode of surgery. Further, they noted that low-risk patients undergoing low-risk surgery may be receiving pharmacologic VTE prophylaxis, thus placing these patients at risk for complications related to such therapy.
This paper by Jorgensen et al. should remind us that VTE prophylaxis should be individualized. Patients may not fit nicely into boxes on our EMR; each clinical decision should be made for each patient and for each clinical scenario. The surgeon’s responsibility is to adopt the evidence-based guidelines that serve each individual patient’s unique risk/benefit profile.
David M. Jaspan, DO, is director of minimally invasive and pelvic surgery and chairman of the department of obstetrics and gynecology at the Einstein Medical Center in Philadelphia. Dr. Jaspan, who was asked to comment on the Jorgenson et al. article, said he had no relevant financial disclosures.
according to a study published in Obstetrics & Gynecology.

The retrospective cohort study looked at data from 37,485 patients who underwent 43,751 gynecologic surgical procedures, including hysterectomy and myomectomy, at two tertiary care academic hospitals.
Overall, 96 patients (0.2%) were diagnosed with postoperative venous thromboembolism. However patients who underwent laparoscopic or vaginal surgery had a significant 78% and 93% lower risk of venous thromboembolism, respectively, than those who underwent laparotomy, even after adjusting for potential confounders such as age, cancer, race, pharmacologic thromboprophylaxis, and surgical time.
The incidence of postoperative thromboembolism was significantly higher among patients undergoing gynecologic surgery for cancer (1.1%). The incidence among those undergoing surgery for benign indications was only 0.2%, and the highest incidence was among patients with cancer who underwent laparotomy (2.2%).
“This study adds to data demonstrating that venous thromboembolism is rare in gynecologic surgery, particularly when a patient undergoes a minimally invasive procedure for benign indications,” wrote Dr. Elisa M. Jorgensen of Beth Israel Deaconess Medical Center, and her coauthors.
Among the 8,273 patients who underwent a hysterectomy, there were 55 cases of venous thromboembolism – representing an 0.7% incidence. However patients who underwent laparotomy had a 1% incidence of postoperative venous thromboembolism, while those who underwent laparoscopic hysterectomy had an 0.3% incidence and those who underwent vaginal hysterectomy had an 0.1% incidence.
Laparotomy was the most common mode of surgery for hysterectomy – accounting for 57% of operations – while 34% were laparoscopic and 9% were vaginal.
However, the authors noted that the use of laparoscopy increased and laparotomy declined over the 9 years of the study. In 2006, 12% of hysterectomies were laparoscopic, compared with 55% in 2015, while over that same period the percentage of laparotomies dropped from 74% to 41%, and the percentage of vaginal procedures declined from 14% to 4%.
“Because current practice guidelines do not account for mode of surgery, we find them to be insufficient for the modern gynecologic surgeon to counsel patients on their individual venous thromboembolism risk or to make ideal decisions regarding selection of thromboprophylaxis,” Dr. Jorgenson and her associates wrote.
Only 5 patients of the 2,851 who underwent myomectomy developed postoperative VTE – an overall incidence of 0.2% – and the authors said numbers were too small to analyze. Vaginal or hysteroscopic myomectomy was the most common surgical method, accounting for 62% of procedures, compared with 23% for laparotomies and 15% for laparoscopies.
More than 90% of patients who experienced postoperative thromboembolism had received some form of thromboprophylaxis before surgery, either mechanical, pharmacologic, or both. In comparison, only 55% of the group who didn’t experience thromboembolism had received thromboprophylaxis.
“The high rate of prophylaxis among patients who developed postoperative venous thromboembolism may reflect surgeons’ abilities to preoperatively identify patients at increased risk, guiding appropriate selection of thromboprophylaxis,” Dr. Jorgenson and her associates wrote.
Addressing the study’s limitations, the authors noted that they were not able to capture data on patients’ body mass index and also were unable to account for patients who might have been diagnosed and treated for postoperative VTE at other hospitals.
No conflicts of interest were declared.
SOURCE: Jorgensen EM et al. Obstet Gynecol. 2018 Nov;132:1275-84.
according to a study published in Obstetrics & Gynecology.

The retrospective cohort study looked at data from 37,485 patients who underwent 43,751 gynecologic surgical procedures, including hysterectomy and myomectomy, at two tertiary care academic hospitals.
Overall, 96 patients (0.2%) were diagnosed with postoperative venous thromboembolism. However patients who underwent laparoscopic or vaginal surgery had a significant 78% and 93% lower risk of venous thromboembolism, respectively, than those who underwent laparotomy, even after adjusting for potential confounders such as age, cancer, race, pharmacologic thromboprophylaxis, and surgical time.
The incidence of postoperative thromboembolism was significantly higher among patients undergoing gynecologic surgery for cancer (1.1%). The incidence among those undergoing surgery for benign indications was only 0.2%, and the highest incidence was among patients with cancer who underwent laparotomy (2.2%).
“This study adds to data demonstrating that venous thromboembolism is rare in gynecologic surgery, particularly when a patient undergoes a minimally invasive procedure for benign indications,” wrote Dr. Elisa M. Jorgensen of Beth Israel Deaconess Medical Center, and her coauthors.
Among the 8,273 patients who underwent a hysterectomy, there were 55 cases of venous thromboembolism – representing an 0.7% incidence. However patients who underwent laparotomy had a 1% incidence of postoperative venous thromboembolism, while those who underwent laparoscopic hysterectomy had an 0.3% incidence and those who underwent vaginal hysterectomy had an 0.1% incidence.
Laparotomy was the most common mode of surgery for hysterectomy – accounting for 57% of operations – while 34% were laparoscopic and 9% were vaginal.
However, the authors noted that the use of laparoscopy increased and laparotomy declined over the 9 years of the study. In 2006, 12% of hysterectomies were laparoscopic, compared with 55% in 2015, while over that same period the percentage of laparotomies dropped from 74% to 41%, and the percentage of vaginal procedures declined from 14% to 4%.
“Because current practice guidelines do not account for mode of surgery, we find them to be insufficient for the modern gynecologic surgeon to counsel patients on their individual venous thromboembolism risk or to make ideal decisions regarding selection of thromboprophylaxis,” Dr. Jorgenson and her associates wrote.
Only 5 patients of the 2,851 who underwent myomectomy developed postoperative VTE – an overall incidence of 0.2% – and the authors said numbers were too small to analyze. Vaginal or hysteroscopic myomectomy was the most common surgical method, accounting for 62% of procedures, compared with 23% for laparotomies and 15% for laparoscopies.
More than 90% of patients who experienced postoperative thromboembolism had received some form of thromboprophylaxis before surgery, either mechanical, pharmacologic, or both. In comparison, only 55% of the group who didn’t experience thromboembolism had received thromboprophylaxis.
“The high rate of prophylaxis among patients who developed postoperative venous thromboembolism may reflect surgeons’ abilities to preoperatively identify patients at increased risk, guiding appropriate selection of thromboprophylaxis,” Dr. Jorgenson and her associates wrote.
Addressing the study’s limitations, the authors noted that they were not able to capture data on patients’ body mass index and also were unable to account for patients who might have been diagnosed and treated for postoperative VTE at other hospitals.
No conflicts of interest were declared.
SOURCE: Jorgensen EM et al. Obstet Gynecol. 2018 Nov;132:1275-84.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Laparoscopic gynecologic surgery is associated with a lower risk of postoperative VTE than laparotomy.
Major finding: Laparoscopic hysterectomy was associated with a 78% lower incidence of postoperative VTE than laparotomy.
Study details: Retrospective cohort study of 37,485 patients who underwent 43,751 gynecologic surgical procedures
Disclosures: No conflicts of interest were declared.
Source: Jorgensen EM et al. Obstet Gynecol. 2018 Nov;132:1275-84.