User login
Veterans don’t have higher risk of leukemia, lymphoma
People who have served in the Armed Forces do not have an increased risk of leukemia or lymphoma, according to research published in Cancer Epidemiology.
Researchers analyzed the long-term risks of developing leukemia, Hodgkin lymphoma (HL), and non-Hodgkin lymphoma (NHL) in veterans living in Scotland.
At a mean 30 years of follow-up, there were no significant differences in the risk of the aforementioned malignancies between veterans and non-veterans in Scotland.
This retrospective study included 56,205 veterans and 172,741 non-veterans.
The veterans’ earliest date of entering service was January 1960, and the latest date of leaving service was December 2012.
At a mean follow-up of 29.3 years, 294 (0.52%) veterans and 974 (0.56%) non-veterans were diagnosed with leukemia, HL, or NHL.
There were 125 (0.22%) cases of leukemia in veterans and 365 (0.21%) in non-veterans. There were 59 (0.10%) cases of HL in veterans and 182 (0.11%) in non-veterans. And there were 144 (0.26%) cases of NHL in veterans and 538 (0.31%) in non-veterans.
There was no significant difference in the risk of all 3 cancer types between the veterans and non-veterans. The unadjusted hazard ratio (HR) was 0.96 (P=0.541).
There were no significant differences in an adjusted analysis either. (The analysis was adjusted for regional deprivation, which takes into account information on income, employment, health, education, housing, crime, and access to services.)
The adjusted HR was 1.03 (P=0.773) for leukemias, 1.19 (P=0.272) for HL, and 0.86 (P=0.110) for NHL.
“This is an important study which provides reassurance that military service in the last 50 years does not increase people’s risk of leukemia overall,” said study author Beverly Bergman, PhD, of the University of Glasgow in the UK.
“The Armed Forces comply with all relevant health and safety legislation and regulations, and we can now see that their risk is no different from the general population.” ![]()
People who have served in the Armed Forces do not have an increased risk of leukemia or lymphoma, according to research published in Cancer Epidemiology.
Researchers analyzed the long-term risks of developing leukemia, Hodgkin lymphoma (HL), and non-Hodgkin lymphoma (NHL) in veterans living in Scotland.
At a mean 30 years of follow-up, there were no significant differences in the risk of the aforementioned malignancies between veterans and non-veterans in Scotland.
This retrospective study included 56,205 veterans and 172,741 non-veterans.
The veterans’ earliest date of entering service was January 1960, and the latest date of leaving service was December 2012.
At a mean follow-up of 29.3 years, 294 (0.52%) veterans and 974 (0.56%) non-veterans were diagnosed with leukemia, HL, or NHL.
There were 125 (0.22%) cases of leukemia in veterans and 365 (0.21%) in non-veterans. There were 59 (0.10%) cases of HL in veterans and 182 (0.11%) in non-veterans. And there were 144 (0.26%) cases of NHL in veterans and 538 (0.31%) in non-veterans.
There was no significant difference in the risk of all 3 cancer types between the veterans and non-veterans. The unadjusted hazard ratio (HR) was 0.96 (P=0.541).
There were no significant differences in an adjusted analysis either. (The analysis was adjusted for regional deprivation, which takes into account information on income, employment, health, education, housing, crime, and access to services.)
The adjusted HR was 1.03 (P=0.773) for leukemias, 1.19 (P=0.272) for HL, and 0.86 (P=0.110) for NHL.
“This is an important study which provides reassurance that military service in the last 50 years does not increase people’s risk of leukemia overall,” said study author Beverly Bergman, PhD, of the University of Glasgow in the UK.
“The Armed Forces comply with all relevant health and safety legislation and regulations, and we can now see that their risk is no different from the general population.” ![]()
People who have served in the Armed Forces do not have an increased risk of leukemia or lymphoma, according to research published in Cancer Epidemiology.
Researchers analyzed the long-term risks of developing leukemia, Hodgkin lymphoma (HL), and non-Hodgkin lymphoma (NHL) in veterans living in Scotland.
At a mean 30 years of follow-up, there were no significant differences in the risk of the aforementioned malignancies between veterans and non-veterans in Scotland.
This retrospective study included 56,205 veterans and 172,741 non-veterans.
The veterans’ earliest date of entering service was January 1960, and the latest date of leaving service was December 2012.
At a mean follow-up of 29.3 years, 294 (0.52%) veterans and 974 (0.56%) non-veterans were diagnosed with leukemia, HL, or NHL.
There were 125 (0.22%) cases of leukemia in veterans and 365 (0.21%) in non-veterans. There were 59 (0.10%) cases of HL in veterans and 182 (0.11%) in non-veterans. And there were 144 (0.26%) cases of NHL in veterans and 538 (0.31%) in non-veterans.
There was no significant difference in the risk of all 3 cancer types between the veterans and non-veterans. The unadjusted hazard ratio (HR) was 0.96 (P=0.541).
There were no significant differences in an adjusted analysis either. (The analysis was adjusted for regional deprivation, which takes into account information on income, employment, health, education, housing, crime, and access to services.)
The adjusted HR was 1.03 (P=0.773) for leukemias, 1.19 (P=0.272) for HL, and 0.86 (P=0.110) for NHL.
“This is an important study which provides reassurance that military service in the last 50 years does not increase people’s risk of leukemia overall,” said study author Beverly Bergman, PhD, of the University of Glasgow in the UK.
“The Armed Forces comply with all relevant health and safety legislation and regulations, and we can now see that their risk is no different from the general population.” ![]()
Selinexor trials placed on partial hold
The US Food and Drug Administration (FDA) has placed a partial clinical hold on all trials of selinexor (KPT-330).
Selinexor is an inhibitor being evaluated in multiple trials of patients with relapsed and/or refractory hematologic and solid tumor malignancies.
While the partial clinical hold remains in effect, patients with stable disease or better may remain on selinexor.
However, no new patients may be enrolled in selinexor trials until the hold is lifted.
The FDA has indicated that the partial clinical hold is due to incomplete information in the existing version of the investigator’s brochure, including an incomplete list of serious adverse events associated with selinexor.
Karyopharm Therapeutics Inc., the company developing selinexor, said it has amended the brochure, updated the informed consent documents accordingly, and submitted the documents to the FDA as requested.
As of March 10, Karyopharm had provided all requested materials to the FDA believed to be required to lift the partial clinical hold. By regulation, the FDA has 30 days from the receipt of Karyopharm’s submission to notify the company whether the partial clinical hold is lifted.
Karyopharm said it is working with the FDA to seek the release of the hold and resume enrollment in its selinexor trials as expeditiously as possible. The company believes its previously disclosed enrollment rates and timelines for its ongoing trials will remain materially unchanged.
About selinexor
Selinexor is a selective inhibitor of nuclear export (SINE) XPO1 antagonist. The drug binds with and inhibits XPO1, leading to the accumulation of tumor suppressor proteins in the cell nucleus. This reinitiates and amplifies their tumor suppressor function and is believed to induce apoptosis in cancer cells while largely sparing normal cells.
To date, more than 1900 patients have been treated with selinexor. The drug is currently being evaluated in several trials across multiple cancer indications.
One of these is the phase 2 SOPRA trial, in which selinexor is being compared to investigator’s choice of therapy (1 of 3 potential salvage therapies). The trial is enrolling patients 60 years of age or older with relapsed or refractory acute myeloid leukemia who are ineligible for standard intensive chemotherapy and/or transplant.
The SADAL study is a phase 2b trial comparing high and low doses of selinexor in patients with relapsed and/or refractory de novo diffuse large B-cell lymphoma who have no therapeutic options of demonstrated clinical benefit.
STORM is a phase 2b trial evaluating selinexor and low-dose dexamethasone in patients with heavily pretreated multiple myeloma (MM). And STOMP is a phase 1b/2 study evaluating selinexor in combination with existing therapies across the broader population in MM.
Karyopharm is also planning a randomized, phase 3 study known as BOSTON. In this trial, researchers will compare selinexor plus bortezomib and low-dose dexamethasone to bortezomib and low-dose dexamethasone in MM patients who have had 1 to 3 prior lines of therapy.
Additional phase 1, 2, and 3 studies are ongoing or currently planned.
The US Food and Drug Administration (FDA) has placed a partial clinical hold on all trials of selinexor (KPT-330).
Selinexor is an inhibitor being evaluated in multiple trials of patients with relapsed and/or refractory hematologic and solid tumor malignancies.
While the partial clinical hold remains in effect, patients with stable disease or better may remain on selinexor.
However, no new patients may be enrolled in selinexor trials until the hold is lifted.
The FDA has indicated that the partial clinical hold is due to incomplete information in the existing version of the investigator’s brochure, including an incomplete list of serious adverse events associated with selinexor.
Karyopharm Therapeutics Inc., the company developing selinexor, said it has amended the brochure, updated the informed consent documents accordingly, and submitted the documents to the FDA as requested.
As of March 10, Karyopharm had provided all requested materials to the FDA believed to be required to lift the partial clinical hold. By regulation, the FDA has 30 days from the receipt of Karyopharm’s submission to notify the company whether the partial clinical hold is lifted.
Karyopharm said it is working with the FDA to seek the release of the hold and resume enrollment in its selinexor trials as expeditiously as possible. The company believes its previously disclosed enrollment rates and timelines for its ongoing trials will remain materially unchanged.
About selinexor
Selinexor is a selective inhibitor of nuclear export (SINE) XPO1 antagonist. The drug binds with and inhibits XPO1, leading to the accumulation of tumor suppressor proteins in the cell nucleus. This reinitiates and amplifies their tumor suppressor function and is believed to induce apoptosis in cancer cells while largely sparing normal cells.
To date, more than 1900 patients have been treated with selinexor. The drug is currently being evaluated in several trials across multiple cancer indications.
One of these is the phase 2 SOPRA trial, in which selinexor is being compared to investigator’s choice of therapy (1 of 3 potential salvage therapies). The trial is enrolling patients 60 years of age or older with relapsed or refractory acute myeloid leukemia who are ineligible for standard intensive chemotherapy and/or transplant.
The SADAL study is a phase 2b trial comparing high and low doses of selinexor in patients with relapsed and/or refractory de novo diffuse large B-cell lymphoma who have no therapeutic options of demonstrated clinical benefit.
STORM is a phase 2b trial evaluating selinexor and low-dose dexamethasone in patients with heavily pretreated multiple myeloma (MM). And STOMP is a phase 1b/2 study evaluating selinexor in combination with existing therapies across the broader population in MM.
Karyopharm is also planning a randomized, phase 3 study known as BOSTON. In this trial, researchers will compare selinexor plus bortezomib and low-dose dexamethasone to bortezomib and low-dose dexamethasone in MM patients who have had 1 to 3 prior lines of therapy.
Additional phase 1, 2, and 3 studies are ongoing or currently planned.
The US Food and Drug Administration (FDA) has placed a partial clinical hold on all trials of selinexor (KPT-330).
Selinexor is an inhibitor being evaluated in multiple trials of patients with relapsed and/or refractory hematologic and solid tumor malignancies.
While the partial clinical hold remains in effect, patients with stable disease or better may remain on selinexor.
However, no new patients may be enrolled in selinexor trials until the hold is lifted.
The FDA has indicated that the partial clinical hold is due to incomplete information in the existing version of the investigator’s brochure, including an incomplete list of serious adverse events associated with selinexor.
Karyopharm Therapeutics Inc., the company developing selinexor, said it has amended the brochure, updated the informed consent documents accordingly, and submitted the documents to the FDA as requested.
As of March 10, Karyopharm had provided all requested materials to the FDA believed to be required to lift the partial clinical hold. By regulation, the FDA has 30 days from the receipt of Karyopharm’s submission to notify the company whether the partial clinical hold is lifted.
Karyopharm said it is working with the FDA to seek the release of the hold and resume enrollment in its selinexor trials as expeditiously as possible. The company believes its previously disclosed enrollment rates and timelines for its ongoing trials will remain materially unchanged.
About selinexor
Selinexor is a selective inhibitor of nuclear export (SINE) XPO1 antagonist. The drug binds with and inhibits XPO1, leading to the accumulation of tumor suppressor proteins in the cell nucleus. This reinitiates and amplifies their tumor suppressor function and is believed to induce apoptosis in cancer cells while largely sparing normal cells.
To date, more than 1900 patients have been treated with selinexor. The drug is currently being evaluated in several trials across multiple cancer indications.
One of these is the phase 2 SOPRA trial, in which selinexor is being compared to investigator’s choice of therapy (1 of 3 potential salvage therapies). The trial is enrolling patients 60 years of age or older with relapsed or refractory acute myeloid leukemia who are ineligible for standard intensive chemotherapy and/or transplant.
The SADAL study is a phase 2b trial comparing high and low doses of selinexor in patients with relapsed and/or refractory de novo diffuse large B-cell lymphoma who have no therapeutic options of demonstrated clinical benefit.
STORM is a phase 2b trial evaluating selinexor and low-dose dexamethasone in patients with heavily pretreated multiple myeloma (MM). And STOMP is a phase 1b/2 study evaluating selinexor in combination with existing therapies across the broader population in MM.
Karyopharm is also planning a randomized, phase 3 study known as BOSTON. In this trial, researchers will compare selinexor plus bortezomib and low-dose dexamethasone to bortezomib and low-dose dexamethasone in MM patients who have had 1 to 3 prior lines of therapy.
Additional phase 1, 2, and 3 studies are ongoing or currently planned.
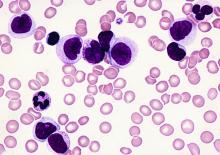
MRD predicts outcome of HSCT in ALL, study suggests
ORLANDO, FL—Minimal residual disease (MRD) measurements before and after hematopoietic stem cell transplant (HSCT) can help predict outcomes in patients with childhood acute lymphoblastic leukemia (ALL), according to researchers.
Their work also suggests several other factors can be used to predict event-free survival (EFS) in this patient population, and the team developed risk scores incorporating these factors.
Michael A. Pulsipher, MD, of Children’s Hospital Los Angeles in California, presented this work as one of the “Best Abstracts” at the 2017 BMT Tandem Meetings (abstract 4*).
“The new risk scores that we were able to develop very nicely predict outcomes post-transplant and can guide study planning,” Dr Pulsipher said.
“MRD pre-transplant was a very powerful predictor of outcome, and MRD post-transplant highlights individual patients at risk.”
For this study, Dr Pulsipher and his colleagues retrospectively analyzed 747 patients treated in Europe, North America, and Australia. The patients received transplants between September 1999 and May 2015.
Most patients had pre-B ALL (78%, n=586), 19% (n=145) had T-cell ALL, 2% had “other” ALLs (n=8) or no data on ALL type (n=8). Sixty-two percent (n=466) were male.
Nearly half of patients were between the ages of 2 and 10 (49%, n=365), 47% (n=351) were older than 10, and 4% (n=31) were younger than 2.
Transplant details
Patients received grafts from matched unrelated donors (42%, n=314), matched sibling donors (30%, n=227), mismatched donors (10%, n=75), and cord blood from unrelated donors (17%, n=128). There was no data on donor type for 3 patients.
Most patients received bone marrow transplants (61%, n=458), 20% (n=147) received cord blood, and 18% (n=131) received peripheral blood stem cells. Eight patients received “other” types of transplants, and 3 patients had no data on stem cell source.
More than half of the patients (55%, n=410) were in their second complete remission (CR) at transplant. Thirty-seven percent were in their first CR (n=275), 7% were in their third or greater CR (n=53), and 1% were not in remission (n=7). Two patients had no data on remission status.
MRD
MRD was assessed before HSCT as well as after—on or near days 30, 60, 90, 180, 365, and beyond.
There were 4 MRD categories:
- MRD negative: No signal
- MRD low: >0 to <10-4 (<0.01%)
- MRD high: ≥10-4 to <10-3 (0.01 to 0.1%)
- MRD very high: ≥10-3 to <10-2 (>0.1%).
Dr Pulsipher noted that, when analyzing MRD pre-HSCT or at 30 days after HSCT, the estimated 5-year EFS was similar for patients in the MRD-negative and MRD-low groups. However, as time went on (at days 90, 180, and 365), any detectable level of MRD was associated with a poor prognosis.
“And patients arriving at day 365 with no detectable MRD had an exceptional prognosis, with survival approaching 90%,” Dr Pulsipher said.
He also pointed out an interaction between acute graft-vs-host disease (aGVHD) and MRD post-HSCT. He and his colleagues observed better survival for MRD-positive patients with aGVHD (grade 1-2) than for MRD-positive patients without aGVHD.
Pre-HSCT risk score
Via an adjusted Cox regression analysis, the researchers identified several pre-transplant factors that predicted EFS at 18 months.
These included remission status, donor type, immunophenotype, and MRD. The researchers assigned points to each of these factors to create a risk score.
Compared to patients in first CR, the hazard ratio (HR) for patients in early second CR was 2.53, and the score was 3. For patients in third CR or greater, the HR was 1.95, and the score was 2.
Compared to patients with a matched sibling donor, the HR for patients with a mismatched donor was 1.41, and the score was 1. For patients who received cord blood from an unrelated donor, the HR was 1.48, and the score was 1.
Compared to patients with T-cell ALL, the HR for patients with pre-B ALL was 1.35, and the score was 1.
Compared to patients with MRD <10-4, the HR for patients with MRD ≥10-4 was 2.32, and the score was 2.
The probability of EFS at 18 months was 78% ± 2% for patients with 0 to 1 points, 54% ± 3% for those with 2 to 3 points, and 46% ± 5% for patients with 4 or more points.
Day 30 post-HSCT risk score
When considering patients at day 30 post-HSCT, factors that predicted 18-month EFS included remission status, donor type, immunophenotype, aGVHD status, and MRD.
The HR for patients in early second CR was 2.51, and the score was 3. For patients in third CR or greater, the HR was 2.09, and the score was 2.
The HR for patients with a mismatched donor was 1.75, and the score was 2. The HR for patients with pre-B ALL was 1.40, and the score was 1.
Compared to patients with grade 1-2 aGVHD, the HR was 2.02 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 3 aGVHD, the HR was 1.44, and the score was 1. For patients with grade 4 aGVHD, the HR was 7.12, and the score was 7.
The researchers evaluated MRD prior to HSCT and MRD at day 30, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 30, the HR was 2.29, and the score was 2.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 30, the HR was 3.17, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 30, the HR was 3.63, and the score was 4.
The probability of EFS at 18 months was 80% ± 2% for patients with 0 to 3 points, 54% ± 4% for those with 4 to 6 points, and 25% ± 6% for those with 7 or more points.
Day 90 post-HSCT risk score
When considering patients at day 90 post-HSCT, factors that predicted 18-month EFS included remission status, aGVHD status, and MRD.
For patients in early second CR, the HR was 2.81, and the score was 3. For those in third CR or greater, the HR was 1.85, and the score was 2.
Compared to patients with grade 1-2 aGVHD, the HR was 1.60 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 4 aGVHD, the HR was 2.49, and the score was 2.
The researchers assessed MRD prior to HSCT and MRD at day 90, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 90, the HR was 6.03, and the score was 6.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 90, the HR was 3.11, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 90, the HR was 4.59, and the score was 5.
The probability of EFS at 18 months was 83% ± 2% for patients with 0 to 2 points, 60% ± 4% for those with 3 to 5 points, and 17% ± 11 for those with 6 or more points. ![]()
*Information in the abstract differs from the presentation.
ORLANDO, FL—Minimal residual disease (MRD) measurements before and after hematopoietic stem cell transplant (HSCT) can help predict outcomes in patients with childhood acute lymphoblastic leukemia (ALL), according to researchers.
Their work also suggests several other factors can be used to predict event-free survival (EFS) in this patient population, and the team developed risk scores incorporating these factors.
Michael A. Pulsipher, MD, of Children’s Hospital Los Angeles in California, presented this work as one of the “Best Abstracts” at the 2017 BMT Tandem Meetings (abstract 4*).
“The new risk scores that we were able to develop very nicely predict outcomes post-transplant and can guide study planning,” Dr Pulsipher said.
“MRD pre-transplant was a very powerful predictor of outcome, and MRD post-transplant highlights individual patients at risk.”
For this study, Dr Pulsipher and his colleagues retrospectively analyzed 747 patients treated in Europe, North America, and Australia. The patients received transplants between September 1999 and May 2015.
Most patients had pre-B ALL (78%, n=586), 19% (n=145) had T-cell ALL, 2% had “other” ALLs (n=8) or no data on ALL type (n=8). Sixty-two percent (n=466) were male.
Nearly half of patients were between the ages of 2 and 10 (49%, n=365), 47% (n=351) were older than 10, and 4% (n=31) were younger than 2.
Transplant details
Patients received grafts from matched unrelated donors (42%, n=314), matched sibling donors (30%, n=227), mismatched donors (10%, n=75), and cord blood from unrelated donors (17%, n=128). There was no data on donor type for 3 patients.
Most patients received bone marrow transplants (61%, n=458), 20% (n=147) received cord blood, and 18% (n=131) received peripheral blood stem cells. Eight patients received “other” types of transplants, and 3 patients had no data on stem cell source.
More than half of the patients (55%, n=410) were in their second complete remission (CR) at transplant. Thirty-seven percent were in their first CR (n=275), 7% were in their third or greater CR (n=53), and 1% were not in remission (n=7). Two patients had no data on remission status.
MRD
MRD was assessed before HSCT as well as after—on or near days 30, 60, 90, 180, 365, and beyond.
There were 4 MRD categories:
- MRD negative: No signal
- MRD low: >0 to <10-4 (<0.01%)
- MRD high: ≥10-4 to <10-3 (0.01 to 0.1%)
- MRD very high: ≥10-3 to <10-2 (>0.1%).
Dr Pulsipher noted that, when analyzing MRD pre-HSCT or at 30 days after HSCT, the estimated 5-year EFS was similar for patients in the MRD-negative and MRD-low groups. However, as time went on (at days 90, 180, and 365), any detectable level of MRD was associated with a poor prognosis.
“And patients arriving at day 365 with no detectable MRD had an exceptional prognosis, with survival approaching 90%,” Dr Pulsipher said.
He also pointed out an interaction between acute graft-vs-host disease (aGVHD) and MRD post-HSCT. He and his colleagues observed better survival for MRD-positive patients with aGVHD (grade 1-2) than for MRD-positive patients without aGVHD.
Pre-HSCT risk score
Via an adjusted Cox regression analysis, the researchers identified several pre-transplant factors that predicted EFS at 18 months.
These included remission status, donor type, immunophenotype, and MRD. The researchers assigned points to each of these factors to create a risk score.
Compared to patients in first CR, the hazard ratio (HR) for patients in early second CR was 2.53, and the score was 3. For patients in third CR or greater, the HR was 1.95, and the score was 2.
Compared to patients with a matched sibling donor, the HR for patients with a mismatched donor was 1.41, and the score was 1. For patients who received cord blood from an unrelated donor, the HR was 1.48, and the score was 1.
Compared to patients with T-cell ALL, the HR for patients with pre-B ALL was 1.35, and the score was 1.
Compared to patients with MRD <10-4, the HR for patients with MRD ≥10-4 was 2.32, and the score was 2.
The probability of EFS at 18 months was 78% ± 2% for patients with 0 to 1 points, 54% ± 3% for those with 2 to 3 points, and 46% ± 5% for patients with 4 or more points.
Day 30 post-HSCT risk score
When considering patients at day 30 post-HSCT, factors that predicted 18-month EFS included remission status, donor type, immunophenotype, aGVHD status, and MRD.
The HR for patients in early second CR was 2.51, and the score was 3. For patients in third CR or greater, the HR was 2.09, and the score was 2.
The HR for patients with a mismatched donor was 1.75, and the score was 2. The HR for patients with pre-B ALL was 1.40, and the score was 1.
Compared to patients with grade 1-2 aGVHD, the HR was 2.02 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 3 aGVHD, the HR was 1.44, and the score was 1. For patients with grade 4 aGVHD, the HR was 7.12, and the score was 7.
The researchers evaluated MRD prior to HSCT and MRD at day 30, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 30, the HR was 2.29, and the score was 2.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 30, the HR was 3.17, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 30, the HR was 3.63, and the score was 4.
The probability of EFS at 18 months was 80% ± 2% for patients with 0 to 3 points, 54% ± 4% for those with 4 to 6 points, and 25% ± 6% for those with 7 or more points.
Day 90 post-HSCT risk score
When considering patients at day 90 post-HSCT, factors that predicted 18-month EFS included remission status, aGVHD status, and MRD.
For patients in early second CR, the HR was 2.81, and the score was 3. For those in third CR or greater, the HR was 1.85, and the score was 2.
Compared to patients with grade 1-2 aGVHD, the HR was 1.60 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 4 aGVHD, the HR was 2.49, and the score was 2.
The researchers assessed MRD prior to HSCT and MRD at day 90, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 90, the HR was 6.03, and the score was 6.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 90, the HR was 3.11, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 90, the HR was 4.59, and the score was 5.
The probability of EFS at 18 months was 83% ± 2% for patients with 0 to 2 points, 60% ± 4% for those with 3 to 5 points, and 17% ± 11 for those with 6 or more points. ![]()
*Information in the abstract differs from the presentation.
ORLANDO, FL—Minimal residual disease (MRD) measurements before and after hematopoietic stem cell transplant (HSCT) can help predict outcomes in patients with childhood acute lymphoblastic leukemia (ALL), according to researchers.
Their work also suggests several other factors can be used to predict event-free survival (EFS) in this patient population, and the team developed risk scores incorporating these factors.
Michael A. Pulsipher, MD, of Children’s Hospital Los Angeles in California, presented this work as one of the “Best Abstracts” at the 2017 BMT Tandem Meetings (abstract 4*).
“The new risk scores that we were able to develop very nicely predict outcomes post-transplant and can guide study planning,” Dr Pulsipher said.
“MRD pre-transplant was a very powerful predictor of outcome, and MRD post-transplant highlights individual patients at risk.”
For this study, Dr Pulsipher and his colleagues retrospectively analyzed 747 patients treated in Europe, North America, and Australia. The patients received transplants between September 1999 and May 2015.
Most patients had pre-B ALL (78%, n=586), 19% (n=145) had T-cell ALL, 2% had “other” ALLs (n=8) or no data on ALL type (n=8). Sixty-two percent (n=466) were male.
Nearly half of patients were between the ages of 2 and 10 (49%, n=365), 47% (n=351) were older than 10, and 4% (n=31) were younger than 2.
Transplant details
Patients received grafts from matched unrelated donors (42%, n=314), matched sibling donors (30%, n=227), mismatched donors (10%, n=75), and cord blood from unrelated donors (17%, n=128). There was no data on donor type for 3 patients.
Most patients received bone marrow transplants (61%, n=458), 20% (n=147) received cord blood, and 18% (n=131) received peripheral blood stem cells. Eight patients received “other” types of transplants, and 3 patients had no data on stem cell source.
More than half of the patients (55%, n=410) were in their second complete remission (CR) at transplant. Thirty-seven percent were in their first CR (n=275), 7% were in their third or greater CR (n=53), and 1% were not in remission (n=7). Two patients had no data on remission status.
MRD
MRD was assessed before HSCT as well as after—on or near days 30, 60, 90, 180, 365, and beyond.
There were 4 MRD categories:
- MRD negative: No signal
- MRD low: >0 to <10-4 (<0.01%)
- MRD high: ≥10-4 to <10-3 (0.01 to 0.1%)
- MRD very high: ≥10-3 to <10-2 (>0.1%).
Dr Pulsipher noted that, when analyzing MRD pre-HSCT or at 30 days after HSCT, the estimated 5-year EFS was similar for patients in the MRD-negative and MRD-low groups. However, as time went on (at days 90, 180, and 365), any detectable level of MRD was associated with a poor prognosis.
“And patients arriving at day 365 with no detectable MRD had an exceptional prognosis, with survival approaching 90%,” Dr Pulsipher said.
He also pointed out an interaction between acute graft-vs-host disease (aGVHD) and MRD post-HSCT. He and his colleagues observed better survival for MRD-positive patients with aGVHD (grade 1-2) than for MRD-positive patients without aGVHD.
Pre-HSCT risk score
Via an adjusted Cox regression analysis, the researchers identified several pre-transplant factors that predicted EFS at 18 months.
These included remission status, donor type, immunophenotype, and MRD. The researchers assigned points to each of these factors to create a risk score.
Compared to patients in first CR, the hazard ratio (HR) for patients in early second CR was 2.53, and the score was 3. For patients in third CR or greater, the HR was 1.95, and the score was 2.
Compared to patients with a matched sibling donor, the HR for patients with a mismatched donor was 1.41, and the score was 1. For patients who received cord blood from an unrelated donor, the HR was 1.48, and the score was 1.
Compared to patients with T-cell ALL, the HR for patients with pre-B ALL was 1.35, and the score was 1.
Compared to patients with MRD <10-4, the HR for patients with MRD ≥10-4 was 2.32, and the score was 2.
The probability of EFS at 18 months was 78% ± 2% for patients with 0 to 1 points, 54% ± 3% for those with 2 to 3 points, and 46% ± 5% for patients with 4 or more points.
Day 30 post-HSCT risk score
When considering patients at day 30 post-HSCT, factors that predicted 18-month EFS included remission status, donor type, immunophenotype, aGVHD status, and MRD.
The HR for patients in early second CR was 2.51, and the score was 3. For patients in third CR or greater, the HR was 2.09, and the score was 2.
The HR for patients with a mismatched donor was 1.75, and the score was 2. The HR for patients with pre-B ALL was 1.40, and the score was 1.
Compared to patients with grade 1-2 aGVHD, the HR was 2.02 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 3 aGVHD, the HR was 1.44, and the score was 1. For patients with grade 4 aGVHD, the HR was 7.12, and the score was 7.
The researchers evaluated MRD prior to HSCT and MRD at day 30, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 30, the HR was 2.29, and the score was 2.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 30, the HR was 3.17, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 30, the HR was 3.63, and the score was 4.
The probability of EFS at 18 months was 80% ± 2% for patients with 0 to 3 points, 54% ± 4% for those with 4 to 6 points, and 25% ± 6% for those with 7 or more points.
Day 90 post-HSCT risk score
When considering patients at day 90 post-HSCT, factors that predicted 18-month EFS included remission status, aGVHD status, and MRD.
For patients in early second CR, the HR was 2.81, and the score was 3. For those in third CR or greater, the HR was 1.85, and the score was 2.
Compared to patients with grade 1-2 aGVHD, the HR was 1.60 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 4 aGVHD, the HR was 2.49, and the score was 2.
The researchers assessed MRD prior to HSCT and MRD at day 90, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 90, the HR was 6.03, and the score was 6.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 90, the HR was 3.11, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 90, the HR was 4.59, and the score was 5.
The probability of EFS at 18 months was 83% ± 2% for patients with 0 to 2 points, 60% ± 4% for those with 3 to 5 points, and 17% ± 11 for those with 6 or more points. ![]()
*Information in the abstract differs from the presentation.
FDA grants mAb orphan designation for MDS
The US Food and Drug Administration (FDA) has granted orphan drug designation for BI 836858, an anti-CD33 monoclonal antibody (mAb), in the treatment of myelodysplastic syndromes (MDS).
BI 836858 previously received orphan designation for the treatment of acute myeloid leukemia (AML).
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases.
This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
About BI 836858
BI 836858 is a fully human, immunoglobulin G1 anti-CD33 mAb. It has been engineered for improved binding to FcgRIIIa to mediate natural killer cell antibody-dependent cellular cytotoxicity against CD33-expressing tumor cells.
BI 836858 is being developed by Boehringer Ingelheim.
A phase 1/2 trial (NCT02240706) of BI 836858 in patients with MDS is ongoing. The phase 1 portion was designed to evaluate various doses of the mAb in patients with low or intermediate-1 risk MDS with symptomatic anemia.
The phase 2 portion was designed to compare BI 836858 plus best supportive care to best supportive care alone in patients with low- or intermediate-1-risk MDS who have symptomatic anemia but do not have a 5q deletion.
BI 836858 is also being tested in combination with decitabine in a phase 1/2 study (NCT02632721) of patients with AML.
The goals of the phase 1 portion and the phase 1 extension are to determine the maximum-tolerated dose/recommended dose, safety, pharmacokinetics, and efficacy of BI 836858 in combination with decitabine.
The goals of the phase 2 portion of the study are to investigate the efficacy, safety, and pharmacokinetics of BI 836858 in combination with decitabine compared to decitabine monotherapy.
BI 836858 was previously evaluated in combination with decitabine in a preclinical study. The combination exhibited activity against AML in vitro. The research was published in Blood last year.
BI 836858 is also being evaluated as part of the Leukemia & Lymphoma Society’s Beat AML Master Trial program to advance treatment for patients with AML.
In this trial, investigators are using genomic technology to identify AML mutations in newly diagnosed patients over the age of 60 and match the patients with an investigational drug or drugs best suited to attack the mutations found. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation for BI 836858, an anti-CD33 monoclonal antibody (mAb), in the treatment of myelodysplastic syndromes (MDS).
BI 836858 previously received orphan designation for the treatment of acute myeloid leukemia (AML).
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases.
This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
About BI 836858
BI 836858 is a fully human, immunoglobulin G1 anti-CD33 mAb. It has been engineered for improved binding to FcgRIIIa to mediate natural killer cell antibody-dependent cellular cytotoxicity against CD33-expressing tumor cells.
BI 836858 is being developed by Boehringer Ingelheim.
A phase 1/2 trial (NCT02240706) of BI 836858 in patients with MDS is ongoing. The phase 1 portion was designed to evaluate various doses of the mAb in patients with low or intermediate-1 risk MDS with symptomatic anemia.
The phase 2 portion was designed to compare BI 836858 plus best supportive care to best supportive care alone in patients with low- or intermediate-1-risk MDS who have symptomatic anemia but do not have a 5q deletion.
BI 836858 is also being tested in combination with decitabine in a phase 1/2 study (NCT02632721) of patients with AML.
The goals of the phase 1 portion and the phase 1 extension are to determine the maximum-tolerated dose/recommended dose, safety, pharmacokinetics, and efficacy of BI 836858 in combination with decitabine.
The goals of the phase 2 portion of the study are to investigate the efficacy, safety, and pharmacokinetics of BI 836858 in combination with decitabine compared to decitabine monotherapy.
BI 836858 was previously evaluated in combination with decitabine in a preclinical study. The combination exhibited activity against AML in vitro. The research was published in Blood last year.
BI 836858 is also being evaluated as part of the Leukemia & Lymphoma Society’s Beat AML Master Trial program to advance treatment for patients with AML.
In this trial, investigators are using genomic technology to identify AML mutations in newly diagnosed patients over the age of 60 and match the patients with an investigational drug or drugs best suited to attack the mutations found. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation for BI 836858, an anti-CD33 monoclonal antibody (mAb), in the treatment of myelodysplastic syndromes (MDS).
BI 836858 previously received orphan designation for the treatment of acute myeloid leukemia (AML).
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases.
This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
About BI 836858
BI 836858 is a fully human, immunoglobulin G1 anti-CD33 mAb. It has been engineered for improved binding to FcgRIIIa to mediate natural killer cell antibody-dependent cellular cytotoxicity against CD33-expressing tumor cells.
BI 836858 is being developed by Boehringer Ingelheim.
A phase 1/2 trial (NCT02240706) of BI 836858 in patients with MDS is ongoing. The phase 1 portion was designed to evaluate various doses of the mAb in patients with low or intermediate-1 risk MDS with symptomatic anemia.
The phase 2 portion was designed to compare BI 836858 plus best supportive care to best supportive care alone in patients with low- or intermediate-1-risk MDS who have symptomatic anemia but do not have a 5q deletion.
BI 836858 is also being tested in combination with decitabine in a phase 1/2 study (NCT02632721) of patients with AML.
The goals of the phase 1 portion and the phase 1 extension are to determine the maximum-tolerated dose/recommended dose, safety, pharmacokinetics, and efficacy of BI 836858 in combination with decitabine.
The goals of the phase 2 portion of the study are to investigate the efficacy, safety, and pharmacokinetics of BI 836858 in combination with decitabine compared to decitabine monotherapy.
BI 836858 was previously evaluated in combination with decitabine in a preclinical study. The combination exhibited activity against AML in vitro. The research was published in Blood last year.
BI 836858 is also being evaluated as part of the Leukemia & Lymphoma Society’s Beat AML Master Trial program to advance treatment for patients with AML.
In this trial, investigators are using genomic technology to identify AML mutations in newly diagnosed patients over the age of 60 and match the patients with an investigational drug or drugs best suited to attack the mutations found. ![]()
Study confirms increased adiposity in HSCT survivors
ORLANDO, FL—A recently conducted study confirms that survivors of hematopoietic stem cell transplant (HSCT) have increased body fat mass and lower lean mass compared to normal controls. And this is despite having a comparable body mass index (BMI).
Researchers say the abnormalities in adipokine levels—leptin and adiponectin—could provide insight into the mechanisms that contribute to the metabolic syndrome and cardiovascular complications that often develop in HSCT survivors.
Leptin and adiponectin are associated with obesity, insulin secretion, insulin resistance, endothelial function, vascular homeostasis, and atherosclerosis.
“So knowing that there is a dynamic interplay between obesity and insulin resistance and cytokine and adipokine profiles and, ultimately, insulin-resistance syndrome, we sought to evaluate, as part of a larger study, how treatment effects, including high-dose chemotherapy and radiation, alter cytokine profiles as well as obesity and body composition,” said Tyler G. Ketterl, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
Dr Ketterl presented the findings at the 2017 BMT Tandem Meetings as abstract 52.*
Study design
The research team compared 151 HSCT recipients who had survived more than 2 years after transplant with 92 sibling controls.
HSCT survivors were randomly recruited from 2 centers—Fred Hutchinson Cancer Research Center and University of Minnesota Masonic Children’s Hospital—and were younger than 21 years when diagnosed.
The researchers evaluated all participants for body composition, cardiovascular risk factors, and adipokines using anthropomorphic measurements, DXA scans for muscle and fat mass, and laboratory bloodwork.
The team stratified the HSCT survivors by the preparative regimen they had received—total body irradiation (TBI) alone, TBI plus cranial radiation (CRT), and chemotherapy alone.
Study population
Males comprised more than half the study population in each arm, 58% of HSCT survivors and 54% of siblings.
Nine percent and 8% in the HSCT and sibling arms, respectively, were non-white and/or Hispanic, and the mean current ages were 24.0 (range, 10-51) for HSCT survivors and 24.2 (range, 10-48) for siblings.
The survivors’ mean age at diagnosis was 9.1 years (range, 0.4–20.6), their mean age at transplant was 11.2 years (range, 0.6–32.6), and the mean time from transplant to study participation was 13.5 years (range, 2.6–32).
Most patients received a transplant for leukemia—54 (36%) for acute myeloid leukemia, 46 (31%) for acute lymphoblastic leukemia, and 15 (10%) for chronic myeloid leukemia. Thirteen (9%) received transplants for myelodysplastic syndromes, 12 (8%) for Hodgkin lymphoma, and 10 (6%) for non-Hodgkin lymphoma.
A little more than half had TBI (85, 56%) as the preparative regimen, 31 (21%) had TBI plus CRT, and 35 (23%) had chemotherapy only.
About three-quarters (116, 77%) had an allogeneic transplant, and 35 (23%) had an autologous transplant.
Results
Overall, HSCT survivors had significantly lower adiponectin levels than siblings (P<0.001).
Survivors who received TBI with or without CRT had significantly lower adiponectin levels than siblings (P<0.001), while survivors who received chemotherapy alone did not (P=0.42).
Adiponectin is involved in insulin sensitization, hepatoprotective action, antiatherogenic action, protection against the development of diabetes, and regulation of lipid metabolism.
Overall, survivors had significantly higher leptin levels than siblings (P<0.001).
This held true regardless of conditioning regimen, although levels for patients who received chemotherapy only were not as significantly high (P=0.02) as for survivors who received TBI (P<0.001).
Leptin helps increase energy expenditure, decrease appetite and food uptake, modify insulin sensitivity on muscles and liver, prevent ectopic lipid deposition, and regulate immune function.
BMI adjusted for age, sex, and Tanner stage was not significantly different between survivors and siblings, but percent fat mass was significantly higher across all conditioning regimens for survivors compared to siblings (P<0.001).
“And this goes along with previous data,” Dr Ketterl said, “that shows sarcopenic obesity is common amongst transplant survivors.”
The researchers believe these significant differences may provide insight into the underlying risk of developing metabolic syndrome and cardiovascular complications in transplant survivors. ![]()
*Some details in the abstract differ from the presentation.
ORLANDO, FL—A recently conducted study confirms that survivors of hematopoietic stem cell transplant (HSCT) have increased body fat mass and lower lean mass compared to normal controls. And this is despite having a comparable body mass index (BMI).
Researchers say the abnormalities in adipokine levels—leptin and adiponectin—could provide insight into the mechanisms that contribute to the metabolic syndrome and cardiovascular complications that often develop in HSCT survivors.
Leptin and adiponectin are associated with obesity, insulin secretion, insulin resistance, endothelial function, vascular homeostasis, and atherosclerosis.
“So knowing that there is a dynamic interplay between obesity and insulin resistance and cytokine and adipokine profiles and, ultimately, insulin-resistance syndrome, we sought to evaluate, as part of a larger study, how treatment effects, including high-dose chemotherapy and radiation, alter cytokine profiles as well as obesity and body composition,” said Tyler G. Ketterl, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
Dr Ketterl presented the findings at the 2017 BMT Tandem Meetings as abstract 52.*
Study design
The research team compared 151 HSCT recipients who had survived more than 2 years after transplant with 92 sibling controls.
HSCT survivors were randomly recruited from 2 centers—Fred Hutchinson Cancer Research Center and University of Minnesota Masonic Children’s Hospital—and were younger than 21 years when diagnosed.
The researchers evaluated all participants for body composition, cardiovascular risk factors, and adipokines using anthropomorphic measurements, DXA scans for muscle and fat mass, and laboratory bloodwork.
The team stratified the HSCT survivors by the preparative regimen they had received—total body irradiation (TBI) alone, TBI plus cranial radiation (CRT), and chemotherapy alone.
Study population
Males comprised more than half the study population in each arm, 58% of HSCT survivors and 54% of siblings.
Nine percent and 8% in the HSCT and sibling arms, respectively, were non-white and/or Hispanic, and the mean current ages were 24.0 (range, 10-51) for HSCT survivors and 24.2 (range, 10-48) for siblings.
The survivors’ mean age at diagnosis was 9.1 years (range, 0.4–20.6), their mean age at transplant was 11.2 years (range, 0.6–32.6), and the mean time from transplant to study participation was 13.5 years (range, 2.6–32).
Most patients received a transplant for leukemia—54 (36%) for acute myeloid leukemia, 46 (31%) for acute lymphoblastic leukemia, and 15 (10%) for chronic myeloid leukemia. Thirteen (9%) received transplants for myelodysplastic syndromes, 12 (8%) for Hodgkin lymphoma, and 10 (6%) for non-Hodgkin lymphoma.
A little more than half had TBI (85, 56%) as the preparative regimen, 31 (21%) had TBI plus CRT, and 35 (23%) had chemotherapy only.
About three-quarters (116, 77%) had an allogeneic transplant, and 35 (23%) had an autologous transplant.
Results
Overall, HSCT survivors had significantly lower adiponectin levels than siblings (P<0.001).
Survivors who received TBI with or without CRT had significantly lower adiponectin levels than siblings (P<0.001), while survivors who received chemotherapy alone did not (P=0.42).
Adiponectin is involved in insulin sensitization, hepatoprotective action, antiatherogenic action, protection against the development of diabetes, and regulation of lipid metabolism.
Overall, survivors had significantly higher leptin levels than siblings (P<0.001).
This held true regardless of conditioning regimen, although levels for patients who received chemotherapy only were not as significantly high (P=0.02) as for survivors who received TBI (P<0.001).
Leptin helps increase energy expenditure, decrease appetite and food uptake, modify insulin sensitivity on muscles and liver, prevent ectopic lipid deposition, and regulate immune function.
BMI adjusted for age, sex, and Tanner stage was not significantly different between survivors and siblings, but percent fat mass was significantly higher across all conditioning regimens for survivors compared to siblings (P<0.001).
“And this goes along with previous data,” Dr Ketterl said, “that shows sarcopenic obesity is common amongst transplant survivors.”
The researchers believe these significant differences may provide insight into the underlying risk of developing metabolic syndrome and cardiovascular complications in transplant survivors. ![]()
*Some details in the abstract differ from the presentation.
ORLANDO, FL—A recently conducted study confirms that survivors of hematopoietic stem cell transplant (HSCT) have increased body fat mass and lower lean mass compared to normal controls. And this is despite having a comparable body mass index (BMI).
Researchers say the abnormalities in adipokine levels—leptin and adiponectin—could provide insight into the mechanisms that contribute to the metabolic syndrome and cardiovascular complications that often develop in HSCT survivors.
Leptin and adiponectin are associated with obesity, insulin secretion, insulin resistance, endothelial function, vascular homeostasis, and atherosclerosis.
“So knowing that there is a dynamic interplay between obesity and insulin resistance and cytokine and adipokine profiles and, ultimately, insulin-resistance syndrome, we sought to evaluate, as part of a larger study, how treatment effects, including high-dose chemotherapy and radiation, alter cytokine profiles as well as obesity and body composition,” said Tyler G. Ketterl, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
Dr Ketterl presented the findings at the 2017 BMT Tandem Meetings as abstract 52.*
Study design
The research team compared 151 HSCT recipients who had survived more than 2 years after transplant with 92 sibling controls.
HSCT survivors were randomly recruited from 2 centers—Fred Hutchinson Cancer Research Center and University of Minnesota Masonic Children’s Hospital—and were younger than 21 years when diagnosed.
The researchers evaluated all participants for body composition, cardiovascular risk factors, and adipokines using anthropomorphic measurements, DXA scans for muscle and fat mass, and laboratory bloodwork.
The team stratified the HSCT survivors by the preparative regimen they had received—total body irradiation (TBI) alone, TBI plus cranial radiation (CRT), and chemotherapy alone.
Study population
Males comprised more than half the study population in each arm, 58% of HSCT survivors and 54% of siblings.
Nine percent and 8% in the HSCT and sibling arms, respectively, were non-white and/or Hispanic, and the mean current ages were 24.0 (range, 10-51) for HSCT survivors and 24.2 (range, 10-48) for siblings.
The survivors’ mean age at diagnosis was 9.1 years (range, 0.4–20.6), their mean age at transplant was 11.2 years (range, 0.6–32.6), and the mean time from transplant to study participation was 13.5 years (range, 2.6–32).
Most patients received a transplant for leukemia—54 (36%) for acute myeloid leukemia, 46 (31%) for acute lymphoblastic leukemia, and 15 (10%) for chronic myeloid leukemia. Thirteen (9%) received transplants for myelodysplastic syndromes, 12 (8%) for Hodgkin lymphoma, and 10 (6%) for non-Hodgkin lymphoma.
A little more than half had TBI (85, 56%) as the preparative regimen, 31 (21%) had TBI plus CRT, and 35 (23%) had chemotherapy only.
About three-quarters (116, 77%) had an allogeneic transplant, and 35 (23%) had an autologous transplant.
Results
Overall, HSCT survivors had significantly lower adiponectin levels than siblings (P<0.001).
Survivors who received TBI with or without CRT had significantly lower adiponectin levels than siblings (P<0.001), while survivors who received chemotherapy alone did not (P=0.42).
Adiponectin is involved in insulin sensitization, hepatoprotective action, antiatherogenic action, protection against the development of diabetes, and regulation of lipid metabolism.
Overall, survivors had significantly higher leptin levels than siblings (P<0.001).
This held true regardless of conditioning regimen, although levels for patients who received chemotherapy only were not as significantly high (P=0.02) as for survivors who received TBI (P<0.001).
Leptin helps increase energy expenditure, decrease appetite and food uptake, modify insulin sensitivity on muscles and liver, prevent ectopic lipid deposition, and regulate immune function.
BMI adjusted for age, sex, and Tanner stage was not significantly different between survivors and siblings, but percent fat mass was significantly higher across all conditioning regimens for survivors compared to siblings (P<0.001).
“And this goes along with previous data,” Dr Ketterl said, “that shows sarcopenic obesity is common amongst transplant survivors.”
The researchers believe these significant differences may provide insight into the underlying risk of developing metabolic syndrome and cardiovascular complications in transplant survivors. ![]()
*Some details in the abstract differ from the presentation.
Imatinib is safe, effective long-term, team says
Long-term follow-up of patients treated with imatinib suggests the drug can remain effective beyond 10 years and does not confer “unacceptable” cumulative toxicity, according to researchers.
The group evaluated data on patients who had newly diagnosed, chronic-phase chronic myeloid leukemia (CML) when they began treatment with imatinib.
The median treatment duration was 8.9 years, and the estimated 10-year survival rate ranged from 64.4% to 84.4%.
The researchers said serious adverse events (AEs) thought to be related to imatinib were uncommon and typically occurred early, within the first year of treatment.
These results were reported in NEJM. The research was funded by Novartis Pharmaceuticals, which markets imatinib as Gleevec.
“The long-term success of this treatment confirms the remarkable success we’ve seen since the very first Gleevec trials,” said study author Brian Druker, MD, a physician-scientist at Oregon Health & Science University in Portland, Oregon, who led the original clinical development of Gleevec.
“This study reinforces the notion that we can create effective and non-toxic therapies.”
The study enrolled 1106 newly diagnosed, chronic-phase CML patients at 177 cancer centers in more than 16 countries. Half were assigned to treatment with imatinib (n=533) and the other half to interferon alfa plus cytarabine.
This study allowed for cross-over between the treatment arms, and 65.6% of patients in the cytarabine/interferon alfa arm ultimately crossed over to the imatinib arm.
However, when assessing the effects of imatinib, the researchers focused only on the patients who were first randomized to receive imatinib.
The median follow-up was 10.9 years (range, 0 to 11.7, which included follow-up after patients discontinued study treatment).
Of the patients randomized to imatinib, 48.3% (n=267) completed treatment with the drug. The median duration of first-line imatinib was 8.9 years (range, <0.1 to 11.7).
For patients who did not complete imatinib treatment, reasons for discontinuation included a lack of efficacy (15.9%), withdrawn consent (10.3%), AEs (6.9%), because they proceeded to transplant (3.8%), death (3.4%), protocol violation (3.1%), loss to follow-up (2.7%), cross over to the interferon arm (2.5%), administrative problems (2.2%), abnormal laboratory values (0.5%), or abnormal procedure (0.4%).
Safety
The incidence of serious AEs considered related to imatinib was 9.3% (51/551).
Drug-related serious AEs occurring in at least 2 patients included abdominal pain (n=4), anemia (n=3), congestive cardiac failure (n=3), gastrointestinal hemorrhage (n=3), vomiting (n=3), alanine aminotransferase increase (n=2), cardiac arrest (n=2), conjunctival hemorrhage (n=2), and melana (n=2).
Six patients had a second neoplasm (benign, malignant, or unspecified).
Response
The cumulative rate of complete cytogenetic response (CCR) at the end of the trial was 82.8%.
In the intent-to-treat population, the rate of CCR went from 52.8% in the first year to 22.2% at year 10.
Among evaluable patients, the rate of CCR went from 70.9% (292/412) in the first year to 91.8% (123/134) in year 10.
In the intent-to-treat population, the rate of major molecular response went from 27.7% in the first year to 34.4% at year 10.
Among evaluable patients, the rate of major molecular response went from 50.2% (153/305) in the first year to 93.1% (190/204) in year 10.
Progression and survival
The rate of progression was 6.9% (38/553) in the intent-to-treat population. Most of these patients (n=34) progressed during the first 4 years.
There were 260 patients who were still alive and receiving imatinib at 10 years and 96 patients who were alive but not receiving imatinib.
The researchers did not know the survival status of 111 patients, and there were 86 known deaths at 10 years (89 by the end of the study).
The estimated 10-year survival rate ranged from 64.4% (assuming all 111 patients with unknown status had died) to 84.4% (assuming all 111 were alive).
The cause of death was CML in 50 patients, a secondary malignant condition in 11, a cardiac disorder/cardiovascular disease in 7, infectious disease in 5, and “other” causes in 16 patients. ![]()
Long-term follow-up of patients treated with imatinib suggests the drug can remain effective beyond 10 years and does not confer “unacceptable” cumulative toxicity, according to researchers.
The group evaluated data on patients who had newly diagnosed, chronic-phase chronic myeloid leukemia (CML) when they began treatment with imatinib.
The median treatment duration was 8.9 years, and the estimated 10-year survival rate ranged from 64.4% to 84.4%.
The researchers said serious adverse events (AEs) thought to be related to imatinib were uncommon and typically occurred early, within the first year of treatment.
These results were reported in NEJM. The research was funded by Novartis Pharmaceuticals, which markets imatinib as Gleevec.
“The long-term success of this treatment confirms the remarkable success we’ve seen since the very first Gleevec trials,” said study author Brian Druker, MD, a physician-scientist at Oregon Health & Science University in Portland, Oregon, who led the original clinical development of Gleevec.
“This study reinforces the notion that we can create effective and non-toxic therapies.”
The study enrolled 1106 newly diagnosed, chronic-phase CML patients at 177 cancer centers in more than 16 countries. Half were assigned to treatment with imatinib (n=533) and the other half to interferon alfa plus cytarabine.
This study allowed for cross-over between the treatment arms, and 65.6% of patients in the cytarabine/interferon alfa arm ultimately crossed over to the imatinib arm.
However, when assessing the effects of imatinib, the researchers focused only on the patients who were first randomized to receive imatinib.
The median follow-up was 10.9 years (range, 0 to 11.7, which included follow-up after patients discontinued study treatment).
Of the patients randomized to imatinib, 48.3% (n=267) completed treatment with the drug. The median duration of first-line imatinib was 8.9 years (range, <0.1 to 11.7).
For patients who did not complete imatinib treatment, reasons for discontinuation included a lack of efficacy (15.9%), withdrawn consent (10.3%), AEs (6.9%), because they proceeded to transplant (3.8%), death (3.4%), protocol violation (3.1%), loss to follow-up (2.7%), cross over to the interferon arm (2.5%), administrative problems (2.2%), abnormal laboratory values (0.5%), or abnormal procedure (0.4%).
Safety
The incidence of serious AEs considered related to imatinib was 9.3% (51/551).
Drug-related serious AEs occurring in at least 2 patients included abdominal pain (n=4), anemia (n=3), congestive cardiac failure (n=3), gastrointestinal hemorrhage (n=3), vomiting (n=3), alanine aminotransferase increase (n=2), cardiac arrest (n=2), conjunctival hemorrhage (n=2), and melana (n=2).
Six patients had a second neoplasm (benign, malignant, or unspecified).
Response
The cumulative rate of complete cytogenetic response (CCR) at the end of the trial was 82.8%.
In the intent-to-treat population, the rate of CCR went from 52.8% in the first year to 22.2% at year 10.
Among evaluable patients, the rate of CCR went from 70.9% (292/412) in the first year to 91.8% (123/134) in year 10.
In the intent-to-treat population, the rate of major molecular response went from 27.7% in the first year to 34.4% at year 10.
Among evaluable patients, the rate of major molecular response went from 50.2% (153/305) in the first year to 93.1% (190/204) in year 10.
Progression and survival
The rate of progression was 6.9% (38/553) in the intent-to-treat population. Most of these patients (n=34) progressed during the first 4 years.
There were 260 patients who were still alive and receiving imatinib at 10 years and 96 patients who were alive but not receiving imatinib.
The researchers did not know the survival status of 111 patients, and there were 86 known deaths at 10 years (89 by the end of the study).
The estimated 10-year survival rate ranged from 64.4% (assuming all 111 patients with unknown status had died) to 84.4% (assuming all 111 were alive).
The cause of death was CML in 50 patients, a secondary malignant condition in 11, a cardiac disorder/cardiovascular disease in 7, infectious disease in 5, and “other” causes in 16 patients. ![]()
Long-term follow-up of patients treated with imatinib suggests the drug can remain effective beyond 10 years and does not confer “unacceptable” cumulative toxicity, according to researchers.
The group evaluated data on patients who had newly diagnosed, chronic-phase chronic myeloid leukemia (CML) when they began treatment with imatinib.
The median treatment duration was 8.9 years, and the estimated 10-year survival rate ranged from 64.4% to 84.4%.
The researchers said serious adverse events (AEs) thought to be related to imatinib were uncommon and typically occurred early, within the first year of treatment.
These results were reported in NEJM. The research was funded by Novartis Pharmaceuticals, which markets imatinib as Gleevec.
“The long-term success of this treatment confirms the remarkable success we’ve seen since the very first Gleevec trials,” said study author Brian Druker, MD, a physician-scientist at Oregon Health & Science University in Portland, Oregon, who led the original clinical development of Gleevec.
“This study reinforces the notion that we can create effective and non-toxic therapies.”
The study enrolled 1106 newly diagnosed, chronic-phase CML patients at 177 cancer centers in more than 16 countries. Half were assigned to treatment with imatinib (n=533) and the other half to interferon alfa plus cytarabine.
This study allowed for cross-over between the treatment arms, and 65.6% of patients in the cytarabine/interferon alfa arm ultimately crossed over to the imatinib arm.
However, when assessing the effects of imatinib, the researchers focused only on the patients who were first randomized to receive imatinib.
The median follow-up was 10.9 years (range, 0 to 11.7, which included follow-up after patients discontinued study treatment).
Of the patients randomized to imatinib, 48.3% (n=267) completed treatment with the drug. The median duration of first-line imatinib was 8.9 years (range, <0.1 to 11.7).
For patients who did not complete imatinib treatment, reasons for discontinuation included a lack of efficacy (15.9%), withdrawn consent (10.3%), AEs (6.9%), because they proceeded to transplant (3.8%), death (3.4%), protocol violation (3.1%), loss to follow-up (2.7%), cross over to the interferon arm (2.5%), administrative problems (2.2%), abnormal laboratory values (0.5%), or abnormal procedure (0.4%).
Safety
The incidence of serious AEs considered related to imatinib was 9.3% (51/551).
Drug-related serious AEs occurring in at least 2 patients included abdominal pain (n=4), anemia (n=3), congestive cardiac failure (n=3), gastrointestinal hemorrhage (n=3), vomiting (n=3), alanine aminotransferase increase (n=2), cardiac arrest (n=2), conjunctival hemorrhage (n=2), and melana (n=2).
Six patients had a second neoplasm (benign, malignant, or unspecified).
Response
The cumulative rate of complete cytogenetic response (CCR) at the end of the trial was 82.8%.
In the intent-to-treat population, the rate of CCR went from 52.8% in the first year to 22.2% at year 10.
Among evaluable patients, the rate of CCR went from 70.9% (292/412) in the first year to 91.8% (123/134) in year 10.
In the intent-to-treat population, the rate of major molecular response went from 27.7% in the first year to 34.4% at year 10.
Among evaluable patients, the rate of major molecular response went from 50.2% (153/305) in the first year to 93.1% (190/204) in year 10.
Progression and survival
The rate of progression was 6.9% (38/553) in the intent-to-treat population. Most of these patients (n=34) progressed during the first 4 years.
There were 260 patients who were still alive and receiving imatinib at 10 years and 96 patients who were alive but not receiving imatinib.
The researchers did not know the survival status of 111 patients, and there were 86 known deaths at 10 years (89 by the end of the study).
The estimated 10-year survival rate ranged from 64.4% (assuming all 111 patients with unknown status had died) to 84.4% (assuming all 111 were alive).
The cause of death was CML in 50 patients, a secondary malignant condition in 11, a cardiac disorder/cardiovascular disease in 7, infectious disease in 5, and “other” causes in 16 patients. ![]()
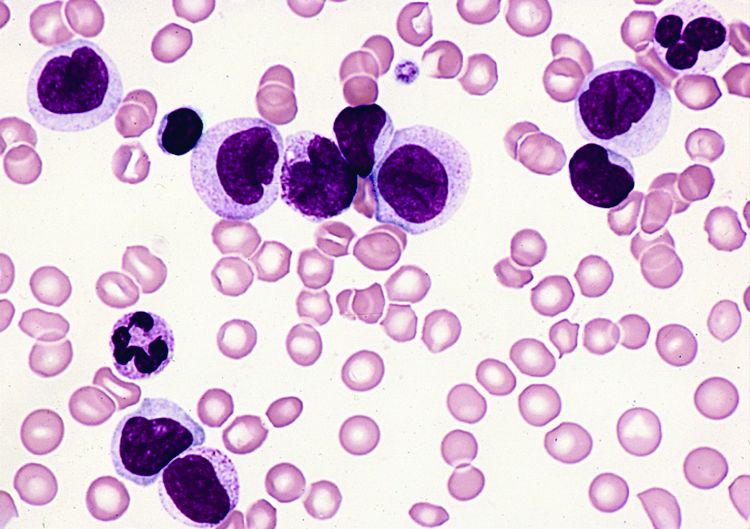
FDA lifts clinical hold on AML trials
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
Post-transplant drug combo eyed for high-risk AML
ORLANDO – Azacitadine and valproic acid can be safely coadministered as maintenance therapy after allogeneic stem cell transplantation in patients with high-risk acute myelogenous leukemia (AML), according to interim findings from an investigator-initiated phase II study.
One-year relapse-free and overall survival rates were about 80%, and no significant toxicities were reported in 28 such patients who began the treatment at least 40 days after transplant and were treated for 4 months, Patrick A. Hagen, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“As we all know, relapse after allogeneic transplant for AML is a huge and ongoing problem. It’s the primary cause of death following transplant, and unfortunately it really hasn’t decreased over the past couple decades,” Dr. Hagen said, adding that relapse is of increasing concern for biologically high-risk patients and is a “pretty ripe area for improved methodologies or approaches.” The decision to pursue maintenance therapy after transplant is complicated: It’s a good opportunity to improve outcomes, but there are many challenges, including problems with drug interactions and myelosuppression, he said.
The study was undertaken based in part on previously reported findings of synergism of a demethylating agent and a histone dacetylase inhibitor in patients with AML, he said.
The maintenance therapy included up to four 28-day cycles of azacitadine at 40 mg/m2 daily on days 1-5, along with oral valproic acid daily throughout the cycle at a 15-mg/kg dose adjusted to achieve a 100-mcg/mL trough level of bound valproic acid as tolerated. Nineteen patients completed all four cycles of treatment.
“The regimen was pretty well tolerated. The vast majority of the toxicities were grade I/II – 70%. The only grade-4 toxicities were cytopenia related and did not lead to a delay in treatment,” he said.
No patients developed acute graft-versus-host disease after therapy, although 11 (39%) developed chronic GVHD, which was extensive in 8, Dr. Hagen said.
Study participants were adults with high-risk AML with no grade 3-4 acute GVHD. All had adequate organ function after allogeneic stem cell transplantation (allo-SCT) performed 40-60 days prior to the start of maintenance therapy. Those with active or uncontrolled infections, low-risk AML in first relapse, neutrophil counts below 1,500, and platelets below 50,000 were excluded, he said.
The patients’ median age was 44 years, they had a median of two prior chemotherapy regimens, and their median Sorror Comorbidity Index was 2.5. Cytogenetics were mostly intermediate and adverse; only one patient had favorable cytogenetics.
Graft type was mixed, with most patients having matched unrelated donors. Conditioning regimens also were mixed, although they “skewed toward myeloablative,” he said. GVHD prophylaxis was standard for the institution and included tacrolimus and methotrexate.
The promising 1-year overall survival and relapse rate without significant dose-limiting toxicities warrants further evaluation in a phase III trial, Dr. Hagen concluded.
He reported having no disclosures.
ORLANDO – Azacitadine and valproic acid can be safely coadministered as maintenance therapy after allogeneic stem cell transplantation in patients with high-risk acute myelogenous leukemia (AML), according to interim findings from an investigator-initiated phase II study.
One-year relapse-free and overall survival rates were about 80%, and no significant toxicities were reported in 28 such patients who began the treatment at least 40 days after transplant and were treated for 4 months, Patrick A. Hagen, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“As we all know, relapse after allogeneic transplant for AML is a huge and ongoing problem. It’s the primary cause of death following transplant, and unfortunately it really hasn’t decreased over the past couple decades,” Dr. Hagen said, adding that relapse is of increasing concern for biologically high-risk patients and is a “pretty ripe area for improved methodologies or approaches.” The decision to pursue maintenance therapy after transplant is complicated: It’s a good opportunity to improve outcomes, but there are many challenges, including problems with drug interactions and myelosuppression, he said.
The study was undertaken based in part on previously reported findings of synergism of a demethylating agent and a histone dacetylase inhibitor in patients with AML, he said.
The maintenance therapy included up to four 28-day cycles of azacitadine at 40 mg/m2 daily on days 1-5, along with oral valproic acid daily throughout the cycle at a 15-mg/kg dose adjusted to achieve a 100-mcg/mL trough level of bound valproic acid as tolerated. Nineteen patients completed all four cycles of treatment.
“The regimen was pretty well tolerated. The vast majority of the toxicities were grade I/II – 70%. The only grade-4 toxicities were cytopenia related and did not lead to a delay in treatment,” he said.
No patients developed acute graft-versus-host disease after therapy, although 11 (39%) developed chronic GVHD, which was extensive in 8, Dr. Hagen said.
Study participants were adults with high-risk AML with no grade 3-4 acute GVHD. All had adequate organ function after allogeneic stem cell transplantation (allo-SCT) performed 40-60 days prior to the start of maintenance therapy. Those with active or uncontrolled infections, low-risk AML in first relapse, neutrophil counts below 1,500, and platelets below 50,000 were excluded, he said.
The patients’ median age was 44 years, they had a median of two prior chemotherapy regimens, and their median Sorror Comorbidity Index was 2.5. Cytogenetics were mostly intermediate and adverse; only one patient had favorable cytogenetics.
Graft type was mixed, with most patients having matched unrelated donors. Conditioning regimens also were mixed, although they “skewed toward myeloablative,” he said. GVHD prophylaxis was standard for the institution and included tacrolimus and methotrexate.
The promising 1-year overall survival and relapse rate without significant dose-limiting toxicities warrants further evaluation in a phase III trial, Dr. Hagen concluded.
He reported having no disclosures.
ORLANDO – Azacitadine and valproic acid can be safely coadministered as maintenance therapy after allogeneic stem cell transplantation in patients with high-risk acute myelogenous leukemia (AML), according to interim findings from an investigator-initiated phase II study.
One-year relapse-free and overall survival rates were about 80%, and no significant toxicities were reported in 28 such patients who began the treatment at least 40 days after transplant and were treated for 4 months, Patrick A. Hagen, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“As we all know, relapse after allogeneic transplant for AML is a huge and ongoing problem. It’s the primary cause of death following transplant, and unfortunately it really hasn’t decreased over the past couple decades,” Dr. Hagen said, adding that relapse is of increasing concern for biologically high-risk patients and is a “pretty ripe area for improved methodologies or approaches.” The decision to pursue maintenance therapy after transplant is complicated: It’s a good opportunity to improve outcomes, but there are many challenges, including problems with drug interactions and myelosuppression, he said.
The study was undertaken based in part on previously reported findings of synergism of a demethylating agent and a histone dacetylase inhibitor in patients with AML, he said.
The maintenance therapy included up to four 28-day cycles of azacitadine at 40 mg/m2 daily on days 1-5, along with oral valproic acid daily throughout the cycle at a 15-mg/kg dose adjusted to achieve a 100-mcg/mL trough level of bound valproic acid as tolerated. Nineteen patients completed all four cycles of treatment.
“The regimen was pretty well tolerated. The vast majority of the toxicities were grade I/II – 70%. The only grade-4 toxicities were cytopenia related and did not lead to a delay in treatment,” he said.
No patients developed acute graft-versus-host disease after therapy, although 11 (39%) developed chronic GVHD, which was extensive in 8, Dr. Hagen said.
Study participants were adults with high-risk AML with no grade 3-4 acute GVHD. All had adequate organ function after allogeneic stem cell transplantation (allo-SCT) performed 40-60 days prior to the start of maintenance therapy. Those with active or uncontrolled infections, low-risk AML in first relapse, neutrophil counts below 1,500, and platelets below 50,000 were excluded, he said.
The patients’ median age was 44 years, they had a median of two prior chemotherapy regimens, and their median Sorror Comorbidity Index was 2.5. Cytogenetics were mostly intermediate and adverse; only one patient had favorable cytogenetics.
Graft type was mixed, with most patients having matched unrelated donors. Conditioning regimens also were mixed, although they “skewed toward myeloablative,” he said. GVHD prophylaxis was standard for the institution and included tacrolimus and methotrexate.
The promising 1-year overall survival and relapse rate without significant dose-limiting toxicities warrants further evaluation in a phase III trial, Dr. Hagen concluded.
He reported having no disclosures.
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: 1-year relapse-free survival and 1-year overall survival were about 80%.
Data source: An interim analysis of data from 28 patients in a phase II study.
Disclosures: Dr. Hagen reported having no disclosures.
CLL boost in PFS came at high cost in side effects
Add-on idelalisib boosted the progression-free survival (PFS) of patients with relapsed and refractory chronic lymphocytic leukemia by over 9 months in a double-blind, placebo-controlled trial of 416 participants. But that improvement came at the price of a 4% absolute increase in treatment-emergent adverse events leading to death.
At a median follow-up of 14 months, the median PFS was 20.8 months in the 207 patients in the idelalisib group and 11.1 months in the 209 patients in the placebo group. However, 11% of patients in the idelalisib group and 7% of those in the placebo group had treatment-related adverse events that resulted in death.
Overall, 68% of those in the idelalisib group, and 44% in the placebo group, had serious adverse events that included febrile neutropenia, pneumonia, and pyrexia. Six deaths resulted from infections in the idelalisib group, and three deaths resulted from infections in the placebo group.
All 416 participants in the international, multicenter study had measurable lymphadenopathy by CT or MRI and progression of chronic lymphocytic leukemia within 36 months of their last therapy. Patients were stratified by high-risk genetic mutations (IGHV, del[17p], or TP53) and refractory versus relapsed disease. Participants were randomly assigned to receive daily idelalisib or placebo, plus a maximum of six cycles of bendamustine and rituximab.
The primary endpoint of PFS was assessed by an independent review committee in the intention-to-treat population.
A 150 mg dose of idelalisib or placebo was given twice daily until disease progressed or drug-related toxicity was intolerable. Bendamustine was given intravenously at 70 mg/m2 on days 1 and 2 for six 28-day cycles. Rituximab was given at 375 mg/m2 on day 1 of cycle 1 and at 500 mg/m2 on day 1 of cycles 2–6.
The trial is ongoing, the researchers reported.
The trial is funded by Gilead Sciences, the maker of idelalisib (Zydelig). Dr. Zelenetz disclosed consulting with multiple drug companies, including Gilead.
[email protected]
On Twitter @maryjodales
Add-on idelalisib boosted the progression-free survival (PFS) of patients with relapsed and refractory chronic lymphocytic leukemia by over 9 months in a double-blind, placebo-controlled trial of 416 participants. But that improvement came at the price of a 4% absolute increase in treatment-emergent adverse events leading to death.
At a median follow-up of 14 months, the median PFS was 20.8 months in the 207 patients in the idelalisib group and 11.1 months in the 209 patients in the placebo group. However, 11% of patients in the idelalisib group and 7% of those in the placebo group had treatment-related adverse events that resulted in death.
Overall, 68% of those in the idelalisib group, and 44% in the placebo group, had serious adverse events that included febrile neutropenia, pneumonia, and pyrexia. Six deaths resulted from infections in the idelalisib group, and three deaths resulted from infections in the placebo group.
All 416 participants in the international, multicenter study had measurable lymphadenopathy by CT or MRI and progression of chronic lymphocytic leukemia within 36 months of their last therapy. Patients were stratified by high-risk genetic mutations (IGHV, del[17p], or TP53) and refractory versus relapsed disease. Participants were randomly assigned to receive daily idelalisib or placebo, plus a maximum of six cycles of bendamustine and rituximab.
The primary endpoint of PFS was assessed by an independent review committee in the intention-to-treat population.
A 150 mg dose of idelalisib or placebo was given twice daily until disease progressed or drug-related toxicity was intolerable. Bendamustine was given intravenously at 70 mg/m2 on days 1 and 2 for six 28-day cycles. Rituximab was given at 375 mg/m2 on day 1 of cycle 1 and at 500 mg/m2 on day 1 of cycles 2–6.
The trial is ongoing, the researchers reported.
The trial is funded by Gilead Sciences, the maker of idelalisib (Zydelig). Dr. Zelenetz disclosed consulting with multiple drug companies, including Gilead.
[email protected]
On Twitter @maryjodales
Add-on idelalisib boosted the progression-free survival (PFS) of patients with relapsed and refractory chronic lymphocytic leukemia by over 9 months in a double-blind, placebo-controlled trial of 416 participants. But that improvement came at the price of a 4% absolute increase in treatment-emergent adverse events leading to death.
At a median follow-up of 14 months, the median PFS was 20.8 months in the 207 patients in the idelalisib group and 11.1 months in the 209 patients in the placebo group. However, 11% of patients in the idelalisib group and 7% of those in the placebo group had treatment-related adverse events that resulted in death.
Overall, 68% of those in the idelalisib group, and 44% in the placebo group, had serious adverse events that included febrile neutropenia, pneumonia, and pyrexia. Six deaths resulted from infections in the idelalisib group, and three deaths resulted from infections in the placebo group.
All 416 participants in the international, multicenter study had measurable lymphadenopathy by CT or MRI and progression of chronic lymphocytic leukemia within 36 months of their last therapy. Patients were stratified by high-risk genetic mutations (IGHV, del[17p], or TP53) and refractory versus relapsed disease. Participants were randomly assigned to receive daily idelalisib or placebo, plus a maximum of six cycles of bendamustine and rituximab.
The primary endpoint of PFS was assessed by an independent review committee in the intention-to-treat population.
A 150 mg dose of idelalisib or placebo was given twice daily until disease progressed or drug-related toxicity was intolerable. Bendamustine was given intravenously at 70 mg/m2 on days 1 and 2 for six 28-day cycles. Rituximab was given at 375 mg/m2 on day 1 of cycle 1 and at 500 mg/m2 on day 1 of cycles 2–6.
The trial is ongoing, the researchers reported.
The trial is funded by Gilead Sciences, the maker of idelalisib (Zydelig). Dr. Zelenetz disclosed consulting with multiple drug companies, including Gilead.
[email protected]
On Twitter @maryjodales
Key clinical point:
Major finding: Add-on idelalisib boosted the progression-free survival of patients with relapsed and refractory chronic lymphocytic leukemia by over 9 months.
Data source: A double-blind, placebo-controlled trial of 416 participants.
Disclosures: Gilead Sciences, the maker of idelalisib (Zydelig), sponsored the study. Dr. Zelenetz disclosed consulting with multiple drug companies, including Gilead.
In CML, imatinib benefits persist at 10 years
In patients with chronic myeloid leukemia (CML), the safety and benefits of imatinib persisted over the course of 10 years in a follow-up study reported online March 9 in the New England Journal of Medicine.
The initial results of the phase III International Randomized Study of Interferon and ST1571 (IRIS) trial “fundamentally changed CML treatment and led to marked improvements in prognosis for patients” when imatinib was shown more effective than interferon plus cytarabine among newly diagnosed patients in the chronic phase of the disease, said Andreas Hochhaus, MD, of the Klinik für Innere Medizin II, Universitätsklinikum Jena (Germany), and his associates. The researchers are now reporting the final follow-up results after a median of 10.9 years for the 553 patients who had been randomly assigned to receive daily oral imatinib in the IRIS trial.
The high rate of crossover to the imatinib group among IRIS study participants precluded a direct comparison of overall survival between the two study groups at 10 years. However, the estimated overall 10-year survival in the imatinib group alone was 83.3%. “A total of 260 patients (47.0%) were alive and still receiving study treatment at 10 years, 96 patients (17.4%) were alive and not receiving study treatment, 86 known deaths (15.6% of patients) had occurred, and 11 patients (20.1%) had unknown survival status,” Dr. Hochhaus and his associates reported (N Engl J Med. 2017 Mar 9. doi: 10.1056/NEJMoa1609324).
Approximately 9% of those in the imatinib group had a serious adverse event during follow-up, including 4 patients (0.7%) in whom the event was considered to be related to the drug. Most occurred during the first year of treatment and declined over time. No new safety signals were observed after the 5-year follow-up.
“These results highlight the safety and efficacy of imatinib therapy, with a clear improvement over the outcomes that were expected n patients who received a diagnosis of CML before the introduction of tyrosine kinase inhibitor therapy, when interferon alfa and hematopoietic stem-cell transplantation were the standard therapies,” the investigators said.
Second-generation tyrosine kinase inhibitors have been developed since the IRIS trial was begun, and “it remains to be seen whether they will have similarly favorable long-term safety. Given the long-term safety and efficacy results with imatinib and the increasing availability of generic imatinib, comparative analyses evaluating the available tyrosine kinase inhibitors for first-line therapy are likely to be forthcoming,” they noted.
In patients with chronic myeloid leukemia (CML), the safety and benefits of imatinib persisted over the course of 10 years in a follow-up study reported online March 9 in the New England Journal of Medicine.
The initial results of the phase III International Randomized Study of Interferon and ST1571 (IRIS) trial “fundamentally changed CML treatment and led to marked improvements in prognosis for patients” when imatinib was shown more effective than interferon plus cytarabine among newly diagnosed patients in the chronic phase of the disease, said Andreas Hochhaus, MD, of the Klinik für Innere Medizin II, Universitätsklinikum Jena (Germany), and his associates. The researchers are now reporting the final follow-up results after a median of 10.9 years for the 553 patients who had been randomly assigned to receive daily oral imatinib in the IRIS trial.
The high rate of crossover to the imatinib group among IRIS study participants precluded a direct comparison of overall survival between the two study groups at 10 years. However, the estimated overall 10-year survival in the imatinib group alone was 83.3%. “A total of 260 patients (47.0%) were alive and still receiving study treatment at 10 years, 96 patients (17.4%) were alive and not receiving study treatment, 86 known deaths (15.6% of patients) had occurred, and 11 patients (20.1%) had unknown survival status,” Dr. Hochhaus and his associates reported (N Engl J Med. 2017 Mar 9. doi: 10.1056/NEJMoa1609324).
Approximately 9% of those in the imatinib group had a serious adverse event during follow-up, including 4 patients (0.7%) in whom the event was considered to be related to the drug. Most occurred during the first year of treatment and declined over time. No new safety signals were observed after the 5-year follow-up.
“These results highlight the safety and efficacy of imatinib therapy, with a clear improvement over the outcomes that were expected n patients who received a diagnosis of CML before the introduction of tyrosine kinase inhibitor therapy, when interferon alfa and hematopoietic stem-cell transplantation were the standard therapies,” the investigators said.
Second-generation tyrosine kinase inhibitors have been developed since the IRIS trial was begun, and “it remains to be seen whether they will have similarly favorable long-term safety. Given the long-term safety and efficacy results with imatinib and the increasing availability of generic imatinib, comparative analyses evaluating the available tyrosine kinase inhibitors for first-line therapy are likely to be forthcoming,” they noted.
In patients with chronic myeloid leukemia (CML), the safety and benefits of imatinib persisted over the course of 10 years in a follow-up study reported online March 9 in the New England Journal of Medicine.
The initial results of the phase III International Randomized Study of Interferon and ST1571 (IRIS) trial “fundamentally changed CML treatment and led to marked improvements in prognosis for patients” when imatinib was shown more effective than interferon plus cytarabine among newly diagnosed patients in the chronic phase of the disease, said Andreas Hochhaus, MD, of the Klinik für Innere Medizin II, Universitätsklinikum Jena (Germany), and his associates. The researchers are now reporting the final follow-up results after a median of 10.9 years for the 553 patients who had been randomly assigned to receive daily oral imatinib in the IRIS trial.
The high rate of crossover to the imatinib group among IRIS study participants precluded a direct comparison of overall survival between the two study groups at 10 years. However, the estimated overall 10-year survival in the imatinib group alone was 83.3%. “A total of 260 patients (47.0%) were alive and still receiving study treatment at 10 years, 96 patients (17.4%) were alive and not receiving study treatment, 86 known deaths (15.6% of patients) had occurred, and 11 patients (20.1%) had unknown survival status,” Dr. Hochhaus and his associates reported (N Engl J Med. 2017 Mar 9. doi: 10.1056/NEJMoa1609324).
Approximately 9% of those in the imatinib group had a serious adverse event during follow-up, including 4 patients (0.7%) in whom the event was considered to be related to the drug. Most occurred during the first year of treatment and declined over time. No new safety signals were observed after the 5-year follow-up.
“These results highlight the safety and efficacy of imatinib therapy, with a clear improvement over the outcomes that were expected n patients who received a diagnosis of CML before the introduction of tyrosine kinase inhibitor therapy, when interferon alfa and hematopoietic stem-cell transplantation were the standard therapies,” the investigators said.
Second-generation tyrosine kinase inhibitors have been developed since the IRIS trial was begun, and “it remains to be seen whether they will have similarly favorable long-term safety. Given the long-term safety and efficacy results with imatinib and the increasing availability of generic imatinib, comparative analyses evaluating the available tyrosine kinase inhibitors for first-line therapy are likely to be forthcoming,” they noted.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Imatinib’s benefits in chronic myeloid leukemia and its safety profile persisted over the long term in a 10-year follow-up study.
Major finding: The estimated overall 10-year survival was 83.3%, and no new safety signals were observed after 5-year follow-up.
Data source: Extended follow-up of an open-label international randomized trial involving 553 adults with CML.
Disclosures: This study was funded by Novartis. Dr. Hochhaus reported ties to Novartis and other drug companies.