User login
Boosting daily exercise after age 70 tied to lower CVD risk
Increasingly active patterns of physical activity were linked with reduced rates of overall mortality and cardiovascular disease (CVD), but early rather than later in late life, in a 20-year follow-up cohort study.
In this population of people older than 65 years, researchers found that physical activity overall was associated with lower rates of incident CVD, particularly among men, and the association was strongest in people 70 to 75 years of age, rather than in older age groups.
They also looked at “trajectories,” or changes in activity over time, and found that a stable-high trajectory of activity was associated with a significantly lower risk for cardiovascular outcomes in men than in those with a stable-low trajectory. For women, more physical activity was consistently associated with lower CVD outcomes, although not statistically significantly so, except for overall mortality, which did reach significance.
Notably, the greatest reduction in cardiovascular risk was reported in people who did more than 20 minutes of physical exercise each day, and it was more pronounced in those 70 years of age.
Physical activity was also associated with a lower incidence of heart failure and coronary heart disease in older people, again especially early on in late life, reported Claudio Barbiellini Amidei, MD, University of Padua, Italy, and colleagues.
The data suggest that physical activity is more effective in preventing CVD onset when implemented early rather than later in life, noted Dr. Amidei in an email.
“The findings of our study are suggestive of a protective effect of physical activity in late-life on cardiovascular health. WHO recommendations for adults and older adults are to practice at least 20 minutes of moderate to vigorous physical activity per day. I believe this is a realistic target, and policy makers should raise awareness on the importance of achieving this goal at all ages, including in late-life,” Dr. Amidei said.
The study was published online Feb. 14 in Heart.
Previous research has demonstrated that the most benefit of high physical activity, compared with low, begins at about 60 years of age, and that is because younger people are at much lower risk, noted Carl “Chip” Lavie MD, FACC, medical director of cardiac rehabilitation and prevention, Ochsner Clinical School–The University of Queensland School of Medicine, New Orleans, who was not involved in the study.
“At quite old ages, for example over age 80, resistance exercise or weight training and balance training may be even more important than aerobic training,” he added.
Activity ‘trajectories’
The benefits of physical activity on cardiovascular risk are well established, the researchers note. Less clear is the role that trajectories of activity over time play, although research to date suggests a reduction in risk with increasing activity from mid-life to early old age, they write.
For the current analysis, the researchers assessed 3,099 Italian participants. Mean age was about 75 years, and baseline data were collected from 1995 to 1997.
Follow-up visits were conducted after 4 years and again after 7 years. Using hospital medical records and mortality data, the researchers were able to collect surveillance data through 2018. Hospital records, surveys, and clinical assessments helped them identify incident and prevalent cardiovascular diseases, such as stroke, coronary heart disease, and heart failure.
Participants’ physical activity patterns were classified as stable-high, low-increasing, high-decreasing, and stable-low. Exposure was evaluated at 70, 75, 80, and 85 years of age.
“In our analyses, we focused on moderate to vigorous physical activity, and these include a broad range of exercises, such as walking very briskly, playing tennis, [and] jogging, but comprise also other activities, such as gardening or doing household chores,” said Dr. Amidei.
Patterns of stable-low physical activity were linked to a significantly greater risk for cardiovascular outcomes in men than patterns of stable-high physical activity (hazard ratio, 0.48; 95% confidence interval, 0.27-0.86; P for trend = .002).
No significant relation was found between physical activity and stroke, the researchers note.
“The benefits of physical activity seem to lessen above the age of 75 years and seem more important in men,” noted Dr. Lavie. “This may be partly due to the higher risk of CVD in men. Women typically lag 13 to 15 years behind men for CVD but start catching up in older years.”
Limitations of the study include lack of information regarding physical activity during mid-life, the limited number of stroke events, the relatively few participants older than 85 years, and potential recall bias, the researchers note.
Another limitation was that the physical activity data were based on patient surveys collected 3 years apart and did not involve the use of an accelerometer, the researchers add.
“Future observational studies are required to confirm our findings and pathophysiological studies are warranted to examine the underlying biological mechanisms. Physical activity is likely to be beneficial at any age, but to summarize our findings, we could say that when it comes to being physically active, the sooner the better,” concluded Dr. Amidei.
Dr. Amidei reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Increasingly active patterns of physical activity were linked with reduced rates of overall mortality and cardiovascular disease (CVD), but early rather than later in late life, in a 20-year follow-up cohort study.
In this population of people older than 65 years, researchers found that physical activity overall was associated with lower rates of incident CVD, particularly among men, and the association was strongest in people 70 to 75 years of age, rather than in older age groups.
They also looked at “trajectories,” or changes in activity over time, and found that a stable-high trajectory of activity was associated with a significantly lower risk for cardiovascular outcomes in men than in those with a stable-low trajectory. For women, more physical activity was consistently associated with lower CVD outcomes, although not statistically significantly so, except for overall mortality, which did reach significance.
Notably, the greatest reduction in cardiovascular risk was reported in people who did more than 20 minutes of physical exercise each day, and it was more pronounced in those 70 years of age.
Physical activity was also associated with a lower incidence of heart failure and coronary heart disease in older people, again especially early on in late life, reported Claudio Barbiellini Amidei, MD, University of Padua, Italy, and colleagues.
The data suggest that physical activity is more effective in preventing CVD onset when implemented early rather than later in life, noted Dr. Amidei in an email.
“The findings of our study are suggestive of a protective effect of physical activity in late-life on cardiovascular health. WHO recommendations for adults and older adults are to practice at least 20 minutes of moderate to vigorous physical activity per day. I believe this is a realistic target, and policy makers should raise awareness on the importance of achieving this goal at all ages, including in late-life,” Dr. Amidei said.
The study was published online Feb. 14 in Heart.
Previous research has demonstrated that the most benefit of high physical activity, compared with low, begins at about 60 years of age, and that is because younger people are at much lower risk, noted Carl “Chip” Lavie MD, FACC, medical director of cardiac rehabilitation and prevention, Ochsner Clinical School–The University of Queensland School of Medicine, New Orleans, who was not involved in the study.
“At quite old ages, for example over age 80, resistance exercise or weight training and balance training may be even more important than aerobic training,” he added.
Activity ‘trajectories’
The benefits of physical activity on cardiovascular risk are well established, the researchers note. Less clear is the role that trajectories of activity over time play, although research to date suggests a reduction in risk with increasing activity from mid-life to early old age, they write.
For the current analysis, the researchers assessed 3,099 Italian participants. Mean age was about 75 years, and baseline data were collected from 1995 to 1997.
Follow-up visits were conducted after 4 years and again after 7 years. Using hospital medical records and mortality data, the researchers were able to collect surveillance data through 2018. Hospital records, surveys, and clinical assessments helped them identify incident and prevalent cardiovascular diseases, such as stroke, coronary heart disease, and heart failure.
Participants’ physical activity patterns were classified as stable-high, low-increasing, high-decreasing, and stable-low. Exposure was evaluated at 70, 75, 80, and 85 years of age.
“In our analyses, we focused on moderate to vigorous physical activity, and these include a broad range of exercises, such as walking very briskly, playing tennis, [and] jogging, but comprise also other activities, such as gardening or doing household chores,” said Dr. Amidei.
Patterns of stable-low physical activity were linked to a significantly greater risk for cardiovascular outcomes in men than patterns of stable-high physical activity (hazard ratio, 0.48; 95% confidence interval, 0.27-0.86; P for trend = .002).
No significant relation was found between physical activity and stroke, the researchers note.
“The benefits of physical activity seem to lessen above the age of 75 years and seem more important in men,” noted Dr. Lavie. “This may be partly due to the higher risk of CVD in men. Women typically lag 13 to 15 years behind men for CVD but start catching up in older years.”
Limitations of the study include lack of information regarding physical activity during mid-life, the limited number of stroke events, the relatively few participants older than 85 years, and potential recall bias, the researchers note.
Another limitation was that the physical activity data were based on patient surveys collected 3 years apart and did not involve the use of an accelerometer, the researchers add.
“Future observational studies are required to confirm our findings and pathophysiological studies are warranted to examine the underlying biological mechanisms. Physical activity is likely to be beneficial at any age, but to summarize our findings, we could say that when it comes to being physically active, the sooner the better,” concluded Dr. Amidei.
Dr. Amidei reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Increasingly active patterns of physical activity were linked with reduced rates of overall mortality and cardiovascular disease (CVD), but early rather than later in late life, in a 20-year follow-up cohort study.
In this population of people older than 65 years, researchers found that physical activity overall was associated with lower rates of incident CVD, particularly among men, and the association was strongest in people 70 to 75 years of age, rather than in older age groups.
They also looked at “trajectories,” or changes in activity over time, and found that a stable-high trajectory of activity was associated with a significantly lower risk for cardiovascular outcomes in men than in those with a stable-low trajectory. For women, more physical activity was consistently associated with lower CVD outcomes, although not statistically significantly so, except for overall mortality, which did reach significance.
Notably, the greatest reduction in cardiovascular risk was reported in people who did more than 20 minutes of physical exercise each day, and it was more pronounced in those 70 years of age.
Physical activity was also associated with a lower incidence of heart failure and coronary heart disease in older people, again especially early on in late life, reported Claudio Barbiellini Amidei, MD, University of Padua, Italy, and colleagues.
The data suggest that physical activity is more effective in preventing CVD onset when implemented early rather than later in life, noted Dr. Amidei in an email.
“The findings of our study are suggestive of a protective effect of physical activity in late-life on cardiovascular health. WHO recommendations for adults and older adults are to practice at least 20 minutes of moderate to vigorous physical activity per day. I believe this is a realistic target, and policy makers should raise awareness on the importance of achieving this goal at all ages, including in late-life,” Dr. Amidei said.
The study was published online Feb. 14 in Heart.
Previous research has demonstrated that the most benefit of high physical activity, compared with low, begins at about 60 years of age, and that is because younger people are at much lower risk, noted Carl “Chip” Lavie MD, FACC, medical director of cardiac rehabilitation and prevention, Ochsner Clinical School–The University of Queensland School of Medicine, New Orleans, who was not involved in the study.
“At quite old ages, for example over age 80, resistance exercise or weight training and balance training may be even more important than aerobic training,” he added.
Activity ‘trajectories’
The benefits of physical activity on cardiovascular risk are well established, the researchers note. Less clear is the role that trajectories of activity over time play, although research to date suggests a reduction in risk with increasing activity from mid-life to early old age, they write.
For the current analysis, the researchers assessed 3,099 Italian participants. Mean age was about 75 years, and baseline data were collected from 1995 to 1997.
Follow-up visits were conducted after 4 years and again after 7 years. Using hospital medical records and mortality data, the researchers were able to collect surveillance data through 2018. Hospital records, surveys, and clinical assessments helped them identify incident and prevalent cardiovascular diseases, such as stroke, coronary heart disease, and heart failure.
Participants’ physical activity patterns were classified as stable-high, low-increasing, high-decreasing, and stable-low. Exposure was evaluated at 70, 75, 80, and 85 years of age.
“In our analyses, we focused on moderate to vigorous physical activity, and these include a broad range of exercises, such as walking very briskly, playing tennis, [and] jogging, but comprise also other activities, such as gardening or doing household chores,” said Dr. Amidei.
Patterns of stable-low physical activity were linked to a significantly greater risk for cardiovascular outcomes in men than patterns of stable-high physical activity (hazard ratio, 0.48; 95% confidence interval, 0.27-0.86; P for trend = .002).
No significant relation was found between physical activity and stroke, the researchers note.
“The benefits of physical activity seem to lessen above the age of 75 years and seem more important in men,” noted Dr. Lavie. “This may be partly due to the higher risk of CVD in men. Women typically lag 13 to 15 years behind men for CVD but start catching up in older years.”
Limitations of the study include lack of information regarding physical activity during mid-life, the limited number of stroke events, the relatively few participants older than 85 years, and potential recall bias, the researchers note.
Another limitation was that the physical activity data were based on patient surveys collected 3 years apart and did not involve the use of an accelerometer, the researchers add.
“Future observational studies are required to confirm our findings and pathophysiological studies are warranted to examine the underlying biological mechanisms. Physical activity is likely to be beneficial at any age, but to summarize our findings, we could say that when it comes to being physically active, the sooner the better,” concluded Dr. Amidei.
Dr. Amidei reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early treatment may delay atherosclerosis in familial hypercholesterolemia
Patients with familial hypercholesterolemia (FH) who start lipid-lowering treatment earlier in life may reduce their cardiovascular risk, compared with those who don’t begin treatment early, according to results of a recent meta-analysis.
They showed a difference in the carotid intima-media thickness (IMT) between patients with and without FH that increased with age, but there was also a difference in IMT seen among patients with FH who started treatment early, compared with untreated patients with FH, Kika van Bergen en Henegouwen, of the departments of pediatrics and epidemiology and data science at Amsterdam University Medical Center, and colleagues wrote in their report, published in the Journal of Clinical Lipidology.
“The fact that the difference in IMT increases with age between FH patients and unaffected controls, and is more pronounced in studies with untreated FH patients than in studies with treated patients, suggests that starting treatment already at a young age in patients with FH is preferred,” the researchers wrote. “However, despite treatment, IMT in treated FH patients is still thicker in comparison to subjects without FH.”
The researchers identified 42 studies with among patients with FH and healthy control groups across the MEDLINE, EMBASE and Trials.gov databases up to a cutoff date of April 2020, with 39 studies specifically examining carotid IMT, 2 studies evaluating carotid and femoral IMT, and 1 study evaluating femoral IMT alone. Overall, the researchers examined IMT measurements in 3,796 patients with FH and 2,363 control group participants.
Although data on age and gender for FH and control groups were not available in 6 studies, the mean age ranged from 9 to 57 years for patients with FH and from 8 to 61 years in the control group. Men comprised just under half of both the FH and control groups.
The mean between-group difference in carotid IMT in 34 studies was 0.11 mm (95% confidence interval, 0.06-0.15 mm; P < .001) for patients with FH, compared with the control group, while the mean difference in femoral IMT in three studies was 0.47 mm (95% CI, 0.19-0.74 mm; P < .001) between FH and control groups.
In 13 studies in which data on differences between partly treated and untreated FH were available, there was a significant between-group difference in carotid IMT with partly treated patients with FH, compared with the control group (0.05 mm; 95% CI, 0.03-0.08 mm; P < .001), but a larger mean between-group difference in carotid IMT among untreated patients with FH, compared with a control group (0.12 mm; 95% CI, 0.03-0.21 mm; P = .009).
The researchers also analyzed how age impacts carotid IMT, and they found patients with FH had a mean increase of 0.0018 mm (95% CI, –0.0007 to 0.0042 mm) over a control group in 34 studies. For patients with partly treated FH, compared with patients with untreated FH, the mean between-group increase per year was smaller (0.0023 mm; 95% CI, 0.0021-0.0025 mm), compared with the control group (0.0104 mm; 95% CI, 0.0100-0.0108 mm).
“This sign of residual risk might suggest that more robust cholesterol-lowering treatment and achieving treatment targets, or earlier treatment initiation, is needed to reduce IMT progression to non-FH conditions,” the researchers said. “Therefore, we must find and diagnose these patients, and treat them according to current guidelines.”
Limitations of the authors’ meta-analyses include heterogeneity among studies, differences in IMT measurement protocols, and inclusion of studies with an open-label design. Although randomized clinical trials would be preferable to compare treatment effect, “since statin therapy is indicated in FH patients to reduce [cardiovascular disease], it would be unethical to have a placebo group,” they said.
The authors reported no relevant financial disclosures.
Patients with familial hypercholesterolemia (FH) who start lipid-lowering treatment earlier in life may reduce their cardiovascular risk, compared with those who don’t begin treatment early, according to results of a recent meta-analysis.
They showed a difference in the carotid intima-media thickness (IMT) between patients with and without FH that increased with age, but there was also a difference in IMT seen among patients with FH who started treatment early, compared with untreated patients with FH, Kika van Bergen en Henegouwen, of the departments of pediatrics and epidemiology and data science at Amsterdam University Medical Center, and colleagues wrote in their report, published in the Journal of Clinical Lipidology.
“The fact that the difference in IMT increases with age between FH patients and unaffected controls, and is more pronounced in studies with untreated FH patients than in studies with treated patients, suggests that starting treatment already at a young age in patients with FH is preferred,” the researchers wrote. “However, despite treatment, IMT in treated FH patients is still thicker in comparison to subjects without FH.”
The researchers identified 42 studies with among patients with FH and healthy control groups across the MEDLINE, EMBASE and Trials.gov databases up to a cutoff date of April 2020, with 39 studies specifically examining carotid IMT, 2 studies evaluating carotid and femoral IMT, and 1 study evaluating femoral IMT alone. Overall, the researchers examined IMT measurements in 3,796 patients with FH and 2,363 control group participants.
Although data on age and gender for FH and control groups were not available in 6 studies, the mean age ranged from 9 to 57 years for patients with FH and from 8 to 61 years in the control group. Men comprised just under half of both the FH and control groups.
The mean between-group difference in carotid IMT in 34 studies was 0.11 mm (95% confidence interval, 0.06-0.15 mm; P < .001) for patients with FH, compared with the control group, while the mean difference in femoral IMT in three studies was 0.47 mm (95% CI, 0.19-0.74 mm; P < .001) between FH and control groups.
In 13 studies in which data on differences between partly treated and untreated FH were available, there was a significant between-group difference in carotid IMT with partly treated patients with FH, compared with the control group (0.05 mm; 95% CI, 0.03-0.08 mm; P < .001), but a larger mean between-group difference in carotid IMT among untreated patients with FH, compared with a control group (0.12 mm; 95% CI, 0.03-0.21 mm; P = .009).
The researchers also analyzed how age impacts carotid IMT, and they found patients with FH had a mean increase of 0.0018 mm (95% CI, –0.0007 to 0.0042 mm) over a control group in 34 studies. For patients with partly treated FH, compared with patients with untreated FH, the mean between-group increase per year was smaller (0.0023 mm; 95% CI, 0.0021-0.0025 mm), compared with the control group (0.0104 mm; 95% CI, 0.0100-0.0108 mm).
“This sign of residual risk might suggest that more robust cholesterol-lowering treatment and achieving treatment targets, or earlier treatment initiation, is needed to reduce IMT progression to non-FH conditions,” the researchers said. “Therefore, we must find and diagnose these patients, and treat them according to current guidelines.”
Limitations of the authors’ meta-analyses include heterogeneity among studies, differences in IMT measurement protocols, and inclusion of studies with an open-label design. Although randomized clinical trials would be preferable to compare treatment effect, “since statin therapy is indicated in FH patients to reduce [cardiovascular disease], it would be unethical to have a placebo group,” they said.
The authors reported no relevant financial disclosures.
Patients with familial hypercholesterolemia (FH) who start lipid-lowering treatment earlier in life may reduce their cardiovascular risk, compared with those who don’t begin treatment early, according to results of a recent meta-analysis.
They showed a difference in the carotid intima-media thickness (IMT) between patients with and without FH that increased with age, but there was also a difference in IMT seen among patients with FH who started treatment early, compared with untreated patients with FH, Kika van Bergen en Henegouwen, of the departments of pediatrics and epidemiology and data science at Amsterdam University Medical Center, and colleagues wrote in their report, published in the Journal of Clinical Lipidology.
“The fact that the difference in IMT increases with age between FH patients and unaffected controls, and is more pronounced in studies with untreated FH patients than in studies with treated patients, suggests that starting treatment already at a young age in patients with FH is preferred,” the researchers wrote. “However, despite treatment, IMT in treated FH patients is still thicker in comparison to subjects without FH.”
The researchers identified 42 studies with among patients with FH and healthy control groups across the MEDLINE, EMBASE and Trials.gov databases up to a cutoff date of April 2020, with 39 studies specifically examining carotid IMT, 2 studies evaluating carotid and femoral IMT, and 1 study evaluating femoral IMT alone. Overall, the researchers examined IMT measurements in 3,796 patients with FH and 2,363 control group participants.
Although data on age and gender for FH and control groups were not available in 6 studies, the mean age ranged from 9 to 57 years for patients with FH and from 8 to 61 years in the control group. Men comprised just under half of both the FH and control groups.
The mean between-group difference in carotid IMT in 34 studies was 0.11 mm (95% confidence interval, 0.06-0.15 mm; P < .001) for patients with FH, compared with the control group, while the mean difference in femoral IMT in three studies was 0.47 mm (95% CI, 0.19-0.74 mm; P < .001) between FH and control groups.
In 13 studies in which data on differences between partly treated and untreated FH were available, there was a significant between-group difference in carotid IMT with partly treated patients with FH, compared with the control group (0.05 mm; 95% CI, 0.03-0.08 mm; P < .001), but a larger mean between-group difference in carotid IMT among untreated patients with FH, compared with a control group (0.12 mm; 95% CI, 0.03-0.21 mm; P = .009).
The researchers also analyzed how age impacts carotid IMT, and they found patients with FH had a mean increase of 0.0018 mm (95% CI, –0.0007 to 0.0042 mm) over a control group in 34 studies. For patients with partly treated FH, compared with patients with untreated FH, the mean between-group increase per year was smaller (0.0023 mm; 95% CI, 0.0021-0.0025 mm), compared with the control group (0.0104 mm; 95% CI, 0.0100-0.0108 mm).
“This sign of residual risk might suggest that more robust cholesterol-lowering treatment and achieving treatment targets, or earlier treatment initiation, is needed to reduce IMT progression to non-FH conditions,” the researchers said. “Therefore, we must find and diagnose these patients, and treat them according to current guidelines.”
Limitations of the authors’ meta-analyses include heterogeneity among studies, differences in IMT measurement protocols, and inclusion of studies with an open-label design. Although randomized clinical trials would be preferable to compare treatment effect, “since statin therapy is indicated in FH patients to reduce [cardiovascular disease], it would be unethical to have a placebo group,” they said.
The authors reported no relevant financial disclosures.
FROM THE JOURNAL OF CLINICAL LIPIDOLOGY
Irregular and long periods linked to NAFLD
Long or irregular menstrual cycles in relatively young women are linked an increased risk of both prevalent and incident nonalcoholic fatty liver disease (NAFLD), according to a cross-sectional study that included data on more than 70,000 women.
“Our results indicate that menstrual irregularity, which is easier to diagnose and usually presented earlier than PCOS [polycystic ovary syndrome] highlights the possibility of identifying premenopausal women at risk of developing NAFLD,” reported a team of authors primarily from Sungkyunkwan University, Seoul, South Korea.
The study evaluated women aged younger than 40 years who were participating in the Kangbuk Samsung Health Study, which involves a comprehensive biennial health examination at health centers in South Korea. Of the 135,090 women enrolled over a 6-year period who had at least one follow-up examination, 72,092 were available for analysis after excluding for a sizable list of confounding factors such as liver disease and infections; exposure to steatogenic medications, such as corticosteroids; hysterectomy; and pregnancy.
NAFLD prevalence climbs with longer menses
Of these women, 36.378 (27.7%) had menstrual cycles of 26-30 days and were identified as the index group. The prevalence of NAFLD in this group was 5.8%. For those with a menstrual cycle of 31-39 days, the prevalence rate climbed to 7.2%. For those with a menstrual cycle of at least 40 days or too irregular to estimate, the prevalence was 9.7%. The prevalence was 7.1% for those with a menstrual cycle less than 21 days.
The results of this study were published in the Journal of Clinical Endocrinology & Metabolism.
In those without NAFLD at baseline who were then followed for a mean of 4.4 years, there were 4,524 incident cases of NAFLD. Incidence density was calculated per 103 patient-years. In the index group, the rate was 18.4. It climbed to 20.2 for those with a menstrual cycle of 31-39 days and then to 22.9 for those with a menstrual cycle of at least 40 days. For those with a cycle of fewer than 21 days, the rate was 26.8.
After adjusting for age, body mass index, insulin resistance, and other confounders, the hazard ratio for incident NAFLD for those with long or irregular menstrual cycles compared with the incident group corresponded with a 22% increased risk (HR, 1.22; 95% confidence interval, 1.14-1.31). When calculated in a time-dependent analysis, the risk of NAFLD was increased by almost 50% (HR, 1.49; 95% CI, 1.38-1.60).
Risk persists with PCOS exclusion
PCOS has previously been associated with increased risk of NAFLD, but the association between long or irregular menstrual cycles and NAFLD persisted after women with PCOS were excluded.
The mechanism that links menstrual irregularity with NAFLD is unclear, but the investigators said that estrogen exposure is implicated. In addition to a previously reported associated between low estradiol levels and antiestrogens such as tamoxifen with increased risk of NAFLD, they cited studies associating estrogen replacement therapy with a reduced risk of NAFLD. The role of estrogen in suppressing inflammation, oxidative stress, and insulin resistance are all activities that might link more regular menses with a reduced risk of NAFLD, the authors contended.
Women older than 40 years were excluded from this analysis to reduce the possibility of perimenopausal changes as a confounding factor.
Of study limitations acknowledged by the investigators, the presence of NAFLD was diagnosed on ultrasonography rather than histology. Information on sex hormone or prolactin levels was not captured in relation to NAFLD incidence, and the lack of exposure to estrogen replacement therapy and oral contraceptives was based on self-reports from the participants.
Still, the large study size and the consistency of results after adjustment for multiple risk factors argue that long and irregular menstrual cycles do identify women at risk for NAFLD. One implication is that irregular menses can be a marker for NAFLD risk.
“Our findings do not prove a causal relationship, but they show that long or irregular menstrual cycles were significantly associated with an increased risk of developing NAFLD,” said Seungho Ryu, MD, PhD, a professor at the Sungkyunkwan University. Senior author of this study, Dr. Ryu emphasized in an interview that the association “was not explained by obesity or any other risk factor for NAFLD.”
Lifestyle changes may lower risk
The message is that “young women with long or irregular menstrual cycles may benefit from lifestyle changes to reduce the risk of NAFLD,” Dr. Ryu stated.
The Study of Women’s Health Across the Nation, which was started in 1994, has not evaluated NAFLD, but it did show a relationship between longer menstrual cycles and more cardiometabolic risk factors, according to Nanette Santoro MD, professor and chair, department of obstetrics & gynecology, University of Colorado at Denver, Aurora.
This suggests that others are “thinking along the same lines,” but in discussing this study with this news organization, she characterized some of the design elements as well as some of the findings in this study as “peculiar.”
In addition to a “very, very narrow definition of regular cycles,” she questioned the consistent hazard ratio for NAFLD for those with long cycles relative to other types of irregular menses. Presuming that the group with longer cycles would have included at least some patients with undiagnosed PCOS, she was would have expected that the risk would have been highest in this group. While conceding that differences in body composition of Korean women is a potential explanation for this apparent discrepancy, “I would like to see confirmed in other samples of women with more detailed metabolic assessments to understand who is at risk,” she said.
Not least problematic for the strength of the conclusions, the hazard ratio for NAFLD among women with long or irregular menstrual cycles was “pretty low.” She described this as a level at which the risk “is very susceptible to confounding and unlikely to influence clinical practice.”
Anuja Dokras, MD, PHD, a professor of obstetrics and gynecology and director of the PCOS Center at the University of Pennsylvania, Philadelphia, also questioned whether undiagnosed PCOS might have skewed the data.
“There is increasing data on the association between PCOS and NAFLD. Irregular menses is a key criterion for PCOS, and PCOS is the commonest reason for anovulation,” she said. Dr. Dokras therefore considered it possible that patients with unrecognized PCOS were included in the study, weakening the claim that risk of NAFLD and long menstrual cycles remains significant after controlling for PCOS.
Dr. Ryu and coinvestigators, Dr. Santoro, and Dr. Dokras reported no potential conflicts of interest.
Long or irregular menstrual cycles in relatively young women are linked an increased risk of both prevalent and incident nonalcoholic fatty liver disease (NAFLD), according to a cross-sectional study that included data on more than 70,000 women.
“Our results indicate that menstrual irregularity, which is easier to diagnose and usually presented earlier than PCOS [polycystic ovary syndrome] highlights the possibility of identifying premenopausal women at risk of developing NAFLD,” reported a team of authors primarily from Sungkyunkwan University, Seoul, South Korea.
The study evaluated women aged younger than 40 years who were participating in the Kangbuk Samsung Health Study, which involves a comprehensive biennial health examination at health centers in South Korea. Of the 135,090 women enrolled over a 6-year period who had at least one follow-up examination, 72,092 were available for analysis after excluding for a sizable list of confounding factors such as liver disease and infections; exposure to steatogenic medications, such as corticosteroids; hysterectomy; and pregnancy.
NAFLD prevalence climbs with longer menses
Of these women, 36.378 (27.7%) had menstrual cycles of 26-30 days and were identified as the index group. The prevalence of NAFLD in this group was 5.8%. For those with a menstrual cycle of 31-39 days, the prevalence rate climbed to 7.2%. For those with a menstrual cycle of at least 40 days or too irregular to estimate, the prevalence was 9.7%. The prevalence was 7.1% for those with a menstrual cycle less than 21 days.
The results of this study were published in the Journal of Clinical Endocrinology & Metabolism.
In those without NAFLD at baseline who were then followed for a mean of 4.4 years, there were 4,524 incident cases of NAFLD. Incidence density was calculated per 103 patient-years. In the index group, the rate was 18.4. It climbed to 20.2 for those with a menstrual cycle of 31-39 days and then to 22.9 for those with a menstrual cycle of at least 40 days. For those with a cycle of fewer than 21 days, the rate was 26.8.
After adjusting for age, body mass index, insulin resistance, and other confounders, the hazard ratio for incident NAFLD for those with long or irregular menstrual cycles compared with the incident group corresponded with a 22% increased risk (HR, 1.22; 95% confidence interval, 1.14-1.31). When calculated in a time-dependent analysis, the risk of NAFLD was increased by almost 50% (HR, 1.49; 95% CI, 1.38-1.60).
Risk persists with PCOS exclusion
PCOS has previously been associated with increased risk of NAFLD, but the association between long or irregular menstrual cycles and NAFLD persisted after women with PCOS were excluded.
The mechanism that links menstrual irregularity with NAFLD is unclear, but the investigators said that estrogen exposure is implicated. In addition to a previously reported associated between low estradiol levels and antiestrogens such as tamoxifen with increased risk of NAFLD, they cited studies associating estrogen replacement therapy with a reduced risk of NAFLD. The role of estrogen in suppressing inflammation, oxidative stress, and insulin resistance are all activities that might link more regular menses with a reduced risk of NAFLD, the authors contended.
Women older than 40 years were excluded from this analysis to reduce the possibility of perimenopausal changes as a confounding factor.
Of study limitations acknowledged by the investigators, the presence of NAFLD was diagnosed on ultrasonography rather than histology. Information on sex hormone or prolactin levels was not captured in relation to NAFLD incidence, and the lack of exposure to estrogen replacement therapy and oral contraceptives was based on self-reports from the participants.
Still, the large study size and the consistency of results after adjustment for multiple risk factors argue that long and irregular menstrual cycles do identify women at risk for NAFLD. One implication is that irregular menses can be a marker for NAFLD risk.
“Our findings do not prove a causal relationship, but they show that long or irregular menstrual cycles were significantly associated with an increased risk of developing NAFLD,” said Seungho Ryu, MD, PhD, a professor at the Sungkyunkwan University. Senior author of this study, Dr. Ryu emphasized in an interview that the association “was not explained by obesity or any other risk factor for NAFLD.”
Lifestyle changes may lower risk
The message is that “young women with long or irregular menstrual cycles may benefit from lifestyle changes to reduce the risk of NAFLD,” Dr. Ryu stated.
The Study of Women’s Health Across the Nation, which was started in 1994, has not evaluated NAFLD, but it did show a relationship between longer menstrual cycles and more cardiometabolic risk factors, according to Nanette Santoro MD, professor and chair, department of obstetrics & gynecology, University of Colorado at Denver, Aurora.
This suggests that others are “thinking along the same lines,” but in discussing this study with this news organization, she characterized some of the design elements as well as some of the findings in this study as “peculiar.”
In addition to a “very, very narrow definition of regular cycles,” she questioned the consistent hazard ratio for NAFLD for those with long cycles relative to other types of irregular menses. Presuming that the group with longer cycles would have included at least some patients with undiagnosed PCOS, she was would have expected that the risk would have been highest in this group. While conceding that differences in body composition of Korean women is a potential explanation for this apparent discrepancy, “I would like to see confirmed in other samples of women with more detailed metabolic assessments to understand who is at risk,” she said.
Not least problematic for the strength of the conclusions, the hazard ratio for NAFLD among women with long or irregular menstrual cycles was “pretty low.” She described this as a level at which the risk “is very susceptible to confounding and unlikely to influence clinical practice.”
Anuja Dokras, MD, PHD, a professor of obstetrics and gynecology and director of the PCOS Center at the University of Pennsylvania, Philadelphia, also questioned whether undiagnosed PCOS might have skewed the data.
“There is increasing data on the association between PCOS and NAFLD. Irregular menses is a key criterion for PCOS, and PCOS is the commonest reason for anovulation,” she said. Dr. Dokras therefore considered it possible that patients with unrecognized PCOS were included in the study, weakening the claim that risk of NAFLD and long menstrual cycles remains significant after controlling for PCOS.
Dr. Ryu and coinvestigators, Dr. Santoro, and Dr. Dokras reported no potential conflicts of interest.
Long or irregular menstrual cycles in relatively young women are linked an increased risk of both prevalent and incident nonalcoholic fatty liver disease (NAFLD), according to a cross-sectional study that included data on more than 70,000 women.
“Our results indicate that menstrual irregularity, which is easier to diagnose and usually presented earlier than PCOS [polycystic ovary syndrome] highlights the possibility of identifying premenopausal women at risk of developing NAFLD,” reported a team of authors primarily from Sungkyunkwan University, Seoul, South Korea.
The study evaluated women aged younger than 40 years who were participating in the Kangbuk Samsung Health Study, which involves a comprehensive biennial health examination at health centers in South Korea. Of the 135,090 women enrolled over a 6-year period who had at least one follow-up examination, 72,092 were available for analysis after excluding for a sizable list of confounding factors such as liver disease and infections; exposure to steatogenic medications, such as corticosteroids; hysterectomy; and pregnancy.
NAFLD prevalence climbs with longer menses
Of these women, 36.378 (27.7%) had menstrual cycles of 26-30 days and were identified as the index group. The prevalence of NAFLD in this group was 5.8%. For those with a menstrual cycle of 31-39 days, the prevalence rate climbed to 7.2%. For those with a menstrual cycle of at least 40 days or too irregular to estimate, the prevalence was 9.7%. The prevalence was 7.1% for those with a menstrual cycle less than 21 days.
The results of this study were published in the Journal of Clinical Endocrinology & Metabolism.
In those without NAFLD at baseline who were then followed for a mean of 4.4 years, there were 4,524 incident cases of NAFLD. Incidence density was calculated per 103 patient-years. In the index group, the rate was 18.4. It climbed to 20.2 for those with a menstrual cycle of 31-39 days and then to 22.9 for those with a menstrual cycle of at least 40 days. For those with a cycle of fewer than 21 days, the rate was 26.8.
After adjusting for age, body mass index, insulin resistance, and other confounders, the hazard ratio for incident NAFLD for those with long or irregular menstrual cycles compared with the incident group corresponded with a 22% increased risk (HR, 1.22; 95% confidence interval, 1.14-1.31). When calculated in a time-dependent analysis, the risk of NAFLD was increased by almost 50% (HR, 1.49; 95% CI, 1.38-1.60).
Risk persists with PCOS exclusion
PCOS has previously been associated with increased risk of NAFLD, but the association between long or irregular menstrual cycles and NAFLD persisted after women with PCOS were excluded.
The mechanism that links menstrual irregularity with NAFLD is unclear, but the investigators said that estrogen exposure is implicated. In addition to a previously reported associated between low estradiol levels and antiestrogens such as tamoxifen with increased risk of NAFLD, they cited studies associating estrogen replacement therapy with a reduced risk of NAFLD. The role of estrogen in suppressing inflammation, oxidative stress, and insulin resistance are all activities that might link more regular menses with a reduced risk of NAFLD, the authors contended.
Women older than 40 years were excluded from this analysis to reduce the possibility of perimenopausal changes as a confounding factor.
Of study limitations acknowledged by the investigators, the presence of NAFLD was diagnosed on ultrasonography rather than histology. Information on sex hormone or prolactin levels was not captured in relation to NAFLD incidence, and the lack of exposure to estrogen replacement therapy and oral contraceptives was based on self-reports from the participants.
Still, the large study size and the consistency of results after adjustment for multiple risk factors argue that long and irregular menstrual cycles do identify women at risk for NAFLD. One implication is that irregular menses can be a marker for NAFLD risk.
“Our findings do not prove a causal relationship, but they show that long or irregular menstrual cycles were significantly associated with an increased risk of developing NAFLD,” said Seungho Ryu, MD, PhD, a professor at the Sungkyunkwan University. Senior author of this study, Dr. Ryu emphasized in an interview that the association “was not explained by obesity or any other risk factor for NAFLD.”
Lifestyle changes may lower risk
The message is that “young women with long or irregular menstrual cycles may benefit from lifestyle changes to reduce the risk of NAFLD,” Dr. Ryu stated.
The Study of Women’s Health Across the Nation, which was started in 1994, has not evaluated NAFLD, but it did show a relationship between longer menstrual cycles and more cardiometabolic risk factors, according to Nanette Santoro MD, professor and chair, department of obstetrics & gynecology, University of Colorado at Denver, Aurora.
This suggests that others are “thinking along the same lines,” but in discussing this study with this news organization, she characterized some of the design elements as well as some of the findings in this study as “peculiar.”
In addition to a “very, very narrow definition of regular cycles,” she questioned the consistent hazard ratio for NAFLD for those with long cycles relative to other types of irregular menses. Presuming that the group with longer cycles would have included at least some patients with undiagnosed PCOS, she was would have expected that the risk would have been highest in this group. While conceding that differences in body composition of Korean women is a potential explanation for this apparent discrepancy, “I would like to see confirmed in other samples of women with more detailed metabolic assessments to understand who is at risk,” she said.
Not least problematic for the strength of the conclusions, the hazard ratio for NAFLD among women with long or irregular menstrual cycles was “pretty low.” She described this as a level at which the risk “is very susceptible to confounding and unlikely to influence clinical practice.”
Anuja Dokras, MD, PHD, a professor of obstetrics and gynecology and director of the PCOS Center at the University of Pennsylvania, Philadelphia, also questioned whether undiagnosed PCOS might have skewed the data.
“There is increasing data on the association between PCOS and NAFLD. Irregular menses is a key criterion for PCOS, and PCOS is the commonest reason for anovulation,” she said. Dr. Dokras therefore considered it possible that patients with unrecognized PCOS were included in the study, weakening the claim that risk of NAFLD and long menstrual cycles remains significant after controlling for PCOS.
Dr. Ryu and coinvestigators, Dr. Santoro, and Dr. Dokras reported no potential conflicts of interest.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
How Lp(a) can help improve ASCVD risk assessment
A look back at a pair of large cohort studies suggests a telling relation between two distinct predictors of atherosclerotic cardiovascular disease (ASCVD) risk and may offer guidance on how to interpret them together.
Elevated levels of lipoprotein(a), or Lp(a), and high coronary artery calcium (CAC) scores were both predictive of ASCVD risk over 10 years, but independent of each other and a host of more traditional cardiovascular risk factors, for example, in the analysis of data from the MESA (Multi-Ethnic Study of Atherosclerosis) and DHS (Dallas Heart Study) longitudinal cohorts.
Notably, the risk when both Lp(a) and CAC scores were high far exceeded that associated with either marker alone. But when CAC scores were less than 100 Agatston units, predicted ASCVD risk wasn’t influenced by levels of Lp(a). Indeed, a CAC score of 0 predicted the lowest levels of ASCVD risk, even with elevated Lp(a).
That is, the findings suggest, the addition of Lp(a) makes a difference to the risk assessment only when CAC scores are high, at least 100 units, and elevated Lp(a) doesn’t mean increased ASCVD risk in the absence of coronary calcium.
“Our novel findings indicate that elevated Lp(a) drives ASCVD risk independent of the subclinical coronary atherosclerosis burden captured by CAC score,” concluded a report on the analysis, published in the Journal of the American College of Cardiology, with lead author Anurag Mehta, MD, Emory University, Atlanta.
There are no formal recommendations on how to interpret Lp(a) and CAC scores together, but the current findings “provide impetus for measuring Lp(a) in more individuals as part of the shared decision-making process,” the authors contended.
“Really, the calcium score carries the majority of the information in terms of risk, except in the highest CAC score group. That is, if you have a high Lp(a) and a high burden of calcium, your risk is significantly higher than if you just have the high calcium score and the normal Lp(a),” senior author Parag H. Joshi, MD, MHS, said in an interview.
“We thought we would see that the group with higher Lp(a) would have more events over 10 years, even among those who didn’t have coronary calcium,” said Dr. Joshi, of the University of Texas Southwestern Medical Center, Dallas. “But we really don’t see that, at least in a statistically significant way.”
A CAC score of 0 would at least support a more conservative approach in a patient with elevated Lp(a) “who is hesitant to be on a statin or to be more aggressive managing their risk,” Dr. Joshi said.
“This study should be very reassuring for a patient like that,” Ron Blankstein, MD, director of cardiac computed tomography at Brigham and Women’s Hospital, Boston, said in an interview.
“If you have a high Lp(a) and you’re concerned, I think this study really supports the role of calcium scoring for further risk assessment,” said Dr. Blankstein, who is not associated with the new report. “We often check Lp(a) in individuals who perhaps have a family history or who come to see us in a preventive cardiology clinic. If it is high and there is concern, a calcium score can be very helpful. If it’s zero, that really means a very low risk of events. And if it’s elevated, I think we’re going to be more concerned about that patient.”
The current analysis suggests “that, when a patient without clinical cardiovascular disease is identified with either CAC ≥100 or Lp(a) >50 mg/dL, the next step in the risk evaluation should be to measure either Lp(a) or CAC, respectively – if not already performed – to identify the patients at highest risk,” Sotirios Tsimikas, MD, director of vascular medicine at University of California, San Diego, wrote in an accompanying editorial.
“Both Lp(a) and CAC should be more broadly applied in clinical care settings in patients without prior ASCVD to identify those that most likely will benefit from more aggressive therapy and, in the future, from Lp(a)-lowering therapies,” he wrote.
The analyses were conducted separately on data from 4,512 initially asymptomatic patients in MESA and 2,078 from the DHS cohort, who were followed for ASCVD events an average of 13 years and 11 years, respectively. Such events included coronary heart disease–related death, nonfatal MI, and fatal or nonfatal stroke.
In the MESA cohort – 52% women, 36.8% White, 29.3% Black, 22.2% Hispanic, and 11.7% Chinese – elevated Lp(a) (quintile 5 vs. quintiles 1-4) and CAC scores of 1-99 and above 100 (both compared with 0) were each independently associated with increased risk for ASCVD events. The hazard ratio was 1.29 (P = .02) for elevated Lp(a), 1.68 (P < .01) for a CAC score of 1-99, and 2.66 (P < .01) for a CAC score of at least 100.
The corresponding HRs in the DHS cohort were 1.54 (P = .07) for Lp(a), 3.32 (P < .01) for a CAC score of 1-99, and 5.21 (P < .01) for a CAC score of at least 100.
Of note, the authors wrote, ASCVD risk among MESA participants with a CAC score of 0 was not significantly different in those with normal and elevated Lp(a).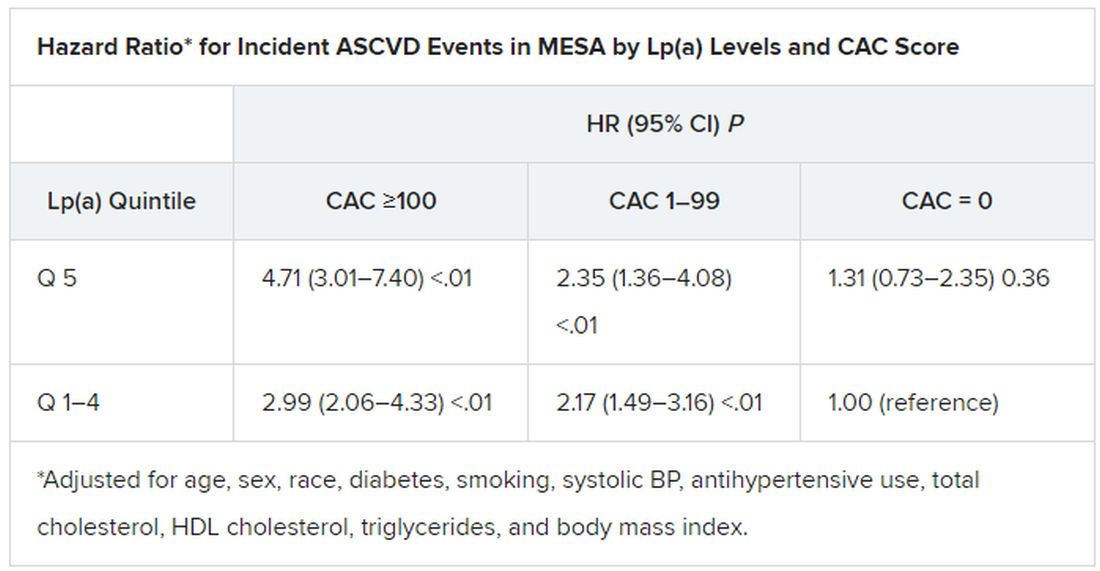
The findings were similar in the corresponding DHS analysis, the authors noted.
When both Lp(a) and CAC scores are considered as dichotomous variables, the highest 10-year ASCVD incidence in MESA was in participants with both elevated Lp(a) (≥50 mg/dL) and a high CAC score (≥100). The lowest risk was seen when Lp(a) was normal (<50 mg/dL) and the CAC score was no more than moderately high (<100).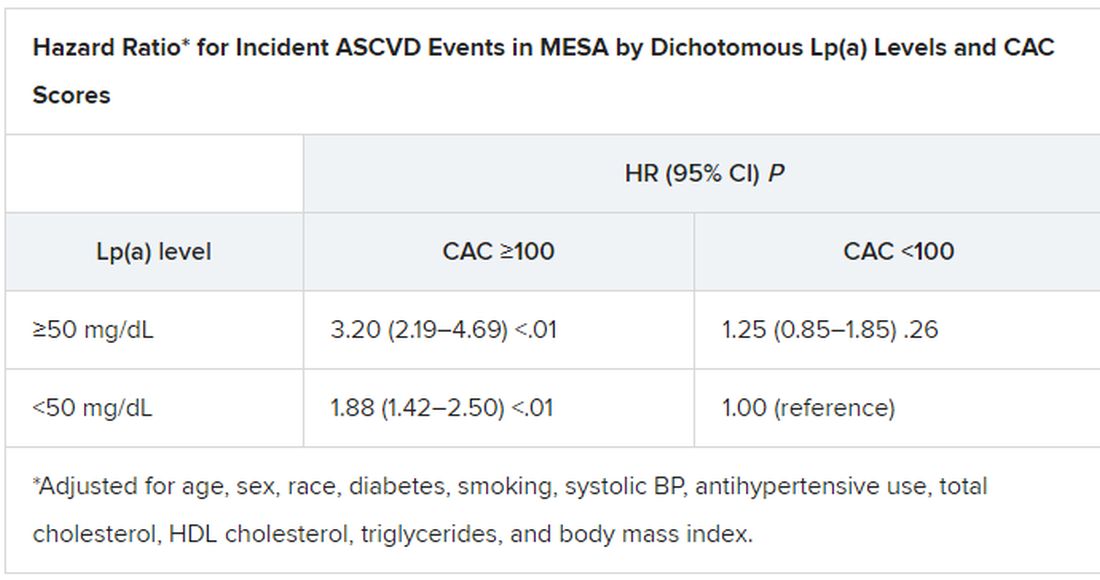
The results in the corresponding DHS analysis, according to the report, again mirrored those from MESA.
“This study has important implications for our patients and also potentially for future clinical trial design,” Dr. Blankstein noted. “A big part of developing a trial in this space is identifying the patients who are at higher risk,” and the current analysis supports CAC scores for identifying the highest-risk patient among those with elevated Lp(a).
Current wisdom is that, for the most part, Lp(a) levels are genetically mediated and are mostly unaffected by interventions such as diet management or exercise. It’s unknown whether reducing elevated Lp(a) levels pharmacologically will cut ASCVD risk, but there are a number of clinical trial programs currently aimed at learning just that. They include the Novartis-sponsored phase 3 HORIZON trial of the antisense agent pelacarsen (TQJ230), with an estimated enrollment of almost 7,700; a randomized, controlled dose-finding study of the small interfering RNA agent olpasiran (AMG890), with 290 patients and funded by Amgen; and an 88-patient phase 1 study of another siRNA agent, SLN360, supported by Silence Therapeutics.
Dr. Mehta reported no relevant relationships. Dr. Joshi has received grant support from Novo Nordisk and consulting income from Bayer and Regeneron; holds equity in G3 Therapeutics; and has served as site investigator for GlaxoSmithKline, Sanofi, AstraZeneca, and Novartis. Dr. Blankstein reported serving as a consultant to Amgen, Novartis, and Silence Therapeutics.
A version of this article first appeared on Medscape.com.
A look back at a pair of large cohort studies suggests a telling relation between two distinct predictors of atherosclerotic cardiovascular disease (ASCVD) risk and may offer guidance on how to interpret them together.
Elevated levels of lipoprotein(a), or Lp(a), and high coronary artery calcium (CAC) scores were both predictive of ASCVD risk over 10 years, but independent of each other and a host of more traditional cardiovascular risk factors, for example, in the analysis of data from the MESA (Multi-Ethnic Study of Atherosclerosis) and DHS (Dallas Heart Study) longitudinal cohorts.
Notably, the risk when both Lp(a) and CAC scores were high far exceeded that associated with either marker alone. But when CAC scores were less than 100 Agatston units, predicted ASCVD risk wasn’t influenced by levels of Lp(a). Indeed, a CAC score of 0 predicted the lowest levels of ASCVD risk, even with elevated Lp(a).
That is, the findings suggest, the addition of Lp(a) makes a difference to the risk assessment only when CAC scores are high, at least 100 units, and elevated Lp(a) doesn’t mean increased ASCVD risk in the absence of coronary calcium.
“Our novel findings indicate that elevated Lp(a) drives ASCVD risk independent of the subclinical coronary atherosclerosis burden captured by CAC score,” concluded a report on the analysis, published in the Journal of the American College of Cardiology, with lead author Anurag Mehta, MD, Emory University, Atlanta.
There are no formal recommendations on how to interpret Lp(a) and CAC scores together, but the current findings “provide impetus for measuring Lp(a) in more individuals as part of the shared decision-making process,” the authors contended.
“Really, the calcium score carries the majority of the information in terms of risk, except in the highest CAC score group. That is, if you have a high Lp(a) and a high burden of calcium, your risk is significantly higher than if you just have the high calcium score and the normal Lp(a),” senior author Parag H. Joshi, MD, MHS, said in an interview.
“We thought we would see that the group with higher Lp(a) would have more events over 10 years, even among those who didn’t have coronary calcium,” said Dr. Joshi, of the University of Texas Southwestern Medical Center, Dallas. “But we really don’t see that, at least in a statistically significant way.”
A CAC score of 0 would at least support a more conservative approach in a patient with elevated Lp(a) “who is hesitant to be on a statin or to be more aggressive managing their risk,” Dr. Joshi said.
“This study should be very reassuring for a patient like that,” Ron Blankstein, MD, director of cardiac computed tomography at Brigham and Women’s Hospital, Boston, said in an interview.
“If you have a high Lp(a) and you’re concerned, I think this study really supports the role of calcium scoring for further risk assessment,” said Dr. Blankstein, who is not associated with the new report. “We often check Lp(a) in individuals who perhaps have a family history or who come to see us in a preventive cardiology clinic. If it is high and there is concern, a calcium score can be very helpful. If it’s zero, that really means a very low risk of events. And if it’s elevated, I think we’re going to be more concerned about that patient.”
The current analysis suggests “that, when a patient without clinical cardiovascular disease is identified with either CAC ≥100 or Lp(a) >50 mg/dL, the next step in the risk evaluation should be to measure either Lp(a) or CAC, respectively – if not already performed – to identify the patients at highest risk,” Sotirios Tsimikas, MD, director of vascular medicine at University of California, San Diego, wrote in an accompanying editorial.
“Both Lp(a) and CAC should be more broadly applied in clinical care settings in patients without prior ASCVD to identify those that most likely will benefit from more aggressive therapy and, in the future, from Lp(a)-lowering therapies,” he wrote.
The analyses were conducted separately on data from 4,512 initially asymptomatic patients in MESA and 2,078 from the DHS cohort, who were followed for ASCVD events an average of 13 years and 11 years, respectively. Such events included coronary heart disease–related death, nonfatal MI, and fatal or nonfatal stroke.
In the MESA cohort – 52% women, 36.8% White, 29.3% Black, 22.2% Hispanic, and 11.7% Chinese – elevated Lp(a) (quintile 5 vs. quintiles 1-4) and CAC scores of 1-99 and above 100 (both compared with 0) were each independently associated with increased risk for ASCVD events. The hazard ratio was 1.29 (P = .02) for elevated Lp(a), 1.68 (P < .01) for a CAC score of 1-99, and 2.66 (P < .01) for a CAC score of at least 100.
The corresponding HRs in the DHS cohort were 1.54 (P = .07) for Lp(a), 3.32 (P < .01) for a CAC score of 1-99, and 5.21 (P < .01) for a CAC score of at least 100.
Of note, the authors wrote, ASCVD risk among MESA participants with a CAC score of 0 was not significantly different in those with normal and elevated Lp(a).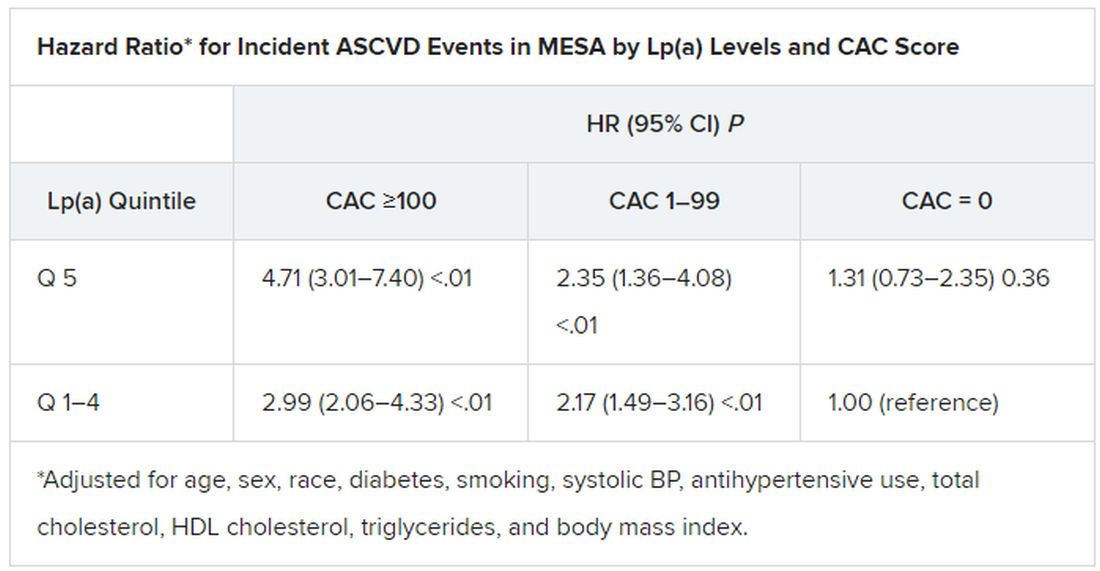
The findings were similar in the corresponding DHS analysis, the authors noted.
When both Lp(a) and CAC scores are considered as dichotomous variables, the highest 10-year ASCVD incidence in MESA was in participants with both elevated Lp(a) (≥50 mg/dL) and a high CAC score (≥100). The lowest risk was seen when Lp(a) was normal (<50 mg/dL) and the CAC score was no more than moderately high (<100).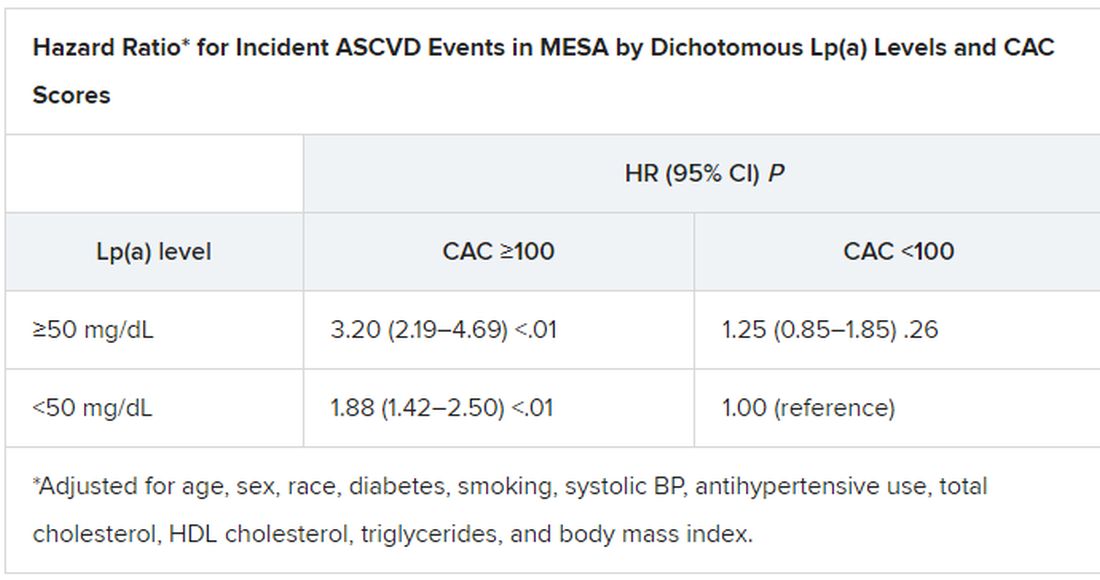
The results in the corresponding DHS analysis, according to the report, again mirrored those from MESA.
“This study has important implications for our patients and also potentially for future clinical trial design,” Dr. Blankstein noted. “A big part of developing a trial in this space is identifying the patients who are at higher risk,” and the current analysis supports CAC scores for identifying the highest-risk patient among those with elevated Lp(a).
Current wisdom is that, for the most part, Lp(a) levels are genetically mediated and are mostly unaffected by interventions such as diet management or exercise. It’s unknown whether reducing elevated Lp(a) levels pharmacologically will cut ASCVD risk, but there are a number of clinical trial programs currently aimed at learning just that. They include the Novartis-sponsored phase 3 HORIZON trial of the antisense agent pelacarsen (TQJ230), with an estimated enrollment of almost 7,700; a randomized, controlled dose-finding study of the small interfering RNA agent olpasiran (AMG890), with 290 patients and funded by Amgen; and an 88-patient phase 1 study of another siRNA agent, SLN360, supported by Silence Therapeutics.
Dr. Mehta reported no relevant relationships. Dr. Joshi has received grant support from Novo Nordisk and consulting income from Bayer and Regeneron; holds equity in G3 Therapeutics; and has served as site investigator for GlaxoSmithKline, Sanofi, AstraZeneca, and Novartis. Dr. Blankstein reported serving as a consultant to Amgen, Novartis, and Silence Therapeutics.
A version of this article first appeared on Medscape.com.
A look back at a pair of large cohort studies suggests a telling relation between two distinct predictors of atherosclerotic cardiovascular disease (ASCVD) risk and may offer guidance on how to interpret them together.
Elevated levels of lipoprotein(a), or Lp(a), and high coronary artery calcium (CAC) scores were both predictive of ASCVD risk over 10 years, but independent of each other and a host of more traditional cardiovascular risk factors, for example, in the analysis of data from the MESA (Multi-Ethnic Study of Atherosclerosis) and DHS (Dallas Heart Study) longitudinal cohorts.
Notably, the risk when both Lp(a) and CAC scores were high far exceeded that associated with either marker alone. But when CAC scores were less than 100 Agatston units, predicted ASCVD risk wasn’t influenced by levels of Lp(a). Indeed, a CAC score of 0 predicted the lowest levels of ASCVD risk, even with elevated Lp(a).
That is, the findings suggest, the addition of Lp(a) makes a difference to the risk assessment only when CAC scores are high, at least 100 units, and elevated Lp(a) doesn’t mean increased ASCVD risk in the absence of coronary calcium.
“Our novel findings indicate that elevated Lp(a) drives ASCVD risk independent of the subclinical coronary atherosclerosis burden captured by CAC score,” concluded a report on the analysis, published in the Journal of the American College of Cardiology, with lead author Anurag Mehta, MD, Emory University, Atlanta.
There are no formal recommendations on how to interpret Lp(a) and CAC scores together, but the current findings “provide impetus for measuring Lp(a) in more individuals as part of the shared decision-making process,” the authors contended.
“Really, the calcium score carries the majority of the information in terms of risk, except in the highest CAC score group. That is, if you have a high Lp(a) and a high burden of calcium, your risk is significantly higher than if you just have the high calcium score and the normal Lp(a),” senior author Parag H. Joshi, MD, MHS, said in an interview.
“We thought we would see that the group with higher Lp(a) would have more events over 10 years, even among those who didn’t have coronary calcium,” said Dr. Joshi, of the University of Texas Southwestern Medical Center, Dallas. “But we really don’t see that, at least in a statistically significant way.”
A CAC score of 0 would at least support a more conservative approach in a patient with elevated Lp(a) “who is hesitant to be on a statin or to be more aggressive managing their risk,” Dr. Joshi said.
“This study should be very reassuring for a patient like that,” Ron Blankstein, MD, director of cardiac computed tomography at Brigham and Women’s Hospital, Boston, said in an interview.
“If you have a high Lp(a) and you’re concerned, I think this study really supports the role of calcium scoring for further risk assessment,” said Dr. Blankstein, who is not associated with the new report. “We often check Lp(a) in individuals who perhaps have a family history or who come to see us in a preventive cardiology clinic. If it is high and there is concern, a calcium score can be very helpful. If it’s zero, that really means a very low risk of events. And if it’s elevated, I think we’re going to be more concerned about that patient.”
The current analysis suggests “that, when a patient without clinical cardiovascular disease is identified with either CAC ≥100 or Lp(a) >50 mg/dL, the next step in the risk evaluation should be to measure either Lp(a) or CAC, respectively – if not already performed – to identify the patients at highest risk,” Sotirios Tsimikas, MD, director of vascular medicine at University of California, San Diego, wrote in an accompanying editorial.
“Both Lp(a) and CAC should be more broadly applied in clinical care settings in patients without prior ASCVD to identify those that most likely will benefit from more aggressive therapy and, in the future, from Lp(a)-lowering therapies,” he wrote.
The analyses were conducted separately on data from 4,512 initially asymptomatic patients in MESA and 2,078 from the DHS cohort, who were followed for ASCVD events an average of 13 years and 11 years, respectively. Such events included coronary heart disease–related death, nonfatal MI, and fatal or nonfatal stroke.
In the MESA cohort – 52% women, 36.8% White, 29.3% Black, 22.2% Hispanic, and 11.7% Chinese – elevated Lp(a) (quintile 5 vs. quintiles 1-4) and CAC scores of 1-99 and above 100 (both compared with 0) were each independently associated with increased risk for ASCVD events. The hazard ratio was 1.29 (P = .02) for elevated Lp(a), 1.68 (P < .01) for a CAC score of 1-99, and 2.66 (P < .01) for a CAC score of at least 100.
The corresponding HRs in the DHS cohort were 1.54 (P = .07) for Lp(a), 3.32 (P < .01) for a CAC score of 1-99, and 5.21 (P < .01) for a CAC score of at least 100.
Of note, the authors wrote, ASCVD risk among MESA participants with a CAC score of 0 was not significantly different in those with normal and elevated Lp(a).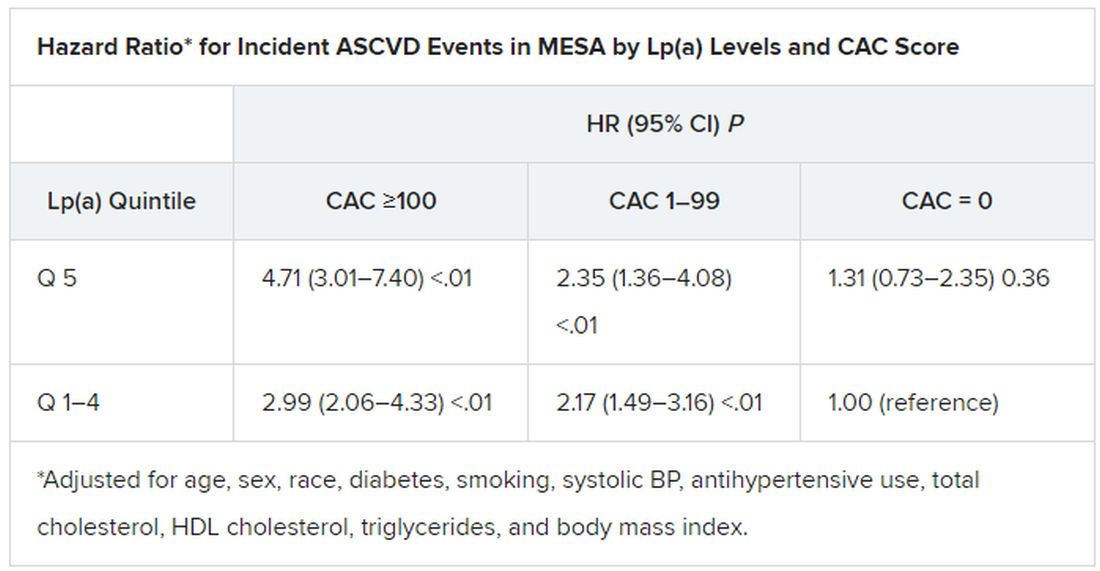
The findings were similar in the corresponding DHS analysis, the authors noted.
When both Lp(a) and CAC scores are considered as dichotomous variables, the highest 10-year ASCVD incidence in MESA was in participants with both elevated Lp(a) (≥50 mg/dL) and a high CAC score (≥100). The lowest risk was seen when Lp(a) was normal (<50 mg/dL) and the CAC score was no more than moderately high (<100).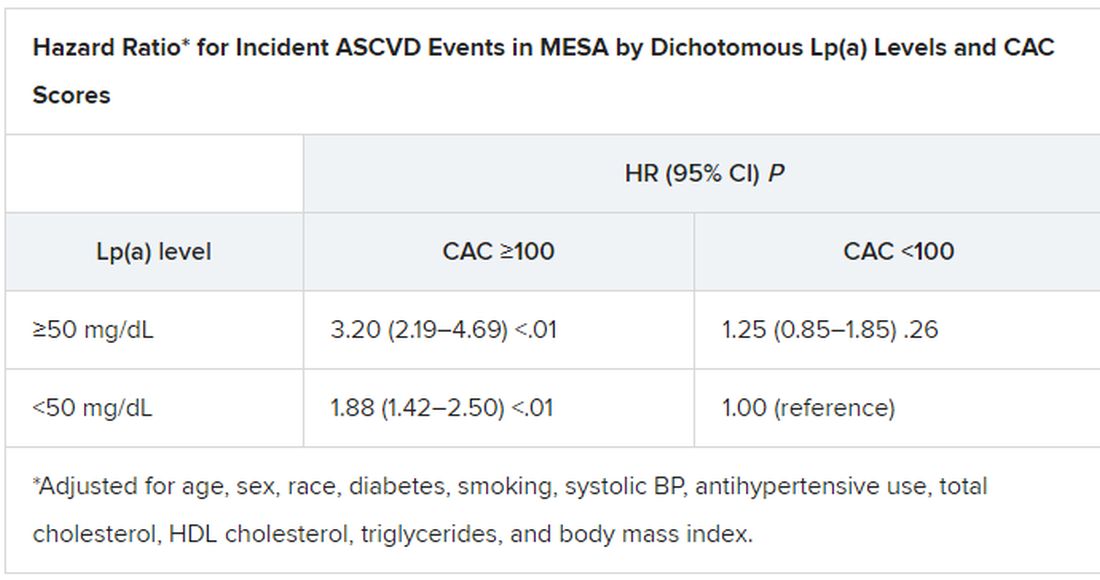
The results in the corresponding DHS analysis, according to the report, again mirrored those from MESA.
“This study has important implications for our patients and also potentially for future clinical trial design,” Dr. Blankstein noted. “A big part of developing a trial in this space is identifying the patients who are at higher risk,” and the current analysis supports CAC scores for identifying the highest-risk patient among those with elevated Lp(a).
Current wisdom is that, for the most part, Lp(a) levels are genetically mediated and are mostly unaffected by interventions such as diet management or exercise. It’s unknown whether reducing elevated Lp(a) levels pharmacologically will cut ASCVD risk, but there are a number of clinical trial programs currently aimed at learning just that. They include the Novartis-sponsored phase 3 HORIZON trial of the antisense agent pelacarsen (TQJ230), with an estimated enrollment of almost 7,700; a randomized, controlled dose-finding study of the small interfering RNA agent olpasiran (AMG890), with 290 patients and funded by Amgen; and an 88-patient phase 1 study of another siRNA agent, SLN360, supported by Silence Therapeutics.
Dr. Mehta reported no relevant relationships. Dr. Joshi has received grant support from Novo Nordisk and consulting income from Bayer and Regeneron; holds equity in G3 Therapeutics; and has served as site investigator for GlaxoSmithKline, Sanofi, AstraZeneca, and Novartis. Dr. Blankstein reported serving as a consultant to Amgen, Novartis, and Silence Therapeutics.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Autoantibodies may underpin clotting effects of COVID-19
Circulating antiphospholipid autoantibodies may contribute to endothelial cell activation and dysfunction in severe COVID-19, researchers report.
In 2020, the same researchers reported results from a preclinical study demonstrating that autoantibodies from patients with active COVID-19 caused clotting in mice.
The new study, published in Arthritis and Rheumatology, found higher-than-expected levels of antiphospholipid autoantibodies in the blood samples of 244 patients hospitalized with COVID-19.
“While endothelial dysfunction has been implicated in the widespread thromboinflammatory complications of COVID-19, the upstream mediators of endotheliopathy remain for the most part cryptic,” write Hui Shi, MD, PhD, and coauthors from the University of Michigan, Ann Arbor, and the National Heart, Lung, and Blood Institute.
When asked for comment on the study, Eline T. Luning Prak, MD, PhD, professor of pathology and laboratory medicine at the Hospital of the University of Pennsylvania in Philadelphia, said, “The autopsy cases for COVID-19 strongly point to thromboembolic complications in many individuals who succumbed to sequelae of the infection.
“Importantly, however, many factors can contribute to this pathology, including the inflammatory milieu, monocyte activation, neutrophil extracellular traps, immune complexes, complement, as well as effects on endothelial cells,” explained Dr. Luning Prak, who was not involved in the study.
“The findings in this paper nicely complement another study by Schmaier et al. that came out recently in JCI Insight that also suggests that endothelial cells can be activated by antibodies, she said.
‘Even stronger connection between autoantibody formation and clotting in COVID-19’
Dr. Shi and her team cultured human endothelial cells in serum or plasma from 244 patients hospitalized with COVID-19 and plasma from 100 patients with non-COVID sepsis. Using in-cell enzyme-linked immunosorbent assay, they measured levels of key cell adhesion molecules.
After analysis, the researchers found that serum from COVID-19 patients activated cultured endothelial cells to express surface adhesion molecules essential to inflammation and thrombosis, particularly E-selectin, ICAM-1, and VCAM-1.
“The presence of circulating antiphospholipid antibodies was a strong marker of the ability of COVID-19 serum to activate endothelium,” they explain.
Further analyses revealed that, for a subset of serum samples from patients with severe infection, this activation could be mitigated by depleting total immunoglobulin G.
In addition, supplementation of control serum with patient IgG was adequate to trigger endothelial activation.
On the basis of these results, the researchers hypothesize that antiphospholipid autoantibodies may characterize antibody profiles in severe COVID-19 that activate the endothelium and transition the usually quiescent blood-vessel wall interface toward inflammation and coagulation.
“[These findings] provide an even stronger connection between autoantibody formation and clotting in COVID-19,” Dr. Shi said in an accompanying press release.
Clinical implications
From a clinical perspective, Dr. Shi and her team question whether patients with severe COVID-19 should be tested for antiphospholipid antibodies to assess their risk of thrombosis and progression to respiratory failure.
Moreover, they question whether patients with high antiphospholipid antibody titers might benefit from therapies used in conventional cases of severe antiphospholipid syndrome, such as plasmapheresis, anticoagulation therapy, and complement inhibition, Dr. Shi added.
The researchers hope to answer these and other remaining questions in future studies. “Eventually, we may be able to repurpose treatments used in traditional cases of antiphospholipid syndrome for COVID-19.
“As we await definitive solutions to the pandemic, these findings add important context to the complex interplay between SARS-CoV-2 infection, the human immune system, and vascular immunobiology,” she concluded.
The study was supported by grants from the Rheumatology Research Foundation, the Michigan Medicine Frankel Cardiovascular Center, and the A. Alfred Taubman Medical Research Institute. One author is an inventor on an unrelated pending patent to the University of Michigan. The other authors and Dr. Luning Prak have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Circulating antiphospholipid autoantibodies may contribute to endothelial cell activation and dysfunction in severe COVID-19, researchers report.
In 2020, the same researchers reported results from a preclinical study demonstrating that autoantibodies from patients with active COVID-19 caused clotting in mice.
The new study, published in Arthritis and Rheumatology, found higher-than-expected levels of antiphospholipid autoantibodies in the blood samples of 244 patients hospitalized with COVID-19.
“While endothelial dysfunction has been implicated in the widespread thromboinflammatory complications of COVID-19, the upstream mediators of endotheliopathy remain for the most part cryptic,” write Hui Shi, MD, PhD, and coauthors from the University of Michigan, Ann Arbor, and the National Heart, Lung, and Blood Institute.
When asked for comment on the study, Eline T. Luning Prak, MD, PhD, professor of pathology and laboratory medicine at the Hospital of the University of Pennsylvania in Philadelphia, said, “The autopsy cases for COVID-19 strongly point to thromboembolic complications in many individuals who succumbed to sequelae of the infection.
“Importantly, however, many factors can contribute to this pathology, including the inflammatory milieu, monocyte activation, neutrophil extracellular traps, immune complexes, complement, as well as effects on endothelial cells,” explained Dr. Luning Prak, who was not involved in the study.
“The findings in this paper nicely complement another study by Schmaier et al. that came out recently in JCI Insight that also suggests that endothelial cells can be activated by antibodies, she said.
‘Even stronger connection between autoantibody formation and clotting in COVID-19’
Dr. Shi and her team cultured human endothelial cells in serum or plasma from 244 patients hospitalized with COVID-19 and plasma from 100 patients with non-COVID sepsis. Using in-cell enzyme-linked immunosorbent assay, they measured levels of key cell adhesion molecules.
After analysis, the researchers found that serum from COVID-19 patients activated cultured endothelial cells to express surface adhesion molecules essential to inflammation and thrombosis, particularly E-selectin, ICAM-1, and VCAM-1.
“The presence of circulating antiphospholipid antibodies was a strong marker of the ability of COVID-19 serum to activate endothelium,” they explain.
Further analyses revealed that, for a subset of serum samples from patients with severe infection, this activation could be mitigated by depleting total immunoglobulin G.
In addition, supplementation of control serum with patient IgG was adequate to trigger endothelial activation.
On the basis of these results, the researchers hypothesize that antiphospholipid autoantibodies may characterize antibody profiles in severe COVID-19 that activate the endothelium and transition the usually quiescent blood-vessel wall interface toward inflammation and coagulation.
“[These findings] provide an even stronger connection between autoantibody formation and clotting in COVID-19,” Dr. Shi said in an accompanying press release.
Clinical implications
From a clinical perspective, Dr. Shi and her team question whether patients with severe COVID-19 should be tested for antiphospholipid antibodies to assess their risk of thrombosis and progression to respiratory failure.
Moreover, they question whether patients with high antiphospholipid antibody titers might benefit from therapies used in conventional cases of severe antiphospholipid syndrome, such as plasmapheresis, anticoagulation therapy, and complement inhibition, Dr. Shi added.
The researchers hope to answer these and other remaining questions in future studies. “Eventually, we may be able to repurpose treatments used in traditional cases of antiphospholipid syndrome for COVID-19.
“As we await definitive solutions to the pandemic, these findings add important context to the complex interplay between SARS-CoV-2 infection, the human immune system, and vascular immunobiology,” she concluded.
The study was supported by grants from the Rheumatology Research Foundation, the Michigan Medicine Frankel Cardiovascular Center, and the A. Alfred Taubman Medical Research Institute. One author is an inventor on an unrelated pending patent to the University of Michigan. The other authors and Dr. Luning Prak have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Circulating antiphospholipid autoantibodies may contribute to endothelial cell activation and dysfunction in severe COVID-19, researchers report.
In 2020, the same researchers reported results from a preclinical study demonstrating that autoantibodies from patients with active COVID-19 caused clotting in mice.
The new study, published in Arthritis and Rheumatology, found higher-than-expected levels of antiphospholipid autoantibodies in the blood samples of 244 patients hospitalized with COVID-19.
“While endothelial dysfunction has been implicated in the widespread thromboinflammatory complications of COVID-19, the upstream mediators of endotheliopathy remain for the most part cryptic,” write Hui Shi, MD, PhD, and coauthors from the University of Michigan, Ann Arbor, and the National Heart, Lung, and Blood Institute.
When asked for comment on the study, Eline T. Luning Prak, MD, PhD, professor of pathology and laboratory medicine at the Hospital of the University of Pennsylvania in Philadelphia, said, “The autopsy cases for COVID-19 strongly point to thromboembolic complications in many individuals who succumbed to sequelae of the infection.
“Importantly, however, many factors can contribute to this pathology, including the inflammatory milieu, monocyte activation, neutrophil extracellular traps, immune complexes, complement, as well as effects on endothelial cells,” explained Dr. Luning Prak, who was not involved in the study.
“The findings in this paper nicely complement another study by Schmaier et al. that came out recently in JCI Insight that also suggests that endothelial cells can be activated by antibodies, she said.
‘Even stronger connection between autoantibody formation and clotting in COVID-19’
Dr. Shi and her team cultured human endothelial cells in serum or plasma from 244 patients hospitalized with COVID-19 and plasma from 100 patients with non-COVID sepsis. Using in-cell enzyme-linked immunosorbent assay, they measured levels of key cell adhesion molecules.
After analysis, the researchers found that serum from COVID-19 patients activated cultured endothelial cells to express surface adhesion molecules essential to inflammation and thrombosis, particularly E-selectin, ICAM-1, and VCAM-1.
“The presence of circulating antiphospholipid antibodies was a strong marker of the ability of COVID-19 serum to activate endothelium,” they explain.
Further analyses revealed that, for a subset of serum samples from patients with severe infection, this activation could be mitigated by depleting total immunoglobulin G.
In addition, supplementation of control serum with patient IgG was adequate to trigger endothelial activation.
On the basis of these results, the researchers hypothesize that antiphospholipid autoantibodies may characterize antibody profiles in severe COVID-19 that activate the endothelium and transition the usually quiescent blood-vessel wall interface toward inflammation and coagulation.
“[These findings] provide an even stronger connection between autoantibody formation and clotting in COVID-19,” Dr. Shi said in an accompanying press release.
Clinical implications
From a clinical perspective, Dr. Shi and her team question whether patients with severe COVID-19 should be tested for antiphospholipid antibodies to assess their risk of thrombosis and progression to respiratory failure.
Moreover, they question whether patients with high antiphospholipid antibody titers might benefit from therapies used in conventional cases of severe antiphospholipid syndrome, such as plasmapheresis, anticoagulation therapy, and complement inhibition, Dr. Shi added.
The researchers hope to answer these and other remaining questions in future studies. “Eventually, we may be able to repurpose treatments used in traditional cases of antiphospholipid syndrome for COVID-19.
“As we await definitive solutions to the pandemic, these findings add important context to the complex interplay between SARS-CoV-2 infection, the human immune system, and vascular immunobiology,” she concluded.
The study was supported by grants from the Rheumatology Research Foundation, the Michigan Medicine Frankel Cardiovascular Center, and the A. Alfred Taubman Medical Research Institute. One author is an inventor on an unrelated pending patent to the University of Michigan. The other authors and Dr. Luning Prak have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
More than half of U.S. women enter pregnancy at higher CVD risk
Less than half of women in the United States enter pregnancy in favorable cardiovascular health, new research suggests.
In 2019, among women aged 20 to 44 years with live births in the United States, only 40.2% were in favorable cardiovascular health prior to pregnancy, defined as normal weight, no diabetes, and no hypertension.
Although all regions and states showed a decline in prepregnancy favorable cardiometabolic health, there were significant differences among geographic regions in the country, the authors report. “These data reveal critical deficiencies and geographic disparities in prepregnancy cardiometabolic health,” they conclude.
“One of the things that we know in the U.S. is that the maternal mortality rate has been increasing, and there are significant differences at the state level in both adverse maternal outcomes, such as maternal mortality, as well as adverse pregnancy outcomes,” corresponding author Sadiya S. Khan, MD, MS, FACC, Northwestern University Feinberg School of Medicine, Chicago, told this news organization.
“These outcomes are often related to health factors that predate pregnancy,” Dr. Khan explained, “and the processes that begin at the very, very beginning of conception are informed by health factors prior to pregnancy, in particular cardiometabolic factors like body mass index or obesity, high blood pressure, and diabetes.”
The results were published online on Feb. 14 in a special “Go Red for Women” spotlight issue of Circulation.
Cardiometabolic health factors
Using maternal birth records from live births in the Centers for Disease Control and Prevention Natality Database between 2016 and 2019, the authors analyzed data on 14,174,625 women with live births aged 20 to 44 years. The majority (81.4%) were 20 to 34 years of age, 22.7% were Hispanic or Latina, and 52.7% were non-Hispanic White.
Favorable cardiometabolic health was defined as a BMI of 18 to 24.9 kg/m2, absence of diabetes, and absence of hypertension.
Although all regions and states experienced a decline in favorable cardiometabolic health during the study period of 2016 to 2019, with a drop overall of 3.2% – from 43.5 to 40.2 per 100 live births – it was especially true of the South and Midwest regions.
In 2019, favorable prepregnancy cardiometabolic health was lowest in the South (38.1%) and Midwest (38.8%) and highest in the West (42.2%) and Northeast (43.6%).
State by state, the lowest prevalence of favorable cardiometabolic health was found in Mississippi, at 31.2%, and highest in Utah, at 47.2%.
They also found a correlation between favorable cardiometabolic health and state-level percentages of high-school education or less and enrollment in Medicaid in 2019.
Similar to what has been seen with cardiovascular disease, “we observe that the states with the lowest prevalence of favorable cardiometabolic health were in the Southeast United States,” said Dr. Khan, “and similar geographic variation was observed with some more patterns in education and Medicaid coverage for birth, and these were used as proxies for socioeconomic status in those areas.”
Although Dr. Khan notes that the relationships cannot be determined to be causal from this analysis, she said that “it does suggest that upstream social determinants of health are important determinants of cardiometabolic health.”
Socioeconomic intervention
Dr. Khan noted that policies at the federal and state level can identify ways to “ensure that individuals who are thinking about pregnancy have access to health care and have access to resources, too, from a broad range of health determinants, including housing stability, food security, as well as access to health care be optimized prior to pregnancy.”
The authors note that this analysis may actually overestimate the prevalence of favorable cardiometabolic health, and data on cholesterol, diet, a distinction between type 1 and type 2 diabetes, and physical activity were not available.
Only individuals with live births were included, which could result in the elimination of a potentially high-risk group; however, late pregnancy losses represent less than 0.3% of all pregnancies, they say.
The authors conclude that “future research is needed to equitably improve health prior to pregnancy and quantify the potential benefits in cardiovascular disease outcomes for birthing individuals and their offspring.”
This work was supported by grants from the National Heart, Lung, and Blood Institute and American Heart Association Transformational Project Award awarded to Sadiya S. Khan.
A version of this article first appeared on Medscape.com.
Less than half of women in the United States enter pregnancy in favorable cardiovascular health, new research suggests.
In 2019, among women aged 20 to 44 years with live births in the United States, only 40.2% were in favorable cardiovascular health prior to pregnancy, defined as normal weight, no diabetes, and no hypertension.
Although all regions and states showed a decline in prepregnancy favorable cardiometabolic health, there were significant differences among geographic regions in the country, the authors report. “These data reveal critical deficiencies and geographic disparities in prepregnancy cardiometabolic health,” they conclude.
“One of the things that we know in the U.S. is that the maternal mortality rate has been increasing, and there are significant differences at the state level in both adverse maternal outcomes, such as maternal mortality, as well as adverse pregnancy outcomes,” corresponding author Sadiya S. Khan, MD, MS, FACC, Northwestern University Feinberg School of Medicine, Chicago, told this news organization.
“These outcomes are often related to health factors that predate pregnancy,” Dr. Khan explained, “and the processes that begin at the very, very beginning of conception are informed by health factors prior to pregnancy, in particular cardiometabolic factors like body mass index or obesity, high blood pressure, and diabetes.”
The results were published online on Feb. 14 in a special “Go Red for Women” spotlight issue of Circulation.
Cardiometabolic health factors
Using maternal birth records from live births in the Centers for Disease Control and Prevention Natality Database between 2016 and 2019, the authors analyzed data on 14,174,625 women with live births aged 20 to 44 years. The majority (81.4%) were 20 to 34 years of age, 22.7% were Hispanic or Latina, and 52.7% were non-Hispanic White.
Favorable cardiometabolic health was defined as a BMI of 18 to 24.9 kg/m2, absence of diabetes, and absence of hypertension.
Although all regions and states experienced a decline in favorable cardiometabolic health during the study period of 2016 to 2019, with a drop overall of 3.2% – from 43.5 to 40.2 per 100 live births – it was especially true of the South and Midwest regions.
In 2019, favorable prepregnancy cardiometabolic health was lowest in the South (38.1%) and Midwest (38.8%) and highest in the West (42.2%) and Northeast (43.6%).
State by state, the lowest prevalence of favorable cardiometabolic health was found in Mississippi, at 31.2%, and highest in Utah, at 47.2%.
They also found a correlation between favorable cardiometabolic health and state-level percentages of high-school education or less and enrollment in Medicaid in 2019.
Similar to what has been seen with cardiovascular disease, “we observe that the states with the lowest prevalence of favorable cardiometabolic health were in the Southeast United States,” said Dr. Khan, “and similar geographic variation was observed with some more patterns in education and Medicaid coverage for birth, and these were used as proxies for socioeconomic status in those areas.”
Although Dr. Khan notes that the relationships cannot be determined to be causal from this analysis, she said that “it does suggest that upstream social determinants of health are important determinants of cardiometabolic health.”
Socioeconomic intervention
Dr. Khan noted that policies at the federal and state level can identify ways to “ensure that individuals who are thinking about pregnancy have access to health care and have access to resources, too, from a broad range of health determinants, including housing stability, food security, as well as access to health care be optimized prior to pregnancy.”
The authors note that this analysis may actually overestimate the prevalence of favorable cardiometabolic health, and data on cholesterol, diet, a distinction between type 1 and type 2 diabetes, and physical activity were not available.
Only individuals with live births were included, which could result in the elimination of a potentially high-risk group; however, late pregnancy losses represent less than 0.3% of all pregnancies, they say.
The authors conclude that “future research is needed to equitably improve health prior to pregnancy and quantify the potential benefits in cardiovascular disease outcomes for birthing individuals and their offspring.”
This work was supported by grants from the National Heart, Lung, and Blood Institute and American Heart Association Transformational Project Award awarded to Sadiya S. Khan.
A version of this article first appeared on Medscape.com.
Less than half of women in the United States enter pregnancy in favorable cardiovascular health, new research suggests.
In 2019, among women aged 20 to 44 years with live births in the United States, only 40.2% were in favorable cardiovascular health prior to pregnancy, defined as normal weight, no diabetes, and no hypertension.
Although all regions and states showed a decline in prepregnancy favorable cardiometabolic health, there were significant differences among geographic regions in the country, the authors report. “These data reveal critical deficiencies and geographic disparities in prepregnancy cardiometabolic health,” they conclude.
“One of the things that we know in the U.S. is that the maternal mortality rate has been increasing, and there are significant differences at the state level in both adverse maternal outcomes, such as maternal mortality, as well as adverse pregnancy outcomes,” corresponding author Sadiya S. Khan, MD, MS, FACC, Northwestern University Feinberg School of Medicine, Chicago, told this news organization.
“These outcomes are often related to health factors that predate pregnancy,” Dr. Khan explained, “and the processes that begin at the very, very beginning of conception are informed by health factors prior to pregnancy, in particular cardiometabolic factors like body mass index or obesity, high blood pressure, and diabetes.”
The results were published online on Feb. 14 in a special “Go Red for Women” spotlight issue of Circulation.
Cardiometabolic health factors
Using maternal birth records from live births in the Centers for Disease Control and Prevention Natality Database between 2016 and 2019, the authors analyzed data on 14,174,625 women with live births aged 20 to 44 years. The majority (81.4%) were 20 to 34 years of age, 22.7% were Hispanic or Latina, and 52.7% were non-Hispanic White.
Favorable cardiometabolic health was defined as a BMI of 18 to 24.9 kg/m2, absence of diabetes, and absence of hypertension.
Although all regions and states experienced a decline in favorable cardiometabolic health during the study period of 2016 to 2019, with a drop overall of 3.2% – from 43.5 to 40.2 per 100 live births – it was especially true of the South and Midwest regions.
In 2019, favorable prepregnancy cardiometabolic health was lowest in the South (38.1%) and Midwest (38.8%) and highest in the West (42.2%) and Northeast (43.6%).
State by state, the lowest prevalence of favorable cardiometabolic health was found in Mississippi, at 31.2%, and highest in Utah, at 47.2%.
They also found a correlation between favorable cardiometabolic health and state-level percentages of high-school education or less and enrollment in Medicaid in 2019.
Similar to what has been seen with cardiovascular disease, “we observe that the states with the lowest prevalence of favorable cardiometabolic health were in the Southeast United States,” said Dr. Khan, “and similar geographic variation was observed with some more patterns in education and Medicaid coverage for birth, and these were used as proxies for socioeconomic status in those areas.”
Although Dr. Khan notes that the relationships cannot be determined to be causal from this analysis, she said that “it does suggest that upstream social determinants of health are important determinants of cardiometabolic health.”
Socioeconomic intervention
Dr. Khan noted that policies at the federal and state level can identify ways to “ensure that individuals who are thinking about pregnancy have access to health care and have access to resources, too, from a broad range of health determinants, including housing stability, food security, as well as access to health care be optimized prior to pregnancy.”
The authors note that this analysis may actually overestimate the prevalence of favorable cardiometabolic health, and data on cholesterol, diet, a distinction between type 1 and type 2 diabetes, and physical activity were not available.
Only individuals with live births were included, which could result in the elimination of a potentially high-risk group; however, late pregnancy losses represent less than 0.3% of all pregnancies, they say.
The authors conclude that “future research is needed to equitably improve health prior to pregnancy and quantify the potential benefits in cardiovascular disease outcomes for birthing individuals and their offspring.”
This work was supported by grants from the National Heart, Lung, and Blood Institute and American Heart Association Transformational Project Award awarded to Sadiya S. Khan.
A version of this article first appeared on Medscape.com.
AHA targets ‘low-value’ heart care in new scientific statement
Low-value health care services that provide little or no benefit to patients are “common, potentially harmful, and costly,” and there is a critical need to reduce this kind of care, the American Heart Association said in a newly released scientific statement.
Each year, nearly half of patients in the United States will receive at least one low-value test or procedure, with the attendant risk of avoidable complications from cascades of care and excess costs to individuals and society, the authors noted. Reducing low-value care is particularly important in cardiology, given the high prevalence and costs of cardiovascular disease in the United States.
The statement was published online Feb. 22, 2022, in Circulation: Cardiovascular Quality and Outcomes.
High burden with uncertain benefit
“Cardiovascular disease is common and can present suddenly, such as a heart attack or abnormal heart rhythm,” Vinay Kini, MD, chair of the statement writing group and assistant professor of medicine at Weill Cornell Medicine, New York, said in a news release.
“Our desire to be vigilant about treating and preventing cardiovascular disease may sometimes lead to use of tests and procedures where the benefits to patients may be uncertain,” Dr. Kini said. “This may impose burdens on patients, in the form of increased risk of physical harm from the low-value procedure or potential complications, as well as follow-up care and out-of-pocket financial costs.”
For example, studies have shown that up to one in five echocardiograms and up to half of all stress tests performed in the United States may be rated as rarely appropriate, based on established guidelines for their use.
In addition, up to 15% of percutaneous coronary interventions (PCIs) are classified as rarely appropriate, the writing group said.
Annually, among Medicare fee-for-service beneficiaries, low-value stress testing in patients with stable coronary artery disease is estimated to cost between $212 million and $2.1 billion, while costs of PCI for stable CAD range from $212 million to $2.8 billion, the writing group noted.
“At best, spending on low-value care potentially diverts resources from higher-value services that would benefit patients more effectively at the same or reduced cost. At worst, low-value care results in physical harm in the form of preventable morbidity and mortality,” they said.
“Thus, reducing low-value care is one of the few patient-centered solutions that directly address both the need to control health care spending and the societal imperative to devote its limited resources to beneficial health care services that improve health,” they added.
The group outlines several ways to reduce low-value cardiovascular care targeting patients, providers, and payers/policymakers.
For patients, education and shared decision-making may help reduce low-value care and dispel misconceptions about the intended purpose of test or treatment, they suggested.
For clinicians, a “layered” approach to reducing low-value care may be most effective, such as through education, audit and feedback, and behavioral science tools (“nudges”) to shift behaviors and practices, they said.
For payers and policy leaders, interventions to reduce low-value care include national insurance coverage determinations; prior authorization; alternative payment models that reward lower costs and higher-quality health care; value-based insurance designs that financially penalize low-value care; and medical liability reform to reduce defensive medical practices.
Low-value cardiovascular care is a complex problem, the writing group acknowledged, and achieving meaningful reductions in low-value cardiovascular care will require a multidisciplinary approach that includes continuous research, implementation, evaluation, and adjustment while ensuring equitable access to care.
“Each approach has benefits and drawbacks,” Dr. Kini said. “For example, prior authorization imposes a large burden on health care professionals to obtain insurance approval for tests and treatments. Prior authorization and some value-based payment models may unintentionally worsen existing racial and ethnic health care disparities.
“A one-size-fits-all approach to reducing low-value care is unlikely to succeed; rather, acting through multiple perspectives and frequently measuring impacts and potential unintended consequences is critical,” he concluded.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA’s Council on Quality of Care and Outcomes Research.
The research had no commercial funding. Dr. Kini disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Low-value health care services that provide little or no benefit to patients are “common, potentially harmful, and costly,” and there is a critical need to reduce this kind of care, the American Heart Association said in a newly released scientific statement.
Each year, nearly half of patients in the United States will receive at least one low-value test or procedure, with the attendant risk of avoidable complications from cascades of care and excess costs to individuals and society, the authors noted. Reducing low-value care is particularly important in cardiology, given the high prevalence and costs of cardiovascular disease in the United States.
The statement was published online Feb. 22, 2022, in Circulation: Cardiovascular Quality and Outcomes.
High burden with uncertain benefit
“Cardiovascular disease is common and can present suddenly, such as a heart attack or abnormal heart rhythm,” Vinay Kini, MD, chair of the statement writing group and assistant professor of medicine at Weill Cornell Medicine, New York, said in a news release.
“Our desire to be vigilant about treating and preventing cardiovascular disease may sometimes lead to use of tests and procedures where the benefits to patients may be uncertain,” Dr. Kini said. “This may impose burdens on patients, in the form of increased risk of physical harm from the low-value procedure or potential complications, as well as follow-up care and out-of-pocket financial costs.”
For example, studies have shown that up to one in five echocardiograms and up to half of all stress tests performed in the United States may be rated as rarely appropriate, based on established guidelines for their use.
In addition, up to 15% of percutaneous coronary interventions (PCIs) are classified as rarely appropriate, the writing group said.
Annually, among Medicare fee-for-service beneficiaries, low-value stress testing in patients with stable coronary artery disease is estimated to cost between $212 million and $2.1 billion, while costs of PCI for stable CAD range from $212 million to $2.8 billion, the writing group noted.
“At best, spending on low-value care potentially diverts resources from higher-value services that would benefit patients more effectively at the same or reduced cost. At worst, low-value care results in physical harm in the form of preventable morbidity and mortality,” they said.
“Thus, reducing low-value care is one of the few patient-centered solutions that directly address both the need to control health care spending and the societal imperative to devote its limited resources to beneficial health care services that improve health,” they added.
The group outlines several ways to reduce low-value cardiovascular care targeting patients, providers, and payers/policymakers.
For patients, education and shared decision-making may help reduce low-value care and dispel misconceptions about the intended purpose of test or treatment, they suggested.
For clinicians, a “layered” approach to reducing low-value care may be most effective, such as through education, audit and feedback, and behavioral science tools (“nudges”) to shift behaviors and practices, they said.
For payers and policy leaders, interventions to reduce low-value care include national insurance coverage determinations; prior authorization; alternative payment models that reward lower costs and higher-quality health care; value-based insurance designs that financially penalize low-value care; and medical liability reform to reduce defensive medical practices.
Low-value cardiovascular care is a complex problem, the writing group acknowledged, and achieving meaningful reductions in low-value cardiovascular care will require a multidisciplinary approach that includes continuous research, implementation, evaluation, and adjustment while ensuring equitable access to care.
“Each approach has benefits and drawbacks,” Dr. Kini said. “For example, prior authorization imposes a large burden on health care professionals to obtain insurance approval for tests and treatments. Prior authorization and some value-based payment models may unintentionally worsen existing racial and ethnic health care disparities.
“A one-size-fits-all approach to reducing low-value care is unlikely to succeed; rather, acting through multiple perspectives and frequently measuring impacts and potential unintended consequences is critical,” he concluded.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA’s Council on Quality of Care and Outcomes Research.
The research had no commercial funding. Dr. Kini disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Low-value health care services that provide little or no benefit to patients are “common, potentially harmful, and costly,” and there is a critical need to reduce this kind of care, the American Heart Association said in a newly released scientific statement.
Each year, nearly half of patients in the United States will receive at least one low-value test or procedure, with the attendant risk of avoidable complications from cascades of care and excess costs to individuals and society, the authors noted. Reducing low-value care is particularly important in cardiology, given the high prevalence and costs of cardiovascular disease in the United States.
The statement was published online Feb. 22, 2022, in Circulation: Cardiovascular Quality and Outcomes.
High burden with uncertain benefit
“Cardiovascular disease is common and can present suddenly, such as a heart attack or abnormal heart rhythm,” Vinay Kini, MD, chair of the statement writing group and assistant professor of medicine at Weill Cornell Medicine, New York, said in a news release.
“Our desire to be vigilant about treating and preventing cardiovascular disease may sometimes lead to use of tests and procedures where the benefits to patients may be uncertain,” Dr. Kini said. “This may impose burdens on patients, in the form of increased risk of physical harm from the low-value procedure or potential complications, as well as follow-up care and out-of-pocket financial costs.”
For example, studies have shown that up to one in five echocardiograms and up to half of all stress tests performed in the United States may be rated as rarely appropriate, based on established guidelines for their use.
In addition, up to 15% of percutaneous coronary interventions (PCIs) are classified as rarely appropriate, the writing group said.
Annually, among Medicare fee-for-service beneficiaries, low-value stress testing in patients with stable coronary artery disease is estimated to cost between $212 million and $2.1 billion, while costs of PCI for stable CAD range from $212 million to $2.8 billion, the writing group noted.
“At best, spending on low-value care potentially diverts resources from higher-value services that would benefit patients more effectively at the same or reduced cost. At worst, low-value care results in physical harm in the form of preventable morbidity and mortality,” they said.
“Thus, reducing low-value care is one of the few patient-centered solutions that directly address both the need to control health care spending and the societal imperative to devote its limited resources to beneficial health care services that improve health,” they added.
The group outlines several ways to reduce low-value cardiovascular care targeting patients, providers, and payers/policymakers.
For patients, education and shared decision-making may help reduce low-value care and dispel misconceptions about the intended purpose of test or treatment, they suggested.
For clinicians, a “layered” approach to reducing low-value care may be most effective, such as through education, audit and feedback, and behavioral science tools (“nudges”) to shift behaviors and practices, they said.
For payers and policy leaders, interventions to reduce low-value care include national insurance coverage determinations; prior authorization; alternative payment models that reward lower costs and higher-quality health care; value-based insurance designs that financially penalize low-value care; and medical liability reform to reduce defensive medical practices.
Low-value cardiovascular care is a complex problem, the writing group acknowledged, and achieving meaningful reductions in low-value cardiovascular care will require a multidisciplinary approach that includes continuous research, implementation, evaluation, and adjustment while ensuring equitable access to care.
“Each approach has benefits and drawbacks,” Dr. Kini said. “For example, prior authorization imposes a large burden on health care professionals to obtain insurance approval for tests and treatments. Prior authorization and some value-based payment models may unintentionally worsen existing racial and ethnic health care disparities.
“A one-size-fits-all approach to reducing low-value care is unlikely to succeed; rather, acting through multiple perspectives and frequently measuring impacts and potential unintended consequences is critical,” he concluded.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA’s Council on Quality of Care and Outcomes Research.
The research had no commercial funding. Dr. Kini disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Could the protective effect on heart disease of eating more veg be exaggerated?
Eating sufficient amounts of vegetables might be good for overall health, but surprising results from a study suggested that their inclusion in the diet might have little or no effect on the risk of developing cardiovascular disease (CVD).
An investigation, led by the Nuffield department of population health at the University of Oxford, found that They said their findings, published in the journal Frontiers in Nutrition might mean that advice on vegetable intake and heart disease in high-income countries should be reappraised.
However, leading experts commented that the findings confirmed that higher overall vegetable consumption did lower the risk of cardiovascular disease.
UK Biobank data
Boosting health through a diet rich in vegetables has been backed by a large body of evidence, with guidelines consistently recommending them as a valuable source of macronutrients and micronutrients, such as dietary fiber, vitamins, and phytochemicals. However, the research team, which included the Chinese University of Hong Kong and the University of Bristol, set out to probe the independent effects of cooked and raw vegetables on health outcomes. Previous epidemiological studies had demonstrated inconsistent findings, they said.
They based their research on 399,586 people with no history of angina, stroke, and myocardial infarction, who enrolled in the UK Biobank. Of those, 55.4% were women, and 90.9% were of White ethnicity. The average body mass index was 27.3.
Raw and cooked vegetables
From their enrollment questionnaire, the mean intake of vegetables was found to be 2.3 heaped tablespoons per day of raw vegetables, and 2.8 of cooked vegetables. During an average follow-up of 12.1 years, 4.5% of the participants went on to develop CVD.
There was an inverse association between incident CVD and total and raw vegetable intake, but not cooked vegetable intake. Those who ate the most vegetables – both cooked and raw – had a 10% lower incidence of CVD, compared with those who ate the least. However, whereas raw vegetable intake was associated with an 11% reduction in CVD for those who ate the most, compared with the least, no reduction was seen for cooked vegetables.
Consuming two or more heaped tablespoons each day of cooked and raw vegetables was associated with a lower risk of dying from CVD, but little evidence was seen that a higher intake increased protection further. Similarly, there was evidence of an inverse association of CVD mortality with raw vegetable intake.
Researcher Qi Feng, from the Nuffield department of population health, said: “Our large study did not find evidence for a protective effect of vegetable intake on the occurrence of CVD. Instead, our analyses show that the seemingly protective effect of vegetable intake against CVD risk is very likely to be accounted for by bias from residual confounding factors, related to differences in socioeconomic situation and lifestyle.”
Expert opinions
Some clinical specialists took issue with the interpretation of the findings.
Dr. Dipender Gill, BMBCh, PhD, National Institute for Health Research clinical lecturer at St George’s, University of London, told the Science Media Centre that: “Many of the considered confounders that were adjusted for may actually represent mediating mechanisms. For example, vegetable consumption may reduce cardiovascular risk by lowering blood pressure and bodyweight, and improving glycaemic control.
“By adjusting for such traits, the authors may inadvertently be negating some of the mechanisms by which vegetable consumption is exerting beneficial effects.”
Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics at King’s College London, said: “The conclusion that cooked vegetables may not be effective in reducing risk of cardiovascular disease may not be justified, especially as the group consuming the highest levels of vegetables were more likely to be receiving medication for high blood cholesterol and high blood pressure (i.e. this group was at higher risk of CVD), compared with those consuming the lowest intake.” He added: “These findings should not be taken to indicate that eating more vegetables has no benefit to health, especially cardiovascular health.”
Naveed Sattar, FMedSci, FRCPath, FRCPGlas, professor of metabolic medicine at the University of Glasgow, agreed. “In short, this paper should in no way change advice to eat at least five portions of fruit and vegetables a day,” he said. “Many living in the U.K. fall well short of this, sadly, and more needs to be done to encourage better intake of vegetables.
“In fact, I suspect we may have underestimated the importance of a healthy diet on health and disease in general.”
A version of this article first appeared on Medscape.com.
Eating sufficient amounts of vegetables might be good for overall health, but surprising results from a study suggested that their inclusion in the diet might have little or no effect on the risk of developing cardiovascular disease (CVD).
An investigation, led by the Nuffield department of population health at the University of Oxford, found that They said their findings, published in the journal Frontiers in Nutrition might mean that advice on vegetable intake and heart disease in high-income countries should be reappraised.
However, leading experts commented that the findings confirmed that higher overall vegetable consumption did lower the risk of cardiovascular disease.
UK Biobank data
Boosting health through a diet rich in vegetables has been backed by a large body of evidence, with guidelines consistently recommending them as a valuable source of macronutrients and micronutrients, such as dietary fiber, vitamins, and phytochemicals. However, the research team, which included the Chinese University of Hong Kong and the University of Bristol, set out to probe the independent effects of cooked and raw vegetables on health outcomes. Previous epidemiological studies had demonstrated inconsistent findings, they said.
They based their research on 399,586 people with no history of angina, stroke, and myocardial infarction, who enrolled in the UK Biobank. Of those, 55.4% were women, and 90.9% were of White ethnicity. The average body mass index was 27.3.
Raw and cooked vegetables
From their enrollment questionnaire, the mean intake of vegetables was found to be 2.3 heaped tablespoons per day of raw vegetables, and 2.8 of cooked vegetables. During an average follow-up of 12.1 years, 4.5% of the participants went on to develop CVD.
There was an inverse association between incident CVD and total and raw vegetable intake, but not cooked vegetable intake. Those who ate the most vegetables – both cooked and raw – had a 10% lower incidence of CVD, compared with those who ate the least. However, whereas raw vegetable intake was associated with an 11% reduction in CVD for those who ate the most, compared with the least, no reduction was seen for cooked vegetables.
Consuming two or more heaped tablespoons each day of cooked and raw vegetables was associated with a lower risk of dying from CVD, but little evidence was seen that a higher intake increased protection further. Similarly, there was evidence of an inverse association of CVD mortality with raw vegetable intake.
Researcher Qi Feng, from the Nuffield department of population health, said: “Our large study did not find evidence for a protective effect of vegetable intake on the occurrence of CVD. Instead, our analyses show that the seemingly protective effect of vegetable intake against CVD risk is very likely to be accounted for by bias from residual confounding factors, related to differences in socioeconomic situation and lifestyle.”
Expert opinions
Some clinical specialists took issue with the interpretation of the findings.
Dr. Dipender Gill, BMBCh, PhD, National Institute for Health Research clinical lecturer at St George’s, University of London, told the Science Media Centre that: “Many of the considered confounders that were adjusted for may actually represent mediating mechanisms. For example, vegetable consumption may reduce cardiovascular risk by lowering blood pressure and bodyweight, and improving glycaemic control.
“By adjusting for such traits, the authors may inadvertently be negating some of the mechanisms by which vegetable consumption is exerting beneficial effects.”
Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics at King’s College London, said: “The conclusion that cooked vegetables may not be effective in reducing risk of cardiovascular disease may not be justified, especially as the group consuming the highest levels of vegetables were more likely to be receiving medication for high blood cholesterol and high blood pressure (i.e. this group was at higher risk of CVD), compared with those consuming the lowest intake.” He added: “These findings should not be taken to indicate that eating more vegetables has no benefit to health, especially cardiovascular health.”
Naveed Sattar, FMedSci, FRCPath, FRCPGlas, professor of metabolic medicine at the University of Glasgow, agreed. “In short, this paper should in no way change advice to eat at least five portions of fruit and vegetables a day,” he said. “Many living in the U.K. fall well short of this, sadly, and more needs to be done to encourage better intake of vegetables.
“In fact, I suspect we may have underestimated the importance of a healthy diet on health and disease in general.”
A version of this article first appeared on Medscape.com.
Eating sufficient amounts of vegetables might be good for overall health, but surprising results from a study suggested that their inclusion in the diet might have little or no effect on the risk of developing cardiovascular disease (CVD).
An investigation, led by the Nuffield department of population health at the University of Oxford, found that They said their findings, published in the journal Frontiers in Nutrition might mean that advice on vegetable intake and heart disease in high-income countries should be reappraised.
However, leading experts commented that the findings confirmed that higher overall vegetable consumption did lower the risk of cardiovascular disease.
UK Biobank data
Boosting health through a diet rich in vegetables has been backed by a large body of evidence, with guidelines consistently recommending them as a valuable source of macronutrients and micronutrients, such as dietary fiber, vitamins, and phytochemicals. However, the research team, which included the Chinese University of Hong Kong and the University of Bristol, set out to probe the independent effects of cooked and raw vegetables on health outcomes. Previous epidemiological studies had demonstrated inconsistent findings, they said.
They based their research on 399,586 people with no history of angina, stroke, and myocardial infarction, who enrolled in the UK Biobank. Of those, 55.4% were women, and 90.9% were of White ethnicity. The average body mass index was 27.3.
Raw and cooked vegetables
From their enrollment questionnaire, the mean intake of vegetables was found to be 2.3 heaped tablespoons per day of raw vegetables, and 2.8 of cooked vegetables. During an average follow-up of 12.1 years, 4.5% of the participants went on to develop CVD.
There was an inverse association between incident CVD and total and raw vegetable intake, but not cooked vegetable intake. Those who ate the most vegetables – both cooked and raw – had a 10% lower incidence of CVD, compared with those who ate the least. However, whereas raw vegetable intake was associated with an 11% reduction in CVD for those who ate the most, compared with the least, no reduction was seen for cooked vegetables.
Consuming two or more heaped tablespoons each day of cooked and raw vegetables was associated with a lower risk of dying from CVD, but little evidence was seen that a higher intake increased protection further. Similarly, there was evidence of an inverse association of CVD mortality with raw vegetable intake.
Researcher Qi Feng, from the Nuffield department of population health, said: “Our large study did not find evidence for a protective effect of vegetable intake on the occurrence of CVD. Instead, our analyses show that the seemingly protective effect of vegetable intake against CVD risk is very likely to be accounted for by bias from residual confounding factors, related to differences in socioeconomic situation and lifestyle.”
Expert opinions
Some clinical specialists took issue with the interpretation of the findings.
Dr. Dipender Gill, BMBCh, PhD, National Institute for Health Research clinical lecturer at St George’s, University of London, told the Science Media Centre that: “Many of the considered confounders that were adjusted for may actually represent mediating mechanisms. For example, vegetable consumption may reduce cardiovascular risk by lowering blood pressure and bodyweight, and improving glycaemic control.
“By adjusting for such traits, the authors may inadvertently be negating some of the mechanisms by which vegetable consumption is exerting beneficial effects.”
Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics at King’s College London, said: “The conclusion that cooked vegetables may not be effective in reducing risk of cardiovascular disease may not be justified, especially as the group consuming the highest levels of vegetables were more likely to be receiving medication for high blood cholesterol and high blood pressure (i.e. this group was at higher risk of CVD), compared with those consuming the lowest intake.” He added: “These findings should not be taken to indicate that eating more vegetables has no benefit to health, especially cardiovascular health.”
Naveed Sattar, FMedSci, FRCPath, FRCPGlas, professor of metabolic medicine at the University of Glasgow, agreed. “In short, this paper should in no way change advice to eat at least five portions of fruit and vegetables a day,” he said. “Many living in the U.K. fall well short of this, sadly, and more needs to be done to encourage better intake of vegetables.
“In fact, I suspect we may have underestimated the importance of a healthy diet on health and disease in general.”
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN NUTRITION
USPSTF tweaks primary prevention statin recommendations in new draft guidance
Given the expansive contemporary role of statins for primary cardiovascular disease (CVD) prevention, the language in the new U.S. Preventive Services Task Force draft guidance on their use in that setting may seem conservative. Even so, the proposed recommendations, open to public comment until March 21, take more recent data into account but don’t substantially vary from the 2016 USPSTF document they are intended to replace.
The task force concluded “with moderate certainty” that a statin prescription will clinically benefit adults aged 40-75 years without CVD but with at least one of several risk factors, such as dyslipidemia or diabetes, who have a 10-year CVD risk of at least 7.5%.
the new report states. That, says an accompanying USPSTF press release, means such people “may benefit from statin use and should decide with their clinician if taking a statin is right for them.”
Also, notes the report, the net benefit of statin therapy is “at least moderate” for individuals with a 10% or greater CVD risk over the next decade who, the press release states, “should take a statin to prevent a first heart attack or stroke.”
The evidence review on which the task force based the guidance, the report says, lacked sufficient basis for determining statin benefit versus risk in adults older than 75 years without a history of CVD. “In the absence of this evidence, clinicians should use their judgment as to whether to offer a statin to a patient in this age group,” according to the press release.
The review focused on 22 clinical trials for data on the statin benefits and saw significantly decreased associated risks for death from any cause, fatal or nonfatal stroke, and fatal or nonfatal myocardial infarction with treatment. The combined trial populations exceeded 85,000 for assessing all-cause mortality and 76,000 for each of the other two endpoints.
To assess any potential statin therapy harms, the evidence review covered 19 clinical trials with a combined enrollment of about 75,000 – two more trials than considered in the 2016 document – plus three observational studies with more than 400,000 participants. Statins were found not to be associated with an increased risk for study withdrawal because of adverse events, nor were there signs of greater risk for myalgia or new-onset diabetes, compared with placebo.
“A majority of the trials reviewed by the USPSTF used moderate-intensity statin therapy,” the report states. “Based on available evidence, use of moderate-intensity statin therapy seems reasonable for the primary prevention of CVD in most persons.”
A version of this article first appeared on Medscape.com.
Given the expansive contemporary role of statins for primary cardiovascular disease (CVD) prevention, the language in the new U.S. Preventive Services Task Force draft guidance on their use in that setting may seem conservative. Even so, the proposed recommendations, open to public comment until March 21, take more recent data into account but don’t substantially vary from the 2016 USPSTF document they are intended to replace.
The task force concluded “with moderate certainty” that a statin prescription will clinically benefit adults aged 40-75 years without CVD but with at least one of several risk factors, such as dyslipidemia or diabetes, who have a 10-year CVD risk of at least 7.5%.
the new report states. That, says an accompanying USPSTF press release, means such people “may benefit from statin use and should decide with their clinician if taking a statin is right for them.”
Also, notes the report, the net benefit of statin therapy is “at least moderate” for individuals with a 10% or greater CVD risk over the next decade who, the press release states, “should take a statin to prevent a first heart attack or stroke.”
The evidence review on which the task force based the guidance, the report says, lacked sufficient basis for determining statin benefit versus risk in adults older than 75 years without a history of CVD. “In the absence of this evidence, clinicians should use their judgment as to whether to offer a statin to a patient in this age group,” according to the press release.
The review focused on 22 clinical trials for data on the statin benefits and saw significantly decreased associated risks for death from any cause, fatal or nonfatal stroke, and fatal or nonfatal myocardial infarction with treatment. The combined trial populations exceeded 85,000 for assessing all-cause mortality and 76,000 for each of the other two endpoints.
To assess any potential statin therapy harms, the evidence review covered 19 clinical trials with a combined enrollment of about 75,000 – two more trials than considered in the 2016 document – plus three observational studies with more than 400,000 participants. Statins were found not to be associated with an increased risk for study withdrawal because of adverse events, nor were there signs of greater risk for myalgia or new-onset diabetes, compared with placebo.
“A majority of the trials reviewed by the USPSTF used moderate-intensity statin therapy,” the report states. “Based on available evidence, use of moderate-intensity statin therapy seems reasonable for the primary prevention of CVD in most persons.”
A version of this article first appeared on Medscape.com.
Given the expansive contemporary role of statins for primary cardiovascular disease (CVD) prevention, the language in the new U.S. Preventive Services Task Force draft guidance on their use in that setting may seem conservative. Even so, the proposed recommendations, open to public comment until March 21, take more recent data into account but don’t substantially vary from the 2016 USPSTF document they are intended to replace.
The task force concluded “with moderate certainty” that a statin prescription will clinically benefit adults aged 40-75 years without CVD but with at least one of several risk factors, such as dyslipidemia or diabetes, who have a 10-year CVD risk of at least 7.5%.
the new report states. That, says an accompanying USPSTF press release, means such people “may benefit from statin use and should decide with their clinician if taking a statin is right for them.”
Also, notes the report, the net benefit of statin therapy is “at least moderate” for individuals with a 10% or greater CVD risk over the next decade who, the press release states, “should take a statin to prevent a first heart attack or stroke.”
The evidence review on which the task force based the guidance, the report says, lacked sufficient basis for determining statin benefit versus risk in adults older than 75 years without a history of CVD. “In the absence of this evidence, clinicians should use their judgment as to whether to offer a statin to a patient in this age group,” according to the press release.
The review focused on 22 clinical trials for data on the statin benefits and saw significantly decreased associated risks for death from any cause, fatal or nonfatal stroke, and fatal or nonfatal myocardial infarction with treatment. The combined trial populations exceeded 85,000 for assessing all-cause mortality and 76,000 for each of the other two endpoints.
To assess any potential statin therapy harms, the evidence review covered 19 clinical trials with a combined enrollment of about 75,000 – two more trials than considered in the 2016 document – plus three observational studies with more than 400,000 participants. Statins were found not to be associated with an increased risk for study withdrawal because of adverse events, nor were there signs of greater risk for myalgia or new-onset diabetes, compared with placebo.
“A majority of the trials reviewed by the USPSTF used moderate-intensity statin therapy,” the report states. “Based on available evidence, use of moderate-intensity statin therapy seems reasonable for the primary prevention of CVD in most persons.”
A version of this article first appeared on Medscape.com.
Full-press therapy rare in diabetes with ASCVD
A high percentage of people with type 2 diabetes also have atherosclerotic cardiovascular disease (ASCVD), but fewer than 1 in 20 get the triumvirate of evidence-based medications – drugs to lower cholesterol, blood pressure, and glucose levels – that can mitigate the dominant health risks they face, a large multicenter cohort study reported.
The cohort consisted of 324,706 patients with diabetes and ASCVD in the National Patient-Centered Clinical Research Network in 2018.
Senior study author Christopher B. Granger, MD, said in an interview that the findings represent “a shocking underuse of treatments proven to improve outcomes in this high-risk population.” For example, he noted that high-intensity statins are “inexpensive, well tolerated, and highly effective, but the fact that they’re only used in 26.8% of this population is really an indictment and embarrassment for our health-care system.”
The study analyzed prescriptions of high-intensity statins to lower cholesterol, ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure, and SGLT2 inhibitors or GLP-1 receptor agonists for hyperglycemia in a population with both diabetes and ASCVD.
This study amplifies the perceived treatment gap in cardiovascular risk reduction in persons with diabetes,” Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., said in an interview. “The unfortunate treatment deficiency documented among 325,000 patients in 12 health systems is carefully quantitated and the message is loud, clear, and simple: There is gross underutilization of agents – ACE inhibitors and ARBs, SGLT-2 inhibitors, GLP-1 receptor agonists, and high-intensity statins – with definitively proven ASCVD benefit.”
In the cohort population, 44% were women and 56% were men; 18.2% were black and 12.8% were Latinx. In terms of care patterns for the 205,885 patients who had specialized visit data from the year before the study, the most (74.8%) saw a primary care physician, while only 8.7% visited an endocrinologist and 26.4% saw a cardiologist.
In terms of the prescriptions they received, 58.6% were on a statin, with less than half on a high-intensity statin; 45.5% were on either an ACE inhibitor or ARB, 3.9% received a GLP-1 receptor agonist, and 2.8% were taking a SGLT2 inhibitor.
The investigators pointed out that figure of 58.6% for patients who got a statin was significantly lower than the 74.6% reported in a study of a database of commercially insured patients, but was more in line with findings a 2018 study of patients with diabetes and ASCVD.
Only 4.8% of patients got all three types of therapies, and a high percentage (42.6%) didn’t get any prescription for the three major risk factors.
Overcoming barriers to prescriptions
The study noted that more work needs to be done to overcome the barriers to more widespread use of these therapies in patients with both diabetes and ASCVD.
Specifically with SGLT2 inhibitors and GLP-1 receptor agonists, cost was more likely to be a barrier than with the other drug groups, but that didn’t explain the low levels of high-intensity statin prescriptions, said Dr. Granger of Duke University, Durham, N.C.
The first barrier he mentioned is what he called “clinical inertia.” He said: “I’m a cardiologist who cares for these patients in my clinic each week, and there are so many different things that we need to be trying to achieve with the brief time we have with each patient in our clinic setting that people tend to miss the opportunity.”
The cost barrier, especially with the glucose-lowering therapies, can be overcome with clinic and health care system programs that aid patients in getting discounted drugs, he noted.
Other barriers Dr. Granger pointed out are lack of education – “So many people think that people with previous muscle aches can’t take a high-intensity statin, and we know that’s not true” – and misinformation, which he called “the more nefarious issue.”
He said, “Part of the problem is that misinformation travels much faster than accurate information. There’s so much out there about statins being toxic, which is just not true.”
Fragmentation of the U.S. health care system and the lack of feedback on quality measures, and physicians deferring decisions on glucose-lowering therapy to endocrinologists also pose barriers to more widespread use of evidence-based therapies in patients with diabetes and ASCVD, Dr. Granger said.
“This is a call to action,” Dr. Granger said. “By clearly describing these gaps, we hope that people will see this as an important opportunity to improve care not only at the level of individual providers, but even more importantly at the level of health systems.”
Dr. Jellinger said the “dismal results” of the study serve as a “wake-up call,” adding that “my own perception among my colleagues, along with the data referred to in this article, point to definitely higher usage among commercially insured patients. However, even in more enriched populations the message is not having its full impact. We have remarkable agents for our patients with diabetes that can make a real impact in diabetes-related morbidity and mortality. Our twofold goal should be to aggressively educate a broad slate of health care professionals and, of course, make patient access easy and affordable without ‘prior authorization.’ ”
The study noted the need to bring the prescribing patterns for patients with both diabetes and ASCVD more in line with evidence-based guidelines. To that end, said Dr. Granger, the researchers are moving ahead on a randomized study of a quality improvement project involving about 45 U.S. cardiology clinics using a feedback loop to apply more consistent prescribing patterns for the three therapy groups. “Hopefully a year from now we’ll have a lot more information about this problem,” Dr. Granger added.
Boehringer Ingelheim and Lilly funded the study. Dr. Granger reported financial relationships with Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Pfizer, Medtronic, Akros Pharma, Apple, AstraZeneca, Daichi-Sankyo, Novartis, AbbVie, Bayer, Boston Scientific, CeleCor, Correvio, Espero, Merck, Novo Nordisk, Rhoshan Pharmaceuticals, and Roche Diagnostics. Dr. Jellinger is on speaker’s bureaus for Esperion and Amgen.
A high percentage of people with type 2 diabetes also have atherosclerotic cardiovascular disease (ASCVD), but fewer than 1 in 20 get the triumvirate of evidence-based medications – drugs to lower cholesterol, blood pressure, and glucose levels – that can mitigate the dominant health risks they face, a large multicenter cohort study reported.
The cohort consisted of 324,706 patients with diabetes and ASCVD in the National Patient-Centered Clinical Research Network in 2018.
Senior study author Christopher B. Granger, MD, said in an interview that the findings represent “a shocking underuse of treatments proven to improve outcomes in this high-risk population.” For example, he noted that high-intensity statins are “inexpensive, well tolerated, and highly effective, but the fact that they’re only used in 26.8% of this population is really an indictment and embarrassment for our health-care system.”
The study analyzed prescriptions of high-intensity statins to lower cholesterol, ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure, and SGLT2 inhibitors or GLP-1 receptor agonists for hyperglycemia in a population with both diabetes and ASCVD.
This study amplifies the perceived treatment gap in cardiovascular risk reduction in persons with diabetes,” Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., said in an interview. “The unfortunate treatment deficiency documented among 325,000 patients in 12 health systems is carefully quantitated and the message is loud, clear, and simple: There is gross underutilization of agents – ACE inhibitors and ARBs, SGLT-2 inhibitors, GLP-1 receptor agonists, and high-intensity statins – with definitively proven ASCVD benefit.”
In the cohort population, 44% were women and 56% were men; 18.2% were black and 12.8% were Latinx. In terms of care patterns for the 205,885 patients who had specialized visit data from the year before the study, the most (74.8%) saw a primary care physician, while only 8.7% visited an endocrinologist and 26.4% saw a cardiologist.
In terms of the prescriptions they received, 58.6% were on a statin, with less than half on a high-intensity statin; 45.5% were on either an ACE inhibitor or ARB, 3.9% received a GLP-1 receptor agonist, and 2.8% were taking a SGLT2 inhibitor.
The investigators pointed out that figure of 58.6% for patients who got a statin was significantly lower than the 74.6% reported in a study of a database of commercially insured patients, but was more in line with findings a 2018 study of patients with diabetes and ASCVD.
Only 4.8% of patients got all three types of therapies, and a high percentage (42.6%) didn’t get any prescription for the three major risk factors.
Overcoming barriers to prescriptions
The study noted that more work needs to be done to overcome the barriers to more widespread use of these therapies in patients with both diabetes and ASCVD.
Specifically with SGLT2 inhibitors and GLP-1 receptor agonists, cost was more likely to be a barrier than with the other drug groups, but that didn’t explain the low levels of high-intensity statin prescriptions, said Dr. Granger of Duke University, Durham, N.C.
The first barrier he mentioned is what he called “clinical inertia.” He said: “I’m a cardiologist who cares for these patients in my clinic each week, and there are so many different things that we need to be trying to achieve with the brief time we have with each patient in our clinic setting that people tend to miss the opportunity.”
The cost barrier, especially with the glucose-lowering therapies, can be overcome with clinic and health care system programs that aid patients in getting discounted drugs, he noted.
Other barriers Dr. Granger pointed out are lack of education – “So many people think that people with previous muscle aches can’t take a high-intensity statin, and we know that’s not true” – and misinformation, which he called “the more nefarious issue.”
He said, “Part of the problem is that misinformation travels much faster than accurate information. There’s so much out there about statins being toxic, which is just not true.”
Fragmentation of the U.S. health care system and the lack of feedback on quality measures, and physicians deferring decisions on glucose-lowering therapy to endocrinologists also pose barriers to more widespread use of evidence-based therapies in patients with diabetes and ASCVD, Dr. Granger said.
“This is a call to action,” Dr. Granger said. “By clearly describing these gaps, we hope that people will see this as an important opportunity to improve care not only at the level of individual providers, but even more importantly at the level of health systems.”
Dr. Jellinger said the “dismal results” of the study serve as a “wake-up call,” adding that “my own perception among my colleagues, along with the data referred to in this article, point to definitely higher usage among commercially insured patients. However, even in more enriched populations the message is not having its full impact. We have remarkable agents for our patients with diabetes that can make a real impact in diabetes-related morbidity and mortality. Our twofold goal should be to aggressively educate a broad slate of health care professionals and, of course, make patient access easy and affordable without ‘prior authorization.’ ”
The study noted the need to bring the prescribing patterns for patients with both diabetes and ASCVD more in line with evidence-based guidelines. To that end, said Dr. Granger, the researchers are moving ahead on a randomized study of a quality improvement project involving about 45 U.S. cardiology clinics using a feedback loop to apply more consistent prescribing patterns for the three therapy groups. “Hopefully a year from now we’ll have a lot more information about this problem,” Dr. Granger added.
Boehringer Ingelheim and Lilly funded the study. Dr. Granger reported financial relationships with Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Pfizer, Medtronic, Akros Pharma, Apple, AstraZeneca, Daichi-Sankyo, Novartis, AbbVie, Bayer, Boston Scientific, CeleCor, Correvio, Espero, Merck, Novo Nordisk, Rhoshan Pharmaceuticals, and Roche Diagnostics. Dr. Jellinger is on speaker’s bureaus for Esperion and Amgen.
A high percentage of people with type 2 diabetes also have atherosclerotic cardiovascular disease (ASCVD), but fewer than 1 in 20 get the triumvirate of evidence-based medications – drugs to lower cholesterol, blood pressure, and glucose levels – that can mitigate the dominant health risks they face, a large multicenter cohort study reported.
The cohort consisted of 324,706 patients with diabetes and ASCVD in the National Patient-Centered Clinical Research Network in 2018.
Senior study author Christopher B. Granger, MD, said in an interview that the findings represent “a shocking underuse of treatments proven to improve outcomes in this high-risk population.” For example, he noted that high-intensity statins are “inexpensive, well tolerated, and highly effective, but the fact that they’re only used in 26.8% of this population is really an indictment and embarrassment for our health-care system.”
The study analyzed prescriptions of high-intensity statins to lower cholesterol, ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure, and SGLT2 inhibitors or GLP-1 receptor agonists for hyperglycemia in a population with both diabetes and ASCVD.
This study amplifies the perceived treatment gap in cardiovascular risk reduction in persons with diabetes,” Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., said in an interview. “The unfortunate treatment deficiency documented among 325,000 patients in 12 health systems is carefully quantitated and the message is loud, clear, and simple: There is gross underutilization of agents – ACE inhibitors and ARBs, SGLT-2 inhibitors, GLP-1 receptor agonists, and high-intensity statins – with definitively proven ASCVD benefit.”
In the cohort population, 44% were women and 56% were men; 18.2% were black and 12.8% were Latinx. In terms of care patterns for the 205,885 patients who had specialized visit data from the year before the study, the most (74.8%) saw a primary care physician, while only 8.7% visited an endocrinologist and 26.4% saw a cardiologist.
In terms of the prescriptions they received, 58.6% were on a statin, with less than half on a high-intensity statin; 45.5% were on either an ACE inhibitor or ARB, 3.9% received a GLP-1 receptor agonist, and 2.8% were taking a SGLT2 inhibitor.
The investigators pointed out that figure of 58.6% for patients who got a statin was significantly lower than the 74.6% reported in a study of a database of commercially insured patients, but was more in line with findings a 2018 study of patients with diabetes and ASCVD.
Only 4.8% of patients got all three types of therapies, and a high percentage (42.6%) didn’t get any prescription for the three major risk factors.
Overcoming barriers to prescriptions
The study noted that more work needs to be done to overcome the barriers to more widespread use of these therapies in patients with both diabetes and ASCVD.
Specifically with SGLT2 inhibitors and GLP-1 receptor agonists, cost was more likely to be a barrier than with the other drug groups, but that didn’t explain the low levels of high-intensity statin prescriptions, said Dr. Granger of Duke University, Durham, N.C.
The first barrier he mentioned is what he called “clinical inertia.” He said: “I’m a cardiologist who cares for these patients in my clinic each week, and there are so many different things that we need to be trying to achieve with the brief time we have with each patient in our clinic setting that people tend to miss the opportunity.”
The cost barrier, especially with the glucose-lowering therapies, can be overcome with clinic and health care system programs that aid patients in getting discounted drugs, he noted.
Other barriers Dr. Granger pointed out are lack of education – “So many people think that people with previous muscle aches can’t take a high-intensity statin, and we know that’s not true” – and misinformation, which he called “the more nefarious issue.”
He said, “Part of the problem is that misinformation travels much faster than accurate information. There’s so much out there about statins being toxic, which is just not true.”
Fragmentation of the U.S. health care system and the lack of feedback on quality measures, and physicians deferring decisions on glucose-lowering therapy to endocrinologists also pose barriers to more widespread use of evidence-based therapies in patients with diabetes and ASCVD, Dr. Granger said.
“This is a call to action,” Dr. Granger said. “By clearly describing these gaps, we hope that people will see this as an important opportunity to improve care not only at the level of individual providers, but even more importantly at the level of health systems.”
Dr. Jellinger said the “dismal results” of the study serve as a “wake-up call,” adding that “my own perception among my colleagues, along with the data referred to in this article, point to definitely higher usage among commercially insured patients. However, even in more enriched populations the message is not having its full impact. We have remarkable agents for our patients with diabetes that can make a real impact in diabetes-related morbidity and mortality. Our twofold goal should be to aggressively educate a broad slate of health care professionals and, of course, make patient access easy and affordable without ‘prior authorization.’ ”
The study noted the need to bring the prescribing patterns for patients with both diabetes and ASCVD more in line with evidence-based guidelines. To that end, said Dr. Granger, the researchers are moving ahead on a randomized study of a quality improvement project involving about 45 U.S. cardiology clinics using a feedback loop to apply more consistent prescribing patterns for the three therapy groups. “Hopefully a year from now we’ll have a lot more information about this problem,” Dr. Granger added.
Boehringer Ingelheim and Lilly funded the study. Dr. Granger reported financial relationships with Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Pfizer, Medtronic, Akros Pharma, Apple, AstraZeneca, Daichi-Sankyo, Novartis, AbbVie, Bayer, Boston Scientific, CeleCor, Correvio, Espero, Merck, Novo Nordisk, Rhoshan Pharmaceuticals, and Roche Diagnostics. Dr. Jellinger is on speaker’s bureaus for Esperion and Amgen.
FROM JAMA OPEN NETWORK