User login
Underprescribed menopause relief: Women suffer needlessly
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
Older women risk overdiagnosis with mammograms: Study
Women who continued breast cancer screenings when they reached age 70 had no lower chance of dying from the disease, and just getting a mammogram could instead set them on a path toward unnecessary risks, according to a new study from Yale University.
The findings, published in Annals of Internal Medicine, suggest that , meaning that the cancer found during the screening would not have caused symptoms in a person’s lifetime. (For context, the average life expectancy of a woman in the U.S. is 79 years, according to the Centers for Disease Control and Prevention.)
Overdiagnosis can be harmful because it carries the risks of complications from overtreatment, plus financial and emotional hardships and unnecessary use of limited resources.
For the study, researchers analyzed data for 54,635 women aged 70 and older and compared the rate of breast cancer diagnosis and death among women who did and did not have mammograms during a 15-year follow-up period.
The rate of breast cancer in the study among women aged 70-74 was 6% for women who were screened and 4% for women who were not screened. The researchers estimated that 31% of the cases were potentially overdiagnosed. Among women aged 75-84, breast cancer was found in 5% of women who were screened, compared to less than 3% of unscreened women. Their estimated overdiagnosis rate was 47%. Finally, 3% of women aged 85 and older who were screened had breast cancer detected, compared with 1% of women in the unscreened group. For the older group, the overdiagnosis rate was 54%.
“While our study focused on overdiagnosis, it is important to acknowledge that overdiagnosis is just one of many considerations when deciding whether to continue screening,” researcher and Yale assistant professor of medicine Ilana Richman, MD, said in a statement. “A patient’s preferences and values, personal risk factors, and the overall balance of risks and benefits from screening are also important to take into account when making screening decisions.”
A version of this article first appeared on WebMD.com.
Women who continued breast cancer screenings when they reached age 70 had no lower chance of dying from the disease, and just getting a mammogram could instead set them on a path toward unnecessary risks, according to a new study from Yale University.
The findings, published in Annals of Internal Medicine, suggest that , meaning that the cancer found during the screening would not have caused symptoms in a person’s lifetime. (For context, the average life expectancy of a woman in the U.S. is 79 years, according to the Centers for Disease Control and Prevention.)
Overdiagnosis can be harmful because it carries the risks of complications from overtreatment, plus financial and emotional hardships and unnecessary use of limited resources.
For the study, researchers analyzed data for 54,635 women aged 70 and older and compared the rate of breast cancer diagnosis and death among women who did and did not have mammograms during a 15-year follow-up period.
The rate of breast cancer in the study among women aged 70-74 was 6% for women who were screened and 4% for women who were not screened. The researchers estimated that 31% of the cases were potentially overdiagnosed. Among women aged 75-84, breast cancer was found in 5% of women who were screened, compared to less than 3% of unscreened women. Their estimated overdiagnosis rate was 47%. Finally, 3% of women aged 85 and older who were screened had breast cancer detected, compared with 1% of women in the unscreened group. For the older group, the overdiagnosis rate was 54%.
“While our study focused on overdiagnosis, it is important to acknowledge that overdiagnosis is just one of many considerations when deciding whether to continue screening,” researcher and Yale assistant professor of medicine Ilana Richman, MD, said in a statement. “A patient’s preferences and values, personal risk factors, and the overall balance of risks and benefits from screening are also important to take into account when making screening decisions.”
A version of this article first appeared on WebMD.com.
Women who continued breast cancer screenings when they reached age 70 had no lower chance of dying from the disease, and just getting a mammogram could instead set them on a path toward unnecessary risks, according to a new study from Yale University.
The findings, published in Annals of Internal Medicine, suggest that , meaning that the cancer found during the screening would not have caused symptoms in a person’s lifetime. (For context, the average life expectancy of a woman in the U.S. is 79 years, according to the Centers for Disease Control and Prevention.)
Overdiagnosis can be harmful because it carries the risks of complications from overtreatment, plus financial and emotional hardships and unnecessary use of limited resources.
For the study, researchers analyzed data for 54,635 women aged 70 and older and compared the rate of breast cancer diagnosis and death among women who did and did not have mammograms during a 15-year follow-up period.
The rate of breast cancer in the study among women aged 70-74 was 6% for women who were screened and 4% for women who were not screened. The researchers estimated that 31% of the cases were potentially overdiagnosed. Among women aged 75-84, breast cancer was found in 5% of women who were screened, compared to less than 3% of unscreened women. Their estimated overdiagnosis rate was 47%. Finally, 3% of women aged 85 and older who were screened had breast cancer detected, compared with 1% of women in the unscreened group. For the older group, the overdiagnosis rate was 54%.
“While our study focused on overdiagnosis, it is important to acknowledge that overdiagnosis is just one of many considerations when deciding whether to continue screening,” researcher and Yale assistant professor of medicine Ilana Richman, MD, said in a statement. “A patient’s preferences and values, personal risk factors, and the overall balance of risks and benefits from screening are also important to take into account when making screening decisions.”
A version of this article first appeared on WebMD.com.
FROM ANNALS OF INTERNAL MEDICINE
Does tamoxifen use increase the risk of endometrial cancer in premenopausal patients?
Ryu KJ, Kim MS, Lee JY, et al. Risk of endometrial polyps, hyperplasia, carcinoma, and uterine cancer after tamoxifen treatment in premenopausal women with breast cancer. JAMA Netw Open. 2022;5:e2243951.
EXPERT COMMENTARY
Tamoxifen is a selective estrogen receptor modulator (SERM) approved by the US Food and Drug Administration (FDA) for both adjuvant treatment of invasive or metastatic breast cancer with hormone receptor (HR)–positive tumors (duration, 5 to 10 years) and for reduction of future breast cancers in certain high-risk individuals (duration, 5 years). It is also occasionally used for non-FDA approved indications, such as cyclic mastodynia.
Because breast cancer is among the most frequently diagnosed cancers in the United States (297,790 new cases expected in 2023) and approximately 80% are HR-positive tumors that will require hormonal adjuvant therapy,1 physicians and other gynecologic clinicians should have a working understanding of tamoxifen, including the risks and benefits associated with its use. Among the recognized serious adverse effects of tamoxifen is the increased risk of endometrial cancer in menopausal patients. This adverse effect creates a potential conundrum for clinicians who may be managing patients with tamoxifen to treat or prevent breast cancer, while also increasing the risk of another cancer. Prior prospective studies of tamoxifen have demonstrated a statistically and clinically significant increased risk of endometrial cancer in menopausal patients but not in premenopausal patients.
A recent study challenged those previous findings, suggesting that the risk of endometrial cancer is similar in both premenopausal and postmenopausal patients taking tamoxifen for treatment of breast cancer.2
Details of the study
The study by Ryu and colleagues used data from the Korean National Health Insurance Service, which covers 97% of the Korean population.2 The authors selected patients being treated for invasive breast cancer from January 1, 2003, through December 31, 2018, who were between the ages of 20 and 50 years when the breast cancer diagnosis was first made. Patients with a diagnostic code entered into their electronic health record that was consistent with menopausal status were excluded, along with any patients with a current or prior history of aromatase inhibitor use (for which one must be naturally, medically, or surgically menopausal to use). Based on these exclusions, the study cohort was then assumed to be premenopausal.
The study group included patients diagnosed with invasive breast cancer who were treated with adjuvant hormonal therapy with tamoxifen (n = 34,637), and the control group included patients with invasive breast cancer who were not treated with adjuvant hormonal therapy (n = 43,683). The primary study end point was the finding of endometrial or uterine pathology, including endometrial polyps, endometrial hyperplasia, endometrial cancer, and other uterine malignant neoplasms not originating in the endometrium (for example, uterine sarcomas).
Because this was a retrospective cohort study that included all eligible patients, the 2 groups were not matched. The treatment group was statistically older, had a higher body mass index (BMI) and a larger waist circumference, were more likely to be hypertensive, and included more patients with diabetes than the control group—all known risk factors for endometrial cancer. However, after adjusting for these 4 factors, an increased risk of endometrial cancer remained in the tamoxifen group compared with the control group (hazard ratio [HR], 3.77; 95% confidence interval [CI], 3.04–4.66). In addition, tamoxifen use was independently associated with an increased risk of endometrial polyps (HR, 3.90; 95% CI, 3.65–4.16), endometrial hyperplasia (HR, 5.56; 95% CI, 5.06–6.12), and other uterine cancers (HR, 2.27; 95% CI, 1.54–3.33). In a subgroup analysis, the risk for endometrial cancer was not higher in patients treated for more than 5 years of tamoxifen compared with those treated for 5 years or less.
Study strengths and limitations
A major strength of this study was the large number of study participants (n = 34,637 tamoxifen; n = 43,683 control), the long duration of follow-up (up to 15 years), and use of a single source of data with coverage of nearly the entire population of Korea. While the 2 study populations (tamoxifen vs no tamoxifen) were initially unbalanced in terms of endometrial cancer risk (age, BMI, concurrent diagnoses of hypertension and diabetes), the authors corrected for this with a multivariate analysis.
Furthermore, while the likely homogeneity of the study population may not make the results generalizable, the authors noted that Korean patients have a higher tendency toward early-onset breast cancer. This observation could make this cohort better suited for a study on premenopausal effects of tamoxifen.
Limitations. These data are provocative as they conflict with level 1 evidence based on multiple well-designed, double-blind, placebo-controlled randomized trials in which tamoxifen use for 5 years did not demonstrate a statistically increased risk of endometrial cancer in patients younger than age 50.3-5 Because of the importance of the question and the implications for many premenopausal women being treated with tamoxifen, we carefully evaluated the study methodology to better understand this discrepancy.
Continue to: Methodological concerns...
Methodological concerns
In the study by Ryu and colleagues, we found the definition of premenopausal to be problematic. Ultimately, if patients did not have a diagnosis of menopause in the problem summary list, they were assumed to be premenopausal if they were between the ages of 20 and 50 and not taking an aromatase inhibitor. However, important considerations in this population include the cancer stage and treatment regimens that can and do directly impact menopausal status.
Data demonstrate that early-onset breast cancer tends to be associated with more biologically aggressive characteristics that frequently require adjuvant or neoadjuvant chemotherapy.6,7 This chemotherapy regimen is comprised most commonly of Adriamycin (doxorubicin), paclitaxel, and cyclophosphamide. Cyclophosphamide is an alkylating agent that is a known gonadotoxin, and it often renders patients either temporarily or permanently menopausal due to chemotherapy-induced ovarian failure. Prior studies have demonstrated that for patients in their 40s, approximately 90% of those treated with cyclophosphamide-containing chemo-therapy for breast cancer will experience chemotherapy-induced amenorrhea (CIA).8 Although some patients in their 40s with CIA will resume ovarian function, the majority will not.8,9
Due to the lack of reliability in diagnosing CIA, blood levels of estradiol and follicle stimulating hormone are often necessary for confirmation and, even so, may be only temporary. One prospective analysis of 4 randomized neoadjuvant/adjuvant breast cancer trials used this approach and demonstrated that 85.1% of the study cohort experienced chemotherapy-induced ovarian failure at the end of their treatment, with some fluctuating back to premenopausal hormonal levels at 6 and 12 months.10
Furthermore, in the study by Ryu and colleagues, there is no description or confirmation of menstrual patterns in the study group to support the diagnosis of ongoing premenopausal status. Data on CIA and loss of ovarian function, therefore, are critical to the accurate categorization of patients as premenopausal or menopausal in this study. The study also relied on consistent and accurate recording of appropriate medical codes to capture a patient’s menopausal status, which is unclear for this particular population and health system.
In evaluating prior research, multiple studies demonstrated no increased risk of endometrial cancer in premenopausal women taking tamoxifen for breast cancer prevention (TABLE).3,5 These breast cancer prevention trials have several major advantages in assessing tamoxifen-associated endometrial cancer risk for premenopausal patients compared with the current study:
- Both studies were prospective double-blind, placebo-controlled randomized clinical breast cancer prevention trials with carefully designed and measured outcomes.
- Since these were breast cancer prevention trials, administration of gonadotoxic chemotherapy was not a concern. As a result, miscategorizing patients with chemotherapy-induced menopause as premenopausal would not be expected, and premature menopause would not be expected at a higher rate than the general population.
- Careful histories were required prior to study entry and throughout the study, including data on menopausal status and menstrual and uterine bleeding histories.11
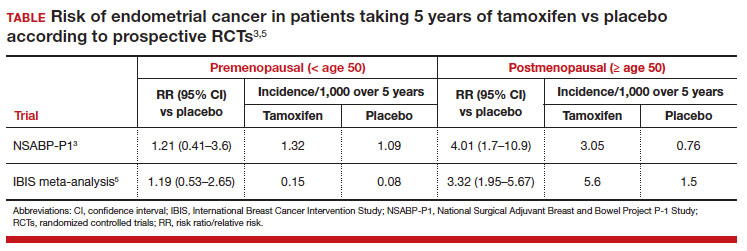
In these prevention trials, the effect of tamoxifen on uterine pathology demonstratedrepeatable evidence that there was a statistically significant increased risk of endometrial cancer in postmenopausal women, but there was no similar increased risk of endometrial cancer in premenopausal women (TABLE).3,5 Interestingly, the magnitude of the endometrial cancer risk found in the premenopausal patients in the study by Ryu and colleagues (RR, 3.77) is comparable to that of the menopausal group in the prevention trials, raising concern that many or most of the patients in the treatment group assumed to be premenopausal may have indeed been “menopausal” for some or all the time they were taking tamoxifen due to the possible aforementioned reasons. ●
While the data from the study by Ryu and colleagues are provocative, the findings that premenopausal women are at an increased risk of endometrial cancer do not agree with those of well-designed previous trials. Our concerns about categorization bias (that is, women in the treatment group may have been menopausal for some or all the time they were taking tamoxifen but were not formally diagnosed) make the conclusion that endometrial cancer risk is increased in truly premenopausal women somewhat specious. In a Committee Opinion (last endorsed in 2020), the American College of Obstetricians and Gynecologists (ACOG) stated the following: “Postmenopausal women taking tamoxifen should be closely monitored for symptoms of endometrial hyperplasia or cancer. Premenopausal women treated with tamoxifen have no known increased risk of uterine cancer and as such require no additional monitoring beyond routine gynecologic care.”12 Based on multiple previously published studies with solid level 1 evidence and the challenges with the current study design, we continue to agree with this ACOG statement.
VERSHA PLEASANT, MD, MPH; MARK D. PEARLMAN, MD
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17-48.
- Ryu KJ, Kim MS, Lee JY, et al. Risk of endometrial polyps, hyperplasia, carcinoma, and uterine cancer after tamoxifen treatment in premenopausal women with breast cancer. JAMA Netw Open. 2022;5:e2243951-e.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371-1388.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 2005;97:1652-1662.
- Iqbal J, Ginsburg OM, Wijeratne TD, et al. Endometrial cancer and venous thromboembolism in women under age 50 who take tamoxifen for prevention of breast cancer: a systematic review. Cancer Treat Rev. 2012;38:318-328.
- Kumar R, Abreu C, Toi M, et al. Oncobiology and treatment of breast cancer in young women. Cancer Metastasis Rev. 2022;41:749-770.
- Tesch ME, Partidge AH. Treatment of breast cancer in young adults. Am Soc Clin Oncol Educ Book. 2022;42:1-12.
- Han HS, Ro J, Lee KS, et al. Analysis of chemotherapy-induced amenorrhea rates by three different anthracycline and taxane containing regimens for early breast cancer. Breast Cancer Res Treat. 2009;115:335-342.
- Henry NL, Xia R, Banerjee M, et al. Predictors of recovery of ovarian function during aromatase inhibitor therapy. Ann Oncol. 2013;24:2011-2016.
- Furlanetto J, Marme F, Seiler S, et al. Chemotherapy-induced ovarian failure in young women with early breast cancer: prospective analysis of four randomised neoadjuvant/ adjuvant breast cancer trials. Eur J Cancer. 2021;152: 193-203.
- Runowicz CD, Costantino JP, Wickerham DL, et al. Gynecologic conditions in participants in the NSABP breast cancer prevention study of tamoxifen and raloxifene (STAR). Am J Obstet Gynecol. 2011;205:535.e1-535.e5.
- American College of Obstetricians and Gynecologists. Committee opinion no. 601: tamoxifen and uterine cancer. Obstet Gynecol. 2014;123:1394-1397.
Ryu KJ, Kim MS, Lee JY, et al. Risk of endometrial polyps, hyperplasia, carcinoma, and uterine cancer after tamoxifen treatment in premenopausal women with breast cancer. JAMA Netw Open. 2022;5:e2243951.
EXPERT COMMENTARY
Tamoxifen is a selective estrogen receptor modulator (SERM) approved by the US Food and Drug Administration (FDA) for both adjuvant treatment of invasive or metastatic breast cancer with hormone receptor (HR)–positive tumors (duration, 5 to 10 years) and for reduction of future breast cancers in certain high-risk individuals (duration, 5 years). It is also occasionally used for non-FDA approved indications, such as cyclic mastodynia.
Because breast cancer is among the most frequently diagnosed cancers in the United States (297,790 new cases expected in 2023) and approximately 80% are HR-positive tumors that will require hormonal adjuvant therapy,1 physicians and other gynecologic clinicians should have a working understanding of tamoxifen, including the risks and benefits associated with its use. Among the recognized serious adverse effects of tamoxifen is the increased risk of endometrial cancer in menopausal patients. This adverse effect creates a potential conundrum for clinicians who may be managing patients with tamoxifen to treat or prevent breast cancer, while also increasing the risk of another cancer. Prior prospective studies of tamoxifen have demonstrated a statistically and clinically significant increased risk of endometrial cancer in menopausal patients but not in premenopausal patients.
A recent study challenged those previous findings, suggesting that the risk of endometrial cancer is similar in both premenopausal and postmenopausal patients taking tamoxifen for treatment of breast cancer.2
Details of the study
The study by Ryu and colleagues used data from the Korean National Health Insurance Service, which covers 97% of the Korean population.2 The authors selected patients being treated for invasive breast cancer from January 1, 2003, through December 31, 2018, who were between the ages of 20 and 50 years when the breast cancer diagnosis was first made. Patients with a diagnostic code entered into their electronic health record that was consistent with menopausal status were excluded, along with any patients with a current or prior history of aromatase inhibitor use (for which one must be naturally, medically, or surgically menopausal to use). Based on these exclusions, the study cohort was then assumed to be premenopausal.
The study group included patients diagnosed with invasive breast cancer who were treated with adjuvant hormonal therapy with tamoxifen (n = 34,637), and the control group included patients with invasive breast cancer who were not treated with adjuvant hormonal therapy (n = 43,683). The primary study end point was the finding of endometrial or uterine pathology, including endometrial polyps, endometrial hyperplasia, endometrial cancer, and other uterine malignant neoplasms not originating in the endometrium (for example, uterine sarcomas).
Because this was a retrospective cohort study that included all eligible patients, the 2 groups were not matched. The treatment group was statistically older, had a higher body mass index (BMI) and a larger waist circumference, were more likely to be hypertensive, and included more patients with diabetes than the control group—all known risk factors for endometrial cancer. However, after adjusting for these 4 factors, an increased risk of endometrial cancer remained in the tamoxifen group compared with the control group (hazard ratio [HR], 3.77; 95% confidence interval [CI], 3.04–4.66). In addition, tamoxifen use was independently associated with an increased risk of endometrial polyps (HR, 3.90; 95% CI, 3.65–4.16), endometrial hyperplasia (HR, 5.56; 95% CI, 5.06–6.12), and other uterine cancers (HR, 2.27; 95% CI, 1.54–3.33). In a subgroup analysis, the risk for endometrial cancer was not higher in patients treated for more than 5 years of tamoxifen compared with those treated for 5 years or less.
Study strengths and limitations
A major strength of this study was the large number of study participants (n = 34,637 tamoxifen; n = 43,683 control), the long duration of follow-up (up to 15 years), and use of a single source of data with coverage of nearly the entire population of Korea. While the 2 study populations (tamoxifen vs no tamoxifen) were initially unbalanced in terms of endometrial cancer risk (age, BMI, concurrent diagnoses of hypertension and diabetes), the authors corrected for this with a multivariate analysis.
Furthermore, while the likely homogeneity of the study population may not make the results generalizable, the authors noted that Korean patients have a higher tendency toward early-onset breast cancer. This observation could make this cohort better suited for a study on premenopausal effects of tamoxifen.
Limitations. These data are provocative as they conflict with level 1 evidence based on multiple well-designed, double-blind, placebo-controlled randomized trials in which tamoxifen use for 5 years did not demonstrate a statistically increased risk of endometrial cancer in patients younger than age 50.3-5 Because of the importance of the question and the implications for many premenopausal women being treated with tamoxifen, we carefully evaluated the study methodology to better understand this discrepancy.
Continue to: Methodological concerns...
Methodological concerns
In the study by Ryu and colleagues, we found the definition of premenopausal to be problematic. Ultimately, if patients did not have a diagnosis of menopause in the problem summary list, they were assumed to be premenopausal if they were between the ages of 20 and 50 and not taking an aromatase inhibitor. However, important considerations in this population include the cancer stage and treatment regimens that can and do directly impact menopausal status.
Data demonstrate that early-onset breast cancer tends to be associated with more biologically aggressive characteristics that frequently require adjuvant or neoadjuvant chemotherapy.6,7 This chemotherapy regimen is comprised most commonly of Adriamycin (doxorubicin), paclitaxel, and cyclophosphamide. Cyclophosphamide is an alkylating agent that is a known gonadotoxin, and it often renders patients either temporarily or permanently menopausal due to chemotherapy-induced ovarian failure. Prior studies have demonstrated that for patients in their 40s, approximately 90% of those treated with cyclophosphamide-containing chemo-therapy for breast cancer will experience chemotherapy-induced amenorrhea (CIA).8 Although some patients in their 40s with CIA will resume ovarian function, the majority will not.8,9
Due to the lack of reliability in diagnosing CIA, blood levels of estradiol and follicle stimulating hormone are often necessary for confirmation and, even so, may be only temporary. One prospective analysis of 4 randomized neoadjuvant/adjuvant breast cancer trials used this approach and demonstrated that 85.1% of the study cohort experienced chemotherapy-induced ovarian failure at the end of their treatment, with some fluctuating back to premenopausal hormonal levels at 6 and 12 months.10
Furthermore, in the study by Ryu and colleagues, there is no description or confirmation of menstrual patterns in the study group to support the diagnosis of ongoing premenopausal status. Data on CIA and loss of ovarian function, therefore, are critical to the accurate categorization of patients as premenopausal or menopausal in this study. The study also relied on consistent and accurate recording of appropriate medical codes to capture a patient’s menopausal status, which is unclear for this particular population and health system.
In evaluating prior research, multiple studies demonstrated no increased risk of endometrial cancer in premenopausal women taking tamoxifen for breast cancer prevention (TABLE).3,5 These breast cancer prevention trials have several major advantages in assessing tamoxifen-associated endometrial cancer risk for premenopausal patients compared with the current study:
- Both studies were prospective double-blind, placebo-controlled randomized clinical breast cancer prevention trials with carefully designed and measured outcomes.
- Since these were breast cancer prevention trials, administration of gonadotoxic chemotherapy was not a concern. As a result, miscategorizing patients with chemotherapy-induced menopause as premenopausal would not be expected, and premature menopause would not be expected at a higher rate than the general population.
- Careful histories were required prior to study entry and throughout the study, including data on menopausal status and menstrual and uterine bleeding histories.11
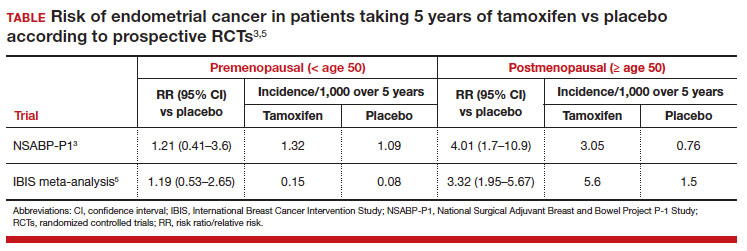
In these prevention trials, the effect of tamoxifen on uterine pathology demonstratedrepeatable evidence that there was a statistically significant increased risk of endometrial cancer in postmenopausal women, but there was no similar increased risk of endometrial cancer in premenopausal women (TABLE).3,5 Interestingly, the magnitude of the endometrial cancer risk found in the premenopausal patients in the study by Ryu and colleagues (RR, 3.77) is comparable to that of the menopausal group in the prevention trials, raising concern that many or most of the patients in the treatment group assumed to be premenopausal may have indeed been “menopausal” for some or all the time they were taking tamoxifen due to the possible aforementioned reasons. ●
While the data from the study by Ryu and colleagues are provocative, the findings that premenopausal women are at an increased risk of endometrial cancer do not agree with those of well-designed previous trials. Our concerns about categorization bias (that is, women in the treatment group may have been menopausal for some or all the time they were taking tamoxifen but were not formally diagnosed) make the conclusion that endometrial cancer risk is increased in truly premenopausal women somewhat specious. In a Committee Opinion (last endorsed in 2020), the American College of Obstetricians and Gynecologists (ACOG) stated the following: “Postmenopausal women taking tamoxifen should be closely monitored for symptoms of endometrial hyperplasia or cancer. Premenopausal women treated with tamoxifen have no known increased risk of uterine cancer and as such require no additional monitoring beyond routine gynecologic care.”12 Based on multiple previously published studies with solid level 1 evidence and the challenges with the current study design, we continue to agree with this ACOG statement.
VERSHA PLEASANT, MD, MPH; MARK D. PEARLMAN, MD
Ryu KJ, Kim MS, Lee JY, et al. Risk of endometrial polyps, hyperplasia, carcinoma, and uterine cancer after tamoxifen treatment in premenopausal women with breast cancer. JAMA Netw Open. 2022;5:e2243951.
EXPERT COMMENTARY
Tamoxifen is a selective estrogen receptor modulator (SERM) approved by the US Food and Drug Administration (FDA) for both adjuvant treatment of invasive or metastatic breast cancer with hormone receptor (HR)–positive tumors (duration, 5 to 10 years) and for reduction of future breast cancers in certain high-risk individuals (duration, 5 years). It is also occasionally used for non-FDA approved indications, such as cyclic mastodynia.
Because breast cancer is among the most frequently diagnosed cancers in the United States (297,790 new cases expected in 2023) and approximately 80% are HR-positive tumors that will require hormonal adjuvant therapy,1 physicians and other gynecologic clinicians should have a working understanding of tamoxifen, including the risks and benefits associated with its use. Among the recognized serious adverse effects of tamoxifen is the increased risk of endometrial cancer in menopausal patients. This adverse effect creates a potential conundrum for clinicians who may be managing patients with tamoxifen to treat or prevent breast cancer, while also increasing the risk of another cancer. Prior prospective studies of tamoxifen have demonstrated a statistically and clinically significant increased risk of endometrial cancer in menopausal patients but not in premenopausal patients.
A recent study challenged those previous findings, suggesting that the risk of endometrial cancer is similar in both premenopausal and postmenopausal patients taking tamoxifen for treatment of breast cancer.2
Details of the study
The study by Ryu and colleagues used data from the Korean National Health Insurance Service, which covers 97% of the Korean population.2 The authors selected patients being treated for invasive breast cancer from January 1, 2003, through December 31, 2018, who were between the ages of 20 and 50 years when the breast cancer diagnosis was first made. Patients with a diagnostic code entered into their electronic health record that was consistent with menopausal status were excluded, along with any patients with a current or prior history of aromatase inhibitor use (for which one must be naturally, medically, or surgically menopausal to use). Based on these exclusions, the study cohort was then assumed to be premenopausal.
The study group included patients diagnosed with invasive breast cancer who were treated with adjuvant hormonal therapy with tamoxifen (n = 34,637), and the control group included patients with invasive breast cancer who were not treated with adjuvant hormonal therapy (n = 43,683). The primary study end point was the finding of endometrial or uterine pathology, including endometrial polyps, endometrial hyperplasia, endometrial cancer, and other uterine malignant neoplasms not originating in the endometrium (for example, uterine sarcomas).
Because this was a retrospective cohort study that included all eligible patients, the 2 groups were not matched. The treatment group was statistically older, had a higher body mass index (BMI) and a larger waist circumference, were more likely to be hypertensive, and included more patients with diabetes than the control group—all known risk factors for endometrial cancer. However, after adjusting for these 4 factors, an increased risk of endometrial cancer remained in the tamoxifen group compared with the control group (hazard ratio [HR], 3.77; 95% confidence interval [CI], 3.04–4.66). In addition, tamoxifen use was independently associated with an increased risk of endometrial polyps (HR, 3.90; 95% CI, 3.65–4.16), endometrial hyperplasia (HR, 5.56; 95% CI, 5.06–6.12), and other uterine cancers (HR, 2.27; 95% CI, 1.54–3.33). In a subgroup analysis, the risk for endometrial cancer was not higher in patients treated for more than 5 years of tamoxifen compared with those treated for 5 years or less.
Study strengths and limitations
A major strength of this study was the large number of study participants (n = 34,637 tamoxifen; n = 43,683 control), the long duration of follow-up (up to 15 years), and use of a single source of data with coverage of nearly the entire population of Korea. While the 2 study populations (tamoxifen vs no tamoxifen) were initially unbalanced in terms of endometrial cancer risk (age, BMI, concurrent diagnoses of hypertension and diabetes), the authors corrected for this with a multivariate analysis.
Furthermore, while the likely homogeneity of the study population may not make the results generalizable, the authors noted that Korean patients have a higher tendency toward early-onset breast cancer. This observation could make this cohort better suited for a study on premenopausal effects of tamoxifen.
Limitations. These data are provocative as they conflict with level 1 evidence based on multiple well-designed, double-blind, placebo-controlled randomized trials in which tamoxifen use for 5 years did not demonstrate a statistically increased risk of endometrial cancer in patients younger than age 50.3-5 Because of the importance of the question and the implications for many premenopausal women being treated with tamoxifen, we carefully evaluated the study methodology to better understand this discrepancy.
Continue to: Methodological concerns...
Methodological concerns
In the study by Ryu and colleagues, we found the definition of premenopausal to be problematic. Ultimately, if patients did not have a diagnosis of menopause in the problem summary list, they were assumed to be premenopausal if they were between the ages of 20 and 50 and not taking an aromatase inhibitor. However, important considerations in this population include the cancer stage and treatment regimens that can and do directly impact menopausal status.
Data demonstrate that early-onset breast cancer tends to be associated with more biologically aggressive characteristics that frequently require adjuvant or neoadjuvant chemotherapy.6,7 This chemotherapy regimen is comprised most commonly of Adriamycin (doxorubicin), paclitaxel, and cyclophosphamide. Cyclophosphamide is an alkylating agent that is a known gonadotoxin, and it often renders patients either temporarily or permanently menopausal due to chemotherapy-induced ovarian failure. Prior studies have demonstrated that for patients in their 40s, approximately 90% of those treated with cyclophosphamide-containing chemo-therapy for breast cancer will experience chemotherapy-induced amenorrhea (CIA).8 Although some patients in their 40s with CIA will resume ovarian function, the majority will not.8,9
Due to the lack of reliability in diagnosing CIA, blood levels of estradiol and follicle stimulating hormone are often necessary for confirmation and, even so, may be only temporary. One prospective analysis of 4 randomized neoadjuvant/adjuvant breast cancer trials used this approach and demonstrated that 85.1% of the study cohort experienced chemotherapy-induced ovarian failure at the end of their treatment, with some fluctuating back to premenopausal hormonal levels at 6 and 12 months.10
Furthermore, in the study by Ryu and colleagues, there is no description or confirmation of menstrual patterns in the study group to support the diagnosis of ongoing premenopausal status. Data on CIA and loss of ovarian function, therefore, are critical to the accurate categorization of patients as premenopausal or menopausal in this study. The study also relied on consistent and accurate recording of appropriate medical codes to capture a patient’s menopausal status, which is unclear for this particular population and health system.
In evaluating prior research, multiple studies demonstrated no increased risk of endometrial cancer in premenopausal women taking tamoxifen for breast cancer prevention (TABLE).3,5 These breast cancer prevention trials have several major advantages in assessing tamoxifen-associated endometrial cancer risk for premenopausal patients compared with the current study:
- Both studies were prospective double-blind, placebo-controlled randomized clinical breast cancer prevention trials with carefully designed and measured outcomes.
- Since these were breast cancer prevention trials, administration of gonadotoxic chemotherapy was not a concern. As a result, miscategorizing patients with chemotherapy-induced menopause as premenopausal would not be expected, and premature menopause would not be expected at a higher rate than the general population.
- Careful histories were required prior to study entry and throughout the study, including data on menopausal status and menstrual and uterine bleeding histories.11
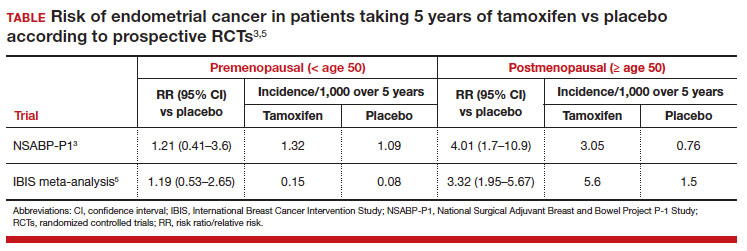
In these prevention trials, the effect of tamoxifen on uterine pathology demonstratedrepeatable evidence that there was a statistically significant increased risk of endometrial cancer in postmenopausal women, but there was no similar increased risk of endometrial cancer in premenopausal women (TABLE).3,5 Interestingly, the magnitude of the endometrial cancer risk found in the premenopausal patients in the study by Ryu and colleagues (RR, 3.77) is comparable to that of the menopausal group in the prevention trials, raising concern that many or most of the patients in the treatment group assumed to be premenopausal may have indeed been “menopausal” for some or all the time they were taking tamoxifen due to the possible aforementioned reasons. ●
While the data from the study by Ryu and colleagues are provocative, the findings that premenopausal women are at an increased risk of endometrial cancer do not agree with those of well-designed previous trials. Our concerns about categorization bias (that is, women in the treatment group may have been menopausal for some or all the time they were taking tamoxifen but were not formally diagnosed) make the conclusion that endometrial cancer risk is increased in truly premenopausal women somewhat specious. In a Committee Opinion (last endorsed in 2020), the American College of Obstetricians and Gynecologists (ACOG) stated the following: “Postmenopausal women taking tamoxifen should be closely monitored for symptoms of endometrial hyperplasia or cancer. Premenopausal women treated with tamoxifen have no known increased risk of uterine cancer and as such require no additional monitoring beyond routine gynecologic care.”12 Based on multiple previously published studies with solid level 1 evidence and the challenges with the current study design, we continue to agree with this ACOG statement.
VERSHA PLEASANT, MD, MPH; MARK D. PEARLMAN, MD
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17-48.
- Ryu KJ, Kim MS, Lee JY, et al. Risk of endometrial polyps, hyperplasia, carcinoma, and uterine cancer after tamoxifen treatment in premenopausal women with breast cancer. JAMA Netw Open. 2022;5:e2243951-e.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371-1388.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 2005;97:1652-1662.
- Iqbal J, Ginsburg OM, Wijeratne TD, et al. Endometrial cancer and venous thromboembolism in women under age 50 who take tamoxifen for prevention of breast cancer: a systematic review. Cancer Treat Rev. 2012;38:318-328.
- Kumar R, Abreu C, Toi M, et al. Oncobiology and treatment of breast cancer in young women. Cancer Metastasis Rev. 2022;41:749-770.
- Tesch ME, Partidge AH. Treatment of breast cancer in young adults. Am Soc Clin Oncol Educ Book. 2022;42:1-12.
- Han HS, Ro J, Lee KS, et al. Analysis of chemotherapy-induced amenorrhea rates by three different anthracycline and taxane containing regimens for early breast cancer. Breast Cancer Res Treat. 2009;115:335-342.
- Henry NL, Xia R, Banerjee M, et al. Predictors of recovery of ovarian function during aromatase inhibitor therapy. Ann Oncol. 2013;24:2011-2016.
- Furlanetto J, Marme F, Seiler S, et al. Chemotherapy-induced ovarian failure in young women with early breast cancer: prospective analysis of four randomised neoadjuvant/ adjuvant breast cancer trials. Eur J Cancer. 2021;152: 193-203.
- Runowicz CD, Costantino JP, Wickerham DL, et al. Gynecologic conditions in participants in the NSABP breast cancer prevention study of tamoxifen and raloxifene (STAR). Am J Obstet Gynecol. 2011;205:535.e1-535.e5.
- American College of Obstetricians and Gynecologists. Committee opinion no. 601: tamoxifen and uterine cancer. Obstet Gynecol. 2014;123:1394-1397.
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17-48.
- Ryu KJ, Kim MS, Lee JY, et al. Risk of endometrial polyps, hyperplasia, carcinoma, and uterine cancer after tamoxifen treatment in premenopausal women with breast cancer. JAMA Netw Open. 2022;5:e2243951-e.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371-1388.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 2005;97:1652-1662.
- Iqbal J, Ginsburg OM, Wijeratne TD, et al. Endometrial cancer and venous thromboembolism in women under age 50 who take tamoxifen for prevention of breast cancer: a systematic review. Cancer Treat Rev. 2012;38:318-328.
- Kumar R, Abreu C, Toi M, et al. Oncobiology and treatment of breast cancer in young women. Cancer Metastasis Rev. 2022;41:749-770.
- Tesch ME, Partidge AH. Treatment of breast cancer in young adults. Am Soc Clin Oncol Educ Book. 2022;42:1-12.
- Han HS, Ro J, Lee KS, et al. Analysis of chemotherapy-induced amenorrhea rates by three different anthracycline and taxane containing regimens for early breast cancer. Breast Cancer Res Treat. 2009;115:335-342.
- Henry NL, Xia R, Banerjee M, et al. Predictors of recovery of ovarian function during aromatase inhibitor therapy. Ann Oncol. 2013;24:2011-2016.
- Furlanetto J, Marme F, Seiler S, et al. Chemotherapy-induced ovarian failure in young women with early breast cancer: prospective analysis of four randomised neoadjuvant/ adjuvant breast cancer trials. Eur J Cancer. 2021;152: 193-203.
- Runowicz CD, Costantino JP, Wickerham DL, et al. Gynecologic conditions in participants in the NSABP breast cancer prevention study of tamoxifen and raloxifene (STAR). Am J Obstet Gynecol. 2011;205:535.e1-535.e5.
- American College of Obstetricians and Gynecologists. Committee opinion no. 601: tamoxifen and uterine cancer. Obstet Gynecol. 2014;123:1394-1397.
Progesterone might benefit women in perimenopause
In a randomized, placebo-controlled trial of about 180 women with vasomotor symptoms (VMS), women who received progesterone perceived a significantly greater decrease in night sweats (P = .023) and improved sleep quality (P = .005), compared with controls. VMS score did not differ significantly by treatment group, however.
“Women who have menstruated within the last year, who are waking twice or more times a week with night sweats and bothered by sleep disturbances would benefit from taking oral micronized progesterone 300 mg at bedtime,” principal investigator Jerilynn C. Prior, MD, professor of endocrinology at the University of British Columbia in Vancouver, British Columbia, Canada, said in an interview.
The study was published online in Scientific Reports.
A neglected group?
The best management for symptoms in perimenopause is an often-neglected topic of research, said Dr. Prior. Yet perimenopause is often associated with significant symptoms for women, including heavy menstrual bleeding, sore breasts, mood swings, night sweats, and insomnia – all when many women are at the peak of their careers.
Dr. Prior herself had a difficult perimenopause. “I began having cyclic night sweats, clustered around flow, when I was still having regular menstrual cycles, plus breast tenderness and sleep problems,” she said. “I knew from my research and my own experience that my estrogen levels were very high. Higher estrogen levels are not suppressible by exogenous estrogen, so it made no sense to me to ask my family doctor for a prescription for estrogen – or hormone replacement therapy, as it was then called. However, medroxyprogesterone acetate had been reported to be effective for menopausal hot flushes. I tried it, and it helped my night sweats and hot flushes but not my sleep. When oral micronized progesterone became available, I switched to that.”
In the current study, which was performed at the UBC Centre for Menstrual Cycle and Ovulation Research, the investigators studied 189 community-dwelling women from across Canada who were aged 35-58 years, had menstruated in the past year, and were bothered by daytime flushes or night sweats at least twice per week.
Participants were randomly assigned to receive either 300 mg of oral micronized progesterone or placebo at bedtime for 3 months. They recorded VMS number and intensity while awake and asleep each day. Some women participated remotely by web conference, telephone, or email. The experimental medicine was delivered to these participants by courier. The primary outcome was VMS score during the 3rd month.
Most (87%) participants were White, and about 57% had a college degree. The population’s average body mass index was 26.7, and 66.7% of participants were in late perimenopause.
The mean baseline VMS score among the women was 12.2. The average frequency of VMS per 24-hour day was 4.9. Average VMS intensity was 2.3 on a scale of 0-4. VMS scores decreased over time in both treatment groups.
At month 3, the VMS score was 5.5 in the progesterone group and 7.1 in the placebo group. The difference between groups was not statistically significant.
Compared with controls, however, women in the progesterone group perceived a significantly greater decrease in night sweats and improved sleep quality. Progesterone also was associated with significantly decreased perception of physical and emotional interference with their daily activities, compared with placebo (P = .017). Moreover, progesterone did not increase depression.
There were no serious adverse events.
“I hope that when women who look young and are still menstruating in their late 30s to early 50s go to the doctor and ask for help with night sweats and sleep problems, they will be told about this trial and offered progesterone therapy. I also hope they won’t be told, ‘You are too young,’ or ‘You are not in menopause,’ with the inference that the issue is all in their minds,” said Dr. Prior.
Useful dosing information
Mitchell S. Kramer, MD, chair of obstetrics and gynecology at Huntington (N.Y.) Hospital Northwell Health, said in a comment that “progesterone has been used for quite a while. I’ve been treating menopausal and perimenopausal hormonal disturbances and VMS for many years, and progesterone has been a real staple of treatment for these symptoms, especially in perimenopausal patients who are not good candidates for estrogen or who won’t accept treatment with estrogen. It’s actually nice to see a study that addresses this issue in a randomized controlled fashion and that confirms the efficacy of progesterone.”
The most helpful aspect of the study is the dosing information, Dr. Kramer added. “They recommend a 300-mg dose of oral micronized progesterone, which is much higher than I normally use. I may start to prescribe the higher dose and perhaps get a better or more complete response. There were no adverse events reported in this study, so the higher dose was enlightening to me,” he said.
Perimenopause is a time that is challenging to manage, said Michelle Jacobson, MD, of the department of obstetrics and gynecology at the University of Toronto, and obstetrician-gynecologist at Women’s College and Mount Sinai Hospitals in Toronto.
“There are so many nuances to the management. Women are suffering oftentimes from classic menopausal symptoms. There are fluctuating levels of estrogen, sometimes high. Sometimes there are complications of bleeding. There is the potential need for contraception because they are still menstruating,” she said in an interview.
“It’s important to specifically study this group of women with their own unique needs. Dr. Prior is a longtime proponent of using progesterone therapy, and kudos to her for doing this study in perimenopausal women, which is a group that is probably underrepresented in the menopause management literature,” she said.
Dr. Prior and Dr. Kramer reported no relevant financial relationships. Dr. Jacobson reported financial relationships with Astellas, AbbVie, Bayer, BioSyent, Duchesnay, Eisai, Lupin, Organon, Pfizer, and Searchlight.
A version of this article first appeared on Medscape.com.
In a randomized, placebo-controlled trial of about 180 women with vasomotor symptoms (VMS), women who received progesterone perceived a significantly greater decrease in night sweats (P = .023) and improved sleep quality (P = .005), compared with controls. VMS score did not differ significantly by treatment group, however.
“Women who have menstruated within the last year, who are waking twice or more times a week with night sweats and bothered by sleep disturbances would benefit from taking oral micronized progesterone 300 mg at bedtime,” principal investigator Jerilynn C. Prior, MD, professor of endocrinology at the University of British Columbia in Vancouver, British Columbia, Canada, said in an interview.
The study was published online in Scientific Reports.
A neglected group?
The best management for symptoms in perimenopause is an often-neglected topic of research, said Dr. Prior. Yet perimenopause is often associated with significant symptoms for women, including heavy menstrual bleeding, sore breasts, mood swings, night sweats, and insomnia – all when many women are at the peak of their careers.
Dr. Prior herself had a difficult perimenopause. “I began having cyclic night sweats, clustered around flow, when I was still having regular menstrual cycles, plus breast tenderness and sleep problems,” she said. “I knew from my research and my own experience that my estrogen levels were very high. Higher estrogen levels are not suppressible by exogenous estrogen, so it made no sense to me to ask my family doctor for a prescription for estrogen – or hormone replacement therapy, as it was then called. However, medroxyprogesterone acetate had been reported to be effective for menopausal hot flushes. I tried it, and it helped my night sweats and hot flushes but not my sleep. When oral micronized progesterone became available, I switched to that.”
In the current study, which was performed at the UBC Centre for Menstrual Cycle and Ovulation Research, the investigators studied 189 community-dwelling women from across Canada who were aged 35-58 years, had menstruated in the past year, and were bothered by daytime flushes or night sweats at least twice per week.
Participants were randomly assigned to receive either 300 mg of oral micronized progesterone or placebo at bedtime for 3 months. They recorded VMS number and intensity while awake and asleep each day. Some women participated remotely by web conference, telephone, or email. The experimental medicine was delivered to these participants by courier. The primary outcome was VMS score during the 3rd month.
Most (87%) participants were White, and about 57% had a college degree. The population’s average body mass index was 26.7, and 66.7% of participants were in late perimenopause.
The mean baseline VMS score among the women was 12.2. The average frequency of VMS per 24-hour day was 4.9. Average VMS intensity was 2.3 on a scale of 0-4. VMS scores decreased over time in both treatment groups.
At month 3, the VMS score was 5.5 in the progesterone group and 7.1 in the placebo group. The difference between groups was not statistically significant.
Compared with controls, however, women in the progesterone group perceived a significantly greater decrease in night sweats and improved sleep quality. Progesterone also was associated with significantly decreased perception of physical and emotional interference with their daily activities, compared with placebo (P = .017). Moreover, progesterone did not increase depression.
There were no serious adverse events.
“I hope that when women who look young and are still menstruating in their late 30s to early 50s go to the doctor and ask for help with night sweats and sleep problems, they will be told about this trial and offered progesterone therapy. I also hope they won’t be told, ‘You are too young,’ or ‘You are not in menopause,’ with the inference that the issue is all in their minds,” said Dr. Prior.
Useful dosing information
Mitchell S. Kramer, MD, chair of obstetrics and gynecology at Huntington (N.Y.) Hospital Northwell Health, said in a comment that “progesterone has been used for quite a while. I’ve been treating menopausal and perimenopausal hormonal disturbances and VMS for many years, and progesterone has been a real staple of treatment for these symptoms, especially in perimenopausal patients who are not good candidates for estrogen or who won’t accept treatment with estrogen. It’s actually nice to see a study that addresses this issue in a randomized controlled fashion and that confirms the efficacy of progesterone.”
The most helpful aspect of the study is the dosing information, Dr. Kramer added. “They recommend a 300-mg dose of oral micronized progesterone, which is much higher than I normally use. I may start to prescribe the higher dose and perhaps get a better or more complete response. There were no adverse events reported in this study, so the higher dose was enlightening to me,” he said.
Perimenopause is a time that is challenging to manage, said Michelle Jacobson, MD, of the department of obstetrics and gynecology at the University of Toronto, and obstetrician-gynecologist at Women’s College and Mount Sinai Hospitals in Toronto.
“There are so many nuances to the management. Women are suffering oftentimes from classic menopausal symptoms. There are fluctuating levels of estrogen, sometimes high. Sometimes there are complications of bleeding. There is the potential need for contraception because they are still menstruating,” she said in an interview.
“It’s important to specifically study this group of women with their own unique needs. Dr. Prior is a longtime proponent of using progesterone therapy, and kudos to her for doing this study in perimenopausal women, which is a group that is probably underrepresented in the menopause management literature,” she said.
Dr. Prior and Dr. Kramer reported no relevant financial relationships. Dr. Jacobson reported financial relationships with Astellas, AbbVie, Bayer, BioSyent, Duchesnay, Eisai, Lupin, Organon, Pfizer, and Searchlight.
A version of this article first appeared on Medscape.com.
In a randomized, placebo-controlled trial of about 180 women with vasomotor symptoms (VMS), women who received progesterone perceived a significantly greater decrease in night sweats (P = .023) and improved sleep quality (P = .005), compared with controls. VMS score did not differ significantly by treatment group, however.
“Women who have menstruated within the last year, who are waking twice or more times a week with night sweats and bothered by sleep disturbances would benefit from taking oral micronized progesterone 300 mg at bedtime,” principal investigator Jerilynn C. Prior, MD, professor of endocrinology at the University of British Columbia in Vancouver, British Columbia, Canada, said in an interview.
The study was published online in Scientific Reports.
A neglected group?
The best management for symptoms in perimenopause is an often-neglected topic of research, said Dr. Prior. Yet perimenopause is often associated with significant symptoms for women, including heavy menstrual bleeding, sore breasts, mood swings, night sweats, and insomnia – all when many women are at the peak of their careers.
Dr. Prior herself had a difficult perimenopause. “I began having cyclic night sweats, clustered around flow, when I was still having regular menstrual cycles, plus breast tenderness and sleep problems,” she said. “I knew from my research and my own experience that my estrogen levels were very high. Higher estrogen levels are not suppressible by exogenous estrogen, so it made no sense to me to ask my family doctor for a prescription for estrogen – or hormone replacement therapy, as it was then called. However, medroxyprogesterone acetate had been reported to be effective for menopausal hot flushes. I tried it, and it helped my night sweats and hot flushes but not my sleep. When oral micronized progesterone became available, I switched to that.”
In the current study, which was performed at the UBC Centre for Menstrual Cycle and Ovulation Research, the investigators studied 189 community-dwelling women from across Canada who were aged 35-58 years, had menstruated in the past year, and were bothered by daytime flushes or night sweats at least twice per week.
Participants were randomly assigned to receive either 300 mg of oral micronized progesterone or placebo at bedtime for 3 months. They recorded VMS number and intensity while awake and asleep each day. Some women participated remotely by web conference, telephone, or email. The experimental medicine was delivered to these participants by courier. The primary outcome was VMS score during the 3rd month.
Most (87%) participants were White, and about 57% had a college degree. The population’s average body mass index was 26.7, and 66.7% of participants were in late perimenopause.
The mean baseline VMS score among the women was 12.2. The average frequency of VMS per 24-hour day was 4.9. Average VMS intensity was 2.3 on a scale of 0-4. VMS scores decreased over time in both treatment groups.
At month 3, the VMS score was 5.5 in the progesterone group and 7.1 in the placebo group. The difference between groups was not statistically significant.
Compared with controls, however, women in the progesterone group perceived a significantly greater decrease in night sweats and improved sleep quality. Progesterone also was associated with significantly decreased perception of physical and emotional interference with their daily activities, compared with placebo (P = .017). Moreover, progesterone did not increase depression.
There were no serious adverse events.
“I hope that when women who look young and are still menstruating in their late 30s to early 50s go to the doctor and ask for help with night sweats and sleep problems, they will be told about this trial and offered progesterone therapy. I also hope they won’t be told, ‘You are too young,’ or ‘You are not in menopause,’ with the inference that the issue is all in their minds,” said Dr. Prior.
Useful dosing information
Mitchell S. Kramer, MD, chair of obstetrics and gynecology at Huntington (N.Y.) Hospital Northwell Health, said in a comment that “progesterone has been used for quite a while. I’ve been treating menopausal and perimenopausal hormonal disturbances and VMS for many years, and progesterone has been a real staple of treatment for these symptoms, especially in perimenopausal patients who are not good candidates for estrogen or who won’t accept treatment with estrogen. It’s actually nice to see a study that addresses this issue in a randomized controlled fashion and that confirms the efficacy of progesterone.”
The most helpful aspect of the study is the dosing information, Dr. Kramer added. “They recommend a 300-mg dose of oral micronized progesterone, which is much higher than I normally use. I may start to prescribe the higher dose and perhaps get a better or more complete response. There were no adverse events reported in this study, so the higher dose was enlightening to me,” he said.
Perimenopause is a time that is challenging to manage, said Michelle Jacobson, MD, of the department of obstetrics and gynecology at the University of Toronto, and obstetrician-gynecologist at Women’s College and Mount Sinai Hospitals in Toronto.
“There are so many nuances to the management. Women are suffering oftentimes from classic menopausal symptoms. There are fluctuating levels of estrogen, sometimes high. Sometimes there are complications of bleeding. There is the potential need for contraception because they are still menstruating,” she said in an interview.
“It’s important to specifically study this group of women with their own unique needs. Dr. Prior is a longtime proponent of using progesterone therapy, and kudos to her for doing this study in perimenopausal women, which is a group that is probably underrepresented in the menopause management literature,” she said.
Dr. Prior and Dr. Kramer reported no relevant financial relationships. Dr. Jacobson reported financial relationships with Astellas, AbbVie, Bayer, BioSyent, Duchesnay, Eisai, Lupin, Organon, Pfizer, and Searchlight.
A version of this article first appeared on Medscape.com.
FROM SCIENTIFIC REPORTS
2023 Update on menopause
This year’s menopause Update highlights a highly effective nonhormonal medication that recently received approval by the US Food and Drug Administration (FDA) for the treatment of bothersome menopausal vasomotor symptoms. In addition, the Update provides guidance regarding how ObGyns should respond when an endometrial biopsy for postmenopausal bleeding reveals proliferative changes.
Breakthrough in women’s health: A new nonhormone therapy for vasomotor symptoms
Johnson KA, Martin N, Nappi RE, et al. Efficacy and safety of fezolinetant in moderate-to-severe vasomotor symptoms associated with menopause: a phase 3 RCT. J Clin Endocrinol Metab. 2023;dgad058. doi:10.1210/clinem/dgad058.
Lederman S, Ottery FD, Cano A, et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): a phase 3 randomised controlled study. Lancet. 2023;401:1091-1102. doi:10.1016/S0140-6736(23)00085-5.
A new oral nonestrogen-containing medication for relief of moderate to severe hot flashes, fezolinetant (Veozah) 45 mg daily, has been approved by the FDA and was expected to be available by the end of May 2023. Fezolinetant is a selective neurokinin 3 (NK3) receptor antagonistthat offers a targeted nonhormonal approach to menopausal vasomotor symptoms (VMS), and it is the first in its class to make it to market.
The decline in estrogen at menopause appears to result in increased signaling at kisspeptin/neurokinin B/dynorphin (KNDy) neurons in the thermoregulatory center within the hypothalamus with resultant increases in hot flashes.1,2 Fezolinetant works by binding to and blocking the activities of the NK3 receptor.3-5
Key study findings
Selective NK3 receptor antagonists, including fezolinetant, effectively reduce the frequency and severity of VMS comparable to that of hormone therapy (HT). Two phase 3 clinical trials, Skylight 1 and 2, confirmed the efficacy and safety of fezolinetant 45 mg in treating VMS,6,7 and an additional 52-week placebo-controlled study, Skylight 4, confirmed long-term safety.8 Onset of action occurs within a week. Reported adverse events occurred in 1% to 2% of healthy menopausal women participating in clinical trials; these included headaches, abdominal pain, diarrhea, insomnia, back pain, hot flushes, and reversible elevated hepatic transaminase levels.6-9
The published phase 2 trials9 and the international randomized controlled trial (RCT) 12-week studies, Skylight 1 and 2,6,7 found that once-daily 30-mg and 45-mg doses of fezolinetant significantly reduced VMS frequency and severity at 12 weeks among women aged 40 to 60 years who reported an average of 7 moderate to severe VMS/day; the reduction in reported VMS was sustained at 40 weeks. Phase 3 data from Skylight 1 and 2 demonstrated fezolinetant’s efficacy in reducing the frequency and severity of VMS and provided information on the safety profile of fezolinetant compared with placebo over 12 weeks and a noncontrolled extension for an additional 40 weeks.6,7
Oral fezolinetant was associated with improved quality of life, including reduced VMS-related interference with daily life.10 Johnson and colleagues, reporting for Skylight 2, found VMS frequency and severity improvement by week 1, which achieved statistical significance at weeks 4 and 12, with this improvement maintained through week 52.6 A 64.3% reduction in mean daily VMS from baseline was seen at 12 weeks for fezolinetant 45 mg compared with a 45.4% reduction for placebo. VMS severity significantly decreased compared with placebo at 4 and 12 weeks.6
Serious treatment-emergent adverse events were infrequent, reported by 2%, 1%, and 0% of those receiving fezolinetant 30 mg, fezolinetant 45 mg, and placebo.6 Increases in levels of alanine aminotransferase (ALT) or aspartate aminotransferase (AST) were noted and were described as asymptomatic, isolated, intermittent, or transient, and these levels returned to baseline during treatment or after discontinuation.6
Of the 5 participants taking fezolinetant in Skyline 1 with ALT or AST levels greater than 3 times the upper limit of normal in the 12-week randomized trial, levels returned to normal range while continuing treatment in 2 participants, with treatment interruption in 2, and with discontinuation in 1. No new safety signals were seen in the 40-week extension trial.6
Fezolinetant offers a much-needed effective and safe selective nonhormone NK3 receptor antagonist therapy that reduces the frequency and severity of menopausal VMS and has been shown to be safe through 52 weeks of treatment.
To read more about how fezolinetant specifically targets the hormone receptor that triggers hot flashes as well as on prescribing hormone therapy for women with menopausal symptoms, see “Focus on menopause: Q&A with Jan Shifren, MD, and Genevieve NealPerry, MD, PhD,” in the December 2022 issue of OBG Management at https://www.mdedge.com/obgyn/article/260380/menopause
Continue to: Endometrial and bone safety...
Endometrial and bone safety
Results from Skylight 4, a phase 3, randomized, double-blind, 52-week safety study, provided additional evidence that confirmed the longer-term safety of fezolinetant over a 52-week treatment period.8
Endometrial safety was assessed in postmenopausal women with normal baseline endometrium (n = 599).8 For fezolinetant 45 mg, 1 of 203 participants had endometrial hyperplasia (EH) (0.5%; upper limit of one-sided 95% confidence interval [CI], 2.3%); no cases of EH were noted in the placebo (0 of 186) or fezolinetant 30-mg (0 of 210) groups. The incidence of EH or malignancy in fezolinetant-treated participants was within prespecified limits, as assessed by blinded, centrally read endometrial biopsies. Endometrial malignancy occurred in 1 of 210 in the fezolinetant 30-mg group (0.5%; 95% CI, 2.2%) with no cases in the other groups, thus meeting FDA requirements for endometrial safety.8
In addition, no significant differences were noted in change from baseline endometrial thickness on transvaginal ultrasonography between fezolinetant-treated and placebo groups. Likewise, no loss of bone density was found on dual-energy x-ray absorptiometry (DEXA) scans or trabecular bone scores.8
Liver safety
Although no cases of severe liver injury were noted, elevations in serum transaminase concentrations greater than 3 times the upper limit of normal were observed in the clinical trials. In Skylight 4, liver enzyme elevations more than 3 times the upper limit of normal occurred in 6 of 583 participants taking placebo, 8 of 590 taking fezolinetant 30 mg, and 12 of 589 taking fezolinetant 45 mg.8
The prescribing information for fezolinetant includes a warning for elevated hepatic transaminases: Fezolinetant should not be started if baseline serum transaminase concentration is equal to or exceeds 2 times the upper limit of normal. Liver tests should be obtained at baseline and repeated every 3 months for the first 9 months and then if symptoms suggest liver injury.11,12
Unmet need for nonhormone treatment of VMS
Vasomotor symptoms affect up to 80% of women, with approximately 25% bothersome enough to warrant treatment. Vasomotor symptoms persist for a median of 7 years, with duration and severity differing by race and ethnicity. Black, Hispanic, and possibly Native American women experience the highest burden of VMS.2 Although VMS, including hot flashes, night sweats, and mood and sleep disturbances, often are considered an annoyance to those with mild symptoms, moderate to severe VMS impact women’s lives, including functioning at home or work, affecting relationships, and decreasing perceived quality of life, and they have been associated with workplace absenteeism and increased health care costs, both direct from medical care and testing and indirect costs from lost work.13-15
Women with 7 or more daily moderate to severe VMS (defined as with sweating or affecting function) reported interference with sleep (94%), concentration (84%), mood (85%), energy (77%), and sexual activity (61%).16 Moderately to severely bothersome VMS have been associated with impaired psychological and general well-being, affecting work performance.17 Based on a Mayo Clinic workplace survey, Faubion and colleagues estimated an annual loss of $1.8 billion in the United States for menopause-related missed work and a $28 billion loss when medical expenses were added.15
Menopausal HT has been the primary treatment for VMS and has been shown to reduce the frequency and severity of hot flashes, with additional benefits on sleep, mood, fatigue, bone loss and reduction of fracture, and genitourinary syndrome of menopause (GSM), and with potential improvement in cardiovascular health with decreased type 2 diabetes.18,19 For healthy women with early menopause and no contraindications, HT has been recommended until at least the age of natural menopause, as observational data suggest that HT prevents osteoporosis, cardiovascular disease, neurodegenerative changes, and sexual dysfunction for these women.19,20 Similarly, for healthy women younger than age 60 or within 10 years of menopause, initiating HT has been shown to be safe and effective in treating bothersome VMS and preventing osteoporotic fractures and genitourinary changes.19,21
Most systemic HT formulations are inexpensive (for example, available as generics), with multiple dosing and formulations available for use alone or combined as oral, transdermal, or vaginal therapies. Despite the fear that arose for clinicians and women from the initial 2002 findings of the Women’s Health Initiative regarding increased risk of breast cancer, stroke, venous thrombosis, cardiovascular disease, and dementia, major medical societies agree that when initiated at or soon after menopause, HT is a safe and effective therapy to relieve VMS, protect against bone loss, and treat genitourinary changes.19,21
Many women, however, cannot take HT, including those with estrogen-sensitive cancers, such as breast or uterine cancers; prior cardiovascular disease, stroke, or venous thrombotic events; severe endometriosis; or migraine headaches with visual auras.2 In addition, many symptomatic menopausal women without health contraindications choose not to take HT.2 Until now, the only FDA-approved VMS nonhormone therapy has been a low-dose 7.5-mg paroxetine salt. Unfortunately, this formulation, along with the off-label use of other antidepressants (selective serotonin reuptake inhibitors and serotonin and norepinephrine reuptake inhibitors), gabapentinoids, oxybutynin, and clonidine, are substantially less effective than HT in treating moderate to severe VMS.
Bottom line
A substantial unmet need remains for effective therapy for moderate to severe VMS for women who cannot or choose not to take menopausal HT to relieve VMS.2,16 Effective, safe nonhormone treatment options such as the new NK3 receptor antagonist fezolinetant will address this clinically important need.
One concern is that the cost of developing and bringing to market the first of a new type of medication will be passed on to consumers, which may put it out of the price range for the many women who need it. However, the development and FDA approval of fezolinetant as the first NK3 receptor antagonist to treat menopausal VMS is potentially a practice changer. It provides a novel, effective, and safe FDA-approved nonhormonal treatment for menopausal women with moderate to severe VMS, particularly for women who cannot or will not take hormone therapy.
Continue to: When endometrial biopsy for postmenopausal bleeding reveals proliferative changes, how should we respond?...
When endometrial biopsy for postmenopausal bleeding reveals proliferative changes, how should we respond?
Abraham C. Proliferative endometrium in menopause: to treat or not to treat? Obstet Gynecol. 2023;141:265-267. doi:10.1097/AOG.0000000000005054.
The following case represents a common scenario for ObGyns.
CASE Patient with proliferative endometrial changes
A menopausal patient with a body mass index (BMI) > 30 kg/m2 presents with uterine bleeding. She does not use systemic menopausal hormone therapy. Endometrial biopsy indicates proliferative changes.
When endometrial biopsy performed for bleeding reveals proliferative changes in menopausal women, we traditionally have responded by reassuring the patient that the findings are benign and advising that she should let us know if future spotting or bleeding occurs.
However, a recent review by Abraham published in Obstetrics and Gynecology details the implications of proliferative endometrial changes in menopausal patients, advising that treatment, as well as monitoring, may be appropriate.22
Endometrial changes and what they suggest
In premenopausal women, proliferative endometrial changes are physiologic and result from ovarian estrogen production early in each cycle, during what is called the proliferative (referring to the endometrium) or follicular (referring to the dominant follicle that synthesizes estrogen) phase. In menopausal women who are not using HT, however, proliferative endometrial changes, with orderly uniform glands seen on histologic evaluation, reflect aromatization of androgens by adipose and other tissues into estrogen.
The next step on the continuum to hyperplasia (benign or atypical) after proliferative endometrium is disordered proliferative endometrium. At this stage, histologic evaluation reveals scattered cystic and dilated glands that have a normal gland-to-stroma ratio with a low gland density overall and without any atypia. Randomly distributed glands may have tubal metaplasia or fibrin thrombi associated with microinfarcts, often presenting with irregular bleeding. This is a noncancerous change that occurs with excess estrogen (endogenous or exogenous).23
Progestins reverse endometrial hyperplasia by activating progesterone receptors, which leads to stromal decidualization with thinning of the endometrium. They have a pronounced effect on the histologic appearance of the endometrium. By contrast, endometrial intraepithelial neoplasia (EIN, previously known as endometrial hyperplasiawith atypia) shows underlying molecular mutations and histologic alterations and represents a sharp transition to true neoplasia, which greatly increases the risk of endometrioid endometrial adenocarcinoma.24
For decades, we have been aware that if women diagnosed with endometrial hyperplasia are not treated with progestational therapy, their future risk of endometrial cancer is elevated. More recently, we also recognize that menopausal women found to have proliferative endometrial changes, if not treated, have an increased risk of endometrial cancer.
In a retrospective cohort study of almost 300 menopausal women who were not treated after endometrial biopsy revealed proliferative changes, investigators followed participants for an average of 11 years.25 These women had a mean BMI of 34 kg/m2. During follow-up, almost 12% of these women were diagnosed with endometrial hyperplasia or cancer. This incidence of endometrial neoplasia was some 4 times higher than for women initially found to have atrophic endometrial changes.25
Progestin treatment
Oral progestin therapy with follow-up endometrial biopsy constitutes traditional management for endometrial hyperplasia. Such therapy minimizes the likelihood that hyperplasia will progress to endometrial cancer.
We now recognize that the convenience, as well as the high endometrial progestin levels achieved, with levonorgestrel-releasing intrauterine devices (LNG-IUDs) have advantages over oral progestin therapy in treating endometrial hyperplasia. Indeed, a recent US report found that among women with EIN managed medically, use of progestin-releasing IUDs has grown from 7.7% in 2008 to 35.6% in 2020.26
Although both oral and intrauterine progestin are highly effective in treating simple hyperplasia, progestin IUDs are substantially more effective than oral progestins in treating EIN.27 Progestin concentrations in the endometrium have been shown to be 100-fold higher after LNG-IUD placement compared with oral progestin use.22 In addition, adverse effects, including bloating, unpleasant mood changes, and increased appetite, are more common with oral than intrauterine progestin therapy.28
Unfortunately, data from randomized trials addressing progestational treatment of proliferative endometrium in menopausal women are not available to support the treatment of proliferative endometrium with either oral progestins or the LNG-IUD.22
Role of ultrasonography
Another concern is relying on a finding of thin endometrial thickness on vaginal ultrasonography. In a simulated retrospective cohort study, use of transvaginal ultrasonography to determine the appropriateness of a biopsy was found not to be sufficiently accurate or racially equitable with regard to Black women.29 In simulated data, transvaginal ultrasonography missed almost 5 times more cases of endometrial cancer among Black women compared with White women due to higher fibroid prevalence and nonendometrioid histologic type malignancies in Black women.29
Assessing risk
If proliferative endometrium is found, Abraham suggests assessing risk using22:
- age
- comorbidities (including obesity)
- endometrial echo thickness on vaginal ultrasonography.
Consider the patient’s risk and tolerance of recurrent bleeding as well as her tolerance for progestational adverse effects if medical therapy is chosen. Discussion about next steps should include reviewing the histologic findings with the patient and discussing the difference in risk of progression to endometrial cancer of a finding of proliferative endometrium compared with a histologic finding of endometrial hyperplasia.
Using this patient-centered approach, observation over time with follow-up endometrial biopsies remains a management option. Although some women may tolerate micronized progesterone over synthetic progestins, there is concern that it may be less effective in suppressing the endometrium than synthetic progestins.30 Accordingly, synthetic progestins represent first-line options in this setting.
In her review, Abraham suggests that when endometrial biopsy reveals proliferative changes in a menopausal woman, we should initiate progestin treatment and perform surveillance endometrial sampling every 3 to 6 months. If such sampling reveals benign but not proliferative endometrium, progestin therapy can be stopped and endometrial biopsy repeated if bleeding recurs.22 ●
ObGyns may choose to adopt Abraham’s approach or to hold off on progestin therapy while performing follow-up endometrial sampling. Either way, the take-home message is that the finding of proliferative endometrial changes on biopsy for postmenopausal bleeding requires proactive management.
- Modi M, Dhillo WS. Neurokinin 3 receptor antagonism: a novel treatment for menopausal hot flushes. Neuroendocrinology. 2019;109:242-248. doi:10.1159/000495889
- Pinkerton JV, Redick DL, Homewood LN, et al. Neurokinin receptor antagonist, fezolinetant, for treatment of menopausal vasomotor symptoms. J Clin Endocrinol Metab. 2023;dgad209. doi:10.1210/clinem/dgad209
- Rance NE, Dacks PA, Mittelman-Smith MA, et al. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: a novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34:211-227. doi:10.1016 /j.yfrne.2013.07.003
- Mittelman-Smith MA, Williams H, Krajewski-Hall SJ, et al. Role for kisspeptin/neurokinin B/dynorphin (KNDy) neurons in cutaneous vasodilatation and the estrogen modulation of body temperature. Proc Natl Acad Sci USA. 2012;109:1984619851. doi:10.1073/pnas.1211517109
- Astellas Pharma. Astellas’ Veozah (fezolinetant) approved by US FDA for treatment of vasomotor symptoms due to menopause. May 12, 2023. PR Newswire. Accessed May 15, 2023. https://www.prnewswire.com/news-releases/astellas-veozah-fezolinetant-approved-by-us-fda-for -treatment-of-vasomotor-symptoms-due-to-menopause -301823639.html
- Johnson KA, Martin N, Nappi RE, et al. Efficacy and safety of fezolinetant in moderate-to-severe vasomotor symptoms associated with menopause: a phase 3 RCT. J Clin Endocrinol Metab. 2023;dgad058. doi:10.1210/clinem/dgad058
- Lederman S, Ottery FD, Cano A, et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): a phase 3 randomised controlled study. Lancet. 2023;401:1091-1102. doi:10.1016 /S0140-6736(23)00085-5
- Neal-Perry G, Cano A, Lederman S, et al. Safety of fezolinetant for vasomotor symptoms associated with menopause: a randomized controlled trial. Obstet Gynecol. 2023;141:737-747. doi:10.1097/AOG.0000000000005114
- Depypere H, Timmerman D, Donders G, et al. Treatment of menopausal vasomotor symptoms with fezolinetant, a neurokinin 3 receptor antagonist: a phase 2a trial. J Clin Endocrinol Metab. 2019;104:5893-5905. doi: 10.1210/jc .2019-00677
- Santoro N, Waldbaum A, Lederman S, et al. Effect of the neurokinin 3 receptor antagonist fezolinetant on patientreported outcomes in postmenopausal women with vasomotor symptoms: results of a randomized, placebo-controlled, double-blind, dose-ranging study (VESTA). Menopause. 2020;27:1350-1356. doi:10.1097/GME.0000000000001621
- FDA approves novel drug to treat moderate to severe hot flashes caused by menopause. May 12, 2023. US Food and Drug Administration. Accessed May 15, 2023. https://www .fda.gov/news-events/press-announcements/fda-approves -novel-drug-treat-moderate-severe-hot-flashes-caused -menopause
- Veozah. Prescribing information. Astellas; 2023. Accessed May 16, 2023. https://www.astellas.com/us/system/files /veozah_uspi.pdf
- Pinkerton JV. Money talks: untreated hot flashes cost women, the workplace, and society. Menopause. 2015;22:254-255. doi:10.1097/GME.0000000000000427
- Sarrel P, Portman D, Lefebvre P, et al. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause. 2015;22(3):260-266. doi:10.1097/GME.0000000000000320
- Faubion SS, Enders F, Hedges MS, et al. Impact of menopause symptoms on women in the workplace. Mayo Clin Proc. 2023;98:833-845. doi:10.1016/j.mayocp.2023.02.025
- Williams RE, Levine KB, Kalilani L, et al. Menopause- specific questionnaire assessment in US populationbased study shows negative impact on health-related quality of life. Maturitas. 2009;62:153-159. doi:10.1016 /j.maturitas.2008.12.006
- Gartoulla P, Bell RJ, Worsley R, et al. Moderate-severely bothersome vasomotor symptoms are associated with lowered psychological general wellbeing in women at midlife. Maturitas. 2015;81:487-492. doi:10.1016 /j.maturitas.2015.06.004
- Manson JE, Kaunitz AM. Menopause management—getting clinical care back on track. N Engl J Med. 2016;374:803-806. doi:10.1056/NEJMp1514242
- 2022 Hormone Therapy Position Statement of the North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of the North American Menopause Society. Menopause. 2022;29:767-794. doi:10.1097/GME.0000000000002028
- Kaunitz AM, Kapoor E, Faubion S. Treatment of women after bilateral salpingo-oophorectomy performed prior to natural menopause. JAMA. 2021;12;326:1429-1430. doi:10.1001 /jama.2021.3305
- Pinkerton JV. Hormone therapy for postmenopausal women. N Engl J Med. 2020;382:446-455. doi:10.1056 /NEJMcp1714787
- Abraham C. Proliferative endometrium in menopause: to treat or not to treat? Obstet Gynecol. 2023;141:265-267. doi:10.1097/AOG.0000000000005054
- Chandra V, Kim JJ, Benbrook DM, et al. Therapeutic options for management of endometrial hyperplasia. J Gynecol Oncol. 2016;27:e8. doi:10.3802/jgo.2016.27.e8
- Owings RA, Quick CM. Endometrial intraepithelial neoplasia. Arch Pathol Lab Med. 2014;138:484-491. doi:10.5858 /arpa.2012-0709-RA
- Rotenberg O, Doulaveris G, Fridman D, et al. Long-term outcome of postmenopausal women with proliferative endometrium on endometrial sampling. Am J Obstet Gynecol. 2020;223:896.e1-896.e7. doi:10.1016/j.ajog.2020.06.045
- Suzuki Y, Chen L, Hou JY, et al. Systemic progestins and progestin-releasing intrauterine device therapy for premenopausal patients with endometrial intraepithelial neoplasia. Obstet Gynecol. 2023;141:979-987. doi:10.1097 /AOG.0000000000005124
- Mandelbaum RS, Ciccone MA, Nusbaum DJ, et al. Progestin therapy for obese women with complex atypical hyperplasia: levonorgestrel-releasing intrauterine device vs systemic therapy. Am J Obstet Gynecol. 2020;223:103.e1-103.e13. doi:10.1016/j.ajog.2019.12.273
- Liu S, Kciuk O, Frank M, et al. Progestins of today and tomorrow. Curr Opin Obstet Gynecol. 2022;34:344-350. doi:10.1097 /GCO.0000000000000819
- Doll KM, Romano SS, Marsh EE, et al. Estimated performance of transvaginal ultrasonography for evaluation of postmenopausal bleeding in a simulated cohort of black and white women in the US. JAMA Oncol. 2021;7:1158-1165. doi:10.1001/jamaoncol.2021.1700
- Gompel A. Progesterone and endometrial cancer. Best Pract Res Clin Obstet Gynaecol. 2020;69:95-107. doi:10.1016 /j.bpobgyn.2020.05.003
This year’s menopause Update highlights a highly effective nonhormonal medication that recently received approval by the US Food and Drug Administration (FDA) for the treatment of bothersome menopausal vasomotor symptoms. In addition, the Update provides guidance regarding how ObGyns should respond when an endometrial biopsy for postmenopausal bleeding reveals proliferative changes.
Breakthrough in women’s health: A new nonhormone therapy for vasomotor symptoms
Johnson KA, Martin N, Nappi RE, et al. Efficacy and safety of fezolinetant in moderate-to-severe vasomotor symptoms associated with menopause: a phase 3 RCT. J Clin Endocrinol Metab. 2023;dgad058. doi:10.1210/clinem/dgad058.
Lederman S, Ottery FD, Cano A, et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): a phase 3 randomised controlled study. Lancet. 2023;401:1091-1102. doi:10.1016/S0140-6736(23)00085-5.
A new oral nonestrogen-containing medication for relief of moderate to severe hot flashes, fezolinetant (Veozah) 45 mg daily, has been approved by the FDA and was expected to be available by the end of May 2023. Fezolinetant is a selective neurokinin 3 (NK3) receptor antagonistthat offers a targeted nonhormonal approach to menopausal vasomotor symptoms (VMS), and it is the first in its class to make it to market.
The decline in estrogen at menopause appears to result in increased signaling at kisspeptin/neurokinin B/dynorphin (KNDy) neurons in the thermoregulatory center within the hypothalamus with resultant increases in hot flashes.1,2 Fezolinetant works by binding to and blocking the activities of the NK3 receptor.3-5
Key study findings
Selective NK3 receptor antagonists, including fezolinetant, effectively reduce the frequency and severity of VMS comparable to that of hormone therapy (HT). Two phase 3 clinical trials, Skylight 1 and 2, confirmed the efficacy and safety of fezolinetant 45 mg in treating VMS,6,7 and an additional 52-week placebo-controlled study, Skylight 4, confirmed long-term safety.8 Onset of action occurs within a week. Reported adverse events occurred in 1% to 2% of healthy menopausal women participating in clinical trials; these included headaches, abdominal pain, diarrhea, insomnia, back pain, hot flushes, and reversible elevated hepatic transaminase levels.6-9
The published phase 2 trials9 and the international randomized controlled trial (RCT) 12-week studies, Skylight 1 and 2,6,7 found that once-daily 30-mg and 45-mg doses of fezolinetant significantly reduced VMS frequency and severity at 12 weeks among women aged 40 to 60 years who reported an average of 7 moderate to severe VMS/day; the reduction in reported VMS was sustained at 40 weeks. Phase 3 data from Skylight 1 and 2 demonstrated fezolinetant’s efficacy in reducing the frequency and severity of VMS and provided information on the safety profile of fezolinetant compared with placebo over 12 weeks and a noncontrolled extension for an additional 40 weeks.6,7
Oral fezolinetant was associated with improved quality of life, including reduced VMS-related interference with daily life.10 Johnson and colleagues, reporting for Skylight 2, found VMS frequency and severity improvement by week 1, which achieved statistical significance at weeks 4 and 12, with this improvement maintained through week 52.6 A 64.3% reduction in mean daily VMS from baseline was seen at 12 weeks for fezolinetant 45 mg compared with a 45.4% reduction for placebo. VMS severity significantly decreased compared with placebo at 4 and 12 weeks.6
Serious treatment-emergent adverse events were infrequent, reported by 2%, 1%, and 0% of those receiving fezolinetant 30 mg, fezolinetant 45 mg, and placebo.6 Increases in levels of alanine aminotransferase (ALT) or aspartate aminotransferase (AST) were noted and were described as asymptomatic, isolated, intermittent, or transient, and these levels returned to baseline during treatment or after discontinuation.6
Of the 5 participants taking fezolinetant in Skyline 1 with ALT or AST levels greater than 3 times the upper limit of normal in the 12-week randomized trial, levels returned to normal range while continuing treatment in 2 participants, with treatment interruption in 2, and with discontinuation in 1. No new safety signals were seen in the 40-week extension trial.6
Fezolinetant offers a much-needed effective and safe selective nonhormone NK3 receptor antagonist therapy that reduces the frequency and severity of menopausal VMS and has been shown to be safe through 52 weeks of treatment.
To read more about how fezolinetant specifically targets the hormone receptor that triggers hot flashes as well as on prescribing hormone therapy for women with menopausal symptoms, see “Focus on menopause: Q&A with Jan Shifren, MD, and Genevieve NealPerry, MD, PhD,” in the December 2022 issue of OBG Management at https://www.mdedge.com/obgyn/article/260380/menopause
Continue to: Endometrial and bone safety...
Endometrial and bone safety
Results from Skylight 4, a phase 3, randomized, double-blind, 52-week safety study, provided additional evidence that confirmed the longer-term safety of fezolinetant over a 52-week treatment period.8
Endometrial safety was assessed in postmenopausal women with normal baseline endometrium (n = 599).8 For fezolinetant 45 mg, 1 of 203 participants had endometrial hyperplasia (EH) (0.5%; upper limit of one-sided 95% confidence interval [CI], 2.3%); no cases of EH were noted in the placebo (0 of 186) or fezolinetant 30-mg (0 of 210) groups. The incidence of EH or malignancy in fezolinetant-treated participants was within prespecified limits, as assessed by blinded, centrally read endometrial biopsies. Endometrial malignancy occurred in 1 of 210 in the fezolinetant 30-mg group (0.5%; 95% CI, 2.2%) with no cases in the other groups, thus meeting FDA requirements for endometrial safety.8
In addition, no significant differences were noted in change from baseline endometrial thickness on transvaginal ultrasonography between fezolinetant-treated and placebo groups. Likewise, no loss of bone density was found on dual-energy x-ray absorptiometry (DEXA) scans or trabecular bone scores.8
Liver safety
Although no cases of severe liver injury were noted, elevations in serum transaminase concentrations greater than 3 times the upper limit of normal were observed in the clinical trials. In Skylight 4, liver enzyme elevations more than 3 times the upper limit of normal occurred in 6 of 583 participants taking placebo, 8 of 590 taking fezolinetant 30 mg, and 12 of 589 taking fezolinetant 45 mg.8
The prescribing information for fezolinetant includes a warning for elevated hepatic transaminases: Fezolinetant should not be started if baseline serum transaminase concentration is equal to or exceeds 2 times the upper limit of normal. Liver tests should be obtained at baseline and repeated every 3 months for the first 9 months and then if symptoms suggest liver injury.11,12
Unmet need for nonhormone treatment of VMS
Vasomotor symptoms affect up to 80% of women, with approximately 25% bothersome enough to warrant treatment. Vasomotor symptoms persist for a median of 7 years, with duration and severity differing by race and ethnicity. Black, Hispanic, and possibly Native American women experience the highest burden of VMS.2 Although VMS, including hot flashes, night sweats, and mood and sleep disturbances, often are considered an annoyance to those with mild symptoms, moderate to severe VMS impact women’s lives, including functioning at home or work, affecting relationships, and decreasing perceived quality of life, and they have been associated with workplace absenteeism and increased health care costs, both direct from medical care and testing and indirect costs from lost work.13-15
Women with 7 or more daily moderate to severe VMS (defined as with sweating or affecting function) reported interference with sleep (94%), concentration (84%), mood (85%), energy (77%), and sexual activity (61%).16 Moderately to severely bothersome VMS have been associated with impaired psychological and general well-being, affecting work performance.17 Based on a Mayo Clinic workplace survey, Faubion and colleagues estimated an annual loss of $1.8 billion in the United States for menopause-related missed work and a $28 billion loss when medical expenses were added.15
Menopausal HT has been the primary treatment for VMS and has been shown to reduce the frequency and severity of hot flashes, with additional benefits on sleep, mood, fatigue, bone loss and reduction of fracture, and genitourinary syndrome of menopause (GSM), and with potential improvement in cardiovascular health with decreased type 2 diabetes.18,19 For healthy women with early menopause and no contraindications, HT has been recommended until at least the age of natural menopause, as observational data suggest that HT prevents osteoporosis, cardiovascular disease, neurodegenerative changes, and sexual dysfunction for these women.19,20 Similarly, for healthy women younger than age 60 or within 10 years of menopause, initiating HT has been shown to be safe and effective in treating bothersome VMS and preventing osteoporotic fractures and genitourinary changes.19,21
Most systemic HT formulations are inexpensive (for example, available as generics), with multiple dosing and formulations available for use alone or combined as oral, transdermal, or vaginal therapies. Despite the fear that arose for clinicians and women from the initial 2002 findings of the Women’s Health Initiative regarding increased risk of breast cancer, stroke, venous thrombosis, cardiovascular disease, and dementia, major medical societies agree that when initiated at or soon after menopause, HT is a safe and effective therapy to relieve VMS, protect against bone loss, and treat genitourinary changes.19,21
Many women, however, cannot take HT, including those with estrogen-sensitive cancers, such as breast or uterine cancers; prior cardiovascular disease, stroke, or venous thrombotic events; severe endometriosis; or migraine headaches with visual auras.2 In addition, many symptomatic menopausal women without health contraindications choose not to take HT.2 Until now, the only FDA-approved VMS nonhormone therapy has been a low-dose 7.5-mg paroxetine salt. Unfortunately, this formulation, along with the off-label use of other antidepressants (selective serotonin reuptake inhibitors and serotonin and norepinephrine reuptake inhibitors), gabapentinoids, oxybutynin, and clonidine, are substantially less effective than HT in treating moderate to severe VMS.
Bottom line
A substantial unmet need remains for effective therapy for moderate to severe VMS for women who cannot or choose not to take menopausal HT to relieve VMS.2,16 Effective, safe nonhormone treatment options such as the new NK3 receptor antagonist fezolinetant will address this clinically important need.
One concern is that the cost of developing and bringing to market the first of a new type of medication will be passed on to consumers, which may put it out of the price range for the many women who need it. However, the development and FDA approval of fezolinetant as the first NK3 receptor antagonist to treat menopausal VMS is potentially a practice changer. It provides a novel, effective, and safe FDA-approved nonhormonal treatment for menopausal women with moderate to severe VMS, particularly for women who cannot or will not take hormone therapy.
Continue to: When endometrial biopsy for postmenopausal bleeding reveals proliferative changes, how should we respond?...
When endometrial biopsy for postmenopausal bleeding reveals proliferative changes, how should we respond?
Abraham C. Proliferative endometrium in menopause: to treat or not to treat? Obstet Gynecol. 2023;141:265-267. doi:10.1097/AOG.0000000000005054.
The following case represents a common scenario for ObGyns.
CASE Patient with proliferative endometrial changes
A menopausal patient with a body mass index (BMI) > 30 kg/m2 presents with uterine bleeding. She does not use systemic menopausal hormone therapy. Endometrial biopsy indicates proliferative changes.
When endometrial biopsy performed for bleeding reveals proliferative changes in menopausal women, we traditionally have responded by reassuring the patient that the findings are benign and advising that she should let us know if future spotting or bleeding occurs.
However, a recent review by Abraham published in Obstetrics and Gynecology details the implications of proliferative endometrial changes in menopausal patients, advising that treatment, as well as monitoring, may be appropriate.22
Endometrial changes and what they suggest
In premenopausal women, proliferative endometrial changes are physiologic and result from ovarian estrogen production early in each cycle, during what is called the proliferative (referring to the endometrium) or follicular (referring to the dominant follicle that synthesizes estrogen) phase. In menopausal women who are not using HT, however, proliferative endometrial changes, with orderly uniform glands seen on histologic evaluation, reflect aromatization of androgens by adipose and other tissues into estrogen.
The next step on the continuum to hyperplasia (benign or atypical) after proliferative endometrium is disordered proliferative endometrium. At this stage, histologic evaluation reveals scattered cystic and dilated glands that have a normal gland-to-stroma ratio with a low gland density overall and without any atypia. Randomly distributed glands may have tubal metaplasia or fibrin thrombi associated with microinfarcts, often presenting with irregular bleeding. This is a noncancerous change that occurs with excess estrogen (endogenous or exogenous).23
Progestins reverse endometrial hyperplasia by activating progesterone receptors, which leads to stromal decidualization with thinning of the endometrium. They have a pronounced effect on the histologic appearance of the endometrium. By contrast, endometrial intraepithelial neoplasia (EIN, previously known as endometrial hyperplasiawith atypia) shows underlying molecular mutations and histologic alterations and represents a sharp transition to true neoplasia, which greatly increases the risk of endometrioid endometrial adenocarcinoma.24
For decades, we have been aware that if women diagnosed with endometrial hyperplasia are not treated with progestational therapy, their future risk of endometrial cancer is elevated. More recently, we also recognize that menopausal women found to have proliferative endometrial changes, if not treated, have an increased risk of endometrial cancer.
In a retrospective cohort study of almost 300 menopausal women who were not treated after endometrial biopsy revealed proliferative changes, investigators followed participants for an average of 11 years.25 These women had a mean BMI of 34 kg/m2. During follow-up, almost 12% of these women were diagnosed with endometrial hyperplasia or cancer. This incidence of endometrial neoplasia was some 4 times higher than for women initially found to have atrophic endometrial changes.25
Progestin treatment
Oral progestin therapy with follow-up endometrial biopsy constitutes traditional management for endometrial hyperplasia. Such therapy minimizes the likelihood that hyperplasia will progress to endometrial cancer.
We now recognize that the convenience, as well as the high endometrial progestin levels achieved, with levonorgestrel-releasing intrauterine devices (LNG-IUDs) have advantages over oral progestin therapy in treating endometrial hyperplasia. Indeed, a recent US report found that among women with EIN managed medically, use of progestin-releasing IUDs has grown from 7.7% in 2008 to 35.6% in 2020.26
Although both oral and intrauterine progestin are highly effective in treating simple hyperplasia, progestin IUDs are substantially more effective than oral progestins in treating EIN.27 Progestin concentrations in the endometrium have been shown to be 100-fold higher after LNG-IUD placement compared with oral progestin use.22 In addition, adverse effects, including bloating, unpleasant mood changes, and increased appetite, are more common with oral than intrauterine progestin therapy.28
Unfortunately, data from randomized trials addressing progestational treatment of proliferative endometrium in menopausal women are not available to support the treatment of proliferative endometrium with either oral progestins or the LNG-IUD.22
Role of ultrasonography
Another concern is relying on a finding of thin endometrial thickness on vaginal ultrasonography. In a simulated retrospective cohort study, use of transvaginal ultrasonography to determine the appropriateness of a biopsy was found not to be sufficiently accurate or racially equitable with regard to Black women.29 In simulated data, transvaginal ultrasonography missed almost 5 times more cases of endometrial cancer among Black women compared with White women due to higher fibroid prevalence and nonendometrioid histologic type malignancies in Black women.29
Assessing risk
If proliferative endometrium is found, Abraham suggests assessing risk using22:
- age
- comorbidities (including obesity)
- endometrial echo thickness on vaginal ultrasonography.
Consider the patient’s risk and tolerance of recurrent bleeding as well as her tolerance for progestational adverse effects if medical therapy is chosen. Discussion about next steps should include reviewing the histologic findings with the patient and discussing the difference in risk of progression to endometrial cancer of a finding of proliferative endometrium compared with a histologic finding of endometrial hyperplasia.
Using this patient-centered approach, observation over time with follow-up endometrial biopsies remains a management option. Although some women may tolerate micronized progesterone over synthetic progestins, there is concern that it may be less effective in suppressing the endometrium than synthetic progestins.30 Accordingly, synthetic progestins represent first-line options in this setting.
In her review, Abraham suggests that when endometrial biopsy reveals proliferative changes in a menopausal woman, we should initiate progestin treatment and perform surveillance endometrial sampling every 3 to 6 months. If such sampling reveals benign but not proliferative endometrium, progestin therapy can be stopped and endometrial biopsy repeated if bleeding recurs.22 ●
ObGyns may choose to adopt Abraham’s approach or to hold off on progestin therapy while performing follow-up endometrial sampling. Either way, the take-home message is that the finding of proliferative endometrial changes on biopsy for postmenopausal bleeding requires proactive management.
This year’s menopause Update highlights a highly effective nonhormonal medication that recently received approval by the US Food and Drug Administration (FDA) for the treatment of bothersome menopausal vasomotor symptoms. In addition, the Update provides guidance regarding how ObGyns should respond when an endometrial biopsy for postmenopausal bleeding reveals proliferative changes.
Breakthrough in women’s health: A new nonhormone therapy for vasomotor symptoms
Johnson KA, Martin N, Nappi RE, et al. Efficacy and safety of fezolinetant in moderate-to-severe vasomotor symptoms associated with menopause: a phase 3 RCT. J Clin Endocrinol Metab. 2023;dgad058. doi:10.1210/clinem/dgad058.
Lederman S, Ottery FD, Cano A, et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): a phase 3 randomised controlled study. Lancet. 2023;401:1091-1102. doi:10.1016/S0140-6736(23)00085-5.
A new oral nonestrogen-containing medication for relief of moderate to severe hot flashes, fezolinetant (Veozah) 45 mg daily, has been approved by the FDA and was expected to be available by the end of May 2023. Fezolinetant is a selective neurokinin 3 (NK3) receptor antagonistthat offers a targeted nonhormonal approach to menopausal vasomotor symptoms (VMS), and it is the first in its class to make it to market.
The decline in estrogen at menopause appears to result in increased signaling at kisspeptin/neurokinin B/dynorphin (KNDy) neurons in the thermoregulatory center within the hypothalamus with resultant increases in hot flashes.1,2 Fezolinetant works by binding to and blocking the activities of the NK3 receptor.3-5
Key study findings
Selective NK3 receptor antagonists, including fezolinetant, effectively reduce the frequency and severity of VMS comparable to that of hormone therapy (HT). Two phase 3 clinical trials, Skylight 1 and 2, confirmed the efficacy and safety of fezolinetant 45 mg in treating VMS,6,7 and an additional 52-week placebo-controlled study, Skylight 4, confirmed long-term safety.8 Onset of action occurs within a week. Reported adverse events occurred in 1% to 2% of healthy menopausal women participating in clinical trials; these included headaches, abdominal pain, diarrhea, insomnia, back pain, hot flushes, and reversible elevated hepatic transaminase levels.6-9
The published phase 2 trials9 and the international randomized controlled trial (RCT) 12-week studies, Skylight 1 and 2,6,7 found that once-daily 30-mg and 45-mg doses of fezolinetant significantly reduced VMS frequency and severity at 12 weeks among women aged 40 to 60 years who reported an average of 7 moderate to severe VMS/day; the reduction in reported VMS was sustained at 40 weeks. Phase 3 data from Skylight 1 and 2 demonstrated fezolinetant’s efficacy in reducing the frequency and severity of VMS and provided information on the safety profile of fezolinetant compared with placebo over 12 weeks and a noncontrolled extension for an additional 40 weeks.6,7
Oral fezolinetant was associated with improved quality of life, including reduced VMS-related interference with daily life.10 Johnson and colleagues, reporting for Skylight 2, found VMS frequency and severity improvement by week 1, which achieved statistical significance at weeks 4 and 12, with this improvement maintained through week 52.6 A 64.3% reduction in mean daily VMS from baseline was seen at 12 weeks for fezolinetant 45 mg compared with a 45.4% reduction for placebo. VMS severity significantly decreased compared with placebo at 4 and 12 weeks.6
Serious treatment-emergent adverse events were infrequent, reported by 2%, 1%, and 0% of those receiving fezolinetant 30 mg, fezolinetant 45 mg, and placebo.6 Increases in levels of alanine aminotransferase (ALT) or aspartate aminotransferase (AST) were noted and were described as asymptomatic, isolated, intermittent, or transient, and these levels returned to baseline during treatment or after discontinuation.6
Of the 5 participants taking fezolinetant in Skyline 1 with ALT or AST levels greater than 3 times the upper limit of normal in the 12-week randomized trial, levels returned to normal range while continuing treatment in 2 participants, with treatment interruption in 2, and with discontinuation in 1. No new safety signals were seen in the 40-week extension trial.6
Fezolinetant offers a much-needed effective and safe selective nonhormone NK3 receptor antagonist therapy that reduces the frequency and severity of menopausal VMS and has been shown to be safe through 52 weeks of treatment.
To read more about how fezolinetant specifically targets the hormone receptor that triggers hot flashes as well as on prescribing hormone therapy for women with menopausal symptoms, see “Focus on menopause: Q&A with Jan Shifren, MD, and Genevieve NealPerry, MD, PhD,” in the December 2022 issue of OBG Management at https://www.mdedge.com/obgyn/article/260380/menopause
Continue to: Endometrial and bone safety...
Endometrial and bone safety
Results from Skylight 4, a phase 3, randomized, double-blind, 52-week safety study, provided additional evidence that confirmed the longer-term safety of fezolinetant over a 52-week treatment period.8
Endometrial safety was assessed in postmenopausal women with normal baseline endometrium (n = 599).8 For fezolinetant 45 mg, 1 of 203 participants had endometrial hyperplasia (EH) (0.5%; upper limit of one-sided 95% confidence interval [CI], 2.3%); no cases of EH were noted in the placebo (0 of 186) or fezolinetant 30-mg (0 of 210) groups. The incidence of EH or malignancy in fezolinetant-treated participants was within prespecified limits, as assessed by blinded, centrally read endometrial biopsies. Endometrial malignancy occurred in 1 of 210 in the fezolinetant 30-mg group (0.5%; 95% CI, 2.2%) with no cases in the other groups, thus meeting FDA requirements for endometrial safety.8
In addition, no significant differences were noted in change from baseline endometrial thickness on transvaginal ultrasonography between fezolinetant-treated and placebo groups. Likewise, no loss of bone density was found on dual-energy x-ray absorptiometry (DEXA) scans or trabecular bone scores.8
Liver safety
Although no cases of severe liver injury were noted, elevations in serum transaminase concentrations greater than 3 times the upper limit of normal were observed in the clinical trials. In Skylight 4, liver enzyme elevations more than 3 times the upper limit of normal occurred in 6 of 583 participants taking placebo, 8 of 590 taking fezolinetant 30 mg, and 12 of 589 taking fezolinetant 45 mg.8
The prescribing information for fezolinetant includes a warning for elevated hepatic transaminases: Fezolinetant should not be started if baseline serum transaminase concentration is equal to or exceeds 2 times the upper limit of normal. Liver tests should be obtained at baseline and repeated every 3 months for the first 9 months and then if symptoms suggest liver injury.11,12
Unmet need for nonhormone treatment of VMS
Vasomotor symptoms affect up to 80% of women, with approximately 25% bothersome enough to warrant treatment. Vasomotor symptoms persist for a median of 7 years, with duration and severity differing by race and ethnicity. Black, Hispanic, and possibly Native American women experience the highest burden of VMS.2 Although VMS, including hot flashes, night sweats, and mood and sleep disturbances, often are considered an annoyance to those with mild symptoms, moderate to severe VMS impact women’s lives, including functioning at home or work, affecting relationships, and decreasing perceived quality of life, and they have been associated with workplace absenteeism and increased health care costs, both direct from medical care and testing and indirect costs from lost work.13-15
Women with 7 or more daily moderate to severe VMS (defined as with sweating or affecting function) reported interference with sleep (94%), concentration (84%), mood (85%), energy (77%), and sexual activity (61%).16 Moderately to severely bothersome VMS have been associated with impaired psychological and general well-being, affecting work performance.17 Based on a Mayo Clinic workplace survey, Faubion and colleagues estimated an annual loss of $1.8 billion in the United States for menopause-related missed work and a $28 billion loss when medical expenses were added.15
Menopausal HT has been the primary treatment for VMS and has been shown to reduce the frequency and severity of hot flashes, with additional benefits on sleep, mood, fatigue, bone loss and reduction of fracture, and genitourinary syndrome of menopause (GSM), and with potential improvement in cardiovascular health with decreased type 2 diabetes.18,19 For healthy women with early menopause and no contraindications, HT has been recommended until at least the age of natural menopause, as observational data suggest that HT prevents osteoporosis, cardiovascular disease, neurodegenerative changes, and sexual dysfunction for these women.19,20 Similarly, for healthy women younger than age 60 or within 10 years of menopause, initiating HT has been shown to be safe and effective in treating bothersome VMS and preventing osteoporotic fractures and genitourinary changes.19,21
Most systemic HT formulations are inexpensive (for example, available as generics), with multiple dosing and formulations available for use alone or combined as oral, transdermal, or vaginal therapies. Despite the fear that arose for clinicians and women from the initial 2002 findings of the Women’s Health Initiative regarding increased risk of breast cancer, stroke, venous thrombosis, cardiovascular disease, and dementia, major medical societies agree that when initiated at or soon after menopause, HT is a safe and effective therapy to relieve VMS, protect against bone loss, and treat genitourinary changes.19,21
Many women, however, cannot take HT, including those with estrogen-sensitive cancers, such as breast or uterine cancers; prior cardiovascular disease, stroke, or venous thrombotic events; severe endometriosis; or migraine headaches with visual auras.2 In addition, many symptomatic menopausal women without health contraindications choose not to take HT.2 Until now, the only FDA-approved VMS nonhormone therapy has been a low-dose 7.5-mg paroxetine salt. Unfortunately, this formulation, along with the off-label use of other antidepressants (selective serotonin reuptake inhibitors and serotonin and norepinephrine reuptake inhibitors), gabapentinoids, oxybutynin, and clonidine, are substantially less effective than HT in treating moderate to severe VMS.
Bottom line
A substantial unmet need remains for effective therapy for moderate to severe VMS for women who cannot or choose not to take menopausal HT to relieve VMS.2,16 Effective, safe nonhormone treatment options such as the new NK3 receptor antagonist fezolinetant will address this clinically important need.
One concern is that the cost of developing and bringing to market the first of a new type of medication will be passed on to consumers, which may put it out of the price range for the many women who need it. However, the development and FDA approval of fezolinetant as the first NK3 receptor antagonist to treat menopausal VMS is potentially a practice changer. It provides a novel, effective, and safe FDA-approved nonhormonal treatment for menopausal women with moderate to severe VMS, particularly for women who cannot or will not take hormone therapy.
Continue to: When endometrial biopsy for postmenopausal bleeding reveals proliferative changes, how should we respond?...
When endometrial biopsy for postmenopausal bleeding reveals proliferative changes, how should we respond?
Abraham C. Proliferative endometrium in menopause: to treat or not to treat? Obstet Gynecol. 2023;141:265-267. doi:10.1097/AOG.0000000000005054.
The following case represents a common scenario for ObGyns.
CASE Patient with proliferative endometrial changes
A menopausal patient with a body mass index (BMI) > 30 kg/m2 presents with uterine bleeding. She does not use systemic menopausal hormone therapy. Endometrial biopsy indicates proliferative changes.
When endometrial biopsy performed for bleeding reveals proliferative changes in menopausal women, we traditionally have responded by reassuring the patient that the findings are benign and advising that she should let us know if future spotting or bleeding occurs.
However, a recent review by Abraham published in Obstetrics and Gynecology details the implications of proliferative endometrial changes in menopausal patients, advising that treatment, as well as monitoring, may be appropriate.22
Endometrial changes and what they suggest
In premenopausal women, proliferative endometrial changes are physiologic and result from ovarian estrogen production early in each cycle, during what is called the proliferative (referring to the endometrium) or follicular (referring to the dominant follicle that synthesizes estrogen) phase. In menopausal women who are not using HT, however, proliferative endometrial changes, with orderly uniform glands seen on histologic evaluation, reflect aromatization of androgens by adipose and other tissues into estrogen.
The next step on the continuum to hyperplasia (benign or atypical) after proliferative endometrium is disordered proliferative endometrium. At this stage, histologic evaluation reveals scattered cystic and dilated glands that have a normal gland-to-stroma ratio with a low gland density overall and without any atypia. Randomly distributed glands may have tubal metaplasia or fibrin thrombi associated with microinfarcts, often presenting with irregular bleeding. This is a noncancerous change that occurs with excess estrogen (endogenous or exogenous).23
Progestins reverse endometrial hyperplasia by activating progesterone receptors, which leads to stromal decidualization with thinning of the endometrium. They have a pronounced effect on the histologic appearance of the endometrium. By contrast, endometrial intraepithelial neoplasia (EIN, previously known as endometrial hyperplasiawith atypia) shows underlying molecular mutations and histologic alterations and represents a sharp transition to true neoplasia, which greatly increases the risk of endometrioid endometrial adenocarcinoma.24
For decades, we have been aware that if women diagnosed with endometrial hyperplasia are not treated with progestational therapy, their future risk of endometrial cancer is elevated. More recently, we also recognize that menopausal women found to have proliferative endometrial changes, if not treated, have an increased risk of endometrial cancer.
In a retrospective cohort study of almost 300 menopausal women who were not treated after endometrial biopsy revealed proliferative changes, investigators followed participants for an average of 11 years.25 These women had a mean BMI of 34 kg/m2. During follow-up, almost 12% of these women were diagnosed with endometrial hyperplasia or cancer. This incidence of endometrial neoplasia was some 4 times higher than for women initially found to have atrophic endometrial changes.25
Progestin treatment
Oral progestin therapy with follow-up endometrial biopsy constitutes traditional management for endometrial hyperplasia. Such therapy minimizes the likelihood that hyperplasia will progress to endometrial cancer.
We now recognize that the convenience, as well as the high endometrial progestin levels achieved, with levonorgestrel-releasing intrauterine devices (LNG-IUDs) have advantages over oral progestin therapy in treating endometrial hyperplasia. Indeed, a recent US report found that among women with EIN managed medically, use of progestin-releasing IUDs has grown from 7.7% in 2008 to 35.6% in 2020.26
Although both oral and intrauterine progestin are highly effective in treating simple hyperplasia, progestin IUDs are substantially more effective than oral progestins in treating EIN.27 Progestin concentrations in the endometrium have been shown to be 100-fold higher after LNG-IUD placement compared with oral progestin use.22 In addition, adverse effects, including bloating, unpleasant mood changes, and increased appetite, are more common with oral than intrauterine progestin therapy.28
Unfortunately, data from randomized trials addressing progestational treatment of proliferative endometrium in menopausal women are not available to support the treatment of proliferative endometrium with either oral progestins or the LNG-IUD.22
Role of ultrasonography
Another concern is relying on a finding of thin endometrial thickness on vaginal ultrasonography. In a simulated retrospective cohort study, use of transvaginal ultrasonography to determine the appropriateness of a biopsy was found not to be sufficiently accurate or racially equitable with regard to Black women.29 In simulated data, transvaginal ultrasonography missed almost 5 times more cases of endometrial cancer among Black women compared with White women due to higher fibroid prevalence and nonendometrioid histologic type malignancies in Black women.29
Assessing risk
If proliferative endometrium is found, Abraham suggests assessing risk using22:
- age
- comorbidities (including obesity)
- endometrial echo thickness on vaginal ultrasonography.
Consider the patient’s risk and tolerance of recurrent bleeding as well as her tolerance for progestational adverse effects if medical therapy is chosen. Discussion about next steps should include reviewing the histologic findings with the patient and discussing the difference in risk of progression to endometrial cancer of a finding of proliferative endometrium compared with a histologic finding of endometrial hyperplasia.
Using this patient-centered approach, observation over time with follow-up endometrial biopsies remains a management option. Although some women may tolerate micronized progesterone over synthetic progestins, there is concern that it may be less effective in suppressing the endometrium than synthetic progestins.30 Accordingly, synthetic progestins represent first-line options in this setting.
In her review, Abraham suggests that when endometrial biopsy reveals proliferative changes in a menopausal woman, we should initiate progestin treatment and perform surveillance endometrial sampling every 3 to 6 months. If such sampling reveals benign but not proliferative endometrium, progestin therapy can be stopped and endometrial biopsy repeated if bleeding recurs.22 ●
ObGyns may choose to adopt Abraham’s approach or to hold off on progestin therapy while performing follow-up endometrial sampling. Either way, the take-home message is that the finding of proliferative endometrial changes on biopsy for postmenopausal bleeding requires proactive management.
- Modi M, Dhillo WS. Neurokinin 3 receptor antagonism: a novel treatment for menopausal hot flushes. Neuroendocrinology. 2019;109:242-248. doi:10.1159/000495889
- Pinkerton JV, Redick DL, Homewood LN, et al. Neurokinin receptor antagonist, fezolinetant, for treatment of menopausal vasomotor symptoms. J Clin Endocrinol Metab. 2023;dgad209. doi:10.1210/clinem/dgad209
- Rance NE, Dacks PA, Mittelman-Smith MA, et al. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: a novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34:211-227. doi:10.1016 /j.yfrne.2013.07.003
- Mittelman-Smith MA, Williams H, Krajewski-Hall SJ, et al. Role for kisspeptin/neurokinin B/dynorphin (KNDy) neurons in cutaneous vasodilatation and the estrogen modulation of body temperature. Proc Natl Acad Sci USA. 2012;109:1984619851. doi:10.1073/pnas.1211517109
- Astellas Pharma. Astellas’ Veozah (fezolinetant) approved by US FDA for treatment of vasomotor symptoms due to menopause. May 12, 2023. PR Newswire. Accessed May 15, 2023. https://www.prnewswire.com/news-releases/astellas-veozah-fezolinetant-approved-by-us-fda-for -treatment-of-vasomotor-symptoms-due-to-menopause -301823639.html
- Johnson KA, Martin N, Nappi RE, et al. Efficacy and safety of fezolinetant in moderate-to-severe vasomotor symptoms associated with menopause: a phase 3 RCT. J Clin Endocrinol Metab. 2023;dgad058. doi:10.1210/clinem/dgad058
- Lederman S, Ottery FD, Cano A, et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): a phase 3 randomised controlled study. Lancet. 2023;401:1091-1102. doi:10.1016 /S0140-6736(23)00085-5
- Neal-Perry G, Cano A, Lederman S, et al. Safety of fezolinetant for vasomotor symptoms associated with menopause: a randomized controlled trial. Obstet Gynecol. 2023;141:737-747. doi:10.1097/AOG.0000000000005114
- Depypere H, Timmerman D, Donders G, et al. Treatment of menopausal vasomotor symptoms with fezolinetant, a neurokinin 3 receptor antagonist: a phase 2a trial. J Clin Endocrinol Metab. 2019;104:5893-5905. doi: 10.1210/jc .2019-00677
- Santoro N, Waldbaum A, Lederman S, et al. Effect of the neurokinin 3 receptor antagonist fezolinetant on patientreported outcomes in postmenopausal women with vasomotor symptoms: results of a randomized, placebo-controlled, double-blind, dose-ranging study (VESTA). Menopause. 2020;27:1350-1356. doi:10.1097/GME.0000000000001621
- FDA approves novel drug to treat moderate to severe hot flashes caused by menopause. May 12, 2023. US Food and Drug Administration. Accessed May 15, 2023. https://www .fda.gov/news-events/press-announcements/fda-approves -novel-drug-treat-moderate-severe-hot-flashes-caused -menopause
- Veozah. Prescribing information. Astellas; 2023. Accessed May 16, 2023. https://www.astellas.com/us/system/files /veozah_uspi.pdf
- Pinkerton JV. Money talks: untreated hot flashes cost women, the workplace, and society. Menopause. 2015;22:254-255. doi:10.1097/GME.0000000000000427
- Sarrel P, Portman D, Lefebvre P, et al. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause. 2015;22(3):260-266. doi:10.1097/GME.0000000000000320
- Faubion SS, Enders F, Hedges MS, et al. Impact of menopause symptoms on women in the workplace. Mayo Clin Proc. 2023;98:833-845. doi:10.1016/j.mayocp.2023.02.025
- Williams RE, Levine KB, Kalilani L, et al. Menopause- specific questionnaire assessment in US populationbased study shows negative impact on health-related quality of life. Maturitas. 2009;62:153-159. doi:10.1016 /j.maturitas.2008.12.006
- Gartoulla P, Bell RJ, Worsley R, et al. Moderate-severely bothersome vasomotor symptoms are associated with lowered psychological general wellbeing in women at midlife. Maturitas. 2015;81:487-492. doi:10.1016 /j.maturitas.2015.06.004
- Manson JE, Kaunitz AM. Menopause management—getting clinical care back on track. N Engl J Med. 2016;374:803-806. doi:10.1056/NEJMp1514242
- 2022 Hormone Therapy Position Statement of the North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of the North American Menopause Society. Menopause. 2022;29:767-794. doi:10.1097/GME.0000000000002028
- Kaunitz AM, Kapoor E, Faubion S. Treatment of women after bilateral salpingo-oophorectomy performed prior to natural menopause. JAMA. 2021;12;326:1429-1430. doi:10.1001 /jama.2021.3305
- Pinkerton JV. Hormone therapy for postmenopausal women. N Engl J Med. 2020;382:446-455. doi:10.1056 /NEJMcp1714787
- Abraham C. Proliferative endometrium in menopause: to treat or not to treat? Obstet Gynecol. 2023;141:265-267. doi:10.1097/AOG.0000000000005054
- Chandra V, Kim JJ, Benbrook DM, et al. Therapeutic options for management of endometrial hyperplasia. J Gynecol Oncol. 2016;27:e8. doi:10.3802/jgo.2016.27.e8
- Owings RA, Quick CM. Endometrial intraepithelial neoplasia. Arch Pathol Lab Med. 2014;138:484-491. doi:10.5858 /arpa.2012-0709-RA
- Rotenberg O, Doulaveris G, Fridman D, et al. Long-term outcome of postmenopausal women with proliferative endometrium on endometrial sampling. Am J Obstet Gynecol. 2020;223:896.e1-896.e7. doi:10.1016/j.ajog.2020.06.045
- Suzuki Y, Chen L, Hou JY, et al. Systemic progestins and progestin-releasing intrauterine device therapy for premenopausal patients with endometrial intraepithelial neoplasia. Obstet Gynecol. 2023;141:979-987. doi:10.1097 /AOG.0000000000005124
- Mandelbaum RS, Ciccone MA, Nusbaum DJ, et al. Progestin therapy for obese women with complex atypical hyperplasia: levonorgestrel-releasing intrauterine device vs systemic therapy. Am J Obstet Gynecol. 2020;223:103.e1-103.e13. doi:10.1016/j.ajog.2019.12.273
- Liu S, Kciuk O, Frank M, et al. Progestins of today and tomorrow. Curr Opin Obstet Gynecol. 2022;34:344-350. doi:10.1097 /GCO.0000000000000819
- Doll KM, Romano SS, Marsh EE, et al. Estimated performance of transvaginal ultrasonography for evaluation of postmenopausal bleeding in a simulated cohort of black and white women in the US. JAMA Oncol. 2021;7:1158-1165. doi:10.1001/jamaoncol.2021.1700
- Gompel A. Progesterone and endometrial cancer. Best Pract Res Clin Obstet Gynaecol. 2020;69:95-107. doi:10.1016 /j.bpobgyn.2020.05.003
- Modi M, Dhillo WS. Neurokinin 3 receptor antagonism: a novel treatment for menopausal hot flushes. Neuroendocrinology. 2019;109:242-248. doi:10.1159/000495889
- Pinkerton JV, Redick DL, Homewood LN, et al. Neurokinin receptor antagonist, fezolinetant, for treatment of menopausal vasomotor symptoms. J Clin Endocrinol Metab. 2023;dgad209. doi:10.1210/clinem/dgad209
- Rance NE, Dacks PA, Mittelman-Smith MA, et al. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: a novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34:211-227. doi:10.1016 /j.yfrne.2013.07.003
- Mittelman-Smith MA, Williams H, Krajewski-Hall SJ, et al. Role for kisspeptin/neurokinin B/dynorphin (KNDy) neurons in cutaneous vasodilatation and the estrogen modulation of body temperature. Proc Natl Acad Sci USA. 2012;109:1984619851. doi:10.1073/pnas.1211517109
- Astellas Pharma. Astellas’ Veozah (fezolinetant) approved by US FDA for treatment of vasomotor symptoms due to menopause. May 12, 2023. PR Newswire. Accessed May 15, 2023. https://www.prnewswire.com/news-releases/astellas-veozah-fezolinetant-approved-by-us-fda-for -treatment-of-vasomotor-symptoms-due-to-menopause -301823639.html
- Johnson KA, Martin N, Nappi RE, et al. Efficacy and safety of fezolinetant in moderate-to-severe vasomotor symptoms associated with menopause: a phase 3 RCT. J Clin Endocrinol Metab. 2023;dgad058. doi:10.1210/clinem/dgad058
- Lederman S, Ottery FD, Cano A, et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): a phase 3 randomised controlled study. Lancet. 2023;401:1091-1102. doi:10.1016 /S0140-6736(23)00085-5
- Neal-Perry G, Cano A, Lederman S, et al. Safety of fezolinetant for vasomotor symptoms associated with menopause: a randomized controlled trial. Obstet Gynecol. 2023;141:737-747. doi:10.1097/AOG.0000000000005114
- Depypere H, Timmerman D, Donders G, et al. Treatment of menopausal vasomotor symptoms with fezolinetant, a neurokinin 3 receptor antagonist: a phase 2a trial. J Clin Endocrinol Metab. 2019;104:5893-5905. doi: 10.1210/jc .2019-00677
- Santoro N, Waldbaum A, Lederman S, et al. Effect of the neurokinin 3 receptor antagonist fezolinetant on patientreported outcomes in postmenopausal women with vasomotor symptoms: results of a randomized, placebo-controlled, double-blind, dose-ranging study (VESTA). Menopause. 2020;27:1350-1356. doi:10.1097/GME.0000000000001621
- FDA approves novel drug to treat moderate to severe hot flashes caused by menopause. May 12, 2023. US Food and Drug Administration. Accessed May 15, 2023. https://www .fda.gov/news-events/press-announcements/fda-approves -novel-drug-treat-moderate-severe-hot-flashes-caused -menopause
- Veozah. Prescribing information. Astellas; 2023. Accessed May 16, 2023. https://www.astellas.com/us/system/files /veozah_uspi.pdf
- Pinkerton JV. Money talks: untreated hot flashes cost women, the workplace, and society. Menopause. 2015;22:254-255. doi:10.1097/GME.0000000000000427
- Sarrel P, Portman D, Lefebvre P, et al. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause. 2015;22(3):260-266. doi:10.1097/GME.0000000000000320
- Faubion SS, Enders F, Hedges MS, et al. Impact of menopause symptoms on women in the workplace. Mayo Clin Proc. 2023;98:833-845. doi:10.1016/j.mayocp.2023.02.025
- Williams RE, Levine KB, Kalilani L, et al. Menopause- specific questionnaire assessment in US populationbased study shows negative impact on health-related quality of life. Maturitas. 2009;62:153-159. doi:10.1016 /j.maturitas.2008.12.006
- Gartoulla P, Bell RJ, Worsley R, et al. Moderate-severely bothersome vasomotor symptoms are associated with lowered psychological general wellbeing in women at midlife. Maturitas. 2015;81:487-492. doi:10.1016 /j.maturitas.2015.06.004
- Manson JE, Kaunitz AM. Menopause management—getting clinical care back on track. N Engl J Med. 2016;374:803-806. doi:10.1056/NEJMp1514242
- 2022 Hormone Therapy Position Statement of the North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of the North American Menopause Society. Menopause. 2022;29:767-794. doi:10.1097/GME.0000000000002028
- Kaunitz AM, Kapoor E, Faubion S. Treatment of women after bilateral salpingo-oophorectomy performed prior to natural menopause. JAMA. 2021;12;326:1429-1430. doi:10.1001 /jama.2021.3305
- Pinkerton JV. Hormone therapy for postmenopausal women. N Engl J Med. 2020;382:446-455. doi:10.1056 /NEJMcp1714787
- Abraham C. Proliferative endometrium in menopause: to treat or not to treat? Obstet Gynecol. 2023;141:265-267. doi:10.1097/AOG.0000000000005054
- Chandra V, Kim JJ, Benbrook DM, et al. Therapeutic options for management of endometrial hyperplasia. J Gynecol Oncol. 2016;27:e8. doi:10.3802/jgo.2016.27.e8
- Owings RA, Quick CM. Endometrial intraepithelial neoplasia. Arch Pathol Lab Med. 2014;138:484-491. doi:10.5858 /arpa.2012-0709-RA
- Rotenberg O, Doulaveris G, Fridman D, et al. Long-term outcome of postmenopausal women with proliferative endometrium on endometrial sampling. Am J Obstet Gynecol. 2020;223:896.e1-896.e7. doi:10.1016/j.ajog.2020.06.045
- Suzuki Y, Chen L, Hou JY, et al. Systemic progestins and progestin-releasing intrauterine device therapy for premenopausal patients with endometrial intraepithelial neoplasia. Obstet Gynecol. 2023;141:979-987. doi:10.1097 /AOG.0000000000005124
- Mandelbaum RS, Ciccone MA, Nusbaum DJ, et al. Progestin therapy for obese women with complex atypical hyperplasia: levonorgestrel-releasing intrauterine device vs systemic therapy. Am J Obstet Gynecol. 2020;223:103.e1-103.e13. doi:10.1016/j.ajog.2019.12.273
- Liu S, Kciuk O, Frank M, et al. Progestins of today and tomorrow. Curr Opin Obstet Gynecol. 2022;34:344-350. doi:10.1097 /GCO.0000000000000819
- Doll KM, Romano SS, Marsh EE, et al. Estimated performance of transvaginal ultrasonography for evaluation of postmenopausal bleeding in a simulated cohort of black and white women in the US. JAMA Oncol. 2021;7:1158-1165. doi:10.1001/jamaoncol.2021.1700
- Gompel A. Progesterone and endometrial cancer. Best Pract Res Clin Obstet Gynaecol. 2020;69:95-107. doi:10.1016 /j.bpobgyn.2020.05.003
HT, even short-term use, linked to dementia risk in women
Short-term and cyclical use of estrogen and progestin therapy for menopausal symptoms is linked to an increased risk of dementia, results of a large observational study show.
(AD) 20 years later, compared with those who didn’t use HT. The risk was present even in women who used HT for brief periods at menopause onset.
However, both the investigators and experts not involved in the research caution that further studies are needed to explore whether the increased risk of dementia stems from HT use or whether women in need of HT have other underlying dementia risk factors.
“We cannot guarantee that our findings illustrate a causal relationship or if they represent underlying disposition to dementia in women in need of [HT],” lead investigator Nelsan Pourhadi, MD, from the Danish Dementia Research Centre at Copenhagen University Hospital Rigshospitalet, told this news organization.
Still, he added, the findings supported evidence from the Women’s Health Initiative Memory Study (WHIMS), the largest randomized trial on menopausal hormone therapy and dementia.
The findings were published online in BMJ.
Conflicting findings
Before WHIMS was published in 2003, HT was widely prescribed to relieve menopausal symptoms. However, WHIMS, which included more than 4,000 women aged 65 years or older, revealed that HT was associated with a twofold increased risk of dementia.
Studies published since then have yielded mixed results, adding to the controversy surrounding the safety of HT.
To discover whether age of initiation or length of duration of HT affects health outcomes, Dr. Pourhadi and his team undertook the observational study.
Between 2000 and 2018, the researchers tracked more than 60,000 Danish women aged 50-60 years using diagnosis and prescription information from Denmark’s National Registry of Patients.
The registry records showed that nearly 5,600 women developed dementia and 56,000 did not develop dementia. Of the 5,600 women with dementia, 1,460 had a diagnosis of AD.
Nearly 18,000 participants in the study sample received HT – 1,790 (29%) in the dementia group and 16,150 (32%) in the control group. Half started treatment before age 53 years and half stopped within 4 years. Roughly 90% used oral medications, which included a combination of estrogen and progestin.
The median age at which participants started HT was 53 years for both cases and controls, and the median duration of use was 4 years.
Longer use equals greater risk
Compared with those who did not use HT, those who used estrogen-progestin therapy had a 24% increased risk of developing all-cause dementia (hazard ratio, 1.24; 95% confidence interval, 1.17-1.44).
The increased dementia risk was similar between continuous (estrogen and progestin taken daily) and cyclic (daily estrogen with progestin taken 10-14 days a month) treatment regimens.
Longer durations of HT use were associated with increased risk, ranging from a 21% increased risk (HR, 1.21; 95% CI, 1.09-1.35) for those who used it for 1 year or less to a 74% increased risk (HR, 1.74; 95% CI, 1.45-2.10) for use lasting 12 years or more.
Women who started HT between the age of 45 and 50 had a 26% increased risk of developing all-cause dementia (HR, 1.26; 95% CI, 1.13-1.41) while women who initiated HT between age 51 and 60 had a 21% greater risk (HR, 1.21; 95% CI, 1.12-1.29).
Progestin-only or vaginal-estrogen-only therapy was not associated with the development of dementia.
The investigators noted that because this is an observational study, “further studies are warranted to explore if the observed association in this study between menopausal hormone therapy use and increased risk of dementia illustrates a causal effect.”
No causal relationship
In an accompanying editorial, Kejal Kantarci, MD, a professor of radiology at the Mayo Clinic, Rochester, Minn., noted that three clinical trials, including the WHIMS of Younger Women (WHIMS-Y) in 2013, did not show a link between cognitive function and HT.
“Although [Dr.] Pourhadi and colleagues’ study was done carefully using national registries, the observed associations could be artefactual and should not be used to infer a causal relationship between hormone therapy and dementia risk. These findings cannot inform shared decision-making about use of hormone therapy for menopausal symptoms,” she states in the editorial.
Also commenting on the findings, Amanda Heslegrave, PhD, a senior research fellow at the U.K. Dementia Research Institute, London, said in a release from the U.K.’s Science Media Centre that while the study “may cause alarm for women taking [HT], it highlights just how much we still don’t know about the effects of hormones on women’s brain health, and with promising treatments on the horizon, it should be a call to action to make this a priority area of research.”
There was no specific funding for the study. Dr. Kantarci reported working on an unpaid educational activity on Alzheimer’s disease for Biogen and is the PI on a study of a PET imaging ligand for Alzheimer’s disease, to which Eli Lilly and Avid Radiopharmaceuticals donated supplies.
A version of this article originally appeared on Medscape.com.
Short-term and cyclical use of estrogen and progestin therapy for menopausal symptoms is linked to an increased risk of dementia, results of a large observational study show.
(AD) 20 years later, compared with those who didn’t use HT. The risk was present even in women who used HT for brief periods at menopause onset.
However, both the investigators and experts not involved in the research caution that further studies are needed to explore whether the increased risk of dementia stems from HT use or whether women in need of HT have other underlying dementia risk factors.
“We cannot guarantee that our findings illustrate a causal relationship or if they represent underlying disposition to dementia in women in need of [HT],” lead investigator Nelsan Pourhadi, MD, from the Danish Dementia Research Centre at Copenhagen University Hospital Rigshospitalet, told this news organization.
Still, he added, the findings supported evidence from the Women’s Health Initiative Memory Study (WHIMS), the largest randomized trial on menopausal hormone therapy and dementia.
The findings were published online in BMJ.
Conflicting findings
Before WHIMS was published in 2003, HT was widely prescribed to relieve menopausal symptoms. However, WHIMS, which included more than 4,000 women aged 65 years or older, revealed that HT was associated with a twofold increased risk of dementia.
Studies published since then have yielded mixed results, adding to the controversy surrounding the safety of HT.
To discover whether age of initiation or length of duration of HT affects health outcomes, Dr. Pourhadi and his team undertook the observational study.
Between 2000 and 2018, the researchers tracked more than 60,000 Danish women aged 50-60 years using diagnosis and prescription information from Denmark’s National Registry of Patients.
The registry records showed that nearly 5,600 women developed dementia and 56,000 did not develop dementia. Of the 5,600 women with dementia, 1,460 had a diagnosis of AD.
Nearly 18,000 participants in the study sample received HT – 1,790 (29%) in the dementia group and 16,150 (32%) in the control group. Half started treatment before age 53 years and half stopped within 4 years. Roughly 90% used oral medications, which included a combination of estrogen and progestin.
The median age at which participants started HT was 53 years for both cases and controls, and the median duration of use was 4 years.
Longer use equals greater risk
Compared with those who did not use HT, those who used estrogen-progestin therapy had a 24% increased risk of developing all-cause dementia (hazard ratio, 1.24; 95% confidence interval, 1.17-1.44).
The increased dementia risk was similar between continuous (estrogen and progestin taken daily) and cyclic (daily estrogen with progestin taken 10-14 days a month) treatment regimens.
Longer durations of HT use were associated with increased risk, ranging from a 21% increased risk (HR, 1.21; 95% CI, 1.09-1.35) for those who used it for 1 year or less to a 74% increased risk (HR, 1.74; 95% CI, 1.45-2.10) for use lasting 12 years or more.
Women who started HT between the age of 45 and 50 had a 26% increased risk of developing all-cause dementia (HR, 1.26; 95% CI, 1.13-1.41) while women who initiated HT between age 51 and 60 had a 21% greater risk (HR, 1.21; 95% CI, 1.12-1.29).
Progestin-only or vaginal-estrogen-only therapy was not associated with the development of dementia.
The investigators noted that because this is an observational study, “further studies are warranted to explore if the observed association in this study between menopausal hormone therapy use and increased risk of dementia illustrates a causal effect.”
No causal relationship
In an accompanying editorial, Kejal Kantarci, MD, a professor of radiology at the Mayo Clinic, Rochester, Minn., noted that three clinical trials, including the WHIMS of Younger Women (WHIMS-Y) in 2013, did not show a link between cognitive function and HT.
“Although [Dr.] Pourhadi and colleagues’ study was done carefully using national registries, the observed associations could be artefactual and should not be used to infer a causal relationship between hormone therapy and dementia risk. These findings cannot inform shared decision-making about use of hormone therapy for menopausal symptoms,” she states in the editorial.
Also commenting on the findings, Amanda Heslegrave, PhD, a senior research fellow at the U.K. Dementia Research Institute, London, said in a release from the U.K.’s Science Media Centre that while the study “may cause alarm for women taking [HT], it highlights just how much we still don’t know about the effects of hormones on women’s brain health, and with promising treatments on the horizon, it should be a call to action to make this a priority area of research.”
There was no specific funding for the study. Dr. Kantarci reported working on an unpaid educational activity on Alzheimer’s disease for Biogen and is the PI on a study of a PET imaging ligand for Alzheimer’s disease, to which Eli Lilly and Avid Radiopharmaceuticals donated supplies.
A version of this article originally appeared on Medscape.com.
Short-term and cyclical use of estrogen and progestin therapy for menopausal symptoms is linked to an increased risk of dementia, results of a large observational study show.
(AD) 20 years later, compared with those who didn’t use HT. The risk was present even in women who used HT for brief periods at menopause onset.
However, both the investigators and experts not involved in the research caution that further studies are needed to explore whether the increased risk of dementia stems from HT use or whether women in need of HT have other underlying dementia risk factors.
“We cannot guarantee that our findings illustrate a causal relationship or if they represent underlying disposition to dementia in women in need of [HT],” lead investigator Nelsan Pourhadi, MD, from the Danish Dementia Research Centre at Copenhagen University Hospital Rigshospitalet, told this news organization.
Still, he added, the findings supported evidence from the Women’s Health Initiative Memory Study (WHIMS), the largest randomized trial on menopausal hormone therapy and dementia.
The findings were published online in BMJ.
Conflicting findings
Before WHIMS was published in 2003, HT was widely prescribed to relieve menopausal symptoms. However, WHIMS, which included more than 4,000 women aged 65 years or older, revealed that HT was associated with a twofold increased risk of dementia.
Studies published since then have yielded mixed results, adding to the controversy surrounding the safety of HT.
To discover whether age of initiation or length of duration of HT affects health outcomes, Dr. Pourhadi and his team undertook the observational study.
Between 2000 and 2018, the researchers tracked more than 60,000 Danish women aged 50-60 years using diagnosis and prescription information from Denmark’s National Registry of Patients.
The registry records showed that nearly 5,600 women developed dementia and 56,000 did not develop dementia. Of the 5,600 women with dementia, 1,460 had a diagnosis of AD.
Nearly 18,000 participants in the study sample received HT – 1,790 (29%) in the dementia group and 16,150 (32%) in the control group. Half started treatment before age 53 years and half stopped within 4 years. Roughly 90% used oral medications, which included a combination of estrogen and progestin.
The median age at which participants started HT was 53 years for both cases and controls, and the median duration of use was 4 years.
Longer use equals greater risk
Compared with those who did not use HT, those who used estrogen-progestin therapy had a 24% increased risk of developing all-cause dementia (hazard ratio, 1.24; 95% confidence interval, 1.17-1.44).
The increased dementia risk was similar between continuous (estrogen and progestin taken daily) and cyclic (daily estrogen with progestin taken 10-14 days a month) treatment regimens.
Longer durations of HT use were associated with increased risk, ranging from a 21% increased risk (HR, 1.21; 95% CI, 1.09-1.35) for those who used it for 1 year or less to a 74% increased risk (HR, 1.74; 95% CI, 1.45-2.10) for use lasting 12 years or more.
Women who started HT between the age of 45 and 50 had a 26% increased risk of developing all-cause dementia (HR, 1.26; 95% CI, 1.13-1.41) while women who initiated HT between age 51 and 60 had a 21% greater risk (HR, 1.21; 95% CI, 1.12-1.29).
Progestin-only or vaginal-estrogen-only therapy was not associated with the development of dementia.
The investigators noted that because this is an observational study, “further studies are warranted to explore if the observed association in this study between menopausal hormone therapy use and increased risk of dementia illustrates a causal effect.”
No causal relationship
In an accompanying editorial, Kejal Kantarci, MD, a professor of radiology at the Mayo Clinic, Rochester, Minn., noted that three clinical trials, including the WHIMS of Younger Women (WHIMS-Y) in 2013, did not show a link between cognitive function and HT.
“Although [Dr.] Pourhadi and colleagues’ study was done carefully using national registries, the observed associations could be artefactual and should not be used to infer a causal relationship between hormone therapy and dementia risk. These findings cannot inform shared decision-making about use of hormone therapy for menopausal symptoms,” she states in the editorial.
Also commenting on the findings, Amanda Heslegrave, PhD, a senior research fellow at the U.K. Dementia Research Institute, London, said in a release from the U.K.’s Science Media Centre that while the study “may cause alarm for women taking [HT], it highlights just how much we still don’t know about the effects of hormones on women’s brain health, and with promising treatments on the horizon, it should be a call to action to make this a priority area of research.”
There was no specific funding for the study. Dr. Kantarci reported working on an unpaid educational activity on Alzheimer’s disease for Biogen and is the PI on a study of a PET imaging ligand for Alzheimer’s disease, to which Eli Lilly and Avid Radiopharmaceuticals donated supplies.
A version of this article originally appeared on Medscape.com.
Does ‘skeletal age’ describe fracture impact on mortality?
Thach Tran, MD, and colleagues introduced the concept of “skeletal age” in a recently published paper that aims to incorporate the impact of fragility, or low trauma, fractures – which can occur in patients with osteoporosis – on mortality risk.
They defined “skeletal age” as the age of the skeleton following a fragility fracture. This is calculated as the chronological age of the individual plus the number of years of “life lost” as a consequence of the specific fracture.
The risk for premature death following fragility fractures is concerning, with 22%-58% of patients with hip fracture dying within a year (Brauer et al.; Rapp et al.). Thus, it’s important to treat osteoporosis in a timely fashion to reduce the risk for such fractures and the excess mortality risk associated with them.
Implementation and uptake of such treatment, however, either before or after a fragility fracture, is far from optimal (Solomon et al). This may be because patients don’t fully understand the consequence of such a fracture, and outcomes measures currently in use (such as relative risk or hazard of mortality) are difficult to communicate to patients.
In the recent paper by Dr. Tran and colleagues, the authors examined the association between fractures and mortality based on sex, age, associated comorbidities, and fracture site. They pooled this information to create a “skeletal age” for each fracture site, using data from the Danish National Hospital Discharge Registry, which documents fractures and related mortality for all Danish people.
They examined mortality over a period of at least 2 years following a fragility fracture in individuals aged 50 or older, and reported that occurrence of any fragility fracture is associated with a 30%-45% increased risk for death, with the highest risk noted for hip and femur fractures (twofold increase). Fractures of the pelvis, vertebrae, humerus, ribs, clavicle, and lower leg were also associated with increased mortality risk, but no increase was seen with fractures of the forearm, knee, ankle, hand, or foot.
The number of years of life lost at any age depending on the fracture site is represented as a linear graph of skeletal age for any chronological age, for specific fracture sites, separated by sex.
For example, the skeletal age of a 50-year-old man who has a hip fracture is 57 years (7 years of life lost as a consequence of the fracture), while that for a 70-year-old man with the same fracture is 75 years (5 years of life lost because of the fracture). Similarly, the skeletal age of a 50-year-old man with a fracture of the pelvis, femur, vertebrae, and humerus is 55 years (5 years of life lost). Fractures of the lower leg, humerus, and clavicle lead to fewer lost years of life.
The authors are to be commended for creating a simple strategy to quantify mortality risk following low-impact or fragility fractures in older individuals; this could enable providers to communicate the importance of osteoporosis treatment more effectively to patients on the basis of their skeletal age, and for patients to better understand this information.
The study design appears reasonably robust as the authors considered many factors that might affect mortality risk, such as sex, age, and comorbidities, and the results are based on information from a very large number of people – 1.6 million.
However, there’s a major issue with the concept of “skeletal age” as proposed by Dr. Tran and colleagues. The term is already in use and defines the maturity of bones in children and adolescents, also called “bone age” (Greulich and Pyle 1959; Skeletal Age, Radiology Key). This is a real oversight and could cause confusion in interpreting “skeletal age.”
Skeletal age as currently defined in children and adolescents is influenced by chronological age, exposure to certain hormones, nutritional deficiencies, and systemic diseases, and is a predictor of adult height based on the skeletal age and current height. This concept is completely different from that being proposed by the authors in this paper. Dr. Tran and colleagues (and the reviewers of this paper) are probably not familiar with the use of the terminology in youth, which is a major oversight; they should consider changing the terminology given this overlap.
Further, fragility fractures can occur from osteoporosis at any age, and this study doesn’t provide information regarding years of life lost from occurrence of fragility fractures at younger ages, or the age at which mortality risk starts to increase (as the study was performed only in those aged 50 or older).
While the study takes into account general comorbidities in developing the model to define years of life lost, it doesn’t account for other factors that can influence fracture risk, such as lifestyle factors, activity level, and genetic risk (family history of osteoporosis, for example). Of note, the impact of additional fractures isn’t considered either and should be factored into future investigations.
Overall, the study is robust and important and provides valuable information regarding mortality risk from a fragility fracture in older people. However, there are some flaws that need to be considered and addressed, the most serious of which is that the term “skeletal age” has been in existence for decades, applied to a much younger age group, and its implications are completely different from those being proposed by the authors here.
A version of this article first appeared on Medscape.com.
Thach Tran, MD, and colleagues introduced the concept of “skeletal age” in a recently published paper that aims to incorporate the impact of fragility, or low trauma, fractures – which can occur in patients with osteoporosis – on mortality risk.
They defined “skeletal age” as the age of the skeleton following a fragility fracture. This is calculated as the chronological age of the individual plus the number of years of “life lost” as a consequence of the specific fracture.
The risk for premature death following fragility fractures is concerning, with 22%-58% of patients with hip fracture dying within a year (Brauer et al.; Rapp et al.). Thus, it’s important to treat osteoporosis in a timely fashion to reduce the risk for such fractures and the excess mortality risk associated with them.
Implementation and uptake of such treatment, however, either before or after a fragility fracture, is far from optimal (Solomon et al). This may be because patients don’t fully understand the consequence of such a fracture, and outcomes measures currently in use (such as relative risk or hazard of mortality) are difficult to communicate to patients.
In the recent paper by Dr. Tran and colleagues, the authors examined the association between fractures and mortality based on sex, age, associated comorbidities, and fracture site. They pooled this information to create a “skeletal age” for each fracture site, using data from the Danish National Hospital Discharge Registry, which documents fractures and related mortality for all Danish people.
They examined mortality over a period of at least 2 years following a fragility fracture in individuals aged 50 or older, and reported that occurrence of any fragility fracture is associated with a 30%-45% increased risk for death, with the highest risk noted for hip and femur fractures (twofold increase). Fractures of the pelvis, vertebrae, humerus, ribs, clavicle, and lower leg were also associated with increased mortality risk, but no increase was seen with fractures of the forearm, knee, ankle, hand, or foot.
The number of years of life lost at any age depending on the fracture site is represented as a linear graph of skeletal age for any chronological age, for specific fracture sites, separated by sex.
For example, the skeletal age of a 50-year-old man who has a hip fracture is 57 years (7 years of life lost as a consequence of the fracture), while that for a 70-year-old man with the same fracture is 75 years (5 years of life lost because of the fracture). Similarly, the skeletal age of a 50-year-old man with a fracture of the pelvis, femur, vertebrae, and humerus is 55 years (5 years of life lost). Fractures of the lower leg, humerus, and clavicle lead to fewer lost years of life.
The authors are to be commended for creating a simple strategy to quantify mortality risk following low-impact or fragility fractures in older individuals; this could enable providers to communicate the importance of osteoporosis treatment more effectively to patients on the basis of their skeletal age, and for patients to better understand this information.
The study design appears reasonably robust as the authors considered many factors that might affect mortality risk, such as sex, age, and comorbidities, and the results are based on information from a very large number of people – 1.6 million.
However, there’s a major issue with the concept of “skeletal age” as proposed by Dr. Tran and colleagues. The term is already in use and defines the maturity of bones in children and adolescents, also called “bone age” (Greulich and Pyle 1959; Skeletal Age, Radiology Key). This is a real oversight and could cause confusion in interpreting “skeletal age.”
Skeletal age as currently defined in children and adolescents is influenced by chronological age, exposure to certain hormones, nutritional deficiencies, and systemic diseases, and is a predictor of adult height based on the skeletal age and current height. This concept is completely different from that being proposed by the authors in this paper. Dr. Tran and colleagues (and the reviewers of this paper) are probably not familiar with the use of the terminology in youth, which is a major oversight; they should consider changing the terminology given this overlap.
Further, fragility fractures can occur from osteoporosis at any age, and this study doesn’t provide information regarding years of life lost from occurrence of fragility fractures at younger ages, or the age at which mortality risk starts to increase (as the study was performed only in those aged 50 or older).
While the study takes into account general comorbidities in developing the model to define years of life lost, it doesn’t account for other factors that can influence fracture risk, such as lifestyle factors, activity level, and genetic risk (family history of osteoporosis, for example). Of note, the impact of additional fractures isn’t considered either and should be factored into future investigations.
Overall, the study is robust and important and provides valuable information regarding mortality risk from a fragility fracture in older people. However, there are some flaws that need to be considered and addressed, the most serious of which is that the term “skeletal age” has been in existence for decades, applied to a much younger age group, and its implications are completely different from those being proposed by the authors here.
A version of this article first appeared on Medscape.com.
Thach Tran, MD, and colleagues introduced the concept of “skeletal age” in a recently published paper that aims to incorporate the impact of fragility, or low trauma, fractures – which can occur in patients with osteoporosis – on mortality risk.
They defined “skeletal age” as the age of the skeleton following a fragility fracture. This is calculated as the chronological age of the individual plus the number of years of “life lost” as a consequence of the specific fracture.
The risk for premature death following fragility fractures is concerning, with 22%-58% of patients with hip fracture dying within a year (Brauer et al.; Rapp et al.). Thus, it’s important to treat osteoporosis in a timely fashion to reduce the risk for such fractures and the excess mortality risk associated with them.
Implementation and uptake of such treatment, however, either before or after a fragility fracture, is far from optimal (Solomon et al). This may be because patients don’t fully understand the consequence of such a fracture, and outcomes measures currently in use (such as relative risk or hazard of mortality) are difficult to communicate to patients.
In the recent paper by Dr. Tran and colleagues, the authors examined the association between fractures and mortality based on sex, age, associated comorbidities, and fracture site. They pooled this information to create a “skeletal age” for each fracture site, using data from the Danish National Hospital Discharge Registry, which documents fractures and related mortality for all Danish people.
They examined mortality over a period of at least 2 years following a fragility fracture in individuals aged 50 or older, and reported that occurrence of any fragility fracture is associated with a 30%-45% increased risk for death, with the highest risk noted for hip and femur fractures (twofold increase). Fractures of the pelvis, vertebrae, humerus, ribs, clavicle, and lower leg were also associated with increased mortality risk, but no increase was seen with fractures of the forearm, knee, ankle, hand, or foot.
The number of years of life lost at any age depending on the fracture site is represented as a linear graph of skeletal age for any chronological age, for specific fracture sites, separated by sex.
For example, the skeletal age of a 50-year-old man who has a hip fracture is 57 years (7 years of life lost as a consequence of the fracture), while that for a 70-year-old man with the same fracture is 75 years (5 years of life lost because of the fracture). Similarly, the skeletal age of a 50-year-old man with a fracture of the pelvis, femur, vertebrae, and humerus is 55 years (5 years of life lost). Fractures of the lower leg, humerus, and clavicle lead to fewer lost years of life.
The authors are to be commended for creating a simple strategy to quantify mortality risk following low-impact or fragility fractures in older individuals; this could enable providers to communicate the importance of osteoporosis treatment more effectively to patients on the basis of their skeletal age, and for patients to better understand this information.
The study design appears reasonably robust as the authors considered many factors that might affect mortality risk, such as sex, age, and comorbidities, and the results are based on information from a very large number of people – 1.6 million.
However, there’s a major issue with the concept of “skeletal age” as proposed by Dr. Tran and colleagues. The term is already in use and defines the maturity of bones in children and adolescents, also called “bone age” (Greulich and Pyle 1959; Skeletal Age, Radiology Key). This is a real oversight and could cause confusion in interpreting “skeletal age.”
Skeletal age as currently defined in children and adolescents is influenced by chronological age, exposure to certain hormones, nutritional deficiencies, and systemic diseases, and is a predictor of adult height based on the skeletal age and current height. This concept is completely different from that being proposed by the authors in this paper. Dr. Tran and colleagues (and the reviewers of this paper) are probably not familiar with the use of the terminology in youth, which is a major oversight; they should consider changing the terminology given this overlap.
Further, fragility fractures can occur from osteoporosis at any age, and this study doesn’t provide information regarding years of life lost from occurrence of fragility fractures at younger ages, or the age at which mortality risk starts to increase (as the study was performed only in those aged 50 or older).
While the study takes into account general comorbidities in developing the model to define years of life lost, it doesn’t account for other factors that can influence fracture risk, such as lifestyle factors, activity level, and genetic risk (family history of osteoporosis, for example). Of note, the impact of additional fractures isn’t considered either and should be factored into future investigations.
Overall, the study is robust and important and provides valuable information regarding mortality risk from a fragility fracture in older people. However, there are some flaws that need to be considered and addressed, the most serious of which is that the term “skeletal age” has been in existence for decades, applied to a much younger age group, and its implications are completely different from those being proposed by the authors here.
A version of this article first appeared on Medscape.com.
A ‘one-stop shop’: New guidance on hormones and aging
The idea of the statement “is to be complete, but also to clarify some misunderstandings. ...We tried to be very clear in the language about what we know, where we can go, where we shouldn’t go, and what we still need to learn,” statement coauthor Cynthia A. Stuenkel, MD, of the University of California, San Diego, said in an interview.
The document is divided into nine parts or axes: growth hormone, adrenal, ovarian, testicular, thyroid, osteoporosis, vitamin D deficiency, type 2 diabetes, and water metabolism. Each section covers natural history and observational data in older individuals, available therapies, clinical trial data on efficacy and safety in older individuals, bulleted “key points,” and research gaps.
“Hormones and Aging: An Endocrine Society Scientific Statement” was presented at the annual meeting of the Endocrine Society and published online in the Journal of Clinical Endocrinology & Metabolism.
During a press briefing, writing group chair Anne R. Cappola, MD, of the University of Pennsylvania, Philadelphia, said the goal is to “provide a really concise summary across each of these areas. ... There are multiple hormonal changes that occur with age, so we really couldn’t limit ourselves to just one gland or the few that we commonly think about. We wanted to cover all the axes.”
The statement tackles several controversial areas, including hormone therapy for menopausal symptoms in women and hypogonadal symptoms in men, diabetes treatment goals in older adults, distinguishing between age-associated changes in thyroid function and early hypothyroidism, and vitamin D supplementation in older adults.
“Hormones have these almost mythical qualities to some people. ... ‘If I just had my hormones back the way they were, it would all work out.’ What we want to do is make sure that patients are being treated appropriately and that their symptoms are being heard and managed and ascribed to the appropriate problems and not necessarily to hormonal problems when they are not. ... Part of what we need to do is [provide] the evidence that we have, which includes evidence of when not to prescribe as well as [when] to prescribe,” Dr. Cappola said.
Not designed to be read all at once
In the menopause section, for example, one “key point” is that menopausal symptoms are common, vary in degree and bother, and can be effectively treated with a variety of therapies proven effective in randomized clinical trials. Another key point is that menopausal hormone therapy is safest for women who are younger than 60 years and less than 10 years since starting menopause.
“It’s almost 20 years since the original Women’s Health Initiative, and that led to an incredible falloff of prescribing hormone therapy and a falloff in teaching of our students, residents, fellows, and practitioners about [menopausal] hormone therapy. ... Hopefully, by issuing this kind of aging statement it gets people to read, think, and learn more. And, hopefully, we can improve the education of physicians. ... Menopause is a universal experience. Clinicians should know about it,” noted Dr. Stuenkel, who chaired the menopause section writing panel.
In the type 2 diabetes section, in the bullet points it is noted that oral glucose tolerance testing may reveal abnormal glucose status in older adults that are not picked up with hemoglobin A1c or fasting glucose levels and that glycemic targets should be individualized.
Asked to comment on the statement, Michele Bellantoni, MD, said: “This was a huge undertaking because there are so many areas of expertise here. I thought they did a very good job of reviewing the literature and showing each of the different hormonal axes. ... It’s a good go-to review.”
“I thought it was a very good attempt to catalog and provide opportunities for policy, and particularly at [the National Institutes of Health], as they look at funding to show where are these gaps and to support appropriate research. I think the most important aspect to come of this is identifying research gaps for funding opportunities. I very much support that,” noted Dr. Bellantoni, who is clinical director of the division of geriatric medicine at Johns Hopkins University, Baltimore.
However, she also said that the 40-page document might be a bit much for busy clinicians, despite the bullet points at the end of each section.
“I would love to see an editorial that puts into perspective the take-home messages or a subsequent article that distills this into every day practice of care of older adults, both preventative and treatment care. ... I think that would be so useful.”
During the briefing, Dr. Cappola noted that the document need not be read all at once.
“It ended up being a large document, but you should not be intimidated by it because each section is only about 2,000 words. So, it’s really a kind of one-stop shop to be able to look across all these axes at once. We also wanted people to think about the common themes that occur across all these axes when considering what’s going on right now and for future research,” she said.
Dr. Stuenkel, Dr. Cappola, and Dr. Bellantoni reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The idea of the statement “is to be complete, but also to clarify some misunderstandings. ...We tried to be very clear in the language about what we know, where we can go, where we shouldn’t go, and what we still need to learn,” statement coauthor Cynthia A. Stuenkel, MD, of the University of California, San Diego, said in an interview.
The document is divided into nine parts or axes: growth hormone, adrenal, ovarian, testicular, thyroid, osteoporosis, vitamin D deficiency, type 2 diabetes, and water metabolism. Each section covers natural history and observational data in older individuals, available therapies, clinical trial data on efficacy and safety in older individuals, bulleted “key points,” and research gaps.
“Hormones and Aging: An Endocrine Society Scientific Statement” was presented at the annual meeting of the Endocrine Society and published online in the Journal of Clinical Endocrinology & Metabolism.
During a press briefing, writing group chair Anne R. Cappola, MD, of the University of Pennsylvania, Philadelphia, said the goal is to “provide a really concise summary across each of these areas. ... There are multiple hormonal changes that occur with age, so we really couldn’t limit ourselves to just one gland or the few that we commonly think about. We wanted to cover all the axes.”
The statement tackles several controversial areas, including hormone therapy for menopausal symptoms in women and hypogonadal symptoms in men, diabetes treatment goals in older adults, distinguishing between age-associated changes in thyroid function and early hypothyroidism, and vitamin D supplementation in older adults.
“Hormones have these almost mythical qualities to some people. ... ‘If I just had my hormones back the way they were, it would all work out.’ What we want to do is make sure that patients are being treated appropriately and that their symptoms are being heard and managed and ascribed to the appropriate problems and not necessarily to hormonal problems when they are not. ... Part of what we need to do is [provide] the evidence that we have, which includes evidence of when not to prescribe as well as [when] to prescribe,” Dr. Cappola said.
Not designed to be read all at once
In the menopause section, for example, one “key point” is that menopausal symptoms are common, vary in degree and bother, and can be effectively treated with a variety of therapies proven effective in randomized clinical trials. Another key point is that menopausal hormone therapy is safest for women who are younger than 60 years and less than 10 years since starting menopause.
“It’s almost 20 years since the original Women’s Health Initiative, and that led to an incredible falloff of prescribing hormone therapy and a falloff in teaching of our students, residents, fellows, and practitioners about [menopausal] hormone therapy. ... Hopefully, by issuing this kind of aging statement it gets people to read, think, and learn more. And, hopefully, we can improve the education of physicians. ... Menopause is a universal experience. Clinicians should know about it,” noted Dr. Stuenkel, who chaired the menopause section writing panel.
In the type 2 diabetes section, in the bullet points it is noted that oral glucose tolerance testing may reveal abnormal glucose status in older adults that are not picked up with hemoglobin A1c or fasting glucose levels and that glycemic targets should be individualized.
Asked to comment on the statement, Michele Bellantoni, MD, said: “This was a huge undertaking because there are so many areas of expertise here. I thought they did a very good job of reviewing the literature and showing each of the different hormonal axes. ... It’s a good go-to review.”
“I thought it was a very good attempt to catalog and provide opportunities for policy, and particularly at [the National Institutes of Health], as they look at funding to show where are these gaps and to support appropriate research. I think the most important aspect to come of this is identifying research gaps for funding opportunities. I very much support that,” noted Dr. Bellantoni, who is clinical director of the division of geriatric medicine at Johns Hopkins University, Baltimore.
However, she also said that the 40-page document might be a bit much for busy clinicians, despite the bullet points at the end of each section.
“I would love to see an editorial that puts into perspective the take-home messages or a subsequent article that distills this into every day practice of care of older adults, both preventative and treatment care. ... I think that would be so useful.”
During the briefing, Dr. Cappola noted that the document need not be read all at once.
“It ended up being a large document, but you should not be intimidated by it because each section is only about 2,000 words. So, it’s really a kind of one-stop shop to be able to look across all these axes at once. We also wanted people to think about the common themes that occur across all these axes when considering what’s going on right now and for future research,” she said.
Dr. Stuenkel, Dr. Cappola, and Dr. Bellantoni reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The idea of the statement “is to be complete, but also to clarify some misunderstandings. ...We tried to be very clear in the language about what we know, where we can go, where we shouldn’t go, and what we still need to learn,” statement coauthor Cynthia A. Stuenkel, MD, of the University of California, San Diego, said in an interview.
The document is divided into nine parts or axes: growth hormone, adrenal, ovarian, testicular, thyroid, osteoporosis, vitamin D deficiency, type 2 diabetes, and water metabolism. Each section covers natural history and observational data in older individuals, available therapies, clinical trial data on efficacy and safety in older individuals, bulleted “key points,” and research gaps.
“Hormones and Aging: An Endocrine Society Scientific Statement” was presented at the annual meeting of the Endocrine Society and published online in the Journal of Clinical Endocrinology & Metabolism.
During a press briefing, writing group chair Anne R. Cappola, MD, of the University of Pennsylvania, Philadelphia, said the goal is to “provide a really concise summary across each of these areas. ... There are multiple hormonal changes that occur with age, so we really couldn’t limit ourselves to just one gland or the few that we commonly think about. We wanted to cover all the axes.”
The statement tackles several controversial areas, including hormone therapy for menopausal symptoms in women and hypogonadal symptoms in men, diabetes treatment goals in older adults, distinguishing between age-associated changes in thyroid function and early hypothyroidism, and vitamin D supplementation in older adults.
“Hormones have these almost mythical qualities to some people. ... ‘If I just had my hormones back the way they were, it would all work out.’ What we want to do is make sure that patients are being treated appropriately and that their symptoms are being heard and managed and ascribed to the appropriate problems and not necessarily to hormonal problems when they are not. ... Part of what we need to do is [provide] the evidence that we have, which includes evidence of when not to prescribe as well as [when] to prescribe,” Dr. Cappola said.
Not designed to be read all at once
In the menopause section, for example, one “key point” is that menopausal symptoms are common, vary in degree and bother, and can be effectively treated with a variety of therapies proven effective in randomized clinical trials. Another key point is that menopausal hormone therapy is safest for women who are younger than 60 years and less than 10 years since starting menopause.
“It’s almost 20 years since the original Women’s Health Initiative, and that led to an incredible falloff of prescribing hormone therapy and a falloff in teaching of our students, residents, fellows, and practitioners about [menopausal] hormone therapy. ... Hopefully, by issuing this kind of aging statement it gets people to read, think, and learn more. And, hopefully, we can improve the education of physicians. ... Menopause is a universal experience. Clinicians should know about it,” noted Dr. Stuenkel, who chaired the menopause section writing panel.
In the type 2 diabetes section, in the bullet points it is noted that oral glucose tolerance testing may reveal abnormal glucose status in older adults that are not picked up with hemoglobin A1c or fasting glucose levels and that glycemic targets should be individualized.
Asked to comment on the statement, Michele Bellantoni, MD, said: “This was a huge undertaking because there are so many areas of expertise here. I thought they did a very good job of reviewing the literature and showing each of the different hormonal axes. ... It’s a good go-to review.”
“I thought it was a very good attempt to catalog and provide opportunities for policy, and particularly at [the National Institutes of Health], as they look at funding to show where are these gaps and to support appropriate research. I think the most important aspect to come of this is identifying research gaps for funding opportunities. I very much support that,” noted Dr. Bellantoni, who is clinical director of the division of geriatric medicine at Johns Hopkins University, Baltimore.
However, she also said that the 40-page document might be a bit much for busy clinicians, despite the bullet points at the end of each section.
“I would love to see an editorial that puts into perspective the take-home messages or a subsequent article that distills this into every day practice of care of older adults, both preventative and treatment care. ... I think that would be so useful.”
During the briefing, Dr. Cappola noted that the document need not be read all at once.
“It ended up being a large document, but you should not be intimidated by it because each section is only about 2,000 words. So, it’s really a kind of one-stop shop to be able to look across all these axes at once. We also wanted people to think about the common themes that occur across all these axes when considering what’s going on right now and for future research,” she said.
Dr. Stuenkel, Dr. Cappola, and Dr. Bellantoni reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ENDO 2023
A new nonhormonal option for menopausal hot flashes: What prescribers should know
This transcript has been edited for clarity.
Hello. I am Dr. JoAnn Pinkerton, professor of obstetrics and gynecology at the University of Virginia and a North American Menopause Society–credentialed menopause specialist.
I am excited to tell you about a brand-new, just-approved non-estrogen therapy for treatment of menopausal symptoms. . The manufacturer, Astellas, is expected to make fezolinetant available at pharmacies before the end of this year. This medication binds to and blocks the neurokinin 3 (NK3) receptor, which plays a role in regulating body temperature, leading to a reduction in hot flashes.
For women suffering from frequent moderate to severe hot flashes, fezolinetant is an exciting breakthrough in women’s health as it is a highly effective nonhormonal treatment that reduces hot flashes and improves quality of life.
In two phase 3 clinical trials (Johnson et al. and Lederman et al.), fezolinetant 45 mg reduced the frequency of vasomotor symptoms by about 65%, significantly more than placebo, and similar to the 75% reduction seen with hormone therapy. Fezolinetant’s efficacy becomes evident within 1 week, reducing both frequency and severity of hot flashes.
With respect to side effects, 1%-2% of the menopausal women participating in clinical trials reported adverse events, including headaches, abdominal pain, diarrhea, insomnia, back pain, hot flushes, and reversible elevated hepatic transaminases. Serious adverse events were infrequent.
Subgroup analysis of data presented at ACOG’s 2023 annual meeting noted fezolinetant’s effectiveness among diverse populations, including White or Black race, body mass index of 30 or higher, those younger or older than age 55, smokers, former smokers, and never smokers, in U.S. as well as in European trial participants.
With respect to safety, a 52-week placebo-controlled safety trial confirmed safety for this time period. Adverse effects on the endometrium were neither seen nor expected, as fezolinetant is a centrally acting non–estrogen-containing medication. In addition, no loss of bone density was seen.
Prior trials of neurokinin receptor antagonists suggested the potential for hepatotoxicity. Increases in ALT or AST noted in one of the phase 3 trials of fezolinetant were described as asymptomatic, isolated, intermittent, or transient and returned to baseline during treatment or after discontinuation. However, the FDA placed a warning about liver injury potential. Package labeling recommends baseline liver function tests before starting fezolinetant and at 3, 6, and 9 months. In addition, concomitant use of moderate CYP1A2 inhibitors, including many antidepressants and cimetidine, should be avoided.
As with other recently approved medications, I am concerned that high cost could prevent appropriate candidates from having access.
Until now, the FDA had approved only one nonhormone therapy for vasomotor symptoms, 7.5 mg paroxetine salt. However, neither this formulation nor off-label use of other SSRIs, SNRIs, gabapentinoids, oxybutynin, or clonidine are as effective as hormone therapy or fezolinetant for moderate to severe vasomotor symptoms.
For women with bothersome menopausal hot flashes who can’t or choose not to use hormone therapy, including those with estrogen-sensitive breast or uterine cancers, fezolinetant offers a much-needed, highly effective, safe, nonhormone/non-estrogen option to treat their hot flashes.
The FDA approved it for treating vasomotor symptoms of menopause (hot flashes and night sweats) but it also appears to improve sleep disruption, mood, and quality of life.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I am Dr. JoAnn Pinkerton, professor of obstetrics and gynecology at the University of Virginia and a North American Menopause Society–credentialed menopause specialist.
I am excited to tell you about a brand-new, just-approved non-estrogen therapy for treatment of menopausal symptoms. . The manufacturer, Astellas, is expected to make fezolinetant available at pharmacies before the end of this year. This medication binds to and blocks the neurokinin 3 (NK3) receptor, which plays a role in regulating body temperature, leading to a reduction in hot flashes.
For women suffering from frequent moderate to severe hot flashes, fezolinetant is an exciting breakthrough in women’s health as it is a highly effective nonhormonal treatment that reduces hot flashes and improves quality of life.
In two phase 3 clinical trials (Johnson et al. and Lederman et al.), fezolinetant 45 mg reduced the frequency of vasomotor symptoms by about 65%, significantly more than placebo, and similar to the 75% reduction seen with hormone therapy. Fezolinetant’s efficacy becomes evident within 1 week, reducing both frequency and severity of hot flashes.
With respect to side effects, 1%-2% of the menopausal women participating in clinical trials reported adverse events, including headaches, abdominal pain, diarrhea, insomnia, back pain, hot flushes, and reversible elevated hepatic transaminases. Serious adverse events were infrequent.
Subgroup analysis of data presented at ACOG’s 2023 annual meeting noted fezolinetant’s effectiveness among diverse populations, including White or Black race, body mass index of 30 or higher, those younger or older than age 55, smokers, former smokers, and never smokers, in U.S. as well as in European trial participants.
With respect to safety, a 52-week placebo-controlled safety trial confirmed safety for this time period. Adverse effects on the endometrium were neither seen nor expected, as fezolinetant is a centrally acting non–estrogen-containing medication. In addition, no loss of bone density was seen.
Prior trials of neurokinin receptor antagonists suggested the potential for hepatotoxicity. Increases in ALT or AST noted in one of the phase 3 trials of fezolinetant were described as asymptomatic, isolated, intermittent, or transient and returned to baseline during treatment or after discontinuation. However, the FDA placed a warning about liver injury potential. Package labeling recommends baseline liver function tests before starting fezolinetant and at 3, 6, and 9 months. In addition, concomitant use of moderate CYP1A2 inhibitors, including many antidepressants and cimetidine, should be avoided.
As with other recently approved medications, I am concerned that high cost could prevent appropriate candidates from having access.
Until now, the FDA had approved only one nonhormone therapy for vasomotor symptoms, 7.5 mg paroxetine salt. However, neither this formulation nor off-label use of other SSRIs, SNRIs, gabapentinoids, oxybutynin, or clonidine are as effective as hormone therapy or fezolinetant for moderate to severe vasomotor symptoms.
For women with bothersome menopausal hot flashes who can’t or choose not to use hormone therapy, including those with estrogen-sensitive breast or uterine cancers, fezolinetant offers a much-needed, highly effective, safe, nonhormone/non-estrogen option to treat their hot flashes.
The FDA approved it for treating vasomotor symptoms of menopause (hot flashes and night sweats) but it also appears to improve sleep disruption, mood, and quality of life.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I am Dr. JoAnn Pinkerton, professor of obstetrics and gynecology at the University of Virginia and a North American Menopause Society–credentialed menopause specialist.
I am excited to tell you about a brand-new, just-approved non-estrogen therapy for treatment of menopausal symptoms. . The manufacturer, Astellas, is expected to make fezolinetant available at pharmacies before the end of this year. This medication binds to and blocks the neurokinin 3 (NK3) receptor, which plays a role in regulating body temperature, leading to a reduction in hot flashes.
For women suffering from frequent moderate to severe hot flashes, fezolinetant is an exciting breakthrough in women’s health as it is a highly effective nonhormonal treatment that reduces hot flashes and improves quality of life.
In two phase 3 clinical trials (Johnson et al. and Lederman et al.), fezolinetant 45 mg reduced the frequency of vasomotor symptoms by about 65%, significantly more than placebo, and similar to the 75% reduction seen with hormone therapy. Fezolinetant’s efficacy becomes evident within 1 week, reducing both frequency and severity of hot flashes.
With respect to side effects, 1%-2% of the menopausal women participating in clinical trials reported adverse events, including headaches, abdominal pain, diarrhea, insomnia, back pain, hot flushes, and reversible elevated hepatic transaminases. Serious adverse events were infrequent.
Subgroup analysis of data presented at ACOG’s 2023 annual meeting noted fezolinetant’s effectiveness among diverse populations, including White or Black race, body mass index of 30 or higher, those younger or older than age 55, smokers, former smokers, and never smokers, in U.S. as well as in European trial participants.
With respect to safety, a 52-week placebo-controlled safety trial confirmed safety for this time period. Adverse effects on the endometrium were neither seen nor expected, as fezolinetant is a centrally acting non–estrogen-containing medication. In addition, no loss of bone density was seen.
Prior trials of neurokinin receptor antagonists suggested the potential for hepatotoxicity. Increases in ALT or AST noted in one of the phase 3 trials of fezolinetant were described as asymptomatic, isolated, intermittent, or transient and returned to baseline during treatment or after discontinuation. However, the FDA placed a warning about liver injury potential. Package labeling recommends baseline liver function tests before starting fezolinetant and at 3, 6, and 9 months. In addition, concomitant use of moderate CYP1A2 inhibitors, including many antidepressants and cimetidine, should be avoided.
As with other recently approved medications, I am concerned that high cost could prevent appropriate candidates from having access.
Until now, the FDA had approved only one nonhormone therapy for vasomotor symptoms, 7.5 mg paroxetine salt. However, neither this formulation nor off-label use of other SSRIs, SNRIs, gabapentinoids, oxybutynin, or clonidine are as effective as hormone therapy or fezolinetant for moderate to severe vasomotor symptoms.
For women with bothersome menopausal hot flashes who can’t or choose not to use hormone therapy, including those with estrogen-sensitive breast or uterine cancers, fezolinetant offers a much-needed, highly effective, safe, nonhormone/non-estrogen option to treat their hot flashes.
The FDA approved it for treating vasomotor symptoms of menopause (hot flashes and night sweats) but it also appears to improve sleep disruption, mood, and quality of life.
A version of this article first appeared on Medscape.com.
Hormone therapies still ‘most effective’ in treating menopausal vasomotor symptoms
Despite new options in non–hormone-based treatments,
This recommendation emerged from an updated position statement from the North American Menopause Society in its first review of the scientific literature since 2015. The statement specifically targets nonhormonal management of symptoms such as hot flashes and night sweats, which occur in as many as 80% of menopausal women but are undertreated. The statement appears in the June issue of the Journal of The North American Menopause Society.
“Women with contraindications or objections to hormone treatment should be informed by professionals of evidence-based effective nonhormone treatment options,” stated a NAMS advisory panel led by Chrisandra L. Shufelt, MD, MS, professor and chair of the division of general internal medicine and associate director of the Women’s Health Research Center at the Mayo Clinic in Jacksonville, Fla. The statement is one of multiple NAMS updates performed at regular intervals, said Dr. Shufelt, also past president of NAMS, in an interview. “But the research has changed, and we wanted to make clinicians aware of new medications. One of our interesting findings was more evidence that off-label use of the nonhormonal overactive bladder drug oxybutynin can lower the rate of hot flashes.”
Dr. Shufelt noted that many of the current update’s findings align with previous research, and stressed that the therapeutic recommendations apply specifically to VMS. “Not all menopause-related symptoms are vasomotor, however,” she said. “While a lot of the lifestyle options such as cooling techniques and exercise are not recommended for controlling hot flashes, diet and exercise changes can be beneficial for other health reasons.”
Although it’s the most effective option for VMS, hormone therapy is not suitable for women with contraindications such as a previous blood clot, an estrogen-dependent cancer, a family history of such cancers, or a personal preference against hormone use, Dr. Shufelt added, so nonhormonal alternatives are important to prevent women from wasting time and money on ineffective remedies. “Women need to know what works and what doesn’t,” she said.
Recommended nonhormonal therapies
Based on a rigorous review of the scientific evidence to date, NAMS found the following therapies to be effective: cognitive-behavioral therapy; clinical hypnosis; SSRIs and serotonin-norepinephrine reuptake inhibitors – which yield mild to moderate improvements; gabapentin – which lessens the frequency and severity of hot flashes; fezolinetant (Veozah), a novel first-in-class neurokinin B antagonist that was Food and Drug Administration–approved in May for VSM; and oxybutynin, an antimuscarinic, anticholinergic drug, that reduces moderate to severe VMS, although long-term use in older adults may be linked to cognitive decline, weight loss, and stellate ganglion block.
Therapies that were ineffective, associated with adverse effects (AEs), or lacking adequate evidence of efficacy and thus not recommended for VMS included: paced respiration; supplemental and herbal remedies such as black cohosh, milk thistle, and evening primrose; cooling techniques; trigger avoidance; exercise and yoga; mindfulness-based intervention and relaxation; suvorexant, a dual orexin-receptor antagonist used for insomnia; soy foods, extracts, and the soy metabolite equol; cannabinoids; acupuncture; calibration of neural oscillations; chiropractics; clonidine, an alpha-2 adrenergic agonist that is associated with significant AEs with no recent evidence of benefit over placebo; dietary modification; and pregabalin – which is associated with significant AEs and has controlled-substance prescribing restrictions.
Ultimately, clinicians should individualize menopause care to each patient. For example, “if a patient says that avoiding caffeine in the morning stops her from having hot flashes in the afternoon, that’s fine,” Dr. Shufelt said.
HT still most effective
“This statement is excellent, comprehensive, and evidence-based,” commented Jill M. Rabin MD, vice chair of education and development, obstetrics and gynecology, at Northshore University Hospital/LIJ Medical Center in Manhasset, N.Y., and professor of obstetrics and gynecology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell Health in Hempstead, N.Y.
Dr. Rabin, coauthor of Mind Over Bladder was not involved in compiling the statement.
She agreed that hormone therapy is the most effective option for VMS and regularly prescribes it for suitable candidates in different forms depending on the type and severity of menopausal symptoms. As for nonhormonal options, Dr. Rabin added in an interview, some of those not recommended in the current NAMS statement could yet prove to be effective as more data accumulate. Suvorexant may be one to watch, for instance, but currently there are not enough data on its effectiveness.
“It’s really important to keep up on this nonhormonal research,” Dr. Rabin said. “As the population ages, more and more women will be in the peri- and postmenopausal periods and some have medical reasons for not taking hormone therapy.” It’s important to recommend nonhormonal therapies of proven benefit according to current high-level evidence, she said, “but also to keep your ear to the ground about those still under investigation.”
As for the lifestyle and alternative remedies of unproven benefit, Dr. Rabin added, there’s little harm in trying them. “As far as I know, no one’s ever died of relaxation and paced breathing.” In addition, a patient’s interaction with and sense of control over her own physiology provided by these techniques may be beneficial in themselves.
Dr. Shufelt reported grant support from the National Institutes of Health. Numerous authors reported consulting fees from and other financial ties to private-sector companies. Dr. Rabin had no relevant competing interests to disclose with regard to her comments.
Despite new options in non–hormone-based treatments,
This recommendation emerged from an updated position statement from the North American Menopause Society in its first review of the scientific literature since 2015. The statement specifically targets nonhormonal management of symptoms such as hot flashes and night sweats, which occur in as many as 80% of menopausal women but are undertreated. The statement appears in the June issue of the Journal of The North American Menopause Society.
“Women with contraindications or objections to hormone treatment should be informed by professionals of evidence-based effective nonhormone treatment options,” stated a NAMS advisory panel led by Chrisandra L. Shufelt, MD, MS, professor and chair of the division of general internal medicine and associate director of the Women’s Health Research Center at the Mayo Clinic in Jacksonville, Fla. The statement is one of multiple NAMS updates performed at regular intervals, said Dr. Shufelt, also past president of NAMS, in an interview. “But the research has changed, and we wanted to make clinicians aware of new medications. One of our interesting findings was more evidence that off-label use of the nonhormonal overactive bladder drug oxybutynin can lower the rate of hot flashes.”
Dr. Shufelt noted that many of the current update’s findings align with previous research, and stressed that the therapeutic recommendations apply specifically to VMS. “Not all menopause-related symptoms are vasomotor, however,” she said. “While a lot of the lifestyle options such as cooling techniques and exercise are not recommended for controlling hot flashes, diet and exercise changes can be beneficial for other health reasons.”
Although it’s the most effective option for VMS, hormone therapy is not suitable for women with contraindications such as a previous blood clot, an estrogen-dependent cancer, a family history of such cancers, or a personal preference against hormone use, Dr. Shufelt added, so nonhormonal alternatives are important to prevent women from wasting time and money on ineffective remedies. “Women need to know what works and what doesn’t,” she said.
Recommended nonhormonal therapies
Based on a rigorous review of the scientific evidence to date, NAMS found the following therapies to be effective: cognitive-behavioral therapy; clinical hypnosis; SSRIs and serotonin-norepinephrine reuptake inhibitors – which yield mild to moderate improvements; gabapentin – which lessens the frequency and severity of hot flashes; fezolinetant (Veozah), a novel first-in-class neurokinin B antagonist that was Food and Drug Administration–approved in May for VSM; and oxybutynin, an antimuscarinic, anticholinergic drug, that reduces moderate to severe VMS, although long-term use in older adults may be linked to cognitive decline, weight loss, and stellate ganglion block.
Therapies that were ineffective, associated with adverse effects (AEs), or lacking adequate evidence of efficacy and thus not recommended for VMS included: paced respiration; supplemental and herbal remedies such as black cohosh, milk thistle, and evening primrose; cooling techniques; trigger avoidance; exercise and yoga; mindfulness-based intervention and relaxation; suvorexant, a dual orexin-receptor antagonist used for insomnia; soy foods, extracts, and the soy metabolite equol; cannabinoids; acupuncture; calibration of neural oscillations; chiropractics; clonidine, an alpha-2 adrenergic agonist that is associated with significant AEs with no recent evidence of benefit over placebo; dietary modification; and pregabalin – which is associated with significant AEs and has controlled-substance prescribing restrictions.
Ultimately, clinicians should individualize menopause care to each patient. For example, “if a patient says that avoiding caffeine in the morning stops her from having hot flashes in the afternoon, that’s fine,” Dr. Shufelt said.
HT still most effective
“This statement is excellent, comprehensive, and evidence-based,” commented Jill M. Rabin MD, vice chair of education and development, obstetrics and gynecology, at Northshore University Hospital/LIJ Medical Center in Manhasset, N.Y., and professor of obstetrics and gynecology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell Health in Hempstead, N.Y.
Dr. Rabin, coauthor of Mind Over Bladder was not involved in compiling the statement.
She agreed that hormone therapy is the most effective option for VMS and regularly prescribes it for suitable candidates in different forms depending on the type and severity of menopausal symptoms. As for nonhormonal options, Dr. Rabin added in an interview, some of those not recommended in the current NAMS statement could yet prove to be effective as more data accumulate. Suvorexant may be one to watch, for instance, but currently there are not enough data on its effectiveness.
“It’s really important to keep up on this nonhormonal research,” Dr. Rabin said. “As the population ages, more and more women will be in the peri- and postmenopausal periods and some have medical reasons for not taking hormone therapy.” It’s important to recommend nonhormonal therapies of proven benefit according to current high-level evidence, she said, “but also to keep your ear to the ground about those still under investigation.”
As for the lifestyle and alternative remedies of unproven benefit, Dr. Rabin added, there’s little harm in trying them. “As far as I know, no one’s ever died of relaxation and paced breathing.” In addition, a patient’s interaction with and sense of control over her own physiology provided by these techniques may be beneficial in themselves.
Dr. Shufelt reported grant support from the National Institutes of Health. Numerous authors reported consulting fees from and other financial ties to private-sector companies. Dr. Rabin had no relevant competing interests to disclose with regard to her comments.
Despite new options in non–hormone-based treatments,
This recommendation emerged from an updated position statement from the North American Menopause Society in its first review of the scientific literature since 2015. The statement specifically targets nonhormonal management of symptoms such as hot flashes and night sweats, which occur in as many as 80% of menopausal women but are undertreated. The statement appears in the June issue of the Journal of The North American Menopause Society.
“Women with contraindications or objections to hormone treatment should be informed by professionals of evidence-based effective nonhormone treatment options,” stated a NAMS advisory panel led by Chrisandra L. Shufelt, MD, MS, professor and chair of the division of general internal medicine and associate director of the Women’s Health Research Center at the Mayo Clinic in Jacksonville, Fla. The statement is one of multiple NAMS updates performed at regular intervals, said Dr. Shufelt, also past president of NAMS, in an interview. “But the research has changed, and we wanted to make clinicians aware of new medications. One of our interesting findings was more evidence that off-label use of the nonhormonal overactive bladder drug oxybutynin can lower the rate of hot flashes.”
Dr. Shufelt noted that many of the current update’s findings align with previous research, and stressed that the therapeutic recommendations apply specifically to VMS. “Not all menopause-related symptoms are vasomotor, however,” she said. “While a lot of the lifestyle options such as cooling techniques and exercise are not recommended for controlling hot flashes, diet and exercise changes can be beneficial for other health reasons.”
Although it’s the most effective option for VMS, hormone therapy is not suitable for women with contraindications such as a previous blood clot, an estrogen-dependent cancer, a family history of such cancers, or a personal preference against hormone use, Dr. Shufelt added, so nonhormonal alternatives are important to prevent women from wasting time and money on ineffective remedies. “Women need to know what works and what doesn’t,” she said.
Recommended nonhormonal therapies
Based on a rigorous review of the scientific evidence to date, NAMS found the following therapies to be effective: cognitive-behavioral therapy; clinical hypnosis; SSRIs and serotonin-norepinephrine reuptake inhibitors – which yield mild to moderate improvements; gabapentin – which lessens the frequency and severity of hot flashes; fezolinetant (Veozah), a novel first-in-class neurokinin B antagonist that was Food and Drug Administration–approved in May for VSM; and oxybutynin, an antimuscarinic, anticholinergic drug, that reduces moderate to severe VMS, although long-term use in older adults may be linked to cognitive decline, weight loss, and stellate ganglion block.
Therapies that were ineffective, associated with adverse effects (AEs), or lacking adequate evidence of efficacy and thus not recommended for VMS included: paced respiration; supplemental and herbal remedies such as black cohosh, milk thistle, and evening primrose; cooling techniques; trigger avoidance; exercise and yoga; mindfulness-based intervention and relaxation; suvorexant, a dual orexin-receptor antagonist used for insomnia; soy foods, extracts, and the soy metabolite equol; cannabinoids; acupuncture; calibration of neural oscillations; chiropractics; clonidine, an alpha-2 adrenergic agonist that is associated with significant AEs with no recent evidence of benefit over placebo; dietary modification; and pregabalin – which is associated with significant AEs and has controlled-substance prescribing restrictions.
Ultimately, clinicians should individualize menopause care to each patient. For example, “if a patient says that avoiding caffeine in the morning stops her from having hot flashes in the afternoon, that’s fine,” Dr. Shufelt said.
HT still most effective
“This statement is excellent, comprehensive, and evidence-based,” commented Jill M. Rabin MD, vice chair of education and development, obstetrics and gynecology, at Northshore University Hospital/LIJ Medical Center in Manhasset, N.Y., and professor of obstetrics and gynecology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell Health in Hempstead, N.Y.
Dr. Rabin, coauthor of Mind Over Bladder was not involved in compiling the statement.
She agreed that hormone therapy is the most effective option for VMS and regularly prescribes it for suitable candidates in different forms depending on the type and severity of menopausal symptoms. As for nonhormonal options, Dr. Rabin added in an interview, some of those not recommended in the current NAMS statement could yet prove to be effective as more data accumulate. Suvorexant may be one to watch, for instance, but currently there are not enough data on its effectiveness.
“It’s really important to keep up on this nonhormonal research,” Dr. Rabin said. “As the population ages, more and more women will be in the peri- and postmenopausal periods and some have medical reasons for not taking hormone therapy.” It’s important to recommend nonhormonal therapies of proven benefit according to current high-level evidence, she said, “but also to keep your ear to the ground about those still under investigation.”
As for the lifestyle and alternative remedies of unproven benefit, Dr. Rabin added, there’s little harm in trying them. “As far as I know, no one’s ever died of relaxation and paced breathing.” In addition, a patient’s interaction with and sense of control over her own physiology provided by these techniques may be beneficial in themselves.
Dr. Shufelt reported grant support from the National Institutes of Health. Numerous authors reported consulting fees from and other financial ties to private-sector companies. Dr. Rabin had no relevant competing interests to disclose with regard to her comments.
FROM THE JOURNAL OF THE NORTH AMERICAN MENOPAUSE SOCIETY















