User login
Tic disorders proliferate in bipolar patients with OCD
Bipolar disorder patients with comorbid obsessive-compulsive disorder were significantly more likely to suffer from tic disorders, as well as hoarding, excoriation, and body dysmorphic disorder, than were those without comorbid OCD, data from 70 patients suggest.
Between 10% and 20% of patients with bipolar disorder (BD) also meet criteria for obsessive-compulsive disorder (OCD), and these patients are more likely to experience treatment resistance and poor prognosis than are BD patients without OCD. In addition, preliminary indications suggest a specific association between OCD and bipolar depression (BP-D) in particular, wrote Leonid Braverman, MD, of Ma’ale HaCarmel Mental Health Center, Tirat Carmel, Israel, and colleagues.
In addition, “there is compelling evidence indicating that OCD-spectrum and tic disorders share with OCD clinical characteristics, familial inheritance, neurobiological underpinnings and some aspects of pharmacotherapy,” and investigations into the clinical characteristics of OCD spectrum behaviors in BP-D patients with and without OCD are ongoing, they said.
In a study published in the Journal of Obsessive-Compulsive and Related Disorders (2021 Mar 21. doi: 10.1016/j.jocrd.2021.100643), the researchers reviewed data from 87 adults who met the DSM-5 criteria for BP-D. Of these, 27 also met criteria for OCD, 17 for subthreshold OCD, and 43 had neither OCD nor subthreshold OCD. The researchers compared the 27 OCD patients and the 43 non-OCD patients; the OCD patients had significantly higher rates overall of body dysmorphic disorder, hoarding disorder, excoriation disorder, and tic disorder, compared with non-OCD patients (P range from < .05-0.01 for all). No differences between the groups appeared for trichotillomania.
Also, the researchers found significant between-group differences in the number of patients with at least one OCD spectrum disorder and tic disorders (13 of 19 patients in the OCD group vs. 3 of 37 patients in the non-OCD group) and in the co-occurrence of two OCD-spectrum and tic disorders (3 of 19 patients in the OCD group vs. 1 patient in the non-OCD group).
The most common comorbid psychiatric disorders in both groups were substance use and combined anxiety disorders, followed by eating disorders, but no between-group differences were found in the frequencies of any of these conditions.
“From the clinical perspective, in BP-D patients,” the researchers noted.
The study findings were limited by several factors, including the small sample size, cross-sectional design, and exclusion of subsyndromic disorders, the researchers noted. However, the results support findings from previous studies, and the study emphasizes the clinical complexity and poor prognosis for these patients. Therefore, additional research is needed in patients with BP-D verse the manic/hypomanic phases of bipolar illness to determine similar patterns, they said. Medication trials are needed to address functional impairments in these patients, given the differences in treatment of BDD, hoarding, excoriation, and tic disorders, compared with “pure” OCD, they concluded.
The study received no outside funding. The researchers reported no financial conflicts.
Bipolar disorder patients with comorbid obsessive-compulsive disorder were significantly more likely to suffer from tic disorders, as well as hoarding, excoriation, and body dysmorphic disorder, than were those without comorbid OCD, data from 70 patients suggest.
Between 10% and 20% of patients with bipolar disorder (BD) also meet criteria for obsessive-compulsive disorder (OCD), and these patients are more likely to experience treatment resistance and poor prognosis than are BD patients without OCD. In addition, preliminary indications suggest a specific association between OCD and bipolar depression (BP-D) in particular, wrote Leonid Braverman, MD, of Ma’ale HaCarmel Mental Health Center, Tirat Carmel, Israel, and colleagues.
In addition, “there is compelling evidence indicating that OCD-spectrum and tic disorders share with OCD clinical characteristics, familial inheritance, neurobiological underpinnings and some aspects of pharmacotherapy,” and investigations into the clinical characteristics of OCD spectrum behaviors in BP-D patients with and without OCD are ongoing, they said.
In a study published in the Journal of Obsessive-Compulsive and Related Disorders (2021 Mar 21. doi: 10.1016/j.jocrd.2021.100643), the researchers reviewed data from 87 adults who met the DSM-5 criteria for BP-D. Of these, 27 also met criteria for OCD, 17 for subthreshold OCD, and 43 had neither OCD nor subthreshold OCD. The researchers compared the 27 OCD patients and the 43 non-OCD patients; the OCD patients had significantly higher rates overall of body dysmorphic disorder, hoarding disorder, excoriation disorder, and tic disorder, compared with non-OCD patients (P range from < .05-0.01 for all). No differences between the groups appeared for trichotillomania.
Also, the researchers found significant between-group differences in the number of patients with at least one OCD spectrum disorder and tic disorders (13 of 19 patients in the OCD group vs. 3 of 37 patients in the non-OCD group) and in the co-occurrence of two OCD-spectrum and tic disorders (3 of 19 patients in the OCD group vs. 1 patient in the non-OCD group).
The most common comorbid psychiatric disorders in both groups were substance use and combined anxiety disorders, followed by eating disorders, but no between-group differences were found in the frequencies of any of these conditions.
“From the clinical perspective, in BP-D patients,” the researchers noted.
The study findings were limited by several factors, including the small sample size, cross-sectional design, and exclusion of subsyndromic disorders, the researchers noted. However, the results support findings from previous studies, and the study emphasizes the clinical complexity and poor prognosis for these patients. Therefore, additional research is needed in patients with BP-D verse the manic/hypomanic phases of bipolar illness to determine similar patterns, they said. Medication trials are needed to address functional impairments in these patients, given the differences in treatment of BDD, hoarding, excoriation, and tic disorders, compared with “pure” OCD, they concluded.
The study received no outside funding. The researchers reported no financial conflicts.
Bipolar disorder patients with comorbid obsessive-compulsive disorder were significantly more likely to suffer from tic disorders, as well as hoarding, excoriation, and body dysmorphic disorder, than were those without comorbid OCD, data from 70 patients suggest.
Between 10% and 20% of patients with bipolar disorder (BD) also meet criteria for obsessive-compulsive disorder (OCD), and these patients are more likely to experience treatment resistance and poor prognosis than are BD patients without OCD. In addition, preliminary indications suggest a specific association between OCD and bipolar depression (BP-D) in particular, wrote Leonid Braverman, MD, of Ma’ale HaCarmel Mental Health Center, Tirat Carmel, Israel, and colleagues.
In addition, “there is compelling evidence indicating that OCD-spectrum and tic disorders share with OCD clinical characteristics, familial inheritance, neurobiological underpinnings and some aspects of pharmacotherapy,” and investigations into the clinical characteristics of OCD spectrum behaviors in BP-D patients with and without OCD are ongoing, they said.
In a study published in the Journal of Obsessive-Compulsive and Related Disorders (2021 Mar 21. doi: 10.1016/j.jocrd.2021.100643), the researchers reviewed data from 87 adults who met the DSM-5 criteria for BP-D. Of these, 27 also met criteria for OCD, 17 for subthreshold OCD, and 43 had neither OCD nor subthreshold OCD. The researchers compared the 27 OCD patients and the 43 non-OCD patients; the OCD patients had significantly higher rates overall of body dysmorphic disorder, hoarding disorder, excoriation disorder, and tic disorder, compared with non-OCD patients (P range from < .05-0.01 for all). No differences between the groups appeared for trichotillomania.
Also, the researchers found significant between-group differences in the number of patients with at least one OCD spectrum disorder and tic disorders (13 of 19 patients in the OCD group vs. 3 of 37 patients in the non-OCD group) and in the co-occurrence of two OCD-spectrum and tic disorders (3 of 19 patients in the OCD group vs. 1 patient in the non-OCD group).
The most common comorbid psychiatric disorders in both groups were substance use and combined anxiety disorders, followed by eating disorders, but no between-group differences were found in the frequencies of any of these conditions.
“From the clinical perspective, in BP-D patients,” the researchers noted.
The study findings were limited by several factors, including the small sample size, cross-sectional design, and exclusion of subsyndromic disorders, the researchers noted. However, the results support findings from previous studies, and the study emphasizes the clinical complexity and poor prognosis for these patients. Therefore, additional research is needed in patients with BP-D verse the manic/hypomanic phases of bipolar illness to determine similar patterns, they said. Medication trials are needed to address functional impairments in these patients, given the differences in treatment of BDD, hoarding, excoriation, and tic disorders, compared with “pure” OCD, they concluded.
The study received no outside funding. The researchers reported no financial conflicts.
FROM THE JOURNAL OF OBSESSIVE-COMPULSIVE AND RELATED DISORDERS
Let’s not criticize off-label prescribing
The public health crisis sparked by COVID-19 has engendered much debate in the realm where politics, journalism, law, and medicine meet.
Doctors have used the media to name other doctors as sources of harmful misinformation, in some cases going so far as to invoke medical practice board oversight as a potential intervention when doctors make public statements deemed too far out of bounds scientifically. Over the past year, some physicians have been harshly criticized for speaking about off-label prescribing, a widely accepted part of everyday medical practice.
The science and ethics of off-label prescribing have not changed; what has changed is the quality of dialogue around it. As psychiatrists, it does not fall within our scope of practice to offer definitive public opinions on the treatment of COVID-19, nor is that our purpose here. However, we can speak to a process that damages patients and doctors alike by undermining trust. All of this heat around bad medical information, in our opinion, amounts to using the methods of other fields to evaluate science and clinical practice. A remedy, then, to improve the quality of public medical intelligence would be to clarify the rules of scientific debate and to once again clearly state that off-label prescribing is part and parcel of the good practice of clinical medicine.
Physicians who work in the field of professional discipline have thought about the limits of propriety in making charges of impropriety. We (R.S.E. and R.S.K.) asked the American Psychiatric Association’s Ethics Committee to expand upon its existing commentary on innovative practice and making allegations of professional misconduct. We used the committee’s answers to our questions as the basis for the arguments we are making in this piece.
The APA’s Ethics Committee uses clear-cut benchmarks to define innovative medical care: “The standards of care ... evolve with evidence from research and observations of practice. Among the expected supports for innovative practice are scientific testing, peer-reviewed publication, replication, and broad or widespread acceptance within a relevant scientific or professional community.” When it comes to off-label prescribing for any medical condition, it is easy enough to ascertain whether clinical reports have appeared in peer-reviewed journals.
Two of the biggest blockbusters in psychiatry, chlorpromazine and lithium, began as drugs used for other conditions almost since the inception of our field. In other words, the use of these drugs for mental illness began, in today’s jargon, as off-label. We practitioners of psychiatry live in the land of off-label prescribing and have always comfortably done so. In fact, almost all of medicine does. The key in today’s world of best-practice medicine is obtaining a truly informed consent.
For COVID-19, our incredible psychotropic molecules may once again be doing some trail-blazing off-label work. Late last year, Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University in St. Louis, reported in a preliminary study of adult outpatients with symptomatic COVID-19 that those treated with fluvoxamine “had a lower likelihood of clinical deterioration over 15 days,” compared with those on placebo (JAMA. 2020;324[22]:2292-300). We were heartened to see Dr. Lenze discuss his work on a recent “60 Minutes” segment. David Seftel, MD, MBA, a clinician who administered fluvoxamine as early treatment for a COVID-19 outbreak that occurred in a community of racetrack employees and their families in the San Francisco Bay Area, also was featured. Rather than waiting for the results of large clinical trials, Dr. Lenze and Dr. Seftel proceeded, based on reports published in peer-reviewed journals, to treat patients whose lives were at risk.
If we find ourselves strongly disagreeing about the science of off-label prescribing, the proper response is to critique methodologies, not the character or competence of colleagues. The APA Ethics Committee discourages use of the media as a forum for making allegations of incompetent or unethical practice: “Judgments regarding violations of established norms of ethical or professional conduct should be made not by individuals but by bodies authorized to take evidence and make informed decisions.”
At least one state legislature is taking action to protect patients’ access to the doctors they trust. In Arizona, SB 1416 passed in the Senate and is now working its way through the House. This bill would prohibit medical boards from disciplining doctors for speaking out about or prescribing off-label drugs when a reasonable basis for use exists.
Psychological research on the “backfire effect” suggests that heavy-handed campaigns to enforce medical consensus will only harden minds in ways that neither advance science nor improve the quality of clinical decision-making.
Medical disciplinary boards and the news media were neither designed nor are they equipped to adjudicate scientific debates. Science is never settled: Hypothesis and theory are always open to testing and revision as new evidence emerges. There is a place in medicine for formal disciplinary processes, as well-delineated by professional bodies such as the APA Ethics Committee. Another important part of protecting the public is to support an environment of scientific inquiry in which diversity of opinion is welcomed. As physicians, we translate science into excellent clinical care every day in our practices, and we advance science by sharing what we learn through friendly collegial communication and collaboration.
Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships. Dr. Kohanski is in private practice in Dayton, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She also is the host and author of Clinical Correlation, a series of the Psychcast. Dr. Kohanski disclosed no relevant financial relationships.
The public health crisis sparked by COVID-19 has engendered much debate in the realm where politics, journalism, law, and medicine meet.
Doctors have used the media to name other doctors as sources of harmful misinformation, in some cases going so far as to invoke medical practice board oversight as a potential intervention when doctors make public statements deemed too far out of bounds scientifically. Over the past year, some physicians have been harshly criticized for speaking about off-label prescribing, a widely accepted part of everyday medical practice.
The science and ethics of off-label prescribing have not changed; what has changed is the quality of dialogue around it. As psychiatrists, it does not fall within our scope of practice to offer definitive public opinions on the treatment of COVID-19, nor is that our purpose here. However, we can speak to a process that damages patients and doctors alike by undermining trust. All of this heat around bad medical information, in our opinion, amounts to using the methods of other fields to evaluate science and clinical practice. A remedy, then, to improve the quality of public medical intelligence would be to clarify the rules of scientific debate and to once again clearly state that off-label prescribing is part and parcel of the good practice of clinical medicine.
Physicians who work in the field of professional discipline have thought about the limits of propriety in making charges of impropriety. We (R.S.E. and R.S.K.) asked the American Psychiatric Association’s Ethics Committee to expand upon its existing commentary on innovative practice and making allegations of professional misconduct. We used the committee’s answers to our questions as the basis for the arguments we are making in this piece.
The APA’s Ethics Committee uses clear-cut benchmarks to define innovative medical care: “The standards of care ... evolve with evidence from research and observations of practice. Among the expected supports for innovative practice are scientific testing, peer-reviewed publication, replication, and broad or widespread acceptance within a relevant scientific or professional community.” When it comes to off-label prescribing for any medical condition, it is easy enough to ascertain whether clinical reports have appeared in peer-reviewed journals.
Two of the biggest blockbusters in psychiatry, chlorpromazine and lithium, began as drugs used for other conditions almost since the inception of our field. In other words, the use of these drugs for mental illness began, in today’s jargon, as off-label. We practitioners of psychiatry live in the land of off-label prescribing and have always comfortably done so. In fact, almost all of medicine does. The key in today’s world of best-practice medicine is obtaining a truly informed consent.
For COVID-19, our incredible psychotropic molecules may once again be doing some trail-blazing off-label work. Late last year, Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University in St. Louis, reported in a preliminary study of adult outpatients with symptomatic COVID-19 that those treated with fluvoxamine “had a lower likelihood of clinical deterioration over 15 days,” compared with those on placebo (JAMA. 2020;324[22]:2292-300). We were heartened to see Dr. Lenze discuss his work on a recent “60 Minutes” segment. David Seftel, MD, MBA, a clinician who administered fluvoxamine as early treatment for a COVID-19 outbreak that occurred in a community of racetrack employees and their families in the San Francisco Bay Area, also was featured. Rather than waiting for the results of large clinical trials, Dr. Lenze and Dr. Seftel proceeded, based on reports published in peer-reviewed journals, to treat patients whose lives were at risk.
If we find ourselves strongly disagreeing about the science of off-label prescribing, the proper response is to critique methodologies, not the character or competence of colleagues. The APA Ethics Committee discourages use of the media as a forum for making allegations of incompetent or unethical practice: “Judgments regarding violations of established norms of ethical or professional conduct should be made not by individuals but by bodies authorized to take evidence and make informed decisions.”
At least one state legislature is taking action to protect patients’ access to the doctors they trust. In Arizona, SB 1416 passed in the Senate and is now working its way through the House. This bill would prohibit medical boards from disciplining doctors for speaking out about or prescribing off-label drugs when a reasonable basis for use exists.
Psychological research on the “backfire effect” suggests that heavy-handed campaigns to enforce medical consensus will only harden minds in ways that neither advance science nor improve the quality of clinical decision-making.
Medical disciplinary boards and the news media were neither designed nor are they equipped to adjudicate scientific debates. Science is never settled: Hypothesis and theory are always open to testing and revision as new evidence emerges. There is a place in medicine for formal disciplinary processes, as well-delineated by professional bodies such as the APA Ethics Committee. Another important part of protecting the public is to support an environment of scientific inquiry in which diversity of opinion is welcomed. As physicians, we translate science into excellent clinical care every day in our practices, and we advance science by sharing what we learn through friendly collegial communication and collaboration.
Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships. Dr. Kohanski is in private practice in Dayton, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She also is the host and author of Clinical Correlation, a series of the Psychcast. Dr. Kohanski disclosed no relevant financial relationships.
The public health crisis sparked by COVID-19 has engendered much debate in the realm where politics, journalism, law, and medicine meet.
Doctors have used the media to name other doctors as sources of harmful misinformation, in some cases going so far as to invoke medical practice board oversight as a potential intervention when doctors make public statements deemed too far out of bounds scientifically. Over the past year, some physicians have been harshly criticized for speaking about off-label prescribing, a widely accepted part of everyday medical practice.
The science and ethics of off-label prescribing have not changed; what has changed is the quality of dialogue around it. As psychiatrists, it does not fall within our scope of practice to offer definitive public opinions on the treatment of COVID-19, nor is that our purpose here. However, we can speak to a process that damages patients and doctors alike by undermining trust. All of this heat around bad medical information, in our opinion, amounts to using the methods of other fields to evaluate science and clinical practice. A remedy, then, to improve the quality of public medical intelligence would be to clarify the rules of scientific debate and to once again clearly state that off-label prescribing is part and parcel of the good practice of clinical medicine.
Physicians who work in the field of professional discipline have thought about the limits of propriety in making charges of impropriety. We (R.S.E. and R.S.K.) asked the American Psychiatric Association’s Ethics Committee to expand upon its existing commentary on innovative practice and making allegations of professional misconduct. We used the committee’s answers to our questions as the basis for the arguments we are making in this piece.
The APA’s Ethics Committee uses clear-cut benchmarks to define innovative medical care: “The standards of care ... evolve with evidence from research and observations of practice. Among the expected supports for innovative practice are scientific testing, peer-reviewed publication, replication, and broad or widespread acceptance within a relevant scientific or professional community.” When it comes to off-label prescribing for any medical condition, it is easy enough to ascertain whether clinical reports have appeared in peer-reviewed journals.
Two of the biggest blockbusters in psychiatry, chlorpromazine and lithium, began as drugs used for other conditions almost since the inception of our field. In other words, the use of these drugs for mental illness began, in today’s jargon, as off-label. We practitioners of psychiatry live in the land of off-label prescribing and have always comfortably done so. In fact, almost all of medicine does. The key in today’s world of best-practice medicine is obtaining a truly informed consent.
For COVID-19, our incredible psychotropic molecules may once again be doing some trail-blazing off-label work. Late last year, Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University in St. Louis, reported in a preliminary study of adult outpatients with symptomatic COVID-19 that those treated with fluvoxamine “had a lower likelihood of clinical deterioration over 15 days,” compared with those on placebo (JAMA. 2020;324[22]:2292-300). We were heartened to see Dr. Lenze discuss his work on a recent “60 Minutes” segment. David Seftel, MD, MBA, a clinician who administered fluvoxamine as early treatment for a COVID-19 outbreak that occurred in a community of racetrack employees and their families in the San Francisco Bay Area, also was featured. Rather than waiting for the results of large clinical trials, Dr. Lenze and Dr. Seftel proceeded, based on reports published in peer-reviewed journals, to treat patients whose lives were at risk.
If we find ourselves strongly disagreeing about the science of off-label prescribing, the proper response is to critique methodologies, not the character or competence of colleagues. The APA Ethics Committee discourages use of the media as a forum for making allegations of incompetent or unethical practice: “Judgments regarding violations of established norms of ethical or professional conduct should be made not by individuals but by bodies authorized to take evidence and make informed decisions.”
At least one state legislature is taking action to protect patients’ access to the doctors they trust. In Arizona, SB 1416 passed in the Senate and is now working its way through the House. This bill would prohibit medical boards from disciplining doctors for speaking out about or prescribing off-label drugs when a reasonable basis for use exists.
Psychological research on the “backfire effect” suggests that heavy-handed campaigns to enforce medical consensus will only harden minds in ways that neither advance science nor improve the quality of clinical decision-making.
Medical disciplinary boards and the news media were neither designed nor are they equipped to adjudicate scientific debates. Science is never settled: Hypothesis and theory are always open to testing and revision as new evidence emerges. There is a place in medicine for formal disciplinary processes, as well-delineated by professional bodies such as the APA Ethics Committee. Another important part of protecting the public is to support an environment of scientific inquiry in which diversity of opinion is welcomed. As physicians, we translate science into excellent clinical care every day in our practices, and we advance science by sharing what we learn through friendly collegial communication and collaboration.
Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships. Dr. Kohanski is in private practice in Dayton, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She also is the host and author of Clinical Correlation, a series of the Psychcast. Dr. Kohanski disclosed no relevant financial relationships.
Antidepressant may help COVID-19 patients avoid serious illness
The antidepressant fluvoxamine shows promise in preventing people infected with coronavirus from developing serious symptoms and having to be hospitalized, according to a nonrandomized study of California racetrack workers.
“What we observed was that of all the patients who received fluvoxamine, none of them had a severe COVID infection that affected their lungs or their respiratory status,” Caline Mattar, MD, told KNBC in Los Angeles. Dr. Mattar is an infectious disease researcher at Washington University in St. Louis who helped conduct the study that was published in Open Forum Infectious Diseases.
Fluvoxamine, which is sold under the brand name Luvox, is a selective serotonin reuptake inhibitor (SSRI) often prescribed for people diagnosed with obsessive-compulsive disorder. It’s been on the market for over a decade.
Two-hundred employees at Golden Gate Fields Racetrack in Berkeley, Calif., tested positive for COVID-19 last November. Track physician David Seftel, MD, offered fluvoxamine to 113 of them, having learned of a previous randomized study of COVID-19 patients that indicated fluvoxamine helped ward off serious illness, Science News said.
The 65 workers who took a 2-week course of the drug didn’t have to be hospitalized, didn’t have serious symptoms, and felt better after 2 weeks, the study said. Six of the 48 workers who turned down fluvoxamine had to be hospitalized, two required intensive care, and one died, the study said.
“Overall, fluvoxamine appears promising as early treatment for COVID-19 to prevent clinical deterioration requiring hospitalization and to prevent possible long haul symptoms persisting beyond 2 weeks,” the study said.
They said their research needed verification from a randomized, controlled trial. Such a study is now being conducted by Washington University and other schools, KNBC said.
The track workers who were infected were predominantly male and Latino, and 30% had chronic medical problems such as diabetes or high blood pressure, Science News said.
A version of this article first appeared on WebMD.com.
The antidepressant fluvoxamine shows promise in preventing people infected with coronavirus from developing serious symptoms and having to be hospitalized, according to a nonrandomized study of California racetrack workers.
“What we observed was that of all the patients who received fluvoxamine, none of them had a severe COVID infection that affected their lungs or their respiratory status,” Caline Mattar, MD, told KNBC in Los Angeles. Dr. Mattar is an infectious disease researcher at Washington University in St. Louis who helped conduct the study that was published in Open Forum Infectious Diseases.
Fluvoxamine, which is sold under the brand name Luvox, is a selective serotonin reuptake inhibitor (SSRI) often prescribed for people diagnosed with obsessive-compulsive disorder. It’s been on the market for over a decade.
Two-hundred employees at Golden Gate Fields Racetrack in Berkeley, Calif., tested positive for COVID-19 last November. Track physician David Seftel, MD, offered fluvoxamine to 113 of them, having learned of a previous randomized study of COVID-19 patients that indicated fluvoxamine helped ward off serious illness, Science News said.
The 65 workers who took a 2-week course of the drug didn’t have to be hospitalized, didn’t have serious symptoms, and felt better after 2 weeks, the study said. Six of the 48 workers who turned down fluvoxamine had to be hospitalized, two required intensive care, and one died, the study said.
“Overall, fluvoxamine appears promising as early treatment for COVID-19 to prevent clinical deterioration requiring hospitalization and to prevent possible long haul symptoms persisting beyond 2 weeks,” the study said.
They said their research needed verification from a randomized, controlled trial. Such a study is now being conducted by Washington University and other schools, KNBC said.
The track workers who were infected were predominantly male and Latino, and 30% had chronic medical problems such as diabetes or high blood pressure, Science News said.
A version of this article first appeared on WebMD.com.
The antidepressant fluvoxamine shows promise in preventing people infected with coronavirus from developing serious symptoms and having to be hospitalized, according to a nonrandomized study of California racetrack workers.
“What we observed was that of all the patients who received fluvoxamine, none of them had a severe COVID infection that affected their lungs or their respiratory status,” Caline Mattar, MD, told KNBC in Los Angeles. Dr. Mattar is an infectious disease researcher at Washington University in St. Louis who helped conduct the study that was published in Open Forum Infectious Diseases.
Fluvoxamine, which is sold under the brand name Luvox, is a selective serotonin reuptake inhibitor (SSRI) often prescribed for people diagnosed with obsessive-compulsive disorder. It’s been on the market for over a decade.
Two-hundred employees at Golden Gate Fields Racetrack in Berkeley, Calif., tested positive for COVID-19 last November. Track physician David Seftel, MD, offered fluvoxamine to 113 of them, having learned of a previous randomized study of COVID-19 patients that indicated fluvoxamine helped ward off serious illness, Science News said.
The 65 workers who took a 2-week course of the drug didn’t have to be hospitalized, didn’t have serious symptoms, and felt better after 2 weeks, the study said. Six of the 48 workers who turned down fluvoxamine had to be hospitalized, two required intensive care, and one died, the study said.
“Overall, fluvoxamine appears promising as early treatment for COVID-19 to prevent clinical deterioration requiring hospitalization and to prevent possible long haul symptoms persisting beyond 2 weeks,” the study said.
They said their research needed verification from a randomized, controlled trial. Such a study is now being conducted by Washington University and other schools, KNBC said.
The track workers who were infected were predominantly male and Latino, and 30% had chronic medical problems such as diabetes or high blood pressure, Science News said.
A version of this article first appeared on WebMD.com.
Let side effects guide treatment choice for refractory OCD
Choosing the most effective treatment for patients with obsessive-compulsive disorder requires flexibility and agility on the part of clinicians, according to Wayne K. Goodman, MD.
“There are no data at this point to suggest that one SSRI is superior to another. It’s really dealer’s choice, and it has to do with really picking medications based upon side effects,” Dr. Goodman said at the Psychopharmacology Update, presented by Current Psychiatry and Global Academy for Medical Education. Clinicians can use family history as a guide, he noted, but pharmacogenetic testing has not been helpful in his experience for selection or dosing of an SSRI.
SSRIs, such as fluvoxamine, are one of two mainstays of treatment for patients with obsessive-compulsive disorder (OCD). The other drug class is serotonin reuptake inhibitors, which include medications such clomipramine. Cognitive-behavioral therapy options, such as Exposure and Response Prevention therapy, also has some, albeit limited, efficacy.
Meanwhile, Dr. Goodman said, antidepressant classes other than SRIs and SSRIs have not been effective in treating obsessive-compulsive symptoms, and some patients do not adhere well to cognitive-behavioral therapy, said Dr. Goodman, who is the D.C. and Irene Ellwood Professor in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston.
Choosing the most effective treatment for patients with obsessive-compulsive disorder requires flexibility and agility on the part of clinicians, according to Wayne K. Goodman, MD.
“There are no data at this point to suggest that one SSRI is superior to another. It’s really dealer’s choice, and it has to do with really picking medications based upon side effects,” Dr. Goodman said at the Psychopharmacology Update, presented by Current Psychiatry and Global Academy for Medical Education. Clinicians can use family history as a guide, he noted, but pharmacogenetic testing has not been helpful in his experience for selection or dosing of an SSRI.
SSRIs, such as fluvoxamine, are one of two mainstays of treatment for patients with obsessive-compulsive disorder (OCD). The other drug class is serotonin reuptake inhibitors, which include medications such clomipramine. Cognitive-behavioral therapy options, such as Exposure and Response Prevention therapy, also has some, albeit limited, efficacy.
Meanwhile, Dr. Goodman said, antidepressant classes other than SRIs and SSRIs have not been effective in treating obsessive-compulsive symptoms, and some patients do not adhere well to cognitive-behavioral therapy, said Dr. Goodman, who is the D.C. and Irene Ellwood Professor in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston.
Choosing the most effective treatment for patients with obsessive-compulsive disorder requires flexibility and agility on the part of clinicians, according to Wayne K. Goodman, MD.
“There are no data at this point to suggest that one SSRI is superior to another. It’s really dealer’s choice, and it has to do with really picking medications based upon side effects,” Dr. Goodman said at the Psychopharmacology Update, presented by Current Psychiatry and Global Academy for Medical Education. Clinicians can use family history as a guide, he noted, but pharmacogenetic testing has not been helpful in his experience for selection or dosing of an SSRI.
SSRIs, such as fluvoxamine, are one of two mainstays of treatment for patients with obsessive-compulsive disorder (OCD). The other drug class is serotonin reuptake inhibitors, which include medications such clomipramine. Cognitive-behavioral therapy options, such as Exposure and Response Prevention therapy, also has some, albeit limited, efficacy.
Meanwhile, Dr. Goodman said, antidepressant classes other than SRIs and SSRIs have not been effective in treating obsessive-compulsive symptoms, and some patients do not adhere well to cognitive-behavioral therapy, said Dr. Goodman, who is the D.C. and Irene Ellwood Professor in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston.
FROM PSYCHOPHARMACOLOGY UPDATE
COVID-19’s psychological impact gets a name
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
During normal times, the U.K.-based charity No Panic offers itself as an easily accessible service to those with anxiety disorders and phobias. Visitors to the website who can receive immediate, remote support from trained volunteers. But this spring was anything but normal, as the reality of COVID-19’s worldwide spread became terrifyingly clear.
COVID-19 cases peaked in the United Kingdom in early April. Nationwide lockdown efforts contributed to a gradual but ultimately substantial decline in cases, yet, despite the favorable trend lines, No Panic has remained busier than ever.
Beyond the physical symptoms associated with COVID-19, the psychological outcomes are vast and, it seems, prolonged. Researchers have now formalized a definition of the long-term mental maladies associated with the pandemic, collectively deeming them “coronaphobia.”
The term is a catch-all phrase for the fear and the emotional and social strain experienced by the general public in response to COVID-19. Obsessive behaviors, distress, avoidance reaction, panic, anxiety, hoarding, paranoia, and depression are some of the responses associated with coronaphobia. On the surface, these appear to be normal, somewhat fitting reactions to this surreal and frightening moment in time. However, for those experiencing coronaphobia, they are distinctly maladaptive and harmful.
“We had a serious rise in the use of our services, notably the helpline and email enquiries,” explained Sarah Floyd, No Panic’s volunteer advisor and social media coordinator. “It has been up and down all along, but more of an up since lockdown is easing.”
The group’s experience offers yet more evidence that the anxieties and fears caused by this global pandemic don’t flatten alongside the curve but instead linger as chronic problems requiring ongoing care.
“Every week in my clinic, I’m seeing people who are experiencing more anxiety and hopelessness and having an emotional response that is perhaps out of proportion to what one would expect, which is directly related to what is going on in the world right now with coronavirus,” said Gregory Scott Brown, MD, founder and director of the Center for Green Psychiatry in West Lake Hills, Tex. “Simply put, I think what we are looking at is adjustment disorder. That is probably how the DSM would define it.”
Adjustment disorder is one of the most frequently diagnosed mental health conditions, although it is also relatively understudied. It is really a set of disorders that follow in the wake of a significant stressor, which can vary from serious illness or the death of a loved one to relocating or experiencing work problems. The resulting dysfunction and distress that the person experiences are considered out of proportion in duration or scale with what would normally be expected. Diagnosing an adjustment disorder is made difficult by the lack of a valid and reliable screening measure.
Recent literature suggests that coronaphobia may be likely to occur in those who feel vulnerable to disease, are predisposed to anxiety, or are intolerant of uncertainty. Preexisting mental health conditions can also be exacerbated by periods of quarantine, self-isolation, and lockdown, which can lead to panic attacks, chronophobia (fear of passing time), and suicidality.
Although imperfect comparisons, findings from earlier 21st century disease outbreaks, such as severe acute respiratory syndrome and the Ebola virus, signal that containment efforts themselves play a role in deteriorating mental health. A recent rapid review found that, in studies comparing persons who had previously undergone quarantines and those who had not, the former were significantly more likely to experience acute stress disorder, posttraumatic stress symptoms, and depression. Quarantine was found to result in long-term behavioral changes, such as avoiding crowds, among the general public and health care practitioners.
That tremendous psychological morbidity should accompany a global pandemic of this scale is not surprising, according to Amit Anand, MD, vice chair for research for the Center for Behavioral Health and director of the Mood and Emotional Disorders Across the Life Span program at the Cleveland Clinic.
“The technical definition of anxiety is an impending sense of doom, and I think all of us are living with that,” Dr. Anand said. “The basic question then becomes, what is normal and when does it become abnormal?”
He added that most classifications of psychiatric disorders are set during periods of relative stability, which the current moment is most certainly not.
“This is such an unusual situation, so I think it will depend on case-by-case basis, keeping the whole context in mind as whether the patient is thinking or behaving with an abnormal amount of anxiety,” Dr. Anand said.
Investigators are currently trying to give clinicians the tools to better make that determination. In the first scientific study of this clinical condition, Sherman Lee, MD, reported that five symptoms – dizziness, sleep disturbances, tonic immobility, appetite loss, and nausea/abdominal distress – were strong factors for distinguishing coronaphobia from otherwise normal concerns about COVID-19 that did not result in functional impairment. Dr. Lee and colleagues have since published further evidence that coronaphobia “is a unique predictor of psychological distress during the COVID-19 crisis.” They are working on validating a self-reported mental health screener for this condition.
Having the tools to identify patients struggling with coronaphobia may go some ways toward addressing another area of declining health. At the outset of the COVID-19 pandemic, there was a question as to whether doctors would be beset by a surge of the “worried well” – persons mistakenly believing themselves to be infected. Now months into the pandemic, the converse phenomenon – a fear of contracting COVID-19 that is driving patients away from practitioners – appears to be the more valid concern.
In early spring, the pandemic’s first surge was accompanied by reports of approximately 40% and 60% drops in visits to EDs and ambulatory centers, respectively. Stories of acute stroke patients avoiding treatment began to appear in the press. Major U.S. cities saw noteworthy declines in 911 calls, indicating a hesitancy to be taken to a hospital. That COVID-19 has been accompanied by mass unemployment and subsequent loss of insurance complicates the notion that fear alone is keeping people from treatment. In other countries, it has been explicitly linked. Investigators in Singapore noted that coronaphobia played a role in reducing willingness to attend in-person visits among adolescents with eating disorders. Similarly, case reports in Israel suggest that coronaphobia has contributed to delays in diagnoses of common pediatric diseases.
There is also a concern, colloquially termed “reentry anxiety,” that mental health problems caused by the pandemic, the accompanying lockdown, self-isolation, and quarantine practices will prove alarmingly durable. Even after this challenging moment in history draws to a close, many people may face substantial stress in returning to the normal activities of life – social, professional, familial – once taken for granted.
“We are in the beginning phase of that now,” said Dr. Anand. “ I think the longer it goes on for, the more difficult it will be.”
In the United States, that day may seem far away. Nonetheless, it is important to begin laying the therapeutic groundwork now, according to Dr. Brown.
“I am recommending unconventional therapies like meet-up groups, online forums,” he said. “Everything has shifted online, and so there are a lot of support groups that patients can participate to learn coping skills and really hear what other people are going through.”
Before reaching that stage, Dr. Brown recommends that clinicians first simply discuss such anxieties with their patients in order to normalize them.
“Realize that everyone essentially is going through some degree of this right now. The coronavirus pandemic is literally impacting every person on the face of the planet. Sometimes just pointing that out to people can really help,” he said.
A version of this article originally appeared on Medscape.com.
Reassuring findings on SSRIs and diabetes risk in children
SSRIs are associated with a much lower risk of type 2 diabetes (T2D) in children and adolescents than previously reported, new research shows.
Investigators found publicly insured patients treated with SSRIs had a 13% increased risk for T2D, compared with those not treated with these agents. In addition, those taking SSRIs continuously (defined as receiving one or more prescriptions every 3 months) had a 33% increased risk of T2D.
On the other hand, privately insured youth had a much lower increased risk – a finding that may be attributable to a lower prevalence of risk factors for T2D in this group.
“We cannot exclude that children and adolescents treated with SSRIs may be at a small increased risk of developing T2D, particularly publicly insured patients, but the magnitude of association was weaker than previous thought and much smaller than other known risk factors for T2DM, such as obesity, race, and poverty,” lead investigator Jenny Sun, PhD, said in an interview.
“When weighing the known benefits and risks of SSRI treatment in children and adolescents, our findings provide reassurance that the risk of T2DM is not as substantial as initially reported,” said Dr. Sun, a postdoctoral research fellow in the department of population medicine at Harvard Medical School’s Harvard Pilgrim Health Care Institute, Boston.
The study was published online Sept. 2 in JAMA Psychiatry.
Limited evidence
Previous research suggested that SSRIs increase the risk of T2D by up to 90% in children and adolescents.
However, the investigators noted, the study reporting this finding was too small to draw conclusions about the SSRI class as a whole also did not examine specific SSRIs.
In addition, although “several studies have reported that antidepressant use may be a risk factor for T2D in adults, evidence was limited in children and adolescents,” said Dr. Sun.
“Rapid changes in growth during childhood and adolescents can alter drugs’ pharmacokinetics and pharmacodynamics, so high-quality, age-specific data are needed to inform prescribing decisions,” she said.
For the current study, the researchers analyzed claims data on almost 1.6 million patients aged 10-19 years (58.3% female; mean age, 15.1 years) from two large claims databases.
The analysis focused on those with a diagnosis warranting treatment with an SSRI, including depression, generalized or social anxiety disorder, obsessive compulsive disorder, PTSD, panic disorder, or bulimia nervosa.
The Medicaid Analytic Extract database consisted of 316,178 patients insured through Medicaid or the Children’s Health Insurance Program. The IBM MarketScan database consisted of 211,460 privately insured patients. Patients were followed up for a mean of 2.3 and 2.2 years, respectively.
Patients who initiated SSRI treatment were compared with those with a similar indication but who were not taking an SSRI. Secondary analyses compared new SSRI users with patients who recently initiated treatment with bupropion, which has no metabolic side effects, or with patients who recently initiated psychotherapy.
“In observational data, it is difficult to mimic a placebo group, often used in RCTs [randomized, controlled trials], therefore several comparator groups were explored to broaden our understanding,” said Dr. Sun.
In addition, the researchers compared the individual SSRI medications, using fluoxetine as a comparator.
A wide range of more than 100 potential confounders or “proxies of confounders,” were taken into account, including demographic characteristics, psychiatric diagnoses, metabolic conditions, concomitant medications, and use of health care services.
The researchers conducted two analyses. They included an intention-to-treat (ITT) analysis that was restricted to patients with one or more additional SSRI prescriptions during the 6 months following the index exposure assessment period.
Close monitoring required
An as-treated analysis estimated the association of continuous SSRI treatment (vs. untreated, bupropion treatment, and psychotherapy), with adherence assessed at 3-month intervals.
Initiation and continuation of SSRI treatment in publicly insured patients were both associated with a considerably higher risk of T2D, compared with untreated patients, and a steeper risk, compared with their privately insured counterparts.
For newly treated publicly insured patients initiated on SSRI treatment, the ITT adjusted hazard ratio was 1.13 (95% confidence interval, 1.04-1.22).
There was an even stronger association among continuously treated publicly insured patients, with an as-treated aHR of 1.33 (95% CI, 1.21-1.47). The authors noted that this corresponds to 6.6 additional T2D cases per 10,000 patients continuously treated for at least 2 years.
The association was weaker in privately insured patients (ITT aHR, 1.01; 95% CI, 0.84-1.23; as-treated aHR, 1.10; 95% CI, 0.88-1.36).
The secondary analyses yielded similar findings: When SSRI treatment was compared with psychotherapy, the as-treated aHR for publicly insured patients was 1.44 (95% CI, 1.25-1.65), whereas the aHR for privately insured patients was lower at 1.21 (95% CI, 0.93-1.57)
The investigators found no increased risk when SSRIs were compared with bupropion, and the within-class analysis showed that none of the SSRIs carried an increased hazard of T2D, compared with fluoxetine.
“Publicly insured patients are enrolled in Medicaid and the Children’s Health Insurance Program, whereas privately insured patients are generally covered by their parent’s employer-sponsored insurance,” said Dr. Sun.
“Publicly insured patients are of lower socioeconomic status and represent a population with greater overall medical burden, more comorbidities, and a higher prevalence of risk factors for T2D, such as obesity, at the time of treatment initiation,” she said.
She added that high-risk children and youth should be closely monitored and clinicians should also consider recommending dietary modifications and increased exercise to offset T2D risk.
Useful ‘real-world data’
William Cooper, MD, MPH, professor of pediatrics and health policy at Vanderbilt University Medical Center in Nashville, Tenn., said that the study “provides a fascinating look at risks of SSRI medications in children and adolescents.”
Dr. Cooper, who was not involved with the study, said that the authors “draw from real-world data representing two different populations and carefully consider factors which might confound the associations.”
The results, he said, “provide important benefits for patients, families, and clinicians as they weigh the risks and benefits of using SSRIs for children who need treatment for depression and anxiety disorders.
The study was supported by a training grant from the program in pharmacoepidemiology at the Harvard School of Public Health. Dr. Sun disclosed no relevant financial relationships. Dr. Cooper disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SSRIs are associated with a much lower risk of type 2 diabetes (T2D) in children and adolescents than previously reported, new research shows.
Investigators found publicly insured patients treated with SSRIs had a 13% increased risk for T2D, compared with those not treated with these agents. In addition, those taking SSRIs continuously (defined as receiving one or more prescriptions every 3 months) had a 33% increased risk of T2D.
On the other hand, privately insured youth had a much lower increased risk – a finding that may be attributable to a lower prevalence of risk factors for T2D in this group.
“We cannot exclude that children and adolescents treated with SSRIs may be at a small increased risk of developing T2D, particularly publicly insured patients, but the magnitude of association was weaker than previous thought and much smaller than other known risk factors for T2DM, such as obesity, race, and poverty,” lead investigator Jenny Sun, PhD, said in an interview.
“When weighing the known benefits and risks of SSRI treatment in children and adolescents, our findings provide reassurance that the risk of T2DM is not as substantial as initially reported,” said Dr. Sun, a postdoctoral research fellow in the department of population medicine at Harvard Medical School’s Harvard Pilgrim Health Care Institute, Boston.
The study was published online Sept. 2 in JAMA Psychiatry.
Limited evidence
Previous research suggested that SSRIs increase the risk of T2D by up to 90% in children and adolescents.
However, the investigators noted, the study reporting this finding was too small to draw conclusions about the SSRI class as a whole also did not examine specific SSRIs.
In addition, although “several studies have reported that antidepressant use may be a risk factor for T2D in adults, evidence was limited in children and adolescents,” said Dr. Sun.
“Rapid changes in growth during childhood and adolescents can alter drugs’ pharmacokinetics and pharmacodynamics, so high-quality, age-specific data are needed to inform prescribing decisions,” she said.
For the current study, the researchers analyzed claims data on almost 1.6 million patients aged 10-19 years (58.3% female; mean age, 15.1 years) from two large claims databases.
The analysis focused on those with a diagnosis warranting treatment with an SSRI, including depression, generalized or social anxiety disorder, obsessive compulsive disorder, PTSD, panic disorder, or bulimia nervosa.
The Medicaid Analytic Extract database consisted of 316,178 patients insured through Medicaid or the Children’s Health Insurance Program. The IBM MarketScan database consisted of 211,460 privately insured patients. Patients were followed up for a mean of 2.3 and 2.2 years, respectively.
Patients who initiated SSRI treatment were compared with those with a similar indication but who were not taking an SSRI. Secondary analyses compared new SSRI users with patients who recently initiated treatment with bupropion, which has no metabolic side effects, or with patients who recently initiated psychotherapy.
“In observational data, it is difficult to mimic a placebo group, often used in RCTs [randomized, controlled trials], therefore several comparator groups were explored to broaden our understanding,” said Dr. Sun.
In addition, the researchers compared the individual SSRI medications, using fluoxetine as a comparator.
A wide range of more than 100 potential confounders or “proxies of confounders,” were taken into account, including demographic characteristics, psychiatric diagnoses, metabolic conditions, concomitant medications, and use of health care services.
The researchers conducted two analyses. They included an intention-to-treat (ITT) analysis that was restricted to patients with one or more additional SSRI prescriptions during the 6 months following the index exposure assessment period.
Close monitoring required
An as-treated analysis estimated the association of continuous SSRI treatment (vs. untreated, bupropion treatment, and psychotherapy), with adherence assessed at 3-month intervals.
Initiation and continuation of SSRI treatment in publicly insured patients were both associated with a considerably higher risk of T2D, compared with untreated patients, and a steeper risk, compared with their privately insured counterparts.
For newly treated publicly insured patients initiated on SSRI treatment, the ITT adjusted hazard ratio was 1.13 (95% confidence interval, 1.04-1.22).
There was an even stronger association among continuously treated publicly insured patients, with an as-treated aHR of 1.33 (95% CI, 1.21-1.47). The authors noted that this corresponds to 6.6 additional T2D cases per 10,000 patients continuously treated for at least 2 years.
The association was weaker in privately insured patients (ITT aHR, 1.01; 95% CI, 0.84-1.23; as-treated aHR, 1.10; 95% CI, 0.88-1.36).
The secondary analyses yielded similar findings: When SSRI treatment was compared with psychotherapy, the as-treated aHR for publicly insured patients was 1.44 (95% CI, 1.25-1.65), whereas the aHR for privately insured patients was lower at 1.21 (95% CI, 0.93-1.57)
The investigators found no increased risk when SSRIs were compared with bupropion, and the within-class analysis showed that none of the SSRIs carried an increased hazard of T2D, compared with fluoxetine.
“Publicly insured patients are enrolled in Medicaid and the Children’s Health Insurance Program, whereas privately insured patients are generally covered by their parent’s employer-sponsored insurance,” said Dr. Sun.
“Publicly insured patients are of lower socioeconomic status and represent a population with greater overall medical burden, more comorbidities, and a higher prevalence of risk factors for T2D, such as obesity, at the time of treatment initiation,” she said.
She added that high-risk children and youth should be closely monitored and clinicians should also consider recommending dietary modifications and increased exercise to offset T2D risk.
Useful ‘real-world data’
William Cooper, MD, MPH, professor of pediatrics and health policy at Vanderbilt University Medical Center in Nashville, Tenn., said that the study “provides a fascinating look at risks of SSRI medications in children and adolescents.”
Dr. Cooper, who was not involved with the study, said that the authors “draw from real-world data representing two different populations and carefully consider factors which might confound the associations.”
The results, he said, “provide important benefits for patients, families, and clinicians as they weigh the risks and benefits of using SSRIs for children who need treatment for depression and anxiety disorders.
The study was supported by a training grant from the program in pharmacoepidemiology at the Harvard School of Public Health. Dr. Sun disclosed no relevant financial relationships. Dr. Cooper disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SSRIs are associated with a much lower risk of type 2 diabetes (T2D) in children and adolescents than previously reported, new research shows.
Investigators found publicly insured patients treated with SSRIs had a 13% increased risk for T2D, compared with those not treated with these agents. In addition, those taking SSRIs continuously (defined as receiving one or more prescriptions every 3 months) had a 33% increased risk of T2D.
On the other hand, privately insured youth had a much lower increased risk – a finding that may be attributable to a lower prevalence of risk factors for T2D in this group.
“We cannot exclude that children and adolescents treated with SSRIs may be at a small increased risk of developing T2D, particularly publicly insured patients, but the magnitude of association was weaker than previous thought and much smaller than other known risk factors for T2DM, such as obesity, race, and poverty,” lead investigator Jenny Sun, PhD, said in an interview.
“When weighing the known benefits and risks of SSRI treatment in children and adolescents, our findings provide reassurance that the risk of T2DM is not as substantial as initially reported,” said Dr. Sun, a postdoctoral research fellow in the department of population medicine at Harvard Medical School’s Harvard Pilgrim Health Care Institute, Boston.
The study was published online Sept. 2 in JAMA Psychiatry.
Limited evidence
Previous research suggested that SSRIs increase the risk of T2D by up to 90% in children and adolescents.
However, the investigators noted, the study reporting this finding was too small to draw conclusions about the SSRI class as a whole also did not examine specific SSRIs.
In addition, although “several studies have reported that antidepressant use may be a risk factor for T2D in adults, evidence was limited in children and adolescents,” said Dr. Sun.
“Rapid changes in growth during childhood and adolescents can alter drugs’ pharmacokinetics and pharmacodynamics, so high-quality, age-specific data are needed to inform prescribing decisions,” she said.
For the current study, the researchers analyzed claims data on almost 1.6 million patients aged 10-19 years (58.3% female; mean age, 15.1 years) from two large claims databases.
The analysis focused on those with a diagnosis warranting treatment with an SSRI, including depression, generalized or social anxiety disorder, obsessive compulsive disorder, PTSD, panic disorder, or bulimia nervosa.
The Medicaid Analytic Extract database consisted of 316,178 patients insured through Medicaid or the Children’s Health Insurance Program. The IBM MarketScan database consisted of 211,460 privately insured patients. Patients were followed up for a mean of 2.3 and 2.2 years, respectively.
Patients who initiated SSRI treatment were compared with those with a similar indication but who were not taking an SSRI. Secondary analyses compared new SSRI users with patients who recently initiated treatment with bupropion, which has no metabolic side effects, or with patients who recently initiated psychotherapy.
“In observational data, it is difficult to mimic a placebo group, often used in RCTs [randomized, controlled trials], therefore several comparator groups were explored to broaden our understanding,” said Dr. Sun.
In addition, the researchers compared the individual SSRI medications, using fluoxetine as a comparator.
A wide range of more than 100 potential confounders or “proxies of confounders,” were taken into account, including demographic characteristics, psychiatric diagnoses, metabolic conditions, concomitant medications, and use of health care services.
The researchers conducted two analyses. They included an intention-to-treat (ITT) analysis that was restricted to patients with one or more additional SSRI prescriptions during the 6 months following the index exposure assessment period.
Close monitoring required
An as-treated analysis estimated the association of continuous SSRI treatment (vs. untreated, bupropion treatment, and psychotherapy), with adherence assessed at 3-month intervals.
Initiation and continuation of SSRI treatment in publicly insured patients were both associated with a considerably higher risk of T2D, compared with untreated patients, and a steeper risk, compared with their privately insured counterparts.
For newly treated publicly insured patients initiated on SSRI treatment, the ITT adjusted hazard ratio was 1.13 (95% confidence interval, 1.04-1.22).
There was an even stronger association among continuously treated publicly insured patients, with an as-treated aHR of 1.33 (95% CI, 1.21-1.47). The authors noted that this corresponds to 6.6 additional T2D cases per 10,000 patients continuously treated for at least 2 years.
The association was weaker in privately insured patients (ITT aHR, 1.01; 95% CI, 0.84-1.23; as-treated aHR, 1.10; 95% CI, 0.88-1.36).
The secondary analyses yielded similar findings: When SSRI treatment was compared with psychotherapy, the as-treated aHR for publicly insured patients was 1.44 (95% CI, 1.25-1.65), whereas the aHR for privately insured patients was lower at 1.21 (95% CI, 0.93-1.57)
The investigators found no increased risk when SSRIs were compared with bupropion, and the within-class analysis showed that none of the SSRIs carried an increased hazard of T2D, compared with fluoxetine.
“Publicly insured patients are enrolled in Medicaid and the Children’s Health Insurance Program, whereas privately insured patients are generally covered by their parent’s employer-sponsored insurance,” said Dr. Sun.
“Publicly insured patients are of lower socioeconomic status and represent a population with greater overall medical burden, more comorbidities, and a higher prevalence of risk factors for T2D, such as obesity, at the time of treatment initiation,” she said.
She added that high-risk children and youth should be closely monitored and clinicians should also consider recommending dietary modifications and increased exercise to offset T2D risk.
Useful ‘real-world data’
William Cooper, MD, MPH, professor of pediatrics and health policy at Vanderbilt University Medical Center in Nashville, Tenn., said that the study “provides a fascinating look at risks of SSRI medications in children and adolescents.”
Dr. Cooper, who was not involved with the study, said that the authors “draw from real-world data representing two different populations and carefully consider factors which might confound the associations.”
The results, he said, “provide important benefits for patients, families, and clinicians as they weigh the risks and benefits of using SSRIs for children who need treatment for depression and anxiety disorders.
The study was supported by a training grant from the program in pharmacoepidemiology at the Harvard School of Public Health. Dr. Sun disclosed no relevant financial relationships. Dr. Cooper disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Evaluate, manage the stress response in susceptible individuals affected by COVID-19
Steroid therapy should be explored for quarantined mental health patients
Psychological First Aid is an innovative program launched by the American Red Cross with the goal of addressing issues of concern such as those stemming from COVID-19–related stress. According to Red Cross mental health volunteer representative Deb Butman-Perkins, the program provides “a general overview of what does stress look like, how do we feel it, how do we recognize it in our bodies ... physical, emotional, spiritual, physiological, where does all that stress occur?”1
The program brings a spotlight to the interdisciplinary nature of the stress response, especially with respect to the importance of developing the necessary coping skills during an ongoing crisis. However, to effectively evaluate and manage the overall stress response for psychiatric patients during quarantine conditions, as well as those who are formally diagnosed with COVID-19, clinicians also will need to revisit what we’ve learned about the hypothalamic-pituitary-adrenal (HPA) axis.
We know that the stress response – which varies somewhat across the spectrum – is necessary to ensure homeostatic regulation. A feedback loop is initiated at the receptor level, involving a myriad of hormones and chemical signals that bring forth the body’s “flight-or-fight” response. Hormones such as epinephrine/norepinephrine and cortisol are secreted by the HPA axis in reaction to the stress response, resulting in a spike in heart rate, blood pressure, and transient hyperglycemia, respectively. In particular, hyperglycemia provides immediate energy to muscles during a perceived crisis.2
In addition, prolonged exposure to living in quarantine can lead to feelings of isolation and estrangement – and excessive anxiety. Combined, those conditions may exert an indelible effect on the HPA axis – leading to a warped pattern of cortisol secretion with respect to baseline.3 (It has been noted in the literature that serum cortisol plays a protective role in thwarting off the effects of PTSD development. Consistent with this line of thinking, military personnel have been preemptively treated with high-dose cortisol during acute exposure.)
Prolonged exposure to psychosocial stressors also increases the overall risk of developing medical comorbidities. Patients who adopt maladaptive responses to traumatic events, for example, may experience dysregulation in eating behaviors and/or disordered sleep.4
In light of those realities, clinicians should explore the role of steroid therapy as a means of treating mental health patients experiencing psychological stress formation tied to ongoing quarantine conditions.
Challenges of neuroendocrine medications for COVID-19
COVID-19, caused by exposure to SARS-CoV-2, adeptly leverages the ACE2 receptor of the lungs as an entry point to evade the host’s defenses. It should be noted that the ACE2 protein is expressed on the cells of multiple organs of the body, including the adrenals, which are largely responsible for coordinating the stress response of the HPA axis.
Postmortem analysis from severe acute respiratory syndrome (SARS-CoV is also from the Coronaviridae family) patients indicates the presence of necrotic adrenal cells, further solidifying the association of the HPA axis to the COVID-19 disease state and pathophysiological course.5 Molecular mimicry of the adrenocorticotropic hormone allows SARS-CoV the ability to infiltrate the host’s defenses, in particular, the ability to mount a clinically apt cortisol stress response (e.g., hypocortisolism).As for those who survived the 2003 SARS outbreak, less than half of the patients have been observed to develop symptoms of frank hypocortisolism within a few months after exposure.
and an ongoing clinical trial is evaluating the safety and efficacy parameters of corticosteroids in COVID-19–exposed patients.
In addition, there is reason to believe that application of prophylactic steroids might affect the overall clinical course of COVID-19, thereby reducing mortality and morbidity rates in patients with severe presentation, such as septic shock. The rationale for this line of thought is based on the ability of glucocorticoids to suppress an ensuing cytokine storm by the virus in question.5,6 In clinical practice, steroids have been used to treat a host of viral diseases, including influenza, respiratory syncytial virus, and Middle East respiratory syndrome coronavirus.
Aside from the selective use of corticosteroids, the medication regimen may incorporate ACE inhibitors and/or angiotensin receptor blockers (ARBs) because of COVID-19’s ability to activate the renin-angiotensin-aldosterone system with respect to the physiological stress response.
The interplay of the HPA axis with the sympathoadrenal system is responsible for adaptive behaviors in the individual. Disrupted feedback loops from prolonged activation are associated with numerous stress-based conditions in mental illness, namely, PTSD, anxiety, and mood disorders. We are concerned about frontline health care workers, who are particularly prone to chronic stress and burnout because of the cumbersome patient load and equipment shortage that have characterized the coronavirus crisis.
Timely administration of corticosteroids on a case-by-case basis would keep the cytokines at bay by precluding their undue activation of the HPA axis and corresponding cascade stress response. Steroids are also known to restore disrupted feedback loops at the level of the immune cells. However, because of conflicting reports concerning viral clearance in some SARS and COVID-19 studies, treatment with steroids may be limited to select patient populations with the necessary dose adjustments. Ongoing clinical trials will further elucidate upon the applicability of steroids as well as the role of other neuroendocrine agents, such as ACE inhibitors or ARBs, in the treatment of COVID-19.
Behavioral manifestations and psychosocial health
As far as the stress response is concerned, an analysis performed by researchers in China after the COVID-19 outbreak found gender disparities in symptom expression. In the study (n = 1,210) the researchers found in female citizens a greater frequency of behavioral manifestations, including acute stress reaction, and symptoms of anxiety and mood disorders – namely, depression.7 Patient perception and awareness of the perils of coronavirus typically varied across the spectrum; some individuals reportedly undermined and devalued their risk of contracting COVID-19 – these patients may benefit from therapeutic modalities, such as cognitive-behavioral therapy (CBT), as a means of challenging their firmly entrenched cognitive distortions. CBT is an effective tool in addressing maladaptive coping responses, because these strategies tend to correspond with poor prognosis with respect to overall mental health. Aside from CBT, the clinician may advise other behavioral techniques, such as relaxation training, with the aim of controlling the symptoms of mood and anxiety disorders.
We often take for granted general pandemic safety precautions, such as maintaining physical distancing coupled with engaging in regular hand hygiene and wearing masks, but these actions also are known to alleviate mental anguish. Access to accurate and easy-to-consume health information regarding COVID-19 is also associated with psychological well-being during the quarantine.8
An intriguing “phenomenon” has emerged in the form of “panic buying.”However, researchers reported in the peer-reviewed journal Nature Human Behaviour that this pattern of behaviors is not typical for those under distress and represents an overstated misnomer of sorts. According to Jay J. Van Bavel, PhD, and associates, prevailing reports from news outlets have skewed the features of a panic. “News stories that employ the language of panic often create the very phenomena that they purport to condemn,” Dr. Van Bavel and associates wrote. “They can foster the very individualism and competitiveness that turn sensible preparations into dysfunctional stockpiling and undermine the sense of collective purpose which facilitates people supporting one another during an emergency.”9
The researchers proceeded to highlight the scope of effective crisis leadership with respect to establishing a sense of communal “self-efficacy and hope.” The influence of organized leadership serves to solidify the structure of the community as a whole, allowing group members the opportunity to address the stressors of interest. Such leadership may mitigate the stress response by fostering a necessary, healthy set for stress management.
Strategies aimed at supporting mental health
Coping and stress management strategies may include the process of building virtual networks (e.g., social media platforms) because physical distancing may contribute toward further isolation and social estrangement. However, it should be noted that ideally social media consumption should be centered upon interactive enrichment activities that provide a suitable substitute for the absence of physical support systems. The goal is to facilitate meaningful relationships and enduring communications that produce healthy and resilient mindsets.
In particular, individuals who possess adaptive mindsets with a realistic view of ongoing psychosocial stressors, be it from the impact of the pandemic or other influential events, are more likely to benefit when moving forward with life. In other words, the individual in question leverages these experiences as a means of “stress-related growth,” thereby enhancing the overall quality of relationships. Tentative studies in stress management have yielded promising support for interventions that aim to modulate mindsets (as a function of the stress response) by proper appraisal of the stress stimuli, according to Dr. Van Bavel and associates.
Employing assessment scales
To mitigate the stress response, clinicians need to use the relevant stress scales for assessing the full impact of distress brought on by COVID-19 and optimizing therapeutic modalities for those who need them most. Again, the stress response would vary, depending on the patient, and may include paranoia, xenophobia, compulsive ritualistic behavior, as well as full-fledged symptoms of acute stress disorder/PTSD.Steven Taylor, PhD, RPsych, and associates, part of a research team funded by the Canadian Institutes of Health Research and the University of Regina (Sask.), formulated their proprietary COVID Stress Scales (CSS) based on 36 items pertaining to individual anxiety and/or stress responses.10
As general purpose pandemic scales, the assessment tools will be transferable to similar outbreaks, and have been examined for validity and reliability. Additional validation scales include the Patient Health Questionnaire–4 for anxiety and depression, the Short Health Anxiety Inventory for anxiety (irrespective of physical condition), and the Marlowe-Crowne Social Desirability Scale–Short Form for psychological well-being based on the presence (or the lack thereof) of desirable characteristics.10 As a composite scale and predictive tool (especially with respect to future pandemics), the CSS allows clinicians a means of identifying the people who are most compliant with safety procedures, social distancing, hygiene expectations, and vaccine protocols – when applicable – reported Dr. Taylor and associates.
Moving forward: The next step in COVID-19 preparedness
As clinicians continue to develop guidelines that are befitting of COVID-19’s “new normal,” a holistic psychosocial framework will need to integrate the various psychometrics gathered from assessment scales, as well as understanding trauma, especially with respect to the HPA axis.
For starters, there is a certain element of “anticipatory anxiety” for those experiencing distress from COVID-19. A highly uncertain future with no immediate cure in the future, isolation and social estrangement, as well as financial setbacks, compound the situation. Moreover, the DSM fails to acknowledge other sources of traumatic experiences that are systemic in nature, such as discriminatory practices, injustice, and/or persecution.
It has also been noted that some distressed individuals experience a hypervigilant state that is comparable with PTSD.11 There may be a push to incorporate machine learning and other modalities to better identify those at risk (for example, health care professionals who perform their duties with limited resources, thereby inducing sleep dysregulation, anxiety, and hopelessness) for mental health deterioration. Interventions may need to be coordinated in a timely manner to disrupt the progression of acute stress disorder to PTSD. Peer support programs and resiliency training – successful therapeutic approaches for PTSD – may prove to have considerable utility for mitigating the overall stress response of COVID-19.12
References
1. “Red Cross offering online course to manage crisis-related stress.” ABC 6 News. kaaltv.com, 2020 Aug 29.
2. Islam FA, Choudhry C. J Psychiatry Psychiatric Disord 2017;1(5): 290-3.
3. Faravelli C et al. World J Psychiatry. 2012 Feb 22;2(1):13-25.
4. Carmassi C et al. Psychiatry Res. 2015 Jan 30;225(1-2):64-9.
5. Pal R. Endocrine. 2020 Apr 28. doi: 10.1007/s12020-020-02325-1.
6. Steenblock C et al. Mol Psychiatry. 2020 May. doi: 10.1038/s41380-020-0758-9.
7. Wang C et al. Int J Environ Res Public Health. 2020 Jan;17(5):1729.
8. Ho CS et al. Ann Acad Med Singap. 2020 Mar 16;49(3):155-60.
9. Van Bavel JJ et al. Nat Hum Behav. 2020 Apr 30. doi: 10.1038/s41562-020-0884-z.
10. Taylor S et al. J Anxiety Disord. 2020 May 4;72:102232.
11. Horesh D, Brown AD. Psychol Trauma. 2020 May;12(4):331-5.
12. Clark H et al. National Health Library and Knowledge Service/Evidence Team. Summary of Evidence: COVID-19, 2020 May 22. Version 2.0.
Dr. Faisal A. Islam is a medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Mohammed S. Islam is a research physician and extern at Interfaith Medical Center, New York. Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. Dr. Jolayemi is an attending psychiatrist at Interfaith Medical Center. No disclosures were reported.
Steroid therapy should be explored for quarantined mental health patients
Steroid therapy should be explored for quarantined mental health patients
Psychological First Aid is an innovative program launched by the American Red Cross with the goal of addressing issues of concern such as those stemming from COVID-19–related stress. According to Red Cross mental health volunteer representative Deb Butman-Perkins, the program provides “a general overview of what does stress look like, how do we feel it, how do we recognize it in our bodies ... physical, emotional, spiritual, physiological, where does all that stress occur?”1
The program brings a spotlight to the interdisciplinary nature of the stress response, especially with respect to the importance of developing the necessary coping skills during an ongoing crisis. However, to effectively evaluate and manage the overall stress response for psychiatric patients during quarantine conditions, as well as those who are formally diagnosed with COVID-19, clinicians also will need to revisit what we’ve learned about the hypothalamic-pituitary-adrenal (HPA) axis.
We know that the stress response – which varies somewhat across the spectrum – is necessary to ensure homeostatic regulation. A feedback loop is initiated at the receptor level, involving a myriad of hormones and chemical signals that bring forth the body’s “flight-or-fight” response. Hormones such as epinephrine/norepinephrine and cortisol are secreted by the HPA axis in reaction to the stress response, resulting in a spike in heart rate, blood pressure, and transient hyperglycemia, respectively. In particular, hyperglycemia provides immediate energy to muscles during a perceived crisis.2
In addition, prolonged exposure to living in quarantine can lead to feelings of isolation and estrangement – and excessive anxiety. Combined, those conditions may exert an indelible effect on the HPA axis – leading to a warped pattern of cortisol secretion with respect to baseline.3 (It has been noted in the literature that serum cortisol plays a protective role in thwarting off the effects of PTSD development. Consistent with this line of thinking, military personnel have been preemptively treated with high-dose cortisol during acute exposure.)
Prolonged exposure to psychosocial stressors also increases the overall risk of developing medical comorbidities. Patients who adopt maladaptive responses to traumatic events, for example, may experience dysregulation in eating behaviors and/or disordered sleep.4
In light of those realities, clinicians should explore the role of steroid therapy as a means of treating mental health patients experiencing psychological stress formation tied to ongoing quarantine conditions.
Challenges of neuroendocrine medications for COVID-19
COVID-19, caused by exposure to SARS-CoV-2, adeptly leverages the ACE2 receptor of the lungs as an entry point to evade the host’s defenses. It should be noted that the ACE2 protein is expressed on the cells of multiple organs of the body, including the adrenals, which are largely responsible for coordinating the stress response of the HPA axis.
Postmortem analysis from severe acute respiratory syndrome (SARS-CoV is also from the Coronaviridae family) patients indicates the presence of necrotic adrenal cells, further solidifying the association of the HPA axis to the COVID-19 disease state and pathophysiological course.5 Molecular mimicry of the adrenocorticotropic hormone allows SARS-CoV the ability to infiltrate the host’s defenses, in particular, the ability to mount a clinically apt cortisol stress response (e.g., hypocortisolism).As for those who survived the 2003 SARS outbreak, less than half of the patients have been observed to develop symptoms of frank hypocortisolism within a few months after exposure.
and an ongoing clinical trial is evaluating the safety and efficacy parameters of corticosteroids in COVID-19–exposed patients.
In addition, there is reason to believe that application of prophylactic steroids might affect the overall clinical course of COVID-19, thereby reducing mortality and morbidity rates in patients with severe presentation, such as septic shock. The rationale for this line of thought is based on the ability of glucocorticoids to suppress an ensuing cytokine storm by the virus in question.5,6 In clinical practice, steroids have been used to treat a host of viral diseases, including influenza, respiratory syncytial virus, and Middle East respiratory syndrome coronavirus.
Aside from the selective use of corticosteroids, the medication regimen may incorporate ACE inhibitors and/or angiotensin receptor blockers (ARBs) because of COVID-19’s ability to activate the renin-angiotensin-aldosterone system with respect to the physiological stress response.
The interplay of the HPA axis with the sympathoadrenal system is responsible for adaptive behaviors in the individual. Disrupted feedback loops from prolonged activation are associated with numerous stress-based conditions in mental illness, namely, PTSD, anxiety, and mood disorders. We are concerned about frontline health care workers, who are particularly prone to chronic stress and burnout because of the cumbersome patient load and equipment shortage that have characterized the coronavirus crisis.
Timely administration of corticosteroids on a case-by-case basis would keep the cytokines at bay by precluding their undue activation of the HPA axis and corresponding cascade stress response. Steroids are also known to restore disrupted feedback loops at the level of the immune cells. However, because of conflicting reports concerning viral clearance in some SARS and COVID-19 studies, treatment with steroids may be limited to select patient populations with the necessary dose adjustments. Ongoing clinical trials will further elucidate upon the applicability of steroids as well as the role of other neuroendocrine agents, such as ACE inhibitors or ARBs, in the treatment of COVID-19.
Behavioral manifestations and psychosocial health
As far as the stress response is concerned, an analysis performed by researchers in China after the COVID-19 outbreak found gender disparities in symptom expression. In the study (n = 1,210) the researchers found in female citizens a greater frequency of behavioral manifestations, including acute stress reaction, and symptoms of anxiety and mood disorders – namely, depression.7 Patient perception and awareness of the perils of coronavirus typically varied across the spectrum; some individuals reportedly undermined and devalued their risk of contracting COVID-19 – these patients may benefit from therapeutic modalities, such as cognitive-behavioral therapy (CBT), as a means of challenging their firmly entrenched cognitive distortions. CBT is an effective tool in addressing maladaptive coping responses, because these strategies tend to correspond with poor prognosis with respect to overall mental health. Aside from CBT, the clinician may advise other behavioral techniques, such as relaxation training, with the aim of controlling the symptoms of mood and anxiety disorders.
We often take for granted general pandemic safety precautions, such as maintaining physical distancing coupled with engaging in regular hand hygiene and wearing masks, but these actions also are known to alleviate mental anguish. Access to accurate and easy-to-consume health information regarding COVID-19 is also associated with psychological well-being during the quarantine.8
An intriguing “phenomenon” has emerged in the form of “panic buying.”However, researchers reported in the peer-reviewed journal Nature Human Behaviour that this pattern of behaviors is not typical for those under distress and represents an overstated misnomer of sorts. According to Jay J. Van Bavel, PhD, and associates, prevailing reports from news outlets have skewed the features of a panic. “News stories that employ the language of panic often create the very phenomena that they purport to condemn,” Dr. Van Bavel and associates wrote. “They can foster the very individualism and competitiveness that turn sensible preparations into dysfunctional stockpiling and undermine the sense of collective purpose which facilitates people supporting one another during an emergency.”9
The researchers proceeded to highlight the scope of effective crisis leadership with respect to establishing a sense of communal “self-efficacy and hope.” The influence of organized leadership serves to solidify the structure of the community as a whole, allowing group members the opportunity to address the stressors of interest. Such leadership may mitigate the stress response by fostering a necessary, healthy set for stress management.
Strategies aimed at supporting mental health
Coping and stress management strategies may include the process of building virtual networks (e.g., social media platforms) because physical distancing may contribute toward further isolation and social estrangement. However, it should be noted that ideally social media consumption should be centered upon interactive enrichment activities that provide a suitable substitute for the absence of physical support systems. The goal is to facilitate meaningful relationships and enduring communications that produce healthy and resilient mindsets.
In particular, individuals who possess adaptive mindsets with a realistic view of ongoing psychosocial stressors, be it from the impact of the pandemic or other influential events, are more likely to benefit when moving forward with life. In other words, the individual in question leverages these experiences as a means of “stress-related growth,” thereby enhancing the overall quality of relationships. Tentative studies in stress management have yielded promising support for interventions that aim to modulate mindsets (as a function of the stress response) by proper appraisal of the stress stimuli, according to Dr. Van Bavel and associates.
Employing assessment scales
To mitigate the stress response, clinicians need to use the relevant stress scales for assessing the full impact of distress brought on by COVID-19 and optimizing therapeutic modalities for those who need them most. Again, the stress response would vary, depending on the patient, and may include paranoia, xenophobia, compulsive ritualistic behavior, as well as full-fledged symptoms of acute stress disorder/PTSD.Steven Taylor, PhD, RPsych, and associates, part of a research team funded by the Canadian Institutes of Health Research and the University of Regina (Sask.), formulated their proprietary COVID Stress Scales (CSS) based on 36 items pertaining to individual anxiety and/or stress responses.10
As general purpose pandemic scales, the assessment tools will be transferable to similar outbreaks, and have been examined for validity and reliability. Additional validation scales include the Patient Health Questionnaire–4 for anxiety and depression, the Short Health Anxiety Inventory for anxiety (irrespective of physical condition), and the Marlowe-Crowne Social Desirability Scale–Short Form for psychological well-being based on the presence (or the lack thereof) of desirable characteristics.10 As a composite scale and predictive tool (especially with respect to future pandemics), the CSS allows clinicians a means of identifying the people who are most compliant with safety procedures, social distancing, hygiene expectations, and vaccine protocols – when applicable – reported Dr. Taylor and associates.
Moving forward: The next step in COVID-19 preparedness
As clinicians continue to develop guidelines that are befitting of COVID-19’s “new normal,” a holistic psychosocial framework will need to integrate the various psychometrics gathered from assessment scales, as well as understanding trauma, especially with respect to the HPA axis.
For starters, there is a certain element of “anticipatory anxiety” for those experiencing distress from COVID-19. A highly uncertain future with no immediate cure in the future, isolation and social estrangement, as well as financial setbacks, compound the situation. Moreover, the DSM fails to acknowledge other sources of traumatic experiences that are systemic in nature, such as discriminatory practices, injustice, and/or persecution.
It has also been noted that some distressed individuals experience a hypervigilant state that is comparable with PTSD.11 There may be a push to incorporate machine learning and other modalities to better identify those at risk (for example, health care professionals who perform their duties with limited resources, thereby inducing sleep dysregulation, anxiety, and hopelessness) for mental health deterioration. Interventions may need to be coordinated in a timely manner to disrupt the progression of acute stress disorder to PTSD. Peer support programs and resiliency training – successful therapeutic approaches for PTSD – may prove to have considerable utility for mitigating the overall stress response of COVID-19.12
References
1. “Red Cross offering online course to manage crisis-related stress.” ABC 6 News. kaaltv.com, 2020 Aug 29.
2. Islam FA, Choudhry C. J Psychiatry Psychiatric Disord 2017;1(5): 290-3.
3. Faravelli C et al. World J Psychiatry. 2012 Feb 22;2(1):13-25.
4. Carmassi C et al. Psychiatry Res. 2015 Jan 30;225(1-2):64-9.
5. Pal R. Endocrine. 2020 Apr 28. doi: 10.1007/s12020-020-02325-1.
6. Steenblock C et al. Mol Psychiatry. 2020 May. doi: 10.1038/s41380-020-0758-9.
7. Wang C et al. Int J Environ Res Public Health. 2020 Jan;17(5):1729.
8. Ho CS et al. Ann Acad Med Singap. 2020 Mar 16;49(3):155-60.
9. Van Bavel JJ et al. Nat Hum Behav. 2020 Apr 30. doi: 10.1038/s41562-020-0884-z.
10. Taylor S et al. J Anxiety Disord. 2020 May 4;72:102232.
11. Horesh D, Brown AD. Psychol Trauma. 2020 May;12(4):331-5.
12. Clark H et al. National Health Library and Knowledge Service/Evidence Team. Summary of Evidence: COVID-19, 2020 May 22. Version 2.0.
Dr. Faisal A. Islam is a medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Mohammed S. Islam is a research physician and extern at Interfaith Medical Center, New York. Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. Dr. Jolayemi is an attending psychiatrist at Interfaith Medical Center. No disclosures were reported.
Psychological First Aid is an innovative program launched by the American Red Cross with the goal of addressing issues of concern such as those stemming from COVID-19–related stress. According to Red Cross mental health volunteer representative Deb Butman-Perkins, the program provides “a general overview of what does stress look like, how do we feel it, how do we recognize it in our bodies ... physical, emotional, spiritual, physiological, where does all that stress occur?”1
The program brings a spotlight to the interdisciplinary nature of the stress response, especially with respect to the importance of developing the necessary coping skills during an ongoing crisis. However, to effectively evaluate and manage the overall stress response for psychiatric patients during quarantine conditions, as well as those who are formally diagnosed with COVID-19, clinicians also will need to revisit what we’ve learned about the hypothalamic-pituitary-adrenal (HPA) axis.
We know that the stress response – which varies somewhat across the spectrum – is necessary to ensure homeostatic regulation. A feedback loop is initiated at the receptor level, involving a myriad of hormones and chemical signals that bring forth the body’s “flight-or-fight” response. Hormones such as epinephrine/norepinephrine and cortisol are secreted by the HPA axis in reaction to the stress response, resulting in a spike in heart rate, blood pressure, and transient hyperglycemia, respectively. In particular, hyperglycemia provides immediate energy to muscles during a perceived crisis.2
In addition, prolonged exposure to living in quarantine can lead to feelings of isolation and estrangement – and excessive anxiety. Combined, those conditions may exert an indelible effect on the HPA axis – leading to a warped pattern of cortisol secretion with respect to baseline.3 (It has been noted in the literature that serum cortisol plays a protective role in thwarting off the effects of PTSD development. Consistent with this line of thinking, military personnel have been preemptively treated with high-dose cortisol during acute exposure.)
Prolonged exposure to psychosocial stressors also increases the overall risk of developing medical comorbidities. Patients who adopt maladaptive responses to traumatic events, for example, may experience dysregulation in eating behaviors and/or disordered sleep.4
In light of those realities, clinicians should explore the role of steroid therapy as a means of treating mental health patients experiencing psychological stress formation tied to ongoing quarantine conditions.
Challenges of neuroendocrine medications for COVID-19
COVID-19, caused by exposure to SARS-CoV-2, adeptly leverages the ACE2 receptor of the lungs as an entry point to evade the host’s defenses. It should be noted that the ACE2 protein is expressed on the cells of multiple organs of the body, including the adrenals, which are largely responsible for coordinating the stress response of the HPA axis.
Postmortem analysis from severe acute respiratory syndrome (SARS-CoV is also from the Coronaviridae family) patients indicates the presence of necrotic adrenal cells, further solidifying the association of the HPA axis to the COVID-19 disease state and pathophysiological course.5 Molecular mimicry of the adrenocorticotropic hormone allows SARS-CoV the ability to infiltrate the host’s defenses, in particular, the ability to mount a clinically apt cortisol stress response (e.g., hypocortisolism).As for those who survived the 2003 SARS outbreak, less than half of the patients have been observed to develop symptoms of frank hypocortisolism within a few months after exposure.
and an ongoing clinical trial is evaluating the safety and efficacy parameters of corticosteroids in COVID-19–exposed patients.
In addition, there is reason to believe that application of prophylactic steroids might affect the overall clinical course of COVID-19, thereby reducing mortality and morbidity rates in patients with severe presentation, such as septic shock. The rationale for this line of thought is based on the ability of glucocorticoids to suppress an ensuing cytokine storm by the virus in question.5,6 In clinical practice, steroids have been used to treat a host of viral diseases, including influenza, respiratory syncytial virus, and Middle East respiratory syndrome coronavirus.
Aside from the selective use of corticosteroids, the medication regimen may incorporate ACE inhibitors and/or angiotensin receptor blockers (ARBs) because of COVID-19’s ability to activate the renin-angiotensin-aldosterone system with respect to the physiological stress response.
The interplay of the HPA axis with the sympathoadrenal system is responsible for adaptive behaviors in the individual. Disrupted feedback loops from prolonged activation are associated with numerous stress-based conditions in mental illness, namely, PTSD, anxiety, and mood disorders. We are concerned about frontline health care workers, who are particularly prone to chronic stress and burnout because of the cumbersome patient load and equipment shortage that have characterized the coronavirus crisis.
Timely administration of corticosteroids on a case-by-case basis would keep the cytokines at bay by precluding their undue activation of the HPA axis and corresponding cascade stress response. Steroids are also known to restore disrupted feedback loops at the level of the immune cells. However, because of conflicting reports concerning viral clearance in some SARS and COVID-19 studies, treatment with steroids may be limited to select patient populations with the necessary dose adjustments. Ongoing clinical trials will further elucidate upon the applicability of steroids as well as the role of other neuroendocrine agents, such as ACE inhibitors or ARBs, in the treatment of COVID-19.
Behavioral manifestations and psychosocial health
As far as the stress response is concerned, an analysis performed by researchers in China after the COVID-19 outbreak found gender disparities in symptom expression. In the study (n = 1,210) the researchers found in female citizens a greater frequency of behavioral manifestations, including acute stress reaction, and symptoms of anxiety and mood disorders – namely, depression.7 Patient perception and awareness of the perils of coronavirus typically varied across the spectrum; some individuals reportedly undermined and devalued their risk of contracting COVID-19 – these patients may benefit from therapeutic modalities, such as cognitive-behavioral therapy (CBT), as a means of challenging their firmly entrenched cognitive distortions. CBT is an effective tool in addressing maladaptive coping responses, because these strategies tend to correspond with poor prognosis with respect to overall mental health. Aside from CBT, the clinician may advise other behavioral techniques, such as relaxation training, with the aim of controlling the symptoms of mood and anxiety disorders.
We often take for granted general pandemic safety precautions, such as maintaining physical distancing coupled with engaging in regular hand hygiene and wearing masks, but these actions also are known to alleviate mental anguish. Access to accurate and easy-to-consume health information regarding COVID-19 is also associated with psychological well-being during the quarantine.8
An intriguing “phenomenon” has emerged in the form of “panic buying.”However, researchers reported in the peer-reviewed journal Nature Human Behaviour that this pattern of behaviors is not typical for those under distress and represents an overstated misnomer of sorts. According to Jay J. Van Bavel, PhD, and associates, prevailing reports from news outlets have skewed the features of a panic. “News stories that employ the language of panic often create the very phenomena that they purport to condemn,” Dr. Van Bavel and associates wrote. “They can foster the very individualism and competitiveness that turn sensible preparations into dysfunctional stockpiling and undermine the sense of collective purpose which facilitates people supporting one another during an emergency.”9
The researchers proceeded to highlight the scope of effective crisis leadership with respect to establishing a sense of communal “self-efficacy and hope.” The influence of organized leadership serves to solidify the structure of the community as a whole, allowing group members the opportunity to address the stressors of interest. Such leadership may mitigate the stress response by fostering a necessary, healthy set for stress management.
Strategies aimed at supporting mental health
Coping and stress management strategies may include the process of building virtual networks (e.g., social media platforms) because physical distancing may contribute toward further isolation and social estrangement. However, it should be noted that ideally social media consumption should be centered upon interactive enrichment activities that provide a suitable substitute for the absence of physical support systems. The goal is to facilitate meaningful relationships and enduring communications that produce healthy and resilient mindsets.
In particular, individuals who possess adaptive mindsets with a realistic view of ongoing psychosocial stressors, be it from the impact of the pandemic or other influential events, are more likely to benefit when moving forward with life. In other words, the individual in question leverages these experiences as a means of “stress-related growth,” thereby enhancing the overall quality of relationships. Tentative studies in stress management have yielded promising support for interventions that aim to modulate mindsets (as a function of the stress response) by proper appraisal of the stress stimuli, according to Dr. Van Bavel and associates.
Employing assessment scales
To mitigate the stress response, clinicians need to use the relevant stress scales for assessing the full impact of distress brought on by COVID-19 and optimizing therapeutic modalities for those who need them most. Again, the stress response would vary, depending on the patient, and may include paranoia, xenophobia, compulsive ritualistic behavior, as well as full-fledged symptoms of acute stress disorder/PTSD.Steven Taylor, PhD, RPsych, and associates, part of a research team funded by the Canadian Institutes of Health Research and the University of Regina (Sask.), formulated their proprietary COVID Stress Scales (CSS) based on 36 items pertaining to individual anxiety and/or stress responses.10
As general purpose pandemic scales, the assessment tools will be transferable to similar outbreaks, and have been examined for validity and reliability. Additional validation scales include the Patient Health Questionnaire–4 for anxiety and depression, the Short Health Anxiety Inventory for anxiety (irrespective of physical condition), and the Marlowe-Crowne Social Desirability Scale–Short Form for psychological well-being based on the presence (or the lack thereof) of desirable characteristics.10 As a composite scale and predictive tool (especially with respect to future pandemics), the CSS allows clinicians a means of identifying the people who are most compliant with safety procedures, social distancing, hygiene expectations, and vaccine protocols – when applicable – reported Dr. Taylor and associates.
Moving forward: The next step in COVID-19 preparedness
As clinicians continue to develop guidelines that are befitting of COVID-19’s “new normal,” a holistic psychosocial framework will need to integrate the various psychometrics gathered from assessment scales, as well as understanding trauma, especially with respect to the HPA axis.
For starters, there is a certain element of “anticipatory anxiety” for those experiencing distress from COVID-19. A highly uncertain future with no immediate cure in the future, isolation and social estrangement, as well as financial setbacks, compound the situation. Moreover, the DSM fails to acknowledge other sources of traumatic experiences that are systemic in nature, such as discriminatory practices, injustice, and/or persecution.
It has also been noted that some distressed individuals experience a hypervigilant state that is comparable with PTSD.11 There may be a push to incorporate machine learning and other modalities to better identify those at risk (for example, health care professionals who perform their duties with limited resources, thereby inducing sleep dysregulation, anxiety, and hopelessness) for mental health deterioration. Interventions may need to be coordinated in a timely manner to disrupt the progression of acute stress disorder to PTSD. Peer support programs and resiliency training – successful therapeutic approaches for PTSD – may prove to have considerable utility for mitigating the overall stress response of COVID-19.12
References
1. “Red Cross offering online course to manage crisis-related stress.” ABC 6 News. kaaltv.com, 2020 Aug 29.
2. Islam FA, Choudhry C. J Psychiatry Psychiatric Disord 2017;1(5): 290-3.
3. Faravelli C et al. World J Psychiatry. 2012 Feb 22;2(1):13-25.
4. Carmassi C et al. Psychiatry Res. 2015 Jan 30;225(1-2):64-9.
5. Pal R. Endocrine. 2020 Apr 28. doi: 10.1007/s12020-020-02325-1.
6. Steenblock C et al. Mol Psychiatry. 2020 May. doi: 10.1038/s41380-020-0758-9.
7. Wang C et al. Int J Environ Res Public Health. 2020 Jan;17(5):1729.
8. Ho CS et al. Ann Acad Med Singap. 2020 Mar 16;49(3):155-60.
9. Van Bavel JJ et al. Nat Hum Behav. 2020 Apr 30. doi: 10.1038/s41562-020-0884-z.
10. Taylor S et al. J Anxiety Disord. 2020 May 4;72:102232.
11. Horesh D, Brown AD. Psychol Trauma. 2020 May;12(4):331-5.
12. Clark H et al. National Health Library and Knowledge Service/Evidence Team. Summary of Evidence: COVID-19, 2020 May 22. Version 2.0.
Dr. Faisal A. Islam is a medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Mohammed S. Islam is a research physician and extern at Interfaith Medical Center, New York. Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. Dr. Jolayemi is an attending psychiatrist at Interfaith Medical Center. No disclosures were reported.
Obsessions or psychosis?
CASE Perseverating on nonexistent sexual assaults
Mr. R, age 17, who has been diagnosed with obsessive-compulsive disorder (OCD), presents to the emergency department (ED) because he thinks that he is being sexually assaulted and is concerned that he is sexually assaulting other people. His family reports that Mr. R has perseverated over these thoughts for months, although there is no evidence to suggest these events have occurred. In order to ameliorate his distress, he performs rituals of looking upwards and repeatedly saying, “It didn’t happen.”
Mr. R is admitted to the inpatient psychiatry unit for further evaluation.
HISTORY Decompensation while attending a PHP
Mr. R had been diagnosed with bipolar disorder and attention-deficit/hyperactivity disorder when he was 13. During that time, he was treated with divalproex sodium and dextroamphetamine. At age 15, Mr. R’s diagnosis was changed to OCD. Seven months before coming to the ED, his symptoms had been getting worse. On one occasion, Mr. R was talking in a nonsensical fashion at school, and the police were called. Mr. R became physically aggressive with the police and was subsequently hospitalized, after which he attended a partial hospitalization program (PHP). At the PHP, Mr. R received exposure and response prevention therapy for OCD, but did not improve, and his symptoms deteriorated until he was unable to brush his teeth or shower regularly. While attending the PHP, Mr. R also developed disorganized speech. The PHP clinicians became concerned that Mr. R’s symptoms may have been prodromal symptoms of schizophrenia because he did not respond to the OCD treatment and his symptoms had worsened over the 3 months he attended the PHP.
EVALUATION Normal laboratory results
Upon admission to the inpatient psychiatric unit, Mr. R is restarted on his home medications, which include
His laboratory workup, including a complete blood count, comprehensive metabolic panel, urine drug screen, and blood ethanol, are all within normal limits. Previous laboratory results, including a thyroid function panel, vitamin D level, and various autoimmune panels, were also within normal limits.
His family reports that Mr. R’s symptoms seem to worsen when he is under increased stress from school and prepping for standardized college admission examinations. The family also says that while he is playing tennis, Mr. R will posture himself in a crouched down position and at times will remain in this position for 30 minutes.
Mr. R says he eventually wants to go to college and have a professional career.
[polldaddy:10600530]
Continue to: The authors' observations
The authors’ observations
When considering Mr. R’s diagnosis, our treatment team considered the possibility of OCD with absent insight/delusional beliefs, OCD with comorbid schizophrenia, bipolar disorder, and psychotic disorder due to another medical condition.
Overlap between OCD and schizophrenia
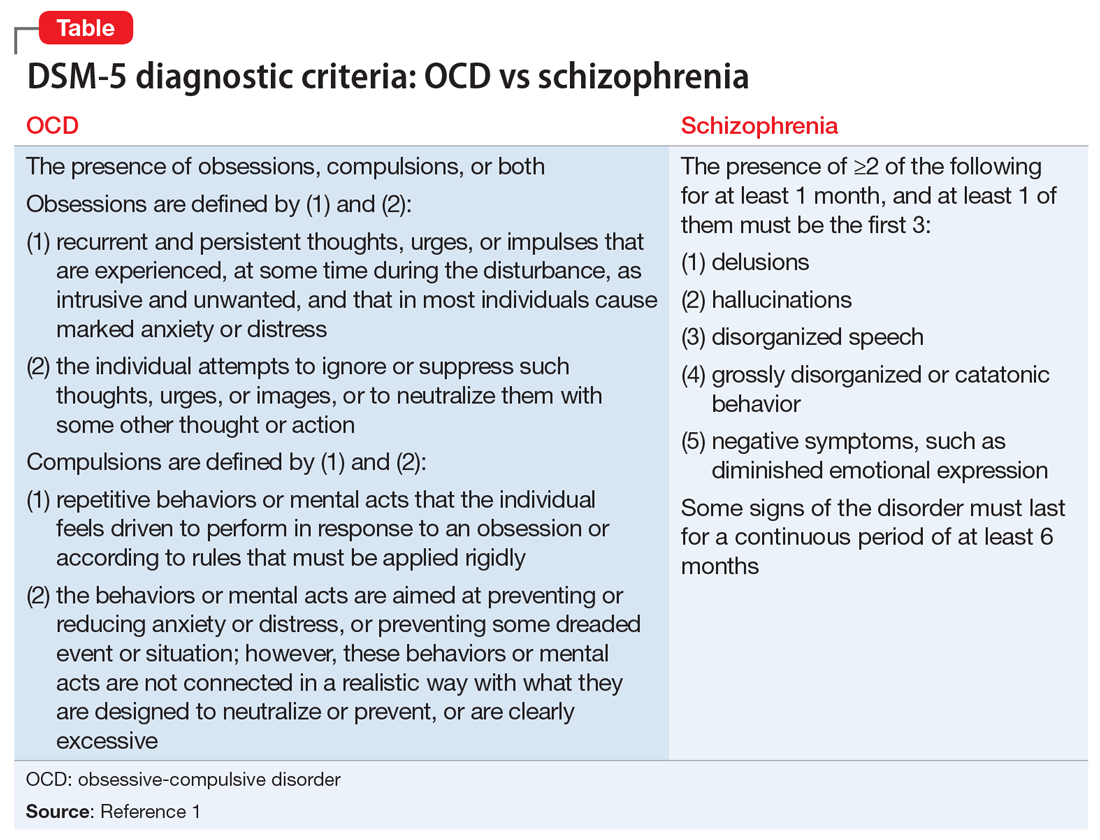
Much of the literature about OCD examines its functional impairment in adults, with findings extrapolated to pediatric patients. Children differ from adults in a variety of meaningful ways. Baytunca et al4 examined adolescents with early-onset schizophrenia, with and without comorbid OCD. Patients with comorbid OCD required higher doses of antipsychotic medication to treat acute psychotic symptoms and maintain a reduction in symptoms. The study controlled for the severity of schizophrenia, and its findings suggest that schizophrenia with comorbid OCD is more treatment-resistant than schizophrenia alone.4
Some researchers have theorized that in adolescents, OCD and psychosis are integrally related such that one disorder could represent a prodrome or a cause of the other disorder. Niendam et al5 studied OCS in the psychosis prodrome. They found that OCS can present as a part of the prodromal picture in youth at high risk for psychosis. However, because none of the patients experiencing OCS converted to full-blown psychosis, these results suggest that OCS may not represent a prodrome to psychosis per se. Instead, these individuals may represent a subset of false positives over the follow-up period.5 Another possible explanation for the increased emergence of pre-psychotic symptoms in adolescents with OCD could be a difference in their threshold of perception. OCS compels adolescents with OCD to self-analyze more critically and frequently. As a result, these patients may more often report depressive symptoms, distress, and exacerbations of pre-psychotic symptoms. These findings highlight that
[polldaddy:10600532]
Continue to: TREATMENT Improvement after switching to haloperidol
TREATMENT Improvement after switching to haloperidol
The treatment team decides to change Mr. R’s medications by cross-titrating risperidone to
The treatment team obtains a consultation on whether electroconvulsive therapy would be appropriate, but this treatment is not recommended. Instead, the team considers
Throughout admission, Mr. R focuses on his lack of improvement and how this episode is negatively impacting his grades and his dream of going to college and having a professional career.
OUTCOME Relief at last
Mr. R improves with the addition of sertraline and tolerates rapid titration well. He continues haloperidol without adverse effects, and is discharged home with close follow-up in a PHP and outpatient psychiatry.
However, after discharge, Mr. R’s symptoms get worse, and he is admitted to a different inpatient facility. At this facility, he continues sertraline, but haloperidol is cross-titrated to
Continue to: Currently...
Currently, Mr. R has greatly improved and is able to function in school. He takes sertraline, 100 mg twice a day, and olanzapine, 7.5 mg twice a day. Mr. R reports his rituals have reduced in frequency to less than 15 minutes each day. His thought processes are organized, and he is confident he will be able to achieve his goals.
The authors’ observations
Given Mr. R’s rapid improvement once an effective pharmacologic regimen was established, we concluded that he had a severe case of OCD with absent insight/delusional beliefs, and that he did not have schizophrenia. Mr. R’s case highlights how a psychiatric diagnosis can produce anxiety as a result of the psychosocial stressors and limitations associated with that diagnosis.
Bottom Line
There is both an epidemiologic and biologic overlap between obsessive-compulsive disorder and schizophrenia. In adolescents, either disorder could represent a prodrome or a cause of the other. It is essential to perform a thorough assessment of individuals with obsessive-compulsive disorder because these patients may exhibit subtle psychotic symptoms.
Related Resources
- Cunill R, Castells X, Simeon D. Relationships between obsessivecompulsive symptomatology and severity of psychosis in schizophrenia: a systematic review and meta-analysis. J Clin Psychiatry. 2009;70(1):70-82.
- Harris E, Delgado SV. Treatment-resistant OCD: there’s more we can do. Current Psychiatry. 2018;17(11):10-12,14-18,51.
Drug Brand Names
Clozapine • Clozaril
Dextroamphetamine • Dexedrine
Divalproex sodium • Depakote
Fluvoxamine • Luvox
Haloperidol • Haldol
Hydroxyzine • Atarax, Vistaril
Lurasidone • Latuda
Olanzapine • Zyprexa
Risperidone • Risperdal
Sertraline • Zoloft
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Schirmbeck F, Swets M, de Haan L. Obsessive-compulsive symptoms in schizophrenia. In: De Haan L, Schirmbeck F, Zink M. Epidemiology: prevalence and clinical characteristics of obsessive-compulsive disorder and obsessive-compulsive symptoms in patients with psychotic disorders. New York, NY: Springer International Publishing; 2015:47-61.
3. de Haan L, Sterk B, Wouters L, et al. The 5-year course of obsessive-compulsive symptoms and obsessive-compulsive disorder in first-episode schizophrenia and related disorders. Schizophr Bull. 2011;39(1):151-160.
4. Baytunca B, Kalyoncu T, Ozel I, et al. Early onset schizophrenia associated with obsessive-compulsive disorder: clinical features and correlates. Clin Neuropharmacol. 2017;40(6):243-245.
5. Niendam TA, Berzak J, Cannon TD, et al. Obsessive compulsive symptoms in the psychosis prodrome: correlates of clinical and functional outcome. Schizophr Res. 2009;108(1-3):170-175.
CASE Perseverating on nonexistent sexual assaults
Mr. R, age 17, who has been diagnosed with obsessive-compulsive disorder (OCD), presents to the emergency department (ED) because he thinks that he is being sexually assaulted and is concerned that he is sexually assaulting other people. His family reports that Mr. R has perseverated over these thoughts for months, although there is no evidence to suggest these events have occurred. In order to ameliorate his distress, he performs rituals of looking upwards and repeatedly saying, “It didn’t happen.”
Mr. R is admitted to the inpatient psychiatry unit for further evaluation.
HISTORY Decompensation while attending a PHP
Mr. R had been diagnosed with bipolar disorder and attention-deficit/hyperactivity disorder when he was 13. During that time, he was treated with divalproex sodium and dextroamphetamine. At age 15, Mr. R’s diagnosis was changed to OCD. Seven months before coming to the ED, his symptoms had been getting worse. On one occasion, Mr. R was talking in a nonsensical fashion at school, and the police were called. Mr. R became physically aggressive with the police and was subsequently hospitalized, after which he attended a partial hospitalization program (PHP). At the PHP, Mr. R received exposure and response prevention therapy for OCD, but did not improve, and his symptoms deteriorated until he was unable to brush his teeth or shower regularly. While attending the PHP, Mr. R also developed disorganized speech. The PHP clinicians became concerned that Mr. R’s symptoms may have been prodromal symptoms of schizophrenia because he did not respond to the OCD treatment and his symptoms had worsened over the 3 months he attended the PHP.
EVALUATION Normal laboratory results
Upon admission to the inpatient psychiatric unit, Mr. R is restarted on his home medications, which include
His laboratory workup, including a complete blood count, comprehensive metabolic panel, urine drug screen, and blood ethanol, are all within normal limits. Previous laboratory results, including a thyroid function panel, vitamin D level, and various autoimmune panels, were also within normal limits.
His family reports that Mr. R’s symptoms seem to worsen when he is under increased stress from school and prepping for standardized college admission examinations. The family also says that while he is playing tennis, Mr. R will posture himself in a crouched down position and at times will remain in this position for 30 minutes.
Mr. R says he eventually wants to go to college and have a professional career.
[polldaddy:10600530]
Continue to: The authors' observations
The authors’ observations
When considering Mr. R’s diagnosis, our treatment team considered the possibility of OCD with absent insight/delusional beliefs, OCD with comorbid schizophrenia, bipolar disorder, and psychotic disorder due to another medical condition.
Overlap between OCD and schizophrenia
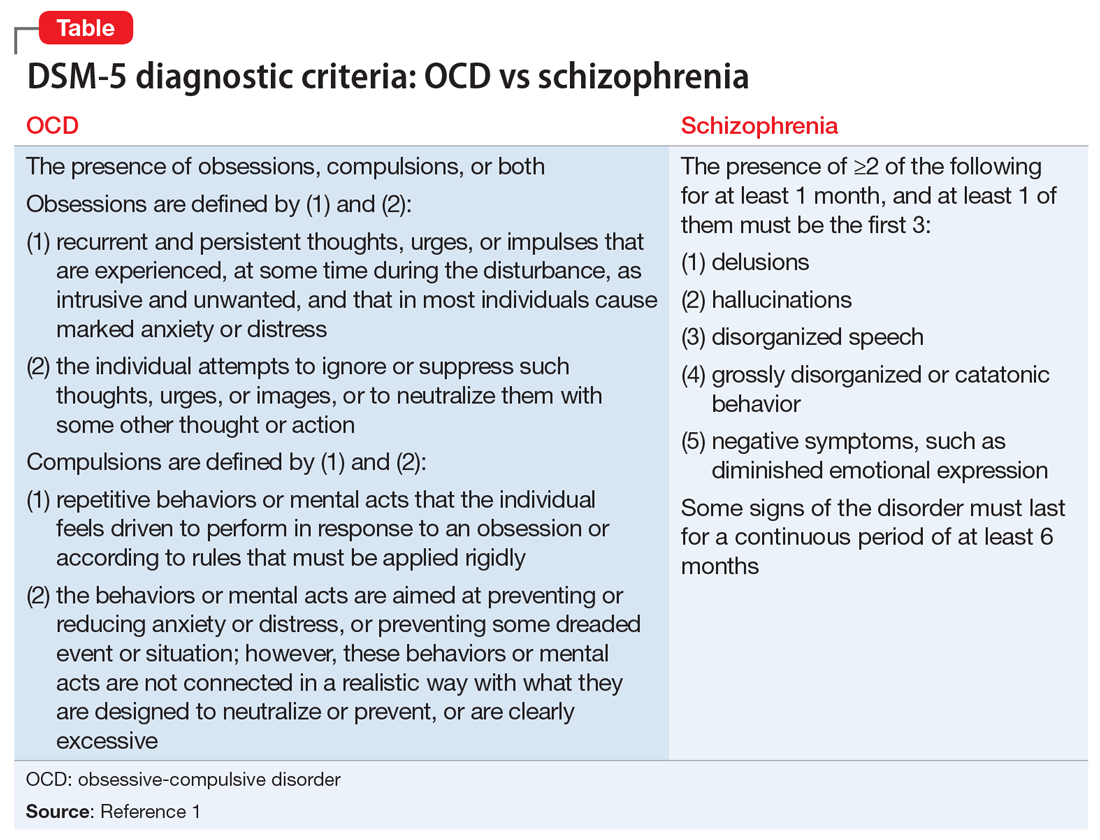
Much of the literature about OCD examines its functional impairment in adults, with findings extrapolated to pediatric patients. Children differ from adults in a variety of meaningful ways. Baytunca et al4 examined adolescents with early-onset schizophrenia, with and without comorbid OCD. Patients with comorbid OCD required higher doses of antipsychotic medication to treat acute psychotic symptoms and maintain a reduction in symptoms. The study controlled for the severity of schizophrenia, and its findings suggest that schizophrenia with comorbid OCD is more treatment-resistant than schizophrenia alone.4
Some researchers have theorized that in adolescents, OCD and psychosis are integrally related such that one disorder could represent a prodrome or a cause of the other disorder. Niendam et al5 studied OCS in the psychosis prodrome. They found that OCS can present as a part of the prodromal picture in youth at high risk for psychosis. However, because none of the patients experiencing OCS converted to full-blown psychosis, these results suggest that OCS may not represent a prodrome to psychosis per se. Instead, these individuals may represent a subset of false positives over the follow-up period.5 Another possible explanation for the increased emergence of pre-psychotic symptoms in adolescents with OCD could be a difference in their threshold of perception. OCS compels adolescents with OCD to self-analyze more critically and frequently. As a result, these patients may more often report depressive symptoms, distress, and exacerbations of pre-psychotic symptoms. These findings highlight that
[polldaddy:10600532]
Continue to: TREATMENT Improvement after switching to haloperidol
TREATMENT Improvement after switching to haloperidol
The treatment team decides to change Mr. R’s medications by cross-titrating risperidone to
The treatment team obtains a consultation on whether electroconvulsive therapy would be appropriate, but this treatment is not recommended. Instead, the team considers
Throughout admission, Mr. R focuses on his lack of improvement and how this episode is negatively impacting his grades and his dream of going to college and having a professional career.
OUTCOME Relief at last
Mr. R improves with the addition of sertraline and tolerates rapid titration well. He continues haloperidol without adverse effects, and is discharged home with close follow-up in a PHP and outpatient psychiatry.
However, after discharge, Mr. R’s symptoms get worse, and he is admitted to a different inpatient facility. At this facility, he continues sertraline, but haloperidol is cross-titrated to
Continue to: Currently...
Currently, Mr. R has greatly improved and is able to function in school. He takes sertraline, 100 mg twice a day, and olanzapine, 7.5 mg twice a day. Mr. R reports his rituals have reduced in frequency to less than 15 minutes each day. His thought processes are organized, and he is confident he will be able to achieve his goals.
The authors’ observations
Given Mr. R’s rapid improvement once an effective pharmacologic regimen was established, we concluded that he had a severe case of OCD with absent insight/delusional beliefs, and that he did not have schizophrenia. Mr. R’s case highlights how a psychiatric diagnosis can produce anxiety as a result of the psychosocial stressors and limitations associated with that diagnosis.
Bottom Line
There is both an epidemiologic and biologic overlap between obsessive-compulsive disorder and schizophrenia. In adolescents, either disorder could represent a prodrome or a cause of the other. It is essential to perform a thorough assessment of individuals with obsessive-compulsive disorder because these patients may exhibit subtle psychotic symptoms.
Related Resources
- Cunill R, Castells X, Simeon D. Relationships between obsessivecompulsive symptomatology and severity of psychosis in schizophrenia: a systematic review and meta-analysis. J Clin Psychiatry. 2009;70(1):70-82.
- Harris E, Delgado SV. Treatment-resistant OCD: there’s more we can do. Current Psychiatry. 2018;17(11):10-12,14-18,51.
Drug Brand Names
Clozapine • Clozaril
Dextroamphetamine • Dexedrine
Divalproex sodium • Depakote
Fluvoxamine • Luvox
Haloperidol • Haldol
Hydroxyzine • Atarax, Vistaril
Lurasidone • Latuda
Olanzapine • Zyprexa
Risperidone • Risperdal
Sertraline • Zoloft
CASE Perseverating on nonexistent sexual assaults
Mr. R, age 17, who has been diagnosed with obsessive-compulsive disorder (OCD), presents to the emergency department (ED) because he thinks that he is being sexually assaulted and is concerned that he is sexually assaulting other people. His family reports that Mr. R has perseverated over these thoughts for months, although there is no evidence to suggest these events have occurred. In order to ameliorate his distress, he performs rituals of looking upwards and repeatedly saying, “It didn’t happen.”
Mr. R is admitted to the inpatient psychiatry unit for further evaluation.
HISTORY Decompensation while attending a PHP
Mr. R had been diagnosed with bipolar disorder and attention-deficit/hyperactivity disorder when he was 13. During that time, he was treated with divalproex sodium and dextroamphetamine. At age 15, Mr. R’s diagnosis was changed to OCD. Seven months before coming to the ED, his symptoms had been getting worse. On one occasion, Mr. R was talking in a nonsensical fashion at school, and the police were called. Mr. R became physically aggressive with the police and was subsequently hospitalized, after which he attended a partial hospitalization program (PHP). At the PHP, Mr. R received exposure and response prevention therapy for OCD, but did not improve, and his symptoms deteriorated until he was unable to brush his teeth or shower regularly. While attending the PHP, Mr. R also developed disorganized speech. The PHP clinicians became concerned that Mr. R’s symptoms may have been prodromal symptoms of schizophrenia because he did not respond to the OCD treatment and his symptoms had worsened over the 3 months he attended the PHP.
EVALUATION Normal laboratory results
Upon admission to the inpatient psychiatric unit, Mr. R is restarted on his home medications, which include
His laboratory workup, including a complete blood count, comprehensive metabolic panel, urine drug screen, and blood ethanol, are all within normal limits. Previous laboratory results, including a thyroid function panel, vitamin D level, and various autoimmune panels, were also within normal limits.
His family reports that Mr. R’s symptoms seem to worsen when he is under increased stress from school and prepping for standardized college admission examinations. The family also says that while he is playing tennis, Mr. R will posture himself in a crouched down position and at times will remain in this position for 30 minutes.
Mr. R says he eventually wants to go to college and have a professional career.
[polldaddy:10600530]
Continue to: The authors' observations
The authors’ observations
When considering Mr. R’s diagnosis, our treatment team considered the possibility of OCD with absent insight/delusional beliefs, OCD with comorbid schizophrenia, bipolar disorder, and psychotic disorder due to another medical condition.
Overlap between OCD and schizophrenia
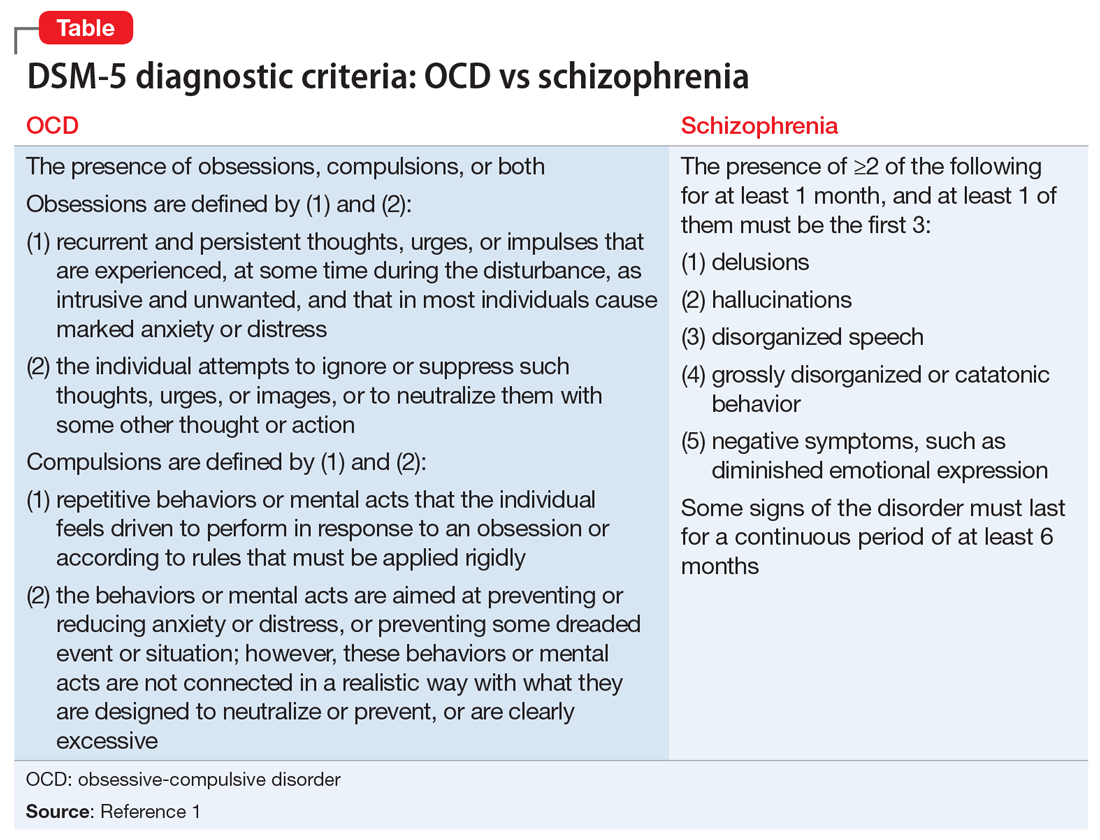
Much of the literature about OCD examines its functional impairment in adults, with findings extrapolated to pediatric patients. Children differ from adults in a variety of meaningful ways. Baytunca et al4 examined adolescents with early-onset schizophrenia, with and without comorbid OCD. Patients with comorbid OCD required higher doses of antipsychotic medication to treat acute psychotic symptoms and maintain a reduction in symptoms. The study controlled for the severity of schizophrenia, and its findings suggest that schizophrenia with comorbid OCD is more treatment-resistant than schizophrenia alone.4
Some researchers have theorized that in adolescents, OCD and psychosis are integrally related such that one disorder could represent a prodrome or a cause of the other disorder. Niendam et al5 studied OCS in the psychosis prodrome. They found that OCS can present as a part of the prodromal picture in youth at high risk for psychosis. However, because none of the patients experiencing OCS converted to full-blown psychosis, these results suggest that OCS may not represent a prodrome to psychosis per se. Instead, these individuals may represent a subset of false positives over the follow-up period.5 Another possible explanation for the increased emergence of pre-psychotic symptoms in adolescents with OCD could be a difference in their threshold of perception. OCS compels adolescents with OCD to self-analyze more critically and frequently. As a result, these patients may more often report depressive symptoms, distress, and exacerbations of pre-psychotic symptoms. These findings highlight that
[polldaddy:10600532]
Continue to: TREATMENT Improvement after switching to haloperidol
TREATMENT Improvement after switching to haloperidol
The treatment team decides to change Mr. R’s medications by cross-titrating risperidone to
The treatment team obtains a consultation on whether electroconvulsive therapy would be appropriate, but this treatment is not recommended. Instead, the team considers
Throughout admission, Mr. R focuses on his lack of improvement and how this episode is negatively impacting his grades and his dream of going to college and having a professional career.
OUTCOME Relief at last
Mr. R improves with the addition of sertraline and tolerates rapid titration well. He continues haloperidol without adverse effects, and is discharged home with close follow-up in a PHP and outpatient psychiatry.
However, after discharge, Mr. R’s symptoms get worse, and he is admitted to a different inpatient facility. At this facility, he continues sertraline, but haloperidol is cross-titrated to
Continue to: Currently...
Currently, Mr. R has greatly improved and is able to function in school. He takes sertraline, 100 mg twice a day, and olanzapine, 7.5 mg twice a day. Mr. R reports his rituals have reduced in frequency to less than 15 minutes each day. His thought processes are organized, and he is confident he will be able to achieve his goals.
The authors’ observations
Given Mr. R’s rapid improvement once an effective pharmacologic regimen was established, we concluded that he had a severe case of OCD with absent insight/delusional beliefs, and that he did not have schizophrenia. Mr. R’s case highlights how a psychiatric diagnosis can produce anxiety as a result of the psychosocial stressors and limitations associated with that diagnosis.
Bottom Line
There is both an epidemiologic and biologic overlap between obsessive-compulsive disorder and schizophrenia. In adolescents, either disorder could represent a prodrome or a cause of the other. It is essential to perform a thorough assessment of individuals with obsessive-compulsive disorder because these patients may exhibit subtle psychotic symptoms.
Related Resources
- Cunill R, Castells X, Simeon D. Relationships between obsessivecompulsive symptomatology and severity of psychosis in schizophrenia: a systematic review and meta-analysis. J Clin Psychiatry. 2009;70(1):70-82.
- Harris E, Delgado SV. Treatment-resistant OCD: there’s more we can do. Current Psychiatry. 2018;17(11):10-12,14-18,51.
Drug Brand Names
Clozapine • Clozaril
Dextroamphetamine • Dexedrine
Divalproex sodium • Depakote
Fluvoxamine • Luvox
Haloperidol • Haldol
Hydroxyzine • Atarax, Vistaril
Lurasidone • Latuda
Olanzapine • Zyprexa
Risperidone • Risperdal
Sertraline • Zoloft
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Schirmbeck F, Swets M, de Haan L. Obsessive-compulsive symptoms in schizophrenia. In: De Haan L, Schirmbeck F, Zink M. Epidemiology: prevalence and clinical characteristics of obsessive-compulsive disorder and obsessive-compulsive symptoms in patients with psychotic disorders. New York, NY: Springer International Publishing; 2015:47-61.
3. de Haan L, Sterk B, Wouters L, et al. The 5-year course of obsessive-compulsive symptoms and obsessive-compulsive disorder in first-episode schizophrenia and related disorders. Schizophr Bull. 2011;39(1):151-160.
4. Baytunca B, Kalyoncu T, Ozel I, et al. Early onset schizophrenia associated with obsessive-compulsive disorder: clinical features and correlates. Clin Neuropharmacol. 2017;40(6):243-245.
5. Niendam TA, Berzak J, Cannon TD, et al. Obsessive compulsive symptoms in the psychosis prodrome: correlates of clinical and functional outcome. Schizophr Res. 2009;108(1-3):170-175.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Schirmbeck F, Swets M, de Haan L. Obsessive-compulsive symptoms in schizophrenia. In: De Haan L, Schirmbeck F, Zink M. Epidemiology: prevalence and clinical characteristics of obsessive-compulsive disorder and obsessive-compulsive symptoms in patients with psychotic disorders. New York, NY: Springer International Publishing; 2015:47-61.
3. de Haan L, Sterk B, Wouters L, et al. The 5-year course of obsessive-compulsive symptoms and obsessive-compulsive disorder in first-episode schizophrenia and related disorders. Schizophr Bull. 2011;39(1):151-160.
4. Baytunca B, Kalyoncu T, Ozel I, et al. Early onset schizophrenia associated with obsessive-compulsive disorder: clinical features and correlates. Clin Neuropharmacol. 2017;40(6):243-245.
5. Niendam TA, Berzak J, Cannon TD, et al. Obsessive compulsive symptoms in the psychosis prodrome: correlates of clinical and functional outcome. Schizophr Res. 2009;108(1-3):170-175.
Why are many of my patients doing better during the pandemic?
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
New guidance to help manage OCD during COVID-19
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.