User login
Company stops development of eryaspase in ALL
Erytech Pharma said it plans to stop development of eryaspase for acute lymphoblastic leukemia (ALL).
This means withdrawal of the European marketing authorization application for eryaspase as a treatment for relapsed and refractory ALL.
However, Erytech will continue development of eryaspase as a treatment for certain solid tumor malignancies.
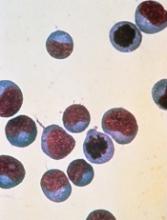
Eryaspase consists of L-asparaginase encapsulated inside donor-derived red blood cells. These enzyme-loaded red blood cells function as bioreactors to eliminate circulating asparagine and “starve” cancer cells, thereby inducing their death.
Erytech noted that eryaspase has produced favorable efficacy and safety results in ALL.
However, based on recent feedback from regulatory agencies in Europe and the US, the company believes significant additional investment would be required to seek regulatory approval of eryaspase for the treatment of ALL. Erytech also believes there would be a limited market opportunity for eryaspase in ALL.
Therefore, the company decided to cease further clinical development efforts in ALL. The resources that will become available as a result of this decision will be allocated to the development of eryaspase in solid tumors.
In 2017, Erytech announced results from a phase 2b clinical trial of eryaspase plus chemotherapy in patients with second-line metastatic pancreatic cancer. The company expects to begin enrollment in a phase 3 trial of this patient population in the third quarter of 2018.
In addition, Erytech is preparing for a pair of phase 2 proof-of-concept trials of eryaspase. One is in first-line pancreatic cancer, and the other is in metastatic triple-negative breast cancer. The company is also evaluating development options in additional solid tumor indications with high unmet medical need.
To ensure an adequate supply of eryaspase, Erytech is constructing a large-scale manufacturing facility in Princeton, New Jersey, and is expanding its manufacturing capacity in Lyon, France. The company expects both facilities to be operational for clinical production at the expanded capacity in the first quarter of 2019.
Erytech Pharma said it plans to stop development of eryaspase for acute lymphoblastic leukemia (ALL).
This means withdrawal of the European marketing authorization application for eryaspase as a treatment for relapsed and refractory ALL.
However, Erytech will continue development of eryaspase as a treatment for certain solid tumor malignancies.
Eryaspase consists of L-asparaginase encapsulated inside donor-derived red blood cells. These enzyme-loaded red blood cells function as bioreactors to eliminate circulating asparagine and “starve” cancer cells, thereby inducing their death.
Erytech noted that eryaspase has produced favorable efficacy and safety results in ALL.
However, based on recent feedback from regulatory agencies in Europe and the US, the company believes significant additional investment would be required to seek regulatory approval of eryaspase for the treatment of ALL. Erytech also believes there would be a limited market opportunity for eryaspase in ALL.
Therefore, the company decided to cease further clinical development efforts in ALL. The resources that will become available as a result of this decision will be allocated to the development of eryaspase in solid tumors.
In 2017, Erytech announced results from a phase 2b clinical trial of eryaspase plus chemotherapy in patients with second-line metastatic pancreatic cancer. The company expects to begin enrollment in a phase 3 trial of this patient population in the third quarter of 2018.
In addition, Erytech is preparing for a pair of phase 2 proof-of-concept trials of eryaspase. One is in first-line pancreatic cancer, and the other is in metastatic triple-negative breast cancer. The company is also evaluating development options in additional solid tumor indications with high unmet medical need.
To ensure an adequate supply of eryaspase, Erytech is constructing a large-scale manufacturing facility in Princeton, New Jersey, and is expanding its manufacturing capacity in Lyon, France. The company expects both facilities to be operational for clinical production at the expanded capacity in the first quarter of 2019.
Erytech Pharma said it plans to stop development of eryaspase for acute lymphoblastic leukemia (ALL).
This means withdrawal of the European marketing authorization application for eryaspase as a treatment for relapsed and refractory ALL.
However, Erytech will continue development of eryaspase as a treatment for certain solid tumor malignancies.
Eryaspase consists of L-asparaginase encapsulated inside donor-derived red blood cells. These enzyme-loaded red blood cells function as bioreactors to eliminate circulating asparagine and “starve” cancer cells, thereby inducing their death.
Erytech noted that eryaspase has produced favorable efficacy and safety results in ALL.
However, based on recent feedback from regulatory agencies in Europe and the US, the company believes significant additional investment would be required to seek regulatory approval of eryaspase for the treatment of ALL. Erytech also believes there would be a limited market opportunity for eryaspase in ALL.
Therefore, the company decided to cease further clinical development efforts in ALL. The resources that will become available as a result of this decision will be allocated to the development of eryaspase in solid tumors.
In 2017, Erytech announced results from a phase 2b clinical trial of eryaspase plus chemotherapy in patients with second-line metastatic pancreatic cancer. The company expects to begin enrollment in a phase 3 trial of this patient population in the third quarter of 2018.
In addition, Erytech is preparing for a pair of phase 2 proof-of-concept trials of eryaspase. One is in first-line pancreatic cancer, and the other is in metastatic triple-negative breast cancer. The company is also evaluating development options in additional solid tumor indications with high unmet medical need.
To ensure an adequate supply of eryaspase, Erytech is constructing a large-scale manufacturing facility in Princeton, New Jersey, and is expanding its manufacturing capacity in Lyon, France. The company expects both facilities to be operational for clinical production at the expanded capacity in the first quarter of 2019.
Avapritinib produces durable responses in SM
STOCKHOLM—The KIT/PDGFRA inhibitor avapritinib has produced durable responses in patients with systemic mastocytosis (SM).
In the phase 1 EXPLORER trial, avapritinib produced an overall response rate of 83%.
Responses have lasted up to 22 months, and 79% of responders remained on avapritinib as of the data cutoff.
The most common treatment-related adverse events (AEs) were periorbital edema, anemia, nausea, and fatigue.
These data were presented in a poster (abstract PF612) at the 23rd Congress of the European Hematology Association (EHA).
The trial was sponsored by Blueprint Medicines Corporation.
As of the data cutoff (April 30, 2018), 52 patients had been treated with avapritinib in the dose-escalation and expansion portions of the EXPLORER trial.
This included 25 patients with aggressive SM (ASM), 15 with advanced SM and an associated hematologic neoplasm (SM-AHN), 5 with mast cell leukemia (MCL), 5 pending central pathology diagnosis, and 2 with smoldering SM.
Thirty-five patients (67%) were previously treated, including 10 (19%) who previously received midostaurin. The patients’ median age was 63 (range, 34-83), and 52% were male.
Treatment
Thirty-two patients were treated in the dose-escalation portion of the study and received avapritinib at doses ranging from 30 mg to 400 mg daily. The 35 patients in the expansion portion received avapritinib at 300 mg daily.
Among all 52 enrolled patients, 42 remained on treatment as of the data cutoff date. Four patients discontinued treatment with avapritinib due to AEs. Three of these were treatment-related, and 1 was unrelated.
Three patients discontinued treatment due to clinical progression as determined by the investigator. None of the patients had documented disease progression by IWG-MRT-ECNM criteria.
Two patients discontinued due to investigator decision, and 1 withdrew consent.
Safety
All 52 patients were evaluable for safety.
Treatment-related AEs included periorbital edema (62%), anemia (33%), nausea (33%), fatigue (31%), peripheral edema (27%), diarrhea (25%), hair color changes (23%), thrombocytopenia (19%), cognitive effects (19%), vomiting (19%), and dizziness (12%).
Grade 3 or higher AEs, regardless of drug relationship, included thrombocytopenia (17%), anemia (15%), fatigue (6%), vomiting (6%), periorbital edema (4%), nausea (4%), diarrhea (2%), hair color changes (2%), and cognitive effects (2%).
Efficacy
As of the data cutoff, 23 patients were evaluable for response by IWG-MRT-ECNM criteria. This included 8 patients with ASM, 10 with SM-AHN, and 5 with MCL.
The overall response rate was 83% (n=19). All responses observed in the dose-escalation portion of the trial have been confirmed, and all responses in the dose-expansion portion of the trial are pending confirmation.
Four patients (17%) had a confirmed complete response with a full (n=1) or partial (n=3) recovery of peripheral blood counts. All of these responses occurred in patients with ASM.
Twelve patients (52%) had a partial response (7 confirmed, 5 pending confirmation). This included 6 patients with SM-AHN, 4 with MCL, and 2 with ASM.
Three patients (13%) had clinical improvement (2 confirmed, 1 pending confirmation), and 4 had stable disease. None of the patients progressed.
The duration of response ranged from 8 months to 22 months, and 79% of responders (15/19) remained on treatment at the data cutoff.
“As a clinician treating patients with this devastating and sometimes fatal rare disease, I’m excited to see that most patients with advanced systemic mastocytosis respond to treatment with avapritinib, and these responses deepen over time and are durable,” said study investigator Michael W. Deininger, MD, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City.
“These data further support avapritinib’s unique approach of selectively targeting D816V mutant KIT, the disease driver in most patients with systemic mastocytosis. If these results are confirmed in the planned phase 2 trial, avapritinib has the potential to become a new standard of care for patients with advanced forms of the disease.”
STOCKHOLM—The KIT/PDGFRA inhibitor avapritinib has produced durable responses in patients with systemic mastocytosis (SM).
In the phase 1 EXPLORER trial, avapritinib produced an overall response rate of 83%.
Responses have lasted up to 22 months, and 79% of responders remained on avapritinib as of the data cutoff.
The most common treatment-related adverse events (AEs) were periorbital edema, anemia, nausea, and fatigue.
These data were presented in a poster (abstract PF612) at the 23rd Congress of the European Hematology Association (EHA).
The trial was sponsored by Blueprint Medicines Corporation.
As of the data cutoff (April 30, 2018), 52 patients had been treated with avapritinib in the dose-escalation and expansion portions of the EXPLORER trial.
This included 25 patients with aggressive SM (ASM), 15 with advanced SM and an associated hematologic neoplasm (SM-AHN), 5 with mast cell leukemia (MCL), 5 pending central pathology diagnosis, and 2 with smoldering SM.
Thirty-five patients (67%) were previously treated, including 10 (19%) who previously received midostaurin. The patients’ median age was 63 (range, 34-83), and 52% were male.
Treatment
Thirty-two patients were treated in the dose-escalation portion of the study and received avapritinib at doses ranging from 30 mg to 400 mg daily. The 35 patients in the expansion portion received avapritinib at 300 mg daily.
Among all 52 enrolled patients, 42 remained on treatment as of the data cutoff date. Four patients discontinued treatment with avapritinib due to AEs. Three of these were treatment-related, and 1 was unrelated.
Three patients discontinued treatment due to clinical progression as determined by the investigator. None of the patients had documented disease progression by IWG-MRT-ECNM criteria.
Two patients discontinued due to investigator decision, and 1 withdrew consent.
Safety
All 52 patients were evaluable for safety.
Treatment-related AEs included periorbital edema (62%), anemia (33%), nausea (33%), fatigue (31%), peripheral edema (27%), diarrhea (25%), hair color changes (23%), thrombocytopenia (19%), cognitive effects (19%), vomiting (19%), and dizziness (12%).
Grade 3 or higher AEs, regardless of drug relationship, included thrombocytopenia (17%), anemia (15%), fatigue (6%), vomiting (6%), periorbital edema (4%), nausea (4%), diarrhea (2%), hair color changes (2%), and cognitive effects (2%).
Efficacy
As of the data cutoff, 23 patients were evaluable for response by IWG-MRT-ECNM criteria. This included 8 patients with ASM, 10 with SM-AHN, and 5 with MCL.
The overall response rate was 83% (n=19). All responses observed in the dose-escalation portion of the trial have been confirmed, and all responses in the dose-expansion portion of the trial are pending confirmation.
Four patients (17%) had a confirmed complete response with a full (n=1) or partial (n=3) recovery of peripheral blood counts. All of these responses occurred in patients with ASM.
Twelve patients (52%) had a partial response (7 confirmed, 5 pending confirmation). This included 6 patients with SM-AHN, 4 with MCL, and 2 with ASM.
Three patients (13%) had clinical improvement (2 confirmed, 1 pending confirmation), and 4 had stable disease. None of the patients progressed.
The duration of response ranged from 8 months to 22 months, and 79% of responders (15/19) remained on treatment at the data cutoff.
“As a clinician treating patients with this devastating and sometimes fatal rare disease, I’m excited to see that most patients with advanced systemic mastocytosis respond to treatment with avapritinib, and these responses deepen over time and are durable,” said study investigator Michael W. Deininger, MD, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City.
“These data further support avapritinib’s unique approach of selectively targeting D816V mutant KIT, the disease driver in most patients with systemic mastocytosis. If these results are confirmed in the planned phase 2 trial, avapritinib has the potential to become a new standard of care for patients with advanced forms of the disease.”
STOCKHOLM—The KIT/PDGFRA inhibitor avapritinib has produced durable responses in patients with systemic mastocytosis (SM).
In the phase 1 EXPLORER trial, avapritinib produced an overall response rate of 83%.
Responses have lasted up to 22 months, and 79% of responders remained on avapritinib as of the data cutoff.
The most common treatment-related adverse events (AEs) were periorbital edema, anemia, nausea, and fatigue.
These data were presented in a poster (abstract PF612) at the 23rd Congress of the European Hematology Association (EHA).
The trial was sponsored by Blueprint Medicines Corporation.
As of the data cutoff (April 30, 2018), 52 patients had been treated with avapritinib in the dose-escalation and expansion portions of the EXPLORER trial.
This included 25 patients with aggressive SM (ASM), 15 with advanced SM and an associated hematologic neoplasm (SM-AHN), 5 with mast cell leukemia (MCL), 5 pending central pathology diagnosis, and 2 with smoldering SM.
Thirty-five patients (67%) were previously treated, including 10 (19%) who previously received midostaurin. The patients’ median age was 63 (range, 34-83), and 52% were male.
Treatment
Thirty-two patients were treated in the dose-escalation portion of the study and received avapritinib at doses ranging from 30 mg to 400 mg daily. The 35 patients in the expansion portion received avapritinib at 300 mg daily.
Among all 52 enrolled patients, 42 remained on treatment as of the data cutoff date. Four patients discontinued treatment with avapritinib due to AEs. Three of these were treatment-related, and 1 was unrelated.
Three patients discontinued treatment due to clinical progression as determined by the investigator. None of the patients had documented disease progression by IWG-MRT-ECNM criteria.
Two patients discontinued due to investigator decision, and 1 withdrew consent.
Safety
All 52 patients were evaluable for safety.
Treatment-related AEs included periorbital edema (62%), anemia (33%), nausea (33%), fatigue (31%), peripheral edema (27%), diarrhea (25%), hair color changes (23%), thrombocytopenia (19%), cognitive effects (19%), vomiting (19%), and dizziness (12%).
Grade 3 or higher AEs, regardless of drug relationship, included thrombocytopenia (17%), anemia (15%), fatigue (6%), vomiting (6%), periorbital edema (4%), nausea (4%), diarrhea (2%), hair color changes (2%), and cognitive effects (2%).
Efficacy
As of the data cutoff, 23 patients were evaluable for response by IWG-MRT-ECNM criteria. This included 8 patients with ASM, 10 with SM-AHN, and 5 with MCL.
The overall response rate was 83% (n=19). All responses observed in the dose-escalation portion of the trial have been confirmed, and all responses in the dose-expansion portion of the trial are pending confirmation.
Four patients (17%) had a confirmed complete response with a full (n=1) or partial (n=3) recovery of peripheral blood counts. All of these responses occurred in patients with ASM.
Twelve patients (52%) had a partial response (7 confirmed, 5 pending confirmation). This included 6 patients with SM-AHN, 4 with MCL, and 2 with ASM.
Three patients (13%) had clinical improvement (2 confirmed, 1 pending confirmation), and 4 had stable disease. None of the patients progressed.
The duration of response ranged from 8 months to 22 months, and 79% of responders (15/19) remained on treatment at the data cutoff.
“As a clinician treating patients with this devastating and sometimes fatal rare disease, I’m excited to see that most patients with advanced systemic mastocytosis respond to treatment with avapritinib, and these responses deepen over time and are durable,” said study investigator Michael W. Deininger, MD, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City.
“These data further support avapritinib’s unique approach of selectively targeting D816V mutant KIT, the disease driver in most patients with systemic mastocytosis. If these results are confirmed in the planned phase 2 trial, avapritinib has the potential to become a new standard of care for patients with advanced forms of the disease.”
EC grants blinatumomab full approval
The European Commission (EC) has granted a full marketing authorization for blinatumomab (BLINCYTO®) as a treatment for adults with Philadelphia chromosome-negative (Ph-), relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
The EC granted blinatumomab conditional authorization for this indication in 2015. Now, the drug has full authorization based on overall survival (OS) data from the phase 3 TOWER study.
This authorization is valid in all European Union and European Economic Area-European Free Trade Association states (Norway, Iceland, and Liechtenstein).
Blinatumomab is a bispecific CD19-directed CD3 T cell engager (BiTE®) immunotherapy construct. It binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of effector T cells.
The TOWER study was a phase 3, randomized trial in which researchers compared blinatumomab to standard of care (SOC) chemotherapy in 405 adults with Ph-, relapsed/refractory B-cell precursor ALL.
Patients were randomized in a 2:1 ratio to receive blinatumomab (n=271) or investigator’s choice of SOC chemotherapy (n=134).
On the recommendation of an independent data monitoring committee, Amgen ended the study early for evidence of superior efficacy in the blinatumomab arm.
The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm (hazard ratio=0.71; P=0.012).
For patients treated in first salvage, the median OS was 11.1 months in the blinatumomab arm and 5.3 months in the SOC arm (hazard ratio=0.6).
Safety results in the blinatumomab arm were comparable to those seen in previous phase 2 studies.
These results were published in NEJM in March 2017.
The European Commission (EC) has granted a full marketing authorization for blinatumomab (BLINCYTO®) as a treatment for adults with Philadelphia chromosome-negative (Ph-), relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
The EC granted blinatumomab conditional authorization for this indication in 2015. Now, the drug has full authorization based on overall survival (OS) data from the phase 3 TOWER study.
This authorization is valid in all European Union and European Economic Area-European Free Trade Association states (Norway, Iceland, and Liechtenstein).
Blinatumomab is a bispecific CD19-directed CD3 T cell engager (BiTE®) immunotherapy construct. It binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of effector T cells.
The TOWER study was a phase 3, randomized trial in which researchers compared blinatumomab to standard of care (SOC) chemotherapy in 405 adults with Ph-, relapsed/refractory B-cell precursor ALL.
Patients were randomized in a 2:1 ratio to receive blinatumomab (n=271) or investigator’s choice of SOC chemotherapy (n=134).
On the recommendation of an independent data monitoring committee, Amgen ended the study early for evidence of superior efficacy in the blinatumomab arm.
The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm (hazard ratio=0.71; P=0.012).
For patients treated in first salvage, the median OS was 11.1 months in the blinatumomab arm and 5.3 months in the SOC arm (hazard ratio=0.6).
Safety results in the blinatumomab arm were comparable to those seen in previous phase 2 studies.
These results were published in NEJM in March 2017.
The European Commission (EC) has granted a full marketing authorization for blinatumomab (BLINCYTO®) as a treatment for adults with Philadelphia chromosome-negative (Ph-), relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
The EC granted blinatumomab conditional authorization for this indication in 2015. Now, the drug has full authorization based on overall survival (OS) data from the phase 3 TOWER study.
This authorization is valid in all European Union and European Economic Area-European Free Trade Association states (Norway, Iceland, and Liechtenstein).
Blinatumomab is a bispecific CD19-directed CD3 T cell engager (BiTE®) immunotherapy construct. It binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of effector T cells.
The TOWER study was a phase 3, randomized trial in which researchers compared blinatumomab to standard of care (SOC) chemotherapy in 405 adults with Ph-, relapsed/refractory B-cell precursor ALL.
Patients were randomized in a 2:1 ratio to receive blinatumomab (n=271) or investigator’s choice of SOC chemotherapy (n=134).
On the recommendation of an independent data monitoring committee, Amgen ended the study early for evidence of superior efficacy in the blinatumomab arm.
The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm (hazard ratio=0.71; P=0.012).
For patients treated in first salvage, the median OS was 11.1 months in the blinatumomab arm and 5.3 months in the SOC arm (hazard ratio=0.6).
Safety results in the blinatumomab arm were comparable to those seen in previous phase 2 studies.
These results were published in NEJM in March 2017.
Gene signature might identify patients at risk of CAR T-associated neurotoxicity
CHICAGO—A specific gene signature might be able to identify patients at risk of CD19 CAR T-cell associated neurotoxicity, according to results of an exploratory analysis presented at the 2018 ASCO Annual Meeting.
The analysis, based on bone marrow samples from patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) treated with JCAR015 in the ROCKET trial, helped identify a set of neurotoxicity-associated genes that separated patients based on molecular subtype.
“These findings suggest that patient risk stratification by molecular subtype of disease or gene expression signature may play a role in identifying patients at elevated risk of neurotoxicity,” said Jae Park, MD, of Memorial Sloan Kettering Cancer Center, New York, New York, in a presentation of the findings (abstract 7007).
The phase 2 ROCKET study included adult patients with relapsed or refractory morphological (>5% blasts in bone marrow) CD-19 positive disease in first salvage or greater, including post allogeneic hematopoietic stem cell transplantation (HSCT). Prior blinatumomab was allowed.
The tumor gene expression study presented at ASCO was based on sequenced RNA from pre-apheresis bone marrow samples available for 31 patients in the ROCKET study.
Investigators identified a set of 10 genes expressed more frequently in bone marrow samples from patients in ROCKET with low (grade 0-1) neurotoxicity, and 7 that were more frequent in those who had severe (grade 4-5) neurotoxicity.
Looking at B-cell ALL samples in public datasets by molecular subtype, they found genes highly expressed in the low neurotoxicity ROCKET patients were also highly expressed in Philadelphia chromosome-positive (Ph+) and Ph-like subtypes.
Conversely, the genes highly expressed in the severe neurotoxicity patients were also highly expressed in non-Ph-like samples.
A total of 16 ROCKET patients were classified as having Ph-like gene expression and 15 as having non-Ph-like expression.
There were no grade 4-5 neurotoxicity events in the Ph-like patients, while both grade 3+ and grade 4+ neurotoxicity were significantly more prevalent in the non-Ph-like patients, investigators reported.
One of the most differentially expressed genes in the set was CCL17, which was higher in the low-neurotoxicity tumor samples, and likewise highly expressed in Ph-like B-cell ALL, according to the report.
“[CCL17] may serve as an early biomarker for differentiating severe neurotoxicity,” Dr Park said.
These findings are now being validated in the previously mentioned data set, as well as other studies to see if the findings can be replicated, according to Dr Park.
Juno Therapeutics, a Celgene company, shut down the phase 2 ROCKET trial of JCAR015 in 2017 after 2 clinical holds in 2016 and 5 patient deaths.
CHICAGO—A specific gene signature might be able to identify patients at risk of CD19 CAR T-cell associated neurotoxicity, according to results of an exploratory analysis presented at the 2018 ASCO Annual Meeting.
The analysis, based on bone marrow samples from patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) treated with JCAR015 in the ROCKET trial, helped identify a set of neurotoxicity-associated genes that separated patients based on molecular subtype.
“These findings suggest that patient risk stratification by molecular subtype of disease or gene expression signature may play a role in identifying patients at elevated risk of neurotoxicity,” said Jae Park, MD, of Memorial Sloan Kettering Cancer Center, New York, New York, in a presentation of the findings (abstract 7007).
The phase 2 ROCKET study included adult patients with relapsed or refractory morphological (>5% blasts in bone marrow) CD-19 positive disease in first salvage or greater, including post allogeneic hematopoietic stem cell transplantation (HSCT). Prior blinatumomab was allowed.
The tumor gene expression study presented at ASCO was based on sequenced RNA from pre-apheresis bone marrow samples available for 31 patients in the ROCKET study.
Investigators identified a set of 10 genes expressed more frequently in bone marrow samples from patients in ROCKET with low (grade 0-1) neurotoxicity, and 7 that were more frequent in those who had severe (grade 4-5) neurotoxicity.
Looking at B-cell ALL samples in public datasets by molecular subtype, they found genes highly expressed in the low neurotoxicity ROCKET patients were also highly expressed in Philadelphia chromosome-positive (Ph+) and Ph-like subtypes.
Conversely, the genes highly expressed in the severe neurotoxicity patients were also highly expressed in non-Ph-like samples.
A total of 16 ROCKET patients were classified as having Ph-like gene expression and 15 as having non-Ph-like expression.
There were no grade 4-5 neurotoxicity events in the Ph-like patients, while both grade 3+ and grade 4+ neurotoxicity were significantly more prevalent in the non-Ph-like patients, investigators reported.
One of the most differentially expressed genes in the set was CCL17, which was higher in the low-neurotoxicity tumor samples, and likewise highly expressed in Ph-like B-cell ALL, according to the report.
“[CCL17] may serve as an early biomarker for differentiating severe neurotoxicity,” Dr Park said.
These findings are now being validated in the previously mentioned data set, as well as other studies to see if the findings can be replicated, according to Dr Park.
Juno Therapeutics, a Celgene company, shut down the phase 2 ROCKET trial of JCAR015 in 2017 after 2 clinical holds in 2016 and 5 patient deaths.
CHICAGO—A specific gene signature might be able to identify patients at risk of CD19 CAR T-cell associated neurotoxicity, according to results of an exploratory analysis presented at the 2018 ASCO Annual Meeting.
The analysis, based on bone marrow samples from patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) treated with JCAR015 in the ROCKET trial, helped identify a set of neurotoxicity-associated genes that separated patients based on molecular subtype.
“These findings suggest that patient risk stratification by molecular subtype of disease or gene expression signature may play a role in identifying patients at elevated risk of neurotoxicity,” said Jae Park, MD, of Memorial Sloan Kettering Cancer Center, New York, New York, in a presentation of the findings (abstract 7007).
The phase 2 ROCKET study included adult patients with relapsed or refractory morphological (>5% blasts in bone marrow) CD-19 positive disease in first salvage or greater, including post allogeneic hematopoietic stem cell transplantation (HSCT). Prior blinatumomab was allowed.
The tumor gene expression study presented at ASCO was based on sequenced RNA from pre-apheresis bone marrow samples available for 31 patients in the ROCKET study.
Investigators identified a set of 10 genes expressed more frequently in bone marrow samples from patients in ROCKET with low (grade 0-1) neurotoxicity, and 7 that were more frequent in those who had severe (grade 4-5) neurotoxicity.
Looking at B-cell ALL samples in public datasets by molecular subtype, they found genes highly expressed in the low neurotoxicity ROCKET patients were also highly expressed in Philadelphia chromosome-positive (Ph+) and Ph-like subtypes.
Conversely, the genes highly expressed in the severe neurotoxicity patients were also highly expressed in non-Ph-like samples.
A total of 16 ROCKET patients were classified as having Ph-like gene expression and 15 as having non-Ph-like expression.
There were no grade 4-5 neurotoxicity events in the Ph-like patients, while both grade 3+ and grade 4+ neurotoxicity were significantly more prevalent in the non-Ph-like patients, investigators reported.
One of the most differentially expressed genes in the set was CCL17, which was higher in the low-neurotoxicity tumor samples, and likewise highly expressed in Ph-like B-cell ALL, according to the report.
“[CCL17] may serve as an early biomarker for differentiating severe neurotoxicity,” Dr Park said.
These findings are now being validated in the previously mentioned data set, as well as other studies to see if the findings can be replicated, according to Dr Park.
Juno Therapeutics, a Celgene company, shut down the phase 2 ROCKET trial of JCAR015 in 2017 after 2 clinical holds in 2016 and 5 patient deaths.
FDA places SB-generated CAR T-cell therapy on clinical hold
The US Food and Drug Administrated (FDA) placed a clinical hold on the phase 1 trial of the Sleeping Beauty (SB)-generated CAR T-cell therapy in relapsed or refractory leukemia and lymphoma patients.
The Sleeping Beauty platform was designed to very rapidly manufacture CD19-specific CAR T cells at the point of care.
All SB-CAR T-cell processing is planned to take place within 2 days at the healthcare facility, thus eliminating shipping cells from hospitals to production sites and back again.
The FDA is requesting more chemistry, manufacturing, and control (CMC) information before allowing the trial to proceed.
The Sleeping Beauty technology, a non-viral transposon/transposase system, has the potential to reduce the costs and complexity associated with recombinant viral vector-based immunotherapy, according to developers.
Ziopharm Oncology, Precigen, Inc, a wholly owned subsidiary of Intrexon Corporation, and the University of Texas MD Anderson Cancer Center, are developing the Sleeping Beauty CAR T cell therapy.
“We know what is needed to address the hold issues and are looking forward to responding to the agency in a timely manner,” said Laurence Cooper, MD, PhD, chief executive officer of Ziopharm, in a corporate release.
“We are undertaking cutting-edge science and are on the verge of a paradigm shift based on our approach to very rapidly manufacture CD19-specific T cells within 2 days using our non-viral approach to CAR-T therapy based on the Sleeping Beauty platform.”
The phase 1 trial in question is a third-generation trial in which the CAR T cells are designed to co-express CD19-specific CAR, membrane-bound interleukin 15, and a safety switch.
The findings from earlier generation phase 1 trials have been previously reported in The Journal of Clinical Investigation.
The US Food and Drug Administrated (FDA) placed a clinical hold on the phase 1 trial of the Sleeping Beauty (SB)-generated CAR T-cell therapy in relapsed or refractory leukemia and lymphoma patients.
The Sleeping Beauty platform was designed to very rapidly manufacture CD19-specific CAR T cells at the point of care.
All SB-CAR T-cell processing is planned to take place within 2 days at the healthcare facility, thus eliminating shipping cells from hospitals to production sites and back again.
The FDA is requesting more chemistry, manufacturing, and control (CMC) information before allowing the trial to proceed.
The Sleeping Beauty technology, a non-viral transposon/transposase system, has the potential to reduce the costs and complexity associated with recombinant viral vector-based immunotherapy, according to developers.
Ziopharm Oncology, Precigen, Inc, a wholly owned subsidiary of Intrexon Corporation, and the University of Texas MD Anderson Cancer Center, are developing the Sleeping Beauty CAR T cell therapy.
“We know what is needed to address the hold issues and are looking forward to responding to the agency in a timely manner,” said Laurence Cooper, MD, PhD, chief executive officer of Ziopharm, in a corporate release.
“We are undertaking cutting-edge science and are on the verge of a paradigm shift based on our approach to very rapidly manufacture CD19-specific T cells within 2 days using our non-viral approach to CAR-T therapy based on the Sleeping Beauty platform.”
The phase 1 trial in question is a third-generation trial in which the CAR T cells are designed to co-express CD19-specific CAR, membrane-bound interleukin 15, and a safety switch.
The findings from earlier generation phase 1 trials have been previously reported in The Journal of Clinical Investigation.
The US Food and Drug Administrated (FDA) placed a clinical hold on the phase 1 trial of the Sleeping Beauty (SB)-generated CAR T-cell therapy in relapsed or refractory leukemia and lymphoma patients.
The Sleeping Beauty platform was designed to very rapidly manufacture CD19-specific CAR T cells at the point of care.
All SB-CAR T-cell processing is planned to take place within 2 days at the healthcare facility, thus eliminating shipping cells from hospitals to production sites and back again.
The FDA is requesting more chemistry, manufacturing, and control (CMC) information before allowing the trial to proceed.
The Sleeping Beauty technology, a non-viral transposon/transposase system, has the potential to reduce the costs and complexity associated with recombinant viral vector-based immunotherapy, according to developers.
Ziopharm Oncology, Precigen, Inc, a wholly owned subsidiary of Intrexon Corporation, and the University of Texas MD Anderson Cancer Center, are developing the Sleeping Beauty CAR T cell therapy.
“We know what is needed to address the hold issues and are looking forward to responding to the agency in a timely manner,” said Laurence Cooper, MD, PhD, chief executive officer of Ziopharm, in a corporate release.
“We are undertaking cutting-edge science and are on the verge of a paradigm shift based on our approach to very rapidly manufacture CD19-specific T cells within 2 days using our non-viral approach to CAR-T therapy based on the Sleeping Beauty platform.”
The phase 1 trial in question is a third-generation trial in which the CAR T cells are designed to co-express CD19-specific CAR, membrane-bound interleukin 15, and a safety switch.
The findings from earlier generation phase 1 trials have been previously reported in The Journal of Clinical Investigation.
Quizartinib can prolong OS in rel/ref, FLT3-ITD AML
STOCKHOLM—Phase 3 results suggest the FLT3 inhibitor quizartinib can prolong overall survival (OS) in patients with relapsed/refractory, FLT3-ITD acute myeloid leukemia (AML).
In the QuANTUM-R study, patients who received single-agent quizartinib had a significantly longer median OS than patients who received salvage chemotherapy.
There was a trend toward improved event-free survival (EFS) with quizartinib as well.
“QuANTUM-R represents the first study that shows a significant improvement in overall survival for a single agent—a FLT3 inhibitor or any other targeted agent—in this population of FLT3-mutated AML patients with refractory or relapsed disease . . .,” said study investigator Jorge Cortes, MD, of MD Anderson Cancer Center in Houston, Texas.
Dr Cortes presented results from QuANTUM-R at the 23rd Congress of the European Hematology Association (EHA). The research was selected as the best late-breaking abstract (LB2600).
The study was funded by Daiichi Sankyo, Inc., and Dr Cortes is a consultant for the company.
Patients and treatment
QuANTUM-R enrolled adults with FLT3-ITD AML (at least 3% FLT3-ITD allelic ratio) who had refractory disease or had relapsed within 6 months of their first complete remission. They had received at least 1 cycle of an induction regimen containing standard-dose anthracycline or mitoxantrone.
Patients were randomized to receive once-daily treatment with quizartinib (n=245) or a salvage chemotherapy regimen (n=122)—low-dose cytarabine (LoDAC, n=29); combination mitoxantrone, etoposide, and cytarabine (MEC, n=40); or combination fludarabine, cytarabine, and idarubicin (FLAG-IDA, n=53).
Responders could proceed to hematopoietic stem cell transplant (HSCT), and those in the quizartinib arm could resume quizartinib after HSCT.
Baseline characteristics were similar between the treatment arms. The median age was 55 (range, 19-81) for patients receiving quizartinib and 58 (range, 18-78) for those receiving chemotherapy.
Thirty-three percent of the quizartinib arm had refractory disease, and 67% had relapsed disease. Thirty-four percent of the chemotherapy arm had refractory disease, and 66% had relapsed disease.
The percentage of patients with a prior allogeneic HSCT was 25% in the quizartinib arm and 23% in the chemotherapy arm. Most patients in both arms had intermediate-risk cytogenetics—78% of the quizartinib arm and 66% of the chemotherapy arm.
In all, 241 patients received quizartinib, and 94 received salvage chemotherapy—LoDAC (n=22), MEC (n=25), and FLAG-IDA (n=47). Of the 28 patients in the chemotherapy group who were not treated, most withdrew consent.
The median treatment duration was 4 cycles (range, 1-3) in the quizartinib arm and 1 cycle (range, 1-2) for patients who received LoDAC, MEC, and FLAG-IDA.
The most common reason for discontinuation of chemotherapy was lack of response/progression (n=49), followed by death (n=6). Twenty-four patients completed salvage chemotherapy.
In the quizarinib arm, the most common reasons for treatment discontinuation were HSCT (n=79), relapse (n=60), or lack of response/progression (n=47).
Thirty-two percent of quizartinib-treated patients and 12% of the chemotherapy group went on to HSCT.
Results
The median follow-up was 23.5 months. The efficacy results include all randomized patients, and the safety results include only those who received their assigned treatment.
The study’s primary endpoint was OS. The median OS was 6.2 months in the quizartinib arm and 4.7 months in the chemotherapy arm (hazard ratio=0.76, P=0.0177). The 1-year OS rate was 27% and 20%, respectively.
The median EFS was 6.0 weeks in the quizartinib arm and 3.7 weeks in the chemotherapy arm (hazard ratio=0.90, P=0.1071). Dr Cortes noted that patients who did not receive treatment were censored on day 1, and partial responses were counted as failures in the EFS analysis.
The overall response rate was 69% in the quizartinib arm and 30% in the chemotherapy arm.
The composite complete response (CR) rate was 48% in the quizartinib arm and 27% in the chemotherapy arm. This includes the CR rate (4% and 1%, respectively), the rate of CR with incomplete platelet recovery (4% and 0%, respectively), and the rate of CR with incomplete hematologic recovery (40% and 26%, respectively). The rate of partial response was 21% and 3%, respectively.
Dr Cortes said rates of treatment-emergent adverse events (TEAEs) were similar between the treatment arms.
Grade 3 or higher hematologic TEAEs occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included thrombocytopenia (35% and 34%), anemia (30% and 29%), neutropenia (32% and 25%), febrile neutropenia (31% and 21%), and leukopenia (17% and 16%).
Grade 3 or higher nonhematologic TEAEs occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included fatigue (8% and 1%), hypokalemia (12% and 9%), sepsis/septic shock (16% and 18%), dyspnea (5% for both), hypophosphatemia (5% for both), and pneumonia (12% and 9%).
Three percent of patients in the quizartinib arm had grade 3 QTcF prolongation, but there were no grade 4 cases. Two patients discontinued quizartinib due to QTcF prolongation.
“The safety of this drug has remained constant across over 1600 patients that have been treated with quizartinib across a variety of studies,” Dr Cortes said.
He added that QuANTUM-R results open up the possibility that quizartinib could be used in other settings. Researchers are already testing standard chemotherapy with and without quizartinib in a phase 3 trial of patients with newly diagnosed, FLT-ITD AML (QuANTUM-First).
STOCKHOLM—Phase 3 results suggest the FLT3 inhibitor quizartinib can prolong overall survival (OS) in patients with relapsed/refractory, FLT3-ITD acute myeloid leukemia (AML).
In the QuANTUM-R study, patients who received single-agent quizartinib had a significantly longer median OS than patients who received salvage chemotherapy.
There was a trend toward improved event-free survival (EFS) with quizartinib as well.
“QuANTUM-R represents the first study that shows a significant improvement in overall survival for a single agent—a FLT3 inhibitor or any other targeted agent—in this population of FLT3-mutated AML patients with refractory or relapsed disease . . .,” said study investigator Jorge Cortes, MD, of MD Anderson Cancer Center in Houston, Texas.
Dr Cortes presented results from QuANTUM-R at the 23rd Congress of the European Hematology Association (EHA). The research was selected as the best late-breaking abstract (LB2600).
The study was funded by Daiichi Sankyo, Inc., and Dr Cortes is a consultant for the company.
Patients and treatment
QuANTUM-R enrolled adults with FLT3-ITD AML (at least 3% FLT3-ITD allelic ratio) who had refractory disease or had relapsed within 6 months of their first complete remission. They had received at least 1 cycle of an induction regimen containing standard-dose anthracycline or mitoxantrone.
Patients were randomized to receive once-daily treatment with quizartinib (n=245) or a salvage chemotherapy regimen (n=122)—low-dose cytarabine (LoDAC, n=29); combination mitoxantrone, etoposide, and cytarabine (MEC, n=40); or combination fludarabine, cytarabine, and idarubicin (FLAG-IDA, n=53).
Responders could proceed to hematopoietic stem cell transplant (HSCT), and those in the quizartinib arm could resume quizartinib after HSCT.
Baseline characteristics were similar between the treatment arms. The median age was 55 (range, 19-81) for patients receiving quizartinib and 58 (range, 18-78) for those receiving chemotherapy.
Thirty-three percent of the quizartinib arm had refractory disease, and 67% had relapsed disease. Thirty-four percent of the chemotherapy arm had refractory disease, and 66% had relapsed disease.
The percentage of patients with a prior allogeneic HSCT was 25% in the quizartinib arm and 23% in the chemotherapy arm. Most patients in both arms had intermediate-risk cytogenetics—78% of the quizartinib arm and 66% of the chemotherapy arm.
In all, 241 patients received quizartinib, and 94 received salvage chemotherapy—LoDAC (n=22), MEC (n=25), and FLAG-IDA (n=47). Of the 28 patients in the chemotherapy group who were not treated, most withdrew consent.
The median treatment duration was 4 cycles (range, 1-3) in the quizartinib arm and 1 cycle (range, 1-2) for patients who received LoDAC, MEC, and FLAG-IDA.
The most common reason for discontinuation of chemotherapy was lack of response/progression (n=49), followed by death (n=6). Twenty-four patients completed salvage chemotherapy.
In the quizarinib arm, the most common reasons for treatment discontinuation were HSCT (n=79), relapse (n=60), or lack of response/progression (n=47).
Thirty-two percent of quizartinib-treated patients and 12% of the chemotherapy group went on to HSCT.
Results
The median follow-up was 23.5 months. The efficacy results include all randomized patients, and the safety results include only those who received their assigned treatment.
The study’s primary endpoint was OS. The median OS was 6.2 months in the quizartinib arm and 4.7 months in the chemotherapy arm (hazard ratio=0.76, P=0.0177). The 1-year OS rate was 27% and 20%, respectively.
The median EFS was 6.0 weeks in the quizartinib arm and 3.7 weeks in the chemotherapy arm (hazard ratio=0.90, P=0.1071). Dr Cortes noted that patients who did not receive treatment were censored on day 1, and partial responses were counted as failures in the EFS analysis.
The overall response rate was 69% in the quizartinib arm and 30% in the chemotherapy arm.
The composite complete response (CR) rate was 48% in the quizartinib arm and 27% in the chemotherapy arm. This includes the CR rate (4% and 1%, respectively), the rate of CR with incomplete platelet recovery (4% and 0%, respectively), and the rate of CR with incomplete hematologic recovery (40% and 26%, respectively). The rate of partial response was 21% and 3%, respectively.
Dr Cortes said rates of treatment-emergent adverse events (TEAEs) were similar between the treatment arms.
Grade 3 or higher hematologic TEAEs occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included thrombocytopenia (35% and 34%), anemia (30% and 29%), neutropenia (32% and 25%), febrile neutropenia (31% and 21%), and leukopenia (17% and 16%).
Grade 3 or higher nonhematologic TEAEs occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included fatigue (8% and 1%), hypokalemia (12% and 9%), sepsis/septic shock (16% and 18%), dyspnea (5% for both), hypophosphatemia (5% for both), and pneumonia (12% and 9%).
Three percent of patients in the quizartinib arm had grade 3 QTcF prolongation, but there were no grade 4 cases. Two patients discontinued quizartinib due to QTcF prolongation.
“The safety of this drug has remained constant across over 1600 patients that have been treated with quizartinib across a variety of studies,” Dr Cortes said.
He added that QuANTUM-R results open up the possibility that quizartinib could be used in other settings. Researchers are already testing standard chemotherapy with and without quizartinib in a phase 3 trial of patients with newly diagnosed, FLT-ITD AML (QuANTUM-First).
STOCKHOLM—Phase 3 results suggest the FLT3 inhibitor quizartinib can prolong overall survival (OS) in patients with relapsed/refractory, FLT3-ITD acute myeloid leukemia (AML).
In the QuANTUM-R study, patients who received single-agent quizartinib had a significantly longer median OS than patients who received salvage chemotherapy.
There was a trend toward improved event-free survival (EFS) with quizartinib as well.
“QuANTUM-R represents the first study that shows a significant improvement in overall survival for a single agent—a FLT3 inhibitor or any other targeted agent—in this population of FLT3-mutated AML patients with refractory or relapsed disease . . .,” said study investigator Jorge Cortes, MD, of MD Anderson Cancer Center in Houston, Texas.
Dr Cortes presented results from QuANTUM-R at the 23rd Congress of the European Hematology Association (EHA). The research was selected as the best late-breaking abstract (LB2600).
The study was funded by Daiichi Sankyo, Inc., and Dr Cortes is a consultant for the company.
Patients and treatment
QuANTUM-R enrolled adults with FLT3-ITD AML (at least 3% FLT3-ITD allelic ratio) who had refractory disease or had relapsed within 6 months of their first complete remission. They had received at least 1 cycle of an induction regimen containing standard-dose anthracycline or mitoxantrone.
Patients were randomized to receive once-daily treatment with quizartinib (n=245) or a salvage chemotherapy regimen (n=122)—low-dose cytarabine (LoDAC, n=29); combination mitoxantrone, etoposide, and cytarabine (MEC, n=40); or combination fludarabine, cytarabine, and idarubicin (FLAG-IDA, n=53).
Responders could proceed to hematopoietic stem cell transplant (HSCT), and those in the quizartinib arm could resume quizartinib after HSCT.
Baseline characteristics were similar between the treatment arms. The median age was 55 (range, 19-81) for patients receiving quizartinib and 58 (range, 18-78) for those receiving chemotherapy.
Thirty-three percent of the quizartinib arm had refractory disease, and 67% had relapsed disease. Thirty-four percent of the chemotherapy arm had refractory disease, and 66% had relapsed disease.
The percentage of patients with a prior allogeneic HSCT was 25% in the quizartinib arm and 23% in the chemotherapy arm. Most patients in both arms had intermediate-risk cytogenetics—78% of the quizartinib arm and 66% of the chemotherapy arm.
In all, 241 patients received quizartinib, and 94 received salvage chemotherapy—LoDAC (n=22), MEC (n=25), and FLAG-IDA (n=47). Of the 28 patients in the chemotherapy group who were not treated, most withdrew consent.
The median treatment duration was 4 cycles (range, 1-3) in the quizartinib arm and 1 cycle (range, 1-2) for patients who received LoDAC, MEC, and FLAG-IDA.
The most common reason for discontinuation of chemotherapy was lack of response/progression (n=49), followed by death (n=6). Twenty-four patients completed salvage chemotherapy.
In the quizarinib arm, the most common reasons for treatment discontinuation were HSCT (n=79), relapse (n=60), or lack of response/progression (n=47).
Thirty-two percent of quizartinib-treated patients and 12% of the chemotherapy group went on to HSCT.
Results
The median follow-up was 23.5 months. The efficacy results include all randomized patients, and the safety results include only those who received their assigned treatment.
The study’s primary endpoint was OS. The median OS was 6.2 months in the quizartinib arm and 4.7 months in the chemotherapy arm (hazard ratio=0.76, P=0.0177). The 1-year OS rate was 27% and 20%, respectively.
The median EFS was 6.0 weeks in the quizartinib arm and 3.7 weeks in the chemotherapy arm (hazard ratio=0.90, P=0.1071). Dr Cortes noted that patients who did not receive treatment were censored on day 1, and partial responses were counted as failures in the EFS analysis.
The overall response rate was 69% in the quizartinib arm and 30% in the chemotherapy arm.
The composite complete response (CR) rate was 48% in the quizartinib arm and 27% in the chemotherapy arm. This includes the CR rate (4% and 1%, respectively), the rate of CR with incomplete platelet recovery (4% and 0%, respectively), and the rate of CR with incomplete hematologic recovery (40% and 26%, respectively). The rate of partial response was 21% and 3%, respectively.
Dr Cortes said rates of treatment-emergent adverse events (TEAEs) were similar between the treatment arms.
Grade 3 or higher hematologic TEAEs occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included thrombocytopenia (35% and 34%), anemia (30% and 29%), neutropenia (32% and 25%), febrile neutropenia (31% and 21%), and leukopenia (17% and 16%).
Grade 3 or higher nonhematologic TEAEs occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included fatigue (8% and 1%), hypokalemia (12% and 9%), sepsis/septic shock (16% and 18%), dyspnea (5% for both), hypophosphatemia (5% for both), and pneumonia (12% and 9%).
Three percent of patients in the quizartinib arm had grade 3 QTcF prolongation, but there were no grade 4 cases. Two patients discontinued quizartinib due to QTcF prolongation.
“The safety of this drug has remained constant across over 1600 patients that have been treated with quizartinib across a variety of studies,” Dr Cortes said.
He added that QuANTUM-R results open up the possibility that quizartinib could be used in other settings. Researchers are already testing standard chemotherapy with and without quizartinib in a phase 3 trial of patients with newly diagnosed, FLT-ITD AML (QuANTUM-First).
Anti-CD22 CAR T rescues kids with ALL after CD19 failure
STOCKHOLM, SWEDEN – A novel chimeric antigen receptor T-cell construct directed against CD22 was able to rescue children with relapsed or refractory B-cell acute lymphoblastic leukemia for whom CD19-directed CAR T therapy had failed, investigators from China reported.
Thirty days after CAR T cell infusion, 12 of 15 children (80%) treated with the unnamed CD22 CAR T product had a complete response (CR) and one (6.7%) had a partial response (PR), for an overall response rate (ORR) of 86.7%, said Jing Pan, MD, from the Beijing Boren Hospital in China.
Surprisingly for a therapy of its type, the CD22 CAR T was well tolerated, with only mild cases of the cytokine release syndrome (CRS), and it could be delivered safely in children with relapsed disease after hematopoietic cell transplants (HCT), she reported in a briefing and in an oral abstract session at the annual congress of the European Hematology Association.
“CD22 CAR T immunotherapy brings hope for patients with refractory or relapsed B-ALL who failed on CD19 CAR T immunotherapy, and we think it’s quite safe. No children died and no children had severe side effects during the study, even in post-HCT patients,” Dr. Pan said.
She noted that in a previous clinical trial by her group, some patients experienced relapses and were resistant to retreatment with CD19-directed CAR T therapy due to mutations or loss of the CD19 antigen (Leukemia. 2017 Dec;31[12]:2587-93).
Since CD22 is highly expressed on leukemic cells in children with B-ALL, the investigators decided to evaluate the safety and efficacy of a CD22 CAR T as a rescue strategy. They enrolled 15 patients who either experienced relapse or did not have a response to CD19 CAR T immunotherapy. The CAR T construct they used contains an anti-CD22 single-chain variable fragment derived from a humanized CD22 antibody.
Patient conditioning with fludarabine and cyclophosphamide was performed simultaneously with CAR T transfection and expansion. After about 7 days, the expanded and transformed CAR T cells were infused at a dose of 8.2 x 105/kg in patients who had not undergone HCT, and 0.9 x 105 in patients who had received a transplant.
The patients ranged from 2 to 18 years old (median 8 years), had a median disease course of 21 months (range 5-84 months), and had a median of 42% bone marrow blasts (range 5%-95.5%).
Four of the 15 patients had relapses following allogeneic HCT, and the remaining 11 had relapses following chemotherapy. Two of the patients were found to be minimal residual disease (MRD)-positive by flow cytometry. Two patients had extramedullary disease only at relapse.
Ten of 11 patients who had experienced a hematologic relapse had either a CR or CR with incomplete recovery of counts (CRi), and of these 10 patients, nine were determined on follow-up to be MRD-negative by flow cytometry.
One of the two patients with extramedullary disease had a CR, and the other had a partial response.
Although two patients had no response to CD22 CAR T therapy, expression of the antigen was strong on leukemia cells from these patients, Dr. Pan said.
All patients experienced CRS, but none had greater than grade 2, Dr. Pan said, although she did not provide give specific numbers. Two patients had grade 1 neurotoxicity, two patients had grade 2 hypoxemia, and one patient had grade 2 liver enzyme elevation.
At a median follow-up of 108 days, six patients had been bridged to allogeneic HCT, and eleven of 12 patients who had a CR or CRi at 30 days had no evidence of disease progression. The remaining patient with an initial CR or CRi had a relapse at day 50. The 6-month progression-free survival rate was 91.7%.
Anton Hagenbeek, MD, PhD, from the Academic Medical Center at the University of Amsterdam, the Netherlands, who moderated the briefing but was not involved in the study, commented that given the high leukemia burden of the patients and the apparent efficacy of the therapy, one would expect to see higher grades of CRS, and asked Dr. Pan whether she could account for the CRS findings in her study, compared with those of trials for CD19-directed CAR T therapy.
It may have to do with differences in density of CD22 expression, compared with CD19 expression on leukemia cells, or on differences in the antibody used to target the cells, Dr. Pan said.
SOURCE: Pan J et al. EHA Congress, Abstract S832.
STOCKHOLM, SWEDEN – A novel chimeric antigen receptor T-cell construct directed against CD22 was able to rescue children with relapsed or refractory B-cell acute lymphoblastic leukemia for whom CD19-directed CAR T therapy had failed, investigators from China reported.
Thirty days after CAR T cell infusion, 12 of 15 children (80%) treated with the unnamed CD22 CAR T product had a complete response (CR) and one (6.7%) had a partial response (PR), for an overall response rate (ORR) of 86.7%, said Jing Pan, MD, from the Beijing Boren Hospital in China.
Surprisingly for a therapy of its type, the CD22 CAR T was well tolerated, with only mild cases of the cytokine release syndrome (CRS), and it could be delivered safely in children with relapsed disease after hematopoietic cell transplants (HCT), she reported in a briefing and in an oral abstract session at the annual congress of the European Hematology Association.
“CD22 CAR T immunotherapy brings hope for patients with refractory or relapsed B-ALL who failed on CD19 CAR T immunotherapy, and we think it’s quite safe. No children died and no children had severe side effects during the study, even in post-HCT patients,” Dr. Pan said.
She noted that in a previous clinical trial by her group, some patients experienced relapses and were resistant to retreatment with CD19-directed CAR T therapy due to mutations or loss of the CD19 antigen (Leukemia. 2017 Dec;31[12]:2587-93).
Since CD22 is highly expressed on leukemic cells in children with B-ALL, the investigators decided to evaluate the safety and efficacy of a CD22 CAR T as a rescue strategy. They enrolled 15 patients who either experienced relapse or did not have a response to CD19 CAR T immunotherapy. The CAR T construct they used contains an anti-CD22 single-chain variable fragment derived from a humanized CD22 antibody.
Patient conditioning with fludarabine and cyclophosphamide was performed simultaneously with CAR T transfection and expansion. After about 7 days, the expanded and transformed CAR T cells were infused at a dose of 8.2 x 105/kg in patients who had not undergone HCT, and 0.9 x 105 in patients who had received a transplant.
The patients ranged from 2 to 18 years old (median 8 years), had a median disease course of 21 months (range 5-84 months), and had a median of 42% bone marrow blasts (range 5%-95.5%).
Four of the 15 patients had relapses following allogeneic HCT, and the remaining 11 had relapses following chemotherapy. Two of the patients were found to be minimal residual disease (MRD)-positive by flow cytometry. Two patients had extramedullary disease only at relapse.
Ten of 11 patients who had experienced a hematologic relapse had either a CR or CR with incomplete recovery of counts (CRi), and of these 10 patients, nine were determined on follow-up to be MRD-negative by flow cytometry.
One of the two patients with extramedullary disease had a CR, and the other had a partial response.
Although two patients had no response to CD22 CAR T therapy, expression of the antigen was strong on leukemia cells from these patients, Dr. Pan said.
All patients experienced CRS, but none had greater than grade 2, Dr. Pan said, although she did not provide give specific numbers. Two patients had grade 1 neurotoxicity, two patients had grade 2 hypoxemia, and one patient had grade 2 liver enzyme elevation.
At a median follow-up of 108 days, six patients had been bridged to allogeneic HCT, and eleven of 12 patients who had a CR or CRi at 30 days had no evidence of disease progression. The remaining patient with an initial CR or CRi had a relapse at day 50. The 6-month progression-free survival rate was 91.7%.
Anton Hagenbeek, MD, PhD, from the Academic Medical Center at the University of Amsterdam, the Netherlands, who moderated the briefing but was not involved in the study, commented that given the high leukemia burden of the patients and the apparent efficacy of the therapy, one would expect to see higher grades of CRS, and asked Dr. Pan whether she could account for the CRS findings in her study, compared with those of trials for CD19-directed CAR T therapy.
It may have to do with differences in density of CD22 expression, compared with CD19 expression on leukemia cells, or on differences in the antibody used to target the cells, Dr. Pan said.
SOURCE: Pan J et al. EHA Congress, Abstract S832.
STOCKHOLM, SWEDEN – A novel chimeric antigen receptor T-cell construct directed against CD22 was able to rescue children with relapsed or refractory B-cell acute lymphoblastic leukemia for whom CD19-directed CAR T therapy had failed, investigators from China reported.
Thirty days after CAR T cell infusion, 12 of 15 children (80%) treated with the unnamed CD22 CAR T product had a complete response (CR) and one (6.7%) had a partial response (PR), for an overall response rate (ORR) of 86.7%, said Jing Pan, MD, from the Beijing Boren Hospital in China.
Surprisingly for a therapy of its type, the CD22 CAR T was well tolerated, with only mild cases of the cytokine release syndrome (CRS), and it could be delivered safely in children with relapsed disease after hematopoietic cell transplants (HCT), she reported in a briefing and in an oral abstract session at the annual congress of the European Hematology Association.
“CD22 CAR T immunotherapy brings hope for patients with refractory or relapsed B-ALL who failed on CD19 CAR T immunotherapy, and we think it’s quite safe. No children died and no children had severe side effects during the study, even in post-HCT patients,” Dr. Pan said.
She noted that in a previous clinical trial by her group, some patients experienced relapses and were resistant to retreatment with CD19-directed CAR T therapy due to mutations or loss of the CD19 antigen (Leukemia. 2017 Dec;31[12]:2587-93).
Since CD22 is highly expressed on leukemic cells in children with B-ALL, the investigators decided to evaluate the safety and efficacy of a CD22 CAR T as a rescue strategy. They enrolled 15 patients who either experienced relapse or did not have a response to CD19 CAR T immunotherapy. The CAR T construct they used contains an anti-CD22 single-chain variable fragment derived from a humanized CD22 antibody.
Patient conditioning with fludarabine and cyclophosphamide was performed simultaneously with CAR T transfection and expansion. After about 7 days, the expanded and transformed CAR T cells were infused at a dose of 8.2 x 105/kg in patients who had not undergone HCT, and 0.9 x 105 in patients who had received a transplant.
The patients ranged from 2 to 18 years old (median 8 years), had a median disease course of 21 months (range 5-84 months), and had a median of 42% bone marrow blasts (range 5%-95.5%).
Four of the 15 patients had relapses following allogeneic HCT, and the remaining 11 had relapses following chemotherapy. Two of the patients were found to be minimal residual disease (MRD)-positive by flow cytometry. Two patients had extramedullary disease only at relapse.
Ten of 11 patients who had experienced a hematologic relapse had either a CR or CR with incomplete recovery of counts (CRi), and of these 10 patients, nine were determined on follow-up to be MRD-negative by flow cytometry.
One of the two patients with extramedullary disease had a CR, and the other had a partial response.
Although two patients had no response to CD22 CAR T therapy, expression of the antigen was strong on leukemia cells from these patients, Dr. Pan said.
All patients experienced CRS, but none had greater than grade 2, Dr. Pan said, although she did not provide give specific numbers. Two patients had grade 1 neurotoxicity, two patients had grade 2 hypoxemia, and one patient had grade 2 liver enzyme elevation.
At a median follow-up of 108 days, six patients had been bridged to allogeneic HCT, and eleven of 12 patients who had a CR or CRi at 30 days had no evidence of disease progression. The remaining patient with an initial CR or CRi had a relapse at day 50. The 6-month progression-free survival rate was 91.7%.
Anton Hagenbeek, MD, PhD, from the Academic Medical Center at the University of Amsterdam, the Netherlands, who moderated the briefing but was not involved in the study, commented that given the high leukemia burden of the patients and the apparent efficacy of the therapy, one would expect to see higher grades of CRS, and asked Dr. Pan whether she could account for the CRS findings in her study, compared with those of trials for CD19-directed CAR T therapy.
It may have to do with differences in density of CD22 expression, compared with CD19 expression on leukemia cells, or on differences in the antibody used to target the cells, Dr. Pan said.
SOURCE: Pan J et al. EHA Congress, Abstract S832.
REPORTING FROM THE EHA CONGRESS
Key clinical point: A CD22-directed chimeric antigen receptor T cell construct may be a highly effective salvage therapy in children with acute lymphoblastic leukemia that has relapsed after, or is resistant to, CD19-direct CAR T therapy.
Major finding: In total, 12 of 15 children (80%) treated with the CD22 CAR T product had a complete response 30 days after infusion.
Study details: Open-label, single-center, single-arm study in 15 children with ALL that is resistant to, or relapsed after, prior CD19 CAR T therapy.
Disclosures: Dr. Pan and colleagues did not disclose a funding source for the study. She reported having no conflicts of interest.
Source: Pan J et al. EHA Congress, Abstract S832.
Efficacy of KTE-C19 CAR T cells not compromised by prior blinatumomab
CHICAGO—Prior exposure to blinatumomab does not appear to affect the successful manufacture of KTE-C19 or its efficacy in patients with relapsed/refractory acute lymphoblastic leukemia (ALL), an investigator reported at the 2018 ASCO Annual Meeting.
The clinical benefit of KTE-C19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, was preserved regardless of whether patients were exposed to blinatumomab, said Bijal D. Shah, MD, of Moffitt Cancer Center in Tampa, Florida.
High rates of complete response and undetectable minimal residual disease (MRD) were independent of exposure to blinatumomab, a CD19/CD3 bispecific T-cell engager.
“We feel the results of these data support KTE-C19 as an effective option for adults with refractory leukemia, regardless of prior exposure to CD19-directed therapy,” Dr Shah reported at the meeting (abstract 7006*).
The current standard of care for adults with relapsed/refractory ALL includes blinatumomab, raising the question of whether prior exposure to this CD19-directed treatment could influence the manufacture or efficacy of KTE-C19.
Sara Cooley, MD, of Masonic Medical Center, University of Minnesota in Minneapolis, said results of this analysis suggest prior blinatumomab should not be a contraindication or concern in the context of KTE-C19.
“This remains to be shown with other CAR T-cell therapies,” she said in a presentation at ASCO on cellular therapy in leukemia.
The analysis by Dr Shah and co-investigators was based on ZUMA-3 (NCT02614066), a phase 1 study including adults with relapsed/refractory ALL who received KTE-C19 at doses of 0.5, 1, or 2 x 106 cells/kg.
They excluded patients in the highest dose cohort, who were required to be blinatumomab naïve, per protocol. That left 23 patients who received 0.5 or 1 x 106 cells/kg, of whom 11 had prior blinatumomab exposure and 12 did not.
Best overall response appeared to be independent of prior blinatumomab treatment, with a CR rate of 72% overall, and 63% and 80% for blinatumomab-exposed and blinatumomab-naïve patients, respectively.
The rate of undetectable MRD was likewise high at 88% in the prior blinatumomab group and 100% in the no-blinatumomab group.
Product characteristics did not vary according to blinatumomab exposure, though there was a trend toward a more differentiated phenotype in those patients who had received prior CD19-directed treatment, he said.
There were no significant differences between groups in the rate of grade 3 or greater cytokine release syndrome. Neurologic events were higher in the blinatumomab-naïve patients, though a higher percentage of those patients received the 1 x 106 cells/kg dose, Dr Shah reported.
Investigators also looked at CAR T levels by treatment.
“We cannot appreciate any significant differences between the blinatumomab-naïve and the blinatumomab-exposed groups,” Dr Shah told ASCO attendees.
The ZUMA-3 trial was sponsored by Kite, a Gilead Company.
*Data in the abstract differ from the presentation.
CHICAGO—Prior exposure to blinatumomab does not appear to affect the successful manufacture of KTE-C19 or its efficacy in patients with relapsed/refractory acute lymphoblastic leukemia (ALL), an investigator reported at the 2018 ASCO Annual Meeting.
The clinical benefit of KTE-C19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, was preserved regardless of whether patients were exposed to blinatumomab, said Bijal D. Shah, MD, of Moffitt Cancer Center in Tampa, Florida.
High rates of complete response and undetectable minimal residual disease (MRD) were independent of exposure to blinatumomab, a CD19/CD3 bispecific T-cell engager.
“We feel the results of these data support KTE-C19 as an effective option for adults with refractory leukemia, regardless of prior exposure to CD19-directed therapy,” Dr Shah reported at the meeting (abstract 7006*).
The current standard of care for adults with relapsed/refractory ALL includes blinatumomab, raising the question of whether prior exposure to this CD19-directed treatment could influence the manufacture or efficacy of KTE-C19.
Sara Cooley, MD, of Masonic Medical Center, University of Minnesota in Minneapolis, said results of this analysis suggest prior blinatumomab should not be a contraindication or concern in the context of KTE-C19.
“This remains to be shown with other CAR T-cell therapies,” she said in a presentation at ASCO on cellular therapy in leukemia.
The analysis by Dr Shah and co-investigators was based on ZUMA-3 (NCT02614066), a phase 1 study including adults with relapsed/refractory ALL who received KTE-C19 at doses of 0.5, 1, or 2 x 106 cells/kg.
They excluded patients in the highest dose cohort, who were required to be blinatumomab naïve, per protocol. That left 23 patients who received 0.5 or 1 x 106 cells/kg, of whom 11 had prior blinatumomab exposure and 12 did not.
Best overall response appeared to be independent of prior blinatumomab treatment, with a CR rate of 72% overall, and 63% and 80% for blinatumomab-exposed and blinatumomab-naïve patients, respectively.
The rate of undetectable MRD was likewise high at 88% in the prior blinatumomab group and 100% in the no-blinatumomab group.
Product characteristics did not vary according to blinatumomab exposure, though there was a trend toward a more differentiated phenotype in those patients who had received prior CD19-directed treatment, he said.
There were no significant differences between groups in the rate of grade 3 or greater cytokine release syndrome. Neurologic events were higher in the blinatumomab-naïve patients, though a higher percentage of those patients received the 1 x 106 cells/kg dose, Dr Shah reported.
Investigators also looked at CAR T levels by treatment.
“We cannot appreciate any significant differences between the blinatumomab-naïve and the blinatumomab-exposed groups,” Dr Shah told ASCO attendees.
The ZUMA-3 trial was sponsored by Kite, a Gilead Company.
*Data in the abstract differ from the presentation.
CHICAGO—Prior exposure to blinatumomab does not appear to affect the successful manufacture of KTE-C19 or its efficacy in patients with relapsed/refractory acute lymphoblastic leukemia (ALL), an investigator reported at the 2018 ASCO Annual Meeting.
The clinical benefit of KTE-C19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, was preserved regardless of whether patients were exposed to blinatumomab, said Bijal D. Shah, MD, of Moffitt Cancer Center in Tampa, Florida.
High rates of complete response and undetectable minimal residual disease (MRD) were independent of exposure to blinatumomab, a CD19/CD3 bispecific T-cell engager.
“We feel the results of these data support KTE-C19 as an effective option for adults with refractory leukemia, regardless of prior exposure to CD19-directed therapy,” Dr Shah reported at the meeting (abstract 7006*).
The current standard of care for adults with relapsed/refractory ALL includes blinatumomab, raising the question of whether prior exposure to this CD19-directed treatment could influence the manufacture or efficacy of KTE-C19.
Sara Cooley, MD, of Masonic Medical Center, University of Minnesota in Minneapolis, said results of this analysis suggest prior blinatumomab should not be a contraindication or concern in the context of KTE-C19.
“This remains to be shown with other CAR T-cell therapies,” she said in a presentation at ASCO on cellular therapy in leukemia.
The analysis by Dr Shah and co-investigators was based on ZUMA-3 (NCT02614066), a phase 1 study including adults with relapsed/refractory ALL who received KTE-C19 at doses of 0.5, 1, or 2 x 106 cells/kg.
They excluded patients in the highest dose cohort, who were required to be blinatumomab naïve, per protocol. That left 23 patients who received 0.5 or 1 x 106 cells/kg, of whom 11 had prior blinatumomab exposure and 12 did not.
Best overall response appeared to be independent of prior blinatumomab treatment, with a CR rate of 72% overall, and 63% and 80% for blinatumomab-exposed and blinatumomab-naïve patients, respectively.
The rate of undetectable MRD was likewise high at 88% in the prior blinatumomab group and 100% in the no-blinatumomab group.
Product characteristics did not vary according to blinatumomab exposure, though there was a trend toward a more differentiated phenotype in those patients who had received prior CD19-directed treatment, he said.
There were no significant differences between groups in the rate of grade 3 or greater cytokine release syndrome. Neurologic events were higher in the blinatumomab-naïve patients, though a higher percentage of those patients received the 1 x 106 cells/kg dose, Dr Shah reported.
Investigators also looked at CAR T levels by treatment.
“We cannot appreciate any significant differences between the blinatumomab-naïve and the blinatumomab-exposed groups,” Dr Shah told ASCO attendees.
The ZUMA-3 trial was sponsored by Kite, a Gilead Company.
*Data in the abstract differ from the presentation.
Ivosidenib active in R/R IDH1-mutated AML patients
CHICAGO—The investigational drug ivosidenib, an inhibitor of the mutant IDH1 enzyme, achieved complete remission (CR) rates of 32% and an overall response rate of 42% in relapsed/refractory (R/R) patients with acute myeloid leukemia (AML) and IDH1 mutation, according to investigators.
In addition, overall survival (OS) in patients who achieved CR more than doubled compared with those in the overall study population.
Fewer patients with CR had febrile neutropenia and infectious complications, and 25% of patients with CR were able to clear the IDH1 clone.
Duration of response was 6.5 months with the investigational drug.
Investigators reported the grade 3/4 toxicities could be managed with supportive care, were not fatal, and some patients still achieved responses.
IDH1 mutation, first identified almost 10 years ago with the sequencing of the first AML cancer genome, is a recurrent mutation in over 10% of patients with AML.
Mutated IDH1, reported in several malignancies, results in impaired cellular differentiation. Ivosidenib is a first-in-class oral therapy designed to inhibit the mutant IDH1 enzyme.
Phase 1 study (NCT02074839)
The phase 1 dose-escalation and dose expansion study specifically enrolled patients with R/RAML with mutated IDH1.
Daniel A. Pollyea, MD, of the Colorado University School of Medicine in Aurora, reported the data from 2 of the dose expansion cohorts as well as 35 patients from the dose escalation cohort at the 2018 ASCO Annual Meeting (abstract 7000).
All patients received ivosidenib 500 mg daily.
CR/CRh (CR with partial hematologic recovery; defined as morphologic remission with recovery of neutrophils to at least 500/mm3 and recovery of platelets to at least 50,000/µL) was the primary efficacy endpoint.
Of 179 patients in the primary efficacy cohort, 10% were still receiving treatment at the time of the presentation.
While most patients discontinued due to disease progression, 10% came off therapy for stem cell transplantation. Median duration of treatment was 4 months.
Patients were a median 67 years of age. Approximately 1/3 had secondary AML.
Patients had received a median of 2 prior therapies and approximately 1/4 had relapsed after transplantation.
Fifty-nine percent were refractory to induction or reinduction therapy.
Toxicity
Dr Pollyea considered adverse events to be as expected for a relapsed/refractory AML population.
However, he called out 3 for special mention—leukocytosis, ECG QT prolongation, and IDH differentiation syndrome—none of which was fatal.
Eight percent of patients had grade 3 or 4 leukocytosis, some of which were mechanistically induced from treatment.
About 10% of patients had grade 3 or 4 QT prolongation.
And grade 3 or 4 differentiation syndrome was reported for approximately 5% of patients.
In 19 patients with any grade differentiation syndrome, CR was reported for 5 patients. The message: patients experiencing this adverse event can be managed with supportive care, continue treatment, and still respond.
All adverse events were managed with supportive care measures, including concomitant medications, and ivosidenib dose modifications as required.
CR/CRh was 32% for the efficacy cohort; median time to response was 2 months and median time of response was 8.2 months. CR rate was 24%. Investigator-reported International Working Group categorized ORR was 42%.
The median OS was 9 months for the entire cohort and 18.8 months for patients who achieved CR/CRh.
Dr Pollyea reported that transfusion independence—defined as no need for transfusion for 56 days—was achieved in all CR patients, 75% of CRh patients, and even in a proportion of nonresponders.
Investigtors observed febrile neutropenia and grade 3 or 4 infectious complications in fewer patients who achieved CR/CRh.
Of note was the observation that 23% of patients who achieved CR/CRh were able to clear the mutant IDH1 clone. Patients who did not respond still harbored the IDH1 clone, Dr Pollyea reported.
These results reported at ASCO are an update from those simultaneously published in NEJM.
The study was supported by Agios Pharmaceuticals.
Ivosidenib is being evaluated alone and in combination in other clinical trials.
CHICAGO—The investigational drug ivosidenib, an inhibitor of the mutant IDH1 enzyme, achieved complete remission (CR) rates of 32% and an overall response rate of 42% in relapsed/refractory (R/R) patients with acute myeloid leukemia (AML) and IDH1 mutation, according to investigators.
In addition, overall survival (OS) in patients who achieved CR more than doubled compared with those in the overall study population.
Fewer patients with CR had febrile neutropenia and infectious complications, and 25% of patients with CR were able to clear the IDH1 clone.
Duration of response was 6.5 months with the investigational drug.
Investigators reported the grade 3/4 toxicities could be managed with supportive care, were not fatal, and some patients still achieved responses.
IDH1 mutation, first identified almost 10 years ago with the sequencing of the first AML cancer genome, is a recurrent mutation in over 10% of patients with AML.
Mutated IDH1, reported in several malignancies, results in impaired cellular differentiation. Ivosidenib is a first-in-class oral therapy designed to inhibit the mutant IDH1 enzyme.
Phase 1 study (NCT02074839)
The phase 1 dose-escalation and dose expansion study specifically enrolled patients with R/RAML with mutated IDH1.
Daniel A. Pollyea, MD, of the Colorado University School of Medicine in Aurora, reported the data from 2 of the dose expansion cohorts as well as 35 patients from the dose escalation cohort at the 2018 ASCO Annual Meeting (abstract 7000).
All patients received ivosidenib 500 mg daily.
CR/CRh (CR with partial hematologic recovery; defined as morphologic remission with recovery of neutrophils to at least 500/mm3 and recovery of platelets to at least 50,000/µL) was the primary efficacy endpoint.
Of 179 patients in the primary efficacy cohort, 10% were still receiving treatment at the time of the presentation.
While most patients discontinued due to disease progression, 10% came off therapy for stem cell transplantation. Median duration of treatment was 4 months.
Patients were a median 67 years of age. Approximately 1/3 had secondary AML.
Patients had received a median of 2 prior therapies and approximately 1/4 had relapsed after transplantation.
Fifty-nine percent were refractory to induction or reinduction therapy.
Toxicity
Dr Pollyea considered adverse events to be as expected for a relapsed/refractory AML population.
However, he called out 3 for special mention—leukocytosis, ECG QT prolongation, and IDH differentiation syndrome—none of which was fatal.
Eight percent of patients had grade 3 or 4 leukocytosis, some of which were mechanistically induced from treatment.
About 10% of patients had grade 3 or 4 QT prolongation.
And grade 3 or 4 differentiation syndrome was reported for approximately 5% of patients.
In 19 patients with any grade differentiation syndrome, CR was reported for 5 patients. The message: patients experiencing this adverse event can be managed with supportive care, continue treatment, and still respond.
All adverse events were managed with supportive care measures, including concomitant medications, and ivosidenib dose modifications as required.
CR/CRh was 32% for the efficacy cohort; median time to response was 2 months and median time of response was 8.2 months. CR rate was 24%. Investigator-reported International Working Group categorized ORR was 42%.
The median OS was 9 months for the entire cohort and 18.8 months for patients who achieved CR/CRh.
Dr Pollyea reported that transfusion independence—defined as no need for transfusion for 56 days—was achieved in all CR patients, 75% of CRh patients, and even in a proportion of nonresponders.
Investigtors observed febrile neutropenia and grade 3 or 4 infectious complications in fewer patients who achieved CR/CRh.
Of note was the observation that 23% of patients who achieved CR/CRh were able to clear the mutant IDH1 clone. Patients who did not respond still harbored the IDH1 clone, Dr Pollyea reported.
These results reported at ASCO are an update from those simultaneously published in NEJM.
The study was supported by Agios Pharmaceuticals.
Ivosidenib is being evaluated alone and in combination in other clinical trials.
CHICAGO—The investigational drug ivosidenib, an inhibitor of the mutant IDH1 enzyme, achieved complete remission (CR) rates of 32% and an overall response rate of 42% in relapsed/refractory (R/R) patients with acute myeloid leukemia (AML) and IDH1 mutation, according to investigators.
In addition, overall survival (OS) in patients who achieved CR more than doubled compared with those in the overall study population.
Fewer patients with CR had febrile neutropenia and infectious complications, and 25% of patients with CR were able to clear the IDH1 clone.
Duration of response was 6.5 months with the investigational drug.
Investigators reported the grade 3/4 toxicities could be managed with supportive care, were not fatal, and some patients still achieved responses.
IDH1 mutation, first identified almost 10 years ago with the sequencing of the first AML cancer genome, is a recurrent mutation in over 10% of patients with AML.
Mutated IDH1, reported in several malignancies, results in impaired cellular differentiation. Ivosidenib is a first-in-class oral therapy designed to inhibit the mutant IDH1 enzyme.
Phase 1 study (NCT02074839)
The phase 1 dose-escalation and dose expansion study specifically enrolled patients with R/RAML with mutated IDH1.
Daniel A. Pollyea, MD, of the Colorado University School of Medicine in Aurora, reported the data from 2 of the dose expansion cohorts as well as 35 patients from the dose escalation cohort at the 2018 ASCO Annual Meeting (abstract 7000).
All patients received ivosidenib 500 mg daily.
CR/CRh (CR with partial hematologic recovery; defined as morphologic remission with recovery of neutrophils to at least 500/mm3 and recovery of platelets to at least 50,000/µL) was the primary efficacy endpoint.
Of 179 patients in the primary efficacy cohort, 10% were still receiving treatment at the time of the presentation.
While most patients discontinued due to disease progression, 10% came off therapy for stem cell transplantation. Median duration of treatment was 4 months.
Patients were a median 67 years of age. Approximately 1/3 had secondary AML.
Patients had received a median of 2 prior therapies and approximately 1/4 had relapsed after transplantation.
Fifty-nine percent were refractory to induction or reinduction therapy.
Toxicity
Dr Pollyea considered adverse events to be as expected for a relapsed/refractory AML population.
However, he called out 3 for special mention—leukocytosis, ECG QT prolongation, and IDH differentiation syndrome—none of which was fatal.
Eight percent of patients had grade 3 or 4 leukocytosis, some of which were mechanistically induced from treatment.
About 10% of patients had grade 3 or 4 QT prolongation.
And grade 3 or 4 differentiation syndrome was reported for approximately 5% of patients.
In 19 patients with any grade differentiation syndrome, CR was reported for 5 patients. The message: patients experiencing this adverse event can be managed with supportive care, continue treatment, and still respond.
All adverse events were managed with supportive care measures, including concomitant medications, and ivosidenib dose modifications as required.
CR/CRh was 32% for the efficacy cohort; median time to response was 2 months and median time of response was 8.2 months. CR rate was 24%. Investigator-reported International Working Group categorized ORR was 42%.
The median OS was 9 months for the entire cohort and 18.8 months for patients who achieved CR/CRh.
Dr Pollyea reported that transfusion independence—defined as no need for transfusion for 56 days—was achieved in all CR patients, 75% of CRh patients, and even in a proportion of nonresponders.
Investigtors observed febrile neutropenia and grade 3 or 4 infectious complications in fewer patients who achieved CR/CRh.
Of note was the observation that 23% of patients who achieved CR/CRh were able to clear the mutant IDH1 clone. Patients who did not respond still harbored the IDH1 clone, Dr Pollyea reported.
These results reported at ASCO are an update from those simultaneously published in NEJM.
The study was supported by Agios Pharmaceuticals.
Ivosidenib is being evaluated alone and in combination in other clinical trials.
Dasatinib outcomes similar to imatinib in pediatric Ph+ ALL
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.