User login
UPDATE ON OBSTETRICS
The authors report no financial relationships relevant to this article.
If there have been overriding themes in obstetrics over the past year, they have been “more,” “sooner,” “faster,” “safer.” Advances in our field have thrilled our scientific curiosity and increased our ability to alleviate suffering—but at what cost? And who will pay that cost?
In this Update, we focus on recent advances in prenatal diagnosis and fetal therapy, as well as the ever-encroaching economic barriers that may limit our ability to get what we want. In particular, we will discuss:
- two technologies in prenatal genetics: noninvasive aneuploidy testing using cell-free DNA and prenatal microarray analysis
- open fetal surgery to reduce mortality and improve the function and quality of life for fetuses with open neural tube defects
- the value and probable impact of bundled payments—that is, one payment for multiple services grouped into one “episode.”
Two noninvasive approaches to prenatal diagnosis offer promise—but practicality and cost are uncertain
Ashoor G, Syngelaki RM, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
Reddy UM, Page GP, Saade GR, et al. Karyotype versus microarray testing for genetic abnormalities after stillbirth. N Engl J Med. 2012;367(23):2185–2193.
Talkowski ME, Ordulu Z, Pillalamarri V, et al. Clinical diagnosis by whole-genome sequencing of a prenatal sample. N Engl J Med. 2012;367(23):2226–2232.
Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367(23):2175–2184.
Genetic screening and testing are a standard part of prenatal care in most developed countries. We have come a long way since a maternal age of 35 years was the only variable separating patients into low- and high-risk categories. This year, two technologies have emerged that may change forever the way we approach prenatal genetics:
One argument for using more accurate genetic screening methods: They limit the number of invasive tests that are needed. Chorionic villus sampling (CVS) and amniocentesis, even when performed by the most experienced of operators, pose a small but real risk of fetal injury and pregnancy loss.
Noninvasive aneuploidy diagnosis is now a reality in high-risk population screening
The holy grail of aneuploidy diagnosis would be a noninvasive way to sample fetal cells. Although we have known for decades that fetal cells enter the maternal circulation, it has been impractical to use them for aneuploidy testing because of their scarcity and longevity. In the 1990s, however, cell-free fetal DNA (cffDNA), a compound of DNA fragments of uncertain origin, was identified in maternal plasma. CffDNA is more plentiful than fetal cells. It also disappears within hours of delivery, demonstrating that it is specific to the current pregnancy.
CffDNA is already used in fetal Rh typing and gender determination in disorders such as congenital adrenal hyperplasia. Several studies in high-risk populations have demonstrated high sensitivity and specificity for the detection of Trisomies 21, 18, and 13. Several commercial tests are now available, although neither their accuracy nor their cost has been determined for use in low-risk population screening, compared with traditional testing.
Microarray analysis, paired with karyotyping, can elucidate ultrasound-identified fetal anomalies
Cytogenetic microarray analysis is also being explored in the prenatal period. Microarray analysis is currently used as a first-line test for infants and children who demonstrate developmental delay, autism spectrum disorders, dysmorphic features, and congenital anomalies. As many as 15% of patients with an otherwise normal karyotype will have a clinically significant copy number variant (CNV) on microarray. This finding has led to the use of microarray analysis in conjunction with karyotyping for fetuses with ultrasound-identified anomalies. Both targeted arrays (for syndromes associated with ultrasound anomalies) and whole-genome arrays are available.

Recent data from a study from the National Institute of Child Health and Human Development (NICHD) reveal that the prenatal detection rates for aneuploidy and unbalanced translocations are comparable between microarray analysis and karyotyping. Microarray analysis did not, however, detect triploidies or balanced translocations. As many as 6% of patients with a normal karyotype and structural anomalies and 1.7% of patients with advanced maternal age or positive screening tests had either a known or potentially clinically relevant CNV. This large study concluded that microarray analysis not only provides equal detection of aneuploidy but also more information in the form of CNVs, compared with karyotyping alone.
Microarray analysis also has been used in the study of pregnancy loss and stillbirth because it does not require viable or intact tissue as a source of DNA—an advantage, compared with traditional karyotyping. A recent study from the Stillbirth Collaborative Research Network demonstrated that genetic results in cases involving stillbirth were obtained more frequently via microarray analysis (87.4%) than by karyotype (70.5%). In addition, more genetic abnormalities (aneuploidy, pathogenic CNVs, and CNVs of unknown clinical significance) were detected by microarray analysis. Investigators concluded that microarray analysis may be especially useful in cases involving stillbirth (when a karyotype cannot be obtained) and structural abnormalities.
We want an accurate, completely risk-free genetic test that can be used for anyone. What we have so far is a technology that must be tested before it can be used in most of our patients—that is, the low-risk ones. We also have access to the fetus’ genetic code on a very specific level.
The total costs of such an approach—test, interpretation, counseling, and long-term follow-up of uncertain results—are unknown at this time and may prove to be unaffordable on a population-wide basis.
Should microarray analysis replace routine prenatal genetic testing?
A major dilemma associated with this technology is the significant amount of time that may be needed to counsel patients when the results are of unclear clinical significance.5 If the fetus has an anomaly, and a related CNV is identified, then counseling of the parents is fairly straightforward. However, if the fetus has an anomaly and a CNV that has not yet been defined, what should the parents be told? Some argue that this information should not be shared with the parents, whereas others recommend full disclosure of all results—even if we do not yet know what to make of them.
Another issue with microarray analysis is its inability to detect balanced translocations, triploidies, and low-level mosaicism, which require either a karyotype or whole-genome sequencing. Microarray analysis is also more expensive than karyotyping, although this may change in the future.
>Fetal therapy involves a complex equation of potential benefits and risks
Adzick NS, Thom EA, Spong CY, et al; MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1104.
Fetal therapy is broadly defined as any intervention administered to or via the mother with a primary indication to improve perinatal or long-term outcomes for the fetus or newborn. The concept of intervening to prevent the death of a fetus by correcting an anatomic anomaly or halting a disease process in utero is not new. Liley performed the first intrauterine fetal transfusion for Rh alloimmunization in the 1960s. Today, we perform fetal interventions routinely to reduce mortality by giving medical therapy to the mother, such as antenatal corticosteroids to enhance fetal lung maturity or anti-arrhythmics for supraventricular tachycardia. More invasive procedures have proved to be lifesaving (placental laser coagulation for twin-twin transfusion syndrome), ameliorating in the short term (shunting for lower urinary tract obstruction to relieve oligohydramnios), or ultimately not helpful (decompression of hydrocephalus).
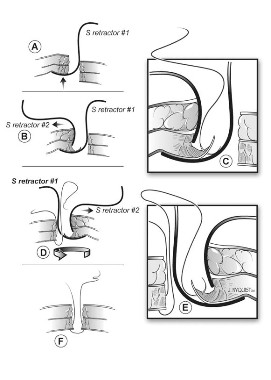
Most recently, open fetal surgery has taken center stage as an intervention focused not only on reducing mortality but on improving function and quality of life for fetuses with open neural tube defects (ONTDs). This anomaly was targeted for fetal intervention because, although ONTDs are not generally considered lethal, a significant number of patients die before the age of 5, the majority of patients require shunts that leave them vulnerable to complications, and ONTDs generally impose lifelong intellectual and physical limitations. Repair during fetal life was proposed to prevent damage to the spinal cord and reverse hindbrain herniation, with the goal of improving long-term neurologic function.
The Management of Myelomeningocele Study (MOMS) is a prospective, multicenter trial that randomly assigned fetuses with isolated ONTDs to open fetal repair of myelomeningocele via hysterotomy or to postnatal repair of the defect. Forty percent of infants who underwent fetal repair required placement of a shunt, compared with 82% of those who had postnatal repair (relative risk, 0.48; 97.7% CI, 0.36 to 0.64; P<.001). Infants in the fetal-repair group also had significantly improved composite scores for mental development and motor function at 30 months (P = .007), as well as improvement in secondary outcomes such as hindbrain herniation and independent walking at 30 months.
As exciting as these results are, open fetal surgery still has significant limitations. The few centers that perform the most complex surgeries often have strict exclusion criteria, including maternal body mass index (BMI) greater than 35 kg/m2 and other medical comorbidities. The surgery also poses real risks for both mother and fetus. In the MOMS trial, the risk of preterm labor increased in the fetal-repair group, compared with postnatal repair (38% vs 14%), as did the risk of premature rupture of membranes (46% vs 8%). The fetal-repair group delivered more than 3 weeks earlier than the postnatal repair group (34 vs 37 weeks). Twenty-five percent of the fetal-repair group had thinning of the uterine scar, with uterine dehiscence seen in 10%. When myelomeningocele is repaired during fetal life, mothers require two hysterotomies during pregnancy and face an increased risk of uterine rupture and preterm delivery in subsequent pregnancies. The use of tocolytics exposes these mothers to an increased risk of pulmonary edema (6% in the fetal-repair group vs 0% for postnatal repair).
Other issues that should be addressed:
- the need for rigorous study of open fetal surgery for other fetal anomalies
- prognostic factors for success and for complications
- long-term outcomes in neurologic development of children and fertility of mothers
- a comparison of costs between fetal and postnatal treatment.
Although we may want to intervene as early in life as possible (that is, the fetal period) to achieve the best outcomes for the child, we need to weigh the short-term benefits of intervention against the known risks that intervention poses for the mother in the current pregnancy as well as the potential implications for future pregnancies (ie, the need for all future deliveries to be by cesarean section), not to mention the unknown long-term effects of intervention on both the child and society.
Bundled payments may help us deliver higher-quality, more efficient, and less costly care
Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Fact Sheet: Bundled Payments for Care Improvement Initiative. Washington, DC: DHS; 2011. http://innovations.cms.gov/Files/fact-sheet/Bundled-Payment-Fact-Sheet.pdf. Accessed December 6, 2012.
There is little question that health care in the United States needs reform. The culture of “more is better” is not sustainable economically—nor does our health as a whole reflect the amount of money that we spend on health care, compared with other countries. Although the future is not yet clear, one proposed mechanism for reform is the institution of bundled payments—the grouping of multiple services into one “episode” for payment purposes. An episode might include inpatient hospitalization for pneumonia, for example, or the grouping of surgery with post-discharge care. In obstetrics, all pregnancy care could be grouped into one episode. The concept behind bundled payments is to provide incentives to institutions and providers to delivery higher-quality, more efficient, and less costly care.
If bundled payments become the reality for obstetric care in the future, how will that affect the way we care for our patients? Instead of blindly ordering all available tests, we need to consider thoroughly whether the patient truly needs a test to improve pregnancy outcomes. We also need to consider whether other measures might be avoided safely to keep costs within the bundle. A few examples:
- Is a screening fetal echocardiogram really necessary in a diabetic woman if the ultrasound anatomy scan is sufficient to rule out any cardiac anomaly that might require intervention in the delivery room?
- How will we integrate the expense of cell-free fetal DNA aneuploidy testing and microarray analysis, not to mention the extended counseling sessions that will be necessary to explain findings of uncertain clinical significance, into the bundle? Will “low-risk” patients need to pay out of pocket?
Few physicians entered medicine to worry about costs. Most of us want to worry about our patients. Yet, the reality is that scientific curiosity and a desire to do more—and to do it sooner, faster, and safer—are no longer sufficient justifications for many clinical decisions. We soon may need to figure out how to get what we need without spending as much in the process. In doing so, we may find ourselves moving away from the computer screen and back to the bedside—where we belong.
- Will a second ultrasound scan to visualize the fetal spine in a patient with a normal alpha-fetoprotein level be included in the bundle or paid for by the patient?
These issues may seem trivial, but we can no longer afford to order every test available. We will need to spend more time examining and counseling our patients so that they feel they are still getting the best care possible.
We want to hear from you! Tell us what you think.
1. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis by fetal nucleic acid analysis in maternal plasma: the coming of age. Semin Fetal Neonatal Med. 2011;16(2):88-93.
2. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis empowered by high-throughput sequencing. Prenat Diagn. 2012;32(4):401-406.
3. Savage MS, Mourad MJ, Wapner RJ. Evolving applications of microarray analysis in prenatal diagnosis. Curr Opin Obstet Gynecol. 2011;23(2):103-108.
4. Dugoff L. Application of genomic technology in prenatal diagnosis [editorial]. N Engl J Med. 2012;367(23):2249-2251.
5. Wapner RJ, Driscoll DA, Simpson JL. Integration of microarray technology into prenatal diagnosis: counseling issues generated during the NICHD clinical trial. Prenat Diagn. 2012;32(4):396-400.
The authors report no financial relationships relevant to this article.
If there have been overriding themes in obstetrics over the past year, they have been “more,” “sooner,” “faster,” “safer.” Advances in our field have thrilled our scientific curiosity and increased our ability to alleviate suffering—but at what cost? And who will pay that cost?
In this Update, we focus on recent advances in prenatal diagnosis and fetal therapy, as well as the ever-encroaching economic barriers that may limit our ability to get what we want. In particular, we will discuss:
- two technologies in prenatal genetics: noninvasive aneuploidy testing using cell-free DNA and prenatal microarray analysis
- open fetal surgery to reduce mortality and improve the function and quality of life for fetuses with open neural tube defects
- the value and probable impact of bundled payments—that is, one payment for multiple services grouped into one “episode.”
Two noninvasive approaches to prenatal diagnosis offer promise—but practicality and cost are uncertain
Ashoor G, Syngelaki RM, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
Reddy UM, Page GP, Saade GR, et al. Karyotype versus microarray testing for genetic abnormalities after stillbirth. N Engl J Med. 2012;367(23):2185–2193.
Talkowski ME, Ordulu Z, Pillalamarri V, et al. Clinical diagnosis by whole-genome sequencing of a prenatal sample. N Engl J Med. 2012;367(23):2226–2232.
Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367(23):2175–2184.
Genetic screening and testing are a standard part of prenatal care in most developed countries. We have come a long way since a maternal age of 35 years was the only variable separating patients into low- and high-risk categories. This year, two technologies have emerged that may change forever the way we approach prenatal genetics:
One argument for using more accurate genetic screening methods: They limit the number of invasive tests that are needed. Chorionic villus sampling (CVS) and amniocentesis, even when performed by the most experienced of operators, pose a small but real risk of fetal injury and pregnancy loss.
Noninvasive aneuploidy diagnosis is now a reality in high-risk population screening
The holy grail of aneuploidy diagnosis would be a noninvasive way to sample fetal cells. Although we have known for decades that fetal cells enter the maternal circulation, it has been impractical to use them for aneuploidy testing because of their scarcity and longevity. In the 1990s, however, cell-free fetal DNA (cffDNA), a compound of DNA fragments of uncertain origin, was identified in maternal plasma. CffDNA is more plentiful than fetal cells. It also disappears within hours of delivery, demonstrating that it is specific to the current pregnancy.
CffDNA is already used in fetal Rh typing and gender determination in disorders such as congenital adrenal hyperplasia. Several studies in high-risk populations have demonstrated high sensitivity and specificity for the detection of Trisomies 21, 18, and 13. Several commercial tests are now available, although neither their accuracy nor their cost has been determined for use in low-risk population screening, compared with traditional testing.
Microarray analysis, paired with karyotyping, can elucidate ultrasound-identified fetal anomalies
Cytogenetic microarray analysis is also being explored in the prenatal period. Microarray analysis is currently used as a first-line test for infants and children who demonstrate developmental delay, autism spectrum disorders, dysmorphic features, and congenital anomalies. As many as 15% of patients with an otherwise normal karyotype will have a clinically significant copy number variant (CNV) on microarray. This finding has led to the use of microarray analysis in conjunction with karyotyping for fetuses with ultrasound-identified anomalies. Both targeted arrays (for syndromes associated with ultrasound anomalies) and whole-genome arrays are available.

Recent data from a study from the National Institute of Child Health and Human Development (NICHD) reveal that the prenatal detection rates for aneuploidy and unbalanced translocations are comparable between microarray analysis and karyotyping. Microarray analysis did not, however, detect triploidies or balanced translocations. As many as 6% of patients with a normal karyotype and structural anomalies and 1.7% of patients with advanced maternal age or positive screening tests had either a known or potentially clinically relevant CNV. This large study concluded that microarray analysis not only provides equal detection of aneuploidy but also more information in the form of CNVs, compared with karyotyping alone.
Microarray analysis also has been used in the study of pregnancy loss and stillbirth because it does not require viable or intact tissue as a source of DNA—an advantage, compared with traditional karyotyping. A recent study from the Stillbirth Collaborative Research Network demonstrated that genetic results in cases involving stillbirth were obtained more frequently via microarray analysis (87.4%) than by karyotype (70.5%). In addition, more genetic abnormalities (aneuploidy, pathogenic CNVs, and CNVs of unknown clinical significance) were detected by microarray analysis. Investigators concluded that microarray analysis may be especially useful in cases involving stillbirth (when a karyotype cannot be obtained) and structural abnormalities.
We want an accurate, completely risk-free genetic test that can be used for anyone. What we have so far is a technology that must be tested before it can be used in most of our patients—that is, the low-risk ones. We also have access to the fetus’ genetic code on a very specific level.
The total costs of such an approach—test, interpretation, counseling, and long-term follow-up of uncertain results—are unknown at this time and may prove to be unaffordable on a population-wide basis.
Should microarray analysis replace routine prenatal genetic testing?
A major dilemma associated with this technology is the significant amount of time that may be needed to counsel patients when the results are of unclear clinical significance.5 If the fetus has an anomaly, and a related CNV is identified, then counseling of the parents is fairly straightforward. However, if the fetus has an anomaly and a CNV that has not yet been defined, what should the parents be told? Some argue that this information should not be shared with the parents, whereas others recommend full disclosure of all results—even if we do not yet know what to make of them.
Another issue with microarray analysis is its inability to detect balanced translocations, triploidies, and low-level mosaicism, which require either a karyotype or whole-genome sequencing. Microarray analysis is also more expensive than karyotyping, although this may change in the future.
>Fetal therapy involves a complex equation of potential benefits and risks
Adzick NS, Thom EA, Spong CY, et al; MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1104.
Fetal therapy is broadly defined as any intervention administered to or via the mother with a primary indication to improve perinatal or long-term outcomes for the fetus or newborn. The concept of intervening to prevent the death of a fetus by correcting an anatomic anomaly or halting a disease process in utero is not new. Liley performed the first intrauterine fetal transfusion for Rh alloimmunization in the 1960s. Today, we perform fetal interventions routinely to reduce mortality by giving medical therapy to the mother, such as antenatal corticosteroids to enhance fetal lung maturity or anti-arrhythmics for supraventricular tachycardia. More invasive procedures have proved to be lifesaving (placental laser coagulation for twin-twin transfusion syndrome), ameliorating in the short term (shunting for lower urinary tract obstruction to relieve oligohydramnios), or ultimately not helpful (decompression of hydrocephalus).
Most recently, open fetal surgery has taken center stage as an intervention focused not only on reducing mortality but on improving function and quality of life for fetuses with open neural tube defects (ONTDs). This anomaly was targeted for fetal intervention because, although ONTDs are not generally considered lethal, a significant number of patients die before the age of 5, the majority of patients require shunts that leave them vulnerable to complications, and ONTDs generally impose lifelong intellectual and physical limitations. Repair during fetal life was proposed to prevent damage to the spinal cord and reverse hindbrain herniation, with the goal of improving long-term neurologic function.
The Management of Myelomeningocele Study (MOMS) is a prospective, multicenter trial that randomly assigned fetuses with isolated ONTDs to open fetal repair of myelomeningocele via hysterotomy or to postnatal repair of the defect. Forty percent of infants who underwent fetal repair required placement of a shunt, compared with 82% of those who had postnatal repair (relative risk, 0.48; 97.7% CI, 0.36 to 0.64; P<.001). Infants in the fetal-repair group also had significantly improved composite scores for mental development and motor function at 30 months (P = .007), as well as improvement in secondary outcomes such as hindbrain herniation and independent walking at 30 months.
As exciting as these results are, open fetal surgery still has significant limitations. The few centers that perform the most complex surgeries often have strict exclusion criteria, including maternal body mass index (BMI) greater than 35 kg/m2 and other medical comorbidities. The surgery also poses real risks for both mother and fetus. In the MOMS trial, the risk of preterm labor increased in the fetal-repair group, compared with postnatal repair (38% vs 14%), as did the risk of premature rupture of membranes (46% vs 8%). The fetal-repair group delivered more than 3 weeks earlier than the postnatal repair group (34 vs 37 weeks). Twenty-five percent of the fetal-repair group had thinning of the uterine scar, with uterine dehiscence seen in 10%. When myelomeningocele is repaired during fetal life, mothers require two hysterotomies during pregnancy and face an increased risk of uterine rupture and preterm delivery in subsequent pregnancies. The use of tocolytics exposes these mothers to an increased risk of pulmonary edema (6% in the fetal-repair group vs 0% for postnatal repair).
Other issues that should be addressed:
- the need for rigorous study of open fetal surgery for other fetal anomalies
- prognostic factors for success and for complications
- long-term outcomes in neurologic development of children and fertility of mothers
- a comparison of costs between fetal and postnatal treatment.
Although we may want to intervene as early in life as possible (that is, the fetal period) to achieve the best outcomes for the child, we need to weigh the short-term benefits of intervention against the known risks that intervention poses for the mother in the current pregnancy as well as the potential implications for future pregnancies (ie, the need for all future deliveries to be by cesarean section), not to mention the unknown long-term effects of intervention on both the child and society.
Bundled payments may help us deliver higher-quality, more efficient, and less costly care
Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Fact Sheet: Bundled Payments for Care Improvement Initiative. Washington, DC: DHS; 2011. http://innovations.cms.gov/Files/fact-sheet/Bundled-Payment-Fact-Sheet.pdf. Accessed December 6, 2012.
There is little question that health care in the United States needs reform. The culture of “more is better” is not sustainable economically—nor does our health as a whole reflect the amount of money that we spend on health care, compared with other countries. Although the future is not yet clear, one proposed mechanism for reform is the institution of bundled payments—the grouping of multiple services into one “episode” for payment purposes. An episode might include inpatient hospitalization for pneumonia, for example, or the grouping of surgery with post-discharge care. In obstetrics, all pregnancy care could be grouped into one episode. The concept behind bundled payments is to provide incentives to institutions and providers to delivery higher-quality, more efficient, and less costly care.
If bundled payments become the reality for obstetric care in the future, how will that affect the way we care for our patients? Instead of blindly ordering all available tests, we need to consider thoroughly whether the patient truly needs a test to improve pregnancy outcomes. We also need to consider whether other measures might be avoided safely to keep costs within the bundle. A few examples:
- Is a screening fetal echocardiogram really necessary in a diabetic woman if the ultrasound anatomy scan is sufficient to rule out any cardiac anomaly that might require intervention in the delivery room?
- How will we integrate the expense of cell-free fetal DNA aneuploidy testing and microarray analysis, not to mention the extended counseling sessions that will be necessary to explain findings of uncertain clinical significance, into the bundle? Will “low-risk” patients need to pay out of pocket?
Few physicians entered medicine to worry about costs. Most of us want to worry about our patients. Yet, the reality is that scientific curiosity and a desire to do more—and to do it sooner, faster, and safer—are no longer sufficient justifications for many clinical decisions. We soon may need to figure out how to get what we need without spending as much in the process. In doing so, we may find ourselves moving away from the computer screen and back to the bedside—where we belong.
- Will a second ultrasound scan to visualize the fetal spine in a patient with a normal alpha-fetoprotein level be included in the bundle or paid for by the patient?
These issues may seem trivial, but we can no longer afford to order every test available. We will need to spend more time examining and counseling our patients so that they feel they are still getting the best care possible.
We want to hear from you! Tell us what you think.
The authors report no financial relationships relevant to this article.
If there have been overriding themes in obstetrics over the past year, they have been “more,” “sooner,” “faster,” “safer.” Advances in our field have thrilled our scientific curiosity and increased our ability to alleviate suffering—but at what cost? And who will pay that cost?
In this Update, we focus on recent advances in prenatal diagnosis and fetal therapy, as well as the ever-encroaching economic barriers that may limit our ability to get what we want. In particular, we will discuss:
- two technologies in prenatal genetics: noninvasive aneuploidy testing using cell-free DNA and prenatal microarray analysis
- open fetal surgery to reduce mortality and improve the function and quality of life for fetuses with open neural tube defects
- the value and probable impact of bundled payments—that is, one payment for multiple services grouped into one “episode.”
Two noninvasive approaches to prenatal diagnosis offer promise—but practicality and cost are uncertain
Ashoor G, Syngelaki RM, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
Reddy UM, Page GP, Saade GR, et al. Karyotype versus microarray testing for genetic abnormalities after stillbirth. N Engl J Med. 2012;367(23):2185–2193.
Talkowski ME, Ordulu Z, Pillalamarri V, et al. Clinical diagnosis by whole-genome sequencing of a prenatal sample. N Engl J Med. 2012;367(23):2226–2232.
Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367(23):2175–2184.
Genetic screening and testing are a standard part of prenatal care in most developed countries. We have come a long way since a maternal age of 35 years was the only variable separating patients into low- and high-risk categories. This year, two technologies have emerged that may change forever the way we approach prenatal genetics:
One argument for using more accurate genetic screening methods: They limit the number of invasive tests that are needed. Chorionic villus sampling (CVS) and amniocentesis, even when performed by the most experienced of operators, pose a small but real risk of fetal injury and pregnancy loss.
Noninvasive aneuploidy diagnosis is now a reality in high-risk population screening
The holy grail of aneuploidy diagnosis would be a noninvasive way to sample fetal cells. Although we have known for decades that fetal cells enter the maternal circulation, it has been impractical to use them for aneuploidy testing because of their scarcity and longevity. In the 1990s, however, cell-free fetal DNA (cffDNA), a compound of DNA fragments of uncertain origin, was identified in maternal plasma. CffDNA is more plentiful than fetal cells. It also disappears within hours of delivery, demonstrating that it is specific to the current pregnancy.
CffDNA is already used in fetal Rh typing and gender determination in disorders such as congenital adrenal hyperplasia. Several studies in high-risk populations have demonstrated high sensitivity and specificity for the detection of Trisomies 21, 18, and 13. Several commercial tests are now available, although neither their accuracy nor their cost has been determined for use in low-risk population screening, compared with traditional testing.
Microarray analysis, paired with karyotyping, can elucidate ultrasound-identified fetal anomalies
Cytogenetic microarray analysis is also being explored in the prenatal period. Microarray analysis is currently used as a first-line test for infants and children who demonstrate developmental delay, autism spectrum disorders, dysmorphic features, and congenital anomalies. As many as 15% of patients with an otherwise normal karyotype will have a clinically significant copy number variant (CNV) on microarray. This finding has led to the use of microarray analysis in conjunction with karyotyping for fetuses with ultrasound-identified anomalies. Both targeted arrays (for syndromes associated with ultrasound anomalies) and whole-genome arrays are available.

Recent data from a study from the National Institute of Child Health and Human Development (NICHD) reveal that the prenatal detection rates for aneuploidy and unbalanced translocations are comparable between microarray analysis and karyotyping. Microarray analysis did not, however, detect triploidies or balanced translocations. As many as 6% of patients with a normal karyotype and structural anomalies and 1.7% of patients with advanced maternal age or positive screening tests had either a known or potentially clinically relevant CNV. This large study concluded that microarray analysis not only provides equal detection of aneuploidy but also more information in the form of CNVs, compared with karyotyping alone.
Microarray analysis also has been used in the study of pregnancy loss and stillbirth because it does not require viable or intact tissue as a source of DNA—an advantage, compared with traditional karyotyping. A recent study from the Stillbirth Collaborative Research Network demonstrated that genetic results in cases involving stillbirth were obtained more frequently via microarray analysis (87.4%) than by karyotype (70.5%). In addition, more genetic abnormalities (aneuploidy, pathogenic CNVs, and CNVs of unknown clinical significance) were detected by microarray analysis. Investigators concluded that microarray analysis may be especially useful in cases involving stillbirth (when a karyotype cannot be obtained) and structural abnormalities.
We want an accurate, completely risk-free genetic test that can be used for anyone. What we have so far is a technology that must be tested before it can be used in most of our patients—that is, the low-risk ones. We also have access to the fetus’ genetic code on a very specific level.
The total costs of such an approach—test, interpretation, counseling, and long-term follow-up of uncertain results—are unknown at this time and may prove to be unaffordable on a population-wide basis.
Should microarray analysis replace routine prenatal genetic testing?
A major dilemma associated with this technology is the significant amount of time that may be needed to counsel patients when the results are of unclear clinical significance.5 If the fetus has an anomaly, and a related CNV is identified, then counseling of the parents is fairly straightforward. However, if the fetus has an anomaly and a CNV that has not yet been defined, what should the parents be told? Some argue that this information should not be shared with the parents, whereas others recommend full disclosure of all results—even if we do not yet know what to make of them.
Another issue with microarray analysis is its inability to detect balanced translocations, triploidies, and low-level mosaicism, which require either a karyotype or whole-genome sequencing. Microarray analysis is also more expensive than karyotyping, although this may change in the future.
>Fetal therapy involves a complex equation of potential benefits and risks
Adzick NS, Thom EA, Spong CY, et al; MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1104.
Fetal therapy is broadly defined as any intervention administered to or via the mother with a primary indication to improve perinatal or long-term outcomes for the fetus or newborn. The concept of intervening to prevent the death of a fetus by correcting an anatomic anomaly or halting a disease process in utero is not new. Liley performed the first intrauterine fetal transfusion for Rh alloimmunization in the 1960s. Today, we perform fetal interventions routinely to reduce mortality by giving medical therapy to the mother, such as antenatal corticosteroids to enhance fetal lung maturity or anti-arrhythmics for supraventricular tachycardia. More invasive procedures have proved to be lifesaving (placental laser coagulation for twin-twin transfusion syndrome), ameliorating in the short term (shunting for lower urinary tract obstruction to relieve oligohydramnios), or ultimately not helpful (decompression of hydrocephalus).
Most recently, open fetal surgery has taken center stage as an intervention focused not only on reducing mortality but on improving function and quality of life for fetuses with open neural tube defects (ONTDs). This anomaly was targeted for fetal intervention because, although ONTDs are not generally considered lethal, a significant number of patients die before the age of 5, the majority of patients require shunts that leave them vulnerable to complications, and ONTDs generally impose lifelong intellectual and physical limitations. Repair during fetal life was proposed to prevent damage to the spinal cord and reverse hindbrain herniation, with the goal of improving long-term neurologic function.
The Management of Myelomeningocele Study (MOMS) is a prospective, multicenter trial that randomly assigned fetuses with isolated ONTDs to open fetal repair of myelomeningocele via hysterotomy or to postnatal repair of the defect. Forty percent of infants who underwent fetal repair required placement of a shunt, compared with 82% of those who had postnatal repair (relative risk, 0.48; 97.7% CI, 0.36 to 0.64; P<.001). Infants in the fetal-repair group also had significantly improved composite scores for mental development and motor function at 30 months (P = .007), as well as improvement in secondary outcomes such as hindbrain herniation and independent walking at 30 months.
As exciting as these results are, open fetal surgery still has significant limitations. The few centers that perform the most complex surgeries often have strict exclusion criteria, including maternal body mass index (BMI) greater than 35 kg/m2 and other medical comorbidities. The surgery also poses real risks for both mother and fetus. In the MOMS trial, the risk of preterm labor increased in the fetal-repair group, compared with postnatal repair (38% vs 14%), as did the risk of premature rupture of membranes (46% vs 8%). The fetal-repair group delivered more than 3 weeks earlier than the postnatal repair group (34 vs 37 weeks). Twenty-five percent of the fetal-repair group had thinning of the uterine scar, with uterine dehiscence seen in 10%. When myelomeningocele is repaired during fetal life, mothers require two hysterotomies during pregnancy and face an increased risk of uterine rupture and preterm delivery in subsequent pregnancies. The use of tocolytics exposes these mothers to an increased risk of pulmonary edema (6% in the fetal-repair group vs 0% for postnatal repair).
Other issues that should be addressed:
- the need for rigorous study of open fetal surgery for other fetal anomalies
- prognostic factors for success and for complications
- long-term outcomes in neurologic development of children and fertility of mothers
- a comparison of costs between fetal and postnatal treatment.
Although we may want to intervene as early in life as possible (that is, the fetal period) to achieve the best outcomes for the child, we need to weigh the short-term benefits of intervention against the known risks that intervention poses for the mother in the current pregnancy as well as the potential implications for future pregnancies (ie, the need for all future deliveries to be by cesarean section), not to mention the unknown long-term effects of intervention on both the child and society.
Bundled payments may help us deliver higher-quality, more efficient, and less costly care
Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Fact Sheet: Bundled Payments for Care Improvement Initiative. Washington, DC: DHS; 2011. http://innovations.cms.gov/Files/fact-sheet/Bundled-Payment-Fact-Sheet.pdf. Accessed December 6, 2012.
There is little question that health care in the United States needs reform. The culture of “more is better” is not sustainable economically—nor does our health as a whole reflect the amount of money that we spend on health care, compared with other countries. Although the future is not yet clear, one proposed mechanism for reform is the institution of bundled payments—the grouping of multiple services into one “episode” for payment purposes. An episode might include inpatient hospitalization for pneumonia, for example, or the grouping of surgery with post-discharge care. In obstetrics, all pregnancy care could be grouped into one episode. The concept behind bundled payments is to provide incentives to institutions and providers to delivery higher-quality, more efficient, and less costly care.
If bundled payments become the reality for obstetric care in the future, how will that affect the way we care for our patients? Instead of blindly ordering all available tests, we need to consider thoroughly whether the patient truly needs a test to improve pregnancy outcomes. We also need to consider whether other measures might be avoided safely to keep costs within the bundle. A few examples:
- Is a screening fetal echocardiogram really necessary in a diabetic woman if the ultrasound anatomy scan is sufficient to rule out any cardiac anomaly that might require intervention in the delivery room?
- How will we integrate the expense of cell-free fetal DNA aneuploidy testing and microarray analysis, not to mention the extended counseling sessions that will be necessary to explain findings of uncertain clinical significance, into the bundle? Will “low-risk” patients need to pay out of pocket?
Few physicians entered medicine to worry about costs. Most of us want to worry about our patients. Yet, the reality is that scientific curiosity and a desire to do more—and to do it sooner, faster, and safer—are no longer sufficient justifications for many clinical decisions. We soon may need to figure out how to get what we need without spending as much in the process. In doing so, we may find ourselves moving away from the computer screen and back to the bedside—where we belong.
- Will a second ultrasound scan to visualize the fetal spine in a patient with a normal alpha-fetoprotein level be included in the bundle or paid for by the patient?
These issues may seem trivial, but we can no longer afford to order every test available. We will need to spend more time examining and counseling our patients so that they feel they are still getting the best care possible.
We want to hear from you! Tell us what you think.
1. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis by fetal nucleic acid analysis in maternal plasma: the coming of age. Semin Fetal Neonatal Med. 2011;16(2):88-93.
2. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis empowered by high-throughput sequencing. Prenat Diagn. 2012;32(4):401-406.
3. Savage MS, Mourad MJ, Wapner RJ. Evolving applications of microarray analysis in prenatal diagnosis. Curr Opin Obstet Gynecol. 2011;23(2):103-108.
4. Dugoff L. Application of genomic technology in prenatal diagnosis [editorial]. N Engl J Med. 2012;367(23):2249-2251.
5. Wapner RJ, Driscoll DA, Simpson JL. Integration of microarray technology into prenatal diagnosis: counseling issues generated during the NICHD clinical trial. Prenat Diagn. 2012;32(4):396-400.
1. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis by fetal nucleic acid analysis in maternal plasma: the coming of age. Semin Fetal Neonatal Med. 2011;16(2):88-93.
2. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis empowered by high-throughput sequencing. Prenat Diagn. 2012;32(4):401-406.
3. Savage MS, Mourad MJ, Wapner RJ. Evolving applications of microarray analysis in prenatal diagnosis. Curr Opin Obstet Gynecol. 2011;23(2):103-108.
4. Dugoff L. Application of genomic technology in prenatal diagnosis [editorial]. N Engl J Med. 2012;367(23):2249-2251.
5. Wapner RJ, Driscoll DA, Simpson JL. Integration of microarray technology into prenatal diagnosis: counseling issues generated during the NICHD clinical trial. Prenat Diagn. 2012;32(4):396-400.
Alcohol: An unfortunate teratogen
Medical students learn early in their education that alcohol is a teratogen. Despite this widespread knowledge, many obstetricians counsel patients about the safety of low doses of alcohol in pregnancy.1 Indeed, the Royal College of Obstetricians and Gynaecologists’ position on this is, “while the safest approach may be to avoid any alcohol during pregnancy, it remains the case that there is no evidence of harm from low levels of alcohol consumption, defined as no more than one or two units of alcohol once or twice a week.”2
Like many providers, I was aware of this controversy, but it became truly personal when a beloved family member was diagnosed with fetal alcohol syndrome (FAS). In this paper, I will review some of the controversy regarding alcohol in pregnancy, highlight findings from the literature, provide tools for prevention, and identify new developments regarding this devastating, preventable condition.
Charlie
To know my nephew Charlie is to fall in love with my nephew Charlie. One of the happiest moments of my life was when I learned my brother and sister-in-law had adopted twins from Kazakhstan. When my little niece and nephew started their new life in the United States, certain medical issues seemed to merit additional attention. Although both were very small for their age and required significant nutritional support, Charlie seemed to be a bit more rambunctious and required additional supervision.
The children were fortunate enough to have incredibly loving, dedicated parents, who have access to exceptional medical care as residents of Philadelphia, Pennsylvania. After extensive testing, it became clear what was causing Charlie’s developmental delay; his pediatric team made the diagnosis of FAS. My brother and sister-in-law became incredibly well-read about this challenging disorder, and threw themselves into national advocacy work to help prevent this unnecessary tragedy.
Recent data point to teratogenicity, but media confuse the issue
Some recent media coverage3 of celebrities who apparently drank while pregnant was in response to an article in the Journal of Epidemiology and Community Health.4 The authors of this study concluded that, “at age 5 years, cohort members born to mothers who drank up to one to two drinks per week or per occasion during pregnancy were not at increased risk of clinically relevant behavioral difficulties or cognitive deficits, compared with children of mothers in the not-in-pregnancy group.”
This is certainly not the first occasion the popular press has covered a published study that seems to indicate no ill effects of alcohol use in pregnancy. A 2008 report by Kelly and colleagues,5 and its subsequent media coverage, prompted the Fetal Alcohol Spectrum Disorders Study Group to state that the panel of experts was “alarmed” by recent newspaper reports suggesting that light drinking during pregnancy may be beneficial for an unborn child.6 They noted misleading and irresponsible media reports of the findings, which suggested that 3-year-old children whose mothers drank “lightly” during pregnancy were not at risk for certain behavioral problems.
What the study authors proceeded to note, however (that the media did not mention), was that the light drinkers in their study had socioeconomic advantages, compared with nondrinkers.5 (Advantaged economic status is established to be beneficial for childhood development.) They also noted that the study involved preschool-aged children, stating “Generally the adverse effects of light drinking during pregnancy are subtle and may go undetected in young children. However, other group studies of more moderate or ‘social’ drinking levels during pregnancy have shown an adverse impact on multiple aspects of development through adolescence and young adulthood, even when important environmental factors are taken into account.” A sentence I thought was most compelling in their statement was, “It is an inconvenient fact of life that alcohol is a teratogen.” Now, this fact is well supported in the literature.7
There are animal studies regarding the use of “low-dose” or “moderate” alcohol in pregnancy that demonstrate adverse behavioral outcomes with exposure to even small doses of alcohol.8,9 It is an American tragedy that, according to the Centers for Disease Control and Prevention (CDC), rates of FAS in this country range from 0.2 to 2.0 cases per 1,000 live births. Indeed, the rates of fetal alcohol spectrum disorders (FASD) might be at least three times this rate.10 As is the case with other disorders, there are health disparities regarding the prevalence of this condition as well.11
FAS: A long history of preventable disease
1973: Identified. FAS was first described in a 1973 Lancet report, “Pattern of malformation in offspring of chronic alcoholic mothers.”12
1996: Call for prevention. In 1995, the US Surgeon General issued a statement regarding alcohol use in pregnancy, noting, “We do not know what, if any, amount of alcohol is safe.”13 In 1996, the Institute of Medicine released a paper calling FAS and FASD “completely preventable birth defects and neurodevelopmental abnormalities.”14
2000: The troubling effects gathered. The American Academy of Pediatrics (AAP) published a monograph on FAS in 2000, defining it as a constellation of physical, behavioral, and cognitive abnormalities.15
These features classically define FAS:
- dysmorphic facial features
- prenatal and postnatal growth abnormalities
- mental retardation.
Approximately 80% of children with this condition have:
- microcephaly
- behavioral abnormalities.
As many as 50% of affected children also exhibit:
- poor coordination
- hypotonia
- attention-deficit hyperactivity disorder
- decreased adipose tissue
- identifiable facial anomalies (such as maxillary hypoplasia, cleft palate, and micrognathia).
Also common:
- cardiac defects
- hemangiomas
- eye or ear abnormalities.
The AAP further noted that data current to the time (and still true today) did not support the concept of a safe level of alcohol consumption by pregnant women below which no damage to a fetus will occur.15

Alcohol intake during pregnancy puts the fetus at risk for cognitive and neuropsychological impairment and physical abnormalities, including dysmorphic facial features (such as micrognathia), restricted prenatal growth, cardiac defects, and eye and ear abnormalities. There is no threshold dose of alcohol that is safe during pregnancy, according to the American College of Obstetricians and Gynecologists.
Despite the knowledge we’ve gained, FAS persists
According to a 2006–2010 CDC analysis involving more than 345,000 women of reproductive age from all 50 states, 7.6% of pregnant women reported alcohol use and 1.4% (or 1 in 71) reported binge drinking (defined, respectively, as at least one alcoholic drink and four or more alcoholic drinks on one occasion in the past 30 days).16 The highest prevalence of obstetric alcohol consumption occurs in women who are:
- aged 35 to 44 years
- white
- college graduates
- employed.
The problem may be bigger than reported. The incidences of alcohol and binge drinking found in the CDC report include women’s self-report—but women drink alcohol without knowing they’re pregnant. Only 40% of women realize they’re pregnant at 4 weeks of gestation, a critical time for organogenesis, and approximately half of all births are unplanned.9
When my brother and sister-in law adopted my beautiful niece and nephew, they were very aware of the risk for conditions like FAS. In an evaluation of 71 children adopted from Eastern Europe at 5 years of age, FAS was diagnosed in 30% of children and “partial FAS” in another 9%.17 Birth defects attributed to alcohol were present in 11% of the children.
Are women’s health providers up to date on FAS education?
In recognition of alcohol’s potentially life-altering consequences for the developing fetus, the American College of Obstetricians and Gynecologists (ACOG) produced an FASD prevention tool kit in 2006 and published a 2011 committee opinion on at-risk drinking and alcohol dependence and their implications for obstetrics and gynecology.18,19 Both guidelines direct clinicians to advise patients to abstain from alcohol during pregnancy.
Results from a 2010 survey of 800 ACOG fellows revealed that only 78% of obstetricians advised abstinence from alcohol during pregnancy. Fifty-eight percent of respondents did not use a validated screening tool for alcohol use in their pregnant patients, and only 72% felt prepared to screen for risky or hazardous drinking.19 (Most were unaware of the ACOG tool kit, which had been published several years earlier.)
In a survey of pediatricians, obstetricians, and family physicians, clinicians said that about 67% of their patients asked about alcohol use in pregnancy, with about 2% of those patients specifically mentioning FAS. About 41% of these same physicians erroneously placed the threshold for FAS at one to three drinks per day,20 when in fact there is no threshold of drinking that has been proven to be safe.
A survey of 1,000 actively practicing ACOG fellows revealed that, while 97% of obstetricians routinely asked their patients about alcohol use, only 20% of providers reported to their patients that abstinence was safest, and 4% of providers didn’t believe that consumption of eight or more drinks weekly posed fetal risk.21
How can we educate our patients about the dangers of alcohol in pregnancy?
Fetal death. A recent Danish study of 79,216 pregnant women revealed that 45% had consumed some alcohol during pregnancy. Two percent reported at least four drinks per week, and 25% admitted to binge drinking during pregnancy. Term infants born to women in the latter two groups had increased neonatal mortality, with hazard ratios of 3.56 (95% confidence interval [CI], 1.15–8.43) and 2.69 (95% CI, 1.27–5.69), respectively.22
Decreased cognitive status. A study by Willford and colleagues evaluated the relationship between prenatal alcohol exposure and cognitive status of 1,360 10-year-old children.23 The authors utilized the Stanford-Binet Intelligence Test, including the composite scores and verbal, abstract/visual, quantitative, and short-term memory scores. After controlling for other variables, among African American offspring they found that, for each additional drink, the average composite score decreased by 1.9 points. This difference was more striking for second-trimester use, and was significant even for one drink daily versus abstention from alcohol.
Impaired neuropsychological development. Another study evaluating light to moderate amounts of prenatal alcohol exposure in 10- and 11-year-old children found significantly worse scores regarding a number of neuropsychological developmental assessments.24
No threshold dose of causation. Results of a 2012 prospective study in California, with data collected on 992 subjects from 1978 until 2005, revealed that many physical FAS features, including microcephaly, smooth philtrum, and thin vermillion border; reduced birth length; and reduced birth weight, were associated with alcohol exposure at specific gestational ages, and were dose-related.25 This paper didn’t reveal any evidence of a threshold dose of causation.
Neurobehavioral outcomes of FAS are not always considered
Another recent study that the media recently highlighted as finding “no association between low or moderate prenatal alcohol exposure and birth defects” was by O’Leary and colleagues.26 Like other similarly limited studies, this one involved only children younger than 6 years and didn’t assess any of the important neurobehavioral outcomes of FAS.
FAS encompasses much more than visible birth defects. As the aforementioned ACOG tool kit stated, “For every child born with FAS, many more children are born with neurobehavioral deficits caused by alcohol exposure but without the physical characteristics of FAS.”
The costs of FAS are felt with dollars, too
The financial cost to our nation is extraordinary. In 1991, Abel and Sokol estimated the incremental annual cost of treating FAS at nearly $75 million, with about three-quarters of that cost associated with FAS cases involving mental retardation.27
A 2002 assessment estimated the lifetime cost for each individual with FAS (adjusting for the change in the cost of medical care services, lost productivity, and inflation) at $2 million. This figure consists of $1.6 million for medical treatment, special education, and residential care for persons with mental retardation, and $0.4 million for productivity losses.28
Where human studies fall short, animal studies can help elucidate causation
Unquestionably, there are flaws in the existing literature on the causation of FAS. Many studies rely on self-reporting by pregnant women, and underreporting in these cases is a real concern. There often are other confounders potentially negatively affecting fetal development, making it difficult to differentiate causation. The animal studies that don’t share these limitations do suggest a causal relationship between antenatal alcohol exposure and poor obstetric outcomes, however.29 These studies suggest mechanisms such as altered gene expression, oxidative stress, and apoptosis (programmed cell death).30
Warren, Hewitt, and Thomas describe how intrauterine alcohol exposure interferes with the function of L1CAM, the L1 cell-adhesion molecule.31 They noted that just one drink could interfere with the ability of L1CAM to mediate cell adhesion and axonal growth. Prenatal alcohol exposure is also thought to contribute to interference in neurotransmitter and N-methyl-D-aspartate receptor coupling, which may have potential therapeutic implications.32
Considerations in FAS identification and treatment
There is a potential to identify alcohol exposure in the womb. The majority of ingested alcohol is eventually converted to carbon dioxide and water in both maternal and fetal circulations, which has hampered the identification of biomarkers for clinical use in FAS. Fatty acid ethyl esters (FAEEs), nonoxidative metabolites of ethanol, may prove to be such markers.33 FAEEs have been measured in a variety of tissues, including blood and meconium. FAEEs can be measured in both neonatal and maternal hair samples.
A study evaluating the utility of such testing in 324 at-risk pregnancies revealed 90% sensitivity and 90% specificity for identifying “excessive drinking” using a cutoff of 0.5 ng/mg.34
Research shows potential therapeutic approaches during pregnancy. While the use of biomarkers has the potential to assist with the identification of at-risk newborns, it merely identifies past alcohol use; it doesn’t necessarily permit identification and prevention of the known negative pediatric sequelae. Preliminary animal studies reveal the potential benefit of neuroprotective peptides to prevent brain damage in alcohol-exposed mice.35 Further research is ongoing.
Treatment: The earlier the better
Early diagnosis and a positive environment improve outcomes. It is well established that early intervention improves outcomes. One comprehensive review of 415 patients with FAS noted troubling outcomes in general for adolescents and adults.36 Over their life spans, the prevalence of such outcomes was:
- 61% for disrupted school experiences
- 60% for trouble with the law
- 50% for confinement (in detention, jail, prison, or a psychiatric or alcohol/drug inpatient setting)
- 49% for inappropriate sexual behaviors on repeated occasions
- 35% for alcohol/drug problems.
The odds of escaping these adverse life outcomes are increased up to fourfold when the individual receives a FAS or FASD diagnosis at an earlier age and is reared in a stable environment.36
Barrier to treatment: A mother’s guilt. One of the challenges I’ve learned from my sister-in-law is the stigma mothers face when they bring their child in for services once the diagnosis of FAS is suspected. While adoptive mothers obviously can’t be held accountable for the intrauterine environment to which a fetus is exposed, the same can’t be said of biologic mothers. Therefore, there is a real risk that a mother who is unwilling or unable to face the potentially devastating news that her baby’s issues might be related to choices she made during pregnancy, might not bring her child in for necessary assessment and treatment. Therefore, prevention is a key proponent of treatment.
Prevent FAS: Provide contraception, screen for alcohol use, intervene
While ObGyns aren’t likely to diagnose many children with FAS, we are in an excellent position to try to prevent this tragedy through our counseling of reproductive-aged women. I suspect that most obstetricians spend a considerable amount of time discussing much less frequent obstetric sequelae, such as listeriosis, in the prenatal care setting. Validated alcohol screening tools take moments to administer, and once patients who might have alcohol problems are identified, either a serious discussion about contraception or an honest discussion of FAS may be appropriate. There have been a number of screening tools developed.
The CAGE screen is frequently taught in medical schools, but it isn’t as sensitive for women or minorities.19
The T-ACE (Tolerance, Annoyed, Cut Down, Eye-opener) tool involves four questions that take less than 1 minute to administer (FIGURE 1).39
TWEAK is another potential tool identified by Russell and colleagues (Tolerance, Worry, Eye opener, Amnesia, and Cut down in drinking).39 Other methods utilized include an AUDIT screen and a CRAFFT screen.40 Regardless of which tool is utilized, screening is not time-consuming and is better than merely inquiring about alcohol consumption in general.
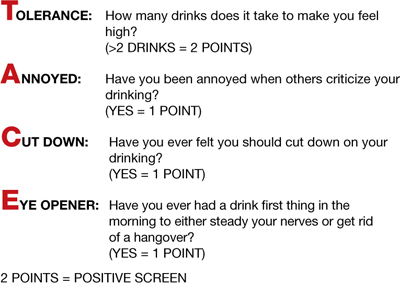
FIGURE 1 T-ACE validated alcohol screening tool
Source: American College of Obstetricians and Gynecologists. At risk drinking and illicit drug use: Ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2008;112(6):1449–1460.
When alcohol use is found, intervene
Once patients with at-risk behavior are identified, obstetric staff should offer brief interventions to influence problem drinking. Miller and Sanchez summarized the key elements that were most successful in these programs with the acronym FRAMES: Feedback, Responsibility, Advice, Menu, Empathy, Self-efficacy (FIGURE 2).41 This approach has been formally evaluated in the CDC’s multisite pilot study entitled Project CHOICES.42
In this motivational intervention, sexually active, fertile women of reproductive age underwent up to four motivational counseling sessions and one visit to a provider. At 6 months, 69% of women reduced their risk for an alcohol-exposed pregnancy—although the women who drank the least amount had the greatest benefit, primarily by choosing effective contraception, but also by reducing alcohol intake.
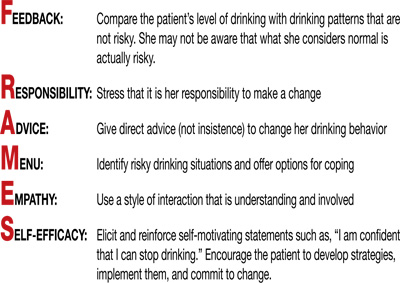
FIGURE 2 FRAMES model to deliver brief interventions
Source: American College of Obstetricians and Gynecologists. Drinking and reproductive health: A fetal alcohol spectrum disorders prevention tool kit. Washington, DC: ACOG; 2006.
A single, brief intervention is effective in already-pregnant women. Chang and colleagues conducted a randomized trial of a single-session brief intervention given to pregnant women with positive T-ACE screens and their partners (FIGURE 3).43 Either the study nurse or physician participated in the intervention, and each single session took 25 minutes on average. The pregnant women with the highest level of alcohol use reduced their drinking the most, and this effect was even larger when their partners participated. Other studies of brief interventions showed similar benefits.44,45
Another study evaluating a brief intervention involving training of health-care providers to improve screening rates revealed improved detection and therapy among at-risk patients.46
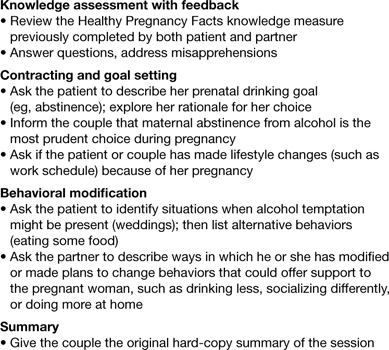
FIGURE 3 Single session, 25-minute intervention for patients and their partners
Source: Chang G, McNamara T, Orav J, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):991–998.
FAS prevention begins with routine counseling and contraception
Although FAS is often thought of in relation to obstetric populations, appointments for preconception counseling or routine health maintenance among women of reproductive age are an essential tool in FAS prevention. As previously mentioned, since approximately half of all pregnancies in this country are unplanned, long-acting reversible contraception is widely available to facilitate improved family planning.
Other contraceptive options also should be discussed. ACOG has teamed up with the CDC to develop a phone app for providers to use at the patient’s bedside to assist with identification and treatment of women at risk for alcohol use during pregnancy.47
The stakes are high, it’s time to step up
As obstetricians, we are powerless to prevent many conditions—such as vasa previa, acute fatty liver of pregnancy, and amniotic band syndrome. FAS is 100% preventable.
There aren’t that many proven teratogens in our profession, and there are none that involve behavior that is more socially acceptable than alcohol consumption. It is time for our profession to encourage women to appreciate how small a percentage of one’s life is spent pregnant, how many more years there are to enjoy an occasional cocktail, and how very high the stakes are during this important period of their lives. Oh, how I wish someone had been able to communicate all of this to sweet Charlie’s biologic mother. I am so grateful he’s getting the exceptional care he’s getting and very optimistic regarding his future. I only hope others in his situation are given the same opportunities.
Prenatal counseling
Louise Wilkins-Haug, MD, PhD (January 2008)
Prevention of fetal alcohol syndrome requires routine screening of all women of reproductive age
We want to hear from you! Tell us what you think.
1. Baram M. Moms-to-be get mixed messages on drinking. ABC News. http://abcnews.go.com/Health/story?id=2654849&page=1#.UM9l-RyeARY. Published November 15 2006. Accessed December 14, 2012.
2. Royal College of Obstetricians and Gynaecologists. Alcohol consumption and the outcomes of pregnancy (RCOG Statement No. 5). London UK: Royal College of Obstetricians and Gynaecologists. January 3, 2006.
3. Pearson C. Alcohol during pregnancy: How dangerous is it really? The Huffington Post. http://www.huffingtonpost.com/2011/04/06/alcohol-during-pregnancy_n_845103.html. Published April 6 2011. Updated September 16, 2011. Accessed December 14, 2012.
4. Kelly YJ, Sacker A, Gray R, et al. Light drinking during pregnancy: still no increased risk for socioemotional difficulties or cognitive deficits at 5 years of age? J Epidemiol Community Health. 2012;66(1):41-48.Epub Oct 5, 2010.
5. Kelly Y, Sacker A, Gray R, Kelly J, Wolke D, Quigley MA. Light drinking in pregnancy a risk for behavioural problems and cognitive deficits at 3 years of age? Int J Epidemiol. 2009;38(1):129-140.Epub Oct 30, 2008.
6. Zhou F. Fetal Alcohol Spectrum Disorders Study Group (FASDSG). Research Society on Alcoholism. http://rsoa.org/fas.html. Updated September 9 2010. Accessed December 14, 2012.
7. Kelly S, Day N, Streissguth AP. Effects of prenatal alcohol exposure on social behavior in humans and other species. Neurotoxicol Teratol. 2000;22(2):143-149.
8. Vaglenova J, Petkov V. Fetal alcohol effects in rats exposed pre-and postnatally to a low dose of ethanol. Alcohol Clin Exp Res. 1998;22(3):697-703.
9. Schneider M, Moore C, Kraemer G. Moderate alcohol during pregnancy: learning and behavior in adolescent rhesus monkeys. Alcohol Clin Exp Res. 2001;25(9):1383-1392.
10. Centers for Disease Control and Prevention. Fetal alcohol spectrum disorders. Data and statistics in the United States. http://www.cdc.gov/ncbddd/fasd/data.html. Updated August 16 2012. Accessed December 14, 2012.
11. Egeland G, Perham-Hestere KA, Gessner BD, Ingle D, Berner JE, Middaugh J. Fetal alcohol syndrome in Alaska 1977 through 1992: an administrative prevalence derived from multiple data sources. Am J Pub Health. 1998;88(5):781-786.
12. Jones K, Smith D, Ulleland C, Streissguth A. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1(7815):1267-1271.
13. Institute of Medicine. Fetal alcohol syndrome: diagnosis epidemiology, prevention, and treatment (1996). http://www.come-over.to/FAS/IOMsummary.htm. Accessed December 14, 2012.
14. Committee of Substance Abuse and Committee on Children with Disabilities. American Academy of Pediatrics. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106(2):358-361.
15. US Department of Health & Human Services. US Surgeon General releases advisory on alcohol use in pregnancy. http://www.surgeongeneral.gov/news/2005/02/sg02222005.html. Published February 21 2005. Accessed December 13, 2012.
16. Centers for Disease Control and Prevention. Alcohol use and binge drinking among women of childbearing age–United States 2006–2010. MMWR. 2012;61(28):534-538.http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6128a4.htm?s_cid=mm6128a4_w. Accessed December 17, 2012.
17. Landgren M, Svensson L, Stromland K, Gronlund M. Prenatal alcohol exposure and neurodvelopmental disorders in children adopted from Eastern Europe. Pediatrics. 2010;125(5):e1178-1185.doi:10.1542/peds.2009-0712.
18. American College of Obstetricians and Gynecologists. Drinking and reproductive health: A fetal alcohol spectrum disorders prevention tool kit. http://www.acog.org/~/media/Departments/Tobacco%20Alcohol%20and%20Substance%20Abuse/FASDToolKit.pdf?dmc=1&ts=20121217T1504384811. Published 2006. Accessed December 14 2012.
19. Anderson B, Dang E, Floyd R, Sokol R, Mahoney J, Schulkin J. Knowledge opinions, and practice patterns of obstetrician-gynecologist regarding their patients’ use of alcohol. J Addiction Med. 2010;4(2):114-121.
20. Abel EL, Kruger M. What do physicians know and say about fetal alcohol syndrome: a survey of obstetricians pediatricians, and family medicine physicians. Alcohol Clin Exp Res. 1998;22(9):1951-1954.
21. Diekman S, Floyd R, Decoufle P, Schulkin J, Ebrahim S, Sokol R. A survey of obstetrician-gynecologists on their patients’ alcohol use during pregnancy. Obstet Gynecol. 2000;95(5):756-763.
22. Strandberg-Larsen K, Gronboek M, Andersen A, Andersen P, Olsen J. Alcohol drinking pattern during pregnancy and risk of infant mortality. Epidemiology. 2009;20(6):884-891.
23. Willford J, Leech S, Day N. Moderate prenatal alcohol exposure and cognitive status of children at age 10. Alcohol Clin Exp Res. 2006;30(6):1051-1059.
24. Richardson G, Ryan C, Willford J, Day N, Goldschmidt. Prenatal alcohol and marijuana exposure: Effects on neuropsychological outcomes at 10 years. Neurotoxicol Teratol. 2002;24(3):309-320.
25. Feldman H, Jones K, Lindsay S, et al. Prenatal alcohol exposure patterns and alcohol-related birth defects and growth deficiencies: a prospective study. Alcohol Clin Exp Res. 2012;36(4):670-676.
26. O’Leary C, Nassar N, Kurinczuk J, et al. Prenatal alcohol exposure and risk of birth defects. Pediatrics. 2010;126(4):e843-850.doi:10.1542/peds.2010-0256.
27. Abel E, Sokol R. A revised conservative estimate of the incidence of FAS and its economic its impact. Alcohol Clin Exp Res. 1991;15(3):514-524.
28. Lupton C. The financial impact of fetal alcohol syndrome. Fetal Alcohol Spectrum Disorders Center for Excellence. www.fasdcenter.samhsa.gov/publications/cost.cfm. Accessed December 14 2012.
29. Bailey B, Sokol R. Prenatal alcohol exposure and miscarriage stillbirth, preterm delivery, and sudden infant death syndrome. Alcohol Res Health. 2011;34(1):86-91.
30. Yelin R, Kot H, Yelin D, Fainsod A. Early molecular effects of ethanol during vertebrate embryogenesis. Differentiation. 2007;75(5):393-403.
31. Warren K, Hewitt B, Thomas J. Fetal alcohol spectrum disorders: research challenges and opportunities. Alcohol Res Health. 2011;34(1):4-15.
32. Ramanathan R, Wilkemeyer M, Mittal B, Perides G, Chamess ME. Alcohol inhibits cell-cell adhesion mediated by human L1. J Cell Biol. 1996;133(2):381-390.
33. Burd L, Hofer R. Biomarkers for detection of prenatal alcohol exposure: a critical review of fatty acid ethyl estsers in meconium. Birth Defects Res A Clin Mol Teratol. 2008;82(7):487-493.
34. Kulaga V, Pragst F, Fulga N, Koren G. Hair análisis of fatty acid esters in the detection of excessive drinking in the context of fetal alcohol spectrum disorders. Ther Drug Monit. 2009;31(2):261-266.
35. Sari Y, Gozes I. Brain deficits associated with fetal alcohol exposure may be protected in part, by peptides derived from activity-dependent neurotrophic factor and activity-dependent neuroprotective protein. Brain Res Rev. 2006;52(1):107-118.
36. Streissguth A, Bookstein F, Barr H, Sampson P, O’malley K, Young J. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25(4):228-238.
37. 19. Committee on Health Care for Underserved Women. American College of Obstetricians and Gynecologists. Committee Opinion No. 496: At-risk drinking and alcohol dependence: Obstetric and gynecologic implications. Obstet Gynecol. 2011;118(2 Pt 1):383-388.
38. Sokol R, Martier S, Ager J. The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol. 1989;160(4):863-868.
39. Chan A, Pristach E, Weite J, Russell M. Use of the TWEAK test in screening for alcoholism/ heavy drinking in three populations. Alcohol Clin Exp Res. 1993;17(6):1188-1192.
40. Floyd R, O’Connor M, Bertrand J, Sokol R. Reducing adverse outcomes from prenatal alcohol exposure: a clinical plan of action. Alcohol Clin Exp Res. 2006;30(8):1271-1275.
41. Miller W, Sanchez V. Motivating young adults for treatment and lifestyle change. In: Howard GS Nathan PE, eds. Alcohol use and misuse by young adults. Notre Dame, IN: University of Notre Dame Press; 1994:55–81.
42. Center for Disease Control and Prevention. Motivational intervention to reduce alcohol-exposed pregnancies—Florida Texas, and Virginia, 1997–2001. MMWR. 2003;52(19):441-444.
43. Chang G, McNamara T, Orav J, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):991-998.
44. Manwell L, Fleming M, Mundt M, Stauffacher E, Barry K. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention trial. Alcohol Clin Exp Res. 2000;24(10):1517-1524.
45. O’Connor M, Whaley S. Brief intervention for alcohol use by pregnant women. Am J Pub Health. 2007;97(2):252-258.
46. Mwansa-Kambafwile J, Rendall-Mkosi K, Jacobs R, Nel E, London L. Evaluation of a service provider short course for prevention of fetal alcohol syndrome. J Stud Alcohol Drugs. 2011;72(4):530-535.
47. American College of Obstetricians and Gynecologists. At-risk alcohol use screening and intervention. http://198.87.1.43/womenalcohol/index.html. Published 2011. Accessed December 16 2012.
Medical students learn early in their education that alcohol is a teratogen. Despite this widespread knowledge, many obstetricians counsel patients about the safety of low doses of alcohol in pregnancy.1 Indeed, the Royal College of Obstetricians and Gynaecologists’ position on this is, “while the safest approach may be to avoid any alcohol during pregnancy, it remains the case that there is no evidence of harm from low levels of alcohol consumption, defined as no more than one or two units of alcohol once or twice a week.”2
Like many providers, I was aware of this controversy, but it became truly personal when a beloved family member was diagnosed with fetal alcohol syndrome (FAS). In this paper, I will review some of the controversy regarding alcohol in pregnancy, highlight findings from the literature, provide tools for prevention, and identify new developments regarding this devastating, preventable condition.
Charlie
To know my nephew Charlie is to fall in love with my nephew Charlie. One of the happiest moments of my life was when I learned my brother and sister-in-law had adopted twins from Kazakhstan. When my little niece and nephew started their new life in the United States, certain medical issues seemed to merit additional attention. Although both were very small for their age and required significant nutritional support, Charlie seemed to be a bit more rambunctious and required additional supervision.
The children were fortunate enough to have incredibly loving, dedicated parents, who have access to exceptional medical care as residents of Philadelphia, Pennsylvania. After extensive testing, it became clear what was causing Charlie’s developmental delay; his pediatric team made the diagnosis of FAS. My brother and sister-in-law became incredibly well-read about this challenging disorder, and threw themselves into national advocacy work to help prevent this unnecessary tragedy.
Recent data point to teratogenicity, but media confuse the issue
Some recent media coverage3 of celebrities who apparently drank while pregnant was in response to an article in the Journal of Epidemiology and Community Health.4 The authors of this study concluded that, “at age 5 years, cohort members born to mothers who drank up to one to two drinks per week or per occasion during pregnancy were not at increased risk of clinically relevant behavioral difficulties or cognitive deficits, compared with children of mothers in the not-in-pregnancy group.”
This is certainly not the first occasion the popular press has covered a published study that seems to indicate no ill effects of alcohol use in pregnancy. A 2008 report by Kelly and colleagues,5 and its subsequent media coverage, prompted the Fetal Alcohol Spectrum Disorders Study Group to state that the panel of experts was “alarmed” by recent newspaper reports suggesting that light drinking during pregnancy may be beneficial for an unborn child.6 They noted misleading and irresponsible media reports of the findings, which suggested that 3-year-old children whose mothers drank “lightly” during pregnancy were not at risk for certain behavioral problems.
What the study authors proceeded to note, however (that the media did not mention), was that the light drinkers in their study had socioeconomic advantages, compared with nondrinkers.5 (Advantaged economic status is established to be beneficial for childhood development.) They also noted that the study involved preschool-aged children, stating “Generally the adverse effects of light drinking during pregnancy are subtle and may go undetected in young children. However, other group studies of more moderate or ‘social’ drinking levels during pregnancy have shown an adverse impact on multiple aspects of development through adolescence and young adulthood, even when important environmental factors are taken into account.” A sentence I thought was most compelling in their statement was, “It is an inconvenient fact of life that alcohol is a teratogen.” Now, this fact is well supported in the literature.7
There are animal studies regarding the use of “low-dose” or “moderate” alcohol in pregnancy that demonstrate adverse behavioral outcomes with exposure to even small doses of alcohol.8,9 It is an American tragedy that, according to the Centers for Disease Control and Prevention (CDC), rates of FAS in this country range from 0.2 to 2.0 cases per 1,000 live births. Indeed, the rates of fetal alcohol spectrum disorders (FASD) might be at least three times this rate.10 As is the case with other disorders, there are health disparities regarding the prevalence of this condition as well.11
FAS: A long history of preventable disease
1973: Identified. FAS was first described in a 1973 Lancet report, “Pattern of malformation in offspring of chronic alcoholic mothers.”12
1996: Call for prevention. In 1995, the US Surgeon General issued a statement regarding alcohol use in pregnancy, noting, “We do not know what, if any, amount of alcohol is safe.”13 In 1996, the Institute of Medicine released a paper calling FAS and FASD “completely preventable birth defects and neurodevelopmental abnormalities.”14
2000: The troubling effects gathered. The American Academy of Pediatrics (AAP) published a monograph on FAS in 2000, defining it as a constellation of physical, behavioral, and cognitive abnormalities.15
These features classically define FAS:
- dysmorphic facial features
- prenatal and postnatal growth abnormalities
- mental retardation.
Approximately 80% of children with this condition have:
- microcephaly
- behavioral abnormalities.
As many as 50% of affected children also exhibit:
- poor coordination
- hypotonia
- attention-deficit hyperactivity disorder
- decreased adipose tissue
- identifiable facial anomalies (such as maxillary hypoplasia, cleft palate, and micrognathia).
Also common:
- cardiac defects
- hemangiomas
- eye or ear abnormalities.
The AAP further noted that data current to the time (and still true today) did not support the concept of a safe level of alcohol consumption by pregnant women below which no damage to a fetus will occur.15

Alcohol intake during pregnancy puts the fetus at risk for cognitive and neuropsychological impairment and physical abnormalities, including dysmorphic facial features (such as micrognathia), restricted prenatal growth, cardiac defects, and eye and ear abnormalities. There is no threshold dose of alcohol that is safe during pregnancy, according to the American College of Obstetricians and Gynecologists.
Despite the knowledge we’ve gained, FAS persists
According to a 2006–2010 CDC analysis involving more than 345,000 women of reproductive age from all 50 states, 7.6% of pregnant women reported alcohol use and 1.4% (or 1 in 71) reported binge drinking (defined, respectively, as at least one alcoholic drink and four or more alcoholic drinks on one occasion in the past 30 days).16 The highest prevalence of obstetric alcohol consumption occurs in women who are:
- aged 35 to 44 years
- white
- college graduates
- employed.
The problem may be bigger than reported. The incidences of alcohol and binge drinking found in the CDC report include women’s self-report—but women drink alcohol without knowing they’re pregnant. Only 40% of women realize they’re pregnant at 4 weeks of gestation, a critical time for organogenesis, and approximately half of all births are unplanned.9
When my brother and sister-in law adopted my beautiful niece and nephew, they were very aware of the risk for conditions like FAS. In an evaluation of 71 children adopted from Eastern Europe at 5 years of age, FAS was diagnosed in 30% of children and “partial FAS” in another 9%.17 Birth defects attributed to alcohol were present in 11% of the children.
Are women’s health providers up to date on FAS education?
In recognition of alcohol’s potentially life-altering consequences for the developing fetus, the American College of Obstetricians and Gynecologists (ACOG) produced an FASD prevention tool kit in 2006 and published a 2011 committee opinion on at-risk drinking and alcohol dependence and their implications for obstetrics and gynecology.18,19 Both guidelines direct clinicians to advise patients to abstain from alcohol during pregnancy.
Results from a 2010 survey of 800 ACOG fellows revealed that only 78% of obstetricians advised abstinence from alcohol during pregnancy. Fifty-eight percent of respondents did not use a validated screening tool for alcohol use in their pregnant patients, and only 72% felt prepared to screen for risky or hazardous drinking.19 (Most were unaware of the ACOG tool kit, which had been published several years earlier.)
In a survey of pediatricians, obstetricians, and family physicians, clinicians said that about 67% of their patients asked about alcohol use in pregnancy, with about 2% of those patients specifically mentioning FAS. About 41% of these same physicians erroneously placed the threshold for FAS at one to three drinks per day,20 when in fact there is no threshold of drinking that has been proven to be safe.
A survey of 1,000 actively practicing ACOG fellows revealed that, while 97% of obstetricians routinely asked their patients about alcohol use, only 20% of providers reported to their patients that abstinence was safest, and 4% of providers didn’t believe that consumption of eight or more drinks weekly posed fetal risk.21
How can we educate our patients about the dangers of alcohol in pregnancy?
Fetal death. A recent Danish study of 79,216 pregnant women revealed that 45% had consumed some alcohol during pregnancy. Two percent reported at least four drinks per week, and 25% admitted to binge drinking during pregnancy. Term infants born to women in the latter two groups had increased neonatal mortality, with hazard ratios of 3.56 (95% confidence interval [CI], 1.15–8.43) and 2.69 (95% CI, 1.27–5.69), respectively.22
Decreased cognitive status. A study by Willford and colleagues evaluated the relationship between prenatal alcohol exposure and cognitive status of 1,360 10-year-old children.23 The authors utilized the Stanford-Binet Intelligence Test, including the composite scores and verbal, abstract/visual, quantitative, and short-term memory scores. After controlling for other variables, among African American offspring they found that, for each additional drink, the average composite score decreased by 1.9 points. This difference was more striking for second-trimester use, and was significant even for one drink daily versus abstention from alcohol.
Impaired neuropsychological development. Another study evaluating light to moderate amounts of prenatal alcohol exposure in 10- and 11-year-old children found significantly worse scores regarding a number of neuropsychological developmental assessments.24
No threshold dose of causation. Results of a 2012 prospective study in California, with data collected on 992 subjects from 1978 until 2005, revealed that many physical FAS features, including microcephaly, smooth philtrum, and thin vermillion border; reduced birth length; and reduced birth weight, were associated with alcohol exposure at specific gestational ages, and were dose-related.25 This paper didn’t reveal any evidence of a threshold dose of causation.
Neurobehavioral outcomes of FAS are not always considered
Another recent study that the media recently highlighted as finding “no association between low or moderate prenatal alcohol exposure and birth defects” was by O’Leary and colleagues.26 Like other similarly limited studies, this one involved only children younger than 6 years and didn’t assess any of the important neurobehavioral outcomes of FAS.
FAS encompasses much more than visible birth defects. As the aforementioned ACOG tool kit stated, “For every child born with FAS, many more children are born with neurobehavioral deficits caused by alcohol exposure but without the physical characteristics of FAS.”
The costs of FAS are felt with dollars, too
The financial cost to our nation is extraordinary. In 1991, Abel and Sokol estimated the incremental annual cost of treating FAS at nearly $75 million, with about three-quarters of that cost associated with FAS cases involving mental retardation.27
A 2002 assessment estimated the lifetime cost for each individual with FAS (adjusting for the change in the cost of medical care services, lost productivity, and inflation) at $2 million. This figure consists of $1.6 million for medical treatment, special education, and residential care for persons with mental retardation, and $0.4 million for productivity losses.28
Where human studies fall short, animal studies can help elucidate causation
Unquestionably, there are flaws in the existing literature on the causation of FAS. Many studies rely on self-reporting by pregnant women, and underreporting in these cases is a real concern. There often are other confounders potentially negatively affecting fetal development, making it difficult to differentiate causation. The animal studies that don’t share these limitations do suggest a causal relationship between antenatal alcohol exposure and poor obstetric outcomes, however.29 These studies suggest mechanisms such as altered gene expression, oxidative stress, and apoptosis (programmed cell death).30
Warren, Hewitt, and Thomas describe how intrauterine alcohol exposure interferes with the function of L1CAM, the L1 cell-adhesion molecule.31 They noted that just one drink could interfere with the ability of L1CAM to mediate cell adhesion and axonal growth. Prenatal alcohol exposure is also thought to contribute to interference in neurotransmitter and N-methyl-D-aspartate receptor coupling, which may have potential therapeutic implications.32
Considerations in FAS identification and treatment
There is a potential to identify alcohol exposure in the womb. The majority of ingested alcohol is eventually converted to carbon dioxide and water in both maternal and fetal circulations, which has hampered the identification of biomarkers for clinical use in FAS. Fatty acid ethyl esters (FAEEs), nonoxidative metabolites of ethanol, may prove to be such markers.33 FAEEs have been measured in a variety of tissues, including blood and meconium. FAEEs can be measured in both neonatal and maternal hair samples.
A study evaluating the utility of such testing in 324 at-risk pregnancies revealed 90% sensitivity and 90% specificity for identifying “excessive drinking” using a cutoff of 0.5 ng/mg.34
Research shows potential therapeutic approaches during pregnancy. While the use of biomarkers has the potential to assist with the identification of at-risk newborns, it merely identifies past alcohol use; it doesn’t necessarily permit identification and prevention of the known negative pediatric sequelae. Preliminary animal studies reveal the potential benefit of neuroprotective peptides to prevent brain damage in alcohol-exposed mice.35 Further research is ongoing.
Treatment: The earlier the better
Early diagnosis and a positive environment improve outcomes. It is well established that early intervention improves outcomes. One comprehensive review of 415 patients with FAS noted troubling outcomes in general for adolescents and adults.36 Over their life spans, the prevalence of such outcomes was:
- 61% for disrupted school experiences
- 60% for trouble with the law
- 50% for confinement (in detention, jail, prison, or a psychiatric or alcohol/drug inpatient setting)
- 49% for inappropriate sexual behaviors on repeated occasions
- 35% for alcohol/drug problems.
The odds of escaping these adverse life outcomes are increased up to fourfold when the individual receives a FAS or FASD diagnosis at an earlier age and is reared in a stable environment.36
Barrier to treatment: A mother’s guilt. One of the challenges I’ve learned from my sister-in-law is the stigma mothers face when they bring their child in for services once the diagnosis of FAS is suspected. While adoptive mothers obviously can’t be held accountable for the intrauterine environment to which a fetus is exposed, the same can’t be said of biologic mothers. Therefore, there is a real risk that a mother who is unwilling or unable to face the potentially devastating news that her baby’s issues might be related to choices she made during pregnancy, might not bring her child in for necessary assessment and treatment. Therefore, prevention is a key proponent of treatment.
Prevent FAS: Provide contraception, screen for alcohol use, intervene
While ObGyns aren’t likely to diagnose many children with FAS, we are in an excellent position to try to prevent this tragedy through our counseling of reproductive-aged women. I suspect that most obstetricians spend a considerable amount of time discussing much less frequent obstetric sequelae, such as listeriosis, in the prenatal care setting. Validated alcohol screening tools take moments to administer, and once patients who might have alcohol problems are identified, either a serious discussion about contraception or an honest discussion of FAS may be appropriate. There have been a number of screening tools developed.
The CAGE screen is frequently taught in medical schools, but it isn’t as sensitive for women or minorities.19
The T-ACE (Tolerance, Annoyed, Cut Down, Eye-opener) tool involves four questions that take less than 1 minute to administer (FIGURE 1).39
TWEAK is another potential tool identified by Russell and colleagues (Tolerance, Worry, Eye opener, Amnesia, and Cut down in drinking).39 Other methods utilized include an AUDIT screen and a CRAFFT screen.40 Regardless of which tool is utilized, screening is not time-consuming and is better than merely inquiring about alcohol consumption in general.
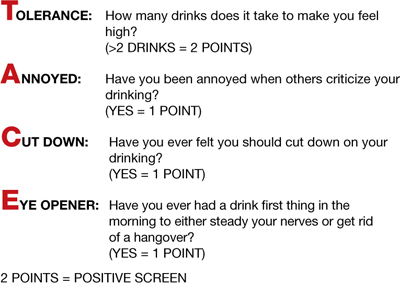
FIGURE 1 T-ACE validated alcohol screening tool
Source: American College of Obstetricians and Gynecologists. At risk drinking and illicit drug use: Ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2008;112(6):1449–1460.
When alcohol use is found, intervene
Once patients with at-risk behavior are identified, obstetric staff should offer brief interventions to influence problem drinking. Miller and Sanchez summarized the key elements that were most successful in these programs with the acronym FRAMES: Feedback, Responsibility, Advice, Menu, Empathy, Self-efficacy (FIGURE 2).41 This approach has been formally evaluated in the CDC’s multisite pilot study entitled Project CHOICES.42
In this motivational intervention, sexually active, fertile women of reproductive age underwent up to four motivational counseling sessions and one visit to a provider. At 6 months, 69% of women reduced their risk for an alcohol-exposed pregnancy—although the women who drank the least amount had the greatest benefit, primarily by choosing effective contraception, but also by reducing alcohol intake.
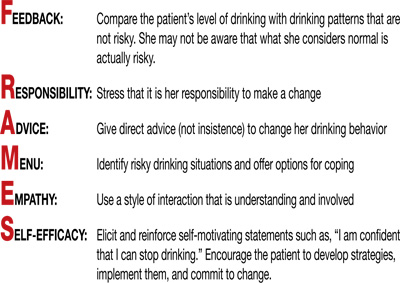
FIGURE 2 FRAMES model to deliver brief interventions
Source: American College of Obstetricians and Gynecologists. Drinking and reproductive health: A fetal alcohol spectrum disorders prevention tool kit. Washington, DC: ACOG; 2006.
A single, brief intervention is effective in already-pregnant women. Chang and colleagues conducted a randomized trial of a single-session brief intervention given to pregnant women with positive T-ACE screens and their partners (FIGURE 3).43 Either the study nurse or physician participated in the intervention, and each single session took 25 minutes on average. The pregnant women with the highest level of alcohol use reduced their drinking the most, and this effect was even larger when their partners participated. Other studies of brief interventions showed similar benefits.44,45
Another study evaluating a brief intervention involving training of health-care providers to improve screening rates revealed improved detection and therapy among at-risk patients.46
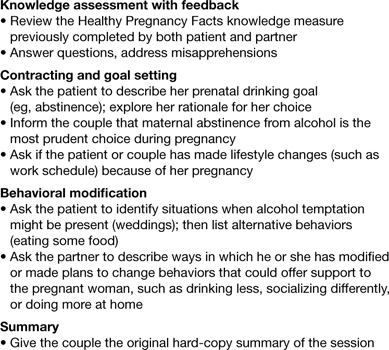
FIGURE 3 Single session, 25-minute intervention for patients and their partners
Source: Chang G, McNamara T, Orav J, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):991–998.
FAS prevention begins with routine counseling and contraception
Although FAS is often thought of in relation to obstetric populations, appointments for preconception counseling or routine health maintenance among women of reproductive age are an essential tool in FAS prevention. As previously mentioned, since approximately half of all pregnancies in this country are unplanned, long-acting reversible contraception is widely available to facilitate improved family planning.
Other contraceptive options also should be discussed. ACOG has teamed up with the CDC to develop a phone app for providers to use at the patient’s bedside to assist with identification and treatment of women at risk for alcohol use during pregnancy.47
The stakes are high, it’s time to step up
As obstetricians, we are powerless to prevent many conditions—such as vasa previa, acute fatty liver of pregnancy, and amniotic band syndrome. FAS is 100% preventable.
There aren’t that many proven teratogens in our profession, and there are none that involve behavior that is more socially acceptable than alcohol consumption. It is time for our profession to encourage women to appreciate how small a percentage of one’s life is spent pregnant, how many more years there are to enjoy an occasional cocktail, and how very high the stakes are during this important period of their lives. Oh, how I wish someone had been able to communicate all of this to sweet Charlie’s biologic mother. I am so grateful he’s getting the exceptional care he’s getting and very optimistic regarding his future. I only hope others in his situation are given the same opportunities.
Prenatal counseling
Louise Wilkins-Haug, MD, PhD (January 2008)
Prevention of fetal alcohol syndrome requires routine screening of all women of reproductive age
We want to hear from you! Tell us what you think.
Medical students learn early in their education that alcohol is a teratogen. Despite this widespread knowledge, many obstetricians counsel patients about the safety of low doses of alcohol in pregnancy.1 Indeed, the Royal College of Obstetricians and Gynaecologists’ position on this is, “while the safest approach may be to avoid any alcohol during pregnancy, it remains the case that there is no evidence of harm from low levels of alcohol consumption, defined as no more than one or two units of alcohol once or twice a week.”2
Like many providers, I was aware of this controversy, but it became truly personal when a beloved family member was diagnosed with fetal alcohol syndrome (FAS). In this paper, I will review some of the controversy regarding alcohol in pregnancy, highlight findings from the literature, provide tools for prevention, and identify new developments regarding this devastating, preventable condition.
Charlie
To know my nephew Charlie is to fall in love with my nephew Charlie. One of the happiest moments of my life was when I learned my brother and sister-in-law had adopted twins from Kazakhstan. When my little niece and nephew started their new life in the United States, certain medical issues seemed to merit additional attention. Although both were very small for their age and required significant nutritional support, Charlie seemed to be a bit more rambunctious and required additional supervision.
The children were fortunate enough to have incredibly loving, dedicated parents, who have access to exceptional medical care as residents of Philadelphia, Pennsylvania. After extensive testing, it became clear what was causing Charlie’s developmental delay; his pediatric team made the diagnosis of FAS. My brother and sister-in-law became incredibly well-read about this challenging disorder, and threw themselves into national advocacy work to help prevent this unnecessary tragedy.
Recent data point to teratogenicity, but media confuse the issue
Some recent media coverage3 of celebrities who apparently drank while pregnant was in response to an article in the Journal of Epidemiology and Community Health.4 The authors of this study concluded that, “at age 5 years, cohort members born to mothers who drank up to one to two drinks per week or per occasion during pregnancy were not at increased risk of clinically relevant behavioral difficulties or cognitive deficits, compared with children of mothers in the not-in-pregnancy group.”
This is certainly not the first occasion the popular press has covered a published study that seems to indicate no ill effects of alcohol use in pregnancy. A 2008 report by Kelly and colleagues,5 and its subsequent media coverage, prompted the Fetal Alcohol Spectrum Disorders Study Group to state that the panel of experts was “alarmed” by recent newspaper reports suggesting that light drinking during pregnancy may be beneficial for an unborn child.6 They noted misleading and irresponsible media reports of the findings, which suggested that 3-year-old children whose mothers drank “lightly” during pregnancy were not at risk for certain behavioral problems.
What the study authors proceeded to note, however (that the media did not mention), was that the light drinkers in their study had socioeconomic advantages, compared with nondrinkers.5 (Advantaged economic status is established to be beneficial for childhood development.) They also noted that the study involved preschool-aged children, stating “Generally the adverse effects of light drinking during pregnancy are subtle and may go undetected in young children. However, other group studies of more moderate or ‘social’ drinking levels during pregnancy have shown an adverse impact on multiple aspects of development through adolescence and young adulthood, even when important environmental factors are taken into account.” A sentence I thought was most compelling in their statement was, “It is an inconvenient fact of life that alcohol is a teratogen.” Now, this fact is well supported in the literature.7
There are animal studies regarding the use of “low-dose” or “moderate” alcohol in pregnancy that demonstrate adverse behavioral outcomes with exposure to even small doses of alcohol.8,9 It is an American tragedy that, according to the Centers for Disease Control and Prevention (CDC), rates of FAS in this country range from 0.2 to 2.0 cases per 1,000 live births. Indeed, the rates of fetal alcohol spectrum disorders (FASD) might be at least three times this rate.10 As is the case with other disorders, there are health disparities regarding the prevalence of this condition as well.11
FAS: A long history of preventable disease
1973: Identified. FAS was first described in a 1973 Lancet report, “Pattern of malformation in offspring of chronic alcoholic mothers.”12
1996: Call for prevention. In 1995, the US Surgeon General issued a statement regarding alcohol use in pregnancy, noting, “We do not know what, if any, amount of alcohol is safe.”13 In 1996, the Institute of Medicine released a paper calling FAS and FASD “completely preventable birth defects and neurodevelopmental abnormalities.”14
2000: The troubling effects gathered. The American Academy of Pediatrics (AAP) published a monograph on FAS in 2000, defining it as a constellation of physical, behavioral, and cognitive abnormalities.15
These features classically define FAS:
- dysmorphic facial features
- prenatal and postnatal growth abnormalities
- mental retardation.
Approximately 80% of children with this condition have:
- microcephaly
- behavioral abnormalities.
As many as 50% of affected children also exhibit:
- poor coordination
- hypotonia
- attention-deficit hyperactivity disorder
- decreased adipose tissue
- identifiable facial anomalies (such as maxillary hypoplasia, cleft palate, and micrognathia).
Also common:
- cardiac defects
- hemangiomas
- eye or ear abnormalities.
The AAP further noted that data current to the time (and still true today) did not support the concept of a safe level of alcohol consumption by pregnant women below which no damage to a fetus will occur.15

Alcohol intake during pregnancy puts the fetus at risk for cognitive and neuropsychological impairment and physical abnormalities, including dysmorphic facial features (such as micrognathia), restricted prenatal growth, cardiac defects, and eye and ear abnormalities. There is no threshold dose of alcohol that is safe during pregnancy, according to the American College of Obstetricians and Gynecologists.
Despite the knowledge we’ve gained, FAS persists
According to a 2006–2010 CDC analysis involving more than 345,000 women of reproductive age from all 50 states, 7.6% of pregnant women reported alcohol use and 1.4% (or 1 in 71) reported binge drinking (defined, respectively, as at least one alcoholic drink and four or more alcoholic drinks on one occasion in the past 30 days).16 The highest prevalence of obstetric alcohol consumption occurs in women who are:
- aged 35 to 44 years
- white
- college graduates
- employed.
The problem may be bigger than reported. The incidences of alcohol and binge drinking found in the CDC report include women’s self-report—but women drink alcohol without knowing they’re pregnant. Only 40% of women realize they’re pregnant at 4 weeks of gestation, a critical time for organogenesis, and approximately half of all births are unplanned.9
When my brother and sister-in law adopted my beautiful niece and nephew, they were very aware of the risk for conditions like FAS. In an evaluation of 71 children adopted from Eastern Europe at 5 years of age, FAS was diagnosed in 30% of children and “partial FAS” in another 9%.17 Birth defects attributed to alcohol were present in 11% of the children.
Are women’s health providers up to date on FAS education?
In recognition of alcohol’s potentially life-altering consequences for the developing fetus, the American College of Obstetricians and Gynecologists (ACOG) produced an FASD prevention tool kit in 2006 and published a 2011 committee opinion on at-risk drinking and alcohol dependence and their implications for obstetrics and gynecology.18,19 Both guidelines direct clinicians to advise patients to abstain from alcohol during pregnancy.
Results from a 2010 survey of 800 ACOG fellows revealed that only 78% of obstetricians advised abstinence from alcohol during pregnancy. Fifty-eight percent of respondents did not use a validated screening tool for alcohol use in their pregnant patients, and only 72% felt prepared to screen for risky or hazardous drinking.19 (Most were unaware of the ACOG tool kit, which had been published several years earlier.)
In a survey of pediatricians, obstetricians, and family physicians, clinicians said that about 67% of their patients asked about alcohol use in pregnancy, with about 2% of those patients specifically mentioning FAS. About 41% of these same physicians erroneously placed the threshold for FAS at one to three drinks per day,20 when in fact there is no threshold of drinking that has been proven to be safe.
A survey of 1,000 actively practicing ACOG fellows revealed that, while 97% of obstetricians routinely asked their patients about alcohol use, only 20% of providers reported to their patients that abstinence was safest, and 4% of providers didn’t believe that consumption of eight or more drinks weekly posed fetal risk.21
How can we educate our patients about the dangers of alcohol in pregnancy?
Fetal death. A recent Danish study of 79,216 pregnant women revealed that 45% had consumed some alcohol during pregnancy. Two percent reported at least four drinks per week, and 25% admitted to binge drinking during pregnancy. Term infants born to women in the latter two groups had increased neonatal mortality, with hazard ratios of 3.56 (95% confidence interval [CI], 1.15–8.43) and 2.69 (95% CI, 1.27–5.69), respectively.22
Decreased cognitive status. A study by Willford and colleagues evaluated the relationship between prenatal alcohol exposure and cognitive status of 1,360 10-year-old children.23 The authors utilized the Stanford-Binet Intelligence Test, including the composite scores and verbal, abstract/visual, quantitative, and short-term memory scores. After controlling for other variables, among African American offspring they found that, for each additional drink, the average composite score decreased by 1.9 points. This difference was more striking for second-trimester use, and was significant even for one drink daily versus abstention from alcohol.
Impaired neuropsychological development. Another study evaluating light to moderate amounts of prenatal alcohol exposure in 10- and 11-year-old children found significantly worse scores regarding a number of neuropsychological developmental assessments.24
No threshold dose of causation. Results of a 2012 prospective study in California, with data collected on 992 subjects from 1978 until 2005, revealed that many physical FAS features, including microcephaly, smooth philtrum, and thin vermillion border; reduced birth length; and reduced birth weight, were associated with alcohol exposure at specific gestational ages, and were dose-related.25 This paper didn’t reveal any evidence of a threshold dose of causation.
Neurobehavioral outcomes of FAS are not always considered
Another recent study that the media recently highlighted as finding “no association between low or moderate prenatal alcohol exposure and birth defects” was by O’Leary and colleagues.26 Like other similarly limited studies, this one involved only children younger than 6 years and didn’t assess any of the important neurobehavioral outcomes of FAS.
FAS encompasses much more than visible birth defects. As the aforementioned ACOG tool kit stated, “For every child born with FAS, many more children are born with neurobehavioral deficits caused by alcohol exposure but without the physical characteristics of FAS.”
The costs of FAS are felt with dollars, too
The financial cost to our nation is extraordinary. In 1991, Abel and Sokol estimated the incremental annual cost of treating FAS at nearly $75 million, with about three-quarters of that cost associated with FAS cases involving mental retardation.27
A 2002 assessment estimated the lifetime cost for each individual with FAS (adjusting for the change in the cost of medical care services, lost productivity, and inflation) at $2 million. This figure consists of $1.6 million for medical treatment, special education, and residential care for persons with mental retardation, and $0.4 million for productivity losses.28
Where human studies fall short, animal studies can help elucidate causation
Unquestionably, there are flaws in the existing literature on the causation of FAS. Many studies rely on self-reporting by pregnant women, and underreporting in these cases is a real concern. There often are other confounders potentially negatively affecting fetal development, making it difficult to differentiate causation. The animal studies that don’t share these limitations do suggest a causal relationship between antenatal alcohol exposure and poor obstetric outcomes, however.29 These studies suggest mechanisms such as altered gene expression, oxidative stress, and apoptosis (programmed cell death).30
Warren, Hewitt, and Thomas describe how intrauterine alcohol exposure interferes with the function of L1CAM, the L1 cell-adhesion molecule.31 They noted that just one drink could interfere with the ability of L1CAM to mediate cell adhesion and axonal growth. Prenatal alcohol exposure is also thought to contribute to interference in neurotransmitter and N-methyl-D-aspartate receptor coupling, which may have potential therapeutic implications.32
Considerations in FAS identification and treatment
There is a potential to identify alcohol exposure in the womb. The majority of ingested alcohol is eventually converted to carbon dioxide and water in both maternal and fetal circulations, which has hampered the identification of biomarkers for clinical use in FAS. Fatty acid ethyl esters (FAEEs), nonoxidative metabolites of ethanol, may prove to be such markers.33 FAEEs have been measured in a variety of tissues, including blood and meconium. FAEEs can be measured in both neonatal and maternal hair samples.
A study evaluating the utility of such testing in 324 at-risk pregnancies revealed 90% sensitivity and 90% specificity for identifying “excessive drinking” using a cutoff of 0.5 ng/mg.34
Research shows potential therapeutic approaches during pregnancy. While the use of biomarkers has the potential to assist with the identification of at-risk newborns, it merely identifies past alcohol use; it doesn’t necessarily permit identification and prevention of the known negative pediatric sequelae. Preliminary animal studies reveal the potential benefit of neuroprotective peptides to prevent brain damage in alcohol-exposed mice.35 Further research is ongoing.
Treatment: The earlier the better
Early diagnosis and a positive environment improve outcomes. It is well established that early intervention improves outcomes. One comprehensive review of 415 patients with FAS noted troubling outcomes in general for adolescents and adults.36 Over their life spans, the prevalence of such outcomes was:
- 61% for disrupted school experiences
- 60% for trouble with the law
- 50% for confinement (in detention, jail, prison, or a psychiatric or alcohol/drug inpatient setting)
- 49% for inappropriate sexual behaviors on repeated occasions
- 35% for alcohol/drug problems.
The odds of escaping these adverse life outcomes are increased up to fourfold when the individual receives a FAS or FASD diagnosis at an earlier age and is reared in a stable environment.36
Barrier to treatment: A mother’s guilt. One of the challenges I’ve learned from my sister-in-law is the stigma mothers face when they bring their child in for services once the diagnosis of FAS is suspected. While adoptive mothers obviously can’t be held accountable for the intrauterine environment to which a fetus is exposed, the same can’t be said of biologic mothers. Therefore, there is a real risk that a mother who is unwilling or unable to face the potentially devastating news that her baby’s issues might be related to choices she made during pregnancy, might not bring her child in for necessary assessment and treatment. Therefore, prevention is a key proponent of treatment.
Prevent FAS: Provide contraception, screen for alcohol use, intervene
While ObGyns aren’t likely to diagnose many children with FAS, we are in an excellent position to try to prevent this tragedy through our counseling of reproductive-aged women. I suspect that most obstetricians spend a considerable amount of time discussing much less frequent obstetric sequelae, such as listeriosis, in the prenatal care setting. Validated alcohol screening tools take moments to administer, and once patients who might have alcohol problems are identified, either a serious discussion about contraception or an honest discussion of FAS may be appropriate. There have been a number of screening tools developed.
The CAGE screen is frequently taught in medical schools, but it isn’t as sensitive for women or minorities.19
The T-ACE (Tolerance, Annoyed, Cut Down, Eye-opener) tool involves four questions that take less than 1 minute to administer (FIGURE 1).39
TWEAK is another potential tool identified by Russell and colleagues (Tolerance, Worry, Eye opener, Amnesia, and Cut down in drinking).39 Other methods utilized include an AUDIT screen and a CRAFFT screen.40 Regardless of which tool is utilized, screening is not time-consuming and is better than merely inquiring about alcohol consumption in general.
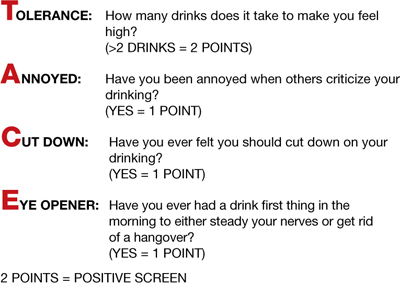
FIGURE 1 T-ACE validated alcohol screening tool
Source: American College of Obstetricians and Gynecologists. At risk drinking and illicit drug use: Ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2008;112(6):1449–1460.
When alcohol use is found, intervene
Once patients with at-risk behavior are identified, obstetric staff should offer brief interventions to influence problem drinking. Miller and Sanchez summarized the key elements that were most successful in these programs with the acronym FRAMES: Feedback, Responsibility, Advice, Menu, Empathy, Self-efficacy (FIGURE 2).41 This approach has been formally evaluated in the CDC’s multisite pilot study entitled Project CHOICES.42
In this motivational intervention, sexually active, fertile women of reproductive age underwent up to four motivational counseling sessions and one visit to a provider. At 6 months, 69% of women reduced their risk for an alcohol-exposed pregnancy—although the women who drank the least amount had the greatest benefit, primarily by choosing effective contraception, but also by reducing alcohol intake.
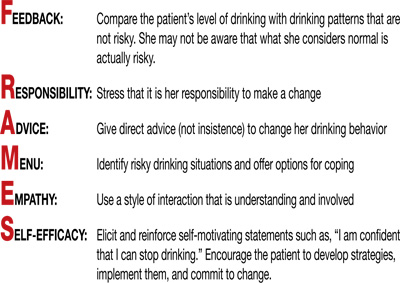
FIGURE 2 FRAMES model to deliver brief interventions
Source: American College of Obstetricians and Gynecologists. Drinking and reproductive health: A fetal alcohol spectrum disorders prevention tool kit. Washington, DC: ACOG; 2006.
A single, brief intervention is effective in already-pregnant women. Chang and colleagues conducted a randomized trial of a single-session brief intervention given to pregnant women with positive T-ACE screens and their partners (FIGURE 3).43 Either the study nurse or physician participated in the intervention, and each single session took 25 minutes on average. The pregnant women with the highest level of alcohol use reduced their drinking the most, and this effect was even larger when their partners participated. Other studies of brief interventions showed similar benefits.44,45
Another study evaluating a brief intervention involving training of health-care providers to improve screening rates revealed improved detection and therapy among at-risk patients.46
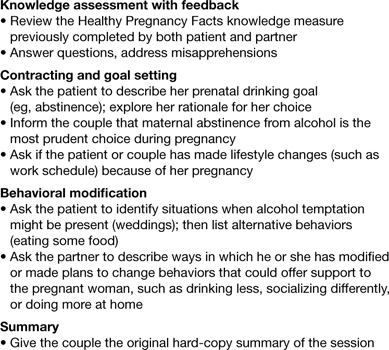
FIGURE 3 Single session, 25-minute intervention for patients and their partners
Source: Chang G, McNamara T, Orav J, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):991–998.
FAS prevention begins with routine counseling and contraception
Although FAS is often thought of in relation to obstetric populations, appointments for preconception counseling or routine health maintenance among women of reproductive age are an essential tool in FAS prevention. As previously mentioned, since approximately half of all pregnancies in this country are unplanned, long-acting reversible contraception is widely available to facilitate improved family planning.
Other contraceptive options also should be discussed. ACOG has teamed up with the CDC to develop a phone app for providers to use at the patient’s bedside to assist with identification and treatment of women at risk for alcohol use during pregnancy.47
The stakes are high, it’s time to step up
As obstetricians, we are powerless to prevent many conditions—such as vasa previa, acute fatty liver of pregnancy, and amniotic band syndrome. FAS is 100% preventable.
There aren’t that many proven teratogens in our profession, and there are none that involve behavior that is more socially acceptable than alcohol consumption. It is time for our profession to encourage women to appreciate how small a percentage of one’s life is spent pregnant, how many more years there are to enjoy an occasional cocktail, and how very high the stakes are during this important period of their lives. Oh, how I wish someone had been able to communicate all of this to sweet Charlie’s biologic mother. I am so grateful he’s getting the exceptional care he’s getting and very optimistic regarding his future. I only hope others in his situation are given the same opportunities.
Prenatal counseling
Louise Wilkins-Haug, MD, PhD (January 2008)
Prevention of fetal alcohol syndrome requires routine screening of all women of reproductive age
We want to hear from you! Tell us what you think.
1. Baram M. Moms-to-be get mixed messages on drinking. ABC News. http://abcnews.go.com/Health/story?id=2654849&page=1#.UM9l-RyeARY. Published November 15 2006. Accessed December 14, 2012.
2. Royal College of Obstetricians and Gynaecologists. Alcohol consumption and the outcomes of pregnancy (RCOG Statement No. 5). London UK: Royal College of Obstetricians and Gynaecologists. January 3, 2006.
3. Pearson C. Alcohol during pregnancy: How dangerous is it really? The Huffington Post. http://www.huffingtonpost.com/2011/04/06/alcohol-during-pregnancy_n_845103.html. Published April 6 2011. Updated September 16, 2011. Accessed December 14, 2012.
4. Kelly YJ, Sacker A, Gray R, et al. Light drinking during pregnancy: still no increased risk for socioemotional difficulties or cognitive deficits at 5 years of age? J Epidemiol Community Health. 2012;66(1):41-48.Epub Oct 5, 2010.
5. Kelly Y, Sacker A, Gray R, Kelly J, Wolke D, Quigley MA. Light drinking in pregnancy a risk for behavioural problems and cognitive deficits at 3 years of age? Int J Epidemiol. 2009;38(1):129-140.Epub Oct 30, 2008.
6. Zhou F. Fetal Alcohol Spectrum Disorders Study Group (FASDSG). Research Society on Alcoholism. http://rsoa.org/fas.html. Updated September 9 2010. Accessed December 14, 2012.
7. Kelly S, Day N, Streissguth AP. Effects of prenatal alcohol exposure on social behavior in humans and other species. Neurotoxicol Teratol. 2000;22(2):143-149.
8. Vaglenova J, Petkov V. Fetal alcohol effects in rats exposed pre-and postnatally to a low dose of ethanol. Alcohol Clin Exp Res. 1998;22(3):697-703.
9. Schneider M, Moore C, Kraemer G. Moderate alcohol during pregnancy: learning and behavior in adolescent rhesus monkeys. Alcohol Clin Exp Res. 2001;25(9):1383-1392.
10. Centers for Disease Control and Prevention. Fetal alcohol spectrum disorders. Data and statistics in the United States. http://www.cdc.gov/ncbddd/fasd/data.html. Updated August 16 2012. Accessed December 14, 2012.
11. Egeland G, Perham-Hestere KA, Gessner BD, Ingle D, Berner JE, Middaugh J. Fetal alcohol syndrome in Alaska 1977 through 1992: an administrative prevalence derived from multiple data sources. Am J Pub Health. 1998;88(5):781-786.
12. Jones K, Smith D, Ulleland C, Streissguth A. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1(7815):1267-1271.
13. Institute of Medicine. Fetal alcohol syndrome: diagnosis epidemiology, prevention, and treatment (1996). http://www.come-over.to/FAS/IOMsummary.htm. Accessed December 14, 2012.
14. Committee of Substance Abuse and Committee on Children with Disabilities. American Academy of Pediatrics. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106(2):358-361.
15. US Department of Health & Human Services. US Surgeon General releases advisory on alcohol use in pregnancy. http://www.surgeongeneral.gov/news/2005/02/sg02222005.html. Published February 21 2005. Accessed December 13, 2012.
16. Centers for Disease Control and Prevention. Alcohol use and binge drinking among women of childbearing age–United States 2006–2010. MMWR. 2012;61(28):534-538.http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6128a4.htm?s_cid=mm6128a4_w. Accessed December 17, 2012.
17. Landgren M, Svensson L, Stromland K, Gronlund M. Prenatal alcohol exposure and neurodvelopmental disorders in children adopted from Eastern Europe. Pediatrics. 2010;125(5):e1178-1185.doi:10.1542/peds.2009-0712.
18. American College of Obstetricians and Gynecologists. Drinking and reproductive health: A fetal alcohol spectrum disorders prevention tool kit. http://www.acog.org/~/media/Departments/Tobacco%20Alcohol%20and%20Substance%20Abuse/FASDToolKit.pdf?dmc=1&ts=20121217T1504384811. Published 2006. Accessed December 14 2012.
19. Anderson B, Dang E, Floyd R, Sokol R, Mahoney J, Schulkin J. Knowledge opinions, and practice patterns of obstetrician-gynecologist regarding their patients’ use of alcohol. J Addiction Med. 2010;4(2):114-121.
20. Abel EL, Kruger M. What do physicians know and say about fetal alcohol syndrome: a survey of obstetricians pediatricians, and family medicine physicians. Alcohol Clin Exp Res. 1998;22(9):1951-1954.
21. Diekman S, Floyd R, Decoufle P, Schulkin J, Ebrahim S, Sokol R. A survey of obstetrician-gynecologists on their patients’ alcohol use during pregnancy. Obstet Gynecol. 2000;95(5):756-763.
22. Strandberg-Larsen K, Gronboek M, Andersen A, Andersen P, Olsen J. Alcohol drinking pattern during pregnancy and risk of infant mortality. Epidemiology. 2009;20(6):884-891.
23. Willford J, Leech S, Day N. Moderate prenatal alcohol exposure and cognitive status of children at age 10. Alcohol Clin Exp Res. 2006;30(6):1051-1059.
24. Richardson G, Ryan C, Willford J, Day N, Goldschmidt. Prenatal alcohol and marijuana exposure: Effects on neuropsychological outcomes at 10 years. Neurotoxicol Teratol. 2002;24(3):309-320.
25. Feldman H, Jones K, Lindsay S, et al. Prenatal alcohol exposure patterns and alcohol-related birth defects and growth deficiencies: a prospective study. Alcohol Clin Exp Res. 2012;36(4):670-676.
26. O’Leary C, Nassar N, Kurinczuk J, et al. Prenatal alcohol exposure and risk of birth defects. Pediatrics. 2010;126(4):e843-850.doi:10.1542/peds.2010-0256.
27. Abel E, Sokol R. A revised conservative estimate of the incidence of FAS and its economic its impact. Alcohol Clin Exp Res. 1991;15(3):514-524.
28. Lupton C. The financial impact of fetal alcohol syndrome. Fetal Alcohol Spectrum Disorders Center for Excellence. www.fasdcenter.samhsa.gov/publications/cost.cfm. Accessed December 14 2012.
29. Bailey B, Sokol R. Prenatal alcohol exposure and miscarriage stillbirth, preterm delivery, and sudden infant death syndrome. Alcohol Res Health. 2011;34(1):86-91.
30. Yelin R, Kot H, Yelin D, Fainsod A. Early molecular effects of ethanol during vertebrate embryogenesis. Differentiation. 2007;75(5):393-403.
31. Warren K, Hewitt B, Thomas J. Fetal alcohol spectrum disorders: research challenges and opportunities. Alcohol Res Health. 2011;34(1):4-15.
32. Ramanathan R, Wilkemeyer M, Mittal B, Perides G, Chamess ME. Alcohol inhibits cell-cell adhesion mediated by human L1. J Cell Biol. 1996;133(2):381-390.
33. Burd L, Hofer R. Biomarkers for detection of prenatal alcohol exposure: a critical review of fatty acid ethyl estsers in meconium. Birth Defects Res A Clin Mol Teratol. 2008;82(7):487-493.
34. Kulaga V, Pragst F, Fulga N, Koren G. Hair análisis of fatty acid esters in the detection of excessive drinking in the context of fetal alcohol spectrum disorders. Ther Drug Monit. 2009;31(2):261-266.
35. Sari Y, Gozes I. Brain deficits associated with fetal alcohol exposure may be protected in part, by peptides derived from activity-dependent neurotrophic factor and activity-dependent neuroprotective protein. Brain Res Rev. 2006;52(1):107-118.
36. Streissguth A, Bookstein F, Barr H, Sampson P, O’malley K, Young J. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25(4):228-238.
37. 19. Committee on Health Care for Underserved Women. American College of Obstetricians and Gynecologists. Committee Opinion No. 496: At-risk drinking and alcohol dependence: Obstetric and gynecologic implications. Obstet Gynecol. 2011;118(2 Pt 1):383-388.
38. Sokol R, Martier S, Ager J. The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol. 1989;160(4):863-868.
39. Chan A, Pristach E, Weite J, Russell M. Use of the TWEAK test in screening for alcoholism/ heavy drinking in three populations. Alcohol Clin Exp Res. 1993;17(6):1188-1192.
40. Floyd R, O’Connor M, Bertrand J, Sokol R. Reducing adverse outcomes from prenatal alcohol exposure: a clinical plan of action. Alcohol Clin Exp Res. 2006;30(8):1271-1275.
41. Miller W, Sanchez V. Motivating young adults for treatment and lifestyle change. In: Howard GS Nathan PE, eds. Alcohol use and misuse by young adults. Notre Dame, IN: University of Notre Dame Press; 1994:55–81.
42. Center for Disease Control and Prevention. Motivational intervention to reduce alcohol-exposed pregnancies—Florida Texas, and Virginia, 1997–2001. MMWR. 2003;52(19):441-444.
43. Chang G, McNamara T, Orav J, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):991-998.
44. Manwell L, Fleming M, Mundt M, Stauffacher E, Barry K. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention trial. Alcohol Clin Exp Res. 2000;24(10):1517-1524.
45. O’Connor M, Whaley S. Brief intervention for alcohol use by pregnant women. Am J Pub Health. 2007;97(2):252-258.
46. Mwansa-Kambafwile J, Rendall-Mkosi K, Jacobs R, Nel E, London L. Evaluation of a service provider short course for prevention of fetal alcohol syndrome. J Stud Alcohol Drugs. 2011;72(4):530-535.
47. American College of Obstetricians and Gynecologists. At-risk alcohol use screening and intervention. http://198.87.1.43/womenalcohol/index.html. Published 2011. Accessed December 16 2012.
1. Baram M. Moms-to-be get mixed messages on drinking. ABC News. http://abcnews.go.com/Health/story?id=2654849&page=1#.UM9l-RyeARY. Published November 15 2006. Accessed December 14, 2012.
2. Royal College of Obstetricians and Gynaecologists. Alcohol consumption and the outcomes of pregnancy (RCOG Statement No. 5). London UK: Royal College of Obstetricians and Gynaecologists. January 3, 2006.
3. Pearson C. Alcohol during pregnancy: How dangerous is it really? The Huffington Post. http://www.huffingtonpost.com/2011/04/06/alcohol-during-pregnancy_n_845103.html. Published April 6 2011. Updated September 16, 2011. Accessed December 14, 2012.
4. Kelly YJ, Sacker A, Gray R, et al. Light drinking during pregnancy: still no increased risk for socioemotional difficulties or cognitive deficits at 5 years of age? J Epidemiol Community Health. 2012;66(1):41-48.Epub Oct 5, 2010.
5. Kelly Y, Sacker A, Gray R, Kelly J, Wolke D, Quigley MA. Light drinking in pregnancy a risk for behavioural problems and cognitive deficits at 3 years of age? Int J Epidemiol. 2009;38(1):129-140.Epub Oct 30, 2008.
6. Zhou F. Fetal Alcohol Spectrum Disorders Study Group (FASDSG). Research Society on Alcoholism. http://rsoa.org/fas.html. Updated September 9 2010. Accessed December 14, 2012.
7. Kelly S, Day N, Streissguth AP. Effects of prenatal alcohol exposure on social behavior in humans and other species. Neurotoxicol Teratol. 2000;22(2):143-149.
8. Vaglenova J, Petkov V. Fetal alcohol effects in rats exposed pre-and postnatally to a low dose of ethanol. Alcohol Clin Exp Res. 1998;22(3):697-703.
9. Schneider M, Moore C, Kraemer G. Moderate alcohol during pregnancy: learning and behavior in adolescent rhesus monkeys. Alcohol Clin Exp Res. 2001;25(9):1383-1392.
10. Centers for Disease Control and Prevention. Fetal alcohol spectrum disorders. Data and statistics in the United States. http://www.cdc.gov/ncbddd/fasd/data.html. Updated August 16 2012. Accessed December 14, 2012.
11. Egeland G, Perham-Hestere KA, Gessner BD, Ingle D, Berner JE, Middaugh J. Fetal alcohol syndrome in Alaska 1977 through 1992: an administrative prevalence derived from multiple data sources. Am J Pub Health. 1998;88(5):781-786.
12. Jones K, Smith D, Ulleland C, Streissguth A. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1(7815):1267-1271.
13. Institute of Medicine. Fetal alcohol syndrome: diagnosis epidemiology, prevention, and treatment (1996). http://www.come-over.to/FAS/IOMsummary.htm. Accessed December 14, 2012.
14. Committee of Substance Abuse and Committee on Children with Disabilities. American Academy of Pediatrics. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106(2):358-361.
15. US Department of Health & Human Services. US Surgeon General releases advisory on alcohol use in pregnancy. http://www.surgeongeneral.gov/news/2005/02/sg02222005.html. Published February 21 2005. Accessed December 13, 2012.
16. Centers for Disease Control and Prevention. Alcohol use and binge drinking among women of childbearing age–United States 2006–2010. MMWR. 2012;61(28):534-538.http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6128a4.htm?s_cid=mm6128a4_w. Accessed December 17, 2012.
17. Landgren M, Svensson L, Stromland K, Gronlund M. Prenatal alcohol exposure and neurodvelopmental disorders in children adopted from Eastern Europe. Pediatrics. 2010;125(5):e1178-1185.doi:10.1542/peds.2009-0712.
18. American College of Obstetricians and Gynecologists. Drinking and reproductive health: A fetal alcohol spectrum disorders prevention tool kit. http://www.acog.org/~/media/Departments/Tobacco%20Alcohol%20and%20Substance%20Abuse/FASDToolKit.pdf?dmc=1&ts=20121217T1504384811. Published 2006. Accessed December 14 2012.
19. Anderson B, Dang E, Floyd R, Sokol R, Mahoney J, Schulkin J. Knowledge opinions, and practice patterns of obstetrician-gynecologist regarding their patients’ use of alcohol. J Addiction Med. 2010;4(2):114-121.
20. Abel EL, Kruger M. What do physicians know and say about fetal alcohol syndrome: a survey of obstetricians pediatricians, and family medicine physicians. Alcohol Clin Exp Res. 1998;22(9):1951-1954.
21. Diekman S, Floyd R, Decoufle P, Schulkin J, Ebrahim S, Sokol R. A survey of obstetrician-gynecologists on their patients’ alcohol use during pregnancy. Obstet Gynecol. 2000;95(5):756-763.
22. Strandberg-Larsen K, Gronboek M, Andersen A, Andersen P, Olsen J. Alcohol drinking pattern during pregnancy and risk of infant mortality. Epidemiology. 2009;20(6):884-891.
23. Willford J, Leech S, Day N. Moderate prenatal alcohol exposure and cognitive status of children at age 10. Alcohol Clin Exp Res. 2006;30(6):1051-1059.
24. Richardson G, Ryan C, Willford J, Day N, Goldschmidt. Prenatal alcohol and marijuana exposure: Effects on neuropsychological outcomes at 10 years. Neurotoxicol Teratol. 2002;24(3):309-320.
25. Feldman H, Jones K, Lindsay S, et al. Prenatal alcohol exposure patterns and alcohol-related birth defects and growth deficiencies: a prospective study. Alcohol Clin Exp Res. 2012;36(4):670-676.
26. O’Leary C, Nassar N, Kurinczuk J, et al. Prenatal alcohol exposure and risk of birth defects. Pediatrics. 2010;126(4):e843-850.doi:10.1542/peds.2010-0256.
27. Abel E, Sokol R. A revised conservative estimate of the incidence of FAS and its economic its impact. Alcohol Clin Exp Res. 1991;15(3):514-524.
28. Lupton C. The financial impact of fetal alcohol syndrome. Fetal Alcohol Spectrum Disorders Center for Excellence. www.fasdcenter.samhsa.gov/publications/cost.cfm. Accessed December 14 2012.
29. Bailey B, Sokol R. Prenatal alcohol exposure and miscarriage stillbirth, preterm delivery, and sudden infant death syndrome. Alcohol Res Health. 2011;34(1):86-91.
30. Yelin R, Kot H, Yelin D, Fainsod A. Early molecular effects of ethanol during vertebrate embryogenesis. Differentiation. 2007;75(5):393-403.
31. Warren K, Hewitt B, Thomas J. Fetal alcohol spectrum disorders: research challenges and opportunities. Alcohol Res Health. 2011;34(1):4-15.
32. Ramanathan R, Wilkemeyer M, Mittal B, Perides G, Chamess ME. Alcohol inhibits cell-cell adhesion mediated by human L1. J Cell Biol. 1996;133(2):381-390.
33. Burd L, Hofer R. Biomarkers for detection of prenatal alcohol exposure: a critical review of fatty acid ethyl estsers in meconium. Birth Defects Res A Clin Mol Teratol. 2008;82(7):487-493.
34. Kulaga V, Pragst F, Fulga N, Koren G. Hair análisis of fatty acid esters in the detection of excessive drinking in the context of fetal alcohol spectrum disorders. Ther Drug Monit. 2009;31(2):261-266.
35. Sari Y, Gozes I. Brain deficits associated with fetal alcohol exposure may be protected in part, by peptides derived from activity-dependent neurotrophic factor and activity-dependent neuroprotective protein. Brain Res Rev. 2006;52(1):107-118.
36. Streissguth A, Bookstein F, Barr H, Sampson P, O’malley K, Young J. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25(4):228-238.
37. 19. Committee on Health Care for Underserved Women. American College of Obstetricians and Gynecologists. Committee Opinion No. 496: At-risk drinking and alcohol dependence: Obstetric and gynecologic implications. Obstet Gynecol. 2011;118(2 Pt 1):383-388.
38. Sokol R, Martier S, Ager J. The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol. 1989;160(4):863-868.
39. Chan A, Pristach E, Weite J, Russell M. Use of the TWEAK test in screening for alcoholism/ heavy drinking in three populations. Alcohol Clin Exp Res. 1993;17(6):1188-1192.
40. Floyd R, O’Connor M, Bertrand J, Sokol R. Reducing adverse outcomes from prenatal alcohol exposure: a clinical plan of action. Alcohol Clin Exp Res. 2006;30(8):1271-1275.
41. Miller W, Sanchez V. Motivating young adults for treatment and lifestyle change. In: Howard GS Nathan PE, eds. Alcohol use and misuse by young adults. Notre Dame, IN: University of Notre Dame Press; 1994:55–81.
42. Center for Disease Control and Prevention. Motivational intervention to reduce alcohol-exposed pregnancies—Florida Texas, and Virginia, 1997–2001. MMWR. 2003;52(19):441-444.
43. Chang G, McNamara T, Orav J, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):991-998.
44. Manwell L, Fleming M, Mundt M, Stauffacher E, Barry K. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention trial. Alcohol Clin Exp Res. 2000;24(10):1517-1524.
45. O’Connor M, Whaley S. Brief intervention for alcohol use by pregnant women. Am J Pub Health. 2007;97(2):252-258.
46. Mwansa-Kambafwile J, Rendall-Mkosi K, Jacobs R, Nel E, London L. Evaluation of a service provider short course for prevention of fetal alcohol syndrome. J Stud Alcohol Drugs. 2011;72(4):530-535.
47. American College of Obstetricians and Gynecologists. At-risk alcohol use screening and intervention. http://198.87.1.43/womenalcohol/index.html. Published 2011. Accessed December 16 2012.
OTC antireflux drugs
Gastroesophageal reflux disease – also called heartburn, pyrosis, or reflux esophagitis – is an uncommon complication in women of reproductive age. However, gastroesophageal reflux disease is a common condition in pregnancy with symptoms usually ending shortly after birth (Gastroenterol. Clin. North Am. 2003;32:235-61).
Not surprisingly, the prevalence of heartburn increases as pregnancy progresses. In one study of 607 pregnant women, 22% had heartburn in the 1st trimester, 39% in the 2nd trimester, and 72% in the 3rd trimester (Br. J. Obstet. Gynaecol. 1992;99:731-4).
The symptoms of gastroesophageal reflux disease (GERD) are related to relaxation of the lower esophageal sphincter and are most pronounced when lying down. Moreover, intraesophageal pressures are lower and intragastric pressures higher in pregnancy.
Typically, the first over-the-counter (OTC) products that pregnant women turn to for relief of heartburn are antacids, such as aluminum hydroxide or carbonate, calcium carbonate, or magnesium hydroxide or oxide. Although readily available and commonly used to relieve the burning sensation of GERD, antacids are not always effective in providing long-lasting relief. In these cases, patients often turn to OTC histamine2 (H2) antagonists or proton-pump inhibitors (PPIs). Interestingly, women also use these agents to reduce reflux symptoms to lessen nausea and vomiting of pregnancy.
There are four OTC histamine2 antagonists: cimetidine (Tagamet), famotidine (Pepcid), nizatidine (Axid), and ranitidine (Zantac). For the PPIs, six are available, but only the first two agents are OTC: lansoprazole (Prevacid), omeprazole (Prilosec), dexlansoprazole (Dexilant), esomeprazole (Nexium), pantoprazole (Protonix), and rabeprazole (AcipHex).
There is a substantial amount of information regarding the use of H2 blockers and PPIs in pregnancy. Two meta-analyses published in 2009, one on H2 blockers and the other on PPIs, found no increased risk of major defects, spontaneous abortions, or preterm birth (Dig. Dis. Sci. 2009;54:1835-8; Am. J. Gastroenterol. 2009;104:1541-5).
In addition, five reviews on the treatment of GERD in pregnancy have concluded that these agents, with the possible exception of nizatidine, are relatively safe (Drug Saf. 1998;19:325-37; Gastroenterol Clin. North Am. 1998;27:153-67; Curr. Treat. Options Gastroenterol. 2002;5:301-10; Gastroenterol. Clin. North Am. 2003;32:235-61; Aliment Pharmacol. Ther. 2005;22:749-57). Nizatidine was not recommended because in a reproduction study with rabbits, abortions and decreased fetal weight were observed. Importantly, the dose that caused this toxicity was about 80 times the recommended human dose based on body surface area, so the results have no relevance to humans.
Among the H2 blockers, cimetidine has the most reported human pregnancy experience, but there is concern that the drug might cause feminization of male offspring. This concern was based on research from one group that observed the following long-lasting toxic effects in male rats exposed throughout gestation: decreased weights of the testicles, prostate gland, and seminal vesicles; reduced testosterone serum levels; a lack of sexual motivation; and decreased sexual performance (Science 1982;218:493-4; Neurobehav. Toxicol. Teratol. 1984;6:313-8; Gastroenterology 1984;86:675-80). However, research from two other groups using the same methodology failed to confirm this toxicity (Fundam. Appl. Toxicol. 1987;8:188-97; Toxicol. Lett. 1988;44:315-29). In addition, feminization of human males exposed in utero has not been reported.
Severe anaphylactoid reactions have been reported in four women receiving intravenous or oral ranitidine during labor (Br. J. Clin. Pract. 1990;44:78; Anaesthesia 1992;47:360-1; Anaesth. Intensive Care 1993;21:702-3; J. Anesth. 2003;17:199-200). Three of the newborns did well, but the fourth infant had seizures and was still receiving phenobarbital at 8 months of age.
A large 2009 Swedish cohort study evaluated the association between gastric acid suppressors during gestation and a diagnosis in the offspring of allergic disease or a prescription for asthma or allergy medications. The drug types included in the study were H2 antagonists, PPIs, prostaglandins, combinations for eradication of Helicobacter pylori, and drugs for peptic ulcer and GERD. Of 585,716 children, 29,490 (5%) met the diagnosis and 5,645 (1%) had been exposed to gastric acid suppression therapy in pregnancy. Of these children, 405 (0.07%) were treated for allergic disease. For developing allergy, the odds ratio (OR) was 1.43, irrespective of the drug, time of exposure during pregnancy, and maternal history of allergy. For developing childhood asthma, but not other allergic diseases, the OR was 1.51 irrespective of the type of acid-suppressive drug and the time of exposure in pregnancy. The authors proposed three possible mechanisms for their findings: Exposure to increased amounts of allergens could cause sensitization to digestion labile antigens in the fetus, the maternal T helper cell type 2 cytokine pattern could promote an allergy-prone phenotype in the fetus, and maternal allergen-specific IgE could cross the placenta and sensitize fetal immune cells to food and airborne allergens (Clin. Exp. Allergy 2009;39:246-53). It was also possible that a general increase in childhood asthma but not necessarily an increase in allergic asthma had occurred during the 10-year (1995-2004) study period. The study results require confirmation.
For breastfeeding, all H2 blockers are compatible, but human experience is limited. Cimetidine and ranitidine are concentrated in milk with concentrations much higher than those in maternal plasma. Famotidine also is concentrated in milk, but to a lesser degree, and the data for nizatidine are too limited to assess. The human data for lansoprazole and omeprazole are limited to one case report. The premature male infant (36 weeks) was breastfed while his mother continued her GERD treatment with omeprazole 20 mg/day. No harm was noted in the infant, who was doing well at 1 year of age. Theoretically, any of these agents could adversely affect a nursing infant’s gastric acidity and have other potentially harmful effects, but such toxicity has not been reported. Nevertheless, because of their potency, avoiding PPIs during breastfeeding should be considered.
Mr. Gerald G. Briggs is a pharmacist clinical specialist at the outpatient clinics of Memorial Care Center for Women at Miller Children’s Hospital in Long Beach, Calif.; a clinical professor of pharmacy at the University of California, San Francisco; and an adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He also is coauthor of "Drugs in Pregnancy and Lactation," and coeditor of "Diseases, Complications, and Drug Therapy in Obstetrics." He said he had no relevant financial disclosures. E-mail him at [email protected].
Gastroesophageal reflux disease – also called heartburn, pyrosis, or reflux esophagitis – is an uncommon complication in women of reproductive age. However, gastroesophageal reflux disease is a common condition in pregnancy with symptoms usually ending shortly after birth (Gastroenterol. Clin. North Am. 2003;32:235-61).
Not surprisingly, the prevalence of heartburn increases as pregnancy progresses. In one study of 607 pregnant women, 22% had heartburn in the 1st trimester, 39% in the 2nd trimester, and 72% in the 3rd trimester (Br. J. Obstet. Gynaecol. 1992;99:731-4).
The symptoms of gastroesophageal reflux disease (GERD) are related to relaxation of the lower esophageal sphincter and are most pronounced when lying down. Moreover, intraesophageal pressures are lower and intragastric pressures higher in pregnancy.
Typically, the first over-the-counter (OTC) products that pregnant women turn to for relief of heartburn are antacids, such as aluminum hydroxide or carbonate, calcium carbonate, or magnesium hydroxide or oxide. Although readily available and commonly used to relieve the burning sensation of GERD, antacids are not always effective in providing long-lasting relief. In these cases, patients often turn to OTC histamine2 (H2) antagonists or proton-pump inhibitors (PPIs). Interestingly, women also use these agents to reduce reflux symptoms to lessen nausea and vomiting of pregnancy.
There are four OTC histamine2 antagonists: cimetidine (Tagamet), famotidine (Pepcid), nizatidine (Axid), and ranitidine (Zantac). For the PPIs, six are available, but only the first two agents are OTC: lansoprazole (Prevacid), omeprazole (Prilosec), dexlansoprazole (Dexilant), esomeprazole (Nexium), pantoprazole (Protonix), and rabeprazole (AcipHex).
There is a substantial amount of information regarding the use of H2 blockers and PPIs in pregnancy. Two meta-analyses published in 2009, one on H2 blockers and the other on PPIs, found no increased risk of major defects, spontaneous abortions, or preterm birth (Dig. Dis. Sci. 2009;54:1835-8; Am. J. Gastroenterol. 2009;104:1541-5).
In addition, five reviews on the treatment of GERD in pregnancy have concluded that these agents, with the possible exception of nizatidine, are relatively safe (Drug Saf. 1998;19:325-37; Gastroenterol Clin. North Am. 1998;27:153-67; Curr. Treat. Options Gastroenterol. 2002;5:301-10; Gastroenterol. Clin. North Am. 2003;32:235-61; Aliment Pharmacol. Ther. 2005;22:749-57). Nizatidine was not recommended because in a reproduction study with rabbits, abortions and decreased fetal weight were observed. Importantly, the dose that caused this toxicity was about 80 times the recommended human dose based on body surface area, so the results have no relevance to humans.
Among the H2 blockers, cimetidine has the most reported human pregnancy experience, but there is concern that the drug might cause feminization of male offspring. This concern was based on research from one group that observed the following long-lasting toxic effects in male rats exposed throughout gestation: decreased weights of the testicles, prostate gland, and seminal vesicles; reduced testosterone serum levels; a lack of sexual motivation; and decreased sexual performance (Science 1982;218:493-4; Neurobehav. Toxicol. Teratol. 1984;6:313-8; Gastroenterology 1984;86:675-80). However, research from two other groups using the same methodology failed to confirm this toxicity (Fundam. Appl. Toxicol. 1987;8:188-97; Toxicol. Lett. 1988;44:315-29). In addition, feminization of human males exposed in utero has not been reported.
Severe anaphylactoid reactions have been reported in four women receiving intravenous or oral ranitidine during labor (Br. J. Clin. Pract. 1990;44:78; Anaesthesia 1992;47:360-1; Anaesth. Intensive Care 1993;21:702-3; J. Anesth. 2003;17:199-200). Three of the newborns did well, but the fourth infant had seizures and was still receiving phenobarbital at 8 months of age.
A large 2009 Swedish cohort study evaluated the association between gastric acid suppressors during gestation and a diagnosis in the offspring of allergic disease or a prescription for asthma or allergy medications. The drug types included in the study were H2 antagonists, PPIs, prostaglandins, combinations for eradication of Helicobacter pylori, and drugs for peptic ulcer and GERD. Of 585,716 children, 29,490 (5%) met the diagnosis and 5,645 (1%) had been exposed to gastric acid suppression therapy in pregnancy. Of these children, 405 (0.07%) were treated for allergic disease. For developing allergy, the odds ratio (OR) was 1.43, irrespective of the drug, time of exposure during pregnancy, and maternal history of allergy. For developing childhood asthma, but not other allergic diseases, the OR was 1.51 irrespective of the type of acid-suppressive drug and the time of exposure in pregnancy. The authors proposed three possible mechanisms for their findings: Exposure to increased amounts of allergens could cause sensitization to digestion labile antigens in the fetus, the maternal T helper cell type 2 cytokine pattern could promote an allergy-prone phenotype in the fetus, and maternal allergen-specific IgE could cross the placenta and sensitize fetal immune cells to food and airborne allergens (Clin. Exp. Allergy 2009;39:246-53). It was also possible that a general increase in childhood asthma but not necessarily an increase in allergic asthma had occurred during the 10-year (1995-2004) study period. The study results require confirmation.
For breastfeeding, all H2 blockers are compatible, but human experience is limited. Cimetidine and ranitidine are concentrated in milk with concentrations much higher than those in maternal plasma. Famotidine also is concentrated in milk, but to a lesser degree, and the data for nizatidine are too limited to assess. The human data for lansoprazole and omeprazole are limited to one case report. The premature male infant (36 weeks) was breastfed while his mother continued her GERD treatment with omeprazole 20 mg/day. No harm was noted in the infant, who was doing well at 1 year of age. Theoretically, any of these agents could adversely affect a nursing infant’s gastric acidity and have other potentially harmful effects, but such toxicity has not been reported. Nevertheless, because of their potency, avoiding PPIs during breastfeeding should be considered.
Mr. Gerald G. Briggs is a pharmacist clinical specialist at the outpatient clinics of Memorial Care Center for Women at Miller Children’s Hospital in Long Beach, Calif.; a clinical professor of pharmacy at the University of California, San Francisco; and an adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He also is coauthor of "Drugs in Pregnancy and Lactation," and coeditor of "Diseases, Complications, and Drug Therapy in Obstetrics." He said he had no relevant financial disclosures. E-mail him at [email protected].
Gastroesophageal reflux disease – also called heartburn, pyrosis, or reflux esophagitis – is an uncommon complication in women of reproductive age. However, gastroesophageal reflux disease is a common condition in pregnancy with symptoms usually ending shortly after birth (Gastroenterol. Clin. North Am. 2003;32:235-61).
Not surprisingly, the prevalence of heartburn increases as pregnancy progresses. In one study of 607 pregnant women, 22% had heartburn in the 1st trimester, 39% in the 2nd trimester, and 72% in the 3rd trimester (Br. J. Obstet. Gynaecol. 1992;99:731-4).
The symptoms of gastroesophageal reflux disease (GERD) are related to relaxation of the lower esophageal sphincter and are most pronounced when lying down. Moreover, intraesophageal pressures are lower and intragastric pressures higher in pregnancy.
Typically, the first over-the-counter (OTC) products that pregnant women turn to for relief of heartburn are antacids, such as aluminum hydroxide or carbonate, calcium carbonate, or magnesium hydroxide or oxide. Although readily available and commonly used to relieve the burning sensation of GERD, antacids are not always effective in providing long-lasting relief. In these cases, patients often turn to OTC histamine2 (H2) antagonists or proton-pump inhibitors (PPIs). Interestingly, women also use these agents to reduce reflux symptoms to lessen nausea and vomiting of pregnancy.
There are four OTC histamine2 antagonists: cimetidine (Tagamet), famotidine (Pepcid), nizatidine (Axid), and ranitidine (Zantac). For the PPIs, six are available, but only the first two agents are OTC: lansoprazole (Prevacid), omeprazole (Prilosec), dexlansoprazole (Dexilant), esomeprazole (Nexium), pantoprazole (Protonix), and rabeprazole (AcipHex).
There is a substantial amount of information regarding the use of H2 blockers and PPIs in pregnancy. Two meta-analyses published in 2009, one on H2 blockers and the other on PPIs, found no increased risk of major defects, spontaneous abortions, or preterm birth (Dig. Dis. Sci. 2009;54:1835-8; Am. J. Gastroenterol. 2009;104:1541-5).
In addition, five reviews on the treatment of GERD in pregnancy have concluded that these agents, with the possible exception of nizatidine, are relatively safe (Drug Saf. 1998;19:325-37; Gastroenterol Clin. North Am. 1998;27:153-67; Curr. Treat. Options Gastroenterol. 2002;5:301-10; Gastroenterol. Clin. North Am. 2003;32:235-61; Aliment Pharmacol. Ther. 2005;22:749-57). Nizatidine was not recommended because in a reproduction study with rabbits, abortions and decreased fetal weight were observed. Importantly, the dose that caused this toxicity was about 80 times the recommended human dose based on body surface area, so the results have no relevance to humans.
Among the H2 blockers, cimetidine has the most reported human pregnancy experience, but there is concern that the drug might cause feminization of male offspring. This concern was based on research from one group that observed the following long-lasting toxic effects in male rats exposed throughout gestation: decreased weights of the testicles, prostate gland, and seminal vesicles; reduced testosterone serum levels; a lack of sexual motivation; and decreased sexual performance (Science 1982;218:493-4; Neurobehav. Toxicol. Teratol. 1984;6:313-8; Gastroenterology 1984;86:675-80). However, research from two other groups using the same methodology failed to confirm this toxicity (Fundam. Appl. Toxicol. 1987;8:188-97; Toxicol. Lett. 1988;44:315-29). In addition, feminization of human males exposed in utero has not been reported.
Severe anaphylactoid reactions have been reported in four women receiving intravenous or oral ranitidine during labor (Br. J. Clin. Pract. 1990;44:78; Anaesthesia 1992;47:360-1; Anaesth. Intensive Care 1993;21:702-3; J. Anesth. 2003;17:199-200). Three of the newborns did well, but the fourth infant had seizures and was still receiving phenobarbital at 8 months of age.
A large 2009 Swedish cohort study evaluated the association between gastric acid suppressors during gestation and a diagnosis in the offspring of allergic disease or a prescription for asthma or allergy medications. The drug types included in the study were H2 antagonists, PPIs, prostaglandins, combinations for eradication of Helicobacter pylori, and drugs for peptic ulcer and GERD. Of 585,716 children, 29,490 (5%) met the diagnosis and 5,645 (1%) had been exposed to gastric acid suppression therapy in pregnancy. Of these children, 405 (0.07%) were treated for allergic disease. For developing allergy, the odds ratio (OR) was 1.43, irrespective of the drug, time of exposure during pregnancy, and maternal history of allergy. For developing childhood asthma, but not other allergic diseases, the OR was 1.51 irrespective of the type of acid-suppressive drug and the time of exposure in pregnancy. The authors proposed three possible mechanisms for their findings: Exposure to increased amounts of allergens could cause sensitization to digestion labile antigens in the fetus, the maternal T helper cell type 2 cytokine pattern could promote an allergy-prone phenotype in the fetus, and maternal allergen-specific IgE could cross the placenta and sensitize fetal immune cells to food and airborne allergens (Clin. Exp. Allergy 2009;39:246-53). It was also possible that a general increase in childhood asthma but not necessarily an increase in allergic asthma had occurred during the 10-year (1995-2004) study period. The study results require confirmation.
For breastfeeding, all H2 blockers are compatible, but human experience is limited. Cimetidine and ranitidine are concentrated in milk with concentrations much higher than those in maternal plasma. Famotidine also is concentrated in milk, but to a lesser degree, and the data for nizatidine are too limited to assess. The human data for lansoprazole and omeprazole are limited to one case report. The premature male infant (36 weeks) was breastfed while his mother continued her GERD treatment with omeprazole 20 mg/day. No harm was noted in the infant, who was doing well at 1 year of age. Theoretically, any of these agents could adversely affect a nursing infant’s gastric acidity and have other potentially harmful effects, but such toxicity has not been reported. Nevertheless, because of their potency, avoiding PPIs during breastfeeding should be considered.
Mr. Gerald G. Briggs is a pharmacist clinical specialist at the outpatient clinics of Memorial Care Center for Women at Miller Children’s Hospital in Long Beach, Calif.; a clinical professor of pharmacy at the University of California, San Francisco; and an adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He also is coauthor of "Drugs in Pregnancy and Lactation," and coeditor of "Diseases, Complications, and Drug Therapy in Obstetrics." He said he had no relevant financial disclosures. E-mail him at [email protected].
Overweight pregnant women can safely gain under 25 pounds
Although overweight or obese women should gain no more than 25 pounds in a singleton pregnancy, there is no harm in their gaining less, as long as the fetus is growing as it should, according to the American College of Obstetricians and Gynecologists.
There is no medical need to increase weight gain just to meet the goals the Institute of Medicine recommended in 2009, ACOG said.
"For an obese pregnant woman who is gaining less weight than recommended, but who has an appropriately growing fetus, no evidence exists that encouraging increased weight to conform with the updated IOM guidelines will improve maternal or fetal outcomes," ACOG’s Committee on Obstetric Practice wrote in the January issue of Obstetrics and Gynecology (2013;121:210-2). The committee made a similar statement about overweight pregnant women.
In examining the IOM recommendations, ACOG reviewed the extant literature on maternal and fetal outcomes in overweight and obese women. The 2009 weight gain recommendations have not been universally embraced, the group said, because many clinicians feel they aren’t strict enough for overweight or obese women.
"The [recommendations] have met with controversial reactions from some physicians who believe that the weight gain targets are too high," the committee wrote. "Also, these perceived high weight gain targets do not address concerns regarding postpartum weight retention. In addition, concerns have been raised that the guidelines do not differentiate degrees of obesity, especially for morbidly obese women."
Setting weight goals for any pregnancy means balancing risks and benefits for two patients simultaneously, the committee noted. Obese mothers are more likely to develop gestational diabetes and preeclampsia. They have more cesarean births, and with those, a greater risk of wound infection and venous thromboembolism.
The infants of these mothers are more likely to have birth defects, including a doubling of the risk for neural tube defects. Stillbirth is more common, as is fetal macrosomia, a prime driver of an increased risk for cesarean section and its attendant maternal risks.
After reviewing both the IOM recommendations and the current literature, ACOG made several of its own recommendations for managing overweight or obese pregnant patients (Obstet. Gynecol. 2013;121:213-7).
In the preconceptional period:
• Include information about the risks obesity poses to both mother and infant, and encourage the patient to lose weight before becoming pregnant.
• Offer a nutritional assessment and exercise prescription.
During pregnancy:
• Assess height, weight, and body mass index at the first prenatal visit, and explain the IOM weight gain recommendations. Review them at each visit.
• Continue with nutritional counseling and exercise.
• For patients who have undergone bariatric surgery, prescribe additional iron, vitamin B12, folate, vitamin D, and calcium.
During labor and delivery:
• Get an early anesthesia consult, as both epidurals and general anesthesia are uniquely challenging in obese patients.
• For patients undergoing a cesarean, consider a higher-than-usual dose of prophylactic antibiotics to ward off wound infections.
• Assess each patient for thromboembolism potential; use pneumatic compression, unfractionated heparin, or low-molecular-weight heparin as indicated.
• Consider suture closure of the subcutaneous fat layer after a cesarean, as this could help reduce the risk of postoperative wound disruption.
Post partum:
• Encourage the patient to lose weight before attempting another pregnancy – enlist the help of a specialist.
All ACOG committee members are required to follow the college’s guidelines for relationships with the health care industry, according to the ACOG website.
Although overweight or obese women should gain no more than 25 pounds in a singleton pregnancy, there is no harm in their gaining less, as long as the fetus is growing as it should, according to the American College of Obstetricians and Gynecologists.
There is no medical need to increase weight gain just to meet the goals the Institute of Medicine recommended in 2009, ACOG said.
"For an obese pregnant woman who is gaining less weight than recommended, but who has an appropriately growing fetus, no evidence exists that encouraging increased weight to conform with the updated IOM guidelines will improve maternal or fetal outcomes," ACOG’s Committee on Obstetric Practice wrote in the January issue of Obstetrics and Gynecology (2013;121:210-2). The committee made a similar statement about overweight pregnant women.
In examining the IOM recommendations, ACOG reviewed the extant literature on maternal and fetal outcomes in overweight and obese women. The 2009 weight gain recommendations have not been universally embraced, the group said, because many clinicians feel they aren’t strict enough for overweight or obese women.
"The [recommendations] have met with controversial reactions from some physicians who believe that the weight gain targets are too high," the committee wrote. "Also, these perceived high weight gain targets do not address concerns regarding postpartum weight retention. In addition, concerns have been raised that the guidelines do not differentiate degrees of obesity, especially for morbidly obese women."
Setting weight goals for any pregnancy means balancing risks and benefits for two patients simultaneously, the committee noted. Obese mothers are more likely to develop gestational diabetes and preeclampsia. They have more cesarean births, and with those, a greater risk of wound infection and venous thromboembolism.
The infants of these mothers are more likely to have birth defects, including a doubling of the risk for neural tube defects. Stillbirth is more common, as is fetal macrosomia, a prime driver of an increased risk for cesarean section and its attendant maternal risks.
After reviewing both the IOM recommendations and the current literature, ACOG made several of its own recommendations for managing overweight or obese pregnant patients (Obstet. Gynecol. 2013;121:213-7).
In the preconceptional period:
• Include information about the risks obesity poses to both mother and infant, and encourage the patient to lose weight before becoming pregnant.
• Offer a nutritional assessment and exercise prescription.
During pregnancy:
• Assess height, weight, and body mass index at the first prenatal visit, and explain the IOM weight gain recommendations. Review them at each visit.
• Continue with nutritional counseling and exercise.
• For patients who have undergone bariatric surgery, prescribe additional iron, vitamin B12, folate, vitamin D, and calcium.
During labor and delivery:
• Get an early anesthesia consult, as both epidurals and general anesthesia are uniquely challenging in obese patients.
• For patients undergoing a cesarean, consider a higher-than-usual dose of prophylactic antibiotics to ward off wound infections.
• Assess each patient for thromboembolism potential; use pneumatic compression, unfractionated heparin, or low-molecular-weight heparin as indicated.
• Consider suture closure of the subcutaneous fat layer after a cesarean, as this could help reduce the risk of postoperative wound disruption.
Post partum:
• Encourage the patient to lose weight before attempting another pregnancy – enlist the help of a specialist.
All ACOG committee members are required to follow the college’s guidelines for relationships with the health care industry, according to the ACOG website.
Although overweight or obese women should gain no more than 25 pounds in a singleton pregnancy, there is no harm in their gaining less, as long as the fetus is growing as it should, according to the American College of Obstetricians and Gynecologists.
There is no medical need to increase weight gain just to meet the goals the Institute of Medicine recommended in 2009, ACOG said.
"For an obese pregnant woman who is gaining less weight than recommended, but who has an appropriately growing fetus, no evidence exists that encouraging increased weight to conform with the updated IOM guidelines will improve maternal or fetal outcomes," ACOG’s Committee on Obstetric Practice wrote in the January issue of Obstetrics and Gynecology (2013;121:210-2). The committee made a similar statement about overweight pregnant women.
In examining the IOM recommendations, ACOG reviewed the extant literature on maternal and fetal outcomes in overweight and obese women. The 2009 weight gain recommendations have not been universally embraced, the group said, because many clinicians feel they aren’t strict enough for overweight or obese women.
"The [recommendations] have met with controversial reactions from some physicians who believe that the weight gain targets are too high," the committee wrote. "Also, these perceived high weight gain targets do not address concerns regarding postpartum weight retention. In addition, concerns have been raised that the guidelines do not differentiate degrees of obesity, especially for morbidly obese women."
Setting weight goals for any pregnancy means balancing risks and benefits for two patients simultaneously, the committee noted. Obese mothers are more likely to develop gestational diabetes and preeclampsia. They have more cesarean births, and with those, a greater risk of wound infection and venous thromboembolism.
The infants of these mothers are more likely to have birth defects, including a doubling of the risk for neural tube defects. Stillbirth is more common, as is fetal macrosomia, a prime driver of an increased risk for cesarean section and its attendant maternal risks.
After reviewing both the IOM recommendations and the current literature, ACOG made several of its own recommendations for managing overweight or obese pregnant patients (Obstet. Gynecol. 2013;121:213-7).
In the preconceptional period:
• Include information about the risks obesity poses to both mother and infant, and encourage the patient to lose weight before becoming pregnant.
• Offer a nutritional assessment and exercise prescription.
During pregnancy:
• Assess height, weight, and body mass index at the first prenatal visit, and explain the IOM weight gain recommendations. Review them at each visit.
• Continue with nutritional counseling and exercise.
• For patients who have undergone bariatric surgery, prescribe additional iron, vitamin B12, folate, vitamin D, and calcium.
During labor and delivery:
• Get an early anesthesia consult, as both epidurals and general anesthesia are uniquely challenging in obese patients.
• For patients undergoing a cesarean, consider a higher-than-usual dose of prophylactic antibiotics to ward off wound infections.
• Assess each patient for thromboembolism potential; use pneumatic compression, unfractionated heparin, or low-molecular-weight heparin as indicated.
• Consider suture closure of the subcutaneous fat layer after a cesarean, as this could help reduce the risk of postoperative wound disruption.
Post partum:
• Encourage the patient to lose weight before attempting another pregnancy – enlist the help of a specialist.
All ACOG committee members are required to follow the college’s guidelines for relationships with the health care industry, according to the ACOG website.
FROM OBSTETRICS AND GYNECOLOGY
Links found between episodes of mood disorders, childbirth
More than 70% of women with mood disorders who become pregnant experience at least one episode of their disorder in association with the birth or, less often, the pregnancy, according to a report published online Dec. 17 in Archives of General Psychiatry.
Given that approximately 40% of all pregnancies are unplanned, the risk of perinatal episodes of mania, hypomania, psychotic depression, and nonpsychotic major depression should be discussed with all women of childbearing age who have mood disorders, even those who are not planning a pregnancy, said Dr. Ian Jones of the Institute of Psychological Medicine and Clinical Neurosciences at Cardiff (Wales) University and his associates.
In addition, "it is important that all professionals providing health care for pregnant women, including midwives, family physicians, and obstetricians, are aware of this increased risk," they wrote.
Dr. Jones and his colleagues assessed the occurrence of a range of psychological disorders associated with childbirth using data from two clinical and genetic studies of mood disorders. One study cohort included 573 women with recurrent major depression occurring in 1998-2004, and the other included 980 women with bipolar I disorder and 232 with bipolar II disorder occurring in 1991-2010.
Data were available regarding 3,017 pregnancies in 1,410 of these women. The prevalence of episodes of mania, hypomania, depression with psychosis, or nonpsychotic major depression either during pregnancy or within 1 year of childbirth was similar across the spectrum of mood disorders: 70.8% for bipolar I disorder, 70.9% for bipolar II disorder, and 73.7% for recurrent major depression.
"The importance of pregnancy and childbirth for women with mood disorders should therefore not be underestimated," the investigators said (Arch. Gen. Psychiatry 2012 Dec. 17 [doi:10.1001/jamapsychiatry.2013.279]).
In this sample, 94% of the episodes of mania or psychotic depression occurred within 4 weeks postpartum.
For women with bipolar I disorder, approximately 20% of deliveries were associated with a postpartum episode of mania or psychotic depression and an additional 25% were associated with an episode of nonpsychotic major depression. Altogether, nearly half of the deliveries in women with bipolar I disorder were associated with "an episode of a major mood disorder of some description," Dr. Jones and his associates reported.
Although the rate of such episodes was lower for both bipolar II disorder and recurrent major depression, "it would be wrong to underestimate the importance" of such episodes in these patient populations, they said. Approximately 40% of deliveries among women with bipolar II disorder or major recurrent depression were associated with episodes of these disorders.
Only a small proportion of psychotic or depressive episodes occurred during pregnancy rather than postpartum in this sample. The rate, however, was roughly twice as high in women with bipolar II disorder (18.4%) than in those with bipolar I disorder (8.6%) or recurrent major depression (11%).
The relatively few episodes of psychosis or depression that developed during pregnancy were equally distributed across the three trimesters.
Similarly, less than 4% of all episodes of psychosis or depression occurred after 6 months postpartum, and the rates were similar across the three types of mood disorder, Dr. Jones and his associates said.
This study was supported by the Wellcome Trust, the Stanley Medical Research Institute, and the Welsh Assembly Government Health Studentship. No financial conflicts were reported.
More than 70% of women with mood disorders who become pregnant experience at least one episode of their disorder in association with the birth or, less often, the pregnancy, according to a report published online Dec. 17 in Archives of General Psychiatry.
Given that approximately 40% of all pregnancies are unplanned, the risk of perinatal episodes of mania, hypomania, psychotic depression, and nonpsychotic major depression should be discussed with all women of childbearing age who have mood disorders, even those who are not planning a pregnancy, said Dr. Ian Jones of the Institute of Psychological Medicine and Clinical Neurosciences at Cardiff (Wales) University and his associates.
In addition, "it is important that all professionals providing health care for pregnant women, including midwives, family physicians, and obstetricians, are aware of this increased risk," they wrote.
Dr. Jones and his colleagues assessed the occurrence of a range of psychological disorders associated with childbirth using data from two clinical and genetic studies of mood disorders. One study cohort included 573 women with recurrent major depression occurring in 1998-2004, and the other included 980 women with bipolar I disorder and 232 with bipolar II disorder occurring in 1991-2010.
Data were available regarding 3,017 pregnancies in 1,410 of these women. The prevalence of episodes of mania, hypomania, depression with psychosis, or nonpsychotic major depression either during pregnancy or within 1 year of childbirth was similar across the spectrum of mood disorders: 70.8% for bipolar I disorder, 70.9% for bipolar II disorder, and 73.7% for recurrent major depression.
"The importance of pregnancy and childbirth for women with mood disorders should therefore not be underestimated," the investigators said (Arch. Gen. Psychiatry 2012 Dec. 17 [doi:10.1001/jamapsychiatry.2013.279]).
In this sample, 94% of the episodes of mania or psychotic depression occurred within 4 weeks postpartum.
For women with bipolar I disorder, approximately 20% of deliveries were associated with a postpartum episode of mania or psychotic depression and an additional 25% were associated with an episode of nonpsychotic major depression. Altogether, nearly half of the deliveries in women with bipolar I disorder were associated with "an episode of a major mood disorder of some description," Dr. Jones and his associates reported.
Although the rate of such episodes was lower for both bipolar II disorder and recurrent major depression, "it would be wrong to underestimate the importance" of such episodes in these patient populations, they said. Approximately 40% of deliveries among women with bipolar II disorder or major recurrent depression were associated with episodes of these disorders.
Only a small proportion of psychotic or depressive episodes occurred during pregnancy rather than postpartum in this sample. The rate, however, was roughly twice as high in women with bipolar II disorder (18.4%) than in those with bipolar I disorder (8.6%) or recurrent major depression (11%).
The relatively few episodes of psychosis or depression that developed during pregnancy were equally distributed across the three trimesters.
Similarly, less than 4% of all episodes of psychosis or depression occurred after 6 months postpartum, and the rates were similar across the three types of mood disorder, Dr. Jones and his associates said.
This study was supported by the Wellcome Trust, the Stanley Medical Research Institute, and the Welsh Assembly Government Health Studentship. No financial conflicts were reported.
More than 70% of women with mood disorders who become pregnant experience at least one episode of their disorder in association with the birth or, less often, the pregnancy, according to a report published online Dec. 17 in Archives of General Psychiatry.
Given that approximately 40% of all pregnancies are unplanned, the risk of perinatal episodes of mania, hypomania, psychotic depression, and nonpsychotic major depression should be discussed with all women of childbearing age who have mood disorders, even those who are not planning a pregnancy, said Dr. Ian Jones of the Institute of Psychological Medicine and Clinical Neurosciences at Cardiff (Wales) University and his associates.
In addition, "it is important that all professionals providing health care for pregnant women, including midwives, family physicians, and obstetricians, are aware of this increased risk," they wrote.
Dr. Jones and his colleagues assessed the occurrence of a range of psychological disorders associated with childbirth using data from two clinical and genetic studies of mood disorders. One study cohort included 573 women with recurrent major depression occurring in 1998-2004, and the other included 980 women with bipolar I disorder and 232 with bipolar II disorder occurring in 1991-2010.
Data were available regarding 3,017 pregnancies in 1,410 of these women. The prevalence of episodes of mania, hypomania, depression with psychosis, or nonpsychotic major depression either during pregnancy or within 1 year of childbirth was similar across the spectrum of mood disorders: 70.8% for bipolar I disorder, 70.9% for bipolar II disorder, and 73.7% for recurrent major depression.
"The importance of pregnancy and childbirth for women with mood disorders should therefore not be underestimated," the investigators said (Arch. Gen. Psychiatry 2012 Dec. 17 [doi:10.1001/jamapsychiatry.2013.279]).
In this sample, 94% of the episodes of mania or psychotic depression occurred within 4 weeks postpartum.
For women with bipolar I disorder, approximately 20% of deliveries were associated with a postpartum episode of mania or psychotic depression and an additional 25% were associated with an episode of nonpsychotic major depression. Altogether, nearly half of the deliveries in women with bipolar I disorder were associated with "an episode of a major mood disorder of some description," Dr. Jones and his associates reported.
Although the rate of such episodes was lower for both bipolar II disorder and recurrent major depression, "it would be wrong to underestimate the importance" of such episodes in these patient populations, they said. Approximately 40% of deliveries among women with bipolar II disorder or major recurrent depression were associated with episodes of these disorders.
Only a small proportion of psychotic or depressive episodes occurred during pregnancy rather than postpartum in this sample. The rate, however, was roughly twice as high in women with bipolar II disorder (18.4%) than in those with bipolar I disorder (8.6%) or recurrent major depression (11%).
The relatively few episodes of psychosis or depression that developed during pregnancy were equally distributed across the three trimesters.
Similarly, less than 4% of all episodes of psychosis or depression occurred after 6 months postpartum, and the rates were similar across the three types of mood disorder, Dr. Jones and his associates said.
This study was supported by the Wellcome Trust, the Stanley Medical Research Institute, and the Welsh Assembly Government Health Studentship. No financial conflicts were reported.
FROM ARCHIVES OF GENERAL PSYCHIATRY
Major Finding: More than 70% of pregnant women with bipolar I disorder, 70.9% of those with bipolar II disorder, and 73.7% of those with recurrent major depression experienced at least one episode of mania, hypomania, psychotic depression, or nonpsychotic major depression in the perinatal or postpartum period.
Data Source: Two clinical and genetic studies of mood disorders involving 1,410 women with bipolar I disorder, bipolar II disorder, or recurrent major depression who had 3,017 pregnancies.
Disclosures: This study was supported by the Wellcome Trust, the Stanley Medical Research Institute, and the Welsh Assembly Government Health Studentship. No financial conflicts were reported.
Care bundles lower birth injuries, claims
Implementing evidence-based protocols related to vacuum-assisted delivery, early elective inductions, and labor augmentation helped reduce complications and liability claims in the first phase of a national perinatal safety initiative.
The Premier Perinatal Safety Initiative, which is a project of the Premier health care alliance, includes 14 hospitals from around the country that adopted team-based communications processes, participated in simulation training, and implemented evidence-based care bundles starting in 2008.
"We went to work on what would be an idealized design for perinatal care," Susan D. DeVore, president and CEO of the Premier health care alliance, said during a press conference to release the phase I results.
The results from phase I of the study (2008-2010) show that the interventions appear to be reducing maternal and neonatal harm.
Participating hospitals reduced birth hypoxia/asphyxia by 25%, dropping the instances of this type of neonatal injury from 1.6 per 1,000 deliveries in 2006-2007 to 1.2 per 1,000 during 2008-2010. Similarly, neonatal birth trauma fell from 1.8 to 1.4 per 1,000 deliveries in the same time periods, a reduction of 22%.
Postpartum hemorrhage, the most common cause of perinatal maternal death in the developed world, dropped 5.4% (from 30.0 to 28.4 instances per 1,000 deliveries) during phase I. Cardiac arrest and other cardiac complications resulting from administration of anesthesia during labor and delivery were reduced from 4.0 instances per 1,000 deliveries during the baseline period to 3.4 instances during phase I, a drop of 15%.
The study intervention also appears to be bringing down liability claims, though it sometimes takes 2 years or more following an injury before a claim is filed, Ms. DeVore said. Preliminary data show that the number of liability claims filed fell from an average of 18 during the baseline period to 10 in 2009; it is trending to be at 8 in 2010. Additionally, more claims were resolved without payment at the end of phase I than during the baseline period, according to Premier.
During phase I of the study, participating hospitals implemented three care bundles on elective induction, labor augmentation, and vacuum-assisted delivery. The hospitals had to show that they were providing all of the elements in the bundle to be considered adherent. For instance, the vacuum bundle requires that alternative labor strategies are considered, the patient is prepared, there is a high probability of success, the maximum application time and number of "pop-offs" is predetermined and documented, and cesarean and resuscitation teams are available at delivery.
Over the course of the study, adherence to the bundles has increased significantly. Compliance with the augmentation bundle rose from 33% at baseline to 72% at the end of phase I. Compliance with the elective induction bundle rose from 58% to 88%. And compliance with the vacuum bundle jumped from 9% at baseline to 51%.
Health care providers in the study also worked on improving communication throughout the labor and delivery team by adopting communication protocols used by the military, including TeamSTEPPS and Situation Background Assessment Recommendation (SBAR). They also performed simulations in which they role played worst-case scenarios using mannequins. "So, in real life, when some of these situations occur, it’s not the first time they’ve responded to it," Ms. DeVore said. "They’ve been through very serious simulations."
Phase II of the study, which will also look at the role of hospital culture in perinatal performance improvement, began in January 2011 and will be completed in December 2012. Premier expects to release final results from the project in the summer or fall of 2013.
Implementing evidence-based protocols related to vacuum-assisted delivery, early elective inductions, and labor augmentation helped reduce complications and liability claims in the first phase of a national perinatal safety initiative.
The Premier Perinatal Safety Initiative, which is a project of the Premier health care alliance, includes 14 hospitals from around the country that adopted team-based communications processes, participated in simulation training, and implemented evidence-based care bundles starting in 2008.
"We went to work on what would be an idealized design for perinatal care," Susan D. DeVore, president and CEO of the Premier health care alliance, said during a press conference to release the phase I results.
The results from phase I of the study (2008-2010) show that the interventions appear to be reducing maternal and neonatal harm.
Participating hospitals reduced birth hypoxia/asphyxia by 25%, dropping the instances of this type of neonatal injury from 1.6 per 1,000 deliveries in 2006-2007 to 1.2 per 1,000 during 2008-2010. Similarly, neonatal birth trauma fell from 1.8 to 1.4 per 1,000 deliveries in the same time periods, a reduction of 22%.
Postpartum hemorrhage, the most common cause of perinatal maternal death in the developed world, dropped 5.4% (from 30.0 to 28.4 instances per 1,000 deliveries) during phase I. Cardiac arrest and other cardiac complications resulting from administration of anesthesia during labor and delivery were reduced from 4.0 instances per 1,000 deliveries during the baseline period to 3.4 instances during phase I, a drop of 15%.
The study intervention also appears to be bringing down liability claims, though it sometimes takes 2 years or more following an injury before a claim is filed, Ms. DeVore said. Preliminary data show that the number of liability claims filed fell from an average of 18 during the baseline period to 10 in 2009; it is trending to be at 8 in 2010. Additionally, more claims were resolved without payment at the end of phase I than during the baseline period, according to Premier.
During phase I of the study, participating hospitals implemented three care bundles on elective induction, labor augmentation, and vacuum-assisted delivery. The hospitals had to show that they were providing all of the elements in the bundle to be considered adherent. For instance, the vacuum bundle requires that alternative labor strategies are considered, the patient is prepared, there is a high probability of success, the maximum application time and number of "pop-offs" is predetermined and documented, and cesarean and resuscitation teams are available at delivery.
Over the course of the study, adherence to the bundles has increased significantly. Compliance with the augmentation bundle rose from 33% at baseline to 72% at the end of phase I. Compliance with the elective induction bundle rose from 58% to 88%. And compliance with the vacuum bundle jumped from 9% at baseline to 51%.
Health care providers in the study also worked on improving communication throughout the labor and delivery team by adopting communication protocols used by the military, including TeamSTEPPS and Situation Background Assessment Recommendation (SBAR). They also performed simulations in which they role played worst-case scenarios using mannequins. "So, in real life, when some of these situations occur, it’s not the first time they’ve responded to it," Ms. DeVore said. "They’ve been through very serious simulations."
Phase II of the study, which will also look at the role of hospital culture in perinatal performance improvement, began in January 2011 and will be completed in December 2012. Premier expects to release final results from the project in the summer or fall of 2013.
Implementing evidence-based protocols related to vacuum-assisted delivery, early elective inductions, and labor augmentation helped reduce complications and liability claims in the first phase of a national perinatal safety initiative.
The Premier Perinatal Safety Initiative, which is a project of the Premier health care alliance, includes 14 hospitals from around the country that adopted team-based communications processes, participated in simulation training, and implemented evidence-based care bundles starting in 2008.
"We went to work on what would be an idealized design for perinatal care," Susan D. DeVore, president and CEO of the Premier health care alliance, said during a press conference to release the phase I results.
The results from phase I of the study (2008-2010) show that the interventions appear to be reducing maternal and neonatal harm.
Participating hospitals reduced birth hypoxia/asphyxia by 25%, dropping the instances of this type of neonatal injury from 1.6 per 1,000 deliveries in 2006-2007 to 1.2 per 1,000 during 2008-2010. Similarly, neonatal birth trauma fell from 1.8 to 1.4 per 1,000 deliveries in the same time periods, a reduction of 22%.
Postpartum hemorrhage, the most common cause of perinatal maternal death in the developed world, dropped 5.4% (from 30.0 to 28.4 instances per 1,000 deliveries) during phase I. Cardiac arrest and other cardiac complications resulting from administration of anesthesia during labor and delivery were reduced from 4.0 instances per 1,000 deliveries during the baseline period to 3.4 instances during phase I, a drop of 15%.
The study intervention also appears to be bringing down liability claims, though it sometimes takes 2 years or more following an injury before a claim is filed, Ms. DeVore said. Preliminary data show that the number of liability claims filed fell from an average of 18 during the baseline period to 10 in 2009; it is trending to be at 8 in 2010. Additionally, more claims were resolved without payment at the end of phase I than during the baseline period, according to Premier.
During phase I of the study, participating hospitals implemented three care bundles on elective induction, labor augmentation, and vacuum-assisted delivery. The hospitals had to show that they were providing all of the elements in the bundle to be considered adherent. For instance, the vacuum bundle requires that alternative labor strategies are considered, the patient is prepared, there is a high probability of success, the maximum application time and number of "pop-offs" is predetermined and documented, and cesarean and resuscitation teams are available at delivery.
Over the course of the study, adherence to the bundles has increased significantly. Compliance with the augmentation bundle rose from 33% at baseline to 72% at the end of phase I. Compliance with the elective induction bundle rose from 58% to 88%. And compliance with the vacuum bundle jumped from 9% at baseline to 51%.
Health care providers in the study also worked on improving communication throughout the labor and delivery team by adopting communication protocols used by the military, including TeamSTEPPS and Situation Background Assessment Recommendation (SBAR). They also performed simulations in which they role played worst-case scenarios using mannequins. "So, in real life, when some of these situations occur, it’s not the first time they’ve responded to it," Ms. DeVore said. "They’ve been through very serious simulations."
Phase II of the study, which will also look at the role of hospital culture in perinatal performance improvement, began in January 2011 and will be completed in December 2012. Premier expects to release final results from the project in the summer or fall of 2013.
Simple technique facilitates laparoscopic port closure
LAS VEGAS – Surgeons have developed a simple new suture technique using two S-retractors to close laparoscopic and robotic surgery ports without sacrificing visualization.
"This method involves minimal training and surgical skill, is quick to perform, and requires no additional instrumentation and no additional cost to the institution, surgeon, or patient," Dr. Homayara Aziz said at the 41st AAGL Global Congress.
No fewer than 29 original methods have been described in the literature for fascial closure, but many use assistance from inside the abdomen or extracorporeal assistance, and require additional ports. Others can be performed without an additional port, but may or may not provide direct visualization when securing the abdominal wall fascia and peritoneum.
With the new technique, devised at the State University of New York at Buffalo, the needle does not enter the peritoneal cavity blindly, where the bowel or other visceral organs may be present, Dr. Aziz said. Instead, the S-retractor functions as a barrier to protect the contents of the abdominal cavity, reducing the risk of visceral injuries.
The S-retractor also provides direct visualization of the different abdominal layers, exposing the needle tip during its course through the fascia. Because there is no needle tip in the intraperitoneal cavity, the procedure is safer, she said.
The two-step process starts with the surgeon inserting an S-retractor through the incision into the peritoneal cavity and then lifting the abdominal layers with the bottom of the retractor, creating a barrier between the fascia and the visceral contents. The assistant uses a second S-retractor to retract the skin, fat, and muscle in the opposite direction to expose the fascia. The surgeon then uses a needle suture to grasp the fascia, Dr. Aziz explained.
The first retractor is then rotated 180 degrees in the peritoneum by the surgeon to allow for work on the opposite side of the fascia. The second retractor, used by the assistant, is also moved to the opposite side of the abdominal wall layers to expose the fascia.
The surgeon again continues to grasp the opposite side of the fascia with the suture. The two ends are tied and the fascia is closed. If the fascial defect is greater than 10 mm, the surgeon may continue the same technique for another interrupted suture, figure of 8, or running closure, said Dr. Aziz, now a clinical instructor of obstetrics, gynecology, and reproductive science at the University of Maryland, Baltimore.
She reported on a prospective, consecutive case series involving 100 private and clinic patients in which this method was used over a 3-year period for fascial closure of total laparoscopic hysterectomies; bilateral or unilateral salpingo-oophorectomy where the port site was more than 12 mm to remove the specimen using an endocatch bag; and any robotic surgery where the ports are generally more than 8 mm.
There were no intraoperative incidents, nor was there added operative time or need to access costly instruments, she said.
No bowel injuries or port-site hernias were reported during a mean follow-up of 6 weeks post surgery and at 12-month annual follow-up.
"Closure of the fascia should remain simple, easy, cost-effective, and quick to apply," Dr. Aziz said. "It should also be safe and without any complications, and this technique described here fulfills all of these criteria."
The technique takes 5 minutes or less to learn, and has been used on at least 200 additional patients at both institutions since the current analysis was performed, Dr. Aziz said in an interview. "Many of my attendings at SUNY Buffalo call it ‘the Aziz technique’ and [it] has gained much popularity."
Dr. Aziz reported no relevant conflicts of interest.
LAS VEGAS – Surgeons have developed a simple new suture technique using two S-retractors to close laparoscopic and robotic surgery ports without sacrificing visualization.
"This method involves minimal training and surgical skill, is quick to perform, and requires no additional instrumentation and no additional cost to the institution, surgeon, or patient," Dr. Homayara Aziz said at the 41st AAGL Global Congress.
No fewer than 29 original methods have been described in the literature for fascial closure, but many use assistance from inside the abdomen or extracorporeal assistance, and require additional ports. Others can be performed without an additional port, but may or may not provide direct visualization when securing the abdominal wall fascia and peritoneum.
With the new technique, devised at the State University of New York at Buffalo, the needle does not enter the peritoneal cavity blindly, where the bowel or other visceral organs may be present, Dr. Aziz said. Instead, the S-retractor functions as a barrier to protect the contents of the abdominal cavity, reducing the risk of visceral injuries.
The S-retractor also provides direct visualization of the different abdominal layers, exposing the needle tip during its course through the fascia. Because there is no needle tip in the intraperitoneal cavity, the procedure is safer, she said.
The two-step process starts with the surgeon inserting an S-retractor through the incision into the peritoneal cavity and then lifting the abdominal layers with the bottom of the retractor, creating a barrier between the fascia and the visceral contents. The assistant uses a second S-retractor to retract the skin, fat, and muscle in the opposite direction to expose the fascia. The surgeon then uses a needle suture to grasp the fascia, Dr. Aziz explained.
The first retractor is then rotated 180 degrees in the peritoneum by the surgeon to allow for work on the opposite side of the fascia. The second retractor, used by the assistant, is also moved to the opposite side of the abdominal wall layers to expose the fascia.
The surgeon again continues to grasp the opposite side of the fascia with the suture. The two ends are tied and the fascia is closed. If the fascial defect is greater than 10 mm, the surgeon may continue the same technique for another interrupted suture, figure of 8, or running closure, said Dr. Aziz, now a clinical instructor of obstetrics, gynecology, and reproductive science at the University of Maryland, Baltimore.
She reported on a prospective, consecutive case series involving 100 private and clinic patients in which this method was used over a 3-year period for fascial closure of total laparoscopic hysterectomies; bilateral or unilateral salpingo-oophorectomy where the port site was more than 12 mm to remove the specimen using an endocatch bag; and any robotic surgery where the ports are generally more than 8 mm.
There were no intraoperative incidents, nor was there added operative time or need to access costly instruments, she said.
No bowel injuries or port-site hernias were reported during a mean follow-up of 6 weeks post surgery and at 12-month annual follow-up.
"Closure of the fascia should remain simple, easy, cost-effective, and quick to apply," Dr. Aziz said. "It should also be safe and without any complications, and this technique described here fulfills all of these criteria."
The technique takes 5 minutes or less to learn, and has been used on at least 200 additional patients at both institutions since the current analysis was performed, Dr. Aziz said in an interview. "Many of my attendings at SUNY Buffalo call it ‘the Aziz technique’ and [it] has gained much popularity."
Dr. Aziz reported no relevant conflicts of interest.
LAS VEGAS – Surgeons have developed a simple new suture technique using two S-retractors to close laparoscopic and robotic surgery ports without sacrificing visualization.
"This method involves minimal training and surgical skill, is quick to perform, and requires no additional instrumentation and no additional cost to the institution, surgeon, or patient," Dr. Homayara Aziz said at the 41st AAGL Global Congress.
No fewer than 29 original methods have been described in the literature for fascial closure, but many use assistance from inside the abdomen or extracorporeal assistance, and require additional ports. Others can be performed without an additional port, but may or may not provide direct visualization when securing the abdominal wall fascia and peritoneum.
With the new technique, devised at the State University of New York at Buffalo, the needle does not enter the peritoneal cavity blindly, where the bowel or other visceral organs may be present, Dr. Aziz said. Instead, the S-retractor functions as a barrier to protect the contents of the abdominal cavity, reducing the risk of visceral injuries.
The S-retractor also provides direct visualization of the different abdominal layers, exposing the needle tip during its course through the fascia. Because there is no needle tip in the intraperitoneal cavity, the procedure is safer, she said.
The two-step process starts with the surgeon inserting an S-retractor through the incision into the peritoneal cavity and then lifting the abdominal layers with the bottom of the retractor, creating a barrier between the fascia and the visceral contents. The assistant uses a second S-retractor to retract the skin, fat, and muscle in the opposite direction to expose the fascia. The surgeon then uses a needle suture to grasp the fascia, Dr. Aziz explained.
The first retractor is then rotated 180 degrees in the peritoneum by the surgeon to allow for work on the opposite side of the fascia. The second retractor, used by the assistant, is also moved to the opposite side of the abdominal wall layers to expose the fascia.
The surgeon again continues to grasp the opposite side of the fascia with the suture. The two ends are tied and the fascia is closed. If the fascial defect is greater than 10 mm, the surgeon may continue the same technique for another interrupted suture, figure of 8, or running closure, said Dr. Aziz, now a clinical instructor of obstetrics, gynecology, and reproductive science at the University of Maryland, Baltimore.
She reported on a prospective, consecutive case series involving 100 private and clinic patients in which this method was used over a 3-year period for fascial closure of total laparoscopic hysterectomies; bilateral or unilateral salpingo-oophorectomy where the port site was more than 12 mm to remove the specimen using an endocatch bag; and any robotic surgery where the ports are generally more than 8 mm.
There were no intraoperative incidents, nor was there added operative time or need to access costly instruments, she said.
No bowel injuries or port-site hernias were reported during a mean follow-up of 6 weeks post surgery and at 12-month annual follow-up.
"Closure of the fascia should remain simple, easy, cost-effective, and quick to apply," Dr. Aziz said. "It should also be safe and without any complications, and this technique described here fulfills all of these criteria."
The technique takes 5 minutes or less to learn, and has been used on at least 200 additional patients at both institutions since the current analysis was performed, Dr. Aziz said in an interview. "Many of my attendings at SUNY Buffalo call it ‘the Aziz technique’ and [it] has gained much popularity."
Dr. Aziz reported no relevant conflicts of interest.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: There were no intraoperative incidents, and no bowel injuries or port site hernias, during a mean follow-up of 6 weeks post surgery and at 12 months follow-up.
Data Source: Prospective, consecutive case series of 100 patients.
Disclosures: Dr. Aziz reported no relevant conflicts of interest.
Microarray Testing Provides More Answers Than Karyotyping in Stillbirth
Microarray testing is more likely to identify a genetic abnormality than is standard karyotyping in cases of stillbirth, according to a report published online Dec. 6 in the New England Journal of Medicine.
Microarray analysis is more productive in such cases chiefly because it can be used on nonviable tissue, even on macerated tissue, with some success, said Dr. Uma M. Reddy of the National Institute of Child Health and Human Development, Bethesda, Md., and her associates.
Until now, only two small studies, involving only 44 stillbirths in all, have assessed the usefulness of microarray testing to identify a cause in stillbirths.
The investigators performed a population-based study of genetic findings in cases of stillbirth using data from the Stillbirth Collaborative Research Network, a racially and ethnically diverse cohort drawn from five geographic catchment areas in the United States. They assessed 532 stillbirths (from 524 pregnancies) that occurred at 59 hospitals during 2006-2008.
Standard karyotyping was attempted on fetal tissue, placental tissue, cord blood, fetal muscle, and/or fetal liver, and results were obtained in 375 (71%) of these stillbirths. A total of 31 were classified as abnormal, with findings including trisomy 21, trisomy 18, trisomy 13, monosomy X, and other sex-chromosome abnormalities.
When microarray testing was performed on the same samples, results were obtained in 465 (87.4%) of the stillbirths, which is a significantly greater yield than that obtained with karyotyping. "We thus were able to obtain a result in 90 more cases (24% more) than we would have done using karyotype analysis alone," the researchers said.
Microarray testing showed no "benign" or "probably benign" chromosomal abnormalities in these stillbirths. It showed aneuploidy in 32, other pathogenic variants in 12, and variants "of unknown significance" in 25.
"Microarray analysis provided improved detection of genomic abnormalities, as compared with karyotype analysis (8.3% vs. 5.8%), a 41.9% increase. ... When we included variants of unknown significance in this comparison, we observed an even greater detection of abnormalities with the use of microarray analysis, as compared with karyotype analysis (13% vs. 5.8%), a 122.6% increase," Dr. Reddy and her colleagues said.
"Of the 157 stillbirths for which karyotype analysis failed to provide a definitive result, 79.6% yielded a definitive microarray result: 73.9% were normal or probably benign, and 5.7% were abnormal," they noted.
Looked at another way, karyotyping either failed altogether or produced normal results in 41% of the 44 stillbirths in which microarray testing demonstrated aneuploidy or a known pathogenic chromosomal variant (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMoa1201569]).
The investigators also performed a subgroup analysis of the 443 antepartum stillbirths in this series. As with the entire study cohort, microarray analysis detected more abnormalities (8.8%) in this subgroup than did karyotyping (6.5%), representing a 35% increase in diagnostic yield.
In a subgroup analysis of the 472 stillbirths in which postmortem examinations were conducted, microarray analysis also detected more abnormalities (29.9%) than did karyotyping (19.4%), which represents a 54% increase in diagnostic yield.
In addition, the microarray technique, but not karyotyping, identified three stillbirths with abnormalities on chromosome 22q11.2, a region that is known to be disrupted in DiGeorge syndrome (also known as velocardiofacial syndrome). One of these fetuses was found to have multiple cardiopulmonary, facial, skeletal, urogenital, and thymic anomalies on postmortem examination.
This result suggests that genomic imbalances in the 22q11.2 region may be associated with stillbirth as well as with DiGeorge syndrome. Identifying such variations in cases of stillbirth would be important so that parental studies can be performed. The risk of recurrence of DiGeorge syndrome in subsequent pregnancies can vary from less than 0.1% in genotypically normal parents to 50% if one parent has a deletion, Dr. Reddy and her associates said.
In another eight stillbirths, the microarray method, but not karyotyping, also identified variations "of unknown significance" in the region of chromosome 19p13.3. This region is known to harbor frequent variations that are not yet understood. No congenital anomalies were present in these eight cases on postmortem examination, but there were "substantially abnormal" placental findings, including chronic deciduitis, villous infarction, chronic cytomegalovirus villitis, and abruption.
Chromosomal variations in this region previously have been associated with disease but not with stillbirth, so the variation identified on microarray testing in these eight stillbirths may be benign or may confer a risk of stillbirth; further research should supply the answer, the investigators said.
This study was supported by NICHD. Dr. Reddy reported no potential financial conflicts of interest, and her associates reported numerous ties to industry sources.
The findings of Dr. Reddy and her colleagues "provide a good rationale for performing microarray analysis in cases of stillbirth, particularly when congenital anomalies are present," Dr. Lorraine Dugoff wrote.
Identifying a genetic abnormality after a stillbirth "may provide comfort, end the search for a cause, and help with the assessment of risk and the development of a plan of care for future" pregnancies, she added.
Dr. Dugoff is with the department of ob.gyn. at the University of Pennsylvania, Philadelphia. She reported a pending research award from PerkinElme. These remarks were taken from her editorial accompanying Dr. Reddy’s report (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMe1212303]).
The findings of Dr. Reddy and her colleagues "provide a good rationale for performing microarray analysis in cases of stillbirth, particularly when congenital anomalies are present," Dr. Lorraine Dugoff wrote.
Identifying a genetic abnormality after a stillbirth "may provide comfort, end the search for a cause, and help with the assessment of risk and the development of a plan of care for future" pregnancies, she added.
Dr. Dugoff is with the department of ob.gyn. at the University of Pennsylvania, Philadelphia. She reported a pending research award from PerkinElme. These remarks were taken from her editorial accompanying Dr. Reddy’s report (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMe1212303]).
The findings of Dr. Reddy and her colleagues "provide a good rationale for performing microarray analysis in cases of stillbirth, particularly when congenital anomalies are present," Dr. Lorraine Dugoff wrote.
Identifying a genetic abnormality after a stillbirth "may provide comfort, end the search for a cause, and help with the assessment of risk and the development of a plan of care for future" pregnancies, she added.
Dr. Dugoff is with the department of ob.gyn. at the University of Pennsylvania, Philadelphia. She reported a pending research award from PerkinElme. These remarks were taken from her editorial accompanying Dr. Reddy’s report (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMe1212303]).
Microarray testing is more likely to identify a genetic abnormality than is standard karyotyping in cases of stillbirth, according to a report published online Dec. 6 in the New England Journal of Medicine.
Microarray analysis is more productive in such cases chiefly because it can be used on nonviable tissue, even on macerated tissue, with some success, said Dr. Uma M. Reddy of the National Institute of Child Health and Human Development, Bethesda, Md., and her associates.
Until now, only two small studies, involving only 44 stillbirths in all, have assessed the usefulness of microarray testing to identify a cause in stillbirths.
The investigators performed a population-based study of genetic findings in cases of stillbirth using data from the Stillbirth Collaborative Research Network, a racially and ethnically diverse cohort drawn from five geographic catchment areas in the United States. They assessed 532 stillbirths (from 524 pregnancies) that occurred at 59 hospitals during 2006-2008.
Standard karyotyping was attempted on fetal tissue, placental tissue, cord blood, fetal muscle, and/or fetal liver, and results were obtained in 375 (71%) of these stillbirths. A total of 31 were classified as abnormal, with findings including trisomy 21, trisomy 18, trisomy 13, monosomy X, and other sex-chromosome abnormalities.
When microarray testing was performed on the same samples, results were obtained in 465 (87.4%) of the stillbirths, which is a significantly greater yield than that obtained with karyotyping. "We thus were able to obtain a result in 90 more cases (24% more) than we would have done using karyotype analysis alone," the researchers said.
Microarray testing showed no "benign" or "probably benign" chromosomal abnormalities in these stillbirths. It showed aneuploidy in 32, other pathogenic variants in 12, and variants "of unknown significance" in 25.
"Microarray analysis provided improved detection of genomic abnormalities, as compared with karyotype analysis (8.3% vs. 5.8%), a 41.9% increase. ... When we included variants of unknown significance in this comparison, we observed an even greater detection of abnormalities with the use of microarray analysis, as compared with karyotype analysis (13% vs. 5.8%), a 122.6% increase," Dr. Reddy and her colleagues said.
"Of the 157 stillbirths for which karyotype analysis failed to provide a definitive result, 79.6% yielded a definitive microarray result: 73.9% were normal or probably benign, and 5.7% were abnormal," they noted.
Looked at another way, karyotyping either failed altogether or produced normal results in 41% of the 44 stillbirths in which microarray testing demonstrated aneuploidy or a known pathogenic chromosomal variant (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMoa1201569]).
The investigators also performed a subgroup analysis of the 443 antepartum stillbirths in this series. As with the entire study cohort, microarray analysis detected more abnormalities (8.8%) in this subgroup than did karyotyping (6.5%), representing a 35% increase in diagnostic yield.
In a subgroup analysis of the 472 stillbirths in which postmortem examinations were conducted, microarray analysis also detected more abnormalities (29.9%) than did karyotyping (19.4%), which represents a 54% increase in diagnostic yield.
In addition, the microarray technique, but not karyotyping, identified three stillbirths with abnormalities on chromosome 22q11.2, a region that is known to be disrupted in DiGeorge syndrome (also known as velocardiofacial syndrome). One of these fetuses was found to have multiple cardiopulmonary, facial, skeletal, urogenital, and thymic anomalies on postmortem examination.
This result suggests that genomic imbalances in the 22q11.2 region may be associated with stillbirth as well as with DiGeorge syndrome. Identifying such variations in cases of stillbirth would be important so that parental studies can be performed. The risk of recurrence of DiGeorge syndrome in subsequent pregnancies can vary from less than 0.1% in genotypically normal parents to 50% if one parent has a deletion, Dr. Reddy and her associates said.
In another eight stillbirths, the microarray method, but not karyotyping, also identified variations "of unknown significance" in the region of chromosome 19p13.3. This region is known to harbor frequent variations that are not yet understood. No congenital anomalies were present in these eight cases on postmortem examination, but there were "substantially abnormal" placental findings, including chronic deciduitis, villous infarction, chronic cytomegalovirus villitis, and abruption.
Chromosomal variations in this region previously have been associated with disease but not with stillbirth, so the variation identified on microarray testing in these eight stillbirths may be benign or may confer a risk of stillbirth; further research should supply the answer, the investigators said.
This study was supported by NICHD. Dr. Reddy reported no potential financial conflicts of interest, and her associates reported numerous ties to industry sources.
Microarray testing is more likely to identify a genetic abnormality than is standard karyotyping in cases of stillbirth, according to a report published online Dec. 6 in the New England Journal of Medicine.
Microarray analysis is more productive in such cases chiefly because it can be used on nonviable tissue, even on macerated tissue, with some success, said Dr. Uma M. Reddy of the National Institute of Child Health and Human Development, Bethesda, Md., and her associates.
Until now, only two small studies, involving only 44 stillbirths in all, have assessed the usefulness of microarray testing to identify a cause in stillbirths.
The investigators performed a population-based study of genetic findings in cases of stillbirth using data from the Stillbirth Collaborative Research Network, a racially and ethnically diverse cohort drawn from five geographic catchment areas in the United States. They assessed 532 stillbirths (from 524 pregnancies) that occurred at 59 hospitals during 2006-2008.
Standard karyotyping was attempted on fetal tissue, placental tissue, cord blood, fetal muscle, and/or fetal liver, and results were obtained in 375 (71%) of these stillbirths. A total of 31 were classified as abnormal, with findings including trisomy 21, trisomy 18, trisomy 13, monosomy X, and other sex-chromosome abnormalities.
When microarray testing was performed on the same samples, results were obtained in 465 (87.4%) of the stillbirths, which is a significantly greater yield than that obtained with karyotyping. "We thus were able to obtain a result in 90 more cases (24% more) than we would have done using karyotype analysis alone," the researchers said.
Microarray testing showed no "benign" or "probably benign" chromosomal abnormalities in these stillbirths. It showed aneuploidy in 32, other pathogenic variants in 12, and variants "of unknown significance" in 25.
"Microarray analysis provided improved detection of genomic abnormalities, as compared with karyotype analysis (8.3% vs. 5.8%), a 41.9% increase. ... When we included variants of unknown significance in this comparison, we observed an even greater detection of abnormalities with the use of microarray analysis, as compared with karyotype analysis (13% vs. 5.8%), a 122.6% increase," Dr. Reddy and her colleagues said.
"Of the 157 stillbirths for which karyotype analysis failed to provide a definitive result, 79.6% yielded a definitive microarray result: 73.9% were normal or probably benign, and 5.7% were abnormal," they noted.
Looked at another way, karyotyping either failed altogether or produced normal results in 41% of the 44 stillbirths in which microarray testing demonstrated aneuploidy or a known pathogenic chromosomal variant (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMoa1201569]).
The investigators also performed a subgroup analysis of the 443 antepartum stillbirths in this series. As with the entire study cohort, microarray analysis detected more abnormalities (8.8%) in this subgroup than did karyotyping (6.5%), representing a 35% increase in diagnostic yield.
In a subgroup analysis of the 472 stillbirths in which postmortem examinations were conducted, microarray analysis also detected more abnormalities (29.9%) than did karyotyping (19.4%), which represents a 54% increase in diagnostic yield.
In addition, the microarray technique, but not karyotyping, identified three stillbirths with abnormalities on chromosome 22q11.2, a region that is known to be disrupted in DiGeorge syndrome (also known as velocardiofacial syndrome). One of these fetuses was found to have multiple cardiopulmonary, facial, skeletal, urogenital, and thymic anomalies on postmortem examination.
This result suggests that genomic imbalances in the 22q11.2 region may be associated with stillbirth as well as with DiGeorge syndrome. Identifying such variations in cases of stillbirth would be important so that parental studies can be performed. The risk of recurrence of DiGeorge syndrome in subsequent pregnancies can vary from less than 0.1% in genotypically normal parents to 50% if one parent has a deletion, Dr. Reddy and her associates said.
In another eight stillbirths, the microarray method, but not karyotyping, also identified variations "of unknown significance" in the region of chromosome 19p13.3. This region is known to harbor frequent variations that are not yet understood. No congenital anomalies were present in these eight cases on postmortem examination, but there were "substantially abnormal" placental findings, including chronic deciduitis, villous infarction, chronic cytomegalovirus villitis, and abruption.
Chromosomal variations in this region previously have been associated with disease but not with stillbirth, so the variation identified on microarray testing in these eight stillbirths may be benign or may confer a risk of stillbirth; further research should supply the answer, the investigators said.
This study was supported by NICHD. Dr. Reddy reported no potential financial conflicts of interest, and her associates reported numerous ties to industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Prenatal Diagnosis: Microarray Analysis Bests Karyotyping
Chromosomal microarray testing is equivalent to standard karyotype testing for prenatal diagnosis of common aneuploidies, and it provides additional clinically relevant information that karyotyping cannot, according to a report published online Dec. 6 in the New England Journal of Medicine.
In a study comparing the yields between these two techniques for routine detection of fetal disorders among more than 4,000 pregnant women, microarray testing identified important genetic anomalies missed by karyotyping in 1.7% of pregnancies with the usual indications for diagnostic testing (such as advanced maternal age) and 6% of cases in which ultrasound had revealed an anomaly.
"These data indicate a benefit to chromosomal microarray analysis as a standard part of prenatal testing, bearing in mind that, as with karyotyping, the detection of variants of uncertain clinical significance presents a challenge for counseling and cause [patients] anxiety," said Dr. Ronald J. Wapner of Columbia University Medical Center, New York, and his associates.
In fact, if microarray testing proves to have a similar yield of positive results in confirmation studies, "offering invasive testing and microarray analysis to all pregnant women would seem to be appropriate. This is consistent with the recommendations of the American Congress of Obstetricians and Gynecologists, who suggest that all women, regardless of their risk, should be offered the option of invasive testing," they noted.
Until now, microarray testing has been assessed as a method for prenatal diagnosis only in small studies of pregnancies with a high likelihood of chromosomal abnormalities, such as those in which the fetus is known to have structural anomalies. But it was not known whether the technique would reliably detect all the chromosomal abnormalities that are identified by standard karyotyping, let alone whether it would detect additional chromosomal abnormalities.
"We conducted a large, prospective study of prenatal diagnostic samples to assess, in blinded fashion, the ability of microarray analysis to diagnose common chromosome abnormalities and to gauge the extent of additional information provided by microarray analysis as compared with standard karyotyping," Dr. Wapner and his associates wrote.
They screened 6,537 women with singleton pregnancies who presented to 29 prenatal diagnostic centers for either chorionic villus sampling (CVS) or amniocentesis in 2008-2011. They then enrolled 4,406 of these women who had indications such as advanced maternal age, a positive result on aneuploidy screening, or fetal structural anomalies detected on ultrasound, and who had adequate samples from CVS (2,275 pregnancies) or amniocentesis (2,131 pregnancies).
Microarray testing was successful in 4,340 (98.8%) of these cases. Fifty-eight of these were then excluded because the samples showed mosaicism on karyotyping.
Standard karyotyping identified common autosomal aneuploidies in 7.4% of the remaining 4,282 samples and sex-chromosome aneuploidies in another 1.3%. Microarray testing also identified all of these aneuploidies. Moreover, the microarray method indicated that another eight of the CVS samples showed probable mosaicism.
More important, microarray analysis identified clinically significant segmental aneuploidies that had not been detected on karyotyping. Overall, 2% of the samples that showed normal karyotypes were found to have clinically significant copy-number variants on microarray testing, the investigators said (N. Engl. J. Med. 2012;367:2175-84).
In the subgroup of 755 samples from pregnancies with suspected growth or structural anomalies, 6% showed clinically relevant findings on microarray that were not detected on karyotyping.
Similarly, in the subgroup of 1,966 pregnancies that didn’t show anomalies on ultrasound but were referred for prenatal testing because of advanced maternal age, microarray analysis detected chromosomal abnormalities in 1.7% that were not detected on karyotyping.
Microarray testing also flagged 130 cases that were normal on karyotyping but showed chromosomal abnormalities "of uncertain significance." In 36 of these, the findings were judged to be "probably benign"; the remaining 94 cases were referred to an expert committee so their clinical relevance could be adjudicated. The committee judged 61 of these cases to be concerning enough that the patient should be informed of the chromosomal abnormality.
However, during the interval since the inception of this study 5 years ago, researchers have made considerable progress in determining whether most of these "uncertain" findings are either benign or clinically significant. If the currently available data had been used to adjudicate these 94 samples, only 56 would have been judged as "of uncertain significance," while 30 would have been categorized as clearly pathogenic and 8 as probably benign.
"With this additional information, the pathogenicity of only 1.5% of copy-number variants detected on microarray in karyotypically normal samples remains ‘uncertain,’ and this number should continue to fall as additional experience is acquired," Dr. Wapner and his associates said.
They added that they are following the offspring from the pregnancies in which copy-number variants were discovered, to establish what, if any, phenotypes develop. They are particularly interested in linking specific chromosomal abnormalities with later diagnoses of developmental delay.
This study was supported by the National Institute of Child Health and Human Development. Agilent Technologies and Affymetrix donated the microarrays and reagents used in the study, and Integrated Genetics was reimbursed for the costs of handling samples and managing cytogenetic data. Dr. Wapner reported no potential financial conflicts of interest, and his associates reported numerous ties to industry sources.
These findings support the use of microarray analysis instead of conventional karyotyping when fetal anomalies have been detected on ultrasound, said Dr. Lorraine Dugoff.
However, it is not yet established whether microarray testing is warranted in cases of advanced maternal age or when Down syndrome is suspected, because the significance of some chromosomal abnormalities remains uncertain. "In such cases ... it is possible that the counseling conundrum may outweigh the value of incremental information provided by the microarray analysis," she said.
"In addition, the increased cost associated with microarray – including the cost of parental studies in some cases – as compared with the cost of conventional karyotyping may be significantly out of proportion to the information gained in these lower-yield cases."
Dr. Dugoff is in the department of obstetrics and gynecology at the University of Pennsylvania, Philadelphia. She reported a pending research award from PerkinElmer for the study of preeclampsia. These remarks were taken from her editorial accompanying Dr. Wapner’s report (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMe1212303]).
These findings support the use of microarray analysis instead of conventional karyotyping when fetal anomalies have been detected on ultrasound, said Dr. Lorraine Dugoff.
However, it is not yet established whether microarray testing is warranted in cases of advanced maternal age or when Down syndrome is suspected, because the significance of some chromosomal abnormalities remains uncertain. "In such cases ... it is possible that the counseling conundrum may outweigh the value of incremental information provided by the microarray analysis," she said.
"In addition, the increased cost associated with microarray – including the cost of parental studies in some cases – as compared with the cost of conventional karyotyping may be significantly out of proportion to the information gained in these lower-yield cases."
Dr. Dugoff is in the department of obstetrics and gynecology at the University of Pennsylvania, Philadelphia. She reported a pending research award from PerkinElmer for the study of preeclampsia. These remarks were taken from her editorial accompanying Dr. Wapner’s report (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMe1212303]).
These findings support the use of microarray analysis instead of conventional karyotyping when fetal anomalies have been detected on ultrasound, said Dr. Lorraine Dugoff.
However, it is not yet established whether microarray testing is warranted in cases of advanced maternal age or when Down syndrome is suspected, because the significance of some chromosomal abnormalities remains uncertain. "In such cases ... it is possible that the counseling conundrum may outweigh the value of incremental information provided by the microarray analysis," she said.
"In addition, the increased cost associated with microarray – including the cost of parental studies in some cases – as compared with the cost of conventional karyotyping may be significantly out of proportion to the information gained in these lower-yield cases."
Dr. Dugoff is in the department of obstetrics and gynecology at the University of Pennsylvania, Philadelphia. She reported a pending research award from PerkinElmer for the study of preeclampsia. These remarks were taken from her editorial accompanying Dr. Wapner’s report (N. Engl. J. Med. 2012 Dec. 6 [doi:10.1056/NEJMe1212303]).
Chromosomal microarray testing is equivalent to standard karyotype testing for prenatal diagnosis of common aneuploidies, and it provides additional clinically relevant information that karyotyping cannot, according to a report published online Dec. 6 in the New England Journal of Medicine.
In a study comparing the yields between these two techniques for routine detection of fetal disorders among more than 4,000 pregnant women, microarray testing identified important genetic anomalies missed by karyotyping in 1.7% of pregnancies with the usual indications for diagnostic testing (such as advanced maternal age) and 6% of cases in which ultrasound had revealed an anomaly.
"These data indicate a benefit to chromosomal microarray analysis as a standard part of prenatal testing, bearing in mind that, as with karyotyping, the detection of variants of uncertain clinical significance presents a challenge for counseling and cause [patients] anxiety," said Dr. Ronald J. Wapner of Columbia University Medical Center, New York, and his associates.
In fact, if microarray testing proves to have a similar yield of positive results in confirmation studies, "offering invasive testing and microarray analysis to all pregnant women would seem to be appropriate. This is consistent with the recommendations of the American Congress of Obstetricians and Gynecologists, who suggest that all women, regardless of their risk, should be offered the option of invasive testing," they noted.
Until now, microarray testing has been assessed as a method for prenatal diagnosis only in small studies of pregnancies with a high likelihood of chromosomal abnormalities, such as those in which the fetus is known to have structural anomalies. But it was not known whether the technique would reliably detect all the chromosomal abnormalities that are identified by standard karyotyping, let alone whether it would detect additional chromosomal abnormalities.
"We conducted a large, prospective study of prenatal diagnostic samples to assess, in blinded fashion, the ability of microarray analysis to diagnose common chromosome abnormalities and to gauge the extent of additional information provided by microarray analysis as compared with standard karyotyping," Dr. Wapner and his associates wrote.
They screened 6,537 women with singleton pregnancies who presented to 29 prenatal diagnostic centers for either chorionic villus sampling (CVS) or amniocentesis in 2008-2011. They then enrolled 4,406 of these women who had indications such as advanced maternal age, a positive result on aneuploidy screening, or fetal structural anomalies detected on ultrasound, and who had adequate samples from CVS (2,275 pregnancies) or amniocentesis (2,131 pregnancies).
Microarray testing was successful in 4,340 (98.8%) of these cases. Fifty-eight of these were then excluded because the samples showed mosaicism on karyotyping.
Standard karyotyping identified common autosomal aneuploidies in 7.4% of the remaining 4,282 samples and sex-chromosome aneuploidies in another 1.3%. Microarray testing also identified all of these aneuploidies. Moreover, the microarray method indicated that another eight of the CVS samples showed probable mosaicism.
More important, microarray analysis identified clinically significant segmental aneuploidies that had not been detected on karyotyping. Overall, 2% of the samples that showed normal karyotypes were found to have clinically significant copy-number variants on microarray testing, the investigators said (N. Engl. J. Med. 2012;367:2175-84).
In the subgroup of 755 samples from pregnancies with suspected growth or structural anomalies, 6% showed clinically relevant findings on microarray that were not detected on karyotyping.
Similarly, in the subgroup of 1,966 pregnancies that didn’t show anomalies on ultrasound but were referred for prenatal testing because of advanced maternal age, microarray analysis detected chromosomal abnormalities in 1.7% that were not detected on karyotyping.
Microarray testing also flagged 130 cases that were normal on karyotyping but showed chromosomal abnormalities "of uncertain significance." In 36 of these, the findings were judged to be "probably benign"; the remaining 94 cases were referred to an expert committee so their clinical relevance could be adjudicated. The committee judged 61 of these cases to be concerning enough that the patient should be informed of the chromosomal abnormality.
However, during the interval since the inception of this study 5 years ago, researchers have made considerable progress in determining whether most of these "uncertain" findings are either benign or clinically significant. If the currently available data had been used to adjudicate these 94 samples, only 56 would have been judged as "of uncertain significance," while 30 would have been categorized as clearly pathogenic and 8 as probably benign.
"With this additional information, the pathogenicity of only 1.5% of copy-number variants detected on microarray in karyotypically normal samples remains ‘uncertain,’ and this number should continue to fall as additional experience is acquired," Dr. Wapner and his associates said.
They added that they are following the offspring from the pregnancies in which copy-number variants were discovered, to establish what, if any, phenotypes develop. They are particularly interested in linking specific chromosomal abnormalities with later diagnoses of developmental delay.
This study was supported by the National Institute of Child Health and Human Development. Agilent Technologies and Affymetrix donated the microarrays and reagents used in the study, and Integrated Genetics was reimbursed for the costs of handling samples and managing cytogenetic data. Dr. Wapner reported no potential financial conflicts of interest, and his associates reported numerous ties to industry sources.
Chromosomal microarray testing is equivalent to standard karyotype testing for prenatal diagnosis of common aneuploidies, and it provides additional clinically relevant information that karyotyping cannot, according to a report published online Dec. 6 in the New England Journal of Medicine.
In a study comparing the yields between these two techniques for routine detection of fetal disorders among more than 4,000 pregnant women, microarray testing identified important genetic anomalies missed by karyotyping in 1.7% of pregnancies with the usual indications for diagnostic testing (such as advanced maternal age) and 6% of cases in which ultrasound had revealed an anomaly.
"These data indicate a benefit to chromosomal microarray analysis as a standard part of prenatal testing, bearing in mind that, as with karyotyping, the detection of variants of uncertain clinical significance presents a challenge for counseling and cause [patients] anxiety," said Dr. Ronald J. Wapner of Columbia University Medical Center, New York, and his associates.
In fact, if microarray testing proves to have a similar yield of positive results in confirmation studies, "offering invasive testing and microarray analysis to all pregnant women would seem to be appropriate. This is consistent with the recommendations of the American Congress of Obstetricians and Gynecologists, who suggest that all women, regardless of their risk, should be offered the option of invasive testing," they noted.
Until now, microarray testing has been assessed as a method for prenatal diagnosis only in small studies of pregnancies with a high likelihood of chromosomal abnormalities, such as those in which the fetus is known to have structural anomalies. But it was not known whether the technique would reliably detect all the chromosomal abnormalities that are identified by standard karyotyping, let alone whether it would detect additional chromosomal abnormalities.
"We conducted a large, prospective study of prenatal diagnostic samples to assess, in blinded fashion, the ability of microarray analysis to diagnose common chromosome abnormalities and to gauge the extent of additional information provided by microarray analysis as compared with standard karyotyping," Dr. Wapner and his associates wrote.
They screened 6,537 women with singleton pregnancies who presented to 29 prenatal diagnostic centers for either chorionic villus sampling (CVS) or amniocentesis in 2008-2011. They then enrolled 4,406 of these women who had indications such as advanced maternal age, a positive result on aneuploidy screening, or fetal structural anomalies detected on ultrasound, and who had adequate samples from CVS (2,275 pregnancies) or amniocentesis (2,131 pregnancies).
Microarray testing was successful in 4,340 (98.8%) of these cases. Fifty-eight of these were then excluded because the samples showed mosaicism on karyotyping.
Standard karyotyping identified common autosomal aneuploidies in 7.4% of the remaining 4,282 samples and sex-chromosome aneuploidies in another 1.3%. Microarray testing also identified all of these aneuploidies. Moreover, the microarray method indicated that another eight of the CVS samples showed probable mosaicism.
More important, microarray analysis identified clinically significant segmental aneuploidies that had not been detected on karyotyping. Overall, 2% of the samples that showed normal karyotypes were found to have clinically significant copy-number variants on microarray testing, the investigators said (N. Engl. J. Med. 2012;367:2175-84).
In the subgroup of 755 samples from pregnancies with suspected growth or structural anomalies, 6% showed clinically relevant findings on microarray that were not detected on karyotyping.
Similarly, in the subgroup of 1,966 pregnancies that didn’t show anomalies on ultrasound but were referred for prenatal testing because of advanced maternal age, microarray analysis detected chromosomal abnormalities in 1.7% that were not detected on karyotyping.
Microarray testing also flagged 130 cases that were normal on karyotyping but showed chromosomal abnormalities "of uncertain significance." In 36 of these, the findings were judged to be "probably benign"; the remaining 94 cases were referred to an expert committee so their clinical relevance could be adjudicated. The committee judged 61 of these cases to be concerning enough that the patient should be informed of the chromosomal abnormality.
However, during the interval since the inception of this study 5 years ago, researchers have made considerable progress in determining whether most of these "uncertain" findings are either benign or clinically significant. If the currently available data had been used to adjudicate these 94 samples, only 56 would have been judged as "of uncertain significance," while 30 would have been categorized as clearly pathogenic and 8 as probably benign.
"With this additional information, the pathogenicity of only 1.5% of copy-number variants detected on microarray in karyotypically normal samples remains ‘uncertain,’ and this number should continue to fall as additional experience is acquired," Dr. Wapner and his associates said.
They added that they are following the offspring from the pregnancies in which copy-number variants were discovered, to establish what, if any, phenotypes develop. They are particularly interested in linking specific chromosomal abnormalities with later diagnoses of developmental delay.
This study was supported by the National Institute of Child Health and Human Development. Agilent Technologies and Affymetrix donated the microarrays and reagents used in the study, and Integrated Genetics was reimbursed for the costs of handling samples and managing cytogenetic data. Dr. Wapner reported no potential financial conflicts of interest, and his associates reported numerous ties to industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: Microarray testing identified all the common aneuploidies and sex-chromosome–linked aneuploidies that were detected by karyotyping, as well as additional genetic anomalies that were missed by karyotyping in approximately 2%-6% of the entire cohort.
Data Source: Results were taken from a prospective study comparing the prenatal diagnostic findings from standard karyotyping of chorionic villus sampling and amniocentesis to those from microarray testing of the same samples in 4,406 pregnancies in 2008-2011.
Disclosures: This study was supported by the National Institute of Child Health and Human Development. Agilent Technologies and Affymetrix donated the microarrays and reagents used in the study, and Integrated Genetics was reimbursed for the costs of handling samples and managing cytogenetic data. Dr. Wapner reported no potential financial conflicts of interest, and his associates reported numerous ties to industry sources.
New Criteria for Gestational Diabetes Could Swamp Providers
A lower cut-point for diagnosing gestational diabetes is a double-edged sword for clinicians.
Adopting more stringent criteria would triple the number of women identified whose abnormal glucose levels could potentially endanger their health and that of their unborn children. Once diagnosed, they could be treated.
But adopting the proposed criteria would skyrocket the number of diagnosed gestational diabetes cases from about 135,000 to more than 500,000 each year, according to Dr. E. Albert Reece, dean of the University of Maryland School of Medicine, Baltimore.
"It’s quite possible that lowering the diagnostic threshold with these criteria could push the incidence of gestational diabetes from about 7% of all pregnancies to more than 20%," Dr. Reece said in an interview. "With that may come the potential for more cesarean sections and their related adverse consequences. It’s not a case of simply diagnosing earlier – it’s diagnosing earlier with a real potential for increased interventions that bring along their own risks."
The American Diabetes Association adopted the new diagnostic criteria last year (Diabetes Care 2011;34:S11-61). Now, the American College of Obstetricians and Gynecologists is contemplating its own move, and Dr. Reece, a well-respected expert on the topic, is urging caution.
If ACOG were to adopt the criteria, he said, obstetric interventions related to the condition would almost certainly rise. Mothers and babies would be at the most direct risk of any additional procedures, but clinicians will face their own set of problems.
As cesarean sections and other invasive procedures increase, lawsuits go up as well. The possibility of these collateral consequences isn’t the only thing to consider, warned Dr. Reece. Even now, clinicians who care for women with gestational diabetes are hard pressed to keep up with their patient load, let alone the tens of thousands more who would be diagnosed under the new criteria.
Associated costs can’t be ignored either, he said, especially at this crucial time in America’s health care history, when affordable care for everyone is now the law of the land.
In theory, the idea of catching more cases earlier seems sensible. But health care policy should rely on more than theory, said Dr. Reece, who is also the John Z. and Akiko K. Bowers Distinguished Professor of Obstetrics and Gynecology at the university.
"If we could be certain that making this diagnosis earlier would actually improve outcomes, we would have a compelling reason to change. But at this point, many are unconvinced that change would result in improved outcomes."
The current diagnostic threshold for gestational diabetes is a positive result on two or more oral glucose tolerance tests, with glucose levels of more than 180 mg/dL at 1 hour; more than 155 mg/dL at 2 hours; and more than 140 mg/dL at 3 hours. This approach is based on data gathered in the 1970s and 1980s.
More recent data from the Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) Study Cooperative Research Group suggest that subclinical hyperglycemia affects additional thousands of pregnant women. The study found positive associations between maternal hyperglycemia and increasing rates of large for gestational age neonates, evidence of fetal hyperinsulinemia, neonatal hypoglycemia, and cesarean delivery.
After the study was published in 2008, the International Association of Diabetes and Pregnancy Study Groups (IADPSG) published its new recommendations for the diagnosis and classification of hyperglycemia during pregnancy. Under the new system, gestational diabetes can be diagnosed after a single abnormal oral glucose tolerance test with the threshold of fasting plasma glucose of more than 92 mg/dL, or, after a single oral test, a level of more than 180 mg/dL at 1 hour and more than 152 mg/dL at 2 hours.
"A key argument for changing the current diagnostic guidelines for gestational diabetes in the United States is that a single diagnostic test – by eliminating the screening phase – will be more convenient for the provider and the patient," Dr. Reece wrote in the October issue of the American Journal of Obstetrics and Gynecology (2012 [doi: 10.1016/j.ajog.2012.10.887]). "Furthermore, because it is more user-friendly, it is argued that the one-step diagnostic test also will be much easier to administer and, thus, the earlier diagnosis and treatment of gestational diabetes will lead to more consistent care, better organized research, and, ultimately, to better outcomes for mothers and their babies."
According to the American Diabetes Association, up to 10% of women with gestational diabetes have underlying undiagnosed diabetes, usually type 2. Women who develop gestational diabetes without underlying disease have a 35%-60% chance of developing it over the next 10-20 years.
Studies also are beginning to uncover long-term risks for babies who develop during a hyperglycemic pregnancy. These infants appear to have double the risk of developing childhood obesity and/or metabolic syndrome, laying the foundation for adulthood rife with obesity- and diabetes-related health problems.
But when researchers examine the overall effect of a more stringent screening and diagnostic protocol, the view is somewhat cloudy, Dr. Reece said.
A 2011 study found that treating mild gestational diabetes was a cost-effective way of improving maternal and neonatal outcomes, including decreasing preeclampsia, cesarean sections, macrosomia, shoulder dystocia, permanent and transient brachial plexus injury, neonatal hypoglycemia, neonatal hyperbilirubinemia, and neonatal intensive care unit admissions (Am. J. Obstet. Gynecol. 2011;205:282.e1-7).
But a more recent study found that treating the condition only saves money when considering the mother’s long-term health.
"Our model demonstrates that [the new criteria] are cost-effective only when post-delivery care reduces diabetes incidence," wrote Dr. Erika Werner.
"When post-delivery care was not accomplished, the ... strategy was no longer cost-effective. ... Although there are potential perinatal benefits associated with the [criteria], these benefits alone do not justify the additional cost associated with tripling the number of GDM diagnoses in the U.S.," the authors wrote (Diabetes Care 2012;35:529-35).
The criteria’s biggest financial bang would come from their ability to detect occult diabetes in the mothers, Dr. Werner said in an interview.
"It would allow us to differentiate those women with underlying diabetes from those with only gestational diabetes. We’re missing these women now because very few ever come back for their postnatal diabetes screening," said Dr. Werner, a maternal fetal medicine specialist at Johns Hopkins University, Baltimore. Intervening early can be assumed to save much of the long-term financial costs of type 2 diabetes.
Her cost analysis isn’t set in stone, though, because it couldn’t control for the financial impact of either increased perinatal interventions – like cesarean sections – or the financial impact of preventing fetal consequences. And there’s no way to predict how many women who did develop diabetes postnatally would require insulin or oral medications, and how many could be conservatively managed with diet and exercise.
"We didn’t control for this because there are not data telling us that controlling glucose in pregnancy improves outcomes for women and neonates. The trends are there, but the confidence intervals are not. Any cost analysis is limited by the data that are out there. And in this case, we need more data," she said.
Dr. Reece agreed, saying only large long-term studies could provide enough of the evidence necessary to support changing the diagnostic algorithm.
But, Dr. Werner said, U.S. physicians might be able to learn from their international colleagues. "Some countries are already moving forward with them, and that will give us some of the additional data that we’re looking for."
Australia is one of those countries. The Australasian Diabetes in Pregnancy Society (www.adips.org) adopted the diagnostic criteria earlier this year, said Prof. Robert Moses, director of the Illawarra Diabetes Service in Wollongong, New South Wales. In a March editorial in the journal Diabetes Care, he likened the controversy over the recommendation to "opening Pandora’s box," adding that he supports the change, but that it needs to be thoughtfully applied, in a "clinically responsible way" (2012;35:461-2).
The change is expected to bump up Australia’s gestational diabetes incidence from 10% to 13%, Dr. Moses said in an interview. Any increase in the cost of managing these women and their pregnancies pales beside the clinical alternative.
"The cost of diagnosing and treating women with gestational diabetes is relatively little compared with other health costs. However, there are unfortunately a lot of potential add-on costs. We know that women with gestational diabetes have more interventions, both obstetric and pediatric."
Even considering those costs, ensuring the long-term health of these mothers and babies is a good investment, he said. To put the cost in perspective, "One course of experimental cancer therapy is likely to cost more than testing 1,000 women and treating the 130 with gestational diabetes. It is all a matter of perspective and priority."
He’s glad that Australia chose to move ahead with the change rather than wait for the official numbers to prove that it works.
"Large studies are difficult to initiate and fund. At some stage, common sense has to prevail. Waiting for the results of trials which will not happen in our lifetime should not be an excuse not to give the best possible maternal and fetal care. This is too important a problem to ignore, especially as the solution is relatively simple and the cost is relatively trivial," he said.
None of the sources named disclosed any financial relationships relative to the topic of this article.
A lower cut-point for diagnosing gestational diabetes is a double-edged sword for clinicians.
Adopting more stringent criteria would triple the number of women identified whose abnormal glucose levels could potentially endanger their health and that of their unborn children. Once diagnosed, they could be treated.
But adopting the proposed criteria would skyrocket the number of diagnosed gestational diabetes cases from about 135,000 to more than 500,000 each year, according to Dr. E. Albert Reece, dean of the University of Maryland School of Medicine, Baltimore.
"It’s quite possible that lowering the diagnostic threshold with these criteria could push the incidence of gestational diabetes from about 7% of all pregnancies to more than 20%," Dr. Reece said in an interview. "With that may come the potential for more cesarean sections and their related adverse consequences. It’s not a case of simply diagnosing earlier – it’s diagnosing earlier with a real potential for increased interventions that bring along their own risks."
The American Diabetes Association adopted the new diagnostic criteria last year (Diabetes Care 2011;34:S11-61). Now, the American College of Obstetricians and Gynecologists is contemplating its own move, and Dr. Reece, a well-respected expert on the topic, is urging caution.
If ACOG were to adopt the criteria, he said, obstetric interventions related to the condition would almost certainly rise. Mothers and babies would be at the most direct risk of any additional procedures, but clinicians will face their own set of problems.
As cesarean sections and other invasive procedures increase, lawsuits go up as well. The possibility of these collateral consequences isn’t the only thing to consider, warned Dr. Reece. Even now, clinicians who care for women with gestational diabetes are hard pressed to keep up with their patient load, let alone the tens of thousands more who would be diagnosed under the new criteria.
Associated costs can’t be ignored either, he said, especially at this crucial time in America’s health care history, when affordable care for everyone is now the law of the land.
In theory, the idea of catching more cases earlier seems sensible. But health care policy should rely on more than theory, said Dr. Reece, who is also the John Z. and Akiko K. Bowers Distinguished Professor of Obstetrics and Gynecology at the university.
"If we could be certain that making this diagnosis earlier would actually improve outcomes, we would have a compelling reason to change. But at this point, many are unconvinced that change would result in improved outcomes."
The current diagnostic threshold for gestational diabetes is a positive result on two or more oral glucose tolerance tests, with glucose levels of more than 180 mg/dL at 1 hour; more than 155 mg/dL at 2 hours; and more than 140 mg/dL at 3 hours. This approach is based on data gathered in the 1970s and 1980s.
More recent data from the Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) Study Cooperative Research Group suggest that subclinical hyperglycemia affects additional thousands of pregnant women. The study found positive associations between maternal hyperglycemia and increasing rates of large for gestational age neonates, evidence of fetal hyperinsulinemia, neonatal hypoglycemia, and cesarean delivery.
After the study was published in 2008, the International Association of Diabetes and Pregnancy Study Groups (IADPSG) published its new recommendations for the diagnosis and classification of hyperglycemia during pregnancy. Under the new system, gestational diabetes can be diagnosed after a single abnormal oral glucose tolerance test with the threshold of fasting plasma glucose of more than 92 mg/dL, or, after a single oral test, a level of more than 180 mg/dL at 1 hour and more than 152 mg/dL at 2 hours.
"A key argument for changing the current diagnostic guidelines for gestational diabetes in the United States is that a single diagnostic test – by eliminating the screening phase – will be more convenient for the provider and the patient," Dr. Reece wrote in the October issue of the American Journal of Obstetrics and Gynecology (2012 [doi: 10.1016/j.ajog.2012.10.887]). "Furthermore, because it is more user-friendly, it is argued that the one-step diagnostic test also will be much easier to administer and, thus, the earlier diagnosis and treatment of gestational diabetes will lead to more consistent care, better organized research, and, ultimately, to better outcomes for mothers and their babies."
According to the American Diabetes Association, up to 10% of women with gestational diabetes have underlying undiagnosed diabetes, usually type 2. Women who develop gestational diabetes without underlying disease have a 35%-60% chance of developing it over the next 10-20 years.
Studies also are beginning to uncover long-term risks for babies who develop during a hyperglycemic pregnancy. These infants appear to have double the risk of developing childhood obesity and/or metabolic syndrome, laying the foundation for adulthood rife with obesity- and diabetes-related health problems.
But when researchers examine the overall effect of a more stringent screening and diagnostic protocol, the view is somewhat cloudy, Dr. Reece said.
A 2011 study found that treating mild gestational diabetes was a cost-effective way of improving maternal and neonatal outcomes, including decreasing preeclampsia, cesarean sections, macrosomia, shoulder dystocia, permanent and transient brachial plexus injury, neonatal hypoglycemia, neonatal hyperbilirubinemia, and neonatal intensive care unit admissions (Am. J. Obstet. Gynecol. 2011;205:282.e1-7).
But a more recent study found that treating the condition only saves money when considering the mother’s long-term health.
"Our model demonstrates that [the new criteria] are cost-effective only when post-delivery care reduces diabetes incidence," wrote Dr. Erika Werner.
"When post-delivery care was not accomplished, the ... strategy was no longer cost-effective. ... Although there are potential perinatal benefits associated with the [criteria], these benefits alone do not justify the additional cost associated with tripling the number of GDM diagnoses in the U.S.," the authors wrote (Diabetes Care 2012;35:529-35).
The criteria’s biggest financial bang would come from their ability to detect occult diabetes in the mothers, Dr. Werner said in an interview.
"It would allow us to differentiate those women with underlying diabetes from those with only gestational diabetes. We’re missing these women now because very few ever come back for their postnatal diabetes screening," said Dr. Werner, a maternal fetal medicine specialist at Johns Hopkins University, Baltimore. Intervening early can be assumed to save much of the long-term financial costs of type 2 diabetes.
Her cost analysis isn’t set in stone, though, because it couldn’t control for the financial impact of either increased perinatal interventions – like cesarean sections – or the financial impact of preventing fetal consequences. And there’s no way to predict how many women who did develop diabetes postnatally would require insulin or oral medications, and how many could be conservatively managed with diet and exercise.
"We didn’t control for this because there are not data telling us that controlling glucose in pregnancy improves outcomes for women and neonates. The trends are there, but the confidence intervals are not. Any cost analysis is limited by the data that are out there. And in this case, we need more data," she said.
Dr. Reece agreed, saying only large long-term studies could provide enough of the evidence necessary to support changing the diagnostic algorithm.
But, Dr. Werner said, U.S. physicians might be able to learn from their international colleagues. "Some countries are already moving forward with them, and that will give us some of the additional data that we’re looking for."
Australia is one of those countries. The Australasian Diabetes in Pregnancy Society (www.adips.org) adopted the diagnostic criteria earlier this year, said Prof. Robert Moses, director of the Illawarra Diabetes Service in Wollongong, New South Wales. In a March editorial in the journal Diabetes Care, he likened the controversy over the recommendation to "opening Pandora’s box," adding that he supports the change, but that it needs to be thoughtfully applied, in a "clinically responsible way" (2012;35:461-2).
The change is expected to bump up Australia’s gestational diabetes incidence from 10% to 13%, Dr. Moses said in an interview. Any increase in the cost of managing these women and their pregnancies pales beside the clinical alternative.
"The cost of diagnosing and treating women with gestational diabetes is relatively little compared with other health costs. However, there are unfortunately a lot of potential add-on costs. We know that women with gestational diabetes have more interventions, both obstetric and pediatric."
Even considering those costs, ensuring the long-term health of these mothers and babies is a good investment, he said. To put the cost in perspective, "One course of experimental cancer therapy is likely to cost more than testing 1,000 women and treating the 130 with gestational diabetes. It is all a matter of perspective and priority."
He’s glad that Australia chose to move ahead with the change rather than wait for the official numbers to prove that it works.
"Large studies are difficult to initiate and fund. At some stage, common sense has to prevail. Waiting for the results of trials which will not happen in our lifetime should not be an excuse not to give the best possible maternal and fetal care. This is too important a problem to ignore, especially as the solution is relatively simple and the cost is relatively trivial," he said.
None of the sources named disclosed any financial relationships relative to the topic of this article.
A lower cut-point for diagnosing gestational diabetes is a double-edged sword for clinicians.
Adopting more stringent criteria would triple the number of women identified whose abnormal glucose levels could potentially endanger their health and that of their unborn children. Once diagnosed, they could be treated.
But adopting the proposed criteria would skyrocket the number of diagnosed gestational diabetes cases from about 135,000 to more than 500,000 each year, according to Dr. E. Albert Reece, dean of the University of Maryland School of Medicine, Baltimore.
"It’s quite possible that lowering the diagnostic threshold with these criteria could push the incidence of gestational diabetes from about 7% of all pregnancies to more than 20%," Dr. Reece said in an interview. "With that may come the potential for more cesarean sections and their related adverse consequences. It’s not a case of simply diagnosing earlier – it’s diagnosing earlier with a real potential for increased interventions that bring along their own risks."
The American Diabetes Association adopted the new diagnostic criteria last year (Diabetes Care 2011;34:S11-61). Now, the American College of Obstetricians and Gynecologists is contemplating its own move, and Dr. Reece, a well-respected expert on the topic, is urging caution.
If ACOG were to adopt the criteria, he said, obstetric interventions related to the condition would almost certainly rise. Mothers and babies would be at the most direct risk of any additional procedures, but clinicians will face their own set of problems.
As cesarean sections and other invasive procedures increase, lawsuits go up as well. The possibility of these collateral consequences isn’t the only thing to consider, warned Dr. Reece. Even now, clinicians who care for women with gestational diabetes are hard pressed to keep up with their patient load, let alone the tens of thousands more who would be diagnosed under the new criteria.
Associated costs can’t be ignored either, he said, especially at this crucial time in America’s health care history, when affordable care for everyone is now the law of the land.
In theory, the idea of catching more cases earlier seems sensible. But health care policy should rely on more than theory, said Dr. Reece, who is also the John Z. and Akiko K. Bowers Distinguished Professor of Obstetrics and Gynecology at the university.
"If we could be certain that making this diagnosis earlier would actually improve outcomes, we would have a compelling reason to change. But at this point, many are unconvinced that change would result in improved outcomes."
The current diagnostic threshold for gestational diabetes is a positive result on two or more oral glucose tolerance tests, with glucose levels of more than 180 mg/dL at 1 hour; more than 155 mg/dL at 2 hours; and more than 140 mg/dL at 3 hours. This approach is based on data gathered in the 1970s and 1980s.
More recent data from the Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) Study Cooperative Research Group suggest that subclinical hyperglycemia affects additional thousands of pregnant women. The study found positive associations between maternal hyperglycemia and increasing rates of large for gestational age neonates, evidence of fetal hyperinsulinemia, neonatal hypoglycemia, and cesarean delivery.
After the study was published in 2008, the International Association of Diabetes and Pregnancy Study Groups (IADPSG) published its new recommendations for the diagnosis and classification of hyperglycemia during pregnancy. Under the new system, gestational diabetes can be diagnosed after a single abnormal oral glucose tolerance test with the threshold of fasting plasma glucose of more than 92 mg/dL, or, after a single oral test, a level of more than 180 mg/dL at 1 hour and more than 152 mg/dL at 2 hours.
"A key argument for changing the current diagnostic guidelines for gestational diabetes in the United States is that a single diagnostic test – by eliminating the screening phase – will be more convenient for the provider and the patient," Dr. Reece wrote in the October issue of the American Journal of Obstetrics and Gynecology (2012 [doi: 10.1016/j.ajog.2012.10.887]). "Furthermore, because it is more user-friendly, it is argued that the one-step diagnostic test also will be much easier to administer and, thus, the earlier diagnosis and treatment of gestational diabetes will lead to more consistent care, better organized research, and, ultimately, to better outcomes for mothers and their babies."
According to the American Diabetes Association, up to 10% of women with gestational diabetes have underlying undiagnosed diabetes, usually type 2. Women who develop gestational diabetes without underlying disease have a 35%-60% chance of developing it over the next 10-20 years.
Studies also are beginning to uncover long-term risks for babies who develop during a hyperglycemic pregnancy. These infants appear to have double the risk of developing childhood obesity and/or metabolic syndrome, laying the foundation for adulthood rife with obesity- and diabetes-related health problems.
But when researchers examine the overall effect of a more stringent screening and diagnostic protocol, the view is somewhat cloudy, Dr. Reece said.
A 2011 study found that treating mild gestational diabetes was a cost-effective way of improving maternal and neonatal outcomes, including decreasing preeclampsia, cesarean sections, macrosomia, shoulder dystocia, permanent and transient brachial plexus injury, neonatal hypoglycemia, neonatal hyperbilirubinemia, and neonatal intensive care unit admissions (Am. J. Obstet. Gynecol. 2011;205:282.e1-7).
But a more recent study found that treating the condition only saves money when considering the mother’s long-term health.
"Our model demonstrates that [the new criteria] are cost-effective only when post-delivery care reduces diabetes incidence," wrote Dr. Erika Werner.
"When post-delivery care was not accomplished, the ... strategy was no longer cost-effective. ... Although there are potential perinatal benefits associated with the [criteria], these benefits alone do not justify the additional cost associated with tripling the number of GDM diagnoses in the U.S.," the authors wrote (Diabetes Care 2012;35:529-35).
The criteria’s biggest financial bang would come from their ability to detect occult diabetes in the mothers, Dr. Werner said in an interview.
"It would allow us to differentiate those women with underlying diabetes from those with only gestational diabetes. We’re missing these women now because very few ever come back for their postnatal diabetes screening," said Dr. Werner, a maternal fetal medicine specialist at Johns Hopkins University, Baltimore. Intervening early can be assumed to save much of the long-term financial costs of type 2 diabetes.
Her cost analysis isn’t set in stone, though, because it couldn’t control for the financial impact of either increased perinatal interventions – like cesarean sections – or the financial impact of preventing fetal consequences. And there’s no way to predict how many women who did develop diabetes postnatally would require insulin or oral medications, and how many could be conservatively managed with diet and exercise.
"We didn’t control for this because there are not data telling us that controlling glucose in pregnancy improves outcomes for women and neonates. The trends are there, but the confidence intervals are not. Any cost analysis is limited by the data that are out there. And in this case, we need more data," she said.
Dr. Reece agreed, saying only large long-term studies could provide enough of the evidence necessary to support changing the diagnostic algorithm.
But, Dr. Werner said, U.S. physicians might be able to learn from their international colleagues. "Some countries are already moving forward with them, and that will give us some of the additional data that we’re looking for."
Australia is one of those countries. The Australasian Diabetes in Pregnancy Society (www.adips.org) adopted the diagnostic criteria earlier this year, said Prof. Robert Moses, director of the Illawarra Diabetes Service in Wollongong, New South Wales. In a March editorial in the journal Diabetes Care, he likened the controversy over the recommendation to "opening Pandora’s box," adding that he supports the change, but that it needs to be thoughtfully applied, in a "clinically responsible way" (2012;35:461-2).
The change is expected to bump up Australia’s gestational diabetes incidence from 10% to 13%, Dr. Moses said in an interview. Any increase in the cost of managing these women and their pregnancies pales beside the clinical alternative.
"The cost of diagnosing and treating women with gestational diabetes is relatively little compared with other health costs. However, there are unfortunately a lot of potential add-on costs. We know that women with gestational diabetes have more interventions, both obstetric and pediatric."
Even considering those costs, ensuring the long-term health of these mothers and babies is a good investment, he said. To put the cost in perspective, "One course of experimental cancer therapy is likely to cost more than testing 1,000 women and treating the 130 with gestational diabetes. It is all a matter of perspective and priority."
He’s glad that Australia chose to move ahead with the change rather than wait for the official numbers to prove that it works.
"Large studies are difficult to initiate and fund. At some stage, common sense has to prevail. Waiting for the results of trials which will not happen in our lifetime should not be an excuse not to give the best possible maternal and fetal care. This is too important a problem to ignore, especially as the solution is relatively simple and the cost is relatively trivial," he said.
None of the sources named disclosed any financial relationships relative to the topic of this article.