User login
Address Nonoperative Limb After Knee Surgery
SAN DIEGO – It’s important to pay attention to both knees – the knee that was operated on as well as the knee that wasn’t operated on – after a unilateral, medial, opening-wedge high tibial osteotomy.
Joint load increases in the nonoperative knee following the procedure, which is used to correct varus malalignment, according to researchers at the University of Western Ontario, London.
The findings apply to a subset of opening wedge high tibial osteotomy (HTO) patients, those who present initially with significant bilateral varus, but in whom symptoms were severe enough to require surgery in only one knee.
In 38 such patients, 2 years after surgery "we noted a 0.25% [of body weight times height] increase in peak knee adduction moment in the non-operative limb," as well as a slight increase in vertical ground reaction force, said lead author and physiotherapist Angelo Boulougouris, a biomechanics doctoral candidate at the school. The external knee adduction moment measured during gait is an indicator of tibiofemoral joint osteoarthritis progression.
"The major point is to pay attention to what’s happening to the opposite knee, to make sure you are not ignoring it and focusing your entire treatment plan on just looking at the operative knee," he said.
An unloader brace, for instance, might be appropriate for the nonoperative knee, among other possible interventions, he said. An unloader brace is designed to lessen the stress on a knee with medial compartment knee osteoarthritis. This use of the unloader brace would be to prevent development of knee OA rather than to ease the discomfort associated with established disease
During HTO, a wedge of the cancellous bone allograft is placed in the proximal end of the tibia, correcting both varus deformity and weight distribution through the knee. "Our surgeons are particularly careful to not over-correct," Mr. Boulougouris said.
Of the 38 patients, 32 were men, the average age was about 50 and average body mass index (BMI) about 27 kg/m2. Varus malalignment in the operative limb was about 11 degrees and Kellgren-Lawrence grades ranged from 1 to 3. Varus malalignment was about 8 degrees in the nonoperative limb, with Kellgren-Lawrence grades ranging from 0 to 1.
Patients did well overall, reporting decreased pain and improved quality of life at 2 years. Varus malalignment was corrected in the operative limb, and unchanged in the nonoperative limb.
Knee adduction moment had also significantly decreased on the operative side (mean change, –1.99 % of body weight times height), but increased slightly on the nonoperative side. Gait changes also increased load on the nonoperative knee, including increased gait speed (mean change, 0.08 m/sec) and decreased trunk lean to the stance-phase limb (mean change, –1.43 degrees). The findings were statistically significant.
The reasons could include the operation itself, disease progression in the nonoperative knee, or the fact that patients had gained an average of about 4.5 pounds at the 2-year follow-up.
Mr. Boulougouris said that he doubts the weight gain had much to do with it. He and his colleagues hope to tease out the contributing factors in a regression analysis.
The study was funded by the Canadian Institute of Health Research. Mr. Boulougouris reported that he had no relevant financial conflicts of interest to disclose.
Joint load, nonoperative knee, varus malalignment, opening wedge high tibial osteotomy, HTO, bilateral varus, knee adduction, Angelo Boulougouris, tibiofemoral joint osteoarthritis, unloader brace, medial compartment knee osteoarthritis,
SAN DIEGO – It’s important to pay attention to both knees – the knee that was operated on as well as the knee that wasn’t operated on – after a unilateral, medial, opening-wedge high tibial osteotomy.
Joint load increases in the nonoperative knee following the procedure, which is used to correct varus malalignment, according to researchers at the University of Western Ontario, London.
The findings apply to a subset of opening wedge high tibial osteotomy (HTO) patients, those who present initially with significant bilateral varus, but in whom symptoms were severe enough to require surgery in only one knee.
In 38 such patients, 2 years after surgery "we noted a 0.25% [of body weight times height] increase in peak knee adduction moment in the non-operative limb," as well as a slight increase in vertical ground reaction force, said lead author and physiotherapist Angelo Boulougouris, a biomechanics doctoral candidate at the school. The external knee adduction moment measured during gait is an indicator of tibiofemoral joint osteoarthritis progression.
"The major point is to pay attention to what’s happening to the opposite knee, to make sure you are not ignoring it and focusing your entire treatment plan on just looking at the operative knee," he said.
An unloader brace, for instance, might be appropriate for the nonoperative knee, among other possible interventions, he said. An unloader brace is designed to lessen the stress on a knee with medial compartment knee osteoarthritis. This use of the unloader brace would be to prevent development of knee OA rather than to ease the discomfort associated with established disease
During HTO, a wedge of the cancellous bone allograft is placed in the proximal end of the tibia, correcting both varus deformity and weight distribution through the knee. "Our surgeons are particularly careful to not over-correct," Mr. Boulougouris said.
Of the 38 patients, 32 were men, the average age was about 50 and average body mass index (BMI) about 27 kg/m2. Varus malalignment in the operative limb was about 11 degrees and Kellgren-Lawrence grades ranged from 1 to 3. Varus malalignment was about 8 degrees in the nonoperative limb, with Kellgren-Lawrence grades ranging from 0 to 1.
Patients did well overall, reporting decreased pain and improved quality of life at 2 years. Varus malalignment was corrected in the operative limb, and unchanged in the nonoperative limb.
Knee adduction moment had also significantly decreased on the operative side (mean change, –1.99 % of body weight times height), but increased slightly on the nonoperative side. Gait changes also increased load on the nonoperative knee, including increased gait speed (mean change, 0.08 m/sec) and decreased trunk lean to the stance-phase limb (mean change, –1.43 degrees). The findings were statistically significant.
The reasons could include the operation itself, disease progression in the nonoperative knee, or the fact that patients had gained an average of about 4.5 pounds at the 2-year follow-up.
Mr. Boulougouris said that he doubts the weight gain had much to do with it. He and his colleagues hope to tease out the contributing factors in a regression analysis.
The study was funded by the Canadian Institute of Health Research. Mr. Boulougouris reported that he had no relevant financial conflicts of interest to disclose.
SAN DIEGO – It’s important to pay attention to both knees – the knee that was operated on as well as the knee that wasn’t operated on – after a unilateral, medial, opening-wedge high tibial osteotomy.
Joint load increases in the nonoperative knee following the procedure, which is used to correct varus malalignment, according to researchers at the University of Western Ontario, London.
The findings apply to a subset of opening wedge high tibial osteotomy (HTO) patients, those who present initially with significant bilateral varus, but in whom symptoms were severe enough to require surgery in only one knee.
In 38 such patients, 2 years after surgery "we noted a 0.25% [of body weight times height] increase in peak knee adduction moment in the non-operative limb," as well as a slight increase in vertical ground reaction force, said lead author and physiotherapist Angelo Boulougouris, a biomechanics doctoral candidate at the school. The external knee adduction moment measured during gait is an indicator of tibiofemoral joint osteoarthritis progression.
"The major point is to pay attention to what’s happening to the opposite knee, to make sure you are not ignoring it and focusing your entire treatment plan on just looking at the operative knee," he said.
An unloader brace, for instance, might be appropriate for the nonoperative knee, among other possible interventions, he said. An unloader brace is designed to lessen the stress on a knee with medial compartment knee osteoarthritis. This use of the unloader brace would be to prevent development of knee OA rather than to ease the discomfort associated with established disease
During HTO, a wedge of the cancellous bone allograft is placed in the proximal end of the tibia, correcting both varus deformity and weight distribution through the knee. "Our surgeons are particularly careful to not over-correct," Mr. Boulougouris said.
Of the 38 patients, 32 were men, the average age was about 50 and average body mass index (BMI) about 27 kg/m2. Varus malalignment in the operative limb was about 11 degrees and Kellgren-Lawrence grades ranged from 1 to 3. Varus malalignment was about 8 degrees in the nonoperative limb, with Kellgren-Lawrence grades ranging from 0 to 1.
Patients did well overall, reporting decreased pain and improved quality of life at 2 years. Varus malalignment was corrected in the operative limb, and unchanged in the nonoperative limb.
Knee adduction moment had also significantly decreased on the operative side (mean change, –1.99 % of body weight times height), but increased slightly on the nonoperative side. Gait changes also increased load on the nonoperative knee, including increased gait speed (mean change, 0.08 m/sec) and decreased trunk lean to the stance-phase limb (mean change, –1.43 degrees). The findings were statistically significant.
The reasons could include the operation itself, disease progression in the nonoperative knee, or the fact that patients had gained an average of about 4.5 pounds at the 2-year follow-up.
Mr. Boulougouris said that he doubts the weight gain had much to do with it. He and his colleagues hope to tease out the contributing factors in a regression analysis.
The study was funded by the Canadian Institute of Health Research. Mr. Boulougouris reported that he had no relevant financial conflicts of interest to disclose.
Joint load, nonoperative knee, varus malalignment, opening wedge high tibial osteotomy, HTO, bilateral varus, knee adduction, Angelo Boulougouris, tibiofemoral joint osteoarthritis, unloader brace, medial compartment knee osteoarthritis,
Joint load, nonoperative knee, varus malalignment, opening wedge high tibial osteotomy, HTO, bilateral varus, knee adduction, Angelo Boulougouris, tibiofemoral joint osteoarthritis, unloader brace, medial compartment knee osteoarthritis,
FROM THE WORLD CONGRESS ON OSTEOARTHRITIS
Major Finding: At 2 years after a unilateral, opening-wedge high tibial osteotomy, 38 patients experienced a mean 0.25% body weight times height increase in peak knee adduction moment in the nonoperative limb.
Data Source: Comparison of baseline values to 2-year postop values.
Disclosures: The study was funded by the Canadian Institute of Health Research. Mr. Boulougouris said he had no disclosures.
Joint Distraction May Delay Need for Knee Replacement
Joint distraction can induce tissue structure modification in knee osteoarthritis, possibly reversing structural damage to cartilage tissue and delaying the need for knee replacement surgery. This is according to results of an open 1-year pilot study reported in the August issue of Annals of the Rheumatic Diseases.
Endoprosthesis currently is the accepted method for treating pain caused by end-stage knee OA. However, the growing number of procedures carries a high price tag, and there is a higher risk of failure in patients aged younger than 65 years.
With that in mind, Dr. Femke Intema of the University Medical Center Utrecht (the Netherlands) and colleagues wanted to determine whether joint distraction could halt and possibly reverse joint degeneration in knee OA (Ann. Rheum. Dis. 2011;70:1441-6).
The study included 11 men and 9 women who had knee OA and in whom knee replacement surgery was indicated in 2006-2008. Patients were an average of 48 years old; 18 of them had predominant OA in the medial compartment; the remaining two had OA in the lateral compartment. Patients had a score of 60 mm or higher on the Visual Analogue Scale (VAS) of pain, as well as radiographic signs of joint damage, and primarily tibiofemoral OA.
Joint distraction was applied for 2 months via an external fixation frame. At the 1-year follow-up, researchers evaluated tissue structure modification according to the following:
• Radiographic analysis. This showed that the mean joint space width (JSW) of the most affected compartment increased from 2.7 mm to 3.6 mm between baseline and 12 months, whereas the minimum JSW increased from 1 mm to 1.9 mm.
• Quantitative MRI analysis. At 1 year, this showed an increase in the mean thickness of cartilage over total area of bone (ThCtAB) from 2.4 mm to 3 mm in the most affected compartment, and a decrease in mean percentage area of denuded bone (dABp) from 22% to 5%. The thickness of cartilage over area of bone covered with cartilage (ThCcAB), a secondary structural outcome parameter, showed a borderline increase from 2.9 mm to 3.1 mm.
• Biomarker analysis on serum and urine samples. These showed an 11% decrease of CTXII (a collagen type II breakdown marker), and a 103% increase in PILANP/CTXII (a collage type II synthesis marker), between 6 and 12 months. These findings suggest a net increase in collagen synthesis, the researchers said.
The primary outcome parameter of this study was the WOMAC (Western Ontario and McMaster Universities) osteoarthritis index questionnaire, which decreased from 55 points at baseline to 23 points at 1 year. In all, 18 of the 20 patients showed a greater-than-10% improvement, and 16 showed a greater-than-25% improvement. There were significant improvements in the individual components of the WOMAC index, namely pain, stiffness, and function.
One secondary measure, the VAS pain score, decreased from 73 mm at baseline to 31 mm at 1 year. Physical examination of the joint, which assessed crepitus, pain on palpation, pain with flexion, and joint effusion, showed improvement from 46% to 75%.
"This study is the first to demonstrate intrinsic tissue structure repair in OA," the researchers said. "Historically, the regenerative capacity of cartilage has been questioned owing to the slow turnover rate of cartilage matrix, especially of collagen. However, this study shows that a significant amount of cartilage tissue is formed within 1 year after the distraction, demonstrating that under certain conditions, cartilage has regenerative capacity."
There is uncertainty as to the underlying mechanism of the structural repair that was seen in this study. One possibility is that temporary distraction prevents mechanical stress on the cartilage, eliminates further wear and tear, and allows tissue repair to begin, the researchers said.
For now, the researchers are unsure which patients may benefit from this procedure, as the study included only those patients who were younger than 50 years, had severe OA, and were likely candidates for joint replacement surgery. Referrals from peripheral hospitals may have led to selection bias, the researchers say.
Safety concerns exist as well. Two patients developed lung emboli and required hospitalization and anticoagulative treatment. Also, 17 patients developed single or multiple pin-tract infections, all of which were successfully treated with antibiotics.
Larger and longer trials in a variety of OA populations are needed to optimize treatment, to determine which patients would benefit the most and for the longest period of time, and to pay attention to reducing the number of complications, the researchers said.
The authors had no relationships to disclose. The Dutch Arthritis Foundation provided financial support for this study.
Joint distraction can induce tissue structure modification in knee osteoarthritis, possibly reversing structural damage to cartilage tissue and delaying the need for knee replacement surgery. This is according to results of an open 1-year pilot study reported in the August issue of Annals of the Rheumatic Diseases.
Endoprosthesis currently is the accepted method for treating pain caused by end-stage knee OA. However, the growing number of procedures carries a high price tag, and there is a higher risk of failure in patients aged younger than 65 years.
With that in mind, Dr. Femke Intema of the University Medical Center Utrecht (the Netherlands) and colleagues wanted to determine whether joint distraction could halt and possibly reverse joint degeneration in knee OA (Ann. Rheum. Dis. 2011;70:1441-6).
The study included 11 men and 9 women who had knee OA and in whom knee replacement surgery was indicated in 2006-2008. Patients were an average of 48 years old; 18 of them had predominant OA in the medial compartment; the remaining two had OA in the lateral compartment. Patients had a score of 60 mm or higher on the Visual Analogue Scale (VAS) of pain, as well as radiographic signs of joint damage, and primarily tibiofemoral OA.
Joint distraction was applied for 2 months via an external fixation frame. At the 1-year follow-up, researchers evaluated tissue structure modification according to the following:
• Radiographic analysis. This showed that the mean joint space width (JSW) of the most affected compartment increased from 2.7 mm to 3.6 mm between baseline and 12 months, whereas the minimum JSW increased from 1 mm to 1.9 mm.
• Quantitative MRI analysis. At 1 year, this showed an increase in the mean thickness of cartilage over total area of bone (ThCtAB) from 2.4 mm to 3 mm in the most affected compartment, and a decrease in mean percentage area of denuded bone (dABp) from 22% to 5%. The thickness of cartilage over area of bone covered with cartilage (ThCcAB), a secondary structural outcome parameter, showed a borderline increase from 2.9 mm to 3.1 mm.
• Biomarker analysis on serum and urine samples. These showed an 11% decrease of CTXII (a collagen type II breakdown marker), and a 103% increase in PILANP/CTXII (a collage type II synthesis marker), between 6 and 12 months. These findings suggest a net increase in collagen synthesis, the researchers said.
The primary outcome parameter of this study was the WOMAC (Western Ontario and McMaster Universities) osteoarthritis index questionnaire, which decreased from 55 points at baseline to 23 points at 1 year. In all, 18 of the 20 patients showed a greater-than-10% improvement, and 16 showed a greater-than-25% improvement. There were significant improvements in the individual components of the WOMAC index, namely pain, stiffness, and function.
One secondary measure, the VAS pain score, decreased from 73 mm at baseline to 31 mm at 1 year. Physical examination of the joint, which assessed crepitus, pain on palpation, pain with flexion, and joint effusion, showed improvement from 46% to 75%.
"This study is the first to demonstrate intrinsic tissue structure repair in OA," the researchers said. "Historically, the regenerative capacity of cartilage has been questioned owing to the slow turnover rate of cartilage matrix, especially of collagen. However, this study shows that a significant amount of cartilage tissue is formed within 1 year after the distraction, demonstrating that under certain conditions, cartilage has regenerative capacity."
There is uncertainty as to the underlying mechanism of the structural repair that was seen in this study. One possibility is that temporary distraction prevents mechanical stress on the cartilage, eliminates further wear and tear, and allows tissue repair to begin, the researchers said.
For now, the researchers are unsure which patients may benefit from this procedure, as the study included only those patients who were younger than 50 years, had severe OA, and were likely candidates for joint replacement surgery. Referrals from peripheral hospitals may have led to selection bias, the researchers say.
Safety concerns exist as well. Two patients developed lung emboli and required hospitalization and anticoagulative treatment. Also, 17 patients developed single or multiple pin-tract infections, all of which were successfully treated with antibiotics.
Larger and longer trials in a variety of OA populations are needed to optimize treatment, to determine which patients would benefit the most and for the longest period of time, and to pay attention to reducing the number of complications, the researchers said.
The authors had no relationships to disclose. The Dutch Arthritis Foundation provided financial support for this study.
Joint distraction can induce tissue structure modification in knee osteoarthritis, possibly reversing structural damage to cartilage tissue and delaying the need for knee replacement surgery. This is according to results of an open 1-year pilot study reported in the August issue of Annals of the Rheumatic Diseases.
Endoprosthesis currently is the accepted method for treating pain caused by end-stage knee OA. However, the growing number of procedures carries a high price tag, and there is a higher risk of failure in patients aged younger than 65 years.
With that in mind, Dr. Femke Intema of the University Medical Center Utrecht (the Netherlands) and colleagues wanted to determine whether joint distraction could halt and possibly reverse joint degeneration in knee OA (Ann. Rheum. Dis. 2011;70:1441-6).
The study included 11 men and 9 women who had knee OA and in whom knee replacement surgery was indicated in 2006-2008. Patients were an average of 48 years old; 18 of them had predominant OA in the medial compartment; the remaining two had OA in the lateral compartment. Patients had a score of 60 mm or higher on the Visual Analogue Scale (VAS) of pain, as well as radiographic signs of joint damage, and primarily tibiofemoral OA.
Joint distraction was applied for 2 months via an external fixation frame. At the 1-year follow-up, researchers evaluated tissue structure modification according to the following:
• Radiographic analysis. This showed that the mean joint space width (JSW) of the most affected compartment increased from 2.7 mm to 3.6 mm between baseline and 12 months, whereas the minimum JSW increased from 1 mm to 1.9 mm.
• Quantitative MRI analysis. At 1 year, this showed an increase in the mean thickness of cartilage over total area of bone (ThCtAB) from 2.4 mm to 3 mm in the most affected compartment, and a decrease in mean percentage area of denuded bone (dABp) from 22% to 5%. The thickness of cartilage over area of bone covered with cartilage (ThCcAB), a secondary structural outcome parameter, showed a borderline increase from 2.9 mm to 3.1 mm.
• Biomarker analysis on serum and urine samples. These showed an 11% decrease of CTXII (a collagen type II breakdown marker), and a 103% increase in PILANP/CTXII (a collage type II synthesis marker), between 6 and 12 months. These findings suggest a net increase in collagen synthesis, the researchers said.
The primary outcome parameter of this study was the WOMAC (Western Ontario and McMaster Universities) osteoarthritis index questionnaire, which decreased from 55 points at baseline to 23 points at 1 year. In all, 18 of the 20 patients showed a greater-than-10% improvement, and 16 showed a greater-than-25% improvement. There were significant improvements in the individual components of the WOMAC index, namely pain, stiffness, and function.
One secondary measure, the VAS pain score, decreased from 73 mm at baseline to 31 mm at 1 year. Physical examination of the joint, which assessed crepitus, pain on palpation, pain with flexion, and joint effusion, showed improvement from 46% to 75%.
"This study is the first to demonstrate intrinsic tissue structure repair in OA," the researchers said. "Historically, the regenerative capacity of cartilage has been questioned owing to the slow turnover rate of cartilage matrix, especially of collagen. However, this study shows that a significant amount of cartilage tissue is formed within 1 year after the distraction, demonstrating that under certain conditions, cartilage has regenerative capacity."
There is uncertainty as to the underlying mechanism of the structural repair that was seen in this study. One possibility is that temporary distraction prevents mechanical stress on the cartilage, eliminates further wear and tear, and allows tissue repair to begin, the researchers said.
For now, the researchers are unsure which patients may benefit from this procedure, as the study included only those patients who were younger than 50 years, had severe OA, and were likely candidates for joint replacement surgery. Referrals from peripheral hospitals may have led to selection bias, the researchers say.
Safety concerns exist as well. Two patients developed lung emboli and required hospitalization and anticoagulative treatment. Also, 17 patients developed single or multiple pin-tract infections, all of which were successfully treated with antibiotics.
Larger and longer trials in a variety of OA populations are needed to optimize treatment, to determine which patients would benefit the most and for the longest period of time, and to pay attention to reducing the number of complications, the researchers said.
The authors had no relationships to disclose. The Dutch Arthritis Foundation provided financial support for this study.
FROM ANNALS OF THE RHEUMATIC DISEASES
Major Finding: Joint distraction can induce tissue structure modification in knee osteoarthritis, as shown on radiography, MRI, and blood work, possibly delaying the need for endoprosthesis.
Data Source: An open, 1-year pilot study of 20 patients with tibiofemoral osteoarthritis who were treated surgically with joint distraction.
Disclosures: The authors had no relationships to disclose. The Dutch Arthritis Foundation provided financial support for this study.
Hereditary Hemochromatosis Linked to Increased Arthropathies and Joint Surgery
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
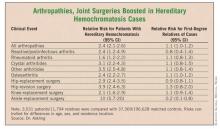
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
LONDON – Patients with hereditary hemochromatosis have a significantly increased prevalence of various arthropathies and an elevated need for joint-replacement surgery, compared with the general population, according to findings from a study of Swedish national registry data.
The analysis also showed that first-degree relatives of people with hereditary hemochromatosis do not have an increased rate of arthropathies or need for joint replacement, even though genetic models predict that a majority of these relatives carry one copy of an autosomal recessive mutation that causes hereditary hemochromatosis.
"This dissociation between the genotype and the phenotype" relative to the risk for arthropathy and need for joint replacement "suggests to me that the gene itself is not involved. It suggests to me that you need more than just the gene" to boost the risk for arthropathy and joint failure, noted Dr. Johan Askling.
Arthropathy is a classic phenotypic feature of patients with hereditary hemochromatosis, a genetic disease in people who carry two mutated copies of the hemochromatosis gene (HFE) associated with iron overload. But the nature of the relationship between the disease and arthropathies remains poorly understood. The new finding that increased arthropathies occur only in homozygous, affected individuals suggests that the risk is linked to iron overload itself, rather than to the causative mutated genes.
Dr. Askling and his associates identified 3,531 patients with a diagnosis of hereditary hemochromatosis from Swedish national records for the period 1999-2006. The investigators also identified another 11,794 first-degree relatives of these patients. They then identified 37,369 people as matched controls for the patients from the general Swedish population and 196,628 people as matched controls for the first-degree relatives.
The researchers then tallied the incidence of consultations or hospitalizations for rheumatoid arthritis, osteoarthritis, and other arthritides in the cases, their first-degree relatives, and the controls during the study period. They calculated a relative risk for these complications in affected people and in their relatives, compared with the controls that adjusted for differences in age, sex, and residence location. The researchers also ran similar analyses for the incidence of various joint-replacement surgeries (see table).
The results showed that the patients with hereditary hemochromatosis had consistent, statistically significant increased rates of arthropathies. For example, for all arthropathies the rate was 2.4-fold higher in the patients than in the controls. But this increased rate did not exist among the first-degree relatives. For all arthropathies, their rate was just 10% higher than among the matched controls, a difference that was not significant, reported Dr. Askling, an epidemiologist at the Karolinska Institute in Stockholm.
A similar pattern existed for joint-replacement surgeries. Hip surgery, for example, was 2.9-fold more frequent among the hereditary hemochromatosis patients than among their matched controls, while among the first-degree relatives the incidence of hip-replacement surgery was 10% less common than among the matched controls, a difference that was not statistically significant.
Dr. Askling said that he had no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: Patients with hereditary hemochromatosis had a 2.4-fold increased prevalence of arthropathies and a 2.9-fold increased rate of hip surgery, compared with matched controls. In contrast, first-degree relatives of hereditary hemochromatosis patients had no significantly different rates for arthropathy or need for joint-replacement surgery, compared with controls.
Data Source: Case-control study of records from Swedish national registries during 1999-2006, with 3,531 patients diagnosed with hereditary hemochromatosis and 37,369 matched controls, and 11,794 first-degree relatives of the patients and 196,628 matched controls.
Disclosures: Dr. Askling said that he had no disclosures.
Gastric Bypass May Increase Long-Term Fracture Risk
Major Finding: The fracture risk for gastric bypass surgery patients was 2.3-fold greater than that for the general population.
Data Source: A retrospective study of 258 patients who underwent bariatric surgery between 1985 and 2004.
Disclosures: Dr. Kennel reported that he and his coinvestigators have no significant financial relationships to report.
BOSTON – Gastric bypass surgery appears to be linked to increased long-term fracture risk, based on a retrospective study of 258 bariatric surgery patients.
“Bariatric surgery results in an increased risk of fractures. We think the important take-home point here is that we need to start looking at the skeleton as one of those key areas for long-term follow-up,” Dr. Kurt Kennel said at the meeting.
The fracture risk for bariatric surgery patients in this study was 2.3 times greater than that for individuals who did not have bariatric surgery, reported Dr. Kennel of the endocrinology department at the Mayo Clinic in Rochester, Minn.
“We have questions about what this means in the long term,” said Dr. Kennel. In this study, the mean time to first fracture was 6 years, with a mean follow-up of 9 years. However, in much of the current literature on bariatric surgery, patients are followed only 1–2 years and the only issues addressed are related to surgery or weight.
“Some issues – like bone, for example – may not show the manifestations of these effects for many years and therefore we may be missing some of those effects,” said Dr. Kennel.
The researchers used data from the Rochester Epidemiology Project to conduct a retrospective study of fracture incidence. REP connects medical records from the Mayo Clinic, local hospitals, and local private practices. The study included data from 258 patients, who underwent a first bariatric surgery between 1985 and 2004 at the Mayo Clinic.
Fractures were expressed in standardized incidence ratios that compare the number of observed fractures to the number of expected fractures by skeletal site.
Expected fracture data were derived by applying age- and sex-specific incidence rates from the local population to the age- and sex-specific person-years of follow-up.
The average age of the bariatric surgery patients was 44 years and most (83%) were female. Following bariatric surgery, 79 patients experienced 132 fractures.
Bariatric surgery patients had an increased risk of fracture at nearly all of the skeletal sites studied, not just in weight-bearing bones.
Also of note, 94% of these patients had undergone gastric bypass procedures. Dr. Kennel attributed this to the time frame used in the study.
Other bariatric surgical procedures – such as adjustable gastric banding and sleeve gastrectomy – are more recent developments. Dr. Kennel acknowledged that different bariatric procedures might yield different fracture risks.
The increased rate of fractures “suggests that structural and biochemical changes in bone that are observed after bariatric surgery are clinically important.
Clinicians should discuss bone health with patients who have undergone or are considering bariatric surgery.”
Major Finding: The fracture risk for gastric bypass surgery patients was 2.3-fold greater than that for the general population.
Data Source: A retrospective study of 258 patients who underwent bariatric surgery between 1985 and 2004.
Disclosures: Dr. Kennel reported that he and his coinvestigators have no significant financial relationships to report.
BOSTON – Gastric bypass surgery appears to be linked to increased long-term fracture risk, based on a retrospective study of 258 bariatric surgery patients.
“Bariatric surgery results in an increased risk of fractures. We think the important take-home point here is that we need to start looking at the skeleton as one of those key areas for long-term follow-up,” Dr. Kurt Kennel said at the meeting.
The fracture risk for bariatric surgery patients in this study was 2.3 times greater than that for individuals who did not have bariatric surgery, reported Dr. Kennel of the endocrinology department at the Mayo Clinic in Rochester, Minn.
“We have questions about what this means in the long term,” said Dr. Kennel. In this study, the mean time to first fracture was 6 years, with a mean follow-up of 9 years. However, in much of the current literature on bariatric surgery, patients are followed only 1–2 years and the only issues addressed are related to surgery or weight.
“Some issues – like bone, for example – may not show the manifestations of these effects for many years and therefore we may be missing some of those effects,” said Dr. Kennel.
The researchers used data from the Rochester Epidemiology Project to conduct a retrospective study of fracture incidence. REP connects medical records from the Mayo Clinic, local hospitals, and local private practices. The study included data from 258 patients, who underwent a first bariatric surgery between 1985 and 2004 at the Mayo Clinic.
Fractures were expressed in standardized incidence ratios that compare the number of observed fractures to the number of expected fractures by skeletal site.
Expected fracture data were derived by applying age- and sex-specific incidence rates from the local population to the age- and sex-specific person-years of follow-up.
The average age of the bariatric surgery patients was 44 years and most (83%) were female. Following bariatric surgery, 79 patients experienced 132 fractures.
Bariatric surgery patients had an increased risk of fracture at nearly all of the skeletal sites studied, not just in weight-bearing bones.
Also of note, 94% of these patients had undergone gastric bypass procedures. Dr. Kennel attributed this to the time frame used in the study.
Other bariatric surgical procedures – such as adjustable gastric banding and sleeve gastrectomy – are more recent developments. Dr. Kennel acknowledged that different bariatric procedures might yield different fracture risks.
The increased rate of fractures “suggests that structural and biochemical changes in bone that are observed after bariatric surgery are clinically important.
Clinicians should discuss bone health with patients who have undergone or are considering bariatric surgery.”
Major Finding: The fracture risk for gastric bypass surgery patients was 2.3-fold greater than that for the general population.
Data Source: A retrospective study of 258 patients who underwent bariatric surgery between 1985 and 2004.
Disclosures: Dr. Kennel reported that he and his coinvestigators have no significant financial relationships to report.
BOSTON – Gastric bypass surgery appears to be linked to increased long-term fracture risk, based on a retrospective study of 258 bariatric surgery patients.
“Bariatric surgery results in an increased risk of fractures. We think the important take-home point here is that we need to start looking at the skeleton as one of those key areas for long-term follow-up,” Dr. Kurt Kennel said at the meeting.
The fracture risk for bariatric surgery patients in this study was 2.3 times greater than that for individuals who did not have bariatric surgery, reported Dr. Kennel of the endocrinology department at the Mayo Clinic in Rochester, Minn.
“We have questions about what this means in the long term,” said Dr. Kennel. In this study, the mean time to first fracture was 6 years, with a mean follow-up of 9 years. However, in much of the current literature on bariatric surgery, patients are followed only 1–2 years and the only issues addressed are related to surgery or weight.
“Some issues – like bone, for example – may not show the manifestations of these effects for many years and therefore we may be missing some of those effects,” said Dr. Kennel.
The researchers used data from the Rochester Epidemiology Project to conduct a retrospective study of fracture incidence. REP connects medical records from the Mayo Clinic, local hospitals, and local private practices. The study included data from 258 patients, who underwent a first bariatric surgery between 1985 and 2004 at the Mayo Clinic.
Fractures were expressed in standardized incidence ratios that compare the number of observed fractures to the number of expected fractures by skeletal site.
Expected fracture data were derived by applying age- and sex-specific incidence rates from the local population to the age- and sex-specific person-years of follow-up.
The average age of the bariatric surgery patients was 44 years and most (83%) were female. Following bariatric surgery, 79 patients experienced 132 fractures.
Bariatric surgery patients had an increased risk of fracture at nearly all of the skeletal sites studied, not just in weight-bearing bones.
Also of note, 94% of these patients had undergone gastric bypass procedures. Dr. Kennel attributed this to the time frame used in the study.
Other bariatric surgical procedures – such as adjustable gastric banding and sleeve gastrectomy – are more recent developments. Dr. Kennel acknowledged that different bariatric procedures might yield different fracture risks.
The increased rate of fractures “suggests that structural and biochemical changes in bone that are observed after bariatric surgery are clinically important.
Clinicians should discuss bone health with patients who have undergone or are considering bariatric surgery.”
Black Osteoarthritis Patients Tend to Balk at Total Knee Replacement
LONDON – The reasons why fewer black than white patients undergo knee replacement as a treatment option for end-stage osteoarthritis remain elusive.
According to the findings of a 725-patient study, women and blacks with knee osteoarthritis (OA) were less willing than men or their white counterparts to consider having total knee replacement (TKR) surgery.
Black patients were also found to be less aware of the benefits of joint replacement and had worse expectations of the outcome than did white patients.
Despite a number of sociocultural differences, however, it is not clear why the uptake of TKR differs among ethnic groups.
"We know that joint replacement is an effective – actually the only effective – intervention for end-stage osteoarthritis," said study author Dr. C. Kent Kwoh, who is professor of medicine, epidemiology and clinical and translational science at the University of Pittsburgh and chief of the rheumatology section at VA Pittsburgh Healthcare System.
"The problem is that there have been many studies that have shown there are disparities in joint replacement; [blacks] get hip and knee replacement much less often than do whites," Dr. Kwoh added in an interview during a poster session at the annual European Congress of Rheumatology. "The question is, Why?"
Previous research has shown that even when faced with very severe and painful OA and a physician recommendation for TKR, black patients are less willing than whites to consider this an option.
The present study was in a much larger community-based sample than has been the case in past investigations, said Dr. Kwoh, and it aimed to identify more specific factors and patient attitudes that might influence the decision to undergo TKR.
Using a cross-sectional survey design, the investigators recruited patients aged 50 years or older who had chronic, frequent knee pain and radiographic evidence of OA.
The study population consisted of 234 black and 491 white patients, with mean respective ages of 58 years and 68 years (P less than .0004).
In addition to being younger, black patients tended to have worse knee pain, with higher total WOMAC (Western Ontario and McMaster Universities) osteoarthritis index scores (54 vs. 43), and OA Pain Assessment scores for constant (7 vs. 11) and intermittent (14 vs. 11) pain than white patients (P less than .0004 for all comparisons).
"There were differences in a number of [other] variables [between whites and blacks], such as income, employment status, education, access to insurance, expectations of outcome, trust in the health system, and religiosity, that may impact the choice for joint replacement" Dr. Kwoh observed.
However, putting all of these variables into a multivariate model didn’t seem to fully explain the disparity in TKR acceptance between the two groups.
The adjusted odds ratio for willingness to undergo TKR was 0.38 comparing black vs. white patients (95% confidence interval, 0.19-0.74; P = .005) and 2.52 for male vs. female sex (95% CI, 1.37-4.66; P = .003).
"We’re left a little bit puzzled at this point," Dr. Kwoh admitted. "Our other studies have shown differences in expectations; that is, if you have worse expectations, you were less likely to consider joint replacement."
In that previous work, however, an adjustment of the findings according to patient expectations seemed to take care of the difference in willingness. "In this study, we weren’t able to show that," Dr. Kwoh said. "So maybe there are other, unmeasured confounders that we have to address."
As to where these findings leave the practicing physician who advises patients, Dr. Kwoh noted that patient education is important and that patients really need to have a good understanding of the risks and benefits.
"Joint replacement is effective, we know that it works very well, it has low morbidity and low mortality, and so patients who really need it should avail themselves to it," Dr. Kwoh advised.
Dr. Kwoh stated that he had no conflicts of interest. The study was funded by the University of Pittsburgh Multidisciplinary Clinical Research Center for Rheumatic and Musculoskeletal Diseases.
LONDON – The reasons why fewer black than white patients undergo knee replacement as a treatment option for end-stage osteoarthritis remain elusive.
According to the findings of a 725-patient study, women and blacks with knee osteoarthritis (OA) were less willing than men or their white counterparts to consider having total knee replacement (TKR) surgery.
Black patients were also found to be less aware of the benefits of joint replacement and had worse expectations of the outcome than did white patients.
Despite a number of sociocultural differences, however, it is not clear why the uptake of TKR differs among ethnic groups.
"We know that joint replacement is an effective – actually the only effective – intervention for end-stage osteoarthritis," said study author Dr. C. Kent Kwoh, who is professor of medicine, epidemiology and clinical and translational science at the University of Pittsburgh and chief of the rheumatology section at VA Pittsburgh Healthcare System.
"The problem is that there have been many studies that have shown there are disparities in joint replacement; [blacks] get hip and knee replacement much less often than do whites," Dr. Kwoh added in an interview during a poster session at the annual European Congress of Rheumatology. "The question is, Why?"
Previous research has shown that even when faced with very severe and painful OA and a physician recommendation for TKR, black patients are less willing than whites to consider this an option.
The present study was in a much larger community-based sample than has been the case in past investigations, said Dr. Kwoh, and it aimed to identify more specific factors and patient attitudes that might influence the decision to undergo TKR.
Using a cross-sectional survey design, the investigators recruited patients aged 50 years or older who had chronic, frequent knee pain and radiographic evidence of OA.
The study population consisted of 234 black and 491 white patients, with mean respective ages of 58 years and 68 years (P less than .0004).
In addition to being younger, black patients tended to have worse knee pain, with higher total WOMAC (Western Ontario and McMaster Universities) osteoarthritis index scores (54 vs. 43), and OA Pain Assessment scores for constant (7 vs. 11) and intermittent (14 vs. 11) pain than white patients (P less than .0004 for all comparisons).
"There were differences in a number of [other] variables [between whites and blacks], such as income, employment status, education, access to insurance, expectations of outcome, trust in the health system, and religiosity, that may impact the choice for joint replacement" Dr. Kwoh observed.
However, putting all of these variables into a multivariate model didn’t seem to fully explain the disparity in TKR acceptance between the two groups.
The adjusted odds ratio for willingness to undergo TKR was 0.38 comparing black vs. white patients (95% confidence interval, 0.19-0.74; P = .005) and 2.52 for male vs. female sex (95% CI, 1.37-4.66; P = .003).
"We’re left a little bit puzzled at this point," Dr. Kwoh admitted. "Our other studies have shown differences in expectations; that is, if you have worse expectations, you were less likely to consider joint replacement."
In that previous work, however, an adjustment of the findings according to patient expectations seemed to take care of the difference in willingness. "In this study, we weren’t able to show that," Dr. Kwoh said. "So maybe there are other, unmeasured confounders that we have to address."
As to where these findings leave the practicing physician who advises patients, Dr. Kwoh noted that patient education is important and that patients really need to have a good understanding of the risks and benefits.
"Joint replacement is effective, we know that it works very well, it has low morbidity and low mortality, and so patients who really need it should avail themselves to it," Dr. Kwoh advised.
Dr. Kwoh stated that he had no conflicts of interest. The study was funded by the University of Pittsburgh Multidisciplinary Clinical Research Center for Rheumatic and Musculoskeletal Diseases.
LONDON – The reasons why fewer black than white patients undergo knee replacement as a treatment option for end-stage osteoarthritis remain elusive.
According to the findings of a 725-patient study, women and blacks with knee osteoarthritis (OA) were less willing than men or their white counterparts to consider having total knee replacement (TKR) surgery.
Black patients were also found to be less aware of the benefits of joint replacement and had worse expectations of the outcome than did white patients.
Despite a number of sociocultural differences, however, it is not clear why the uptake of TKR differs among ethnic groups.
"We know that joint replacement is an effective – actually the only effective – intervention for end-stage osteoarthritis," said study author Dr. C. Kent Kwoh, who is professor of medicine, epidemiology and clinical and translational science at the University of Pittsburgh and chief of the rheumatology section at VA Pittsburgh Healthcare System.
"The problem is that there have been many studies that have shown there are disparities in joint replacement; [blacks] get hip and knee replacement much less often than do whites," Dr. Kwoh added in an interview during a poster session at the annual European Congress of Rheumatology. "The question is, Why?"
Previous research has shown that even when faced with very severe and painful OA and a physician recommendation for TKR, black patients are less willing than whites to consider this an option.
The present study was in a much larger community-based sample than has been the case in past investigations, said Dr. Kwoh, and it aimed to identify more specific factors and patient attitudes that might influence the decision to undergo TKR.
Using a cross-sectional survey design, the investigators recruited patients aged 50 years or older who had chronic, frequent knee pain and radiographic evidence of OA.
The study population consisted of 234 black and 491 white patients, with mean respective ages of 58 years and 68 years (P less than .0004).
In addition to being younger, black patients tended to have worse knee pain, with higher total WOMAC (Western Ontario and McMaster Universities) osteoarthritis index scores (54 vs. 43), and OA Pain Assessment scores for constant (7 vs. 11) and intermittent (14 vs. 11) pain than white patients (P less than .0004 for all comparisons).
"There were differences in a number of [other] variables [between whites and blacks], such as income, employment status, education, access to insurance, expectations of outcome, trust in the health system, and religiosity, that may impact the choice for joint replacement" Dr. Kwoh observed.
However, putting all of these variables into a multivariate model didn’t seem to fully explain the disparity in TKR acceptance between the two groups.
The adjusted odds ratio for willingness to undergo TKR was 0.38 comparing black vs. white patients (95% confidence interval, 0.19-0.74; P = .005) and 2.52 for male vs. female sex (95% CI, 1.37-4.66; P = .003).
"We’re left a little bit puzzled at this point," Dr. Kwoh admitted. "Our other studies have shown differences in expectations; that is, if you have worse expectations, you were less likely to consider joint replacement."
In that previous work, however, an adjustment of the findings according to patient expectations seemed to take care of the difference in willingness. "In this study, we weren’t able to show that," Dr. Kwoh said. "So maybe there are other, unmeasured confounders that we have to address."
As to where these findings leave the practicing physician who advises patients, Dr. Kwoh noted that patient education is important and that patients really need to have a good understanding of the risks and benefits.
"Joint replacement is effective, we know that it works very well, it has low morbidity and low mortality, and so patients who really need it should avail themselves to it," Dr. Kwoh advised.
Dr. Kwoh stated that he had no conflicts of interest. The study was funded by the University of Pittsburgh Multidisciplinary Clinical Research Center for Rheumatic and Musculoskeletal Diseases.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: The adjusted odds ratio for willingness to undergo TKR was 0.38 comparing black vs. white patients (95% CI, 0.19-0.74; P = .005).
Data Source: A cross-sectional survey of more than 700 patients with severe knee OA to assess attitudes to total knee replacement.
Disclosures: Dr. Kwoh stated that he had no conflicts of interest. The study was funded by the University of Pittsburgh Multidisciplinary Clinical Research Center for Rheumatic and Musculoskeletal Diseases.
Zoledronic Acid Relieves Knee OA Pain and Shrinks Bone Marrow Lesions
LONDON – A single 5-mg infusion of zoledronic acid, a bisphosphonate, in patients with knee osteoarthritis led to significant pain reduction and shrinkage of bone marrow lesions in a randomized, placebo-controlled study with 59 patients.
The zoledronic acid treatment led to an average 15-point drop in pain (on a visual analog scale of 0-100) beyond what occurred in the placebo group, and the active treatment was also linked with an average 170-mm2 reduction in maximal bone marrow lesion (BML) area beyond the placebo-treated patients, which was a cut in BML area of about 37%, compared with the starting BML area, Dr. Graeme Jones said at the annual European Congress of Rheumatology. Dr. Jones visualizes BMLs using MRI knee scans.
"This is the first intervention shown to work on BMLs" in patients with osteoarthritis (OA), said Dr. Jones, professor of rheumatology and epidemiology and head of the musculoskeletal unit at the Menzies Research Institute Tasmania, Hobart, Australia.
"This is exciting for treating existing OA. It is one of the first positive structure modification trials," commented Dr. Philip Conaghan, professor and chairman of musculoskeletal medicine at the University of Leeds (England).
"Results from several studies have linked BMLs with pain and cartilage damage in OA patients. The larger the BML, the faster the cartilage loss and the worse the pain," Dr. Jones said in an interview. Based on studies his group has done, about 20% of BMLs that are associated with knee OA spontaneously enlarge over the course of 3 years, another 20% shrink in size, and about 60% remain the same, he said. Their earlier research findings also showed that BMLs are independently linked with fast progression of OA and the need for knee replacement. "If you reduce BMLs, it should produce good outcomes in patients," he said.
"The next step is to show that treatment with zoledronic acid not only reduces BML size but also slows cartilage loss. Sixty patients followed for 12 months were not enough to assess cartilage. We will need about 400 patients followed for 2 years," Dr. Jones added.
Despite not yet having information on cartilage effects, he said that his results so far have convinced him that treatment with zoledronic acid is reasonable for patients with painful knee OA and BMLs.
"I use it off label. Patients need to know it’s off label, and they [therefore] must be willing to pay for it, but I use it. It’s been shown to work, and nothing else works. Zoledronic acid [Reclast] is available, we know about its safety, and it’s been used for a long time to treat osteoporosis and cancers. If you have OA patients with BMLs, this is something to actively consider for them. Patients with OA have very limited treatment options. This can make a large difference in their pain, and it has long-lasting benefit so it can be given once a year," Dr. Jones said.
He recommended an infusion of 5 mg of zoledronic acid for patients who are at least 50 years old with knee OA that fulfills the American College of Rheumatology clinical criteria, and knee BMLs that are visible on an MRI scan of the affected knee. In his experience, 88% of these knee OA patients have BMLs. Dr. Jones noted that he does not use a maximal BML area threshold for initiating treatment, although in his study the average maximal BML area was about 465 mm2. About one-third of people aged 50 years or older with no clinical evidence of OA also have BMLs, he noted.
The benefits of zoledronic acid that were seen in his study might be a class effect that may be replicated by treatment with another bisphosphonate, but zoledronic acid is more potent than oral bisphosphonates and hence the drug’s beneficial effect on pain and BML shrinkage may exceed the effect that other bisphosphonates might have, he said.
The pain benefit appeared to start wearing off about a year after the zoledronic acid injection. Dr. Jones said that he has a small number of patients whom he has infused a second time, which produced a second round of pain reduction. He has not yet given any OA patients a third dose of the drug.
The 59 patients who were enrolled in the study had an average age of about 60 years, with an average knee pain score of about 52 on the visual analog scale; all patients had BMLs as seen on MRI scans of their affected knees. In all, 31 patients received a 5-mg infusion of zoledronic acid and 28 patients received a placebo infusion. All patients also continued their conventional pain medication regimens. The zoledronic acid infusion was well tolerated: Although infusion reactions were reported in 90% of the patients who received the drug and in 43% of the placebo patients, serious adverse effects occurred in only 19% of the patients who received zoledronic acid and in 4% of the placebo patients.
The Food and Drug Administration has approved zoledronic acid under a number of brand names to prevent or treat osteoporosis in postmenopausal women or patients who are at risk for osteoporosis because they are taking or have taken corticosteroid therapy; to manage Paget disease; and to prevent chemotherapy-induced bone fractures or fractures in patients with multiple myeloma or cancer that has metastasized to the bones from other locations.
The study was funded by Novartis, which markets zoledronic acid (Reclast). Dr. Jones and Dr. Conaghan said that they had no disclosures.
*Correction, 6/6/2011: An earlier version of this story incorrectly stated that Dr. Jones had no disclosures. Dr. Jones has received speaker fees, travel sponsorship, and research support from Novartis and from several other drug companies.
LONDON – A single 5-mg infusion of zoledronic acid, a bisphosphonate, in patients with knee osteoarthritis led to significant pain reduction and shrinkage of bone marrow lesions in a randomized, placebo-controlled study with 59 patients.
The zoledronic acid treatment led to an average 15-point drop in pain (on a visual analog scale of 0-100) beyond what occurred in the placebo group, and the active treatment was also linked with an average 170-mm2 reduction in maximal bone marrow lesion (BML) area beyond the placebo-treated patients, which was a cut in BML area of about 37%, compared with the starting BML area, Dr. Graeme Jones said at the annual European Congress of Rheumatology. Dr. Jones visualizes BMLs using MRI knee scans.
"This is the first intervention shown to work on BMLs" in patients with osteoarthritis (OA), said Dr. Jones, professor of rheumatology and epidemiology and head of the musculoskeletal unit at the Menzies Research Institute Tasmania, Hobart, Australia.
"This is exciting for treating existing OA. It is one of the first positive structure modification trials," commented Dr. Philip Conaghan, professor and chairman of musculoskeletal medicine at the University of Leeds (England).
"Results from several studies have linked BMLs with pain and cartilage damage in OA patients. The larger the BML, the faster the cartilage loss and the worse the pain," Dr. Jones said in an interview. Based on studies his group has done, about 20% of BMLs that are associated with knee OA spontaneously enlarge over the course of 3 years, another 20% shrink in size, and about 60% remain the same, he said. Their earlier research findings also showed that BMLs are independently linked with fast progression of OA and the need for knee replacement. "If you reduce BMLs, it should produce good outcomes in patients," he said.
"The next step is to show that treatment with zoledronic acid not only reduces BML size but also slows cartilage loss. Sixty patients followed for 12 months were not enough to assess cartilage. We will need about 400 patients followed for 2 years," Dr. Jones added.
Despite not yet having information on cartilage effects, he said that his results so far have convinced him that treatment with zoledronic acid is reasonable for patients with painful knee OA and BMLs.
"I use it off label. Patients need to know it’s off label, and they [therefore] must be willing to pay for it, but I use it. It’s been shown to work, and nothing else works. Zoledronic acid [Reclast] is available, we know about its safety, and it’s been used for a long time to treat osteoporosis and cancers. If you have OA patients with BMLs, this is something to actively consider for them. Patients with OA have very limited treatment options. This can make a large difference in their pain, and it has long-lasting benefit so it can be given once a year," Dr. Jones said.
He recommended an infusion of 5 mg of zoledronic acid for patients who are at least 50 years old with knee OA that fulfills the American College of Rheumatology clinical criteria, and knee BMLs that are visible on an MRI scan of the affected knee. In his experience, 88% of these knee OA patients have BMLs. Dr. Jones noted that he does not use a maximal BML area threshold for initiating treatment, although in his study the average maximal BML area was about 465 mm2. About one-third of people aged 50 years or older with no clinical evidence of OA also have BMLs, he noted.
The benefits of zoledronic acid that were seen in his study might be a class effect that may be replicated by treatment with another bisphosphonate, but zoledronic acid is more potent than oral bisphosphonates and hence the drug’s beneficial effect on pain and BML shrinkage may exceed the effect that other bisphosphonates might have, he said.
The pain benefit appeared to start wearing off about a year after the zoledronic acid injection. Dr. Jones said that he has a small number of patients whom he has infused a second time, which produced a second round of pain reduction. He has not yet given any OA patients a third dose of the drug.
The 59 patients who were enrolled in the study had an average age of about 60 years, with an average knee pain score of about 52 on the visual analog scale; all patients had BMLs as seen on MRI scans of their affected knees. In all, 31 patients received a 5-mg infusion of zoledronic acid and 28 patients received a placebo infusion. All patients also continued their conventional pain medication regimens. The zoledronic acid infusion was well tolerated: Although infusion reactions were reported in 90% of the patients who received the drug and in 43% of the placebo patients, serious adverse effects occurred in only 19% of the patients who received zoledronic acid and in 4% of the placebo patients.
The Food and Drug Administration has approved zoledronic acid under a number of brand names to prevent or treat osteoporosis in postmenopausal women or patients who are at risk for osteoporosis because they are taking or have taken corticosteroid therapy; to manage Paget disease; and to prevent chemotherapy-induced bone fractures or fractures in patients with multiple myeloma or cancer that has metastasized to the bones from other locations.
The study was funded by Novartis, which markets zoledronic acid (Reclast). Dr. Jones and Dr. Conaghan said that they had no disclosures.
*Correction, 6/6/2011: An earlier version of this story incorrectly stated that Dr. Jones had no disclosures. Dr. Jones has received speaker fees, travel sponsorship, and research support from Novartis and from several other drug companies.
LONDON – A single 5-mg infusion of zoledronic acid, a bisphosphonate, in patients with knee osteoarthritis led to significant pain reduction and shrinkage of bone marrow lesions in a randomized, placebo-controlled study with 59 patients.
The zoledronic acid treatment led to an average 15-point drop in pain (on a visual analog scale of 0-100) beyond what occurred in the placebo group, and the active treatment was also linked with an average 170-mm2 reduction in maximal bone marrow lesion (BML) area beyond the placebo-treated patients, which was a cut in BML area of about 37%, compared with the starting BML area, Dr. Graeme Jones said at the annual European Congress of Rheumatology. Dr. Jones visualizes BMLs using MRI knee scans.
"This is the first intervention shown to work on BMLs" in patients with osteoarthritis (OA), said Dr. Jones, professor of rheumatology and epidemiology and head of the musculoskeletal unit at the Menzies Research Institute Tasmania, Hobart, Australia.
"This is exciting for treating existing OA. It is one of the first positive structure modification trials," commented Dr. Philip Conaghan, professor and chairman of musculoskeletal medicine at the University of Leeds (England).
"Results from several studies have linked BMLs with pain and cartilage damage in OA patients. The larger the BML, the faster the cartilage loss and the worse the pain," Dr. Jones said in an interview. Based on studies his group has done, about 20% of BMLs that are associated with knee OA spontaneously enlarge over the course of 3 years, another 20% shrink in size, and about 60% remain the same, he said. Their earlier research findings also showed that BMLs are independently linked with fast progression of OA and the need for knee replacement. "If you reduce BMLs, it should produce good outcomes in patients," he said.
"The next step is to show that treatment with zoledronic acid not only reduces BML size but also slows cartilage loss. Sixty patients followed for 12 months were not enough to assess cartilage. We will need about 400 patients followed for 2 years," Dr. Jones added.
Despite not yet having information on cartilage effects, he said that his results so far have convinced him that treatment with zoledronic acid is reasonable for patients with painful knee OA and BMLs.
"I use it off label. Patients need to know it’s off label, and they [therefore] must be willing to pay for it, but I use it. It’s been shown to work, and nothing else works. Zoledronic acid [Reclast] is available, we know about its safety, and it’s been used for a long time to treat osteoporosis and cancers. If you have OA patients with BMLs, this is something to actively consider for them. Patients with OA have very limited treatment options. This can make a large difference in their pain, and it has long-lasting benefit so it can be given once a year," Dr. Jones said.
He recommended an infusion of 5 mg of zoledronic acid for patients who are at least 50 years old with knee OA that fulfills the American College of Rheumatology clinical criteria, and knee BMLs that are visible on an MRI scan of the affected knee. In his experience, 88% of these knee OA patients have BMLs. Dr. Jones noted that he does not use a maximal BML area threshold for initiating treatment, although in his study the average maximal BML area was about 465 mm2. About one-third of people aged 50 years or older with no clinical evidence of OA also have BMLs, he noted.
The benefits of zoledronic acid that were seen in his study might be a class effect that may be replicated by treatment with another bisphosphonate, but zoledronic acid is more potent than oral bisphosphonates and hence the drug’s beneficial effect on pain and BML shrinkage may exceed the effect that other bisphosphonates might have, he said.
The pain benefit appeared to start wearing off about a year after the zoledronic acid injection. Dr. Jones said that he has a small number of patients whom he has infused a second time, which produced a second round of pain reduction. He has not yet given any OA patients a third dose of the drug.
The 59 patients who were enrolled in the study had an average age of about 60 years, with an average knee pain score of about 52 on the visual analog scale; all patients had BMLs as seen on MRI scans of their affected knees. In all, 31 patients received a 5-mg infusion of zoledronic acid and 28 patients received a placebo infusion. All patients also continued their conventional pain medication regimens. The zoledronic acid infusion was well tolerated: Although infusion reactions were reported in 90% of the patients who received the drug and in 43% of the placebo patients, serious adverse effects occurred in only 19% of the patients who received zoledronic acid and in 4% of the placebo patients.
The Food and Drug Administration has approved zoledronic acid under a number of brand names to prevent or treat osteoporosis in postmenopausal women or patients who are at risk for osteoporosis because they are taking or have taken corticosteroid therapy; to manage Paget disease; and to prevent chemotherapy-induced bone fractures or fractures in patients with multiple myeloma or cancer that has metastasized to the bones from other locations.
The study was funded by Novartis, which markets zoledronic acid (Reclast). Dr. Jones and Dr. Conaghan said that they had no disclosures.
*Correction, 6/6/2011: An earlier version of this story incorrectly stated that Dr. Jones had no disclosures. Dr. Jones has received speaker fees, travel sponsorship, and research support from Novartis and from several other drug companies.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: A 5-mg infusion of zoledronic acid given to 31 patients with knee OA and associated bone marrow lesions reduced pain by 15 points more on a visual analogue scale than did placebo, and reduced maximal bone marrow lesion area by 170-mm2 after 6 months, compared with patients who received a placebo infusion.
Data Source: A single-center, randomized study with 31 patients who received a zoledronic acid infusion and 28 patients who received a placebo infusion.
Disclosures: The study was funded by Novartis, which markets zoledronic acid. Dr. Jones and Dr. Conaghan said that they had no disclosures.
WHO Data Shows Worldwide Uptick in Osteoarthritis
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: All musculoskeletal disorders combined had a prevalence of 2.1% of the
worldwide population and ranked 12th in disability-adjusted life-year (DALY) burden among all disorders. Preliminary data from the 2005 study show trends
toward increases in the prevalence of osteoarthritis of the knee and
hip, rheumatoid arthritis, and other musculoskeletal disease.
Data Source: The Global Burden of Diseases, Injuries, and Risk Factors Study investigating the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions.
Disclosures: Dr. March had no disclosures to report. The study received funding from
the Bill and Melinda Gates Foundation and the Australian Commonwealth
Government’s Department of Health and Aging.
Chondroitin Prevented Joint Destruction in Knee OA
Chondroitin sulfate slows the progression of knee osteoarthritis, according to findings from a pilot study that used magnetic resonance imaging to assess joint structural changes.
"It’s reassuring to see that the four major x-rays studies are now confirmed by high technology in the assessment of disease progression," said the study’s lead author Dr. Jean-Pierre Pelletier, in an interview. (Osteoarthr. Cartil. 1998;6:39-46), (Osteoarthr. Cartil. 2004;12:269-76), (Arthritis Rheum. 2005;52:779-86), (Arthritis Rheum. 2009;60:524-33).
The randomized, double-blind, placebo-controlled study showed that chondroitin sulfate reduced the cartilage loss volume in 69 patients with knee OA in as early as 6 months. (Ann. Rheum. Dis. 2011 March 1)
The findings show that "[MRI] is a good quantitative technique to find answers in shorter period of time with smaller number of patients," said Dr. Roy D. Altman, professor of medicine at the University of California, Los Angeles, who is not involved with the study.
The effect of disease-modifying drug chondroitin sulfate on cartilage volume loss, bone marrow lesions (BML), and disease symptoms has been controversial (BMJ 2010;341:c4675). However, the authors of this study said that the MRI findings provided additional evidence on the joint structure protective effect of chondroitin sulfate.
Several studies have also shown that MRI can quantitatively and reliably assess the volume and cartilage thickness in addition to joint structural changes in subchondral bone, menisci, and synovium, the authors reported.
"MRI provides you with direct visualization of the cartilage," said Dr. Pelletier, director of the osteoarthritis research unit at the University of Montreal Hospital Research Centre. "And the beauty of MRI is that it not only it provides assessment of progression of change in cartilage, but also in many other tissues of the joint, like the subchondral bone and the synovium.
"In addition, the pronounced reduction in OA cartilage loss found in patients treated with chondroitin sulfate was also associated with a reduction in the size of BML. This finding is most interesting as BML are believed to be associated with the progression of OA cartilage lesions," according to a number of studies, said Dr. Pelletier.
The study also showed that patients who were being treated with NSAIDs in addition to chondroitin sulfate showed a significant reduction in synovial membrane thickness (1.3 plus or minus 0.3 mm in 6 months vs. 1.6 plus or minus 0.3 mm placebo) and a lower incidence of joint swelling, compared with the placebo group (0% in chondroitin sulfate vs. 11.4% in placebo). The finding "is interesting with practical clinical impact, and definitely needs future exploration," the authors wrote.
Researchers recruited 69 patients of both sexes between 40 and 80 years of age from rheumatology clinics in Quebec province. All patients had clinical signs of synovitis.
The study had two phases. For the double-blind phase, the patients were randomly assigned to once-daily placebo or 800 mg of chondroitin sulfate for 6 months. During the following 6 months, or the open-label phase, both groups received 800 mg of chondroitin sulfate daily.
Cartilage volume and BML were assessed by MRI at baseline, 6 months, and 12 months. Synovial membrane thickness was assessed at baseline and 6 months.
Patients who took a daily oral dose of chondroitin sulfate had a significant reduction in cartilage volume loss at 6 months (–2.87%) and 12 months (–3.71%) in the global knee compared to the placebo group (–4.67% at 6 months and -6.12% at 12 months).
There were no differences in BML during the first 6 months. But, at 12 months reduction in BML were observed in the chondroitin sulfate group (–0.57%), especially in the lateral compartment (–0.13%) and the lateral condyle (–0.43). The additional 6-months needed to see the change could suggest that "BML are consequential to cartilage degradation and thus reducing cartilage lesions could lead to fewer BML. Alternatively, BML were shown to be involved in an inflammatory/catabolic process on which chondroitin sulfate could act directly, leading to structural repair," according to the study.
No significant difference in disease symptoms were measured by visual analog scale and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaires. "The main aim of the study was not the symptoms. The main goal was to find out whether chondroitin sulfate can reduce progression of knee OA," said Dr. Pelletier.
The study had limitations, including a small sample size. In addition, the system used did not allow the detection of the cartilage in the patella, researchers reported. They added that long-term studies are needed to find the impact of CS in disease symptoms.
Whether the quantitive MRI technique will eventually replace X-ray technology in such studies is unclear, said Dr. Pelletier. "That’s for regulatory bodies to decide," he said. "But it’s quite clear that MRI is the technology of the future. It’s very helpful, because you can truly speed up drug development in the field of OA and with less expense, using smaller number of patients and in a shorter period of time."
Dr. Jean-Pierre Pelletier and Dr. Johanne Martel-Pelletier are consultants for and shareholders in ArthroLab Inc. and ArthroVision Inc. Jean-Pierre Raynauld is a consultant for ArthroVision. Dr. André Beaulieu, Dr. Louis Bassette, and Dr. Frédéric Morin received honoraria from ArthroLab. François Abram is an employee of ArthroVision. Marc Dorais is a consultant for ArthroVision. Dr. Altman had no relevant financial conflicts of interest.
Chondroitin sulfate slows the progression of knee osteoarthritis, according to findings from a pilot study that used magnetic resonance imaging to assess joint structural changes.
"It’s reassuring to see that the four major x-rays studies are now confirmed by high technology in the assessment of disease progression," said the study’s lead author Dr. Jean-Pierre Pelletier, in an interview. (Osteoarthr. Cartil. 1998;6:39-46), (Osteoarthr. Cartil. 2004;12:269-76), (Arthritis Rheum. 2005;52:779-86), (Arthritis Rheum. 2009;60:524-33).
The randomized, double-blind, placebo-controlled study showed that chondroitin sulfate reduced the cartilage loss volume in 69 patients with knee OA in as early as 6 months. (Ann. Rheum. Dis. 2011 March 1)
The findings show that "[MRI] is a good quantitative technique to find answers in shorter period of time with smaller number of patients," said Dr. Roy D. Altman, professor of medicine at the University of California, Los Angeles, who is not involved with the study.
The effect of disease-modifying drug chondroitin sulfate on cartilage volume loss, bone marrow lesions (BML), and disease symptoms has been controversial (BMJ 2010;341:c4675). However, the authors of this study said that the MRI findings provided additional evidence on the joint structure protective effect of chondroitin sulfate.
Several studies have also shown that MRI can quantitatively and reliably assess the volume and cartilage thickness in addition to joint structural changes in subchondral bone, menisci, and synovium, the authors reported.
"MRI provides you with direct visualization of the cartilage," said Dr. Pelletier, director of the osteoarthritis research unit at the University of Montreal Hospital Research Centre. "And the beauty of MRI is that it not only it provides assessment of progression of change in cartilage, but also in many other tissues of the joint, like the subchondral bone and the synovium.
"In addition, the pronounced reduction in OA cartilage loss found in patients treated with chondroitin sulfate was also associated with a reduction in the size of BML. This finding is most interesting as BML are believed to be associated with the progression of OA cartilage lesions," according to a number of studies, said Dr. Pelletier.
The study also showed that patients who were being treated with NSAIDs in addition to chondroitin sulfate showed a significant reduction in synovial membrane thickness (1.3 plus or minus 0.3 mm in 6 months vs. 1.6 plus or minus 0.3 mm placebo) and a lower incidence of joint swelling, compared with the placebo group (0% in chondroitin sulfate vs. 11.4% in placebo). The finding "is interesting with practical clinical impact, and definitely needs future exploration," the authors wrote.
Researchers recruited 69 patients of both sexes between 40 and 80 years of age from rheumatology clinics in Quebec province. All patients had clinical signs of synovitis.
The study had two phases. For the double-blind phase, the patients were randomly assigned to once-daily placebo or 800 mg of chondroitin sulfate for 6 months. During the following 6 months, or the open-label phase, both groups received 800 mg of chondroitin sulfate daily.
Cartilage volume and BML were assessed by MRI at baseline, 6 months, and 12 months. Synovial membrane thickness was assessed at baseline and 6 months.
Patients who took a daily oral dose of chondroitin sulfate had a significant reduction in cartilage volume loss at 6 months (–2.87%) and 12 months (–3.71%) in the global knee compared to the placebo group (–4.67% at 6 months and -6.12% at 12 months).
There were no differences in BML during the first 6 months. But, at 12 months reduction in BML were observed in the chondroitin sulfate group (–0.57%), especially in the lateral compartment (–0.13%) and the lateral condyle (–0.43). The additional 6-months needed to see the change could suggest that "BML are consequential to cartilage degradation and thus reducing cartilage lesions could lead to fewer BML. Alternatively, BML were shown to be involved in an inflammatory/catabolic process on which chondroitin sulfate could act directly, leading to structural repair," according to the study.
No significant difference in disease symptoms were measured by visual analog scale and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaires. "The main aim of the study was not the symptoms. The main goal was to find out whether chondroitin sulfate can reduce progression of knee OA," said Dr. Pelletier.
The study had limitations, including a small sample size. In addition, the system used did not allow the detection of the cartilage in the patella, researchers reported. They added that long-term studies are needed to find the impact of CS in disease symptoms.
Whether the quantitive MRI technique will eventually replace X-ray technology in such studies is unclear, said Dr. Pelletier. "That’s for regulatory bodies to decide," he said. "But it’s quite clear that MRI is the technology of the future. It’s very helpful, because you can truly speed up drug development in the field of OA and with less expense, using smaller number of patients and in a shorter period of time."
Dr. Jean-Pierre Pelletier and Dr. Johanne Martel-Pelletier are consultants for and shareholders in ArthroLab Inc. and ArthroVision Inc. Jean-Pierre Raynauld is a consultant for ArthroVision. Dr. André Beaulieu, Dr. Louis Bassette, and Dr. Frédéric Morin received honoraria from ArthroLab. François Abram is an employee of ArthroVision. Marc Dorais is a consultant for ArthroVision. Dr. Altman had no relevant financial conflicts of interest.
Chondroitin sulfate slows the progression of knee osteoarthritis, according to findings from a pilot study that used magnetic resonance imaging to assess joint structural changes.
"It’s reassuring to see that the four major x-rays studies are now confirmed by high technology in the assessment of disease progression," said the study’s lead author Dr. Jean-Pierre Pelletier, in an interview. (Osteoarthr. Cartil. 1998;6:39-46), (Osteoarthr. Cartil. 2004;12:269-76), (Arthritis Rheum. 2005;52:779-86), (Arthritis Rheum. 2009;60:524-33).
The randomized, double-blind, placebo-controlled study showed that chondroitin sulfate reduced the cartilage loss volume in 69 patients with knee OA in as early as 6 months. (Ann. Rheum. Dis. 2011 March 1)
The findings show that "[MRI] is a good quantitative technique to find answers in shorter period of time with smaller number of patients," said Dr. Roy D. Altman, professor of medicine at the University of California, Los Angeles, who is not involved with the study.
The effect of disease-modifying drug chondroitin sulfate on cartilage volume loss, bone marrow lesions (BML), and disease symptoms has been controversial (BMJ 2010;341:c4675). However, the authors of this study said that the MRI findings provided additional evidence on the joint structure protective effect of chondroitin sulfate.
Several studies have also shown that MRI can quantitatively and reliably assess the volume and cartilage thickness in addition to joint structural changes in subchondral bone, menisci, and synovium, the authors reported.
"MRI provides you with direct visualization of the cartilage," said Dr. Pelletier, director of the osteoarthritis research unit at the University of Montreal Hospital Research Centre. "And the beauty of MRI is that it not only it provides assessment of progression of change in cartilage, but also in many other tissues of the joint, like the subchondral bone and the synovium.
"In addition, the pronounced reduction in OA cartilage loss found in patients treated with chondroitin sulfate was also associated with a reduction in the size of BML. This finding is most interesting as BML are believed to be associated with the progression of OA cartilage lesions," according to a number of studies, said Dr. Pelletier.
The study also showed that patients who were being treated with NSAIDs in addition to chondroitin sulfate showed a significant reduction in synovial membrane thickness (1.3 plus or minus 0.3 mm in 6 months vs. 1.6 plus or minus 0.3 mm placebo) and a lower incidence of joint swelling, compared with the placebo group (0% in chondroitin sulfate vs. 11.4% in placebo). The finding "is interesting with practical clinical impact, and definitely needs future exploration," the authors wrote.
Researchers recruited 69 patients of both sexes between 40 and 80 years of age from rheumatology clinics in Quebec province. All patients had clinical signs of synovitis.
The study had two phases. For the double-blind phase, the patients were randomly assigned to once-daily placebo or 800 mg of chondroitin sulfate for 6 months. During the following 6 months, or the open-label phase, both groups received 800 mg of chondroitin sulfate daily.
Cartilage volume and BML were assessed by MRI at baseline, 6 months, and 12 months. Synovial membrane thickness was assessed at baseline and 6 months.
Patients who took a daily oral dose of chondroitin sulfate had a significant reduction in cartilage volume loss at 6 months (–2.87%) and 12 months (–3.71%) in the global knee compared to the placebo group (–4.67% at 6 months and -6.12% at 12 months).
There were no differences in BML during the first 6 months. But, at 12 months reduction in BML were observed in the chondroitin sulfate group (–0.57%), especially in the lateral compartment (–0.13%) and the lateral condyle (–0.43). The additional 6-months needed to see the change could suggest that "BML are consequential to cartilage degradation and thus reducing cartilage lesions could lead to fewer BML. Alternatively, BML were shown to be involved in an inflammatory/catabolic process on which chondroitin sulfate could act directly, leading to structural repair," according to the study.
No significant difference in disease symptoms were measured by visual analog scale and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaires. "The main aim of the study was not the symptoms. The main goal was to find out whether chondroitin sulfate can reduce progression of knee OA," said Dr. Pelletier.
The study had limitations, including a small sample size. In addition, the system used did not allow the detection of the cartilage in the patella, researchers reported. They added that long-term studies are needed to find the impact of CS in disease symptoms.
Whether the quantitive MRI technique will eventually replace X-ray technology in such studies is unclear, said Dr. Pelletier. "That’s for regulatory bodies to decide," he said. "But it’s quite clear that MRI is the technology of the future. It’s very helpful, because you can truly speed up drug development in the field of OA and with less expense, using smaller number of patients and in a shorter period of time."
Dr. Jean-Pierre Pelletier and Dr. Johanne Martel-Pelletier are consultants for and shareholders in ArthroLab Inc. and ArthroVision Inc. Jean-Pierre Raynauld is a consultant for ArthroVision. Dr. André Beaulieu, Dr. Louis Bassette, and Dr. Frédéric Morin received honoraria from ArthroLab. François Abram is an employee of ArthroVision. Marc Dorais is a consultant for ArthroVision. Dr. Altman had no relevant financial conflicts of interest.
FROM ANNALS OF THE RHEUMATIC DISEASES
Treat Bone Injuries Early in Brain Trauma Patients
BUENOS AIRES — Treatment of orthopedic injuries in patients with traumatic brain injury should not be delayed, Dr. Ivan Rubel said at the annual conference of the International Society of Orthopaedic Surgery and Traumatology.
A population-based study conducted in the Twin Cities area of Minnesota found that most patients who were seen in an emergency department for traumatic brain injury had received the injury from sports and recreational activities (Minn. Med. 2006;89:40–4). The traumatic brain injuries that trauma surgeons are more likely to encounter, however, come from falls or car accidents, said Dr. Rubel, director of the orthopedics and traumatology department at FLENI Institute in Buenos Aires.
Pelvic and extremity fractures are common in patients with traumatic brain injury. Many skeletal injuries are not given priority, or might even be missed. However, as the survival rate of patients with traumatic brain injury has increased, there is a greater emphasis on minimizing dysfunction and disability in these patients, particularly when the dysfunction and disability arise from concomitant orthopedic trauma.
In a study of health-related quality of life in pediatric patients during the first year following a traumatic brain injury, the treatment of associated injuries was shown to have a greater impact than other factors such as patient or family characteristics (Arch. Pediatr. Adolesc. Med. 2006;160:252–60). “With the recent advances in intensive care medicine, most of these patients survive,” said Dr. Rubel. “We have to focus on minimizing the dysfunction and disability.”
The main question concerns when to operate on orthopedic injuries in a patient with traumatic brain injury, explained Dr. Rubel. Early fracture fixation in blunt trauma patients is generally recommended, but many doctors are hesitant to perform early fixation in patients with severe brain trauma. There is a widespread view that fracture fixation should be postponed to protect the injured brain.
This view was challenged by a study examining the timing of fracture fixation in blunt trauma patients with severe head injuries (Am. J. Surg. 1998;176:324–9). Investigators reviewed records of 47 consecutive blunt trauma patients with both severe head injuries and long bone fractures requiring surgical fixation. Twenty-two patients had undergone early fracture fixation within 24 hours of hospital admission (mean time 17 hours), and 25 patients had undergone delayed treatment (mean time 143 hours). Review of patient records revealed that there were no significant differences between the two groups in terms of neurologic or orthopedic complications, length of hospital stay, or mortality. Thus, delay of fracture fixation did not protect the injured brain in this study population.
Dr. Rubel described a young patient who was treated at FLENI Institute for a severe traumatic head injury and multiple fractures. The head injury required decompression with a wide craniotomy. The patient remained in a coma for 6 weeks, and CT scans showed cerebral edema. Radiography revealed a huge intrapelvic calcification affecting the bladder and rectum, malunion of the pelvis, malunion of the tibia, and a radio-ulnar synostosis. She was placed in long arm and leg casts and was told that she could not have pelvic surgery because of the likelihood that she would die during the procedure.
“Once at our institution, the malunion of the tibia was corrected upon admission, and she was allowed to exercise on a rehabilitation bicycle,” said Dr. Rubel. The second step was resection of the forearm synostosis, which improved the position of the hand for daily activities and allowed her to rehabilitate her writing capabilities, he said. As the brain edema resolved, the patient gradually improved both in cognition and in function. Restoration of the pelvic malunion with serial osteotomies was the last surgical intervention.
“It's hard for patients to understand not to put weight on the leg, since the brain is still inflamed,” said Dr. Rubel. Rehabilitation was performed in a pool with chest-deep water. At 6 months from the accident, she returned to her normal activities.
Immediately after trauma, there is a window of opportunity when treatment of orthopedic injuries is optimal. Use that window of opportunity around trauma and start helping the patients right away to minimize their skeletal and psychological and cognitive dysfunction, advised Dr. Rubel.
BUENOS AIRES — Treatment of orthopedic injuries in patients with traumatic brain injury should not be delayed, Dr. Ivan Rubel said at the annual conference of the International Society of Orthopaedic Surgery and Traumatology.
A population-based study conducted in the Twin Cities area of Minnesota found that most patients who were seen in an emergency department for traumatic brain injury had received the injury from sports and recreational activities (Minn. Med. 2006;89:40–4). The traumatic brain injuries that trauma surgeons are more likely to encounter, however, come from falls or car accidents, said Dr. Rubel, director of the orthopedics and traumatology department at FLENI Institute in Buenos Aires.
Pelvic and extremity fractures are common in patients with traumatic brain injury. Many skeletal injuries are not given priority, or might even be missed. However, as the survival rate of patients with traumatic brain injury has increased, there is a greater emphasis on minimizing dysfunction and disability in these patients, particularly when the dysfunction and disability arise from concomitant orthopedic trauma.
In a study of health-related quality of life in pediatric patients during the first year following a traumatic brain injury, the treatment of associated injuries was shown to have a greater impact than other factors such as patient or family characteristics (Arch. Pediatr. Adolesc. Med. 2006;160:252–60). “With the recent advances in intensive care medicine, most of these patients survive,” said Dr. Rubel. “We have to focus on minimizing the dysfunction and disability.”
The main question concerns when to operate on orthopedic injuries in a patient with traumatic brain injury, explained Dr. Rubel. Early fracture fixation in blunt trauma patients is generally recommended, but many doctors are hesitant to perform early fixation in patients with severe brain trauma. There is a widespread view that fracture fixation should be postponed to protect the injured brain.
This view was challenged by a study examining the timing of fracture fixation in blunt trauma patients with severe head injuries (Am. J. Surg. 1998;176:324–9). Investigators reviewed records of 47 consecutive blunt trauma patients with both severe head injuries and long bone fractures requiring surgical fixation. Twenty-two patients had undergone early fracture fixation within 24 hours of hospital admission (mean time 17 hours), and 25 patients had undergone delayed treatment (mean time 143 hours). Review of patient records revealed that there were no significant differences between the two groups in terms of neurologic or orthopedic complications, length of hospital stay, or mortality. Thus, delay of fracture fixation did not protect the injured brain in this study population.
Dr. Rubel described a young patient who was treated at FLENI Institute for a severe traumatic head injury and multiple fractures. The head injury required decompression with a wide craniotomy. The patient remained in a coma for 6 weeks, and CT scans showed cerebral edema. Radiography revealed a huge intrapelvic calcification affecting the bladder and rectum, malunion of the pelvis, malunion of the tibia, and a radio-ulnar synostosis. She was placed in long arm and leg casts and was told that she could not have pelvic surgery because of the likelihood that she would die during the procedure.
“Once at our institution, the malunion of the tibia was corrected upon admission, and she was allowed to exercise on a rehabilitation bicycle,” said Dr. Rubel. The second step was resection of the forearm synostosis, which improved the position of the hand for daily activities and allowed her to rehabilitate her writing capabilities, he said. As the brain edema resolved, the patient gradually improved both in cognition and in function. Restoration of the pelvic malunion with serial osteotomies was the last surgical intervention.
“It's hard for patients to understand not to put weight on the leg, since the brain is still inflamed,” said Dr. Rubel. Rehabilitation was performed in a pool with chest-deep water. At 6 months from the accident, she returned to her normal activities.
Immediately after trauma, there is a window of opportunity when treatment of orthopedic injuries is optimal. Use that window of opportunity around trauma and start helping the patients right away to minimize their skeletal and psychological and cognitive dysfunction, advised Dr. Rubel.
BUENOS AIRES — Treatment of orthopedic injuries in patients with traumatic brain injury should not be delayed, Dr. Ivan Rubel said at the annual conference of the International Society of Orthopaedic Surgery and Traumatology.
A population-based study conducted in the Twin Cities area of Minnesota found that most patients who were seen in an emergency department for traumatic brain injury had received the injury from sports and recreational activities (Minn. Med. 2006;89:40–4). The traumatic brain injuries that trauma surgeons are more likely to encounter, however, come from falls or car accidents, said Dr. Rubel, director of the orthopedics and traumatology department at FLENI Institute in Buenos Aires.
Pelvic and extremity fractures are common in patients with traumatic brain injury. Many skeletal injuries are not given priority, or might even be missed. However, as the survival rate of patients with traumatic brain injury has increased, there is a greater emphasis on minimizing dysfunction and disability in these patients, particularly when the dysfunction and disability arise from concomitant orthopedic trauma.
In a study of health-related quality of life in pediatric patients during the first year following a traumatic brain injury, the treatment of associated injuries was shown to have a greater impact than other factors such as patient or family characteristics (Arch. Pediatr. Adolesc. Med. 2006;160:252–60). “With the recent advances in intensive care medicine, most of these patients survive,” said Dr. Rubel. “We have to focus on minimizing the dysfunction and disability.”
The main question concerns when to operate on orthopedic injuries in a patient with traumatic brain injury, explained Dr. Rubel. Early fracture fixation in blunt trauma patients is generally recommended, but many doctors are hesitant to perform early fixation in patients with severe brain trauma. There is a widespread view that fracture fixation should be postponed to protect the injured brain.
This view was challenged by a study examining the timing of fracture fixation in blunt trauma patients with severe head injuries (Am. J. Surg. 1998;176:324–9). Investigators reviewed records of 47 consecutive blunt trauma patients with both severe head injuries and long bone fractures requiring surgical fixation. Twenty-two patients had undergone early fracture fixation within 24 hours of hospital admission (mean time 17 hours), and 25 patients had undergone delayed treatment (mean time 143 hours). Review of patient records revealed that there were no significant differences between the two groups in terms of neurologic or orthopedic complications, length of hospital stay, or mortality. Thus, delay of fracture fixation did not protect the injured brain in this study population.
Dr. Rubel described a young patient who was treated at FLENI Institute for a severe traumatic head injury and multiple fractures. The head injury required decompression with a wide craniotomy. The patient remained in a coma for 6 weeks, and CT scans showed cerebral edema. Radiography revealed a huge intrapelvic calcification affecting the bladder and rectum, malunion of the pelvis, malunion of the tibia, and a radio-ulnar synostosis. She was placed in long arm and leg casts and was told that she could not have pelvic surgery because of the likelihood that she would die during the procedure.
“Once at our institution, the malunion of the tibia was corrected upon admission, and she was allowed to exercise on a rehabilitation bicycle,” said Dr. Rubel. The second step was resection of the forearm synostosis, which improved the position of the hand for daily activities and allowed her to rehabilitate her writing capabilities, he said. As the brain edema resolved, the patient gradually improved both in cognition and in function. Restoration of the pelvic malunion with serial osteotomies was the last surgical intervention.
“It's hard for patients to understand not to put weight on the leg, since the brain is still inflamed,” said Dr. Rubel. Rehabilitation was performed in a pool with chest-deep water. At 6 months from the accident, she returned to her normal activities.
Immediately after trauma, there is a window of opportunity when treatment of orthopedic injuries is optimal. Use that window of opportunity around trauma and start helping the patients right away to minimize their skeletal and psychological and cognitive dysfunction, advised Dr. Rubel.