User login
Ultrasound, cystoscopy combo tops CT for asymptomatic microscopic hematuria
Combining renal ultrasound and bladder cystoscopy is the most cost-effective approach for the initial evaluation of asymptomatic microscopic hematuria, even among patients at risk for genitourinary malignancy, according to a report published online April 17 in JAMA Internal Medicine.
“The superiority of this approach over the use of CT plus cystoscopy is driven primarily by higher costs of CT and the associated complications, albeit rare,” said Joshua A. Halpern, MD, of the department of urology, CornellUniversity, New York, and his associates. “Given the low prevalence of upper-tract malignant abnormalities in patients with asymptomatic microscopic hematuria, the small advantage in the sensitivity of CT imaging does not compensate for the significant additional costs.”
Every year, hundreds of thousands of patients undergo urinalysis for a variety of indications, and an estimated 40% are found to have microscopic hematuria in the absence of any urinary symptoms. This finding requires further evaluation because of one particular possible cause: a genitourinary malignancy. An estimated 11% of people with asymptomatic microscopic hematuria are found to have malignant abnormalities, the investigators said.
They assessed the cost-effectiveness of four common follow-up evaluations by creating a decision-analysis model to simulate the rates of cancer detection in adults with no history of cancer and with negative urine cultures that ruled out UTI as the cause of the hematuria.
The model was based on data from real-world experience in the medical literature and incorporated information on cancer incidence, diagnostic test accuracy, and complications.
The four approaches they examined were CT plus cystoscopy, which is considered the preferred method of diagnostic work-up by the American Urological Association; renal ultrasound plus cystoscopy, which many clinicians in the United States and other countries use instead; cystoscopy alone; and CT alone.
Compared with no follow-up evaluation, CT alone detected the fewest cancers (221 per 10,000 patients) at the highest cost ($9,300,000 per 10,000 patients). Cystoscopy alone detected 222 cancers per 10,000 at a cost of $10,287 per 10,000. Ultrasound plus cystoscopy detected 23 additional cancers per 10,000 patients at a relatively low cost of $53,810 per 10,000. Replacing ultrasound with CT detected just one additional cancer but cost an additional $6,480,484 per 10,000 patients.
The findings were similar in several sensitivity analyses, as well as in a subgroup analysis involving only higher-risk patients – men, smokers, and patients aged 50 years and older, the investigators noted (JAMA Intern Med. 2017 Apr 17. doi: 10.1001/jamaintenmed.2017.0739).
Dr. Halpern and his associates also applied their results to nationwide 2012 statistics for 485,222 patient visits to urologists to assess microscopic hematuria. If all urologists complied with AUA guidelines and used CT instead of ultrasound plus cystoscopy to assess these patients, they would have detected only 60 additional cancers, at an additional cost of $389,914,648.
Given these findings, renal ultrasound plus bladder cystoscopy should be considered the first-line assessment for these patients, Dr. Halpern and his associates said. Rewriting practice guidelines accordingly “will substantially reduce national expenditures associated with asymptomatic microscopic hematuria evaluation by up to $390 million.”
Moreover, recommending ultrasound rather than CT might have the unintended but beneficial consequence of improving compliance with further evaluation, because many primary care physicians are reluctant to refer these patients for radiocontrast CT studies, the researchers noted.
No sponsor was cited for this study. Dr. Halpern and his associates reported having no relevant financial disclosures.
The substantial differences between ultrasound and CT in cost per cancer detected, combined with the harm from CT-related contrast reactions and radiation exposure, strongly support renal ultrasound plus cystoscopy as the preferred first-line approach to assessing asymptomatic microscopic hematuria.
According to Halpern et al., this approach would cost approximately $54,000 per cancer detected. Replacing ultrasound with CT would detect just 1 additional cancer per 10,000 assessments, at an incremental cost of $6.5 million.
Leslee L. Subak, MD, and Deborah Grady, MD, are in the departments of obstetrics, gynecology, and reproductive sciences; urology; and epidemiology and biostatistics at the University of California, San Francisco. Dr. Subak reported receiving funding from Astellas to research urinary incontinence. Dr. Subak and Dr. Grady made these remarks in an invited commentary accompanying Dr. Halpern’s report (JAMA Intern Med. 2017 Apr 17. doi: 10.1001/jamainternmed.2017.0758).
The substantial differences between ultrasound and CT in cost per cancer detected, combined with the harm from CT-related contrast reactions and radiation exposure, strongly support renal ultrasound plus cystoscopy as the preferred first-line approach to assessing asymptomatic microscopic hematuria.
According to Halpern et al., this approach would cost approximately $54,000 per cancer detected. Replacing ultrasound with CT would detect just 1 additional cancer per 10,000 assessments, at an incremental cost of $6.5 million.
Leslee L. Subak, MD, and Deborah Grady, MD, are in the departments of obstetrics, gynecology, and reproductive sciences; urology; and epidemiology and biostatistics at the University of California, San Francisco. Dr. Subak reported receiving funding from Astellas to research urinary incontinence. Dr. Subak and Dr. Grady made these remarks in an invited commentary accompanying Dr. Halpern’s report (JAMA Intern Med. 2017 Apr 17. doi: 10.1001/jamainternmed.2017.0758).
The substantial differences between ultrasound and CT in cost per cancer detected, combined with the harm from CT-related contrast reactions and radiation exposure, strongly support renal ultrasound plus cystoscopy as the preferred first-line approach to assessing asymptomatic microscopic hematuria.
According to Halpern et al., this approach would cost approximately $54,000 per cancer detected. Replacing ultrasound with CT would detect just 1 additional cancer per 10,000 assessments, at an incremental cost of $6.5 million.
Leslee L. Subak, MD, and Deborah Grady, MD, are in the departments of obstetrics, gynecology, and reproductive sciences; urology; and epidemiology and biostatistics at the University of California, San Francisco. Dr. Subak reported receiving funding from Astellas to research urinary incontinence. Dr. Subak and Dr. Grady made these remarks in an invited commentary accompanying Dr. Halpern’s report (JAMA Intern Med. 2017 Apr 17. doi: 10.1001/jamainternmed.2017.0758).
Combining renal ultrasound and bladder cystoscopy is the most cost-effective approach for the initial evaluation of asymptomatic microscopic hematuria, even among patients at risk for genitourinary malignancy, according to a report published online April 17 in JAMA Internal Medicine.
“The superiority of this approach over the use of CT plus cystoscopy is driven primarily by higher costs of CT and the associated complications, albeit rare,” said Joshua A. Halpern, MD, of the department of urology, CornellUniversity, New York, and his associates. “Given the low prevalence of upper-tract malignant abnormalities in patients with asymptomatic microscopic hematuria, the small advantage in the sensitivity of CT imaging does not compensate for the significant additional costs.”
Every year, hundreds of thousands of patients undergo urinalysis for a variety of indications, and an estimated 40% are found to have microscopic hematuria in the absence of any urinary symptoms. This finding requires further evaluation because of one particular possible cause: a genitourinary malignancy. An estimated 11% of people with asymptomatic microscopic hematuria are found to have malignant abnormalities, the investigators said.
They assessed the cost-effectiveness of four common follow-up evaluations by creating a decision-analysis model to simulate the rates of cancer detection in adults with no history of cancer and with negative urine cultures that ruled out UTI as the cause of the hematuria.
The model was based on data from real-world experience in the medical literature and incorporated information on cancer incidence, diagnostic test accuracy, and complications.
The four approaches they examined were CT plus cystoscopy, which is considered the preferred method of diagnostic work-up by the American Urological Association; renal ultrasound plus cystoscopy, which many clinicians in the United States and other countries use instead; cystoscopy alone; and CT alone.
Compared with no follow-up evaluation, CT alone detected the fewest cancers (221 per 10,000 patients) at the highest cost ($9,300,000 per 10,000 patients). Cystoscopy alone detected 222 cancers per 10,000 at a cost of $10,287 per 10,000. Ultrasound plus cystoscopy detected 23 additional cancers per 10,000 patients at a relatively low cost of $53,810 per 10,000. Replacing ultrasound with CT detected just one additional cancer but cost an additional $6,480,484 per 10,000 patients.
The findings were similar in several sensitivity analyses, as well as in a subgroup analysis involving only higher-risk patients – men, smokers, and patients aged 50 years and older, the investigators noted (JAMA Intern Med. 2017 Apr 17. doi: 10.1001/jamaintenmed.2017.0739).
Dr. Halpern and his associates also applied their results to nationwide 2012 statistics for 485,222 patient visits to urologists to assess microscopic hematuria. If all urologists complied with AUA guidelines and used CT instead of ultrasound plus cystoscopy to assess these patients, they would have detected only 60 additional cancers, at an additional cost of $389,914,648.
Given these findings, renal ultrasound plus bladder cystoscopy should be considered the first-line assessment for these patients, Dr. Halpern and his associates said. Rewriting practice guidelines accordingly “will substantially reduce national expenditures associated with asymptomatic microscopic hematuria evaluation by up to $390 million.”
Moreover, recommending ultrasound rather than CT might have the unintended but beneficial consequence of improving compliance with further evaluation, because many primary care physicians are reluctant to refer these patients for radiocontrast CT studies, the researchers noted.
No sponsor was cited for this study. Dr. Halpern and his associates reported having no relevant financial disclosures.
Combining renal ultrasound and bladder cystoscopy is the most cost-effective approach for the initial evaluation of asymptomatic microscopic hematuria, even among patients at risk for genitourinary malignancy, according to a report published online April 17 in JAMA Internal Medicine.
“The superiority of this approach over the use of CT plus cystoscopy is driven primarily by higher costs of CT and the associated complications, albeit rare,” said Joshua A. Halpern, MD, of the department of urology, CornellUniversity, New York, and his associates. “Given the low prevalence of upper-tract malignant abnormalities in patients with asymptomatic microscopic hematuria, the small advantage in the sensitivity of CT imaging does not compensate for the significant additional costs.”
Every year, hundreds of thousands of patients undergo urinalysis for a variety of indications, and an estimated 40% are found to have microscopic hematuria in the absence of any urinary symptoms. This finding requires further evaluation because of one particular possible cause: a genitourinary malignancy. An estimated 11% of people with asymptomatic microscopic hematuria are found to have malignant abnormalities, the investigators said.
They assessed the cost-effectiveness of four common follow-up evaluations by creating a decision-analysis model to simulate the rates of cancer detection in adults with no history of cancer and with negative urine cultures that ruled out UTI as the cause of the hematuria.
The model was based on data from real-world experience in the medical literature and incorporated information on cancer incidence, diagnostic test accuracy, and complications.
The four approaches they examined were CT plus cystoscopy, which is considered the preferred method of diagnostic work-up by the American Urological Association; renal ultrasound plus cystoscopy, which many clinicians in the United States and other countries use instead; cystoscopy alone; and CT alone.
Compared with no follow-up evaluation, CT alone detected the fewest cancers (221 per 10,000 patients) at the highest cost ($9,300,000 per 10,000 patients). Cystoscopy alone detected 222 cancers per 10,000 at a cost of $10,287 per 10,000. Ultrasound plus cystoscopy detected 23 additional cancers per 10,000 patients at a relatively low cost of $53,810 per 10,000. Replacing ultrasound with CT detected just one additional cancer but cost an additional $6,480,484 per 10,000 patients.
The findings were similar in several sensitivity analyses, as well as in a subgroup analysis involving only higher-risk patients – men, smokers, and patients aged 50 years and older, the investigators noted (JAMA Intern Med. 2017 Apr 17. doi: 10.1001/jamaintenmed.2017.0739).
Dr. Halpern and his associates also applied their results to nationwide 2012 statistics for 485,222 patient visits to urologists to assess microscopic hematuria. If all urologists complied with AUA guidelines and used CT instead of ultrasound plus cystoscopy to assess these patients, they would have detected only 60 additional cancers, at an additional cost of $389,914,648.
Given these findings, renal ultrasound plus bladder cystoscopy should be considered the first-line assessment for these patients, Dr. Halpern and his associates said. Rewriting practice guidelines accordingly “will substantially reduce national expenditures associated with asymptomatic microscopic hematuria evaluation by up to $390 million.”
Moreover, recommending ultrasound rather than CT might have the unintended but beneficial consequence of improving compliance with further evaluation, because many primary care physicians are reluctant to refer these patients for radiocontrast CT studies, the researchers noted.
No sponsor was cited for this study. Dr. Halpern and his associates reported having no relevant financial disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Combining renal ultrasound and bladder cystoscopy is the most cost-effective approach for the initial evaluation of asymptomatic microscopic hematuria.
Major finding: If all urologists complied with AUA guidelines and used CT instead of ultrasound plus cystoscopy to assess the 485,222 patients who were seen for asymptomatic microscopic hematuria in 2012, they would have detected only 60 additional cancers, at an additional cost of $389,914,648.
Data source: Decision-analysis modeling of four common approaches to assessing asymptomatic microscopic hematuria.
Disclosures: No sponsor was cited for this study. Dr. Halpern and his associates reported having no relevant financial disclosures.
When to Discontinue RAAS Therapy in CKD Patients
Q) A speaker at a meeting I attended said that ACEis/ARBs can be used in all stages of CKD. But locally, our nephrologists discontinue use when the GFR falls below 20 mL/min. Who is correct?
Definitive data on whether to continue use of ACE inhibitors (ACEis) and angiotensin-II receptor blockers (ARBs) in patients with chronic kidney disease (CKD) is lacking.¹ At this time, it is difficult to prove that the renoprotective effects of renin-angiotensin-aldosterone system (RAAS) inhibitors are separate from their antihypertensive effects. Few studies have investigated the effects of RAAS therapy on patients with advanced CKD at baseline (CKD stage 4 or 5; glomerular filtration rate [GFR], < 30 mL/min).2
ACEis and ARBs are indicated for use in CKD patients with hypertension, proteinuria/albuminuria, heart failure with reduced ejection fraction, and left ventricle dysfunction post–myocardial infarction.3 While these medications are the main pharmacologic therapy for reducing albuminuria in CKD patients, they increase serum creatinine by 20% to 30% and thereby decrease GFR.2,4
The decision to continue or discontinue ACEi/ARB use when patients reach CKD stage 4 or 5 is controversial. On one hand, risks associated with continuation include hyperkalemia, metabolic acidosis, and possible reduction in GFR. The decision to discontinue these medications may result in increased GFR, improved kidney function, and delayed onset of kidney failure or need for dialysis.3,4 In a 2011 study examining outcomes in patients with stage 4 CKD two years after stopping their ACEis/ARBs, the researchers found that patients who were alive without renal replacement therapy were hypertensive but had the highest GFRs.3
On the other hand, ACEis/ARBs have been shown to reduce incidence of cardiovascular disease (CVD) in patients without CKD. It is widely known that patients with CKD have increased risk for CVD, though there is little data examining the effects of RAAS inhibitors on CVD in this population.¹ A recent study found a reduced risk for fatal CVD in peritoneal dialysis patients treated with ACEis.5 Another study reported improved renal outcomes in nondiabetic patients with advanced CKD who were treated with ACEis.6 The National Kidney Foundation/Kidney Disease Outcomes Quality Initiative Clinical Practice Guidelines on Hypertension currently state that with careful monitoring, most patients with advanced CKD can continue taking ACEis/ARBs.7
More studies are needed to confidently close this controversial debate. Fortunately, the STOP-ACEi study, a three-year trial that began in 2014 in the UK, is examining the effects of ACEi/ARB use in patients with advanced CKD. It aims to determine whether discontinuation of ACEis/ARBs in these patients can help to stabilize or improve renal function, compared to continued use. By maintaining good blood pressure control in these patients, the researchers hope to distinguish the antihypertensive effects from other potential benefits of the RAAS inhibitors.2 The results of this trial may provide additional clarity for making decisions about ACEi/ARB treatment in our patients with advanced CKD. —RVR, SMR
Rebecca V. Rokosky, MSN, APRN, FNP-BC
Sub Investigator in the Clinical Advancement Center, PPLC, San Antonio, Texas
Shannon M. Rice, MS, PA-C
Division of Nephrology and Hypertension, Department of Medicine, University of California, San Diego
1. Ahmed A, Jorna T, Bhandari S. Should we STOP angiotensin converting enzyme inhibitors/angiotensin receptor blockers in advanced kidney disease? Nephron. 2016; 133(3):147-158.
2. Bhandari S, Ives N, Brettell EA, et al. Multicentre randomized controlled trial of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker withdrawal in advanced renal disease: the STOP-ACEi trial. Nephrol Dial Transplant. 2016; 31(2):255-261.
3. Gonclaves A, Khwaja A, Ahmed A, et al. Stopping renin-angiotensin system inhibitors in chronic kidney disease: predictors of response. Nephron Clin Pract. 2011;119(4):348-354.
4. Zuber K, Gilmartin C, Davis J. Managing hypertension in patients with chronic kidney disease. JAAPA. 2014;27(9):37-46.
5. Shen JI, Saxena AB, Montez-Rath ME, et al. Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker use and cardiovascular outcomes in patients initiating peritoneal dialysis. Nephrol Dial Transplant. 2016 Apr 13. [Epub ahead of print]
6. Hou F, Zhang X, Zhang GH, et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med. 2006;354(2):131-140.
7. Kidney Disease Outcomes Quality Initiative (K/DOQI). K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1-S290.
Q) A speaker at a meeting I attended said that ACEis/ARBs can be used in all stages of CKD. But locally, our nephrologists discontinue use when the GFR falls below 20 mL/min. Who is correct?
Definitive data on whether to continue use of ACE inhibitors (ACEis) and angiotensin-II receptor blockers (ARBs) in patients with chronic kidney disease (CKD) is lacking.¹ At this time, it is difficult to prove that the renoprotective effects of renin-angiotensin-aldosterone system (RAAS) inhibitors are separate from their antihypertensive effects. Few studies have investigated the effects of RAAS therapy on patients with advanced CKD at baseline (CKD stage 4 or 5; glomerular filtration rate [GFR], < 30 mL/min).2
ACEis and ARBs are indicated for use in CKD patients with hypertension, proteinuria/albuminuria, heart failure with reduced ejection fraction, and left ventricle dysfunction post–myocardial infarction.3 While these medications are the main pharmacologic therapy for reducing albuminuria in CKD patients, they increase serum creatinine by 20% to 30% and thereby decrease GFR.2,4
The decision to continue or discontinue ACEi/ARB use when patients reach CKD stage 4 or 5 is controversial. On one hand, risks associated with continuation include hyperkalemia, metabolic acidosis, and possible reduction in GFR. The decision to discontinue these medications may result in increased GFR, improved kidney function, and delayed onset of kidney failure or need for dialysis.3,4 In a 2011 study examining outcomes in patients with stage 4 CKD two years after stopping their ACEis/ARBs, the researchers found that patients who were alive without renal replacement therapy were hypertensive but had the highest GFRs.3
On the other hand, ACEis/ARBs have been shown to reduce incidence of cardiovascular disease (CVD) in patients without CKD. It is widely known that patients with CKD have increased risk for CVD, though there is little data examining the effects of RAAS inhibitors on CVD in this population.¹ A recent study found a reduced risk for fatal CVD in peritoneal dialysis patients treated with ACEis.5 Another study reported improved renal outcomes in nondiabetic patients with advanced CKD who were treated with ACEis.6 The National Kidney Foundation/Kidney Disease Outcomes Quality Initiative Clinical Practice Guidelines on Hypertension currently state that with careful monitoring, most patients with advanced CKD can continue taking ACEis/ARBs.7
More studies are needed to confidently close this controversial debate. Fortunately, the STOP-ACEi study, a three-year trial that began in 2014 in the UK, is examining the effects of ACEi/ARB use in patients with advanced CKD. It aims to determine whether discontinuation of ACEis/ARBs in these patients can help to stabilize or improve renal function, compared to continued use. By maintaining good blood pressure control in these patients, the researchers hope to distinguish the antihypertensive effects from other potential benefits of the RAAS inhibitors.2 The results of this trial may provide additional clarity for making decisions about ACEi/ARB treatment in our patients with advanced CKD. —RVR, SMR
Rebecca V. Rokosky, MSN, APRN, FNP-BC
Sub Investigator in the Clinical Advancement Center, PPLC, San Antonio, Texas
Shannon M. Rice, MS, PA-C
Division of Nephrology and Hypertension, Department of Medicine, University of California, San Diego
Q) A speaker at a meeting I attended said that ACEis/ARBs can be used in all stages of CKD. But locally, our nephrologists discontinue use when the GFR falls below 20 mL/min. Who is correct?
Definitive data on whether to continue use of ACE inhibitors (ACEis) and angiotensin-II receptor blockers (ARBs) in patients with chronic kidney disease (CKD) is lacking.¹ At this time, it is difficult to prove that the renoprotective effects of renin-angiotensin-aldosterone system (RAAS) inhibitors are separate from their antihypertensive effects. Few studies have investigated the effects of RAAS therapy on patients with advanced CKD at baseline (CKD stage 4 or 5; glomerular filtration rate [GFR], < 30 mL/min).2
ACEis and ARBs are indicated for use in CKD patients with hypertension, proteinuria/albuminuria, heart failure with reduced ejection fraction, and left ventricle dysfunction post–myocardial infarction.3 While these medications are the main pharmacologic therapy for reducing albuminuria in CKD patients, they increase serum creatinine by 20% to 30% and thereby decrease GFR.2,4
The decision to continue or discontinue ACEi/ARB use when patients reach CKD stage 4 or 5 is controversial. On one hand, risks associated with continuation include hyperkalemia, metabolic acidosis, and possible reduction in GFR. The decision to discontinue these medications may result in increased GFR, improved kidney function, and delayed onset of kidney failure or need for dialysis.3,4 In a 2011 study examining outcomes in patients with stage 4 CKD two years after stopping their ACEis/ARBs, the researchers found that patients who were alive without renal replacement therapy were hypertensive but had the highest GFRs.3
On the other hand, ACEis/ARBs have been shown to reduce incidence of cardiovascular disease (CVD) in patients without CKD. It is widely known that patients with CKD have increased risk for CVD, though there is little data examining the effects of RAAS inhibitors on CVD in this population.¹ A recent study found a reduced risk for fatal CVD in peritoneal dialysis patients treated with ACEis.5 Another study reported improved renal outcomes in nondiabetic patients with advanced CKD who were treated with ACEis.6 The National Kidney Foundation/Kidney Disease Outcomes Quality Initiative Clinical Practice Guidelines on Hypertension currently state that with careful monitoring, most patients with advanced CKD can continue taking ACEis/ARBs.7
More studies are needed to confidently close this controversial debate. Fortunately, the STOP-ACEi study, a three-year trial that began in 2014 in the UK, is examining the effects of ACEi/ARB use in patients with advanced CKD. It aims to determine whether discontinuation of ACEis/ARBs in these patients can help to stabilize or improve renal function, compared to continued use. By maintaining good blood pressure control in these patients, the researchers hope to distinguish the antihypertensive effects from other potential benefits of the RAAS inhibitors.2 The results of this trial may provide additional clarity for making decisions about ACEi/ARB treatment in our patients with advanced CKD. —RVR, SMR
Rebecca V. Rokosky, MSN, APRN, FNP-BC
Sub Investigator in the Clinical Advancement Center, PPLC, San Antonio, Texas
Shannon M. Rice, MS, PA-C
Division of Nephrology and Hypertension, Department of Medicine, University of California, San Diego
1. Ahmed A, Jorna T, Bhandari S. Should we STOP angiotensin converting enzyme inhibitors/angiotensin receptor blockers in advanced kidney disease? Nephron. 2016; 133(3):147-158.
2. Bhandari S, Ives N, Brettell EA, et al. Multicentre randomized controlled trial of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker withdrawal in advanced renal disease: the STOP-ACEi trial. Nephrol Dial Transplant. 2016; 31(2):255-261.
3. Gonclaves A, Khwaja A, Ahmed A, et al. Stopping renin-angiotensin system inhibitors in chronic kidney disease: predictors of response. Nephron Clin Pract. 2011;119(4):348-354.
4. Zuber K, Gilmartin C, Davis J. Managing hypertension in patients with chronic kidney disease. JAAPA. 2014;27(9):37-46.
5. Shen JI, Saxena AB, Montez-Rath ME, et al. Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker use and cardiovascular outcomes in patients initiating peritoneal dialysis. Nephrol Dial Transplant. 2016 Apr 13. [Epub ahead of print]
6. Hou F, Zhang X, Zhang GH, et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med. 2006;354(2):131-140.
7. Kidney Disease Outcomes Quality Initiative (K/DOQI). K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1-S290.
1. Ahmed A, Jorna T, Bhandari S. Should we STOP angiotensin converting enzyme inhibitors/angiotensin receptor blockers in advanced kidney disease? Nephron. 2016; 133(3):147-158.
2. Bhandari S, Ives N, Brettell EA, et al. Multicentre randomized controlled trial of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker withdrawal in advanced renal disease: the STOP-ACEi trial. Nephrol Dial Transplant. 2016; 31(2):255-261.
3. Gonclaves A, Khwaja A, Ahmed A, et al. Stopping renin-angiotensin system inhibitors in chronic kidney disease: predictors of response. Nephron Clin Pract. 2011;119(4):348-354.
4. Zuber K, Gilmartin C, Davis J. Managing hypertension in patients with chronic kidney disease. JAAPA. 2014;27(9):37-46.
5. Shen JI, Saxena AB, Montez-Rath ME, et al. Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker use and cardiovascular outcomes in patients initiating peritoneal dialysis. Nephrol Dial Transplant. 2016 Apr 13. [Epub ahead of print]
6. Hou F, Zhang X, Zhang GH, et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med. 2006;354(2):131-140.
7. Kidney Disease Outcomes Quality Initiative (K/DOQI). K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 suppl 1):S1-S290.
New Drugs to Treat Hyperkalemia
Q)I have heard talk about the development of new drugs to treat hyperkalemia. What is the status of these?
Hyperkalemia is a commonly seen electrolyte imbalance in clinical practice. Risks associated with moderate-to-severe hyperkalemia include potentially fatal cardiac conduction abnormalities/arrhythmias, making identification and management critical. An in-depth discussion of hyperkalemia diagnosis can be found in our March 2017 CE/CME activity (2017;27[3]:40-49).
Risk factors for hyperkalemia include excess intake or supplementation of potassium, type 2 diabetes, liver cirrhosis, congestive heart failure (CHF), and chronic kidney disease (CKD). The kidneys excrete 90% to 95% of ingested potassium, and the gut excretes the rest. Normal kidneys take six to 12 hours to excrete an acute potassium load. As kidney function decreases, risk for hyperkalemia increases.1 Hyperkalemia rates as high as 26% have been observed in patients with CKD stages 3 to 5 (glomerular filtration rate [GFR], < 60 mL/min).2
Renin-angiotensin-aldosterone system (RAAS) inhibitors—including ACE inhibitors (ACEis), angiotensin-receptor blockers, and aldosterone agonists—are associated with hyperkalemia. While RAAS therapy can play an important role in the management of CKD and cardiovascular disease (CVD), the development of hyperkalemia can necessitate a dose reduction or discontinuation of these medications, limiting their therapeutic benefit. Other medications that elevate risk for hyperkalemia include NSAIDs, heparin, cyclosporine, amiloride, triamterene, and nonselective ß-blockers.1
Therapeutic options for nonurgent treatment of hyperkalemia are limited. In addition to reducing or discontinuing associated medications, strategies include use of diuretics (as appropriate), treatment of metabolic acidosis, and dietary restrictions (ie, limiting high-potassium foods).1 Pharmacologically, there has been one (less than ideal) option—until recently.
Sodium polystyrene sulfonate (SPS), an ion-exchange resin approved in 1958, can be used to treat hyperkalemia.3 It comes in an enema and an oral form; the former has a faster onset, but the latter is more effective, with an onset of action of one to two hours and a duration of four to six hours.1 However, each gram of SPS contains 100 g of sodium, and the typical dose of SPS is 15 g to 60 g.4 The resulting increase in sodium load can be a concern for patients with CHF, severe hypertension, or severe edema.5
Data from randomized controlled trials (RCTs) are limited; however, one double-blind RCT investigated the effect of SPS on 33 patients with CKD and mild-to-moderate hyperkalemia (potassium level, 5 mEq/L to 5.9 mEq/L). The researchers found that patients who took 30 g/d of SPS for seven days experienced a 73% reduction in serum potassium, compared with a 38% reduction in patients who took a placebo. Of note, more gastrointestinal issues were observed in the SPS group.6
Additionally, a retrospective chart review of 14 patients with CKD and heart disease found low-dose SPS to be safe and effective when used as a secondary measure for hyperkalemia prevention in those taking RAAS therapy.7 However, a systematic review found that SPS use with and without concurrent sorbitol may be associated with serious and fatal gastrointestinal injuries.8 In 2011, the FDA issued a black box warning regarding increased risk for intestinal necrosis when SPS is used with sorbitol.9 In 2015, the FDA recommended separating SPS from other oral medications by at least six hours, due to its potential to bind with other medications.10
Patiromer, a new potassium binder, was approved by the FDA in 2015. This sodium-free, nonabsorbed, spherical polymer uses calcium as the exchange cation to bind potassium in the gastrointestinal tract. Its onset of action is seven hours, with a 24-hour duration of action. It is not approved for emergency use. There are no renal dosing adjustment considerations with patiromer.
In RCTs, patiromer has been associated with a significant reduction in serum potassium in patients with CKD (with or without diabetes) taking RAAS therapy. The starting dose is 8.4 g/d mixed with water, taken with food; this can be increased by 8.4 g each week as needed, to a maximum dosage of 25.2 g/d. Patiromer binds between 8.5 mEq to 8.8 mEq of potassium per gram of polymer.
The original approval included a black box warning to take patiromer six hours before and after other medications, due to concern for binding with certain medications. However, after an additional study in 2016, the FDA removed this warning and approved a change in administration to three hours before and after taking other medications.
Use of patiromer is not advised in those with severe constipation, bowel obstruction/impaction, or allergies to any of its components.11 Adverse reactions associated with patiromer include constipation (which generally improves with time), hypomagnesemia, diarrhea, nausea, abdominal discomfort, and flatulence. A 52-week RCT of 304 patients with CKD on RAAS found the most common adverse event to be mild-to-moderate constipation (6.3% of patients), with two patients discontinuing therapy as a result.4 In clinical trials, 9% of patients developed hypomagnesemia (serum magnesium value, < 1.4 mg/dL). It is recommended that serum magnesium levels be monitored and supplementation offered, when appropriate.11
Sodium zirconium cyclosilicate (ZS-9) is among the potassium-lowering medications on the horizon. In 2016, the FDA accepted a new drug application for this insoluble, unabsorbed cation exchanger that also works in the GI tract and uses sodium and hydrogen as exchange cations.12
For now, however, dietary education remains a mainstay of treatment for patients with elevated serum potassium levels. It is particularly important to inform your patients that many salt substitutes and low-sodium products contain potassium chloride. They should therefore exercise caution when incorporating sodium-reducing components into their diet. —CS
Cynthia Smith, DNP, CNN-NP, APRN, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virginia
1. Gilbert S, Weiner D, Gipson D, eds; National Kidney Foundation. Primer on Kidney Diseases. 6th ed. Philadelphia, PA: Saunders Elsevier; 2014.
2. Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156-1162.
3. Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol: a preliminary report. N Engl J Med. 1961;264:111-115.
4. Dunn JD, Benton WW, Orozco-Torrentera E, Adamson RT. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 suppl): s307-s315.
5. Li L, Harrison SD, Cope MJ, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21(5):456-465.
6. Lepage L, Dufour AC, Doiron J, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015; 10(12):2136-2142.
7. Chernin G, Gal-Oz A, Ben-Assa E, et al. Secondary prevention of hyperkalemia with sodium polystyrene sulfonate in cardiac and kidney patients on renin-angiotensin-aldosterone system inhibition therapy. Clin Cardiol. 2012;35(1):32-36.
8. Harel Z, Harel S, Shah PS, et al. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126(3):264.e9-e24.
9. FDA. Safety warning: Kayexalate (sodium polystyrene sulfonate) powder. www.fda.gov/Safety/MedWatch/SafetyInformation/ucm186845.htm. Accessed February 15, 2017.
10. FDA. FDA drug safety communication: FDA required drug interaction studies with potassium-lowering drug Kayexalate (sodium polystyrene sulfonate). www.fda.gov/Drugs/DrugSafety/ucm468035.htm. Accessed March 1, 2017.
11. Veltassa® (patiromer) [package insert]. Redwood City, CA: Relypsa, Inc; 2016. www.veltassa.com/pi.pdf. Accessed March 1, 2017.
12. AstraZeneca. FDA accepts for review New Drug Application for sodium zirconium cyclosilicate (ZS-9) for the treatment of hyperkalaemia. www.astrazeneca.com/investor-relations/Stock-exchange-announcements/fda-accepts-for-review-new-drug-application-for-sodium-zirconium-18102016.html. Accessed March 1, 2017.
Q)I have heard talk about the development of new drugs to treat hyperkalemia. What is the status of these?
Hyperkalemia is a commonly seen electrolyte imbalance in clinical practice. Risks associated with moderate-to-severe hyperkalemia include potentially fatal cardiac conduction abnormalities/arrhythmias, making identification and management critical. An in-depth discussion of hyperkalemia diagnosis can be found in our March 2017 CE/CME activity (2017;27[3]:40-49).
Risk factors for hyperkalemia include excess intake or supplementation of potassium, type 2 diabetes, liver cirrhosis, congestive heart failure (CHF), and chronic kidney disease (CKD). The kidneys excrete 90% to 95% of ingested potassium, and the gut excretes the rest. Normal kidneys take six to 12 hours to excrete an acute potassium load. As kidney function decreases, risk for hyperkalemia increases.1 Hyperkalemia rates as high as 26% have been observed in patients with CKD stages 3 to 5 (glomerular filtration rate [GFR], < 60 mL/min).2
Renin-angiotensin-aldosterone system (RAAS) inhibitors—including ACE inhibitors (ACEis), angiotensin-receptor blockers, and aldosterone agonists—are associated with hyperkalemia. While RAAS therapy can play an important role in the management of CKD and cardiovascular disease (CVD), the development of hyperkalemia can necessitate a dose reduction or discontinuation of these medications, limiting their therapeutic benefit. Other medications that elevate risk for hyperkalemia include NSAIDs, heparin, cyclosporine, amiloride, triamterene, and nonselective ß-blockers.1
Therapeutic options for nonurgent treatment of hyperkalemia are limited. In addition to reducing or discontinuing associated medications, strategies include use of diuretics (as appropriate), treatment of metabolic acidosis, and dietary restrictions (ie, limiting high-potassium foods).1 Pharmacologically, there has been one (less than ideal) option—until recently.
Sodium polystyrene sulfonate (SPS), an ion-exchange resin approved in 1958, can be used to treat hyperkalemia.3 It comes in an enema and an oral form; the former has a faster onset, but the latter is more effective, with an onset of action of one to two hours and a duration of four to six hours.1 However, each gram of SPS contains 100 g of sodium, and the typical dose of SPS is 15 g to 60 g.4 The resulting increase in sodium load can be a concern for patients with CHF, severe hypertension, or severe edema.5
Data from randomized controlled trials (RCTs) are limited; however, one double-blind RCT investigated the effect of SPS on 33 patients with CKD and mild-to-moderate hyperkalemia (potassium level, 5 mEq/L to 5.9 mEq/L). The researchers found that patients who took 30 g/d of SPS for seven days experienced a 73% reduction in serum potassium, compared with a 38% reduction in patients who took a placebo. Of note, more gastrointestinal issues were observed in the SPS group.6
Additionally, a retrospective chart review of 14 patients with CKD and heart disease found low-dose SPS to be safe and effective when used as a secondary measure for hyperkalemia prevention in those taking RAAS therapy.7 However, a systematic review found that SPS use with and without concurrent sorbitol may be associated with serious and fatal gastrointestinal injuries.8 In 2011, the FDA issued a black box warning regarding increased risk for intestinal necrosis when SPS is used with sorbitol.9 In 2015, the FDA recommended separating SPS from other oral medications by at least six hours, due to its potential to bind with other medications.10
Patiromer, a new potassium binder, was approved by the FDA in 2015. This sodium-free, nonabsorbed, spherical polymer uses calcium as the exchange cation to bind potassium in the gastrointestinal tract. Its onset of action is seven hours, with a 24-hour duration of action. It is not approved for emergency use. There are no renal dosing adjustment considerations with patiromer.
In RCTs, patiromer has been associated with a significant reduction in serum potassium in patients with CKD (with or without diabetes) taking RAAS therapy. The starting dose is 8.4 g/d mixed with water, taken with food; this can be increased by 8.4 g each week as needed, to a maximum dosage of 25.2 g/d. Patiromer binds between 8.5 mEq to 8.8 mEq of potassium per gram of polymer.
The original approval included a black box warning to take patiromer six hours before and after other medications, due to concern for binding with certain medications. However, after an additional study in 2016, the FDA removed this warning and approved a change in administration to three hours before and after taking other medications.
Use of patiromer is not advised in those with severe constipation, bowel obstruction/impaction, or allergies to any of its components.11 Adverse reactions associated with patiromer include constipation (which generally improves with time), hypomagnesemia, diarrhea, nausea, abdominal discomfort, and flatulence. A 52-week RCT of 304 patients with CKD on RAAS found the most common adverse event to be mild-to-moderate constipation (6.3% of patients), with two patients discontinuing therapy as a result.4 In clinical trials, 9% of patients developed hypomagnesemia (serum magnesium value, < 1.4 mg/dL). It is recommended that serum magnesium levels be monitored and supplementation offered, when appropriate.11
Sodium zirconium cyclosilicate (ZS-9) is among the potassium-lowering medications on the horizon. In 2016, the FDA accepted a new drug application for this insoluble, unabsorbed cation exchanger that also works in the GI tract and uses sodium and hydrogen as exchange cations.12
For now, however, dietary education remains a mainstay of treatment for patients with elevated serum potassium levels. It is particularly important to inform your patients that many salt substitutes and low-sodium products contain potassium chloride. They should therefore exercise caution when incorporating sodium-reducing components into their diet. —CS
Cynthia Smith, DNP, CNN-NP, APRN, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virginia
Q)I have heard talk about the development of new drugs to treat hyperkalemia. What is the status of these?
Hyperkalemia is a commonly seen electrolyte imbalance in clinical practice. Risks associated with moderate-to-severe hyperkalemia include potentially fatal cardiac conduction abnormalities/arrhythmias, making identification and management critical. An in-depth discussion of hyperkalemia diagnosis can be found in our March 2017 CE/CME activity (2017;27[3]:40-49).
Risk factors for hyperkalemia include excess intake or supplementation of potassium, type 2 diabetes, liver cirrhosis, congestive heart failure (CHF), and chronic kidney disease (CKD). The kidneys excrete 90% to 95% of ingested potassium, and the gut excretes the rest. Normal kidneys take six to 12 hours to excrete an acute potassium load. As kidney function decreases, risk for hyperkalemia increases.1 Hyperkalemia rates as high as 26% have been observed in patients with CKD stages 3 to 5 (glomerular filtration rate [GFR], < 60 mL/min).2
Renin-angiotensin-aldosterone system (RAAS) inhibitors—including ACE inhibitors (ACEis), angiotensin-receptor blockers, and aldosterone agonists—are associated with hyperkalemia. While RAAS therapy can play an important role in the management of CKD and cardiovascular disease (CVD), the development of hyperkalemia can necessitate a dose reduction or discontinuation of these medications, limiting their therapeutic benefit. Other medications that elevate risk for hyperkalemia include NSAIDs, heparin, cyclosporine, amiloride, triamterene, and nonselective ß-blockers.1
Therapeutic options for nonurgent treatment of hyperkalemia are limited. In addition to reducing or discontinuing associated medications, strategies include use of diuretics (as appropriate), treatment of metabolic acidosis, and dietary restrictions (ie, limiting high-potassium foods).1 Pharmacologically, there has been one (less than ideal) option—until recently.
Sodium polystyrene sulfonate (SPS), an ion-exchange resin approved in 1958, can be used to treat hyperkalemia.3 It comes in an enema and an oral form; the former has a faster onset, but the latter is more effective, with an onset of action of one to two hours and a duration of four to six hours.1 However, each gram of SPS contains 100 g of sodium, and the typical dose of SPS is 15 g to 60 g.4 The resulting increase in sodium load can be a concern for patients with CHF, severe hypertension, or severe edema.5
Data from randomized controlled trials (RCTs) are limited; however, one double-blind RCT investigated the effect of SPS on 33 patients with CKD and mild-to-moderate hyperkalemia (potassium level, 5 mEq/L to 5.9 mEq/L). The researchers found that patients who took 30 g/d of SPS for seven days experienced a 73% reduction in serum potassium, compared with a 38% reduction in patients who took a placebo. Of note, more gastrointestinal issues were observed in the SPS group.6
Additionally, a retrospective chart review of 14 patients with CKD and heart disease found low-dose SPS to be safe and effective when used as a secondary measure for hyperkalemia prevention in those taking RAAS therapy.7 However, a systematic review found that SPS use with and without concurrent sorbitol may be associated with serious and fatal gastrointestinal injuries.8 In 2011, the FDA issued a black box warning regarding increased risk for intestinal necrosis when SPS is used with sorbitol.9 In 2015, the FDA recommended separating SPS from other oral medications by at least six hours, due to its potential to bind with other medications.10
Patiromer, a new potassium binder, was approved by the FDA in 2015. This sodium-free, nonabsorbed, spherical polymer uses calcium as the exchange cation to bind potassium in the gastrointestinal tract. Its onset of action is seven hours, with a 24-hour duration of action. It is not approved for emergency use. There are no renal dosing adjustment considerations with patiromer.
In RCTs, patiromer has been associated with a significant reduction in serum potassium in patients with CKD (with or without diabetes) taking RAAS therapy. The starting dose is 8.4 g/d mixed with water, taken with food; this can be increased by 8.4 g each week as needed, to a maximum dosage of 25.2 g/d. Patiromer binds between 8.5 mEq to 8.8 mEq of potassium per gram of polymer.
The original approval included a black box warning to take patiromer six hours before and after other medications, due to concern for binding with certain medications. However, after an additional study in 2016, the FDA removed this warning and approved a change in administration to three hours before and after taking other medications.
Use of patiromer is not advised in those with severe constipation, bowel obstruction/impaction, or allergies to any of its components.11 Adverse reactions associated with patiromer include constipation (which generally improves with time), hypomagnesemia, diarrhea, nausea, abdominal discomfort, and flatulence. A 52-week RCT of 304 patients with CKD on RAAS found the most common adverse event to be mild-to-moderate constipation (6.3% of patients), with two patients discontinuing therapy as a result.4 In clinical trials, 9% of patients developed hypomagnesemia (serum magnesium value, < 1.4 mg/dL). It is recommended that serum magnesium levels be monitored and supplementation offered, when appropriate.11
Sodium zirconium cyclosilicate (ZS-9) is among the potassium-lowering medications on the horizon. In 2016, the FDA accepted a new drug application for this insoluble, unabsorbed cation exchanger that also works in the GI tract and uses sodium and hydrogen as exchange cations.12
For now, however, dietary education remains a mainstay of treatment for patients with elevated serum potassium levels. It is particularly important to inform your patients that many salt substitutes and low-sodium products contain potassium chloride. They should therefore exercise caution when incorporating sodium-reducing components into their diet. —CS
Cynthia Smith, DNP, CNN-NP, APRN, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virginia
1. Gilbert S, Weiner D, Gipson D, eds; National Kidney Foundation. Primer on Kidney Diseases. 6th ed. Philadelphia, PA: Saunders Elsevier; 2014.
2. Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156-1162.
3. Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol: a preliminary report. N Engl J Med. 1961;264:111-115.
4. Dunn JD, Benton WW, Orozco-Torrentera E, Adamson RT. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 suppl): s307-s315.
5. Li L, Harrison SD, Cope MJ, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21(5):456-465.
6. Lepage L, Dufour AC, Doiron J, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015; 10(12):2136-2142.
7. Chernin G, Gal-Oz A, Ben-Assa E, et al. Secondary prevention of hyperkalemia with sodium polystyrene sulfonate in cardiac and kidney patients on renin-angiotensin-aldosterone system inhibition therapy. Clin Cardiol. 2012;35(1):32-36.
8. Harel Z, Harel S, Shah PS, et al. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126(3):264.e9-e24.
9. FDA. Safety warning: Kayexalate (sodium polystyrene sulfonate) powder. www.fda.gov/Safety/MedWatch/SafetyInformation/ucm186845.htm. Accessed February 15, 2017.
10. FDA. FDA drug safety communication: FDA required drug interaction studies with potassium-lowering drug Kayexalate (sodium polystyrene sulfonate). www.fda.gov/Drugs/DrugSafety/ucm468035.htm. Accessed March 1, 2017.
11. Veltassa® (patiromer) [package insert]. Redwood City, CA: Relypsa, Inc; 2016. www.veltassa.com/pi.pdf. Accessed March 1, 2017.
12. AstraZeneca. FDA accepts for review New Drug Application for sodium zirconium cyclosilicate (ZS-9) for the treatment of hyperkalaemia. www.astrazeneca.com/investor-relations/Stock-exchange-announcements/fda-accepts-for-review-new-drug-application-for-sodium-zirconium-18102016.html. Accessed March 1, 2017.
1. Gilbert S, Weiner D, Gipson D, eds; National Kidney Foundation. Primer on Kidney Diseases. 6th ed. Philadelphia, PA: Saunders Elsevier; 2014.
2. Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156-1162.
3. Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol: a preliminary report. N Engl J Med. 1961;264:111-115.
4. Dunn JD, Benton WW, Orozco-Torrentera E, Adamson RT. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 suppl): s307-s315.
5. Li L, Harrison SD, Cope MJ, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21(5):456-465.
6. Lepage L, Dufour AC, Doiron J, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015; 10(12):2136-2142.
7. Chernin G, Gal-Oz A, Ben-Assa E, et al. Secondary prevention of hyperkalemia with sodium polystyrene sulfonate in cardiac and kidney patients on renin-angiotensin-aldosterone system inhibition therapy. Clin Cardiol. 2012;35(1):32-36.
8. Harel Z, Harel S, Shah PS, et al. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126(3):264.e9-e24.
9. FDA. Safety warning: Kayexalate (sodium polystyrene sulfonate) powder. www.fda.gov/Safety/MedWatch/SafetyInformation/ucm186845.htm. Accessed February 15, 2017.
10. FDA. FDA drug safety communication: FDA required drug interaction studies with potassium-lowering drug Kayexalate (sodium polystyrene sulfonate). www.fda.gov/Drugs/DrugSafety/ucm468035.htm. Accessed March 1, 2017.
11. Veltassa® (patiromer) [package insert]. Redwood City, CA: Relypsa, Inc; 2016. www.veltassa.com/pi.pdf. Accessed March 1, 2017.
12. AstraZeneca. FDA accepts for review New Drug Application for sodium zirconium cyclosilicate (ZS-9) for the treatment of hyperkalaemia. www.astrazeneca.com/investor-relations/Stock-exchange-announcements/fda-accepts-for-review-new-drug-application-for-sodium-zirconium-18102016.html. Accessed March 1, 2017.
MicroRNAs linked to treatment response in lupus nephritis
MELBOURNE – Researchers have identified six microRNAs that may indicate a better likelihood of response to cyclophosphamide in patients with lupus nephritis, according to a study presented at an international conference on systemic lupus erythematosus.
“MicroRNA has been shown to be important in systemic lupus in several studies, and they’ve identified several microRNA that have been shown to affect the outcome measures in patients,” said Sarfaraz Hasni, MD, director of the Lupus Clinical Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases in Bethesda, Md., who presented a poster on the study at the meeting.
The aim of this study, involving 71 patients with lupus nephritis, was to look for microRNAs associated with treatment response to cyclophosphamide.
The first stage of the study involved isolating microRNAs from kidney biopsies taken from a first cohort of 17 responders and 15 nonresponders.
Responders were patients who, after 2 years of intravenous cyclophosphamide, showed no active urinary sediments, less than five red blood cells or white blood cells in urine, and proteinuria below 1 g/24 hours.
After analyzing 300-400 microRNAs in these biopsies, the investigators identified 6 that were significantly upregulated in association with treatment outcome in both the first cohort as well as a second validation cohort of 22 responders and 17 nonresponders.
When the researchers looked at the most likely genetic targets of these microRNAs, they identified genes associated with G2/M DNA damage checkpoint regulation, which points to a link with cyclophosphamide efficacy, as well as associations with immunological disease and renal inflammation.
Dr. Hasni said that previous studies of microRNA had looked in the peripheral blood but suggested this may not necessarily reflect what was happening in the kidney.
The next step for researchers is to see if upregulation of these microRNAs is predictive of treatment response.
“If you are giving cyclophosphamide for 2 years, it comes with a high risk of side effects, especially in young women because there is potential for premature ovarian failure,” Dr. Hasni said in an interview. “If we can predict that this patient is not going to respond to cyclophosphamide or will not have a good outcome, we can use alternative therapy, or perhaps use more aggressive or a combination therapy approach rather than keep doing the same thing and 2 years later find out the patient is not going to respond.”
The researchers are also keen to investigate whether these same microRNAs can be isolated from serum or urine, which would reduce the need for kidney biopsy.
“The testing for microRNA is not that hard – it’s the biopsy and extracting the tissue from the biopsy... that’s obviously cumbersome and can only be done in a research setting.”
No conflicts of interest were declared.
MELBOURNE – Researchers have identified six microRNAs that may indicate a better likelihood of response to cyclophosphamide in patients with lupus nephritis, according to a study presented at an international conference on systemic lupus erythematosus.
“MicroRNA has been shown to be important in systemic lupus in several studies, and they’ve identified several microRNA that have been shown to affect the outcome measures in patients,” said Sarfaraz Hasni, MD, director of the Lupus Clinical Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases in Bethesda, Md., who presented a poster on the study at the meeting.
The aim of this study, involving 71 patients with lupus nephritis, was to look for microRNAs associated with treatment response to cyclophosphamide.
The first stage of the study involved isolating microRNAs from kidney biopsies taken from a first cohort of 17 responders and 15 nonresponders.
Responders were patients who, after 2 years of intravenous cyclophosphamide, showed no active urinary sediments, less than five red blood cells or white blood cells in urine, and proteinuria below 1 g/24 hours.
After analyzing 300-400 microRNAs in these biopsies, the investigators identified 6 that were significantly upregulated in association with treatment outcome in both the first cohort as well as a second validation cohort of 22 responders and 17 nonresponders.
When the researchers looked at the most likely genetic targets of these microRNAs, they identified genes associated with G2/M DNA damage checkpoint regulation, which points to a link with cyclophosphamide efficacy, as well as associations with immunological disease and renal inflammation.
Dr. Hasni said that previous studies of microRNA had looked in the peripheral blood but suggested this may not necessarily reflect what was happening in the kidney.
The next step for researchers is to see if upregulation of these microRNAs is predictive of treatment response.
“If you are giving cyclophosphamide for 2 years, it comes with a high risk of side effects, especially in young women because there is potential for premature ovarian failure,” Dr. Hasni said in an interview. “If we can predict that this patient is not going to respond to cyclophosphamide or will not have a good outcome, we can use alternative therapy, or perhaps use more aggressive or a combination therapy approach rather than keep doing the same thing and 2 years later find out the patient is not going to respond.”
The researchers are also keen to investigate whether these same microRNAs can be isolated from serum or urine, which would reduce the need for kidney biopsy.
“The testing for microRNA is not that hard – it’s the biopsy and extracting the tissue from the biopsy... that’s obviously cumbersome and can only be done in a research setting.”
No conflicts of interest were declared.
MELBOURNE – Researchers have identified six microRNAs that may indicate a better likelihood of response to cyclophosphamide in patients with lupus nephritis, according to a study presented at an international conference on systemic lupus erythematosus.
“MicroRNA has been shown to be important in systemic lupus in several studies, and they’ve identified several microRNA that have been shown to affect the outcome measures in patients,” said Sarfaraz Hasni, MD, director of the Lupus Clinical Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases in Bethesda, Md., who presented a poster on the study at the meeting.
The aim of this study, involving 71 patients with lupus nephritis, was to look for microRNAs associated with treatment response to cyclophosphamide.
The first stage of the study involved isolating microRNAs from kidney biopsies taken from a first cohort of 17 responders and 15 nonresponders.
Responders were patients who, after 2 years of intravenous cyclophosphamide, showed no active urinary sediments, less than five red blood cells or white blood cells in urine, and proteinuria below 1 g/24 hours.
After analyzing 300-400 microRNAs in these biopsies, the investigators identified 6 that were significantly upregulated in association with treatment outcome in both the first cohort as well as a second validation cohort of 22 responders and 17 nonresponders.
When the researchers looked at the most likely genetic targets of these microRNAs, they identified genes associated with G2/M DNA damage checkpoint regulation, which points to a link with cyclophosphamide efficacy, as well as associations with immunological disease and renal inflammation.
Dr. Hasni said that previous studies of microRNA had looked in the peripheral blood but suggested this may not necessarily reflect what was happening in the kidney.
The next step for researchers is to see if upregulation of these microRNAs is predictive of treatment response.
“If you are giving cyclophosphamide for 2 years, it comes with a high risk of side effects, especially in young women because there is potential for premature ovarian failure,” Dr. Hasni said in an interview. “If we can predict that this patient is not going to respond to cyclophosphamide or will not have a good outcome, we can use alternative therapy, or perhaps use more aggressive or a combination therapy approach rather than keep doing the same thing and 2 years later find out the patient is not going to respond.”
The researchers are also keen to investigate whether these same microRNAs can be isolated from serum or urine, which would reduce the need for kidney biopsy.
“The testing for microRNA is not that hard – it’s the biopsy and extracting the tissue from the biopsy... that’s obviously cumbersome and can only be done in a research setting.”
No conflicts of interest were declared.
AT LUPUS 2017
Key clinical point:
Major finding: Researchers have identified six microRNAs from kidney biopsies that are significantly upregulated in patients who respond to cyclophosphamide treatment for lupus nephritis.
Data source: Prospective cohort study in 71 patients with lupus nephritis.
Disclosures: No conflicts of interest were declared.
Lupus nephritis expert offers management tips
MELBOURNE – Multidisciplinary management of comorbidities is one of the most important aspects of the care of patients with lupus nephritis, Frédéric Houssiau, MD, PhD, said at an international congress on systemic lupus erythematosus.
In his presentation describing his top 10 tips for the management of lupus nephritis, Dr. Houssiau said traditional risk factors do not explain the two- to threefold higher risk of cardiovascular disease in patients with lupus, making it important to address known cardiovascular disease risk factors.
Dr. Houssiau also stressed the importance of paying attention to clotting disorders, preventing glucocorticoid-related intraocular pressure, ensuring patients are immunized against influenza, and enabling patient access to an intensive care unit in the event of severe sepsis.
He also called for physicians to “unmask” nonadherence to therapy, saying it was the most common cause of treatment failure.
“We don’t look enough to nonadherence to therapy, and we have no good clue to sort that out,” he said in an interview. “We can identify nonadherent patients, but it’s very difficult to change their mind, to make them adherent, and we have nurses, nurse-practitioners, questionnaires for adherence, but none of them, I think, so far have changed practice.”
Dr. Houssiau argued for the importance of having a good connection with a nephrologist and always performing a renal biopsy in patients with lupus nephritis.
“The reason for that is first to identify the immune deposits, either mesangial or subendothelial or subepithelial, and another reason is clearly not to miss the antiphospholipid syndrome,” he told the audience. “The third very good reason to perform the renal biopsy is clearly to classify the patient.”
Echoing other presentations at the conference, Dr. Houssiau said there was a need to define treatment targets in lupus nephritis.
“In diabetes, in hypertension, in rheumatoid arthritis, the target is well known by all of us,” he said. “What is the target that we should achieve in the lupus nephritis patient? That is much more difficult.”
He cited data from the recent MAINTAIN trial, which suggested that proteinuria levels at 12 months after initiation of treatment were highly predictive of patients who were likely to have a good renal prognosis. Patients with a 24-hour proteinuria level of around 0.7-0.8 g/day had a significantly greater likelihood of normal serum creatinine 7 years later, he said.
“Yet, we need more, we need better markers, because the negative predictive value is very bad, which means that a lot of patients who do not reach that target still, fortunately, will end up without renal failure.”
Dr. Houssiau also emphasized the need to minimize the use of steroids where possible, as data from an inception cohort run by him and his colleagues have shown that patients who failed to taper down to 4 mg of prednisone or less, after 1 year, had significantly more damage accrual.
He also advocated using either mycophenolate mofetil or intravenous cyclophosphamide as induction therapy based on data suggesting the two are equally efficacious at 6 months. Dr. Houssiau suggested favoring intravenous cyclophosphamide if fertility was a concern because it has been shown to not affect ovarian reserve and has the added advantage of better compliance.
Maintaining immunosuppression is also vital, Dr. Houssiau told the conference, and patients should be treated with immunosuppressants for at least 5, and possibly even up to 10, years.
“There is a small study showing an inverse correlation between the length of therapy and remission on the one hand, and risk of relapse, so the more you treat, the more the period of remission is long, the lower risk of relapse,” he said. However, there are little trial data on withdrawing immunosuppression or trials of immunosuppressant withdrawal, he noted.
Commenting on the future prospects for new treatments for lupus nephritis, Dr. Houssiau advised keeping faith in targeted therapies and precision medicine despite a slew of failed phase III clinical trials, and watching the development of calcineurin inhibitors, such as voclosporin.
Dr. Houssiau declared receiving research grants and honoraria from AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Lilly, Roche, Serono, and UCB.
MELBOURNE – Multidisciplinary management of comorbidities is one of the most important aspects of the care of patients with lupus nephritis, Frédéric Houssiau, MD, PhD, said at an international congress on systemic lupus erythematosus.
In his presentation describing his top 10 tips for the management of lupus nephritis, Dr. Houssiau said traditional risk factors do not explain the two- to threefold higher risk of cardiovascular disease in patients with lupus, making it important to address known cardiovascular disease risk factors.
Dr. Houssiau also stressed the importance of paying attention to clotting disorders, preventing glucocorticoid-related intraocular pressure, ensuring patients are immunized against influenza, and enabling patient access to an intensive care unit in the event of severe sepsis.
He also called for physicians to “unmask” nonadherence to therapy, saying it was the most common cause of treatment failure.
“We don’t look enough to nonadherence to therapy, and we have no good clue to sort that out,” he said in an interview. “We can identify nonadherent patients, but it’s very difficult to change their mind, to make them adherent, and we have nurses, nurse-practitioners, questionnaires for adherence, but none of them, I think, so far have changed practice.”
Dr. Houssiau argued for the importance of having a good connection with a nephrologist and always performing a renal biopsy in patients with lupus nephritis.
“The reason for that is first to identify the immune deposits, either mesangial or subendothelial or subepithelial, and another reason is clearly not to miss the antiphospholipid syndrome,” he told the audience. “The third very good reason to perform the renal biopsy is clearly to classify the patient.”
Echoing other presentations at the conference, Dr. Houssiau said there was a need to define treatment targets in lupus nephritis.
“In diabetes, in hypertension, in rheumatoid arthritis, the target is well known by all of us,” he said. “What is the target that we should achieve in the lupus nephritis patient? That is much more difficult.”
He cited data from the recent MAINTAIN trial, which suggested that proteinuria levels at 12 months after initiation of treatment were highly predictive of patients who were likely to have a good renal prognosis. Patients with a 24-hour proteinuria level of around 0.7-0.8 g/day had a significantly greater likelihood of normal serum creatinine 7 years later, he said.
“Yet, we need more, we need better markers, because the negative predictive value is very bad, which means that a lot of patients who do not reach that target still, fortunately, will end up without renal failure.”
Dr. Houssiau also emphasized the need to minimize the use of steroids where possible, as data from an inception cohort run by him and his colleagues have shown that patients who failed to taper down to 4 mg of prednisone or less, after 1 year, had significantly more damage accrual.
He also advocated using either mycophenolate mofetil or intravenous cyclophosphamide as induction therapy based on data suggesting the two are equally efficacious at 6 months. Dr. Houssiau suggested favoring intravenous cyclophosphamide if fertility was a concern because it has been shown to not affect ovarian reserve and has the added advantage of better compliance.
Maintaining immunosuppression is also vital, Dr. Houssiau told the conference, and patients should be treated with immunosuppressants for at least 5, and possibly even up to 10, years.
“There is a small study showing an inverse correlation between the length of therapy and remission on the one hand, and risk of relapse, so the more you treat, the more the period of remission is long, the lower risk of relapse,” he said. However, there are little trial data on withdrawing immunosuppression or trials of immunosuppressant withdrawal, he noted.
Commenting on the future prospects for new treatments for lupus nephritis, Dr. Houssiau advised keeping faith in targeted therapies and precision medicine despite a slew of failed phase III clinical trials, and watching the development of calcineurin inhibitors, such as voclosporin.
Dr. Houssiau declared receiving research grants and honoraria from AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Lilly, Roche, Serono, and UCB.
MELBOURNE – Multidisciplinary management of comorbidities is one of the most important aspects of the care of patients with lupus nephritis, Frédéric Houssiau, MD, PhD, said at an international congress on systemic lupus erythematosus.
In his presentation describing his top 10 tips for the management of lupus nephritis, Dr. Houssiau said traditional risk factors do not explain the two- to threefold higher risk of cardiovascular disease in patients with lupus, making it important to address known cardiovascular disease risk factors.
Dr. Houssiau also stressed the importance of paying attention to clotting disorders, preventing glucocorticoid-related intraocular pressure, ensuring patients are immunized against influenza, and enabling patient access to an intensive care unit in the event of severe sepsis.
He also called for physicians to “unmask” nonadherence to therapy, saying it was the most common cause of treatment failure.
“We don’t look enough to nonadherence to therapy, and we have no good clue to sort that out,” he said in an interview. “We can identify nonadherent patients, but it’s very difficult to change their mind, to make them adherent, and we have nurses, nurse-practitioners, questionnaires for adherence, but none of them, I think, so far have changed practice.”
Dr. Houssiau argued for the importance of having a good connection with a nephrologist and always performing a renal biopsy in patients with lupus nephritis.
“The reason for that is first to identify the immune deposits, either mesangial or subendothelial or subepithelial, and another reason is clearly not to miss the antiphospholipid syndrome,” he told the audience. “The third very good reason to perform the renal biopsy is clearly to classify the patient.”
Echoing other presentations at the conference, Dr. Houssiau said there was a need to define treatment targets in lupus nephritis.
“In diabetes, in hypertension, in rheumatoid arthritis, the target is well known by all of us,” he said. “What is the target that we should achieve in the lupus nephritis patient? That is much more difficult.”
He cited data from the recent MAINTAIN trial, which suggested that proteinuria levels at 12 months after initiation of treatment were highly predictive of patients who were likely to have a good renal prognosis. Patients with a 24-hour proteinuria level of around 0.7-0.8 g/day had a significantly greater likelihood of normal serum creatinine 7 years later, he said.
“Yet, we need more, we need better markers, because the negative predictive value is very bad, which means that a lot of patients who do not reach that target still, fortunately, will end up without renal failure.”
Dr. Houssiau also emphasized the need to minimize the use of steroids where possible, as data from an inception cohort run by him and his colleagues have shown that patients who failed to taper down to 4 mg of prednisone or less, after 1 year, had significantly more damage accrual.
He also advocated using either mycophenolate mofetil or intravenous cyclophosphamide as induction therapy based on data suggesting the two are equally efficacious at 6 months. Dr. Houssiau suggested favoring intravenous cyclophosphamide if fertility was a concern because it has been shown to not affect ovarian reserve and has the added advantage of better compliance.
Maintaining immunosuppression is also vital, Dr. Houssiau told the conference, and patients should be treated with immunosuppressants for at least 5, and possibly even up to 10, years.
“There is a small study showing an inverse correlation between the length of therapy and remission on the one hand, and risk of relapse, so the more you treat, the more the period of remission is long, the lower risk of relapse,” he said. However, there are little trial data on withdrawing immunosuppression or trials of immunosuppressant withdrawal, he noted.
Commenting on the future prospects for new treatments for lupus nephritis, Dr. Houssiau advised keeping faith in targeted therapies and precision medicine despite a slew of failed phase III clinical trials, and watching the development of calcineurin inhibitors, such as voclosporin.
Dr. Houssiau declared receiving research grants and honoraria from AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Lilly, Roche, Serono, and UCB.
EXPERT ANALYSIS FROM LUPUS 2017
Vascular involvement may signify worse outcomes in lupus nephritis
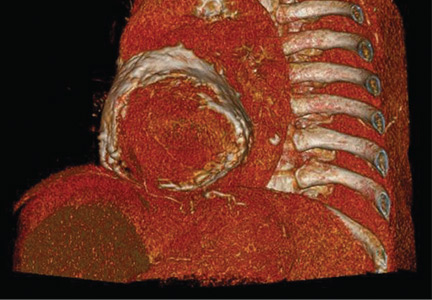
MELBOURNE – Vascular involvement in patients with lupus nephritis is associated with poorer outcomes and could be a trigger for a more aggressive treatment approach, according to observational study results reported at an international congress on systemic lupus erythematosus.
Manish Rathi, MD, a nephrologist at the Postgraduate Institution of Medical Education & Research in Chandigarh, India, reported the results of a 5-year prospective cohort study in 241 patients with biopsy-proven lupus nephritis.
Researchers found that patients with vascular involvement had significantly higher serum creatinine at baseline than did those without it. At follow-up, they also had significantly higher proteinuria and serum creatinine, as well as significantly lower serum albumin.
This group was also less likely to achieve complete remission, compared with patients without vascular involvement (38.2% vs. 61.9%; P = .006), and had treatment-refractory disease almost twice as often (26.3% vs. 14.3%; P = .02).
Overall, vascular involvement was seen in 32.3% of patients, with the most common form being arteriosclerosis (22.8%), followed by vascular thrombotic microangiopathy (11.2%), asymptomatic vascular immune deposits (5.3%), vasculopathy (2%), and vasculitis (0.8%).
Three-quarters of all patients had nephrotic syndrome, and 41.9% were identified as Class IV, 18.7% as Class V, 10.4% as Class III, and 3.7% as Class II.
When researchers examined the presentation and outcomes among these subgroups, they found that patients with vascular thrombotic microangiopathy had a significantly higher serum creatinine and were less likely to respond to treatment, compared with patients without vascular thrombotic microangiopathy (60% vs. 79.1%).
Similarly, patients with arteriosclerosis had significantly lower incidence of complete remission, compared with those without arteriosclerosis (37.7% vs. 58.8%) although they had significantly higher rates of partial remission (35.8% vs. 19.4%).
“Lupus patients, if they had involvement of vascular compartment, they had more severe presentation at the time of presentation as well as poorer outcomes despite giving the standard therapy,” Dr. Rathi said.
In an interview, Dr. Rathi said the results had already influenced their own treatment approach with these patients.
“What we have started doing now is – if there is vascular involvement, particularly the thrombotic microangiopathy – we treat them as severe lupus nephritis [patients], so even if their class of lupus nephritis is less severe, we’ll be treating them as severe,” he said.
Commenting on the presentation, Frederic Houssiau, MD, PhD, a professor of rheumatology at the Cliniques Universitaires Saint-Luc in Brussels, said he agreed that vascular involvement was neglected in the current classification of lupus nephritis and that it should be taken into account.
“Maybe we should not only consider the class but also look in more detail to the pathophysiological findings,” Dr. Houssiau said in an interview. “When you have a lot of inflammation in the vessels, for instance, maybe we should use cyclophosphamide.”
No conflicts of interest were disclosed.
MELBOURNE – Vascular involvement in patients with lupus nephritis is associated with poorer outcomes and could be a trigger for a more aggressive treatment approach, according to observational study results reported at an international congress on systemic lupus erythematosus.
Manish Rathi, MD, a nephrologist at the Postgraduate Institution of Medical Education & Research in Chandigarh, India, reported the results of a 5-year prospective cohort study in 241 patients with biopsy-proven lupus nephritis.
Researchers found that patients with vascular involvement had significantly higher serum creatinine at baseline than did those without it. At follow-up, they also had significantly higher proteinuria and serum creatinine, as well as significantly lower serum albumin.
This group was also less likely to achieve complete remission, compared with patients without vascular involvement (38.2% vs. 61.9%; P = .006), and had treatment-refractory disease almost twice as often (26.3% vs. 14.3%; P = .02).
Overall, vascular involvement was seen in 32.3% of patients, with the most common form being arteriosclerosis (22.8%), followed by vascular thrombotic microangiopathy (11.2%), asymptomatic vascular immune deposits (5.3%), vasculopathy (2%), and vasculitis (0.8%).
Three-quarters of all patients had nephrotic syndrome, and 41.9% were identified as Class IV, 18.7% as Class V, 10.4% as Class III, and 3.7% as Class II.
When researchers examined the presentation and outcomes among these subgroups, they found that patients with vascular thrombotic microangiopathy had a significantly higher serum creatinine and were less likely to respond to treatment, compared with patients without vascular thrombotic microangiopathy (60% vs. 79.1%).
Similarly, patients with arteriosclerosis had significantly lower incidence of complete remission, compared with those without arteriosclerosis (37.7% vs. 58.8%) although they had significantly higher rates of partial remission (35.8% vs. 19.4%).
“Lupus patients, if they had involvement of vascular compartment, they had more severe presentation at the time of presentation as well as poorer outcomes despite giving the standard therapy,” Dr. Rathi said.
In an interview, Dr. Rathi said the results had already influenced their own treatment approach with these patients.
“What we have started doing now is – if there is vascular involvement, particularly the thrombotic microangiopathy – we treat them as severe lupus nephritis [patients], so even if their class of lupus nephritis is less severe, we’ll be treating them as severe,” he said.
Commenting on the presentation, Frederic Houssiau, MD, PhD, a professor of rheumatology at the Cliniques Universitaires Saint-Luc in Brussels, said he agreed that vascular involvement was neglected in the current classification of lupus nephritis and that it should be taken into account.
“Maybe we should not only consider the class but also look in more detail to the pathophysiological findings,” Dr. Houssiau said in an interview. “When you have a lot of inflammation in the vessels, for instance, maybe we should use cyclophosphamide.”
No conflicts of interest were disclosed.
MELBOURNE – Vascular involvement in patients with lupus nephritis is associated with poorer outcomes and could be a trigger for a more aggressive treatment approach, according to observational study results reported at an international congress on systemic lupus erythematosus.
Manish Rathi, MD, a nephrologist at the Postgraduate Institution of Medical Education & Research in Chandigarh, India, reported the results of a 5-year prospective cohort study in 241 patients with biopsy-proven lupus nephritis.
Researchers found that patients with vascular involvement had significantly higher serum creatinine at baseline than did those without it. At follow-up, they also had significantly higher proteinuria and serum creatinine, as well as significantly lower serum albumin.
This group was also less likely to achieve complete remission, compared with patients without vascular involvement (38.2% vs. 61.9%; P = .006), and had treatment-refractory disease almost twice as often (26.3% vs. 14.3%; P = .02).
Overall, vascular involvement was seen in 32.3% of patients, with the most common form being arteriosclerosis (22.8%), followed by vascular thrombotic microangiopathy (11.2%), asymptomatic vascular immune deposits (5.3%), vasculopathy (2%), and vasculitis (0.8%).
Three-quarters of all patients had nephrotic syndrome, and 41.9% were identified as Class IV, 18.7% as Class V, 10.4% as Class III, and 3.7% as Class II.
When researchers examined the presentation and outcomes among these subgroups, they found that patients with vascular thrombotic microangiopathy had a significantly higher serum creatinine and were less likely to respond to treatment, compared with patients without vascular thrombotic microangiopathy (60% vs. 79.1%).
Similarly, patients with arteriosclerosis had significantly lower incidence of complete remission, compared with those without arteriosclerosis (37.7% vs. 58.8%) although they had significantly higher rates of partial remission (35.8% vs. 19.4%).
“Lupus patients, if they had involvement of vascular compartment, they had more severe presentation at the time of presentation as well as poorer outcomes despite giving the standard therapy,” Dr. Rathi said.
In an interview, Dr. Rathi said the results had already influenced their own treatment approach with these patients.
“What we have started doing now is – if there is vascular involvement, particularly the thrombotic microangiopathy – we treat them as severe lupus nephritis [patients], so even if their class of lupus nephritis is less severe, we’ll be treating them as severe,” he said.
Commenting on the presentation, Frederic Houssiau, MD, PhD, a professor of rheumatology at the Cliniques Universitaires Saint-Luc in Brussels, said he agreed that vascular involvement was neglected in the current classification of lupus nephritis and that it should be taken into account.
“Maybe we should not only consider the class but also look in more detail to the pathophysiological findings,” Dr. Houssiau said in an interview. “When you have a lot of inflammation in the vessels, for instance, maybe we should use cyclophosphamide.”
No conflicts of interest were disclosed.
AT LUPUS 2017
Key clinical point:
Major finding: Patients with vascular involvement in lupus nephritis are significantly less likely to achieve complete remission and have higher rates of treatment-refractory disease.
Data source: An observational cohort study in 241 patients with biopsy-proven lupus nephritis.
Disclosures: No conflicts of interest were declared.
Biomarker combination may forecast remission in lupus nephritis
MELBOURNE – A reduction in urinary protein creatinine ratio and normalization of inflammatory biomarkers early in treatment of lupus nephritis may predict response rates at 24 and 48 weeks, according to data from the AURION study presented at an international congress on systemic lupus erythematosus.
The AURION study was a single-arm exploratory study assessing the value of an early reduction in proteinuria in 10 patients with active lupus nephritis. The patients were treated with novel calcineurin inhibitor voclosporin (23.7 mg twice daily) in addition to usual care with mycophenolate mofetil and low-dose steroids. The treatment protocol also included a forced steroid taper from 0.5 g at day 0 to 2.5 mg from week 12.
The 48-week study examined the biomarkers of a 25% reduction in urinary protein creatinine ratio and normalization of inflammatory lupus biomarkers C3, C4, and anti–double stranded DNA at 8 weeks, and explored their relationship to remission rates at 24 and 48 weeks. Overall, by week 24, 70% of patients had achieved complete remission, and by week 48, 5 of 7 (71%) had achieved complete remission. Three patients dropped out of the study before week 48: one because of decreased estimated glomerular filtration rate, one because of a systemic lupus erythematosus flare, and one at the discretion of an investigator.
All patients showed a 25% reduction in urinary protein creatinine ratio at week 8, with a mean decrease of 61% by week 24. Researchers also saw a 22% increase in mean C3 levels and a 58% increase in mean C4 from baseline to week 24. There was also a decrease in anti–double stranded DNA.
When researchers examined the specificity and sensitivities of these biomarkers at week 8 in predicting renal response at weeks 24 and 48, they found that a 25% reduction in urinary protein creatinine ratio had a good sensitivity (71% and 75% at 24 and 48 weeks, respectively), but low specificity (33% and 24%).
In contrast, normalization of C4 and C3 by week 8 both showed a specificity of 100% by week 24 and 75% by week 48, but a sensitivity of 29% for week 24 and 25% for week 48.
Normalization of anti–double stranded DNA had a sensitivity of 57% at week 24 and 50% at week 48, and a specificity of 100% at week 24 and 50% at week 48.
“Certainly if you use C3, C4, and urinary protein creatinine ratio, you can say to the patient after week 8, ‘I don’t think this is going to work for you. You need to come off this therapy and move to something else,’ ” he said in an interview.
Mr. Huizinga said the company, which recently released 48-week data from the larger AURA-LV study of the same regimen in 265 patients, was now building this week-8 analysis into its studies, and hoped it would also provide an early predictive marker for other clinical trials.
Commenting on the findings, Brad Rovin, MD, professor of nephrology and pathology at Ohio State University, Columbus, and also an adviser to Aurinia, said this predictive ability would be extremely useful for clinicians.
“If a patient isn’t responding appropriately and you can really know that with some degree of certainty at 8 weeks, then instead of waiting 6 months to change therapy, maybe you should change earlier,” Dr. Rovin said in an interview.
This was particularly important in lupus nephritis, as the longer inflammation is allowed to continue, the greater the likelihood that it might tip over into fibrosis, he noted.
The study was funded by Aurinia.
MELBOURNE – A reduction in urinary protein creatinine ratio and normalization of inflammatory biomarkers early in treatment of lupus nephritis may predict response rates at 24 and 48 weeks, according to data from the AURION study presented at an international congress on systemic lupus erythematosus.
The AURION study was a single-arm exploratory study assessing the value of an early reduction in proteinuria in 10 patients with active lupus nephritis. The patients were treated with novel calcineurin inhibitor voclosporin (23.7 mg twice daily) in addition to usual care with mycophenolate mofetil and low-dose steroids. The treatment protocol also included a forced steroid taper from 0.5 g at day 0 to 2.5 mg from week 12.
The 48-week study examined the biomarkers of a 25% reduction in urinary protein creatinine ratio and normalization of inflammatory lupus biomarkers C3, C4, and anti–double stranded DNA at 8 weeks, and explored their relationship to remission rates at 24 and 48 weeks. Overall, by week 24, 70% of patients had achieved complete remission, and by week 48, 5 of 7 (71%) had achieved complete remission. Three patients dropped out of the study before week 48: one because of decreased estimated glomerular filtration rate, one because of a systemic lupus erythematosus flare, and one at the discretion of an investigator.
All patients showed a 25% reduction in urinary protein creatinine ratio at week 8, with a mean decrease of 61% by week 24. Researchers also saw a 22% increase in mean C3 levels and a 58% increase in mean C4 from baseline to week 24. There was also a decrease in anti–double stranded DNA.
When researchers examined the specificity and sensitivities of these biomarkers at week 8 in predicting renal response at weeks 24 and 48, they found that a 25% reduction in urinary protein creatinine ratio had a good sensitivity (71% and 75% at 24 and 48 weeks, respectively), but low specificity (33% and 24%).
In contrast, normalization of C4 and C3 by week 8 both showed a specificity of 100% by week 24 and 75% by week 48, but a sensitivity of 29% for week 24 and 25% for week 48.
Normalization of anti–double stranded DNA had a sensitivity of 57% at week 24 and 50% at week 48, and a specificity of 100% at week 24 and 50% at week 48.
“Certainly if you use C3, C4, and urinary protein creatinine ratio, you can say to the patient after week 8, ‘I don’t think this is going to work for you. You need to come off this therapy and move to something else,’ ” he said in an interview.
Mr. Huizinga said the company, which recently released 48-week data from the larger AURA-LV study of the same regimen in 265 patients, was now building this week-8 analysis into its studies, and hoped it would also provide an early predictive marker for other clinical trials.
Commenting on the findings, Brad Rovin, MD, professor of nephrology and pathology at Ohio State University, Columbus, and also an adviser to Aurinia, said this predictive ability would be extremely useful for clinicians.
“If a patient isn’t responding appropriately and you can really know that with some degree of certainty at 8 weeks, then instead of waiting 6 months to change therapy, maybe you should change earlier,” Dr. Rovin said in an interview.
This was particularly important in lupus nephritis, as the longer inflammation is allowed to continue, the greater the likelihood that it might tip over into fibrosis, he noted.
The study was funded by Aurinia.
MELBOURNE – A reduction in urinary protein creatinine ratio and normalization of inflammatory biomarkers early in treatment of lupus nephritis may predict response rates at 24 and 48 weeks, according to data from the AURION study presented at an international congress on systemic lupus erythematosus.
The AURION study was a single-arm exploratory study assessing the value of an early reduction in proteinuria in 10 patients with active lupus nephritis. The patients were treated with novel calcineurin inhibitor voclosporin (23.7 mg twice daily) in addition to usual care with mycophenolate mofetil and low-dose steroids. The treatment protocol also included a forced steroid taper from 0.5 g at day 0 to 2.5 mg from week 12.
The 48-week study examined the biomarkers of a 25% reduction in urinary protein creatinine ratio and normalization of inflammatory lupus biomarkers C3, C4, and anti–double stranded DNA at 8 weeks, and explored their relationship to remission rates at 24 and 48 weeks. Overall, by week 24, 70% of patients had achieved complete remission, and by week 48, 5 of 7 (71%) had achieved complete remission. Three patients dropped out of the study before week 48: one because of decreased estimated glomerular filtration rate, one because of a systemic lupus erythematosus flare, and one at the discretion of an investigator.
All patients showed a 25% reduction in urinary protein creatinine ratio at week 8, with a mean decrease of 61% by week 24. Researchers also saw a 22% increase in mean C3 levels and a 58% increase in mean C4 from baseline to week 24. There was also a decrease in anti–double stranded DNA.
When researchers examined the specificity and sensitivities of these biomarkers at week 8 in predicting renal response at weeks 24 and 48, they found that a 25% reduction in urinary protein creatinine ratio had a good sensitivity (71% and 75% at 24 and 48 weeks, respectively), but low specificity (33% and 24%).
In contrast, normalization of C4 and C3 by week 8 both showed a specificity of 100% by week 24 and 75% by week 48, but a sensitivity of 29% for week 24 and 25% for week 48.
Normalization of anti–double stranded DNA had a sensitivity of 57% at week 24 and 50% at week 48, and a specificity of 100% at week 24 and 50% at week 48.
“Certainly if you use C3, C4, and urinary protein creatinine ratio, you can say to the patient after week 8, ‘I don’t think this is going to work for you. You need to come off this therapy and move to something else,’ ” he said in an interview.
Mr. Huizinga said the company, which recently released 48-week data from the larger AURA-LV study of the same regimen in 265 patients, was now building this week-8 analysis into its studies, and hoped it would also provide an early predictive marker for other clinical trials.
Commenting on the findings, Brad Rovin, MD, professor of nephrology and pathology at Ohio State University, Columbus, and also an adviser to Aurinia, said this predictive ability would be extremely useful for clinicians.
“If a patient isn’t responding appropriately and you can really know that with some degree of certainty at 8 weeks, then instead of waiting 6 months to change therapy, maybe you should change earlier,” Dr. Rovin said in an interview.
This was particularly important in lupus nephritis, as the longer inflammation is allowed to continue, the greater the likelihood that it might tip over into fibrosis, he noted.
The study was funded by Aurinia.
AT LUPUS 2017
Key clinical point: Early reduction in urinary protein creatinine ratio and normalization of inflammatory biomarkers may predict 24- and 48-week lupus nephritis treatment response rates.
Major finding: A 25% reduction in urine protein creatinine ratio, and normalization of C3 or C4 levels at 8 weeks may be predictive of complete remission at 48 weeks.
Data source: The single-center exploratory AURION study of 10 patients with active lupus nephritis.
Disclosures: Mr. Huizinga is vice president of clinical affairs for Aurinia Pharmaceuticals, which funded the study.
AKI seen in 64% of children hospitalized with diabetic ketoacidosis
A high proportion of children with type 1 diabetes who are hospitalized for diabetic ketoacidosis (DKA) develop acute kidney injury (AKI), according to results from a study.
Researchers reviewing records from a Canadian hospital found that in a cohort of 165 children hospitalized for DKA during a 5-year period (2008-2013), 64% developed the complication. Severe forms of AKI (stage 2 or 3) were common, representing 45% and 20%, respectively, of children with AKI. Two patients in the cohort required dialysis.
“We hypothesized that, because DKA is associated with both volume depletion and conservative fluid administration upon presentation, these children are potentially at high risk for AKI, above the level of risk expected by the rare reported cases in the literature,” Dr. Hursh and his colleagues wrote (JAMA Pediatr. 2017 Mar 13. doi: 10.1001/jamapediatrics.2017.0020).
The investigators found that lower serum bicarbonate levels and elevated heart rates were indeed associated with increased risk of severe AKI. Serum bicarbonate level of less than 10 mEq/L was associated with a fivefold increase in the odds of severe (stage 2 or 3) AKI (adjusted odds ratio, 5.22; 95% confidence interval, 1.35-20.22). Each increase of 5 bpm in initial heart rate was associated with a 22% increase in the odds of severe AKI (aOR, 1.22; 95% CI, 1.07-1.39).
Dr. Hursh and his colleagues defined AKI using serum creatinine values. As baseline values prior to hospital admission were not available, the researchers used estimated normal value ranges from published studies, choosing a glomerular filtration rate of 120 mL/min per 1.73 m2 as a standard baseline value. Urine output was not used as a measure because of inconsistent records.
Of particular concern was that more than 40% of patients with AKI “did not have documented resolution of AKI prior to discharge or arrangements for follow-up in the nephrology clinic. Of note, the final AKI stage was severe for 50% of these children,” the researchers wrote in their analysis.
The findings suggest that clinicians “should consider AKI as a frequent complication that accompanies pediatric DKA and should be especially alert to its presence in severe presentations of DKA,” they said. AKI is underrecognized “both because of a lack of awareness of AKI as a complication of DKA and because the serum creatinine level in pediatric patients must be interpreted in the context of the child’s age and height. It is crucial to develop or have in place systems that identify and monitor abnormal markers of renal function in this population.”
The researchers acknowledged as limitations of their study its retrospective design, the absence of baseline serum creatinine values, and the lack of urine output data for use in AKI severity grading. And prospective longitudinal studies, they wrote, “are needed to assess the effect of these AKI episodes on the trajectory of renal disease in children with diabetes.”
The researchers reported no outside funding or relevant financial disclosures.
With the lack of targeted therapies to prevent AKI or decrease its associated consequences, supportive care is the mainstay of treatment and focuses on fluid and electrolyte management, nutrition, prevention of further injury through close attention to medication dosing, and, when needed, renal replacement therapy. At first glance, these findings may not appear to be overly surprising or significant; children with volume depletion have decreased renal blood flow, leading to AKI, which corrects with fluid administration. However, the authors appropriately suggest that this issue is not a simple one and that fluid management should be carefully considered in these patients. Because of severe hyperglycemia and derangements in serum sodium concentration, children with DKA are at risk of potentially catastrophic cerebral edema, leading to recommendations for cautious administration of fluids in this high-risk population.
These findings may lead clinicians and investigators to question established practices related to aggressive fluid administration in the sickest children. While awaiting more research to determine the sweet spot for fluid management in children with AKI, it seems reasonable to give fluids to patients with AKI secondary to volume depletion while quickly shifting to more restrictive strategies in those who do not respond to volume and have decreasing urine output. This may be especially important for children with DKA, as conservative fluid management may decrease central nervous system complications.
We commend the authors for exploring AKI in a novel pediatric population, expanding our knowledge on whom kidney function should be more diligently examined, providing insights on relevant fluid strategies, and increasing awareness for a group of patients who may benefit from closer long-term nephrology follow-up.
Benjamin L. Laskin, MD , is at the Children’s Hospital of Philadelphia, and Jens Goebel, MD , is at Children’s Hospital Colorado, Aurora. Dr. Laskin’s and Dr. Goebel’s comments are excerpted from an editorial accompanying the study by Hursh et al. (JAMA Pediatr. 2017 Mar 13. doi: 10.1001/jamapediatrics.2017.0009). Dr Laskin is supported by a National Institutes of Health grant. The editorialists had no other relevant financial disclosures.
With the lack of targeted therapies to prevent AKI or decrease its associated consequences, supportive care is the mainstay of treatment and focuses on fluid and electrolyte management, nutrition, prevention of further injury through close attention to medication dosing, and, when needed, renal replacement therapy. At first glance, these findings may not appear to be overly surprising or significant; children with volume depletion have decreased renal blood flow, leading to AKI, which corrects with fluid administration. However, the authors appropriately suggest that this issue is not a simple one and that fluid management should be carefully considered in these patients. Because of severe hyperglycemia and derangements in serum sodium concentration, children with DKA are at risk of potentially catastrophic cerebral edema, leading to recommendations for cautious administration of fluids in this high-risk population.
These findings may lead clinicians and investigators to question established practices related to aggressive fluid administration in the sickest children. While awaiting more research to determine the sweet spot for fluid management in children with AKI, it seems reasonable to give fluids to patients with AKI secondary to volume depletion while quickly shifting to more restrictive strategies in those who do not respond to volume and have decreasing urine output. This may be especially important for children with DKA, as conservative fluid management may decrease central nervous system complications.
We commend the authors for exploring AKI in a novel pediatric population, expanding our knowledge on whom kidney function should be more diligently examined, providing insights on relevant fluid strategies, and increasing awareness for a group of patients who may benefit from closer long-term nephrology follow-up.
Benjamin L. Laskin, MD , is at the Children’s Hospital of Philadelphia, and Jens Goebel, MD , is at Children’s Hospital Colorado, Aurora. Dr. Laskin’s and Dr. Goebel’s comments are excerpted from an editorial accompanying the study by Hursh et al. (JAMA Pediatr. 2017 Mar 13. doi: 10.1001/jamapediatrics.2017.0009). Dr Laskin is supported by a National Institutes of Health grant. The editorialists had no other relevant financial disclosures.
With the lack of targeted therapies to prevent AKI or decrease its associated consequences, supportive care is the mainstay of treatment and focuses on fluid and electrolyte management, nutrition, prevention of further injury through close attention to medication dosing, and, when needed, renal replacement therapy. At first glance, these findings may not appear to be overly surprising or significant; children with volume depletion have decreased renal blood flow, leading to AKI, which corrects with fluid administration. However, the authors appropriately suggest that this issue is not a simple one and that fluid management should be carefully considered in these patients. Because of severe hyperglycemia and derangements in serum sodium concentration, children with DKA are at risk of potentially catastrophic cerebral edema, leading to recommendations for cautious administration of fluids in this high-risk population.
These findings may lead clinicians and investigators to question established practices related to aggressive fluid administration in the sickest children. While awaiting more research to determine the sweet spot for fluid management in children with AKI, it seems reasonable to give fluids to patients with AKI secondary to volume depletion while quickly shifting to more restrictive strategies in those who do not respond to volume and have decreasing urine output. This may be especially important for children with DKA, as conservative fluid management may decrease central nervous system complications.
We commend the authors for exploring AKI in a novel pediatric population, expanding our knowledge on whom kidney function should be more diligently examined, providing insights on relevant fluid strategies, and increasing awareness for a group of patients who may benefit from closer long-term nephrology follow-up.
Benjamin L. Laskin, MD , is at the Children’s Hospital of Philadelphia, and Jens Goebel, MD , is at Children’s Hospital Colorado, Aurora. Dr. Laskin’s and Dr. Goebel’s comments are excerpted from an editorial accompanying the study by Hursh et al. (JAMA Pediatr. 2017 Mar 13. doi: 10.1001/jamapediatrics.2017.0009). Dr Laskin is supported by a National Institutes of Health grant. The editorialists had no other relevant financial disclosures.
A high proportion of children with type 1 diabetes who are hospitalized for diabetic ketoacidosis (DKA) develop acute kidney injury (AKI), according to results from a study.
Researchers reviewing records from a Canadian hospital found that in a cohort of 165 children hospitalized for DKA during a 5-year period (2008-2013), 64% developed the complication. Severe forms of AKI (stage 2 or 3) were common, representing 45% and 20%, respectively, of children with AKI. Two patients in the cohort required dialysis.
“We hypothesized that, because DKA is associated with both volume depletion and conservative fluid administration upon presentation, these children are potentially at high risk for AKI, above the level of risk expected by the rare reported cases in the literature,” Dr. Hursh and his colleagues wrote (JAMA Pediatr. 2017 Mar 13. doi: 10.1001/jamapediatrics.2017.0020).
The investigators found that lower serum bicarbonate levels and elevated heart rates were indeed associated with increased risk of severe AKI. Serum bicarbonate level of less than 10 mEq/L was associated with a fivefold increase in the odds of severe (stage 2 or 3) AKI (adjusted odds ratio, 5.22; 95% confidence interval, 1.35-20.22). Each increase of 5 bpm in initial heart rate was associated with a 22% increase in the odds of severe AKI (aOR, 1.22; 95% CI, 1.07-1.39).
Dr. Hursh and his colleagues defined AKI using serum creatinine values. As baseline values prior to hospital admission were not available, the researchers used estimated normal value ranges from published studies, choosing a glomerular filtration rate of 120 mL/min per 1.73 m2 as a standard baseline value. Urine output was not used as a measure because of inconsistent records.
Of particular concern was that more than 40% of patients with AKI “did not have documented resolution of AKI prior to discharge or arrangements for follow-up in the nephrology clinic. Of note, the final AKI stage was severe for 50% of these children,” the researchers wrote in their analysis.
The findings suggest that clinicians “should consider AKI as a frequent complication that accompanies pediatric DKA and should be especially alert to its presence in severe presentations of DKA,” they said. AKI is underrecognized “both because of a lack of awareness of AKI as a complication of DKA and because the serum creatinine level in pediatric patients must be interpreted in the context of the child’s age and height. It is crucial to develop or have in place systems that identify and monitor abnormal markers of renal function in this population.”
The researchers acknowledged as limitations of their study its retrospective design, the absence of baseline serum creatinine values, and the lack of urine output data for use in AKI severity grading. And prospective longitudinal studies, they wrote, “are needed to assess the effect of these AKI episodes on the trajectory of renal disease in children with diabetes.”
The researchers reported no outside funding or relevant financial disclosures.
A high proportion of children with type 1 diabetes who are hospitalized for diabetic ketoacidosis (DKA) develop acute kidney injury (AKI), according to results from a study.
Researchers reviewing records from a Canadian hospital found that in a cohort of 165 children hospitalized for DKA during a 5-year period (2008-2013), 64% developed the complication. Severe forms of AKI (stage 2 or 3) were common, representing 45% and 20%, respectively, of children with AKI. Two patients in the cohort required dialysis.
“We hypothesized that, because DKA is associated with both volume depletion and conservative fluid administration upon presentation, these children are potentially at high risk for AKI, above the level of risk expected by the rare reported cases in the literature,” Dr. Hursh and his colleagues wrote (JAMA Pediatr. 2017 Mar 13. doi: 10.1001/jamapediatrics.2017.0020).
The investigators found that lower serum bicarbonate levels and elevated heart rates were indeed associated with increased risk of severe AKI. Serum bicarbonate level of less than 10 mEq/L was associated with a fivefold increase in the odds of severe (stage 2 or 3) AKI (adjusted odds ratio, 5.22; 95% confidence interval, 1.35-20.22). Each increase of 5 bpm in initial heart rate was associated with a 22% increase in the odds of severe AKI (aOR, 1.22; 95% CI, 1.07-1.39).
Dr. Hursh and his colleagues defined AKI using serum creatinine values. As baseline values prior to hospital admission were not available, the researchers used estimated normal value ranges from published studies, choosing a glomerular filtration rate of 120 mL/min per 1.73 m2 as a standard baseline value. Urine output was not used as a measure because of inconsistent records.
Of particular concern was that more than 40% of patients with AKI “did not have documented resolution of AKI prior to discharge or arrangements for follow-up in the nephrology clinic. Of note, the final AKI stage was severe for 50% of these children,” the researchers wrote in their analysis.
The findings suggest that clinicians “should consider AKI as a frequent complication that accompanies pediatric DKA and should be especially alert to its presence in severe presentations of DKA,” they said. AKI is underrecognized “both because of a lack of awareness of AKI as a complication of DKA and because the serum creatinine level in pediatric patients must be interpreted in the context of the child’s age and height. It is crucial to develop or have in place systems that identify and monitor abnormal markers of renal function in this population.”
The researchers acknowledged as limitations of their study its retrospective design, the absence of baseline serum creatinine values, and the lack of urine output data for use in AKI severity grading. And prospective longitudinal studies, they wrote, “are needed to assess the effect of these AKI episodes on the trajectory of renal disease in children with diabetes.”
The researchers reported no outside funding or relevant financial disclosures.
FROM JAMA PEDIATRICS
Key clinical point: Acute kidney injury may occur in up to two-thirds of children hospitalized for diabetic ketoacidosis.
Major finding: In a cohort of 165 children hospitalized with DKA, 64% developed AKI. Of these, 45% had stage 2 AKI and 20% had stage 3.
Data source: A retrospective single-site cohort study of records from 165 children with DKA hospitalized from 2008 to 2013.
Disclosures: The researchers disclosed no outside funding or relevant financial conflicts of interest.
Voclosporin linked to threefold increase in lupus nephritis remission
Treatment with the investigational calcineurin inhibitor voclosporin is associated with a significant, threefold-higher rate of complete remission for lupus nephritis, compared with the current standard of care, according to 48-week data from the AURA-LV (Aurinia Urinary Protein Reduction Active–Lupus With Voclosporin) study.
In a company release, manufacturer Aurinia Pharmaceuticals presented the results of the international phase IIb controlled trial involving 265 patients with active lupus nephritis from 20 countries, which they say has now met its primary and secondary endpoints.
After 48 weeks, 49% of patients in the low-dose group and 40% in the high-dose group had achieved complete remission, compared with 24% in the control group (P less than .001 for low-dose vs. control; P = .026 for high-dose vs. control). This represented a threefold-higher remission rate for the low-dose group (odds ratio, 3.21) and a twofold-higher rate for the high-dose group (OR, 2.1), compared with controls.
Complete remission was defined as a composite endpoint that included urine protein/creatinine ratio of 0.5 mg/mg or less; normal, stable renal function; presence of sustained, low dose steroids; and no administration of rescue medications.
Partial remission – defined as at least a 50% reduction in urine protein/creatinine ratio with no concomitant use of rescue medication – was seen in 68% of patients in the low-dose voclosporin group, 72% of patients in the high-dose group, and 48% of patients in the control arm (P = .007 for low-dose vs. control; P = .002 for high-dose vs. control).
Investigators said there were no unexpected safety signals from voclosporin, but there were three deaths and one malignancy reported in the control arm after the study treatment period ended.
Brad Rovin, MD, of Ohio State University in Columbus said in the company’s statement that current treatments for this severe complication of systemic lupus erythematosus are toxic, and complete renal response rates are low.
“The AURA trial’s long-term results convincingly demonstrate that the addition of voclosporin to standard of care treatment is superior to standard of care alone,” Dr. Rovin said. “This is an impressive renal response rate, and these results may shift the treatment paradigm of lupus nephritis.”
Aurinia’s chief medical officer, Neil Solomons, MD, said in the release that the results provide the company with confidence that they can now execute a successful phase III program.
The 24-week results of the study – in which all primary and the 24-week secondary endpoints were also met – were released in November 2016.
Treatment with the investigational calcineurin inhibitor voclosporin is associated with a significant, threefold-higher rate of complete remission for lupus nephritis, compared with the current standard of care, according to 48-week data from the AURA-LV (Aurinia Urinary Protein Reduction Active–Lupus With Voclosporin) study.
In a company release, manufacturer Aurinia Pharmaceuticals presented the results of the international phase IIb controlled trial involving 265 patients with active lupus nephritis from 20 countries, which they say has now met its primary and secondary endpoints.
After 48 weeks, 49% of patients in the low-dose group and 40% in the high-dose group had achieved complete remission, compared with 24% in the control group (P less than .001 for low-dose vs. control; P = .026 for high-dose vs. control). This represented a threefold-higher remission rate for the low-dose group (odds ratio, 3.21) and a twofold-higher rate for the high-dose group (OR, 2.1), compared with controls.
Complete remission was defined as a composite endpoint that included urine protein/creatinine ratio of 0.5 mg/mg or less; normal, stable renal function; presence of sustained, low dose steroids; and no administration of rescue medications.
Partial remission – defined as at least a 50% reduction in urine protein/creatinine ratio with no concomitant use of rescue medication – was seen in 68% of patients in the low-dose voclosporin group, 72% of patients in the high-dose group, and 48% of patients in the control arm (P = .007 for low-dose vs. control; P = .002 for high-dose vs. control).
Investigators said there were no unexpected safety signals from voclosporin, but there were three deaths and one malignancy reported in the control arm after the study treatment period ended.
Brad Rovin, MD, of Ohio State University in Columbus said in the company’s statement that current treatments for this severe complication of systemic lupus erythematosus are toxic, and complete renal response rates are low.
“The AURA trial’s long-term results convincingly demonstrate that the addition of voclosporin to standard of care treatment is superior to standard of care alone,” Dr. Rovin said. “This is an impressive renal response rate, and these results may shift the treatment paradigm of lupus nephritis.”
Aurinia’s chief medical officer, Neil Solomons, MD, said in the release that the results provide the company with confidence that they can now execute a successful phase III program.
The 24-week results of the study – in which all primary and the 24-week secondary endpoints were also met – were released in November 2016.
Treatment with the investigational calcineurin inhibitor voclosporin is associated with a significant, threefold-higher rate of complete remission for lupus nephritis, compared with the current standard of care, according to 48-week data from the AURA-LV (Aurinia Urinary Protein Reduction Active–Lupus With Voclosporin) study.
In a company release, manufacturer Aurinia Pharmaceuticals presented the results of the international phase IIb controlled trial involving 265 patients with active lupus nephritis from 20 countries, which they say has now met its primary and secondary endpoints.
After 48 weeks, 49% of patients in the low-dose group and 40% in the high-dose group had achieved complete remission, compared with 24% in the control group (P less than .001 for low-dose vs. control; P = .026 for high-dose vs. control). This represented a threefold-higher remission rate for the low-dose group (odds ratio, 3.21) and a twofold-higher rate for the high-dose group (OR, 2.1), compared with controls.
Complete remission was defined as a composite endpoint that included urine protein/creatinine ratio of 0.5 mg/mg or less; normal, stable renal function; presence of sustained, low dose steroids; and no administration of rescue medications.
Partial remission – defined as at least a 50% reduction in urine protein/creatinine ratio with no concomitant use of rescue medication – was seen in 68% of patients in the low-dose voclosporin group, 72% of patients in the high-dose group, and 48% of patients in the control arm (P = .007 for low-dose vs. control; P = .002 for high-dose vs. control).
Investigators said there were no unexpected safety signals from voclosporin, but there were three deaths and one malignancy reported in the control arm after the study treatment period ended.
Brad Rovin, MD, of Ohio State University in Columbus said in the company’s statement that current treatments for this severe complication of systemic lupus erythematosus are toxic, and complete renal response rates are low.
“The AURA trial’s long-term results convincingly demonstrate that the addition of voclosporin to standard of care treatment is superior to standard of care alone,” Dr. Rovin said. “This is an impressive renal response rate, and these results may shift the treatment paradigm of lupus nephritis.”
Aurinia’s chief medical officer, Neil Solomons, MD, said in the release that the results provide the company with confidence that they can now execute a successful phase III program.
The 24-week results of the study – in which all primary and the 24-week secondary endpoints were also met – were released in November 2016.
Key clinical point:
Major finding: Nearly half of patients treated with the lower dose of investigational calcineurin inhibitor voclosporin achieved complete remission compared to one-quarter of patients in the control group.
Data source: The AURA-LV phase IIb controlled study involving 265 patients with active lupus nephritis.
Disclosures: The results were presented in a company release from manufacturer Aurinia Pharmaceuticals.
Porcelain heart in a uremic patient
A 58-year-old man with end-stage renal disease due to diabetic nephropathy was admitted with aggravated exertional dyspnea and intermittent chest pain for 1 week. He had been on hemodialysis for 15 years.
His blood pressure was 124/69 mm Hg, pulse 96 beats per minute, and temperature 35.8°C. On physical examination, he had bilateral diffuse crackles, elevated jugular venous pressure (9.5 cm H2O) with positive hepatojugular reflux, and apparent dependent pedal edema. The Kussmaul sign was not observed.
Cardiac enzymes were in the normal range (creatine kinase 73 U/L, troponin I 0.032 ng/mL), but the brain-natriuretic peptide level was elevated at 340 pg/mL. Other laboratory findings included calcium 9 mg/dL (reference range 8.4–10.2 mg/dL), inorganic phosphate 5 mg/dL (2.5–4.5 mg/dL), and intact parathyroid hormone 1,457 pg/mL (10–69 pg/mL).
Electrocardiography showed sinus tachycardia with low voltage in diffuse leads and generalized flattening of the T wave. Chest radiography showed a bilateral reticulonodular pattern, mild costophrenic angle obliteration, and notable calcifications along the cardiac contour. Thoracic computed tomography showed a porcelain-like encasement of the heart (Figure 1). Transthoracic echocardiography showed thickened pericardium, pericardial calcification, and mild interventricular septal bounce in diastole, with no dyskinesia of ventricular wall motion. We decided not to perform an invasive hemodynamic assessment.
CAUSES OF PERICARDIAL CALCIFICATION
Pericardial calcification, abnormal calcium deposits in response to inflammation,1 has become more widely reported as the use of chest computed tomography has become more widespread. The common identifiable causes of pericardial calcification include recurrent or chronic pericarditis, radiation therapy for Hodgkin lymphoma or breast cancer, tuberculosis, and end-stage kidney disease.2,3 Other possible causes are retention of uremic metabolites, metastatic calcification induced by secondary hyperparathyroidism, and calcium-phosphate deposition induced by hyperphosphatemia.4
In chronic kidney disease, the amount of pericardial fluid and fibrinous pericardial deposition is thought to contribute to increased pericardial thickness and constriction. In some patients, pericardial calcification and thickening would lead to constrictive pericarditis, which could be confirmed by echocardiography and cardiac catheterization. About 25% to 50% of cases of pericardial calcification are complicated by constrictive pericarditis.5,6 Constrictive pericarditis occurs in up to 4% of patients with end-stage renal disease, even with successful dialysis.7
Partial clinical improvement may be obtained with intensive hemodialysis, strict volume control, and decreased catabolism in patients with multiple comorbidities.8 However, the definite treatment is total pericardiectomy, which reduces symptoms substantially and offers a favorable long-term outcome.7
SECONDARY HYPERPARATHYROIDISM
Secondary hyperparathyroidism is a common complication in patients with end-stage renal disease and is characterized by derangements in the homeostasis of calcium, phosphorus, and vitamin D.9
Because renal function is decreased, phosphate is retained and calcitriol synthesis is reduced, resulting in hypocalcemia, which induces parathyroid gland hyperplasia and parathyroid hormone secretion.10 Moreover, some patents with long-standing secondary hyperparathyroidism may develop tertiary hyperparathyroidism associated with autonomous parathyroid hormone secretion, hypercalcemia, and hyperphosphatemia.11
The Kidney Disease: Improving Global Outcomes (KDIGO) Work Group recommends screening for and managing secondary hyperparathyroidism in all patients with stage 3 chronic kidney disease (estimated glomerular filtration rate < 60 mL/min). In patients with stage 5 chronic kidney disease or on dialysis, the serum calcium and phosphorus levels should be monitored every 1 to 3 months and the parathyroid hormone levels every 3 to 6 months.12
According to KDIGO guidelines, the target level of calcium is less than 10.2 mg/dL, and the target phosphorus level is less than 4.6 mg/dL. The level of parathyroid hormone should be maintained at 2 to 9 times the upper limit of normal for the assay.
The management of secondary hyperparathyroidism includes a low-phosphorus diet, calcium-containing or calcium-free phosphate binders, a calcitriol supplement, and calcimimetics. If medical treatment fails and manifestations are significant, parathyroidectomy may be indicated.13
- Alpert MA, Ravenscraft MD. Pericardial involvement in end-stage renal disease. Am J Med Sci 2003; 325:228–236.
- Gowda RM, Boxt LM. Calcifications of the heart. Radiol Clin North Am 2004; 42:603–617.
- Kleynberg RL, Kleynberg VM, Kleynberg LM, Farahmandian D. Chronic constrictive pericarditis in association with end-stage renal disease. Int J Nephrol 2011; 2011:469602.
- Rao N, Crail S. Metastatic calcification and long-term hemodialysis. N Engl J Med 2013; 368:2415.
- Ling LH, Oh JK, Schaff HV, et al. Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy. Circulation 1999; 100:1380–1386.
- Bergman M, Vitrai J, Salman H. Constrictive pericarditis: a reminder of a not so rare disease. Eur J Intern Med 2006; 17:457–464.
- Szabó G, Schmack B, Bulut C, et al. Constrictive pericarditis: risks, aetiologies and outcomes after total pericardiectomy: 24 years of experience. Eur J Cardiothorac Surg 2013; 44:1023–1028.
- Feldman V, Dovrish Z, Weisenberg N, Neuman Y, Amital H. Uremic pericarditis. Isr Med Assoc J 2011; 13:256–257.
- Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 2007; 71:31–38.
- Martin KJ, Gonzalez EA. Metabolic bone disease in chronic kidney disease. J Am Soc Nephrol 2007; 18:875–885.
- Kerby J, Rue LW, Blair H, Hudson S, Sellers MT, Diethelm AG. Operative treatment of tertiary hyperparathyroidism: a single-center experience. Ann Surg 1998; 227:878–886.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKDMBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease—mineral and bone disorder (CKD-MBD). Kidney Int Suppl 2009; 76:S1–130.
- National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 2003; 42(4 suppl 3):S1–201.
A 58-year-old man with end-stage renal disease due to diabetic nephropathy was admitted with aggravated exertional dyspnea and intermittent chest pain for 1 week. He had been on hemodialysis for 15 years.
His blood pressure was 124/69 mm Hg, pulse 96 beats per minute, and temperature 35.8°C. On physical examination, he had bilateral diffuse crackles, elevated jugular venous pressure (9.5 cm H2O) with positive hepatojugular reflux, and apparent dependent pedal edema. The Kussmaul sign was not observed.
Cardiac enzymes were in the normal range (creatine kinase 73 U/L, troponin I 0.032 ng/mL), but the brain-natriuretic peptide level was elevated at 340 pg/mL. Other laboratory findings included calcium 9 mg/dL (reference range 8.4–10.2 mg/dL), inorganic phosphate 5 mg/dL (2.5–4.5 mg/dL), and intact parathyroid hormone 1,457 pg/mL (10–69 pg/mL).
Electrocardiography showed sinus tachycardia with low voltage in diffuse leads and generalized flattening of the T wave. Chest radiography showed a bilateral reticulonodular pattern, mild costophrenic angle obliteration, and notable calcifications along the cardiac contour. Thoracic computed tomography showed a porcelain-like encasement of the heart (Figure 1). Transthoracic echocardiography showed thickened pericardium, pericardial calcification, and mild interventricular septal bounce in diastole, with no dyskinesia of ventricular wall motion. We decided not to perform an invasive hemodynamic assessment.
CAUSES OF PERICARDIAL CALCIFICATION
Pericardial calcification, abnormal calcium deposits in response to inflammation,1 has become more widely reported as the use of chest computed tomography has become more widespread. The common identifiable causes of pericardial calcification include recurrent or chronic pericarditis, radiation therapy for Hodgkin lymphoma or breast cancer, tuberculosis, and end-stage kidney disease.2,3 Other possible causes are retention of uremic metabolites, metastatic calcification induced by secondary hyperparathyroidism, and calcium-phosphate deposition induced by hyperphosphatemia.4
In chronic kidney disease, the amount of pericardial fluid and fibrinous pericardial deposition is thought to contribute to increased pericardial thickness and constriction. In some patients, pericardial calcification and thickening would lead to constrictive pericarditis, which could be confirmed by echocardiography and cardiac catheterization. About 25% to 50% of cases of pericardial calcification are complicated by constrictive pericarditis.5,6 Constrictive pericarditis occurs in up to 4% of patients with end-stage renal disease, even with successful dialysis.7
Partial clinical improvement may be obtained with intensive hemodialysis, strict volume control, and decreased catabolism in patients with multiple comorbidities.8 However, the definite treatment is total pericardiectomy, which reduces symptoms substantially and offers a favorable long-term outcome.7
SECONDARY HYPERPARATHYROIDISM
Secondary hyperparathyroidism is a common complication in patients with end-stage renal disease and is characterized by derangements in the homeostasis of calcium, phosphorus, and vitamin D.9
Because renal function is decreased, phosphate is retained and calcitriol synthesis is reduced, resulting in hypocalcemia, which induces parathyroid gland hyperplasia and parathyroid hormone secretion.10 Moreover, some patents with long-standing secondary hyperparathyroidism may develop tertiary hyperparathyroidism associated with autonomous parathyroid hormone secretion, hypercalcemia, and hyperphosphatemia.11
The Kidney Disease: Improving Global Outcomes (KDIGO) Work Group recommends screening for and managing secondary hyperparathyroidism in all patients with stage 3 chronic kidney disease (estimated glomerular filtration rate < 60 mL/min). In patients with stage 5 chronic kidney disease or on dialysis, the serum calcium and phosphorus levels should be monitored every 1 to 3 months and the parathyroid hormone levels every 3 to 6 months.12
According to KDIGO guidelines, the target level of calcium is less than 10.2 mg/dL, and the target phosphorus level is less than 4.6 mg/dL. The level of parathyroid hormone should be maintained at 2 to 9 times the upper limit of normal for the assay.
The management of secondary hyperparathyroidism includes a low-phosphorus diet, calcium-containing or calcium-free phosphate binders, a calcitriol supplement, and calcimimetics. If medical treatment fails and manifestations are significant, parathyroidectomy may be indicated.13
A 58-year-old man with end-stage renal disease due to diabetic nephropathy was admitted with aggravated exertional dyspnea and intermittent chest pain for 1 week. He had been on hemodialysis for 15 years.
His blood pressure was 124/69 mm Hg, pulse 96 beats per minute, and temperature 35.8°C. On physical examination, he had bilateral diffuse crackles, elevated jugular venous pressure (9.5 cm H2O) with positive hepatojugular reflux, and apparent dependent pedal edema. The Kussmaul sign was not observed.
Cardiac enzymes were in the normal range (creatine kinase 73 U/L, troponin I 0.032 ng/mL), but the brain-natriuretic peptide level was elevated at 340 pg/mL. Other laboratory findings included calcium 9 mg/dL (reference range 8.4–10.2 mg/dL), inorganic phosphate 5 mg/dL (2.5–4.5 mg/dL), and intact parathyroid hormone 1,457 pg/mL (10–69 pg/mL).
Electrocardiography showed sinus tachycardia with low voltage in diffuse leads and generalized flattening of the T wave. Chest radiography showed a bilateral reticulonodular pattern, mild costophrenic angle obliteration, and notable calcifications along the cardiac contour. Thoracic computed tomography showed a porcelain-like encasement of the heart (Figure 1). Transthoracic echocardiography showed thickened pericardium, pericardial calcification, and mild interventricular septal bounce in diastole, with no dyskinesia of ventricular wall motion. We decided not to perform an invasive hemodynamic assessment.
CAUSES OF PERICARDIAL CALCIFICATION
Pericardial calcification, abnormal calcium deposits in response to inflammation,1 has become more widely reported as the use of chest computed tomography has become more widespread. The common identifiable causes of pericardial calcification include recurrent or chronic pericarditis, radiation therapy for Hodgkin lymphoma or breast cancer, tuberculosis, and end-stage kidney disease.2,3 Other possible causes are retention of uremic metabolites, metastatic calcification induced by secondary hyperparathyroidism, and calcium-phosphate deposition induced by hyperphosphatemia.4
In chronic kidney disease, the amount of pericardial fluid and fibrinous pericardial deposition is thought to contribute to increased pericardial thickness and constriction. In some patients, pericardial calcification and thickening would lead to constrictive pericarditis, which could be confirmed by echocardiography and cardiac catheterization. About 25% to 50% of cases of pericardial calcification are complicated by constrictive pericarditis.5,6 Constrictive pericarditis occurs in up to 4% of patients with end-stage renal disease, even with successful dialysis.7
Partial clinical improvement may be obtained with intensive hemodialysis, strict volume control, and decreased catabolism in patients with multiple comorbidities.8 However, the definite treatment is total pericardiectomy, which reduces symptoms substantially and offers a favorable long-term outcome.7
SECONDARY HYPERPARATHYROIDISM
Secondary hyperparathyroidism is a common complication in patients with end-stage renal disease and is characterized by derangements in the homeostasis of calcium, phosphorus, and vitamin D.9
Because renal function is decreased, phosphate is retained and calcitriol synthesis is reduced, resulting in hypocalcemia, which induces parathyroid gland hyperplasia and parathyroid hormone secretion.10 Moreover, some patents with long-standing secondary hyperparathyroidism may develop tertiary hyperparathyroidism associated with autonomous parathyroid hormone secretion, hypercalcemia, and hyperphosphatemia.11
The Kidney Disease: Improving Global Outcomes (KDIGO) Work Group recommends screening for and managing secondary hyperparathyroidism in all patients with stage 3 chronic kidney disease (estimated glomerular filtration rate < 60 mL/min). In patients with stage 5 chronic kidney disease or on dialysis, the serum calcium and phosphorus levels should be monitored every 1 to 3 months and the parathyroid hormone levels every 3 to 6 months.12
According to KDIGO guidelines, the target level of calcium is less than 10.2 mg/dL, and the target phosphorus level is less than 4.6 mg/dL. The level of parathyroid hormone should be maintained at 2 to 9 times the upper limit of normal for the assay.
The management of secondary hyperparathyroidism includes a low-phosphorus diet, calcium-containing or calcium-free phosphate binders, a calcitriol supplement, and calcimimetics. If medical treatment fails and manifestations are significant, parathyroidectomy may be indicated.13
- Alpert MA, Ravenscraft MD. Pericardial involvement in end-stage renal disease. Am J Med Sci 2003; 325:228–236.
- Gowda RM, Boxt LM. Calcifications of the heart. Radiol Clin North Am 2004; 42:603–617.
- Kleynberg RL, Kleynberg VM, Kleynberg LM, Farahmandian D. Chronic constrictive pericarditis in association with end-stage renal disease. Int J Nephrol 2011; 2011:469602.
- Rao N, Crail S. Metastatic calcification and long-term hemodialysis. N Engl J Med 2013; 368:2415.
- Ling LH, Oh JK, Schaff HV, et al. Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy. Circulation 1999; 100:1380–1386.
- Bergman M, Vitrai J, Salman H. Constrictive pericarditis: a reminder of a not so rare disease. Eur J Intern Med 2006; 17:457–464.
- Szabó G, Schmack B, Bulut C, et al. Constrictive pericarditis: risks, aetiologies and outcomes after total pericardiectomy: 24 years of experience. Eur J Cardiothorac Surg 2013; 44:1023–1028.
- Feldman V, Dovrish Z, Weisenberg N, Neuman Y, Amital H. Uremic pericarditis. Isr Med Assoc J 2011; 13:256–257.
- Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 2007; 71:31–38.
- Martin KJ, Gonzalez EA. Metabolic bone disease in chronic kidney disease. J Am Soc Nephrol 2007; 18:875–885.
- Kerby J, Rue LW, Blair H, Hudson S, Sellers MT, Diethelm AG. Operative treatment of tertiary hyperparathyroidism: a single-center experience. Ann Surg 1998; 227:878–886.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKDMBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease—mineral and bone disorder (CKD-MBD). Kidney Int Suppl 2009; 76:S1–130.
- National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 2003; 42(4 suppl 3):S1–201.
- Alpert MA, Ravenscraft MD. Pericardial involvement in end-stage renal disease. Am J Med Sci 2003; 325:228–236.
- Gowda RM, Boxt LM. Calcifications of the heart. Radiol Clin North Am 2004; 42:603–617.
- Kleynberg RL, Kleynberg VM, Kleynberg LM, Farahmandian D. Chronic constrictive pericarditis in association with end-stage renal disease. Int J Nephrol 2011; 2011:469602.
- Rao N, Crail S. Metastatic calcification and long-term hemodialysis. N Engl J Med 2013; 368:2415.
- Ling LH, Oh JK, Schaff HV, et al. Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy. Circulation 1999; 100:1380–1386.
- Bergman M, Vitrai J, Salman H. Constrictive pericarditis: a reminder of a not so rare disease. Eur J Intern Med 2006; 17:457–464.
- Szabó G, Schmack B, Bulut C, et al. Constrictive pericarditis: risks, aetiologies and outcomes after total pericardiectomy: 24 years of experience. Eur J Cardiothorac Surg 2013; 44:1023–1028.
- Feldman V, Dovrish Z, Weisenberg N, Neuman Y, Amital H. Uremic pericarditis. Isr Med Assoc J 2011; 13:256–257.
- Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 2007; 71:31–38.
- Martin KJ, Gonzalez EA. Metabolic bone disease in chronic kidney disease. J Am Soc Nephrol 2007; 18:875–885.
- Kerby J, Rue LW, Blair H, Hudson S, Sellers MT, Diethelm AG. Operative treatment of tertiary hyperparathyroidism: a single-center experience. Ann Surg 1998; 227:878–886.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKDMBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease—mineral and bone disorder (CKD-MBD). Kidney Int Suppl 2009; 76:S1–130.
- National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 2003; 42(4 suppl 3):S1–201.