User login
COVID vaccination rates among pregnant people remain low
COVID vaccination rates among pregnant people remain low, despite data that shows the vaccines can prevent the high risk of severe disease during pregnancy.
About 30% of pregnant people are vaccinated, according to the latest CDC data, with only 18% obtaining a dose during pregnancy. Health officials have been tracking the timing of vaccination before and during pregnancy.
The vaccination rates are even lower among pregnant Black people, CDC data shows. About 15% are fully vaccinated, compared with 25% of pregnant Hispanic and Latino people, 34% of pregnant White people, and 46% of pregnant Asian people.
“This puts them at severe risk of severe disease from COVID-19,” Rochelle Walensky, MD, the CDC director, said during a news briefing with the White House COVID-19 Response Team.
“We know that pregnant women are at increased risk of severe disease, of hospitalization and ventilation,” she said. “They’re also at increased risk for adverse events to their baby.”
Those who give birth while infected with COVID-19 had “significantly higher rates” of intensive care unit admission, intubation, ventilation, and death, according to a recent study published in JAMA Network Open.
Dr. Walensky said on Sept. 28 that studies show COVID-19 vaccines can be taken at any time while pregnant or breastfeeding. She noted that the vaccines are safe for both mothers and their babies.
“We’ve actually seen that some antibody from the vaccine traverses [the placenta] to the baby and, in fact, could potentially protect the baby,” she said.
Public health officials say the low vaccination rates can be attributed to caution around the time of pregnancy, concern for the baby, barriers to health care, and misinformation promoted online.
“Pregnancy is a precious time. It’s also a time that a lot of women have fear,” Pam Oliver, MD, an obstetrics and gynecology doctor and executive vice president of North Carolina’s Novant Health, told USA Today.
“It is natural to have questions,” she said. “So, let’s talk about what we know, let’s put it in perspective.”
A version of this article first appeared on Medscape.com.
COVID vaccination rates among pregnant people remain low, despite data that shows the vaccines can prevent the high risk of severe disease during pregnancy.
About 30% of pregnant people are vaccinated, according to the latest CDC data, with only 18% obtaining a dose during pregnancy. Health officials have been tracking the timing of vaccination before and during pregnancy.
The vaccination rates are even lower among pregnant Black people, CDC data shows. About 15% are fully vaccinated, compared with 25% of pregnant Hispanic and Latino people, 34% of pregnant White people, and 46% of pregnant Asian people.
“This puts them at severe risk of severe disease from COVID-19,” Rochelle Walensky, MD, the CDC director, said during a news briefing with the White House COVID-19 Response Team.
“We know that pregnant women are at increased risk of severe disease, of hospitalization and ventilation,” she said. “They’re also at increased risk for adverse events to their baby.”
Those who give birth while infected with COVID-19 had “significantly higher rates” of intensive care unit admission, intubation, ventilation, and death, according to a recent study published in JAMA Network Open.
Dr. Walensky said on Sept. 28 that studies show COVID-19 vaccines can be taken at any time while pregnant or breastfeeding. She noted that the vaccines are safe for both mothers and their babies.
“We’ve actually seen that some antibody from the vaccine traverses [the placenta] to the baby and, in fact, could potentially protect the baby,” she said.
Public health officials say the low vaccination rates can be attributed to caution around the time of pregnancy, concern for the baby, barriers to health care, and misinformation promoted online.
“Pregnancy is a precious time. It’s also a time that a lot of women have fear,” Pam Oliver, MD, an obstetrics and gynecology doctor and executive vice president of North Carolina’s Novant Health, told USA Today.
“It is natural to have questions,” she said. “So, let’s talk about what we know, let’s put it in perspective.”
A version of this article first appeared on Medscape.com.
COVID vaccination rates among pregnant people remain low, despite data that shows the vaccines can prevent the high risk of severe disease during pregnancy.
About 30% of pregnant people are vaccinated, according to the latest CDC data, with only 18% obtaining a dose during pregnancy. Health officials have been tracking the timing of vaccination before and during pregnancy.
The vaccination rates are even lower among pregnant Black people, CDC data shows. About 15% are fully vaccinated, compared with 25% of pregnant Hispanic and Latino people, 34% of pregnant White people, and 46% of pregnant Asian people.
“This puts them at severe risk of severe disease from COVID-19,” Rochelle Walensky, MD, the CDC director, said during a news briefing with the White House COVID-19 Response Team.
“We know that pregnant women are at increased risk of severe disease, of hospitalization and ventilation,” she said. “They’re also at increased risk for adverse events to their baby.”
Those who give birth while infected with COVID-19 had “significantly higher rates” of intensive care unit admission, intubation, ventilation, and death, according to a recent study published in JAMA Network Open.
Dr. Walensky said on Sept. 28 that studies show COVID-19 vaccines can be taken at any time while pregnant or breastfeeding. She noted that the vaccines are safe for both mothers and their babies.
“We’ve actually seen that some antibody from the vaccine traverses [the placenta] to the baby and, in fact, could potentially protect the baby,” she said.
Public health officials say the low vaccination rates can be attributed to caution around the time of pregnancy, concern for the baby, barriers to health care, and misinformation promoted online.
“Pregnancy is a precious time. It’s also a time that a lot of women have fear,” Pam Oliver, MD, an obstetrics and gynecology doctor and executive vice president of North Carolina’s Novant Health, told USA Today.
“It is natural to have questions,” she said. “So, let’s talk about what we know, let’s put it in perspective.”
A version of this article first appeared on Medscape.com.
USPSTF expands criteria for those at risk of developing preeclampsia
The U.S. Preventive Services Task Force continues to recommend that pregnant women at risk of developing preeclampsia take low-dose aspirin daily, and has expanded the criteria for those at risk.
“I think that this issue has been one that people have talked about and thought about for a long time, but it hasn’t kind of leapt into the front for all practitioners,” Aaron B. Caughey, MD, MPH, PhD, a USPSTF member, said in an interview. “We think it’s really important that all providers and all pregnant persons are aware that folks at an increased risk for preeclampsia can receive a reduction in the risk of preeclampsia from receiving baby aspirin starting after 12 weeks of gestation.”
The task force concluded with moderate certainty that a daily dose of 81 milligrams of aspirin after 12 weeks of pregnancy could reduce the risk for preeclampsia, preterm birth, and stillbirths in pregnant persons at high risk for preeclampsia. The recommendations, which were published in JAMA, are identical to the panel’s 2014 recommendations.
However, the new draft includes a suggestion that expands the list of pregnant patients at risk of developing preeclampsia. In 2014, the USPSTF recommended that clinicians prescribe low-dose daily aspirin to those who had at least two moderate-risk factors related to disparity – first pregnancy, obesity, family history of preeclampsia, lower income, age of 35 years or older, of African descent, and previous adverse pregnancy outcomes. The recent update suggests clinicians consider prescribing low-dose aspirin to patients with just one of the moderate risk factors. The task force also added “in vitro fertilization” as a moderate risk factor.
Dr. Caughey said the motivation for this addition was out of concern for disparities in outcomes for people who have less access to care and to help curb the racial disparity in the prevalence of preeclampsia in Black women and other disadvantaged groups. “[In an effort] to prevent the development of preeclampsia in such individuals that have historically had worse health outcomes, we wanted to emphasize that should at least be considered by clinicians,” Dr. Caughey said.
This change is a “major one,” according to Victor Klein, MD, MBA, CPHRM, a specialist in high-risk pregnancy.
“That’s probably three-quarters of my patients. The majority of my patients will now be candidates [to receive a low-dose aspirin prescription to prevent preeclampsia],” Dr. Klein, vice chairman of obstetrics and gynecology at North Shore University Hospital, Manhasset, N.Y., said in an interview. “[This] may increase the amount of people who will be getting the aspirin and therefore decrease the chance of preeclampsia or developing preeclampsia.”
Preeclampsia is a condition characterized by high blood pressure and signs of problems with the kidneys, liver, and other organs during pregnancy, according to the Centers for Disease Control and Prevention. The condition occurs in about 1 in 25 pregnancies in the United States and can cause serious and fatal complications for both the mother and child.
Although the update reaffirms that aspirin is safe and effective in preventing preeclampsia, Dr. Klein believes the dosage they are recommending is too low, as he has had patients develop preeclampsia while taking 81 mg of aspirin daily. Dr. Klein says he prescribes two daily doses of 81 mg aspirin to some of his patients.
“The majority of us in the field of high-risk pregnancies feel that 81 milligrams is not enough,” Dr. Klein said. “So I am disappointed that [they] didn’t talk about consideration for higher doses. I have patients taking two baby aspirins who developed preeclampsia.”
However, the systematic review that the USPSTF’s recommendation was based on did not “really find evidence to suggest that a higher dose was necessarily better than the lower dose,” Dr. Caughey said. However, this may be something they look at again in the near future.
“I know of clinicians that are asking if we should be using a higher dose,” Dr. Caughey explained. “If more evidence accumulates then absolutely we will look at that issue again.”
In their draft, the task force said there’s limited evidence on the side effects of low-dose aspirin on long-term child developmental outcomes and said the evidence report found no physical or developmental differences in infants at age 12 and 18 months.
USPSTF said comparative effectiveness trials are needed to identify “specific aspirin protocols” and evaluate which dosage, timing, and time of day will have the greatest benefit. The task force also said more research is needed to improve identification of those at an increased risk of developing preeclampsia.
Dr. Caughey and Dr. Klein disclosed no conflicts of interest.
The U.S. Preventive Services Task Force continues to recommend that pregnant women at risk of developing preeclampsia take low-dose aspirin daily, and has expanded the criteria for those at risk.
“I think that this issue has been one that people have talked about and thought about for a long time, but it hasn’t kind of leapt into the front for all practitioners,” Aaron B. Caughey, MD, MPH, PhD, a USPSTF member, said in an interview. “We think it’s really important that all providers and all pregnant persons are aware that folks at an increased risk for preeclampsia can receive a reduction in the risk of preeclampsia from receiving baby aspirin starting after 12 weeks of gestation.”
The task force concluded with moderate certainty that a daily dose of 81 milligrams of aspirin after 12 weeks of pregnancy could reduce the risk for preeclampsia, preterm birth, and stillbirths in pregnant persons at high risk for preeclampsia. The recommendations, which were published in JAMA, are identical to the panel’s 2014 recommendations.
However, the new draft includes a suggestion that expands the list of pregnant patients at risk of developing preeclampsia. In 2014, the USPSTF recommended that clinicians prescribe low-dose daily aspirin to those who had at least two moderate-risk factors related to disparity – first pregnancy, obesity, family history of preeclampsia, lower income, age of 35 years or older, of African descent, and previous adverse pregnancy outcomes. The recent update suggests clinicians consider prescribing low-dose aspirin to patients with just one of the moderate risk factors. The task force also added “in vitro fertilization” as a moderate risk factor.
Dr. Caughey said the motivation for this addition was out of concern for disparities in outcomes for people who have less access to care and to help curb the racial disparity in the prevalence of preeclampsia in Black women and other disadvantaged groups. “[In an effort] to prevent the development of preeclampsia in such individuals that have historically had worse health outcomes, we wanted to emphasize that should at least be considered by clinicians,” Dr. Caughey said.
This change is a “major one,” according to Victor Klein, MD, MBA, CPHRM, a specialist in high-risk pregnancy.
“That’s probably three-quarters of my patients. The majority of my patients will now be candidates [to receive a low-dose aspirin prescription to prevent preeclampsia],” Dr. Klein, vice chairman of obstetrics and gynecology at North Shore University Hospital, Manhasset, N.Y., said in an interview. “[This] may increase the amount of people who will be getting the aspirin and therefore decrease the chance of preeclampsia or developing preeclampsia.”
Preeclampsia is a condition characterized by high blood pressure and signs of problems with the kidneys, liver, and other organs during pregnancy, according to the Centers for Disease Control and Prevention. The condition occurs in about 1 in 25 pregnancies in the United States and can cause serious and fatal complications for both the mother and child.
Although the update reaffirms that aspirin is safe and effective in preventing preeclampsia, Dr. Klein believes the dosage they are recommending is too low, as he has had patients develop preeclampsia while taking 81 mg of aspirin daily. Dr. Klein says he prescribes two daily doses of 81 mg aspirin to some of his patients.
“The majority of us in the field of high-risk pregnancies feel that 81 milligrams is not enough,” Dr. Klein said. “So I am disappointed that [they] didn’t talk about consideration for higher doses. I have patients taking two baby aspirins who developed preeclampsia.”
However, the systematic review that the USPSTF’s recommendation was based on did not “really find evidence to suggest that a higher dose was necessarily better than the lower dose,” Dr. Caughey said. However, this may be something they look at again in the near future.
“I know of clinicians that are asking if we should be using a higher dose,” Dr. Caughey explained. “If more evidence accumulates then absolutely we will look at that issue again.”
In their draft, the task force said there’s limited evidence on the side effects of low-dose aspirin on long-term child developmental outcomes and said the evidence report found no physical or developmental differences in infants at age 12 and 18 months.
USPSTF said comparative effectiveness trials are needed to identify “specific aspirin protocols” and evaluate which dosage, timing, and time of day will have the greatest benefit. The task force also said more research is needed to improve identification of those at an increased risk of developing preeclampsia.
Dr. Caughey and Dr. Klein disclosed no conflicts of interest.
The U.S. Preventive Services Task Force continues to recommend that pregnant women at risk of developing preeclampsia take low-dose aspirin daily, and has expanded the criteria for those at risk.
“I think that this issue has been one that people have talked about and thought about for a long time, but it hasn’t kind of leapt into the front for all practitioners,” Aaron B. Caughey, MD, MPH, PhD, a USPSTF member, said in an interview. “We think it’s really important that all providers and all pregnant persons are aware that folks at an increased risk for preeclampsia can receive a reduction in the risk of preeclampsia from receiving baby aspirin starting after 12 weeks of gestation.”
The task force concluded with moderate certainty that a daily dose of 81 milligrams of aspirin after 12 weeks of pregnancy could reduce the risk for preeclampsia, preterm birth, and stillbirths in pregnant persons at high risk for preeclampsia. The recommendations, which were published in JAMA, are identical to the panel’s 2014 recommendations.
However, the new draft includes a suggestion that expands the list of pregnant patients at risk of developing preeclampsia. In 2014, the USPSTF recommended that clinicians prescribe low-dose daily aspirin to those who had at least two moderate-risk factors related to disparity – first pregnancy, obesity, family history of preeclampsia, lower income, age of 35 years or older, of African descent, and previous adverse pregnancy outcomes. The recent update suggests clinicians consider prescribing low-dose aspirin to patients with just one of the moderate risk factors. The task force also added “in vitro fertilization” as a moderate risk factor.
Dr. Caughey said the motivation for this addition was out of concern for disparities in outcomes for people who have less access to care and to help curb the racial disparity in the prevalence of preeclampsia in Black women and other disadvantaged groups. “[In an effort] to prevent the development of preeclampsia in such individuals that have historically had worse health outcomes, we wanted to emphasize that should at least be considered by clinicians,” Dr. Caughey said.
This change is a “major one,” according to Victor Klein, MD, MBA, CPHRM, a specialist in high-risk pregnancy.
“That’s probably three-quarters of my patients. The majority of my patients will now be candidates [to receive a low-dose aspirin prescription to prevent preeclampsia],” Dr. Klein, vice chairman of obstetrics and gynecology at North Shore University Hospital, Manhasset, N.Y., said in an interview. “[This] may increase the amount of people who will be getting the aspirin and therefore decrease the chance of preeclampsia or developing preeclampsia.”
Preeclampsia is a condition characterized by high blood pressure and signs of problems with the kidneys, liver, and other organs during pregnancy, according to the Centers for Disease Control and Prevention. The condition occurs in about 1 in 25 pregnancies in the United States and can cause serious and fatal complications for both the mother and child.
Although the update reaffirms that aspirin is safe and effective in preventing preeclampsia, Dr. Klein believes the dosage they are recommending is too low, as he has had patients develop preeclampsia while taking 81 mg of aspirin daily. Dr. Klein says he prescribes two daily doses of 81 mg aspirin to some of his patients.
“The majority of us in the field of high-risk pregnancies feel that 81 milligrams is not enough,” Dr. Klein said. “So I am disappointed that [they] didn’t talk about consideration for higher doses. I have patients taking two baby aspirins who developed preeclampsia.”
However, the systematic review that the USPSTF’s recommendation was based on did not “really find evidence to suggest that a higher dose was necessarily better than the lower dose,” Dr. Caughey said. However, this may be something they look at again in the near future.
“I know of clinicians that are asking if we should be using a higher dose,” Dr. Caughey explained. “If more evidence accumulates then absolutely we will look at that issue again.”
In their draft, the task force said there’s limited evidence on the side effects of low-dose aspirin on long-term child developmental outcomes and said the evidence report found no physical or developmental differences in infants at age 12 and 18 months.
USPSTF said comparative effectiveness trials are needed to identify “specific aspirin protocols” and evaluate which dosage, timing, and time of day will have the greatest benefit. The task force also said more research is needed to improve identification of those at an increased risk of developing preeclampsia.
Dr. Caughey and Dr. Klein disclosed no conflicts of interest.
FROM JAMA
Diabetes drug may extend pregnancy in women with preeclampsia
New evidence suggests a drug used to lower blood sugar levels may also help extend the duration of preterm pregnancies in women with preeclampsia.
The findings from a small clinical trial, published Sept. 23 in the BMJ, showed that pregnant women who received the diabetes medication metformin prolonged their pregnancy by a week compared to those who received a placebo. Although this finding was not statistically significant, researchers said they are “cautiously optimistic” about the treatment of preterm preeclampsia.
“We hope that it will encourage others to test not only metformin but also other promising therapeutic candidates to treat and prevent preeclampsia,” study author Catherine Cluver, MBChB, FCOG, PhD, associate professor in the department of obstetrics and gynecology at Stellenbosch University in South Africa, said in an interview.
Preeclampsia, a condition that occurs about 1 in 25 pregnancies in the United States, happens when a woman develops high blood pressure and protein in her urine, according to the Centers for Disease Control and Prevention.
Preterm preeclampsia is a severe variant affecting 0.5% of all pregnancies, or 10% of those with preeclampsia, researchers wrote in the study. The condition is associated with more maternal and neonatal death and increases their risks of developing an illness.
Dr. Cluver said that when a mother develops preeclampsia, the lining of her blood vessels, or the endothelium, is affected and there are specific proteins in the blood that increase. Dr. Cluver’s preclinical study found that metformin improved endothelial function and decreased these biomarkers in laboratory work.
“We therefore set out to see if metformin could be used to prolong gestation in preterm preeclampsia,” she said.
For the study, Dr. Cluver and colleagues performed a double-blind, placebo-controlled clinical trial to compare the prolongation of pregnancies among women who were at least 26 months pregnant with preterm preeclampsia. They were treated with either 3 grams of extended-release metformin (90 women), or a matching placebo (90 women).*
In the treatment group, the average time from the start of the study to delivery was 17.7 days, compared to 10.1 days in the placebo group. The median difference was 7.6 days.
The researchers also found that 40% of women in the metformin group reached 34 weeks’ gestation compared with 28% of those in the placebo group. Fewer women in the metformin group delivered because of fetal indications such as fetal distress or other issues – 33% vs. 44%. However, the researchers said those results were not statistically significant.
They said they were cautiously optimistic when they found that the median time for prolongation of pregnancy in the metformin group was 17.5 days compared with 7.9 days in the placebo group, findings that were statistically significant.
Some adverse effects participants experienced while taking metformin during their pregnancy included diarrhea and an increase in nausea.
Although the study is important in maternal-fetal medicine and is a novel approach to preterm preeclampsia, the findings weren’t strong enough, but they point to the need for further study, said Victor Klein, MD, MBA, CPHRM, a specialist in high-risk pregnancy who was not involved in the study.
“Even though they did have an improved outcome, it wasn’t strong enough. It wasn’t long enough to prove that the medicine was useful or efficacious,” said Dr. Klein, vice chairman of obstetrics and gynecology at North Shore University Hospital, New York.
Metformin is also used to treat gestational diabetes, which is an “advantage of repurposing the drug is that it is likely to be safe,” the researchers wrote. They said longer term follow-up data might be worthwhile in future trials.
None of the experts had conflicts of interest to disclose.
*This story was updated on 10/6/2021.
New evidence suggests a drug used to lower blood sugar levels may also help extend the duration of preterm pregnancies in women with preeclampsia.
The findings from a small clinical trial, published Sept. 23 in the BMJ, showed that pregnant women who received the diabetes medication metformin prolonged their pregnancy by a week compared to those who received a placebo. Although this finding was not statistically significant, researchers said they are “cautiously optimistic” about the treatment of preterm preeclampsia.
“We hope that it will encourage others to test not only metformin but also other promising therapeutic candidates to treat and prevent preeclampsia,” study author Catherine Cluver, MBChB, FCOG, PhD, associate professor in the department of obstetrics and gynecology at Stellenbosch University in South Africa, said in an interview.
Preeclampsia, a condition that occurs about 1 in 25 pregnancies in the United States, happens when a woman develops high blood pressure and protein in her urine, according to the Centers for Disease Control and Prevention.
Preterm preeclampsia is a severe variant affecting 0.5% of all pregnancies, or 10% of those with preeclampsia, researchers wrote in the study. The condition is associated with more maternal and neonatal death and increases their risks of developing an illness.
Dr. Cluver said that when a mother develops preeclampsia, the lining of her blood vessels, or the endothelium, is affected and there are specific proteins in the blood that increase. Dr. Cluver’s preclinical study found that metformin improved endothelial function and decreased these biomarkers in laboratory work.
“We therefore set out to see if metformin could be used to prolong gestation in preterm preeclampsia,” she said.
For the study, Dr. Cluver and colleagues performed a double-blind, placebo-controlled clinical trial to compare the prolongation of pregnancies among women who were at least 26 months pregnant with preterm preeclampsia. They were treated with either 3 grams of extended-release metformin (90 women), or a matching placebo (90 women).*
In the treatment group, the average time from the start of the study to delivery was 17.7 days, compared to 10.1 days in the placebo group. The median difference was 7.6 days.
The researchers also found that 40% of women in the metformin group reached 34 weeks’ gestation compared with 28% of those in the placebo group. Fewer women in the metformin group delivered because of fetal indications such as fetal distress or other issues – 33% vs. 44%. However, the researchers said those results were not statistically significant.
They said they were cautiously optimistic when they found that the median time for prolongation of pregnancy in the metformin group was 17.5 days compared with 7.9 days in the placebo group, findings that were statistically significant.
Some adverse effects participants experienced while taking metformin during their pregnancy included diarrhea and an increase in nausea.
Although the study is important in maternal-fetal medicine and is a novel approach to preterm preeclampsia, the findings weren’t strong enough, but they point to the need for further study, said Victor Klein, MD, MBA, CPHRM, a specialist in high-risk pregnancy who was not involved in the study.
“Even though they did have an improved outcome, it wasn’t strong enough. It wasn’t long enough to prove that the medicine was useful or efficacious,” said Dr. Klein, vice chairman of obstetrics and gynecology at North Shore University Hospital, New York.
Metformin is also used to treat gestational diabetes, which is an “advantage of repurposing the drug is that it is likely to be safe,” the researchers wrote. They said longer term follow-up data might be worthwhile in future trials.
None of the experts had conflicts of interest to disclose.
*This story was updated on 10/6/2021.
New evidence suggests a drug used to lower blood sugar levels may also help extend the duration of preterm pregnancies in women with preeclampsia.
The findings from a small clinical trial, published Sept. 23 in the BMJ, showed that pregnant women who received the diabetes medication metformin prolonged their pregnancy by a week compared to those who received a placebo. Although this finding was not statistically significant, researchers said they are “cautiously optimistic” about the treatment of preterm preeclampsia.
“We hope that it will encourage others to test not only metformin but also other promising therapeutic candidates to treat and prevent preeclampsia,” study author Catherine Cluver, MBChB, FCOG, PhD, associate professor in the department of obstetrics and gynecology at Stellenbosch University in South Africa, said in an interview.
Preeclampsia, a condition that occurs about 1 in 25 pregnancies in the United States, happens when a woman develops high blood pressure and protein in her urine, according to the Centers for Disease Control and Prevention.
Preterm preeclampsia is a severe variant affecting 0.5% of all pregnancies, or 10% of those with preeclampsia, researchers wrote in the study. The condition is associated with more maternal and neonatal death and increases their risks of developing an illness.
Dr. Cluver said that when a mother develops preeclampsia, the lining of her blood vessels, or the endothelium, is affected and there are specific proteins in the blood that increase. Dr. Cluver’s preclinical study found that metformin improved endothelial function and decreased these biomarkers in laboratory work.
“We therefore set out to see if metformin could be used to prolong gestation in preterm preeclampsia,” she said.
For the study, Dr. Cluver and colleagues performed a double-blind, placebo-controlled clinical trial to compare the prolongation of pregnancies among women who were at least 26 months pregnant with preterm preeclampsia. They were treated with either 3 grams of extended-release metformin (90 women), or a matching placebo (90 women).*
In the treatment group, the average time from the start of the study to delivery was 17.7 days, compared to 10.1 days in the placebo group. The median difference was 7.6 days.
The researchers also found that 40% of women in the metformin group reached 34 weeks’ gestation compared with 28% of those in the placebo group. Fewer women in the metformin group delivered because of fetal indications such as fetal distress or other issues – 33% vs. 44%. However, the researchers said those results were not statistically significant.
They said they were cautiously optimistic when they found that the median time for prolongation of pregnancy in the metformin group was 17.5 days compared with 7.9 days in the placebo group, findings that were statistically significant.
Some adverse effects participants experienced while taking metformin during their pregnancy included diarrhea and an increase in nausea.
Although the study is important in maternal-fetal medicine and is a novel approach to preterm preeclampsia, the findings weren’t strong enough, but they point to the need for further study, said Victor Klein, MD, MBA, CPHRM, a specialist in high-risk pregnancy who was not involved in the study.
“Even though they did have an improved outcome, it wasn’t strong enough. It wasn’t long enough to prove that the medicine was useful or efficacious,” said Dr. Klein, vice chairman of obstetrics and gynecology at North Shore University Hospital, New York.
Metformin is also used to treat gestational diabetes, which is an “advantage of repurposing the drug is that it is likely to be safe,” the researchers wrote. They said longer term follow-up data might be worthwhile in future trials.
None of the experts had conflicts of interest to disclose.
*This story was updated on 10/6/2021.
COVID-19 vaccines in pregnancy may protect baby, too
Women who receive COVID-19 vaccines during pregnancy pass antibodies to their babies, which could protect newborns from the disease, research has shown.
.
Researchers with New York University Langone Health conducted a study that included pregnant women who had received at least one dose of an mRNA COVID-19 vaccine (Pfizer/BioNTech or Moderna) by June 4.
All neonates had antibodies to the spike protein at high titers, the researchers found.
Unlike similar prior studies, the researchers also looked for antibodies to the nucleocapsid protein, which would have indicated the presence of antibodies from natural COVID-19 infection. They did not detect antibodies to the nucleocapsid protein, and the lack of these antibodies suggests that the antibodies to the spike protein resulted from vaccination and not from prior infection, the researchers said.
The participants had a median time from completion of the vaccine series to delivery of 13 weeks. The study was published online in the American Journal of Obstetrics & Gynecology MFM.
“The presence of these anti-spike antibodies in the cord blood should, at least in theory, offer these newborns some degree of protection,” said study investigator Ashley S. Roman, MD, director of the division of maternal-fetal medicine at NYU Langone Health. “While the primary rationale for vaccination during pregnancy is to keep moms healthy and keep moms out of the hospital, the outstanding question to us was whether there is any fetal or neonatal benefit conferred by receiving the vaccine during pregnancy.”
Questions remain about the degree and durability of protection for newborns from these antibodies. An ongoing study, MOMI-VAX, aims to systematically measure antibody levels in mothers who receive COVID-19 vaccines during pregnancy and in their babies over time.
The present study contributes welcome preliminary evidence suggesting a benefit to infants, said Emily Adhikari, MD, of the University of Texas Southwestern Medical Center in Dallas, who was not involved in the study.
Still, “the main concern and our priority as obstetricians is to vaccinate pregnant women to protect them from severe or critical illness,” she said.
Although most individuals infected with SARS-CoV-2 recover, a significant portion of pregnant women get seriously sick, Dr. Adhikari said. “With this recent Delta surge, we are seeing more pregnant patients who are sicker,” said Dr. Adhikari, who has published research from one hospital describing this trend.
When weighing whether patients should receive COVID-19 vaccines in pregnancy, the risks from infection have outweighed any risk from vaccination to such an extent that there is “not a comparison to make,” Dr. Adhikari said. “The risks of the infection are so much higher.
“For me, it is a matter of making sure that my patient understands that we have really good safety data on these vaccines and there is no reason to think that a pregnant person would be harmed by them. On the contrary, the benefit is to protect and maybe even save your life,” Dr. Adhikari said. “And now we have more evidence that the fetus may also benefit.”
The rationale for vaccinations during pregnancy can vary, Dr. Roman said. Flu shots in pregnancy mainly are intended to protect the mother, though they confer protection for newborns as well. With the whooping cough vaccine given in the third trimester, however, the primary aim is to protect the baby from whooping cough in the first months of life, Dr. Roman said.
“I think it is really important for pregnant women to understand that antibodies crossing the placenta is a good thing,” she added.
As patients who already have received COVID-19 vaccines become pregnant and may become eligible for a booster dose, Dr. Adhikari will offer it, she said, though she has confidence in the protection provided by the initial immune response.
Dr. Roman and Dr. Adhikari had no disclosures.
Women who receive COVID-19 vaccines during pregnancy pass antibodies to their babies, which could protect newborns from the disease, research has shown.
.
Researchers with New York University Langone Health conducted a study that included pregnant women who had received at least one dose of an mRNA COVID-19 vaccine (Pfizer/BioNTech or Moderna) by June 4.
All neonates had antibodies to the spike protein at high titers, the researchers found.
Unlike similar prior studies, the researchers also looked for antibodies to the nucleocapsid protein, which would have indicated the presence of antibodies from natural COVID-19 infection. They did not detect antibodies to the nucleocapsid protein, and the lack of these antibodies suggests that the antibodies to the spike protein resulted from vaccination and not from prior infection, the researchers said.
The participants had a median time from completion of the vaccine series to delivery of 13 weeks. The study was published online in the American Journal of Obstetrics & Gynecology MFM.
“The presence of these anti-spike antibodies in the cord blood should, at least in theory, offer these newborns some degree of protection,” said study investigator Ashley S. Roman, MD, director of the division of maternal-fetal medicine at NYU Langone Health. “While the primary rationale for vaccination during pregnancy is to keep moms healthy and keep moms out of the hospital, the outstanding question to us was whether there is any fetal or neonatal benefit conferred by receiving the vaccine during pregnancy.”
Questions remain about the degree and durability of protection for newborns from these antibodies. An ongoing study, MOMI-VAX, aims to systematically measure antibody levels in mothers who receive COVID-19 vaccines during pregnancy and in their babies over time.
The present study contributes welcome preliminary evidence suggesting a benefit to infants, said Emily Adhikari, MD, of the University of Texas Southwestern Medical Center in Dallas, who was not involved in the study.
Still, “the main concern and our priority as obstetricians is to vaccinate pregnant women to protect them from severe or critical illness,” she said.
Although most individuals infected with SARS-CoV-2 recover, a significant portion of pregnant women get seriously sick, Dr. Adhikari said. “With this recent Delta surge, we are seeing more pregnant patients who are sicker,” said Dr. Adhikari, who has published research from one hospital describing this trend.
When weighing whether patients should receive COVID-19 vaccines in pregnancy, the risks from infection have outweighed any risk from vaccination to such an extent that there is “not a comparison to make,” Dr. Adhikari said. “The risks of the infection are so much higher.
“For me, it is a matter of making sure that my patient understands that we have really good safety data on these vaccines and there is no reason to think that a pregnant person would be harmed by them. On the contrary, the benefit is to protect and maybe even save your life,” Dr. Adhikari said. “And now we have more evidence that the fetus may also benefit.”
The rationale for vaccinations during pregnancy can vary, Dr. Roman said. Flu shots in pregnancy mainly are intended to protect the mother, though they confer protection for newborns as well. With the whooping cough vaccine given in the third trimester, however, the primary aim is to protect the baby from whooping cough in the first months of life, Dr. Roman said.
“I think it is really important for pregnant women to understand that antibodies crossing the placenta is a good thing,” she added.
As patients who already have received COVID-19 vaccines become pregnant and may become eligible for a booster dose, Dr. Adhikari will offer it, she said, though she has confidence in the protection provided by the initial immune response.
Dr. Roman and Dr. Adhikari had no disclosures.
Women who receive COVID-19 vaccines during pregnancy pass antibodies to their babies, which could protect newborns from the disease, research has shown.
.
Researchers with New York University Langone Health conducted a study that included pregnant women who had received at least one dose of an mRNA COVID-19 vaccine (Pfizer/BioNTech or Moderna) by June 4.
All neonates had antibodies to the spike protein at high titers, the researchers found.
Unlike similar prior studies, the researchers also looked for antibodies to the nucleocapsid protein, which would have indicated the presence of antibodies from natural COVID-19 infection. They did not detect antibodies to the nucleocapsid protein, and the lack of these antibodies suggests that the antibodies to the spike protein resulted from vaccination and not from prior infection, the researchers said.
The participants had a median time from completion of the vaccine series to delivery of 13 weeks. The study was published online in the American Journal of Obstetrics & Gynecology MFM.
“The presence of these anti-spike antibodies in the cord blood should, at least in theory, offer these newborns some degree of protection,” said study investigator Ashley S. Roman, MD, director of the division of maternal-fetal medicine at NYU Langone Health. “While the primary rationale for vaccination during pregnancy is to keep moms healthy and keep moms out of the hospital, the outstanding question to us was whether there is any fetal or neonatal benefit conferred by receiving the vaccine during pregnancy.”
Questions remain about the degree and durability of protection for newborns from these antibodies. An ongoing study, MOMI-VAX, aims to systematically measure antibody levels in mothers who receive COVID-19 vaccines during pregnancy and in their babies over time.
The present study contributes welcome preliminary evidence suggesting a benefit to infants, said Emily Adhikari, MD, of the University of Texas Southwestern Medical Center in Dallas, who was not involved in the study.
Still, “the main concern and our priority as obstetricians is to vaccinate pregnant women to protect them from severe or critical illness,” she said.
Although most individuals infected with SARS-CoV-2 recover, a significant portion of pregnant women get seriously sick, Dr. Adhikari said. “With this recent Delta surge, we are seeing more pregnant patients who are sicker,” said Dr. Adhikari, who has published research from one hospital describing this trend.
When weighing whether patients should receive COVID-19 vaccines in pregnancy, the risks from infection have outweighed any risk from vaccination to such an extent that there is “not a comparison to make,” Dr. Adhikari said. “The risks of the infection are so much higher.
“For me, it is a matter of making sure that my patient understands that we have really good safety data on these vaccines and there is no reason to think that a pregnant person would be harmed by them. On the contrary, the benefit is to protect and maybe even save your life,” Dr. Adhikari said. “And now we have more evidence that the fetus may also benefit.”
The rationale for vaccinations during pregnancy can vary, Dr. Roman said. Flu shots in pregnancy mainly are intended to protect the mother, though they confer protection for newborns as well. With the whooping cough vaccine given in the third trimester, however, the primary aim is to protect the baby from whooping cough in the first months of life, Dr. Roman said.
“I think it is really important for pregnant women to understand that antibodies crossing the placenta is a good thing,” she added.
As patients who already have received COVID-19 vaccines become pregnant and may become eligible for a booster dose, Dr. Adhikari will offer it, she said, though she has confidence in the protection provided by the initial immune response.
Dr. Roman and Dr. Adhikari had no disclosures.
FROM AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY MFM
Consensus statement warns against acetaminophen use during pregnancy
Pregnant women should use paracetamol/acetaminophen only with a medical indication and at the lowest effective dose for the shortest possible time, according to an international consensus statement published online Sept. 23 in Nature Reviews Endocrinology.
With global rates of use high and risks considered negligible, the expert panel of 13 U.S. and European authors call for focused research into how this analgesic and febrifuge may impair fetal development and lead to adverse outcomes in children. They outline several precautionary measures to be taken in the meantime.
According to first author and epidemiologist Ann Z. Bauer, ScD, a postdoctoral research fellow at the University of Massachusetts in Lowell, and colleagues, this drug is used by an estimated 65% of pregnant women in the United States, and more than 50% worldwide. It is currently the active ingredient in more than 600 prescription and nonprescription medications, including Tylenol, which historically has been deemed safe in all trimesters of pregnancy.
But a growing body of experimental and epidemiological evidence suggests prenatal exposure to paracetamol (N-acetyl-p-aminophenol, or APAP) might alter fetal development and elevate the risks of neurodevelopmental, reproductive and urogenital disorders in both sexes. Exposure in utero has been linked, for example, to potential behavioral problems in children.
The new recommendations are based on a review of experimental animal and cell-based research as well as human epidemiological data published from January 1995 to October 2020. The authors include clinicians, epidemiologists, and scientists specializing in toxicology, endocrinology, reproductive medicine and neurodevelopment.
Recommendations
Although the new guidance does not differ markedly from current advice, the authors believe stronger communication and greater awareness of risks are needed. In addition to restricting use of this medication to low doses for short periods when medically necessary, expectant mothers should receive counseling before conception or early in pregnancy. If uncertain about its use, they should consult their physicians or pharmacists.
In other recommendations, the panel said:
- The 2015 FDA Drug Safety Communication recommendations should be updated based on evaluation of all available scientific evidence.
- The European Medicines Agency Pharmacovigilance Risk Assessment Committee should review the most recent epidemiologic and experimental research and issue an updated Drug Safety Communication.
- Obstetric and gynecological associations should update their guidance after reviewing all available research.
- The Acetaminophen Awareness Coalition (“Know Your Dose” Campaign) should add standardized warnings and specifically advise pregnant women to forgo APAP unless it’s medically indicated.
- All sales of APAP-containing medications should be accompanied by recommendations specifically for use in pregnancy. This information should include warning labels on packaging, and if possible, APAP should be sold only in pharmacies (as in France).
Mechanism of action
APAP is an endocrine disruptor (Neuroscientist. 2020 Sep 11. doi: 10.1177/1073858420952046). “Chemicals that disrupt the endocrine system are concerning because they can interfere with the activity of endogenous hormones that are essential for healthy neurological, urogenital, and reproductive development,” researchers wrote.
“The precise mechanism is not clear but its toxicity is thought to be due mainly to hormone disruption,” Dr. Bauer said in an interview.
Moreover, APAP readily crosses the placenta and blood–brain barrier, and changes in APAP metabolism during pregnancy might make women and their fetuses more vulnerable to its toxic effects. For instance, the molar dose fraction of APAP converted to the oxidative metabolite N-acetyl-p-benzoquinone imine increases during pregnancy. In addition to its hepatotoxicity, this poisonous byproduct is thought to be a genotoxin that increases DNA cleavage by acting on the enzyme topoisomerase II.
Asked for her perspective on the statement, Kjersti Aagaard, MD, PhD, a professor of obstetrics and gynecology at Baylor College of Medicine and Texas Children’s Hospital in Houston, called the expert panel’s statement thoughtful and comprehensive, but she urged caution in interpreting the role of acetaminophen.
The challenge in linking any commonly used medication to adverse effects and congenital defects, she said, is “teasing out an association from causation. Given the commonality of the use of acetaminophen with the relative rarity of the outcomes, it is clear that not all cases of exposure result in adverse outcomes.”
As for judicious use, she said, one would be to reduce a high fever, which can cause miscarriage, neural tube defects, and potential heart disease in adulthood. Acetaminophen is the drug of choice in this case since nonsteroidal anti-inflammatory drugs such as ibuprofen are not recommended owing to their known risks to the fetal heart.
Dr. Aagaard emphasized that while acetaminophen use is temporally associated with learning and behavioral problems, and urogenital disorders at birth in male infants such as like hypospadias, so is exposure to multiple environmental chemicals and pollutants, as well as climate change. “It would be a real mistake with real life implications if we associated any congenital disease or disorder with a commonly used medication with known benefits if the true causal link lies elsewhere.”
She said the precautionary statements fall into the time-honored therapeutic principle of first do no harm. “However, the call for research action must be undertaken earnestly and sincerely.”
According to Dr. Bauer, the statement’s essential take-home message is that “physicians should educate themselves and educate women about what we’re learning about the risks of acetaminophen in pregnancy.” Risk can be minimized by using the lowest effective dose for the shortest time and only when medically indicated. “Pregnant women should speak to their physicians about acetaminophen. It’s about empowerment and making smart decisions,” she said.
This study received no specific funding. Coauthor Dr. R.T. Mitchell is supported by a UK Research Institute fellowship.
Pregnant women should use paracetamol/acetaminophen only with a medical indication and at the lowest effective dose for the shortest possible time, according to an international consensus statement published online Sept. 23 in Nature Reviews Endocrinology.
With global rates of use high and risks considered negligible, the expert panel of 13 U.S. and European authors call for focused research into how this analgesic and febrifuge may impair fetal development and lead to adverse outcomes in children. They outline several precautionary measures to be taken in the meantime.
According to first author and epidemiologist Ann Z. Bauer, ScD, a postdoctoral research fellow at the University of Massachusetts in Lowell, and colleagues, this drug is used by an estimated 65% of pregnant women in the United States, and more than 50% worldwide. It is currently the active ingredient in more than 600 prescription and nonprescription medications, including Tylenol, which historically has been deemed safe in all trimesters of pregnancy.
But a growing body of experimental and epidemiological evidence suggests prenatal exposure to paracetamol (N-acetyl-p-aminophenol, or APAP) might alter fetal development and elevate the risks of neurodevelopmental, reproductive and urogenital disorders in both sexes. Exposure in utero has been linked, for example, to potential behavioral problems in children.
The new recommendations are based on a review of experimental animal and cell-based research as well as human epidemiological data published from January 1995 to October 2020. The authors include clinicians, epidemiologists, and scientists specializing in toxicology, endocrinology, reproductive medicine and neurodevelopment.
Recommendations
Although the new guidance does not differ markedly from current advice, the authors believe stronger communication and greater awareness of risks are needed. In addition to restricting use of this medication to low doses for short periods when medically necessary, expectant mothers should receive counseling before conception or early in pregnancy. If uncertain about its use, they should consult their physicians or pharmacists.
In other recommendations, the panel said:
- The 2015 FDA Drug Safety Communication recommendations should be updated based on evaluation of all available scientific evidence.
- The European Medicines Agency Pharmacovigilance Risk Assessment Committee should review the most recent epidemiologic and experimental research and issue an updated Drug Safety Communication.
- Obstetric and gynecological associations should update their guidance after reviewing all available research.
- The Acetaminophen Awareness Coalition (“Know Your Dose” Campaign) should add standardized warnings and specifically advise pregnant women to forgo APAP unless it’s medically indicated.
- All sales of APAP-containing medications should be accompanied by recommendations specifically for use in pregnancy. This information should include warning labels on packaging, and if possible, APAP should be sold only in pharmacies (as in France).
Mechanism of action
APAP is an endocrine disruptor (Neuroscientist. 2020 Sep 11. doi: 10.1177/1073858420952046). “Chemicals that disrupt the endocrine system are concerning because they can interfere with the activity of endogenous hormones that are essential for healthy neurological, urogenital, and reproductive development,” researchers wrote.
“The precise mechanism is not clear but its toxicity is thought to be due mainly to hormone disruption,” Dr. Bauer said in an interview.
Moreover, APAP readily crosses the placenta and blood–brain barrier, and changes in APAP metabolism during pregnancy might make women and their fetuses more vulnerable to its toxic effects. For instance, the molar dose fraction of APAP converted to the oxidative metabolite N-acetyl-p-benzoquinone imine increases during pregnancy. In addition to its hepatotoxicity, this poisonous byproduct is thought to be a genotoxin that increases DNA cleavage by acting on the enzyme topoisomerase II.
Asked for her perspective on the statement, Kjersti Aagaard, MD, PhD, a professor of obstetrics and gynecology at Baylor College of Medicine and Texas Children’s Hospital in Houston, called the expert panel’s statement thoughtful and comprehensive, but she urged caution in interpreting the role of acetaminophen.
The challenge in linking any commonly used medication to adverse effects and congenital defects, she said, is “teasing out an association from causation. Given the commonality of the use of acetaminophen with the relative rarity of the outcomes, it is clear that not all cases of exposure result in adverse outcomes.”
As for judicious use, she said, one would be to reduce a high fever, which can cause miscarriage, neural tube defects, and potential heart disease in adulthood. Acetaminophen is the drug of choice in this case since nonsteroidal anti-inflammatory drugs such as ibuprofen are not recommended owing to their known risks to the fetal heart.
Dr. Aagaard emphasized that while acetaminophen use is temporally associated with learning and behavioral problems, and urogenital disorders at birth in male infants such as like hypospadias, so is exposure to multiple environmental chemicals and pollutants, as well as climate change. “It would be a real mistake with real life implications if we associated any congenital disease or disorder with a commonly used medication with known benefits if the true causal link lies elsewhere.”
She said the precautionary statements fall into the time-honored therapeutic principle of first do no harm. “However, the call for research action must be undertaken earnestly and sincerely.”
According to Dr. Bauer, the statement’s essential take-home message is that “physicians should educate themselves and educate women about what we’re learning about the risks of acetaminophen in pregnancy.” Risk can be minimized by using the lowest effective dose for the shortest time and only when medically indicated. “Pregnant women should speak to their physicians about acetaminophen. It’s about empowerment and making smart decisions,” she said.
This study received no specific funding. Coauthor Dr. R.T. Mitchell is supported by a UK Research Institute fellowship.
Pregnant women should use paracetamol/acetaminophen only with a medical indication and at the lowest effective dose for the shortest possible time, according to an international consensus statement published online Sept. 23 in Nature Reviews Endocrinology.
With global rates of use high and risks considered negligible, the expert panel of 13 U.S. and European authors call for focused research into how this analgesic and febrifuge may impair fetal development and lead to adverse outcomes in children. They outline several precautionary measures to be taken in the meantime.
According to first author and epidemiologist Ann Z. Bauer, ScD, a postdoctoral research fellow at the University of Massachusetts in Lowell, and colleagues, this drug is used by an estimated 65% of pregnant women in the United States, and more than 50% worldwide. It is currently the active ingredient in more than 600 prescription and nonprescription medications, including Tylenol, which historically has been deemed safe in all trimesters of pregnancy.
But a growing body of experimental and epidemiological evidence suggests prenatal exposure to paracetamol (N-acetyl-p-aminophenol, or APAP) might alter fetal development and elevate the risks of neurodevelopmental, reproductive and urogenital disorders in both sexes. Exposure in utero has been linked, for example, to potential behavioral problems in children.
The new recommendations are based on a review of experimental animal and cell-based research as well as human epidemiological data published from January 1995 to October 2020. The authors include clinicians, epidemiologists, and scientists specializing in toxicology, endocrinology, reproductive medicine and neurodevelopment.
Recommendations
Although the new guidance does not differ markedly from current advice, the authors believe stronger communication and greater awareness of risks are needed. In addition to restricting use of this medication to low doses for short periods when medically necessary, expectant mothers should receive counseling before conception or early in pregnancy. If uncertain about its use, they should consult their physicians or pharmacists.
In other recommendations, the panel said:
- The 2015 FDA Drug Safety Communication recommendations should be updated based on evaluation of all available scientific evidence.
- The European Medicines Agency Pharmacovigilance Risk Assessment Committee should review the most recent epidemiologic and experimental research and issue an updated Drug Safety Communication.
- Obstetric and gynecological associations should update their guidance after reviewing all available research.
- The Acetaminophen Awareness Coalition (“Know Your Dose” Campaign) should add standardized warnings and specifically advise pregnant women to forgo APAP unless it’s medically indicated.
- All sales of APAP-containing medications should be accompanied by recommendations specifically for use in pregnancy. This information should include warning labels on packaging, and if possible, APAP should be sold only in pharmacies (as in France).
Mechanism of action
APAP is an endocrine disruptor (Neuroscientist. 2020 Sep 11. doi: 10.1177/1073858420952046). “Chemicals that disrupt the endocrine system are concerning because they can interfere with the activity of endogenous hormones that are essential for healthy neurological, urogenital, and reproductive development,” researchers wrote.
“The precise mechanism is not clear but its toxicity is thought to be due mainly to hormone disruption,” Dr. Bauer said in an interview.
Moreover, APAP readily crosses the placenta and blood–brain barrier, and changes in APAP metabolism during pregnancy might make women and their fetuses more vulnerable to its toxic effects. For instance, the molar dose fraction of APAP converted to the oxidative metabolite N-acetyl-p-benzoquinone imine increases during pregnancy. In addition to its hepatotoxicity, this poisonous byproduct is thought to be a genotoxin that increases DNA cleavage by acting on the enzyme topoisomerase II.
Asked for her perspective on the statement, Kjersti Aagaard, MD, PhD, a professor of obstetrics and gynecology at Baylor College of Medicine and Texas Children’s Hospital in Houston, called the expert panel’s statement thoughtful and comprehensive, but she urged caution in interpreting the role of acetaminophen.
The challenge in linking any commonly used medication to adverse effects and congenital defects, she said, is “teasing out an association from causation. Given the commonality of the use of acetaminophen with the relative rarity of the outcomes, it is clear that not all cases of exposure result in adverse outcomes.”
As for judicious use, she said, one would be to reduce a high fever, which can cause miscarriage, neural tube defects, and potential heart disease in adulthood. Acetaminophen is the drug of choice in this case since nonsteroidal anti-inflammatory drugs such as ibuprofen are not recommended owing to their known risks to the fetal heart.
Dr. Aagaard emphasized that while acetaminophen use is temporally associated with learning and behavioral problems, and urogenital disorders at birth in male infants such as like hypospadias, so is exposure to multiple environmental chemicals and pollutants, as well as climate change. “It would be a real mistake with real life implications if we associated any congenital disease or disorder with a commonly used medication with known benefits if the true causal link lies elsewhere.”
She said the precautionary statements fall into the time-honored therapeutic principle of first do no harm. “However, the call for research action must be undertaken earnestly and sincerely.”
According to Dr. Bauer, the statement’s essential take-home message is that “physicians should educate themselves and educate women about what we’re learning about the risks of acetaminophen in pregnancy.” Risk can be minimized by using the lowest effective dose for the shortest time and only when medically indicated. “Pregnant women should speak to their physicians about acetaminophen. It’s about empowerment and making smart decisions,” she said.
This study received no specific funding. Coauthor Dr. R.T. Mitchell is supported by a UK Research Institute fellowship.
Survey: Nursing shortages affect safety during labor and delivery
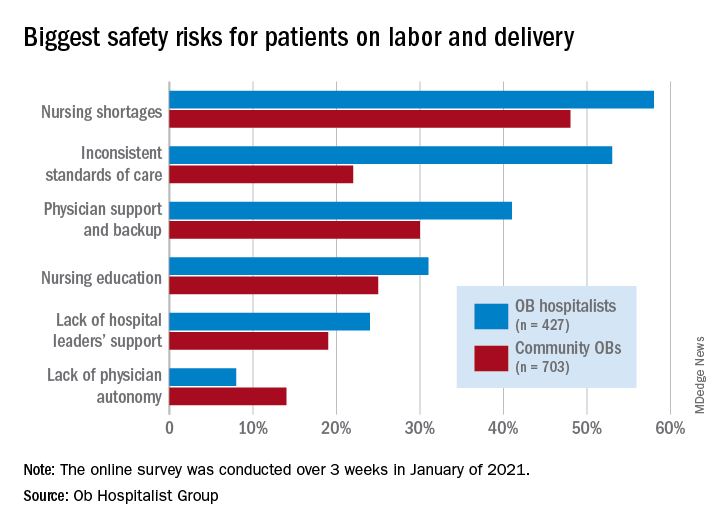
Just over 58% of the 1,130 respondents put nursing shortages ahead of physician support and backup (39.0%), inconsistent standards of care (38.5%), and nursing education (31.1%) as the most important challenge to patient safety, the Ob Hospitalist Group (OBHG) said in a new report.
“The survey reveals some startling gaps in physician and patient support all along the care continuum in obstetrics and OB hospitalist programs filling them,” said Lenny Castiglione, the CEO of OBHG, a national network of over 1,000 obstetric hospitalists. “As pressure builds on ob. units to improve care and reduce costs, and as clinical resources are stretched in the continuing battle against COVID-19 and its variants, health systems need to take serious measures to fill these gaps through staff recruitment, retention, and training.”
The national shortage of nurses is expected to get worse over the coming years as Baby Boomers’ need for health care increases and the large population (over 1 million) of older registered nurses retires by 2030, the OBHG said based on projections from the American Association of Colleges of Nursing.
Ob. hospitalists were somewhat more likely to see the nursing shortage as a major problem, compared with community-based Obs (58% vs. 48%), but the biggest difference in perception of safety risk between the two groups (53% for hospitalists vs. 22% for community physicians) involved inconsistent standards of care. “This is likely due to the ob. hospitalists’ 24/7 presence on the unit, and their visibility into the care provided across the unit,” the report noted.
Priorities for the future
Participants also were asked to rank each of seven focus areas on a scale of 0 (lowest priority) to 3 (highest) by its importance in the next 5 years. Maternal mortality was identified as the highest priority by 59.2% of physicians, followed by gaps in access to care between patient populations (38.0%), rural health care (26.5%), and ob.gyn. shortage (26.4%), the OBHG said.
A number of respondents noted the increase in high-risk patients, many of whom are obese and/or older and have comorbidities. “We know that the risk of C-sections increases relative to maternal weight. We need to focus on maternal morbidity and mortality,” one physician wrote in the open-ended response section.
When compared with the community obs., the hospitalists were much more likely to assign top priority over the next 5 years to maternal mortality (73% vs. 50%) and to gaps in access between patient populations (51% vs. 30%), according to the OBHG survey, which was conducted in January of 2021.
How will practice change in 5 years?
As for changes coming to obstetrical care over the next 5 years, respondents gave their strongest prediction to increased use of telemedicine, with 81.2% saying it would increase and just 14.4% predicting no change. The focus on subspecialization is expected to increase by 79.4% of participants (16.5% said no change), and 75.7% said that use of mid-level providers would rise (20.6% said no change), the survey data show.
The move toward mid-level providers was noted in many of the open-ended responses. “There is nothing mid-level about the midwifery care my colleagues provide our patients. They are experts in their field,” one physician wrote, but another said, “just because I foresee a shift toward increasing utilization of mid-levels and primary care practitioners for women’s health does not mean I endorse this trend.”
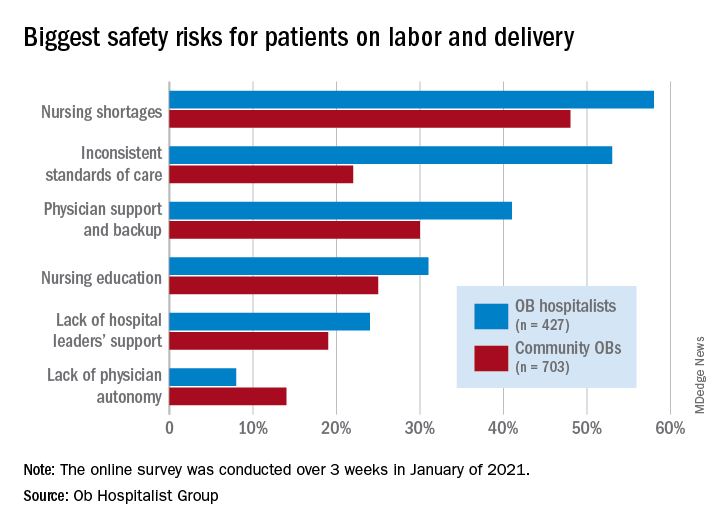
Just over 58% of the 1,130 respondents put nursing shortages ahead of physician support and backup (39.0%), inconsistent standards of care (38.5%), and nursing education (31.1%) as the most important challenge to patient safety, the Ob Hospitalist Group (OBHG) said in a new report.
“The survey reveals some startling gaps in physician and patient support all along the care continuum in obstetrics and OB hospitalist programs filling them,” said Lenny Castiglione, the CEO of OBHG, a national network of over 1,000 obstetric hospitalists. “As pressure builds on ob. units to improve care and reduce costs, and as clinical resources are stretched in the continuing battle against COVID-19 and its variants, health systems need to take serious measures to fill these gaps through staff recruitment, retention, and training.”
The national shortage of nurses is expected to get worse over the coming years as Baby Boomers’ need for health care increases and the large population (over 1 million) of older registered nurses retires by 2030, the OBHG said based on projections from the American Association of Colleges of Nursing.
Ob. hospitalists were somewhat more likely to see the nursing shortage as a major problem, compared with community-based Obs (58% vs. 48%), but the biggest difference in perception of safety risk between the two groups (53% for hospitalists vs. 22% for community physicians) involved inconsistent standards of care. “This is likely due to the ob. hospitalists’ 24/7 presence on the unit, and their visibility into the care provided across the unit,” the report noted.
Priorities for the future
Participants also were asked to rank each of seven focus areas on a scale of 0 (lowest priority) to 3 (highest) by its importance in the next 5 years. Maternal mortality was identified as the highest priority by 59.2% of physicians, followed by gaps in access to care between patient populations (38.0%), rural health care (26.5%), and ob.gyn. shortage (26.4%), the OBHG said.
A number of respondents noted the increase in high-risk patients, many of whom are obese and/or older and have comorbidities. “We know that the risk of C-sections increases relative to maternal weight. We need to focus on maternal morbidity and mortality,” one physician wrote in the open-ended response section.
When compared with the community obs., the hospitalists were much more likely to assign top priority over the next 5 years to maternal mortality (73% vs. 50%) and to gaps in access between patient populations (51% vs. 30%), according to the OBHG survey, which was conducted in January of 2021.
How will practice change in 5 years?
As for changes coming to obstetrical care over the next 5 years, respondents gave their strongest prediction to increased use of telemedicine, with 81.2% saying it would increase and just 14.4% predicting no change. The focus on subspecialization is expected to increase by 79.4% of participants (16.5% said no change), and 75.7% said that use of mid-level providers would rise (20.6% said no change), the survey data show.
The move toward mid-level providers was noted in many of the open-ended responses. “There is nothing mid-level about the midwifery care my colleagues provide our patients. They are experts in their field,” one physician wrote, but another said, “just because I foresee a shift toward increasing utilization of mid-levels and primary care practitioners for women’s health does not mean I endorse this trend.”
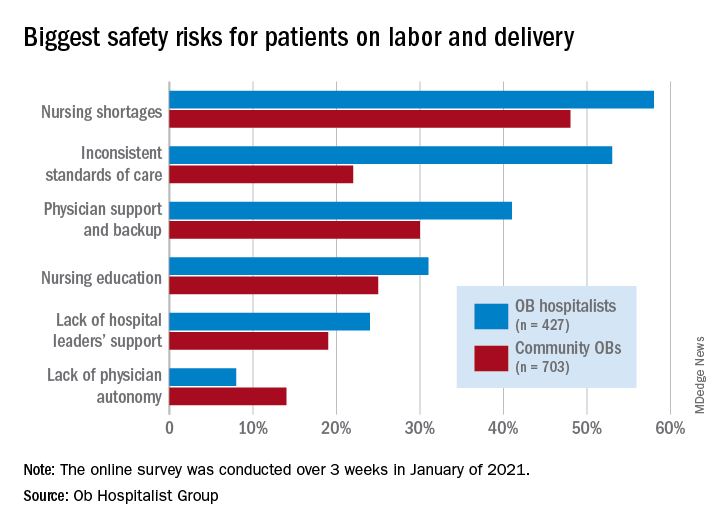
Just over 58% of the 1,130 respondents put nursing shortages ahead of physician support and backup (39.0%), inconsistent standards of care (38.5%), and nursing education (31.1%) as the most important challenge to patient safety, the Ob Hospitalist Group (OBHG) said in a new report.
“The survey reveals some startling gaps in physician and patient support all along the care continuum in obstetrics and OB hospitalist programs filling them,” said Lenny Castiglione, the CEO of OBHG, a national network of over 1,000 obstetric hospitalists. “As pressure builds on ob. units to improve care and reduce costs, and as clinical resources are stretched in the continuing battle against COVID-19 and its variants, health systems need to take serious measures to fill these gaps through staff recruitment, retention, and training.”
The national shortage of nurses is expected to get worse over the coming years as Baby Boomers’ need for health care increases and the large population (over 1 million) of older registered nurses retires by 2030, the OBHG said based on projections from the American Association of Colleges of Nursing.
Ob. hospitalists were somewhat more likely to see the nursing shortage as a major problem, compared with community-based Obs (58% vs. 48%), but the biggest difference in perception of safety risk between the two groups (53% for hospitalists vs. 22% for community physicians) involved inconsistent standards of care. “This is likely due to the ob. hospitalists’ 24/7 presence on the unit, and their visibility into the care provided across the unit,” the report noted.
Priorities for the future
Participants also were asked to rank each of seven focus areas on a scale of 0 (lowest priority) to 3 (highest) by its importance in the next 5 years. Maternal mortality was identified as the highest priority by 59.2% of physicians, followed by gaps in access to care between patient populations (38.0%), rural health care (26.5%), and ob.gyn. shortage (26.4%), the OBHG said.
A number of respondents noted the increase in high-risk patients, many of whom are obese and/or older and have comorbidities. “We know that the risk of C-sections increases relative to maternal weight. We need to focus on maternal morbidity and mortality,” one physician wrote in the open-ended response section.
When compared with the community obs., the hospitalists were much more likely to assign top priority over the next 5 years to maternal mortality (73% vs. 50%) and to gaps in access between patient populations (51% vs. 30%), according to the OBHG survey, which was conducted in January of 2021.
How will practice change in 5 years?
As for changes coming to obstetrical care over the next 5 years, respondents gave their strongest prediction to increased use of telemedicine, with 81.2% saying it would increase and just 14.4% predicting no change. The focus on subspecialization is expected to increase by 79.4% of participants (16.5% said no change), and 75.7% said that use of mid-level providers would rise (20.6% said no change), the survey data show.
The move toward mid-level providers was noted in many of the open-ended responses. “There is nothing mid-level about the midwifery care my colleagues provide our patients. They are experts in their field,” one physician wrote, but another said, “just because I foresee a shift toward increasing utilization of mid-levels and primary care practitioners for women’s health does not mean I endorse this trend.”
Maryland reduces cesarean delivery rates
A statewide educational initiative in Maryland was associated with a significant reduction in cesarean delivery rates over 30 months, although program implementation was widely variable across participating hospitals, according to investigators.
Cesarean deliveries dropped 1.6% among nulliparous, term, singleton, vertex births, falling short of the 3.2% reduction recently achieved by a similar program in California, reported lead author Jennifer A. Callaghan-Koru, PhD, of the University of Maryland, Baltimore County, and colleagues.
“Although cesarean delivery can be lifesaving, evidence suggests that there is no benefit to maternal health when national cesarean delivery rates are higher than 20 per 100 live births,” the investigators wrote in Obstetrics & Gynecology.
They noted that cesarean delivery rates in the United States rose dramatically between 1996 and 2006, from 20.7% to 32.9%, before falling back to 31.7% in 2019.
According to the investigators, high cesarean delivery rates have drawn action from a roster of stakeholders, including the American College of Obstetricians and Gynecologists (ACOG), the Society for Maternal-Fetal Medicine (SMFM), the Department of Health and Human Services, the Joint Commission, and the Council on Patient Safety in Women’s Health Care.
The latter group created an evidence-based obstetric patient safety bundle that was used in the present study. The investigators recruited 31 out of 32 birthing hospitals in Maryland, and over the course of 30 months, educated the participating hospitals on the practices recommended by the bundle, via in-person and remote training.
To measure implementation and associated outcomes, the investigators used a data portal provided by the ACOG Alliance for Innovation in Maternal Health (AIM) program, which supports adoption of the council’s safety bundle nationwide. Data included number of births; number of cesarean births; overall cesarean delivery rates; cesarean rates among nulliparous, term, singleton, vertex births; cesarean rates among nulliparous, term, singleton, vertex inductions; as well as severe maternal morbidity rates.
Among the 26 safety practices in the bundle, hospitals reported current use of 7 (median) before the program began, with a range from 0 to 23. During the 30-month collaboration, hospitals added a median of 4 practices, ranging from 0 to 17.
Concurrently, cesarean delivery rates for nulliparous, term, singleton, vertex births dropped from 26.9% to 28.5% (P = .011), while rates for inductions dropped to a greater degree, from 36.1% to 31.3% (P less than .001). Further analysis showed that greater reductions in rates of cesarean delivery were associated with adoption of practices in the “Response” domain.
“The Response domain has the largest number of practices that standardize clinical care, including induction scheduling, diagnosis and treatment of labor dystocia and failed induction, and interpretation of fetal heart rate patterns,” the investigators wrote. “The important role of standardizing care is consistent with a Cochrane review that found moderately strong evidence that the implementation of clinical practice guidelines, alongside feedback to clinicians (e.g., second opinions, audit and feedback of rates), can reduce cesarean delivery.”
Dr. Callaghan-Koru and colleagues noted the high variability of implementation among hospitals, which could explain why statewide reductions weren’t more dramatic.
“Other evaluations of perinatal quality improvement collaboratives have also found that some hospitals get left behind in these efforts, without making considerable progress and improving outcomes,” they wrote. “Given that work by state perinatal quality improvement collaboratives represents a primary national strategy for reducing maternal morbidity and mortality, it is critically important to conduct further implementation research to identify determinants of success and strategies to support all participating hospitals to make improvements.”
According to Iris Krishna, MD, of Emory University, Atlanta, each state’s starting point may predict how successful similar programs will be.
“The safe reduction in the cesarean delivery rate will vary by state,” Dr. Krishna said in a written comment. “States that have a well-established perinatal quality collaborative that have the support on the provider, hospital, and statewide level are more likely to successfully implement strategies and see a statistically significant decrease.”
She went on to emphasize the importance of collaboration across multiple levels of organization, and across a variety of health care providers and administrators.
“Successful implementation requires a multidisciplinary team (physicians, nurses, quality improvement officers) and a multifaceted approach (statewide policies),” Dr. Krishna said. “Key stakeholders will need to ‘buy in’ or be willing to support the policy and practice change to ensure its success. To address obstacles, initiatives to support vaginal birth are important, such as provider training on labor and support techniques, criteria for diagnosis of and management of labor dystocia and arrest disorders, standard responses to abnormal fetal heart rate patterns, and availability of expertise to lessen the need for cesarean delivery, such as breech version, instrumented delivery, and twin delivery protocols. It is also important for hospitals to a have a mentor model of quality improvement and shared learning strategies that work.”
Dr. Krishna agreed with the investigators that more work is necessary to determine best strategies for future intervention.
“Research is needed in identifying determinants of success and sustainment,” she said.
Dr. Burke received funding from her employer, Trinity Health, to conduct a pilot study concerning blood loss.
A statewide educational initiative in Maryland was associated with a significant reduction in cesarean delivery rates over 30 months, although program implementation was widely variable across participating hospitals, according to investigators.
Cesarean deliveries dropped 1.6% among nulliparous, term, singleton, vertex births, falling short of the 3.2% reduction recently achieved by a similar program in California, reported lead author Jennifer A. Callaghan-Koru, PhD, of the University of Maryland, Baltimore County, and colleagues.
“Although cesarean delivery can be lifesaving, evidence suggests that there is no benefit to maternal health when national cesarean delivery rates are higher than 20 per 100 live births,” the investigators wrote in Obstetrics & Gynecology.
They noted that cesarean delivery rates in the United States rose dramatically between 1996 and 2006, from 20.7% to 32.9%, before falling back to 31.7% in 2019.
According to the investigators, high cesarean delivery rates have drawn action from a roster of stakeholders, including the American College of Obstetricians and Gynecologists (ACOG), the Society for Maternal-Fetal Medicine (SMFM), the Department of Health and Human Services, the Joint Commission, and the Council on Patient Safety in Women’s Health Care.
The latter group created an evidence-based obstetric patient safety bundle that was used in the present study. The investigators recruited 31 out of 32 birthing hospitals in Maryland, and over the course of 30 months, educated the participating hospitals on the practices recommended by the bundle, via in-person and remote training.
To measure implementation and associated outcomes, the investigators used a data portal provided by the ACOG Alliance for Innovation in Maternal Health (AIM) program, which supports adoption of the council’s safety bundle nationwide. Data included number of births; number of cesarean births; overall cesarean delivery rates; cesarean rates among nulliparous, term, singleton, vertex births; cesarean rates among nulliparous, term, singleton, vertex inductions; as well as severe maternal morbidity rates.
Among the 26 safety practices in the bundle, hospitals reported current use of 7 (median) before the program began, with a range from 0 to 23. During the 30-month collaboration, hospitals added a median of 4 practices, ranging from 0 to 17.
Concurrently, cesarean delivery rates for nulliparous, term, singleton, vertex births dropped from 26.9% to 28.5% (P = .011), while rates for inductions dropped to a greater degree, from 36.1% to 31.3% (P less than .001). Further analysis showed that greater reductions in rates of cesarean delivery were associated with adoption of practices in the “Response” domain.
“The Response domain has the largest number of practices that standardize clinical care, including induction scheduling, diagnosis and treatment of labor dystocia and failed induction, and interpretation of fetal heart rate patterns,” the investigators wrote. “The important role of standardizing care is consistent with a Cochrane review that found moderately strong evidence that the implementation of clinical practice guidelines, alongside feedback to clinicians (e.g., second opinions, audit and feedback of rates), can reduce cesarean delivery.”
Dr. Callaghan-Koru and colleagues noted the high variability of implementation among hospitals, which could explain why statewide reductions weren’t more dramatic.
“Other evaluations of perinatal quality improvement collaboratives have also found that some hospitals get left behind in these efforts, without making considerable progress and improving outcomes,” they wrote. “Given that work by state perinatal quality improvement collaboratives represents a primary national strategy for reducing maternal morbidity and mortality, it is critically important to conduct further implementation research to identify determinants of success and strategies to support all participating hospitals to make improvements.”
According to Iris Krishna, MD, of Emory University, Atlanta, each state’s starting point may predict how successful similar programs will be.
“The safe reduction in the cesarean delivery rate will vary by state,” Dr. Krishna said in a written comment. “States that have a well-established perinatal quality collaborative that have the support on the provider, hospital, and statewide level are more likely to successfully implement strategies and see a statistically significant decrease.”
She went on to emphasize the importance of collaboration across multiple levels of organization, and across a variety of health care providers and administrators.
“Successful implementation requires a multidisciplinary team (physicians, nurses, quality improvement officers) and a multifaceted approach (statewide policies),” Dr. Krishna said. “Key stakeholders will need to ‘buy in’ or be willing to support the policy and practice change to ensure its success. To address obstacles, initiatives to support vaginal birth are important, such as provider training on labor and support techniques, criteria for diagnosis of and management of labor dystocia and arrest disorders, standard responses to abnormal fetal heart rate patterns, and availability of expertise to lessen the need for cesarean delivery, such as breech version, instrumented delivery, and twin delivery protocols. It is also important for hospitals to a have a mentor model of quality improvement and shared learning strategies that work.”
Dr. Krishna agreed with the investigators that more work is necessary to determine best strategies for future intervention.
“Research is needed in identifying determinants of success and sustainment,” she said.
Dr. Burke received funding from her employer, Trinity Health, to conduct a pilot study concerning blood loss.
A statewide educational initiative in Maryland was associated with a significant reduction in cesarean delivery rates over 30 months, although program implementation was widely variable across participating hospitals, according to investigators.
Cesarean deliveries dropped 1.6% among nulliparous, term, singleton, vertex births, falling short of the 3.2% reduction recently achieved by a similar program in California, reported lead author Jennifer A. Callaghan-Koru, PhD, of the University of Maryland, Baltimore County, and colleagues.
“Although cesarean delivery can be lifesaving, evidence suggests that there is no benefit to maternal health when national cesarean delivery rates are higher than 20 per 100 live births,” the investigators wrote in Obstetrics & Gynecology.
They noted that cesarean delivery rates in the United States rose dramatically between 1996 and 2006, from 20.7% to 32.9%, before falling back to 31.7% in 2019.
According to the investigators, high cesarean delivery rates have drawn action from a roster of stakeholders, including the American College of Obstetricians and Gynecologists (ACOG), the Society for Maternal-Fetal Medicine (SMFM), the Department of Health and Human Services, the Joint Commission, and the Council on Patient Safety in Women’s Health Care.
The latter group created an evidence-based obstetric patient safety bundle that was used in the present study. The investigators recruited 31 out of 32 birthing hospitals in Maryland, and over the course of 30 months, educated the participating hospitals on the practices recommended by the bundle, via in-person and remote training.
To measure implementation and associated outcomes, the investigators used a data portal provided by the ACOG Alliance for Innovation in Maternal Health (AIM) program, which supports adoption of the council’s safety bundle nationwide. Data included number of births; number of cesarean births; overall cesarean delivery rates; cesarean rates among nulliparous, term, singleton, vertex births; cesarean rates among nulliparous, term, singleton, vertex inductions; as well as severe maternal morbidity rates.
Among the 26 safety practices in the bundle, hospitals reported current use of 7 (median) before the program began, with a range from 0 to 23. During the 30-month collaboration, hospitals added a median of 4 practices, ranging from 0 to 17.
Concurrently, cesarean delivery rates for nulliparous, term, singleton, vertex births dropped from 26.9% to 28.5% (P = .011), while rates for inductions dropped to a greater degree, from 36.1% to 31.3% (P less than .001). Further analysis showed that greater reductions in rates of cesarean delivery were associated with adoption of practices in the “Response” domain.
“The Response domain has the largest number of practices that standardize clinical care, including induction scheduling, diagnosis and treatment of labor dystocia and failed induction, and interpretation of fetal heart rate patterns,” the investigators wrote. “The important role of standardizing care is consistent with a Cochrane review that found moderately strong evidence that the implementation of clinical practice guidelines, alongside feedback to clinicians (e.g., second opinions, audit and feedback of rates), can reduce cesarean delivery.”
Dr. Callaghan-Koru and colleagues noted the high variability of implementation among hospitals, which could explain why statewide reductions weren’t more dramatic.
“Other evaluations of perinatal quality improvement collaboratives have also found that some hospitals get left behind in these efforts, without making considerable progress and improving outcomes,” they wrote. “Given that work by state perinatal quality improvement collaboratives represents a primary national strategy for reducing maternal morbidity and mortality, it is critically important to conduct further implementation research to identify determinants of success and strategies to support all participating hospitals to make improvements.”
According to Iris Krishna, MD, of Emory University, Atlanta, each state’s starting point may predict how successful similar programs will be.
“The safe reduction in the cesarean delivery rate will vary by state,” Dr. Krishna said in a written comment. “States that have a well-established perinatal quality collaborative that have the support on the provider, hospital, and statewide level are more likely to successfully implement strategies and see a statistically significant decrease.”
She went on to emphasize the importance of collaboration across multiple levels of organization, and across a variety of health care providers and administrators.
“Successful implementation requires a multidisciplinary team (physicians, nurses, quality improvement officers) and a multifaceted approach (statewide policies),” Dr. Krishna said. “Key stakeholders will need to ‘buy in’ or be willing to support the policy and practice change to ensure its success. To address obstacles, initiatives to support vaginal birth are important, such as provider training on labor and support techniques, criteria for diagnosis of and management of labor dystocia and arrest disorders, standard responses to abnormal fetal heart rate patterns, and availability of expertise to lessen the need for cesarean delivery, such as breech version, instrumented delivery, and twin delivery protocols. It is also important for hospitals to a have a mentor model of quality improvement and shared learning strategies that work.”
Dr. Krishna agreed with the investigators that more work is necessary to determine best strategies for future intervention.
“Research is needed in identifying determinants of success and sustainment,” she said.
Dr. Burke received funding from her employer, Trinity Health, to conduct a pilot study concerning blood loss.
FROM OBSTETRICS & GYNECOLOGY
HPV infection during pregnancy ups risk of premature birth
Persistent human papillomavirus (HPV) 16 and HPV 18 during a pregnancy may be associated with an increased risk of premature birth.
Findings published online in JAMA Network Open found that 15.9% of individuals who had a persistent HPV 16 or 18 infection during the first and third trimesters of their pregnancy gave birth prematurely, compared with 5.6% of those who did not have an HPV infection at all.
The findings prompted the question of “the pathophysiology of HPV in pregnancy and how the virus is affecting the placenta,” said Lisette Davidson Tanner, MD, MPH, FACOG, who was not involved in the study.
Researchers said the findings are the first to show the association between preterm birth and HPV, which is an incurable virus that most sexually active individuals will get at some point in their lives, according to the Centers for Disease Control and Prevention.
“The results of this study are very important in helping us understand the burden caused by HPV in pregnancy,” study author Helen Trottier, MSc, PhD, researcher at the Centre Hospitalier Universitaire Sainte-Justine, said in an interview. “We may have just pinpointed an important cause of preterm birth that has so far been unexplained.”
Dr. Trottier and colleagues examined data from 1,052 pregnant women from three university-affiliated health care centers in Montreal between Nov. 8, 2010, and Oct. 16, 2016.
Only 5.6% of those who did not have an HPV infection had a premature birth, compared with 6.9% of those who tested positive for any HPV infection in the first trimester.
When looking at the first trimester, researchers found 12% of those diagnosed with HPV 16 and 18 had a preterm birth, compared to 4.9% of those who had a high-risk HPV infection other than HPV 16/18. When looking at the third trimester, researchers found that 15.9% of those with HPV 16/18 had an increased risk of giving birth prematurely, compared to those who had other high-risk HPV infections.
When researchers looked at the persistence of these HPV infections, they found that most HPV infections detected in the first trimester persist to the third trimester. The findings also revealed that persistent vaginal HPV 16/18 detection was significantly associated with all preterm births and spontaneous preterm births. This association was also found among those who had HPV infections detected in their placentas.
Meanwhile, 5.8% of those who had an HPV infection only during the first trimester experienced a preterm birth.
The researchers also found that HPV infections were frequent in pregnancy even among populations “considered to be at low risk based on sociodemographic and sexual history characteristics,” they wrote. Dr. Trottier said she hopes the findings will strengthen support for HPV vaccination.
Dr. Trottier’s study adds to a growing body of research regarding the adverse effects of HPV, according to Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “It is already well known that HPV is associated with a number of anogenital and oropharyngeal cancers,” Dr. Tanner said in an interview. “The potential association with preterm birth only adds weight to the recommendations to screen for and prevent HPV infection.”
HPV 16 and 18 are high-risk types that cause about 70% of cervical cancers and precancerous cervical lesions, according to the World Health Organization. However, there are three HPV vaccines – 9-valent HPV vaccine (Gardasil), quadrivalent HPV vaccine (Gardasil®, 4vHPV), and bivalent HPV vaccine (Cervarix) – that help protect against HPV 16/18.
The findings strengthen the benefits of HPV vaccination, Dr. Trottier explained. “There is no cure when the HPV infection is present,” Dr. Trottier said. “If the link [between preterm birth and HPV infections] is indeed causal, we can expect a greater risk of preterm delivery in these women. The effective tool we have is the HPV vaccination, but it should ideally be received before the start of sexual activity in order to prevent future infections that could occur in women.”
The American College of Obstetricians and Gynecologists recommends HPV vaccination for girls and women between the ages of 11 and 26 years old. However, Dr. Tanner said, women aged 27-45 who were previously unvaccinated may still receive benefit from the vaccine.
“Despite the known efficacy of the vaccine, only 50% of patients are up to date with their HPV vaccination,” Dr. Tanner explained. “This study further highlights the need to educate and encourage patients to be vaccinated.”
The researchers said future studies should investigate the association of HPV vaccination and vaccination programs with the risk of preterm birth.
The experts disclosed no conflicts of interest.
Persistent human papillomavirus (HPV) 16 and HPV 18 during a pregnancy may be associated with an increased risk of premature birth.
Findings published online in JAMA Network Open found that 15.9% of individuals who had a persistent HPV 16 or 18 infection during the first and third trimesters of their pregnancy gave birth prematurely, compared with 5.6% of those who did not have an HPV infection at all.
The findings prompted the question of “the pathophysiology of HPV in pregnancy and how the virus is affecting the placenta,” said Lisette Davidson Tanner, MD, MPH, FACOG, who was not involved in the study.
Researchers said the findings are the first to show the association between preterm birth and HPV, which is an incurable virus that most sexually active individuals will get at some point in their lives, according to the Centers for Disease Control and Prevention.
“The results of this study are very important in helping us understand the burden caused by HPV in pregnancy,” study author Helen Trottier, MSc, PhD, researcher at the Centre Hospitalier Universitaire Sainte-Justine, said in an interview. “We may have just pinpointed an important cause of preterm birth that has so far been unexplained.”
Dr. Trottier and colleagues examined data from 1,052 pregnant women from three university-affiliated health care centers in Montreal between Nov. 8, 2010, and Oct. 16, 2016.
Only 5.6% of those who did not have an HPV infection had a premature birth, compared with 6.9% of those who tested positive for any HPV infection in the first trimester.
When looking at the first trimester, researchers found 12% of those diagnosed with HPV 16 and 18 had a preterm birth, compared to 4.9% of those who had a high-risk HPV infection other than HPV 16/18. When looking at the third trimester, researchers found that 15.9% of those with HPV 16/18 had an increased risk of giving birth prematurely, compared to those who had other high-risk HPV infections.
When researchers looked at the persistence of these HPV infections, they found that most HPV infections detected in the first trimester persist to the third trimester. The findings also revealed that persistent vaginal HPV 16/18 detection was significantly associated with all preterm births and spontaneous preterm births. This association was also found among those who had HPV infections detected in their placentas.
Meanwhile, 5.8% of those who had an HPV infection only during the first trimester experienced a preterm birth.
The researchers also found that HPV infections were frequent in pregnancy even among populations “considered to be at low risk based on sociodemographic and sexual history characteristics,” they wrote. Dr. Trottier said she hopes the findings will strengthen support for HPV vaccination.
Dr. Trottier’s study adds to a growing body of research regarding the adverse effects of HPV, according to Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “It is already well known that HPV is associated with a number of anogenital and oropharyngeal cancers,” Dr. Tanner said in an interview. “The potential association with preterm birth only adds weight to the recommendations to screen for and prevent HPV infection.”
HPV 16 and 18 are high-risk types that cause about 70% of cervical cancers and precancerous cervical lesions, according to the World Health Organization. However, there are three HPV vaccines – 9-valent HPV vaccine (Gardasil), quadrivalent HPV vaccine (Gardasil®, 4vHPV), and bivalent HPV vaccine (Cervarix) – that help protect against HPV 16/18.
The findings strengthen the benefits of HPV vaccination, Dr. Trottier explained. “There is no cure when the HPV infection is present,” Dr. Trottier said. “If the link [between preterm birth and HPV infections] is indeed causal, we can expect a greater risk of preterm delivery in these women. The effective tool we have is the HPV vaccination, but it should ideally be received before the start of sexual activity in order to prevent future infections that could occur in women.”
The American College of Obstetricians and Gynecologists recommends HPV vaccination for girls and women between the ages of 11 and 26 years old. However, Dr. Tanner said, women aged 27-45 who were previously unvaccinated may still receive benefit from the vaccine.
“Despite the known efficacy of the vaccine, only 50% of patients are up to date with their HPV vaccination,” Dr. Tanner explained. “This study further highlights the need to educate and encourage patients to be vaccinated.”
The researchers said future studies should investigate the association of HPV vaccination and vaccination programs with the risk of preterm birth.
The experts disclosed no conflicts of interest.
Persistent human papillomavirus (HPV) 16 and HPV 18 during a pregnancy may be associated with an increased risk of premature birth.
Findings published online in JAMA Network Open found that 15.9% of individuals who had a persistent HPV 16 or 18 infection during the first and third trimesters of their pregnancy gave birth prematurely, compared with 5.6% of those who did not have an HPV infection at all.
The findings prompted the question of “the pathophysiology of HPV in pregnancy and how the virus is affecting the placenta,” said Lisette Davidson Tanner, MD, MPH, FACOG, who was not involved in the study.
Researchers said the findings are the first to show the association between preterm birth and HPV, which is an incurable virus that most sexually active individuals will get at some point in their lives, according to the Centers for Disease Control and Prevention.
“The results of this study are very important in helping us understand the burden caused by HPV in pregnancy,” study author Helen Trottier, MSc, PhD, researcher at the Centre Hospitalier Universitaire Sainte-Justine, said in an interview. “We may have just pinpointed an important cause of preterm birth that has so far been unexplained.”
Dr. Trottier and colleagues examined data from 1,052 pregnant women from three university-affiliated health care centers in Montreal between Nov. 8, 2010, and Oct. 16, 2016.
Only 5.6% of those who did not have an HPV infection had a premature birth, compared with 6.9% of those who tested positive for any HPV infection in the first trimester.
When looking at the first trimester, researchers found 12% of those diagnosed with HPV 16 and 18 had a preterm birth, compared to 4.9% of those who had a high-risk HPV infection other than HPV 16/18. When looking at the third trimester, researchers found that 15.9% of those with HPV 16/18 had an increased risk of giving birth prematurely, compared to those who had other high-risk HPV infections.
When researchers looked at the persistence of these HPV infections, they found that most HPV infections detected in the first trimester persist to the third trimester. The findings also revealed that persistent vaginal HPV 16/18 detection was significantly associated with all preterm births and spontaneous preterm births. This association was also found among those who had HPV infections detected in their placentas.
Meanwhile, 5.8% of those who had an HPV infection only during the first trimester experienced a preterm birth.
The researchers also found that HPV infections were frequent in pregnancy even among populations “considered to be at low risk based on sociodemographic and sexual history characteristics,” they wrote. Dr. Trottier said she hopes the findings will strengthen support for HPV vaccination.
Dr. Trottier’s study adds to a growing body of research regarding the adverse effects of HPV, according to Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “It is already well known that HPV is associated with a number of anogenital and oropharyngeal cancers,” Dr. Tanner said in an interview. “The potential association with preterm birth only adds weight to the recommendations to screen for and prevent HPV infection.”
HPV 16 and 18 are high-risk types that cause about 70% of cervical cancers and precancerous cervical lesions, according to the World Health Organization. However, there are three HPV vaccines – 9-valent HPV vaccine (Gardasil), quadrivalent HPV vaccine (Gardasil®, 4vHPV), and bivalent HPV vaccine (Cervarix) – that help protect against HPV 16/18.
The findings strengthen the benefits of HPV vaccination, Dr. Trottier explained. “There is no cure when the HPV infection is present,” Dr. Trottier said. “If the link [between preterm birth and HPV infections] is indeed causal, we can expect a greater risk of preterm delivery in these women. The effective tool we have is the HPV vaccination, but it should ideally be received before the start of sexual activity in order to prevent future infections that could occur in women.”
The American College of Obstetricians and Gynecologists recommends HPV vaccination for girls and women between the ages of 11 and 26 years old. However, Dr. Tanner said, women aged 27-45 who were previously unvaccinated may still receive benefit from the vaccine.
“Despite the known efficacy of the vaccine, only 50% of patients are up to date with their HPV vaccination,” Dr. Tanner explained. “This study further highlights the need to educate and encourage patients to be vaccinated.”
The researchers said future studies should investigate the association of HPV vaccination and vaccination programs with the risk of preterm birth.
The experts disclosed no conflicts of interest.
FROM JAMA NETWORK OPEN
Infants breathe better when pregnant moms exercise
Lung function in early infancy may be influenced by the mother’s level of physical activity during pregnancy, results of a study from Sweden suggest.
Low-lung function at 3 months of age, as measured by the ratio of time to peak tidal expiratory flow to expiratory time (tPTEF/tE), was more frequent among children whose mothers were physically inactive during the first half of pregnancy compared with those who exercised either moderately or strenuously, reported Hrefna Katrin Gudmundsdottir, MD, a pediatrician and PhD candidate at the University of Oslo, Norway. The results were based on a prospective observational study of 841 mother-child pairs.
“The potential link between maternal inactivity and low lung function in infancy adds to the importance of advising pregnant women and women of childbearing age on physical activity,” she said in an oral abstract presented during the virtual European Respiratory Society (ERS) International Congress.
Jonathan Grigg, MD, professor of pediatric respiratory and environmental medicine at Queen Mary University of London, who was not involved in the study, commented that it “offers a fascinating hint that increased physical activity of mothers is associated with better lung function in their babies and, therefore, possibly their health in later life. More research is needed to confirm this link, but it is important that women feel supported by their health care providers to be active in a way that is comfortable and accessible to them.”
Impaired lung function in infancy is associated with wheezing and asthma in childhood, and lower lung function later in life, Dr. Gudmundsdottir said. She also noted that impaired lung function begins in utero and is related to fetal and infant size, family history of asthma, and/or maternal smoking.
Physical activity during pregnancy has been demonstrated to reduce the risk of preterm birth and cesarean birth and of children being born either abnormally small or abnormally large for their gestational age, she explained.
To see where physical inactivity in the first half of pregnancy is associated with lower lung function in otherwise healthy 3-month old infants, Dr. Gudmundsdottir and colleagues looked at data on a mother-child cohort from the prospective population-based PreventADALL study, which was designed to study prevention of atopic dermatitis and allergies in children in Norway and Sweden.
A total of 814 infants (49% female) had available measures of tidal flow volume in the awake state at 3 months, as well as mother-reported data on physical activity at 18 weeks of pregnancy.
The investigators categorized the mothers as inactive, with either no or only low-intensity physical activity, “fairly” active, or “very” active based on self reporting.
The average tPTEF/tE value among all infants in the study was 0.391. The average value for 290 infants born to inactive mothers was 0.387, compared with 0.394 for 299 infants born to very active mothers, a difference that was not statistically significant.
Maternal physical activity level was not significantly associated with continuous tPTEF/tE, but the investigators did find that the offspring of inactive mothers were significantly more likely than the children of fairly or very active mothers to have a tPTEF/tE below 0.25 in both univariate analysis (odds ratio, 2.15; P = .011), and in multivariate analysis controlling for maternal age, education, parity, prepregnancy body-mass index, parental atopy, and in-utero exposure to nicotine (OR, 2.18; P = .013).
In univariate but not multivariate analysis, children of inactive mothers were significantly more likely than infants of more active mothers to have tPTEF/tE values below the 50th percentile (OR, 1.35; P = .042).
“We observed a trend that adds to the importance of advising women of childbearing age and pregnant women about physical activity. However, there may be factors that affect both maternal physical activity and lung function in offspring that we have not accounted for and could affect the results, so more research is needed,” Dr. Gudmundsdottir said in a statement.
Dr. Grigg pointed out that “it’s also worth keeping in mind that the single most important thing that mothers can do for their own health and that of their baby is to ensure that they do not smoke or use other tobacco products before, during, and after pregnancy. A smoke-free home has the biggest impact on lung function and health in childhood and later life.”
The study was supported by the University of Oslo. Dr. Gudmundsdottir and Dr. Grigg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Lung function in early infancy may be influenced by the mother’s level of physical activity during pregnancy, results of a study from Sweden suggest.
Low-lung function at 3 months of age, as measured by the ratio of time to peak tidal expiratory flow to expiratory time (tPTEF/tE), was more frequent among children whose mothers were physically inactive during the first half of pregnancy compared with those who exercised either moderately or strenuously, reported Hrefna Katrin Gudmundsdottir, MD, a pediatrician and PhD candidate at the University of Oslo, Norway. The results were based on a prospective observational study of 841 mother-child pairs.
“The potential link between maternal inactivity and low lung function in infancy adds to the importance of advising pregnant women and women of childbearing age on physical activity,” she said in an oral abstract presented during the virtual European Respiratory Society (ERS) International Congress.
Jonathan Grigg, MD, professor of pediatric respiratory and environmental medicine at Queen Mary University of London, who was not involved in the study, commented that it “offers a fascinating hint that increased physical activity of mothers is associated with better lung function in their babies and, therefore, possibly their health in later life. More research is needed to confirm this link, but it is important that women feel supported by their health care providers to be active in a way that is comfortable and accessible to them.”
Impaired lung function in infancy is associated with wheezing and asthma in childhood, and lower lung function later in life, Dr. Gudmundsdottir said. She also noted that impaired lung function begins in utero and is related to fetal and infant size, family history of asthma, and/or maternal smoking.
Physical activity during pregnancy has been demonstrated to reduce the risk of preterm birth and cesarean birth and of children being born either abnormally small or abnormally large for their gestational age, she explained.
To see where physical inactivity in the first half of pregnancy is associated with lower lung function in otherwise healthy 3-month old infants, Dr. Gudmundsdottir and colleagues looked at data on a mother-child cohort from the prospective population-based PreventADALL study, which was designed to study prevention of atopic dermatitis and allergies in children in Norway and Sweden.
A total of 814 infants (49% female) had available measures of tidal flow volume in the awake state at 3 months, as well as mother-reported data on physical activity at 18 weeks of pregnancy.
The investigators categorized the mothers as inactive, with either no or only low-intensity physical activity, “fairly” active, or “very” active based on self reporting.
The average tPTEF/tE value among all infants in the study was 0.391. The average value for 290 infants born to inactive mothers was 0.387, compared with 0.394 for 299 infants born to very active mothers, a difference that was not statistically significant.
Maternal physical activity level was not significantly associated with continuous tPTEF/tE, but the investigators did find that the offspring of inactive mothers were significantly more likely than the children of fairly or very active mothers to have a tPTEF/tE below 0.25 in both univariate analysis (odds ratio, 2.15; P = .011), and in multivariate analysis controlling for maternal age, education, parity, prepregnancy body-mass index, parental atopy, and in-utero exposure to nicotine (OR, 2.18; P = .013).
In univariate but not multivariate analysis, children of inactive mothers were significantly more likely than infants of more active mothers to have tPTEF/tE values below the 50th percentile (OR, 1.35; P = .042).
“We observed a trend that adds to the importance of advising women of childbearing age and pregnant women about physical activity. However, there may be factors that affect both maternal physical activity and lung function in offspring that we have not accounted for and could affect the results, so more research is needed,” Dr. Gudmundsdottir said in a statement.
Dr. Grigg pointed out that “it’s also worth keeping in mind that the single most important thing that mothers can do for their own health and that of their baby is to ensure that they do not smoke or use other tobacco products before, during, and after pregnancy. A smoke-free home has the biggest impact on lung function and health in childhood and later life.”
The study was supported by the University of Oslo. Dr. Gudmundsdottir and Dr. Grigg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Lung function in early infancy may be influenced by the mother’s level of physical activity during pregnancy, results of a study from Sweden suggest.
Low-lung function at 3 months of age, as measured by the ratio of time to peak tidal expiratory flow to expiratory time (tPTEF/tE), was more frequent among children whose mothers were physically inactive during the first half of pregnancy compared with those who exercised either moderately or strenuously, reported Hrefna Katrin Gudmundsdottir, MD, a pediatrician and PhD candidate at the University of Oslo, Norway. The results were based on a prospective observational study of 841 mother-child pairs.
“The potential link between maternal inactivity and low lung function in infancy adds to the importance of advising pregnant women and women of childbearing age on physical activity,” she said in an oral abstract presented during the virtual European Respiratory Society (ERS) International Congress.
Jonathan Grigg, MD, professor of pediatric respiratory and environmental medicine at Queen Mary University of London, who was not involved in the study, commented that it “offers a fascinating hint that increased physical activity of mothers is associated with better lung function in their babies and, therefore, possibly their health in later life. More research is needed to confirm this link, but it is important that women feel supported by their health care providers to be active in a way that is comfortable and accessible to them.”
Impaired lung function in infancy is associated with wheezing and asthma in childhood, and lower lung function later in life, Dr. Gudmundsdottir said. She also noted that impaired lung function begins in utero and is related to fetal and infant size, family history of asthma, and/or maternal smoking.
Physical activity during pregnancy has been demonstrated to reduce the risk of preterm birth and cesarean birth and of children being born either abnormally small or abnormally large for their gestational age, she explained.
To see where physical inactivity in the first half of pregnancy is associated with lower lung function in otherwise healthy 3-month old infants, Dr. Gudmundsdottir and colleagues looked at data on a mother-child cohort from the prospective population-based PreventADALL study, which was designed to study prevention of atopic dermatitis and allergies in children in Norway and Sweden.
A total of 814 infants (49% female) had available measures of tidal flow volume in the awake state at 3 months, as well as mother-reported data on physical activity at 18 weeks of pregnancy.
The investigators categorized the mothers as inactive, with either no or only low-intensity physical activity, “fairly” active, or “very” active based on self reporting.
The average tPTEF/tE value among all infants in the study was 0.391. The average value for 290 infants born to inactive mothers was 0.387, compared with 0.394 for 299 infants born to very active mothers, a difference that was not statistically significant.
Maternal physical activity level was not significantly associated with continuous tPTEF/tE, but the investigators did find that the offspring of inactive mothers were significantly more likely than the children of fairly or very active mothers to have a tPTEF/tE below 0.25 in both univariate analysis (odds ratio, 2.15; P = .011), and in multivariate analysis controlling for maternal age, education, parity, prepregnancy body-mass index, parental atopy, and in-utero exposure to nicotine (OR, 2.18; P = .013).
In univariate but not multivariate analysis, children of inactive mothers were significantly more likely than infants of more active mothers to have tPTEF/tE values below the 50th percentile (OR, 1.35; P = .042).
“We observed a trend that adds to the importance of advising women of childbearing age and pregnant women about physical activity. However, there may be factors that affect both maternal physical activity and lung function in offspring that we have not accounted for and could affect the results, so more research is needed,” Dr. Gudmundsdottir said in a statement.
Dr. Grigg pointed out that “it’s also worth keeping in mind that the single most important thing that mothers can do for their own health and that of their baby is to ensure that they do not smoke or use other tobacco products before, during, and after pregnancy. A smoke-free home has the biggest impact on lung function and health in childhood and later life.”
The study was supported by the University of Oslo. Dr. Gudmundsdottir and Dr. Grigg have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Medical power couple launch robot that helps in the labor room
Medical Power Couples is a new series highlighting spouses or domestic partners prominent in health care. Both have achieved high-level professional success and have made significant contributions to their respective fields.
Julie Shah, PhD, and Neel Shah, MD
Ob.gyn. Neel Shah was telling his wife how challenging it was for labor and delivery nurses to make room assignments: to delegate available beds, predict the timing of patient progression from one room to another, and pair patients with staff nurses, equipment, and resources.
Julie Shah, a roboticist with Massachusetts Institute of Technology, Cambridge, compared the head nurses to air traffic controllers, but without near the decision support. Julie had previously worked for aerospace giant Boeing, where she helped design a set of algorithmic techniques to give decision support to manufacturing personnel and embed robots to aid their work.
Suddenly the Shahs had an idea.
The robot, tested in 2018 at a Boston tertiary care center, produced high-quality recommendations accepted by nurses and physicians 90% of the time. The android was taught to observe actual performances of human tasks – what was done and not done in certain situations – and develop a scheduling policy. The Shahs and their team were the first to field a robotic system on a labor and delivery unit to aid in the coordination of resources required for patient care.
“For the first time, we were able to develop a novel machine-learning technique that could learn from demonstration or observation, heuristics, or strategies for solving resource allocation and scheduling problems, which was really exciting,” Julie said. “We were able to show also how that system could be embedded to offer decision support to reduce the cognitive burden of nurses.”
Neel and Julie joke that their first collaboration dates back to middle school when they sang together in chorus. The Shahs grew up in the same small New Jersey town and met as 14-year-olds.
Though the Shahs have known each other more than half their lives, they haven’t always lived side by side. After they married, Julie accepted an opportunity in Seattle, while Neel remained 3,000 miles away in Boston.
“He does all the cooking, so I did not eat well,” Julie recalled with a laugh. “It was not great.”
“I don’t self-regulate well,” Neel adds. “I just worked 24/7. I started a nonprofit that year, so externally, it looked like I was crushing it, but …”
“He was lonely,” Julie says.
Now back in the same city, the Shahs are doting parents to two toddlers aged 2 and 4, and also serve as heads of house at an MIT graduate dorm.
Julie, 39, is an associate professor in the department of aeronautics and astronautics at MIT and leads the Interactive Robotics Group of the Computer Science and Artificial Intelligence Laboratory. She is renowned for her innovative methods for enabling fluid human-robot teamwork in time- and safety-critical environments such as surgery, manufacturing, and space exploration. In 2014, she was recognized by the MIT Technology Review as one of the world’s top innovators under 35, and her work on industrial human-robot collaboration was recognized as one of the 10 breakthrough technologies of 2013.
Neel, 39, is an assistant professor of obstetrics, gynecology and reproductive biology at Harvard Medical School in Boston and chief medical officer of Maven Clinic, a virtual clinic for women’s and family health. A scientist and entrepreneur, Neel is globally recognized for designing solutions to improve health care. He is founder of Costs of Care, an NGO that curates insights from clinicians and patients to help delivery systems provide better care.
He also cofounded the March for Moms Association, a coalition of organizations that works to raise public and private investment in mothers’ well-being. Most recently, Neel and his team designed TeamBirth, an intrapartum care process that aims to improve the safety and dignity of childbirth care and promote communication and teamwork.
The Shahs say their personalities are sometimes opposite, but that they balance each other well.
“Julie thinks in lists, which sometimes drives me crazy, and I think in exploding clouds, which I think drives her crazy, but the combination usually works out,” Neel said. “We seem to be good complements for each other.”
In their own words
What is one food that your spouse eats that you can’t stand?
Neel: She eats raisins, and I hate raisins. Raisins are a crime against humanity. They’re wrong. The chocolate-covered raisins are even grosser.
What is one parenting difference you have?
Julie: Safety. I hover around the kids around safety hazards, and Neel is very relaxed.
What’s one quirky thing about your partner?
Neel: She has a parrot that predates our marriage. He started out as an illegal dorm bird. He just screeches and poops. If you’re developing a character in a book or a movie and you want to make them seem slightly off, you make them a bird owner. Think about it.
Julie: He’s 19 and his name is Bolivar, after the South American revolutionary. He’s very sweet.
Neel: I live in a Hitchcock movie.
If you weren’t a physician/scientist, what is a dream job you might have?
Julie: I would be a dolphin trainer. That was my childhood dream.
Neel: I’d want to do something creative. I’ve always wanted to be a better musician. I play the guitar and piano.
A version of this article first appeared on Medscape.com.
Medical Power Couples is a new series highlighting spouses or domestic partners prominent in health care. Both have achieved high-level professional success and have made significant contributions to their respective fields.
Julie Shah, PhD, and Neel Shah, MD
Ob.gyn. Neel Shah was telling his wife how challenging it was for labor and delivery nurses to make room assignments: to delegate available beds, predict the timing of patient progression from one room to another, and pair patients with staff nurses, equipment, and resources.
Julie Shah, a roboticist with Massachusetts Institute of Technology, Cambridge, compared the head nurses to air traffic controllers, but without near the decision support. Julie had previously worked for aerospace giant Boeing, where she helped design a set of algorithmic techniques to give decision support to manufacturing personnel and embed robots to aid their work.
Suddenly the Shahs had an idea.
The robot, tested in 2018 at a Boston tertiary care center, produced high-quality recommendations accepted by nurses and physicians 90% of the time. The android was taught to observe actual performances of human tasks – what was done and not done in certain situations – and develop a scheduling policy. The Shahs and their team were the first to field a robotic system on a labor and delivery unit to aid in the coordination of resources required for patient care.
“For the first time, we were able to develop a novel machine-learning technique that could learn from demonstration or observation, heuristics, or strategies for solving resource allocation and scheduling problems, which was really exciting,” Julie said. “We were able to show also how that system could be embedded to offer decision support to reduce the cognitive burden of nurses.”
Neel and Julie joke that their first collaboration dates back to middle school when they sang together in chorus. The Shahs grew up in the same small New Jersey town and met as 14-year-olds.
Though the Shahs have known each other more than half their lives, they haven’t always lived side by side. After they married, Julie accepted an opportunity in Seattle, while Neel remained 3,000 miles away in Boston.
“He does all the cooking, so I did not eat well,” Julie recalled with a laugh. “It was not great.”
“I don’t self-regulate well,” Neel adds. “I just worked 24/7. I started a nonprofit that year, so externally, it looked like I was crushing it, but …”
“He was lonely,” Julie says.
Now back in the same city, the Shahs are doting parents to two toddlers aged 2 and 4, and also serve as heads of house at an MIT graduate dorm.
Julie, 39, is an associate professor in the department of aeronautics and astronautics at MIT and leads the Interactive Robotics Group of the Computer Science and Artificial Intelligence Laboratory. She is renowned for her innovative methods for enabling fluid human-robot teamwork in time- and safety-critical environments such as surgery, manufacturing, and space exploration. In 2014, she was recognized by the MIT Technology Review as one of the world’s top innovators under 35, and her work on industrial human-robot collaboration was recognized as one of the 10 breakthrough technologies of 2013.
Neel, 39, is an assistant professor of obstetrics, gynecology and reproductive biology at Harvard Medical School in Boston and chief medical officer of Maven Clinic, a virtual clinic for women’s and family health. A scientist and entrepreneur, Neel is globally recognized for designing solutions to improve health care. He is founder of Costs of Care, an NGO that curates insights from clinicians and patients to help delivery systems provide better care.
He also cofounded the March for Moms Association, a coalition of organizations that works to raise public and private investment in mothers’ well-being. Most recently, Neel and his team designed TeamBirth, an intrapartum care process that aims to improve the safety and dignity of childbirth care and promote communication and teamwork.
The Shahs say their personalities are sometimes opposite, but that they balance each other well.
“Julie thinks in lists, which sometimes drives me crazy, and I think in exploding clouds, which I think drives her crazy, but the combination usually works out,” Neel said. “We seem to be good complements for each other.”
In their own words
What is one food that your spouse eats that you can’t stand?
Neel: She eats raisins, and I hate raisins. Raisins are a crime against humanity. They’re wrong. The chocolate-covered raisins are even grosser.
What is one parenting difference you have?
Julie: Safety. I hover around the kids around safety hazards, and Neel is very relaxed.
What’s one quirky thing about your partner?
Neel: She has a parrot that predates our marriage. He started out as an illegal dorm bird. He just screeches and poops. If you’re developing a character in a book or a movie and you want to make them seem slightly off, you make them a bird owner. Think about it.
Julie: He’s 19 and his name is Bolivar, after the South American revolutionary. He’s very sweet.
Neel: I live in a Hitchcock movie.
If you weren’t a physician/scientist, what is a dream job you might have?
Julie: I would be a dolphin trainer. That was my childhood dream.
Neel: I’d want to do something creative. I’ve always wanted to be a better musician. I play the guitar and piano.
A version of this article first appeared on Medscape.com.
Medical Power Couples is a new series highlighting spouses or domestic partners prominent in health care. Both have achieved high-level professional success and have made significant contributions to their respective fields.
Julie Shah, PhD, and Neel Shah, MD
Ob.gyn. Neel Shah was telling his wife how challenging it was for labor and delivery nurses to make room assignments: to delegate available beds, predict the timing of patient progression from one room to another, and pair patients with staff nurses, equipment, and resources.
Julie Shah, a roboticist with Massachusetts Institute of Technology, Cambridge, compared the head nurses to air traffic controllers, but without near the decision support. Julie had previously worked for aerospace giant Boeing, where she helped design a set of algorithmic techniques to give decision support to manufacturing personnel and embed robots to aid their work.
Suddenly the Shahs had an idea.
The robot, tested in 2018 at a Boston tertiary care center, produced high-quality recommendations accepted by nurses and physicians 90% of the time. The android was taught to observe actual performances of human tasks – what was done and not done in certain situations – and develop a scheduling policy. The Shahs and their team were the first to field a robotic system on a labor and delivery unit to aid in the coordination of resources required for patient care.
“For the first time, we were able to develop a novel machine-learning technique that could learn from demonstration or observation, heuristics, or strategies for solving resource allocation and scheduling problems, which was really exciting,” Julie said. “We were able to show also how that system could be embedded to offer decision support to reduce the cognitive burden of nurses.”
Neel and Julie joke that their first collaboration dates back to middle school when they sang together in chorus. The Shahs grew up in the same small New Jersey town and met as 14-year-olds.
Though the Shahs have known each other more than half their lives, they haven’t always lived side by side. After they married, Julie accepted an opportunity in Seattle, while Neel remained 3,000 miles away in Boston.
“He does all the cooking, so I did not eat well,” Julie recalled with a laugh. “It was not great.”
“I don’t self-regulate well,” Neel adds. “I just worked 24/7. I started a nonprofit that year, so externally, it looked like I was crushing it, but …”
“He was lonely,” Julie says.
Now back in the same city, the Shahs are doting parents to two toddlers aged 2 and 4, and also serve as heads of house at an MIT graduate dorm.
Julie, 39, is an associate professor in the department of aeronautics and astronautics at MIT and leads the Interactive Robotics Group of the Computer Science and Artificial Intelligence Laboratory. She is renowned for her innovative methods for enabling fluid human-robot teamwork in time- and safety-critical environments such as surgery, manufacturing, and space exploration. In 2014, she was recognized by the MIT Technology Review as one of the world’s top innovators under 35, and her work on industrial human-robot collaboration was recognized as one of the 10 breakthrough technologies of 2013.
Neel, 39, is an assistant professor of obstetrics, gynecology and reproductive biology at Harvard Medical School in Boston and chief medical officer of Maven Clinic, a virtual clinic for women’s and family health. A scientist and entrepreneur, Neel is globally recognized for designing solutions to improve health care. He is founder of Costs of Care, an NGO that curates insights from clinicians and patients to help delivery systems provide better care.
He also cofounded the March for Moms Association, a coalition of organizations that works to raise public and private investment in mothers’ well-being. Most recently, Neel and his team designed TeamBirth, an intrapartum care process that aims to improve the safety and dignity of childbirth care and promote communication and teamwork.
The Shahs say their personalities are sometimes opposite, but that they balance each other well.
“Julie thinks in lists, which sometimes drives me crazy, and I think in exploding clouds, which I think drives her crazy, but the combination usually works out,” Neel said. “We seem to be good complements for each other.”
In their own words
What is one food that your spouse eats that you can’t stand?
Neel: She eats raisins, and I hate raisins. Raisins are a crime against humanity. They’re wrong. The chocolate-covered raisins are even grosser.
What is one parenting difference you have?
Julie: Safety. I hover around the kids around safety hazards, and Neel is very relaxed.
What’s one quirky thing about your partner?
Neel: She has a parrot that predates our marriage. He started out as an illegal dorm bird. He just screeches and poops. If you’re developing a character in a book or a movie and you want to make them seem slightly off, you make them a bird owner. Think about it.
Julie: He’s 19 and his name is Bolivar, after the South American revolutionary. He’s very sweet.
Neel: I live in a Hitchcock movie.
If you weren’t a physician/scientist, what is a dream job you might have?
Julie: I would be a dolphin trainer. That was my childhood dream.
Neel: I’d want to do something creative. I’ve always wanted to be a better musician. I play the guitar and piano.
A version of this article first appeared on Medscape.com.