User login
Characteristics of mucinous adenocarcinoma highlighted
CORONADO, CALIF. – Head and neck mucinous adenocarcinoma is commonly diagnosed at a low tumor stage with no nodal involvement but with the potential for distant metastases.
The findings come from the largest study of its kind to date, which was presented by Neel R. Sangal at the Triological Society’s Combined Sections Meeting.
“Mucinous carcinoma was previously classified as colloid carcinoma, which leads to increased confusion in the nomenclature,” said Mr. Sangal, a 4th-year student at New Jersey Medical School, Newark.
“This changed in the 1980s, which led to difficulty in characterizing the disease over time. This histology is well studied in the GI system, in the lungs, and in the breast, but the head and neck presentation is extremely rare, and it lacks comprehensive study.
“It commonly presents as a slow-growing, painless, nonulcerated nodule. From case reports, it’s typically low-grade and indolent, but it commonly recurs, and it does have metastatic potential,” he said. “Histologically, it’s characterized by nets of aggressive epithelial cells that are accompanied by significant extracellular mucin.”
In an effort to understand the demographic, clinicopathologic, treatment, and survival characteristics of mucinous adenocarcinoma, the researchers evaluated cases from the Surveillance, Epidemiology, and End Results Program (SEER) database between 1973 and 2014. They selected patients based on their International Classification of Diseases morphological code specific for mucinous adenocarcinoma and ICD primary site code consistent for cancers of the head and neck.
In all, 583 cases met criteria, “which highlights how rare this disease is,” Mr. Sangal said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
The mean age at diagnosis was 64.8 years; 55.2% of cases were male, 64.5% were white, 15.4% were black, 8.7% were Hispanic, 6.7% were Asian, and the remaining 5% were from other ethnicities. The four most frequent primary sites were the eyelid (29.8%), followed by skin of the face (22.6%), skin of the scalp and neck (12.2%), and the parotid gland (8.7%). Most of the lesions lacked nodal involvement and metastasis (94.1% and 96.2%, respectively). Histology presented mainly at lower stages. Specifically, 68% had T0-1 disease, 21.5% had T2-3 disease, and 10.5% had T4 disease.
When the researchers stratified treatment frequency by various clinical pathologic characteristics, they found large differences in the type of treatment received by the primary site. “Those on the salivary gland tended to receive radiation at a much higher percentage than those of the skin, which mostly received surgery alone,” Mr. Sangal said. “We also found a linear correlation between T stage and increased use of radiation alongside surgery. Similarly, those with nodal involvement and distant metastasis had increased rates of radiation with surgery.”
Disease-specific survival and overall survival rates were 92.2% and 80.5%, respectively. Advanced age at diagnosis was a significant predictor of survival. In addition, Hispanics had the highest rates of survival, while the white and black patients had similar survival curves. “ Mr. Sangal added. “We also found a linear correlation between T stage and survival. Similarly, those with nodal involvement and distant metastasis also had decreased survival.”
He acknowledged certain limitations of the study, including the potential for inconsistent coding in the SEER database.
Samer T. Elsamna was lead author on the study. None of the researchers reported having financial disclosures.
SOURCE: Elsamna ST et al. Triological CSM 2019, Abstracts.
CORONADO, CALIF. – Head and neck mucinous adenocarcinoma is commonly diagnosed at a low tumor stage with no nodal involvement but with the potential for distant metastases.
The findings come from the largest study of its kind to date, which was presented by Neel R. Sangal at the Triological Society’s Combined Sections Meeting.
“Mucinous carcinoma was previously classified as colloid carcinoma, which leads to increased confusion in the nomenclature,” said Mr. Sangal, a 4th-year student at New Jersey Medical School, Newark.
“This changed in the 1980s, which led to difficulty in characterizing the disease over time. This histology is well studied in the GI system, in the lungs, and in the breast, but the head and neck presentation is extremely rare, and it lacks comprehensive study.
“It commonly presents as a slow-growing, painless, nonulcerated nodule. From case reports, it’s typically low-grade and indolent, but it commonly recurs, and it does have metastatic potential,” he said. “Histologically, it’s characterized by nets of aggressive epithelial cells that are accompanied by significant extracellular mucin.”
In an effort to understand the demographic, clinicopathologic, treatment, and survival characteristics of mucinous adenocarcinoma, the researchers evaluated cases from the Surveillance, Epidemiology, and End Results Program (SEER) database between 1973 and 2014. They selected patients based on their International Classification of Diseases morphological code specific for mucinous adenocarcinoma and ICD primary site code consistent for cancers of the head and neck.
In all, 583 cases met criteria, “which highlights how rare this disease is,” Mr. Sangal said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
The mean age at diagnosis was 64.8 years; 55.2% of cases were male, 64.5% were white, 15.4% were black, 8.7% were Hispanic, 6.7% were Asian, and the remaining 5% were from other ethnicities. The four most frequent primary sites were the eyelid (29.8%), followed by skin of the face (22.6%), skin of the scalp and neck (12.2%), and the parotid gland (8.7%). Most of the lesions lacked nodal involvement and metastasis (94.1% and 96.2%, respectively). Histology presented mainly at lower stages. Specifically, 68% had T0-1 disease, 21.5% had T2-3 disease, and 10.5% had T4 disease.
When the researchers stratified treatment frequency by various clinical pathologic characteristics, they found large differences in the type of treatment received by the primary site. “Those on the salivary gland tended to receive radiation at a much higher percentage than those of the skin, which mostly received surgery alone,” Mr. Sangal said. “We also found a linear correlation between T stage and increased use of radiation alongside surgery. Similarly, those with nodal involvement and distant metastasis had increased rates of radiation with surgery.”
Disease-specific survival and overall survival rates were 92.2% and 80.5%, respectively. Advanced age at diagnosis was a significant predictor of survival. In addition, Hispanics had the highest rates of survival, while the white and black patients had similar survival curves. “ Mr. Sangal added. “We also found a linear correlation between T stage and survival. Similarly, those with nodal involvement and distant metastasis also had decreased survival.”
He acknowledged certain limitations of the study, including the potential for inconsistent coding in the SEER database.
Samer T. Elsamna was lead author on the study. None of the researchers reported having financial disclosures.
SOURCE: Elsamna ST et al. Triological CSM 2019, Abstracts.
CORONADO, CALIF. – Head and neck mucinous adenocarcinoma is commonly diagnosed at a low tumor stage with no nodal involvement but with the potential for distant metastases.
The findings come from the largest study of its kind to date, which was presented by Neel R. Sangal at the Triological Society’s Combined Sections Meeting.
“Mucinous carcinoma was previously classified as colloid carcinoma, which leads to increased confusion in the nomenclature,” said Mr. Sangal, a 4th-year student at New Jersey Medical School, Newark.
“This changed in the 1980s, which led to difficulty in characterizing the disease over time. This histology is well studied in the GI system, in the lungs, and in the breast, but the head and neck presentation is extremely rare, and it lacks comprehensive study.
“It commonly presents as a slow-growing, painless, nonulcerated nodule. From case reports, it’s typically low-grade and indolent, but it commonly recurs, and it does have metastatic potential,” he said. “Histologically, it’s characterized by nets of aggressive epithelial cells that are accompanied by significant extracellular mucin.”
In an effort to understand the demographic, clinicopathologic, treatment, and survival characteristics of mucinous adenocarcinoma, the researchers evaluated cases from the Surveillance, Epidemiology, and End Results Program (SEER) database between 1973 and 2014. They selected patients based on their International Classification of Diseases morphological code specific for mucinous adenocarcinoma and ICD primary site code consistent for cancers of the head and neck.
In all, 583 cases met criteria, “which highlights how rare this disease is,” Mr. Sangal said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
The mean age at diagnosis was 64.8 years; 55.2% of cases were male, 64.5% were white, 15.4% were black, 8.7% were Hispanic, 6.7% were Asian, and the remaining 5% were from other ethnicities. The four most frequent primary sites were the eyelid (29.8%), followed by skin of the face (22.6%), skin of the scalp and neck (12.2%), and the parotid gland (8.7%). Most of the lesions lacked nodal involvement and metastasis (94.1% and 96.2%, respectively). Histology presented mainly at lower stages. Specifically, 68% had T0-1 disease, 21.5% had T2-3 disease, and 10.5% had T4 disease.
When the researchers stratified treatment frequency by various clinical pathologic characteristics, they found large differences in the type of treatment received by the primary site. “Those on the salivary gland tended to receive radiation at a much higher percentage than those of the skin, which mostly received surgery alone,” Mr. Sangal said. “We also found a linear correlation between T stage and increased use of radiation alongside surgery. Similarly, those with nodal involvement and distant metastasis had increased rates of radiation with surgery.”
Disease-specific survival and overall survival rates were 92.2% and 80.5%, respectively. Advanced age at diagnosis was a significant predictor of survival. In addition, Hispanics had the highest rates of survival, while the white and black patients had similar survival curves. “ Mr. Sangal added. “We also found a linear correlation between T stage and survival. Similarly, those with nodal involvement and distant metastasis also had decreased survival.”
He acknowledged certain limitations of the study, including the potential for inconsistent coding in the SEER database.
Samer T. Elsamna was lead author on the study. None of the researchers reported having financial disclosures.
SOURCE: Elsamna ST et al. Triological CSM 2019, Abstracts.
REPORTING FROM TRIOLOGICAL CSM
Key clinical point: Head and neck adenocarcinoma is mostly indolent with a favorable outcome.
Major finding: Disease-specific survival and overall survival rates were 92.2% and 80.5%, respectively.
Study details: An evaluation of 583 head and neck mucinous adenocarcinoma cases from the Surveillance, Epidemiology, and End Results (SEER) database between 1973 and 2014.
Disclosures: The researchers reported having no financial disclosures.
Source: Elsamna ST et al. Triological CSM 2019, Abstracts.
Enoblituzumab plus pembrolizumab shows promise for select solid tumors
WASHINGTON – Combination enoblituzumab and pembrolizumab showed acceptable safety and encouraging antitumor activity in select patients with B7-H3-expressing non–small-cell lung cancer (NSCLC), squamous cell carcinoma of the head and neck (SCCHN), and other solid tumors in a phase 1 dose-escalation and expansion study.
Of note, the combination showed activity in patients anticipated to be poorly responsive to checkpoint inhibitor therapy alone, Charu Aggarwal, MD, of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the Society for Immunotherapy of Cancer.
In all, 133 patients were treated weekly with 3, 10 or 15 mg/kg intravenous doses of the investigational anti-B7-H3 monoclonal antibody enoblituzumab plus 2 mg/kg intravenous doses of the programmed death-1 (PD-1) inhibitor pembrolizumab every 3 weeks (the standard dose at the time) for up to 1 year in the open-label dose-escalation study. Of those, 85% experienced treatment-related adverse events (AEs), and 27.1% experienced grade 3 or higher AEs, Dr. Aggarwal said.
These AEs were mostly infusion-related reactions typically seen with the first dose, and they were not usually cumulative, she said, noting that the rates of immune-related adverse events were less than 5%, about 7% of patients discontinued treatment because of a drug-related AE, and 1 treatment-related death due to pneumonitis occurred.
“No maximum tolerated dose was reached,” she added. “What I want to emphasize is that this is a combination immunotherapy approach, and what we found was that despite a combination approach, the nature, rate, and incidence of immune-related adverse events was not different than what is expected compared to single-agent [therapy] alone.”
Patients were then divided into disease-specific dose-expansion cohorts and the SCCHN and NSCLC cohorts were further stratified based on whether or not they had prior exposure to PD-1 inhibitor therapy.
Antitumor activity was noted in anti-PD-1-naive SCCHN patients, and objective responses were also seen in NSCLC patient with tumor programmed death-ligand 1 (PD-L1) expression of less than 1% and patients with checkpoint inhibitor–refractory urothelial carcinoma.
“We saw a 33.3% response rate in IO [immunotherapy]-naive head and neck cancer patients, and a 35.7% response rate in patients with PD-L1-negative immunotherapy-naive non–small-cell lung cancer patients,” she said.
No objective radiographic responses were seen in the IO-exposed SCCHN patients, but a few were seen in the other tumor cohorts, she noted.
“What was more interesting is this prolonged and high level of stable disease that we found in patients who had been previously treated with IO and had actually experienced significant clinical and radiographic progression then experienced stability with this combination,” she said, noting that “a fair amount of stable disease” was also seen in the IO-naive SCCHN and NSCLC patients.
In the immunotherapy-naive SCCHN patients, responses were seen regardless of human papillomavirus status, and four are still on treatment. One had a confirmed complete response.
“The majority of our patients on our trial and in this cohort were B7-H3-positive, she said, adding that the responses that were seen, including in those with stable disease, were “sustained and durable.”
Responses were similar in the immunotherapy-naive NSCLC patients who were PD-L1 negative, she said.
“Responses were seen irrespective of histology ... and many of these patients are still on treatment,” she added, noting that most were B7-H3-positive, which “seems to select our patients who have an even higher response rate of about 45%.”
The responses in that cohort also occurred early, were durable, and are sustained, and some patients remain on treatment and “are enjoying the clinical benefit afforded by this combination,” she said.
The findings are notable, because B7-H3 is highly expressed in many solid tumors, and monotherapy with enoblituzumab, which targets B7-H3 and is engineered to enhance antibody-dependent cell-mediated cytotoxicity, has demonstrated antitumor activity with an acceptable safety profile in patients with selected solid tumors.
In this study it was combined with pembrolizumab to test the hypothesis that coordinated engagement of both innate and adaptive immunity via the targeting of two distinct members of the B7 family could achieve greater antitumor activity than either agent alone, she explained.
The results “benchmark favorably” versus prior experience with PD-1 agents; pembrolizumab and nivolumab each lead to activity of about 13%-16%, she said.
“We acknowledge that our study has very small numbers. Nevertheless, these are encouraging data ... in this very tough-to-treat population,” Dr. Aggarwal said, adding that “further investigation of enoblituzumab with an anti-PD-1 molecule is warranted in both head and neck and lung cancer patients, perhaps including in combination with chemotherapy.”
Further, given the expression patterns of B7-H3 on a wide variety of solid tumors, further investigation of this combination ... is warranted in other tumor types, including in both checkpoint-naive and -treated populations, she concluded.
This study was sponsored by MacroGenics. Dr. Aggarwal reported receiving consulting fees from BMS.
SOURCE: Aggarwal C et al., SITC 2018 Abstract O24.
WASHINGTON – Combination enoblituzumab and pembrolizumab showed acceptable safety and encouraging antitumor activity in select patients with B7-H3-expressing non–small-cell lung cancer (NSCLC), squamous cell carcinoma of the head and neck (SCCHN), and other solid tumors in a phase 1 dose-escalation and expansion study.
Of note, the combination showed activity in patients anticipated to be poorly responsive to checkpoint inhibitor therapy alone, Charu Aggarwal, MD, of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the Society for Immunotherapy of Cancer.
In all, 133 patients were treated weekly with 3, 10 or 15 mg/kg intravenous doses of the investigational anti-B7-H3 monoclonal antibody enoblituzumab plus 2 mg/kg intravenous doses of the programmed death-1 (PD-1) inhibitor pembrolizumab every 3 weeks (the standard dose at the time) for up to 1 year in the open-label dose-escalation study. Of those, 85% experienced treatment-related adverse events (AEs), and 27.1% experienced grade 3 or higher AEs, Dr. Aggarwal said.
These AEs were mostly infusion-related reactions typically seen with the first dose, and they were not usually cumulative, she said, noting that the rates of immune-related adverse events were less than 5%, about 7% of patients discontinued treatment because of a drug-related AE, and 1 treatment-related death due to pneumonitis occurred.
“No maximum tolerated dose was reached,” she added. “What I want to emphasize is that this is a combination immunotherapy approach, and what we found was that despite a combination approach, the nature, rate, and incidence of immune-related adverse events was not different than what is expected compared to single-agent [therapy] alone.”
Patients were then divided into disease-specific dose-expansion cohorts and the SCCHN and NSCLC cohorts were further stratified based on whether or not they had prior exposure to PD-1 inhibitor therapy.
Antitumor activity was noted in anti-PD-1-naive SCCHN patients, and objective responses were also seen in NSCLC patient with tumor programmed death-ligand 1 (PD-L1) expression of less than 1% and patients with checkpoint inhibitor–refractory urothelial carcinoma.
“We saw a 33.3% response rate in IO [immunotherapy]-naive head and neck cancer patients, and a 35.7% response rate in patients with PD-L1-negative immunotherapy-naive non–small-cell lung cancer patients,” she said.
No objective radiographic responses were seen in the IO-exposed SCCHN patients, but a few were seen in the other tumor cohorts, she noted.
“What was more interesting is this prolonged and high level of stable disease that we found in patients who had been previously treated with IO and had actually experienced significant clinical and radiographic progression then experienced stability with this combination,” she said, noting that “a fair amount of stable disease” was also seen in the IO-naive SCCHN and NSCLC patients.
In the immunotherapy-naive SCCHN patients, responses were seen regardless of human papillomavirus status, and four are still on treatment. One had a confirmed complete response.
“The majority of our patients on our trial and in this cohort were B7-H3-positive, she said, adding that the responses that were seen, including in those with stable disease, were “sustained and durable.”
Responses were similar in the immunotherapy-naive NSCLC patients who were PD-L1 negative, she said.
“Responses were seen irrespective of histology ... and many of these patients are still on treatment,” she added, noting that most were B7-H3-positive, which “seems to select our patients who have an even higher response rate of about 45%.”
The responses in that cohort also occurred early, were durable, and are sustained, and some patients remain on treatment and “are enjoying the clinical benefit afforded by this combination,” she said.
The findings are notable, because B7-H3 is highly expressed in many solid tumors, and monotherapy with enoblituzumab, which targets B7-H3 and is engineered to enhance antibody-dependent cell-mediated cytotoxicity, has demonstrated antitumor activity with an acceptable safety profile in patients with selected solid tumors.
In this study it was combined with pembrolizumab to test the hypothesis that coordinated engagement of both innate and adaptive immunity via the targeting of two distinct members of the B7 family could achieve greater antitumor activity than either agent alone, she explained.
The results “benchmark favorably” versus prior experience with PD-1 agents; pembrolizumab and nivolumab each lead to activity of about 13%-16%, she said.
“We acknowledge that our study has very small numbers. Nevertheless, these are encouraging data ... in this very tough-to-treat population,” Dr. Aggarwal said, adding that “further investigation of enoblituzumab with an anti-PD-1 molecule is warranted in both head and neck and lung cancer patients, perhaps including in combination with chemotherapy.”
Further, given the expression patterns of B7-H3 on a wide variety of solid tumors, further investigation of this combination ... is warranted in other tumor types, including in both checkpoint-naive and -treated populations, she concluded.
This study was sponsored by MacroGenics. Dr. Aggarwal reported receiving consulting fees from BMS.
SOURCE: Aggarwal C et al., SITC 2018 Abstract O24.
WASHINGTON – Combination enoblituzumab and pembrolizumab showed acceptable safety and encouraging antitumor activity in select patients with B7-H3-expressing non–small-cell lung cancer (NSCLC), squamous cell carcinoma of the head and neck (SCCHN), and other solid tumors in a phase 1 dose-escalation and expansion study.
Of note, the combination showed activity in patients anticipated to be poorly responsive to checkpoint inhibitor therapy alone, Charu Aggarwal, MD, of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the Society for Immunotherapy of Cancer.
In all, 133 patients were treated weekly with 3, 10 or 15 mg/kg intravenous doses of the investigational anti-B7-H3 monoclonal antibody enoblituzumab plus 2 mg/kg intravenous doses of the programmed death-1 (PD-1) inhibitor pembrolizumab every 3 weeks (the standard dose at the time) for up to 1 year in the open-label dose-escalation study. Of those, 85% experienced treatment-related adverse events (AEs), and 27.1% experienced grade 3 or higher AEs, Dr. Aggarwal said.
These AEs were mostly infusion-related reactions typically seen with the first dose, and they were not usually cumulative, she said, noting that the rates of immune-related adverse events were less than 5%, about 7% of patients discontinued treatment because of a drug-related AE, and 1 treatment-related death due to pneumonitis occurred.
“No maximum tolerated dose was reached,” she added. “What I want to emphasize is that this is a combination immunotherapy approach, and what we found was that despite a combination approach, the nature, rate, and incidence of immune-related adverse events was not different than what is expected compared to single-agent [therapy] alone.”
Patients were then divided into disease-specific dose-expansion cohorts and the SCCHN and NSCLC cohorts were further stratified based on whether or not they had prior exposure to PD-1 inhibitor therapy.
Antitumor activity was noted in anti-PD-1-naive SCCHN patients, and objective responses were also seen in NSCLC patient with tumor programmed death-ligand 1 (PD-L1) expression of less than 1% and patients with checkpoint inhibitor–refractory urothelial carcinoma.
“We saw a 33.3% response rate in IO [immunotherapy]-naive head and neck cancer patients, and a 35.7% response rate in patients with PD-L1-negative immunotherapy-naive non–small-cell lung cancer patients,” she said.
No objective radiographic responses were seen in the IO-exposed SCCHN patients, but a few were seen in the other tumor cohorts, she noted.
“What was more interesting is this prolonged and high level of stable disease that we found in patients who had been previously treated with IO and had actually experienced significant clinical and radiographic progression then experienced stability with this combination,” she said, noting that “a fair amount of stable disease” was also seen in the IO-naive SCCHN and NSCLC patients.
In the immunotherapy-naive SCCHN patients, responses were seen regardless of human papillomavirus status, and four are still on treatment. One had a confirmed complete response.
“The majority of our patients on our trial and in this cohort were B7-H3-positive, she said, adding that the responses that were seen, including in those with stable disease, were “sustained and durable.”
Responses were similar in the immunotherapy-naive NSCLC patients who were PD-L1 negative, she said.
“Responses were seen irrespective of histology ... and many of these patients are still on treatment,” she added, noting that most were B7-H3-positive, which “seems to select our patients who have an even higher response rate of about 45%.”
The responses in that cohort also occurred early, were durable, and are sustained, and some patients remain on treatment and “are enjoying the clinical benefit afforded by this combination,” she said.
The findings are notable, because B7-H3 is highly expressed in many solid tumors, and monotherapy with enoblituzumab, which targets B7-H3 and is engineered to enhance antibody-dependent cell-mediated cytotoxicity, has demonstrated antitumor activity with an acceptable safety profile in patients with selected solid tumors.
In this study it was combined with pembrolizumab to test the hypothesis that coordinated engagement of both innate and adaptive immunity via the targeting of two distinct members of the B7 family could achieve greater antitumor activity than either agent alone, she explained.
The results “benchmark favorably” versus prior experience with PD-1 agents; pembrolizumab and nivolumab each lead to activity of about 13%-16%, she said.
“We acknowledge that our study has very small numbers. Nevertheless, these are encouraging data ... in this very tough-to-treat population,” Dr. Aggarwal said, adding that “further investigation of enoblituzumab with an anti-PD-1 molecule is warranted in both head and neck and lung cancer patients, perhaps including in combination with chemotherapy.”
Further, given the expression patterns of B7-H3 on a wide variety of solid tumors, further investigation of this combination ... is warranted in other tumor types, including in both checkpoint-naive and -treated populations, she concluded.
This study was sponsored by MacroGenics. Dr. Aggarwal reported receiving consulting fees from BMS.
SOURCE: Aggarwal C et al., SITC 2018 Abstract O24.
REPORTING FROM SITC 2018
Key clinical point: Enoblituzumab plus pembrolizumab shows promise in select patients with B7-H3-expressing solid tumors.
Major finding: The ORRs were 33.3% in IO-naive SCCHN patients and 35.7% in PD-L1-negative IO-naive NSCLC patients.
Study details: A phase 1 dose-escalation and expansion study of 133 patients.
Disclosures: This study was sponsored by MacroGenics. Dr. Aggarwal reported receiving consulting fees from BMS.
Source: Aggarwal C et al. SITC 2018 Abstract O24.
Prevalence of Suspicious Ultrasound Features in Hot Thyroid Nodules (FULL)
Although historically associated with a low risk of malignancy, hyperthyroidism is no longer thought to be protective against the occurrence of thyroid cancer. The incidence of malignancy has been reported in Graves disease at 2% and as high as 9% in toxic multinodular goiters.1,2
In evaluating patients with thyroid nodules and low thyroid stimulating hormone (TSH), which may indicate hyperthyroidism, the American Thyroid Association (ATA) recommends a radioiodine thyroid scan to determine whether a thyroid nodule is autonomous (hot) or nonfunctional (cold).3 Hot thyroid nodules are nodular areas of hyperfunctioning activity on radioiodine scan where tracer uptake is greater than the surrounding normal thyroid.
Historically, hot nodules have been associated with a low risk of malignancy and typically did not receive further ultrasound evaluation. However, recent studies have documented that the incidence of thyroid cancer in hot nodules may be underestimated. Mirfakhraee and colleagues performed a literature review in 2013 that revealed the prevalence of thyroid carcinoma in hot nodules managed by thyroidectomy ranged from 0% to 12.5% and averaged 3.1%.4 These findings may underestimate the prevalence of malignancy, because most hot nodules are not managed by thyroidectomy.
Given findings of hot nodules harboring malignancy, the authors investigated the role of thyroid ultrasound in patients with hyperthyroidism to identify suspicious features concerning for possible malignancies. The study objective was to estimate the prevalence of hot nodules with sonographic features concerning for malignancy in patients with hyperthyroidism in a Department of Veterans Affairs (VA) health care system.
Methods
This retrospective chart review consisted of 149,549 patients seen between January 2010 and December 2015 at the VA Northern California Health Care System (VANCHCS). The institutional review board approved the study and informed consent was waived.
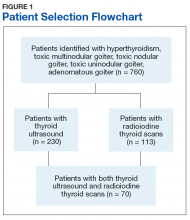
Seven hundred sixty veterans were identified in the Computerized Patient Record System (CPRS) using the following ICD-9 codes: 242.9 (hyperthyroidism), 242.2 (toxic multinodular goiter), 242.3 (toxic nodular goiter), 242.1 (toxic uninodular goiter), and 241.9 (adenomatous goiter) (Figure 1).
Manual review of thyroid ultrasound scans for suspicious characteristics concerning for thyroid carcinoma were based on the 2015 ATA Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer.3 Per the ATA guidelines, sonographic patterns that are highly suspicious for malignancy were solid hypoechoic nodule or solid hypoechoic component of a partially cystic nodule with one or more of the following features: irregular margins (infiltrative, microlobulated), microcalcifications, taller than wide on transverse view, and rim calcifications with small extrusive soft-tissue component. Sonographic patterns with intermediate suspicion were hypoechoic solid nodule with smooth margins without microcalcifications, extrathyroidal extension, or taller than wide shape.3
Results
Of the 760 identified veterans, 230 had thyroid ultrasounds, and 113 had radioiodine thyroid scans. Of these, 70 patients had both ultrasound and radioiodine thyroid scans. This cohort consisted of 84.3% (59) males and 15.7% women (11). Ages ranged from 32 to 93 (mean age 62.9) years.
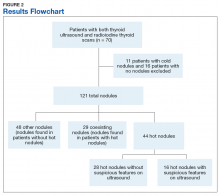
A total of 121 nodules were identified among the remaining 43 patients (11 individuals with cold thyroid scans and 16 individuals with no nodules were excluded). Of the 121 nodules, 44 were hot nodules, 29 were coexisting nodules found in patients with hot nodules, and 48 were other nodules found in patients without coexisting hot nodules (Figure 2).
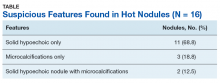
Of the 44 hot nodules, the analysis identified 16 hot nodules with suspicious features on ultrasound and 28 nodules without suspicious findings. Breakdown of specific suspicious features included 11 that were solid hypoechoic, 3 nodules that had microcalcifications, and 2 nodules that had both characteristics (Table).
Twelve patients had hot nodules with suspicious ultrasound findings. Of this group, 6 patients had no further workup, 1 patient was lost to follow-up, and 1 patient was planned for fine needle aspiration (FNA) biopsy. Four patients underwent FNA, and all results were benign.
Discussion
Although most veterans identified with hyperthyroidism did not undergo imaging studies, of those who did, a remarkable number had unexpected ultrasonographically suspicious nodules. Of the 44 hot nodules identified on radioiodine studies, 16 had suspicious ultrasound findings that raised concern for malignancy based on the most recent ATA guidelines. In contrast to recent studies that have suggested an increased incidence of thyroid carcinoma in hot nodules, no cancers were detected in this cohort.4 However, only 4 patients in this study underwent FNA.
Worth noting is that the most common suspicious feature found in this study’s cohort was hypoechoic solid nodules, which is a feature that has a sensitivity of 81% however a low specificity of 53% in detecting thyroid malignancy.5 This appearance also is found in 55% of benign thyroid nodules.6 The overlap of hypoechoic nodules as a feature in both benign and malignant thyroid nodules can present as a diagnostic challenge in differentiating between the two.
The 2015 ATA guideline recommends that low TSH warrants a radioiodine scan, and FNA should be considered for isofunctioning or nonfunctioning nodules with suspicious sonographic features. Hot nodules found on scintigraphy need no further cytologic evaluation because they are mostly benign.3 There is no clear stance on the use of ultrasound in hot nodules.
The answer to whether patients with hot nodules should undergo ultrasound still remains unclear. This study showed a surprising number of hot nodules with worrisome architecture found on ultrasound. However, whether that correlates to actual malignant findings remains unknown as most individuals in the cohort did not undergo biopsy. Also, given the high prevalence of suspicious findings, it may be difficult to use ultrasound as a diagnostic tool in patients with hot nodules as false positives may lead to unnecessary interventions such as biopsy.
Limitations
The patient population consisted mostly of men (84.3%) and cannot be applied to the general population. Thyroid nodules are 4 times more common in women than they are in men.7 Another limitation was the lack of data on patients’ radiation exposure while in military service or as civilians. Finally, as a retrospective study, there was unavoidable selection bias.
Conclusion
The prevalence of suspicious findings concerning for malignancy in hot nodules was 36.3% (16/44) based on the 2015 ATA guidelines. This study’s preliminary observation suggests that although ultrasound is a noninvasive and relatively inexpensive diagnostic modality, it has a limited role in the evaluation of hot nodules given the high prevalence of suspicious findings. Clinicians may still consider its use in patients who also have high-risk historic features. This was a thought-generating, retrospective study, and further prospective studies in larger populations are needed to validate the study’s results.
1. Stocker DJ, Burch HB. Thyroid cancer yield in patients with Graves’ disease. Minerva Endocrinol. 2003;28(3):205-212.
2. Cerci C, Cerci SS, Eroglu E, et al. Thyroid cancer in toxic and non-toxic multinodular goiter. J Postgrad Med. 2007;53(3):157-160.
3. Haugen BRM, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.
4. Mirfakhraee S, Mathews D, Peng L, Woodruff S, Zigman JM. A solitary hyperfunctioning thyroid nodule harboring thyroid carcinoma: review of the literature. Thyroid Res. 2013;6(1):7.
5. Papini E, Guglielmi R, Bianchini A, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002;87(5):1941-1946.
6. Mazzaferri EL. Management of a solitary thyroid nodule. N Engl J Med. 1993;328(8):553-559.
7. Fish SA, Langer JE, Mandel SJ. Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am. 2008;37(2):401-417.
Although historically associated with a low risk of malignancy, hyperthyroidism is no longer thought to be protective against the occurrence of thyroid cancer. The incidence of malignancy has been reported in Graves disease at 2% and as high as 9% in toxic multinodular goiters.1,2
In evaluating patients with thyroid nodules and low thyroid stimulating hormone (TSH), which may indicate hyperthyroidism, the American Thyroid Association (ATA) recommends a radioiodine thyroid scan to determine whether a thyroid nodule is autonomous (hot) or nonfunctional (cold).3 Hot thyroid nodules are nodular areas of hyperfunctioning activity on radioiodine scan where tracer uptake is greater than the surrounding normal thyroid.
Historically, hot nodules have been associated with a low risk of malignancy and typically did not receive further ultrasound evaluation. However, recent studies have documented that the incidence of thyroid cancer in hot nodules may be underestimated. Mirfakhraee and colleagues performed a literature review in 2013 that revealed the prevalence of thyroid carcinoma in hot nodules managed by thyroidectomy ranged from 0% to 12.5% and averaged 3.1%.4 These findings may underestimate the prevalence of malignancy, because most hot nodules are not managed by thyroidectomy.
Given findings of hot nodules harboring malignancy, the authors investigated the role of thyroid ultrasound in patients with hyperthyroidism to identify suspicious features concerning for possible malignancies. The study objective was to estimate the prevalence of hot nodules with sonographic features concerning for malignancy in patients with hyperthyroidism in a Department of Veterans Affairs (VA) health care system.
Methods
This retrospective chart review consisted of 149,549 patients seen between January 2010 and December 2015 at the VA Northern California Health Care System (VANCHCS). The institutional review board approved the study and informed consent was waived.
Seven hundred sixty veterans were identified in the Computerized Patient Record System (CPRS) using the following ICD-9 codes: 242.9 (hyperthyroidism), 242.2 (toxic multinodular goiter), 242.3 (toxic nodular goiter), 242.1 (toxic uninodular goiter), and 241.9 (adenomatous goiter) (Figure 1).
Manual review of thyroid ultrasound scans for suspicious characteristics concerning for thyroid carcinoma were based on the 2015 ATA Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer.3 Per the ATA guidelines, sonographic patterns that are highly suspicious for malignancy were solid hypoechoic nodule or solid hypoechoic component of a partially cystic nodule with one or more of the following features: irregular margins (infiltrative, microlobulated), microcalcifications, taller than wide on transverse view, and rim calcifications with small extrusive soft-tissue component. Sonographic patterns with intermediate suspicion were hypoechoic solid nodule with smooth margins without microcalcifications, extrathyroidal extension, or taller than wide shape.3
Results
Of the 760 identified veterans, 230 had thyroid ultrasounds, and 113 had radioiodine thyroid scans. Of these, 70 patients had both ultrasound and radioiodine thyroid scans. This cohort consisted of 84.3% (59) males and 15.7% women (11). Ages ranged from 32 to 93 (mean age 62.9) years.
A total of 121 nodules were identified among the remaining 43 patients (11 individuals with cold thyroid scans and 16 individuals with no nodules were excluded). Of the 121 nodules, 44 were hot nodules, 29 were coexisting nodules found in patients with hot nodules, and 48 were other nodules found in patients without coexisting hot nodules (Figure 2).
Of the 44 hot nodules, the analysis identified 16 hot nodules with suspicious features on ultrasound and 28 nodules without suspicious findings. Breakdown of specific suspicious features included 11 that were solid hypoechoic, 3 nodules that had microcalcifications, and 2 nodules that had both characteristics (Table).
Twelve patients had hot nodules with suspicious ultrasound findings. Of this group, 6 patients had no further workup, 1 patient was lost to follow-up, and 1 patient was planned for fine needle aspiration (FNA) biopsy. Four patients underwent FNA, and all results were benign.
Discussion
Although most veterans identified with hyperthyroidism did not undergo imaging studies, of those who did, a remarkable number had unexpected ultrasonographically suspicious nodules. Of the 44 hot nodules identified on radioiodine studies, 16 had suspicious ultrasound findings that raised concern for malignancy based on the most recent ATA guidelines. In contrast to recent studies that have suggested an increased incidence of thyroid carcinoma in hot nodules, no cancers were detected in this cohort.4 However, only 4 patients in this study underwent FNA.
Worth noting is that the most common suspicious feature found in this study’s cohort was hypoechoic solid nodules, which is a feature that has a sensitivity of 81% however a low specificity of 53% in detecting thyroid malignancy.5 This appearance also is found in 55% of benign thyroid nodules.6 The overlap of hypoechoic nodules as a feature in both benign and malignant thyroid nodules can present as a diagnostic challenge in differentiating between the two.
The 2015 ATA guideline recommends that low TSH warrants a radioiodine scan, and FNA should be considered for isofunctioning or nonfunctioning nodules with suspicious sonographic features. Hot nodules found on scintigraphy need no further cytologic evaluation because they are mostly benign.3 There is no clear stance on the use of ultrasound in hot nodules.
The answer to whether patients with hot nodules should undergo ultrasound still remains unclear. This study showed a surprising number of hot nodules with worrisome architecture found on ultrasound. However, whether that correlates to actual malignant findings remains unknown as most individuals in the cohort did not undergo biopsy. Also, given the high prevalence of suspicious findings, it may be difficult to use ultrasound as a diagnostic tool in patients with hot nodules as false positives may lead to unnecessary interventions such as biopsy.
Limitations
The patient population consisted mostly of men (84.3%) and cannot be applied to the general population. Thyroid nodules are 4 times more common in women than they are in men.7 Another limitation was the lack of data on patients’ radiation exposure while in military service or as civilians. Finally, as a retrospective study, there was unavoidable selection bias.
Conclusion
The prevalence of suspicious findings concerning for malignancy in hot nodules was 36.3% (16/44) based on the 2015 ATA guidelines. This study’s preliminary observation suggests that although ultrasound is a noninvasive and relatively inexpensive diagnostic modality, it has a limited role in the evaluation of hot nodules given the high prevalence of suspicious findings. Clinicians may still consider its use in patients who also have high-risk historic features. This was a thought-generating, retrospective study, and further prospective studies in larger populations are needed to validate the study’s results.
Although historically associated with a low risk of malignancy, hyperthyroidism is no longer thought to be protective against the occurrence of thyroid cancer. The incidence of malignancy has been reported in Graves disease at 2% and as high as 9% in toxic multinodular goiters.1,2
In evaluating patients with thyroid nodules and low thyroid stimulating hormone (TSH), which may indicate hyperthyroidism, the American Thyroid Association (ATA) recommends a radioiodine thyroid scan to determine whether a thyroid nodule is autonomous (hot) or nonfunctional (cold).3 Hot thyroid nodules are nodular areas of hyperfunctioning activity on radioiodine scan where tracer uptake is greater than the surrounding normal thyroid.
Historically, hot nodules have been associated with a low risk of malignancy and typically did not receive further ultrasound evaluation. However, recent studies have documented that the incidence of thyroid cancer in hot nodules may be underestimated. Mirfakhraee and colleagues performed a literature review in 2013 that revealed the prevalence of thyroid carcinoma in hot nodules managed by thyroidectomy ranged from 0% to 12.5% and averaged 3.1%.4 These findings may underestimate the prevalence of malignancy, because most hot nodules are not managed by thyroidectomy.
Given findings of hot nodules harboring malignancy, the authors investigated the role of thyroid ultrasound in patients with hyperthyroidism to identify suspicious features concerning for possible malignancies. The study objective was to estimate the prevalence of hot nodules with sonographic features concerning for malignancy in patients with hyperthyroidism in a Department of Veterans Affairs (VA) health care system.
Methods
This retrospective chart review consisted of 149,549 patients seen between January 2010 and December 2015 at the VA Northern California Health Care System (VANCHCS). The institutional review board approved the study and informed consent was waived.
Seven hundred sixty veterans were identified in the Computerized Patient Record System (CPRS) using the following ICD-9 codes: 242.9 (hyperthyroidism), 242.2 (toxic multinodular goiter), 242.3 (toxic nodular goiter), 242.1 (toxic uninodular goiter), and 241.9 (adenomatous goiter) (Figure 1).
Manual review of thyroid ultrasound scans for suspicious characteristics concerning for thyroid carcinoma were based on the 2015 ATA Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer.3 Per the ATA guidelines, sonographic patterns that are highly suspicious for malignancy were solid hypoechoic nodule or solid hypoechoic component of a partially cystic nodule with one or more of the following features: irregular margins (infiltrative, microlobulated), microcalcifications, taller than wide on transverse view, and rim calcifications with small extrusive soft-tissue component. Sonographic patterns with intermediate suspicion were hypoechoic solid nodule with smooth margins without microcalcifications, extrathyroidal extension, or taller than wide shape.3
Results
Of the 760 identified veterans, 230 had thyroid ultrasounds, and 113 had radioiodine thyroid scans. Of these, 70 patients had both ultrasound and radioiodine thyroid scans. This cohort consisted of 84.3% (59) males and 15.7% women (11). Ages ranged from 32 to 93 (mean age 62.9) years.
A total of 121 nodules were identified among the remaining 43 patients (11 individuals with cold thyroid scans and 16 individuals with no nodules were excluded). Of the 121 nodules, 44 were hot nodules, 29 were coexisting nodules found in patients with hot nodules, and 48 were other nodules found in patients without coexisting hot nodules (Figure 2).
Of the 44 hot nodules, the analysis identified 16 hot nodules with suspicious features on ultrasound and 28 nodules without suspicious findings. Breakdown of specific suspicious features included 11 that were solid hypoechoic, 3 nodules that had microcalcifications, and 2 nodules that had both characteristics (Table).
Twelve patients had hot nodules with suspicious ultrasound findings. Of this group, 6 patients had no further workup, 1 patient was lost to follow-up, and 1 patient was planned for fine needle aspiration (FNA) biopsy. Four patients underwent FNA, and all results were benign.
Discussion
Although most veterans identified with hyperthyroidism did not undergo imaging studies, of those who did, a remarkable number had unexpected ultrasonographically suspicious nodules. Of the 44 hot nodules identified on radioiodine studies, 16 had suspicious ultrasound findings that raised concern for malignancy based on the most recent ATA guidelines. In contrast to recent studies that have suggested an increased incidence of thyroid carcinoma in hot nodules, no cancers were detected in this cohort.4 However, only 4 patients in this study underwent FNA.
Worth noting is that the most common suspicious feature found in this study’s cohort was hypoechoic solid nodules, which is a feature that has a sensitivity of 81% however a low specificity of 53% in detecting thyroid malignancy.5 This appearance also is found in 55% of benign thyroid nodules.6 The overlap of hypoechoic nodules as a feature in both benign and malignant thyroid nodules can present as a diagnostic challenge in differentiating between the two.
The 2015 ATA guideline recommends that low TSH warrants a radioiodine scan, and FNA should be considered for isofunctioning or nonfunctioning nodules with suspicious sonographic features. Hot nodules found on scintigraphy need no further cytologic evaluation because they are mostly benign.3 There is no clear stance on the use of ultrasound in hot nodules.
The answer to whether patients with hot nodules should undergo ultrasound still remains unclear. This study showed a surprising number of hot nodules with worrisome architecture found on ultrasound. However, whether that correlates to actual malignant findings remains unknown as most individuals in the cohort did not undergo biopsy. Also, given the high prevalence of suspicious findings, it may be difficult to use ultrasound as a diagnostic tool in patients with hot nodules as false positives may lead to unnecessary interventions such as biopsy.
Limitations
The patient population consisted mostly of men (84.3%) and cannot be applied to the general population. Thyroid nodules are 4 times more common in women than they are in men.7 Another limitation was the lack of data on patients’ radiation exposure while in military service or as civilians. Finally, as a retrospective study, there was unavoidable selection bias.
Conclusion
The prevalence of suspicious findings concerning for malignancy in hot nodules was 36.3% (16/44) based on the 2015 ATA guidelines. This study’s preliminary observation suggests that although ultrasound is a noninvasive and relatively inexpensive diagnostic modality, it has a limited role in the evaluation of hot nodules given the high prevalence of suspicious findings. Clinicians may still consider its use in patients who also have high-risk historic features. This was a thought-generating, retrospective study, and further prospective studies in larger populations are needed to validate the study’s results.
1. Stocker DJ, Burch HB. Thyroid cancer yield in patients with Graves’ disease. Minerva Endocrinol. 2003;28(3):205-212.
2. Cerci C, Cerci SS, Eroglu E, et al. Thyroid cancer in toxic and non-toxic multinodular goiter. J Postgrad Med. 2007;53(3):157-160.
3. Haugen BRM, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.
4. Mirfakhraee S, Mathews D, Peng L, Woodruff S, Zigman JM. A solitary hyperfunctioning thyroid nodule harboring thyroid carcinoma: review of the literature. Thyroid Res. 2013;6(1):7.
5. Papini E, Guglielmi R, Bianchini A, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002;87(5):1941-1946.
6. Mazzaferri EL. Management of a solitary thyroid nodule. N Engl J Med. 1993;328(8):553-559.
7. Fish SA, Langer JE, Mandel SJ. Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am. 2008;37(2):401-417.
1. Stocker DJ, Burch HB. Thyroid cancer yield in patients with Graves’ disease. Minerva Endocrinol. 2003;28(3):205-212.
2. Cerci C, Cerci SS, Eroglu E, et al. Thyroid cancer in toxic and non-toxic multinodular goiter. J Postgrad Med. 2007;53(3):157-160.
3. Haugen BRM, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.
4. Mirfakhraee S, Mathews D, Peng L, Woodruff S, Zigman JM. A solitary hyperfunctioning thyroid nodule harboring thyroid carcinoma: review of the literature. Thyroid Res. 2013;6(1):7.
5. Papini E, Guglielmi R, Bianchini A, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002;87(5):1941-1946.
6. Mazzaferri EL. Management of a solitary thyroid nodule. N Engl J Med. 1993;328(8):553-559.
7. Fish SA, Langer JE, Mandel SJ. Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am. 2008;37(2):401-417.
Clinical trial: The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma trial is an interventional study recruiting patients with human papillomavirus (HPV)–positive oropharyngeal cancer.
Patients who are recruited will undergo robotic surgery after being screened for poor prognosis. Patients with good prognosis will be followed without receiving postoperative radiation. Those in this group who experience a recurrence will receive either more surgery and postoperative radiotherapy or postoperative chemoradiotherapy alone. Patients with poor prognosis will receive reduced-dose radiotherapy or chemoradiotherapy based on pathology.
Few trials have examined deescalation using surgery alone in intermediate- and early-stage HPV-positive cancer, the investigators noted, adding that they expect more than half of participants will undergo curative treatment with surgery alone and that withholding radiation in these patients will not noticeably affect their long-term survival.
Patients are eligible for the study if they have early- or intermediate-stage, resectable, HPV-positive oropharyngeal cancer. Patients must be at aged at least 18 years; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1; have a limiting serious illness; and have had previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Secondary outcome measures include overall survival, toxicity rates, quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma trial is an interventional study recruiting patients with human papillomavirus (HPV)–positive oropharyngeal cancer.
Patients who are recruited will undergo robotic surgery after being screened for poor prognosis. Patients with good prognosis will be followed without receiving postoperative radiation. Those in this group who experience a recurrence will receive either more surgery and postoperative radiotherapy or postoperative chemoradiotherapy alone. Patients with poor prognosis will receive reduced-dose radiotherapy or chemoradiotherapy based on pathology.
Few trials have examined deescalation using surgery alone in intermediate- and early-stage HPV-positive cancer, the investigators noted, adding that they expect more than half of participants will undergo curative treatment with surgery alone and that withholding radiation in these patients will not noticeably affect their long-term survival.
Patients are eligible for the study if they have early- or intermediate-stage, resectable, HPV-positive oropharyngeal cancer. Patients must be at aged at least 18 years; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1; have a limiting serious illness; and have had previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Secondary outcome measures include overall survival, toxicity rates, quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma trial is an interventional study recruiting patients with human papillomavirus (HPV)–positive oropharyngeal cancer.
Patients who are recruited will undergo robotic surgery after being screened for poor prognosis. Patients with good prognosis will be followed without receiving postoperative radiation. Those in this group who experience a recurrence will receive either more surgery and postoperative radiotherapy or postoperative chemoradiotherapy alone. Patients with poor prognosis will receive reduced-dose radiotherapy or chemoradiotherapy based on pathology.
Few trials have examined deescalation using surgery alone in intermediate- and early-stage HPV-positive cancer, the investigators noted, adding that they expect more than half of participants will undergo curative treatment with surgery alone and that withholding radiation in these patients will not noticeably affect their long-term survival.
Patients are eligible for the study if they have early- or intermediate-stage, resectable, HPV-positive oropharyngeal cancer. Patients must be at aged at least 18 years; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1; have a limiting serious illness; and have had previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Secondary outcome measures include overall survival, toxicity rates, quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
Immunotherapy may hold the key to defeating virally associated cancers
Infection with certain viruses has been causally linked to the development of cancer. In recent years, an improved understanding of the unique pathology and molecular underpinnings of these virally associated cancers has prompted the development of more personalized treatment strategies, with a particular focus on immunotherapy. Here, we describe some of the latest developments.
The link between viruses and cancer
Suspicions about a possible role of viral infections in the development of cancer were first aroused in the early 1900s. The seminal discovery is traced back to Peyton Rous, who showed that a malignant tumor growing in a chicken could be transferred to a healthy bird by injecting it with tumor extracts that contained no actual tumor cells.1
The infectious etiology of human cancer, however, remained controversial until many years later when the first cancer-causing virus, Epstein-Barr virus (EBV), was identified in cell cultures from patients with Burkitt lymphoma. Shortly afterward, the Rous sarcoma virus was unveiled as the oncogenic agent behind Rous’ observations.2Seven viruses have now been linked to the development of cancers and are thought to be responsible for around 12% of all cancer cases worldwide. The burden is likely to increase as technological advancements make it easier to establish a causal link between viruses and cancer development.3
In addition to making these links, researchers have also made significant headway in understanding how viruses cause cancer. Cancerous transformation of host cells occurs in only a minority of those who are infected with oncogenic viruses and often occurs in the setting of chronic infection.
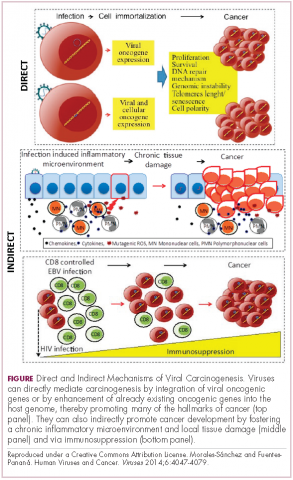
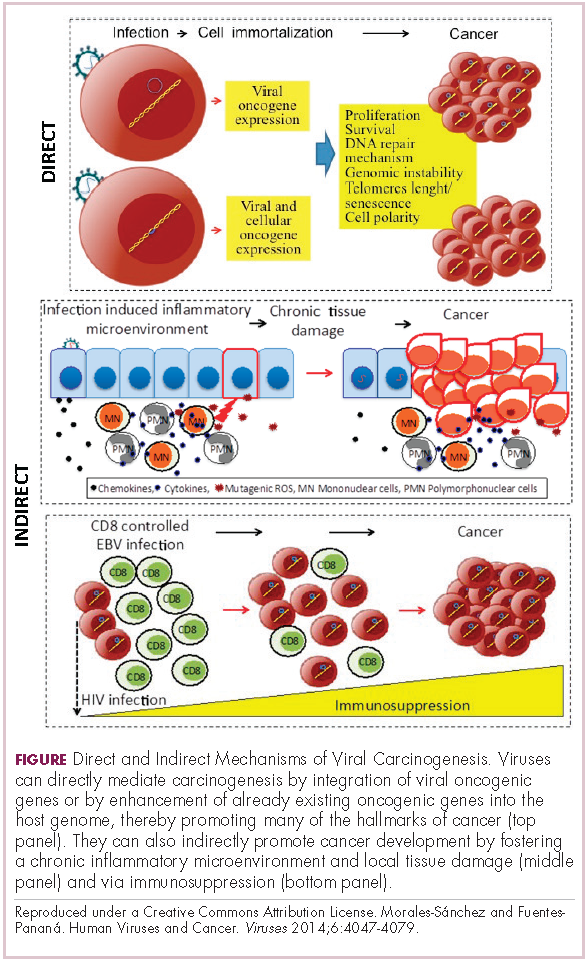
Viruses can mediate carcinogenesis by direct and/or indirect mechanisms (Figure 1). Many of the hallmarks of cancer, the key attributes that drive the transformation from a normal cell to a malignant one, are compatible with the virus’s needs, such as needing to avoid cell death, increasing cell proliferation, and avoiding detection by the immune system.
Viruses hijack the cellular machinery to meet those needs and they can do this either by producing viral proteins that have an oncogenic effect or by integrating their genetic material into the host cell genome. When the latter occurs, the process of integration can also cause damage to the DNA, which further increases the risk of cancer-promoting changes occurring in the host genome.
Viruses can indirectly contribute to carcinogenesis by fostering a microenvironment of chronic inflammation, causing oxidative stress and local tissue damage, and by suppressing the antitumor immune response.4,5
Screening and prevention efforts have helped to reduce the burden of several different virally associated cancers. However, for the substantial proportion of patients who are still affected by these cancers, there is a pressing need for new therapeutic options, particularly since genome sequencing studies have revealed that these cancers can often have distinct underlying molecular mechanisms.
Vaccines lead the charge in HPV-driven cancers
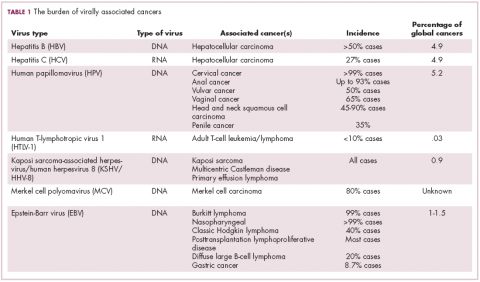
German virologist Harald zur Hausen received the Nobel Prize in 2008 for his discovery of the oncogenic role of human papillomaviruses (HPVs), a large family of more than 100 DNA viruses that infect the epithelial cells of the skin and mucous membranes. They are responsible for the largest number of virally associated cancer cases globally – around 5% (Table 1).
A number of different cancer types are linked to HPV infection, but it is best known as the cause of cervical cancer. The development of diagnostic blood tests and prophylactic vaccines for prevention and early intervention in HPV infection has helped to reduce the incidence of cervical cancer. Conversely, another type of HPV-associated cancer, head and neck squamous cell carcinoma (HNSCC), has seen increased incidence in recent years.
HPVs are categorized according to their oncogenic potential as high, intermediate, or low risk. The high-risk HPV16 and HPV18 strains are most commonly associated with cancer. They are thought to cause cancer predominantly through integration into the host genome. The HPV genome is composed of 8 genes encoding proteins that regulate viral replication and assembly. The E6 and E7 genes are the most highly oncogenic; as the HPV DNA is inserted into the host genome, the transcriptional regulator of E6/E7 is lost, leading to their increased expression. These genes have significant oncogenic potential because of their interaction with 2 tumor suppressor proteins, p53 and pRb.6,7
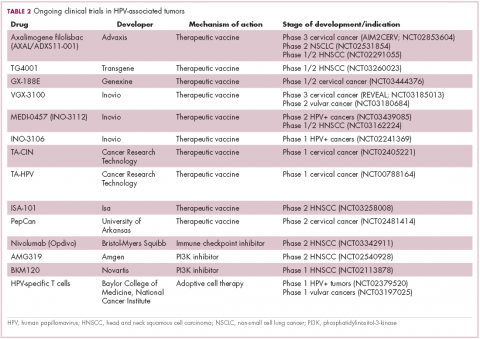
The largest investment in therapeutic development for HPV-positive cancers has been in the realm of immunotherapy in an effort to boost the anti-tumor immune response. In particular, there has been a focus on the development of therapeutic vaccines, designed to prime the anti-tumor immune response to recognize viral antigens. A variety of different types of vaccines are being developed, including live, attenuated and inactivated vaccines that are protein, DNA, or peptide based. Most developed to date target the E6/E7 proteins from the HPV16/18 strains (Table 2).8,9
Other immunotherapies are also being evaluated, including immune checkpoint inhibitors, antibodies designed to target one of the principal mechanisms of immune evasion exploited by cancer cells. The combination of immune checkpoint inhibitors with vaccines is a particularly promising strategy in HPV-associated cancers. At the European Society for Medical Oncology Congress in 2017, the results of a phase 2 trial of nivolumab in combination with ISA-101 were presented.
Among 24 patients with HPV-positive tumors, the majority oropharyngeal cancers, the combination elicited an overall response rate (ORR) of 33%, including 2 complete responses (CRs). Most adverse events (AEs) were mild to moderate in severity and included fever, injection site reactions, fatigue and nausea.14
Hepatocellular carcinoma: a tale of two viruses
The hepatitis viruses are a group of 5 unrelated viruses that causes inflammation of the liver. Hepatitis B (HBV), a DNA virus, and hepatitis C (HCV), an RNA virus, are also oncoviruses; HBV in particular is one of the main causes of hepatocellular carcinoma (HCC), the most common type of liver cancer.
The highly inflammatory environment fostered by HBV and HCV infection causes liver damage that often leads to cirrhosis. Continued infection can drive permanent damage to the hepatocytes, leading to genetic and epigenetic damage and driving oncogenesis. As an RNA virus, HCV doesn’t integrate into the genome and no confirmed viral oncoproteins have been identified to date, therefore it mostly drives cancer through these indirect mechanisms, which is also reflected in the fact that HCV-associated HCC predominantly occurs against a backdrop of liver cirrhosis.
HBV does integrate into the host genome. Genome sequencing studies revealed hundreds of integration sites, but most commonly they disrupted host genes involved in telomere stability and cell cycle regulation, providing some insight into the mechanisms by which HBV-associated HCC develops. In addition, HBV produces several oncoproteins, including HBx, which disrupts gene transcription, cell signaling pathways, cell cycle progress, apoptosis and other cellular processes.15,16
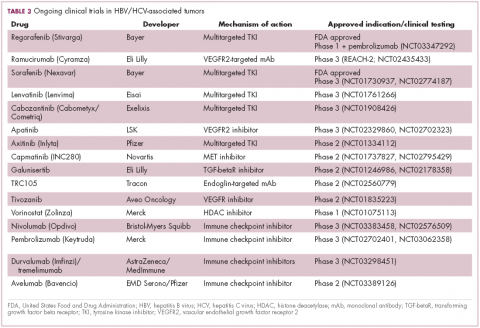
Multitargeted tyrosine kinase inhibitors (TKIs) have been the focal point of therapeutic development in HCC. However, following the approval of sorafenib in 2008, there was a dearth of effective new treatment options despite substantial efforts and numerous phase 3 trials. More recently, immunotherapy has also come to the forefront, especially immune checkpoint inhibitors.
Last year marked the first new drug approvals in nearly a decade – the TKI regorafenib (Stivarga) and immune checkpoint inhibitor nivolumab (Opdivo), both in the second-line setting after failure of sorafenib. Treatment options in this setting may continue to expand, with the TKIs cabozantinib and lenvatinib and the immune checkpoint inhibitor pembrolizumab and the combination of durvalumab and tremelimumab hot on their heels.17-20 Many of these drugs are also being evaluated in the front-line setting in comparison with sorafenib (Table 3).
At the current time, the treatment strategy for patients with HCC is independent of etiology, however, there are significant ongoing efforts to try to tease out the implications of infection for treatment efficacy. A recent meta-analysis of patients treated with sorafenib in 3 randomized phase 3 trials (n = 3,526) suggested that it improved overall survival (OS) among patients who were HCV-positive, but HBV-negative.21
Studies of the vascular endothelial growth factor receptor 2-targeting monoclonal antibody ramucirumab, on the other hand, suggested that it may have a greater OS benefit in patients with HBV, while regorafenib seemed to have a comparable OS benefit in both subgroups.22-25 The immune checkpoint inhibitors studied thus far seem to elicit responses irrespective of infection status.
A phase 2 trial of the immune checkpoint inhibitor tremelimumab was conducted specifically in patients with advanced HCC and chronic HCV infection. The disease control rate (DCR) was 76.4%, with 17.6% partial response (PR) rate. There was also a significant drop in viral load, suggesting that tremelimumab may have antiviral effects.26,27,28
Adoptive cell therapy promising in EBV-positive cancers
More than 90% of the global population is infected with EBV, making it one of the most common human viruses. It is a member of the herpesvirus family that is probably best known as the cause of infectious mononucleosis. On rare occasions, however, EBV can cause tumor development, though our understanding of its exact pathogenic role in cancer is still incomplete.
EBV is a DNA virus that doesn’t tend to integrate into the host genome, but instead remains in the nucleus in the form of episomes and produces several oncoproteins, including latent membrane protein-1. It is associated with a range of different cancer types, including Burkitt lymphoma and other B-cell malignancies. It also infects epithelial cells and can cause nasopharyngeal carcinoma and gastric cancer, however, much less is known about the molecular underpinnings of these EBV-positive cancer types.26,27Gastric cancers actually comprise the largest group of EBV-associated tumors because of the global incidence of this cancer type. The Cancer Genome Atlas Research Network recently characterized gastric cancer on a molecular level and identified an EBV-positive subgroup as a distinct clinical entity with unique molecular characteristics.29
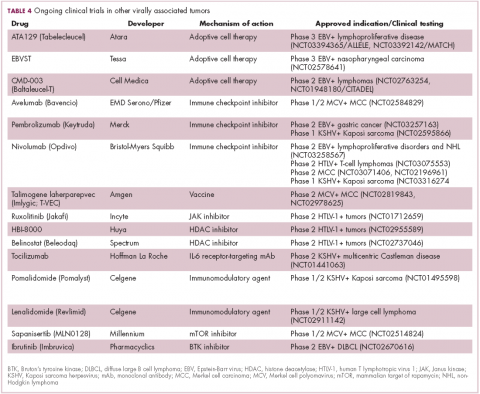
The focus of therapeutic development has again been on immunotherapy, however in this case the idea of collecting the patients T cells, engineering them to recognize EBV, and then reinfusing them into the patient – adoptive cell therapy – has gained the most traction (Table 4).
Two presentations at the American Society of Hematology annual meeting in 2017 detailed ongoing clinical trials of Atara Biotherapeutics’ ATA129 and Cell Medica’s CMD-003. ATA129 was associated with a high response rate and a low rate of serious AEs in patients with posttransplant lymphoproliferative disorder; ORR was 80% in 6 patients treated after hematopoietic stem cell transplantation, and 83% in 6 patients after solid organ transplant.30
CMD-003, meanwhile, demonstrated preliminary signs of activity and safety in patients with relapsed extranodal NK/T-cell lymphoma, according to early results from the phase 2 CITADEL trial. Among 6 evaluable patients, the ORR was 50% and the DCR was 67%.31
Newest oncovirus on the block
The most recently discovered cancer-associated virus is Merkel cell polyomavirus (MCV), a DNA virus that was identified in 2008. Like EBV, virtually the whole global adult population is infected with MCV. It is linked to the development of a highly aggressive and lethal, though rare, form of skin cancer – Merkel cell carcinoma.
MCV is found in around 80% of MCC cases and in fewer than 10% of melanomas and other skin cancers. Thus far, several direct mechanisms of oncogenesis have been described, including integration of MCV into the host genome and the production of viral oncogenes, though their precise function is as yet unclear.32-34
The American Cancer Society estimates that only 1500 cases of MCC are diagnosed each year in the United States.35 Its rarity makes it difficult to conduct clinical trials with sufficient power, yet some headway has still been made.
Around half of MCCs express the programmed cell death ligand 1 (PD-L1) on their surface, making them a logical candidate for immune checkpoint inhibition. In 2017, avelumab became the first FDA-approved drug for the treatment of MCC. Approval was based on the JAVELIN Merkel 200 study in which 88 patients received avelumab. After 1 year of follow-up the ORR was 31.8%, with a CR rate of 9%.36
Genome sequencing studies suggest that the mutational profile of MCV-positive tumors is quite different to those that are MCV-negative, which could have therapeutic implications. To date, these implications have not been delineated, given the challenge of small patient numbers, however an ongoing phase 1/2 trial is evaluating the combination of avelumab and radiation therapy or recombinant interferon beta, with or without MCV-specific cytotoxic T cells in patients with MCC and MCV infection.
The 2 other known cancer-causing viruses are human T-lymphotropic virus 1 (HTLV-1), a retrovirus associated with adult T-cell leukemia/lymphoma (ATL) and Kaposi sarcoma herpesvirus (KSHV). The latter is the causative agent of Kaposi sarcoma, often in combination with human immunodeficiency virus (HIV), a rare skin tumor that became renowned in the 1980s as an AIDS-defining illness.
The incidence of HTLV-1- and KSHV-positive tumors is substantially lower than the other virally associated cancers and, like MCC, this makes studying them and conducting clinical trials of novel therapeutic options a challenge. Nonetheless, several trials of targeted therapies and immunotherapies are underway.
1. Rous PA. Transmissible avain neoplasm. (Sarcoma of the common fowl). J Exp Med. 1910;12(5):696-705.
2. Epstein MA, Achong BG, Barr YM. Virus particles in cultured lymphoblasts from Burkitt's lymphoma. Lancet. 1964;1(7335):702-703.
3. Mesri Enrique A, Feitelson MA, Munger K. Human viral oncogenesis: a cancer hallmarks analysis. Cell Host & Microbe. 2014;15(3):266-282.
4. Santana-Davila R, Bhatia S, Chow LQ. Harnessing the immune system as a therapeutic tool in virus-associated cancers. JAMA Oncol. 2017;3(1):106-112.
5. Tashiro H, Brenner MK. Immunotherapy against cancer-related viruses. Cell Res. 2017;27(1):59-73.
6. Brianti P, De Flammineis E, Mercuri SR. Review of HPV-related diseases and cancers. New Microbiol. 2017;40(2):80-85.
7. Tulay P, Serakinci N. The route to HPV-associated neoplastic transformation: a review of the literature. Crit Rev Eukaryot Gene Expr. 2016;26(1):27-39.
8. Smola S. Immunopathogenesis of HPV-associated cancers and prospects for immunotherapy. Viruses. 2017;9(9).
9. Rosales R, Rosales C. Immune therapy for human papillomaviruses-related cancers. World Journal of Clinical Oncology. 2014;5(5):1002-1019.
10. Miles B, Safran HP, Monk BJ. Therapeutic options for treatment of human papillomavirus-associated cancers - novel immunologic vaccines: ADXS11-001. Gynecol Oncol Res Pract. 2017;4:10.
11. Miles BA, Monk BJ, Safran HP. Mechanistic insights into ADXS11-001 human papillomavirus-associated cancer immunotherapy. Gynecol Oncol Res Pract. 2017;4:9.
12. Huh W, Dizon D, Powell M, Landrum L, Leath C. A prospective phase II trial of the listeria-based human papillomavirus immunotherapy axalimogene filolisbac in second and third-line metastatic cervical cancer: A NRG oncology group trial. Paper presented at: Annual Meeting on Women's Cancer; March 12-15, 2017, 2017; National Harbor, MD.
13. Petit RG, Mehta A, Jain M, et al. ADXS11-001 immunotherapy targeting HPV-E7: final results from a Phase II study in Indian women with recurrent cervical cancer. Journal for Immunotherapy of Cancer. 2014;2(Suppl 3):P92-P92.
14. Glisson B, Massarelli E, William W, et al. Nivolumab and ISA 101 HPV vaccine in incurable HPV-16+ cancer. Ann Oncol. 2017;28(suppl_5):v403-v427.
15. Ding X-X, Zhu Q-G, Zhang S-M, et al. Precision medicine for hepatocellular carcinoma: driver mutations and targeted therapy. Oncotarget. 2017;8(33):55715-55730.
16. Ringehan M, McKeating JA, Protzer U. Viral hepatitis and liver cancer. Philosophical Transactions of the Royal Society B: Biological Sciences. 2017;372(1732):20160274.
17. Abou-Alfa G, Meyer T, Cheng AL, et al. Cabozantinib (C) versus placebo (P) in patients (pts) with advanced hepatocellular carcinoma (HCC) who have received prior sorafenib: results from the randomized phase III CELESTIAL trial. J Clin Oncol. 2017;36(Suppl 4S):abstr 207.
18. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018.
19. Zhu AX, Finn RS, Cattan S, et al. KEYNOTE-224: Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib. J Clin Oncol. 2018;36(Suppl 4S):Abstr 209.
20. Kelley RK, Abou-Alfa GK, Bendell JC, et al. Phase I/II study of durvalumab and tremelimumab in patients with unresectable hepatocellular carcinoma (HCC): Phase I safety and efficacy analyses. Journal of Clinical Oncology. 2017;35(15_suppl):4073-4073.
21. Jackson R, Psarelli E-E, Berhane S, Khan H, Johnson P. Impact of Viral Status on Survival in Patients Receiving Sorafenib for Advanced Hepatocellular Cancer: A Meta-Analysis of Randomized Phase III Trials. Journal of Clinical Oncology. 2017;35(6):622-628.
22. Kudo M. Molecular Targeted Agents for Hepatocellular Carcinoma: Current Status and Future Perspectives. Liver Cancer. 2017;6(2):101-112.
23. zur Hausen H, Meinhof W, Scheiber W, Bornkamm GW. Attempts to detect virus-secific DNA in human tumors. I. Nucleic acid hybridizations with complementary RNA of human wart virus. Int J Cancer. 1974;13(5):650-656.
24. Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56-66.
25. Bruix J, Tak WY, Gasbarrini A, et al. Regorafenib as second-line therapy for intermediate or advanced hepatocellular carcinoma: multicentre, open-label, phase II safety study. Eur J Cancer. 2013;49(16):3412-3419.
26. Neparidze N, Lacy J. Malignancies associated with epstein-barr virus: pathobiology, clinical features, and evolving treatments. Clin Adv Hematol Oncol. 2014;12(6):358-371.
27. Ozoya OO, Sokol L, Dalia S. EBV-Related Malignancies, Outcomes and Novel Prevention Strategies. Infect Disord Drug Targets. 2016;16(1):4-21.
28. Sangro B, Gomez-Martin C, de la Mata M, et al. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J Hepatol. 2013;59(1):81-88.
29. The Cancer Genome Atlas Research N. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202.
30. Prockop S, Li A, Baiocchi R, et al. Efficacy and safety of ATA129, partially matched allogeneic third-party Epstein-Barr virus-targeted cytotoxic T lymphocytes in a multicenter study for post-transplant lymphoproliferative disorder. Paper presented at: 59th Annual Meeting of the American Society of Hematology; December 9-12, 2017, 2017; Atlanta, GA.
31. Kim W, Ardeshna K, Lin Y, et al. Autologous EBV-specific T cells (CMD-003): Early results from a multicenter, multinational Phase 2 trial for treatment of EBV-associated NK/T-cell lymphoma. Paper presented at: 59th Annual Meeting of the American Society of Hematology; December 9-12, 2017, 2017; Atlanta, GA.
32. Schadendorf D, Lebbé C, zur Hausen A, et al. Merkel cell carcinoma: Epidemiology, prognosis, therapy and unmet medical needs. European Journal of Cancer. 2017;71:53-69.
33. Spurgeon ME, Lambert PF. Merkel cell polyomavirus: a newly discovered human virus with oncogenic potential. Virology. 2013;435(1):118-130.
34. Tello TL, Coggshall K, Yom SS, Yu SS. Merkel cell carcinoma: An update and review: Current and future therapy. J Am Acad Dermatol. 2018;78(3):445-454.
35. American Cancer Society. Key Statistics for Merkel Cell Carcinoma. 2015; https://www.cancer.org/cancer/merkel-cell-skin-cancer/about/key-statistics.html#written_by. Accessed March 7th, 2017.
36. Kaufman HL, Russell J, Hamid O, et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. The Lancet Oncology.17(10):1374-1385.
Infection with certain viruses has been causally linked to the development of cancer. In recent years, an improved understanding of the unique pathology and molecular underpinnings of these virally associated cancers has prompted the development of more personalized treatment strategies, with a particular focus on immunotherapy. Here, we describe some of the latest developments.
The link between viruses and cancer
Suspicions about a possible role of viral infections in the development of cancer were first aroused in the early 1900s. The seminal discovery is traced back to Peyton Rous, who showed that a malignant tumor growing in a chicken could be transferred to a healthy bird by injecting it with tumor extracts that contained no actual tumor cells.1
The infectious etiology of human cancer, however, remained controversial until many years later when the first cancer-causing virus, Epstein-Barr virus (EBV), was identified in cell cultures from patients with Burkitt lymphoma. Shortly afterward, the Rous sarcoma virus was unveiled as the oncogenic agent behind Rous’ observations.2Seven viruses have now been linked to the development of cancers and are thought to be responsible for around 12% of all cancer cases worldwide. The burden is likely to increase as technological advancements make it easier to establish a causal link between viruses and cancer development.3
In addition to making these links, researchers have also made significant headway in understanding how viruses cause cancer. Cancerous transformation of host cells occurs in only a minority of those who are infected with oncogenic viruses and often occurs in the setting of chronic infection.
Viruses can mediate carcinogenesis by direct and/or indirect mechanisms (Figure 1). Many of the hallmarks of cancer, the key attributes that drive the transformation from a normal cell to a malignant one, are compatible with the virus’s needs, such as needing to avoid cell death, increasing cell proliferation, and avoiding detection by the immune system.
Viruses hijack the cellular machinery to meet those needs and they can do this either by producing viral proteins that have an oncogenic effect or by integrating their genetic material into the host cell genome. When the latter occurs, the process of integration can also cause damage to the DNA, which further increases the risk of cancer-promoting changes occurring in the host genome.
Viruses can indirectly contribute to carcinogenesis by fostering a microenvironment of chronic inflammation, causing oxidative stress and local tissue damage, and by suppressing the antitumor immune response.4,5
Screening and prevention efforts have helped to reduce the burden of several different virally associated cancers. However, for the substantial proportion of patients who are still affected by these cancers, there is a pressing need for new therapeutic options, particularly since genome sequencing studies have revealed that these cancers can often have distinct underlying molecular mechanisms.
Vaccines lead the charge in HPV-driven cancers
German virologist Harald zur Hausen received the Nobel Prize in 2008 for his discovery of the oncogenic role of human papillomaviruses (HPVs), a large family of more than 100 DNA viruses that infect the epithelial cells of the skin and mucous membranes. They are responsible for the largest number of virally associated cancer cases globally – around 5% (Table 1).
A number of different cancer types are linked to HPV infection, but it is best known as the cause of cervical cancer. The development of diagnostic blood tests and prophylactic vaccines for prevention and early intervention in HPV infection has helped to reduce the incidence of cervical cancer. Conversely, another type of HPV-associated cancer, head and neck squamous cell carcinoma (HNSCC), has seen increased incidence in recent years.
HPVs are categorized according to their oncogenic potential as high, intermediate, or low risk. The high-risk HPV16 and HPV18 strains are most commonly associated with cancer. They are thought to cause cancer predominantly through integration into the host genome. The HPV genome is composed of 8 genes encoding proteins that regulate viral replication and assembly. The E6 and E7 genes are the most highly oncogenic; as the HPV DNA is inserted into the host genome, the transcriptional regulator of E6/E7 is lost, leading to their increased expression. These genes have significant oncogenic potential because of their interaction with 2 tumor suppressor proteins, p53 and pRb.6,7
The largest investment in therapeutic development for HPV-positive cancers has been in the realm of immunotherapy in an effort to boost the anti-tumor immune response. In particular, there has been a focus on the development of therapeutic vaccines, designed to prime the anti-tumor immune response to recognize viral antigens. A variety of different types of vaccines are being developed, including live, attenuated and inactivated vaccines that are protein, DNA, or peptide based. Most developed to date target the E6/E7 proteins from the HPV16/18 strains (Table 2).8,9
Other immunotherapies are also being evaluated, including immune checkpoint inhibitors, antibodies designed to target one of the principal mechanisms of immune evasion exploited by cancer cells. The combination of immune checkpoint inhibitors with vaccines is a particularly promising strategy in HPV-associated cancers. At the European Society for Medical Oncology Congress in 2017, the results of a phase 2 trial of nivolumab in combination with ISA-101 were presented.
Among 24 patients with HPV-positive tumors, the majority oropharyngeal cancers, the combination elicited an overall response rate (ORR) of 33%, including 2 complete responses (CRs). Most adverse events (AEs) were mild to moderate in severity and included fever, injection site reactions, fatigue and nausea.14
Hepatocellular carcinoma: a tale of two viruses
The hepatitis viruses are a group of 5 unrelated viruses that causes inflammation of the liver. Hepatitis B (HBV), a DNA virus, and hepatitis C (HCV), an RNA virus, are also oncoviruses; HBV in particular is one of the main causes of hepatocellular carcinoma (HCC), the most common type of liver cancer.
The highly inflammatory environment fostered by HBV and HCV infection causes liver damage that often leads to cirrhosis. Continued infection can drive permanent damage to the hepatocytes, leading to genetic and epigenetic damage and driving oncogenesis. As an RNA virus, HCV doesn’t integrate into the genome and no confirmed viral oncoproteins have been identified to date, therefore it mostly drives cancer through these indirect mechanisms, which is also reflected in the fact that HCV-associated HCC predominantly occurs against a backdrop of liver cirrhosis.
HBV does integrate into the host genome. Genome sequencing studies revealed hundreds of integration sites, but most commonly they disrupted host genes involved in telomere stability and cell cycle regulation, providing some insight into the mechanisms by which HBV-associated HCC develops. In addition, HBV produces several oncoproteins, including HBx, which disrupts gene transcription, cell signaling pathways, cell cycle progress, apoptosis and other cellular processes.15,16
Multitargeted tyrosine kinase inhibitors (TKIs) have been the focal point of therapeutic development in HCC. However, following the approval of sorafenib in 2008, there was a dearth of effective new treatment options despite substantial efforts and numerous phase 3 trials. More recently, immunotherapy has also come to the forefront, especially immune checkpoint inhibitors.
Last year marked the first new drug approvals in nearly a decade – the TKI regorafenib (Stivarga) and immune checkpoint inhibitor nivolumab (Opdivo), both in the second-line setting after failure of sorafenib. Treatment options in this setting may continue to expand, with the TKIs cabozantinib and lenvatinib and the immune checkpoint inhibitor pembrolizumab and the combination of durvalumab and tremelimumab hot on their heels.17-20 Many of these drugs are also being evaluated in the front-line setting in comparison with sorafenib (Table 3).
At the current time, the treatment strategy for patients with HCC is independent of etiology, however, there are significant ongoing efforts to try to tease out the implications of infection for treatment efficacy. A recent meta-analysis of patients treated with sorafenib in 3 randomized phase 3 trials (n = 3,526) suggested that it improved overall survival (OS) among patients who were HCV-positive, but HBV-negative.21
Studies of the vascular endothelial growth factor receptor 2-targeting monoclonal antibody ramucirumab, on the other hand, suggested that it may have a greater OS benefit in patients with HBV, while regorafenib seemed to have a comparable OS benefit in both subgroups.22-25 The immune checkpoint inhibitors studied thus far seem to elicit responses irrespective of infection status.
A phase 2 trial of the immune checkpoint inhibitor tremelimumab was conducted specifically in patients with advanced HCC and chronic HCV infection. The disease control rate (DCR) was 76.4%, with 17.6% partial response (PR) rate. There was also a significant drop in viral load, suggesting that tremelimumab may have antiviral effects.26,27,28
Adoptive cell therapy promising in EBV-positive cancers
More than 90% of the global population is infected with EBV, making it one of the most common human viruses. It is a member of the herpesvirus family that is probably best known as the cause of infectious mononucleosis. On rare occasions, however, EBV can cause tumor development, though our understanding of its exact pathogenic role in cancer is still incomplete.
EBV is a DNA virus that doesn’t tend to integrate into the host genome, but instead remains in the nucleus in the form of episomes and produces several oncoproteins, including latent membrane protein-1. It is associated with a range of different cancer types, including Burkitt lymphoma and other B-cell malignancies. It also infects epithelial cells and can cause nasopharyngeal carcinoma and gastric cancer, however, much less is known about the molecular underpinnings of these EBV-positive cancer types.26,27Gastric cancers actually comprise the largest group of EBV-associated tumors because of the global incidence of this cancer type. The Cancer Genome Atlas Research Network recently characterized gastric cancer on a molecular level and identified an EBV-positive subgroup as a distinct clinical entity with unique molecular characteristics.29
The focus of therapeutic development has again been on immunotherapy, however in this case the idea of collecting the patients T cells, engineering them to recognize EBV, and then reinfusing them into the patient – adoptive cell therapy – has gained the most traction (Table 4).
Two presentations at the American Society of Hematology annual meeting in 2017 detailed ongoing clinical trials of Atara Biotherapeutics’ ATA129 and Cell Medica’s CMD-003. ATA129 was associated with a high response rate and a low rate of serious AEs in patients with posttransplant lymphoproliferative disorder; ORR was 80% in 6 patients treated after hematopoietic stem cell transplantation, and 83% in 6 patients after solid organ transplant.30
CMD-003, meanwhile, demonstrated preliminary signs of activity and safety in patients with relapsed extranodal NK/T-cell lymphoma, according to early results from the phase 2 CITADEL trial. Among 6 evaluable patients, the ORR was 50% and the DCR was 67%.31
Newest oncovirus on the block
The most recently discovered cancer-associated virus is Merkel cell polyomavirus (MCV), a DNA virus that was identified in 2008. Like EBV, virtually the whole global adult population is infected with MCV. It is linked to the development of a highly aggressive and lethal, though rare, form of skin cancer – Merkel cell carcinoma.
MCV is found in around 80% of MCC cases and in fewer than 10% of melanomas and other skin cancers. Thus far, several direct mechanisms of oncogenesis have been described, including integration of MCV into the host genome and the production of viral oncogenes, though their precise function is as yet unclear.32-34
The American Cancer Society estimates that only 1500 cases of MCC are diagnosed each year in the United States.35 Its rarity makes it difficult to conduct clinical trials with sufficient power, yet some headway has still been made.
Around half of MCCs express the programmed cell death ligand 1 (PD-L1) on their surface, making them a logical candidate for immune checkpoint inhibition. In 2017, avelumab became the first FDA-approved drug for the treatment of MCC. Approval was based on the JAVELIN Merkel 200 study in which 88 patients received avelumab. After 1 year of follow-up the ORR was 31.8%, with a CR rate of 9%.36
Genome sequencing studies suggest that the mutational profile of MCV-positive tumors is quite different to those that are MCV-negative, which could have therapeutic implications. To date, these implications have not been delineated, given the challenge of small patient numbers, however an ongoing phase 1/2 trial is evaluating the combination of avelumab and radiation therapy or recombinant interferon beta, with or without MCV-specific cytotoxic T cells in patients with MCC and MCV infection.
The 2 other known cancer-causing viruses are human T-lymphotropic virus 1 (HTLV-1), a retrovirus associated with adult T-cell leukemia/lymphoma (ATL) and Kaposi sarcoma herpesvirus (KSHV). The latter is the causative agent of Kaposi sarcoma, often in combination with human immunodeficiency virus (HIV), a rare skin tumor that became renowned in the 1980s as an AIDS-defining illness.
The incidence of HTLV-1- and KSHV-positive tumors is substantially lower than the other virally associated cancers and, like MCC, this makes studying them and conducting clinical trials of novel therapeutic options a challenge. Nonetheless, several trials of targeted therapies and immunotherapies are underway.
Infection with certain viruses has been causally linked to the development of cancer. In recent years, an improved understanding of the unique pathology and molecular underpinnings of these virally associated cancers has prompted the development of more personalized treatment strategies, with a particular focus on immunotherapy. Here, we describe some of the latest developments.
The link between viruses and cancer
Suspicions about a possible role of viral infections in the development of cancer were first aroused in the early 1900s. The seminal discovery is traced back to Peyton Rous, who showed that a malignant tumor growing in a chicken could be transferred to a healthy bird by injecting it with tumor extracts that contained no actual tumor cells.1
The infectious etiology of human cancer, however, remained controversial until many years later when the first cancer-causing virus, Epstein-Barr virus (EBV), was identified in cell cultures from patients with Burkitt lymphoma. Shortly afterward, the Rous sarcoma virus was unveiled as the oncogenic agent behind Rous’ observations.2Seven viruses have now been linked to the development of cancers and are thought to be responsible for around 12% of all cancer cases worldwide. The burden is likely to increase as technological advancements make it easier to establish a causal link between viruses and cancer development.3
In addition to making these links, researchers have also made significant headway in understanding how viruses cause cancer. Cancerous transformation of host cells occurs in only a minority of those who are infected with oncogenic viruses and often occurs in the setting of chronic infection.
Viruses can mediate carcinogenesis by direct and/or indirect mechanisms (Figure 1). Many of the hallmarks of cancer, the key attributes that drive the transformation from a normal cell to a malignant one, are compatible with the virus’s needs, such as needing to avoid cell death, increasing cell proliferation, and avoiding detection by the immune system.
Viruses hijack the cellular machinery to meet those needs and they can do this either by producing viral proteins that have an oncogenic effect or by integrating their genetic material into the host cell genome. When the latter occurs, the process of integration can also cause damage to the DNA, which further increases the risk of cancer-promoting changes occurring in the host genome.
Viruses can indirectly contribute to carcinogenesis by fostering a microenvironment of chronic inflammation, causing oxidative stress and local tissue damage, and by suppressing the antitumor immune response.4,5
Screening and prevention efforts have helped to reduce the burden of several different virally associated cancers. However, for the substantial proportion of patients who are still affected by these cancers, there is a pressing need for new therapeutic options, particularly since genome sequencing studies have revealed that these cancers can often have distinct underlying molecular mechanisms.
Vaccines lead the charge in HPV-driven cancers
German virologist Harald zur Hausen received the Nobel Prize in 2008 for his discovery of the oncogenic role of human papillomaviruses (HPVs), a large family of more than 100 DNA viruses that infect the epithelial cells of the skin and mucous membranes. They are responsible for the largest number of virally associated cancer cases globally – around 5% (Table 1).
A number of different cancer types are linked to HPV infection, but it is best known as the cause of cervical cancer. The development of diagnostic blood tests and prophylactic vaccines for prevention and early intervention in HPV infection has helped to reduce the incidence of cervical cancer. Conversely, another type of HPV-associated cancer, head and neck squamous cell carcinoma (HNSCC), has seen increased incidence in recent years.
HPVs are categorized according to their oncogenic potential as high, intermediate, or low risk. The high-risk HPV16 and HPV18 strains are most commonly associated with cancer. They are thought to cause cancer predominantly through integration into the host genome. The HPV genome is composed of 8 genes encoding proteins that regulate viral replication and assembly. The E6 and E7 genes are the most highly oncogenic; as the HPV DNA is inserted into the host genome, the transcriptional regulator of E6/E7 is lost, leading to their increased expression. These genes have significant oncogenic potential because of their interaction with 2 tumor suppressor proteins, p53 and pRb.6,7
The largest investment in therapeutic development for HPV-positive cancers has been in the realm of immunotherapy in an effort to boost the anti-tumor immune response. In particular, there has been a focus on the development of therapeutic vaccines, designed to prime the anti-tumor immune response to recognize viral antigens. A variety of different types of vaccines are being developed, including live, attenuated and inactivated vaccines that are protein, DNA, or peptide based. Most developed to date target the E6/E7 proteins from the HPV16/18 strains (Table 2).8,9
Other immunotherapies are also being evaluated, including immune checkpoint inhibitors, antibodies designed to target one of the principal mechanisms of immune evasion exploited by cancer cells. The combination of immune checkpoint inhibitors with vaccines is a particularly promising strategy in HPV-associated cancers. At the European Society for Medical Oncology Congress in 2017, the results of a phase 2 trial of nivolumab in combination with ISA-101 were presented.
Among 24 patients with HPV-positive tumors, the majority oropharyngeal cancers, the combination elicited an overall response rate (ORR) of 33%, including 2 complete responses (CRs). Most adverse events (AEs) were mild to moderate in severity and included fever, injection site reactions, fatigue and nausea.14
Hepatocellular carcinoma: a tale of two viruses
The hepatitis viruses are a group of 5 unrelated viruses that causes inflammation of the liver. Hepatitis B (HBV), a DNA virus, and hepatitis C (HCV), an RNA virus, are also oncoviruses; HBV in particular is one of the main causes of hepatocellular carcinoma (HCC), the most common type of liver cancer.
The highly inflammatory environment fostered by HBV and HCV infection causes liver damage that often leads to cirrhosis. Continued infection can drive permanent damage to the hepatocytes, leading to genetic and epigenetic damage and driving oncogenesis. As an RNA virus, HCV doesn’t integrate into the genome and no confirmed viral oncoproteins have been identified to date, therefore it mostly drives cancer through these indirect mechanisms, which is also reflected in the fact that HCV-associated HCC predominantly occurs against a backdrop of liver cirrhosis.
HBV does integrate into the host genome. Genome sequencing studies revealed hundreds of integration sites, but most commonly they disrupted host genes involved in telomere stability and cell cycle regulation, providing some insight into the mechanisms by which HBV-associated HCC develops. In addition, HBV produces several oncoproteins, including HBx, which disrupts gene transcription, cell signaling pathways, cell cycle progress, apoptosis and other cellular processes.15,16
Multitargeted tyrosine kinase inhibitors (TKIs) have been the focal point of therapeutic development in HCC. However, following the approval of sorafenib in 2008, there was a dearth of effective new treatment options despite substantial efforts and numerous phase 3 trials. More recently, immunotherapy has also come to the forefront, especially immune checkpoint inhibitors.
Last year marked the first new drug approvals in nearly a decade – the TKI regorafenib (Stivarga) and immune checkpoint inhibitor nivolumab (Opdivo), both in the second-line setting after failure of sorafenib. Treatment options in this setting may continue to expand, with the TKIs cabozantinib and lenvatinib and the immune checkpoint inhibitor pembrolizumab and the combination of durvalumab and tremelimumab hot on their heels.17-20 Many of these drugs are also being evaluated in the front-line setting in comparison with sorafenib (Table 3).
At the current time, the treatment strategy for patients with HCC is independent of etiology, however, there are significant ongoing efforts to try to tease out the implications of infection for treatment efficacy. A recent meta-analysis of patients treated with sorafenib in 3 randomized phase 3 trials (n = 3,526) suggested that it improved overall survival (OS) among patients who were HCV-positive, but HBV-negative.21
Studies of the vascular endothelial growth factor receptor 2-targeting monoclonal antibody ramucirumab, on the other hand, suggested that it may have a greater OS benefit in patients with HBV, while regorafenib seemed to have a comparable OS benefit in both subgroups.22-25 The immune checkpoint inhibitors studied thus far seem to elicit responses irrespective of infection status.
A phase 2 trial of the immune checkpoint inhibitor tremelimumab was conducted specifically in patients with advanced HCC and chronic HCV infection. The disease control rate (DCR) was 76.4%, with 17.6% partial response (PR) rate. There was also a significant drop in viral load, suggesting that tremelimumab may have antiviral effects.26,27,28
Adoptive cell therapy promising in EBV-positive cancers
More than 90% of the global population is infected with EBV, making it one of the most common human viruses. It is a member of the herpesvirus family that is probably best known as the cause of infectious mononucleosis. On rare occasions, however, EBV can cause tumor development, though our understanding of its exact pathogenic role in cancer is still incomplete.
EBV is a DNA virus that doesn’t tend to integrate into the host genome, but instead remains in the nucleus in the form of episomes and produces several oncoproteins, including latent membrane protein-1. It is associated with a range of different cancer types, including Burkitt lymphoma and other B-cell malignancies. It also infects epithelial cells and can cause nasopharyngeal carcinoma and gastric cancer, however, much less is known about the molecular underpinnings of these EBV-positive cancer types.26,27Gastric cancers actually comprise the largest group of EBV-associated tumors because of the global incidence of this cancer type. The Cancer Genome Atlas Research Network recently characterized gastric cancer on a molecular level and identified an EBV-positive subgroup as a distinct clinical entity with unique molecular characteristics.29
The focus of therapeutic development has again been on immunotherapy, however in this case the idea of collecting the patients T cells, engineering them to recognize EBV, and then reinfusing them into the patient – adoptive cell therapy – has gained the most traction (Table 4).
Two presentations at the American Society of Hematology annual meeting in 2017 detailed ongoing clinical trials of Atara Biotherapeutics’ ATA129 and Cell Medica’s CMD-003. ATA129 was associated with a high response rate and a low rate of serious AEs in patients with posttransplant lymphoproliferative disorder; ORR was 80% in 6 patients treated after hematopoietic stem cell transplantation, and 83% in 6 patients after solid organ transplant.30
CMD-003, meanwhile, demonstrated preliminary signs of activity and safety in patients with relapsed extranodal NK/T-cell lymphoma, according to early results from the phase 2 CITADEL trial. Among 6 evaluable patients, the ORR was 50% and the DCR was 67%.31
Newest oncovirus on the block
The most recently discovered cancer-associated virus is Merkel cell polyomavirus (MCV), a DNA virus that was identified in 2008. Like EBV, virtually the whole global adult population is infected with MCV. It is linked to the development of a highly aggressive and lethal, though rare, form of skin cancer – Merkel cell carcinoma.
MCV is found in around 80% of MCC cases and in fewer than 10% of melanomas and other skin cancers. Thus far, several direct mechanisms of oncogenesis have been described, including integration of MCV into the host genome and the production of viral oncogenes, though their precise function is as yet unclear.32-34
The American Cancer Society estimates that only 1500 cases of MCC are diagnosed each year in the United States.35 Its rarity makes it difficult to conduct clinical trials with sufficient power, yet some headway has still been made.
Around half of MCCs express the programmed cell death ligand 1 (PD-L1) on their surface, making them a logical candidate for immune checkpoint inhibition. In 2017, avelumab became the first FDA-approved drug for the treatment of MCC. Approval was based on the JAVELIN Merkel 200 study in which 88 patients received avelumab. After 1 year of follow-up the ORR was 31.8%, with a CR rate of 9%.36
Genome sequencing studies suggest that the mutational profile of MCV-positive tumors is quite different to those that are MCV-negative, which could have therapeutic implications. To date, these implications have not been delineated, given the challenge of small patient numbers, however an ongoing phase 1/2 trial is evaluating the combination of avelumab and radiation therapy or recombinant interferon beta, with or without MCV-specific cytotoxic T cells in patients with MCC and MCV infection.
The 2 other known cancer-causing viruses are human T-lymphotropic virus 1 (HTLV-1), a retrovirus associated with adult T-cell leukemia/lymphoma (ATL) and Kaposi sarcoma herpesvirus (KSHV). The latter is the causative agent of Kaposi sarcoma, often in combination with human immunodeficiency virus (HIV), a rare skin tumor that became renowned in the 1980s as an AIDS-defining illness.
The incidence of HTLV-1- and KSHV-positive tumors is substantially lower than the other virally associated cancers and, like MCC, this makes studying them and conducting clinical trials of novel therapeutic options a challenge. Nonetheless, several trials of targeted therapies and immunotherapies are underway.
1. Rous PA. Transmissible avain neoplasm. (Sarcoma of the common fowl). J Exp Med. 1910;12(5):696-705.
2. Epstein MA, Achong BG, Barr YM. Virus particles in cultured lymphoblasts from Burkitt's lymphoma. Lancet. 1964;1(7335):702-703.
3. Mesri Enrique A, Feitelson MA, Munger K. Human viral oncogenesis: a cancer hallmarks analysis. Cell Host & Microbe. 2014;15(3):266-282.
4. Santana-Davila R, Bhatia S, Chow LQ. Harnessing the immune system as a therapeutic tool in virus-associated cancers. JAMA Oncol. 2017;3(1):106-112.
5. Tashiro H, Brenner MK. Immunotherapy against cancer-related viruses. Cell Res. 2017;27(1):59-73.
6. Brianti P, De Flammineis E, Mercuri SR. Review of HPV-related diseases and cancers. New Microbiol. 2017;40(2):80-85.
7. Tulay P, Serakinci N. The route to HPV-associated neoplastic transformation: a review of the literature. Crit Rev Eukaryot Gene Expr. 2016;26(1):27-39.
8. Smola S. Immunopathogenesis of HPV-associated cancers and prospects for immunotherapy. Viruses. 2017;9(9).
9. Rosales R, Rosales C. Immune therapy for human papillomaviruses-related cancers. World Journal of Clinical Oncology. 2014;5(5):1002-1019.
10. Miles B, Safran HP, Monk BJ. Therapeutic options for treatment of human papillomavirus-associated cancers - novel immunologic vaccines: ADXS11-001. Gynecol Oncol Res Pract. 2017;4:10.
11. Miles BA, Monk BJ, Safran HP. Mechanistic insights into ADXS11-001 human papillomavirus-associated cancer immunotherapy. Gynecol Oncol Res Pract. 2017;4:9.
12. Huh W, Dizon D, Powell M, Landrum L, Leath C. A prospective phase II trial of the listeria-based human papillomavirus immunotherapy axalimogene filolisbac in second and third-line metastatic cervical cancer: A NRG oncology group trial. Paper presented at: Annual Meeting on Women's Cancer; March 12-15, 2017, 2017; National Harbor, MD.
13. Petit RG, Mehta A, Jain M, et al. ADXS11-001 immunotherapy targeting HPV-E7: final results from a Phase II study in Indian women with recurrent cervical cancer. Journal for Immunotherapy of Cancer. 2014;2(Suppl 3):P92-P92.
14. Glisson B, Massarelli E, William W, et al. Nivolumab and ISA 101 HPV vaccine in incurable HPV-16+ cancer. Ann Oncol. 2017;28(suppl_5):v403-v427.
15. Ding X-X, Zhu Q-G, Zhang S-M, et al. Precision medicine for hepatocellular carcinoma: driver mutations and targeted therapy. Oncotarget. 2017;8(33):55715-55730.
16. Ringehan M, McKeating JA, Protzer U. Viral hepatitis and liver cancer. Philosophical Transactions of the Royal Society B: Biological Sciences. 2017;372(1732):20160274.
17. Abou-Alfa G, Meyer T, Cheng AL, et al. Cabozantinib (C) versus placebo (P) in patients (pts) with advanced hepatocellular carcinoma (HCC) who have received prior sorafenib: results from the randomized phase III CELESTIAL trial. J Clin Oncol. 2017;36(Suppl 4S):abstr 207.
18. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018.
19. Zhu AX, Finn RS, Cattan S, et al. KEYNOTE-224: Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib. J Clin Oncol. 2018;36(Suppl 4S):Abstr 209.
20. Kelley RK, Abou-Alfa GK, Bendell JC, et al. Phase I/II study of durvalumab and tremelimumab in patients with unresectable hepatocellular carcinoma (HCC): Phase I safety and efficacy analyses. Journal of Clinical Oncology. 2017;35(15_suppl):4073-4073.
21. Jackson R, Psarelli E-E, Berhane S, Khan H, Johnson P. Impact of Viral Status on Survival in Patients Receiving Sorafenib for Advanced Hepatocellular Cancer: A Meta-Analysis of Randomized Phase III Trials. Journal of Clinical Oncology. 2017;35(6):622-628.
22. Kudo M. Molecular Targeted Agents for Hepatocellular Carcinoma: Current Status and Future Perspectives. Liver Cancer. 2017;6(2):101-112.
23. zur Hausen H, Meinhof W, Scheiber W, Bornkamm GW. Attempts to detect virus-secific DNA in human tumors. I. Nucleic acid hybridizations with complementary RNA of human wart virus. Int J Cancer. 1974;13(5):650-656.
24. Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56-66.
25. Bruix J, Tak WY, Gasbarrini A, et al. Regorafenib as second-line therapy for intermediate or advanced hepatocellular carcinoma: multicentre, open-label, phase II safety study. Eur J Cancer. 2013;49(16):3412-3419.
26. Neparidze N, Lacy J. Malignancies associated with epstein-barr virus: pathobiology, clinical features, and evolving treatments. Clin Adv Hematol Oncol. 2014;12(6):358-371.
27. Ozoya OO, Sokol L, Dalia S. EBV-Related Malignancies, Outcomes and Novel Prevention Strategies. Infect Disord Drug Targets. 2016;16(1):4-21.
28. Sangro B, Gomez-Martin C, de la Mata M, et al. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J Hepatol. 2013;59(1):81-88.
29. The Cancer Genome Atlas Research N. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202.
30. Prockop S, Li A, Baiocchi R, et al. Efficacy and safety of ATA129, partially matched allogeneic third-party Epstein-Barr virus-targeted cytotoxic T lymphocytes in a multicenter study for post-transplant lymphoproliferative disorder. Paper presented at: 59th Annual Meeting of the American Society of Hematology; December 9-12, 2017, 2017; Atlanta, GA.
31. Kim W, Ardeshna K, Lin Y, et al. Autologous EBV-specific T cells (CMD-003): Early results from a multicenter, multinational Phase 2 trial for treatment of EBV-associated NK/T-cell lymphoma. Paper presented at: 59th Annual Meeting of the American Society of Hematology; December 9-12, 2017, 2017; Atlanta, GA.
32. Schadendorf D, Lebbé C, zur Hausen A, et al. Merkel cell carcinoma: Epidemiology, prognosis, therapy and unmet medical needs. European Journal of Cancer. 2017;71:53-69.
33. Spurgeon ME, Lambert PF. Merkel cell polyomavirus: a newly discovered human virus with oncogenic potential. Virology. 2013;435(1):118-130.
34. Tello TL, Coggshall K, Yom SS, Yu SS. Merkel cell carcinoma: An update and review: Current and future therapy. J Am Acad Dermatol. 2018;78(3):445-454.
35. American Cancer Society. Key Statistics for Merkel Cell Carcinoma. 2015; https://www.cancer.org/cancer/merkel-cell-skin-cancer/about/key-statistics.html#written_by. Accessed March 7th, 2017.
36. Kaufman HL, Russell J, Hamid O, et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. The Lancet Oncology.17(10):1374-1385.
1. Rous PA. Transmissible avain neoplasm. (Sarcoma of the common fowl). J Exp Med. 1910;12(5):696-705.
2. Epstein MA, Achong BG, Barr YM. Virus particles in cultured lymphoblasts from Burkitt's lymphoma. Lancet. 1964;1(7335):702-703.
3. Mesri Enrique A, Feitelson MA, Munger K. Human viral oncogenesis: a cancer hallmarks analysis. Cell Host & Microbe. 2014;15(3):266-282.
4. Santana-Davila R, Bhatia S, Chow LQ. Harnessing the immune system as a therapeutic tool in virus-associated cancers. JAMA Oncol. 2017;3(1):106-112.
5. Tashiro H, Brenner MK. Immunotherapy against cancer-related viruses. Cell Res. 2017;27(1):59-73.
6. Brianti P, De Flammineis E, Mercuri SR. Review of HPV-related diseases and cancers. New Microbiol. 2017;40(2):80-85.
7. Tulay P, Serakinci N. The route to HPV-associated neoplastic transformation: a review of the literature. Crit Rev Eukaryot Gene Expr. 2016;26(1):27-39.
8. Smola S. Immunopathogenesis of HPV-associated cancers and prospects for immunotherapy. Viruses. 2017;9(9).
9. Rosales R, Rosales C. Immune therapy for human papillomaviruses-related cancers. World Journal of Clinical Oncology. 2014;5(5):1002-1019.
10. Miles B, Safran HP, Monk BJ. Therapeutic options for treatment of human papillomavirus-associated cancers - novel immunologic vaccines: ADXS11-001. Gynecol Oncol Res Pract. 2017;4:10.
11. Miles BA, Monk BJ, Safran HP. Mechanistic insights into ADXS11-001 human papillomavirus-associated cancer immunotherapy. Gynecol Oncol Res Pract. 2017;4:9.
12. Huh W, Dizon D, Powell M, Landrum L, Leath C. A prospective phase II trial of the listeria-based human papillomavirus immunotherapy axalimogene filolisbac in second and third-line metastatic cervical cancer: A NRG oncology group trial. Paper presented at: Annual Meeting on Women's Cancer; March 12-15, 2017, 2017; National Harbor, MD.
13. Petit RG, Mehta A, Jain M, et al. ADXS11-001 immunotherapy targeting HPV-E7: final results from a Phase II study in Indian women with recurrent cervical cancer. Journal for Immunotherapy of Cancer. 2014;2(Suppl 3):P92-P92.
14. Glisson B, Massarelli E, William W, et al. Nivolumab and ISA 101 HPV vaccine in incurable HPV-16+ cancer. Ann Oncol. 2017;28(suppl_5):v403-v427.
15. Ding X-X, Zhu Q-G, Zhang S-M, et al. Precision medicine for hepatocellular carcinoma: driver mutations and targeted therapy. Oncotarget. 2017;8(33):55715-55730.
16. Ringehan M, McKeating JA, Protzer U. Viral hepatitis and liver cancer. Philosophical Transactions of the Royal Society B: Biological Sciences. 2017;372(1732):20160274.
17. Abou-Alfa G, Meyer T, Cheng AL, et al. Cabozantinib (C) versus placebo (P) in patients (pts) with advanced hepatocellular carcinoma (HCC) who have received prior sorafenib: results from the randomized phase III CELESTIAL trial. J Clin Oncol. 2017;36(Suppl 4S):abstr 207.
18. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018.
19. Zhu AX, Finn RS, Cattan S, et al. KEYNOTE-224: Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib. J Clin Oncol. 2018;36(Suppl 4S):Abstr 209.
20. Kelley RK, Abou-Alfa GK, Bendell JC, et al. Phase I/II study of durvalumab and tremelimumab in patients with unresectable hepatocellular carcinoma (HCC): Phase I safety and efficacy analyses. Journal of Clinical Oncology. 2017;35(15_suppl):4073-4073.
21. Jackson R, Psarelli E-E, Berhane S, Khan H, Johnson P. Impact of Viral Status on Survival in Patients Receiving Sorafenib for Advanced Hepatocellular Cancer: A Meta-Analysis of Randomized Phase III Trials. Journal of Clinical Oncology. 2017;35(6):622-628.
22. Kudo M. Molecular Targeted Agents for Hepatocellular Carcinoma: Current Status and Future Perspectives. Liver Cancer. 2017;6(2):101-112.
23. zur Hausen H, Meinhof W, Scheiber W, Bornkamm GW. Attempts to detect virus-secific DNA in human tumors. I. Nucleic acid hybridizations with complementary RNA of human wart virus. Int J Cancer. 1974;13(5):650-656.
24. Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56-66.
25. Bruix J, Tak WY, Gasbarrini A, et al. Regorafenib as second-line therapy for intermediate or advanced hepatocellular carcinoma: multicentre, open-label, phase II safety study. Eur J Cancer. 2013;49(16):3412-3419.
26. Neparidze N, Lacy J. Malignancies associated with epstein-barr virus: pathobiology, clinical features, and evolving treatments. Clin Adv Hematol Oncol. 2014;12(6):358-371.
27. Ozoya OO, Sokol L, Dalia S. EBV-Related Malignancies, Outcomes and Novel Prevention Strategies. Infect Disord Drug Targets. 2016;16(1):4-21.
28. Sangro B, Gomez-Martin C, de la Mata M, et al. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J Hepatol. 2013;59(1):81-88.
29. The Cancer Genome Atlas Research N. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202.
30. Prockop S, Li A, Baiocchi R, et al. Efficacy and safety of ATA129, partially matched allogeneic third-party Epstein-Barr virus-targeted cytotoxic T lymphocytes in a multicenter study for post-transplant lymphoproliferative disorder. Paper presented at: 59th Annual Meeting of the American Society of Hematology; December 9-12, 2017, 2017; Atlanta, GA.
31. Kim W, Ardeshna K, Lin Y, et al. Autologous EBV-specific T cells (CMD-003): Early results from a multicenter, multinational Phase 2 trial for treatment of EBV-associated NK/T-cell lymphoma. Paper presented at: 59th Annual Meeting of the American Society of Hematology; December 9-12, 2017, 2017; Atlanta, GA.
32. Schadendorf D, Lebbé C, zur Hausen A, et al. Merkel cell carcinoma: Epidemiology, prognosis, therapy and unmet medical needs. European Journal of Cancer. 2017;71:53-69.
33. Spurgeon ME, Lambert PF. Merkel cell polyomavirus: a newly discovered human virus with oncogenic potential. Virology. 2013;435(1):118-130.
34. Tello TL, Coggshall K, Yom SS, Yu SS. Merkel cell carcinoma: An update and review: Current and future therapy. J Am Acad Dermatol. 2018;78(3):445-454.
35. American Cancer Society. Key Statistics for Merkel Cell Carcinoma. 2015; https://www.cancer.org/cancer/merkel-cell-skin-cancer/about/key-statistics.html#written_by. Accessed March 7th, 2017.
36. Kaufman HL, Russell J, Hamid O, et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. The Lancet Oncology.17(10):1374-1385.
Monalizumab-cetuximab combo shows promise in advanced head and neck SCC
WASHINGTON – and associated with deep and durable responses in patients with recurrent or metastatic squamous cell carcinoma (SCC) of the head and neck, according to data from an ongoing cohort expansion study.
As of Aug. 21, 2018, the primary study endpoint of overall response rate in 40 evaluable patients enrolled in the single-arm, nonrandomized phase 1/2 study was 27.5%, Roger Cohen, MD, reported at the annual meeting of the Society for Immunotherapy of Cancer.
There were 11 confirmed responses, including 1 complete response and 10 partial responses at a median follow-up of 8 months, said Dr. Cohen, a professor of medicine at the Hospital of the University of Pennsylvania and director of clinical research at the Abramson Cancer Center, Philadelphia.
Median progression-free survival and overall survival were 5.0 months and 10.3 months, respectively.
“We observed responses in patients who were naive to immunotherapy, as well as patients who had received and progressed after immunotherapy. We observed responses in patients who were platinum resistant, and we also saw responses in [human papillomavirus (HPV)]–positive and –negative patients,” he said, adding that responses occurred relatively early at a median of 1.6 months, and that there was little difference between those who had and had not received prior immunotherapy with programmed death-1 (PD-1) antibodies.
A number of the responses, as well as the stable diseases, were durable for “a considerable period of time.” The median duration of response was 5.6 months, he said.
Study participants were mainly middle-aged men with recurrent or metastatic HPV-positive or -negative advanced disease and “decent” performance status. They received monalizumab at a dose of 10 mg/kg every 2 weeks plus cetuximab at the labeled loading dose of 400 mg/m2 once weekly then 250 mg/m2 once weekly. All had progressed after prior platinum-based chemotherapy and had no more than two prior lines of therapy in the recurrent/metastatic setting; 17 (43%) had prior anti–programmed death-ligand 1 (PD-L1) therapy, 5 (13%) had prior cetuximab, but none of those patients were cetuximab resistant.
They were treated until disease progression or unacceptable toxicity and were assessed every 8 weeks for response per Response Evaluation Criteria in Solid Tumors (RECIST) criteria, he said.
This treatment combination was shown in the phase 1 portion of the study to have a favorable safety profile, and the safety profile was confirmed in this expansion cohort; adverse events related to the combination were dominated by EGFR antibody–related side effects in the skin, as well as hypomagnesemia. Most adverse events associated with monalizumab were grade 1-2.
“Serious adverse events are in the single digits,” Dr. Cohen said.
Monalizumab is a first-in-class humanized immunoglobulin-G4 monoclonal antibody against the human natural killer group 2A (NKG2A), which is the receptor for the NKG2A ligand, HLA-E.
“The HLA-E NKG2A diad shuts down NK cells and tumor-infiltrating CD8-positive T-cells,” he explained, adding that “the concept behind the antibody is that by blocking the interaction of the receptor for the ligand you can reduce this inhibitory signaling by NK cells and thereby unleash their ability to target tumor.”
Cetuximab is an established and approved EGFR inhibitor for the treatment of patients with head and neck SCC who progress after platinum-based chemotherapy. It has been associated with a 13% response rate.
“The therapeutic hypothesis is that dual targeting with these two antibodies will allow us to realize greater antitumor activity in head and neck cancer than is seen with cetuximab alone,” he said, later adding that “the combination of monalizumab and cetuximab results in early, deep, and durable responses in patients with squamous cell cancer of the head and neck ... and the activity indeed is higher than cetuximab alone, compared with historical data.”
Additionally, the safety is acceptable, and preliminary translational analyses do show some immunological proof-of-concept – mainly that infiltration of the tumor stroma with NK and CD8-positive T cells is correlated with response, he said.
“Importantly, this study is continuing to enroll patients, and taking account of the ever-changing landscape in the treatment of patients with advanced cancer, we are going to enroll another 40 patients, except this time we will require them to be platinum, as well as PD-1 antibody exposed. These patients still represent an enormous unmet medical need.
“We think these results do warrant further development of the combo of monalizumab and cetuximab in patients with advanced SCC of the head and neck,” he concluded.
Dr. Cohen reported receiving consulting fees and/or research funding from Cantargia, Celldex, Genocea, Innate, HEAT, Kyntherapeutics, Merck, Takeda Macrogenics, and Tmunity.
SOURCE: Cohen R et al. SITC 2018, Abstract 051.
WASHINGTON – and associated with deep and durable responses in patients with recurrent or metastatic squamous cell carcinoma (SCC) of the head and neck, according to data from an ongoing cohort expansion study.
As of Aug. 21, 2018, the primary study endpoint of overall response rate in 40 evaluable patients enrolled in the single-arm, nonrandomized phase 1/2 study was 27.5%, Roger Cohen, MD, reported at the annual meeting of the Society for Immunotherapy of Cancer.
There were 11 confirmed responses, including 1 complete response and 10 partial responses at a median follow-up of 8 months, said Dr. Cohen, a professor of medicine at the Hospital of the University of Pennsylvania and director of clinical research at the Abramson Cancer Center, Philadelphia.
Median progression-free survival and overall survival were 5.0 months and 10.3 months, respectively.
“We observed responses in patients who were naive to immunotherapy, as well as patients who had received and progressed after immunotherapy. We observed responses in patients who were platinum resistant, and we also saw responses in [human papillomavirus (HPV)]–positive and –negative patients,” he said, adding that responses occurred relatively early at a median of 1.6 months, and that there was little difference between those who had and had not received prior immunotherapy with programmed death-1 (PD-1) antibodies.
A number of the responses, as well as the stable diseases, were durable for “a considerable period of time.” The median duration of response was 5.6 months, he said.
Study participants were mainly middle-aged men with recurrent or metastatic HPV-positive or -negative advanced disease and “decent” performance status. They received monalizumab at a dose of 10 mg/kg every 2 weeks plus cetuximab at the labeled loading dose of 400 mg/m2 once weekly then 250 mg/m2 once weekly. All had progressed after prior platinum-based chemotherapy and had no more than two prior lines of therapy in the recurrent/metastatic setting; 17 (43%) had prior anti–programmed death-ligand 1 (PD-L1) therapy, 5 (13%) had prior cetuximab, but none of those patients were cetuximab resistant.
They were treated until disease progression or unacceptable toxicity and were assessed every 8 weeks for response per Response Evaluation Criteria in Solid Tumors (RECIST) criteria, he said.
This treatment combination was shown in the phase 1 portion of the study to have a favorable safety profile, and the safety profile was confirmed in this expansion cohort; adverse events related to the combination were dominated by EGFR antibody–related side effects in the skin, as well as hypomagnesemia. Most adverse events associated with monalizumab were grade 1-2.
“Serious adverse events are in the single digits,” Dr. Cohen said.
Monalizumab is a first-in-class humanized immunoglobulin-G4 monoclonal antibody against the human natural killer group 2A (NKG2A), which is the receptor for the NKG2A ligand, HLA-E.
“The HLA-E NKG2A diad shuts down NK cells and tumor-infiltrating CD8-positive T-cells,” he explained, adding that “the concept behind the antibody is that by blocking the interaction of the receptor for the ligand you can reduce this inhibitory signaling by NK cells and thereby unleash their ability to target tumor.”
Cetuximab is an established and approved EGFR inhibitor for the treatment of patients with head and neck SCC who progress after platinum-based chemotherapy. It has been associated with a 13% response rate.
“The therapeutic hypothesis is that dual targeting with these two antibodies will allow us to realize greater antitumor activity in head and neck cancer than is seen with cetuximab alone,” he said, later adding that “the combination of monalizumab and cetuximab results in early, deep, and durable responses in patients with squamous cell cancer of the head and neck ... and the activity indeed is higher than cetuximab alone, compared with historical data.”
Additionally, the safety is acceptable, and preliminary translational analyses do show some immunological proof-of-concept – mainly that infiltration of the tumor stroma with NK and CD8-positive T cells is correlated with response, he said.
“Importantly, this study is continuing to enroll patients, and taking account of the ever-changing landscape in the treatment of patients with advanced cancer, we are going to enroll another 40 patients, except this time we will require them to be platinum, as well as PD-1 antibody exposed. These patients still represent an enormous unmet medical need.
“We think these results do warrant further development of the combo of monalizumab and cetuximab in patients with advanced SCC of the head and neck,” he concluded.
Dr. Cohen reported receiving consulting fees and/or research funding from Cantargia, Celldex, Genocea, Innate, HEAT, Kyntherapeutics, Merck, Takeda Macrogenics, and Tmunity.
SOURCE: Cohen R et al. SITC 2018, Abstract 051.
WASHINGTON – and associated with deep and durable responses in patients with recurrent or metastatic squamous cell carcinoma (SCC) of the head and neck, according to data from an ongoing cohort expansion study.
As of Aug. 21, 2018, the primary study endpoint of overall response rate in 40 evaluable patients enrolled in the single-arm, nonrandomized phase 1/2 study was 27.5%, Roger Cohen, MD, reported at the annual meeting of the Society for Immunotherapy of Cancer.
There were 11 confirmed responses, including 1 complete response and 10 partial responses at a median follow-up of 8 months, said Dr. Cohen, a professor of medicine at the Hospital of the University of Pennsylvania and director of clinical research at the Abramson Cancer Center, Philadelphia.
Median progression-free survival and overall survival were 5.0 months and 10.3 months, respectively.
“We observed responses in patients who were naive to immunotherapy, as well as patients who had received and progressed after immunotherapy. We observed responses in patients who were platinum resistant, and we also saw responses in [human papillomavirus (HPV)]–positive and –negative patients,” he said, adding that responses occurred relatively early at a median of 1.6 months, and that there was little difference between those who had and had not received prior immunotherapy with programmed death-1 (PD-1) antibodies.
A number of the responses, as well as the stable diseases, were durable for “a considerable period of time.” The median duration of response was 5.6 months, he said.
Study participants were mainly middle-aged men with recurrent or metastatic HPV-positive or -negative advanced disease and “decent” performance status. They received monalizumab at a dose of 10 mg/kg every 2 weeks plus cetuximab at the labeled loading dose of 400 mg/m2 once weekly then 250 mg/m2 once weekly. All had progressed after prior platinum-based chemotherapy and had no more than two prior lines of therapy in the recurrent/metastatic setting; 17 (43%) had prior anti–programmed death-ligand 1 (PD-L1) therapy, 5 (13%) had prior cetuximab, but none of those patients were cetuximab resistant.
They were treated until disease progression or unacceptable toxicity and were assessed every 8 weeks for response per Response Evaluation Criteria in Solid Tumors (RECIST) criteria, he said.
This treatment combination was shown in the phase 1 portion of the study to have a favorable safety profile, and the safety profile was confirmed in this expansion cohort; adverse events related to the combination were dominated by EGFR antibody–related side effects in the skin, as well as hypomagnesemia. Most adverse events associated with monalizumab were grade 1-2.
“Serious adverse events are in the single digits,” Dr. Cohen said.
Monalizumab is a first-in-class humanized immunoglobulin-G4 monoclonal antibody against the human natural killer group 2A (NKG2A), which is the receptor for the NKG2A ligand, HLA-E.
“The HLA-E NKG2A diad shuts down NK cells and tumor-infiltrating CD8-positive T-cells,” he explained, adding that “the concept behind the antibody is that by blocking the interaction of the receptor for the ligand you can reduce this inhibitory signaling by NK cells and thereby unleash their ability to target tumor.”
Cetuximab is an established and approved EGFR inhibitor for the treatment of patients with head and neck SCC who progress after platinum-based chemotherapy. It has been associated with a 13% response rate.
“The therapeutic hypothesis is that dual targeting with these two antibodies will allow us to realize greater antitumor activity in head and neck cancer than is seen with cetuximab alone,” he said, later adding that “the combination of monalizumab and cetuximab results in early, deep, and durable responses in patients with squamous cell cancer of the head and neck ... and the activity indeed is higher than cetuximab alone, compared with historical data.”
Additionally, the safety is acceptable, and preliminary translational analyses do show some immunological proof-of-concept – mainly that infiltration of the tumor stroma with NK and CD8-positive T cells is correlated with response, he said.
“Importantly, this study is continuing to enroll patients, and taking account of the ever-changing landscape in the treatment of patients with advanced cancer, we are going to enroll another 40 patients, except this time we will require them to be platinum, as well as PD-1 antibody exposed. These patients still represent an enormous unmet medical need.
“We think these results do warrant further development of the combo of monalizumab and cetuximab in patients with advanced SCC of the head and neck,” he concluded.
Dr. Cohen reported receiving consulting fees and/or research funding from Cantargia, Celldex, Genocea, Innate, HEAT, Kyntherapeutics, Merck, Takeda Macrogenics, and Tmunity.
SOURCE: Cohen R et al. SITC 2018, Abstract 051.
REPORTING FROM SITC 2018
Key clinical point: Monalizumab + cetuximab is safe, active in recurrent or metastatic SCC of the head and neck.
Major finding: Overall response rate in 40 evaluable patients was 27.5%,with 1 CR and 10 PRs at 8 weeks.
Study details: A cohort expansion of 40 patients in the single-arm, non-randomized phase 1/2 study.
Disclosures: Dr. Cohen reported receiving consulting fees and/or research funding from Cantargia, Celldex, Genocea, Innate, HEAT, Kyntherapeutics, Merck, Takeda Macrogenics, and Tmunity.
Source: Cohen R et al. SITC 2018, Abstract 051.
Adding pembrolizumab to cisplatin-based CRT shows promise in HPV+ head and neck cancers
WASHINGTON – according to Steven F. Powell, MD.
Of 34 patients with a mean age of 59 years and stage III-IVb disease enrolled as part of an expansion cohort following a prior study demonstrating the safety of the regimen, 85% had a complete response (CR) at a median follow-up of 21 months based on imaging or salvage surgery, and an additional 2 patients had no clinical evidence of disease, Dr. Powell reported in a late-breaking oral abstract session at the annual meeting of the Society for Immunotherapy of Cancer.
About 80% of the patients had intermediate-risk disease, which is “higher risk than your standard HPV-related cancers,” said Dr. Powell of Sanford Cancer Center, Sioux Falls, S.D.
“On posttreatment imaging ... we showed a 62% complete response rate based on [RECIST 1.1 CT criteria], with 11 patients having a partial response and 2 felt to have a partial response based on CT imaging. Looking at Hopkins criteria [for PET scans] alone – 78% of our patients had a complete response,” he said.
Of the patients with a partial response based on either criteria, 11 were negative for disease on PET and 1 that was positive based on Hopkins criteria underwent neck dissection and had only inflammatory tissue; these 12 patients were also considered to have had a CR.
Additionally, of the two patients with progressive disease, one had a positive PET scan, but all biopsies were negative for ongoing disease, thus that patient was also considered to have a CR, for the overall CR rate of 85%, Dr. Powell said.
Two of the four other patients with a partial response were found at surgery to have “nothing to biopsy or resect,” so it was felt that they had a complete response clinically, and the remaining two had partial responses locoregionally and had residual disease, including residual disease at the primary site in one patient, and nodal disease in one patient.
It is important to consider the challenges of PET imaging in this study, he noted, explaining that in one patient with progressive disease, a posttreatment PET appeared to show bone and dermal metastases, but biopsies of all the areas showed that those were granulomatous disease – most likely sarcoidosis that was not present prior to the treatment.
“This ended up resolving over a year and the PET scan became negative, so I think this highlights that as we move into the curative intent setting we need to be very careful that with PET scanning we need to confirm with biopsy [in patients treated with immuno-oncology] therapies,” Dr. Powell said.
As for survival, the early data are “very encouraging,” with only one patient progressing to date (progression-free survival, 97.1%), but he cautioned that follow-up is “still only 23 months.”
The patient who progressed developed distant metastases and died from their disease, he said.
Treatment in this study included 40 mg/m2 of cisplatin weekly (six planned doses), 200 mg of pembrolizumab every 3 weeks (eight planned doses) and radiation therapy at 2 Gy once daily for 35 fractions (total of 70 Gy). The primary efficacy endpoint was complete response at 100 days after completion of chemoradiotherapy (CRT).
“Looking at safety ... we did not see any new safety signals. We had two dose discontinuations due to immune-related adverse events, which resolved on their own without therapy. Two patients stopped early due to protocol reasons,” Dr. Powell said, noting that the discontinuation rate was comparable with that seen in pembrolizumab monotherapy studies.
Standard therapy compliance was also good, with the chemotherapy goal dose reached in 88% of patients. The CRT dose was reached in all patients with no major delays in treatment.
“So adding CRT did not impact the safety of giving standard therapy,” he said.
Enrollment in this ongoing study was completed as of August, and data for the HPV-negative cohort should be available sometime in 2019. Several correlative research projects are also underway, he said.
The findings thus far show that pembrolizumab can be safely given with CRT in both HPV-positive and HPV-negative disease, with “encouraging response and progression-free survival in predominantly higher-risk patients,” Dr. Powell said.
“It is important to know that PET may pose challenges as we move into big phase 3, randomized trials, and I would strongly recommend biopsy to confirm PET findings,” he said, adding that it will be “interesting to see how this pans out in high-risk disease.
“I’m hopeful that our correlative research will help guide how we time therapy and how we move ahead in this field,” he said.
The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
WASHINGTON – according to Steven F. Powell, MD.
Of 34 patients with a mean age of 59 years and stage III-IVb disease enrolled as part of an expansion cohort following a prior study demonstrating the safety of the regimen, 85% had a complete response (CR) at a median follow-up of 21 months based on imaging or salvage surgery, and an additional 2 patients had no clinical evidence of disease, Dr. Powell reported in a late-breaking oral abstract session at the annual meeting of the Society for Immunotherapy of Cancer.
About 80% of the patients had intermediate-risk disease, which is “higher risk than your standard HPV-related cancers,” said Dr. Powell of Sanford Cancer Center, Sioux Falls, S.D.
“On posttreatment imaging ... we showed a 62% complete response rate based on [RECIST 1.1 CT criteria], with 11 patients having a partial response and 2 felt to have a partial response based on CT imaging. Looking at Hopkins criteria [for PET scans] alone – 78% of our patients had a complete response,” he said.
Of the patients with a partial response based on either criteria, 11 were negative for disease on PET and 1 that was positive based on Hopkins criteria underwent neck dissection and had only inflammatory tissue; these 12 patients were also considered to have had a CR.
Additionally, of the two patients with progressive disease, one had a positive PET scan, but all biopsies were negative for ongoing disease, thus that patient was also considered to have a CR, for the overall CR rate of 85%, Dr. Powell said.
Two of the four other patients with a partial response were found at surgery to have “nothing to biopsy or resect,” so it was felt that they had a complete response clinically, and the remaining two had partial responses locoregionally and had residual disease, including residual disease at the primary site in one patient, and nodal disease in one patient.
It is important to consider the challenges of PET imaging in this study, he noted, explaining that in one patient with progressive disease, a posttreatment PET appeared to show bone and dermal metastases, but biopsies of all the areas showed that those were granulomatous disease – most likely sarcoidosis that was not present prior to the treatment.
“This ended up resolving over a year and the PET scan became negative, so I think this highlights that as we move into the curative intent setting we need to be very careful that with PET scanning we need to confirm with biopsy [in patients treated with immuno-oncology] therapies,” Dr. Powell said.
As for survival, the early data are “very encouraging,” with only one patient progressing to date (progression-free survival, 97.1%), but he cautioned that follow-up is “still only 23 months.”
The patient who progressed developed distant metastases and died from their disease, he said.
Treatment in this study included 40 mg/m2 of cisplatin weekly (six planned doses), 200 mg of pembrolizumab every 3 weeks (eight planned doses) and radiation therapy at 2 Gy once daily for 35 fractions (total of 70 Gy). The primary efficacy endpoint was complete response at 100 days after completion of chemoradiotherapy (CRT).
“Looking at safety ... we did not see any new safety signals. We had two dose discontinuations due to immune-related adverse events, which resolved on their own without therapy. Two patients stopped early due to protocol reasons,” Dr. Powell said, noting that the discontinuation rate was comparable with that seen in pembrolizumab monotherapy studies.
Standard therapy compliance was also good, with the chemotherapy goal dose reached in 88% of patients. The CRT dose was reached in all patients with no major delays in treatment.
“So adding CRT did not impact the safety of giving standard therapy,” he said.
Enrollment in this ongoing study was completed as of August, and data for the HPV-negative cohort should be available sometime in 2019. Several correlative research projects are also underway, he said.
The findings thus far show that pembrolizumab can be safely given with CRT in both HPV-positive and HPV-negative disease, with “encouraging response and progression-free survival in predominantly higher-risk patients,” Dr. Powell said.
“It is important to know that PET may pose challenges as we move into big phase 3, randomized trials, and I would strongly recommend biopsy to confirm PET findings,” he said, adding that it will be “interesting to see how this pans out in high-risk disease.
“I’m hopeful that our correlative research will help guide how we time therapy and how we move ahead in this field,” he said.
The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
WASHINGTON – according to Steven F. Powell, MD.
Of 34 patients with a mean age of 59 years and stage III-IVb disease enrolled as part of an expansion cohort following a prior study demonstrating the safety of the regimen, 85% had a complete response (CR) at a median follow-up of 21 months based on imaging or salvage surgery, and an additional 2 patients had no clinical evidence of disease, Dr. Powell reported in a late-breaking oral abstract session at the annual meeting of the Society for Immunotherapy of Cancer.
About 80% of the patients had intermediate-risk disease, which is “higher risk than your standard HPV-related cancers,” said Dr. Powell of Sanford Cancer Center, Sioux Falls, S.D.
“On posttreatment imaging ... we showed a 62% complete response rate based on [RECIST 1.1 CT criteria], with 11 patients having a partial response and 2 felt to have a partial response based on CT imaging. Looking at Hopkins criteria [for PET scans] alone – 78% of our patients had a complete response,” he said.
Of the patients with a partial response based on either criteria, 11 were negative for disease on PET and 1 that was positive based on Hopkins criteria underwent neck dissection and had only inflammatory tissue; these 12 patients were also considered to have had a CR.
Additionally, of the two patients with progressive disease, one had a positive PET scan, but all biopsies were negative for ongoing disease, thus that patient was also considered to have a CR, for the overall CR rate of 85%, Dr. Powell said.
Two of the four other patients with a partial response were found at surgery to have “nothing to biopsy or resect,” so it was felt that they had a complete response clinically, and the remaining two had partial responses locoregionally and had residual disease, including residual disease at the primary site in one patient, and nodal disease in one patient.
It is important to consider the challenges of PET imaging in this study, he noted, explaining that in one patient with progressive disease, a posttreatment PET appeared to show bone and dermal metastases, but biopsies of all the areas showed that those were granulomatous disease – most likely sarcoidosis that was not present prior to the treatment.
“This ended up resolving over a year and the PET scan became negative, so I think this highlights that as we move into the curative intent setting we need to be very careful that with PET scanning we need to confirm with biopsy [in patients treated with immuno-oncology] therapies,” Dr. Powell said.
As for survival, the early data are “very encouraging,” with only one patient progressing to date (progression-free survival, 97.1%), but he cautioned that follow-up is “still only 23 months.”
The patient who progressed developed distant metastases and died from their disease, he said.
Treatment in this study included 40 mg/m2 of cisplatin weekly (six planned doses), 200 mg of pembrolizumab every 3 weeks (eight planned doses) and radiation therapy at 2 Gy once daily for 35 fractions (total of 70 Gy). The primary efficacy endpoint was complete response at 100 days after completion of chemoradiotherapy (CRT).
“Looking at safety ... we did not see any new safety signals. We had two dose discontinuations due to immune-related adverse events, which resolved on their own without therapy. Two patients stopped early due to protocol reasons,” Dr. Powell said, noting that the discontinuation rate was comparable with that seen in pembrolizumab monotherapy studies.
Standard therapy compliance was also good, with the chemotherapy goal dose reached in 88% of patients. The CRT dose was reached in all patients with no major delays in treatment.
“So adding CRT did not impact the safety of giving standard therapy,” he said.
Enrollment in this ongoing study was completed as of August, and data for the HPV-negative cohort should be available sometime in 2019. Several correlative research projects are also underway, he said.
The findings thus far show that pembrolizumab can be safely given with CRT in both HPV-positive and HPV-negative disease, with “encouraging response and progression-free survival in predominantly higher-risk patients,” Dr. Powell said.
“It is important to know that PET may pose challenges as we move into big phase 3, randomized trials, and I would strongly recommend biopsy to confirm PET findings,” he said, adding that it will be “interesting to see how this pans out in high-risk disease.
“I’m hopeful that our correlative research will help guide how we time therapy and how we move ahead in this field,” he said.
The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
REPORTING FROM SITC 2018
Key clinical point: Adding pembrolizumab to weekly low-dose cisplatin-based chemoradiotherapy shows promise in human papillomavirus–associated head and neck squamous cell carcinoma.
Major finding: A total of 85% of patients had a complete response at the 21-month follow-up; progression-free survival was 97.1%.
Study details: An expansion cohort of 34 patients.
Disclosures: The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
Pembrolizumab extends survival of head and neck cancer
MUNICH – In patients with recurrent or metastatic head and neck squamous cell carcinoma expressing programmed death ligand-1 (PDL-1), the immune checkpoint inhibitor pembrolizumab alone or in combination with chemotherapy improved overall survival, compared with the EXTREME chemotherapy regimen, reported investigators in the Keynote 048 trial.
Overall survival (OS) among patients with a PD-L1 combined positive score (CPS) of 20 or greater treated with pembrolizumab (Keytruda) monotherapy was 14.9 months compared with 10.7 months for patients treated with the EXTREME regimen, a combination of cetuximab (Erbitux), carboplatin or cisplatin, and 5-fluorouracil.
A similar overall survival benefit was seen in patients with a CPS of 1 or greater, and in the total population of patients treated with pembrolizumab plus chemotherapy followed by pembrolizumab maintenance compared with EXTREME chemotherapy, Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn.
There were no differences in response rates between either pembrolizumab monotherapy or in combination compared with chemotherapy alone, but responses were more durable with the checkpoint inhibitor than with chemotherapy.
“Pembrolizumab alone and pembrolizumab given with platinum and 5-fluorouracil should represent new standards of care for the first-line treatment of metastatic head and neck carcinoma. Immune checkpoint monotherapy with pembrolizumab allows patients to live longer and has a better safety profile than the previous standard for those patients whose tumors express PD-L1,” she said at a briefing prior to her presentation of the data in a presidential symposium at the European Society for Medical Oncology Congress.
“This is the first time since 10 years that we show an improvement in survival for this group of patients,” said Jean-Pascal Machiels, MD, of University Clinic Saint-Luc, Brussels, the invited discussant for the briefing and the symposium.
The CPS is a ratio of PD-L1-positive tumor cells, lymphocytes, and macrophages to the total numbers of cells counted multiplied by 100. The investigators looked at progression-free survival (PFS) and OS in three cohorts of patients with squamous cell carcinomas of the oropharynx, oral cavity, hypopharynx, or larynx that were recurrent or metastatic and were incurable by local therapies. They compared pembrolizumab monotherapy with the EXTREME regimen, and pembrolizumab plus chemotherapy (as described in the following paragraph) with EXTREME.
A total of 882 patients were enrolled and stratified by PD-L1 expression (on 50% or greater of tumor cells, or less than 50%), p16 positive or negative status in the oropharynx, and Eastern Cooperative Oncology Group performance status of 0 or 1. The patients were then randomly assigned on a 1:1:1 basis to either pembrolizumab monotherapy at 200 mg every 3 weeks for up to 35 cycles, pembrolizumab plus a standard chemotherapy regimen (carboplatin to an area-under-the curve [AUC] of 5 or cisplatin 100 mg/m2 plus 5-FU 1000 mg/m2 per day for 4 days for six cycles, followed by pembrolizumab maintenance for up to 35 cycles or EXTREME (cetuximab at a loading dose of 400 mg/m2 followed by 250 mg/m2 once weekly plus the chemotherapy regimen described above, followed by maintenance cetuximab).
Pembrolizumab monotherapy vs. EXTREME
For the coprimary endpoint of OS in the CPS 20 or greater population, pembrolizumab was associated with significantly better survival than EXTREME at both the 12- and 24-month time points (56.9% vs. 44.9%, and 38.3% vs. 22,1%, respectively). After a minimum follow-up of 17 months, the median OS was 14.9 months with pembrolizumab, vs. 10.7 months for EXTREME. The hazard ratio (HR) for death with pembrolizumab was 0.61 (P = .0007).
The median OS in the CPS 1 or greater population was 12.3 months and 10.3 months, respectively (HR 0.78, P = .0086).
There were no differences between the arms in PFS, however, either in the CPS 20 or greater or CPS 1 or greater populations.
Although, as noted, response rates did not differ between the groups, the median duration of response was 20.9 months with pembrolizumab in both the CPS 20 and CPS 1 populations, compared with 4.2 and 4.5 months, respectively, for EXTREME.
Treatment-related adverse events of any grade occurred in 58% of patients in the monotherapy arm, vs. 96.9% in the EXTREME arm. Fatal adverse events occurred in 1% vs. 2.8%, and events leading to drug discontinuation occurred in 4.7% vs. 19.9%, respectively. There were more immune-mediated events in the pembrolizumab arm, including one death (from pneumonitis) vs. no deaths from immune-related causes in the EXTREME arm.
Pembrolizumab plus chemo vs. EXTREME
The combination of pembrolizumab was also superior to EXTREME in the total population, with 12- and 24-month OS rates of 53% vs. 43.9%, and 29% vs. 18.7%, respectively. The median OS was 13 months with the pembrolizumab/chemo combination, vs. 10.7 months for EXTREME, translating into an HR of 0.77 (P = .0034). In this analysis as well as in the pembrolizumab monotherapy combination, there was no difference in PFS or response rates, but responses in the pembrolizumab arm were more durable.
In this comparison, treatment-related adverse events were generally similar between the groups, although there were 10 treatment-related deaths with pembrolizumab, compared with eight in the EXTREME arm.
There was one immune-related death, from pneumonitis, in the pembrolizumab arm, vs. none in the EXTREME arm. Hypothyroidism, pneumonitis, hyperthyroidism and colitis were more frequent with pembrolizumab, whereas infusion reactions and severe skin reactions were more frequent with EXTREME.
“There are further analyses of biomarker and clinical predictors that will be forthcoming from this study, and these may eventually optimally guide the choice of whether to administer pembrolizumab alone or in the novel combination, Dr. Burtness said at the briefing.
“What’s extremely important also is that for a subgroup of patients with high expression of PD-L1, we can probably remove the cisplatin and have a good outcome with immunotherapy alone,” Dr. Machiels said.
He said that more work needs to be done to determine which patients are most likely to benefit from immunotherapy in the recurrent/metastatic setting, and “we have to see how we can now bring this active drug to the curative treatment of the patient, in combination with chemoradiation.”
The study was funded by Merck Sharp & Dohme. Dr. Burtness disclosed being and advisory board member and receiving travel expenses from MSD and others. Dr. Machiels disclosed speaker honoraria, travel expenses, and an uncompensated advisory role with MSD.
SOURCE: Burtness B et al. ESMO 2018. Abstract LBA8_PR.
MUNICH – In patients with recurrent or metastatic head and neck squamous cell carcinoma expressing programmed death ligand-1 (PDL-1), the immune checkpoint inhibitor pembrolizumab alone or in combination with chemotherapy improved overall survival, compared with the EXTREME chemotherapy regimen, reported investigators in the Keynote 048 trial.
Overall survival (OS) among patients with a PD-L1 combined positive score (CPS) of 20 or greater treated with pembrolizumab (Keytruda) monotherapy was 14.9 months compared with 10.7 months for patients treated with the EXTREME regimen, a combination of cetuximab (Erbitux), carboplatin or cisplatin, and 5-fluorouracil.
A similar overall survival benefit was seen in patients with a CPS of 1 or greater, and in the total population of patients treated with pembrolizumab plus chemotherapy followed by pembrolizumab maintenance compared with EXTREME chemotherapy, Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn.
There were no differences in response rates between either pembrolizumab monotherapy or in combination compared with chemotherapy alone, but responses were more durable with the checkpoint inhibitor than with chemotherapy.
“Pembrolizumab alone and pembrolizumab given with platinum and 5-fluorouracil should represent new standards of care for the first-line treatment of metastatic head and neck carcinoma. Immune checkpoint monotherapy with pembrolizumab allows patients to live longer and has a better safety profile than the previous standard for those patients whose tumors express PD-L1,” she said at a briefing prior to her presentation of the data in a presidential symposium at the European Society for Medical Oncology Congress.
“This is the first time since 10 years that we show an improvement in survival for this group of patients,” said Jean-Pascal Machiels, MD, of University Clinic Saint-Luc, Brussels, the invited discussant for the briefing and the symposium.
The CPS is a ratio of PD-L1-positive tumor cells, lymphocytes, and macrophages to the total numbers of cells counted multiplied by 100. The investigators looked at progression-free survival (PFS) and OS in three cohorts of patients with squamous cell carcinomas of the oropharynx, oral cavity, hypopharynx, or larynx that were recurrent or metastatic and were incurable by local therapies. They compared pembrolizumab monotherapy with the EXTREME regimen, and pembrolizumab plus chemotherapy (as described in the following paragraph) with EXTREME.
A total of 882 patients were enrolled and stratified by PD-L1 expression (on 50% or greater of tumor cells, or less than 50%), p16 positive or negative status in the oropharynx, and Eastern Cooperative Oncology Group performance status of 0 or 1. The patients were then randomly assigned on a 1:1:1 basis to either pembrolizumab monotherapy at 200 mg every 3 weeks for up to 35 cycles, pembrolizumab plus a standard chemotherapy regimen (carboplatin to an area-under-the curve [AUC] of 5 or cisplatin 100 mg/m2 plus 5-FU 1000 mg/m2 per day for 4 days for six cycles, followed by pembrolizumab maintenance for up to 35 cycles or EXTREME (cetuximab at a loading dose of 400 mg/m2 followed by 250 mg/m2 once weekly plus the chemotherapy regimen described above, followed by maintenance cetuximab).
Pembrolizumab monotherapy vs. EXTREME
For the coprimary endpoint of OS in the CPS 20 or greater population, pembrolizumab was associated with significantly better survival than EXTREME at both the 12- and 24-month time points (56.9% vs. 44.9%, and 38.3% vs. 22,1%, respectively). After a minimum follow-up of 17 months, the median OS was 14.9 months with pembrolizumab, vs. 10.7 months for EXTREME. The hazard ratio (HR) for death with pembrolizumab was 0.61 (P = .0007).
The median OS in the CPS 1 or greater population was 12.3 months and 10.3 months, respectively (HR 0.78, P = .0086).
There were no differences between the arms in PFS, however, either in the CPS 20 or greater or CPS 1 or greater populations.
Although, as noted, response rates did not differ between the groups, the median duration of response was 20.9 months with pembrolizumab in both the CPS 20 and CPS 1 populations, compared with 4.2 and 4.5 months, respectively, for EXTREME.
Treatment-related adverse events of any grade occurred in 58% of patients in the monotherapy arm, vs. 96.9% in the EXTREME arm. Fatal adverse events occurred in 1% vs. 2.8%, and events leading to drug discontinuation occurred in 4.7% vs. 19.9%, respectively. There were more immune-mediated events in the pembrolizumab arm, including one death (from pneumonitis) vs. no deaths from immune-related causes in the EXTREME arm.
Pembrolizumab plus chemo vs. EXTREME
The combination of pembrolizumab was also superior to EXTREME in the total population, with 12- and 24-month OS rates of 53% vs. 43.9%, and 29% vs. 18.7%, respectively. The median OS was 13 months with the pembrolizumab/chemo combination, vs. 10.7 months for EXTREME, translating into an HR of 0.77 (P = .0034). In this analysis as well as in the pembrolizumab monotherapy combination, there was no difference in PFS or response rates, but responses in the pembrolizumab arm were more durable.
In this comparison, treatment-related adverse events were generally similar between the groups, although there were 10 treatment-related deaths with pembrolizumab, compared with eight in the EXTREME arm.
There was one immune-related death, from pneumonitis, in the pembrolizumab arm, vs. none in the EXTREME arm. Hypothyroidism, pneumonitis, hyperthyroidism and colitis were more frequent with pembrolizumab, whereas infusion reactions and severe skin reactions were more frequent with EXTREME.
“There are further analyses of biomarker and clinical predictors that will be forthcoming from this study, and these may eventually optimally guide the choice of whether to administer pembrolizumab alone or in the novel combination, Dr. Burtness said at the briefing.
“What’s extremely important also is that for a subgroup of patients with high expression of PD-L1, we can probably remove the cisplatin and have a good outcome with immunotherapy alone,” Dr. Machiels said.
He said that more work needs to be done to determine which patients are most likely to benefit from immunotherapy in the recurrent/metastatic setting, and “we have to see how we can now bring this active drug to the curative treatment of the patient, in combination with chemoradiation.”
The study was funded by Merck Sharp & Dohme. Dr. Burtness disclosed being and advisory board member and receiving travel expenses from MSD and others. Dr. Machiels disclosed speaker honoraria, travel expenses, and an uncompensated advisory role with MSD.
SOURCE: Burtness B et al. ESMO 2018. Abstract LBA8_PR.
MUNICH – In patients with recurrent or metastatic head and neck squamous cell carcinoma expressing programmed death ligand-1 (PDL-1), the immune checkpoint inhibitor pembrolizumab alone or in combination with chemotherapy improved overall survival, compared with the EXTREME chemotherapy regimen, reported investigators in the Keynote 048 trial.
Overall survival (OS) among patients with a PD-L1 combined positive score (CPS) of 20 or greater treated with pembrolizumab (Keytruda) monotherapy was 14.9 months compared with 10.7 months for patients treated with the EXTREME regimen, a combination of cetuximab (Erbitux), carboplatin or cisplatin, and 5-fluorouracil.
A similar overall survival benefit was seen in patients with a CPS of 1 or greater, and in the total population of patients treated with pembrolizumab plus chemotherapy followed by pembrolizumab maintenance compared with EXTREME chemotherapy, Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn.
There were no differences in response rates between either pembrolizumab monotherapy or in combination compared with chemotherapy alone, but responses were more durable with the checkpoint inhibitor than with chemotherapy.
“Pembrolizumab alone and pembrolizumab given with platinum and 5-fluorouracil should represent new standards of care for the first-line treatment of metastatic head and neck carcinoma. Immune checkpoint monotherapy with pembrolizumab allows patients to live longer and has a better safety profile than the previous standard for those patients whose tumors express PD-L1,” she said at a briefing prior to her presentation of the data in a presidential symposium at the European Society for Medical Oncology Congress.
“This is the first time since 10 years that we show an improvement in survival for this group of patients,” said Jean-Pascal Machiels, MD, of University Clinic Saint-Luc, Brussels, the invited discussant for the briefing and the symposium.
The CPS is a ratio of PD-L1-positive tumor cells, lymphocytes, and macrophages to the total numbers of cells counted multiplied by 100. The investigators looked at progression-free survival (PFS) and OS in three cohorts of patients with squamous cell carcinomas of the oropharynx, oral cavity, hypopharynx, or larynx that were recurrent or metastatic and were incurable by local therapies. They compared pembrolizumab monotherapy with the EXTREME regimen, and pembrolizumab plus chemotherapy (as described in the following paragraph) with EXTREME.
A total of 882 patients were enrolled and stratified by PD-L1 expression (on 50% or greater of tumor cells, or less than 50%), p16 positive or negative status in the oropharynx, and Eastern Cooperative Oncology Group performance status of 0 or 1. The patients were then randomly assigned on a 1:1:1 basis to either pembrolizumab monotherapy at 200 mg every 3 weeks for up to 35 cycles, pembrolizumab plus a standard chemotherapy regimen (carboplatin to an area-under-the curve [AUC] of 5 or cisplatin 100 mg/m2 plus 5-FU 1000 mg/m2 per day for 4 days for six cycles, followed by pembrolizumab maintenance for up to 35 cycles or EXTREME (cetuximab at a loading dose of 400 mg/m2 followed by 250 mg/m2 once weekly plus the chemotherapy regimen described above, followed by maintenance cetuximab).
Pembrolizumab monotherapy vs. EXTREME
For the coprimary endpoint of OS in the CPS 20 or greater population, pembrolizumab was associated with significantly better survival than EXTREME at both the 12- and 24-month time points (56.9% vs. 44.9%, and 38.3% vs. 22,1%, respectively). After a minimum follow-up of 17 months, the median OS was 14.9 months with pembrolizumab, vs. 10.7 months for EXTREME. The hazard ratio (HR) for death with pembrolizumab was 0.61 (P = .0007).
The median OS in the CPS 1 or greater population was 12.3 months and 10.3 months, respectively (HR 0.78, P = .0086).
There were no differences between the arms in PFS, however, either in the CPS 20 or greater or CPS 1 or greater populations.
Although, as noted, response rates did not differ between the groups, the median duration of response was 20.9 months with pembrolizumab in both the CPS 20 and CPS 1 populations, compared with 4.2 and 4.5 months, respectively, for EXTREME.
Treatment-related adverse events of any grade occurred in 58% of patients in the monotherapy arm, vs. 96.9% in the EXTREME arm. Fatal adverse events occurred in 1% vs. 2.8%, and events leading to drug discontinuation occurred in 4.7% vs. 19.9%, respectively. There were more immune-mediated events in the pembrolizumab arm, including one death (from pneumonitis) vs. no deaths from immune-related causes in the EXTREME arm.
Pembrolizumab plus chemo vs. EXTREME
The combination of pembrolizumab was also superior to EXTREME in the total population, with 12- and 24-month OS rates of 53% vs. 43.9%, and 29% vs. 18.7%, respectively. The median OS was 13 months with the pembrolizumab/chemo combination, vs. 10.7 months for EXTREME, translating into an HR of 0.77 (P = .0034). In this analysis as well as in the pembrolizumab monotherapy combination, there was no difference in PFS or response rates, but responses in the pembrolizumab arm were more durable.
In this comparison, treatment-related adverse events were generally similar between the groups, although there were 10 treatment-related deaths with pembrolizumab, compared with eight in the EXTREME arm.
There was one immune-related death, from pneumonitis, in the pembrolizumab arm, vs. none in the EXTREME arm. Hypothyroidism, pneumonitis, hyperthyroidism and colitis were more frequent with pembrolizumab, whereas infusion reactions and severe skin reactions were more frequent with EXTREME.
“There are further analyses of biomarker and clinical predictors that will be forthcoming from this study, and these may eventually optimally guide the choice of whether to administer pembrolizumab alone or in the novel combination, Dr. Burtness said at the briefing.
“What’s extremely important also is that for a subgroup of patients with high expression of PD-L1, we can probably remove the cisplatin and have a good outcome with immunotherapy alone,” Dr. Machiels said.
He said that more work needs to be done to determine which patients are most likely to benefit from immunotherapy in the recurrent/metastatic setting, and “we have to see how we can now bring this active drug to the curative treatment of the patient, in combination with chemoradiation.”
The study was funded by Merck Sharp & Dohme. Dr. Burtness disclosed being and advisory board member and receiving travel expenses from MSD and others. Dr. Machiels disclosed speaker honoraria, travel expenses, and an uncompensated advisory role with MSD.
SOURCE: Burtness B et al. ESMO 2018. Abstract LBA8_PR.
REPORTING FROM ESMO 2018
Key clinical point: Pembrolizumab alone or in combination with chemotherapy was associated with better overall survival of squamous cell head and neck cancer, compared with the EXTREME chemotherapy regimen.
Major finding: Overall survival among patients with a PD-L1 combined positive score of 20 or greater treated with pembrolizumab (Keytruda) monotherapy was 14.9 compared with 10.7 months for patients treated with the EXTREME regimen.
Study details: Randomized phase 3 trial of 882 patients with recurrent or metastatic squamous cell carcinoma of the head and neck.
Disclosures: The study was funded by Merck Sharp & Dohme. Dr. Burtness disclosed being and advisory board member and receiving travel expenses from MSD and others. Dr. Machiels disclosed speaker honoraria, travel expenses, and an uncompensated advisory role with MSD.
Source: Burtness B et al. ESMO 2018. Abstract LBA8_PR.
Worse OS, control of low-risk oropharyngeal cancer with cetuximab
MUNICH – The term “practice-changing trial” usually implies change for the better, but results of a study comparing two regimens for patients with low-risk human papillomavirus–positive oropharyngeal cancer showed that cetuximab plus radiation was associated with worse local control and worse overall survival than the older standard of cisplatin plus radiation, investigators in the De-Escalate HPV trial reported.
Although rates of severe toxicity, the primary endpoint, were similar between cisplatin and radiation and cetuximab (Erbitux) plus radiation, 2-year overall survival was significantly worse with cetuximab, a finding that caught the investigators off guard, admitted Hisham Mehanna, PhD, a surgeon at the Institute of Head and Neck Studies and Education at the University of Birmingham (England).
“This difference in overall survival was underpinned by a significantly higher recurrence rate with cetuximab,” he said at the European Society of Medical Oncology Congress. “And that recurrence rate was both in locoregional control as well as in distant control.”
The results of the study reaffirm that cisplatin remains the standard of care in patients with low-risk human papillomavirus (HPV)–positive oropharyngeal cancer, and highlight the vital importance of carefully controlled clinical trials.
“I think there’s a salutary lesson: Changes in standard of care really should only be done of the basis of high-level, phase 3 comparative evidence, even, as was in our case, when treatments have been approved by regulatory bodies,” he said.
The trial raises the question of whether deintensification strategies should continue to be used in locally advanced HPV-positive oropharyngeal cancer, and suggests that clinicians should rethink the use of targeted agents in these patients in the absence of predictive biomarkers, commented Amanda Psyrri, MD, PhD, from the University of Athens and Attikon University Hospital.
The standard of care for patients with head and neck cancers is radiotherapy with concomitant cisplatin, which has been shown to improve absolute overall survival at the cost of increases in both acute and late severe toxicities.
The De-Escalate HPV trial was designed to see whether replacing cisplatin with cetuximab, a tyrosine kinase inhibitor targeted against the epidermal growth factor receptor, could be associated with less toxicity, better quality of life, and better swallowing in patients with low-risk HPV-positive oropharyngeal cancer.
The investigators enrolled 334 patients from 32 centers in the United Kingdom, Ireland, and the Netherlands, and randomly assigned them to therapy with 70 Gy radiotherapy given in 35 fractions over 7 weeks, plus either intravenous cisplatin 100 mg/m2 per day on days 1, 22, and 43, or IV cetuximab at a 400 mg pretreatment loading dose, then 250 mg weekly.
There were no significant differences between treatment arms in the primary endpoint of toxicity, either severe (grade 3-5) or all grades of toxicity (1-5). In addition, there were no significant differences between the treatment arms in global health status assessed by the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire – Core Questionnaire (EORTC QLQ-C30) or in swallowing as evaluated by the MD Anderson Dysphagia Inventory-Global.
There were, however, significantly more serious adverse events in the cisplatin arm, at 162 versus 95 in the cetuximab arm.
But as noted before, the investigators were surprised to see that 2-year overall survival was worse with cetuximab at 89.4%, compared with 97.5% for cisplatin (P = .001). The hazard ratio for death with cetuximab was 4.99 and the adjusted HR was 5.94 (P = .001). Dr. Mehanna did not report factors considered in the adjusted HR.
The number needed to treat for harm was 12.
“Our study was not powered to identify a difference in survival, and hence our surprise to find a significantly worse overall survival with cetuximab,” he said.
The 2-year recurrence rates were 6.0% in the cisplatin arm versus 16.1% in the cetuximab arm (HR, 3.39; P = .0007).
Locoregional recurrence rates were 3% in the cisplatin arm versus 12% in the cetuximab arm and rates of distant recurrence were 3% versus 9%, respectively.
The results suggest that clinicians should be cautious when considering deescalation treatments that reduce the use of systemic chemotherapy, either with radiotherapy alone or with surgery, Dr. Mehanna said.
In a briefing prior to the presentation of the data in a presidential symposium, discussant Jean-Pascal Machiels, MD, from the University Clinic Saint-Luc in Brussels, said that, prior to this study, “the common belief was that [cetuximab and radiation] could be used, maybe, instead of chemoradiation in these patients, because also we believed that this may decrease toxicity.
“But clearly we have a signal that the chemoradiation has more activity in this setting, and it should remain the standard of care,” he continued.
Dr. Machiels cautioned that the findings cannot be extrapolated to patients with HPV-negative disease.
The study was sponsored by the University of Warwick (England), University of Birmingham, University of Oxford (England), and Cancer Research UK. Dr. Mehanna reported honoraria from AstraZeneca, MSD, Sanofi Pasteur, and Merck, and is a director and stockholder of the Warwickshire Head and Neck Clinic. Dr. Psyrri reported honoraria from Merck Serono, Roche, MSD, AstraZeneca, Bristol-Myers Squibb, Bayer, Pfizer, Medscape, and Prime Oncology. Dr. Machiels reported a consulting or advisory role with Boehringer Ingelheim, Debiopharm Group, Innate Pharma, Merck, Nanobiotix, and Pfizer, and research funding from Bayer, Janssen Pharmaceuticals, Novartis, and Sanofi.
SOURCE: Mehanna H et al. ESMO 2018, Abstract LBA9_PR.
MUNICH – The term “practice-changing trial” usually implies change for the better, but results of a study comparing two regimens for patients with low-risk human papillomavirus–positive oropharyngeal cancer showed that cetuximab plus radiation was associated with worse local control and worse overall survival than the older standard of cisplatin plus radiation, investigators in the De-Escalate HPV trial reported.
Although rates of severe toxicity, the primary endpoint, were similar between cisplatin and radiation and cetuximab (Erbitux) plus radiation, 2-year overall survival was significantly worse with cetuximab, a finding that caught the investigators off guard, admitted Hisham Mehanna, PhD, a surgeon at the Institute of Head and Neck Studies and Education at the University of Birmingham (England).
“This difference in overall survival was underpinned by a significantly higher recurrence rate with cetuximab,” he said at the European Society of Medical Oncology Congress. “And that recurrence rate was both in locoregional control as well as in distant control.”
The results of the study reaffirm that cisplatin remains the standard of care in patients with low-risk human papillomavirus (HPV)–positive oropharyngeal cancer, and highlight the vital importance of carefully controlled clinical trials.
“I think there’s a salutary lesson: Changes in standard of care really should only be done of the basis of high-level, phase 3 comparative evidence, even, as was in our case, when treatments have been approved by regulatory bodies,” he said.
The trial raises the question of whether deintensification strategies should continue to be used in locally advanced HPV-positive oropharyngeal cancer, and suggests that clinicians should rethink the use of targeted agents in these patients in the absence of predictive biomarkers, commented Amanda Psyrri, MD, PhD, from the University of Athens and Attikon University Hospital.
The standard of care for patients with head and neck cancers is radiotherapy with concomitant cisplatin, which has been shown to improve absolute overall survival at the cost of increases in both acute and late severe toxicities.
The De-Escalate HPV trial was designed to see whether replacing cisplatin with cetuximab, a tyrosine kinase inhibitor targeted against the epidermal growth factor receptor, could be associated with less toxicity, better quality of life, and better swallowing in patients with low-risk HPV-positive oropharyngeal cancer.
The investigators enrolled 334 patients from 32 centers in the United Kingdom, Ireland, and the Netherlands, and randomly assigned them to therapy with 70 Gy radiotherapy given in 35 fractions over 7 weeks, plus either intravenous cisplatin 100 mg/m2 per day on days 1, 22, and 43, or IV cetuximab at a 400 mg pretreatment loading dose, then 250 mg weekly.
There were no significant differences between treatment arms in the primary endpoint of toxicity, either severe (grade 3-5) or all grades of toxicity (1-5). In addition, there were no significant differences between the treatment arms in global health status assessed by the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire – Core Questionnaire (EORTC QLQ-C30) or in swallowing as evaluated by the MD Anderson Dysphagia Inventory-Global.
There were, however, significantly more serious adverse events in the cisplatin arm, at 162 versus 95 in the cetuximab arm.
But as noted before, the investigators were surprised to see that 2-year overall survival was worse with cetuximab at 89.4%, compared with 97.5% for cisplatin (P = .001). The hazard ratio for death with cetuximab was 4.99 and the adjusted HR was 5.94 (P = .001). Dr. Mehanna did not report factors considered in the adjusted HR.
The number needed to treat for harm was 12.
“Our study was not powered to identify a difference in survival, and hence our surprise to find a significantly worse overall survival with cetuximab,” he said.
The 2-year recurrence rates were 6.0% in the cisplatin arm versus 16.1% in the cetuximab arm (HR, 3.39; P = .0007).
Locoregional recurrence rates were 3% in the cisplatin arm versus 12% in the cetuximab arm and rates of distant recurrence were 3% versus 9%, respectively.
The results suggest that clinicians should be cautious when considering deescalation treatments that reduce the use of systemic chemotherapy, either with radiotherapy alone or with surgery, Dr. Mehanna said.
In a briefing prior to the presentation of the data in a presidential symposium, discussant Jean-Pascal Machiels, MD, from the University Clinic Saint-Luc in Brussels, said that, prior to this study, “the common belief was that [cetuximab and radiation] could be used, maybe, instead of chemoradiation in these patients, because also we believed that this may decrease toxicity.
“But clearly we have a signal that the chemoradiation has more activity in this setting, and it should remain the standard of care,” he continued.
Dr. Machiels cautioned that the findings cannot be extrapolated to patients with HPV-negative disease.
The study was sponsored by the University of Warwick (England), University of Birmingham, University of Oxford (England), and Cancer Research UK. Dr. Mehanna reported honoraria from AstraZeneca, MSD, Sanofi Pasteur, and Merck, and is a director and stockholder of the Warwickshire Head and Neck Clinic. Dr. Psyrri reported honoraria from Merck Serono, Roche, MSD, AstraZeneca, Bristol-Myers Squibb, Bayer, Pfizer, Medscape, and Prime Oncology. Dr. Machiels reported a consulting or advisory role with Boehringer Ingelheim, Debiopharm Group, Innate Pharma, Merck, Nanobiotix, and Pfizer, and research funding from Bayer, Janssen Pharmaceuticals, Novartis, and Sanofi.
SOURCE: Mehanna H et al. ESMO 2018, Abstract LBA9_PR.
MUNICH – The term “practice-changing trial” usually implies change for the better, but results of a study comparing two regimens for patients with low-risk human papillomavirus–positive oropharyngeal cancer showed that cetuximab plus radiation was associated with worse local control and worse overall survival than the older standard of cisplatin plus radiation, investigators in the De-Escalate HPV trial reported.
Although rates of severe toxicity, the primary endpoint, were similar between cisplatin and radiation and cetuximab (Erbitux) plus radiation, 2-year overall survival was significantly worse with cetuximab, a finding that caught the investigators off guard, admitted Hisham Mehanna, PhD, a surgeon at the Institute of Head and Neck Studies and Education at the University of Birmingham (England).
“This difference in overall survival was underpinned by a significantly higher recurrence rate with cetuximab,” he said at the European Society of Medical Oncology Congress. “And that recurrence rate was both in locoregional control as well as in distant control.”
The results of the study reaffirm that cisplatin remains the standard of care in patients with low-risk human papillomavirus (HPV)–positive oropharyngeal cancer, and highlight the vital importance of carefully controlled clinical trials.
“I think there’s a salutary lesson: Changes in standard of care really should only be done of the basis of high-level, phase 3 comparative evidence, even, as was in our case, when treatments have been approved by regulatory bodies,” he said.
The trial raises the question of whether deintensification strategies should continue to be used in locally advanced HPV-positive oropharyngeal cancer, and suggests that clinicians should rethink the use of targeted agents in these patients in the absence of predictive biomarkers, commented Amanda Psyrri, MD, PhD, from the University of Athens and Attikon University Hospital.
The standard of care for patients with head and neck cancers is radiotherapy with concomitant cisplatin, which has been shown to improve absolute overall survival at the cost of increases in both acute and late severe toxicities.
The De-Escalate HPV trial was designed to see whether replacing cisplatin with cetuximab, a tyrosine kinase inhibitor targeted against the epidermal growth factor receptor, could be associated with less toxicity, better quality of life, and better swallowing in patients with low-risk HPV-positive oropharyngeal cancer.
The investigators enrolled 334 patients from 32 centers in the United Kingdom, Ireland, and the Netherlands, and randomly assigned them to therapy with 70 Gy radiotherapy given in 35 fractions over 7 weeks, plus either intravenous cisplatin 100 mg/m2 per day on days 1, 22, and 43, or IV cetuximab at a 400 mg pretreatment loading dose, then 250 mg weekly.
There were no significant differences between treatment arms in the primary endpoint of toxicity, either severe (grade 3-5) or all grades of toxicity (1-5). In addition, there were no significant differences between the treatment arms in global health status assessed by the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire – Core Questionnaire (EORTC QLQ-C30) or in swallowing as evaluated by the MD Anderson Dysphagia Inventory-Global.
There were, however, significantly more serious adverse events in the cisplatin arm, at 162 versus 95 in the cetuximab arm.
But as noted before, the investigators were surprised to see that 2-year overall survival was worse with cetuximab at 89.4%, compared with 97.5% for cisplatin (P = .001). The hazard ratio for death with cetuximab was 4.99 and the adjusted HR was 5.94 (P = .001). Dr. Mehanna did not report factors considered in the adjusted HR.
The number needed to treat for harm was 12.
“Our study was not powered to identify a difference in survival, and hence our surprise to find a significantly worse overall survival with cetuximab,” he said.
The 2-year recurrence rates were 6.0% in the cisplatin arm versus 16.1% in the cetuximab arm (HR, 3.39; P = .0007).
Locoregional recurrence rates were 3% in the cisplatin arm versus 12% in the cetuximab arm and rates of distant recurrence were 3% versus 9%, respectively.
The results suggest that clinicians should be cautious when considering deescalation treatments that reduce the use of systemic chemotherapy, either with radiotherapy alone or with surgery, Dr. Mehanna said.
In a briefing prior to the presentation of the data in a presidential symposium, discussant Jean-Pascal Machiels, MD, from the University Clinic Saint-Luc in Brussels, said that, prior to this study, “the common belief was that [cetuximab and radiation] could be used, maybe, instead of chemoradiation in these patients, because also we believed that this may decrease toxicity.
“But clearly we have a signal that the chemoradiation has more activity in this setting, and it should remain the standard of care,” he continued.
Dr. Machiels cautioned that the findings cannot be extrapolated to patients with HPV-negative disease.
The study was sponsored by the University of Warwick (England), University of Birmingham, University of Oxford (England), and Cancer Research UK. Dr. Mehanna reported honoraria from AstraZeneca, MSD, Sanofi Pasteur, and Merck, and is a director and stockholder of the Warwickshire Head and Neck Clinic. Dr. Psyrri reported honoraria from Merck Serono, Roche, MSD, AstraZeneca, Bristol-Myers Squibb, Bayer, Pfizer, Medscape, and Prime Oncology. Dr. Machiels reported a consulting or advisory role with Boehringer Ingelheim, Debiopharm Group, Innate Pharma, Merck, Nanobiotix, and Pfizer, and research funding from Bayer, Janssen Pharmaceuticals, Novartis, and Sanofi.
SOURCE: Mehanna H et al. ESMO 2018, Abstract LBA9_PR.
REPORTING FROM ESMO 2018
Key clinical point: Radiation and concomitant cisplatin remains the standard of care for patients with low-risk human papillomavirus–positive oropharyngeal cancer.
Major finding: The 2-year overall survival was 97.5% with cisplatin versus 89.4% with cetuximab (P = .001).
Study details: A randomized trial in 334 patients with low-risk oropharyngeal cancer.
Disclosures: The study was sponsored by the University of Warwick (England), University of Birmingham, University of Oxford (England), and Cancer Research UK. Dr. Mehanna reported honoraria from AstraZeneca, MSD, Sanofi Pasteur, and Merck, and is a director and stockholder of the Warwickshire Head and Neck Clinic. Dr. Psyrri reported honoraria from Merck Serono, Roche, MSD, AstraZeneca, Bristol-Myers Squibb, Bayer, Pfizer, Medscape, and Prime Oncology. Dr. Machiels reported a consulting or advisory role with Boehringer Ingelheim, Debiopharm Group, Innate Pharma, Merck, Nanobiotix, and Pfizer, and research funding from Bayer, Janssen Pharmaceuticals, Novartis, and Sanofi.
Source: Mehanna H et al. ESMO 2018, Abstract LBA9_PR.
ESMO 2018: First look at immunotherapy as first-line treatment for HNSCC
for first-line treatment of recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) will be presented during a presidential symposium at the European Society for Medical Oncology Congress.
The drug is currently approved for second-line treatment of HNSCC. Merck, the maker of the anti–programmed cell death protein therapy, announced in July that the primary endpoint of overall survival as monotherapy in the first-line setting of advanced HNSCC had been met in patients whose tumors expressed programmed death–ligand 1.
More than 800 patients in KEYNOTE-048 were randomized to receive pembrolizumab as monotherapy or in combination with cisplatin or carboplatin and 5-FU, or cetuximab plus cisplatin or carboplatin and 5-FU.
The dual primary endpoints were overall survival and progression-free survival. The secondary endpoints of the study were PFS (at 6 months and 12 months), objective response rate, and time to deterioration in Quality of Life Global Health Status/Quality of Life Scales of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, according to the company.
Further details from the interim analysis of KEYNOTE-048 will be presented by Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn., during Presidential Symposium 3 at ESMO 2018 on Oct. 22 in Munich.
for first-line treatment of recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) will be presented during a presidential symposium at the European Society for Medical Oncology Congress.
The drug is currently approved for second-line treatment of HNSCC. Merck, the maker of the anti–programmed cell death protein therapy, announced in July that the primary endpoint of overall survival as monotherapy in the first-line setting of advanced HNSCC had been met in patients whose tumors expressed programmed death–ligand 1.
More than 800 patients in KEYNOTE-048 were randomized to receive pembrolizumab as monotherapy or in combination with cisplatin or carboplatin and 5-FU, or cetuximab plus cisplatin or carboplatin and 5-FU.
The dual primary endpoints were overall survival and progression-free survival. The secondary endpoints of the study were PFS (at 6 months and 12 months), objective response rate, and time to deterioration in Quality of Life Global Health Status/Quality of Life Scales of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, according to the company.
Further details from the interim analysis of KEYNOTE-048 will be presented by Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn., during Presidential Symposium 3 at ESMO 2018 on Oct. 22 in Munich.
for first-line treatment of recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) will be presented during a presidential symposium at the European Society for Medical Oncology Congress.
The drug is currently approved for second-line treatment of HNSCC. Merck, the maker of the anti–programmed cell death protein therapy, announced in July that the primary endpoint of overall survival as monotherapy in the first-line setting of advanced HNSCC had been met in patients whose tumors expressed programmed death–ligand 1.
More than 800 patients in KEYNOTE-048 were randomized to receive pembrolizumab as monotherapy or in combination with cisplatin or carboplatin and 5-FU, or cetuximab plus cisplatin or carboplatin and 5-FU.
The dual primary endpoints were overall survival and progression-free survival. The secondary endpoints of the study were PFS (at 6 months and 12 months), objective response rate, and time to deterioration in Quality of Life Global Health Status/Quality of Life Scales of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, according to the company.
Further details from the interim analysis of KEYNOTE-048 will be presented by Barbara Burtness, MD, of Yale Cancer Center, New Haven, Conn., during Presidential Symposium 3 at ESMO 2018 on Oct. 22 in Munich.