User login
EC expands indication for arsenic trioxide in APL

Image courtesy of the Armed
Forces Institute of Pathology
The European Commission (EC) has extended the approved indication for arsenic trioxide (Trisenox®) in patients with acute promyelocytic leukemia (APL).
The drug is now approved for use in combination with all-trans-retinoic acid (ATRA) to induce remission and for consolidation in adults with newly diagnosed low- to intermediate-risk APL (white blood cell count, ≤ 10 x 103/μL) characterized by the presence of the t(15;17) translocation and/or the presence of the PML/RARα gene.
Arsenic trioxide was previously approved by the EC to induce remission and as consolidation in adults with relapsed/refractory APL, which is characterized by the presence of the t(15;17) translocation and/or the presence of the PML/RARα gene, whose previous treatment included a retinoid and chemotherapy.
“This [expanded] approval by the European Commission is good news for APL patients, as we now have access to a cure for an acute leukemia without using chemotherapy,” said Francesco Lo-Coco, MD, of University of Rome Tor Vergata in Italy.
“Moreover, this decision is a very positive endorsement by the European Commission, as it was made based solely on published academic research and studies.”
Arsenic trioxide is marketed by Teva Pharmaceutical Industries Ltd.
Phase 3 study results
The EC’s expanded approval of arsenic trioxide is based on results from the APL0406 Intergroup GIMEMA-AMLSG-SAL study. Previous results from this phase 3 study were published in NEJM in 2013.
Updated results include 276 adults (ages 18 to 71) with newly diagnosed, low- or intermediate-risk APL. Patients were randomized to receive ATRA plus arsenic trioxide or ATRA plus chemotherapy.
A total of 263 patients were evaluable for response to induction. One hundred percent of patients in the arsenic trioxide arm (127/127) achieved a complete response (CR), as did 97% (132/136) of patients in the chemotherapy arm (P=0.12).
After a median follow-up of 40.6 months, the event-free survival was 97.3% in the arsenic trioxide arm and 80% in the chemotherapy arm (P<0.001). The cumulative incidence of relapse was 1.9% and 13.9%, respectively (P=0.0013).
At 50 months, the overall survival was 99.2% in the arsenic trioxide arm and 92.6% in the chemotherapy arm (P=0.0073).
After induction, there were 2 relapses and 1 death in CR in the arsenic trioxide arm.
In the chemotherapy arm, there were 2 instances of molecular resistance after third consolidation, 15 relapses, 5 deaths in CR, and 2 patients who developed a therapy-related myeloid neoplasm. ![]()

Image courtesy of the Armed
Forces Institute of Pathology
The European Commission (EC) has extended the approved indication for arsenic trioxide (Trisenox®) in patients with acute promyelocytic leukemia (APL).
The drug is now approved for use in combination with all-trans-retinoic acid (ATRA) to induce remission and for consolidation in adults with newly diagnosed low- to intermediate-risk APL (white blood cell count, ≤ 10 x 103/μL) characterized by the presence of the t(15;17) translocation and/or the presence of the PML/RARα gene.
Arsenic trioxide was previously approved by the EC to induce remission and as consolidation in adults with relapsed/refractory APL, which is characterized by the presence of the t(15;17) translocation and/or the presence of the PML/RARα gene, whose previous treatment included a retinoid and chemotherapy.
“This [expanded] approval by the European Commission is good news for APL patients, as we now have access to a cure for an acute leukemia without using chemotherapy,” said Francesco Lo-Coco, MD, of University of Rome Tor Vergata in Italy.
“Moreover, this decision is a very positive endorsement by the European Commission, as it was made based solely on published academic research and studies.”
Arsenic trioxide is marketed by Teva Pharmaceutical Industries Ltd.
Phase 3 study results
The EC’s expanded approval of arsenic trioxide is based on results from the APL0406 Intergroup GIMEMA-AMLSG-SAL study. Previous results from this phase 3 study were published in NEJM in 2013.
Updated results include 276 adults (ages 18 to 71) with newly diagnosed, low- or intermediate-risk APL. Patients were randomized to receive ATRA plus arsenic trioxide or ATRA plus chemotherapy.
A total of 263 patients were evaluable for response to induction. One hundred percent of patients in the arsenic trioxide arm (127/127) achieved a complete response (CR), as did 97% (132/136) of patients in the chemotherapy arm (P=0.12).
After a median follow-up of 40.6 months, the event-free survival was 97.3% in the arsenic trioxide arm and 80% in the chemotherapy arm (P<0.001). The cumulative incidence of relapse was 1.9% and 13.9%, respectively (P=0.0013).
At 50 months, the overall survival was 99.2% in the arsenic trioxide arm and 92.6% in the chemotherapy arm (P=0.0073).
After induction, there were 2 relapses and 1 death in CR in the arsenic trioxide arm.
In the chemotherapy arm, there were 2 instances of molecular resistance after third consolidation, 15 relapses, 5 deaths in CR, and 2 patients who developed a therapy-related myeloid neoplasm. ![]()

Image courtesy of the Armed
Forces Institute of Pathology
The European Commission (EC) has extended the approved indication for arsenic trioxide (Trisenox®) in patients with acute promyelocytic leukemia (APL).
The drug is now approved for use in combination with all-trans-retinoic acid (ATRA) to induce remission and for consolidation in adults with newly diagnosed low- to intermediate-risk APL (white blood cell count, ≤ 10 x 103/μL) characterized by the presence of the t(15;17) translocation and/or the presence of the PML/RARα gene.
Arsenic trioxide was previously approved by the EC to induce remission and as consolidation in adults with relapsed/refractory APL, which is characterized by the presence of the t(15;17) translocation and/or the presence of the PML/RARα gene, whose previous treatment included a retinoid and chemotherapy.
“This [expanded] approval by the European Commission is good news for APL patients, as we now have access to a cure for an acute leukemia without using chemotherapy,” said Francesco Lo-Coco, MD, of University of Rome Tor Vergata in Italy.
“Moreover, this decision is a very positive endorsement by the European Commission, as it was made based solely on published academic research and studies.”
Arsenic trioxide is marketed by Teva Pharmaceutical Industries Ltd.
Phase 3 study results
The EC’s expanded approval of arsenic trioxide is based on results from the APL0406 Intergroup GIMEMA-AMLSG-SAL study. Previous results from this phase 3 study were published in NEJM in 2013.
Updated results include 276 adults (ages 18 to 71) with newly diagnosed, low- or intermediate-risk APL. Patients were randomized to receive ATRA plus arsenic trioxide or ATRA plus chemotherapy.
A total of 263 patients were evaluable for response to induction. One hundred percent of patients in the arsenic trioxide arm (127/127) achieved a complete response (CR), as did 97% (132/136) of patients in the chemotherapy arm (P=0.12).
After a median follow-up of 40.6 months, the event-free survival was 97.3% in the arsenic trioxide arm and 80% in the chemotherapy arm (P<0.001). The cumulative incidence of relapse was 1.9% and 13.9%, respectively (P=0.0013).
At 50 months, the overall survival was 99.2% in the arsenic trioxide arm and 92.6% in the chemotherapy arm (P=0.0073).
After induction, there were 2 relapses and 1 death in CR in the arsenic trioxide arm.
In the chemotherapy arm, there were 2 instances of molecular resistance after third consolidation, 15 relapses, 5 deaths in CR, and 2 patients who developed a therapy-related myeloid neoplasm. ![]()
Acute-onset hypokalemic paralysis with arsenic trioxide therapy in patient with acute promyelocytic leukemia
Acute myeloid leukemia (AML) is characterized by clonal proliferation of myeloid precursors with a reduced capacity to differentiate into mature cellular components.1 Acute promyeloctic leukemia (APL; previously called AML-M3), a subtype of AML, is further characterized by a balanced translocation t(15;17) (q24.1;q21.1). It is an interesting model in cancer research because it responds to the differentiation and apoptosis induction therapy using arsenic trioxide (ATO) and all-trans retinoic acid (ATRA).2
Click on the PDF icon at the top of this introduction to read the full article.
Acute myeloid leukemia (AML) is characterized by clonal proliferation of myeloid precursors with a reduced capacity to differentiate into mature cellular components.1 Acute promyeloctic leukemia (APL; previously called AML-M3), a subtype of AML, is further characterized by a balanced translocation t(15;17) (q24.1;q21.1). It is an interesting model in cancer research because it responds to the differentiation and apoptosis induction therapy using arsenic trioxide (ATO) and all-trans retinoic acid (ATRA).2
Click on the PDF icon at the top of this introduction to read the full article.
Acute myeloid leukemia (AML) is characterized by clonal proliferation of myeloid precursors with a reduced capacity to differentiate into mature cellular components.1 Acute promyeloctic leukemia (APL; previously called AML-M3), a subtype of AML, is further characterized by a balanced translocation t(15;17) (q24.1;q21.1). It is an interesting model in cancer research because it responds to the differentiation and apoptosis induction therapy using arsenic trioxide (ATO) and all-trans retinoic acid (ATRA).2
Click on the PDF icon at the top of this introduction to read the full article.
Outcome of tumor lysis syndrome in pediatric patients with hematologic malignancies – a single-center experience from Pakistan
Background Tumor lysis syndrome (TLS) is serious complication of anticancer chemotherapy, leading to substantial morbidity and mortality in adults and pediatric patients.
Objective To report the incidence and outcomes of TLS in pediatric patients with hematologic malignancies at a center in Pakistan.
Methods Retrospective chart review of 317 pediatric patients with hematologic malignancies during January 2008-December 2013. Demographic features and clinical and laboratory parameters of TLS, with immediate and 6-month outcomes were determined using a semi-structured questionnaire.
Results Median age at diagnosis was 9 years, with the 79.2% patients being male. Laboratory TLS was present in 36 patients (11.4%), with 27 (8.5%) developing clinical TLS and 13 (4.1%) requiring intensive care support. Hyperphosphatemia was the most frequent metabolic abnormality (14.2%), followed by hypocalcemia (13.9%), hyperuricemia (12.6%), and hyperkalemia (1.3%). 45 patients (14.2%) developed acute kidney injury (AKI). Patients who developed TLS had a signficantly higher white blood cell count at initiation of chemotherapy (142.0 x 109/L [SD, 173.1] vs 31.5 x 109/L [SD, 58.0]; P = .01) and a higher incidence of AKI (58.3% vs 8.5% of patients; P < .001).
Limitations Retrospective design of study, high rate of loss to follow-up, and unavailability of lactate dehydrogenase levels in a majority of patients.
Conclusion The incidence of TLS pediatric hematologic malignancies was 11.4% at our center. The main cause of death was sepsis. Hyperphosphatemia was the common metabolic derangement and hyperkalemia was the least common. TLS warrants intensive supportive care to prevent further morbidity and decrease mortality.
Click on the PDF icon at the top of this introduction to read the full article.
Background Tumor lysis syndrome (TLS) is serious complication of anticancer chemotherapy, leading to substantial morbidity and mortality in adults and pediatric patients.
Objective To report the incidence and outcomes of TLS in pediatric patients with hematologic malignancies at a center in Pakistan.
Methods Retrospective chart review of 317 pediatric patients with hematologic malignancies during January 2008-December 2013. Demographic features and clinical and laboratory parameters of TLS, with immediate and 6-month outcomes were determined using a semi-structured questionnaire.
Results Median age at diagnosis was 9 years, with the 79.2% patients being male. Laboratory TLS was present in 36 patients (11.4%), with 27 (8.5%) developing clinical TLS and 13 (4.1%) requiring intensive care support. Hyperphosphatemia was the most frequent metabolic abnormality (14.2%), followed by hypocalcemia (13.9%), hyperuricemia (12.6%), and hyperkalemia (1.3%). 45 patients (14.2%) developed acute kidney injury (AKI). Patients who developed TLS had a signficantly higher white blood cell count at initiation of chemotherapy (142.0 x 109/L [SD, 173.1] vs 31.5 x 109/L [SD, 58.0]; P = .01) and a higher incidence of AKI (58.3% vs 8.5% of patients; P < .001).
Limitations Retrospective design of study, high rate of loss to follow-up, and unavailability of lactate dehydrogenase levels in a majority of patients.
Conclusion The incidence of TLS pediatric hematologic malignancies was 11.4% at our center. The main cause of death was sepsis. Hyperphosphatemia was the common metabolic derangement and hyperkalemia was the least common. TLS warrants intensive supportive care to prevent further morbidity and decrease mortality.
Click on the PDF icon at the top of this introduction to read the full article.
Background Tumor lysis syndrome (TLS) is serious complication of anticancer chemotherapy, leading to substantial morbidity and mortality in adults and pediatric patients.
Objective To report the incidence and outcomes of TLS in pediatric patients with hematologic malignancies at a center in Pakistan.
Methods Retrospective chart review of 317 pediatric patients with hematologic malignancies during January 2008-December 2013. Demographic features and clinical and laboratory parameters of TLS, with immediate and 6-month outcomes were determined using a semi-structured questionnaire.
Results Median age at diagnosis was 9 years, with the 79.2% patients being male. Laboratory TLS was present in 36 patients (11.4%), with 27 (8.5%) developing clinical TLS and 13 (4.1%) requiring intensive care support. Hyperphosphatemia was the most frequent metabolic abnormality (14.2%), followed by hypocalcemia (13.9%), hyperuricemia (12.6%), and hyperkalemia (1.3%). 45 patients (14.2%) developed acute kidney injury (AKI). Patients who developed TLS had a signficantly higher white blood cell count at initiation of chemotherapy (142.0 x 109/L [SD, 173.1] vs 31.5 x 109/L [SD, 58.0]; P = .01) and a higher incidence of AKI (58.3% vs 8.5% of patients; P < .001).
Limitations Retrospective design of study, high rate of loss to follow-up, and unavailability of lactate dehydrogenase levels in a majority of patients.
Conclusion The incidence of TLS pediatric hematologic malignancies was 11.4% at our center. The main cause of death was sepsis. Hyperphosphatemia was the common metabolic derangement and hyperkalemia was the least common. TLS warrants intensive supportive care to prevent further morbidity and decrease mortality.
Click on the PDF icon at the top of this introduction to read the full article.
Fourth approved indication for ofatumumab in chronic lymphocytic leukemia
The recent decision by the US Food and Drug Administration to approve ofatumumab in combination with fludarabine and cyclophosphamide in relapsed disease marks a fourth approved indication for this drug in patients with chronic lymphocytic leukemia (CLL). Ofatumumab is a fully human monoclonal antibody that targets the CD20 protein on the surface of B cells, first approved for the treatment of CLL back in 2009.
Click on the PDF icon at the top of this introduction to read the full article.
The recent decision by the US Food and Drug Administration to approve ofatumumab in combination with fludarabine and cyclophosphamide in relapsed disease marks a fourth approved indication for this drug in patients with chronic lymphocytic leukemia (CLL). Ofatumumab is a fully human monoclonal antibody that targets the CD20 protein on the surface of B cells, first approved for the treatment of CLL back in 2009.
Click on the PDF icon at the top of this introduction to read the full article.
The recent decision by the US Food and Drug Administration to approve ofatumumab in combination with fludarabine and cyclophosphamide in relapsed disease marks a fourth approved indication for this drug in patients with chronic lymphocytic leukemia (CLL). Ofatumumab is a fully human monoclonal antibody that targets the CD20 protein on the surface of B cells, first approved for the treatment of CLL back in 2009.
Click on the PDF icon at the top of this introduction to read the full article.
ALL subtype ‘highly prevalent’ in adults

Photo courtesy of St. Jude
Children’s Research Hospital
Researchers have found evidence to suggest that a high-risk subtype of acute lymphoblastic leukemia (ALL) is “highly prevalent” in adults with ALL.
In a study of nearly 800 adults with ALL, roughly a quarter of the patients had Philadelphia chromosome-like (Ph-like) ALL.
Patients with Ph-like ALL had inferior overall survival (OS) and event-free survival (EFS), but most of them also had kinase-activating alterations that suggest they might respond well to tyrosine kinase inhibitors.
The researchers reported these findings in the Journal of Clinical Oncology.
“This study establishes that a large percentage of adults with ALL have this high-risk subtype,” said study author Charles Mullighan, MD, MBBS, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The finding provides a compelling reason to identify those with Ph-like ALL and move forward with clinical trials of these targeted therapies in combination with current chemotherapeutic regimens.”
This study builds on previous research, which suggested that Ph-like ALL becomes more common with age, is associated with poor prognosis, and is characterized by genomic alterations that appear to make patients responsive to treatment with tyrosine kinase inhibitors.
“Our 2014 findings that the prevalence of Ph-like ALL increased with age and was particularly common in young adults generated tremendous interest because adult ALL is difficult to treat,” Dr Mullighan said. “In this study, we determined that the prevalence remains high across the age spectrum of adults with ALL.”
Prevalence and outcomes
The study included 798 adults who were between the ages of 21 and 86 when diagnosed with ALL. A total of 194 patients (24%) had Ph-like ALL.
The incidence of Ph-like ALL was 27.9% among young adults (ages 21 to 39), 20.4% in adults (ages 40 to 59), and 24.0% in older adults (ages 60 to 86).
Patients with Ph-like ALL had significantly inferior 5-year OS compared to patients with non-Ph-like ALL—23.8% and 52.4%, respectively (P<0.001). The same was true for 5-year EFS—22.5% and 49.3%, respectively (P<0.001).
Among Ph-like ALL patients, the 5-year EFS rates were 40.4% for young adults, 29.8% for adults, and 18.9% for older adults. The 5-year OS rates were 45.2%, 35.1%, and 16.2%, respectively.
Genomic analysis
The researchers performed genomic analysis of 180 of the Ph-like ALL cases and found that 88% had kinase-activating alterations.
This included CRLF2 rearrangements in 51% of cases, JAK2 or EPOR rearrangements in 12.4%, ABL class fusions in 9.8%, other JAK-STAT sequence mutations in 7.2%, other kinase alterations in 4.1%, and Ras pathway mutations in 3.6%.
“Our comprehensive sequencing showed that Ph-like ALL in adults is the most genetically diverse subtype of leukemia that has been described,” said study author Kathryn Roberts, PhD, of St. Jude.
“Cumulatively, more than 50 different chromosomal rearrangements involving 15 different kinases and cytokine receptors have been identified. In this study, we identified 11 chromosomal rearrangements that are new to Ph-like ALL.”
These 11 rearrangements are FIP1L1-PDGFRA, SNX29-PDGFRB, SMU1-JAK2, ZNF340-JAK2, THADA-EPOR, SMARCA4-TYK2, ZNF340-TYK2, ZYMM2-FLT3, DNTT-BLNK, TMEM2-PTK2B, and KANK1-CBL1.
The diversity of kinase-activating alterations in Ph-like ALL has important clinical implications, said study author Hagop Kantarjian, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“It is important that we now identify patients with Ph-like ALL at diagnosis to provide optimal treatment with targeted agents,” he said.
The findings also highlight the importance of centralized comprehensive genomic sequencing for patients, said study author Elisabeth Paietta, PhD, of the Montefiore Health System and Albert Einstein College of Medicine in Bronx, New York.
“Lymphoblasts from almost half of the patients with Ph-like ALL harbor a genomic rearrangement of CRLF2, which can be detected by flow cytometry using an antibody to CRLF2,” Dr Paietta said. “This is very important as it allows a quick characterization of this Ph-like ALL subtype prior to any detailed sequencing.” ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
Researchers have found evidence to suggest that a high-risk subtype of acute lymphoblastic leukemia (ALL) is “highly prevalent” in adults with ALL.
In a study of nearly 800 adults with ALL, roughly a quarter of the patients had Philadelphia chromosome-like (Ph-like) ALL.
Patients with Ph-like ALL had inferior overall survival (OS) and event-free survival (EFS), but most of them also had kinase-activating alterations that suggest they might respond well to tyrosine kinase inhibitors.
The researchers reported these findings in the Journal of Clinical Oncology.
“This study establishes that a large percentage of adults with ALL have this high-risk subtype,” said study author Charles Mullighan, MD, MBBS, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The finding provides a compelling reason to identify those with Ph-like ALL and move forward with clinical trials of these targeted therapies in combination with current chemotherapeutic regimens.”
This study builds on previous research, which suggested that Ph-like ALL becomes more common with age, is associated with poor prognosis, and is characterized by genomic alterations that appear to make patients responsive to treatment with tyrosine kinase inhibitors.
“Our 2014 findings that the prevalence of Ph-like ALL increased with age and was particularly common in young adults generated tremendous interest because adult ALL is difficult to treat,” Dr Mullighan said. “In this study, we determined that the prevalence remains high across the age spectrum of adults with ALL.”
Prevalence and outcomes
The study included 798 adults who were between the ages of 21 and 86 when diagnosed with ALL. A total of 194 patients (24%) had Ph-like ALL.
The incidence of Ph-like ALL was 27.9% among young adults (ages 21 to 39), 20.4% in adults (ages 40 to 59), and 24.0% in older adults (ages 60 to 86).
Patients with Ph-like ALL had significantly inferior 5-year OS compared to patients with non-Ph-like ALL—23.8% and 52.4%, respectively (P<0.001). The same was true for 5-year EFS—22.5% and 49.3%, respectively (P<0.001).
Among Ph-like ALL patients, the 5-year EFS rates were 40.4% for young adults, 29.8% for adults, and 18.9% for older adults. The 5-year OS rates were 45.2%, 35.1%, and 16.2%, respectively.
Genomic analysis
The researchers performed genomic analysis of 180 of the Ph-like ALL cases and found that 88% had kinase-activating alterations.
This included CRLF2 rearrangements in 51% of cases, JAK2 or EPOR rearrangements in 12.4%, ABL class fusions in 9.8%, other JAK-STAT sequence mutations in 7.2%, other kinase alterations in 4.1%, and Ras pathway mutations in 3.6%.
“Our comprehensive sequencing showed that Ph-like ALL in adults is the most genetically diverse subtype of leukemia that has been described,” said study author Kathryn Roberts, PhD, of St. Jude.
“Cumulatively, more than 50 different chromosomal rearrangements involving 15 different kinases and cytokine receptors have been identified. In this study, we identified 11 chromosomal rearrangements that are new to Ph-like ALL.”
These 11 rearrangements are FIP1L1-PDGFRA, SNX29-PDGFRB, SMU1-JAK2, ZNF340-JAK2, THADA-EPOR, SMARCA4-TYK2, ZNF340-TYK2, ZYMM2-FLT3, DNTT-BLNK, TMEM2-PTK2B, and KANK1-CBL1.
The diversity of kinase-activating alterations in Ph-like ALL has important clinical implications, said study author Hagop Kantarjian, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“It is important that we now identify patients with Ph-like ALL at diagnosis to provide optimal treatment with targeted agents,” he said.
The findings also highlight the importance of centralized comprehensive genomic sequencing for patients, said study author Elisabeth Paietta, PhD, of the Montefiore Health System and Albert Einstein College of Medicine in Bronx, New York.
“Lymphoblasts from almost half of the patients with Ph-like ALL harbor a genomic rearrangement of CRLF2, which can be detected by flow cytometry using an antibody to CRLF2,” Dr Paietta said. “This is very important as it allows a quick characterization of this Ph-like ALL subtype prior to any detailed sequencing.” ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
Researchers have found evidence to suggest that a high-risk subtype of acute lymphoblastic leukemia (ALL) is “highly prevalent” in adults with ALL.
In a study of nearly 800 adults with ALL, roughly a quarter of the patients had Philadelphia chromosome-like (Ph-like) ALL.
Patients with Ph-like ALL had inferior overall survival (OS) and event-free survival (EFS), but most of them also had kinase-activating alterations that suggest they might respond well to tyrosine kinase inhibitors.
The researchers reported these findings in the Journal of Clinical Oncology.
“This study establishes that a large percentage of adults with ALL have this high-risk subtype,” said study author Charles Mullighan, MD, MBBS, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The finding provides a compelling reason to identify those with Ph-like ALL and move forward with clinical trials of these targeted therapies in combination with current chemotherapeutic regimens.”
This study builds on previous research, which suggested that Ph-like ALL becomes more common with age, is associated with poor prognosis, and is characterized by genomic alterations that appear to make patients responsive to treatment with tyrosine kinase inhibitors.
“Our 2014 findings that the prevalence of Ph-like ALL increased with age and was particularly common in young adults generated tremendous interest because adult ALL is difficult to treat,” Dr Mullighan said. “In this study, we determined that the prevalence remains high across the age spectrum of adults with ALL.”
Prevalence and outcomes
The study included 798 adults who were between the ages of 21 and 86 when diagnosed with ALL. A total of 194 patients (24%) had Ph-like ALL.
The incidence of Ph-like ALL was 27.9% among young adults (ages 21 to 39), 20.4% in adults (ages 40 to 59), and 24.0% in older adults (ages 60 to 86).
Patients with Ph-like ALL had significantly inferior 5-year OS compared to patients with non-Ph-like ALL—23.8% and 52.4%, respectively (P<0.001). The same was true for 5-year EFS—22.5% and 49.3%, respectively (P<0.001).
Among Ph-like ALL patients, the 5-year EFS rates were 40.4% for young adults, 29.8% for adults, and 18.9% for older adults. The 5-year OS rates were 45.2%, 35.1%, and 16.2%, respectively.
Genomic analysis
The researchers performed genomic analysis of 180 of the Ph-like ALL cases and found that 88% had kinase-activating alterations.
This included CRLF2 rearrangements in 51% of cases, JAK2 or EPOR rearrangements in 12.4%, ABL class fusions in 9.8%, other JAK-STAT sequence mutations in 7.2%, other kinase alterations in 4.1%, and Ras pathway mutations in 3.6%.
“Our comprehensive sequencing showed that Ph-like ALL in adults is the most genetically diverse subtype of leukemia that has been described,” said study author Kathryn Roberts, PhD, of St. Jude.
“Cumulatively, more than 50 different chromosomal rearrangements involving 15 different kinases and cytokine receptors have been identified. In this study, we identified 11 chromosomal rearrangements that are new to Ph-like ALL.”
These 11 rearrangements are FIP1L1-PDGFRA, SNX29-PDGFRB, SMU1-JAK2, ZNF340-JAK2, THADA-EPOR, SMARCA4-TYK2, ZNF340-TYK2, ZYMM2-FLT3, DNTT-BLNK, TMEM2-PTK2B, and KANK1-CBL1.
The diversity of kinase-activating alterations in Ph-like ALL has important clinical implications, said study author Hagop Kantarjian, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“It is important that we now identify patients with Ph-like ALL at diagnosis to provide optimal treatment with targeted agents,” he said.
The findings also highlight the importance of centralized comprehensive genomic sequencing for patients, said study author Elisabeth Paietta, PhD, of the Montefiore Health System and Albert Einstein College of Medicine in Bronx, New York.
“Lymphoblasts from almost half of the patients with Ph-like ALL harbor a genomic rearrangement of CRLF2, which can be detected by flow cytometry using an antibody to CRLF2,” Dr Paietta said. “This is very important as it allows a quick characterization of this Ph-like ALL subtype prior to any detailed sequencing.” ![]()
Novel CLL drugs could greatly increase costs

New research suggests the increasing use of oral targeted therapies for chronic lymphocytic leukemia (CLL) could raise US treatment costs for the disease by almost 600%.
Investigators modeled the evolving management of CLL from 2011 to 2025 and found that increasing use of the oral targeted therapies ibrutinib and idelalisib could greatly increase costs for both patients and payers.
The team detailed these findings in the Journal of Clinical Oncology.
“The rising cost of cancer care is a serious concern,” said study author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital in Boston.
“The average cost of annual cancer treatment, which was below $10,000 per patient before 2000, has now increased to more than $100,000. Such increasing trends can limit access to new therapies, potentially undermining their clinical effectiveness. These new drugs are highly effective, but their high costs motivated us to project their changing economic burden and affordability.”
Dr Chhatwal and his colleagues noted that ibrutinib and idelalisib each cost around $130,000 per year, and treatment with these drugs may be continued indefinitely.
So the team set out to determine the potential financial impact of the drugs on payers’ budgets, as well as on Medicare-enrolled patients, who represent the majority of CLL patients in the US.
The investigators developed a model to simulate the evolving management of CLL from 2011 to 2025.
In one scenario, chemoimmunotherapy was the standard of care before 2014, while oral targeted therapies were used for patients with del(17p) and relapsed CLL from 2014 onward and for first-line treatment of CLL from 2016 onward.
The team also modeled a scenario in which chemoimmunotherapy was the standard of care throughout the entire time period and compared the costs between these scenarios.
The model projects that:
- Per-patient lifetime costs for CLL treatment will increase from $147,000 to $604,000 from 2016 onward
- The total out-of-pocket costs for Medicare patients will increase from $9200 to $57,000 for patients initiating treatment from 2016 onward
- The total annual cost of CLL management in the US will rise from $0.74 billion in 2011 to $5.13 billion in 2025, an increase of 590%.
“Such substantial increases in the cost are mainly driven by high drug prices, prolonged treatment duration, and the increase in the number of patients living with CLL,” said study author Qiushi Chen, PhD, of Massachusetts General Hospital.
The investigators also noted that the standard measure used to determine the cost-effectiveness of a medical intervention is whether it costs less than $100,000 for each additional year of life gained. The projected cost-effectiveness ratio of oral targeted therapy in CLL is $189,000 for each year gained.
“At the current average wholesale prices, oral targeted therapies for CLL are not cost-effective, and prices would need to drop by 50% to 70% to become cost-effective,” Dr Chhatwal said.
“We are not recommending that clinicians choose less effective CLL management strategies that do not include oral targeted therapies,” said study author Nitin Jain, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Instead, we propose that the prices of these drugs need to be reduced to make the treatment cost-effective and more affordable, something we hope may happen with all cancer drugs. We also believe more research is needed to explore whether we can discontinue targeted treatment of patients who have responded well without risking worsening of their health.” ![]()

New research suggests the increasing use of oral targeted therapies for chronic lymphocytic leukemia (CLL) could raise US treatment costs for the disease by almost 600%.
Investigators modeled the evolving management of CLL from 2011 to 2025 and found that increasing use of the oral targeted therapies ibrutinib and idelalisib could greatly increase costs for both patients and payers.
The team detailed these findings in the Journal of Clinical Oncology.
“The rising cost of cancer care is a serious concern,” said study author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital in Boston.
“The average cost of annual cancer treatment, which was below $10,000 per patient before 2000, has now increased to more than $100,000. Such increasing trends can limit access to new therapies, potentially undermining their clinical effectiveness. These new drugs are highly effective, but their high costs motivated us to project their changing economic burden and affordability.”
Dr Chhatwal and his colleagues noted that ibrutinib and idelalisib each cost around $130,000 per year, and treatment with these drugs may be continued indefinitely.
So the team set out to determine the potential financial impact of the drugs on payers’ budgets, as well as on Medicare-enrolled patients, who represent the majority of CLL patients in the US.
The investigators developed a model to simulate the evolving management of CLL from 2011 to 2025.
In one scenario, chemoimmunotherapy was the standard of care before 2014, while oral targeted therapies were used for patients with del(17p) and relapsed CLL from 2014 onward and for first-line treatment of CLL from 2016 onward.
The team also modeled a scenario in which chemoimmunotherapy was the standard of care throughout the entire time period and compared the costs between these scenarios.
The model projects that:
- Per-patient lifetime costs for CLL treatment will increase from $147,000 to $604,000 from 2016 onward
- The total out-of-pocket costs for Medicare patients will increase from $9200 to $57,000 for patients initiating treatment from 2016 onward
- The total annual cost of CLL management in the US will rise from $0.74 billion in 2011 to $5.13 billion in 2025, an increase of 590%.
“Such substantial increases in the cost are mainly driven by high drug prices, prolonged treatment duration, and the increase in the number of patients living with CLL,” said study author Qiushi Chen, PhD, of Massachusetts General Hospital.
The investigators also noted that the standard measure used to determine the cost-effectiveness of a medical intervention is whether it costs less than $100,000 for each additional year of life gained. The projected cost-effectiveness ratio of oral targeted therapy in CLL is $189,000 for each year gained.
“At the current average wholesale prices, oral targeted therapies for CLL are not cost-effective, and prices would need to drop by 50% to 70% to become cost-effective,” Dr Chhatwal said.
“We are not recommending that clinicians choose less effective CLL management strategies that do not include oral targeted therapies,” said study author Nitin Jain, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Instead, we propose that the prices of these drugs need to be reduced to make the treatment cost-effective and more affordable, something we hope may happen with all cancer drugs. We also believe more research is needed to explore whether we can discontinue targeted treatment of patients who have responded well without risking worsening of their health.” ![]()

New research suggests the increasing use of oral targeted therapies for chronic lymphocytic leukemia (CLL) could raise US treatment costs for the disease by almost 600%.
Investigators modeled the evolving management of CLL from 2011 to 2025 and found that increasing use of the oral targeted therapies ibrutinib and idelalisib could greatly increase costs for both patients and payers.
The team detailed these findings in the Journal of Clinical Oncology.
“The rising cost of cancer care is a serious concern,” said study author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital in Boston.
“The average cost of annual cancer treatment, which was below $10,000 per patient before 2000, has now increased to more than $100,000. Such increasing trends can limit access to new therapies, potentially undermining their clinical effectiveness. These new drugs are highly effective, but their high costs motivated us to project their changing economic burden and affordability.”
Dr Chhatwal and his colleagues noted that ibrutinib and idelalisib each cost around $130,000 per year, and treatment with these drugs may be continued indefinitely.
So the team set out to determine the potential financial impact of the drugs on payers’ budgets, as well as on Medicare-enrolled patients, who represent the majority of CLL patients in the US.
The investigators developed a model to simulate the evolving management of CLL from 2011 to 2025.
In one scenario, chemoimmunotherapy was the standard of care before 2014, while oral targeted therapies were used for patients with del(17p) and relapsed CLL from 2014 onward and for first-line treatment of CLL from 2016 onward.
The team also modeled a scenario in which chemoimmunotherapy was the standard of care throughout the entire time period and compared the costs between these scenarios.
The model projects that:
- Per-patient lifetime costs for CLL treatment will increase from $147,000 to $604,000 from 2016 onward
- The total out-of-pocket costs for Medicare patients will increase from $9200 to $57,000 for patients initiating treatment from 2016 onward
- The total annual cost of CLL management in the US will rise from $0.74 billion in 2011 to $5.13 billion in 2025, an increase of 590%.
“Such substantial increases in the cost are mainly driven by high drug prices, prolonged treatment duration, and the increase in the number of patients living with CLL,” said study author Qiushi Chen, PhD, of Massachusetts General Hospital.
The investigators also noted that the standard measure used to determine the cost-effectiveness of a medical intervention is whether it costs less than $100,000 for each additional year of life gained. The projected cost-effectiveness ratio of oral targeted therapy in CLL is $189,000 for each year gained.
“At the current average wholesale prices, oral targeted therapies for CLL are not cost-effective, and prices would need to drop by 50% to 70% to become cost-effective,” Dr Chhatwal said.
“We are not recommending that clinicians choose less effective CLL management strategies that do not include oral targeted therapies,” said study author Nitin Jain, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Instead, we propose that the prices of these drugs need to be reduced to make the treatment cost-effective and more affordable, something we hope may happen with all cancer drugs. We also believe more research is needed to explore whether we can discontinue targeted treatment of patients who have responded well without risking worsening of their health.” ![]()
Targeted therapies predicted to blow out costs for CLL
The lifetime cost of treating chronic lymphocytic leukemia is forecast to rise precipitously for patients diagnosed today, as oral targeted therapies take over as the first-line treatment option, according to a study published November 21 in the Journal of Clinical Oncology.
The conclusion is based on economic models that also indicated the annual cost in the United States of managing chronic lymphocytic leukemia (CLL) will increase from its current level of $0.74 billion to $5.13 billion by 2025 (J Clin Oncol. 2016 Nov 21. doi: 10.1200/JCO.2016.68.2856).
While the majority of patients with CLL are covered by Medicare in the United States, they still currently pay $9,200 in out-of-pocket costs for oral agents. This figure is forecast to increase to $57,000 for those who start treatment in 2016 due to the increased costs of oral targeted therapeutics.
“Such an economic impact could result in financial toxicity, limited access, and lower adherence to the oral therapies, which may undermine their clinical effectiveness,” Qiushi Chen, from the Georgia Institute of Technology, Atlanta, and his coauthors wrote. They called for a more sustainable pricing strategy for oral targeted therapies, rather than have clinicians be forced to choose less effective but more affordable management strategies.
The researchers developed a microsimulation model of CLL, simulating the dynamics of the patient population under given management strategies from 2011-2025.
Around 130,000 patients live with CLL in the United States and around 15,000 new cases are diagnosed each year. By 2025, the authors forecast that 199,000 people will be living with the disease; a 55% increase that is both the result of new diagnoses and of improved survival with new oral targeted therapies.
Chemoimmunotherapy regimens – such as fludarabine, cyclophosphamide, and rituximab – have long been the standard first-line approach to CLL. But in recent years, new oral targeted agents such as ibrutinib and idelalisib have significantly improved progression-free survival and overall survival in CLL.
Ibrutinib is approved for first-line management of CLL, idelalisib is approved in combination with rituximab for patients with relapsed/refractory chronic lymphocytic leukemia, and venetoclax is approved for patients with relapsed chronic lymphocytic leukemia with del(17p).
“Both ibrutinib and idelalisib are priced at approximately $130,000 per [CLL patient per] year and are recommended until patients have progressive disease or significant toxicities,” the authors wrote. “In contrast, the costs for chemoimmunotherapy-based treatments range from $60,000 to $100,000 for a finite duration, that is, a typical six-cycle course that lasts for approximately 6 months.”
The higher costs will add up to additional annual spending of $29 billion to 2025, compared with around $1.12 billion annually for chemoimmunotherapy alone.
“Compared with the CIT scenario, the oral targeted therapy scenario resulted in an increase of 107,000 person–quality-adjusted life-years (149,000 person–life years), with additional discounted costs of $20.2 billion,” the authors reported.
The annual cost of cancer care in the United States is increasing across the board, from $143 billion in 2010 to $180 billion in 2020, but the cost of care for CLL is increasing more significantly than for other cancers. For example, breast and prostate cancers are forecast to have a 24%-38% increase in annual cost by 2020, while CLL is predicted to increase by 500%.
Seven authors declared research funding, honoraria and consultancy funding from a range of pharmaceutical companies including those involved in the manufacture of therapies for chronic lymphocytic leukemia. Two authors had no conflicts to declare.
The lifetime cost of treating chronic lymphocytic leukemia is forecast to rise precipitously for patients diagnosed today, as oral targeted therapies take over as the first-line treatment option, according to a study published November 21 in the Journal of Clinical Oncology.
The conclusion is based on economic models that also indicated the annual cost in the United States of managing chronic lymphocytic leukemia (CLL) will increase from its current level of $0.74 billion to $5.13 billion by 2025 (J Clin Oncol. 2016 Nov 21. doi: 10.1200/JCO.2016.68.2856).
While the majority of patients with CLL are covered by Medicare in the United States, they still currently pay $9,200 in out-of-pocket costs for oral agents. This figure is forecast to increase to $57,000 for those who start treatment in 2016 due to the increased costs of oral targeted therapeutics.
“Such an economic impact could result in financial toxicity, limited access, and lower adherence to the oral therapies, which may undermine their clinical effectiveness,” Qiushi Chen, from the Georgia Institute of Technology, Atlanta, and his coauthors wrote. They called for a more sustainable pricing strategy for oral targeted therapies, rather than have clinicians be forced to choose less effective but more affordable management strategies.
The researchers developed a microsimulation model of CLL, simulating the dynamics of the patient population under given management strategies from 2011-2025.
Around 130,000 patients live with CLL in the United States and around 15,000 new cases are diagnosed each year. By 2025, the authors forecast that 199,000 people will be living with the disease; a 55% increase that is both the result of new diagnoses and of improved survival with new oral targeted therapies.
Chemoimmunotherapy regimens – such as fludarabine, cyclophosphamide, and rituximab – have long been the standard first-line approach to CLL. But in recent years, new oral targeted agents such as ibrutinib and idelalisib have significantly improved progression-free survival and overall survival in CLL.
Ibrutinib is approved for first-line management of CLL, idelalisib is approved in combination with rituximab for patients with relapsed/refractory chronic lymphocytic leukemia, and venetoclax is approved for patients with relapsed chronic lymphocytic leukemia with del(17p).
“Both ibrutinib and idelalisib are priced at approximately $130,000 per [CLL patient per] year and are recommended until patients have progressive disease or significant toxicities,” the authors wrote. “In contrast, the costs for chemoimmunotherapy-based treatments range from $60,000 to $100,000 for a finite duration, that is, a typical six-cycle course that lasts for approximately 6 months.”
The higher costs will add up to additional annual spending of $29 billion to 2025, compared with around $1.12 billion annually for chemoimmunotherapy alone.
“Compared with the CIT scenario, the oral targeted therapy scenario resulted in an increase of 107,000 person–quality-adjusted life-years (149,000 person–life years), with additional discounted costs of $20.2 billion,” the authors reported.
The annual cost of cancer care in the United States is increasing across the board, from $143 billion in 2010 to $180 billion in 2020, but the cost of care for CLL is increasing more significantly than for other cancers. For example, breast and prostate cancers are forecast to have a 24%-38% increase in annual cost by 2020, while CLL is predicted to increase by 500%.
Seven authors declared research funding, honoraria and consultancy funding from a range of pharmaceutical companies including those involved in the manufacture of therapies for chronic lymphocytic leukemia. Two authors had no conflicts to declare.
The lifetime cost of treating chronic lymphocytic leukemia is forecast to rise precipitously for patients diagnosed today, as oral targeted therapies take over as the first-line treatment option, according to a study published November 21 in the Journal of Clinical Oncology.
The conclusion is based on economic models that also indicated the annual cost in the United States of managing chronic lymphocytic leukemia (CLL) will increase from its current level of $0.74 billion to $5.13 billion by 2025 (J Clin Oncol. 2016 Nov 21. doi: 10.1200/JCO.2016.68.2856).
While the majority of patients with CLL are covered by Medicare in the United States, they still currently pay $9,200 in out-of-pocket costs for oral agents. This figure is forecast to increase to $57,000 for those who start treatment in 2016 due to the increased costs of oral targeted therapeutics.
“Such an economic impact could result in financial toxicity, limited access, and lower adherence to the oral therapies, which may undermine their clinical effectiveness,” Qiushi Chen, from the Georgia Institute of Technology, Atlanta, and his coauthors wrote. They called for a more sustainable pricing strategy for oral targeted therapies, rather than have clinicians be forced to choose less effective but more affordable management strategies.
The researchers developed a microsimulation model of CLL, simulating the dynamics of the patient population under given management strategies from 2011-2025.
Around 130,000 patients live with CLL in the United States and around 15,000 new cases are diagnosed each year. By 2025, the authors forecast that 199,000 people will be living with the disease; a 55% increase that is both the result of new diagnoses and of improved survival with new oral targeted therapies.
Chemoimmunotherapy regimens – such as fludarabine, cyclophosphamide, and rituximab – have long been the standard first-line approach to CLL. But in recent years, new oral targeted agents such as ibrutinib and idelalisib have significantly improved progression-free survival and overall survival in CLL.
Ibrutinib is approved for first-line management of CLL, idelalisib is approved in combination with rituximab for patients with relapsed/refractory chronic lymphocytic leukemia, and venetoclax is approved for patients with relapsed chronic lymphocytic leukemia with del(17p).
“Both ibrutinib and idelalisib are priced at approximately $130,000 per [CLL patient per] year and are recommended until patients have progressive disease or significant toxicities,” the authors wrote. “In contrast, the costs for chemoimmunotherapy-based treatments range from $60,000 to $100,000 for a finite duration, that is, a typical six-cycle course that lasts for approximately 6 months.”
The higher costs will add up to additional annual spending of $29 billion to 2025, compared with around $1.12 billion annually for chemoimmunotherapy alone.
“Compared with the CIT scenario, the oral targeted therapy scenario resulted in an increase of 107,000 person–quality-adjusted life-years (149,000 person–life years), with additional discounted costs of $20.2 billion,” the authors reported.
The annual cost of cancer care in the United States is increasing across the board, from $143 billion in 2010 to $180 billion in 2020, but the cost of care for CLL is increasing more significantly than for other cancers. For example, breast and prostate cancers are forecast to have a 24%-38% increase in annual cost by 2020, while CLL is predicted to increase by 500%.
Seven authors declared research funding, honoraria and consultancy funding from a range of pharmaceutical companies including those involved in the manufacture of therapies for chronic lymphocytic leukemia. Two authors had no conflicts to declare.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The high cost of oral therapies for chronic lymphocytic leukemia could result in financial toxicity, limited access, and lower adherence, which may undermine their clinical effectiveness.
Major finding: The cost of treating chronic lymphocytic leukemia is forecast to increase from its current level of $0.74 billion to $5.13 billion by 2025.
Data source: Microsimulation model of chronic lymphocytic leukemia treatment from 2010-2025.
Disclosures: Seven authors declared research funding, honoraria, and consultancy funding from a range of pharmaceutical companies including those involved in the manufacture of therapies for chronic lymphocytic leukemia. Two authors had no conflicts to declare.
Large-scale tumor profiling deemed feasible, but challenges remain

Photo courtesy of the
National Institute of
General Medical Sciences
New research suggests large-scale genomic profiling is technically feasible in a broad population of cancer patients.
However, the study also revealed challenges and barriers to widespread implementation of precision medicine, according to researchers.
Specifically, half of the patients studied did not receive results of genomic profiling due to insufficient samples or sequencing failure.
Most patients who did receive results did not see a change in their care.
However, genomic profiling provided an accurate diagnosis and changed treatment for a handful of the patients studied.
Lynette M. Sholl, MD, of Brigham and Women’s Hospital in Boston, Massachusetts, and her colleagues reported these findings in JCI Insight.
The report contains data on pediatric and adult patients with a range of malignancies.
Patient samples were analyzed using OncoPanel. This platform sequences hundreds of known cancer-related genes to look for alterations that drive tumors and might be helpful in guiding treatment choice or enrolling the patient in an appropriate clinical trial.
This study began with 7397 patients, but many of these individuals did not have specimens adequate for sequencing. This left 3892 patients (53%) to undergo genomic profiling, but sequencing failed in 165 (4%) of them. So sequencing was successful in 3727 patients, or 50% of the overall population.
Of the 3727 patients in whom sequencing was successful, 73% had at least 1 genetic alteration that was considered “clinically actionable or informative” by the researchers.
This included 54% of patients with alterations that might be used to inform diagnosis or recommend enrollment in a clinical trial. It also included 19% of patients who had an alteration that “would inform standard-of-care therapeutic decision-making,” according to the researchers.
The team provided several examples of how genomic testing clarified or changed a patient’s diagnosis, which, in turn, altered treatment and prognosis.
One example was a patient who was originally diagnosed with peripheral T-cell lymphoma, which was later revised to myeloid sarcoma. Sequencing results suggested the patient actually had FIP1L1-PDGFRA-driven acute myeloid leukemia, which predicted responsiveness to imatinib.
The patient was treated with imatinib and experienced a “dramatic and sustained clinical response.” He then proceeded to allogeneic transplant and had no evidence of disease at 1 year of follow-up.
The researchers concluded that genomic sequencing results may alter the management of cancer patients in some cases, but certain barriers must be overcome to enable precision cancer medicine on a large scale. ![]()

Photo courtesy of the
National Institute of
General Medical Sciences
New research suggests large-scale genomic profiling is technically feasible in a broad population of cancer patients.
However, the study also revealed challenges and barriers to widespread implementation of precision medicine, according to researchers.
Specifically, half of the patients studied did not receive results of genomic profiling due to insufficient samples or sequencing failure.
Most patients who did receive results did not see a change in their care.
However, genomic profiling provided an accurate diagnosis and changed treatment for a handful of the patients studied.
Lynette M. Sholl, MD, of Brigham and Women’s Hospital in Boston, Massachusetts, and her colleagues reported these findings in JCI Insight.
The report contains data on pediatric and adult patients with a range of malignancies.
Patient samples were analyzed using OncoPanel. This platform sequences hundreds of known cancer-related genes to look for alterations that drive tumors and might be helpful in guiding treatment choice or enrolling the patient in an appropriate clinical trial.
This study began with 7397 patients, but many of these individuals did not have specimens adequate for sequencing. This left 3892 patients (53%) to undergo genomic profiling, but sequencing failed in 165 (4%) of them. So sequencing was successful in 3727 patients, or 50% of the overall population.
Of the 3727 patients in whom sequencing was successful, 73% had at least 1 genetic alteration that was considered “clinically actionable or informative” by the researchers.
This included 54% of patients with alterations that might be used to inform diagnosis or recommend enrollment in a clinical trial. It also included 19% of patients who had an alteration that “would inform standard-of-care therapeutic decision-making,” according to the researchers.
The team provided several examples of how genomic testing clarified or changed a patient’s diagnosis, which, in turn, altered treatment and prognosis.
One example was a patient who was originally diagnosed with peripheral T-cell lymphoma, which was later revised to myeloid sarcoma. Sequencing results suggested the patient actually had FIP1L1-PDGFRA-driven acute myeloid leukemia, which predicted responsiveness to imatinib.
The patient was treated with imatinib and experienced a “dramatic and sustained clinical response.” He then proceeded to allogeneic transplant and had no evidence of disease at 1 year of follow-up.
The researchers concluded that genomic sequencing results may alter the management of cancer patients in some cases, but certain barriers must be overcome to enable precision cancer medicine on a large scale. ![]()

Photo courtesy of the
National Institute of
General Medical Sciences
New research suggests large-scale genomic profiling is technically feasible in a broad population of cancer patients.
However, the study also revealed challenges and barriers to widespread implementation of precision medicine, according to researchers.
Specifically, half of the patients studied did not receive results of genomic profiling due to insufficient samples or sequencing failure.
Most patients who did receive results did not see a change in their care.
However, genomic profiling provided an accurate diagnosis and changed treatment for a handful of the patients studied.
Lynette M. Sholl, MD, of Brigham and Women’s Hospital in Boston, Massachusetts, and her colleagues reported these findings in JCI Insight.
The report contains data on pediatric and adult patients with a range of malignancies.
Patient samples were analyzed using OncoPanel. This platform sequences hundreds of known cancer-related genes to look for alterations that drive tumors and might be helpful in guiding treatment choice or enrolling the patient in an appropriate clinical trial.
This study began with 7397 patients, but many of these individuals did not have specimens adequate for sequencing. This left 3892 patients (53%) to undergo genomic profiling, but sequencing failed in 165 (4%) of them. So sequencing was successful in 3727 patients, or 50% of the overall population.
Of the 3727 patients in whom sequencing was successful, 73% had at least 1 genetic alteration that was considered “clinically actionable or informative” by the researchers.
This included 54% of patients with alterations that might be used to inform diagnosis or recommend enrollment in a clinical trial. It also included 19% of patients who had an alteration that “would inform standard-of-care therapeutic decision-making,” according to the researchers.
The team provided several examples of how genomic testing clarified or changed a patient’s diagnosis, which, in turn, altered treatment and prognosis.
One example was a patient who was originally diagnosed with peripheral T-cell lymphoma, which was later revised to myeloid sarcoma. Sequencing results suggested the patient actually had FIP1L1-PDGFRA-driven acute myeloid leukemia, which predicted responsiveness to imatinib.
The patient was treated with imatinib and experienced a “dramatic and sustained clinical response.” He then proceeded to allogeneic transplant and had no evidence of disease at 1 year of follow-up.
The researchers concluded that genomic sequencing results may alter the management of cancer patients in some cases, but certain barriers must be overcome to enable precision cancer medicine on a large scale. ![]()
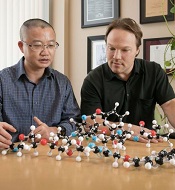
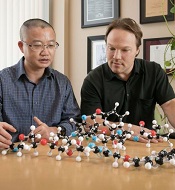
Compound could treat leukemia, other cancers
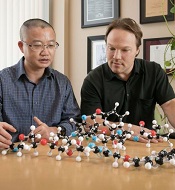
and Patrick Harran with
a model of DZ-2384
Photo courtesy of
Reed Hutchinson/UCLA
A new compound holds promise for treating leukemia and other cancers, according to researchers.
The compound, DZ-2384, is a synthetic version of diazonamide A, a toxin isolated from a marine animal.
DZ-2384 is a microtubule-targeting agent (MTA). It binds to and alters the stability of microtubules, disrupting the normal function of the mitotic spindle and arresting cell-cycle progression at mitosis, ultimately leading to cell death.
However, researchers found that DZ-2384 behaves somewhat differently from other MTAs.
They reported these findings in Science Translational Medicine. The research was supported, in part, by Diazon Pharmaceuticals Inc.
The researchers tested DZ-2384 in mouse models of various cancers, including adult Philadelphia chromosome–negative acute lymphocytic leukemia.
In animals receiving DZ-2384, tumors shrank as much as or more than when a conventional MTA was used, but with much less toxicity at effective doses.
In particular, animals receiving DZ-2384 had markedly less peripheral neuropathy than those that received docetaxel, a conventional MTA. Peripheral neuropathy is one of the chief side effects of MTAs and can prompt treatment discontinuation.
“We have good reason to expect that human clinical trials of DZ-2384 will show that, at doses effective for treating a person’s cancer, there will be much less risk of the peripheral neuropathy that can force clinicians to stop treatment,” said study author Patrick Harran, PhD, of the University of California, Los Angeles.
Dr Harran believes clinical trials of DZ-2384 could begin within 2 years.
How this study began
Dr Harran began his work with diazonamides as a fundamental chemistry research problem.
In 1991, a group of researchers described diazonamides A and B, which they had isolated from the marine animal Diazona chinensis.
But Dr Harran and his colleagues found the described structure of diazonamide A was incorrect. In 2001, the team published a study that corrected the chemical structure of diazonamide A, and, 2 years later, they had synthesized the true structure in their lab.
Next, they began studying what the molecule might be doing to stop cells from dividing. In 2007, they discovered that the synthetic diazonamides they had produced minimized undesirable toxic effects that are commonly associated with chemotherapy.
Specifically, the compounds had an unusually large therapeutic window. In experiment after experiment, Dr Harran said, the researchers found that synthetic diazonamides’ therapeutic window was at least 10 times larger than that of traditional MTAs.
A key finding
In 2015, researchers prepared a form of DZ-2384 that was engineered with a molecular-scale “tracking device” so they could monitor its activity and better understand how it worked.
That helped the team confirm what they had come to suspect: that the compound binds to tubulin, which is a building block of mitotic spindles and a common target of MTAs.
Armed with this information, the researchers used X-ray crystallography to determine the structure of DZ-2384 bound to tubulin.
Their work offers a possible explanation for how DZ-2384 could disrupt dynamic tubulin polymers during cell division but spare those polymers in resting cells like neurons in the peripheral nervous system.
And that is what appears to allow the compound to attack growing cancer cells while minimizing damage to healthy cells. ![]()
and Patrick Harran with
a model of DZ-2384
Photo courtesy of
Reed Hutchinson/UCLA
A new compound holds promise for treating leukemia and other cancers, according to researchers.
The compound, DZ-2384, is a synthetic version of diazonamide A, a toxin isolated from a marine animal.
DZ-2384 is a microtubule-targeting agent (MTA). It binds to and alters the stability of microtubules, disrupting the normal function of the mitotic spindle and arresting cell-cycle progression at mitosis, ultimately leading to cell death.
However, researchers found that DZ-2384 behaves somewhat differently from other MTAs.
They reported these findings in Science Translational Medicine. The research was supported, in part, by Diazon Pharmaceuticals Inc.
The researchers tested DZ-2384 in mouse models of various cancers, including adult Philadelphia chromosome–negative acute lymphocytic leukemia.
In animals receiving DZ-2384, tumors shrank as much as or more than when a conventional MTA was used, but with much less toxicity at effective doses.
In particular, animals receiving DZ-2384 had markedly less peripheral neuropathy than those that received docetaxel, a conventional MTA. Peripheral neuropathy is one of the chief side effects of MTAs and can prompt treatment discontinuation.
“We have good reason to expect that human clinical trials of DZ-2384 will show that, at doses effective for treating a person’s cancer, there will be much less risk of the peripheral neuropathy that can force clinicians to stop treatment,” said study author Patrick Harran, PhD, of the University of California, Los Angeles.
Dr Harran believes clinical trials of DZ-2384 could begin within 2 years.
How this study began
Dr Harran began his work with diazonamides as a fundamental chemistry research problem.
In 1991, a group of researchers described diazonamides A and B, which they had isolated from the marine animal Diazona chinensis.
But Dr Harran and his colleagues found the described structure of diazonamide A was incorrect. In 2001, the team published a study that corrected the chemical structure of diazonamide A, and, 2 years later, they had synthesized the true structure in their lab.
Next, they began studying what the molecule might be doing to stop cells from dividing. In 2007, they discovered that the synthetic diazonamides they had produced minimized undesirable toxic effects that are commonly associated with chemotherapy.
Specifically, the compounds had an unusually large therapeutic window. In experiment after experiment, Dr Harran said, the researchers found that synthetic diazonamides’ therapeutic window was at least 10 times larger than that of traditional MTAs.
A key finding
In 2015, researchers prepared a form of DZ-2384 that was engineered with a molecular-scale “tracking device” so they could monitor its activity and better understand how it worked.
That helped the team confirm what they had come to suspect: that the compound binds to tubulin, which is a building block of mitotic spindles and a common target of MTAs.
Armed with this information, the researchers used X-ray crystallography to determine the structure of DZ-2384 bound to tubulin.
Their work offers a possible explanation for how DZ-2384 could disrupt dynamic tubulin polymers during cell division but spare those polymers in resting cells like neurons in the peripheral nervous system.
And that is what appears to allow the compound to attack growing cancer cells while minimizing damage to healthy cells. ![]()
and Patrick Harran with
a model of DZ-2384
Photo courtesy of
Reed Hutchinson/UCLA
A new compound holds promise for treating leukemia and other cancers, according to researchers.
The compound, DZ-2384, is a synthetic version of diazonamide A, a toxin isolated from a marine animal.
DZ-2384 is a microtubule-targeting agent (MTA). It binds to and alters the stability of microtubules, disrupting the normal function of the mitotic spindle and arresting cell-cycle progression at mitosis, ultimately leading to cell death.
However, researchers found that DZ-2384 behaves somewhat differently from other MTAs.
They reported these findings in Science Translational Medicine. The research was supported, in part, by Diazon Pharmaceuticals Inc.
The researchers tested DZ-2384 in mouse models of various cancers, including adult Philadelphia chromosome–negative acute lymphocytic leukemia.
In animals receiving DZ-2384, tumors shrank as much as or more than when a conventional MTA was used, but with much less toxicity at effective doses.
In particular, animals receiving DZ-2384 had markedly less peripheral neuropathy than those that received docetaxel, a conventional MTA. Peripheral neuropathy is one of the chief side effects of MTAs and can prompt treatment discontinuation.
“We have good reason to expect that human clinical trials of DZ-2384 will show that, at doses effective for treating a person’s cancer, there will be much less risk of the peripheral neuropathy that can force clinicians to stop treatment,” said study author Patrick Harran, PhD, of the University of California, Los Angeles.
Dr Harran believes clinical trials of DZ-2384 could begin within 2 years.
How this study began
Dr Harran began his work with diazonamides as a fundamental chemistry research problem.
In 1991, a group of researchers described diazonamides A and B, which they had isolated from the marine animal Diazona chinensis.
But Dr Harran and his colleagues found the described structure of diazonamide A was incorrect. In 2001, the team published a study that corrected the chemical structure of diazonamide A, and, 2 years later, they had synthesized the true structure in their lab.
Next, they began studying what the molecule might be doing to stop cells from dividing. In 2007, they discovered that the synthetic diazonamides they had produced minimized undesirable toxic effects that are commonly associated with chemotherapy.
Specifically, the compounds had an unusually large therapeutic window. In experiment after experiment, Dr Harran said, the researchers found that synthetic diazonamides’ therapeutic window was at least 10 times larger than that of traditional MTAs.
A key finding
In 2015, researchers prepared a form of DZ-2384 that was engineered with a molecular-scale “tracking device” so they could monitor its activity and better understand how it worked.
That helped the team confirm what they had come to suspect: that the compound binds to tubulin, which is a building block of mitotic spindles and a common target of MTAs.
Armed with this information, the researchers used X-ray crystallography to determine the structure of DZ-2384 bound to tubulin.
Their work offers a possible explanation for how DZ-2384 could disrupt dynamic tubulin polymers during cell division but spare those polymers in resting cells like neurons in the peripheral nervous system.
And that is what appears to allow the compound to attack growing cancer cells while minimizing damage to healthy cells. ![]()
Team develops model of common infant ALL

Photo by Petr Kratochvil
After trying for nearly 2 decades, researchers have created a mouse model of t(4;11) pro-B acute lymphoblastic
leukemia (ALL).
The team said this model, described in Cancer Cell, mimics the human disease phenotypically and molecularly.
This type of ALL, which is common in infants, results from the translocation t(4;11)(q21;q23), which fuses the mixed-lineage leukemia (MLL) gene on chromosome 11 to the ALL-1 fused gene on chromosome 4 (AF4).
“For 20 years, scientists have repeatedly tried and consistently failed to make a model of MLL-AF4 pro-B acute lymphoblastic leukemia,” said study author Michael Thirman, MD, of the University of Chicago in Illinois.
“Even though we understood the basic genetic flaw, no one had been able create a mouse model that mimicked the human disease, which is crucial for evaluating potential therapies.”
That frustrated many researchers, who shifted their focus to test alternative hypotheses on the causes of t(4;11) pro-B ALL or refocused their laboratories to study different aspects of the disease.
However, Dr Thirman and his colleagues began working on this problem “years ago,” he said, and stayed with it.
The team identified 2 hurdles. The first was a problem with the retrovirus used to insert the MLL-AF4 fusion gene into mouse cells.
“We soon discovered that the virus wasn’t working,” Dr Thirman explained. “We knew that certain parts of human DNA can decrease viral titers. So we switched from the human version of AF4 to the mouse version, Af4, which is slightly different. This increased viral titers 30-fold.”
That worked, but it led to the second hurdle. The mice injected with virus transporting MLL-Af4 developed leukemia, but it was acute myeloid leukemia.
So the researchers inserted the fused MLL-Af4 gene into human CD34 cells, which were derived from cord blood or peripheral blood from volunteer donors.
The team then transferred those cells to mice, and, this time, the mice developed t(4;11) pro-B ALL.
The researchers said this model “fully recapitulates the immunophenotypic and molecular aspects” of human t(4;11) pro-B ALL and will therefore be “a valuable tool” for studying the disease. ![]()

Photo by Petr Kratochvil
After trying for nearly 2 decades, researchers have created a mouse model of t(4;11) pro-B acute lymphoblastic
leukemia (ALL).
The team said this model, described in Cancer Cell, mimics the human disease phenotypically and molecularly.
This type of ALL, which is common in infants, results from the translocation t(4;11)(q21;q23), which fuses the mixed-lineage leukemia (MLL) gene on chromosome 11 to the ALL-1 fused gene on chromosome 4 (AF4).
“For 20 years, scientists have repeatedly tried and consistently failed to make a model of MLL-AF4 pro-B acute lymphoblastic leukemia,” said study author Michael Thirman, MD, of the University of Chicago in Illinois.
“Even though we understood the basic genetic flaw, no one had been able create a mouse model that mimicked the human disease, which is crucial for evaluating potential therapies.”
That frustrated many researchers, who shifted their focus to test alternative hypotheses on the causes of t(4;11) pro-B ALL or refocused their laboratories to study different aspects of the disease.
However, Dr Thirman and his colleagues began working on this problem “years ago,” he said, and stayed with it.
The team identified 2 hurdles. The first was a problem with the retrovirus used to insert the MLL-AF4 fusion gene into mouse cells.
“We soon discovered that the virus wasn’t working,” Dr Thirman explained. “We knew that certain parts of human DNA can decrease viral titers. So we switched from the human version of AF4 to the mouse version, Af4, which is slightly different. This increased viral titers 30-fold.”
That worked, but it led to the second hurdle. The mice injected with virus transporting MLL-Af4 developed leukemia, but it was acute myeloid leukemia.
So the researchers inserted the fused MLL-Af4 gene into human CD34 cells, which were derived from cord blood or peripheral blood from volunteer donors.
The team then transferred those cells to mice, and, this time, the mice developed t(4;11) pro-B ALL.
The researchers said this model “fully recapitulates the immunophenotypic and molecular aspects” of human t(4;11) pro-B ALL and will therefore be “a valuable tool” for studying the disease. ![]()

Photo by Petr Kratochvil
After trying for nearly 2 decades, researchers have created a mouse model of t(4;11) pro-B acute lymphoblastic
leukemia (ALL).
The team said this model, described in Cancer Cell, mimics the human disease phenotypically and molecularly.
This type of ALL, which is common in infants, results from the translocation t(4;11)(q21;q23), which fuses the mixed-lineage leukemia (MLL) gene on chromosome 11 to the ALL-1 fused gene on chromosome 4 (AF4).
“For 20 years, scientists have repeatedly tried and consistently failed to make a model of MLL-AF4 pro-B acute lymphoblastic leukemia,” said study author Michael Thirman, MD, of the University of Chicago in Illinois.
“Even though we understood the basic genetic flaw, no one had been able create a mouse model that mimicked the human disease, which is crucial for evaluating potential therapies.”
That frustrated many researchers, who shifted their focus to test alternative hypotheses on the causes of t(4;11) pro-B ALL or refocused their laboratories to study different aspects of the disease.
However, Dr Thirman and his colleagues began working on this problem “years ago,” he said, and stayed with it.
The team identified 2 hurdles. The first was a problem with the retrovirus used to insert the MLL-AF4 fusion gene into mouse cells.
“We soon discovered that the virus wasn’t working,” Dr Thirman explained. “We knew that certain parts of human DNA can decrease viral titers. So we switched from the human version of AF4 to the mouse version, Af4, which is slightly different. This increased viral titers 30-fold.”
That worked, but it led to the second hurdle. The mice injected with virus transporting MLL-Af4 developed leukemia, but it was acute myeloid leukemia.
So the researchers inserted the fused MLL-Af4 gene into human CD34 cells, which were derived from cord blood or peripheral blood from volunteer donors.
The team then transferred those cells to mice, and, this time, the mice developed t(4;11) pro-B ALL.
The researchers said this model “fully recapitulates the immunophenotypic and molecular aspects” of human t(4;11) pro-B ALL and will therefore be “a valuable tool” for studying the disease. ![]()