User login
Building owners, managers must do more to prevent Legionnaires’ disease
Building owners, managers, and administrators of hospitals and other health care facilities around the country are being urged to shore up their water system management facilities to prevent further outbreaks of Legionnaires’ disease, which is the focus of the Center for Disease Control and Prevention’s latest Vital Signs report.
“Almost all Legionnaires’ disease outbreaks are preventable with improvements in water system management,” explained CDC Director Tom Frieden, adding that “At the end of the day, building owners and managers need to take steps to reduce the risk of Legionnaires’ disease [and] work together to reduce this risk and limit the number of people exposed, infected, and hospitalized or, potentially, fatally infected.”
For the report, the CDC investigated 27 outbreaks of Legionnaires’ disease in the United States from 2000 through 2014, which involved a total of 415 cases and 65 fatalities. In each outbreak analysis, the location, source of exposure, and problems with environmental controls of Legionella – the bacterium that causes the disease – were evaluated.
Hotels and resorts accounted for 44% of all outbreaks over the 15-year period, followed by long-term care facilities (19%) and hospitals (15%). However, outbreaks at the latter two location types accounted for 85% of all deaths, while outbreaks at hotels and resorts accounted for only 6%. Potable water was the most common direct cause of Legionella infections, followed by water from cooling towers, hot tubs, industrial equipment, and decorative fountains.
Additionally, 23 of the investigations yielded enough information to determine the exact cause of the outbreak, all of which were caused by at least one of 4 issues. The first was process failures, such as not having a proper water system management program in place to handle Legionella; this was found in two-thirds of the outbreaks. The second major cause was human error, such as not replacing filters or tubing as recommended by manufacturers, which was a cause in half of the outbreaks. The third was equipment breakdown, which was found in one-third of the outbreaks. Finally, reasons external to the buildings themselves – such as water main breaks or disruptions caused by nearby construction – factored into one-third of the outbreaks.
“Large, recent outbreaks of Legionnaires’ disease in New York City and Flint, Michigan, have brought attention to the disease and highlight the need for us to understand why these outbreaks happen and how best to prevent them, [which is] why this Vital Signs is targeted to a specific audience that we in public health don’t talk [to] often enough: building owners and managers,” Dr. Frieden said. “It’s not a traditional public health audience, [but] they are the key to environmental controls in buildings that we live in, get our health care in, and work in everyday.”
To that end, Dr. Frieden announced the release of a new CDC toolkit entitled “Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings: A Practical Guide to Implementing Industry Standards,” which building owners, managers, and administrators can turn to for guidance on how to implement effective water system management protocols in their buildings.
Legionnaires’ disease is a serious lung infection caused by inhalation of the bacteria Legionella, which can be found in water and inhaled as airborne mist. Elderly individuals, as well as those with suppressed immune systems because of underlying illnesses, are at a heightened risk for Legionnaires’ disease, which would explain the higher death rates observed at hospitals and long-term care facilities. Dr. Frieden stated that outbreaks and cases of Legionnaires’ disease are on the rise nationally, with about 5,000 infections and 20 outbreaks occurring annually; roughly 10% of infections result in death.
The uptick in recent cases is likely because of “the aging of the population, the increase in chronic illness, [an] increase in immunosuppression through use of medication to treat a variety of conditions [and] an aging plumbing infrastructure and that makes maintenance all the more challenging,” according to Dr. Frieden. “It is also possible that increased use of diagnostic tests and more reliable reporting are contributing to some of the rising rates.”
Building owners, managers, and administrators of hospitals and other health care facilities around the country are being urged to shore up their water system management facilities to prevent further outbreaks of Legionnaires’ disease, which is the focus of the Center for Disease Control and Prevention’s latest Vital Signs report.
“Almost all Legionnaires’ disease outbreaks are preventable with improvements in water system management,” explained CDC Director Tom Frieden, adding that “At the end of the day, building owners and managers need to take steps to reduce the risk of Legionnaires’ disease [and] work together to reduce this risk and limit the number of people exposed, infected, and hospitalized or, potentially, fatally infected.”
For the report, the CDC investigated 27 outbreaks of Legionnaires’ disease in the United States from 2000 through 2014, which involved a total of 415 cases and 65 fatalities. In each outbreak analysis, the location, source of exposure, and problems with environmental controls of Legionella – the bacterium that causes the disease – were evaluated.
Hotels and resorts accounted for 44% of all outbreaks over the 15-year period, followed by long-term care facilities (19%) and hospitals (15%). However, outbreaks at the latter two location types accounted for 85% of all deaths, while outbreaks at hotels and resorts accounted for only 6%. Potable water was the most common direct cause of Legionella infections, followed by water from cooling towers, hot tubs, industrial equipment, and decorative fountains.
Additionally, 23 of the investigations yielded enough information to determine the exact cause of the outbreak, all of which were caused by at least one of 4 issues. The first was process failures, such as not having a proper water system management program in place to handle Legionella; this was found in two-thirds of the outbreaks. The second major cause was human error, such as not replacing filters or tubing as recommended by manufacturers, which was a cause in half of the outbreaks. The third was equipment breakdown, which was found in one-third of the outbreaks. Finally, reasons external to the buildings themselves – such as water main breaks or disruptions caused by nearby construction – factored into one-third of the outbreaks.
“Large, recent outbreaks of Legionnaires’ disease in New York City and Flint, Michigan, have brought attention to the disease and highlight the need for us to understand why these outbreaks happen and how best to prevent them, [which is] why this Vital Signs is targeted to a specific audience that we in public health don’t talk [to] often enough: building owners and managers,” Dr. Frieden said. “It’s not a traditional public health audience, [but] they are the key to environmental controls in buildings that we live in, get our health care in, and work in everyday.”
To that end, Dr. Frieden announced the release of a new CDC toolkit entitled “Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings: A Practical Guide to Implementing Industry Standards,” which building owners, managers, and administrators can turn to for guidance on how to implement effective water system management protocols in their buildings.
Legionnaires’ disease is a serious lung infection caused by inhalation of the bacteria Legionella, which can be found in water and inhaled as airborne mist. Elderly individuals, as well as those with suppressed immune systems because of underlying illnesses, are at a heightened risk for Legionnaires’ disease, which would explain the higher death rates observed at hospitals and long-term care facilities. Dr. Frieden stated that outbreaks and cases of Legionnaires’ disease are on the rise nationally, with about 5,000 infections and 20 outbreaks occurring annually; roughly 10% of infections result in death.
The uptick in recent cases is likely because of “the aging of the population, the increase in chronic illness, [an] increase in immunosuppression through use of medication to treat a variety of conditions [and] an aging plumbing infrastructure and that makes maintenance all the more challenging,” according to Dr. Frieden. “It is also possible that increased use of diagnostic tests and more reliable reporting are contributing to some of the rising rates.”
Building owners, managers, and administrators of hospitals and other health care facilities around the country are being urged to shore up their water system management facilities to prevent further outbreaks of Legionnaires’ disease, which is the focus of the Center for Disease Control and Prevention’s latest Vital Signs report.
“Almost all Legionnaires’ disease outbreaks are preventable with improvements in water system management,” explained CDC Director Tom Frieden, adding that “At the end of the day, building owners and managers need to take steps to reduce the risk of Legionnaires’ disease [and] work together to reduce this risk and limit the number of people exposed, infected, and hospitalized or, potentially, fatally infected.”
For the report, the CDC investigated 27 outbreaks of Legionnaires’ disease in the United States from 2000 through 2014, which involved a total of 415 cases and 65 fatalities. In each outbreak analysis, the location, source of exposure, and problems with environmental controls of Legionella – the bacterium that causes the disease – were evaluated.
Hotels and resorts accounted for 44% of all outbreaks over the 15-year period, followed by long-term care facilities (19%) and hospitals (15%). However, outbreaks at the latter two location types accounted for 85% of all deaths, while outbreaks at hotels and resorts accounted for only 6%. Potable water was the most common direct cause of Legionella infections, followed by water from cooling towers, hot tubs, industrial equipment, and decorative fountains.
Additionally, 23 of the investigations yielded enough information to determine the exact cause of the outbreak, all of which were caused by at least one of 4 issues. The first was process failures, such as not having a proper water system management program in place to handle Legionella; this was found in two-thirds of the outbreaks. The second major cause was human error, such as not replacing filters or tubing as recommended by manufacturers, which was a cause in half of the outbreaks. The third was equipment breakdown, which was found in one-third of the outbreaks. Finally, reasons external to the buildings themselves – such as water main breaks or disruptions caused by nearby construction – factored into one-third of the outbreaks.
“Large, recent outbreaks of Legionnaires’ disease in New York City and Flint, Michigan, have brought attention to the disease and highlight the need for us to understand why these outbreaks happen and how best to prevent them, [which is] why this Vital Signs is targeted to a specific audience that we in public health don’t talk [to] often enough: building owners and managers,” Dr. Frieden said. “It’s not a traditional public health audience, [but] they are the key to environmental controls in buildings that we live in, get our health care in, and work in everyday.”
To that end, Dr. Frieden announced the release of a new CDC toolkit entitled “Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings: A Practical Guide to Implementing Industry Standards,” which building owners, managers, and administrators can turn to for guidance on how to implement effective water system management protocols in their buildings.
Legionnaires’ disease is a serious lung infection caused by inhalation of the bacteria Legionella, which can be found in water and inhaled as airborne mist. Elderly individuals, as well as those with suppressed immune systems because of underlying illnesses, are at a heightened risk for Legionnaires’ disease, which would explain the higher death rates observed at hospitals and long-term care facilities. Dr. Frieden stated that outbreaks and cases of Legionnaires’ disease are on the rise nationally, with about 5,000 infections and 20 outbreaks occurring annually; roughly 10% of infections result in death.
The uptick in recent cases is likely because of “the aging of the population, the increase in chronic illness, [an] increase in immunosuppression through use of medication to treat a variety of conditions [and] an aging plumbing infrastructure and that makes maintenance all the more challenging,” according to Dr. Frieden. “It is also possible that increased use of diagnostic tests and more reliable reporting are contributing to some of the rising rates.”
FROM CDC VITAL SIGNS
Bezlotoxumab beats placebo at preventing recurrent C. difficile infections in high-risk patients
SAN DIEGO – Bezlotoxumab prevented recurrent Clostridium difficile infections (CDIs) among high-risk patients even more effectively than in the overall populations of the placebo-controlled MODIFY I and MODIFY II trials, according to a report at the annual Digestive Disease Week.
“In those key subpopulations at high risk for recurrence [of C. difficile infection], bezlotoxumab both reduced recurrence and increased rates of global cure,” said Dr. Ciaran P. Kelly of Harvard Medical School and Beth Israel Deaconess Medical Center in Boston. The biologic was especially effective among older adults and patients with at least one recent episode of CDI, Dr. Kelly and his associates found.
Bezlotoxumab is a monoclonal antibody targeting Clostridium difficile toxin B. The international, randomized, double-blind, 12-week MODIFY I and II trials included 2,656 patients with laboratory-confirmed CDI who were randomly assigned to receive either a single intravenous dose of the biologic (10 mg per kg) or placebo in addition to standard care antibiotics – that is, oral metronidazole and vancomycin; intravenous metronidazole with oral vancomycin; oral fidaxomicin; or oral fidaxomicin with intravenous metronidazole.
In both trials, bezlotoxumab was associated with a 10% decrease in rates of recurrent CDI, compared with placebo (P = .0003). Bezlotoxumab also achieved a 9.7% increase in rates of global cure, defined as clinical cure of the initial episode with no recurrence, Dr. Kelly said.
For the current analysis, he and his associates examined the efficacy of bezlotoxumab among patients at increased risk for recurrent CDI. These patients were older than 65 years, were immunocompromised, had a history of recurrent CDI, had been diagnosed with CDI within 6 months, and/or had severe CDI or were infected with hypervirulent, binary toxin positive strain. Most patients in the trials fell into at least one of these categories, Dr. Kelly said.
For each subgroup, bezlotoxumab was associated with lower rates of CDI recurrence and higher rates of global cure than in the overall study population, he emphasized. Compared with placebo, the most dramatic improvements in recurrence and global cure rates were among older patients (a 16% decrease and a 16% increase, respectively), patients with recent CDI (a 16% increase and a 12% decrease), patients with a history of recurrent CDI (a 13% decrease and a 12% increase) and immunocompromised patients (a 13% decrease and a 15% increase).
Neither trial generated a concerning safety signal, according to Dr. Kelly. There were “slight increases” in infusion reactions in the bezlotoxumab arms, but these were mostly minor and short lived, he added. “Serious adverse events were, in fact, slightly more common in the placebo group, mainly because of adverse events related to recurrence.”
The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
SAN DIEGO – Bezlotoxumab prevented recurrent Clostridium difficile infections (CDIs) among high-risk patients even more effectively than in the overall populations of the placebo-controlled MODIFY I and MODIFY II trials, according to a report at the annual Digestive Disease Week.
“In those key subpopulations at high risk for recurrence [of C. difficile infection], bezlotoxumab both reduced recurrence and increased rates of global cure,” said Dr. Ciaran P. Kelly of Harvard Medical School and Beth Israel Deaconess Medical Center in Boston. The biologic was especially effective among older adults and patients with at least one recent episode of CDI, Dr. Kelly and his associates found.
Bezlotoxumab is a monoclonal antibody targeting Clostridium difficile toxin B. The international, randomized, double-blind, 12-week MODIFY I and II trials included 2,656 patients with laboratory-confirmed CDI who were randomly assigned to receive either a single intravenous dose of the biologic (10 mg per kg) or placebo in addition to standard care antibiotics – that is, oral metronidazole and vancomycin; intravenous metronidazole with oral vancomycin; oral fidaxomicin; or oral fidaxomicin with intravenous metronidazole.
In both trials, bezlotoxumab was associated with a 10% decrease in rates of recurrent CDI, compared with placebo (P = .0003). Bezlotoxumab also achieved a 9.7% increase in rates of global cure, defined as clinical cure of the initial episode with no recurrence, Dr. Kelly said.
For the current analysis, he and his associates examined the efficacy of bezlotoxumab among patients at increased risk for recurrent CDI. These patients were older than 65 years, were immunocompromised, had a history of recurrent CDI, had been diagnosed with CDI within 6 months, and/or had severe CDI or were infected with hypervirulent, binary toxin positive strain. Most patients in the trials fell into at least one of these categories, Dr. Kelly said.
For each subgroup, bezlotoxumab was associated with lower rates of CDI recurrence and higher rates of global cure than in the overall study population, he emphasized. Compared with placebo, the most dramatic improvements in recurrence and global cure rates were among older patients (a 16% decrease and a 16% increase, respectively), patients with recent CDI (a 16% increase and a 12% decrease), patients with a history of recurrent CDI (a 13% decrease and a 12% increase) and immunocompromised patients (a 13% decrease and a 15% increase).
Neither trial generated a concerning safety signal, according to Dr. Kelly. There were “slight increases” in infusion reactions in the bezlotoxumab arms, but these were mostly minor and short lived, he added. “Serious adverse events were, in fact, slightly more common in the placebo group, mainly because of adverse events related to recurrence.”
The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
SAN DIEGO – Bezlotoxumab prevented recurrent Clostridium difficile infections (CDIs) among high-risk patients even more effectively than in the overall populations of the placebo-controlled MODIFY I and MODIFY II trials, according to a report at the annual Digestive Disease Week.
“In those key subpopulations at high risk for recurrence [of C. difficile infection], bezlotoxumab both reduced recurrence and increased rates of global cure,” said Dr. Ciaran P. Kelly of Harvard Medical School and Beth Israel Deaconess Medical Center in Boston. The biologic was especially effective among older adults and patients with at least one recent episode of CDI, Dr. Kelly and his associates found.
Bezlotoxumab is a monoclonal antibody targeting Clostridium difficile toxin B. The international, randomized, double-blind, 12-week MODIFY I and II trials included 2,656 patients with laboratory-confirmed CDI who were randomly assigned to receive either a single intravenous dose of the biologic (10 mg per kg) or placebo in addition to standard care antibiotics – that is, oral metronidazole and vancomycin; intravenous metronidazole with oral vancomycin; oral fidaxomicin; or oral fidaxomicin with intravenous metronidazole.
In both trials, bezlotoxumab was associated with a 10% decrease in rates of recurrent CDI, compared with placebo (P = .0003). Bezlotoxumab also achieved a 9.7% increase in rates of global cure, defined as clinical cure of the initial episode with no recurrence, Dr. Kelly said.
For the current analysis, he and his associates examined the efficacy of bezlotoxumab among patients at increased risk for recurrent CDI. These patients were older than 65 years, were immunocompromised, had a history of recurrent CDI, had been diagnosed with CDI within 6 months, and/or had severe CDI or were infected with hypervirulent, binary toxin positive strain. Most patients in the trials fell into at least one of these categories, Dr. Kelly said.
For each subgroup, bezlotoxumab was associated with lower rates of CDI recurrence and higher rates of global cure than in the overall study population, he emphasized. Compared with placebo, the most dramatic improvements in recurrence and global cure rates were among older patients (a 16% decrease and a 16% increase, respectively), patients with recent CDI (a 16% increase and a 12% decrease), patients with a history of recurrent CDI (a 13% decrease and a 12% increase) and immunocompromised patients (a 13% decrease and a 15% increase).
Neither trial generated a concerning safety signal, according to Dr. Kelly. There were “slight increases” in infusion reactions in the bezlotoxumab arms, but these were mostly minor and short lived, he added. “Serious adverse events were, in fact, slightly more common in the placebo group, mainly because of adverse events related to recurrence.”
The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
AT DDW® 2016
Key clinical point: The monoclonal antibody bezlotoxumab prevented recurrent CDIs among patients at high risk for this outcome.
Major finding: Compared with placebo, bezlotoxumab achieved the most dramatic differences in rates of CDI recurrence and global cure for older patients (a 16% decrease and a 16% increase, respectively).
Data source: An analysis of the international, randomized, double-blind, 12-week MODIFY I and II trials, which included 2,656 patients with laboratory-confirmed CDI.
Disclosures: The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
Improvement needed for U.S. acute care hospitals implementing ASPs
There is more room for improving U.S. acute care hospitals’ antibiotic stewardship programs (ASPs) and implementing the seven core elements, according to findings from the 2014 National Healthcare Safety Network (NHSN) Annual Hospital Survey.
In univariate analyses, Dr. Lori A. Pollack, of the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention, and her associates looked at 4,184 acute care hospitals. Of those acute care hospitals, 1,642 (39%) reported implementing all seven CDC-defined core elements – leadership commitment, a single program leader responsible for outcomes, a pharmacy leader, specific interventions to improve prescribing, tracking antibiotic use and resistance, reporting data back to provider, and education – for hospital ASPs. In the hospitals with more than 200 beds, 775 (56%) were more likely to report all seven core elements, compared with 672 (39%) hospitals with 51-200 beds, and 328 (22%) of hospitals with 50 or fewer beds.
The hospitals with 50 or fewer beds were less likely to report leadership support (40%) or antibiotic stewardship education (46%), compared with facilities with greater than 50 beds (69% leadership, 69% education). Also, the major teaching hospitals were more likely to report all seven core elements (54%) than were hospitals that had only undergraduate education or no teaching affiliation (34%).
The study also conducted a final multivariate model and found that the strongest predictor for meeting all seven core elements was support from the facility administration (adjusted relative risk, 7.2; P less than .0001).
“Our findings suggest that many hospitals need to add infrastructure and measurement support to their current actions to improve antibiotic use,” the researchers concluded. “CDC is committed to on-going work with partners to help all hospitals implement effective antibiotic stewardship programs, and future years of this survey will help monitor progress toward that goal.”
Read the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw323).
There is more room for improving U.S. acute care hospitals’ antibiotic stewardship programs (ASPs) and implementing the seven core elements, according to findings from the 2014 National Healthcare Safety Network (NHSN) Annual Hospital Survey.
In univariate analyses, Dr. Lori A. Pollack, of the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention, and her associates looked at 4,184 acute care hospitals. Of those acute care hospitals, 1,642 (39%) reported implementing all seven CDC-defined core elements – leadership commitment, a single program leader responsible for outcomes, a pharmacy leader, specific interventions to improve prescribing, tracking antibiotic use and resistance, reporting data back to provider, and education – for hospital ASPs. In the hospitals with more than 200 beds, 775 (56%) were more likely to report all seven core elements, compared with 672 (39%) hospitals with 51-200 beds, and 328 (22%) of hospitals with 50 or fewer beds.
The hospitals with 50 or fewer beds were less likely to report leadership support (40%) or antibiotic stewardship education (46%), compared with facilities with greater than 50 beds (69% leadership, 69% education). Also, the major teaching hospitals were more likely to report all seven core elements (54%) than were hospitals that had only undergraduate education or no teaching affiliation (34%).
The study also conducted a final multivariate model and found that the strongest predictor for meeting all seven core elements was support from the facility administration (adjusted relative risk, 7.2; P less than .0001).
“Our findings suggest that many hospitals need to add infrastructure and measurement support to their current actions to improve antibiotic use,” the researchers concluded. “CDC is committed to on-going work with partners to help all hospitals implement effective antibiotic stewardship programs, and future years of this survey will help monitor progress toward that goal.”
Read the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw323).
There is more room for improving U.S. acute care hospitals’ antibiotic stewardship programs (ASPs) and implementing the seven core elements, according to findings from the 2014 National Healthcare Safety Network (NHSN) Annual Hospital Survey.
In univariate analyses, Dr. Lori A. Pollack, of the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention, and her associates looked at 4,184 acute care hospitals. Of those acute care hospitals, 1,642 (39%) reported implementing all seven CDC-defined core elements – leadership commitment, a single program leader responsible for outcomes, a pharmacy leader, specific interventions to improve prescribing, tracking antibiotic use and resistance, reporting data back to provider, and education – for hospital ASPs. In the hospitals with more than 200 beds, 775 (56%) were more likely to report all seven core elements, compared with 672 (39%) hospitals with 51-200 beds, and 328 (22%) of hospitals with 50 or fewer beds.
The hospitals with 50 or fewer beds were less likely to report leadership support (40%) or antibiotic stewardship education (46%), compared with facilities with greater than 50 beds (69% leadership, 69% education). Also, the major teaching hospitals were more likely to report all seven core elements (54%) than were hospitals that had only undergraduate education or no teaching affiliation (34%).
The study also conducted a final multivariate model and found that the strongest predictor for meeting all seven core elements was support from the facility administration (adjusted relative risk, 7.2; P less than .0001).
“Our findings suggest that many hospitals need to add infrastructure and measurement support to their current actions to improve antibiotic use,” the researchers concluded. “CDC is committed to on-going work with partners to help all hospitals implement effective antibiotic stewardship programs, and future years of this survey will help monitor progress toward that goal.”
Read the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw323).
FROM CLINICAL INFECTIOUS DISEASES
Ultrasound improves early diagnosis of ventilator-associated pneumonia
The use of lung ultrasound, both alone and in combination with clinical and microbiologic data, can improve the early diagnosis of ventilator-associated pneumonia (VAP), according to the results of a study published in Chest.
The early diagnosis of VAP is challenging, and leaves intensivists with two options. The first is waiting for positive results from patients’ specimens, which delays treatment and increases mortality risk. The other is to administer antibiotics to all patients suspected of having VAP, which may be inappropriate and can lead to the development of multiresistant bacteria. “A pressing need therefore exists for reliable diagnostic tools to diagnose VAP early so that antibiotics can be promptly initiated, avoiding two extreme approaches,” wrote Dr. Silvia Mongodi of the Fondazione IRCCS Policlinico San Matteo in Pavia, Italy, and her colleagues.
Based on the results of previous research, the investigators hypothesized that lung ultrasound (LUS) could be used to diagnose VAP early and help to avoid treatment delays or mistakes. To test this hypothesis, the diagnostic performance of LUS alone and in combination with clinical and microbiologic data was evaluated prospectively in 99 patients with suspected VAP in ICUs at Saint Joseph Hospital (Paris), Fondazione IRCCS Policlinico San Matteo, and Centre Hospitalier de l’Université de Montréal (Chest. 2016 Apr;149[4]:969-80. doi: 10.1016/j.chest.2015.12.012).
The study results showed that subpleural consolidations and dynamic linear/arborescent air bronchograms were the principal LUS signs of VAP, and that the presence of both in the same individual made the diagnosis highly specific (88%), with a high positive predictive value (86%) and a positive likelihood ratio of 2.9. Furthermore, the addition of data from either of two different endotracheal aspirate assessment techniques (EAgram [direct Gram stain examination] or EAquant [direct Gram stain culture]) to the data from the principal LUS signs showed 97% specificity with each technique and positive likelihood ratios of 6.6 and 7.1, respectively, Dr. Mongodi and her associates reported.
Dr. Mongodi and her colleagues said that their results were encouraging but would need to be validated in larger clinical trials.
No funding was received for this study. The authors reported no conflicts of interest.
Dr. Daniel Ouellette, FCCP comments: Ultrasound techniques are increasingly being used in the intensive care unit to direct physician decisions. A report by Mongodi and colleagues suggests that ultrasound may be employed to diagnose ventilator-associated pneumonia in critically ill patients. While promising, this study is limited by small patient numbers and by the fact that reliable criteria to diagnose VAP are lacking. Further research is needed before this technique can be used reliably in the ICU.
Dr. Daniel Ouellette, FCCP comments: Ultrasound techniques are increasingly being used in the intensive care unit to direct physician decisions. A report by Mongodi and colleagues suggests that ultrasound may be employed to diagnose ventilator-associated pneumonia in critically ill patients. While promising, this study is limited by small patient numbers and by the fact that reliable criteria to diagnose VAP are lacking. Further research is needed before this technique can be used reliably in the ICU.
Dr. Daniel Ouellette, FCCP comments: Ultrasound techniques are increasingly being used in the intensive care unit to direct physician decisions. A report by Mongodi and colleagues suggests that ultrasound may be employed to diagnose ventilator-associated pneumonia in critically ill patients. While promising, this study is limited by small patient numbers and by the fact that reliable criteria to diagnose VAP are lacking. Further research is needed before this technique can be used reliably in the ICU.
The use of lung ultrasound, both alone and in combination with clinical and microbiologic data, can improve the early diagnosis of ventilator-associated pneumonia (VAP), according to the results of a study published in Chest.
The early diagnosis of VAP is challenging, and leaves intensivists with two options. The first is waiting for positive results from patients’ specimens, which delays treatment and increases mortality risk. The other is to administer antibiotics to all patients suspected of having VAP, which may be inappropriate and can lead to the development of multiresistant bacteria. “A pressing need therefore exists for reliable diagnostic tools to diagnose VAP early so that antibiotics can be promptly initiated, avoiding two extreme approaches,” wrote Dr. Silvia Mongodi of the Fondazione IRCCS Policlinico San Matteo in Pavia, Italy, and her colleagues.
Based on the results of previous research, the investigators hypothesized that lung ultrasound (LUS) could be used to diagnose VAP early and help to avoid treatment delays or mistakes. To test this hypothesis, the diagnostic performance of LUS alone and in combination with clinical and microbiologic data was evaluated prospectively in 99 patients with suspected VAP in ICUs at Saint Joseph Hospital (Paris), Fondazione IRCCS Policlinico San Matteo, and Centre Hospitalier de l’Université de Montréal (Chest. 2016 Apr;149[4]:969-80. doi: 10.1016/j.chest.2015.12.012).
The study results showed that subpleural consolidations and dynamic linear/arborescent air bronchograms were the principal LUS signs of VAP, and that the presence of both in the same individual made the diagnosis highly specific (88%), with a high positive predictive value (86%) and a positive likelihood ratio of 2.9. Furthermore, the addition of data from either of two different endotracheal aspirate assessment techniques (EAgram [direct Gram stain examination] or EAquant [direct Gram stain culture]) to the data from the principal LUS signs showed 97% specificity with each technique and positive likelihood ratios of 6.6 and 7.1, respectively, Dr. Mongodi and her associates reported.
Dr. Mongodi and her colleagues said that their results were encouraging but would need to be validated in larger clinical trials.
No funding was received for this study. The authors reported no conflicts of interest.
The use of lung ultrasound, both alone and in combination with clinical and microbiologic data, can improve the early diagnosis of ventilator-associated pneumonia (VAP), according to the results of a study published in Chest.
The early diagnosis of VAP is challenging, and leaves intensivists with two options. The first is waiting for positive results from patients’ specimens, which delays treatment and increases mortality risk. The other is to administer antibiotics to all patients suspected of having VAP, which may be inappropriate and can lead to the development of multiresistant bacteria. “A pressing need therefore exists for reliable diagnostic tools to diagnose VAP early so that antibiotics can be promptly initiated, avoiding two extreme approaches,” wrote Dr. Silvia Mongodi of the Fondazione IRCCS Policlinico San Matteo in Pavia, Italy, and her colleagues.
Based on the results of previous research, the investigators hypothesized that lung ultrasound (LUS) could be used to diagnose VAP early and help to avoid treatment delays or mistakes. To test this hypothesis, the diagnostic performance of LUS alone and in combination with clinical and microbiologic data was evaluated prospectively in 99 patients with suspected VAP in ICUs at Saint Joseph Hospital (Paris), Fondazione IRCCS Policlinico San Matteo, and Centre Hospitalier de l’Université de Montréal (Chest. 2016 Apr;149[4]:969-80. doi: 10.1016/j.chest.2015.12.012).
The study results showed that subpleural consolidations and dynamic linear/arborescent air bronchograms were the principal LUS signs of VAP, and that the presence of both in the same individual made the diagnosis highly specific (88%), with a high positive predictive value (86%) and a positive likelihood ratio of 2.9. Furthermore, the addition of data from either of two different endotracheal aspirate assessment techniques (EAgram [direct Gram stain examination] or EAquant [direct Gram stain culture]) to the data from the principal LUS signs showed 97% specificity with each technique and positive likelihood ratios of 6.6 and 7.1, respectively, Dr. Mongodi and her associates reported.
Dr. Mongodi and her colleagues said that their results were encouraging but would need to be validated in larger clinical trials.
No funding was received for this study. The authors reported no conflicts of interest.
Key clinical point: The specificity of the examination for ventilator-associated pneumonia diagnosis could be increased with daily lung-ultrasound monitoring of ICU patients.
Major finding: Lung ultrasound reliably improved the diagnosis of ventilator-associated pneumonia with high specificity (88%), high positive predictive value (86%), and a positive likelihood ratio of 2.9.
Data sources: Patients with suspected ventilator-associated pneumonia in ICUs in France, Italy, and Canada.
Disclosures: No funding was received for this study. The authors reported no conflicts of interest.
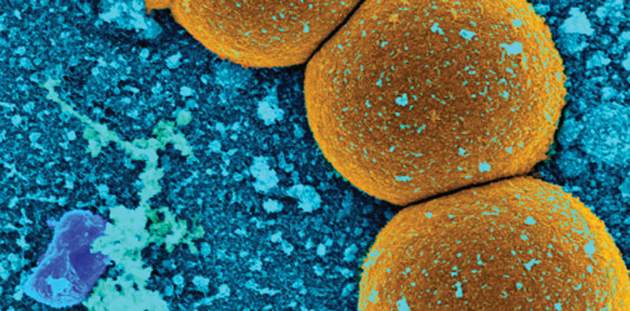
Study: Number of MRSA cases in Japan may be underestimated
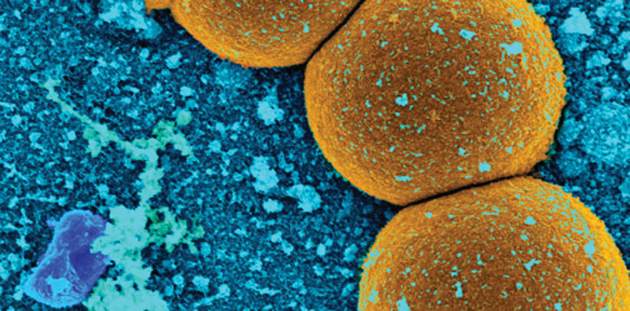
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
Key clinical point: Sentinel surveillance systems may substantially underestimate the number of methicillin-resistant Staphylococcus aureus cases in Japan.
Major finding: Direct notification to the Japan Nosocomial Infections Surveillance system regarding methicillin-resistant Staphylococcus aureus patients was not affected by patients’ age, and information from health insurance claims was useful for evaluation of the sentinel infection surveillance system.
Data sources: The Japan Nosocomial Infections Surveillance system and the National Health Insurance Organization.
Disclosures: Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
FDA warns against routine fluoroquinolone use
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
Daptomycin beats infective endocarditis caused by several pathogens
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
Key clinical point: Daptomycin had a high cure rate for infective endocarditis caused by MRSA, MSSA, coagulase-negative staph, and enterococci.
Major finding: The 2-year clinical cure rate was 90% for S. aureus infections.
Data source: Retrospective analysis of EUCORE, which comprised 198 patients.
Disclosures: Dr. Guleri had no financial disclosures.
MRSA prevalence in asymptomatic athletes comparable to dialysis, HIV patients
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is comparable to that among individuals with chronic illnesses.
Major finding: The prevalence of MRSA colonization was 8% among U.S. athletes and 13% among U.S. collegiate athletes. The prevalence of MRSA in the total athletic population was comparable to MRSA in patients with illnesses such as kidney disease and HIV.
Data source: A PubMed and EMBASE search yielded 382 studies and was narrowed to 15 analyses.
Disclosures: The investigators declared no conflicts of interest.
Patients with HAIs have more readmissions, higher mortality rates
Patients with a health care-acquired infection had a larger proportion of readmissions, greater associated costs, and higher mortality rates compared to patients with no HAI, according to a study published in the American Journal of Infection Control.
Investigators at Linköping (Sweden) University examined the effects of HAIs by calculating the difference in hospital length of stay (LOS) and actual direct health care costs for patients with an HAI compared with patients without HAI. They used data from the Swedish National Point Prevalence Surveys of HAI 2010-2012, merged with cost-per-patient data from the Health Care Register of the Swedish county of Östergötland. Extended LOS and costs related to an HAI were adjusted for sex, age, intensive care unit use, and surgery.
The average prevalence of HAI for all 7,981 patients in the study was 10.8%, although for the 7,062 patients in the main analyses the prevalence of HAI in the Point Prevalence Survey was 9.9%. Those patients with HAI (732 patients) had a larger proportion of readmissions compared with patients with no HAI (29.0% vs 16.5%), a significant difference, said Mikael Rahmqvist, Ph.D., of the department of medical and health sciences at Linköping University, and lead author of the study.
Of the total hospital bed days occupied by patients in the study population, 9.3% was considered to be excess days, attributed to the group of patients with an HAI. This excess LOS comprised 11.4% of total health care costs (95% confidence interval, 10.2-12.7). The 1-year overall mortality rate for patients with HAI in comparison to all other patients was 1.75 (95% CI, 1.45-2.11). The coauthors said all of the differences measured were statistically significant (P less than .001).
“Our results imply that a reduction of HAI prevalence to a significant degree could reduce health care costs, lessen patient suffering, and also increase patients’ long-term survival,” said Dr. Rahmqvist and his coauthors.
They reported having no conflicts.
Read the full study in the American Journal of Infection Control (doi:10.1016/j.ajic.2016.01.035).
On Twitter @richpizzi
Patients with a health care-acquired infection had a larger proportion of readmissions, greater associated costs, and higher mortality rates compared to patients with no HAI, according to a study published in the American Journal of Infection Control.
Investigators at Linköping (Sweden) University examined the effects of HAIs by calculating the difference in hospital length of stay (LOS) and actual direct health care costs for patients with an HAI compared with patients without HAI. They used data from the Swedish National Point Prevalence Surveys of HAI 2010-2012, merged with cost-per-patient data from the Health Care Register of the Swedish county of Östergötland. Extended LOS and costs related to an HAI were adjusted for sex, age, intensive care unit use, and surgery.
The average prevalence of HAI for all 7,981 patients in the study was 10.8%, although for the 7,062 patients in the main analyses the prevalence of HAI in the Point Prevalence Survey was 9.9%. Those patients with HAI (732 patients) had a larger proportion of readmissions compared with patients with no HAI (29.0% vs 16.5%), a significant difference, said Mikael Rahmqvist, Ph.D., of the department of medical and health sciences at Linköping University, and lead author of the study.
Of the total hospital bed days occupied by patients in the study population, 9.3% was considered to be excess days, attributed to the group of patients with an HAI. This excess LOS comprised 11.4% of total health care costs (95% confidence interval, 10.2-12.7). The 1-year overall mortality rate for patients with HAI in comparison to all other patients was 1.75 (95% CI, 1.45-2.11). The coauthors said all of the differences measured were statistically significant (P less than .001).
“Our results imply that a reduction of HAI prevalence to a significant degree could reduce health care costs, lessen patient suffering, and also increase patients’ long-term survival,” said Dr. Rahmqvist and his coauthors.
They reported having no conflicts.
Read the full study in the American Journal of Infection Control (doi:10.1016/j.ajic.2016.01.035).
On Twitter @richpizzi
Patients with a health care-acquired infection had a larger proportion of readmissions, greater associated costs, and higher mortality rates compared to patients with no HAI, according to a study published in the American Journal of Infection Control.
Investigators at Linköping (Sweden) University examined the effects of HAIs by calculating the difference in hospital length of stay (LOS) and actual direct health care costs for patients with an HAI compared with patients without HAI. They used data from the Swedish National Point Prevalence Surveys of HAI 2010-2012, merged with cost-per-patient data from the Health Care Register of the Swedish county of Östergötland. Extended LOS and costs related to an HAI were adjusted for sex, age, intensive care unit use, and surgery.
The average prevalence of HAI for all 7,981 patients in the study was 10.8%, although for the 7,062 patients in the main analyses the prevalence of HAI in the Point Prevalence Survey was 9.9%. Those patients with HAI (732 patients) had a larger proportion of readmissions compared with patients with no HAI (29.0% vs 16.5%), a significant difference, said Mikael Rahmqvist, Ph.D., of the department of medical and health sciences at Linköping University, and lead author of the study.
Of the total hospital bed days occupied by patients in the study population, 9.3% was considered to be excess days, attributed to the group of patients with an HAI. This excess LOS comprised 11.4% of total health care costs (95% confidence interval, 10.2-12.7). The 1-year overall mortality rate for patients with HAI in comparison to all other patients was 1.75 (95% CI, 1.45-2.11). The coauthors said all of the differences measured were statistically significant (P less than .001).
“Our results imply that a reduction of HAI prevalence to a significant degree could reduce health care costs, lessen patient suffering, and also increase patients’ long-term survival,” said Dr. Rahmqvist and his coauthors.
They reported having no conflicts.
Read the full study in the American Journal of Infection Control (doi:10.1016/j.ajic.2016.01.035).
On Twitter @richpizzi
FROM AMERICAN JOURNAL OF INFECTION CONTROL
Kawasaki disease and infections aren’t mutually exclusive
CHICAGO – Kawasaki disease and concurrent bacterial or viral infection are by no means mutually exclusive, Dr. Cathie-Kim Le cautioned at the annual meeting of the American College of Cardiology.
“Recognizing that both can coexist will ensure timely IVIg [intravenous immunoglobulin] treatment and appropriate containment of coronary artery complications,” said Dr. Le of Sainte-Justine University Hospital in Montreal.
She presented a retrospective study of 128 patients, mean age 3.4 years, admitted to the pediatric academic tertiary care center with a discharge diagnosis of Kawasaki disease. During their hospitalization all of them underwent a work-up for bacterial and viral infectious diseases, which proved positive in 33% of cases. Roughly 40% of subjects had incomplete Kawasaki disease, meaning they lacked a sufficient number of signs of mucocutaneous inflammation to fulfill the epidemiologic case definition; however, their prevalence of concomitant infection was similar to that of the group with classic Kawasaki disease.
Among the most common types of infections in patients with Kawasaki disease were otitis media, which accounted for 17% of the infections; upper respiratory infections, 21%; and group A streptococcal pharyngitis and pneumonia, which accounted for 14% each.
There were no differences in clinical presentation or laboratory values between children with or without concomitant infection. Nor was myocardial profiling useful in differentiating patients with concomitant infection from those without: Ventricular shortening fraction scores and N-terminal probrain natriuretic peptide levels were similar in the two groups of Kawasaki disease patients.
Acute coronary dilatation occurred in 26% of Kawasaki disease patients with concomitant infection and similarly in 30% of those without infection. Coronary aneurysm, the most serious complication of Kawasaki disease, occurred in 14% of patients with infection and an identical proportion of the uninfected.
Almost all patients received IVIg. Resistance to the effects of IVIg occurred in 36% of patients with concomitant infection, a rate twice that seen in the group without infection. Coronary aneurysms and dilatations were significantly more common in IVIg-resistant patients, regardless of their infection status.
Dr. Le reported having no relevant financial conflicts.
CHICAGO – Kawasaki disease and concurrent bacterial or viral infection are by no means mutually exclusive, Dr. Cathie-Kim Le cautioned at the annual meeting of the American College of Cardiology.
“Recognizing that both can coexist will ensure timely IVIg [intravenous immunoglobulin] treatment and appropriate containment of coronary artery complications,” said Dr. Le of Sainte-Justine University Hospital in Montreal.
She presented a retrospective study of 128 patients, mean age 3.4 years, admitted to the pediatric academic tertiary care center with a discharge diagnosis of Kawasaki disease. During their hospitalization all of them underwent a work-up for bacterial and viral infectious diseases, which proved positive in 33% of cases. Roughly 40% of subjects had incomplete Kawasaki disease, meaning they lacked a sufficient number of signs of mucocutaneous inflammation to fulfill the epidemiologic case definition; however, their prevalence of concomitant infection was similar to that of the group with classic Kawasaki disease.
Among the most common types of infections in patients with Kawasaki disease were otitis media, which accounted for 17% of the infections; upper respiratory infections, 21%; and group A streptococcal pharyngitis and pneumonia, which accounted for 14% each.
There were no differences in clinical presentation or laboratory values between children with or without concomitant infection. Nor was myocardial profiling useful in differentiating patients with concomitant infection from those without: Ventricular shortening fraction scores and N-terminal probrain natriuretic peptide levels were similar in the two groups of Kawasaki disease patients.
Acute coronary dilatation occurred in 26% of Kawasaki disease patients with concomitant infection and similarly in 30% of those without infection. Coronary aneurysm, the most serious complication of Kawasaki disease, occurred in 14% of patients with infection and an identical proportion of the uninfected.
Almost all patients received IVIg. Resistance to the effects of IVIg occurred in 36% of patients with concomitant infection, a rate twice that seen in the group without infection. Coronary aneurysms and dilatations were significantly more common in IVIg-resistant patients, regardless of their infection status.
Dr. Le reported having no relevant financial conflicts.
CHICAGO – Kawasaki disease and concurrent bacterial or viral infection are by no means mutually exclusive, Dr. Cathie-Kim Le cautioned at the annual meeting of the American College of Cardiology.
“Recognizing that both can coexist will ensure timely IVIg [intravenous immunoglobulin] treatment and appropriate containment of coronary artery complications,” said Dr. Le of Sainte-Justine University Hospital in Montreal.
She presented a retrospective study of 128 patients, mean age 3.4 years, admitted to the pediatric academic tertiary care center with a discharge diagnosis of Kawasaki disease. During their hospitalization all of them underwent a work-up for bacterial and viral infectious diseases, which proved positive in 33% of cases. Roughly 40% of subjects had incomplete Kawasaki disease, meaning they lacked a sufficient number of signs of mucocutaneous inflammation to fulfill the epidemiologic case definition; however, their prevalence of concomitant infection was similar to that of the group with classic Kawasaki disease.
Among the most common types of infections in patients with Kawasaki disease were otitis media, which accounted for 17% of the infections; upper respiratory infections, 21%; and group A streptococcal pharyngitis and pneumonia, which accounted for 14% each.
There were no differences in clinical presentation or laboratory values between children with or without concomitant infection. Nor was myocardial profiling useful in differentiating patients with concomitant infection from those without: Ventricular shortening fraction scores and N-terminal probrain natriuretic peptide levels were similar in the two groups of Kawasaki disease patients.
Acute coronary dilatation occurred in 26% of Kawasaki disease patients with concomitant infection and similarly in 30% of those without infection. Coronary aneurysm, the most serious complication of Kawasaki disease, occurred in 14% of patients with infection and an identical proportion of the uninfected.
Almost all patients received IVIg. Resistance to the effects of IVIg occurred in 36% of patients with concomitant infection, a rate twice that seen in the group without infection. Coronary aneurysms and dilatations were significantly more common in IVIg-resistant patients, regardless of their infection status.
Dr. Le reported having no relevant financial conflicts.
AT ACC 16
Key clinical point: One-third of Kawasaki patients have a concomitant common infection that may delay timely diagnosis.
Major finding: Coronary aneurysm, the most serious complication of Kawasaki disease, occurred in 14% of patients with an infection and in 14% of the uninfected.
Data source: A retrospective study of 128 children with Kawasaki disease.
Disclosures: The study presenter reported having no relevant financial conflicts.