User login
Worse survival seen among black patients with MCL
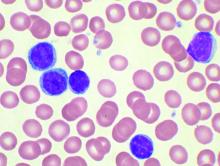
Black non-Hispanic patients with mantle cell lymphoma (MCL) have a lower rate of 5-year overall survival, compared with white non-Hispanic and Hispanic patients, according to a retrospective analysis of more than 18,000 cases.
However, black patients were also most likely to receive treatment at an academic center, which was an independent predictor of better survival, reported Nikesh N. Shah, MD, of Emory University, Atlanta, and his colleagues. This finding suggests that even academic centers still need to focus on overcoming demographic disparities.
“Racial and socioeconomic differences have been reported in many malignancies and certain lymphomas; however, few studies report on disparities in MCL,” the investigators wrote in Clinical Lymphoma, Myeloma & Leukemia. “To our knowledge this is the first such study to assess racial and socioeconomic disparities in this disease.”
The investigators reviewed 18,120 patients with MCL diagnosed between 2004 and 2013; data were drawn from the National Cancer Database. The primary endpoint was overall survival from the time of diagnosis, with analyses conducted to assess various associations with race/ethnicity, facility type, clinical/tumor characteristics, cancer stage, insurance type, and other factors.
Results showed that Hispanic patients had the highest rate of overall survival, at 55.8%, followed by white patients, at 50.1%. Trailing behind these groups were black patients (46.8%) and patients of other races/ethnicities (46.0%).
Along with survival disparities, race/ethnicity was tied to certain clinical and treatment characteristics. Compared with white patients, black patients were more likely to experience B symptoms (28% vs. 25%) and have Medicaid or lack insurance (15% vs. 5%). Black and Hispanic patients were also less likely than white non-Hispanic patients to receive stem cell transplant (13% vs. 10% vs. 10%).
Although black patients were more likely than white patients to receive treatment at an academic center (51% vs. 38%), a factor independently associated with best survival among center types, whatever advantage provided apparently did not exceed disadvantages associated with race.
“We report inferior overall survival in black patients after accounting for socioeconomic status, as seen in other malignancies,” the investigators wrote. “Surprisingly, these patients were more likely to be treated at academic centers, which independently showed improved overall survival in multivariable analysis that controlled for age, disease stage, insurance status, and other socioeconomic factors.”
The researchers cited a number of steps that could help close the survival gap, including providing more comprehensive supportive care between physician visits and enrollment of patients from diverse racial background on clinical trials.
The study was funded by the National Institutes of Health. The researchers reported having no conflicts of interest.
SOURCE: Shah NN et al. Clin Lymphoma Myeloma Leuk. 2019 Mar 11. doi: 10.1016/j.clml.2019.03.006.
Black non-Hispanic patients with mantle cell lymphoma (MCL) have a lower rate of 5-year overall survival, compared with white non-Hispanic and Hispanic patients, according to a retrospective analysis of more than 18,000 cases.
However, black patients were also most likely to receive treatment at an academic center, which was an independent predictor of better survival, reported Nikesh N. Shah, MD, of Emory University, Atlanta, and his colleagues. This finding suggests that even academic centers still need to focus on overcoming demographic disparities.
“Racial and socioeconomic differences have been reported in many malignancies and certain lymphomas; however, few studies report on disparities in MCL,” the investigators wrote in Clinical Lymphoma, Myeloma & Leukemia. “To our knowledge this is the first such study to assess racial and socioeconomic disparities in this disease.”
The investigators reviewed 18,120 patients with MCL diagnosed between 2004 and 2013; data were drawn from the National Cancer Database. The primary endpoint was overall survival from the time of diagnosis, with analyses conducted to assess various associations with race/ethnicity, facility type, clinical/tumor characteristics, cancer stage, insurance type, and other factors.
Results showed that Hispanic patients had the highest rate of overall survival, at 55.8%, followed by white patients, at 50.1%. Trailing behind these groups were black patients (46.8%) and patients of other races/ethnicities (46.0%).
Along with survival disparities, race/ethnicity was tied to certain clinical and treatment characteristics. Compared with white patients, black patients were more likely to experience B symptoms (28% vs. 25%) and have Medicaid or lack insurance (15% vs. 5%). Black and Hispanic patients were also less likely than white non-Hispanic patients to receive stem cell transplant (13% vs. 10% vs. 10%).
Although black patients were more likely than white patients to receive treatment at an academic center (51% vs. 38%), a factor independently associated with best survival among center types, whatever advantage provided apparently did not exceed disadvantages associated with race.
“We report inferior overall survival in black patients after accounting for socioeconomic status, as seen in other malignancies,” the investigators wrote. “Surprisingly, these patients were more likely to be treated at academic centers, which independently showed improved overall survival in multivariable analysis that controlled for age, disease stage, insurance status, and other socioeconomic factors.”
The researchers cited a number of steps that could help close the survival gap, including providing more comprehensive supportive care between physician visits and enrollment of patients from diverse racial background on clinical trials.
The study was funded by the National Institutes of Health. The researchers reported having no conflicts of interest.
SOURCE: Shah NN et al. Clin Lymphoma Myeloma Leuk. 2019 Mar 11. doi: 10.1016/j.clml.2019.03.006.
Black non-Hispanic patients with mantle cell lymphoma (MCL) have a lower rate of 5-year overall survival, compared with white non-Hispanic and Hispanic patients, according to a retrospective analysis of more than 18,000 cases.
However, black patients were also most likely to receive treatment at an academic center, which was an independent predictor of better survival, reported Nikesh N. Shah, MD, of Emory University, Atlanta, and his colleagues. This finding suggests that even academic centers still need to focus on overcoming demographic disparities.
“Racial and socioeconomic differences have been reported in many malignancies and certain lymphomas; however, few studies report on disparities in MCL,” the investigators wrote in Clinical Lymphoma, Myeloma & Leukemia. “To our knowledge this is the first such study to assess racial and socioeconomic disparities in this disease.”
The investigators reviewed 18,120 patients with MCL diagnosed between 2004 and 2013; data were drawn from the National Cancer Database. The primary endpoint was overall survival from the time of diagnosis, with analyses conducted to assess various associations with race/ethnicity, facility type, clinical/tumor characteristics, cancer stage, insurance type, and other factors.
Results showed that Hispanic patients had the highest rate of overall survival, at 55.8%, followed by white patients, at 50.1%. Trailing behind these groups were black patients (46.8%) and patients of other races/ethnicities (46.0%).
Along with survival disparities, race/ethnicity was tied to certain clinical and treatment characteristics. Compared with white patients, black patients were more likely to experience B symptoms (28% vs. 25%) and have Medicaid or lack insurance (15% vs. 5%). Black and Hispanic patients were also less likely than white non-Hispanic patients to receive stem cell transplant (13% vs. 10% vs. 10%).
Although black patients were more likely than white patients to receive treatment at an academic center (51% vs. 38%), a factor independently associated with best survival among center types, whatever advantage provided apparently did not exceed disadvantages associated with race.
“We report inferior overall survival in black patients after accounting for socioeconomic status, as seen in other malignancies,” the investigators wrote. “Surprisingly, these patients were more likely to be treated at academic centers, which independently showed improved overall survival in multivariable analysis that controlled for age, disease stage, insurance status, and other socioeconomic factors.”
The researchers cited a number of steps that could help close the survival gap, including providing more comprehensive supportive care between physician visits and enrollment of patients from diverse racial background on clinical trials.
The study was funded by the National Institutes of Health. The researchers reported having no conflicts of interest.
SOURCE: Shah NN et al. Clin Lymphoma Myeloma Leuk. 2019 Mar 11. doi: 10.1016/j.clml.2019.03.006.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
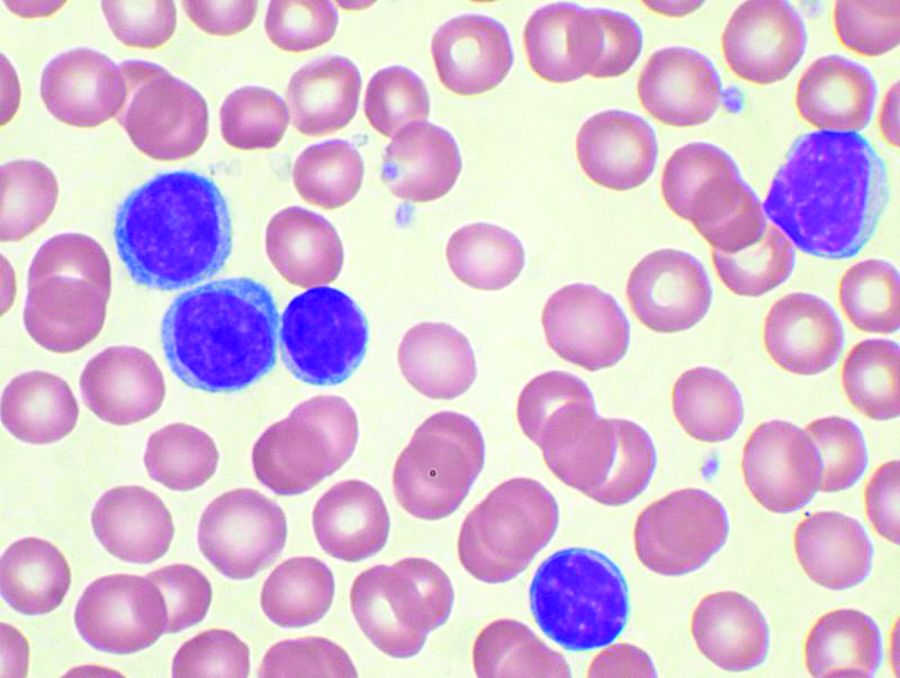
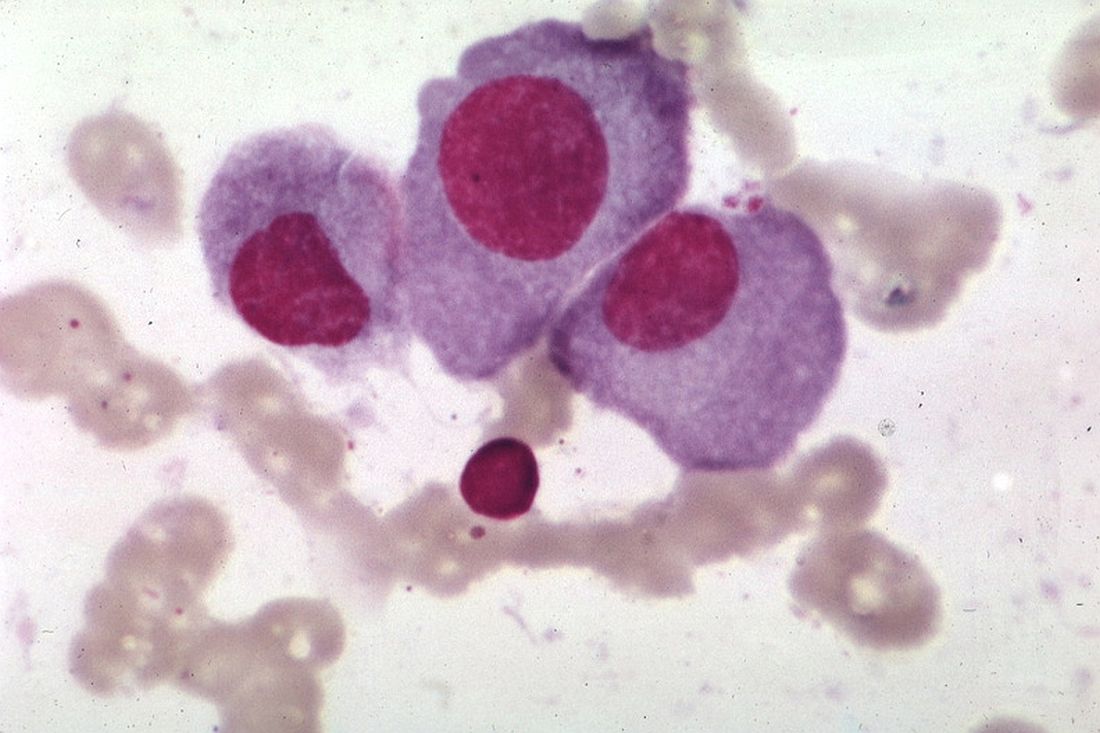
Short telomeres predict poorer response to chemo in CLL
A telomere-length analysis tool appears to identify reliably which chronic lymphocytic leukemia (CLL) patients will benefit from frontline chemotherapy, according to an analysis of 260 patients across two separate trials.
The analysis compared the use of high-throughput, single telomere–length analysis (HTSTELA) with other commonly used markers including beta-2 microglobulin, fluorescence-in-situ hybridization (FISH) cytogenetics, CD38 expression, ZAP70 expression, and IGHV mutation status. The researchers looked specifically at whether telomere length could predict response to frontline treatment with fludarabine, cyclophosphamide, rituximab (FCR)–based regimens.
“[T]elomere length is a powerful predictor of both [progression-free survival] and [overall survival] in patients treated with FCR-based therapies. In contrast, CD38 expression and beta-2 microglobulin expression were not predictive, and IGHV mutation status was only predictive of PFS (progression-free survival),” Kevin Norris, PhD, of Cardiff (Wales) University and his colleagues wrote in Leukemia.
Previous studies have shown that telomere-length analysis offers independent prognostic information in all stages of CLL. In the present study, the researchers used HTSTELA to analyze patient samples taken from two concurrent, phase 2 clinical trials of frontline FCR-based treatment – ARCTIC and ADMIRE.
The researchers divided the cohort based on a threshold of telomere dysfunction – the point at which the chromosome end-capping function is lost and there is genomic instability. Shorter telomeres are inside the fusogenic range (TL-IFR) and longer telomeres are outside fusogenic range (TL-OFR).
Patients with TL-IFR had significantly shorter PFS on FCR-based treatment (P less than .0001). They also had reduced overall survival (OS; P = .0002). In the same cohort of patients, IGHV mutation status was predictive of PFS (P = .0016), but it was not predictive for OS (P = .38), while CD38 and beta-2 microglobulin were not predictive of PFS or OS.
The researchers also looked at the value of telomere length in predicting outcomes among IGHV-mutated and -unmutated patients.
Patients with IGHV-mutated disease and TL-IFR had worse PFS and OS than did patients with TL-OFR. TL-IFR patients in this cohort were more likely to progress (hazard ratio, 4.35; P less than .0001) and more likely to die from their disease (HR, 3.81; P = .006).
“Although the number of IGHV-mutated patients with TL-IFR was relatively small (n = 16), our data suggests that telomere length can identify a subset of “bad risk” IGHV-mutated patients who do not respond well to FCR,” the researchers wrote.
Among IGHV unmutated patients, those with short telomeres had worse PFS (HR, 1.48; P = .08) and OS (HR, 2.18; P = .025) than did those with longer telomeres.
In multivariate modeling of all the potential markers, telomere length was the statistically significant dominant covariable for both PFS and OS.
The study was funded by a Bloodwise grant and the Wales Cancer Research Center. Dr. Norris and three coauthors reported that they are coinventors of patents relevant to the study and hold shares in a company set to provide telomere length testing.
SOURCE: Norris K et al. Leukemia. 2019 Jan 30. doi: 10.1038/s41375-019-0389-9.
A telomere-length analysis tool appears to identify reliably which chronic lymphocytic leukemia (CLL) patients will benefit from frontline chemotherapy, according to an analysis of 260 patients across two separate trials.
The analysis compared the use of high-throughput, single telomere–length analysis (HTSTELA) with other commonly used markers including beta-2 microglobulin, fluorescence-in-situ hybridization (FISH) cytogenetics, CD38 expression, ZAP70 expression, and IGHV mutation status. The researchers looked specifically at whether telomere length could predict response to frontline treatment with fludarabine, cyclophosphamide, rituximab (FCR)–based regimens.
“[T]elomere length is a powerful predictor of both [progression-free survival] and [overall survival] in patients treated with FCR-based therapies. In contrast, CD38 expression and beta-2 microglobulin expression were not predictive, and IGHV mutation status was only predictive of PFS (progression-free survival),” Kevin Norris, PhD, of Cardiff (Wales) University and his colleagues wrote in Leukemia.
Previous studies have shown that telomere-length analysis offers independent prognostic information in all stages of CLL. In the present study, the researchers used HTSTELA to analyze patient samples taken from two concurrent, phase 2 clinical trials of frontline FCR-based treatment – ARCTIC and ADMIRE.
The researchers divided the cohort based on a threshold of telomere dysfunction – the point at which the chromosome end-capping function is lost and there is genomic instability. Shorter telomeres are inside the fusogenic range (TL-IFR) and longer telomeres are outside fusogenic range (TL-OFR).
Patients with TL-IFR had significantly shorter PFS on FCR-based treatment (P less than .0001). They also had reduced overall survival (OS; P = .0002). In the same cohort of patients, IGHV mutation status was predictive of PFS (P = .0016), but it was not predictive for OS (P = .38), while CD38 and beta-2 microglobulin were not predictive of PFS or OS.
The researchers also looked at the value of telomere length in predicting outcomes among IGHV-mutated and -unmutated patients.
Patients with IGHV-mutated disease and TL-IFR had worse PFS and OS than did patients with TL-OFR. TL-IFR patients in this cohort were more likely to progress (hazard ratio, 4.35; P less than .0001) and more likely to die from their disease (HR, 3.81; P = .006).
“Although the number of IGHV-mutated patients with TL-IFR was relatively small (n = 16), our data suggests that telomere length can identify a subset of “bad risk” IGHV-mutated patients who do not respond well to FCR,” the researchers wrote.
Among IGHV unmutated patients, those with short telomeres had worse PFS (HR, 1.48; P = .08) and OS (HR, 2.18; P = .025) than did those with longer telomeres.
In multivariate modeling of all the potential markers, telomere length was the statistically significant dominant covariable for both PFS and OS.
The study was funded by a Bloodwise grant and the Wales Cancer Research Center. Dr. Norris and three coauthors reported that they are coinventors of patents relevant to the study and hold shares in a company set to provide telomere length testing.
SOURCE: Norris K et al. Leukemia. 2019 Jan 30. doi: 10.1038/s41375-019-0389-9.
A telomere-length analysis tool appears to identify reliably which chronic lymphocytic leukemia (CLL) patients will benefit from frontline chemotherapy, according to an analysis of 260 patients across two separate trials.
The analysis compared the use of high-throughput, single telomere–length analysis (HTSTELA) with other commonly used markers including beta-2 microglobulin, fluorescence-in-situ hybridization (FISH) cytogenetics, CD38 expression, ZAP70 expression, and IGHV mutation status. The researchers looked specifically at whether telomere length could predict response to frontline treatment with fludarabine, cyclophosphamide, rituximab (FCR)–based regimens.
“[T]elomere length is a powerful predictor of both [progression-free survival] and [overall survival] in patients treated with FCR-based therapies. In contrast, CD38 expression and beta-2 microglobulin expression were not predictive, and IGHV mutation status was only predictive of PFS (progression-free survival),” Kevin Norris, PhD, of Cardiff (Wales) University and his colleagues wrote in Leukemia.
Previous studies have shown that telomere-length analysis offers independent prognostic information in all stages of CLL. In the present study, the researchers used HTSTELA to analyze patient samples taken from two concurrent, phase 2 clinical trials of frontline FCR-based treatment – ARCTIC and ADMIRE.
The researchers divided the cohort based on a threshold of telomere dysfunction – the point at which the chromosome end-capping function is lost and there is genomic instability. Shorter telomeres are inside the fusogenic range (TL-IFR) and longer telomeres are outside fusogenic range (TL-OFR).
Patients with TL-IFR had significantly shorter PFS on FCR-based treatment (P less than .0001). They also had reduced overall survival (OS; P = .0002). In the same cohort of patients, IGHV mutation status was predictive of PFS (P = .0016), but it was not predictive for OS (P = .38), while CD38 and beta-2 microglobulin were not predictive of PFS or OS.
The researchers also looked at the value of telomere length in predicting outcomes among IGHV-mutated and -unmutated patients.
Patients with IGHV-mutated disease and TL-IFR had worse PFS and OS than did patients with TL-OFR. TL-IFR patients in this cohort were more likely to progress (hazard ratio, 4.35; P less than .0001) and more likely to die from their disease (HR, 3.81; P = .006).
“Although the number of IGHV-mutated patients with TL-IFR was relatively small (n = 16), our data suggests that telomere length can identify a subset of “bad risk” IGHV-mutated patients who do not respond well to FCR,” the researchers wrote.
Among IGHV unmutated patients, those with short telomeres had worse PFS (HR, 1.48; P = .08) and OS (HR, 2.18; P = .025) than did those with longer telomeres.
In multivariate modeling of all the potential markers, telomere length was the statistically significant dominant covariable for both PFS and OS.
The study was funded by a Bloodwise grant and the Wales Cancer Research Center. Dr. Norris and three coauthors reported that they are coinventors of patents relevant to the study and hold shares in a company set to provide telomere length testing.
SOURCE: Norris K et al. Leukemia. 2019 Jan 30. doi: 10.1038/s41375-019-0389-9.
FROM LEUKEMIA
Oral triplet deemed effective in relapsed/refractory myeloma
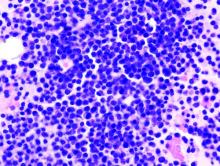
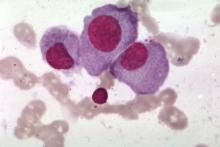
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
FROM BLOOD ADVANCES
Therapeutic dosing of busulfan helps reduce relapse in ASCT
HOUSTON – Compared with weight-based dosing, pharmacokinetic-directed therapeutic dose monitoring of busulfan used in combination with cyclophosphamide and etoposide reduced relapse risk in non-Hodgkin lymphoma (NHL) patients undergoing autologous stem cell transplantation (ASCT), according to a review of 336 cases.
This was particularly true in patients with less than a complete response at the time of transplant, Brian T. Hill, MD, PhD, reported at the Transplantation & Cellular Therapy Meetings.
The relapse rate at 24 months after ASCT was 19% in 78 adult NHL patients who underwent ASCT with pharmacokinetic-guided therapeutic dose monitoring (PK-TDM), compared with 38% in 258 patients who received weight-based-dosing (WBD) of busulfan with cyclophosphamide and etoposide.
Progression-free survival (PFS) improved with PK-TDM vs. WBD (69% vs. 55%) but overall survival (OS) did not differ between the groups, most likely because of subsequent therapy given at the time of relapse, said Dr. Hill, director of the lymphoid malignancies program and a staff physician at the Cleveland Clinic Taussig Cancer Institute, Ohio.
The findings are from a retrospective comparison of outcomes in patients treated between 2014 and 2017 when PK-TDM was the standard practice, and patients treated between 2007 and 2013 when fixed weight-based dosing was standard, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“In 2013 we began a program of therapeutic dose monitoring at our site,” Dr. Hill said, explaining that with TDM the goal is to eliminate the low and high levels seen with weight-based dosing, and “to get the maximum number of patients into the therapeutic zone.”
TDM became the preferred approach for busulfan dosing because of the drug’s “unpredictable and widely variable pharmacokinetics,” and ASBMT guidelines now call for consideration of TDM with first-line busulfan to minimize the potential complications, he noted.
“But it’s noteworthy that ... there are really no data to show that TDM can reduce the rates of relapse,” he added.
For this study, WBD busulfan dosing was 2.8 mg/kg every 24 hours on day –9 to –6 of ASCT. For PK-TDM, plasma busulfan concentration was serially determined using a previously described and externally validated in-house liquid chromatography–tandem mass spectrometry assay, he said, explaining that busulfan area under the curve (AUC) after first dose was calculated for each patient and used to adjust subsequent doses to target a daily AUC of 4,500 micromol/min.
To account for baseline differences in the two groups, including a higher number of prior chemotherapy regimens in the WBD group and a higher proportion of aggressive B-cell and T-cell lymphoma in the TDM group, two propensity-matched cohorts of 47 patients each were derived via logistic regression analysis.
“In the propensity-matched cohorts we saw a similar pattern, with therapeutic dose monitoring patients having lower relapse and improved progression-free survival, but no change in the nonrelapse mortality or the overall survival,” Dr. Hill said.
Notably, PFS did not differ between the groups when the researchers looked only at those in complete remission at transplant, but a significant improvement in PFS was seen in the TDM vs. WBD cohorts when they looked only at patients with partial remission, stable disease, or progressive disease (collectively considered as those in less than CR at transplant), he said (P = .79 vs. .08, respectively).
On multivariate analysis, less than CR status was associated with an increased risk of relapse after ASCT (hazard ratio, 2.0), and TDM vs. WBD was associated with a decreased risk of relapse (HR, 0.5).
No differences were seen between the groups with respect to changes in pulmonary or liver function from baseline, or in treatment-related mortality rates, Dr. Hill noted.
The findings support the use of PK-TDM for NHL patients undergoing ASCT with busulfan, but further study is needed, he concluded.
Dr. Hill reported having no relevant financial disclosures.
SOURCE: Hill B et al. TCT 2019, Abstract 39.
HOUSTON – Compared with weight-based dosing, pharmacokinetic-directed therapeutic dose monitoring of busulfan used in combination with cyclophosphamide and etoposide reduced relapse risk in non-Hodgkin lymphoma (NHL) patients undergoing autologous stem cell transplantation (ASCT), according to a review of 336 cases.
This was particularly true in patients with less than a complete response at the time of transplant, Brian T. Hill, MD, PhD, reported at the Transplantation & Cellular Therapy Meetings.
The relapse rate at 24 months after ASCT was 19% in 78 adult NHL patients who underwent ASCT with pharmacokinetic-guided therapeutic dose monitoring (PK-TDM), compared with 38% in 258 patients who received weight-based-dosing (WBD) of busulfan with cyclophosphamide and etoposide.
Progression-free survival (PFS) improved with PK-TDM vs. WBD (69% vs. 55%) but overall survival (OS) did not differ between the groups, most likely because of subsequent therapy given at the time of relapse, said Dr. Hill, director of the lymphoid malignancies program and a staff physician at the Cleveland Clinic Taussig Cancer Institute, Ohio.
The findings are from a retrospective comparison of outcomes in patients treated between 2014 and 2017 when PK-TDM was the standard practice, and patients treated between 2007 and 2013 when fixed weight-based dosing was standard, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“In 2013 we began a program of therapeutic dose monitoring at our site,” Dr. Hill said, explaining that with TDM the goal is to eliminate the low and high levels seen with weight-based dosing, and “to get the maximum number of patients into the therapeutic zone.”
TDM became the preferred approach for busulfan dosing because of the drug’s “unpredictable and widely variable pharmacokinetics,” and ASBMT guidelines now call for consideration of TDM with first-line busulfan to minimize the potential complications, he noted.
“But it’s noteworthy that ... there are really no data to show that TDM can reduce the rates of relapse,” he added.
For this study, WBD busulfan dosing was 2.8 mg/kg every 24 hours on day –9 to –6 of ASCT. For PK-TDM, plasma busulfan concentration was serially determined using a previously described and externally validated in-house liquid chromatography–tandem mass spectrometry assay, he said, explaining that busulfan area under the curve (AUC) after first dose was calculated for each patient and used to adjust subsequent doses to target a daily AUC of 4,500 micromol/min.
To account for baseline differences in the two groups, including a higher number of prior chemotherapy regimens in the WBD group and a higher proportion of aggressive B-cell and T-cell lymphoma in the TDM group, two propensity-matched cohorts of 47 patients each were derived via logistic regression analysis.
“In the propensity-matched cohorts we saw a similar pattern, with therapeutic dose monitoring patients having lower relapse and improved progression-free survival, but no change in the nonrelapse mortality or the overall survival,” Dr. Hill said.
Notably, PFS did not differ between the groups when the researchers looked only at those in complete remission at transplant, but a significant improvement in PFS was seen in the TDM vs. WBD cohorts when they looked only at patients with partial remission, stable disease, or progressive disease (collectively considered as those in less than CR at transplant), he said (P = .79 vs. .08, respectively).
On multivariate analysis, less than CR status was associated with an increased risk of relapse after ASCT (hazard ratio, 2.0), and TDM vs. WBD was associated with a decreased risk of relapse (HR, 0.5).
No differences were seen between the groups with respect to changes in pulmonary or liver function from baseline, or in treatment-related mortality rates, Dr. Hill noted.
The findings support the use of PK-TDM for NHL patients undergoing ASCT with busulfan, but further study is needed, he concluded.
Dr. Hill reported having no relevant financial disclosures.
SOURCE: Hill B et al. TCT 2019, Abstract 39.
HOUSTON – Compared with weight-based dosing, pharmacokinetic-directed therapeutic dose monitoring of busulfan used in combination with cyclophosphamide and etoposide reduced relapse risk in non-Hodgkin lymphoma (NHL) patients undergoing autologous stem cell transplantation (ASCT), according to a review of 336 cases.
This was particularly true in patients with less than a complete response at the time of transplant, Brian T. Hill, MD, PhD, reported at the Transplantation & Cellular Therapy Meetings.
The relapse rate at 24 months after ASCT was 19% in 78 adult NHL patients who underwent ASCT with pharmacokinetic-guided therapeutic dose monitoring (PK-TDM), compared with 38% in 258 patients who received weight-based-dosing (WBD) of busulfan with cyclophosphamide and etoposide.
Progression-free survival (PFS) improved with PK-TDM vs. WBD (69% vs. 55%) but overall survival (OS) did not differ between the groups, most likely because of subsequent therapy given at the time of relapse, said Dr. Hill, director of the lymphoid malignancies program and a staff physician at the Cleveland Clinic Taussig Cancer Institute, Ohio.
The findings are from a retrospective comparison of outcomes in patients treated between 2014 and 2017 when PK-TDM was the standard practice, and patients treated between 2007 and 2013 when fixed weight-based dosing was standard, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“In 2013 we began a program of therapeutic dose monitoring at our site,” Dr. Hill said, explaining that with TDM the goal is to eliminate the low and high levels seen with weight-based dosing, and “to get the maximum number of patients into the therapeutic zone.”
TDM became the preferred approach for busulfan dosing because of the drug’s “unpredictable and widely variable pharmacokinetics,” and ASBMT guidelines now call for consideration of TDM with first-line busulfan to minimize the potential complications, he noted.
“But it’s noteworthy that ... there are really no data to show that TDM can reduce the rates of relapse,” he added.
For this study, WBD busulfan dosing was 2.8 mg/kg every 24 hours on day –9 to –6 of ASCT. For PK-TDM, plasma busulfan concentration was serially determined using a previously described and externally validated in-house liquid chromatography–tandem mass spectrometry assay, he said, explaining that busulfan area under the curve (AUC) after first dose was calculated for each patient and used to adjust subsequent doses to target a daily AUC of 4,500 micromol/min.
To account for baseline differences in the two groups, including a higher number of prior chemotherapy regimens in the WBD group and a higher proportion of aggressive B-cell and T-cell lymphoma in the TDM group, two propensity-matched cohorts of 47 patients each were derived via logistic regression analysis.
“In the propensity-matched cohorts we saw a similar pattern, with therapeutic dose monitoring patients having lower relapse and improved progression-free survival, but no change in the nonrelapse mortality or the overall survival,” Dr. Hill said.
Notably, PFS did not differ between the groups when the researchers looked only at those in complete remission at transplant, but a significant improvement in PFS was seen in the TDM vs. WBD cohorts when they looked only at patients with partial remission, stable disease, or progressive disease (collectively considered as those in less than CR at transplant), he said (P = .79 vs. .08, respectively).
On multivariate analysis, less than CR status was associated with an increased risk of relapse after ASCT (hazard ratio, 2.0), and TDM vs. WBD was associated with a decreased risk of relapse (HR, 0.5).
No differences were seen between the groups with respect to changes in pulmonary or liver function from baseline, or in treatment-related mortality rates, Dr. Hill noted.
The findings support the use of PK-TDM for NHL patients undergoing ASCT with busulfan, but further study is needed, he concluded.
Dr. Hill reported having no relevant financial disclosures.
SOURCE: Hill B et al. TCT 2019, Abstract 39.
REPORTING FROM TCT 2019
Case report may link gluteal implants to lymphoma
Patients with textured silicone gluteal implants could be at risk of anaplastic large cell lymphoma, based on a possible case of ALCL in a patient diagnosed 1 year after implant placement.
The 49-year-old woman was initially diagnosed with anaplastic lymphoma kinase–negative ALCL via a lung mass and pleural fluid before bilateral gluteal ulceration occurred 1 month later, reported Orr Shauly of the University of Southern California in Los Angeles, and his colleagues.
Soft-tissue disease and fluid accumulation around the gluteal implants suggested that the lung mass had metastasized from primary neoplasia in the gluteal region. If ALCL did originate at the site of the gluteal implants, it would represent a first for silicone implant–associated ALCL, which has historically been associated exclusively with breast implants.
“As many as 200 cases of [breast implant-associated ALCL] have been described worldwide, with a majority in the context of cosmetic primary breast augmentation or cancer-related breast reconstruction with the use of a textured implant (57% of all cases),” the investigators wrote in Aesthetic Surgery Journal. “Recently however, it has been hypothesized that the relationship of ALCL with the placement of textured silicone implants may not [be] limited to the breast due to its multifactorial nature and association with texturization of the implant surface.”
During the initial work-up, a CT showed fluid collection and enhancement around the gluteal implants. Following ALCL diagnosis via lung mass biopsy and histopathology, the patient was transferred to a different facility for chemotherapy. When the patient presented 1 month later to the original facility with gluteal ulceration, the oncology team suspected infection; however, all cultures from fluid around the implants were negative.
Because of the possibility of false-negative tests, the patient was started on a regimen of acyclovir, vancomycin, metronidazole, and isavuconazole. Explantation was planned, but before this could occur, the patient deteriorated rapidly and died of respiratory and renal failure.
ALCL was not confirmed via cytology or histopathology in the gluteal region, and the patient’s family did not consent to autopsy, so a definitive diagnosis of gluteal implant–associated ALCL remained elusive.
“In this instance, it can only be concluded that the patient’s condition may have been associated with placement of textured silicone gluteal implants, but [we] still lack evidence of causation,” the investigators wrote. “It should also be noted that ALCL does not typically present with skin ulceration, and this may be a unique disease process in this patient or as a result of her bedridden state given the late stage of her disease. Furthermore, this presentation was uniquely aggressive and presented extremely quickly after placement of the gluteal implants. In most patients, ALCL develops and presents approximately 10 years after implantation.”
The investigators cautioned that “care should be taken to avoid sensationalizing all implant-associated ALCL.”
The authors reported having no conflicts of interest and the study did not receive funding.
SOURCE: Shauly O et al. Aesthet Surg J. 2019 Feb 15. doi: 10.1093/asj/sjz044.
Patients with textured silicone gluteal implants could be at risk of anaplastic large cell lymphoma, based on a possible case of ALCL in a patient diagnosed 1 year after implant placement.
The 49-year-old woman was initially diagnosed with anaplastic lymphoma kinase–negative ALCL via a lung mass and pleural fluid before bilateral gluteal ulceration occurred 1 month later, reported Orr Shauly of the University of Southern California in Los Angeles, and his colleagues.
Soft-tissue disease and fluid accumulation around the gluteal implants suggested that the lung mass had metastasized from primary neoplasia in the gluteal region. If ALCL did originate at the site of the gluteal implants, it would represent a first for silicone implant–associated ALCL, which has historically been associated exclusively with breast implants.
“As many as 200 cases of [breast implant-associated ALCL] have been described worldwide, with a majority in the context of cosmetic primary breast augmentation or cancer-related breast reconstruction with the use of a textured implant (57% of all cases),” the investigators wrote in Aesthetic Surgery Journal. “Recently however, it has been hypothesized that the relationship of ALCL with the placement of textured silicone implants may not [be] limited to the breast due to its multifactorial nature and association with texturization of the implant surface.”
During the initial work-up, a CT showed fluid collection and enhancement around the gluteal implants. Following ALCL diagnosis via lung mass biopsy and histopathology, the patient was transferred to a different facility for chemotherapy. When the patient presented 1 month later to the original facility with gluteal ulceration, the oncology team suspected infection; however, all cultures from fluid around the implants were negative.
Because of the possibility of false-negative tests, the patient was started on a regimen of acyclovir, vancomycin, metronidazole, and isavuconazole. Explantation was planned, but before this could occur, the patient deteriorated rapidly and died of respiratory and renal failure.
ALCL was not confirmed via cytology or histopathology in the gluteal region, and the patient’s family did not consent to autopsy, so a definitive diagnosis of gluteal implant–associated ALCL remained elusive.
“In this instance, it can only be concluded that the patient’s condition may have been associated with placement of textured silicone gluteal implants, but [we] still lack evidence of causation,” the investigators wrote. “It should also be noted that ALCL does not typically present with skin ulceration, and this may be a unique disease process in this patient or as a result of her bedridden state given the late stage of her disease. Furthermore, this presentation was uniquely aggressive and presented extremely quickly after placement of the gluteal implants. In most patients, ALCL develops and presents approximately 10 years after implantation.”
The investigators cautioned that “care should be taken to avoid sensationalizing all implant-associated ALCL.”
The authors reported having no conflicts of interest and the study did not receive funding.
SOURCE: Shauly O et al. Aesthet Surg J. 2019 Feb 15. doi: 10.1093/asj/sjz044.
Patients with textured silicone gluteal implants could be at risk of anaplastic large cell lymphoma, based on a possible case of ALCL in a patient diagnosed 1 year after implant placement.
The 49-year-old woman was initially diagnosed with anaplastic lymphoma kinase–negative ALCL via a lung mass and pleural fluid before bilateral gluteal ulceration occurred 1 month later, reported Orr Shauly of the University of Southern California in Los Angeles, and his colleagues.
Soft-tissue disease and fluid accumulation around the gluteal implants suggested that the lung mass had metastasized from primary neoplasia in the gluteal region. If ALCL did originate at the site of the gluteal implants, it would represent a first for silicone implant–associated ALCL, which has historically been associated exclusively with breast implants.
“As many as 200 cases of [breast implant-associated ALCL] have been described worldwide, with a majority in the context of cosmetic primary breast augmentation or cancer-related breast reconstruction with the use of a textured implant (57% of all cases),” the investigators wrote in Aesthetic Surgery Journal. “Recently however, it has been hypothesized that the relationship of ALCL with the placement of textured silicone implants may not [be] limited to the breast due to its multifactorial nature and association with texturization of the implant surface.”
During the initial work-up, a CT showed fluid collection and enhancement around the gluteal implants. Following ALCL diagnosis via lung mass biopsy and histopathology, the patient was transferred to a different facility for chemotherapy. When the patient presented 1 month later to the original facility with gluteal ulceration, the oncology team suspected infection; however, all cultures from fluid around the implants were negative.
Because of the possibility of false-negative tests, the patient was started on a regimen of acyclovir, vancomycin, metronidazole, and isavuconazole. Explantation was planned, but before this could occur, the patient deteriorated rapidly and died of respiratory and renal failure.
ALCL was not confirmed via cytology or histopathology in the gluteal region, and the patient’s family did not consent to autopsy, so a definitive diagnosis of gluteal implant–associated ALCL remained elusive.
“In this instance, it can only be concluded that the patient’s condition may have been associated with placement of textured silicone gluteal implants, but [we] still lack evidence of causation,” the investigators wrote. “It should also be noted that ALCL does not typically present with skin ulceration, and this may be a unique disease process in this patient or as a result of her bedridden state given the late stage of her disease. Furthermore, this presentation was uniquely aggressive and presented extremely quickly after placement of the gluteal implants. In most patients, ALCL develops and presents approximately 10 years after implantation.”
The investigators cautioned that “care should be taken to avoid sensationalizing all implant-associated ALCL.”
The authors reported having no conflicts of interest and the study did not receive funding.
SOURCE: Shauly O et al. Aesthet Surg J. 2019 Feb 15. doi: 10.1093/asj/sjz044.
FROM AESTHETIC SURGERY JOURNAL
Myeloma risk score has treatment-planning potential
A proposed clinical scoring system using readily available laboratory data, rather than complex formulas, can be used to predict risk for overall survival and help with clinical decision making for patients with multiple myeloma who are ineligible for stem cell transplants, the system’s creators claim.
When applied to data from two clinical trials that enrolled patients with transplant-ineligible multiple myeloma, the UK Myeloma Research Alliance Risk Profile (MRP) was shown to accurately group patients into low-, medium- and high-risk categories and was prognostic of overall survival, reported Gordon Cook, PhD, of the University of Leeds, England, and his colleagues.
“The ability of clinical scoring systems, such as that proposed here, to predict whether a patient is likely to stop treatment early because of treatment intolerability, could enable preemptive, upfront dose adjustments in patients with multiple myeloma, preventing toxicity and potentially enabling patients to stay on therapy for longer,” they wrote in the Lancet Haematology.
The investigators used data on 1,852 newly diagnosed patients recruited to the non–intensive treatment pathway of the UK’s National Cancer Research Institute Myeloma XI study (NCRI-XI, ISRCTN49407852) for a training dataset and internal validation dataset, and 520 patients recruited into the Medical Research Council Myeloma IX study (MRC-IX, ISRCTN68454111) for the test dataset.
Patient characteristics, biochemical measurements, and hematological data were plugged into univariate and multivariate models to determine their potential as prognostic variables.
The final model for the test and validation datasets included World Health Organization performance status, the multiple myeloma International Staging System, patient age, and C-reactive protein concentrations.
As noted before, the scoring algorithm groups patients into low-, medium- and high-risk categories, with each of the prognostic variables increasing in severity across the three groups in both clinical trials.
In the NCRI-XI trial, median overall survival for patients in the MRP low-risk group was 60 months, compared with 44 months in the medium-risk group, and 25 months in the high-risk group.
Similarly, in the MRC-IX trial, the respective median overall survival was 49, 34, and 20 months.
The risk groups also were associated with progression-free survival in each trial, although not as robustly as the association with overall survival.
The investigators also found that, the higher the risk group, the greater the likelihood that the median percentage of protocol dose delivered would be lower, and both a decrease in protocol dose delivered and quality of life at baseline were associated with increased risk.
The MRP categories were prognostic in patients treated with various therapeutic regimens and in patients with high-risk cytogenetics.
“None of the risk scoring systems previously developed in myeloma are dynamic, making them unable to accommodate changes in disease-related frailty that might be minimized by effective anti-myeloma therapy. There is therefore scope to improve clinical risk scores by the addition of a suitable frailty biomarker, which is currently still in developmental stages,” Dr. Cook and his colleagues wrote.
The study was funded by the Medical Research Council, Novartis, Schering Health Care, Chugai, Pharmion, Celgene, Ortho Biotech, Cancer Research UK, Celgene, Merck Sharp & Dohme, and Amgen. Dr. Cook reported grants and nonfinancial support from Celgene, Amgen, and Merck Sharp & Dohme, during the conduct of the study and personal fees from other companies outside the submitted work.
SOURCE: Cook G et al. Lancet Haematol. 2019 Mar;6(3):e154-66.
A proposed clinical scoring system using readily available laboratory data, rather than complex formulas, can be used to predict risk for overall survival and help with clinical decision making for patients with multiple myeloma who are ineligible for stem cell transplants, the system’s creators claim.
When applied to data from two clinical trials that enrolled patients with transplant-ineligible multiple myeloma, the UK Myeloma Research Alliance Risk Profile (MRP) was shown to accurately group patients into low-, medium- and high-risk categories and was prognostic of overall survival, reported Gordon Cook, PhD, of the University of Leeds, England, and his colleagues.
“The ability of clinical scoring systems, such as that proposed here, to predict whether a patient is likely to stop treatment early because of treatment intolerability, could enable preemptive, upfront dose adjustments in patients with multiple myeloma, preventing toxicity and potentially enabling patients to stay on therapy for longer,” they wrote in the Lancet Haematology.
The investigators used data on 1,852 newly diagnosed patients recruited to the non–intensive treatment pathway of the UK’s National Cancer Research Institute Myeloma XI study (NCRI-XI, ISRCTN49407852) for a training dataset and internal validation dataset, and 520 patients recruited into the Medical Research Council Myeloma IX study (MRC-IX, ISRCTN68454111) for the test dataset.
Patient characteristics, biochemical measurements, and hematological data were plugged into univariate and multivariate models to determine their potential as prognostic variables.
The final model for the test and validation datasets included World Health Organization performance status, the multiple myeloma International Staging System, patient age, and C-reactive protein concentrations.
As noted before, the scoring algorithm groups patients into low-, medium- and high-risk categories, with each of the prognostic variables increasing in severity across the three groups in both clinical trials.
In the NCRI-XI trial, median overall survival for patients in the MRP low-risk group was 60 months, compared with 44 months in the medium-risk group, and 25 months in the high-risk group.
Similarly, in the MRC-IX trial, the respective median overall survival was 49, 34, and 20 months.
The risk groups also were associated with progression-free survival in each trial, although not as robustly as the association with overall survival.
The investigators also found that, the higher the risk group, the greater the likelihood that the median percentage of protocol dose delivered would be lower, and both a decrease in protocol dose delivered and quality of life at baseline were associated with increased risk.
The MRP categories were prognostic in patients treated with various therapeutic regimens and in patients with high-risk cytogenetics.
“None of the risk scoring systems previously developed in myeloma are dynamic, making them unable to accommodate changes in disease-related frailty that might be minimized by effective anti-myeloma therapy. There is therefore scope to improve clinical risk scores by the addition of a suitable frailty biomarker, which is currently still in developmental stages,” Dr. Cook and his colleagues wrote.
The study was funded by the Medical Research Council, Novartis, Schering Health Care, Chugai, Pharmion, Celgene, Ortho Biotech, Cancer Research UK, Celgene, Merck Sharp & Dohme, and Amgen. Dr. Cook reported grants and nonfinancial support from Celgene, Amgen, and Merck Sharp & Dohme, during the conduct of the study and personal fees from other companies outside the submitted work.
SOURCE: Cook G et al. Lancet Haematol. 2019 Mar;6(3):e154-66.
A proposed clinical scoring system using readily available laboratory data, rather than complex formulas, can be used to predict risk for overall survival and help with clinical decision making for patients with multiple myeloma who are ineligible for stem cell transplants, the system’s creators claim.
When applied to data from two clinical trials that enrolled patients with transplant-ineligible multiple myeloma, the UK Myeloma Research Alliance Risk Profile (MRP) was shown to accurately group patients into low-, medium- and high-risk categories and was prognostic of overall survival, reported Gordon Cook, PhD, of the University of Leeds, England, and his colleagues.
“The ability of clinical scoring systems, such as that proposed here, to predict whether a patient is likely to stop treatment early because of treatment intolerability, could enable preemptive, upfront dose adjustments in patients with multiple myeloma, preventing toxicity and potentially enabling patients to stay on therapy for longer,” they wrote in the Lancet Haematology.
The investigators used data on 1,852 newly diagnosed patients recruited to the non–intensive treatment pathway of the UK’s National Cancer Research Institute Myeloma XI study (NCRI-XI, ISRCTN49407852) for a training dataset and internal validation dataset, and 520 patients recruited into the Medical Research Council Myeloma IX study (MRC-IX, ISRCTN68454111) for the test dataset.
Patient characteristics, biochemical measurements, and hematological data were plugged into univariate and multivariate models to determine their potential as prognostic variables.
The final model for the test and validation datasets included World Health Organization performance status, the multiple myeloma International Staging System, patient age, and C-reactive protein concentrations.
As noted before, the scoring algorithm groups patients into low-, medium- and high-risk categories, with each of the prognostic variables increasing in severity across the three groups in both clinical trials.
In the NCRI-XI trial, median overall survival for patients in the MRP low-risk group was 60 months, compared with 44 months in the medium-risk group, and 25 months in the high-risk group.
Similarly, in the MRC-IX trial, the respective median overall survival was 49, 34, and 20 months.
The risk groups also were associated with progression-free survival in each trial, although not as robustly as the association with overall survival.
The investigators also found that, the higher the risk group, the greater the likelihood that the median percentage of protocol dose delivered would be lower, and both a decrease in protocol dose delivered and quality of life at baseline were associated with increased risk.
The MRP categories were prognostic in patients treated with various therapeutic regimens and in patients with high-risk cytogenetics.
“None of the risk scoring systems previously developed in myeloma are dynamic, making them unable to accommodate changes in disease-related frailty that might be minimized by effective anti-myeloma therapy. There is therefore scope to improve clinical risk scores by the addition of a suitable frailty biomarker, which is currently still in developmental stages,” Dr. Cook and his colleagues wrote.
The study was funded by the Medical Research Council, Novartis, Schering Health Care, Chugai, Pharmion, Celgene, Ortho Biotech, Cancer Research UK, Celgene, Merck Sharp & Dohme, and Amgen. Dr. Cook reported grants and nonfinancial support from Celgene, Amgen, and Merck Sharp & Dohme, during the conduct of the study and personal fees from other companies outside the submitted work.
SOURCE: Cook G et al. Lancet Haematol. 2019 Mar;6(3):e154-66.
FROM THE LANCET HAEMATOLOGY
Bendamustine-rituximab shines in frontline treatment of MCL, iNHL
Frontline treatment with patients in the BRIGHT study.
The bendamustine-rituximab (BR) regimen had superior 5-year progression-free survival rates, event-free survival, and duration of response, compared with either rituximab with cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine, and prednisone (R-CVP). The follow-up study did not find a significant difference in overall survival, however.
While the cumulative evidence from BRIGHT and other studies supports BR as a first-line treatment option for patients with indolent non-Hodgkin lymphoma (iNHL) and mantle cell lymphoma (MCL), the lack of an overall survival benefit indicates that the sequence of BR and R-CHOP or R-CVP “may not be critical,” Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville, and his colleagues wrote in the Journal of Clinical Oncology.
“[The] choice of regimen for the initial treatment of iNHL may be driven more by patient preferences regarding the differences in toxicity profile,” the researchers wrote.
Initial results from the BRIGHT study found that BR was noninferior to R-CHOP/R-CVP in terms of complete response rate (P = .0225 for noninferiority). The present study includes outcomes data for at least 5 years after completion of the study treatment.
For the entire study, the median follow-up was 65.0 months for patients in the BR group and 64.1 months for patients in the R-CHOP/R-CVP group. Overall, the intention-to-treat population included 224 patients receiving BR and 223 patients receiving R-CHOP and R-CVP.
The median time to progression was not reached in either treatment group. The 5-year progression-free survival (PFS) rates were 65.5% in the BR group and 55.8% in the R-CHOP/R-CVP group. The difference between these rates was significant, with a hazard ratio of 0.61 (95% confidence interval, 0.45-0.85; P = .0025).
Similarly, event-free survival was better in the BR group versus the R-CHOP/R-CVP group (HR, 0.63; 95% CI, 0.46-0.84; P = .0020). Duration of response also favored the BR treatment regimen (HR, 0.66; 95% CI, 0.47-0.92; P = .0134).
The long-term follow-up showed no significant difference in overall survival, with an HR of 1.15 for BR versus R-CHOP/R-CVP (95% CI, 0.72-1.84; P = .5461). Overall, there were 40 deaths in the BR treatment group and 32 deaths in the R-CHOP/R-CVP group.
Whether patients received maintenance rituximab did not affect the overall survival between groups. Similarly, there was no difference in overall survival by lymphoma type.
“Benefit from BR treatment did not translate to prolonged [overall survival], possibly because of the subsequent lines of therapy, including the use of BR in patients in the R-CHOP/R-CVP group,” the researchers wrote.
In terms of safety, the follow-up data showed no significant difference in early non–disease-related mortality between the treatment groups. However, the BRIGHT study showed higher rates of secondary malignancies in the BR group, compared with R-CHOP/R-CVP. That finding was not seen in the Study Group of Indolent Lymphomas Non-Hodgkin Lymphoma (StiL NHL) 1 trial, and the authors could not provide an explanation for the increase in their research.
This study was supported by Teva Pharmaceuticals. Dr. Flinn reported receiving institutional research funding from Teva and receiving institutional research funding from or serving as a consultant to several other companies.
SOURCE: Flinn IW et al. J Clin Oncol. 2019 Feb 27. doi: 10.1200/JCO.18.00605.
Frontline treatment with patients in the BRIGHT study.
The bendamustine-rituximab (BR) regimen had superior 5-year progression-free survival rates, event-free survival, and duration of response, compared with either rituximab with cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine, and prednisone (R-CVP). The follow-up study did not find a significant difference in overall survival, however.
While the cumulative evidence from BRIGHT and other studies supports BR as a first-line treatment option for patients with indolent non-Hodgkin lymphoma (iNHL) and mantle cell lymphoma (MCL), the lack of an overall survival benefit indicates that the sequence of BR and R-CHOP or R-CVP “may not be critical,” Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville, and his colleagues wrote in the Journal of Clinical Oncology.
“[The] choice of regimen for the initial treatment of iNHL may be driven more by patient preferences regarding the differences in toxicity profile,” the researchers wrote.
Initial results from the BRIGHT study found that BR was noninferior to R-CHOP/R-CVP in terms of complete response rate (P = .0225 for noninferiority). The present study includes outcomes data for at least 5 years after completion of the study treatment.
For the entire study, the median follow-up was 65.0 months for patients in the BR group and 64.1 months for patients in the R-CHOP/R-CVP group. Overall, the intention-to-treat population included 224 patients receiving BR and 223 patients receiving R-CHOP and R-CVP.
The median time to progression was not reached in either treatment group. The 5-year progression-free survival (PFS) rates were 65.5% in the BR group and 55.8% in the R-CHOP/R-CVP group. The difference between these rates was significant, with a hazard ratio of 0.61 (95% confidence interval, 0.45-0.85; P = .0025).
Similarly, event-free survival was better in the BR group versus the R-CHOP/R-CVP group (HR, 0.63; 95% CI, 0.46-0.84; P = .0020). Duration of response also favored the BR treatment regimen (HR, 0.66; 95% CI, 0.47-0.92; P = .0134).
The long-term follow-up showed no significant difference in overall survival, with an HR of 1.15 for BR versus R-CHOP/R-CVP (95% CI, 0.72-1.84; P = .5461). Overall, there were 40 deaths in the BR treatment group and 32 deaths in the R-CHOP/R-CVP group.
Whether patients received maintenance rituximab did not affect the overall survival between groups. Similarly, there was no difference in overall survival by lymphoma type.
“Benefit from BR treatment did not translate to prolonged [overall survival], possibly because of the subsequent lines of therapy, including the use of BR in patients in the R-CHOP/R-CVP group,” the researchers wrote.
In terms of safety, the follow-up data showed no significant difference in early non–disease-related mortality between the treatment groups. However, the BRIGHT study showed higher rates of secondary malignancies in the BR group, compared with R-CHOP/R-CVP. That finding was not seen in the Study Group of Indolent Lymphomas Non-Hodgkin Lymphoma (StiL NHL) 1 trial, and the authors could not provide an explanation for the increase in their research.
This study was supported by Teva Pharmaceuticals. Dr. Flinn reported receiving institutional research funding from Teva and receiving institutional research funding from or serving as a consultant to several other companies.
SOURCE: Flinn IW et al. J Clin Oncol. 2019 Feb 27. doi: 10.1200/JCO.18.00605.
Frontline treatment with patients in the BRIGHT study.
The bendamustine-rituximab (BR) regimen had superior 5-year progression-free survival rates, event-free survival, and duration of response, compared with either rituximab with cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine, and prednisone (R-CVP). The follow-up study did not find a significant difference in overall survival, however.
While the cumulative evidence from BRIGHT and other studies supports BR as a first-line treatment option for patients with indolent non-Hodgkin lymphoma (iNHL) and mantle cell lymphoma (MCL), the lack of an overall survival benefit indicates that the sequence of BR and R-CHOP or R-CVP “may not be critical,” Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville, and his colleagues wrote in the Journal of Clinical Oncology.
“[The] choice of regimen for the initial treatment of iNHL may be driven more by patient preferences regarding the differences in toxicity profile,” the researchers wrote.
Initial results from the BRIGHT study found that BR was noninferior to R-CHOP/R-CVP in terms of complete response rate (P = .0225 for noninferiority). The present study includes outcomes data for at least 5 years after completion of the study treatment.
For the entire study, the median follow-up was 65.0 months for patients in the BR group and 64.1 months for patients in the R-CHOP/R-CVP group. Overall, the intention-to-treat population included 224 patients receiving BR and 223 patients receiving R-CHOP and R-CVP.
The median time to progression was not reached in either treatment group. The 5-year progression-free survival (PFS) rates were 65.5% in the BR group and 55.8% in the R-CHOP/R-CVP group. The difference between these rates was significant, with a hazard ratio of 0.61 (95% confidence interval, 0.45-0.85; P = .0025).
Similarly, event-free survival was better in the BR group versus the R-CHOP/R-CVP group (HR, 0.63; 95% CI, 0.46-0.84; P = .0020). Duration of response also favored the BR treatment regimen (HR, 0.66; 95% CI, 0.47-0.92; P = .0134).
The long-term follow-up showed no significant difference in overall survival, with an HR of 1.15 for BR versus R-CHOP/R-CVP (95% CI, 0.72-1.84; P = .5461). Overall, there were 40 deaths in the BR treatment group and 32 deaths in the R-CHOP/R-CVP group.
Whether patients received maintenance rituximab did not affect the overall survival between groups. Similarly, there was no difference in overall survival by lymphoma type.
“Benefit from BR treatment did not translate to prolonged [overall survival], possibly because of the subsequent lines of therapy, including the use of BR in patients in the R-CHOP/R-CVP group,” the researchers wrote.
In terms of safety, the follow-up data showed no significant difference in early non–disease-related mortality between the treatment groups. However, the BRIGHT study showed higher rates of secondary malignancies in the BR group, compared with R-CHOP/R-CVP. That finding was not seen in the Study Group of Indolent Lymphomas Non-Hodgkin Lymphoma (StiL NHL) 1 trial, and the authors could not provide an explanation for the increase in their research.
This study was supported by Teva Pharmaceuticals. Dr. Flinn reported receiving institutional research funding from Teva and receiving institutional research funding from or serving as a consultant to several other companies.
SOURCE: Flinn IW et al. J Clin Oncol. 2019 Feb 27. doi: 10.1200/JCO.18.00605.
FROM JOURNAL OF CLINICAL ONCOLOGY
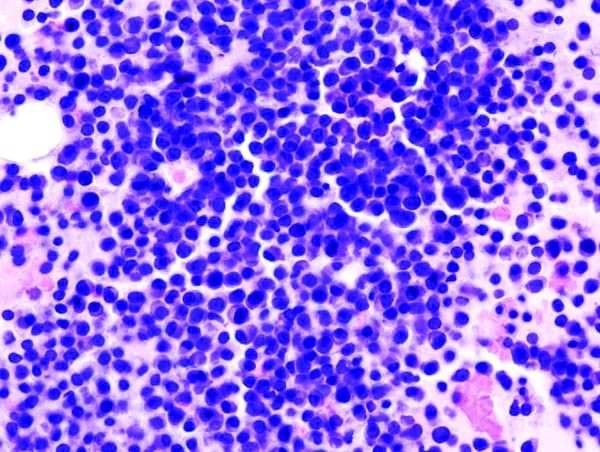
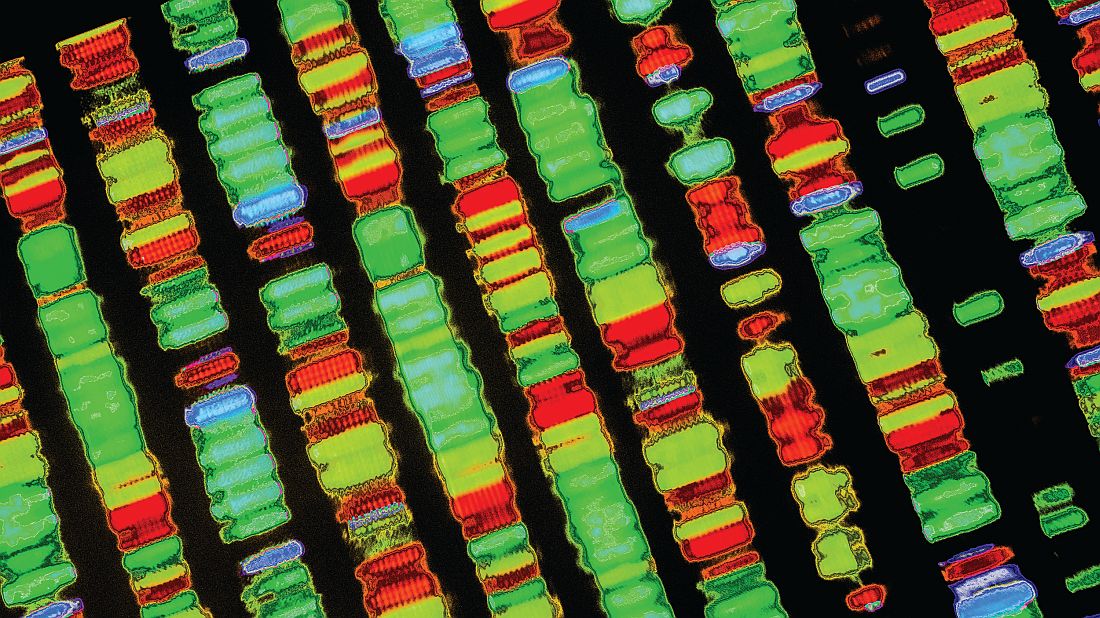
Analysis suggests ‘Burkitt-like lymphoma’ is a misnomer
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
REPORTING FROM HAEMATOLOGICA
Gene expression signature reveals high-grade GCB DLBCL
New research suggests a gene expression signature can distinguish high-grade diffuse large B-cell lymphomas (DLBCLs) from other germinal center B-cell–like (GCB) DLBCLs.
Researchers identified GCB DLBCL patients with this 104-gene signature who had a “distinct mutational landscape” and inferior treatment outcomes. David W. Scott, MBChB, PhD, of the British Columbia Cancer Research Centre in Vancouver, and his colleagues described these patients in the Journal of Clinical Oncology.
The findings were published alongside a related editorial and a similar study from another group.
Dr. Scott and his colleagues began their study by analyzing data from 157 patients with de novo GCB DLBCL. Twenty-five of these patients had double- or triple-hit high-grade B-cell lymphoma with BCL2 translocations (HGBL-DH/TH-BCL2).
The researchers identified 104 genes that were the “most significantly differentially expressed between HGBL-DH/TH-BCL2 and other GCB DLBCLs” to create their double-hit gene signature (DHITsig).
The signature divided the patients into two groups — 42 patients (27%) whose tumors were positive for the DHITsig and 115 (73%) whose tumors were negative. Notably, 22 of the 25 HGBL-DH/TH-BCL2 tumors were DHITsig-positive and 3 were negative.
The DHITsig was not associated with clinical variables such as tumor volume, but it was associated with prognosis. Treatment outcomes were inferior in patients who were DHITsig-positive.
The 5-year time to progression rate was 81% in patients who were DHITsig-negative and 57% in those who were positive (P less than .001). The 5-year overall survival rate was 81% and 60%, respectively (P = .001).
The researchers observed similar results in a validation cohort of 262 patients with GCB-DLBCL who received rituximab-based therapy. The 5-year overall survival rate was 76% in patients who were DHITsig-negative and 49% in those who were positive (P less than .001).
Dr. Scott and his colleagues also evaluated the DHITsig in a second validation cohort of 162 patients with GCB DLBCL.
In analyzing data from all three cohorts, the researchers found that mutations in MYC, BCL2, CREBBP, EZH2Y646, DDX3X, TP53, and KMT2D were more frequent in DHITsig-positive patients and mutations in TNFAIP3, KLHL6, NFKBIE, TET2, CD58, and STAT3 were more common in DHITsig-negative patients.
Additional analyses suggested the cell of origin for DHITsig-positive tumors comes from the intermediate zone or dark zone of the germinal center.
Finally, the researchers found they could use a “clinically relevant assay” to detect the DHITsig. They added a 30-gene module to the Lymph3Cx assay to create a NanoString-based assay called DLBCL90.
The team tested DLBCL90 in 171 GCB DLBCL patients. In this group, 26% of patients were DHITsig-positive, 64% were negative, and 10% were indeterminate. The prognostic significance of the signature was maintained with the assay results, according to the researchers.
Dr. Scott and his colleagues also wanted to validate the association between the DHITsig and HGBL-DH/TH-BCL2, so they tested the DLBCL90 assay in two additional groups of patients.
First, the assay was used in 88 patients who had transformed follicular lymphoma with DLBCL morphology. Eleven of the 25 DHITsig-positive tumors and 4 of the 13 DHITsig-indeterminate tumors were HGBL-DH/TH-BCL2. However, none of the 50 DHITsig-negative tumors were HGBL-DH/TH-BCL2.
The researchers then used the DLBCL90 assay on 26 HGBL tumors. Twenty-three of these were DHITsig-positive and 3 were indeterminate.
This research was supported by the Canadian Cancer Society Research Institute and other organizations. The researchers reported relationships with Seattle Genetics, Roche, Janssen, Celgene, and various other companies.
SOURCE: Scott DW et al. J Clin Oncol. 2019 Jan 20;37(3):190-201.
New research suggests a gene expression signature can distinguish high-grade diffuse large B-cell lymphomas (DLBCLs) from other germinal center B-cell–like (GCB) DLBCLs.
Researchers identified GCB DLBCL patients with this 104-gene signature who had a “distinct mutational landscape” and inferior treatment outcomes. David W. Scott, MBChB, PhD, of the British Columbia Cancer Research Centre in Vancouver, and his colleagues described these patients in the Journal of Clinical Oncology.
The findings were published alongside a related editorial and a similar study from another group.
Dr. Scott and his colleagues began their study by analyzing data from 157 patients with de novo GCB DLBCL. Twenty-five of these patients had double- or triple-hit high-grade B-cell lymphoma with BCL2 translocations (HGBL-DH/TH-BCL2).
The researchers identified 104 genes that were the “most significantly differentially expressed between HGBL-DH/TH-BCL2 and other GCB DLBCLs” to create their double-hit gene signature (DHITsig).
The signature divided the patients into two groups — 42 patients (27%) whose tumors were positive for the DHITsig and 115 (73%) whose tumors were negative. Notably, 22 of the 25 HGBL-DH/TH-BCL2 tumors were DHITsig-positive and 3 were negative.
The DHITsig was not associated with clinical variables such as tumor volume, but it was associated with prognosis. Treatment outcomes were inferior in patients who were DHITsig-positive.
The 5-year time to progression rate was 81% in patients who were DHITsig-negative and 57% in those who were positive (P less than .001). The 5-year overall survival rate was 81% and 60%, respectively (P = .001).
The researchers observed similar results in a validation cohort of 262 patients with GCB-DLBCL who received rituximab-based therapy. The 5-year overall survival rate was 76% in patients who were DHITsig-negative and 49% in those who were positive (P less than .001).
Dr. Scott and his colleagues also evaluated the DHITsig in a second validation cohort of 162 patients with GCB DLBCL.
In analyzing data from all three cohorts, the researchers found that mutations in MYC, BCL2, CREBBP, EZH2Y646, DDX3X, TP53, and KMT2D were more frequent in DHITsig-positive patients and mutations in TNFAIP3, KLHL6, NFKBIE, TET2, CD58, and STAT3 were more common in DHITsig-negative patients.
Additional analyses suggested the cell of origin for DHITsig-positive tumors comes from the intermediate zone or dark zone of the germinal center.
Finally, the researchers found they could use a “clinically relevant assay” to detect the DHITsig. They added a 30-gene module to the Lymph3Cx assay to create a NanoString-based assay called DLBCL90.
The team tested DLBCL90 in 171 GCB DLBCL patients. In this group, 26% of patients were DHITsig-positive, 64% were negative, and 10% were indeterminate. The prognostic significance of the signature was maintained with the assay results, according to the researchers.
Dr. Scott and his colleagues also wanted to validate the association between the DHITsig and HGBL-DH/TH-BCL2, so they tested the DLBCL90 assay in two additional groups of patients.
First, the assay was used in 88 patients who had transformed follicular lymphoma with DLBCL morphology. Eleven of the 25 DHITsig-positive tumors and 4 of the 13 DHITsig-indeterminate tumors were HGBL-DH/TH-BCL2. However, none of the 50 DHITsig-negative tumors were HGBL-DH/TH-BCL2.
The researchers then used the DLBCL90 assay on 26 HGBL tumors. Twenty-three of these were DHITsig-positive and 3 were indeterminate.
This research was supported by the Canadian Cancer Society Research Institute and other organizations. The researchers reported relationships with Seattle Genetics, Roche, Janssen, Celgene, and various other companies.
SOURCE: Scott DW et al. J Clin Oncol. 2019 Jan 20;37(3):190-201.
New research suggests a gene expression signature can distinguish high-grade diffuse large B-cell lymphomas (DLBCLs) from other germinal center B-cell–like (GCB) DLBCLs.
Researchers identified GCB DLBCL patients with this 104-gene signature who had a “distinct mutational landscape” and inferior treatment outcomes. David W. Scott, MBChB, PhD, of the British Columbia Cancer Research Centre in Vancouver, and his colleagues described these patients in the Journal of Clinical Oncology.
The findings were published alongside a related editorial and a similar study from another group.
Dr. Scott and his colleagues began their study by analyzing data from 157 patients with de novo GCB DLBCL. Twenty-five of these patients had double- or triple-hit high-grade B-cell lymphoma with BCL2 translocations (HGBL-DH/TH-BCL2).
The researchers identified 104 genes that were the “most significantly differentially expressed between HGBL-DH/TH-BCL2 and other GCB DLBCLs” to create their double-hit gene signature (DHITsig).
The signature divided the patients into two groups — 42 patients (27%) whose tumors were positive for the DHITsig and 115 (73%) whose tumors were negative. Notably, 22 of the 25 HGBL-DH/TH-BCL2 tumors were DHITsig-positive and 3 were negative.
The DHITsig was not associated with clinical variables such as tumor volume, but it was associated with prognosis. Treatment outcomes were inferior in patients who were DHITsig-positive.
The 5-year time to progression rate was 81% in patients who were DHITsig-negative and 57% in those who were positive (P less than .001). The 5-year overall survival rate was 81% and 60%, respectively (P = .001).
The researchers observed similar results in a validation cohort of 262 patients with GCB-DLBCL who received rituximab-based therapy. The 5-year overall survival rate was 76% in patients who were DHITsig-negative and 49% in those who were positive (P less than .001).
Dr. Scott and his colleagues also evaluated the DHITsig in a second validation cohort of 162 patients with GCB DLBCL.
In analyzing data from all three cohorts, the researchers found that mutations in MYC, BCL2, CREBBP, EZH2Y646, DDX3X, TP53, and KMT2D were more frequent in DHITsig-positive patients and mutations in TNFAIP3, KLHL6, NFKBIE, TET2, CD58, and STAT3 were more common in DHITsig-negative patients.
Additional analyses suggested the cell of origin for DHITsig-positive tumors comes from the intermediate zone or dark zone of the germinal center.
Finally, the researchers found they could use a “clinically relevant assay” to detect the DHITsig. They added a 30-gene module to the Lymph3Cx assay to create a NanoString-based assay called DLBCL90.
The team tested DLBCL90 in 171 GCB DLBCL patients. In this group, 26% of patients were DHITsig-positive, 64% were negative, and 10% were indeterminate. The prognostic significance of the signature was maintained with the assay results, according to the researchers.
Dr. Scott and his colleagues also wanted to validate the association between the DHITsig and HGBL-DH/TH-BCL2, so they tested the DLBCL90 assay in two additional groups of patients.
First, the assay was used in 88 patients who had transformed follicular lymphoma with DLBCL morphology. Eleven of the 25 DHITsig-positive tumors and 4 of the 13 DHITsig-indeterminate tumors were HGBL-DH/TH-BCL2. However, none of the 50 DHITsig-negative tumors were HGBL-DH/TH-BCL2.
The researchers then used the DLBCL90 assay on 26 HGBL tumors. Twenty-three of these were DHITsig-positive and 3 were indeterminate.
This research was supported by the Canadian Cancer Society Research Institute and other organizations. The researchers reported relationships with Seattle Genetics, Roche, Janssen, Celgene, and various other companies.
SOURCE: Scott DW et al. J Clin Oncol. 2019 Jan 20;37(3):190-201.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Priority review granted to lenalidomide for FL, MZL
The Food and Drug Administration has granted priority review to a supplemental new drug application (sNDA) for lenalidomide (Revlimid).
Celgene is seeking approval for lenalidomide in combination with rituximab to treat patients with previously treated follicular lymphoma (FL) or marginal zone lymphoma (MZL).
The FDA plans to make a decision on the sNDA by June 27, 2019.
The FDA aims to take action on a priority review application within 6 months of receiving it rather than the standard 10 months. The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The sNDA for lenalidomide is supported by the phase 3 AUGMENT study (NCT01938001) in which researchers compared rituximab plus lenalidomide to rituximab plus placebo in patients with relapsed/refractory FL or MZL.
Results from AUGMENT were presented at the 2018 annual meeting of the American Society of Hematology (Blood 2018 Nov 29;132:445).
According to the ASH abstract, the trial included 358 patients who were randomized to receive rituximab plus lenalidomide (n = 178) or rituximab plus placebo (n = 180).
At a median follow-up of 28.3 months, the overall response rate was 78% in the lenalidomide arm and 53% in the placebo arm (P less than .0001). The complete response rate was 34% and 18%, respectively (P = .001).
The median progression-free survival was 39.4 months in the lenalidomide arm and 14.1 months in the placebo arm. Overall survival data were not mature, but there were 16 deaths reported in the lenalidomide arm and 26 deaths in the placebo arm.
Treatment-emergent adverse events that were more common in the lenalidomide arm than the placebo arm included infections, cutaneous reactions, constipation, thrombocytopenia, and tumor flare reaction.
The Food and Drug Administration has granted priority review to a supplemental new drug application (sNDA) for lenalidomide (Revlimid).
Celgene is seeking approval for lenalidomide in combination with rituximab to treat patients with previously treated follicular lymphoma (FL) or marginal zone lymphoma (MZL).
The FDA plans to make a decision on the sNDA by June 27, 2019.
The FDA aims to take action on a priority review application within 6 months of receiving it rather than the standard 10 months. The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The sNDA for lenalidomide is supported by the phase 3 AUGMENT study (NCT01938001) in which researchers compared rituximab plus lenalidomide to rituximab plus placebo in patients with relapsed/refractory FL or MZL.
Results from AUGMENT were presented at the 2018 annual meeting of the American Society of Hematology (Blood 2018 Nov 29;132:445).
According to the ASH abstract, the trial included 358 patients who were randomized to receive rituximab plus lenalidomide (n = 178) or rituximab plus placebo (n = 180).
At a median follow-up of 28.3 months, the overall response rate was 78% in the lenalidomide arm and 53% in the placebo arm (P less than .0001). The complete response rate was 34% and 18%, respectively (P = .001).
The median progression-free survival was 39.4 months in the lenalidomide arm and 14.1 months in the placebo arm. Overall survival data were not mature, but there were 16 deaths reported in the lenalidomide arm and 26 deaths in the placebo arm.
Treatment-emergent adverse events that were more common in the lenalidomide arm than the placebo arm included infections, cutaneous reactions, constipation, thrombocytopenia, and tumor flare reaction.
The Food and Drug Administration has granted priority review to a supplemental new drug application (sNDA) for lenalidomide (Revlimid).
Celgene is seeking approval for lenalidomide in combination with rituximab to treat patients with previously treated follicular lymphoma (FL) or marginal zone lymphoma (MZL).
The FDA plans to make a decision on the sNDA by June 27, 2019.
The FDA aims to take action on a priority review application within 6 months of receiving it rather than the standard 10 months. The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The sNDA for lenalidomide is supported by the phase 3 AUGMENT study (NCT01938001) in which researchers compared rituximab plus lenalidomide to rituximab plus placebo in patients with relapsed/refractory FL or MZL.
Results from AUGMENT were presented at the 2018 annual meeting of the American Society of Hematology (Blood 2018 Nov 29;132:445).
According to the ASH abstract, the trial included 358 patients who were randomized to receive rituximab plus lenalidomide (n = 178) or rituximab plus placebo (n = 180).
At a median follow-up of 28.3 months, the overall response rate was 78% in the lenalidomide arm and 53% in the placebo arm (P less than .0001). The complete response rate was 34% and 18%, respectively (P = .001).
The median progression-free survival was 39.4 months in the lenalidomide arm and 14.1 months in the placebo arm. Overall survival data were not mature, but there were 16 deaths reported in the lenalidomide arm and 26 deaths in the placebo arm.
Treatment-emergent adverse events that were more common in the lenalidomide arm than the placebo arm included infections, cutaneous reactions, constipation, thrombocytopenia, and tumor flare reaction.