User login
Survey explores mental health, services use in police officers
New research shows that about a quarter of police officers in one large force report past or present mental health problems.
Responding to a survey, 26% of police officers on the Dallas police department screened positive for depression, anxiety, PTSD, or symptoms of suicide ideation or self-harm.
Mental illness rates were particularly high among female officers, those who were divorced, widowed, or separated, and those with military experience.
The study also showed that concerns over confidentiality and stigma may prevent officers with mental illness from seeking treatment.
The results underscored the need to identify police officers with psychiatric problems and to connect them to the most appropriate individualized care, author Katelyn K. Jetelina, PhD, assistant professor in the department of epidemiology, human genetics, and environmental sciences, University of Texas Health Science Center, Dallas, said in an interview.
“This is a very hard-to-reach population, and because of that, we need to be innovative in reaching them for services,” she said.
The study was published online Oct. 7 in JAMA Network Open.
Dr. Jetelina and colleagues are investigating various aspects of police officers’ well-being, including their nutritional needs and their occupational, physical, and mental health.
The current study included 434 members of the Dallas police department, the ninth largest in the United States. The mean age of the participants was 37 years, 82% were men, and about half were White. The 434 officers represented 97% of those invited to participate (n = 446) and 31% of the total patrol population of the Dallas police department (n = 1,413).
These officers completed a short survey on their smartphone that asked about lifetime diagnoses of depression, anxiety, and PTSD. They were also asked whether they experienced suicidal ideation or self-harm during the previous 2 weeks.
Overall, 12% of survey respondents reported having been diagnosed with a mental illness. This, said Jetelina, is slightly lower than the rate reported in the general population.
Study participants who had not currently been diagnosed with a mental illness completed the Patient Health Questionnaire–2 (PHQ-2), the Generalized Anxiety Disorder–2 (GAD-2), and the Primary Care–Posttraumatic Stress Disorder (PC-PTSD).
Officers were considered to have a positive result if they had a score of 3 or more (PHQ-2, sensitivity of 83% and specificity of 92%; PC-PTSD-5, sensitivity of 93% and specificity of 85%; GAD-2, sensitivity of 86% and specificity of 83%).
About 26% of respondents had a positive screening for mental illness symptoms, mainly PTSD and depression, which Dr. Jetelina noted is a higher percentage than in the general population.
This rate of mental health symptoms is “high and concerning,” but not surprising because of the work of police officers, which could include attending to sometimes violent car crashes, domestic abuse situations, and armed conflicts, said Dr. Jetelina.
“They’re constantly exposed to traumatic calls for service; they see people on their worst day, 8 hours a day, 5 days a week. That stress and exposure will have a detrimental effect on mental health, and we have to pay more attention to that,” she said.
Dr. Jetelina pointed out that the surveys were completed in January and February 2020, before COVID-19 had become a cause of stress for everyone and before the increase in calls for defunding police amid a resurgence of Black Lives Matter demonstrations.
However, she stressed that racial biases and occupational stress among police officers are “nothing new for them.” For example, in 2016, five Dallas police officers were killed during Black Lives Matter protests because of their race/ethnicity.
More at risk
The study showed that certain subgroups of officers were more at risk for mental illness. After adjustment for confounders, including demographic characteristics, marital status, and educational level, the odds of being diagnosed with a mental illness during the course of one’s life were significantly higher among female officers than male officers (adjusted odds ratio, 3.20; 95% confidence interval, 1.18-8.68).
Officers who were divorced, widowed, or separated and those who had more experience and held a higher rank were also at greater risk for mental illness.
As well, (aOR, 3.25; 95% CI, 1.38-7.67).
The study also asked participants about use of mental health care services over the past 12 months. About 35% of those who had a current mental health diagnosis and 17% of those who screened positive for mental health symptoms reported using such services.
The study also asked those who screened positive about their interest in seeking such services. After adjustments, officers with suicidal ideation or self-harm were significantly more likely to be interested in getting help, compared with officers who did not report suicidal ideation or self-harm (aOR, 7.66; 95% CI, 1.70-34.48).
Dr. Jetelina was impressed that so many officers were keen to seek help, which “is a big positive,” she said. “It’s just a matter of better detecting who needs the help and better connecting them to medical services that meet their needs.”
Mindfulness exercise
Dr. Jetelina and colleagues are conducting a pilot test of the use by police officers of smartwatches that monitor heart rate and oxygen levels. If measurements with these devices reach a predetermined threshold, the officers are “pinged” and are instructed to perform a mindfulness exercise in the field, she said.
Results so far “are really exciting,” said Dr. Jetelina. “Officers have found this extremely helpful and feasible, and so the next step is to test if this truly impacts mental illness over time.”
Routine mental health screening of officers might be beneficial, but only if it’s conducted in a manner “respectful of the officers’ needs and wants,” said Dr. Jetelina.
She pointed out that although psychological assessments are routinely carried out following an extreme traumatic call, such as one involving an officer-involved shooting, the “in-between” calls could have a more severe cumulative impact on mental health.
It’s important to provide officers with easy-to-access services tailored for their individual needs, said Dr. Jetelina.
‘Numb to it’
Eighteen patrol officers also participated in a focus group, during which several themes regarding the use of mental health care services emerged. One theme was the inability of officers to identify when they’re personally experiencing a mental health problem.
Participants said they had become “numb” to the traumatic events on the job, which is “concerning,” Dr. Jetelina said. “They think that having nightmares every week is completely normal, but it’s not, and this needs to be addressed.”
Other themes that emerged from focus groups included the belief that psychologists can’t relate to police stressors; concerns about confidentiality (one sentiment that was expressed was “you’re an idiot” if you “trust this department”); and stigma for officers who seek mental health care (participants talked about “reprisal” from seeing “a shrink,” including being labeled as “a nutter” and losing their job).
Dr. Jetelina noted that some “champion” officers revealed their mental health journey during focus groups, which tended to “open a Pandora’s box” for others to discuss their experience. She said these champions could be leveraged throughout the police department to help reduce stigma.
The study included participants from only one police department, although rigorous data collection allows for generalizability to the entire patrol department, say the authors. Although the study included only brief screens of mental illness symptoms, these short versions of screening tests have high sensitivity and specificity for mental illness in primary care, they noted.
The next step for the researchers is to study how mental illness and symptoms affect job performance, said Dr. Jetelina. “Does this impact excessive use of force? Does this impact workers’ compensation? Does this impact dispatch times, the time it takes for a police officer to respond to [a] 911 call?”
Possible underrepresentation
Anthony T. Ng, MD, regional medical director, East Region Hartford HealthCare Behavioral Health Network in Mansfield, Conn., and member of the American Psychiatric Association’s Council on Communications, found the study “helpful.”
However, the 26% who tested positive for mental illness may be an “underrepresentation” of the true picture, inasmuch as police officers might minimize or be less than truthful about their mental health status, said Dr. Ng.
Law enforcement has “never been easy,” but stressors may have escalated recently as police forces deal with shortages of staff and jails, said Dr. Ng.
He also noted that officers might face stressors at home. “Evidence shows that domestic violence is quite high – or higher than average – among law enforcement,” he said. “All these things add up.”
Psychiatrists and other mental health professionals should be “aware of the unique challenges” that police officers face and be “proactively involved” in providing guidance and education on mitigating stress, said Dr. Ng.
“You have police officers wearing body armor, so why can’t you give them some training to learn how to have psychiatric or psychological body armor?” he said. But it’s a two-way street; police forces should be open to outreach from mental health professionals. “We have to meet halfway.”
Compassion fatigue
In an accompanying commentary, John M. Violanti, PhD, of the department of epidemiology and environmental health at the State University of New York at Buffalo, said the article helps bring “to the forefront” the issue of the psychological dangers of police work.
There is conjecture as to why police experience mental distress, said Dr. Violanti, who pointed to a study of New York City police suicides during the 1930s that suggested that police have a “social license” for aggressive behavior but are restrained as part of public trust, placing them in a position of “psychological strain.”
“This situation may be reflective of the same situation police find themselves today,” said Dr. Violanti.
“Compassion fatigue,” a feeling of mental exhaustion caused by the inability to care for all persons in trouble, may also be a factor, as could the constant stress that leaves police officers feeling “cynical and isolated from others,” he wrote.
“The socialization process of becoming a police officer is associated with constrictive reasoning, viewing the world as either right or wrong, which leaves no middle ground for alternatives to deal with mental distress,” Dr. Violanti said.
He noted that police officers may abuse alcohol because of stress, peer pressure, isolation, and a culture that approves of alcohol use. “Officers tend to drink together and reinforce their own values.”.
Although no prospective studies have linked police mental health problems with childhood abuse or neglect, some mental health professionals estimate that about 25% of their police clients have a history of childhood abuse or neglect, said Dr. Violanti.
He agreed that mindfulness may help manage stress and increase cognitive flexibility in dealing with trauma and crises.
A possible way to ensure confidentiality is a peer support program that allows distressed officers to first talk privately with a trained and trusted peer officer and to then seek professional help if necessary, said Dr. Violanti.
The study was funded by a grant from the National Institute of Occupational Health and Safety. Dr. Jetelina, Dr. Ng, and Dr. Violanti disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New research shows that about a quarter of police officers in one large force report past or present mental health problems.
Responding to a survey, 26% of police officers on the Dallas police department screened positive for depression, anxiety, PTSD, or symptoms of suicide ideation or self-harm.
Mental illness rates were particularly high among female officers, those who were divorced, widowed, or separated, and those with military experience.
The study also showed that concerns over confidentiality and stigma may prevent officers with mental illness from seeking treatment.
The results underscored the need to identify police officers with psychiatric problems and to connect them to the most appropriate individualized care, author Katelyn K. Jetelina, PhD, assistant professor in the department of epidemiology, human genetics, and environmental sciences, University of Texas Health Science Center, Dallas, said in an interview.
“This is a very hard-to-reach population, and because of that, we need to be innovative in reaching them for services,” she said.
The study was published online Oct. 7 in JAMA Network Open.
Dr. Jetelina and colleagues are investigating various aspects of police officers’ well-being, including their nutritional needs and their occupational, physical, and mental health.
The current study included 434 members of the Dallas police department, the ninth largest in the United States. The mean age of the participants was 37 years, 82% were men, and about half were White. The 434 officers represented 97% of those invited to participate (n = 446) and 31% of the total patrol population of the Dallas police department (n = 1,413).
These officers completed a short survey on their smartphone that asked about lifetime diagnoses of depression, anxiety, and PTSD. They were also asked whether they experienced suicidal ideation or self-harm during the previous 2 weeks.
Overall, 12% of survey respondents reported having been diagnosed with a mental illness. This, said Jetelina, is slightly lower than the rate reported in the general population.
Study participants who had not currently been diagnosed with a mental illness completed the Patient Health Questionnaire–2 (PHQ-2), the Generalized Anxiety Disorder–2 (GAD-2), and the Primary Care–Posttraumatic Stress Disorder (PC-PTSD).
Officers were considered to have a positive result if they had a score of 3 or more (PHQ-2, sensitivity of 83% and specificity of 92%; PC-PTSD-5, sensitivity of 93% and specificity of 85%; GAD-2, sensitivity of 86% and specificity of 83%).
About 26% of respondents had a positive screening for mental illness symptoms, mainly PTSD and depression, which Dr. Jetelina noted is a higher percentage than in the general population.
This rate of mental health symptoms is “high and concerning,” but not surprising because of the work of police officers, which could include attending to sometimes violent car crashes, domestic abuse situations, and armed conflicts, said Dr. Jetelina.
“They’re constantly exposed to traumatic calls for service; they see people on their worst day, 8 hours a day, 5 days a week. That stress and exposure will have a detrimental effect on mental health, and we have to pay more attention to that,” she said.
Dr. Jetelina pointed out that the surveys were completed in January and February 2020, before COVID-19 had become a cause of stress for everyone and before the increase in calls for defunding police amid a resurgence of Black Lives Matter demonstrations.
However, she stressed that racial biases and occupational stress among police officers are “nothing new for them.” For example, in 2016, five Dallas police officers were killed during Black Lives Matter protests because of their race/ethnicity.
More at risk
The study showed that certain subgroups of officers were more at risk for mental illness. After adjustment for confounders, including demographic characteristics, marital status, and educational level, the odds of being diagnosed with a mental illness during the course of one’s life were significantly higher among female officers than male officers (adjusted odds ratio, 3.20; 95% confidence interval, 1.18-8.68).
Officers who were divorced, widowed, or separated and those who had more experience and held a higher rank were also at greater risk for mental illness.
As well, (aOR, 3.25; 95% CI, 1.38-7.67).
The study also asked participants about use of mental health care services over the past 12 months. About 35% of those who had a current mental health diagnosis and 17% of those who screened positive for mental health symptoms reported using such services.
The study also asked those who screened positive about their interest in seeking such services. After adjustments, officers with suicidal ideation or self-harm were significantly more likely to be interested in getting help, compared with officers who did not report suicidal ideation or self-harm (aOR, 7.66; 95% CI, 1.70-34.48).
Dr. Jetelina was impressed that so many officers were keen to seek help, which “is a big positive,” she said. “It’s just a matter of better detecting who needs the help and better connecting them to medical services that meet their needs.”
Mindfulness exercise
Dr. Jetelina and colleagues are conducting a pilot test of the use by police officers of smartwatches that monitor heart rate and oxygen levels. If measurements with these devices reach a predetermined threshold, the officers are “pinged” and are instructed to perform a mindfulness exercise in the field, she said.
Results so far “are really exciting,” said Dr. Jetelina. “Officers have found this extremely helpful and feasible, and so the next step is to test if this truly impacts mental illness over time.”
Routine mental health screening of officers might be beneficial, but only if it’s conducted in a manner “respectful of the officers’ needs and wants,” said Dr. Jetelina.
She pointed out that although psychological assessments are routinely carried out following an extreme traumatic call, such as one involving an officer-involved shooting, the “in-between” calls could have a more severe cumulative impact on mental health.
It’s important to provide officers with easy-to-access services tailored for their individual needs, said Dr. Jetelina.
‘Numb to it’
Eighteen patrol officers also participated in a focus group, during which several themes regarding the use of mental health care services emerged. One theme was the inability of officers to identify when they’re personally experiencing a mental health problem.
Participants said they had become “numb” to the traumatic events on the job, which is “concerning,” Dr. Jetelina said. “They think that having nightmares every week is completely normal, but it’s not, and this needs to be addressed.”
Other themes that emerged from focus groups included the belief that psychologists can’t relate to police stressors; concerns about confidentiality (one sentiment that was expressed was “you’re an idiot” if you “trust this department”); and stigma for officers who seek mental health care (participants talked about “reprisal” from seeing “a shrink,” including being labeled as “a nutter” and losing their job).
Dr. Jetelina noted that some “champion” officers revealed their mental health journey during focus groups, which tended to “open a Pandora’s box” for others to discuss their experience. She said these champions could be leveraged throughout the police department to help reduce stigma.
The study included participants from only one police department, although rigorous data collection allows for generalizability to the entire patrol department, say the authors. Although the study included only brief screens of mental illness symptoms, these short versions of screening tests have high sensitivity and specificity for mental illness in primary care, they noted.
The next step for the researchers is to study how mental illness and symptoms affect job performance, said Dr. Jetelina. “Does this impact excessive use of force? Does this impact workers’ compensation? Does this impact dispatch times, the time it takes for a police officer to respond to [a] 911 call?”
Possible underrepresentation
Anthony T. Ng, MD, regional medical director, East Region Hartford HealthCare Behavioral Health Network in Mansfield, Conn., and member of the American Psychiatric Association’s Council on Communications, found the study “helpful.”
However, the 26% who tested positive for mental illness may be an “underrepresentation” of the true picture, inasmuch as police officers might minimize or be less than truthful about their mental health status, said Dr. Ng.
Law enforcement has “never been easy,” but stressors may have escalated recently as police forces deal with shortages of staff and jails, said Dr. Ng.
He also noted that officers might face stressors at home. “Evidence shows that domestic violence is quite high – or higher than average – among law enforcement,” he said. “All these things add up.”
Psychiatrists and other mental health professionals should be “aware of the unique challenges” that police officers face and be “proactively involved” in providing guidance and education on mitigating stress, said Dr. Ng.
“You have police officers wearing body armor, so why can’t you give them some training to learn how to have psychiatric or psychological body armor?” he said. But it’s a two-way street; police forces should be open to outreach from mental health professionals. “We have to meet halfway.”
Compassion fatigue
In an accompanying commentary, John M. Violanti, PhD, of the department of epidemiology and environmental health at the State University of New York at Buffalo, said the article helps bring “to the forefront” the issue of the psychological dangers of police work.
There is conjecture as to why police experience mental distress, said Dr. Violanti, who pointed to a study of New York City police suicides during the 1930s that suggested that police have a “social license” for aggressive behavior but are restrained as part of public trust, placing them in a position of “psychological strain.”
“This situation may be reflective of the same situation police find themselves today,” said Dr. Violanti.
“Compassion fatigue,” a feeling of mental exhaustion caused by the inability to care for all persons in trouble, may also be a factor, as could the constant stress that leaves police officers feeling “cynical and isolated from others,” he wrote.
“The socialization process of becoming a police officer is associated with constrictive reasoning, viewing the world as either right or wrong, which leaves no middle ground for alternatives to deal with mental distress,” Dr. Violanti said.
He noted that police officers may abuse alcohol because of stress, peer pressure, isolation, and a culture that approves of alcohol use. “Officers tend to drink together and reinforce their own values.”.
Although no prospective studies have linked police mental health problems with childhood abuse or neglect, some mental health professionals estimate that about 25% of their police clients have a history of childhood abuse or neglect, said Dr. Violanti.
He agreed that mindfulness may help manage stress and increase cognitive flexibility in dealing with trauma and crises.
A possible way to ensure confidentiality is a peer support program that allows distressed officers to first talk privately with a trained and trusted peer officer and to then seek professional help if necessary, said Dr. Violanti.
The study was funded by a grant from the National Institute of Occupational Health and Safety. Dr. Jetelina, Dr. Ng, and Dr. Violanti disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New research shows that about a quarter of police officers in one large force report past or present mental health problems.
Responding to a survey, 26% of police officers on the Dallas police department screened positive for depression, anxiety, PTSD, or symptoms of suicide ideation or self-harm.
Mental illness rates were particularly high among female officers, those who were divorced, widowed, or separated, and those with military experience.
The study also showed that concerns over confidentiality and stigma may prevent officers with mental illness from seeking treatment.
The results underscored the need to identify police officers with psychiatric problems and to connect them to the most appropriate individualized care, author Katelyn K. Jetelina, PhD, assistant professor in the department of epidemiology, human genetics, and environmental sciences, University of Texas Health Science Center, Dallas, said in an interview.
“This is a very hard-to-reach population, and because of that, we need to be innovative in reaching them for services,” she said.
The study was published online Oct. 7 in JAMA Network Open.
Dr. Jetelina and colleagues are investigating various aspects of police officers’ well-being, including their nutritional needs and their occupational, physical, and mental health.
The current study included 434 members of the Dallas police department, the ninth largest in the United States. The mean age of the participants was 37 years, 82% were men, and about half were White. The 434 officers represented 97% of those invited to participate (n = 446) and 31% of the total patrol population of the Dallas police department (n = 1,413).
These officers completed a short survey on their smartphone that asked about lifetime diagnoses of depression, anxiety, and PTSD. They were also asked whether they experienced suicidal ideation or self-harm during the previous 2 weeks.
Overall, 12% of survey respondents reported having been diagnosed with a mental illness. This, said Jetelina, is slightly lower than the rate reported in the general population.
Study participants who had not currently been diagnosed with a mental illness completed the Patient Health Questionnaire–2 (PHQ-2), the Generalized Anxiety Disorder–2 (GAD-2), and the Primary Care–Posttraumatic Stress Disorder (PC-PTSD).
Officers were considered to have a positive result if they had a score of 3 or more (PHQ-2, sensitivity of 83% and specificity of 92%; PC-PTSD-5, sensitivity of 93% and specificity of 85%; GAD-2, sensitivity of 86% and specificity of 83%).
About 26% of respondents had a positive screening for mental illness symptoms, mainly PTSD and depression, which Dr. Jetelina noted is a higher percentage than in the general population.
This rate of mental health symptoms is “high and concerning,” but not surprising because of the work of police officers, which could include attending to sometimes violent car crashes, domestic abuse situations, and armed conflicts, said Dr. Jetelina.
“They’re constantly exposed to traumatic calls for service; they see people on their worst day, 8 hours a day, 5 days a week. That stress and exposure will have a detrimental effect on mental health, and we have to pay more attention to that,” she said.
Dr. Jetelina pointed out that the surveys were completed in January and February 2020, before COVID-19 had become a cause of stress for everyone and before the increase in calls for defunding police amid a resurgence of Black Lives Matter demonstrations.
However, she stressed that racial biases and occupational stress among police officers are “nothing new for them.” For example, in 2016, five Dallas police officers were killed during Black Lives Matter protests because of their race/ethnicity.
More at risk
The study showed that certain subgroups of officers were more at risk for mental illness. After adjustment for confounders, including demographic characteristics, marital status, and educational level, the odds of being diagnosed with a mental illness during the course of one’s life were significantly higher among female officers than male officers (adjusted odds ratio, 3.20; 95% confidence interval, 1.18-8.68).
Officers who were divorced, widowed, or separated and those who had more experience and held a higher rank were also at greater risk for mental illness.
As well, (aOR, 3.25; 95% CI, 1.38-7.67).
The study also asked participants about use of mental health care services over the past 12 months. About 35% of those who had a current mental health diagnosis and 17% of those who screened positive for mental health symptoms reported using such services.
The study also asked those who screened positive about their interest in seeking such services. After adjustments, officers with suicidal ideation or self-harm were significantly more likely to be interested in getting help, compared with officers who did not report suicidal ideation or self-harm (aOR, 7.66; 95% CI, 1.70-34.48).
Dr. Jetelina was impressed that so many officers were keen to seek help, which “is a big positive,” she said. “It’s just a matter of better detecting who needs the help and better connecting them to medical services that meet their needs.”
Mindfulness exercise
Dr. Jetelina and colleagues are conducting a pilot test of the use by police officers of smartwatches that monitor heart rate and oxygen levels. If measurements with these devices reach a predetermined threshold, the officers are “pinged” and are instructed to perform a mindfulness exercise in the field, she said.
Results so far “are really exciting,” said Dr. Jetelina. “Officers have found this extremely helpful and feasible, and so the next step is to test if this truly impacts mental illness over time.”
Routine mental health screening of officers might be beneficial, but only if it’s conducted in a manner “respectful of the officers’ needs and wants,” said Dr. Jetelina.
She pointed out that although psychological assessments are routinely carried out following an extreme traumatic call, such as one involving an officer-involved shooting, the “in-between” calls could have a more severe cumulative impact on mental health.
It’s important to provide officers with easy-to-access services tailored for their individual needs, said Dr. Jetelina.
‘Numb to it’
Eighteen patrol officers also participated in a focus group, during which several themes regarding the use of mental health care services emerged. One theme was the inability of officers to identify when they’re personally experiencing a mental health problem.
Participants said they had become “numb” to the traumatic events on the job, which is “concerning,” Dr. Jetelina said. “They think that having nightmares every week is completely normal, but it’s not, and this needs to be addressed.”
Other themes that emerged from focus groups included the belief that psychologists can’t relate to police stressors; concerns about confidentiality (one sentiment that was expressed was “you’re an idiot” if you “trust this department”); and stigma for officers who seek mental health care (participants talked about “reprisal” from seeing “a shrink,” including being labeled as “a nutter” and losing their job).
Dr. Jetelina noted that some “champion” officers revealed their mental health journey during focus groups, which tended to “open a Pandora’s box” for others to discuss their experience. She said these champions could be leveraged throughout the police department to help reduce stigma.
The study included participants from only one police department, although rigorous data collection allows for generalizability to the entire patrol department, say the authors. Although the study included only brief screens of mental illness symptoms, these short versions of screening tests have high sensitivity and specificity for mental illness in primary care, they noted.
The next step for the researchers is to study how mental illness and symptoms affect job performance, said Dr. Jetelina. “Does this impact excessive use of force? Does this impact workers’ compensation? Does this impact dispatch times, the time it takes for a police officer to respond to [a] 911 call?”
Possible underrepresentation
Anthony T. Ng, MD, regional medical director, East Region Hartford HealthCare Behavioral Health Network in Mansfield, Conn., and member of the American Psychiatric Association’s Council on Communications, found the study “helpful.”
However, the 26% who tested positive for mental illness may be an “underrepresentation” of the true picture, inasmuch as police officers might minimize or be less than truthful about their mental health status, said Dr. Ng.
Law enforcement has “never been easy,” but stressors may have escalated recently as police forces deal with shortages of staff and jails, said Dr. Ng.
He also noted that officers might face stressors at home. “Evidence shows that domestic violence is quite high – or higher than average – among law enforcement,” he said. “All these things add up.”
Psychiatrists and other mental health professionals should be “aware of the unique challenges” that police officers face and be “proactively involved” in providing guidance and education on mitigating stress, said Dr. Ng.
“You have police officers wearing body armor, so why can’t you give them some training to learn how to have psychiatric or psychological body armor?” he said. But it’s a two-way street; police forces should be open to outreach from mental health professionals. “We have to meet halfway.”
Compassion fatigue
In an accompanying commentary, John M. Violanti, PhD, of the department of epidemiology and environmental health at the State University of New York at Buffalo, said the article helps bring “to the forefront” the issue of the psychological dangers of police work.
There is conjecture as to why police experience mental distress, said Dr. Violanti, who pointed to a study of New York City police suicides during the 1930s that suggested that police have a “social license” for aggressive behavior but are restrained as part of public trust, placing them in a position of “psychological strain.”
“This situation may be reflective of the same situation police find themselves today,” said Dr. Violanti.
“Compassion fatigue,” a feeling of mental exhaustion caused by the inability to care for all persons in trouble, may also be a factor, as could the constant stress that leaves police officers feeling “cynical and isolated from others,” he wrote.
“The socialization process of becoming a police officer is associated with constrictive reasoning, viewing the world as either right or wrong, which leaves no middle ground for alternatives to deal with mental distress,” Dr. Violanti said.
He noted that police officers may abuse alcohol because of stress, peer pressure, isolation, and a culture that approves of alcohol use. “Officers tend to drink together and reinforce their own values.”.
Although no prospective studies have linked police mental health problems with childhood abuse or neglect, some mental health professionals estimate that about 25% of their police clients have a history of childhood abuse or neglect, said Dr. Violanti.
He agreed that mindfulness may help manage stress and increase cognitive flexibility in dealing with trauma and crises.
A possible way to ensure confidentiality is a peer support program that allows distressed officers to first talk privately with a trained and trusted peer officer and to then seek professional help if necessary, said Dr. Violanti.
The study was funded by a grant from the National Institute of Occupational Health and Safety. Dr. Jetelina, Dr. Ng, and Dr. Violanti disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Repurposing cardiovascular drugs for serious mental illness
One of the hottest topics now in psychiatry is the possibility of repurposing long-established cardiovascular medications for treatment of patients with serious mental illness, Livia De Picker, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.

The appeal is multifold. A huge unmet need exists in psychiatry for new and better treatments with novel mechanisms of action. Many guideline-recommended cardiovascular medications have a long track record, including a well-established safety profile with no surprises, and are available in generic versions. They can be developed for a new indication at minimal cost, noted Dr. De Picker, a psychiatrist at the University of Antwerp (Belgium).
The idea of psychiatric repurposing of drugs originally developed for nonpsychiatric indications is nothing new, she added. Examples include lithium for gout, valproate for epilepsy, and ketamine for anesthesiology.
One hitch in efforts to repurpose cardiovascular medications is that, when psychiatric patients have been included in randomized trials of the drugs’ cardiovascular effects, the psychiatric outcomes often went untallied.
Indeed, the only high-quality randomized trial evidence of psychiatric benefits for any class of cardiovascular medications is for statins, where a modest-sized meta-analysis of six placebo-controlled trials in 339 patients with schizophrenia showed the lipid-lowering agents had benefit for both positive and negative symptoms (Psychiatry Res. 2018 Apr;262:84-93). But that’s not a body of data of sufficient size to be definitive, in Dr. De Picker’s view.
Much of the recent enthusiasm for exploring the potential of cardiovascular drugs for psychiatric conditions comes from hypothesis-generating big data analyses drawn from Scandinavian national patient registries. Danish investigators scrutinized all 1.6 million Danes exposed to six classes of drugs of interest during 2005-2015 and determined that those on long-term statins, low-dose aspirin, ACE inhibitors, angiotensin receptor blockers, or allopurinol were associated with a decreased rate of new-onset depression, while high-dose aspirin and non-aspirin NSAIDs were associated with an increased rate, compared with a 30% random sample of the country’s population (Acta Psychiatr Scand. 2019 Jan;1391:68-77).
Similarly, the Danish group found that continued use of statins, angiotensin agents, or low-dose aspirin was associated with a decreased rate of new-onset bipolar disorder, while high-dose aspirin and other NSAIDs were linked to increased risk (Bipolar Disord. 2019 Aug;[15]:410-8). What these agents have in common, the investigators observed, is that they act on inflammation and potentially on the stress response system.
Meanwhile, Swedish investigators examined the course of 142,691 Swedes with a diagnosis of bipolar disorder, schizophrenia, or nonaffective psychosis during 2005-2016. They determined that, during periods when those individuals were on a statin, calcium channel blocker, or metformin, they had reduced rates of psychiatric hospitalization and self-harm (JAMA Psychiatry. 2019 Apr 1;76[4]:382-90).
Scottish researchers analyzed the health records of 144,066 patients placed on monotherapy for hypertension and determined that the lowest risk for hospitalization for a mood disorder during follow-up was in those prescribed an ACE inhibitor or angiotensin receptor blocker. The risk was significantly higher in patients on a beta-blocker or calcium channel blocker, and intermediate in those on a thiazide diuretic (Hypertension. 2016 Nov;68[5:1132-8).
“Obviously, this is all at a very macro scale and we have no idea whatsoever what this means for individual patients, number needed to treat, or which type of patients would benefit, but it does provide us with some guidance for future research,” according to Dr. De Picker.
In the meantime, while physicians await definitive evidence of any impact of cardiovascular drugs might have on psychiatric outcomes, abundant data exist underscoring what she called “shockingly high levels” of inadequate management of cardiovascular risk factors in patients with serious mental illness. That problem needs to be addressed, and Dr. De Picker offered her personal recommendations for doing so in a manner consistent with the evidence to date suggestive of potential mental health benefits of some cardiovascular medications.
She advised that, for treatment of hypertension in patients with bipolar disorder or major depression, an ACE inhibitor or angiotensin-converting enzyme inhibitor is preferred as first-line. There is some evidence to suggest lipophilic beta-blockers, which cross the blood-brain barrier, improve anxiety symptoms and panic attacks, and prevent memory consolidation in patients with posttraumatic stress disorder. But the Scottish data suggest that they may worsen mood disorders.
“I would be careful in using beta-blockers as first-line treatment for hypertension. They’re not in the guidelines for anxiety disorders. British guidelines recommend them to prevent memory consolidation in PTSD, but do not use them as first-line in patients with major depressive disorder or bipolar disorder,” she said. As for calcium channel blockers, the jury is still out, with mixed and inconsistent evidence to date as to the impact of this drug class on mental illness outcomes.
She recommended a very low threshold for prescribing statin therapy in patients with serious mental illness in light of the superb risk/benefit ratio for this drug class. In her younger patients, she turns for guidance to an online calculator of an individual’s 10-year risk of a first acute MI or stroke.
Metformin has been shown to be beneficial for addressing the weight gain and other adverse metabolic effects caused by antipsychotic agents, and there is some preliminary evidence of improved psychiatric outcomes in patients with serious mental illness.
Christian Otte, MD, who also spoke at the session, noted that not only do emerging data point to the possibility that cardiovascular drugs might have benefit in terms of psychiatric outcomes, there is also some evidence, albeit mixed, that the converse is true: that is, psychiatric drugs may have cardiovascular benefits. He pointed to a South Korean trial in which 300 patients with a recent acute coronary syndrome and major depression were randomized to 24 weeks of escitalopram or placebo. At median 8.1 years of follow-up, the group that received the SSRI had a 31% relative risk reduction in the primary composite endpoint of all-cause mortality, acute MI, or percutaneous coronary intervention (JAMA. 2018 Jul 24; 320[4]:350–7).
“Potentially independent of their antidepressant effects, some SSRIs’ antiplatelet effects could be beneficial for patients with coronary heart disease, although the jury is still open regarding this question, with evidence in both directions,” said Dr. Otte, professor of psychiatry at Charite University Medical Center in Berlin.
Dr. De Picker offered an example as well: Finnish psychiatrists recently reported that cardiovascular mortality was reduced by an adjusted 38% during periods when 62,250 Finnish schizophrenia patients were on antipsychotic agents, compared with periods of nonuse of the drugs in a national study with a median 14.1 years of follow-up (World Psychiatry. 2020 Feb;19[1]:61-8).
“What they discovered – and this is quite contrary to what we are used to hearing about antipsychotic medication and cardiovascular risk – is that while the number of cardiovascular hospitalizations was not different in periods with or without antipsychotic use, the cardiovascular mortality was quite strikingly reduced when patients were on antipsychotic medication,” she said.
Asked by an audience member whether she personally prescribes metformin, Dr. De Picker replied: “Well, yes, why not? One of the very nice things about metformin is that it is actually a very safe drug, even in the hands of nonspecialists.
“I understand that maybe psychiatrists may not feel very comfortable in starting patients on metformin due to a lack of experience. But there are really only two things you need to take into account. About one-quarter of patients will experience GI side effects – nausea, vomiting, abdominal discomfort – and this can be reduced by gradually uptitrating the dose, dosing at mealtime, and using an extended-release formulation. And the second thing is that metformin can impair vitamin B12 absorption, so I think, especially in psychiatric patients, it would be good to do an annual measurement of vitamin B12 level and, if necessary, administer intramuscular supplements,” Dr. De Picker said.
She reported having no financial conflicts regarding her presentation.
SOURCE: De Picker L. ECNP 2020. Session EDU.05.
One of the hottest topics now in psychiatry is the possibility of repurposing long-established cardiovascular medications for treatment of patients with serious mental illness, Livia De Picker, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.

The appeal is multifold. A huge unmet need exists in psychiatry for new and better treatments with novel mechanisms of action. Many guideline-recommended cardiovascular medications have a long track record, including a well-established safety profile with no surprises, and are available in generic versions. They can be developed for a new indication at minimal cost, noted Dr. De Picker, a psychiatrist at the University of Antwerp (Belgium).
The idea of psychiatric repurposing of drugs originally developed for nonpsychiatric indications is nothing new, she added. Examples include lithium for gout, valproate for epilepsy, and ketamine for anesthesiology.
One hitch in efforts to repurpose cardiovascular medications is that, when psychiatric patients have been included in randomized trials of the drugs’ cardiovascular effects, the psychiatric outcomes often went untallied.
Indeed, the only high-quality randomized trial evidence of psychiatric benefits for any class of cardiovascular medications is for statins, where a modest-sized meta-analysis of six placebo-controlled trials in 339 patients with schizophrenia showed the lipid-lowering agents had benefit for both positive and negative symptoms (Psychiatry Res. 2018 Apr;262:84-93). But that’s not a body of data of sufficient size to be definitive, in Dr. De Picker’s view.
Much of the recent enthusiasm for exploring the potential of cardiovascular drugs for psychiatric conditions comes from hypothesis-generating big data analyses drawn from Scandinavian national patient registries. Danish investigators scrutinized all 1.6 million Danes exposed to six classes of drugs of interest during 2005-2015 and determined that those on long-term statins, low-dose aspirin, ACE inhibitors, angiotensin receptor blockers, or allopurinol were associated with a decreased rate of new-onset depression, while high-dose aspirin and non-aspirin NSAIDs were associated with an increased rate, compared with a 30% random sample of the country’s population (Acta Psychiatr Scand. 2019 Jan;1391:68-77).
Similarly, the Danish group found that continued use of statins, angiotensin agents, or low-dose aspirin was associated with a decreased rate of new-onset bipolar disorder, while high-dose aspirin and other NSAIDs were linked to increased risk (Bipolar Disord. 2019 Aug;[15]:410-8). What these agents have in common, the investigators observed, is that they act on inflammation and potentially on the stress response system.
Meanwhile, Swedish investigators examined the course of 142,691 Swedes with a diagnosis of bipolar disorder, schizophrenia, or nonaffective psychosis during 2005-2016. They determined that, during periods when those individuals were on a statin, calcium channel blocker, or metformin, they had reduced rates of psychiatric hospitalization and self-harm (JAMA Psychiatry. 2019 Apr 1;76[4]:382-90).
Scottish researchers analyzed the health records of 144,066 patients placed on monotherapy for hypertension and determined that the lowest risk for hospitalization for a mood disorder during follow-up was in those prescribed an ACE inhibitor or angiotensin receptor blocker. The risk was significantly higher in patients on a beta-blocker or calcium channel blocker, and intermediate in those on a thiazide diuretic (Hypertension. 2016 Nov;68[5:1132-8).
“Obviously, this is all at a very macro scale and we have no idea whatsoever what this means for individual patients, number needed to treat, or which type of patients would benefit, but it does provide us with some guidance for future research,” according to Dr. De Picker.
In the meantime, while physicians await definitive evidence of any impact of cardiovascular drugs might have on psychiatric outcomes, abundant data exist underscoring what she called “shockingly high levels” of inadequate management of cardiovascular risk factors in patients with serious mental illness. That problem needs to be addressed, and Dr. De Picker offered her personal recommendations for doing so in a manner consistent with the evidence to date suggestive of potential mental health benefits of some cardiovascular medications.
She advised that, for treatment of hypertension in patients with bipolar disorder or major depression, an ACE inhibitor or angiotensin-converting enzyme inhibitor is preferred as first-line. There is some evidence to suggest lipophilic beta-blockers, which cross the blood-brain barrier, improve anxiety symptoms and panic attacks, and prevent memory consolidation in patients with posttraumatic stress disorder. But the Scottish data suggest that they may worsen mood disorders.
“I would be careful in using beta-blockers as first-line treatment for hypertension. They’re not in the guidelines for anxiety disorders. British guidelines recommend them to prevent memory consolidation in PTSD, but do not use them as first-line in patients with major depressive disorder or bipolar disorder,” she said. As for calcium channel blockers, the jury is still out, with mixed and inconsistent evidence to date as to the impact of this drug class on mental illness outcomes.
She recommended a very low threshold for prescribing statin therapy in patients with serious mental illness in light of the superb risk/benefit ratio for this drug class. In her younger patients, she turns for guidance to an online calculator of an individual’s 10-year risk of a first acute MI or stroke.
Metformin has been shown to be beneficial for addressing the weight gain and other adverse metabolic effects caused by antipsychotic agents, and there is some preliminary evidence of improved psychiatric outcomes in patients with serious mental illness.
Christian Otte, MD, who also spoke at the session, noted that not only do emerging data point to the possibility that cardiovascular drugs might have benefit in terms of psychiatric outcomes, there is also some evidence, albeit mixed, that the converse is true: that is, psychiatric drugs may have cardiovascular benefits. He pointed to a South Korean trial in which 300 patients with a recent acute coronary syndrome and major depression were randomized to 24 weeks of escitalopram or placebo. At median 8.1 years of follow-up, the group that received the SSRI had a 31% relative risk reduction in the primary composite endpoint of all-cause mortality, acute MI, or percutaneous coronary intervention (JAMA. 2018 Jul 24; 320[4]:350–7).
“Potentially independent of their antidepressant effects, some SSRIs’ antiplatelet effects could be beneficial for patients with coronary heart disease, although the jury is still open regarding this question, with evidence in both directions,” said Dr. Otte, professor of psychiatry at Charite University Medical Center in Berlin.
Dr. De Picker offered an example as well: Finnish psychiatrists recently reported that cardiovascular mortality was reduced by an adjusted 38% during periods when 62,250 Finnish schizophrenia patients were on antipsychotic agents, compared with periods of nonuse of the drugs in a national study with a median 14.1 years of follow-up (World Psychiatry. 2020 Feb;19[1]:61-8).
“What they discovered – and this is quite contrary to what we are used to hearing about antipsychotic medication and cardiovascular risk – is that while the number of cardiovascular hospitalizations was not different in periods with or without antipsychotic use, the cardiovascular mortality was quite strikingly reduced when patients were on antipsychotic medication,” she said.
Asked by an audience member whether she personally prescribes metformin, Dr. De Picker replied: “Well, yes, why not? One of the very nice things about metformin is that it is actually a very safe drug, even in the hands of nonspecialists.
“I understand that maybe psychiatrists may not feel very comfortable in starting patients on metformin due to a lack of experience. But there are really only two things you need to take into account. About one-quarter of patients will experience GI side effects – nausea, vomiting, abdominal discomfort – and this can be reduced by gradually uptitrating the dose, dosing at mealtime, and using an extended-release formulation. And the second thing is that metformin can impair vitamin B12 absorption, so I think, especially in psychiatric patients, it would be good to do an annual measurement of vitamin B12 level and, if necessary, administer intramuscular supplements,” Dr. De Picker said.
She reported having no financial conflicts regarding her presentation.
SOURCE: De Picker L. ECNP 2020. Session EDU.05.
One of the hottest topics now in psychiatry is the possibility of repurposing long-established cardiovascular medications for treatment of patients with serious mental illness, Livia De Picker, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.

The appeal is multifold. A huge unmet need exists in psychiatry for new and better treatments with novel mechanisms of action. Many guideline-recommended cardiovascular medications have a long track record, including a well-established safety profile with no surprises, and are available in generic versions. They can be developed for a new indication at minimal cost, noted Dr. De Picker, a psychiatrist at the University of Antwerp (Belgium).
The idea of psychiatric repurposing of drugs originally developed for nonpsychiatric indications is nothing new, she added. Examples include lithium for gout, valproate for epilepsy, and ketamine for anesthesiology.
One hitch in efforts to repurpose cardiovascular medications is that, when psychiatric patients have been included in randomized trials of the drugs’ cardiovascular effects, the psychiatric outcomes often went untallied.
Indeed, the only high-quality randomized trial evidence of psychiatric benefits for any class of cardiovascular medications is for statins, where a modest-sized meta-analysis of six placebo-controlled trials in 339 patients with schizophrenia showed the lipid-lowering agents had benefit for both positive and negative symptoms (Psychiatry Res. 2018 Apr;262:84-93). But that’s not a body of data of sufficient size to be definitive, in Dr. De Picker’s view.
Much of the recent enthusiasm for exploring the potential of cardiovascular drugs for psychiatric conditions comes from hypothesis-generating big data analyses drawn from Scandinavian national patient registries. Danish investigators scrutinized all 1.6 million Danes exposed to six classes of drugs of interest during 2005-2015 and determined that those on long-term statins, low-dose aspirin, ACE inhibitors, angiotensin receptor blockers, or allopurinol were associated with a decreased rate of new-onset depression, while high-dose aspirin and non-aspirin NSAIDs were associated with an increased rate, compared with a 30% random sample of the country’s population (Acta Psychiatr Scand. 2019 Jan;1391:68-77).
Similarly, the Danish group found that continued use of statins, angiotensin agents, or low-dose aspirin was associated with a decreased rate of new-onset bipolar disorder, while high-dose aspirin and other NSAIDs were linked to increased risk (Bipolar Disord. 2019 Aug;[15]:410-8). What these agents have in common, the investigators observed, is that they act on inflammation and potentially on the stress response system.
Meanwhile, Swedish investigators examined the course of 142,691 Swedes with a diagnosis of bipolar disorder, schizophrenia, or nonaffective psychosis during 2005-2016. They determined that, during periods when those individuals were on a statin, calcium channel blocker, or metformin, they had reduced rates of psychiatric hospitalization and self-harm (JAMA Psychiatry. 2019 Apr 1;76[4]:382-90).
Scottish researchers analyzed the health records of 144,066 patients placed on monotherapy for hypertension and determined that the lowest risk for hospitalization for a mood disorder during follow-up was in those prescribed an ACE inhibitor or angiotensin receptor blocker. The risk was significantly higher in patients on a beta-blocker or calcium channel blocker, and intermediate in those on a thiazide diuretic (Hypertension. 2016 Nov;68[5:1132-8).
“Obviously, this is all at a very macro scale and we have no idea whatsoever what this means for individual patients, number needed to treat, or which type of patients would benefit, but it does provide us with some guidance for future research,” according to Dr. De Picker.
In the meantime, while physicians await definitive evidence of any impact of cardiovascular drugs might have on psychiatric outcomes, abundant data exist underscoring what she called “shockingly high levels” of inadequate management of cardiovascular risk factors in patients with serious mental illness. That problem needs to be addressed, and Dr. De Picker offered her personal recommendations for doing so in a manner consistent with the evidence to date suggestive of potential mental health benefits of some cardiovascular medications.
She advised that, for treatment of hypertension in patients with bipolar disorder or major depression, an ACE inhibitor or angiotensin-converting enzyme inhibitor is preferred as first-line. There is some evidence to suggest lipophilic beta-blockers, which cross the blood-brain barrier, improve anxiety symptoms and panic attacks, and prevent memory consolidation in patients with posttraumatic stress disorder. But the Scottish data suggest that they may worsen mood disorders.
“I would be careful in using beta-blockers as first-line treatment for hypertension. They’re not in the guidelines for anxiety disorders. British guidelines recommend them to prevent memory consolidation in PTSD, but do not use them as first-line in patients with major depressive disorder or bipolar disorder,” she said. As for calcium channel blockers, the jury is still out, with mixed and inconsistent evidence to date as to the impact of this drug class on mental illness outcomes.
She recommended a very low threshold for prescribing statin therapy in patients with serious mental illness in light of the superb risk/benefit ratio for this drug class. In her younger patients, she turns for guidance to an online calculator of an individual’s 10-year risk of a first acute MI or stroke.
Metformin has been shown to be beneficial for addressing the weight gain and other adverse metabolic effects caused by antipsychotic agents, and there is some preliminary evidence of improved psychiatric outcomes in patients with serious mental illness.
Christian Otte, MD, who also spoke at the session, noted that not only do emerging data point to the possibility that cardiovascular drugs might have benefit in terms of psychiatric outcomes, there is also some evidence, albeit mixed, that the converse is true: that is, psychiatric drugs may have cardiovascular benefits. He pointed to a South Korean trial in which 300 patients with a recent acute coronary syndrome and major depression were randomized to 24 weeks of escitalopram or placebo. At median 8.1 years of follow-up, the group that received the SSRI had a 31% relative risk reduction in the primary composite endpoint of all-cause mortality, acute MI, or percutaneous coronary intervention (JAMA. 2018 Jul 24; 320[4]:350–7).
“Potentially independent of their antidepressant effects, some SSRIs’ antiplatelet effects could be beneficial for patients with coronary heart disease, although the jury is still open regarding this question, with evidence in both directions,” said Dr. Otte, professor of psychiatry at Charite University Medical Center in Berlin.
Dr. De Picker offered an example as well: Finnish psychiatrists recently reported that cardiovascular mortality was reduced by an adjusted 38% during periods when 62,250 Finnish schizophrenia patients were on antipsychotic agents, compared with periods of nonuse of the drugs in a national study with a median 14.1 years of follow-up (World Psychiatry. 2020 Feb;19[1]:61-8).
“What they discovered – and this is quite contrary to what we are used to hearing about antipsychotic medication and cardiovascular risk – is that while the number of cardiovascular hospitalizations was not different in periods with or without antipsychotic use, the cardiovascular mortality was quite strikingly reduced when patients were on antipsychotic medication,” she said.
Asked by an audience member whether she personally prescribes metformin, Dr. De Picker replied: “Well, yes, why not? One of the very nice things about metformin is that it is actually a very safe drug, even in the hands of nonspecialists.
“I understand that maybe psychiatrists may not feel very comfortable in starting patients on metformin due to a lack of experience. But there are really only two things you need to take into account. About one-quarter of patients will experience GI side effects – nausea, vomiting, abdominal discomfort – and this can be reduced by gradually uptitrating the dose, dosing at mealtime, and using an extended-release formulation. And the second thing is that metformin can impair vitamin B12 absorption, so I think, especially in psychiatric patients, it would be good to do an annual measurement of vitamin B12 level and, if necessary, administer intramuscular supplements,” Dr. De Picker said.
She reported having no financial conflicts regarding her presentation.
SOURCE: De Picker L. ECNP 2020. Session EDU.05.
FROM ECNP 2020
Divergent COVID-19 mental health impacts seen in Spain and China
Spain and China used very different public health responses to the COVID-19 crisis, and that has had significant consequences in terms of the mental health as well as physical health of the two countries’ citizens, Roger Ho, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
Dr. Ho, a psychiatrist at the National University of Singapore, presented a first-of-its-kind cross-cultural comparative study of the impact of the COVID-19 pandemic in two epicenters on opposite sides of the world. A total of 1,539 participants drawn from the general populations in the two countries completed the online National University of Singapore COVID-19 Questionnaire. The survey was conducted in late February/early March in China and in mid-April in Spain, times of intense disease activity in the countries.
The questionnaire assesses knowledge and concerns about COVID, precautionary measures taken in the last 14 days, contact history, and physical symptoms related to COVID in the last 14 days. The pandemic’s psychological impact was evaluated using the Impact of Event Scale–Revised (IES-R). Participants also completed the Depression, Anxiety, and Stress-21 Scale (DASS-21).
Of note, the pandemic has taken a vastly greater physical toll in Spain than China. As of May 5, there were 83,000 confirmed cases of COVID-19 in China, with a population of 1.39 billion, compared with 248,000 in Spain, with a population of 46.9 million. The Spanish case rate of 5,500 per 1 million population was 100 times greater than China’s; the Spanish mortality rate of 585 per million was 185-fold greater.
Mental health findings
Spaniards experienced significantly higher levels of stress and depression as reflected in DASS-21 subscale scores of 14.22 and 8.65, respectively, compared with 7.86 and 6.38, in Chinese respondents. Spanish subjects also reported greater anxiety levels than the Chinese on the DASS-21 anxiety subscale, although not to a statistically significant extent. Yet, counterintuitively, given the DASS-21 results, the pandemic had a greater adverse psychological impact on the Chinese subjects as reflected in their significantly higher average IES-D score of 30.76 versus 27.64 in Spain. Dr. Ho offered a hypothesis as to why: The survey documented that many Chinese respondents felt socially stigmatized, and that their nation had been discriminated against by the rest of the world because the pandemic started in China.
Satisfaction with the public health response
Spanish respondents reported less confidence in their COVID-related medical services.
“This could be due to the rising number of infected health care workers in Spain. In contrast, the Chinese had more confidence in their medical services, probably because the government quickly deployed medical personnel and treated COVID-19 patients at rapidly built hospitals,” according to Dr. Ho.
Spain and other European countries shared four shortcomings in their pandemic response, he continued: lack of personal protective equipment for health care workers, delay in developing response strategies, a shortage of hospital beds, and inability to protect vulnerable elderly individuals from infection in nursing homes.
Experiencing cough, shortness of breath, myalgia, or other physical symptoms potentially associated with COVID-19 within the past 14 days was associated with worse depression, anxiety, and stress scores in both China and Spain. This underscores from a mental health standpoint the importance of rapid and accurate testing for the infection, Dr. Ho said.
Significantly more Spanish respondents felt there was too much unnecessary worry about COVID-19, suggesting a need for better health education regarding the pandemic.
Use of face masks
Consistent use of face masks regardless of the presence or absence of symptoms was far more common in the Chinese epicenter, where, unlike in Spain, this precautionary measure was associated with significantly lower IES-R and DASS-21 scores.
but for the Spanish, wearing a face mask was associated with higher IES-R scores,” Dr. Ho said. “We understand that it is difficult for Europeans to accept the need to use masks for healthy people because mask-wearing suggests vulnerability to sickness and concealment of identity. The Chinese have a collective culture. They believe they should wear a face mask to protect their health and that of other people.”
Dr. Ho reported no financial conflicts regarding his study, conducted with coinvestigators at Huaibei (China) Normal University and Complutense University of Madrid.
SOURCE: Ho R. ECNP 2020, Session ISE01.
Spain and China used very different public health responses to the COVID-19 crisis, and that has had significant consequences in terms of the mental health as well as physical health of the two countries’ citizens, Roger Ho, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
Dr. Ho, a psychiatrist at the National University of Singapore, presented a first-of-its-kind cross-cultural comparative study of the impact of the COVID-19 pandemic in two epicenters on opposite sides of the world. A total of 1,539 participants drawn from the general populations in the two countries completed the online National University of Singapore COVID-19 Questionnaire. The survey was conducted in late February/early March in China and in mid-April in Spain, times of intense disease activity in the countries.
The questionnaire assesses knowledge and concerns about COVID, precautionary measures taken in the last 14 days, contact history, and physical symptoms related to COVID in the last 14 days. The pandemic’s psychological impact was evaluated using the Impact of Event Scale–Revised (IES-R). Participants also completed the Depression, Anxiety, and Stress-21 Scale (DASS-21).
Of note, the pandemic has taken a vastly greater physical toll in Spain than China. As of May 5, there were 83,000 confirmed cases of COVID-19 in China, with a population of 1.39 billion, compared with 248,000 in Spain, with a population of 46.9 million. The Spanish case rate of 5,500 per 1 million population was 100 times greater than China’s; the Spanish mortality rate of 585 per million was 185-fold greater.
Mental health findings
Spaniards experienced significantly higher levels of stress and depression as reflected in DASS-21 subscale scores of 14.22 and 8.65, respectively, compared with 7.86 and 6.38, in Chinese respondents. Spanish subjects also reported greater anxiety levels than the Chinese on the DASS-21 anxiety subscale, although not to a statistically significant extent. Yet, counterintuitively, given the DASS-21 results, the pandemic had a greater adverse psychological impact on the Chinese subjects as reflected in their significantly higher average IES-D score of 30.76 versus 27.64 in Spain. Dr. Ho offered a hypothesis as to why: The survey documented that many Chinese respondents felt socially stigmatized, and that their nation had been discriminated against by the rest of the world because the pandemic started in China.
Satisfaction with the public health response
Spanish respondents reported less confidence in their COVID-related medical services.
“This could be due to the rising number of infected health care workers in Spain. In contrast, the Chinese had more confidence in their medical services, probably because the government quickly deployed medical personnel and treated COVID-19 patients at rapidly built hospitals,” according to Dr. Ho.
Spain and other European countries shared four shortcomings in their pandemic response, he continued: lack of personal protective equipment for health care workers, delay in developing response strategies, a shortage of hospital beds, and inability to protect vulnerable elderly individuals from infection in nursing homes.
Experiencing cough, shortness of breath, myalgia, or other physical symptoms potentially associated with COVID-19 within the past 14 days was associated with worse depression, anxiety, and stress scores in both China and Spain. This underscores from a mental health standpoint the importance of rapid and accurate testing for the infection, Dr. Ho said.
Significantly more Spanish respondents felt there was too much unnecessary worry about COVID-19, suggesting a need for better health education regarding the pandemic.
Use of face masks
Consistent use of face masks regardless of the presence or absence of symptoms was far more common in the Chinese epicenter, where, unlike in Spain, this precautionary measure was associated with significantly lower IES-R and DASS-21 scores.
but for the Spanish, wearing a face mask was associated with higher IES-R scores,” Dr. Ho said. “We understand that it is difficult for Europeans to accept the need to use masks for healthy people because mask-wearing suggests vulnerability to sickness and concealment of identity. The Chinese have a collective culture. They believe they should wear a face mask to protect their health and that of other people.”
Dr. Ho reported no financial conflicts regarding his study, conducted with coinvestigators at Huaibei (China) Normal University and Complutense University of Madrid.
SOURCE: Ho R. ECNP 2020, Session ISE01.
Spain and China used very different public health responses to the COVID-19 crisis, and that has had significant consequences in terms of the mental health as well as physical health of the two countries’ citizens, Roger Ho, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
Dr. Ho, a psychiatrist at the National University of Singapore, presented a first-of-its-kind cross-cultural comparative study of the impact of the COVID-19 pandemic in two epicenters on opposite sides of the world. A total of 1,539 participants drawn from the general populations in the two countries completed the online National University of Singapore COVID-19 Questionnaire. The survey was conducted in late February/early March in China and in mid-April in Spain, times of intense disease activity in the countries.
The questionnaire assesses knowledge and concerns about COVID, precautionary measures taken in the last 14 days, contact history, and physical symptoms related to COVID in the last 14 days. The pandemic’s psychological impact was evaluated using the Impact of Event Scale–Revised (IES-R). Participants also completed the Depression, Anxiety, and Stress-21 Scale (DASS-21).
Of note, the pandemic has taken a vastly greater physical toll in Spain than China. As of May 5, there were 83,000 confirmed cases of COVID-19 in China, with a population of 1.39 billion, compared with 248,000 in Spain, with a population of 46.9 million. The Spanish case rate of 5,500 per 1 million population was 100 times greater than China’s; the Spanish mortality rate of 585 per million was 185-fold greater.
Mental health findings
Spaniards experienced significantly higher levels of stress and depression as reflected in DASS-21 subscale scores of 14.22 and 8.65, respectively, compared with 7.86 and 6.38, in Chinese respondents. Spanish subjects also reported greater anxiety levels than the Chinese on the DASS-21 anxiety subscale, although not to a statistically significant extent. Yet, counterintuitively, given the DASS-21 results, the pandemic had a greater adverse psychological impact on the Chinese subjects as reflected in their significantly higher average IES-D score of 30.76 versus 27.64 in Spain. Dr. Ho offered a hypothesis as to why: The survey documented that many Chinese respondents felt socially stigmatized, and that their nation had been discriminated against by the rest of the world because the pandemic started in China.
Satisfaction with the public health response
Spanish respondents reported less confidence in their COVID-related medical services.
“This could be due to the rising number of infected health care workers in Spain. In contrast, the Chinese had more confidence in their medical services, probably because the government quickly deployed medical personnel and treated COVID-19 patients at rapidly built hospitals,” according to Dr. Ho.
Spain and other European countries shared four shortcomings in their pandemic response, he continued: lack of personal protective equipment for health care workers, delay in developing response strategies, a shortage of hospital beds, and inability to protect vulnerable elderly individuals from infection in nursing homes.
Experiencing cough, shortness of breath, myalgia, or other physical symptoms potentially associated with COVID-19 within the past 14 days was associated with worse depression, anxiety, and stress scores in both China and Spain. This underscores from a mental health standpoint the importance of rapid and accurate testing for the infection, Dr. Ho said.
Significantly more Spanish respondents felt there was too much unnecessary worry about COVID-19, suggesting a need for better health education regarding the pandemic.
Use of face masks
Consistent use of face masks regardless of the presence or absence of symptoms was far more common in the Chinese epicenter, where, unlike in Spain, this precautionary measure was associated with significantly lower IES-R and DASS-21 scores.
but for the Spanish, wearing a face mask was associated with higher IES-R scores,” Dr. Ho said. “We understand that it is difficult for Europeans to accept the need to use masks for healthy people because mask-wearing suggests vulnerability to sickness and concealment of identity. The Chinese have a collective culture. They believe they should wear a face mask to protect their health and that of other people.”
Dr. Ho reported no financial conflicts regarding his study, conducted with coinvestigators at Huaibei (China) Normal University and Complutense University of Madrid.
SOURCE: Ho R. ECNP 2020, Session ISE01.
FROM ECNP 2020
Mental illness tied to increased mortality in COVID-19
A psychiatric diagnosis for patients hospitalized with COVID-19 is linked to a significantly increased risk for death, new research shows.
Investigators found that patients who were hospitalized with COVID-19 and who had been diagnosed with a psychiatric disorder had a 50% increased risk for a COVID-related death in comparison with COVID-19 patients who had not received a psychiatric diagnosis.
“Pay attention and potentially address/treat a prior psychiatric diagnosis if a patient is hospitalized for COVID-19, as this risk factor can impact the patient’s outcome – death – while in the hospital,” lead investigator Luming Li, MD, assistant professor of psychiatry and associate medical director of quality improvement, Yale New Haven Psychiatric Hospital, New Haven, Conn., said in an interview.
The study was published Sept. 30 in JAMA Network Open.
Negative impact
“We were interested to learn more about the impact of psychiatric diagnoses on COVID-19 mortality, as prior large cohort studies included neurological and other medical conditions but did not assess for a priori psychiatric diagnoses,” said Dr. Li.
“We know from the literature that prior psychiatric diagnoses can have a negative impact on the outcomes of medical conditions, and therefore we tested our hypothesis on a cohort of patients who were hospitalized with COVID-19,” she added.
To investigate, the researchers analyzed data on 1,685 patients hospitalized with COVID-19 between Feb. 15 and April 25, 2020, and whose cases were followed to May 27, 2020. The patients (mean age, 65.2 years; 52.6% men) were drawn from the Yale New Haven Health System.
The median follow-up period was 8 days (interquartile range, 4-16 days) .
Of these patients, 28% had received a psychiatric diagnosis prior to hospitalization. (i.e., cancer, cerebrovascular disease, heart failure, diabetes, kidney disease, liver disease, MI, and/or HIV).
Psychiatric diagnoses were defined in accordance with ICD codes that included mental and behavioral health, Alzheimer’s disease, and self-injury.
Vulnerability to stress
In the unadjusted model, the risk for COVID-19–related hospital death was greater for those who had received any psychiatric diagnosis, compared with those had not (hazard ratio, 2.3; 95% CI, 1.8-2.9; P < .001).
In the adjusted model that controlled for demographic characteristics, other medical comorbidities, and hospital location, the mortality risk somewhat decreased but still remained significantly higher (HR, 1.5; 95% CI, 1.1-1.9; P = .003).
Dr. Li noted a number of factors that might account for the higher mortality rate among psychiatric patients who had COVID-19 in comparison with COVD-19 patients who did not have a psychiatric disorder. These included “potential inflammatory and stress responses that the body experiences related to prior psychiatric conditions,” she said.
Having been previously diagnosed with a psychiatric disorder may also “reflect existing neurochemical differences, compared to those who do not have a prior psychiatric diagnosis, [and] these differences may make the population with the prior psychiatric diagnosis more vulnerable to respond to an acute stressor such as COVID-19,” she said.
Quality care
Harold Pincus, MD, professor and vice chair of the department of psychiatry at Columbia University, New York, said it “adds to the fairly well-known and well-established phenomenon that people with mental illnesses have a high risk of all sorts of morbidity and mortality for non–mental health conditions.”
The researchers “adjusted for various expected [mortality] risks that would be independent of the presence of COVID-19,” so “there was something else going on associated with mortality,” said Dr. Pincus, who is also codirector of the Irving Institute for Clinical and Translation Research. He was not involved with the study.
Beyond the possibility of “some basic immunologic process affected by the presence of a mental disorder,” it is possible that the vulnerability is “related to access to quality care for the comorbid general condition that is not being effectively treated,” he said.
“The take-home message is that people with mental disorders are at higher risk for death, and we need to make sure that, irrespective of COVID-19, they get adequate preventive and chronic-disease care, which would be the most effective way to intervene and protect the impact of a serious disease like COVID-19,” he noted. This would include being appropriately vaccinated and receiving preventive healthcare to reduce smoking and encourage weight loss.
No source of funding for the study was provided. Dr. Li reported receiving grants from a Health and Aging Policy Fellowship during the conduct of the study. Dr. Pincus reported no relevant financial relationships.
A psychiatric diagnosis for patients hospitalized with COVID-19 is linked to a significantly increased risk for death, new research shows.
Investigators found that patients who were hospitalized with COVID-19 and who had been diagnosed with a psychiatric disorder had a 50% increased risk for a COVID-related death in comparison with COVID-19 patients who had not received a psychiatric diagnosis.
“Pay attention and potentially address/treat a prior psychiatric diagnosis if a patient is hospitalized for COVID-19, as this risk factor can impact the patient’s outcome – death – while in the hospital,” lead investigator Luming Li, MD, assistant professor of psychiatry and associate medical director of quality improvement, Yale New Haven Psychiatric Hospital, New Haven, Conn., said in an interview.
The study was published Sept. 30 in JAMA Network Open.
Negative impact
“We were interested to learn more about the impact of psychiatric diagnoses on COVID-19 mortality, as prior large cohort studies included neurological and other medical conditions but did not assess for a priori psychiatric diagnoses,” said Dr. Li.
“We know from the literature that prior psychiatric diagnoses can have a negative impact on the outcomes of medical conditions, and therefore we tested our hypothesis on a cohort of patients who were hospitalized with COVID-19,” she added.
To investigate, the researchers analyzed data on 1,685 patients hospitalized with COVID-19 between Feb. 15 and April 25, 2020, and whose cases were followed to May 27, 2020. The patients (mean age, 65.2 years; 52.6% men) were drawn from the Yale New Haven Health System.
The median follow-up period was 8 days (interquartile range, 4-16 days) .
Of these patients, 28% had received a psychiatric diagnosis prior to hospitalization. (i.e., cancer, cerebrovascular disease, heart failure, diabetes, kidney disease, liver disease, MI, and/or HIV).
Psychiatric diagnoses were defined in accordance with ICD codes that included mental and behavioral health, Alzheimer’s disease, and self-injury.
Vulnerability to stress
In the unadjusted model, the risk for COVID-19–related hospital death was greater for those who had received any psychiatric diagnosis, compared with those had not (hazard ratio, 2.3; 95% CI, 1.8-2.9; P < .001).
In the adjusted model that controlled for demographic characteristics, other medical comorbidities, and hospital location, the mortality risk somewhat decreased but still remained significantly higher (HR, 1.5; 95% CI, 1.1-1.9; P = .003).
Dr. Li noted a number of factors that might account for the higher mortality rate among psychiatric patients who had COVID-19 in comparison with COVD-19 patients who did not have a psychiatric disorder. These included “potential inflammatory and stress responses that the body experiences related to prior psychiatric conditions,” she said.
Having been previously diagnosed with a psychiatric disorder may also “reflect existing neurochemical differences, compared to those who do not have a prior psychiatric diagnosis, [and] these differences may make the population with the prior psychiatric diagnosis more vulnerable to respond to an acute stressor such as COVID-19,” she said.
Quality care
Harold Pincus, MD, professor and vice chair of the department of psychiatry at Columbia University, New York, said it “adds to the fairly well-known and well-established phenomenon that people with mental illnesses have a high risk of all sorts of morbidity and mortality for non–mental health conditions.”
The researchers “adjusted for various expected [mortality] risks that would be independent of the presence of COVID-19,” so “there was something else going on associated with mortality,” said Dr. Pincus, who is also codirector of the Irving Institute for Clinical and Translation Research. He was not involved with the study.
Beyond the possibility of “some basic immunologic process affected by the presence of a mental disorder,” it is possible that the vulnerability is “related to access to quality care for the comorbid general condition that is not being effectively treated,” he said.
“The take-home message is that people with mental disorders are at higher risk for death, and we need to make sure that, irrespective of COVID-19, they get adequate preventive and chronic-disease care, which would be the most effective way to intervene and protect the impact of a serious disease like COVID-19,” he noted. This would include being appropriately vaccinated and receiving preventive healthcare to reduce smoking and encourage weight loss.
No source of funding for the study was provided. Dr. Li reported receiving grants from a Health and Aging Policy Fellowship during the conduct of the study. Dr. Pincus reported no relevant financial relationships.
A psychiatric diagnosis for patients hospitalized with COVID-19 is linked to a significantly increased risk for death, new research shows.
Investigators found that patients who were hospitalized with COVID-19 and who had been diagnosed with a psychiatric disorder had a 50% increased risk for a COVID-related death in comparison with COVID-19 patients who had not received a psychiatric diagnosis.
“Pay attention and potentially address/treat a prior psychiatric diagnosis if a patient is hospitalized for COVID-19, as this risk factor can impact the patient’s outcome – death – while in the hospital,” lead investigator Luming Li, MD, assistant professor of psychiatry and associate medical director of quality improvement, Yale New Haven Psychiatric Hospital, New Haven, Conn., said in an interview.
The study was published Sept. 30 in JAMA Network Open.
Negative impact
“We were interested to learn more about the impact of psychiatric diagnoses on COVID-19 mortality, as prior large cohort studies included neurological and other medical conditions but did not assess for a priori psychiatric diagnoses,” said Dr. Li.
“We know from the literature that prior psychiatric diagnoses can have a negative impact on the outcomes of medical conditions, and therefore we tested our hypothesis on a cohort of patients who were hospitalized with COVID-19,” she added.
To investigate, the researchers analyzed data on 1,685 patients hospitalized with COVID-19 between Feb. 15 and April 25, 2020, and whose cases were followed to May 27, 2020. The patients (mean age, 65.2 years; 52.6% men) were drawn from the Yale New Haven Health System.
The median follow-up period was 8 days (interquartile range, 4-16 days) .
Of these patients, 28% had received a psychiatric diagnosis prior to hospitalization. (i.e., cancer, cerebrovascular disease, heart failure, diabetes, kidney disease, liver disease, MI, and/or HIV).
Psychiatric diagnoses were defined in accordance with ICD codes that included mental and behavioral health, Alzheimer’s disease, and self-injury.
Vulnerability to stress
In the unadjusted model, the risk for COVID-19–related hospital death was greater for those who had received any psychiatric diagnosis, compared with those had not (hazard ratio, 2.3; 95% CI, 1.8-2.9; P < .001).
In the adjusted model that controlled for demographic characteristics, other medical comorbidities, and hospital location, the mortality risk somewhat decreased but still remained significantly higher (HR, 1.5; 95% CI, 1.1-1.9; P = .003).
Dr. Li noted a number of factors that might account for the higher mortality rate among psychiatric patients who had COVID-19 in comparison with COVD-19 patients who did not have a psychiatric disorder. These included “potential inflammatory and stress responses that the body experiences related to prior psychiatric conditions,” she said.
Having been previously diagnosed with a psychiatric disorder may also “reflect existing neurochemical differences, compared to those who do not have a prior psychiatric diagnosis, [and] these differences may make the population with the prior psychiatric diagnosis more vulnerable to respond to an acute stressor such as COVID-19,” she said.
Quality care
Harold Pincus, MD, professor and vice chair of the department of psychiatry at Columbia University, New York, said it “adds to the fairly well-known and well-established phenomenon that people with mental illnesses have a high risk of all sorts of morbidity and mortality for non–mental health conditions.”
The researchers “adjusted for various expected [mortality] risks that would be independent of the presence of COVID-19,” so “there was something else going on associated with mortality,” said Dr. Pincus, who is also codirector of the Irving Institute for Clinical and Translation Research. He was not involved with the study.
Beyond the possibility of “some basic immunologic process affected by the presence of a mental disorder,” it is possible that the vulnerability is “related to access to quality care for the comorbid general condition that is not being effectively treated,” he said.
“The take-home message is that people with mental disorders are at higher risk for death, and we need to make sure that, irrespective of COVID-19, they get adequate preventive and chronic-disease care, which would be the most effective way to intervene and protect the impact of a serious disease like COVID-19,” he noted. This would include being appropriately vaccinated and receiving preventive healthcare to reduce smoking and encourage weight loss.
No source of funding for the study was provided. Dr. Li reported receiving grants from a Health and Aging Policy Fellowship during the conduct of the study. Dr. Pincus reported no relevant financial relationships.
COVID-19’s psychological impact gets a name
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
Suicide in America: The urban-rural divide
The gap in suicide rates between rural and urban areas has widened since 2000 for both males and females, according to a recent report from the National Center for Health Statistics.

After remaining stable from 2000 to 2007, the suicide rate for rural males rose 34% from 2007 to 2018, versus 17% among urban males over the same period. Suicide rates for females were significantly lower than those of men, but the changes were larger. For rural females, the rate increased 91% from 2000 to 2018, compared with 51% for urban females, Kristen Pettrone, MD, MPH, and Sally C. Curtin, MA, said in an NCHS Data Brief.
For 2018, the last year with available data, the age-adjusted rates look like this: 21.5 per 100,000 population for urban males, 30.7 for rural males, 5.9 per 100,000 for urban females, and 8.0 for rural females. The overall rate for the United States was 14.2 per 100,000, with combined male/female rates of 13.4 in urban areas and 19.4 in rural areas, the researchers said.
Methods of suicide also varied by sex and urban-rural status. Firearms were the leading method for males in both rural and urban areas, but females split between firearms in rural areas and suffocation (including hangings) in urban areas, said Dr. Pettrone of the Centers for Disease Control and Prevention and Ms. Curtin of the NCHS.
Suffocation, however, was the fastest-growing method from 2000 to 2018, regardless of sex or location. Suffocation-related suicide rates more than quadrupled for rural females, and more than doubled for urban females and rural males, while rates rose 85% among males in urban areas, based on data from the National Vital Statistics System.
“Suicide has remained the 10th leading cause of death in the United States since 2008,” they wrote, and
SOURCE: Pettrone K, Curtin SC. 2020 Aug. NCHS Data Brief, No 373.
The gap in suicide rates between rural and urban areas has widened since 2000 for both males and females, according to a recent report from the National Center for Health Statistics.

After remaining stable from 2000 to 2007, the suicide rate for rural males rose 34% from 2007 to 2018, versus 17% among urban males over the same period. Suicide rates for females were significantly lower than those of men, but the changes were larger. For rural females, the rate increased 91% from 2000 to 2018, compared with 51% for urban females, Kristen Pettrone, MD, MPH, and Sally C. Curtin, MA, said in an NCHS Data Brief.
For 2018, the last year with available data, the age-adjusted rates look like this: 21.5 per 100,000 population for urban males, 30.7 for rural males, 5.9 per 100,000 for urban females, and 8.0 for rural females. The overall rate for the United States was 14.2 per 100,000, with combined male/female rates of 13.4 in urban areas and 19.4 in rural areas, the researchers said.
Methods of suicide also varied by sex and urban-rural status. Firearms were the leading method for males in both rural and urban areas, but females split between firearms in rural areas and suffocation (including hangings) in urban areas, said Dr. Pettrone of the Centers for Disease Control and Prevention and Ms. Curtin of the NCHS.
Suffocation, however, was the fastest-growing method from 2000 to 2018, regardless of sex or location. Suffocation-related suicide rates more than quadrupled for rural females, and more than doubled for urban females and rural males, while rates rose 85% among males in urban areas, based on data from the National Vital Statistics System.
“Suicide has remained the 10th leading cause of death in the United States since 2008,” they wrote, and
SOURCE: Pettrone K, Curtin SC. 2020 Aug. NCHS Data Brief, No 373.
The gap in suicide rates between rural and urban areas has widened since 2000 for both males and females, according to a recent report from the National Center for Health Statistics.

After remaining stable from 2000 to 2007, the suicide rate for rural males rose 34% from 2007 to 2018, versus 17% among urban males over the same period. Suicide rates for females were significantly lower than those of men, but the changes were larger. For rural females, the rate increased 91% from 2000 to 2018, compared with 51% for urban females, Kristen Pettrone, MD, MPH, and Sally C. Curtin, MA, said in an NCHS Data Brief.
For 2018, the last year with available data, the age-adjusted rates look like this: 21.5 per 100,000 population for urban males, 30.7 for rural males, 5.9 per 100,000 for urban females, and 8.0 for rural females. The overall rate for the United States was 14.2 per 100,000, with combined male/female rates of 13.4 in urban areas and 19.4 in rural areas, the researchers said.
Methods of suicide also varied by sex and urban-rural status. Firearms were the leading method for males in both rural and urban areas, but females split between firearms in rural areas and suffocation (including hangings) in urban areas, said Dr. Pettrone of the Centers for Disease Control and Prevention and Ms. Curtin of the NCHS.
Suffocation, however, was the fastest-growing method from 2000 to 2018, regardless of sex or location. Suffocation-related suicide rates more than quadrupled for rural females, and more than doubled for urban females and rural males, while rates rose 85% among males in urban areas, based on data from the National Vital Statistics System.
“Suicide has remained the 10th leading cause of death in the United States since 2008,” they wrote, and
SOURCE: Pettrone K, Curtin SC. 2020 Aug. NCHS Data Brief, No 373.
Cognitive impairments in major depression cluster in three patterns
Objective neuropsychological tests can be used to subclassify the cognitive symptoms present in patients with major depression into three patterns having implications for treatment responsiveness, Gitte Moos Knudsen, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Our data highlight the importance of assessing and targeting cognitive symptoms,” said Dr. Knudsen, the ECNP president and professor of neurology at the University of Copenhagen.
She was a coauthor of the Danish NeuroPharm study, in which 92 antidepressant-free patients with moderate or severe major depressive disorder and 103 healthy controls completed a comprehensive neuropsychological test battery. The testing included a validation study of the EMOTICOM test battery, a novel neuropsychological test battery developed specifically to assess what has been called “hot” cognition, such as emotion processing, social cognition, and affective verbal memory.
Overall, the depressed patients collectively showed moderate increases in measures of guilt and shame, moderate deficits in working and verbal memory, moderately slowed reaction time, and mild to moderate negative affective bias, compared with controls. No correlation was found between performance on any of the individual cognitive domains and depression severity as measured using the Hamilton Depression Rating Scale, underscoring the concept that cognitive impairment is a distinct component of depressive pathology rather than an extension of the classic mood and somatic symptoms of major depression.
Cluster analysis revealed three distinct patterns of cognitive impairment in the study population. Unlike the individual cognitive domains, these cognitive clusters did correlate with depression severity. The implication is that as they become available.
Investigators classified 38 of the 92 patients with major depressive disorder as falling within Cluster A. That is, they exhibited marked deficits in hot cognition expressed in a greatly impaired ability to accurately identify facial emotions on photographs, with resultant high scores for emotion recognition bias and emotion misattribution bias. This impairment in hot cognition was accompanied by minimal guilt and shame and little or no deficits in the cold cognitive domains of verbal and working memory.
Cluster B, composed of 28 patients, was characterized by generally good cognitive function, with positive biases in emotion processing, near-normal guilt and shame ratings, but moderate deficits across the cold cognition domains, making for a mirror image of Cluster A.
The 26 patients in Cluster C demonstrated large deficits in both the hot and cold cognition domains, with particularly pronounced guilt and shame scores.
The three clusters didn’t differ in terms of age or sex. However, patients in Cluster C had significantly more severe core depressive symptoms as measured by Hamilton scores than in Clusters A and B.
This analysis from the NeuroPharm study was cross-sectional. Dr. Knudsen cited a recent large Chinese longitudinal study to underscore how the prevalence of patient-reported cognitive deficits in major depressive disorder is high. And while those deficits decrease over time, they nonetheless remain substantial after 6 months on antidepressant therapy.
That study included 598 Chinese outpatients with major depressive disorder. At baseline, 77% had cognitive symptoms as evidenced by a total score of 21 or more on the self-rated Perceived Deficits Questionnaire–Depression (PDQ-D). One month after going on antidepressant monotherapy, the prevalence of cognitive symptoms had dropped to 59%. At 2 months, the rate was 45%. And at month 6, a PDQ-D score of 21 or greater was still present in 32.4% of patients. High baseline PDQ-D scores were associated with worse clinical outcomes, including a lower treatment response rate at 1 month and a lower remission rate at 2 months. Moreover, high PDQ-D scores at 2 months were associated with lower remission and higher relapse rates at 6 months.
Dr. Knudsen reported having no financial conflicts regarding the NeuroPharm study, which was conducted free of commercial support. She serves as an adviser to Sage Therapeutics and Sanos.
Objective neuropsychological tests can be used to subclassify the cognitive symptoms present in patients with major depression into three patterns having implications for treatment responsiveness, Gitte Moos Knudsen, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Our data highlight the importance of assessing and targeting cognitive symptoms,” said Dr. Knudsen, the ECNP president and professor of neurology at the University of Copenhagen.
She was a coauthor of the Danish NeuroPharm study, in which 92 antidepressant-free patients with moderate or severe major depressive disorder and 103 healthy controls completed a comprehensive neuropsychological test battery. The testing included a validation study of the EMOTICOM test battery, a novel neuropsychological test battery developed specifically to assess what has been called “hot” cognition, such as emotion processing, social cognition, and affective verbal memory.
Overall, the depressed patients collectively showed moderate increases in measures of guilt and shame, moderate deficits in working and verbal memory, moderately slowed reaction time, and mild to moderate negative affective bias, compared with controls. No correlation was found between performance on any of the individual cognitive domains and depression severity as measured using the Hamilton Depression Rating Scale, underscoring the concept that cognitive impairment is a distinct component of depressive pathology rather than an extension of the classic mood and somatic symptoms of major depression.
Cluster analysis revealed three distinct patterns of cognitive impairment in the study population. Unlike the individual cognitive domains, these cognitive clusters did correlate with depression severity. The implication is that as they become available.
Investigators classified 38 of the 92 patients with major depressive disorder as falling within Cluster A. That is, they exhibited marked deficits in hot cognition expressed in a greatly impaired ability to accurately identify facial emotions on photographs, with resultant high scores for emotion recognition bias and emotion misattribution bias. This impairment in hot cognition was accompanied by minimal guilt and shame and little or no deficits in the cold cognitive domains of verbal and working memory.
Cluster B, composed of 28 patients, was characterized by generally good cognitive function, with positive biases in emotion processing, near-normal guilt and shame ratings, but moderate deficits across the cold cognition domains, making for a mirror image of Cluster A.
The 26 patients in Cluster C demonstrated large deficits in both the hot and cold cognition domains, with particularly pronounced guilt and shame scores.
The three clusters didn’t differ in terms of age or sex. However, patients in Cluster C had significantly more severe core depressive symptoms as measured by Hamilton scores than in Clusters A and B.
This analysis from the NeuroPharm study was cross-sectional. Dr. Knudsen cited a recent large Chinese longitudinal study to underscore how the prevalence of patient-reported cognitive deficits in major depressive disorder is high. And while those deficits decrease over time, they nonetheless remain substantial after 6 months on antidepressant therapy.
That study included 598 Chinese outpatients with major depressive disorder. At baseline, 77% had cognitive symptoms as evidenced by a total score of 21 or more on the self-rated Perceived Deficits Questionnaire–Depression (PDQ-D). One month after going on antidepressant monotherapy, the prevalence of cognitive symptoms had dropped to 59%. At 2 months, the rate was 45%. And at month 6, a PDQ-D score of 21 or greater was still present in 32.4% of patients. High baseline PDQ-D scores were associated with worse clinical outcomes, including a lower treatment response rate at 1 month and a lower remission rate at 2 months. Moreover, high PDQ-D scores at 2 months were associated with lower remission and higher relapse rates at 6 months.
Dr. Knudsen reported having no financial conflicts regarding the NeuroPharm study, which was conducted free of commercial support. She serves as an adviser to Sage Therapeutics and Sanos.
Objective neuropsychological tests can be used to subclassify the cognitive symptoms present in patients with major depression into three patterns having implications for treatment responsiveness, Gitte Moos Knudsen, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Our data highlight the importance of assessing and targeting cognitive symptoms,” said Dr. Knudsen, the ECNP president and professor of neurology at the University of Copenhagen.
She was a coauthor of the Danish NeuroPharm study, in which 92 antidepressant-free patients with moderate or severe major depressive disorder and 103 healthy controls completed a comprehensive neuropsychological test battery. The testing included a validation study of the EMOTICOM test battery, a novel neuropsychological test battery developed specifically to assess what has been called “hot” cognition, such as emotion processing, social cognition, and affective verbal memory.
Overall, the depressed patients collectively showed moderate increases in measures of guilt and shame, moderate deficits in working and verbal memory, moderately slowed reaction time, and mild to moderate negative affective bias, compared with controls. No correlation was found between performance on any of the individual cognitive domains and depression severity as measured using the Hamilton Depression Rating Scale, underscoring the concept that cognitive impairment is a distinct component of depressive pathology rather than an extension of the classic mood and somatic symptoms of major depression.
Cluster analysis revealed three distinct patterns of cognitive impairment in the study population. Unlike the individual cognitive domains, these cognitive clusters did correlate with depression severity. The implication is that as they become available.
Investigators classified 38 of the 92 patients with major depressive disorder as falling within Cluster A. That is, they exhibited marked deficits in hot cognition expressed in a greatly impaired ability to accurately identify facial emotions on photographs, with resultant high scores for emotion recognition bias and emotion misattribution bias. This impairment in hot cognition was accompanied by minimal guilt and shame and little or no deficits in the cold cognitive domains of verbal and working memory.
Cluster B, composed of 28 patients, was characterized by generally good cognitive function, with positive biases in emotion processing, near-normal guilt and shame ratings, but moderate deficits across the cold cognition domains, making for a mirror image of Cluster A.
The 26 patients in Cluster C demonstrated large deficits in both the hot and cold cognition domains, with particularly pronounced guilt and shame scores.
The three clusters didn’t differ in terms of age or sex. However, patients in Cluster C had significantly more severe core depressive symptoms as measured by Hamilton scores than in Clusters A and B.
This analysis from the NeuroPharm study was cross-sectional. Dr. Knudsen cited a recent large Chinese longitudinal study to underscore how the prevalence of patient-reported cognitive deficits in major depressive disorder is high. And while those deficits decrease over time, they nonetheless remain substantial after 6 months on antidepressant therapy.
That study included 598 Chinese outpatients with major depressive disorder. At baseline, 77% had cognitive symptoms as evidenced by a total score of 21 or more on the self-rated Perceived Deficits Questionnaire–Depression (PDQ-D). One month after going on antidepressant monotherapy, the prevalence of cognitive symptoms had dropped to 59%. At 2 months, the rate was 45%. And at month 6, a PDQ-D score of 21 or greater was still present in 32.4% of patients. High baseline PDQ-D scores were associated with worse clinical outcomes, including a lower treatment response rate at 1 month and a lower remission rate at 2 months. Moreover, high PDQ-D scores at 2 months were associated with lower remission and higher relapse rates at 6 months.
Dr. Knudsen reported having no financial conflicts regarding the NeuroPharm study, which was conducted free of commercial support. She serves as an adviser to Sage Therapeutics and Sanos.
FROM ECNP 2020
Listening to Tim Ferriss
Let me tell you about Tim Ferriss. A few years ago, I started reading his best-selling book, The 4-Hour Body. Ferris detailed how he made himself into a one-man experiment – he’d make changes to his diet, checked his weight and his labs, maybe he even had metabolic studies done.
He’d take these measures after soaking in hot baths, then ice baths, and while I admired his discipline, he did lose me during the chapter where he was using steroids. In the end, he advised a dairy-free, low-carbohydrate diet of green vegetables, beans or lentils, and protein for four meals a day, 6 days a week, with free-for-all eating on the 7th day. Then, there was a weight-lifting routine with kettle bells and ice packs to be placed on your shoulders for a set amount of time each day.
I may not remember the program’s details, but something about Ferris fascinated me. He brands himself as being a “human guinea pig,” about “lifestyle design,” and whatever that is, I like it. Perhaps I am attracted to the idea that we might control the trajectories of our generally uncontrollable lives.
Tim Ferriss graduated from Princeton, he’s written five best-selling books and has a popular podcast, he’s been a TED speaker, and he’s been on Fortune’s “40 under 40” list – and there’s so much more. Ferriss is brilliant, innovative, handsome, charismatic, prolific, extraordinarily athletic. I may have forgotten to mention that he was the National Chinese Kickboxing Champion and was a semifinalist in the World Champion Tango competition in Buenos Aires. He’s adventuresome and fearless, and if that isn’t enough, he speaks five languages. In the genetic dice roll, Mr. Ferriss did well, and he’s a driven and energetic hard worker who is open to new experiences.
I subscribe to the Tim Ferriss podcast – as of this writing, there are 466 episodes, with an incredible lineup of interviews with famous and successful guests. I also subscribe to his “5-Bullet Friday” email list where he mentions the interesting things he is reading, watching, learning about, or eating, and the products he is trying – single-ply toilet paper gets a thumbs down – then ends with a thought-provoking quote. This gentleman spends a tremendous amount of time searching and striving, working on himself and his own emotional growth and self-improvement, and yet he still has time for incredible explorations and experiences.
A search for psychic peace
Honestly, were it not for a few little details, I would like to be Tim Ferriss. Who wouldn’t? But what stops me from actually wanting to be Ferriss is that early on while listening to him, I realized that his drive has been fueled by intense psychic pain. He talks openly about being very close to suicide in college, about a tormenting mood disorder, demons to tame, and productivity as an antidote to a fear of failure, not always as a joy for life. There are moments that I have felt so sad for this remarkable stranger. Tim Ferriss is a searcher and what I believe he searches for most is his own psychic peace.
In a forum for psychiatrists, I wish I could write that Ferriss has found solace with our Food and Drug Administration–approved pharmaceuticals and with psychotherapy, but that’s not what he says. What Ferriss has found helpful, however, is psychedelics, and a wide variety of psychological and philosophical teachings ranging from meditation to Stoicism. And most notably, Ferriss has been an advocate for using hallucinogens as a legal medical intervention. Ferriss was one of four philanthropists who donated a total of $17 million to fund the Johns Hopkins Center for Psychedelic & Consciousness Research. He’s helped to move this field forward and to improve its credibility.
On Sept. 14, 2020, Tim Ferriss released a podcast he recorded with his dance partner and close friend, Debbie Millman, and when he recorded it, he was not certain he would release it. None of his usual sponsors endorsed during the podcast. He starts Episode #464 with, “For me, this is the most important podcast episode I’ve ever published. In it, I describe the most life-shaping, certainly the most difficult, and certainly the most transformative journey of my 43 years on this planet. I’ve never shared it before.”
by a babysitter’s son. He worried about how this would affect his family, if they would be left feeling guilty or devastated. He says, “Please note that I expect to be completely overwhelmed emotionally and otherwise when this is published and please understand if I’m not able to reply to any outreach.”
Ferriss and Millman had a long discussion about their sexual abuse as children. Millman was abused by her stepfather at the age of 9, and she talks about confronting him many years later. Ferriss has not confronted his perpetrator, though he has contemplated doing so.
Sexual violence and violation at any age leaves people scarred. In a recent letter to the New York Times in response to President Trump’s words of support to Ghislaine Maxwell, the woman who helped Jeffrey Epstein find his victims, Baltimore psychiatrist Robin Weiss wrote, “Thirty-eight years ago, when I was 32, I was raped. I was married, I was a doctor – you might say I was in pretty stable shape. Yet the shame and guilt I felt were overwhelming. Why didn’t I fight harder? How did I let this happen? I knew better, yet it took me years to overcome those irrational feelings.” These feelings of shame, guilt, self-doubt, and self-blame are nearly universal in survivors of sexual trauma. In children, they can be even worse, as children often don’t have an understanding that what is being done to them is wrong. They lack the language and the maturity to process the events, and ongoing abuse may be accompanied by threats to life of the child or their family members if they tell others, as was the case with Millman. She chose to process her abuse and the consequent difficulties she had by seeking psychiatric care. She took antidepressants and has been in psychoanalysis, both of which she has found to be helpful. Her treatment has tamed her demons, it is ongoing decades later and those demons have not vanished.
Abuse comes back in ‘a tidal wave’
Not surprisingly, Ferriss struggled with whether to make these events public. While so much of his story feels familiar to those of us who help patients process their trauma, it’s not completely typical. Ferriss remembered these episodes of sexual abuse “in high resolution,” while using ayahuasca, a hallucinogen, about 5 years ago. He describes suppressing and discounting these memories until he attended a 10-day silent retreat where he used psilocybin. I found it interesting that Ferriss fasted for 5 days before attending the retreat “to increase the depth of the experience.” He goes on to say, “Around day 6 of this silent retreat, all of this abuse came back to me like a tidal wave and it was replaying as if I was wearing a virtual reality headset. I was immersed, I wasn’t an observer, it was as though I was being traumatized and retraumatized 24/7.” He describes an excruciating and horrifying experience and he referred to it as a “psychotic break.”
Ferriss goes on to talk about how bringing these memories to light has affected him, how it’s explained many of his behaviors and ways of relating in a way that has helped him organize and understand his life.
“It was at the tail end of the retreat that I realized that these 17 seemingly inexplicable behaviors of mine – these vicious cycles or triggers that I had been treating like separate problems to be solved, were all downstream of this trauma. Oh, now that you click that puzzle piece into place, these really strange behaviors – this self-loathing, this rage that was seemingly so exaggerated and disproportionate – leading to the near-suicide I had in college – all these things fell into places making sense.” It gave him a sense of relief but was simultaneously overwhelming.
Both Ferriss and Millman talk about books and treatments that have been helpful to them. Their knowledge of trauma treatments and resources is impressive and can be found at: Tim Ferriss – My Healing Journey After Childhood Abuse (Includes Extensive Resource List). Their wish is to share their suffering as a way to help others, impart hope, and better connect.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Let me tell you about Tim Ferriss. A few years ago, I started reading his best-selling book, The 4-Hour Body. Ferris detailed how he made himself into a one-man experiment – he’d make changes to his diet, checked his weight and his labs, maybe he even had metabolic studies done.
He’d take these measures after soaking in hot baths, then ice baths, and while I admired his discipline, he did lose me during the chapter where he was using steroids. In the end, he advised a dairy-free, low-carbohydrate diet of green vegetables, beans or lentils, and protein for four meals a day, 6 days a week, with free-for-all eating on the 7th day. Then, there was a weight-lifting routine with kettle bells and ice packs to be placed on your shoulders for a set amount of time each day.
I may not remember the program’s details, but something about Ferris fascinated me. He brands himself as being a “human guinea pig,” about “lifestyle design,” and whatever that is, I like it. Perhaps I am attracted to the idea that we might control the trajectories of our generally uncontrollable lives.
Tim Ferriss graduated from Princeton, he’s written five best-selling books and has a popular podcast, he’s been a TED speaker, and he’s been on Fortune’s “40 under 40” list – and there’s so much more. Ferriss is brilliant, innovative, handsome, charismatic, prolific, extraordinarily athletic. I may have forgotten to mention that he was the National Chinese Kickboxing Champion and was a semifinalist in the World Champion Tango competition in Buenos Aires. He’s adventuresome and fearless, and if that isn’t enough, he speaks five languages. In the genetic dice roll, Mr. Ferriss did well, and he’s a driven and energetic hard worker who is open to new experiences.
I subscribe to the Tim Ferriss podcast – as of this writing, there are 466 episodes, with an incredible lineup of interviews with famous and successful guests. I also subscribe to his “5-Bullet Friday” email list where he mentions the interesting things he is reading, watching, learning about, or eating, and the products he is trying – single-ply toilet paper gets a thumbs down – then ends with a thought-provoking quote. This gentleman spends a tremendous amount of time searching and striving, working on himself and his own emotional growth and self-improvement, and yet he still has time for incredible explorations and experiences.
A search for psychic peace
Honestly, were it not for a few little details, I would like to be Tim Ferriss. Who wouldn’t? But what stops me from actually wanting to be Ferriss is that early on while listening to him, I realized that his drive has been fueled by intense psychic pain. He talks openly about being very close to suicide in college, about a tormenting mood disorder, demons to tame, and productivity as an antidote to a fear of failure, not always as a joy for life. There are moments that I have felt so sad for this remarkable stranger. Tim Ferriss is a searcher and what I believe he searches for most is his own psychic peace.
In a forum for psychiatrists, I wish I could write that Ferriss has found solace with our Food and Drug Administration–approved pharmaceuticals and with psychotherapy, but that’s not what he says. What Ferriss has found helpful, however, is psychedelics, and a wide variety of psychological and philosophical teachings ranging from meditation to Stoicism. And most notably, Ferriss has been an advocate for using hallucinogens as a legal medical intervention. Ferriss was one of four philanthropists who donated a total of $17 million to fund the Johns Hopkins Center for Psychedelic & Consciousness Research. He’s helped to move this field forward and to improve its credibility.
On Sept. 14, 2020, Tim Ferriss released a podcast he recorded with his dance partner and close friend, Debbie Millman, and when he recorded it, he was not certain he would release it. None of his usual sponsors endorsed during the podcast. He starts Episode #464 with, “For me, this is the most important podcast episode I’ve ever published. In it, I describe the most life-shaping, certainly the most difficult, and certainly the most transformative journey of my 43 years on this planet. I’ve never shared it before.”
by a babysitter’s son. He worried about how this would affect his family, if they would be left feeling guilty or devastated. He says, “Please note that I expect to be completely overwhelmed emotionally and otherwise when this is published and please understand if I’m not able to reply to any outreach.”
Ferriss and Millman had a long discussion about their sexual abuse as children. Millman was abused by her stepfather at the age of 9, and she talks about confronting him many years later. Ferriss has not confronted his perpetrator, though he has contemplated doing so.
Sexual violence and violation at any age leaves people scarred. In a recent letter to the New York Times in response to President Trump’s words of support to Ghislaine Maxwell, the woman who helped Jeffrey Epstein find his victims, Baltimore psychiatrist Robin Weiss wrote, “Thirty-eight years ago, when I was 32, I was raped. I was married, I was a doctor – you might say I was in pretty stable shape. Yet the shame and guilt I felt were overwhelming. Why didn’t I fight harder? How did I let this happen? I knew better, yet it took me years to overcome those irrational feelings.” These feelings of shame, guilt, self-doubt, and self-blame are nearly universal in survivors of sexual trauma. In children, they can be even worse, as children often don’t have an understanding that what is being done to them is wrong. They lack the language and the maturity to process the events, and ongoing abuse may be accompanied by threats to life of the child or their family members if they tell others, as was the case with Millman. She chose to process her abuse and the consequent difficulties she had by seeking psychiatric care. She took antidepressants and has been in psychoanalysis, both of which she has found to be helpful. Her treatment has tamed her demons, it is ongoing decades later and those demons have not vanished.
Abuse comes back in ‘a tidal wave’
Not surprisingly, Ferriss struggled with whether to make these events public. While so much of his story feels familiar to those of us who help patients process their trauma, it’s not completely typical. Ferriss remembered these episodes of sexual abuse “in high resolution,” while using ayahuasca, a hallucinogen, about 5 years ago. He describes suppressing and discounting these memories until he attended a 10-day silent retreat where he used psilocybin. I found it interesting that Ferriss fasted for 5 days before attending the retreat “to increase the depth of the experience.” He goes on to say, “Around day 6 of this silent retreat, all of this abuse came back to me like a tidal wave and it was replaying as if I was wearing a virtual reality headset. I was immersed, I wasn’t an observer, it was as though I was being traumatized and retraumatized 24/7.” He describes an excruciating and horrifying experience and he referred to it as a “psychotic break.”
Ferriss goes on to talk about how bringing these memories to light has affected him, how it’s explained many of his behaviors and ways of relating in a way that has helped him organize and understand his life.
“It was at the tail end of the retreat that I realized that these 17 seemingly inexplicable behaviors of mine – these vicious cycles or triggers that I had been treating like separate problems to be solved, were all downstream of this trauma. Oh, now that you click that puzzle piece into place, these really strange behaviors – this self-loathing, this rage that was seemingly so exaggerated and disproportionate – leading to the near-suicide I had in college – all these things fell into places making sense.” It gave him a sense of relief but was simultaneously overwhelming.
Both Ferriss and Millman talk about books and treatments that have been helpful to them. Their knowledge of trauma treatments and resources is impressive and can be found at: Tim Ferriss – My Healing Journey After Childhood Abuse (Includes Extensive Resource List). Their wish is to share their suffering as a way to help others, impart hope, and better connect.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Let me tell you about Tim Ferriss. A few years ago, I started reading his best-selling book, The 4-Hour Body. Ferris detailed how he made himself into a one-man experiment – he’d make changes to his diet, checked his weight and his labs, maybe he even had metabolic studies done.
He’d take these measures after soaking in hot baths, then ice baths, and while I admired his discipline, he did lose me during the chapter where he was using steroids. In the end, he advised a dairy-free, low-carbohydrate diet of green vegetables, beans or lentils, and protein for four meals a day, 6 days a week, with free-for-all eating on the 7th day. Then, there was a weight-lifting routine with kettle bells and ice packs to be placed on your shoulders for a set amount of time each day.
I may not remember the program’s details, but something about Ferris fascinated me. He brands himself as being a “human guinea pig,” about “lifestyle design,” and whatever that is, I like it. Perhaps I am attracted to the idea that we might control the trajectories of our generally uncontrollable lives.
Tim Ferriss graduated from Princeton, he’s written five best-selling books and has a popular podcast, he’s been a TED speaker, and he’s been on Fortune’s “40 under 40” list – and there’s so much more. Ferriss is brilliant, innovative, handsome, charismatic, prolific, extraordinarily athletic. I may have forgotten to mention that he was the National Chinese Kickboxing Champion and was a semifinalist in the World Champion Tango competition in Buenos Aires. He’s adventuresome and fearless, and if that isn’t enough, he speaks five languages. In the genetic dice roll, Mr. Ferriss did well, and he’s a driven and energetic hard worker who is open to new experiences.
I subscribe to the Tim Ferriss podcast – as of this writing, there are 466 episodes, with an incredible lineup of interviews with famous and successful guests. I also subscribe to his “5-Bullet Friday” email list where he mentions the interesting things he is reading, watching, learning about, or eating, and the products he is trying – single-ply toilet paper gets a thumbs down – then ends with a thought-provoking quote. This gentleman spends a tremendous amount of time searching and striving, working on himself and his own emotional growth and self-improvement, and yet he still has time for incredible explorations and experiences.
A search for psychic peace
Honestly, were it not for a few little details, I would like to be Tim Ferriss. Who wouldn’t? But what stops me from actually wanting to be Ferriss is that early on while listening to him, I realized that his drive has been fueled by intense psychic pain. He talks openly about being very close to suicide in college, about a tormenting mood disorder, demons to tame, and productivity as an antidote to a fear of failure, not always as a joy for life. There are moments that I have felt so sad for this remarkable stranger. Tim Ferriss is a searcher and what I believe he searches for most is his own psychic peace.
In a forum for psychiatrists, I wish I could write that Ferriss has found solace with our Food and Drug Administration–approved pharmaceuticals and with psychotherapy, but that’s not what he says. What Ferriss has found helpful, however, is psychedelics, and a wide variety of psychological and philosophical teachings ranging from meditation to Stoicism. And most notably, Ferriss has been an advocate for using hallucinogens as a legal medical intervention. Ferriss was one of four philanthropists who donated a total of $17 million to fund the Johns Hopkins Center for Psychedelic & Consciousness Research. He’s helped to move this field forward and to improve its credibility.
On Sept. 14, 2020, Tim Ferriss released a podcast he recorded with his dance partner and close friend, Debbie Millman, and when he recorded it, he was not certain he would release it. None of his usual sponsors endorsed during the podcast. He starts Episode #464 with, “For me, this is the most important podcast episode I’ve ever published. In it, I describe the most life-shaping, certainly the most difficult, and certainly the most transformative journey of my 43 years on this planet. I’ve never shared it before.”
by a babysitter’s son. He worried about how this would affect his family, if they would be left feeling guilty or devastated. He says, “Please note that I expect to be completely overwhelmed emotionally and otherwise when this is published and please understand if I’m not able to reply to any outreach.”
Ferriss and Millman had a long discussion about their sexual abuse as children. Millman was abused by her stepfather at the age of 9, and she talks about confronting him many years later. Ferriss has not confronted his perpetrator, though he has contemplated doing so.
Sexual violence and violation at any age leaves people scarred. In a recent letter to the New York Times in response to President Trump’s words of support to Ghislaine Maxwell, the woman who helped Jeffrey Epstein find his victims, Baltimore psychiatrist Robin Weiss wrote, “Thirty-eight years ago, when I was 32, I was raped. I was married, I was a doctor – you might say I was in pretty stable shape. Yet the shame and guilt I felt were overwhelming. Why didn’t I fight harder? How did I let this happen? I knew better, yet it took me years to overcome those irrational feelings.” These feelings of shame, guilt, self-doubt, and self-blame are nearly universal in survivors of sexual trauma. In children, they can be even worse, as children often don’t have an understanding that what is being done to them is wrong. They lack the language and the maturity to process the events, and ongoing abuse may be accompanied by threats to life of the child or their family members if they tell others, as was the case with Millman. She chose to process her abuse and the consequent difficulties she had by seeking psychiatric care. She took antidepressants and has been in psychoanalysis, both of which she has found to be helpful. Her treatment has tamed her demons, it is ongoing decades later and those demons have not vanished.
Abuse comes back in ‘a tidal wave’
Not surprisingly, Ferriss struggled with whether to make these events public. While so much of his story feels familiar to those of us who help patients process their trauma, it’s not completely typical. Ferriss remembered these episodes of sexual abuse “in high resolution,” while using ayahuasca, a hallucinogen, about 5 years ago. He describes suppressing and discounting these memories until he attended a 10-day silent retreat where he used psilocybin. I found it interesting that Ferriss fasted for 5 days before attending the retreat “to increase the depth of the experience.” He goes on to say, “Around day 6 of this silent retreat, all of this abuse came back to me like a tidal wave and it was replaying as if I was wearing a virtual reality headset. I was immersed, I wasn’t an observer, it was as though I was being traumatized and retraumatized 24/7.” He describes an excruciating and horrifying experience and he referred to it as a “psychotic break.”
Ferriss goes on to talk about how bringing these memories to light has affected him, how it’s explained many of his behaviors and ways of relating in a way that has helped him organize and understand his life.
“It was at the tail end of the retreat that I realized that these 17 seemingly inexplicable behaviors of mine – these vicious cycles or triggers that I had been treating like separate problems to be solved, were all downstream of this trauma. Oh, now that you click that puzzle piece into place, these really strange behaviors – this self-loathing, this rage that was seemingly so exaggerated and disproportionate – leading to the near-suicide I had in college – all these things fell into places making sense.” It gave him a sense of relief but was simultaneously overwhelming.
Both Ferriss and Millman talk about books and treatments that have been helpful to them. Their knowledge of trauma treatments and resources is impressive and can be found at: Tim Ferriss – My Healing Journey After Childhood Abuse (Includes Extensive Resource List). Their wish is to share their suffering as a way to help others, impart hope, and better connect.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Suicidality jumped in Israel during spring COVID-19 lockdown
Suicidality appears to have increased sharply in Israel during the initial nationwide lockdown implemented in response to the COVID-19 pandemic, Gil Zalsman, MD, MHA, reported at the virtual congress of the European College of Neuropsychopharmacology.
He presented highlights from a soon-to-be-published analysis of the content of online chat sessions fielded by a national crisis hotline (Sahar.org.il) during the first 6 months of 2020, compared with January through June 2019, in the pre-COVID-19 era.
It’s far too early to say whether actual deaths tied to suicide rose significantly during the spring lockdown, since medical examiners often take a long time before ruling suicide as cause of death. But this much is clear: The number of suicide-related chat sessions recorded at the volunteer-staffed national hotline during April 2020 was two-and-a-half times greater than in April 2019, and threefold greater in May 2020 than a year earlier, according to Dr. Zalsman, professor of psychiatry at Tel Aviv University and director of the Geha Mental Health Center in Petach Tikva, Israel, where he also directs an adolescent day unit.
The proportion of chats handled at the crisis hotline, many of them concerned with the standard topics – relationships, stress, fears, anxiety, and other non–suicide-related issues – was 48% greater in the first half of 2020, compared with a year earlier. Indeed, the pandemic is putting an enormous strain on crisis hotlines the world over.
“Everybody who is working hotlines knows that they’re falling apart. There are too many calls, too many chats. They need to multiply their volunteers,” Dr. Zalsman said.
The number of suicide-related online chats jumped the week of March 12, when schools closed across Israel and a partial lockdown began. The peak in suicide-related chats occurred beginning the week of April 17, when the forced total lockdown was declared.
“Everything was closed. You couldn’t go out or the police would arrest you,” Dr. Zalsman recalled.
The suicide-related chat count started to drop off in mid-May, when schools reopened, and continued to decline through the end of June.
Only a small percentage of suicide-related chats were deemed by crisis hotline volunteers and their supervisors to be truly life-threatening situations necessitating a call to the police. But the number of such exchanges was significantly greater in April and May 2020 than in January and February, or in April and May 2019.
Use of the crisis hotline is ordinarily skewed toward tech-savvy young people, or as Dr. Zalsman called them, “kids who live inside their computers.” He note that the psychological impact of the pandemic on children and adolescents is largely unexplored research territory to date.
“ You can kill your grandfather by coughing,” Dr. Zalsman said.
Older people also seek help
A finding that he and his coinvestigators didn’t anticipate was the significantly increased use of the service by individuals aged 65 and older during the pandemic. This underscores the increased vulnerability of older people, which stems in part from their heightened risk for severe infection and consequent need for prolonged physical isolation, he said.
The conventional thinking among suicidologists is that during times of crisis – wars, natural disasters – suicidality plunges, then rises quickly afterward.
“People withhold themselves. When there’s a big danger from outside they ignore the danger from inside. And once the danger from outside is gone, they’re left with emptiness, unemployment, economic crisis, and they start” taking their own lives, Dr. Zalsman explained. He expects suicidality to increase after the pandemic, or as the Israeli crisis hotline data suggest, perhaps even during it, for multiple reasons. Patients with preexisting psychiatric disorders are often going untreated. The prolonged physical isolation causes emotional difficulties for some people, especially when accompanied by social isolation and loneliness. There is grief over the loss of friends and relatives because of COVID-19. And there is an expectation of looming economic hardship, with mounting unemployment and bankruptcies.
Dr. Zalsman reported having no financial conflicts regarding his study, conducted free of commercial support.
SOURCE: Zalsman G. ECNP 2020, Session TP.06.
Suicidality appears to have increased sharply in Israel during the initial nationwide lockdown implemented in response to the COVID-19 pandemic, Gil Zalsman, MD, MHA, reported at the virtual congress of the European College of Neuropsychopharmacology.
He presented highlights from a soon-to-be-published analysis of the content of online chat sessions fielded by a national crisis hotline (Sahar.org.il) during the first 6 months of 2020, compared with January through June 2019, in the pre-COVID-19 era.
It’s far too early to say whether actual deaths tied to suicide rose significantly during the spring lockdown, since medical examiners often take a long time before ruling suicide as cause of death. But this much is clear: The number of suicide-related chat sessions recorded at the volunteer-staffed national hotline during April 2020 was two-and-a-half times greater than in April 2019, and threefold greater in May 2020 than a year earlier, according to Dr. Zalsman, professor of psychiatry at Tel Aviv University and director of the Geha Mental Health Center in Petach Tikva, Israel, where he also directs an adolescent day unit.
The proportion of chats handled at the crisis hotline, many of them concerned with the standard topics – relationships, stress, fears, anxiety, and other non–suicide-related issues – was 48% greater in the first half of 2020, compared with a year earlier. Indeed, the pandemic is putting an enormous strain on crisis hotlines the world over.
“Everybody who is working hotlines knows that they’re falling apart. There are too many calls, too many chats. They need to multiply their volunteers,” Dr. Zalsman said.
The number of suicide-related online chats jumped the week of March 12, when schools closed across Israel and a partial lockdown began. The peak in suicide-related chats occurred beginning the week of April 17, when the forced total lockdown was declared.
“Everything was closed. You couldn’t go out or the police would arrest you,” Dr. Zalsman recalled.
The suicide-related chat count started to drop off in mid-May, when schools reopened, and continued to decline through the end of June.
Only a small percentage of suicide-related chats were deemed by crisis hotline volunteers and their supervisors to be truly life-threatening situations necessitating a call to the police. But the number of such exchanges was significantly greater in April and May 2020 than in January and February, or in April and May 2019.
Use of the crisis hotline is ordinarily skewed toward tech-savvy young people, or as Dr. Zalsman called them, “kids who live inside their computers.” He note that the psychological impact of the pandemic on children and adolescents is largely unexplored research territory to date.
“ You can kill your grandfather by coughing,” Dr. Zalsman said.
Older people also seek help
A finding that he and his coinvestigators didn’t anticipate was the significantly increased use of the service by individuals aged 65 and older during the pandemic. This underscores the increased vulnerability of older people, which stems in part from their heightened risk for severe infection and consequent need for prolonged physical isolation, he said.
The conventional thinking among suicidologists is that during times of crisis – wars, natural disasters – suicidality plunges, then rises quickly afterward.
“People withhold themselves. When there’s a big danger from outside they ignore the danger from inside. And once the danger from outside is gone, they’re left with emptiness, unemployment, economic crisis, and they start” taking their own lives, Dr. Zalsman explained. He expects suicidality to increase after the pandemic, or as the Israeli crisis hotline data suggest, perhaps even during it, for multiple reasons. Patients with preexisting psychiatric disorders are often going untreated. The prolonged physical isolation causes emotional difficulties for some people, especially when accompanied by social isolation and loneliness. There is grief over the loss of friends and relatives because of COVID-19. And there is an expectation of looming economic hardship, with mounting unemployment and bankruptcies.
Dr. Zalsman reported having no financial conflicts regarding his study, conducted free of commercial support.
SOURCE: Zalsman G. ECNP 2020, Session TP.06.
Suicidality appears to have increased sharply in Israel during the initial nationwide lockdown implemented in response to the COVID-19 pandemic, Gil Zalsman, MD, MHA, reported at the virtual congress of the European College of Neuropsychopharmacology.
He presented highlights from a soon-to-be-published analysis of the content of online chat sessions fielded by a national crisis hotline (Sahar.org.il) during the first 6 months of 2020, compared with January through June 2019, in the pre-COVID-19 era.
It’s far too early to say whether actual deaths tied to suicide rose significantly during the spring lockdown, since medical examiners often take a long time before ruling suicide as cause of death. But this much is clear: The number of suicide-related chat sessions recorded at the volunteer-staffed national hotline during April 2020 was two-and-a-half times greater than in April 2019, and threefold greater in May 2020 than a year earlier, according to Dr. Zalsman, professor of psychiatry at Tel Aviv University and director of the Geha Mental Health Center in Petach Tikva, Israel, where he also directs an adolescent day unit.
The proportion of chats handled at the crisis hotline, many of them concerned with the standard topics – relationships, stress, fears, anxiety, and other non–suicide-related issues – was 48% greater in the first half of 2020, compared with a year earlier. Indeed, the pandemic is putting an enormous strain on crisis hotlines the world over.
“Everybody who is working hotlines knows that they’re falling apart. There are too many calls, too many chats. They need to multiply their volunteers,” Dr. Zalsman said.
The number of suicide-related online chats jumped the week of March 12, when schools closed across Israel and a partial lockdown began. The peak in suicide-related chats occurred beginning the week of April 17, when the forced total lockdown was declared.
“Everything was closed. You couldn’t go out or the police would arrest you,” Dr. Zalsman recalled.
The suicide-related chat count started to drop off in mid-May, when schools reopened, and continued to decline through the end of June.
Only a small percentage of suicide-related chats were deemed by crisis hotline volunteers and their supervisors to be truly life-threatening situations necessitating a call to the police. But the number of such exchanges was significantly greater in April and May 2020 than in January and February, or in April and May 2019.
Use of the crisis hotline is ordinarily skewed toward tech-savvy young people, or as Dr. Zalsman called them, “kids who live inside their computers.” He note that the psychological impact of the pandemic on children and adolescents is largely unexplored research territory to date.
“ You can kill your grandfather by coughing,” Dr. Zalsman said.
Older people also seek help
A finding that he and his coinvestigators didn’t anticipate was the significantly increased use of the service by individuals aged 65 and older during the pandemic. This underscores the increased vulnerability of older people, which stems in part from their heightened risk for severe infection and consequent need for prolonged physical isolation, he said.
The conventional thinking among suicidologists is that during times of crisis – wars, natural disasters – suicidality plunges, then rises quickly afterward.
“People withhold themselves. When there’s a big danger from outside they ignore the danger from inside. And once the danger from outside is gone, they’re left with emptiness, unemployment, economic crisis, and they start” taking their own lives, Dr. Zalsman explained. He expects suicidality to increase after the pandemic, or as the Israeli crisis hotline data suggest, perhaps even during it, for multiple reasons. Patients with preexisting psychiatric disorders are often going untreated. The prolonged physical isolation causes emotional difficulties for some people, especially when accompanied by social isolation and loneliness. There is grief over the loss of friends and relatives because of COVID-19. And there is an expectation of looming economic hardship, with mounting unemployment and bankruptcies.
Dr. Zalsman reported having no financial conflicts regarding his study, conducted free of commercial support.
SOURCE: Zalsman G. ECNP 2020, Session TP.06.
FROM ECNP 2020
Suicide rates up significantly among adolescents, young adults
Suicide rates in young people aged 10-24 years increased significantly in 42 states from 2007-2009 to 2016-2018, according to a recent analysis from the National Center for Health Statistics.
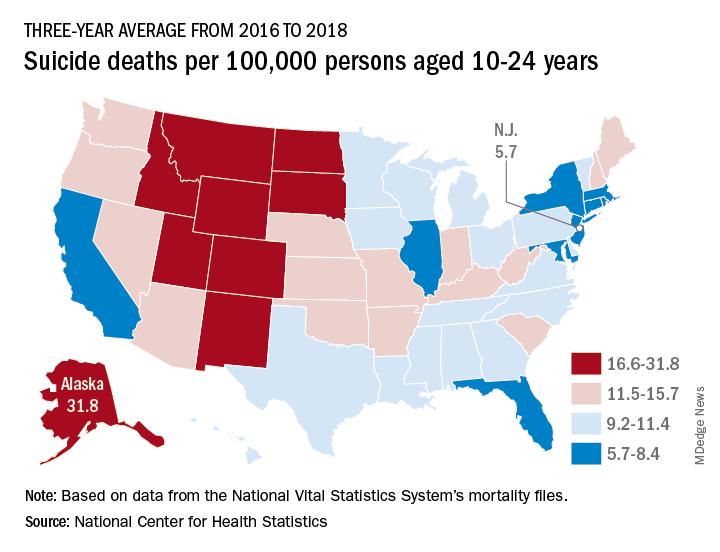
Nationally, the suicide rate jumped 47%, based on the averages for the two 3-year periods, rising from 7.0 per 100,000 persons aged 10-24 years to 10.3 per 100,000. For all ages, the corresponding increase was 47%, Sally C. Curtin, MA, of the NCHS, said in a National Vital Statistics Report.
There was no state with a decrease in suicide rates for adolescents and young adults, as the other eight all had nonsignificant increases, the smallest being 14% in South Dakota. Three-year averages were used to increase statistical power for states with relatively small numbers of deaths but were still not enough to show significance for some large increases, such as the 48% rise in Delaware, Ms. Curtin noted.
In 2016-2018, Alaska’s suicide rate of 31.8 per 100,000 persons aged 10-24 years was the highest in the country, followed by South Dakota (23.6), Montana (23.2), and Wyoming (20.5). New Jersey had the lowest rate at 5.7 per 100,000, with New York and Rhode Island both slightly higher at 5.9 and Connecticut at 6.3, based on data from the National Vital Statistics System.
Even the low numbers, however, hide some large changes, as New Jersey (up by 39%) and New York (up by 44%) were among the 42 states with statistically significant increases, which ranged from 21.7% in Maryland to 110% in New Hampshire, Ms. Curtin said in the report. The increases seen in this analysis contrast with data from the preceding time period, as “the suicide rate among persons aged 10-24 was statistically stable from 2000 to 2007.”
SOURCE: Curtin SC. National Vital Statistics Reports. 2020;69(11)1-9.
Suicide rates in young people aged 10-24 years increased significantly in 42 states from 2007-2009 to 2016-2018, according to a recent analysis from the National Center for Health Statistics.
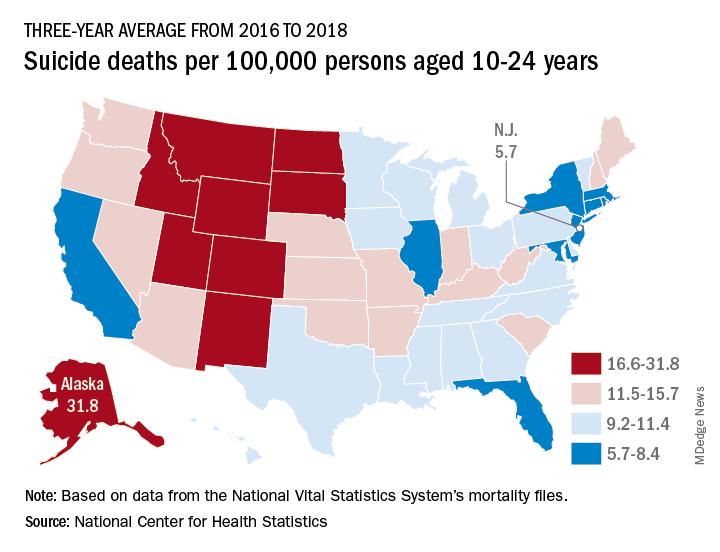
Nationally, the suicide rate jumped 47%, based on the averages for the two 3-year periods, rising from 7.0 per 100,000 persons aged 10-24 years to 10.3 per 100,000. For all ages, the corresponding increase was 47%, Sally C. Curtin, MA, of the NCHS, said in a National Vital Statistics Report.
There was no state with a decrease in suicide rates for adolescents and young adults, as the other eight all had nonsignificant increases, the smallest being 14% in South Dakota. Three-year averages were used to increase statistical power for states with relatively small numbers of deaths but were still not enough to show significance for some large increases, such as the 48% rise in Delaware, Ms. Curtin noted.
In 2016-2018, Alaska’s suicide rate of 31.8 per 100,000 persons aged 10-24 years was the highest in the country, followed by South Dakota (23.6), Montana (23.2), and Wyoming (20.5). New Jersey had the lowest rate at 5.7 per 100,000, with New York and Rhode Island both slightly higher at 5.9 and Connecticut at 6.3, based on data from the National Vital Statistics System.
Even the low numbers, however, hide some large changes, as New Jersey (up by 39%) and New York (up by 44%) were among the 42 states with statistically significant increases, which ranged from 21.7% in Maryland to 110% in New Hampshire, Ms. Curtin said in the report. The increases seen in this analysis contrast with data from the preceding time period, as “the suicide rate among persons aged 10-24 was statistically stable from 2000 to 2007.”
SOURCE: Curtin SC. National Vital Statistics Reports. 2020;69(11)1-9.
Suicide rates in young people aged 10-24 years increased significantly in 42 states from 2007-2009 to 2016-2018, according to a recent analysis from the National Center for Health Statistics.
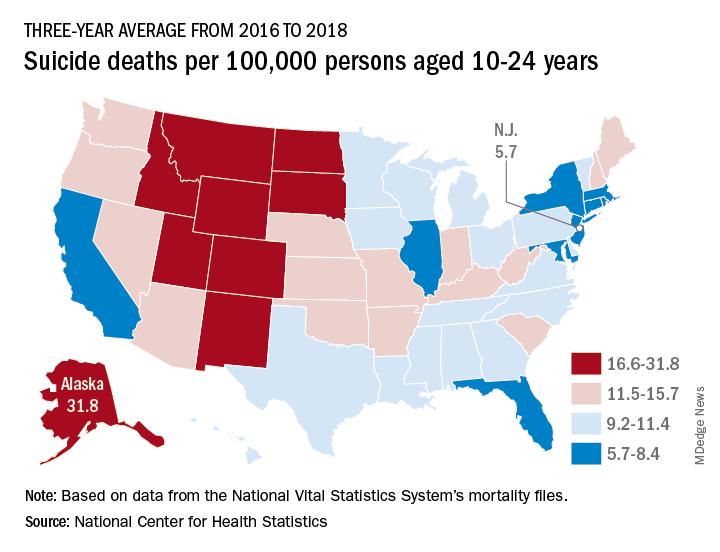
Nationally, the suicide rate jumped 47%, based on the averages for the two 3-year periods, rising from 7.0 per 100,000 persons aged 10-24 years to 10.3 per 100,000. For all ages, the corresponding increase was 47%, Sally C. Curtin, MA, of the NCHS, said in a National Vital Statistics Report.
There was no state with a decrease in suicide rates for adolescents and young adults, as the other eight all had nonsignificant increases, the smallest being 14% in South Dakota. Three-year averages were used to increase statistical power for states with relatively small numbers of deaths but were still not enough to show significance for some large increases, such as the 48% rise in Delaware, Ms. Curtin noted.
In 2016-2018, Alaska’s suicide rate of 31.8 per 100,000 persons aged 10-24 years was the highest in the country, followed by South Dakota (23.6), Montana (23.2), and Wyoming (20.5). New Jersey had the lowest rate at 5.7 per 100,000, with New York and Rhode Island both slightly higher at 5.9 and Connecticut at 6.3, based on data from the National Vital Statistics System.
Even the low numbers, however, hide some large changes, as New Jersey (up by 39%) and New York (up by 44%) were among the 42 states with statistically significant increases, which ranged from 21.7% in Maryland to 110% in New Hampshire, Ms. Curtin said in the report. The increases seen in this analysis contrast with data from the preceding time period, as “the suicide rate among persons aged 10-24 was statistically stable from 2000 to 2007.”
SOURCE: Curtin SC. National Vital Statistics Reports. 2020;69(11)1-9.






