User login
Early menopause, delayed HT tied to Alzheimer’s pathology
Investigators found elevated levels of tau protein in the brains of women who initiated HT more than 5 years after menopause onset, while those who started the therapy earlier had normal levels.
Tau levels were also higher in women who started menopause before age 45, either naturally or following surgery, but only in those who already had high levels of beta-amyloid.
The findings were published online in JAMA Neurology.
Hotly debated
Previous research has suggested the timing of menopause and HT initiation may be associated with AD. However, the current research is the first to suggest tau deposition may explain that link.
“There have been a lot of conflicting findings around whether HT induces risk for Alzheimer’s disease dementia or not, and – at least in our hands – our observational evidence suggests that any risk is fairly limited to those rarer cases when women might delay their initiation of HT considerably,” senior investigator Rachel Buckley, PhD, assistant investigator in neurology at Massachusetts General Hospital and assistant professor of neurology at Harvard Medical School, Boston, told this news organization.
The link between HT, dementia, and cognitive decline has been hotly debated since the initial release of findings from the Women’s Health Initiative Memory Study, reported 20 years ago.
Since then, dozens of studies have yielded conflicting evidence about HT and AD risk, with some showing a protective effect and others showing the treatment may increase AD risk.
For this study, researchers analyzed data from 292 cognitively unimpaired participants (66.1% female) in the Wisconsin Registry for Alzheimer Prevention. About half of the women had received HT.
Women had higher levels of tau measured on PET imaging than age-matched males, even after adjustment for APOE status and other potential confounders.
Higher tau levels were found in those with an earlier age at menopause (P < .001) and HT use (P = .008) compared with male sex; later menopause onset; or HT nonuse – but only in patients who also had a higher beta-amyloid burden.
Late initiation of HT (> 5 years following age at menopause) was associated with higher tau compared with early initiation (P = .001), regardless of amyloid levels.
Surprising finding
Although researchers expected to find that surgical history (specifically oophorectomy) might have a greater impact on risk, that wasn’t the case.
“Given that bilateral oophorectomy involves the removal of both ovaries, and the immediate ceasing of estrogen production, I had expected this to be the primary driver of higher tau levels,” Dr. Buckley said. “But early age at menopause – regardless of whether the genesis was natural or surgical – seemed to have similar impacts.”
These findings are the latest from Dr. Buckley’s group that indicate that women tend to have higher levels of tau than men, regardless of preexisting amyloid burden in the brain.
“We see this in healthy older women, women with dementia, and even in postmortem cases,” Dr. Buckley said. “It really remains to be seen whether women tend to accumulate tau faster in the brain than men, or whether this is simply a one-shot phenomenon that we see in observational studies at the baseline.”
“One could really flip this finding on its head and suggest that women are truly resilient to the disease,” she continued. “That is, they can hold much more tau in their brain and remain well enough to be studied, unlike men.”
Among the study’s limitations is that the data were collected at a single time point and did not include information on subsequent Alzheimer’s diagnosis or cognitive decline.
“It is important to remember that the participants in this study were not as representative of the general population in the United States, so we cannot extrapolate our findings to women from a range of socioeconomic, racial and ethnic backgrounds or education levels,” she said.
The study’s observational design left researchers unable to demonstrate causation. What’s more, the findings don’t support the assertion that hormone therapy may protect against AD, Dr. Buckley added.
“I would more confidently say that evidence from our work, and that of many others, seems to suggest that HT initiated around the time of menopause may be benign – not providing benefit or risk, at least in the context of Alzheimer’s disease risk,” she said.
Another important takeaway from the study, Dr. Buckley said, is that not all women are at high risk for AD.
“Often the headlines might make you think that most women are destined to progress to dementia, but this simply is not the case,” Dr. Buckley said. “We are now starting to really drill down on what might elevate risk for AD in women and use this information to better inform clinical trials and doctors on how best to think about treating these higher-risk groups.”
New mechanism?
Commenting on the findings, Pauline Maki, PhD, professor of psychiatry, psychology and obstetrics & gynecology at the University of Illinois at Chicago, called the study “interesting.”
“It identifies a new mechanism in humans that could underlie a possible link between sex hormones and dementia,” Dr. Maki said.
However, Dr. Maki noted that the study wasn’t randomized and information about menopause onset was self-reported.
“We must remember that many of the hypotheses about hormone therapy and brain health that came from observational studies were not validated in randomized trials, including the hypothesis that hormone therapy prevents dementia,” she said.
The findings don’t resolve the debate over hormone therapy and AD risk and point to the need for randomized, prospective studies on the topic, Dr. Maki added. Still, she said, they underscore the gender disparity in AD risk.
“It’s a good reminder to clinicians that women have a higher lifetime risk of Alzheimer’s disease and should be advised on factors that might lower their risk,” she said.
The study was funded by the National Institutes of Health. Dr. Buckley reports no relevant financial conflicts. Dr. Maki serves on the advisory boards for Astellas, Bayer, Johnson & Johnson, consults for Pfizer and Mithra, and has equity in Estrigenix, Midi-Health, and Alloy.
A version of this article originally appeared on Medscape.com.
Investigators found elevated levels of tau protein in the brains of women who initiated HT more than 5 years after menopause onset, while those who started the therapy earlier had normal levels.
Tau levels were also higher in women who started menopause before age 45, either naturally or following surgery, but only in those who already had high levels of beta-amyloid.
The findings were published online in JAMA Neurology.
Hotly debated
Previous research has suggested the timing of menopause and HT initiation may be associated with AD. However, the current research is the first to suggest tau deposition may explain that link.
“There have been a lot of conflicting findings around whether HT induces risk for Alzheimer’s disease dementia or not, and – at least in our hands – our observational evidence suggests that any risk is fairly limited to those rarer cases when women might delay their initiation of HT considerably,” senior investigator Rachel Buckley, PhD, assistant investigator in neurology at Massachusetts General Hospital and assistant professor of neurology at Harvard Medical School, Boston, told this news organization.
The link between HT, dementia, and cognitive decline has been hotly debated since the initial release of findings from the Women’s Health Initiative Memory Study, reported 20 years ago.
Since then, dozens of studies have yielded conflicting evidence about HT and AD risk, with some showing a protective effect and others showing the treatment may increase AD risk.
For this study, researchers analyzed data from 292 cognitively unimpaired participants (66.1% female) in the Wisconsin Registry for Alzheimer Prevention. About half of the women had received HT.
Women had higher levels of tau measured on PET imaging than age-matched males, even after adjustment for APOE status and other potential confounders.
Higher tau levels were found in those with an earlier age at menopause (P < .001) and HT use (P = .008) compared with male sex; later menopause onset; or HT nonuse – but only in patients who also had a higher beta-amyloid burden.
Late initiation of HT (> 5 years following age at menopause) was associated with higher tau compared with early initiation (P = .001), regardless of amyloid levels.
Surprising finding
Although researchers expected to find that surgical history (specifically oophorectomy) might have a greater impact on risk, that wasn’t the case.
“Given that bilateral oophorectomy involves the removal of both ovaries, and the immediate ceasing of estrogen production, I had expected this to be the primary driver of higher tau levels,” Dr. Buckley said. “But early age at menopause – regardless of whether the genesis was natural or surgical – seemed to have similar impacts.”
These findings are the latest from Dr. Buckley’s group that indicate that women tend to have higher levels of tau than men, regardless of preexisting amyloid burden in the brain.
“We see this in healthy older women, women with dementia, and even in postmortem cases,” Dr. Buckley said. “It really remains to be seen whether women tend to accumulate tau faster in the brain than men, or whether this is simply a one-shot phenomenon that we see in observational studies at the baseline.”
“One could really flip this finding on its head and suggest that women are truly resilient to the disease,” she continued. “That is, they can hold much more tau in their brain and remain well enough to be studied, unlike men.”
Among the study’s limitations is that the data were collected at a single time point and did not include information on subsequent Alzheimer’s diagnosis or cognitive decline.
“It is important to remember that the participants in this study were not as representative of the general population in the United States, so we cannot extrapolate our findings to women from a range of socioeconomic, racial and ethnic backgrounds or education levels,” she said.
The study’s observational design left researchers unable to demonstrate causation. What’s more, the findings don’t support the assertion that hormone therapy may protect against AD, Dr. Buckley added.
“I would more confidently say that evidence from our work, and that of many others, seems to suggest that HT initiated around the time of menopause may be benign – not providing benefit or risk, at least in the context of Alzheimer’s disease risk,” she said.
Another important takeaway from the study, Dr. Buckley said, is that not all women are at high risk for AD.
“Often the headlines might make you think that most women are destined to progress to dementia, but this simply is not the case,” Dr. Buckley said. “We are now starting to really drill down on what might elevate risk for AD in women and use this information to better inform clinical trials and doctors on how best to think about treating these higher-risk groups.”
New mechanism?
Commenting on the findings, Pauline Maki, PhD, professor of psychiatry, psychology and obstetrics & gynecology at the University of Illinois at Chicago, called the study “interesting.”
“It identifies a new mechanism in humans that could underlie a possible link between sex hormones and dementia,” Dr. Maki said.
However, Dr. Maki noted that the study wasn’t randomized and information about menopause onset was self-reported.
“We must remember that many of the hypotheses about hormone therapy and brain health that came from observational studies were not validated in randomized trials, including the hypothesis that hormone therapy prevents dementia,” she said.
The findings don’t resolve the debate over hormone therapy and AD risk and point to the need for randomized, prospective studies on the topic, Dr. Maki added. Still, she said, they underscore the gender disparity in AD risk.
“It’s a good reminder to clinicians that women have a higher lifetime risk of Alzheimer’s disease and should be advised on factors that might lower their risk,” she said.
The study was funded by the National Institutes of Health. Dr. Buckley reports no relevant financial conflicts. Dr. Maki serves on the advisory boards for Astellas, Bayer, Johnson & Johnson, consults for Pfizer and Mithra, and has equity in Estrigenix, Midi-Health, and Alloy.
A version of this article originally appeared on Medscape.com.
Investigators found elevated levels of tau protein in the brains of women who initiated HT more than 5 years after menopause onset, while those who started the therapy earlier had normal levels.
Tau levels were also higher in women who started menopause before age 45, either naturally or following surgery, but only in those who already had high levels of beta-amyloid.
The findings were published online in JAMA Neurology.
Hotly debated
Previous research has suggested the timing of menopause and HT initiation may be associated with AD. However, the current research is the first to suggest tau deposition may explain that link.
“There have been a lot of conflicting findings around whether HT induces risk for Alzheimer’s disease dementia or not, and – at least in our hands – our observational evidence suggests that any risk is fairly limited to those rarer cases when women might delay their initiation of HT considerably,” senior investigator Rachel Buckley, PhD, assistant investigator in neurology at Massachusetts General Hospital and assistant professor of neurology at Harvard Medical School, Boston, told this news organization.
The link between HT, dementia, and cognitive decline has been hotly debated since the initial release of findings from the Women’s Health Initiative Memory Study, reported 20 years ago.
Since then, dozens of studies have yielded conflicting evidence about HT and AD risk, with some showing a protective effect and others showing the treatment may increase AD risk.
For this study, researchers analyzed data from 292 cognitively unimpaired participants (66.1% female) in the Wisconsin Registry for Alzheimer Prevention. About half of the women had received HT.
Women had higher levels of tau measured on PET imaging than age-matched males, even after adjustment for APOE status and other potential confounders.
Higher tau levels were found in those with an earlier age at menopause (P < .001) and HT use (P = .008) compared with male sex; later menopause onset; or HT nonuse – but only in patients who also had a higher beta-amyloid burden.
Late initiation of HT (> 5 years following age at menopause) was associated with higher tau compared with early initiation (P = .001), regardless of amyloid levels.
Surprising finding
Although researchers expected to find that surgical history (specifically oophorectomy) might have a greater impact on risk, that wasn’t the case.
“Given that bilateral oophorectomy involves the removal of both ovaries, and the immediate ceasing of estrogen production, I had expected this to be the primary driver of higher tau levels,” Dr. Buckley said. “But early age at menopause – regardless of whether the genesis was natural or surgical – seemed to have similar impacts.”
These findings are the latest from Dr. Buckley’s group that indicate that women tend to have higher levels of tau than men, regardless of preexisting amyloid burden in the brain.
“We see this in healthy older women, women with dementia, and even in postmortem cases,” Dr. Buckley said. “It really remains to be seen whether women tend to accumulate tau faster in the brain than men, or whether this is simply a one-shot phenomenon that we see in observational studies at the baseline.”
“One could really flip this finding on its head and suggest that women are truly resilient to the disease,” she continued. “That is, they can hold much more tau in their brain and remain well enough to be studied, unlike men.”
Among the study’s limitations is that the data were collected at a single time point and did not include information on subsequent Alzheimer’s diagnosis or cognitive decline.
“It is important to remember that the participants in this study were not as representative of the general population in the United States, so we cannot extrapolate our findings to women from a range of socioeconomic, racial and ethnic backgrounds or education levels,” she said.
The study’s observational design left researchers unable to demonstrate causation. What’s more, the findings don’t support the assertion that hormone therapy may protect against AD, Dr. Buckley added.
“I would more confidently say that evidence from our work, and that of many others, seems to suggest that HT initiated around the time of menopause may be benign – not providing benefit or risk, at least in the context of Alzheimer’s disease risk,” she said.
Another important takeaway from the study, Dr. Buckley said, is that not all women are at high risk for AD.
“Often the headlines might make you think that most women are destined to progress to dementia, but this simply is not the case,” Dr. Buckley said. “We are now starting to really drill down on what might elevate risk for AD in women and use this information to better inform clinical trials and doctors on how best to think about treating these higher-risk groups.”
New mechanism?
Commenting on the findings, Pauline Maki, PhD, professor of psychiatry, psychology and obstetrics & gynecology at the University of Illinois at Chicago, called the study “interesting.”
“It identifies a new mechanism in humans that could underlie a possible link between sex hormones and dementia,” Dr. Maki said.
However, Dr. Maki noted that the study wasn’t randomized and information about menopause onset was self-reported.
“We must remember that many of the hypotheses about hormone therapy and brain health that came from observational studies were not validated in randomized trials, including the hypothesis that hormone therapy prevents dementia,” she said.
The findings don’t resolve the debate over hormone therapy and AD risk and point to the need for randomized, prospective studies on the topic, Dr. Maki added. Still, she said, they underscore the gender disparity in AD risk.
“It’s a good reminder to clinicians that women have a higher lifetime risk of Alzheimer’s disease and should be advised on factors that might lower their risk,” she said.
The study was funded by the National Institutes of Health. Dr. Buckley reports no relevant financial conflicts. Dr. Maki serves on the advisory boards for Astellas, Bayer, Johnson & Johnson, consults for Pfizer and Mithra, and has equity in Estrigenix, Midi-Health, and Alloy.
A version of this article originally appeared on Medscape.com.
FROM JAMA NEUROLOGY
Obstructive sleep apnea linked to early cognitive decline
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
FROM FRONTIERS IN SLEEP
Food insecurity linked to more rapid cognitive decline in seniors
Food insecurity is linked to a more rapid decline in executive function in older adults, a new study shows.
The findings were reported just weeks after a pandemic-era expansion in Supplemental Nutrition Assistance Program benefits ended, leading to less food assistance for about 5 million people over age 60 who participate in the program.
“Even though we found only a very small association between food insecurity and executive function, it’s still meaningful, because food insecurity is something we can prevent,” lead investigator Boeun Kim, PhD, MPH, RN, postdoctoral fellow at Johns Hopkins University School of Nursing, Baltimore, told this news organization.
The findings were published online in JAMA Network Open.
National data
The number of Americans over 60 with food insecurity has more than doubled since 2007, with an estimated 5.2 million older adults reporting food insecurity in 2020.
Prior studies have linked malnutrition and food insecurity to a decline in cognitive function. Participating in food assistance programs such as SNAP is associated with slower memory decline in older adults.
However, to date, there has been no longitudinal study that has used data from a nationally representative sample of older Americans, which, Dr. Kim said, could limit generalizability of the findings.
To address that issue, investigators analyzed data from 3,037 participants in the National Health and Aging Trends Study, which includes community dwellers age 65 and older who receive Medicare.
Participants reported food insecurity over 7 years, from 2012 to 2019. Data on immediate memory, delayed memory, and executive function were from 2013 to 2020.
Food insecurity was defined as going without groceries due to limited ability or social support; a lack of hot meals related to functional limitation or no help; going without eating because of the inability to feed oneself or no available support; skipping meals due to insufficient food or money; or skipping meals for 5 days or more.
Immediate and delayed recall were assessed using a 10-item word-list memory task, and executive function was measured using a clock drawing test. Each year’s cognitive functions were linked to the prior year’s food insecurity data.
Over 7 years, 417 people, or 12.1%, experienced food insecurity at least once.
Those with food insecurity were more likely to be older, female, part of racial and ethnic minority groups, living alone, obese, and have a lower income and educational attainment, depressive symptoms, social isolation and disability, compared with those without food insecurity.
After adjusting for age, sex, race/ethnicity, educational level, income, marital status, body mass index, functional disability, social isolation, and other potential confounders, researchers found that food insecurity was associated with a more rapid decline in executive function (mean difference in annual change in executive function score, −0.04; 95% confidence interval, −0.09 to −0.003).
Food insecurity was not associated with baseline cognitive function scores or changes in immediate or delayed recall.
“Clinicians should be aware of the experience of food insecurity and the higher risk of cognitive decline so maybe they could do universal screening and refer people with food insecurity to programs that can help them access nutritious meals,” Dr. Kim said.
A sign of other problems?
Thomas Vidic, MD, said food insecurity often goes hand-in-hand with lack of medication adherence, lack of regular medical care, and a host of other issues. Dr. Vidic is a neurologist at the Elkhart Clinic, Ind., and an adjunct clinical professor of neurology at Indiana University.
“When a person has food insecurity, they likely have other problems, and they’re going to degenerate faster,” said Dr. Vidic, who was not part of the study. “This is one important component, and it’s one more way of getting a handle on people who are failing.”
Dr. Vidic, who has dealt with the issue of food insecurity with his own patients, said he suspects the self-report nature of the study may hide the true scale of the problem.
“I suspect the numbers might actually be higher,” he said, adding that the study fills a gap in the literature with a large, nationally representative sample.
“We’re looking for issues to help with the elderly as far as what can we do to keep dementia from progressing,” he said. “There are some things that make sense, but we’ve never had this kind of data before.”
The study was funded by the National Institute on Aging. Dr. Kim and Dr. Vidic have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Food insecurity is linked to a more rapid decline in executive function in older adults, a new study shows.
The findings were reported just weeks after a pandemic-era expansion in Supplemental Nutrition Assistance Program benefits ended, leading to less food assistance for about 5 million people over age 60 who participate in the program.
“Even though we found only a very small association between food insecurity and executive function, it’s still meaningful, because food insecurity is something we can prevent,” lead investigator Boeun Kim, PhD, MPH, RN, postdoctoral fellow at Johns Hopkins University School of Nursing, Baltimore, told this news organization.
The findings were published online in JAMA Network Open.
National data
The number of Americans over 60 with food insecurity has more than doubled since 2007, with an estimated 5.2 million older adults reporting food insecurity in 2020.
Prior studies have linked malnutrition and food insecurity to a decline in cognitive function. Participating in food assistance programs such as SNAP is associated with slower memory decline in older adults.
However, to date, there has been no longitudinal study that has used data from a nationally representative sample of older Americans, which, Dr. Kim said, could limit generalizability of the findings.
To address that issue, investigators analyzed data from 3,037 participants in the National Health and Aging Trends Study, which includes community dwellers age 65 and older who receive Medicare.
Participants reported food insecurity over 7 years, from 2012 to 2019. Data on immediate memory, delayed memory, and executive function were from 2013 to 2020.
Food insecurity was defined as going without groceries due to limited ability or social support; a lack of hot meals related to functional limitation or no help; going without eating because of the inability to feed oneself or no available support; skipping meals due to insufficient food or money; or skipping meals for 5 days or more.
Immediate and delayed recall were assessed using a 10-item word-list memory task, and executive function was measured using a clock drawing test. Each year’s cognitive functions were linked to the prior year’s food insecurity data.
Over 7 years, 417 people, or 12.1%, experienced food insecurity at least once.
Those with food insecurity were more likely to be older, female, part of racial and ethnic minority groups, living alone, obese, and have a lower income and educational attainment, depressive symptoms, social isolation and disability, compared with those without food insecurity.
After adjusting for age, sex, race/ethnicity, educational level, income, marital status, body mass index, functional disability, social isolation, and other potential confounders, researchers found that food insecurity was associated with a more rapid decline in executive function (mean difference in annual change in executive function score, −0.04; 95% confidence interval, −0.09 to −0.003).
Food insecurity was not associated with baseline cognitive function scores or changes in immediate or delayed recall.
“Clinicians should be aware of the experience of food insecurity and the higher risk of cognitive decline so maybe they could do universal screening and refer people with food insecurity to programs that can help them access nutritious meals,” Dr. Kim said.
A sign of other problems?
Thomas Vidic, MD, said food insecurity often goes hand-in-hand with lack of medication adherence, lack of regular medical care, and a host of other issues. Dr. Vidic is a neurologist at the Elkhart Clinic, Ind., and an adjunct clinical professor of neurology at Indiana University.
“When a person has food insecurity, they likely have other problems, and they’re going to degenerate faster,” said Dr. Vidic, who was not part of the study. “This is one important component, and it’s one more way of getting a handle on people who are failing.”
Dr. Vidic, who has dealt with the issue of food insecurity with his own patients, said he suspects the self-report nature of the study may hide the true scale of the problem.
“I suspect the numbers might actually be higher,” he said, adding that the study fills a gap in the literature with a large, nationally representative sample.
“We’re looking for issues to help with the elderly as far as what can we do to keep dementia from progressing,” he said. “There are some things that make sense, but we’ve never had this kind of data before.”
The study was funded by the National Institute on Aging. Dr. Kim and Dr. Vidic have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Food insecurity is linked to a more rapid decline in executive function in older adults, a new study shows.
The findings were reported just weeks after a pandemic-era expansion in Supplemental Nutrition Assistance Program benefits ended, leading to less food assistance for about 5 million people over age 60 who participate in the program.
“Even though we found only a very small association between food insecurity and executive function, it’s still meaningful, because food insecurity is something we can prevent,” lead investigator Boeun Kim, PhD, MPH, RN, postdoctoral fellow at Johns Hopkins University School of Nursing, Baltimore, told this news organization.
The findings were published online in JAMA Network Open.
National data
The number of Americans over 60 with food insecurity has more than doubled since 2007, with an estimated 5.2 million older adults reporting food insecurity in 2020.
Prior studies have linked malnutrition and food insecurity to a decline in cognitive function. Participating in food assistance programs such as SNAP is associated with slower memory decline in older adults.
However, to date, there has been no longitudinal study that has used data from a nationally representative sample of older Americans, which, Dr. Kim said, could limit generalizability of the findings.
To address that issue, investigators analyzed data from 3,037 participants in the National Health and Aging Trends Study, which includes community dwellers age 65 and older who receive Medicare.
Participants reported food insecurity over 7 years, from 2012 to 2019. Data on immediate memory, delayed memory, and executive function were from 2013 to 2020.
Food insecurity was defined as going without groceries due to limited ability or social support; a lack of hot meals related to functional limitation or no help; going without eating because of the inability to feed oneself or no available support; skipping meals due to insufficient food or money; or skipping meals for 5 days or more.
Immediate and delayed recall were assessed using a 10-item word-list memory task, and executive function was measured using a clock drawing test. Each year’s cognitive functions were linked to the prior year’s food insecurity data.
Over 7 years, 417 people, or 12.1%, experienced food insecurity at least once.
Those with food insecurity were more likely to be older, female, part of racial and ethnic minority groups, living alone, obese, and have a lower income and educational attainment, depressive symptoms, social isolation and disability, compared with those without food insecurity.
After adjusting for age, sex, race/ethnicity, educational level, income, marital status, body mass index, functional disability, social isolation, and other potential confounders, researchers found that food insecurity was associated with a more rapid decline in executive function (mean difference in annual change in executive function score, −0.04; 95% confidence interval, −0.09 to −0.003).
Food insecurity was not associated with baseline cognitive function scores or changes in immediate or delayed recall.
“Clinicians should be aware of the experience of food insecurity and the higher risk of cognitive decline so maybe they could do universal screening and refer people with food insecurity to programs that can help them access nutritious meals,” Dr. Kim said.
A sign of other problems?
Thomas Vidic, MD, said food insecurity often goes hand-in-hand with lack of medication adherence, lack of regular medical care, and a host of other issues. Dr. Vidic is a neurologist at the Elkhart Clinic, Ind., and an adjunct clinical professor of neurology at Indiana University.
“When a person has food insecurity, they likely have other problems, and they’re going to degenerate faster,” said Dr. Vidic, who was not part of the study. “This is one important component, and it’s one more way of getting a handle on people who are failing.”
Dr. Vidic, who has dealt with the issue of food insecurity with his own patients, said he suspects the self-report nature of the study may hide the true scale of the problem.
“I suspect the numbers might actually be higher,” he said, adding that the study fills a gap in the literature with a large, nationally representative sample.
“We’re looking for issues to help with the elderly as far as what can we do to keep dementia from progressing,” he said. “There are some things that make sense, but we’ve never had this kind of data before.”
The study was funded by the National Institute on Aging. Dr. Kim and Dr. Vidic have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Self-fitted and audiologist-fitted hearing aids equal for mild to moderate hearing loss
Self-fitted over-the-counter (OTC) hearing aids may be an effective option for individuals with mild to moderate hearing loss, a small randomized effectiveness trial reports. OTC devices yielded 6-week patient-perceived and clinical outcomes comparable to those with audiologist-fitted hearing aids, In fact, at week 2, the self-fitted group had a small but meaningful advantage on two of the four study outcome measures.
“After support and fine-tuning were provided to the self-fitting (remote support) and audiologist-fitted groups, no clinically meaningful differences were evident in any outcome measures at the end of the 6-week trial,” wrote researchers led by Karina C. De Sousa, PhD, a postdoctoral researcher in the department of speech-language pathology and audiology at the University of Pretoria, South Africa.
Their findings appear in JAMA Otolaryngology–Head & Neck Surgery.
Hearing aid uptake is low even in populations with adequate access to audiological resources, the authors noted, with hearing aid use in U.S. adults who could benefit estimated at about 20%. Currently, an estimated 22.9 million older Americans with audiometric hearing loss do not use hearing aids.
Major barriers have been access and affordability, Dr. De Sousa and associates wrote, and until recently, people with hearing loss could obtain hearing aids only after consultation with a credentialed dispenser. “The World Health Organization estimates that over 2.5 billion people will experience some degree of hearing loss by 2050,” Dr. De Sousa said in an interview. “This new category of self-fitting hearing aids opens up newer care pathways for people with mild to moderate hearing loss.”
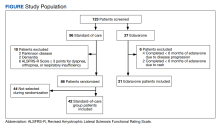
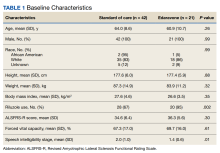
The study
From April to August 2022 the trial recruited 68 participants (51.6% men) with mild-to-moderate self-reported hearing loss, a mean age of 63.6 years, and no ear disease within the past 90 days. They were randomized to a self-fitted commercially available device (Lexi Lumen), with instructional material on set-up and remote support, or to the same unit fitted by an audiologist. The majority in both arms were new users and were similar in age and baseline hearing scores.
The primary outcome measure was patient-reported hearing aid benefit, measured by the Abbreviated Profile of Hearing Aid Benefit (APHAB) questionnaire. This scale evaluates auditory acuity before and after amplification by such criteria as ease of communication, background noise, reverberation, aversiveness, and global hearing status.
Secondary measures included the International Outcome Inventory for Hearing Aids (IOI-HA) and speech recognition in noise measured using an abbreviated speech-in-noise test and a digits-in-noise test. Measures were taken at baseline, week 2, and week 6 after fitting. After the 2-week field trial, the self-fitting arm had an initial advantage on the self-reported APHAB: difference, Cohen d = −.5 (95% confidence interval [CI], −1.0 to 0). It also fared better on the IOI-HA: effect size, r = 0.3 (95% CI, .0 to –.5), but not on speech recognition in noise.
One member of the self-fitting arm withdrew owing to an unrelated middle-ear infection.
“While these results are promising, it is essential to note that OTC hearing aids are not a one-size-fits-all approach,” Dr. De Sousa said. “If a person has ear disease symptoms or hearing loss that is too severe, they have to consult a trained hearing health care professional.” She added that proper use of a self-fitted OTC hearing aid requires a degree of digital proficiency, as many devices are set up using a smartphone.
This study was supported by the National Institutes of Health and by the hearX Group, which provided the Lexie Lumen devices and software support for data collection. Dr. De Sousa reported nonfinancial support from hearX as well as consulting fees from hearX outside of the submitted work. A coauthor reported grant support from the UK’s National Institute for Health and Care Research Manchester Biomedical Research Centre, and fees from hearX during and outside of the study. Another coauthor disclosed fees, equity, and grant support from hearX during the conduct of the study.
Self-fitted over-the-counter (OTC) hearing aids may be an effective option for individuals with mild to moderate hearing loss, a small randomized effectiveness trial reports. OTC devices yielded 6-week patient-perceived and clinical outcomes comparable to those with audiologist-fitted hearing aids, In fact, at week 2, the self-fitted group had a small but meaningful advantage on two of the four study outcome measures.
“After support and fine-tuning were provided to the self-fitting (remote support) and audiologist-fitted groups, no clinically meaningful differences were evident in any outcome measures at the end of the 6-week trial,” wrote researchers led by Karina C. De Sousa, PhD, a postdoctoral researcher in the department of speech-language pathology and audiology at the University of Pretoria, South Africa.
Their findings appear in JAMA Otolaryngology–Head & Neck Surgery.
Hearing aid uptake is low even in populations with adequate access to audiological resources, the authors noted, with hearing aid use in U.S. adults who could benefit estimated at about 20%. Currently, an estimated 22.9 million older Americans with audiometric hearing loss do not use hearing aids.
Major barriers have been access and affordability, Dr. De Sousa and associates wrote, and until recently, people with hearing loss could obtain hearing aids only after consultation with a credentialed dispenser. “The World Health Organization estimates that over 2.5 billion people will experience some degree of hearing loss by 2050,” Dr. De Sousa said in an interview. “This new category of self-fitting hearing aids opens up newer care pathways for people with mild to moderate hearing loss.”
The study
From April to August 2022 the trial recruited 68 participants (51.6% men) with mild-to-moderate self-reported hearing loss, a mean age of 63.6 years, and no ear disease within the past 90 days. They were randomized to a self-fitted commercially available device (Lexi Lumen), with instructional material on set-up and remote support, or to the same unit fitted by an audiologist. The majority in both arms were new users and were similar in age and baseline hearing scores.
The primary outcome measure was patient-reported hearing aid benefit, measured by the Abbreviated Profile of Hearing Aid Benefit (APHAB) questionnaire. This scale evaluates auditory acuity before and after amplification by such criteria as ease of communication, background noise, reverberation, aversiveness, and global hearing status.
Secondary measures included the International Outcome Inventory for Hearing Aids (IOI-HA) and speech recognition in noise measured using an abbreviated speech-in-noise test and a digits-in-noise test. Measures were taken at baseline, week 2, and week 6 after fitting. After the 2-week field trial, the self-fitting arm had an initial advantage on the self-reported APHAB: difference, Cohen d = −.5 (95% confidence interval [CI], −1.0 to 0). It also fared better on the IOI-HA: effect size, r = 0.3 (95% CI, .0 to –.5), but not on speech recognition in noise.
One member of the self-fitting arm withdrew owing to an unrelated middle-ear infection.
“While these results are promising, it is essential to note that OTC hearing aids are not a one-size-fits-all approach,” Dr. De Sousa said. “If a person has ear disease symptoms or hearing loss that is too severe, they have to consult a trained hearing health care professional.” She added that proper use of a self-fitted OTC hearing aid requires a degree of digital proficiency, as many devices are set up using a smartphone.
This study was supported by the National Institutes of Health and by the hearX Group, which provided the Lexie Lumen devices and software support for data collection. Dr. De Sousa reported nonfinancial support from hearX as well as consulting fees from hearX outside of the submitted work. A coauthor reported grant support from the UK’s National Institute for Health and Care Research Manchester Biomedical Research Centre, and fees from hearX during and outside of the study. Another coauthor disclosed fees, equity, and grant support from hearX during the conduct of the study.
Self-fitted over-the-counter (OTC) hearing aids may be an effective option for individuals with mild to moderate hearing loss, a small randomized effectiveness trial reports. OTC devices yielded 6-week patient-perceived and clinical outcomes comparable to those with audiologist-fitted hearing aids, In fact, at week 2, the self-fitted group had a small but meaningful advantage on two of the four study outcome measures.
“After support and fine-tuning were provided to the self-fitting (remote support) and audiologist-fitted groups, no clinically meaningful differences were evident in any outcome measures at the end of the 6-week trial,” wrote researchers led by Karina C. De Sousa, PhD, a postdoctoral researcher in the department of speech-language pathology and audiology at the University of Pretoria, South Africa.
Their findings appear in JAMA Otolaryngology–Head & Neck Surgery.
Hearing aid uptake is low even in populations with adequate access to audiological resources, the authors noted, with hearing aid use in U.S. adults who could benefit estimated at about 20%. Currently, an estimated 22.9 million older Americans with audiometric hearing loss do not use hearing aids.
Major barriers have been access and affordability, Dr. De Sousa and associates wrote, and until recently, people with hearing loss could obtain hearing aids only after consultation with a credentialed dispenser. “The World Health Organization estimates that over 2.5 billion people will experience some degree of hearing loss by 2050,” Dr. De Sousa said in an interview. “This new category of self-fitting hearing aids opens up newer care pathways for people with mild to moderate hearing loss.”
The study
From April to August 2022 the trial recruited 68 participants (51.6% men) with mild-to-moderate self-reported hearing loss, a mean age of 63.6 years, and no ear disease within the past 90 days. They were randomized to a self-fitted commercially available device (Lexi Lumen), with instructional material on set-up and remote support, or to the same unit fitted by an audiologist. The majority in both arms were new users and were similar in age and baseline hearing scores.
The primary outcome measure was patient-reported hearing aid benefit, measured by the Abbreviated Profile of Hearing Aid Benefit (APHAB) questionnaire. This scale evaluates auditory acuity before and after amplification by such criteria as ease of communication, background noise, reverberation, aversiveness, and global hearing status.
Secondary measures included the International Outcome Inventory for Hearing Aids (IOI-HA) and speech recognition in noise measured using an abbreviated speech-in-noise test and a digits-in-noise test. Measures were taken at baseline, week 2, and week 6 after fitting. After the 2-week field trial, the self-fitting arm had an initial advantage on the self-reported APHAB: difference, Cohen d = −.5 (95% confidence interval [CI], −1.0 to 0). It also fared better on the IOI-HA: effect size, r = 0.3 (95% CI, .0 to –.5), but not on speech recognition in noise.
One member of the self-fitting arm withdrew owing to an unrelated middle-ear infection.
“While these results are promising, it is essential to note that OTC hearing aids are not a one-size-fits-all approach,” Dr. De Sousa said. “If a person has ear disease symptoms or hearing loss that is too severe, they have to consult a trained hearing health care professional.” She added that proper use of a self-fitted OTC hearing aid requires a degree of digital proficiency, as many devices are set up using a smartphone.
This study was supported by the National Institutes of Health and by the hearX Group, which provided the Lexie Lumen devices and software support for data collection. Dr. De Sousa reported nonfinancial support from hearX as well as consulting fees from hearX outside of the submitted work. A coauthor reported grant support from the UK’s National Institute for Health and Care Research Manchester Biomedical Research Centre, and fees from hearX during and outside of the study. Another coauthor disclosed fees, equity, and grant support from hearX during the conduct of the study.
FROM JAMA OTOLARYNGOLOGY–HEAD & NECK SURGERY
Urban green and blue spaces linked to less psychological distress
The findings of the study, which was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology, build on a growing understanding of the relationship between types and qualities of urban environments and dementia risk.
Adithya Vegaraju, a student at Washington State University, Spokane, led the study, which looked at data from the Washington State Behavioral Risk Factor Surveillance System to assess prevalence of serious psychological distress among 42,980 Washington state residents aged 65 and over.
The data, collected between 2011 and 2019, used a self-reported questionnaire to determine serious psychological distress, which is defined as a level of mental distress considered debilitating enough to warrant treatment.
Mr. Vegaraju and his coauthor Solmaz Amiri, DDes, also of Washington State University, used ZIP codes, along with U.S. census data, to approximate the urban adults’ proximity to green and blue spaces.
After controlling for potential confounders of age, sex, ethnicity, education, and marital status, the investigators found that people living within half a mile of green or blue spaces had a 17% lower risk of experiencing serious psychological distress, compared with people living farther from these spaces, the investigators said in a news release.
Implications for cognitive decline and dementia?
Psychological distress in adults has been linked in population-based longitudinal studies to later cognitive decline and dementia. One study in older adults found the risk of dementia to be more than 50% higher among adults aged 50-70 with persistent depression. Blue and green spaces have also been investigated in relation to neurodegenerative disease among older adults; a 2022 study looking at data from some 62 million Medicare beneficiaries found those living in areas with more vegetation saw lower risk of hospitalizations for Alzheimer’s disease and related dementias.
“Since we lack effective prevention methods or treatments for mild cognitive impairment and dementia, we need to get creative in how we look at these issues,” Dr. Amiri commented in a press statement about her and Mr. Vegaraju’s findings. “Our hope is that this study showing better mental health among people living close to parks and water will trigger other studies about how these benefits work and whether this proximity can help prevent or delay mild cognitive impairment and dementia.”
The investigators acknowledged that their findings were limited by reliance on a self-reported measure of psychological distress.
A bidirectional connection with depression and dementia
In a comment, Anjum Hajat, PhD, an epidemiologist at University of Washington School of Public Health in Seattle who has also studied the relationship between green space and dementia risk in older adults, noted some further apparent limitations of the new study, for which only an abstract was available at publication.
“It has been shown that people with depression are at higher risk for dementia, but the opposite is also true,” Dr. Hajat commented. “Those with dementia are more likely to develop depression. This bidirectionality makes this study abstract difficult to interpret since the study is based on cross-sectional data: Individuals are not followed over time to see which develops first, dementia or depression.”
Additionally, Dr. Hajat noted, the data used to determine proximity to green and blue spaces did not allow for the calculation of precise distances between subjects’ homes and these spaces.
Mr. Vegaraju and Dr. Amiri’s study had no outside support, and the investigators declared no conflicts of interest. Dr. Hajat declared no conflicts of interest.
The findings of the study, which was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology, build on a growing understanding of the relationship between types and qualities of urban environments and dementia risk.
Adithya Vegaraju, a student at Washington State University, Spokane, led the study, which looked at data from the Washington State Behavioral Risk Factor Surveillance System to assess prevalence of serious psychological distress among 42,980 Washington state residents aged 65 and over.
The data, collected between 2011 and 2019, used a self-reported questionnaire to determine serious psychological distress, which is defined as a level of mental distress considered debilitating enough to warrant treatment.
Mr. Vegaraju and his coauthor Solmaz Amiri, DDes, also of Washington State University, used ZIP codes, along with U.S. census data, to approximate the urban adults’ proximity to green and blue spaces.
After controlling for potential confounders of age, sex, ethnicity, education, and marital status, the investigators found that people living within half a mile of green or blue spaces had a 17% lower risk of experiencing serious psychological distress, compared with people living farther from these spaces, the investigators said in a news release.
Implications for cognitive decline and dementia?
Psychological distress in adults has been linked in population-based longitudinal studies to later cognitive decline and dementia. One study in older adults found the risk of dementia to be more than 50% higher among adults aged 50-70 with persistent depression. Blue and green spaces have also been investigated in relation to neurodegenerative disease among older adults; a 2022 study looking at data from some 62 million Medicare beneficiaries found those living in areas with more vegetation saw lower risk of hospitalizations for Alzheimer’s disease and related dementias.
“Since we lack effective prevention methods or treatments for mild cognitive impairment and dementia, we need to get creative in how we look at these issues,” Dr. Amiri commented in a press statement about her and Mr. Vegaraju’s findings. “Our hope is that this study showing better mental health among people living close to parks and water will trigger other studies about how these benefits work and whether this proximity can help prevent or delay mild cognitive impairment and dementia.”
The investigators acknowledged that their findings were limited by reliance on a self-reported measure of psychological distress.
A bidirectional connection with depression and dementia
In a comment, Anjum Hajat, PhD, an epidemiologist at University of Washington School of Public Health in Seattle who has also studied the relationship between green space and dementia risk in older adults, noted some further apparent limitations of the new study, for which only an abstract was available at publication.
“It has been shown that people with depression are at higher risk for dementia, but the opposite is also true,” Dr. Hajat commented. “Those with dementia are more likely to develop depression. This bidirectionality makes this study abstract difficult to interpret since the study is based on cross-sectional data: Individuals are not followed over time to see which develops first, dementia or depression.”
Additionally, Dr. Hajat noted, the data used to determine proximity to green and blue spaces did not allow for the calculation of precise distances between subjects’ homes and these spaces.
Mr. Vegaraju and Dr. Amiri’s study had no outside support, and the investigators declared no conflicts of interest. Dr. Hajat declared no conflicts of interest.
The findings of the study, which was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology, build on a growing understanding of the relationship between types and qualities of urban environments and dementia risk.
Adithya Vegaraju, a student at Washington State University, Spokane, led the study, which looked at data from the Washington State Behavioral Risk Factor Surveillance System to assess prevalence of serious psychological distress among 42,980 Washington state residents aged 65 and over.
The data, collected between 2011 and 2019, used a self-reported questionnaire to determine serious psychological distress, which is defined as a level of mental distress considered debilitating enough to warrant treatment.
Mr. Vegaraju and his coauthor Solmaz Amiri, DDes, also of Washington State University, used ZIP codes, along with U.S. census data, to approximate the urban adults’ proximity to green and blue spaces.
After controlling for potential confounders of age, sex, ethnicity, education, and marital status, the investigators found that people living within half a mile of green or blue spaces had a 17% lower risk of experiencing serious psychological distress, compared with people living farther from these spaces, the investigators said in a news release.
Implications for cognitive decline and dementia?
Psychological distress in adults has been linked in population-based longitudinal studies to later cognitive decline and dementia. One study in older adults found the risk of dementia to be more than 50% higher among adults aged 50-70 with persistent depression. Blue and green spaces have also been investigated in relation to neurodegenerative disease among older adults; a 2022 study looking at data from some 62 million Medicare beneficiaries found those living in areas with more vegetation saw lower risk of hospitalizations for Alzheimer’s disease and related dementias.
“Since we lack effective prevention methods or treatments for mild cognitive impairment and dementia, we need to get creative in how we look at these issues,” Dr. Amiri commented in a press statement about her and Mr. Vegaraju’s findings. “Our hope is that this study showing better mental health among people living close to parks and water will trigger other studies about how these benefits work and whether this proximity can help prevent or delay mild cognitive impairment and dementia.”
The investigators acknowledged that their findings were limited by reliance on a self-reported measure of psychological distress.
A bidirectional connection with depression and dementia
In a comment, Anjum Hajat, PhD, an epidemiologist at University of Washington School of Public Health in Seattle who has also studied the relationship between green space and dementia risk in older adults, noted some further apparent limitations of the new study, for which only an abstract was available at publication.
“It has been shown that people with depression are at higher risk for dementia, but the opposite is also true,” Dr. Hajat commented. “Those with dementia are more likely to develop depression. This bidirectionality makes this study abstract difficult to interpret since the study is based on cross-sectional data: Individuals are not followed over time to see which develops first, dementia or depression.”
Additionally, Dr. Hajat noted, the data used to determine proximity to green and blue spaces did not allow for the calculation of precise distances between subjects’ homes and these spaces.
Mr. Vegaraju and Dr. Amiri’s study had no outside support, and the investigators declared no conflicts of interest. Dr. Hajat declared no conflicts of interest.
FROM AAN 2023
Phototherapy a safe, effective, inexpensive new option for dementia?
It may be “one of the most promising interventions for improving core symptoms” of the disease.
A new meta-analysis shows that patients with dementia who received phototherapy experienced significant cognitive improvement, compared with those who received usual treatment. However, there were no differences between study groups in terms of improved depression, agitation, or sleep problems.
“Our meta-analysis indicates that phototherapy improved cognitive function in patients with dementia. ... This suggests that phototherapy may be one of the most promising non-pharmacological interventions for improving core symptoms of dementia,” wrote the investigators, led by Xinlian Lu, Peking University, Beijing.
The study was published online in Brain and Behavior.
A new treatment option?
“As drug treatment for dementia has limitations such as medical contraindications, limited efficacy, and adverse effects, nonpharmacological therapy has been increasingly regarded as a critical part of comprehensive dementia care,” the investigators noted.
Phototherapy, which utilizes full-spectrum bright light (usually > 600 lux) or wavelength-specific light (for example, blue-enriched or blue-green), is a “promising nonpharmacological therapy” that is noninvasive, inexpensive, and safe.
Most studies of phototherapy have focused on sleep. Findings have shown “high heterogeneity” among the interventions and the populations in the studies, and results have been “inconsistent.” In addition, the effect of phototherapy on cognitive function and behavioral and psychological symptoms of dementia (BPSD) “still need to be clarified.”
In the systematic review and meta-analysis, the investigators examined the effects of phototherapy on cognitive function, BPSD, and sleep in older adults with dementia.
They searched several databases for randomized controlled trials that investigated phototherapy interventions for elderly patients. The primary outcome was cognitive function, which was assessed via the Mini-Mental State Examination (MMSE).
Secondary outcomes included BPSD, including agitation, anxiety, irritability, depression, anxiety, and sleep disturbances, as assessed by the Cornell Scale for Depression in Dementia (CSDD), the Cohen-Mansfield Agitation Inventory (CMAI), the Neuropsychiatric Inventory (NPI), and measures of sleep, including total sleep time (TST), sleep efficiency (SE), and sleep disorders, as assessed by the Sleep Disorder Inventory (SDI).
To be included in the analysis, individual studies had to focus on elderly adults who had some form of dementia. In addition, a group receiving a phototherapy intervention had to be compared with a nonintervention group, and the study had to specify one of the above-defined outcomes.
The review included phototherapy interventions of all forms, frequencies, and durations, including use of bright light, LED light, and blue or blue-green light.
Regulating circadian rhythm
Twelve studies met the researchers’ criteria. They included a total of 766 patients with dementia – 426 in the intervention group and 340 in the control group. The mean ages ranged from 73.73 to 85.9 years, and there was a greater number of female than male participants.
Of the studies, seven employed routine daily light in the control group, while the others used either dim light (≤ 50 lux) or devices without light.
The researchers found “significant positive intervention effects” for global cognitive function. Improvements in postintervention MMSE scores differed significantly between the experimental groups and control groups (mean difference, 2.68; 95% confidence interval, 1.38-3.98; I2 = 0%).
No significant differences were found in the effects of intervention on depression symptoms, as evidenced in CSDD scores (MD, −0.70; 95% CI, −3.10 to 1.70; I2 = 81%).
Among patients with higher CMAI scores, which indicate more severe agitation behaviors, there was a “trend of decreasing CMAI scores” after phototherapy (MD, −3.12; 95% CI, −8.05 to 1.82; I2 = 0%). No significant difference in NPI scores was observed between the two groups.
Similarly, no significant difference was found between the two groups in TST, SE, or SDI scores.
Adverse effects were infrequent and were not severe. Two of the 426 patients in the intervention group experienced mild ocular irritation, and one experienced slight transient redness of the forehead.
Light “may compensate for the reduction in the visual sensory input of patients with dementia and stimulate specific neurons in the suprachiasmatic nucleus of the hypothalamus to regulate circadian rhythm,” the researchers suggested.
“As circadian rhythms are involved in optimal brain function, light supplementation may act on the synchronizing/phase-shifting effects of circadian rhythms to improve cognitive function,” they added.
They note that the light box is the “most commonly used device in phototherapy.” Light boxes provide full-spectrum bright light, usually greater than 2,500 lux. The duration is 30 minutes in the daytime, and treatment lasts 4-8 weeks.
The investigators cautioned that the light box should be placed 60 cm away from the patient or above the patient’s eye level. They said that a ceiling-mounted light is a “good choice” for providing whole-day phototherapy, since such lights do not interfere with the patient’s daily routine, reduce the demand on staff, and contribute to better adherence.
Phototherapy helmets and glasses are also available. These portable devices “allow for better control of light intensity and are ergonomic without interfering with patients’ normal activities.”
The researchers noted that “further well-designed studies are needed to explore the most effective clinical implementation conditions, including device type, duration, frequency, and time.”
Easy to use
Mariana Figueiro, PhD, professor and director of the Light and Health Research Center, department of population health medicine, Icahn School of Medicine at Mount Sinai, New York, said light is the “major stimulus for the circadian system, and a robust light-dark pattern daily (which can be given by light therapy during the day) improves sleep and behavior and reduces depression and agitation.”
Dr. Figueiro, who was not involved with the current study, noted that patients with dementia “have sleep issues, which can further affect their cognition; improvement in sleep leads to improvement in cognition,” and this may be an underlying mechanism associated with these results.
The clinical significance of the study “is that this is a nonpharmacological intervention and can be easily applied in the homes or controlled facilities, and it can be used with any other medication,” she pointed out.
“More importantly, sleep medications have negative side effects, so the use of nonpharmacological interventions improving sleep and cognition is great for clinical practice,” she added.
However, she took issue with the finding that phototherapy was not effective for depression and agitation, noting that there were “too few studies to say for sure that light therapy is ineffective at improving these outcomes.”
The research received no external funding. The authors and Dr. Figueiro disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It may be “one of the most promising interventions for improving core symptoms” of the disease.
A new meta-analysis shows that patients with dementia who received phototherapy experienced significant cognitive improvement, compared with those who received usual treatment. However, there were no differences between study groups in terms of improved depression, agitation, or sleep problems.
“Our meta-analysis indicates that phototherapy improved cognitive function in patients with dementia. ... This suggests that phototherapy may be one of the most promising non-pharmacological interventions for improving core symptoms of dementia,” wrote the investigators, led by Xinlian Lu, Peking University, Beijing.
The study was published online in Brain and Behavior.
A new treatment option?
“As drug treatment for dementia has limitations such as medical contraindications, limited efficacy, and adverse effects, nonpharmacological therapy has been increasingly regarded as a critical part of comprehensive dementia care,” the investigators noted.
Phototherapy, which utilizes full-spectrum bright light (usually > 600 lux) or wavelength-specific light (for example, blue-enriched or blue-green), is a “promising nonpharmacological therapy” that is noninvasive, inexpensive, and safe.
Most studies of phototherapy have focused on sleep. Findings have shown “high heterogeneity” among the interventions and the populations in the studies, and results have been “inconsistent.” In addition, the effect of phototherapy on cognitive function and behavioral and psychological symptoms of dementia (BPSD) “still need to be clarified.”
In the systematic review and meta-analysis, the investigators examined the effects of phototherapy on cognitive function, BPSD, and sleep in older adults with dementia.
They searched several databases for randomized controlled trials that investigated phototherapy interventions for elderly patients. The primary outcome was cognitive function, which was assessed via the Mini-Mental State Examination (MMSE).
Secondary outcomes included BPSD, including agitation, anxiety, irritability, depression, anxiety, and sleep disturbances, as assessed by the Cornell Scale for Depression in Dementia (CSDD), the Cohen-Mansfield Agitation Inventory (CMAI), the Neuropsychiatric Inventory (NPI), and measures of sleep, including total sleep time (TST), sleep efficiency (SE), and sleep disorders, as assessed by the Sleep Disorder Inventory (SDI).
To be included in the analysis, individual studies had to focus on elderly adults who had some form of dementia. In addition, a group receiving a phototherapy intervention had to be compared with a nonintervention group, and the study had to specify one of the above-defined outcomes.
The review included phototherapy interventions of all forms, frequencies, and durations, including use of bright light, LED light, and blue or blue-green light.
Regulating circadian rhythm
Twelve studies met the researchers’ criteria. They included a total of 766 patients with dementia – 426 in the intervention group and 340 in the control group. The mean ages ranged from 73.73 to 85.9 years, and there was a greater number of female than male participants.
Of the studies, seven employed routine daily light in the control group, while the others used either dim light (≤ 50 lux) or devices without light.
The researchers found “significant positive intervention effects” for global cognitive function. Improvements in postintervention MMSE scores differed significantly between the experimental groups and control groups (mean difference, 2.68; 95% confidence interval, 1.38-3.98; I2 = 0%).
No significant differences were found in the effects of intervention on depression symptoms, as evidenced in CSDD scores (MD, −0.70; 95% CI, −3.10 to 1.70; I2 = 81%).
Among patients with higher CMAI scores, which indicate more severe agitation behaviors, there was a “trend of decreasing CMAI scores” after phototherapy (MD, −3.12; 95% CI, −8.05 to 1.82; I2 = 0%). No significant difference in NPI scores was observed between the two groups.
Similarly, no significant difference was found between the two groups in TST, SE, or SDI scores.
Adverse effects were infrequent and were not severe. Two of the 426 patients in the intervention group experienced mild ocular irritation, and one experienced slight transient redness of the forehead.
Light “may compensate for the reduction in the visual sensory input of patients with dementia and stimulate specific neurons in the suprachiasmatic nucleus of the hypothalamus to regulate circadian rhythm,” the researchers suggested.
“As circadian rhythms are involved in optimal brain function, light supplementation may act on the synchronizing/phase-shifting effects of circadian rhythms to improve cognitive function,” they added.
They note that the light box is the “most commonly used device in phototherapy.” Light boxes provide full-spectrum bright light, usually greater than 2,500 lux. The duration is 30 minutes in the daytime, and treatment lasts 4-8 weeks.
The investigators cautioned that the light box should be placed 60 cm away from the patient or above the patient’s eye level. They said that a ceiling-mounted light is a “good choice” for providing whole-day phototherapy, since such lights do not interfere with the patient’s daily routine, reduce the demand on staff, and contribute to better adherence.
Phototherapy helmets and glasses are also available. These portable devices “allow for better control of light intensity and are ergonomic without interfering with patients’ normal activities.”
The researchers noted that “further well-designed studies are needed to explore the most effective clinical implementation conditions, including device type, duration, frequency, and time.”
Easy to use
Mariana Figueiro, PhD, professor and director of the Light and Health Research Center, department of population health medicine, Icahn School of Medicine at Mount Sinai, New York, said light is the “major stimulus for the circadian system, and a robust light-dark pattern daily (which can be given by light therapy during the day) improves sleep and behavior and reduces depression and agitation.”
Dr. Figueiro, who was not involved with the current study, noted that patients with dementia “have sleep issues, which can further affect their cognition; improvement in sleep leads to improvement in cognition,” and this may be an underlying mechanism associated with these results.
The clinical significance of the study “is that this is a nonpharmacological intervention and can be easily applied in the homes or controlled facilities, and it can be used with any other medication,” she pointed out.
“More importantly, sleep medications have negative side effects, so the use of nonpharmacological interventions improving sleep and cognition is great for clinical practice,” she added.
However, she took issue with the finding that phototherapy was not effective for depression and agitation, noting that there were “too few studies to say for sure that light therapy is ineffective at improving these outcomes.”
The research received no external funding. The authors and Dr. Figueiro disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It may be “one of the most promising interventions for improving core symptoms” of the disease.
A new meta-analysis shows that patients with dementia who received phototherapy experienced significant cognitive improvement, compared with those who received usual treatment. However, there were no differences between study groups in terms of improved depression, agitation, or sleep problems.
“Our meta-analysis indicates that phototherapy improved cognitive function in patients with dementia. ... This suggests that phototherapy may be one of the most promising non-pharmacological interventions for improving core symptoms of dementia,” wrote the investigators, led by Xinlian Lu, Peking University, Beijing.
The study was published online in Brain and Behavior.
A new treatment option?
“As drug treatment for dementia has limitations such as medical contraindications, limited efficacy, and adverse effects, nonpharmacological therapy has been increasingly regarded as a critical part of comprehensive dementia care,” the investigators noted.
Phototherapy, which utilizes full-spectrum bright light (usually > 600 lux) or wavelength-specific light (for example, blue-enriched or blue-green), is a “promising nonpharmacological therapy” that is noninvasive, inexpensive, and safe.
Most studies of phototherapy have focused on sleep. Findings have shown “high heterogeneity” among the interventions and the populations in the studies, and results have been “inconsistent.” In addition, the effect of phototherapy on cognitive function and behavioral and psychological symptoms of dementia (BPSD) “still need to be clarified.”
In the systematic review and meta-analysis, the investigators examined the effects of phototherapy on cognitive function, BPSD, and sleep in older adults with dementia.
They searched several databases for randomized controlled trials that investigated phototherapy interventions for elderly patients. The primary outcome was cognitive function, which was assessed via the Mini-Mental State Examination (MMSE).
Secondary outcomes included BPSD, including agitation, anxiety, irritability, depression, anxiety, and sleep disturbances, as assessed by the Cornell Scale for Depression in Dementia (CSDD), the Cohen-Mansfield Agitation Inventory (CMAI), the Neuropsychiatric Inventory (NPI), and measures of sleep, including total sleep time (TST), sleep efficiency (SE), and sleep disorders, as assessed by the Sleep Disorder Inventory (SDI).
To be included in the analysis, individual studies had to focus on elderly adults who had some form of dementia. In addition, a group receiving a phototherapy intervention had to be compared with a nonintervention group, and the study had to specify one of the above-defined outcomes.
The review included phototherapy interventions of all forms, frequencies, and durations, including use of bright light, LED light, and blue or blue-green light.
Regulating circadian rhythm
Twelve studies met the researchers’ criteria. They included a total of 766 patients with dementia – 426 in the intervention group and 340 in the control group. The mean ages ranged from 73.73 to 85.9 years, and there was a greater number of female than male participants.
Of the studies, seven employed routine daily light in the control group, while the others used either dim light (≤ 50 lux) or devices without light.
The researchers found “significant positive intervention effects” for global cognitive function. Improvements in postintervention MMSE scores differed significantly between the experimental groups and control groups (mean difference, 2.68; 95% confidence interval, 1.38-3.98; I2 = 0%).
No significant differences were found in the effects of intervention on depression symptoms, as evidenced in CSDD scores (MD, −0.70; 95% CI, −3.10 to 1.70; I2 = 81%).
Among patients with higher CMAI scores, which indicate more severe agitation behaviors, there was a “trend of decreasing CMAI scores” after phototherapy (MD, −3.12; 95% CI, −8.05 to 1.82; I2 = 0%). No significant difference in NPI scores was observed between the two groups.
Similarly, no significant difference was found between the two groups in TST, SE, or SDI scores.
Adverse effects were infrequent and were not severe. Two of the 426 patients in the intervention group experienced mild ocular irritation, and one experienced slight transient redness of the forehead.
Light “may compensate for the reduction in the visual sensory input of patients with dementia and stimulate specific neurons in the suprachiasmatic nucleus of the hypothalamus to regulate circadian rhythm,” the researchers suggested.
“As circadian rhythms are involved in optimal brain function, light supplementation may act on the synchronizing/phase-shifting effects of circadian rhythms to improve cognitive function,” they added.
They note that the light box is the “most commonly used device in phototherapy.” Light boxes provide full-spectrum bright light, usually greater than 2,500 lux. The duration is 30 minutes in the daytime, and treatment lasts 4-8 weeks.
The investigators cautioned that the light box should be placed 60 cm away from the patient or above the patient’s eye level. They said that a ceiling-mounted light is a “good choice” for providing whole-day phototherapy, since such lights do not interfere with the patient’s daily routine, reduce the demand on staff, and contribute to better adherence.
Phototherapy helmets and glasses are also available. These portable devices “allow for better control of light intensity and are ergonomic without interfering with patients’ normal activities.”
The researchers noted that “further well-designed studies are needed to explore the most effective clinical implementation conditions, including device type, duration, frequency, and time.”
Easy to use
Mariana Figueiro, PhD, professor and director of the Light and Health Research Center, department of population health medicine, Icahn School of Medicine at Mount Sinai, New York, said light is the “major stimulus for the circadian system, and a robust light-dark pattern daily (which can be given by light therapy during the day) improves sleep and behavior and reduces depression and agitation.”
Dr. Figueiro, who was not involved with the current study, noted that patients with dementia “have sleep issues, which can further affect their cognition; improvement in sleep leads to improvement in cognition,” and this may be an underlying mechanism associated with these results.
The clinical significance of the study “is that this is a nonpharmacological intervention and can be easily applied in the homes or controlled facilities, and it can be used with any other medication,” she pointed out.
“More importantly, sleep medications have negative side effects, so the use of nonpharmacological interventions improving sleep and cognition is great for clinical practice,” she added.
However, she took issue with the finding that phototherapy was not effective for depression and agitation, noting that there were “too few studies to say for sure that light therapy is ineffective at improving these outcomes.”
The research received no external funding. The authors and Dr. Figueiro disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BRAIN AND BEHAVIOR
Disordered sleep tied to a marked increase in stroke risk
Results of a large international study show stroke risk was more than three times higher in those who slept too little, more than twice as high in those who sleep too much, and two to three times higher in those with symptoms of severe obstructive sleep apnea.
The study also showed that the greater the number of sleep disorder symptoms, the greater the stroke risk. The 11% of study participants with five or more symptoms of disordered sleep had a fivefold increased risk for stroke.
Although the study data do not show a causal link between disordered sleep and stroke, the association between the two was strong.
“Given the association, sleep disturbance may represent a marker of somebody at increased risk of stroke, and further interventional studies are required to see if management can reduce this risk,” lead investigator Christine McCarthy, MD, PhD, a geriatric and stroke medicine physician and researcher with the University of Galway (Ireland), told this news organization. “In the interim, however, management of sleep disturbance may have a positive impact on a patient’s quality of life.”
The findings were published online in the journal Neurology.
More symptoms, more risk
Previous research shows severe OSA doubles the risk of stroke and increases the chance of recurrent stroke. A 2019 study showed that people with insomnia had a small increased risk of stroke.
“Both snoring and extremes of sleep duration have been previously associated with an increased risk of stroke in observational research, but less is known about other symptoms of sleep impairment, with less consistent findings,” Dr. McCarthy said.
Prior studies have also generally come from a single geographic region, which Dr. McCarthy noted could limit their generalizability.
For this effort, investigators used data from 4,496 participants in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. About half of the participants had a history of stroke.
Using information collected from a survey of sleep habits, researchers found an elevated stroke risk in those who received less than 5 hours of sleep per night (odds ratio, 3.15; 95% confidence interval, 2.09-4.76) or more than 9 hours of sleep per night (OR, 2.67; 95% CI, 1.89-3.78), compared with those who slept 7 hours a night.
Participants who took unplanned naps or naps lasting an hour or more (OR, 2.46; 95% CI, 1.69-3.57) and participants who reported poor quality sleep (OR,1.52; 95% CI, 1.32-1.75) were also at an increased risk for stroke.
Symptoms of OSA were also strongly associated with increased stroke risk, including snoring (OR, 1.91; 95% CI, 1.62-2.24), snorting (OR, 2.64; 95% CI, 2.17-3.20), and breathing cessation (OR, 2.87; 95% CI, 2.28-2.60).
Stroke risk increased as the number of sleep disturbance symptoms rose, with the greatest risk in the 11% of participants who had five or more symptoms (OR, 5.38; 95% CI, 4.03-7.18).
“This study finds an association between a broad range of sleep impairment symptoms and stroke, and a graded association with increasing symptoms, in an international setting,” Dr. McCarthy said.
Researchers aren’t sure what’s driving the higher stroke risk among people with sleep disturbances. Although the study did control for potential confounders, it wasn’t designed to get at what’s driving the association.
“Sleep disturbance may also have a bi-directional relationship with many stroke risk factors; for example, sleep disturbance may be a symptom of disease and exacerbate disease,” Dr. McCarthy said. “Future interventional studies are required to determine the true direction of the relationship.”
A marker of stroke risk
Daniel Lackland, DrPH, professor of neurology at the Medical University of South Carolina, Charleston, said the findings provide additional evidence of the link between sleep and stroke risk.
“The results confirm sleep disorders as a potential marker and part of the risk profile,” he said.
Collecting information about sleep using a validated assessment tool is an important piece of clinical care, Dr. Lackland said, especially among patients with other stroke risk factors.
One limitation of the study was that data on sleep was collected only at one point, and participants were not followed over time to see if changes in sleep affected stroke risk.
“This is an important point and should be a focus for future studies, as it is critical in the design of interventions,” Dr. Lackland said.
The INTERSTROKE study is funded by the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, Canadian Stroke Network, Swedish Research Council, Swedish Heart and Lung Foundation, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, Astra Zeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), MERCK, Sharp and Dohme, Swedish Heart and Lung Foundation, U.K. Chest, and U.K. Heart and Stroke. Dr. McCarthy and Lackland report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large international study show stroke risk was more than three times higher in those who slept too little, more than twice as high in those who sleep too much, and two to three times higher in those with symptoms of severe obstructive sleep apnea.
The study also showed that the greater the number of sleep disorder symptoms, the greater the stroke risk. The 11% of study participants with five or more symptoms of disordered sleep had a fivefold increased risk for stroke.
Although the study data do not show a causal link between disordered sleep and stroke, the association between the two was strong.
“Given the association, sleep disturbance may represent a marker of somebody at increased risk of stroke, and further interventional studies are required to see if management can reduce this risk,” lead investigator Christine McCarthy, MD, PhD, a geriatric and stroke medicine physician and researcher with the University of Galway (Ireland), told this news organization. “In the interim, however, management of sleep disturbance may have a positive impact on a patient’s quality of life.”
The findings were published online in the journal Neurology.
More symptoms, more risk
Previous research shows severe OSA doubles the risk of stroke and increases the chance of recurrent stroke. A 2019 study showed that people with insomnia had a small increased risk of stroke.
“Both snoring and extremes of sleep duration have been previously associated with an increased risk of stroke in observational research, but less is known about other symptoms of sleep impairment, with less consistent findings,” Dr. McCarthy said.
Prior studies have also generally come from a single geographic region, which Dr. McCarthy noted could limit their generalizability.
For this effort, investigators used data from 4,496 participants in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. About half of the participants had a history of stroke.
Using information collected from a survey of sleep habits, researchers found an elevated stroke risk in those who received less than 5 hours of sleep per night (odds ratio, 3.15; 95% confidence interval, 2.09-4.76) or more than 9 hours of sleep per night (OR, 2.67; 95% CI, 1.89-3.78), compared with those who slept 7 hours a night.
Participants who took unplanned naps or naps lasting an hour or more (OR, 2.46; 95% CI, 1.69-3.57) and participants who reported poor quality sleep (OR,1.52; 95% CI, 1.32-1.75) were also at an increased risk for stroke.
Symptoms of OSA were also strongly associated with increased stroke risk, including snoring (OR, 1.91; 95% CI, 1.62-2.24), snorting (OR, 2.64; 95% CI, 2.17-3.20), and breathing cessation (OR, 2.87; 95% CI, 2.28-2.60).
Stroke risk increased as the number of sleep disturbance symptoms rose, with the greatest risk in the 11% of participants who had five or more symptoms (OR, 5.38; 95% CI, 4.03-7.18).
“This study finds an association between a broad range of sleep impairment symptoms and stroke, and a graded association with increasing symptoms, in an international setting,” Dr. McCarthy said.
Researchers aren’t sure what’s driving the higher stroke risk among people with sleep disturbances. Although the study did control for potential confounders, it wasn’t designed to get at what’s driving the association.
“Sleep disturbance may also have a bi-directional relationship with many stroke risk factors; for example, sleep disturbance may be a symptom of disease and exacerbate disease,” Dr. McCarthy said. “Future interventional studies are required to determine the true direction of the relationship.”
A marker of stroke risk
Daniel Lackland, DrPH, professor of neurology at the Medical University of South Carolina, Charleston, said the findings provide additional evidence of the link between sleep and stroke risk.
“The results confirm sleep disorders as a potential marker and part of the risk profile,” he said.
Collecting information about sleep using a validated assessment tool is an important piece of clinical care, Dr. Lackland said, especially among patients with other stroke risk factors.
One limitation of the study was that data on sleep was collected only at one point, and participants were not followed over time to see if changes in sleep affected stroke risk.
“This is an important point and should be a focus for future studies, as it is critical in the design of interventions,” Dr. Lackland said.
The INTERSTROKE study is funded by the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, Canadian Stroke Network, Swedish Research Council, Swedish Heart and Lung Foundation, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, Astra Zeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), MERCK, Sharp and Dohme, Swedish Heart and Lung Foundation, U.K. Chest, and U.K. Heart and Stroke. Dr. McCarthy and Lackland report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large international study show stroke risk was more than three times higher in those who slept too little, more than twice as high in those who sleep too much, and two to three times higher in those with symptoms of severe obstructive sleep apnea.
The study also showed that the greater the number of sleep disorder symptoms, the greater the stroke risk. The 11% of study participants with five or more symptoms of disordered sleep had a fivefold increased risk for stroke.
Although the study data do not show a causal link between disordered sleep and stroke, the association between the two was strong.
“Given the association, sleep disturbance may represent a marker of somebody at increased risk of stroke, and further interventional studies are required to see if management can reduce this risk,” lead investigator Christine McCarthy, MD, PhD, a geriatric and stroke medicine physician and researcher with the University of Galway (Ireland), told this news organization. “In the interim, however, management of sleep disturbance may have a positive impact on a patient’s quality of life.”
The findings were published online in the journal Neurology.
More symptoms, more risk
Previous research shows severe OSA doubles the risk of stroke and increases the chance of recurrent stroke. A 2019 study showed that people with insomnia had a small increased risk of stroke.
“Both snoring and extremes of sleep duration have been previously associated with an increased risk of stroke in observational research, but less is known about other symptoms of sleep impairment, with less consistent findings,” Dr. McCarthy said.
Prior studies have also generally come from a single geographic region, which Dr. McCarthy noted could limit their generalizability.
For this effort, investigators used data from 4,496 participants in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. About half of the participants had a history of stroke.
Using information collected from a survey of sleep habits, researchers found an elevated stroke risk in those who received less than 5 hours of sleep per night (odds ratio, 3.15; 95% confidence interval, 2.09-4.76) or more than 9 hours of sleep per night (OR, 2.67; 95% CI, 1.89-3.78), compared with those who slept 7 hours a night.
Participants who took unplanned naps or naps lasting an hour or more (OR, 2.46; 95% CI, 1.69-3.57) and participants who reported poor quality sleep (OR,1.52; 95% CI, 1.32-1.75) were also at an increased risk for stroke.
Symptoms of OSA were also strongly associated with increased stroke risk, including snoring (OR, 1.91; 95% CI, 1.62-2.24), snorting (OR, 2.64; 95% CI, 2.17-3.20), and breathing cessation (OR, 2.87; 95% CI, 2.28-2.60).
Stroke risk increased as the number of sleep disturbance symptoms rose, with the greatest risk in the 11% of participants who had five or more symptoms (OR, 5.38; 95% CI, 4.03-7.18).
“This study finds an association between a broad range of sleep impairment symptoms and stroke, and a graded association with increasing symptoms, in an international setting,” Dr. McCarthy said.
Researchers aren’t sure what’s driving the higher stroke risk among people with sleep disturbances. Although the study did control for potential confounders, it wasn’t designed to get at what’s driving the association.
“Sleep disturbance may also have a bi-directional relationship with many stroke risk factors; for example, sleep disturbance may be a symptom of disease and exacerbate disease,” Dr. McCarthy said. “Future interventional studies are required to determine the true direction of the relationship.”
A marker of stroke risk
Daniel Lackland, DrPH, professor of neurology at the Medical University of South Carolina, Charleston, said the findings provide additional evidence of the link between sleep and stroke risk.
“The results confirm sleep disorders as a potential marker and part of the risk profile,” he said.
Collecting information about sleep using a validated assessment tool is an important piece of clinical care, Dr. Lackland said, especially among patients with other stroke risk factors.
One limitation of the study was that data on sleep was collected only at one point, and participants were not followed over time to see if changes in sleep affected stroke risk.
“This is an important point and should be a focus for future studies, as it is critical in the design of interventions,” Dr. Lackland said.
The INTERSTROKE study is funded by the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, Canadian Stroke Network, Swedish Research Council, Swedish Heart and Lung Foundation, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, Astra Zeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), MERCK, Sharp and Dohme, Swedish Heart and Lung Foundation, U.K. Chest, and U.K. Heart and Stroke. Dr. McCarthy and Lackland report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Seven ‘simple’ cardiovascular health measures linked to reduced dementia risk in women
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
FROM AAN 2023
Assessment of IV Edaravone Use in the Management of Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS) is an incurable neurodegenerative disorder that results in progressive deterioration of motor neurons in the ventral horn of the spinal cord, which results in loss of voluntary muscle movements.1 Eventually, typical daily tasks become difficult to perform, and as the disease progresses, the ability to eat and breathe is impaired.2 Reports from 2015 show the annual incidence of ALS is 5 cases per 100,000 people, with the total number of cases reported at more than 16,000 in the United States.3 In clinical practice, disease progression is routinely assessed by the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R). Typical decline is 1 point per month.4
Unfortunately, at this time, ALS care focuses on symptom management, including prevention of weight loss; implementation of communication strategies; and management of pain, constipation, excess secretions, cramping, and breathing. Despite copious research into treatment options, few exist. Riluzole is an oral medication administered twice daily and has been on the market since 1995.5-7 Efficacy was demonstrated in a study showing statistically significant survival at 12 months compared with controls (74% vs 58%, respectively; P = .014).6 Since its approval, riluzole has become part of standard-of-care ALS management.
In 2017, the US Food and Drug Administration (FDA) approved edaravone, an IV medication that was found to slow the progression of ALS in some patients.8-12 Oxidative stress caused by free radicals is hypothesized to increase the progression of ALS by motor neuron degradation.13 Edaravone works as a free radical and peroxynitrite scavenger and has been shown to eliminate lipid peroxides and hydroxyl radicals known to damage endothelial and neuronal cells.12
Given the mechanism of action of edaravone, it seemed to be a promising option to slow the progression of ALS. A 2019 systematic review analyzed 3 randomized studies with 367 patients and found a statistically significant difference in change in ALSFRS-R scores between patients treated with edaravone for 24 weeks compared with patients treated with the placebo (mean difference, 1.63; 95% CI, 0.26-3.00; P = .02).12 Secondary endpoints evaluated included percent forced vital capacity (%FVC), grip strength, and pinch strength: All showing no significant difference when comparing IV edaravone with placebo.
A 2022 postmarketing study of 324 patients with ALS evaluated the safety and efficacy of long-term edaravone treatment. IV edaravone therapy for > 24 weeks was well tolerated, although it was not associated with any disease-modifying benefit when comparing ALSFRS-R scores with patients not receiving edaravone over a median 13.9 months (ALSFRS-R points/month, -0.91 vs -0.85; P = .37).13 A third ALS treatment medication, sodium phenylbutyrate/taurursodiol was approved in 2022 but not available during our study period and not included here.14,15
Studies have shown an increased incidence of ALS in the veteran population. Veterans serving in the Gulf War were nearly twice as likely to develop ALS as those not serving in the Gulf.16 However, existing literature regarding the effectiveness of edaravone does not specifically examine the effect on this unique population. The objective of this study was to assess the effect of IV edaravone on ALS progression in veterans compared with veterans who received standard of care.
Methods
This study was conducted at a large, academic US Department of Veterans Affairs (VA) medical center. Patients with ALS are followed by a multidisciplinary clinic composed of a neurologist, pulmonologist, clinical pharmacist, social worker, speech therapist, physical therapist, occupational therapist, dietician, clinical psychologist, wheelchair clinic representative, and benefits representative. Patients are typically seen for a half-day appointment about every 3 months. During these visits, a comprehensive review of disease progression is performed. This review entails completion of the ALSFRS-R, physical examination, and pulmonary function testing. Speech intelligibility stage (SIS) is assessed by a speech therapist as well. SIS is scored from 1 (no detectable speech disorder) to 5 (no functional speech). All patients followed in this multidisciplinary ALS clinic receive standard-of-care treatment. This includes the discussion of treatment options that if appropriate are provided to help manage a wide range of complications associated with this disease (eg, pain, cramping, constipation, excessive secretions, weight loss, dysphagia). As a part of these personal discussions, treatment with riluzole is also offered as a standard-of-care pharmacologic option.
Study Design
This retrospective case-control study was conducted using electronic health record data to compare ALS progression in patients on IV edaravone therapy with standard of care. The Indiana University/Purdue University, Indianapolis Institutional Review Board and the VA Research and Development Committee approved the study. The control cohort received the standard of care. Patients in the case cohort received standard of care and edaravone 60 mg infusions daily for an initial cycle of 14 days on treatment, followed by 14 days off. All subsequent cycles were 10 of 14 days on treatment followed by 14 days off. The initial 2 doses were administered in the outpatient infusion clinic to monitor for a hypersensitivity reaction. Patients then had a peripherally inserted central catheter line placed and received doses on days 3 through 14 at home. A port was placed for subsequent cycles, which were also completed at home. Appropriateness of edaravone therapy was assessed by the neurologist at each follow-up appointment. Therapy was then discontinued if warranted based on disease progression or patient preference.
Study Population
Patients included were aged 18 to 75 years with diagnosed ALS. Patients with complications that might influence evaluation of medication efficacy (eg, Parkinson disease, schizophrenia, significant dementia, other major medical morbidity) were excluded. Patients were also excluded if they were on continuous bilevel positive airway pressure and/or had a total score of ≤ 3 points on ALSFRS-R items for dyspnea, orthopnea, or respiratory insufficiency. Due to our small sample size, patients were excluded if treatment was < 6 months, which is the gold standard of therapy duration established by clinical trials.9,11,12
The standard-of-care cohort included patients enrolled in the multidisciplinary clinic September 1, 2014 to August 31, 2017. These patients were compared in a 2:1 ratio with patients who received IV edaravone. The edaravone cohort included patients who initiated treatment with IV edaravone between September 1, 2017, and August 31, 2020. This date range prior to the approval of edaravone was chosen to compare patients at similar stages of disease progression and to have the largest sample size possible.
Data Collection
Data were obtained for eligible patients using the VA Computerized Patient Record System. Demographic data gathered for each patient included age, sex, weight, height, body mass index (BMI), race, and riluzole use.
The primary endpoint was the change in ALSFRS-R score after 6 months of IV edaravone compared with standard-of-care ALS management. Secondary outcomes included change in ALSFRS-R scores 3, 12, 18, and 24 months after therapy initiation, change in %FVC and SIS 3, 6, 12, 18, and 24 months after therapy initiation, duration of edaravone completed (months), time to death (months), and adverse events.
Statistical Analysis
Comparisons between the edaravone and control groups for differences in patient characteristics were made using χ2 and 2-sample t tests for categorical and continuous variables, respectively. Comparisons between the 2 groups for differences in study outcomes (ALSFRS-R scores, %FVC, SIS) at each time point were evaluated using 2-sample t tests. Adverse events and adverse drug reactions were compared between groups using χ2 tests. Statistical significance was set at 0.05.
We estimated that a sample size of 21 subjects in the edaravone (case) group and 42 in the standard-of-care (control) group would be needed to achieve 80% power to detect a difference of 6.5 between the 2 groups for the change in ALSFRS-R scores. This 80% power was calculated based on a 2-sample t test, and assuming a 2-sided 5% significance level and a within-group SD of 8.5.9 Statistical analysis was conducted using Microsoft Excel.
Results
Of the 96 patients, 10 met exclusion criteria. From the remaining 86, 42 were randomly selected for the standard-of-care group. A total of 27 patients seen in multidisciplinary ALS clinic between September 1, 2017, and August 31, 2020, received at least 1 dose of IV edaravone. Of the 27 edaravone patients, 6 were excluded for not completing a total of 6 months of edaravone. Two of the 6 excluded developed a rash, which resolved within 1 week after discontinuing edaravone. The other 4 discontinued edaravone before 6 months because of disease progression.
Baseline Characteristics
Efficacy
Discussion
This 24-month, case-control retrospective study assessed efficacy and safety of IV edaravone for the management of ALS. Although the landmark edaravone study showed slowed progression of ALS at 6 and 12 months, the effectiveness of edaravone outside the clinical trial setting has been less compelling.9-11,13 A later study showed no difference in change in ALSFRS-R score at 6 months compared with that of the placebo group.7 In our study, no statistically significant difference was found for change in ALSFRS-R scores at 6 months.
Our study was unique given we evaluated a veteran population. The link between the military and ALS is largely unknown, although studies have shown increased incidence of ALS in people with a military history compared with that of the general population.16-18 Our study was also unique because it was single-centered in design and allowed for outcome assessments, including ALSFRS-R scores, SIS, and %FVC measurements, to all be conducted by the same practitioner to limit variability. Unfortunately, our sample size resulted in a cohort that was underpowered at 12, 18, and 24 months. In addition, there was a lack of data on chart review for SIS and %FVC measurements at 24 months. As ALS progresses toward end stage, SIS and %FVC measurements can become difficult and burdensome on the patient to obtain, and the ALS multidisciplinary team may decide not to gather these data points as ALS progresses. As a result, change in SIS and %FVC measurements were unable to be reported due to lack of gathering this information at the 24-month mark in the edaravone group. Due to the cost and administration burden associated with edaravone, it is important that assessment of disease progression is performed regularly to assess benefit and appropriateness of continued therapy. The oral formulation of edaravone was approved in 2022, shortly after the completion of data collection for this study.19,20 Although our study did not analyze oral edaravone, the administration burden of treatment would be reduced with the oral formulation, and we hypothesize there will be increased patient interest in ALS management with oral vs IV edaravone. Evaluation of long-term treatment for efficacy and safety beyond 24 months has not been evaluated. Future studies should continue to evaluate edaravone use in a larger veteran population.
Limitations
One limitation for our study alluded to earlier in the discussion was sample size. Although this study met power at the 6-month mark, it was limited by the number of patients who received more than 6 months of edaravone (n = 21). As a result, statistical analyses between treatment groups were underpowered at 12, 18, and 24 months. Our study had 80% power to detect a difference of 6.5 between the groups for the change in ALSFRS-R scores. Previous studies detected a statistically significant difference in ALSFRS-R scores, with a difference in ALSFRS-R scores of 2.49 between groups.8 Future studies should evaluate a larger sample size of patients who are prescribed edaravone.
Another limitation was that the edaravone and standard-of-care group data were gathered from different time periods. Two different time frames were selected to increase sample size by gathering data over a longer period and to account for patients who may have qualified for IV edaravone but could not receive it as it was not yet available on the market. There were no known changes to the standard of care between the time periods that would affect results. As noted previously, the standard-of-care group had fewer patients taking riluzole compared with the edaravone group, which may have confounded our results. We concluded patients opting for edaravone were more likely to trial riluzole, taken by mouth twice daily, before starting edaravone, a once-daily IV infusion.
Conclusions
No difference in the rate of ALS progression was noted between patients who received IV edaravone vs standard of care at 6 months. In addition, no difference was noted in other objective measures of disease progression, including %FVC, SIS, and time to death. As a result, the decision to initiate and continue edaravone therapy should be made on an individualized basis according to a prescriber’s clinical judgment and a patient’s goals. Edaravone therapy should be discontinued when disease progression occurs or when medication administration becomes a burden.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at Veteran Health Indiana.
1. Kiernan MC, Vucic S, Cheah BC, et al. Amyotrophic lateral sclerosis. Lancet. 2011;377(9769):942-955. doi:10.1016/S0140-6736(10)61156-7
2. Rowland LP, Shneider NA. Amyotrophic lateral sclerosis. N Engl J Med. 2001;344(22):1688-1700. doi:0.1056/NEJM200105313442207
3. Mehta P, Kaye W, Raymond J, et al. Prevalence of amyotrophic lateral sclerosis–United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(46):1285-1289. doi:10.15585/mmwr.mm6746a1
4. Castrillo-Viguera C, Grasso DL, Simpson E, Shefner J, Cudkowicz ME. Clinical significance in the change of decline in ALSFRS-R. Amyotroph Lateral Scler. 2010;11(1-2):178-180. doi:10.3109/17482960903093710
5. Rilutek. Package insert. Covis Pharmaceuticals; 1995.
6. Bensimon G, Lacomblez L, Meininger V. A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N Engl J Med. 1994;330(9):585-591. doi:10.1056/NEJM199403033300901
7. Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V. Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet. 1996;347(9013):1425-1431. doi:10.1016/s0140-6736(96)91680-3
8. Radicava. Package insert. MT Pharma America Inc; 2017.
9. Abe K, Itoyama Y, Sobue G, et al. Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(7-8):610-617. doi:10.3109/21678421.2014.959024
10. Writing Group; Edaravone (MCI-186) ALS 19 Study Group. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(7):505-512. doi:10.1016/S1474-4422(17)30115-1
11. Writing Group; Edaravone (MCI-186) ALS 19 Study Group. Exploratory double-blind, parallel-group, placebo-controlled study of edaravone (MCI-186) in amyotrophic lateral sclerosis (Japan ALS severity classification: Grade 3, requiring assistance for eating, excretion or ambulation). Amyotroph Lateral Scler Frontotemporal Degener. 2017;18(suppl 1):40-48. doi:10.1080/21678421.2017.1361441
12. Luo L, Song Z, Li X, et al. Efficacy and safety of edaravone in treatment of amyotrophic lateral sclerosis–a systematic review and meta-analysis. Neurol Sci. 2019;40(2):235-241. doi:10.1007/s10072-018-3653-2
13. Witzel S, Maier A, Steinbach R, et al; German Motor Neuron Disease Network (MND-NET). Safety and effectiveness of long-term intravenous administration of edaravone for treatment of patients with amyotrophic lateral sclerosis. JAMA Neurol. 2022;79(2):121-130. doi:10.1001/jamaneurol.2021.4893
14. Paganoni S, Macklin EA, Hendrix S, et al. Trial of sodium phenylbutyrate-taurursodiol for amyotrophic lateral sclerosis. N Engl J Med. 2020;383(10):919-930. doi:10.1056/NEJMoa1916945
15. Relyvrio. Package insert. Amylyx Pharmaceuticals Inc; 2022.
16. McKay KA, Smith KA, Smertinaite L, Fang F, Ingre C, Taube F. Military service and related risk factors for amyotrophic lateral sclerosis. Acta Neurol Scand. 2021;143(1):39-50. doi:10.1111/ane.13345
17. Watanabe K, Tanaka M, Yuki S, Hirai M, Yamamoto Y. How is edaravone effective against acute ischemic stroke and amyotrophic lateral sclerosis? J Clin Biochem Nutr. 2018;62(1):20-38. doi:10.3164/jcbn.17-62
18. Horner RD, Kamins KG, Feussner JR, et al. Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology. 2003;61(6):742-749. doi:10.1212/01.wnl.0000069922.32557.ca
19. Radicava ORS. Package insert. Mitsubishi Tanabe Pharma America Inc; 2022.
20. Shimizu H, Nishimura Y, Shiide Y, et al. Bioequivalence study of oral suspension and intravenous formulation of edaravone in healthy adult subjects. Clin Pharmacol Drug Dev. 2021;10(10):1188-1197. doi:10.1002/cpdd.952
Amyotrophic lateral sclerosis (ALS) is an incurable neurodegenerative disorder that results in progressive deterioration of motor neurons in the ventral horn of the spinal cord, which results in loss of voluntary muscle movements.1 Eventually, typical daily tasks become difficult to perform, and as the disease progresses, the ability to eat and breathe is impaired.2 Reports from 2015 show the annual incidence of ALS is 5 cases per 100,000 people, with the total number of cases reported at more than 16,000 in the United States.3 In clinical practice, disease progression is routinely assessed by the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R). Typical decline is 1 point per month.4
Unfortunately, at this time, ALS care focuses on symptom management, including prevention of weight loss; implementation of communication strategies; and management of pain, constipation, excess secretions, cramping, and breathing. Despite copious research into treatment options, few exist. Riluzole is an oral medication administered twice daily and has been on the market since 1995.5-7 Efficacy was demonstrated in a study showing statistically significant survival at 12 months compared with controls (74% vs 58%, respectively; P = .014).6 Since its approval, riluzole has become part of standard-of-care ALS management.
In 2017, the US Food and Drug Administration (FDA) approved edaravone, an IV medication that was found to slow the progression of ALS in some patients.8-12 Oxidative stress caused by free radicals is hypothesized to increase the progression of ALS by motor neuron degradation.13 Edaravone works as a free radical and peroxynitrite scavenger and has been shown to eliminate lipid peroxides and hydroxyl radicals known to damage endothelial and neuronal cells.12
Given the mechanism of action of edaravone, it seemed to be a promising option to slow the progression of ALS. A 2019 systematic review analyzed 3 randomized studies with 367 patients and found a statistically significant difference in change in ALSFRS-R scores between patients treated with edaravone for 24 weeks compared with patients treated with the placebo (mean difference, 1.63; 95% CI, 0.26-3.00; P = .02).12 Secondary endpoints evaluated included percent forced vital capacity (%FVC), grip strength, and pinch strength: All showing no significant difference when comparing IV edaravone with placebo.
A 2022 postmarketing study of 324 patients with ALS evaluated the safety and efficacy of long-term edaravone treatment. IV edaravone therapy for > 24 weeks was well tolerated, although it was not associated with any disease-modifying benefit when comparing ALSFRS-R scores with patients not receiving edaravone over a median 13.9 months (ALSFRS-R points/month, -0.91 vs -0.85; P = .37).13 A third ALS treatment medication, sodium phenylbutyrate/taurursodiol was approved in 2022 but not available during our study period and not included here.14,15
Studies have shown an increased incidence of ALS in the veteran population. Veterans serving in the Gulf War were nearly twice as likely to develop ALS as those not serving in the Gulf.16 However, existing literature regarding the effectiveness of edaravone does not specifically examine the effect on this unique population. The objective of this study was to assess the effect of IV edaravone on ALS progression in veterans compared with veterans who received standard of care.
Methods
This study was conducted at a large, academic US Department of Veterans Affairs (VA) medical center. Patients with ALS are followed by a multidisciplinary clinic composed of a neurologist, pulmonologist, clinical pharmacist, social worker, speech therapist, physical therapist, occupational therapist, dietician, clinical psychologist, wheelchair clinic representative, and benefits representative. Patients are typically seen for a half-day appointment about every 3 months. During these visits, a comprehensive review of disease progression is performed. This review entails completion of the ALSFRS-R, physical examination, and pulmonary function testing. Speech intelligibility stage (SIS) is assessed by a speech therapist as well. SIS is scored from 1 (no detectable speech disorder) to 5 (no functional speech). All patients followed in this multidisciplinary ALS clinic receive standard-of-care treatment. This includes the discussion of treatment options that if appropriate are provided to help manage a wide range of complications associated with this disease (eg, pain, cramping, constipation, excessive secretions, weight loss, dysphagia). As a part of these personal discussions, treatment with riluzole is also offered as a standard-of-care pharmacologic option.
Study Design
This retrospective case-control study was conducted using electronic health record data to compare ALS progression in patients on IV edaravone therapy with standard of care. The Indiana University/Purdue University, Indianapolis Institutional Review Board and the VA Research and Development Committee approved the study. The control cohort received the standard of care. Patients in the case cohort received standard of care and edaravone 60 mg infusions daily for an initial cycle of 14 days on treatment, followed by 14 days off. All subsequent cycles were 10 of 14 days on treatment followed by 14 days off. The initial 2 doses were administered in the outpatient infusion clinic to monitor for a hypersensitivity reaction. Patients then had a peripherally inserted central catheter line placed and received doses on days 3 through 14 at home. A port was placed for subsequent cycles, which were also completed at home. Appropriateness of edaravone therapy was assessed by the neurologist at each follow-up appointment. Therapy was then discontinued if warranted based on disease progression or patient preference.
Study Population
Patients included were aged 18 to 75 years with diagnosed ALS. Patients with complications that might influence evaluation of medication efficacy (eg, Parkinson disease, schizophrenia, significant dementia, other major medical morbidity) were excluded. Patients were also excluded if they were on continuous bilevel positive airway pressure and/or had a total score of ≤ 3 points on ALSFRS-R items for dyspnea, orthopnea, or respiratory insufficiency. Due to our small sample size, patients were excluded if treatment was < 6 months, which is the gold standard of therapy duration established by clinical trials.9,11,12
The standard-of-care cohort included patients enrolled in the multidisciplinary clinic September 1, 2014 to August 31, 2017. These patients were compared in a 2:1 ratio with patients who received IV edaravone. The edaravone cohort included patients who initiated treatment with IV edaravone between September 1, 2017, and August 31, 2020. This date range prior to the approval of edaravone was chosen to compare patients at similar stages of disease progression and to have the largest sample size possible.
Data Collection
Data were obtained for eligible patients using the VA Computerized Patient Record System. Demographic data gathered for each patient included age, sex, weight, height, body mass index (BMI), race, and riluzole use.
The primary endpoint was the change in ALSFRS-R score after 6 months of IV edaravone compared with standard-of-care ALS management. Secondary outcomes included change in ALSFRS-R scores 3, 12, 18, and 24 months after therapy initiation, change in %FVC and SIS 3, 6, 12, 18, and 24 months after therapy initiation, duration of edaravone completed (months), time to death (months), and adverse events.
Statistical Analysis
Comparisons between the edaravone and control groups for differences in patient characteristics were made using χ2 and 2-sample t tests for categorical and continuous variables, respectively. Comparisons between the 2 groups for differences in study outcomes (ALSFRS-R scores, %FVC, SIS) at each time point were evaluated using 2-sample t tests. Adverse events and adverse drug reactions were compared between groups using χ2 tests. Statistical significance was set at 0.05.
We estimated that a sample size of 21 subjects in the edaravone (case) group and 42 in the standard-of-care (control) group would be needed to achieve 80% power to detect a difference of 6.5 between the 2 groups for the change in ALSFRS-R scores. This 80% power was calculated based on a 2-sample t test, and assuming a 2-sided 5% significance level and a within-group SD of 8.5.9 Statistical analysis was conducted using Microsoft Excel.
Results
Of the 96 patients, 10 met exclusion criteria. From the remaining 86, 42 were randomly selected for the standard-of-care group. A total of 27 patients seen in multidisciplinary ALS clinic between September 1, 2017, and August 31, 2020, received at least 1 dose of IV edaravone. Of the 27 edaravone patients, 6 were excluded for not completing a total of 6 months of edaravone. Two of the 6 excluded developed a rash, which resolved within 1 week after discontinuing edaravone. The other 4 discontinued edaravone before 6 months because of disease progression.
Baseline Characteristics
Efficacy
Discussion
This 24-month, case-control retrospective study assessed efficacy and safety of IV edaravone for the management of ALS. Although the landmark edaravone study showed slowed progression of ALS at 6 and 12 months, the effectiveness of edaravone outside the clinical trial setting has been less compelling.9-11,13 A later study showed no difference in change in ALSFRS-R score at 6 months compared with that of the placebo group.7 In our study, no statistically significant difference was found for change in ALSFRS-R scores at 6 months.
Our study was unique given we evaluated a veteran population. The link between the military and ALS is largely unknown, although studies have shown increased incidence of ALS in people with a military history compared with that of the general population.16-18 Our study was also unique because it was single-centered in design and allowed for outcome assessments, including ALSFRS-R scores, SIS, and %FVC measurements, to all be conducted by the same practitioner to limit variability. Unfortunately, our sample size resulted in a cohort that was underpowered at 12, 18, and 24 months. In addition, there was a lack of data on chart review for SIS and %FVC measurements at 24 months. As ALS progresses toward end stage, SIS and %FVC measurements can become difficult and burdensome on the patient to obtain, and the ALS multidisciplinary team may decide not to gather these data points as ALS progresses. As a result, change in SIS and %FVC measurements were unable to be reported due to lack of gathering this information at the 24-month mark in the edaravone group. Due to the cost and administration burden associated with edaravone, it is important that assessment of disease progression is performed regularly to assess benefit and appropriateness of continued therapy. The oral formulation of edaravone was approved in 2022, shortly after the completion of data collection for this study.19,20 Although our study did not analyze oral edaravone, the administration burden of treatment would be reduced with the oral formulation, and we hypothesize there will be increased patient interest in ALS management with oral vs IV edaravone. Evaluation of long-term treatment for efficacy and safety beyond 24 months has not been evaluated. Future studies should continue to evaluate edaravone use in a larger veteran population.
Limitations
One limitation for our study alluded to earlier in the discussion was sample size. Although this study met power at the 6-month mark, it was limited by the number of patients who received more than 6 months of edaravone (n = 21). As a result, statistical analyses between treatment groups were underpowered at 12, 18, and 24 months. Our study had 80% power to detect a difference of 6.5 between the groups for the change in ALSFRS-R scores. Previous studies detected a statistically significant difference in ALSFRS-R scores, with a difference in ALSFRS-R scores of 2.49 between groups.8 Future studies should evaluate a larger sample size of patients who are prescribed edaravone.
Another limitation was that the edaravone and standard-of-care group data were gathered from different time periods. Two different time frames were selected to increase sample size by gathering data over a longer period and to account for patients who may have qualified for IV edaravone but could not receive it as it was not yet available on the market. There were no known changes to the standard of care between the time periods that would affect results. As noted previously, the standard-of-care group had fewer patients taking riluzole compared with the edaravone group, which may have confounded our results. We concluded patients opting for edaravone were more likely to trial riluzole, taken by mouth twice daily, before starting edaravone, a once-daily IV infusion.
Conclusions
No difference in the rate of ALS progression was noted between patients who received IV edaravone vs standard of care at 6 months. In addition, no difference was noted in other objective measures of disease progression, including %FVC, SIS, and time to death. As a result, the decision to initiate and continue edaravone therapy should be made on an individualized basis according to a prescriber’s clinical judgment and a patient’s goals. Edaravone therapy should be discontinued when disease progression occurs or when medication administration becomes a burden.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at Veteran Health Indiana.
Amyotrophic lateral sclerosis (ALS) is an incurable neurodegenerative disorder that results in progressive deterioration of motor neurons in the ventral horn of the spinal cord, which results in loss of voluntary muscle movements.1 Eventually, typical daily tasks become difficult to perform, and as the disease progresses, the ability to eat and breathe is impaired.2 Reports from 2015 show the annual incidence of ALS is 5 cases per 100,000 people, with the total number of cases reported at more than 16,000 in the United States.3 In clinical practice, disease progression is routinely assessed by the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R). Typical decline is 1 point per month.4
Unfortunately, at this time, ALS care focuses on symptom management, including prevention of weight loss; implementation of communication strategies; and management of pain, constipation, excess secretions, cramping, and breathing. Despite copious research into treatment options, few exist. Riluzole is an oral medication administered twice daily and has been on the market since 1995.5-7 Efficacy was demonstrated in a study showing statistically significant survival at 12 months compared with controls (74% vs 58%, respectively; P = .014).6 Since its approval, riluzole has become part of standard-of-care ALS management.
In 2017, the US Food and Drug Administration (FDA) approved edaravone, an IV medication that was found to slow the progression of ALS in some patients.8-12 Oxidative stress caused by free radicals is hypothesized to increase the progression of ALS by motor neuron degradation.13 Edaravone works as a free radical and peroxynitrite scavenger and has been shown to eliminate lipid peroxides and hydroxyl radicals known to damage endothelial and neuronal cells.12
Given the mechanism of action of edaravone, it seemed to be a promising option to slow the progression of ALS. A 2019 systematic review analyzed 3 randomized studies with 367 patients and found a statistically significant difference in change in ALSFRS-R scores between patients treated with edaravone for 24 weeks compared with patients treated with the placebo (mean difference, 1.63; 95% CI, 0.26-3.00; P = .02).12 Secondary endpoints evaluated included percent forced vital capacity (%FVC), grip strength, and pinch strength: All showing no significant difference when comparing IV edaravone with placebo.
A 2022 postmarketing study of 324 patients with ALS evaluated the safety and efficacy of long-term edaravone treatment. IV edaravone therapy for > 24 weeks was well tolerated, although it was not associated with any disease-modifying benefit when comparing ALSFRS-R scores with patients not receiving edaravone over a median 13.9 months (ALSFRS-R points/month, -0.91 vs -0.85; P = .37).13 A third ALS treatment medication, sodium phenylbutyrate/taurursodiol was approved in 2022 but not available during our study period and not included here.14,15
Studies have shown an increased incidence of ALS in the veteran population. Veterans serving in the Gulf War were nearly twice as likely to develop ALS as those not serving in the Gulf.16 However, existing literature regarding the effectiveness of edaravone does not specifically examine the effect on this unique population. The objective of this study was to assess the effect of IV edaravone on ALS progression in veterans compared with veterans who received standard of care.
Methods
This study was conducted at a large, academic US Department of Veterans Affairs (VA) medical center. Patients with ALS are followed by a multidisciplinary clinic composed of a neurologist, pulmonologist, clinical pharmacist, social worker, speech therapist, physical therapist, occupational therapist, dietician, clinical psychologist, wheelchair clinic representative, and benefits representative. Patients are typically seen for a half-day appointment about every 3 months. During these visits, a comprehensive review of disease progression is performed. This review entails completion of the ALSFRS-R, physical examination, and pulmonary function testing. Speech intelligibility stage (SIS) is assessed by a speech therapist as well. SIS is scored from 1 (no detectable speech disorder) to 5 (no functional speech). All patients followed in this multidisciplinary ALS clinic receive standard-of-care treatment. This includes the discussion of treatment options that if appropriate are provided to help manage a wide range of complications associated with this disease (eg, pain, cramping, constipation, excessive secretions, weight loss, dysphagia). As a part of these personal discussions, treatment with riluzole is also offered as a standard-of-care pharmacologic option.
Study Design
This retrospective case-control study was conducted using electronic health record data to compare ALS progression in patients on IV edaravone therapy with standard of care. The Indiana University/Purdue University, Indianapolis Institutional Review Board and the VA Research and Development Committee approved the study. The control cohort received the standard of care. Patients in the case cohort received standard of care and edaravone 60 mg infusions daily for an initial cycle of 14 days on treatment, followed by 14 days off. All subsequent cycles were 10 of 14 days on treatment followed by 14 days off. The initial 2 doses were administered in the outpatient infusion clinic to monitor for a hypersensitivity reaction. Patients then had a peripherally inserted central catheter line placed and received doses on days 3 through 14 at home. A port was placed for subsequent cycles, which were also completed at home. Appropriateness of edaravone therapy was assessed by the neurologist at each follow-up appointment. Therapy was then discontinued if warranted based on disease progression or patient preference.
Study Population
Patients included were aged 18 to 75 years with diagnosed ALS. Patients with complications that might influence evaluation of medication efficacy (eg, Parkinson disease, schizophrenia, significant dementia, other major medical morbidity) were excluded. Patients were also excluded if they were on continuous bilevel positive airway pressure and/or had a total score of ≤ 3 points on ALSFRS-R items for dyspnea, orthopnea, or respiratory insufficiency. Due to our small sample size, patients were excluded if treatment was < 6 months, which is the gold standard of therapy duration established by clinical trials.9,11,12
The standard-of-care cohort included patients enrolled in the multidisciplinary clinic September 1, 2014 to August 31, 2017. These patients were compared in a 2:1 ratio with patients who received IV edaravone. The edaravone cohort included patients who initiated treatment with IV edaravone between September 1, 2017, and August 31, 2020. This date range prior to the approval of edaravone was chosen to compare patients at similar stages of disease progression and to have the largest sample size possible.
Data Collection
Data were obtained for eligible patients using the VA Computerized Patient Record System. Demographic data gathered for each patient included age, sex, weight, height, body mass index (BMI), race, and riluzole use.
The primary endpoint was the change in ALSFRS-R score after 6 months of IV edaravone compared with standard-of-care ALS management. Secondary outcomes included change in ALSFRS-R scores 3, 12, 18, and 24 months after therapy initiation, change in %FVC and SIS 3, 6, 12, 18, and 24 months after therapy initiation, duration of edaravone completed (months), time to death (months), and adverse events.
Statistical Analysis
Comparisons between the edaravone and control groups for differences in patient characteristics were made using χ2 and 2-sample t tests for categorical and continuous variables, respectively. Comparisons between the 2 groups for differences in study outcomes (ALSFRS-R scores, %FVC, SIS) at each time point were evaluated using 2-sample t tests. Adverse events and adverse drug reactions were compared between groups using χ2 tests. Statistical significance was set at 0.05.
We estimated that a sample size of 21 subjects in the edaravone (case) group and 42 in the standard-of-care (control) group would be needed to achieve 80% power to detect a difference of 6.5 between the 2 groups for the change in ALSFRS-R scores. This 80% power was calculated based on a 2-sample t test, and assuming a 2-sided 5% significance level and a within-group SD of 8.5.9 Statistical analysis was conducted using Microsoft Excel.
Results
Of the 96 patients, 10 met exclusion criteria. From the remaining 86, 42 were randomly selected for the standard-of-care group. A total of 27 patients seen in multidisciplinary ALS clinic between September 1, 2017, and August 31, 2020, received at least 1 dose of IV edaravone. Of the 27 edaravone patients, 6 were excluded for not completing a total of 6 months of edaravone. Two of the 6 excluded developed a rash, which resolved within 1 week after discontinuing edaravone. The other 4 discontinued edaravone before 6 months because of disease progression.
Baseline Characteristics
Efficacy
Discussion
This 24-month, case-control retrospective study assessed efficacy and safety of IV edaravone for the management of ALS. Although the landmark edaravone study showed slowed progression of ALS at 6 and 12 months, the effectiveness of edaravone outside the clinical trial setting has been less compelling.9-11,13 A later study showed no difference in change in ALSFRS-R score at 6 months compared with that of the placebo group.7 In our study, no statistically significant difference was found for change in ALSFRS-R scores at 6 months.
Our study was unique given we evaluated a veteran population. The link between the military and ALS is largely unknown, although studies have shown increased incidence of ALS in people with a military history compared with that of the general population.16-18 Our study was also unique because it was single-centered in design and allowed for outcome assessments, including ALSFRS-R scores, SIS, and %FVC measurements, to all be conducted by the same practitioner to limit variability. Unfortunately, our sample size resulted in a cohort that was underpowered at 12, 18, and 24 months. In addition, there was a lack of data on chart review for SIS and %FVC measurements at 24 months. As ALS progresses toward end stage, SIS and %FVC measurements can become difficult and burdensome on the patient to obtain, and the ALS multidisciplinary team may decide not to gather these data points as ALS progresses. As a result, change in SIS and %FVC measurements were unable to be reported due to lack of gathering this information at the 24-month mark in the edaravone group. Due to the cost and administration burden associated with edaravone, it is important that assessment of disease progression is performed regularly to assess benefit and appropriateness of continued therapy. The oral formulation of edaravone was approved in 2022, shortly after the completion of data collection for this study.19,20 Although our study did not analyze oral edaravone, the administration burden of treatment would be reduced with the oral formulation, and we hypothesize there will be increased patient interest in ALS management with oral vs IV edaravone. Evaluation of long-term treatment for efficacy and safety beyond 24 months has not been evaluated. Future studies should continue to evaluate edaravone use in a larger veteran population.
Limitations
One limitation for our study alluded to earlier in the discussion was sample size. Although this study met power at the 6-month mark, it was limited by the number of patients who received more than 6 months of edaravone (n = 21). As a result, statistical analyses between treatment groups were underpowered at 12, 18, and 24 months. Our study had 80% power to detect a difference of 6.5 between the groups for the change in ALSFRS-R scores. Previous studies detected a statistically significant difference in ALSFRS-R scores, with a difference in ALSFRS-R scores of 2.49 between groups.8 Future studies should evaluate a larger sample size of patients who are prescribed edaravone.
Another limitation was that the edaravone and standard-of-care group data were gathered from different time periods. Two different time frames were selected to increase sample size by gathering data over a longer period and to account for patients who may have qualified for IV edaravone but could not receive it as it was not yet available on the market. There were no known changes to the standard of care between the time periods that would affect results. As noted previously, the standard-of-care group had fewer patients taking riluzole compared with the edaravone group, which may have confounded our results. We concluded patients opting for edaravone were more likely to trial riluzole, taken by mouth twice daily, before starting edaravone, a once-daily IV infusion.
Conclusions
No difference in the rate of ALS progression was noted between patients who received IV edaravone vs standard of care at 6 months. In addition, no difference was noted in other objective measures of disease progression, including %FVC, SIS, and time to death. As a result, the decision to initiate and continue edaravone therapy should be made on an individualized basis according to a prescriber’s clinical judgment and a patient’s goals. Edaravone therapy should be discontinued when disease progression occurs or when medication administration becomes a burden.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at Veteran Health Indiana.
1. Kiernan MC, Vucic S, Cheah BC, et al. Amyotrophic lateral sclerosis. Lancet. 2011;377(9769):942-955. doi:10.1016/S0140-6736(10)61156-7
2. Rowland LP, Shneider NA. Amyotrophic lateral sclerosis. N Engl J Med. 2001;344(22):1688-1700. doi:0.1056/NEJM200105313442207
3. Mehta P, Kaye W, Raymond J, et al. Prevalence of amyotrophic lateral sclerosis–United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(46):1285-1289. doi:10.15585/mmwr.mm6746a1
4. Castrillo-Viguera C, Grasso DL, Simpson E, Shefner J, Cudkowicz ME. Clinical significance in the change of decline in ALSFRS-R. Amyotroph Lateral Scler. 2010;11(1-2):178-180. doi:10.3109/17482960903093710
5. Rilutek. Package insert. Covis Pharmaceuticals; 1995.
6. Bensimon G, Lacomblez L, Meininger V. A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N Engl J Med. 1994;330(9):585-591. doi:10.1056/NEJM199403033300901
7. Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V. Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet. 1996;347(9013):1425-1431. doi:10.1016/s0140-6736(96)91680-3
8. Radicava. Package insert. MT Pharma America Inc; 2017.
9. Abe K, Itoyama Y, Sobue G, et al. Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(7-8):610-617. doi:10.3109/21678421.2014.959024
10. Writing Group; Edaravone (MCI-186) ALS 19 Study Group. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(7):505-512. doi:10.1016/S1474-4422(17)30115-1
11. Writing Group; Edaravone (MCI-186) ALS 19 Study Group. Exploratory double-blind, parallel-group, placebo-controlled study of edaravone (MCI-186) in amyotrophic lateral sclerosis (Japan ALS severity classification: Grade 3, requiring assistance for eating, excretion or ambulation). Amyotroph Lateral Scler Frontotemporal Degener. 2017;18(suppl 1):40-48. doi:10.1080/21678421.2017.1361441
12. Luo L, Song Z, Li X, et al. Efficacy and safety of edaravone in treatment of amyotrophic lateral sclerosis–a systematic review and meta-analysis. Neurol Sci. 2019;40(2):235-241. doi:10.1007/s10072-018-3653-2
13. Witzel S, Maier A, Steinbach R, et al; German Motor Neuron Disease Network (MND-NET). Safety and effectiveness of long-term intravenous administration of edaravone for treatment of patients with amyotrophic lateral sclerosis. JAMA Neurol. 2022;79(2):121-130. doi:10.1001/jamaneurol.2021.4893
14. Paganoni S, Macklin EA, Hendrix S, et al. Trial of sodium phenylbutyrate-taurursodiol for amyotrophic lateral sclerosis. N Engl J Med. 2020;383(10):919-930. doi:10.1056/NEJMoa1916945
15. Relyvrio. Package insert. Amylyx Pharmaceuticals Inc; 2022.
16. McKay KA, Smith KA, Smertinaite L, Fang F, Ingre C, Taube F. Military service and related risk factors for amyotrophic lateral sclerosis. Acta Neurol Scand. 2021;143(1):39-50. doi:10.1111/ane.13345
17. Watanabe K, Tanaka M, Yuki S, Hirai M, Yamamoto Y. How is edaravone effective against acute ischemic stroke and amyotrophic lateral sclerosis? J Clin Biochem Nutr. 2018;62(1):20-38. doi:10.3164/jcbn.17-62
18. Horner RD, Kamins KG, Feussner JR, et al. Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology. 2003;61(6):742-749. doi:10.1212/01.wnl.0000069922.32557.ca
19. Radicava ORS. Package insert. Mitsubishi Tanabe Pharma America Inc; 2022.
20. Shimizu H, Nishimura Y, Shiide Y, et al. Bioequivalence study of oral suspension and intravenous formulation of edaravone in healthy adult subjects. Clin Pharmacol Drug Dev. 2021;10(10):1188-1197. doi:10.1002/cpdd.952
1. Kiernan MC, Vucic S, Cheah BC, et al. Amyotrophic lateral sclerosis. Lancet. 2011;377(9769):942-955. doi:10.1016/S0140-6736(10)61156-7
2. Rowland LP, Shneider NA. Amyotrophic lateral sclerosis. N Engl J Med. 2001;344(22):1688-1700. doi:0.1056/NEJM200105313442207
3. Mehta P, Kaye W, Raymond J, et al. Prevalence of amyotrophic lateral sclerosis–United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(46):1285-1289. doi:10.15585/mmwr.mm6746a1
4. Castrillo-Viguera C, Grasso DL, Simpson E, Shefner J, Cudkowicz ME. Clinical significance in the change of decline in ALSFRS-R. Amyotroph Lateral Scler. 2010;11(1-2):178-180. doi:10.3109/17482960903093710
5. Rilutek. Package insert. Covis Pharmaceuticals; 1995.
6. Bensimon G, Lacomblez L, Meininger V. A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N Engl J Med. 1994;330(9):585-591. doi:10.1056/NEJM199403033300901
7. Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V. Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet. 1996;347(9013):1425-1431. doi:10.1016/s0140-6736(96)91680-3
8. Radicava. Package insert. MT Pharma America Inc; 2017.
9. Abe K, Itoyama Y, Sobue G, et al. Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(7-8):610-617. doi:10.3109/21678421.2014.959024
10. Writing Group; Edaravone (MCI-186) ALS 19 Study Group. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(7):505-512. doi:10.1016/S1474-4422(17)30115-1
11. Writing Group; Edaravone (MCI-186) ALS 19 Study Group. Exploratory double-blind, parallel-group, placebo-controlled study of edaravone (MCI-186) in amyotrophic lateral sclerosis (Japan ALS severity classification: Grade 3, requiring assistance for eating, excretion or ambulation). Amyotroph Lateral Scler Frontotemporal Degener. 2017;18(suppl 1):40-48. doi:10.1080/21678421.2017.1361441
12. Luo L, Song Z, Li X, et al. Efficacy and safety of edaravone in treatment of amyotrophic lateral sclerosis–a systematic review and meta-analysis. Neurol Sci. 2019;40(2):235-241. doi:10.1007/s10072-018-3653-2
13. Witzel S, Maier A, Steinbach R, et al; German Motor Neuron Disease Network (MND-NET). Safety and effectiveness of long-term intravenous administration of edaravone for treatment of patients with amyotrophic lateral sclerosis. JAMA Neurol. 2022;79(2):121-130. doi:10.1001/jamaneurol.2021.4893
14. Paganoni S, Macklin EA, Hendrix S, et al. Trial of sodium phenylbutyrate-taurursodiol for amyotrophic lateral sclerosis. N Engl J Med. 2020;383(10):919-930. doi:10.1056/NEJMoa1916945
15. Relyvrio. Package insert. Amylyx Pharmaceuticals Inc; 2022.
16. McKay KA, Smith KA, Smertinaite L, Fang F, Ingre C, Taube F. Military service and related risk factors for amyotrophic lateral sclerosis. Acta Neurol Scand. 2021;143(1):39-50. doi:10.1111/ane.13345
17. Watanabe K, Tanaka M, Yuki S, Hirai M, Yamamoto Y. How is edaravone effective against acute ischemic stroke and amyotrophic lateral sclerosis? J Clin Biochem Nutr. 2018;62(1):20-38. doi:10.3164/jcbn.17-62
18. Horner RD, Kamins KG, Feussner JR, et al. Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology. 2003;61(6):742-749. doi:10.1212/01.wnl.0000069922.32557.ca
19. Radicava ORS. Package insert. Mitsubishi Tanabe Pharma America Inc; 2022.
20. Shimizu H, Nishimura Y, Shiide Y, et al. Bioequivalence study of oral suspension and intravenous formulation of edaravone in healthy adult subjects. Clin Pharmacol Drug Dev. 2021;10(10):1188-1197. doi:10.1002/cpdd.952
Acute Painful Horner Syndrome as the First Presenting Sign of Carotid Artery Dissection
Horner syndrome is a rare condition that has no sex or race predilection and is characterized by the clinical triad of a miosis, anhidrosis, and small, unilateral ptosis. The prompt diagnosis and determination of the etiology of Horner syndrome are of utmost importance, as the condition can result from many life-threatening systemic complications. Horner syndrome is often asymptomatic but can have distinct, easily identified characteristics seen with an ophthalmic examination. This report describes a patient who presented with Horner syndrome resulting from an internal carotid artery dissection.
Case Presentation
A 61-year-old woman presented with periorbital pain with onset 3 days prior. The patient described the pain as 7 of 10 that had been worsening and was localized around and behind the right eye. She reported new-onset headaches on the right side over the past week with associated intermittent vision blurriness in the right eye. She had a history of mobility issues and had fallen backward about 1 week before, hitting the back of her head on the floor without direct trauma to the eye. She was symptomatic for light sensitivity, syncope, and dizziness, with reports of a recent history of transient ischemic attacks (TIAs) of unknown etiology, which had occurred in the months preceding her examination. She reported no jaw claudication, scalp tenderness, and neck or shoulder pain. She was unaware of any changes in her perspiration pattern on the right side of her face but mentioned that she had noticed her right upper eyelid drooping while looking in the mirror.
This patient had a routine eye examination 2 months before, which was remarkable for stable, nonfoveal involving adult-onset vitelliform dystrophy in the left eye and nuclear sclerotic cataracts and mild refractive error in both eyes. No iris heterochromia was noted, and her pupils were equal, round, and reactive to light. Her history was remarkable for chest pain, obesity, bipolar disorder, vertigo, transient cerebral ischemia, hypertension, hypercholesterolemia, alcohol use disorder, cocaine use disorder, and asthma. A carotid ultrasound had been performed 1 month before the onset of symptoms due to her history of TIAs, which showed no hemodynamically significant stenosis (> 50% stenosis) of either carotid artery. Her medications included oxybutynin chloride, amlodipine, acetaminophen, sertraline hydrochloride, lidocaine, albuterol, risperidone, hydroxyzine hydrochloride, lisinopril, omeprazole, once-daily baby aspirin, atorvastatin, and calcium.
At the time of presentation, an ophthalmic examination revealed no decrease in visual acuity with a best-corrected visual acuity of 20/20 in the right and left eyes. The patient’s pupil sizes were unequal, with a smaller, more miotic right pupil with a greater difference between the pupil sizes in dim illumination (Figure 1).
As the patient had pathologic miosis, conditions causing pathologic mydriasis, such as Adie tonic pupil and cranial nerve III palsy, were ruled out. The presence of an acute, slight ptosis with pathologic miosis and pain in the ipsilateral eye with no reports of exposure to miotic pharmaceutical agents and no history of trauma to the globe or orbit eliminated other differentials, leading to a diagnosis of right-sided Horner syndrome. Due to concerns of acute onset periorbital and retrobulbar pain, she was referred to the emergency department with recommendations for computed tomography angiography (CTA), magnetic resonance imaging (MRI), and magnetic resonance angiogram (MRA) of the head and neck to rule out a carotid artery dissection.
CTA revealed a focal linear filling defect in the right midinternal carotid artery, likely related to an internal carotid artery vascular flap. There was no evidence of proximal intracranial occlusive disease. MRI revealed a linear area of high-intensity signal projecting over the mid and distal right internal carotid artery lumen (Figure 2A).
Imaging suggested an internal carotid artery dissection, and the patient was admitted to the hospital for observation for 4 days. During this time, the patient was instructed to continue taking 81mg aspirin daily and to begin taking 75 mg clopidogrel bisulfate daily to prevent a cerebrovascular accident. Once stability was established, the patient was discharged with instructions to follow up with neurology and neuro-ophthalmology.
Discussion
Anisocoria is defined as a difference in pupil sizes between the eyes.1 This difference can be physiologic with no underlying pathology as an etiology of the condition. If underlying pathology causes anisocoria, it can result in dysfunction with mydriasis, leading to a more miotic pupil, or it can result from issues with miosis, leading to a more mydriatic pupil.1
To determine whether anisocoria is physiologic or pathologic, one must assess the patient’s pupil sizes in dim and bright illumination. If the difference in the pupil size is the same in both room illuminations (ie, the anisocoria is 2 mm in both bright and dim illumination, pupillary constriction and dilation are functioning normally), then the patient has physiologic anisocoria.1 If anisocoria is different in bright and dim illumination (ie, the anisocoria is 1 mm in bright and 3 mm in dim settings or 3 mm in bright and 1 mm in dim settings), the condition is related to pathology. To determine the underlying pathology of anisocoria in cases that are not physiologic, it is important to first determine whether the anisocoria is related to miotic or mydriatic dysfunction.1
If the anisocoria is greater in dim illumination, this suggests mydriatic dysfunction and could be a result of damage to the sympathetic pupillary pathway.1 The smaller or more miotic pupil in this instance is the pathologic pupil. If the anisocoria is greater in bright illumination, this suggests miotic dysfunction and could be a result of damage to the parasympathetic pathway.1 The larger or more mydriatic pupil in this instance is the pathologic pupil. Congenital abnormalities, such as iris colobomas, aniridia, and ectopic pupils, can result in a wide range of pupil sizes and shapes, including miotic or mydriatic pupils.1
Pathologic Mydriasis
Pathologic mydriatic pupils can result from dysfunction in the parasympathetic nervous system, which results in a pupil that is not sufficiently able to dilate with the removal of a light stimulus. Mydriatic pupils can be related to Adie tonic pupil, Argyll-Robertson pupil, third nerve palsy, trauma, surgeries, or pharmacologic mydriasis.2 The conditions that cause mydriasis can be readily differentiated from one another based on clinical examination.
Adie tonic pupil results from damage to the ciliary ganglion.2 While pupillary constriction in response to light will be absent or sluggish in an Adie pupil, the patient will have an intact but sluggish accommodative pupillary response; therefore, the pupil will still constrict with accommodation and convergence to focus on near objects, although slowly. This is known as light-near dissociation.2
Argyll-Robertson pupils are caused by damage to the Edinger-Westphal nucleus in the rostral midbrain.3 Lesions to this area of the brain are typically associated with neurosyphilis but also can be a result of Lyme disease, multiple sclerosis, encephalitis, neurosarcoidosis, herpes zoster, diabetes mellitus, and chronic alcohol misuse.3 Argyll Robertson pupils can appear very similar to a tonic pupil in that this condition will also have a dilated pupil and light-near dissociation.3 These pupils will differ in that they also tend to have an irregular shape (dyscoria), and the pupils will constrict briskly when focusing on near objects and dilate briskly when focusing on distant objects, not sluggishly, as in Adie tonic pupil.3
Mydriasis due to a third nerve palsy will present with ptosis and extraocular muscle dysfunction (including deficits to the superior rectus, medial rectus, inferior oblique, and inferior rectus), with the classic presentation of a completed palsy with the eye positioned “down and out” or the patient’s inability to look medially and superiorly with the affected eye.2
As in cases of pathologic mydriasis, a thorough and in-depth history can help determine traumatic, surgical and pharmacologic etiologies of a mydriatic pupil. It should be determined whether the patient has had any previous trauma or surgeries to the eye or has been in contact with any of the following: acetylcholine receptor antagonists (atropine, scopolamine, homatropine, cyclopentolate, and tropicamide), motion sickness patches (scopolamine), nasal vasoconstrictors, glycopyrrolate deodorants, and/or various plants (Jimson weed or plants belonging to the digitalis family, such as foxglove).2
Pathologic Miosis
Pathologic miotic pupils can result from dysfunction in the sympathetic nervous system and can be related to blunt or penetrating trauma to the orbit, Horner syndrome, and pharmacologic miosis.2 Horner syndrome will be accompanied by a slight ptosis and sometimes anhidrosis on the ipsilateral side of the face. To differentiate between traumatic and pharmacologic miosis, a detailed history should be obtained, paying close attention to injuries to the eyes or head and/or possible exposure to chemical or pharmaceutical agents, including prostaglandins, pilocarpine, organophosphates, and opiates.2
Horner Syndrome
Horner syndrome is a neurologic condition that results from damage to the oculosympathetic pathway.4 The oculosympathetic pathway is a 3-neuron pathway that begins in the hypothalamus and follows a circuitous route to ultimately innervate the facial sweat glands, the smooth muscles of the blood vessels in the orbit and face, the iris dilator muscle, and the Müller muscles of the superior and inferior eyelids.1,5 Therefore, this pathway’s functions include vasoconstriction of facial blood vessels, facial diaphoresis (sweating), pupillary dilation, and maintaining an open position of the eyelids.1
Oculosympathetic pathway anatomy. To understand the findings associated with Horner syndrome, it is necessary to understand the anatomy of this 3-neuron pathway.5 First-order neurons, or central neurons, arise in the posterolateral aspect of the hypothalamus, where they then descend through the midbrain, pons, medulla, and cervical spinal cord via the intermediolateral gray column.6 The fibers then synapse in the ciliospinal center of Budge at the level of cervical vertebra C8 to thoracic vertebra T2, which give rise to the preganglionic, or second-order neurons.6
Second-order neurons begin at the ciliospinal center of Budge and exit the spinal cord via the central roots, most at the level of thoracic vertebra T1, with the remainder leaving at the levels of cervical vertebra C8 and thoracic vertebra T2.7 After exiting the spinal cord, the second-order neurons loop around the subclavian artery, where they then ascend close to the apex of the lung to synapse with the cell bodies of the third-order neurons at the superior cervical ganglion near cervical vertebrae C2 and C3.7
After arising at the superior cervical ganglion, third-order neurons diverge to follow 2 different courses.7 A portion of the neurons travels along the external carotid artery to ultimately innervate the facial sweat glands, while the other portion of the neurons combines with the carotid plexus and travels within the walls of the internal carotid artery and through the cavernous sinus.7 The fibers then briefly join the abducens nerve before anastomosing with the ophthalmic division of the trigeminal nerve.7 After coursing through the superior orbital fissure, the fibers innervate the iris dilator and Müller muscles via the long ciliary nerves.7
Symptoms and signs. Patients with Horner syndrome can present with a variety of symptoms and signs. Patients may be largely asymptomatic or they may complain of a droopy eyelid and blurry vision. The full Horner syndrome triad consists of ipsilateral miosis, anhidrosis of the face, and mild ptosis of the upper eyelid with reverse ptosis of the lower eyelid.8 The difference in pupil size is greatest 4 to 5 seconds after switching from bright to dim room illumination due to dilation lag in the miotic pupil from poor innervation.1
Although the classical triad of ptosis, miosis, and anhidrosis is emphasized in the literature, the full triad may not always be present.4 This variation is due to the anatomy of the oculosympathetic pathway with branches of the nerve system separating at the superior cervical ganglion and following different pathways along the internal and external carotid arteries, resulting in anhidrosis only in Horner syndrome caused by lesions to the first- or second-order neurons.4,5 Because of this deviation of the nerve fibers in the pathway, the presence of miosis and a slight ptosis in the absence of anhidrosis should still strongly suggest Horner syndrome.
In addition to the classic triad, Horner syndrome can present with other ophthalmic findings, including conjunctival injection, changes in accommodation, and a small decrease in intraocular pressure usually by no more than 1 to 2 mm Hg.4 Congenital Horner syndrome is unique in that it can result in iris heterochromia, with the lighter eye being the affected eye.4
Due to the long and circuitous nature of the oculosympathetic pathway, damage can occur due to a wide variety of conditions (Table) and can present with many neurologic findings.7
Localization of lesions. In Horner syndrome, 13% of lesions were present at first-order neurons, 44% at second-order neurons, and 43% at third-order neurons.7 While all these lesions have similar clinical presentations that can be difficult to differentiate, localization of the lesion within the oculosympathetic pathway is important to determine the underlying cause. This determination can be readily achieved in office with pharmacologic pupil testing (Figure 3).
Management. All acute Horner syndrome presentations should be referred for same-day evaluation to rule out potentially life-threatening conditions, such as a cerebrovascular accident, carotid artery dissection or aneurysm, and giant cell arteritis.10 The urgent evaluation should include CTA and MRI/MRA of the head and neck.5 If giant cell arteritis is suspected, it is also recommended to obtain urgent bloodwork, which should include complete blood count with differential, erythrocyte sedimentation rate, and C-reactive protein.5 Carotid angiography and CT of the chest also are indicated if the aforementioned tests are noncontributory, but these are less urgent and can be deferred for evaluation within 1 to 2 days after the initial diagnosis.10
In this patient’s case, an immediate neurologic evaluation was appropriate due to the acute and painful nature of her presentation. Ultimately, her Horner syndrome was determined to result from an internal carotid artery dissection. As indicated by Schievink, all acute Horner syndrome cases should be considered a result of a carotid artery dissection until proven otherwise, despite the presence or absence of any other signs or symptoms.11 This consideration is not only because of the potentially life-threatening sequelae associated with carotid dissections, but also because dissections have been shown to be the most common cause of ischemic strokes in young and middle-aged patients, accounting for 10% to 25% of all ischemic strokes.4,11
Carotid Artery Dissection
An artery dissection is typically the result of a tear of the
There are many causes of carotid artery dissections, such as structural defects of the arterial wall, fibromuscular dysplasia, cystic medial necrosis, and connective tissue disorders, including Ehlers-Danlos syndrome type IV, Marfan syndrome, autosomal dominant polycystic kidney disease, and osteogenesis imperfecta type I.13 Many environmental factors also can induce a carotid artery dissection, such as a history of anesthesia use, resuscitation with classic cardiopulmonary resuscitation techniques, head or neck trauma, chiropractic manipulation of the neck, and hyperextension or rotation of the neck, which can occur in activities such as yoga, painting a ceiling, coughing, vomiting, or sneezing.11
Patients with an internal carotid artery dissection typically present with pain on one side of the neck, face, or head, which can be accompanied by a partial Horner syndrome that results from damage to the oculosympathetic neurons traveling with the carotid plexus in the internal carotid artery wall.9,10 Unilateral facial or orbital pain has been noted to be present in half of patients and is typically accompanied by an ipsilateral headache.9 These symptoms are typically followed by cerebral or retinal ischemia within hours or days of onset and other ophthalmic conditions that can cause blindness, such as ischemic optic neuropathy or retinal artery occlusions, although these are rare.9
Due to the potential complications that can arise, carotid artery dissections require prompt treatment with antithrombotic therapy for 3 to 6 months to prevent carotid artery occlusion, which can result in a hemispheric cerebrovascular accident or TIAs.15 The options for antithrombotic therapy include anticoagulants, such as warfarin, and antiplatelets, such as aspirin. Studies have found similar rates of recurrent ischemic strokes in treatment with anticoagulants compared with antiplatelets, so both are reasonable therapeutic options.15,16 Following a carotid artery dissection diagnosis, patients should be evaluated by neurology to minimize other cardiovascular risk factors and prevent other complications.
Conclusions
Due to the potential life-threatening complications that can arise from conditions resulting in Horner syndrome, it is imperative that clinicians have a thorough understanding of the condition and its appropriate treatment and management modalities. Understanding the need for immediate testing to determine the underlying etiology of Horner syndrome can help prevent a decrease in a patient’s vision or quality of life, and in some cases, prevent death.
Acknowledgments
The author recognizes and thanks Kyle Stuard for his invaluable assistance in the editing of this manuscript
1. Yanoff M, Duker J. Ophthalmology. 5th ed. Elsevier; 2019.
2. Payne WN, Blair K, Barrett MJ. Anisocoria. StatPearls Publishing; 2022. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK470384
3. Lee A, Bindiganavile SH, Fan J, Al-Zubidi N, Bhatti MT. Argyll Robertson pupils. Accessed February 1, 2023. https://eyewiki.aao.org/Argyll_Robertson_Pupils
4. Kedar S, Prakalapakorn G, Yen M, et al. Horner syndrome. American Academy of Optometry. 2021. Accessed February 1, 2023. https://eyewiki.aao.org/Horner_Syndrome
5. Daroff R, Bradley W, Jankovic J. Bradley and Daroff’s Neurology in Clinical Practice. 8th ed. Elsevier; 2022.
6. Kanagalingam S, Miller NR. Horner syndrome: clinical perspectives. Eye Brain. 2015;7:35-46. doi:10.2147/EB.S63633
7. Lykstad J, Reddy V, Hanna A. Neuroanatomy, Pupillary Dilation Pathway. StatPearls Publishing; 2022. Updated August 11, 2021. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK535421
8. Friedman N, Kaiser P, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 5th ed. Elsevier; 2020.
9. Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995;45(8):1517-1522. doi:10.1212/wnl.45.8.1517
10. Gervasio K, Peck T. The Will’s Eye Manual. 8th ed. Walters Kluwer; 2022.
11. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001;344(12):898-906. doi:10.1056/NEJM200103223441206
12. Hart RG, Easton JD. Dissections of cervical and cerebral arteries. Neurol Clin. 1983;1(1):155-182.
13. Goodfriend SD, Tadi P, Koury R. Carotid Artery Dissection. StatPearls Publishing; 2022. Updated December 24, 2021. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK430835
14. Blum CA, Yaghi S. Cervical artery dissection: a review of the epidemiology, pathophysiology, treatment, and outcome. Arch Neurosci. 2015;2(4):e26670. doi:10.5812/archneurosci.26670
15. Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(1):227-276. doi:10.1161/STR.0b013e3181f7d043
16. Mohr JP, Thompson JL, Lazar RM, et al; Warfarin-Aspirin Recurrent Stroke Study Group. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001;345(20):1444-1451. doi:10.1056/NEJMoa011258
17. Davagnanam I, Fraser CL, Miszkiel K, Daniel CS, Plant GT. Adult Horner’s syndrome: a combined clinical, pharmacological, and imaging algorithm. Eye (Lond). 2013;27(3):291-298. doi:10.1038/eye.2012.281
Horner syndrome is a rare condition that has no sex or race predilection and is characterized by the clinical triad of a miosis, anhidrosis, and small, unilateral ptosis. The prompt diagnosis and determination of the etiology of Horner syndrome are of utmost importance, as the condition can result from many life-threatening systemic complications. Horner syndrome is often asymptomatic but can have distinct, easily identified characteristics seen with an ophthalmic examination. This report describes a patient who presented with Horner syndrome resulting from an internal carotid artery dissection.
Case Presentation
A 61-year-old woman presented with periorbital pain with onset 3 days prior. The patient described the pain as 7 of 10 that had been worsening and was localized around and behind the right eye. She reported new-onset headaches on the right side over the past week with associated intermittent vision blurriness in the right eye. She had a history of mobility issues and had fallen backward about 1 week before, hitting the back of her head on the floor without direct trauma to the eye. She was symptomatic for light sensitivity, syncope, and dizziness, with reports of a recent history of transient ischemic attacks (TIAs) of unknown etiology, which had occurred in the months preceding her examination. She reported no jaw claudication, scalp tenderness, and neck or shoulder pain. She was unaware of any changes in her perspiration pattern on the right side of her face but mentioned that she had noticed her right upper eyelid drooping while looking in the mirror.
This patient had a routine eye examination 2 months before, which was remarkable for stable, nonfoveal involving adult-onset vitelliform dystrophy in the left eye and nuclear sclerotic cataracts and mild refractive error in both eyes. No iris heterochromia was noted, and her pupils were equal, round, and reactive to light. Her history was remarkable for chest pain, obesity, bipolar disorder, vertigo, transient cerebral ischemia, hypertension, hypercholesterolemia, alcohol use disorder, cocaine use disorder, and asthma. A carotid ultrasound had been performed 1 month before the onset of symptoms due to her history of TIAs, which showed no hemodynamically significant stenosis (> 50% stenosis) of either carotid artery. Her medications included oxybutynin chloride, amlodipine, acetaminophen, sertraline hydrochloride, lidocaine, albuterol, risperidone, hydroxyzine hydrochloride, lisinopril, omeprazole, once-daily baby aspirin, atorvastatin, and calcium.
At the time of presentation, an ophthalmic examination revealed no decrease in visual acuity with a best-corrected visual acuity of 20/20 in the right and left eyes. The patient’s pupil sizes were unequal, with a smaller, more miotic right pupil with a greater difference between the pupil sizes in dim illumination (Figure 1).
As the patient had pathologic miosis, conditions causing pathologic mydriasis, such as Adie tonic pupil and cranial nerve III palsy, were ruled out. The presence of an acute, slight ptosis with pathologic miosis and pain in the ipsilateral eye with no reports of exposure to miotic pharmaceutical agents and no history of trauma to the globe or orbit eliminated other differentials, leading to a diagnosis of right-sided Horner syndrome. Due to concerns of acute onset periorbital and retrobulbar pain, she was referred to the emergency department with recommendations for computed tomography angiography (CTA), magnetic resonance imaging (MRI), and magnetic resonance angiogram (MRA) of the head and neck to rule out a carotid artery dissection.
CTA revealed a focal linear filling defect in the right midinternal carotid artery, likely related to an internal carotid artery vascular flap. There was no evidence of proximal intracranial occlusive disease. MRI revealed a linear area of high-intensity signal projecting over the mid and distal right internal carotid artery lumen (Figure 2A).
Imaging suggested an internal carotid artery dissection, and the patient was admitted to the hospital for observation for 4 days. During this time, the patient was instructed to continue taking 81mg aspirin daily and to begin taking 75 mg clopidogrel bisulfate daily to prevent a cerebrovascular accident. Once stability was established, the patient was discharged with instructions to follow up with neurology and neuro-ophthalmology.
Discussion
Anisocoria is defined as a difference in pupil sizes between the eyes.1 This difference can be physiologic with no underlying pathology as an etiology of the condition. If underlying pathology causes anisocoria, it can result in dysfunction with mydriasis, leading to a more miotic pupil, or it can result from issues with miosis, leading to a more mydriatic pupil.1
To determine whether anisocoria is physiologic or pathologic, one must assess the patient’s pupil sizes in dim and bright illumination. If the difference in the pupil size is the same in both room illuminations (ie, the anisocoria is 2 mm in both bright and dim illumination, pupillary constriction and dilation are functioning normally), then the patient has physiologic anisocoria.1 If anisocoria is different in bright and dim illumination (ie, the anisocoria is 1 mm in bright and 3 mm in dim settings or 3 mm in bright and 1 mm in dim settings), the condition is related to pathology. To determine the underlying pathology of anisocoria in cases that are not physiologic, it is important to first determine whether the anisocoria is related to miotic or mydriatic dysfunction.1
If the anisocoria is greater in dim illumination, this suggests mydriatic dysfunction and could be a result of damage to the sympathetic pupillary pathway.1 The smaller or more miotic pupil in this instance is the pathologic pupil. If the anisocoria is greater in bright illumination, this suggests miotic dysfunction and could be a result of damage to the parasympathetic pathway.1 The larger or more mydriatic pupil in this instance is the pathologic pupil. Congenital abnormalities, such as iris colobomas, aniridia, and ectopic pupils, can result in a wide range of pupil sizes and shapes, including miotic or mydriatic pupils.1
Pathologic Mydriasis
Pathologic mydriatic pupils can result from dysfunction in the parasympathetic nervous system, which results in a pupil that is not sufficiently able to dilate with the removal of a light stimulus. Mydriatic pupils can be related to Adie tonic pupil, Argyll-Robertson pupil, third nerve palsy, trauma, surgeries, or pharmacologic mydriasis.2 The conditions that cause mydriasis can be readily differentiated from one another based on clinical examination.
Adie tonic pupil results from damage to the ciliary ganglion.2 While pupillary constriction in response to light will be absent or sluggish in an Adie pupil, the patient will have an intact but sluggish accommodative pupillary response; therefore, the pupil will still constrict with accommodation and convergence to focus on near objects, although slowly. This is known as light-near dissociation.2
Argyll-Robertson pupils are caused by damage to the Edinger-Westphal nucleus in the rostral midbrain.3 Lesions to this area of the brain are typically associated with neurosyphilis but also can be a result of Lyme disease, multiple sclerosis, encephalitis, neurosarcoidosis, herpes zoster, diabetes mellitus, and chronic alcohol misuse.3 Argyll Robertson pupils can appear very similar to a tonic pupil in that this condition will also have a dilated pupil and light-near dissociation.3 These pupils will differ in that they also tend to have an irregular shape (dyscoria), and the pupils will constrict briskly when focusing on near objects and dilate briskly when focusing on distant objects, not sluggishly, as in Adie tonic pupil.3
Mydriasis due to a third nerve palsy will present with ptosis and extraocular muscle dysfunction (including deficits to the superior rectus, medial rectus, inferior oblique, and inferior rectus), with the classic presentation of a completed palsy with the eye positioned “down and out” or the patient’s inability to look medially and superiorly with the affected eye.2
As in cases of pathologic mydriasis, a thorough and in-depth history can help determine traumatic, surgical and pharmacologic etiologies of a mydriatic pupil. It should be determined whether the patient has had any previous trauma or surgeries to the eye or has been in contact with any of the following: acetylcholine receptor antagonists (atropine, scopolamine, homatropine, cyclopentolate, and tropicamide), motion sickness patches (scopolamine), nasal vasoconstrictors, glycopyrrolate deodorants, and/or various plants (Jimson weed or plants belonging to the digitalis family, such as foxglove).2
Pathologic Miosis
Pathologic miotic pupils can result from dysfunction in the sympathetic nervous system and can be related to blunt or penetrating trauma to the orbit, Horner syndrome, and pharmacologic miosis.2 Horner syndrome will be accompanied by a slight ptosis and sometimes anhidrosis on the ipsilateral side of the face. To differentiate between traumatic and pharmacologic miosis, a detailed history should be obtained, paying close attention to injuries to the eyes or head and/or possible exposure to chemical or pharmaceutical agents, including prostaglandins, pilocarpine, organophosphates, and opiates.2
Horner Syndrome
Horner syndrome is a neurologic condition that results from damage to the oculosympathetic pathway.4 The oculosympathetic pathway is a 3-neuron pathway that begins in the hypothalamus and follows a circuitous route to ultimately innervate the facial sweat glands, the smooth muscles of the blood vessels in the orbit and face, the iris dilator muscle, and the Müller muscles of the superior and inferior eyelids.1,5 Therefore, this pathway’s functions include vasoconstriction of facial blood vessels, facial diaphoresis (sweating), pupillary dilation, and maintaining an open position of the eyelids.1
Oculosympathetic pathway anatomy. To understand the findings associated with Horner syndrome, it is necessary to understand the anatomy of this 3-neuron pathway.5 First-order neurons, or central neurons, arise in the posterolateral aspect of the hypothalamus, where they then descend through the midbrain, pons, medulla, and cervical spinal cord via the intermediolateral gray column.6 The fibers then synapse in the ciliospinal center of Budge at the level of cervical vertebra C8 to thoracic vertebra T2, which give rise to the preganglionic, or second-order neurons.6
Second-order neurons begin at the ciliospinal center of Budge and exit the spinal cord via the central roots, most at the level of thoracic vertebra T1, with the remainder leaving at the levels of cervical vertebra C8 and thoracic vertebra T2.7 After exiting the spinal cord, the second-order neurons loop around the subclavian artery, where they then ascend close to the apex of the lung to synapse with the cell bodies of the third-order neurons at the superior cervical ganglion near cervical vertebrae C2 and C3.7
After arising at the superior cervical ganglion, third-order neurons diverge to follow 2 different courses.7 A portion of the neurons travels along the external carotid artery to ultimately innervate the facial sweat glands, while the other portion of the neurons combines with the carotid plexus and travels within the walls of the internal carotid artery and through the cavernous sinus.7 The fibers then briefly join the abducens nerve before anastomosing with the ophthalmic division of the trigeminal nerve.7 After coursing through the superior orbital fissure, the fibers innervate the iris dilator and Müller muscles via the long ciliary nerves.7
Symptoms and signs. Patients with Horner syndrome can present with a variety of symptoms and signs. Patients may be largely asymptomatic or they may complain of a droopy eyelid and blurry vision. The full Horner syndrome triad consists of ipsilateral miosis, anhidrosis of the face, and mild ptosis of the upper eyelid with reverse ptosis of the lower eyelid.8 The difference in pupil size is greatest 4 to 5 seconds after switching from bright to dim room illumination due to dilation lag in the miotic pupil from poor innervation.1
Although the classical triad of ptosis, miosis, and anhidrosis is emphasized in the literature, the full triad may not always be present.4 This variation is due to the anatomy of the oculosympathetic pathway with branches of the nerve system separating at the superior cervical ganglion and following different pathways along the internal and external carotid arteries, resulting in anhidrosis only in Horner syndrome caused by lesions to the first- or second-order neurons.4,5 Because of this deviation of the nerve fibers in the pathway, the presence of miosis and a slight ptosis in the absence of anhidrosis should still strongly suggest Horner syndrome.
In addition to the classic triad, Horner syndrome can present with other ophthalmic findings, including conjunctival injection, changes in accommodation, and a small decrease in intraocular pressure usually by no more than 1 to 2 mm Hg.4 Congenital Horner syndrome is unique in that it can result in iris heterochromia, with the lighter eye being the affected eye.4
Due to the long and circuitous nature of the oculosympathetic pathway, damage can occur due to a wide variety of conditions (Table) and can present with many neurologic findings.7
Localization of lesions. In Horner syndrome, 13% of lesions were present at first-order neurons, 44% at second-order neurons, and 43% at third-order neurons.7 While all these lesions have similar clinical presentations that can be difficult to differentiate, localization of the lesion within the oculosympathetic pathway is important to determine the underlying cause. This determination can be readily achieved in office with pharmacologic pupil testing (Figure 3).
Management. All acute Horner syndrome presentations should be referred for same-day evaluation to rule out potentially life-threatening conditions, such as a cerebrovascular accident, carotid artery dissection or aneurysm, and giant cell arteritis.10 The urgent evaluation should include CTA and MRI/MRA of the head and neck.5 If giant cell arteritis is suspected, it is also recommended to obtain urgent bloodwork, which should include complete blood count with differential, erythrocyte sedimentation rate, and C-reactive protein.5 Carotid angiography and CT of the chest also are indicated if the aforementioned tests are noncontributory, but these are less urgent and can be deferred for evaluation within 1 to 2 days after the initial diagnosis.10
In this patient’s case, an immediate neurologic evaluation was appropriate due to the acute and painful nature of her presentation. Ultimately, her Horner syndrome was determined to result from an internal carotid artery dissection. As indicated by Schievink, all acute Horner syndrome cases should be considered a result of a carotid artery dissection until proven otherwise, despite the presence or absence of any other signs or symptoms.11 This consideration is not only because of the potentially life-threatening sequelae associated with carotid dissections, but also because dissections have been shown to be the most common cause of ischemic strokes in young and middle-aged patients, accounting for 10% to 25% of all ischemic strokes.4,11
Carotid Artery Dissection
An artery dissection is typically the result of a tear of the
There are many causes of carotid artery dissections, such as structural defects of the arterial wall, fibromuscular dysplasia, cystic medial necrosis, and connective tissue disorders, including Ehlers-Danlos syndrome type IV, Marfan syndrome, autosomal dominant polycystic kidney disease, and osteogenesis imperfecta type I.13 Many environmental factors also can induce a carotid artery dissection, such as a history of anesthesia use, resuscitation with classic cardiopulmonary resuscitation techniques, head or neck trauma, chiropractic manipulation of the neck, and hyperextension or rotation of the neck, which can occur in activities such as yoga, painting a ceiling, coughing, vomiting, or sneezing.11
Patients with an internal carotid artery dissection typically present with pain on one side of the neck, face, or head, which can be accompanied by a partial Horner syndrome that results from damage to the oculosympathetic neurons traveling with the carotid plexus in the internal carotid artery wall.9,10 Unilateral facial or orbital pain has been noted to be present in half of patients and is typically accompanied by an ipsilateral headache.9 These symptoms are typically followed by cerebral or retinal ischemia within hours or days of onset and other ophthalmic conditions that can cause blindness, such as ischemic optic neuropathy or retinal artery occlusions, although these are rare.9
Due to the potential complications that can arise, carotid artery dissections require prompt treatment with antithrombotic therapy for 3 to 6 months to prevent carotid artery occlusion, which can result in a hemispheric cerebrovascular accident or TIAs.15 The options for antithrombotic therapy include anticoagulants, such as warfarin, and antiplatelets, such as aspirin. Studies have found similar rates of recurrent ischemic strokes in treatment with anticoagulants compared with antiplatelets, so both are reasonable therapeutic options.15,16 Following a carotid artery dissection diagnosis, patients should be evaluated by neurology to minimize other cardiovascular risk factors and prevent other complications.
Conclusions
Due to the potential life-threatening complications that can arise from conditions resulting in Horner syndrome, it is imperative that clinicians have a thorough understanding of the condition and its appropriate treatment and management modalities. Understanding the need for immediate testing to determine the underlying etiology of Horner syndrome can help prevent a decrease in a patient’s vision or quality of life, and in some cases, prevent death.
Acknowledgments
The author recognizes and thanks Kyle Stuard for his invaluable assistance in the editing of this manuscript
Horner syndrome is a rare condition that has no sex or race predilection and is characterized by the clinical triad of a miosis, anhidrosis, and small, unilateral ptosis. The prompt diagnosis and determination of the etiology of Horner syndrome are of utmost importance, as the condition can result from many life-threatening systemic complications. Horner syndrome is often asymptomatic but can have distinct, easily identified characteristics seen with an ophthalmic examination. This report describes a patient who presented with Horner syndrome resulting from an internal carotid artery dissection.
Case Presentation
A 61-year-old woman presented with periorbital pain with onset 3 days prior. The patient described the pain as 7 of 10 that had been worsening and was localized around and behind the right eye. She reported new-onset headaches on the right side over the past week with associated intermittent vision blurriness in the right eye. She had a history of mobility issues and had fallen backward about 1 week before, hitting the back of her head on the floor without direct trauma to the eye. She was symptomatic for light sensitivity, syncope, and dizziness, with reports of a recent history of transient ischemic attacks (TIAs) of unknown etiology, which had occurred in the months preceding her examination. She reported no jaw claudication, scalp tenderness, and neck or shoulder pain. She was unaware of any changes in her perspiration pattern on the right side of her face but mentioned that she had noticed her right upper eyelid drooping while looking in the mirror.
This patient had a routine eye examination 2 months before, which was remarkable for stable, nonfoveal involving adult-onset vitelliform dystrophy in the left eye and nuclear sclerotic cataracts and mild refractive error in both eyes. No iris heterochromia was noted, and her pupils were equal, round, and reactive to light. Her history was remarkable for chest pain, obesity, bipolar disorder, vertigo, transient cerebral ischemia, hypertension, hypercholesterolemia, alcohol use disorder, cocaine use disorder, and asthma. A carotid ultrasound had been performed 1 month before the onset of symptoms due to her history of TIAs, which showed no hemodynamically significant stenosis (> 50% stenosis) of either carotid artery. Her medications included oxybutynin chloride, amlodipine, acetaminophen, sertraline hydrochloride, lidocaine, albuterol, risperidone, hydroxyzine hydrochloride, lisinopril, omeprazole, once-daily baby aspirin, atorvastatin, and calcium.
At the time of presentation, an ophthalmic examination revealed no decrease in visual acuity with a best-corrected visual acuity of 20/20 in the right and left eyes. The patient’s pupil sizes were unequal, with a smaller, more miotic right pupil with a greater difference between the pupil sizes in dim illumination (Figure 1).
As the patient had pathologic miosis, conditions causing pathologic mydriasis, such as Adie tonic pupil and cranial nerve III palsy, were ruled out. The presence of an acute, slight ptosis with pathologic miosis and pain in the ipsilateral eye with no reports of exposure to miotic pharmaceutical agents and no history of trauma to the globe or orbit eliminated other differentials, leading to a diagnosis of right-sided Horner syndrome. Due to concerns of acute onset periorbital and retrobulbar pain, she was referred to the emergency department with recommendations for computed tomography angiography (CTA), magnetic resonance imaging (MRI), and magnetic resonance angiogram (MRA) of the head and neck to rule out a carotid artery dissection.
CTA revealed a focal linear filling defect in the right midinternal carotid artery, likely related to an internal carotid artery vascular flap. There was no evidence of proximal intracranial occlusive disease. MRI revealed a linear area of high-intensity signal projecting over the mid and distal right internal carotid artery lumen (Figure 2A).
Imaging suggested an internal carotid artery dissection, and the patient was admitted to the hospital for observation for 4 days. During this time, the patient was instructed to continue taking 81mg aspirin daily and to begin taking 75 mg clopidogrel bisulfate daily to prevent a cerebrovascular accident. Once stability was established, the patient was discharged with instructions to follow up with neurology and neuro-ophthalmology.
Discussion
Anisocoria is defined as a difference in pupil sizes between the eyes.1 This difference can be physiologic with no underlying pathology as an etiology of the condition. If underlying pathology causes anisocoria, it can result in dysfunction with mydriasis, leading to a more miotic pupil, or it can result from issues with miosis, leading to a more mydriatic pupil.1
To determine whether anisocoria is physiologic or pathologic, one must assess the patient’s pupil sizes in dim and bright illumination. If the difference in the pupil size is the same in both room illuminations (ie, the anisocoria is 2 mm in both bright and dim illumination, pupillary constriction and dilation are functioning normally), then the patient has physiologic anisocoria.1 If anisocoria is different in bright and dim illumination (ie, the anisocoria is 1 mm in bright and 3 mm in dim settings or 3 mm in bright and 1 mm in dim settings), the condition is related to pathology. To determine the underlying pathology of anisocoria in cases that are not physiologic, it is important to first determine whether the anisocoria is related to miotic or mydriatic dysfunction.1
If the anisocoria is greater in dim illumination, this suggests mydriatic dysfunction and could be a result of damage to the sympathetic pupillary pathway.1 The smaller or more miotic pupil in this instance is the pathologic pupil. If the anisocoria is greater in bright illumination, this suggests miotic dysfunction and could be a result of damage to the parasympathetic pathway.1 The larger or more mydriatic pupil in this instance is the pathologic pupil. Congenital abnormalities, such as iris colobomas, aniridia, and ectopic pupils, can result in a wide range of pupil sizes and shapes, including miotic or mydriatic pupils.1
Pathologic Mydriasis
Pathologic mydriatic pupils can result from dysfunction in the parasympathetic nervous system, which results in a pupil that is not sufficiently able to dilate with the removal of a light stimulus. Mydriatic pupils can be related to Adie tonic pupil, Argyll-Robertson pupil, third nerve palsy, trauma, surgeries, or pharmacologic mydriasis.2 The conditions that cause mydriasis can be readily differentiated from one another based on clinical examination.
Adie tonic pupil results from damage to the ciliary ganglion.2 While pupillary constriction in response to light will be absent or sluggish in an Adie pupil, the patient will have an intact but sluggish accommodative pupillary response; therefore, the pupil will still constrict with accommodation and convergence to focus on near objects, although slowly. This is known as light-near dissociation.2
Argyll-Robertson pupils are caused by damage to the Edinger-Westphal nucleus in the rostral midbrain.3 Lesions to this area of the brain are typically associated with neurosyphilis but also can be a result of Lyme disease, multiple sclerosis, encephalitis, neurosarcoidosis, herpes zoster, diabetes mellitus, and chronic alcohol misuse.3 Argyll Robertson pupils can appear very similar to a tonic pupil in that this condition will also have a dilated pupil and light-near dissociation.3 These pupils will differ in that they also tend to have an irregular shape (dyscoria), and the pupils will constrict briskly when focusing on near objects and dilate briskly when focusing on distant objects, not sluggishly, as in Adie tonic pupil.3
Mydriasis due to a third nerve palsy will present with ptosis and extraocular muscle dysfunction (including deficits to the superior rectus, medial rectus, inferior oblique, and inferior rectus), with the classic presentation of a completed palsy with the eye positioned “down and out” or the patient’s inability to look medially and superiorly with the affected eye.2
As in cases of pathologic mydriasis, a thorough and in-depth history can help determine traumatic, surgical and pharmacologic etiologies of a mydriatic pupil. It should be determined whether the patient has had any previous trauma or surgeries to the eye or has been in contact with any of the following: acetylcholine receptor antagonists (atropine, scopolamine, homatropine, cyclopentolate, and tropicamide), motion sickness patches (scopolamine), nasal vasoconstrictors, glycopyrrolate deodorants, and/or various plants (Jimson weed or plants belonging to the digitalis family, such as foxglove).2
Pathologic Miosis
Pathologic miotic pupils can result from dysfunction in the sympathetic nervous system and can be related to blunt or penetrating trauma to the orbit, Horner syndrome, and pharmacologic miosis.2 Horner syndrome will be accompanied by a slight ptosis and sometimes anhidrosis on the ipsilateral side of the face. To differentiate between traumatic and pharmacologic miosis, a detailed history should be obtained, paying close attention to injuries to the eyes or head and/or possible exposure to chemical or pharmaceutical agents, including prostaglandins, pilocarpine, organophosphates, and opiates.2
Horner Syndrome
Horner syndrome is a neurologic condition that results from damage to the oculosympathetic pathway.4 The oculosympathetic pathway is a 3-neuron pathway that begins in the hypothalamus and follows a circuitous route to ultimately innervate the facial sweat glands, the smooth muscles of the blood vessels in the orbit and face, the iris dilator muscle, and the Müller muscles of the superior and inferior eyelids.1,5 Therefore, this pathway’s functions include vasoconstriction of facial blood vessels, facial diaphoresis (sweating), pupillary dilation, and maintaining an open position of the eyelids.1
Oculosympathetic pathway anatomy. To understand the findings associated with Horner syndrome, it is necessary to understand the anatomy of this 3-neuron pathway.5 First-order neurons, or central neurons, arise in the posterolateral aspect of the hypothalamus, where they then descend through the midbrain, pons, medulla, and cervical spinal cord via the intermediolateral gray column.6 The fibers then synapse in the ciliospinal center of Budge at the level of cervical vertebra C8 to thoracic vertebra T2, which give rise to the preganglionic, or second-order neurons.6
Second-order neurons begin at the ciliospinal center of Budge and exit the spinal cord via the central roots, most at the level of thoracic vertebra T1, with the remainder leaving at the levels of cervical vertebra C8 and thoracic vertebra T2.7 After exiting the spinal cord, the second-order neurons loop around the subclavian artery, where they then ascend close to the apex of the lung to synapse with the cell bodies of the third-order neurons at the superior cervical ganglion near cervical vertebrae C2 and C3.7
After arising at the superior cervical ganglion, third-order neurons diverge to follow 2 different courses.7 A portion of the neurons travels along the external carotid artery to ultimately innervate the facial sweat glands, while the other portion of the neurons combines with the carotid plexus and travels within the walls of the internal carotid artery and through the cavernous sinus.7 The fibers then briefly join the abducens nerve before anastomosing with the ophthalmic division of the trigeminal nerve.7 After coursing through the superior orbital fissure, the fibers innervate the iris dilator and Müller muscles via the long ciliary nerves.7
Symptoms and signs. Patients with Horner syndrome can present with a variety of symptoms and signs. Patients may be largely asymptomatic or they may complain of a droopy eyelid and blurry vision. The full Horner syndrome triad consists of ipsilateral miosis, anhidrosis of the face, and mild ptosis of the upper eyelid with reverse ptosis of the lower eyelid.8 The difference in pupil size is greatest 4 to 5 seconds after switching from bright to dim room illumination due to dilation lag in the miotic pupil from poor innervation.1
Although the classical triad of ptosis, miosis, and anhidrosis is emphasized in the literature, the full triad may not always be present.4 This variation is due to the anatomy of the oculosympathetic pathway with branches of the nerve system separating at the superior cervical ganglion and following different pathways along the internal and external carotid arteries, resulting in anhidrosis only in Horner syndrome caused by lesions to the first- or second-order neurons.4,5 Because of this deviation of the nerve fibers in the pathway, the presence of miosis and a slight ptosis in the absence of anhidrosis should still strongly suggest Horner syndrome.
In addition to the classic triad, Horner syndrome can present with other ophthalmic findings, including conjunctival injection, changes in accommodation, and a small decrease in intraocular pressure usually by no more than 1 to 2 mm Hg.4 Congenital Horner syndrome is unique in that it can result in iris heterochromia, with the lighter eye being the affected eye.4
Due to the long and circuitous nature of the oculosympathetic pathway, damage can occur due to a wide variety of conditions (Table) and can present with many neurologic findings.7
Localization of lesions. In Horner syndrome, 13% of lesions were present at first-order neurons, 44% at second-order neurons, and 43% at third-order neurons.7 While all these lesions have similar clinical presentations that can be difficult to differentiate, localization of the lesion within the oculosympathetic pathway is important to determine the underlying cause. This determination can be readily achieved in office with pharmacologic pupil testing (Figure 3).
Management. All acute Horner syndrome presentations should be referred for same-day evaluation to rule out potentially life-threatening conditions, such as a cerebrovascular accident, carotid artery dissection or aneurysm, and giant cell arteritis.10 The urgent evaluation should include CTA and MRI/MRA of the head and neck.5 If giant cell arteritis is suspected, it is also recommended to obtain urgent bloodwork, which should include complete blood count with differential, erythrocyte sedimentation rate, and C-reactive protein.5 Carotid angiography and CT of the chest also are indicated if the aforementioned tests are noncontributory, but these are less urgent and can be deferred for evaluation within 1 to 2 days after the initial diagnosis.10
In this patient’s case, an immediate neurologic evaluation was appropriate due to the acute and painful nature of her presentation. Ultimately, her Horner syndrome was determined to result from an internal carotid artery dissection. As indicated by Schievink, all acute Horner syndrome cases should be considered a result of a carotid artery dissection until proven otherwise, despite the presence or absence of any other signs or symptoms.11 This consideration is not only because of the potentially life-threatening sequelae associated with carotid dissections, but also because dissections have been shown to be the most common cause of ischemic strokes in young and middle-aged patients, accounting for 10% to 25% of all ischemic strokes.4,11
Carotid Artery Dissection
An artery dissection is typically the result of a tear of the
There are many causes of carotid artery dissections, such as structural defects of the arterial wall, fibromuscular dysplasia, cystic medial necrosis, and connective tissue disorders, including Ehlers-Danlos syndrome type IV, Marfan syndrome, autosomal dominant polycystic kidney disease, and osteogenesis imperfecta type I.13 Many environmental factors also can induce a carotid artery dissection, such as a history of anesthesia use, resuscitation with classic cardiopulmonary resuscitation techniques, head or neck trauma, chiropractic manipulation of the neck, and hyperextension or rotation of the neck, which can occur in activities such as yoga, painting a ceiling, coughing, vomiting, or sneezing.11
Patients with an internal carotid artery dissection typically present with pain on one side of the neck, face, or head, which can be accompanied by a partial Horner syndrome that results from damage to the oculosympathetic neurons traveling with the carotid plexus in the internal carotid artery wall.9,10 Unilateral facial or orbital pain has been noted to be present in half of patients and is typically accompanied by an ipsilateral headache.9 These symptoms are typically followed by cerebral or retinal ischemia within hours or days of onset and other ophthalmic conditions that can cause blindness, such as ischemic optic neuropathy or retinal artery occlusions, although these are rare.9
Due to the potential complications that can arise, carotid artery dissections require prompt treatment with antithrombotic therapy for 3 to 6 months to prevent carotid artery occlusion, which can result in a hemispheric cerebrovascular accident or TIAs.15 The options for antithrombotic therapy include anticoagulants, such as warfarin, and antiplatelets, such as aspirin. Studies have found similar rates of recurrent ischemic strokes in treatment with anticoagulants compared with antiplatelets, so both are reasonable therapeutic options.15,16 Following a carotid artery dissection diagnosis, patients should be evaluated by neurology to minimize other cardiovascular risk factors and prevent other complications.
Conclusions
Due to the potential life-threatening complications that can arise from conditions resulting in Horner syndrome, it is imperative that clinicians have a thorough understanding of the condition and its appropriate treatment and management modalities. Understanding the need for immediate testing to determine the underlying etiology of Horner syndrome can help prevent a decrease in a patient’s vision or quality of life, and in some cases, prevent death.
Acknowledgments
The author recognizes and thanks Kyle Stuard for his invaluable assistance in the editing of this manuscript
1. Yanoff M, Duker J. Ophthalmology. 5th ed. Elsevier; 2019.
2. Payne WN, Blair K, Barrett MJ. Anisocoria. StatPearls Publishing; 2022. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK470384
3. Lee A, Bindiganavile SH, Fan J, Al-Zubidi N, Bhatti MT. Argyll Robertson pupils. Accessed February 1, 2023. https://eyewiki.aao.org/Argyll_Robertson_Pupils
4. Kedar S, Prakalapakorn G, Yen M, et al. Horner syndrome. American Academy of Optometry. 2021. Accessed February 1, 2023. https://eyewiki.aao.org/Horner_Syndrome
5. Daroff R, Bradley W, Jankovic J. Bradley and Daroff’s Neurology in Clinical Practice. 8th ed. Elsevier; 2022.
6. Kanagalingam S, Miller NR. Horner syndrome: clinical perspectives. Eye Brain. 2015;7:35-46. doi:10.2147/EB.S63633
7. Lykstad J, Reddy V, Hanna A. Neuroanatomy, Pupillary Dilation Pathway. StatPearls Publishing; 2022. Updated August 11, 2021. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK535421
8. Friedman N, Kaiser P, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 5th ed. Elsevier; 2020.
9. Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995;45(8):1517-1522. doi:10.1212/wnl.45.8.1517
10. Gervasio K, Peck T. The Will’s Eye Manual. 8th ed. Walters Kluwer; 2022.
11. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001;344(12):898-906. doi:10.1056/NEJM200103223441206
12. Hart RG, Easton JD. Dissections of cervical and cerebral arteries. Neurol Clin. 1983;1(1):155-182.
13. Goodfriend SD, Tadi P, Koury R. Carotid Artery Dissection. StatPearls Publishing; 2022. Updated December 24, 2021. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK430835
14. Blum CA, Yaghi S. Cervical artery dissection: a review of the epidemiology, pathophysiology, treatment, and outcome. Arch Neurosci. 2015;2(4):e26670. doi:10.5812/archneurosci.26670
15. Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(1):227-276. doi:10.1161/STR.0b013e3181f7d043
16. Mohr JP, Thompson JL, Lazar RM, et al; Warfarin-Aspirin Recurrent Stroke Study Group. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001;345(20):1444-1451. doi:10.1056/NEJMoa011258
17. Davagnanam I, Fraser CL, Miszkiel K, Daniel CS, Plant GT. Adult Horner’s syndrome: a combined clinical, pharmacological, and imaging algorithm. Eye (Lond). 2013;27(3):291-298. doi:10.1038/eye.2012.281
1. Yanoff M, Duker J. Ophthalmology. 5th ed. Elsevier; 2019.
2. Payne WN, Blair K, Barrett MJ. Anisocoria. StatPearls Publishing; 2022. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK470384
3. Lee A, Bindiganavile SH, Fan J, Al-Zubidi N, Bhatti MT. Argyll Robertson pupils. Accessed February 1, 2023. https://eyewiki.aao.org/Argyll_Robertson_Pupils
4. Kedar S, Prakalapakorn G, Yen M, et al. Horner syndrome. American Academy of Optometry. 2021. Accessed February 1, 2023. https://eyewiki.aao.org/Horner_Syndrome
5. Daroff R, Bradley W, Jankovic J. Bradley and Daroff’s Neurology in Clinical Practice. 8th ed. Elsevier; 2022.
6. Kanagalingam S, Miller NR. Horner syndrome: clinical perspectives. Eye Brain. 2015;7:35-46. doi:10.2147/EB.S63633
7. Lykstad J, Reddy V, Hanna A. Neuroanatomy, Pupillary Dilation Pathway. StatPearls Publishing; 2022. Updated August 11, 2021. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK535421
8. Friedman N, Kaiser P, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 5th ed. Elsevier; 2020.
9. Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995;45(8):1517-1522. doi:10.1212/wnl.45.8.1517
10. Gervasio K, Peck T. The Will’s Eye Manual. 8th ed. Walters Kluwer; 2022.
11. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001;344(12):898-906. doi:10.1056/NEJM200103223441206
12. Hart RG, Easton JD. Dissections of cervical and cerebral arteries. Neurol Clin. 1983;1(1):155-182.
13. Goodfriend SD, Tadi P, Koury R. Carotid Artery Dissection. StatPearls Publishing; 2022. Updated December 24, 2021. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK430835
14. Blum CA, Yaghi S. Cervical artery dissection: a review of the epidemiology, pathophysiology, treatment, and outcome. Arch Neurosci. 2015;2(4):e26670. doi:10.5812/archneurosci.26670
15. Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(1):227-276. doi:10.1161/STR.0b013e3181f7d043
16. Mohr JP, Thompson JL, Lazar RM, et al; Warfarin-Aspirin Recurrent Stroke Study Group. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001;345(20):1444-1451. doi:10.1056/NEJMoa011258
17. Davagnanam I, Fraser CL, Miszkiel K, Daniel CS, Plant GT. Adult Horner’s syndrome: a combined clinical, pharmacological, and imaging algorithm. Eye (Lond). 2013;27(3):291-298. doi:10.1038/eye.2012.281