User login
ASNC rejects new chest pain guideline it helped create
It was Oct. 28 when the two big North American cardiology societies issued a joint practice guideline on evaluating and managing chest pain that was endorsed by five other subspecialty groups. The next day, another group that had taken part in the document’s genesis explained why it wasn’t one of those five.
Although the American Society of Nuclear Cardiology (ASNC) was “actively engaged at every stage of the guideline-writing and review process,” the society “could not endorse the guideline,” the society announced in a statement released to clinicians and the media. The most prominent cited reason: It doesn’t adequately “support the principle of Patient First Imaging.”
The guideline was published in Circulation and the Journal of the American College of Cardiology, flagship journals of the American Heart Association and American College of Cardiology, respectively.
The document notes at least two clinicians represented ASNC as peer reviewers, and another was on the writing committee, but the organization does not appear in the list of societies endorsing the document.
“We believe that the document fails to provide unbiased guidance to health care professionals on the optimal evaluation of patients with chest pain,” contends an editorial ASNC board members have scheduled for the Jan. 10 issue of the Journal of Nuclear Medicine but is available now on an open-access preprint server.
“Despite the many important and helpful recommendations in the new guideline, there are several recommendations that we could not support,” it states.
“The ASNC board of directors reviewed the document twice during the endorsement process,” and the society “offered substantive comments after the first endorsement review, several of which were addressed,” Randall C. Thompson, MD, St. Luke’s Mid America Heart Institute and University of Missouri–Kansas City, said in an interview.
“However, some of the board’s concerns went unresolved. It was after the board’s second review, when the document had been declared finalized, that they voted not to endorse,” said Dr. Thompson, who is ASNC president.
“When we gather multiple organizations together to review and summarize the evidence, we work collaboratively to interpret the extensive catalog of peer-reviewed, published literature and create clinical practice recommendations,” Guideline Writing Committee Chair Martha Gulati, MD, University of Arizona, Phoenix, told this news organization in a prepared statement.
“The ASNC had a representative on the writing committee who is a coauthor on the paper and actively participated throughout the writing process the past 4 years,” she said. “The final guideline reflects the latest evidence-based recommendations for the evaluation and diagnosis of chest pain, as agreed by the seven endorsing organizations.”
The document does not clearly note that an ASNC representative was on the writing committee. However, ASNC confirmed that Renee Bullock-Palmer, MD, Deborah Heart and Lung Center, Browns Mills, N.J., is a fellow of the ASNC and had represented the group as one of the coauthors. Two “official reviewers” of the document, however, are listed as ASNC representatives.
Points of contention
“The decision about which test to order can be a nuanced one, and cardiac imaging tests tend to be complementary,” elaborates the editorial on the issue of patient-centered management.
Careful patient selection for different tests is important, “and physician and technical local expertise, availability, quality of equipment, and patient preference are extremely important factors to consider. There is not enough emphasis on this important point,” contend the authors. “This is an important limitation of the guideline.”
Other issues of concern include “lack of balance in the document’s presentation of the science on FFR-CT [fractional flow reserve assessment with computed tomography] and its inappropriately prominent endorsement,” the editorial states.
The U.S. Food and Drug Administration–recognized “limitations and contraindications” to FFR-CT tend to be glossed over in the document, Dr. Thompson said. And most ASNC board members were “concerned with the prominent location of the recommendations for FFR-CT in various tables – especially since there was minimal-to-no discussion of the fact that it is currently provided by only one company, that it is not widely available nor covered routinely by health insurance carriers, and [that] the accuracy in the most relevant population is disputed.”
In other concerns, the document “inadequately discusses the benefit” of combining coronary artery calcium (CAC) scores with functional testing, which ASNC said it supports. For example, adding CAC scores to myocardial perfusion imaging improves its diagnostic accuracy and prognostic power.
Functional vs. anatomic testing?
Moreover, “it is no longer appropriate to bundle all types of stress testing together. All stress imaging tests have their unique advantages and limitations.” Yet, “the concept of the dichotomy of functional testing versus anatomic testing is a common theme in the guideline in many important patient groups,” the editorial states. That could overemphasize CT angiography and thus “blur distinction between different types of functional tests.”
Such concerns about “imbalance” in the portrayals of the two kinds of tests were “amplified by the problem of health insurance companies and radiologic benefits managers inappropriately substituting a test that was ordered by a physician with a different test,” Dr. Thompson elaborated. “There is the impression that some of them ‘cherry-pick’ certain guidelines and that this practice is harmful to patients.”
The ASNC currently does not plan its own corresponding guideline, he said. But the editorial says that “over the coming weeks and months ASNC will offer a series of webinars and other programs that address specific patient populations and dilemmas.” Also, “we will enhance our focus on programs to address quality and efficiency to support a patient-first approach to imaging.”
The five subspecialty groups that have endorsed the document are the American Society of Echocardiography, American College of Chest Physicians, Society for Academic Emergency Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance.
Dr. Thompson has reported no relevant financial relationships. Statements of disclosure for the other editorial writers are listed in the publication.
A version of this article first appeared on Medscape.com.
It was Oct. 28 when the two big North American cardiology societies issued a joint practice guideline on evaluating and managing chest pain that was endorsed by five other subspecialty groups. The next day, another group that had taken part in the document’s genesis explained why it wasn’t one of those five.
Although the American Society of Nuclear Cardiology (ASNC) was “actively engaged at every stage of the guideline-writing and review process,” the society “could not endorse the guideline,” the society announced in a statement released to clinicians and the media. The most prominent cited reason: It doesn’t adequately “support the principle of Patient First Imaging.”
The guideline was published in Circulation and the Journal of the American College of Cardiology, flagship journals of the American Heart Association and American College of Cardiology, respectively.
The document notes at least two clinicians represented ASNC as peer reviewers, and another was on the writing committee, but the organization does not appear in the list of societies endorsing the document.
“We believe that the document fails to provide unbiased guidance to health care professionals on the optimal evaluation of patients with chest pain,” contends an editorial ASNC board members have scheduled for the Jan. 10 issue of the Journal of Nuclear Medicine but is available now on an open-access preprint server.
“Despite the many important and helpful recommendations in the new guideline, there are several recommendations that we could not support,” it states.
“The ASNC board of directors reviewed the document twice during the endorsement process,” and the society “offered substantive comments after the first endorsement review, several of which were addressed,” Randall C. Thompson, MD, St. Luke’s Mid America Heart Institute and University of Missouri–Kansas City, said in an interview.
“However, some of the board’s concerns went unresolved. It was after the board’s second review, when the document had been declared finalized, that they voted not to endorse,” said Dr. Thompson, who is ASNC president.
“When we gather multiple organizations together to review and summarize the evidence, we work collaboratively to interpret the extensive catalog of peer-reviewed, published literature and create clinical practice recommendations,” Guideline Writing Committee Chair Martha Gulati, MD, University of Arizona, Phoenix, told this news organization in a prepared statement.
“The ASNC had a representative on the writing committee who is a coauthor on the paper and actively participated throughout the writing process the past 4 years,” she said. “The final guideline reflects the latest evidence-based recommendations for the evaluation and diagnosis of chest pain, as agreed by the seven endorsing organizations.”
The document does not clearly note that an ASNC representative was on the writing committee. However, ASNC confirmed that Renee Bullock-Palmer, MD, Deborah Heart and Lung Center, Browns Mills, N.J., is a fellow of the ASNC and had represented the group as one of the coauthors. Two “official reviewers” of the document, however, are listed as ASNC representatives.
Points of contention
“The decision about which test to order can be a nuanced one, and cardiac imaging tests tend to be complementary,” elaborates the editorial on the issue of patient-centered management.
Careful patient selection for different tests is important, “and physician and technical local expertise, availability, quality of equipment, and patient preference are extremely important factors to consider. There is not enough emphasis on this important point,” contend the authors. “This is an important limitation of the guideline.”
Other issues of concern include “lack of balance in the document’s presentation of the science on FFR-CT [fractional flow reserve assessment with computed tomography] and its inappropriately prominent endorsement,” the editorial states.
The U.S. Food and Drug Administration–recognized “limitations and contraindications” to FFR-CT tend to be glossed over in the document, Dr. Thompson said. And most ASNC board members were “concerned with the prominent location of the recommendations for FFR-CT in various tables – especially since there was minimal-to-no discussion of the fact that it is currently provided by only one company, that it is not widely available nor covered routinely by health insurance carriers, and [that] the accuracy in the most relevant population is disputed.”
In other concerns, the document “inadequately discusses the benefit” of combining coronary artery calcium (CAC) scores with functional testing, which ASNC said it supports. For example, adding CAC scores to myocardial perfusion imaging improves its diagnostic accuracy and prognostic power.
Functional vs. anatomic testing?
Moreover, “it is no longer appropriate to bundle all types of stress testing together. All stress imaging tests have their unique advantages and limitations.” Yet, “the concept of the dichotomy of functional testing versus anatomic testing is a common theme in the guideline in many important patient groups,” the editorial states. That could overemphasize CT angiography and thus “blur distinction between different types of functional tests.”
Such concerns about “imbalance” in the portrayals of the two kinds of tests were “amplified by the problem of health insurance companies and radiologic benefits managers inappropriately substituting a test that was ordered by a physician with a different test,” Dr. Thompson elaborated. “There is the impression that some of them ‘cherry-pick’ certain guidelines and that this practice is harmful to patients.”
The ASNC currently does not plan its own corresponding guideline, he said. But the editorial says that “over the coming weeks and months ASNC will offer a series of webinars and other programs that address specific patient populations and dilemmas.” Also, “we will enhance our focus on programs to address quality and efficiency to support a patient-first approach to imaging.”
The five subspecialty groups that have endorsed the document are the American Society of Echocardiography, American College of Chest Physicians, Society for Academic Emergency Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance.
Dr. Thompson has reported no relevant financial relationships. Statements of disclosure for the other editorial writers are listed in the publication.
A version of this article first appeared on Medscape.com.
It was Oct. 28 when the two big North American cardiology societies issued a joint practice guideline on evaluating and managing chest pain that was endorsed by five other subspecialty groups. The next day, another group that had taken part in the document’s genesis explained why it wasn’t one of those five.
Although the American Society of Nuclear Cardiology (ASNC) was “actively engaged at every stage of the guideline-writing and review process,” the society “could not endorse the guideline,” the society announced in a statement released to clinicians and the media. The most prominent cited reason: It doesn’t adequately “support the principle of Patient First Imaging.”
The guideline was published in Circulation and the Journal of the American College of Cardiology, flagship journals of the American Heart Association and American College of Cardiology, respectively.
The document notes at least two clinicians represented ASNC as peer reviewers, and another was on the writing committee, but the organization does not appear in the list of societies endorsing the document.
“We believe that the document fails to provide unbiased guidance to health care professionals on the optimal evaluation of patients with chest pain,” contends an editorial ASNC board members have scheduled for the Jan. 10 issue of the Journal of Nuclear Medicine but is available now on an open-access preprint server.
“Despite the many important and helpful recommendations in the new guideline, there are several recommendations that we could not support,” it states.
“The ASNC board of directors reviewed the document twice during the endorsement process,” and the society “offered substantive comments after the first endorsement review, several of which were addressed,” Randall C. Thompson, MD, St. Luke’s Mid America Heart Institute and University of Missouri–Kansas City, said in an interview.
“However, some of the board’s concerns went unresolved. It was after the board’s second review, when the document had been declared finalized, that they voted not to endorse,” said Dr. Thompson, who is ASNC president.
“When we gather multiple organizations together to review and summarize the evidence, we work collaboratively to interpret the extensive catalog of peer-reviewed, published literature and create clinical practice recommendations,” Guideline Writing Committee Chair Martha Gulati, MD, University of Arizona, Phoenix, told this news organization in a prepared statement.
“The ASNC had a representative on the writing committee who is a coauthor on the paper and actively participated throughout the writing process the past 4 years,” she said. “The final guideline reflects the latest evidence-based recommendations for the evaluation and diagnosis of chest pain, as agreed by the seven endorsing organizations.”
The document does not clearly note that an ASNC representative was on the writing committee. However, ASNC confirmed that Renee Bullock-Palmer, MD, Deborah Heart and Lung Center, Browns Mills, N.J., is a fellow of the ASNC and had represented the group as one of the coauthors. Two “official reviewers” of the document, however, are listed as ASNC representatives.
Points of contention
“The decision about which test to order can be a nuanced one, and cardiac imaging tests tend to be complementary,” elaborates the editorial on the issue of patient-centered management.
Careful patient selection for different tests is important, “and physician and technical local expertise, availability, quality of equipment, and patient preference are extremely important factors to consider. There is not enough emphasis on this important point,” contend the authors. “This is an important limitation of the guideline.”
Other issues of concern include “lack of balance in the document’s presentation of the science on FFR-CT [fractional flow reserve assessment with computed tomography] and its inappropriately prominent endorsement,” the editorial states.
The U.S. Food and Drug Administration–recognized “limitations and contraindications” to FFR-CT tend to be glossed over in the document, Dr. Thompson said. And most ASNC board members were “concerned with the prominent location of the recommendations for FFR-CT in various tables – especially since there was minimal-to-no discussion of the fact that it is currently provided by only one company, that it is not widely available nor covered routinely by health insurance carriers, and [that] the accuracy in the most relevant population is disputed.”
In other concerns, the document “inadequately discusses the benefit” of combining coronary artery calcium (CAC) scores with functional testing, which ASNC said it supports. For example, adding CAC scores to myocardial perfusion imaging improves its diagnostic accuracy and prognostic power.
Functional vs. anatomic testing?
Moreover, “it is no longer appropriate to bundle all types of stress testing together. All stress imaging tests have their unique advantages and limitations.” Yet, “the concept of the dichotomy of functional testing versus anatomic testing is a common theme in the guideline in many important patient groups,” the editorial states. That could overemphasize CT angiography and thus “blur distinction between different types of functional tests.”
Such concerns about “imbalance” in the portrayals of the two kinds of tests were “amplified by the problem of health insurance companies and radiologic benefits managers inappropriately substituting a test that was ordered by a physician with a different test,” Dr. Thompson elaborated. “There is the impression that some of them ‘cherry-pick’ certain guidelines and that this practice is harmful to patients.”
The ASNC currently does not plan its own corresponding guideline, he said. But the editorial says that “over the coming weeks and months ASNC will offer a series of webinars and other programs that address specific patient populations and dilemmas.” Also, “we will enhance our focus on programs to address quality and efficiency to support a patient-first approach to imaging.”
The five subspecialty groups that have endorsed the document are the American Society of Echocardiography, American College of Chest Physicians, Society for Academic Emergency Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance.
Dr. Thompson has reported no relevant financial relationships. Statements of disclosure for the other editorial writers are listed in the publication.
A version of this article first appeared on Medscape.com.
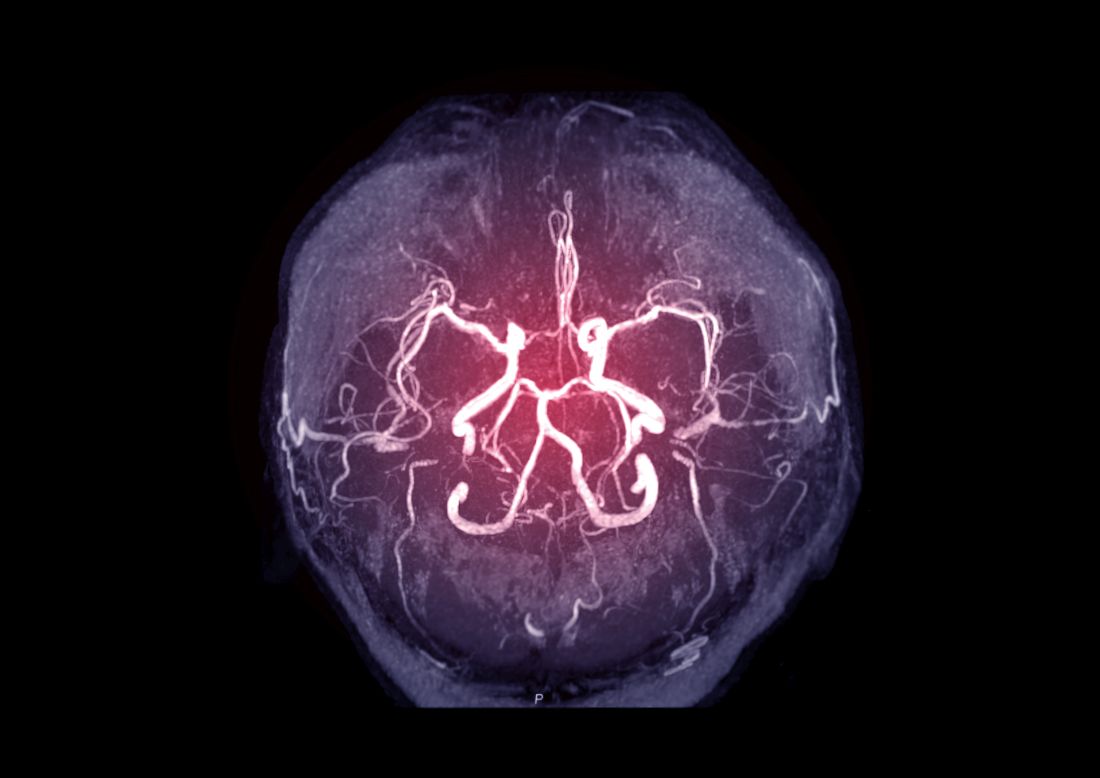
Neuroimaging may predict cognitive decline after chemotherapy for breast cancer
“Cognitive decline is frequently observed after chemotherapy,” according to Michiel B. de Ruiter, PhD, a research scientist with the Netherlands Cancer Institute in Amsterdam. He specializes in cognitive neuroscience and was the lead author of a study published online Sept. 30, 2021, in the Journal of Clinical Oncology. Dr. de Ruiter and colleagues found that fractional anisotropy may demonstrate a low brain white-matter reserve which could be a risk factor for cognitive decline after chemotherapy for breast cancer treatment.
Cognitive decline after chemotherapy has been reported in 20%-40% of patients with cancer affecting quality of life and daily living skills. Studies have suggested that genetic makeup, advanced age, fatigue, and premorbid intelligence quotient are risk factors for chemotherapy-associated cognitive decline. Changes in the microstructure of brain white matter, known as brain reserve, have been reported after exposure to chemotherapy, but its link to cognitive decline is understudied. Several studies outside of oncology have used MRI to derive fractional anisotropy as a measure for brain reserve.
In the new JCO study, researchers examined fractional anisotropy, as measured by MRI, before chemotherapy. The analysis included 49 patients who underwent neuropsychological tests before treatment with anthracycline-based chemotherapy, then again at 6 months and 2 years after chemotherapy.
The results were compared with those of patients with breast cancer who did not receive systemic therapy and then with a control group consisting of patients without cancer.
A low fractional anisotropy score suggested cognitive decline more than 3 years after receiving chemotherapy treatment. The finding was independent of age, premorbid intelligence quotient, baseline fatigue and baseline cognitive complaints. And, having low premorbid intelligence quotient was an independent risk factor for chemotherapy-associated cognitive decline, which the authors said is in line with previous findings.
Fractional anisotropy did not predict cognitive decline in patients who did not receive systemic therapy, as well as patients in the control group.
The findings could possibly lead to the development a pretreatment assessment to screen for patients who may at risk for cognitive decline, the authors wrote. “Clinically validated assessments of white-matter reserve as assessed with an MRI scan may be part of a pretreatment screening. This could also aid in early identification of cognitive decline after chemotherapy, allowing targeted and early interventions to improve cognitive problems,” such as psychoeducation and cognitive rehabilitation.
No potential conflicts of interest were reported.
“Cognitive decline is frequently observed after chemotherapy,” according to Michiel B. de Ruiter, PhD, a research scientist with the Netherlands Cancer Institute in Amsterdam. He specializes in cognitive neuroscience and was the lead author of a study published online Sept. 30, 2021, in the Journal of Clinical Oncology. Dr. de Ruiter and colleagues found that fractional anisotropy may demonstrate a low brain white-matter reserve which could be a risk factor for cognitive decline after chemotherapy for breast cancer treatment.
Cognitive decline after chemotherapy has been reported in 20%-40% of patients with cancer affecting quality of life and daily living skills. Studies have suggested that genetic makeup, advanced age, fatigue, and premorbid intelligence quotient are risk factors for chemotherapy-associated cognitive decline. Changes in the microstructure of brain white matter, known as brain reserve, have been reported after exposure to chemotherapy, but its link to cognitive decline is understudied. Several studies outside of oncology have used MRI to derive fractional anisotropy as a measure for brain reserve.
In the new JCO study, researchers examined fractional anisotropy, as measured by MRI, before chemotherapy. The analysis included 49 patients who underwent neuropsychological tests before treatment with anthracycline-based chemotherapy, then again at 6 months and 2 years after chemotherapy.
The results were compared with those of patients with breast cancer who did not receive systemic therapy and then with a control group consisting of patients without cancer.
A low fractional anisotropy score suggested cognitive decline more than 3 years after receiving chemotherapy treatment. The finding was independent of age, premorbid intelligence quotient, baseline fatigue and baseline cognitive complaints. And, having low premorbid intelligence quotient was an independent risk factor for chemotherapy-associated cognitive decline, which the authors said is in line with previous findings.
Fractional anisotropy did not predict cognitive decline in patients who did not receive systemic therapy, as well as patients in the control group.
The findings could possibly lead to the development a pretreatment assessment to screen for patients who may at risk for cognitive decline, the authors wrote. “Clinically validated assessments of white-matter reserve as assessed with an MRI scan may be part of a pretreatment screening. This could also aid in early identification of cognitive decline after chemotherapy, allowing targeted and early interventions to improve cognitive problems,” such as psychoeducation and cognitive rehabilitation.
No potential conflicts of interest were reported.
“Cognitive decline is frequently observed after chemotherapy,” according to Michiel B. de Ruiter, PhD, a research scientist with the Netherlands Cancer Institute in Amsterdam. He specializes in cognitive neuroscience and was the lead author of a study published online Sept. 30, 2021, in the Journal of Clinical Oncology. Dr. de Ruiter and colleagues found that fractional anisotropy may demonstrate a low brain white-matter reserve which could be a risk factor for cognitive decline after chemotherapy for breast cancer treatment.
Cognitive decline after chemotherapy has been reported in 20%-40% of patients with cancer affecting quality of life and daily living skills. Studies have suggested that genetic makeup, advanced age, fatigue, and premorbid intelligence quotient are risk factors for chemotherapy-associated cognitive decline. Changes in the microstructure of brain white matter, known as brain reserve, have been reported after exposure to chemotherapy, but its link to cognitive decline is understudied. Several studies outside of oncology have used MRI to derive fractional anisotropy as a measure for brain reserve.
In the new JCO study, researchers examined fractional anisotropy, as measured by MRI, before chemotherapy. The analysis included 49 patients who underwent neuropsychological tests before treatment with anthracycline-based chemotherapy, then again at 6 months and 2 years after chemotherapy.
The results were compared with those of patients with breast cancer who did not receive systemic therapy and then with a control group consisting of patients without cancer.
A low fractional anisotropy score suggested cognitive decline more than 3 years after receiving chemotherapy treatment. The finding was independent of age, premorbid intelligence quotient, baseline fatigue and baseline cognitive complaints. And, having low premorbid intelligence quotient was an independent risk factor for chemotherapy-associated cognitive decline, which the authors said is in line with previous findings.
Fractional anisotropy did not predict cognitive decline in patients who did not receive systemic therapy, as well as patients in the control group.
The findings could possibly lead to the development a pretreatment assessment to screen for patients who may at risk for cognitive decline, the authors wrote. “Clinically validated assessments of white-matter reserve as assessed with an MRI scan may be part of a pretreatment screening. This could also aid in early identification of cognitive decline after chemotherapy, allowing targeted and early interventions to improve cognitive problems,” such as psychoeducation and cognitive rehabilitation.
No potential conflicts of interest were reported.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Study points to ideal age for CAC testing in young adults
New risk equations can help determine the need for a first coronary artery calcium (CAC) scan in young adults to identify those most at risk for premature atherosclerosis, researchers say.
“To our knowledge this is the first time to derive a clinical risk equation for the initial conversion from CAC 0, which can be used actually to guide the timing of CAC testing in young adults,” Omar Dzaye, MD, MPH, PhD, Johns Hopkins University School of Medicine, Baltimore, said in an interview.
CAC is an independent predictor of adverse atherosclerotic cardiovascular disease (ASCVD), but routine screening is not recommended in low-risk groups. U.S. guidelines say CAC testing may be considered (class IIa) for risk stratification in adults 40 to 75 years at intermediate risk (estimated 10-year ASCVD risk 7.5% to 20%) when the decision to start preventive therapies is unclear.
The new sex-specific risk equations were derived from 22,346 adults 30 to 50 years of age who underwent CAC testing between 1991 and 2010 for ASCVD risk prediction at four high-volume centers in the CAC Consortium. The average age was 43.5 years, 25% were women, and 12.3% were non-White.
The participants were free of clinical ASCVD or CV symptoms at the time of scanning but had underlying traditional ASCVD risk factors (dyslipidemia in 49.6%, hypertension in 20.0%, active smokers 11.0%, and diabetes in 4.0%), an intermediate 10-year ASCVD risk (2.6%), and/or a significant family history of CHD (49.3%).
As reported in the Journal of the American College of Cardiology, 92.7% of participants had a low 10-year ASCVD risk below 5%, but 34.4% had CAC scores above 0 (median, 20 Agatston units).
Assuming a 25% testing yield (number needed to scan equals four to detect one CAC score above 0), the optimal age for a first scan in young men without risk factors was 42.3 years, and for women it was 57.6 years.
Young adults with one or more risk factors, however, would convert to CAC above 0 at least 3.3 years earlier on average. Diabetes had the strongest influence on the probability of conversion, with men and women predicted to develop incident CAC a respective 5.5 years and 7.3 years earlier on average.
The findings build on previous observations by the team showing that diabetes confers a 40% reduction in the so-called “warranty period” of a CAC score of 0, Dr. Dzaye noted. The National Lipid Association 2020 statement on CAC scoring also suggests it’s reasonable to obtain a CAC scan in people with diabetes aged 30 to 39 years.
“The predicted utility of CAC for ASCVD outcomes is similar in type 1 and type 2 diabetes; however, individuals with type 1 diabetes may actually develop CAC as young as 17 years of age,” he said. “Therefore, definitely, CAC studies in this population are required.”
In contrast, hypertension, dyslipidemia, active smoking, and a family history of CHD were individually associated with the development of CAC 3.3 to 4.3 years earlier. In general, the time to premature CAC was longer for women than for men with a given risk-factor profile.
The predicted age for a first CAC was 37.5 years for men and 48.9 years for women with an intermediate risk-factor profile (for example, smoking plus hypertension) and 33.8 years and 44.7 years, respectively, for those with a high-risk profile (for example, diabetes plus dyslipidemia).
Asked whether the risk equations can be used to guide CAC scanning in clinical practice, Dr. Dzaye said, “we very much believe that this can be used because for the process we published the internal validation, and we also did an external validation that is not published at the moment in [the] MESA [trial].”
He pointed out that study participants did not have a second CAC scan for true modeling of longitudinal CAC and do not represent the general population but, rather, a general cardiology referral population enriched with ASCVD risk factors. Future studies are needed that incorporate a more diverse population, multiple CAC scans, and genetic risk factors.
“This is helpful from a descriptive, epidemiologic point of view and helps us understand the approximate prevalence of coronary calcium greater than 0 in younger men and women, but I’m not convinced that it will or should change clinical practice,” cardiologist Philip Greenland, MD, a professor of preventive medicine and professor of medicine at Northwestern University in Chicago, said in an interview.
Dr. Greenland, who coauthored a review on CAC testing earlier this month, said CAC is the strongest tool we have to improve risk prediction beyond standard risk scores but does involve radiation exposure and some added costs. CAC testing is especially useful as a tiebreaker in older intermediate-risk patients who may be on the fence about starting primary prevention medications but could fall short among “younger, low-risk patients where, as they show here, the proportion of people who have a positive test is well below half.”
“So that means you’re going to have a very large number of people who are CAC 0, which is what we would expect in relatively younger people, but I wouldn’t be happy to try to explain that to a patient: ‘We’re not seeing coronary atherosclerosis right now, but we still want to treat your risk factors.’ That’s kind of a dissonant message,” Dr. Greenland said.
An accompanying editorial suggests “the study has filled an important clinical gap, providing highly actionable data that could help guide clinical decision making for ASCVD prevention.”
Nevertheless, Tasneem Naqvi, MD, Mayo Clinic, Scottsdale, Arizona, and Tamar Polonsky, MD, University of Chicago, question the generalizability of the results and point out that CAC screening at the authors’ recommended ages “could still miss a substantial number of young women with incident MI.”
Exposure to ionizing radiation with CAC is lower than that used in screening mammography for breast cancer but, they agree, should be considered, particularly in young women.
“Alternatively, ultrasonography avoids radiation altogether and can detect plaque earlier than the development of CAC,” write Dr. Naqvi and Dr. Polonsky. Further, the 2019 European Society of Cardiology guidelines for CV risk give ultrasound assessment of carotid artery and femoral plaque a class IIa recommendation and CAC a class IIb recommendation.
Commenting for this news organization, Roger Blumenthal, MD, director of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, said the class IIb recommendation “never really made any sense because the data with coronary calcium is so much stronger than it is with carotid ultrasound.”
“Sometimes smart scientists and researchers differ, but in my strong opinion, the European Society of Cardiology in 2019 did not give it the right classification, while the group I was part of, the American Heart Association/American College of Cardiology [2019 guideline], got it right and emphasized that this is the most cost-effective and useful way to improve risk assessment.”
Dr. Blumenthal, who was not part of the study, noted that U.S. guidelines say CAC measurement is not intended as a screening test for everyone but may be used selectively as a decision aid.
“This study adds to the information about how to use that type of testing. So, I personally think it will be a highly referenced article in the next set of guidelines that the American Heart Association, American College of Cardiology, and other organizations have.”
The study was supported in part by a research grant from the National Institutes of Health National Heart, Lung, and Blood Institute. Dr. Dzaye, Dr. Blumenthal, Dr. Naqvi, and Dr. Polonsky report having no relevant financial relationships.
A version of this article appeared on Medscape.com.
New risk equations can help determine the need for a first coronary artery calcium (CAC) scan in young adults to identify those most at risk for premature atherosclerosis, researchers say.
“To our knowledge this is the first time to derive a clinical risk equation for the initial conversion from CAC 0, which can be used actually to guide the timing of CAC testing in young adults,” Omar Dzaye, MD, MPH, PhD, Johns Hopkins University School of Medicine, Baltimore, said in an interview.
CAC is an independent predictor of adverse atherosclerotic cardiovascular disease (ASCVD), but routine screening is not recommended in low-risk groups. U.S. guidelines say CAC testing may be considered (class IIa) for risk stratification in adults 40 to 75 years at intermediate risk (estimated 10-year ASCVD risk 7.5% to 20%) when the decision to start preventive therapies is unclear.
The new sex-specific risk equations were derived from 22,346 adults 30 to 50 years of age who underwent CAC testing between 1991 and 2010 for ASCVD risk prediction at four high-volume centers in the CAC Consortium. The average age was 43.5 years, 25% were women, and 12.3% were non-White.
The participants were free of clinical ASCVD or CV symptoms at the time of scanning but had underlying traditional ASCVD risk factors (dyslipidemia in 49.6%, hypertension in 20.0%, active smokers 11.0%, and diabetes in 4.0%), an intermediate 10-year ASCVD risk (2.6%), and/or a significant family history of CHD (49.3%).
As reported in the Journal of the American College of Cardiology, 92.7% of participants had a low 10-year ASCVD risk below 5%, but 34.4% had CAC scores above 0 (median, 20 Agatston units).
Assuming a 25% testing yield (number needed to scan equals four to detect one CAC score above 0), the optimal age for a first scan in young men without risk factors was 42.3 years, and for women it was 57.6 years.
Young adults with one or more risk factors, however, would convert to CAC above 0 at least 3.3 years earlier on average. Diabetes had the strongest influence on the probability of conversion, with men and women predicted to develop incident CAC a respective 5.5 years and 7.3 years earlier on average.
The findings build on previous observations by the team showing that diabetes confers a 40% reduction in the so-called “warranty period” of a CAC score of 0, Dr. Dzaye noted. The National Lipid Association 2020 statement on CAC scoring also suggests it’s reasonable to obtain a CAC scan in people with diabetes aged 30 to 39 years.
“The predicted utility of CAC for ASCVD outcomes is similar in type 1 and type 2 diabetes; however, individuals with type 1 diabetes may actually develop CAC as young as 17 years of age,” he said. “Therefore, definitely, CAC studies in this population are required.”
In contrast, hypertension, dyslipidemia, active smoking, and a family history of CHD were individually associated with the development of CAC 3.3 to 4.3 years earlier. In general, the time to premature CAC was longer for women than for men with a given risk-factor profile.
The predicted age for a first CAC was 37.5 years for men and 48.9 years for women with an intermediate risk-factor profile (for example, smoking plus hypertension) and 33.8 years and 44.7 years, respectively, for those with a high-risk profile (for example, diabetes plus dyslipidemia).
Asked whether the risk equations can be used to guide CAC scanning in clinical practice, Dr. Dzaye said, “we very much believe that this can be used because for the process we published the internal validation, and we also did an external validation that is not published at the moment in [the] MESA [trial].”
He pointed out that study participants did not have a second CAC scan for true modeling of longitudinal CAC and do not represent the general population but, rather, a general cardiology referral population enriched with ASCVD risk factors. Future studies are needed that incorporate a more diverse population, multiple CAC scans, and genetic risk factors.
“This is helpful from a descriptive, epidemiologic point of view and helps us understand the approximate prevalence of coronary calcium greater than 0 in younger men and women, but I’m not convinced that it will or should change clinical practice,” cardiologist Philip Greenland, MD, a professor of preventive medicine and professor of medicine at Northwestern University in Chicago, said in an interview.
Dr. Greenland, who coauthored a review on CAC testing earlier this month, said CAC is the strongest tool we have to improve risk prediction beyond standard risk scores but does involve radiation exposure and some added costs. CAC testing is especially useful as a tiebreaker in older intermediate-risk patients who may be on the fence about starting primary prevention medications but could fall short among “younger, low-risk patients where, as they show here, the proportion of people who have a positive test is well below half.”
“So that means you’re going to have a very large number of people who are CAC 0, which is what we would expect in relatively younger people, but I wouldn’t be happy to try to explain that to a patient: ‘We’re not seeing coronary atherosclerosis right now, but we still want to treat your risk factors.’ That’s kind of a dissonant message,” Dr. Greenland said.
An accompanying editorial suggests “the study has filled an important clinical gap, providing highly actionable data that could help guide clinical decision making for ASCVD prevention.”
Nevertheless, Tasneem Naqvi, MD, Mayo Clinic, Scottsdale, Arizona, and Tamar Polonsky, MD, University of Chicago, question the generalizability of the results and point out that CAC screening at the authors’ recommended ages “could still miss a substantial number of young women with incident MI.”
Exposure to ionizing radiation with CAC is lower than that used in screening mammography for breast cancer but, they agree, should be considered, particularly in young women.
“Alternatively, ultrasonography avoids radiation altogether and can detect plaque earlier than the development of CAC,” write Dr. Naqvi and Dr. Polonsky. Further, the 2019 European Society of Cardiology guidelines for CV risk give ultrasound assessment of carotid artery and femoral plaque a class IIa recommendation and CAC a class IIb recommendation.
Commenting for this news organization, Roger Blumenthal, MD, director of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, said the class IIb recommendation “never really made any sense because the data with coronary calcium is so much stronger than it is with carotid ultrasound.”
“Sometimes smart scientists and researchers differ, but in my strong opinion, the European Society of Cardiology in 2019 did not give it the right classification, while the group I was part of, the American Heart Association/American College of Cardiology [2019 guideline], got it right and emphasized that this is the most cost-effective and useful way to improve risk assessment.”
Dr. Blumenthal, who was not part of the study, noted that U.S. guidelines say CAC measurement is not intended as a screening test for everyone but may be used selectively as a decision aid.
“This study adds to the information about how to use that type of testing. So, I personally think it will be a highly referenced article in the next set of guidelines that the American Heart Association, American College of Cardiology, and other organizations have.”
The study was supported in part by a research grant from the National Institutes of Health National Heart, Lung, and Blood Institute. Dr. Dzaye, Dr. Blumenthal, Dr. Naqvi, and Dr. Polonsky report having no relevant financial relationships.
A version of this article appeared on Medscape.com.
New risk equations can help determine the need for a first coronary artery calcium (CAC) scan in young adults to identify those most at risk for premature atherosclerosis, researchers say.
“To our knowledge this is the first time to derive a clinical risk equation for the initial conversion from CAC 0, which can be used actually to guide the timing of CAC testing in young adults,” Omar Dzaye, MD, MPH, PhD, Johns Hopkins University School of Medicine, Baltimore, said in an interview.
CAC is an independent predictor of adverse atherosclerotic cardiovascular disease (ASCVD), but routine screening is not recommended in low-risk groups. U.S. guidelines say CAC testing may be considered (class IIa) for risk stratification in adults 40 to 75 years at intermediate risk (estimated 10-year ASCVD risk 7.5% to 20%) when the decision to start preventive therapies is unclear.
The new sex-specific risk equations were derived from 22,346 adults 30 to 50 years of age who underwent CAC testing between 1991 and 2010 for ASCVD risk prediction at four high-volume centers in the CAC Consortium. The average age was 43.5 years, 25% were women, and 12.3% were non-White.
The participants were free of clinical ASCVD or CV symptoms at the time of scanning but had underlying traditional ASCVD risk factors (dyslipidemia in 49.6%, hypertension in 20.0%, active smokers 11.0%, and diabetes in 4.0%), an intermediate 10-year ASCVD risk (2.6%), and/or a significant family history of CHD (49.3%).
As reported in the Journal of the American College of Cardiology, 92.7% of participants had a low 10-year ASCVD risk below 5%, but 34.4% had CAC scores above 0 (median, 20 Agatston units).
Assuming a 25% testing yield (number needed to scan equals four to detect one CAC score above 0), the optimal age for a first scan in young men without risk factors was 42.3 years, and for women it was 57.6 years.
Young adults with one or more risk factors, however, would convert to CAC above 0 at least 3.3 years earlier on average. Diabetes had the strongest influence on the probability of conversion, with men and women predicted to develop incident CAC a respective 5.5 years and 7.3 years earlier on average.
The findings build on previous observations by the team showing that diabetes confers a 40% reduction in the so-called “warranty period” of a CAC score of 0, Dr. Dzaye noted. The National Lipid Association 2020 statement on CAC scoring also suggests it’s reasonable to obtain a CAC scan in people with diabetes aged 30 to 39 years.
“The predicted utility of CAC for ASCVD outcomes is similar in type 1 and type 2 diabetes; however, individuals with type 1 diabetes may actually develop CAC as young as 17 years of age,” he said. “Therefore, definitely, CAC studies in this population are required.”
In contrast, hypertension, dyslipidemia, active smoking, and a family history of CHD were individually associated with the development of CAC 3.3 to 4.3 years earlier. In general, the time to premature CAC was longer for women than for men with a given risk-factor profile.
The predicted age for a first CAC was 37.5 years for men and 48.9 years for women with an intermediate risk-factor profile (for example, smoking plus hypertension) and 33.8 years and 44.7 years, respectively, for those with a high-risk profile (for example, diabetes plus dyslipidemia).
Asked whether the risk equations can be used to guide CAC scanning in clinical practice, Dr. Dzaye said, “we very much believe that this can be used because for the process we published the internal validation, and we also did an external validation that is not published at the moment in [the] MESA [trial].”
He pointed out that study participants did not have a second CAC scan for true modeling of longitudinal CAC and do not represent the general population but, rather, a general cardiology referral population enriched with ASCVD risk factors. Future studies are needed that incorporate a more diverse population, multiple CAC scans, and genetic risk factors.
“This is helpful from a descriptive, epidemiologic point of view and helps us understand the approximate prevalence of coronary calcium greater than 0 in younger men and women, but I’m not convinced that it will or should change clinical practice,” cardiologist Philip Greenland, MD, a professor of preventive medicine and professor of medicine at Northwestern University in Chicago, said in an interview.
Dr. Greenland, who coauthored a review on CAC testing earlier this month, said CAC is the strongest tool we have to improve risk prediction beyond standard risk scores but does involve radiation exposure and some added costs. CAC testing is especially useful as a tiebreaker in older intermediate-risk patients who may be on the fence about starting primary prevention medications but could fall short among “younger, low-risk patients where, as they show here, the proportion of people who have a positive test is well below half.”
“So that means you’re going to have a very large number of people who are CAC 0, which is what we would expect in relatively younger people, but I wouldn’t be happy to try to explain that to a patient: ‘We’re not seeing coronary atherosclerosis right now, but we still want to treat your risk factors.’ That’s kind of a dissonant message,” Dr. Greenland said.
An accompanying editorial suggests “the study has filled an important clinical gap, providing highly actionable data that could help guide clinical decision making for ASCVD prevention.”
Nevertheless, Tasneem Naqvi, MD, Mayo Clinic, Scottsdale, Arizona, and Tamar Polonsky, MD, University of Chicago, question the generalizability of the results and point out that CAC screening at the authors’ recommended ages “could still miss a substantial number of young women with incident MI.”
Exposure to ionizing radiation with CAC is lower than that used in screening mammography for breast cancer but, they agree, should be considered, particularly in young women.
“Alternatively, ultrasonography avoids radiation altogether and can detect plaque earlier than the development of CAC,” write Dr. Naqvi and Dr. Polonsky. Further, the 2019 European Society of Cardiology guidelines for CV risk give ultrasound assessment of carotid artery and femoral plaque a class IIa recommendation and CAC a class IIb recommendation.
Commenting for this news organization, Roger Blumenthal, MD, director of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, said the class IIb recommendation “never really made any sense because the data with coronary calcium is so much stronger than it is with carotid ultrasound.”
“Sometimes smart scientists and researchers differ, but in my strong opinion, the European Society of Cardiology in 2019 did not give it the right classification, while the group I was part of, the American Heart Association/American College of Cardiology [2019 guideline], got it right and emphasized that this is the most cost-effective and useful way to improve risk assessment.”
Dr. Blumenthal, who was not part of the study, noted that U.S. guidelines say CAC measurement is not intended as a screening test for everyone but may be used selectively as a decision aid.
“This study adds to the information about how to use that type of testing. So, I personally think it will be a highly referenced article in the next set of guidelines that the American Heart Association, American College of Cardiology, and other organizations have.”
The study was supported in part by a research grant from the National Institutes of Health National Heart, Lung, and Blood Institute. Dr. Dzaye, Dr. Blumenthal, Dr. Naqvi, and Dr. Polonsky report having no relevant financial relationships.
A version of this article appeared on Medscape.com.
POCUS in hospital pediatrics
PHM 2021 Session
Safe and (Ultra)sound: Why you should use POCUS in your Pediatric Practice
Presenter
Ria Dancel, MD, FAAP, FACP
Session summary
Dr. Ria Dancel and her colleagues from the University of North Carolina at Chapel Hill presented a broad overview of point-of-care ultrasound (POCUS) applications in the field of pediatric hospital medicine. They discussed its advantages and potential uses, ranging from common scenarios to critical care to procedural guidance. Using illustrative scenarios and interactive cases, she discussed the bedside applications to improve care of hospitalized children. The benefits and risks of radiography and POCUS were reviewed.
The session highlighted the use of POCUS in SSTI (skin and soft tissue infection) to help with differentiating cellulitis from abscesses. Use of POCUS for safer incision and drainages and making day-to-day changes in management was discussed. The ease and benefits of performing real-time lung ultrasound in different pathologies (like pneumonia, effusion, COVID-19) was presented. The speakers discussed the use of POCUS in emergency situations like hypotension and different types of shock. The use of ultrasound in common bedside procedures (bladder catheterization, lumbar ultrasound, peripheral IV placement) were also highlighted. Current literature and evidence were reviewed.
Key takeaways
- Pediatric POCUS is an extremely valuable bedside tool in pediatric hospital medicine.
- It can be used to guide clinical care for many conditions including SSTI, pneumonia, and shock.
- It can be used for procedural guidance for bladder catheterization, lumbar puncture, and intravenous access.
Dr. Patra is a pediatric hospitalist at West Virginia University Children’s Hospital, Morgantown, and associate professor at West Virginia University School of Medicine. He is interested in medical education, quality improvement and clinical research. He is a member of the Executive Council of the Pediatric Special Interest Group of the Society of Hospital Medicine.
PHM 2021 Session
Safe and (Ultra)sound: Why you should use POCUS in your Pediatric Practice
Presenter
Ria Dancel, MD, FAAP, FACP
Session summary
Dr. Ria Dancel and her colleagues from the University of North Carolina at Chapel Hill presented a broad overview of point-of-care ultrasound (POCUS) applications in the field of pediatric hospital medicine. They discussed its advantages and potential uses, ranging from common scenarios to critical care to procedural guidance. Using illustrative scenarios and interactive cases, she discussed the bedside applications to improve care of hospitalized children. The benefits and risks of radiography and POCUS were reviewed.
The session highlighted the use of POCUS in SSTI (skin and soft tissue infection) to help with differentiating cellulitis from abscesses. Use of POCUS for safer incision and drainages and making day-to-day changes in management was discussed. The ease and benefits of performing real-time lung ultrasound in different pathologies (like pneumonia, effusion, COVID-19) was presented. The speakers discussed the use of POCUS in emergency situations like hypotension and different types of shock. The use of ultrasound in common bedside procedures (bladder catheterization, lumbar ultrasound, peripheral IV placement) were also highlighted. Current literature and evidence were reviewed.
Key takeaways
- Pediatric POCUS is an extremely valuable bedside tool in pediatric hospital medicine.
- It can be used to guide clinical care for many conditions including SSTI, pneumonia, and shock.
- It can be used for procedural guidance for bladder catheterization, lumbar puncture, and intravenous access.
Dr. Patra is a pediatric hospitalist at West Virginia University Children’s Hospital, Morgantown, and associate professor at West Virginia University School of Medicine. He is interested in medical education, quality improvement and clinical research. He is a member of the Executive Council of the Pediatric Special Interest Group of the Society of Hospital Medicine.
PHM 2021 Session
Safe and (Ultra)sound: Why you should use POCUS in your Pediatric Practice
Presenter
Ria Dancel, MD, FAAP, FACP
Session summary
Dr. Ria Dancel and her colleagues from the University of North Carolina at Chapel Hill presented a broad overview of point-of-care ultrasound (POCUS) applications in the field of pediatric hospital medicine. They discussed its advantages and potential uses, ranging from common scenarios to critical care to procedural guidance. Using illustrative scenarios and interactive cases, she discussed the bedside applications to improve care of hospitalized children. The benefits and risks of radiography and POCUS were reviewed.
The session highlighted the use of POCUS in SSTI (skin and soft tissue infection) to help with differentiating cellulitis from abscesses. Use of POCUS for safer incision and drainages and making day-to-day changes in management was discussed. The ease and benefits of performing real-time lung ultrasound in different pathologies (like pneumonia, effusion, COVID-19) was presented. The speakers discussed the use of POCUS in emergency situations like hypotension and different types of shock. The use of ultrasound in common bedside procedures (bladder catheterization, lumbar ultrasound, peripheral IV placement) were also highlighted. Current literature and evidence were reviewed.
Key takeaways
- Pediatric POCUS is an extremely valuable bedside tool in pediatric hospital medicine.
- It can be used to guide clinical care for many conditions including SSTI, pneumonia, and shock.
- It can be used for procedural guidance for bladder catheterization, lumbar puncture, and intravenous access.
Dr. Patra is a pediatric hospitalist at West Virginia University Children’s Hospital, Morgantown, and associate professor at West Virginia University School of Medicine. He is interested in medical education, quality improvement and clinical research. He is a member of the Executive Council of the Pediatric Special Interest Group of the Society of Hospital Medicine.
In all-comer approach, FFR adds no value to angiography: RIPCORD 2
Study confirms selective application
In patients with coronary artery disease scheduled for a percutaneous intervention (PCI), fractional flow reserve (FFR) assessment at the time of angiography significantly improves outcome, but it has no apparent value as a routine study in all CAD patients, according to the randomized RIPCORD 2 trial.
When compared to angiography alone in an all comer-strategy, the addition of FFR did not significantly change management or lower costs, but it was associated with a longer time for diagnostic assessment and more complications, Nicholas P. Curzen, BM, PhD, reported at the annual congress of the European Society of Cardiology.
As a tool for evaluating stenotic lesions in diseased vessels, FFR, also known as pressure wire assessment, allows interventionalists to target those vessels that induce ischemia without unnecessarily treating vessels with lesions that are hemodynamically nonsignificant. It is guideline recommended for patients with scheduled PCI on the basis of several randomized trials, including the landmark FAME trial.
“The results of these trials were spectacular. The clinical outcomes were significantly better in the FFR group despite less stents being placed and fewer vessels being stented. And there was significantly less resource utilization in the FFR group,” said Dr. Curzen, professor of interventional cardiology, University of Southampton, England.
Hypothesis: All-comers benefit from FFR
This prompted the new trial, called RIPCORD 2. The hypothesis was that systematic FFR early in the diagnosis of CAD would reduce resource utilization and improve quality of life relative to angiography alone. Both were addressed as primary endpoints. A reduction in clinical events at 12 months was a secondary endpoint.
The 1,136 participants, all scheduled for angiographic evaluation for stable angina or non-ST elevated myocardial infarction (NSTEMI), were randomized at 17 participating centers in the United Kingdom. All underwent angiography, but the experimental arm also underwent FFR for all arteries of a size suitable for revascularization.
Resource utilization evaluated through hospital costs at 12 months was somewhat higher in the FFR group, but the difference was not significant (P =.137). There was also no significant difference (P = 0.88) between the groups in quality of life, which was measured with EQ-5D-5L, an instrument for expressing five dimensions of health on a visual analog scale.
No impact from FFR on clinical events
Furthermore, there was no difference in the rate of clinical events, whether measured by a composite endpoint of major adverse cardiac events (MACE) (P = .64) or by the components of death, stroke, myocardial infarction, and unplanned revascularization, according to Dr. Curzen.
Finally, FFR did not appear to influence subsequent management. When the intervention and control groups were compared, the proportions triaged to optimal medical therapy, optimal medical therapy plus PCI, or optimal medical therapy plus bypass grafting did not differ significantly.
Given the lack of significant differences for FFR plus angiography relative to angiography alone for any clinically relevant outcome, the addition of FFR provides "no overall advantage" in this all comer study population, Dr. Curzen concluded.
However, FFR was associated with some relative disadvantages. These included significantly longer mean procedure times (69 vs. 42.4 minutes; P < .001), significantly greater mean use of contrast (206 vs. 146.3 mL; P < .001), and a significantly higher mean radiation dose (6608.7 vs. 5029.7 cGY/cm2; P < .001). There were 10 complications (1.8%) associated with FFR.
RIPCORD 1 results provided study rationale
In the previously published nonrandomized RIPCORD 1 study, interventionalists were asked to develop a management plan on the basis of angiography alone in 200 patients with stable chest pain. When these interventionalists were then provided with FFR results, the new information resulted in a change of management plan in 36% of cases.
According to Dr. Curzen, it was this study that raised all-comer FFR as a “logical and clinically plausible question.” RIPCORD 2 provided the answer.
While he is now conducting an evaluation of a subgroup of RIPCORD 2 patients with more severe disease, “it appears that the atheroma burden on angiography is adequate” to make an appropriate management determination in most or all cases.
The invited discussant for this study, Robert Byrne, MD, BCh, PhD, director of cardiology, Mater Private Hospital, Dublin, pointed out that more angiography-alone patients in RIPCORD 2 required additional evaluation to develop a management strategy (14.7% vs. 1.8%), but he agreed that FFR offered “no reasonable benefit” in the relatively low-risk patients who were enrolled.
Results do not alter FFR indications
However, he emphasized that the lack of an advantage in this trial should in no way diminish the evidence of benefit for selective FFR use as currently recommended in guidelines. This was echoed strongly in remarks by two other interventionalists who served on the same panel after the RIPCORD 2 results were presented.
“I want to make sure that our audience does not walk away thinking that FFR is useless. This is not what was shown,” said Roxana Mehran, MD, director of interventional cardiovascular research at Icahn School of Medicine at Mount Sinai, New York. She emphasized that this was a study that found no value in a low-risk, all-comer population and is not relevant to the populations where it now has an indication.
Marco Roffi, MD, director of the interventional cardiology unit, Geneva University Hospitals, made the same point.
“These results do not take away the value of FFR in a more selected population [than that enrolled in RIPCORD 2],” Dr. Roffi said. He did not rule out the potential for benefit from adding FFR to angiography even in early disease assessment if a benefit can be demonstrated in a higher-risk population.
Dr. Curzen reports financial relationships with Abbott, Beckman Coulter, HeartFlow, and Boston Scientific, which provided funding for RIPCORD 2. Dr. Byrne reported financial relationships with the trial sponsor as well as Abbott, Biosensors, and Biotronik. Dr. Mehran reports financial relationships with more than 15 medical product companies including the sponsor of this trial. Dr. Roffi reports no relevant financial disclosures.
Study confirms selective application
Study confirms selective application
In patients with coronary artery disease scheduled for a percutaneous intervention (PCI), fractional flow reserve (FFR) assessment at the time of angiography significantly improves outcome, but it has no apparent value as a routine study in all CAD patients, according to the randomized RIPCORD 2 trial.
When compared to angiography alone in an all comer-strategy, the addition of FFR did not significantly change management or lower costs, but it was associated with a longer time for diagnostic assessment and more complications, Nicholas P. Curzen, BM, PhD, reported at the annual congress of the European Society of Cardiology.
As a tool for evaluating stenotic lesions in diseased vessels, FFR, also known as pressure wire assessment, allows interventionalists to target those vessels that induce ischemia without unnecessarily treating vessels with lesions that are hemodynamically nonsignificant. It is guideline recommended for patients with scheduled PCI on the basis of several randomized trials, including the landmark FAME trial.
“The results of these trials were spectacular. The clinical outcomes were significantly better in the FFR group despite less stents being placed and fewer vessels being stented. And there was significantly less resource utilization in the FFR group,” said Dr. Curzen, professor of interventional cardiology, University of Southampton, England.
Hypothesis: All-comers benefit from FFR
This prompted the new trial, called RIPCORD 2. The hypothesis was that systematic FFR early in the diagnosis of CAD would reduce resource utilization and improve quality of life relative to angiography alone. Both were addressed as primary endpoints. A reduction in clinical events at 12 months was a secondary endpoint.
The 1,136 participants, all scheduled for angiographic evaluation for stable angina or non-ST elevated myocardial infarction (NSTEMI), were randomized at 17 participating centers in the United Kingdom. All underwent angiography, but the experimental arm also underwent FFR for all arteries of a size suitable for revascularization.
Resource utilization evaluated through hospital costs at 12 months was somewhat higher in the FFR group, but the difference was not significant (P =.137). There was also no significant difference (P = 0.88) between the groups in quality of life, which was measured with EQ-5D-5L, an instrument for expressing five dimensions of health on a visual analog scale.
No impact from FFR on clinical events
Furthermore, there was no difference in the rate of clinical events, whether measured by a composite endpoint of major adverse cardiac events (MACE) (P = .64) or by the components of death, stroke, myocardial infarction, and unplanned revascularization, according to Dr. Curzen.
Finally, FFR did not appear to influence subsequent management. When the intervention and control groups were compared, the proportions triaged to optimal medical therapy, optimal medical therapy plus PCI, or optimal medical therapy plus bypass grafting did not differ significantly.
Given the lack of significant differences for FFR plus angiography relative to angiography alone for any clinically relevant outcome, the addition of FFR provides "no overall advantage" in this all comer study population, Dr. Curzen concluded.
However, FFR was associated with some relative disadvantages. These included significantly longer mean procedure times (69 vs. 42.4 minutes; P < .001), significantly greater mean use of contrast (206 vs. 146.3 mL; P < .001), and a significantly higher mean radiation dose (6608.7 vs. 5029.7 cGY/cm2; P < .001). There were 10 complications (1.8%) associated with FFR.
RIPCORD 1 results provided study rationale
In the previously published nonrandomized RIPCORD 1 study, interventionalists were asked to develop a management plan on the basis of angiography alone in 200 patients with stable chest pain. When these interventionalists were then provided with FFR results, the new information resulted in a change of management plan in 36% of cases.
According to Dr. Curzen, it was this study that raised all-comer FFR as a “logical and clinically plausible question.” RIPCORD 2 provided the answer.
While he is now conducting an evaluation of a subgroup of RIPCORD 2 patients with more severe disease, “it appears that the atheroma burden on angiography is adequate” to make an appropriate management determination in most or all cases.
The invited discussant for this study, Robert Byrne, MD, BCh, PhD, director of cardiology, Mater Private Hospital, Dublin, pointed out that more angiography-alone patients in RIPCORD 2 required additional evaluation to develop a management strategy (14.7% vs. 1.8%), but he agreed that FFR offered “no reasonable benefit” in the relatively low-risk patients who were enrolled.
Results do not alter FFR indications
However, he emphasized that the lack of an advantage in this trial should in no way diminish the evidence of benefit for selective FFR use as currently recommended in guidelines. This was echoed strongly in remarks by two other interventionalists who served on the same panel after the RIPCORD 2 results were presented.
“I want to make sure that our audience does not walk away thinking that FFR is useless. This is not what was shown,” said Roxana Mehran, MD, director of interventional cardiovascular research at Icahn School of Medicine at Mount Sinai, New York. She emphasized that this was a study that found no value in a low-risk, all-comer population and is not relevant to the populations where it now has an indication.
Marco Roffi, MD, director of the interventional cardiology unit, Geneva University Hospitals, made the same point.
“These results do not take away the value of FFR in a more selected population [than that enrolled in RIPCORD 2],” Dr. Roffi said. He did not rule out the potential for benefit from adding FFR to angiography even in early disease assessment if a benefit can be demonstrated in a higher-risk population.
Dr. Curzen reports financial relationships with Abbott, Beckman Coulter, HeartFlow, and Boston Scientific, which provided funding for RIPCORD 2. Dr. Byrne reported financial relationships with the trial sponsor as well as Abbott, Biosensors, and Biotronik. Dr. Mehran reports financial relationships with more than 15 medical product companies including the sponsor of this trial. Dr. Roffi reports no relevant financial disclosures.
In patients with coronary artery disease scheduled for a percutaneous intervention (PCI), fractional flow reserve (FFR) assessment at the time of angiography significantly improves outcome, but it has no apparent value as a routine study in all CAD patients, according to the randomized RIPCORD 2 trial.
When compared to angiography alone in an all comer-strategy, the addition of FFR did not significantly change management or lower costs, but it was associated with a longer time for diagnostic assessment and more complications, Nicholas P. Curzen, BM, PhD, reported at the annual congress of the European Society of Cardiology.
As a tool for evaluating stenotic lesions in diseased vessels, FFR, also known as pressure wire assessment, allows interventionalists to target those vessels that induce ischemia without unnecessarily treating vessels with lesions that are hemodynamically nonsignificant. It is guideline recommended for patients with scheduled PCI on the basis of several randomized trials, including the landmark FAME trial.
“The results of these trials were spectacular. The clinical outcomes were significantly better in the FFR group despite less stents being placed and fewer vessels being stented. And there was significantly less resource utilization in the FFR group,” said Dr. Curzen, professor of interventional cardiology, University of Southampton, England.
Hypothesis: All-comers benefit from FFR
This prompted the new trial, called RIPCORD 2. The hypothesis was that systematic FFR early in the diagnosis of CAD would reduce resource utilization and improve quality of life relative to angiography alone. Both were addressed as primary endpoints. A reduction in clinical events at 12 months was a secondary endpoint.
The 1,136 participants, all scheduled for angiographic evaluation for stable angina or non-ST elevated myocardial infarction (NSTEMI), were randomized at 17 participating centers in the United Kingdom. All underwent angiography, but the experimental arm also underwent FFR for all arteries of a size suitable for revascularization.
Resource utilization evaluated through hospital costs at 12 months was somewhat higher in the FFR group, but the difference was not significant (P =.137). There was also no significant difference (P = 0.88) between the groups in quality of life, which was measured with EQ-5D-5L, an instrument for expressing five dimensions of health on a visual analog scale.
No impact from FFR on clinical events
Furthermore, there was no difference in the rate of clinical events, whether measured by a composite endpoint of major adverse cardiac events (MACE) (P = .64) or by the components of death, stroke, myocardial infarction, and unplanned revascularization, according to Dr. Curzen.
Finally, FFR did not appear to influence subsequent management. When the intervention and control groups were compared, the proportions triaged to optimal medical therapy, optimal medical therapy plus PCI, or optimal medical therapy plus bypass grafting did not differ significantly.
Given the lack of significant differences for FFR plus angiography relative to angiography alone for any clinically relevant outcome, the addition of FFR provides "no overall advantage" in this all comer study population, Dr. Curzen concluded.
However, FFR was associated with some relative disadvantages. These included significantly longer mean procedure times (69 vs. 42.4 minutes; P < .001), significantly greater mean use of contrast (206 vs. 146.3 mL; P < .001), and a significantly higher mean radiation dose (6608.7 vs. 5029.7 cGY/cm2; P < .001). There were 10 complications (1.8%) associated with FFR.
RIPCORD 1 results provided study rationale
In the previously published nonrandomized RIPCORD 1 study, interventionalists were asked to develop a management plan on the basis of angiography alone in 200 patients with stable chest pain. When these interventionalists were then provided with FFR results, the new information resulted in a change of management plan in 36% of cases.
According to Dr. Curzen, it was this study that raised all-comer FFR as a “logical and clinically plausible question.” RIPCORD 2 provided the answer.
While he is now conducting an evaluation of a subgroup of RIPCORD 2 patients with more severe disease, “it appears that the atheroma burden on angiography is adequate” to make an appropriate management determination in most or all cases.
The invited discussant for this study, Robert Byrne, MD, BCh, PhD, director of cardiology, Mater Private Hospital, Dublin, pointed out that more angiography-alone patients in RIPCORD 2 required additional evaluation to develop a management strategy (14.7% vs. 1.8%), but he agreed that FFR offered “no reasonable benefit” in the relatively low-risk patients who were enrolled.
Results do not alter FFR indications
However, he emphasized that the lack of an advantage in this trial should in no way diminish the evidence of benefit for selective FFR use as currently recommended in guidelines. This was echoed strongly in remarks by two other interventionalists who served on the same panel after the RIPCORD 2 results were presented.
“I want to make sure that our audience does not walk away thinking that FFR is useless. This is not what was shown,” said Roxana Mehran, MD, director of interventional cardiovascular research at Icahn School of Medicine at Mount Sinai, New York. She emphasized that this was a study that found no value in a low-risk, all-comer population and is not relevant to the populations where it now has an indication.
Marco Roffi, MD, director of the interventional cardiology unit, Geneva University Hospitals, made the same point.
“These results do not take away the value of FFR in a more selected population [than that enrolled in RIPCORD 2],” Dr. Roffi said. He did not rule out the potential for benefit from adding FFR to angiography even in early disease assessment if a benefit can be demonstrated in a higher-risk population.
Dr. Curzen reports financial relationships with Abbott, Beckman Coulter, HeartFlow, and Boston Scientific, which provided funding for RIPCORD 2. Dr. Byrne reported financial relationships with the trial sponsor as well as Abbott, Biosensors, and Biotronik. Dr. Mehran reports financial relationships with more than 15 medical product companies including the sponsor of this trial. Dr. Roffi reports no relevant financial disclosures.
FROM ESC CONGRESS 2021
Use of point-of-care ultrasound (POCUS) for heart failure
Case
A 65-year-old woman presents to the emergency department with a chief complaint of shortness of breath for 3 days. Medical history is notable for moderate chronic obstructive pulmonary disorder, systolic heart failure with last known ejection fraction (EF) of 35% and type 2 diabetes complicated by hyperglycemia when on steroids. You are talking the case over with colleagues and they suggest point-of-care ultrasound (POCUS) would be useful in her case.
Brief overview of the issue
Once mainly used by ED and critical care physicians, POCUS is now a tool that many hospitalists are using at the bedside. POCUS differs from traditional comprehensive ultrasounds in the following ways: POCUS is designed to answer a specific clinical question (as opposed to evaluating all organs in a specific region), POCUS exams are performed by the clinician who is formulating the clinical question (as opposed to by a consultative service such as cardiology and radiology), and POCUS can evaluate multiple organ systems (such as by evaluating a patient’s heart, lungs, and inferior vena cava to determine the etiology of hypoxia).
Hospitalist use of POCUS may include guiding procedures, aiding in diagnosis, and assessing effectiveness of treatment. Many high-quality studies have been published that support the use of POCUS and have proven that POCUS can decrease medical errors, help reach diagnoses in a more expedited fashion, and complement or replace more advanced imaging.
A challenge of POCUS is that it is user dependent and there are no established standards for hospitalists in POCUS training. As the Society of Hospital Medicine position statement on POCUS points out, there is a significant difference between skill levels required to obtain a certificate of completion for POCUS training and a certificate of competency in POCUS. Therefore, it is recommended hospitalists work with local credentialing committees to delineate the requirements for POCUS use.
Overview of the data
POCUS for initial assessment and diagnosis of heart failure (HF)
Use of POCUS in cases of suspected HF includes examination of the heart, lungs, and inferior vena cava (IVC). Cardiac ultrasound provides an estimated ejection fraction. Lung ultrasound (LUS) functions to examine for B lines and pleural effusions. The presence of more than three B lines per thoracic zone bilaterally suggests cardiogenic pulmonary edema. Scanning the IVC provides a noninvasive way to assess volume status and is especially helpful when body habitus prevents accurate assessment of jugular venous pressure.
Several studies have addressed the utility of bedside ultrasound in the initial assessment or diagnosis of acute decompensated heart failure (ADHF) in patients presenting with dyspnea in emergency or inpatient settings. Positive B lines are a useful finding, with high sensitivities, high specificities, and positive likelihood ratios. One large multicenter prospective study found LUS to have a sensitivity of 90.5%, specificity of 93.5%, and positive and negative LRs of 14.0 and 0.10, respectively.1 Another large multicenter prospective cohort study showed that LUS was more sensitive and more specific than chest x-ray (CXR) and brain natriuretic peptide in detecting ADHF.2 Additional POCUS findings that have shown relatively high sensitivities and specificities in the initial diagnosis of ADHF include pleural effusion, reduced left ventricular ejection fraction (LVEF), increased left ventricular end-diastolic dimension, and jugular venous distention.
Data also exists on assessments of ADHF using combinations of POCUS findings; for example, lung and cardiac ultrasound (LuCUS) protocols include an evaluation for B lines, assessment of IVC size and collapsibility, and determination of LVEF, although this has mainly been examined in ED patients. For patients who presented to the ED with undifferentiated dyspnea, one such study showed a specificity of 100% when a LuCUS protocol was used to diagnose ADHF while another study showed that the use of a LuCUS protocol changed management in 47% of patients.3,4 Of note, although each LuCUS protocol integrated the use of lung findings, IVC collapsibility, and LVEF, the exact protocols varied by institution. Finally, it has been established in multiple studies that LUS used in addition to standard workup including history and physical, labs, and electrocardiogram has been shown to increase diagnostic accuracy.2,5
Using POCUS to guide diuretic therapy in HF
To date, there have been multiple small studies published on the utility of daily POCUS in hospitalized patients with ADHF to help assess response to treatment and guide diuresis by looking for reduction in B lines on LUS or a change in IVC size or collapsibility. Volpicelli and colleagues showed that daily LUS was at least as good as daily CXR in monitoring response to therapy.6 Similarly, Mozzini and colleagues performed a randomized controlled trial of 120 patients admitted for ADHF who were randomized to a CXR group (who had a CXR performed on admission and discharge) and a LUS group (which was performed at admission, 24 hours, 48 hours, 72 hours, and discharge).7 This study found that the LUS group underwent a significantly higher number of diuretic dose adjustments as compared with the CXR group (P < .001) and had a modest improvement in LOS, compared with the CXR group. Specifically, median LOS was 8 days in CXR group (range, 4-17 days) and 7 days in the LUS group (range, 3-10 days; P < .001).
The impact of POCUS on length of stay (LOS) and readmissions
There is increasing data that POCUS can have meaningful impacts on patient-centered outcomes (morbidity, mortality, and readmission) while exposing patients to minimal discomfort, no venipuncture, and no radiation exposure. First, multiple studies looked at whether performing focused cardiac US of the IVC as a marker of volume status could predict readmission in patients hospitalized for ADHF.8,9 Both of these trials showed that plethoric, noncollapsible IVC at discharge were statistically significant predictors of readmission. In fact, Goonewardena and colleagues demonstrated that patients who required readmission had an enlarged IVC at discharge nearly 3 times more frequently (21% vs. 61%, P < .001) and abnormal IVC collapsibility 1.5 times more frequently (41% vs. 71%, P = .01) as compared with patients who remained out of the hospital.9
Similarly, a subsequent trial looked at whether IVC size on admission was of prognostic importance in patients hospitalized for ADHF and showed that admission IVC diameter was an independent predictor of both 90-day mortality (hazard ratio, 5.88; 95% confidence interval, 1.21-28.10; P = .025) and 90-day readmission (HR, 3.20; 95% CI, 1.24-8.21; P = .016).10 Additionally, LUS heart failure assessment for pulmonary congestion by counting B lines also showed that having more than 15 B lines prior to discharge was an independent predictor of readmission for ADHF at 6 months (HR, 11.74; 95% CI, 1.30-106.16).11
A challenge of POCUS: Obtaining competency
As previously noted, there are not yet any established standards for training and assessing hospitalists in POCUS. The SHM Position Statement on POCUS recommends the following criteria for training5: the training environment should be similar to the location in which the trainee will practice, training and feedback should occur in real time, the trainee should be taught specific applications of POCUS (such as cardiac US, LUS, and IVC US) as each application comes with unique skills and knowledge, clinical competence must be achieved and demonstrated, and continued education and feedback are necessary once competence is obtained.12 SHM recommends residency-based training pathways, training through a local or national program such as the SHM POCUS certificate program, or training through other medical societies for hospitalists already in practice.
Application of the data to our original case
Targeted POCUS using the LuCUS protocol is performed and reveals three B lines in two lung zones bilaterally, moderate bilateral pleural effusions, EF 20%, and a noncollapsible IVC leading to a diagnosis of ADHF. Her ADHF is treated with intravenous diuresis. She is continued on her chronic maintenance chronic obstructive pulmonary disorder regimen but does not receive steroids, avoiding hyperglycemia that has complicated prior admissions. Over the next few days her respiratory and cardiac status is monitored using POCUS to assess her response to therapy and titrate her diuretics to her true dry weight, which was several pounds lower than her previously assumed dry weight. At discharge she is instructed to use the new dry weight which may avoid readmissions for HF.
Bottom line
POCUS improves diagnostic accuracy and facilitates volume assessment and management in acute decompensated heart failure.
Dr. Farber is a medical instructor at Duke University and hospitalist at Duke Regional Hospital, both in Durham, N.C. Dr. Marcantonio is a medical instructor in the department of internal medicine and department of pediatrics at Duke University and hospitalist at Duke University Hospital and Duke Regional Hospital. Dr. Stafford and Dr. Brooks are assistant professors of medicine and hospitalists at Duke Regional Hospital. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor at Duke University. Dr. Menon is a hospitalist at Duke University. Dr. Sharma is associate medical director for clinical education at Duke Regional Hospital and associate professor of medicine at Duke University.
References
1. Pivetta E et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: A randomized controlled trial. Eur J Heart Fail. 2019 Jun;21(6):754-66. doi: 10.1002/ejhf.1379.
2. Pivetta E et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest. 2015;148(1):202-10. doi: 10.1378/chest.14-2608.
3. Anderson KL et al. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31:1208-14. doi: 10.1016/j.ajem.2013.05.007.
4. Russell FM et al. Diagnosing acute heart failure in patients with undifferentiated dyspnea: A lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med. 2015;22(2):182-91. doi:10.1111/acem.12570.
5. Maw AM et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: A systematic review and meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703. doi:10.1001/jamanetworkopen.2019.0703.
6. Volpicelli G et al. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008 Jun;26(5):585-91. doi:10.1016/j.ajem.2007.09.014.
7. Mozzini C et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med. 2018 Jan;13(1):27-33. doi: 10.1007/s11739-017-1738-1.
8. Laffin LJ et al. Focused cardiac ultrasound as a predictor of readmission in acute decompensated heart failure. Int J Cardiovasc Imaging. 2018;34(7):1075-9. doi:10.1007/s10554-018-1317-1.
9. Goonewardena SN et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595-601. doi:10.1016/j.jcmg.2008.06.005.
10. Cubo-Romano P et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016 Nov;11(11):778-84. doi: 10.1002/jhm.2620.
11. Gargani L et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: A lung ultrasound study. Cardiovasc Ultrasound. 2015 Sep 4;13:40. doi: 10.1186/s12947-015-0033-4.
12. Soni NJ et al. Point-of-care ultrasound for hospitalists: A Position Statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2;14:E1-6. doi: 10.12788/jhm.3079.
Key points
- Studies have found POCUS improves the diagnosis of acute decompensated heart failure in patients presenting with dyspnea.
- Daily evaluation with POCUS has decreased length of stay in acute decompensated heart failure.
- Credentialing requirements for hospitalists to use POCUS for clinical care vary by hospital.
Additional reading
Maw AM and Soni NJ. Annals for hospitalists inpatient notes – why should hospitalists use point-of-care ultrasound? Ann Intern Med. 2018 Apr 17;168(8):HO2-HO3. doi: 10.7326/M18-0367.
Lewiss RE. “The ultrasound looked fine”: Point of care ultrasound and patient safety. AHRQ’s Patient Safety Network. WebM&M: Case Studies. 2018 Jul 1. https://psnet.ahrq.gov/web-mm/ultrasound-looked-fine-point-care-ultrasound-and-patient-safety.
Quiz: Testing your POCUS knowledge
POCUS is increasingly prevalent in hospital medicine, but use varies among different disease processes. Which organ system ultrasound or lab test would be most helpful in the following scenario?
An acutely dyspneic patient with no past medical history presents to the ED. Chest x-ray is equivocal. Of the following, which study best confirms a diagnosis of acute decompensated heart failure?
A. Brain natriuretic peptide
B. Point-of-care cardiac ultrasound
C. Point-of-care lung ultrasound
D. Point-of-care inferior vena cava ultrasound
Answer
C. Point-of-care lung ultrasound
Multiple studies, including three systematic reviews, have shown that point-of-care lung ultrasound has high sensitivity and specificity to evaluate for B lines as a marker for cardiogenic pulmonary edema. Point-of-care ultrasound of ejection fraction and inferior vena cava have not been evaluated by systematic review although one randomized, controlled trial showed that an EF less than 45% had 74% specificity and 77% sensitivity and IVC collapsibility index less than 20% had an 86% specificity and 52% sensitivity for detection of acute decompensated heart failure. This same study showed that the combination of cardiac, lung, and IVC point-of-care ultrasound had 100% specificity for diagnosing acute decompensated heart failure. In the future, health care providers could rely on this multiorgan evaluation with point-of-care ultrasound to confirm a diagnosis of acute decompensated heart failure in a dyspneic patient.
Case
A 65-year-old woman presents to the emergency department with a chief complaint of shortness of breath for 3 days. Medical history is notable for moderate chronic obstructive pulmonary disorder, systolic heart failure with last known ejection fraction (EF) of 35% and type 2 diabetes complicated by hyperglycemia when on steroids. You are talking the case over with colleagues and they suggest point-of-care ultrasound (POCUS) would be useful in her case.
Brief overview of the issue
Once mainly used by ED and critical care physicians, POCUS is now a tool that many hospitalists are using at the bedside. POCUS differs from traditional comprehensive ultrasounds in the following ways: POCUS is designed to answer a specific clinical question (as opposed to evaluating all organs in a specific region), POCUS exams are performed by the clinician who is formulating the clinical question (as opposed to by a consultative service such as cardiology and radiology), and POCUS can evaluate multiple organ systems (such as by evaluating a patient’s heart, lungs, and inferior vena cava to determine the etiology of hypoxia).
Hospitalist use of POCUS may include guiding procedures, aiding in diagnosis, and assessing effectiveness of treatment. Many high-quality studies have been published that support the use of POCUS and have proven that POCUS can decrease medical errors, help reach diagnoses in a more expedited fashion, and complement or replace more advanced imaging.
A challenge of POCUS is that it is user dependent and there are no established standards for hospitalists in POCUS training. As the Society of Hospital Medicine position statement on POCUS points out, there is a significant difference between skill levels required to obtain a certificate of completion for POCUS training and a certificate of competency in POCUS. Therefore, it is recommended hospitalists work with local credentialing committees to delineate the requirements for POCUS use.
Overview of the data
POCUS for initial assessment and diagnosis of heart failure (HF)
Use of POCUS in cases of suspected HF includes examination of the heart, lungs, and inferior vena cava (IVC). Cardiac ultrasound provides an estimated ejection fraction. Lung ultrasound (LUS) functions to examine for B lines and pleural effusions. The presence of more than three B lines per thoracic zone bilaterally suggests cardiogenic pulmonary edema. Scanning the IVC provides a noninvasive way to assess volume status and is especially helpful when body habitus prevents accurate assessment of jugular venous pressure.
Several studies have addressed the utility of bedside ultrasound in the initial assessment or diagnosis of acute decompensated heart failure (ADHF) in patients presenting with dyspnea in emergency or inpatient settings. Positive B lines are a useful finding, with high sensitivities, high specificities, and positive likelihood ratios. One large multicenter prospective study found LUS to have a sensitivity of 90.5%, specificity of 93.5%, and positive and negative LRs of 14.0 and 0.10, respectively.1 Another large multicenter prospective cohort study showed that LUS was more sensitive and more specific than chest x-ray (CXR) and brain natriuretic peptide in detecting ADHF.2 Additional POCUS findings that have shown relatively high sensitivities and specificities in the initial diagnosis of ADHF include pleural effusion, reduced left ventricular ejection fraction (LVEF), increased left ventricular end-diastolic dimension, and jugular venous distention.
Data also exists on assessments of ADHF using combinations of POCUS findings; for example, lung and cardiac ultrasound (LuCUS) protocols include an evaluation for B lines, assessment of IVC size and collapsibility, and determination of LVEF, although this has mainly been examined in ED patients. For patients who presented to the ED with undifferentiated dyspnea, one such study showed a specificity of 100% when a LuCUS protocol was used to diagnose ADHF while another study showed that the use of a LuCUS protocol changed management in 47% of patients.3,4 Of note, although each LuCUS protocol integrated the use of lung findings, IVC collapsibility, and LVEF, the exact protocols varied by institution. Finally, it has been established in multiple studies that LUS used in addition to standard workup including history and physical, labs, and electrocardiogram has been shown to increase diagnostic accuracy.2,5
Using POCUS to guide diuretic therapy in HF
To date, there have been multiple small studies published on the utility of daily POCUS in hospitalized patients with ADHF to help assess response to treatment and guide diuresis by looking for reduction in B lines on LUS or a change in IVC size or collapsibility. Volpicelli and colleagues showed that daily LUS was at least as good as daily CXR in monitoring response to therapy.6 Similarly, Mozzini and colleagues performed a randomized controlled trial of 120 patients admitted for ADHF who were randomized to a CXR group (who had a CXR performed on admission and discharge) and a LUS group (which was performed at admission, 24 hours, 48 hours, 72 hours, and discharge).7 This study found that the LUS group underwent a significantly higher number of diuretic dose adjustments as compared with the CXR group (P < .001) and had a modest improvement in LOS, compared with the CXR group. Specifically, median LOS was 8 days in CXR group (range, 4-17 days) and 7 days in the LUS group (range, 3-10 days; P < .001).
The impact of POCUS on length of stay (LOS) and readmissions
There is increasing data that POCUS can have meaningful impacts on patient-centered outcomes (morbidity, mortality, and readmission) while exposing patients to minimal discomfort, no venipuncture, and no radiation exposure. First, multiple studies looked at whether performing focused cardiac US of the IVC as a marker of volume status could predict readmission in patients hospitalized for ADHF.8,9 Both of these trials showed that plethoric, noncollapsible IVC at discharge were statistically significant predictors of readmission. In fact, Goonewardena and colleagues demonstrated that patients who required readmission had an enlarged IVC at discharge nearly 3 times more frequently (21% vs. 61%, P < .001) and abnormal IVC collapsibility 1.5 times more frequently (41% vs. 71%, P = .01) as compared with patients who remained out of the hospital.9
Similarly, a subsequent trial looked at whether IVC size on admission was of prognostic importance in patients hospitalized for ADHF and showed that admission IVC diameter was an independent predictor of both 90-day mortality (hazard ratio, 5.88; 95% confidence interval, 1.21-28.10; P = .025) and 90-day readmission (HR, 3.20; 95% CI, 1.24-8.21; P = .016).10 Additionally, LUS heart failure assessment for pulmonary congestion by counting B lines also showed that having more than 15 B lines prior to discharge was an independent predictor of readmission for ADHF at 6 months (HR, 11.74; 95% CI, 1.30-106.16).11
A challenge of POCUS: Obtaining competency
As previously noted, there are not yet any established standards for training and assessing hospitalists in POCUS. The SHM Position Statement on POCUS recommends the following criteria for training5: the training environment should be similar to the location in which the trainee will practice, training and feedback should occur in real time, the trainee should be taught specific applications of POCUS (such as cardiac US, LUS, and IVC US) as each application comes with unique skills and knowledge, clinical competence must be achieved and demonstrated, and continued education and feedback are necessary once competence is obtained.12 SHM recommends residency-based training pathways, training through a local or national program such as the SHM POCUS certificate program, or training through other medical societies for hospitalists already in practice.
Application of the data to our original case
Targeted POCUS using the LuCUS protocol is performed and reveals three B lines in two lung zones bilaterally, moderate bilateral pleural effusions, EF 20%, and a noncollapsible IVC leading to a diagnosis of ADHF. Her ADHF is treated with intravenous diuresis. She is continued on her chronic maintenance chronic obstructive pulmonary disorder regimen but does not receive steroids, avoiding hyperglycemia that has complicated prior admissions. Over the next few days her respiratory and cardiac status is monitored using POCUS to assess her response to therapy and titrate her diuretics to her true dry weight, which was several pounds lower than her previously assumed dry weight. At discharge she is instructed to use the new dry weight which may avoid readmissions for HF.
Bottom line
POCUS improves diagnostic accuracy and facilitates volume assessment and management in acute decompensated heart failure.
Dr. Farber is a medical instructor at Duke University and hospitalist at Duke Regional Hospital, both in Durham, N.C. Dr. Marcantonio is a medical instructor in the department of internal medicine and department of pediatrics at Duke University and hospitalist at Duke University Hospital and Duke Regional Hospital. Dr. Stafford and Dr. Brooks are assistant professors of medicine and hospitalists at Duke Regional Hospital. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor at Duke University. Dr. Menon is a hospitalist at Duke University. Dr. Sharma is associate medical director for clinical education at Duke Regional Hospital and associate professor of medicine at Duke University.
References
1. Pivetta E et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: A randomized controlled trial. Eur J Heart Fail. 2019 Jun;21(6):754-66. doi: 10.1002/ejhf.1379.
2. Pivetta E et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest. 2015;148(1):202-10. doi: 10.1378/chest.14-2608.
3. Anderson KL et al. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31:1208-14. doi: 10.1016/j.ajem.2013.05.007.
4. Russell FM et al. Diagnosing acute heart failure in patients with undifferentiated dyspnea: A lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med. 2015;22(2):182-91. doi:10.1111/acem.12570.
5. Maw AM et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: A systematic review and meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703. doi:10.1001/jamanetworkopen.2019.0703.
6. Volpicelli G et al. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008 Jun;26(5):585-91. doi:10.1016/j.ajem.2007.09.014.
7. Mozzini C et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med. 2018 Jan;13(1):27-33. doi: 10.1007/s11739-017-1738-1.
8. Laffin LJ et al. Focused cardiac ultrasound as a predictor of readmission in acute decompensated heart failure. Int J Cardiovasc Imaging. 2018;34(7):1075-9. doi:10.1007/s10554-018-1317-1.
9. Goonewardena SN et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595-601. doi:10.1016/j.jcmg.2008.06.005.
10. Cubo-Romano P et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016 Nov;11(11):778-84. doi: 10.1002/jhm.2620.
11. Gargani L et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: A lung ultrasound study. Cardiovasc Ultrasound. 2015 Sep 4;13:40. doi: 10.1186/s12947-015-0033-4.
12. Soni NJ et al. Point-of-care ultrasound for hospitalists: A Position Statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2;14:E1-6. doi: 10.12788/jhm.3079.
Key points
- Studies have found POCUS improves the diagnosis of acute decompensated heart failure in patients presenting with dyspnea.
- Daily evaluation with POCUS has decreased length of stay in acute decompensated heart failure.
- Credentialing requirements for hospitalists to use POCUS for clinical care vary by hospital.
Additional reading
Maw AM and Soni NJ. Annals for hospitalists inpatient notes – why should hospitalists use point-of-care ultrasound? Ann Intern Med. 2018 Apr 17;168(8):HO2-HO3. doi: 10.7326/M18-0367.
Lewiss RE. “The ultrasound looked fine”: Point of care ultrasound and patient safety. AHRQ’s Patient Safety Network. WebM&M: Case Studies. 2018 Jul 1. https://psnet.ahrq.gov/web-mm/ultrasound-looked-fine-point-care-ultrasound-and-patient-safety.
Quiz: Testing your POCUS knowledge
POCUS is increasingly prevalent in hospital medicine, but use varies among different disease processes. Which organ system ultrasound or lab test would be most helpful in the following scenario?
An acutely dyspneic patient with no past medical history presents to the ED. Chest x-ray is equivocal. Of the following, which study best confirms a diagnosis of acute decompensated heart failure?
A. Brain natriuretic peptide
B. Point-of-care cardiac ultrasound
C. Point-of-care lung ultrasound
D. Point-of-care inferior vena cava ultrasound
Answer
C. Point-of-care lung ultrasound
Multiple studies, including three systematic reviews, have shown that point-of-care lung ultrasound has high sensitivity and specificity to evaluate for B lines as a marker for cardiogenic pulmonary edema. Point-of-care ultrasound of ejection fraction and inferior vena cava have not been evaluated by systematic review although one randomized, controlled trial showed that an EF less than 45% had 74% specificity and 77% sensitivity and IVC collapsibility index less than 20% had an 86% specificity and 52% sensitivity for detection of acute decompensated heart failure. This same study showed that the combination of cardiac, lung, and IVC point-of-care ultrasound had 100% specificity for diagnosing acute decompensated heart failure. In the future, health care providers could rely on this multiorgan evaluation with point-of-care ultrasound to confirm a diagnosis of acute decompensated heart failure in a dyspneic patient.
Case
A 65-year-old woman presents to the emergency department with a chief complaint of shortness of breath for 3 days. Medical history is notable for moderate chronic obstructive pulmonary disorder, systolic heart failure with last known ejection fraction (EF) of 35% and type 2 diabetes complicated by hyperglycemia when on steroids. You are talking the case over with colleagues and they suggest point-of-care ultrasound (POCUS) would be useful in her case.
Brief overview of the issue
Once mainly used by ED and critical care physicians, POCUS is now a tool that many hospitalists are using at the bedside. POCUS differs from traditional comprehensive ultrasounds in the following ways: POCUS is designed to answer a specific clinical question (as opposed to evaluating all organs in a specific region), POCUS exams are performed by the clinician who is formulating the clinical question (as opposed to by a consultative service such as cardiology and radiology), and POCUS can evaluate multiple organ systems (such as by evaluating a patient’s heart, lungs, and inferior vena cava to determine the etiology of hypoxia).
Hospitalist use of POCUS may include guiding procedures, aiding in diagnosis, and assessing effectiveness of treatment. Many high-quality studies have been published that support the use of POCUS and have proven that POCUS can decrease medical errors, help reach diagnoses in a more expedited fashion, and complement or replace more advanced imaging.
A challenge of POCUS is that it is user dependent and there are no established standards for hospitalists in POCUS training. As the Society of Hospital Medicine position statement on POCUS points out, there is a significant difference between skill levels required to obtain a certificate of completion for POCUS training and a certificate of competency in POCUS. Therefore, it is recommended hospitalists work with local credentialing committees to delineate the requirements for POCUS use.
Overview of the data
POCUS for initial assessment and diagnosis of heart failure (HF)
Use of POCUS in cases of suspected HF includes examination of the heart, lungs, and inferior vena cava (IVC). Cardiac ultrasound provides an estimated ejection fraction. Lung ultrasound (LUS) functions to examine for B lines and pleural effusions. The presence of more than three B lines per thoracic zone bilaterally suggests cardiogenic pulmonary edema. Scanning the IVC provides a noninvasive way to assess volume status and is especially helpful when body habitus prevents accurate assessment of jugular venous pressure.
Several studies have addressed the utility of bedside ultrasound in the initial assessment or diagnosis of acute decompensated heart failure (ADHF) in patients presenting with dyspnea in emergency or inpatient settings. Positive B lines are a useful finding, with high sensitivities, high specificities, and positive likelihood ratios. One large multicenter prospective study found LUS to have a sensitivity of 90.5%, specificity of 93.5%, and positive and negative LRs of 14.0 and 0.10, respectively.1 Another large multicenter prospective cohort study showed that LUS was more sensitive and more specific than chest x-ray (CXR) and brain natriuretic peptide in detecting ADHF.2 Additional POCUS findings that have shown relatively high sensitivities and specificities in the initial diagnosis of ADHF include pleural effusion, reduced left ventricular ejection fraction (LVEF), increased left ventricular end-diastolic dimension, and jugular venous distention.
Data also exists on assessments of ADHF using combinations of POCUS findings; for example, lung and cardiac ultrasound (LuCUS) protocols include an evaluation for B lines, assessment of IVC size and collapsibility, and determination of LVEF, although this has mainly been examined in ED patients. For patients who presented to the ED with undifferentiated dyspnea, one such study showed a specificity of 100% when a LuCUS protocol was used to diagnose ADHF while another study showed that the use of a LuCUS protocol changed management in 47% of patients.3,4 Of note, although each LuCUS protocol integrated the use of lung findings, IVC collapsibility, and LVEF, the exact protocols varied by institution. Finally, it has been established in multiple studies that LUS used in addition to standard workup including history and physical, labs, and electrocardiogram has been shown to increase diagnostic accuracy.2,5
Using POCUS to guide diuretic therapy in HF
To date, there have been multiple small studies published on the utility of daily POCUS in hospitalized patients with ADHF to help assess response to treatment and guide diuresis by looking for reduction in B lines on LUS or a change in IVC size or collapsibility. Volpicelli and colleagues showed that daily LUS was at least as good as daily CXR in monitoring response to therapy.6 Similarly, Mozzini and colleagues performed a randomized controlled trial of 120 patients admitted for ADHF who were randomized to a CXR group (who had a CXR performed on admission and discharge) and a LUS group (which was performed at admission, 24 hours, 48 hours, 72 hours, and discharge).7 This study found that the LUS group underwent a significantly higher number of diuretic dose adjustments as compared with the CXR group (P < .001) and had a modest improvement in LOS, compared with the CXR group. Specifically, median LOS was 8 days in CXR group (range, 4-17 days) and 7 days in the LUS group (range, 3-10 days; P < .001).
The impact of POCUS on length of stay (LOS) and readmissions
There is increasing data that POCUS can have meaningful impacts on patient-centered outcomes (morbidity, mortality, and readmission) while exposing patients to minimal discomfort, no venipuncture, and no radiation exposure. First, multiple studies looked at whether performing focused cardiac US of the IVC as a marker of volume status could predict readmission in patients hospitalized for ADHF.8,9 Both of these trials showed that plethoric, noncollapsible IVC at discharge were statistically significant predictors of readmission. In fact, Goonewardena and colleagues demonstrated that patients who required readmission had an enlarged IVC at discharge nearly 3 times more frequently (21% vs. 61%, P < .001) and abnormal IVC collapsibility 1.5 times more frequently (41% vs. 71%, P = .01) as compared with patients who remained out of the hospital.9
Similarly, a subsequent trial looked at whether IVC size on admission was of prognostic importance in patients hospitalized for ADHF and showed that admission IVC diameter was an independent predictor of both 90-day mortality (hazard ratio, 5.88; 95% confidence interval, 1.21-28.10; P = .025) and 90-day readmission (HR, 3.20; 95% CI, 1.24-8.21; P = .016).10 Additionally, LUS heart failure assessment for pulmonary congestion by counting B lines also showed that having more than 15 B lines prior to discharge was an independent predictor of readmission for ADHF at 6 months (HR, 11.74; 95% CI, 1.30-106.16).11
A challenge of POCUS: Obtaining competency
As previously noted, there are not yet any established standards for training and assessing hospitalists in POCUS. The SHM Position Statement on POCUS recommends the following criteria for training5: the training environment should be similar to the location in which the trainee will practice, training and feedback should occur in real time, the trainee should be taught specific applications of POCUS (such as cardiac US, LUS, and IVC US) as each application comes with unique skills and knowledge, clinical competence must be achieved and demonstrated, and continued education and feedback are necessary once competence is obtained.12 SHM recommends residency-based training pathways, training through a local or national program such as the SHM POCUS certificate program, or training through other medical societies for hospitalists already in practice.
Application of the data to our original case
Targeted POCUS using the LuCUS protocol is performed and reveals three B lines in two lung zones bilaterally, moderate bilateral pleural effusions, EF 20%, and a noncollapsible IVC leading to a diagnosis of ADHF. Her ADHF is treated with intravenous diuresis. She is continued on her chronic maintenance chronic obstructive pulmonary disorder regimen but does not receive steroids, avoiding hyperglycemia that has complicated prior admissions. Over the next few days her respiratory and cardiac status is monitored using POCUS to assess her response to therapy and titrate her diuretics to her true dry weight, which was several pounds lower than her previously assumed dry weight. At discharge she is instructed to use the new dry weight which may avoid readmissions for HF.
Bottom line
POCUS improves diagnostic accuracy and facilitates volume assessment and management in acute decompensated heart failure.
Dr. Farber is a medical instructor at Duke University and hospitalist at Duke Regional Hospital, both in Durham, N.C. Dr. Marcantonio is a medical instructor in the department of internal medicine and department of pediatrics at Duke University and hospitalist at Duke University Hospital and Duke Regional Hospital. Dr. Stafford and Dr. Brooks are assistant professors of medicine and hospitalists at Duke Regional Hospital. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor at Duke University. Dr. Menon is a hospitalist at Duke University. Dr. Sharma is associate medical director for clinical education at Duke Regional Hospital and associate professor of medicine at Duke University.
References
1. Pivetta E et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: A randomized controlled trial. Eur J Heart Fail. 2019 Jun;21(6):754-66. doi: 10.1002/ejhf.1379.
2. Pivetta E et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest. 2015;148(1):202-10. doi: 10.1378/chest.14-2608.
3. Anderson KL et al. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31:1208-14. doi: 10.1016/j.ajem.2013.05.007.
4. Russell FM et al. Diagnosing acute heart failure in patients with undifferentiated dyspnea: A lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med. 2015;22(2):182-91. doi:10.1111/acem.12570.
5. Maw AM et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: A systematic review and meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703. doi:10.1001/jamanetworkopen.2019.0703.
6. Volpicelli G et al. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008 Jun;26(5):585-91. doi:10.1016/j.ajem.2007.09.014.
7. Mozzini C et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med. 2018 Jan;13(1):27-33. doi: 10.1007/s11739-017-1738-1.
8. Laffin LJ et al. Focused cardiac ultrasound as a predictor of readmission in acute decompensated heart failure. Int J Cardiovasc Imaging. 2018;34(7):1075-9. doi:10.1007/s10554-018-1317-1.
9. Goonewardena SN et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595-601. doi:10.1016/j.jcmg.2008.06.005.
10. Cubo-Romano P et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016 Nov;11(11):778-84. doi: 10.1002/jhm.2620.
11. Gargani L et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: A lung ultrasound study. Cardiovasc Ultrasound. 2015 Sep 4;13:40. doi: 10.1186/s12947-015-0033-4.
12. Soni NJ et al. Point-of-care ultrasound for hospitalists: A Position Statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2;14:E1-6. doi: 10.12788/jhm.3079.
Key points
- Studies have found POCUS improves the diagnosis of acute decompensated heart failure in patients presenting with dyspnea.
- Daily evaluation with POCUS has decreased length of stay in acute decompensated heart failure.
- Credentialing requirements for hospitalists to use POCUS for clinical care vary by hospital.
Additional reading
Maw AM and Soni NJ. Annals for hospitalists inpatient notes – why should hospitalists use point-of-care ultrasound? Ann Intern Med. 2018 Apr 17;168(8):HO2-HO3. doi: 10.7326/M18-0367.
Lewiss RE. “The ultrasound looked fine”: Point of care ultrasound and patient safety. AHRQ’s Patient Safety Network. WebM&M: Case Studies. 2018 Jul 1. https://psnet.ahrq.gov/web-mm/ultrasound-looked-fine-point-care-ultrasound-and-patient-safety.
Quiz: Testing your POCUS knowledge
POCUS is increasingly prevalent in hospital medicine, but use varies among different disease processes. Which organ system ultrasound or lab test would be most helpful in the following scenario?
An acutely dyspneic patient with no past medical history presents to the ED. Chest x-ray is equivocal. Of the following, which study best confirms a diagnosis of acute decompensated heart failure?
A. Brain natriuretic peptide
B. Point-of-care cardiac ultrasound
C. Point-of-care lung ultrasound
D. Point-of-care inferior vena cava ultrasound
Answer
C. Point-of-care lung ultrasound
Multiple studies, including three systematic reviews, have shown that point-of-care lung ultrasound has high sensitivity and specificity to evaluate for B lines as a marker for cardiogenic pulmonary edema. Point-of-care ultrasound of ejection fraction and inferior vena cava have not been evaluated by systematic review although one randomized, controlled trial showed that an EF less than 45% had 74% specificity and 77% sensitivity and IVC collapsibility index less than 20% had an 86% specificity and 52% sensitivity for detection of acute decompensated heart failure. This same study showed that the combination of cardiac, lung, and IVC point-of-care ultrasound had 100% specificity for diagnosing acute decompensated heart failure. In the future, health care providers could rely on this multiorgan evaluation with point-of-care ultrasound to confirm a diagnosis of acute decompensated heart failure in a dyspneic patient.
Intracranial atherosclerosis finding on MRA linked to stroke
An incidental diagnosis of intracranial atherosclerotic stenosis in stroke-free individuals should trigger a thorough assessment of vascular health, according to the authors of a study identifying risk factors and vascular event risk in asymptomatic ICAS.
That conclusion emerged from data collected on more than 1,000 stroke-free participants in NOMAS (Northern Manhattan Study), a trial that prospectively followed participants who underwent a brain magnetic resonance angiogram (MRA) during 2003-2008.
In ICAS patients with stenosis of at least 70%, even with aggressive medical therapy, the annual stroke recurrence rate is 10%-20% in those with occlusions and at least three or more vascular risk factors. This high rate of recurrent vascular events in patients with stroke caused by ICAS warrants greater focus on primary prevention and targeted interventions for stroke-free individuals at highest risk for ICAS-related events, the investigators concluded.
Identify high-risk ICAS
Using NOMAS data, the investigators, led by Jose Gutierrez, MD, MPH, tested the hypothesis that stroke-free subjects at high risk of stroke and vascular events could be identified through the presence of asymptomatic ICAS. NOMAS is an ongoing, population-based epidemiologic study among randomly selected people with home telephones living in northern Manhattan.
During 2003-2008, investigators invited participants who were at least 50 years old, stroke free, and without contraindications to undergo brain MRA. The 1,211 study members were followed annually via telephone and in-person adjudication of events. A control group of 79 patients with no MRA was also identified with similar rates of hypertension, diabetes, hypercholesterolemia and current smoking.
Mean age was about 71 years (59% female, 65% Hispanic, 45% any stenosis). At the time of MRA, 78% had hypertension, 25% had diabetes, 81% had hypercholesterolemia, and 11% were current smokers.
Researchers rated stenoses in 11 brain arteries as 0, with no stenosis; 1, with less than 50% stenosis or luminal irregularities; 2, 50%-69% stenosis; and 3, at least 70% stenosis or flow gap. Outcomes included vascular death, myocardial infarction, ischemic stroke, cardioembolic stroke, intracranial artery disease stroke (which combined intracranial small and large artery disease strokes), and any vascular events (defined as a composite of vascular death, any stroke, or MI).
Greater stenosis denotes higher risk
Analysis found ICAS to be associated with older age (odds ratio, 1.02 per year; 95% confidence interval, 1.01-1.04), hypertension duration (OR, 1.01 per year; 95% CI, 1.00-1.02), higher number of glucose-lowering drugs (OR, 1.64 per each medication; 95% CI, 1.24-2.15), and HDL cholesterol(OR, 0.96 per mg/dL; 95% CI, 0.92-0.99). Event risk was greater among participants with ICAS of at least 70% (5.5% annual risk of vascular events; HR, 2.1; 95% CI, 1.4-3.2; compared with those with no ICAS), the investigators reported in the Journal of the American College of Cardiology.
Furthermore, 80% of incident strokes initially classified as small artery disease occurred among individuals with evidence of any degree of ICAS at their baseline MRI, the investigators noted. They found also that individuals with ICAS who had a primary care physician at the time of their initial MRI had a lower risk of events. Frequent primary care visits, they observed, might imply greater control of risk factors and other unmeasured confounders, such as health literacy, health care trust, access, and availability.
Incidental ICAS should trigger vascular assessment
An incidental diagnosis of ICAS in stroke-free subjects should trigger a thorough assessment of vascular health, the investigators concluded. They commented also that prophylaxis of first-ever stroke at this asymptomatic stage “may magnify the societal benefits of vascular prevention and decrease stroke-related disability and vascular death in our communities.”
“The big gap in our knowledge,” Tanya N. Turan, MD, professor of neurology at Medical University of South Carolina, Charleston, wrote in an accompanying editorial “is understanding the pathophysiological triggers for an asymptomatic stenosis to become a high-risk symptomatic stenosis. Until that question is answered, screening for asymptomatic ICAS is unlikely to change management among patients with known vascular risk factors.” In an interview, she observed further that “MRI plaque imaging could be a useful research tool to see if certain plaque features in an asymptomatic lesion are high risk for causing stroke. If that were proven, then it would make more sense to screen for ICAS and develop specific therapeutic strategies targeting high-risk asymptomatic plaque.”
Focus on recurrent stroke misplaced
Dr. Gutierrez said in an interview: “In the stroke world, most of what we do focuses on preventing recurrent stroke. Nonetheless, three-fourths of strokes in this country are new strokes, so to me it doesn’t make much sense to spend most of our efforts and attention to prevent the smallest fractions of strokes that occur in our society.”
He stressed that “the first immediate application of our results is that if people having a brain MRA for other reasons are found to have incidental, and therefore asymptomatic, ICAS, then they should be aggressively treated for vascular risk factors.” Secondly, “we hope to identify the patients at the highest risk of prevalent ICAS before they have a stroke. Among them, a brain MRI/MRA evaluating the phenotype would determine how aggressively to treat LDL.”
Dr. Gutierrez, professor of neurology at Columbia University Irving Medical Center, New York, noted that educating patients of their underlying high risk of events may have the effect of engaging them more in their own care. “There is evidence that actually showing people scans increases compliance and health literacy. It’s not yet standard of care, but we hope our future projects will help advance the field in the primary prevention direction,” he said.
This work was supported by the National Institutes of Health. The authors reported that they had no relevant financial disclosures.
An incidental diagnosis of intracranial atherosclerotic stenosis in stroke-free individuals should trigger a thorough assessment of vascular health, according to the authors of a study identifying risk factors and vascular event risk in asymptomatic ICAS.
That conclusion emerged from data collected on more than 1,000 stroke-free participants in NOMAS (Northern Manhattan Study), a trial that prospectively followed participants who underwent a brain magnetic resonance angiogram (MRA) during 2003-2008.
In ICAS patients with stenosis of at least 70%, even with aggressive medical therapy, the annual stroke recurrence rate is 10%-20% in those with occlusions and at least three or more vascular risk factors. This high rate of recurrent vascular events in patients with stroke caused by ICAS warrants greater focus on primary prevention and targeted interventions for stroke-free individuals at highest risk for ICAS-related events, the investigators concluded.
Identify high-risk ICAS
Using NOMAS data, the investigators, led by Jose Gutierrez, MD, MPH, tested the hypothesis that stroke-free subjects at high risk of stroke and vascular events could be identified through the presence of asymptomatic ICAS. NOMAS is an ongoing, population-based epidemiologic study among randomly selected people with home telephones living in northern Manhattan.
During 2003-2008, investigators invited participants who were at least 50 years old, stroke free, and without contraindications to undergo brain MRA. The 1,211 study members were followed annually via telephone and in-person adjudication of events. A control group of 79 patients with no MRA was also identified with similar rates of hypertension, diabetes, hypercholesterolemia and current smoking.
Mean age was about 71 years (59% female, 65% Hispanic, 45% any stenosis). At the time of MRA, 78% had hypertension, 25% had diabetes, 81% had hypercholesterolemia, and 11% were current smokers.
Researchers rated stenoses in 11 brain arteries as 0, with no stenosis; 1, with less than 50% stenosis or luminal irregularities; 2, 50%-69% stenosis; and 3, at least 70% stenosis or flow gap. Outcomes included vascular death, myocardial infarction, ischemic stroke, cardioembolic stroke, intracranial artery disease stroke (which combined intracranial small and large artery disease strokes), and any vascular events (defined as a composite of vascular death, any stroke, or MI).
Greater stenosis denotes higher risk
Analysis found ICAS to be associated with older age (odds ratio, 1.02 per year; 95% confidence interval, 1.01-1.04), hypertension duration (OR, 1.01 per year; 95% CI, 1.00-1.02), higher number of glucose-lowering drugs (OR, 1.64 per each medication; 95% CI, 1.24-2.15), and HDL cholesterol(OR, 0.96 per mg/dL; 95% CI, 0.92-0.99). Event risk was greater among participants with ICAS of at least 70% (5.5% annual risk of vascular events; HR, 2.1; 95% CI, 1.4-3.2; compared with those with no ICAS), the investigators reported in the Journal of the American College of Cardiology.
Furthermore, 80% of incident strokes initially classified as small artery disease occurred among individuals with evidence of any degree of ICAS at their baseline MRI, the investigators noted. They found also that individuals with ICAS who had a primary care physician at the time of their initial MRI had a lower risk of events. Frequent primary care visits, they observed, might imply greater control of risk factors and other unmeasured confounders, such as health literacy, health care trust, access, and availability.
Incidental ICAS should trigger vascular assessment
An incidental diagnosis of ICAS in stroke-free subjects should trigger a thorough assessment of vascular health, the investigators concluded. They commented also that prophylaxis of first-ever stroke at this asymptomatic stage “may magnify the societal benefits of vascular prevention and decrease stroke-related disability and vascular death in our communities.”
“The big gap in our knowledge,” Tanya N. Turan, MD, professor of neurology at Medical University of South Carolina, Charleston, wrote in an accompanying editorial “is understanding the pathophysiological triggers for an asymptomatic stenosis to become a high-risk symptomatic stenosis. Until that question is answered, screening for asymptomatic ICAS is unlikely to change management among patients with known vascular risk factors.” In an interview, she observed further that “MRI plaque imaging could be a useful research tool to see if certain plaque features in an asymptomatic lesion are high risk for causing stroke. If that were proven, then it would make more sense to screen for ICAS and develop specific therapeutic strategies targeting high-risk asymptomatic plaque.”
Focus on recurrent stroke misplaced
Dr. Gutierrez said in an interview: “In the stroke world, most of what we do focuses on preventing recurrent stroke. Nonetheless, three-fourths of strokes in this country are new strokes, so to me it doesn’t make much sense to spend most of our efforts and attention to prevent the smallest fractions of strokes that occur in our society.”
He stressed that “the first immediate application of our results is that if people having a brain MRA for other reasons are found to have incidental, and therefore asymptomatic, ICAS, then they should be aggressively treated for vascular risk factors.” Secondly, “we hope to identify the patients at the highest risk of prevalent ICAS before they have a stroke. Among them, a brain MRI/MRA evaluating the phenotype would determine how aggressively to treat LDL.”
Dr. Gutierrez, professor of neurology at Columbia University Irving Medical Center, New York, noted that educating patients of their underlying high risk of events may have the effect of engaging them more in their own care. “There is evidence that actually showing people scans increases compliance and health literacy. It’s not yet standard of care, but we hope our future projects will help advance the field in the primary prevention direction,” he said.
This work was supported by the National Institutes of Health. The authors reported that they had no relevant financial disclosures.
An incidental diagnosis of intracranial atherosclerotic stenosis in stroke-free individuals should trigger a thorough assessment of vascular health, according to the authors of a study identifying risk factors and vascular event risk in asymptomatic ICAS.
That conclusion emerged from data collected on more than 1,000 stroke-free participants in NOMAS (Northern Manhattan Study), a trial that prospectively followed participants who underwent a brain magnetic resonance angiogram (MRA) during 2003-2008.
In ICAS patients with stenosis of at least 70%, even with aggressive medical therapy, the annual stroke recurrence rate is 10%-20% in those with occlusions and at least three or more vascular risk factors. This high rate of recurrent vascular events in patients with stroke caused by ICAS warrants greater focus on primary prevention and targeted interventions for stroke-free individuals at highest risk for ICAS-related events, the investigators concluded.
Identify high-risk ICAS
Using NOMAS data, the investigators, led by Jose Gutierrez, MD, MPH, tested the hypothesis that stroke-free subjects at high risk of stroke and vascular events could be identified through the presence of asymptomatic ICAS. NOMAS is an ongoing, population-based epidemiologic study among randomly selected people with home telephones living in northern Manhattan.
During 2003-2008, investigators invited participants who were at least 50 years old, stroke free, and without contraindications to undergo brain MRA. The 1,211 study members were followed annually via telephone and in-person adjudication of events. A control group of 79 patients with no MRA was also identified with similar rates of hypertension, diabetes, hypercholesterolemia and current smoking.
Mean age was about 71 years (59% female, 65% Hispanic, 45% any stenosis). At the time of MRA, 78% had hypertension, 25% had diabetes, 81% had hypercholesterolemia, and 11% were current smokers.
Researchers rated stenoses in 11 brain arteries as 0, with no stenosis; 1, with less than 50% stenosis or luminal irregularities; 2, 50%-69% stenosis; and 3, at least 70% stenosis or flow gap. Outcomes included vascular death, myocardial infarction, ischemic stroke, cardioembolic stroke, intracranial artery disease stroke (which combined intracranial small and large artery disease strokes), and any vascular events (defined as a composite of vascular death, any stroke, or MI).
Greater stenosis denotes higher risk
Analysis found ICAS to be associated with older age (odds ratio, 1.02 per year; 95% confidence interval, 1.01-1.04), hypertension duration (OR, 1.01 per year; 95% CI, 1.00-1.02), higher number of glucose-lowering drugs (OR, 1.64 per each medication; 95% CI, 1.24-2.15), and HDL cholesterol(OR, 0.96 per mg/dL; 95% CI, 0.92-0.99). Event risk was greater among participants with ICAS of at least 70% (5.5% annual risk of vascular events; HR, 2.1; 95% CI, 1.4-3.2; compared with those with no ICAS), the investigators reported in the Journal of the American College of Cardiology.
Furthermore, 80% of incident strokes initially classified as small artery disease occurred among individuals with evidence of any degree of ICAS at their baseline MRI, the investigators noted. They found also that individuals with ICAS who had a primary care physician at the time of their initial MRI had a lower risk of events. Frequent primary care visits, they observed, might imply greater control of risk factors and other unmeasured confounders, such as health literacy, health care trust, access, and availability.
Incidental ICAS should trigger vascular assessment
An incidental diagnosis of ICAS in stroke-free subjects should trigger a thorough assessment of vascular health, the investigators concluded. They commented also that prophylaxis of first-ever stroke at this asymptomatic stage “may magnify the societal benefits of vascular prevention and decrease stroke-related disability and vascular death in our communities.”
“The big gap in our knowledge,” Tanya N. Turan, MD, professor of neurology at Medical University of South Carolina, Charleston, wrote in an accompanying editorial “is understanding the pathophysiological triggers for an asymptomatic stenosis to become a high-risk symptomatic stenosis. Until that question is answered, screening for asymptomatic ICAS is unlikely to change management among patients with known vascular risk factors.” In an interview, she observed further that “MRI plaque imaging could be a useful research tool to see if certain plaque features in an asymptomatic lesion are high risk for causing stroke. If that were proven, then it would make more sense to screen for ICAS and develop specific therapeutic strategies targeting high-risk asymptomatic plaque.”
Focus on recurrent stroke misplaced
Dr. Gutierrez said in an interview: “In the stroke world, most of what we do focuses on preventing recurrent stroke. Nonetheless, three-fourths of strokes in this country are new strokes, so to me it doesn’t make much sense to spend most of our efforts and attention to prevent the smallest fractions of strokes that occur in our society.”
He stressed that “the first immediate application of our results is that if people having a brain MRA for other reasons are found to have incidental, and therefore asymptomatic, ICAS, then they should be aggressively treated for vascular risk factors.” Secondly, “we hope to identify the patients at the highest risk of prevalent ICAS before they have a stroke. Among them, a brain MRI/MRA evaluating the phenotype would determine how aggressively to treat LDL.”
Dr. Gutierrez, professor of neurology at Columbia University Irving Medical Center, New York, noted that educating patients of their underlying high risk of events may have the effect of engaging them more in their own care. “There is evidence that actually showing people scans increases compliance and health literacy. It’s not yet standard of care, but we hope our future projects will help advance the field in the primary prevention direction,” he said.
This work was supported by the National Institutes of Health. The authors reported that they had no relevant financial disclosures.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
No prehydration prior to contrast-enhanced CT in patients with stage 3 CKD
Background: Postcontrast acute kidney injury (PC-AKI) is known to have a mild, often self-limiting, clinical course. Despite this, preventative measures are advised by international guidelines in high-risk patients.
Study design: The Kompas trial was a multicenter, open-label, noninferiority randomized clinical trial in which 523 patients with stage 3 CKD were randomized to receive no hydration or prehydration with 250 mL of 1.4% sodium bicarbonate in a 1-hour infusion before undergoing elective contrast-enhanced CT. The primary endpoint was the mean relative increase in serum creatinine 2-5 days after contrast administration, compared with baseline.
Setting: Six hospitals in the Netherlands during April 2013–September 2016.
Synopsis: Of the 523 patients, (median age, 74 years), the mean relative increase in creatinine level 2-5 days after contrast administration compared with baseline was 3.0% in the no-prehydration group vs. 3.5% in the prehydration group. This demonstrates that withholding prehydration is noninferior to administrating prehydration. PC-AKI occurred in 7 of 262 patients in the no-prehydration group and 4 of 261 patients in the prehydration group and no patients required dialysis or developed heart failure. These results reassure us that prehydration with sodium bicarbonate can be safely omitted in patients with stage 3 CKD who undergo contrast-enhanced CT.
Bottom line: Prehydration with sodium bicarbonate is not needed to prevent additional renal injury in patients with CKD stage 3 undergoing contrast-enhanced CT imaging.
Citation: Timal RJ et al. Effect of no prehydration vs sodium bicarbonate prehydration prior to contrast-enhanced computed tomography in the prevention of postcontrast acute kidney injury in adults with chronic kidney disease: The Kompas Randomized Clinical Trial. JAMA Intern Med. 2020 Feb 17. doi: 10.1001/jamainternmed.2019.7428.
Dr. Moulder is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Postcontrast acute kidney injury (PC-AKI) is known to have a mild, often self-limiting, clinical course. Despite this, preventative measures are advised by international guidelines in high-risk patients.
Study design: The Kompas trial was a multicenter, open-label, noninferiority randomized clinical trial in which 523 patients with stage 3 CKD were randomized to receive no hydration or prehydration with 250 mL of 1.4% sodium bicarbonate in a 1-hour infusion before undergoing elective contrast-enhanced CT. The primary endpoint was the mean relative increase in serum creatinine 2-5 days after contrast administration, compared with baseline.
Setting: Six hospitals in the Netherlands during April 2013–September 2016.
Synopsis: Of the 523 patients, (median age, 74 years), the mean relative increase in creatinine level 2-5 days after contrast administration compared with baseline was 3.0% in the no-prehydration group vs. 3.5% in the prehydration group. This demonstrates that withholding prehydration is noninferior to administrating prehydration. PC-AKI occurred in 7 of 262 patients in the no-prehydration group and 4 of 261 patients in the prehydration group and no patients required dialysis or developed heart failure. These results reassure us that prehydration with sodium bicarbonate can be safely omitted in patients with stage 3 CKD who undergo contrast-enhanced CT.
Bottom line: Prehydration with sodium bicarbonate is not needed to prevent additional renal injury in patients with CKD stage 3 undergoing contrast-enhanced CT imaging.
Citation: Timal RJ et al. Effect of no prehydration vs sodium bicarbonate prehydration prior to contrast-enhanced computed tomography in the prevention of postcontrast acute kidney injury in adults with chronic kidney disease: The Kompas Randomized Clinical Trial. JAMA Intern Med. 2020 Feb 17. doi: 10.1001/jamainternmed.2019.7428.
Dr. Moulder is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Postcontrast acute kidney injury (PC-AKI) is known to have a mild, often self-limiting, clinical course. Despite this, preventative measures are advised by international guidelines in high-risk patients.
Study design: The Kompas trial was a multicenter, open-label, noninferiority randomized clinical trial in which 523 patients with stage 3 CKD were randomized to receive no hydration or prehydration with 250 mL of 1.4% sodium bicarbonate in a 1-hour infusion before undergoing elective contrast-enhanced CT. The primary endpoint was the mean relative increase in serum creatinine 2-5 days after contrast administration, compared with baseline.
Setting: Six hospitals in the Netherlands during April 2013–September 2016.
Synopsis: Of the 523 patients, (median age, 74 years), the mean relative increase in creatinine level 2-5 days after contrast administration compared with baseline was 3.0% in the no-prehydration group vs. 3.5% in the prehydration group. This demonstrates that withholding prehydration is noninferior to administrating prehydration. PC-AKI occurred in 7 of 262 patients in the no-prehydration group and 4 of 261 patients in the prehydration group and no patients required dialysis or developed heart failure. These results reassure us that prehydration with sodium bicarbonate can be safely omitted in patients with stage 3 CKD who undergo contrast-enhanced CT.
Bottom line: Prehydration with sodium bicarbonate is not needed to prevent additional renal injury in patients with CKD stage 3 undergoing contrast-enhanced CT imaging.
Citation: Timal RJ et al. Effect of no prehydration vs sodium bicarbonate prehydration prior to contrast-enhanced computed tomography in the prevention of postcontrast acute kidney injury in adults with chronic kidney disease: The Kompas Randomized Clinical Trial. JAMA Intern Med. 2020 Feb 17. doi: 10.1001/jamainternmed.2019.7428.
Dr. Moulder is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Analysis supports CAC for personalizing statin use
In patients with intermediate risk of atherosclerotic cardiovascular disease along with risk-enhancing factors, coronary artery calcium scoring may help more precisely calculate their need for statin therapy.
Furthermore, when the need for statin treatment isn’t so clear and patients need additional risk assessment, the scoring can provide further information to personalize clinical decision making, according to a cross-sectional study of 1,688 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) published in JAMA Cardiology.
And regardless of coronary artery calcium (CAC), a low ankle brachial index (ABI) score is a marker for statin therapy, the study found.
The study looked at CAC scoring in the context of ABI and other risk-enhancing factors identified in the 2018 American Heart Association/American College of Cardiology cholesterol management guidelines: a family history of premature atherosclerotic cardiovascular disease (ASCVD), lipid and inflammatory biomarkers, chronic kidney disease, chronic inflammatory conditions, premature menopause or preeclampsia, and South Asian ancestry.
Any number of these factors can indicate the need for statins in people with borderline or intermediate risk. The guidelines also call for selective use of CAC to aid the decision-making process for statin therapy when the risk for developing atherosclerosis isn’t so clear.
“The novel risk-enhancing factors are not perfect,” said lead author Jaideep Patel, MD, director of preventive cardiology at Johns Hopkins Heart Center at Greater Baltimore Medical Center. He noted that the 2018 dyslipidemia guidelines suggested the risk for cardiovascular events rises when new risk-enhancing factors emerge, and that it was difficult to predict the extent to which each enhancer could change the 10-year risk.
Utility of CAC
“In this setting, the most significant finding that supports the utility of CAC scoring is when CAC is absent – a CAC of 0 – even in the setting of any of these enhancers, whether it be single or multiple, the 10-year risk remains extremely low – at the very least below the accepted threshold to initiate statin therapy,” Dr. Patel said.
That threshold is below the 7.5% 10-year ASCVD incidence rate. Over the 12-year mean study follow-up, the ASCVD incidence rate among patients with a CAC score of 0 for all risk-enhancing factors was 7.5 events per 1,000 person years, with one exception: ABI had an incidence rate of 10.4 events per 1,000 person years. “A low ABI score should trigger statin initiation irrespective of CAC score,” Dr. Patel said.
The study found a CAC score of 0 in 45.7% of those with one or two risk-enhancing factors versus 40.3% in those with three or more. “Across all the risk enhancers (except low ABI), the prevalence of CAC of 0 was greater than 50% in women; that is, enhancers overestimate risk,” Dr. Patel said. “The prevalence of CAC of 0 was approximately 40% across all risk enhancers; that is, enhancers overestimate risk.”
Dr. Patel said previous studies have suggested the risk of a major cardiovascular event was almost identical for statin and nonstatin users with a CAC score of 0. “If there is uncertainty about statin use after the physician-patient risk discussion,” he said, “CAC scoring may be helpful to guide the use of statin therapy.”
Senior author Mahmoud Al Rifai, MD, MPH, added: “For example, if CAC was absent, a statin could be deprescribed if there’s disutility on the part of the patient, with ongoing lifestyle and risk factor modification efforts.” Dr. Al Rifai is a cardiology fellow at Baylor College of Medicine, Houston.
Dr. Patel said: “Alternatively, if CAC was present, then it would be prudent to continue statin therapy.”
While South Asian ethnicity is a risk enhancing factor, the investigators acknowledged that MESA didn’t recruit this population group.
Study confirms guidelines
The study “supports the contention of the [AHA/ACC] guidelines that, in people who are in this intermediate risk range, there may be factors that either favor statin treatment or suggest that statin treatment could be deferred,” said Neil J. Stone, MD, of Northwestern University, Chicago, and author of the 2013 ASCVD risk calculator. “The guidelines pointed out that risk-enhancing factors may be associated with an increase in lifetime risk, not necessarily short term, and so could inform a more personalized risk discussion.”
The study findings validate the utility of CAC for guiding statin therapy, Dr. Stone said. “For those who have felt that a calcium score is not useful,” he said, “this is additional evidence to show that, in the context of making a decision in those at intermediate risk as proposed by the guidelines, a calcium score is indeed very useful.”
Dr. Stone added: “An important clinical point not mentioned by the authors is that, when the patient has a CAC score of 0 and risk factors, this may be exactly the time to be aggressive with lifestyle to prevent them from developing a positive CAC score and atherosclerosis, because once atherosclerosis is present, treatment may not restore the risk back to the original lower state.”
Dr. Patel, Dr. Al Rifai, and Dr. Stone have no relevant relationships to disclose. A number of study coauthors disclosed multiple financial relationships.
In patients with intermediate risk of atherosclerotic cardiovascular disease along with risk-enhancing factors, coronary artery calcium scoring may help more precisely calculate their need for statin therapy.
Furthermore, when the need for statin treatment isn’t so clear and patients need additional risk assessment, the scoring can provide further information to personalize clinical decision making, according to a cross-sectional study of 1,688 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) published in JAMA Cardiology.
And regardless of coronary artery calcium (CAC), a low ankle brachial index (ABI) score is a marker for statin therapy, the study found.
The study looked at CAC scoring in the context of ABI and other risk-enhancing factors identified in the 2018 American Heart Association/American College of Cardiology cholesterol management guidelines: a family history of premature atherosclerotic cardiovascular disease (ASCVD), lipid and inflammatory biomarkers, chronic kidney disease, chronic inflammatory conditions, premature menopause or preeclampsia, and South Asian ancestry.
Any number of these factors can indicate the need for statins in people with borderline or intermediate risk. The guidelines also call for selective use of CAC to aid the decision-making process for statin therapy when the risk for developing atherosclerosis isn’t so clear.
“The novel risk-enhancing factors are not perfect,” said lead author Jaideep Patel, MD, director of preventive cardiology at Johns Hopkins Heart Center at Greater Baltimore Medical Center. He noted that the 2018 dyslipidemia guidelines suggested the risk for cardiovascular events rises when new risk-enhancing factors emerge, and that it was difficult to predict the extent to which each enhancer could change the 10-year risk.
Utility of CAC
“In this setting, the most significant finding that supports the utility of CAC scoring is when CAC is absent – a CAC of 0 – even in the setting of any of these enhancers, whether it be single or multiple, the 10-year risk remains extremely low – at the very least below the accepted threshold to initiate statin therapy,” Dr. Patel said.
That threshold is below the 7.5% 10-year ASCVD incidence rate. Over the 12-year mean study follow-up, the ASCVD incidence rate among patients with a CAC score of 0 for all risk-enhancing factors was 7.5 events per 1,000 person years, with one exception: ABI had an incidence rate of 10.4 events per 1,000 person years. “A low ABI score should trigger statin initiation irrespective of CAC score,” Dr. Patel said.
The study found a CAC score of 0 in 45.7% of those with one or two risk-enhancing factors versus 40.3% in those with three or more. “Across all the risk enhancers (except low ABI), the prevalence of CAC of 0 was greater than 50% in women; that is, enhancers overestimate risk,” Dr. Patel said. “The prevalence of CAC of 0 was approximately 40% across all risk enhancers; that is, enhancers overestimate risk.”
Dr. Patel said previous studies have suggested the risk of a major cardiovascular event was almost identical for statin and nonstatin users with a CAC score of 0. “If there is uncertainty about statin use after the physician-patient risk discussion,” he said, “CAC scoring may be helpful to guide the use of statin therapy.”
Senior author Mahmoud Al Rifai, MD, MPH, added: “For example, if CAC was absent, a statin could be deprescribed if there’s disutility on the part of the patient, with ongoing lifestyle and risk factor modification efforts.” Dr. Al Rifai is a cardiology fellow at Baylor College of Medicine, Houston.
Dr. Patel said: “Alternatively, if CAC was present, then it would be prudent to continue statin therapy.”
While South Asian ethnicity is a risk enhancing factor, the investigators acknowledged that MESA didn’t recruit this population group.
Study confirms guidelines
The study “supports the contention of the [AHA/ACC] guidelines that, in people who are in this intermediate risk range, there may be factors that either favor statin treatment or suggest that statin treatment could be deferred,” said Neil J. Stone, MD, of Northwestern University, Chicago, and author of the 2013 ASCVD risk calculator. “The guidelines pointed out that risk-enhancing factors may be associated with an increase in lifetime risk, not necessarily short term, and so could inform a more personalized risk discussion.”
The study findings validate the utility of CAC for guiding statin therapy, Dr. Stone said. “For those who have felt that a calcium score is not useful,” he said, “this is additional evidence to show that, in the context of making a decision in those at intermediate risk as proposed by the guidelines, a calcium score is indeed very useful.”
Dr. Stone added: “An important clinical point not mentioned by the authors is that, when the patient has a CAC score of 0 and risk factors, this may be exactly the time to be aggressive with lifestyle to prevent them from developing a positive CAC score and atherosclerosis, because once atherosclerosis is present, treatment may not restore the risk back to the original lower state.”
Dr. Patel, Dr. Al Rifai, and Dr. Stone have no relevant relationships to disclose. A number of study coauthors disclosed multiple financial relationships.
In patients with intermediate risk of atherosclerotic cardiovascular disease along with risk-enhancing factors, coronary artery calcium scoring may help more precisely calculate their need for statin therapy.
Furthermore, when the need for statin treatment isn’t so clear and patients need additional risk assessment, the scoring can provide further information to personalize clinical decision making, according to a cross-sectional study of 1,688 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) published in JAMA Cardiology.
And regardless of coronary artery calcium (CAC), a low ankle brachial index (ABI) score is a marker for statin therapy, the study found.
The study looked at CAC scoring in the context of ABI and other risk-enhancing factors identified in the 2018 American Heart Association/American College of Cardiology cholesterol management guidelines: a family history of premature atherosclerotic cardiovascular disease (ASCVD), lipid and inflammatory biomarkers, chronic kidney disease, chronic inflammatory conditions, premature menopause or preeclampsia, and South Asian ancestry.
Any number of these factors can indicate the need for statins in people with borderline or intermediate risk. The guidelines also call for selective use of CAC to aid the decision-making process for statin therapy when the risk for developing atherosclerosis isn’t so clear.
“The novel risk-enhancing factors are not perfect,” said lead author Jaideep Patel, MD, director of preventive cardiology at Johns Hopkins Heart Center at Greater Baltimore Medical Center. He noted that the 2018 dyslipidemia guidelines suggested the risk for cardiovascular events rises when new risk-enhancing factors emerge, and that it was difficult to predict the extent to which each enhancer could change the 10-year risk.
Utility of CAC
“In this setting, the most significant finding that supports the utility of CAC scoring is when CAC is absent – a CAC of 0 – even in the setting of any of these enhancers, whether it be single or multiple, the 10-year risk remains extremely low – at the very least below the accepted threshold to initiate statin therapy,” Dr. Patel said.
That threshold is below the 7.5% 10-year ASCVD incidence rate. Over the 12-year mean study follow-up, the ASCVD incidence rate among patients with a CAC score of 0 for all risk-enhancing factors was 7.5 events per 1,000 person years, with one exception: ABI had an incidence rate of 10.4 events per 1,000 person years. “A low ABI score should trigger statin initiation irrespective of CAC score,” Dr. Patel said.
The study found a CAC score of 0 in 45.7% of those with one or two risk-enhancing factors versus 40.3% in those with three or more. “Across all the risk enhancers (except low ABI), the prevalence of CAC of 0 was greater than 50% in women; that is, enhancers overestimate risk,” Dr. Patel said. “The prevalence of CAC of 0 was approximately 40% across all risk enhancers; that is, enhancers overestimate risk.”
Dr. Patel said previous studies have suggested the risk of a major cardiovascular event was almost identical for statin and nonstatin users with a CAC score of 0. “If there is uncertainty about statin use after the physician-patient risk discussion,” he said, “CAC scoring may be helpful to guide the use of statin therapy.”
Senior author Mahmoud Al Rifai, MD, MPH, added: “For example, if CAC was absent, a statin could be deprescribed if there’s disutility on the part of the patient, with ongoing lifestyle and risk factor modification efforts.” Dr. Al Rifai is a cardiology fellow at Baylor College of Medicine, Houston.
Dr. Patel said: “Alternatively, if CAC was present, then it would be prudent to continue statin therapy.”
While South Asian ethnicity is a risk enhancing factor, the investigators acknowledged that MESA didn’t recruit this population group.
Study confirms guidelines
The study “supports the contention of the [AHA/ACC] guidelines that, in people who are in this intermediate risk range, there may be factors that either favor statin treatment or suggest that statin treatment could be deferred,” said Neil J. Stone, MD, of Northwestern University, Chicago, and author of the 2013 ASCVD risk calculator. “The guidelines pointed out that risk-enhancing factors may be associated with an increase in lifetime risk, not necessarily short term, and so could inform a more personalized risk discussion.”
The study findings validate the utility of CAC for guiding statin therapy, Dr. Stone said. “For those who have felt that a calcium score is not useful,” he said, “this is additional evidence to show that, in the context of making a decision in those at intermediate risk as proposed by the guidelines, a calcium score is indeed very useful.”
Dr. Stone added: “An important clinical point not mentioned by the authors is that, when the patient has a CAC score of 0 and risk factors, this may be exactly the time to be aggressive with lifestyle to prevent them from developing a positive CAC score and atherosclerosis, because once atherosclerosis is present, treatment may not restore the risk back to the original lower state.”
Dr. Patel, Dr. Al Rifai, and Dr. Stone have no relevant relationships to disclose. A number of study coauthors disclosed multiple financial relationships.
FROM JAMA CARDIOLOGY
Abnormal exercise EKG in the setting of normal stress echo linked with increased CV risk
Background: Exercise EKG is often integrated with stress echocardiography, but discordance with +EKG/–Echo has unknown significance.
Study design: Observational cohort study.
Setting: Duke University Medical Center, Durham, N.C.
Synopsis: 47,944 patients without known coronary artery disease underwent exercise stress echocardiogram (Echo) with stress EKG. Of those patients, 8.5% had +EKG/–Echo results, which was associated with annualized event rate of adverse cardiac events of 1.72%, which is higher than the 0.89% of patients with –EKG/–Echo results. This was most significant for composite major adverse cardiovascular events less than 30 days out, with an adjusted hazard ratio of 8.06 (95% confidence interval, 5.02-12.94). For major adverse cardiovascular events greater than 30 days out, HR was 1.25 (95% CI 1.02-1.53).
Bottom line: Patients with +EKG/–Echo findings appear to be at higher risk of adverse cardiac events, especially in the short term.
Citation: Daubert MA et al. Implications of abnormal exercise electrocardiography with normal stress echocardiography. JAMA Intern Med. 2020 Jan 27. doi: 10.1001/jamainternmed.2019.6958.
Dr. Ho is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Exercise EKG is often integrated with stress echocardiography, but discordance with +EKG/–Echo has unknown significance.
Study design: Observational cohort study.
Setting: Duke University Medical Center, Durham, N.C.
Synopsis: 47,944 patients without known coronary artery disease underwent exercise stress echocardiogram (Echo) with stress EKG. Of those patients, 8.5% had +EKG/–Echo results, which was associated with annualized event rate of adverse cardiac events of 1.72%, which is higher than the 0.89% of patients with –EKG/–Echo results. This was most significant for composite major adverse cardiovascular events less than 30 days out, with an adjusted hazard ratio of 8.06 (95% confidence interval, 5.02-12.94). For major adverse cardiovascular events greater than 30 days out, HR was 1.25 (95% CI 1.02-1.53).
Bottom line: Patients with +EKG/–Echo findings appear to be at higher risk of adverse cardiac events, especially in the short term.
Citation: Daubert MA et al. Implications of abnormal exercise electrocardiography with normal stress echocardiography. JAMA Intern Med. 2020 Jan 27. doi: 10.1001/jamainternmed.2019.6958.
Dr. Ho is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Exercise EKG is often integrated with stress echocardiography, but discordance with +EKG/–Echo has unknown significance.
Study design: Observational cohort study.
Setting: Duke University Medical Center, Durham, N.C.
Synopsis: 47,944 patients without known coronary artery disease underwent exercise stress echocardiogram (Echo) with stress EKG. Of those patients, 8.5% had +EKG/–Echo results, which was associated with annualized event rate of adverse cardiac events of 1.72%, which is higher than the 0.89% of patients with –EKG/–Echo results. This was most significant for composite major adverse cardiovascular events less than 30 days out, with an adjusted hazard ratio of 8.06 (95% confidence interval, 5.02-12.94). For major adverse cardiovascular events greater than 30 days out, HR was 1.25 (95% CI 1.02-1.53).
Bottom line: Patients with +EKG/–Echo findings appear to be at higher risk of adverse cardiac events, especially in the short term.
Citation: Daubert MA et al. Implications of abnormal exercise electrocardiography with normal stress echocardiography. JAMA Intern Med. 2020 Jan 27. doi: 10.1001/jamainternmed.2019.6958.
Dr. Ho is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.