User login
Two-drug dolutegravir treatment noninferior to 3/4 drug regimen
A two-drug fixed-dose tablet therapy of dolutegravir/lamivudine (Dovato, ViiV Healthcare; DTG/3TC) shows noninferiority in viral suppression among people with HIV-1 who switch from any type of three- or four-drug antiretroviral (ART) regimens. But, presented at the virtual meeting of the International AIDS Society.
The results on the switch to DTG/3TC are from the phase 3 SALSA trial, which compared patients with HIV-1 who either remained on any current three- or four-drug ART regimen or who switched to the two-drug dolutegravir option.
For the primary endpoint, rates of virologic failure at 48 weeks were noninferior in the DTG/3TC group versus the three- or four-drug regimen (.4% vs. 1.2; adjusted difference: –.8% [95% confidence interval, –2.4%, .8%]).
In addition, rates of virologic suppression at week 48 were noninferior, with 94.3% of patients achieving HIV-1 RNA < 50 c/mL in the DTG/3TC group versus 92.7% in the three- or four-drug regimen (adjusted difference: 1.6% [95% CI, –2.8%, 5.9%).
“These data build upon the previous TANGO study and support DTG/3TC as a robust switch option with high levels of efficacy, good safety and tolerability, and a high barrier of resistance,” first author Josep M. Llibre, MD, PhD, consultant, infectious diseases department, Germans Trias i Pujol University Hospital, Barcelona, said in presenting the findings.
The two-drug dolutegravir-based regimen had previously been shown in the phase 3 GEMINI-1 and GEMINI-2 trials to have virologic noninferiority and safety compared with three- or four-drug DTG plus tenofovir/emtricitabine (TDF/FTC) ART regimens in treatment-naive individuals, and, in the subsequent TANGO trial, the regimen was also noninferior versus tenofovir alafenamide–based regimens among treatment-experienced patients, at 144 weeks in both studies.
Trial details
The new SALSA trial, designed to broaden the comparison to treatment with any current three- or four-drug ART regimen, involved 493 patients at 120 study sites in 17 countries.
All patients were initially on a three- or four-drug regimen, with HIV-1 RNA of less than 50 c/mL for more than 6 months, and without prior virologic failure or nucleoside reverse transcriptase inhibitors or dolutegravir resistance-associated mutations.
The participants were randomized 1:1 to remain on their current regimen (n = 247) or to switch to the once-daily, fixed-dose tablet two-drug combination of dolutegravir 50 mg/lamivudine 300 mg (n = 246) for 52 weeks.
In addition to the noninferior virologic outcomes, there were no serious drug-related adverse events, no confirmed virologic withdrawals, and no resistance mutations in either group.
Of note, weight increase was higher in the DTG/3TC group (8%; n = 20) versus the current ART arm (2%; n = 5), as has been observed in previous studies. The adjusted mean change in weight from baseline to week 48 in the DTG arm was 2.1 kg versus 0.6 kg in the current ART arm.
Dr. Llibre pointed out that many of the participants who switched were discontinuing regimens such as TDF and efavirenz that are associated with weight loss, “so discontinuation could be more related to weight gain than the introduction of dolutegravir, but this deserves further study,” he noted.
There were no significant differences in changes in eGFR and fasting lipids, or in changes in inflammatory biomarkers between the groups.
Bone and renal biomarkers were more favorable in the dolutegravir two-drug arm, suggesting that bone and renal function was either maintained or even improved with the drug switch, Dr. Llibre noted.
Commenting on the research, Alexandra Calmy, PhD, of the HIV/AIDS Unit and LIPO & metabolism group, infectious disease division, Geneva University Hospitals, said that data on quality of life and patient satisfaction measures would be of particular interest.
“Indeed, it is not absolutely clear how a two-in-one versus a three-in-one pill may really influence treatment satisfaction and/or quality of life,” she said in an interview. “Validated scales and patient-reported outcomes with regards to treatment satisfaction would have been an added value to the study.”
Dr. Calmy coauthored a previous study looking at weight change and pharmacokinetic parameters in patients with HIV who switched to DTG-based regimens, and also found weight changes were increased with the DTG regimens. However, the weight gain was not associated with DTG plasma levels, thus supporting Dr. Llibre’s suggestion of possible withdrawal effects from other drugs.
STAT trial: Feasibility of two-drug DTG/3TC as first-line treatment
In further findings presented at the meeting on the STAT trial, researchers evaluated the feasibility not of switching to, but of initiating patients on, the two-drug DTG treatment as a first-line therapy, within 14 days of HIV-1 diagnosis.
The “test-and-treat” approach counters common belief that the regimen should be started only after the traditional three-drug regimens, because of the potential of transmitted resistance and baseline hepatitis B virus coinfection.
In the study of 131 patients, at week 48, 82% (107/131) of all participants and 97% (107/110) of those with available data achieved HIV-1 RNA levels of < 50 c/mL.
While two participants had confirmed virologic failure in the study, there were no treatment-emergent resistance-associated mutations, and neither patient discontinued the two-drug DTG treatment. There were low rates of drug-related adverse events (8%) and they were not serious.
“The STAT data is important as it shows us, for the first time, that in patients where potentially very little is known prior to treatment initiation, DTG/3TC can be very effectively used as a first-line regimen in a ‘test-and-treat’ approach without compromising on patient safety,” first author Charlotte-Paige Rolle, MD, director of research operations, Orlando (Fla.) Immunology Center, said in an interview.
Dr. Rolle added that “with careful monitoring of test results in the first weeks of therapy, we can appropriately and safely adjust therapy from DTG/3TC to a three-drug regimen if needed for patients that have transmitted drug resistance to DTG or 3TC, or hepatitis B coinfection, with both of these occurring at very low rates regardless.”
The SALSA and STAT studies received funding from ViiV Healthcare. Dr. Llibre has received honoraria or consultation fees from ViiV Healthcare, Gilead Sciences and Janssen-Cilag. Dr. Rolle has received grants from and served on advisory boards/speakers bureaus for ViiV Healthcare, Gilead, and Janssen. Dr. Calmy had no disclosures to report.
A two-drug fixed-dose tablet therapy of dolutegravir/lamivudine (Dovato, ViiV Healthcare; DTG/3TC) shows noninferiority in viral suppression among people with HIV-1 who switch from any type of three- or four-drug antiretroviral (ART) regimens. But, presented at the virtual meeting of the International AIDS Society.
The results on the switch to DTG/3TC are from the phase 3 SALSA trial, which compared patients with HIV-1 who either remained on any current three- or four-drug ART regimen or who switched to the two-drug dolutegravir option.
For the primary endpoint, rates of virologic failure at 48 weeks were noninferior in the DTG/3TC group versus the three- or four-drug regimen (.4% vs. 1.2; adjusted difference: –.8% [95% confidence interval, –2.4%, .8%]).
In addition, rates of virologic suppression at week 48 were noninferior, with 94.3% of patients achieving HIV-1 RNA < 50 c/mL in the DTG/3TC group versus 92.7% in the three- or four-drug regimen (adjusted difference: 1.6% [95% CI, –2.8%, 5.9%).
“These data build upon the previous TANGO study and support DTG/3TC as a robust switch option with high levels of efficacy, good safety and tolerability, and a high barrier of resistance,” first author Josep M. Llibre, MD, PhD, consultant, infectious diseases department, Germans Trias i Pujol University Hospital, Barcelona, said in presenting the findings.
The two-drug dolutegravir-based regimen had previously been shown in the phase 3 GEMINI-1 and GEMINI-2 trials to have virologic noninferiority and safety compared with three- or four-drug DTG plus tenofovir/emtricitabine (TDF/FTC) ART regimens in treatment-naive individuals, and, in the subsequent TANGO trial, the regimen was also noninferior versus tenofovir alafenamide–based regimens among treatment-experienced patients, at 144 weeks in both studies.
Trial details
The new SALSA trial, designed to broaden the comparison to treatment with any current three- or four-drug ART regimen, involved 493 patients at 120 study sites in 17 countries.
All patients were initially on a three- or four-drug regimen, with HIV-1 RNA of less than 50 c/mL for more than 6 months, and without prior virologic failure or nucleoside reverse transcriptase inhibitors or dolutegravir resistance-associated mutations.
The participants were randomized 1:1 to remain on their current regimen (n = 247) or to switch to the once-daily, fixed-dose tablet two-drug combination of dolutegravir 50 mg/lamivudine 300 mg (n = 246) for 52 weeks.
In addition to the noninferior virologic outcomes, there were no serious drug-related adverse events, no confirmed virologic withdrawals, and no resistance mutations in either group.
Of note, weight increase was higher in the DTG/3TC group (8%; n = 20) versus the current ART arm (2%; n = 5), as has been observed in previous studies. The adjusted mean change in weight from baseline to week 48 in the DTG arm was 2.1 kg versus 0.6 kg in the current ART arm.
Dr. Llibre pointed out that many of the participants who switched were discontinuing regimens such as TDF and efavirenz that are associated with weight loss, “so discontinuation could be more related to weight gain than the introduction of dolutegravir, but this deserves further study,” he noted.
There were no significant differences in changes in eGFR and fasting lipids, or in changes in inflammatory biomarkers between the groups.
Bone and renal biomarkers were more favorable in the dolutegravir two-drug arm, suggesting that bone and renal function was either maintained or even improved with the drug switch, Dr. Llibre noted.
Commenting on the research, Alexandra Calmy, PhD, of the HIV/AIDS Unit and LIPO & metabolism group, infectious disease division, Geneva University Hospitals, said that data on quality of life and patient satisfaction measures would be of particular interest.
“Indeed, it is not absolutely clear how a two-in-one versus a three-in-one pill may really influence treatment satisfaction and/or quality of life,” she said in an interview. “Validated scales and patient-reported outcomes with regards to treatment satisfaction would have been an added value to the study.”
Dr. Calmy coauthored a previous study looking at weight change and pharmacokinetic parameters in patients with HIV who switched to DTG-based regimens, and also found weight changes were increased with the DTG regimens. However, the weight gain was not associated with DTG plasma levels, thus supporting Dr. Llibre’s suggestion of possible withdrawal effects from other drugs.
STAT trial: Feasibility of two-drug DTG/3TC as first-line treatment
In further findings presented at the meeting on the STAT trial, researchers evaluated the feasibility not of switching to, but of initiating patients on, the two-drug DTG treatment as a first-line therapy, within 14 days of HIV-1 diagnosis.
The “test-and-treat” approach counters common belief that the regimen should be started only after the traditional three-drug regimens, because of the potential of transmitted resistance and baseline hepatitis B virus coinfection.
In the study of 131 patients, at week 48, 82% (107/131) of all participants and 97% (107/110) of those with available data achieved HIV-1 RNA levels of < 50 c/mL.
While two participants had confirmed virologic failure in the study, there were no treatment-emergent resistance-associated mutations, and neither patient discontinued the two-drug DTG treatment. There were low rates of drug-related adverse events (8%) and they were not serious.
“The STAT data is important as it shows us, for the first time, that in patients where potentially very little is known prior to treatment initiation, DTG/3TC can be very effectively used as a first-line regimen in a ‘test-and-treat’ approach without compromising on patient safety,” first author Charlotte-Paige Rolle, MD, director of research operations, Orlando (Fla.) Immunology Center, said in an interview.
Dr. Rolle added that “with careful monitoring of test results in the first weeks of therapy, we can appropriately and safely adjust therapy from DTG/3TC to a three-drug regimen if needed for patients that have transmitted drug resistance to DTG or 3TC, or hepatitis B coinfection, with both of these occurring at very low rates regardless.”
The SALSA and STAT studies received funding from ViiV Healthcare. Dr. Llibre has received honoraria or consultation fees from ViiV Healthcare, Gilead Sciences and Janssen-Cilag. Dr. Rolle has received grants from and served on advisory boards/speakers bureaus for ViiV Healthcare, Gilead, and Janssen. Dr. Calmy had no disclosures to report.
A two-drug fixed-dose tablet therapy of dolutegravir/lamivudine (Dovato, ViiV Healthcare; DTG/3TC) shows noninferiority in viral suppression among people with HIV-1 who switch from any type of three- or four-drug antiretroviral (ART) regimens. But, presented at the virtual meeting of the International AIDS Society.
The results on the switch to DTG/3TC are from the phase 3 SALSA trial, which compared patients with HIV-1 who either remained on any current three- or four-drug ART regimen or who switched to the two-drug dolutegravir option.
For the primary endpoint, rates of virologic failure at 48 weeks were noninferior in the DTG/3TC group versus the three- or four-drug regimen (.4% vs. 1.2; adjusted difference: –.8% [95% confidence interval, –2.4%, .8%]).
In addition, rates of virologic suppression at week 48 were noninferior, with 94.3% of patients achieving HIV-1 RNA < 50 c/mL in the DTG/3TC group versus 92.7% in the three- or four-drug regimen (adjusted difference: 1.6% [95% CI, –2.8%, 5.9%).
“These data build upon the previous TANGO study and support DTG/3TC as a robust switch option with high levels of efficacy, good safety and tolerability, and a high barrier of resistance,” first author Josep M. Llibre, MD, PhD, consultant, infectious diseases department, Germans Trias i Pujol University Hospital, Barcelona, said in presenting the findings.
The two-drug dolutegravir-based regimen had previously been shown in the phase 3 GEMINI-1 and GEMINI-2 trials to have virologic noninferiority and safety compared with three- or four-drug DTG plus tenofovir/emtricitabine (TDF/FTC) ART regimens in treatment-naive individuals, and, in the subsequent TANGO trial, the regimen was also noninferior versus tenofovir alafenamide–based regimens among treatment-experienced patients, at 144 weeks in both studies.
Trial details
The new SALSA trial, designed to broaden the comparison to treatment with any current three- or four-drug ART regimen, involved 493 patients at 120 study sites in 17 countries.
All patients were initially on a three- or four-drug regimen, with HIV-1 RNA of less than 50 c/mL for more than 6 months, and without prior virologic failure or nucleoside reverse transcriptase inhibitors or dolutegravir resistance-associated mutations.
The participants were randomized 1:1 to remain on their current regimen (n = 247) or to switch to the once-daily, fixed-dose tablet two-drug combination of dolutegravir 50 mg/lamivudine 300 mg (n = 246) for 52 weeks.
In addition to the noninferior virologic outcomes, there were no serious drug-related adverse events, no confirmed virologic withdrawals, and no resistance mutations in either group.
Of note, weight increase was higher in the DTG/3TC group (8%; n = 20) versus the current ART arm (2%; n = 5), as has been observed in previous studies. The adjusted mean change in weight from baseline to week 48 in the DTG arm was 2.1 kg versus 0.6 kg in the current ART arm.
Dr. Llibre pointed out that many of the participants who switched were discontinuing regimens such as TDF and efavirenz that are associated with weight loss, “so discontinuation could be more related to weight gain than the introduction of dolutegravir, but this deserves further study,” he noted.
There were no significant differences in changes in eGFR and fasting lipids, or in changes in inflammatory biomarkers between the groups.
Bone and renal biomarkers were more favorable in the dolutegravir two-drug arm, suggesting that bone and renal function was either maintained or even improved with the drug switch, Dr. Llibre noted.
Commenting on the research, Alexandra Calmy, PhD, of the HIV/AIDS Unit and LIPO & metabolism group, infectious disease division, Geneva University Hospitals, said that data on quality of life and patient satisfaction measures would be of particular interest.
“Indeed, it is not absolutely clear how a two-in-one versus a three-in-one pill may really influence treatment satisfaction and/or quality of life,” she said in an interview. “Validated scales and patient-reported outcomes with regards to treatment satisfaction would have been an added value to the study.”
Dr. Calmy coauthored a previous study looking at weight change and pharmacokinetic parameters in patients with HIV who switched to DTG-based regimens, and also found weight changes were increased with the DTG regimens. However, the weight gain was not associated with DTG plasma levels, thus supporting Dr. Llibre’s suggestion of possible withdrawal effects from other drugs.
STAT trial: Feasibility of two-drug DTG/3TC as first-line treatment
In further findings presented at the meeting on the STAT trial, researchers evaluated the feasibility not of switching to, but of initiating patients on, the two-drug DTG treatment as a first-line therapy, within 14 days of HIV-1 diagnosis.
The “test-and-treat” approach counters common belief that the regimen should be started only after the traditional three-drug regimens, because of the potential of transmitted resistance and baseline hepatitis B virus coinfection.
In the study of 131 patients, at week 48, 82% (107/131) of all participants and 97% (107/110) of those with available data achieved HIV-1 RNA levels of < 50 c/mL.
While two participants had confirmed virologic failure in the study, there were no treatment-emergent resistance-associated mutations, and neither patient discontinued the two-drug DTG treatment. There were low rates of drug-related adverse events (8%) and they were not serious.
“The STAT data is important as it shows us, for the first time, that in patients where potentially very little is known prior to treatment initiation, DTG/3TC can be very effectively used as a first-line regimen in a ‘test-and-treat’ approach without compromising on patient safety,” first author Charlotte-Paige Rolle, MD, director of research operations, Orlando (Fla.) Immunology Center, said in an interview.
Dr. Rolle added that “with careful monitoring of test results in the first weeks of therapy, we can appropriately and safely adjust therapy from DTG/3TC to a three-drug regimen if needed for patients that have transmitted drug resistance to DTG or 3TC, or hepatitis B coinfection, with both of these occurring at very low rates regardless.”
The SALSA and STAT studies received funding from ViiV Healthcare. Dr. Llibre has received honoraria or consultation fees from ViiV Healthcare, Gilead Sciences and Janssen-Cilag. Dr. Rolle has received grants from and served on advisory boards/speakers bureaus for ViiV Healthcare, Gilead, and Janssen. Dr. Calmy had no disclosures to report.
FROM IAS 2021
Delta variant among the most infectious respiratory viruses, CDC says
.
“Today, I want to speak about our need to come together against a common enemy. SARS-CoV-2 and the Delta variant is spreading with incredible efficiency, and now represents more than 83% of the virus circulating in the U.S.,” Dr. Walensky said at a news briefing July 22. “It is one of the most infectious respiratory viruses we know of and that I have seen in my 20-year career.”
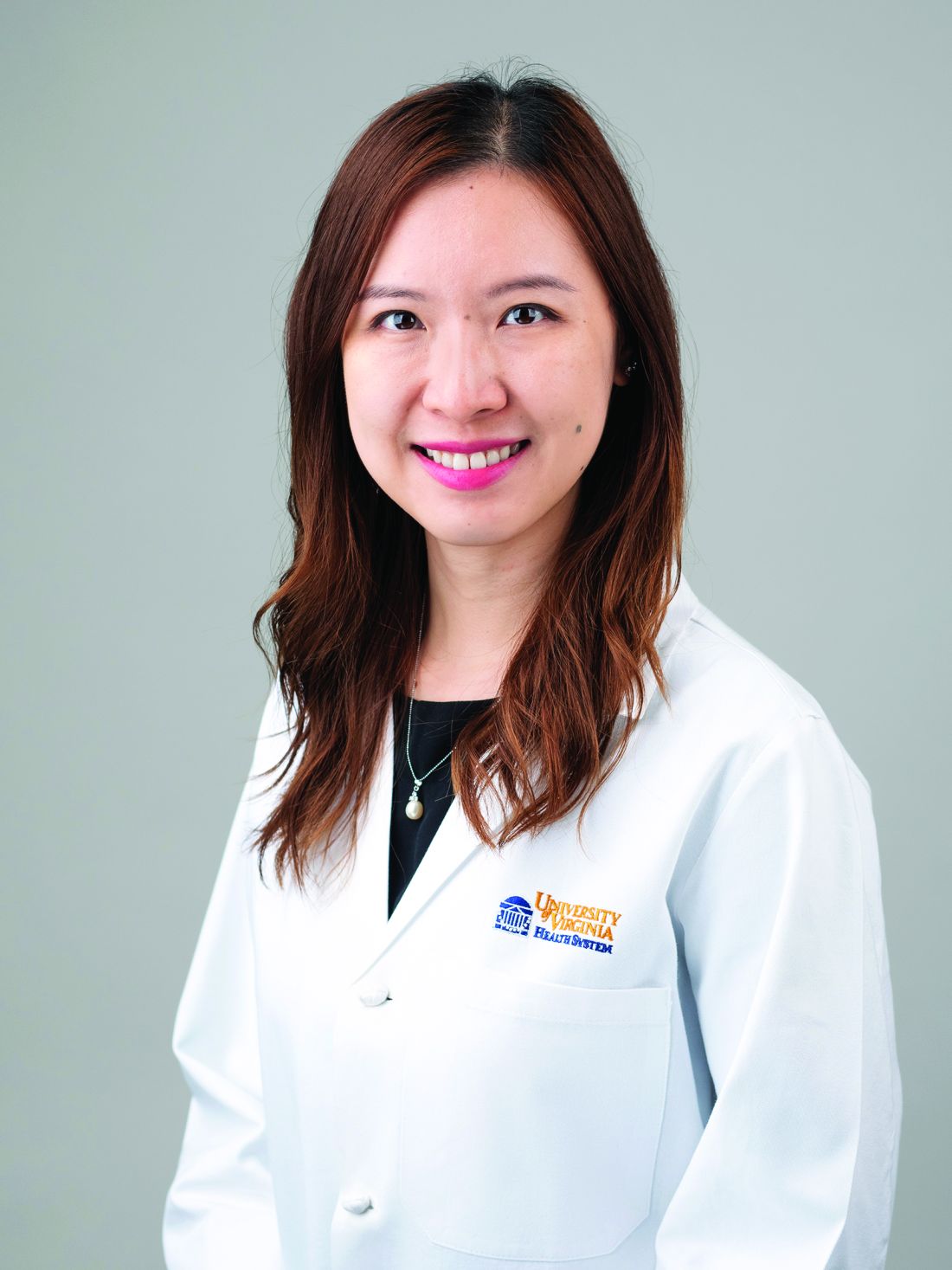
Dr. Walensky said there were 46,318 cases of COVID-19 reported July 21, with a 7-day average of 37,700 cases per day -- up 53% from the previous week. Hospital admissions average about 3,500 per day, an increase of 32%. The 7-day average of deaths is 237 -- a 19% increase from the previous week.
Meanwhile, there are now 162 million Americans who are fully vaccinated against COVID-19.
Areas with low vaccination coverage continue to have the highest case numbers, she reported, with unvaccinated people accounting for 97% of hospitalizations and deaths.
But there may be early signs of progress. The four states with the highest case rates -- Arkansas, Florida, Louisiana, and Nevada -- had a higher rate of new vaccinations, compared with the national average over the past week, White House COVID-19 Response Coordinator Jeff Zients said.
He also announced that the administration will send $100 million to nearly 2,000 rural health clinics to support vaccine education and outreach efforts.
Dr. Walensky said despite the rising numbers, the CDC mask guidance remains the same, but she encouraged vaccinated people to wear masks if they choose.
“Whether you are vaccinated or not, please know we together are not out of the woods yet,” she said. “We are yet at another pivotal moment in this pandemic, with cases rising again and hospitals reaching their capacity in some areas.”
A version of this article first appeared on WebMD.com.
.
“Today, I want to speak about our need to come together against a common enemy. SARS-CoV-2 and the Delta variant is spreading with incredible efficiency, and now represents more than 83% of the virus circulating in the U.S.,” Dr. Walensky said at a news briefing July 22. “It is one of the most infectious respiratory viruses we know of and that I have seen in my 20-year career.”
Dr. Walensky said there were 46,318 cases of COVID-19 reported July 21, with a 7-day average of 37,700 cases per day -- up 53% from the previous week. Hospital admissions average about 3,500 per day, an increase of 32%. The 7-day average of deaths is 237 -- a 19% increase from the previous week.
Meanwhile, there are now 162 million Americans who are fully vaccinated against COVID-19.
Areas with low vaccination coverage continue to have the highest case numbers, she reported, with unvaccinated people accounting for 97% of hospitalizations and deaths.
But there may be early signs of progress. The four states with the highest case rates -- Arkansas, Florida, Louisiana, and Nevada -- had a higher rate of new vaccinations, compared with the national average over the past week, White House COVID-19 Response Coordinator Jeff Zients said.
He also announced that the administration will send $100 million to nearly 2,000 rural health clinics to support vaccine education and outreach efforts.
Dr. Walensky said despite the rising numbers, the CDC mask guidance remains the same, but she encouraged vaccinated people to wear masks if they choose.
“Whether you are vaccinated or not, please know we together are not out of the woods yet,” she said. “We are yet at another pivotal moment in this pandemic, with cases rising again and hospitals reaching their capacity in some areas.”
A version of this article first appeared on WebMD.com.
.
“Today, I want to speak about our need to come together against a common enemy. SARS-CoV-2 and the Delta variant is spreading with incredible efficiency, and now represents more than 83% of the virus circulating in the U.S.,” Dr. Walensky said at a news briefing July 22. “It is one of the most infectious respiratory viruses we know of and that I have seen in my 20-year career.”
Dr. Walensky said there were 46,318 cases of COVID-19 reported July 21, with a 7-day average of 37,700 cases per day -- up 53% from the previous week. Hospital admissions average about 3,500 per day, an increase of 32%. The 7-day average of deaths is 237 -- a 19% increase from the previous week.
Meanwhile, there are now 162 million Americans who are fully vaccinated against COVID-19.
Areas with low vaccination coverage continue to have the highest case numbers, she reported, with unvaccinated people accounting for 97% of hospitalizations and deaths.
But there may be early signs of progress. The four states with the highest case rates -- Arkansas, Florida, Louisiana, and Nevada -- had a higher rate of new vaccinations, compared with the national average over the past week, White House COVID-19 Response Coordinator Jeff Zients said.
He also announced that the administration will send $100 million to nearly 2,000 rural health clinics to support vaccine education and outreach efforts.
Dr. Walensky said despite the rising numbers, the CDC mask guidance remains the same, but she encouraged vaccinated people to wear masks if they choose.
“Whether you are vaccinated or not, please know we together are not out of the woods yet,” she said. “We are yet at another pivotal moment in this pandemic, with cases rising again and hospitals reaching their capacity in some areas.”
A version of this article first appeared on WebMD.com.
Acid suppression therapy increases intestinal colonization of MDROs
Background: Acid suppressants inhibit gastric acid secretion and disrupt the intestinal microbiome, but whether that facilitates colonization and infection with MDROs is unclear.
Study design: Systematic review and meta-analysis.
Setting: Observational studies searched from database through July 2019.
Synopsis: A total of 26 observational studies published during 1996-2019 with 29,382 patients were included in this meta-analysis. Of those, 24 studies directly measured intestinal MDRO carriage and 2 used urinary tract infections (UTIs) as the outcome measure, since most UTIs are caused by bacteria that colonize the intestinal tract. Target MDROs included multidrug-resistant Enterobacteriaceae (MRD-E) and vancomycin-resistant enterococci (VRE). Meta-analysis demonstrated that acid suppression is associated with increased odds of intestinal MDRO colonization (MDR-E: odds ratio, 1.60; 95% confidence interval, 1.33-1.92; VRE: OR, 1.97; 95% CI, 1.49-2.60), in both community and health care settings. The risk was similar for colonization with MDR-E and VRE. Regarding the effect of acid suppression by drug class, results were mixed with some studies demonstrating increased risk of MDRO in PPI users only while others reported increased risk only with H2-receptor antagonists.
Bottom line: Acid suppression therapy is associated with increased odds of MDRO colonization. While observational studies cannot prove causation, it is wise to avoid excessive use of acid suppressants.
Citation: Willems RPJ et al. Evaluation of the association between gastric acid suppression and risk of intestinal colonization with multidrug-resistant microorganisms: A systematic review and meta-analysis. JAMA Intern Med. 2020 Feb 24;180(4):561-71.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Acid suppressants inhibit gastric acid secretion and disrupt the intestinal microbiome, but whether that facilitates colonization and infection with MDROs is unclear.
Study design: Systematic review and meta-analysis.
Setting: Observational studies searched from database through July 2019.
Synopsis: A total of 26 observational studies published during 1996-2019 with 29,382 patients were included in this meta-analysis. Of those, 24 studies directly measured intestinal MDRO carriage and 2 used urinary tract infections (UTIs) as the outcome measure, since most UTIs are caused by bacteria that colonize the intestinal tract. Target MDROs included multidrug-resistant Enterobacteriaceae (MRD-E) and vancomycin-resistant enterococci (VRE). Meta-analysis demonstrated that acid suppression is associated with increased odds of intestinal MDRO colonization (MDR-E: odds ratio, 1.60; 95% confidence interval, 1.33-1.92; VRE: OR, 1.97; 95% CI, 1.49-2.60), in both community and health care settings. The risk was similar for colonization with MDR-E and VRE. Regarding the effect of acid suppression by drug class, results were mixed with some studies demonstrating increased risk of MDRO in PPI users only while others reported increased risk only with H2-receptor antagonists.
Bottom line: Acid suppression therapy is associated with increased odds of MDRO colonization. While observational studies cannot prove causation, it is wise to avoid excessive use of acid suppressants.
Citation: Willems RPJ et al. Evaluation of the association between gastric acid suppression and risk of intestinal colonization with multidrug-resistant microorganisms: A systematic review and meta-analysis. JAMA Intern Med. 2020 Feb 24;180(4):561-71.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Acid suppressants inhibit gastric acid secretion and disrupt the intestinal microbiome, but whether that facilitates colonization and infection with MDROs is unclear.
Study design: Systematic review and meta-analysis.
Setting: Observational studies searched from database through July 2019.
Synopsis: A total of 26 observational studies published during 1996-2019 with 29,382 patients were included in this meta-analysis. Of those, 24 studies directly measured intestinal MDRO carriage and 2 used urinary tract infections (UTIs) as the outcome measure, since most UTIs are caused by bacteria that colonize the intestinal tract. Target MDROs included multidrug-resistant Enterobacteriaceae (MRD-E) and vancomycin-resistant enterococci (VRE). Meta-analysis demonstrated that acid suppression is associated with increased odds of intestinal MDRO colonization (MDR-E: odds ratio, 1.60; 95% confidence interval, 1.33-1.92; VRE: OR, 1.97; 95% CI, 1.49-2.60), in both community and health care settings. The risk was similar for colonization with MDR-E and VRE. Regarding the effect of acid suppression by drug class, results were mixed with some studies demonstrating increased risk of MDRO in PPI users only while others reported increased risk only with H2-receptor antagonists.
Bottom line: Acid suppression therapy is associated with increased odds of MDRO colonization. While observational studies cannot prove causation, it is wise to avoid excessive use of acid suppressants.
Citation: Willems RPJ et al. Evaluation of the association between gastric acid suppression and risk of intestinal colonization with multidrug-resistant microorganisms: A systematic review and meta-analysis. JAMA Intern Med. 2020 Feb 24;180(4):561-71.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
HIV-associated cryptococcal meningitis: Single-dose regimen found non-inferior
A single high dose of the antifungal agent liposomal amphotericin B (L-AmB; AmBisome, Gilead Sciences), with a background regimen of flucytosine and fluconazole, is non-inferior and significantly safer in preventing mortality in HIV-associated cryptococcal meningitis than a conventional seven-day regimen that is the current standard of care, according to a new study.
“The results of this phase 3 [AMBITION-cm] trial make it clear that this approach is just as good as the current World Health Organization-recommended first-line treatment in preventing death,” first author David S. Lawrence, MD, AMBITION study lead clinician, of the London School of Hygiene and Tropical Medicine, United Kingdom, said in an interview.
“The fact that this was the largest ever trial [on HIV-associated cryptococcal meningitis] conducted to date… gives us a high level of confidence in these results,” he said of the study, which was presented at the virtual annual meeting of the International AIDS Society.
“We believe that this should become the WHO-recommended first-line regimen,” he emphasized.
In commenting on the study, Meg Doherty, MD, PhD, director of global HIV, hepatitis, and STI programs at WHO, agreed that a shorter regimen could be vital, particularly in settings with limited resources.
“The results from the AMBITION trial are important for low- and middle-income countries, where the cost and complexity of implementing the current standard seven-day course of L-ambisome or cryptococcal meningitis treatment can put this out of reach for many,” she told this news organization.
“Simplification that maintains the highest quality of care is an important component of the public health approach for HIV treatment and care,” she added.
Dr. Doherty could not comment on any possible changes to WHO recommendations, which are formulated by an independent guideline development group, but a spokesperson said that “WHO is preparing an updated review of the evidence for treating cryptococcal disease as a first step towards updating guidance.”
Conventional treatment toxicities
Cryptococcal meningitis is a leading cause of death in HIV, and the conventional treatment of amphotericin B deoxycholate, though less expensive than L-AmB, is more toxic, causing anemia, renal impairment, and electrolyte abnormalities, Dr. Lawrence explained
Having previously shown a single 10 mg/kg dose of L-AmB to be as effective as the longer regimen of 14 daily doses in terms of clearing cryptococcus from the cerebrospinal fluid, Dr. Lawrence and his colleagues conducted the phase 3 AMBITION-Cm trial to evaluate the effect on mortality, enrolling 844 patients in Botswana, Malawi, South Africa, Uganda, and Zimbabwe who were HIV-positive and had a first episode of cryptococcal meningitis.
Participants in the study were randomized to treatment either with single, high-dose L-AmB (10 mg/kg), combined with 14 days of flucytosine 100 mg/kg/day and fluconazole 1,200 mg/day or to a control group receiving 7 daily doses of AmB deoxycholate (1 mg/kg) plus 7 days of flucytosine 100 mg/kg/day, followed by 7 days of fluconazole 1,200 mg/day.
All patients were also provided with consolidation therapy of fluconazole 800 mg/day for eight weeks. Of the patients, 60.2% were male, their median age was 37, and their median CD4 count was 27 cells/mm3.
For the primary endpoint in the intention-to-treat analysis of 814 patients, the 10-week mortality rate in the single-dose L-AmB group was 24.82% (101 of 407) and 28.75% (117 of 407) in the control arm, for a difference (-3.93%) that was well within the pre-specified non-inferiority margin of 10%.
As expected, the safety measures were significantly improved with the single-dose of L-AmB: Rates of grade 3 or 4 adverse events within the initial 21 days of treatment in the single-dose L-AmB group were 50% versus 62.3% in the control group, and severe anemia occurred in just 13% of single-dose L-AmB participants, compared with 41% in the AmB deoxycholate control arm (both P < .001), Dr. Lawrence reported.
Furthermore, the average decline in hemoglobin over the first week was 0.3 g/dL in the single-dose L-AmB arm and 1.9 g/dL in the control arm, resulting in the need for more blood transfusions in the control arm (P < .001).
The impact on kidney function was also worse in the higher dose arm, with an average increase in creatinine over the first week of 20.2% in the L-AmB group versus 49.7% in the control group, while hypokalemia and thrombophlebitis were also more common with the higher dose group, Dr. Lawrence noted.
In the adjusted analysis, the single-dose L-AmB measures were in fact superior after adjusting for factors including research site, age, sex, baseline Glasgow Coma Scale, CD4 count, CSF cryptococcal colony-forming units/mL, antiretroviral therapy status, hemoglobin, and CSF opening pressure.
Mortality rate still high – but significantly reduced
The mortality rate of about 25% in the study after the treatment is still significantly higher than typically seen in high-income countries such as the United States, where HIV-associated cryptococcal meningitis is less common and associated with a mortality of roughly 10-15%, Dr. Lawrence noted.
The rate is nevertheless among the lowest mortality rates ever reported within a clinical trial conducted in resource-limited settings, he explained.
“These results are a step in the right direction and a significant improvement on the rates of 40% to 45% reported with two-week L-AmB-based regimens in African settings,” Dr. Lawrence underscored.
Higher cost — but potentially more cost-effective
With a higher cost than AmB deoxycholate, L-AmB’s utilization in resource-limited settings has been a challenge: A single vial of L-AmB ranges from $80 to $200, according to some reports, and while 14-day dosing requires as many as 42 vials of L-AmB, even a 7-day regimen still requires 21 vials.
In comparison, the single-dose L-AmB regimen only requires an average of 10 to 11 vials per patient, but the regimen’s higher safety could translate to far greater cost savings, Dr. Lawrence explained.
“While the AmBisome regimen is technically more expensive in terms of drugs, we expect it to be cost-effective or possibly cost-saving when taking into account that there is less toxicity, fewer blood tests, less transfusions, etc., and possibly shorter duration of hospital admission,” he said.
Cost, supply controversy: ‘Black fungus’-related demand
The drug’s cost — as well as supply issues — have meanwhile become even more of a problem as L-AmB has unexpectedly also become urgently needed in the treatment of mucormycosis in India and Nepal, where the otherwise rare fungal disease, commonly known as “black fungus,” has been increasingly affecting COVID-19 patients and survivors.
Gilead had previously announced in 2018 its intention to make L-AmB more widely available at a price of $16.25 per vial, but “implementation of this has been slow,” Dr. Lawrence said.
As a result, Gilead is facing heightened pressure to implement the lower prices – and also improve substantial supply issues, with Médecins Sans Frontières (Doctors Without Borders) and dozens of other global organizations issuing an open letter to Gilead and partner Viatris in June calling for immediate action to implement the lower price and improve supply of L-AmB.
In a company statement, Gilead responded, detailing its “commit[ment] to the non-profit pricing for the treatment of cryptococcal meningitis” and to efforts to improve the public health crisis in India.
For their part, Dr. Lawrence and his colleagues are working on producing more research on the issue.
“We hope that the conclusive results of the AMBITION trial will give a much needed push to implement this program,” he said.
“We are also currently completing the cost-effectiveness analysis of the study, which we hope will provide additional evidence to support widespread implementation of this regimen and highlight further the urgent need to broaden access to AmBisome and flucytosine,” he said.
The trial was supported by a grant through the European Developing Countries Clinical Trials Partnership (EDCTP), the Swedish International Development Cooperation Agency (SIDA) (TRIA2015-1092), and the Wellcome Trust / Medical Research Council (UK)/UKAID Joint Global Health Trials (MR/P006922/1. The AmBisome was donated by Gilead Sciences. Dr. Lawrence had no disclosures to report.
A single high dose of the antifungal agent liposomal amphotericin B (L-AmB; AmBisome, Gilead Sciences), with a background regimen of flucytosine and fluconazole, is non-inferior and significantly safer in preventing mortality in HIV-associated cryptococcal meningitis than a conventional seven-day regimen that is the current standard of care, according to a new study.
“The results of this phase 3 [AMBITION-cm] trial make it clear that this approach is just as good as the current World Health Organization-recommended first-line treatment in preventing death,” first author David S. Lawrence, MD, AMBITION study lead clinician, of the London School of Hygiene and Tropical Medicine, United Kingdom, said in an interview.
“The fact that this was the largest ever trial [on HIV-associated cryptococcal meningitis] conducted to date… gives us a high level of confidence in these results,” he said of the study, which was presented at the virtual annual meeting of the International AIDS Society.
“We believe that this should become the WHO-recommended first-line regimen,” he emphasized.
In commenting on the study, Meg Doherty, MD, PhD, director of global HIV, hepatitis, and STI programs at WHO, agreed that a shorter regimen could be vital, particularly in settings with limited resources.
“The results from the AMBITION trial are important for low- and middle-income countries, where the cost and complexity of implementing the current standard seven-day course of L-ambisome or cryptococcal meningitis treatment can put this out of reach for many,” she told this news organization.
“Simplification that maintains the highest quality of care is an important component of the public health approach for HIV treatment and care,” she added.
Dr. Doherty could not comment on any possible changes to WHO recommendations, which are formulated by an independent guideline development group, but a spokesperson said that “WHO is preparing an updated review of the evidence for treating cryptococcal disease as a first step towards updating guidance.”
Conventional treatment toxicities
Cryptococcal meningitis is a leading cause of death in HIV, and the conventional treatment of amphotericin B deoxycholate, though less expensive than L-AmB, is more toxic, causing anemia, renal impairment, and electrolyte abnormalities, Dr. Lawrence explained
Having previously shown a single 10 mg/kg dose of L-AmB to be as effective as the longer regimen of 14 daily doses in terms of clearing cryptococcus from the cerebrospinal fluid, Dr. Lawrence and his colleagues conducted the phase 3 AMBITION-Cm trial to evaluate the effect on mortality, enrolling 844 patients in Botswana, Malawi, South Africa, Uganda, and Zimbabwe who were HIV-positive and had a first episode of cryptococcal meningitis.
Participants in the study were randomized to treatment either with single, high-dose L-AmB (10 mg/kg), combined with 14 days of flucytosine 100 mg/kg/day and fluconazole 1,200 mg/day or to a control group receiving 7 daily doses of AmB deoxycholate (1 mg/kg) plus 7 days of flucytosine 100 mg/kg/day, followed by 7 days of fluconazole 1,200 mg/day.
All patients were also provided with consolidation therapy of fluconazole 800 mg/day for eight weeks. Of the patients, 60.2% were male, their median age was 37, and their median CD4 count was 27 cells/mm3.
For the primary endpoint in the intention-to-treat analysis of 814 patients, the 10-week mortality rate in the single-dose L-AmB group was 24.82% (101 of 407) and 28.75% (117 of 407) in the control arm, for a difference (-3.93%) that was well within the pre-specified non-inferiority margin of 10%.
As expected, the safety measures were significantly improved with the single-dose of L-AmB: Rates of grade 3 or 4 adverse events within the initial 21 days of treatment in the single-dose L-AmB group were 50% versus 62.3% in the control group, and severe anemia occurred in just 13% of single-dose L-AmB participants, compared with 41% in the AmB deoxycholate control arm (both P < .001), Dr. Lawrence reported.
Furthermore, the average decline in hemoglobin over the first week was 0.3 g/dL in the single-dose L-AmB arm and 1.9 g/dL in the control arm, resulting in the need for more blood transfusions in the control arm (P < .001).
The impact on kidney function was also worse in the higher dose arm, with an average increase in creatinine over the first week of 20.2% in the L-AmB group versus 49.7% in the control group, while hypokalemia and thrombophlebitis were also more common with the higher dose group, Dr. Lawrence noted.
In the adjusted analysis, the single-dose L-AmB measures were in fact superior after adjusting for factors including research site, age, sex, baseline Glasgow Coma Scale, CD4 count, CSF cryptococcal colony-forming units/mL, antiretroviral therapy status, hemoglobin, and CSF opening pressure.
Mortality rate still high – but significantly reduced
The mortality rate of about 25% in the study after the treatment is still significantly higher than typically seen in high-income countries such as the United States, where HIV-associated cryptococcal meningitis is less common and associated with a mortality of roughly 10-15%, Dr. Lawrence noted.
The rate is nevertheless among the lowest mortality rates ever reported within a clinical trial conducted in resource-limited settings, he explained.
“These results are a step in the right direction and a significant improvement on the rates of 40% to 45% reported with two-week L-AmB-based regimens in African settings,” Dr. Lawrence underscored.
Higher cost — but potentially more cost-effective
With a higher cost than AmB deoxycholate, L-AmB’s utilization in resource-limited settings has been a challenge: A single vial of L-AmB ranges from $80 to $200, according to some reports, and while 14-day dosing requires as many as 42 vials of L-AmB, even a 7-day regimen still requires 21 vials.
In comparison, the single-dose L-AmB regimen only requires an average of 10 to 11 vials per patient, but the regimen’s higher safety could translate to far greater cost savings, Dr. Lawrence explained.
“While the AmBisome regimen is technically more expensive in terms of drugs, we expect it to be cost-effective or possibly cost-saving when taking into account that there is less toxicity, fewer blood tests, less transfusions, etc., and possibly shorter duration of hospital admission,” he said.
Cost, supply controversy: ‘Black fungus’-related demand
The drug’s cost — as well as supply issues — have meanwhile become even more of a problem as L-AmB has unexpectedly also become urgently needed in the treatment of mucormycosis in India and Nepal, where the otherwise rare fungal disease, commonly known as “black fungus,” has been increasingly affecting COVID-19 patients and survivors.
Gilead had previously announced in 2018 its intention to make L-AmB more widely available at a price of $16.25 per vial, but “implementation of this has been slow,” Dr. Lawrence said.
As a result, Gilead is facing heightened pressure to implement the lower prices – and also improve substantial supply issues, with Médecins Sans Frontières (Doctors Without Borders) and dozens of other global organizations issuing an open letter to Gilead and partner Viatris in June calling for immediate action to implement the lower price and improve supply of L-AmB.
In a company statement, Gilead responded, detailing its “commit[ment] to the non-profit pricing for the treatment of cryptococcal meningitis” and to efforts to improve the public health crisis in India.
For their part, Dr. Lawrence and his colleagues are working on producing more research on the issue.
“We hope that the conclusive results of the AMBITION trial will give a much needed push to implement this program,” he said.
“We are also currently completing the cost-effectiveness analysis of the study, which we hope will provide additional evidence to support widespread implementation of this regimen and highlight further the urgent need to broaden access to AmBisome and flucytosine,” he said.
The trial was supported by a grant through the European Developing Countries Clinical Trials Partnership (EDCTP), the Swedish International Development Cooperation Agency (SIDA) (TRIA2015-1092), and the Wellcome Trust / Medical Research Council (UK)/UKAID Joint Global Health Trials (MR/P006922/1. The AmBisome was donated by Gilead Sciences. Dr. Lawrence had no disclosures to report.
A single high dose of the antifungal agent liposomal amphotericin B (L-AmB; AmBisome, Gilead Sciences), with a background regimen of flucytosine and fluconazole, is non-inferior and significantly safer in preventing mortality in HIV-associated cryptococcal meningitis than a conventional seven-day regimen that is the current standard of care, according to a new study.
“The results of this phase 3 [AMBITION-cm] trial make it clear that this approach is just as good as the current World Health Organization-recommended first-line treatment in preventing death,” first author David S. Lawrence, MD, AMBITION study lead clinician, of the London School of Hygiene and Tropical Medicine, United Kingdom, said in an interview.
“The fact that this was the largest ever trial [on HIV-associated cryptococcal meningitis] conducted to date… gives us a high level of confidence in these results,” he said of the study, which was presented at the virtual annual meeting of the International AIDS Society.
“We believe that this should become the WHO-recommended first-line regimen,” he emphasized.
In commenting on the study, Meg Doherty, MD, PhD, director of global HIV, hepatitis, and STI programs at WHO, agreed that a shorter regimen could be vital, particularly in settings with limited resources.
“The results from the AMBITION trial are important for low- and middle-income countries, where the cost and complexity of implementing the current standard seven-day course of L-ambisome or cryptococcal meningitis treatment can put this out of reach for many,” she told this news organization.
“Simplification that maintains the highest quality of care is an important component of the public health approach for HIV treatment and care,” she added.
Dr. Doherty could not comment on any possible changes to WHO recommendations, which are formulated by an independent guideline development group, but a spokesperson said that “WHO is preparing an updated review of the evidence for treating cryptococcal disease as a first step towards updating guidance.”
Conventional treatment toxicities
Cryptococcal meningitis is a leading cause of death in HIV, and the conventional treatment of amphotericin B deoxycholate, though less expensive than L-AmB, is more toxic, causing anemia, renal impairment, and electrolyte abnormalities, Dr. Lawrence explained
Having previously shown a single 10 mg/kg dose of L-AmB to be as effective as the longer regimen of 14 daily doses in terms of clearing cryptococcus from the cerebrospinal fluid, Dr. Lawrence and his colleagues conducted the phase 3 AMBITION-Cm trial to evaluate the effect on mortality, enrolling 844 patients in Botswana, Malawi, South Africa, Uganda, and Zimbabwe who were HIV-positive and had a first episode of cryptococcal meningitis.
Participants in the study were randomized to treatment either with single, high-dose L-AmB (10 mg/kg), combined with 14 days of flucytosine 100 mg/kg/day and fluconazole 1,200 mg/day or to a control group receiving 7 daily doses of AmB deoxycholate (1 mg/kg) plus 7 days of flucytosine 100 mg/kg/day, followed by 7 days of fluconazole 1,200 mg/day.
All patients were also provided with consolidation therapy of fluconazole 800 mg/day for eight weeks. Of the patients, 60.2% were male, their median age was 37, and their median CD4 count was 27 cells/mm3.
For the primary endpoint in the intention-to-treat analysis of 814 patients, the 10-week mortality rate in the single-dose L-AmB group was 24.82% (101 of 407) and 28.75% (117 of 407) in the control arm, for a difference (-3.93%) that was well within the pre-specified non-inferiority margin of 10%.
As expected, the safety measures were significantly improved with the single-dose of L-AmB: Rates of grade 3 or 4 adverse events within the initial 21 days of treatment in the single-dose L-AmB group were 50% versus 62.3% in the control group, and severe anemia occurred in just 13% of single-dose L-AmB participants, compared with 41% in the AmB deoxycholate control arm (both P < .001), Dr. Lawrence reported.
Furthermore, the average decline in hemoglobin over the first week was 0.3 g/dL in the single-dose L-AmB arm and 1.9 g/dL in the control arm, resulting in the need for more blood transfusions in the control arm (P < .001).
The impact on kidney function was also worse in the higher dose arm, with an average increase in creatinine over the first week of 20.2% in the L-AmB group versus 49.7% in the control group, while hypokalemia and thrombophlebitis were also more common with the higher dose group, Dr. Lawrence noted.
In the adjusted analysis, the single-dose L-AmB measures were in fact superior after adjusting for factors including research site, age, sex, baseline Glasgow Coma Scale, CD4 count, CSF cryptococcal colony-forming units/mL, antiretroviral therapy status, hemoglobin, and CSF opening pressure.
Mortality rate still high – but significantly reduced
The mortality rate of about 25% in the study after the treatment is still significantly higher than typically seen in high-income countries such as the United States, where HIV-associated cryptococcal meningitis is less common and associated with a mortality of roughly 10-15%, Dr. Lawrence noted.
The rate is nevertheless among the lowest mortality rates ever reported within a clinical trial conducted in resource-limited settings, he explained.
“These results are a step in the right direction and a significant improvement on the rates of 40% to 45% reported with two-week L-AmB-based regimens in African settings,” Dr. Lawrence underscored.
Higher cost — but potentially more cost-effective
With a higher cost than AmB deoxycholate, L-AmB’s utilization in resource-limited settings has been a challenge: A single vial of L-AmB ranges from $80 to $200, according to some reports, and while 14-day dosing requires as many as 42 vials of L-AmB, even a 7-day regimen still requires 21 vials.
In comparison, the single-dose L-AmB regimen only requires an average of 10 to 11 vials per patient, but the regimen’s higher safety could translate to far greater cost savings, Dr. Lawrence explained.
“While the AmBisome regimen is technically more expensive in terms of drugs, we expect it to be cost-effective or possibly cost-saving when taking into account that there is less toxicity, fewer blood tests, less transfusions, etc., and possibly shorter duration of hospital admission,” he said.
Cost, supply controversy: ‘Black fungus’-related demand
The drug’s cost — as well as supply issues — have meanwhile become even more of a problem as L-AmB has unexpectedly also become urgently needed in the treatment of mucormycosis in India and Nepal, where the otherwise rare fungal disease, commonly known as “black fungus,” has been increasingly affecting COVID-19 patients and survivors.
Gilead had previously announced in 2018 its intention to make L-AmB more widely available at a price of $16.25 per vial, but “implementation of this has been slow,” Dr. Lawrence said.
As a result, Gilead is facing heightened pressure to implement the lower prices – and also improve substantial supply issues, with Médecins Sans Frontières (Doctors Without Borders) and dozens of other global organizations issuing an open letter to Gilead and partner Viatris in June calling for immediate action to implement the lower price and improve supply of L-AmB.
In a company statement, Gilead responded, detailing its “commit[ment] to the non-profit pricing for the treatment of cryptococcal meningitis” and to efforts to improve the public health crisis in India.
For their part, Dr. Lawrence and his colleagues are working on producing more research on the issue.
“We hope that the conclusive results of the AMBITION trial will give a much needed push to implement this program,” he said.
“We are also currently completing the cost-effectiveness analysis of the study, which we hope will provide additional evidence to support widespread implementation of this regimen and highlight further the urgent need to broaden access to AmBisome and flucytosine,” he said.
The trial was supported by a grant through the European Developing Countries Clinical Trials Partnership (EDCTP), the Swedish International Development Cooperation Agency (SIDA) (TRIA2015-1092), and the Wellcome Trust / Medical Research Council (UK)/UKAID Joint Global Health Trials (MR/P006922/1. The AmBisome was donated by Gilead Sciences. Dr. Lawrence had no disclosures to report.
REPORTING FROM IAS 2021
Empirical anti-MRSA therapy does not improve mortality in patients with pneumonia
Background: Empirical broad-spectrum antibiotics including anti-MRSA therapy are often selected because of concerns for resistant organisms. However, the outcomes of empirical anti-MRSA therapy among patients with pneumonia are unknown.
Study design: A national retrospective multicenter cohort study of hospitalizations for pneumonia.
Setting: This cohort study included 88,605 hospitalizations for pneumonia in the Veterans Health Administration health care system during 2008-2013, in which patients received either anti-MRSA or standard therapy for community-onset pneumonia.
Synopsis: Among 88,605 hospitalizations for pneumonia, 38% of the patients received empirical anti-MRSA therapy within the first day of hospitalization and vancomycin accounted for 98% of the therapy. The primary outcome was 30-day all-cause mortality after adjustment for patient comorbidities, vital signs, and laboratory results. Three treatment groups were studied: patients receiving anti-MRSA therapy (vancomycin hydrochloride or linezolid) plus guideline-recommended standard antibiotics (beta-lactam and macrolide or tetracycline hydrochloride, or fluoroquinolone); patients receiving anti-MRSA therapy without standard antibiotics; and patients receiving standard therapy alone. There was no mortality benefit of empirical anti-MRSA therapy versus standard antibiotics, even in those with risk factors for MRSA or in those whose clinical severity warranted admission to the ICU. Empirical anti-MRSA treatment was associated with greater 30-day mortality compared with standard therapy alone, with an adjusted risk ratio of 1.4 (95% confidence interval, 1.3-1.5) versus empirical anti-MRSA treatment plus standard therapy and 1.5 (1.4-1.6) versus empirical anti-MRSA treatment without standard therapy.
Bottom line: Empirical anti-MRSA therapy does not improve mortality and should not be routinely used in patients hospitalized for community-onset pneumonia, even in those with MRSA risk factors.
Citation: Jones BE et al. Empirical anti-MRSA vs. standard antibiotic therapy and risk of 30-day mortality in patients hospitalized for pneumonia. JAMA Intern Med. 2020 Feb 17;180(4):552-60.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Empirical broad-spectrum antibiotics including anti-MRSA therapy are often selected because of concerns for resistant organisms. However, the outcomes of empirical anti-MRSA therapy among patients with pneumonia are unknown.
Study design: A national retrospective multicenter cohort study of hospitalizations for pneumonia.
Setting: This cohort study included 88,605 hospitalizations for pneumonia in the Veterans Health Administration health care system during 2008-2013, in which patients received either anti-MRSA or standard therapy for community-onset pneumonia.
Synopsis: Among 88,605 hospitalizations for pneumonia, 38% of the patients received empirical anti-MRSA therapy within the first day of hospitalization and vancomycin accounted for 98% of the therapy. The primary outcome was 30-day all-cause mortality after adjustment for patient comorbidities, vital signs, and laboratory results. Three treatment groups were studied: patients receiving anti-MRSA therapy (vancomycin hydrochloride or linezolid) plus guideline-recommended standard antibiotics (beta-lactam and macrolide or tetracycline hydrochloride, or fluoroquinolone); patients receiving anti-MRSA therapy without standard antibiotics; and patients receiving standard therapy alone. There was no mortality benefit of empirical anti-MRSA therapy versus standard antibiotics, even in those with risk factors for MRSA or in those whose clinical severity warranted admission to the ICU. Empirical anti-MRSA treatment was associated with greater 30-day mortality compared with standard therapy alone, with an adjusted risk ratio of 1.4 (95% confidence interval, 1.3-1.5) versus empirical anti-MRSA treatment plus standard therapy and 1.5 (1.4-1.6) versus empirical anti-MRSA treatment without standard therapy.
Bottom line: Empirical anti-MRSA therapy does not improve mortality and should not be routinely used in patients hospitalized for community-onset pneumonia, even in those with MRSA risk factors.
Citation: Jones BE et al. Empirical anti-MRSA vs. standard antibiotic therapy and risk of 30-day mortality in patients hospitalized for pneumonia. JAMA Intern Med. 2020 Feb 17;180(4):552-60.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Empirical broad-spectrum antibiotics including anti-MRSA therapy are often selected because of concerns for resistant organisms. However, the outcomes of empirical anti-MRSA therapy among patients with pneumonia are unknown.
Study design: A national retrospective multicenter cohort study of hospitalizations for pneumonia.
Setting: This cohort study included 88,605 hospitalizations for pneumonia in the Veterans Health Administration health care system during 2008-2013, in which patients received either anti-MRSA or standard therapy for community-onset pneumonia.
Synopsis: Among 88,605 hospitalizations for pneumonia, 38% of the patients received empirical anti-MRSA therapy within the first day of hospitalization and vancomycin accounted for 98% of the therapy. The primary outcome was 30-day all-cause mortality after adjustment for patient comorbidities, vital signs, and laboratory results. Three treatment groups were studied: patients receiving anti-MRSA therapy (vancomycin hydrochloride or linezolid) plus guideline-recommended standard antibiotics (beta-lactam and macrolide or tetracycline hydrochloride, or fluoroquinolone); patients receiving anti-MRSA therapy without standard antibiotics; and patients receiving standard therapy alone. There was no mortality benefit of empirical anti-MRSA therapy versus standard antibiotics, even in those with risk factors for MRSA or in those whose clinical severity warranted admission to the ICU. Empirical anti-MRSA treatment was associated with greater 30-day mortality compared with standard therapy alone, with an adjusted risk ratio of 1.4 (95% confidence interval, 1.3-1.5) versus empirical anti-MRSA treatment plus standard therapy and 1.5 (1.4-1.6) versus empirical anti-MRSA treatment without standard therapy.
Bottom line: Empirical anti-MRSA therapy does not improve mortality and should not be routinely used in patients hospitalized for community-onset pneumonia, even in those with MRSA risk factors.
Citation: Jones BE et al. Empirical anti-MRSA vs. standard antibiotic therapy and risk of 30-day mortality in patients hospitalized for pneumonia. JAMA Intern Med. 2020 Feb 17;180(4):552-60.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Twice-a-year lenacapavir shows viral suppression in drug-resistant HIV at 26 weeks
With regulatory approval, lenacapavir could become the only HIV-1 treatment option given every 6 months.
“These data support the use of lenacapavir in patients with multidrug-resistant viruses, and according to its long half-life of two subcutaneous injections per year, [it] could help reduce pill burden,” first author Jean-Michel Molina, MD, PhD, professor of infectious diseases and head of the infectious diseases department at the Saint-Louis and Lariboisière Hospitals, Paris, said in an interview.
Presenting the updated findings from the phase 2/3 CAPELLA trial at the virtual annual meeting of the International AIDS Society conference, Dr. Molina underscored the need for longer-term treatments.
“These patients with multidrug resistances are usually those who have not been fully adherent to their regimen,” he said. “Being able to provide the drug, given every 6 months subcutaneously, provides an ideal treatment for overcoming resistance and lack of adherence.”
The study showed that, after 26 weeks, 81% of heavily treatment-experienced people with HIV in a randomized cohort who were treated with a subcutaneous injection of lenacapavir (927 mg) combined with an optimized background antiretroviral regimen achieved sustained virologic suppression, with an undetectable viral load (<50 copies/mL).
In addition, the lenacapavir-treated patients had a clinically meaningful mean increase in CD4 counts of 81 cells/mcL over the 26 weeks.
The drug was well tolerated, with no drug-related serious adverse events or adverse events leading to discontinuation. The most common adverse events were injection-site reactions, which occurred in 56% of participants, with most being mild or moderate.
Importantly, four participants developed emergent resistances to lenacapavir. One was suppressed with a change in the background regimen and two others were suppressed without a change in regimen.
“We know that these mutations affect viral fitness,” Dr. Molina said in an interview. “We need more studies to assess the real impact of these mutations.”
Dr. Molina noted that a phase 2 study is already underway to evaluate how a pairing of lenacapavir with fellow investigational long-acting drug islatravir (Merck) could offset the risk of developing resistances.
Asked by an audience member whether a two-drug regimen with something like islatravir is likely to successfully prevent resistances, Dr. Molina responded that “it’s too early to know what’s going to happen with [combinations], but these first results are really encouraging when you see the very high rate of being fully suppressed after 26 weeks. The efficacy that we’ve seen after [a previous 2-week analysis] is long lasting.”
Lenacapavir targets multiple viral stages
Unlike other antiviral drugs that target just a single stage of viral replication, lenacapavir takes aim at multiple steps in the viral life cycle, including capsid-mediated uptake of HIV-1 proviral DNA, virus assembly and release, and capsid core formation, Dr. Molina explained.
The CAPELLA trial included participants at research centers in North America, Europe, and Asia, with a median age of 52 years; 25% were female, 38% were Black, and their mean HIV-1 RNA (viral load) was 4.17 log copies/mL.
Overall, 72 patients were divided into two cohorts of 36 patients each, including a randomized and nonrandomized cohort. Dr. Molina primarily reported results from the randomized group.
In that group, patients received either a lead-in of oral lenacapavir (600 mg on day 1 and 2 and 300 mg on day 8) or placebo, in combination with patients’ current failing drug regimens in both groups.
At day 15, all participants were switched to the investigator-selected, optimized background treatment regimen, tailored according to patients’ drug-resistance profiles, and those in the lenacapavir group received the subcutaneous injection of lenacapavir; those in the placebo group were switched to the oral lead-in, followed by subcutaneous lenacapavir every 6 months.
Combined data that included six patients from the nonrandomized cohort showed that 79% of patients had a viral load of less than 50 copies/mL at week 26. The 81% viral suppression rate represented the randomized group (29 of 36).
International AIDS Society cochair Hendrik Streeck, MD, director of the Institute of Virology and Institute for HIV Research at the University Bonn (Germany), said a twice-a-year drug could possibly have profound benefits with a reduction in daily pill burden.
“What makes this an interesting drug is that it is long acting, so one can imagine it has the potential to treat individuals such as those who are not very adherent to the antiretroviral therapy, or who can’t easily access treatment, for example in resource-limited settings,” he said in an interview. “The option to treat patients for the next months in advance could be a very important next step.”
Further data from CALIBRATE
Additional data on lenacapavir from the phase 2 CALIBRATE study, presented in a separate session, further showed the drug, given orally or subcutaneously in combination with oral daily emtricitabine/tenofovir alafenamide, resulted in high rates of viral suppression among 94% of 157 treatment-naive patients after 28 weeks.
Commenting on the research, session moderator Alexandra Calmy, MD, PhD, of the HIV/AIDS unit and LIPO & Metabolism group, infectious diseases division, Geneva University Hospitals, noted the study offered “interesting data indeed” – with some caveats: “Why position a new drug class in naive patients [when] we already have good options, available for a large range of various populations?”
Dr. Calmy noted that, in general, lenacapavir “would certainly be an added value with an adapted 6-monthly companion drug.”
But she raised another key issue: “When will we have data on pregnancy that would allow lenacapavir to really be a game changer worldwide?”
The study was funded by Gilead Sciences. Dr. Molina reported receiving research funding from Gilead and being on advisory boards for Gilead, Merck, ViiV, and Janssen. Dr. Calmy and Dr. Streeck reported no relevant financial relationships.
With regulatory approval, lenacapavir could become the only HIV-1 treatment option given every 6 months.
“These data support the use of lenacapavir in patients with multidrug-resistant viruses, and according to its long half-life of two subcutaneous injections per year, [it] could help reduce pill burden,” first author Jean-Michel Molina, MD, PhD, professor of infectious diseases and head of the infectious diseases department at the Saint-Louis and Lariboisière Hospitals, Paris, said in an interview.
Presenting the updated findings from the phase 2/3 CAPELLA trial at the virtual annual meeting of the International AIDS Society conference, Dr. Molina underscored the need for longer-term treatments.
“These patients with multidrug resistances are usually those who have not been fully adherent to their regimen,” he said. “Being able to provide the drug, given every 6 months subcutaneously, provides an ideal treatment for overcoming resistance and lack of adherence.”
The study showed that, after 26 weeks, 81% of heavily treatment-experienced people with HIV in a randomized cohort who were treated with a subcutaneous injection of lenacapavir (927 mg) combined with an optimized background antiretroviral regimen achieved sustained virologic suppression, with an undetectable viral load (<50 copies/mL).
In addition, the lenacapavir-treated patients had a clinically meaningful mean increase in CD4 counts of 81 cells/mcL over the 26 weeks.
The drug was well tolerated, with no drug-related serious adverse events or adverse events leading to discontinuation. The most common adverse events were injection-site reactions, which occurred in 56% of participants, with most being mild or moderate.
Importantly, four participants developed emergent resistances to lenacapavir. One was suppressed with a change in the background regimen and two others were suppressed without a change in regimen.
“We know that these mutations affect viral fitness,” Dr. Molina said in an interview. “We need more studies to assess the real impact of these mutations.”
Dr. Molina noted that a phase 2 study is already underway to evaluate how a pairing of lenacapavir with fellow investigational long-acting drug islatravir (Merck) could offset the risk of developing resistances.
Asked by an audience member whether a two-drug regimen with something like islatravir is likely to successfully prevent resistances, Dr. Molina responded that “it’s too early to know what’s going to happen with [combinations], but these first results are really encouraging when you see the very high rate of being fully suppressed after 26 weeks. The efficacy that we’ve seen after [a previous 2-week analysis] is long lasting.”
Lenacapavir targets multiple viral stages
Unlike other antiviral drugs that target just a single stage of viral replication, lenacapavir takes aim at multiple steps in the viral life cycle, including capsid-mediated uptake of HIV-1 proviral DNA, virus assembly and release, and capsid core formation, Dr. Molina explained.
The CAPELLA trial included participants at research centers in North America, Europe, and Asia, with a median age of 52 years; 25% were female, 38% were Black, and their mean HIV-1 RNA (viral load) was 4.17 log copies/mL.
Overall, 72 patients were divided into two cohorts of 36 patients each, including a randomized and nonrandomized cohort. Dr. Molina primarily reported results from the randomized group.
In that group, patients received either a lead-in of oral lenacapavir (600 mg on day 1 and 2 and 300 mg on day 8) or placebo, in combination with patients’ current failing drug regimens in both groups.
At day 15, all participants were switched to the investigator-selected, optimized background treatment regimen, tailored according to patients’ drug-resistance profiles, and those in the lenacapavir group received the subcutaneous injection of lenacapavir; those in the placebo group were switched to the oral lead-in, followed by subcutaneous lenacapavir every 6 months.
Combined data that included six patients from the nonrandomized cohort showed that 79% of patients had a viral load of less than 50 copies/mL at week 26. The 81% viral suppression rate represented the randomized group (29 of 36).
International AIDS Society cochair Hendrik Streeck, MD, director of the Institute of Virology and Institute for HIV Research at the University Bonn (Germany), said a twice-a-year drug could possibly have profound benefits with a reduction in daily pill burden.
“What makes this an interesting drug is that it is long acting, so one can imagine it has the potential to treat individuals such as those who are not very adherent to the antiretroviral therapy, or who can’t easily access treatment, for example in resource-limited settings,” he said in an interview. “The option to treat patients for the next months in advance could be a very important next step.”
Further data from CALIBRATE
Additional data on lenacapavir from the phase 2 CALIBRATE study, presented in a separate session, further showed the drug, given orally or subcutaneously in combination with oral daily emtricitabine/tenofovir alafenamide, resulted in high rates of viral suppression among 94% of 157 treatment-naive patients after 28 weeks.
Commenting on the research, session moderator Alexandra Calmy, MD, PhD, of the HIV/AIDS unit and LIPO & Metabolism group, infectious diseases division, Geneva University Hospitals, noted the study offered “interesting data indeed” – with some caveats: “Why position a new drug class in naive patients [when] we already have good options, available for a large range of various populations?”
Dr. Calmy noted that, in general, lenacapavir “would certainly be an added value with an adapted 6-monthly companion drug.”
But she raised another key issue: “When will we have data on pregnancy that would allow lenacapavir to really be a game changer worldwide?”
The study was funded by Gilead Sciences. Dr. Molina reported receiving research funding from Gilead and being on advisory boards for Gilead, Merck, ViiV, and Janssen. Dr. Calmy and Dr. Streeck reported no relevant financial relationships.
With regulatory approval, lenacapavir could become the only HIV-1 treatment option given every 6 months.
“These data support the use of lenacapavir in patients with multidrug-resistant viruses, and according to its long half-life of two subcutaneous injections per year, [it] could help reduce pill burden,” first author Jean-Michel Molina, MD, PhD, professor of infectious diseases and head of the infectious diseases department at the Saint-Louis and Lariboisière Hospitals, Paris, said in an interview.
Presenting the updated findings from the phase 2/3 CAPELLA trial at the virtual annual meeting of the International AIDS Society conference, Dr. Molina underscored the need for longer-term treatments.
“These patients with multidrug resistances are usually those who have not been fully adherent to their regimen,” he said. “Being able to provide the drug, given every 6 months subcutaneously, provides an ideal treatment for overcoming resistance and lack of adherence.”
The study showed that, after 26 weeks, 81% of heavily treatment-experienced people with HIV in a randomized cohort who were treated with a subcutaneous injection of lenacapavir (927 mg) combined with an optimized background antiretroviral regimen achieved sustained virologic suppression, with an undetectable viral load (<50 copies/mL).
In addition, the lenacapavir-treated patients had a clinically meaningful mean increase in CD4 counts of 81 cells/mcL over the 26 weeks.
The drug was well tolerated, with no drug-related serious adverse events or adverse events leading to discontinuation. The most common adverse events were injection-site reactions, which occurred in 56% of participants, with most being mild or moderate.
Importantly, four participants developed emergent resistances to lenacapavir. One was suppressed with a change in the background regimen and two others were suppressed without a change in regimen.
“We know that these mutations affect viral fitness,” Dr. Molina said in an interview. “We need more studies to assess the real impact of these mutations.”
Dr. Molina noted that a phase 2 study is already underway to evaluate how a pairing of lenacapavir with fellow investigational long-acting drug islatravir (Merck) could offset the risk of developing resistances.
Asked by an audience member whether a two-drug regimen with something like islatravir is likely to successfully prevent resistances, Dr. Molina responded that “it’s too early to know what’s going to happen with [combinations], but these first results are really encouraging when you see the very high rate of being fully suppressed after 26 weeks. The efficacy that we’ve seen after [a previous 2-week analysis] is long lasting.”
Lenacapavir targets multiple viral stages
Unlike other antiviral drugs that target just a single stage of viral replication, lenacapavir takes aim at multiple steps in the viral life cycle, including capsid-mediated uptake of HIV-1 proviral DNA, virus assembly and release, and capsid core formation, Dr. Molina explained.
The CAPELLA trial included participants at research centers in North America, Europe, and Asia, with a median age of 52 years; 25% were female, 38% were Black, and their mean HIV-1 RNA (viral load) was 4.17 log copies/mL.
Overall, 72 patients were divided into two cohorts of 36 patients each, including a randomized and nonrandomized cohort. Dr. Molina primarily reported results from the randomized group.
In that group, patients received either a lead-in of oral lenacapavir (600 mg on day 1 and 2 and 300 mg on day 8) or placebo, in combination with patients’ current failing drug regimens in both groups.
At day 15, all participants were switched to the investigator-selected, optimized background treatment regimen, tailored according to patients’ drug-resistance profiles, and those in the lenacapavir group received the subcutaneous injection of lenacapavir; those in the placebo group were switched to the oral lead-in, followed by subcutaneous lenacapavir every 6 months.
Combined data that included six patients from the nonrandomized cohort showed that 79% of patients had a viral load of less than 50 copies/mL at week 26. The 81% viral suppression rate represented the randomized group (29 of 36).
International AIDS Society cochair Hendrik Streeck, MD, director of the Institute of Virology and Institute for HIV Research at the University Bonn (Germany), said a twice-a-year drug could possibly have profound benefits with a reduction in daily pill burden.
“What makes this an interesting drug is that it is long acting, so one can imagine it has the potential to treat individuals such as those who are not very adherent to the antiretroviral therapy, or who can’t easily access treatment, for example in resource-limited settings,” he said in an interview. “The option to treat patients for the next months in advance could be a very important next step.”
Further data from CALIBRATE
Additional data on lenacapavir from the phase 2 CALIBRATE study, presented in a separate session, further showed the drug, given orally or subcutaneously in combination with oral daily emtricitabine/tenofovir alafenamide, resulted in high rates of viral suppression among 94% of 157 treatment-naive patients after 28 weeks.
Commenting on the research, session moderator Alexandra Calmy, MD, PhD, of the HIV/AIDS unit and LIPO & Metabolism group, infectious diseases division, Geneva University Hospitals, noted the study offered “interesting data indeed” – with some caveats: “Why position a new drug class in naive patients [when] we already have good options, available for a large range of various populations?”
Dr. Calmy noted that, in general, lenacapavir “would certainly be an added value with an adapted 6-monthly companion drug.”
But she raised another key issue: “When will we have data on pregnancy that would allow lenacapavir to really be a game changer worldwide?”
The study was funded by Gilead Sciences. Dr. Molina reported receiving research funding from Gilead and being on advisory boards for Gilead, Merck, ViiV, and Janssen. Dr. Calmy and Dr. Streeck reported no relevant financial relationships.
FROM IAS 2021
Children and COVID: New vaccinations increase as cases continue to climb
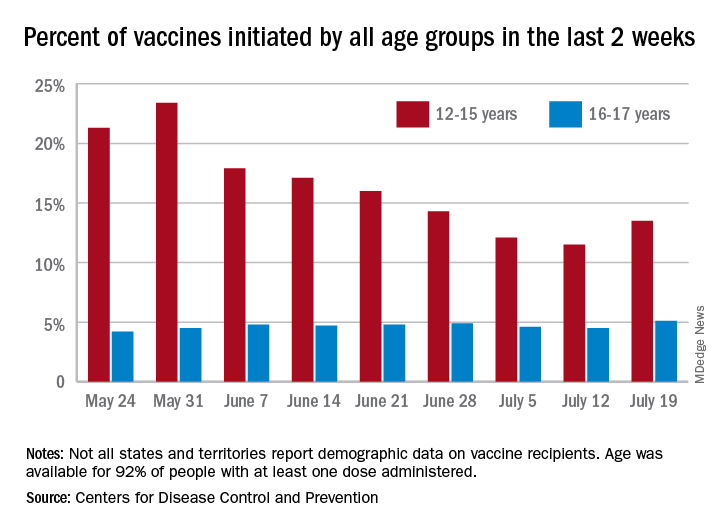
Children aged 12-15 years represented 13.5% of all first vaccinations received during the 2 weeks ending July 19, compared with 11.5% for the 2 weeks ending July 12, marking the first increase since the end of May. First vaccinations in 16- and 17-year-olds, who make up a much smaller share of the U.S. population, also went up, topping 5%, the Centers for Disease Control and Prevention said in its COVID Data Tracker.
The total number of vaccine initiations was almost 250,000 for the week ending July 19, after dropping to a low of 201,000 the previous week. Before that, first vaccinations had fallen in 5 of the previous 6 weeks, going from 1.4 million on May 24 to 307,000 on July 5, the CDC said.
New cases of COVID-19, unfortunately, continued to follow the trend among the larger population: As of July 15, weekly cases in children were up by 179% since dropping to 8,400 on June 24, the American Academy of Pediatrics and the Children’s Hospital Association said in a joint report. The 23,551 new cases in children for the week ending July 15 were 15.9% of all cases reported.
With those new cases, the total number of children infected with COVID-19 comes to almost 4.1 million since the start of the pandemic, the AAP and CHA said. The CDC data indicate that just over 5.35 million children aged 12-15 years and 3.53 million 16- and 17-year-olds have received at least one dose of the COVID-19 vaccine and that 6.8 million children aged 12-17 are fully vaccinated.
Fully vaccinated children represent 26.4% of all 12- to 15-year-olds and 38.3% of the 16- 17-year-olds as of July 19. The corresponding numbers for those who have received at least one dose are 35.2% (ages 12-15) and 46.8% (16-17), the CDC said.
The AAP recently recommended in-person learning with universal masking in schools this fall “because a significant portion of the student population is not yet eligible for vaccines. ... Many schools will not have a system to monitor vaccine status of students, teachers and staff, and some communities overall have low vaccination uptake where the virus may be circulating more prominently.”
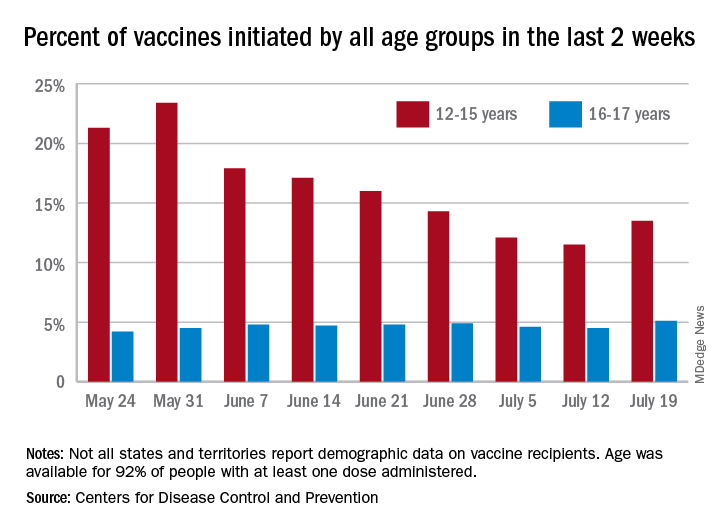
Children aged 12-15 years represented 13.5% of all first vaccinations received during the 2 weeks ending July 19, compared with 11.5% for the 2 weeks ending July 12, marking the first increase since the end of May. First vaccinations in 16- and 17-year-olds, who make up a much smaller share of the U.S. population, also went up, topping 5%, the Centers for Disease Control and Prevention said in its COVID Data Tracker.
The total number of vaccine initiations was almost 250,000 for the week ending July 19, after dropping to a low of 201,000 the previous week. Before that, first vaccinations had fallen in 5 of the previous 6 weeks, going from 1.4 million on May 24 to 307,000 on July 5, the CDC said.
New cases of COVID-19, unfortunately, continued to follow the trend among the larger population: As of July 15, weekly cases in children were up by 179% since dropping to 8,400 on June 24, the American Academy of Pediatrics and the Children’s Hospital Association said in a joint report. The 23,551 new cases in children for the week ending July 15 were 15.9% of all cases reported.
With those new cases, the total number of children infected with COVID-19 comes to almost 4.1 million since the start of the pandemic, the AAP and CHA said. The CDC data indicate that just over 5.35 million children aged 12-15 years and 3.53 million 16- and 17-year-olds have received at least one dose of the COVID-19 vaccine and that 6.8 million children aged 12-17 are fully vaccinated.
Fully vaccinated children represent 26.4% of all 12- to 15-year-olds and 38.3% of the 16- 17-year-olds as of July 19. The corresponding numbers for those who have received at least one dose are 35.2% (ages 12-15) and 46.8% (16-17), the CDC said.
The AAP recently recommended in-person learning with universal masking in schools this fall “because a significant portion of the student population is not yet eligible for vaccines. ... Many schools will not have a system to monitor vaccine status of students, teachers and staff, and some communities overall have low vaccination uptake where the virus may be circulating more prominently.”
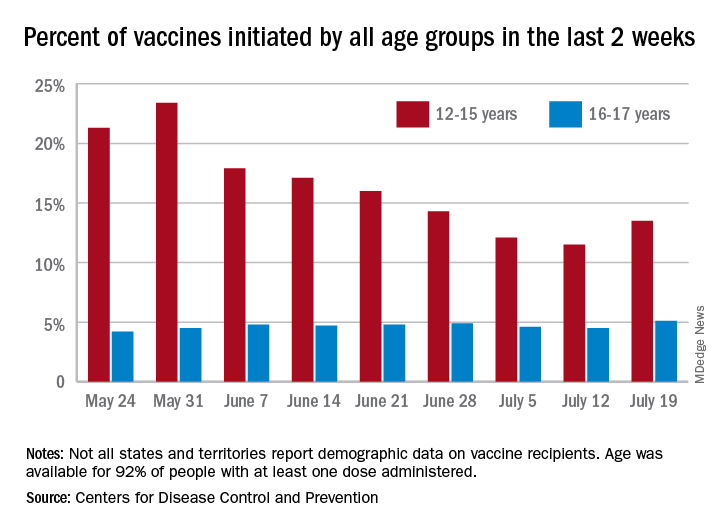
Children aged 12-15 years represented 13.5% of all first vaccinations received during the 2 weeks ending July 19, compared with 11.5% for the 2 weeks ending July 12, marking the first increase since the end of May. First vaccinations in 16- and 17-year-olds, who make up a much smaller share of the U.S. population, also went up, topping 5%, the Centers for Disease Control and Prevention said in its COVID Data Tracker.
The total number of vaccine initiations was almost 250,000 for the week ending July 19, after dropping to a low of 201,000 the previous week. Before that, first vaccinations had fallen in 5 of the previous 6 weeks, going from 1.4 million on May 24 to 307,000 on July 5, the CDC said.
New cases of COVID-19, unfortunately, continued to follow the trend among the larger population: As of July 15, weekly cases in children were up by 179% since dropping to 8,400 on June 24, the American Academy of Pediatrics and the Children’s Hospital Association said in a joint report. The 23,551 new cases in children for the week ending July 15 were 15.9% of all cases reported.
With those new cases, the total number of children infected with COVID-19 comes to almost 4.1 million since the start of the pandemic, the AAP and CHA said. The CDC data indicate that just over 5.35 million children aged 12-15 years and 3.53 million 16- and 17-year-olds have received at least one dose of the COVID-19 vaccine and that 6.8 million children aged 12-17 are fully vaccinated.
Fully vaccinated children represent 26.4% of all 12- to 15-year-olds and 38.3% of the 16- 17-year-olds as of July 19. The corresponding numbers for those who have received at least one dose are 35.2% (ages 12-15) and 46.8% (16-17), the CDC said.
The AAP recently recommended in-person learning with universal masking in schools this fall “because a significant portion of the student population is not yet eligible for vaccines. ... Many schools will not have a system to monitor vaccine status of students, teachers and staff, and some communities overall have low vaccination uptake where the virus may be circulating more prominently.”
HIV: Could another two-drug regimen be on the horizon?
Headache was the most common adverse event (AE) people experienced in 72 weeks of taking the once-daily investigational two-drug HIV treatment islatravir (ISL; Merck) plus doravirine (DOR; Merck), and those AEs were short-lived and mild, according to a safety analysis presented at the International AIDS Society (IAS) Conference 2021.
That finding, combined with other data showing few changes in metabolic markers, is potentially good news for people living with HIV, inasmuch as two-drug regimens generally have fewer side effects than traditional three- or four-drug regimens, said Jean-Michel Molina, MD, PhD, of Sant-Louis and Lariboisière Hospitals, Paris, who previously presented efficacy data on the combination at the HIV Glasgow 2020 Virtual Conference.
“At this point, it’s encouraging,” Dr. Molina told this news organization. “Safety is good, efficacy seems good. But the data are limited, and it’s too early to tell.”
If it makes it to the clinic, IS/DOR would be the fourth two-drug regimen approved for HIV treatment, following the U.S. Food and Drug Administration approval of dolutegravir/lamivudine (Dovato), dolutegravir/rilpivirine (Juluca), and the monthly injectable cabotegravir long-acting/rilpivirine long-acting (Cabenuva).
DOR, a non-nucleoside reverse transcriptase inhibitor (NNRTI), is currently approved and is part of the three-drug single-pill regimen Delstrigo (doravirine/lamivudine/tenofovir disoproxil fumarate, DOR/3TC/TDF, Merck). ISL is still under development for treatment and prevention. Dr. Molina had previously presented data showing that 81.1% of people living with HIV maintained undetectable viral loads (defined as <50 copies/mL) compared to 80.6% of people who continued treatment with DOR/3TC/TDF. Data on ISL/DOR versus DOR/3TC/TDF for people new to HIV treatment were published May 14 in The Lancet HIV.
The ISL/DOR trial was designed to assess the safety of three doses of ISL with 100 mg of DOR – 0.25 mg, 0.75 mg, and 2.25 mg – as a daily treatment. The investigators randomly assigned 29, 30, and 31 participants, respectively, to each of the dual-therapy arms and 31 people to the DOR/3TC/TDF arm after a 24-week lead-in course of DOR/3TC/TDF. At week 60, everyone in the two-drug arms received 0.75 mg of ISL with DOR.
At HIV Glasgow, Dr. Molina didn’t present details about the safety profile of the two-drug combination. Douglas Cunningham, DO, a primary care provider at Pueblo Family Physicians, Phoenix, presented such data at IAS 2021. What he showed was that over the first 96 weeks of the trial, there were a total of 118 AEs among the 90 participants in the ISL plus DOR arms and 42 among the 31 participants in the three-drug regimen arm, but there were only seven drug-related AEs for people in the ISL plus DOR arm, and all of those occurred during the first 48 weeks. There were none from weeks 48 to 96.
In total, there were no drug-related serious AEs for ISL/DOR; there was one in the DOR/3TC/TDF arm. The most common AE was headache, which occurred in a total of 10 participants in the ISL/DOR arms. There were nine cases of vitamin D deficiency, eight cases of nausea, seven cases of arthralgia, diarrhea, sinus pain, and vomiting, and six cases each of anxiety and rash. Four people experienced pain in their extremities.
In the three-drug combination arm, side effects were far fewer – just 18 occurred in at least 10% of participants. The most common AE among people on the three-drug combination was diarrhea, which occurred in six participants. Nausea occurred in three; vomiting and headache in two; and there was one instance each of vitamin D deficiency, arthralgia, sinus pain, rash, and pain in extremities.
“The majority of these events were mild, transient, and not related to study drug,” Dr. Cunningham said.
Three ISL/DOR participants experienced an increase in fasting triglyceride level of >500-1,000 mg/dL, and six patients experienced grade 4 changes in creatine kinase level of ≥20 IU/L. Dr. Cunningham said that all but one of the cases of an increase in creatinine level were the result of physical exertion by the participants, and all of those changes were found to have resolved at future visits. The bottom line is that the two-drug combination was safe.
“In the islatravir and doravirine arm, there were no serious drug related serious AEs and no discontinuations due to drug-related AEs from week 48 to week 96,” said Dr. Cunningham. “Islatravir in combination with doravirine was generally well tolerated through week 96 with few drug-related AEs.”
Still, the value of this combination is unclear for Laura Waters, MD, consulting physician in HIV and sexual health at Central and Northwest London NHS Trust. She pointed out that the data are preliminary and that islatravir hasn’t yet been shown to lessen the chances of development of treatment-resistant mutations – a big deal for two-drug regimens, inasmuch as early attempts at using only two drugs resulted in incomplete suppression of the virus and resistance. Merck is planning a study of the combination in heavily pretreated individuals.
Merck presented data at IAS on another NNRTI, the investigational MK-8507, in combination with islatravir. MK-8507 has the potential to be used weekly instead of daily. Dr. Waters said she suspects that this trial is just a proof of concept of islatravir in combination with an NNRTI. Merck has signed an agreement with Gilead Sciences to co-develop islatravir with long-acting lenacapravir. Additionally, the two-drug combination of dolutegravir and lamivudine has been very successful.
“I’d be surprised if they developed islatravir/doravirine as a usable combo,” she said. “It’s just too soon to say. My personal view is that people are a bit too overoptimistic about it.”
The study was funded by Merck. Dr. Molina has received grants from Gilead Sciences, Merck, ViiV Healthcare, and Sanofi. Dr. Waters has received speaker or advisory fees during the past 2 years from Gilead Sciences, ViiV Healthcare, Merck, Janssen, Theratech, Sipla, and Mylan.
A version of this article first appeared on Medscape.com.
Headache was the most common adverse event (AE) people experienced in 72 weeks of taking the once-daily investigational two-drug HIV treatment islatravir (ISL; Merck) plus doravirine (DOR; Merck), and those AEs were short-lived and mild, according to a safety analysis presented at the International AIDS Society (IAS) Conference 2021.
That finding, combined with other data showing few changes in metabolic markers, is potentially good news for people living with HIV, inasmuch as two-drug regimens generally have fewer side effects than traditional three- or four-drug regimens, said Jean-Michel Molina, MD, PhD, of Sant-Louis and Lariboisière Hospitals, Paris, who previously presented efficacy data on the combination at the HIV Glasgow 2020 Virtual Conference.
“At this point, it’s encouraging,” Dr. Molina told this news organization. “Safety is good, efficacy seems good. But the data are limited, and it’s too early to tell.”
If it makes it to the clinic, IS/DOR would be the fourth two-drug regimen approved for HIV treatment, following the U.S. Food and Drug Administration approval of dolutegravir/lamivudine (Dovato), dolutegravir/rilpivirine (Juluca), and the monthly injectable cabotegravir long-acting/rilpivirine long-acting (Cabenuva).
DOR, a non-nucleoside reverse transcriptase inhibitor (NNRTI), is currently approved and is part of the three-drug single-pill regimen Delstrigo (doravirine/lamivudine/tenofovir disoproxil fumarate, DOR/3TC/TDF, Merck). ISL is still under development for treatment and prevention. Dr. Molina had previously presented data showing that 81.1% of people living with HIV maintained undetectable viral loads (defined as <50 copies/mL) compared to 80.6% of people who continued treatment with DOR/3TC/TDF. Data on ISL/DOR versus DOR/3TC/TDF for people new to HIV treatment were published May 14 in The Lancet HIV.
The ISL/DOR trial was designed to assess the safety of three doses of ISL with 100 mg of DOR – 0.25 mg, 0.75 mg, and 2.25 mg – as a daily treatment. The investigators randomly assigned 29, 30, and 31 participants, respectively, to each of the dual-therapy arms and 31 people to the DOR/3TC/TDF arm after a 24-week lead-in course of DOR/3TC/TDF. At week 60, everyone in the two-drug arms received 0.75 mg of ISL with DOR.
At HIV Glasgow, Dr. Molina didn’t present details about the safety profile of the two-drug combination. Douglas Cunningham, DO, a primary care provider at Pueblo Family Physicians, Phoenix, presented such data at IAS 2021. What he showed was that over the first 96 weeks of the trial, there were a total of 118 AEs among the 90 participants in the ISL plus DOR arms and 42 among the 31 participants in the three-drug regimen arm, but there were only seven drug-related AEs for people in the ISL plus DOR arm, and all of those occurred during the first 48 weeks. There were none from weeks 48 to 96.
In total, there were no drug-related serious AEs for ISL/DOR; there was one in the DOR/3TC/TDF arm. The most common AE was headache, which occurred in a total of 10 participants in the ISL/DOR arms. There were nine cases of vitamin D deficiency, eight cases of nausea, seven cases of arthralgia, diarrhea, sinus pain, and vomiting, and six cases each of anxiety and rash. Four people experienced pain in their extremities.
In the three-drug combination arm, side effects were far fewer – just 18 occurred in at least 10% of participants. The most common AE among people on the three-drug combination was diarrhea, which occurred in six participants. Nausea occurred in three; vomiting and headache in two; and there was one instance each of vitamin D deficiency, arthralgia, sinus pain, rash, and pain in extremities.
“The majority of these events were mild, transient, and not related to study drug,” Dr. Cunningham said.
Three ISL/DOR participants experienced an increase in fasting triglyceride level of >500-1,000 mg/dL, and six patients experienced grade 4 changes in creatine kinase level of ≥20 IU/L. Dr. Cunningham said that all but one of the cases of an increase in creatinine level were the result of physical exertion by the participants, and all of those changes were found to have resolved at future visits. The bottom line is that the two-drug combination was safe.
“In the islatravir and doravirine arm, there were no serious drug related serious AEs and no discontinuations due to drug-related AEs from week 48 to week 96,” said Dr. Cunningham. “Islatravir in combination with doravirine was generally well tolerated through week 96 with few drug-related AEs.”
Still, the value of this combination is unclear for Laura Waters, MD, consulting physician in HIV and sexual health at Central and Northwest London NHS Trust. She pointed out that the data are preliminary and that islatravir hasn’t yet been shown to lessen the chances of development of treatment-resistant mutations – a big deal for two-drug regimens, inasmuch as early attempts at using only two drugs resulted in incomplete suppression of the virus and resistance. Merck is planning a study of the combination in heavily pretreated individuals.
Merck presented data at IAS on another NNRTI, the investigational MK-8507, in combination with islatravir. MK-8507 has the potential to be used weekly instead of daily. Dr. Waters said she suspects that this trial is just a proof of concept of islatravir in combination with an NNRTI. Merck has signed an agreement with Gilead Sciences to co-develop islatravir with long-acting lenacapravir. Additionally, the two-drug combination of dolutegravir and lamivudine has been very successful.
“I’d be surprised if they developed islatravir/doravirine as a usable combo,” she said. “It’s just too soon to say. My personal view is that people are a bit too overoptimistic about it.”
The study was funded by Merck. Dr. Molina has received grants from Gilead Sciences, Merck, ViiV Healthcare, and Sanofi. Dr. Waters has received speaker or advisory fees during the past 2 years from Gilead Sciences, ViiV Healthcare, Merck, Janssen, Theratech, Sipla, and Mylan.
A version of this article first appeared on Medscape.com.
Headache was the most common adverse event (AE) people experienced in 72 weeks of taking the once-daily investigational two-drug HIV treatment islatravir (ISL; Merck) plus doravirine (DOR; Merck), and those AEs were short-lived and mild, according to a safety analysis presented at the International AIDS Society (IAS) Conference 2021.
That finding, combined with other data showing few changes in metabolic markers, is potentially good news for people living with HIV, inasmuch as two-drug regimens generally have fewer side effects than traditional three- or four-drug regimens, said Jean-Michel Molina, MD, PhD, of Sant-Louis and Lariboisière Hospitals, Paris, who previously presented efficacy data on the combination at the HIV Glasgow 2020 Virtual Conference.
“At this point, it’s encouraging,” Dr. Molina told this news organization. “Safety is good, efficacy seems good. But the data are limited, and it’s too early to tell.”
If it makes it to the clinic, IS/DOR would be the fourth two-drug regimen approved for HIV treatment, following the U.S. Food and Drug Administration approval of dolutegravir/lamivudine (Dovato), dolutegravir/rilpivirine (Juluca), and the monthly injectable cabotegravir long-acting/rilpivirine long-acting (Cabenuva).
DOR, a non-nucleoside reverse transcriptase inhibitor (NNRTI), is currently approved and is part of the three-drug single-pill regimen Delstrigo (doravirine/lamivudine/tenofovir disoproxil fumarate, DOR/3TC/TDF, Merck). ISL is still under development for treatment and prevention. Dr. Molina had previously presented data showing that 81.1% of people living with HIV maintained undetectable viral loads (defined as <50 copies/mL) compared to 80.6% of people who continued treatment with DOR/3TC/TDF. Data on ISL/DOR versus DOR/3TC/TDF for people new to HIV treatment were published May 14 in The Lancet HIV.
The ISL/DOR trial was designed to assess the safety of three doses of ISL with 100 mg of DOR – 0.25 mg, 0.75 mg, and 2.25 mg – as a daily treatment. The investigators randomly assigned 29, 30, and 31 participants, respectively, to each of the dual-therapy arms and 31 people to the DOR/3TC/TDF arm after a 24-week lead-in course of DOR/3TC/TDF. At week 60, everyone in the two-drug arms received 0.75 mg of ISL with DOR.
At HIV Glasgow, Dr. Molina didn’t present details about the safety profile of the two-drug combination. Douglas Cunningham, DO, a primary care provider at Pueblo Family Physicians, Phoenix, presented such data at IAS 2021. What he showed was that over the first 96 weeks of the trial, there were a total of 118 AEs among the 90 participants in the ISL plus DOR arms and 42 among the 31 participants in the three-drug regimen arm, but there were only seven drug-related AEs for people in the ISL plus DOR arm, and all of those occurred during the first 48 weeks. There were none from weeks 48 to 96.
In total, there were no drug-related serious AEs for ISL/DOR; there was one in the DOR/3TC/TDF arm. The most common AE was headache, which occurred in a total of 10 participants in the ISL/DOR arms. There were nine cases of vitamin D deficiency, eight cases of nausea, seven cases of arthralgia, diarrhea, sinus pain, and vomiting, and six cases each of anxiety and rash. Four people experienced pain in their extremities.
In the three-drug combination arm, side effects were far fewer – just 18 occurred in at least 10% of participants. The most common AE among people on the three-drug combination was diarrhea, which occurred in six participants. Nausea occurred in three; vomiting and headache in two; and there was one instance each of vitamin D deficiency, arthralgia, sinus pain, rash, and pain in extremities.
“The majority of these events were mild, transient, and not related to study drug,” Dr. Cunningham said.
Three ISL/DOR participants experienced an increase in fasting triglyceride level of >500-1,000 mg/dL, and six patients experienced grade 4 changes in creatine kinase level of ≥20 IU/L. Dr. Cunningham said that all but one of the cases of an increase in creatinine level were the result of physical exertion by the participants, and all of those changes were found to have resolved at future visits. The bottom line is that the two-drug combination was safe.
“In the islatravir and doravirine arm, there were no serious drug related serious AEs and no discontinuations due to drug-related AEs from week 48 to week 96,” said Dr. Cunningham. “Islatravir in combination with doravirine was generally well tolerated through week 96 with few drug-related AEs.”
Still, the value of this combination is unclear for Laura Waters, MD, consulting physician in HIV and sexual health at Central and Northwest London NHS Trust. She pointed out that the data are preliminary and that islatravir hasn’t yet been shown to lessen the chances of development of treatment-resistant mutations – a big deal for two-drug regimens, inasmuch as early attempts at using only two drugs resulted in incomplete suppression of the virus and resistance. Merck is planning a study of the combination in heavily pretreated individuals.
Merck presented data at IAS on another NNRTI, the investigational MK-8507, in combination with islatravir. MK-8507 has the potential to be used weekly instead of daily. Dr. Waters said she suspects that this trial is just a proof of concept of islatravir in combination with an NNRTI. Merck has signed an agreement with Gilead Sciences to co-develop islatravir with long-acting lenacapravir. Additionally, the two-drug combination of dolutegravir and lamivudine has been very successful.
“I’d be surprised if they developed islatravir/doravirine as a usable combo,” she said. “It’s just too soon to say. My personal view is that people are a bit too overoptimistic about it.”
The study was funded by Merck. Dr. Molina has received grants from Gilead Sciences, Merck, ViiV Healthcare, and Sanofi. Dr. Waters has received speaker or advisory fees during the past 2 years from Gilead Sciences, ViiV Healthcare, Merck, Janssen, Theratech, Sipla, and Mylan.
A version of this article first appeared on Medscape.com.
HIV increases risk for severe COVID-19
according to a report from the World Health Organization on COVID-19 outcomes among people living with HIV. The study primarily included people from South Africa but also some data from other parts of the world, including the United States.
However, the report, presented at the 11th IAS Conference on HIV Science (IAS 2021), couldn’t answer some crucial questions clinicians have been wondering about since the COVID-19 pandemic began. For example, was the increase in COVID risk a result of the presence of HIV or because of the immune compromise caused by untreated HIV?
The report didn’t include data on viral load or CD counts, both used to evaluate the health of a person’s immune system. On effective treatment, people living with HIV have a lifespan close to their HIV-negative peers. And effective treatment causes undetectable viral loads which, when maintained for 6 months or more, eliminates transmission of HIV to sexual partners.
What’s clear is that in people with HIV, as in people without HIV, older people, men, and people with diabetes, hypertension, or obesity had the worst outcomes and were most likely to die from COVID-19.
For David Malebranche, MD, MPH, an internal medicine doctor who provides primary care for people in Atlanta, and who was not involved in the study, the WHO study didn’t add anything new. He already recommends the COVID-19 vaccine for all of his patients, HIV-positive or not.
“We don’t have any information from this about the T-cell counts [or] the rates of viral suppression, which I think is tremendously important,” he told this news organization. “To bypass that and not include that in any of the discussion puts the results in a questionable place for me.”
The results come from the WHO Clinical Platform, which culls data from WHO member country surveillance as well as manual case reports from all over the world. By April 29, data on 268,412 people hospitalized with COVID-19 from 37 countries were reported to the platform. Of those, 22,640 people are from the U.S.
A total of 15,522 participants worldwide were living with HIV, 664 in the United States. All U.S. cases were reported from the New York City Health and Hospitals system, Henry Ford Hospital in Detroit, and BronxCare Health System in New York City. Almost all of the remaining participants lived in South Africa – 14,682 of the 15,522, or 94.5%.
Of the 15,522 people living with HIV in the overall group, 37.1% of participants were male, and their median age was 45 years. More than 1 in 3 (36.2%) were admitted with severe or critical COVID-19, and nearly one quarter – 23.1% – with a known outcome died. More than half had one or more chronic conditions, including those that themselves are associated with worse COVID-19 outcomes, such as hypertension (in 33.2% of the participants), diabetes (22.7%), and BMIs above 30 (16.9%). In addition, 8.9% were smokers, 6.6% had chronic pulmonary disease, and 4.3% had chronic heart disease.
After adjusting for those chronic conditions, age, and sex, people living with HIV had a 6% higher rate of severe or critical COVID-19 illness. When investigators adjusted the analysis additionally to differentiate outcomes based on not just the presence of comorbid conditions but the number of them a person had, that increased risk rose to 13%. HIV itself is a comorbid condition, though it wasn’t counted as one in this adjusted analysis.
It didn’t matter whether researchers looked at risk for severe outcomes or deaths after removing the significant co-occurring conditions or if they looked at number of chronic illnesses (aside from HIV), said Silvia Bertagnolio, MD, medical officer at the World Health Organization and co-author of the analysis.
“Both models show almost identical [adjusted odds ratios], meaning that HIV was independently significantly associated with severe/critical presentation,” she told this news organization.
As for death, the analysis showed that, overall, people living with HIV were 30% more likely to die of COVID-19 compared with those not living with HIV. And while this held true even when they adjusted the data for comorbidities, people with HIV were more likely to die if they were over age 65 (risk increased by 82%), male (risk increased by 21%), had diabetes (risk increased by 50%), or had hypertension (risk increased by 26%).
When they broke down the data by WHO region – Africa, Europe, the Americas – investigators found that the increased risk for death held true in Africa. But there were not enough data from the other regions to model mortality risk. What’s more, when they broke the data down by country and excluded South Africa, they found that the elevated risk for death in people living with HIV did not reach statistical significance. Dr. Bertagnolio said she suspects that the small sample sizes from other regions made it impossible to detect a difference, but one could still be present.
One thing conspicuously absent from the analysis was information on viral load, CD4 T-cell count, progression of HIV to AIDS, and whether individuals were in HIV care. The first three factors were not reported in the platform, and the fourth was available for 60% of participants but was not included in the analysis. Dr. Bertagnolio pointed out that, for those 60% of participants, 91.8% were on antiretroviral treatment (ART).
“The majority of patients come from South Africa, and we know that in South Africa, over 90% of people receiving ART are virologically suppressed,” she told this news organization. “So we could speculate that this effect persists despite the use of ART, in a population likely to be virally suppressed, although we cannot assess this with certainty through the data set we had.”
A much smaller study of 749 people living with HIV and diagnosed with SARS-CoV-2, also presented at the conference, found that detectable HIV viral load was significantly associated with a slightly higher risk of severe outcomes (P < .039), but CD4 counts less than 200 cells/mm3 was not (P = .15).
And although both Dr. Bertagnolio and conference organizers presented this data as proof that HIV increases the risk for poor COVID-19 outcomes, Dr. Malebranche isn’t so sure. He estimates that only about half his patients have received the COVID-19 vaccine. But this study is unlikely to make him forcefully recommend a COVID-19 vaccination with young, otherwise healthy, and undetectable people in his care who express particular concern about long-term effects of the vaccine. He also manages a lot of people with HIV who have undetectable viral loads and CD4 counts of up to 1,200 but are older, with diabetes, obesity, and high blood pressure. Those are the people he will target with stronger messages regarding the vaccine.
“The young patients who are healthy, virally suppressed, and doing well may very much argue with me, ‘I’m not going to push it,’ but I will bring it up on the next visit,” he said. The analysis “just helps reinforce in me that I need to have these conversations and be a little bit more persuasive to my older patients with comorbid conditions.”
Dr. Bertagnolio has disclosed no relevant financial relationships. Dr. Malebranche serves on the pre-exposure prophylaxis (PrEP) speakers bureau for Gilead Sciences and has consulted and advised for ViiV Healthcare. This study was funded by the World Health Organization.
A version of this article first appeared on Medscape.com.
according to a report from the World Health Organization on COVID-19 outcomes among people living with HIV. The study primarily included people from South Africa but also some data from other parts of the world, including the United States.
However, the report, presented at the 11th IAS Conference on HIV Science (IAS 2021), couldn’t answer some crucial questions clinicians have been wondering about since the COVID-19 pandemic began. For example, was the increase in COVID risk a result of the presence of HIV or because of the immune compromise caused by untreated HIV?
The report didn’t include data on viral load or CD counts, both used to evaluate the health of a person’s immune system. On effective treatment, people living with HIV have a lifespan close to their HIV-negative peers. And effective treatment causes undetectable viral loads which, when maintained for 6 months or more, eliminates transmission of HIV to sexual partners.
What’s clear is that in people with HIV, as in people without HIV, older people, men, and people with diabetes, hypertension, or obesity had the worst outcomes and were most likely to die from COVID-19.
For David Malebranche, MD, MPH, an internal medicine doctor who provides primary care for people in Atlanta, and who was not involved in the study, the WHO study didn’t add anything new. He already recommends the COVID-19 vaccine for all of his patients, HIV-positive or not.
“We don’t have any information from this about the T-cell counts [or] the rates of viral suppression, which I think is tremendously important,” he told this news organization. “To bypass that and not include that in any of the discussion puts the results in a questionable place for me.”
The results come from the WHO Clinical Platform, which culls data from WHO member country surveillance as well as manual case reports from all over the world. By April 29, data on 268,412 people hospitalized with COVID-19 from 37 countries were reported to the platform. Of those, 22,640 people are from the U.S.
A total of 15,522 participants worldwide were living with HIV, 664 in the United States. All U.S. cases were reported from the New York City Health and Hospitals system, Henry Ford Hospital in Detroit, and BronxCare Health System in New York City. Almost all of the remaining participants lived in South Africa – 14,682 of the 15,522, or 94.5%.
Of the 15,522 people living with HIV in the overall group, 37.1% of participants were male, and their median age was 45 years. More than 1 in 3 (36.2%) were admitted with severe or critical COVID-19, and nearly one quarter – 23.1% – with a known outcome died. More than half had one or more chronic conditions, including those that themselves are associated with worse COVID-19 outcomes, such as hypertension (in 33.2% of the participants), diabetes (22.7%), and BMIs above 30 (16.9%). In addition, 8.9% were smokers, 6.6% had chronic pulmonary disease, and 4.3% had chronic heart disease.
After adjusting for those chronic conditions, age, and sex, people living with HIV had a 6% higher rate of severe or critical COVID-19 illness. When investigators adjusted the analysis additionally to differentiate outcomes based on not just the presence of comorbid conditions but the number of them a person had, that increased risk rose to 13%. HIV itself is a comorbid condition, though it wasn’t counted as one in this adjusted analysis.
It didn’t matter whether researchers looked at risk for severe outcomes or deaths after removing the significant co-occurring conditions or if they looked at number of chronic illnesses (aside from HIV), said Silvia Bertagnolio, MD, medical officer at the World Health Organization and co-author of the analysis.
“Both models show almost identical [adjusted odds ratios], meaning that HIV was independently significantly associated with severe/critical presentation,” she told this news organization.
As for death, the analysis showed that, overall, people living with HIV were 30% more likely to die of COVID-19 compared with those not living with HIV. And while this held true even when they adjusted the data for comorbidities, people with HIV were more likely to die if they were over age 65 (risk increased by 82%), male (risk increased by 21%), had diabetes (risk increased by 50%), or had hypertension (risk increased by 26%).
When they broke down the data by WHO region – Africa, Europe, the Americas – investigators found that the increased risk for death held true in Africa. But there were not enough data from the other regions to model mortality risk. What’s more, when they broke the data down by country and excluded South Africa, they found that the elevated risk for death in people living with HIV did not reach statistical significance. Dr. Bertagnolio said she suspects that the small sample sizes from other regions made it impossible to detect a difference, but one could still be present.
One thing conspicuously absent from the analysis was information on viral load, CD4 T-cell count, progression of HIV to AIDS, and whether individuals were in HIV care. The first three factors were not reported in the platform, and the fourth was available for 60% of participants but was not included in the analysis. Dr. Bertagnolio pointed out that, for those 60% of participants, 91.8% were on antiretroviral treatment (ART).
“The majority of patients come from South Africa, and we know that in South Africa, over 90% of people receiving ART are virologically suppressed,” she told this news organization. “So we could speculate that this effect persists despite the use of ART, in a population likely to be virally suppressed, although we cannot assess this with certainty through the data set we had.”
A much smaller study of 749 people living with HIV and diagnosed with SARS-CoV-2, also presented at the conference, found that detectable HIV viral load was significantly associated with a slightly higher risk of severe outcomes (P < .039), but CD4 counts less than 200 cells/mm3 was not (P = .15).
And although both Dr. Bertagnolio and conference organizers presented this data as proof that HIV increases the risk for poor COVID-19 outcomes, Dr. Malebranche isn’t so sure. He estimates that only about half his patients have received the COVID-19 vaccine. But this study is unlikely to make him forcefully recommend a COVID-19 vaccination with young, otherwise healthy, and undetectable people in his care who express particular concern about long-term effects of the vaccine. He also manages a lot of people with HIV who have undetectable viral loads and CD4 counts of up to 1,200 but are older, with diabetes, obesity, and high blood pressure. Those are the people he will target with stronger messages regarding the vaccine.
“The young patients who are healthy, virally suppressed, and doing well may very much argue with me, ‘I’m not going to push it,’ but I will bring it up on the next visit,” he said. The analysis “just helps reinforce in me that I need to have these conversations and be a little bit more persuasive to my older patients with comorbid conditions.”
Dr. Bertagnolio has disclosed no relevant financial relationships. Dr. Malebranche serves on the pre-exposure prophylaxis (PrEP) speakers bureau for Gilead Sciences and has consulted and advised for ViiV Healthcare. This study was funded by the World Health Organization.
A version of this article first appeared on Medscape.com.
according to a report from the World Health Organization on COVID-19 outcomes among people living with HIV. The study primarily included people from South Africa but also some data from other parts of the world, including the United States.
However, the report, presented at the 11th IAS Conference on HIV Science (IAS 2021), couldn’t answer some crucial questions clinicians have been wondering about since the COVID-19 pandemic began. For example, was the increase in COVID risk a result of the presence of HIV or because of the immune compromise caused by untreated HIV?
The report didn’t include data on viral load or CD counts, both used to evaluate the health of a person’s immune system. On effective treatment, people living with HIV have a lifespan close to their HIV-negative peers. And effective treatment causes undetectable viral loads which, when maintained for 6 months or more, eliminates transmission of HIV to sexual partners.
What’s clear is that in people with HIV, as in people without HIV, older people, men, and people with diabetes, hypertension, or obesity had the worst outcomes and were most likely to die from COVID-19.
For David Malebranche, MD, MPH, an internal medicine doctor who provides primary care for people in Atlanta, and who was not involved in the study, the WHO study didn’t add anything new. He already recommends the COVID-19 vaccine for all of his patients, HIV-positive or not.
“We don’t have any information from this about the T-cell counts [or] the rates of viral suppression, which I think is tremendously important,” he told this news organization. “To bypass that and not include that in any of the discussion puts the results in a questionable place for me.”
The results come from the WHO Clinical Platform, which culls data from WHO member country surveillance as well as manual case reports from all over the world. By April 29, data on 268,412 people hospitalized with COVID-19 from 37 countries were reported to the platform. Of those, 22,640 people are from the U.S.
A total of 15,522 participants worldwide were living with HIV, 664 in the United States. All U.S. cases were reported from the New York City Health and Hospitals system, Henry Ford Hospital in Detroit, and BronxCare Health System in New York City. Almost all of the remaining participants lived in South Africa – 14,682 of the 15,522, or 94.5%.
Of the 15,522 people living with HIV in the overall group, 37.1% of participants were male, and their median age was 45 years. More than 1 in 3 (36.2%) were admitted with severe or critical COVID-19, and nearly one quarter – 23.1% – with a known outcome died. More than half had one or more chronic conditions, including those that themselves are associated with worse COVID-19 outcomes, such as hypertension (in 33.2% of the participants), diabetes (22.7%), and BMIs above 30 (16.9%). In addition, 8.9% were smokers, 6.6% had chronic pulmonary disease, and 4.3% had chronic heart disease.
After adjusting for those chronic conditions, age, and sex, people living with HIV had a 6% higher rate of severe or critical COVID-19 illness. When investigators adjusted the analysis additionally to differentiate outcomes based on not just the presence of comorbid conditions but the number of them a person had, that increased risk rose to 13%. HIV itself is a comorbid condition, though it wasn’t counted as one in this adjusted analysis.
It didn’t matter whether researchers looked at risk for severe outcomes or deaths after removing the significant co-occurring conditions or if they looked at number of chronic illnesses (aside from HIV), said Silvia Bertagnolio, MD, medical officer at the World Health Organization and co-author of the analysis.
“Both models show almost identical [adjusted odds ratios], meaning that HIV was independently significantly associated with severe/critical presentation,” she told this news organization.
As for death, the analysis showed that, overall, people living with HIV were 30% more likely to die of COVID-19 compared with those not living with HIV. And while this held true even when they adjusted the data for comorbidities, people with HIV were more likely to die if they were over age 65 (risk increased by 82%), male (risk increased by 21%), had diabetes (risk increased by 50%), or had hypertension (risk increased by 26%).
When they broke down the data by WHO region – Africa, Europe, the Americas – investigators found that the increased risk for death held true in Africa. But there were not enough data from the other regions to model mortality risk. What’s more, when they broke the data down by country and excluded South Africa, they found that the elevated risk for death in people living with HIV did not reach statistical significance. Dr. Bertagnolio said she suspects that the small sample sizes from other regions made it impossible to detect a difference, but one could still be present.
One thing conspicuously absent from the analysis was information on viral load, CD4 T-cell count, progression of HIV to AIDS, and whether individuals were in HIV care. The first three factors were not reported in the platform, and the fourth was available for 60% of participants but was not included in the analysis. Dr. Bertagnolio pointed out that, for those 60% of participants, 91.8% were on antiretroviral treatment (ART).
“The majority of patients come from South Africa, and we know that in South Africa, over 90% of people receiving ART are virologically suppressed,” she told this news organization. “So we could speculate that this effect persists despite the use of ART, in a population likely to be virally suppressed, although we cannot assess this with certainty through the data set we had.”
A much smaller study of 749 people living with HIV and diagnosed with SARS-CoV-2, also presented at the conference, found that detectable HIV viral load was significantly associated with a slightly higher risk of severe outcomes (P < .039), but CD4 counts less than 200 cells/mm3 was not (P = .15).
And although both Dr. Bertagnolio and conference organizers presented this data as proof that HIV increases the risk for poor COVID-19 outcomes, Dr. Malebranche isn’t so sure. He estimates that only about half his patients have received the COVID-19 vaccine. But this study is unlikely to make him forcefully recommend a COVID-19 vaccination with young, otherwise healthy, and undetectable people in his care who express particular concern about long-term effects of the vaccine. He also manages a lot of people with HIV who have undetectable viral loads and CD4 counts of up to 1,200 but are older, with diabetes, obesity, and high blood pressure. Those are the people he will target with stronger messages regarding the vaccine.
“The young patients who are healthy, virally suppressed, and doing well may very much argue with me, ‘I’m not going to push it,’ but I will bring it up on the next visit,” he said. The analysis “just helps reinforce in me that I need to have these conversations and be a little bit more persuasive to my older patients with comorbid conditions.”
Dr. Bertagnolio has disclosed no relevant financial relationships. Dr. Malebranche serves on the pre-exposure prophylaxis (PrEP) speakers bureau for Gilead Sciences and has consulted and advised for ViiV Healthcare. This study was funded by the World Health Organization.
A version of this article first appeared on Medscape.com.
Pandemic drives drop in prescription drugs for children
The amount of prescription drugs given to children in the United States decreased by 27.1% between April and December 2020, compared with the same period in 2019, based on data from a national database.
Overall, dispensing of prescription drugs to all patients in the United States decreased in the wake of COVID-19 but has since rebounded, wrote Kao-Ping Chua, MD, of the University of Michigan, Ann Arbor, and colleagues. “However, whether these same trends occurred for children is unknown.”
In a study published in Pediatrics, the researchers used the IQVIA National Prescription Audit, a database that contains monthly dispensing details from 92% of retail pharmacies in the United States. They compared changes in the dispensing of prescriptions with children aged 0-19 years during 2018-2020.
In the April 2020–December 2020 time period, prescriptions for children aged 1-2 years, 3-9 years, and 10-19 years decreased by 48.7%, 40.6%, and 16.8%, respectively, compared with the same time period in 2019.
The overall dispensing total for children from April 2020 to December 2020 was 160,630,406, representing a 27.1% reduction, compared with the 220,284,613 total from April 2019 to December 2019.
By drug class, prescriptions for antibiotics, ADHD medications, and antidepressants decreased by 55.6%, 11.8%, and 0.1%, respectively, in comparing the two time periods. Prescriptions for drug classes used typically for acute infections decreased by 51.3%, and those used for chronic diseases decreased by 17.4%.
From January 2018 to February 2020, a median of 25,744,758 prescriptions were dispensed to children aged 0-19 years each month. The total prescriptions decreased from 25,684,219 in March 2020 to 16,742,568 in April 2020, increased to 19,657,289 in October 2020, and decreased again to 15,821,914 during December 2020.
In a subgroup analysis, the decline in prescriptions was greater in children aged 0-9 years, compared with those aged 10-19 years. “Because young children have a higher rate of antibiotic use than older children, declines in antibiotic dispensing might affect overall dispensing totals to a greater degree in young children,” the researchers said.
The study findings were limited by several factors including the lack of information on clinical outcomes, disease severity, and details of new versus ongoing prescriptions, as well as the possible heterogeneity in indications within drug classes, and lack of data from small pharmacies, the researchers noted. However, the results were strengthened by the use of a national all-payer database that including most prescriptions dispensed in the United States, and the use of objective measurements of prescribing practices rather than self-reports.
Despite concerns for the decreased dispensing of chronic disease drugs to children during the pandemic, “declines in dispensing of infection-related drugs, such as antitussives and antibiotics, may be welcome developments,” the researchers said. “These declines reveal that substantial reductions in prescribing of these drugs are possible,” and ongoing monitoring is needed to follow whether the reductions continue long term.
COVID precautions contributed to prescription declines
The mask-wearing and social distancing imposed by the COVID-19 pandemic has contributed to reduced rates of other illnesses, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
“On the surface, with masks and social isolation, we have seen a drastic reduction in infectious disease,” she said. Fewer infections mean a reduced need for prescriptions to treat them. However, Dr. Kinsella expects the situation to change as more venues and activities open. “I expect that, as things continue to open, we will continue to see more infectious disease,” which will likely lead to more prescription drug use.
Part of the study data were provided through the IQVIA Institute’s Human Data Science Research Collaborative. Lead author Dr. Chua was supported by a career development award from the National Institute on Drug Abuse, but had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves as a member of the Pediatric News editorial advisory board.
The amount of prescription drugs given to children in the United States decreased by 27.1% between April and December 2020, compared with the same period in 2019, based on data from a national database.
Overall, dispensing of prescription drugs to all patients in the United States decreased in the wake of COVID-19 but has since rebounded, wrote Kao-Ping Chua, MD, of the University of Michigan, Ann Arbor, and colleagues. “However, whether these same trends occurred for children is unknown.”
In a study published in Pediatrics, the researchers used the IQVIA National Prescription Audit, a database that contains monthly dispensing details from 92% of retail pharmacies in the United States. They compared changes in the dispensing of prescriptions with children aged 0-19 years during 2018-2020.
In the April 2020–December 2020 time period, prescriptions for children aged 1-2 years, 3-9 years, and 10-19 years decreased by 48.7%, 40.6%, and 16.8%, respectively, compared with the same time period in 2019.
The overall dispensing total for children from April 2020 to December 2020 was 160,630,406, representing a 27.1% reduction, compared with the 220,284,613 total from April 2019 to December 2019.
By drug class, prescriptions for antibiotics, ADHD medications, and antidepressants decreased by 55.6%, 11.8%, and 0.1%, respectively, in comparing the two time periods. Prescriptions for drug classes used typically for acute infections decreased by 51.3%, and those used for chronic diseases decreased by 17.4%.
From January 2018 to February 2020, a median of 25,744,758 prescriptions were dispensed to children aged 0-19 years each month. The total prescriptions decreased from 25,684,219 in March 2020 to 16,742,568 in April 2020, increased to 19,657,289 in October 2020, and decreased again to 15,821,914 during December 2020.
In a subgroup analysis, the decline in prescriptions was greater in children aged 0-9 years, compared with those aged 10-19 years. “Because young children have a higher rate of antibiotic use than older children, declines in antibiotic dispensing might affect overall dispensing totals to a greater degree in young children,” the researchers said.
The study findings were limited by several factors including the lack of information on clinical outcomes, disease severity, and details of new versus ongoing prescriptions, as well as the possible heterogeneity in indications within drug classes, and lack of data from small pharmacies, the researchers noted. However, the results were strengthened by the use of a national all-payer database that including most prescriptions dispensed in the United States, and the use of objective measurements of prescribing practices rather than self-reports.
Despite concerns for the decreased dispensing of chronic disease drugs to children during the pandemic, “declines in dispensing of infection-related drugs, such as antitussives and antibiotics, may be welcome developments,” the researchers said. “These declines reveal that substantial reductions in prescribing of these drugs are possible,” and ongoing monitoring is needed to follow whether the reductions continue long term.
COVID precautions contributed to prescription declines
The mask-wearing and social distancing imposed by the COVID-19 pandemic has contributed to reduced rates of other illnesses, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
“On the surface, with masks and social isolation, we have seen a drastic reduction in infectious disease,” she said. Fewer infections mean a reduced need for prescriptions to treat them. However, Dr. Kinsella expects the situation to change as more venues and activities open. “I expect that, as things continue to open, we will continue to see more infectious disease,” which will likely lead to more prescription drug use.
Part of the study data were provided through the IQVIA Institute’s Human Data Science Research Collaborative. Lead author Dr. Chua was supported by a career development award from the National Institute on Drug Abuse, but had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves as a member of the Pediatric News editorial advisory board.
The amount of prescription drugs given to children in the United States decreased by 27.1% between April and December 2020, compared with the same period in 2019, based on data from a national database.
Overall, dispensing of prescription drugs to all patients in the United States decreased in the wake of COVID-19 but has since rebounded, wrote Kao-Ping Chua, MD, of the University of Michigan, Ann Arbor, and colleagues. “However, whether these same trends occurred for children is unknown.”
In a study published in Pediatrics, the researchers used the IQVIA National Prescription Audit, a database that contains monthly dispensing details from 92% of retail pharmacies in the United States. They compared changes in the dispensing of prescriptions with children aged 0-19 years during 2018-2020.
In the April 2020–December 2020 time period, prescriptions for children aged 1-2 years, 3-9 years, and 10-19 years decreased by 48.7%, 40.6%, and 16.8%, respectively, compared with the same time period in 2019.
The overall dispensing total for children from April 2020 to December 2020 was 160,630,406, representing a 27.1% reduction, compared with the 220,284,613 total from April 2019 to December 2019.
By drug class, prescriptions for antibiotics, ADHD medications, and antidepressants decreased by 55.6%, 11.8%, and 0.1%, respectively, in comparing the two time periods. Prescriptions for drug classes used typically for acute infections decreased by 51.3%, and those used for chronic diseases decreased by 17.4%.
From January 2018 to February 2020, a median of 25,744,758 prescriptions were dispensed to children aged 0-19 years each month. The total prescriptions decreased from 25,684,219 in March 2020 to 16,742,568 in April 2020, increased to 19,657,289 in October 2020, and decreased again to 15,821,914 during December 2020.
In a subgroup analysis, the decline in prescriptions was greater in children aged 0-9 years, compared with those aged 10-19 years. “Because young children have a higher rate of antibiotic use than older children, declines in antibiotic dispensing might affect overall dispensing totals to a greater degree in young children,” the researchers said.
The study findings were limited by several factors including the lack of information on clinical outcomes, disease severity, and details of new versus ongoing prescriptions, as well as the possible heterogeneity in indications within drug classes, and lack of data from small pharmacies, the researchers noted. However, the results were strengthened by the use of a national all-payer database that including most prescriptions dispensed in the United States, and the use of objective measurements of prescribing practices rather than self-reports.
Despite concerns for the decreased dispensing of chronic disease drugs to children during the pandemic, “declines in dispensing of infection-related drugs, such as antitussives and antibiotics, may be welcome developments,” the researchers said. “These declines reveal that substantial reductions in prescribing of these drugs are possible,” and ongoing monitoring is needed to follow whether the reductions continue long term.
COVID precautions contributed to prescription declines
The mask-wearing and social distancing imposed by the COVID-19 pandemic has contributed to reduced rates of other illnesses, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
“On the surface, with masks and social isolation, we have seen a drastic reduction in infectious disease,” she said. Fewer infections mean a reduced need for prescriptions to treat them. However, Dr. Kinsella expects the situation to change as more venues and activities open. “I expect that, as things continue to open, we will continue to see more infectious disease,” which will likely lead to more prescription drug use.
Part of the study data were provided through the IQVIA Institute’s Human Data Science Research Collaborative. Lead author Dr. Chua was supported by a career development award from the National Institute on Drug Abuse, but had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves as a member of the Pediatric News editorial advisory board.
FROM PEDIATRICS