User login
The Vampire Study, pathogenic puppies, and carbonated cannabis
What the duck?
Turns out it’s flu shot season for our feathered friends, too. After the bird flu pandemics that began in 2013, Chinese health officials worked hard to vaccinate their chickens and quell the spread of the disease. However, the ducks have outsmarted them: Two new genetic variations of the H7N9 and H7N2 flu subtypes have been found in unvaccinated ducks.
China consumes about 3 billion ducks per year, so officials are working rapidly to eliminate the virus. At press time, there was no word on whether the virus had affected any beloved rubber duckies, but we advise you to use caution when approaching bath time.
Toke-a-Cola
Cannabis is the world’s favorite illicit drug. And Coca-Cola makes the world’s favorite cola. Now there’s news of potential nuptials uniting these two global giants. BNN Bloomberg reports that Coke is talking tie-up with Canada’s Aurora Cannabis in a union that could give birth to cannabis-infused “wellness beverages.”
The fizzy federation would feature products containing cannabidiol, or CBD. Unlike its wilder psychoactive sibling tetrahydrocannabinol, or THC, the more sober-minded CBD is a nonpsychoactive cannabis compound credited with antidepressant, anxiolytic, and anti-inflammatory powers.
And what of Coca-Cola’s mortal cola enemy, Pepsi? Will the Choice of a New Generation let the Real Thing Bogart all the possible market opportunities? Sure, you could soon have a CBD Coke and a smile. But smiles are free. Frito-Lay’s parent, PepsiCo, could offer consumers a doubly profitable, Jeff Spicoli–approved pairing: carbonated cannabinoids and Cheetos.
I vant to suck MY blood
It’s not Halloween quite yet, but get into the spirit with the recently published and aptly named “Vampire Study.” Performed in Zürich, a team of researchers from the division of gastroenterology at Triemli Hospital convinced participants to ingest their own blood, all in the name of science.
Some lucky vamps drank their blood, while others ingested it via nasogastric tube. This isn’t “Saw 17,” though; there was a method to this madness. Researchers were investigating whether the ingestion of blood (as in gastrointestinal bleeding) can result in an increase in fecal calprotectin. Safe to say, though, the ingestion of blood is rarely a good sign – unless your name happens to be Nosferatu.
And they call it Campylobacter love
As any fan of Charles Schulz’s “Peanuts” comic strip can tell you, happiness is a warm puppy. Know what else warm puppies are? Carriers of Campylobacter jejuni.
Every year in the United States, Campylobacter causes an estimated 1.3 million diarrheal illnesses. A recent multistate investigation revealed that 118 people in 18 states across the nation – including 29 employees of an unnamed national pet store chain based in Ohio – got the puppy-borne bug between early 2016 and early 2018.
And the not-so-cuddly infections were resistant to all the antibiotics commonly used to quell Campylobacter. Why? Turns out, of the 149 puppies investigated by health officials, 55% of them got the drugs prophylactically – an approach that may have fueled the resistance. Stung by the canine controversy, the Daisy Hill Puppy Farm has assured Charlie Brown that it never slipped metronidazole into Snoopy’s water bowl.
What the duck?
Turns out it’s flu shot season for our feathered friends, too. After the bird flu pandemics that began in 2013, Chinese health officials worked hard to vaccinate their chickens and quell the spread of the disease. However, the ducks have outsmarted them: Two new genetic variations of the H7N9 and H7N2 flu subtypes have been found in unvaccinated ducks.
China consumes about 3 billion ducks per year, so officials are working rapidly to eliminate the virus. At press time, there was no word on whether the virus had affected any beloved rubber duckies, but we advise you to use caution when approaching bath time.
Toke-a-Cola
Cannabis is the world’s favorite illicit drug. And Coca-Cola makes the world’s favorite cola. Now there’s news of potential nuptials uniting these two global giants. BNN Bloomberg reports that Coke is talking tie-up with Canada’s Aurora Cannabis in a union that could give birth to cannabis-infused “wellness beverages.”
The fizzy federation would feature products containing cannabidiol, or CBD. Unlike its wilder psychoactive sibling tetrahydrocannabinol, or THC, the more sober-minded CBD is a nonpsychoactive cannabis compound credited with antidepressant, anxiolytic, and anti-inflammatory powers.
And what of Coca-Cola’s mortal cola enemy, Pepsi? Will the Choice of a New Generation let the Real Thing Bogart all the possible market opportunities? Sure, you could soon have a CBD Coke and a smile. But smiles are free. Frito-Lay’s parent, PepsiCo, could offer consumers a doubly profitable, Jeff Spicoli–approved pairing: carbonated cannabinoids and Cheetos.
I vant to suck MY blood
It’s not Halloween quite yet, but get into the spirit with the recently published and aptly named “Vampire Study.” Performed in Zürich, a team of researchers from the division of gastroenterology at Triemli Hospital convinced participants to ingest their own blood, all in the name of science.
Some lucky vamps drank their blood, while others ingested it via nasogastric tube. This isn’t “Saw 17,” though; there was a method to this madness. Researchers were investigating whether the ingestion of blood (as in gastrointestinal bleeding) can result in an increase in fecal calprotectin. Safe to say, though, the ingestion of blood is rarely a good sign – unless your name happens to be Nosferatu.
And they call it Campylobacter love
As any fan of Charles Schulz’s “Peanuts” comic strip can tell you, happiness is a warm puppy. Know what else warm puppies are? Carriers of Campylobacter jejuni.
Every year in the United States, Campylobacter causes an estimated 1.3 million diarrheal illnesses. A recent multistate investigation revealed that 118 people in 18 states across the nation – including 29 employees of an unnamed national pet store chain based in Ohio – got the puppy-borne bug between early 2016 and early 2018.
And the not-so-cuddly infections were resistant to all the antibiotics commonly used to quell Campylobacter. Why? Turns out, of the 149 puppies investigated by health officials, 55% of them got the drugs prophylactically – an approach that may have fueled the resistance. Stung by the canine controversy, the Daisy Hill Puppy Farm has assured Charlie Brown that it never slipped metronidazole into Snoopy’s water bowl.
What the duck?
Turns out it’s flu shot season for our feathered friends, too. After the bird flu pandemics that began in 2013, Chinese health officials worked hard to vaccinate their chickens and quell the spread of the disease. However, the ducks have outsmarted them: Two new genetic variations of the H7N9 and H7N2 flu subtypes have been found in unvaccinated ducks.
China consumes about 3 billion ducks per year, so officials are working rapidly to eliminate the virus. At press time, there was no word on whether the virus had affected any beloved rubber duckies, but we advise you to use caution when approaching bath time.
Toke-a-Cola
Cannabis is the world’s favorite illicit drug. And Coca-Cola makes the world’s favorite cola. Now there’s news of potential nuptials uniting these two global giants. BNN Bloomberg reports that Coke is talking tie-up with Canada’s Aurora Cannabis in a union that could give birth to cannabis-infused “wellness beverages.”
The fizzy federation would feature products containing cannabidiol, or CBD. Unlike its wilder psychoactive sibling tetrahydrocannabinol, or THC, the more sober-minded CBD is a nonpsychoactive cannabis compound credited with antidepressant, anxiolytic, and anti-inflammatory powers.
And what of Coca-Cola’s mortal cola enemy, Pepsi? Will the Choice of a New Generation let the Real Thing Bogart all the possible market opportunities? Sure, you could soon have a CBD Coke and a smile. But smiles are free. Frito-Lay’s parent, PepsiCo, could offer consumers a doubly profitable, Jeff Spicoli–approved pairing: carbonated cannabinoids and Cheetos.
I vant to suck MY blood
It’s not Halloween quite yet, but get into the spirit with the recently published and aptly named “Vampire Study.” Performed in Zürich, a team of researchers from the division of gastroenterology at Triemli Hospital convinced participants to ingest their own blood, all in the name of science.
Some lucky vamps drank their blood, while others ingested it via nasogastric tube. This isn’t “Saw 17,” though; there was a method to this madness. Researchers were investigating whether the ingestion of blood (as in gastrointestinal bleeding) can result in an increase in fecal calprotectin. Safe to say, though, the ingestion of blood is rarely a good sign – unless your name happens to be Nosferatu.
And they call it Campylobacter love
As any fan of Charles Schulz’s “Peanuts” comic strip can tell you, happiness is a warm puppy. Know what else warm puppies are? Carriers of Campylobacter jejuni.
Every year in the United States, Campylobacter causes an estimated 1.3 million diarrheal illnesses. A recent multistate investigation revealed that 118 people in 18 states across the nation – including 29 employees of an unnamed national pet store chain based in Ohio – got the puppy-borne bug between early 2016 and early 2018.
And the not-so-cuddly infections were resistant to all the antibiotics commonly used to quell Campylobacter. Why? Turns out, of the 149 puppies investigated by health officials, 55% of them got the drugs prophylactically – an approach that may have fueled the resistance. Stung by the canine controversy, the Daisy Hill Puppy Farm has assured Charlie Brown that it never slipped metronidazole into Snoopy’s water bowl.
The oncologist’s dilemma
The textbook answer would have been straightforward: No additional chemotherapy. Focus on palliative care.
But Max (not his real name) was not a textbook case. He was a person, and he was terrified of dying.
When I met him in clinic, four lines of chemotherapy had not slowed the spread of his rare cancer that was already metastatic at the time of diagnosis. His skin was yellow. His hair had fallen out in clumps. His legs were swollen to the point that he couldn’t walk. He had trouble transferring from his wheelchair on his own.
All this was offset by the college hoodie he wore, a disarming display of his youth. I had to look at the chart to remind myself. He was only 19 years old.
“Will Dr. D give Max chemotherapy?” his mother asked me, referring to the attending oncologist who had been caring for her son since the beginning. “I think he needs it right away,” she said. She was holding back tears.
Protected by the fact that I was a visiting fellow in her clinic for the day, and I was just meeting Max, I deferred the decision to Dr. D.
Dr. D and I reviewed Max’s case outside the room, scrolling through his PET scans showing spread of cancer in his liver, lungs, and bones in only 2 short months. We recounted the multiple lines of chemotherapy and immunotherapy he had tried and that had failed him.
Palliative care? I offered. She agreed.
But as we went back in together, it was harder. Max’s mother began to cry as Dr. D tried to broach the option. To her, palliative care meant death. That was not something she could swallow. Her questions turned back only to the next chemotherapy we would be giving.
I learned that Max’s father worked in a hospital. He knew how serious it was. “He calls me every day, crying,” my attending later told me solemnly. Begging her to do something. Pleading for more chemotherapy.
After some painful back and forth in the room, we didn’t come to a resolution. Dr. D would call them later, she said.
It was a busy clinic day, and we saw the rest of her patients.
“What are we going to do about Max?” I asked at the end of the day. I was writing the note in his chart. We still didn’t have a plan.
More chemotherapy, from any technical and data-based standpoint, was not the right choice. We had no evidence it would improve survival. We did have evidence that it could worsen the quality of life when time was limited. If we gave him more chemotherapy, it would be beyond guidelines, beyond evidence. We would be off the grid.
I thought about the conversations I’d been privy to about giving toxic therapies near the end of life. While a handful felt productive, others were uncomfortably strained. The latter involved a tension that manifests when the goals of the patient and the oncologist are misaligned. The words may be slightly different each time, but the theme is the same.
The oncologist says: “More chemotherapy is not going to work.”
The patient says: “But we don’t know. It’s better than doing nothing. Can’t we try?”
This can be excruciatingly challenging because both sides are correct. Both sides are logical, and yet they are talking past each other.
From the point of view of the person desperate to survive, anything is worth a try. Without trying some form of treatment, there’s a zero percent chance of surviving. Low odds of something working are still better than zero percent odds.
But it’s not an issue of logic. For people like Max’s parents, the questions come from a place of helplessness. The cognitive dissonance sets in because our job is to help and we struggle when we feel we cannot. We want to say yes. I wish we had a treatment to slow Max’s cancer, too. I wish more chemotherapy would help him.
What I’ve learned from these conversations is the importance of defining terms. Specifically, what do we mean when we say a treatment will or will not “work”? What are we trying to achieve? To prolong life by weeks? By months or years? To make your pain go away? To help you feel stronger? To allow you to spend time doing what you love?
The relevant question is not: Will this treatment work? It is: What are your goals, and will this treatment help you achieve them?
Defining terms in that way can mean the difference of a conversation where two sides are talking past one another to one that comes to a mutual understanding – even if the ultimate conclusion is painful for everyone.
Yet sometimes, even for the most skilled communicators, there may be compromise. There may be an agreement to trial Nth-line chemotherapy, even without evidence that it will achieve a person’s goals. It will require nuanced informed consent from both sides. And it will come from a place of compassion.
This is what I thought about as I signed chemotherapy orders for Max that evening. I felt for him, for his parents, and for his oncologist.
Because even though I suspected the treatment wouldn’t work the way they all hoped it would, I also wasn’t the one fielding daily phone calls from a father, begging his oncologist to do something, anything at all, to save his son’s life.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
The textbook answer would have been straightforward: No additional chemotherapy. Focus on palliative care.
But Max (not his real name) was not a textbook case. He was a person, and he was terrified of dying.
When I met him in clinic, four lines of chemotherapy had not slowed the spread of his rare cancer that was already metastatic at the time of diagnosis. His skin was yellow. His hair had fallen out in clumps. His legs were swollen to the point that he couldn’t walk. He had trouble transferring from his wheelchair on his own.
All this was offset by the college hoodie he wore, a disarming display of his youth. I had to look at the chart to remind myself. He was only 19 years old.
“Will Dr. D give Max chemotherapy?” his mother asked me, referring to the attending oncologist who had been caring for her son since the beginning. “I think he needs it right away,” she said. She was holding back tears.
Protected by the fact that I was a visiting fellow in her clinic for the day, and I was just meeting Max, I deferred the decision to Dr. D.
Dr. D and I reviewed Max’s case outside the room, scrolling through his PET scans showing spread of cancer in his liver, lungs, and bones in only 2 short months. We recounted the multiple lines of chemotherapy and immunotherapy he had tried and that had failed him.
Palliative care? I offered. She agreed.
But as we went back in together, it was harder. Max’s mother began to cry as Dr. D tried to broach the option. To her, palliative care meant death. That was not something she could swallow. Her questions turned back only to the next chemotherapy we would be giving.
I learned that Max’s father worked in a hospital. He knew how serious it was. “He calls me every day, crying,” my attending later told me solemnly. Begging her to do something. Pleading for more chemotherapy.
After some painful back and forth in the room, we didn’t come to a resolution. Dr. D would call them later, she said.
It was a busy clinic day, and we saw the rest of her patients.
“What are we going to do about Max?” I asked at the end of the day. I was writing the note in his chart. We still didn’t have a plan.
More chemotherapy, from any technical and data-based standpoint, was not the right choice. We had no evidence it would improve survival. We did have evidence that it could worsen the quality of life when time was limited. If we gave him more chemotherapy, it would be beyond guidelines, beyond evidence. We would be off the grid.
I thought about the conversations I’d been privy to about giving toxic therapies near the end of life. While a handful felt productive, others were uncomfortably strained. The latter involved a tension that manifests when the goals of the patient and the oncologist are misaligned. The words may be slightly different each time, but the theme is the same.
The oncologist says: “More chemotherapy is not going to work.”
The patient says: “But we don’t know. It’s better than doing nothing. Can’t we try?”
This can be excruciatingly challenging because both sides are correct. Both sides are logical, and yet they are talking past each other.
From the point of view of the person desperate to survive, anything is worth a try. Without trying some form of treatment, there’s a zero percent chance of surviving. Low odds of something working are still better than zero percent odds.
But it’s not an issue of logic. For people like Max’s parents, the questions come from a place of helplessness. The cognitive dissonance sets in because our job is to help and we struggle when we feel we cannot. We want to say yes. I wish we had a treatment to slow Max’s cancer, too. I wish more chemotherapy would help him.
What I’ve learned from these conversations is the importance of defining terms. Specifically, what do we mean when we say a treatment will or will not “work”? What are we trying to achieve? To prolong life by weeks? By months or years? To make your pain go away? To help you feel stronger? To allow you to spend time doing what you love?
The relevant question is not: Will this treatment work? It is: What are your goals, and will this treatment help you achieve them?
Defining terms in that way can mean the difference of a conversation where two sides are talking past one another to one that comes to a mutual understanding – even if the ultimate conclusion is painful for everyone.
Yet sometimes, even for the most skilled communicators, there may be compromise. There may be an agreement to trial Nth-line chemotherapy, even without evidence that it will achieve a person’s goals. It will require nuanced informed consent from both sides. And it will come from a place of compassion.
This is what I thought about as I signed chemotherapy orders for Max that evening. I felt for him, for his parents, and for his oncologist.
Because even though I suspected the treatment wouldn’t work the way they all hoped it would, I also wasn’t the one fielding daily phone calls from a father, begging his oncologist to do something, anything at all, to save his son’s life.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
The textbook answer would have been straightforward: No additional chemotherapy. Focus on palliative care.
But Max (not his real name) was not a textbook case. He was a person, and he was terrified of dying.
When I met him in clinic, four lines of chemotherapy had not slowed the spread of his rare cancer that was already metastatic at the time of diagnosis. His skin was yellow. His hair had fallen out in clumps. His legs were swollen to the point that he couldn’t walk. He had trouble transferring from his wheelchair on his own.
All this was offset by the college hoodie he wore, a disarming display of his youth. I had to look at the chart to remind myself. He was only 19 years old.
“Will Dr. D give Max chemotherapy?” his mother asked me, referring to the attending oncologist who had been caring for her son since the beginning. “I think he needs it right away,” she said. She was holding back tears.
Protected by the fact that I was a visiting fellow in her clinic for the day, and I was just meeting Max, I deferred the decision to Dr. D.
Dr. D and I reviewed Max’s case outside the room, scrolling through his PET scans showing spread of cancer in his liver, lungs, and bones in only 2 short months. We recounted the multiple lines of chemotherapy and immunotherapy he had tried and that had failed him.
Palliative care? I offered. She agreed.
But as we went back in together, it was harder. Max’s mother began to cry as Dr. D tried to broach the option. To her, palliative care meant death. That was not something she could swallow. Her questions turned back only to the next chemotherapy we would be giving.
I learned that Max’s father worked in a hospital. He knew how serious it was. “He calls me every day, crying,” my attending later told me solemnly. Begging her to do something. Pleading for more chemotherapy.
After some painful back and forth in the room, we didn’t come to a resolution. Dr. D would call them later, she said.
It was a busy clinic day, and we saw the rest of her patients.
“What are we going to do about Max?” I asked at the end of the day. I was writing the note in his chart. We still didn’t have a plan.
More chemotherapy, from any technical and data-based standpoint, was not the right choice. We had no evidence it would improve survival. We did have evidence that it could worsen the quality of life when time was limited. If we gave him more chemotherapy, it would be beyond guidelines, beyond evidence. We would be off the grid.
I thought about the conversations I’d been privy to about giving toxic therapies near the end of life. While a handful felt productive, others were uncomfortably strained. The latter involved a tension that manifests when the goals of the patient and the oncologist are misaligned. The words may be slightly different each time, but the theme is the same.
The oncologist says: “More chemotherapy is not going to work.”
The patient says: “But we don’t know. It’s better than doing nothing. Can’t we try?”
This can be excruciatingly challenging because both sides are correct. Both sides are logical, and yet they are talking past each other.
From the point of view of the person desperate to survive, anything is worth a try. Without trying some form of treatment, there’s a zero percent chance of surviving. Low odds of something working are still better than zero percent odds.
But it’s not an issue of logic. For people like Max’s parents, the questions come from a place of helplessness. The cognitive dissonance sets in because our job is to help and we struggle when we feel we cannot. We want to say yes. I wish we had a treatment to slow Max’s cancer, too. I wish more chemotherapy would help him.
What I’ve learned from these conversations is the importance of defining terms. Specifically, what do we mean when we say a treatment will or will not “work”? What are we trying to achieve? To prolong life by weeks? By months or years? To make your pain go away? To help you feel stronger? To allow you to spend time doing what you love?
The relevant question is not: Will this treatment work? It is: What are your goals, and will this treatment help you achieve them?
Defining terms in that way can mean the difference of a conversation where two sides are talking past one another to one that comes to a mutual understanding – even if the ultimate conclusion is painful for everyone.
Yet sometimes, even for the most skilled communicators, there may be compromise. There may be an agreement to trial Nth-line chemotherapy, even without evidence that it will achieve a person’s goals. It will require nuanced informed consent from both sides. And it will come from a place of compassion.
This is what I thought about as I signed chemotherapy orders for Max that evening. I felt for him, for his parents, and for his oncologist.
Because even though I suspected the treatment wouldn’t work the way they all hoped it would, I also wasn’t the one fielding daily phone calls from a father, begging his oncologist to do something, anything at all, to save his son’s life.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
TV and mental health story lines; when doctors don’t listen – to women
Turn on the television, and chances are good that popular dramas (especially hospital-oriented shows) will be showing an episode revolving around a mental health issue.
, in time for a commercial. Real life is messier.
“Unfortunately mental health story lines are much more likely to be fear-mongering and wildly wrong. As a psychiatrist, this both piques my interest and upends my work-life balance,” Dr. Gold writes. “Whether I’m watching everyone’s favorite medical drama or ‘reality TV,’ it’s impossible not to switch into physician mode, angry on behalf of all of my patients and the many viewers who are being misled.”
Do physicians hear women?
“Rebecca continues to be paranoid.”
That was a note written by someone involved in the medical care of a 30-something woman diagnosed with stage IIB cervical cancer, according to an article in New York magazine.
“There’s a whiff of old ‘female hysteria’ to [the note], with more than a hint of dismissal,” writes the patient’s sister, Kate Beaton. “Becky was scared, and perhaps that was the main takeaway that day. But she was also right.”
The article tells the story of a vibrant woman who, according to her sister, asked her doctors lots of questions, wrote everything down, and faced years of being dismissed when she explained her symptoms. Becky’s sister says she is telling her sister’s story in an effort to make a difference in the lives of other patients.
“[Becky] did not want anyone to go through what she went through, ever again,” Ms. Beaton writes.
Letting children roam free
Children of the 1950s and 1960s can remember tearing out the door after dinner with the parental order to be home before dark. Where we went and what we did was known only to us. Our parents trusted we knew how to look out after ourselves.
In that tradition, as explained by National Public Radio, some parents are actively turning away from the to-the-second scheduling of their children’s lives and Teflon coating them against the perceived danger of everyday life. Instead, they are letting their children be independent. It can be a powerful life benefit for a child. But it can come at a cost to parents. Parents in several states have been arrested for actions that include letting their children walk to school unattended.
“This very pessimistic, fearful way of looking at childhood isn’t based in reality,” says Leonore Skenazy in a story on NPR. “It is something that we have been taught.” Ms. Skenazy is founder of Free Range Kids, a group that promotes childhood independence.
Boundaries and remote work
More and more Americans are working from home, according to a 2017 Gallup survey. The survey says that 43% of people worked remotely for part of the time in 2016, compared with 39% in 2012.
But for parents who work remotely, separating their business and family lives is especially challenging, Marie Elizabeth Oliver writes in an article published in The Washington Post.
“Being a parent is isolating, but being a parent and working from home is really isolating,” author Karen Alpert says. “Especially as a mom, there’s so much pressure to do your job as fast and efficiently as possible.”
Experts advise setting boundaries by taking steps such as setting timers and checking in every hour, for example. Or using clothes to make the mental shifts between being on the clock, so to speak, and being in leisure mode.
“It’s not that you have to dress up,” author David Heinemeier Hansson says in the article, describing one of his employees who came up with a system that enabled him to set these boundaries using clothes. “It’s just that he knew, ‘I have my home slippers on right now, so I’m not responding to this email.’ “
Neuroscience as a remedy to heartbreak
The end of a romance can be both frustrating and embarrassing. A person may wallow in the emotional muck for a long time.
Such was the case for Dessa, a well-known rapper, singer, and writer from Minneapolis, who carried the emotional baggage of an ex-boyfriend.
“You’re not only suffering,” she comments in an interview on NPR. “You’re just sort of ridiculous. Discipline and dedication are my strong suits – it really bothered me that, no matter how much effort I tried to expend in trying to solve this problem, I was stuck.”
The stalemate ended when she viewed a TED Talk by Helen Fisher, PhD, a biological anthropologist and visiting research associate at Rutgers University, New Brunswick, N.J. Dr. Fisher used functional MRI to examine some people in the throes of lost love. The examinations revealed revved-up activity of certain parts of their brains.
This prompted the idea that techniques of neurofeedback could be used to wipe the pangs of love from the brain circuitry. It seems to have worked for Dessa, although a placebo effect cannot be ruled out.
“Before [the feedback], I felt that I was really under the thumb of a fixation and a compulsion,” she says. “And now it feels like those feelings have been scaled down.”
Turn on the television, and chances are good that popular dramas (especially hospital-oriented shows) will be showing an episode revolving around a mental health issue.
, in time for a commercial. Real life is messier.
“Unfortunately mental health story lines are much more likely to be fear-mongering and wildly wrong. As a psychiatrist, this both piques my interest and upends my work-life balance,” Dr. Gold writes. “Whether I’m watching everyone’s favorite medical drama or ‘reality TV,’ it’s impossible not to switch into physician mode, angry on behalf of all of my patients and the many viewers who are being misled.”
Do physicians hear women?
“Rebecca continues to be paranoid.”
That was a note written by someone involved in the medical care of a 30-something woman diagnosed with stage IIB cervical cancer, according to an article in New York magazine.
“There’s a whiff of old ‘female hysteria’ to [the note], with more than a hint of dismissal,” writes the patient’s sister, Kate Beaton. “Becky was scared, and perhaps that was the main takeaway that day. But she was also right.”
The article tells the story of a vibrant woman who, according to her sister, asked her doctors lots of questions, wrote everything down, and faced years of being dismissed when she explained her symptoms. Becky’s sister says she is telling her sister’s story in an effort to make a difference in the lives of other patients.
“[Becky] did not want anyone to go through what she went through, ever again,” Ms. Beaton writes.
Letting children roam free
Children of the 1950s and 1960s can remember tearing out the door after dinner with the parental order to be home before dark. Where we went and what we did was known only to us. Our parents trusted we knew how to look out after ourselves.
In that tradition, as explained by National Public Radio, some parents are actively turning away from the to-the-second scheduling of their children’s lives and Teflon coating them against the perceived danger of everyday life. Instead, they are letting their children be independent. It can be a powerful life benefit for a child. But it can come at a cost to parents. Parents in several states have been arrested for actions that include letting their children walk to school unattended.
“This very pessimistic, fearful way of looking at childhood isn’t based in reality,” says Leonore Skenazy in a story on NPR. “It is something that we have been taught.” Ms. Skenazy is founder of Free Range Kids, a group that promotes childhood independence.
Boundaries and remote work
More and more Americans are working from home, according to a 2017 Gallup survey. The survey says that 43% of people worked remotely for part of the time in 2016, compared with 39% in 2012.
But for parents who work remotely, separating their business and family lives is especially challenging, Marie Elizabeth Oliver writes in an article published in The Washington Post.
“Being a parent is isolating, but being a parent and working from home is really isolating,” author Karen Alpert says. “Especially as a mom, there’s so much pressure to do your job as fast and efficiently as possible.”
Experts advise setting boundaries by taking steps such as setting timers and checking in every hour, for example. Or using clothes to make the mental shifts between being on the clock, so to speak, and being in leisure mode.
“It’s not that you have to dress up,” author David Heinemeier Hansson says in the article, describing one of his employees who came up with a system that enabled him to set these boundaries using clothes. “It’s just that he knew, ‘I have my home slippers on right now, so I’m not responding to this email.’ “
Neuroscience as a remedy to heartbreak
The end of a romance can be both frustrating and embarrassing. A person may wallow in the emotional muck for a long time.
Such was the case for Dessa, a well-known rapper, singer, and writer from Minneapolis, who carried the emotional baggage of an ex-boyfriend.
“You’re not only suffering,” she comments in an interview on NPR. “You’re just sort of ridiculous. Discipline and dedication are my strong suits – it really bothered me that, no matter how much effort I tried to expend in trying to solve this problem, I was stuck.”
The stalemate ended when she viewed a TED Talk by Helen Fisher, PhD, a biological anthropologist and visiting research associate at Rutgers University, New Brunswick, N.J. Dr. Fisher used functional MRI to examine some people in the throes of lost love. The examinations revealed revved-up activity of certain parts of their brains.
This prompted the idea that techniques of neurofeedback could be used to wipe the pangs of love from the brain circuitry. It seems to have worked for Dessa, although a placebo effect cannot be ruled out.
“Before [the feedback], I felt that I was really under the thumb of a fixation and a compulsion,” she says. “And now it feels like those feelings have been scaled down.”
Turn on the television, and chances are good that popular dramas (especially hospital-oriented shows) will be showing an episode revolving around a mental health issue.
, in time for a commercial. Real life is messier.
“Unfortunately mental health story lines are much more likely to be fear-mongering and wildly wrong. As a psychiatrist, this both piques my interest and upends my work-life balance,” Dr. Gold writes. “Whether I’m watching everyone’s favorite medical drama or ‘reality TV,’ it’s impossible not to switch into physician mode, angry on behalf of all of my patients and the many viewers who are being misled.”
Do physicians hear women?
“Rebecca continues to be paranoid.”
That was a note written by someone involved in the medical care of a 30-something woman diagnosed with stage IIB cervical cancer, according to an article in New York magazine.
“There’s a whiff of old ‘female hysteria’ to [the note], with more than a hint of dismissal,” writes the patient’s sister, Kate Beaton. “Becky was scared, and perhaps that was the main takeaway that day. But she was also right.”
The article tells the story of a vibrant woman who, according to her sister, asked her doctors lots of questions, wrote everything down, and faced years of being dismissed when she explained her symptoms. Becky’s sister says she is telling her sister’s story in an effort to make a difference in the lives of other patients.
“[Becky] did not want anyone to go through what she went through, ever again,” Ms. Beaton writes.
Letting children roam free
Children of the 1950s and 1960s can remember tearing out the door after dinner with the parental order to be home before dark. Where we went and what we did was known only to us. Our parents trusted we knew how to look out after ourselves.
In that tradition, as explained by National Public Radio, some parents are actively turning away from the to-the-second scheduling of their children’s lives and Teflon coating them against the perceived danger of everyday life. Instead, they are letting their children be independent. It can be a powerful life benefit for a child. But it can come at a cost to parents. Parents in several states have been arrested for actions that include letting their children walk to school unattended.
“This very pessimistic, fearful way of looking at childhood isn’t based in reality,” says Leonore Skenazy in a story on NPR. “It is something that we have been taught.” Ms. Skenazy is founder of Free Range Kids, a group that promotes childhood independence.
Boundaries and remote work
More and more Americans are working from home, according to a 2017 Gallup survey. The survey says that 43% of people worked remotely for part of the time in 2016, compared with 39% in 2012.
But for parents who work remotely, separating their business and family lives is especially challenging, Marie Elizabeth Oliver writes in an article published in The Washington Post.
“Being a parent is isolating, but being a parent and working from home is really isolating,” author Karen Alpert says. “Especially as a mom, there’s so much pressure to do your job as fast and efficiently as possible.”
Experts advise setting boundaries by taking steps such as setting timers and checking in every hour, for example. Or using clothes to make the mental shifts between being on the clock, so to speak, and being in leisure mode.
“It’s not that you have to dress up,” author David Heinemeier Hansson says in the article, describing one of his employees who came up with a system that enabled him to set these boundaries using clothes. “It’s just that he knew, ‘I have my home slippers on right now, so I’m not responding to this email.’ “
Neuroscience as a remedy to heartbreak
The end of a romance can be both frustrating and embarrassing. A person may wallow in the emotional muck for a long time.
Such was the case for Dessa, a well-known rapper, singer, and writer from Minneapolis, who carried the emotional baggage of an ex-boyfriend.
“You’re not only suffering,” she comments in an interview on NPR. “You’re just sort of ridiculous. Discipline and dedication are my strong suits – it really bothered me that, no matter how much effort I tried to expend in trying to solve this problem, I was stuck.”
The stalemate ended when she viewed a TED Talk by Helen Fisher, PhD, a biological anthropologist and visiting research associate at Rutgers University, New Brunswick, N.J. Dr. Fisher used functional MRI to examine some people in the throes of lost love. The examinations revealed revved-up activity of certain parts of their brains.
This prompted the idea that techniques of neurofeedback could be used to wipe the pangs of love from the brain circuitry. It seems to have worked for Dessa, although a placebo effect cannot be ruled out.
“Before [the feedback], I felt that I was really under the thumb of a fixation and a compulsion,” she says. “And now it feels like those feelings have been scaled down.”
Slowing down
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Burnout may jeopardize patient care
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Burnout among physicians was associated with lower quality of care because of unprofessionalism, reduced patient satisfaction, and an increased risk of patient safety issues.
Major finding: Physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85).
Study details: A systematic review and meta-analysis of 42,473 physicians from 47 different studies.
Disclosures: The study was funded by the United Kingdom National Institute of Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors reported no relevant conflicts of interest.
Source: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
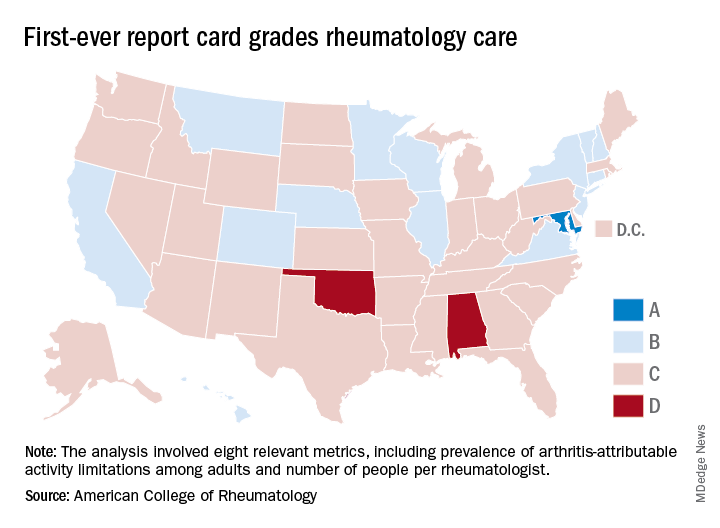
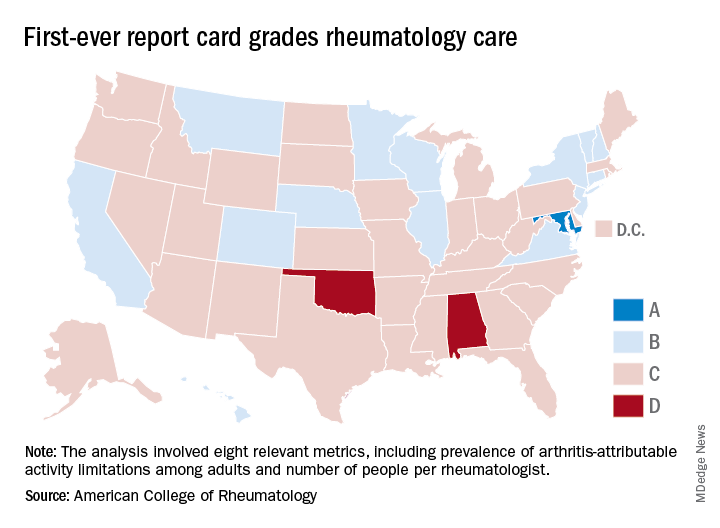
Maryland gets an A on ‘Rheumatic Disease Report Card’
Maryland is alone at the top of the rheumatology care class, but the number of failing states is even smaller, according to the American College of Rheumatology.
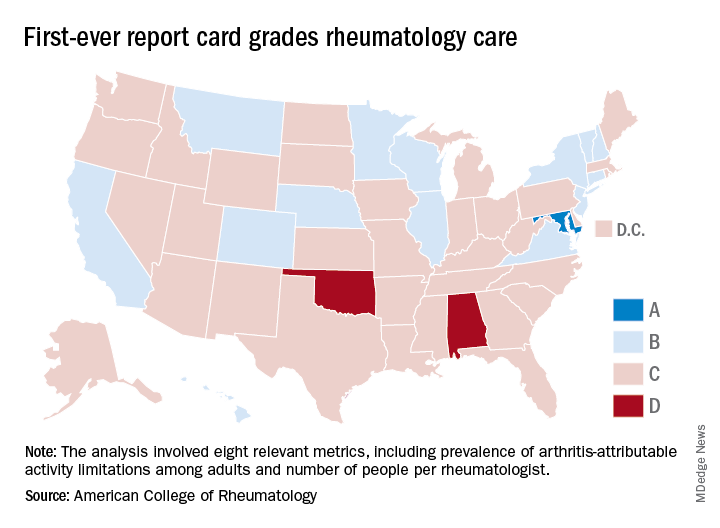
Maryland was the only state to earn an A on the “Rheumatic Disease Report Card,” and while no state failed, two – Alabama and Oklahoma – did receive Ds. Among the 47 other states and the District of Columbia, there were 14 Bs and 34 Cs.
Maryland posted strong scores in all three of the report card’s broad categories of care: 38.25 out of 50 points (third among all states) for access, 35 out of 50 (tied for first with New York) for affordability, and 40 out of 50 (tied for ninth) for activity/lifestyle. Arkansas had the highest score (42.25) for access and Nebraska got 50 out of 50 for activity/lifestyle. Inferiority, however, turned out to be a lot more widespread, as eight states were tied for the low of 10 points in the access category, 26 states got a 0 for affordability, and six states earned 15 points for activity/lifestyle, the ACR said.
Arkansas’s high marks for access were based primarily on “state lawmakers’ recent efforts to address [pharmacy benefit manager] transparency by enacting legislation that should serve as a model for future action in other states looking to address this issue,” ACR officials said in a statement. Nebraska did well in both of the measures used in the activity/lifestyle category – age-adjusted prevalence of arthritis attributable activity limitations among adults and percent of adults who are physically inactive; it also did well because it is home to at least one YMCA-sponsored and one National Recreation and Park Association–sponsored arthritis intervention program funded in part by the Centers for Disease Control and Prevention.
as demand increases and supply decreases. The college’s projections show that almost 6,800 rheumatologists will be needed by 2020 but less than 4,500 will be available, and by 2030 the demand will rise to need for almost 8,200 rheumatologists, while supply is expected to drop below 3,500, according to the report.
“We are at a critical juncture in rheumatology care. The rheumatology workforce is not growing fast enough to keep up with demand and too many of our patients struggle to access and afford the breakthrough therapies they need to manage pain and avoid long-term disability,” ACR President David Daikh, MD, PhD wrote in the report.
Maryland is alone at the top of the rheumatology care class, but the number of failing states is even smaller, according to the American College of Rheumatology.
Maryland was the only state to earn an A on the “Rheumatic Disease Report Card,” and while no state failed, two – Alabama and Oklahoma – did receive Ds. Among the 47 other states and the District of Columbia, there were 14 Bs and 34 Cs.
Maryland posted strong scores in all three of the report card’s broad categories of care: 38.25 out of 50 points (third among all states) for access, 35 out of 50 (tied for first with New York) for affordability, and 40 out of 50 (tied for ninth) for activity/lifestyle. Arkansas had the highest score (42.25) for access and Nebraska got 50 out of 50 for activity/lifestyle. Inferiority, however, turned out to be a lot more widespread, as eight states were tied for the low of 10 points in the access category, 26 states got a 0 for affordability, and six states earned 15 points for activity/lifestyle, the ACR said.
Arkansas’s high marks for access were based primarily on “state lawmakers’ recent efforts to address [pharmacy benefit manager] transparency by enacting legislation that should serve as a model for future action in other states looking to address this issue,” ACR officials said in a statement. Nebraska did well in both of the measures used in the activity/lifestyle category – age-adjusted prevalence of arthritis attributable activity limitations among adults and percent of adults who are physically inactive; it also did well because it is home to at least one YMCA-sponsored and one National Recreation and Park Association–sponsored arthritis intervention program funded in part by the Centers for Disease Control and Prevention.
as demand increases and supply decreases. The college’s projections show that almost 6,800 rheumatologists will be needed by 2020 but less than 4,500 will be available, and by 2030 the demand will rise to need for almost 8,200 rheumatologists, while supply is expected to drop below 3,500, according to the report.
“We are at a critical juncture in rheumatology care. The rheumatology workforce is not growing fast enough to keep up with demand and too many of our patients struggle to access and afford the breakthrough therapies they need to manage pain and avoid long-term disability,” ACR President David Daikh, MD, PhD wrote in the report.
Maryland is alone at the top of the rheumatology care class, but the number of failing states is even smaller, according to the American College of Rheumatology.
Maryland was the only state to earn an A on the “Rheumatic Disease Report Card,” and while no state failed, two – Alabama and Oklahoma – did receive Ds. Among the 47 other states and the District of Columbia, there were 14 Bs and 34 Cs.
Maryland posted strong scores in all three of the report card’s broad categories of care: 38.25 out of 50 points (third among all states) for access, 35 out of 50 (tied for first with New York) for affordability, and 40 out of 50 (tied for ninth) for activity/lifestyle. Arkansas had the highest score (42.25) for access and Nebraska got 50 out of 50 for activity/lifestyle. Inferiority, however, turned out to be a lot more widespread, as eight states were tied for the low of 10 points in the access category, 26 states got a 0 for affordability, and six states earned 15 points for activity/lifestyle, the ACR said.
Arkansas’s high marks for access were based primarily on “state lawmakers’ recent efforts to address [pharmacy benefit manager] transparency by enacting legislation that should serve as a model for future action in other states looking to address this issue,” ACR officials said in a statement. Nebraska did well in both of the measures used in the activity/lifestyle category – age-adjusted prevalence of arthritis attributable activity limitations among adults and percent of adults who are physically inactive; it also did well because it is home to at least one YMCA-sponsored and one National Recreation and Park Association–sponsored arthritis intervention program funded in part by the Centers for Disease Control and Prevention.
as demand increases and supply decreases. The college’s projections show that almost 6,800 rheumatologists will be needed by 2020 but less than 4,500 will be available, and by 2030 the demand will rise to need for almost 8,200 rheumatologists, while supply is expected to drop below 3,500, according to the report.
“We are at a critical juncture in rheumatology care. The rheumatology workforce is not growing fast enough to keep up with demand and too many of our patients struggle to access and afford the breakthrough therapies they need to manage pain and avoid long-term disability,” ACR President David Daikh, MD, PhD wrote in the report.
AAP cautions against marijuana use during pregnancy, breastfeeding
, according to a recent clinical report published in the journal Pediatrics.
“The fact that marijuana is legal in many states may give the impression the drug is harmless during pregnancy, especially with stories swirling on social media about using it for nausea with morning sickness,” Sheryl A. Ryan, MD, FAAP, Chair of the American Academy of Pediatrics (AAP) Committee on Substance Use and Prevention, stated in a press release. “But in fact, this is still a big question. We do not have good safety data on prenatal exposure to marijuana. Based on the limited data that do exist, as pediatricians, we believe there is cause to be concerned about how the drug will impact the long-term development of children.”
The rate of marijuana use is increasing among pregnant women 18 years to 44 years old is increasing, the committee said, with 3.84% of women in 2014 within that age range using marijuana within the past month compared with 2.37% in 2002. Among women who were between 18 years and 25 years old, the rate of marijuana use within the past month was 7.47% in 2014.
The committee also noted research has shown cannabidiol exposure in the short term may impact placental permeability to “pharmacologic agents and recreational substances, potentially placing the fetus at risk from these agents or drugs.” A more well-known substance in marijuana, delta-9-tetrahydrocannabinol (THC) crosses the placental barrier and can appear in fetal blood. Studies have reported any level of marijuana use among pregnant women put the mothers at risk of anemia, while their newborns had an increased risk of low-birth weight and neonatal intensive care unit (NICU) use. Further research has shown impaired mental development, executive function deficits, increased impulsivity and hyperactivity, behavioral problems, depressive symptoms, and greater rates of substance abuse among children exposed to marijuana.
“Many of these effects may not show up right away, but they can impact how well a child can maneuver in the world,” Dr. Ryan stated in the release. “Children’s and teens’ cognitive ability to manage their time and school work might be harmed down the line from marijuana use during their mother’s pregnancy.”
In a related study, Kerri A. Bertrand, MPH, from the department of pediatrics at the University of California in San Diego, Calif., and her colleagues studied cannabinoid concentrations in breastmilk donated to a human milk biorepository. The investigators analyzed 54 samples donated by 50 women who used marijuana while breastfeeding between 2014 and 2017 and determined whether substances such as delta-9-THC, 11-hydroxy-delta-9-tetrahydrocannabinol (11-OH-THC), cannabidiol, and cannabinol were present in breastmilk by performing liquid chromatography mass spectrometry electrospray ionization on the samples.
They found 34 of 54 samples (64%) had detectable delta-9-THC approximately 6 days after marijuana use (median concentration, 9.47 ng/mL; range, 1.01-323 ng/mL), while 5 of 54 samples (9%) had measurable concentrations of 11-OH-THC (range, 1.33-12.80 ng/mL) and 5 of 54 samples (9%) contained measurable cannabidiol (range, 1.32-8.56 ng/mL). Predictors of log delta-9-THC concentrations included number of hours since last use (-0.03; 95% confidence interval, -0.04 to -0.01; P equals .005), the number of times per day marijuana was used (0.51; 95% CI, 0.03-0.99; P equals .039), and the amount of time between sample donation and analysis (0.08; 95% CI, 0.00-0.15; P equals .038), researchers said.
“Because marijuana is the most commonly used recreational drug among breastfeeding women, information regarding risks to breastfeeding infants is urgently needed,” Dr. Bertrand and colleagues wrote in their study.
The authors of the AAP clinical report acknowledge no relevant conflicts of interest. The study by Bertrand and colleagues was supported by the University of California San Diego Center for Better Beginnings, a grant from the National Institutes of Health, and the Gerber Foundation.
SOURCE: Bertrand KA et al. Pediatrics. 2018 Aug 27;doi:10.1542/peds.2018-1076.
The study by Bertrand and colleagues should be commended for being among the first to analyze cannabinoids in breast milk, but there are still very important questions to be answered about marijuana use among women who breast-feed, Sheryl A. Ryan, MD, FAAP, wrote in a related editorial.
Questions remain about why one-third of participants in the study had no detectable cannabinoids in their breast milk, and a frame of reference is needed for the levels that did appear in the study, Dr. Ryan said. Data are also needed on how the cannabinoids “accumulate in the infant, how the infant metabolizes these substances, how quickly they are excreted, whether they accumulate, and thus how long these metabolites remain in the infant,” she said.
Dr. Ryan also questioned what to tell mothers who use marijuana but want to breastfeed their newborns, and noted guidelines from the AAP and the American College of Obstetricians currently recommend avoiding marijuana use entirely while breastfeeding.
“With their study, Bertrand et al. have provided additional and valuable support for those current recommendations. But the picture is incomplete without our understanding of what is happening at the level of those infants exposed to cannabinoid–containing breast milk,” Dr. Ryan said. “Hopefully, the calls for research to answer these important questions will not go unheeded.”
Dr. Ryan is from the Division of Adolescent Medicine and Department of Pediatrics at Penn State Health Children’s Hospital in Hershey, Penn. These comments summarize her editorial in response to Bertrand and colleagues. She reports no relevant conflicts of interest (Ryan SA. Pediatrics. 2018;142[3]:e20181921).
The study by Bertrand and colleagues should be commended for being among the first to analyze cannabinoids in breast milk, but there are still very important questions to be answered about marijuana use among women who breast-feed, Sheryl A. Ryan, MD, FAAP, wrote in a related editorial.
Questions remain about why one-third of participants in the study had no detectable cannabinoids in their breast milk, and a frame of reference is needed for the levels that did appear in the study, Dr. Ryan said. Data are also needed on how the cannabinoids “accumulate in the infant, how the infant metabolizes these substances, how quickly they are excreted, whether they accumulate, and thus how long these metabolites remain in the infant,” she said.
Dr. Ryan also questioned what to tell mothers who use marijuana but want to breastfeed their newborns, and noted guidelines from the AAP and the American College of Obstetricians currently recommend avoiding marijuana use entirely while breastfeeding.
“With their study, Bertrand et al. have provided additional and valuable support for those current recommendations. But the picture is incomplete without our understanding of what is happening at the level of those infants exposed to cannabinoid–containing breast milk,” Dr. Ryan said. “Hopefully, the calls for research to answer these important questions will not go unheeded.”
Dr. Ryan is from the Division of Adolescent Medicine and Department of Pediatrics at Penn State Health Children’s Hospital in Hershey, Penn. These comments summarize her editorial in response to Bertrand and colleagues. She reports no relevant conflicts of interest (Ryan SA. Pediatrics. 2018;142[3]:e20181921).
The study by Bertrand and colleagues should be commended for being among the first to analyze cannabinoids in breast milk, but there are still very important questions to be answered about marijuana use among women who breast-feed, Sheryl A. Ryan, MD, FAAP, wrote in a related editorial.
Questions remain about why one-third of participants in the study had no detectable cannabinoids in their breast milk, and a frame of reference is needed for the levels that did appear in the study, Dr. Ryan said. Data are also needed on how the cannabinoids “accumulate in the infant, how the infant metabolizes these substances, how quickly they are excreted, whether they accumulate, and thus how long these metabolites remain in the infant,” she said.
Dr. Ryan also questioned what to tell mothers who use marijuana but want to breastfeed their newborns, and noted guidelines from the AAP and the American College of Obstetricians currently recommend avoiding marijuana use entirely while breastfeeding.
“With their study, Bertrand et al. have provided additional and valuable support for those current recommendations. But the picture is incomplete without our understanding of what is happening at the level of those infants exposed to cannabinoid–containing breast milk,” Dr. Ryan said. “Hopefully, the calls for research to answer these important questions will not go unheeded.”
Dr. Ryan is from the Division of Adolescent Medicine and Department of Pediatrics at Penn State Health Children’s Hospital in Hershey, Penn. These comments summarize her editorial in response to Bertrand and colleagues. She reports no relevant conflicts of interest (Ryan SA. Pediatrics. 2018;142[3]:e20181921).
, according to a recent clinical report published in the journal Pediatrics.
“The fact that marijuana is legal in many states may give the impression the drug is harmless during pregnancy, especially with stories swirling on social media about using it for nausea with morning sickness,” Sheryl A. Ryan, MD, FAAP, Chair of the American Academy of Pediatrics (AAP) Committee on Substance Use and Prevention, stated in a press release. “But in fact, this is still a big question. We do not have good safety data on prenatal exposure to marijuana. Based on the limited data that do exist, as pediatricians, we believe there is cause to be concerned about how the drug will impact the long-term development of children.”
The rate of marijuana use is increasing among pregnant women 18 years to 44 years old is increasing, the committee said, with 3.84% of women in 2014 within that age range using marijuana within the past month compared with 2.37% in 2002. Among women who were between 18 years and 25 years old, the rate of marijuana use within the past month was 7.47% in 2014.
The committee also noted research has shown cannabidiol exposure in the short term may impact placental permeability to “pharmacologic agents and recreational substances, potentially placing the fetus at risk from these agents or drugs.” A more well-known substance in marijuana, delta-9-tetrahydrocannabinol (THC) crosses the placental barrier and can appear in fetal blood. Studies have reported any level of marijuana use among pregnant women put the mothers at risk of anemia, while their newborns had an increased risk of low-birth weight and neonatal intensive care unit (NICU) use. Further research has shown impaired mental development, executive function deficits, increased impulsivity and hyperactivity, behavioral problems, depressive symptoms, and greater rates of substance abuse among children exposed to marijuana.
“Many of these effects may not show up right away, but they can impact how well a child can maneuver in the world,” Dr. Ryan stated in the release. “Children’s and teens’ cognitive ability to manage their time and school work might be harmed down the line from marijuana use during their mother’s pregnancy.”
In a related study, Kerri A. Bertrand, MPH, from the department of pediatrics at the University of California in San Diego, Calif., and her colleagues studied cannabinoid concentrations in breastmilk donated to a human milk biorepository. The investigators analyzed 54 samples donated by 50 women who used marijuana while breastfeeding between 2014 and 2017 and determined whether substances such as delta-9-THC, 11-hydroxy-delta-9-tetrahydrocannabinol (11-OH-THC), cannabidiol, and cannabinol were present in breastmilk by performing liquid chromatography mass spectrometry electrospray ionization on the samples.
They found 34 of 54 samples (64%) had detectable delta-9-THC approximately 6 days after marijuana use (median concentration, 9.47 ng/mL; range, 1.01-323 ng/mL), while 5 of 54 samples (9%) had measurable concentrations of 11-OH-THC (range, 1.33-12.80 ng/mL) and 5 of 54 samples (9%) contained measurable cannabidiol (range, 1.32-8.56 ng/mL). Predictors of log delta-9-THC concentrations included number of hours since last use (-0.03; 95% confidence interval, -0.04 to -0.01; P equals .005), the number of times per day marijuana was used (0.51; 95% CI, 0.03-0.99; P equals .039), and the amount of time between sample donation and analysis (0.08; 95% CI, 0.00-0.15; P equals .038), researchers said.
“Because marijuana is the most commonly used recreational drug among breastfeeding women, information regarding risks to breastfeeding infants is urgently needed,” Dr. Bertrand and colleagues wrote in their study.
The authors of the AAP clinical report acknowledge no relevant conflicts of interest. The study by Bertrand and colleagues was supported by the University of California San Diego Center for Better Beginnings, a grant from the National Institutes of Health, and the Gerber Foundation.
SOURCE: Bertrand KA et al. Pediatrics. 2018 Aug 27;doi:10.1542/peds.2018-1076.
, according to a recent clinical report published in the journal Pediatrics.
“The fact that marijuana is legal in many states may give the impression the drug is harmless during pregnancy, especially with stories swirling on social media about using it for nausea with morning sickness,” Sheryl A. Ryan, MD, FAAP, Chair of the American Academy of Pediatrics (AAP) Committee on Substance Use and Prevention, stated in a press release. “But in fact, this is still a big question. We do not have good safety data on prenatal exposure to marijuana. Based on the limited data that do exist, as pediatricians, we believe there is cause to be concerned about how the drug will impact the long-term development of children.”
The rate of marijuana use is increasing among pregnant women 18 years to 44 years old is increasing, the committee said, with 3.84% of women in 2014 within that age range using marijuana within the past month compared with 2.37% in 2002. Among women who were between 18 years and 25 years old, the rate of marijuana use within the past month was 7.47% in 2014.
The committee also noted research has shown cannabidiol exposure in the short term may impact placental permeability to “pharmacologic agents and recreational substances, potentially placing the fetus at risk from these agents or drugs.” A more well-known substance in marijuana, delta-9-tetrahydrocannabinol (THC) crosses the placental barrier and can appear in fetal blood. Studies have reported any level of marijuana use among pregnant women put the mothers at risk of anemia, while their newborns had an increased risk of low-birth weight and neonatal intensive care unit (NICU) use. Further research has shown impaired mental development, executive function deficits, increased impulsivity and hyperactivity, behavioral problems, depressive symptoms, and greater rates of substance abuse among children exposed to marijuana.
“Many of these effects may not show up right away, but they can impact how well a child can maneuver in the world,” Dr. Ryan stated in the release. “Children’s and teens’ cognitive ability to manage their time and school work might be harmed down the line from marijuana use during their mother’s pregnancy.”
In a related study, Kerri A. Bertrand, MPH, from the department of pediatrics at the University of California in San Diego, Calif., and her colleagues studied cannabinoid concentrations in breastmilk donated to a human milk biorepository. The investigators analyzed 54 samples donated by 50 women who used marijuana while breastfeeding between 2014 and 2017 and determined whether substances such as delta-9-THC, 11-hydroxy-delta-9-tetrahydrocannabinol (11-OH-THC), cannabidiol, and cannabinol were present in breastmilk by performing liquid chromatography mass spectrometry electrospray ionization on the samples.
They found 34 of 54 samples (64%) had detectable delta-9-THC approximately 6 days after marijuana use (median concentration, 9.47 ng/mL; range, 1.01-323 ng/mL), while 5 of 54 samples (9%) had measurable concentrations of 11-OH-THC (range, 1.33-12.80 ng/mL) and 5 of 54 samples (9%) contained measurable cannabidiol (range, 1.32-8.56 ng/mL). Predictors of log delta-9-THC concentrations included number of hours since last use (-0.03; 95% confidence interval, -0.04 to -0.01; P equals .005), the number of times per day marijuana was used (0.51; 95% CI, 0.03-0.99; P equals .039), and the amount of time between sample donation and analysis (0.08; 95% CI, 0.00-0.15; P equals .038), researchers said.
“Because marijuana is the most commonly used recreational drug among breastfeeding women, information regarding risks to breastfeeding infants is urgently needed,” Dr. Bertrand and colleagues wrote in their study.
The authors of the AAP clinical report acknowledge no relevant conflicts of interest. The study by Bertrand and colleagues was supported by the University of California San Diego Center for Better Beginnings, a grant from the National Institutes of Health, and the Gerber Foundation.
SOURCE: Bertrand KA et al. Pediatrics. 2018 Aug 27;doi:10.1542/peds.2018-1076.
PEDIATRICS
Key clinical point: More studies are needed to analyze the long-term effects marijuana has on mother and child during pregnancy and while breastfeeding.
Major finding: Of women between 18 years and 44 years old, 3.84% used marijuana during pregnancy in 2014 compared with 2.37% in 2002; 64% of samples in Bertrand and colleagues’ study had THC traceable in breastmilk approximately 6 days after marijuana use.
Study details:A clinical report on marijuana use during pregnancy and while breastfeeding, and a study of 50 women who used marijuana while breastfeeding and donated samples to a human milk biorepository.
Disclosures:The authors of the AAP clinical report no relevant conflicts of interest. The study by Bertrand and colleagues was supported by the University of California San Diego Center for Better Beginnings, a grant from the National Institutes of Health, and the Gerber Foundation.
Source: Ryan SA et al. Pediatrics. 2018 Aug 27;doi:10.1542/peds.2018-1889. Bertrand KA et al. Pediatrics. 2018 Aug 27;doi:10.1542/peds.2018-1076.
Study examines the world of alcohol use
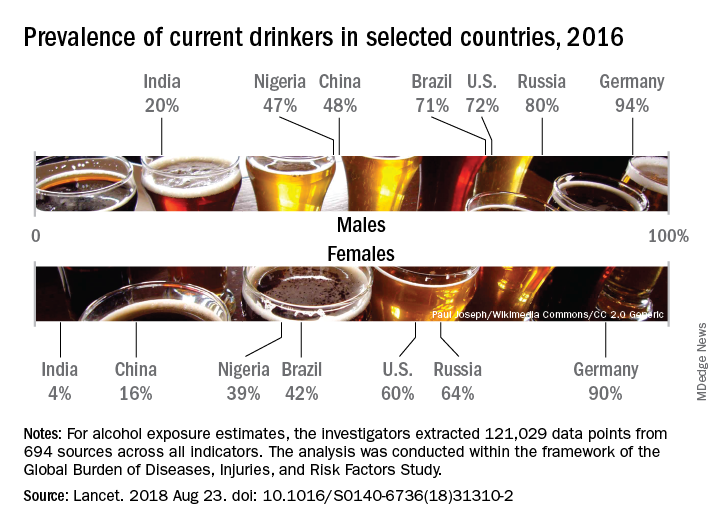
Considerable variations were seen in alcohol consumption. In 2016, males overall consumed more than twice as many standard drinks per day as females: 1.70 versus 0.73. Alcohol consumption in those aged 15-95 years was highest in the top quintile of countries according to sociodemographic development for both males (2.9 drinks per day) and females (1.9) and lowest in the bottom quintile of countries for males (1.4) and the second-lowest quintile for females (0.3), Max G. Griswold, MA, of the University of Washington, Seattle, and his associates said in the Lancet.
Denmark had the highest prevalence of current drinkers of any country for both males (97%) and females (95%) in 2016; Pakistan was lowest for males (0.8%) and Bangladesh was lowest for females (0.3%). The United States had a prevalence of 72% for males and 60% for females, along with consumption rates of 3.2 drinks per day for males and 1.9 for females. Alcohol-related diseases caused 6.7% of male deaths and 2.3% of female deaths in the United States, both close to the global numbers of 6.8% for males and 2.2% for females, the investigators said.
The analysis, conducted within the framework of the Global Burden of Diseases, Injuries, and Risk Factors Study, showed that even a single alcoholic drink a day increases the risk of developing 1 of the 23 alcohol-related health problems by 0.5% a year for people aged 15-95 years, which translates into a rate of 918 per 100,000 population, compared with 914 per 100,000 for nondrinkers. Consuming two drinks a day raises the risk to 7%, which would be an incidence of 977 per 100,000, and those who have five drinks a day increase their risk by 37%, which works out to 1,252 people per 100,000 who would develop an alcohol-related disease, Mr. Griswold and his associates said.
In an editorial comment, Robyn Burton, PhD, of King’s College London and Nick Sheron, MD, of the University of Southampton (England), wrote that “the conclusions of the study are clear and unambiguous: Alcohol is a colossal global health issue and small reductions in health-related harms at low levels of alcohol intake are outweighed by the increased risk of other health-related harms, including cancer. … These diseases of unhealthy behaviors, facilitated by unhealthy environments and fueled by commercial interests putting shareholder value ahead of the tragic human consequences, are the dominant health issue of the 21st century. The solutions are straightforward: Increasing taxation creates income for hard-pressed health ministries, and reducing the exposure of children to alcohol marketing has no downsides.”
The study was funded by the Bill and Melinda Gates Foundation. Mr. Griswold did not have any conflicts to disclose, but six of his several hundred coauthors did make such disclosures.
SOURCE: Griswold MG et al. Lancet. 2018 Aug 23. doi: 10.1016/S0140-6736(18)31310-2.
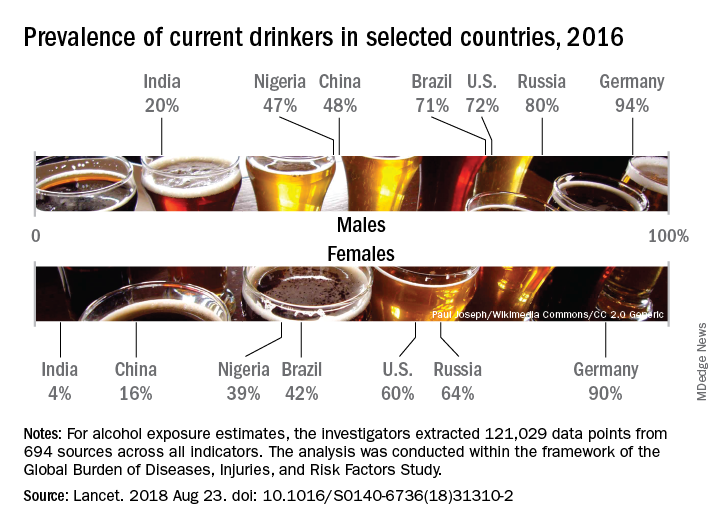
Considerable variations were seen in alcohol consumption. In 2016, males overall consumed more than twice as many standard drinks per day as females: 1.70 versus 0.73. Alcohol consumption in those aged 15-95 years was highest in the top quintile of countries according to sociodemographic development for both males (2.9 drinks per day) and females (1.9) and lowest in the bottom quintile of countries for males (1.4) and the second-lowest quintile for females (0.3), Max G. Griswold, MA, of the University of Washington, Seattle, and his associates said in the Lancet.
Denmark had the highest prevalence of current drinkers of any country for both males (97%) and females (95%) in 2016; Pakistan was lowest for males (0.8%) and Bangladesh was lowest for females (0.3%). The United States had a prevalence of 72% for males and 60% for females, along with consumption rates of 3.2 drinks per day for males and 1.9 for females. Alcohol-related diseases caused 6.7% of male deaths and 2.3% of female deaths in the United States, both close to the global numbers of 6.8% for males and 2.2% for females, the investigators said.
The analysis, conducted within the framework of the Global Burden of Diseases, Injuries, and Risk Factors Study, showed that even a single alcoholic drink a day increases the risk of developing 1 of the 23 alcohol-related health problems by 0.5% a year for people aged 15-95 years, which translates into a rate of 918 per 100,000 population, compared with 914 per 100,000 for nondrinkers. Consuming two drinks a day raises the risk to 7%, which would be an incidence of 977 per 100,000, and those who have five drinks a day increase their risk by 37%, which works out to 1,252 people per 100,000 who would develop an alcohol-related disease, Mr. Griswold and his associates said.
In an editorial comment, Robyn Burton, PhD, of King’s College London and Nick Sheron, MD, of the University of Southampton (England), wrote that “the conclusions of the study are clear and unambiguous: Alcohol is a colossal global health issue and small reductions in health-related harms at low levels of alcohol intake are outweighed by the increased risk of other health-related harms, including cancer. … These diseases of unhealthy behaviors, facilitated by unhealthy environments and fueled by commercial interests putting shareholder value ahead of the tragic human consequences, are the dominant health issue of the 21st century. The solutions are straightforward: Increasing taxation creates income for hard-pressed health ministries, and reducing the exposure of children to alcohol marketing has no downsides.”
The study was funded by the Bill and Melinda Gates Foundation. Mr. Griswold did not have any conflicts to disclose, but six of his several hundred coauthors did make such disclosures.
SOURCE: Griswold MG et al. Lancet. 2018 Aug 23. doi: 10.1016/S0140-6736(18)31310-2.
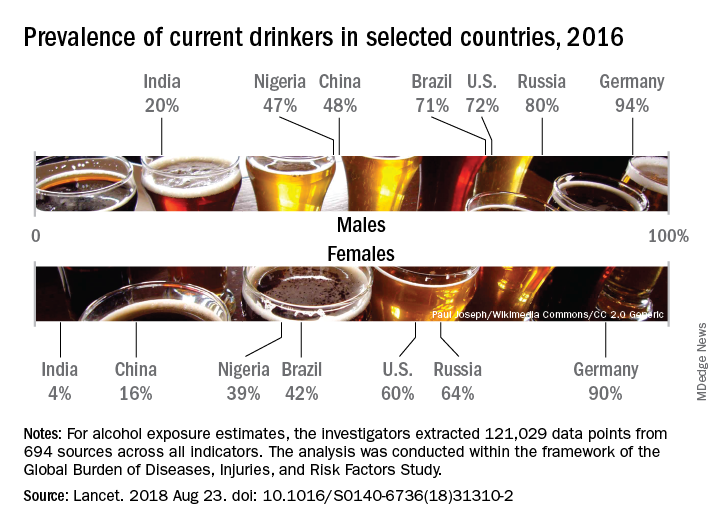
Considerable variations were seen in alcohol consumption. In 2016, males overall consumed more than twice as many standard drinks per day as females: 1.70 versus 0.73. Alcohol consumption in those aged 15-95 years was highest in the top quintile of countries according to sociodemographic development for both males (2.9 drinks per day) and females (1.9) and lowest in the bottom quintile of countries for males (1.4) and the second-lowest quintile for females (0.3), Max G. Griswold, MA, of the University of Washington, Seattle, and his associates said in the Lancet.
Denmark had the highest prevalence of current drinkers of any country for both males (97%) and females (95%) in 2016; Pakistan was lowest for males (0.8%) and Bangladesh was lowest for females (0.3%). The United States had a prevalence of 72% for males and 60% for females, along with consumption rates of 3.2 drinks per day for males and 1.9 for females. Alcohol-related diseases caused 6.7% of male deaths and 2.3% of female deaths in the United States, both close to the global numbers of 6.8% for males and 2.2% for females, the investigators said.
The analysis, conducted within the framework of the Global Burden of Diseases, Injuries, and Risk Factors Study, showed that even a single alcoholic drink a day increases the risk of developing 1 of the 23 alcohol-related health problems by 0.5% a year for people aged 15-95 years, which translates into a rate of 918 per 100,000 population, compared with 914 per 100,000 for nondrinkers. Consuming two drinks a day raises the risk to 7%, which would be an incidence of 977 per 100,000, and those who have five drinks a day increase their risk by 37%, which works out to 1,252 people per 100,000 who would develop an alcohol-related disease, Mr. Griswold and his associates said.
In an editorial comment, Robyn Burton, PhD, of King’s College London and Nick Sheron, MD, of the University of Southampton (England), wrote that “the conclusions of the study are clear and unambiguous: Alcohol is a colossal global health issue and small reductions in health-related harms at low levels of alcohol intake are outweighed by the increased risk of other health-related harms, including cancer. … These diseases of unhealthy behaviors, facilitated by unhealthy environments and fueled by commercial interests putting shareholder value ahead of the tragic human consequences, are the dominant health issue of the 21st century. The solutions are straightforward: Increasing taxation creates income for hard-pressed health ministries, and reducing the exposure of children to alcohol marketing has no downsides.”
The study was funded by the Bill and Melinda Gates Foundation. Mr. Griswold did not have any conflicts to disclose, but six of his several hundred coauthors did make such disclosures.
SOURCE: Griswold MG et al. Lancet. 2018 Aug 23. doi: 10.1016/S0140-6736(18)31310-2.
FROM THE LANCET
Creating positive patient experiences
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Pediatricians doing good globally
Do the images of Syrian refugee children kindle a desire to leave the privileged suburban-dwelling patients in your practice for just a few weeks and donate your clinical skills to help the victims of political conflict? Or, are you looking for a way to give your post-retirement life some meaning by volunteering on a typhoon-ravaged island in Southeast Asia?
Before you ask your partners for a 1-month leave of absence or try to convince your spouse that camping out in a refugee camp would be a better way to spend this year’s travel budget, I urge you to read Pediatricians and Global Health: Opportunities and Considerations for Meaningful Engagement, published in Pediatrics. This lengthy and thorough report by the American Board of Pediatrics Global Health Task Force will give you pause and should serve as an important reality check before you run off to buy the plane tickets for your personal mission of mercy.
Gitanjli Arora, MD, of the Children’s Hospital of Los Angeles, and her coauthors point out that, just because there appears to be a need for people with clinical expertise does not mean that your little black bag of skills honed in the privileged bubble of a first-world country is going to be of much help. This question is one I have pondered on several occasions when I have been offered what might be called “medical voluntourism” opportunities.
If I have distinguished myself as a clinician, that skill has been based on my ability to listen and communicate. Dropped into a community where I have little or no language facility and cultural awareness, I would need to rely on my observational skills. While I pride myself on my ability to make a visual diagnosis, the truth is that my diagnostic successes based solely on observation are almost exclusively dermatologic ones. And, let me add, my familiarity with tropical skin rashes is severely limited. I’m sure I could learn but not in a stay as short as a month.
Taking a history and communicating a treatment plan would force me to rely on the skills of a translator. In settings dominated by upheaval, many of the presenting complaints are going to be the result of, or at least heavily colored by, the chaos induced by anxiety. The ability to sort out where the mind and body connect is difficult enough in a community in which I have spent 40 years and speak the language. Regardless of how much sympathy I feel for the victims of tragic events, my clinical skills would have little value in the short term. Even worse, I would probably just be in the way. As the Task Force points out, my presence could also be squandering local resources as on-site providers worked to get me up to speed.
The authors also explore the numerous other complicating factors that must be considered by those of us who feel the pull to help the victims of global strife and natural disaster. While the authors discourage physicians like you and me from “dropping in” to help, they offer an abundance of suggestions on how we can act globally and stay locally.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Do the images of Syrian refugee children kindle a desire to leave the privileged suburban-dwelling patients in your practice for just a few weeks and donate your clinical skills to help the victims of political conflict? Or, are you looking for a way to give your post-retirement life some meaning by volunteering on a typhoon-ravaged island in Southeast Asia?
Before you ask your partners for a 1-month leave of absence or try to convince your spouse that camping out in a refugee camp would be a better way to spend this year’s travel budget, I urge you to read Pediatricians and Global Health: Opportunities and Considerations for Meaningful Engagement, published in Pediatrics. This lengthy and thorough report by the American Board of Pediatrics Global Health Task Force will give you pause and should serve as an important reality check before you run off to buy the plane tickets for your personal mission of mercy.
Gitanjli Arora, MD, of the Children’s Hospital of Los Angeles, and her coauthors point out that, just because there appears to be a need for people with clinical expertise does not mean that your little black bag of skills honed in the privileged bubble of a first-world country is going to be of much help. This question is one I have pondered on several occasions when I have been offered what might be called “medical voluntourism” opportunities.
If I have distinguished myself as a clinician, that skill has been based on my ability to listen and communicate. Dropped into a community where I have little or no language facility and cultural awareness, I would need to rely on my observational skills. While I pride myself on my ability to make a visual diagnosis, the truth is that my diagnostic successes based solely on observation are almost exclusively dermatologic ones. And, let me add, my familiarity with tropical skin rashes is severely limited. I’m sure I could learn but not in a stay as short as a month.
Taking a history and communicating a treatment plan would force me to rely on the skills of a translator. In settings dominated by upheaval, many of the presenting complaints are going to be the result of, or at least heavily colored by, the chaos induced by anxiety. The ability to sort out where the mind and body connect is difficult enough in a community in which I have spent 40 years and speak the language. Regardless of how much sympathy I feel for the victims of tragic events, my clinical skills would have little value in the short term. Even worse, I would probably just be in the way. As the Task Force points out, my presence could also be squandering local resources as on-site providers worked to get me up to speed.
The authors also explore the numerous other complicating factors that must be considered by those of us who feel the pull to help the victims of global strife and natural disaster. While the authors discourage physicians like you and me from “dropping in” to help, they offer an abundance of suggestions on how we can act globally and stay locally.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Do the images of Syrian refugee children kindle a desire to leave the privileged suburban-dwelling patients in your practice for just a few weeks and donate your clinical skills to help the victims of political conflict? Or, are you looking for a way to give your post-retirement life some meaning by volunteering on a typhoon-ravaged island in Southeast Asia?
Before you ask your partners for a 1-month leave of absence or try to convince your spouse that camping out in a refugee camp would be a better way to spend this year’s travel budget, I urge you to read Pediatricians and Global Health: Opportunities and Considerations for Meaningful Engagement, published in Pediatrics. This lengthy and thorough report by the American Board of Pediatrics Global Health Task Force will give you pause and should serve as an important reality check before you run off to buy the plane tickets for your personal mission of mercy.
Gitanjli Arora, MD, of the Children’s Hospital of Los Angeles, and her coauthors point out that, just because there appears to be a need for people with clinical expertise does not mean that your little black bag of skills honed in the privileged bubble of a first-world country is going to be of much help. This question is one I have pondered on several occasions when I have been offered what might be called “medical voluntourism” opportunities.
If I have distinguished myself as a clinician, that skill has been based on my ability to listen and communicate. Dropped into a community where I have little or no language facility and cultural awareness, I would need to rely on my observational skills. While I pride myself on my ability to make a visual diagnosis, the truth is that my diagnostic successes based solely on observation are almost exclusively dermatologic ones. And, let me add, my familiarity with tropical skin rashes is severely limited. I’m sure I could learn but not in a stay as short as a month.
Taking a history and communicating a treatment plan would force me to rely on the skills of a translator. In settings dominated by upheaval, many of the presenting complaints are going to be the result of, or at least heavily colored by, the chaos induced by anxiety. The ability to sort out where the mind and body connect is difficult enough in a community in which I have spent 40 years and speak the language. Regardless of how much sympathy I feel for the victims of tragic events, my clinical skills would have little value in the short term. Even worse, I would probably just be in the way. As the Task Force points out, my presence could also be squandering local resources as on-site providers worked to get me up to speed.
The authors also explore the numerous other complicating factors that must be considered by those of us who feel the pull to help the victims of global strife and natural disaster. While the authors discourage physicians like you and me from “dropping in” to help, they offer an abundance of suggestions on how we can act globally and stay locally.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].