User login
Mortality Risk Greater in Young Obese Dialysis Patients
DENVER – Obese dialysis patients younger than age 65 years were 1.6 times more likely to die within 7 years, compared with their younger, normal-weight dialysis counterparts.
In addition, young and elderly dialysis patients alike who were underweight faced about a twofold increased risk of dying within the same time frame.
The findings come from the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD), a prospective analysis of 1,749 dialysis patients at 38 centers who were at least 18 years old at their first dialysis treatment and were followed until death, transplantation, or a maximum of 7 years.
"Mortality patterns of body mass index differ between young and elderly dialysis patients," Dr. Ellen K. Hoogeveen said during a press briefing Nov. 18 at the annual meeting of the American Society of Nephrology, where the findings were presented. "Obesity may be harmful in patients younger than 65 years. For patients younger than 65 years starting with dialysis, it is important to strive for normal weight."
At baseline, the researchers classified patients into one of two age groups: young (younger than age 65) and elderly (age 65 and older). They also classified them into one of four weight groups based on body mass index: underweight (less than 20 kg/m2), normal weight (20-25 kg/m2), overweight (25-30 kg/m2), and obese (30 kg/m2 or higher). They used Cox regression analysis to calculate hazard ratios associated with BMI categories, and used normal weight as the reference category
Dr. Hoogeveen, of the department of nephrology at Jeroen Bosch Hospital, Den Bosch, the Netherlands, reported that the mean age of the younger patients was 51 years, while the mean age of elderly patients was 73 years. The mean BMI of both groups was 24 kg/m2, and more than half were men (62% in each group).
The 7-year mortality rate for all patients was 67%. When the researchers adjusted for age, gender, smoking, cardiovascular disease, and modality of dialysis, they found that younger patients who were obese at baseline were 1.6 times more likely to die within 7 years than were younger, normal-weight patients. Elderly obese patients were 1.1 times more likely to die within 7 years than were younger, normal-weight patients, a statistically significant difference.
In addition, young and elderly dialysis patients alike who were underweight at baseline were at significantly increased risk of dying within 7 years, compared with younger patients who had a normal BMI (hazard ratios of 2.2 and 1.6, respectively).
One of the study authors, Dr. Elisabeth Boeschoten, is a consultant for Amgen and Baxter and receives grants/research support from Abbott, Amgen, Baxter, Genzyme, Roche, and Shire. All of the other authors reported no relevant financial disclosures.
DENVER – Obese dialysis patients younger than age 65 years were 1.6 times more likely to die within 7 years, compared with their younger, normal-weight dialysis counterparts.
In addition, young and elderly dialysis patients alike who were underweight faced about a twofold increased risk of dying within the same time frame.
The findings come from the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD), a prospective analysis of 1,749 dialysis patients at 38 centers who were at least 18 years old at their first dialysis treatment and were followed until death, transplantation, or a maximum of 7 years.
"Mortality patterns of body mass index differ between young and elderly dialysis patients," Dr. Ellen K. Hoogeveen said during a press briefing Nov. 18 at the annual meeting of the American Society of Nephrology, where the findings were presented. "Obesity may be harmful in patients younger than 65 years. For patients younger than 65 years starting with dialysis, it is important to strive for normal weight."
At baseline, the researchers classified patients into one of two age groups: young (younger than age 65) and elderly (age 65 and older). They also classified them into one of four weight groups based on body mass index: underweight (less than 20 kg/m2), normal weight (20-25 kg/m2), overweight (25-30 kg/m2), and obese (30 kg/m2 or higher). They used Cox regression analysis to calculate hazard ratios associated with BMI categories, and used normal weight as the reference category
Dr. Hoogeveen, of the department of nephrology at Jeroen Bosch Hospital, Den Bosch, the Netherlands, reported that the mean age of the younger patients was 51 years, while the mean age of elderly patients was 73 years. The mean BMI of both groups was 24 kg/m2, and more than half were men (62% in each group).
The 7-year mortality rate for all patients was 67%. When the researchers adjusted for age, gender, smoking, cardiovascular disease, and modality of dialysis, they found that younger patients who were obese at baseline were 1.6 times more likely to die within 7 years than were younger, normal-weight patients. Elderly obese patients were 1.1 times more likely to die within 7 years than were younger, normal-weight patients, a statistically significant difference.
In addition, young and elderly dialysis patients alike who were underweight at baseline were at significantly increased risk of dying within 7 years, compared with younger patients who had a normal BMI (hazard ratios of 2.2 and 1.6, respectively).
One of the study authors, Dr. Elisabeth Boeschoten, is a consultant for Amgen and Baxter and receives grants/research support from Abbott, Amgen, Baxter, Genzyme, Roche, and Shire. All of the other authors reported no relevant financial disclosures.
DENVER – Obese dialysis patients younger than age 65 years were 1.6 times more likely to die within 7 years, compared with their younger, normal-weight dialysis counterparts.
In addition, young and elderly dialysis patients alike who were underweight faced about a twofold increased risk of dying within the same time frame.
The findings come from the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD), a prospective analysis of 1,749 dialysis patients at 38 centers who were at least 18 years old at their first dialysis treatment and were followed until death, transplantation, or a maximum of 7 years.
"Mortality patterns of body mass index differ between young and elderly dialysis patients," Dr. Ellen K. Hoogeveen said during a press briefing Nov. 18 at the annual meeting of the American Society of Nephrology, where the findings were presented. "Obesity may be harmful in patients younger than 65 years. For patients younger than 65 years starting with dialysis, it is important to strive for normal weight."
At baseline, the researchers classified patients into one of two age groups: young (younger than age 65) and elderly (age 65 and older). They also classified them into one of four weight groups based on body mass index: underweight (less than 20 kg/m2), normal weight (20-25 kg/m2), overweight (25-30 kg/m2), and obese (30 kg/m2 or higher). They used Cox regression analysis to calculate hazard ratios associated with BMI categories, and used normal weight as the reference category
Dr. Hoogeveen, of the department of nephrology at Jeroen Bosch Hospital, Den Bosch, the Netherlands, reported that the mean age of the younger patients was 51 years, while the mean age of elderly patients was 73 years. The mean BMI of both groups was 24 kg/m2, and more than half were men (62% in each group).
The 7-year mortality rate for all patients was 67%. When the researchers adjusted for age, gender, smoking, cardiovascular disease, and modality of dialysis, they found that younger patients who were obese at baseline were 1.6 times more likely to die within 7 years than were younger, normal-weight patients. Elderly obese patients were 1.1 times more likely to die within 7 years than were younger, normal-weight patients, a statistically significant difference.
In addition, young and elderly dialysis patients alike who were underweight at baseline were at significantly increased risk of dying within 7 years, compared with younger patients who had a normal BMI (hazard ratios of 2.2 and 1.6, respectively).
One of the study authors, Dr. Elisabeth Boeschoten, is a consultant for Amgen and Baxter and receives grants/research support from Abbott, Amgen, Baxter, Genzyme, Roche, and Shire. All of the other authors reported no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF NEPHROLOGY
Major Finding: Patients on dialysis who were younger than 65 years of age and obese had a 1.6-fold increased risk of dying within 7 years, compared with their normal-weight counterparts.
Data Source: An analysis of 1,749 dialysis patients in the Netherlands who were followed for 7 years.
Disclosures: One of the study authors, Dr. Elisabeth Boeschoten, is a consultant for Amgen and Baxter and receives grants/research support from Abbott, Amgen, Baxter, Genzyme, Roche, and Shire. All of the other authors reported no relevant financial disclosures.
Provenge Data Found Not Supportive of Off-Label Uses
The existing clinical data on Dendreon’s prostate cancer vaccine Provenge (sipuleucel-T) cannot be "generalizable" to off-label uses, most members of the Medicare Evidence Development & Coverage Advisory Committee agreed at a Nov. 17 meeting.
The meeting was called by the Centers for Medicare and Medicaid Services to consider whether Provenge is a "reasonable and necessary" therapy and thus eligible for Medicare coverage. The treatment is approved for treating asymptomatic or minimally symptomatic prostate cancer that is metastatic and resistant to standard hormone treatment.
The committee’s review is part of a national coverage analysis on Provenge and may be followed by a national coverage determination. Off-label use is one significant issue for the agency. A proposed decision on the agency’s analysis is scheduled to be released by March 3, 2011, and a final decision will be released in June 2011.
The committee voted on a number of questions designed to probe the strength of the available evidence for both off-label and on-label use. In answering questions posed by CMS, members were asked to rate their confidence in the data on a scale ranging from "low" to "high."
The majority of members signaled that the data could not support use of the therapy in patients whose prostate cancer has not metastasized; in patients who have metastatic, castrate-resistant disease but whose symptoms are more severe than minimally symptomatic; or in patients who have metastatic prostate cancer but who have not failed hormonal therapy.
The committee was more confident about the data supporting on-label uses. The majority voted that the data are reasonably adequate to conclude Provenge improves overall patient survival and can help to avoid the "burdens," including side effects, associated with chemotherapy. The committee expressed less confidence that the data conclusively show Provenge improves the control of disease-related symptoms.
MEDCAC members felt the clinical trial data can be extrapolated to use of Provenge in community-based settings and were moderately confident that the research findings were generalizable to demographic groups underrepresented by the patients participating in the studies, including Medicare beneficiaries and minorities, such as African Americans.
"The Pink Sheet" and Hospitalist News Digital Network are both owned by Elsevier.
The existing clinical data on Dendreon’s prostate cancer vaccine Provenge (sipuleucel-T) cannot be "generalizable" to off-label uses, most members of the Medicare Evidence Development & Coverage Advisory Committee agreed at a Nov. 17 meeting.
The meeting was called by the Centers for Medicare and Medicaid Services to consider whether Provenge is a "reasonable and necessary" therapy and thus eligible for Medicare coverage. The treatment is approved for treating asymptomatic or minimally symptomatic prostate cancer that is metastatic and resistant to standard hormone treatment.
The committee’s review is part of a national coverage analysis on Provenge and may be followed by a national coverage determination. Off-label use is one significant issue for the agency. A proposed decision on the agency’s analysis is scheduled to be released by March 3, 2011, and a final decision will be released in June 2011.
The committee voted on a number of questions designed to probe the strength of the available evidence for both off-label and on-label use. In answering questions posed by CMS, members were asked to rate their confidence in the data on a scale ranging from "low" to "high."
The majority of members signaled that the data could not support use of the therapy in patients whose prostate cancer has not metastasized; in patients who have metastatic, castrate-resistant disease but whose symptoms are more severe than minimally symptomatic; or in patients who have metastatic prostate cancer but who have not failed hormonal therapy.
The committee was more confident about the data supporting on-label uses. The majority voted that the data are reasonably adequate to conclude Provenge improves overall patient survival and can help to avoid the "burdens," including side effects, associated with chemotherapy. The committee expressed less confidence that the data conclusively show Provenge improves the control of disease-related symptoms.
MEDCAC members felt the clinical trial data can be extrapolated to use of Provenge in community-based settings and were moderately confident that the research findings were generalizable to demographic groups underrepresented by the patients participating in the studies, including Medicare beneficiaries and minorities, such as African Americans.
"The Pink Sheet" and Hospitalist News Digital Network are both owned by Elsevier.
The existing clinical data on Dendreon’s prostate cancer vaccine Provenge (sipuleucel-T) cannot be "generalizable" to off-label uses, most members of the Medicare Evidence Development & Coverage Advisory Committee agreed at a Nov. 17 meeting.
The meeting was called by the Centers for Medicare and Medicaid Services to consider whether Provenge is a "reasonable and necessary" therapy and thus eligible for Medicare coverage. The treatment is approved for treating asymptomatic or minimally symptomatic prostate cancer that is metastatic and resistant to standard hormone treatment.
The committee’s review is part of a national coverage analysis on Provenge and may be followed by a national coverage determination. Off-label use is one significant issue for the agency. A proposed decision on the agency’s analysis is scheduled to be released by March 3, 2011, and a final decision will be released in June 2011.
The committee voted on a number of questions designed to probe the strength of the available evidence for both off-label and on-label use. In answering questions posed by CMS, members were asked to rate their confidence in the data on a scale ranging from "low" to "high."
The majority of members signaled that the data could not support use of the therapy in patients whose prostate cancer has not metastasized; in patients who have metastatic, castrate-resistant disease but whose symptoms are more severe than minimally symptomatic; or in patients who have metastatic prostate cancer but who have not failed hormonal therapy.
The committee was more confident about the data supporting on-label uses. The majority voted that the data are reasonably adequate to conclude Provenge improves overall patient survival and can help to avoid the "burdens," including side effects, associated with chemotherapy. The committee expressed less confidence that the data conclusively show Provenge improves the control of disease-related symptoms.
MEDCAC members felt the clinical trial data can be extrapolated to use of Provenge in community-based settings and were moderately confident that the research findings were generalizable to demographic groups underrepresented by the patients participating in the studies, including Medicare beneficiaries and minorities, such as African Americans.
"The Pink Sheet" and Hospitalist News Digital Network are both owned by Elsevier.
FROM A MEETING OF THE MEDICARE EVIDENCE DEVELOPMENT AND COVERAGE ADVISORY COMMITTEE
Provenge Data Found Not Supportive of Off-Label Uses
The existing clinical data on Dendreon’s prostate cancer vaccine Provenge (sipuleucel-T) cannot be "generalizable" to off-label uses, most members of the Medicare Evidence Development & Coverage Advisory Committee agreed at a Nov. 17 meeting.
The meeting was called by the Centers for Medicare and Medicaid Services to consider whether Provenge is a "reasonable and necessary" therapy and thus eligible for Medicare coverage. The treatment is approved for treating asymptomatic or minimally symptomatic prostate cancer that is metastatic and resistant to standard hormone treatment.
The committee’s review is part of a national coverage analysis on Provenge and may be followed by a national coverage determination. Off-label use is one significant issue for the agency. A proposed decision on the agency’s analysis is scheduled to be released by March 3, 2011, and a final decision will be released in June 2011.
The committee voted on a number of questions designed to probe the strength of the available evidence for both off-label and on-label use. In answering questions posed by CMS, members were asked to rate their confidence in the data on a scale ranging from "low" to "high."
The majority of members signaled that the data could not support use of the therapy in patients whose prostate cancer has not metastasized; in patients who have metastatic, castrate-resistant disease but whose symptoms are more severe than minimally symptomatic; or in patients who have metastatic prostate cancer but who have not failed hormonal therapy.
The committee was more confident about the data supporting on-label uses. The majority voted that the data are reasonably adequate to conclude Provenge improves overall patient survival and can help to avoid the "burdens," including side effects, associated with chemotherapy. The committee expressed less confidence that the data conclusively show Provenge improves the control of disease-related symptoms.
MEDCAC members felt the clinical trial data can be extrapolated to use of Provenge in community-based settings and were moderately confident that the research findings were generalizable to demographic groups underrepresented by the patients participating in the studies, including Medicare beneficiaries and minorities, such as African Americans.
"The Pink Sheet" and Internal Medicine News Digital Network are both owned by Elsevier.
The existing clinical data on Dendreon’s prostate cancer vaccine Provenge (sipuleucel-T) cannot be "generalizable" to off-label uses, most members of the Medicare Evidence Development & Coverage Advisory Committee agreed at a Nov. 17 meeting.
The meeting was called by the Centers for Medicare and Medicaid Services to consider whether Provenge is a "reasonable and necessary" therapy and thus eligible for Medicare coverage. The treatment is approved for treating asymptomatic or minimally symptomatic prostate cancer that is metastatic and resistant to standard hormone treatment.
The committee’s review is part of a national coverage analysis on Provenge and may be followed by a national coverage determination. Off-label use is one significant issue for the agency. A proposed decision on the agency’s analysis is scheduled to be released by March 3, 2011, and a final decision will be released in June 2011.
The committee voted on a number of questions designed to probe the strength of the available evidence for both off-label and on-label use. In answering questions posed by CMS, members were asked to rate their confidence in the data on a scale ranging from "low" to "high."
The majority of members signaled that the data could not support use of the therapy in patients whose prostate cancer has not metastasized; in patients who have metastatic, castrate-resistant disease but whose symptoms are more severe than minimally symptomatic; or in patients who have metastatic prostate cancer but who have not failed hormonal therapy.
The committee was more confident about the data supporting on-label uses. The majority voted that the data are reasonably adequate to conclude Provenge improves overall patient survival and can help to avoid the "burdens," including side effects, associated with chemotherapy. The committee expressed less confidence that the data conclusively show Provenge improves the control of disease-related symptoms.
MEDCAC members felt the clinical trial data can be extrapolated to use of Provenge in community-based settings and were moderately confident that the research findings were generalizable to demographic groups underrepresented by the patients participating in the studies, including Medicare beneficiaries and minorities, such as African Americans.
"The Pink Sheet" and Internal Medicine News Digital Network are both owned by Elsevier.
The existing clinical data on Dendreon’s prostate cancer vaccine Provenge (sipuleucel-T) cannot be "generalizable" to off-label uses, most members of the Medicare Evidence Development & Coverage Advisory Committee agreed at a Nov. 17 meeting.
The meeting was called by the Centers for Medicare and Medicaid Services to consider whether Provenge is a "reasonable and necessary" therapy and thus eligible for Medicare coverage. The treatment is approved for treating asymptomatic or minimally symptomatic prostate cancer that is metastatic and resistant to standard hormone treatment.
The committee’s review is part of a national coverage analysis on Provenge and may be followed by a national coverage determination. Off-label use is one significant issue for the agency. A proposed decision on the agency’s analysis is scheduled to be released by March 3, 2011, and a final decision will be released in June 2011.
The committee voted on a number of questions designed to probe the strength of the available evidence for both off-label and on-label use. In answering questions posed by CMS, members were asked to rate their confidence in the data on a scale ranging from "low" to "high."
The majority of members signaled that the data could not support use of the therapy in patients whose prostate cancer has not metastasized; in patients who have metastatic, castrate-resistant disease but whose symptoms are more severe than minimally symptomatic; or in patients who have metastatic prostate cancer but who have not failed hormonal therapy.
The committee was more confident about the data supporting on-label uses. The majority voted that the data are reasonably adequate to conclude Provenge improves overall patient survival and can help to avoid the "burdens," including side effects, associated with chemotherapy. The committee expressed less confidence that the data conclusively show Provenge improves the control of disease-related symptoms.
MEDCAC members felt the clinical trial data can be extrapolated to use of Provenge in community-based settings and were moderately confident that the research findings were generalizable to demographic groups underrepresented by the patients participating in the studies, including Medicare beneficiaries and minorities, such as African Americans.
"The Pink Sheet" and Internal Medicine News Digital Network are both owned by Elsevier.
FROM A MEETING OF THE MEDICARE EVIDENCE DEVELOPMENT AND COVERAGE ADVISORY COMMITTEE
Renal Dysfunction May Predict Heart Risk in RA
ATLANTA – Renal dysfunction is independently associated with incident cardiovascular disease in patients with rheumatoid arthritis, according to findings from a prospective Dutch cohort study.
Of 353 RA patients who were part of the Cardiovascular Research and Rheumatoid Arthritis (CARRE) study and who were followed for at least 3 years, 23 developed a cardiovascular event. Serum creatinine levels and glomerular filtration rate (GFR) findings were unfavorable in the patients who had a cardiovascular event, compared with those who did not, Dr. Alper M. van Sijl reported at the annual meeting of the American College of Rheumatology.
Patients with a cardiovascular event had a mean serum creatinine level of 101, compared with 88 micromol/L in the unaffected group; GFR as measured using the Cockcroft-Gault (CG) formula was 63 vs. 80 mL/min, and GFR as measured using the Modification of Diet in Renal Disease (MDRD) formula was 59 vs. 78 mL/min, in the groups, respectively, said Dr. van Sijl of the Jan van Breemen Institute and VU Medical Center, Amsterdam.
Dr. van Sijl and his colleagues used logistic regression analysis to calculate whether incremental increases of 5 micromol/L in serum creatinine level, and incremental decreases of 5 mL/min in glomerular filtration rate as measured using both the CG and MDRD formulas were associated with incident cardiovascular disease. Indeed, all were significantly positively associated with incident cardiovascular disease (odds ratios of 1.13, 1.12, and 1.21, respectively).
"When adjusted for age, gender, body mass index, and prior cardiovascular disease, the association remains. And when adjusted additionally for traditional cardiovascular risk factors, the association becomes even stronger," he said, explaining that a decrease in GFR of 5 mL/min was associated with a 30%-35% increased risk of cardiovascular disease, independent of traditional cardiovascular risk factors.
By comparison, a prior cohort study showed that diabetes patients have about a 20% cardiovascular disease risk increase for every 5-mL/min decrease in GFR, he noted.
The findings of the current study suggest that renal dysfunction might be a "missing link" in the established, but only partially defined, connection between RA and cardiovascular disease, he said.
RA patients are known to have an increased risk of mortality, compared with the general population, and much of that risk has been shown to be attributable to cardiovascular disease. However, standard cardiovascular risk factors – particularly hypercholesterolemia, hypertension, and insulin resistance – explain only part of this association.
Furthermore, renal dysfunction has been shown to be associated with cardiovascular disease in the general population, although findings from landmark studies have shown that risk depends on coexisting hypertension, prior cardiovascular disease, and diabetes, Dr. van Sijl said.
Study findings have shown an association between renal dysfunction and RA. Renal dysfunction in the RA population has been attributed to extra-articular manifestations, NSAID use, and chronic inflammation. At least one study showed an association between renal function and prevalent cardiovascular disease in RA, he said.
Although the current findings do support the idea that decreased renal function can help identify RA patients at increased risk for future cardiovascular disease, further study is needed to determine whether chronic inflammation causes the decreases in GFR, and whether GFR can accurately predict cardiovascular disease occurrence in RA, he said.
"Also still unknown to us is whether possible residual confounding is still present in the form of newly discovered markers of both renal dysfunction and cardiovascular disease such as uric acid, endothelial dysfunction, and cumulative inflammatory burden," he said.
Dr. van Sijl said he had no disclosures to report.
ATLANTA – Renal dysfunction is independently associated with incident cardiovascular disease in patients with rheumatoid arthritis, according to findings from a prospective Dutch cohort study.
Of 353 RA patients who were part of the Cardiovascular Research and Rheumatoid Arthritis (CARRE) study and who were followed for at least 3 years, 23 developed a cardiovascular event. Serum creatinine levels and glomerular filtration rate (GFR) findings were unfavorable in the patients who had a cardiovascular event, compared with those who did not, Dr. Alper M. van Sijl reported at the annual meeting of the American College of Rheumatology.
Patients with a cardiovascular event had a mean serum creatinine level of 101, compared with 88 micromol/L in the unaffected group; GFR as measured using the Cockcroft-Gault (CG) formula was 63 vs. 80 mL/min, and GFR as measured using the Modification of Diet in Renal Disease (MDRD) formula was 59 vs. 78 mL/min, in the groups, respectively, said Dr. van Sijl of the Jan van Breemen Institute and VU Medical Center, Amsterdam.
Dr. van Sijl and his colleagues used logistic regression analysis to calculate whether incremental increases of 5 micromol/L in serum creatinine level, and incremental decreases of 5 mL/min in glomerular filtration rate as measured using both the CG and MDRD formulas were associated with incident cardiovascular disease. Indeed, all were significantly positively associated with incident cardiovascular disease (odds ratios of 1.13, 1.12, and 1.21, respectively).
"When adjusted for age, gender, body mass index, and prior cardiovascular disease, the association remains. And when adjusted additionally for traditional cardiovascular risk factors, the association becomes even stronger," he said, explaining that a decrease in GFR of 5 mL/min was associated with a 30%-35% increased risk of cardiovascular disease, independent of traditional cardiovascular risk factors.
By comparison, a prior cohort study showed that diabetes patients have about a 20% cardiovascular disease risk increase for every 5-mL/min decrease in GFR, he noted.
The findings of the current study suggest that renal dysfunction might be a "missing link" in the established, but only partially defined, connection between RA and cardiovascular disease, he said.
RA patients are known to have an increased risk of mortality, compared with the general population, and much of that risk has been shown to be attributable to cardiovascular disease. However, standard cardiovascular risk factors – particularly hypercholesterolemia, hypertension, and insulin resistance – explain only part of this association.
Furthermore, renal dysfunction has been shown to be associated with cardiovascular disease in the general population, although findings from landmark studies have shown that risk depends on coexisting hypertension, prior cardiovascular disease, and diabetes, Dr. van Sijl said.
Study findings have shown an association between renal dysfunction and RA. Renal dysfunction in the RA population has been attributed to extra-articular manifestations, NSAID use, and chronic inflammation. At least one study showed an association between renal function and prevalent cardiovascular disease in RA, he said.
Although the current findings do support the idea that decreased renal function can help identify RA patients at increased risk for future cardiovascular disease, further study is needed to determine whether chronic inflammation causes the decreases in GFR, and whether GFR can accurately predict cardiovascular disease occurrence in RA, he said.
"Also still unknown to us is whether possible residual confounding is still present in the form of newly discovered markers of both renal dysfunction and cardiovascular disease such as uric acid, endothelial dysfunction, and cumulative inflammatory burden," he said.
Dr. van Sijl said he had no disclosures to report.
ATLANTA – Renal dysfunction is independently associated with incident cardiovascular disease in patients with rheumatoid arthritis, according to findings from a prospective Dutch cohort study.
Of 353 RA patients who were part of the Cardiovascular Research and Rheumatoid Arthritis (CARRE) study and who were followed for at least 3 years, 23 developed a cardiovascular event. Serum creatinine levels and glomerular filtration rate (GFR) findings were unfavorable in the patients who had a cardiovascular event, compared with those who did not, Dr. Alper M. van Sijl reported at the annual meeting of the American College of Rheumatology.
Patients with a cardiovascular event had a mean serum creatinine level of 101, compared with 88 micromol/L in the unaffected group; GFR as measured using the Cockcroft-Gault (CG) formula was 63 vs. 80 mL/min, and GFR as measured using the Modification of Diet in Renal Disease (MDRD) formula was 59 vs. 78 mL/min, in the groups, respectively, said Dr. van Sijl of the Jan van Breemen Institute and VU Medical Center, Amsterdam.
Dr. van Sijl and his colleagues used logistic regression analysis to calculate whether incremental increases of 5 micromol/L in serum creatinine level, and incremental decreases of 5 mL/min in glomerular filtration rate as measured using both the CG and MDRD formulas were associated with incident cardiovascular disease. Indeed, all were significantly positively associated with incident cardiovascular disease (odds ratios of 1.13, 1.12, and 1.21, respectively).
"When adjusted for age, gender, body mass index, and prior cardiovascular disease, the association remains. And when adjusted additionally for traditional cardiovascular risk factors, the association becomes even stronger," he said, explaining that a decrease in GFR of 5 mL/min was associated with a 30%-35% increased risk of cardiovascular disease, independent of traditional cardiovascular risk factors.
By comparison, a prior cohort study showed that diabetes patients have about a 20% cardiovascular disease risk increase for every 5-mL/min decrease in GFR, he noted.
The findings of the current study suggest that renal dysfunction might be a "missing link" in the established, but only partially defined, connection between RA and cardiovascular disease, he said.
RA patients are known to have an increased risk of mortality, compared with the general population, and much of that risk has been shown to be attributable to cardiovascular disease. However, standard cardiovascular risk factors – particularly hypercholesterolemia, hypertension, and insulin resistance – explain only part of this association.
Furthermore, renal dysfunction has been shown to be associated with cardiovascular disease in the general population, although findings from landmark studies have shown that risk depends on coexisting hypertension, prior cardiovascular disease, and diabetes, Dr. van Sijl said.
Study findings have shown an association between renal dysfunction and RA. Renal dysfunction in the RA population has been attributed to extra-articular manifestations, NSAID use, and chronic inflammation. At least one study showed an association between renal function and prevalent cardiovascular disease in RA, he said.
Although the current findings do support the idea that decreased renal function can help identify RA patients at increased risk for future cardiovascular disease, further study is needed to determine whether chronic inflammation causes the decreases in GFR, and whether GFR can accurately predict cardiovascular disease occurrence in RA, he said.
"Also still unknown to us is whether possible residual confounding is still present in the form of newly discovered markers of both renal dysfunction and cardiovascular disease such as uric acid, endothelial dysfunction, and cumulative inflammatory burden," he said.
Dr. van Sijl said he had no disclosures to report.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Renal Denervation Slashed Blood Pressure in Drug-Resistant Hypertensives
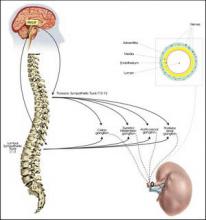
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
Renal Denervation Slashed Blood Pressure in Drug-Resistant Hypertensives
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
Myofascial Physical Therapy Appears Beneficial in Patients With Interstitial Cystitis
CHICAGO – Results of a second randomized trial confirm that significantly more women with interstitial cystitis respond to myofascial physical therapy than traditional massage therapy.
Among 81 women with interstitial cystitis and moderate to severe pain or urgency, global response assessment (GRA) rates at 12 weeks were 59% with myofascial physical therapy versus 26% with global massage therapy consisting of full-body Western massage.
This is the second positive randomized controlled trial for a disorder in desperate need of new treatment options, Rhonda Kotarinos, a physical therapist in Oakbrook Terrace, Ill., said at the annual meeting of the International Pelvic Pain Society.
There is no cure for interstitial cystitis (IC), also referred to as painful bladder syndrome. Treatments include eliminating dietary triggers and reproductive organ triggers, anesthetic instillations, physical therapy, and use of pain medications such as opioids, nonsteroidal anti-inflammatory agents, and tricyclic antidepressants.
The prevalence of IC also varies greatly. A widely cited study reports that 1.1% of 1,218 women presenting for a routine primary care office visit had IC based on the O’Leary-Sant Interstitial Cystitis Symptom and Problem Index, while 12.6% had IC based on responses to the PUF (Pelvic Pain and Urgency/Frequency Patient Symptom Scale) questionnaire. The authors concluded that "the true prevalence of IC in women may be somewhere between these two extremes," (J. Urol. 2005;174:2231-4).
The feasibility of myofascial physical therapy (MPT) was evaluated by the same group of researchers in a pilot trial involving 44 men and women with urologic chronic pelvic pain syndrome, including IC. As in the current study, MPT consisted of connective tissue manipulation to all body wall tissues in the abdominal wall, thighs, back, and buttocks that clinically were found to contain connective tissue abnormalities or painful myofascial trigger points. Myofascial manipulation focused on trigger points and restrictive bands.
Patients also were assigned to 10 1-hour sessions of MPT or global massage therapy (GMT), and asked to rate their overall symptoms using the 7-point global response assessment (GRA), with 1 being "markedly worse" and 7 being "markedly improved."
GRA rates were significantly higher at 57% with MPT vs. 21% with massage therapy (J. Urol. 2009;182:570-80). Subgroup analyses revealed a striking difference in the response to standard massage therapy between the all-male patients with chronic pelvic pain syndrome (CPPS) and women with IC (40% vs. 7%), suggesting that patients with CPPS or men respond differently to massage therapy.
The pilot study was the first and only positive trial in 10 years of research in urologic CPPS funded by the National Institute of Diabetes and Digestive and Kidney Diseases, Ms. Kotarinos said.
The current trial was conducted at 11 centers in the United States and Canada, and included 81 women with IC for less than 3 years who had moderate to severe pelvic pain (95%) or moderate to severe urgency (93%). Their mean age was 43 years; 84% were white, 5% were black, and ethnicity for the remaining 11% was not provided.
The secondary end points did not confirm the primary results, Ms. Kotarinos said. The MPT arm had greater mean changes in symptom scores than did the GMT arm on the Interstitial Cystitis Symptom Index (-3.2 vs. -2.2), Interstitial Cystitis Problem Index (-3.6 vs. -2.4), Likert Pain scale (-2.2 vs. -1.5), and Likert Urge Scale (-2.1 vs. -1.4), but the differences did not reach statistical significance.
In all, 85% of patients in both arms completed therapy, which was well tolerated, she said. This is important as myofascial PT can be painful or seen as unduly invasive. Adverse events of any kind were reported in 64% of the MPT group and 60% of the GMT group, and serious adverse events in 15% vs. 14%, respectively. Serious adverse events among MPT patients included four cases of pain and one case each of dehydration, vomiting, and other genitourinary symptoms.
Ms. Kotarinos pointed out that the study included a small group of highly select patients, and that blinding was ineffective, as nearly all patients correctly guessed their treatment arm.
She suggests that future research is warranted to investigate the lack of response in secondary outcomes and to define the role of MPT in the broader IC population, the optimal patient selection criteria, and optimal treatment parameters.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Ms. Kotarinos disclosed no conflicts of interest.
CHICAGO – Results of a second randomized trial confirm that significantly more women with interstitial cystitis respond to myofascial physical therapy than traditional massage therapy.
Among 81 women with interstitial cystitis and moderate to severe pain or urgency, global response assessment (GRA) rates at 12 weeks were 59% with myofascial physical therapy versus 26% with global massage therapy consisting of full-body Western massage.
This is the second positive randomized controlled trial for a disorder in desperate need of new treatment options, Rhonda Kotarinos, a physical therapist in Oakbrook Terrace, Ill., said at the annual meeting of the International Pelvic Pain Society.
There is no cure for interstitial cystitis (IC), also referred to as painful bladder syndrome. Treatments include eliminating dietary triggers and reproductive organ triggers, anesthetic instillations, physical therapy, and use of pain medications such as opioids, nonsteroidal anti-inflammatory agents, and tricyclic antidepressants.
The prevalence of IC also varies greatly. A widely cited study reports that 1.1% of 1,218 women presenting for a routine primary care office visit had IC based on the O’Leary-Sant Interstitial Cystitis Symptom and Problem Index, while 12.6% had IC based on responses to the PUF (Pelvic Pain and Urgency/Frequency Patient Symptom Scale) questionnaire. The authors concluded that "the true prevalence of IC in women may be somewhere between these two extremes," (J. Urol. 2005;174:2231-4).
The feasibility of myofascial physical therapy (MPT) was evaluated by the same group of researchers in a pilot trial involving 44 men and women with urologic chronic pelvic pain syndrome, including IC. As in the current study, MPT consisted of connective tissue manipulation to all body wall tissues in the abdominal wall, thighs, back, and buttocks that clinically were found to contain connective tissue abnormalities or painful myofascial trigger points. Myofascial manipulation focused on trigger points and restrictive bands.
Patients also were assigned to 10 1-hour sessions of MPT or global massage therapy (GMT), and asked to rate their overall symptoms using the 7-point global response assessment (GRA), with 1 being "markedly worse" and 7 being "markedly improved."
GRA rates were significantly higher at 57% with MPT vs. 21% with massage therapy (J. Urol. 2009;182:570-80). Subgroup analyses revealed a striking difference in the response to standard massage therapy between the all-male patients with chronic pelvic pain syndrome (CPPS) and women with IC (40% vs. 7%), suggesting that patients with CPPS or men respond differently to massage therapy.
The pilot study was the first and only positive trial in 10 years of research in urologic CPPS funded by the National Institute of Diabetes and Digestive and Kidney Diseases, Ms. Kotarinos said.
The current trial was conducted at 11 centers in the United States and Canada, and included 81 women with IC for less than 3 years who had moderate to severe pelvic pain (95%) or moderate to severe urgency (93%). Their mean age was 43 years; 84% were white, 5% were black, and ethnicity for the remaining 11% was not provided.
The secondary end points did not confirm the primary results, Ms. Kotarinos said. The MPT arm had greater mean changes in symptom scores than did the GMT arm on the Interstitial Cystitis Symptom Index (-3.2 vs. -2.2), Interstitial Cystitis Problem Index (-3.6 vs. -2.4), Likert Pain scale (-2.2 vs. -1.5), and Likert Urge Scale (-2.1 vs. -1.4), but the differences did not reach statistical significance.
In all, 85% of patients in both arms completed therapy, which was well tolerated, she said. This is important as myofascial PT can be painful or seen as unduly invasive. Adverse events of any kind were reported in 64% of the MPT group and 60% of the GMT group, and serious adverse events in 15% vs. 14%, respectively. Serious adverse events among MPT patients included four cases of pain and one case each of dehydration, vomiting, and other genitourinary symptoms.
Ms. Kotarinos pointed out that the study included a small group of highly select patients, and that blinding was ineffective, as nearly all patients correctly guessed their treatment arm.
She suggests that future research is warranted to investigate the lack of response in secondary outcomes and to define the role of MPT in the broader IC population, the optimal patient selection criteria, and optimal treatment parameters.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Ms. Kotarinos disclosed no conflicts of interest.
CHICAGO – Results of a second randomized trial confirm that significantly more women with interstitial cystitis respond to myofascial physical therapy than traditional massage therapy.
Among 81 women with interstitial cystitis and moderate to severe pain or urgency, global response assessment (GRA) rates at 12 weeks were 59% with myofascial physical therapy versus 26% with global massage therapy consisting of full-body Western massage.
This is the second positive randomized controlled trial for a disorder in desperate need of new treatment options, Rhonda Kotarinos, a physical therapist in Oakbrook Terrace, Ill., said at the annual meeting of the International Pelvic Pain Society.
There is no cure for interstitial cystitis (IC), also referred to as painful bladder syndrome. Treatments include eliminating dietary triggers and reproductive organ triggers, anesthetic instillations, physical therapy, and use of pain medications such as opioids, nonsteroidal anti-inflammatory agents, and tricyclic antidepressants.
The prevalence of IC also varies greatly. A widely cited study reports that 1.1% of 1,218 women presenting for a routine primary care office visit had IC based on the O’Leary-Sant Interstitial Cystitis Symptom and Problem Index, while 12.6% had IC based on responses to the PUF (Pelvic Pain and Urgency/Frequency Patient Symptom Scale) questionnaire. The authors concluded that "the true prevalence of IC in women may be somewhere between these two extremes," (J. Urol. 2005;174:2231-4).
The feasibility of myofascial physical therapy (MPT) was evaluated by the same group of researchers in a pilot trial involving 44 men and women with urologic chronic pelvic pain syndrome, including IC. As in the current study, MPT consisted of connective tissue manipulation to all body wall tissues in the abdominal wall, thighs, back, and buttocks that clinically were found to contain connective tissue abnormalities or painful myofascial trigger points. Myofascial manipulation focused on trigger points and restrictive bands.
Patients also were assigned to 10 1-hour sessions of MPT or global massage therapy (GMT), and asked to rate their overall symptoms using the 7-point global response assessment (GRA), with 1 being "markedly worse" and 7 being "markedly improved."
GRA rates were significantly higher at 57% with MPT vs. 21% with massage therapy (J. Urol. 2009;182:570-80). Subgroup analyses revealed a striking difference in the response to standard massage therapy between the all-male patients with chronic pelvic pain syndrome (CPPS) and women with IC (40% vs. 7%), suggesting that patients with CPPS or men respond differently to massage therapy.
The pilot study was the first and only positive trial in 10 years of research in urologic CPPS funded by the National Institute of Diabetes and Digestive and Kidney Diseases, Ms. Kotarinos said.
The current trial was conducted at 11 centers in the United States and Canada, and included 81 women with IC for less than 3 years who had moderate to severe pelvic pain (95%) or moderate to severe urgency (93%). Their mean age was 43 years; 84% were white, 5% were black, and ethnicity for the remaining 11% was not provided.
The secondary end points did not confirm the primary results, Ms. Kotarinos said. The MPT arm had greater mean changes in symptom scores than did the GMT arm on the Interstitial Cystitis Symptom Index (-3.2 vs. -2.2), Interstitial Cystitis Problem Index (-3.6 vs. -2.4), Likert Pain scale (-2.2 vs. -1.5), and Likert Urge Scale (-2.1 vs. -1.4), but the differences did not reach statistical significance.
In all, 85% of patients in both arms completed therapy, which was well tolerated, she said. This is important as myofascial PT can be painful or seen as unduly invasive. Adverse events of any kind were reported in 64% of the MPT group and 60% of the GMT group, and serious adverse events in 15% vs. 14%, respectively. Serious adverse events among MPT patients included four cases of pain and one case each of dehydration, vomiting, and other genitourinary symptoms.
Ms. Kotarinos pointed out that the study included a small group of highly select patients, and that blinding was ineffective, as nearly all patients correctly guessed their treatment arm.
She suggests that future research is warranted to investigate the lack of response in secondary outcomes and to define the role of MPT in the broader IC population, the optimal patient selection criteria, and optimal treatment parameters.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Ms. Kotarinos disclosed no conflicts of interest.
FROM THE ANNUAL MEETING OF THE INTERNATIONAL PELVIC PAIN SOCIETY
Myofascial Physical Therapy Appears Beneficial in Patients With Interstitial Cystitis
CHICAGO – Results of a second randomized trial confirm that significantly more women with interstitial cystitis respond to myofascial physical therapy than traditional massage therapy.
Among 81 women with interstitial cystitis and moderate to severe pain or urgency, global response assessment (GRA) rates at 12 weeks were 59% with myofascial physical therapy versus 26% with global massage therapy consisting of full-body Western massage.
This is the second positive randomized controlled trial for a disorder in desperate need of new treatment options, Rhonda Kotarinos, a physical therapist in Oakbrook Terrace, Ill., said at the annual meeting of the International Pelvic Pain Society.
There is no cure for interstitial cystitis (IC), also referred to as painful bladder syndrome. Treatments include eliminating dietary triggers and reproductive organ triggers, anesthetic instillations, physical therapy, and use of pain medications such as opioids, nonsteroidal anti-inflammatory agents, and tricyclic antidepressants.
The prevalence of IC also varies greatly. A widely cited study reports that 1.1% of 1,218 women presenting for a routine primary care office visit had IC based on the O’Leary-Sant Interstitial Cystitis Symptom and Problem Index, while 12.6% had IC based on responses to the PUF (Pelvic Pain and Urgency/Frequency Patient Symptom Scale) questionnaire. The authors concluded that "the true prevalence of IC in women may be somewhere between these two extremes," (J. Urol. 2005;174:2231-4).
The feasibility of myofascial physical therapy (MPT) was evaluated by the same group of researchers in a pilot trial involving 44 men and women with urologic chronic pelvic pain syndrome, including IC. As in the current study, MPT consisted of connective tissue manipulation to all body wall tissues in the abdominal wall, thighs, back, and buttocks that clinically were found to contain connective tissue abnormalities or painful myofascial trigger points. Myofascial manipulation focused on trigger points and restrictive bands.
Patients also were assigned to 10 1-hour sessions of MPT or global massage therapy (GMT), and asked to rate their overall symptoms using the 7-point global response assessment (GRA), with 1 being "markedly worse" and 7 being "markedly improved."
GRA rates were significantly higher at 57% with MPT vs. 21% with massage therapy (J. Urol. 2009;182:570-80). Subgroup analyses revealed a striking difference in the response to standard massage therapy between the all-male patients with chronic pelvic pain syndrome (CPPS) and women with IC (40% vs. 7%), suggesting that patients with CPPS or men respond differently to massage therapy.
The pilot study was the first and only positive trial in 10 years of research in urologic CPPS funded by the National Institute of Diabetes and Digestive and Kidney Diseases, Ms. Kotarinos said.
The current trial was conducted at 11 centers in the United States and Canada, and included 81 women with IC for less than 3 years who had moderate to severe pelvic pain (95%) or moderate to severe urgency (93%). Their mean age was 43 years; 84% were white, 5% were black, and ethnicity for the remaining 11% was not provided.
The secondary end points did not confirm the primary results, Ms. Kotarinos said. The MPT arm had greater mean changes in symptom scores than did the GMT arm on the Interstitial Cystitis Symptom Index (-3.2 vs. -2.2), Interstitial Cystitis Problem Index (-3.6 vs. -2.4), Likert Pain scale (-2.2 vs. -1.5), and Likert Urge Scale (-2.1 vs. -1.4), but the differences did not reach statistical significance.
In all, 85% of patients in both arms completed therapy, which was well tolerated, she said. This is important as myofascial PT can be painful or seen as unduly invasive. Adverse events of any kind were reported in 64% of the MPT group and 60% of the GMT group, and serious adverse events in 15% vs. 14%, respectively. Serious adverse events among MPT patients included four cases of pain and one case each of dehydration, vomiting, and other genitourinary symptoms.
Ms. Kotarinos pointed out that the study included a small group of highly select patients, and that blinding was ineffective, as nearly all patients correctly guessed their treatment arm.
She suggests that future research is warranted to investigate the lack of response in secondary outcomes and to define the role of MPT in the broader IC population, the optimal patient selection criteria, and optimal treatment parameters.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Ms. Kotarinos disclosed no conflicts of interest.
CHICAGO – Results of a second randomized trial confirm that significantly more women with interstitial cystitis respond to myofascial physical therapy than traditional massage therapy.
Among 81 women with interstitial cystitis and moderate to severe pain or urgency, global response assessment (GRA) rates at 12 weeks were 59% with myofascial physical therapy versus 26% with global massage therapy consisting of full-body Western massage.
This is the second positive randomized controlled trial for a disorder in desperate need of new treatment options, Rhonda Kotarinos, a physical therapist in Oakbrook Terrace, Ill., said at the annual meeting of the International Pelvic Pain Society.
There is no cure for interstitial cystitis (IC), also referred to as painful bladder syndrome. Treatments include eliminating dietary triggers and reproductive organ triggers, anesthetic instillations, physical therapy, and use of pain medications such as opioids, nonsteroidal anti-inflammatory agents, and tricyclic antidepressants.
The prevalence of IC also varies greatly. A widely cited study reports that 1.1% of 1,218 women presenting for a routine primary care office visit had IC based on the O’Leary-Sant Interstitial Cystitis Symptom and Problem Index, while 12.6% had IC based on responses to the PUF (Pelvic Pain and Urgency/Frequency Patient Symptom Scale) questionnaire. The authors concluded that "the true prevalence of IC in women may be somewhere between these two extremes," (J. Urol. 2005;174:2231-4).
The feasibility of myofascial physical therapy (MPT) was evaluated by the same group of researchers in a pilot trial involving 44 men and women with urologic chronic pelvic pain syndrome, including IC. As in the current study, MPT consisted of connective tissue manipulation to all body wall tissues in the abdominal wall, thighs, back, and buttocks that clinically were found to contain connective tissue abnormalities or painful myofascial trigger points. Myofascial manipulation focused on trigger points and restrictive bands.
Patients also were assigned to 10 1-hour sessions of MPT or global massage therapy (GMT), and asked to rate their overall symptoms using the 7-point global response assessment (GRA), with 1 being "markedly worse" and 7 being "markedly improved."
GRA rates were significantly higher at 57% with MPT vs. 21% with massage therapy (J. Urol. 2009;182:570-80). Subgroup analyses revealed a striking difference in the response to standard massage therapy between the all-male patients with chronic pelvic pain syndrome (CPPS) and women with IC (40% vs. 7%), suggesting that patients with CPPS or men respond differently to massage therapy.
The pilot study was the first and only positive trial in 10 years of research in urologic CPPS funded by the National Institute of Diabetes and Digestive and Kidney Diseases, Ms. Kotarinos said.
The current trial was conducted at 11 centers in the United States and Canada, and included 81 women with IC for less than 3 years who had moderate to severe pelvic pain (95%) or moderate to severe urgency (93%). Their mean age was 43 years; 84% were white, 5% were black, and ethnicity for the remaining 11% was not provided.
The secondary end points did not confirm the primary results, Ms. Kotarinos said. The MPT arm had greater mean changes in symptom scores than did the GMT arm on the Interstitial Cystitis Symptom Index (-3.2 vs. -2.2), Interstitial Cystitis Problem Index (-3.6 vs. -2.4), Likert Pain scale (-2.2 vs. -1.5), and Likert Urge Scale (-2.1 vs. -1.4), but the differences did not reach statistical significance.
In all, 85% of patients in both arms completed therapy, which was well tolerated, she said. This is important as myofascial PT can be painful or seen as unduly invasive. Adverse events of any kind were reported in 64% of the MPT group and 60% of the GMT group, and serious adverse events in 15% vs. 14%, respectively. Serious adverse events among MPT patients included four cases of pain and one case each of dehydration, vomiting, and other genitourinary symptoms.
Ms. Kotarinos pointed out that the study included a small group of highly select patients, and that blinding was ineffective, as nearly all patients correctly guessed their treatment arm.
She suggests that future research is warranted to investigate the lack of response in secondary outcomes and to define the role of MPT in the broader IC population, the optimal patient selection criteria, and optimal treatment parameters.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Ms. Kotarinos disclosed no conflicts of interest.
CHICAGO – Results of a second randomized trial confirm that significantly more women with interstitial cystitis respond to myofascial physical therapy than traditional massage therapy.
Among 81 women with interstitial cystitis and moderate to severe pain or urgency, global response assessment (GRA) rates at 12 weeks were 59% with myofascial physical therapy versus 26% with global massage therapy consisting of full-body Western massage.
This is the second positive randomized controlled trial for a disorder in desperate need of new treatment options, Rhonda Kotarinos, a physical therapist in Oakbrook Terrace, Ill., said at the annual meeting of the International Pelvic Pain Society.
There is no cure for interstitial cystitis (IC), also referred to as painful bladder syndrome. Treatments include eliminating dietary triggers and reproductive organ triggers, anesthetic instillations, physical therapy, and use of pain medications such as opioids, nonsteroidal anti-inflammatory agents, and tricyclic antidepressants.
The prevalence of IC also varies greatly. A widely cited study reports that 1.1% of 1,218 women presenting for a routine primary care office visit had IC based on the O’Leary-Sant Interstitial Cystitis Symptom and Problem Index, while 12.6% had IC based on responses to the PUF (Pelvic Pain and Urgency/Frequency Patient Symptom Scale) questionnaire. The authors concluded that "the true prevalence of IC in women may be somewhere between these two extremes," (J. Urol. 2005;174:2231-4).
The feasibility of myofascial physical therapy (MPT) was evaluated by the same group of researchers in a pilot trial involving 44 men and women with urologic chronic pelvic pain syndrome, including IC. As in the current study, MPT consisted of connective tissue manipulation to all body wall tissues in the abdominal wall, thighs, back, and buttocks that clinically were found to contain connective tissue abnormalities or painful myofascial trigger points. Myofascial manipulation focused on trigger points and restrictive bands.
Patients also were assigned to 10 1-hour sessions of MPT or global massage therapy (GMT), and asked to rate their overall symptoms using the 7-point global response assessment (GRA), with 1 being "markedly worse" and 7 being "markedly improved."
GRA rates were significantly higher at 57% with MPT vs. 21% with massage therapy (J. Urol. 2009;182:570-80). Subgroup analyses revealed a striking difference in the response to standard massage therapy between the all-male patients with chronic pelvic pain syndrome (CPPS) and women with IC (40% vs. 7%), suggesting that patients with CPPS or men respond differently to massage therapy.
The pilot study was the first and only positive trial in 10 years of research in urologic CPPS funded by the National Institute of Diabetes and Digestive and Kidney Diseases, Ms. Kotarinos said.
The current trial was conducted at 11 centers in the United States and Canada, and included 81 women with IC for less than 3 years who had moderate to severe pelvic pain (95%) or moderate to severe urgency (93%). Their mean age was 43 years; 84% were white, 5% were black, and ethnicity for the remaining 11% was not provided.
The secondary end points did not confirm the primary results, Ms. Kotarinos said. The MPT arm had greater mean changes in symptom scores than did the GMT arm on the Interstitial Cystitis Symptom Index (-3.2 vs. -2.2), Interstitial Cystitis Problem Index (-3.6 vs. -2.4), Likert Pain scale (-2.2 vs. -1.5), and Likert Urge Scale (-2.1 vs. -1.4), but the differences did not reach statistical significance.
In all, 85% of patients in both arms completed therapy, which was well tolerated, she said. This is important as myofascial PT can be painful or seen as unduly invasive. Adverse events of any kind were reported in 64% of the MPT group and 60% of the GMT group, and serious adverse events in 15% vs. 14%, respectively. Serious adverse events among MPT patients included four cases of pain and one case each of dehydration, vomiting, and other genitourinary symptoms.
Ms. Kotarinos pointed out that the study included a small group of highly select patients, and that blinding was ineffective, as nearly all patients correctly guessed their treatment arm.
She suggests that future research is warranted to investigate the lack of response in secondary outcomes and to define the role of MPT in the broader IC population, the optimal patient selection criteria, and optimal treatment parameters.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Ms. Kotarinos disclosed no conflicts of interest.
FROM THE ANNUAL MEETING OF THE INTERNATIONAL PELVIC PAIN SOCIETY
Major Finding: At 12 weeks, global response assessment rates were 59% with myofascial physical therapy vs. 26% with global massage therapy consisting of full-body Western massage.
Data Source: Randomized trial conducted at 11 centers in the United States and Canada in 81 women with interstitial cystitis.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Ms. Kotarinos disclosed no conflicts of interest.
Sunscreens May Help--Or Hurt
Sunscreens are an important part of a dermatologist’s tool kit, but they’re not a panacea for UV-induced damage, according to Dr. Timothy Berger.
Although sunscreens work well in laboratory testing, almost no one applies them in a way that will provide the advertised UV protection, Dr. Berger noted at the seminar sponsored by Skin Disease Education Foundation (SDEF). And for some patients, sunscreens can exacerbate their UV-induced problems.
Sunscreens themselves, not the vehicular preservatives, are usually the culprit when a patient presents with a complaint of being allergic to sunscreens, said Dr. Berger, a professor of dermatology at the University of California, San Francisco.
"You will usually find that the dermatitis only occurs in areas touched by the sun," he said in an interview. "The problem is often an allergy to the PABA or PABA-related substances in the sunscreen they are using."
For patients like this, the best alternative is a PABA-free sunscreen that contains zinc and titanium oxide – inert compounds that are physical barriers against UV light, rather than chemical barriers.
And although SPF ratings might look great in advertisements, it is almost a sure bet that sun-seeking patients are not getting nearly the protection promised, Dr. Berger noted. "Some interesting recent studies have looked at what SPF you actually get what you put on sunscreen. The amount used in testing is actually about four times more than what people really use."
One study found that most people apply about 0.5 mg/cm2, while the lab tests use a volume of 2 mg/cm2 to achieve the advertised SPF (J. Am. Acad. Dermatol. 2010;62:218-22). "The problem is, efficacy falls off in a very sharp way," Dr. Berger said. "If you apply SPF 30 sun block [at one-quarter the recommended amount], you only end up with an actual SPF of about 3."
"We need to make sure our patients understand this. And while most people are still not going to use the necessary amount, we can stress the importance of reapplying frequently, which can help keep the protective value up somewhat," he said.
Light Therapy for Atopy
UV light therapy is a frequent treatment for eczema and other atopic dermatoses, but for about 3% of patients, it the wrong thing to offer, Dr. Berger said. "For this small population, sun exposure actually makes the condition worse. Put them in the light box and the eczema will flare."
More than a cursory skin exam should be performed on patients with atopic dermatitis, he recommended. "Have them remove their clothing at least from the waist up. Look for eczema that has a photo distribution: It might be worse on the face and side of the neck, but beneath the chin the skin could be spared. If it looks like a photo-distributed rash, and they report a history of flare with sun exposure, then prescribing aggressive sun protection might make a big difference."
A frequently missed diagnosis in young children – particularly infants – is erythropoietic protoporphyria (EPP). "The first time these infants go out into the sun, they will start screaming, because their skin is burning," Dr. Berger said. As quickly as 1 hour after sun exposure, they may develop erythema, edema, urticarial lesions, or purpura on exposed skin.
Europeans are somewhat ahead in drug research for treating EPP, Dr. Berger noted, but the United States is catching up. The University of California is one of six U.S. study sites participating in a phase II placebo-controlled trial of afamelanotide, a synthetically produced analog of human alpha-melanocytic–stimulating hormone (alpha-MSH).
"The hope is that the drug will stimulate the production of melanin, which actually has two benefits," Dr. Berger said. "First, it’s a photo protectant, but it’s also an antioxidant."
When porphyrins absorb UV rays, they release free radicals that lead to the acute and chronic damage that occurs on EPP patient skin. The porphyrins can accumulate and damage other tissues – including the liver, which causes problems for about 20% of EPP patients. The extra melanin can help neutralize these highly reactive oxygen species and provide protection from the acute symptoms patients suffer when skin is exposed.
While afamelanotide can never cure EPP, Dr. Berger said, it might afford patients the opportunity to live a more normal life. "While they will never be going out looking for a tan, at least they may be able to enjoy being outdoors without having to be completely encased in clothing."
Dr. Berger disclosed serving as a consultant for Prescription Solutions. SDEF and this news organization are owned by Elsevier.
Sunscreens are an important part of a dermatologist’s tool kit, but they’re not a panacea for UV-induced damage, according to Dr. Timothy Berger.
Although sunscreens work well in laboratory testing, almost no one applies them in a way that will provide the advertised UV protection, Dr. Berger noted at the seminar sponsored by Skin Disease Education Foundation (SDEF). And for some patients, sunscreens can exacerbate their UV-induced problems.
Sunscreens themselves, not the vehicular preservatives, are usually the culprit when a patient presents with a complaint of being allergic to sunscreens, said Dr. Berger, a professor of dermatology at the University of California, San Francisco.
"You will usually find that the dermatitis only occurs in areas touched by the sun," he said in an interview. "The problem is often an allergy to the PABA or PABA-related substances in the sunscreen they are using."
For patients like this, the best alternative is a PABA-free sunscreen that contains zinc and titanium oxide – inert compounds that are physical barriers against UV light, rather than chemical barriers.
And although SPF ratings might look great in advertisements, it is almost a sure bet that sun-seeking patients are not getting nearly the protection promised, Dr. Berger noted. "Some interesting recent studies have looked at what SPF you actually get what you put on sunscreen. The amount used in testing is actually about four times more than what people really use."
One study found that most people apply about 0.5 mg/cm2, while the lab tests use a volume of 2 mg/cm2 to achieve the advertised SPF (J. Am. Acad. Dermatol. 2010;62:218-22). "The problem is, efficacy falls off in a very sharp way," Dr. Berger said. "If you apply SPF 30 sun block [at one-quarter the recommended amount], you only end up with an actual SPF of about 3."
"We need to make sure our patients understand this. And while most people are still not going to use the necessary amount, we can stress the importance of reapplying frequently, which can help keep the protective value up somewhat," he said.
Light Therapy for Atopy
UV light therapy is a frequent treatment for eczema and other atopic dermatoses, but for about 3% of patients, it the wrong thing to offer, Dr. Berger said. "For this small population, sun exposure actually makes the condition worse. Put them in the light box and the eczema will flare."
More than a cursory skin exam should be performed on patients with atopic dermatitis, he recommended. "Have them remove their clothing at least from the waist up. Look for eczema that has a photo distribution: It might be worse on the face and side of the neck, but beneath the chin the skin could be spared. If it looks like a photo-distributed rash, and they report a history of flare with sun exposure, then prescribing aggressive sun protection might make a big difference."
A frequently missed diagnosis in young children – particularly infants – is erythropoietic protoporphyria (EPP). "The first time these infants go out into the sun, they will start screaming, because their skin is burning," Dr. Berger said. As quickly as 1 hour after sun exposure, they may develop erythema, edema, urticarial lesions, or purpura on exposed skin.
Europeans are somewhat ahead in drug research for treating EPP, Dr. Berger noted, but the United States is catching up. The University of California is one of six U.S. study sites participating in a phase II placebo-controlled trial of afamelanotide, a synthetically produced analog of human alpha-melanocytic–stimulating hormone (alpha-MSH).
"The hope is that the drug will stimulate the production of melanin, which actually has two benefits," Dr. Berger said. "First, it’s a photo protectant, but it’s also an antioxidant."
When porphyrins absorb UV rays, they release free radicals that lead to the acute and chronic damage that occurs on EPP patient skin. The porphyrins can accumulate and damage other tissues – including the liver, which causes problems for about 20% of EPP patients. The extra melanin can help neutralize these highly reactive oxygen species and provide protection from the acute symptoms patients suffer when skin is exposed.
While afamelanotide can never cure EPP, Dr. Berger said, it might afford patients the opportunity to live a more normal life. "While they will never be going out looking for a tan, at least they may be able to enjoy being outdoors without having to be completely encased in clothing."
Dr. Berger disclosed serving as a consultant for Prescription Solutions. SDEF and this news organization are owned by Elsevier.
Sunscreens are an important part of a dermatologist’s tool kit, but they’re not a panacea for UV-induced damage, according to Dr. Timothy Berger.
Although sunscreens work well in laboratory testing, almost no one applies them in a way that will provide the advertised UV protection, Dr. Berger noted at the seminar sponsored by Skin Disease Education Foundation (SDEF). And for some patients, sunscreens can exacerbate their UV-induced problems.
Sunscreens themselves, not the vehicular preservatives, are usually the culprit when a patient presents with a complaint of being allergic to sunscreens, said Dr. Berger, a professor of dermatology at the University of California, San Francisco.
"You will usually find that the dermatitis only occurs in areas touched by the sun," he said in an interview. "The problem is often an allergy to the PABA or PABA-related substances in the sunscreen they are using."
For patients like this, the best alternative is a PABA-free sunscreen that contains zinc and titanium oxide – inert compounds that are physical barriers against UV light, rather than chemical barriers.
And although SPF ratings might look great in advertisements, it is almost a sure bet that sun-seeking patients are not getting nearly the protection promised, Dr. Berger noted. "Some interesting recent studies have looked at what SPF you actually get what you put on sunscreen. The amount used in testing is actually about four times more than what people really use."
One study found that most people apply about 0.5 mg/cm2, while the lab tests use a volume of 2 mg/cm2 to achieve the advertised SPF (J. Am. Acad. Dermatol. 2010;62:218-22). "The problem is, efficacy falls off in a very sharp way," Dr. Berger said. "If you apply SPF 30 sun block [at one-quarter the recommended amount], you only end up with an actual SPF of about 3."
"We need to make sure our patients understand this. And while most people are still not going to use the necessary amount, we can stress the importance of reapplying frequently, which can help keep the protective value up somewhat," he said.
Light Therapy for Atopy
UV light therapy is a frequent treatment for eczema and other atopic dermatoses, but for about 3% of patients, it the wrong thing to offer, Dr. Berger said. "For this small population, sun exposure actually makes the condition worse. Put them in the light box and the eczema will flare."
More than a cursory skin exam should be performed on patients with atopic dermatitis, he recommended. "Have them remove their clothing at least from the waist up. Look for eczema that has a photo distribution: It might be worse on the face and side of the neck, but beneath the chin the skin could be spared. If it looks like a photo-distributed rash, and they report a history of flare with sun exposure, then prescribing aggressive sun protection might make a big difference."
A frequently missed diagnosis in young children – particularly infants – is erythropoietic protoporphyria (EPP). "The first time these infants go out into the sun, they will start screaming, because their skin is burning," Dr. Berger said. As quickly as 1 hour after sun exposure, they may develop erythema, edema, urticarial lesions, or purpura on exposed skin.
Europeans are somewhat ahead in drug research for treating EPP, Dr. Berger noted, but the United States is catching up. The University of California is one of six U.S. study sites participating in a phase II placebo-controlled trial of afamelanotide, a synthetically produced analog of human alpha-melanocytic–stimulating hormone (alpha-MSH).
"The hope is that the drug will stimulate the production of melanin, which actually has two benefits," Dr. Berger said. "First, it’s a photo protectant, but it’s also an antioxidant."
When porphyrins absorb UV rays, they release free radicals that lead to the acute and chronic damage that occurs on EPP patient skin. The porphyrins can accumulate and damage other tissues – including the liver, which causes problems for about 20% of EPP patients. The extra melanin can help neutralize these highly reactive oxygen species and provide protection from the acute symptoms patients suffer when skin is exposed.
While afamelanotide can never cure EPP, Dr. Berger said, it might afford patients the opportunity to live a more normal life. "While they will never be going out looking for a tan, at least they may be able to enjoy being outdoors without having to be completely encased in clothing."
Dr. Berger disclosed serving as a consultant for Prescription Solutions. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE SDEF LAS VEGAS DERMATOLOGY SEMINAR
Sexual Function Improves With Successful Stress Incontinence Treatment
LONG BEACH, CALIF. – Women with urinary incontinence who were successfully treated nonsurgically showed significantly greater improvement in sexual function than women whose incontinence did not improve, a study has shown.
Three months after treatment with behavioral therapy, a continence pessary, or both, women whose treatment was successful had a 2.3-point mean improvement in their score on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Women whose incontinence treatment was not successful had a 0.5-point mean improvement on the PISQ-12. The difference was statistically significant, said Dr. Victoria L. Handa of Johns Hopkins University, Baltimore.
Dr. Handa’s study was a planned, prospective secondary analysis of results from the Ambulatory Treatments for Leakage Associated With Stress (ATLAS) trial. That trial involved 445 women with stress urinary incontinence (SUI) or mixed incontinence in which SUI predominated. The women were randomized to receive behavioral therapy, consisting mostly of pelvic muscle training; a continence pessary; or both. The women were a mean of 50 years old, and about 46% had SUI only.
At baseline, women with mixed incontinence scored significantly worse on the PISQ-12 than those with SUI. In particular, they were more likely to report urinary incontinence with sexual activity, and to say that they restricted their sexual activity because of fears of incontinence.
After 3 months of follow-up, there were no significant differences among the three treatment groups on any measure of sexual function.
"I think there is this perception that Kegel exercises are good for sexual function, but in a separate analysis, we didn’t see any association between improvement in pelvic muscle function as measured by Brink score and any measure of sexual function," Dr. Handa said at the annual meeting of the American Urogynecologic Society.
In addition to showing significant improvements in total PISQ-12 scores, women who were successfully treated had significant improvements in two specific symptoms. They were less likely to report urinary incontinence with sexual activity, and less likely to say that they restricted their sexual activity because of fears of incontinence.
The National Institute of Child Health and Human Development sponsored the trial. Dr. Handa said she had no financial disclosures.
Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire, PISQ-12, Dr. Victoria L. Handa, Johns Hopkins University, Ambulatory Treatments for Leakage Associated With Stress trial, ATLAS, stress urinary incontinence, SUI, mixed incontinence
LONG BEACH, CALIF. – Women with urinary incontinence who were successfully treated nonsurgically showed significantly greater improvement in sexual function than women whose incontinence did not improve, a study has shown.
Three months after treatment with behavioral therapy, a continence pessary, or both, women whose treatment was successful had a 2.3-point mean improvement in their score on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Women whose incontinence treatment was not successful had a 0.5-point mean improvement on the PISQ-12. The difference was statistically significant, said Dr. Victoria L. Handa of Johns Hopkins University, Baltimore.
Dr. Handa’s study was a planned, prospective secondary analysis of results from the Ambulatory Treatments for Leakage Associated With Stress (ATLAS) trial. That trial involved 445 women with stress urinary incontinence (SUI) or mixed incontinence in which SUI predominated. The women were randomized to receive behavioral therapy, consisting mostly of pelvic muscle training; a continence pessary; or both. The women were a mean of 50 years old, and about 46% had SUI only.
At baseline, women with mixed incontinence scored significantly worse on the PISQ-12 than those with SUI. In particular, they were more likely to report urinary incontinence with sexual activity, and to say that they restricted their sexual activity because of fears of incontinence.
After 3 months of follow-up, there were no significant differences among the three treatment groups on any measure of sexual function.
"I think there is this perception that Kegel exercises are good for sexual function, but in a separate analysis, we didn’t see any association between improvement in pelvic muscle function as measured by Brink score and any measure of sexual function," Dr. Handa said at the annual meeting of the American Urogynecologic Society.
In addition to showing significant improvements in total PISQ-12 scores, women who were successfully treated had significant improvements in two specific symptoms. They were less likely to report urinary incontinence with sexual activity, and less likely to say that they restricted their sexual activity because of fears of incontinence.
The National Institute of Child Health and Human Development sponsored the trial. Dr. Handa said she had no financial disclosures.
LONG BEACH, CALIF. – Women with urinary incontinence who were successfully treated nonsurgically showed significantly greater improvement in sexual function than women whose incontinence did not improve, a study has shown.
Three months after treatment with behavioral therapy, a continence pessary, or both, women whose treatment was successful had a 2.3-point mean improvement in their score on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Women whose incontinence treatment was not successful had a 0.5-point mean improvement on the PISQ-12. The difference was statistically significant, said Dr. Victoria L. Handa of Johns Hopkins University, Baltimore.
Dr. Handa’s study was a planned, prospective secondary analysis of results from the Ambulatory Treatments for Leakage Associated With Stress (ATLAS) trial. That trial involved 445 women with stress urinary incontinence (SUI) or mixed incontinence in which SUI predominated. The women were randomized to receive behavioral therapy, consisting mostly of pelvic muscle training; a continence pessary; or both. The women were a mean of 50 years old, and about 46% had SUI only.
At baseline, women with mixed incontinence scored significantly worse on the PISQ-12 than those with SUI. In particular, they were more likely to report urinary incontinence with sexual activity, and to say that they restricted their sexual activity because of fears of incontinence.
After 3 months of follow-up, there were no significant differences among the three treatment groups on any measure of sexual function.
"I think there is this perception that Kegel exercises are good for sexual function, but in a separate analysis, we didn’t see any association between improvement in pelvic muscle function as measured by Brink score and any measure of sexual function," Dr. Handa said at the annual meeting of the American Urogynecologic Society.
In addition to showing significant improvements in total PISQ-12 scores, women who were successfully treated had significant improvements in two specific symptoms. They were less likely to report urinary incontinence with sexual activity, and less likely to say that they restricted their sexual activity because of fears of incontinence.
The National Institute of Child Health and Human Development sponsored the trial. Dr. Handa said she had no financial disclosures.
Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire, PISQ-12, Dr. Victoria L. Handa, Johns Hopkins University, Ambulatory Treatments for Leakage Associated With Stress trial, ATLAS, stress urinary incontinence, SUI, mixed incontinence
Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire, PISQ-12, Dr. Victoria L. Handa, Johns Hopkins University, Ambulatory Treatments for Leakage Associated With Stress trial, ATLAS, stress urinary incontinence, SUI, mixed incontinence
FROM THE ANNUAL MEETING OF THE AMERICAN UROGYNECOLOGIC SOCIETY
Major Finding: Three months after successful nonsurgical treatment for stress incontinence, women had a 2.3-point mean improvement in scores on the PISQ-12, while women whose treatment was not successful had a 0.5-point improvement.
Data Source: Planned prospective supplementary study of 445 women with stress or mixed urinary incontinence participating in the ATLAS trial.
Disclosures: The National Institute of Child Health and Human Development sponsored the trial. Dr. Handa said she had no financial disclosures.